Medical Student Guide For Critical Thinking

Critical thinking is an essential cognitive skill for every individual but is a crucial component for healthcare professionals such as doctors, nurses and dentists. It is a skill that should be developed and trained, not just during your career as a doctor, but before that when you are still a medical student.
To be more effective in their studies, students must think their way through abstract problems, work in teams and separate high quality from low quality information. These are the same qualities that today's medical students are supposed to possess regardless of whether they graduate in the UK or study medicine in Europe .
In both well-defined and ill-defined medical emergencies, doctors are expected to make competent decisions. Critical thinking can help medical students and doctors achieve improved productivity, better clinical decision making, higher grades and much more.
This article will explain why critical thinking is a must for people in the medical field.

Definition of Critical Thinking
You can find a variety of definitions of Critical Thinking (CT). It is a term that goes back to the Ancient Greek philosopher Socrates and his teaching practice and vision. Critical thinking and its meaning have changed over the years, but at its core always will be the pursuit of proper judgment.
We can agree on one thing. Critical thinkers question every idea, assumption, and possibility rather than accepting them at once.
The most basic definition of CT is provided by Beyer (1995):
"Critical thinking means making reasoned judgements."
In other words, it is the ability to think logically about what to do and/or believe. It also includes the ability to think critically and independently. CT is the process of identifying, analysing, and then making decisions about a particular topic, advice, opinion or challenge that we are facing.
Steps to critical thinking
There is no universal standard for becoming a critical thinker. It is more like a unique journey for each individual. But as a medical student, you have already so much going on in your academic and personal life. This is why we created a list with 6 steps that will help you develop the necessary skills for critical thinking.
1. Determine the issue or question
The first step is to answer the following questions:
- What is the problem?
- Why is it important?
- Why do we need to find a solution?
- Who is involved?
By answering them, you will define the situation and acquire a deeper understanding of the problem and of any factors that may impact it.
Only after you have a clear picture of the issue and people involved can you start to dive deeper into the problem and search for a solution.
2. Research
Nowadays, we are flooded with information. We have an unlimited source of knowledge – the Internet.
Before choosing which medical schools to apply to, most applicants researched their desired schools online. Some of the areas you might have researched include:
- If the degree is recognised worldwide
- Tuition fees
- Living costs
- Entry requirements
- Competition for entry
- Number of exams
- Programme style
Having done the research, you were able to make an informed decision about your medical future based on the gathered information. Our list may be a little different to yours but that's okay. You know what factors are most important and relevant to you as a person.
The process you followed when choosing which medical school to apply to also applies to step 2 of critical thinking. As a medical student and doctor, you will face situations when you have to compare different arguments and opinions about an issue. Independent research is the key to the right clinical decisions. Medical and dentistry students have to be especially careful when learning from online sources. You shouldn't believe everything you read and take it as the absolute truth. So, here is what you need to do when facing a medical/study argument:
- Gather relevant information from all available reputable sources
- Pay attention to the salient points
- Evaluate the quality of the information and the level of evidence (is it just an opinion, or is it based upon a clinical trial?)
Once you have all the information needed, you can start the process of analysing it. It’s helpful to write down the strong and weak points of the various recommendations and identify the most evidence-based approach.
Here is an example of a comparison between two online course platforms , which shows their respective strengths and weaknesses.
When recommendations or conclusions are contradictory, you will need to make a judgement call on which point of view has the strongest level of evidence to back it up. You should leave aside your feelings and analyse the problem from every angle possible. In the end, you should aim to make your decision based on the available evidence, not assumptions or bias.
4. Be careful about confirmation bias
It is in our nature to want to confirm our existing ideas rather than challenge them. You should try your best to strive for objectivity while evaluating information.
Often, you may find yourself reading articles that support your ideas, but why not broaden your horizons by learning about the other viewpoint?
By doing so, you will have the opportunity to get closer to the truth and may even find unexpected support and evidence for your conclusion.
Curiosity will keep you on the right path. However, if you find yourself searching for information or confirmation that aligns only with your opinion, then it’s important to take a step back. Take a short break, acknowledge your bias, clear your mind and start researching all over.
5. Synthesis
As we have already mentioned a couple of times, medical students are preoccupied with their studies. Therefore, you have to learn how to synthesise information. This is where you take information from multiple sources and bring the information together. Learning how to do this effectively will save you time and help you make better decisions faster.
You will have already located and evaluated your sources in the previous steps. You now have to organise the data into a logical argument that backs up your position on the problem under consideration.
6. Make a decision
Once you have gathered and evaluated all the available evidence, your last step is to make a logical and well-reasoned conclusion.
By following this process you will ensure that whatever decision you make can be backed up if challenged
Why is critical thinking so important for medical students?
The first and most important reason for mastering critical thinking is that it will help you to avoid medical and clinical errors during your studies and future medical career.
Another good reason is that you will be able to identify better alternative options for diagnoses and treatments. You will be able to find the best solution for the patient as a whole which may be different to generic advice specific to the disease.
Furthermore, thinking critically as a medical student will boost your confidence and improve your knowledge and understanding of subjects.
In conclusion, critical thinking is a skill that can be learned and improved. It will encourage you to be the best version of yourself and teach you to take responsibility for your actions.
Critical thinking has become an essential for future health care professionals and you will find it an invaluable skill throughout your career.
We’ll keep you updated
The Premed Competencies for Entering Medical Students
New section.
Medical students must possess a broad range of competencies to successfully learn and develop in medical school and become effective physicians. The premed competency model includes professional, thinking and reasoning, and science competencies, and serves as a roadmap for students as they prepare to succeed in medical school.
The premed competencies, formerly core competencies for entering medical students (view previous competencies ), were updated in 2023 to reflect expectations for medical students. Medical schools will begin using these competencies in the 2024-2025 application cycle to evaluate applicants’ readiness for medical school. ( View the printer-friendly Premed Competencies .)
To learn how the premed competencies were updated in 2022-2023, read Refreshing the Premed Competencies: The Process Used to Update the Core Competencies for Entering Medical Students .
Practices continuous personal and professional growth for improvement, including setting and communicating goals for learning and development; reflects on successes, challenges, and mistakes; pursues opportunities to improve knowledge and understanding; and asks for and incorporates feedback to learn and grow.
Appreciates how historical, sociocultural, political, and economic factors affect others’ interactions, behaviors, and well-being; values diversity; and demonstrates a desire to learn about different cultures, beliefs, and values.
Seeks out and engages diverse and divergent perspectives with a desire to understand and willingness to adjust one’s mindset; understands a situation or idea from alternative viewpoints; reflects on one’s values, beliefs, and identities and how they may affect others; reflects on and addresses bias in oneself and others; and fosters a supportive environment that values inclusivity.
Effectively conveys information to others using spoken words and sentences; actively listens to understand the meaning and intent behind what others say; and recognizes potential communication barriers and adjusts approach or clarifies information as needed.
Demonstrates accountability for performance and responsibilities to self and others; prioritizes and fulfills obligations in a timely and satisfactory manner; and understands consequences of not fulfilling one’s responsibilities to self and others.
Shows a commitment to something larger than oneself; demonstrates dedication to service and a commitment to making meaningful contributions that meet the needs of communities.
Applies knowledge of the self, others, and social systems to solve problems related to the psychological, sociocultural, and biological factors that influence health and well-being.
Applies knowledge and skill in the natural sciences to solve problems related to molecular and macro systems, including biomolecules, molecules, cells, and organs.
Uses logic and reasoning to identify the strengths and weaknesses of alternative solutions, conclusions, or approaches to problems.
Applies quantitative reasoning and appropriate mathematics to describe or explain phenomena in the natural world.
Applies knowledge of the scientific process to integrate and synthesize information, solve problems, and formulate research questions and hypotheses; is facile in the language of the sciences and uses it to participate in the discourse of science and explain how scientific knowledge is discovered and validated.
Effectively conveys information to others by using written words and sentences.
Originally created in 2011, the premed competencies were updated in 2023 through a joint effort between the AAMC and members of the academic medicine community to reflect current and future expectations for new medical students. Medical school representatives across MD- and DO-granting schools from admissions, student affairs, diversity affairs, faculty, and students, as well as prehealth advisors and competency experts contributed. The 17 premed competencies highlight essential knowledge, abilities, and skills that medical schools consider to be important for entering medical students and evaluate in each applicant through a holistic review of the application.
- Architecture and Design
- Asian and Pacific Studies
- Business and Economics
- Classical and Ancient Near Eastern Studies
- Computer Sciences
- Cultural Studies
- Engineering
- General Interest
- Geosciences
- Industrial Chemistry
- Islamic and Middle Eastern Studies
- Jewish Studies
- Library and Information Science, Book Studies
- Life Sciences
- Linguistics and Semiotics
- Literary Studies
- Materials Sciences
- Mathematics
- Social Sciences
- Sports and Recreation
- Theology and Religion
- Publish your article
- The role of authors
- Promoting your article
- Abstracting & indexing
- Publishing Ethics
- Why publish with De Gruyter
- How to publish with De Gruyter
- Our book series
- Our subject areas
- Your digital product at De Gruyter
- Contribute to our reference works
- Product information
- Tools & resources
- Product Information
- Promotional Materials
- Orders and Inquiries
- FAQ for Library Suppliers and Book Sellers
- Repository Policy
- Free access policy
- Open Access agreements
- Database portals
- For Authors
- Customer service
- People + Culture
- Journal Management
- How to join us
- Working at De Gruyter
- Mission & Vision
- De Gruyter Foundation
- De Gruyter Ebound
- Our Responsibility
- Partner publishers

Your purchase has been completed. Your documents are now available to view.
A systematic review on critical thinking in medical education
Background:.
Critical thinking is the ability to raise discriminating questions in an attempt to search for better ideas, a deeper understanding and better solutions relating to a given issue.
This systematic review provides a summary of efforts that have been made to enhance and assess critical thinking in medical education.
Nine databases [Ovid MEDLINE(R), AMED, Academic Search Premier, ERIC, CINAHL, Web of Science, JSTOR, SCOPUS and PsycINFO] were searched to identify journal articles published from the start of each database to October 2012.
A total of 41 articles published from 1981 to 2012 were categorised into two main themes: (i) evaluation of current education on critical thinking and (ii) development of new strategies about critical thinking. Under each theme, the teaching strategies, assessment tools, uses of multimedia and stakeholders were analysed.
Discussion:
While a majority of studies developed teaching strategies and multimedia tools, a further examination of their quality and variety could yield some insights. The articles on assessment placed a greater focus on learning outcomes than on learning processes. It is expected that more research will be conducted on teacher development and students’ voices.
1. Scott JN, Markert RJ, Dunn, MM. Critical thinking: change during medical school and relationship to performance in clinical clerkships. Med Educ 1998;32:14–8. 10.1046/j.1365-2923.1998.00701.x Search in Google Scholar PubMed
2. Jenicek M, Croskerry P, Hitchcock DL. Evidence and its uses in health care and research: the role of critical thinking. Med Sci Monit 2011;17:RA12–7. 10.12659/MSM.881321 Search in Google Scholar PubMed
3. Holden RJ. Lean Thinking in emergency departments: a critical review. Ann Emerg Med 2011;57:265–78. 10.1016/j.annemergmed.2010.08.001 Search in Google Scholar PubMed
4. Finn P. Critical thinking: knowledge and skills for evidence-based practice. Lang Speech Hear Serv Sch 2011;42:69–72. 10.1044/0161-1461(2010/09-0037) Search in Google Scholar PubMed
5. Browne MN, Keeley SM. Asking the right questions. a guide to critical thinking. Englewood Cliffs, NJ: Prentice, 1990. Search in Google Scholar
6. Borglin G. Promoting critical thinking and academic writing skills in nurse education. Nurse Educ Today 2011;32:611–3. 10.1016/j.nedt.2011.06.009 Search in Google Scholar PubMed
7. Chang MJ, Chang YJ, Kuo SH, Yang YH, Chou FH. Relationships between critical thinking ability and nursing competence in clinical nurses. J Clin Nurs 2011;20:3224–32. 10.1111/j.1365-2702.2010.03593.x Search in Google Scholar PubMed
8. Rye KJ. Critical thinking in respiratory therapy. Respir Care 2011;56:364–5. 10.4187/respcare.01245 Search in Google Scholar PubMed
9. Jenkins SD. Cross-cultural perspectives on critical thinking. J Nurs Educ 2011;50:268–74. 10.3928/01484834-20110228-02 Search in Google Scholar PubMed
10. Kowalczyk N. Review of teaching methods and critical thinking skills. Radiol Technol 2011;83:120–32. Search in Google Scholar PubMed
11. Koontz NA, Gunderman RB. Radiation safety and medical education: development and integration of a dedicated educational module into a radiology clerkship, outcomes assessment, and survey of medical students’ perceptions. Acad Radiol 2012;19:491–7. 10.1016/j.acra.2011.12.013 Search in Google Scholar PubMed
12. Amgad M, Shash E, Gaafar R. Cancer education for medical students in developing countries: where do we stand and how to improve? Crit Rev Oncol Hematol 2012;84:122–9. 10.1016/j.critrevonc.2012.01.003 Search in Google Scholar PubMed
13. Ray S, Udumyan R, Rajput-Ray M, Thompson B, Lodge KM, et al. Evaluation of a novel nutrition education intervention for medical students from across England. Br Med J Open 2012;2:e000417–7. 10.1136/bmjopen-2011-000417 Search in Google Scholar PubMed PubMed Central
14. Brashers V, Owen J, Blackhall L, Erickson J, Peterson C. A program design for full integration and assessment of clinically relevant interprofessional education into the clinical/clerkship year for nursing and medical students. J Interprof Care 2012;26:242–4. 10.3109/13561820.2011.653610 Search in Google Scholar PubMed
15. Mutto EM, Cantoni MN, Rabhansl MM, Villar MJ. A perspective of end-of-life care education in undergraduate medical and nursing students in Buenos Aires, Argentina. J Palliat Med 2012;15:93–8. 10.1089/jpm.2011.0238 Search in Google Scholar PubMed
16. Chang YT, Hayter M, Wu SC. A systematic review and meta-ethnography of the qualitative literature: experiences of the menarche. J Clin Nurs 2010;19:447–60. 10.1111/j.1365-2702.2009.03019.x Search in Google Scholar PubMed
17. Glasziou P. Systematic reviews in health care: a practical guide. Cambridge, NY: Cambridge University Press, 2001. 10.1017/CBO9780511543500 Search in Google Scholar
18. Dluhy NM. Mapping knowledge in chronic illness. J Adv Nurs 1995;21:1051–8. 10.1046/j.1365-2648.1995.21061051.x Search in Google Scholar PubMed
19. Schreiber R, Crooks D, Stern PN. Qualitative meta-analysis. In: Morse JM, editor. Completing a qualitative project: details and dialogue. Thousand Oaks, CA: Sage Publications, 1997:311–26. Search in Google Scholar
20. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. PLoS Med 2009;6:e1000097–7. 10.1371/journal.pmed.1000097 Search in Google Scholar PubMed PubMed Central
21. Abdelmoneim I. Students perception of the various teaching methods used in the primary health care course in the Abha, College of Medicine. Saudi Med J 2003;24:1188–91. Search in Google Scholar
22. Abraham R, Ramnarayan K, Kamath A. Validating the effectiveness of Clinically Oriented Physiology Teaching (COPT) in undergraduate physiology curriculum. BMC Med Educ 2008;8:1–17. 10.1186/1472-6920-8-40 Search in Google Scholar PubMed PubMed Central
23. Abraham RR, Upadhya S, Torke S, Ramnarayan K. Student perspectives of assessment by TEMM model in physiology. Adv Physiol Educ 2005;29:94–7. 10.1152/advan.00051.2004 Search in Google Scholar PubMed
24. Abraham RR, Upadhya S, Torke S, Ramnarayan K. Clinically oriented physiology teaching: strategy for developing critical-thinking skills in undergraduate medical students. Adv Physiol Educ 2004;28:102–4. 10.1152/advan.00001.2004 Search in Google Scholar PubMed
25. Abraham RR, Kamath A, Upadhya S, Ramnarayan K. Learning approaches to physiology of undergraduates in an Indian medical school. Med Educ 2006;40:916–23. 10.1111/j.1365-2929.2006.02547.x Search in Google Scholar PubMed
26. Ahmed SA, Van DM. Student perception of peer critique of student-selected study components in a forensic medicine curriculum. J Med Biomed Sci 2010;11:22–30. Search in Google Scholar
27. Alur P, Fatima K, Joseph R. Medical teaching websites: do they reflect the learning paradigm? Med Teach 2002;24:422–4. 10.1080/01421590220145815 Search in Google Scholar PubMed
28. Alweshahi Y, Harley D, Cook DA. Students’ perception of the characteristics of effective bedside teachers. Med Teach 2007;29:204–9. 10.1080/01421590701271818 Search in Google Scholar PubMed
29. Antepohl W, Domeij E, Forsberg P, Ludvigsson J. A follow-up of medical graduates of a problem-based learning curriculum. Med Educ 2003;37:155–162. 10.1046/j.1365-2923.2003.01401.x Search in Google Scholar PubMed
30. Basu Roy R, McMahon GT. Video-based cases disrupt deep critical thinking in problem-based learning. Med Educ 2012;46:426–35. 10.1111/j.1365-2923.2011.04197.x Search in Google Scholar PubMed
31. Birgegård G, Lindquist U. Change in student attitudes to medical school after the introduction of problem-based learning in spite of low ratings. Med Educ 1998;32:46–9. 10.1046/j.1365-2923.1998.00157.x Search in Google Scholar PubMed
32. Chamberlain NR, Stuart MK, Singh VK, Sargentini NJ. Utilization of case presentations in medical microbiology to enhance relevance of basic science for medical students. Med Educ Online 2012;17. doi:10.3402/meo.v17i0.15943. 10.3402/meo.v17i0.15943 Search in Google Scholar PubMed PubMed Central
33. Curet MJ, Mennin SP. The effect of longterm vs shortterm tutors on the quality of the tutorial process and student performance. Adv Health Sci Educ 2003;8:117–26. 10.1023/A:1024991128083 Search in Google Scholar
34. D’Antoni AV, Zipp GP, Olson VG, Cahill TF. Does the mind map learning strategy facilitate information retrieval and critical thinking in medical students? BMC Med Educ 2010;10:1–10. 10.1186/1472-6920-10-61 Search in Google Scholar PubMed PubMed Central
35. de Leng BA, Dolmans DHJM, Jöbsis R, Muijtjens AMM, van der Vleuten CPM. Exploration of an e-learning model to foster critical thinking on basic science concepts during work placements. Comput Educ 2009;53:1–13. 10.1016/j.compedu.2008.12.012 Search in Google Scholar
36. Elizondo-Montemayor L, Cid-García A, Pérez-Rodríguez BA, Alarcón-Fuentes G, Pérez-García I, et al. Outcome-based national profile of Mexico’s medical graduates. Med Teach 2007;29:691–8. 10.1080/01421590701691411 Search in Google Scholar PubMed
37. Foster PJ. Clinical discussion groups: verbal participation and outcomes. J Med Educ 1981;56:831–8. 10.1097/00001888-198110000-00005 Search in Google Scholar PubMed
38. Graffam B. Deriving better questions: creating better clinical instruction. Clin Teach 2008;5:98–102. 10.1111/j.1743-498X.2008.00212.x Search in Google Scholar
39. Hoag K, Lillie J, Hoppe R. Piloting case-based instruction in a didactic clinical immunology course. Clin Lab Sci 2005;18:213–20. Search in Google Scholar
40. Kamin C, O’Sullivan P, Deterding R, Younger M. A comparison of critical thinking in groups of third-year medical students in text, video, and virtual PBL case modalities. Acad Med 2003;78:204–11. 10.1097/00001888-200302000-00018 Search in Google Scholar PubMed
41. Kamin C, O’Sullivan P, Younger M, Deterding R. Measuring critical thinking in problem-based learning discourse. Teach Learn Med 2001;13:27–35. 10.1207/S15328015TLM1301_6 Search in Google Scholar PubMed
42. Kim S, Kolko BE, Greer TH. Web-based problem solving learning: third-year medical students’ participation in end-of-life care virtual clinic. Comput Hum Behav 2002;18:761–72. 10.1016/S0747-5632(02)00029-8 Search in Google Scholar
43. Kumta SM, Tsang PL, Hung LK, Cheng JCY. Fostering critical thinking skills through a web-based tutorial programme for final year medical students – a randomized controlled study. J Educ Multimed Hypermed 2003;12:267–73. Search in Google Scholar
44. Lieberman SA, Trumble JM, Smith ER. The impact of structured student debates on critical thinking and informatics skills of second-year medical students. Acad Med 2000;75(10 Suppl):S84–6. 10.1097/00001888-200010001-00027 Search in Google Scholar PubMed
45. Lindblom-Ylänne S, Lonka K, Leskinen E. On the predictive value of entry-level skills for successful studying in medical school. High Educ 1999;37:239–58. 10.1023/A:1003574125457 Search in Google Scholar
46. Loy G, Gelula M, Vontver L. Teaching students to question. Obstet Gynecol 2004;191:1752–6. 10.1016/j.ajog.2004.07.071 Search in Google Scholar PubMed
47. Lumlertgul N, Kijpaisalratana N, Pityaratstian N, Wangsaturaka D. Cinemeducation: a pilot student project using movies to help students learn medical professionalism. Med Teach 2009;31:327–32. 10.1080/01421590802637941 Search in Google Scholar PubMed
48. Mala-Maung, Abdullah A, Abas ZW. Appreciation of learning environment and development of higher-order learning skills in a problem-based learning medical curriculum. Med J Malaysia 2011;66:435–9. Search in Google Scholar
49. Manzoor I, Mukhtar F, Hashmi NR. Medical students’ perspective about role-plays as a teaching strategy in community medicine. J Coll Physicians Surg Pak 2012;22:222–5. Search in Google Scholar PubMed
50. Miller DA, Sadler JZ, Mohl PC. Critical thinking in preclinical course examinations. Acad Med 1993;68:303–5. 10.1097/00001888-199304000-00020 Search in Google Scholar PubMed
51. Ortiz N, Pedrogo Y, Bonet N. Integration of high-fidelity simulator in third-year paediatrics clerkship. Clin Teach 2011;8:105–8. 10.1111/j.1743-498X.2011.00438.x Search in Google Scholar PubMed
52. Plack MM, Driscoll M, Marquez M, Greenberg L. Peer-facilitated virtual action learning: reflecting on critical incidents during a pediatric clerkship. Acad Pediatr 2010;10:146–52. 10.1016/j.acap.2009.11.007 Search in Google Scholar PubMed
53. Rehman R, Iqbal A, Rehan R. Do adults learn by experience; student’s perceptions and performance in neuro physiology lab course. Rawal Med J 2012;37:206–10. Search in Google Scholar
54. Saalu LC, Abraham AA, Aina WO. Quantitative evaluation of third year medical students’ perception and satisfaction from problem based learning in anatomy: a pilot study of the introduction of problem based learning into the traditional didactic medical curriculum in Nigeria. Educ Res Rev 2010;5:193–200. Search in Google Scholar
55. Scott JN, Markert RJ. Relationship between critical thinking skills and success in preclinical courses. Acad Med 1994;69:920–4. 10.1097/00001888-199411000-00015 Search in Google Scholar PubMed
56. Shafi R, Quadri KHM, Ahmed W, Mahmud SN, Iqbal M. Experience with a theme-based integrated renal module for a second-year MBBS class. Adv Physiol Educ 2010;34:15–9. 10.1152/advan.00069.2009 Search in Google Scholar PubMed
57. Taradi S, Taradi M. Expanding the traditional physiology class with asynchronous online discussions and collaborative projects. Adv Physiol Educ 2004;28:73–8. 10.1152/advan.00017.2003 Search in Google Scholar PubMed
58. Torok HM, Torre D, Elnicki DM. Themes and characteristics of medical students’ self-identified clerkship learning goals: a quasi-statistical qualitative study. Acad Med 2009;84(Suppl 10):S58–62. 10.1097/ACM.0b013e3181b38c71 Search in Google Scholar PubMed
59. Torre DM, Daley B, Stark-Schweitzer T, Siddartha S, Petkova J, et al. A qualitative evaluation of medical student learning with concept maps. Med Teach 2007;29:949–55. 10.1080/01421590701689506 Search in Google Scholar PubMed
60. Wee LE, Koh GC, Lim VKG. Caring for underserved patients through neighborhood health screening: outcomes of a longitudinal, interprofessional, student-run home visit program in Singapore. Acad Med 2011;86:829–39. 10.1097/ACM.0b013e31821d841d Search in Google Scholar PubMed
61. Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol 2008;8:45–54. 10.1186/1471-2288-8-45 Search in Google Scholar PubMed PubMed Central
62. Boyatzis RE. Transforming qualitative information: thematic analysis and code development. Thousand Oaks, CA: Sage Publications, 1998. Search in Google Scholar
63. Vuchetich PJ, Hamilton WR, Ahmad SO, Makoid MC. Analyzing course objectives: assessing critical thinking in the pharmacy curriculum. J Allied Health 2006;35:e253–75. Search in Google Scholar PubMed
64. Bulson JA, Bulson T. Nursing process and critical thinking linked to disaster preparedness. J Emerg Nurs 2011;37:477–83. 10.1016/j.jen.2010.07.011 Search in Google Scholar PubMed
65. Marchigiano G, Eduljee N, Harvey K. Developing critical thinking skills from clinical assignments: a pilot study on nursing students’ self-reported perceptions. J Nurs Manag 2011;19:143–52. 10.1111/j.1365-2834.2010.01191.x Search in Google Scholar PubMed
66. Hobaugh CF. Critical thinking skills: do we have any? Critical thinking skills of faculty teaching medical subjects in a military environment. US Army Med Dep J 2010;10–12:48–62. Search in Google Scholar
67. Helsdingen AS, van den Bosch K, van Gog T, van Merrienboer JJ. The effects of critical thinking instruction on training complex decision making. Hum Factors 2010;52:537–45. 10.1177/0018720810377069 Search in Google Scholar PubMed
68. Hwang SY, Yen M, Lee BO, Huang MC, Tseng HF. A critical thinking disposition scale for nurses: short form. J Clin Nurs 2010;19:3171–6. 10.1111/j.1365-2702.2010.03343.x Search in Google Scholar PubMed
Supplemental Material:
The online version of this article (DOI: https://doi.org/10.1515/ijamh-2015-0117 ) offers supplementary material, available to authorized users.
©2018 Walter de Gruyter GmbH, Berlin/Boston
- X / Twitter
Supplementary Materials
- Supplementary material
Please login or register with De Gruyter to order this product.
Journal and Issue
Articles in the same issue.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Educ Health Promot
The trend of critical thinking disposition in medical students and its relationship with their academic performance
Abdolhussein shakurnia.
Department of Immunology, Medical Faculty, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
Tayebe Fazelinia
1 Department of Medicine, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
Nasrin Khajeali
2 Department of Medical Education, Ahvaz Jundishapur University of Medical Science, Ahvaz, Iran
BACKGROUND:
Critical thinking is one of the important skills required for medical students. It is considered as a main component in medical education and training competent physicians. The current study aimed to investigate the trend of critical thinking disposition of medical students and its association with their academic performance.
MATERIALS AND METHODS:
This descriptive cross sectional study was conducted in 2019 on 315 medical students of Ahvaz Jundishapur University of Medical sciences. A two-section questionnaire was used for data collection. The first section dealt with demographic characteristics and the second section included Ricketts critical thinking disposition inventory using t -test, analysis of variance, and Pearson correlation coefficient.
Mean and standard deviation of critical thinking disposition of medical students was 121.85 ± 11.32. No significant difference was observed between the mean score of critical thinking disposition and years of study ( P = 0.74, F = 0.590). Pearson correlation test also showed no significant association between critical thinking disposition and the students’ grade point average ( P = 0.89, r = 0.007).
CONCLUSIONS:
The results of the current study showed that medical students’ level of critical thinking disposition is above average, and there is no significant correlation between critical thinking disposition and years of study and academic performance of the students. It seems that the educational process in medical school has not been effective in improving the level of students’ critical thinking disposition.
Introduction
Medical faculties involved in training of health-care manpower are always worried about improvement of quality of graduates in providing health care. Physicians in health-care system are faced with unprecedented problems in workplace to which there is no unique and absolutely correct answer. Therefore, they should often make clinical decisions regarding complicated matters with little guidance and limited time and resources. The problem-solving ability in patient bedside is invaluable. Critical thinking can provide a wider view, creative solutions, and multiple paths when dealing with problems.[ 1 , 2 , 3 ]
According to the evidences, critical thinking skills have been linked to improved patient outcomes, better quality patient care, and improved health outcomes in health-care system. Critical thinking is one the important skills in clinical decision-making. Reinforcement of critical thinking skill lets the physician provide the best health-care services by making informed decision.[ 4 , 5 ] In this regard, world federation for medical education (WFME) introduces critical thinking as the main skill for medical students to be achieved during their educational courses.[ 6 ]
Critical thinking is a reasonable, systematic, effective, logical, and outcome-based thinking which analyzes and investigates the information scientifically. Critical thinking consists of two aspects of skill and disposition. Aspect of skill of critical thinking emphasizes cognitive strategies. Without positive disposition regarding critical thinking, this type of thinking does not manifest itself, it is an attribute or habit of mind that is integrated into one's beliefs or actions to effectively solve problems and make decisions as a product of thinking.[ 7 , 8 ] Skills are not enough to enable a person to think critically; if that person does not have the disposition or motivation to do them, there will be no critical thinking.[ 9 ] Therefore, critical thinking disposition is a vital part of critical thinking process.
Since medical training system is now faced with many challenges in satisfying the expectations of society in promoting health. The necessity of training creative, thoughtful, and efficient graduates with high potential of decision-making is indispensable. Naturally, critical thinking provides this opportunity for physicians to provide more valuable services in caring process through making accurate decisions.[ 9 , 10 ]
Experts of medical education consider the development of critical thinking skills necessary for medical students to improve quality of medical education and introduce this skill as one of the medical education standards accreditation of schools of medicine.[ 4 , 11 ]
Training medical students to provide appropriate care for patients in today's developed world needs education which reinforces critical thinking. Therefore, to be aware of the quality of education provided in universities, it is necessary to evaluate the growth and development of critical thinking in students. Despite the importance of critical thinking in the educational process, the results of various studies indicate that in general, students’ ability to use critical thinking skills is low. The trend toward critical thinking in university students has yielded different results. Some studies have reported an increasing trend in the level of students “critical thinking and some other studies have reported a lack of difference in the level of students” critical thinking in different years and a descending trend.[ 12 , 13 , 14 , 15 ]
Training medical students to provide appropriate care for patients needs education which reinforces critical thinking. Therefore, to be aware of the quality of education provided in universities, it is necessary to evaluate the growth and development of critical thinking in students. The finding of Taheri et al. study showed a difference among critical thinking disposition of first and last semester and critical thinking disposition in students of last semester was greater than that of the first semester students.[ 12 ] Barkhordary, Shakurnia and Baniasad, and Kaya et al. in their studies on students of nursing and medicine found no significant statistical difference among critical thinking disposition based on the year of study.[ 13 , 14 , 15 ] Results of the study by Fathiazar et al. and Lei et al. indicate that the trend of mean critical thinking disposition in students is descending.[ 16 , 17 ] Numerous factors for the difference or lack of difference in critical thinking among students during study years in university are reported which necessitates performing further studies in this regard to clarify its reasons.[ 16 , 18 , 19 ]
Findings of the studies conducted on the relationship between critical thinking and educational performance have also showed different results. While some studies point to the positive association between critical thinking disposition and educational performance, results of other studies report lack of such association between these two variables.[ 20 , 21 , 22 ] Therefore, due to heterogeneity of results, further studies in this regard can be helpful. Given the importance and role of critical thinking in the future profession of medical students and in the diagnosis and treatment of diseases, and the necessity of having the ability to analyze and critically think in the complicated and vital environment of health system in which they will be employed after graduation, critical thinking is important for diagnosis and treatment of diseases due to , without critical thinking, physicians are prone to cognitive errors, Cognitive errors can lead to diagnostic errors, which result in increased patient morbidity and mortality.
A diagnostic errors leads to error treatment and since there is no comprehensive research regarding critical thinking disposition of medical students in this university, this study aimed to investigate the status of critical thinking disposition in students of medical fields, its trend during education in university, and its association with educational performance.
Materials and Methods
Study design and setting.
This research is a descriptive cross-sectional study which investigates the trend of critical thinking disposition and its association with educational performance of medical students.
Study participants and sampling
Study population was all medical students studying at Ahvaz Jundishapur University of Medical Sciences in academic year of 2019–2020, and their number was 1759 individuals based on the reports by educational office of the faculty of medicine.
Sample size in this study was estimated to be 317 using Morgan and Krejcie table. Due to probability of incomplete questionnaires and considering 5% of attrition rate, 332 students were considered as study sample.
Data collection tool and technique
Willingness to participate in the study and informed completion of the questionnaire were considered as inclusion criteria and lack of willingness to participate in the study and not completing the questionnaire were considered as exclusion criteria.
Data gathering tool in the study was a two-section questionnaire. The first section consists of demographic characteristics of students. The second section is the Ricketts critical thinking disposition inventory. This questionnaire is a self-assessment tool which examines critical thinking disposition in students. The questionnaire consists of 33 questions in three subscales of innovation (11 phrases); maturation (9 phrases) and involvement (13 phrases), and is graded as 5-scale Likert from[ 1 ] absolutely disagree to[ 5 ] absolutely agree.[ 23 ]
Validity and reliability of the questionnaire have been assessed and confirmed in previous studies.[ 24 ] In Iran, Pakmehr et al. confirmed the validity and reliability of the Persian version of the questionnaire using factorial analysis and calculating Cronbach's alpha coefficient.[ 25 ] In the current study, validity and reliability of the questionnaire were assessed using the opinion of experts (face validity) and calculating Cronbach's alpha coefficient, and Cronbach's alpha achieved for whole questionnaire was 0.828 and for items of innovation, maturation, and involvement, it was 0.730, 0.542, and 0.819, respectively.
Range of scores is among 33–165 with a mean of 99, and the score of 99 is considered an average level in assessment of the level of critical thinking disposition. These values are between 1 and 55 with an average of 33 for the subscale of innovation, between 9 and 45 with an average of 27 for the subscale of maturation, and between 13 and 65 with an average of 39 for the subscale of involvement.
In this study, the grade point average (GPA) value of the students was considered as index and criterion for assessment of educational achievement. Classification of students into two groups with high and low educational achievement based on cut-off point of GPA of students in this study which obtained at 15.93 was done.
The researcher uploaded the questionnaire to a website and sent its link for 332 medical students after obtaining ethical approval and permission from the school of medicine. After being briefed on the objectives of the study, the students were asked to respond the questions one by one and to send the filled questionnaire for the researcher.
The questionnaires were anonymous and the students were assured that their information would remain confidential.
To assess normality of the variables, Kolmogorov–Smirnov test was used. Result of this test showed that data distribution was normal ( P = 0.43). Data were analyzed after coding using SPSS version 18 (IBM Corporation, Armonk, NY, USA). To analyze data, descriptive, and inferential methods were used. Mean, standard deviation, and frequency were used to analyze data descriptively, and to compare groups, analysis of variance (ANOVA) and t -test were used. Pearson correlation coefficient was used to determine probable association between the students’ score of critical thinking disposition and their GPA. P < 0.05 was considered as statistically significant in all tests.
Ethical consideration
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all participants for being included in the study.
Most students were female (61%) and the rest were male (39%). The mean grade point average of the students was 15.91; 179 students had GPA higher than the mean value (57%). The mean total score of critical thinking disposition of the students was 121.85 ± 11.32.
Table 1 shows the mean and standard deviation of critical thinking disposition score and its subscales of innovation, maturation, and involvement. According to the findings, the mean score of critical thinking disposition was greater than the average in the students.
Mean and standard deviation of critical thinking disposition of medical students
SD=Standard deviation
ANOVA test showed no significant difference between the educational years and mean score of critical thinking disposition ( P = ‒0.74, F = 0.590).
Comparison of mean scores of students in subscales also showed no significant difference in the subscales except for maturation subscale which showed significant difference in various years of education ( F = 2.333, P = 0.032) [ Table 2 ].
Comparison of mean of critical thinking disposition of medical students by educational year
Out of the 332 questionnaires distributed among students, 315 questionnaires were completely filled and returned (response rate of 94.6%). Mean age of students was 23.43 years with standard deviation of 2.46 (19 to 29 years).
Mean of critical thinking disposition in males and females was 122.83 ± 11.44 and 121.23 ± 11.23, respectively. Comparing the mean scores of critical thinking disposition and its subscales using independent t -test showed no significant difference between critical thinking disposition by gender ( P = 0.22) [ Figure 1 ].

Mean scores of critical thinking disposition and its sub-scales during years of education
Mean scores of critical thinking disposition in students with low and high GPA were 122.13 ± 11.60 and 121.64 ± 11.60, respectively; and the result of independent t -test indicates that there is no significant difference between in two groups of students ( P = 0.70). Pearson correlation test also showed that there is no significant correlation between the students’ critical thinking disposition and GPA ( P = 0.89, r = 0.007).
In the current study that the trend of critical thinking disposition of medical students was evaluated, the results showed that mean score of critical thinking disposition of the medical students was 121.85 ± 11.32 which is greater than the average level, given the score range of 33–165. Results of the studies conducted in Tehran and Isfahan Universities of Medical Sciences also showed the level of critical thinking disposition of the medical students to be at an average level[ 12 , 26 ] which is in line with the current study. In explaining this result, it can be argued that medical students need to strengthen the level of their critical thinking disposition compared to other students. This is because the level of critical thinking disposition of medical students is far from the desired level and because in medical sciences, students’ future careers require the ability to solve problems and make decisions about patient problems to provide appropriate services. Therefore, appropriate measures need to be taken in educational programs so that this skill is maximized in these students.
Other results of the current study indicate that as medical students go to proceed in their educational programs, their score of critical thinking disposition does not increase. Although it is expected that the critical thinking disposition will increase in higher years of study at university when the students become more experienced, the findings indicate that there is no significant relationship between the critical thinking disposition and academic years. It seems that the educational process in medical school has not been effective in improving the level of students’ critical thinking disposition. Probably, since in the educational programs of medical students, the category of critical thinking disposition has not received special attention, and new educational facilities and methods of medical education are not employed to strengthen this principle. Not surprisingly, no significant difference in critical thinking disposition of students during the study period can be expected. In fact, neglecting the reinforcement of critical thinking disposition in medical education at university has led to unchanged in critical thinking disposition of students, which should be taken as a serious warning. Numerous factors can play a role in justifying the lack of growth in critical thinking disposition in universities, especially Iranian universities during the years of study. For example, in most universities, the lecture method is used predominantly in teaching and less emphasis on active teaching methods. Lecture as a dominant method, in many universities, promotes a passive method of teaching in which critical thinking is either only implicitly taught or barely taught. Researchers suggest that to improve the critical thinking disposition, teachers should pay more attention to active methods such as problem-based learning, simulation, concept map, and appropriate assessment methods.[ 4 , 26 ]
In field of medical sciences, researchers have compared the level of critical thinking disposition during years of education in medical students and have reported different results. The results of the current study were in line with the findings of the studies by Barkhordary, Shakurnia and Baniasad, Athari, and Kaya et al. which did not report any significant difference among critical thinking disposition and years of education.[ 10 , 13 , 14 , 15 ] However, our results are not in line with those of Taheri et al. [ 12 ] and Mslm[ 27 ] which reported an ascending trend between critical thinking disposition and years of education and those of Fathiazar et al. [ 16 ] and Huang et al. [ 28 ] which reported a descending trend. These discrepancies can be the result of factors such as training environment, training method, methods of assessment, and various cultural factors.
According to the results, there was no significant association between critical thinking disposition and educational performance. This issue can be a result of dominance of traditional training method of assessment of students in Iranian universities where in the assessment of students, the skill of critical thinking and analysis is not considered, and memorization is more emphasized. Ranjbar and Esmaili[ 29 ] investigated critical thinking disposition in nursing and midwifery students and its association with the educational status, and their results did not show any significant association, which was in line with the current study.
According to the findings of a research by Mirzaie and Mirzaie, there was a significant association between elements of curriculum and critical thinking disposition, such that reinforcing each of the elements of curriculum (content, objective, method, and assessment) was accompanied with reinforcement of critical thinking disposition in students.[ 30 ] Pakmehr et al. also showed that there is a significant association between quality of training and critical thinking disposition of the students.[ 31 ]
Therefore, any targeted attempt to promote quality of teaching methods should be performed considering other elements of medical curriculum. Importance of developing critical thinking skills is so important that some experts consider critical thinking as the major objective of university education and experiences and believe training is teaching critical thinking to the student.
Unfortunately, the methods of teaching and learning in the Iranian Universities pay more attention to increasing and strengthening memorization, and less to training and developing the skills of critical thinking. Therefore, to fulfill its mission, the higher education system needs to review the goals, content and educational materials, teaching-learning methods and assessment system, and everything related to the curriculum.
Limitation and recommendation
The most important limitation of this research is that the study sample was limited to medical students of Ahvaz Jundishapur University of Medical Sciences, so the generalizing of the results should be done cautiously. It is recommended to select a larger study sample from universities of medical sciences of the country in further studies. In addition, design of the current study was cross-sectional, and there is no possibility of assessment of changes in critical thinking disposition level in students from the entry to university until graduation.
Conclusions
The findings showed that critical thinking disposition in medical students is higher than average, and there is no significant association between critical thinking disposition and years of education and educational performance of the students. Given the positive relationship between curriculum elements and students’ critical thinking disposition, it is necessary to review the curriculum and its elements, especially in the field of teaching-learning strategies.
The curriculum should be organized in a way that strengthens the critical thinking disposition and skills of in medical students. It is suggested that more comprehensive research be conducted in other universities of medical sciences by considering other variables related to the critical thinking disposition to identify the factors and variables predicting the critical thinking disposition levels in students.
Financial support and sponsorship
Conflicts of interest.
There are no conflicts of interest.
Acknowledgements
This article was extracted from the thesis of the general physician degree with the code of IR.AJUMS.REC.1398.871 which was approved by Ethics Committee of Ahvaz Jundishapur University of Medical Sciences. Researchers appreciate the cooperation of all medical students of Ahvaz Jundishapur University of Medical Sciences who participated in this research.
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- Critical thinking in...
Critical thinking in healthcare and education
- Related content
- Peer review
- Jonathan M Sharples , professor 1 ,
- Andrew D Oxman , research director 2 ,
- Kamal R Mahtani , clinical lecturer 3 ,
- Iain Chalmers , coordinator 4 ,
- Sandy Oliver , professor 1 ,
- Kevan Collins , chief executive 5 ,
- Astrid Austvoll-Dahlgren , senior researcher 2 ,
- Tammy Hoffmann , professor 6
- 1 EPPI-Centre, UCL Department of Social Science, London, UK
- 2 Global Health Unit, Norwegian Institute of Public Health, Oslo, Norway
- 3 Centre for Evidence-Based Medicine, Oxford University, Oxford, UK
- 4 James Lind Initiative, Oxford, UK
- 5 Education Endowment Foundation, London, UK
- 6 Centre for Research in Evidence-Based Practice, Bond University, Gold Coast, Australia
- Correspondence to: J M Sharples Jonathan.Sharples{at}eefoundation.org.uk
Critical thinking is just one skill crucial to evidence based practice in healthcare and education, write Jonathan Sharples and colleagues , who see exciting opportunities for cross sector collaboration
Imagine you are a primary care doctor. A patient comes into your office with acute, atypical chest pain. Immediately you consider the patient’s sex and age, and you begin to think about what questions to ask and what diagnoses and diagnostic tests to consider. You will also need to think about what treatments to consider and how to communicate with the patient and potentially with the patient’s family and other healthcare providers. Some of what you do will be done reflexively, with little explicit thought, but caring for most patients also requires you to think critically about what you are going to do.
Critical thinking, the ability to think clearly and rationally about what to do or what to believe, is essential for the practice of medicine. Few doctors are likely to argue with this. Yet, until recently, the UK regulator the General Medical Council and similar bodies in North America did not mention “critical thinking” anywhere in their standards for licensing and accreditation, 1 and critical thinking is not explicitly taught or assessed in most education programmes for health professionals. 2
Moreover, although more than 2800 articles indexed by PubMed have “critical thinking” in the title or abstract, most are about nursing. We argue that it is important for clinicians and patients to learn to think critically and that the teaching and learning of these skills should be considered explicitly. Given the shared interest in critical thinking with broader education, we also highlight why healthcare and education professionals and researchers need to work together to enable people to think critically about the health choices they make throughout life.
Essential skills for doctors and patients
Critical thinking is not a new concept in education: at the beginning of the last century the US educational reformer John Dewey identified the need to help students “to think well.” 3 Critical thinking encompasses a broad set of skills and dispositions, including cognitive skills (such as analysis, inference, and self regulation); approaches to specific questions or problems (orderliness, diligence, and reasonableness); and approaches to life in general (inquisitiveness, concern with being well informed, and open mindedness). 4
An increasing body of evidence highlights that developing critical thinking skills can benefit academic outcomes as well as wider reasoning and problem solving capabilities. 5 For example, the Thinking, Doing, Talking Science programme trains teachers in a repertoire of strategies that encourage pupils to use critical thinking skills in primary school science lessons. An independently conducted randomised trial of this approach found that it had a positive impact on pupils’ science attainment, with signs that it was particularly beneficial for pupils from poorer families. 6
In medicine, increasing attention has been paid to “critical appraisal” in the past 40 years. Critical appraisal is a subset of critical thinking that focuses on how to use research evidence to inform health decisions. 7 8 9 The need for critical appraisal in medicine was recognised at least 75 years ago, 10 and critical appraisal has been recognised for some decades as an essential competency for healthcare professionals. 11 The General Medical Council’s Good Medical Practice guidance includes the need for doctors to be able to “provide effective treatments based on the best available evidence.” 12
If patients and the public are to make well informed health choices, they must also be able to assess the reliability of health claims and information. This is something that most people struggle to do, and it is becoming increasingly important because patients are taking on a bigger role in managing their health and making healthcare decisions, 13 while needing to cope with more and more health information, much of which is not reliable. 14 15 16 17
Teaching critical thinking
Although critical thinking skills are given limited explicit attention in standards for medical education, they are included as a key competency in most frameworks for national curriculums for primary and secondary schools in many countries. 18 Nonetheless, much health and science education, and education generally, still tends towards rote learning rather than the promotion of critical thinking. 19 20 This matters because the ability to think critically is an essential life skill relevant to decision making in many circumstances. The capacity to think critically is, like a lot of learning, developed in school and the home: parental influence creates advantage for pupils who live in homes where they are encouraged to think and talk about what they are doing. This, importantly, goes beyond simply completing tasks to creating deeper understanding of learning processes. As such, the “critical thinking gap” between children from disadvantaged communities and their more advantaged peers requires attention as early as possible.
Although it is possible to teach critical thinking to adults, it is likely to be more productive if the grounds for this have been laid down in an educational environment early in life, starting in primary school. Erroneous beliefs, attitudes, and behaviours developed during childhood may be difficult to change later. 21 22 This also applies to medical education and to health professionals. It becomes increasingly difficult to teach these skills without a foundation to build on and adequate time to learn them.
Strategies for teaching students to think critically have been evaluated in health and medical education; in science, technology, engineering, and maths; and in other subjects. 23 These studies suggest that critical thinking skills can be taught and that in the absence of explicit teaching of critical thinking, important deficiencies emerge in the abilities of students to make sound judgments. In healthcare studies, many medical students score poorly on tests that measure the ability to think critically , and the ability to think critically is correlated with academic success. 24 25
Evaluations of strategies for teaching critical thinking in medicine have focused primarily on critical appraisal skills as part of evidence based healthcare. An overview of systematic reviews of these studies suggests that improving evidence based healthcare competencies is likely to require multifaceted, clinically integrated approaches that include assessment. 26
Cross sector collaboration
Informed Health Choices, an international project aiming to improve decision making, shows the opportunities and benefits of cross sector collaboration between education and health. 27 This project has brought together people working in education and healthcare to develop a curriculum and learning resources for critical thinking about any action that is claimed to improve health. It aims to develop, identify, and promote the use of effective learning resources, beginning at primary school, to help people to make well informed choices as patients and health professionals, and well informed decisions as citizens and policy makers.
The project has drawn on several approaches used in education, including the development of a “spiral curriculum,” measurement tools, and the design of learning resources. A spiral curriculum begins with determining what people should know and be able to do, and outlines where they should begin and how they should progress to reach these goals. The basic ideas are revisited repeatedly, building on them until the student has grasped a deep understanding of the concepts. 28 29 The project has also drawn on educational research and methods to develop reliable and valid tools for measuring the extent to which those goals have been achieved. 30 31 32 The development of learning resources to teach these skills has been informed by educational research, including educational psychology, motivational psychology, and research and methods for developing learning games. 33 34 35 It has also built on the traditions of clinical epidemiology and evidence based medicine to identify the key concepts required to assess health claims. 29
It is difficult to teach critical thinking abstractly, so focusing on health may have advantages beyond the public health benefits of increasing health literacy. 36 Nearly everyone is interested in health, including children, making it easy to engage learners. It is also immediately relevant to students. As reported by one 10 year old in a school that piloted primary school resources, this is about “things we might actually use instead of things we might use when we are all grown up and by then we’ll forget.” Although the current evaluation of the project is focusing on outcomes relating to appraisal of treatment claims, if the intervention shows promise the next step could be to explore how these skills translate to wider educational contexts and outcomes.
Beyond critical thinking
Exciting opportunities for cross sector collaboration are emerging between healthcare and education. Although critical thinking is a useful example of this, other themes cross the education and healthcare domains, including nutrition, exercise, educational neuroscience, learning disabilities and special education needs, and mental health.
In addition to shared topics, several common methodological and conceptual issues also provide opportunities for sharing ideas and innovations and learning from mistakes and successes. For example, the Education Endowment Foundation is the UK government’s What Works Centre for education, aiming to improve evidence based decision making. Discussions hosted by the foundation are exploring how methods to develop guidelines in healthcare can be adapted and applied in education and other sectors.
Similarly, the foundation’s universal use of independent evaluation for teaching and learning interventions is an approach that should be explored, adapted, and applied in healthcare. Since the development and evaluation of educational interventions are separated, evaluators have no vested interested in the results of the assessment, all results are published, and bias and spin in how results are analysed and presented are reduced. By contrast, industry sponsorship of drug and device studies consistently produces results that favour the manufacturer. 37
Another example of joint working between educators and health is the Best Evidence Medical Education Collaboration, an international collaboration focused on improving education of health professionals. 38 And in the UK, the Centre for Evidence Based Medicine coordinates Evidence in School Teaching (Einstein), a project that supports introducing evidence based medicine as part of wider science activities in schools. 39 It aims to engage students, teachers, and the public in evidence based medicine and develop critical thinking to assess health claims and make better choices.
Collaboration has also been important in the development of the Critical Thinking and Appraisal Resource Library (CARL), 40 a set of resources designed to help people understand fair comparisons of treatments. An important aim of CARL is to promote evaluation of these critical thinking resources and interventions, some of which are currently under way at the Education Endowment Foundation. On 22 May 2017, the foundation is also cohosting an event with the Royal College of Paediatrics and Child Health that will focus on their shared interest in critical thinking and appraisal skills.
Education and healthcare have overlapping interests. Doctors, teachers, researchers, patients, learners, and the public can all benefit from working together to help people to think critically about the choices they make. Events such as the global evidence summit in September 2017 ( https://globalevidencesummit.org ) can help bring people together and build on current international experience.
Contributors and sources: This article reflects conclusions from discussions during 2016 among education and health service researchers exploring opportunities for cross sector collaboration and learning. This group includes people with a longstanding interest in evidence informed policy and practice, with expertise in evaluation design, reviewing methodology, knowledge mobilisation, and critical thinking and appraisal.
Competing interests: We have read and understood BMJ policy on declaration of interests and declare that we have no competing interests.
Provenance and peer review: Not commissioned; externally peer reviewed.
- ↵ Krupat E, Sprague JM, Wolpaw D, Haidet P, Hatem D, O’Brien B. Thinking critically about critical thinking: ability, disposition or both? Med Educ 2011 ; 357 : 625 - 35 . doi:10.1111/j.1365-2923.2010.03910.x pmid:21564200 . OpenUrl
- ↵ Huang GC, Newman LR, Schwartzstein RM. Critical thinking in health professions education: summary and consensus statements of the millennium conference 2011. Teach Learn Med 2014 ; 357 : 95 - 102 . doi:10.1080/10401334.2013.857335 pmid:24405353 . OpenUrl
- ↵ Dewey J. How we think. D C Heath, 1910 . https://archive.org/details/howwethink000838mbp doi:10.1037/10903-000 .
- ↵ Facione PA. Critical thinking: a statement of expert consensus for purposes of educational assessment and instruction. Research findings and recommendations. American Philosophical Association, 1990 , http://files.eric.ed.gov/fulltext/ED315423.pdf .
- ↵ Higgins S, Katsipataki M, Coleman R, et al. The Sutton Trust-Education Endowment Foundation Teaching and Learning Toolkit. Education Endowment Foundation, 2015 .
- ↵ Hanley P, Slavin RE, Elliot L. Thinking, doing, talking science. Evaluation report and executive summary. Education Endowment Foundation, 2015 , https://v1.educationendowmentfoundation.org.uk/uploads/pdf/Oxford_Science.pdf .
- ↵ Sackett DL. How to read clinical journals: I. why to read them and how to start reading them critically . Can Med Assoc J 1981 ; 357 : 555 - 8 . pmid:7471000 . OpenUrl
- ↵ Guyatt G, Cairns J, Churchill D, et al. Evidence-Based Medicine Working Group. Evidence-based medicine. A new approach to teaching the practice of medicine . JAMA 1992 ; 357 : 2420 - 5 . doi:10.1001/jama.1992.03490170092032 pmid:1404801 . OpenUrl
- ↵ Oxman AD, Sackett DL, Guyatt GH. The Evidence-Based Medicine Working Group. Users’ guides to the medical literature. I. How to get started . JAMA 1993 ; 357 : 2093 - 5 . doi:10.1001/jama.1993.03510170083036 pmid:8411577 . OpenUrl
- ↵ Rynearson EH. Endocrinology: a critical appraisal . Cal West Med 1940 ; 357 : 257 - 9 . pmid:18745588 . OpenUrl
- ↵ General Medical Council. Tomorrow's doctors. General Medical Council, 1993. http://www.gmc-uk.org/10a_annex_a.pdf_25398162.pdf
- ↵ General Medical Council. Good medical practice. General Medical Council, 2013. http://www.gmc-uk.org/static/documents/content/GMP_.pdf
- ↵ Edwards A, Elwyn G. Shared decision-making in health care: achieving evidence-based patient choice. 2nd ed . Oxford University Press, 2009 .
- ↵ Sumner P, Vivian-Griffiths S, Boivin J, et al. Exaggerations and caveats in press releases and health-related science news. PLoS One 2016 ; 357 : e0168217 . doi:10.1371/journal.pone.0168217 pmid:27978540 . OpenUrl
- ↵ Schwartz LM, Woloshin S, Andrews A, Stukel TA. Influence of medical journal press releases on the quality of associated newspaper coverage: retrospective cohort study. BMJ 2012 ; 357 : d8164 . doi:10.1136/bmj.d8164 . pmid:22286507 . OpenUrl
- ↵ Glenton C, Paulsen EJ, Oxman AD. Portals to Wonderland: health portals lead to confusing information about the effects of health care. BMC Med Inform Decis Mak 2005 ; 357 : 7 . doi:10.1186/1472-6947-5-7 pmid:15769291 . OpenUrl
- ↵ Moynihan R, Bero L, Ross-Degnan D, et al. Coverage by the news media of the benefits and risks of medications . N Engl J Med 2000 ; 357 : 1645 - 50 . doi:10.1056/NEJM200006013422206 pmid:10833211 . OpenUrl
- ↵ Voogt J, Roblin NP. A comparative analysis of international frameworks for 21st century competences: implications for national curriculum policies. J Curric Stud 2012 ; 357 : 299 - 321 doi:10.1080/00220272.2012.668938 . OpenUrl
- ↵ National Research Council. Taking science to school: learning and teaching science in grades K-8. National Academies Press, 2007 .
- ↵ Nordheim L, Pettersen KS, Flottorp S, Hjälmhult E. Critical appraisal of health claims: science teachers’ perceptions and practices . Health Educ J 2016 ; 357 : 449 - 66 doi:10.1108/HE-04-2015-0016 . OpenUrl
- ↵ Committee on Science Learning. Kindergarten through eighth grade. How children learn science. In: Duschl RA, Schweingruber A, Shouse AW, eds. Taking science to school: learning and teaching science in grades K-8. National Academies Press, 2007 .
- ↵ Vosniadou S. International handbook of research on conceptual change. 2nd ed . Routledge, 2013 .
- ↵ Abrami PC, Bernard RM, Borokhovski E, Waddington DI, Wade CA, Persson T. Strategies for teaching students to think critically a meta-analysis. Rev Educ Res 2015 ; 357 : 275 - 314 . OpenUrl
- ↵ Ross D, Schipper S, Westbury C, et al. Examining critical thinking skills in family medicine residents . Fam Med 2016 ; 357 : 121 - 6 . pmid:26950783 . OpenUrl
- ↵ Ross D, Loeffler K, Schipper S, Vandermeer B, Allan GM. Do scores on three commonly used measures of critical thinking correlate with academic success of health professions trainees? A systematic review and meta-analysis. Acad Med 2013 ; 357 : 724 - 34 . doi:10.1097/ACM.0b013e31828b0823 pmid:23524925 . OpenUrl
- ↵ Young T, Rohwer A, Volmink J, Clarke M. What are the effects of teaching evidence-based health care (EBHC)? Overview of systematic reviews. PLoS One 2014 ; 357 : e86706 . doi:10.1371/journal.pone.0086706 pmid:24489771 . OpenUrl
- ↵ Informed Health Choices Group. Informed health choices. www.informedhealthchoices.org
- ↵ Harden RM, Stamper N. What is a spiral curriculum? Med Teach 1999 ; 357 : 141 - 3 . doi:10.1080/01421599979752 pmid:21275727 . OpenUrl
- ↵ Austvoll-Dahlgren A, Oxman AD, Chalmers I, et al. Key concepts that people need to understand to assess claims about treatment effects. J Evid Based Med 2015 ; 357 : 112 - 25 . doi:10.1111/jebm.12160 pmid:26107552 . OpenUrl
- ↵ Austvoll-Dahlgren A, Nsangi A, Semakula D. Interventions and assessment tools addressing key concepts people need to know to appraise claims about treatment effects: a systematic mapping review. Syst Rev 2016 ; 357 : 215 . doi:10.1186/s13643-016-0389-z pmid:28034307 . OpenUrl
- ↵ Austvoll-Dahlgren A, Semakula D, Nsangi A, et al. The development of the “claim evaluation tools”: assessing critical thinking about effects. BMJ Open forthcoming .
- ↵ Austvoll-Dahlgren A, Guttersrud Ø, Semakula D, Nsangi A, Oxman AD. Measuring ability to assess claims about treatment effects: a latent trait analysis of the claim evaluation tools using Rasch modelling. BMJ Open [ forthcoming ].
- ↵ Sandoval WA, Sodian B, Koerber S, Wong J. Developing children’s early competencies to engage with science . Educ Psychol 2014 ; 357 : 139 - 52 doi:10.1080/00461520.2014.917589 . OpenUrl
- ↵ Pintrich PR. A motivational science perspective on the role of student motivation in learning and teaching contexts . J Educ Psychol 2003 ; 357 : 667 - 86 doi:10.1037/0022-0663.95.4.667 . OpenUrl
- ↵ Clark DB, Tanner-Smith EE, Killingsworth SS. Digital games, design, and learning: a systematic review and meta-analysis . Rev Educ Res 2016 ; 357 : 79 - 122 . doi:10.3102/0034654315582065 pmid:26937054 . OpenUrl
- ↵ Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review . Ann Intern Med 2011 ; 357 : 97 - 107 . doi:10.7326/0003-4819-155-2-201107190-00005 pmid:21768583 . OpenUrl
- ↵ Lundh A, Sismondo S, Lexchin J, Busuioc OA, Bero L. Industry sponsorship and research outcome. Cochrane Database Syst Rev 2012 ; 357 : MR000033 . pmid:23235689 . OpenUrl
- ↵ Thistlethwaite J, Hammick M, The Best Evidence Medical Education (BEME) Collaboration: into the next decade. Med Teach 2010 ; 357 : 880 - 2 . doi:10.3109/0142159X.2010.519068 pmid:21039096 . OpenUrl
- ↵ Centre for Evidence Based Medicine. Einstein—taking EBM to schools. http://www.cebm.net/taking-ebm-schools
- ↵ Castle JC, Chalmers I, Atkinson P, et al. Establishing a library of resources to help people understand key concepts in assessing treatment claims—the Critical Thinking and Appraisal Resource Library (CARL). PLoS One forthcoming .
Critical Thinking in Medical School Exams
Cite this chapter.
- T. M. Scott 2 &
- L. L. Chafe 2
47 Accesses
1 Citations
Questions from the exams in the first three years of the medical curriculum at Memorial University medical school were categorised using a simple taxonomy. The three-point taxonomy was developed by examining the range of questions present in question banks. It was found that most questions tested simple recall. These were assigned to the lowest category. The second category was assigned to questions that used the basic information obtained from recall to make generalizations. Questions that demanded interpretation of data and other higher level activities such as synthesis and evaluation were grouped as the third category. Although the third category had a broad range it was found unnecessary to subdivide it since few questions in the question banks tested beyond interpretation of data. The taxonomy was applied to anatomy, biochemistry and genetics exams from first year, cardiovascular, renal, respiratory and neuroscience exams from second year, and neurology exams from third year. In all years questions demanding simple recall dominated exams. In one genetics exam from first year the category 1 questions formed 91% of the exam. Although teaching becomes more clinical by third year the nature of the exam questions did not change. In the third year neurology exam bank the category 1 questions formed 96%. Despite the widely held belief that physicians should be critical thinkers, that skill is not tested in our medical school exams.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Similar content being viewed by others

Mindful Medical Practice and the Good Doctor

Developing Multiple-Choice Questions for Anatomy Examinations

Dual processing theory and expertsʼ reasoning: exploring thinking on national multiple-choice questions
Dobrzykowski TM. Teaching strategies to promote critical thinking skills in nursing staff. Journal of Continuing Education in Nursing 1994;25:272–276.
Google Scholar
McGuire C. A process approach to the construction and analysis of medical examinations. Journal of Medical Education 1963;38:556–563.
Bloom BS, Engelhart MD, Furst EJ, Hill WH, Krathwol DR. The taxonomy of educational objectives. New York: David McKay, 1956.
Buckwalter JA, Schumacher R, Albright JP, Cooper RR. Use of an educational taxonomy for evaluation of cognitive performance. Journal of Medical Education 1981;56:115–121.
Miller DA, Sadler JZ, Mohl PC, Melchiode GA. The cognitive context of examinations in psychiatry using Bloom’s taxonomy. Medical Education 1991;25:480–484.
Article Google Scholar
Norris SP. Format effects on critical thinking test performance. Alberta Journal of Educational Research 1995;41:378–406.
Glen S. Developing critical thinking in higher education. Nurse Education Today 1995;15:170–176.
Reynolds A. Patho-flow diagramming: a strategy for critical thinking and clinical decision making. Journal of Nursing Education 1994;33:333–336.
Case B. Walking around the elephant: a critical-thinking strategy for decision making. Journal of Continuing Education in Nursing 1994;25:101–109.
Hurd PD. Questions and critical thinking. American Journal of Pharmaceutical Education 1994;58:422–423.
Hobson EH, Schafermeyer KW. Writing and critical thinking: writing to learn in large classes. American Journal of Pharmaceutical Education 1994;58:423–427.
McMillan JH. Enhancing college students’ critical thinking: a review of studies. Research in Higher Education 1987;26:3–19.
Rogers JC, Swee DE, Ullian JA. Teaching medical decision making and students’ clinical problem solving skills. Medical Teacher 1991;13:157–164.
Morin S, Barberis-Ryan C. Competency Assessment. Nursing Management 1995;26:40–44.
King A. Inquiring minds really do want to know: using questions to teach critical thinking. Teaching of Psychology 1995;22:13–17.
Regan-Smith MG, Obenshain SS, Woodward C, Richards B, Zeitz HJ, Small PA. Rote learning in medical school. JAMA 1994;272:1380–1381.
Download references
Author information
Authors and affiliations.
Memorial University of Newfoundland, Canada
T. M. Scott & L. L. Chafe
You can also search for this author in PubMed Google Scholar
Editor information
Editors and affiliations.
Maastricht University, The Netherlands
A. J. J. A. Scherpbier , C. P. M. van der Vleuten , J. J. Rethans & A. F. W. van der Steeg , , &
Rights and permissions
Reprints and permissions
Copyright information
© 1997 Springer Science+Business Media Dordrecht
About this chapter
Scott, T.M., Chafe, L.L. (1997). Critical Thinking in Medical School Exams. In: Scherpbier, A.J.J.A., van der Vleuten, C.P.M., Rethans, J.J., van der Steeg, A.F.W. (eds) Advances in Medical Education. Springer, Dordrecht. https://doi.org/10.1007/978-94-011-4886-3_117
Download citation
DOI : https://doi.org/10.1007/978-94-011-4886-3_117
Publisher Name : Springer, Dordrecht
Print ISBN : 978-94-010-6048-6
Online ISBN : 978-94-011-4886-3
eBook Packages : Springer Book Archive
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Critical thinking: change during medical school and relationship to performance in clinical clerkships
Affiliation.
- 1 Department of Anatomy, School of Medicine, Wright State University, Dayton, OH, USA.
- PMID: 9624394
- DOI: 10.1046/j.1365-2923.1998.00701.x
The development of critical thinking, the ability to solve problems by assessing evidence using valid inferences, abstractions, and generalizations, is one of the global goals advocated by most medical schools. This study determined changes in critical thinking skills between entry and near the end of the third year of medical school, assessed the predictive ability of a test of critical thinking skills, and assessed the concurrent validity of clerkship components and final grade. The Watson-Glaser Critical Thinking Assessment (WGCTA) was administered to one class of students at entry to medical school and near the end of year 3. Performance data for those students who completed their clinical clerkships on schedule were also recorded. Critical thinking improved modestly but significantly from entry to medical school to near the end of year 3. The ability of a critical thinking test to predict clerkship performance was limited; the correlation between WGCTA total score at entry and the components and final grade of five major clerkships ranged from near 0 to 0.34. The concurrent validity of clerkship components and final grade was also limited; correlations with WGCTA total score near the end of year 3 ranged between 0.08 and 0.49. The correlation between WGCTA total score and United States Medical Licensing Examination Step 2 was higher at year 3 than at medical school entry. Critical thinking skills improve moderately during medical school. Used alone, tests of critical thinking may be of limited value in predicting which students will be successful in clinical clerkships. Clerkship evaluation components and final grade have limited concurrent validity when a test of critical thinking is the criterion.
- Clinical Clerkship*
- Education, Medical, Undergraduate*
- Educational Measurement*
- Problem Solving
- Students, Medical
- History, Facts & Figures
- YSM Dean & Deputy Deans
- YSM Administration
- Department Chairs
- YSM Executive Group
- YSM Board of Permanent Officers
- FAC Documents
- Current FAC Members
- Appointments & Promotions Committees
- Ad Hoc Committees and Working Groups
- Chair Searches
- Leadership Searches
- Organization Charts
- Faculty Demographic Data
- Professionalism Reporting Data
- 2022 Diversity Engagement Survey
- State of the School Archive
- Faculty Climate Survey: YSM Results
- Strategic Planning
- Mission Statement & Process
- Beyond Sterling Hall
- COVID-19 Series Workshops
- Previous Workshops
- Departments & Centers
- Find People
- Biomedical Data Science
- Health Equity
- Inflammation
- Neuroscience
- Global Health
- Diabetes and Metabolism
- Policies & Procedures
- Media Relations
- A to Z YSM Lab Websites
- A-Z Faculty List
- A-Z Staff List
- A to Z Abbreviations
- Dept. Diversity Vice Chairs & Champions
- Dean’s Advisory Council on Lesbian, Gay, Bisexual, Transgender, Queer and Intersex Affairs Website
- Minority Organization for Retention and Expansion Website
- Office for Women in Medicine and Science
- Committee on the Status of Women in Medicine Website
- Director of Scientist Diversity and Inclusion
- Diversity Supplements
- Frequently Asked Questions
- Recruitment
- By Department & Program
- News & Events
- Executive Committee
- Aperture: Women in Medicine
- Self-Reflection
- Portraits of Strength
- Mindful: Mental Health Through Art
- Event Photo Galleries
- Additional Support
- MD-PhD Program
- PA Online Program
- Joint MD Programs
- How to Apply
- Advanced Health Sciences Research
- Clinical Informatics & Data Science
- Clinical Investigation
- Medical Education
- Visiting Student Programs
- Special Programs & Student Opportunities
- Residency & Fellowship Programs
- Center for Med Ed
- Organizational Chart
- Leadership & Staff
- Committee Procedural Info (Login Required)
- Faculty Affairs Department Teams
- Recent Appointments & Promotions
- Academic Clinician Track
- Clinician Educator-Scholar Track
- Clinican-Scientist Track
- Investigator Track
- Traditional Track
- Research Ranks
- Instructor/Lecturer
- Social Work Ranks
- Voluntary Ranks
- Adjunct Ranks
- Other Appt Types
- Appointments
- Reappointments
- Transfer of Track
- Term Extensions
- Timeline for A&P Processes
- Interfolio Faculty Search
- Interfolio A&P Processes
- Yale CV Part 1 (CV1)
- Yale CV Part 2 (CV2)
- Samples of Scholarship
- Teaching Evaluations
- Letters of Evaluation
- Dept A&P Narrative
- A&P Voting
- Faculty Affairs Staff Pages
- OAPD Faculty Workshops
- Leadership & Development Seminars
- List of Faculty Mentors
- Incoming Faculty Orientation
- Faculty Onboarding
- Past YSM Award Recipients
- Past PA Award Recipients
- Past YM Award Recipients
- International Award Recipients
- Nominations Calendar
- OAPD Newsletter
- Fostering a Shared Vision of Professionalism
- Academic Integrity
- Addressing Professionalism Concerns
- Consultation Support for Chairs & Section Chiefs
- Policies & Codes of Conduct
- First Fridays
- Fund for Physician-Scientist Mentorship
- Grant Library
- Grant Writing Course
- Mock Study Section
- Research Paper Writing
- Establishing a Thriving Research Program
- Funding Opportunities
- Join Our Voluntary Faculty
- Child Mental Health: Fostering Wellness in Children
- Faculty Resources
- Research by Keyword
- Research by Department
- Research by Global Location
- Translational Research
- Research Cores & Services
- Program for the Promotion of Interdisciplinary Team Science (POINTS)
- CEnR Steering Committee
- Experiential Learning Subcommittee
- Goals & Objectives
- Issues List
- Print Magazine PDFs
- Print Newsletter PDFs
- YSM Events Newsletter
- Social Media
- Patient Care
INFORMATION FOR
- Residents & Fellows
- Researchers
Educators in academic surgery on managing expectations for surgery clerkship
Critical thinking, problem-solving, and emotional intelligence are a few of the skills medical students can learn during their surgical rotations. r. peter manes, md, saral mehra, md mba, kelly olino, md, and david stitelman, md, from the yale department of surgery discuss what makes a rewarding surgery clerkship experience..
In this series, Department of Surgery faculty, who were voted as top educators by the Yale School of Medicine's Class of 2024, share reflections on the role of academic surgeons in shaping medical education.
How do you engage and inspire students in the clerkshipexperience, while recognizing that the majority of students will not pursue surgery?
Tailor the educational experience.
R. Peter Manes: While many students are not interested in surgery, they all are curious, inquisitive individuals. It’s important to tailor the educational experience to the learner’s interests, while at the same time highlighting important concepts that every physician needs to know, no matter what career they pursue.
Use the Socratic method
Saral Mehra: I sometimes see students treated as invisible observers. If a student in my operating room or clinic made it this far in life; he/she is clearly a smart, educated, driven individual as clinical educators we need to see them as such. They are real people. Say good morning, ask questions, and make them feel a part of what is going on. Little acts and acknowledgements can go a long way to making students feel engaged and feel as though they belong.
In the operating room, and clinic, I like to use the Socratic method to teach. First, I warn them of my technique, and acknowledge I don’t expect them to know the answers to everything; it’s okay to not have an answer – but they must think. In this way, I can assess their current knowledge base, and adjust my questions to what will benefit them. I also have them write me diagrams and flow charts as they think through anatomy and differential diagnoses – the marking pens and sterile sheets make great writing apparatus.
In the clinic, or when not scrubbed in the operating room, I'll even tell them; it's okay to use your phone and resources to answer my questions- but take 5-10 minutes, figure out the answer, and then teach me. A little secret: if I ask a question for which I don't know the answer (or if a student asks me a question I can’t answer); I ask them to look it up and either tell me the next day or send me an email with the answer.
Success beyond a surgery rotation
Kelly Olino: Each student who comes in is trying to figure out how they belong and have to do this every single month. I think having a one-on-one meeting to begin each rotation and explaining the value of the opportunity they are being given and how valuable the time is to be dedicated to learning is key. We also discuss strategies for success beyond a surgery rotation- pursuing a love of knowledge, pushing for continuous improvement, and understanding that caring is the key to be a great doctor.
Create a shared vision
David Stitelman: Before cases, I like to discuss steps and anatomy with the resident and medical student. This helps us have a shared vision of what happens during cases. In terms of engagement, I also like to ask about undergraduate major, future plans and mentorship. In the Yale system, having a mentor is a big deal and making sure there is a faculty member watching out for the student is vital.
Featured in this article
- R Peter Manes, MD, FACS Associate Professor of Surgery (Otolaryngology); Residency Program Director, Otolaryngology Surgery; Clinical Site Director (YPB), Otolaryngology Surgery
- Saral Mehra, MD, MBA, FACS Associate Professor of Surgery (Otolaryngology); Section Chief, Head and Neck Surgery, Otolaryngology Surgery; Director, Head and Neck Oncologic and Reconstructive Surgery Fellowship, Surgery
- Kelly Olino, MD, FACS Assistant Professor of Surgery (Oncology); Leader, Skin Cancer Surgery, Melanoma Program; Clinical Director of the Smilow Melanoma Program, Yale Cancer Center; Co-Director Cutaneous Malignancy Tumor Board, Yale Cancer Center; Medical Student Clerkship Liaison for Division of Surgical Oncology, Surgery
- David Stitelman, MD Associate Professor of Surgery (Pediatrics)
Related Links
- Educators in academic surgery on giving and receiving feedback
- Educators in academic surgery on balancing education with other responsibilities
- Open access
- Published: 20 March 2023
Thinking more wisely: using the Socratic method to develop critical thinking skills amongst healthcare students
- Yueh-Ren Ho 1 , 2 ,
- Bao-Yu Chen 3 &
- Chien-Ming Li 2 , 4
BMC Medical Education volume 23 , Article number: 173 ( 2023 ) Cite this article
11k Accesses
7 Citations
7 Altmetric
Metrics details
In medicine, critical thinking is required for managing and tolerating medical uncertainty, as well as solving professional problems and treating diseases. However, the core of Confucianism, teacher-centered and exam-oriented settings in middle and high school education may pose challenges to developing critical thinking in Han Chinese or Taiwanese students. Students may be adversely affected by these pedagogies since student-centered settings were more effective in stimulating their critical and reflective thinking, as well as a sense of responsibility, in the ever-changing world. Therefore, guiding students with less stable foundations of critical thinking might require a different approach. A review article highlighted the potential utility of the Socratic method as a tool for teaching critical thinking in the healthcare field. The method involves posing a series of questions to students. More importantly, medical students and residents in clinical teaching are familiar with the method. Almost all healthcare students must complete a biochemistry laboratory course as part of their basic science training. Thus, we aimed to train students to develop critical thinking in the biochemistry laboratory course by using learning sheets and teacher guidance based on the Socratic method and questioning.
We recruited second-year students from a medical school, of whom 32 had medical science and biotechnology majors (MSB), 27 had pharmaceutical science majors (PS), and 85 were medical undergraduate (MU) students. An exercise in critical thinking was conducted during a biochemistry laboratory course, which consisted of five different biochemical experiments, along with learning sheets that contained three or four critical thinking questions. Then, the teacher evaluated the students’ ability to think critically based on nine intellectual dimensions (clarity, accuracy, precision, relevance, depth, breadth, logic, fairness, and significance) based on the universal intellectual standards developed by Prof. Linda Elder and Richard Paul. In the following analysis, regression models and multivariate analysis were used to determine how students improved over time, and trajectory analysis were carried out in order to observe the trends in students’ critical thinking skills construction.
Clarity and logic dimensions were identified as the key elements to facilitate the development of critical thinking skills through learning sheets and teacher guidance in students across all three different healthcare majors. The results showed that metacognitive monitoring via Socratic questioning learning sheets have demonstrated potential encourage students to develop critical thinking skills in all dimensions. Another unique contribution of current study was present the heterogeneous learning patterns and progress trajectories of clarity and logic dimensions within classes.
Using the Socratic learning model could effectively develop students’ critical thinking skills so they can more effectively care for their patients.
Peer Review reports
Introduction
Emerging trends in information technology requires that the new generation of medical students become critical thinkers [ 1 ]. The General Medical Council (GMC) of the United Kingdom encourages teachers to facilitate the acquisition of critical thinking skills by students in the medical and health professions [ 2 ]. Decades of research have proven that critical thinkers can present dispositions like flexibility, persistence, and willingness when faced with a range of tasks; they display meta-cognitive monitoring and a willingness to self-correct to seek long-term consensus[ 3 ]. Although, critical thinking is constructed from childhood in most Western countries and are valued by higher education as a necessary skill for coping with society [ 4 ]. However, critical thinking constructing and teaching has attracted little attention in Eastern education systems until recently [ 5 , 6 ].
Aside from the development of critical thinking skills is a key component of educational systems, recent educational philosophy also emphasizes both thinking processes as well as metacognitive integration skills [ 7 ]. Metacognitive monitoring includes making ease-of-learning judgments (i.e., processing fluency and beliefs), judgments of learning, feeling-of-knowing judgments (i.e., assessing the familiarity of the cue and the question itself or the domain of the question), and having confidence in the retrieved answers [ 8 , 9 ]. It is an adaptive skill of personal insight that health-profession students need to succeed in the rapidly changing and challenging healthcare industry [ 2 , 10 ]. Despite this, higher education curriculum does not emphasize on teaching these skills [ 7 ]. Additionally, any attempts to change the standards in higher education are generally met with resistance and challenges since they are require to encourage teachers to create new curriculum and change the current teaching content by researchers in current study who have more than 40 years’ teaching experience observaions. Healthcare curriculum, in general, remains conservative; Taiwan is not an exception.
Critical thinking is a fundamental component of innovative thinking and has thus become the fundamental skill for cultivating innovative talents in Western education [ 11 ]. Western scholars have asserted that teaching critical thinking should start at an early age and that its foundations should be laid in elementary and secondary schools. There are many ways to define critical thinking. A leading educational expert, Prof. Dewey, defined critical thinking as inclusive of reflective thinking and argued that the thinking process should also be taken as one of the objectives of education [ 12 ]. There are a few general dispositions that an ideal critical thinker would present according to Prof. Ennis’ observation of the constitutive abilities, such as (1) provide a clear statement of the conclusion or question; (2) provide clear reasons and be specific about their relationships with each other; (3) try to be well informed; (4) always seek and use credible sources, observations and mention them frequently; (5) consider the entire situation; (6) be mindful of the context’s primary concern; (7) be aware of alternative options; (8) be open-minded toward other points of view and refrain from making a judgment when there are insufficient evidence and reasons; (9) be willing to change your position when sufficient evidence and reasons support it; (10) seek as much precision as the nature of the subject admits; (11) whenever possible, seek the truth, and more broadly, strive to “get it right”; and (12) utilize their critical thinking abilities and dispositions [ 13 , 14 , 15 , 16 ]. In the eyes of Profs. Dewey and Ennis, critical thinking is a process of careful thought and reflection before a decision is made [ 17 ].
Nevertheless, the measurement or evaluation of critical thinking skills and abilities does not seem easy. Based on another perspective on critical thinking, intellectual standards are evolving [ 18 ]. According to Profs. Elder and Paul, critical thinking is the ability to use the most appropriate reasoning in any situation [ 18 ]. To evaluate these abilities, they established nine dimensions of critical thinking to represent different aspects of critical thinking: clarity, accuracy, precision, relevance, depth, breadth, logic, significance, and fairness [ 18 ]. As Profs. Elder and Paul concluded, those who possess discipline and critical thinking skills would make use of intellectual standards every day; thus, people should target these standards when they ask questions during the thinking process [ 18 , 19 ]. As a result of teachers’ regular introduction of the tools of critical thinking in their classrooms, the Socratic questioning and discussions become more productive and disciplined, thereby enabling students to realize the significance of questioning during the learning process [ 20 , 21 , 22 ].
According to a review article, teaching critical thinking to healthcare students (primarily medical and pharmacy students) through Socratic methods is more effective in developing critical thinking for a number of reasons [ 23 ]. In particular, Socratic questioning provides students with the opportunity to justify their own preconceived beliefs and thoughts after a series of specific, targeted inquiries [ 24 ]. Using Socratic questioning can also assist healthcare students, interns, or residents in thinking critically by understanding the “deep structure” of the question, i.e., deconstructing the question and understanding its true meaning [ 23 ]. The effectiveness of Socratic questioning lies in ascertaining the current knowledge of the students [ 25 ] and establishing a foundation for teaching at their level [ 26 ]. The teacher can accomplish this probing by asking progressively more challenging questions until the limits of the students’ knowledge are discovered [ 25 , 27 , 28 ], as well as by allowing students to express their existing knowledge, which in turn will allow them to synthesize new knowledge [ 26 ], and the dialogue represents the Socratic method [ 29 ]. Alternatively, a critical thinker is more likely to engage in certain established metacognitive strategies under the Socratic paradigm and/or channel the intellectual dimensions of critical thinking [ 17 ].
Unfortunately, Han Chinese students have struggled with learning critical thinking, which is thought to be part of their characterological profile [ 30 ]. This struggle has been faced by students studying abroad [ 11 ] and in students enrolled in the Han Chinese education system, which mainly cultivates Confucianism [ 31 ]. There are at least two types of problems with developing critical thinking in Han Chinese or Taiwanese education. The first involves the core of Confucianism, where foreign teachers have tried to promote critical thinking in elementary and high schools but sensed ethical concerns from the students who refused to participate. This is likely because if they chose to participate, they would have felt obligated to express disagreement and negative feelings to the instructor. The Han Chinese culture values harmony and “not losing face,” emphasizing a holistic perspective and collective good. Thus, students would feel uncomfortable because disagreeing with someone’s opinion in public is consciously or often avoided [ 30 ]. Therefore, encouraging the student to participate in healthy discussions and respectfully challenge their teachers is the starting point for promoting critical thinking in students enrolled in the Han Chinese educational system.
Second, in the Western education approach, learners take an active role in and are responsible for their learning process. On the contrary, the Han Chinese and Taiwan education systems are teacher-centered and exam-oriented; students are expected to follow their teachers’ instructions and perform well in class. More importantly, the textbook or teacher-centered framework lacks half of Ennis’s twelve constitutive abilities for critical thinking [ 13 , 14 , 15 ], such as judging the credibility of a source, observing and judging observation reports, drawing explanatory conclusions (including hypotheses), making and judging value judgments, and attributing unstated assumptions. As a result, Han Chinese students may find it difficult to develop critical thinking skills and present key traits and dispositions that are indicative of an ideal critical thinker. Hence, guiding and evaluating critical thinking in students might not be implemented through the same approach in Eastern educational circumstances as in the West. By understanding the difficulties that Han Chinese students face in developing critical thinking, the current study aims to design a set of critical thinking models that are suitable for Han Chinese students as a starting point for reform teaching.
Research questions, hypotheses and objectives
Research has shown that the laboratory class is not just limited to a step-wise approach to experimentation. It also allows students to develop their critical thinking skills by repeatedly engaging a simple learning framework [ 32 ]. To explore this further, the current study’s primary purpose is to use Socratic questioning in a biochemistry laboratory course with specifically designed learning sheets and feedback from teacher to guide students to improve their critical thinking skills. The learning sheets were evaluated following the universal intellectual standards for critical thinking developed by Prof. Elder and Paul [ 19 , 33 ]. For this study, we hypothesized that students with different healthcare majors might present different improvement trajectories in their intellectual dimensions according to the years of teaching observations in the three healthcare majors. Based on the research and rationale described above, the intervention effect of Socratic questioning in a biochemistry laboratory course was hypothesized as follows (see Fig. 1 ):
Pre-intervention critical thinking abilities are different amongst students of different healthcare majors, especially in each intellectual dimension (H1a). Post-intervention critical thinking abilities would develop in students from each healthcare major after using the Socratic method (H1b).
Critical thinking abilities differs significantly between pre- and post-assessments of the intellectual dimensions of students with the three different healthcare majors (H2).
After clarifying the relation of Socratic method interventions in the class, we aim to scrutinize the trajectories of students between majors further to understand the learning style in class (Aim 1). Furthermore, we also aim to identify the key intellectual dimensions that could lead to an overall improvement in the critical thinking of students in each major (Aim 2). Additionally, we observed improvement trajectories of specific intellectual dimensions within major (Aim 3).
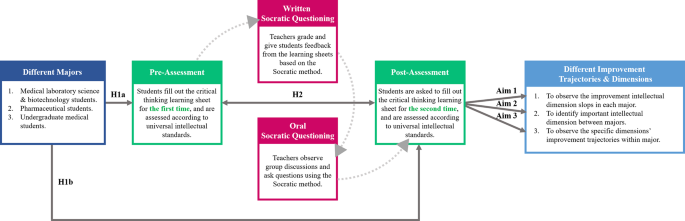
Socratic method framework and structure of the research hypotheses behind the biochemistry laboratory course
Literature review
Critical thinking engagement in the eastern and western medical education.
Over the last decade, medical education has been undergoing a variety of approaches for effectiveness teaching and transformation [ 34 ]. Many paradigms of active teaching/learning methodologies have been adopted in both Eastern and Western medical education systems, some of which are used partially (actual or conceptual similar) Socratic questioning to challenge students’ critical thinking. In this regard, the primary philosophy of case-based learning (CBL) established in the 1920s by Harvard Medical School is to guide students to apply their acquired knowledge base via critical thinking to make clinical decisions to solve the problems that they may encounter in the healthcare environment [ 35 ]. A meta-analysis study of China’s dental education reported that the CBL was a practical pedagogical method across the Chinese dental education system [ 36 ]. The results showed that the CBL method significantly increased knowledge scores, skill scores, comprehensive ability scores, and teaching satisfaction compared with the traditional lecture-based learning (LBL) mode in 2,356 dental students. Hence, there is an urgent need to change the traditional didactic lecture or teacher-centered classroom setting in which students are passive listeners instead of active participants.
Healthcare professionals are also required to solve complex problems and efficiently integrate didactic preclinical knowledge into actual clinical application in patient care [ 35 ]. On the other hand, the design thinking process may enhance both creativity and innovation so that healthcare professionals can respond to clinical problems effectively [ 37 , 38 ]. Problem-based learning (PBL) is a pedagogical approach widely accepted in medical education. It promotes active learning and results in better outcomes [ 39 , 40 , 41 ]. PBL focuses on active lifelong learning by triggering problems, directing student focus, and facilitating tutor involvement [ 39 , 42 , 43 , 44 ]. However, it is noteworthy that some hybrid PBL models have become less effective over time, as well as less aligned with the intended philosophy of student-centered learning [ 45 ]. Another alternative blended learning approach of PBL is team-based learning (TBL), which allows medical educators to provide students with pre-class work, in-class initial tests with immediate feedback, and real clinical problem-solving activities [ 46 ]. In the year-one studies of the Sydney Medical Program, a greater level of engagement in learning, a deeper understanding of concepts, and a sense of responsibility were shown among the medical students working in a TBL setting than among those in a PBL setting [ 47 , 48 ].
Medical educators face another significant challenge with the millennial generation, which has ubiquitous information technology access throughout its education. Thus, it is extremely important to improve students’ motivation to learn through hands-on instruction or teacher–student interaction and then stimulate students’ thinking and learning. In recent years, gamification has been successfully integrated into medical and scientific endeavors, enhancing motivation, participation, and time commitment across a variety of settings [ 49 , 50 , 51 ]. Another healthcare curriculum reform to stimulate active learning is flipped classroom (FC), which assigns learners didactic material, creating opportunities of longitudinal and interprofessional learning experiences for students during class participation [ 52 ] to encourage extracurricular learning, such as critical thinking. As part of the FC model, medical educators also develop formative and diagnostic assessments to identify learning gaps. According to these teaching modules, encouraging students to participate, emphasizing their learning, and observing their development trajectory are the core ideas in recent educational designs [ 53 ].
Although most of above-mentioned studies have been performed in the Eastern and Western education systems, however, without mentioning the differences between cultures and learning styles. Most importantly, the cultivation and foundations of critical thinking neglect the fact that Eastern and Western education systems emerged from very different learning and thinking patterns. Moreover, clinical reasoning and decision achievements depend on established critical thinking skills, therefore, it becomes more important to construct critical thinking early and comprehensively [ 54 ]. While Han Chinese students are not familiar with the core of critical thinking, the most effective approach to teaching critical thinking is still a highly debated topic in medical schools. Taken Taiwan medical education as an example, most clinical courses focuses on professional skills, problem solving, and disease treatment rather than construct critical mindset and metacognitive skills. Education strategies often emphasize the outcome while neglecting the process. Nevertheless, medical educators should also emphasize the process of forming students’ critical thinking when instructing and guiding them in this regard. Consequently, using metacognitive monitoring to enhance critical thinking in healthcare education would be appropriate, especially for Han Chinese systems with a Confucianist outlook. Thus, critical thinking via metacognitive monitoring is important in healthcare education, especially in Han Chinese systems with a Confucianist background.

Proficiency in the art of socratic questioning to enhance students’ critical thinking
Socratic questioning is a disciplined method of engaging in content-driven discourse that can be applied for various purposes: analyzing concepts, finding out the truth, examining assumptions, uncovering assumptions, understanding concepts, distinguishing knowledge from ignorance, and following the logical implications of thought. The scholars who established the intellectual standards of critical thinking have consistently indicated that “The key to distinguishing it from other types of questioning is that the Socratic questioning is systemic, disciplined, and deep and usually focus on foundational concepts, principles, theories, issues, or problems [ 20 , 21 , 22 ].” In short, the Socratic method is a questioning method that stimulates personal understanding. More importantly, the core principle of learning from the unknown fits best within healthcare environments.
Numerous studies have consistently urged teachers to develop Socratic dialogue in their classrooms, regardless of their learning stages and situations [ 55 , 56 , 57 ]. Using enhancement exercises in an elementary school, a study introduced a Socratic questioning strategy to provide guidance and hints to students so that they could think more deeply about an issue or problem before sharing their thoughts [ 55 ]. The lecturer of a speech course in higher education demonstrated how Socratic questioning could help students learn when confronted with a series of questions [ 56 ]. The process improves students’ ability to ask and answer questions and helps them overcome some obstacles related to their lack of self-confidence. In the book Socratic circles: Fostering critical and creative thinking in middle and high school , Dr. Matt Copeland stated that, in middle and high schools, teachers must facilitate discussions by asking questions [ 58 ]. Furthermore, this method could be applied not only to elementary school, middle school, high school but also to higher education classes [ 59 ]. During the Covid-19 pandemic, synchronous discussions in online learning demonstrated that the Socratic questioning strategy successfully improves students’ critical thinking skills [ 57 ].
The incorporation of Socratic questioning in healthcare education curriculum is under development, including for general medical education [ 60 ], medical [ 61 ], pharmacy [ 54 , 62 ], and nursing students [ 63 ]. A review article of revisiting the Socratic method as a tool for teaching critical thinking in healthcare professions revels few advantages of Socratic questioning [ 23 ]. Three type of Socratic questions were mention and could commonly used in different clinical situations [ 23 ], such as procedure question would use in those with correct answers (e.g., Which of the following medications has antithrombotic function? ); preference question can apply in those with no correct answers (e.g., What type of consultation is most suitable for this patient? ); judgment question would be the most challenge critical thinking within a Socratic paradigm by integrating different domain knowledge and skills (e.g., Does this patient require antibiotic treatment? ). It is necessary to apply and analyze information in a logical manner as well as self-regulate and use critical thinking in order to achieve the best outcome for patients. For medical doctors, pharmacists or clinical laboratory technicians to provide high quality health care across all disciplines, critical thinking is inherently required.
In medical school, the emphasis is laid on training learners in meta-capabilities, such as self-driven pattern recognition, ideally as part of an apprenticeship under the supervision of an expert diagnostician [ 61 ]. An in-depth study of the current trends in developing critical thinking amongst medical students demonstrated the use of dialogue for proper questioning and how it directs the learner’s thinking [ 64 ]. Moreover, another study confirmed that critical thinking occurs only when students are motivated and challenged to engage in higher-level thought processes [ 65 ]. In the pharmacy classroom, educators can play a significant role in influencing their students’ mindsets. Growth mindsets can be cultivated through the creation of an environment that encourages it. [ 62 ]. The Socratic questioning method can facilitate critical thinking in nursing education. One study showed that problem solving using critical thinking skills can be facilitated in both educational and practice settings by using Socratic inquiry [ 63 ].
The Socratic method has been adapted in different ways to different domains, but it has become closely associated with many areas, such as basic scientific thinking training, legal dialectical guidance, and clinical teaching. Some adaptations are helpful, some are not. The adaptations can be looked at through reasoning-focused lenses with varying degrees of magnification —a high-magnification adaptation rigorously and precisely tracks or guides the path of reasoning. Thus, how to use the Socratic method to direct students onto the path of critical thinking with appropriate guidance, but not revealing answers becomes an art that tests instructors’ teaching experience and proficiency in questioning.
Critical thinking and reflection exercises in the laboratory course
Medical schools have increasingly encouraged students to become life-long, self-directed learners because of the continual changes in the evidence-based healthcare environment. Science is often applied in everyday life, including translating knowledge from scholarly fields [ 66 ]. However, there is a vast gap between what is taught in medical schools and what is actually required in practice has increasingly widened in this information era. The majority of healthcare professionals are not considered to be real scientists. [ 2 ]. Nevertheless, they need to know how to apply scientific knowledge to their practice. Therefore, a science curriculum in medical school, such as a biochemistry laboratory course, should provide an opportunity to learn scientific methods and conceptual frameworks. It should also promote critical reasoning, providing healthcare students with problem-solving skills.
Medical educators need to accept that critical thinking is important for healthcare students and know how to teach it effectively [ 67 ]. Medical educators are now faced with a dilemma: should they develop a new course or adapt old course to develop critical thinking skills? An effective learning model should promote and stimulate students’ development of such skills [ 67 ]. One of the most common compulsory courses for healthcare students is the biochemistry laboratory course [ 68 , 69 ]. These courses are specifically designed to introduce students to prescribed experiments, requiring them to complete stepwise protocols by themselves [ 68 , 70 ]. The students are expected to understand the concepts behind the methods, procedures, and assays. However, this type of curriculum construction often fails to provide students with adequate opportunities to monitor their critical thinking and thus reduces the chances of developing problem-solving skills [ 70 ]. In order to provide students with more opportunities to think critically, previous studies have also adapted laboratory, basic science, and science fusion courses to help students develop critical thinking skills [ 67 , 68 , 71 , 72 , 73 ].
Several studies have demonstrated that students need critical thinking skills to interpret data and formulate arguments. Thus, science education, particularly in the laboratory setting, is designed to teach quantitative critical thinking (i.e. interpretation and critical evaluation of statistical reports), but the evidence has suggested that this is seldom, if ever, achieved [ 74 , 75 , 76 , 77 , 78 , 79 ]. By providing multiple opportunities for students to participate in critical thinking in the physics laboratory classes at Stanford University, scholars engaged the students to improve the experiment and modify the model repeatedly [ 32 ]. Additionally, a simple learning framework using decision-making cycles and demonstrating experts’ critical thinking significantly improved students’ critical thinking. We thus argue that students should engage in critical thinking exercises with repeated comparisons, decisions, and teacher guidance that are meant to construct their critical thinking in each of their disciplines.
Participants
This research was conducted during the 2017–2018 academic year. The participants were second-year students in the College of Medicine at the National Cheng Kung University (NCKU) of Taiwan. A total of 144 students participated in this study, of whom 32 had medical science and biotechnology majors (hereafter, MSB), 27 had pharmaceutical science majors (hereafter, PS), and 85 were medical undergraduate (hereafter, MU) students. The biochemistry laboratory course was compulsory for these three majors.
For each biochemistry laboratory class, the teacher assembled five to six groups of four to five students each. The course contained five different biochemical experiments: (1) Plasmid DNA (deoxyribonucleic acid) extraction and purification; (2) restriction enzyme digestion and electrophoresis of plasmid DNA; (3) polymerase chain reaction (PCR) amplification of plasmid DNA; (4) recombinant protein expression in Escherichia coli ; and (5) quantification of recombinant protein. The experimental learning sheets included three or four critical thinking questions (Table S1 ), encouraging students to explore experimental principles and alternative explanations further. To facilitate discussion, students were organized into small groups of four to five students seated around a single table, discussing and answering the questions. At this time, the students would pen down their first answers to the critical thinking questions, and the teacher would grade them based on the universal intellectual standards (learning sheets, first evaluation).
Furthermore, according to the students’ answers, the teacher offered a response by asking more questions according to the Socratic method to encourage students to think deeper rather than provide the correct answers. At the following week’s class, the teacher returned the learning sheet and supervised the ongoing activity, clarifying any questions raised by students and encouraging them to re-discuss and re-answer the critical thinking questions according to the teacher’s suggestions. The objective was to create a highly interactive environment to engage students in learning the relevant principles of each laboratory, including troubleshooting experiments and formulating critical concepts and skills. After the discussion, the teacher reexamined the students’ responses and assessed them based on the universal intellectual standards for subsequent grading (learning sheets, second evaluation).
The biochemistry laboratory courses and the Socratic method in current study are performed and taught by a senior biochemistry teacher (PhD in Institute of Basic Medical Science, NCKU) who has 40 years teaching experience. The teacher has long focused on teaching critical thinking skills to students, and also offers four senior clinical case related courses by practicing the Socratic method, such as clinical concept, critical thinking in medicine, clinical reasoning and special topics in clinical reasoning with more than 20 years of experience. Therefore, in the course, teacher will often ask a series of questions for students to think about the relevance of biochemical science and clinical practice.
Assessment development
The research team designed the learning sheets to guide discussion on the key issues concerning five biochemical experiments. The learning sheets were assessed according to the universal intellectual standards for critical thinking [ 33 ]. However, the assessment was adapted to include nine intellectual dimensions to assess student reasoning [ 19 , 33 ]: clarity, accuracy, precision, relevance, depth, breadth, logic, fairness, and significance (Table S2 ). Each dimension was evaluated using a binary score (0 = does not present the skill; 1 = presents the skill) for each question in the learning sheets for both the first and second evaluations. The students received the teacher’s guidance following the first evaluation, providing them with the opportunity to reconsider their reasoning and revise their answers. Our goal was to improve our students’ learning by stimulating the teaching process; at the same time, we were committed to allowing students to speak freely so that we could more effectively facilitate prospective discussions. Thus, the critical thinking scoring system based on nine intellectual dimensions was only for the purpose of the research, without consequences on students’ study progress. In this regard, students were not able to know their intellectual scores. As a result, their course grades were not determined by the learning sheets; rather, they were determined by the general operation, experiment report, and the learning attitude demonstrated during the experiments.
Statistical analysis
Descriptive statistics and variable tests.
We calculated the differences between the performance means for the first and second evaluations using paired t -tests. The mean differences between the students from the three majors were analyzed using a one-way analysis of variance (ANOVA). For the improvement slope for each universal intellectual dimension, we used the second evaluation scores of each experiment as the point with which to construct a quadratic equation curve in one variable (dimension) and then access the slope to represent the students’ improvement. The higher the slope score, the greater the students’ progress on that dimension.
Multivariate analysis
We used traditional analytical methods to observe and analyze the students’ improvement in the five experiments. Data from the second evaluation scores of each experiment served as the multi-time point measurement data. The Cox regression model for multivariate analysis was used to investigate the effect of several variables upon the time during which a specified outcome happened [ 80 ]. For each dimension, the model’s outcome determined that a student’s improvement slope was defined as minor progress if it was lower than the improvement slopes of their peers in the same major overall. However, if the student’s improvement slope was higher than the overall progress intercept of their peers, then it was defined as greater progress. The Cox regression models’ outcomes for each dimension were divided into two groups: minor and more progress. For this model’s outcome, (1) we calculated all dimensions’ slopes mean from each major (MSB: 0.369; PS: 0.405; MU: 0.401); (2) then compared the mean slope of the individual students with the mean slope of major; (3) if the student’s individual improvement slope was lower than mean slope of major, then defined as minor progress; if the student’s individual improvement slope was higher than mean slope of major, then defined as greater progress. From the analysis at this point, we understood that teacher could help students from different majors develop the different dimensions of critical thinking with the use of Socratic methods and simple repeated thinking framework practice. Additionally, we wanted to represent the improvement of intellectual dimensions between the students of different majors and their heterogeneity in critical thinking.
Dimension identification and comparison
To understand which intellectual dimensions were most representative of student improvement across majors, the analysis was divided into three sections: (1) to identify the progress percentage of all nine intellectual dimensions; (2) to identify the progress percentage of statistically significant intellectual dimensions; (3) to compare the differences among all nine dimensions, the significant dimensions, and the reciprocal dimensions. This analysis offered a better understanding of what dimensions represented the overall improvement of students’ critical thinking. Our first step was to calculate the percentage of improvement for each experiment by determining the results of the first and second evaluations for each intellectual dimension. Second, we took average percentage of improvements for each dimension. Finally, we used Student’s t -test to compare the differences among the average of all nine dimensions, the significant dimensions, and the reciprocal dimensions.
Trajectory analysis
In this study, we also hypothesized that each student’s learning and progress trajectories were heterogeneous across different majors. Depending on the major, there may also be differences between students in the same class. To focus our observations on the students’ use of the clarity and logic dimensions, we used a trajectory-tracking analysis [ 81 , 82 ] and categorized the students into two groups based on the participants’ improvement levels within the same major.
Descriptive data
We recruited 144 second-year students from three majors in the College of Medicine, among which 32 were MSB, 27 were PS, and 85 were MU students. All participants’ first and second evaluations were compared in all five biochemistry experiments. The statistically significant between-group differences in the mean initial evaluation results for each dimension are presented in Table 1 .
Overall improvement from the initial to second evaluations throughout the five experiments (H1, H2, and Aim 1)
Table 1 presents the mean results of the first and second evaluations; the five experiments exhibited statistically significant differences ( p < 0.05) across all study groups and dimensions. More detailed analyses revealed significant differences in performance in the second evaluation between the groups after all five biochemistry experiments in the clarity ( p = 0.0019), depth ( p = 0.0097), breadth ( p < 0.0001), logic ( p = 0.0371), and significance ( p = 0.0037) dimensions. However, for some of the dimensions (clarity, accuracy, precision, logic, and fairness), the initial evaluation results differ significantly between the MU and the MSB students, but this was not the case for the secondary evaluation results. The MSB students exhibited the best progress (2nd mean score minus 1st mean score) in the clarity dimension across all experiments. The PS students exhibited the best performance in the logic dimension ( p < 0.05) in the second evaluation after the five experiments.
The results of the MSB students improved steeply in most dimensions in the five experiments, especially depth (slope: 0.472), logic (0.455), and clarity (0.410) (Table 2 ). Time had a stronger effect on several of the dimensions in the multivariate analysis, specifically clarity ( p = 0.0012), relevance ( p = 0.0007), and logic ( p < 0.0001). By contrast, the PS students showed a significant overall improvement in the clarity (slope: 0.212, p < 0.0001), accuracy (0.539, p = 0.0063), precision (0.381, p = 0.0085), relevance (0.216, p < 0.0001), breadth (0.426, p = 0.0045), and logic (0.515, p = 0.0027) dimensions over the observation period (Table 3 ). Finally, the MU students showed a significant overall improvement in six dimensions: clarity (slope: 0.277, p < 0.0001), accuracy (0.520, p = 0.0003), depth (0.459, p = 0.0092), breadth (0.356, p = 0.0100), logic (0.544, p = 0.0190), and significance (0.327, p = 0.0225) (Table 4 ).
Trajectory tracking of the overall, significant, and reciprocal dimensions (Aim 2 and Aim 3)
Figure 2 a illustrates the overall improvement of students across the three majors in all nine dimensions, as assessed via trajectory analysis. The trajectory-tracking algorithm revealed that the significant dimensions for each group were as follows: MSB students—clarity, relevance, and logic; PS students—clarity, accuracy, precision, relevance, breadth, and logic; and MU students—clarity, accuracy, depth, breadth, logic, and significance (Tables 2 , 3 and 4 ; Fig. 2 b). The comparison of each group’s average percentage of improvement between the nine dimensions, the significant dimensions, and the reciprocal dimensions (clarity and logic) is summarized in Fig. 2 c. Figure 2 d–i depicts the students’ improvement in clarity and logic within the different majors using group-based trajectory modeling.
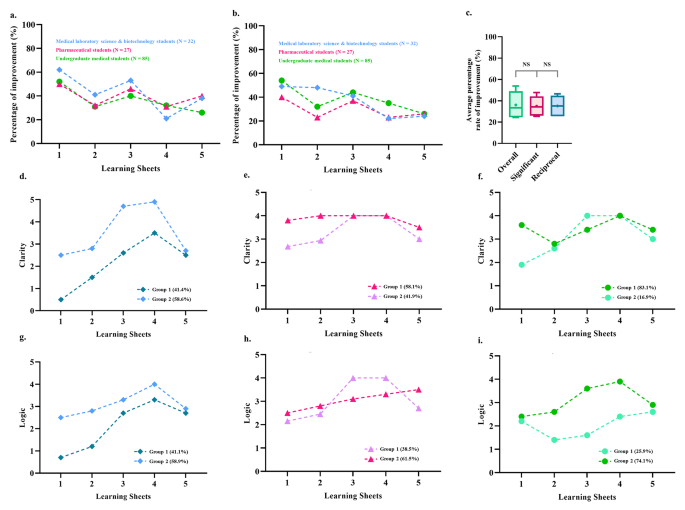
Overall improvement comparison between the students of three majors using a trajectory-tracking analysis approach . ( a ) The mean evaluation scores from the second evaluation minus those from the first evaluation for the nine dimensions were considered an improvement. They were converted to percentages to compare them to the performance in the first evaluation. ( b ) The mean evaluation scores from the second evaluation minus those from the first evaluation for the significant dimensions (within the students of each major, Tables 2 – 4 ) were considered to represent improvement and were converted to percentages to compare them to the performance in the first evaluation. ( c ) Comparison of the average percentage improvement among all nine dimensions, the significant dimensions, and the reciprocal dimensions (i.e., clarity and logic). ( d ) Trajectory analysis to assess the progress of the two subgroups of medical laboratory science and biotechnology students in the clarity dimension. ( e ) Trajectory analysis to assess the progress of the two subgroups of pharmaceutical students in the clarity dimension. ( f ) Trajectory analysis to assess the progress of the two subgroups of undergraduate medical students in the clarity dimension. ( g ) Trajectory analysis to identify the progress of the two subgroups of medical laboratory science and biotechnology students in the logic dimension. ( h ) Trajectory analysis to assess the progress of the two subgroups of pharmaceutical students in the logic dimension. ( i ) Trajectory analysis to assess the progress of the two subgroups of undergraduate medical students in the logic dimension
Empirical contributions
The Han Chinese educational system relies on the passive transmission of knowledge, as evidenced by the years of preparation by students’ through paper-based exams. By adopting this approach during teaching and learning, students do not develop a critical thinking mindset. Our experience has shown that when we encounter first-year students who have just graduated from high school, their previous education failed to develop critical thinking skills. Many foreign and Western teachers have the same experience when they encounter Asian students studying abroad for the first time. Thus, this research aims to provide clinical teachers with guidance on reducing the blind spots that students face when introduced to critical thinking. Moreover, this research aims to provide teachers with a simple teaching model and structure to guide students with less stable foundations in critical thinking. For the teaching structure and process, please refer to the procedure paragraph in the methods section and the teaching flow chart in Fig. 1 . Furthermore, the scoring system shown in the assessment development paragraph in the methods, as well as the scoring rubric is presented in Table S1 .
To our knowledge, this is the first study that uses the Socratic method and the universal intellectual standards to assess and improve critical thinking skills in biochemistry laboratory courses across different healthcare majors. We also used a novel design for teaching critical thinking, with multi-timepoint assessments and trajectory-tracking analysis to observe the students’ process and the improvement intheir critical thinking. This Socratic method, combined with critical thinking-based learning sheets, significantly improved the students’ critical thinking in all nine dimensions of the universal intellectual standards, according to the first and second evaluations conducted in each of the five sessions. Another unique contribution of this study is that it analyzed the progression results at multiple time points in the critical thinking performance of students across different majors. According to the results of comparing the average percentage improvement between all nine dimensions, the significant and reciprocal dimensions (i.e., clarity and logic) do not significantly differ from each other statistically speaking. By reducing the nine intellectual dimensions scoring system, medical educators can focus more on establishing clarity and logic skills in students. In sum, our most important finding was the identification of the clarity and logic dimensions as key elements that facilitate the development of critical thinking skills via the Socratic method in students across three different healthcare majors.
The trajectories of outcomes for students of medical science and biotechnology majors
Understanding what we learn has been identified as the starting point in the professional-development journey [ 2 ]. In principle, if thinking and decision making can be taught, educational intervention is possible. Nevertheless, for a science class like biochemistry, abductive reasoning requires a deep understanding of knowledge, and thinking must be inspired through stimulation.
In this study, the evaluation scores for MSB students did not improve significantly in almost any dimension at the beginning of the course. At first, most students felt uncomfortable with criticizing others, disagreeing with others, or challenging teacher’s knowledge and authority when they spoke their minds. Other MSB students believed that their ability to find answers and make decisions was inadequate and expected the teacher to provide the correct answers. However, preclinical medical technologists must gradually develop their critical thinking skills. Thus, the teacher provided critical thinking cues during the class and monitored the group discussions.
On the other hand, teachers must encourage these types of students, enabling them to accomplish simpler learning goals by providing them with easier-to-attempt clues. The joy of discovering answers on their own rather than the frustration of not achieving high goals should be encouraged. This coaching process improved the MSB students’ willingness to think and explore, leading to greater relevance and breadth of coverage.
The teacher used generation, conceptualization, optimization, and implementation [ 33 ] with the Socratic method to stimulate critical thinking in a four-step cycle in the five experiments. When the spontaneous discussion started in the generation phase, they tried to clarify their knowledge of the theme and identify the problem from the learning sheet. The following step was to conceptualize the problem, and the students drafted all of the possibilities and problems. Teacher frequently asked the students, ‘ What are other possible reasons? ’ Finally, the teacher provided feedback to help the MSB students reach a proper solution and implement it. The teacher would also ask the students leading questions like ‘ What relevant theories can be confirmed more precisely? ’ These guiding processes sharpened their logic and helped them better understand what they had learned. In sum, the benefits of this process included an enhanced ability to think logically, clarification of questions and knowledge gaps, and improvements in the thought process about the theme discussed.
The steady improvement of critical thinking in the students of pharmaceutical science
Currently, pharmacists are seeing their roles and responsibilities shift to becoming patient counselors and educators on the rational use of medicine. Pharmacists are trained to focus on patient-centered care and resolve current and potential drug-related problems [ 83 , 84 ]. Critical thinking, clinical reasoning, and decision-making skills are needed to solve these problems. Nowadays, pharmacists are not just responsible for carrying out doctor’s orders, while there are always alternative treatment options available for them to recommend. Teacher therefore repeatedly emphasized the link between critical thinking and pharmacist practice and encouraged students to ask questions and find out the best alternative through Socratic method in the classroom.
During class, the PS students were required to exert considerable mental effort to conduct an inquiry to solve the learning sheet questions. Instead of providing students with clues or information to help them solve the problems, the teacher guided the PS students on how to seek the information they needed for themselves. The question for the PS students was be ‘ What are the possibly executable strategies? ’ The teacher also joined the students in discussion, using the Socratic method to stimulate critical thinking and draw out ideas and underlying suppositions. In high-quality cooperative argumentative dialogue, teacher should not direct or refer learning, nor should they ask students for the correct answers as in a traditional classroom. The hints that teacher would provide were more like ‘ The narrative explanation can be more precise. ’ Thus, asking high-quality questions and providing feedback also challenges the instructors’ teaching experience.
The PS students were guided not only toward the development of critical thinking skills but also toward solving problems using evidence-based knowledge and decision-making skills. The Socratic method process meets the student where they are on the educational spectrum and encourages and helps them advance. Using this method, the PS students engaged in student-to-student interaction to build knowledge as a group and individually. The course of five experiments conducted via the learning sheets improved many aspects of the students’ critical thinking, including their clarity, relevance, breadth, and logic. In sum, the abilities that they developed in the course should help them focus more on the possible outcomes of pharmacotherapy, medication surveillance, and proper communication and therefore improve the quality of their professional future.
The advanced construction of critical thinking skills in undergraduate medical students
In medical education, “ better thinking and learning skills grounded in understanding ” are recommended for future doctors [ 2 ]. Practicing medicine requires an ability to address current and future diseases using new diagnostic and therapeutic methods [ 10 ]. Therefore, problem solving is not the only core medical skill; the ability to deal with complex, insoluble health issues is also required [ 83 ]. In this domain, critical thinking skills have proven essential in tackling difficult, complex, interdisciplinary health problems [ 10 ].
In our study, the MU students began with high-performance scores in almost all dimensions. As a result, teachers needed to create a more challenging and thought-provoking learning environment to encourage them to think more broadly and deeply. Thus, the teacher would give students advice like ‘ Searching for more relevant information can increase the breadth of knowledge ’ and ‘ If the result is true, what is the relevant theory? ’ Most MU students were faster than other majors at defining and constructing critical thinking. However, another phenomenon often observed in the classroom was that the MU students were more reluctant to express their reasoning than the students of other majors. In other words, MU students were afraid to speak openly about their reasoning and thinking, probably due to the excessive pursuit of the correct answer. In sum, the course of five experiments conducted via the learning sheets enhanced abilities of clarity, accuracy, depth, breadth, logic, and significance in MU students.
Apart from providing structure for their critical thinking, as was done with the other preclinical students, the teacher guided the MU students to use advanced critical thinking skills by regularly analyze their thinking processes, reflecting on the decision-making and thinking process [ 84 ]. Researchers have suggested that reflective practice is key to successful medical professionalism [ 85 ] and humanism [ 86 , 87 ]; but more importantly, it may help medical professionals develop better physician–patient relationships [ 88 ]. Therefore, to advance the critical thinking experience of the MU students, teacher should encourage them to gather ideas, analyze, evaluate, and synthesize information. The teacher guided them to reflect on their plan and solve the questions on the learning sheets using their thoughts and words. These reflective practices could involve various biases in the thinking process and outcome, such as the base-rate fallacy, bias blind spot, or choice-supportive bias. The Socratic debate is a common way to model a complex thinking situation and may help teachers inspire students to become critical thinkers. MU students improved their abilities in the clarity, accuracy, depth, breadth, logic, and significance dimensions in the five experiments. This kind of training in thinking should help preclinical students constantly challenge and critically appraise evidence within their context, as well as their patients’ and their own belief and value systems.
Limitations
This study provides a model for developing a specific learning environment like a biochemistry laboratory class into one that will help students develop their critical thinking skills through inquiry. Our results have shown this method to be feasible and effective. However, there were a few limitations to this study. First, although it included students from three different majors, there was no interdisciplinary collaboration that would have simulated collaborations and communication among other healthcare professionals from different fields, as occurs in clinical practice. Introducing such collaboration may have produced more exciting and comprehensive ideas for solving the problems. Training in these professions is specialized to a considerable extent, so inter-professional collaboration should improve therapeutic outcomes and optimize patient care. Second, the original scoring system was time-consuming. However, one of our study objectives was to modify and reduce the nine intellectual dimensions scoring system into the clarity and logic dimensions. Based on the analysis in the current study, the clarity and logic dimensions were sufficient for monitoring the growth of students’ critical thinking.
The present curriculum innovation aimed to teach critical thinking skills to preclinical students in various medical majors using a Socratic questioning learning model instead of a cookbook approach to learning in laboratory courses. The development of problem-solving and critical thinking skills, in addition to process-related skills, in biochemistry laboratory courses supplements traditional curriculum in a helpful way. The curriculum innovation that we described and proposed may represent an incremental step forward for the discipline; it is a novel educational approach for promoting critical thinking skills, fostering an appreciation of the affective domain, and enabling reflective practice by using small-group processing skill instruction and one-on-one Socratic questioning. The current study results are based on training critical thinking skills that should enable students to engage in the “reflection-on-action” process, which might provide an additional bridge between basic medical knowledge and clinical practice. More importantly, reconstructive mental reviews may indirectly shape preclinical students’ future actions in the challenging healthcare industry characterized by uncertainty and novel circumstances.
Data Availability
Due to conditions on participant consent and other ethical restrictions, the datasets used and analysed in the current study are not publicly available. If you have any database data requirements, please contact the corresponding author of this study.
Art-in S. Current situation and need in learning management for developing the analytical thinking of teachers in basic education of Thailand. Procedia-Social and Behavioral Sciences. 2015;197:1494–500.
Article Google Scholar
Maudsley G, Strivens J. Science’,‘critical thinking’and ‘competence’for tomorrow’s doctors. A review of terms and concepts. Med Educ. 2000;34:53–60.
Halpern DF. Thought and knowledge: an introduction to critical thinking. Psychology Press;2013.
Davies M, Barnett R. The Palgrave handbook of critical thinking in higher education. Springer;2015.
Sit HHW. Characteristics of Chinese students’ learning styles. Int Proc Econ Dev Res. 2013;62:36.
He Y. The roles of thinking styles in learning and achievement among Chinese university students.The University of Hong Kong Libraries.
Nordin S, Yunus K. Exploring Metacognitive Awareness among Teachers. Int J Acad Res Progress Educ Dev. 2020;9:462–72
Nelson TO, Narens L. Why investigate metacognition. Metacognition: Knowing about knowing. 1994;13:1–25.
Google Scholar
Dinsmore DL. Examining the ontological and epistemic assumptions of research on metacognition, self-regulation and self-regulated learning. Educational Psychol. 2017;37:1125–53.
Maudsley G, Strivens J. Promoting professional knowledge, experiential learning and critical thinking for medical students. Med Educ. 2000;34:535–44.
Zhong W, Cheng M. Developing critical thinking: experiences of Chinese International Students in a Post-1992 University in England. Chin Educ Soc. 2021;54:95–106.
Dewey J. How we think. In.: D C Heath; 1910.
Book Google Scholar
Ennis R. Critical thinking: a streamlined conception. Teach Philos. 1991;14:5–24.
Ennis RH. Is critical thinking culturally biased? Teach Philos. 1998;21:15–33.
Ennis R. Critical thinking: reflection and perspective part II. Inquiry: Crit Think Disciplines. 2011;26:5–19.
Ennis RH. A taxonomy of critical thinking dispositions and abilities. 1987. https://education.illinois.edu/docs/default-source/faculty-documents/robert-ennis/thenatureofcriticalthinking_51711_000.pdf
Zare P, Mukundan J. The use of socratic method as a teaching/learning tool to develop students’ critical thinking: a review of literature. Lang India. 2015;15:256–65.
Elder L, Paul R. Critical thinking: Tools for taking charge of your professional and personal life. The Foundation for Critical Thinking;2005.
Paul R, Elder L. Critical thinking: intellectual Standards essential to reasoning well within every domain of human thought, part two. J Dev Educ. 2013;37:32.
Elder L, Paul R. Critical thinking: the art of socratic questioning, part II. J Dev Educ. 2007;31:32.
Paul R, Elder L. Critical thinking: the art of socratic questioning. J Dev Educ. 2007;31:36.
Paul R, Elder L. Critical thinking: the art of socratic questioning, part III. J Dev Educ. 2008;31:34–5.
Oyler DR, Romanelli F. The Fact of Ignorance Revisiting the Socratic Method as a Tool for Teaching Critical Thinking. Am J Pharm Educ. 2014;78.
Paul R, Elder L, Bartell T. A Brief History of the Idea of Critical Thinking, The Critical Thinking Community. In.; 1997.
Tofade T, Elsner J, Haines ST. Best practice strategies for effective use of questions as a teaching tool. Am J Pharm Educ. 2013;77:1–7.
Vygotsky L. Zone of proximal development. Mind in society: The development of higher psychological processes 1987;5291:157.
Rud AG Jr. The Use and Abuse of Socrates in Present Day Teaching;1990.
Oh RC. The socratic method in medicine-the labor of delivering medical truths. For the Office-based Teacher of Family Medicine. 2005;37:537–9.
Stoddard HA, O’Dell DV. Would Socrates have actually used the “Socratic Method” for clinical teaching? J Gen Intern Med. 2016;31:1092–6.
Ku KY, Ho IT. Dispositional factors predicting chinese students’ critical thinking performance. Pers Indiv Differ. 2010;48:54–8.
Liu OL, Shaw A, Gu L, Li G, Hu S, Yu N, Ma L, Xu C, Guo F, Su Q. Assessing college critical thinking: preliminary results from the chinese HEIghten ® critical thinking assessment. High Educ Res Dev. 2018;37:999–1014.
Holmes NG, Wieman CE, Bonn D. Teaching critical thinking. Proc Natl Acad Sci. 2015, 112(36):11199–11204.
Elder L, Paul R. The aspiring thinker’s guide to critical thinking. Rowman & Littlefield; 2019.
Cooke M, Irby DM, Sullivan W, Ludmerer KM. American Medical Education 100 years after the Flexner Report. N Engl J Med. 2006;355:1339–44.
Behar-Horenstein LS, Catalanotto FA, Nascimento MM. Anticipated and actual implementation of case-based learning by Dental Faculty Members during and after training. J Dent Educ. 2015;79:1049–60.
Dong H, Guo C, Zhou L, Zhao J, Wu X, Zhang X, Zhang X. Effectiveness of case-based learning in chinese dental education: a systematic review and meta-analysis. BMJ Open. 2022;12:e048497–7.
Sandars J, Goh P-S. Design thinking in Medical Education: the key features and practical application. J Med Educ Curric Dev. 2020;7:2382120520926518–8.
Khan S, Vandermorris A, Shepherd J, Begun JW, Lanham HJ, Uhl-Bien M, Berta W. Embracing uncertainty, managing complexity: applying complexity thinking principles to transformation efforts in healthcare systems. BMC Health Serv Res. 2018;18:192–2.
Preeti B, Ashish A, Shriram G. Problem based learning (PBL)-an effective approach to improve learning outcomes in medical teaching. J Clin Diagn research: JCDR. 2013;7:2896–7.
Ibrahim ME, Al-Shahrani AM, Abdalla ME, Abubaker IM, Mohamed ME. The effectiveness of problem-based learning in Acquisition of Knowledge, soft skills during basic and preclinical sciences: medical students’ points of view. Acta Informatica Medica. 2018;26:119–24.
Servant-Miklos VF. Problem solving skills versus knowledge acquisition: the historical dispute that split problem-based learning into two camps. Adv Health Sci Educ. 2019;24:619–35.
Bjork RA, Dunlosky J, Kornell N. Self-regulated learning: beliefs, techniques, and illusions. Ann Rev Psychol. 2013;64:417–44.
Colliver JA. Effectiveness of problem-based learning curricula: research and theory. Acad Med. 2000;75:259–66.
Bate E, Hommes J, Duvivier R, Taylor DC. Problem-based learning (PBL): Getting the most out of your students–Their roles and responsibilities: AMEE Guide No. 84. Medical teacher 2013.
Lim WK. Dysfunctional problem-based learning curricula: resolving the problem. BMC Med Educ. 2012;12:89–9.
Burgess AW, McGregor DM. Use of established guidelines when reporting on Interprofessional Team-Based learning in Health Professions Student Education: a systematic review. Acad Med. 2021;97:143–51.
Burgess A, Bleasel J, Haq I, Roberts C, Garsia R, Robertson T, Mellis C. Team-based learning (TBL) in the medical curriculum: better than PBL? BMC Med Educ. 2017;17:243.
Burgess A, Ayton T, Mellis C. Implementation of team-based learning in year 1 of a PBL based medical program: a pilot study. BMC Med Educ. 2016;16:49–9.
Schrope M. Solving tough problems with games. Proc Natl Acad Sci. 2013;110:7104–6.
Nessler M. Three Ways virtual Technologies are making a difference in HR. Employ Relations Today. 2014;40:47–52.
Nevin CR, Westfall AO, Rodriguez JM, Dempsey DM, Cherrington A, Roy B, Patel M, Willig JH. Gamification as a tool for enhancing graduate medical education. Postgrad Med J. 2014;90:685–93.
Technologies in Medical Education. In. The SAGE Encyclopedia of Educational Technology. edn.: SAGE Publications, Inc.; 2015.
Hurtubise L, Hall E, Sheridan L, Han H. The Flipped Classroom in Medical Education: Engaging Students to Build Competency. J Med Educ Curric Dev. 2015;2:JMECD.S23895.
Persky AM, Medina MS, Castleberry AN. Developing critical thinking skills in pharmacy students. Am J Pharm Educ. 2019;83.
Chew SW, Lin I-H, Chen N-S. Using Socratic questioning strategy to enhance critical thinking skill of elementary school students. In: 2019 IEEE 19th International Conference on Advanced Learning Technologies (ICALT): 2019 : IEEE; 2019;290–294.
Manurung YH, Siregar FS. Developing students’ critical thinking on speaking through socratic questioning method. Adv Social Sci Educ Humanit Res. 2018;263:212–6.
Wediyantoro PL, Lailiyah M, Yustisia KK. Synchronous discussion in online learning: investigating students’ critical thinking. En Jour Me. (English Journal of Merdeka): Culture Language and Teaching of English. 2020;5:196–203.
Copeland M. Socratic circles: fostering critical and creative thinking in middle and high school. Stenhouse Publishers; 2005.
Tweed RG, Lehman DR. Learning considered within a cultural context: confucian and socratic approaches. Am Psychol. 2002;57:89–99.
Wilberding E. Socratic methods in the classroom: encouraging critical thinking and problem solving through dialogue. Routledge; 2021.
Sanchez-Lara PA, Grand K, Haanpää MK, Curry CJ, Wang R, Ezgü F, Rose CM, D’Cunha Burkardt D, Conway RL, Relan A. Thinking outside “The Box”: Case‐based didactics for medical education and the instructional legacy of Dr John M. Graham, Jr. Am J Med Genet Part A. 2021;185:2636–45.
Cooley JH, Larson S. Promoting a growth mindset in pharmacy educators and students. Curr Pharm Teach Learn. 2018;10:675–9.
Makhene A. The use of the Socratic inquiry to facilitate critical thinking in nursing education. Health SA Gesondheid. 2019;24.
Harasym PH, Tsai T-C, Hemmati P. Current trends in developing medical students’ critical thinking abilities. Kaohsiung J Med Sci. 2008;24:341–55.
Roberts TG, Dyer JE. The relationship of self-efficacy, motivation, and critical thinking disposition to achievement and attitudes when an illustrated web lecture is used in an online learning environment. J agricultural Educ. 2005;46:12–23.
Chalmers AF. What is this thing called science? Hackett Publishing; 2013.
Zain AR. Effectiveness of guided inquiry based on blended learning in physics instruction to improve critical thinking skills of the senior high school student. In: Journal of Physics: Conference Series : 2018: IOP Publishing; 2018: 012015.
Goodey NM, Talgar CP. Guided inquiry in a biochemistry laboratory course improves experimental design ability. Chem Educ Res Pract. 2016;17:1127–44.
Talgar CP, Goodey NM. Views from academia and industry on skills needed for the modern research environment. Biochem Mol Biol Educ. 2015;43:324–32.
Handelsman J, Ebert-May D, Beichner R, Bruns P, Chang A, DeHaan R, Gentile J, Lauffer S, Stewart J, Tilghman SM. Education. Scientific teaching. Science. 2004;304:521-2.
Thaiposri P, Wannapiroon P. Enhancing students’ critical thinking skills through teaching and learning by inquiry-based learning activities using social network and cloud computing. Procedia-Social and Behavioral Sciences. 2015;174:2137–44.
Hirschberg CB. A course in critical thinking for PhD students in biomolecular sciences and biotechnology: classical experiments in biochemistry;2016.
Van Winkle LJ, Cornell S, Fjortoft N, Bjork BC, Chandar N, Green JM, La Salle S, Viselli SM, Burdick P, Lynch SM. Critical thinking and reflection exercises in a biochemistry course to improve prospective health professions students’ attitudes toward physician-pharmacist collaboration. Am J Pharm Educ. 2013;77.
Kanari Z, Millar R. Reasoning from data: how students collect and interpret data in science investigations. J Res Sci Teach. 2004;41:748–69.
Kumassah E, Ampiah J, Adjei E. An investigation into senior high school (shs3) physics students understanding of data processing of length and time of scientific measurement in the Volta region of Ghana. Int. J. Educ. Technol. High. Educ. 2014;37–61.
Kung RL, Linder C. University students’ ideas about data processing and data comparison in a physics laboratory course. Nordic Stud Sci Educ. 2006;2:40–53.
Ryder J, Leach J. Interpreting experimental data: the views of upper secondary school and university science students. Int J Sci Educ. 2000;22:1069–84.
Ryder J. Data interpretation activities and students’ views of the epistemology of science during a university earth sciences field study course. Teaching and Learning in the Science Laboratory.edn. Springer;2002. p.151–162.
Séré MG, Journeaux R, Larcher C. Learning the statistical analysis of measurement errors. Int J Sci Educ. 1993;15:427–38.
Lunn M, McNeil D. Applying Cox regression to competing risks. Biometrics. 1995;524–532.
Haviland A, Nagin DS, Rosenbaum PR. Combining propensity score matching and group-based trajectory analysis in an observational study. Psychol Methods. 2007;12:247–67.
Helland-Hansen W, Hampson G. Trajectory analysis: concepts and applications. Basin Res. 2009;21:454–83.
Barrows HS, Tamblyn RM. Problem-based learning: an approach to medical education. Volume 1. Springer;1980.
Jensen G, Denton B. Teaching physical therapy students to reflect: a suggestion for clinical education. J Phys Therapy Educ. 1991;5:33–8.
Stern DT, Papadakis M. The developing physician—becoming a professional. N Engl J Med. 2006;355:1794–9.
Gracey CF, Haidet P, Branch WT, Weissmann P, Kern DE, Mitchell G, Frankel R, Inui T. Precepting humanism: strategies for fostering the human dimensions of care in ambulatory settings. Acad Med. 2005;80:21–8.
Branch WT Jr, Kern D, Haidet P, Weissmann P, Gracey CF, Mitchell G, Inui T. Teaching the human dimensions of care in clinical settings. JAMA. 2001;286:1067–74.
Wald HS, Davis SW, Reis SP, Monroe AD, Borkan JM. Reflecting on reflections: enhancement of medical education curriculum with structured field notes and guided feedback. Acad Med. 2009;84:830–7.
Download references
Acknowledgements
The authors wish to thank Chi-Her Lin, MD for their encouragement and support in the writing of this manuscript, and Prof. Woei-Jer Chuang, Hung-Chi Cheng, Chang-Shi Chen, Po-Hsin J. Huang, Chien-hung Yu, and Wen-Tsan Chang for their help with the experimental design. Special thanks to Tanvi Gupta for her help with the improving reading fluency.
This work was supported by the Teaching Practice Research Program, Ministry of Education, Taiwan (Grant No: PMN1110350, PMN1100853, PMN1090364, PMN108075, PMN107018).
Author information
Authors and affiliations.
Department of Biochemistry and Molecular Biology, College of Medicine, National Cheng Kung University, University Road No.1, East District 701, Tainan City, Taiwan (R.O.C.)
Yueh-Ren Ho
School of Medicine, College of Medicine, National Cheng Kung University, University Road No.1, East District 701, Tainan City, Taiwan (R.O.C.)
Yueh-Ren Ho & Chien-Ming Li
Institute of Clinical Medicine, College of Medicine, National Cheng Kung University, University Road No.1, East District 701, Tainan City, Taiwan (R.O.C.)
Bao-Yu Chen
Division of Infectious Diseases, Department of Internal Medicine, Chi Mei Medical Center, Zhonghua Raod No.901, Yongkang District 710, Tainan City, Taiwan (R.O.C.)
Chien-Ming Li
You can also search for this author in PubMed Google Scholar
Contributions
Yueh-Ren Ho: substantially contributed to the conception, data curation, interpretation, drafting and critical revision of the paper. She has given final approval to the manuscript and agrees to be accountable for the work. Bao-Yu Chen: substantially contributed to the conception, formal analysis, methodology, visualization, and writing and editing the manuscript. Chien-Ming Li: substantially contributed to the conception, data curation, review and editing the manuscript.
Corresponding author
Correspondence to Yueh-Ren Ho .
Ethics declarations
Ethics approval and consent to participate.
Students participating in this course will be informed before the class begins that their results will be used for educational academic research, and their written informed consent were obtained. The methodology of the study including the content analysis of literature on data curation activities were approved and funded by Teaching Practice Research Program, Ministry of Education, Taiwan. Throughout the study, all methods followed the approved methodology and adhered to the relevant guidelines and regulations. According to Human Subjects Research Act, Chap. 2, article 5: The Ministry of Education review current study nature and announced the principal investigator shall not submit the research protocol for review and approval by the Institutional Review Board. Please refer to the source of law in the website of Laws & Regulations Database of The Republic of China (Taiwan) ( https://law.moj.gov.tw/ENG/LawClass/LawAll.aspx?pcode=L0020176 ).
Consent for publication
Not applicable.
Competing interests
The authors have declared that there are no conflicts of interest in relation to the subject of this study.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ho, YR., Chen, BY. & Li, CM. Thinking more wisely: using the Socratic method to develop critical thinking skills amongst healthcare students. BMC Med Educ 23 , 173 (2023). https://doi.org/10.1186/s12909-023-04134-2
Download citation
Received : 20 September 2022
Accepted : 02 March 2023
Published : 20 March 2023
DOI : https://doi.org/10.1186/s12909-023-04134-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Biochemistry experiment
- Critical thinking
- Socratic method
- Medical education
- Metacognition
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]

“The Doctor as a Humanist”: The Viewpoint of the Students
Conference Report and Reflection by Poposki Ognen (University Pompeu Fabra); Castillo Gualda Paula (University of Balearic Islands); Barbero Pablos Enrique (University Autonoma de Madrid); Pogosyan Mariam (Sechenov University); Yusupova Diana (Sechenov University); and Ahire Akash (Sechenov University)

The practice of Medicine as a profession has become very technical; doctors rely on fancy investigations, treatment algorithms and standardized guidelines in treating patients. In a lot of universities, medical students and residents are trained without appreciating the importance of art and the humanities in delivering good care to patients and their families. Factual knowledge is imposed on us, as students, from scientific evidence delivered by highly specialized professionals: those who know more and more about niche subjects.
As a result, when someone decides to become a doctor , it seems that scientific training is the sole priority, with most attention being given to the disease-treatment model. As medical students, we are taught very specific subjects, leaving little or no space or time for any cultural enrichment programs. And yet, Personal growth as a doctor and a human being cannot be achieved unless one is exposed to the whole range of human experience. Learning from art and artists can be one such means of gaining these enriching experiences. We can learn from historians, and from eminent painters, sculptors, and writers, as well as from great scientists. How do we achieve these ends? The following essay summarizes and reviews one attempt at providing answers. The 2nd “Doctor as a Humanist” Symposium took place at Sechenov University in Moscow from the 1 st to the 3 rd of April, 2019, to explore the holistic perspective of interpersonal treatment.
To begin our essay, we would like to clarify some key concepts, such as culture, humanism and humanities, as they were employed at the conference. Culture is a complex phenomenon that includes knowledge, beliefs, artistic production, morals, customs and skills acquired by being part of a society, which can be transmitted consciously or unconsciously, by individuals to others and through different generations.
The humanities are academic disciplines that study the cultural aspects and frailties of being human, and use methods that are primarily analytical, critical, or speculative, which distinguish them from the approaches of the natural sciences. Humanism is the practice of making the human story central. Consequently, the studies of humanities, so invested in human stories, is one aspect of practicing humanism.
Technological and practical progress in medicine has been impressive in the past fifty years. Nevertheless, patients still suffer from chronic conditions such as heart failure, chronic lung disease, depression, and many others. These are conditions where technology cannot significantly change the outcomes or reverse the underlying condition. One of the ways to alleviate suffering is through compassion and empathy where the doctor is a professional who listens to, understands and comforts the patient, as well as engaging the patient as a fellow human being. We need arts and humanities as doctors’ tools to comfort and, perhaps, even to heal. We also need them to remind us that we are ‘merely human’ ourselves, and that we share our humanity with our patients, as equals.
Unquestionably, there are fundamental requirements that every physician must internalize; the conference goal was to explain that one such requirement is the humanistic view. Opera, poetry, philosophy, history, the study of dialectics, biographical readings, and even volunteering abroad can be means of engaging the world for positive change. Sometimes called “soft” skills, these are in fact necessary and valuable qualities to empower ourselves as persons, as well as doctors. The 2nd The Doctor as a Humanist Symposium placed the corner stone in a global project that aims to understand medicine as a multidisciplinary subject, and to establish the concept of humanistic medicine both as a science and an art where the patient and the doctor are human beings working together.

STUDENT PARTICIPATION
The event united experts in Medicine and the Humanities from all over the world. The speakers (doctors, nurses and students) were from Russia, the USA, the UK, Spain, Italy, Germany, Mexico and more. Each day’s program was both intense and diverse, and included plenary lectures and panel sessions. Medical students were highly involved in all parts of the conference, offering us a great chance to introduce our projects, share our opinions on various topics, and discuss our questions connected with the role of the humanities in medicine.We participated in roundtable discussions, which were chaired by experts from different countries. Even though this made us nervous, at the same time it was very important for us, as students, to be a part of it. We discussed the future of medical humanities from various perspectives, and above all our thoughts and ideas were listened to and commented on, on an equal basis with the world’s experts. For once, we could see that our views were being taken into consideration, and we hope that in the future this will be the norm and NOT the exception. We are the future of medicine, and our voices should be heard, too.
At the end of the first day there was a students’ session, where we gave our opinions on the relative importance of the medical humanities from a multicultural viewpoint, and on this particular roundtable there were students from Russia, Spain, Iran, Mexico, Italy, as well as a Nursing resident. One of the students during the session shared her view that “I would like to see medicine through the lens of humanism and empathy, and also implement all its principles in my professional life on a daily basis”. All participants agreed, and although we were representing different countries and cultures there was no disagreement about this. Even though we have not yet faced many of the obstacles of the world of medicine, we can see the role of compassion in clinical practice better perhaps than our seniors. We shared our points of view about this question and its relevance in the different countries. It was an incredible moment, as experts and professors demonstrated a great interest in our ideas.
The program was extremely diverse; however, the main idea that most speakers expressed was how to find, sustain and not lose humanist goals. Brandy Schillace gave an impressive presentation entitled “Medical Humanities today: a publisher’s perspective”, which studied the importance of writing and publishing not only clinical trials, but also papers from historians, literary scholars, sociologists, and patients with personal experiences. The nurses Pilar d’Agosto and Maria Arias made a presentation on the topic of the Nursing Perspective that is one of the main pillars of medical practice. Professor Jacek Mostwin (Johns Hopkins University) shared his thoughts on patients’ memoirs. An Italian student, Benedetta Ronchi presented the results of an interview on medical humanities posed to the participants and speakers during the symposium. The plurality of perspectives made this conference an enriching event and showed us how diverse ideas can help us become better doctors. More importantly, it reminded us of our common humanity.
A significant part of the symposium was dedicated to Medicine and Art. Prof Josep Baños and Irene Canbra Badii spoke about the portrayal of physicians in TV medical dramas during the last fifty years. The book “The role of the humanities in the teaching of medical students” was presented by these authors and then given to participants as gifts. Dr Ourania Varsou showed how Poetry can influence human senses through her own experience in communicating with patients. She believed that many of the opinions and knowledge that we have internalized should be unlearned in order to have a better understanding of the human mind. The stimulus of poetry makes this possible. Poetry allows us to find new ways to express ourselves, and thus increase our emotional intelligence and understanding of other people’s feelings.
One of the most impressive lectures was by Dr Joan.B Soriano, who spoke about “Doctors and Patients in Opera” and showed how the leading roles of physicians in opera have changed over the centuries. People used to consider the doctor as the antihero, but with time this view has transformed into a positive one that plays a huge role in history.
It is important to be professional in your medical career, but also to be passionate about the life surrounding you; for instance, Dr Soriano is also a professional baritone singer. For students, this Symposium was full of obvious and hidden messages, which gave us much lot of food for thought. As Edmund Pellegrino, the founding editor of the Journal of Medicine and Philosophy , said: “Medicine is the most humane of sciences, the most empiric of arts, and the most scientific of humanities.”

CHOOSING ONE WORD
To conclude our summary of the students’ viewpoint each of us chose One word to encapsulate our thoughts about the symposium.
The Doctor as a Humanist is a multicultural event where everyone can learn and contribute to this global necessity to put the heart and soul back into medicine. Of course, we are aware and delighted that other organizations are championing the cause of the Humanities in Medicine, and in some cases, such as https://www.dur.ac.uk/imh/ , they have been doing so for many years.
As medical students, we appreciate how we have been placed at the centre of the symposium, which we believe has made this new initiative rather special. We hope that students of Medicine and from other disciplines come and participate in future symposia.
If you want to learn more, and see how you can participate, please contact the International student representatives, Mariam ( [email protected] ) and David ( [email protected] ).
Acknowledgements
Assistance provided by Jonathan McFarland (c) and Joan B. Soriano (University Autonoma de Madrid) was greatly appreciated during the planning and the development of the article.
Analysis and discussion of research | Updates on the latest issues | Open debate
All BMJ blog posts are published under a CC-BY-NC licence
BMJ Journals
Main navigation
- Our Articles
- Dr. Joe's Books
- Media and Press
- Our History
- Public Lectures
- Past Newsletters
Subscribe to the OSS Weekly Newsletter!
Register for the oss 25th anniversary event, twisting facts about cancer.

- Add to calendar
- Tweet Widget
Let’s start with some facts. Antiperspirants, cell phones, root canals or wired bras do not cause cancer. Sugar or dairy products do not “feed” the disease. You cannot cure cancer with an alkaline diet, crystals, juices, shark cartilage, apricot pits, magnets, mistletoe, soursop, chlorella, black walnuts, coconut oil, cesium chloride, reiki, psychic surgery, baking soda, antineoplastons, bioresonance machines, orgone accumulators, Rife frequency generators or coffee enemas.
All of this comes to mind now because I was forwarded a link to a document entitled “Everyday Products Linked to Cancer” which also offers solutions to the problem. So, I clicked. I quickly learned that the discoverer of “the missing link” to “conquering cancer” is identified as a “natural health researcher and certified holistic cancer coach.” That immediately set my alarm bells ringing. This is not terminology that would ever be used to describe a legitimate scientist. And those bells really started to clamor when I encountered phrases like “groundbreaking,” “unveil cancer care known only to a few,” “challenge the one-sided, conventional understanding and offer more effective ways to conquer cancer,” “discover the proven protocols that have helped hundreds of thousands of people prevent and conquer cancer,” and “discover why many cancer treatments and prevention protocols fail.”
It seems Nathan Crane, also described as a “plant-based athlete,” has found the secret that has eluded thousands and thousands of researchers around the globe and is now equipped to “pave the way for future generations to live cancer free.” A search for this sage’s educational background reveals only that he went to Belgrade High School in Montana.
What is the key to living cancer-free? Staying away from “toxic household and personal care products” and “turning to nature” for replacements. Of course, we also need to fortify our body against toxins. How? By making use of “the power of nature’s detoxifiers.” Let me point out that the term “detoxify” is generally indicative of pseudoscience since the toxins being removed are never identified nor is the mechanism by which they are eliminated elucidated.
There is nothing novel in this “Conquering Cancer” manuscript. The Internet and bookstores brim with articles and books about purported carcinogens in everyday products and secret cures hidden by “Big Pharma” for fear of losing profits from the sale of ineffective, toxic chemotherapeutic agents. The idea of secret cures is nonsense, but when it comes to chemicals found in consumer products, there are some legitimate issues. However, fear-mongering documents, such as this one, generally smack of an ignorance of dose-response relationships and claim to have greater knowledge of the impact of these chemicals on health than what actually exists. Suppositions are presented as facts.
Some personal care products and cleaning agents contain chemicals that can be classified as endocrine disruptors or carcinogens. Furthermore, some of these can be detected in our bloodstream and urine. But it is critical to understand that the presence of a chemical cannot be equated to the presence of risk. Labeling a substance as an endocrine disruptor or carcinogen is in general based on cell culture or animal studies that use amounts far greater than what humans can possibly encounter. This does not mean that concerns about the likes of phthalates, bisphenol A, dioxane and nonylphenol ethoxylates should be swept under the carpet, but proclamations that “we’re poisoning ourselves” by using products that contain traces of these substances magnify whatever risk they may pose in an unrealistic fashion.
While reducing our use of products that contain chemicals that have the shadow of carcinogen or endocrine disruptor hanging over them has merit, the claim that turmeric, ginger, cayenne pepper, cinnamon, frankincense, Camu Camu or blueberries are “nature’s detoxifiers” and protect us from cancer is not evidence-based.
However, my biggest problem with this publication is the simplistic view it presents about preventing cancer. This is a very complex disease in which genetics, diet, infections, overweight, smoking, alcohol consumption, certain chemicals, exposure to ionizing radiation, changes in hormone levels, physical activity and age can all play roles. Suggestions that cancer risk can be significantly reduced by adding turmeric to the diet or replacing a commercial cleaning agent with vinegar, or switching from store-bought shampoo to a homemade concoction of aloe vera gel, coconut milk and castile soap, are naïve.
Something else is bothersome about this publication. The talk about “dangerous” everyday products and the use of herbs to “bolster our natural defenses” seems to be just bait to hook people to click on a link to a docuseries about “Conquering Cancer.” We are asked if we are “ready to explore the hidden cause of cancer that has eluded experts for years” and told that we will discover “how to starve your cancer cells without chemo, radiation or surgery.” The latter is a hallmark of quackery.
I did not take the bait because I follow cancer research closely and know that there are no hidden causes or magical cures. Certainly not any that have been discovered by a “certified holistic cancer coach.” I also suspect that if I were to click on the link for a “free ticket” to the series that promises to reveal “how natural, proven methods have helped over 591,753 people prevent and treat this life-threatening disease,” I might at some point be prompted to dig out my credit card for some over-hyped dietary supplement or a book with an assortment of twisted facts. But that’s just a guess.
@JoeSchwarcz
What to read next
Processed foods have many faces 17 may 2024.

Reports of the Death of Dental Cavities Are Greatly Exaggerated 17 May 2024

Methylene Chloride Can Strip Paint but Can Also Strip Years Off Your Life 15 May 2024

No, Eating French Fries is Not the Same as Smoking Cigarettes 10 May 2024

Navigating the Twisted World of Varicose Veins 10 May 2024
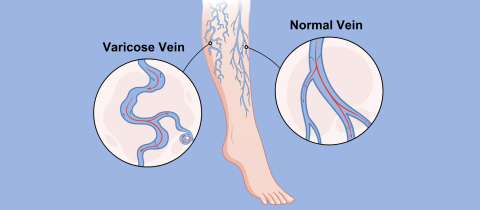
Pass on the Salt: Should We Ask for Potassium Chloride at the Dinner Table Instead? 17 May 2024

Department and University Information
Office for science and society.

- Augsburg.edu
- Inside Augsburg
Search Strommen Center for Meaningful Work
- Faculty & Staff
- Graduate Students
- First Generation
- International
- Students With Disabilities
- Undocumented
- Business & Finance
- Culture and Language
- Environmental Sustainability
- Government, Law & Policy
- Health Professions
- Human & Social Services
- Information Technology & Data
- Marketing, Media & Communications
- Resumes and Cover Letters
- Expand Your Network / Mentor
- Explore Your Interests / Self Assessment
- Negotiate an Offer
- Prepare for an Interview
- Prepare for Graduate School
- Search for a Job / Internship
- Job Fair Preparation
- Start Your Internship
- Choosing a Major
- Career Collaborative
- Travelers EDGE
- Meet the Team
Critical Thinking: A Simple Guide and Why It’s Important
- Share This: Share Critical Thinking: A Simple Guide and Why It’s Important on Facebook Share Critical Thinking: A Simple Guide and Why It’s Important on LinkedIn Share Critical Thinking: A Simple Guide and Why It’s Important on X
Critical Thinking: A Simple Guide and Why It’s Important was originally published on Ivy Exec .
Strong critical thinking skills are crucial for career success, regardless of educational background. It embodies the ability to engage in astute and effective decision-making, lending invaluable dimensions to professional growth.
At its essence, critical thinking is the ability to analyze, evaluate, and synthesize information in a logical and reasoned manner. It’s not merely about accumulating knowledge but harnessing it effectively to make informed decisions and solve complex problems. In the dynamic landscape of modern careers, honing this skill is paramount.
The Impact of Critical Thinking on Your Career
☑ problem-solving mastery.
Visualize critical thinking as the Sherlock Holmes of your career journey. It facilitates swift problem resolution akin to a detective unraveling a mystery. By methodically analyzing situations and deconstructing complexities, critical thinkers emerge as adept problem solvers, rendering them invaluable assets in the workplace.
☑ Refined Decision-Making
Navigating dilemmas in your career path resembles traversing uncertain terrain. Critical thinking acts as a dependable GPS, steering you toward informed decisions. It involves weighing options, evaluating potential outcomes, and confidently choosing the most favorable path forward.
☑ Enhanced Teamwork Dynamics
Within collaborative settings, critical thinkers stand out as proactive contributors. They engage in scrutinizing ideas, proposing enhancements, and fostering meaningful contributions. Consequently, the team evolves into a dynamic hub of ideas, with the critical thinker recognized as the architect behind its success.
☑ Communication Prowess
Effective communication is the cornerstone of professional interactions. Critical thinking enriches communication skills, enabling the clear and logical articulation of ideas. Whether in emails, presentations, or casual conversations, individuals adept in critical thinking exude clarity, earning appreciation for their ability to convey thoughts seamlessly.
☑ Adaptability and Resilience
Perceptive individuals adept in critical thinking display resilience in the face of unforeseen challenges. Instead of succumbing to panic, they assess situations, recalibrate their approaches, and persist in moving forward despite adversity.
☑ Fostering Innovation
Innovation is the lifeblood of progressive organizations, and critical thinking serves as its catalyst. Proficient critical thinkers possess the ability to identify overlooked opportunities, propose inventive solutions, and streamline processes, thereby positioning their organizations at the forefront of innovation.
☑ Confidence Amplification
Critical thinkers exude confidence derived from honing their analytical skills. This self-assurance radiates during job interviews, presentations, and daily interactions, catching the attention of superiors and propelling career advancement.
So, how can one cultivate and harness this invaluable skill?
✅ developing curiosity and inquisitiveness:.
Embrace a curious mindset by questioning the status quo and exploring topics beyond your immediate scope. Cultivate an inquisitive approach to everyday situations. Encourage a habit of asking “why” and “how” to deepen understanding. Curiosity fuels the desire to seek information and alternative perspectives.
✅ Practice Reflection and Self-Awareness:
Engage in reflective thinking by assessing your thoughts, actions, and decisions. Regularly introspect to understand your biases, assumptions, and cognitive processes. Cultivate self-awareness to recognize personal prejudices or cognitive biases that might influence your thinking. This allows for a more objective analysis of situations.
✅ Strengthening Analytical Skills:
Practice breaking down complex problems into manageable components. Analyze each part systematically to understand the whole picture. Develop skills in data analysis, statistics, and logical reasoning. This includes understanding correlation versus causation, interpreting graphs, and evaluating statistical significance.
✅ Engaging in Active Listening and Observation:
Actively listen to diverse viewpoints without immediately forming judgments. Allow others to express their ideas fully before responding. Observe situations attentively, noticing details that others might overlook. This habit enhances your ability to analyze problems more comprehensively.
✅ Encouraging Intellectual Humility and Open-Mindedness:
Foster intellectual humility by acknowledging that you don’t know everything. Be open to learning from others, regardless of their position or expertise. Cultivate open-mindedness by actively seeking out perspectives different from your own. Engage in discussions with people holding diverse opinions to broaden your understanding.
✅ Practicing Problem-Solving and Decision-Making:
Engage in regular problem-solving exercises that challenge you to think creatively and analytically. This can include puzzles, riddles, or real-world scenarios. When making decisions, consciously evaluate available information, consider various alternatives, and anticipate potential outcomes before reaching a conclusion.
✅ Continuous Learning and Exposure to Varied Content:
Read extensively across diverse subjects and formats, exposing yourself to different viewpoints, cultures, and ways of thinking. Engage in courses, workshops, or seminars that stimulate critical thinking skills. Seek out opportunities for learning that challenge your existing beliefs.
✅ Engage in Constructive Disagreement and Debate:
Encourage healthy debates and discussions where differing opinions are respectfully debated.
This practice fosters the ability to defend your viewpoints logically while also being open to changing your perspective based on valid arguments. Embrace disagreement as an opportunity to learn rather than a conflict to win. Engaging in constructive debate sharpens your ability to evaluate and counter-arguments effectively.
✅ Utilize Problem-Based Learning and Real-World Applications:
Engage in problem-based learning activities that simulate real-world challenges. Work on projects or scenarios that require critical thinking skills to develop practical problem-solving approaches. Apply critical thinking in real-life situations whenever possible.
This could involve analyzing news articles, evaluating product reviews, or dissecting marketing strategies to understand their underlying rationale.
In conclusion, critical thinking is the linchpin of a successful career journey. It empowers individuals to navigate complexities, make informed decisions, and innovate in their respective domains. Embracing and honing this skill isn’t just an advantage; it’s a necessity in a world where adaptability and sound judgment reign supreme.
So, as you traverse your career path, remember that the ability to think critically is not just an asset but the differentiator that propels you toward excellence.
Calculate for all schools
Your chance of acceptance, your chancing factors, extracurriculars, what are the best undergrad degrees for pre-med students.
I'm super interested in pursuing medicine, but I'm not sure what major to choose for my undergraduate degree. Which degrees are recommended to prep for medical school and a career as a doctor?
Choosing a major for your undergraduate degree is an important decision, especially when you have a clear goal of pursuing medicine. While there is no single best major for a pre-med student, there are a few popular options known for their strong preparation for medical school. These degrees typically provide a solid foundation in the sciences, ensuring you have the necessary prerequisites and a deep understanding of the subjects you will encounter in medical school. Some commonly recommended majors include:
1. Biology: This major covers a wide range of topics related to living organisms and will give you an excellent understanding of the human body, genetics, and other essential subjects in medicine.
2. Biochemistry: As a biochemistry major, you will study the chemical processes occurring in living organisms. This field combines the principles of both biology and chemistry, giving you a deeper understanding of the biochemical processes at play in the human body.
3. Chemistry: This major will familiarize you with various chemical principles and laboratory techniques. It can be particularly beneficial if you are considering a career in pharmacology or clinical research.
4. Biomedical Engineering: Biomedical engineering is the application of engineering principles and design concepts to medicine and biology. As a biomedical engineering major, you will learn how to develop medical devices and technologies, which can provide a unique perspective as a medical professional.
5. Neuroscience: If you're interested in the brain and nervous system, a major in neuroscience will provide a comprehensive understanding of the subject, which can be beneficial if you are considering a specialization in neurology or psychiatry.
6. Psychology: As a psychology major, you will learn about human behavior and cognitive processes. This knowledge can be helpful in understanding patients' mental health and behavior in a clinical setting.
Bear in mind that while these majors are frequently pursued by pre-med students, medical schools generally do not require applicants to have a specific major. In fact, some medical schools encourage a diverse range of academic backgrounds among their students. The key is to make sure you complete the required prerequisite courses (biology, chemistry, physics, and math) as part of your undergraduate degree.
Ultimately, the best major for a pre-med student is the one in which they can excel academically, develop critical thinking skills, and maintain a strong GPA. Consider your interests and strengths, and remember that there are successful medical students from various academic backgrounds.
About CollegeVine’s Expert FAQ
CollegeVine’s Q&A seeks to offer informed perspectives on commonly asked admissions questions. Every answer is refined and validated by our team of admissions experts to ensure it resonates with trusted knowledge in the field.

- About the Program
- CME Programs/Publications
- Medical School Curriculum
Elena Atochina-Vasserman, MD

Dr. Atochina earned her M.D. from Tomsk Medical School and a Ph.D. in Biochemistry in 1990 from Russian Cardiology Research Center, Moscow, Russia. She completed post-doctoral training at the University of Miami with Dr. James Ryan and at the University of Pennsylvania with Dr. Aron B. Fisher and Dr. Vladimir Muzykantov at the Institute for Environmental Medicine. Following three years as a Research Associate in the laboratory of Dr. Michael F. Beers, she was appointed as a Senior Laboratory Investigator and now directs the Lung Host Defense and Inflammation Core in Dr Beers' laboratory.
Dr. Atochina-Vasserman's early work included studies of selective vascular (in vivo) targeting of enzyme therapeutics for containment of oxidative and vascular stress, inflammation, endothelial injury and ischemia-reperfusion. More recently her work has focused primarily on the study of the response of the lung to a variety of challenges including Pneumocystis murina, Aspergilllus fumigatus, bleomycin, and hyperoxia. She has also examined the interrelationship between surfactant protein D and macrophage function with a special emphasis on the biochemistry of the structure-function changes induced by post translational modification of SP-D by nitric oxide.
About the Program | CME Programs and Publications Medical School Curriculum | Faculty | Resources | Contact Us | Home
Ukraine war latest: Ukraine 'destroys Russian Black Sea minesweeper'
Ukraine's navy says it has destroyed a Russian Black Sea fleet minesweeper. Meanwhile, an attack on a residential area in Kharkiv left six civilians injured - with Ukraine saying it is investigating the bombing as a potential war crime.
Sunday 19 May 2024 12:26, UK
Please use Chrome browser for a more accessible video player
- Two killed in Russian strikes on Kherson | Five dead in Kharkiv
- Ukraine investigating 'potential war crime' after civilians wounded
- Ukrainian soldiers reveal how they were secretly moved ahead of Russian invasion
- Russia takes control of village in Kharkiv - defence ministry
- Live reporting by Josephine Franks
A seven-month pregnant woman was among five people killed in strikes on a Kharkiv recreation area, local police said.
At least 16 people were injured; eight of them are in a serious condition, police said.
An 8-year-old child received minor injuries and a police officer and paramedic were injured in the second strike, they added.
You can see some photos from the scene in this Facebook post from Kharkiv police...
President Salome Zourabichvili has vetoed a controversial bill which sparked weeks of mass protests Georgia - but it is likely her veto will be overturned by the government majority.
The "foreign agents" bill passed by parliament earlier this week would force media and non-governmental organisations and other non-profit groups to register as "pursuing the interests of a foreign power" if they receive more than 20% of funding from abroad.
The president said the bill, which the US has described as a "Kremlin style law", contradicts Georgia's constitution and "all European standards", adding it "must be abolished".
She is increasingly at odds with the ruling party, Georgian Dream, considered by many as pro-Russian.
Read more about the rule and what the president's veto means below...
The number of people killed in Russian airstrikes in a recreation area just outside Kharkiv has risen to five, and at least 16 are injured.
Kharkiv mayor Ihor Terekhov gave update on Telegram, saying: "The explosions heard in Kharkiv around noon occurred in a nearby suburb.
"Two Russian missiles hit a recreation centre where people were relaxing, killing five people and injuring sixteen others."
Yaroslav Trofimko, an inspector with the local police department, said there "never any soldiers here".
"It was a Sunday, people were supposed to be here to rest, children were supposed to he here, pregnant women, resting, enjoying a normal way of life."
He arrived on the scene after the first blast, and was there when the second strike hit the same scene around 20 minutes later.
Ukraine has frequently accused Russia of using "double tap" strikes to kill or injure emergency workers at the scene of strike impacts.
Kharkiv's governor Oleh Syniehubov earlier said a paramedic was among those injured.
Russian air defences downed 103 Ukrainian drones and 12 United States-made ATACMS missiles over the past 24 hours, the Russian defence ministry said .
Russian officials earlier said that Ukraine had fired nine ATACMS at Crimea and attacked Russian regions with at least 60 drones, forcing one oil refinery in southern Russia to halt operations.
We're getting more news from the scene of a Russian strike in a northern suburb of Kharkiv where four people were killed, as reported in our 10.30 post.
The number of people reported injured has risen from eight to 15.
A recreation area was destroyed, according to Reuters correspondents at the site.
Rescuers described a powerful blast, followed by a second, "double tap" strike about fifteen minutes later.
A man's corpse lay under the rubble of what just over an hour previously was a busy lakeside restaurant area on a sunny day.
A woman stumbled around in shock looking for her handbag in the wreckage.
"The occupiers attacked the area where local residents were relaxing," Kharkiv's governor, Oleh Syniehubov, said on Telegram.
In recent weeks, Kharkiv city and the region of the same name have been under constant attack by Russian missiles and guided bombs as Russian troops have launched an offensive in the northeast of the region.
Ukraine fired long-range missiles at Crimea and attacked Russia with at least 60 drones in a major attack last night.
Meanwhile Ukraine says it destroyed more than 30 Russian drones.
Russian air defences shot down 57 Ukrainian drones over its southern Krasnodar region, the country's defence ministry said.
As we reported in our 8.26 post, an oil refinery hit by debris had to halt operations, with local military officials saying there was no fire or damage.
Local news outlet Astra published videos appearing to show an explosion at the refinery as it was hit by a drone. The videos could not be independently verified.
Nine long-range ballistic missiles and a drone were destroyed over the Russia-occupied Crimean Peninsula following Friday morning’s massive Ukrainian drone attack that cut off power in the city of Sevastopol.
The Russian-installed governor of Ukraine's partially occupied Kherson region, Vladimir Saldo, said one person died and 16 were wounded when a Ukrainian drone hit a minibus on Sunday morning.
In Ukraine, air force officials said air defence shot down all 37 Russian drones launched against the country overnight (more in our 7.20 post).
Four people have been killed and at least eight more injured in a Russian airstrike on Kharkiv, Ukrainian officials say.
Kharkiv's governor Oleh Syniehubov said the strike hit the residential area of Malodanyliv.
A paramedic was among those injured, he said on Telegram.
Kharkiv has been the target of frequent airstrikes since Russia began its new offensive on the northeastern region late last week.
Residential buildings have been destroyed and Ukraine has accused Russia of targeting civilians, saying it is investigating this as a "potential war crime".
Governor Oleh Syniehubov said this morning that one person died and 11 were wounded as a result of shelling on Saturday.
Here are some of the latest pictures from the city...
Ukrainian forces have destroyed Russian Black Sea fleet minesweeper, a statement from the Ukrainian navy said.
"Last night the Ukrainian Defence Forces destroyed the Russian Black Sea Fleet's Project 266-M Kovrovets minesweeper," it said on Telegram.
As Russia’s new invasion of northern Ukraine ticks into its second week, Trevor Philips asks Defence Secretary Grant Shapps if we are creating a stalemate in the war with Russia.
It comes after Volodymyr Zelenskyy said this week: "We are in a nonsense situation where the West is afraid that Russia will lose the war. And it does not want Ukraine to lose it."
Grant Shapps says he went to Ukraine earlier this year and made the point that "by delaying what we should be doing - and in fact now have, through particularly what [the US] Congress has done - we are running the risk of doing exactly what President Zelensky is concerned about".
He goes on: "I think this is completely nonsensical for the West. We have to understand we are in an existential battle about the way we run the world order and about democracy itself."
He accuses autocratic countries of trying to "impose" their systems on "free and democratic countries", declaring: "We have to stand up to that."
Be the first to get Breaking News
Install the Sky News app for free


IMAGES
VIDEO
COMMENTS
the need for fostering critical thinking amongmedical practitioners. This article attempts to provide a conceptual analysis of critical thinking with reference to medical education along with measures to foster critical thinking through relevant teaching learning and assessment methods. Key words: Critical thinking, medical education, quality
Medistudents team. August 18, 2021. Critical thinking is an essential cognitive skill for every individual but is a crucial component for healthcare professionals such as doctors, nurses and dentists. It is a skill that should be developed and trained, not just during your career as a doctor, but before that when you are still a medical student.
Critical thinking is an essential cognitive skill for the individuals involved in various healthcare domains such as doctors, nurses, lab assistants, patients and so on, as is emphasized by the Authors. Recent evidence suggests that critical thinking is being perceived/evaluated as a domain-general construct and it is less distinguishable from ...
Medical students must possess a broad range of competencies to successfully learn and develop in medical school and become effective physicians. The premed competency model includes professional, thinking and reasoning, and science competencies, and serves as a roadmap for students as they prepare to succeed in medical school.
This is a qualitative study aiming to explain the barriers of critical thinking in the medical school curriculum. In this study, using the qualitative research approach, critical thinking barriers in the medical school curriculum were explained from the viewpoint of medical education experts of Shiraz University of Medical Sciences.
Pathways. Pathways incorporates pedagogical approaches that foster active learning and critical thinking; earlier clinical experience; and advanced clinical and student-tailored basic/population science experiences that will provide customized pathways for every student. In the Pathways curriculum, the core basic/population science needed to ...
At a national conference in 2011, teams from nine medical schools defined critical thinking as "the ability to apply higher cognitive skills (eg, analysis, synthesis, self-reflection, perspective taking) and/or the disposition to be deliberative about thinking (being open-minded or intellectually honest) that leads to action that is logical ...
To meet these goals, current challenges, motivations, and educational models at the medical school and graduate medical education levels related to formal training in nonclinical aspects of medicine, especially critical thinking, are reviewed. Our diagnostic radiology training program is presented as a "case study" to frame the review.
Research and consensus guidelines now recommend formal critical thinking training. A gap in the literature exists with respect to how to incorporate critical thinking education in a pediatric training environment. Objectives: This study was a targeted needs assessment for developing a formal curriculum on critical thinking for pediatric residents.
Background: Critical thinking is the ability to raise discriminating questions in an attempt to search for better ideas, a deeper understanding and better solutions relating to a given issue. Objective: This systematic review provides a summary of efforts that have been made to enhance and assess critical thinking in medical education. Design: Nine databases [Ovid MEDLINE(R), AMED, Academic ...
The mean grade point average of the students was 15.91; 179 students had GPA higher than the mean value (57%). The mean total score of critical thinking disposition of the students was 121.85 ± 11.32. Table 1 shows the mean and standard deviation of critical thinking disposition score and its subscales of innovation, maturation, and ...
Critical thinking is just one skill crucial to evidence based practice in healthcare and education, write Jonathan Sharples and colleagues , who see exciting opportunities for cross sector collaboration Imagine you are a primary care doctor. A patient comes into your office with acute, atypical chest pain. Immediately you consider the patient's sex and age, and you begin to think about what ...
Teaching and Assessing Critical Thinking and Clinical Reasoning Skills in Medical Education. of teaching which dates back to 470-399 BC dur ing Socrates era (Paul, Elder, & Bartell, 1997). This ...
Medical educators, on the other hand, have not fully integrated critical thinking as part of their curriculum [10, 11]. Bloom's taxonomy has often been used to define curriculum [ 12 ]. The usefulness and importance of Bloom's taxonomy is not to be underestimated; however, its limitations must also be addressed.
Questions from the exams in the first three years of the medical curriculum at Memorial University medical school were categorised using a simple taxonomy. ... Critical Thinking in Medical School Exams. In: Scherpbier, A.J.J.A., van der Vleuten, C.P.M., Rethans, J.J., van der Steeg, A.F.W. (eds) Advances in Medical Education. Springer ...
Critical thinking skills improve moderately during medical school. Used alone, tests of critical thinking may be of limited value in predicting which students will be successful in clinical clerkships. Clerkship evaluation components and final grade have limited concurrent validity when a test of critical thinking is the criterion.
As medical education shifts from a focus on content transfer to the development of critical thinking and problem-solving skills, educators must push learners to develop and practice the skills needed to reason from foundational principles and concepts to explain the history, physical examination, and laboratory data for a given patient. 67, 68 ...
Critical thinking, problem-solving, and emotional intelligence are a few of the skills medical students can learn during their surgical rotations. R. Peter Manes, MD, Saral Mehra, MD MBA, Kelly Olino, MD, and David Stitelman, MD, from the Yale Department of Surgery discuss what makes a rewarding surgery clerkship experience.
In medicine, critical thinking is required for managing and tolerating medical uncertainty, as well as solving professional problems and treating diseases. However, the core of Confucianism, teacher-centered and exam-oriented settings in middle and high school education may pose challenges to developing critical thinking in Han Chinese or Taiwanese students.
The 2nd "Doctor as a Humanist" Symposium took place at Sechenov University in Moscow from the 1 st to the 3 rd of April, 2019, to explore the holistic perspective of interpersonal treatment. To begin our essay, we would like to clarify some key concepts, such as culture, humanism and humanities, as they were employed at the conference.
Is medical school unintellectual? I was having a conversation the other day with a friend who basically said that while medical school is definitely academically rigorous, it is not an intellectual endeavor in the form of critical thinking due to its basis on memorization. For those in medical school or now in practice, is this true?
But twisting science snarls my mind. Particularly when it comes to mangling facts about the causes and treatment of cancer. Let's start with some facts. Antiperspirants, cell phones, root canals or wired bras do not cause cancer. Sugar or dairy products do not "feed" the disease. You cannot cure cancer with an alkaline diet, crystals ...
Apply critical thinking in real-life situations whenever possible. This could involve analyzing news articles, evaluating product reviews, or dissecting marketing strategies to understand their underlying rationale. In conclusion, critical thinking is the linchpin of a successful career journey.
Ultimately, the best major for a pre-med student is the one in which they can excel academically, develop critical thinking skills, and maintain a strong GPA. Consider your interests and strengths, and remember that there are successful medical students from various academic backgrounds.
Elena Atochina-Vasserman, M.D.,Ph.D, is a Senior Laboratory Investigator in the Pulmonary, Allergy, and Critical Care Division (PACCD) of the Department of Medicine at the University of Pennsylvania. Dr. Atochina earned her M.D. from Tomsk Medical School and a Ph.D. in Biochemistry in 1990 from Russian Cardiology Research Center, Moscow, Russia.
Critical thinking has been identified as a crucial general skill contributing to academic and career success in the twenty-first century. With the increasing demands of the modern workplace and a global trend of accountability in higher education, educators and employers pay great attention to the development of students' critical thinking ...
Welcome to FMSMU. I.M. Sechenov First Moscow State Medical University is the oldest leading medical university in Russia that has become a cradle of most medical schools and scientific societies of our country. For decades it has been unofficially known as "First Med".University success is based on a blend of glorious traditions and actual ...
The northeastern Ukrainian city of Kharkiv came under attack once again overnight, according to officials. This one lasted more than 16 hours, according to reports. Meanwhile, Vladimir Putin is in ...