Get science-backed answers as you write with Paperpal's Research feature

How to Write a Conclusion for Research Papers (with Examples)
The conclusion of a research paper is a crucial section that plays a significant role in the overall impact and effectiveness of your research paper. However, this is also the section that typically receives less attention compared to the introduction and the body of the paper. The conclusion serves to provide a concise summary of the key findings, their significance, their implications, and a sense of closure to the study. Discussing how can the findings be applied in real-world scenarios or inform policy, practice, or decision-making is especially valuable to practitioners and policymakers. The research paper conclusion also provides researchers with clear insights and valuable information for their own work, which they can then build on and contribute to the advancement of knowledge in the field.
The research paper conclusion should explain the significance of your findings within the broader context of your field. It restates how your results contribute to the existing body of knowledge and whether they confirm or challenge existing theories or hypotheses. Also, by identifying unanswered questions or areas requiring further investigation, your awareness of the broader research landscape can be demonstrated.
Remember to tailor the research paper conclusion to the specific needs and interests of your intended audience, which may include researchers, practitioners, policymakers, or a combination of these.
Table of Contents
What is a conclusion in a research paper, summarizing conclusion, editorial conclusion, externalizing conclusion, importance of a good research paper conclusion, how to write a conclusion for your research paper, research paper conclusion examples.
- How to write a research paper conclusion with Paperpal?
Frequently Asked Questions
A conclusion in a research paper is the final section where you summarize and wrap up your research, presenting the key findings and insights derived from your study. The research paper conclusion is not the place to introduce new information or data that was not discussed in the main body of the paper. When working on how to conclude a research paper, remember to stick to summarizing and interpreting existing content. The research paper conclusion serves the following purposes: 1
- Warn readers of the possible consequences of not attending to the problem.
- Recommend specific course(s) of action.
- Restate key ideas to drive home the ultimate point of your research paper.
- Provide a “take-home” message that you want the readers to remember about your study.

Types of conclusions for research papers
In research papers, the conclusion provides closure to the reader. The type of research paper conclusion you choose depends on the nature of your study, your goals, and your target audience. I provide you with three common types of conclusions:
A summarizing conclusion is the most common type of conclusion in research papers. It involves summarizing the main points, reiterating the research question, and restating the significance of the findings. This common type of research paper conclusion is used across different disciplines.
An editorial conclusion is less common but can be used in research papers that are focused on proposing or advocating for a particular viewpoint or policy. It involves presenting a strong editorial or opinion based on the research findings and offering recommendations or calls to action.
An externalizing conclusion is a type of conclusion that extends the research beyond the scope of the paper by suggesting potential future research directions or discussing the broader implications of the findings. This type of conclusion is often used in more theoretical or exploratory research papers.
Align your conclusion’s tone with the rest of your research paper. Start Writing with Paperpal Now!
The conclusion in a research paper serves several important purposes:
- Offers Implications and Recommendations : Your research paper conclusion is an excellent place to discuss the broader implications of your research and suggest potential areas for further study. It’s also an opportunity to offer practical recommendations based on your findings.
- Provides Closure : A good research paper conclusion provides a sense of closure to your paper. It should leave the reader with a feeling that they have reached the end of a well-structured and thought-provoking research project.
- Leaves a Lasting Impression : Writing a well-crafted research paper conclusion leaves a lasting impression on your readers. It’s your final opportunity to leave them with a new idea, a call to action, or a memorable quote.

Writing a strong conclusion for your research paper is essential to leave a lasting impression on your readers. Here’s a step-by-step process to help you create and know what to put in the conclusion of a research paper: 2
- Research Statement : Begin your research paper conclusion by restating your research statement. This reminds the reader of the main point you’ve been trying to prove throughout your paper. Keep it concise and clear.
- Key Points : Summarize the main arguments and key points you’ve made in your paper. Avoid introducing new information in the research paper conclusion. Instead, provide a concise overview of what you’ve discussed in the body of your paper.
- Address the Research Questions : If your research paper is based on specific research questions or hypotheses, briefly address whether you’ve answered them or achieved your research goals. Discuss the significance of your findings in this context.
- Significance : Highlight the importance of your research and its relevance in the broader context. Explain why your findings matter and how they contribute to the existing knowledge in your field.
- Implications : Explore the practical or theoretical implications of your research. How might your findings impact future research, policy, or real-world applications? Consider the “so what?” question.
- Future Research : Offer suggestions for future research in your area. What questions or aspects remain unanswered or warrant further investigation? This shows that your work opens the door for future exploration.
- Closing Thought : Conclude your research paper conclusion with a thought-provoking or memorable statement. This can leave a lasting impression on your readers and wrap up your paper effectively. Avoid introducing new information or arguments here.
- Proofread and Revise : Carefully proofread your conclusion for grammar, spelling, and clarity. Ensure that your ideas flow smoothly and that your conclusion is coherent and well-structured.
Write your research paper conclusion 2x faster with Paperpal. Try it now!
Remember that a well-crafted research paper conclusion is a reflection of the strength of your research and your ability to communicate its significance effectively. It should leave a lasting impression on your readers and tie together all the threads of your paper. Now you know how to start the conclusion of a research paper and what elements to include to make it impactful, let’s look at a research paper conclusion sample.

How to write a research paper conclusion with Paperpal?
A research paper conclusion is not just a summary of your study, but a synthesis of the key findings that ties the research together and places it in a broader context. A research paper conclusion should be concise, typically around one paragraph in length. However, some complex topics may require a longer conclusion to ensure the reader is left with a clear understanding of the study’s significance. Paperpal, an AI writing assistant trusted by over 800,000 academics globally, can help you write a well-structured conclusion for your research paper.
- Sign Up or Log In: Create a new Paperpal account or login with your details.
- Navigate to Features : Once logged in, head over to the features’ side navigation pane. Click on Templates and you’ll find a suite of generative AI features to help you write better, faster.
- Generate an outline: Under Templates, select ‘Outlines’. Choose ‘Research article’ as your document type.
- Select your section: Since you’re focusing on the conclusion, select this section when prompted.
- Choose your field of study: Identifying your field of study allows Paperpal to provide more targeted suggestions, ensuring the relevance of your conclusion to your specific area of research.
- Provide a brief description of your study: Enter details about your research topic and findings. This information helps Paperpal generate a tailored outline that aligns with your paper’s content.
- Generate the conclusion outline: After entering all necessary details, click on ‘generate’. Paperpal will then create a structured outline for your conclusion, to help you start writing and build upon the outline.
- Write your conclusion: Use the generated outline to build your conclusion. The outline serves as a guide, ensuring you cover all critical aspects of a strong conclusion, from summarizing key findings to highlighting the research’s implications.
- Refine and enhance: Paperpal’s ‘Make Academic’ feature can be particularly useful in the final stages. Select any paragraph of your conclusion and use this feature to elevate the academic tone, ensuring your writing is aligned to the academic journal standards.
By following these steps, Paperpal not only simplifies the process of writing a research paper conclusion but also ensures it is impactful, concise, and aligned with academic standards. Sign up with Paperpal today and write your research paper conclusion 2x faster .
The research paper conclusion is a crucial part of your paper as it provides the final opportunity to leave a strong impression on your readers. In the research paper conclusion, summarize the main points of your research paper by restating your research statement, highlighting the most important findings, addressing the research questions or objectives, explaining the broader context of the study, discussing the significance of your findings, providing recommendations if applicable, and emphasizing the takeaway message. The main purpose of the conclusion is to remind the reader of the main point or argument of your paper and to provide a clear and concise summary of the key findings and their implications. All these elements should feature on your list of what to put in the conclusion of a research paper to create a strong final statement for your work.
A strong conclusion is a critical component of a research paper, as it provides an opportunity to wrap up your arguments, reiterate your main points, and leave a lasting impression on your readers. Here are the key elements of a strong research paper conclusion: 1. Conciseness : A research paper conclusion should be concise and to the point. It should not introduce new information or ideas that were not discussed in the body of the paper. 2. Summarization : The research paper conclusion should be comprehensive enough to give the reader a clear understanding of the research’s main contributions. 3 . Relevance : Ensure that the information included in the research paper conclusion is directly relevant to the research paper’s main topic and objectives; avoid unnecessary details. 4 . Connection to the Introduction : A well-structured research paper conclusion often revisits the key points made in the introduction and shows how the research has addressed the initial questions or objectives. 5. Emphasis : Highlight the significance and implications of your research. Why is your study important? What are the broader implications or applications of your findings? 6 . Call to Action : Include a call to action or a recommendation for future research or action based on your findings.
The length of a research paper conclusion can vary depending on several factors, including the overall length of the paper, the complexity of the research, and the specific journal requirements. While there is no strict rule for the length of a conclusion, but it’s generally advisable to keep it relatively short. A typical research paper conclusion might be around 5-10% of the paper’s total length. For example, if your paper is 10 pages long, the conclusion might be roughly half a page to one page in length.
In general, you do not need to include citations in the research paper conclusion. Citations are typically reserved for the body of the paper to support your arguments and provide evidence for your claims. However, there may be some exceptions to this rule: 1. If you are drawing a direct quote or paraphrasing a specific source in your research paper conclusion, you should include a citation to give proper credit to the original author. 2. If your conclusion refers to or discusses specific research, data, or sources that are crucial to the overall argument, citations can be included to reinforce your conclusion’s validity.
The conclusion of a research paper serves several important purposes: 1. Summarize the Key Points 2. Reinforce the Main Argument 3. Provide Closure 4. Offer Insights or Implications 5. Engage the Reader. 6. Reflect on Limitations
Remember that the primary purpose of the research paper conclusion is to leave a lasting impression on the reader, reinforcing the key points and providing closure to your research. It’s often the last part of the paper that the reader will see, so it should be strong and well-crafted.
- Makar, G., Foltz, C., Lendner, M., & Vaccaro, A. R. (2018). How to write effective discussion and conclusion sections. Clinical spine surgery, 31(8), 345-346.
- Bunton, D. (2005). The structure of PhD conclusion chapters. Journal of English for academic purposes , 4 (3), 207-224.
Paperpal is a comprehensive AI writing toolkit that helps students and researchers achieve 2x the writing in half the time. It leverages 21+ years of STM experience and insights from millions of research articles to provide in-depth academic writing, language editing, and submission readiness support to help you write better, faster.
Get accurate academic translations, rewriting support, grammar checks, vocabulary suggestions, and generative AI assistance that delivers human precision at machine speed. Try for free or upgrade to Paperpal Prime starting at US$19 a month to access premium features, including consistency, plagiarism, and 30+ submission readiness checks to help you succeed.
Experience the future of academic writing – Sign up to Paperpal and start writing for free!
Related Reads:
- 5 Reasons for Rejection After Peer Review
- Ethical Research Practices For Research with Human Subjects
7 Ways to Improve Your Academic Writing Process
- Paraphrasing in Academic Writing: Answering Top Author Queries
Preflight For Editorial Desk: The Perfect Hybrid (AI + Human) Assistance Against Compromised Manuscripts
You may also like, how to write a high-quality conference paper, academic editing: how to self-edit academic text with..., measuring academic success: definition & strategies for excellence, phd qualifying exam: tips for success , ai in education: it’s time to change the..., is it ethical to use ai-generated abstracts without..., what are journal guidelines on using generative ai..., quillbot review: features, pricing, and free alternatives, what is an academic paper types and elements , should you use ai tools like chatgpt for....
- Privacy Policy

Home » Research Paper Conclusion – Writing Guide and Examples
Research Paper Conclusion – Writing Guide and Examples
Table of Contents

Research Paper Conclusion
Definition:
A research paper conclusion is the final section of a research paper that summarizes the key findings, significance, and implications of the research. It is the writer’s opportunity to synthesize the information presented in the paper, draw conclusions, and make recommendations for future research or actions.
The conclusion should provide a clear and concise summary of the research paper, reiterating the research question or problem, the main results, and the significance of the findings. It should also discuss the limitations of the study and suggest areas for further research.
Parts of Research Paper Conclusion
The parts of a research paper conclusion typically include:
Restatement of the Thesis
The conclusion should begin by restating the thesis statement from the introduction in a different way. This helps to remind the reader of the main argument or purpose of the research.
Summary of Key Findings
The conclusion should summarize the main findings of the research, highlighting the most important results and conclusions. This section should be brief and to the point.
Implications and Significance
In this section, the researcher should explain the implications and significance of the research findings. This may include discussing the potential impact on the field or industry, highlighting new insights or knowledge gained, or pointing out areas for future research.
Limitations and Recommendations
It is important to acknowledge any limitations or weaknesses of the research and to make recommendations for how these could be addressed in future studies. This shows that the researcher is aware of the potential limitations of their work and is committed to improving the quality of research in their field.
Concluding Statement
The conclusion should end with a strong concluding statement that leaves a lasting impression on the reader. This could be a call to action, a recommendation for further research, or a final thought on the topic.
How to Write Research Paper Conclusion
Here are some steps you can follow to write an effective research paper conclusion:
- Restate the research problem or question: Begin by restating the research problem or question that you aimed to answer in your research. This will remind the reader of the purpose of your study.
- Summarize the main points: Summarize the key findings and results of your research. This can be done by highlighting the most important aspects of your research and the evidence that supports them.
- Discuss the implications: Discuss the implications of your findings for the research area and any potential applications of your research. You should also mention any limitations of your research that may affect the interpretation of your findings.
- Provide a conclusion : Provide a concise conclusion that summarizes the main points of your paper and emphasizes the significance of your research. This should be a strong and clear statement that leaves a lasting impression on the reader.
- Offer suggestions for future research: Lastly, offer suggestions for future research that could build on your findings and contribute to further advancements in the field.
Remember that the conclusion should be brief and to the point, while still effectively summarizing the key findings and implications of your research.
Example of Research Paper Conclusion
Here’s an example of a research paper conclusion:
Conclusion :
In conclusion, our study aimed to investigate the relationship between social media use and mental health among college students. Our findings suggest that there is a significant association between social media use and increased levels of anxiety and depression among college students. This highlights the need for increased awareness and education about the potential negative effects of social media use on mental health, particularly among college students.
Despite the limitations of our study, such as the small sample size and self-reported data, our findings have important implications for future research and practice. Future studies should aim to replicate our findings in larger, more diverse samples, and investigate the potential mechanisms underlying the association between social media use and mental health. In addition, interventions should be developed to promote healthy social media use among college students, such as mindfulness-based approaches and social media detox programs.
Overall, our study contributes to the growing body of research on the impact of social media on mental health, and highlights the importance of addressing this issue in the context of higher education. By raising awareness and promoting healthy social media use among college students, we can help to reduce the negative impact of social media on mental health and improve the well-being of young adults.
Purpose of Research Paper Conclusion
The purpose of a research paper conclusion is to provide a summary and synthesis of the key findings, significance, and implications of the research presented in the paper. The conclusion serves as the final opportunity for the writer to convey their message and leave a lasting impression on the reader.
The conclusion should restate the research problem or question, summarize the main results of the research, and explain their significance. It should also acknowledge the limitations of the study and suggest areas for future research or action.
Overall, the purpose of the conclusion is to provide a sense of closure to the research paper and to emphasize the importance of the research and its potential impact. It should leave the reader with a clear understanding of the main findings and why they matter. The conclusion serves as the writer’s opportunity to showcase their contribution to the field and to inspire further research and action.
When to Write Research Paper Conclusion
The conclusion of a research paper should be written after the body of the paper has been completed. It should not be written until the writer has thoroughly analyzed and interpreted their findings and has written a complete and cohesive discussion of the research.
Before writing the conclusion, the writer should review their research paper and consider the key points that they want to convey to the reader. They should also review the research question, hypotheses, and methodology to ensure that they have addressed all of the necessary components of the research.
Once the writer has a clear understanding of the main findings and their significance, they can begin writing the conclusion. The conclusion should be written in a clear and concise manner, and should reiterate the main points of the research while also providing insights and recommendations for future research or action.
Characteristics of Research Paper Conclusion
The characteristics of a research paper conclusion include:
- Clear and concise: The conclusion should be written in a clear and concise manner, summarizing the key findings and their significance.
- Comprehensive: The conclusion should address all of the main points of the research paper, including the research question or problem, the methodology, the main results, and their implications.
- Future-oriented : The conclusion should provide insights and recommendations for future research or action, based on the findings of the research.
- Impressive : The conclusion should leave a lasting impression on the reader, emphasizing the importance of the research and its potential impact.
- Objective : The conclusion should be based on the evidence presented in the research paper, and should avoid personal biases or opinions.
- Unique : The conclusion should be unique to the research paper and should not simply repeat information from the introduction or body of the paper.
Advantages of Research Paper Conclusion
The advantages of a research paper conclusion include:
- Summarizing the key findings : The conclusion provides a summary of the main findings of the research, making it easier for the reader to understand the key points of the study.
- Emphasizing the significance of the research: The conclusion emphasizes the importance of the research and its potential impact, making it more likely that readers will take the research seriously and consider its implications.
- Providing recommendations for future research or action : The conclusion suggests practical recommendations for future research or action, based on the findings of the study.
- Providing closure to the research paper : The conclusion provides a sense of closure to the research paper, tying together the different sections of the paper and leaving a lasting impression on the reader.
- Demonstrating the writer’s contribution to the field : The conclusion provides the writer with an opportunity to showcase their contribution to the field and to inspire further research and action.
Limitations of Research Paper Conclusion
While the conclusion of a research paper has many advantages, it also has some limitations that should be considered, including:
- I nability to address all aspects of the research: Due to the limited space available in the conclusion, it may not be possible to address all aspects of the research in detail.
- Subjectivity : While the conclusion should be objective, it may be influenced by the writer’s personal biases or opinions.
- Lack of new information: The conclusion should not introduce new information that has not been discussed in the body of the research paper.
- Lack of generalizability: The conclusions drawn from the research may not be applicable to other contexts or populations, limiting the generalizability of the study.
- Misinterpretation by the reader: The reader may misinterpret the conclusions drawn from the research, leading to a misunderstanding of the findings.
About the author
Muhammad Hassan
Researcher, Academic Writer, Web developer
You may also like

How to Cite Research Paper – All Formats and...

Data Collection – Methods Types and Examples

Delimitations in Research – Types, Examples and...

Research Paper Format – Types, Examples and...

Research Process – Steps, Examples and Tips

Research Design – Types, Methods and Examples
- USC Libraries
- Research Guides
Organizing Your Social Sciences Research Paper
- 9. The Conclusion
- Purpose of Guide
- Design Flaws to Avoid
- Independent and Dependent Variables
- Glossary of Research Terms
- Reading Research Effectively
- Narrowing a Topic Idea
- Broadening a Topic Idea
- Extending the Timeliness of a Topic Idea
- Academic Writing Style
- Applying Critical Thinking
- Choosing a Title
- Making an Outline
- Paragraph Development
- Research Process Video Series
- Executive Summary
- The C.A.R.S. Model
- Background Information
- The Research Problem/Question
- Theoretical Framework
- Citation Tracking
- Content Alert Services
- Evaluating Sources
- Primary Sources
- Secondary Sources
- Tiertiary Sources
- Scholarly vs. Popular Publications
- Qualitative Methods
- Quantitative Methods
- Insiderness
- Using Non-Textual Elements
- Limitations of the Study
- Common Grammar Mistakes
- Writing Concisely
- Avoiding Plagiarism
- Footnotes or Endnotes?
- Further Readings
- Generative AI and Writing
- USC Libraries Tutorials and Other Guides
- Bibliography
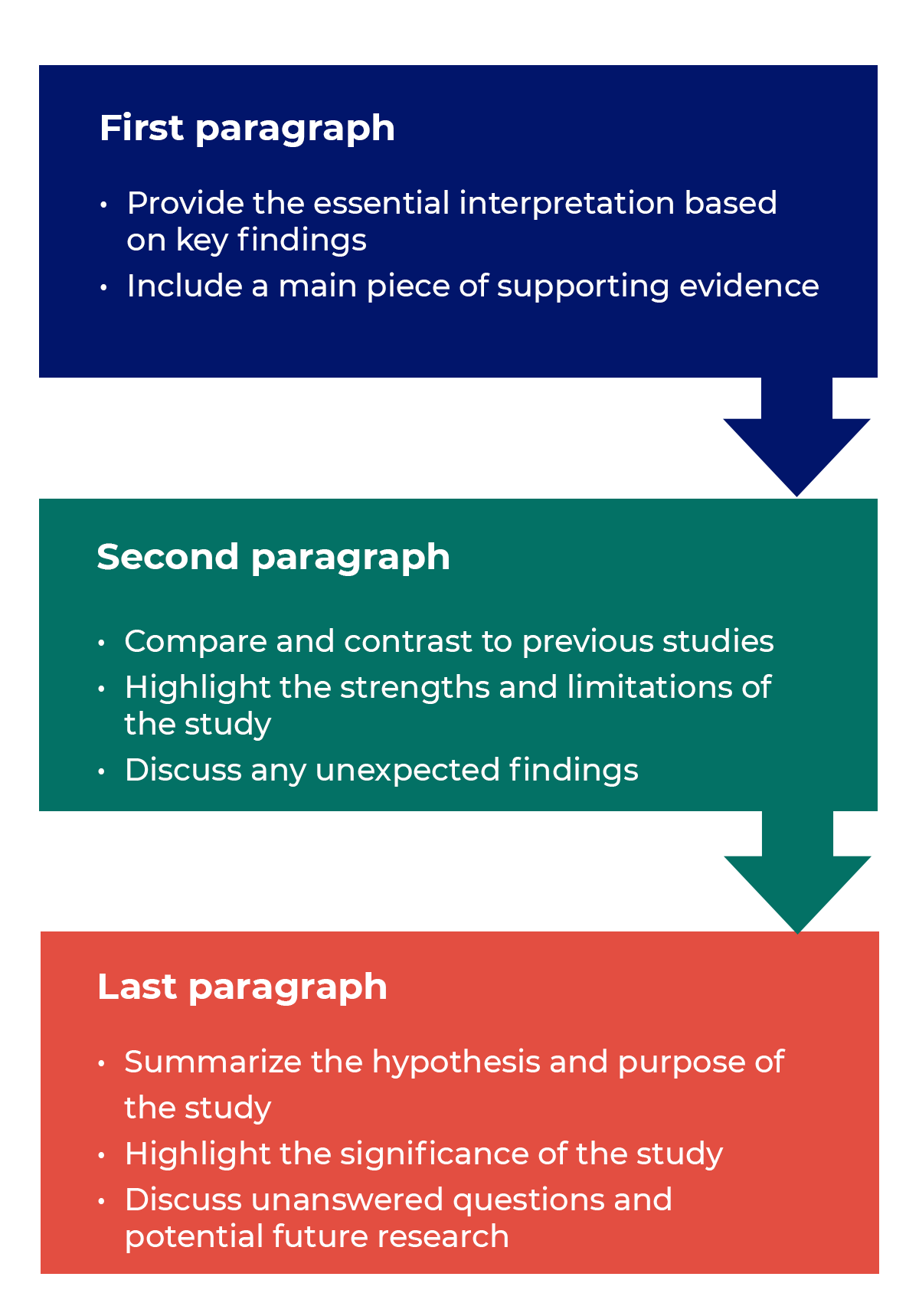
The conclusion is intended to help the reader understand why your research should matter to them after they have finished reading the paper. A conclusion is not merely a summary of the main topics covered or a re-statement of your research problem, but a synthesis of key points derived from the findings of your study and, if applicable, where you recommend new areas for future research. For most college-level research papers, two or three well-developed paragraphs is sufficient for a conclusion, although in some cases, more paragraphs may be required in describing the key findings and their significance.
Conclusions. The Writing Center. University of North Carolina; Conclusions. The Writing Lab and The OWL. Purdue University.
Importance of a Good Conclusion
A well-written conclusion provides you with important opportunities to demonstrate to the reader your understanding of the research problem. These include:
- Presenting the last word on the issues you raised in your paper . Just as the introduction gives a first impression to your reader, the conclusion offers a chance to leave a lasting impression. Do this, for example, by highlighting key findings in your analysis that advance new understanding about the research problem, that are unusual or unexpected, or that have important implications applied to practice.
- Summarizing your thoughts and conveying the larger significance of your study . The conclusion is an opportunity to succinctly re-emphasize your answer to the "So What?" question by placing the study within the context of how your research advances past research about the topic.
- Identifying how a gap in the literature has been addressed . The conclusion can be where you describe how a previously identified gap in the literature [first identified in your literature review section] has been addressed by your research and why this contribution is significant.
- Demonstrating the importance of your ideas . Don't be shy. The conclusion offers an opportunity to elaborate on the impact and significance of your findings. This is particularly important if your study approached examining the research problem from an unusual or innovative perspective.
- Introducing possible new or expanded ways of thinking about the research problem . This does not refer to introducing new information [which should be avoided], but to offer new insight and creative approaches for framing or contextualizing the research problem based on the results of your study.
Bunton, David. “The Structure of PhD Conclusion Chapters.” Journal of English for Academic Purposes 4 (July 2005): 207–224; Conclusions. The Writing Center. University of North Carolina; Kretchmer, Paul. Twelve Steps to Writing an Effective Conclusion. San Francisco Edit, 2003-2008; Conclusions. The Writing Lab and The OWL. Purdue University; Assan, Joseph. "Writing the Conclusion Chapter: The Good, the Bad and the Missing." Liverpool: Development Studies Association (2009): 1-8.
Structure and Writing Style
I. General Rules
The general function of your paper's conclusion is to restate the main argument . It reminds the reader of the strengths of your main argument(s) and reiterates the most important evidence supporting those argument(s). Do this by clearly summarizing the context, background, and necessity of pursuing the research problem you investigated in relation to an issue, controversy, or a gap found in the literature. However, make sure that your conclusion is not simply a repetitive summary of the findings. This reduces the impact of the argument(s) you have developed in your paper.
When writing the conclusion to your paper, follow these general rules:
- Present your conclusions in clear, concise language. Re-state the purpose of your study, then describe how your findings differ or support those of other studies and why [i.e., what were the unique, new, or crucial contributions your study made to the overall research about your topic?].
- Do not simply reiterate your findings or the discussion of your results. Provide a synthesis of arguments presented in the paper to show how these converge to address the research problem and the overall objectives of your study.
- Indicate opportunities for future research if you haven't already done so in the discussion section of your paper. Highlighting the need for further research provides the reader with evidence that you have an in-depth awareness of the research problem but that further investigations should take place beyond the scope of your investigation.
Consider the following points to help ensure your conclusion is presented well:
- If the argument or purpose of your paper is complex, you may need to summarize the argument for your reader.
- If, prior to your conclusion, you have not yet explained the significance of your findings or if you are proceeding inductively, use the end of your paper to describe your main points and explain their significance.
- Move from a detailed to a general level of consideration that returns the topic to the context provided by the introduction or within a new context that emerges from the data [this is opposite of the introduction, which begins with general discussion of the context and ends with a detailed description of the research problem].
The conclusion also provides a place for you to persuasively and succinctly restate the research problem, given that the reader has now been presented with all the information about the topic . Depending on the discipline you are writing in, the concluding paragraph may contain your reflections on the evidence presented. However, the nature of being introspective about the research you have conducted will depend on the topic and whether your professor wants you to express your observations in this way. If asked to think introspectively about the topics, do not delve into idle speculation. Being introspective means looking within yourself as an author to try and understand an issue more deeply, not to guess at possible outcomes or make up scenarios not supported by the evidence.
II. Developing a Compelling Conclusion
Although an effective conclusion needs to be clear and succinct, it does not need to be written passively or lack a compelling narrative. Strategies to help you move beyond merely summarizing the key points of your research paper may include any of the following:
- If your essay deals with a critical, contemporary problem, warn readers of the possible consequences of not attending to the problem proactively.
- Recommend a specific course or courses of action that, if adopted, could address a specific problem in practice or in the development of new knowledge leading to positive change.
- Cite a relevant quotation or expert opinion already noted in your paper in order to lend authority and support to the conclusion(s) you have reached [a good source would be from your literature review].
- Explain the consequences of your research in a way that elicits action or demonstrates urgency in seeking change.
- Restate a key statistic, fact, or visual image to emphasize the most important finding of your paper.
- If your discipline encourages personal reflection, illustrate your concluding point by drawing from your own life experiences.
- Return to an anecdote, an example, or a quotation that you presented in your introduction, but add further insight derived from the findings of your study; use your interpretation of results from your study to recast it in new or important ways.
- Provide a "take-home" message in the form of a succinct, declarative statement that you want the reader to remember about your study.
III. Problems to Avoid
Failure to be concise Your conclusion section should be concise and to the point. Conclusions that are too lengthy often have unnecessary information in them. The conclusion is not the place for details about your methodology or results. Although you should give a summary of what was learned from your research, this summary should be relatively brief, since the emphasis in the conclusion is on the implications, evaluations, insights, and other forms of analysis that you make. Strategies for writing concisely can be found here .
Failure to comment on larger, more significant issues In the introduction, your task was to move from the general [the field of study] to the specific [the research problem]. However, in the conclusion, your task is to move from a specific discussion [your research problem] back to a general discussion framed around the implications and significance of your findings [i.e., how your research contributes new understanding or fills an important gap in the literature]. In short, the conclusion is where you should place your research within a larger context [visualize your paper as an hourglass--start with a broad introduction and review of the literature, move to the specific analysis and discussion, conclude with a broad summary of the study's implications and significance].
Failure to reveal problems and negative results Negative aspects of the research process should never be ignored. These are problems, deficiencies, or challenges encountered during your study. They should be summarized as a way of qualifying your overall conclusions. If you encountered negative or unintended results [i.e., findings that are validated outside the research context in which they were generated], you must report them in the results section and discuss their implications in the discussion section of your paper. In the conclusion, use negative results as an opportunity to explain their possible significance and/or how they may form the basis for future research.
Failure to provide a clear summary of what was learned In order to be able to discuss how your research fits within your field of study [and possibly the world at large], you need to summarize briefly and succinctly how it contributes to new knowledge or a new understanding about the research problem. This element of your conclusion may be only a few sentences long.
Failure to match the objectives of your research Often research objectives in the social and behavioral sciences change while the research is being carried out. This is not a problem unless you forget to go back and refine the original objectives in your introduction. As these changes emerge they must be documented so that they accurately reflect what you were trying to accomplish in your research [not what you thought you might accomplish when you began].
Resist the urge to apologize If you've immersed yourself in studying the research problem, you presumably should know a good deal about it [perhaps even more than your professor!]. Nevertheless, by the time you have finished writing, you may be having some doubts about what you have produced. Repress those doubts! Don't undermine your authority as a researcher by saying something like, "This is just one approach to examining this problem; there may be other, much better approaches that...." The overall tone of your conclusion should convey confidence to the reader about the study's validity and realiability.
Assan, Joseph. "Writing the Conclusion Chapter: The Good, the Bad and the Missing." Liverpool: Development Studies Association (2009): 1-8; Concluding Paragraphs. College Writing Center at Meramec. St. Louis Community College; Conclusions. The Writing Center. University of North Carolina; Conclusions. The Writing Lab and The OWL. Purdue University; Freedman, Leora and Jerry Plotnick. Introductions and Conclusions. The Lab Report. University College Writing Centre. University of Toronto; Leibensperger, Summer. Draft Your Conclusion. Academic Center, the University of Houston-Victoria, 2003; Make Your Last Words Count. The Writer’s Handbook. Writing Center. University of Wisconsin Madison; Miquel, Fuster-Marquez and Carmen Gregori-Signes. “Chapter Six: ‘Last but Not Least:’ Writing the Conclusion of Your Paper.” In Writing an Applied Linguistics Thesis or Dissertation: A Guide to Presenting Empirical Research . John Bitchener, editor. (Basingstoke,UK: Palgrave Macmillan, 2010), pp. 93-105; Tips for Writing a Good Conclusion. Writing@CSU. Colorado State University; Kretchmer, Paul. Twelve Steps to Writing an Effective Conclusion. San Francisco Edit, 2003-2008; Writing Conclusions. Writing Tutorial Services, Center for Innovative Teaching and Learning. Indiana University; Writing: Considering Structure and Organization. Institute for Writing Rhetoric. Dartmouth College.
Writing Tip
Don't Belabor the Obvious!
Avoid phrases like "in conclusion...," "in summary...," or "in closing...." These phrases can be useful, even welcome, in oral presentations. But readers can see by the tell-tale section heading and number of pages remaining that they are reaching the end of your paper. You'll irritate your readers if you belabor the obvious.
Assan, Joseph. "Writing the Conclusion Chapter: The Good, the Bad and the Missing." Liverpool: Development Studies Association (2009): 1-8.
Another Writing Tip
New Insight, Not New Information!
Don't surprise the reader with new information in your conclusion that was never referenced anywhere else in the paper. This why the conclusion rarely has citations to sources. If you have new information to present, add it to the discussion or other appropriate section of the paper. Note that, although no new information is introduced, the conclusion, along with the discussion section, is where you offer your most "original" contributions in the paper; the conclusion is where you describe the value of your research, demonstrate that you understand the material that you’ve presented, and position your findings within the larger context of scholarship on the topic, including describing how your research contributes new insights to that scholarship.
Assan, Joseph. "Writing the Conclusion Chapter: The Good, the Bad and the Missing." Liverpool: Development Studies Association (2009): 1-8; Conclusions. The Writing Center. University of North Carolina.
- << Previous: Limitations of the Study
- Next: Appendices >>
- Last Updated: May 15, 2024 9:53 AM
- URL: https://libguides.usc.edu/writingguide
When you choose to publish with PLOS, your research makes an impact. Make your work accessible to all, without restrictions, and accelerate scientific discovery with options like preprints and published peer review that make your work more Open.
- PLOS Biology
- PLOS Climate
- PLOS Complex Systems
- PLOS Computational Biology
- PLOS Digital Health
- PLOS Genetics
- PLOS Global Public Health
- PLOS Medicine
- PLOS Mental Health
- PLOS Neglected Tropical Diseases
- PLOS Pathogens
- PLOS Sustainability and Transformation
- PLOS Collections
- How to Write Discussions and Conclusions

The discussion section contains the results and outcomes of a study. An effective discussion informs readers what can be learned from your experiment and provides context for the results.
What makes an effective discussion?
When you’re ready to write your discussion, you’ve already introduced the purpose of your study and provided an in-depth description of the methodology. The discussion informs readers about the larger implications of your study based on the results. Highlighting these implications while not overstating the findings can be challenging, especially when you’re submitting to a journal that selects articles based on novelty or potential impact. Regardless of what journal you are submitting to, the discussion section always serves the same purpose: concluding what your study results actually mean.
A successful discussion section puts your findings in context. It should include:
- the results of your research,
- a discussion of related research, and
- a comparison between your results and initial hypothesis.
Tip: Not all journals share the same naming conventions.
You can apply the advice in this article to the conclusion, results or discussion sections of your manuscript.
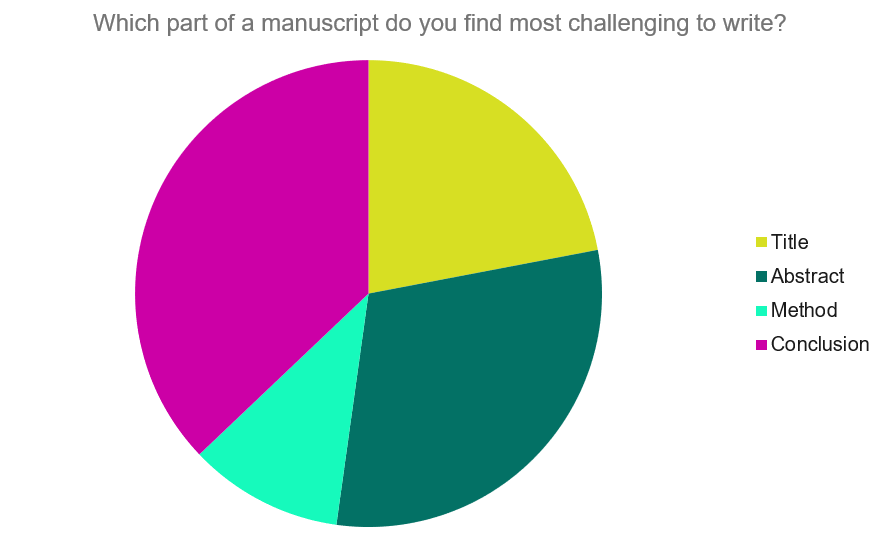
Our Early Career Researcher community tells us that the conclusion is often considered the most difficult aspect of a manuscript to write. To help, this guide provides questions to ask yourself, a basic structure to model your discussion off of and examples from published manuscripts.
Questions to ask yourself:
- Was my hypothesis correct?
- If my hypothesis is partially correct or entirely different, what can be learned from the results?
- How do the conclusions reshape or add onto the existing knowledge in the field? What does previous research say about the topic?
- Why are the results important or relevant to your audience? Do they add further evidence to a scientific consensus or disprove prior studies?
- How can future research build on these observations? What are the key experiments that must be done?
- What is the “take-home” message you want your reader to leave with?
How to structure a discussion
Trying to fit a complete discussion into a single paragraph can add unnecessary stress to the writing process. If possible, you’ll want to give yourself two or three paragraphs to give the reader a comprehensive understanding of your study as a whole. Here’s one way to structure an effective discussion:
Writing Tips
While the above sections can help you brainstorm and structure your discussion, there are many common mistakes that writers revert to when having difficulties with their paper. Writing a discussion can be a delicate balance between summarizing your results, providing proper context for your research and avoiding introducing new information. Remember that your paper should be both confident and honest about the results!

- Read the journal’s guidelines on the discussion and conclusion sections. If possible, learn about the guidelines before writing the discussion to ensure you’re writing to meet their expectations.
- Begin with a clear statement of the principal findings. This will reinforce the main take-away for the reader and set up the rest of the discussion.
- Explain why the outcomes of your study are important to the reader. Discuss the implications of your findings realistically based on previous literature, highlighting both the strengths and limitations of the research.
- State whether the results prove or disprove your hypothesis. If your hypothesis was disproved, what might be the reasons?
- Introduce new or expanded ways to think about the research question. Indicate what next steps can be taken to further pursue any unresolved questions.
- If dealing with a contemporary or ongoing problem, such as climate change, discuss possible consequences if the problem is avoided.
- Be concise. Adding unnecessary detail can distract from the main findings.

Don’t
- Rewrite your abstract. Statements with “we investigated” or “we studied” generally do not belong in the discussion.
- Include new arguments or evidence not previously discussed. Necessary information and evidence should be introduced in the main body of the paper.
- Apologize. Even if your research contains significant limitations, don’t undermine your authority by including statements that doubt your methodology or execution.
- Shy away from speaking on limitations or negative results. Including limitations and negative results will give readers a complete understanding of the presented research. Potential limitations include sources of potential bias, threats to internal or external validity, barriers to implementing an intervention and other issues inherent to the study design.
- Overstate the importance of your findings. Making grand statements about how a study will fully resolve large questions can lead readers to doubt the success of the research.
Snippets of Effective Discussions:
Consumer-based actions to reduce plastic pollution in rivers: A multi-criteria decision analysis approach
Identifying reliable indicators of fitness in polar bears
- How to Write a Great Title
- How to Write an Abstract
- How to Write Your Methods
- How to Report Statistics
- How to Edit Your Work
The contents of the Peer Review Center are also available as a live, interactive training session, complete with slides, talking points, and activities. …
The contents of the Writing Center are also available as a live, interactive training session, complete with slides, talking points, and activities. …
There’s a lot to consider when deciding where to submit your work. Learn how to choose a journal that will help your study reach its audience, while reflecting your values as a researcher…
In a short paper—even a research paper—you don’t need to provide an exhaustive summary as part of your conclusion. But you do need to make some kind of transition between your final body paragraph and your concluding paragraph. This may come in the form of a few sentences of summary. Or it may come in the form of a sentence that brings your readers back to your thesis or main idea and reminds your readers where you began and how far you have traveled.
So, for example, in a paper about the relationship between ADHD and rejection sensitivity, Vanessa Roser begins by introducing readers to the fact that researchers have studied the relationship between the two conditions and then provides her explanation of that relationship. Here’s her thesis: “While socialization may indeed be an important factor in RS, I argue that individuals with ADHD may also possess a neurological predisposition to RS that is exacerbated by the differing executive and emotional regulation characteristic of ADHD.”
In her final paragraph, Roser reminds us of where she started by echoing her thesis: “This literature demonstrates that, as with many other conditions, ADHD and RS share a delicately intertwined pattern of neurological similarities that is rooted in the innate biology of an individual’s mind, a connection that cannot be explained in full by the behavioral mediation hypothesis.”
Highlight the “so what”
At the beginning of your paper, you explain to your readers what’s at stake—why they should care about the argument you’re making. In your conclusion, you can bring readers back to those stakes by reminding them why your argument is important in the first place. You can also draft a few sentences that put those stakes into a new or broader context.
In the conclusion to her paper about ADHD and RS, Roser echoes the stakes she established in her introduction—that research into connections between ADHD and RS has led to contradictory results, raising questions about the “behavioral mediation hypothesis.”
She writes, “as with many other conditions, ADHD and RS share a delicately intertwined pattern of neurological similarities that is rooted in the innate biology of an individual’s mind, a connection that cannot be explained in full by the behavioral mediation hypothesis.”
Leave your readers with the “now what”
After the “what” and the “so what,” you should leave your reader with some final thoughts. If you have written a strong introduction, your readers will know why you have been arguing what you have been arguing—and why they should care. And if you’ve made a good case for your thesis, then your readers should be in a position to see things in a new way, understand new questions, or be ready for something that they weren’t ready for before they read your paper.
In her conclusion, Roser offers two “now what” statements. First, she explains that it is important to recognize that the flawed behavioral mediation hypothesis “seems to place a degree of fault on the individual. It implies that individuals with ADHD must have elicited such frequent or intense rejection by virtue of their inadequate social skills, erasing the possibility that they may simply possess a natural sensitivity to emotion.” She then highlights the broader implications for treatment of people with ADHD, noting that recognizing the actual connection between rejection sensitivity and ADHD “has profound implications for understanding how individuals with ADHD might best be treated in educational settings, by counselors, family, peers, or even society as a whole.”
To find your own “now what” for your essay’s conclusion, try asking yourself these questions:
- What can my readers now understand, see in a new light, or grapple with that they would not have understood in the same way before reading my paper? Are we a step closer to understanding a larger phenomenon or to understanding why what was at stake is so important?
- What questions can I now raise that would not have made sense at the beginning of my paper? Questions for further research? Other ways that this topic could be approached?
- Are there other applications for my research? Could my questions be asked about different data in a different context? Could I use my methods to answer a different question?
- What action should be taken in light of this argument? What action do I predict will be taken or could lead to a solution?
- What larger context might my argument be a part of?
What to avoid in your conclusion
- a complete restatement of all that you have said in your paper.
- a substantial counterargument that you do not have space to refute; you should introduce counterarguments before your conclusion.
- an apology for what you have not said. If you need to explain the scope of your paper, you should do this sooner—but don’t apologize for what you have not discussed in your paper.
- fake transitions like “in conclusion” that are followed by sentences that aren’t actually conclusions. (“In conclusion, I have now demonstrated that my thesis is correct.”)
- picture_as_pdf Conclusions
How to write a strong conclusion for your research paper
Last updated
17 February 2024
Reviewed by
Writing a research paper is a chance to share your knowledge and hypothesis. It's an opportunity to demonstrate your many hours of research and prove your ability to write convincingly.
Ideally, by the end of your research paper, you'll have brought your readers on a journey to reach the conclusions you've pre-determined. However, if you don't stick the landing with a good conclusion, you'll risk losing your reader’s trust.
Writing a strong conclusion for your research paper involves a few important steps, including restating the thesis and summing up everything properly.
Find out what to include and what to avoid, so you can effectively demonstrate your understanding of the topic and prove your expertise.
- Why is a good conclusion important?
A good conclusion can cement your paper in the reader’s mind. Making a strong impression in your introduction can draw your readers in, but it's the conclusion that will inspire them.
- What to include in a research paper conclusion
There are a few specifics you should include in your research paper conclusion. Offer your readers some sense of urgency or consequence by pointing out why they should care about the topic you have covered. Discuss any common problems associated with your topic and provide suggestions as to how these problems can be solved or addressed.
The conclusion should include a restatement of your initial thesis. Thesis statements are strengthened after you’ve presented supporting evidence (as you will have done in the paper), so make a point to reintroduce it at the end.
Finally, recap the main points of your research paper, highlighting the key takeaways you want readers to remember. If you've made multiple points throughout the paper, refer to the ones with the strongest supporting evidence.
- Steps for writing a research paper conclusion
Many writers find the conclusion the most challenging part of any research project . By following these three steps, you'll be prepared to write a conclusion that is effective and concise.
- Step 1: Restate the problem
Always begin by restating the research problem in the conclusion of a research paper. This serves to remind the reader of your hypothesis and refresh them on the main point of the paper.
When restating the problem, take care to avoid using exactly the same words you employed earlier in the paper.
- Step 2: Sum up the paper
After you've restated the problem, sum up the paper by revealing your overall findings. The method for this differs slightly, depending on whether you're crafting an argumentative paper or an empirical paper.
Argumentative paper: Restate your thesis and arguments
Argumentative papers involve introducing a thesis statement early on. In crafting the conclusion for an argumentative paper, always restate the thesis, outlining the way you've developed it throughout the entire paper.
It might be appropriate to mention any counterarguments in the conclusion, so you can demonstrate how your thesis is correct or how the data best supports your main points.
Empirical paper: Summarize research findings
Empirical papers break down a series of research questions. In your conclusion, discuss the findings your research revealed, including any information that surprised you.
Be clear about the conclusions you reached, and explain whether or not you expected to arrive at these particular ones.
- Step 3: Discuss the implications of your research
Argumentative papers and empirical papers also differ in this part of a research paper conclusion. Here are some tips on crafting conclusions for argumentative and empirical papers.
Argumentative paper: Powerful closing statement
In an argumentative paper, you'll have spent a great deal of time expressing the opinions you formed after doing a significant amount of research. Make a strong closing statement in your argumentative paper's conclusion to share the significance of your work.
You can outline the next steps through a bold call to action, or restate how powerful your ideas turned out to be.
Empirical paper: Directions for future research
Empirical papers are broader in scope. They usually cover a variety of aspects and can include several points of view.
To write a good conclusion for an empirical paper, suggest the type of research that could be done in the future, including methods for further investigation or outlining ways other researchers might proceed.
If you feel your research had any limitations, even if they were outside your control, you could mention these in your conclusion.
After you finish outlining your conclusion, ask someone to read it and offer feedback. In any research project you're especially close to, it can be hard to identify problem areas. Having a close friend or someone whose opinion you value read the research paper and provide honest feedback can be invaluable. Take note of any suggested edits and consider incorporating them into your paper if they make sense.
- Things to avoid in a research paper conclusion
Keep these aspects to avoid in mind as you're writing your conclusion and refer to them after you've created an outline.
Dry summary
Writing a memorable, succinct conclusion is arguably more important than a strong introduction. Take care to avoid just rephrasing your main points, and don't fall into the trap of repeating dry facts or citations.
You can provide a new perspective for your readers to think about or contextualize your research. Either way, make the conclusion vibrant and interesting, rather than a rote recitation of your research paper’s highlights.
Clichéd or generic phrasing
Your research paper conclusion should feel fresh and inspiring. Avoid generic phrases like "to sum up" or "in conclusion." These phrases tend to be overused, especially in an academic context and might turn your readers off.
The conclusion also isn't the time to introduce colloquial phrases or informal language. Retain a professional, confident tone consistent throughout your paper’s conclusion so it feels exciting and bold.
New data or evidence
While you should present strong data throughout your paper, the conclusion isn't the place to introduce new evidence. This is because readers are engaged in actively learning as they read through the body of your paper.
By the time they reach the conclusion, they will have formed an opinion one way or the other (hopefully in your favor!). Introducing new evidence in the conclusion will only serve to surprise or frustrate your reader.
Ignoring contradictory evidence
If your research reveals contradictory evidence, don't ignore it in the conclusion. This will damage your credibility as an expert and might even serve to highlight the contradictions.
Be as transparent as possible and admit to any shortcomings in your research, but don't dwell on them for too long.
Ambiguous or unclear resolutions
The point of a research paper conclusion is to provide closure and bring all your ideas together. You should wrap up any arguments you introduced in the paper and tie up any loose ends, while demonstrating why your research and data are strong.
Use direct language in your conclusion and avoid ambiguity. Even if some of the data and sources you cite are inconclusive or contradictory, note this in your conclusion to come across as confident and trustworthy.
- Examples of research paper conclusions
Your research paper should provide a compelling close to the paper as a whole, highlighting your research and hard work. While the conclusion should represent your unique style, these examples offer a starting point:
Ultimately, the data we examined all point to the same conclusion: Encouraging a good work-life balance improves employee productivity and benefits the company overall. The research suggests that when employees feel their personal lives are valued and respected by their employers, they are more likely to be productive when at work. In addition, company turnover tends to be reduced when employees have a balance between their personal and professional lives. While additional research is required to establish ways companies can support employees in creating a stronger work-life balance, it's clear the need is there.
Social media is a primary method of communication among young people. As we've seen in the data presented, most young people in high school use a variety of social media applications at least every hour, including Instagram and Facebook. While social media is an avenue for connection with peers, research increasingly suggests that social media use correlates with body image issues. Young girls with lower self-esteem tend to use social media more often than those who don't log onto social media apps every day. As new applications continue to gain popularity, and as more high school students are given smartphones, more research will be required to measure the effects of prolonged social media use.
What are the different kinds of research paper conclusions?
There are no formal types of research paper conclusions. Ultimately, the conclusion depends on the outline of your paper and the type of research you’re presenting. While some experts note that research papers can end with a new perspective or commentary, most papers should conclude with a combination of both. The most important aspect of a good research paper conclusion is that it accurately represents the body of the paper.
Can I present new arguments in my research paper conclusion?
Research paper conclusions are not the place to introduce new data or arguments. The body of your paper is where you should share research and insights, where the reader is actively absorbing the content. By the time a reader reaches the conclusion of the research paper, they should have formed their opinion. Introducing new arguments in the conclusion can take a reader by surprise, and not in a positive way. It might also serve to frustrate readers.
How long should a research paper conclusion be?
There's no set length for a research paper conclusion. However, it's a good idea not to run on too long, since conclusions are supposed to be succinct. A good rule of thumb is to keep your conclusion around 5 to 10 percent of the paper's total length. If your paper is 10 pages, try to keep your conclusion under one page.
What should I include in a research paper conclusion?
A good research paper conclusion should always include a sense of urgency, so the reader can see how and why the topic should matter to them. You can also note some recommended actions to help fix the problem and some obstacles they might encounter. A conclusion should also remind the reader of the thesis statement, along with the main points you covered in the paper. At the end of the conclusion, add a powerful closing statement that helps cement the paper in the mind of the reader.
Should you be using a customer insights hub?
Do you want to discover previous research faster?
Do you share your research findings with others?
Do you analyze research data?
Start for free today, add your research, and get to key insights faster
Editor’s picks
Last updated: 11 January 2024
Last updated: 15 January 2024
Last updated: 17 January 2024
Last updated: 12 May 2023
Last updated: 30 April 2024
Last updated: 18 May 2023
Last updated: 25 November 2023
Last updated: 13 May 2024
Latest articles
Related topics, .css-je19u9{-webkit-align-items:flex-end;-webkit-box-align:flex-end;-ms-flex-align:flex-end;align-items:flex-end;display:-webkit-box;display:-webkit-flex;display:-ms-flexbox;display:flex;-webkit-flex-direction:row;-ms-flex-direction:row;flex-direction:row;-webkit-box-flex-wrap:wrap;-webkit-flex-wrap:wrap;-ms-flex-wrap:wrap;flex-wrap:wrap;-webkit-box-pack:center;-ms-flex-pack:center;-webkit-justify-content:center;justify-content:center;row-gap:0;text-align:center;max-width:671px;}@media (max-width: 1079px){.css-je19u9{max-width:400px;}.css-je19u9>span{white-space:pre;}}@media (max-width: 799px){.css-je19u9{max-width:400px;}.css-je19u9>span{white-space:pre;}} decide what to .css-1kiodld{max-height:56px;display:-webkit-box;display:-webkit-flex;display:-ms-flexbox;display:flex;-webkit-align-items:center;-webkit-box-align:center;-ms-flex-align:center;align-items:center;}@media (max-width: 1079px){.css-1kiodld{display:none;}} build next, decide what to build next.

Users report unexpectedly high data usage, especially during streaming sessions.

Users find it hard to navigate from the home page to relevant playlists in the app.

It would be great to have a sleep timer feature, especially for bedtime listening.

I need better filters to find the songs or artists I’m looking for.
Log in or sign up
Get started for free
- Link to facebook
- Link to linkedin
- Link to twitter
- Link to youtube
- Writing Tips
How to Write a Conclusion for a Research Paper
3-minute read
- 29th August 2023
If you’re writing a research paper, the conclusion is your opportunity to summarize your findings and leave a lasting impression on your readers. In this post, we’ll take you through how to write an effective conclusion for a research paper and how you can:
· Reword your thesis statement
· Highlight the significance of your research
· Discuss limitations
· Connect to the introduction
· End with a thought-provoking statement
Rewording Your Thesis Statement
Begin your conclusion by restating your thesis statement in a way that is slightly different from the wording used in the introduction. Avoid presenting new information or evidence in your conclusion. Just summarize the main points and arguments of your essay and keep this part as concise as possible. Remember that you’ve already covered the in-depth analyses and investigations in the main body paragraphs of your essay, so it’s not necessary to restate these details in the conclusion.
Find this useful?
Subscribe to our newsletter and get writing tips from our editors straight to your inbox.
Highlighting the Significance of Your Research
The conclusion is a good place to emphasize the implications of your research . Avoid ambiguous or vague language such as “I think” or “maybe,” which could weaken your position. Clearly explain why your research is significant and how it contributes to the broader field of study.
Here’s an example from a (fictional) study on the impact of social media on mental health:
Discussing Limitations
Although it’s important to emphasize the significance of your study, you can also use the conclusion to briefly address any limitations you discovered while conducting your research, such as time constraints or a shortage of resources. Doing this demonstrates a balanced and honest approach to your research.
Connecting to the Introduction
In your conclusion, you can circle back to your introduction , perhaps by referring to a quote or anecdote you discussed earlier. If you end your paper on a similar note to how you began it, you will create a sense of cohesion for the reader and remind them of the meaning and significance of your research.
Ending With a Thought-Provoking Statement
Consider ending your paper with a thought-provoking and memorable statement that relates to the impact of your research questions or hypothesis. This statement can be a call to action, a philosophical question, or a prediction for the future (positive or negative). Here’s an example that uses the same topic as above (social media and mental health):
Expert Proofreading Services
Ensure that your essay ends on a high note by having our experts proofread your research paper. Our team has experience with a wide variety of academic fields and subjects and can help make your paper stand out from the crowd – get started today and see the difference it can make in your work.
Share this article:
Post A New Comment
Got content that needs a quick turnaround? Let us polish your work. Explore our editorial business services.
9-minute read
How to Use Infographics to Boost Your Presentation
Is your content getting noticed? Capturing and maintaining an audience’s attention is a challenge when...
8-minute read
Why Interactive PDFs Are Better for Engagement
Are you looking to enhance engagement and captivate your audience through your professional documents? Interactive...
7-minute read
Seven Key Strategies for Voice Search Optimization
Voice search optimization is rapidly shaping the digital landscape, requiring content professionals to adapt their...
4-minute read
Five Creative Ways to Showcase Your Digital Portfolio
Are you a creative freelancer looking to make a lasting impression on potential clients or...
How to Ace Slack Messaging for Contractors and Freelancers
Effective professional communication is an important skill for contractors and freelancers navigating remote work environments....
How to Insert a Text Box in a Google Doc
Google Docs is a powerful collaborative tool, and mastering its features can significantly enhance your...

Make sure your writing is the best it can be with our expert English proofreading and editing.
- PRO Courses Guides New Tech Help Pro Expert Videos About wikiHow Pro Upgrade Sign In
- EDIT Edit this Article
- EXPLORE Tech Help Pro About Us Random Article Quizzes Request a New Article Community Dashboard This Or That Game Popular Categories Arts and Entertainment Artwork Books Movies Computers and Electronics Computers Phone Skills Technology Hacks Health Men's Health Mental Health Women's Health Relationships Dating Love Relationship Issues Hobbies and Crafts Crafts Drawing Games Education & Communication Communication Skills Personal Development Studying Personal Care and Style Fashion Hair Care Personal Hygiene Youth Personal Care School Stuff Dating All Categories Arts and Entertainment Finance and Business Home and Garden Relationship Quizzes Cars & Other Vehicles Food and Entertaining Personal Care and Style Sports and Fitness Computers and Electronics Health Pets and Animals Travel Education & Communication Hobbies and Crafts Philosophy and Religion Work World Family Life Holidays and Traditions Relationships Youth
- Browse Articles
- Learn Something New
- Quizzes Hot
- This Or That Game
- Train Your Brain
- Explore More
- Support wikiHow
- About wikiHow
- Log in / Sign up
- Education and Communications
- College University and Postgraduate
- Academic Writing
- Research Papers
How to Write a Conclusion for a Research Paper
Last Updated: May 8, 2024 Approved
This article was co-authored by Christopher Taylor, PhD . Christopher Taylor is an Adjunct Assistant Professor of English at Austin Community College in Texas. He received his PhD in English Literature and Medieval Studies from the University of Texas at Austin in 2014. wikiHow marks an article as reader-approved once it receives enough positive feedback. This article received 42 testimonials and 83% of readers who voted found it helpful, earning it our reader-approved status. This article has been viewed 2,259,372 times.
The conclusion of a research paper needs to summarize the content and purpose of the paper without seeming too wooden or dry. Every basic conclusion must share several key elements, but there are also several tactics you can play around with to craft a more effective conclusion and several you should avoid to prevent yourself from weakening your paper's conclusion. Here are some writing tips to keep in mind when creating a conclusion for your next research paper.
Sample Conclusions
Writing a basic conclusion.

- Do not spend a great amount of time or space restating your topic.
- A good research paper will make the importance of your topic apparent, so you do not need to write an elaborate defense of your topic in the conclusion.
- Usually a single sentence is all you need to restate your topic.
- An example would be if you were writing a paper on the epidemiology of infectious disease, you might say something like "Tuberculosis is a widespread infectious disease that affects millions of people worldwide every year."
- Yet another example from the humanities would be a paper about the Italian Renaissance: "The Italian Renaissance was an explosion of art and ideas centered around artists, writers, and thinkers in Florence."

- A thesis is a narrowed, focused view on the topic at hand.
- This statement should be rephrased from the thesis you included in your introduction. It should not be identical or too similar to the sentence you originally used.
- Try re-wording your thesis statement in a way that complements your summary of the topic of your paper in your first sentence of your conclusion.
- An example of a good thesis statement, going back to the paper on tuberculosis, would be "Tuberculosis is a widespread disease that affects millions of people worldwide every year. Due to the alarming rate of the spread of tuberculosis, particularly in poor countries, medical professionals are implementing new strategies for the diagnosis, treatment, and containment of this disease ."

- A good way to go about this is to re-read the topic sentence of each major paragraph or section in the body of your paper.
- Find a way to briefly restate each point mentioned in each topic sentence in your conclusion. Do not repeat any of the supporting details used within your body paragraphs.
- Under most circumstances, you should avoid writing new information in your conclusion. This is especially true if the information is vital to the argument or research presented in your paper.
- For example, in the TB paper you could summarize the information. "Tuberculosis is a widespread disease that affects millions of people worldwide. Due to the alarming rate of the spread of tuberculosis, particularly in poor countries, medical professionals are implementing new strategies for the diagnosis, treatment, and containment of this disease. In developing countries, such as those in Africa and Southeast Asia, the rate of TB infections is soaring. Crowded conditions, poor sanitation, and lack of access to medical care are all compounding factors in the spread of the disease. Medical experts, such as those from the World Health Organization are now starting campaigns to go into communities in developing countries and provide diagnostic testing and treatments. However, the treatments for TB are very harsh and have many side effects. This leads to patient non-compliance and spread of multi-drug resistant strains of the disease."

- Note that this is not needed for all research papers.
- If you already fully explained what the points in your paper mean or why they are significant, you do not need to go into them in much detail in your conclusion. Simply restating your thesis or the significance of your topic should suffice.
- It is always best practice to address important issues and fully explain your points in the body of your paper. The point of a conclusion to a research paper is to summarize your argument for the reader and, perhaps, to call the reader to action if needed.

- Note that a call for action is not essential to all conclusions. A research paper on literary criticism, for instance, is less likely to need a call for action than a paper on the effect that television has on toddlers and young children.
- A paper that is more likely to call readers to action is one that addresses a public or scientific need. Let's go back to our example of tuberculosis. This is a very serious disease that is spreading quickly and with antibiotic-resistant forms.
- A call to action in this research paper would be a follow-up statement that might be along the lines of "Despite new efforts to diagnose and contain the disease, more research is needed to develop new antibiotics that will treat the most resistant strains of tuberculosis and ease the side effects of current treatments."

- For example, if you are writing a history paper, then you might discuss how the historical topic you discussed matters today. If you are writing about a foreign country, then you might use the conclusion to discuss how the information you shared may help readers understand their own country.
Making Your Conclusion as Effective as Possible

- Since this sort of conclusion is so basic, you must aim to synthesize the information rather than merely summarizing it.
- Instead of merely repeating things you already said, rephrase your thesis and supporting points in a way that ties them all together.
- By doing so, you make your research paper seem like a "complete thought" rather than a collection of random and vaguely related ideas.

- Ask a question in your introduction. In your conclusion, restate the question and provide a direct answer.
- Write an anecdote or story in your introduction but do not share the ending. Instead, write the conclusion to the anecdote in the conclusion of your paper.
- For example, if you wanted to get more creative and put a more humanistic spin on a paper on tuberculosis, you might start your introduction with a story about a person with the disease, and refer to that story in your conclusion. For example, you could say something like this before you re-state your thesis in your conclusion: "Patient X was unable to complete the treatment for tuberculosis due to severe side effects and unfortunately succumbed to the disease."
- Use the same concepts and images introduced in your introduction in your conclusion. The images may or may not appear at other points throughout the research paper.

- Include enough information about your topic to back the statement up but do not get too carried away with excess detail.
- If your research did not provide you with a clear-cut answer to a question posed in your thesis, do not be afraid to indicate as much.
- Restate your initial hypothesis and indicate whether you still believe it or if the research you performed has begun swaying your opinion.
- Indicate that an answer may still exist and that further research could shed more light on the topic at hand.

- This may not be appropriate for all types of research papers. Most research papers, such as one on effective treatment for diseases, will have the information to make the case for a particular argument already in the paper.
- A good example of a paper that might ask a question of the reader in the ending is one about a social issue, such as poverty or government policy.
- Ask a question that will directly get at the heart or purpose of the paper. This question is often the same question, or some version of it, that you may have started with when you began your research.
- Make sure that the question can be answered by the evidence presented in your paper.
- If desired you can briefly summarize the answer after stating the question. You could also leave the question hanging for the reader to answer, though.

- Even without a call to action, you can still make a recommendation to your reader.
- For instance, if you are writing about a topic like third-world poverty, you can various ways for the reader to assist in the problem without necessarily calling for more research.
- Another example would be, in a paper about treatment for drug-resistant tuberculosis, you could suggest donating to the World Health Organization or research foundations that are developing new treatments for the disease.
Avoiding Common Pitfalls

- These sayings usually sound stiff, unnatural, or trite when used in writing.
- Moreover, using a phrase like "in conclusion" to begin your conclusion is a little too straightforward and tends to lead to a weak conclusion. A strong conclusion can stand on its own without being labeled as such.

- Always state the main argument or thesis in the introduction. A research paper is an analytical discussion of an academic topic, not a mystery novel.
- A good, effective research paper will allow your reader to follow your main argument from start to finish.
- This is why it is best practice to start your paper with an introduction that states your main argument and to end the paper with a conclusion that re-states your thesis for re-iteration.

- All significant information should be introduced in the body of the paper.
- Supporting evidence expands the topic of your paper by making it appear more detailed. A conclusion should narrow the topic to a more general point.
- A conclusion should only summarize what you have already stated in the body of your paper.
- You may suggest further research or a call to action, but you should not bring in any new evidence or facts in the conclusion.

- Most often, a shift in tone occurs when a research paper with an academic tone gives an emotional or sentimental conclusion.
- Even if the topic of the paper is of personal significance for you, you should not indicate as much in your paper.
- If you want to give your paper a more humanistic slant, you could start and end your paper with a story or anecdote that would give your topic more personal meaning to the reader.
- This tone should be consistent throughout the paper, however.

- Apologetic statements include phrases like "I may not be an expert" or "This is only my opinion."
- Statements like this can usually be avoided by refraining from writing in the first-person.
- Avoid any statements in the first-person. First-person is generally considered to be informal and does not fit with the formal tone of a research paper.
Community Q&A
You Might Also Like

- ↑ http://owl.english.purdue.edu/owl/resource/724/04/
- ↑ http://www.crlsresearchguide.org/18_Writing_Conclusion.asp
- ↑ http://writing.wisc.edu/Handbook/PlanResearchPaper.html#conclusion
- ↑ http://writingcenter.unc.edu/handouts/conclusions/
- ↑ http://writing2.richmond.edu/writing/wweb/conclude.html
About This Article

To write a conclusion for a research paper, start by restating your thesis statement to remind your readers what your main topic is and bring everything full circle. Then, briefly summarize all of the main points you made throughout your paper, which will help remind your readers of everything they learned. You might also want to include a call to action if you think more research or work needs to be done on your topic by writing something like, "Despite efforts to contain the disease, more research is needed to develop antibiotics." Finally, end your conclusion by explaining the broader context of your topic and why your readers should care about it, which will help them understand why your topic is relevant and important. For tips from our Academic co-author, like how to avoid common pitfalls when writing your conclusion, scroll down! Did this summary help you? Yes No
- Send fan mail to authors
Reader Success Stories
Ummay Aimen
Sep 30, 2016
Did this article help you?
Oct 22, 2017
Sally Larrin
Mar 17, 2018
Maya Loeven
Jun 4, 2017
Sep 26, 2016

Featured Articles

Trending Articles

Watch Articles

- Terms of Use
- Privacy Policy
- Do Not Sell or Share My Info
- Not Selling Info
Get all the best how-tos!
Sign up for wikiHow's weekly email newsletter
Reference management. Clean and simple.
How to write an excellent thesis conclusion [with examples]

Restate the thesis
Review or reiterate key points of your work, explain why your work is relevant, a take-away for the reader, more resources on writing thesis conclusions, frequently asked questions about writing an excellent thesis conclusion, related articles.
At this point in your writing, you have most likely finished your introduction and the body of your thesis, dissertation, or research paper . While this is a reason to celebrate, you should not underestimate the importance of your conclusion. The conclusion is the last thing that your reader will see, so it should be memorable.
A good conclusion will review the key points of the thesis and explain to the reader why the information is relevant, applicable, or related to the world as a whole. Make sure to dedicate enough of your writing time to the conclusion and do not put it off until the very last minute.
This article provides an effective technique for writing a conclusion adapted from Erika Eby’s The College Student's Guide to Writing a Good Research Paper: 101 Easy Tips & Tricks to Make Your Work Stand Out .
While the thesis introduction starts out with broad statements about the topic, and then narrows it down to the thesis statement , a thesis conclusion does the same in the opposite order.
- Restate the thesis.
- Review or reiterate key points of your work.
- Explain why your work is relevant.
- Include a core take-away message for the reader.
Tip: Don’t just copy and paste your thesis into your conclusion. Restate it in different words.
The best way to start a conclusion is simply by restating the thesis statement. That does not mean just copying and pasting it from the introduction, but putting it into different words.
You will need to change the structure and wording of it to avoid sounding repetitive. Also, be firm in your conclusion just as you were in the introduction. Try to avoid sounding apologetic by using phrases like "This paper has tried to show..."
The conclusion should address all the same parts as the thesis while making it clear that the reader has reached the end. You are telling the reader that your research is finished and what your findings are.
I have argued throughout this work that the point of critical mass for biopolitical immunity occurred during the Romantic period because of that era's unique combination of post-revolutionary politics and innovations in smallpox prevention. In particular, I demonstrated that the French Revolution and the discovery of vaccination in the 1790s triggered a reconsideration of the relationship between bodies and the state.
Tip: Try to reiterate points from your introduction in your thesis conclusion.
The next step is to review the main points of the thesis as a whole. Look back at the body of of your project and make a note of the key ideas. You can reword these ideas the same way you reworded your thesis statement and then incorporate that into the conclusion.
You can also repeat striking quotations or statistics, but do not use more than two. As the conclusion represents your own closing thoughts on the topic , it should mainly consist of your own words.
In addition, conclusions can contain recommendations to the reader or relevant questions that further the thesis. You should ask yourself:
- What you would ideally like to see your readers do in reaction to your paper?
- Do you want them to take a certain action or investigate further?
- Is there a bigger issue that your paper wants to draw attention to?
Also, try to reference your introduction in your conclusion. You have already taken a first step by restating your thesis. Now, check whether there are other key words, phrases or ideas that are mentioned in your introduction that fit into your conclusion. Connecting the introduction to the conclusion in this way will help readers feel satisfied.
I explored how Mary Wollstonecraft, in both her fiction and political writings, envisions an ideal medico-political state, and how other writers like William Wordsworth and Mary Shelley increasingly imagined the body politic literally, as an incorporated political collective made up of bodies whose immunity to political and medical ills was essential to a healthy state.
Tip: Make sure to explain why your thesis is relevant to your field of research.
Although you can encourage readers to question their opinions and reflect on your topic, do not leave loose ends. You should provide a sense of resolution and make sure your conclusion wraps up your argument. Make sure you explain why your thesis is relevant to your field of research and how your research intervenes within, or substantially revises, existing scholarly debates.
This project challenged conventional ideas about the relationship among Romanticism, medicine, and politics by reading the unfolding of Romantic literature and biopolitical immunity as mutual, co-productive processes. In doing so, this thesis revises the ways in which biopolitics has been theorized by insisting on the inherent connections between Romantic literature and the forms of biopower that characterize early modernity.
Tip: If you began your thesis with an anecdote or historical example, you may want to return to that in your conclusion.
End your conclusion with something memorable, such as:
- a call to action
- a recommendation
- a gesture towards future research
- a brief explanation of how the problem or idea you covered remains relevant
Ultimately, you want readers to feel more informed, or ready to act, as they read your conclusion.
Yet, the Romantic period is only the beginning of modern thought on immunity and biopolitics. Victorian writers, doctors, and politicians upheld the Romantic idea that a "healthy state" was a literal condition that could be achieved by combining politics and medicine, but augmented that idea through legislation and widespread public health measures. While many nineteenth-century efforts to improve citizens' health were successful, the fight against disease ultimately changed course in the twentieth century as global immunological threats such as SARS occupied public consciousness. Indeed, as subsequent public health events make apparent, biopolitical immunity persists as a viable concept for thinking about the relationship between medicine and politics in modernity.
Need more advice? Read our 5 additional tips on how to write a good thesis conclusion.
The conclusion is the last thing that your reader will see, so it should be memorable. To write a great thesis conclusion you should:
The basic content of a conclusion is to review the main points from the paper. This part represents your own closing thoughts on the topic. It should mainly consist of the outcome of the research in your own words.
The length of the conclusion will depend on the length of the whole thesis. Usually, a conclusion should be around 5-7% of the overall word count.
End your conclusion with something memorable, such as a question, warning, or call to action. Depending on the topic, you can also end with a recommendation.
In Open Access: Theses and Dissertations you can find thousands of completed works. Take a look at any of the theses or dissertations for real-life examples of conclusions that were already approved.
Conclusions
What this handout is about.
This handout will explain the functions of conclusions, offer strategies for writing effective ones, help you evaluate conclusions you’ve drafted, and suggest approaches to avoid.
About conclusions
Introductions and conclusions can be difficult to write, but they’re worth investing time in. They can have a significant influence on a reader’s experience of your paper.
Just as your introduction acts as a bridge that transports your readers from their own lives into the “place” of your analysis, your conclusion can provide a bridge to help your readers make the transition back to their daily lives. Such a conclusion will help them see why all your analysis and information should matter to them after they put the paper down.
Your conclusion is your chance to have the last word on the subject. The conclusion allows you to have the final say on the issues you have raised in your paper, to synthesize your thoughts, to demonstrate the importance of your ideas, and to propel your reader to a new view of the subject. It is also your opportunity to make a good final impression and to end on a positive note.
Your conclusion can go beyond the confines of the assignment. The conclusion pushes beyond the boundaries of the prompt and allows you to consider broader issues, make new connections, and elaborate on the significance of your findings.
Your conclusion should make your readers glad they read your paper. Your conclusion gives your reader something to take away that will help them see things differently or appreciate your topic in personally relevant ways. It can suggest broader implications that will not only interest your reader, but also enrich your reader’s life in some way. It is your gift to the reader.
Strategies for writing an effective conclusion
One or more of the following strategies may help you write an effective conclusion:
- Play the “So What” Game. If you’re stuck and feel like your conclusion isn’t saying anything new or interesting, ask a friend to read it with you. Whenever you make a statement from your conclusion, ask the friend to say, “So what?” or “Why should anybody care?” Then ponder that question and answer it. Here’s how it might go: You: Basically, I’m just saying that education was important to Douglass. Friend: So what? You: Well, it was important because it was a key to him feeling like a free and equal citizen. Friend: Why should anybody care? You: That’s important because plantation owners tried to keep slaves from being educated so that they could maintain control. When Douglass obtained an education, he undermined that control personally. You can also use this strategy on your own, asking yourself “So What?” as you develop your ideas or your draft.
- Return to the theme or themes in the introduction. This strategy brings the reader full circle. For example, if you begin by describing a scenario, you can end with the same scenario as proof that your essay is helpful in creating a new understanding. You may also refer to the introductory paragraph by using key words or parallel concepts and images that you also used in the introduction.
- Synthesize, don’t summarize. Include a brief summary of the paper’s main points, but don’t simply repeat things that were in your paper. Instead, show your reader how the points you made and the support and examples you used fit together. Pull it all together.
- Include a provocative insight or quotation from the research or reading you did for your paper.
- Propose a course of action, a solution to an issue, or questions for further study. This can redirect your reader’s thought process and help them to apply your info and ideas to their own life or to see the broader implications.
- Point to broader implications. For example, if your paper examines the Greensboro sit-ins or another event in the Civil Rights Movement, you could point out its impact on the Civil Rights Movement as a whole. A paper about the style of writer Virginia Woolf could point to her influence on other writers or on later feminists.
Strategies to avoid
- Beginning with an unnecessary, overused phrase such as “in conclusion,” “in summary,” or “in closing.” Although these phrases can work in speeches, they come across as wooden and trite in writing.
- Stating the thesis for the very first time in the conclusion.
- Introducing a new idea or subtopic in your conclusion.
- Ending with a rephrased thesis statement without any substantive changes.
- Making sentimental, emotional appeals that are out of character with the rest of an analytical paper.
- Including evidence (quotations, statistics, etc.) that should be in the body of the paper.
Four kinds of ineffective conclusions
- The “That’s My Story and I’m Sticking to It” Conclusion. This conclusion just restates the thesis and is usually painfully short. It does not push the ideas forward. People write this kind of conclusion when they can’t think of anything else to say. Example: In conclusion, Frederick Douglass was, as we have seen, a pioneer in American education, proving that education was a major force for social change with regard to slavery.
- The “Sherlock Holmes” Conclusion. Sometimes writers will state the thesis for the very first time in the conclusion. You might be tempted to use this strategy if you don’t want to give everything away too early in your paper. You may think it would be more dramatic to keep the reader in the dark until the end and then “wow” them with your main idea, as in a Sherlock Holmes mystery. The reader, however, does not expect a mystery, but an analytical discussion of your topic in an academic style, with the main argument (thesis) stated up front. Example: (After a paper that lists numerous incidents from the book but never says what these incidents reveal about Douglass and his views on education): So, as the evidence above demonstrates, Douglass saw education as a way to undermine the slaveholders’ power and also an important step toward freedom.
- The “America the Beautiful”/”I Am Woman”/”We Shall Overcome” Conclusion. This kind of conclusion usually draws on emotion to make its appeal, but while this emotion and even sentimentality may be very heartfelt, it is usually out of character with the rest of an analytical paper. A more sophisticated commentary, rather than emotional praise, would be a more fitting tribute to the topic. Example: Because of the efforts of fine Americans like Frederick Douglass, countless others have seen the shining beacon of light that is education. His example was a torch that lit the way for others. Frederick Douglass was truly an American hero.
- The “Grab Bag” Conclusion. This kind of conclusion includes extra information that the writer found or thought of but couldn’t integrate into the main paper. You may find it hard to leave out details that you discovered after hours of research and thought, but adding random facts and bits of evidence at the end of an otherwise-well-organized essay can just create confusion. Example: In addition to being an educational pioneer, Frederick Douglass provides an interesting case study for masculinity in the American South. He also offers historians an interesting glimpse into slave resistance when he confronts Covey, the overseer. His relationships with female relatives reveal the importance of family in the slave community.
Works consulted
We consulted these works while writing this handout. This is not a comprehensive list of resources on the handout’s topic, and we encourage you to do your own research to find additional publications. Please do not use this list as a model for the format of your own reference list, as it may not match the citation style you are using. For guidance on formatting citations, please see the UNC Libraries citation tutorial . We revise these tips periodically and welcome feedback.
Douglass, Frederick. 1995. Narrative of the Life of Frederick Douglass, an American Slave, Written by Himself. New York: Dover.
Hamilton College. n.d. “Conclusions.” Writing Center. Accessed June 14, 2019. https://www.hamilton.edu//academics/centers/writing/writing-resources/conclusions .
Holewa, Randa. 2004. “Strategies for Writing a Conclusion.” LEO: Literacy Education Online. Last updated February 19, 2004. https://leo.stcloudstate.edu/acadwrite/conclude.html.
You may reproduce it for non-commercial use if you use the entire handout and attribute the source: The Writing Center, University of North Carolina at Chapel Hill
Make a Gift
How to Write a Conclusion for a Research Paper

When you're wrapping up a research paper, the conclusion is like the grand finale of a fireworks show – it's your chance to leave a lasting impression. In this article, we'll break down the steps to help you write a winning research paper conclusion that not only recaps your main points but also ties everything together. Consider it the "So what?" moment – why should people care about your research? Our professional essay writers will guide you through making your conclusion strong, clear, and something that sticks with your readers long after they've put down your paper. So, let's dive in and ensure your research ends on a high note!
What Is a Conclusion in a Research Paper
In a research paper, the conclusion serves as the final segment, where you summarize the main points and findings of your study. It's not just a repetition of what you've already said but rather a chance to tie everything together and highlight the significance of your research. As you learn how to start a research paper , a good conclusion also often discusses the implications of your findings, suggests potential areas for further research, and leaves the reader with a lasting impression of the importance and relevance of your work in the broader context of the field. Essentially, it's your last opportunity to make a strong impact and leave your readers with a clear understanding of the significance of your research. Here’s a research paper conclusion example:
In conclusion, this research paper has navigated the intricacies of sustainable urban development, shedding light on the pivotal role of community engagement and innovative planning strategies. Through applying qualitative and quantitative research methods, we've uncovered valuable insights into the challenges and opportunities inherent in fostering environmentally friendly urban spaces. The implications of these findings extend beyond the confines of this study, emphasizing the imperative for continued exploration in the realms of urban planning and environmental sustainability. By emphasizing both the practical applications and theoretical contributions, this research underscores the significance of community involvement and forward-thinking strategies in shaping the future of urban landscapes. As cities evolve, incorporating these insights into planning and development practices will create resilient and harmonious urban environments.
Conclusion Outline for Research Paper
This outline for a research paper conclusion provides a structured framework to ensure that your ending effectively summarizes the key elements of your research paper and leaves a lasting impression on your readers. Adjust the content based on the specific requirements and focus of your research.
Restate the Thesis Statement
- Briefly restate the main thesis or research question.
- Emphasize the core objective or purpose of the study.
Summarize Key Findings
- Recap the main points and key findings from each section of the paper.
- Provide a concise overview of the research journey.
Discuss Implications
- Explore the broader implications of the research findings.
- Discuss how the results contribute to the existing body of knowledge in the field.
Address Limitations
- Acknowledge any limitations or constraints encountered during the research process.
- Explain how these limitations may impact the interpretation of the findings.
Suggest Areas for Future Research
- Propose potential directions for future studies related to the topic.
- Identify gaps in the current research that warrant further exploration.
Reaffirm Significance
- Reaffirm the importance and relevance of the research in the broader context.
- Highlight the practical applications or real-world implications of the study.
Concluding Statement
- Craft a strong, memorable closing statement that leaves a lasting impression.
- Sum up the overall impact of the research and its potential contribution to the field.
Study the full guide on how to make a research paper outline here, which will also specify the conclusion writing specifics to improve your general prowess.
Tips on How to Make a Conclusion in Research
Here are key considerations regarding a conclusion for research paper to not only recap the primary ideas in your work but also delve deeper to earn a higher grade:
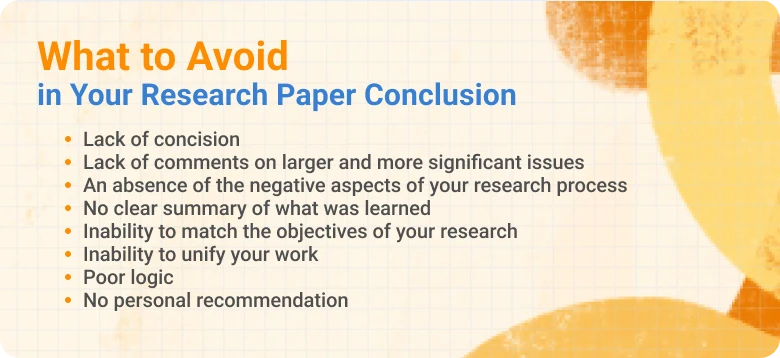
- Provide a concise recap of your main research outcomes.
- Remind readers of your research goals and their accomplishments.
- Stick to summarizing existing content; refrain from adding new details.
- Emphasize why your research matters and its broader implications.
- Clearly explain the practical or theoretical impact of your findings.
- Prompt readers to reflect on how your research influences their perspective.
- Briefly discuss the robustness of your research methods.
- End with a suggestion for future research or a practical application.
- Transparently address any constraints or biases in your study.
- End on a powerful note, leaving a memorable impression on your readers.
.webp)
For your inspiration, we’ve also prepared this research proposal example APA , which dwells on another important aspect of research writing.
How to Write a Research Paper Conclusion
As you finish your research paper, the conclusion takes center stage. In this section, we've got five practical tips for writing a conclusion for a research paper. We'll guide you through summarizing your key findings, revisiting your research goals, discussing the bigger picture, addressing any limitations, and ending on a powerful note. Think of it as your roadmap to creating a conclusion that not only wraps up your research but also leaves a lasting impact on your readers. Let's dive in and make sure your conclusion stands out for all the right reasons!
.webp)
Synthesize Core Discoveries. Initiate your conclusion by synthesizing the essential discoveries of your research. Offer a succinct recapitulation of the primary points and outcomes you have elucidated in your paper. This aids in reinforcing the gravity of your work and reiterates the pivotal information you have presented.
Revisit Research Objectives. Revisit the research objectives or questions you outlined at the beginning of your paper. Assess whether you have successfully addressed these objectives and if your findings align with the initial goals of your research. This reflection helps tie your conclusion back to the purpose of your study.
Discuss Implications and Contributions. Discuss the broader implications of your research and its potential contributions to the field. Consider how your findings might impact future research, applications, or understanding of the subject matter. This demonstrates the significance of your work and places it within a larger context.
Address Limitations and Future Research. Acknowledge any limitations in your study, such as constraints in data collection or potential biases. Briefly discuss how these limitations might have affected your results. Additionally, suggest areas for future research that could build upon your work, addressing any unanswered questions or unexplored aspects. This demonstrates a thoughtful approach to your research.
End with a Strong Conclusion Statement. Conclude your research paper with a strong and memorable statement that reinforces the key message you want readers to take away. This could be a call to action, a proposal for further investigation, or a reflection on the broader significance of your findings. Leave your readers with a lasting impression that emphasizes the importance of your research. Remember that you can buy a research paper anytime if you lack time or get stuck in writer’s block.
Want to Enjoy the Benefits of Academic Freedom?
With our top-notch writers and 24/7 support, you can relax and focus on what really matters
Stylistic Devices to Use in a Conclusion
Discover distinctive stylistic insights that you can apply when writing a conclusion for a research paper:
- Rhetorical Questions. When using rhetorical questions, strategically place them to engage readers' minds. For instance, you might pose a question that prompts reflection on the broader implications of your findings, leaving your audience with something to ponder.
- Powerful Language. Incorporate strong language to convey a sense of conviction and importance. Choose words that resonate with the overall tone of your research and amplify the significance of your conclusions. This adds weight to your key messages.
- Repetitions. Repetitions can be employed to reinforce essential ideas. Reiterate key phrases or concepts in a way that emphasizes their importance without sounding redundant. This technique serves to drive home your main points.
- Anecdotes. Integrating anecdotes into your conclusion can provide a human touch. Share a brief and relevant story that connects with your research, making the information more relatable and memorable for your audience.
- Vivid Imagery. Lastly, use vivid imagery to paint a picture in the minds of your readers. Appeal to their senses by describing scenarios or outcomes related to your research. This creates a more immersive and lasting impression.
If you have a larger paper to write, for example a thesis, use our custom dissertation writing can help you in no time.
How to Make a Conclusion Logically Appealing
Knowing how to write a conclusion for a research paper that is logically appealing is important for leaving a lasting impression on your readers. Here are some tips to achieve this:
Logical Sequencing
- Present your conclusion in a structured manner, following the natural flow of your paper. Readers should effortlessly follow your thought process, making your conclusion more accessible and persuasive.
Reinforce Main Arguments
- Emphasize the core arguments and findings from your research. By reinforcing key points, you solidify your stance and provide a logical culmination to your paper.
Address Counterarguments
- Acknowledge and address potential counterarguments or limitations in your research. Demonstrate intellectual honesty and strengthen your conclusion by preemptively addressing potential doubts.
Connect with Introduction
- Revisit themes or concepts introduced in your introduction to create a cohesive narrative, allowing readers to trace the logical progression of your research from start to finish.
Propose Actionable Insights
- Suggest practical applications or recommendations based on your findings. This will add a forward-looking dimension, making your conclusion more relevant and compelling.
Highlight Significance
- Clearly articulate the broader implications of your research to convey the importance of your work and its potential impact on the field, making your conclusion logically compelling.
Are you ready to produce an A-grade assignment? If not, opt for a custom research paper from our skilled writers across various disciplines.
Avoid These Things When Writing a Research Paper Conclusion
As you write your conclusion of research paper, there’s a list of things professional writers don’t recommend doing. Consider these issues carefully:
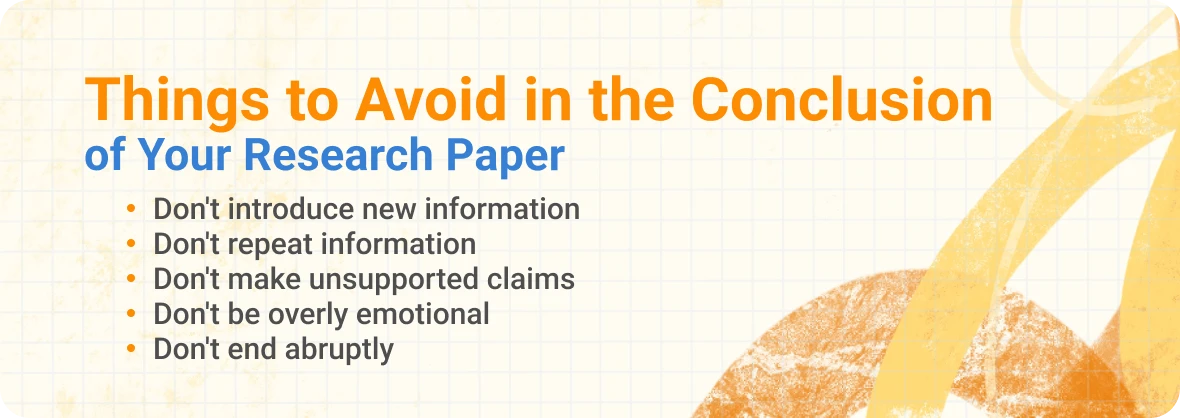
- Repetition of Exact Phrases
- Repetitively using the same phrases or sentences from the main body. Repetition can make your conclusion seem redundant and less engaging.
- Overly Lengthy Summaries
- Providing excessively detailed summaries of each section of your paper. Readers may lose interest if the conclusion becomes too long and detailed.
- Unclear Connection to the Introduction
- Failing to connect the conclusion back to the introduction. A lack of continuity may make the paper feel disjointed.
- Adding New Arguments or Ideas
- Introducing new arguments or ideas that were not addressed in the body. This can confuse the reader and disrupt the coherence of your paper.
- Overuse of Complex Jargon
- Using excessively complex or technical language without clarification. Clear communication is essential in the conclusion, ensuring broad understanding.
- Apologizing or Undermining Confidence
- Apologizing for limitations or expressing doubt about your work. Maintain a confident tone; if limitations exist, present them objectively without undermining your research.
- Sweeping Generalizations
- Making overly broad or unsupported generalizations. Such statements can weaken the credibility of your conclusion.
- Neglecting the Significance
- Failing to emphasize the broader significance of your research. Readers need to understand why your findings matter in a larger context.
- Abrupt Endings
- Concluding abruptly without a strong closing statement. A powerful ending leaves a lasting impression; avoid a sudden or weak conclusion.
Research Paper Conclusion Example
That covers the essential aspects of summarizing a research paper. The only remaining step is to review the conclusion examples for research paper provided by our team.
Like our examples? Order our research proposal writing service to write paper according to your instructions to avoid plagiarizing and to keep your academic integrity strong.
Final Thoughts
In conclusion, the knowledge of how to write the conclusion of a research paper is pivotal for presenting your findings and leaving a lasting impression on your readers. By summarizing the key points, reiterating the significance of your research, and offering avenues for future exploration, you can create a conclusion that not only reinforces the value of your study but also encourages further academic discourse. Remember to balance brevity and completeness, ensuring your conclusion is concise yet comprehensive. Emphasizing the practical implications of your research and connecting it to the broader academic landscape will help solidify the impact of your work. Pay someone to write a research paper if you are having a hard time finishing your coursework on time.
Tired of Stressing Over Endless Essays and Deadlines?
Let us take the load off your shoulders! Order your custom research paper today and experience the relief of knowing that your assignment is in expert hands
How To Write A Conclusion For A Research Paper?
What should the conclusion of a research paper contain, how to start a conclusion paragraph for a research paper.

Daniel Parker
is a seasoned educational writer focusing on scholarship guidance, research papers, and various forms of academic essays including reflective and narrative essays. His expertise also extends to detailed case studies. A scholar with a background in English Literature and Education, Daniel’s work on EssayPro blog aims to support students in achieving academic excellence and securing scholarships. His hobbies include reading classic literature and participating in academic forums.

is an expert in nursing and healthcare, with a strong background in history, law, and literature. Holding advanced degrees in nursing and public health, his analytical approach and comprehensive knowledge help students navigate complex topics. On EssayPro blog, Adam provides insightful articles on everything from historical analysis to the intricacies of healthcare policies. In his downtime, he enjoys historical documentaries and volunteering at local clinics.

Related Articles
%20(3).webp)

- Walden University
- Faculty Portal
Writing a Paper: Conclusions
Writing a conclusion.
A conclusion is an important part of the paper; it provides closure for the reader while reminding the reader of the contents and importance of the paper. It accomplishes this by stepping back from the specifics in order to view the bigger picture of the document. In other words, it is reminding the reader of the main argument. For most course papers, it is usually one paragraph that simply and succinctly restates the main ideas and arguments, pulling everything together to help clarify the thesis of the paper. A conclusion does not introduce new ideas; instead, it should clarify the intent and importance of the paper. It can also suggest possible future research on the topic.
An Easy Checklist for Writing a Conclusion
It is important to remind the reader of the thesis of the paper so he is reminded of the argument and solutions you proposed.
Think of the main points as puzzle pieces, and the conclusion is where they all fit together to create a bigger picture. The reader should walk away with the bigger picture in mind.
Make sure that the paper places its findings in the context of real social change.
Make sure the reader has a distinct sense that the paper has come to an end. It is important to not leave the reader hanging. (You don’t want her to have flip-the-page syndrome, where the reader turns the page, expecting the paper to continue. The paper should naturally come to an end.)
No new ideas should be introduced in the conclusion. It is simply a review of the material that is already present in the paper. The only new idea would be the suggesting of a direction for future research.
Conclusion Example
As addressed in my analysis of recent research, the advantages of a later starting time for high school students significantly outweigh the disadvantages. A later starting time would allow teens more time to sleep--something that is important for their physical and mental health--and ultimately improve their academic performance and behavior. The added transportation costs that result from this change can be absorbed through energy savings. The beneficial effects on the students’ academic performance and behavior validate this decision, but its effect on student motivation is still unknown. I would encourage an in-depth look at the reactions of students to such a change. This sort of study would help determine the actual effects of a later start time on the time management and sleep habits of students.
Related Webinar
Didn't find what you need? Email us at [email protected] .
- Previous Page: Thesis Statements
- Next Page: Writer's Block
- Office of Student Disability Services
Walden Resources
Departments.
- Academic Residencies
- Academic Skills
- Career Planning and Development
- Customer Care Team
- Field Experience
- Military Services
- Student Success Advising
- Writing Skills
Centers and Offices
- Center for Social Change
- Office of Academic Support and Instructional Services
- Office of Degree Acceleration
- Office of Research and Doctoral Services
- Office of Student Affairs
Student Resources
- Doctoral Writing Assessment
- Form & Style Review
- Quick Answers
- ScholarWorks
- SKIL Courses and Workshops
- Walden Bookstore
- Walden Catalog & Student Handbook
- Student Safety/Title IX
- Legal & Consumer Information
- Website Terms and Conditions
- Cookie Policy
- Accessibility
- Accreditation
- State Authorization
- Net Price Calculator
- Contact Walden
Walden University is a member of Adtalem Global Education, Inc. www.adtalem.com Walden University is certified to operate by SCHEV © 2024 Walden University LLC. All rights reserved.
Purdue Online Writing Lab Purdue OWL® College of Liberal Arts
Conclusions

Welcome to the Purdue OWL
This page is brought to you by the OWL at Purdue University. When printing this page, you must include the entire legal notice.
Copyright ©1995-2018 by The Writing Lab & The OWL at Purdue and Purdue University. All rights reserved. This material may not be published, reproduced, broadcast, rewritten, or redistributed without permission. Use of this site constitutes acceptance of our terms and conditions of fair use.
Conclusions wrap up what you have been discussing in your paper. After moving from general to specific information in the introduction and body paragraphs, your conclusion should begin pulling back into more general information that restates the main points of your argument. Conclusions may also call for action or overview future possible research. The following outline may help you conclude your paper:
In a general way,
- Restate your topic and why it is important,
- Restate your thesis/claim,
- Address opposing viewpoints and explain why readers should align with your position,
- Call for action or overview future research possibilities.
Remember that once you accomplish these tasks, unless otherwise directed by your instructor, you are finished. Done. Complete. Don't try to bring in new points or end with a whiz bang(!) conclusion or try to solve world hunger in the final sentence of your conclusion. Simplicity is best for a clear, convincing message.
The preacher's maxim is one of the most effective formulas to follow for argument papers:
Tell what you're going to tell them (introduction).
Tell them (body).
Tell them what you told them (conclusion).
Research Implications & Recommendations
A Plain-Language Explainer With Examples + FREE Template
By: Derek Jansen (MBA) | Reviewers: Dr Eunice Rautenbach | May 2024

The research implications and recommendations are closely related but distinctly different concepts that often trip students up. Here, we’ll unpack them using plain language and loads of examples , so that you can approach your project with confidence.
Overview: Implications & Recommendations
- What are research implications ?
- What are research recommendations ?
- Examples of implications and recommendations
- The “ Big 3 ” categories
- How to write the implications and recommendations
- Template sentences for both sections
- Key takeaways
Implications & Recommendations 101
Let’s start with the basics and define our terms.
At the simplest level, research implications refer to the possible effects or outcomes of a study’s findings. More specifically, they answer the question, “ What do these findings mean?” . In other words, the implications section is where you discuss the broader impact of your study’s findings on theory, practice and future research.
This discussion leads us to the recommendations section , which is where you’ll propose specific actions based on your study’s findings and answer the question, “ What should be done next?” . In other words, the recommendations are practical steps that stakeholders can take to address the key issues identified by your study.
In a nutshell, then, the research implications discuss the broader impact and significance of a study’s findings, while recommendations provide specific actions to take, based on those findings. So, while both of these components are deeply rooted in the findings of the study, they serve different functions within the write up.
Need a helping hand?
Examples: Implications & Recommendations
The distinction between research implications and research recommendations might still feel a bit conceptual, so let’s look at one or two practical examples:
Let’s assume that your study finds that interactive learning methods significantly improve student engagement compared to traditional lectures. In this case, one of your recommendations could be that schools incorporate more interactive learning techniques into their curriculums to enhance student engagement.
Let’s imagine that your study finds that patients who receive personalised care plans have better health outcomes than those with standard care plans. One of your recommendations might be that healthcare providers develop and implement personalised care plans for their patients.
Now, these are admittedly quite simplistic examples, but they demonstrate the difference (and connection ) between the research implications and the recommendations. Simply put, the implications are about the impact of the findings, while the recommendations are about proposed actions, based on the findings.
The “Big 3” Categories
Now that we’ve defined our terms, let’s dig a little deeper into the implications – specifically, the different types or categories of research implications that exist.
Broadly speaking, implications can be divided into three categories – theoretical implications, practical implications and implications for future research .
Theoretical implications relate to how your study’s findings contribute to or challenge existing theories. For example, if a study on social behaviour uncovers new patterns, it might suggest that modifications to current psychological theories are necessary.
Practical implications , on the other hand, focus on how your study’s findings can be applied in real-world settings. For example, if your study demonstrated the effectiveness of a new teaching method, this would imply that educators should consider adopting this method to improve learning outcomes.
Practical implications can also involve policy reconsiderations . For example, if a study reveals significant health benefits from a particular diet, an implication might be that public health guidelines be re-evaluated.
Last but not least, there are the implications for future research . As the name suggests, this category of implications highlights the research gaps or new questions raised by your study. For example, if your study finds mixed results regarding a relationship between two variables, it might imply the need for further investigation to clarify these findings.
To recap then, the three types of implications are the theoretical, the practical and the implications on future research. Regardless of the category, these implications feed into and shape the recommendations , laying the foundation for the actions you’ll propose.
How To Write The Sections
Now that we’ve laid the foundations, it’s time to explore how to write up the implications and recommendations sections respectively.
Let’s start with the “ where ” before digging into the “ how ”. Typically, the implications will feature in the discussion section of your document, while the recommendations will be located in the conclusion . That said, layouts can vary between disciplines and institutions, so be sure to check with your university what their preferences are.
For the implications section, a common approach is to structure the write-up based on the three categories we looked at earlier – theoretical, practical and future research implications. In practical terms, this discussion will usually follow a fairly formulaic sentence structure – for example:
This research provides new insights into [theoretical aspect], indicating that…
The study’s outcomes highlight the potential benefits of adopting [specific practice] in..
This study raises several questions that warrant further investigation, such as…
Moving onto the recommendations section, you could again structure your recommendations using the three categories. Alternatively, you could structure the discussion per stakeholder group – for example, policymakers, organisations, researchers, etc.
Again, you’ll likely use a fairly formulaic sentence structure for this section. Here are some examples for your inspiration:
Based on the findings, [specific group] should consider adopting [new method] to improve…
To address the issues identified, it is recommended that legislation should be introduced to…
Researchers should consider examining [specific variable] to build on the current study’s findings.
Remember, you can grab a copy of our tried and tested templates for both the discussion and conclusion sections over on the Grad Coach blog. You can find the links to those, as well as loads of other free resources, in the description 🙂
FAQs: Implications & Recommendations
How do i determine the implications of my study.
To do this, you’ll need to consider how your findings address gaps in the existing literature, how they could influence theory, practice, or policy, and the potential societal or economic impacts.
When thinking about your findings, it’s also a good idea to revisit your introduction chapter, where you would have discussed the potential significance of your study more broadly. This section can help spark some additional ideas about what your findings mean in relation to your original research aims.
Should I discuss both positive and negative implications?
Absolutely. You’ll need to discuss both the positive and negative implications to provide a balanced view of how your findings affect the field and any limitations or potential downsides.
Can my research implications be speculative?
Yes and no. While implications are somewhat more speculative than recommendations and can suggest potential future outcomes, they should be grounded in your data and analysis. So, be careful to avoid overly speculative claims.
How do I formulate recommendations?
Ideally, you should base your recommendations on the limitations and implications of your study’s findings. So, consider what further research is needed, how policies could be adapted, or how practices could be improved – and make proposals in this respect.
How specific should my recommendations be?
Your recommendations should be as specific as possible, providing clear guidance on what actions or research should be taken next. As mentioned earlier, the implications can be relatively broad, but the recommendations should be very specific and actionable. Ideally, you should apply the SMART framework to your recommendations.
Can I recommend future research in my recommendations?
Absolutely. Highlighting areas where further research is needed is a key aspect of the recommendations section. Naturally, these recommendations should link to the respective section of your implications (i.e., implications for future research).
Wrapping Up: Key Takeaways
We’ve covered quite a bit of ground here, so let’s quickly recap.
- Research implications refer to the possible effects or outcomes of a study’s findings.
- The recommendations section, on the other hand, is where you’ll propose specific actions based on those findings.
- You can structure your implications section based on the three overarching categories – theoretical, practical and future research implications.
- You can carry this structure through to the recommendations as well, or you can group your recommendations by stakeholder.
Remember to grab a copy of our tried and tested free dissertation template, which covers both the implications and recommendations sections. If you’d like 1:1 help with your research project, be sure to check out our private coaching service, where we hold your hand throughout the research journey, step by step.

Psst... there’s more!
This post was based on one of our popular Research Bootcamps . If you're working on a research project, you'll definitely want to check this out ...
You Might Also Like:
Submit a Comment Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- Print Friendly
Social Representativeness and Intervention Adherence—A Systematic Review of Clinical Physical Activity Trials in Breast Cancer Patients

- 1 Department of Circulation and Medical Imaging, Norwegian University of Technology and Science (NTNU), Trondheim, Norway
- 2 Department of Neuromedicine and Movement Science, Norwegian University of Technology and Science (NTNU), Trondheim, Norway
Objectives: Representativeness in physical activity randomised controlled trials (RCT) in breast cancer patients is essential to analyses of feasibility and validity considering privileged- social groups. A step-by-step exclusion of less privileged groups through the trial process could reinforce health inequality. This study aimed at examining representativeness in breast cancer (BC) physical activity trials, investigate associations between socio-economic status (SES) and intervention adherence, and explore associations between representativeness and the relationship between SES and intervention adherence.
Methods: Systematic, computerised searches were performed in PubMed, CINAHL, AMED, EMBASE and PsycINFO. Additional citation-based searches retrieved 37 articles. Distributions of education level, ethnicity, and marital status in study samples were compared to national populations data to estimate representativeness in less privileged groups.
Results: A preponderance of studies favoured educated, married and white patients. Only six studies reported SES-adherence associations, hampering conclusions on this relationship and possible associations between representativeness and an SES-adherence relationship.
Conclusion: Less educated, unmarried and non-white individuals may be underrepresented in BC physical activity RCTs, while SES-adherence associations in such trials are inconclusive. Unintentional social misrepresentations may indicate that disguised inequity warrants revived attention.
Introduction
Clinical trials in breast cancer (BC) research have contributed significantly to improved treatments, health-related quality of life, and survival probability for BC patients [ 1 ]. For example, numerous clinical physical activity (PA) trials have been conducted. Nevertheless, faced with the reality of social health inequalities [ 2 , 3 ], it is essential to ensure that the results of these trials benefit all, not exclusively the most privileged. Previous analyses have concluded that study samples only slightly represent real-world patient populations [ 4 ] due to participants having better health status, lower age, and a dominant ethnicity. However, research inequity on the part of socioeconomic status (SES)-groups has been scarcely investigated. As PA appears to improve physical fitness [ 5 – 8 ], fatigue [ 5 , 6 , 9 , 10 ], and physical functioning [ 5 , 9 , 11 ] in BC patients and survivors, knowledge about representativeness across SES and privilege in randomised controlled trials (RCT) with PA is warranted.
Privilege refers to (often unrecognised) advantages that benefit people belonging to certain groups based on factors like their SES, ethnicity, age, gender identity [ 12 ]. High-SES individuals, for example, are considered to have health benefits as a result of their belonging to a privileged social group [ 13 ]. SES, is ideally measured as the combination of an individual’s or groups’ education, income and occupation [ 14 ] and it is often used to examine social health inequalities [ 15 ]. In the case of BC, there is an excess risk associated with increased education, in both men [ 16 ] and women [ 17 ]. Unmarried women, who face a multitude of hardships and less privilege [ 18 ], may have a higher risk of developing BC [ 19 ]. Similarly, less privileged non-whites have higher odds of being diagnosed with aggressive BC [ 20 ]. However, BC in men and less privileged women is generally diagnosed later, making these cases more severe compared to BC diagnosed in privileged women [ 21 ]. Despite higher incidence rates of early BC, higher survival rates and better health-related quality of life after diagnosis [ 22 ] are associated with higher education [ 23 ]. In young men with invasive BC, overall survival is found to decrease in groups living in ZIP-code areas associated with low SES [ 24 ]. Presumably because <1% of all BC incidents occur in men [ 25 ], most PA research concern women. Female patients often report weight gain, which is associated with undesirable BC-outcomes [ 26 – 28 ]. Thus, it is often recommended that they pursue regular PA [ 29 ]. An inactive lifestyle is suggested to be a significant social determinant of decreased BC survival probability in low-SES groups [ 30 ], and according to Boer et al., there is strong evidence that BC recurrence and mortality are strongly associated with leisure-time PA (LTPA) due to the biological mechanisms affected [ 31 ].
PA is defined as any bodily movement produced by skeletal muscles that results in energy expenditure [ 32 ] and includes the active transport-, leisure time- (including exercise), job-related-, and household PA domains [ 33 ]. The relationship between PA and the risk of BC is well documented [ 34 – 44 ] and is evident for LTPA in postmenopausal BC [ 45 , 46 ]. However, it has been found that different SES-groups in general are inclined to different domains of PA, with high-SES groups being more physically active within the LTPA domain [ 47 ]. Comparable results are reported in studies of women with BC [ 48 – 51 ]. Hence, for RCTs with LTPA, there is a risk of selection bias, which is also acknowledged in the Exercise guidelines for cancer survivors: “ …the individuals enrolled in studies commonly meet prespecified eligibility criteria (…) and were willing to take part in research. This often results in a sample that is healthier or with higher physical function and exercise motivation that may not fully generalize to the broader population of cancer survivors. ” [ 52 ].
Moreover, if there are SES-differences in PA among women with BC in general, participation and adherence to PA trials may differ accordingly. Studies have shown different PA barriers across SES [ 53 , 54 ], partly explaining variances in activity levels [ 55 – 59 ]. If low-SES individuals perform less LTPA than high-SES individuals [ 47 ], the former may be prone to lower participation and adherence rates in exercise RCTs. In addition to findings of better exercise trial adherence in high-SES groups [ 60 , 61 ], less privileged individuals less frequently volunteer to participate in research [ 62 , 63 ], due to barriers to access [ 62 ], lower health literacy and negative attitudes towards research, additional costs, or disease status [ 64 ]. These findings may imply that RCTs with which a privileged group is more familiar and motivated for the provided intervention (i.e., LTPA/exercise) run higher risks of selection bias than RCTs for which compliance is less affected by social grouping.
Hence, the external validity of LTPA trials for BC patients may be impaired, albeit unintendedly, by a stepwise exclusion of less privileged patients; they appear to be recruited and participate less frequently, and may also have lower adherence rates [ 65 ]. The general view is that RCT samples must be homogeneous to gain internal validity and reliable results [ 66 , 67 ]. Simultaneously, the declarations of Helsinki [ 68 ], legitimately and necessarily, prevents researchers from obliging participation for the purpose of representativeness. Consequently, social biases may be fortified [ 64 , 65 ].
The credibility and success of medical progress depend on transparent reporting [ 69 ]. Thus, the CONSORT guidelines developed to improve RCT-articles [ 70 ]. Nevertheless, participant attributes, such as SES-indicators, are seldomly reported [ 71 , 72 ], impeding successful assessments of equitable research [ 72 ]. A reasonable alternative may be to employ the available variables that indicate, or strongly correlate with, privilege and SES. Previous reviews of PA-SES associations have found that education is the most reported SES-indicator [ 47 , 73 , 74 ]. Furthermore, frequently reported characteristics, such as ethnicity and marital status, both reflect social privilege and correlate with SES, thus they may be considered fair representations of privilege in the absence of precise SES-indicators.
The objective of this systematic review was to study previous PA RCTs on BC patients with the intention of examining a) SES-related information and representativeness, b) associations between SES-related indicators and PA intervention adherence, and c) associations between representativeness and reported relationships between SES and intervention adherences. There are, of course, real obstacles to recruting less privileged patients, so non-representative samples should not be seen as researchers’ unwillingness or lack of effort to include the less privileged. The overall aim of the study was not to evaluate single studies conducted for purposes other than representativeness per se , but rather to highlight disguised patterns across comparable studies [ 75 ]. Furthermore, the aim was not to provide meta-analyses and precise sample- vs real-world ratios; however, the study may render a departure point for improving representativeness on the part of less privileged groups.
Systematic, computerised searches were conducted in the PubMed, CINAHL, AMED, EMBASE and PsycINFO databases. The first round followed a traditional method [ 76 ]; we specified a search query by a set and combinations of words, and all publications indexed in the databases that contained those words were returned. “Compliance,” “persistence,” “fidelity,” “maintenance” and “concordance” were used as synonyms for the variable “adherence.” Similarly, “physical,” “exercise,” “fitness,” “sport” and “training” were used as synonyms, in addition to exercise-specific terms, such as “dance,” “swim,” “walk” and “yoga,” to cover any type of PA intervention. An asterisk (*) was attached to the roots of the words to broaden the search, and to retrieve variations on these terms. Because the terms are used interchangeably in the literature, both “ patients ” and “ survivors ” were used to cover relevant study samples. As recommended by Bramer et al. [ 77 ]. Boolean combinations were used to construct suitable search queries in combination with the basic term “breast cancer” (see Figure 1 ). There were no search limits as to publication year.
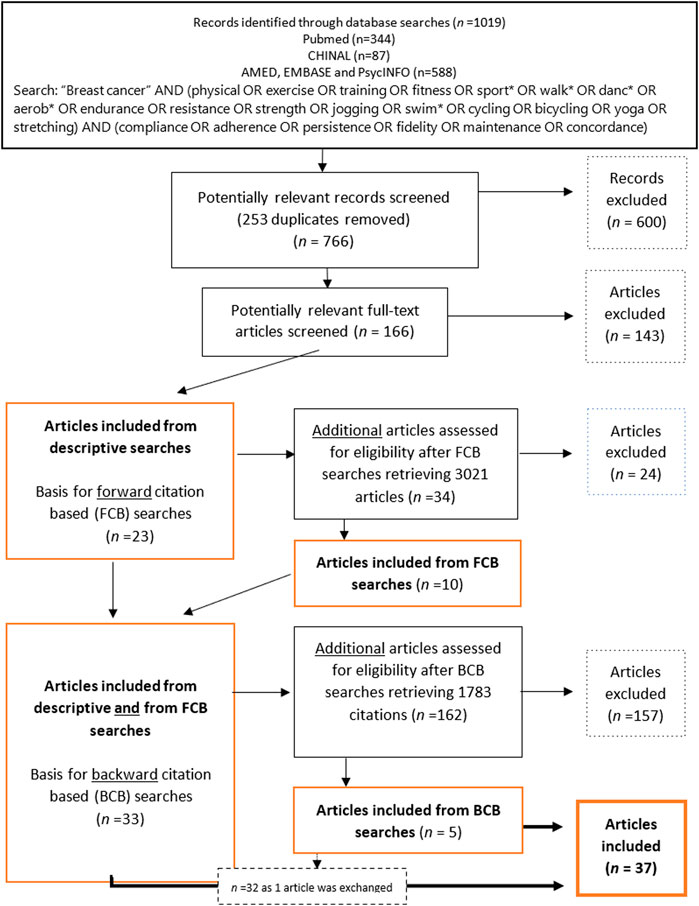
Figure 1 . Flow chart of inclusion and exclusion of articles through descriptive- and citation-based searches (Global, 2000–2020).
The following criteria guided the inclusion and exclusion process, defining the final dataset:
Inclusion Criteria
a) Empirical studies
b) …reporting RCTs including a PA intervention.
c) …including individuals undergoing BC treatment within one-year postdiagnosis.
d) …reporting adherence to the PA intervention.
e) …presenting a comprehensible calculation of adherence.
f) …written in English.
Exclusion Criteria
a) Reviews, theoretical and descriptive papers, books, theses, letters to editor or editorials.
b) …reporting on multiple cancer diagnoses (even if BC was included).
c) …not reporting any SES-related characteristics of the sample … written in any non-English language.
The descriptive searches retrieved 1,019 articles. After excluding immediate duplicates, 766 articles were manually examined and deemed potentially relevant based on a screening of titles and abstracts. This left, 166 potentially relevant articles that were examined to establish their eligibility according to the criteria. An algorithm for all variables was implemented using Python3 to ensure the eligibility of the articles selected. In total, 143 articles were excluded for a total of 23 remaining articles ( Figure 1 ).
To retrieve all possible relevant studies, thus reducing the risk of missing information [ 78 ], citation-based searches (described by Hu et al. [ 79 ], but implemented in Rysstad and Pedersen [ 80 ] and Darvik et al. [ 81 ]) were performed based on the 23 articles found in the descriptive searches. A forward citation-based (FCB) search of articles that cited the articles included in the descriptive searches was first reviewed for eligibility, and 34 potentially relevant articles were identified, 24 of which were excluded. A backwards citation-based (BCB) search, where the reference lists in the 33 articles already included in the material were scanned for eligible studies, retrieved 5 articles of which one replaced a previously included article, following the inclusion criteria.
In cases in which an article reported on two different parent trials, the article was included on the condition that at least one of the parent studies met inclusion criteria c. If two articles were reporting on the same parent RCT sample and overlapped in their data, the earliest article was included. If, however, only one of them reported adherence rates, the article omitting adherence rates was excluded. Nevertheless, the included article had to report on SES-related patient characteristics. In the subsequent step of the inclusion/exclusion process, only articles reporting the samples’ SES distributions were included for further analyses.
The second author performed the database searches but conferred with the first author to discuss any cases of doubt about the potentially relevant articles returned from the query.
Data Extraction and Analysis
The following variables were extracted from the articles: sample descriptions, intervention designs, aims of the studies, measures of SES or privilege, their distributions, and adherence calculations and -rates. For studies that investigated the associations between adherence and SES-related factors, the reported results were registered.
The SES-related distribution in the sample was compared with the corresponding distribution within the country in which the study was conducted, at the matching time of publication. Because adherence to intervention protocols was embedded in our study objectives, only intervention group characteristics were analysed. Due to third-party researchers’ limited access to patient population data, SES-related distribution in a country population, in the corresponding age groups, was used as a proxy for the patient population. For the education variable, the percentage of the study sample holding any tertiary education (no degree required) was compared with the percentage of the country population holding the same educational level (i.e., all formal postsecondary education, including public and private universities, colleges, technical training institutes, and vocational schools [ 82 ]), using public statistics for reference [ 83 – 86 ] (see Supplementary Files S2, S3 for details). Because the final data set included articles about women exclusively, all statistics retrieved and analysed, were relevant to women.
Similarly, the proportion of married women in the study samples and in the associated country populations was compared using United Nations World Marriage Data (age 45–49) [ 87 ] and a corresponding analysis for ethnicity based on national censuses [ 88 – 92 ]. Frequencies in the white alone and non-indigenous and non-visible minority categories from accessible censuses were used to estimate figures for intercensal years by interpolation. The relative differences between the study samples and the associated countries were calculated as follows:
Studies reporting on the association between SES-related factors and adherence to the PA intervention were further explored, and variations in adherence calculations were examined.
The preliminary screening excluded 20%–25% of all potentially relevant articles due to a lack of information about SES-related characteristics. The subsequent selection process, following descriptive, FBC- and BCB-searches, retrieved 37 eligible articles ( Figure 1 ).
A total of 28 (76%) of the included studies were published between 2010 and 2020, and the oldest article was published in 2002 [ 93 ]. Most studies (81%) were conducted in Western countries: 18 in the United States, 5 in Canada, two in the Netherlands, and one each in Spain, France, the United Kingdom, Denmark and Sweden. Six (16%) studies were Asian, including one Indian, two Chinese and three Taiwanese studies. In addition, one Brazilian study was included. The (full) sample sizes ranged from 14 [ 94 ] to 301 [ 95 ], including 11 studies with <50 participants, 15 studies with 50–96 participants, and 11 studies with 100–301 participants. The mean age ranged from 42.1 to 63.2 years (total mean = 51 years) ( Table 1 ). All included studies were of female BC patients.
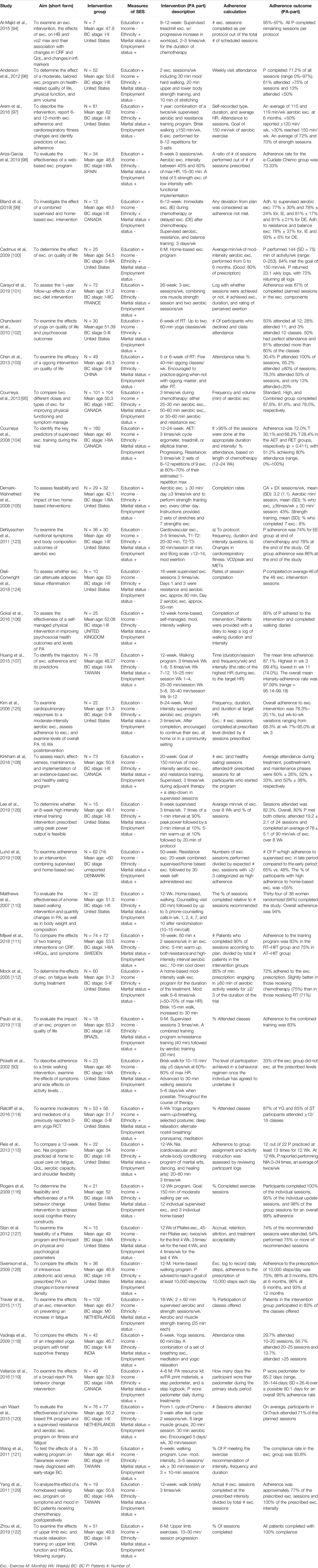
Table 1 . Study aim, sample, SES and intervention descriptions, adherence formula, and adherence outcome in included studies. (Global, 2000–2020).
Education was the most frequently used indicator of privilege and was found in 30 (81%) of the articles [ 93 – 122 ] ( Table 1 ). Marital status was reported in 28 (76%) [ 93 – 95 , 97 – 99 , 101 – 109 , 111 – 115 , 122 ], ethnicity in 22 articles (59%) [ 93 – 95 , 102 , 105 , 108 , 110 , 112 , 114 – 116 , 119 , 123 – 128 ] employment status in 25 articles (68%) [ 93 – 95 , 98 , 101 , 102 , 104 , 106 – 111 , 113 – 115 , 118 , 119 ], and income in eight articles (22%) [ 95 , 96 , 103 , 104 , 114 , 116 , 122 , 123 ]. Two articles [ 95 , 114 ] reported five indicators, and four [ 124 , 126 , 127 , 129 ] reported one. Ethnicity was reported in all 18 USA studies, as well as in four of the five Canadian studies, but it was not reported in the remaining studies. For the rest of the indicators, no geographical patterns were identified.
There was no uniform definition of adherence although the most common calculation was attendance rates relative to total, or weekly, prescribed, or possible, PA sessions. The mean adherence rate for these studies was 78.9% (30.4%–100%). All studies reported on patients diagnosed with BC in stages 0–III.*. Most studies reported the feasibility or effect of a PA intervention on patients undergoing radiation-, chemotherapy, or both.
The PA-interventions were designed differently in terms of PA type (e.g., walking, exercise including endurance and strength, yoga, aerobics, martial arts, dancing, cycling, qigong, balance training, Pilates), intensity (e.g., according to Ainsworth et al. [ 130 ], yoga is performed at 2.5 METs, whereas bicycling could require 4–16 METs), duration (10–60 min/session, 6 weeks–12 months/intervention) and frequency (voluntarily–5 bouts/week).
Privileged Groups and Adherence to PA Interventions
Some articles were feasibility studies centred on adherence; others reported adherence as a sub-analysis. Six studies reported on the relationship between SES-related factors and adherence to or completion of the intervention [ 97 , 104 , 107 , 109 , 111 , 114 ]. However, two of these studies reported no significant difference in participant characteristics between withdrawers and completers [ 111 ] or between those with 75% attendance and other participants [ 114 ], without specified SES-indicators. Three of these six studies indicated a positive, however weak, association between adherence to an aerobic- and strength training protocol and educational level [ 97 , 104 , 109 ]. One study [ 107 ] noted that employment status was associated with adherence measured as intensity, but not when adherence was assessed in terms of exercise time. No differences in adherence across educational levels were reported in this study.
Representativeness in terms of Research Participants’ Education, Ethnicity and Marital Status
Figure 2 displays the sample-country differences in educational level. Eight studies had a lower proportion of individuals with higher education compared to the country population [ 97 – 99 , 101 , 106 , 107 , 114 , 121 ], whereas 21 studies showed the opposite trend. In 11 of these studies, the proportion of participants who had tertiary education in the population was >25% lower compared to the sample [ 94 , 96 , 100 , 102 – 105 , 109 , 111 , 120 , 122 ]. Four studies had a difference ≤10% [ 93 , 95 , 108 , 115 ] ( Figure 2 ; Table 1 in Supplementary Files S1–S3 ).
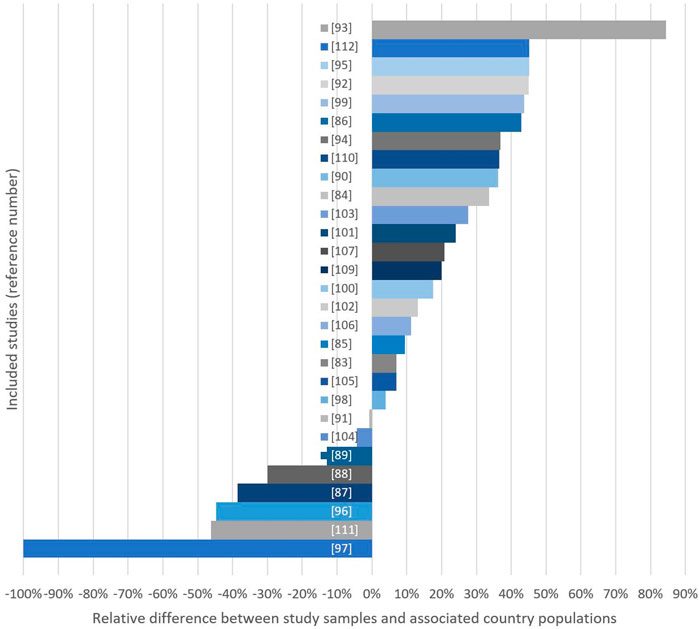
Figure 2 . Relative differences (%) between study samples and country populations considering either mean years of education (*) or % of women with >1 year of high education in study sample. Bars extending the right side indicate studies with high-education group overrepresentation (Global, 2000–2020).
The mean proportion of married women in the relevant samples was 71.9% (SD = 11.68), while the corresponding number was 73.9 (SD = 7.32) for the country populations ( Figure 3 ; Table 2 in Supplementary File S1 ). Sixteen of the studies using marital status reported their results on samples with a lower proportion of married women compared to the country population [ 93 , 95 , 97 , 98 , 103 , 104 , 107 , 108 , 111 – 115 , 121 , 122 , 125 ], while 11 examined samples with a higher proportion of married women compared to the country population [ 94 , 99 , 101 , 102 , 106 , 109 , 117 – 119 , 123 , 131 ]. One study [ 105 ] showed no difference (Tables 2, 3 in Supplementary File S1 ).
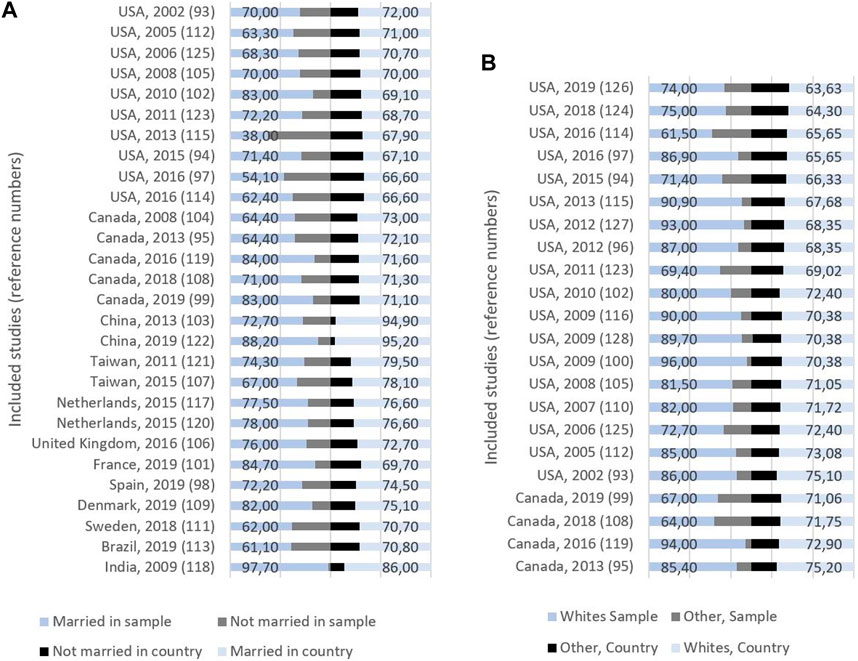
Figure 3 . (A) Study origin, publication year, and proportion (%) of married and non-married women in sample (left) and country (right). (B) Study origin, publication year, and proportion (%) of whites and other ethnicities in sample (left) and country (right) (Global, 2000–2020).
In the 22 studies that reported ethnicity , the mean proportion of whites was 81%: 77.6% Canadian studies, and 81.8% American studies ( Figure 3 ; Table 3 in Supplementary File S1 ). Three of these studies reported their results on samples with a lower proportion of whites compared with the country population, while the remaining 19 studies had samples with a higher proportion of whites. There was a difference between samples and countries of 10%–25% in 15 of these studies (Table 3 in Supplementary File S1 ).
Representativeness and Adherence
There was no clear relationship between the registered representativeness and the associations between indicators of SES and adherence. Three of the six mentioned studies reporting such associations [ 97 , 107 , 114 ] had samples with a lower proportion of high-SES BC patients compared to their country populations, while the other three [ 104 , 109 , 111 ] had samples with a higher proportion of high-SES patients.
To our knowledge, this is the first systematic review to report the social representativeness of RCTs examining the effects of PA on BC-related outcomes. In the included dataset, there was a preponderance of studies overrepresenting groups associated with higher privilege, supporting previous results indicating social bias [ 132 ]. Misrepresentations were found across different indicators of privilege, likely because different indicators tend to interrelate [ 133 ]. Our findings coincide with earlier observations that low-SES patients are less inclined to participate in research than high-SES patients [ 62 , 63 ], as well as with previous findings of obstacles to recruiting less privileged populations to cancer RCTs [ 64 ].
The most pronounced findings were based on studies that reported participants’ education. However, in six studies that did not record education but rather recorded ethnicity/race, as in the total dataset, there was a preponderance of white participants. In agreement with previous reports [ 62 , 132 , 134 ], this was interpreted as recruitment bias, although these analyses were based on less accurate data compared to the analyses on education. All 22 studies reporting ethnicity were from the USA and Canada, where the ethnic distribution varies over time and space, particularly in the United States [ 91 ]. Although education and income relate to ethnicity [ 135 ], our results on the representativeness of ethnic groups are unclear due to inaccurate data and increased confusion among the populations regarding ethnic categories. In general, it may appear inappropriate to use the category white as an exclusive indicator of social privilege in global comparative analyses such as the current study. Nonetheless, in the overall discussion of representativeness in RCTs, research favouring certain ethnicities over others should not be supported.
Representativeness was further assessed by marital status, and the mean difference between the study samples and the associated country populations was small. However, the differences ranged from −78% to 17.7%, and only 9 studies differed less than 5% from the country population. This means that although marital status is considered a measure of whether people have the social and financial benefits of being coupled, it could affect the possibility of being included in a PA trial.
What is considered an acceptable level of representativeness in RCT samples is difficult to decide. Recruitment issues may lead to sample biases, as patient populations often differ across social groups due to their diagnoses or hospital characteristics. However, the body of articles from the current dataset that employed education as the SES-indicator included eight studies with ( “negative” differences from the country population and 22 studies with “positive” differences (including 11 samples with >25% difference from the country population), which are significant findings. The fact that studies with a negative deviation from the country’s corresponding distribution in this subgroup were published after 2015 could be an effect of the CONSORT guidelines [ 70 ] and the Belmont report [ 136 ], which emphasised the implications of selection biases. However, our screening and analyses clearly show that there is still a potential for improvement among researchers in their attention to social distribution in samples.
Our results may have been more valid if baseline characteristics were compared with a real-world patient population and a patient sample (see [ 4 ]). However, such analyses require that third-party researchers also have access to exact data about the patient populations within each region, at the precise time of the studies, in addition to which patients are eligible according to each of the RCT criteria. The primary aim of the present study was to revive the question of external validity and feasibility from a perspective of social health inequalities in PA research. Therefore, status distribution in the respective age groups within the country populations served as an acceptable proxy for the distribution in the patient population.
Another objection may be that, for a patient to be considered eligible for a PA RCT, their cancer must be at a stage compatible with physical exertion and that more advanced BCs are associated with lower privilege [ 137 ]. Hence, RCTs with exercise often include patients with higher SES (education) because they have less advanced BC. However, this claim confirms the importance of putting focus on representativeness in RCTs targeting an already socially skewed patient population; it is important to be even more aware of sample representativeness to avoid excessive bias by favouring the already privileged. Likewise, employing already skewed patient populations as a reference could promote further social inequalities in health. Nonetheless, if the reference ratio for assessing representativeness was 1.22 [ 17 ], it would be possible to accept 22% more high-education patients before claiming misrepresentation of less privileged groups. However, according to our results, based on patients’ educational levels, approximately 45% of the included studies would still be considered biased in favour of the most privileged patients.
SES and PA Intervention Adherence
A proper body of articles with analyses of the association between SES-related characteristics and adherence was expected, and also that these articles would provide a basis for a synthesised examination of this relationship. However, the fact that only 6 studies investigated this association suggests that this question is perceived to be of little relevance in the field of BC and PA research. A previous review on the representativeness of RCTs reported no socioeconomic misrepresentation in oncology studies [ 4 ] however, our interpretation is supported by the fact that the review included only articles that provided a representativeness analysis, which the oncology articles had omitted in the case of SES.
No clear trend of associations between SES-related factors and adherence was seen across the six aforementioned studies, and the small number of studies and the differences between them hampered a clear conclusion. Previous studies have argued that poor representativeness may explain a lack of associations between SES and adherence rates [ 138 , 139 ]. In the current data set, there was no clear association between representativeness and SES-adherence associations. However, the small number of relevant articles formed an overly scarce base for reliable and conclusive analyses of this research question.
A tendency for studies that found a positive relationship between SES-related factors and adherence to report on longer interventions and to calculate adherence in terms of rates of attendance was observed. Three studies reported that the adherence rates decreased over time [ 97 , 104 , 107 ]. Previous results support the interpretation that time is a barrier to participation in PA interventions [ 53 , 140 ]. Strazdin et al. have substantiated how availability of time may have a larger impact on low-SES women in general [ 141 , 142 ]. Hence, the limited availability of time over a prolonged period may partly explain why less privileged patients have poorer adherence in such trials than their privileged counterparts.
Reasons for refusing to participate, or reasons for withdrawing, were not registered in our study. We should not ignore the fact that researchers experience real obstacles in recruiting of less privileged patients, so non-representative samples should not be seen as unwillingness or lack of effort to include the less privileged. There are reasons to believe that reasons for refusal to participate in the articles included coincide with the most common barriers previously reported [ 10 , 64 , 131 ] . However, although participation is voluntary and individual motivation or barriers are relevant, the adherence rates and the current social group distribution of patients in RCTs with PA may also be affected by the intervention design and the inclusion criteria defined by the researchers of each individual study [ 64 ].
All the included studies reported LTPA interventions. Considering that low-SES groups engage less in LTPA [ 47 ], it is reasonable to expect that low-SES patients were less inclined to participate in, and complete, such RCTs. Hence, a preponderance of RCTs employing exercise interventions could be perceived as being in favour of privileged patients. The searches of the current study did not, however, include search terms covering other PA domains and may thereby have strengthened the impression that LTPA is the prevailing protocol in RCTs of PA in BC patients. However, although many patients return to work during their first-year post diagnosis, RCTs designed for other PA-domains would not be verifiable as the patients’ level of PA would differ too much to control. In addition, the control group would have to be inactive within these PA-domains, which would be a requirement almost impossible to implement. The probability that many published RCTs of other types of PA exist, thus altering our results, is therefore small.
Consequences of Enhanced Selection Bias in Favour of Privileged Patients
Provided that our results reflect reality as they are based on synthesised data from a large set of systematically selected articles, social equity is a challenge to PA trials in BC patients. A stepwise, albeit unintended, social exclusion process causes attrition bias and a successive decrease in external validity, (i.e., the results are even less valid for individuals in other social groups than those who have completed the intervention when the intervention is finalised) [ 65 ]. Thus, PA-treatment is also less adaptable to patients in the same groups as those who withdraw. Drawing on the fundamental cause theory [ 143 ], these mechanisms show how affluent people could benefit more, in this case, from PA research, because studies serve the interests of these groups more than they care for all SES-groups. In addition, insignificant results from sub-analyses of social group-differences may be misinterpreted because the distribution of social groups in the samples does not mirror real life. This may disguise the possible fact that although all patients, by policy, should have equal access to health services, PA treatment interventions may not be suitable for all. An “inverse PA research law” analogous to the “inverse healthcare law” [ 144 ] describes how PA research interventions, initiated with the intention to treat a patient population, regardless of social status, nevertheless attend to privileged groups more than the less privileged who initially are prone to poorer health and thus more entitled to clinical research.
Strengths and Limitations
The major strength of this research is the thorough and systematic search of eligible studies, including traditional, and both BCB and FCB searches. To avoid our searches and not be included, an article would have to be published in a journal that is not indexed in any of the chosen databases, not be identified by the search terms, not be included in either the reference lists of the articles included from the descriptive searches or not have cited the articles included from the descriptive searches. It is possible that some articles were lost. However, it is less likely that any articles not included would be systematically more representative compared with the articles included.
The sample sizes in one-third of the studies were <50, seemingly decreasing the validity of our conclusions. However, rather than being a shortcoming of our study, the limitation is applicable to each RCT because the small samples, among other factors, hamper representativeness analyses such as ours. Hence, our analyses were based on the publication reality, whatever flawed original data materials.
SES and social privilege classifications vary across cultures, research fields, and public statistics, and they may cause imprecise standards for comparisons between studies of different origins. Nevertheless, our results present the big picture of misrepresentation across social groups with a precision sufficient to boost the debate within the scientific community.
Less educated, unmarried and non--white individuals may be underrepresented in BC PA RCTs, and SES-adherence associations in such trials are inconclusive. Unintentional social misrepresentation may create disguised inequity, warranting revived attention to this issue.
The current study provides a departure point for intensified attention to representativeness in RCTs. It should act as motivation both for seeking improved external validity, and for reconsidering whether LTPA in BC treatment is suitable for all.
Author Contributions
RS and MD made substantial contributions to the study: RS conceived the idea of the study, including its design, methodology and analysis. MD and RS performed descriptive- and FC searches, and BC searches, respectively, and the subsequent inclusion/exclusion of articles. RS and MD performed the analyses. RS drafted the manuscript. RS and MD reviewed and edited the manuscript and approved the final version. All authors contributed to the article and approved the submitted version.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of Interest
The authors declare that they do not have any conflicts of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.ssph-journal.org/articles/10.3389/ijph.2024.1607002/full#supplementary-material
1. Wickerham, DL, O'Connell, MJ, Costantino, JP, Cronin, WM, Paik, S, and Geyer, CE. The Half century of Clinical Trials of the National Surgical Adjuvant Breast and Bowel Project. In: Seminars in Oncology . Amsterdam, Netherlands: Elsevier (2008).
CrossRef Full Text | Google Scholar
2. Marmot, M, and Bell, R. Social Inequalities in Health: A Proper Concern of Epidemiology. Ann Epidemiol (2016) 26(4):238–40. doi:10.1016/j.annepidem.2016.02.003
PubMed Abstract | CrossRef Full Text | Google Scholar
3. Mackenbach, JP. Persistence of Social Inequalities in Modern Welfare States: Explanation of a Paradox. Scand J Public Health (2017) 45(2):113–20. doi:10.1177/1403494816683878
4. Kennedy-Martin, T, Curtis, S, Faries, D, Robinson, S, and Johnston, J. A Literature Review on the Representativeness of Randomized Controlled Trial Samples and Implications for the External Validity of Trial Results. Trials (2015) 16(1):495–14. doi:10.1186/s13063-015-1023-4
5. Dantzer, R, Meagher, MW, and Cleeland, CS. Translational Approaches to Treatment-Induced Symptoms in Cancer Patients. Nat Rev Clin Oncol (2012) 9(7):414–26. doi:10.1038/nrclinonc.2012.88
6. Furmaniak, AC, Menig, M, and Markes, MH. Exercise for Women Receiving Adjuvant Therapy for Breast Cancer. Cochrane Database Syst Rev (2016) 9:CD005001. doi:10.1002/14651858.CD005001.pub3
7. Irwin, ML, Crumley, D, McTiernan, A, Bernstein, L, Baumgartner, R, Gilliland, FD, et al. Physical Activity Levels before and after a Diagnosis of Breast Carcinoma: The Health, Eating, Activity, and Lifestyle (HEAL) Study. Cancer Interdiscip Int J Am Cancer Soc (2003) 97(7):1746–57. doi:10.1002/cncr.11227
8. Protani, M, Coory, M, and Martin, JH. Effect of Obesity on Survival of Women with Breast Cancer: Systematic Review and Meta-Analysis. Breast Cancer Res Treat (2010) 123(3):627–35. doi:10.1007/s10549-010-0990-0
9. Husebo, AML, Karlsen, B, Allan, H, Soreide, JA, and Bru, E. Factors Perceived to Influence Exercise Adherence in Women with Breast Cancer Participating in an Exercise Programme during Adjuvant Chemotherapy: A Focus Group Study. J Clin Nurs (2015) 24(3-4):500–10. doi:10.1111/jocn.12633
10. Maddocks, M, Mockett, S, and Wilcock, A. Is Exercise an Acceptable and Practical Therapy for People with or Cured of Cancer? A Systematic Review. Cancer Treat Rev (2009) 35(4):383–90. doi:10.1016/j.ctrv.2008.11.008
11. Bhute, VJ, Ma, Y, Bao, X, and Palecek, SP. The Poly (ADP-Ribose) Polymerase Inhibitor Veliparib and Radiation Cause Significant Cell Line Dependent Metabolic Changes in Breast Cancer Cells. Sci Rep-uk (2016) 6(1):36061. doi:10.1038/srep36061
12. Black, LL, and Stone, D. Expanding the Definition of Privilege: The Concept of Social Privilege. J Multicultural Couns Dev (2005) 33(4):243–55. doi:10.1002/j.2161-1912.2005.tb00020.x
13. Reynolds, MM. Health Power Resources Theory: A Relational Approach to the Study of Health Inequalities. J Health Soc Behav (2021) 62(4):493–511. doi:10.1177/00221465211025963
14. Lampert, T, Hoebel, J, Kuntz, B, Müters, S, and Kroll, LE. Socioeconomic Status and Subjective Social Status Measurement in KiGGS Wave 2. J Health Monit (2018) 3(1):108–25. doi:10.17886/RKI-GBE-2018-033
15. Braveman, PA, Cubbin, C, Egerter, S, Chideya, S, Marchi, KS, Metzler, M, et al. Socioeconomic Status in Health Research: One Size Does Not Fit All. JAMA (2005) 294(22):2879–88. doi:10.1001/jama.294.22.2879
16. D'Avanzo, B, and La Vecchia, C. Risk Factors for Male Breast Cancer. Br J Cancer (1995) 71(6):1359–62. doi:10.1038/bjc.1995.264
17. Dong, J-Y, and Qin, L-Q. Education Level and Breast Cancer Incidence: A Meta-Analysis of Cohort Studies. Menopause (2020) 27(1):113–8. doi:10.1097/GME.0000000000001425
18. Kearney, MS. The Two-Parent Privilege: How the Decline in Marriage Has Increased Inequality and Lowered Social Mobility, and what We Can Do about it . Great Britain: Swift Press (2023).
Google Scholar
19. Li, M, Han, M, Chen, Z, Tang, Y, Ma, J, Zhang, Z, et al. Does Marital Status Correlate With the Female Breast Cancer Risk? A Systematic Review and Meta-Analysis of Observational Studies. PLoS One (2020) 15(3):e0229899.
20. Sineshaw, HM, Gaudet, M, Ward, EM, Flanders, WD, Desantis, C, Lin, CC, et al. Association of Race/ethnicity, Socioeconomic Status, and Breast Cancer Subtypes in the National Cancer Data Base (2010–2011). Breast Cancer Res Tr (2014) 145(3):753–63. doi:10.1007/s10549-014-2976-9
21. Krieger, N, Wright, E, Chen, JT, Waterman, PD, Huntley, ER, and Arcaya, M. Cancer Stage at Diagnosis, Historical Redlining, and Current Neighborhood Characteristics: Breast, Cervical, Lung, and Colorectal Cancers, Massachusetts, 2001–2015. Am J Epidemiol (2020) 189(10):1065–75. doi:10.1093/aje/kwaa045
22. Klassen, AC, and Smith, KC. The Enduring and Evolving Relationship between Social Class and Breast Cancer burden: A Review of the Literature. Cancer Epidemiol (2011) 35(3):217–34. doi:10.1016/j.canep.2011.02.009
23. Trewin, CB, Johansson, ALV, Hjerkind, KV, Strand, BH, Kiserud, CE, and Ursin, G. Stage-Specific Survival Has Improved for Young Breast Cancer Patients since 2000: But Not Equally. Breast Cancer Res Tr (2020) 182:477–89. doi:10.1007/s10549-020-05698-z
24. Flaherty, DC, Bawa, R, Burton, C, and Goldfarb, M. Breast Cancer in Male Adolescents and Young Adults. Ann Surg Oncol (2017) 24(1):84–90. doi:10.1245/s10434-016-5586-4
25. Siegel, RL, Miller, KD, and Jemal, A. Cancer Statistics, 2018. CA: a Cancer J clinicians (2018) 68(1):7–30. doi:10.3322/caac.21442
26. Patterson, RE, Cadmus, LA, Emond, JA, and Pierce, JP. Physical Activity, Diet, Adiposity and Female Breast Cancer Prognosis: A Review of the Epidemiologic Literature. Maturitas (2010) 66(1):5–15. doi:10.1016/j.maturitas.2010.01.004
27. Nichols, HB, Trentham-Dietz, A, Egan, KM, Titus-Ernstoff, L, Holmes, MD, Bersch, AJ, et al. Body Mass index before and after Breast Cancer Diagnosis: Associations with All-Cause, Breast Cancer, and Cardiovascular Disease Mortality. Cancer Epidemiol Biomarkers Prev (2009) 18(5):1403–9. doi:10.1158/1055-9965.EPI-08-1094
28. Healy, L, Ryan, A, Carroll, P, Ennis, D, Crowley, V, Boyle, T, et al. Metabolic Syndrome, central Obesity and Insulin Resistance Are Associated with Adverse Pathological Features in Postmenopausal Breast Cancer. Clin Oncol-uk (2010) 22(4):281–8. doi:10.1016/j.clon.2010.02.001
29. Rock, CL, Doyle, C, Demark-Wahnefried, W, Meyerhardt, J, Courneya, KS, Schwartz, AL, et al. Nutrition and Physical Activity Guidelines for Cancer Survivors. CA: A Cancer J Clinicians (2012) 62(4):243–74. doi:10.3322/caac.21142
30. Lundqvist, A, Andersson, E, Ahlberg, I, Nilbert, M, and Gerdtham, U Socioeconomic Inequalities in Breast Cancer Incidence and Mortality in Europe-A Systematic Review and Meta-Analysis. Eur J Public Health (2016) 26(5):804–13. doi:10.1093/eurpub/ckw070
31. de Boer, MC, Wörner, EA, Verlaan, D, and van Leeuwen, PA. The Mechanisms and Effects of Physical Activity on Breast Cancer. Clin Breast Cancer (2017) 17(4):272–8. doi:10.1016/j.clbc.2017.01.006
32. Caspersen, CJPK, and Christenson, GM. Physical Activity, Exercise, and Physical Fitness: Definitions and Distinctions for Health-Related Research. Public Health Rep (1985) 100(2):126–31.
PubMed Abstract | Google Scholar
33. Warren, JM, Ekelund, U, Besson, H, Mezzani, A, Geladas, N, Vanhees, L, et al. Assessment of Physical Activity – A Review of Methodologies with Reference to Epidemiological Research: A Report of the Exercise Physiology Section of the European Association of Cardiovascular Prevention and Rehabilitation. Eur J Cardiovasc Prev Rehabil (2010) 17(2):127–39. doi:10.1097/HJR.0b013e32832ed875
34. Dorgan, JF, Brown, C, Barrett, M, Splansky, GL, Kreger, BE, D'Agostino, RB, et al. Physical Activity and Risk of Breast Cancer in the Framingham Heart Study. Am J Epidemiol (1994) 139(7):662–9. doi:10.1093/oxfordjournals.aje.a117056
35. Fraser, GE, and Shavlik, D. Risk Factors, Lifetime Risk, and Age at Onset of Breast Cancer. Ann Epidemiol (1997) 7(6):375–82. doi:10.1016/s1047-2797(97)00042-2
36. Cerhan, JR, Chiu, BC, Wallace, RB, Lemke, JH, Lynch, CF, Torner, JC, et al. Physical Activity, Physical Function, and the Risk of Breast Cancer in a Prospective Study Among Elderly Women. J Gerontol Ser A: Biol Sci Med Sci (1998) 53(4):M251–6. doi:10.1093/gerona/53a.4.m251
37. Rockhill, B, Willett, WC, Hunter, DJ, Manson, JE, Hankinson, SE, and Colditz, GA. A Prospective Study of Recreational Physical Activity and Breast Cancer Risk. Arch Intern Med (1999) 159(19):2290–6. doi:10.1001/archinte.159.19.2290
38. Thune, I, Brenn, T, Lund, E, and Gaard, M. Physical Activity and the Risk of Breast Cancer. N Engl J Med (1997) 336(18):1269–75. doi:10.1056/NEJM199705013361801
39. Mittendorf, R. Strenuous Physical Activity in Young Adulthood and Risk of Breast Cancer (United States) (Vol 6, Pg 352, 1996). Cancer Cause Control (1996) 7(2):291.
40. Bernstein, L, Henderson, BE, Hanisch, R, Sullivan-Halley, J, and Ross, RK. Physical Exercise and Reduced Risk of Breast Cancer in Young Women. J Natl Cancer (1994) 86(18):1403–8. doi:10.1093/jnci/86.18.1403
41. Friedenreich, CM, and Rohan, TE. Physical Activity and Risk of Breast Cancer. Eur J Cancer Prev (1995) 4(2):145–51. doi:10.1097/00008469-199504000-00004
42. McTiernan, A, Stanford, JL, Weiss, NS, Daling, JR, and Voigt, LF. Occurrence of Breast Cancer in Relation to Recreational Exercise in Women Age 50-64 Years. Epidemiology (1996) 7(6):598–604. doi:10.1097/00001648-199611000-00006
43. Chen, CL, White, E, Malone, KE, and Daling, JR. Leisure-Time Physical Activity in Relation to Breast Cancer Among Young Women (Washington, United States). Cancer Causes Control (1997) 8(1):77–84. doi:10.1023/a:1018439306604
44. Gammon, MD, John, EM, and Britton, JA. Recreational and Occupational Physical Activities and Risk of Breast Cancer. J Natl Cancer Inst (1998) 90(2):100–17. doi:10.1093/jnci/90.2.100
45. Monninkhof, EM, Elias, SG, Vlems, FA, van der Tweel, I, Schuit, AJ, Voskuil, DW, et al. Physical Activity and Breast Cancer - A Systematic Review. Epidemiology (2007) 18(1):137–57. doi:10.1097/01.ede.0000251167.75581.98
46. Friedenreich, CM. Physical Activity and Breast Cancer: Review of the Epidemiologic Evidence and Biologic Mechanisms. Recent Results Cancer Res (2011) 188:125–39. doi:10.1007/978-3-642-10858-7_11
47. Stalsberg, R, and Pedersen, AV. Are Differences in Physical Activity across Socioeconomic Groups Associated with Choice of Physical Activity Variables to Report? Int J Environ Res Public Health (2018) 15(5):922. doi:10.3390/ijerph15050922
48. Hong, S, Bardwell, WA, Natarajan, L, Flatt, SW, Rock, CL, Newman, VA, et al. Correlates of Physical Activity Level in Breast Cancer Survivors Participating in the Women's Healthy Eating and Living (WHEL) Study. Breast Cancer Res Tr (2007) 101(2):225–32. doi:10.1007/s10549-006-9284-y
49. Bertram, LA, Stefanick, ML, Saquib, N, Natarajan, L, Patterson, RE, Bardwell, W, et al. Physical Activity, Additional Breast Cancer Events, and Mortality Among Early-Stage Breast Cancer Survivors: Findings from the WHEL Study. Cancer Causes Control (2011) 22(3):427–35. doi:10.1007/s10552-010-9714-3
50. Keegan, TH, Shariff-Marco, S, Sangaramoorthy, M, Koo, J, Hertz, A, Schupp, CW, et al. Neighborhood Influences on Recreational Physical Activity and Survival after Breast Cancer. Cancer Causes Control (2014) 25(10):1295–308. doi:10.1007/s10552-014-0431-1
51. Boyle, T, Vallance, JK, Ransom, EK, and Lynch, BM. How Sedentary and Physically Active Are Breast Cancer Survivors, and Which Population Subgroups Have Higher or Lower Levels of These Behaviors? Support Care Cancer (2016) 24(5):2181–90. doi:10.1007/s00520-015-3011-3
52. Campbell, KL, Winters-Stone, KM, Wiskemann, J, May, AM, Schwartz, AL, Courneya, KS, et al. Exercise Guidelines for Cancer Survivors: Consensus Statement from International Multidisciplinary Roundtable. Med Sci Sports Exerc (2019) 51(11):2375–90. doi:10.1249/MSS.0000000000002116
53. Oyekanmi, G, and Paxton, RJ. Barriers to Physical Activity Among African American Breast Cancer Survivors. Psycho-Oncology (2014) 23(11):1314–7. doi:10.1002/pon.3527
54. Owusu, C, Antognoli, E, Nock, N, Hergenroeder, P, Austin, K, Bennet, E, et al. Perspective of Older African-American and Non-Hispanic white Breast Cancer Survivors from Diverse Socioeconomic Backgrounds toward Physical Activity: A Qualitative Study. J Geriatr Oncol (2018) 9(3):235–42. doi:10.1016/j.jgo.2017.12.003
55. Grzywacz, JG, and Marks, NF. Social Inequalities and Exercise during Adulthood: Toward an Ecological Perspective. J Health Soc Behav (2001) 42(June):202–20. doi:10.2307/3090178
56. Lee, RE, and Cubbin, C. Neighborhood Context and Youth Cardiovascular Health Behaviors. Am J Public Health (2002) 92(3):428–36. doi:10.2105/ajph.92.3.428
57. Varo, JJ, Martinez-Gonzalez, MA, de Irala-Estevez, J, Kearney, J, Gibney, M, and Martinez, JA. Distribution and Determinants of Sedentary Lifestyles in the European Union. Int J Epidemiol (2003) 32(1):138–46. doi:10.1093/ije/dyg116
58. Jenum, AK, Lorentzen, CAN, and Ommundsen, Y. Targeting Physical Activity in a Low Socioeconomic Status Population: Observations from the Norwegian “Romsås in Motion” Study. Br J Sport Med (2009) 43(1):64–9. doi:10.1136/bjsm.2008.053637
59. Trost, SG, Owen, N, Bauman, AE, Sallis, JF, and Brown, W. Correlates of Adults’ Participation in Physical Activity: Review and Update. Med Sci Sports Exerc (2002) 34(12):1996–2001. doi:10.1097/00005768-200212000-00020
60. Austin, JL, Smith, JE, Gianini, L, and Campos-Melady, M. Attitudinal Familism Predicts Weight Management Adherence in Mexican–American Women. J Behav Med (2013) 36(3):259–69. doi:10.1007/s10865-012-9420-6
61. Lemstra, M, and Rogers, MR. The Importance of Community Consultation and Social Support in Adhering to an Obesity Reduction Program: Results from the Healthy Weights Initiative. Patient Preference and Adherence (2015) 9:1473–80. doi:10.2147/PPA.S91912
62. Sharrocks, K, Spicer, J, Camidge, DR, and Papa, S. The Impact of Socioeconomic Status on Access to Cancer Clinical Trials. Br J Cancer (2014) 111(9):1684–7. doi:10.1038/bjc.2014.108
63. Langhammer, A, Krokstad, S, Romundstad, P, Heggland, J, and Holmen, J. The HUNT Study: Participation Is Associated with Survival and Depends on Socioeconomic Status, Diseases and Symptoms. BMC Med Res Methodol (2012) 12(1):143. doi:10.1186/1471-2288-12-143
64. Ford, JG, Howerton, MW, Lai, GY, Gary, TL, Bolen, S, Gibbons, MC, et al. Barriers to Recruiting Underrepresented Populations to Cancer Clinical Trials: A Systematic Review. Cancer (2008) 112(2):228–42. doi:10.1002/cncr.23157
65. Stalsberg, R. Social Inequalities in Physical Activity Implications of Research Practices–The Case of Studying Breast Cancer Survivors [Doctoral Thesis] . Trondheim: Norwegian university of science and technology (2021).
66. Akobeng, AK. Assessing the Validity of Clinical Trials. J Pediatr Gastroenterol Nutr (2008) 47(3):277–82. doi:10.1097/MPG.0b013e31816c749f
67. Campbell, DT. Factors Relevant to the Validity of Experiments in Social Settings. Psychol Bull (1957) 54(4):297–312. doi:10.1037/h0040950
68. World Medical Association. World Medical Association Declaration of helsinki: Ethical Principles for Medical Research Involving Human Subjects. JAMA (2013) 310(20):2191–4. doi:10.1001/jama.2013.281053
69. Rennie, DJJ. CONSORT Revised—Improving the Reporting of Randomized Trials. JAMA (2001) 285(15):2006–7.doi:10.1001/jama.285.15.2006
70. Schulz, KF, Altman, DG, and Moher, D, CONSORT Group. CONSORT 2010 Statement: Updated Guidelines for Reporting Parallel Group Randomised Trials. BMC Med (2010) 8:18. doi:10.1186/1741-7015-8-18
71. Speck, RM, Courneya, KS, Masse, LC, Duval, S, and Schmitz, KH. An Update of Controlled Physical Activity Trials in Cancer Survivors: A Systematic Review and Meta-Analysis. J Cancer Survivorship (2010) 4(2):87–100. doi:10.1007/s11764-009-0110-5
72. Furler, J, Magin, P, Pirotta, M, and van Driel, M. Participant Demographics Reported in "Table 1" of Randomised Controlled Trials: A Case of "inverse Evidence. Int J Equity Health (2012) 11:14. doi:10.1186/1475-9276-11-14
73. Stalsberg, R, and Pedersen, AV. Effects of Socioeconomic Status on the Physical Activity in Adolescents: A Systematic Review of the Evidence. Scand J Med Sci Sports (2010) 20(3):368–83. doi:10.1111/j.1600-0838.2009.01047.x
74. Gidlow, C, Johnston, LH, Crone, D, Ellis, N, and James, D. A Systematic Review of the Relationship between Socio-Economic Position and Physical Activity. Health Edu J (2006) 65(4):338–67. doi:10.1177/0017896906069378
75. Evans, JA, and Foster, JG. Metaknowledge. Science (2011) 331(6018):721–5. doi:10.1126/science.1201765
76. Schatz, BR. Information Retrieval in Digital Libraries: Bringing Search to the Net. Science (1997) 275(5298):327–34. doi:10.1126/science.275.5298.327
77. Bramer, WM, De Jonge, GB, Rethlefsen, ML, Mast, F, and Kleijnen, J. A Systematic Approach to Searching: An Efficient and Complete Method to Develop Literature Searches. J Med Libr Assoc JMLA. (2018) 106(4):531–41. doi:10.5195/jmla.2018.283
78. Horsley, T, Dingwall, O, and Sampson, M. Checking Reference Lists to Find Additional Studies for Systematic Reviews. Cochrane Db Syst Rev (2011) 2011(8):MR000026. doi:10.1002/14651858.MR000026.pub2
79. Hu, X, Rousseau, R, and Chen, J. On the Definition of Forward and Backward Citation Generations. J Informetrics (2011) 5(1):27–36. doi:10.1016/j.joi.2010.07.004
80. Rysstad, AL, and Pedersen, AV. Brief Report: Non-right-Handedness within the Autism Spectrum Disorder. J autism Dev Disord (2016) 46(3):1110–7. doi:10.1007/s10803-015-2631-2
81. Darvik, M, Lorås, HW, and Pedersen, AV. The Prevalence of Left-Handedness Is Higher Among Individuals with Developmental Coordination Disorder Than in the General Population. Front Psychol (2018) 9:1948–11. doi:10.3389/fpsyg.2018.01948
82. The World Bank. Higher Education. THE WORLD BANK (2021). Available from: https://www.worldbank.org/en/topic/tertiaryeducation (Accessed December 1, 2023).
83. World Bank – processed by Our World in Data. Average Years of Schooling for Women [dataset]. World Bank, World Bank Education Statistics (EdStats) (2023). Available from: https://ourworldindata.org/grapher/mean-years-of-schooling-female?tab=table&time=2004.2005 (Accessed November 7, 2023).
84. World Bank – processed by Our World in Data. Average Years of Schooling for Women [dataset]. World Bank, World Bank Education Statistics (EdStats) (2023). Available from: https://ourworldindata.org/grapher/mean-years-of-schooling-female?tab=table&time=2006.2009 (Accessed November 7, 2023).
85. OECD. Educational Attainment and Labour-Force Status: Trends in Educational Attainment, by Educational Attainment and Age Group: OECD.Stat (2023). Available from: https://stats.oecd.org/Index.aspx?QueryId=93191 (Accessed November 7, 2023).
86. Ministry of Education, Republic of China (Taiwan). Enrollment Rates of School - Total Net Enrollment Rates: Ministry of Education (2022). Available from: https://stats.moe.gov.tw/files/ebook/indicators/13.pdf (Accessed May 04, 2022).
87. United Nations. Department of Economic and Social Affairs Population Division: Estimates and Projections of Women of Reproductive Age Who Are Married or in a Union (2022). Available from: https://population.un.org/dataportal/data/indicators/44/locations/840,124,156,158,250,528,826,724,208,752,76/start/2000/end/2020/table/pivotbyvariant (Accessed November 7, 2023).
88. Statistics Canada. Canada (Code 01) (Table). National Household Survey (NHS) Profile. 2011 National Household Survey. Statistics Canada Catalogue No. 99-004-XWE (2013). Available from: https://www12.statcan.gc.ca/nhs-enm/2011/dp-pd/prof/details/page.cfm?Lang=E&Geo1=PR&Code1=01&Data=Count&SearchText=Canada&SearchType=Begins&SearchPR=01&A1=All&B1=All&Custom=&TABID=1 (Accessed September 11, 2013).
89. Statistics Canada. Canada [Country] and Canada [Country] (Table). Census Profile. 2016 Census. Statistics Canada Catalogue No. 98-316-X2016001 (2017). Available from: https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/prof/details/page.cfm?Lang=E&Geo1=PR&Code1=01&Geo2=PR&Code2=01&Data=Count&SearchText=canada&SearchType=Begins&SearchPR=01&B1=All&TABID=1 (Accessed November 29, 2017).
90. Statistics Canada. Visible Minority and Population Group by Generation Status: Canada, Provinces and Territories, Census Metropolitan Areas and Census Agglomerations with Parts. Table: 98-10-0324-01 (2023). Available from: https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=9810032401 (Accessed October 26, 2023).
91. United States Census Bureau. Race and Ethnicity in the United States: 2010 Census and 2020 Census 2021 (2021). Available from: https://www.census.gov/library/visualizations/interactive/race-and-ethnicity-in-the-united-state-2010-and-2020-census.html (Accessed November 29, 2023).
92. United States Census Bureau. "Profile of General Demographic Characteristics: 2000." Decennial Census, DEC State Legislative District Demographic Profile (100-Percent) (2000). Available from: https://data.census.gov/table?y=2000 (Accessed November 29, 2023).
93. Pickett, M, Mock, V, Ropka, ME, Cameron, L, Coleman, M, and Podewils, L. Adherence to Moderate-Intensity Exercise during Breast Cancer Therapy. Cancer Pract (2002) 10(6):284–92. doi:10.1046/j.1523-5394.2002.106006.x
94. Al-Majid, S, Wilson, LD, Rakovski, C, and Coburn, JW. Effects of Exercise on Biobehavioral Outcomes of Fatigue during Cancer Treatment: Results of a Feasibility Study. Biol Res Nurs (2015) 17(1):40–8. doi:10.1177/1099800414523489
95. Courneya, KS, McKenzie, DC, Mackey, JR, Gelmon, K, Friedenreich, CM, Yasui, Y, et al. Effects of Exercise Dose and Type during Breast Cancer Chemotherapy: Multicenter Randomized Trial. J Natl Cancer (2013) 105(23):1821–32. doi:10.1093/jnci/djt297
96. Anderson, RT, Kimmick, GG, McCoy, TP, Hopkins, J, Levine, E, Miller, G, et al. A Randomized Trial of Exercise on Well-Being and Function Following Breast Cancer Surgery: The RESTORE Trial. J Cancer Survivorship-Research Pract (2012) 6(2):172–81. doi:10.1007/s11764-011-0208-4
97. Arem, H, Sorkin, M, Cartmel, B, Fiellin, M, Capozza, S, Harrigan, M, et al. Exercise Adherence in a Randomized Trial of Exercise on Aromatase Inhibitor Arthralgias in Breast Cancer Survivors: The Hormones and Physical Exercise (HOPE) Study. J Cancer Survivorship (2016) 10(4):654–62. doi:10.1007/s11764-015-0511-6
98. Ariza-Garcia, A, Lozano-Lozano, M, Galiano-Castillo, N, Postigo-Martin, P, Arroyo-Morales, M, and Cantarero-Villanueva, I. A Web-Based Exercise System (E-CuidateChemo) to Counter the Side Effects of Chemotherapy in Patients with Breast Cancer: Randomized Controlled Trial. J Med Internet Res (2019) 21(7):e14418. doi:10.2196/14418
99. Bland, KA, Kirkham, AA, Bovard, J, Shenkier, T, Zucker, D, McKenzie, DC, et al. Effect of Exercise on Taxane Chemotherapy–Induced Peripheral Neuropathy in Women with Breast Cancer: A Randomized Controlled Trial. Clin Breast Cancer (2019) 19(6):411–22. doi:10.1016/j.clbc.2019.05.013
100. Cadmus, LA, Salovey, P, Yu, H, Chung, G, Kasl, S, and Irwin, ML. Exercise and Quality of Life during and after Treatment for Breast Cancer: Results of Two Randomized Controlled Trials. Psycho-Oncology (2009) 18(4):343–52. doi:10.1002/pon.1525
101. Carayol, M, Ninot, G, Senesse, P, Bleuse, J-P, Gourgou, S, Sancho-Garnier, H, et al. Short and Long-Term Impact of Adapted Physical Activity and Diet Counseling during Adjuvant Breast Cancer Therapy: The “APAD1” Randomized Controlled Trial. BMC cancer (2019) 19(1):737–20. doi:10.1186/s12885-019-5896-6
102. Chandwani, KD, Thornton, B, Perkins, GH, Arun, B, Raghuram, N, Nagendra, H, et al. Yoga Improves Quality of Life and Benefit Finding in Women Undergoing Radiotherapy for Breast Cancer. J Soc Integr Oncol (2010) 8(2):43–55.
103. Chen, Z, Meng, Z, Milbury, K, Bei, W, Zhang, Y, Thornton, B, et al. Qigong Improves Quality of Life in Women Undergoing Radiotherapy for Breast Cancer: Results of a Randomized Controlled Trial. Cancer (2013) 119(9):1690–8. doi:10.1002/cncr.27904
104. Courneya, KS, Segal, RJ, Gelmon, K, Reid, RD, Mackey, JR, Friedenreich, CM, et al. Predictors of Supervised Exercise Adherence during Breast Cancer Chemotherapy. Med Sci Sports Exerc (2008) 40:1180–7. doi:10.1249/MSS.0b013e318168da45
105. Demark-Wahnefried, W, Case, LD, Blackwell, K, Marcom, PK, Kraus, W, Aziz, N, et al. Results of a Diet/exercise Feasibility Trial to Prevent Adverse Body Composition Change in Breast Cancer Patients on Adjuvant Chemotherapy. Clin Breast Cancer (2008) 8(1):70–9. doi:10.3816/CBC.2008.n.005
106. Gokal, K, Wallis, D, Ahmed, S, Boiangiu, I, Kancherla, K, and Munir, F. Effects of a Self-Managed home-Based Walking Intervention on Psychosocial Health Outcomes for Breast Cancer Patients Receiving Chemotherapy: A Randomised Controlled Trial. Support Care Cancer (2016) 24(3):1139–66. doi:10.1007/s00520-015-2884-5
107. Huang, HP, Wen, FH, Tsai, JC, Lin, YC, Shun, SC, Chang, HK, et al. Adherence to Prescribed Exercise Time and Intensity Declines as the Exercise Program Proceeds: Findings from Women under Treatment for Breast Cancer. Support Care Cancer (2015) 23(7):2061–71. doi:10.1007/s00520-014-2567-7
108. Kirkham, AA, Van Patten, CL, Gelmon, KA, McKenzie, DC, Bonsignore, A, Bland, KA, et al. Effectiveness of Oncologist-Referred Exercise and Healthy Eating Programming as a Part of Supportive Adjuvant Care for Early Breast Cancer. Oncologist (2018) 23(1):105–15. doi:10.1634/theoncologist.2017-0141
109. Lund, LW, Ammitzbøll, G, Hansen, DG, Andersen, EAW, and Dalton, SO. Adherence to a Long-Term Progressive Resistance Training Program, Combining Supervised and home-Based Exercise for Breast Cancer Patients during Adjuvant Treatment. Acta Oncologica (2019) 58(5):650–7. doi:10.1080/0284186X.2018.1560497
110. Matthews, CE, Wilcox, S, Hanby, CL, Ananian, CD, Heiney, SP, Gebretsadik, T, et al. Evaluation of a 12-Week home-Based Walking Intervention for Breast Cancer Survivors. Support Care Cancer (2007) 15(2):203–11. doi:10.1007/s00520-006-0122-x
111. Mijwel, S, Backman, M, Bolam, KA, Jervaeus, A, Sundberg, CJ, Margolin, S, et al. Adding High-Intensity Interval Training to Conventional Training Modalities: Optimizing Health-Related Outcomes during Chemotherapy for Breast Cancer: The OptiTrain Randomized Controlled Trial. Breast Cancer Res Tr (2018) 168(1):79–93. doi:10.1007/s10549-017-4571-3
112. Mock, V, Frangakis, C, Davidson, NE, Ropka, ME, Pickett, M, Poniatowski, B, et al. Exercise Manages Fatigue during Breast Cancer Treatment: A Randomized Controlled Trial. Psycho-Oncology (2005) 14(6):464–77. doi:10.1002/pon.863
113. Paulo, TR, Rossi, FE, Viezel, J, Tosello, GT, Seidinger, SC, Simões, RR, et al. The Impact of an Exercise Program on Quality of Life in Older Breast Cancer Survivors Undergoing Aromatase Inhibitor Therapy: A Randomized Controlled Trial. Health Qual Life Out (2019) 17(1):17–2. doi:10.1186/s12955-019-1090-4
114. Ratcliff, CG, Milbury, K, Chandwani, KD, Chaoul, A, Perkins, G, Nagarathna, R, et al. Examining Mediators and Moderators of Yoga for Women with Breast Cancer Undergoing Radiotherapy. Integr Cancer Therapies (2016) 15(3):250–62. doi:10.1177/1534735415624141
115. D Reis, ME Walsh, S Young-McCaughan, and T Jones, Effects of Nia Exercise in Women Receiving Radiation Therapy for Breast Cancer . Oncol Nurs Forum (2013).
116. Rogers, LQ, Hopkins-Price, P, Vicari, S, Pamenter, R, Courneya, KS, Markwell, S, et al. A Randomized Trial to Increase Physical Activity in Breast Cancer Survivors. Med Sci Sports Exerc (2009) 41(4):935–46. doi:10.1249/MSS.0b013e31818e0e1b
117. Travier, N, Velthuis, MJ, Bisschop, CNS, van den Buijs, B, Monninkhof, EM, Backx, F, et al. Effects of an 18-Week Exercise Programme Started Early during Breast Cancer Treatment: A Randomised Controlled Trial. Bmc Med (2015) 13:121. doi:10.1186/s12916-015-0362-z
118. Vadiraja, SH, Rao, MR, Nagendra, RH, Nagarathna, R, Rekha, M, Vanitha, N, et al. Effects of Yoga on Symptom Management in Breast Cancer Patients: A Randomized Controlled Trial. Int J Yoga (2009) 2(2):73–9. doi:10.4103/0973-6131.60048
119. Vallance, JK, Friedenreich, CM, Lavallee, CM, Culos-Reed, N, Mackey, JR, Walley, B, et al. Exploring the Feasibility of a Broad-Reach Physical Activity Behavior Change Intervention for Women Receiving Chemotherapy for Breast Cancer: A Randomized Trial. Cancer Epidemiol Biomarkers Prev (2016) 25(2):391–8. doi:10.1158/1055-9965.EPI-15-0812
120. van Waart, H, Stuiver, MM, van Harten, WH, Geleijn, E, Kieffer, JM, Buffart, LM, et al. Effect of Low-Intensity Physical Activity and Moderate to High-Intensity Physical Exercise during Adjuvant Chemotherapy on Physical Fitness, Fatigue, and Chemotherapy Completion Rates: Results of the PACES Randomized Clinical Trial. J Clin Oncol (2015) 33(17):1918–27. doi:10.1200/JCO.2014.59.1081
121. Wang, YJ, Boehmke, M, Wu, YW, Dickerson, SS, and Fisher, N. Effects of a 6-Week Walking Program on Taiwanese Women Newly Diagnosed with Early-Stage Breast Cancer. Cancer Nurs (2011) 34(2):E1–13. doi:10.1097/NCC.0b013e3181e4588d
122. Zhou, K, Wang, W, An, J, Li, M, Li, J, and Li, X. Effects of Progressive Upper Limb Exercises and Muscle Relaxation Training on Upper Limb Function and Health-Related Quality of Life Following Surgery in Women with Breast Cancer: A Clinical Randomized Controlled Trial. Ann Surg Oncol (2019) 26(7):2156–65. doi:10.1245/s10434-019-07305-y
123. DeNysschen, CA, Brown, JK, Cho, MH, and Dodd, MJ. Nutritional Symptom and Body Composition Outcomes of Aerobic Exercise in Women with Breast Cancer. Clin Nurs Res (2011) 20(1):29–46. doi:10.1177/1054773810379402
124. Dieli-Conwright, CM, Parmentier, J-H, Sami, N, Lee, K, Spicer, D, Mack, WJ, et al. Adipose Tissue Inflammation in Breast Cancer Survivors: Effects of a 16-Week Combined Aerobic and Resistance Exercise Training Intervention. Breast Cancer Res Tr (2018) 168(1):147–57. doi:10.1007/s10549-017-4576-y
125. Kim, C-J, Kang, D-H, Smith, BA, and Landers, KA. Cardiopulmonary Responses and Adherence to Exercise in Women Newly Diagnosed with Breast Cancer Undergoing Adjuvant Therapy. Cancer Nurs (2006) 29(2):156–65. doi:10.1097/00002820-200603000-00013
126. Lee, K, Kang, I, Mack, WJ, Mortimer, J, Sattler, F, Salem, G, et al. Feasibility of High Intensity Interval Training in Patients with Breast Cancer Undergoing Anthracycline Chemotherapy: A Randomized Pilot Trial. BMC cancer (2019) 19(1):653–9. doi:10.1186/s12885-019-5887-7
127. Stan, DL, Kathleen Sundt, R, Cheville, AL, Youdas, JW, Krause, DA, Boughey, JC, et al. Pilates for Breast Cancer Survivors: Impact on Physical Parameters and Quality of Life after Mastectomy. Clin J Oncol Nurs (2012) 16(2):131–41. doi:10.1188/12.CJON.131-141
128. Swenson, KK, Nissen, MJ, Anderson, E, Shapiro, A, Schousboe, J, and Leach, J. Effects of Exercise vs Bisphosphonates on Bone mineral Density in Breast Cancer Patients Receiving Chemotherapy. J Support Oncol (2009) 7(3):101–7.
129. Yang, CY, Tsai, JC, Huang, YC, and Lin, CC. Effects of a home-Based Walking Program on Perceived Symptom and Mood Status in Postoperative Breast Cancer Women Receiving Adjuvant Chemotherapy. J Adv Nurs (2011) 67(1):158–68. doi:10.1111/j.1365-2648.2010.05492.x
130. Ainsworth, BE, Haskell, WL, Herrmann, SD, Meckes, N, Bassett, DR, Tudor-Locke, C, et al. 2011 Compendium of Physical Activities: A Second Update of Codes and MET Values. Med Sci Sports Exerc (2011) 43(8):1575–81. doi:10.1249/MSS.0b013e31821ece12
131. van Waart, H, van Harten, WH, Buffart, LM, Sonke, GS, Stuiver, MM, and Aaronson, NK. Why Do Patients Choose (Not) to Participate in an Exercise Trial during Adjuvant Chemotherapy for Breast Cancer? Psycho-Oncology (2016) 25(8):964–70. doi:10.1002/pon.3936
132. Susukida, R, Crum, RM, Stuart, EA, Ebnesajjad, C, and Mojtabai, R. Assessing Sample Representativeness in Randomized Controlled Trials: Application to the National Institute of Drug Abuse Clinical Trials Network. Addiction (2016) 111(7):1226–34. doi:10.1111/add.13327
133. Galobardes, B, Shaw, M, Lawlor, DA, Lynch, JW, and Smith, GD. Indicators of Socioeconomic Position (Part 1). J Epidemiol Community Health (2006) 60(1):7–12. doi:10.1136/jech.2004.023531
134. Murthy, VH, Krumholz, HM, and Gross, CP. Participation in Cancer Clinical Trials: Race, Sex, and Age-Based Disparities. Jama (2004) 291(22):2720–6. doi:10.1001/jama.291.22.2720
135. Semega, J, and Kollar, M. Income in the United States: 2021 . United States: U.S. CENSUS BUREAU (2022).
136. Sims, JM. A Brief Review of the Belmont Report. Dimensions Crit Care Nurs (2010) 29(4):173–4. doi:10.1097/DCC.0b013e3181de9ec5
137. Coughlin, SS. Social Determinants of Breast Cancer Risk, Stage, and Survival. Breast Cancer Res Treat (2019) 177:537–48. doi:10.1007/s10549-019-05340-7
138. Stalsberg, R, Bertheussen, GF, Børset, H, Thomsen, SN, Husøy, A, Flote, VG, et al. Do Breast Cancer Patients Manage to Participate in an Outdoor, Tailored, Physical Activity Program during Adjuvant Breast Cancer Treatment, Independent of Health and Socio-Demographic Characteristics? J Clin Med (2022) 11(3):843. doi:10.3390/jcm11030843
139. Daley, AJ, Crank, H, Mutrie, N, Saxton, JM, and Coleman, R. Determinants of Adherence to Exercise in Women Treated for Breast Cancer. Eur J Oncol Nurs (2007) 11(5):392–9. doi:10.1016/j.ejon.2007.03.001
140. Brunet, J, Taran, S, Burke, S, and Sabiston, CM. A Qualitative Exploration of Barriers and Motivators to Physical Activity Participation in Women Treated for Breast Cancer. Disabil Rehabil (2013) 35(24):2038–45. doi:10.3109/09638288.2013.802378
141. Strazdins, L, Griffin, AL, Broom, DH, Banwell, C, Korda, R, Dixon, J, et al. Time Scarcity: Another Health Inequality? Environ Plann A: Economy Space (2011) 43(3):545–59. doi:10.1068/a4360
142. Strazdins, L, Welsh, J, Korda, R, Broom, D, and Paolucci, F. Not All Hours Are Equal: Could Time Be a Social Determinant of Health? Sociol Health Ill (2016) 38(1):21–42. doi:10.1111/1467-9566.12300
143. Phelan, JC, Link, BG, Diez-Roux, A, Kawachi, I, and Levin, B. “Fundamental Causes” of Social Inequalities in Mortality: A Test of the Theory. J Health Soc Behav (2004) 45(3):265–85. doi:10.1177/002214650404500303
144. Hart, T. The Inverse Care Law. The Lancet (1971) 297(7696):405–12.
Keywords: sampling bias, social validity, research equity, exercise trials, breast cancer, mammae cancer, meta-analysis
Citation: Stalsberg R and Darvik MD (2024) Social Representativeness and Intervention Adherence—A Systematic Review of Clinical Physical Activity Trials in Breast Cancer Patients. Int J Public Health 69:1607002. doi: 10.3389/ijph.2024.1607002
Received: 21 December 2023; Accepted: 10 April 2024; Published: 09 May 2024.
Reviewed by:
Copyright © 2024 Stalsberg and Darvik. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ragna Stalsberg, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
- Open access
- Published: 15 May 2024
The association between ultra-processed food and common pregnancy adverse outcomes: a dose-response systematic review and meta-analysis
- Sepide Talebi 1 , 2 ,
- Sanaz Mehrabani 3 ,
- Seyed Mojtaba Ghoreishy 4 , 5 ,
- Alexei Wong 6 ,
- Aliasghar Moghaddam 7 ,
- Peyman Rahimi Feyli 7 ,
- Parsa Amirian 8 ,
- Mahsa Zarpoosh 8 ,
- Mohammad Ali Hojjati Kermani 9 &
- Sajjad Moradi 10
BMC Pregnancy and Childbirth volume 24 , Article number: 369 ( 2024 ) Cite this article
Metrics details
Given the increasing incidence of negative outcomes during pregnancy, our research team conducted a dose-response systematic review and meta-analysis to investigate the relationship between ultra-processed foods (UPFs) consumption and common adverse pregnancy outcomes including gestational diabetes mellitus (GDM), preeclampsia (PE), preterm birth (PTB), low birth weight (LBW), and small for gestational age (SGA) infants. UPFs are described as formulations of food substances often modified by chemical processes and then assembled into ready-to-consume hyper-palatable food and drink products using flavors, colors, emulsifiers, and other cosmetic additives. Examples include savory snacks, reconstituted meat products, frozen meals that have already been made, and soft drinks.
A comprehensive search was performed using the Scopus, PubMed, and Web of Science databases up to December 2023. We pooled relative risk (RR) and 95% confidence intervals (CI) using a random-effects model.
Our analysis (encompassing 54 studies with 552,686 individuals) revealed a significant association between UPFs intake and increased risks of GDM (RR = 1.19; 95% CI: 1.10, 1.27; I 2 = 77.5%; p < 0.001; studies = 44; number of participants = 180,824), PE (RR = 1.28; 95% CI: 1.03, 1.59; I 2 = 80.0%; p = 0.025; studies = 12; number of participants = 54,955), while no significant relationships were found for PTB, LBW and SGA infants. Importantly, a 100 g increment in UPFs intake was related to a 27% increase in GDM risk (RR = 1.27; 95% CI: 1.07, 1.51; I 2 = 81.0%; p = 0.007; studies = 9; number of participants = 39,812). The non-linear dose-response analysis further indicated a positive, non-linear relationship between UPFs intake and GDM risk P nonlinearity = 0.034, P dose-response = 0.034), although no such relationship was observed for PE (P nonlinearity = 0.696, P dose-response = 0.812).
In summary, both prior to and during pregnancy, chronic and excessive intake of UPFs is associated with an increased risk of GDM and PE. However, further observational studies, particularly among diverse ethnic groups with precise UPFs consumption measurement tools, are imperative for a more comprehensive understanding.
Peer Review reports
Introduction
The Centers for Disease Control and Prevention’s (CDC’s) 2022 National Center for Health Statistics report alarmingly indicates a persistent rise in pregnancy-related mortality in the US across three decades, highlighting significant disparities in “race” and maternal age [ 1 ]. This trend underscores the pivotal role of addressing common pregnancy adverse outcomes as a critical component of maternal morbidity and mortality prevention strategies [ 2 ].
Promoting healthy dietary habits during pregnancy is imperative to meet the increased physiological needs of expectant mothers. The phenomenon of “nutritional transition”, characterized by a shift towards high-calorie, low-micronutrient foods, culminates in malnutrition and obesity [ 3 ]. The significance of maternal nutrition in prenatal care is heavily emphasized by researchers as a preventive measure against adverse pregnancy outcomes [ 4 ]. The consumption of diets rich in refined carbohydrates, fats, and sweets is linked to an increased risk of gestational diabetes mellitus (GDM) and preterm birth (PTB) [ 5 ]. Moreover, such dietary patterns adversely affect women’s health by exacerbating hypertensive disorders and contributing to conditions like preeclampsia (PE), low birth weight (LBW), and small-for-gestational-age (SGA) infants [ 6 ]. Recognizing the detrimental impact of these unhealthy dietary patterns, it becomes crucial to consider the role of food processing in the maternal diet.
The NOVA classification, a framework for grouping edible substances, categorizes foods into four groups based on the extent and purpose of food processing applied, ranging from unprocessed or minimally processed foods to ultra-processed foods (UPFs) [ 7 , 8 ]. UPFs are characterized by their high content of additives such as preservatives, artificial flavors, colors, and sweeteners, and are typically devoid of whole or minimally processed ingredients [ 9 ]. The consumption of UPFs has been associated with higher risks of obesity, hypertension, cancer, and other chronic diseases [ 8 , 10 , 11 , 12 ]. These foods are implicated in disrupting insulin signaling, promoting excessive energy intake, weight gain, and increased urinary concentrations of phthalate metabolites, which act as endocrine disruptors [ 13 , 14 ]. In the context of adverse pregnancy outcomes, recent meta-analytic work highlighted a heightened risk of GDM (odds ratio (OR): 1.48; 95% confidence interval (CI): 1.17, 1.87) and PE (OR: 1.28; 95% CI: 1.15, 1.42) among high UPFs consumers, with no significant associations observed in LBW, PTB, and Large for Gestational Age (LGA) [ 15 ]. However, the previous meta-analysis did not encompass a comprehensive set of extant studies for each adverse outcome (as evidenced by the inclusion of only 10 studies for GDM in contrast to the 44 studies incorporated in our current investigation), thereby underscoring the challenge posed by the unutilized data in previous analyses. Additionally, recent studies of relevance have emerged [ 16 , 17 , 18 ] and the preceding meta-analytic work did not include a dose-response analysis [ 15 ]. The integration of dose-response analysis offers benefits such as facilitating the formulation of public health directives, augmenting precision, and quantifying the dose-response relationship. Consequently, we decided to conduct an updated dose-response systematic review and meta-analysis to rigorously evaluate the association between UPFs consumption and common adverse pregnancy outcomes, including GDM, SGA, LBW, PTB, and PE.
This systematic review and meta-analysis was conducted according to the guidelines specified in the 2020 Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [ 19 ]. The study protocol was registered with the International Prospective Register of Systematic Reviews Database (PROSPERO) under the registration number CRD42023486135.
Literature search and selection
A systematic literature search was done employing PubMed/MEDLINE, ISI Web of Science and Scopus, with no date restrictions, up to December 6, 2023. The search keywords and strategy are reported in Supplementary Table 1 . Data from grey literature sources such as notes, conference abstracts, reviews, case reports, letters, short surveys, and reports were obtained from a manual search of references mentioned in original research articles published in one of these databases. To augment the breadth of research identified, references within reviews and pertinent studies that met eligibility criteria were further subjected to manual examination.
Inclusion and exclusion criteria
Inclusion criteria were defined as follows: a) observational studies (cohort, case-control, or cross-sectional,) in adult subjects (≥18 years) reporting data on the association between UPFs intake and the risk of adverse pregnancy outcomes (including GDM PE, PTB, LBW, and SGA infants), and reporting effect estimates in the form of hazard ratio (HR), relative risk (RR), or odds ratios (OR), each with at least 95% confidence interval (95% CI). Exclusion criteria included: a) studies done in children and adolescents (< 18 years), b) studies without sufficient data (for instance, those failing to report effect sizes or 95% CIs, instead reporting beta coefficients), and c) those with no relevant exposure. Study titles and abstracts, as well as full-text reviews from database searches meeting the inclusion criteria, were assessed by two reviewers (ST and SM). Any disagreements regarding study inclusion/exclusion criteria were resolved by consensus following discussion. The PICOS tool for each article was reported in Supplementary Table 2 .
Data extraction
Two investigators (FJ and SM) extracted the following data, based on a standardized extraction form, from the studies that met the inclusion criteria: a) first author’s name, year of publication, and country of origin; b) study characteristics (design, follow-up period, and source of data on health status); c) participant characteristics (number of participants/cases, age and sex); d) methods of evaluating UPFs intake; e) the risk of adverse pregnancy outcomes; f) main study results (outcomes), and g) covariates utilized for adjustments in multivariate analyses. Any disagreement regarding data extraction characteristics was decided by consensus following the discussion.
Quality assessment
Applying the Newcastle-Ottawa Scale (NOS) [ 20 ], two investigators assessed the quality of each shortlisted study. The NOS was specifically chosen due to its comprehensive framework designed to evaluate the quality of non-randomized studies. This scale excels in its design, content, and user-friendliness, making it particularly suitable for integrating quality assessments into the interpretation of meta-analytic results. The NOS scale for systematic reviews or meta-analyses, allocating up to 9 points across three domains: study group selection (four points), study group comparability (two points), and exposure and outcomes ascertainment for case-control or cohort studies (three points). Studies scoring 7–9 are deemed high quality/low risk of bias, whereas a score of 0–3 indicates a high risk of bias. Table 1 shows the consensus from this assessment.
Statistical analyses and data synthesis
Statistical analyses were performed applying STATA version 14.0 (StataCorp, College Station, TX, USA) and SPSS version 25.0 (IBM, Armonk, NY, USA). The RR and 95% CI were established as overall effect sizes in this work, similar to effect estimates reported in observational articles meeting the inclusion criteria for this meta-analysis [ 21 ]. The synthesized effect estimates were reported as pooled RR with 95% CI. Due to anticipated heterogeneity between studies, effect estimates were calculated using the DerSimonian-Laird weighted random-effects model [ 22 ]. A pairwise meta-analysis combined the effect size results for the highest and lowest categories of UPFs intake. Heterogeneity among the articles was examined by the Cochran Q and I-squared (I 2 ) statistics, with the I 2 value estimated from [(Q-df)/Q × 100%]; where Q is the χ 2 value and df the corresponding degrees of freedom. Between-study heterogeneity was considered significant when the Cochran Q statistic was significant ( p < 0.05) or if I 2 > 50%; specifically, low, moderate, high, and extreme heterogeneity was defined based on the I 2 statistics cut-offs of < 25%, 25–50%, 50–75%, and >75%, respectively.
Furthermore, subgroup analyses were conducted to evaluate any potential effects due to the study design (cross-sectional, case-control, or cohort), UPFs classification method (NOVA food classification, Western-type diet pattern, fast-food, or sweets consumption), the study region of origin (North America, South America, Asia, Europe, and Australia), pre-pregnancy body mass index (< 25 kg/m 2 and ≥ 25 kg/m 2 ) [ 23 , 24 ], age (< 30 years and ≥ 30 years) [ 24 ], number of cases (< 100 or ≥ 100), number of participants (< 1000 or ≥ 1000), dietary assessment method (food frequency questionnaires [FFQ], 24 h recall, or food records), dietary assessment period (pre-pregnancy, early pregnancy, mid-pregnancy), and other covariate adjustments. Sensitivity analysis was conducted by omitting each study and evaluating the remaining pooled effect estimates. Publication bias was evaluated by visual inspection of funnel plots, and formal testing using Egger’s regression asymmetry and Begg’s rank correlation tests [ 25 , 26 ], with outcomes considered as significant at p < 0.05.
A dose-response meta-analysis was completed to estimate the RRs per 100 g increment in UPFs intake, based on the method introduced by Greenland and colleagues [ 27 , 28 ]. For this process, studies needed to report the number of cases (i.e., participants with incidence) and non-cases (i.e., participants without incidence) or person-years (i.e., the number of people in the study and the duration of their participation) as well as the median point of UPFs intake across more than three categories of intake. Ultimately, a one-stage linear mixed-effects meta-analysis was undertaken to model the dose-response associations, estimating and combining study-specific slope lines to obtain an average slope in a single stage. This linear mixed-effects meta-analysis includes studies with two categories of exposures (at least two effect sizes) in the dose-response analysis.
Quality of evidence
The quality of evidence across articles was ranked employing the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) working group guidelines. The GRADE criteria categorize evidence quality into high, moderate, low, or very low levels [ 29 ].
Study characteristics
Our systematic search and examination of reference lists yielded a total of 3433 records. After omitting duplicates, 2787 articles remained for assessment (Fig. 1 ). A title and abstract review led to the removal of 2707 articles. Subsequent full-text assessment of the 80 remaining studies resulted in the exclusion of a further 26 articles for the following reasons: five articles reported outcomes not relevant to our research scope, six lacked sufficient data, and 15 did not focus on relevant exposure (Supplemental Table 3 ). Consequently, 54 studies met our inclusion criteria and were selected in the present meta-analysis [ 16 , 17 , 18 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 ].
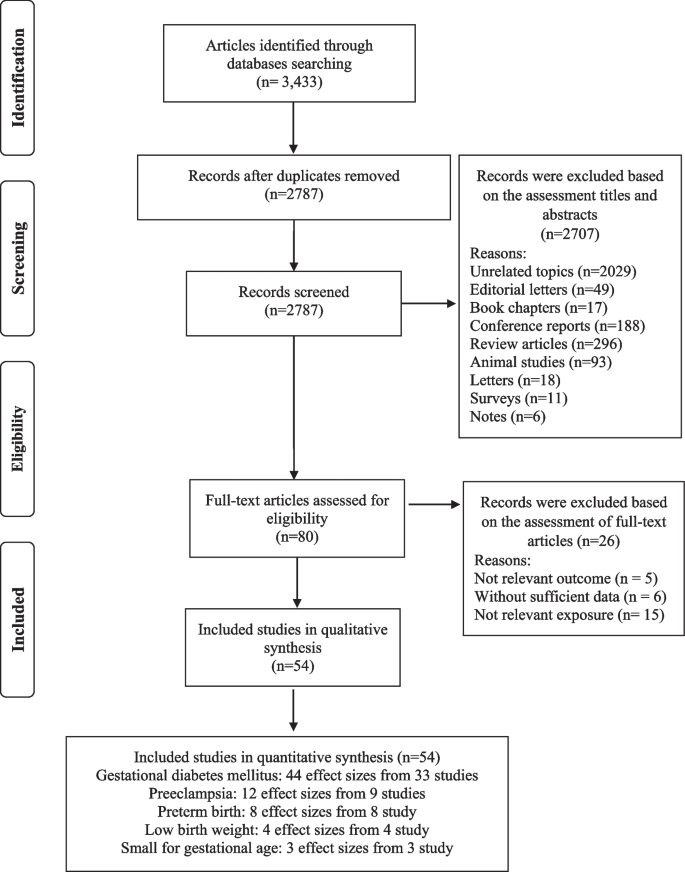
Flow chart of the process of the study selection
The selected studies (detailed in Supplemental Table 4 ) encompass 38 cohort studies [ 16 , 31 , 33 , 34 , 35 , 36 , 37 , 39 , 40 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 51 , 52 , 54 , 55 , 57 , 58 , 59 , 60 , 61 , 62 , 65 , 66 , 67 , 69 , 70 , 71 , 73 , 74 , 75 , 78 ], 11 case-control studies [ 17 , 18 , 30 , 32 , 34 , 50 , 63 , 66 , 68 , 72 , 77 ], and five cross-sectional studies [ 38 , 46 , 64 , 76 , 79 ]. These articles, conducted between 1988 and 2023, originated from different countries including the USA [ 33 , 36 , 53 , 58 , 60 , 62 , 69 , 74 , 78 ], the UK [ 16 ], China [ 43 , 49 , 51 , 71 , 73 ], Brazil [ 31 , 59 , 63 , 64 , 68 , 79 ], Spain [ 39 , 40 , 42 , 55 , 57 ], Iran [ 17 , 18 , 30 , 32 , 48 , 54 , 66 , 76 , 77 ], Malaysia [ 75 ], Palestine [ 72 ], Australia [ 45 , 46 , 65 ], Singapore [ 37 , 38 ], Norway [ 35 , 44 , 47 ], Japan [ 41 , 67 ], Czech Republic [ 34 ], Iceland [ 70 ] and Denmark [ 61 ]. The study-specific, maximally adjusted RR was reported for 552,686 individuals across the included articles and was pooled for meta-analysis to assess the association between UPFs and the risk GDM [ 16 , 32 , 33 , 34 , 36 , 38 , 39 , 40 , 41 , 43 , 48 , 49 , 50 , 51 , 53 , 54 , 55 , 56 , 59 , 60 , 64 , 65 , 66 , 70 , 71 , 72 , 73 , 74 , 75 , 77 , 78 , 79 ], PE [ 17 , 18 , 30 , 35 , 48 , 52 , 62 , 69 , 74 , 76 ], PTB [ 31 , 37 , 44 , 45 , 46 , 48 , 52 , 58 , 61 , 67 ], LBW [ 45 , 63 , 67 ] and SGA infants [ 46 , 67 , 68 ]. The Newcastle-Ottawa grade (used for quality assessment) categorized 27 studies as high quality [ 17 , 33 , 35 , 36 , 37 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 47 , 51 , 53 , 55 , 57 , 58 , 60 , 62 , 65 , 67 , 69 , 74 , 75 , 78 ] and 27 as medium quality [ 16 , 18 , 30 , 31 , 32 , 34 , 38 , 46 , 48 , 49 , 50 , 52 , 54 , 56 , 59 , 61 , 63 , 64 , 66 , 68 , 70 , 71 , 72 , 73 , 76 , 77 , 79 ]. Moreover, the outcomes revealed that the level of agreement between investigators for data collection as well as for quality assessment was appropriate (Kappa = 0.897).
Ultra-processed food and common adverse pregnancy outcomes
Our results suggested a significant relationship between higher UPF intake and an increased risk of GDM (RR = 1.19; 95% CI: 1.10, 1.27; I 2 = 77.5%; p < 0.001; n = 44), PE (RR = 1.28; 95% CI: 1.03, 1.59; I 2 = 80.0%; p = 0.025; n = 12), but not PTB (RR = 1.06; 95% CI: 0.97, 1.17; I 2 = 34.2%; p = 0.231; n = 8), LBW (RR = 1.01; 95% CI: 0.91, 1.12; I 2 = 52.2%; p = 0.905; n = 4) and SGA infants (RR = 1.11; 95% CI: 0.81, 1.52; I 2 = 66.3%; p = 0.532; n = 3), (Refer to Table 1 , Supplementary Fig. 1 ).
In the context of GDM, subgroup analysis showed that a greater UPFs intake was significantly associated with an enhanced risk in cohort studies (vs. cross-sectional) (RR = 1.18; 95% CI: 1.09, 1.27; I 2 = 79.3%; p < 0.001; n = 31) and case-control studies (RR = 2.06; 95% CI: 1.31, 3.35; I 2 = 77.7%; p = 0.002; n = 10), particularly in studies assessed western dietary pattern (RR = 1.34; 95% CI: 1.01, 1.76; I 2 = 43.0%; p = 0.040; n = 7) or fast-foods (RR = 1.32; 95% CI: 1.15, 1.51; I 2 = 79.3%; p < 0.001; n = 22), (vs. NOVA classification or sweets consumption), in North America (vs. Europe, South America, Asia and Australia) (RR = 1.43; 95% CI: 1.27, 1.53; I 2 = 45.4%; p < 0.001; n = 10), and across studies with > 100 number of case (RR = 1.38; 95% CI: 1.21, 1.58; I 2 = 74.8%; p < 0.001; n = 12)(vs. < 100 number of case), in studies with > 1000 number of participants (RR = 1.33; 95% CI: 1.15, 1.54; I 2 = 76.9%; p < 0.001; n = 21)(vs. < 1000 number of participants), in studies used FFQ for dietary assessment (RR = 1.27; 95% CI: 1.14, 1.43; I 2 = 78.6%; p < 0.001; n = 34) (vs. 24 h recall or food record), particularly in studies where the period of dietary assessment was at early pregnancy (RR = 1.26; 95% CI: 1.09, 1.46; I 2 = 80.5%; p = 0.002; n = 19) (vs. pre-pregnancy or mid-pregnancy). Moreover, subgroup analysis for covariates adjustment showed that BMI and physical activity may influence the association between UPF intake and the risk of GDM (Table 2 ).
For PE, the subgroup analysis also highlighted that greater UPFs intake was significantly associated with an enhanced risk in studies assessed western dietary pattern (RR = 2.51; 95% CI: 1.13, 5.57; I 2 = 91.1%; p = 0.023; n = 3) or NOVA classification (RR = 1.22; 95% CI: 1.04, 1.42; I 2 = 0.0%; p = 0.013; n = 3), (vs. sweets consumption), in Asia (vs. Europe or US areas) (RR = 1.65; 95% CI: 1.07, 2.55; I 2 = 86.1%; p < 0.001; n = 6), and across studies with > 100 number of case (RR = 1.57; 95% CI: 1.03, 2.40; I 2 = 93.2%; p < 0.001; n = 4)(vs. < 100 number of case), in studies with number of < 1000 participants (RR = 1.65; 95% CI: 1.07, 2.55; I 2 = 86.1%; p = 0.023; n = 6)(vs. > 1000 number of participants), in participants aged ≥30 years (RR = 1.28; 95% CI: 1.07, 1.54; I 2 = 50.4%; p = 0.089; n = 5)(vs. participants aged < 30 years), in participants with pre-pregnancy-BMI > 25 (RR = 1.52; 95% CI: 1.07, 2.15; I 2 = 84.7%; p = 0.021; n = 1)(vs. participants with pre-pregnancy-BMI ≤ 25), in studies used FFQ for dietary assessment (RR = 1.38; 95% CI: 1.10, 1.72; I 2 = 82.6%; p = 0.005; n = 10) (vs. questions), and particularly in studies where the period of dietary assessment was at mid-pregnancy (RR = 1.23; 95% CI: 1.05, 1.43; I 2 = 38.8%; p = 0.009; n = 3) (vs. early pregnancy). Furthermore, subgroup analysis for covariates adjustment showed that BMI and physical activity may influence the association between UPF intake and the risk of PE (Table 3 ).
Linear and non-linear dose-response analysis
The linear dose-response analysis (refer to Table 1 and Fig. 2 ) indicates a 27% increase in GDM risk per 100 g increment in UPF intake RR = 1.27; 95% CI: 1.07, 1.51; I 2 = 81.0%; p = 0.007; n = 9). However, the linear dose-response analysis for other outcomes was not undertaken due to the limited number of studies available.
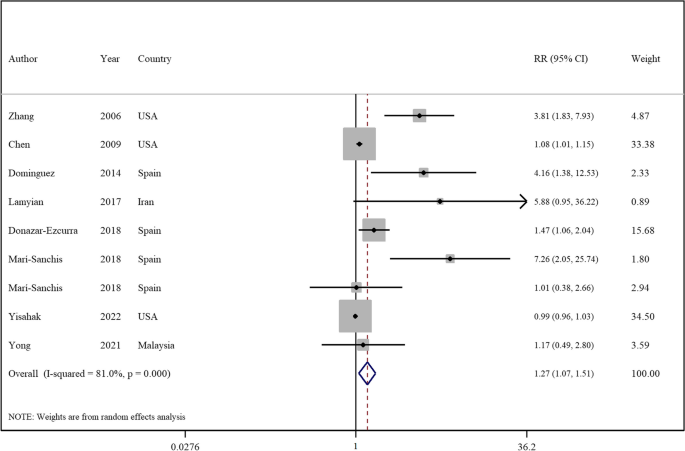
Forest plots showing the linear dose-response meta-analysis of mortality risk for 100 g change in ultra-processed food consumption in daily intake and risk of gestational diabetes mellitus
The non-linear dose-response analysis revealed a positive non-linear relationship between UPFs intake and GDM risk (P nonlinearity = 0.034, P dose-response = 0.034, Fig. 3 ), but not for PE (P nonlinearity = 0.696, P dose-response = 0.812, Fig. 4 ). The non-linear dose-response analysis was not conducted for other outcomes due to insufficient studies.
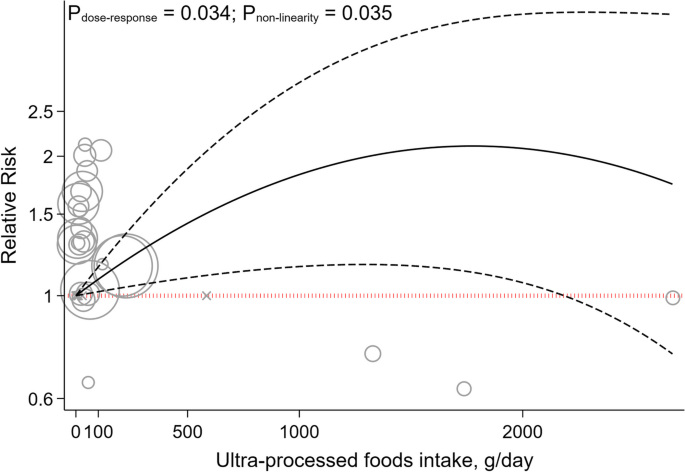
Non-linear dose-response indicated associations between UPF intake and the risk of gestational diabetes mellitus
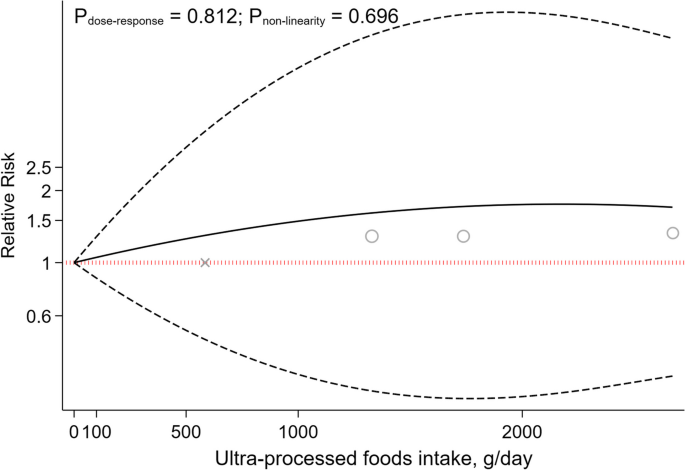
Non-linear dose-response indicated associations between UPF intake and the risk of preeclampsia
Sensitivity analyses and publication bias
Sensitivity analysis across the highest to the lowest meta-analysis for GDM, PE, PTB, LBW and SGA infants showed no significant influence of any single study (Supplemental Fig. 2 ).
No evidence of publication bias was found in articles related to the association with an increased risk of PE ( p = 0.529, Egger’s test; p = 0.891, Begg’s), PTB ( p = 0.458, Egger’s test; p = 0.473, Begg’s), LBW ( p = 0.905, Egger’s test; p = 1.00, Begg’s test), and SGA infants ( p = 0.348, Egger’s test; p = 1.00, Begg’s test). Although, for GDM, Egger’s test indicated potential publication bias ( p < 0.001), not corroborated by Begg’s test ( p = 0.241). As illustrated in Supplemental Fig. 3 , the funnel plot was symmetrical for the association between the UPFs intake and all outcomes, except for studies that reported the risk of GDM disease.
Utilizing the GRADE scale for quality evaluation, we detected the evidence for associations between UPFs intake and risk of GDM, PE, PTB, LBW and SGA infants was classified as moderate (Refer to Table 1 ).
In the realm of maternal and fetal health, the quality of dietary intake during pregnancy is of paramount significance. Accumulating evidence suggests a correlation between the consumption of UPFs and the deterioration of diet quality, potentially elevating the risk of various health complications [ 80 , 81 , 82 ]. This systematic review and meta-analysis aimed to elucidate the relationship between UPFs intake and adverse pregnancy outcomes including GDM, SGA, LBW, PTB, and PE, through an integrative analysis of existing studies. Our outcomes indicate a significant association between UPFs consumption and increased risks of PE, and GDM either prior to or during pregnancy. However, no significant association was found between UPFs intake and the risks of LBW, SGA, and PTB. Importantly, a 27% increment in the incidence of GDM was linked to a 100 g increase in UPF intake. Furthermore, a positive, non-linear relationship between UPF intake and GDM risk was identified through non-linear dose-response analysis, albeit no analogous association was found for PE.
The results of the current work showed a positive association between UPFs consumption and the risk of PE. In addition, subgroup analysis revealed this relationship to be more pronounced in studies using the NOVA-food classification and a Western dietary pattern for UPFs intake assessment, compared to those focusing on sweet intake. The NOVA classification categorizes foods based on the extent of processing, encompassing various UPFs. Moreover, the association between UPFs consumption and the risk of PE was significant in studies conducted in Asia (vs other regions). Prevalence of PE varies globally, ranging from 0.2–6.7% in Asia, 2.8–9.2% in Oceania, 2.8–5.2% in Europe, 2.6–4.0% in North America, and 1.8–7.7% in South America and the Caribbean [ 83 ]. However, the high heterogeneity in Asian studies should be noted when interpreting this result. Furthermore, a significant association was observed in studies involving women aged 30 years or older, aligning with the increased PE risk associated with advanced maternal age [ 84 ]. Additionally, a significant association was identified between PE risk and UPFs intake in women with pre-pregnancy BMI higher than 25 kg/m 2 (vs BMI ≤25). This aligns with previous findings linking excessive weight gain in expectant mothers to an elevated PE risk, with overweight and obese mothers facing substantially higher risks [ 85 ].
The association between UPFs intake and PE can be elucidated through several mechanisms. The risk factors for PE, including GDM, maternal obesity, and advanced maternal age, are extensively documented in the literature [ 84 , 85 , 86 ]. It has been established that adopting healthy lifestyle habits (including dietary patterns) can mitigate these risk factors [ 87 ]. A higher intake of UPFs is associated with a diminished dietary quality, marked by an increased consumption of sugars and fats, alongside a decrease in fiber, protein, vitamins, and minerals [ 88 , 89 ]. UPFs are known to contain elevated levels of pro-inflammatory agents such as refined sugars, salt, and trans fats. The ingestion of these inflammatory components can precipitate oxidative stress and systemic inflammation [ 90 , 91 , 92 ], which are implicated in the pathogenesis of preeclampsia [ 93 , 94 ]. Additionally, the presence of trans fatty acids, added phosphates, and a high salt content in UPFs may impair endothelial function [ 95 , 96 , 97 ], a critical factor in the pathophysiology of hypertension observed in preeclampsia [ 98 ]. Furthermore, the intake of UPFs can alter the composition and diversity of the gut microbiota [ 99 ]. Studies have shown that food additives commonly found in UPFs, such as emulsifiers, sweeteners, and colorants, adversely affect the gut flora [ 100 ]. The interplay between the gut microbiota and the placenta, referred to as the “gut–placenta” axis, is crucial for understanding the etiology of PE. Dysbiosis of the gut microbiota and bacterial products like lipopolysaccharide (LPS) have been identified as promotive of PE [ 101 , 102 ]. According to Kell et al., microbial infection, particularly through bacterial products such as LPS (also known as endotoxin), which is highly inflammatory, can initiate an innate immune response that exacerbates inflammation [ 103 ]. Hence, it is hypothesized that dysbiosis induced by UPFs consumption may play a significant role in the promotion of preeclampsia. Moreover, UPFs intake is positively associated with a risk of obesity [ 104 ], a condition marked by insulin resistance and hyperinsulinemia, crucial factors in PE development [ 105 ]. Pregnant women with obesity and PE exhibit higher leptin levels, correlating with increased Tumor Necrosis Factor-Alfa (TNF-α), Interleukin 6 (IL-6), and C-reactive protein concentrations [ 106 , 107 ]. Additionally, excessive adipose tissue near the reproductive tract is the source of increased complement components and fragments in preeclamptic pregnancies. These complement proteins may promote an imbalance in angiogenic factors (characterized by increased production of antiangiogenic factors and a decrease in proangiogenic factors). This imbalance leads to placental injury, resulting in decreased blood flow to the tissue, and is accompanied by changes in cytokines levels (decreased IL-10 and increased TNF-α) before the onset of PE [ 108 ].
Our pooled analysis also revealed that higher UPFs intake was related to an increased risk of GDM. This association was significant in studies employing cohort and case-control designs (as opposed to those with cross-sectional methodologies). The inherent recall bias in cross-sectional studies that rely on self-reporting, is a notable limitation affecting the reliability of outcomes [ 109 ]. Moreover, this association was more pronounced in studies that used Western dietary patterns and fast-food consumption for the assessment of UPFs intake (vs those employing NOVA food classification and sweet consumption metrics). The concept of a dietary pattern, which represents the aggregate of eating and drinking habits, is critical as it exerts a greater impact on health and chronic diseases than any individual food item [ 110 ]. Additionally, the application of the NOVA food classification in existing studies is less frequent, suggesting the need for further research utilizing this methodology to derive more meaningful results. Geographical variations were also evident, with significant associations observed in studies conducted in America, compared to those in Asia and Europe. This is in context with the differing regional prevalences of GDM: 7.1% in North America and the Caribbean, 7.8% in Europe and 20.8% in South-East Asia [ 111 ]. Despite the higher prevalence of GDM in Asian populations, the greater intake of UPFs in American and European cohorts may have influenced the study outcomes [ 112 , 113 , 114 , 115 ]. Additionally, a positive association between UPFs intake and GDM risk was observed in studies focusing on women with a pre-pregnancy BMI > 25. Previous research indicates that being overweight or obese before and during pregnancy is a significant risk factor for GDM [ 116 , 117 , 118 ]. However, the scarcity of studies in women with pre-pregnancy BMI > 25 kg/m 2 kg/m suggests the need for more research in this demographic for robust conclusions.
Our outcomes also indicated that a 100 g increase in UPF intake was associated with a 27% increase in the risk of GDM. Moreover, the non-linear dose-response analysis similarly showed a positive, non-linear association between the consumption of UPFs and the risk of GDM. These findings underscore the significant impact that UPF consumption can have on GDM risk. The evidence points towards a robust and worrying correlation where even moderate increases in UPF intake can precipitate a marked rise in GDM risk, highlighting the critical need for dietary awareness and intervention among pregnant women. This aligns with broader nutritional science, emphasizing the importance of minimizing UPF consumption to mitigate not only GDM risk but potentially other metabolic disorders as well, given the multitude of adverse mechanisms through which UPFs affect glucose metabolism and insulin sensitivity.
Pathophysiologically, UPFs intake may increase GDM risk through several mechanisms. In pregnant women with GDM, pre-pregnancy reduced insulin sensitivity and β-cell dysfunction lead to hyperglycemia [ 119 , 120 ]. The hypothesis that excessive sugar intake may augment body mass, thereby indirectly precipitating insulin resistance and subsequent diabetes, is widely recognized. Moreover, the liver’s capacity to assimilate and metabolize refined sugars prevalent in UPFs (such as fructose and sucrose) may be compromised, leading to augmented fat deposition and deteriorated insulin sensitivity [ 121 ]. Furthermore, insulin resistance may be induced by cosmetic ingredients present in UPFs. For example, dietary additives like carrageenan, employed as a thickening and stabilizing agent, may interfere with insulin signaling and thus foster insulin resistance [ 122 ]. Additionally, UPFs intake correlates with increased production of reactive oxygen species and inflammatory biomarkers [ 123 ], inducing insulin resistance through molecular pathways such as β-cell and mitochondrial dysfunction, decreased GLUT4 expression, impaired insulin signaling and heightened inflammatory responses [ 124 ]. Furthermore, UPFs often contain packaging materials like phthalates and bisphenol A, known to have endocrine disruption properties that may contribute to insulin resistance and diabetes development [ 125 , 126 ]. The ingestion of substantial quantities of UPFs also elevates inflammation, a pivotal factor in the genesis of insulin resistance, culminating in hyperglycemia and the development of GDM [ 127 ]. A diet replete with saturated fats, trans fats, sugars, and salt, characteristic of high UPFs consumption, may contribute to chronic inflammation [ 128 ]. Furthermore, excessive UPFs consumption may supplant essential components of a balanced and nutritious diet. For instance, fruits and vegetables are associated with an anti-inflammatory effect [ 129 ]. In addition, the leaching of chemicals from food packaging into UPFs could introduce non-nutritional elements such as phthalates or bisphenol A, potentially eliciting an inflammatory response [ 130 ].
The present study did not establish a significant association between UPFs consumption and the risk of LBW. This result may be attributable to several factors. Firstly, a limited number of studies have evaluated the association between UPFs intake and LBW risk. Additionally, the intake of high-sugar foods (such as sugar-sweetened beverages) has been correlated with an increased risk of LBW in non-GDM subjects [ 34 , 40 ]. This could be attributed to impaired fetal nutrition due to reduced vascular function, potentially induced by oxidative stress, inflammation, and endothelial dysfunction associated with high sugar consumption [ 131 ]. However, in GDM subjects this association may not be found due to the higher glucose loads in the fetus [ 47 ]. Therefore, additional research is warranted in both GDM and non-GDM populations to elucidate these relationships comprehensively.
Moreover, SGA was not associated with the intake of UPFs according to the pooled analysis of conducted studies. Although additional studies are necessary to explore this relationship further, existing evidence suggests that a fast-food dietary pattern may lead to increased fat intake and a reduced intake of essential micronutrients crucial for fetal development [ 132 ]. Maternal UPFs intake is linked to lower protein intake, reduced overall nutrition quality, and higher intake of trans fats, carbohydrates and saturated fats, which may increase the risk of neonatal adiposity [ 133 , 134 , 135 ]. Furthermore, higher fast-food intake during pregnancy has been linked with an elevated risk of maternal obesity, which in turn, may increase the likelihood of LGA babies [ 132 , 136 ].
Regarding PTB, the current study found no association with UPFs consumption. Previous research has indicated that dietary patterns rich in fruits and vegetables are associated with a lower risk of PTB [ 37 , 45 ]. Inadequate nutrition before and during pregnancy can lead to health issues for both the mother and fetus, increasing the risk of preterm delivery and intrauterine growth retardation [ 137 ]. The absence of an association between UPFs consumption and preterm delivery in this study could be due to various factors, including the need for a higher UPFs consumption threshold during pregnancy to manifest negative impacts on preterm birth. Additionally, the varied diet of pregnant women, typically including beneficial foods such as fruits, vegetables and nuts, may mitigate the adverse effects of UPFs.
The current investigation has several crucial strengths that make its findings highly significant. Firstly, by pooling all available observational data on the topic, the study provides a comprehensive and robust analysis of the relationship between UPFs intake and adverse pregnancy outcomes. Secondly, the study’s use of a dose-response analysis adds further weight to its conclusions and bolsters our understanding of the link between these two factors. However, there are limitations to consider. These include potential information and recall biases due to the self-reported nature of dietary intake assessments (such as the FFQ) and the absence of specific dietary tools for assessing UPFs consumption. Additionally, this meta-analysis included studies that did not use NOVA’s specialized dietary assessments. Moreover, dietary changes following pregnancy discovery could affect results, and the observational nature of the included studies precludes causal inference. Despite the inclusion of numerous confounding variables, several factors must be cautiously considered in the interpretation of the research findings. For instance, the socio-economic status of participants influences their dietary habits, while race and ethnicity may affect pregnancy outcomes. Furthermore, disparities in access to healthcare services can impact dietary choices and pregnancy outcomes. Other health statuses, such as mental health conditions among pregnant subjects, also influence dietary selections and pregnancy results [ 138 , 139 ]. Finally, the availability of data on broader categories such as diabetes in pregnancy and hypertensive disorders was limited, hindering our ability to conduct a comprehensive analysis on these broader categories.
Our outcomes indicate that prior to or during pregnancy, UPFs intake is associated with a higher risk of GDM and PE. However, no significant link tying UPFs intake to SGA, LWB and PTB was established. Importantly, a 100 g increment in UPFs intake was related to a 27% increase in GDM risk. This study aligns with global trends, where a rise in adverse pregnancy outcomes seems to align with the escalation of industrialization and the corresponding surge in UPFs production and consumption. Investigating the potential linkage between UPFs intake and the rise of adverse pregnancy outcomes may help in the development of nutrition-centric policies for expecting mothers and promote more health-conscious decision-making. To further substantiate these findings, extensive empirical research is required. Future studies should encompass observational research across diverse ethnic groups. Moreover, the adoption of more precise tools for measuring UPFs consumption is imperative. In observational research, it may be challenging to ascertain whether the consumption of UPFs directly contributes to adverse pregnancy outcomes or if it serves as an indicator of other underlying factors. Components of UPFs may escalate the risk of negative pregnancy outcomes. Moreover, UPF consumption could be part of a complex interplay affecting other variables that directly result in adverse outcomes. For instance, UPF intake could influence gestational weight gain, potentially leading to insulin resistance, which is known to correlate with unfavorable pregnancy outcomes, including GDM. Additionally, the consumption of UPFs may not only diminish dietary quality but also be linked with various lifestyle and dietary factors, such as poor diet quality, thereby increasing the risk of adverse pregnancy outcomes [ 140 ]. The bidirectional correlation between UPF consumption and unfavorable pregnancy outcomes also merits consideration. For example, individuals experiencing depression or other health conditions might alter their dietary patterns to include a higher intake of UPFs [ 138 ]. Evaluating changes in UPF consumption over time, utilizing precise questionnaires that assess food items classified as UPFs according to the NOVA food classification system, and their association with other health outcomes affecting pregnancy, such as obesity, could offer insights into this relationship. Considering these approaches is essential to enhance the depth and accuracy of investigations into the potential association between UPFs intake and the incidence of adverse pregnancy outcomes.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due but are available from the corresponding author on reasonable request.
Hoyert DL, Miniño AM. Maternal Mortality in the United States: Changes in Coding, Publication, and Data Release, 2018. Natl Vital Stat Rep. 2020;69(2):1–18.
PubMed Google Scholar
Parikh NI, Gonzalez JM, Anderson CA, Judd SE, Rexrode KM, Hlatky MA, et al. Adverse pregnancy outcomes and cardiovascular disease risk: unique opportunities for cardiovascular disease prevention in women: a scientific statement from the American Heart Association. Circulation. 2021;143(18):e902–e16.
Article CAS PubMed Google Scholar
Hashmi AH, Solomon N, Lee SJ, Min AM, Gilder ME, Wiladphaingern J, et al. Nutrition in transition: historical cohort analysis summarising trends in under-and over-nutrition among pregnant women in a marginalised population along the Thailand–Myanmar border from 1986 to 2016. Br J Nutr. 2019;121(12):1413–23.
Lind JM, Hennessy A, McLean M. Cardiovascular disease in women: the significance of hypertension and gestational diabetes during pregnancy. Curr Opin Cardiol. 2014;29(5):447–53.
Article PubMed Google Scholar
Englund-Ögge L, Birgisdottir BE, Sengpiel V, Brantsæter AL, Haugen M, Myhre R, et al. Meal frequency patterns and glycemic properties of maternal diet in relation to preterm delivery: results from a large prospective cohort study. PLoS One. 2017;12(3):e0172896.
Article PubMed PubMed Central Google Scholar
Mekie M, Mekonnen W, Assegid M. Cohabitation duration, obstetric, behavioral and nutritional factors predict preeclampsia among nulliparous women in West Amhara zones of Ethiopia: age matched case control study. PLoS One. 2020;15(1):e0228127.
Article CAS PubMed PubMed Central Google Scholar
Monteiro CA, Cannon G, Levy R, Moubarac J-C, Jaime P, Martins AP, et al. NOVA The star shines bright. World Nutrition. 2016;7(1–3):28–38.
Google Scholar
da Costa Louzada ML, Baraldi LG, Steele EM, Martins APB, Canella DS, Moubarac J-C, et al. Consumption of ultra-processed foods and obesity in Brazilian adolescents and adults. Prev Med. 2015;81:9–15.
Article Google Scholar
Monteiro CA, Levy RB, Claro RM, Castro IRR, Cannon G. A new classification of foods based on the extent and purpose of their processing. Cadernos de saude publica. 2010;26:2039–49.
Mendonça RD, Pimenta AM, Gea A, de la Fuente-Arrillaga C, Martinez-Gonzalez MA, Lopes ACS, et al. Ultraprocessed food consumption and risk of overweight and obesity: the University of Navarra Follow-up (SUN) cohort study. Am J Clin Nutr. 2016;104(5):1433–40.
Mendonça RD, Lopes ACS, Pimenta AM, Gea A, Martinez-Gonzalez MA, Bes-Rastrollo M. Ultra-processed food consumption and the incidence of hypertension in a Mediterranean cohort: the Seguimiento Universidad de Navarra project. Am J Hypertens. 2017;30(4):358–66.
Fiolet T, Srour B, Sellem L, Kesse-Guyot E, Allès B, Méjean C, Deschasaux M, Fassier P, Latino-Martel P, Beslay M, Hercberg S, Lavalette C, Monteiro CA, Julia C, Touvier M. Consumption of ultra-processed foods and cancer risk: results from NutriNet-Santé prospective cohort. BMJ. 2018;360:k322. https://doi.org/10.1136/bmj.k322 .
Bhattacharyya S, Feferman L, Tobacman JK. Carrageenan inhibits insulin signaling through GRB10-mediated decrease in Tyr (P)-IRS1 and through inflammation-induced increase in Ser (P) 307-IRS1. J Biol Chem. 2015;290(17):10764–74.
Buckley JP, Kim H, Wong E, Rebholz CM. Ultra-processed food consumption and exposure to phthalates and bisphenols in the US National Health and nutrition examination survey, 2013–2014. Environ Int. 2019;131:105057.
Paula WO, Patriota ES, Gonçalves VS, Pizato N. Maternal consumption of ultra-processed foods-rich diet and perinatal outcomes: a systematic review and meta-analysis. Nutrients. 2022;14(15):3242.
Mahendra A, Kehoe SH, Kumaran K, Krishnaveni GV, Arun N, Pidaparthy P, et al. Periconceptional diet and the risk of gestational diabetes in south Indian women: findings from the BAngalore nutrition gestational diabetes LiFEstyle study (BANGLES). Lancet Glob Health. 2023;11:S4.
Kooshki A, Sovizi B, Mahmoudi R, Ghezi S, Foroumandi E. The association between food groups and preeclampsia: a case-control study. Hyperten Pregnancy. 2022;41(1):64–9.
Article CAS Google Scholar
Moradi M, Niazi A, Selajgeh F, Mazloumi E. Comparing dietary patterns during pregnancy in women with preeclampsia and healthy women: a case-control study. J Midwife Reproduct Health. 2022;10(1)
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Oxford: Ottawa Hospital Research Institute; 2000.
Symons M, Moore D. Hazard rate ratio and prospective epidemiological studies. J Clin Epidemiol. 2002;55(9):893–9.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88.
Jayedi A, Soltani S, Zargar MS, Khan TA, Shab-Bidar SJB. Central fatness and risk of all cause mortality: systematic review and dose-response meta-analysis of 72 prospective cohort studies. 2020;370.
Song C, Lyu Y, Li C, Liu P, Li J, Ma R, et al. Long-term risk of diabetes in women at varying durations after gestational diabetes: a systematic review and meta-analysis with more than 2 million women 2018;19(3):421–9.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–101.
Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ (Clin res ed). 1997;315(7109):629–34.
Berlin JA, Longnecker MP, Greenland S. Meta-analysis of epidemiologic dose-response data. Epidemiology. 1993;4(3):218–28. https://doi.org/10.1097/00001648-199305000-00005 .
Orsini N, Bellocco R, Greenland SJTsj. Generalized least squares for trend estimation of summarized dose–response data 2006;6(1):40–57.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. Bmj. 2008;336(7650):924–6.
Abbasi R, Bakhshimoghaddam F, Alizadeh M. Major dietary patterns in relation to preeclampsia among Iranian pregnant women: a case–control study. J Matern Fetal Neonatal Med. 2021;34(21):3529–36.
Alves-Santos NH, Cocate PG, Benaim C, Farias DR, Emmett PM, Kac G. Prepregnancy dietary patterns and their association with perinatal outcomes: a prospective cohort study. J Acad Nutr Diet. 2019;119(9):1439–51.
Asadi M, Shahzeidi M, Nadjarzadeh A, Hashemi Yusefabad H, Mansoori A. The relationship between pre-pregnancy dietary patterns adherence and risk of gestational diabetes mellitus in Iran: a case–control study. Nutr Diet. 2019;76(5):597–603.
Bao W, Tobias DK, Olsen SF, Zhang C. Pre-pregnancy fried food consumption and the risk of gestational diabetes mellitus: a prospective cohort study. Diabetol. 2014;57(12):2485–91.
Bartáková V, Kuricová K, Zlámal F, Bělobrádková J, Kaňková K. Differences in food intake and genetic variability in taste receptors between Czech pregnant women with and without gestational diabetes mellitus. Eur J Nutr. 2018;57(2):513–21.
Brantsæter AL, Haugen M, Samuelsen SO, Torjusen H, Trogstad L, Alexander J, et al. A dietary pattern characterized by high intake of vegetables, fruits, and vegetable oils is associated with reduced risk of preeclampsia in nulliparous pregnant Norwegian women. J Nutr. 2009;139(6):1162–8.
Chen LW, Hu FB, Yeung E, Willett W, Zhang CL. Prospective study of pre-gravid sugar-sweetened beverage consumption and the risk of gestational diabetes mellitus. Diabetes Care. 2009;32(12):2236–41.
Chia AR, de Seymour JV, Colega M, Chen LW, Chan YH, Aris IM, et al. A vegetable, fruit, and white rice dietary pattern during pregnancy is associated with a lower risk of preterm birth and larger birth size in a multiethnic Asian cohort: the growing up in Singapore towards healthy outcomes (GUSTO) cohort study. Am J Clin Nutr. 2016;104(5):1416–23.
de Seymour J, Chia AR, Colega M, Jones B, McKenzie E, Cai SR, et al. Maternal dietary patterns and gestational diabetes mellitus in a multi-ethnic Asian cohort: the GUSTO study. Nutrients. 2016;8(9)
Dominguez LJ, Martinez-Gonzalez MA, Basterra-Gortari FJ, Gea A, Barbagallo M, Bes-Rastrollo M. Fast food consumption and gestational diabetes incidence in the SUN project. PLoS One. 2014;9(9):e106627.
Donazar-Ezcurra M, Lopez-del Burgo C, Martinez-Gonzalez MA, Basterra-Gortari FJ, de Irala J, Bes-Rastrollo M. Soft drink consumption and gestational diabetes risk in the SUN project. Clin Nutr. 2018;37(2):638–45.
Dong JY, Kimura T, Ikehara S, Cui M, Kawanishi Y, Yamagishi K, et al. Chocolate consumption and risk of gestational diabetes mellitus: the Japan environment and Children's study. Br J Nutr. 2019;122(8):936–41.
Drozd-Dąbrowska M, Trusewicz R, Ganczak M. Selected risk factors of developmental delay in polish infants: a case-control study. Int J Environ Res Public Health. 2018;15(12)
Du HY, Jiang H, Karmin O, Bo C, Xu LJ, Liu SP, et al. Association of dietary pattern during pregnancy and gestational diabetes mellitus: a prospective cohort study in northern China. Biomed Environ Sci. 2017;30(12):887–97.
CAS PubMed Google Scholar
Englund-Ögge L, Brantsæter AL, Sengpiel V, Haugen M, Birgisdottir BE, Myhre R, et al. Maternal dietary patterns and preterm delivery: Results from large prospective cohort study. BMJ (Online). 2014;348
Gete DG, Waller M, Mishra GD. Prepregnancy dietary patterns and risk of preterm birth and low birth weight: findings from the Australian longitudinal study on Women's health. Am J Clin Nutr. 2020;111(5):1048–58.
Grieger JA, Grzeskowiak LE, Clifton VL. Preconception dietary patterns in human pregnancies are associated with preterm delivery. J Nutr. 2014;144(7):1075–80.
Grundt JH, Eide GE, Brantsæter AL, Haugen M, Markestad T. Is consumption of sugar-sweetened soft drinks during pregnancy associated with birth weight? Mater Child Nutrit. 2017;13(4):e12405.
Hajianfar H, Esmaillzadeh A, Feizi A, Shahshahan Z, Azadbakht L. The association between major dietary patterns and pregnancy-related complications. Archiv Iran Med. 2018;21(10):443–51.
Hehua Z, Yang X, Qing C, Shanyan G, Yuhong Z. Dietary patterns and associations between air pollution and gestational diabetes mellitus. Environ Int. 2021;147
Hezaveh ZS, Feizy Z, Dehghani F, Sarbakhsh P, Moini A, Vafa M. The association between maternal dietary protein intake and risk of gestational diabetes mellitus. International journal of. Prev Med. 2019;10(1)
Hu JJ, Oken E, Aris IM, Lin PID, Ma YA, Ding N, et al. Dietary patterns during pregnancy are associated with the risk of gestational diabetes mellitus: evidence from a Chinese prospective birth cohort study. Nutrients. 2019;11(2)
Ikem E, Halldorsson TI, Birgisdóttir BE, Rasmussen MA, Olsen SF, Maslova E. Dietary patterns and the risk of pregnancy-associated hypertension in the Danish National Birth Cohort: a prospective longitudinal study. BJOG: An Int J Obstetr Gynaecol. 2019;126(5):663–73.
Kahr MK, Suter MA, Ballas J, Ramin SM, Monga M, Lee W, et al. Geospatial analysis of food environment demonstrates associations with gestational diabetes. Am J Obstet Gynecol. 2016;214(1):110.e1-.e9.
Lamyian M, Hosseinpour-Niazi S, Mirmiran P, Banaem LM, Goshtasebi A, Azizi F. Pre-pregnancy fast food consumption is associated with gestational diabetes mellitus among tehranian women. Nutrients. 2017;9(3)
Leone A, Martínez-González M, Craig W, Fresán U, Gómez-Donoso C, Bes-Rastrollo M. Pre-gestational consumption of ultra-processed foods and risk of gestational diabetes in a Mediterranean cohort. The SUN project. Nutrients. 2021;13(7)
Lotfi MH, Fallahzadeh H, Rahmanian M, Hosseinzadeh M, Lashkardoost H, Doaei S, et al. Association of food groups intake and physical activity with gestational diabetes mellitus in Iranian women. J Mater -Fetal Neonatal Med. 2020;33(21):3559–64.
Marí-Sanchis A, Díaz-Jurado G, Basterra-Gortari FJ, de la Fuente-Arrillaga C, Martínez-González MA, Bes-Rastrollo M. Association between pre-pregnancy consumption of meat, iron intake, and the risk of gestational diabetes: the SUN project. Eur J Nutr. 2018;57(3):939–49.
Martin CL, Sotres-Alvarez D, Siega-Riz AM. Maternal dietary patterns during the second trimester are associated with preterm birth. J Nutr. 2015;145(8):1857–64.
Nascimento GR, Alves LV, Fonseca CL, Figueiroa JN, Alves JG. Dietary patterns and gestational diabetes mellitus in a low income pregnant women population in Brazil - a cohort study. Archivos Latinoamericanos de Nutricion. 2016;66(4):301–8.
Osorio-Yáñez C, Gelaye B, Qiu C, Bao W, Cardenas A, Enquobahrie DA, et al. Maternal intake of fried foods and risk of gestational diabetes mellitus. Ann Epidemiol. 2017;27(6):384–90.e1.
Rasmussen MA, Maslova E, Halldorsson TI, Olsen SF. Characterization of dietary patterns in the Danish National Birth Cohort in relation to preterm birth. PLoS One. 2014;9(4)
Saftlas AF, Triche EW, Beydoun H, Bracken MB. Does chocolate intake during pregnancy reduce the risks of preeclampsia and gestational hypertension? Ann Epidemiol. 2010;20(8):584–91.
Santos IS, Victora CG, Huttly S, Carvalhal JB. Caffeine intake and low birth weight: a population-based case-control study. Am J Epidemiol. 1998;147(7):620–7.
Sartorelli DS, Crivellenti LC, Zuccolotto DCC, Franco LJ. Relationship between minimally and ultra-processed food intake during pregnancy with obesity and gestational diabetes mellitus. Cadernos de Saude Publica. 2019;35(4)
Schoenaker DA, Soedamah-Muthu SS, Callaway LK, Mishra GD. Pre-pregnancy dietary patterns and risk of gestational diabetes mellitus: results from an Australian population-based prospective cohort study. Diabetol. 2015;58(12):2726–35. https://doi.org/10.1007/s00125-015-3742-1 . Epub 2015 Sep 10.
Sedaghat F, Akhoondan M, Ehteshami M, Aghamohammadi V, Ghanei N, Mirmiran P, Rashidkhani B. Maternal Dietary Patterns and Gestational Diabetes Risk: A Case-Control Study. J Diabetes Res. 2017;2017:5173926. https://doi.org/10.1155/2017/5173926 . Epub 2017 Dec 6.
Tamada H, Ebara T, Matsuki T, Kato S, Sato H, Ito Y, et al. Ready-meal consumption during pregnancy is a risk factor for stillbirth: the Japan environment and Children’s study (JECS). Japan environment and Children’s study, Ready-Meal Consumption During Pregnancy is a Risk Factor for Stillbirth: The Japan Environment and Children’s Study (JECS).
Teixeira JA, Hoffman DJ, Castro TG, Saldiva S, Francisco RPV, Vieira SE, et al. Pre-pregnancy dietary pattern is associated with newborn size: results from ProcriAr study. Br J Nutr. 2021;126(6):903–12.
Triche EW, Grosso LM, Belanger K, Darefsky AS, Benowitz NL, Bracken MB. Chocolate consumption in pregnancy and reduced likelihood of preeclampsia. Epidemiol. 2008;19(3):459–64.
Tryggvadottir EA, Medek H, Birgisdottir BE, Geirsson RT, Gunnarsdottir I. Association between healthy maternal dietary pattern and risk for gestational diabetes mellitus. Eur J Clin Nutr. 2016;70(2):237–42.
Tsoi KY, Chan RSM, Tam CH, Li LS, Tam WH, Ma RCW. Dietary patterns of Chinese pregnant women in Hong Kong. Asia Pac J Clin Nutr. 2022;31(3):378–93.
Wahedy K, El Bilbeisi AHH, Bakry MJ. DIETARY PATTERNS and THEIR ASSOCIATION with GLYCEMIC CONTROL and RISK of GESTATIONAL DIABETES MELLITUS in GAZA STRIP, PALESTINE: a CASE-CONTROL STUDY. Bullet Pharmaceut Sci Assiut. 2021;44(2):537–49.
Wen L, Ge H, Qiao J, Zhang L, Chen X, Kilby MD, et al. Maternal dietary patterns and risk of gestational diabetes mellitus in twin pregnancies: a longitudinal twin pregnancies birth cohort study. Nutr J. 2020;19(1)
Yisahak SF, Hinkle SN, Mumford SL, Gleason JL, Grantz KL, Zhang C, et al. Periconceptional and first trimester Ultraprocessed food intake and maternal Cardiometabolic outcomes. Diabetes Care. 2022;45(9):2028–36.
Yong HY, Mohd Shariff Z, Mohd Yusof BN, Rejali Z, Tee YYS, Bindels J, van der Beek EM. Beverage Intake and the Risk of Gestational Diabetes Mellitus: The SECOST. Nutrients. 2021;13(7):2208. https://doi.org/10.3390/nu13072208 .
Zareei S, Homayounfar R, Naghizadeh MM, Ehrampoush E, Amiri Z, Rahimi M, et al. Dietary pattern in patients with preeclampsia in Fasa. Iran Shiraz E Med J. 2019;20(11)
Zareei S, Homayounfar R, Naghizadeh MM, Ehrampoush E, Rahimi M. Dietary pattern in pregnancy and risk of gestational diabetes mellitus (GDM). Diabet Metabol Syndrome: Clin Res Rev. 2018;12(3):399–404.
Zhang C, Schulze MB, Solomon CG, Hu FB. A prospective study of dietary patterns, meat intake and the risk of gestational diabetes mellitus. Diabetologia. 2006;49(11):2604-13. https://doi.org/10.1007/s00125-006-0422-1 . Epub 2006 Sep 7.
Zuccolotto DCC, Crivellenti LC, Franco LJ, Sarotelli DS. Dietary patterns of pregnant women, maternal excessive body weight and gestational diabetes. Revista de Saude Publica. 2019;53.
Moradi S, Hojjati Kermani MA, Bagheri R, Mohammadi H, Jayedi A, Lane MM, et al. Ultra-processed food consumption and adult diabetes risk: a systematic review and dose-response Meta-analysis. Nutrients. 2021;13(12)
Suksatan W, Moradi S, Naeini F, Bagheri R, Mohammadi H, Talebi S, Mehrabani S, Hojjati Kermani MA, Suzuki K. Ultra-Processed Food Consumption and Adult Mortality Risk: A Systematic Review and Dose-Response Meta-Analysis of 207,291 Participants. Nutrients. 2021;14(1):174. https://doi.org/10.3390/nu14010174 .
Babaei A, Pourmotabbed A, Talebi S, Mehrabani S, Bagheri R, Ghoreishy SM, et al. The association of ultra-processed food consumption with adult inflammatory bowel disease risk: a systematic review and dose-response meta-analysis of 4 035 694 participants. Nutr Rev. 2023;
Umesawa M, Kobashi G. Epidemiology of hypertensive disorders in pregnancy: prevalence, risk factors, predictors and prognosis. Hyperten res: official j Japan Soc Hypert. 2017;40(3):213–20.
Sutan R, Aminuddin NA, Mahdy ZA. Prevalence, maternal characteristics, and birth outcomes of preeclampsia: a cross-sectional study in a single tertiary healthcare center in greater Kuala Lumpur Malaysia. Front Public Health. 2022;10:973271.
Bodnar LM, Ness RB, Markovic N, Roberts JM. The risk of preeclampsia rises with increasing prepregnancy body mass index. Ann Epidemiol. 2005;15(7):475–82.
Catalano PM, McIntyre HD, Cruickshank JK, McCance DR, Dyer AR, Metzger BE, et al. The hyperglycemia and adverse pregnancy outcome study: associations of GDM and obesity with pregnancy outcomes. Diabetes Care. 2012;35(4):780–6.
Perry A, Stephanou A, Rayman MP. Dietary factors that affect the risk of pre-eclampsia. BMJ nutrit prevent health. 2022;5(1):118–33.
Martini D, Godos J, Bonaccio M, Vitaglione P, Grosso G. Ultra-processed foods and nutritional dietary profile: a Meta-analysis of nationally representative samples. Nutrients. 2021;13(10)
Maldonado-Pereira L, Barnaba C, de Los CG, Medina-Meza IG. Evaluation of the nutritional quality of ultra-processed foods (ready to eat + fast food): fatty acids, sugar, and sodium. J Food Sci. 2022;87(8):3659–76.
Monguchi T, Hara T, Hasokawa M, Nakajima H, Mori K, Toh R, et al. Excessive intake of trans fatty acid accelerates atherosclerosis through promoting inflammation and oxidative stress in a mouse model of hyperlipidemia. J Cardiol. 2017;70(2):121–7.
Ma X, Nan F, Liang H, Shu P, Fan X, Song X, et al. Excessive intake of sugar: an accomplice of inflammation. Front Immunol. 2022;13:988481.
Wojcik M, Krawczyk M, Zieleniak A, Mac Marcjanek K, Wozniak LA. Chapter 14 - associations of high blood sugar with oxidative stress and inflammation in patients with type 2 diabetes. In: Preuss HG, Bagchi D, editors. Dietary Sugar Salt and Fat in Human Health. Academic Press; 2020. p. 305–23.
Chapter Google Scholar
Chiarello DI, Abad C, Rojas D, Toledo F, Vázquez CM, Mate A, et al. Oxidative stress: Normal pregnancy versus preeclampsia. Biochim Biophys Acta (BBA)-Mol Basis Dis. 2020;1866(2):165354.
Harmon AC, Cornelius DC, Amaral LM, Faulkner JL, Cunningham MW, Jr., Wallace K, et al. The role of inflammation in the pathology of preeclampsia. Clinical science (London, England : 1979). 2016;130(6):409–19.
Patik JC, Lennon SL, Farquhar WB, Edwards DG. Mechanisms of dietary sodium-induced impairments in Endothelial function and potential countermeasures. Nutrients. 2021;13(1)
Shuto E, Taketani Y, Tanaka R, Harada N, Isshiki M, Sato M, et al. Dietary phosphorus acutely impairs endothelial function. J Am Soc Nephrol: JASN. 2009;20(7):1504–12.
Lopez-Garcia E, Schulze MB, Meigs JB, Manson JE, Rifai N, Stampfer MJ, et al. Consumption of trans fatty acids is related to plasma biomarkers of inflammation and Endothelial Dysfunction1. J Nutr. 2005;135(3):562–6.
Lamarca B. Endothelial dysfunction. An important mediator in the pathophysiology of hypertension during pre-eclampsia. Minerva Ginecol 2012;64(4):309–20.
Fernandes AE, Rosa PWL, Melo ME, Martins RCR, Santin FGO, Moura AMSH, et al. Differences in the gut microbiota of women according to ultra-processed food consumption. Nutr Metab Cardiovasc Dis. 2023;33(1):84–9. https://doi.org/10.1016/j.numecd.2022.09.025 . Epub 2022 Oct 11.
Whelan K, Bancil AS, Lindsay JO, Chassaing B. Ultra-processed foods and food additives in gut health and disease. Nat Rev Gastroenterol Hepatol. 2024;22:1–22.
Fan M, Li X, Gao X, Dong L, Xin G, Chen L, et al. LPS induces preeclampsia-like phenotype in rats and HTR8/SVneo cells dysfunction through TLR4/p38 MAPK pathway. Front Physiol. 2019;10:1030.
Jin J, Gao L, Zou X, Zhang Y, Zheng Z, Zhang X, et al. Gut Dysbiosis promotes preeclampsia by regulating macrophages and trophoblasts. Circ Res. 2022;131(6):492–506.
Kell DB, Kenny LC. A dormant microbial component in the development of preeclampsia. Front Med. 2016;3:60.
Rauber F, Chang K, Vamos EP, da Costa Louzada ML, Monteiro CA, Millett C, et al. Ultra-processed food consumption and risk of obesity: a prospective cohort study of UK biobank. Eur J Nutr. 2021;60(4):2169–80.
Wondmkun YT. Obesity, insulin resistance, and type 2 diabetes: associations and therapeutic implications. Diabet metab syndrome obes: targets therapy. 2020;13:3611–6.
Teran E, Escudero C, Moya W, Flores M, Vallance P, Lopez-Jaramillo P. Elevated C-reactive protein and pro-inflammatory cytokines in Andean women with pre-eclampsia. Int J Gynecol Obstet. 2001;75(3):243–9.
Palei AC, Spradley FT, Granger JP. Chronic hyperleptinemia results in the development of hypertension in pregnant rats. Am J Phys Regul Integr Comp Phys. 2015;308(10):R855–R61.
CAS Google Scholar
Olson KN, Redman LM, Sones JL. Obesity "complements" preeclampsia. Physiol Genom. 2019;51(3):73–6.
Wang X, Cheng Z. Cross-sectional studies: strengths, weaknesses, and recommendations. Chest. 2020;158(1 Supplement):S65–71.
Mozaffarian D, Ludwig DS. Dietary guidelines in the 21st century—a time for food. Jama. 2010;304(6):681–2.
Wang H, Li N, Chivese T, Werfalli M, Sun H, Yuen L, et al. IDF diabetes atlas: estimation of global and regional gestational diabetes mellitus prevalence for 2021 by International Association of Diabetes in pregnancy study Group's criteria. Diabetes Res Clin Pract. 2022;183:109050.
Kityo A, Lee SA. The intake of ultra-processed foods and prevalence of chronic kidney disease: the health examinees study. Nutrients. 2022;14(17)
Nardocci M, Leclerc B-S, Louzada M-L, Monteiro CA, Batal M, Moubarac J-C. Consumption of ultra-processed foods and obesity in Canada. Can J Public Health. 2019;110:4–14.
Rauber F, Louzada MLC, Steele EM, Millett C, Monteiro CA, Levy RB. Ultra-processed food consumption and chronic non-communicable diseases-related dietary nutrient profile in the UK (2008–2014). Nutrients. 2018;10(5):587.
Lavigne-Robichaud M, Moubarac J-C, Lantagne-Lopez S, Johnson-Down L, Batal M, Sidi EAL, et al. Diet quality indices in relation to metabolic syndrome in an indigenous Cree (Eeyouch) population in northern Québec. Canada Pub health nutrit. 2018;21(1):172–80.
Sun Y, Shen Z, Zhan Y, Wang Y, Ma S, Zhang S, et al. Effects of pre-pregnancy body mass index and gestational weight gain on maternal and infant complications. BMC pregnan childbirth. 2020;20(1):1–13.
Linder T, Eder A, Monod C, Rosicky I, Eppel D, Redling K, et al. Impact of prepregnancy overweight and obesity on treatment modality and pregnancy outcome in women with gestational diabetes mellitus. Front Endocrinol. 2022;13:799625.
Najafi F, Hasani J, Izadi N, Hashemi-Nazari S-S, Namvar Z, Shamsi H, et al. Risk of gestational diabetes mellitus by pre-pregnancy body mass index: a systematic review and meta-analysis. Diabet Metab Syndrome: Clin Res Rev. 2021;15(4):102181.
McIntyre HD, Catalano P, Zhang C, Desoye G, Mathiesen ER, Damm P. Gestational diabetes mellitus. Nat Rev Dis Primers. 2019;5(1):47.
Plows JF, Stanley JL, Baker PN, Reynolds CM, Vickers MH. The pathophysiology of gestational diabetes mellitus. Int J Mol Sci. 2018;19(11):3342.
Stanhope KL. Sugar consumption, metabolic disease and obesity: the state of the controversy. Crit Rev Clin Lab Sci. 2016;53(1):52–67.
Bhattacharyya S, I OS, Katyal S, Unterman T, Tobacman JK. Exposure to the common food additive carrageenan leads to glucose intolerance, insulin resistance and inhibition of insulin signalling in HepG2 cells and C57BL/6J mice. Diabetologia. 2012;55(1):194–203.
Quetglas-Llabrés MM, Monserrat-Mesquida M, Bouzas C, Mateos D, Ugarriza L, Gómez C, et al. Oxidative stress and inflammatory biomarkers are related to high intake of ultra-processed food in old adults with metabolic syndrome. Antioxidants (Basel, Switzerland). 2023;12(8).
Yaribeygi H, Sathyapalan T, Atkin SL, Sahebkar A. Molecular mechanisms linking oxidative stress and diabetes mellitus. Oxidative Med Cell Longev. 2020;2020:8609213.
Bertoli S, Leone A, Battezzati A. Human bisphenol a exposure and the “diabesity phenotype”. Dose-Response. 2015;13(3):1559325815599173.
Rolfo A, Nuzzo AM, De Amicis R, Moretti L, Bertoli S, Leone A. Fetal–maternal exposure to endocrine disruptors: correlation with diet intake and pregnancy outcomes. Nutrients. 2020;12(6):1744.
Lorenzo PI, Martín-Montalvo A, Cobo Vuilleumier N, Gauthier BR. Molecular modelling of islet β-cell adaptation to inflammation in pregnancy and gestational diabetes mellitus. Int J Mol Sci. 2019;20(24)
Christ A, Lauterbach M, Latz E. Western diet and the immune system: an inflammatory connection. Immunity. 2019;51(5):794–811.
Neale E, Batterham M, Tapsell LC. Consumption of a healthy dietary pattern results in significant reductions in C-reactive protein levels in adults: a meta-analysis. Nutr Res. 2016;36(5):391–401.
Liu Z, Lu Y, Zhong K, Wang C, Xu X. The associations between endocrine disrupting chemicals and markers of inflammation and immune responses: a systematic review and meta-analysis. Ecotoxicol Environ Saf. 2022;234:113382.
Node K, Inoue T. Postprandial hyperglycemia as an etiological factor in vascular failure. Cardiovasc Diabetol. 2009;8:23.
Hu Z, Tylavsky FA, Kocak M, Fowke JH, Han JC, Davis RL, et al. Effects of maternal dietary patterns during pregnancy on early childhood growth trajectories and obesity risk: the CANDLE study. Nutrients. 2020;12(2)
Wang Y, Wang K, Du M, Khandpur N, Rossato SL, Lo C-H, et al. Maternal consumption of ultra-processed foods and subsequent risk of offspring overweight or obesity: results from three prospective cohort studies. Bmj. 2022:379.
Paula WO, Gonçalves VSS, Patriota ESO, Franceschini SCC, Pizato N. Impact of ultra-processed food consumption on quality of diet among Brazilian pregnant women assisted in primary health care. Int J Environ Res Public Health. 2023;20(2)
Crume TL, Brinton JT, Shapiro A, Kaar J, Glueck DH, Siega-Riz AM, et al. Maternal dietary intake during pregnancy and offspring body composition: the healthy start study. Am J Obstet Gynecol. 2016;215(5):609–e1-e8.
Article PubMed Central Google Scholar
Wan Y, Chen Y, Wu X, Yin A, Tian F, Zhang H, et al. Mediation effect of maternal triglyceride and fasting glucose level on the relationship between maternal overweight/ obesity and fetal growth: a prospective cohort study. BMC Pregnancy and Childbirth. 2023;23(1):449.
Akbari Z, Mansourian M, Kelishadi R. Relationship of the intake of different food groups by pregnant mothers with the birth weight and gestational age: need for public and individual educational programs. J educ health promot. 2015;4:23.
Fischer S, Morales-Suárez-Varela M. The bidirectional relationship between gestational diabetes and depression in pregnant women: a systematic search and review. Healthcare (Basel, Switzerland). 2023;11(3).
Khan R, Waqas A, Bilal A, Mustehsan ZH, Omar J, Rahman A. Association of Maternal depression with diet: a systematic review. Asian J Psychiatr. 2020;52:102098.
Ancira-Moreno M, O'Neill MS, Rivera-Dommarco J, Batis C, Rodríguez Ramírez S, Sánchez BN, et al. Dietary patterns and diet quality during pregnancy and low birthweight: the PRINCESA cohort. Matern Child Nutr. 2020;16(3):e12972.
Download references
Acknowledgments
Author information, authors and affiliations.
Students’ Scientific Research Center (SSRC), Tehran University of Medical Sciences, Tehran, Iran
Sepide Talebi
Department of Clinical Nutrition, School of Nutritional Sciences and Dietetics, Tehran University of Medical Sciences, Tehran, Iran
Food Security Research Center, Isfahan University of Medical Sciences, Isfahan, Iran
Sanaz Mehrabani
Department of Nutrition, School of Public Health, Iran University of Medical Sciences, Tehran, Iran
Seyed Mojtaba Ghoreishy
Student research committee, School of Public Health, Iran University of Medical Sciences, Tehran, Iran
Department of Health and Human Performance, Marymount University, Arlington, VA, USA
Alexei Wong
Department of Clinical Sciences, Faculty of Veterinary Medicine, Razi University, Kermanshah, Iran
Aliasghar Moghaddam & Peyman Rahimi Feyli
General Practitioner, Kermanshah University of Medical Sciences (KUMS), Kermanshah, Iran
Parsa Amirian & Mahsa Zarpoosh
Clinical Tuberculosis and Epidemiology Research Center, National Research Institute of Tuberculosis and Lung Diseases (NRITLD), Masih Daneshvari Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Mohammad Ali Hojjati Kermani
Department of Nutrition and Food Sciences, Research Center for Evidence-Based Health Management, Maragheh University of Medical Sciences, Maragheh, Iran
Sajjad Moradi
You can also search for this author in PubMed Google Scholar
Contributions
SM and ST designed this study. SM, MZ and PA contributed to the conduct of the search. SM and ST performed the statistical analysis and interpreted the results. SM, SM-GH, Sanaz Merabani, and MA-HK wrote the initial manuscript. AW, AM and PR_F critically revised the manuscript and contributed to the subsequent drafts of the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Correspondence to Sajjad Moradi .
Ethics declarations
Ethics approval and consent to participate.
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., supplementary material 3., supplementary material 4., supplementary material 5., supplementary material 6., supplementary material 7., supplementary material 8., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Talebi, S., Mehrabani, S., Ghoreishy, S.M. et al. The association between ultra-processed food and common pregnancy adverse outcomes: a dose-response systematic review and meta-analysis. BMC Pregnancy Childbirth 24 , 369 (2024). https://doi.org/10.1186/s12884-024-06489-w
Download citation
Received : 18 January 2024
Accepted : 07 April 2024
Published : 15 May 2024
DOI : https://doi.org/10.1186/s12884-024-06489-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Ultra-processed foods
- Gestational diabetes mellitus
- Preeclampsia
- Preterm birth
BMC Pregnancy and Childbirth
ISSN: 1471-2393
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Open access
- Published: 09 May 2024
Overlooked by the obstetric gaze – how women with persistent health problems due to severe perineal trauma experience encounters with healthcare services: a qualitative study
- Katharina Tjernström 1 ,
- Inger Lindberg 1 ,
- Maria Wiklund 2 &
- Margareta Persson 1
BMC Health Services Research volume 24 , Article number: 610 ( 2024 ) Cite this article
102 Accesses
Metrics details
During the first year postpartum, about 25 per cent of Swedish women with severe perineal trauma (SPT), i.e., a third- or fourth-degree perineal laceration at childbirth, are unsatisfied with their healthcare contacts. Further, there is a lack of research on the more long-term experiences of healthcare encounters among women with persistent SPT-related health problems. This study explores how women with self-reported persistent SPT-related health problems experience their contact with healthcare services 18 months to five years after childbirth when the SPT occurred.
In this descriptive qualitative study, a purposive sample of twelve women with self-reported persistent health problems after SPT were individually interviewed from November 2020 – February 2022. The data was analysed using inductive qualitative content analysis.
Our results showed a paradoxical situation for women with persistent health problems due to SPT. They struggled with their traumatised body, but healthcare professionals rejected their health problems as postpartum normalities. This paradox highlighted the women’s difficulties in accessing postpartum healthcare, rehabilitation, and sick leave, which left them with neglected healthcare needs, diminished emotional well-being, and loss of financial and social status. Our results indicated that these health problems did not diminish over time. Consequently, the women had to search relentlessly for a ‘key person’ in healthcare who acknowledged their persistent problems as legitimate to access needed care, rehabilitation, and sick leave, thus feeling empowered.
Conclusions
Our study revealed that women with persistent SPT-related health problems experienced complex health challenges. Additionally, their needs for medical care, rehabilitation, and sick leave were largely neglected. Thus, the study highlights an inequitable provision of SPT-related healthcare services in Sweden, including regional disparities in access to care. Hence, the authors suggest that Swedish national guidelines for SPT-related care need to be developed and implemented, applying a woman-centered approach, to ensure equitable, effective, and accessible healthcare.
Peer Review reports
Intrapartum and postpartum healthcare should ideally be high-quality, evidence-based, and a positive experience stemming from woman-centred care with a holistic approach based on human rights [ 1 ]. This approach acknowledges each woman’s articulated needs and expectations in her social, emotional, physical, spiritual, and cultural context [ 2 ]. Nevertheless, during the first year postpartum, about one in four Swedish women with severe perineal trauma (SPT) [ 3 ], i.e., a third- or fourth-degree perineal laceration involving the anal sphincter muscle and anorectal mucosa at vaginal childbirth [ 4 ], are dissatisfied with their care and one in three women report ongoing health problems related to their SPT. Women with SPT may suffer from various physiological and psychological consequences such as pain [ 5 , 6 ] , incontinence [ 7 ], defecation problems [ 8 ], vaginal prolapse [ 5 ], sexual dysfunction [ 9 ] or depression and anxiety [ 10 , 11 , 12 ].
Reducing physical symptoms is essential to support emotional and social recovery after any perineal trauma [ 13 , 14 ]. Women with SPT emphasise that professional, competent, and respectful attitudes from healthcare professionals (HCPs), including individual and adapted information, facilitate, and promote their postpartum recovery. Thus, the HCPs’ competence and knowledge of treatment options is a prerequisite for women to access needed care [ 15 ]. An additional problem in the Swedish context is the lack of national recommendations or guidelines, which enables each of the 21 regions to develop own regional and local guidelines. An audit of the existing regional and local guidelines for prevention and care of SPT shows an unexpected diversity or lack of evidence-based recommendations [ 16 ]. However, dissatisfaction with access to healthcare has been expressed by women with persistent, i.e., beyond one year postpartum, SPT-related health problems [ 6 , 17 ]. Furthermore, women criticise inadequate or absent support [ 6 , 18 ], poor information and education [ 6 , 10 , 18 ], and lack of follow-up care regarding SPT and its potential psychological and social consequences [ 6 , 10 ]. Postpartum care focuses more on the baby than the mother’s well-being [ 18 , 19 ]. Also, the available treatment options are perceived as limited and outdated by those with access to needed care [ 17 , 18 ]. Moreover, women with SPT describe that some HCPs tend to normalise their SPT-related problems [ 10 , 17 , 18 , 19 , 20 , 21 , 22 ], and women are met in unprofessional and disrespectful ways [ 17 , 23 ], where HCPs are perceived as ignorant, nonchalant, and questioning women’s symptoms [ 10 , 17 ]. Previous research [ 24 ] indicates an institutional objectification of women with SPT by Swedish healthcare providers hindering access to healthcare, sick leave, and occupational rehabilitation after SPT. In contrast, women also report being acknowledged and liberated when HCPs have a professional and empathic approach and provide continuity of care that enables access to care for persistent SPT-related health problems [ 17 , 18 , 19 , 25 ]. Thus, several women who sustained an SPT during childbirth do not experience access to needed and necessary care, a fact that needs further exploration.
Globally, sexual and reproductive health and rights (SRHR) are crucial for individual health and gender equality [ 26 ]. Current issues within SRHR and midwifery are controlled by the institutional power in health institutions, i.e., medical power [ 27 ], connected to the still-existing economic and educational disadvantages of women globally, which are also feminist issues [ 26 , 28 ]. As midwife stands for ‘with woman’ [ 28 ], gender or feminist approaches are used in advancing midwifery theory [ 27 , 29 ] and various aspects of SRHR topics such as breastfeeding promotion [ 30 ], birth plans [ 31 ] and attitudes towards contraceptives [ 32 ]. In midwifery and feminist approaches, the biological material body and the socially constructed gendered body are viewed as intertwined [ 33 ]. Moreover, midwifery care is recommended to be woman-centred [ 1 , 2 ], focusing on the individual woman’s needs and transferring control from the institution to the woman herself. However, despite the different organisations of sexual and reproductive healthcare between countries, international research shows similar results regarding women’s diverging experiences with postpartum SPT-related healthcare [ 6 , 15 , 17 , 18 ].
In sum, there is growing evidence showing that many women with persisting health problems caused by SPT are often, but not always, met with mistrust and ignorance when seeking care for their problems. Even though there may be national, regional, or local protocols or guidelines for care after SPT, women with persistent SPT-related problems still raise their voices about the difficulty of getting access to competent quality care. This indicates a potential gender bias [ 34 ] and a need for gender theoretical perspectives in midwifery [ 28 ], as utilized in this study. Additionally, few studies explore the care-seeking experience among this group of women in a longer time perspective after childbirth when the SPT occurred.
The aim of this study is to explore how women with self-reported persistent SPT-related health problems experience their contact with healthcare services 18 months to five years after childbirth when the SPT occurred.
Study design and context
The present study is part of a larger research project investigating the long-term consequences of SPT on quality of life, working life, and healthcare contacts. This study had an inductive qualitative interview study design applying qualitative content analysis to analyse data [ 35 , 36 , 37 ]. This method searches for patterns, e.g., by identifying similarities and differences in the data. The researchers obtain an in-depth understanding of the studied phenomenon through abstraction and interpretation [ 36 ]; thus, an appropriate method to apply to capture women’s experiences of their healthcare encounters when seeking medical help and support. Throughout the research process, the recommendations for qualitative research according to ‘Consolidated criteria for reporting qualitative research’ (COREQ) were followed [ 38 ].
Sweden has 21 partly independent regions primarily responsible for providing healthcare services to the population. Healthcare services are tax-funded, and the regions have extensive autonomy to decide upon the healthcare services within each region based on the frameworks of the Health and Medical Service Act [ 39 ]. Additionally, within the Swedish social security system, 480 days of paid parental leave are allocated to each child in Sweden and can be utilised by their legal guardian(s) until the child is twelve years old. Of these 480 days, 60 days are specifically assigned to each parent, and the remaining days are split between parents as desired. The financial compensation is based on the parent’s income and is financed by taxes [ 40 ].
In Sweden, midwives are the primary care providers to women with normal pregnancies, births, and postpartum care. In case of complications to pregnancy and childbirth, midwives collaborate with other medical professionals, especially obstetricians. For example, midwives suture first- and second-degree perineal lacerations, while obstetricians are responsible for all SPT repairs [ 41 ]. Generally, in Sweden, women who sustain an SPT during childbirth are offered a check-up with the obstetrician responsible for the repair before discharge and should also have a follow-up with an obstetrician or sometimes a physiotherapist within the postnatal period. Thereafter, women with no mayor initial healing problems are advised to contact relevant healthcare services if any health issues related to the SPT should arise in the future. Women presenting with complicated healing are treated accordingly. Additionally, women with second- to fourth-degree perineal lacerations are assessed with questionnaires three times during the first year postpartum by the National Perineal Laceration Register. However, there are no recommendations in Sweden for prolonged check-ups for women with SPT after the postnatal period and no guidelines on organised check-ups for women with prolonged symptoms due to SPT exist [ 42 , 43 ].
Women with persistent SPT-related health problems and characteristics were purposively recruited to achieve a heterogeneous sample reflecting multiple experiences. An overview of inclusion and exclusion criteria can be found in Table 1 .
The closed Swedish Facebook community ‘Förlossningsskadad? Du är inte ensam!’ [‘Injured at childbirth? You are not alone!’] functioned as a recruitment platform for a national sample of women reporting persistent SPT-related health problems. The Facebook community is secluded to women with SPT and started in 2014. During the data collection period (Nov 2020 – Feb 2022), the group had over 7,600 members; today, the community has grown to include over 9,500 members [ 44 ].
In late November 2020, the administrators of the Facebook community pinned a digital poster with study information and a link to the study homepage in the group feed. The study homepage contained written information on the research project and contact details for the research group if any women wanted additional information about the study. Interested potential participants contacted the research group via a contact form on the homepage, and the first author (KT) confirmed that the potential participants met the inclusion criteria via telephone. Thirteen participants from different parts of Sweden showed interest in participating and left their contact information. One woman never responded to our efforts to reach her. The remaining twelve women fulfilled the inclusion criteria and were invited to an interview. Before the interview, the women answered a digital survey on background data (such as demographic data, education, employment, sick leave, and childbirth history) distributed via REDCap ® , a web-based application to create secure online questionnaires and research databases [ 45 ]. The interviews were finalised in February 2022.
Data collection
We collected data via individual open-ended interviews [ 46 ], supported by a semi-structured interview guide [see Additional file 1 ]. The interview guide, developed by KT and MP with input from MW and IL, was based on literature reviews, our awareness of gender as a social construct [ 33 ], and the clinical pre-understanding within the research group. After a pilot interview conducted by KT (not included in the data), minor adjustments were made to the interview guide. The final interview guide covered the topics of everyday life experiences, work, and general functioning. However, despite the mentioned interview topics, the emergent study design and the ability to speak freely about what was perceived as important for their daily functioning, the contacts with healthcare services was brought up in vivid and extensive narratives by all participants as part of their descriptions of their challenges in everyday life and their ability to function at work. Hence, the experiences the women made of the healthcare services played an important role for the women in their daily management of SPT-related health problems.
As data collection occurred during the COVID-19 pandemic, all participants were interviewed digitally via Zoom ® [ 47 , 48 ]. With the participant’s consent, the interviews were audio-recorded via Zoom ® and a separate digital recorder (as backup). Any Zoom video files automatically generated were deleted directly after the termination of the interview to protect participants’ identities. The first author interviewed all women; in two interviews, co-authors (IL or MW) also attended. The authors had no professional or personal affiliation with the enrolled participants . Detailed interviews ranging from 29 – 112 minutes (median: 61.5 minutes) gave extensive data. All interviews were performed in Swedish and transcribed verbatim. After that, the first author validated the transcripts for accuracy by reviewing the text while listening to the recordings.
Authors’ pre-understanding and theoretical positionality
The research group comprises three midwives (KT, IL, MP) and one physiotherapist (MW). We all have extensive professional experiences from clinical practice in primary and in-patient care, where three authors (KT, IL, MP) have specific professional experiences of caring for women with SPT. Additionally, we are women, feminists, and mothers with various birth experiences. Further, the group holds expertise in gender studies and qualitative research within midwifery science, such as perineal trauma and medical sociology. Hence, we stem from a social constructivist research standpoint and utilise ourselves as co-constructors in the analysis process. As feminist researchers, we apply a gender theoretical lens to the data.
Data analysis
The interviews were analysed using qualitative content analysis with an inductive and stepwise approach focusing on the manifest and latent content [ 35 , 36 , 37 ]. The interviews, transcripts, and analysis steps were performed in Swedish.
The analytical procedure started with reading the transcripts multiple times while highlighting text, meaning units, with content relevant to the aim of this study. Then, identified meaning units were condensed, focusing on preserving their core meaning and labelled with manifest codes [ 35 , 36 , 37 ]. Initially, KT coded one interview and triangulated those codes with the principal investigator (MP). KT then coded the rest of the interviews. In the next step, similar codes were clustered, forming subcategories based on the manifest content. Moving towards an interpretation of the content, categories were created by the abstraction of subcategories. This was done by KT and MP separately and then triangulated to identify significant concepts. Next, the preliminary categories and subcategories were triangulated with the whole research group until a consensus was obtained. To answer the question of ‘what?’ and ‘how?’ within the data, the latent content and thread of meaning were identified by clustering and abstracting the emerging findings to form subthemes and a theme [ 36 , 37 ]. The emerging findings were also peer-reviewed and discussed at a research seminar. The finalisation of the analysis resulted in an overarching theme and four subthemes. The translation of categories, subthemes, theme and inserted citations from Swedish into English was performed as a last step. The translation and choice of words were discussed between authors (all knowledgeable in English) to reach a consensus and minimise translation bias.
During the coding process, the researchers used MAXQDA ® [ 49 ], a software for organising, transcribing, analysing, and visualising qualitative research data, and Microsoft Excel ® [ 50 ] as aids to organise the codes.
Demographics of included participants
The background characteristics of the twelve participants in the final sample are presented in Table 2 .
The participants identified themselves as cis women, i.e., their gender identity matched their sex assigned at birth [ 51 ], and are thus referred to as ‘women’ in this paper. All women were in a partner relationship. The women reported a broad spectrum of physical and phycological health problems following the SPT at childbirth, e.g., urine or anal incontinence, pain in the lower abdomen, sexual dysfunction, and depression. Thirty per cent of the women had full-time employment, and the proportion of parental leave varied from 12% to 100% (three women had an ongoing parental leave with subsequent children at the interview). Further, 60% of the women had a sedentary occupation. Five women had been on sick leave after reconstructive surgery, and five reported sick leave for other reasons than their SPT.
The analysis resulted in one theme, ‘Overlooked by the obstetric gaze – living the paradox of a normalised but traumatised postpartum body’, with related subthemes ‘Questioning whether it’s all in my head’, ‘Fighting persistently for access and legitimacy in no (wo)man's-land’, ‘Facing multidimensional losses when no help in sight’, and ‘Depending on other’s advocacy to navigate an arbitrary system’. An overview of the findings is presented in Table 3 . The findings are presented as an overarching theme and thereafter, the related subthemes and categories. Citations from the participants illustrate the findings. All women have been allocated pseudonyms in the result presentation.
Overlooked by the obstetric gaze – living the paradox of a normalised but traumatised postpartum body
The latent theme ‘Overlooked by the obstetric gaze – living the paradox of a normalised but traumatised postpartum body’ represented the women’s experiences of healthcare encounters covering HCPs’ diminishing attitudes towards women’s persistent SPT-related health problems and the women’s difficulties accessing healthcare and sick leave. We interpreted that the women were assessed by the HCPs’ ‘obstetric gaze’, i.e., a medical gaze in postpartum healthcare normalising their persistent health problems and judging the women’s lower abdomen as ‘fine’ by their looks. The obstetric gaze put the women in a paradoxical situation where HCPs normalised tangible symptoms to be a natural part of childbirth. With no medical legitimacy of the health problems, the women also felt labelled as ‘hysterical’ (exaggerating health problems) by the HCPs. As a result, on the one hand, they had to continue facing persistent and tangible health problems such as incontinence, pain or prolapses. On the other hand, no acknowledgement by HCPs of their health problems led them to question whether their problems were merely a product of their imagination and, thus, only existed ‘in their head’. The theme also comprised women’s struggle for legitimacy in a gendered healthcare system - a no-(wo)man's land. They experienced that healthcare services and social insurance systems were challenging to access and demanded a tenacious and extensive fight to obtain legitimacy for their health problems. Consequently, the women had to put up with neglected healthcare needs, negatively impacting their physical and emotional well-being, and financial and social status when no medical help or rehabilitation was available. However, some women had encountered an HCP who was empathic and understanding, hence not guided by the obstetric gaze. Such encounters legitimised persistent problems and were crucial for accessing needed care, sick leave, and rehabilitation.
Questioning whether it’s all in my head
The subtheme ‘Questioning whether it’s all in my head’ focused on the women’s experiences of facing ignoration and no confirmation of perceived health problems and thus being labelled as a hysterical woman. The related categories referred to a normalisation process that the women experienced in their encounters with HCPs, which made them question their bodily perceptions. Furthermore, the women felt accused of exaggerating symptoms because their persistent SPT-related health problems did not match HPCs’ views of acceptable postpartum symptoms. Thus, it could be understood that the women found themselves in a paradox of suffering from tangible physical consequences after SPT, which were normalised by HCPs and their ‘obstetric gaze’.
Facing HCP's ignoration of perceived problems
The women experienced the HCPs defining their persistent health problems after the SPT as ‘normal’. The HCPs assured the women that their problems would disappear with time or that transient motherhood-related aspects, such as breastfeeding or fragile vaginal mucosa, were the cause of the problem. One woman expressed:
“Then I felt, ‘It should not feel like this; this is something wrong’, and I sought medical attention and was seen by multiple physicians […] They thought my vaginal mucous membrane was not ready for intercourse. I was still breastfeeding, so they thought I should stop breastfeeding. Then maybe the mucous membrane would be restored, which was causing me the pain. I was not listened to at all. I was treated very poorly by one physician in particular, and despite second opinions and so on, nobody… nobody took me seriously.” (Linda)
Consequently, the women perceived that their concerns were ignored. They also learned that the HCPs saw their prolonged physical problems after SPT as an inevitable part of childbirth, which the women should accept. One woman resigned:
“But then [the physician] says something like this: ’Well, that's completely normal’, but I felt like, ‘Yes, but it doesn't feel normal'.” (Emma)
After the genital and pelvic floor examinations, the HCPs often guaranteed the women that ‘everything looked fine’, i.e., reinforcing the normality of the genital area. Although the women described to the HCPs that they struggled with SPT-related problems, their concerns were met with a comment on the physical appearance rather than a comprehensive examination of the pelvic floor's functionality.
One woman responded:
“They think ‘everything looks fine’ and ‘everything looks good and repaired’. I still have problems. I was also referred to a surgeon, who did a rectoscopy, and ‘it looked so nice’. Then, I was referred to a urotherapist to learn how to pinch my muscles because ‘everything would be so good’. She helped me get a second opinion in XX [town], where they discovered that there was still damage." (Jin)
Another woman expressed:
”I couldn’t care less what it [genital area] looks like. Nobody will be down there watching. I only need it [genital area] to function as intended.” (Anna)
Consequently, the women felt ignored and unheard in their contact with healthcare services. They perceived that HCPs did not listen to them, leaving them feeling invisible, sometimes even having severe health problems.
“I was hospitalised with sepsis before someone listened to me.” (Josefin)
Being labelled as a hysterical woman
The women also experienced being labelled as the ‘hysterical woman’ who exaggerated their persistent symptoms and had mental health problems. The women described how the HCPs accused them of imagining their SPT-related health problems. One woman indignantly revealed that the HCP she encountered said, 'These problems only exist in your head’ (Joanna), i.e., suggesting that the perceived symptoms did not exist and rejecting the health concerns. Hence, this attitude made some women believe their problems were a product of their imagination and sometimes made them even question their sanity.
Moreover, the HCPs’ condescending attitudes towards the women made them feel dismissed and devalued. For example, the women shared that HCPs laughed at them or were rough or cold during the examination. Moreover, HCPs expressed that they had ‘seen worse’ (Amanda). Some women also conveyed that they were advised ‘to drink some wine to feel better’ (Elin) when discussing painful intercourses due to their SPT-related health problems.
“You are constantly dismissed, ‘No, but everything looks fine, you have no problems’. Then you start to think you’re imagining things. And then you may not dare to talk about the injuries.” (Jin)
Fighting persistently for access and legitimacy in no (wo)man's-land
The subtheme ‘Fighting persistently for access and legitimacy in no (wo)man's-land’ referred to the women’s experience of gender constructs related to inaccessible healthcare services and their often year-long struggles to access this gendered healthcare and linked social insurance systems. The difficulties in accessing care created negative attitudes towards the healthcare services, making the women wish for general improvements in women’s healthcare.
Struggling to access the gendered healthcare and social insurance systems
The women pointed out that after giving birth, they needed more extensive information on their injury, precautions, available help (follow-up care or re-operation), and sick leave. To overcome the lack of required information, they had to request or actively search for it on their own, which also led to uncertainty about where and when to seek further help if needed.
“I was sent home with a brochure and a pat on the shoulder.” (Amanda)
The women also experienced a lack of adequate healthcare services targeted at their SPT-related health problems. For example, many women did not have access to a pelvic floor clinic or had to travel long distances to see specialists. Hence, their place of residence decided the quality of care the women received. Moreover, some women problematised the organisation of postpartum care as they missed out on follow-up care and even, in some cases, were denied follow-up care or referrals to specialised care were lost. As a result, some women had no opportunity to talk to the operating physician or experienced no follow-up care, although they requested it.
“They said it can take up to a year to get better. So, when that year had passed, and before starting to work again, I called different places in the hospital and asked: What should I do now? […] It took several months before I got an appointment with the surgeon for an assessment. And then I had to get a second opinion. So, it took like seven months before I got an appointment at [a specialist clinic].” (Hawa)
For the women, access to healthcare services, sick leave certificates, and HCPs’ dismissive attitudes were perceived as gender-related, i.e., difficulties in obtaining help from women’s healthcare services would not exist if the services were more women-oriented. One woman illustrated this by expressing: ‘If men gave birth to babies, the situation would not be like this’ (Joanna). Moreover, they perceived that women’s healthcare services were not prioritised. They explicitly stated that the absence of sick leave certificates and benefits was related to their gender. The women were expected to cope without sick leave benefits because vaginal and perineal lacerations of any scope were viewed as a natural part of childbirth, a normal process of a woman’s body. Thus, sequelae thereof did not exist or were taboo in society.
“Everything that happens during and after childbirth and related injuries has been a taboo discussion topic, so it has been completely ‘normal’ to suffer from persistent pain.” (Anna)
“I have applied for compensation from the national patient insurance. I got rejection after rejection; nothing has gone wrong. I was told: 'You simply must expect these things in childbirth. And a caesarean section is not less risky'.” (Hawa)
Thus, the women argued that society and the government did not invest needed resources in women’s healthcare. In addition, those few women receiving a short period of sick cash benefits had it immediately after giving birth or after re-operation, but not for prolonged problems. Further, the women noted that they were not offered sick leave certificates due to persistent physical SPT-related health problems but instead due to mental issues, such as depression or anxiety.
“I've heard about women who have been mentally unwell and have hurt their children. So maybe physicians get cautious and put women on sick leave if they say, ‘I'm not feeling mentally well’. Then they act quickly because they think it's so important. But they don't think about the physical injuries because that's part of [childbirth].” (Jenny)
However, the women shared how they fought long and hard for acknowledgement and care and made demands; for many, this process had covered years. They had to repeatedly insist that something was wrong and felt pressure to prove their health problems to the HCPs. In some women, this led to their persistent problems being diagnosed and acknowledged after several years of delay. The struggle for care involved countless visits and referrals to different HCPs, demanding much strength and persistence, which exhausted them. Sometimes, the sequelae had to develop into an acute health situation, or some women decided to pay for private care to access the proper treatment and rehabilitation. Further, with time, they also became explicit about their demands for sick leave certificates and benefits.
“Well, it [short sick leave period because of birth traumas] just feels like scorn. To me, it is not a sufficient length of sick leave.” (Elin)
Wishing for improvement in women's healthcare
The perceived lack of adequate care and rehabilitation, access to sick leave benefits, and HCPs’ attitude negatively influenced the women’s opinions on healthcare services, especially postpartum healthcare. In addition, the women perceived many HCPs as unprofessional, indifferent, and unstructured. As a result, the women mistrusted the HCPs and lost hope in healthcare services. Thus, they were reluctant to seek further care and were anxious about receiving proper treatment or that HCPs would miss important things.
“I am not being listened to in women's healthcare. This is partly why I feel so disappointed.” (Linda) “You just don't trust the healthcare system. […] Some people have been struggling with their injuries for like 18 years. But the [specialist clinic] – I finally received fantastic treatment, and what if it could be available everywhere [in Sweden]?” (Hawa)
Moreover, the women described a struggle for their rights when deciding whether to report the HCPs to the authorities and pointed out the need to improve women’s healthcare. Reporting HCPs was perceived as complicated as the women did not want to blame specific individuals. The women saw that the major problem lay within the healthcare system and with individual HCPs.
“In the end, I met a fantastic person [healthcare professional]. She wanted me to report the mistreatment when I eventually had the strength. Because no one listened when I said I was ill. So, she has offered to help me if I want to, but I don't know if I have the strength to file a complaint.” (Josefin)
A wish to improve women’s healthcare services was articulated, especially regarding personal follow-up care beyond one year postpartum and the possibility of full-time or part-time sick leave certificates and benefits for persistent problems on equal terms. This wish also strengthened their decision not to give up searching for help and to raise their voices to help themselves and other women.
“I received physiotherapy and the follow-up surveys [the Perineal Laceration Register] during the first year, but thereafter I would have liked to have an annual follow-up for the next years to ensure the status and potential re-operations. […] I can google, but I want to have that information in dialog with a living person, but you do not get that.” (Jenny)
Partaking in developing educational material for HCPs or starting a career within women’s healthcare were some women’s ways to contribute and increase competency in persistent SPT-related health problems.
“One of my strategies since I got the injury is also to try to influence. Being able to be involved and influence what postpartum care should consist of.” (Jin)
Facing multidimensional losses when no help in sight
The subtheme ‘Facing multidimensional losses when no help in sight’ covered physical and mental health consequences and the financial and social losses the participating women faced when no support or access to needed care and rehabilitation was provided.
Being physically victimised by HCP's malpractice
The women’s experiences covered either being misdiagnosed during the suturing after birth or in the following years when seeking help for persistent SPT-related health problems. Further, they shared how physicians had incorrectly sutured vaginal and perineal muscles after childbirth, leading the women to live with incontinence, pain, prolapses, or sexual dysfunction if their vaginas were sutured too tight. They also described how they endured infections, wound ruptures, sepsis, necrosis, and re-operations. Additionally, the women perceived a general lack of competency regarding communication and persistent SPT-related health problems, including problems related to sex life and sexual functioning, besides a more specific lack regarding suturing techniques and ultrasound examinations.
“I was referred to a specialist clinic. And they found out that all the muscles were separated, the internal and external sphincters were torn, and my pinching ability was kind of weak. So, it was quite the opposite, really, quite the opposite. None of what the other physician had said was true [laughs]. Absolutely incredible. And she is supposed to be a specialist.” (Hawa)
Aching inside
Living with troubled postpartum bodies and the absence of HCPs’ legitimation of the women´s problems made them struggle mentally, feeling speechless and silenced. This neglect reinforced irritation, anger, distress, bitterness, and disappointment towards the HCPs and the healthcare services. One woman illustrated the emotional struggle in this way:
“It's just that the health services don’t believe you, which makes you feel terrible. It's a big deal that no one listens.” (Josefin)
Moreover, the women felt uncertain about their health status due to a default medical diagnosis with concerns for their future and which staff to trust. Consequently, some had to bite the bullet, put up with their situation, and try to think positively. Other women were denying or diminishing their SPT-related health problems, accepting that their symptoms would improve, even disappear or that their condition was ‘normal’ as they had been told. Further, the women described despair because their neglected health problems caused by their SPT made them feel exposed, unsure, and hopeless. In some, this desperation resulted in a mental breakdown, a fear of losing custody of their child due to mental illness or suicidal thoughts.
“Something broke inside of me that day. I felt entirely omitted; I was close to leaving my son and committing suicide. Nobody understood how bad everything was.” (Elin)
Additionally, the women suffered emotionally when motherhood was crushed. Their partner had to take the primary responsibility for the family, and the children had to come in second place as the mothers suffered from various physical and mental health problems. As a result, the women felt they missed their children’s development and could not use their parental social security benefits as desired.
“I feel devasted because people tell me, ‘You are on maternity leave’. I’m not on maternity leave; I’m sick. I should be on sick leave.” (Jaanika)
Suffering financial and societal losses
Moreover, the women suffered financially and societally due to persistent health problems. Some women were denied financial compensation from Patient Insurance (a national insurance system where patients can seek compensation for care injuries). The Social Security Agency and the HCPs were perceived as obstacles to receiving sick cash benefits. They noted that ‘extensive’ health problems were required to receive sick cash benefits and that their health problems paradoxically were not seen as extensive or even a problem per se by the HCPs; hence, no sick leave certificates were issued.
“He [the physician] tried to argue and clarify my pain situation in the sick leave certificate to meet the requirements for a sick leave benefit at the Social Security Agency. I was in so much pain and had to lie down to breastfeed. But, no, ‘If you can manage to hold the baby when breastfeeding, then you are on maternity leave, not sick leave benefit’ [mimicking the official at the Social Security Agency who rejected the certificate and consequently also the sick cash benefit]”. (Jaanika)
Furthermore, the women were set back financially and societally because they could not work full-time due to their persistent health problems. Therefore, some women chose to compensate for their work absence with part-time parental benefits to diminish their working hours and cover their inability to work due to persistent SPT-related health problems. Without a sick leave certificate, i.e., the physicians or the officials at the Social Security Agency’s acknowledgement of a ‘true’ health problem, partners or other relatives were obliged to adjust their work schedules to support or unburden the woman’s suffering and inability to work full-time. This reduction in working hours for the SPT-affected women and, in some cases, their partners was expressed to potentially negatively affect their upcoming careers and pensions. As a result, the women experienced being caught between stools in the social insurance systems:
“[…] You end up in a position where you are neither on sick leave nor unemployment benefits and at the same time cannot perform any offered work [due to persistent problems]. But multiple societal bodies demand and expect you to be a part of the working force, and nobody really listens.” (Elin)
Depending on other’s advocacy to navigate an arbitrary system
The last subtheme, ‘Depending on other’s advocacy to navigate an arbitrary system’, highlights the women’s experiences of, often by chance, finding a single devoted professional, i.e., a ‘key person’, to access needed care and rehabilitation. Such a ‘key person’ was vital to recognising persistent problems, legitimating symptoms, and enabling access to needed care, sick leave, and rehabilitation. The women who finally had legitimation for their health problems described that the medical diagnosis also came with a feeling of sanity and empowerment, relieving them of their paradoxical situation.
Encountering a ‘key person’ to receive needed care
A support system was a prerequisite for enduring their health problems and finding the strength to fight for access to care. This system could be a partner, other family members, or friends who gave the women power and courage, but most importantly – encountering a professional who saw their problems and provided referrals or other options to obtain the needed help and support. In most cases, women would search for years for competent HCPs, such as midwives, physicians, or physiotherapists, who would listen and acknowledge persistent problems. This ‘key person’ showed empathy and trustworthiness, creating relief and security. Further, the ‘key person’ was portrayed as competent, attentive, professional, and respectful. The ‘key persons’ also shared women’s outrage at the mistreatment and default healthcare they endured. Additionally, these ‘key persons’ were surprised that the women were not on sick cash benefits due to their symptoms and that they had to compensate for their financial situation with parental benefits or reduced working hours and lower salaries. Consequently, finding this ‘key person’, often by chance or word of mouth, was crucial for accessing care and marked a significant turning point in the women’s recovery.
“I sought help from another midwife, as I felt something was wrong. This midwife referred me to the physiotherapist, who referred me to a specialist, who then referred me to surgery and rehabilitation.” (Malin)
Some women received follow-up care for their persistent SPT-related health problems during the first year postpartum. If persistent problems occurred and were acknowledged, the women were offered different surgical approaches with various outcomes, consultations by colon specialists, physiotherapy, and psychiatric care. They were grateful for the help they received but felt more comprehensive care was needed.
Feeling sane and empowered
Confirmation of persistent SPT-related health problems was expressed as liberating, strengthening and, as one woman put it, a ‘win’ (Elin). Receiving a medical diagnosis and appurtenant treatment was relieving because the medical confirmation of the symptoms released a considerable burden. These women described being acknowledged, and the diagnosis proved that health problems existed, and the struggles were not in vain. Furthermore, it explicitly stated to everyone, including themselves, that they were not ‘crazy’, ‘imagining things’ or ‘hysterical’.
“So, my laceration has been classified as an injury caused by the healthcare services. This was somehow a confirmation. It's not just that it's in my head, but it has been established that it is a medical injury, and it could have been avoided.” (Jin)
Alongside feelings of sanity and being legitimised, the women experienced empowerment. The women felt supported and confident. Thus, finding an agency to address the taboo of their SPT by talking openly about it and helping others in the same situation was also seen as therapeutic. Further, the legitimation of the sequelae and access to appropriate care gave them time to heal and process their trauma. Receiving sick leave certificates and benefits was seen as a part of the empowerment and legitimacy of their persistent SPT-related health problems, reducing stress, and easing the financial burden. Furthermore, access to occupational rehabilitation and understanding at work became available. Thus, the women who had received the help they needed after a struggle to obtain it were hopeful about the future and possible recovery.
“I have regained my authority to speak up. It [SPT-related health problems] should be out in the open, not withheld.” (Jaanika)
Our main finding was that women with persistent health problems due to SPT at childbirth were caught in a paradox of living in a normalised but traumatised body, and their health problems were rejected as postpartum normalities. Furthermore, our results elucidated the difficulties in accessing postpartum healthcare, rehabilitation, and sick leave benefits. Therefore, the women struggled with neglected healthcare needs, diminished emotional well-being, and loss of financial and social status. Our study highlighted experiences up to 5 years after sustaining SPT, which showed that some women’s SPT-related health problems do not diminish with time. They faced challenges functioning in daily life, at work, and in society. In contrast, finding a ‘key person’, i.e., a professional who acknowledged the women’s persistent problems as legitimate, was a prerequisite for accessing all the needed care and sick leave and enhancing empowerment for the women. Thus, this ‘key person’ was not blinded by the obstetric gaze and instead used their agency and advocacy as support.
In the following, we will discuss our findings related to other empirical studies and problematise them with theoretical reflections.
The paradox of normalising the postpartum body
In our findings, the paradox arose when the HCPs dismissed physical health problems after SPT despite women’s perceived symptoms. Central in this context was a normalisation process where health problems were regarded as ‘normal’ by HCPs, a phenomenon also found in prior research on SPT [ 17 , 18 , 19 , 20 , 21 , 22 ]. The HCPs’ normalisation of women’s health problems can also be found regarding other medical conditions affecting women, such as pelvic organ prolapse [ 52 ], menstrual pain [ 53 ], endometriosis [ 54 ] or nausea and vomiting during pregnancy [ 55 ]. In light of the medicalisation of women’s healthcare, where the medical field has sought to pathologise natural bodily processes such as pregnancy and childbirth [ 33 ], actual medical conditions such as persistent SPT-related health problems are paradoxically normalised. Our findings, therefore, highlight the need to challenge HCPs’ views of what constitutes a ‘normal postpartum body’ or ‘normal postpartum symptoms’ after sustaining SPT.
The key to healthcare
In the context of denied legitimacy of health problems and neglected needs, it appeared that the women became dependent on the goodwill of a ‘key person’, personified as the respectful, competent, and empathetic HCP. Prior research on SPT has also found women struggling with accessing healthcare [ 6 , 17 ] and specific HCPs as enablers of care [ 12 ]. The dependency on a ‘key person’ to access adequate care might highlight a structural problem within the provision of postpartum SPT-related healthcare. Globally, there are a few national guidelines on SPT management and prevention [ 56 ]. Additionally, no national guidelines regarding postpartum care of SPT exist in Sweden, and pelvic floor teams are only available in some Swedish regions [ 16 ]. In our study, the women lacked information, and competent HCPs were hard to find or located far away. Other studies have shown poor patient information and education as a postpartum problem [ 6 , 10 , 18 ], indicating a need to develop targeted oral and written information on wound healing and recovery. Further, women in Australia describe similar challenges to accessing SPT-related healthcare when having persistent SPT-related health problems [ 18 ]. The absence of national Australian guidelines may have led to inconsistent care, failing to meet women’s healthcare needs. Further, women from rural areas have had additional difficulties accessing needed care. In 2021, a clinical standard for SPT was implemented in Australia, comprising care standards for follow-up [ 57 ]. Thus, to improve the national situation in Sweden, more research and resources must be allocated to develop evidence-based recommendations, preferably internationally accepted guidelines [ 56 ]. Moreover, the accessibility of SPT-related healthcare, such as pelvic floor clinics, needs to be expanded so that women can easily meet their ‘key person’ if required.
Woman-(de)centred care?
We found that HCPs were obstructed by their obstetric gaze when assessing women with persistent SPT-related health problems. Obstetric gaze derives from the medical gaze notions [ 58 ], suggesting a gaze that splits the individual from the body, constructing the care-seeker as a medical object or condition instead of an individual with a social context. This gaze blinded HCPs who normalised obvious health problems. Recent advances in women’s healthcare in industrial countries and midwifery research show development towards continuity of care models with a woman-centred approach in different caseload-midwifery projects and informed choice regarding place of childbirth [ 28 , 59 , 60 , 61 ]. Wom e n-centred care [ 2 ] is a widespread care philosophy within midwifery that advocates for providing individualised care to women. Further, wom a n-centred care emphasises the individual woman’s healthcare needs and situation, incorporating the concepts of choice, control, continuity of caregiver, and self-determination. It can be argued that the obstetric gaze obstructed HCPs in providing wom a n-centred care because they did not acknowledge the women’s healthcare needs. Consequently, the women did not have control over their health situation. Making women feel empowered [ 2 , 62 ] is crucial in woman-centred care. Hence, the ‘key persons’ in our study managed to provide wom a n-centred care where acknowledgement of problems as real medical problems and access to care made the women experience empowerment. Therefore, we argue that guidelines regarding follow-up care after SPT should ideally be developed with wom a n-centred care as its core.
Everything looks fine
The biomedical model has traditionally focused on normality and abnormality rather than health [ 63 ]. Theoretically, the ‘obstetric gaze’ is closely tied to the ‘medical gaze’ and the ‘male gaze’, referring to the biomedical paradigm and its power [ 27 , 58 ]. In our study, the obstetric gaze judged the women’s persistent health problems due to SPT as ‘normal’ and the appearance of their genital area as ‘fine’, which created a paradoxical situation regarding the legitimacy of their ongoing health problems after SPT. Generally, the healthcare sector is critiqued for reducing the body to only incorporating organs and tissue, i.e., focusing on physical symptoms [ 27 ].
The women in our study, of which most showed more than one significant symptom after SPT, noted that HCPs would comment on the physical appearance of the perineal area rather than its functionality by telling them that ‘everything looked fine’. The focus on looks rather than functionality regarding SPT-related health problems aligns with the findings presented by others [ 17 ]. Having women describe how their persistent physical pelvic floor problems after SPT during childbirth are trivialised, normalised, questioned, and labelled as mental health issues is of utmost concern. This implies the need for rapid improvements in HCPs’ knowledge and organisation of care but also raises the question of what is considered a normal status and recovery after any perineal laceration in the short- and long-term perspective. A similar discursive focus on women’s appearance instead of their health problems has also been found among HCPs when women seek care for chronic pain [ 64 ]. The sentence ‘Everything looks fine’ can be interpreted as an objectifying, gendered discourse in an obstetric context. This discourse may reinforce the obstetric gaze and, in the broader sense, the medical gaze [ 58 ]. The Swedish Health and Medical Care Act [ 39 ] advocates for the respectful treatment of patients. Hence, it is noteworthy that the women experienced being judged by the looks of their genital area in their medical encounters rather than HCPs addressing the functionality. Such treatment does not align with the legislation and calls for a discourse analysis of the attitudes of HCPs towards women with persistent SPT-related health problems and their experiences of providing care for affected women.
Being subjected to obstetric gaslighting
In light of the women’s perception of their dismissal as dramatic, illegitimate, and irrational patients, we argue that they faced so-called ‘gaslighting’ in an obstetric context [ 65 , 66 ]. Thus, the women experienced being offered sick leave for mental problems instead of their perceived physical health problems, depicting them as hysterical women who exaggerated their condition. Gaslighting is a concept used in medicine in general [ 66 ] and in obstetrics regarding traumatic childbirth experiences [ 65 ]. The concept of hysteria, i.e., a prior medical diagnosis and historical concept theoretically linked to femininity [ 67 , 68 ] and ‘obstetric gaslighting’ [ 65 ], has also been found in research on women’s chronic pain [ 64 ] and endometriosis [ 69 ]. Men with chronic pain are perceived as brave, and women in pain are hysterical, emotional, whining, malingering, or imagining pain [ 64 ]. Further, women with endometriosis are viewed as ‘reproductive bodies’ with a proneness for hysteria [ 69 ]. Obstetric gaslighting, enforced by the normalisation of SPT-related health problems and the gendered stereotype of women as hysterical patients, puts women with SPT in an inferior position towards HCPs and can, therefore, be interpreted as a demonstration of institutional power [ 65 ]. Hence, being overlooked by the obstetric gaze might constitute a form of obstetric gaslighting, a concept that has not been applied to SPT before.
Implications and significance
Our study indicated that women continue to have problems accessing healthcare for persistent SPT-related health problems several years postpartum. Additionally, women with persistent SPT-related health problems often depended on a ‘key person’ with the competence to open the doors to comprehensive care, as shown in our findings. The Swedish Government launched a multi-million project from 2015 to 2022 to improve and promote women’s health [ 70 ]. Despite this investment, the depicted experiences of the included women reflect upon remaining structural and clinical problems within Swedish healthcare, which need further attention, investigation, and actions. Additionally, there are considerable differences in reported satisfaction and prevalence of complications at the one-year follow-up between the regions [ 3 ], indicating that there are suboptimal healthcare services. With a significant variation in satisfaction and recovery at one year, there are reasons to believe that women with prolonged problems may experience problems getting access to needed care.
Our study also showed that SPT-related healthcare services are not available on equal terms to women with persistent SPT-related health problems. In general, many women within this group had problems accessing care and sick leave for years. However, depending on where the women reside, not all women have access to specialised care. This inequity may be explained by Sweden having 21 self-governing health regions, and in the absence of national guidelines regarding SPT care and follow-up, the healthcare provision for affected women varies. To secure access to postpartum care for women with SPT in general and those with different prerequisites within this group, implementation studies are needed to develop and evaluate the effect of national guidelines for follow-up care regarding SPT.
Strengths and limitations
This study has strengths and limitations that need to be addressed. A significant strength, enhancing credibility and transferability, was providing a clear context and thick descriptions of our results, where we thoroughly portrayed the women’s voices using quotations [ 35 ]. Further, our detailed account of the study context, data collection, and data analysis process facilitated the transferability of our study. Including three women born outside of Sweden added to the variety of the sample and thus improved credibility because qualitative research often overlooks immigrants' experiences. However, the migrant women spoke Swedish well enough to participate in an interview, indicating that they have been living in Sweden for some time and might be familiar with the healthcare system. Finally, the credibility and dependability of this study were also strengthened by the frequent use of interdisciplinary triangulation between the authors throughout data analysis and the writing process, as well as peer review at a research seminar.
A potential limitation was that this study may not have fully explored the situation of women with fourth-degree lacerations or those with lower education, as most participants had third-degree perineal lacerations and higher education. Further, we could not include non-binary persons and same-sex or single parents, which may be a weakness; consequently, future studies should focus on the under-represented participant groups and migrant women needing an interpreter. Additionally, all women responded voluntarily to the study invitation. Thus, our participants might be particularly outspoken about their problems or interested in raising their voices or experiences. However, they represented a variety of persistent SPT-related health problems of various severity, and some had been able to get access to medical help, whereas others had not. Additionally, our findings cohered to similar studies [ 12 , 17 ] covering shorter periods after the SPT, which may indicate that the experiences of the challenging search for needed help remain over time. Therefore, our findings may reflect other women’s experiences seeking care for SPT-related health problems and may be transferable to other women’s experiences with persistent health problems of a rare condition.
The data for this study was comprehensive and rich. Information power in qualitative research is an ongoing discussion, and the number of participants and their representativity can be seen as a limitation of credibility and transferability [ 71 , 72 ]. Graneheim, Lindgren and Lundman [ 36 ] argue that sample size should be determined by the study’s aim and the data’s quality so that variations in experiences can be captured. They do, therefore, not recommend a specific number of participants, but others do [ 71 ]. With this in mind, the authors believe that the women’s detailed descriptions of the included concepts and the extensive length of the conducted interviews enabled us to achieve sufficient information power based on the richness of the data [ 72 ].
By qualitatively exploring how women with persistent SPT-related health problems experienced their healthcare encounters, we interpreted that they faced a paradox of being reassured of normality by HCPs despite reporting sequelae symptoms. Thus, women’s needs for medical care, rehabilitation, and sick leave were largely neglected. Further, our study might indicate a structural problem within women’s postpartum healthcare, indicating that access to care depended on encountering a ‘key person’, a professional who acknowledged persistent problems as real symptoms. Access to quality care provided with a professional attitude was essential for the future well-being of women with persistent SPT-related health problems. Thus, it should not depend on meeting a single ‘key person’. Therefore, national guidelines for long-term postpartum care of persistent SPT-related health problems must be developed in Sweden. Additionally, to ensure that healthcare services meet the individual needs of women with persistent SPT-related health problems, it is crucial to consider arranging the organisation and availability of quality care for these women from a woman-centred perspective.
Availability of data and materials
The original recordings and transcripts from the current study are not publicly available due to securing the individual privacy and confidentiality of the participants. Data are available from the corresponding author upon reasonable request.
Abbreviations
Healthcare professionals
Interquartile range
Strategic Research Area Health Care Science
- Severe perineal trauma
Sexual and reproductive health and rights
World Health Organisation
World Health Organization (WHO). WHO recommendations: Intrapartum care for a positive childbirth experience. Geneva: WHO; 2018. Cited 2024 Feb 14. Available from: https://www.who.int/publications/i/item/9789241550215 .
Leap N. Woman-centred or women-centred care: does it matter? Br J Midwifery. 2009;17(1):12–6.
Article Google Scholar
Uustal E. Bristning vid förlossning grad 3 - 4. Årsrapport från GynOp-registret avseende operationer utförda år 2022. [Laceration at childbirth, grade 3 - 4, Annual Report of surgeries 2022]. Umeå: The Swedish National Quality Register of Gynecological Surgery; 2023. Cited 2024 Maj 8. Available from: https://www.gynop.se/rapporter/arsrapporter/ .
World Health Organization (WHO). International statistical classification of diseases and related health problems (ICD) 10th revision. Geneva: WHO; 2019. Cited 2024 Maj 8. Available from: https://icd.who.int/browse10/2019/en .
d’Almeida I. Women’s experiences following obstetric anal sphincter injury. J Pelvic Obstet Gynaecol Physiother. 2020;127:39–50.
Google Scholar
Darmody E, Bradshaw C, Atkinson S. Women’s experience of obstetric anal sphincter injury following childbirth: An integrated review. Midwifery. 2020;91:102820.
Article PubMed Google Scholar
LaCross A, Groff M, Smaldone A. Obstetric anal sphincter injury and anal incontinence following vaginal birth: a systematic review and meta-analysis. J Midwifery Women’s Health. 2015;60(1):37–47.
Samarasekera DN, Bekhit MT, Wright Y, Lowndes RH, Stanley KP, Preston JP, et al. Long-term anal continence and quality of life following postpartum anal sphincter injury. Colorectal Dis. 2008;10(8):793–9.
Article CAS PubMed Google Scholar
Andreucci CB, Bussadori JC, Pacagnella RC, Chou D, Filippi V, Say L, et al. Sexual life and dysfunction after maternal morbidity: a systematic review. BMC Pregnancy Childbirth. 2015;15:307.
Article PubMed PubMed Central Google Scholar
Beck CT. Effects of fourth-degree perineal lacerations on women’s physical and mental health. J Obstet Gynecol Neonatal Nurs. 2021;50(2):133–42.
Keighley MR, Perston Y, Bradshaw E, Hayes J, Keighley DM, Webb S. The social, psychological, emotional morbidity and adjustment techniques for women with anal incontinence following Obstetric Anal Sphincter Injury: use of a word picture to identify a hidden syndrome. BMC Pregnancy Childbirth. 2016;16(1):275.
Article CAS PubMed PubMed Central Google Scholar
Lindqvist M, Lindberg I, Nilsson M, Uustal E, Persson M. “Struggling to settle with a damaged body” - A Swedish qualitative study of women’s experiences one year after obstetric anal sphincter muscle injury (OASIS) at childbirth. Sex Reprod Healthc. 2019;19:36–41.
Shoorab NJ, Taghipour A, Mirteimouri M, Roudsari RL. Social recovery: a neglected dimension of caring for women with perineal trauma in Iran. Iran J Nurs Midwifery Res. 2020;25(4):333–40.
Jahani Shoorab N, Mirteimouri M, Taghipour A, Latifnejad Roudsari R. Women’s experiences of emotional recovery from childbirth-related perineal trauma: a qualitative content analysis. Int J Community Based Nurs Midwifery. 2019;7(3):181–91.
PubMed Google Scholar
Swedish Agency for Health Technology Assessment and Assessment of Social Services. Practices to improve detection of perineal tears and women’s views and experiences of healthcare providers following sustained perineal tear. A systematic review. 2021. Report No.: 323.
Persson M, Lindberg I, Ohman A. Regional and clinical guidelines for prevention and care of obstetric anal sphincter injuries - A critical frame analysis. Midwifery. 2023;119:103608.
Huber M, Tunon K, Lindqvist M. “From hell to healed” - A qualitative study on women’s experience of recovery, relationships and sexuality after severe obstetric perineal injury. Sex Reprod Healthc. 2022;33:100736.
Priddis HS, Schmied V, Kettle C, Sneddon A, Dahlen HG. “A patchwork of services”–caring for women who sustain severe perineal trauma in New South Wales–from the perspective of women and midwives. BMC Pregnancy Childbirth. 2014;14:236.
Priddis H, Schmied V, Dahlen H. Women’s experiences following severe perineal trauma: a qualitative study. BMC Womens Health. 2014;14(1):32.
Williams A, Lavender T, Richmond DH, Tincello DG. Women’s experiences after a third-degree obstetric anal sphincter tear: a qualitative study. Birth. 2005;32(2):129–36.
Herron-Marx S, Williams A, Hicks C. A Q methodology study of women’s experience of enduring postnatal perineal and pelvic floor morbidity. Midwifery. 2007;23(3):322–34.
Crookall R, Fowler G, Wood C, Slade P. A systematic mixed studies review of women’s experiences of perineal trauma sustained during childbirth. J Adv Nurs. 2018;74(9):2038–52.
Priddis H, Dahlen H, Schmied V. Women’s experiences following severe perineal trauma: a meta-ethnographic synthesis. J Adv Nurs. 2013;69(4):748–59.
Tjernström K, Lindberg I, Wiklund M, Persson M. Negotiating the ambiguity of an (in)authentic working life: a grounded theory study into severe perineal trauma. BMC Women’s Health. 2023;23(1):47.
Lindqvist M, Persson M, Nilsson M, Uustal E, Lindberg I. “A worse nightmare than expected” - a Swedish qualitative study of women’s experiences two months after obstetric anal sphincter muscle injury. Midwifery. 2018;61:22–8.
United Nations. The Sustainable Development Goals Report 2022. New York City: United Nations; 2022. Cited 2024 Feb 24. Available from: https://unstats.un.org/sdgs/report/2022/ .
Fahy K, Foureur M, Hastie C. Birth territory and midwifery guardianship : theory for practice, education, and research. Edinburgh: Books for Midwives; 2008.
Walsh D, Christianson M, Stewart M. Why midwives should be feminists. Midirs Midwifery Digest. 2015;25(2):154–60.
Buchanan K, Newnham E, Geraghty S, Whitehead L. Navigating midwifery solidarity: a feminist participatory action research framework. Women Birth. 2023;36(1):e169–74.
Benoit B, Goldberg L, Campbell-Yeo M. Infant feeding and maternal guilt: The application of a feminist phenomenological framework to guide clinician practices in breast feeding promotion. Midwifery. 2016;34:58–65.
Westergren A, Edin K, Walsh D, Christianson M. Autonomous and dependent-The dichotomy of birth: a feminist analysis of birth plans in Sweden. Midwifery. 2019;68:56–64.
Alspaugh A, Barroso J, Reibel M, Phillips S. Women’s contraceptive perceptions, beliefs, and attitudes: an integrative review of qualitative research. J Midwifery Womens Health. 2020;65(1):64–84.
Davis DL, Walker K. Re-discovering the material body in midwifery through an exploration of theories of embodiment. Midwifery. 2010;26(4):457–62.
Govender V, Penn-Kekana L. Gender biases and discrimination: a review of health care interpersonal interactions. Global Public Health. 2008;3(sup1):90–103.
Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(2):105–12.
Graneheim UH, Lindgren BM, Lundman B. Methodological challenges in qualitative content analysis: a discussion paper. Nurse Educ Today. 2017;56:29–34.
Lindgren BM, Lundman B, Graneheim UH. Abstraction and interpretation during the qualitative content analysis process. Int J Nurs Stud. 2020;108:103632.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57.
Ministry of Health and Social Affairs. Hälso- och sjukvårdslag (2017:30) [Health and Medical Care Act]. Stockholm: The Swedish Riksdag; 2017. Cited 2024 Maj 8. Available from: https://www.riksdagen.se/sv/dokument-och-lagar/dokument/svensk-forfattningssamling/halso-och-sjukvardslag-201730_sfs-2017-30/ .
The Swedish Social Insurance Agency. Parental benefits. 2023. Cited 2024 Feb 20. Available from: https://www.forsakringskassan.se/english/parents/when-the-child-is-born/parental-benefit .
The Swedish Association of Midwives. Kompetensbeskrivning för legitimerad barnmorska [Description of competences for registered midwives]. Stockholm: The Swedish Association of Midwives; 2018. Updated 2019 Jan. Cited 2024 Feb 20. Available from: https://storage.googleapis.com/barnmorskeforbundet-se/uploads/2020/04/Kompetensbeskrivning-for-legitimerad-barnmorska.pdf .
Bäckenbottenutbildning [Pelvic floor education]. Utbildningsmaterial: Uppföljning [Educational material: Follow-up]. 2022. Cited 2024 Maj 8. Available from: https://backenbottenutbildning.se/index.php/utbildningsmaterial/uppfoljning .
GynOp [The Swedish National Quality Register of Gynecological Surgery]. About GynOp. 2023. Cited 2024 Feb 20. Available from: https://www.gynop.se/home/about-gynop/ .
Öhman H, Schesny S, Bearth L, Löwendahl J. Förlossningsskadad? Du är inte ensam! [Injured at childbirth? You are not alone!’]. 2014. Cited 2024 Feb 20. Available from: https://www.facebook.com/groups/forlossningsskadad/ .
Vanderbilt University. About REDCap. Nashville: Vanderbilt; 2023. Updated 2023. Cited 2024 Feb 20. Available from: https://projectredcap.org/about/ .
Kvale S, Brinkmann S. Interviews: learning the craft of qualitative research interviewing. 2nd ed. Los Angeles: Sage Publications; 2009.
Keen S, Lomeli-Rodriguez M, Joffe H. From challenge to opportunity: virtual qualitative research during COVID-19 and beyond. Int J Qual Methods. 2022;21:16094069221105076.
Thunberg S, Arnell L. Pioneering the use of technologies in qualitative research - A research review of the use of digital interviews. Int J Soc Res Methodol. 2022;25(6):757–68.
MAXQDA. Why MAXQDA? Berlin: VERBI Software GmbH; 2024. Cited 2024 Maj 8. Available from: https://www.maxqda.com/why-maxqda .
Microsoft. Microsoft Excel. Redmond: Microsoft; 2024. Cited 2024 Maj 8. Available from: https://www.microsoft.com/sv-se/microsoft-365/excel?market=se .
Griffin GA. Dictionary of Gender Studies. Oxford: Oxford University Press; 2017.
Book Google Scholar
Abhyankar P, Uny I, Semple K, Wane S, Hagen S, Wilkinson J, et al. Women’s experiences of receiving care for pelvic organ prolapse: a qualitative study. BMC Womens Health. 2019;19(1):45.
Scott KD, Hintz EA, Harris TM. “Having pain is normal”: How talk about chronic pelvic and genital pain reflects messages from menarche. Health Commun. 2022;37(3):296–306.
Pettersson A, Bertero CM. How women with endometriosis experience health care encounters. Womens Health Rep (New Rochelle). 2020;1(1):529–42.
Heitmann K, Svendsen HC, Sporsheim IH, Holst L. Nausea in pregnancy: attitudes among pregnant women and general practitioners on treatment and pregnancy care. Scand J Prim Health Care. 2016;34(1):13–20.
Roper JC, Amber N, Wan OYK, Sultan AH, Thakar R. Review of available national guidelines for obstetric anal sphincter injury. Int Urogynecol J. 2020;31(11):2247–59.
The Australian Commission on Safety and Quality in Health Care. Third and Fourth Degree Perineal Tears Clinical Care Standard. Sydney: The Australian Commission on Safety and Quality in Health Care; 2021. Cited 2024 Feb 20. Available from: https://www.safetyandquality.gov.au/standards/clinical-care-standards/third-and-fourth-degree-perineal-tears-clinical-care-standard .
Foucault M, Sheridan A. The birth of the clinic: an archaeology of medical perception. 3rd ed. London: Routledge; 2003.
Scarf VL, Rossiter C, Vedam S, Dahlen HG, Ellwood D, Forster D, et al. Maternal and perinatal outcomes by planned place of birth among women with low-risk pregnancies in high-income countries: a systematic review and meta-analysis. Midwifery. 2018;62:240–55.
Offerhaus P, Jans S, Hukkelhoven C, de Vries R, Nieuwenhuijze M. Women’s characteristics and care outcomes of caseload midwifery care in the Netherlands: a retrospective cohort study. BMC Pregnancy Childbirth. 2020;20(1):517.
Forster DA, McLachlan HL, Davey MA, Biro MA, Farrell T, Gold L, et al. Continuity of care by a primary midwife (caseload midwifery) increases women’s satisfaction with antenatal, intrapartum and postpartum care: results from the COSMOS randomised controlled trial. BMC Pregnancy Childbirth. 2016;16:28.
Brady S, Lee N, Gibbons K, Bogossian F. Woman-centred care: an integrative review of the empirical literature. Int J Nurs Stud. 2019;94:107–19.
Findlay D. The medical gaze: medical models, power, and women’s health. Atlantis. 1992;18(1&2):104–24.
Samulowitz A, Gremyr I, Eriksson E, Hensing G. “Brave Men” and “Emotional Women”: a theory-guided literature review on gender bias in health care and gendered norms towards patients with chronic pain. Pain Res Manag. 2018;2018:6358624.
Fielding-Singh P, Dmowska A. Obstetric gaslighting and the denial of mothers’ realities. Soc Sci Med (1982). 2022;301:114938.
Sebring JCH. Towards a sociological understanding of medical gaslighting in western health care. Sociol Health Ill. 2021;43(9):1951–64.
Jones CE. Wandering wombs and “female troubles”: the hysterical origins, symptoms, and treatments of endometriosis. Women Stud. 2015;44(8):1083–113.
Tasca C, Rapetti M, Carta MG, Fadda B. Women and hysteria in the history of mental health. Clin Pract Epidemiol Ment Health. 2012;8:110–9.
Young K, Fisher J, Kirkman M. “Do mad people get endo or does endo make you mad?”: Clinicians’ discursive constructions of Medicine and women with endometriosis. Fem Psychol. 2019;29(3):337–56.
The Swedish Ministry of Health and Social Affairs. Överenskommelse om en förbättrad förlossningsvård och insatser för kvinnors hälsa [Agreement on improving maternity care and women's health] [Internet]. Stockholm: The Swedish Government; 2015. S2015/07777/FS. [cited 2024 Maj 8]. Available from: https://www.regeringen.se/overenskommelser-och-avtal/2015/12/overenskommelse-om-en-forbattrad-forlossningsvard-och-insatser-for-kvinnors-halsa/ .
Boddy CR. Sample size for qualitative research. Qual Mark Res. 2016;19(4):426–32.
Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies: guided by information power. Qual Health Res. 2016;26(13):1753–60.
Download references
Acknowledgements
We want to thank the participating women for generously sharing their experiences.
Open access funding provided by Umea University. This work was supported by the Research Lift (SWE: Forskningslyftet) and Strategic Research Area Health Care Science (SFO-V), Umeå University. The funders had no specific role in the conceptualisation, design, data collection, analysis, publication decision, or manuscript preparation.
Author information
Authors and affiliations.
Department of Nursing, Umeå University, 901 87, Umeå, Sweden
Katharina Tjernström, Inger Lindberg & Margareta Persson
Department of Community Medicine and Rehabilitation, Section of Physiotherapy, Umeå University, 901 87, Umeå, Sweden
Maria Wiklund
You can also search for this author in PubMed Google Scholar
Contributions
KT: conceptualisation; data curation; formal analysis; investigation; methodology; validation; visualisation; writing - original draft; writing - review & editing. IL: conceptualisation; methodology; supervision; visualisation; writing - review & editing. MW: conceptualisation; methodology; supervision; visualisation; writing - review & editing. MP: conceptualisation; data curation; funding acquisition; methodology; project administration; supervision; visualisation; writing - review & editing. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Katharina Tjernström .
Ethics declarations
Ethics approval and consent to participate.
The Swedish Ethical Review Authority approved the study. An amendment to the original ethical approval of the research project to further explore the experiences of encounters with healthcare services was obtained (Dnr: 2020-035410908 and Dnr: 2022-02784-02). The study was undertaken in compliance with research ethics guidelines. All participation was voluntary, and participants received oral and written information about the study and provided written informed consent before the interviews. No interview questions were mandatory, and the women decided if and how detailed they wanted to share their experiences.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
12913_2024_11037_moesm1_esm.pdf.
Additional file 1. Semi-structured interview guide for individual interviews; contains interview questions aimed at highlighting the experience of everyday life and working life after suffering 3 rd or 4 th degree perineal laceration at childbirth (i.e., severe perineal trauma [SPT]).
Additional file 2. Consolidated criteria for reporting qualitative studies (COREQ): 32-item checklist.
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Tjernström, K., Lindberg, I., Wiklund, M. et al. Overlooked by the obstetric gaze – how women with persistent health problems due to severe perineal trauma experience encounters with healthcare services: a qualitative study. BMC Health Serv Res 24 , 610 (2024). https://doi.org/10.1186/s12913-024-11037-5
Download citation
Received : 11 September 2023
Accepted : 23 April 2024
Published : 09 May 2024
DOI : https://doi.org/10.1186/s12913-024-11037-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Persistent health problems
- Qualitative content analysis
- Healthcare encounters
- Postpartum healthcare
- Normalisation
- Access to care
- Empowerment
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
- How to recruit?
- Internship calendars
- Post an offer
- How to give
- Ways to give
- 2019-2024 campaign
- News and publications
- Annual Report
- Build your brand
- Work with our students
- Become a partner
- Our corporate partners
Adolescence and Social Media: the Slippery Sands of Research on a Global Phenomenon
2024 marks 20 years since the birth of social media. Since then, it has become a major communication force in the lives of teenagers - a 2024 Pew survey claims that 93% of American youth use it, for example. Unsurprisingly, research on its impact has followed suit. But just how reliable are the conclusions in this new field of studies? In April 2024, HEC Professors Tina Lowrey and L.J. Shrum co-authored a research paper with their former doctoral student Elena Fumagalli (H18), showing conflicting findings on the negative and positive effects of social media on youth. They warn against major policies and lawsuits founded on inconclusive studies and contradictory scientific research. Professors Lowrey and Shrum share with Breakthroughs their study to try to make sense of a subject matter inflaming public debate. Extracts.

HEC Paris Marketing Professors L.J. Shrum and Tina M. Lowrey
listen to the breakthroughs podcast:
External content from acast has been blocked. access privacy settings.
In this publication, your stated objective was to make sense of a plethora of research on social media and its impact on teenagers. You also hoped to create a template for consumer researchers working on this topic. Indeed, you claim that academics are not unanimous on this impact. Could you elaborate?
L.J. Shrum: Sure. What people need to remember is that everything's in constant flux. Researchers in this field of new technology have a good term for it: the moving target problem. So, for example, what Facebook was when it started is not what Facebook is now, right? Even its name has changed. So, how do you make sense of research on Facebook 10 years ago and 15 years ago in comparison to now? Even the name has changed. And the same thing is true for almost every single social media platform. It's very difficult to define. In our approach, we focused primarily on the last five years, which is when some huge breakthroughs have happened in terms of acquiring good data and doing the proper analyses.
This is a selective review of research on 13- to 21-year-olds. Why choose this age category, Tina?
Tina Lowrey: We wanted to look at adolescence, and thought it was important to include older adolescents who are starting to become young adults just because the research that was out there was showing certain patterns of impact based on age. For females, the largest vulnerable age group is 11 to 13, and for males, it's more like 14 to 15. And so, we just felt like that was a good age range to capture.
Despite this dearth of quality research and its very unequal quality, politicians and journalists appear to be very categorical in the decisions they make or the articles they publish. We've seen, for example, the Kids Off Social Media Act. That’s a bipartisan attempt to ban social media for children under the age of 13 in the United States. L.J., you're not just a consumer psychologist; you also have a PhD in communications. How would you explain the fact that people are making major decisions based on research that's divided?
L.J. Shrum: Politicians and journalists often make some blanket statements, and, for the most part, they’re not far off target, to be fair. But the devil is in the details. And, so, what we're finding in the research that's coming out is that it's not just how old you are, it's not just what gender you are, it's also how you use it and the type of social media that you use. Those are nuances that are very difficult to make a sound bite out of, and also to legislate on.
Politicians and journalists often make some blanket statements. They’re not far off target, but the devil is in the details: it's not just how old and what gender you are, it's also how you use social media and the type of social media that you use.
Tina Lowrey, there is nevertheless a certain convergence of the research that you looked at. Let's start with one: it seems that social media is negative for young girls. Could you elaborate?
Tina Lowrey: Yes. So, I think that part of the reason is the onset of puberty. There are a lot of things going on, it’s a rough time, it was this way even before social media existed.
But social media can exacerbate some of the body image issues that young women have. Again, social media didn't create this problem. But social media ratchets up the impact with considerable negative impact on young teenage girls. And I think that the other issue L.J. mentioned, is that it depends on which social media we're talking about and how you're using it. And previous research does not really account for causality. Someone who has lower self-esteem might be using social media differently to someone with higher self-esteem. Which raises the question: which came first, the social media usage or the self-esteem level? So, it's very complicated, but newer research that's more longitudinal in nature partially addresses that concern of causality.
L.J. Shrum: Coming back to the first point. We can see the same phenomenon with boys. Research seems to concur that the negative impact just happens to map onto puberty. We’re not sure whether it is causal, but that's pretty elegant. As for later on, what research seems to suggest strongly is also an increase in negative effects at around age 19 for both boys and girls. Well, that just happens to correlate or coincide with big sociological changes: we're moving out of the nest, we're going to college, we're going to work. And those these times are very anxious. And so, I think that's when you see the exacerbation that Tina refers to. That age group is about transitioning from adolescence into young adulthood. Negative well-being in that period has been around for decades. But I think again, social media just exacerbates these problems.
Tina Lowrey: And it's also very targeted. We know from some whistleblowers that the social media platforms are intentionally making it addictive. I do think that television and radio pale in comparison to how targeted social media can be. Finally, I think it’s there all the time; it’s ubiquitous - you can be completely on it 23 hours a day if you don't need any sleep. (Laugh)
There’s also a very pragmatic side to your research paper. For example, you call for more research on the underlying factors of social media usage on well-being, and you also are calling for more long-term studies on the impact on people. Could you explain how you feel this can be implemented?
L.J. Shrum: Sure. It became obvious during our analysis that more recent research points to what we call moderators. These are factors which cause greater or lesser negative impact. Now, we have this definition of social media that's very broad and scholars can't even agree on how to define it. Research shows there are different types of social media: Instagram is different than Twitter. One is very image based; the other is word based. There are ones that have different purposes. And so, what's starting to come out is that certain types of social media may have negative effects at a young age. If you take Instagram, it may have a bigger negative effect, let's say, on adolescent body image, whereas other types of social media may have none of the effects you would predict. So, understanding which social media are causing a problem, what kinds of problems they're causing, and also how you use it is essential. Yet, there’s just not enough research accurately defining social media. We also suggest further research on what we refer to as active or passive uses. Are you posting, and are you engaging, or are you just lurking and looking? These usages seem to have different effects on adolescents. Active is associated with a more positive impact on self-esteem than the more passive use of social media where you're not actively engaged, so you're being negatively impacted by what you see and hear.

Tina Lowrey’s research interests include children's understanding of brand symbolism, gift giving and ritual, and the application of psycholinguistic...

L. J. Shrum is a consumer psychologist whose research applies social cognition concepts to understand the determinants of consumer judgments. He has...
Related content on Marketing

Holding Advertisers to Account May Help Reduce Infant Deaths Linked to Unsafe Sleeping
By Anne Laure Sellier

Going Circular to Align Business Models with Planetary Boundaries
By Daniel Halbheer

COMMENTS
Research Paper Conclusion Examples; Summarizing Conclusion: Impact of social media on adolescents' mental health: In conclusion, our study has shown that increased usage of social media is significantly associated with higher levels of anxiety and depression among adolescents. These findings highlight the importance of understanding the ...
Table of contents. Step 1: Restate the problem. Step 2: Sum up the paper. Step 3: Discuss the implications. Research paper conclusion examples. Frequently asked questions about research paper conclusions.
Example of Research Paper Conclusion. Here's an example of a research paper conclusion: Conclusion: In conclusion, our study aimed to investigate the relationship between social media use and mental health among college students. Our findings suggest that there is a significant association between social media use and increased levels of ...
The conclusion is intended to help the reader understand why your research should matter to them after they have finished reading the paper. A conclusion is not merely a summary of the main topics covered or a re-statement of your research problem, but a synthesis of key points derived from the findings of your study and, if applicable, where you recommend new areas for future research.
Begin with a clear statement of the principal findings. This will reinforce the main take-away for the reader and set up the rest of the discussion. Explain why the outcomes of your study are important to the reader. Discuss the implications of your findings realistically based on previous literature, highlighting both the strengths and ...
For example, while the conclusion to a STEM paper could focus on questions for further study, the conclusion of a literature paper could include a quotation from your central text that can now be understood differently in light of what has been discussed in the paper. ... In a short paper—even a research paper—you don't need to provide an ...
Step 1: Restate the problem. Always begin by restating the research problem in the conclusion of a research paper. This serves to remind the reader of your hypothesis and refresh them on the main point of the paper. When restating the problem, take care to avoid using exactly the same words you employed earlier in the paper.
Step 1: Answer your research question. Step 2: Summarize and reflect on your research. Step 3: Make future recommendations. Step 4: Emphasize your contributions to your field. Step 5: Wrap up your thesis or dissertation. Full conclusion example. Conclusion checklist. Other interesting articles.
Begin your conclusion by restating your thesis statement in a way that is slightly different from the wording used in the introduction. Avoid presenting new information or evidence in your conclusion. Just summarize the main points and arguments of your essay and keep this part as concise as possible. Remember that you've already covered the ...
Step 1: Return to your thesis. To begin your conclusion, signal that the essay is coming to an end by returning to your overall argument. Don't just repeat your thesis statement—instead, try to rephrase your argument in a way that shows how it has been developed since the introduction.. Example: Returning to the thesis Braille paved the way for dramatic cultural changes in the way blind ...
A conclusion is the final paragraph of a research paper and serves to help the reader understand why your research should matter to them. The conclusion of a conclusion should: Restate your topic and why it is important. Restate your thesis/claim. Address opposing viewpoints and explain why readers should align with your position.
The point of a conclusion to a research paper is to summarize your argument for the reader and, perhaps, to call the reader to action if needed. 5. Make a call to action when appropriate. If and when needed, you can state to your readers that there is a need for further research on your paper's topic.
This article provides an effective technique for writing a conclusion adapted from Erika Eby's The College Student's Guide to Writing a Good Research Paper: 101 Easy Tips & Tricks to Make Your Work Stand Out.. While the thesis introduction starts out with broad statements about the topic, and then narrows it down to the thesis statement, a thesis conclusion does the same in the opposite order.
Example: In conclusion, Frederick Douglass was, as we have seen, a pioneer in American education, proving that education was a major force for social change with regard to slavery. ... You may find it hard to leave out details that you discovered after hours of research and thought, but adding random facts and bits of evidence at the end of an ...
Some universities will prefer that you cover some of these points in the discussion chapter, or that you cover the points at different levels in different chapters. Step 1: Craft a brief introduction section. As with all chapters in your dissertation or thesis, the conclusions chapter needs to start with a brief introduction.
Present your conclusion in a structured manner, following the natural flow of your paper. Readers should effortlessly follow your thought process, making your conclusion more accessible and persuasive. Reinforce Main Arguments. Emphasize the core arguments and findings from your research.
Research paper conclusion examples. Below, we've created basic templates showing the key parts of a research paper conclusion. Keep in mind that the length of your conclusion will depend on the length of your paper. The order of the parts may vary, too; these templates only demonstrate how to tie them together. 1. Empirical research paper ...
The only new idea would be the suggesting of a direction for future research. Conclusion Example. As addressed in my analysis of recent research, the advantages of a later starting time for high school students significantly outweigh the disadvantages. A later starting time would allow teens more time to sleep--something that is important for ...
Conclusions wrap up what you have been discussing in your paper. After moving from general to specific information in the introduction and body paragraphs, your conclusion should begin pulling back into more general information that restates the main points of your argument. Conclusions may also call for action or overview future possible research.
Strong conclusion examples pave the way for the perfect paper ending. See how to write a good conclusion for a project, essay or paper to get the grade. ... Some might argue that a conclusion is one of the most important components of any research paper or article. It's your last opportunity to make a good impression on your reader. If you can ...
1. Restate the thesis. An effective conclusion brings the reader back to the main point, reminding the reader of the purpose of the essay. However, avoid repeating the thesis verbatim. Paraphrase your argument slightly while still preserving the primary point. 2. Reiterate supporting points.
Research implications refer to the possible effects or outcomes of a study's findings. The recommendations section, on the other hand, is where you'll propose specific actions based on those findings. You can structure your implications section based on the three overarching categories - theoretical, practical and future research ...
Only six studies reported SES-adherence associations, hampering conclusions on this relationship and possible associations between representativeness and an SES-adherence relationship. ... and were willing to take part in research. This often results in a sample that is healthier or with higher physical function and exercise motivation that may ...
To describe the sample and examine research culture, descriptive statistics (frequencies, proportion, M ... Conclusions. There is ample room for much needed development in research capacity and culture for nurses and allied health professionals working in mental health services. There are indications that the need for development is perhaps ...
Previous research indicates that being overweight or obese before and during pregnancy is a significant risk factor for GDM [116,117,118]. However, the scarcity of studies in women with pre-pregnancy BMI > 25 kg/m 2 kg/m suggests the need for more research in this demographic for robust conclusions.
As an example, Bridge2AI Voice is a National Institutes of Health-funded consortium with the aim of building a large-scale data bank of 30,000 voices linked to health metadata and creating best practices in terms of voice data collection to fuel artificial intelligence (AI) research.
Background During the first year postpartum, about 25 per cent of Swedish women with severe perineal trauma (SPT), i.e., a third- or fourth-degree perineal laceration at childbirth, are unsatisfied with their healthcare contacts. Further, there is a lack of research on the more long-term experiences of healthcare encounters among women with persistent SPT-related health problems. This study ...
2024 marks 20 years since the birth of social media. Since then, it has become a major communication force in the lives of teenagers - a 2024 Pew survey claims that 93% of American youth use it, for example. Unsurprisingly, research on its impact has followed suit. But just how reliable are the conclusions in this new field of studies? In April 2024, HEC Professors Tina Lowrey and L.J. Shrum ...