The Value of Critical Thinking in Nursing

- How Nurses Use Critical Thinking
- How to Improve Critical Thinking
- Common Mistakes

Some experts describe a person’s ability to question belief systems, test previously held assumptions, and recognize ambiguity as evidence of critical thinking. Others identify specific skills that demonstrate critical thinking, such as the ability to identify problems and biases, infer and draw conclusions, and determine the relevance of information to a situation.
Nicholas McGowan, BSN, RN, CCRN, has been a critical care nurse for 10 years in neurological trauma nursing and cardiovascular and surgical intensive care. He defines critical thinking as “necessary for problem-solving and decision-making by healthcare providers. It is a process where people use a logical process to gather information and take purposeful action based on their evaluation.”
“This cognitive process is vital for excellent patient outcomes because it requires that nurses make clinical decisions utilizing a variety of different lenses, such as fairness, ethics, and evidence-based practice,” he says.

How Do Nurses Use Critical Thinking?
Successful nurses think beyond their assigned tasks to deliver excellent care for their patients. For example, a nurse might be tasked with changing a wound dressing, delivering medications, and monitoring vital signs during a shift. However, it requires critical thinking skills to understand how a difference in the wound may affect blood pressure and temperature and when those changes may require immediate medical intervention.
Nurses care for many patients during their shifts. Strong critical thinking skills are crucial when juggling various tasks so patient safety and care are not compromised.
Jenna Liphart Rhoads, Ph.D., RN, is a nurse educator with a clinical background in surgical-trauma adult critical care, where critical thinking and action were essential to the safety of her patients. She talks about examples of critical thinking in a healthcare environment, saying:
“Nurses must also critically think to determine which patient to see first, which medications to pass first, and the order in which to organize their day caring for patients. Patient conditions and environments are continually in flux, therefore nurses must constantly be evaluating and re-evaluating information they gather (assess) to keep their patients safe.”
The COVID-19 pandemic created hospital care situations where critical thinking was essential. It was expected of the nurses on the general floor and in intensive care units. Crystal Slaughter is an advanced practice nurse in the intensive care unit (ICU) and a nurse educator. She observed critical thinking throughout the pandemic as she watched intensive care nurses test the boundaries of previously held beliefs and master providing excellent care while preserving resources.
“Nurses are at the patient’s bedside and are often the first ones to detect issues. Then, the nurse needs to gather the appropriate subjective and objective data from the patient in order to frame a concise problem statement or question for the physician or advanced practice provider,” she explains.
Top 5 Ways Nurses Can Improve Critical Thinking Skills
We asked our experts for the top five strategies nurses can use to purposefully improve their critical thinking skills.
Case-Based Approach
Slaughter is a fan of the case-based approach to learning critical thinking skills.
In much the same way a detective would approach a mystery, she mentors her students to ask questions about the situation that help determine the information they have and the information they need. “What is going on? What information am I missing? Can I get that information? What does that information mean for the patient? How quickly do I need to act?”
Consider forming a group and working with a mentor who can guide you through case studies. This provides you with a learner-centered environment in which you can analyze data to reach conclusions and develop communication, analytical, and collaborative skills with your colleagues.
Practice Self-Reflection
Rhoads is an advocate for self-reflection. “Nurses should reflect upon what went well or did not go well in their workday and identify areas of improvement or situations in which they should have reached out for help.” Self-reflection is a form of personal analysis to observe and evaluate situations and how you responded.
This gives you the opportunity to discover mistakes you may have made and to establish new behavior patterns that may help you make better decisions. You likely already do this. For example, after a disagreement or contentious meeting, you may go over the conversation in your head and think about ways you could have responded.
It’s important to go through the decisions you made during your day and determine if you should have gotten more information before acting or if you could have asked better questions.
During self-reflection, you may try thinking about the problem in reverse. This may not give you an immediate answer, but can help you see the situation with fresh eyes and a new perspective. How would the outcome of the day be different if you planned the dressing change in reverse with the assumption you would find a wound infection? How does this information change your plan for the next dressing change?
Develop a Questioning Mind
McGowan has learned that “critical thinking is a self-driven process. It isn’t something that can simply be taught. Rather, it is something that you practice and cultivate with experience. To develop critical thinking skills, you have to be curious and inquisitive.”
To gain critical thinking skills, you must undergo a purposeful process of learning strategies and using them consistently so they become a habit. One of those strategies is developing a questioning mind. Meaningful questions lead to useful answers and are at the core of critical thinking .
However, learning to ask insightful questions is a skill you must develop. Faced with staff and nursing shortages , declining patient conditions, and a rising number of tasks to be completed, it may be difficult to do more than finish the task in front of you. Yet, questions drive active learning and train your brain to see the world differently and take nothing for granted.
It is easier to practice questioning in a non-stressful, quiet environment until it becomes a habit. Then, in the moment when your patient’s care depends on your ability to ask the right questions, you can be ready to rise to the occasion.
Practice Self-Awareness in the Moment
Critical thinking in nursing requires self-awareness and being present in the moment. During a hectic shift, it is easy to lose focus as you struggle to finish every task needed for your patients. Passing medication, changing dressings, and hanging intravenous lines all while trying to assess your patient’s mental and emotional status can affect your focus and how you manage stress as a nurse .
Staying present helps you to be proactive in your thinking and anticipate what might happen, such as bringing extra lubricant for a catheterization or extra gloves for a dressing change.
By staying present, you are also better able to practice active listening. This raises your assessment skills and gives you more information as a basis for your interventions and decisions.
Use a Process
As you are developing critical thinking skills, it can be helpful to use a process. For example:
- Ask questions.
- Gather information.
- Implement a strategy.
- Evaluate the results.
- Consider another point of view.
These are the fundamental steps of the nursing process (assess, diagnose, plan, implement, evaluate). The last step will help you overcome one of the common problems of critical thinking in nursing — personal bias.
Common Critical Thinking Pitfalls in Nursing
Your brain uses a set of processes to make inferences about what’s happening around you. In some cases, your unreliable biases can lead you down the wrong path. McGowan places personal biases at the top of his list of common pitfalls to critical thinking in nursing.
“We all form biases based on our own experiences. However, nurses have to learn to separate their own biases from each patient encounter to avoid making false assumptions that may interfere with their care,” he says. Successful critical thinkers accept they have personal biases and learn to look out for them. Awareness of your biases is the first step to understanding if your personal bias is contributing to the wrong decision.
New nurses may be overwhelmed by the transition from academics to clinical practice, leading to a task-oriented mindset and a common new nurse mistake ; this conflicts with critical thinking skills.
“Consider a patient whose blood pressure is low but who also needs to take a blood pressure medication at a scheduled time. A task-oriented nurse may provide the medication without regard for the patient’s blood pressure because medication administration is a task that must be completed,” Slaughter says. “A nurse employing critical thinking skills would address the low blood pressure, review the patient’s blood pressure history and trends, and potentially call the physician to discuss whether medication should be withheld.”
Fear and pride may also stand in the way of developing critical thinking skills. Your belief system and worldview provide comfort and guidance, but this can impede your judgment when you are faced with an individual whose belief system or cultural practices are not the same as yours. Fear or pride may prevent you from pursuing a line of questioning that would benefit the patient. Nurses with strong critical thinking skills exhibit:
- Learn from their mistakes and the mistakes of other nurses
- Look forward to integrating changes that improve patient care
- Treat each patient interaction as a part of a whole
- Evaluate new events based on past knowledge and adjust decision-making as needed
- Solve problems with their colleagues
- Are self-confident
- Acknowledge biases and seek to ensure these do not impact patient care
An Essential Skill for All Nurses
Critical thinking in nursing protects patient health and contributes to professional development and career advancement. Administrative and clinical nursing leaders are required to have strong critical thinking skills to be successful in their positions.
By using the strategies in this guide during your daily life and in your nursing role, you can intentionally improve your critical thinking abilities and be rewarded with better patient outcomes and potential career advancement.
Frequently Asked Questions About Critical Thinking in Nursing
How are critical thinking skills utilized in nursing practice.
Nursing practice utilizes critical thinking skills to provide the best care for patients. Often, the patient’s cause of pain or health issue is not immediately clear. Nursing professionals need to use their knowledge to determine what might be causing distress, collect vital information, and make quick decisions on how best to handle the situation.
How does nursing school develop critical thinking skills?
Nursing school gives students the knowledge professional nurses use to make important healthcare decisions for their patients. Students learn about diseases, anatomy, and physiology, and how to improve the patient’s overall well-being. Learners also participate in supervised clinical experiences, where they practice using their critical thinking skills to make decisions in professional settings.
Do only nurse managers use critical thinking?
Nurse managers certainly use critical thinking skills in their daily duties. But when working in a health setting, anyone giving care to patients uses their critical thinking skills. Everyone — including licensed practical nurses, registered nurses, and advanced nurse practitioners —needs to flex their critical thinking skills to make potentially life-saving decisions.
Meet Our Contributors

Crystal Slaughter, DNP, APRN, ACNS-BC, CNE
Crystal Slaughter is a core faculty member in Walden University’s RN-to-BSN program. She has worked as an advanced practice registered nurse with an intensivist/pulmonary service to provide care to hospitalized ICU patients and in inpatient palliative care. Slaughter’s clinical interests lie in nursing education and evidence-based practice initiatives to promote improving patient care.

Jenna Liphart Rhoads, Ph.D., RN
Jenna Liphart Rhoads is a nurse educator and freelance author and editor. She earned a BSN from Saint Francis Medical Center College of Nursing and an MS in nursing education from Northern Illinois University. Rhoads earned a Ph.D. in education with a concentration in nursing education from Capella University where she researched the moderation effects of emotional intelligence on the relationship of stress and GPA in military veteran nursing students. Her clinical background includes surgical-trauma adult critical care, interventional radiology procedures, and conscious sedation in adult and pediatric populations.

Nicholas McGowan, BSN, RN, CCRN
Nicholas McGowan is a critical care nurse with 10 years of experience in cardiovascular, surgical intensive care, and neurological trauma nursing. McGowan also has a background in education, leadership, and public speaking. He is an online learner who builds on his foundation of critical care nursing, which he uses directly at the bedside where he still practices. In addition, McGowan hosts an online course at Critical Care Academy where he helps nurses achieve critical care (CCRN) certification.
Probing the Relationship Between Evidence-Based Practice Implementation Models and Critical Thinking in Applied Nursing Practice
- PMID: 27031030
- DOI: 10.3928/00220124-20160322-05
HOW TO OBTAIN CONTACT HOURS BY READING THIS ISSUE Instructions: 1.2 contact hours will be awarded by Villanova University College of Nursing upon successful completion of this activity. A contact hour is a unit of measurement that denotes 60 minutes of an organized learning activity. This is a learner-based activity. Villanova University College of Nursing does not require submission of your answers to the quiz. A contact hour certificate will be awarded after you register, pay the registration fee, and complete the evaluation form online at http://goo.gl/gMfXaf. In order to obtain contact hours you must: 1. Read the article, "Probing the Relationship Between Evidence-Based Practice Implementation Models and Critical Thinking in Applied Nursing Practice," found on pages 161-168, carefully noting any tables and other illustrative materials that are included to enhance your knowledge and understanding of the content. Be sure to keep track of the amount of time (number of minutes) you spend reading the article and completing the quiz. 2. Read and answer each question on the quiz. After completing all of the questions, compare your answers to those provided within this issue. If you have incorrect answers, return to the article for further study. 3. Go to the Villanova website to register for contact hour credit. You will be asked to provide your name, contact information, and a VISA, MasterCard, or Discover card number for payment of the $20.00 fee. Once you complete the online evaluation, a certificate will be automatically generated. This activity is valid for continuing education credit until March 31, 2019. CONTACT HOURS This activity is co-provided by Villanova University College of Nursing and SLACK Incorporated. Villanova University College of Nursing is accredited as a provider of continuing nursing education by the American Nurses Credentialing Center's Commission on Accreditation.
Objectives: • Describe the key components and characteristics related to evidence-based practice and critical thinking. • Identify the relationship between evidence-based practice and critical thinking. DISCLOSURE STATEMENT Neither the planners nor the author have any conflicts of interest to disclose. Evidence-based practice is not a new concept to the profession of nursing, yet its application and sustainability is inconsistent in nursing practice. Despite the expansion of efforts to teach evidence-based practice and practically apply evidence at the bedside, a research-practice gap still exists. Several critical factors contribute to the successful application of evidence into practice, including critical thinking. The purpose of this article is to discuss the relationship between critical thinking and the current evidence-based practice implementation models. Understanding this relationship will help nurse educators and clinicians in cultivating critical thinking skills in nursing staff to most effectively apply evidence at the bedside. Critical thinking is a key element and is essential to the learning and implementation of evidence-based practice, as demonstrated by its integration into evidence-based practice implementation models.
Copyright 2016, SLACK Incorporated.
- Attitude of Health Personnel
- Clinical Competence*
- Education, Nursing, Continuing / organization & administration*
- Evidence-Based Nursing / education*
- Models, Nursing
- Nursing Education Research
- Nursing Staff, Hospital / education*
- United States
Promoting critical thinking through an evidence-based skills fair intervention
Journal of Research in Innovative Teaching & Learning
ISSN : 2397-7604
Article publication date: 23 November 2020
Issue publication date: 1 April 2022
The lack of critical thinking in new graduates has been a concern to the nursing profession. The purpose of this study was to investigate the effects of an innovative, evidence-based skills fair intervention on nursing students' achievements and perceptions of critical thinking skills development.
Design/methodology/approach
The explanatory sequential mixed-methods design was employed for this study.
The findings indicated participants perceived the intervention as a strategy for developing critical thinking.
Originality/value
The study provides educators helpful information in planning their own teaching practice in educating students.
Critical thinking
Evidence-based practice, skills fair intervention.
Gonzalez, H.C. , Hsiao, E.-L. , Dees, D.C. , Noviello, S.R. and Gerber, B.L. (2022), "Promoting critical thinking through an evidence-based skills fair intervention", Journal of Research in Innovative Teaching & Learning , Vol. 15 No. 1, pp. 41-54. https://doi.org/10.1108/JRIT-08-2020-0041
Emerald Publishing Limited
Copyright © 2020, Heidi C. Gonzalez, E-Ling Hsiao, Dianne C. Dees, Sherri R. Noviello and Brian L. Gerber
Published in Journal of Research in Innovative Teaching & Learning . Published by Emerald Publishing Limited. This article is published under the Creative Commons Attribution (CC BY 4.0) licence. Anyone may reproduce, distribute, translate and create derivative works of this article (for both commercial and non-commercial purposes), subject to full attribution to the original publication and authors. The full terms of this licence may be seen at http://creativecommons.org/licences/by/4.0/legalcode
Introduction
Critical thinking (CT) was defined as “cognitive skills of analyzing, applying standards, discriminating, information seeking, logical reasoning, predicting, and transforming knowledge” ( Scheffer and Rubenfeld, 2000 , p. 357). Critical thinking is the basis for all professional decision-making ( Moore, 2007 ). The lack of critical thinking in student nurses and new graduates has been a concern to the nursing profession. It would negatively affect the quality of service and directly relate to the high error rates in novice nurses that influence patient safety ( Arli et al. , 2017 ; Saintsing et al. , 2011 ). It was reported that as many as 88% of novice nurses commit medication errors with 30% of these errors due to a lack of critical thinking ( Ebright et al. , 2004 ). Failure to rescue is another type of error common for novice nurses, reported as high as 37% ( Saintsing et al. , 2011 ). The failure to recognize trends or complications promptly or take action to stabilize the patient occurs when health-care providers do not recognize signs and symptoms of the early warnings of distress ( Garvey and CNE series, 2015 ). Internationally, this lack of preparedness and critical thinking attributes to the reported 35–60% attrition rate of new graduate nurses in their first two years of practice ( Goodare, 2015 ). The high attrition rate of new nurses has expensive professional and economic costs of $82,000 or more per nurse and negatively affects patient care ( Twibell et al. , 2012 ). Facione and Facione (2013) reported the failure to utilize critical thinking skills not only interferes with learning but also results in poor decision-making and unclear communication between health-care professionals, which ultimately leads to patient deaths.
Due to the importance of critical thinking, many nursing programs strive to infuse critical thinking into their curriculum to better prepare graduates for the realities of clinical practice that involves ever-changing, complex clinical situations and bridge the gap between education and practice in nursing ( Benner et al. , 2010 ; Kim et al. , 2019 ; Park et al. , 2016 ; Newton and Moore, 2013 ; Nibert, 2011 ). To help develop students' critical thinking skills, nurse educators must change the way they teach nursing, so they can prepare future nurses to be effective communicators, critical thinkers and creative problem solvers ( Rieger et al. , 2015 ). Nursing leaders also need to redefine teaching practice and educational guidelines that drive innovation in undergraduate nursing programs.
Evidence-based practice has been advocated to promote critical thinking and help reduce the research-practice gap ( Profetto-McGrath, 2005 ; Stanley and Dougherty, 2010 ). Evidence-based practice was defined as “the conscientious, explicit, and judicious use of current best evidence in making decisions about the care of the individual patient” ( Sackett et al. , 1996 , p. 71). Skills fair intervention, one type of evidence-based practice, can be used to engage students, promote active learning and develop critical thinking ( McCausland and Meyers, 2013 ; Roberts et al. , 2009 ). Skills fair intervention helps promote a consistent teaching practice of the psychomotor skills to the novice nurse that decreased anxiety, gave clarity of expectations to the students in the clinical setting and increased students' critical thinking skills ( Roberts et al. , 2009 ). The researchers of this study had an opportunity to create an active, innovative skills fair intervention for a baccalaureate nursing program in one southeastern state. This intervention incorporated evidence-based practice rationale with critical thinking prompts using Socratic questioning, evidence-based practice videos to the psychomotor skill rubrics, group work, guided discussions, expert demonstration followed by guided practice and blended learning in an attempt to promote and develop critical thinking in nursing students ( Hsu and Hsieh, 2013 ; Oermann et al. , 2011 ; Roberts et al. , 2009 ). The effects of an innovative skills fair intervention on senior baccalaureate nursing students' achievements and their perceptions of critical thinking development were examined in the study.
Literature review
The ability to use reasoned opinion focusing equally on processes and outcomes over emotions is called critical thinking ( Paul and Elder, 2008 ). Critical thinking skills are desired in almost every discipline and play a major role in decision-making and daily judgments. The roots of critical thinking date back to Socrates 2,500 years ago and can be traced to the ancient philosopher Aristotle ( Paul and Elder, 2012 ). Socrates challenged others by asking inquisitive questions in an attempt to challenge their knowledge. In the 1980s, critical thinking gained nationwide recognition as a behavioral science concept in the educational system ( Robert and Petersen, 2013 ). Many researchers in both education and nursing have attempted to define, measure and teach critical thinking for decades. However, a theoretical definition has yet to be accepted and established by the nursing profession ( Romeo, 2010 ). The terms critical literacy, CT, reflective thinking, systems thinking, clinical judgment and clinical reasoning are used synonymously in the reviewed literature ( Clarke and Whitney, 2009 ; Dykstra, 2008 ; Jones, 2010 ; Swing, 2014 ; Turner, 2005 ).
Watson and Glaser (1980) viewed critical thinking not only as cognitive skills but also as a combination of skills, knowledge and attitudes. Paul (1993) , the founder of the Foundation for Critical Thinking, offered several definitions of critical thinking and identified three essential components of critical thinking: elements of thought, intellectual standards and affective traits. Brunt (2005) stated critical thinking is a process of being practical and considered it to be “the process of purposeful thinking and reflective reasoning where practitioners examine ideas, assumptions, principles, conclusions, beliefs, and actions in the contexts of nursing practice” (p. 61). In an updated definition, Ennis (2011) described critical thinking as, “reasonable reflective thinking focused on deciding what to believe or do” (para. 1).
The most comprehensive attempt to define critical thinking was under the direction of Facione and sponsored by the American Philosophical Association ( Scheffer and Rubenfeld, 2000 ). Facione (1990) surveyed 53 experts from the arts and sciences using the Delphi method to define critical thinking as a “purposeful, self-regulatory judgment which results in interpretation, analysis, evaluation, and inference, as well as an explanation of the evidential, conceptual, methodological, criteriological, or contextual considerations upon which judgment, is based” (p. 2).
To come to a consensus definition for critical thinking, Scheffer and Rubenfeld (2000) also conducted a Delphi study. Their study consisted of an international panel of nurses who completed five rounds of sequenced questions to arrive at a consensus definition. Critical thinking was defined as “habits of mind” and “cognitive skills.” The elements of habits of mind included “confidence, contextual perspective, creativity, flexibility, inquisitiveness, intellectual integrity, intuition, open-mindedness, perseverance, and reflection” ( Scheffer and Rubenfeld, 2000 , p. 352). The elements of cognitive skills were recognized as “analyzing, applying standards, discriminating, information seeking, logical reasoning, predicting, and transforming knowledge” ( Scheffer and Rubenfeld, 2000 , p. 352). In addition, Ignatavicius (2001) defined the development of critical thinking as a long-term process that must be practiced, nurtured and reinforced over time. Ignatavicius believed that a critical thinker required six cognitive skills: interpretation, analysis, evaluation, inference, explanation and self-regulation ( Chun-Chih et al. , 2015 ). According to Ignatavicius (2001) , the development of critical thinking is difficult to measure or describe because it is a formative rather than summative process.
Fero et al. (2009) noted that patient safety might be compromised if a nurse cannot provide clinically competent care due to a lack of critical thinking. The Institute of Medicine (2001) recommended five health care competencies: patient-centered care, interdisciplinary team care, evidence-based practice, informatics and quality improvement. Understanding the development and attainment of critical thinking is the key for gaining these future competencies ( Scheffer and Rubenfeld, 2000 ). The development of a strong scientific foundation for nursing practice depends on habits such as contextual perspective, inquisitiveness, creativity, analysis and reasoning skills. Therefore, the need to better understand how these critical thinking habits are developed in nursing students needs to be explored through additional research ( Fero et al. , 2009 ). Despite critical thinking being listed since the 1980s as an accreditation outcome criteria for baccalaureate programs by the National League for Nursing, very little improvement has been observed in practice ( McMullen and McMullen, 2009 ). James (2013) reported the number of patient harm incidents associated with hospital care is much higher than previously thought. James' study indicated that between 210,000 and 440,000 patients each year go to the hospital for care and end up suffering some preventable harm that contributes to their death. James' study of preventable errors is attributed to other sources besides nursing care, but having a nurse in place who can advocate and critically think for patients will make a positive impact on improving patient safety ( James, 2013 ; Robert and Peterson, 2013 ).
Adopting teaching practice to promote CT is a crucial component of nursing education. Research by Nadelson and Nadelson (2014) suggested evidence-based practice is best learned when integrated into multiple areas of the curriculum. Evidence-based practice developed its roots through evidence-based medicine, and the philosophical origins extend back to the mid-19th century ( Longton, 2014 ). Florence Nightingale, the pioneer of modern nursing, used evidence-based practice during the Crimean War when she recognized a connection between poor sanitary conditions and rising mortality rates of wounded soldiers ( Rahman and Applebaum, 2011 ). In professional nursing practice today, a commonly used definition of evidence-based practice is derived from Dr. David Sackett: the conscientious, explicit and judicious use of current best evidence in making decisions about the care of the individual patient ( Sackett et al. , 1996 , p. 71). As professional nurses, it is imperative for patient safety to remain inquisitive and ask if the care provided is based on available evidence. One of the core beliefs of the American Nephrology Nurses' Association's (2019) 2019–2020 Strategic Plan is “Anna must support research to develop evidence-based practice, as well as to advance nursing science, and that as individual members, we must support, participate in, and apply evidence-based research that advances our own skills, as well as nursing science” (p. 1). Longton (2014) reported the lack of evidence-based practice in nursing resulted in negative outcomes for patients. In fact, when evidence-based practice was implemented, changes in policies and procedures occurred that resulted in decreased reports of patient harm and associated health-care costs. The Institute of Medicine (2011) recommendations included nurses being leaders in the transformation of the health-care system and achieving higher levels of education that will provide the ability to critically analyze data to improve the quality of care for patients. Student nurses must be taught to connect and integrate CT and evidence-based practice throughout their program of study and continue that practice throughout their careers.
One type of evidence-based practice that can be used to engage students, promote active learning and develop critical thinking is skills fair intervention ( McCausland and Meyers, 2013 ; Roberts et al. , 2009 ). Skills fair intervention promoted a consistent teaching approach of the psychomotor skills to the novice nurse that decreased anxiety, gave clarity of expectations to the students in the clinical setting and increased students' critical thinking skills ( Roberts et al. , 2009 ). The skills fair intervention used in this study is a teaching strategy that incorporated CT prompts, Socratic questioning, group work, guided discussions, return demonstrations and blended learning in an attempt to develop CT in nursing students ( Hsu and Hsieh, 2013 ; Roberts et al. , 2009 ). It melded evidence-based practice with simulated CT opportunities while students practiced essential psychomotor skills.
Research methodology
Context – skills fair intervention.
According to Roberts et al. (2009) , psychomotor skills decline over time even among licensed experienced professionals within as little as two weeks and may need to be relearned within two months without performing a skill. When applying this concept to student nurses for whom each skill is new, it is no wonder their competency result is diminished after having a summer break from nursing school. This skills fair intervention is a one-day event to assist baccalaureate students who had taken the summer off from their studies in nursing and all faculty participated in operating the stations. It incorporated evidence-based practice rationale with critical thinking prompts using Socratic questioning, evidence-based practice videos to the psychomotor skill rubrics, group work, guided discussions, expert demonstration followed by guided practice and blended learning in an attempt to promote and develop critical thinking in baccalaureate students.
Students were scheduled and placed randomly into eight teams based on attributes of critical thinking as described by Wittmann-Price (2013) : Team A – Perseverance, Team B – Flexibility, Team C – Confidence, Team D – Creativity, Team E – Inquisitiveness, Team F – Reflection, Team G – Analyzing and Team H – Intuition. The students rotated every 20 minutes through eight stations: Medication Administration: Intramuscular and Subcutaneous Injections, Initiating Intravenous Therapy, ten-minute Focused Physical Assessment, Foley Catheter Insertion, Nasogastric Intubation, Skin Assessment/Braden Score and Restraints, Vital Signs and a Safety Station. When the students completed all eight stations, they went to the “Check-Out” booth to complete a simple evaluation to determine their perceptions of the effectiveness of the innovative intervention. When the evaluations were complete, each of the eight critical thinking attribute teams placed their index cards into a hat, and a student won a small prize. All Junior 2, Senior 1 and Senior 2 students were required to attend the Skills Fair. The Skills Fair Team strove to make the event as festive as possible, engaging nursing students with balloons, candy, tri-boards, signs and fun pre and postactivities. The Skills Fair rubrics, scheduling and instructions were shared electronically with students and faculty before the skills fair intervention to ensure adequate preparation and continuous resource availability as students move forward into their future clinical settings.
Research design
Institutional review board (IRB) approval was obtained from XXX University to conduct this study and protect human subject rights. The explanatory sequential mixed-methods design was employed for this study. The design was chosen to identify what effects a skills fair intervention that had on senior baccalaureate nursing students' achievements on the Kaplan Critical Thinking Integrated Test (KCTIT) and then follow up with individual interviews to explore those test results in more depth. In total, 52 senior nursing students completed the KCTIT; 30 of them participated in the skills fair intervention and 22 of them did not participate. The KCTIT is a computerized 85-item exam in which 85 equates to 100%, making each question worth one point. It has high reliability and validity ( Kaplan Nursing, 2012 ; Swing, 2014 ). The reliability value of the KCTIT ranged from 0.72 to 0.89. A t -test was used to analyze the test results.
A total of 11 participants were purposefully selected based on a range of six high achievers and five low achievers on the KCTIT for open-ended one-on-one interviews. Each interview was conducted individually and lasted for about 60 minutes. An open-ended interview protocol was used to guide the flow of data collection. The interviewees' ages ranged from 21 to 30 years, with an average of 24 years. One of 11 interviewees was male. Among them, seven were White, three were Black and one was Indian American. The data collected were used to answer the following research questions: (1) What was the difference in achievements on the KCTIT among senior baccalaureate nursing students who participated in the skills fair intervention and students who did not participate? (2) What were the senior baccalaureate nursing students' perceptions of internal and external factors impacting the development of critical thinking skills during the skills fair intervention? and (3) What were the senior baccalaureate nursing students' perceptions of the skills fair intervention as a critical thinking developmental strategy?
Inductive content analysis was used to analyze interview data by starting with the close reading of the transcripts and writing memos for initial coding, followed by an analysis of patterns and relationships among the data for focused coding. The intercoder reliability was established for qualitative data analysis with a nursing expert. The lead researcher and the expert read the transcript several times and assigned a code to significant units of text that corresponded with answering the research questions. The codes were compared based on differences and similarities and sorted into subcategories and categories. Then, headings and subheadings were used based on similar comments to develop central themes and patterns. The process of establishing intercoder reliability helped to increase dependability, conformability and credibility of the findings ( Graneheim and Lundman, 2004 ). In addition, methods of credibility, confirmability, dependability and transferability were applied to increase the trustworthiness of this study ( Graneheim and Lundman, 2004 ). First, reflexivity was observed by keeping journals and memos. This practice allowed the lead researcher to reflect on personal views to minimize bias. Data saturation was reached through following the recommended number of participants as well as repeated immersion in the data during analysis until no new data surfaced. Member checking was accomplished through returning the transcript and the interpretation to the participants to check the accuracy and truthfulness of the findings. Finally, proper documentation was conducted to allow accurate crossreferencing throughout the study.
Quantitative results
Results for the quantitative portion showed there was no difference in scores on the KCTIT between senior nursing students who participated in the skills fair intervention and senior nursing students who did not participate, t (50) = −0.174, p = 0.86 > 0.05. The test scores between the nonparticipant group ( M = 67.59, SD = 5.81) and the participant group ( M = 67.88, SD = 5.99) were almost equal.
Qualitative results
Initial coding.
The results from the initial coding and generated themes are listed in Table 1 . First, the participants perceived the skills fair intervention as “promoting experience” and “confidence” by practicing previously learned knowledge and reinforcing it with active learning strategies. Second, the participants perceived the skills fair intervention as a relaxed, nonthreatening learning environment due to the festive atmosphere, especially in comparison to other learning experiences in the nursing program. The nonthreatening environment of the skills fair intervention allowed students to learn without fear. Third, the majority of participants believed their critical thinking was strengthened after participating. Several participants believed their perception of critical thinking was “enhanced” or “reinforced” rather than significantly changed.
Focused coding results
The final themes were derived from the analysis of patterns and relationships among the content of the data using inductive content analysis ( Saldana, 2009 ). The following was examined across the focused coding process: (1) factors impacting critical thinking skills development during skills fair intervention and (2) skills fair intervention a critical thinking skills developmental strategy.
Factors impacting critical thinking skills development . The factors impacting the development of critical thinking during the skills fair intervention were divided into two themes: internal factors and external factors. The internal factors were characteristics innate to the students. The identified internal factors were (1) confidence and anxiety levels, (2) attitude and (3) age. The external factors were the outside influences that affected the students. The external factors were (1) experience and practice, (2) faculty involvement, (3) positive learning environment and (4) faculty prompts.
I think that confidence and anxiety definitely both have a huge impact on your ability to be able to really critically think. If you start getting anxious and panicking you cannot think through the process like you need too. I do not really think gender or age necessarily would have anything to do with critical thinking.
Definitely the confidence level, I think, the more advanced you get in the program, your confidence just keeps on growing. Level of anxiety, definitely… I think the people who were in the Skills Fair for the first time, had more anxiety because they did not really know to think, they did not know how strict it was going to be, or if they really had to know everything by the book. I think the Skills Fair helped everyone's confidence levels, but especially the Jr. 2's.
Attitude was an important factor in the development of critical thinking skills during the skills fair intervention as participants believed possessing a pleasant and positive attitude meant a student was eager to learn, participate, accept responsibility for completing duties and think seriously. Participant 6 believed attitude contributed to performance in the Skills Fair.
I feel like, certain things bring critical thinking out in you. And since I'm a little bit older than some of the other students, I have had more life experiences and am able to figure stuff out better. Older students have had more time to learn by trial and error, and this and that.
Like when I had clinical with you, you'd always tell us to know our patients' medications. To always know and be prepared to answer questions – because at first as a Junior 1 we did not do that in the clinical setting… and as a Junior 2, I did not really have to know my medications, but with you as a Senior 1, I started to realize that the patients do ask about their meds, so I was making sure that I knew everything before they asked it. And just having more practice with IVs – at first, I was really nervous, but when I got to my preceptorship – I had done so many IVs and with all of the practice, it just built up my confidence with that skill so when I performed that skill during the Fair, I was confident due to my clinical experiences and able to think and perform better.
I think teachers will always affect the ability to critically think just because you want [to] get the right answer because they are there and you want to seem smart to them [Laugh]. Also, if you are leading in the wrong direction of your thinking – they help steer you back to [in] the right direction so I think that was very helpful.
You could tell the faculty really tried to make it more laid back and fun, so everybody would have a good experience. The faculty had a good attitude. I think making it fun and active helped keep people positive. You know if people are negative and not motivated, nothing gets accomplished. The faculty did an amazing job at making the Skills Fair a positive atmosphere.
However, for some of the participants, a positive learning environment depended on their fellow students. The students were randomly assigned alphabetically to groups, and the groups were assigned to starting stations at the Skills Fair. The participants claimed some students did not want to participate and displayed cynicism toward the intervention. The participants believed their cynicism affected the positive learning environment making critical thinking more difficult during the Skills Fair.
Okay, when [instructor name] was demonstrating the Chevron technique right after we inserted the IV catheter and we were trying to secure the catheter, put on the extension set, and flush the line at what seemed to be all at the same time. I forgot about how you do not want to put the tape right over the hub of the catheter because when you go back in and try to assess the IV site – you're trying to assess whether or not it is patent or infiltrated – you have to visualize the insertion site. That was one of the things that I had been doing wrong because I was just so excited that I got the IV in the vein in the first place – that I did not think much about the tape or the tegaderm for sterility. So I think an important part of critical thinking is to be able to recognize when you've made a mistake and stop, stop yourself from doing it in the future (see Table 2 ).
Skills fair intervention as a developmental strategy for critical thinking . The participants identified the skills fair intervention was effective as a developmental strategy for critical thinking, as revealed in two themes: (1) develops alternative thinking and (2) thinking before doing (See Table 3 ).
Develops alternative thinking . The participants perceived the skills fair intervention helped enhance critical thinking and confidence by developing alternative thinking. Alternative thinking was described as quickly thinking of alternative solutions to problems based on the latest evidence and using that information to determine what actions were warranted to prevent complications and prevent injury. It helped make better connections through the learning of rationale between knowledge and skills and then applying that knowledge to prevent complications and errors to ensure the safety of patients. The participants stated the learning of rationale for certain procedures provided during the skills fair intervention such as the evidence and critical thinking prompts included in the rubrics helped reinforce this connection. The participants also shared they developed alternative thinking after participating in the skills fair intervention by noticing trends in data to prevent potential complications from the faculty prompts. Participant 1 stated her instructor prompted her alternative thinking through questioning about noticing trends to prevent potential complications. She said the following:
Another way critical thinking occurred during the skills fair was when [instructor name] was teaching and prompted us about what it would be like to care for a patient with a fractured hip – I think this was at the 10-minute focused assessment station, but I could be wrong. I remember her asking, “What do you need to be on the look-out for? What can go wrong?” I automatically did not think critically very well and was only thinking circulation in the leg, dah, dah, dah. But she was prompting us to think about mobility alterations and its effect on perfusion and oxygenation. She was trying to help us build those connections. And I think that's a lot of the aspects of critical thinking that gets overlooked with the nursing student – trouble making connections between our knowledge and applying it in practice.
Thinking before doing . The participants perceived thinking before doing, included thinking of how and why certain procedures, was necessary through self-examination prior to taking action. The hands-on situational learning allowed the participants in the skills fair intervention to better notice assessment data and think at a higher level as their previous learning of the skills was perceived as memorization of steps. This higher level of learning allowed participants to consider different future outcomes and analyze pertinent data before taking action.
I think what helped me the most is considering outcomes of my actions before I do anything. For instance, if you're thinking, “Okay. Well, I need to check their blood pressure before I administer this blood pressure medication – or the blood pressure could potentially bottom out.” I really do not want my patient to bottom out and get hypotensive because I administered a medication that was ordered, but not safe to give. I could prevent problems from happening if I know what to be on alert for and act accordingly. So ultimately knowing that in the clinical setting, I can prevent complications from happening and I save myself, my license, and promote patient safety. I think knowing that I've seen the importance of critical thinking already in practice has helped me value and understand why I should be critically thinking. Yes, we use the 5-rights of medication safety – but we also have to think. For instance, if I am going to administer insulin – what do I need to know or do to give this safely? What is the current blood sugar? Has the patient been eating? When is the next meal scheduled? Is the patient NPO for a procedure? Those are examples of questions to consider and the level of thinking that needs to take place prior to taking actions in the clinical setting.
Although the results of quantitative data showed no significant difference in scores on the KCTIT between the participant and nonparticipant groups, during the interviews some participants attributed this result to the test not being part of a course grade and believed students “did not try very hard to score well.” However, the participants who attended interviews did identify the skills fair intervention as a developmental strategy for critical thinking by helping them develop alternative thinking and thinking before doing. The findings are supported in the literature as (1) nurses must recognize signs of clinical deterioration and take action promptly to prevent potential complications ( Garvey and CNE series 2015 ) and (2) nurses must analyze pertinent data and consider all possible solutions before deciding on the most appropriate action for each patient ( Papathanasiou et al. , 2014 ).
The skills fair intervention also enhanced the development of self-confidence by participants practicing previously learned skills in a controlled, safe environment. The nonthreatening environment of the skills fair intervention allowed students to learn without fear and the majority of participants believed their critical thinking was strengthened after participating. The interview data also revealed a combination of internal and external factors that influenced the development of critical thinking during the skills fair intervention including confidence and anxiety levels, attitude, age, experience and practice, faculty involvement, positive learning environment and faculty prompts. These factors should be considered when addressing the promotion and development of critical thinking.
Conclusions, limitations and recommendations
A major concern in the nursing profession is the lack of critical thinking in student nurses and new graduates, which influences the decision-making of novice nurses and directly affects patient care and safety ( Saintsing et al. , 2011 ). Nurse educators must use evidence-based practice to prepare students to critically think with the complicated and constantly evolving environment of health care today ( Goodare, 2015 ; Newton and Moore, 2013 ). Evidence-based practice has been advocated to promote critical thinking ( Profetto-McGrath, 2005 ; Stanley and Dougherty, 2010 ). The skills fair intervention can be one type of evidence-based practice used to promote critical thinking ( McCausland and Meyers, 2013 ; Roberts et al. , 2009 ). The Intervention used in this study incorporated evidence-based practice rationale with critical thinking prompts using Socratic questioning, evidence-based practice videos to the psychomotor skill rubrics, group work, guided discussions, expert demonstration followed by guided practice and blended learning in an attempt to promote and develop critical thinking in nursing students.
The explanatory sequential mixed-methods design was employed to investigate the effects of the innovative skills fair intervention on senior baccalaureate nursing students' achievements and their perceptions of critical thinking skills development. Although the quantitative results showed no significant difference in scores on the KCTIT between students who participated in the skills fair intervention and those who did not, those who attended the interviews perceived their critical thinking was reinforced after the skills fair intervention and believed it was an effective developmental strategy for critical thinking, as it developed alternative thinking and thinking before doing. This information is useful for nurse educators who plan their own teaching practice to promote critical thinking and improve patient outcomes. The findings also provide schools and educators information that helps review their current approach in educating nursing students. As evidenced in the findings, the importance of developing critical thinking skills is crucial for becoming a safe, professional nurse. Internal and external factors impacting the development of critical thinking during the skills fair intervention were identified including confidence and anxiety levels, attitude, age, experience and practice, faculty involvement, positive learning environment and faculty prompts. These factors should be considered when addressing the promotion and development of critical thinking.
There were several limitations to this study. One of the major limitations of the study was the limited exposure of students' time of access to the skills fair intervention, as it was a one-day learning intervention. Another limitation was the sample selection and size. The skills fair intervention was limited to only one baccalaureate nursing program in one southeastern state. As such, the findings of the study cannot be generalized as it may not be representative of baccalaureate nursing programs in general. In addition, this study did not consider students' critical thinking achievements prior to the skills fair intervention. Therefore, no baseline measurement of critical thinking was available for a before and after comparison. Other factors in the nursing program could have affected the students' scores on the KCTIT, such as anxiety or motivation that was not taken into account in this study.
The recommendations for future research are to expand the topic by including other regions, larger samples and other baccalaureate nursing programs. In addition, future research should consider other participant perceptions, such as nurse educators, to better understand the development and growth of critical thinking skills among nursing students. Finally, based on participant perceptions, future research should include a more rigorous skills fair intervention to develop critical thinking and explore the link between confidence and critical thinking in nursing students.
Initial coding results
Factors impacting critical thinking skill development during skills fair intervention
Skills fair intervention as a developmental strategy for critical thinking
American Nephrology Nurses Association (ANNA) ( 2019 ), “ Learning, leading, connecting, and playing at the intersection of nephrology and nursing-2019–2020 strategic plan ”, viewed 3 Aug 2019, available at: https://www.annanurse.org/download/reference/association/strategicPlan.pdf .
Arli , S.D. , Bakan , A.B. , Ozturk , S. , Erisik , E. and Yildirim , Z. ( 2017 ), “ Critical thinking and caring in nursing students ”, International Journal of Caring Sciences , Vol. 10 No. 1 , pp. 471 - 478 .
Benner , P. , Sutphen , M. , Leonard , V. and Day , L. ( 2010 ), Educating Nurses: A Call for Radical Transformation , Jossey-Bass , San Francisco .
Brunt , B. ( 2005 ), “ Critical thinking in nursing: an integrated review ”, The Journal of Continuing Education in Nursing , Vol. 36 No. 2 , pp. 60 - 67 .
Chun-Chih , L. , Chin-Yen , H. , I-Ju , P. and Li-Chin , C. ( 2015 ), “ The teaching-learning approach and critical thinking development: a qualitative exploration of Taiwanese nursing students ”, Journal of Professional Nursing , Vol. 31 No. 2 , pp. 149 - 157 , doi: 10.1016/j.profnurs.2014.07.001 .
Clarke , L.W. and Whitney , E. ( 2009 ), “ Walking in their shoes: using multiple-perspectives texts as a bridge to critical literacy ”, The Reading Teacher , Vol. 62 No. 6 , pp. 530 - 534 , doi: 10.1598/RT.62.6.7 .
Dykstra , D. ( 2008 ), “ Integrating critical thinking and memorandum writing into course curriculum using the internet as a research tool ”, College Student Journal , Vol. 42 No. 3 , pp. 920 - 929 , doi: 10.1007/s10551-010-0477-2 .
Ebright , P. , Urden , L. , Patterson , E. and Chalko , B. ( 2004 ), “ Themes surrounding novice nurse near-miss and adverse-event situations ”, The Journal of Nursing Administration: The Journal of Nursing Administration , Vol. 34 , pp. 531 - 538 , doi: 10.1097/00005110-200411000-00010 .
Ennis , R. ( 2011 ), “ The nature of critical thinking: an outline of critical thinking dispositions and abilities ”, viewed 3 May 2017, available at: https://education.illinois.edu/docs/default-source/faculty-documents/robert-ennis/thenatureofcriticalthinking_51711_000.pdf .
Facione , P.A. ( 1990 ), Critical Thinking: A Statement of Expert Consensus for Purposes of Educational Assessment and Instruction , The California Academic Press , Millbrae .
Facione , N.C. and Facione , P.A. ( 2013 ), The Health Sciences Reasoning Test: Test Manual , The California Academic Press , Millbrae .
Fero , L.J. , Witsberger , C.M. , Wesmiller , S.W. , Zullo , T.G. and Hoffman , L.A. ( 2009 ), “ Critical thinking ability of new graduate and experienced nurses ”, Journal of Advanced Nursing , Vol. 65 No. 1 , pp. 139 - 148 , doi: 10.1111/j.1365-2648.2008.04834.x .
Garvey , P.K. and CNE series ( 2015 ), “ Failure to rescue: the nurse's impact ”, Medsurg Nursing , Vol. 24 No. 3 , pp. 145 - 149 .
Goodare , P. ( 2015 ), “ Literature review: ‘are you ok there?’ The socialization of student and graduate nurses: do we have it right? ”, Australian Journal of Advanced Nursing , Vol. 33 No. 1 , pp. 38 - 43 .
Graneheim , U.H. and Lundman , B. ( 2014 ), “ Qualitative content analysis in nursing research: concepts, procedures, and measures to achieve trustworthiness ”, Nurse Education Today , Vol. 24 No. 2 , pp. 105 - 12 , doi: 10.1016/j.nedt.2003.10.001 .
Hsu , L. and Hsieh , S. ( 2013 ), “ Factors affecting metacognition of undergraduate nursing students in a blended learning environment ”, International Journal of Nursing Practice , Vol. 20 No. 3 , pp. 233 - 241 , doi: 10.1111/ijn.12131 .
Ignatavicius , D. ( 2001 ), “ Six critical thinking skills for at-the-bedside success ”, Dimensions of Critical Care Nursing , Vol. 20 No. 2 , pp. 30 - 33 .
Institute of Medicine ( 2001 ), Crossing the Quality Chasm: A New Health System for the 21st Century , National Academy Press , Washington .
James , J. ( 2013 ), “ A new, evidence-based estimate of patient harms associated with hospital care ”, Journal of Patient Safety , Vol. 9 No. 3 , pp. 122 - 128 , doi: 10.1097/PTS.0b013e3182948a69 .
Jones , J.H. ( 2010 ), “ Developing critical thinking in the perioperative environment ”, AORN Journal , Vol. 91 No. 2 , pp. 248 - 256 , doi: 10.1016/j.aorn.2009.09.025 .
Kaplan Nursing ( 2012 ), Kaplan Nursing Integrated Testing Program Faculty Manual , Kaplan Nursing , New York, NY .
Kim , J.S. , Gu , M.O. and Chang , H.K. ( 2019 ), “ Effects of an evidence-based practice education program using multifaceted interventions: a quasi-experimental study with undergraduate nursing students ”, BMC Medical Education , Vol. 19 , doi: 10.1186/s12909-019-1501-6 .
Longton , S. ( 2014 ), “ Utilizing evidence-based practice for patient safety ”, Nephrology Nursing Journal , Vol. 41 No. 4 , pp. 343 - 344 .
McCausland , L.L. and Meyers , C.C. ( 2013 ), “ An interactive skills fair to prepare undergraduate nursing students for clinical experience ”, Nursing Education Perspectives , Vol. 34 No. 6 , pp. 419 - 420 , doi: 10.5480/1536-5026-34.6.419 .
McMullen , M.A. and McMullen , W.F. ( 2009 ), “ Examining patterns of change in the critical thinking skills of graduate nursing students ”, Journal of Nursing Education , Vol. 48 No. 6 , pp. 310 - 318 , doi: 10.3928/01484834-20090515-03 .
Moore , Z.E. ( 2007 ), “ Critical thinking and the evidence-based practice of sport psychology ”, Journal of Clinical Sport Psychology , Vol. 1 , pp. 9 - 22 , doi: 10.1123/jcsp.1.1.9 .
Nadelson , S. and Nadelson , L.S. ( 2014 ), “ Evidence-based practice article reviews using CASP tools: a method for teaching EBP ”, Worldviews on Evidence-Based Nursing , Vol. 11 No. 5 , pp. 344 - 346 , doi: 10.1111/wvn.12059 .
Newton , S.E. and Moore , G. ( 2013 ), “ Critical thinking skills of basic baccalaureate and accelerated second-degree nursing students ”, Nursing Education Perspectives , Vol. 34 No. 3 , pp. 154 - 158 , doi: 10.5480/1536-5026-34.3.154 .
Nibert , A. ( 2011 ), “ Nursing education and practice: bridging the gap ”, Advance Healthcare Network , viewed 3 May 2017, available at: https://www.elitecme.com/resource-center/nursing/nursing-education-practice-bridging-the-gap/ .
Oermann , M.H. , Kardong-Edgren , S. , Odom-Maryon , T. , Hallmark , B.F. , Hurd , D. , Rogers , N. and Smart , D.A. ( 2011 ), “ Deliberate practice of motor skills in nursing education: CPR as exemplar ”, Nursing Education Perspectives , Vol. 32 No. 5 , pp. 311 - 315 , doi: 10.5480/1536-5026-32.5.311 .
Papathanasiou , I.V. , Kleisiaris , C.F. , Fradelos , E.C. , Kakou , K. and Kourkouta , L. ( 2014 ), “ Critical thinking: the development of an essential skill for nursing students ”, Acta Informatica Medica , Vol. 22 No. 4 , pp. 283 - 286 , doi: 10.5455/aim.2014.22.283-286 .
Park , M.Y. , Conway , J. and McMillan , M. ( 2016 ), “ Enhancing critical thinking through simulation ”, Journal of Problem-Based Learning , Vol. 3 No. 1 , pp. 31 - 40 , doi: 10.24313/jpbl.2016.3.1.31 .
Paul , R. ( 1993 ), Critical Thinking: How to Prepare Students for a Rapidly Changing World , The Foundation for Critical Thinking , Santa Rosa .
Paul , R. and Elder , L. ( 2008 ), “ Critical thinking: the art of socratic questioning, part III ”, Journal of Developmental Education , Vol. 31 No. 3 , pp. 34 - 35 .
Paul , R. and Elder , L. ( 2012 ), Critical Thinking: Tools for Taking Charge of Your Learning and Your Life , 3rd ed. , Pearson/Prentice Hall , Boston .
Profetto-McGrath , J. ( 2005 ), “ Critical thinking and evidence-based practice ”, Journal of Professional Nursing , Vol. 21 No. 6 , pp. 364 - 371 , doi: 10.1016/j.profnurs.2005.10.002 .
Rahman , A. and Applebaum , R. ( 2011 ), “ What's all this about evidence-based practice? The roots, the controversies, and why it matters ”, American Society on Aging , viewed 3 May 2017, available at: https://www.asaging.org/blog/whats-all-about-evidence-based-practice-roots-controversies-and-why-it-matters .
Rieger , K. , Chernomas , W. , McMillan , D. , Morin , F. and Demczuk , L. ( 2015 ), “ The effectiveness and experience of arts‐based pedagogy among undergraduate nursing students: a comprehensive systematic review protocol ”, JBI Database of Systematic Reviews and Implementation Reports , Vol. 13 No. 2 , pp. 101 - 124 , doi: 10.11124/jbisrir-2015-1891 .
Robert , R.R. and Petersen , S. ( 2013 ), “ Critical thinking at the bedside: providing safe passage to patients ”, Medsurg Nursing , Vol. 22 No. 2 , pp. 85 - 118 .
Roberts , S.T. , Vignato , J.A. , Moore , J.L. and Madden , C.A. ( 2009 ), “ Promoting skill building and confidence in freshman nursing students with a skills-a-thon ”, Educational Innovations , Vol. 48 No. 8 , pp. 460 - 464 , doi: 10.3928/01484834-20090518-05 .
Romeo , E. ( 2010 ), “ Quantitative research on critical thinking and predicting nursing students' NCLEX-RN performance ”, Journal of Nursing Education , Vol. 49 No. 7 , pp. 378 - 386 , doi: 10.3928/01484834-20100331-05 .
Sackett , D. , Rosenberg , W. , Gray , J. , Haynes , R. and Richardson , W. ( 1996 ), “ Evidence-based medicine: what it is and what it isn't ”, British Medical Journal , Vol. 312 No. 7023 , pp. 71 - 72 , doi: 10.1136/bmj.312.7023.71 .
Saintsing , D. , Gibson , L.M. and Pennington , A.W. ( 2011 ), “ The novice nurse and clinical decision-making: how to avoid errors ”, Journal of Nursing Management , Vol. 19 No. 3 , pp. 354 - 359 .
Saldana , J. ( 2009 ), The Coding Manual for Qualitative Researchers , Sage , Los Angeles .
Scheffer , B. and Rubenfeld , M. ( 2000 ), “ A consensus statement on critical thinking in nursing ”, Journal of Nursing Education , Vol. 39 No. 8 , pp. 352 - 359 .
Stanley , M.C. and Dougherty , J.P. ( 2010 ), “ Nursing education model. A paradigm shift in nursing education: a new model ”, Nursing Education Perspectives , Vol. 31 No. 6 , pp. 378 - 380 , doi: 10.1043/1536-5026-31.6.378 .
Swing , V.K. ( 2014 ), “ Early identification of transformation in the proficiency level of critical thinking skills (CTS) for the first-semester associate degree nursing (ADN) student ”, doctoral thesis , Capella University , Minneapolis , viewed 3 May 2017, ProQuest Dissertations & Theses database .
Turner , P. ( 2005 ), “ Critical thinking in nursing education and practice as defined in the literature ”, Nursing Education Perspectives , Vol. 26 No. 5 , pp. 272 - 277 .
Twibell , R. , St Pierre , J. , Johnson , D. , Barton , D. , Davis , C. and Kidd , M. ( 2012 ), “ Tripping over the welcome mat: why new nurses don't stay and what the evidence says we can do about it ”, American Nurse Today , Vol. 7 No. 6 , pp. 1 - 10 .
Watson , G. and Glaser , E.M. ( 1980 ), Watson Glaser Critical Thinking Appraisal , Psychological Corporation , San Antonio .
Wittmann-Price , R.A. ( 2013 ), “ Facilitating learning in the classroom setting ”, in Wittmann-Price , R.A. , Godshall , M. and Wilson , L. (Eds), Certified Nurse Educator (CNE) Review Manual , Springer Publishing , New York, NY , pp. 19 - 70 .
Corresponding author
Related articles, we’re listening — tell us what you think, something didn’t work….
Report bugs here
All feedback is valuable
Please share your general feedback
Join us on our journey
Platform update page.
Visit emeraldpublishing.com/platformupdate to discover the latest news and updates
Questions & More Information
Answers to the most commonly asked questions here
What is Evidence-Based Practice in Nursing? (With Examples, Benefits, & Challenges)

Are you a nurse looking for ways to increase patient satisfaction, improve patient outcomes, and impact the profession? Have you found yourself caught between traditional nursing approaches and new patient care practices? Although evidence-based practices have been used for years, this concept is the focus of patient care today more than ever. Perhaps you are wondering, “What is evidence-based practice in nursing?” In this article, I will share information to help you begin understanding evidence-based practice in nursing + 10 examples about how to implement EBP.
What Is Evidence-Based Practice In Nursing?
When was evidence-based practice first introduced in nursing, who introduced evidence-based practice in nursing, what is the difference between evidence-based practice in nursing and research in nursing, what are the benefits of evidence-based practice in nursing, top 5 benefits to the patient, top 5 benefits to the nurse, top 5 benefits to the healthcare organization, 10 strategies nursing schools employ to teach evidence-based practices, 1. assigning case studies:, 2. journal clubs:, 3. clinical presentations:, 4. quizzes:, 5. on-campus laboratory intensives:, 6. creating small work groups:, 7. interactive lectures:, 8. teaching research methods:, 9. requiring collaboration with a clinical preceptor:, 10. research papers:, what are the 5 main skills required for evidence-based practice in nursing, 1. critical thinking:, 2. scientific mindset:, 3. effective written and verbal communication:, 4. ability to identify knowledge gaps:, 5. ability to integrate findings into practice relevant to the patient’s problem:, what are 5 main components of evidence-based practice in nursing, 1. clinical expertise:, 2. management of patient values, circumstances, and wants when deciding to utilize evidence for patient care:, 3. practice management:, 4. decision-making:, 5. integration of best available evidence:, what are some examples of evidence-based practice in nursing, 1. elevating the head of a patient’s bed between 30 and 45 degrees, 2. implementing measures to reduce impaired skin integrity, 3. implementing techniques to improve infection control practices, 4. administering oxygen to a client with chronic obstructive pulmonary disease (copd), 5. avoiding frequently scheduled ventilator circuit changes, 6. updating methods for bathing inpatient bedbound clients, 7. performing appropriate patient assessments before and after administering medication, 8. restricting the use of urinary catheterizations, when possible, 9. encouraging well-balanced diets as soon as possible for children with gastrointestinal symptoms, 10. implementing and educating patients about safety measures at home and in healthcare facilities, how to use evidence-based knowledge in nursing practice, step #1: assessing the patient and developing clinical questions:, step #2: finding relevant evidence to answer the clinical question:, step #3: acquire evidence and validate its relevance to the patient’s specific situation:, step #4: appraise the quality of evidence and decide whether to apply the evidence:, step #5: apply the evidence to patient care:, step #6: evaluating effectiveness of the plan:, 10 major challenges nurses face in the implementation of evidence-based practice, 1. not understanding the importance of the impact of evidence-based practice in nursing:, 2. fear of not being accepted:, 3. negative attitudes about research and evidence-based practice in nursing and its impact on patient outcomes:, 4. lack of knowledge on how to carry out research:, 5. resource constraints within a healthcare organization:, 6. work overload:, 7. inaccurate or incomplete research findings:, 8. patient demands do not align with evidence-based practices in nursing:, 9. lack of internet access while in the clinical setting:, 10. some nursing supervisors/managers may not support the concept of evidence-based nursing practices:, 12 ways nurse leaders can promote evidence-based practice in nursing, 1. be open-minded when nurses on your teams make suggestions., 2. mentor other nurses., 3. support and promote opportunities for educational growth., 4. ask for increased resources., 5. be research-oriented., 6. think of ways to make your work environment research-friendly., 7. promote ebp competency by offering strategy sessions with staff., 8. stay up-to-date about healthcare issues and research., 9. actively use information to demonstrate ebp within your team., 10. create opportunities to reinforce skills., 11. develop templates or other written tools that support evidence-based decision-making., 12. review evidence for its relevance to your organization., bonus 8 top suggestions from a nurse to improve your evidence-based practices in nursing, 1. subscribe to nursing journals., 2. offer to be involved with research studies., 3. be intentional about learning., 4. find a mentor., 5. ask questions, 6. attend nursing workshops and conferences., 7. join professional nursing organizations., 8. be honest with yourself about your ability to independently implement evidence-based practice in nursing., useful resources to stay up to date with evidence-based practices in nursing, professional organizations & associations, blogs/websites, youtube videos, my final thoughts, frequently asked questions answered by our expert, 1. what did nurses do before evidence-based practice, 2. how did florence nightingale use evidence-based practice, 3. what is the main limitation of evidence-based practice in nursing, 4. what are the common misconceptions about evidence-based practice in nursing, 5. are all types of nurses required to use evidence-based knowledge in their nursing practice, 6. will lack of evidence-based knowledge impact my nursing career, 7. i do not have access to research databases, how do i improve my evidence-based practice in nursing, 7. are there different levels of evidence-based practices in nursing.
• Level One: Meta-analysis of random clinical trials and experimental studies • Level Two: Quasi-experimental studies- These are focused studies used to evaluate interventions. • Level Three: Non-experimental or qualitative studies. • Level Four: Opinions of nationally recognized experts based on research. • Level Five: Opinions of individual experts based on non-research evidence such as literature reviews, case studies, organizational experiences, and personal experiences.
8. How Can I Assess My Evidence-Based Knowledge In Nursing Practice?

This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search
Search menu
Brechin A. Introducing critical practice. In: Brechin A, Brown H, Eby MA (eds). London: Sage/Open University; 2000
Introduction to evidence informed decision making. 2012. https://cihr-irsc.gc.ca/e/45245.html (accessed 8 March 2022)
Cullen L, Adams SL. Planning for implementation of evidence-based practice. JONA: The Journal of Nursing Administration. 2012; 42:(4)222-230 https://doi.org/10.1097/NNA.0b013e31824ccd0a
DiCenso A, Guyatt G, Ciliska D. Evidence-based nursing. A guide to clinical practice.St. Louis (MO): Mosby; 2005
Implementing evidence-informed practice: International perspectives. In: Dill K, Shera W (eds). Toronto, Canada: Canadian Scholars Press; 2012
Dufault M. Testing a collaborative research utilization model to translate best practices in pain management. Worldviews Evid Based Nurs. 2004; 1:S26-S32 https://doi.org/10.1111/j.1524-475X.2004.04049.x
Epstein I. Promoting harmony where there is commonly conflict: evidence-informed practice as an integrative strategy. Soc Work Health Care. 2009; 48:(3)216-231 https://doi.org/10.1080/00981380802589845
Epstein I. Reconciling evidence-based practice, evidence-informed practice, and practice-based research: the role of clinical data-mining. Social Work. 2011; 56:(3)284-288 https://doi.org/10.1093/sw/56.3.284
Implementation research: a synthesis of the literature. 2005. https://tinyurl.com/mwpf4be4 (accessed 6 March 2022)
Graham ID, Logan J, Harrison MB Lost in knowledge translation: time for a map?. J Contin Educ Health Prof. 2006; 26:(1)13-24 https://doi.org/10.1002/chp.47
Greenhalgh T, Robert G, Bate P, MacFarlane F, Kyriakidou O. Diffusion of innovations in health service organisations. A systematic literature review.Malden (MA): Blackwell; 2005
Greenhalgh T, Howick J, Maskrey N. Evidence based medicine: a movement in crisis?. BMJ. 2014; 348 https://doi.org/10.1136/bmj.g3725
Haynes RB, Devereaux PJ, Guyatt GH. Clinical expertise in the era of evidence-based medicine and patient choice. BMJ Evidence-Based Medicine. 2002; 7:36-38 https://doi.org/10.1136/ebm.7.2.36
Hitch D, Nicola-Richmond K. Instructional practices for evidence-based practice with pre-registration allied health students: a review of recent research and developments. Adv Health Sci Educ Theory Pract. 2017; 22:(4)1031-1045 https://doi.org/10.1007/s10459-016-9702-9
Jerkert J. Negative mechanistic reasoning in medical intervention assessment. Theor Med Bioeth. 2015; 36:(6)425-437 https://doi.org/10.1007/s11017-015-9348-2
McSherry R, Artley A, Holloran J. Research awareness: an important factor for evidence-based practice?. Worldviews Evid Based Nurs. 2006; 3:(3)103-115 https://doi.org/10.1111/j.1741-6787.2006.00059.x
McSherry R, Simmons M, Pearce P. An introduction to evidence-informed nursing. In: McSherry R, Simmons M, Abbott P London: Routledge; 2002
Implementing excellence in your health care organization: managing, leading and collaborating. In: McSherry R, Warr J (eds). Maidenhead: Open University Press; 2010
Melnyk BM, Fineout-Overholt E, Stillwell SB, Williamson KM. Evidence-based practice: step by step: the seven steps of evidence-based practice. AJN, American Journal of Nursing. 2010; 110:(1)51-53 https://doi.org/10.1097/01.NAJ.0000366056.06605.d2
Implementing evidence-based practices: six ‘drivers’ of success. Part 3 in a Series on Fostering the Adoption of Evidence-Based Practices in Out-Of-School Time Programs. 2007. https://tinyurl.com/mu2y6ahk (accessed 8 March 2022)
Muir-Gray JA. Evidence-based healthcare. How to make health policy and management decisions.Edinburgh: Churchill Livingstone; 1997
Nevo I, Slonim-Nevo V. The myth of evidence-based practice: towards evidence-informed practice. British Journal of Social Work. 2011; 41:(6)1176-1197 https://doi.org/10.1093/bjsw/bcq149
Newhouse RP, Dearholt S, Poe S, Pugh LC, White K. The Johns Hopkins Nursing Evidence-based Practice Rating Scale.: The Johns Hopkins Hospital: Johns Hopkins University School of Nursing; 2005
Nursing and Midwifery Council. The Code. 2018. https://www.nmc.org.uk/standards/code (accessed 7 March 2022)
Nutley S, Walter I, Davies HTO. Promoting evidence-based practice: models and mechanisms from cross-sector review. Research on Social Work Practice. 2009; 19:(5)552-559 https://doi.org/10.1177/1049731509335496
Reed JE, Howe C, Doyle C, Bell D. Successful Healthcare Improvements From Translating Evidence in complex systems (SHIFT-Evidence): simple rules to guide practice and research. Int J Qual Health Care. 2019; 31:(3)238-244 https://doi.org/10.1093/intqhc/mzy160
Rosswurm MA, Larrabee JH. A model for change to evidence-based practice. Image J Nurs Sch. 1999; 31:(4)317-322 https://doi.org/10.1111/j.1547-5069.1999.tb00510.x
Rubin A. Improving the teaching of evidence-based practice: introduction to the special issue. Research on Social Work Practice. 2007; 17:(5)541-547 https://doi.org/10.1177/1049731507300145
Shlonsky A, Mildon R. Methodological pluralism in the age of evidence-informed practice and policy. Scand J Public Health. 2014; 42:18-27 https://doi.org/10.1177/1403494813516716
Straus SE, Tetroe J, Graham I. Defining knowledge translation. CMAJ. 2009; 181:(3-4)165-168 https://doi.org/10.1503/cmaj.081229
Titler MG, Everett LQ. Translating research into practice. Considerations for critical care investigators. Crit Care Nurs Clin North Am. 2001; 13:(4)587-604 https://doi.org/10.1016/S0899-5885(18)30026-1
Titler MG, Kleiber C, Steelman V Infusing research into practice to promote quality care. Nurs Res. 1994; 43:(5)307-313 https://doi.org/10.1097/00006199-199409000-00009
Titler MG, Kleiber C, Steelman VJ The Iowa model of evidence-based practice to promote quality care. Crit Care Nurs Clin North Am. 2001; 13:(4)497-509 https://doi.org/10.1016/S0899-5885(18)30017-0
Ubbink DT, Guyatt GH, Vermeulen H. Framework of policy recommendations for implementation of evidence-based practice: a systematic scoping review. BMJ Open. 2013; 3:(1) https://doi.org/10.1136/bmjopen-2012-001881
Wang LP, Jiang XL, Wang L, Wang GR, Bai YJ. Barriers to and facilitators of research utilization: a survey of registered nurses in China. PLoS One. 2013; 8:(11) https://doi.org/10.1371/journal.pone.0081908
Warren JI, McLaughlin M, Bardsley J, Eich J, Esche CA, Kropkowski L, Risch S. The strengths and challenges of implementing EBP in healthcare systems. Worldviews Evid Based Nurs. 2016; 13:(1)15-24 https://doi.org/10.1111/wvn.12149
Webber M, Carr S. Applying research evidence in social work practice: Seeing beyond paradigms. In: Webber M (ed). London: Palgrave; 2015
Evidence-based practice vs. evidence-based practice: what's the difference?. 2014. https://tinyurl.com/2p8msjaf (accessed 8 March 2022)

Evidence-informed practice: simplifying and applying the concept for nursing students and academics
Elizabeth Adjoa Kumah
Nurse Researcher, Faculty of Health and Social Care, University of Chester, Chester
View articles · Email Elizabeth Adjoa
Robert McSherry
Professor of Nursing and Practice Development, Faculty of Health and Social Care, University of Chester, Chester
View articles
Josette Bettany-Saltikov
Senior Lecturer, School of Health and Social Care, Teesside University, Middlesbrough
Paul van Schaik
Professor of Research, School of Social Sciences, Humanities and Law, Teesside University, Middlesbrough

Background:
Nurses' ability to apply evidence effectively in practice is a critical factor in delivering high-quality patient care. Evidence-based practice (EBP) is recognised as the gold standard for the delivery of safe and effective person-centred care. However, decades following its inception, nurses continue to encounter difficulties in implementing EBP and, although models for its implementation offer stepwise approaches, factors, such as the context of care and its mechanistic nature, act as barriers to effective and consistent implementation. It is, therefore, imperative to find a solution to the way evidence is applied in practice. Evidence-informed practice (EIP) has been mooted as an alternative to EBP, prompting debate as to which approach better enables the transfer of evidence into practice. Although there are several EBP models and educational interventions, research on the concept of EIP is limited. This article seeks to clarify the concept of EIP and provide an integrated systems-based model of EIP for the application of evidence in clinical nursing practice, by presenting the systems and processes of the EIP model. Two scenarios are used to demonstrate the factors and elements of the EIP model and define how it facilitates the application of evidence to practice. The EIP model provides a framework to deliver clinically effective care, and the ability to justify the processes used and the service provided by referring to reliable evidence.
Evidence-based practice (EBP) was first mentioned in the literature by Muir-Gray, who defined EBP as ‘an approach to decision-making in which the clinician uses the best available evidence in consultation with the patient to decide upon the option which suits the patient best’ (1997:97). Since this initial definition was set out in 1997, EBP has gained prominence as the gold standard for the delivery of safe and effective health care.
There are several models for implementing EBP. Examples include:
- Rosswurm and Larrabee's (1999) model
- The Iowa model ( Titler et al, 2001 )
- Collaborative research utilisation model ( Dufault, 2004 ); DiCenso et al's (2005) model
- Greenhalgh et al's (2005) model
- Johns Hopkins Nursing model ( Newhouse et al, 2005 )
- Melnyk et al's (2010) model.
Although a comprehensive review of these models is beyond the scope of this article, a brief assessment reveals some commonalities among them. These include a) asking or selecting a practice question, b) searching for the best evidence, c) critically appraising and applying the evidence, d) evaluating the outcome(s) of patient care delivery, and e) disseminating the outcome(s).
Regardless of the benefits of EBP, and the existence of multiple EBP models intended to facilitate the application of evidence into practice, health professionals, including nurses, continue to struggle to implement it effectively ( Ubbink et al, 2013 ). Critics of EBP have questioned its validity ( Rubin, 2007 ; Nevo and Slonim-Nevo, 2011 ); the best practice and setting to support its use ( Nutley et al, 2009 ); its failure to address the complexity of health and health care, as well as the patient's context ( Muir-Gray, 1997 ; Reed et al, 2019 ), and its mechanistic approach ( Epstein, 2009 ; Jerkert, 2015 ). Some of these criticisms are outlined below.
For example, previous studies have reported the barriers health professionals face to successfully implement EBP. Ubbink et al (2013) conducted a systematic review to determine nurses' and doctors' views on knowledge, attitudes, skills, barriers, and behaviour required to implement EBP. The review included 31 studies from 17 countries: eight from North America and 11 from Europe. The results revealed that organisational and individual barriers prevent uptake of EBP among nurses and doctors. These barriers included the lack of material and human resources, and lack of support from managers and leaders; individual barriers included knowledge deficit regarding EBP, time and workload ( Ubbink et al, 2013 ). Researchers such as Hitch and Nicola-Richmond (2017) and Warren et al (2016) found similar barriers to implementing EBP reported by health professionals.
Effective and consistent implementation of EBP in healthcare settings depends on complex interdependent factors, such as the characteristics of an organisation (eg the internal and external healthcare environment, and organisational structures and values); the EBP intervention (eg reduction of hospital-acquired infections); and the attitudes of the individual practitioner towards EBP ( Titler and Everett, 2001 ; Cullen and Adams, 2012 ). Yet, existing approaches of EBP have been ineffective in facilitating its implementation ( Greenhalgh et al, 2014 ).
Consequently, authors such as Cullen and Adams (2012) and Greenhalgh et al (2014) have called for a resurgence of the concept, especially concerning the components of EBP associated with involving patients in decision-making, and with expert judgement and experience. Greenhalgh et al (2014:3) consider it is time to return to implementing ‘real EBP’, where person-centred care is the priority, and health professionals and their patients ‘are free to make appropriate care decisions that may not match what best evidence seems to suggest’. Nonetheless, researchers including McSherry et al (2002) , Epstein (2009) and Nevo and Slonim-Nevo (2011) have proposed an alternative, holistic approach to the application of evidence into practice, termed evidence-informed practice (EIP).
Journey towards evidence-informed practice
The problems with the uptake and effective implementation of EBP led to the emergence of the EIP concept. This concept is based on the premise that healthcare practice should, as a matter of principle, be informed by, rather than based on, evidence ( Nevo and Slonim-Nevo, 2011 ). This implies that other forms of evidence (for example, patient experiences, the nurse's expertise and experiences), not just the ‘research evidence’, should be considered in applying evidence in practice.
McSherry et al (2002) defined EIP as the assimilation of professional judgment and research evidence regarding the efficiency of interventions. This definition was further elaborated as an approach to patient care where:
‘Practitioners are encouraged to be knowledgeable about findings coming from all types of studies and to use them in an integrative manner, taking into consideration clinical experience and judgment, clients' preferences and values, and context of the interventions.’
Nevo and Slonim-Nevo (2011:18)
It has been over two decades since EIP emerged in the literature, however, primary research on the concept has been limited. Hence, although the term EIP has gained momentum in recent times, the methods needed to implement it effectively are not widely known ( McSherry, 2007 ; Woodbury and Kuhnke, 2014 ). While some proponents of EIP (eg Epstein 2011 ; Webber and Carr 2015 ) have identified significant differences between EBP and EIP, most researchers (eg Ciliska, 2012 ; Shlonsky and Mildon, 2014 ) have used the terms interchangeably.
Ciliska (2012) , for instance, developed an evidence-informed decision making (EIDM) module, but referred to the steps of EBP (ie Ask, Acquire, Appraise, Integrate, Adapt, Apply, Analyse) as the processes to be followed in implementing EIDM. Ciliska (2012) explained that the term EIDM was adopted to signify that other types of evidence are useful in clinical decision-making and to attempt to get beyond the criticisms of EBP. This notwithstanding, the author maintained the existing process for implementing EBP. Similarly, Shlonsky and Mildon (2014) used the terms EBP and EIP interchangeably, as they consistently referred to an EBP approach as EIP. Examples include referring to the steps of EBP as ‘the steps of EIP’ ( Shlonsky and Mildon, 2014:3 ) and referring to Haynes et al's (2002) expanded EBP model as a ‘revised EIP model’ ( Shlonsky and Mildon, 2014:2 ).
Another term that is often used interchangeably with EIP is ‘knowledge translation’. This term has been explored extensively. For example, the Canadian Institute of Health Research (CIHR) has adopted knowledge translation to signify the use of high-quality research evidence to make informed decisions ( Straus et al, 2009 ). The CIHR ( Graham et al, 2006 ) developed a ‘knowledge to action’ model intended to integrate the creation and application of knowledge. The model acknowledges the non-linear process of applying evidence in practice, where each stage is influenced by the next, as well as the preceding, stage. In a typical clinical setting, the actual process of applying evidence in practice is not linear, as acknowledged by the proponents of EBP, but cyclical and interdependent. Ciliska (2012) linked Graham et al's (2006) model to the components of evidence-informed decision-making. According to Ciliska (2012:7) , the knowledge-to-action model ‘fits with the steps of evidence-informed decision-making’. However, like EBP, the term ‘knowledge translation’, differs significantly from the EIP concept because it focuses on the ‘research evidence’ in decision-making.
The apparent confusion surrounding EIP is due to inadequate information about its components and the methods involved in implementing the concept. To foster a culture of EIP among health professionals, they must first be made aware of the actual components of the concept and the strategies involved in its successful implementation. The following section uses case scenarios to provide a description of the factors and elements of the EIP model and defines how it facilitates the application of evidence into clinical nursing practice.
Systems thinking
The clinical setting within which nurses work is a complex system made up of several interdependent and inter-related parts. Problems with healthcare delivery and management must therefore be perceived as a consequence of the exchanges between elements of the systems, instead of an outcome or the malfunctioning of a particular element. This, McSherry and Warr (2010) , have referred to as ‘systems thinking’.
Effective implementation of EIP demands an understanding of the various parts of the system that come together to aid the application of evidence in practice.
The evidence-informed practice model
The original model.
The earliest version of the evidence-informed practice model is depicted in Figure 1 . This was developed specifically for nurses and was originally named ‘the evidence-informed nursing model’. The model presented in Figure 1 was developed through PhD research conducted by Robert McSherry (2007) , with the aim to explore, through a mixed-methods study design, why the use of research as evidence in support of clinical nursing practice remains problematic. Study participants were registered nurses practising in a hospital trust located in north-east England.
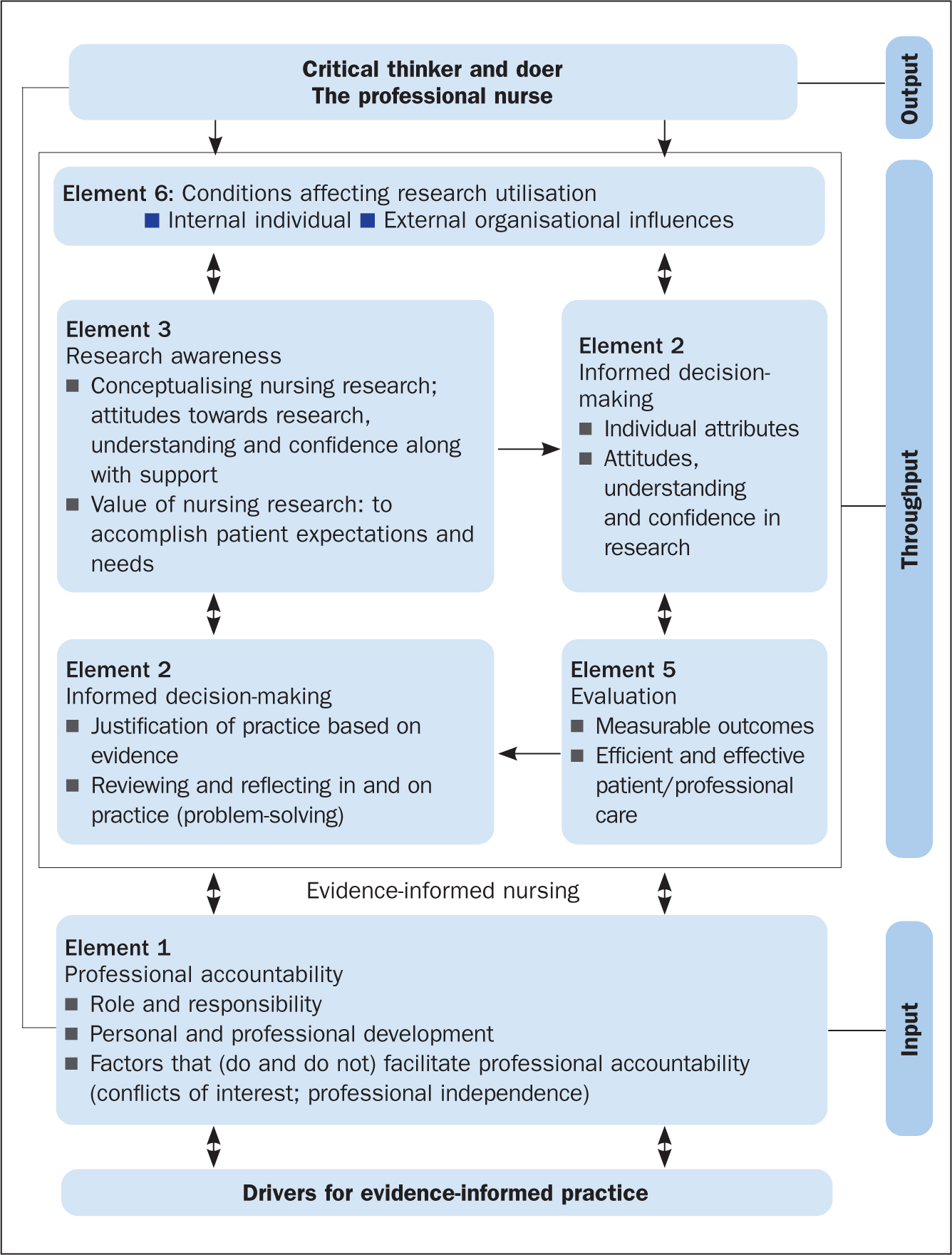
The results of McSherry's (2007) study showed that, to effectively apply evidence in clinical nursing practice, nurses needed to be informed of, and be able to interact with, several key elements. The evidence-informed nursing model was developed as an alternative framework for facilitating the application of evidence in clinical nursing practice and was grounded in the principles and practices of systems thinking. This is because, primarily, the model provided an integrated process to applying evidence into practice, consisting of:
- A clearly defined input; to encourage nurses to use evidence in practice
- Throughput; facilitation of the processes associated with the elements
- Output; improved standards of professional practice
The revised model
The evidence-informed nursing model has been adapted to the evidence-informed practice model. The new model ( Figure 2 ) is adapted in several ways. First, it has been modified to be all-inclusive, so it could be applied to any health profession. Second, the model has been simplified to show the interconnectedness of the various factors and elements that enable a professional to use evidence in support of their clinical decision-making. Third, the model demonstrates the ongoing complexity that health professionals find themselves working in, in the quest to apply evidence to clinical practice. Last, the EIP model incorporates the principles and components of EBP, which is particularly evident in the EIP cycle (the throughput phase of the model).
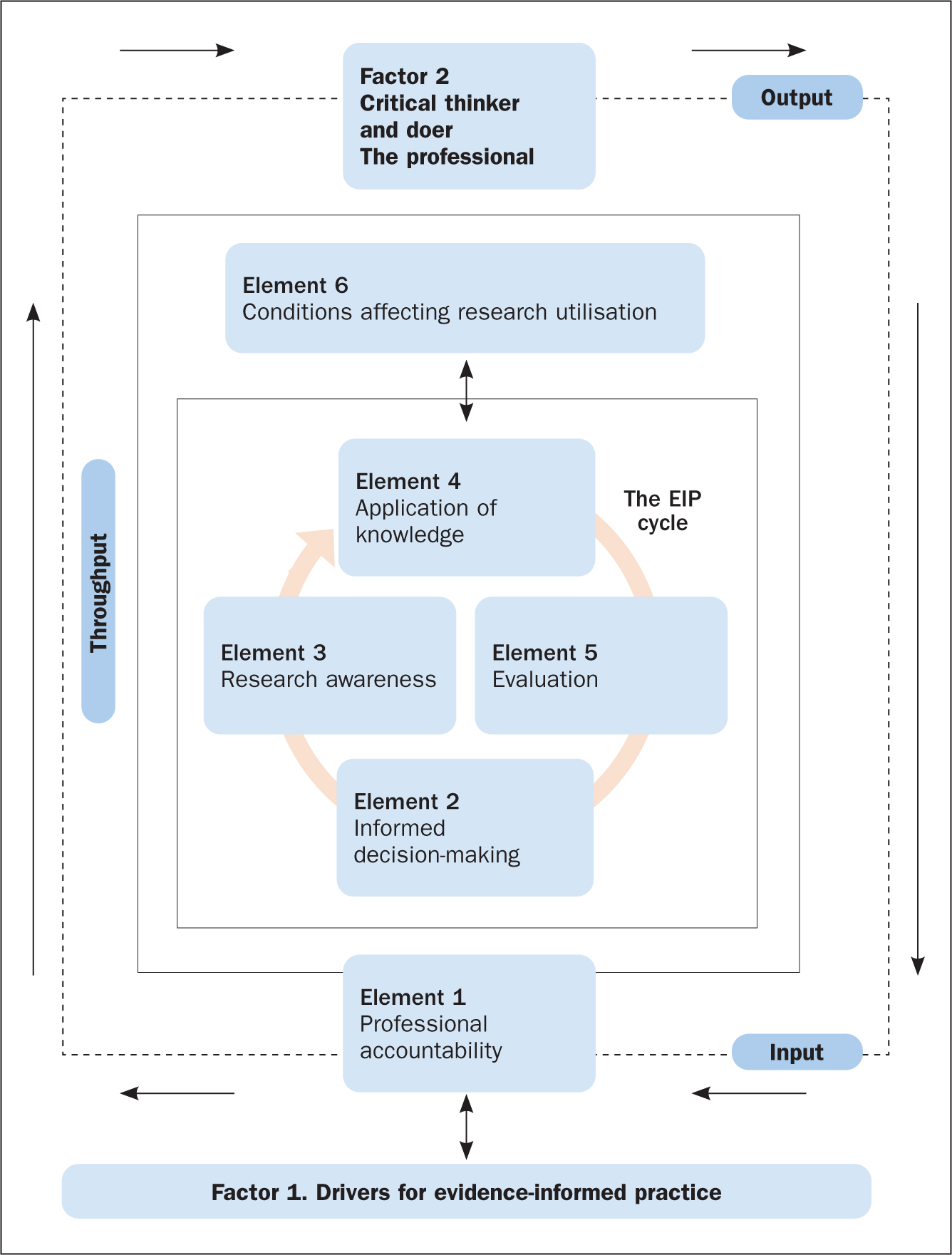
The factors and elements of the EIP model ( Figure 2 ) are explored in more detail below with reference to two scenarios, which are used to apply the EIP model to clinical nursing practice within both a scientific and the wider context within which nursing care takes place.
The first factor of the EIP model is ‘Factor 1. Drivers for evidence-informed practice’ ( Figure 2 ). In order for nurses to enhance patient care and experiences, along with improving their knowledge and skills of the patient's condition and associated signs and symptoms, they need to be aware of what EIP is, what it involves, and the principles required to make it happen. Applying the scenarios, it is essential that the nurse understands and can identify the key elements that drive successful implementation of the EIP concept. This is referred to as the drivers for EIP, which are illustrated in Figure 3 and discussed below.
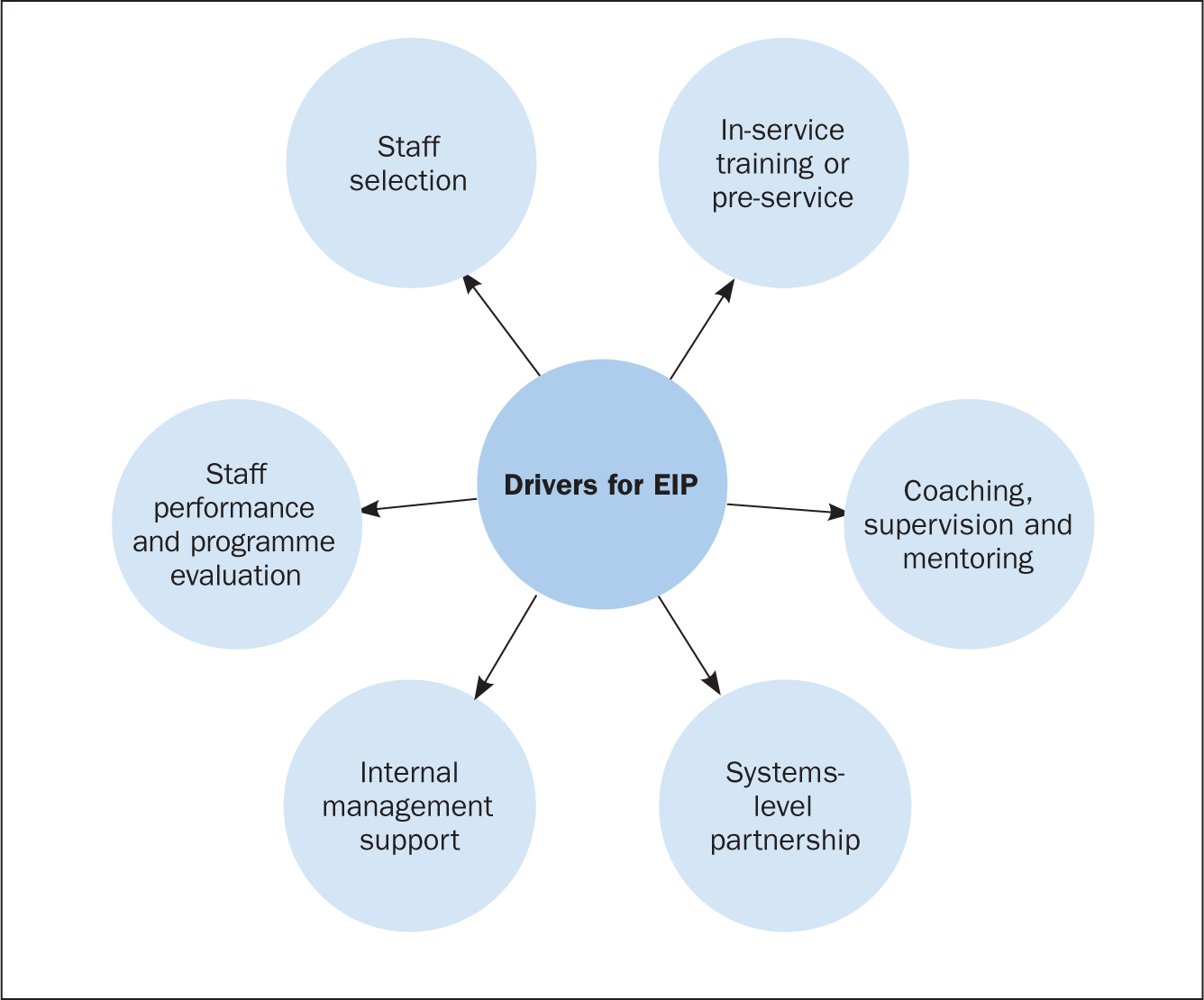
Drivers for EIP
Staff selection.
Recruiting, interviewing and redeploying existing staff or hiring new staff are part of the staff selection process ( Dill and Shera, 2012 ). The importance of this driver is to identify personnel who qualify to implement the EIP programme or model. Additionally, it aims at selecting individuals within the organisation (for example coaches, supervisors, and trainers), who will ensure that the required organisational changes to support nurses in the effective implementation of EIP are done.
In-service training or pre-service
Training on EIP programmes involves activities that are related to offering instruction, providing specialist information or skills development in a structured manner to nurses and other key healthcare staff involved in the EIP programme. Nurses, as well as other members of staff, must learn when, how, where, and with whom to use new approaches and skills in applying evidence to practice ( Metz et al, 2007 ).
Coaching, supervision and mentoring
The coaching and mentoring approach enables new skills to be introduced to nurses on the ward with the support of a coach. The duty of a coach is to offer expert information and support, together with encouragement, opportunities and advice to practise and apply skills that are specific to the EIP programme. Effective implementation of human service interventions (such as EIP) requires changes in behaviour at administrative, supervisory and practitioner levels ( Dill and Shera, 2012 ). Coaching and mentoring are the main ways to bring about a change in behaviour for staff who have been successfully involved in the beginning stage of the implementation process and throughout the life of the EIP programme.
Systems-level partnership
This refers to the improvement of partnerships with the broader and immediate systems to ensure access to required funds, and institutional and human resources necessary to support nurses' work. The immediate systems-level partnership refers to working with individuals or organisations that directly influence healthcare delivery (for example, nurses and doctors).
Partnerships within the broader system, on the other hand, refer to policymakers, funders or other organisations that may support the EIP programme, but are not directly involved in delivering health care. A variety of activities may be conducted as part of the development of systems-level partnerships to aid the implementation of EIP. These may include fundraising activities to support the implementation of EIP programmes, as well as the use of external coaches and consultants to assist with mentoring, technical assistance and training on an ongoing basis.
Internal management support
This involves activities that are associated with establishing processes and structures within an EIP programme to enhance effective implementation of the programme. This is necessary in order to inform healthcare decision-making as well as keep staff organised and focussed on desired care outcomes ( Fixsen et al, 2005 ). Instances of internal management support include the formation of institutional structures and processes, the allocation of resources to support selection of suitable staff, and administrative support for efficient training.
Staff performance and programme evaluation
This involves evaluation of staff performance and the overall EIP programme to determine whether the objectives of the programme have been achieved. To do this effectively, it is important to evaluate the outcomes of the above-defined drivers, in particular, staff selection, in-service training, as well as coaching and mentoring. This will offer managers and stakeholders insight about the effectiveness of staff selection, training, and mentoring in facilitating the application of evidence into clinical practice ( Dill and Shera, 2012 ).
Elements of the EIP model
The first element of the EIP model is professional accountability, depicted as an ‘input’ in Figure 2 . This is an essential part of a nurse's roles and responsibilities and is reaffirmed in the nursing Code ( Nursing and Midwifery Council, 2018 ) of professional practice, the contract of employment and job description. In both case scenarios involving Mitchell and Yvonne ( Box 1 ), professional accountability is evident on several fronts: the nurse must establish a caring, compassionate and therapeutic relationship with the patients by involving and engaging them in shared decision-making regarding all aspects of their care, treatments, and interventions; the nurse is accountable and answerable to the patient and his or her professional colleagues throughout the patient's journey.
Box 1.Patient scenariosScenario 1Yvonne, aged 31, is admitted to the emergency medical unit following a visit to her GP for a non-healing wound to her right big toe. The GP also reported that Yvonne has had a recurring sore throat, extreme tiredness and a low white blood cell count.The GP requested an urgent investigation of these symptoms. Yvonne was placed in a side room for precaution.Scenario 2Mitchell, aged 58, arrives in the emergency department complaining of severe chest pain. He is diaphoretic (sweating excessively) and says his pain is radiating down his left arm and up into his jaw, and he adds that he feels nauseated. A few minutes after admission, he suffers a cardiac arrest.He is resuscitated and transferred to the intensive care unit. He is intubated, is placed on a ventilator and has a central line catheter in place.
Throughput: the evidence-informed practice cycle
The EIP cycle (located in the ‘throughput’ of Figure 2 ) involves the processes or methods through which nurses apply evidence in support of their decision-making in clinical nursing practice. This often occurs in a clinical nursing environment that is complex, constantly changing, and involves numerous members of the multidisciplinary team, patients and their family. Effective communication (verbal and written) is essential for ensuring that the various elements are interchanging, interconnecting and communicating between, and with, each other. For example, the case of Yvonne in scenario 1 ( Box 1 ) can be used as an example to underline the importance of good communication. It is important to explain to the patient and her family the reason for nursing her in a side room rather than the main ward. In this situation, avoiding and preventing cross-infection is essential to safeguard Yvonne from harm.
To ensure the EIP cycle proceeds effectively requires that the nurse (the health professional) acts as the conduit for the interplay between the different elements of the model (ie Element 2: informed decision-making; Element 3: research awareness; Element 4: application of knowledge; and Element 5: evaluation). These elements will be further explored.
Element 2. Informed decision-making
This involves two-way communication between the nurse and the patient(s), and is critical in ensuring there is a robust relationship (honesty, openness, transparency) founded on the principles of person-centred care ( McSherry and Warr, 2010 ). It reaffirms the ethical principle of a patient's right to make an informed decision about what is suitable for them, and takes into account their beliefs, values, priorities and personal circumstances. In case scenario 2, applying the EIP model, the critical care nurse will be expected to involve Mitchell's (the patient's) relatives, medical staff and other members of the healthcare team in making decisions about, for example, ventilator management and care of the central line catheter. However, decision-making in an intensive care unit can be complex, and some of the decisions may involve the nurse only. Similarly, applying the EIP model in case scenario 1, the nurse will be expected to communicate with the patient (Yvonne), carers and colleagues about the importance of hand hygiene, wound care and the importance of using precautions to avoid hospital-acquired infections when caring for the patient.
In both case scenarios, the nurse must endeavour to involve the patient/family members in the process of decision-making by providing them with timely, appropriate and relevant information needed to make often complex and life-changing decisions.
Element 3. Research awareness
This element refers to motivating practitioners to acquire skills and knowledge, as well as to conceptualise what research and evidence involves and the significance they have in improving standards of healthcare practice ( McSherry et al, 2006 ). Research awareness is reliant on the nurse's attitudes towards research, the acquisition of knowledge and confidence about the value of research to practice, and on having supportive managers and colleagues.
This element of the EIP cycle, contained within the model, incorporates three of the steps (Research awareness) of EBP: ask a clinical question, search the literature for research evidence to answer the question, and critically appraise the evidence obtained). Although the nurse is not required to be a researcher to implement the EIP model effectively, they must be knowledgeable about relevant databases and search engines (such as Medline and Google), as well as critical appraisal tools, in order to be able to include high-quality research evidence when making patient care decisions.
However, the EIP model acknowledges the fact that research evidence may not always be readily available, and nurses may not have the necessary hardware and software in the care environment to enable them to search for research evidence. Hence, recommendations by Greenhalgh et al (2014) led to inclusion, within the EIP model, of nurses as critical thinkers and doers which, therefore, allows them to make appropriate care decisions based on patient preferences and actions, the clinical state, clinical setting and circumstances, and advocates that nurses apply their own knowledge, expertise and clinical experiences in clinical decision-making, which may not necessarily match what the research evidence seems to suggest.
With reference to scenario 2 (and similarly for scenario 1), to adhere to the EIP model the nurse would take the following steps:
- Update his/her knowledge about Mitchell's clinical presentation
- Search Medline for research evidence on ‘chest pain’, and ‘cardiac arrest’ and its associated symptoms. Based on the number of articles obtained, the nurse reads the titles and abstracts, and then, the full text of selected articles to exclude irrelevant articles. The remaining articles are then critically appraised to include the best research evidence in patient care decisions.
In situations where the above steps are not possible, the model advocates that the nurse endeavours to make the best care decisions possible based on patient preferences, clinical state, context and circumstances, and the nurse's own expertise and experience, as well as the experience of the patient and family members where possible.
Element 4. Application of knowledge
This is a complex element that requires the gathering and assimilation of various sources of information, evidence, quality and standards, and policy and guidance, to support the nurse's decision-making in clinical practice. In relation to both scenarios, the nurse would need to:
- Apply knowledge acquired from the patients (Mitchell and Yvonne), along with information from their relatives
- Apply evidence from reviewing the findings from research
- Take into account information gleaned from engaging with the multidisciplinary team
- Ensure they follow recommended local and national guidance and policy on the management of each patient's condition.
It is imperative that the nurse is experienced, knowledgeable, and competent in order to make the most appropriate care decisions together with the patient, the family and the wider multidisciplinary team. To do this effectively, the nurse requires certain personal attributes, it is also important for the organisation within which the nurse works to have specific institutional characteristics. Institutional features include culture, education and training, and workload/skill mix, whereas personal characteristics include improved confidence, attitude, understanding and behaviour towards the application of evidence into practice.
Element 5. Evaluation
This element of the EIP cycle within the model measures the effects of decision-making and actions of the nurse on care outcomes and in creating an optimal care environment. In both scenarios, the nurse would need to periodically evaluate specific processes and outcomes of care. For example, with regards to scenario 2, this would include:
- Monitoring how Mitchell is performing on the ventilator
- Taking the necessary infection prevention precautions to avoid the development of infections related to the insertion of a central line and transmission of hospital-acquired infection
- Monitoring improvement in Mitchell's general wellbeing.
Depending on the outcome of the evaluation, Mitchell's care plan would be either revised or continued.
Element 6. Conditions affecting research utilisation
Research utilisation involves critically appraising research findings, disseminating, and using the knowledge obtained from research to cause changes in an existing healthcare practice ( Titler et al, 1994 ). The conditions that affect research utilisation are grouped into five domains ( Wang et al, 2013 ):
- The process involved in utilising research findings
- Accessibility to research
- The quality of research
- The knowledge and attitudes of the nurse (health professional) regarding the use of research findings
- The organisation within which the findings of research are to be implemented.
In the two scenarios ( Box 1 ), the nurse needs to be aware of the potential barriers to research utilisation and identify ways to overcome these in order to effectively apply evidence to healthcare practice. In addition, the clinical environment within which nurses work must provide sufficient support in order to enhance the effective and consistent application of evidence to practice. Nurses must be supported to acquire the necessary knowledge, skills, and understanding needed to practise safely (ie competently and confidently). In addition, the resources necessary to obtain research evidence, such as IT (computers and internet), must be readily available in the clinical setting for easy access to information.
Factor 2 (Output). Critical thinker and doer, the professional nurse
To ensure that nurses inform their decisions with the best available evidence, it is imperative that they have a sound understanding and knowledge of what constitutes the EIP model ( Figure 2 ). Successfully engaging with the various factors and elements of this model will lead to the desired outcome—that of a professional who is a critical thinker and doer, a professional nurse who, as argued by Brechin (2000:44) , is ‘knowledgeable and skilled, yet welcomes alternative ideas and belief systems, appreciating and respecting alternative views’. In this context, it is about creating a caring and compassionate environment in which excellence in nursing practice occurs. This can only be exemplified by ensuring that decisions and actions are based on the best available evidence.
The benefits of the EIP model for the nurse, patient and family are that it simplifies a highly complex series of systems and processes pertaining to how evidence is used to support decisions made in clinical practice. The EIP model simply illustrates the why, the how and the sequencing of getting evidence into clinical practice. It also complements the evidence-based movement by offering a holistic systems-based approach to facilitating the application of evidence into clinical practice.
EIP is a holistic integrated approach to applying evidence into practice, which incorporates the steps of EBP within its system and processes. In other words, EBP is a subset of the EIP model, made explicit within the EIP cycle. Thus, EIP is neither an alternative to, nor a replacement for, EBP. The EIP model provides a framework for nurses (indeed all health practitioners) to deliver clinically effective care and enable them to justify the processes used and the service provided by referring to reliable evidence. Using two scenarios, this article demonstrated how the EIP model can be applied to clinical nursing practice. Future initiatives should focus on developing EIP educational interventions and determining the effects of such interventions on healthcare students' knowledge of, and attitudes towards, the application of evidence to practice.
- Two main concepts have been associated with the application of evidence into practice: evidence-based practice (EBP) and evidence-informed practice (EIP)
- The main feature that distinguishes EIP from EBP is the processes used in implementing the concepts
- EIP provides the mechanisms or processes to follow in implementing EBP
- EIP is not a substitute or replacement for EBP. EIP is an integrated approach to applying evidence to practice, which incorporates the steps of EBP in its processes
CPD reflective questions
- Make a list of the challenges you encounter in implementing EBP
- Use the same list and indicate how these challenges prevent you from using evidence to support your nursing clinical decisions and actions in practice
- How does viewing health and healthcare delivery as a complex system impact on your patient care?
- Make a list of the drivers that are encouraging you to support your clinical nursing decisions and actions with evidence
- Using your own experience to date and the information presented in the text, make a list of why and how you think evidence-informed practice forms part of your professional accountability and professional registration
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008 Apr.

Patient Safety and Quality: An Evidence-Based Handbook for Nurses.
Chapter 7 the evidence for evidence-based practice implementation.
Marita G. Titler .
Affiliations
Overview of evidence-based practice.
Evidence-based health care practices are available for a number of conditions such as asthma, heart failure, and diabetes. However, these practices are not always implemented in care delivery, and variation in practices abound. 1–4 Traditionally, patient safety research has focused on data analyses to identify patient safety issues and to demonstrate that a new practice will lead to improved quality and patient safety. 5 Much less research attention has been paid to how to implement practices. Yet, only by putting into practice what is learned from research will care be made safer. 5 Implementing evidence-based safety practices are difficult and need strategies that address the complexity of systems of care, individual practitioners, senior leadership, and—ultimately—changing health care cultures to be evidence-based safety practice environments. 5
Nursing has a rich history of using research in practice, pioneered by Florence Nightingale. 6–9 Although during the early and mid-1900s, few nurses contributed to this foundation initiated by Nightingale, 10 the nursing profession has more recently provided major leadership for improving care through application of research findings in practice. 11
Evidence-based practice (EBP) is the conscientious and judicious use of current best evidence in conjunction with clinical expertise and patient values to guide health care decisions. 12–15 Best evidence includes empirical evidence from randomized controlled trials; evidence from other scientific methods such as descriptive and qualitative research; as well as use of information from case reports, scientific principles, and expert opinion. When enough research evidence is available, the practice should be guided by research evidence in conjunction with clinical expertise and patient values. In some cases, however, a sufficient research base may not be available, and health care decision making is derived principally from nonresearch evidence sources such as expert opinion and scientific principles. 16 As more research is done in a specific area, the research evidence must be incorporated into the EBP. 15
Models of Evidence-Based Practice
Multiple models of EBP are available and have been used in a variety of clinical settings. 16–36 Although review of these models is beyond the scope of this chapter, common elements of these models are selecting a practice topic (e.g., discharge instructions for individuals with heart failure), critique and syntheses of evidence, implementation, evaluation of the impact on patient care and provider performance, and consideration of the context/setting in which the practice is implemented. 15 , 17 The learning that occurs during the process of translating research into practice is valuable information to capture and feed back into the process, so that others can adapt the evidence-based guideline and/or the implementation strategies.
A recent conceptual framework for maximizing and accelerating the transfer of research results from the Agency for Healthcare Research and Quality (AHRQ) patient safety research portfolio to health care delivery was developed by the dissemination subcommittee of the AHRQ Patient Safety Research Coordinating Committee. 37 This model is a synthesis of concepts from scientific information on knowledge transfer, social marketing, social and organizational innovation, and behavior change (see Figure 1 ). 37 Although the framework is portrayed as a series of stages, the authors of this framework do not believe that the knowledge transfer process is linear; rather, activities occur simultaneously or in different sequences, with implementation of EBPs being a multifaceted process with many actors and systems.
AHRQ Model of Knowledge Transfer Adapted from Nieva, V., Murphy, R., Ridley, N., et al. Used with permission. http://www.ahrq.gov/qual/advances/
Steps of Evidence-Based Practice
Steps of promoting adoption of EBPs can be viewed from the perspective of those who conduct research or generate knowledge, 23 , 37 those who use the evidence-based information in practice, 16 , 31 and those who serve as boundary spanners to link knowledge generators with knowledge users. 19
Steps of knowledge transfer in the AHRQ model 37 represent three major stages: (1) knowledge creation and distillation, (2) diffusion and dissemination, and (3) organizational adoption and implementation. These stages of knowledge transfer are viewed through the lens of researchers/creators of new knowledge and begin with determining what findings from the patient safety portfolio or individual research projects ought to be disseminated.
Knowledge creation and distillation is conducting research (with expected variation in readiness for use in health care delivery systems) and then packaging relevant research findings into products that can be put into action—such as specific practice recommendations—thereby increasing the likelihood that research evidence will find its way into practice. 37 It is essential that the knowledge distillation process be informed and guided by end users for research findings to be implemented in care delivery. The criteria used in knowledge distillation should include perspectives of the end users (e.g., transportability to the real-world health care setting, feasibility, volume of evidence needed by health care organizations and clinicians), as well as traditional knowledge generation considerations (e.g., strength of the evidence, generalizability).
Diffusion and dissemination involves partnering with professional opinion leaders and health care organizations to disseminate knowledge that can form the basis of action (e.g., essential elements for discharge teaching for hospitalized patient with heart failure) to potential users. Dissemination partnerships link researchers with intermediaries that can function as knowledge brokers and connectors to the practitioners and health care delivery organizations. Intermediaries can be professional organizations such as the National Patient Safety Foundation or multidisciplinary knowledge transfer teams such as those that are effective in disseminating research-based cancer prevention programs. In this model, dissemination partnerships provide an authoritative seal of approval for new knowledge and help identify influential groups and communities that can create a demand for application of the evidence in practice. Both mass communication and targeted dissemination are used to reach audiences with the anticipation that early users will influence the latter adopters of the new usable, evidence-based research findings. Targeted dissemination efforts must use multifaceted dissemination strategies, with an emphasis on channels and media that are most effective for particular user segments (e.g., nurses, physicians, pharmacists).
End user adoption, implementation, and institutionalization is the final stage of the knowledge transfer process. 37 This stage focuses on getting organizations, teams, and individuals to adopt and consistently use evidence-based research findings and innovations in everyday practice. Implementing and sustaining EBPs in health care settings involves complex interrelationships among the EBP topic (e.g., reduction of medication errors), the organizational social system characteristics (such as operational structures and values, the external health care environment), and the individual clinicians. 35 , 37–39 A variety of strategies for implementation include using a change champion in the organization who can address potential implementation challenges, piloting/trying the change in a particular patient care area of the organization, and using multidisciplinary implementation teams to assist in the practical aspects of embedding innovations into ongoing organizational processes. 35 , 37 Changing practice takes considerable effort at both the individual and organizational level to apply evidence-based information and products in a particular context. 22 When improvements in care are demonstrated in the pilot studies and communicated to other relevant units in the organization, key personnel may then agree to fully adopt and sustain the change in practice. Once the EBP change is incorporated into the structure of the organization, the change is no longer considered an innovation but a standard of care. 22 , 37
In comparison, other models of EBP (e.g., Iowa Model of Evidence-based Practice to Promote Quality of Care 16 ) view the steps of the EBP process from the perspective of clinicians and/or organizational/clinical contexts of care delivery. When viewing steps of the EBP process through the lens of an end user, the process begins with selecting an area for improving care based on evidence (rather than asking what findings ought to be disseminated); determining the priority of the potential topic for the organization; formulating an EBP team composed of key stakeholders; finding, critiquing, and synthesizing the evidence; setting forth EBP recommendations, with the type and strength of evidence used to support each clearly documented; determining if the evidence findings are appropriate for use in practice; writing an EBP standard specific to the organization; piloting the change in practice; implementing changes in practice in other relevant practice areas (depending on the outcome of the pilot); evaluating the EBP changes; and transitioning ongoing quality improvement (QI) monitoring, staff education, and competency review of the EBP topic to appropriate organizational groups as defined by the organizational structure. 15 , 40 The work of EBP implementation from the perspective of the end user is greatly facilitated by efforts of AHRQ, professional nursing organizations (e.g., Oncology Nursing Society), and others that distill and package research findings into useful products and tools for use at the point of care delivery.
When the clinical questions of end users can be addressed through use of existing evidence that is packaged with end users in mind, steps of the EBP process take less time and more effort can be directed toward the implementation, evaluation, and sustainability components of the process. For example, finding, critiquing, and synthesizing the evidence; setting forth EBP recommendations with documentation of the type and strength of evidence for each recommendation; and determining appropriateness of the evidence for use in practice are accelerated when the knowledge-based information is readily available. Some distilled research findings also include quick reference guides that can be used at the point of care and/or integrated into health care information systems, which also helps with implementation. 41 , 42
Translation Science: An Overview
Translation science is the investigation of methods, interventions, and variables that influence adoption by individuals and organizations of EBPs to improve clinical and operational decisionmaking in health care. 35 , 43–46 This includes testing the effect of interventions on promoting and sustaining adoption of EBPs. Examples of translation studies include describing facilitators and barriers to knowledge uptake and use, organizational predictors of adherence to EBP guidelines, attitudes toward EBPs, and defining the structure of the scientific field. 11 , 47–49
Translation science must be guided by a conceptual model that organizes the strategies being tested, elucidates the extraneous variables (e.g., behaviors and facilitators) that may influence adoption of EBPs (e.g., organizational size, characteristics of users), and builds a scientific knowledge base for this field of inquiry. 15 , 50 Conceptual models used in the translating-research-into-practice studies funded by AHRQ were adult learning, health education, social influence, marketing, and organizational and behavior theories. 51 Investigators have used Rogers’s Diffusion of Innovation model, 35 , 39 , 52–55 the Promoting Action on Research Implementation in Health Services (PARIHS) model, 29 the push/pull framework, 23 , 56 , 57 the decisionmaking framework, 58 and the Institute for Healthcare Improvement (IHI) model 59 in translation science.
Study findings regarding evidence-based practices in a diversity of health care settings are building an empirical foundation of translation science. 19 , 43 , 51 , 60–83 These investigations and others 18 , 84–86 provide initial scientific knowledge to guide us in how to best promote use of evidence in practice. To advance knowledge about promoting and sustaining adoption of EBPs in health care, translation science needs more studies that test translating research into practice (TRIP) interventions: studies that investigate what TRIP interventions work, for whom, in what circumstances, in what types of settings; and studies that explain the underlying mechanisms of effective TRIP interventions. 35 , 49 , 79 , 87 Partnership models, which encourage ongoing interaction between researchers and practitioners, may be the way forward to carry out such studies. 56 Challenges, issues, methods, and instruments used in translation research are described elsewhere. 11 , 19 , 49 , 78 , 88–97
- Research Evidence
What Is Known About Implementing Evidence-Based Practices?
Multifaceted implementation strategies are needed to promote use of research evidence in clinical and administrative health care decisionmaking. 15 , 22 , 37 , 45 , 64 , 72 , 77 , 79 , 98 , 99 Although Grimshaw and colleagues 65 suggest that multifaceted interventions are no more effective than single interventions, context (site of care delivery) was not incorporated in the synthesis methodology. As noted by others, the same TRIP intervention may meet with varying degrees of effectiveness when applied in different contexts. 35 , 49 , 79 , 80 , 87 , 100 , 101 Implementation strategies also need to address both the individual practitioner and organizational perspective. 15 , 22 , 37 , 64 , 72 , 77 , 79 , 98 When practitioners decide individually what evidence to use in practice, considerable variability in practice patterns result, 71 potentially resulting in adverse patient outcomes.
For example, an “individual” perspective of EBP would leave the decision about use of evidence-based endotracheal suctioning techniques to each nurse and respiratory therapist. Some individuals may be familiar with the research findings for endotracheal suctioning while others may not. This is likely to result in different and conflicting practices being used as people change shifts every 8 to 12 hours. From an organizational perspective, endotracheal suctioning policies and procedures based on research are written, the evidence-based information is integrated into the clinical information systems, and adoption of these practices by nurses and other practitioners is systematically promoted in the organization. This includes assuring that practitioners have the necessary knowledge, skills, and equipment to carry out the evidence-based endotracheal suctioning practice. The organizational governance supports use of these practices through various councils and committees such as the Practice Committee, Staff Education Committee, and interdisciplinary EBP work groups.
The Translation Research Model, 35 built on Rogers’s seminal work on diffusion of innovations, 39 provides a guiding framework for testing and selecting strategies to promote adoption of EBPs. According to the Translation Research Model, adoption of innovations such as EBPs are influenced by the nature of the innovation (e.g., the type and strength of evidence, the clinical topic) and the manner in which it is communicated (disseminated) to members (nurses) of a social system (organization, nursing profession). 35 Strategies for promoting adoption of EBPs must address these four areas (nature of the EBP topic; users of the evidence; communication; social system) within a context of participative change (see Figure 2 ). This model provided the framework for a multisite study that tested the effectiveness of a multifaceted TRIP intervention designed to promote adoption of evidence-based acute pain management practices for hospitalized older adults. The intervention improved the quality of acute pain management practices and reduced costs. 81 The model is currently being used to test the effectiveness of a multifaceted TRIP intervention to promote evidence-based cancer pain management of older adults in home hospice settings. * This guiding framework is used herein to overview what is known about implementation interventions to promote use of EBPs in health care systems (see Evidence Table ).
*Implementation Model Redrawn from Rogers EM. Diffusion of innovations. 5th ed. New York: The Free Press; 2003; Titler MG, Everett LQ. Translating research into practice: considerations for critical care investigators. Crit Care Nurs Clin North Am 2001a;13(4):587-604. (more...)
Evidence Table
Evidence-Based Practice in Nursing
Nature of the Innovation or Evidence-Based Practice
Characteristics of an innovation or EBP topic that affect adoption include the relative advantage of the EBP (e.g., effectiveness, relevance to the task, social prestige); the compatibility with values, norms, work, and perceived needs of users; and complexity of the EBP topic. 39 For example, EBP topics that are perceived by users as relatively simple (e.g., influenza vaccines for older adults) are more easily adopted in less time than those that are more complex (acute pain management for hospitalized older adults). Strategies to promote adoption of EBPs related to characteristics of the topic include practitioner review and “reinvention” of the EBP guideline to fit the local context, use of quick reference guides and decision aids, and use of clinical reminders. 53 , 59 , 60 , 65 , 74 , 82 , 102–107 An important principle to remember when planning implementation of an EBP is that the attributes of the EBP topic as perceived by users and stakeholders (e.g., ease of use, valued part of practice) are neither stable features nor sure determinants of their adoption. Rather it is the interaction among the characteristics of the EBP topic, the intended users, and a particular context of practice that determines the rate and extent of adoption. 22 , 35 , 39
Studies suggest that clinical systems, computerized decision support, and prompts that support practice (e.g., decisionmaking algorithms, paper reminders) have a positive effect on aligning practices with the evidence base. 15 , 51 , 65 , 74 , 80 , 82 , 102 , 104 , 107–110 Computerized knowledge management has consistently demonstrated significant improvements in provider performance and patient outcomes. 82 Feldman and colleagues, using a just-in-time e-mail reminder in home health care, have demonstrated (1) improvements in evidence-based care and outcomes for patients with heart failure, 64 , 77 and (2) reduced pain intensity for cancer patients. 75 Clinical information systems should deploy the evidence base to the point of care and incorporate computer decision-support software that integrates evidence for use in clinical decisionmaking about individual patients. 40 , 104 , 111–114 There is still much to learn about the “best” manner of deploying evidence-based information through electronic clinical information systems to support evidence-based care. 115
Methods of Communication
Interpersonal communication channels, methods of communication, and influence among social networks of users affect adoption of EBPs. 39 Use of mass media, opinion leaders, change champions, and consultation by experts along with education are among strategies tested to promote use of EBPs. Education is necessary but not sufficient to change practice, and didactic continuing education alone does little to change practice behavior. 61 , 116 There is little evidence that interprofessional education as compared to discipline-specific education improves EBP. 117 Interactive education, used in combination with other practice-reinforcing strategies, has more positive effects on improving EBP than didactic education alone. 66 , 68 , 71 , 74 , 118 , 119 There is evidence that mass media messages (e.g., television, radio, newspapers, leaflets, posters and pamphlets), targeted at the health care consumer population, have some effect on use of health services for the targeted behavior (e.g., colorectal cancer screening). However, little empirical evidence is available to guide framing of messages communicated through planned mass media campaigns to achieve the intended change. 120
Several studies have demonstrated that opinion leaders are effective in changing behaviors of health care practitioners, 22 , 68 , 79 , 100 , 116 , 121–123 especially in combination with educational outreach or performance feedback. Opinion leaders are from the local peer group, viewed as a respected source of influence, considered by associates as technically competent, and trusted to judge the fit between the innovation and the local situation. 39 , 116 , 121 , 124–127 With their wide sphere of influence across several microsystems/units, opinion leaders’ use of the innovation influences peers and alters group norms. 39 , 128 The key characteristic of an opinion leader is that he or she is trusted to evaluate new information in the context of group norms. Opinion leadership is multifaceted and complex, with role functions varying by the circumstances, but few successful projects to implement innovations in organizations have managed without the input of identifiable opinion leaders. 22 , 35 , 39 , 81 , 96 Social interactions such as “hallway chats,” one-on-one discussions, and addressing questions are important, yet often overlooked components of translation. 39 , 59 Thus, having local opinion leaders discuss the EBPs with members of their peer group is necessary to translate research into practice. If the EBP that is being implemented is interdisciplinary in nature, discipline-specific opinion leaders should be used to promote the change in practice. 39
Change champions are also helpful for implementing innovations. 39 , 49 , 81 , 129–131 They are practitioners within the local group setting (e.g., clinic, patient care unit) who are expert clinicians, passionate about the innovation, committed to improving quality of care, and have a positive working relationship with other health care professionals. 39 , 125 , 131 , 132 They circulate information, encourage peers to adopt the innovation, arrange demonstrations, and orient staff to the innovation. 49 , 130 The change champion believes in an idea; will not take “no” for an answer; is undaunted by insults and rebuffs; and, above all, persists. 133 Because nurses prefer interpersonal contact and communication with colleagues rather than Internet or traditional sources of practice knowledge, 134–137 it is imperative that one or two change champions be identified for each patient care unit or clinic where the change is being made for EBPs to be enacted by direct care providers. 81 , 138 Conferencing with opinion leaders and change champions periodically during implementation is helpful to address questions and provide guidance as needed. 35 , 66 , 81 , 106
Because nurses’ preferred information source is through peers and social interactions, 134–137 , 139 , 140 using a core group in conjunction with change champions is also helpful for implementing the practice change. 16 , 110 , 141 A core group is a select group of practitioners with the mutual goal of disseminating information regarding a practice change and facilitating the change by other staff in their unit/microsystem. 142 Core group members represent various shifts and days of the week and become knowledgeable about the scientific basis for the practice; the change champion educates and assists them in using practices that are aligned with the evidence. Each member of the core group, in turn, takes the responsibility for imparting evidence-based information and effecting practice change with two or three of their peers. Members assist the change champion and opinion leader with disseminating the EBP information to other staff, reinforce the practice change on a daily basis, and provide positive feedback to those who align their practice with the evidence base. 15 Using a core-group approach in conjunction with a change champion results in a critical mass of practitioners promoting adoption of the EBP. 39
Educational outreach, also known as academic detailing, promotes positive changes in practice behaviors of nurses and physicians. 22 , 64 , 66 , 71 , 74 , 75 , 77 , 81 , 119 , 143 Academic detailing is done by a topic expert, knowledgeable of the research base (e.g., cancer pain management), who may be external to the practice setting; he or she meets one-on-one with practitioners in their setting to provide information about the EBP topic. These individuals are able to explain the research base for the EBPs to others and are able to respond convincingly to challenges and debates. 22 This strategy may include providing feedback on provider or team performance with respect to selected EBP indicators (e.g., frequency of pain assessment). 66 , 81 , 119
Users of the Innovation or Evidence-Based Practice
Members of a social system (e.g., nurses, physicians, clerical staff) influence how quickly and widely EBPs are adopted. 39 Audit and feedback, performance gap assessment (PGA), and trying the EBP are strategies that have been tested. 15 , 22 , 65 , 66 , 70–72 , 81 , 98 , 124 , 144 PGA and audit and feedback have consistently shown a positive effect on changing practice behavior of providers. 65 , 66 , 70 , 72 , 81 , 98 , 124 , 144 , 145 PGA (baseline practice performance) informs members, at the beginning of change, about a practice performance and opportunities for improvement. Specific practice indicators selected for PGA are related to the practices that are the focus of evidence-based practice change, such as every-4-hour pain assessment for acute pain management. 15 , 66 , 81
Auditing and feedback are ongoing processes of using and assessing performance indicators (e.g., every-4-hour pain assessment), aggregating data into reports, and discussing the findings with practitioners during the practice change. 22 , 49 , 66 , 70 , 72 , 81 , 98 , 145 This strategy helps staff know and see how their efforts to improve care and patient outcomes are progressing throughout the implementation process. Although there is no clear empirical evidence for how to provide audit and feedback, 70 , 146 effects may be larger when clinicians are active participants in implementing change and discuss the data rather than being passive recipients of feedback reports. 67 , 70 Qualitative studies provide some insight into use of audit and feedback. 60 , 67 One study on use of data feedback for improving treatment of acute myocardial infarction found that (1) feedback data must be perceived by physicians as important and valid, (2) the data source and timeliness of data feedback are critical to perceived validity, (3) time is required to establish credibility of data within a hospital, (4) benchmarking improves the validity of the data feedback, and (5) physician leaders can enhance the effectiveness of data feedback. Data feedback that profiles an individual physician’s practices can be effective but may be perceived as punitive; data feedback must persist to sustain improved performance; and effectiveness of data feedback is intertwined with the organizational context, including physician leadership and organizational culture. 60 Hysong and colleagues 67 found that high-performing institutions provided timely, individualized, nonpunitive feedback to providers, whereas low performers were more variable in their timeliness and nonpunitiveness and relied more on standardized, facility-level reports. The concept of useful feedback emerged as the core concept around which timeliness, individualization, nonpunitiveness, and customizability are important.
Users of an innovation usually try it for a period of time before adopting it in their practice. 22 , 39 , 147 When “trying an EBP” (piloting the change) is incorporated as part of the implementation process, users have an opportunity to use it for a period of time, provide feedback to those in charge of implementation, and modify the practice if necessary. 148 Piloting the EBP as part of implementation has a positive influence on the extent of adoption of the new practice. 22 , 39 , 148
Characteristics of users such as educational preparation, practice specialty, and views on innovativeness may influence adoption of an EBP, although findings are equivocal. 27 , 39 , 130 , 149–153 Nurses’ disposition to critical thinking is, however, positively correlated with research use, 154 and those in clinical educator roles are more likely to use research than staff nurses or nurse managers. 155
Social System
Clearly, the social system or context of care delivery matters when implementing EBPs. 2 , 30 , 33 , 39 , 60 , 84 , 85 , 91 , 92 , 101 , 156–163 For example, investigators demonstrated the effectiveness of a prompted voiding intervention for urinary incontinence in nursing homes, but sustaining the intervention in day-to-day practice was limited when the responsibility of carrying out the intervention was shifted to nursing home staff (rather than the investigative team) and required staffing levels in excess of a majority of nursing home settings. 164 This illustrates the importance of embedding interventions into ongoing processes of care.
Several organizational factors affect adoption of EBPs. 22 , 39 , 79 , 134 , 165–167 Vaughn and colleagues 101 demonstrated that organizational resources, physician full-time employees (FTEs) per 1,000 patient visits, organizational size, and whether the facility was located in or near a city affected use of evidence in the health care system of the Department of Veterans Affairs (VA). Large, mature, functionally differentiated organizations (e.g., divided into semiautonomous departments and units) that are specialized, with a focus of professional knowledge, slack resources to channel into new projects, decentralized decisionmaking, and low levels of formalization will more readily adopt innovations such as new practices based on evidence. Larger organizations are generally more innovative because size increases the likelihood that other predictors of innovation adoption—such as slack financial and human resources and differentiation—will be present. However, these organizational determinants account for only about 15 percent of the variation in innovation adoption between comparable organizations. 22 Adler and colleagues 168 hypothesize that while more structurally complex organizations may be more innovative and hence adopt EBPs relatively early, less structurally complex organizations may be able to diffuse EBPs more effectively. Establishing semiautonomous teams is associated with successful implementation of EBPs, and thus should be considered in managing organizational units. 168–170
As part of the work of implementing EBPs, it is important that the social system—unit, service line, or clinic—ensures that policies, procedures, standards, clinical pathways, and documentation systems support the use of the EBPs. 49 , 68 , 72 , 73 , 103 , 140 , 171 Documentation forms or clinical information systems may need revision to support changes in practice; documentation systems that fail to readily support the new practice thwart change. 82
Absorptive capacity for new knowledge is another social system factor that affects adoption of EBPs. Absorptive capacity is the knowledge and skills to enact the EBPs; the strength of evidence alone will not promote adoption. An organization that is able to systematically identify, capture, interpret, share, reframe, and recodify new knowledge, and put it to appropriate use, will be better able to assimilate EBPs. 82 , 103 , 172 , 173 A learning organizational culture and proactive leadership that promotes knowledge sharing are important components of building absorptive capacity for new knowledge. 66 , 139 , 142 , 174 Components of a receptive context for EBP include strong leadership, clear strategic vision, good managerial relations, visionary staff in key positions, a climate conducive to experimentation and risk taking, and effective data capture systems. Leadership is critical in encouraging organizational members to break out of the convergent thinking and routines that are the norm in large, well-established organizations. 4 , 22 , 39 , 122 , 148 , 163 , 175
An organization may be generally amenable to innovations but not ready or willing to assimilate a particular EBP. Elements of system readiness include tension for change, EBP-system fit, assessment of implications, support and advocacy for the EBP, dedicated time and resources, and capacity to evaluate the impact of the EBP during and following implementation. If there is tension around specific work or clinical issues and staff perceive that the situation is intolerable, a potential EBP is likely to be assimilated if it can successfully address the issues, and thereby reduce the tension. 22 , 175
Assessing and structuring workflow to fit with a potential EBP is an important component of fostering adoption. If implications of the EBP are fully assessed, anticipated, and planned for, the practice is more likely to be adopted. 148 , 162 , 176 If supporters for a specific EBP outnumber and are more strategically placed within the organizational power base than opponents, the EBP is more likely to be adopted by the organization. 60 , 175 Organizations that have the capacity to evaluate the impact of the EBP change are more likely to assimilate it. Effective implementation needs both a receptive climate and a good fit between the EBP and intended adopters’ needs and values. 22 , 60 , 140 , 175 , 177
Leadership support is critical for promoting use of EBPs. 33 , 59 , 72 , 85 , 98 , 122 , 178–181 This support, which is expressed verbally, provides necessary resources, materials, and time to fulfill assigned responsibilities. 148 , 171 , 182 , 183 Senior leaders need to create an organizational mission, vision, and strategic plan that incorporate EBP; implement performance expectations for staff that include EBP work; integrate the work of EBP into the governance structure of the health care system; demonstrate the value of EBPs through administrative behaviors; and establish explicit expectations that nurse leaders will create microsystems that value and support clinical inquiry. 122 , 183 , 184
A recent review of organizational interventions to implement EBPs for improving patient care examined five major aspects of patient care. The review suggests that revision of professional roles (changing responsibilities and work of health professionals such as expanding roles of nurses and pharmacists) improved processes of care, but it was less clear about the effect on improvement of patient outcomes. Multidisciplinary teams (collaborative practice teams of physicians, nurses, and allied health professionals) treating mostly patients with prevalent chronic diseases resulted in improved patient outcomes. Integrated care services (e.g., disease management and case management) resulted in improved patient outcomes and cost savings. Interventions aimed at knowledge management (principally via use of technology to support patient care) resulted in improved adherence to EBPs and patient outcomes. The last aspect, quality management, had the fewest reviews available, with the results uncertain. A number of organizational interventions were not included in this review (e.g., leadership, process redesign, organizational learning), and the authors note that the lack of a widely accepted taxonomy of organizational interventions is a problem in examining effectiveness across studies. 82
An organizational intervention that is receiving increasing attention is tailored interventions to overcome barriers to change. 162 , 175 , 185 This type of intervention focuses on first assessing needs in terms of what is causing the gap between current practice and EBP for a specified topic, what behaviors and/or mechanism need to change, what organizational units and persons should be involved, and identification of ways to facilitate the changes. This information is then used in tailoring an intervention for the setting that will promote use of the specified EBP. Based on a recent systematic review, effectiveness of tailored implementation interventions remains uncertain. 185
In summary, making an evidence-based change in practice involves a series of action steps and a complex, nonlinear process. Implementing the change will take several weeks to months, depending on the nature of the practice change. Increasing staff knowledge about a specific EBP and passive dissemination strategies are not likely to work, particularly in complex health care settings. Strategies that seem to have a positive effect on promoting use of EBPs include audit and feedback, use of clinical reminders and practice prompts, opinion leaders, change champions, interactive education, mass media, educational outreach/academic detailing, and characteristics of the context of care delivery (e.g., leadership, learning, questioning). It is important that senior leadership and those leading EBP improvements are aware of change as a process and continue to encourage and teach peers about the change in practice. The new practice must be continually reinforced and sustained or the practice change will be intermittent and soon fade, allowing more traditional methods of care to return. 15
- Practice Implications From Translation Science
Principles of Evidence-Based Practice for Patient Safety
Several translation science principles are informative for implementing patient safety initiatives:
- First, consider the context and engage health care personnel who are at the point of care in selecting and prioritizing patient safety initiatives, clearly communicating the evidence base (strength and type) for the patient safety practice topic(s) and the conditions or setting to which it applies. These communication messages need to be carefully designed and targeted to each stakeholder user group.
- Second, illustrate, through qualitative or quantitative data (e.g., near misses, sentinel events, adverse events, injuries from adverse events), the reason the organization and individuals within the organization should commit to an evidence-based safety practice topic. Clinicians tend to be more engaged in adopting patient safety initiatives when they understand the evidence base of the practice, in contrast to administrators saying, “We must do this because it is an external regulatory requirement.” For example, it is critical to converse with busy clinicians about the evidence-based rationale for doing fall-risk assessment, and to help them understand that fall-risk assessment is an external regulatory agency expectation because the strength of the evidence supports this patient safety practice.
- Third, didactic education alone is never enough to change practice; one-time education on a specific safety initiative is not enough. Simply improving knowledge does not necessarily improve practice. Rather, organizations must invest in the tools and skills needed to create a culture of evidence-based patient safety practices where questions are encouraged and systems are created to make it easy to do the right thing.
- Fourth, the context of EBP improvements in patient safety need to be addressed at each step of the implementation process; piloting the change in practice is essential to determine the fit between the EBP patient safety information/innovation and the setting of care delivery. There is no one way to implement, and what works in one agency may need modification to fit the organizational culture of another context.
- Finally, it is important to evaluate the processes and outcomes of implementation. Users and stakeholders need to know that the efforts to improve patient safety have a positive impact on quality of care. For example, if a new barcoding system is being used to administer blood products, it is imperative to know that the steps in the process are being followed (process indicators) and that the change in practice is resulting in fewer blood product transfusion errors (outcome indicators).
Research Implications
Translation science is young, and although there is a growing body of knowledge in this area, we have, to date, many unanswered questions. These include the type of audit and feedback (e.g., frequency, content, format) strategies that are most effective, the characteristics of opinion leaders that are critical for success, the role of specific context variables, and the combination of strategies that are most effective. We also know very little about use of tailored implementation interventions, or the key context attributes to assess and use in developing and testing tailored interventions. The types of clinical reminders that are most effective for making EBP knowledge available at the point of care require further empirical explanation. We also know very little about the intensity and intervention dose of single and multifaceted strategies that are effective for promoting and sustaining use of EBPs or how the effectiveness differs by type of topic (e.g., simple versus complex). Only recently has the context of care delivery been acknowledged as affecting use of evidence, and further empirical work is needed in this area to understand how complex adaptive systems of practice incorporate knowledge acquisition and use. Lastly, we do not know what strategies or combination of strategies work for whom, in what context, why they work in some settings or cases and not others, and what is the mechanism by which these strategies or combination of strategies work.
This is an exciting area of investigation that has a direct impact on implementing patient safety practices. In planning investigations, researchers must use a conceptual model to guide the research and add to the empirical and theoretical understanding of this field of inquiry. Additionally, funding is needed for implementation studies that focus on evidence-based patient safety practices as the topic of concern. To generalize empirical findings from patient safety implementation studies, we must have a better understanding of what implementation strategies work, with whom, and in what types of settings, and we must investigate the underlying mechanisms of these strategies. This is likely to require mixed methods, a better understanding of complexity science, and greater appreciation for nontraditional methods and realistic inquiry. 87
Although the science of translating research into practice is fairly new, there is some guiding evidence of what implementation interventions to use in promoting patient safety practices. However, there is no magic bullet for translating what is known from research into practice. To move evidence-based interventions into practice, several strategies may be needed. Additionally, what works in one context of care may or may not work in another setting, thereby suggesting that context variables matter in implementation. 80
- Search Strategy
Several electronic databases were searched (MEDLINE ® , CINAHL ® , PubMed ® ) using terms of evidence-based practice research, implementation research, and patient safety. (The terms “quality improvement” or “quality improvement intervention research” were not used.) The Cochrane Collaboration–Cochrane Reviews was also searched to look for systematic reviews of specific implementation strategies, and the Journal of Implementation Science was also reviewed. I also requested the final reports of the TRIP I and TRIP II studies funded by AHRQ. Classic articles known to the author were also included in this chapter (e.g.,Locock et al. 123 ).
*Principal Investigator: Keela Herr (R01 grant no. CA115363-01; National Cancer Institute (NCI))Background
- Cite this Page Titler MG. The Evidence for Evidence-Based Practice Implementation. In: Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008 Apr. Chapter 7.
- PDF version of this page (470K)
In this Page
Other titles in this collection.
- Advances in Patient Safety
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- It Is Not That Simple nor Compelling! Comment on "Translating Evidence Into Healthcare Policy and Practice: Single Versus Multi-faceted Implementation Strategies - Is There a Simple Answer to a Complex Question?". [Int J Health Policy Manag. 2015] It Is Not That Simple nor Compelling! Comment on "Translating Evidence Into Healthcare Policy and Practice: Single Versus Multi-faceted Implementation Strategies - Is There a Simple Answer to a Complex Question?". Bucknall T, Fossum M. Int J Health Policy Manag. 2015 Jul 28; 4(11):787-8. Epub 2015 Jul 28.
- Nursing implementation science: how evidence-based nursing requires evidence-based implementation. [J Nurs Scholarsh. 2008] Nursing implementation science: how evidence-based nursing requires evidence-based implementation. van Achterberg T, Schoonhoven L, Grol R. J Nurs Scholarsh. 2008; 40(4):302-10.
- Review The science of implementation: changing the practice of critical care. [Curr Opin Crit Care. 2008] Review The science of implementation: changing the practice of critical care. Weinert CR, Mann HJ. Curr Opin Crit Care. 2008 Aug; 14(4):460-5.
- Review Integrative review of implementation strategies for translation of research-based evidence by nurses. [Clin Nurse Spec. 2014] Review Integrative review of implementation strategies for translation of research-based evidence by nurses. Wuchner SS. Clin Nurse Spec. 2014 Jul-Aug; 28(4):214-23.
- Review A realist analysis of hospital patient safety in Wales: applied learning for alternative contexts from a multisite case study [ 2015] Review A realist analysis of hospital patient safety in Wales: applied learning for alternative contexts from a multisite case study Herepath A, Kitchener M, Waring J. 2015 Sep
Recent Activity
- The Evidence for Evidence-Based Practice Implementation - Patient Safety and Qua... The Evidence for Evidence-Based Practice Implementation - Patient Safety and Quality
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

IMAGES
VIDEO
COMMENTS
Here are five ways to nurture your critical-thinking skills: Be a lifelong learner. Continuous learning through educational courses and professional development lets you stay current with evidence-based practice. That knowledge helps you make informed decisions in stressful moments. Practice reflection.
5 min read • June, 01 2023. Evidence-based practice in nursing involves providing holistic, quality care based on the most up-to-date research and knowledge rather than traditional methods, advice from colleagues, or personal beliefs. Nurses can expand their knowledge and improve their clinical practice experience by collecting, processing ...
CRITICAL THINKING (CT) is vital in developing evidence-based nursing practice. Evidence-based practice (EBP) supports nursing care that can be "individualized to patients and their families, is more effective, streamlined, and dynamic, and maximizes effects of clinical judgment" ( Youngblut & Brooten, 2001, p. 468).
Critical thinking is a complex, dynamic process formed by attitudes and strategic skills, with the aim of achieving a specific goal or objective. The attitudes, including the critical thinking attitudes, constitute an important part of the idea of good care, of the good professional. It could be said that they become a virtue of the nursing ...
Background. The Institute of Medicine (IOM) has recommended that Evidence-Based Practice (EBP) be used in 90% of clinical decisions by 2020 [].EBP has become a popular buzzword in the healthcare industry [1, 2].This concept is defined as a problem-solving process in clinical decision making, which combines best research evidence with clinical expertise, patient preference, and clinical guidelines.
Critical Thinking. Nursing education has emphasized critical thinking as an essential nursing skill for more than 50 years. 1 The definitions of critical thinking have evolved over the years. There are several key definitions for critical thinking to consider. ... This implies that evidence-based practice, indicative of expertise in practice, ...
Critical thinking (CT) is vital to evidence-based nursing practice. Evidence-based practice (EBP) supports nursing care and can contribute positively to patient outcomes across a variety of settings and geographic locations. The nature of EBP, its relevance to nursing, and the skills needed to support it should be required components of ...
4. IMPLEMENTATION OF CRITICAL THINKING IN NURSING PRACTICE. In their shifts nurses act effectively without using critical thinking as many decisions are mainly based on habit and have a minimum reflection. Thus, higher critical thinking skills are put into operation, when some new ideas or needs are displayed to take a decision beyond routine.
This scoping review examined literature related to teaching, learning, assessment and implementation of EBP and application of CT by nursing students and graduates and found innovative teaching methods required to promote learning. Evidence-Based Practice (EBP) in health is important for patient safety and quality care while Critical Thinking (CT) is a vital prerequisite to evidence based nursing.
PDF | On Nov 30, 2022, Patricia Katowa-Mukwato and others published Evidence based practice and critical thinking in nursing education and practice: A scoping review of literature | Find, read and ...
Critical thinking in nursing clinical practice, education and research: From attitudes to virtue. Anna Falcó ... Based on selective analysis of the descriptive and empirical literature that addresses conceptual review of critical thinking, we conducted an analysis of this topic in the settings of clinical practice, training and research from ...
Nursing practice utilizes critical thinking skills to provide the best care for patients. Often, the patient's cause of pain or health issue is not immediately clear. ... Slaughter's clinical interests lie in nursing education and evidence-based practice initiatives to promote improving patient care. Jenna Liphart Rhoads, Ph.D., RN.
Evidence-Based Practice (EBP) in health is important for patient safety and quality care while Critical Thinking (CT) is a vital prerequisite to evidence based nursing. Despite their importance, in some settings neither EBP nor CT is taught assessed or implemented. This scoping review examined literature related to teaching, learning, assessment and implementation of EBP and application of CT ...
Read the article, "Probing the Relationship Between Evidence-Based Practice Implementation Models and Critical Thinking in Applied Nursing Practice," found on pages 161-168, carefully noting any tables and other illustrative materials that are included to enhance your knowledge and understanding of the content.
Evidence-based practice is now widely recognized as the key to improving healthcare quality and patient outcomes. Although the purposes of nursing research (conducting research to generate new knowledge) and evidence-based nursing practice (utilizing best evidence as basis of nursing practice) seem quite different, an increasing number of research studies have been conducted with the goal of ...
One type of evidence-based practice that can be used to engage students, promote active learning and develop critical thinking is skills fair intervention ( McCausland and Meyers, 2013; Roberts et al., 2009 ). Skills fair intervention promoted a consistent teaching approach of the psychomotor skills to the novice nurse that decreased anxiety ...
Critical thinking (CT) is vital to evidence-based nursing practice. Evidence-based practice (EBP) supports nursing care and can contribute positively to patient outcomes across a variety of settings and geographic locations. The nature of EBP, its relevance to nursing, and the skills needed to support it should be required components of baccalaureate education and must be introduced early in ...
The impact of evidence-based practice (EBP) has echoed across nursing practice, education, and science. The call for evidence-based quality improvement and healthcare transformation underscores the need for redesigning care that is effective, safe, and efficient. In line with multiple direction-setting recommendations from national experts, nurses have responded to launch initiatives that ...
Critical Thinking: Evidence-based practices in nursing require having the ability to evaluate data logically and weigh the evidence. 2. Scientific Mindset: ... Evidence-based practice in nursing involves several components such as creating answerable clinical questions, using resources to find the best evidence to answer the clinical question(s ...
Evidence-based practice is "integrating the best available evidence with the healthcare educator's expertise and the client's needs while considering the practice environment.[1] One of the roles of the NPD practitioner in the 2022 edition of the Nursing Scope and Standards of Practice is a champion for scientific inquiry. In this role, the NPD practitioner promotes a spirit of inquiry ...
Thus, Evidence based nursing practice is an important aspect of Critical Thinking in nursing practice. Evidence Based Nursing Practice: Evidence based practice is the conscientious, explicit and judicious use of current best evidence in making decisions about the case of individual patients (Sackett, 1996).
The problems with the uptake and effective implementation of EBP led to the emergence of the EIP concept. This concept is based on the premise that healthcare practice should, as a matter of principle, be informed by, rather than based on, evidence (Nevo and Slonim-Nevo, 2011). This implies that other forms of evidence (for example, patient experiences, the nurse's expertise and experiences ...
Models of Evidence-Based Practice. Multiple models of EBP are available and have been used in a variety of clinical settings. 16-36 Although review of these models is beyond the scope of this chapter, common elements of these models are selecting a practice topic (e.g., discharge instructions for individuals with heart failure), critique and syntheses of evidence, implementation, evaluation ...