- Português Br
- Journalist Pass

Mayo Clinic Minute: Game-changing treatment for chronic kidney disease could slow down progression of the disease
Share this:.

About 15% of adults in the U.S. are estimated to have chronic kidney disease — that's about 37 million people.
What if those people could be treated with medication that could slow the progression of their disease, and help avoid the need for dialysis and kidney transplantation altogether?
Dr. Naim Issa , a Mayo Clinic transplant nephrologist says there is a class of medications to help people with chronic kidney disease that does just that. He says Mayo Clinic has been incorporating these medications to help patients for the last few years.
March 9 is World Kidney Day, a day aimed at raising awareness about the importance of the kidneys.
Watch: The Mayo Clinic Minute
Journalists: Broadcast-quality video (1:03) is in the downloads at the end of this post. Please courtesy: "Mayo Clinic News Network." Read the script .
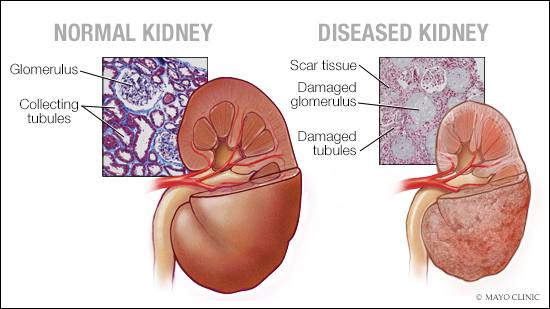
Most people don't have symptoms of chronic kidney disease until it's at an advanced stage.
"Early detection of chronic kidney disease may help us actually treat and prevent patients ahead of time before the need for dialysis or kidney transplantation," says Dr. Issa.
He says a new class of drugs, SGLT2 inhibitors , is being called a game changer. The drugs were originally designed to treat diabetes — a main cause of chronic kidney disease.
Medicines in the SGLT2 inhibitor class include canagliflozin , dapagliflozin and empagliflozin.
"In large trials , we observed groundbreaking success with those medications in slowing down the progression of chronic kidney disease, to the extent of avoiding dialysis and the need for kidney transplantation," Dr. Issa says.
The medications are used whether the patient is diabetic or not.
"They are actually game-changer medications that help us prevent the progression of chronic kidney disease," says Dr. Issa.
You can help yourself by following a low-sodium, moderate-protein diet, avoid smoking and getting plenty of exercise.
Dr. Issa says it is important that patients with chronic kidney disease work with their primary care physician and health care team to monitor and check blood pressure, urine analysis and bloodwork.
Related posts:
- Lifestyle changes can be critical for kidney transplant patients’ long-term survival
- Mayo Clinic Minute: What is chronic kidney disease?
- Diets higher in calcium and potassium may help prevent recurrent symptomatic kidney stones, Mayo Clinic study finds
For the safety of its patients, staff and visitors, Mayo Clinic has strict masking policies in place. Anyone shown without a mask was recorded prior to COVID-19 or recorded in an area not designated for patient care, where safety protocols were followed.
- Cauliflower: A versatile nutrition superstar Mayo Clinic Q and A: Metabolic syndrome and lifestyle changes
Related Articles

- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
February 2, 2023
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
Scientists first in the world to regenerate diseased kidney cells
by Federico Graciano, Duke-NUS Medical School
In a world first, scientists at Duke-NUS Medical School, the National Heart Center Singapore (NHCS) and colleagues in Germany have shown that regenerative therapy to restore impaired kidney function may soon be a possibility.
In a preclinical study reported in Nature Communications , the team found that blocking a damaging and scar-regulating protein called interleukin-11 (IL-11) enables damaged kidney cells to regenerate, restoring impaired kidney function due to disease and acute injuries.
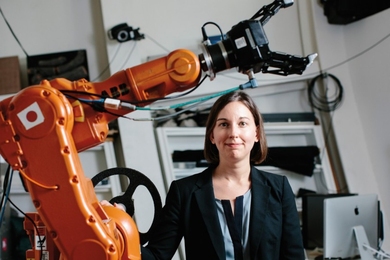
"Kidney failure is a global epidemic," said Assistant Professor Anissa Widjaja, a molecular biologist with Duke-NUS' Cardiovascular & Metabolic Disorders (CVMD) Signature Research Program. "Closer to home, Singapore ranks first in the world for diabetes-induced kidney failure and fourth in terms of kidney failure prevalence. The contribution of chronic kidney disease to mortality is rapidly increasing, suggesting there are shortcomings in current therapeutic approaches."
Searching for ways to restore the kidney's ability to regenerate damaged cells, Widjaja worked with Professor Stuart Cook, Tanoto Foundation Professor of Cardiovascular Medicine at the SingHealth Duke-NUS Academic Medical Center and the CVMD Program, and Clinician Scientist and Senior Consultant with the Department of Cardiology, NHCS, and Duke-NUS Dean Professor Thomas Coffman, a world-leading nephrologist. They teamed up with scientists in Germany to investigate the role of IL-11, which is known to trigger scarring in other organs, including the liver, lungs and heart, in acute and chronic kidney disease.
Their findings implicate the protein in triggering a cascade of molecular processes in response to kidney injury that leads to inflammation, fibrosis (scarring) and loss of function. They also discovered that inhibiting IL-11 with a neutralizing antibody can prevent and even reverse kidney damage in this setting.
"We found that IL-11 is detrimental to kidney function and triggers the development of chronic kidney disease," said Cook. "We also showed that anti-IL11 therapy can treat kidney failure, reverse established chronic kidney disease, and restore kidney function by promoting regeneration in mice, while being safe for long term use."
More specifically, the researchers showed that renal tubular cells, which line the tiny tubes inside kidneys, release IL-11 in response to kidney damage . This turns on a signaling cascade that ultimately leads to increased expression of a gene, called Snail Family Transcriptional Repressor 1 (SNAI1), which arrests cellular growth and promotes kidney dysfunction.
In a preclinical model of human diabetic kidney disease, turning off this process by administering an antibody that binds to IL-11 led to proliferation of the kidney tubule cells and reversal of fibrosis and inflammation, resulting in the regeneration of the injured kidney and the restoration of renal function.
While clinical trials of an antibody that binds to another pro-fibrotic molecule called transforming growth factor beta have been unsuccessful, this new approach brings hope of a new target.
"By boosting the kidney's intrinsic capability to regenerate, Prof. Cook and Asst. Prof. Widjaja have shown that we can restore function to a damaged kidney," said Coffman, who is also the principal investigator of the Diabetes Study in Nephropathy and other Microvascular Complications (DYNAMO), a large collaborative study that aims to find new solutions for the prevention and treatment of diabetic kidney disease.
"This discovery could be a real game-changer in the treatment of chronic kidney disease —which is a major public health concern in Singapore and globally—bringing us one step closer to delivering the benefits promised by regenerative medicine."
Explore further
Feedback to editors

New study finds genetic markers that explain up to 12% of the differences between two people's blood pressure

Microbiome researchers challenge the state of the art in colon cancer biomarker discovery

X-chromosome inactivation may reduce autism risk, study in mice suggests
2 hours ago

Microarray patches safe and effective for vaccinating children, trial shows
12 hours ago

Healthy lifestyle may offset effects of life-shortening genes by more than 60%

Fentanyl inhalation may cause potentially irreversible brain damage, warn doctors

Frequent teen vaping might boost risk of toxic lead and uranium exposure

Study in Haiti suggests early-onset heart failure is prevalent form of heart disease in low-income countries
14 hours ago

AI algorithms can determine how well newborns nurse, study shows
15 hours ago

Kaposi sarcoma discovery and mouse model could facilitate drug development
Related stories.

Turning off the damaging signals from a genetic syndrome that causes debilitating kidney disease
Mar 9, 2022

Analysis links impaired kidney function with cognitive disorders
Nov 3, 2022

Diabetes drug slows kidney function decline
Nov 6, 2021

Protecting the injured kidney
Jun 5, 2020

Mayo Clinic Minute: What is chronic kidney disease?
Mar 13, 2020

Scientists make a major breakthrough to treat fibrotic diseases that cause organ failure
Nov 13, 2017
Recommended for you

Blood samples enhance B-cell lymphoma diagnostics and prognosis, study shows
19 hours ago

Scientists develop new organoid model to study thymus function

Blood test finds knee osteoarthritis up to eight years before it appears on X-rays
Apr 26, 2024

Robotic nerve 'cuffs' could help treat a range of neurological conditions

Using stem cell-derived heart muscle cells to advance heart regenerative therapy

Nanomaterial that mimics proteins could be basis for new neurodegenerative disease treatments
Apr 25, 2024
Let us know if there is a problem with our content
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
Suggestions or feedback?
MIT News | Massachusetts Institute of Technology
- Machine learning
- Social justice
- Black holes
- Classes and programs
Departments
- Aeronautics and Astronautics
- Brain and Cognitive Sciences
- Architecture
- Political Science
- Mechanical Engineering
Centers, Labs, & Programs
- Abdul Latif Jameel Poverty Action Lab (J-PAL)
- Picower Institute for Learning and Memory
- Lincoln Laboratory
- School of Architecture + Planning
- School of Engineering
- School of Humanities, Arts, and Social Sciences
- Sloan School of Management
- School of Science
- MIT Schwarzman College of Computing
A new drug candidate can shrink kidney cysts
Press contact :, media download.
*Terms of Use:
Images for download on the MIT News office website are made available to non-commercial entities, press and the general public under a Creative Commons Attribution Non-Commercial No Derivatives license . You may not alter the images provided, other than to crop them to size. A credit line must be used when reproducing images; if one is not provided below, credit the images to "MIT."
Previous image Next image
Autosomal dominant polycystic kidney disease (ADPKD), the most common form of polycystic kidney disease, can lead to kidney enlargement and eventual loss of function. The disease affects more than 12 million people worldwide, and many patients end up needing dialysis or a kidney transplant by the time they reach their 60s.
Researchers at MIT and Yale University School of Medicine have now found that a compound originally developed as a potential cancer treatment holds promise for treating ADPKD. The drug works by exploiting kidney cyst cells’ vulnerability to oxidative stress — a state of imbalance between damaging free radicals and beneficial antioxidants.
In a study employing two mouse models of the disease, the researchers found that the drug dramatically shrank kidney cysts without harming healthy kidney cells.
“We really believe this has potential to impact the field and provide a different treatment paradigm for this important disease,” says Bogdan Fedeles, a research scientist and program manager in MIT’s Center for Environmental Health Sciences and the lead author of the study, which appears this week in the Proceedings of the National Academy of Sciences .
John Essigmann, the William R. and Betsy P. Leitch Professor of Biological Engineering and Chemistry at MIT; Sorin Fedeles, executive director of the Polycystic Kidney Disease Outcomes Consortium and assistant professor (adjunct) at Yale University School of Medicine; and Stefan Somlo, the C.N.H. Long Professor of Medicine and Genetics and chief of nephrology at Yale University School of Medicine, are the senior authors of the paper .
Cells under stress
ADPKD typically progresses slowly. Often diagnosed when patients are in their 30s, it usually doesn’t cause serious impairment of kidney function until patients reach their 60s. The only drug that is FDA-approved to treat the disease, tolvaptan, slows growth of the cysts but has side effects that include frequent urination and possible liver damage.
Essigmann’s lab did not originally set out to study PKD; the new study grew out of work on potential new drugs for cancer. Nearly 25 years ago, MIT research scientist Robert Croy, also an author of the new PNAS study, designed compounds that contain a DNA-damaging agent known as an aniline mustard, which can induce cell death in cancer cells.
In the mid 2000s, Fedeles, then a grad student in Essigmann’s lab, along with Essigmann and Croy, discovered that in addition to damaging DNA, these compounds also induce oxidative stress by interfering with mitochondria — the organelles that generate energy for cells.
Tumor cells are already under oxidative stress because of their abnormal metabolism. When they are treated with these compounds, known as 11beta compounds, the additional disruption helps to kill the cells. In a study published in 2011, Fedeles reported that treatment with 11beta compounds significantly suppressed the growth of prostate tumors implanted in mice.
A conversation with his brother, Sorin Fedeles, who studies polycystic kidney disease, led the pair to theorize that these compounds might also be good candidates for treating kidney cysts. At the time, research in ADPKD was beginning to suggest that kidney cyst cells also experience oxidative stress, due to an abnormal metabolism that resembles that of cancer cells.
“We were talking about a mechanism of what would be a good drug for polycystic kidney disease, and we had this intuition that the compounds that I was working with might actually have an impact in ADPKD,” Bogdan Fedeles says.
The 11beta compounds work by disrupting the mitochondria’s ability to generate ATP (the molecules that cells use to store energy), as well as a cofactor known as NADPH, which can act as an antioxidant to help cells neutralize damaging free radicals. Tumor cells and kidney cyst cells tend to produce increased levels of free radicals because of the oxidative stress they’re under. When these cells are treated with 11beta compounds, the extra oxidative stress, including the further depletion of NADPH, pushes the cells over the edge.
“A little bit of oxidative stress is OK, but the cystic cells have a low threshold for tolerating it. Whereas normal cells survive treatment, the cystic cells will die because they exceed the threshold,” Essigmann says.
Shrinking cysts
Using two different mouse models of ADPKD, the researchers showed that 11beta-dichloro could significantly reduce the size of kidney cysts and improve kidney function.
The researchers also synthesized a “defanged” version of the compound called 11beta-dipropyl, which does not include any direct DNA-damaging ability and could potentially be safer for use in humans. They tested this compound in the early-onset model of PKD and found that it was as effective as 11beta-dichloro.
In all of the experiments, healthy kidney cells did not appear to be affected by the treatment. That’s because healthy cells are able to withstand a small increase in oxidative stress, unlike the diseased cells, which are highly susceptible to any new disturbances, the researchers say. In addition to restoring kidney function, the treatment also ameliorated other clinical features of ADPKD; biomarkers for tissue inflammation and fibrosis were decreased in the treated mice compared to the control animals.
The results also suggest that in patients, treatment with 11beta compounds once every few months, or even once a year, could significantly delay disease progression, and thus avoid the need for continuous, burdensome antiproliferative therapies such as tolvaptan.
“Based on what we know about the cyst growth paradigm, you could in theory treat patients in a pulsatile manner — once a year, or perhaps even less often — and have a meaningful impact on total kidney volume and kidney function,” Sorin Fedeles says.
The researchers now hope to run further tests on 11beta-dipropyl, as well as develop ways to produce it on a larger scale. They also plan to explore related compounds that could be good drug candidates for PKD.
Other MIT authors who contributed to this work include Research Scientist Nina Gubina, former postdoc Sakunchai Khumsubdee, former postdoc Denise Andrade, and former undergraduates Sally S. Liu ’20 and co-op student Jake Campolo. The research was funded by the PKD Foundation, the U.S. Department of Defense, the National Institutes of Health, and the National Institute of Environmental Health Sciences through the Center for Environmental Health Sciences at MIT.
Share this news article on:
Related links.
- John Essigmann
- Center for Environmental Health Sciences
- Department of Biological Engineering
- Department of Chemistry
Related Topics
- Biological engineering
- Center for Environmental Health Sciences (CEHS)
- National Institutes of Health (NIH)
Related Articles
Detecting mutations could lead to earlier liver cancer diagnosis
New evidence for how a rare form of liver cancer arises
Forced mutations doom HIV
Previous item Next item
More MIT News

Offering clean energy around the clock
Read full story →

Now corporate boards have responsibility for cybersecurity, too
An AI dataset carves new paths to tornado detection

MIT faculty, instructors, students experiment with generative AI in teaching and learning
Julie Shah named head of the Department of Aeronautics and Astronautics

Remembering Chasity Nunez, a shining star at MIT Health
- More news on MIT News homepage →
Massachusetts Institute of Technology 77 Massachusetts Avenue, Cambridge, MA, USA
- Map (opens in new window)
- Events (opens in new window)
- People (opens in new window)
- Careers (opens in new window)
- Accessibility
- Social Media Hub
- MIT on Facebook
- MIT on YouTube
- MIT on Instagram
Kidney Disease News
Top headlines, latest headlines.
- Mini Kidneys and Kidney Disease
- Healthy Sleep and Blood Sugar
- Ultrasound Imaging: Ultrafast Tech
- Accurate Blood Markers for Acute Kidney Injury
- Ketogenic Diet for Polycystic Kidney Disease
- Kidney: CRISPR Could Repair Genetic Defect
- Kidney Stone Prevention
- Kidney Failure Breakthrough
- Measuring Biological Aging
- Testosterone and Vulnerability of Male Kidneys
Earlier Headlines
Wednesday, january 31, 2024.
- Diabetes Medication Class Tied to Lower Risk of Kidney Stones
Tuesday, December 5, 2023
- Eye Scans Provide Crucial Insights Into Kidney Health
Thursday, August 31, 2023
- AI Helps ID Cancer Risk Factors
Wednesday, August 30, 2023
- Antibody Shows Promise for Preventing Organ Rejection After Transplantation
Tuesday, August 29, 2023
- Can an Artificial Kidney Finally Free Patients from Dialysis?
Thursday, August 24, 2023
- Metabolite in Urine Predicts Diabetic Kidney Failure 5-10 Years Early; Oral Therapeutic Drug Shows Promise in Mice
Monday, August 21, 2023
- Simple Blood Test May Predict Future Heart, Kidney Risk for People With Type 2 Diabetes
Wednesday, August 16, 2023
- Pig Kidney Xenotransplantation Performing Optimally After 32 Days in Human Body
Monday, August 14, 2023
- Study Brings Insight to Kidney Cancer With Gene Mutation
Thursday, August 10, 2023
- Gene Therapy Hope for Children With Kidney Disease
Tuesday, August 1, 2023
- Predicting Heart Failure With Longitudinal Urine Patterns and Its Changing
Monday, July 24, 2023
- Scientists Find That Supplementation With a Special Omega-3 Lipid Could Treat Acute Kidney Injury
Wednesday, July 19, 2023
- Single-Cell Atlas of the Human Kidney Provides New Resources to Study Kidney Disease
Thursday, July 13, 2023
- Researchers' Sweeping Discovery Shows How Kidney Cells Self-Renew
Friday, June 23, 2023
- Source of Common Kidney Disease Lies Outside the Kidney, Study Suggests
Tuesday, February 28, 2023
- Ultrasound Device May Offer New Treatment Option for Hypertension
Sunday, February 5, 2023
- During Dolphin Research, Engineer Discovers New Method to Possibly Improve Pharmaceuticals
Monday, January 30, 2023
- New Mathematical Model Shows How the Body Regulates Potassium
Friday, December 2, 2022
- Systems Analysis of Kidney Metabolism Reveals Unexpected Links to Viral Protection
Wednesday, November 30, 2022
- Existing Drug Could Reduce Side Effects of Popular Cancer Treatment
Wednesday, November 9, 2022
- Early Diagnosis Tool for Childhood Kidney Disease
Tuesday, November 8, 2022
- Protected from a Form of Cell Death, Women Are More Resilient to Kidney Disease
Monday, October 31, 2022
- Study Assesses Symptom Trajectories and Outcomes in Patients With Kidney Disease
Tuesday, October 25, 2022
- Common, Usually Harmless Group of Bacteria Associated With Higher Death Rates in Kidney Patients
Tuesday, October 18, 2022
- Scientists Illuminate How Virus Attacks Cat Kidney, Could Jump to Humans
Monday, October 17, 2022
- Gene Signature Points to Prognosis in Kidney Cancer
Friday, October 7, 2022
- Awake Patients Can Have Kidney Stones Moved, Blasted
Tuesday, September 20, 2022
- For Black Patients, Nixing 'race Adjustment' May Improve Kidney Transplant Odds, Study Finds
Friday, September 16, 2022
- Is It Really Healthy to Restrict Protein Intake for Kidney Transplant Recipients?
- Researchers Identify a Gene Therapy Target for Polycystic Kidney Disease
Monday, September 12, 2022
- Recommended Blood Sugar Levels to Avoid Diabetes-Related Damage
Wednesday, August 31, 2022
- African-Caribbean People With Type 1 Diabetes More Likely to Develop Kidney Disease, Study Finds
Tuesday, August 16, 2022
- Detection of Rare Genetic Mutation in One Family Could Lead to Better Diabetes Treatments
Thursday, August 11, 2022
- Leaving Small Kidney Stones Behind Causes Problems Later
Monday, August 1, 2022
- Diets Higher in Calcium and Potassium May Help Prevent Recurrent Symptomatic Kidney Stones
Friday, July 29, 2022
- New DNA Repair-Kit Successfully Fixes Hereditary Disease in Patient-Derived Cells
Monday, July 18, 2022
- Anti-Rejection Medication and Immunotherapy Kicks Cancer and Protects Kidney Transplants
Wednesday, July 13, 2022
- Study Results Challenge Current Thinking About Autosomal Dominant Polycystic Kidney Disease
Thursday, July 7, 2022
- Scientists Use Mini-Kidney Models to Identify Potential Drugs for Polycystic Kidney Disease
Monday, June 27, 2022
- New Approach to Treatment of Deadly Kidney Cancer
Thursday, June 16, 2022
- Genetic Screening Algorithm Could Identify People With Kidney Disease Risk
Thursday, June 2, 2022
- Coffee Consumption Link to Reduced Risk of Acute Kidney Injury, Study Finds
Wednesday, May 25, 2022
- Epigenetic Markers Predict Complications in Patients With Type 2 Diabetes
Thursday, May 19, 2022
- Standard Test for Multiple Myeloma Provides Clues of a Rare, More Deadly Type
Thursday, May 5, 2022
- Combining Certain Meds With Ibuprofen Can Permanently Injure Kidneys
Monday, April 25, 2022
- Living Kidney Donor Surgery Is Low Risk for Most Patients
- Researchers Identify Key Regulators of Urinary Concentration in the Kidney
Thursday, April 21, 2022
- COVID-19 Can Directly Infect and Damage Human Kidney Cells
Tuesday, April 12, 2022
- Low-Dose Lithium May Slow Kidney Aging
Monday, April 11, 2022
- Research in Human Kidney Organoids Reveals Target to Prevent Irreversible Kidney Damage
Friday, March 25, 2022
- Reduced Kidney Function Increases Bleeding Risk in Antithrombotic Therapy
Wednesday, March 23, 2022
- Improving Prognosis in Chronic Kidney Disease
Wednesday, March 9, 2022
- Turning Off the Damaging Signals from a Genetic Syndrome That Causes Debilitating Kidney Disease
Tuesday, February 1, 2022
- Complex Three-Dimensional Kidney Tissue Generated in the Lab from the Scratch
Thursday, January 20, 2022
- First Clinical-Grade Transplant of Gene-Edited Pig Kidneys Into Brain-Dead Human
Wednesday, January 19, 2022
- High Protein Diet May Harm Polar Bears
Wednesday, January 12, 2022
- Long-Term Use of Blood Pressure Drugs May Cause Kidney Damage, Study Suggests
Wednesday, January 5, 2022
- Immuno-CRISPR Assay Could Help Diagnose Kidney Transplant Rejection Early on
Monday, December 13, 2021
- Cannabis Use Could Cause Harmful Drug Interactions
Wednesday, December 8, 2021
- D-Serine Is Useful for the Rapid and Precise Measurement of Kidney Function
Thursday, November 11, 2021
- Low-Cost Medicine Effective in Treating High Blood Pressure for Some
Monday, November 8, 2021
- Galectin-1 Linked to Increased Risk of Type 2 Diabetes
Friday, November 5, 2021
- New Insights Into Kidney Disease With Tropical Frog Models
Thursday, November 4, 2021
- Blood Metabolites Associated With Coffee Consumption May Affect Kidney Disease Risk
Wednesday, November 3, 2021
- Inflammatory Cytokine Levels May Predict Outcomes in Orthopedic Trauma Patients
Thursday, October 21, 2021
- Targeted Drug Shows Activity Against Brain Metastases in Kidney Cancer
Thursday, October 14, 2021
- Pesticide Linked to Chronic Kidney Disease
Saturday, October 2, 2021
- Details Behind Kidney Transplant Recipients' Immune Response to the Virus That Causes COVID-19
Wednesday, September 1, 2021
- COVID-19 Long-Haulers at Risk of Developing Kidney Damage, Disease
Monday, August 30, 2021
- Finerenone Improves Outcomes in Patients With Mild-to-Moderate Kidney Disease and Diabetes
Monday, August 23, 2021
- Blueprints for How Human Kidneys Form Their Filtering Units
- New Air Routes Are Vital for Organ Transplants
Friday, August 6, 2021
- Trials Reveal Efficacy and Safety of Oral Drug for Treating Anemia Associated With Kidney Disease
- Do Vitamin D Supplements Offer Kidney-Related Benefits for Individuals With High Diabetes Risk?
Wednesday, August 4, 2021
- Artificial Pancreas Trialled for Outpatients With Type 2 Diabetes
Thursday, July 22, 2021
- 'Missing Self' Contributes to Organ Rejection After Transplantation
Wednesday, June 23, 2021
- Cellular Signatures of Kidney Tumors Discovered
Tuesday, June 15, 2021
- Stem Cell Scientists Make Big Progress in Building Mini-Kidneys
Monday, June 14, 2021
- Does Zinc Inhibit or Promote Growth of Kidney Stones? Well, Both
Thursday, June 10, 2021
- Study Examines the Effects of COVID-19 on Human Kidney Cells
Friday, May 28, 2021
- Depressive Symptoms Linked to Rapid Kidney Function Decline
Tuesday, May 25, 2021
- Geology Helps Map Kidney Stone Formation from Tiny to Troublesome
Monday, May 17, 2021
- Lipid Droplets Help Protect Kidney Cells from Damage
Tuesday, May 4, 2021
- Changes in Proteins Play Important Role in Aging Kidneys
- The Enzyme That Could Help Curb Chronic Kidney Disease
- LATEST NEWS
- Health & Medicine
- Diseases & Conditions
- Alzheimer's Research
- Amyotrophic Lateral Sclerosis
- Attention Deficit Disorder
- Back and Neck Pain
- Birth Defects
- Bladder Disorders
- Blood Clots
- COVID and SARS
- Cervical Cancer
- Bladder Cancer
- Multiple Myeloma
- Pancreatic Cancer
- Brain Tumor
- Colon Cancer
- Breast Cancer
- Ovarian Cancer
- Lung Cancer
- Mesothelioma
- Skin Cancer
- Prostate Cancer
- Cerebral Palsy
- Chikungunya
- Chronic Fatigue Syndrome
- Cold and Flu
- Crohn's Disease
- Cystic Fibrosis
- Dengue Fever
- Down Syndrome
- Eating Disorder Research
- Encephalitis
- Epilepsy Research
- Erectile Dysfunction
- Fibromyalgia
- Gastrointestinal Problems
- HIV and AIDS
- Headache Research
- Hearing Loss
- Heart Health
- Cholesterol
- Stroke Prevention
- Heart Disease
- Hormone Disorders
- Hypertension
- Infectious Diseases
- Insomnia Research
- Irritable Bowel Syndrome
- Kidney Disease
- Liver Disease
- Lung Disease
- Lyme Disease
- Mental Health Research
- Multiple Sclerosis Research
- Mumps, Measles, Rubella
- Muscular Dystrophy
- Osteoporosis
- Parkinson's Research
- Prostate Health
- Restless Leg Syndrome
- Sickle Cell Anemia
- Sleep Disorder Research
- Thyroid Disease
- Triglycerides
- Tuberculosis
- Medical Topics
- Accident and Trauma
- Alternative Medicine
- Birth Control
- Bone and Spine
- Chronic Illness
- Controlled Substances
- Dietary Supplements and Minerals
- Epigenetics
- Food Additives
- Foodborne Illness
- Foot Health
- Gene Therapy
- Health Policy
- Human Biology
- Immune System
- Joint Health
- Medical Imaging
- Nervous System
- Pain Control
- Personalized Medicine
- Pharmacology
- Psychology Research
- Wounds and Healing
- PHYSICAL/TECH
- ENVIRONMENT
- SOCIETY & EDUCATION
- Long Snouts Protect Foxes Diving Into Snow
- Promising Experimental Type 1 Diabetes Drug
- Giant, Prehistoric Salmon Had Tusk-Like Teeth
- Plants On the Menu of Ancient Hunter-Gatherers
- Unexpected Differences in Binary Stars: Origin
- Flexitarian: Invasive Species With Veggies
- T. Rex Not as Smart as Previously Claimed
- Asteroid Ryugu and Interplanetary Space
- Mice Think Like Babies
- Ancient Maya Blessed Their Ballcourts
Trending Topics
Strange & offbeat.
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Advances in the...
Advances in the management of chronic kidney disease
- Related content
- Peer review
- Teresa K Chen , assistant professor 1 ,
- Melanie P Hoenig , associate professor 2 ,
- Dorothea Nitsch , professor 3 ,
- Morgan E Grams , professor 4
- 1 Kidney Health Research Collaborative and Division of Nephrology, Department of Medicine, University of California San Francisco; and San Francisco VA Health Care System, San Francisco, CA, USA
- 2 Division of Nephrology, Department of Medicine, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA, USA
- 3 Department of Non-Communicable Disease Epidemiology, Faculty of Epidemiology and Population Health, London School of Hygiene and Tropical Medicine, London, UK
- 4 Department of Medicine, New York University Langone School of Medicine, New York, NY, USA
- Correspondence to: M E Grams Morgan.Grams{at}nyulangone.org
Chronic kidney disease (CKD) represents a global public health crisis, but awareness by patients and providers is poor. Defined as persistent abnormalities in kidney structure or function for more than three months, manifested as either low glomerular filtration rate or presence of a marker of kidney damage such as albuminuria, CKD can be identified through readily available blood and urine tests. Early recognition of CKD is crucial for harnessing major advances in staging, prognosis, and treatment. This review discusses the evidence behind the general principles of CKD management, such as blood pressure and glucose control, renin-angiotensin-aldosterone system blockade, statin therapy, and dietary management. It additionally describes individualized approaches to treatment based on risk of kidney failure and cause of CKD. Finally, it reviews novel classes of kidney protective agents including sodium-glucose cotransporter-2 inhibitors, glucagon-like peptide-1 receptor agonists, non-steroidal selective mineralocorticoid receptor antagonists, and endothelin receptor antagonists. Appropriate, widespread implementation of these highly effective therapies should improve the lives of people with CKD and decrease the worldwide incidence of kidney failure.
Introduction
Chronic kidney disease (CKD) affects approximately 10% of the world’s population and is associated with substantial morbidity and mortality. 1 Risks of kidney failure, acute kidney injury, heart failure, cardiovascular disease, and hospital admissions are all heightened in people with CKD. 2 The Global Burden of Disease Consortium projects that CKD will be in the top five conditions contributing to years of life lost by 2040. 3 However, CKD remains under-recognized by both patients and providers. 1 A diverse entity, CKD is most commonly attributed to diabetes or high blood pressure, but many other causes exist, from genetic causes to adverse effects of drugs to autoimmune processes. 2 In this review, we summarize the evidence for current paradigms of disease identification and classification, discuss new equations developed for estimating glomerular filtration rate (GFR) and harmonizing different measures of albuminuria, report major progress in individualized risk estimation of kidney failure and other adverse outcomes both for CKD in general and within specific disease entities, and describe longstanding and novel treatment strategies. Notable advances have been made in both general and cause specific therapies, including sodium-glucose cotransporter-2 (SGLT-2) inhibitors, glucagon-like peptide-1 (GLP-1) receptor agonists, non-steroidal selective mineralocorticoid receptor antagonists (MRA), and endothelin receptor antagonists. Finally, we describe major guidelines in CKD and highlight common themes as well as differences in their recommendations.
Sources and selection criteria
We searched PubMed for peer reviewed articles in the English language from 1 January 2010 to 14 July 2023 using the keywords listed in the web appendix. We additionally reviewed reference lists of selected articles, prioritizing randomized controlled trials, systematic reviews, and meta-analyses when possible but also including observational studies and reviews that were of high quality. We included older articles if we deemed them to be of high importance. Finally, we reviewed guidelines from websites of professional societies and advisory committees (for example, the National Institute for Health and Care Excellence (NICE), Kidney Disease: Improving Global Outcomes (KDIGO), US Centers for Disease Control and Prevention, US Department of Health and Human Services, and International Society of Hypertension).
Epidemiology
CKD is a global public health crisis. Recent estimates suggest that more than 700 million people have CKD, with greater burdens in low income and middle income countries. 1 4 Determining the global, regional, and national burden of disease is challenging owing to inconsistent use of estimating equations for GFR, laboratory assay standardization, and albuminuria testing. Despite this, some important observations can still be made. The prevalence of CKD increases with age and is greatest in people over 70 years. 2 In the US, compared with White people, Black people have substantially higher rates of kidney failure, followed by Native Americans, people of Hispanic ethnicity, and people of Asian descent. 5
The most commonly reported risk factors for CKD are diabetes mellitus and hypertension. 6 7 Social determinants of health are also important and likely contribute to racial disparities in kidney disease. Specific genetic variants increase risk of CKD, including variants in the APOL1 and HBB genes that are present in far greater proportions among people of African ancestry. 8 9 10 11 In Central America, Sri Lanka, Egypt, and Central India, defined geographic areas exist where many cases of CKD of unknown cause have been identified. 12 Some experts postulate that heat stress or pesticides may contribute.
Whereas the incidence of CKD is difficult to estimate, reliant as it is on testing for GFR and albuminuria, the incidence of kidney failure with the receipt of replacement therapy (KFRT) is more readily captured. Many countries have developed national registries of patients with kidney failure, allowing comparison of incidence across ages and countries. 13 For example, the countries with the highest incidence of treated kidney failure in 2020 were Taiwan, the US, and Singapore, whereas the countries with the highest prevalence were Taiwan, the Republic of Korea, and Japan. 5
Definition and classification of CKD: cause, GFR, and albuminuria staging
CKD is defined as persistent abnormalities in kidney structure or function for more than three months, manifest as either low GFR or presence of a marker of kidney damage. 2 Specifically, diagnosis requires one or more of the following: albuminuria, defined as an albumin-to-creatinine ratio (ACR) ≥30 mg per gram of creatinine (approximately ≥3 mg/mmol) or albumin excretion of ≥30 mg/day; GFR <60 mL/min/1.73 m 2 ; abnormalities on urine sediment, histology, or imaging; electrolyte or other abnormalities attributed to tubular disorders; or history of kidney transplantation. The KDIGO heat map helps with understanding of overall risk (low, moderately increased, high, and very high) of patients according to level of albuminuria (A category), level of GFR (G category), and cause of disease ( fig 1 ), such that people with normal estimated GFR but higher albuminuria have a similar risk to people with moderately reduced estimated GFR and no albuminuria.

Kidney Disease: Improving Global Outcomes heat map with guidance on monitoring. 2 Numbers in boxes indicate recommended frequency of monitoring (number of times per year). Colors denote risk as follows: green (low risk), yellow (moderately increased risk), orange (high risk), and red (very high risk). CKD=chronic kidney disease; GFR=glomerular filtration rate
- Download figure
- Open in new tab
- Download powerpoint
Clinical manifestations of CKD
Albuminuria.
Albuminuria is often the first sign of kidney damage, and its detection drives many treatment decisions. 2 The prevalence of albuminuria in people with diabetes or hypertension is estimated to be 32% and 22%, respectively. 14 However, only a minority of patients receive urine screening tests. 14 15 For example, the mean albuminuria screening rates across health systems in the US were 35% among adults with diabetes and 4% among adults with hypertension. 14
The gold standard for assessing albuminuria is either a sample collected mid-stream from an early morning urine void or a 24 hour urine collection; however, in situations where this is not possible, a spot collection is reasonable. 2 Quantification of albumin is preferred over that of total protein. 2 16 This preference is because the sensitivity of the total protein assay to different protein components can vary by laboratory, as well as the fact that proteinuria assessments do not easily discriminate A1 and A2 categories. Both urine albumin and urine protein are typically indexed to urine creatinine to account for differences in dilution, as urine ACR or urine protein-to-creatinine ratio (PCR). Dipstick protein assessment is generally more economical than both methods; however, like PCR, dipstick assessment can be insensitive in A1 and A2 categories. Although conversion calculators exist to aid in the harmonization of ACR and PCR measures; they do not work well at lower ranges of albuminuria. 17 18
The second axis for CKD classification focuses on GFR. 2 The gold standard for assessing GFR is direct measurement from clearance of an exogenous filtration marker such as iohexol or iothalamate; however, this is relatively cumbersome and rarely done in clinical practice. Instead, GFR is usually estimated by using plasma or serum concentrations of endogenous filtration markers, such as creatinine and cystatin C, and demographic variables. Early equations for adults, such as Modification of Diet in Renal Disease (MDRD) and CKD Epidemiology Collaboration (CKD-EPI) 2009 equations, used filtration markers along with age, sex, and race (Black versus non-Black) to estimate GFR. 19 20 21 The newer European Kidney Function Consortium equation, which allows for seamless GFR evaluation from infancy to old age, uses a population specific divisor to adjust creatinine values (for example, separate values for Black European and White European populations). 22 However, the use of race in GFR estimation has faced strong criticism and, in 2021, the US based American Society of Nephrology-National Kidney Foundation Task Force on Reassessing the Inclusion of Race in Diagnosing Kidney Disease recommended immediate adoption of the race-free CKD-EPI 2021 estimating equations, which exist for creatinine alone (eGFRcr) as well as for creatinine and cystatin C (eGFRcr-cys). 23 24 25 Cystatin C has distinct confounders (non-GFR determinants) of its relation with GFR compared with creatinine ( fig 2 ). 2 26 Thus, eGFRcr-cys is a more accurate estimate of GFR than eGFRcr alone, irrespective of equation used, in most scenarios, including those in which large differences exist between eGFRcr and that estimated solely using cystatin C (eGFRcys). 25 27 28 However, the newest GFR estimating equations have not been tested extensively in Asian populations. 29 30

Common non-glomerular filtration rate (GFR) determinants of blood concentrations of creatinine and cystatin C. 2 26 eGFR=estimated glomerular filtration rate
The third axis for classification is cause of CKD, which is generally ascertained through imaging, assessment of extrarenal manifestations and biomarkers, or kidney biopsy. 2 Classification of cause typically hinges on the presence or absence of systemic disease (for example, obesity, diabetes, hypertension, systemic autoimmune disease) and the specific location of the kidney pathology (for example, glomeruli, tubulointerstitium, vasculature, or cystic/congenital abnormality). Unfortunately, the cause of CKD is often unknown, limiting its utility. Molecular phenotyping and genetic testing are increasingly being used to assign cause of disease. Targeted gene panels offered commercially may have high diagnostic yields in select populations, such as patients with glomerular disease, nephrotic syndrome, or congenital anomalies of the kidney and urinary tract. 31 One study suggested that for appropriately selected patients, 34% had disease either reclassified or assigned on the basis of genetic testing, thus changing clinical management. 32 The European Renal Association and the European Rare Kidney Disease Reference Network have issued a joint statement providing recommendations for how to provide genetic testing, including specific settings in which it may be considered ( box 1 ). 33
European Renal Association and European Rare Kidney Disease Reference Network recommendations for settings in which genetic testing might be considered 33
Most tubulopathies
Glomerulopathies:
Congenital nephrotic syndrome
Nephrotic syndrome refractory to standard steroid therapy
Multi-organ phenotypes suggestive of syndromic steroid resistant nephrotic syndrome
Complement disorders:
Immune complex mediated membranoproliferative glomerulonephritis
C3 glomerulopathy
Atypical hemolytic uremic syndrome
Renal ciliopathies
Congenital anomalies of the kidney and urinary tract
Patients aged <50 years with severe CKD of unknown cause
Patients aged >50 years with adult onset CKD and family history of CKD
CKD=chronic kidney disease
Individualized prognosis and treatment
Identifying the cause of CKD is critical as different causes of CKD carry different prognoses and can have distinct treatments. 2 For example, autosomal dominant polycystic kidney disease (ADPKD) is the most common genetic cause of CKD and is typically associated with faster progression than other disease entities. 32 34 Individualized prognosis is often determined by using disease specific risk classification or calculators (for example, the Mayo classification or the ADPKD Prognostic Tool), and screening and treatment recommendations such as increased fluid intake and tolvaptan are unique to this entity. 35 36 37 38 IgA nephropathy, the most common type of glomerulonephritis worldwide, particularly in East Asian and Pacific Asian countries, 39 has its own prognostic aids, such as the International IgA Nephropathy Prediction Tool, 40 41 and treatments specific to IgA nephropathy are in various stages of development. 42 The APOL1 high risk genotypes confer about twofold higher risk of kidney failure in the general population and are common in people of African ancestry. 8 43 44 45 A recently published phase 2A study of targeted therapy for APOL1 related disease showed promising reductions in albuminuria; the phase 3 study is ongoing. 46 Other disease specific therapies are increasingly available, such as belimumab in lupus nephritis and lumasiran for primary hyperoxaluria type 1. 47 48
Individualized risk prediction is also available for more general populations of patients with CKD. The most widely known and validated is the kidney failure risk equation (KFRE), which is used in patients with GFR <60 mL/min/1.73 m 2 . 49 Tested in more than 30 countries and 700 000 people, the tool provides probabilities of kidney failure at two years and five years based on age, sex, and estimated GFR and albuminuria levels. 50 Like all risk equations, the KFRE may perform better with recalibration to absolute risk levels of local populations, but the discriminatory ability (that is, distinguishing people at high risk from those at low risk) has been extremely consistent across all studies. The KFRE has also been validated in recipients of kidney transplants. 51 52 Although the KFRE does not explicitly take into account the competing risk of death, estimates are quite accurate except among the members of the oldest segments of the population at the highest risk. 53 One study suggested that the KFRE provides more accurate prediction of kidney failure than both patients and providers. 54 Even within categories of GFR and urine ACR, the KFRE provides a wide estimate of risk prediction, which can be helpful in the counseling and referral of patients ( fig 3 ). Some centers will refer patients with a two year risk of kidney failure greater than 20-40% for vascular access and kidney transplantation evaluation, on the basis that tools that incorporate albuminuria provide more accurate and unbiased time to kidney failure than does estimated GFR alone. 55 Studies suggest that the KFRE is robust to different GFR equations (specifically, CKD-EPI 2009 and CKD-EPI 2021) and that many patients value being counseled using this information. 53 56

Range of predicted risk of kidney failure using the kidney failure risk equation (KFRE) within G and A categories of chronic kidney disease (CKD). The KFRE ( ckdpcrisk.org/kidneyfailurerisk ) was used to estimate two year risk of kidney failure in 350 232 patients with estimated glomerular filtration rate (eGFR) <60 mL/min/1.73 m 2 from the Optum Laboratories Data Warehouse (OLDW). OLDW is a longitudinal, real world data asset with deidentified administrative claims and electronic health record data. Patients with eGFR and albuminuria (urine albumin-to-creatinine ratio (ACR), protein-to-creatinine ratio, or dipstick protein) within a two year window were included in this analysis. Different measures of albuminuria were harmonized to ACR levels for A categories ( ckdpcrisk.org/pcr2acr )
Other risk equations exist to predict the risk of cardiovascular disease and death in CKD; some of these do consider the competing risk of death ( www.ckdpcrisk.org ). For example, the advanced CKD risk tool provides simultaneous estimates of kidney failure, cardiovascular disease, and death for patients with estimated GFR <30 mL/min/1.73 m 2 , which can inform decisions on access placement and reinforce the importance of cardiovascular risk reduction. 57 Estimating risks of cardiovascular disease is particularly relevant given that many more patients with CKD have cardiovascular disease events than need KFRT. 58 Other efforts incorporate estimated GFR and albuminuria into existing tools, such as SCORE2 and the pooled cohort equation for the prediction of cardiovascular disease. 59 60
Patient specific prognostic clues may stem from discrepant estimated GFR values between eGFRcr and eGFRcys. 61 62 63 When eGFRcys is substantially lower than eGFRcr, the risk for kidney related laboratory abnormalities (for example, anemia, hyperuricemia, and hyperphosphatemia) and subsequent adverse outcomes (for example, kidney failure, heart failure, and mortality) is higher. 61 64 65 By contrast, having a lower eGFRcr than eGFRcys is associated with lower risk of adverse outcomes. 66 Risk factors for having a discrepancy between eGFRcr and eGFRcys include older age, female sex, higher body mass index, recent weight loss, and smoking.
General principles of management
The mainstays of therapy for patients with CKD include treating the underlying cause if known, and correcting risk factors (for example, albuminuria) for CKD progression and other CKD related complications ( fig 4 ). 2

Comprehensive care of patients with chronic kidney disease (CKD), irrespective of cause
Blood pressure targets
The three major studies for evaluating the optimal blood pressure target in CKD were the Modification of Diet in Renal Disease Study (MDRD), African American Study of Kidney Disease and Hypertension (AASK), and Systolic Blood Pressure Intervention Trial (SPRINT). 67 68 69 In both MDRD and AASK, intensive blood pressure control did not slow GFR decline overall. 67 68 However, in MDRD, participants with baseline proteinuria of ≥3 g/day seemed to benefit from intensive blood pressure control, with slower mean rates of GFR decline compared with their counterparts in the usual blood pressure control group. 67 Among SPRINT participants with baseline CKD (n=2646), aiming for a systolic blood pressure goal of <120 mm Hg versus <140 mm Hg did not significantly reduce the risk for a composite kidney outcome that included a ≥50% reduction in estimated GFR, long term dialysis, or kidney transplant. 69 70 However, benefits of intensive blood pressure control were seen with respect to prevention of the composite cardiovascular outcome (defined as myocardial infarction, acute coronary syndrome, stroke, heart failure, or death from cardiovascular causes—hazard ratio 0.75, 95% confidence interval 0.64 to 0.89) and all cause mortality (hazard ratio 0.73, 0.60 to 0.90), regardless of CKD status. 69 Blood pressure control can also reduce albuminuria, as shown in the Chlorthalidone in Chronic Kidney Disease (CLICK) trial of chlorthalidone in advanced CKD. 71
Glycemic targets
Among patients with diabetes and CKD, glycemic control is an important component of comprehensive care. 72 The Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation (ADVANCE) was the largest trial of intensive glucose control to enroll patients with CKD. 73 Among the 11 140 trial participants, 19% had an estimated GFR <60 mL/min/1.73 m 2 and 31% had albuminuria at baseline. 74 Compared with standard glucose control, intensive glucose control was associated with 9% (hazard ratio 0.91, 0.85 to 0.98), 30% (0.70, 0.57 to 0.85), and 65% (0.35, 0.15 to 0.83) lower risks of developing new onset ACR 30-300 mg/g, ACR >300 mg/g, and end stage kidney disease (ESKD), respectively.
Specific classes of therapy
Angiotensin converting enzyme inhibitors and angiotensin receptor blockers.
When choosing antihypertensive agents, those that act by inhibiting the renin-angiotensin-aldosterone system (RAAS) have particular relevance in CKD. A 2001 meta-analysis of 11 studies suggested that, for non-diabetic CKD, the use of angiotensin converting enzyme (ACE) inhibitors resulted in a 30% reduction in risk of KFRT or doubling of serum creatinine. 75 Clinical trials in populations with CKD and diabetes (for example, IDNT, RENAAL) have also shown benefit of angiotensin receptor blockers (ARB) in preventing CKD progression ( table 1 ). 77 78 RAAS inhibition also plays a role in prevention of cardiovascular disease. The Heart Outcomes Prevention Evaluation (HOPE) study showed that ACE inhibitors reduced the risks of myocardial infarction, stroke, and cardiovascular death in populations at high risk for cardiovascular disease, including those with diabetes and albuminuria. 80 The Ongoing Telmisartan Alone and in Combination with Ramipril Global Endpoint Trial (ONTARGET) showed that ACE inhibitors and ARB were generally equivalent in the prevention of cardiovascular events. 81 Because of the increased risk of hyperkalemia and acute kidney injury, dual therapy with both an ACE inhibitor and an ARB is typically avoided. 82
Landmark randomized clinical trials on angiotensin converting enzyme inhibitors or angiotensin receptor blockers in chronic kidney disease
- View inline
When GFR declines, providers often grapple with whether RAAS inhibitors should be continued. The Benazepril in Advanced CKD study showed that benazepril reduced the risk of the primary composite kidney endpoint by 43% compared with placebo, thus suggesting that RAAS inhibitors are beneficial even in advanced CKD (baseline serum creatinine 3.1-5.0 mg/dL). 79 Three recent reports further explored this question, also examining the benefits in prevention of death and cardiovascular events associated with continuation of RAAS inhibitors. 83 84 85 A retrospective, propensity score matched study of patients with estimated GFR <30 mL/min/1.73 m 2 showed higher risk of all cause mortality and major adverse cardiovascular events in those who stopped RAAS inhibitors compared with those who continued them, 83 as did a Swedish trial emulation study. 84 The risk of kidney replacement therapy associated with cessation of RAAS inhibitors was not statistically significant in the first study and lower in the second study. 83 84 In an open label randomized trial, cessation of RAAS inhibitors did not show significant between group differences in long term decline in estimated GFR or initiation of kidney replacement therapy, providing reassurance that RAAS inhibitors can be safely continued as GFR declines. 85
SGLT-2 inhibitors
One of the biggest advancements in CKD management over the past decade was the discovery that SGLT-2 inhibitors have robust protective effects on the heart and kidneys in patients with and without diabetes. Recent trials showed an approximate 30% reduction in risk for diverse kidney outcomes among patients with baseline estimated GFR values as low as 20 mL/min/1.73 m 2 ( table 2 ). 86 88 89 91 Importantly, the three trials designed with primary kidney outcomes (Canagliflozin and Renal Events in Diabetes and Established Nephropathy Clinical Evaluation (CREDENCE), Dapagliflozin and Prevention of Adverse Outcomes in Chronic Kidney Disease (DAPA-CKD), and Study of Heart and Kidney Protection with Empagliflozin (EMPA-KIDNEY)) were terminated early because pre-specified efficacy criteria were met, with median follow-up times ranging from 2.0 to 2.6 years. 88 89 91 The overwhelming majority of trial participants were taking an ACE inhibitor or ARB before randomization, showing that the benefits of SGLT-2 inhibitors on slowing CKD progression are additive to those of RAAS inhibitors. One simulation study estimated that a 50 year old adult with non-diabetic albuminuric CKD would have seven extra years free from doubling of serum creatinine, kidney failure, or all cause mortality if treated with an SGLT-2 inhibitor and RAAS inhibitor. 92
Landmark randomized clinical trials on sodium-glucose co-transporter 2 inhibitors in chronic kidney disease (CKD)
Subgroup analyses of the DAPA-CKD and EMPA-KIDNEY trials have provided additional insights on the wide range of patients who are likely to benefit from SGLT-2 inhibitors. 89 91 In DAPA-CKD, dapagliflozin was favored over placebo in all pre-specified subgroups by baseline age, sex, race, diabetes status, systolic blood pressure, estimated GFR (<45 v ≥45 mL/min/1.73 m 2 ), and ACR (≤1000 v >1000 mg/g or ≤113 v >113 mg/mmol). 89 Similarly, in EMPA-KIDNEY, empagliflozin was associated with lower risk of the primary composite outcome compared with placebo regardless of baseline diabetes status or estimated GFR (<30 v ≥30 mL/min/1.73 m 2 to <45 v ≥45 mL/min/1.73 m 2 ). 91 The risk of the primary outcome was not lower among patients with ACR ≤300 mg/g (approximately ≤30 mg/mmol). In exploratory analyses, however, empagliflozin was associated with slower annual rates of decline in estimated GFR compared with placebo among participants with ACR between 30 and 300 mg/g (approximately 3-30 mg/mmol) and slower chronic slope (from two months to the final follow-up visit) among all ACR subgroups.
The DAPA-CKD trial also showed that the kidney protective effects of SGLT-2 inhibitors extend to patients with IgA nephropathy and perhaps also those with focal segmental glomerulosclerosis (FSGS). 93 94 Among 270 participants with IgA nephropathy (mean estimated GFR 44 mL/min/1.73 m 2 ; median ACR 900 mg/g (102 mg/mmol)), dapagliflozin was associated with a 71% lower risk of developing the primary outcome and a 70% lower risk of ESKD compared with placebo. 93 Among the 104 participants with FSGS (mean estimated GFR 42 mL/min/1.73 m 2 ; median ACR 1248 mg/g (141 mg/mmol)), dapagliflozin was not associated with a lower risk of the primary composite outcome, although this analysis was limited in power (only 11 events). 94 In exploratory analyses, dapagliflozin was associated with slower chronic decline in estimated GFR in the FSGS population. Investigations on the use of SGLT-2 inhibitors in other patient populations, such as those with polycystic kidney disease and kidney transplant recipients, are ongoing (clinicaltrials.gov).
SGLT-2 inhibitors, which act at the level of the proximal tubule to block the reabsorption of glucose and sodium, 95 are generally safe to use in patients with CKD. Early signals of heightened risks of volume depletion, serious genital infections, bone fractures, and need for limb amputation in the Canagliflozin Cardiovascular Assessment Study (CANVAS) were not observed in subsequent studies—CREDENCE, DAPA-CKD, and EMPA-KIDNEY—thus assuaging these concerns ( table 3 ). 86 88 89 91 A pooled analysis of 15 081 participants with type 2 diabetes and CKD G3-4 showed similar rates of serious adverse events for empagliflozin versus placebo, with a higher rate only of mild genital infections with the SGLT-2 inhibitor. 96 A real world study of patients receiving SGLT-2 inhibitors compared with dipeptidyl peptidase-4 (DPP-4) inhibitors found no increased risk of outpatient urinary tract infections or severe urinary tract infection events requiring hospital admission. 97
Adverse effects of SGLT-2 inhibitors * in CANVAS, CREDENCE, DAPA-CKD, and EMPA-KIDNEY trials
GLP-1 receptor agonists
GLP-1 receptor agonists have also been shown to improve kidney outcomes among patients with type 2 diabetes, albeit in trials that were designed for primary cardiac outcomes ( table 4 ). 98 99 100 101 102 103 104 105 106 107 108 109 The reduction in risk of kidney outcomes, which included albuminuria, ranged from 15% to 36%. A large meta-analysis of approximately 44 000 participants from the six trials in table 4 reported that use of GLP-1 receptor agonists was associated with a 21% lower risk of developing the composite kidney outcome, defined as new onset albuminuria >300 mg/g, doubling of serum creatinine, ≥40% decline in estimated GFR, kidney replacement therapy, or death due to kidney causes, compared with placebo. 100 This risk reduction seemed to be driven by the reduction in incident albuminuria >300 mg/g; associations between GLP-1 receptor agonists and CKD progression and kidney failure were not statistically significant. However, results were more promising in A Study Comparing Dulaglutide with Insulin Glargine on Glycemic Control in Participants with Type 2 Diabetes and Moderate or Severe Chronic Kidney Disease (AWARD-7), a clinical trial designed to evaluate change in glycated hemoglobin. 110 Among 577 adults with type 2 diabetes and CKD G3-4 randomized to open label dulaglutide 1.5 mg once weekly, dulaglutide 0.75 mg once weekly, or insulin glargine daily, both dulaglutide groups had slower estimated GFR declines compared with the insulin glargine group; among participants with baseline albuminuria >300 mg/g, dulaglutide was associated with greater ACR reductions in a dose dependent manner over the one year follow-up.
Landmark randomized clinical trials on associations of glucagon-like peptide-1 (GLP-1) receptor agonists with secondary kidney outcomes among patients with type 2 diabetes mellitus
Exact mechanisms by which the GLP-1 receptor agonists slow decline in estimated GFR and/or reduce albuminuria are not entirely clear, but proposed mechanisms include improved glycemic control, weight loss, increased natriuresis, and reduced inflammation and oxidative stress. 111 112 113 Adverse effects observed with this class of drugs have included diarrhea, nausea, and vomiting. 103 104 107 109 110
Mineralocorticoid receptor antagonists
Several MRAs are available and can be useful adjuncts to RAAS inhibitors, particularly among populations with albuminuria and/or diabetes. Two common steroidal non-selective MRAs, spironolactone and eplerenone, both lower albuminuria. 72 In a meta-analysis of 372 participants from seven trials, combination therapy with a non-selective MRA and an ACE inhibitor and/or ARB was associated with a significant reduction in proteinuria, albeit with a higher risk of hyperkalemia. 114 Finerenone, a non-steroidal selective MRA, was also recently approved. 115 Compared with the steroidal non-selective MRAs, finerenone has a stronger selectivity for the mineralocorticoid receptor, a shorter half life, less of a blood pressure lowering effect, and a more favorable side effect profile, as well as potentially greater anti-inflammatory and antifibrotic effects. 115 116 117 The Finerenone in Reducing Kidney Failure and Disease Progression in Diabetic Kidney Disease (FIDELIO-DKD) trial and the Finerenone in Reducing Cardiovascular Mortality and Morbidity in Diabetic Kidney Disease (FIGARO-DKD) trial were two complementary phase 3 clinical trials designed to investigate the kidney and cardiovascular benefits of finerenone, respectively, in people with albuminuria levels ≥30 mg/g and type 2 diabetes ( table 5 ). 116 118 Both trials included patients taking maximally tolerated ACE inhibitor or ARB, with participants in FIDELIO-DKD generally having more severe baseline CKD. In a pooled analysis of the two trials, finerenone was associated with a 15-23% lower risk of developing the kidney composite outcomes and a 32% lower mean change in ACR from baseline to four months. 119 Hyperkalemia was more frequent among patients randomized to finerenone (14%) compared with placebo (7%). In pre-specified analyses, baseline SGLT-2 inhibitor use (n=877) or GLP-1 receptor agonist use (n=944) did not modify the beneficial effect of finerenone on the kidney composite outcome, thus suggesting a potential role for dual therapy (for example, finerenone plus SGLT-2 inhibitor or GLP-1 receptor agonist) among patients with type 2 diabetes and CKD.
Landmark randomized clinical trials on finerenone in chronic kidney disease
Endothelin receptor antagonists
Endothelin receptor antagonists have emerged as novel treatments for a variety of kidney diseases. The Study of Diabetic Nephropathy with Atrasentan (SONAR) evaluated the effect of atrasentan on a composite kidney outcome (defined as a doubling of serum creatinine or ESKD) among adults with type 2 diabetes, estimated GFR 25-75 mL/min/1.73 m 2 , and urine ACR 300-5000 mg/g taking a stable dose of ACE inhibitor or ARB. 120 After a six week enrichment period during which all participants received atrasentan 0.75 mg daily (n=5517), those who responded (defined as a ≥30% reduction in urine ACR without the development of substantial fluid retention or increase in serum creatinine by >0.5 mg/dL and 20% from baseline; n=2648) were randomized to receive atrasentan or placebo. Over a median follow-up of 2.2 years, the atrasentan group had a 35% lower risk of developing the composite kidney outcome compared with the placebo group, although fluid retention and anemia were more frequent in the former. Of note, the frequency of hyperkalemia was low (1%) in both treatment groups. Sparsentan, a dual endothelin and angiotensin II receptor antagonist, is also being investigated as a treatment for FSGS and IgA nephropathy. 121 122 In a phase 2, randomized, double blind, active control trial, 109 adults with biopsy proven FSGS (estimated GFR >30 mL/min/1.73 m 2 and urine PCR ≥1 g/g) received varying doses of sparsentan (200, 400, or 800 mg daily) or irbesartan 300 mg daily. 121 At eight weeks, participants receiving sparsentan had greater reductions in urine PCR compared with those receiving irbesartan. In an interim analysis of the PROTECT phase 3 trial, adults with biopsy proven IgA nephropathy (urine PCR ≥1 g/day) randomized to sparsentan 400 mg daily had a 41% greater reduction in urine PCR over 36 weeks and threefold higher odds of achieving complete remission of proteinuria at any point compared with their counterparts who were randomized to irbesartan 300 mg daily. 122 Based in part on the results of this study, the US Food and Drug Administration (FDA) granted accelerated approval for the use of this drug in adults with primary IgA nephropathy considered to be at risk of rapid disease progression. 123
Endothelin 1 has been implicated in the pathogenesis of kidney disease via various mechanisms including vasoconstriction, vascular hypertrophy, endothelial and podocyte injury, inflammation, cell proliferation, extracellular matrix accumulation, and fibrosis. 124 Systemic and local kidney production of endothelin 1 is augmented in CKD.
Other nephroprotective and cardiovascular risk reduction strategies
A bidirectional association exists between CKD and cardiovascular disease: cardiovascular disease is both a risk factor for CKD and a common outcome in patients with CKD. 125 126 Thus, patients with CKD are likely to benefit from efforts at cardiovascular risk reduction including administration of a statin as well as the gamut of lifestyle changes. 2 127
Lipid management
The Study of Heart and Renal Protection (SHARP) trial evaluated the efficacy of ezetimibe and simvastatin combination therapy in patients with moderate to severe CKD (33% on dialysis; 67% not on dialysis with mean estimated GFR of 27 mL/min/1.73 m 2 ). 128 Treatment with these low density lipoprotein (LDL) cholesterol lowering agents led to a 17% risk reduction for development of a first major atherosclerotic event compared with placebo, although this benefit was seen only in the patients not requiring maintenance dialysis. Those at very high risk (for example, with previous major atherosclerotic cardiovascular disease events) may benefit from additional therapies to lower LDL cholesterol, including evolocumab. 129 Evolocumab is a monoclonal antibody for proprotein convertase subtilisin/kexin type 9, which increases LDL cholesterol receptors and hence clearance of LDL; this novel therapy also seems to be safe and efficacious in patients with CKD. 129 130

Physical activity
Exercise has been shown to benefit patients with CKD. Several small, randomized trials have reported that exercise training programs in patients with moderate to severe CKD are safe, feasible, and effective in improving physical activity levels, cardiorespiratory fitness, and quality of life. 131 132 133 134 135 Whether these interventions also slow CKD progression remains to be determined, as many of these studies were underpowered for this outcome.
For patients with obesity, weight loss may reduce the risk of CKD progression, whether it comes from intensive lifestyle intervention such as in the Look AHEAD (Action for Health in Diabetes) trial or, as in observational studies, from bariatric surgery. 136 137 138 Micronutrient and macronutrient composition of diets may also matter. 139
Traditional recommendations about diet in the setting of CKD have focused on limiting protein and dietary acid intake. Experimental evidence suggests that protein intake can increase intraglomerular pressure and cause glomerular hyperfiltration. 140 141 142 Observational data from large cohort studies suggest that the type of protein may be important; a diet high in animal protein may increase risk, whereas protein from plant sources may be better tolerated. 143 144 For example, an observational study in Singapore found a strong correlation between red meat intake and risk of ESKD. 145 Little clinical trial evidence for protein restriction exists. The MDRD study randomized patients to different levels of protein restriction but found no statistically significant difference in the rate of GFR decline. 67
A second line of investigation has been into the benefits of increasing nutritional alkali intake, with a body of open label trials suggesting benefits on kidney function and prevention of starting dialysis. 146 A phase 3 double blinded, placebo controlled trial reported that veverimer (a potent acid binder that acts in the intestine) was effective in raising or normalizing serum bicarbonate among patients with CKD and chronic metabolic acidosis. 147 Other double blinded studies using veverimer suggested that treating acidosis in CKD improves quality of life and overall physical function. 148 However, a recent trial evaluating veverimer in slowing progression of CKD was negative. 149
Although patients with CKD are prone to hyperkalemia, potassium intake has a beneficial effect on blood pressure, cardiovascular disease, and death independent of and opposite to that of sodium intake. 150 151 152 153 One large randomized controlled trial suggested that substituting 25% of sodium chloride intake with potassium chloride reduced the risk of major adverse cardiovascular events by 13% in the general population. 154 Similarly, small studies suggest that diets rich in potassium may be beneficial in CKD. A feeding trial in people with CKD G3 observed that 100 mmol compared with 40 mmol of dietary potassium per day increased serum potassium by 0.21 mmol/L, 155 similar to the increase seen with finerenone. 156 Many dietary studies have evaluated patterns of diet rather than potassium alone: for example, plant based diets tend to be rich in not only potassium but also alkali and fiber. Observational data from prospective cohorts suggest that plant based diets are associated with less CKD progression. 143 157 158 Evidence is also emerging to suggest that increasing fiber intake benefits the gut microbiome, decreases inflammation, and possibly slows CKD progression. 159
Appropriate drug dosing and nephrotoxin avoidance
An important component of care for patients with CKD is avoidance of additional insults. Many drugs are cleared by glomerular filtration or tubular secretion by the kidney, and reduced GFR can lead to accumulation of the drug or its metabolites resulting in adverse effects. 160 Careful estimation of GFR is generally a first step in determining dosage for renally excreted drugs. 161 The US FDA guidance to industry suggests that estimated GFR based on serum creatinine may be used in pharmacokinetic studies. 162 If drugs are dosed on the basis of estimated GFR (rather than estimated creatinine clearance from the Cockcroft-Gault equation, an equation that is known to be flawed), estimated GFR must be “de-indexed” by multiplying the standardized estimated GFR by the individual’s calculated body surface area and dividing by 1.73 m 2 . 163 164 165 This is because drug clearance is thought to be proportional to a person’s GFR and not the GFR standardized to body surface area. Antibiotics and antiviral agents, direct oral anticoagulants, drugs for diabetes mellitus, and chemotherapeutic agents are the most common drugs that require attention to dosing in CKD. 2 160 164
Some drugs should be avoided or minimized in CKD because of their potential to worsen kidney function. For example, non-steroidal anti-inflammatory drugs (NSAIDs) can exacerbate hypertension, cause fluid retention, and contribute to the risk of acute kidney injury. 166 Particularly when used with RAAS inhibitors and diuretics, NSAIDs are ideally avoided. 167 In select patients with CKD, however, some clinicians will prescribe an abbreviated course of NSAIDs given that the most common alternative, opioids, also have significant adverse effects. 168 Proton pump inhibitors can lead to acute or chronic interstitial nephritis and have been associated with incident CKD, progression of CKD, and ESKD. 169 170 Although the mechanism by which proton pump inhibitors contribute to CKD remains unclear, most experts agree that these agents should be used judiciously.
Emerging treatments
Many phase 3-4 clinical trials are ongoing to evaluate emerging treatments for kidney disease (clinicaltrials.gov). These include, but are not limited to, investigations on the use of dapagliflozin in advanced CKD (for example, estimated GFR <25 mL/min/1.73 m 2 , on maintenance dialysis with residual daily urine output of >500 mL, and kidney transplant recipients with estimated GFR ≤45 mL/min/1.73 m 2 ; NCT05374291 ); finerenone in non-diabetic CKD ( NCT05047263 ); and monteluklast ( NCT05362474 ) and pentoxyifylline ( NCT03625648 ) in diabetic CKD. Several therapies are also being tested for rarer causes of kidney disease: obinutuzumab ( NCT04629248 ), zanubrutinib ( NCT05707377 ), and SNP-ACTH (1-39) gel ( NCT05696613 ) in membranous nephropathy; voclosporin ( NCT05288855 ), atacicept ( NCT05609812 ), anifrolumab ( NCT05138133 ), inanalumab ( NCT05126277 ), secukinumab ( NCT04181762 ), obinutuzumab ( NCT04221477 ), and ACTHar gel ( NCT02226341 ) in lupus nephritis; VX-147 in APOL1 related kidney disease ( NCT05312879 ); imlifidase in antiglomerular basement membrane disease ( NCT05679401 ); sparsentan in focal segmental glomerulosclerosis ( NCT03493685 ); and pegcetacoplan ( NCT05067127 ) in immune complex glomerulonephritis. IgA nephropathy, in particular, is an area of high interest, as recent work suggests that disease activity may be driven by the overproduction of galactose deficient IgA antibodies that are recognized as autoantigens, triggering glomerular deposition of immune complexes. 171 Monoclonal antibodies to signaling molecules that enhance IgA production are in phase 3 trials, as are immunosuppressive and non-immunosuppressive agents (for example, those acting on the endothelin-1 and angiotensin II pathways): budesonide ( NCT03643965 ), sparsentan ( NCT03762850 ), atrasentan ( NCT04573478 ), LNP023 ( NCT04578834 ), RO7434656 ( NCT05797610 ), atacicept ( NCT04716231 ), and sibeprenlimab ( NCT05248646 ; NCT05248659 ).
Major guidelines in CKD are issued by the international KDIGO group ( https://kdigo.org/ ), and locally in the UK by NICE ( www.nice.org.uk/guidance/ng28/chapter/Recommendations#chronic-kidney-disease ), with the most recent issuances primarily from 2023 (currently in public review) and 2021, respectively. KDIGO publishes guidelines on the evaluation and management of patients with CKD in general, as well as myriad other aspects (for example, diabetes, blood pressure, lipids, anemia, mineral and bone disease, hepatitis C, ADPKD, glomerular diseases). With the expansion of therapeutic options, both organizations are updating recommendations frequently. Other guideline producing organizations such as the American College of Cardiology, the American Heart Association, the European Society of Cardiology, the European Society of Hypertension, the International Society of Hypertension, and the American Diabetes Association (ADA) provide more limited statements of recommendation for the specific aspects of the management of patients with CKD. 172 173 174 175
Annual screening for CKD (including testing for albuminuria) is widely recommended in people with diabetes. 72 174 175 176 177 Guidelines in hypertension are less clear. 178 The 2020 Global Hypertension Practice Guideline from the International Society of Hypertension is a notable exception and now recommends routine assessment of albuminuria in addition to estimated GFR in people with hypertension. 173 KDIGO and NICE also recommend testing anyone who is at risk for CKD, which includes those with hypertension, cardiovascular disease, diabetes, and previous acute kidney injury, along with multiple other, less common conditions. 179 For CKD, the KDIGO guidelines recommend at least annual albuminuria testing with greater frequency in higher risk categories ( fig 1 ). 2 The NICE guidelines, on the other hand, recommend annual ACR testing with individualization based on clinical characteristics, risk of progression, and whether a change in ACR would lead to a change in management. 16
KDIGO guidelines and those from NICE differ slightly on staging CKD. KDIGO recommends using a validated equation for GFR estimation and suggests that using “race as a distinct variable in the computation of GFR” is not appropriate. 179 NICE recommends using the CKD-EPI 2009 equation, which did include race, but using the computed value for non-Black people for everyone, a position that is also endorsed by other European groups. 16 180 181 The KDIGO guidelines recommend staging CKD by eGFRcr-cys when cystatin C is available, as well as when precise estimates of GFR are needed for clinical decision making. 2 179 The NICE guidelines recommend direct measurement of GFR rather than the use of cystatin C in clinical situations requiring additional precision. 16
Both KDIGO and NICE emphasize the importance of risk assessment in patients with CKD. The NICE guidelines suggest that primary care providers should counsel patients using the KFRE five year risk estimate, with referral to a specialist if risk is greater than 5%. 16 KDIGO 2023 additionally suggests that the two year risk estimate can drive referral for multidisciplinary care (>10%) and preparation for kidney replacement therapy, including vascular access planning and referral for transplantation (>40%). 179 The KDIGO 2023 guidelines also emphasize the importance of cardiovascular risk assessment using equations developed in people with CKD or that encompasses estimated GFR and albuminuria and the use of disease specific tools in IgA nephropathy and ADPKD. 179
Multiple guidelines comment on target blood pressures in the setting of CKD. The NICE guidelines recommend a target of <140/90 mm Hg, or <130/80 mm Hg if ACR is ≥70 mg/mmol (approximately 700 mg/g). 16 Guidelines from the American College of Cardiology, American Heart Association, European Society of Cardiology, and European Society of Hypertension recommend a systolic blood pressure target of <130 mm Hg as a best practice target, with the European Society of Cardiology and European Society of Hypertension specifically advising against lower targets. 172 The KDIGO guidelines on hypertension in CKD advocate for a systolic blood pressure goal of <120 mm Hg, as assessed using standardized office measurements. 182 This recommendation is based largely on data from SPRINT and the observed benefits in cardiovascular endpoints and survival rather than benefits in kidney endpoints. 70
Of note, disparate guideline recommendations may reflect different emphasis on standardized blood pressure measurement techniques, which can result in measured blood pressure that is substantially lower than measurement in an uncontrolled setting. 183 Joint statements from several international groups including KDIGO stress the importance of proper technique when assessing blood pressure. 184 Both NICE and KDIGO recommend RAAS inhibitors (either ACE inhibitor or ARB) as first line antihypertensive treatment for people without diabetes but with albuminuria (NICE: urine ACR >70 mg/mmol; KDIGO: A3) as well as those with diabetes and CKD G1-G4, A2-A3. 16 182 KDIGO 2023 suggests continuation of RAAS inhibitors even when estimated GFR is <30 mL/min/1.73 m 2 . 179
For patients with diabetes and CKD not treated with dialysis, KDIGO recommends a hemoglobin A 1c target ranging from <6.5% to <8%. 72 NICE does not provide specific recommendations for people with CKD, instead emphasizing shared decision making but a general goal of hemoglobin A 1c <7% for people with diabetes treated with drugs associated with hypoglycemia and <6.5% for people with diabetes managed by lifestyle or a single drug not associated with hypoglycemia. 185
KDIGO and ADA guidelines recommend SGLT-2 inhibitors as first line drug therapy for all people with type 2 diabetes, CKD, and an estimated GFR ≥20 mL/min/1.73 m 2 ( fig 5 ). 72 174 175 179 The NICE guidelines recommend that an SGLT-2 inhibitor should be offered when ACR is >30 mg/mmol (approximately >300 mg/g) and considered when ACR is between 3 and 30 mg/mmol (approximately 30 to 300 mg/g) in patients with type 2 diabetes and CKD who are already taking an ACE inhibitor or ARB and meet estimated GFR thresholds. 185 The NICE guidelines further specify that dapagliflozin should also be considered in people with estimated GFR 25-75 mL/min/1.73 m 2 and ACR ≥22.6 mg/mmol (approximately 200 mg/g) regardless of diabetes status 186 ; KDIGO is broader and recommends SGLT-2 inhibitors in general in people with ACR ≥200 mg/g and estimated GFR ≥20 mL/min/1.73 m 2 , as well as in those with CKD and heart failure. 179 KDIGO further specifies that once started, a SGLT-2 inhibitor can be continued even if the estimated GFR drops below 20 mL/min/1.73 m 2 , as long as it is tolerated and kidney replacement therapy has not yet been started. 72 179 The KDIGO and ADA guidelines recommend the use of GLP-1 receptor agonists in patients with type 2 diabetes and CKD who are unable to tolerate metformin or an SGLT-2 inhibitor or do not meet their individualized glycemic target with these drugs. 72 174 175 179

Kidney Disease: Improving Global Outcomes/American Diabetes Association recommendations on the management of diabetes in populations with chronic kidney disease. 72 174 ACR=albumin-to-creatinine ratio; ASCVD=atherosclerotic cardiovascular disease; BP=blood pressure; CCB=calcium channel blocker; CVD=cardiovascular disease; eGFR=estimated glomerular filtration rate; GLP-1 RA=glucagon-like peptide-1 receptor agonist; HTN=hypertension; MRA=mineralocorticoid receptor antagonist; PCSK9i=proprotein convertase subtilisin/kexin type 9 inhibitor; RAS=renin-angiotensin system; SGLT2i=sodium-glucose cotransporter-2 inhibitor
In patients with diabetes and CKD, the KDIGO and ADA guidelines recommend that finerenone should be used as add-on therapy to maximally tolerated ACE inhibitor or ARB if ACR is ≥30 mg/g (approximately ≥3 mg/mmol) and potassium is within normal limits (that is, ≤4.8 mmol/L based on trial and ≤5.0 mmol/L as per FDA). 72 174 175 179 More specifically, the starting dose should be 10 mg daily when estimated GFR is 25-59 mL/min/1.73 m 2 and 20 mg daily when it is ≥60 mL/min/1.73 m 2 . The guidelines also recommend that potassium concentration should be checked at four weeks after starting treatment, with each dose change, and routinely during treatment. If potassium is >5.5 mmol/L, the drug should be stopped and restarted at the lower dose of 10 mg daily when potassium is ≤5.0 mmol/L. Additionally, finerenone need not be stopped when estimated GFR falls below 25 mL/min/1.73 m 2 as long as the patient is normokalemic. 174 175
With respect to cardiovascular risk reduction, the KDIGO guidelines suggest that all patients aged over 50 with CKD G3-G5 but not treated with chronic dialysis or kidney transplantation should be treated with a statin, irrespective of cholesterol concentrations or a statin/ezetimide combination. 179 187 The NICE recommendation is broader, recommending starting atorvastatin 20 mg for all people with CKD. 188 KDIGO recommends regular physical activity for people with CKD, for at least 150 minutes a week of moderate intensity exercise. 179 NICE simply suggests providing lifestyle advice, including encouragement of exercise, maintenance of healthy weight, and smoking cessation, and specifically recommends against offering low protein diets (defined as dietary protein intake <0.8 g/kg/day). 16 KDIGO recommends maintaining sodium intake <2 g/day and a protein intake of 0.8 g/kg/day but no higher than 1.3 g/kg/day. 179
People with CKD face high risks of many adverse outcomes, including requirement for kidney replacement therapy, cardiovascular events, and death. Fortunately, major advances have been made in the field of CKD over the past decade. Estimating equations for GFR and ACR have evolved for more precise classification of disease. Individualized risk prediction tools exist to assist in the counseling, referral, and treatment of patients. Novel therapies build on the fundamentals—a healthy lifestyle, blood pressure and glucose control, and statin therapy and RAAS blockade—to provide effective preventive strategies for CKD progression and cardiovascular events.
Glossary of abbreviations
ACE—angiotensin converting enzyme
ACR—albumin-to-creatinine ratio
ADA—American Diabetes Association
ADPKD—autosomal dominant polycystic kidney disease
ARB—angiotensin receptor blockers
CKD—chronic kidney disease
CKD-EPI—CKD Epidemiology Collaboration
DPP-4—dipeptidyl peptidase-4
eGFRcr—estimated glomerular filtration rate using creatinine
eGFRcr-cys—estimated glomerular filtration rate using creatinine and cystatin C
eGFRcys—estimated glomerular filtration rate using cystatin C
ESKD—end stage kidney disease
FDA—Food and Drug Administration
FSGS—focal segmental glomerulosclerosis
GFR—glomerular filtration rate
GLP-1—glucagon-like peptide-1
KDIGO—Kidney Disease: Improving Global Outcomes
KFRE—kidney failure risk equation
KFRT—kidney failure with replacement therapy
LDL—low density lipoprotein
MDRD—Modification of Diet in Renal Disease
MRA—mineralocorticoid receptor antagonists
NICE—National Institute for Health and Care Excellence
NSAID—non-steroidal anti-inflammatory drug
PCR—protein-to-creatinine ratio
RAAS—renin-angiotensin-aldosterone system
SGLT-2—sodium-glucose cotransporter-2
Questions for future research
How do the race-free estimating equations perform in global populations?
Where can genetic testing add value in patient care?
Can cause of chronic kidney disease be incorporated into risk prediction tools?
How can medical therapy be best tailored for the individual patient with chronic kidney disease?
Patient perspective
Increasing awareness of chronic kidney disease is key to empowering patients to make lifestyle changes and seek treatments to improve their health outcomes. We are pleased to offer our perspective as husband and wife, and as physicians, who have been affected by kidney disease. Roberta M Falke is a patient with autosomal dominant polycystic kidney disease (ADPKD), a kidney transplant recipient, and a retired hematologist-oncologist. Andrew S Levey is a kidney donor and a nephrologist. Our knowledge of Roberta’s family history enabled early diagnosis and treatment. 189 Although we have benefited from our training and positions in the healthcare system, all patients can benefit from early diagnosis.
RMF —My ADPKD was diagnosed when I developed pyelonephritis at age 22 years. Thereafter, I had prophylaxis and prompt treatment of recurrent urinary tract infections and, as the disease progressed, complications of kidney and liver cysts, hypertension, hyperparathyroidism, vitamin D deficiency, acidosis, hyperkalemia, and ultimately kidney failure, with fatigue, dietary restrictions, and a long list of medications to take every day. I had always known that living donor kidney transplantation would be the best treatment for my kidney failure. Over time, family members without ADPKD donated to others, and when I was ready at age 60 years no family members were available. Fortunately, Andy stepped up. I felt better immediately after the transplant, and in the 13 years since then I have continued to take medications daily but have had few complications. I am grateful to all those who have cared for me for many years and enabled me to make the best choices I could to help myself, and I’m especially grateful to Andy who gave me the gift of life.
ASL —I knew that Roberta would develop kidney failure and hoped that a living kidney donor would be available for her. I wanted to donate, but our blood group incompatibility was an obstacle, so it was exciting when paired donor exchange was conceived and implemented in our region. I believe that kidney donors benefit from donation, not only by fulfilling their spirit of altruism but by improving their own lives. In my case, donating has been life changing. Roberta and I have been able to have an active, fulfilling life for more than a decade after the transplant, without the demands and complications of kidney failure or dialysis. I hope that we will have many more years together. I am also grateful to all those who enabled me to achieve my goal and to Roberta, who always takes full responsibility for caring for her kidney disease.
Acknowledgments
We thank Andrew S Levey and Roberta M Falke for providing both their perspective as patients affected by kidney disease and their input on the manuscript itself. We also acknowledge Alix Rosenberg and Yingying Sang for their help with the boxes and figures.
Series explanation: State of the Art Reviews are commissioned on the basis of their relevance to academics and specialists in the US and internationally. For this reason they are written predominantly by US authors
Contributors: All authors were involved in the conception, writing, and revision of the manuscript. MEG is the guarantor.
Funding: TKC is supported by NIH/NIDDK K08DK117068; MEG is supported by NIH/NIDDK R01DK108803, R01DK100446, R01DK115534, R01DK124399, and NIH/NHLBI K24HL155861.
Competing interests: We have read and understood the BMJ policy on declaration of interests and declare the following interests: TKC and MEG received an honorarium from the American Society of Nephrology (nephSAP).
Patient involvement: We invited a husband and wife, Andrew S Levey and Roberta M Falke, who are affected by chronic kidney disease, to write a patient perspective together. They also reviewed and provided input on the penultimate draft of the paper.
Provenance and peer review: Commissioned; externally peer reviewed.
- GBD Chronic Kidney Disease Collaboration
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group
- Foreman KJ ,
- Marquez N ,
- Dolgert A ,
- Kovesdy C ,
- Langham R ,
- Rosenberg M ,
- ↵ United States Renal Data System. 2022 USRDS Annual Data Report: Epidemiology of kidney disease in the United States. 2022. https://adr.usrds.org/2022 .
- Garcia-Garcia G ,
- Friedman DJ ,
- Derebail VK ,
- Genovese G ,
- Johnson RJ ,
- Wesseling C ,
- Johnson DW ,
- O’Shaughnessy MM ,
- CKD Prognosis Consortium
- Shlipak MG ,
- ↵ National Institute for Health and Care Excellence. NICE guideline [NG203]: Chronic kidney disease: assessment and management. 2021. www.nice.org.uk/guidance/ng203 .
- Nadkarni GN ,
- Chronic Kidney Disease Prognosis Consortium
- Weaver RG ,
- Modification of Diet in Renal Disease Study Group
- Chronic Kidney Disease Epidemiology Collaboration
- Stevens LA ,
- Schmid CH ,
- CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration)
- Delgado C ,
- Eneanya ND ,
- ↵ Chen DC, Potok OA, Rifkin D, Estrella MM. Advantages, Limitations, and Clinical Considerations in Using Cystatin C to Estimate GFR. Kidney360 2022;3:1807-1814.
- Khandpur S ,
- Awasthi A ,
- Behera MR ,
- Nestor JG ,
- Groopman EE ,
- Cameron-Christie S ,
- Antignac C ,
- Bergmann C ,
- Sexton DJ ,
- Collins AJ ,
- Torres VE ,
- Chapman AB ,
- Devuyst O ,
- TEMPO 3:4 Trial Investigators
- Müller RU ,
- Messchendorp AL ,
- Irazabal MV ,
- Rangel LJ ,
- Bergstralh EJ ,
- CRISP Investigators
- ↵ QxMD. Total Kidney Volume (height-adjusted) Calculator & ADPKD Prognostic Tool using Kidney Dimensions calculator. https://qxmd.com/calculate/calculator_490/total-kidney-volume-height-adjusted-calculator-adpkd-prognostic-tool-using-kidney-dimensions .
- Rodrigues JC ,
- ↵ QxMD. International IgAN Prediction Tool at biopsy - adults. https://qxmd.com/calculate/calculator_499/international-igan-prediction-tool-at-biopsy-adults .
- Barbour SJ ,
- International IgA Nephropathy Network
- Selvaskandan H ,
- Gonzalez-Martin G ,
- Barratt J ,
- Foster MC ,
- Fornage M ,
- AASK Study Investigators ,
- CRIC Study Investigators
- Zimmerman B ,
- VX19-147-101 Study Group
- Houssiau F ,
- Garrelfs SF ,
- Frishberg Y ,
- Hulton SA ,
- ILLUMINATE-A Collaborators
- Griffith J ,
- Ferguson TW ,
- Fallahzadeh MK ,
- McCulloch CE ,
- Brunskill NJ ,
- Ballew SH ,
- Nguyen HA ,
- Abdelmalek JA ,
- Woodell TB ,
- Greene TH ,
- Sparkes D ,
- Harasemiw O ,
- Thorsteinsdottir B ,
- Matsushita K ,
- Kaptoge S ,
- Hageman SHJ ,
- Jassal SK ,
- Scherzer R ,
- Farrington DK ,
- Surapaneni A ,
- Seegmiller JC ,
- Carrero JJ ,
- Wright JT Jr . ,
- African American Study of Kidney Disease and Hypertension Study Group
- Williamson JD ,
- Whelton PK ,
- SPRINT Research Group
- Agarwal R ,
- Cramer AE ,
- Kidney Disease: Improving Global Outcomes (KDIGO) Diabetes Work Group
- MacMahon S ,
- Chalmers J ,
- ADVANCE Collaborative Group
- Perkovic V ,
- Heerspink HL ,
- The GISEN Group (Gruppo Italiano di Studi Epidemiologici in Nefrologia)
- Brenner BM ,
- Cooper ME ,
- de Zeeuw D ,
- RENAAL Study Investigators
- Hunsicker LG ,
- Clarke WR ,
- Collaborative Study Group
- Sleight P ,
- Dagenais G ,
- Heart Outcomes Prevention Evaluation Study Investigators
- ONTARGET Investigators
- Emanuele N ,
- VA NEPHRON-D Investigators
- Bhandari S ,
- STOP ACEi Trial Investigators
- Mahaffey KW ,
- CANVAS Program Collaborative Group
- Jardine MJ ,
- CREDENCE Trial Investigators
- Heerspink HJL ,
- Stefánsson BV ,
- Correa-Rotter R ,
- DAPA-CKD Trial Committees and Investigators
- Wheeler DC ,
- Stefansson BV ,
- Batiushin M ,
- Herrington WG ,
- Staplin N ,
- The EMPA-KIDNEY Collaborative Group
- Vaduganathan M ,
- DeFronzo RA ,
- Reeves WB ,
- Tuttle KR ,
- Nangaku M ,
- Schneeweiss S ,
- Fralick M ,
- Muskiet MHA ,
- Tonneijck L ,
- Pfeffer MA ,
- Claggett B ,
- ELIXA Investigators
- Kristensen SL ,
- Bentley-Lewis R ,
- Aguilar D ,
- Riddle MC ,
- Ørsted DD ,
- Brown-Frandsen K ,
- LEADER Steering Committee and Investigators
- Daniels GH ,
- LEADER Steering Committee ,
- LEADER Trial Investigators
- Consoli A ,
- SUSTAIN-6 Investigators
- Holman RR ,
- Bethel MA ,
- EXSCEL Study Group
- Merrill P ,
- Gerstein HC ,
- Colhoun HM ,
- Dagenais GR ,
- REWIND Investigators
- REWIND Trial Investigators
- Rosenstock J ,
- AMPLITUDE-O Trial Investigators
- Lakshmanan MC ,
- Dieter BP ,
- Alicic RZ ,
- O’Neil PM ,
- Birkenfeld AL ,
- McGowan B ,
- Pratley R ,
- PIONEER 4 investigators
- Navaneethan SD ,
- Nigwekar SU ,
- Sehgal AR ,
- Strippoli GF
- Epstein M ,
- Kovesdy CP ,
- Pecoits-Filho R
- Bakris GL ,
- FIDELIO-DKD Investigators
- Barrera-Chimal J ,
- Lima-Posada I ,
- Filippatos G ,
- FIGARO-DKD Investigators
- FIDELIO-DKD and FIGARO-DKD investigators
- Parving HH ,
- Andress DL ,
- SONAR Committees and Investigators
- Trachtman H ,
- DUET Study Group
- Radhakrishnan J ,
- Alpers CE ,
- PROTECT Investigators
- ↵ US Food and Drug Administration. Highlights of prescribing information: Filspari. 2023. https://www.accessdata.fda.gov/drugsatfda_docs/label/2023/216403s000lbl.pdf .
- Kalyesubula R ,
- Schaeffner E ,
- Ishigami J ,
- Trevisan M ,
- Grundy SM ,
- Bailey AL ,
- Baigent C ,
- Landray MJ ,
- SHARP Investigators
- Lloyd-Jones DM ,
- Morris PB ,
- Ballantyne CM ,
- Writing Committee
- Charytan DM ,
- Sabatine MS ,
- Pedersen TR ,
- FOURIER Steering Committee and Investigators
- Weiner DE ,
- Uchiyama K ,
- Muraoka K ,
- Beetham KS ,
- Krishnasamy R ,
- Stanton T ,
- Howden EJ ,
- Coombes JS ,
- Douglas B ,
- Campbell KL ,
- Ikizler TA ,
- Robinson-Cohen C ,
- Look AHEAD Research Group
- Sadeghirad B ,
- Hostetter TH
- Caulfield LE ,
- Garcia-Larsen V ,
- Bushinsky DA
- Wesson DE ,
- Mathur VS ,
- ↵ Tangri N, Mathur VS, Bushinsky DA, Inker LA, et al. VALOR-CKD: A Multicenter, Randomized, Double-Blind Placebo-Controlled Trial Evaluating Veverimer in Slowing Progression of CKD in Patients With Metabolic Acidosis. 2022, Florida. https://www.asn-online.org/education/kidneyweek/2022/program-abstract.aspx?controlId=3801835 .
- Aburto NJ ,
- Gutierrez H ,
- Elliott P ,
- Cappuccio FP
- Narasaki Y ,
- O’Donnell M ,
- Rangarajan S ,
- PURE Investigators
- Juraschek SP ,
- Miller ER 3rd . ,
- Fioretto P ,
- Anderson CAM ,
- Whittaker CF ,
- Miklich MA ,
- Matzke GR ,
- Aronoff GR ,
- Atkinson AJ Jr . ,
- ↵ US Food and Drug Administration, Center for Drug Evaluation and Research. Pharmacokinetics in patients with impaired renal function - study design, data analysis, and impact on dosing. 2020. https://www.fda.gov/media/78573/download .
- Vondracek SF ,
- Teitelbaum I ,
- Hudson JQ ,
- Perazella MA
- Azoulay L ,
- Nessim SJ ,
- Doerfler RM ,
- Lazarus B ,
- Wilson FP ,
- Balasubramanian S ,
- Pattrapornpisut P ,
- Avila-Casado C ,
- Charchar F ,
- de Boer IH ,
- Sadusky T ,
- Tummalapalli SL ,
- Boulware LE ,
- Conference Participants
- American Diabetes Association Professional Practice Committee
- ↵ Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2023 Clinical Practice Guideline For the Evaluation and Management of Chronic Kidney Disease - Public Review Draft July 2023. 2023. https://kdigo.org/wp-content/uploads/2017/02/KDIGO-2023-CKD-Guideline-Public-Review-Draft_5-July-2023.pdf .
- Gansevoort RT ,
- Anders HJ ,
- Cozzolino M ,
- Delanaye P ,
- Kidney Disease: Improving Global Outcomes (KDIGO) Blood Pressure Work Group
- Muntner P ,
- Einhorn PT ,
- Cushman WC ,
- 2017 National Heart, Lung, and Blood Institute Working Group
- Cheung AK ,
- ↵ National Institute for Health and Care Excellence. NICE guideline [NG28]: Type 2 diabetes in adults: management. 2022. https://www.nice.org.uk/guidance/ng28/chapter/Recommendations#chronic-kidney-disease .
- ↵ National Institute for Health and Care Excellence. Technology appraisal guidance [TA775]: Dapagliflozin for treating chronic kidney disease. 2022. https://www.nice.org.uk/guidance/ta775/chapter/1-Recommendations .
- Kidney Disease: Improving Global Outcomes (KDIGO) Lipid Work Group
- ↵ National Institute for Health and Care Excellence. NICE guideline [CG181]: Cardiovascular disease: risk assessment and reduction, including lipid modification. 2023. https://www.nice.org.uk/guidance/cg181/chapter/Recommendations#lipid-modification-therapy-for-the-primary-and-secondary-prevention-of-cardiovascular-disease .
- Share full article
Advertisement
Supported by
Personal Health
Are Too Many Older Adults Told They Have Kidney Disease?
Many men and women with “failing kidneys” may not have anything more than a normal age-related decline in kidney function.

By Jane E. Brody
If the public has learned anything about medicine during the Covid-19 pandemic, it is that science is constantly evolving. New findings can change how experts define a given illness, as well as how they diagnose, prevent and treat it.
Such is the case, a new study suggests, with chronic kidney disease. A growing cadre of physicians are combating what they call an over-diagnosis of this condition in the elderly. According to these doctors, many older adults who’ve been told their kidneys are on the road to failure may not have anything more than a normal age-related decline in kidney function. For many, their kidney disease is unlikely to become a medical problem during their remaining years of life.
This, in fact, is exactly what happened to a friend’s mother who was told she had kidney disease in her late 70s. She received drug treatment for the disorder and recently died at 92 of a combination of old age, malnutrition and bedsores, but with kidneys that still worked perfectly.
Yet being told that organs as important as one’s kidneys are functioning poorly may cause older people needless emotional distress. In addition, doctors may too readily prescribe medications, including drugs that lower blood pressure, that have financial costs and side effects.
Life-sustaining filtration
Most people are born with two kidneys, which work as the body’s filtration system. Each bean-shaped organ has about a million units called nephrons. And each nephron contains a glomerulus, a tuft of tiny vessels that filters the blood as it passes through, and a tubule that sends cleansed blood and essential nutrients back into circulation. In the course of a day, some 150 quarts of blood normally pass through the kidneys, with only a quart or two of liquid waste leaving the body as urine.
Health care workers typically assess how well someone’s kidneys work by starting with a blood test for the glomerular filtration rate, or G.F.R., an estimate of how much blood passes through the glomeruli every minute. If the estimated G.F.R. is abnormally low, the patient’s urine is analyzed for the level of protein, or albumin, being excreted. If that is high, it could indicate poorly functioning kidneys.
According to current guidelines, an estimated G.F.R. below 60 for three months or longer is considered an indication of chronic kidney disease. While a rate below 60 would indeed be worrisome for a 50-year-old, for people in their 70s and 80s it may simply reflect the normal slowing of a bodily function with age, the new research suggests.
What the study found
The new research, published in JAMA Internal Medicine in August , found that many people over 65 with a low estimated G.F.R. and no elevated protein in their urine did not have increased health risks.
For the study, Dr. Pietro Ravani, a nephrologist at the Cumming School of Medicine at the University of Calgary in Alberta, and his co-authors analyzed health data collected from 127,132 men and women in Canada. They compared the risk of kidney disease and death over five years based on their G.F.R.
The fate of those with a G.F.R. of less than 60 — which would result in a diagnosis of chronic kidney disease using current guidelines — was then assessed according to two different criteria. One was based on the fixed rate of 60, and the other with a sliding G.F.R. that was adjusted for age, ranging from younger than 40 to older than 65.
The researchers found that in younger adults, a G.F.R. of 45 to 59 would indicate declining kidney function that warrants careful monitoring and treatment. But in older adults, particularly those in their 80s and beyond, the risk of kidney failure associated with such a low G.F.R. was essentially the same as those with a G.F.R. of 60 or above. In fact, the risk of death from kidney failure up to and beyond age 100 was no different at any age over 65.
“When old patients come to the clinic all worried about kidney disease, I most often tell them their kidneys will not die before they do,” Dr. Ravani said.
Evolving guidelines
Debate about the over-diagnosis of kidney disease is not new. Thirteen years ago, two nephrologists debunked the supposed “epidemic” of chronic kidney disease that stemmed from diagnostic guidelines issued in 2002 . Although revised guidelines in 2012 further narrowed the definition of who has chronic kidney disease, the new study suggests those guidelines still result in far too many older adults being told they have the condition.
The new research demonstrated that the commonly used benchmark for defining kidney disease — a glomerular filtration rate of less than 60 milliliters per minute — often results in older adults receiving a diagnosis and treatment for a condition that will never cause symptoms or hasten their death.
The findings suggest that the diagnostic guidelines for chronic kidney disease needs yet another refinement that would significantly “reduce the burden of kidney disease” in the elderly, Dr. Ravani said.
Competing interests
In an editorial accompanying the new report , Dr. Ann M. O’Hare, a nephrologist at the University of Washington and the VA Puget Sound Health Care System in Seattle, noted that there is ongoing resistance to changing current diagnostic guidelines. Much of this resistance, she argued, is based less on science than on the financial, personal and professional stakes many decision makers have in maintaining the status quo.
She explained that various groups — including pharmaceutical and biotechnology companies, health systems, professional organizations that develop medical guidelines, and even patient advocacy groups — benefit directly or indirectly from the current definition of disease that unnecessarily labels hundreds of thousands of older adults with a diagnosis of chronic kidney disease.
The forces driving over-diagnosis can be subtle and not always financial, Dr. O’Hare said in an interview. Some groups believe strongly that everything possible should be done to avoid kidney failure down the road, no matter how unlikely it may be in an elderly person. But the new study showed that the current diagnostic cutoff “labels a large number of people with having a disease when they have nothing more than a natural decline in kidney function with age,” she said.
Too often, Dr. Ravani said, doctors give credit for the patient’s survival to the medication that was prescribed, when in fact it really made no difference. Before agreeing to take a medication, he suggested that patients ask what effect it is likely to have on their lives.
Jane Brody is the Personal Health columnist, a position she has held since 1976. She has written more than a dozen books including the best sellers “Jane Brody’s Nutrition Book” and “Jane Brody’s Good Food Book.” More about Jane E. Brody
A Guide to Aging Well
Looking to grow old gracefully we can help..
Researchers are investigating how our biology changes as we grow older — and whether there are ways to stop it .
You need more than strength to age well — you also need power. Here’s how to measure how much power you have and here’s how to increase yours .
Ignore the hyperbaric chambers and infrared light: These are the evidence-backed secrets to aging well .
Your body’s need for fuel shifts as you get older. Your eating habits should shift , too.
People who think positively about getting older often live longer, healthier lives. These tips can help you reconsider your perspective .
The sun’s rays cause the majority of skin changes as you grow older. Here’s how sunscreen helps prevent the damage .
Joint pain, stiffness and swelling aren’t always inevitable results of aging, experts say. Here’s what you can do to reduce your risk for arthritis .
- Mission and Vision
- Department Leadership
- Community and Culture
- Department History
- Accreditation
- Graduate Program
- Undergraduate Program
- Bachelor's/Master's Integrated Program
- Student Community
- Faculty Directory
- Staff Directory
- Job Openings
- External Advisory Committee
- Research Centers
- Research Partners
- Student Research Opportunities
- Research Poster Resources
- In the Media
- PULSE Newsletter
- Alumni Profiles
News and Events
- Closer Look: Biomechanics
Novel MRI Approach Aims to Spot Kidney Disease in All Populations

Magnetic Resonance Imaging (MRI) has been a vital diagnostic tool for decades, aiding in detecting and treating conditions spanning from brain disorders to foot injuries. Despite the benefits, accessibility and affordability continue to pose significant challenges for many.
A new grant from the National Institutes of Health will support the development of novel MRI scans for detecting kidney disease. Led by Adam Bush, assistant professor in the Cockrell School of Engineering’s Department of Biomedical Engineering, and Jon Tamir, assistant professor in the Chandra Family Department of Electrical and Computer Engineering, the five-year, $2.6 million project will focus specifically on Black populations, where kidney disease and its complications are more common.
Why it Matters: Kidney disease is a leading cause of death in the U.S. and affects 1 in 7 adults — 90% of whom are unaware they even have the disease. Hypertension and diabetes are the most common causes of kidney disease, and the CDC estimates that treatment in 2019 cost Americans more than $100 billion.
Glomerular filtration rate (GFR) measures how well kidneys filter waste from blood to create urine, and it is the most common way to assess kidney function. However, GFR tests done through blood samples can be inaccurate, and more elaborate methods are cumbersome, costly, time-consuming and less safe.
Consequently, early stages of kidney disease often go undetected and are rarely studied.
Black Americans are at particular risk. Kidney disease is 15% more common among Black Americans and they are three times more likely to develop end-stage renal disease compared to non-Black Americans. Black Americans also have higher rates of hypertension and diabetes, yet the exact mechanism of kidney disease in this population is understudied.
"I'm eager to work together with Jon and move MRI technology forward in a manner that no one, regardless of their ethnicity, background, or income, cannot receive a proper diagnosis that could potentially save their life," said Bush.
The Goal: Bush and Tamir aim to develop safe and rapid ways of measuring kidney function using MRI. The technology is widely used to assess the brain but is used in the body to a lesser degree. Key limitations for body MRI applications include physical variation and motion.
Bush and Tamir aim to solve technical challenges with imaging the kidney, including long scan times and subject movement. The key to their approach is the design of fast and motion-robust sampling combined with advanced biophysical modeling of the kidney.
The researchers believe these methods can create improved indicators for kidney health that are safer, simpler and more precise than current methods for measuring kidney function.
"Imaging the kidneys is challenging, but we've assembled a fantastic team, and we're eager to improve equity and broaden access to historically underserved populations," said Tamir.
WRITTEN BY JOSHUA KLEINSTREUER
- Room Reservations
- Equipment Reservations
- Faculty and Staff Resources
- Communications Guidelines
- BME Students Canvas
- ENGR Direct
- UT Directory
Follow Texas BME
- U.S. Department of Health & Human Services

- Virtual Tour
- Staff Directory
- En Español
You are here
News releases.
Media Advisory
Friday, April 26, 2024
Analysis identifies 50 new genomic regions associated with kidney cancer risk
In a new analysis of genetic susceptibility to kidney cancer, an international team of researchers has identified 50 new areas across the genome that are associated with the risk of developing kidney cancer. These insights could one day be used to advance our understanding of the molecular basis of kidney cancer, inform screening efforts for those at highest risk, and identify new drug targets. The study was led by scientists at the National Cancer Institute (NCI), part of the National Institutes of Health (NIH).
A previous genome-wide association study (GWAS) of people of European ancestry identified 13 regions of the genome that are associated with kidney cancer risk. However, the study population was not diverse. To identify additional regions, researchers conducted a GWAS in participants of many different genetic ancestries that included 29,020 people with kidney cancer and 835,670 people without kidney cancer. Analysis of the data, which came from published studies, biobanks, and a new study, resulted in the identification of 50 new regions associated with the risk of developing kidney cancer, bringing the total number of such regions to 63.
Among the newly identified genetic variants were several associated with a risk of developing papillary renal cell carcinoma, the second most common subtype of renal cell carcinoma. Another variant, in the VHL gene, was common in individuals of African ancestry and was associated with an estimated three times higher risk of developing clear cell renal cell carcinoma, the most common type of kidney cancer.
Finally, the researchers used the study data to develop a measure of an individual’s overall risk of developing kidney cancer, known as a polygenic risk score , that can be combined with established risk factors—such as high blood pressure, smoking, and a high body-mass index measurement—to possibly enable earlier detection of the disease.
Mark P. Purdue, Ph.D., Division of Cancer Epidemiology and Genetics , National Cancer Institute
“ Multi-ancestry genome-wide association study of kidney cancer identifies 63 susceptibility regions ” appears April 26, 2024, in Nature Genetics .
About the National Cancer Institute (NCI): NCI leads the National Cancer Program and NIH’s efforts to dramatically reduce the prevalence of cancer and improve the lives of people with cancer. NCI supports a wide range of cancer research and training extramurally through grants and contracts. NCI’s intramural research program conducts innovative, transdisciplinary basic, translational, clinical, and epidemiological research on the causes of cancer, avenues for prevention, risk prediction, early detection, and treatment, including research at the NIH Clinical Center—the world’s largest research hospital. Learn more about the intramural research done in NCI’s Division of Cancer Epidemiology and Genetics . For more information about cancer, please visit the NCI website at cancer.gov or call NCI’s contact center at 1-800-4-CANCER (1-800-422-6237).
About the National Institutes of Health (NIH): NIH, the nation's medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit www.nih.gov .
NIH…Turning Discovery Into Health ®
Connect with Us
- More Social Media from NIH
- Skip to main content
- Skip to FDA Search
- Skip to in this section menu
- Skip to footer links

The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
U.S. Food and Drug Administration
- Search
- Menu
- News & Events
- FDA Newsroom
- Press Announcements
FDA Approves Treatment for Chronic Kidney Disease
FDA News Release
Approval is First to Cover Many Causes of Disease
Today, the U.S. Food and Drug Administration approved Farxiga (dapagliflozin) oral tablets to reduce the risk of kidney function decline, kidney failure, cardiovascular death and hospitalization for heart failure in adults with chronic kidney disease who are at risk of disease progression.
“Chronic kidney disease is an important public health issue, and there is a significant unmet need for therapies that slow disease progression and improve outcomes,” said Aliza Thompson, M.D., M.S., deputy director of the Division of Cardiology and Nephrology in the FDA’s Center for Drug Evaluation and Research. “Today’s approval of Farxiga for the treatment of chronic kidney disease is an important step forward in helping people living with kidney disease.”
Chronic kidney disease occurs when the kidneys are damaged and cannot filter blood normally. Due to this defective filtering, patients can have complications related to fluid, electrolytes (minerals required for many bodily processes), and waste build-up in the body. Chronic kidney disease sometimes can progress to kidney failure. Patients also are at high risk of cardiovascular disease, including heart disease and stroke.
The efficacy of Farxiga to improve kidney outcomes and reduce cardiovascular death in patients with chronic kidney disease was evaluated in a multicenter, double-blind study. In this study, 4,304 patients were randomly assigned to receive either Farxiga or a placebo. The study compared the two groups for the number of patients whose disease progressed to a composite (or combined) endpoint that included at least a 50% reduction in kidney function, progression to kidney failure, or cardiovascular or kidney death. Results showed that 197 of the 2,152 patients who received Farxiga had at least one of the composite endpoint events compared to 312 of the 2,152 patients who received a placebo. The study also compared the two groups for the number of patients who were hospitalized for heart failure or died from cardiovascular disease. A total of 100 patients who received Farxiga were hospitalized or died compared to 138 patients who received a placebo.
Farxiga was not studied, nor is expected to be effective, in treating chronic kidney disease among patients with autosomal dominant or recessive polycystic (characterized by multiple cysts) kidney disease or among patients who require or have recently used immunosuppressive therapy to treat kidney disease.
Patients should not use Farxiga if they have a history of serious hypersensitivity reactions to the medication or if they are on dialysis treatment. Serious, life-threatening cases of Fournier’s Gangrene have occurred in patients with diabetes taking Farxiga. Patients should consider a lower dose of insulin or insulin secretagogue to reduce the risk of hypoglycemia (low blood sugar) if they are also taking Farxiga. Farxiga can cause dehydration, serious urinary tract infections, genital yeast infections, and metabolic acidosis or ketoacidosis (acid build-up in the blood). Patients should be assessed for their volume status and kidney function before starting Farxiga.
Farxiga was originally approved in 2014 to improve glycemic control in adults with type 2 diabetes in addition to diet and exercise.
Farxiga received Fast Track , Breakthrough Therapy and Priority Review designations for the indication being approved today. Fast track is designed to facilitate the development and expedite the review of drugs to treat serious conditions and fill an unmet medical need. Breakthrough therapy designation is designed to expedite the development and review of drugs that are intended to treat a serious condition and preliminary clinical evidence indicates that the drug may demonstrate substantial improvement over available therapy on a clinically significant endpoint(s). Priority review directs overall attention and resources to the evaluation of applications for drugs that, if approved, would be significant improvements in the safety or effectiveness of the treatment, diagnosis or prevention of serious conditions when compared to standard applications.
The FDA granted the approval of Farxiga to AstraZeneca.
Related Information
- NIH: Chronic Kidney Disease
The FDA, an agency within the U.S. Department of Health and Human Services, protects the public health by assuring the safety, effectiveness, and security of human and veterinary drugs, vaccines and other biological products for human use, and medical devices. The agency also is responsible for the safety and security of our nation’s food supply, cosmetics, dietary supplements, products that give off electronic radiation, and for regulating tobacco products.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Kidney Int Suppl (2011)
- v.12(1); 2022 Apr
Epidemiology of chronic kidney disease: an update 2022
Csaba p. kovesdy.
1 Division of Nephrology, Department of Medicine, University of Tennessee Health Science Center, Memphis, Tennessee, USA
Chronic kidney disease is a progressive condition that affects >10% of the general population worldwide, amounting to >800 million individuals. Chronic kidney disease is more prevalent in older individuals, women, racial minorities, and in people experiencing diabetes mellitus and hypertension. Chronic kidney disease represents an especially large burden in low- and middle-income countries, which are least equipped to deal with its consequences. Chronic kidney disease has emerged as one of the leading causes of mortality worldwide, and it is one of a small number of non-communicable diseases that have shown an increase in associated deaths over the past 2 decades. The high number of affected individuals and the significant adverse impact of chronic kidney disease should prompt enhanced efforts for better prevention and treatment.
Graphical abstract

Chronic kidney disease (CKD) has emerged as one of the most prominent causes of death and suffering in the 21 st century. Due in part to the rise in risk factors, such as obesity and diabetes mellitus, the number of patients affected by CKD has also been increasing, affecting an estimated 843.6 million individuals worldwide in 2017. 1 Although mortality has declined in patients with end-stage kidney disease (ESKD), 2 the Global Burden of Disease (GBD) studies have shown that CKD has emerged as a leading cause of worldwide mortality. 3 , 4 It is, therefore, paramount that CKD is identified, monitored, and treated, and that preventative and therapeutic measures addressing CKD are systematically implemented worldwide. This narrative review summarizes information about global CKD prevalence, its trends over time, its various determinants, and its associated mortality. Other aspects of kidney disease epidemiology, such as CKD in pediatric patients, CKD incidence, progression to ESKD, or various clinical (e.g., cardiovascular disease) and patient-reported outcomes caused by CKD, are mentioned briefly or not discussed.
Definitions of CKD and its pitfalls in epidemiologic studies
The diagnosis of CKD is made by laboratory testing, most often by estimating glomerular filtration rate (GFR) from a filtration marker, such as serum creatinine or cystatin C, using various formulas, or by testing urine for the presence of albumin or protein (or a combination of these). 5 The classification schemas advocated by various professional organizations in the past 2 decades 5 have laid the groundwork for the systematic detection and monitoring of CKD worldwide, resulting in an improved understanding of its prevalence and the resulting impact on outcomes, such as mortality. Most studies have used estimated GFR (eGFR) to determine the presence of CKD (and, therefore, report on the prevalence of CKD stages 3–5), whereas other studies have combined albuminuria (typically defined as an albumin-to-creatinine ratio of >30 mg/g) and decreased eGFR to report on CKD stages 1–5. Finally, to differentiate CKD (which is considered to be a chronic progressive disease) from conditions such as acute kidney injury or from transient fluctuations in kidney function unrelated to kidney damage, the standard definition of CKD includes a so-called “chronicity criterion” (i.e., that the low eGFR or elevated urine albumin should be detectable for at least 90 days, requiring the presence of repeated measurements over time). 5 There is currently no consensus on the length of time used in the assessment of CKD when applying the chronicity criterion, with epidemiologic studies applying various algorithms, from single measurements to any repeated measurements past 90 days, or limiting the repeated measurement(s) to 90 to 365 days, and from requiring consecutive repeated markers of CKD to accepting CKD markers interspersed with markers not conforming to CKD criteria. The potential impact of using 6 different definition algorithms (5 laboratory measurement based and one based on International Classification of Diseases [ICD] diagnostic codes) to ascertain the prevalence of CKD was recently examined in a population-based cohort from Northern Denmark. 6 The prevalence of CKD varied considerably between the various laboratory-based definitions, ranging from 8327 cases per 100,000 population when using a single eGFR value to 4637 cases per 100,000 population when using a time-limited repeated eGFR-based definition. Furthermore, when using an ICD diagnostic code-based definition, the prevalence of CKD was markedly lower, at 775 cases per 100,000 population. Studies assessing the prevalence of CKD have applied a variety of definitions of CKD, and thus their results (and especially the results of studies aggregating their findings, as described below) must be interpreted with caution.
Prevalence and global burden of CKD
The prevalence of CKD has been reported in an increasing number of studies worldwide (the individual discussion of which is beyond the scope of this review), which has made it possible to aggregate their findings and to derive information about global CKD prevalence overall, as well as in various patient subgroups and geographic regions. A study assessing the prevalence and burden of CKD in 2010 pooled the results of 33 population-based representative studies from around the world and reported an age-standardized global prevalence of CKD stages 1–5 in individuals aged ≥20 years of 10.4% among men and 11.8% among women. 7 The study reported important differences by geographic region classified by income level, with a CKD age-standardized prevalence of 8.6% and 9.6% in men and women, respectively, in high-income countries, and 10.6% and 12.5% in men and women, respectively, in low- and middle-income countries. The age-standardized global prevalence of CKD stages 3–5 in adults aged ≥20 years in the same study was 4.7% in men and 5.8% in women. A more recent study performed a comprehensive systematic review and meta-analysis of 100 studies comprising 6,908,440 patients, and reported a global prevalence of 13.4% for CKD stages 1–5 and 10.6% for CKD stages 3–5. 8 The prevalence of the individual CKD stages was 3.5% (stage 1), 3.9% (stage 2), 7.6% (stage 3), 0.4% (stage 4), and 0.1% (stage 5). 8 On the basis of the results of studies examining the global prevalence of CKD, the current total number of individuals affected by CKD stages 1–5 worldwide was estimated to be 843.6 million. 1
Changes in CKD prevalence over time
There are significantly fewer studies examining changes in CKD prevalence over time, as this requires a reassessment of the same population using similar methods. In the United States, the Centers for Disease Control and Prevention CKD Surveillance System reported that the prevalence of CKD stages 1–4 was 11.8% in 1988 to 1994, and it increased to 14.2% in 2015 to 2016. 9 This increase was not linear, as was reported by a study examining data from the National Health and Nutrition Examination Survey; this study showed that although the prevalence of CKD stage 3–4 increased from the 1990s to the 2000s, it has remained largely stable since. 10 A similarly stable prevalence of CKD stages 1–5 was reported in Norway for the time period between 1995 and 2008. 11 Interestingly, the prevalence of CKD stages 3–5 declined significantly over 7 years in the United Kingdom based on the nationally representative Health Survey for England. In this study, the adjusted odds ratio of an eGFR <60 ml/min per 1.73 m 2 comparing 2003 with 2009/2010 was 0.73 (95% confidence interval, 0.57–0.93). 12 The reasons for recently reported stabilized or improved CKD prevalence are unclear. These trends have occurred despite a concomitant increase in common risk factors of CKD, such as diabetes and obesity, although hypertension control has improved over this time period. 12 It is worth mentioning that, due to population growth, a stable trend in CKD prevalence still represents an increase in the absolute number of patients with CKD. The reason(s) for the observed dynamic changes in CKD prevalence (and the discrepancies observed between the data from different countries) is difficult to determine. Disease prevalence could vary due to changes in disease incidence, but information about CKD incidence is much sparser in the literature, and the results of published studies cannot be interpreted in the context of prevalence estimates performed in different populations and different eras, 13 , 14 , 15 , 16 , 17 due to the major impact of characteristics, such as age, sex, or race, on incidence values. Prevalence can also change because of changes in survival or longer lifetime duration of diagnosed CKD (e.g., from better screening); it is possible that the aggregate change in CKD prevalence may be the result of a combination of factors.
Effect of patient characteristics and comorbidities on CKD prevalence
The prevalence of CKD is affected by both its definition and its pathophysiology. Because most CKD cases are identified using eGFR, its determinants will impact the estimates of CKD prevalence. Most important, higher age results in lower eGFR independent of the other components of the equation; hence, even with a stable serum creatinine concentration, an individual can develop CKD as a result of advancing age due to the assumption that age-related losses in muscle mass will obscure the decrease in age-associated losses in GFR. Indeed, the aforementioned meta-analysis by Hill et al. assessed the impact of age on CKD prevalence and reported a linearly higher prevalence for CKD stages 1–5 associated with advancing age, ranging from 13.7% in the 30- to 40-year-old group to 27.9% in patients aged >70 to 80 years. 8 Similar trends were reported in the United States during 2015 to 2016, where the prevalence of CKD stages 1–4 was 5.6% among individuals aged 20 to 39 years and 44% among those aged >70 years. 9 Notwithstanding the biological plausibility of age-associated loss of GFR, the pathologic significance of early-stage (i.e., stage 3a) CKD that is solely a result of advanced age (and characterized by normal urine albumin and serum creatinine values) continues to be debated. 18
The prevalence of CKD has been reported to be higher in females than in males. In the United States, the age-adjusted prevalence of CKD stages 1–4 in 2015 to 2016 was 14.9% in females and 12.3% in males, 9 similar to the sex-based differences reported in the global studies mentioned above. 7 , 8 The reasons for these differences are unclear and are likely to be complex. Although GFR estimating equations include a correction factor for sex, a single cutoff of <60 ml/min per 1.73 m 2 for CKD definition may result in overdiagnosing CKD in women. 19 The higher CKD prevalence described in women also contrasts with experimental data showing the protective effects of estrogen and potential deleterious effects of testosterone on nondiabetic CKD, 20 as well as data that indicate a higher incidence of kidney failure in men. 21 , 22 A meta-analysis of 30 studies examining sex-stratified data concluded that CKD progression was faster in men compared with women, 23 although other studies have cautioned that such differences may be due to nonbiological factors, such as lifestyle, cultural, and socioeconomic factors. 24 Better characterization of the effects of sex on CKD incidence, prevalence, and progression requires further examination, including the study of potential development of sex-specific disease markers. 19
Racial differences in the incidence and prevalence of CKD and kidney failure are well described in the United States, 25 , 26 , 27 but a global and systematic evaluation of such differences is difficult because variances between countries are complex and represent a combination of risk factors (including differences in race). Furthermore, within-country comparisons may not always be possible due to racial/ethnic homogeneities and/or local restrictions on reporting individuals’ race and ethnicity. An additional challenge is the inaccuracy of GFR estimation formulas in individuals of different races, and an ongoing debate in the United States over the exclusion of the correction factor for self-reported African American race from the existing estimation formulas as a means to alleviate racial disparities. 28 In the United States, the age-adjusted prevalence of CKD stages 1–4 among non-Hispanic Whites, non-Hispanic Blacks, and Mexican Americans in 2015 to 2016 was 13%, 16.5%, and 15.3%, respectively. 9 The reasons for race-associated differences are complex, and include differences in the prevalence of CKD risk factors (such as diabetes mellitus, hypertension, and obesity), genetic causes, lifestyle and cultural differences, and socioeconomic disparities. 29 , 30 , 31 , 32
Diabetes mellitus has emerged as the most important risk factor for CKD in the developed world; this is reflected in studies examining CKD prevalence. In the United States, the prevalence of CKD stages 3–4 among diagnosed diabetics was 24.5% in 2011 to 2014, whereas in prediabetics it was 14.3% and in nondiabetics it was 4.9%. 9 The association between diabetes mellitus and the prevalence of CKD was also reported in a meta-analysis that included 82 global studies. 8 The effect of diabetes mellitus on kidney function and on the development and progression of CKD is well established. 33 Nevertheless, epidemiologic studies examining CKD in diabetics have to contend with the fact that diabetic populations (especially type 2 diabetics) often experience multiple other comorbid conditions, such as hypertension or vascular disease, which are themselves independent risk factors for CKD. A study examining a national cohort of US veterans with newly diagnosed type 2 diabetes mellitus reported a crude prevalence of CKD stages 1–5 of 31.6%, half of whom had CKD stages 3–5. 34 Although the timing of incident type 2 diabetes mellitus is difficult to ascertain, the high prevalence of CKD in this study suggests that at least some of the CKD cases diagnosed in diabetics may not be a direct result of diabetes-related mechanisms.
Hypertension is the strongest cardiovascular risk factor worldwide and is also closely associated with CKD. 35 The prevalence of CKD among hypertensive US adults was 35.8% in 2011 to 2014, compared with a prevalence of 14.4% in prehypertensives and 10.2% among nonhypertensive individuals. 9 A significant association between hypertension and the prevalence of CKD was also reported in a meta-analysis that included 75 global studies. 8
Mortality associated with CKD
CKD is now widely recognized as one of the leading causes of death worldwide. The GBD reports have been tracking causes of death across the globe for the past decade. The 2013 GBD report indicated that although relative death rates decreased for most communicable and noncommunicable diseases, CKD (defined as all stages, including patients on dialysis) was one of only a handful of conditions to show an increase since 1990. 3 , 4 The global all-age mortality rate attributed to CKD increased by 41.5% between 1990 and 2017. 36 Besides being one of the leading causes of death, CKD also became the 19th leading cause of years of life lost (which is calculated from the number of deaths attributable to CKD and the life expectancy of individuals in various age groups at the time of their death from CKD 3 ) in 2013, compared with being the 36th leading cause in 1990. 3 Subsequent GBD reports indicate that the rise of CKD among the list of causes of death has continued, occupying the 13th place in 2016 37 and 12th place in 2017, 36 with predictions suggesting that it will become the fifth highest cause of years of life lost globally by 2040. 38 The GBD reports also shed light on the disproportionate nature of the burden imparted by CKD-associated death in different world regions, with Latin America, the Caribbean region, Southeast Asia and East Asia, Oceania, North Africa, and the Middle East being especially affected. Among high-income nations, CKD was among the top 10 causes of death in Singapore, Greece, and Israel ( Figure 1 ). 3 , 4 These reports are especially noteworthy when considering that they did not include deaths that were caused indirectly by CKD, such as those related to acute kidney injury or to various cardiovascular causes, both of which can be caused or potentiated by CKD. 4

Regions and countries where chronic kidney disease is in the top 10 causes of years of life lost in 2013. On the basis of data from the Global Burden of Disease Study 2013. 3
Conclusions
CKD is extremely common and has emerged as one of the leading noncommunicable causes of death worldwide. It is projected to affect an increasing number of individuals over time and to further rise in importance among the various global causes of death. CKD affects populations in different regions of the world unequally, likely as a result of differences in population demographic characteristics, their comorbidities, and access to health care resources. The common nature and devastating effects of CKD should prompt major efforts to develop and implement effective preventative and therapeutic efforts aimed at lowering the development of CKD and slowing its progression.
This article is published as part of a supplement sponsored by Bayer AG.
CPK is a consultant for Abbott, Akebia, AstraZeneca, Bayer, Cara Therapeutics, CSL Behring, Dr. Schar, Reata, Rockwell, Takeda, Tricida and Vifor. CPK received no personal funding for this article.
Acknowledgments
Development of this article was funded by an unrestricted educational grant from Bayer AG. CPK would like to acknowledge Jo Luscombe, PhD, of Chameleon Communications International, who provided editorial assistance with funding via an unrestricted educational grant from Bayer AG.
An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Entire Site
- Research & Funding
- Health Information
- About NIDDK
- Research Areas
Kidney Disease

Normal, healthy kidneys filter about 200 quarts of blood each day, generating about 2 quarts of excess fluid, salts, and waste products that are excreted as urine. Loss of function of these organs, even for a short period of time or due to gradual deterioration, can result in life-threatening complications. Loss of kidney function is an important health challenge whether it occurs suddenly or over a long period of time.
The NIDDK supports basic and clinical research on kidney development; the causes of kidney disease; improving kidney health equity and reducing kidney health disparities; the underlying mechanisms leading to progression of kidney disease; and the development and testing of possible treatments to prevent or slow progression of kidney disease. Also of interest are studies of inherited diseases such as polycystic kidney disease, congenital kidney disorders, and immune-related kidney diseases such as IgA nephropathy and hemolytic uremic syndrome.
It has been estimated that 37 million American adults have chronic kidney disease (CKD). CKD has two main causes: high blood pressure and diabetes. CKD, especially if undetected, can progress to irreversible kidney failure. People with kidney failure require dialysis or a kidney transplant to live. Minority populations, particularly African Americans, Hispanic and Latino Americans, and American Indians and Alaska Natives, bear a disproportionate burden of CKD and kidney failure.
In addition, NIDDK has congressional authorization for the National Kidney and Urologic Diseases Information Clearinghouse , which provides services via the NIDDK Health Information Center. NIDDK responds to questions and provides health information about kidney disease to people with kidney disease and to their families, health professionals, and the public.
Research Updates and News
- Scientists discover potential treatment approaches for polycystic kidney disease
- Alternatives to Race-Based Kidney Function Calculations
- New atlas of human kidney cells to help unlock kidney disease research
- Being hospitalized with acute kidney injury may increase risk for rehospitalization and death
- A Potential Explanation for Differences in Susceptibility to Kidney Complications of Diabetes
View More News Articles
Select Landmark Studies
- Chronic Kidney Disease in Children Study: CKiD
- Effects of Chronic Kidney Disease in Adults Study: CRIC
To achieve its mission, NIDDK supports, conducts, coordinates, and plans research. NIDDK also provides data and samples from NIDDK-funded studies and explains research findings to health professionals and the public.
Support Research
NIDDK invests in basic, clinical and translational research and training at colleges, universities and other institutions.
- Acute Kidney Injury
- Chronic Kidney Disease
- Diabetic Kidney Disease
- End-Stage Renal Disease
- Kidney Bioengineering, Biotechnology, and Imaging
- Kidney Clinical Research and Epidemiology
- Kidney Developmental Biology and Aging
Conduct Research
NIDDK investigators conduct biomedical research and training in the Institute's laboratories and clinical facilities in Maryland and Arizona.
- Kidney Diseases Branch
Coordinate & Plan Research
NIDDK takes multiple approaches to research planning and priority setting.
Meetings & Workshops
- Gut Microbiota and Kidney Disease
Strategic Plans & Reports
- U.S. Renal Data System
- NIDDK Strategic Plan for Research
- Kidney Research National Dialogue (KRND) Summary
Provide Access to Research Resources
NIDDK makes publicly supported resources, data sets, and studies available to researchers.
Provide Health Information
NIDDK provides patient education information, practice tools for diagnosis and treatment, and statistics.
- Kidney Disease Statistics
- Health Information about Kidney Diseases
- Kidney Disease for Health Professionals
- Advanced Health Information Search
Kidney disease ends here .

New resource drives vital research in chronic kidney disease
A new publication from NURTuRE – the first national UK chronic kidney disease cohort study with a linked biobank, developed as a collaboration between Kidney Research UK, research groups and pharmaceuticals companies – has been published in Nephrology, Dialysis and Transplantation . Alongside highlighting important patterns in kidney function and use of prescription medications in chronic kidney disease patients, this new study clearly demonstrates the potential for NURTuRE to support vital new breakthroughs in kidney medicine.
Meeting the growing need for innovation in kidney disease management
Chronic kidney disease (CKD) impacts more than 3 million people in the UK, often with serious outcomes. There is an increasing understanding that to better manage kidney disease we need to look closely at the many pathways and mechanisms that can lead to a diagnosis of CKD. This new NURTuRE paper presents results on the number of CKD patients enrolled in the biobank, age, gender and other demographic characteristics, alongside detailed clinical and biological information.

Professor Maarten Taal, lead author on the paper, commented
“NURTuRE (the National Unified Renal Translational Research Enterprise) offers researchers a unique opportunity to improve our knowledge of factors related to poor outcomes in CKD patients, potentially supporting earlier identification of the most at-risk patients and more effective treatment choices. NURTuRE should also help us find new treatment targets.”
Introducing NURTuRE
NURTuRE contains information from patients living with different types of kidney disease in the UK, providing a unique resource to support important new research. To date, patients diagnosed with chronic kidney disease (CKD) and idiopathic nephrotic syndrome (INS) have been recruited, with acute kidney injury (AKI) scheduled to begin soon.
The NURTuRE team collected and securely stored biological samples from approximately 3,000 patients with CKD and plan to include up to 800 patients with idiopathic nephrotic syndrome (INS). This type of collection of samples for research is known as a ‘biobank’. In addition to samples of plasma, serum, urine, DNA and tissue, NURTuRE will link to long-term clinical (healthcare) data, through the UK Renal Registry and NHS Digital. The information in NURTuRE will support crucial new research, offering hope to many patients living with kidney diseases.
A rich source of information to support vital future research
Results from Professor Taal’s paper showed that of the 2,996 patients in the CKD cohort, more than half were aged 65 years or greater, just less than 60% were male and most were of white ethnicity (84%). The four most common causes of CKD included glomerular disease (relating to the filters within the kidney), diabetes and hereditary diseases but in a large proportion the cause was unknown. The team also found differences between males and females enrolled in NURTuRE. Results showed that females in the CKD group were younger and less likely to be diagnosed with diabetes or heart disease. Females were also less likely to be treated with medications called renin-angiotensin system inhibitors and statins, and had a lower predicted risk of needing to start dialysis. The reasons for these differences will be explored in future studies.
Participants with lower kidney function were more likely to be older, male, of white ethnicity and have a diabetes diagnosis, alongside differences in biochemical measures. Results also showed that nearly 70% of patients would be classed as ‘high-risk’ based on the available risk assessments. Professor Taal commented “These early results show important differences within the CKD population, highlighting the need to look at individualised management. The long-term follow-up data, and detailed patient information in NURTuRE, will support future research designed to allow a more personalised approach to CKD care.”
Next steps for NURTuRE
From late 2023/early 2024, researchers not involved in the initial collaboration will be able apply to access NURTuRE samples and data for their own research, subject to approval. Plans are also underway to include new types of kidney diseases in the NURTuRE programme.
Michael Nation, director of NURTuRE at Kidney Research UK added, “Everyone involved in the NURTuRE collaborative should be proud of the progress that we have made. We have an exciting year ahead as the biobank opens for external research applications and we begin recruitment of our third patient cohort. I’d like to thank everyone who has supported us, but particularly the patients who joined and advised us enabling the progress we see today.”

Our research news

New £10.4M research centre will unlock new tests, treatments and cures for people living with rare kidney diseases

Can we support new approaches to kidney care by looking more closely at personalised care? The NURTuRE perspective

Pregnancy and Alport syndrome: a new way to look at the kidney filters

Study highlights potential early intervention for diabetic patients at risk of kidney disease

Study suggests rare kidney diseases treatments could dramatically reduce the burden of kidney disease on patients and the NHS

Survey highlights gaps in mental health care for UK kidney patients

Study shows promise of creating mini kidneys for personalised prenatal care

Unravelling inherited kidney diseases: an International Women’s Day conversation with Dr Melanie Chan

New results from the MELODY study highlight the variations in care experienced by transplant patients at different hospitals

Can sugar patterns help to predict kidney disease?

Unlocking the potential of kidney blood vessels in the treatment of childhood kidney disease

Can diabetic eye disease treatments affect kidney function?

Understanding the link between genetics and the immune system in the development of idiopathic nephrotic syndrome

Can stem cells help us improve the condition of donor kidneys?

Diabetes and kidney research charities team up to tackle diabetic kidney disease

Ground-breaking clinical trial offers treatment hope for IgA nephropathy

Meet Professor Claire Sharpe

Identifying a new drug target for diabetic kidney disease

Understanding the genetic causes of common childhood kidney disease

Exploring the role of BK virus in kidney transplant patients’ cancer risk: a World Cancer Day conversation with Dr Simon Baker
Why not make a donation now.
(Every £ counts)
Privacy Overview
Accelerating New Clinical Trials and Treatments for Kidney Disease
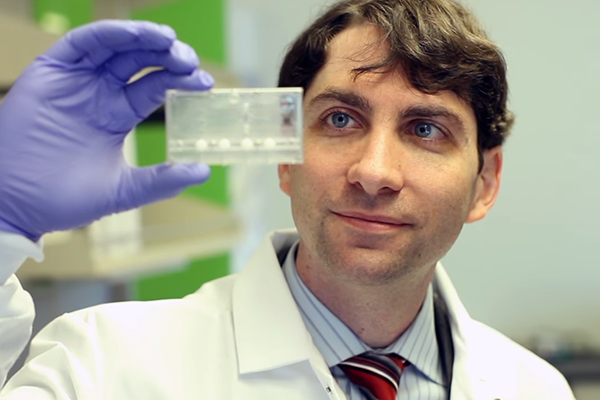
News and features
New £10.4 million research centre will unlock new tests, treatments and cures for people living with rare kidney diseases.

Press release issued: 23 April 2024
Thousands of people living with rare kidney disease will get access to improved diagnostics, treatments and potentially cures, thanks to the creation of a new research centre, involving experts from the University of Bristol.
In 2023, a major report from Kidney Research UK showed that kidney failure could overwhelm the health care system within ten years. The LifeArc-Kidney Research UK Centre for Rare Kidney Diseases is being launched to provide urgent focus and resource. It will unite researchers, patients and healthcare professionals and build on strong established resources, including the national registry of rare kidney diseases (RaDaR), the national renal sample biobank (NURTuRE) and care guidelines. It will signal the start of a transformation in all of the 13 of the UK’s children’s kidney centres to embed a culture of research by connecting the systems to accelerate discoveries and advance the treatment of rare kidney diseases.
The new translational centre is jointly funded by the medical research charity, LifeArc, who are investing £9.4 million in partnership with Kidney Research UK which is contributing an additional £1 million to be used to support the work of the centre over the next five years. It will be led by Dr Louise Oni, Senior Lecturer in Paediatric Nephrology at the University of Liverpool and honorary consultant paediatric nephrologist at Alder Hey Children’s Hospital.
Dr Louise Oni said: “It is a privilege to be leading this exciting transformation on behalf of the entire kidney community. We are incredibly grateful for the opportunity to establish the LifeArc-Kidney Research UK Centre for Rare Kidney Diseases with the support of our charity partners Kidney Research UK. This UK wide project aims to create a culture of constant learning to bring rapid advances to patients of all ages living with kidney diseases. The project will start by focusing on children with rare kidney diseases to attempt to halt the journey to kidney failure and then upscale into adult patients. Through collaboration, the templates presented by these rare disease centres will support mass transformation to benefit many other patients.”
Dr Aisling McMahon, executive director of research at Kidney Research UK, said: “Ensuring that everyone has equal access to innovations and new therapies designed to benefit kidney patients is a key priority for Kidney Research UK. We are delighted to be co-funding this new centre with LifeArc and working in partnership with them and the renal research community to deliver this exciting project. This new collaboration will ensure that patients of all ages with rare kidney diseases not only benefit from new approaches to prevention, diagnosis and treatment, but also become active partners in the research process.”
Kathryn Croker faced kidney failure after being diagnosed with the rare disease IgA vasculitis, aged just 13. Following a successful kidney transplant from her dad in 2013, she went on to volunteer with Kidney Research UK and now shares her own experiences to help shape research projects, including this new centre. She said: “If there was a way to treat rare diseases before they get to that point of causing kidney failure and needing a transplant, that would just be incredible because it changes the course of your life. It’s exciting to be involved in a project with doctors and researchers focused on kidney disease in children, as typically research involves adults. Hopefully in the next 20 years or less, what I’ve experienced since childhood will be a thing of the past because I don’t want anyone to go through what I have. This new research centre is an exciting opportunity to achieve that.”
Moin Saleem , Professor of Paediatric Renal Medicine at Bristol Medical School: Translational Health Sciences (THS) and Director of Bristol Renal , and one of the Bristol leads for the new centre added: “The Bristol team are delighted to be core part of this transformative project. The kidney community in the UK (patients, clinicians, researchers) has several unique world-leading strengths, and is perfectly poised for this collaborative lead from Dr Oni to bring together these resources into a cohesive unit.
“Bristol Renal was the originator of the UK renal rare disease registry as well as the national biobank (NURTuRE), and contributes world-leading translational science in kidney disease. Rare disease requires cooperation above all, and this exciting collaboration will markedly accelerate key scientific and infrastructure advances for the benefit of patients who have a huge unmet need."
The new LifeArc-Kidney Research UK Centre for Rare Kidney Diseases is one of four new centres to be funded by the non-profit medical charity, LifeArc, with the aim of overcoming these barriers that ordinarily prevent new tests and treatments reaching patients. Globally, there are more than 300 million people living with rare diseases. However, rare disease research can be fragmented. Researchers can lack access to specialist facilities, as well as advice on regulation, trial designs, preclinical regulatory requirements, and translational project management, which are vital in getting new innovations to patients.
Dr Catriona Crombie , Head of Rare Disease at LifeArc, continued: “We are extremely proud to be launching four new LifeArc Translational Centres for Rare Diseases. Each centre has been awarded funding because it holds real promise for delivering change for people living with rare diseases. These centres also have the potential to create a blueprint for accelerating improvements across other disease areas, including common diseases.”
Premium Content

- MIND, BODY, WONDER
The unexpected health benefits of Ozempic and Mounjaro
Research is showing that these new weight-loss drugs can help treat conditions from addiction to kidney disease—and may even be contributing to a boom of “Ozempic babies.”
Casey Arnold, who lives in a suburb of Houston, spent years trying to quit smoking. She’d tried nicotine patches. That failed. She tried quitting cold turkey but that made her short tempered. On other occasions the idea of quitting made her so anxious, she smoked more to ease her fears.
By the time she permanently gave up cigarettes in the winter of 2023, at age 55, she’d been smoking for four decades and was up to two packs a day. But this time it was a new type of weight loss drug that helped her quit.
GLP-1, short for glucagon-like peptide 1, is a natural hormone that stimulates the production and release of insulin, slows digestion, curbs appetite, and blunts the brain’s focus on food. GLP-1 agonist drugs, like exanetide, tirzepatide and semaglutide, mimic this hormone. They were originally developed as diabetes treatments, but as more people began taking them, researchers observed these medications are effective for many more conditions than just diabetes and weight loss.
The FDA recently approved semaglutide, the active ingredient of Wegovy, for the treatment of obesity and for reducing the risk of heart attack and stroke in patients with obesity and heart disease . But as the number of people taking these drugs grows, physicians and researchers are learning about unanticipated health benefits for conditions where treatments have been limited, such as addiction, heart failure, and kidney disease.
( Ozempic is a serious drug with serious risks. Here’s what to know. )
Arnold quit smoking while participating in a clinical trial examining the potential of GLP-1 agonists as a treatment for smoking addiction.
“It was totally opposite of when I tried to quit in my previous years,” Arnold says. “I was shocked at how calm I was, compared to how I used to think about quitting.” Instead of anxiety and rage, she felt at peace, and her cravings faded.
“It’s just been an avalanche across the different patient populations,” says Mark Petrie , a cardiologist at the University of Glasgow, whose research focuses on the use of GLP-1 agonists in patients with heart failure. “It’s just good news all around.”
Heart failure with preserved ejection fraction
More than six million Americans are living with heart failure , a condition where the heart progressively loses the ability to pump enough blood to the rest of the body. Of these patients, approximately half have a type known as heart failure with preserved ejection fraction , in which the heart can pump normally but is too stiff to fill up with blood.
In a study published last year , researchers tested semaglutide as a treatment for heart failure with preserved ejection fraction in patients who were not diabetic. The result: patients who received the drug showed fewer symptoms and reported a better quality of life, compared to those who received the placebo. Patients who received the drug had lower levels of C-reactive protein, which is a marker for inflammation.
“This is a big finding,” says James de Lemos, a cardiologist at UT Southwestern Medical Center, in Dallas, Texas, who was not associated with the study. The study was too small to determine if semaglutide can reduce the risk of hospitalization or death but given the stark improvement in patient quality of life, it’s promising.
Although some of these benefits are likely due to weight loss, that’s just part of what makes this treatment effective.
These medications are also cardioprotective and reduce inflammation, which is known to be a driver of heart failure, says Amanda Vest , a cardiologist at the Cleveland Clinic, who specializes in treating patients with heart failure. “We must continue to think more expansively than just about the number on the scale,” Vest says.
For patients with the other major type of heart failure—heart failure with reduced ejection fraction—there is less evidence, so far, that these drugs are effective. More trials are in the works to determine which types of patients will benefit from the use of these medications.
Kidney disease
An estimated 850 million people worldwide are living with chronic kidney disease , but there are few effective treatments. Historically, the main strategy has been to stall kidney failure for as long as possible and then move the patient to dialysis or wait for a kidney transplant. But nine out of 10 patients die of complications before reaching that point.
For patients with severe chronic kidney disease, “you are looking at a mortality rate that’s 10 to 20 percent a year,” says Katherine Tuttle , a nephrologist at the University of Washington Medicine. “This is on par with the worst malignancies.”
As a couple of recent studies have shown , the GLP-1 agonist dulaglutide helps patients who suffer from chronic kidney disease and diabetes. In a recent trial looking at the effect of semaglutide on patients with chronic kidney disease and type 2 diabetes, the treatment was so effective at delaying the progression of chronic kidney disease that the clinical trial was stopped early so that all the trial patients could benefit from the drug.
“It’s the only semaglutide trial that was stopped early for efficacy,” says Tuttle, who is on the executive committee for the trial. “To stop a trial early for efficacy, the bar is set really high,” which includes strong enough evidence for its efficacy that it would be no longer considered ethical to continue giving patients the placebo.
( New obesity drugs are coming. Here's how they could change everything. )
You May Also Like
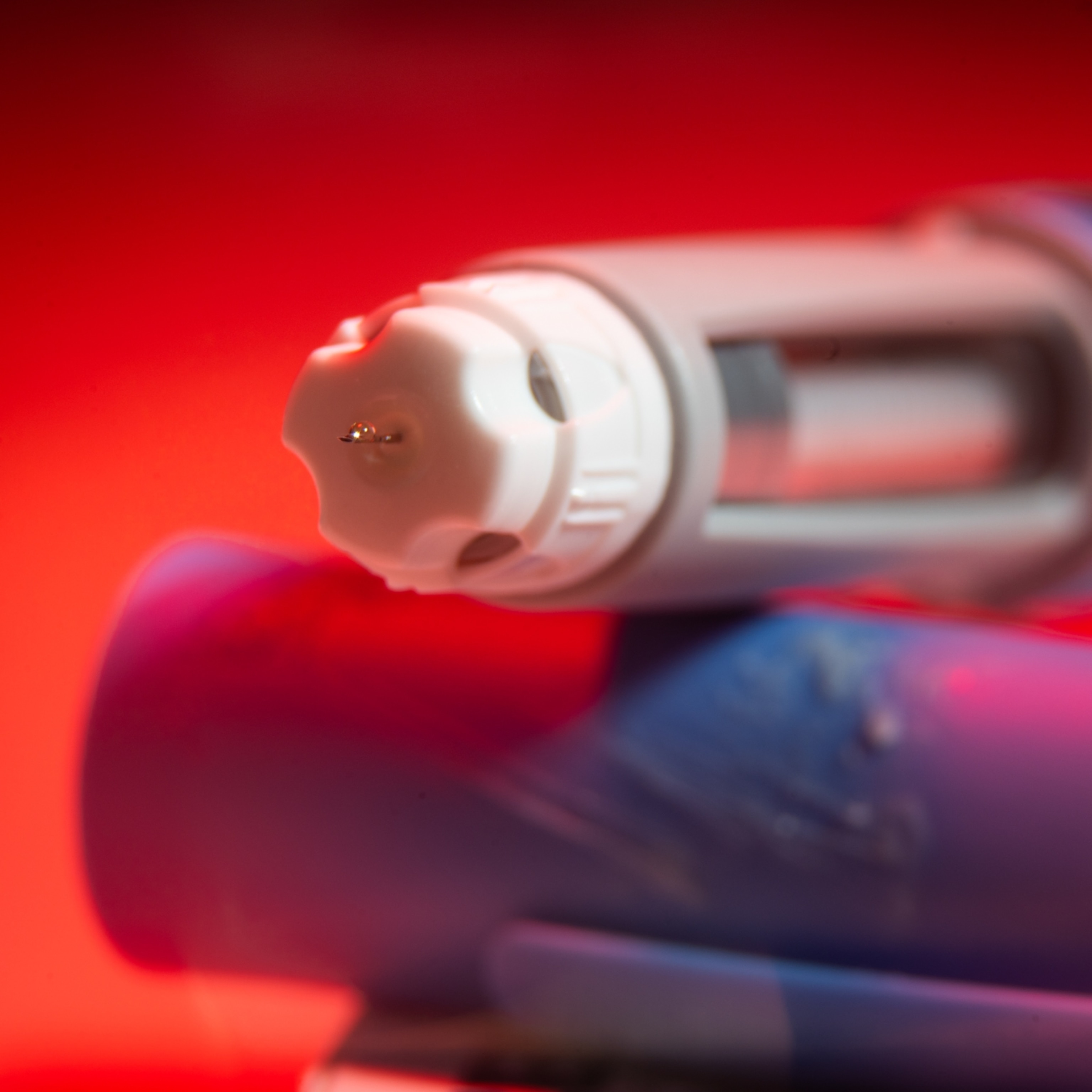
Ozempic and Mounjaro have another benefit: treating inflammation

Scientists are finally studying women’s bodies. This is what we’re learning.
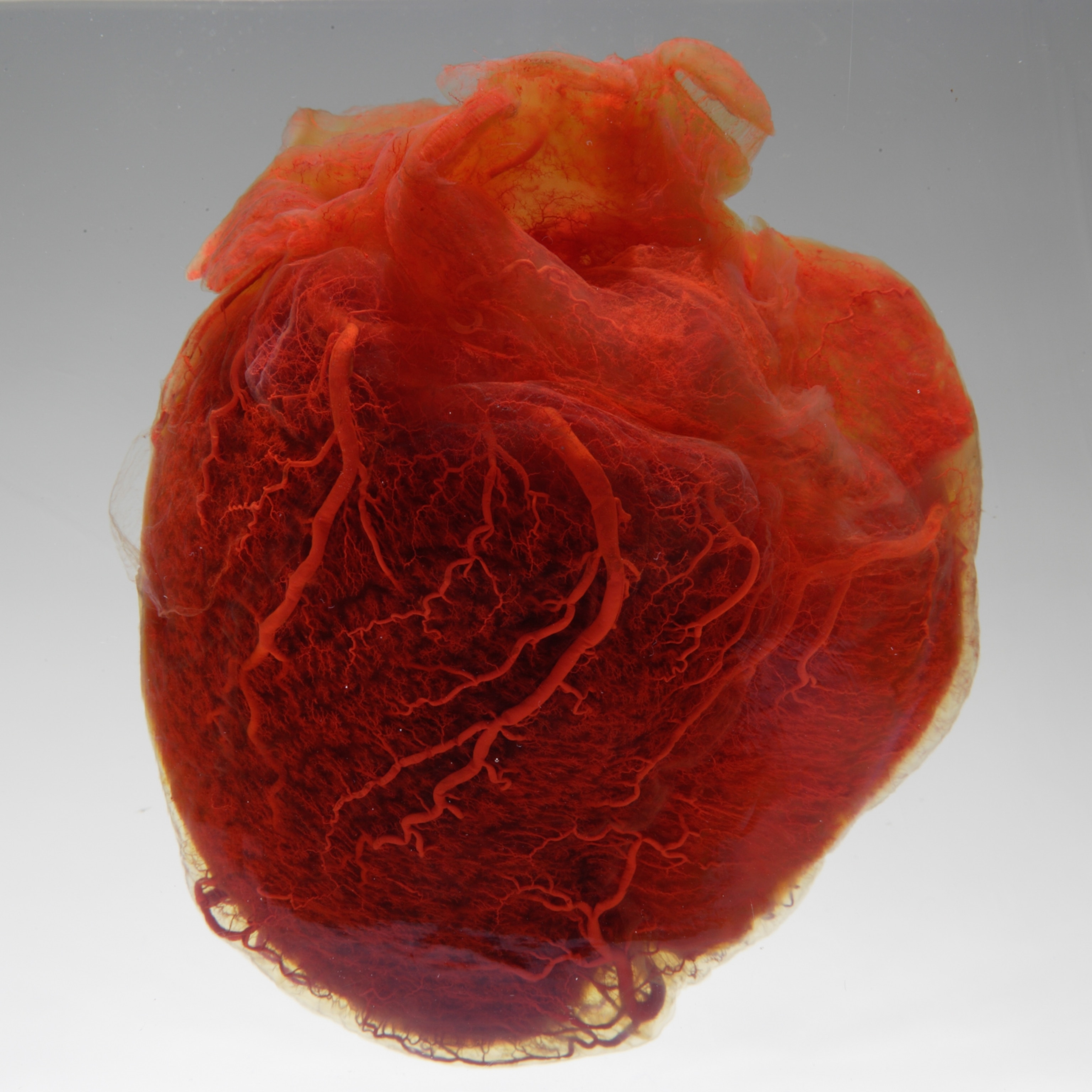
In a first, microplastic particles have been linked to heart disease
As Tuttle notes, the effects on the kidneys is only partially due to reductions in risk factors such as blood pressure, blood sugar, and weight. Other benefits are likely to result from reduced inflammation.
“They have a profound anti-inflammatory effect,” Tuttle says. “Our field is really under recognizing the importance of inflammation, particularly in kidney damage caused by diabetes.”
Results from the trial will be published later this year.
Effects on fertility
For a growing number of patients on GLP-1 agonists, such as Ozempic or Mounjaro, one surprising side effect has been unexpected pregnancy, which for some patients, has come after years of struggling with infertility. Although more research is needed to explore the link between GLP-1 agonists and pregnancy, it’s become enough of a phenomenon that ‘Ozempic babies’ has become a trending phrase. Meanwhile, experts think there are several factors responsible.
The first factor is the fact that GLP-1 agonists cause a delayed gastric emptying, which can cause oral contraception pills to be absorbed by the body at a slower rate. “These drugs are altering that particular part of the drug absorption phase,” says Archana Sadhu , an endocrinologist at Houston Methodist Hospital, adding that this effect can be particularly prominent during dosage increases. This means that oral birth control may not be as effective.
The second factor is the link between polycystic ovarian syndrome (PCOS)—the leading cause of infertility in women—and insulin resistance.
“Insulin resistance will dysregulate the ovarian cycle,” Sadhu says. Insulin resistance can lead to infertility by disrupting hormones such as estrogen and testosterone, which are related to fertility; and it can affect the release of eggs from the ovaries. When patients start taking GLP-1 agonists, this reduces their insulin resistance, which boosts fertility.
However, the effects of these drugs on pregnancy are still unknown, which means that it’s important for patients to talk with their doctors about any plans for becoming pregnant, as well as strategies for contraception, which may include adding in a second method to augment oral contraceptive pills, or switching to a different method.
Treating addiction
Since Ozempic and Mounjaro have been become more common, patients have been reporting several unexpected side effects, such as a diminished desire to smoke or drink. Although more research is needed, it’s thought that the part of the brain that is responsible for food cravings overlaps with the part of the brain that is responsible for cravings for substances of abuse, says Luba Yammine, an addiction researcher at UTHealth Houston.
For doctors working in the field, earlier versions of these GLP-1 drugs showed tremendous potential as anti-addiction medications.
“We have far fewer medications available” for treating addiction and many patients report difficulties accessing these, says Christian Hendershot, an addiction researcher at the University of North Carolina School of Medicine. The field also receives less research funding compared with other diseases.
For Yammine, she first became interested in studying the effect of GLP-1 agonists on addiction while working in primary care, where she had several patients who were smokers with diabetes. Yammine would counsel her patients on quitting smoking, prescribing nicotine patches or the medication buproprion, to help them quit. But most of the time these strategies failed.
“It’s hard to quit smoking, period,” Yammine says. “The vast majority of smokers want to quit, but even with the use of these therapies, many of them are not successful.”
To help these smokers with their diabetes she would prescribe GLP-1 agonist medications, only to discover when they returned for a follow-up that they had quit smoking. When she asked them what happened, their answer was that suddenly their cravings vanished. “That was a very interesting finding,” Yammine says.
This happened often enough that Yammine decided to explore the impact of these GLP-1 receptor agonists on addiction through a clinical trial.
Yammine and her collaborators led a pilot study , in which 46 percent of the participants who received exanetide, plus nicotine patches and smoking cessation counseling, were able to quit, compared to 26 percent of participants who received nicotine patches, counseling, and a placebo. Yammine and her collaborators are now following up with a larger trial. They are also planning a separate trial with semaglutide.
For the patients in the study who received exanetide, their post-cessation weight was 5.6 pounds lower than those who received the placebo, a side effect that can help offset the weight gain that is often associated with quitting smoking.
“This weight gain is very problematic,” Yammine says, adding that many patients are either afraid to quit or relapse due to concerns about weight gain, while it can also put them at heightened risk for developing weight-related conditions, such as type 2 diabetes.
For Arnold, who was enrolled in a follow up trial that Yammine is conducting, the months in which she was participating in the trial was characterized both by a calmness surrounding her efforts to quit, as well as minimal weight gain. Since the trial has ended, she’s been able to maintain her efforts to quit smoking, although she gained a little weight. “I don’t have cravings,” Arnold says. “It’s this weight gain that is bothering me.”
Arnold, who works for an HVAC company, would really like to go back on exanetide, but as is the case with so many other patients who have experienced benefits from GLP-1 receptor agonists, she’s finding that it’s too expensive to do so. Just one month’s supply costs about $1,000, and without FDA approval for its use as an anti-addiction drug, most health insurance companies won’t pay for it.
Related Topics

How ultra-processed food harms the body and brain

Here's what happens to your body when you quit smoking

Just one pregnancy can add months to your biological age

Why heart attacks are rising in young adults—and what to watch out for

These common U.S. snack ingredients are banned or restricted abroad
- Environment
- Perpetual Planet
History & Culture
- History & Culture
- Mind, Body, Wonder
- Paid Content
- Terms of Use
- Privacy Policy
- Your US State Privacy Rights
- Children's Online Privacy Policy
- Interest-Based Ads
- About Nielsen Measurement
- Do Not Sell or Share My Personal Information
- Nat Geo Home
- Attend a Live Event
- Book a Trip
- Inspire Your Kids
- Shop Nat Geo
- Visit the D.C. Museum
- Learn About Our Impact
- Support Our Mission
- Advertise With Us
- Customer Service
- Renew Subscription
- Manage Your Subscription
- Work at Nat Geo
- Sign Up for Our Newsletters
- Contribute to Protect the Planet
Copyright © 1996-2015 National Geographic Society Copyright © 2015-2024 National Geographic Partners, LLC. All rights reserved
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
Kidney diseases articles within Nature Reviews Nephrology
Research Highlight | 29 April 2024
Role of the gut microbiota in the pathogenesis of IgA nephropathy
- Ellen F. Carney
Research Highlight | 26 April 2024
Progression and outcomes of rare kidney diseases
- Susan J. Allison
Review Article | 26 April 2024
Applications of SGLT2 inhibitors beyond glycaemic control
Here, the authors discuss the beneficial effects of sodium–glucose cotransporter 2 (SGLT2) inhibitors for a range of clinical outcomes beyond glucose lowering, including kidney and cardiovascular protection. They also discuss the need for implementation and adherence initiatives to help translate the benefits of these agents into real-world clinical outcomes.
- Daniel V. O’Hara
- , Carolyn S. P. Lam
- & Meg J. Jardine
Review Article | 25 April 2024
Post-translational modifications in kidney diseases and associated cardiovascular risk
Chronic kidney disease (CKD) is associated with several alterations in protein post-translational modifications. Here, the authors examine the evidence of these alterations, their links with CKD progression and cardiovascular risk in patients with CKD, and their potential clinical applications.
- Heidi Noels
- , Vera Jankowski
- & Joachim Jankowski
News & Views | 24 April 2024
Not every organ ticks the same
A new study describes the development of proteomics-based ageing clocks that calculate the biological age of specific organs and define features of extreme ageing associated with age-related diseases. Their findings support the notion that plasma proteins can be used to monitor the ageing rates of specific organs and disease progression.
- Khaoula Talbi
- & Anette Melk
Comment | 23 April 2024
Considerations of sex as a binary variable in clinical algorithms
Clinical algorithms that are used to guide medical decision-making often include sex as a variable. However, binary considerations of sex and/or gender might introduce bias due to potentially inaccurate assumptions about sex and gender-specific physiology, hormones and exposures. An equity-focused approach to sex and gender is essential when using clinical algorithms to ensure health equity across populations.
- Dinushika Mohottige
- , Samira Farouk
- & Selma Feldman Witchel
Review Article | 19 April 2024
Calcium signalling and transport in the kidney
Calcium reabsorption along the nephron is essential for calcium homeostasis and whole-body electrolyte balance. Here, Staruschenko et al. highlight signalling pathways and molecules involved in renal calcium handling in health and disease, and discuss progress in the integration of systems-level and molecular understanding of calcium transport and regulation.
- Alexander Staruschenko
- , R. Todd Alexander
- & Daria V. Ilatovskaya
Comment | 17 April 2024
Thiazides in kidney transplant recipients: skin in the game
Clinical trial data suggest that thiazides and thiazide-like drugs could be beneficial for blood-pressure lowering in patients with severe chronic kidney disease. However, prolonged exposure to these photosensitizing drugs could translate into increased risk of squamous cell carcinoma and post-transplant diabetes in the already extremely vulnerable kidney transplant population.
- Steven Van Laecke
Review Article | 17 April 2024
Epithelial cell states associated with kidney and allograft injury
This Review describes parallels in the injury mechanisms that underlie acute kidney injury, chronic kidney disease and allograft injury, and explains how our understanding of the molecular changes that occur in epithelia in the context of kidney disease may contribute to the therapeutic targeting of specific epithelial cell phenotypes for the treatment of transplantation complications.
- Christian Hinze
- , Svjetlana Lovric
- & Kai M. Schmidt-Ott
Editorial | 03 April 2024
Kidney disease: a global health priority
The prevalence of kidney disease and its associated morbidity and mortality continue to rise. This crisis cannot be tackled unless kidney disease is made a global public health priority.
Review Article | 03 April 2024
Combination therapy for kidney disease in people with diabetes mellitus
Several new drug classes have been demonstrated to improve kidney outcomes in people with diabetes mellitus. Here, the authors examine the evidence for the efficacy and safety of combination treatment to reduce the progression of diabetic kidney disease.
- Daniël H. van Raalte
- , Petter Bjornstad
- & Hiddo J. L. Heerspink
Consensus Statement | 03 April 2024
Chronic kidney disease and the global public health agenda: an international consensus
Addressing the burden of non-communicable diseases is a global public health priority. In this joint Consensus Statement, the American Society of Nephrology, the European Renal Association and the International Society of Nephrology highlight the need to recognize kidney disease as a key driver of premature mortality, in addition to other non-communicable diseases already prioritized by the World Health Organization.
- Anna Francis
- , Meera N. Harhay
- & Vivekanand Jha
Comment | 02 April 2024
The global landscape of kidney registries: immense challenges and unique opportunities
Kidney registries are essential to understanding the burden of kidney disease and facilitating the development of sustainable and effective programs for kidney disease prevention and care. Key barriers to implementation of registries at a global scale include funding and data quality. These issues warrant the attention of the global nephrology community.
- Christopher H. Grant
- , Fergus J. Caskey
- & Samira Bell
Research Highlight | 28 March 2024
Sex differences in kidney metabolism and DKD
Research Highlight | 26 March 2024
Switching off SOX9 for epithelial recovery after AKI
- Monica Wang
Clonal haematopoiesis and AKI
Consensus Statement | 05 March 2024
Clinical practice recommendations for kidney involvement in tuberous sclerosis complex: a consensus statement by the ERKNet Working Group for Autosomal Dominant Structural Kidney Disorders and the ERA Genes & Kidney Working Group
Care for patients with tuberous sclerosis complex (TSC) should be coordinated by a multidisciplinary team. This Consensus Statement, which involved input from nephrologists, urologists, geneticists, radiologists, interventional radiologists and pathologists as well as patient representatives, provides an overview of TSC-associated kidney manifestations and outlines current recommendations for the management of kidney involvement in TSC.
- Djalila Mekahli
- , Roman-Ulrich Müller
- & John Bissler
Review Article | 05 March 2024
Role of biophysics and mechanobiology in podocyte physiology
In this Review, the authors examine the biophysical and biomechanical properties that influence podocyte physiology as they integrate and adapt to stimuli from their dynamic environment within the glomerular capillaries. The authors also discuss how dysregulation and loss of biomechanical resilience in podocytes can contribute to kidney disease.
- Jonathan Haydak
- & Evren U. Azeloglu
Research Highlight | 29 February 2024
The renal glucagon receptor is essential to kidney metabolic and homeostatic functions
Research Highlight | 28 February 2024
A CAAR NK cell approach to eliminate pathogenic autoantibody-secreting cells
Research Highlight | 26 February 2024
Pericyte–stem cell crosstalk in ccRCC
Review Article | 06 February 2024
Sirtuins in kidney health and disease
This Review summarizes the roles of sirtuins in kidney development, physiological processes and the pathogenesis of acute and chronic kidney diseases. The authors also highlight the potential of sirtuins as therapeutic targets to limit human kidney disease and renal ageing.
- Luca Perico
- , Giuseppe Remuzzi
- & Ariela Benigni
Research Highlight | 01 February 2024
Macrophages clean out the tubules
Research Highlight | 30 January 2024
Effects of SGLT2 inhibitors on the metabolic environment and uraemic toxins
News & Views | 29 January 2024
A united vision for cardiovascular–kidney–metabolic health
Improved understanding of the interrelated nature of cardiovascular, kidney and metabolic (CKM) health, the development of novel risk prediction equations, and the availability of powerful new therapies provide an opportunity to change the course of CKM health. Achieving such change at a population level will require additional advances to deliver equitable interdisciplinary care.
- Susan E. Quaggin
- & Benjamin Magod
Review Article | 29 January 2024
The multifaceted links between hearing loss and chronic kidney disease
Chronic kidney disease is associated with a graded and independent excess risk of sensorineural hearing loss. This Review describes how disruption of shared signalling pathways that are important for the development of both the ear and the kidney and/or the presence of clinical drivers, such as specific medications or treatments, may underlie these associations.
- Dina Greenberg
- , Norman D. Rosenblum
- & Marcello Tonelli
Review Article | 25 January 2024
The changing landscape of HIV-associated kidney disease
The availability of antiretroviral therapy has led to a transformation in the spectrum of kidney diseases associated with HIV infection. This Review describes the changing pattern of kidney diseases associated with HIV infection, their risk factors, methods of evaluating kidney function in patients with HIV and current therapeutic approaches.
- Nina E. Diana
- & Saraladevi Naicker
Comment | 22 January 2024
Amplifying the voices of patients with kidney disease
All patients with kidney disease have the right to have a say in their own clinical care, the provision of health services and research into kidney disease. Patient empowerment and advocacy, especially for those whose views are seldom heard, can be enhanced by working together in communities.
- Miranda Scanlon
Review Article | 22 January 2024
Metabolic alterations in hereditary and sporadic renal cell carcinoma
Renal cell carcinoma is a metabolic disease linked to a variety of alterations in genes that regulate cellular metabolism. Here, the authors examine cell-intrinsic metabolic alterations in hereditary and sporadic renal cell carcinoma, and how they can be exploited to develop novel therapeutic interventions.
- Nathan J. Coffey
- & M. Celeste Simon
Comment | 18 January 2024
Health policy for universal, sustainable and equitable kidney care
Treatment of chronic kidney disease requires a comprehensive approach including universal access to early diagnosis and to medications that can slow disease progression. Such equitable access is not only an ethical requirement but can also reduce the financial and human costs of advancing kidney and cardiovascular disease.
- Ricardo Silvariño
- & Laura Solá
Review Article | 02 January 2024
Translating B cell immunology to the treatment of antibody-mediated allograft rejection
Antibody-mediated rejection is a key mechanism in allograft loss. Here, the authors examine advances in B cell biology and how they can inform the development of new therapies to prevent or mitigate antibody-mediated rejection, with the goal of improving transplantation outcomes.
- Peter S. Heeger
- , Maria Carrera Haro
- & Stanley Jordan
Viewpoint | 02 January 2024
New and emerging therapies for diabetic kidney disease
The theme of World Kidney Day 2024 is “kidney health for all — advancing equitable access to care and optimal medication practice”. To mark this event, Nature Reviews Nephrology invited five researchers from different geographical regions worldwide to discuss the impact of new and emerging therapies for diabetic kidney disease on patient care as well as the barriers that must be overcome to ensure equitable access to these therapies.
- Ricardo Correa-Rotter
- , Louise J. Maple-Brown
- & Ifeoma I. Ulasi
Year in Review | 21 December 2023
Single-cell genomics sheds light on kidney tissue immunity
The widespread availability of single-cell and single-nuclear genomic tools has enabled unbiased and high-dimensional assessment of tissue immunity in the kidney. The application of these technologies to human and mouse kidney samples, combined with spatial transcriptomics, has yielded unexpected insights into how resident and infiltrating immune cells maintain tissue homeostasis and drive disease.
- Andrew P. Stewart
- & Menna R. Clatworthy
Year in Review | 20 December 2023
Reaping the rewards of mechanistic discovery in glomerular disease
Several successfully completed clinical trials of novel therapies in glomerular disease were reported in 2023. Building on important mechanistic discoveries about disease onset and progression over the past several years, these therapies raise hope that multiple options will be available to reduce the risk of kidney failure in glomerular disease.
- Arpita Joshi
- & Laura H. Mariani
Year in Review | 14 December 2023
New evidence of the impact of mitochondria on kidney health and disease
Several publications from 2023 have substantiated the importance of altered NAD synthesis in kidney injury and disease progression. Now, NAD deficiency has been linked to the release of mitochondrial RNA and activation of pathways that induce inflammation. Another enzyme that governs mitochondrial function, PCK1, has also now been linked to kidney disease.
- Thomas Verissimo
- & Sophie de Seigneux
Year in Review | 01 December 2023
Targeted identification of risk and treatment of diabetic kidney disease
Basic discovery and clinical trials in diabetic kidney disease (DKD) have continued to be reported in 2023 despite the disruption of research activity by COVID-19 in recent years. Advances in clinical trials and emerging ways to diagnose, monitor and treat DKD dominate the current literature.
- Sarah J. Glastras
- & Carol A. Pollock
Research Highlight | 27 November 2023
Renoprotective effects of sparsentan: clinical trial evidence in IgA nephropathy and FSGS
Targeting april to slow progression of iga nephropathy.
Review Article | 22 November 2023
Mechanisms and consequences of sex differences in immune responses
Sex differences in immune cell function and immune responses affect the development and outcome of diverse diseases. Here, the authors review current understanding of sex differences in immunity. They describe the key mechanisms that mediate sex differences in immune responses and discuss the functional relevance of such differences for immune-related diseases.
- Shannon E. Dunn
- , Whitney A. Perry
- & Sabra L. Klein
Review Article | 20 November 2023
Differences in the epidemiology, management and outcomes of kidney disease in men and women
Improved understanding of kidney disease from a sex- and gender-specific perspective is needed to improve patient care. Here, the authors discuss differences in the epidemiology, management and outcomes of acute kidney injury, chronic kidney disease and kidney failure in men and women.
- Nicholas C. Chesnaye
- , Juan Jesus Carrero
- & Kitty J. Jager
News & Views | 16 November 2023
Kidney xenotransplantation edges closer to the clinic
The demand for kidney transplants is far from met by human donors — a problem that may be solved by the clinical translation of porcine kidney xenotransplantation. A new paper describes the development of genetically ‘humanized’ pigs, the kidneys of which kept nephrectomized cynomolgus macaques alive for up to 2 years.
- Eckhard Wolf
- & Bruno Reichart
Review Article | 26 October 2023
Clonal haematopoiesis, ageing and kidney disease
Clonal haematopoiesis of indeterminate potential (CHIP) is associated with increased risk of disease, including cardiovascular and kidney disease. Here, the authors discuss the consequences of CHIP across various organ systems, including direct and indirect effects on kidney health.
- Caitlyn Vlasschaert
- , Matthew B. Lanktree
- & Pradeep Natarajan
Research Highlight | 25 October 2023
Taking kidney temperatures to detect rejection
Review Article | 23 October 2023
Transport and barrier mechanisms that regulate ciliary compartmentalization and ciliopathies
The compartmentalized structure of primary cilia is maintained via interconnected barrier and active transport systems and underlies its unique composition and function. This Review describes the major compartmentalizing pathways that occur at the cilium and how insights into cilia transport and barrier mechanisms have shed light on the mechanisms underlying ciliary diseases.
- Ailis L. Moran
- , Laura Louzao-Martinez
- & Oliver E. Blacque
Review Article | 19 October 2023
Oxidative stress and the role of redox signalling in chronic kidney disease
Although potentially harmful in excess, reactive oxygen species (ROS) also act as signalling molecules and contribute to cell survival. This Review describes the relevance of ROS to physiological processes and disease pathogenesis with a focus on the kidney. The authors also outline the current status of clinical trials that aim to target ROS signalling in humans.
- Seiji Kishi
- , Hajime Nagasu
- & Naoki Kashihara
Review Article | 18 October 2023
TRPM channels in health and disease
The family of melastatin-like transient receptor potential (TRPM) channels comprises eight multifunctional cation channels. Here, the authors examine the functional role of each TRPM channel, including insights from channelopathies, and discuss the implications for kidney homeostasis and pathology.
- Vladimir Chubanov
- , Michael Köttgen
- & Thomas Gudermann
News & Views | 02 October 2023
MSC therapy for diabetic kidney disease and nephrotic syndrome
New clinical studies suggest that mesenchymal stem cell (MSC) therapy can have positive clinical effects, potentially via immunomodulation, in patients with diabetic nephropathy or nephrotic syndrome. These trials suggest that the therapy is safe, but adverse reactions highlight the need to examine the source and functional attributes of MSCs closely.
- & Lilach O. Lerman
Review Article | 27 September 2023
Acute kidney injury in patients with burns
Here, the authors discuss the pathophysiology of acute kidney injury (AKI) in patients with burns, approaches to prevention and management of AKI in this population and the application of AKI biomarkers and artificial intelligence approaches to guide treatment and predict short-term and long-term outcomes.
- Matthieu Legrand
- , Audra T. Clark
- & Marlies Ostermann
Research Highlight | 25 September 2023
Gene therapy in a model of nephrotic syndrome
Research Highlight | 21 September 2023
Use of kidneys from SARS-CoV-2 infected donors
Browse broader subjects
Browse narrower subjects.
- Acid, base, fluid, electrolyte disorders
- Acute kidney injury
- Chronic kidney disease
- Fanconi syndrome
- Glomerular diseases
- Interstitial disease
- Lupus nephritis
- Nephrosclerosis
- Obstructive nephropathy
- Paediatric kidney disease
- Phosphorus metabolism disorders
- Polycystic kidney disease
- Renal artery stenosis
- Renal calculi
- Renal cancer
- Renal fibrosis
- Thrombotic microangiopathies
- Toxin-induced nephropathy
- Urinary tract infection
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Newsletters and Deep Dive digital magazine
Spotlight on kidney disease: Driving change for patients

Katherine Forbes, director of innovation and enterprise at Kidney Research UK, discusses the unique, evolving role of medical research charities in facilitating collaborative partnerships and new ways of working to accelerate research and drive innovations designed to improve patient outcomes.
The figures are stark. The number of patients with, or at risk of, kidney disease is growing and threatens to overwhelm an already stretched health and care system in the UK.
The recently published health economics report, ’Kidney Disease: a UK public health emergency’, commissioned by Kidney Research UK, estimates there are 7.2 million people in the UK currently living with chronic kidney disease - more than 10% of the entire population. Furthermore, over three million people are living with later stages of chronic kidney disease (CKD, stages 3-5) and almost four million are believed to have as yet undiagnosed early-stage kidney disease, which could progress and require treatment.
The total economic burden of kidney disease in the UK is £7 billion, with £6.4 billion attributable to direct costs to the NHS – about 3.2% of NHS budgets across the four nations. There is currently a further estimated £372 million in productivity loss to the UK economy from missed work due to dialysis alone. This is on top of the significant impact on and huge reduction in quality of life for patients with advanced CKD.
Fast forward to 2033, and the number of patients with end stage kidney disease requiring dialysis could increase by nearly 400% to 143,000 and the total economic burden of kidney disease on the UK could rise to a staggering £13.9 billion.
The challenge is not just for more effective, personalised treatment options for those patients who have kidney disease, but we also urgently require improved approaches to diagnostics, risk prediction, and prevention. To achieve all of this, we must focus not only on discovery, but also accelerating these new innovations to the clinic, where they will improve patient experiences and outcomes. We also need to pilot new approaches to transforming the patient pathway, taking a whole system approach. No single organisation can do this alone.
New approaches to drive innovation for kidney patients
Gone are the days when medical research charities only funded research. This remains their core business, as it provides much needed scientific progress, while building expertise and capacity for the future.
Today, medical research charities also recognise the urgent role they can play in driving and progressing research and - crucially - supporting the translation of this research to bridge the gap between basic scientific discoveries and their practical application that will benefit patients in clinical settings. Medical research charities provide and unlock an unrivalled depth of knowledge and expertise in their disease areas: both in-house and through their networks of researchers, whether academic or clinical, alongside patient advisers. We recognise that patient-led research is at the epicentre of driving innovation and new, collaborative approaches are needed if we are to going to reduce health inequalities and achieve better health outcomes.
The awards and categories of research grant calls, such as Fellowships, PhD awards, whilst creating a pipeline of translational research, also helps to build and sustain career pathways for those researchers who may be our future innovators, or become globally respected key opinion leaders. But charities are also at the cutting edge of understanding advancements in technologies, such as artificial intelligence (AI) and imaging and, importantly, the gaps in infrastructure required to support the research community (academic, clinical, or commercial) to accelerate innovation. For example, the recent launch of the Kidney Data Science Catalyst - a partnership between the British Heart Foundation (BHF) Data Science Centre at Health Data Research UK and Kidney Research UK - is designed to further enable approved researchers to securely access, link, and analyse existing UK health data, which will expedite the search for better ways to prevent, diagnose, and treat kidney disease.
Often overlooked, medical research charities are an essential component in the health innovation ecosystem, providing insight, resources, expertise, networks, and guidance to accelerate research and drive innovation. We recognise the urgent need to maximise the impact of research and support early-stage innovation, particularly in the context of increasing healthcare challenges and health system pressures.
Many charities (alongside angel investors, incubators, accelerators, and early-stage venture funds) are providing pre- seed and seed funding to start-ups in their earliest stages or, alternatively, supporting the advancement of technologies through philanthropic means, bringing together business and investment expertise - advisers, clinicians, and academics - to evaluate innovations, providing investor confidence now and in the future.
Beyond finance, early-stage innovators face significant hurdles, with successful translation depending on a combination of skills and expertise to deliver clinical validation, regulatory compliance, IP protection, market fit, market access, funding, and clinical and scientific excellence. Accelerator programmes, commercial upskilling, and support are essential to equip researchers with the best chance of success.
Putting patients at the centre of research
New products, diagnostics, and treatments would not be possible without patient involvement and engagement. Patient involvement is integral to the commercialisation journey and post-market surveillance of medical innovations. And at the heart of every medical research charity lies a “patient first” philosophy; our missions are inherently centred around improving the health and well-being of individuals living with specific medical conditions. This patient-centric approach shapes strategy, funding decisions, and ultimately the decision on which research initiatives to support.
Through awareness campaigns, policy advocacy, and patient engagement initiatives, medical research charities mobilise the patient community, ensuring that their collective voice is heard by researchers, developers, and decision-makers. This first-hand knowledge allows charities to inform and influence the direction of research and innovation. But patient involvement doesn’t stop there. The patient community also wants to help drive and accelerate innovation, whether through participation in clinical trials, patient-focused clinical study protocol reviews, or independent patient studies to evidence the impact of symptoms or need for new treatments. Additionally, in providing written or oral evidence of the need for new drugs and treatments at NICE HTA committees.
Collaboration is key. As with many medical research charities, at Kidney Research UK, we recognise our role as a ‘trusted broker’, a facilitator, a convenor, and driver of change. Across the public, private, academic, and health sectors forces must unite to harness the collective power to change the lives of patients for the better.

kidney research
BMS, J&J challenges to Medicare negotiations are thrown out
In another setback for the pharma industry, a US federal judge has rejected a bid to overturn the Medicare pricing negotiation brought by Bristol-Myers Squibb and Johnson

Innovation as Strategy: Enabling life sciences of the future
Explore “Innovation as Strategy” framework, providing a guide for employing innovative strategies in life sciences.

Deep Dive: Market Access 2024
In this edition of Deep Dive, Unpacking complex choreography in the biologics patent dance, Alexion examines the urgent need for accelerated access programmes for rare disease treatments, and Putna

How doctors are interacting with content in 10 data trends
It will come as no surprise to anyone in the healthcare space that doctors today are under an inordinate amount of pressure.

Patient Centricity to Integration: Enhancing Cancer Outcomes
We are living in an era of unprecedented advances in cancer treatments with transformative therapies being regularly approved.
2nd ADC Toxicity Summit 2024
Improving Prediction & Translation of ADC Toxicities to Drive More Tolerable ADCs Successfully Into & Through Clinical Development

15th World Bispecific Summit 2024
Radically Optimize Bi, Tri & Multispecific Antibodies to Enhance Target Discovery, Mechanistic Diversity & Clinical Translation to Maximize the Therapeutic Index & Enhance Combi
Get in-depth news, opinions and features on pharma and healthcare sent straight to your inbox
Kidney Research UK
Research charities.
Katherine Forbes is director of innovation and enterprise at Kidney Research UK. Her prior career spanned the private, public, and health sectors, primarily in strategy development and partnership roles in economic development, innovation, and health and life sciences. Forbes is passionate about the role the charity sector can play in driving innovation and supporting economic growth.
Editor's Picks
Enter xaira, with $1bn for its ai in drug discovery platform, bms preps for car-t growth with $380m cellares deal, eu approves pfizer antibiotic for superbug infections, endeavor raises $132.5m for fibrosis, cancer drugs, fda initiative puts ar/vr at heart of home health drive.
California to sell state-branded Narcan generic to cut costs
California has said it will start selling its own generic version of overdose reversal agent naloxone in another example of the use of government-level purchasing power to

Fixing clinical trial data management
It’s 2024, and in most clinical trials, data is still being moved from the EHR to the EDC manually – with employees reading data from one screen and typing it onto another.

IMAGES
VIDEO
COMMENTS
Here are nine of the biggest headlines from the nephrology research field from 2023. Breakthrough #1: New atlas of human kidney cells to help unlock kidney disease research | National Institutes of Health (NIH) In July, the National Institutes of Health (NIH) announced it had created a "comprehensive atlas of the human kidney."
Kidney Research Institute, New York, NY, USA. Peter Kotanko. ... Harold Simmons Center for Kidney Disease Research and Epidemiology, California, USA. Kamyar Kalantar-Zadeh.
He says a new class of drugs, SGLT2 inhibitors, is being called a game changer.The drugs were originally designed to treat diabetes — a main cause of chronic kidney disease.. Medicines in the SGLT2 inhibitor class include canagliflozin, dapagliflozin and empagliflozin. "In large trials, we observed groundbreaking success with those medications in slowing down the progression of chronic ...
Kidney diseases are hereditary and nonhereditary disorders that affect the kidney. Diabetes mellitus and high blood pressure are important risk factors for kidney disease. A new study describes ...
Atom. RSS Feed. Chronic kidney disease (CKD) is defined as a progressive loss of renal function that lasts for more than 3 months, and is classified according to the degree of kidney damage ...
Adjuvant pembrolizumab therapy after surgery for renal-cell carcinoma was approved on the basis of a significant improvement in disease-free survival in the KEYNOTE-564 trial. Whether the results r...
A total of 6609 patients underwent randomization. During a median of 2.0 years of follow-up, progression of kidney disease or death from cardiovascular causes occurred in 432 of 3304 patients (13. ...
More specifically, the researchers showed that renal tubular cells, which line the tiny tubes inside kidneys, release IL-11 in response to kidney damage.This turns on a signaling cascade that ...
The drug works by exploiting kidney cyst cells' vulnerability to oxidative stress — a state of imbalance between damaging free radicals and beneficial antioxidants. In a study employing two mouse models of the disease, the researchers found that the drug dramatically shrank kidney cysts without harming healthy kidney cells.
INTRODUCTION. Kidney disease is a prevalent global health problem. A new analysis suggested that the global prevalence of chronic kidney disease (CKD) in the year 2017, was 9.1% (697.5 million cases)[1,2].The World Health Organization has estimated that as many as 5 to 10 million people die annually from kidney diseases worldwide[].By 2040, CKD is projected to be the fifth leading cause of ...
New Genetic Variants for Chronic Kidney Disease Identified. Feb. 7, 2024 — Scientists have identified new genes that may play a role in chronic kidney disease. They analyzed data from more than ...
The lack of human kidney models has limited the ability to develop new drugs to treat or prevent kidney disease. The Kidney Tissue Atlas comprises maps of 51 main kidney cell types that include rare and novel cell populations, 28 kidney cellular states that represent injury or disease, a repository of raw gene data, and interactive 3D models of ...
Chronic kidney disease (CKD) represents a global public health crisis, but awareness by patients and providers is poor. Defined as persistent abnormalities in kidney structure or function for more than three months, manifested as either low glomerular filtration rate or presence of a marker of kidney damage such as albuminuria, CKD can be identified through readily available blood and urine tests.
The new research demonstrated that the commonly used benchmark for defining kidney disease — a glomerular filtration rate of less than 60 milliliters per minute — often results in older adults ...
Why it Matters: Kidney disease is a leading cause of death in the U.S. and affects 1 in 7 adults — 90% of whom are unaware they even have the disease. Hypertension and diabetes are the most common causes of kidney disease, and the CDC estimates that treatment in 2019 cost Americans more than $100 billion.
Chronic kidney disease: highlights from research Sponsor feature: CKD is a hidden threat, but the treatment landscape is evolving Subjects. Diseases ... News & Views 24 APR 24.
P. AugustN Engl J Med 2023;388:179-180. Chronic kidney disease (CKD) will be the fifth highest cause of years of life lost worldwide by 2040. 1 CKD is defined as a sustained estimated glomerular ...
Media Advisory. Friday, April 26, 2024. Analysis identifies 50 new genomic regions associated with kidney cancer risk. What. In a new analysis of genetic susceptibility to kidney cancer, an international team of researchers has identified 50 new areas across the genome that are associated with the risk of developing kidney cancer. These insights could one day be used to advance our ...
April 30, 2021. Today, the U.S. Food and Drug Administration approved Farxiga (dapagliflozin) oral tablets to reduce the risk of kidney function decline, kidney failure, cardiovascular death and ...
Chronic kidney disease (CKD) has emerged as one of the most prominent causes of death and suffering in the 21 st century. Due in part to the rise in risk factors, such as obesity and diabetes mellitus, the number of patients affected by CKD has also been increasing, affecting an estimated 843.6 million individuals worldwide in 2017. 1 Although ...
New research in mice has identified a genetic factor that might help explain why some people with diabetes are more prone than others to kidney complications of the disease. Between 10 and 30 percent of people with either type 1 or type 2 diabetes develop diabetic kidney disease (DKD), making diabetes a major risk factor for loss of kidney ...
Research Updates and News. Scientists discover potential treatment approaches for polycystic kidney disease; New atlas of human kidney cells to help unlock kidney disease research; Being hospitalized with acute kidney injury may increase risk for rehospitalization and death; Resolving key details of polycystic kidney disease genetics
A new publication from NURTuRE - the first national UK chronic kidney disease cohort study with a linked biobank, developed as a collaboration between Kidney Research UK, research groups and pharmaceuticals companies - has been published in Nephrology, Dialysis and Transplantation.Alongside highlighting important patterns in kidney function and use of prescription medications in chronic ...
Silver Spring, MD—March 16, 2018—Today, the National Kidney Foundation (NKF), along with the Food and Drug Administration (FDA) and the European Medicines Agency (EMA) concluded a scientific workshop collaboration to review the results of a major, multi-year meta-analysis examining the largest compilation of data ever collected on chronic kidney disease (CKD).
Chronic kidney disease: highlights from research. Illuminating genetic risk, disrupting fibrosis and intercepting inflammation. A kidney organoid containing nephron epithelial cells and stromal ...
The new LifeArc-Kidney Research UK Centre for Rare Kidney Diseases is one of four new centres to be funded by the non-profit medical charity, LifeArc, with the aim of overcoming these barriers that ordinarily prevent new tests and treatments reaching patients. Globally, there are more than 300 million people living with rare diseases.
Research is showing that these new weight-loss drugs can help treat conditions from addiction to kidney disease—and may even be contributing to a boom of "Ozempic babies." By Rachel Fairbank ...
New research published in the American Journal of Kidney Diseases suggests that a higher intake of plant-based protein could reduce the risk of developing chronic kidney disease (CKD). In the ...
Basic discovery and clinical trials in diabetic kidney disease (DKD) have continued to be reported in 2023 despite the disruption of research activity by COVID-19 in recent years.
The recently published health economics report, 'Kidney Disease: a UK public health emergency', commissioned by Kidney Research UK, estimates there are 7.2 million people in the UK currently ...