An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Hypertens
- v.2017; 2017


Prevalence and Associated Risk Factors of Hypertension: A Cross-Sectional Study in Urban Varanasi
Shikha singh.
1 Department of Community Medicine, Institute of Medical Sciences, Banaras Hindu University, Varanasi 221005, India
Ravi Shankar
Gyan prakash singh.
2 Division of Biostatistics, Department of Community Medicine, Institute of Medical Sciences, Banaras Hindu University, Varanasi 221005, India
Hypertension is a major public health problem and important area of research due to its high prevalence and being major risk factor for cardiovascular diseases and other complications. Objectives . (1) To assess the prevalence of hypertension and its associated factors and (2) to estimate awareness, treatment, and adequacy of control of hypertension among study subjects. Methods and Materials . A community based cross-sectional study with multistage sampling design was conducted among urban population of Varanasi. A modified WHO STEPS interview schedule on 640 study subjects aged 25–64 years was used. Results . The prevalence of hypertension was 32.9% (male: 40.9%, female: 26.0%). Mean systolic and diastolic BP were 124.25 ± 15.05 mmHg and 83.45 ± 9.49 mmHg, respectively. Higher odds of being hypertensive were found in male subjects, eldest age group, married subjects, subjects of upper socioeconomic status, illiterate subjects, and retired subjects. Tobacco and alcohol consumption, overweight, obesity, and abdominal obesity were also associated with hypertension. Out of the total hypertensive 211 subjects, only 81 (38.4%) were aware about their hypertension status; out of those, 57 (70.4%) were seeking treatment and 20 (35.08%) had their blood pressure adequately controlled. Conclusion . Around one-third of the subjects were hypertensive and half of the study subjects were prehypertensive in this area. The awareness, treatment, and control of high blood pressure were also very low.
1. Introduction
Hypertension is a major public health problem due to its high prevalence all around the globe [ 1 – 4 ]. Around 7.5 million deaths or 12.8% of the total of all annual deaths worldwide occur due to high blood pressure [ 5 ]. It is predicted to be increased to 1.56 billion adults with hypertension in 2025 [ 6 ].
Raised blood pressure is a major risk factor for chronic heart disease, stroke, and coronary heart disease. Elevated BP is positively correlated to the risk of stroke and coronary heart disease. Other than coronary heart disease and stroke, its complications include heart failure, peripheral vascular disease, renal impairment, retinal hemorrhage, and visual impairment [ 5 ].
Hypertension (or HTN) or high blood pressure is defined as abnormally high arterial blood pressure. According to the Joint National Committee 7 (JNC7), normal blood pressure is a systolic BP < 120 mmHg and diastolic BP < 80 mm Hg. Hypertension is defined as systolic BP level of ≥140 mmHg and/or diastolic BP level ≥ 90 mmHg. The grey area falling between 120–139 mmHg systolic BP and 80–89 mmHg diastolic BP is defined as “prehypertension” [ 7 , 8 ]. Although prehypertension is not a medical condition in itself, prehypertensive subjects are at more risk of developing HTN [ 1 ].
It is a silent killer as very rarely any symptom can be seen in its early stages until a severe medical crisis takes place like heart attack, stroke, or chronic kidney disease [ 8 – 10 ]. Since people are unaware of excessive blood pressure, it is only through measurements that detection can be done. Although majority of patients with hypertension remain asymptomatic, some people with HTN report headaches, lightheadedness, vertigo, altered vision, or fainting episode [ 11 ].
There are several factors predisposing to hypertension. These factors vary from country to country and even there is difference between urban and rural regions of the same place [ 12 ]. Realizing the effect of urbanization on our collective health, World Health Organization has chosen “Urbanization and Health” as the theme for World Health Day 2010 [ 13 ]. Urbanization is considered a determinant of health and one of the key drivers of noncommunicable diseases (NCDs), especially in low- and middle-income countries (LMICs) [ 14 ]. Urban people are more at risk of these diseases as compared to their rural counterparts. As per the findings of National Family Health Survey (NFHS-4), the prevalence of hypertension, obesity, and blood glucose in urban area of Uttar Pradesh was 10.5%, 23.9, and 9.9%, respectively. However, the prevalence of the same phenomenon was 8.3%, 10.8%, and 8.2%, respectively in rural area [ 15 ]. It is clear that all the parameters are having higher prevalence in urban area as compared to rural area. Rapid urbanization, increasing elderly population, mechanization, sedentary life, and dietary changes act together as a web of risk factors which entangles people in it and leads to several chronic diseases. In order to take effective prevention measures, identification of the risk factors is an essential prerequisite. This study intends to generate information on prevalence of hypertension and their associated risk factors in urban area of Varanasi. In addition, it will also look into the awareness and control of hypertension among the study subjects.
2. Materials and Methods
2.1. study area.
Varanasi is an Indian city on the bank of Ganges in Uttar Pradesh. It has total population of 3676841 as per Census 2011. As per Census 2011, out of total population, 52% people live in urban areas, while 48% live in the rural areas. There are 90 Census enumeration wards in Varanasi district. Out of these 90 wards, 5 wards were selected by using simple random sampling.
2.2. Study Design and Sample Size
A community based cross-sectional study was carried out among the people aged 25 to 64 years living in the selected study area. The sample size for the present study was calculated by taking most probable prevalence of hypertension as 50% and permissible error as 5% with 95% confidence interval. Fixing the permissible error as 50%, the minimum sample size was calculated as n = 384. Since sampling procedure was multistage, hence considering the design effect, the sample size was further increased by one and half times. Considering the nonresponse rate of 10% the final sample size in study was fixed as 640. In the present study, a prior written informed consent was also taken from the participants. Prior written informed consent was taken by the participants.
2.3. Sampling Methodology
A multistage sampling was used for this study. There were three stages and for each stage different sampling design was used.
At first, out of these 90 wards, 5 wards were selected by using simple random sampling. At second stage, from each selected ward the households were further selected by using systematic random sampling and probability proportional to size was done. At the third stage, one member of target age group was interviewed from selected household. If the selected family has more than one available eligible person then one was chosen randomly by using lottery method. In case of nonavailability of eligible person in a selected household, at the time of survey, the adjacent household was selected.
2.4. Selection of Study Subjects
2.4.1. inclusion criteria.
Individuals aged 25–64 years in the selected study area who gave consent for participation were considered.
2.4.2. Exclusion Criteria
Individuals who are unable to give response due to serious physical or mental illness and with whom anthropometry measurements cannot be performed were excluded from the study.
2.5. Tools of the Study
Interview schedule [modified and pretested WHO stepwise approach to chronic disease risk factor surveillance (STEPS)], Libra weighing machine, steel anthropometry rod, measuring tape, and Omron BP Machine were used.
2.6. Techniques of the Study
In all study participants, a structured and pretested interview schedule was administered to obtain data on sociodemographic parameters.
2.6.1. Blood Pressure Measurement
Blood pressure was measured two times on the right arm of the selected subject using automatic electronic device (OMRON HEM-7261). The average of two readings was used.
2.6.2. Anthropometric Measurements
All the anthropometric measurements were done by the following standardized technique. Weight was measured by Libra weighing machine having an accuracy of 0.1 kg and height was measured by using a steel anthropometry rod with accuracy of 0.1 cm using standard techniques. Body Mass Index was calculated using the following formula: BMI = weight (kg)/height (mt) 2 . Based on BMI obtained, the subjects were classified into different categories according to the WHO global classification [ 16 ]. Waist circumference (in cm) was measured using a nonstretchable measuring tape. Waist circumference was measured at the smallest horizontal girth between the costal margins and the iliac crest at the end of expiration. Hip circumference (in cm) was measured at the broadest part of the hips by using nonstretchable measuring tape. Waist-to-hip circumference (WHR) was calculated by dividing waist circumference by hip circumference [ 17 ].
2.7. Ethical Consideration
Ethical approval was obtained from the Institute Ethical Committee of the Institute of Medical Sciences, Banaras Hindu University Varanasi. Prior written consent was taken from the subjects who volunteered to participate in the study. Identified hypertensive subjects were referred to the nearby clinic for treatment.
2.8. Definitions Used
- (i) Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) classification was used for hypertension [ 8 ].
- (ii) Hypertension is defined as systolic BP level of ≥140 mmHg and/or diastolic BP level of ≥90 mmHg or being previously diagnosed as hypertensive by any health professional. The area falling between 120–139 mmHg systolic BP and 80–89 mmHg diastolic BP is defined as “prehypertension” [ 8 ].
- (iii) Isolated diastolic hypertension (IDH) having a systolic blood pressure ≤ 140 mmHg and diastolic blood pressure ≥ 90 mmHg and isolated systolic hypertension (ISH) having a systolic blood pressure ≥ 140 mmHg and diastolic blood pressure < 90 mmHg was used to diagnose IDH and ISH, respectively.
- (iv) Awareness was defined as history of hypertension based on diagnosis by a healthcare provider. Treatment was defined as taking any medication or other treatment for hypertension in the last two weeks prior to the survey and control was defined as blood pressure < 140 and <90 mmHg in subjects who were taking medications
- (v) WHO International BMI classification: BMI < 18.5 was classified as “underweight”; <16.00, “severe thinness”; 16.00–16.99, “moderate thinness”; 17.00–18.49, “mild thinness”; 18.50–24.99, “normal range”; BMI ≥ 25.00, “overweight” ; 25.0–29.99, “preobese” ; ≥30.00, “obese” ; 30.00–34.99, “obese class I” ; 35.00–39.99, “obese class II”; and >40.00, “obese class III.”
Revised modified BG Prasad socioeconomic classification scale, January 2014.
- (vii) Current daily smokers are defined as those who were currently smoking cigarettes, bidis, or hookah daily. Current daily smokeless tobacco users are defined as those who were currently using chewable tobacco products, gutka, naswar, khaini, or zarda paan daily. Current alcohol drinkers are defined as those who reported to consuming alcohol within the past one year [ 17 ].
- (viii) Physical activity was measured in three domains that is activity at work, to and from places, and recreational activities as well as time spent sitting. The interview schedule also covered type of activity (vigorous and moderate) at work and for recreational activities. Information was also collected on the number of days in a week spent on different activities and time spent in a day for each activity was also recorded [ 17 ]. Those who were not active in any domain were defined as “inactive,” those who were vigorously active in any category were defined as “vigorously active,” and the rest were “moderately active.”
2.9. Data Processing
The information obtained from the survey was entered into a database developed for the study, using SPSS 16.0 program. Descriptive statistics (mean and standard deviation) were calculated for continuous variables and frequencies and percentages were calculated to summarize qualitative data. Other statistical tests like chi-square test and ANOVA were applied. Logistic regression was applied to identify the risk factors for hypertension. A significance level of 0.05 was used.
A total of 640 study subjects were interviewed for the survey. Out of these, 301 (47%) were male subjects and 339 (53%) were female. The median age (±SD) of the study subjects was 39.0 (±11.9) years and for male and female it was 40.0 (±11.9) years and 38 (±11.8) years, respectively. Regarding religion and caste of the study subjects, around 96% subjects were Hindu and majority of the subjects were in general category, respectively. Majority of the study subjects were married and one-third of the subjects belonged to the upper socioeconomic class. Mean (±SD) BMI of the study subjects was 24.11 ± 3.94 kg/m 2 ; for men it was 23.78 ± 3.95 kg/m 2 and for women it was 24.41 ± 3.92 kg/m 2 . According to Body Mass Index (BMI), more than one-third of the study subjects were either overweight or obese. With regard to abdominal obesity as measured by waist circumference, 40% subjects were at risk ( Table 2 ).
Background characteristics of the study subjects ( N 640).
Table 3 depicts the mean values of systolic and diastolic BP according to age and gender. The mean systolic and diastolic BP of all the study subjects were 124.2 ± 15.0 mmHg and 83.4 ± 9.5 mmHg, respectively. In men, the highest mean systolic BP and mean diastolic BP were among the eldest age group and preceding eldest age group (45–54 years), respectively, while in female the highest mean value of systolic and diastolic BP both were among the 45–54-year age group. With regard to systolic BP, there was significant difference among all the age groups among both male and female study subjects and the same was with diastolic BP as well. The prevalence of isolated systolic BP was found to be 10.6% [95% CI: (8.27–13.37)] and isolated diastolic BP was 19.7% [95% CI: 16.6–23.18]. The proportion was higher in male (14.8%) as compared to female (6.8%). Among both groups (male and female), prevalence was higher among the eldest age group. The prevalence of isolated diastolic BP was higher among male subjects (28.1) against female subjects (12.2%). It was the highest among the second oldest age group among male and oldest age group in female subjects. With regard to systolic BP, age was associated with hypertension status among both genders, whereas diastolic BP was associated with age in male subjects only. There was no association between age and diastolic BP in female subjects.
Mean systolic and diastolic blood pressure (mm hg) and prevalence (%) of isolated systolic hypertensive and isolated diastolic hypertensive by age and gender.
# Excluding known hypertensive.
The overall prevalence of hypertension was 32.96% [95% CI: (29.4–36.7)]. The sex specific prevalence was 40.9% [95% CI: 35.5–46.5] for male and 26.0% [95% CI: 21.6–30.9] for female. Prehypertension was prevalent in 45.9% [95% CI: (40.3–51.5)] of men and 38.05% [95% CI: (33.0–43.2)] of women. In men, hypertension was significantly associated with age but in women, age does not have any effect on their hypertension status. History of hypertension or the prediagnosed cases of hypertension was more among female (6.7%) as compared to male (5.9%) subjects ( Table 4 ).
Prevalence of hypertension and prehypertension by gender and age groups among the study subjects ( N 640).
Table 5 shows the associated factors of prehypertension and hypertension. Gender, age, marital status, occupation, education status, tobacco use, and physical activity were significantly associated with the hypertension status of the study subjects ( p < 0.05). Both the rate of prehypertension and hypertension were higher among male. Hypertension was more prevalent in the 45–54 years, while prehypertension was more in the 35–44-year age group. Being married and government servant were found to be risk factors for both hypertension and prehypertension. Hypertension was found to be more among illiterate subjects, and with regard to prehypertension, primary educated subjects suffered more. Study subjects from lower and upper socioeconomic status were almost equal victims of hypertension. Tobacco use and alcohol use were found to be risk factors for being hypertensive in the study subjects. Although alcohol use was not significantly associated with hypertension status but rate of hypertension was higher among the alcohol users.
Prevalence of prehypertension and hypertension ∗ according to sociodemographic characteristics and behavioral risk factors.
∗ Excluding known hypertensive.
The binary logistic regression analysis showed that odds of being hypertensive were higher among the male subjects (OR: 1.97), eldest age group (OR: 6.49), married subjects (OR: 2.34), uneducated subjects (OR: 1.17), retired subjects (OR: 3.66), and those who were from upper socioeconomic status (1.31). With regard to anthropometric risk factors, being overweight (OR: 1.99), being obese (OR: 3.57), and having abdominal obesity (OR: 1.73) had higher odds of hypertension. Tobacco use (OR: 1.86), alcohol use (OR: 1.55), and nonvegetarian diet (OR: 1.10) also had higher odds of being hypertensive. Gender, age, marital status, occupation, BMI, abdominal obesity, and tobacco use were significantly associated with hypertension. Education, socioeconomic status, and alcohol use were not statistically associated with hypertension. Being female, younger in age, unmarried, highly educated, and staying away from any kind of addiction could serve as protective factors against hypertension ( Table 6 ).
Univariate analysis for the association of hypertension and sociodemographic characteristics, anthropometric measurements, and behavioral risk factors ( N 640).
Out of the total subjects with hypertension, around one-third of the subjects were aware of their condition. Out of those who were aware, 70% were seeking treatment. Only a third of the treated subjects with hypertension had their blood pressure adequately controlled ( Figure 1 ). Females were marginally more aware of their hypertensive status as compared to male counterparts (see Table 4 , history of hypertension). As age, education status, and socioeconomic status were advancing, the awareness of hypertensive status among study subjects was also increasing (not shown in the table).

Flow diagram showing awareness, treatment, and adequacy of control of hypertension among study subjects.
4. Discussion
India is a developing country and like other developing countries, it is going through a rapid demographic and epidemiological transition. In all such transitions, nutrition is the key ingredient and plays prime role. This cross-sectional community based study identified a high prevalence of prehypertension and hypertension in urban areas of Varanasi, which was 41.7% and 32.96%, respectively. Only a quarter of subjects were in the normal category, which highlights the escalating burden of this silent killer.
The prevalence of hypertension in the present study (32.96%) was higher in comparison with the prevalence reported in other studies [ 4 , 6 , 10 , 19 – 22 ]. Few studies reported the results in line with the present study [ 23 , 24 ]. According to World Health Organization (2015), the overall prevalence of hypertension in India was 23.5% and gender specific prevalence was 24.2% and 22.7% among the men and women, respectively [ 25 ].
The prevalence of prehypertension in the present study was 41.7% (male: 45.9% and female: 38.05%). The prevalence estimated in the present study was much higher than that estimated by Nellore (22.3%) [ 10 ] and Bihar (37.95%) [ 20 ]. The difference of prevalence observed between the present study and other studies with respect to hypertension and prehypertension could be due to social and cultural differences, dietary and lifestyle factors, and also the age span as well as the research methodology used.
Men exhibit higher prevalence of hypertension and prehypertension than their female counterparts (M: 40.9% and F: 26.0%) and (M: 45.9% and F: 38.05%), respectively. Similarly, various studies came out with the higher percentage of hypertension in men than women [ 20 , 22 , 23 , 26 – 29 ]. One of the possible explanations for this gender disparity in hypertension prevalence could be partially due to biological sex difference and partially due to behavioral risk factors like smoking, alcohol consumption, or physical activity. We speculate that absentia from alcohol and smoking might be few of those protective factors against hypertension in women. Other than that, women are more interested in health care services utilization and also more frequently report their poor health and therefore they are more likely to have better health [ 6 , 30 ].
Age was found to be an important risk factor for hypertension. As the age was advancing so did the prevalence of hypertension among both the sexes. Similar findings were reported by few other studies also where advancing age was positively related to hypertension [ 1 , 6 , 19 , 21 , 22 , 26 , 31 , 32 ]. With increasing age, the aorta and arteries walls will be stiffened and this contributes to the high prevalence of hypertension in older age groups [ 4 ].
In the present study, marital status, education, occupation, socioeconomic status, BMI, abdominal obesity, tobacco use, alcohol use, and physical activity were significantly associated with the hypertension.
Low literacy level and being too rich were associated with hypertension. The higher education level was negatively correlated to hypertension in the present study. These studies also supported this finding [ 6 , 12 , 33 ]. We speculate that it could be due to the reason that higher education imparts better knowledge and information about hypertension and subsequently those people with higher education had a healthier lifestyle.
Table 5 revealed that education was significantly associated with hypertension ( χ 2 = 17.049, df = 6 and p value = 0.009); however, when adjusted effect of education on hypertension was observed by logistic regression, then no statistical association was observed. Though some studies had shown a significant association of these two variables [ 6 , 12 ], in the study performed in the state of Kerala [ 33 ], insignificant association between education and hypertension was observed. We speculate that this insignificant association could be due to very few subjects in the illiterate and less educated category. There are so many studies which do not refute the finding of the present study that higher socioeconomic status is a risk for hypertension [ 3 , 22 , 24 , 32 , 34 – 36 ]. We assume that better socioeconomic status imparts people with more purchasing power on fast and convenience foods and less physical activity which are already proven to be contributing risk factors for overweight and obesity that subsequently linked to hypertension.
The different anthropometric measurements like BMI, waist circumference, and hip circumference were taken into account to measure overweight, obesity, and central or abdominal obesity. This study showed that overweight and obesity measured by both BMI and waist circumference were major modifiable risk factors to develop hypertension. Overweight subjects had twofold risk of being hypertensive and obese had more than threefold risk for the same in comparison to underweight subjects in this study. There was positive relation observed between increasing BMI and increasing rate of hypertension, which was consistent with other studies [ 1 – 4 , 6 , 12 , 20 , 21 , 23 , 32 , 36 – 39 ]. South Asians have tendency of developing centralized obesity without developing generalized obesity and because of this waist circumference and waist-hip ratio are better measures of body fat [ 40 ]. Abdominal obesity (OR: 1.73) also found to be positively linked to high blood pressure in the present study. Various epidemiological and pathophysiological mechanisms explained the link between obesity and hypertension. One of the probable reasons behind this positive relation between obesity and hypertension could be that increased weight increases cardiac output and increased peripheral resistance of arterioles. Other than that, urbanization is also a cause of changes in dietary habits and reduced physical activity which leads to obesity and subsequently results in hypertension [ 4 ].
Interestingly, we have found inverse association between physical activity and hypertension. Hypertension was more among physically active subjects as compared to inactive subjects (OR: 0.63) but no statistically significant difference was found. Similar result was reported by other study conducted in Turkey [ 1 ]. The exact reason behind this is unknown and yet to be explored. We speculate that they had started physical activity probably under medical advice after being diagnosed for hypertension or other risk factors like overweight or obesity.
As per WHO report, alcohol consumption was the third largest risk factor in the developed countries and tobacco use was being the second major cause of death worldwide [ 17 ]. This study indicated the positive association between alcohol and tobacco use and hypertension. Hypertension was more prevalent in tobacco users (OR: 1.86) and alcohol users (OR: 1.55) as compared to nonusers. This finding is supported by other studies also [ 19 , 23 , 32 , 36 ]. But there are several other studies with contradictory findings [ 1 , 21 , 41 ]. Although not statistically significant, odds of being hypertensive were more among nonvegetarian (OR: 1.10) subjects, while vegetarian diet was proved to be protective against hypertension in this study. Several other studies reported the same result [ 3 , 19 , 33 , 34 ]. A study conducted in Bihar [ 20 ] refutes this finding and reported that vegetarian diet was positively associated with hypertension.
A recent review study revealed that hypertension awareness rate has been doubled from less than 30% in 1980s to around 60% in present among urban populations and less than 10% in 1980s to 35–40% presently among rural population. However, the treatment and control status is still low at around 30% in urban and 20% in rural areas [ 42 ]. Rate of awareness, treatment, and control in the present study was observed as 38.4%, 70.4%, and 35.08%, respectively. Previous study conducted in rural Varanasi reported hypertension awareness, treatment, and control (26.5%, 55.6%, and 40%), respectively [ 7 ].
5. Conclusion & Recommendation
From the results of this study, it can be concluded that the prevalence of both prehypertension and hypertension is very high in urban Varanasi. This makes the people of this area vulnerable to several chronic diseases and other unbearable health consequences. Specifically men are at more risk of being hypertensive than female. Increasing age is proved to be an independent risk factor for hypertension. Programs are needed to improve the surveillance systems and implementation of community based screening programs for early detection of hypertension is also needed. As the awareness of the hypertension status among hypertensive cases was very poor, improving health literacy to increase the awareness of hypertension is also the need of the hour. Interventions like weight management, increased physical activity, increased fruits and vegetables consumption, and reduction in tobacco and alcohol use are required and recommended.
Acknowledgments
The authors would like to thank all the participants for participating in the study.
Additional Points
Limitations of the Study . This study suffers from few of the following limitations. (i) One of the main limitations of this study was the cross-sectional design of the study which restricts examining causal associations. (ii) The study was only conducted in urban areas. (iii) Stress is a major risk factor for hypertension. It could also be considered in the present study for better results.
Conflicts of Interest
There were no conflicts of interest regarding the publication of this article.
- Open access
- Published: 01 May 2022
Interventions in hypertension: systematic review and meta-analysis of natural and quasi-experiments
- Tong Xia ORCID: orcid.org/0000-0001-7136-8361 1 ,
- Fan Zhao ORCID: orcid.org/0000-0002-1261-5841 1 &
- Roch A. Nianogo ORCID: orcid.org/0000-0001-5932-6169 1 , 2
Clinical Hypertension volume 28 , Article number: 13 ( 2022 ) Cite this article
7593 Accesses
6 Citations
3 Altmetric
Metrics details
Hypertension is an urgent public health problem. Consistent summary from natural and quasi-experiments employed to evaluate interventions that aim at preventing or controlling hypertension is lacking in the current literature. This study aims to summarize the evidence from natural and quasi-experiments that evaluated interventions used to prevent or control hypertension.
We searched PubMed, Embase and Web of Science for natural and quasi-experiments evaluating interventions used to prevent hypertension, improve blood pressure control or reduce blood pressure levels from January 2008 to November 2018. Descriptions of studies and interventions were systematically summarized, and a meta-analysis was conducted.
Thirty studies were identified, and all used quasi-experimental designs including a difference-in-difference, a pre-post with a control group or a propensity score matching design. Education and counseling on lifestyle modifications such as promoting physical activity (PA), promoting a healthy diet and smoking cessation consultations could help prevent hypertension in healthy people. The use of computerized clinical practice guidelines by general practitioners, education and management of hypertension, the screening for cardiovascular disease (CVD) goals and referral could help improve hypertension control in patients with hypertension. The educating and counseling on PA and diet, the monitoring of patients’ metabolic factors and chronic diseases, the combination of education on lifestyles with management of hypertension, the screening for economic risk factors, medical needs, and CVD risk factors and referral all could help reduce blood pressure. In the meta-analysis, the largest reduction in blood pressure was seen for interventions which combined education, counseling and management strategies: weighted mean difference in systolic blood pressure was − 5.34 mmHg (95% confidence interval [CI], − 7.35 to − 3.33) and in diastolic blood pressure was − 3.23 mmHg (95% CI, − 5.51 to − 0.96).
Conclusions
Interventions that used education and counseling strategies; those that used management strategies; those that used combined education, counseling and management strategies and those that used screening and referral strategies were beneficial in preventing, controlling hypertension and reducing blood pressure levels. The combination of education, counseling and management strategies appeared to be the most beneficial intervention to reduce blood pressure levels.
Cardiovascular diseases (CVD) represent the leading cause of death, accounting for one in three deaths in the United States (US) and worldwide [ 1 , 2 , 3 ]. One of their most potent risk factors, hypertension (also known as high blood pressure), is a common risk factor for CVD [ 3 , 4 ]. Approximately 40% of adults aged 25 and over had elevated blood pressure in 2008 [ 3 ]. What is more, hypertension is responsible for at least 45% of deaths due to heart diseases and 51% of deaths due to stroke worldwide [ 3 , 4 ]. In the US alone, the direct medical and indirect expenses from CVDs were estimated at approximately $329 billion in 2013 to 2014 [ 5 ]. Effective large-scale interventions to prevent or treat hypertension are therefore urgently needed to reverse this trend. Yet, as new and promising interventions are surfacing every day, the need for rigorous evaluation of these interventions to inform evidence-based policies and clinical practice is ever growing.
To this effect, several randomized clinical trials (RCT) have been conducted to evaluate interventions used to prevent hypertension or improve its control [ 6 , 7 , 8 ]. However, although RCTs represent the gold standard for evaluating the efficacy (i.e., impact under ideal conditions) of most health interventions because of their high internal validity [ 9 , 10 ], they are not always feasible, appropriate or ethical for the evaluation of certain types of interventions. Furthermore, results from RCTs are not always generalizable to populations or settings of interest due to the highly selected sample and because the intervention is generally conducted under more stringent conditions ( low external validity ) [ 11 ]. To evaluate the effectiveness of an intervention (i.e., impact under real conditions) and to increase the uptake and implementation of evidence-based health interventions in the communities of interests, other types of experimental designs have been proposed. One such example is natural and quasi-experiments. The terms “natural experiments” and “quasi-experiments” are sometimes used interchangeably. In this study, and as described by others [ 12 ], we will distinguish these two concepts. Natural and quasi-experiments are similar in that, in both cases, there is no randomization of treatments or exposures (i.e., no random assignment). They differ, however, in that, natural experiments are those that involve naturally occurring or unplanned events (e.g., a national policy, new law), while quasi-experiments involve intentional or planned interventions implemented (typically for the purpose of research/evaluation) to change a specific outcome of interest (e.g., a community intervention program). Furthermore, in natural experiments, the investigator does not have control over the treatment assignment whereas in quasi-experiments, the investigator has control over the treatment assignment [ 12 ]. These experiments include difference-in-difference (DID) designs, synthetic controls and regression discontinuity designs to name a few [ 13 , 14 , 15 ].
As utilization of natural and quasi-experiments is increasing in public health and in the biomedical field [ 13 , 14 , 15 ], more natural and quasi-experiments are being conducted to evaluate interventions targeted to prevent or control hypertension [ 16 , 17 , 18 , 19 ]. This could be due to recent development or the reframing of classical approaches for determining causality in natural and quasi- experiments [ 13 , 14 , 15 , 20 ]. However, unlike RCTs of interventions aiming to prevent hypertension or improve its control [ 6 , 7 , 8 ], consistent summary and synthesis of evidence from natural and quasi- experiments is lacking in the current literature. The primary aim of the current systematic review is to summarize the evidence from natural and quasi-experiments that have evaluated interventions used to prevent, control hypertension or reduce blood pressure levels. A secondary aim of this study is to conduct a meta-analysis to summarize intervention effectiveness.
Data sources and strategy
We searched PubMed, Embase and Web of Science from January 2008 to November 2018. This time frame was selected to encompass studies that would have likely benefited from recent development and improvement in natural and quasi- experiments [ 13 , 20 ]. Briefly, the search strategy consisted in intersecting keywords related to the study methods (e.g., natural experiments, quasi-experiments, DID, synthetic control, interrupted time series, etc.) with the environment or settings (e.g., community, nation, organization, etc.) and the outcome (e.g., hypertension, elevated blood pressure, etc.). The full search strategy is described in Table S 1 . This systematic review and meta-analysis were conducted according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) statement [ 21 ] (Fig. 1 ).
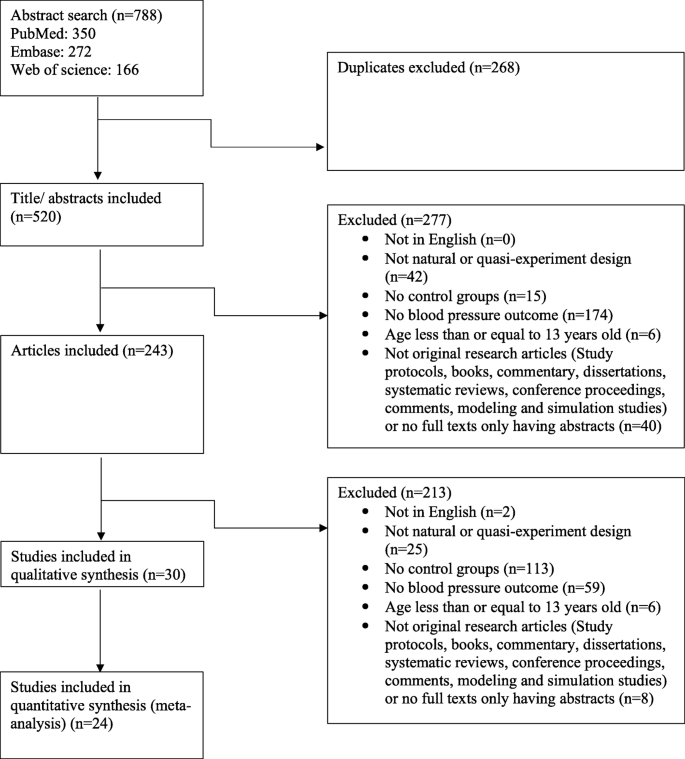
Study search and selection flow
Study selection
Two trained members (TX, FZ) screened abstracts and full-text articles. Disagreements were decided by a third member (RN). We included studies that used natural and quasi-experiments to evaluate interventions aimed at preventing hypertension, controlling hypertension or reducing blood pressure levels. The outcome measures were prevalence of hypertension and changes in mean blood pressure. Studies were excluded if they were not in English, were not a natural experiment or a quasi-experimental design, did not include a control group (as it has higher risk to internal validity due to the absence of comparison to adjust for time trends and confounding) [ 22 ], did not include blood pressure or hypertension as their outcome or included participants that were 13 years old or younger. In addition, we excluded studies that were not original research articles (e.g., study protocol, books, commentary, dissertations, conference proceedings, comments, systematic reviews, modeling and simulation studies), or had no full text available.
Data extraction and quality assessment
The following information was extracted: study design, sample size, study duration, data source, geographic location, participants’ socio-demographic characteristics, intervention types, intervention levels (e.g., individuals, community, school, clinic and national levels as suggested by the socio-ecological model [ 23 ]), behavior targeted and outcome measures (prevalence of hypertension or mean blood pressure change) (Table 1 , Table S 2 ).
The interventions were classified by strategies into four types:
Education and counseling: This subcategory includes strategies that aim at educating and providing knowledge and counseling to participants on lifestyle modifications (e.g., increasing physical activity (PA), eating better, avoiding or stopping smoking, etc.).
Management: This subcategory includes strategies that aim at monitoring patients’ metabolic factors and chronic diseases (e.g., blood pressure, cholesterol level, etc.) as well as patients’ adherence to medication. These strategies are generally done or facilitated by physicians, general practitioners (e.g., by assessing computerized clinical guidelines in the electronic health record management system), nurses, other staffs, or patients themselves.
Education, counseling and management: This subcategory combines education and counseling strategies with management strategies as described above.
Screening and referral for management: This subcategory includes strategies that aim at screening for (i.e., checking for the presence of) economic risk factors, medical needs, and CVD risk factors, followed by the referral of participants who screened positive to professionals who specialize in the management of those needs.
We also classified the interventions by settings into (1) community level; (2) health center level (i.e., primary care center or general practices), (3) organization level and (4) nationwide. In addition, we have classified the intervention by duration of the study into short-term (i.e., participants were followed for less than 12 months) and long-term (i.e., participants were followed for longer than or equal to 12 months).
We implemented the Cochrane Risk of Bias Tool for risk of bias and used the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) approach to assess the quality of the evidence for mean blood pressure change outcome [ 50 ], since the meta-analysis focused on this outcome. The risk of bias for studies included in this review could be found in Table S 3 and the quality of studies has also been summarized in Table S 4 .
Meta-analysis
To summarize the effectiveness of interventions on mean blood pressure changes, we also conducted a meta-analysis. Due to the high heterogeneity in the studies and interventions, we undertook a random-effects model and only summarized the effectiveness of intervention strategies by subgroup defined by intervention types, settings and duration. We estimated the weighted mean difference (WMD) of blood pressure and 95% confidence intervals (CIs). The studies included in the meta-analysis were only those whose outcomes were mean differences (MDs) in blood pressure ( n = 27) [ 16 , 19 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 ] as these studies provided the data needed for performing the meta-analysis. Three studies [ 38 , 39 , 43 ] were excluded as they did not provide enough information to compute the standard errors (SEs). To estimate the average effect of the intervention when not directly provided, we subtracted the before-and-after change in the intervention group from that in the control group or subtracted the intervention-to-control difference at follow-up to that at baseline (pre-post design with a control group). Methods to calculate intervention impact and SEs were outlined in the appendix (Figs. S 1 , S 2 , Table S 5 ).
We presented the meta-analysis results using forest plots (Table 2 , Fig. 2 , Figs. S 3 , S 4 ). We assessed the heterogeneity by using the I 2 (Table 2 , Fig. 2 , Figs. S 3 , S 4 ). We did not perform meta-regression as it is not recommended when the number of studies is small (< 10 studies per covariate) [ 51 ]. We assessed publication bias by using funnel plots of SEs (Figs. S 5 , S 6 , S 7 ). To test the robustness of our results, we performed sensitivity analyses by removing one study at a time from the pool of studies to assess its impact on the findings (Tables S 6 , S 7 , S 8 , Figs. S 8 , S 9 , S 10 ). Data were analyzed with Stata 15.1 (StataCorp LLC, College Station, TX, USA).
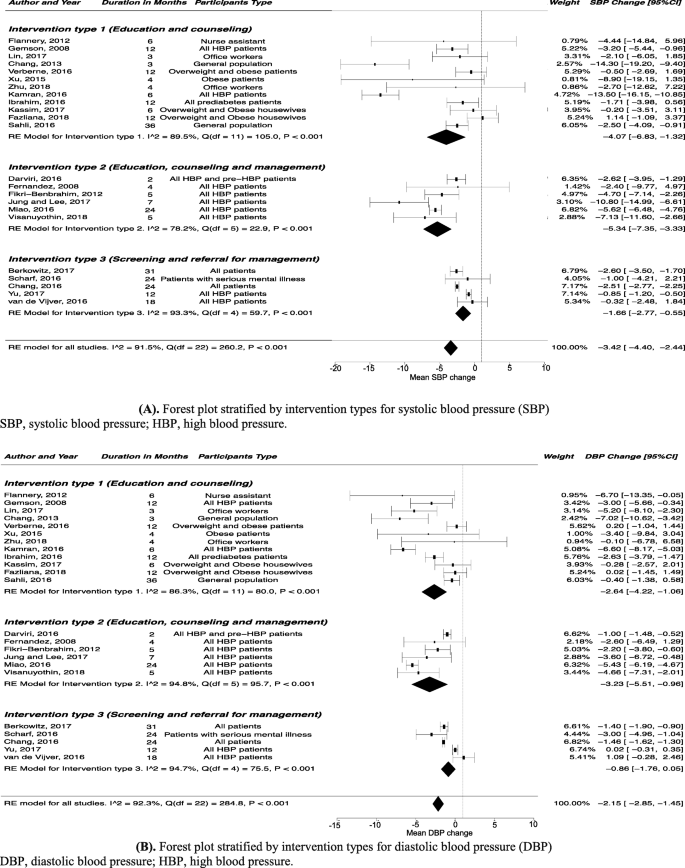
Forest plot stratified by intervention types for blood pressure. A Forest plot stratified by intervention types for systolic blood pressure (SBP). B Forest plot stratified by intervention types for diastolic blood pressure (DBP)
Overall, 788 titles of potentially relevant studies were identified and screened. In total, 545 were excluded and 243 full papers were retrieved, then 30 studies were included in the final sample ( Fig. 1 ) .
Study characteristics
Of the 30 studies included in this review [ 16 , 17 , 18 , 19 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 ], three studies reported changes in hypertension prevalence, among which one study reported preventing hypertension in the general population [ 24 ] and two studies reported blood pressure control in patients with hypertension [ 17 , 18 ]; 25 studies reported mean blood pressure changes [ 16 , 19 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 ]; two studies reported both outcome measures (changes in hypertension prevalence and mean blood pressure changes) [ 25 , 26 ]. Thirteen studies used education and counseling intervention strategies [ 24 , 25 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 ]; four studies used management intervention strategies [ 18 , 19 , 38 , 39 ]; seven studies combined education, counseling and management intervention strategies [ 26 , 40 , 41 , 42 , 43 , 44 , 45 ]; and six studies used screening and referral for management intervention strategies [ 16 , 17 , 46 , 47 , 48 , 49 ]. Fourteen studies followed participants for less than 12 months (i.e., short-term interventions) [ 17 , 26 , 27 , 29 , 30 , 32 , 33 , 34 , 36 , 40 , 41 , 42 , 43 , 45 ]. Twelve studies were conducted in the US [ 16 , 17 , 19 , 24 , 27 , 28 , 32 , 33 , 39 , 41 , 43 , 46 ] and most studies included both genders [ 16 , 17 , 18 , 19 , 24 , 25 , 26 , 28 , 29 , 30 , 31 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 ] and all racial/ethnic groups [ 16 , 17 , 18 , 19 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 ]. We found no natural experiments according to the definition used in this study (Table 1 , Table S 2 ).
Quality ratings
According to the Cochrane Risk of Bias Tool, most studies included in this review were found to have a high risk of bias ( Table S 3 ). This was so because the Cochrane Risk of Bias Tool was mostly designed for RCTs. Studies included in this review only used quasi-experiment designs and as such did not use randomization, allocation concealment, blinding of participants and personnel, and blinding of outcome assessment. Using the GRADE approach, the quality of evidence was deemed of low quality for the mean systolic blood pressure (SBP) and diastolic blood pressure (DBP) change outcome (Table S 4 ).
Studies that reported prevalence of hypertension in the general population or changes in the prevalence of controlled blood pressure in hypertension patients after intervention
Outcome of interest: prevention of hypertension in healthy people, education and counseling intervention strategies.
Two studies evaluated the education and counseling intervention strategies, and both found that those strategies could help prevent hypertension in healthy people [ 24 , 25 ]. One study in the US found that nutritional education and giving access to fruits and vegetables through community gardens helped reduce hypertension prevalence (61.0% vs. 45.0%; P < 0.01), whereas the prevalence of hypertension in the control group did not change (46.7% vs. 49.8%; P = 0.39) [ 24 ]. The other study in Africa showed that an education strategy which promoted PA and healthy diet and combined with free smoking cessation consultations could help reduce the prevalence of hypertension (22.8% vs. 16.2%; P = 0.01), compared to that in control group (14.0% vs. 15.1%; P = 0.52) [ 25 ].
Outcome of interest: improvement of hypertension control in patients with hypertension
Management intervention strategies.
A study in the US showed that patients whose general practitioners accessed the computerized clinical practice guideline at least twice a day improved their hypertension control compared to the patients whose general practitioners never accessed the computerized clinical practice guideline ( P < 0.001) [ 18 ].
Education, counseling and management intervention strategies
A study in the US found that patients who received education about hypertension and did home blood pressure monitoring had a better control of their hypertension compared to the control group ( P = 0.03) [ 26 ].
Screening and referral for management intervention strategies
A study in the US showed that for White patients, interventions which involved a coordinator who identified and reached out to patients not meeting CVD goals and linked them to management programs could improve the odds of blood pressure control (odds ratio, 1.13; 95% CI, 1.05 to 1.22) compared to no intervention [ 17 ].
Studies that reported mean blood pressure changes after intervention
Outcome of interest: reduction in mean blood pressure.
Seven [ 25 , 27 , 28 , 29 , 30 , 34 , 35 ] of twelve [ 25 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 ] (58.3%) studies showed that the education and counseling intervention strategies could help reduce mean blood pressure compared to the control group. Education and counseling interventions targeting lifestyle modifications (e.g., diet and PA) have been found effective in reducing blood pressure in the workplace. A study in US female nursing assistants found that combining education and continuing motivation (e.g., counseling on questions of interventions and receiving feedback) on diet and PA led to more reduction in DBP compared to the control group who only received the education (MD, − 6.70 mmHg; 95% CI, − 13.35 to − 0.05) [ 27 ]. Two other studies also found that multi-component lifestyle interventions in the workplace including sharing health information by messages, putting up posters, using pedometers, and giving education on PA could help healthy employees or employees with hypertension lower blood pressure [ 28 , 29 ]. Besides the workplace, interventions implemented in a community setting also appeared to work in reducing blood pressure. A study that included participants age 55 years or more in Asia found that people who attended 60-min Tai Chi three times per week for 12 weeks had a larger reduction in SBP (MD, − 14.30 mmHg; 95% CI, − 19.20 to − 9.40) and in DBP (MD, − 7.02 mmHg; 95% CI, − 10.62 to − 3.42) compared to people maintaining usual daily activities [ 30 ]. Another study among patients with hypertension in Asia found that education about the nutritional behavior and guidelines from dietary approaches to stop hypertension (DASH) approach could help reduce blood pressure more in the intervention group compared to the control group who only received the instruction booklets used in intervention group (SBP: MD, − 13.50 mmHg; 95% CI, − 16.15 to − 10.85; DBP: MD, − 6.60 mmHg; 95% CI, − 8.17 to − 5.03) [ 34 ]. One study in Africa also showed that education on promoting PA and healthy diet, combined with free smoking cessation consultations could help reduce SBP in the intervention group [ 25 ].
Two [ 19 , 39 ] of three [ 19 , 38 , 39 ] (66.7%) studies showed that the management intervention strategies could help reduce mean blood pressure compared to the control group. A study in the US showed that supporting diabetes patients’ self-management of hypertension by team-based chronic models (e.g., proactive patient outreach, depression screening, and health coaching) could decrease more DBP over a 6-month period compared to the usual care (MD, − 1.13 mmHg; 95% CI, − 2.23 to − 0.04) [ 19 ]. A study among hypertension patients in Asia showed that improving the social health insurance system by increasing outpatient expenditure reimbursement ratio could help reduce more SBP (MD, − 2.9 mmHg; P = 0.01) compared to outpatient expense not covered [ 38 ]. The other study among diabetes patients in the US also showed that team-based treatment with trained staff on medical management and self-management helped lower SBP (MD, − 0.88 mmHg; P = 0.01), but it did not compare the MD between treatment and control group [ 39 ].
Six [ 26 , 40 , 42 , 43 , 44 , 45 ] of seven [ 26 , 40 , 41 , 42 , 43 , 44 , 45 ] (85.7%) studies showed that the combination of education, counseling and management intervention strategies led to more blood pressure reduction compared to the control group. One study among hypertension patients in Europe found that management of stress by biofeedback-assisted relaxation and lifestyle counseling on diet and PA reduced more SBP (MD, − 2.62 mmHg; 95% CI, − 3.96 to − 1.29) and DBP (MD, − 1.00 mmHg; 95% CI, − 1.90 to − 0.93) compared to the control group [ 40 ]. One study among hypertension patients in the US also found that education about hypertension and home blood pressure monitoring could help reduce more SBP (MD, − 4.70 mmHg; 95% CI, − 7.14 to − 2.26) and DBP (MD, − 2.20 mmHg; 95% CI, − 3.80 to − 0.60) compared to controls [ 26 ]. A study among 65-year-and-older hypertension patients in Asia found that the intervention group who received education on hypertension management, community-based eHealth monitoring, and monthly telephone counseling had more reduction in SBP (MD, − 10.80 mmHg; 95% CI, − 14.99 to − 6.61) compared to the control group who only received a poster about hypertension management [ 42 ]. A study among hypertension patients in the US also showed that interventions on lifestyle modifications, and nutritional, pharmacological therapies as well as medication adherence lowered SBP and DBP compared to the control group [ 43 ]. A study among hypertension patients in Asia found that integration of preventive-curative services delivery and cooperation among village-town-county physicians for education on lifestyle modifications, taking blood pressure drugs regularly and monitoring the blood pressure could help reduce blood pressure more in the intervention group [ 44 ]. The other study in Asia also found that integrated program with health education on home blood pressure monitoring and hypertension measurement skills could help reduce blood pressure more in the intervention group [ 45 ].
Four [ 16 , 46 , 47 , 48 ] of five [ 16 , 46 , 47 , 48 , 49 ] (80.0%) studies showed that the screening and referral for management intervention strategies could help reduce more blood pressure compared to the control group. Screening for medical or economic needs followed by offering treatment and resources has been found helpful. One study in the US found that screening for unmet needs in primary care and offering those who screened positive some resources could reduce SBP (MD, − 2.6 mmHg; 95% CI, − 3.5 to − 1.7]) and DBP (MD, − 1.4 mmHg; 95% CI, − 1.9 to − 0.9) in patients [ 16 ]. The other study among patients with serious mental illness in the US also found that using registry for general medical needs and outcomes, screening and referral for general medical illness prevention and treatment could help reduce more DBP compared to controls (MD, − 3.00 mmHg; 95% CI, − 4.96 to − 1.04) [ 46 ]. Assessing and screening CVD risk followed by a management program has also been found beneficial to reduce blood pressure. A study in Europe showed that participating in CVD risk assessment and management program, including screening and tailored strategies for lifestyle advice on CVD risk factors could reduce more SBP (MD, − 2.51 mmHg; 95% CI, − 2.77 to − 2.25) and DBP (MD, − 1.46 mmHg; 95% CI, − 1.62 to − 1.29) compared to controls [ 47 ]. A study among hypertension patients in Asia also found that a standardized CVD-risk assessment, a hypertension complication screening and adherence to medications could help reduce more blood pressure compared to the usual care [ 48 ].
Meta-analysis of the effectiveness of interventions on mean blood pressure change
Intervention type sub-group analysis.
The largest blood pressure reduction (SBP: WMD, − 5.34 mmHg; 95% CI, − 7.35 to − 3.33; DBP: WMD, − 3.23 mmHg; 95% CI, − 5.51 to − 0.96) was seen for interventions that combined education, counseling and management intervention strategies (Table 2 , Fig. 2 ).
Intervention setting sub-group analysis
Participants who experienced interventions implemented in community settings (WMD, − 3.77 mmHg; 95% CI, − 6.17 to − 1.37) and in health center settings (WMD, − 3.77 mmHg; 95% CI, − 5.78 to − 1.76) had large SBP reduction. Participants experienced interventions implemented in organization settings had large DBP reduction (WMD, − 3.92 mmHg; 95% CI, − 5.80 to − 2.04) (Table 2 , Fig. S 3 ).
Intervention duration sub-group analysis
Participants who were followed for less than 12 months (i.e., short-term interventions) had a large reduction in blood pressure (SBP: WMD, − 6.25 mmHg; 95% CI, − 9.28 to − 3.21; DBP: WMD, − 3.54 mmHg; 95% CI, − 5.21 to − 1.87) and participants who were followed for longer than or equal to 12 months (i.e., long-term interventions) had a moderate reduction in blood pressure (SBP: WMD, − 1.89 mmHg; 95% CI, − 2.80 to − 0.97; DBP: WMD, − 1.33 mmHg; 95% CI, − 2.11 to − 0.55) (Table 2 , Fig. S 4 ).
We summarized the evidence from quasi-experiments that have evaluated interventions used to (1) prevent hypertension in the general population, (2) improve hypertension control in patients with hypertension or (3) reduce blood pressure levels in both the general population and patients.
In this systematic review, we found that the intervention strategies such as (1) education and counseling, (2) management, (3) education, counseling and management and (4) screening and referral for management were beneficial in preventing, controlling hypertension or reducing blood pressure levels. In particular, we found that education and counseling on lifestyle modifications (i.e., promoting PA, healthy diet, smoking cessation consultations) could help prevent hypertension in healthy people. The use of computerized clinical practice guidelines by general practitioners, education and management of hypertension, screening for CVD goals and referral to management could help improve hypertension control in patients with hypertension. The education and counseling on lifestyle modifications, the monitoring of patients’ metabolic factors and chronic diseases (e.g., blood pressure, cholesterol level, etc.) as well as patients’ adherence to medication, the combined education and management of hypertension, the screening for economic risk factors, medical needs, and CVD risk factors, followed by the referral to management all could help reduce blood pressure levels. Our study is one of the few systematic reviews that have summarized the evidence from quasi-experiments on hypertension prevention and control. A previous systematic review [ 52 ] which summarized evidence from cluster-randomized trials and quasi-experimental studies had been conducted and found that education, counseling and management strategies were also beneficial in controlling hypertension and reducing blood pressure. It showed that educating healthcare providers and patients, facilitating relay of clinical data to providers, promoting patients’ accesses to resources were associated with improved hypertension control and decreased blood pressure [ 52 ]. Another systematic review which summarized evidence from RCTs found that several interventions including blood pressure self-monitoring, educational strategies, improving the delivery of care, and appointment reminder systems could help control hypertension and reduce blood pressure [ 6 ]. Another study also found that community-based health workers interventions including health education and counseling, navigating the health care system, managing care, as well as giving social services and support had a significant effect on improving hypertension control and decreasing blood pressure [ 53 ]. A review from observational studies and RCT evidence from the US Preventive Services Task Force found that office measurement of blood pressure could effectively screen adults for hypertension [ 7 ].
Our review did not find natural experiments studies according to the definition used in this study. Quasi-experimental designs included DID, propensity score matching and pre-post designs with a control group (PPCG). While PPCG designs generally involve two groups (intervention and control) and two different time points (before and after the intervention), DID designs generally involve two or more intervention and control groups and multiple time points [ 13 ]. In this review, we did not include pre-post without a control group design because of its higher risk to internal validity due to the absence of comparison to adjust for time trends and confounding [ 22 ]. The findings in this review, highlight that, quasi-experiments are increasingly used to evaluate the effectiveness of health interventions for hypertension management when RCTs are not feasible or appropriate. For instance, several studies included in our systematic review often indicated that RCTs would have been difficult to be implemented given that the intervention was conducted in a particular setting such as a pragmatic clinical setting [ 16 , 43 , 45 , 48 ], a community setting [ 24 , 35 , 36 , 42 ], or a real-world organizational setting [ 33 ] because of ethical concerns and human resources issues. Another reason why quasi-experiments were chosen had to do with the need for translation and generalizability of the evidence in a specific community setting [ 32 ]. In fact, RCTs are not always generalizable to the communities or settings of interests [ 11 ]. The growing interest in and hence the increase in the use of natural and quasi-experiments in public health may be due to the recognition and realization of its usefulness in evaluating health interventions [ 14 , 54 ].
Given that there was high heterogeneity in the studies included in this systematic review, we have performed a random effects model and have only presented the subgroup analysis by intervention types, settings and duration of the study. Overall, our study suggested that interventions that combined education, counseling and management strategies appeared to show a relatively large beneficial effect for reducing blood pressure. However, our finding should be interpreted with caution due to the high-risk of bias and lower quality of evidence given the quasi-experimental nature of the designs (as opposed to evidence from randomized experiments). Nevertheless, the findings here can give us some insights on the benefit of interventions such as education, counseling and management, especially given that our findings are in line with previous studies [ 6 , 8 , 52 , 55 ]. Given that RCTs are not always feasible or appropriate, scientists should develop more rigorous methods to increase the internal validity of non-randomized studies. Compared to previous studies, one systematic review with meta-analysis including cluster-randomized trials and quasi-experiment studies showed that multi-component interventions which incorporated education of health care providers and patients, facilitating relay of clinical data to providers, and promoting patients’ accesses to resources could reduce more blood pressure compared to controls [ 52 ]. A recent systematic review with meta-analysis of RCTs also reported that interventions which included blood pressure self-monitoring, appointment reminder systems, educational strategies, and improving the delivery of care showed beneficial effects on lowering blood pressure [ 6 ]. Another systematic review and meta-analysis of RCTs also showed that self-measured blood pressure monitoring lowered SBP by 3.9 mmHg and DBP by 2.4 mmHg at 6 months compared to the usual care group [ 8 ]. One systematic review and meta-analysis of RCTs found that diet improvement, aerobic exercise, alcohol and sodium restriction, and fish oil supplements reduced blood pressure as well [ 55 ].
Limitations
This review has some limitations. First, the definition of natural and quasi-experiments is not consistent across fields. Second, the main limitation in most if not all the quasi-experimental study designs noted in this review was the potential for unobserved and uncontrolled confounding, which is a threat to internal validity and could lead to biased findings. Third, our findings may not be generalizable to all countries and settings as we only included studies published in the English language in this review. Fourth, as is the case in most other reviews, we could have missed relevant studies despite our best attempt to conduct a thorough search of the literature. Fifth, we found that most studies included in this study had a high risk of bias. It might be because we used the Cochrane Risk of Bias Tool to assess bias which was designed for examining RCTs. Studies in this review only used quasi-experiment designs and did not have randomization, allocation concealment, blinding of participants and personnel, and blinding of outcome assessment. Sixth, studies generally reported the measure of intervention impact differently across studies, making it difficult to combine the findings. In addition, studies were highly heterogeneous in terms of the types of individuals included in the study (e.g., healthy individuals and patients). We conducted the subgroup meta-analysis to reduce the heterogeneity, but the high heterogeneity still existed. Therefore, the results from meta-analysis need to be interpreted with caution. The individual impact reported for each individual study and the results from systematic review should be given more consideration.
In this systematic review, interventions that used education and counseling strategies; those that used management strategies; those that combined education, counseling and management strategies and those that used screening and referral for management strategies were beneficial in preventing, controlling hypertension and reducing blood pressure levels. The combination of education, counseling and management strategies appeared to be the most beneficial intervention to reduce blood pressure levels. The findings in this review, highlight that, a number of interventions that aim at preventing, controlling hypertension or reducing blood pressure levels are being evaluated through the use of quasi-experimental studies. Given that RCTs are not always feasible or appropriate, scientists should develop more rigorous methods to increase the internal validity of such quasi-experimental studies.

Availability of data and materials
The data supporting the conclusions of this article is included within the article and the additional file.
Abbreviations
Confidence interval
Cardiovascular disease
Dietary approaches to stop hypertension
Diastolic blood pressure
Difference-in-difference
Grading of Recommendations, Assessment, Development, and Evaluation
Mean difference
Physical activity
Pre-post designs with a control group
Randomized clinical trial
Systolic blood pressure
Standard error
United States
Weighted mean difference
National Center for Health Statistics & Heron, M. Deaths: Leading Causes for 2018. Atlanta: CDC; 2021.
Lewington S, Lacey B, Clarke R, Guo Y, Kong XL, Yang L, et al. The burden of hypertension and associated risk for cardiovascular mortality in China. JAMA Intern Med. 2016;176:524–32.
Article PubMed Google Scholar
World Health Organization (WHO). A global brief on hypertension: silent killer, global public health crisis: World Health Day 2013. Geneva: WHO; 2013.
Sun D, Liu J, Xiao L, Liu Y, Wang Z, Li C, et al. Recent development of risk-prediction models for incident hypertension: an updated systematic review. PLoS One. 2017;12:e0187240.
Article PubMed PubMed Central Google Scholar
Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, et al. Heart disease and stroke statistics-2018 update: a report from the American Heart Association. Circulation. 2018;137:e67–492.
Glynn LG, Murphy AW, Smith SM, Schroeder K, Fahey T. Interventions used to improve control of blood pressure in patients with hypertension. Cochrane Database Syst Rev. 2010;3:CD005182.
Google Scholar
Sheridan S, Pignone M, Donahue K. Screening for high blood pressure: a review of the evidence for the U.S. preventive services task force. Am J Prev Med. 2003;25:151–8.
Uhlig K, Patel K, Ip S, Kitsios GD, Balk EM. Self-measured blood pressure monitoring in the management of hypertension: a systematic review and meta-analysis. Ann Intern Med. 2013;159:185–94.
de Simone G, Izzo R, Verdecchia P. Are observational studies more informative than randomized controlled trials in hypertension? Pro side of the argument. Hypertension. 2013;62:463–9.
Li DZ, Zhou Y, Yang YN, Ma YT, Li XM, Yu J, et al. Acupuncture for essential hypertension: a meta-analysis of randomized sham-controlled clinical trials. Evid Based Complement Alternat Med. 2014;2014:279478.
Murthy VH, Krumholz HM, Gross CP. Participation in cancer clinical trials: race-, sex-, and age-based disparities. JAMA. 2004;291:2720–6.
Article CAS PubMed Google Scholar
Remler DK, Van Ryzin GG. Research methods in practice: strategies for description and causation. 2nd ed. SAGE: Los Angeles; 2014.
Handley MA, Lyles CR, McCulloch C, Cattamanchi A. Selecting and improving quasi-experimental designs in effectiveness and implementation research. Annu Rev Public Health. 2018;39:5–25.
Basu S, Meghani A, Siddiqi A. Evaluating the health impact of large-scale public policy changes: classical and novel approaches. Annu Rev Public Health. 2017;38:351–70.
Craig P, Katikireddi SV, Leyland A, Popham F. Natural experiments: an overview of methods, approaches, and contributions to public health intervention research. Annu Rev Public Health. 2017;38:39–56.
Berkowitz SA, Hulberg AC, Standish S, Reznor G, Atlas SJ. Addressing unmet basic resource needs as part of chronic cardiometabolic disease management. JAMA Intern Med. 2017;177:244–52.
James A, Berkowitz SA, Ashburner JM, Chang Y, Horn DM, O’Keefe SM, et al. Impact of a population health management intervention on disparities in cardiovascular disease control. J Gen Intern Med. 2018;33:463–70.
Comin E, Catalan-Ramos A, Iglesias-Rodal M, Grau M, Del Val JL, Consola A, et al. Impact of implementing electronic clinical practice guidelines for the diagnosis, control and treatment of cardiovascular risk factors: a pre-post controlled study. Aten Primaria. 2017;49:389–98.
Panattoni L, Hurlimann L, Wilson C, Durbin M, Tai-Seale M. Workflow standardization of a novel team care model to improve chronic care: a quasi-experimental study. BMC Health Serv Res. 2017;17:286.
Bor J. Capitalizing on natural experiments to improve our understanding of population health. Am J Public Health. 2016;106:1388–9.
Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097.
Ho AM, Phelan R, Mizubuti GB, Murdoch JAC, Wickett S, Ho AK, et al. Bias in before-after studies: narrative overview for anesthesiologists. Anesth Analg. 2018;126:1755–62.
Bronfenbrenner U. The ecology of human development: experiments by nature and design. Cambridge: Harvard University Press; 1979.
Barnidge EK, Baker EA, Schootman M, Motton F, Sawicki M, Rose F. The effect of education plus access on perceived fruit and vegetable consumption in a rural African American community intervention. Health Educ Res. 2015;30:773–85.
Article CAS PubMed PubMed Central Google Scholar
Sahli J, Maatoug J, Harrabi I, Ben Fredj S, Dendana E, Ghannem H. Effectiveness of a community-based intervention program to reduce hypertension prevalence among adults: results of a quasiexperimental study with control group in the region of Sousse. Tunisia Glob Heart. 2016;11:131–7.
Fikri-Benbrahim N, Faus MJ, Martínez-Martínez F, Alsina DG, Sabater-Hernandez D. Effect of a pharmacist intervention in Spanish community pharmacies on blood pressure control in hypertensive patients. Am J Health Syst Pharm. 2012;69:1311–8.
Flannery K, Resnick B, Galik E, Lipscomb J, McPhaul K, Shaughnessy M. The worksite heart health improvement project (WHHIP): feasibility and efficacy. Public Health Nurs. 2012;29:455–66.
Gemson DH, Commisso R, Fuente J, Newman J, Benson S. Promoting weight loss and blood pressure control at work: impact of an education and intervention program. J Occup Environ Med. 2008;50:272–81.
Lin YP, Lin CC, Chen MM, Lee KC. Short-term efficacy of a “sit less, walk more” workplace intervention on improving cardiometabolic health and work productivity in office workers. J Occup Environ Med. 2017;59:327–34.
Chang MY, Yeh SC, Chu MC, Wu TM, Huang TH. Associations between Tai chi Chung program, anxiety, and cardiovascular risk factors. Am J Health Promot. 2013;28:16–22.
Verberne LD, Hendriks MR, Rutten GM, Spronk I, Savelberg HH, Veenhof C, et al. Evaluation of a combined lifestyle intervention for overweight and obese patients in primary health care: a quasi-experimental design. Fam Pract. 2016;33:671–7.
Xu F, Letendre J, Bekke J, Beebe N, Mahler L, Lofgren IE, et al. Impact of a program of Tai chi plus behaviorally based dietary weight loss on physical functioning and coronary heart disease risk factors: a community-based study in obese older women. J Nutr Gerontol Geriatr. 2015;34:50–65.
Zhu W, Gutierrez M, Toledo MJ, Mullane S, Stella AP, Diemar R, et al. Long-term effects of sit-stand workstations on workplace sitting: a natural experiment. J Sci Med Sport. 2018;21:811–6.
Kamran A, Sharifirad G, Heydari H, Sharifian E. The effect of theory based nutritional education on fat intake, weight and blood lipids. Electron Physician. 2016;8:3333–42.
Ibrahim N, Ming Moy F, Awalludin IA, Mohd Ali Z, Ismail IS. Effects of a community-based healthy lifestyle intervention program (co-HELP) among adults with prediabetes in a developing country: a quasi-experimental study. PLoS One. 2016;11:e0167123.
Kassim MSA, Manaf MRA, Nor NSM, Ambak R. Effects of lifestyle intervention towards obesity and blood pressure among housewives in Klang Valley: a quasi-experimental study. Malays J Med Sci. 2017;24:83–91.
PubMed PubMed Central Google Scholar
Fazliana M, Liyana AZ, Omar A, Ambak R, Mohamad Nor NS, Shamsudin UK, et al. Effects of weight loss intervention on body composition and blood pressure among overweight and obese women: findings from the MyBFF@home study. BMC Womens Health. 2018;18(Suppl 1):93.
Miao Y, Gu J, Zhang L, He R, Sandeep S, Wu J. Improving the performance of social health insurance system through increasing outpatient expenditure reimbursement ratio: a quasi-experimental evaluation study from rural China. Int J Equity Health. 2018;17:89.
Scanlon DP, Hollenbeak CS, Beich J, Dyer AM, Gabbay RA, Milstein A. Financial and clinical impact of team-based treatment for medicaid enrollees with diabetes in a federally qualified health center. Diabetes Care. 2008;31:2160–5.
Darviri C, Artemiadis AK, Protogerou A, Soldatos P, Kranioutou C, Vasdekis S, et al. A HEALth promotion and STRESS management program (HEAL-STRESS study) for prehypertensive and hypertensive patients: a quasi-experimental study in Greece. J Hum Hypertens. 2016;30:397–403.
Fernandez S, Scales KL, Pineiro JM, Schoenthaler AM, Ogedegbe G. A senior center-based pilot trial of the effect of lifestyle intervention on blood pressure in minority elderly people with hypertension. J Am Geriatr Soc. 2008;56:1860–6.
Jung H, Lee JE. The impact of community-based eHealth self-management intervention among elderly living alone with hypertension. J Telemed Telecare. 2017;23:167–73.
Hussain T, Franz W, Brown E, Kan A, Okoye M, Dietz K, et al. The role of care management as a population health intervention to address disparities and control hypertension: a quasi-experimental observational study. Ethn Dis. 2016;26:285–94.
Miao Y, Zhang L, Sparring V, Sandeep S, Tang W, Sun X, et al. Improving health related quality of life among rural hypertensive patients through the integrative strategy of health services delivery: a quasi-experimental trial from Chongqing. China Int J Equity Health. 2016;15:132.
Visanuyothin S, Plianbangchang S, Somrongthong R. An integrated program with home blood-pressure monitoring and village health volunteers for treating poorly controlled hypertension at the primary care level in an urban community of Thailand. Integr Blood Press Control. 2018;11:25–35.
Scharf DM, Schmidt Hackbarth N, Eberhart NK, Horvitz-Lennon M, Beckman R, Han B, et al. General medical outcomes from the primary and behavioral health care integration grant program. Psychiatr Serv. 2016;67:1226–32.
Chang KC, Lee JT, Vamos EP, Soljak M, Johnston D, Khunti K, et al. Impact of the National Health Service Health Check on cardiovascular disease risk: a difference-in-differences matching analysis. CMAJ. 2016;188:E228–38.
Yu EY, Wan EY, Wong CK, Chan AK, Chan KH, Ho SY, et al. Effects of risk assessment and management programme for hypertension on clinical outcomes and cardiovascular disease risks after 12 months: a population-based matched cohort study. J Hypertens. 2017;35:627–36.
van de Vijver S, Oti SO, Gomez GB, Agyemang C, Egondi T, Moll van Charante E, et al. Impact evaluation of a community-based intervention for prevention of cardiovascular diseases in the slums of Nairobi. the SCALE-UP study Glob Health Action. 2016;9:30922.
Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions. 2nd ed. Wiley-Blackwell: Hoboken; 2020.
Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to meta-analysis. Chichester: John Wiley & Sons; 2009.
Book Google Scholar
Walsh JM, McDonald KM, Shojania KG, Sundaram V, Nayak S, Lewis R, et al. Quality improvement strategies for hypertension management: a systematic review. Med Care. 2006;44:646–57.
Kim K, Choi JS, Choi E, Nieman CL, Joo JH, Lin FR, et al. Effects of community-based health worker interventions to improve chronic disease management and care among vulnerable populations: a systematic review. Am J Public Health. 2016;106:e3–28.
Rehkopf DH, Basu S. A new tool for case studies in epidemiology-the synthetic control method. Epidemiology. 2018;29:503–5.
Dickinson HO, Mason JM, Nicolson DJ, Campbell F, Beyer FR, Cook JV, et al. Lifestyle interventions to reduce raised blood pressure: a systematic review of randomized controlled trials. J Hypertens. 2006;24:215–33.
Download references
Acknowledgments
Not applicable.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and affiliations.
Department of Epidemiology, Fielding School of Public Health, University of California, Los Angeles (UCLA), 650 Charles E. Young Drive South, Los Angeles, CA, 90095, USA
Tong Xia, Fan Zhao & Roch A. Nianogo
California Center for Population Research (CCPR), 337 Charles E. Young Drive East, Los Angeles, CA, 90095, USA
Roch A. Nianogo
You can also search for this author in PubMed Google Scholar
Contributions
TX participated in the study conception, design and analysis and wrote the initial first draft of the article. FZ participated in the study conception, design and reviewed the first draft of the article. RN conceived and supervised the design and analysis, finalized the first draft and critically reviewed and revised the manuscript. All authors provided critical input and insights into the development and writing of the article and approved the final manuscript as submitted.
Corresponding author
Correspondence to Roch A. Nianogo .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: table s1..
Search words. Table S2. Summary of the characteristics of the studies included in this review ( n = 30). Table S3. Risk of Bias Tool Assessments Across Studies (n = 30). Table S4. GRADE Evidence Profiles Across Studies in Meta-analysis ( n = 24). Table S5. Estimates and parameters in studies that reported on the mean difference in blood pressure ( n = 27). Table S6. Sensitivity analysis for systolic blood pressure (SBP) and diastolic blood pressure (DBP) in meta-analysis stratified by intervention type. Table S7. Sensitivity analysis for systolic blood pressure (SBP) and diastolic blood pressure (DBP) in meta-analysis stratified by intervention setting. Table S8. Sensitivity analysis for systolic blood pressure (SBP) and diastolic blood pressure (DBP) in meta-analysis stratified by intervention duration. Fig. S1. Methods to calculate mean differences (MD). Fig. S2. Methods to calculate standard errors (SE). Fig. S3. Forest plot stratified by intervention settings for blood pressure. (A) Forest plot stratified by intervention settings for systolic blood pressure (SBP). (B) Forest plot stratified by intervention settings for diastolic blood pressure (DBP). Fig. S4. Forest plot stratified by intervention duration for blood pressure. ( A) Forest plot stratified by intervention duration for systolic blood pressure (SBP). ( B) Forest plot stratified by intervention duration for diastolic blood pressure (DBP). Fig. S5. Funnel plot of systolic blood pressure (SBP), diastolic blood pressure (DBP) stratified by intervention types. Fig. S6. Funnel plot of systolic blood pressure (SBP), diastolic blood pressure (DBP) stratified by intervention settings. Fig. S7. Funnel plot of systolic blood pressure (SBP), diastolic blood pressure (DBP) stratified by intervention duration. Fig. S8. Sensitivity analysis of systolic blood pressure (SBP), diastolic blood pressure (DBP) stratified by intervention types. Fig. S9. Sensitivity analysis of systolic blood pressure (SBP), diastolic blood pressure (DBP) stratified by intervention settings. Fig. S10. Sensitivity analysis of systolic blood pressure (SBP), diastolic blood pressure (DBP) stratified by intervention duration
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Xia, T., Zhao, F. & Nianogo, R.A. Interventions in hypertension: systematic review and meta-analysis of natural and quasi-experiments. Clin Hypertens 28 , 13 (2022). https://doi.org/10.1186/s40885-022-00198-2
Download citation
Received : 19 February 2021
Accepted : 21 January 2022
Published : 01 May 2022
DOI : https://doi.org/10.1186/s40885-022-00198-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Hypertension
- Non-randomized controlled trials as topic
- Comparative effectiveness research
Clinical Hypertension
ISSN: 2056-5909
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
Join JSH, Free to Read Hypertension Research!
All members are entitled to access the electronic version of the Hypertension Research. Why don’t you join the Japanese Society of Hypertension?
Current issue
Preface-various factors in the management of blood pressure.
- Masaki Mogi
- Satoshi Hoshide
- Kazuomi Kario
Possible relationship between primary aldosteronism and small vessel disease
- Tatsuya Haze
- Kouichi Tamura
Blood pressure variability in acute ischemic stroke
- Kenichi Todo
Systemic hemodynamic atherothrombotic syndrome: from hypothesis to evidence
- Yusuke Ishiyama
The association between depressive symptoms and masked hypertension in participants with normotension measured at research center
- Sayuri Tokioka
- Naoki Nakaya
- Atsushi Hozawa
The impact of clinical inertia on uncontrolled blood pressure in treated hypertension: real-world, longitudinal data from Japan
- Michihiro Satoh
- Tomoko Muroya
- Hirohito Metoki

Announcements
Showcase of graphical abstracts.
Please enjoy our fantastic Graphical Abstracts!
Guidelines and Specific Topics
Collections
We are pleased to share with you a collection of papers published as Review Series. We hope you enjoy.
Open Access Articles
You can find open access articles of this journal.
Guide To Authors

About the Journal
Japanese Society of Hypertension

Advertisement
Browse articles
Blood pressure in the longevous population with different status of hypertension and frailty
- Takeo Ishii
The effect of different treatment strategies on glycolipid metabolism disorders and cardiovascular events in primary aldosteronism
- Shiting Zhou
Predicting cognitive function and dementia risk in patients with hypertension
- Gustavo H. Cerezo
- Ruth A. Fernández
- Facundo Risso Patrón
24-h central pressure is a valuable predictor for left ventricular hypertrophy in non-dialysis patients with chronic kidney disease
- Lingling Liu
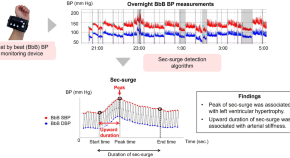
Development of beat-by-beat blood pressure monitoring device and nocturnal sec-surge detection algorithm
- Ayako Kokubo
- Mitsuo Kuwabara
Prediction of endogenous mineralocorticoid receptor activity by depressor effects of mineralocorticoid receptor antagonists in patients with primary aldosteronism
- Makiko Ikemoto
- Satoshi Morimoto
- Atsuhiro Ichihara
Accumulating evidence suggests the potential of selective adrenal artery embolization as a standard treatment for primary aldosteronism
- Toshifumi Nakamura
- Kaori Hayashi
Impact of nocturnal blood pressure dipping on recurrence of atrial fibrillation after pulmonary vein isolation
- Tomonori Watanabe
Akkermansia muciniphila extracellular vesicles have a protective effect against hypertension
- Jee Young Kim
- Cheong-Wun Kim
- Inkyeom Kim
Trending - Altmetric
The effects of exercise training on hypertensive older adults: an umbrella meta-analysis
Antihypertensive effects of Ocimum basilicum L. (OBL) on blood pressure in renovascular hypertensive rats
An evidence review project for food with function claims ~Challenges of the Japan society for vascular failure for the promotion of adequate evidences for food with function claims
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

IMAGES
COMMENTS
1. Introduction. Hypertension is a major public health problem due to its high prevalence all around the globe [1-4].Around 7.5 million deaths or 12.8% of the total of all annual deaths worldwide occur due to high blood pressure [].It is predicted to be increased to 1.56 billion adults with hypertension in 2025 [].Raised blood pressure is a major risk factor for chronic heart disease, stroke ...
Introduction. Essential or primary hypertension, the world's leading risk factor for global disease burden, is expected to cause more than half of the estimated 17 million deaths per year resulting from cardiovascular disease (CVD) worldwide. 1 Defined as an elevation of blood pressure (BP) beyond 140/90 mm Hg, hypertension is strongly correlated with adverse outcomes such as stroke ...
Abstract. Dr Irvine Page proposed the Mosaic Theory of Hypertension in the 1940s advocating that hypertension is the result of many factors that interact to raise blood pressure and cause end-organ damage. Over the years, Dr Page modified his paradigm, and new concepts regarding oxidative stress, inflammation, genetics, sodium homeostasis, and ...
Abstract. Fragmented investigation has masked the overall picture for causes of cardiovascular disease (CVD). Among the risk factors for CVD, high blood pressure (BP) is associated with the strongest evidence for causation and it has a high prevalence of exposure. Biologically, normal levels of BP are considerably lower than what has typically ...
Improvements in the detection, treatment, and control of hypertension have varied substantially across countries, with some middle-income countries now outperforming most high-income nations. The dual approach of reducing hypertension prevalence through primary prevention and enhancing its treatment and control is achievable not only in high-income countries but also in low-income and middle ...
Hypertension Research (2023) In 2021, 217 excellent manuscripts were published in Hypertension Research. Editorial teams greatly appreciate the authors' contribution to hypertension research ...
The journal consistently attracts the most important and highly innovative papers from the current research; our commitment to rapid publication ensures that these are published in the fastest time possible. In addition to primary papers from world-renowned experts, the Journal contains authoritative reviews that summarize and evaluate the most significant recent developments.
Hypertension is an urgent public health problem. Consistent summary from natural and quasi-experiments employed to evaluate interventions that aim at preventing or controlling hypertension is lacking in the current literature. This study aims to summarize the evidence from natural and quasi-experiments that evaluated interventions used to prevent or control hypertension.
Results: Among adults aged 20 to 79 years, 24% of males and 23% of females had hypertension, de ned as measured BP ≥140/90 mm Hg or past-month use. of antihypertensive medication. Hyper tension ...
Blood pressure lowering and safety improvements with liver angiotensinogen inhibition in models of hypertension and kidney injury. Hypertension. 2017; 70:566-576. doi: 10.1161/HYPERTENSIONAHA.117.09755 Link Google Scholar; 58. Uijl E, Mirabito Colafella KM, Sun Y, Ren L, van Veghel R, Garrelds IM, de Vries R, Poglitsch M, Zlatev I, Kim JB, et al.
Hypertension is high blood pressure. It is generally defined in adults as systolic blood pressure greater than or equal to 140mmHg and/or diastolic blood pressure greater than or equal to 90mmHg.
In Hypertension Research 2020, papers on the association of uric acid with CKD and CVD from cohort studies in the Japanese general population such as BOREAS-CKD2, CIRCS, and the Hisayama Study ...
Cuff blood pressure (BP) is recommended for guiding hypertension management. However, central BP has been proposed as a superior clinical measurement. This study aimed to determine whether controlling hypertension as measured by central BP was beneficial in reducing left ventricular mass index beyond control of standard cuff hypertension.
This mini-review focuses on recent topics on basic research in hypertension from the several points of view. The recent topics indicate that interorgan communication has received particular ...
Hypertension—Vision and Mission. My vision for Hypertension is to ensure that it remains the foremost and most prestigious journal in the field internationally and that it is agile enough to adapt to rapid developments in hypertension research and biomedical science as well as new publishing and communications technologies. It must be the preferred place to publish the highest quality ...
Uncontrolled hypertension is the greatest challenge worldwide [ 2 ]. In particular, uncontrolled hypertension is more common in Asian countries, except in South Korea and Taiwan [ 2, 3 ], although ...
In January 2015, the average time from submission to first decision for all original research papers submitted to Circulation Research was 14.7 days. Correspondence to Suzanne Oparil, MD, Vascular Biology and Hypertension Program, 1720 2nd Ave South, ZRB 1034, Birmingham, AL 35294. E-mail [email protected].
In the present study entitled " Blood pressure in the very old with different status of hypertension and frailty", in the Hypertension Research, Wang et al. aimed to determine antihypertensive ...
Collections. Hypertension Research, official publication of the Japanese Society of Hypertension, publishes papers reporting original clinical and experimental research in the field of ...