- Search Menu
- Volume 2024, Issue 3, March 2024 (In Progress)
- Volume 2024, Issue 2, February 2024
- Case of the Year
- MSF Case Reports
- Audiovestibular medicine
- Cardiology and cardiovascular systems
- Critical care medicine
- Dermatology
- Emergency medicine
- Endocrinology and metabolism
- Gastroenterology and hepatology
- Geriatrics and gerontology
- Haematology
- Infectious diseases and tropical medicine
- Medical ophthalmology
- Medical disorders in pregnancy
- Paediatrics
- Palliative medicine
- Pharmacology and pharmacy
- Radiology, nuclear medicine, and medical imaging
- Respiratory disorders
- Rheumatology
- Sexual and reproductive health
- Sports medicine
- Substance abuse
- Author Guidelines
- Submission Site
- Open Access
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Answer to part 1, answer to part 2, answer to part 3, answer to part 4, answer to part 5.
- < Previous
Educational Case: A 57-year-old man with chest pain
Contributed equally.
- Article contents
- Figures & tables
- Supplementary Data
Nikhil Aggarwal, Subothini Selvendran, Vassilios Vassiliou, Educational Case: A 57-year-old man with chest pain, Oxford Medical Case Reports , Volume 2016, Issue 4, April 2016, Pages 62–65, https://doi.org/10.1093/omcr/omw008
- Permissions Icon Permissions
This is an educational case report including multiple choice questions and their answers. For the best educational experience we recommend the interactive web version of the exercise which is available via the following link: http://www.oxfordjournals.org/our_journals/omcr/ec01p1.html
A 57 year-old male lorry driver, presented to his local emergency department with a 20-minute episode of diaphoresis and chest pain. The chest pain was central, radiating to the left arm and crushing in nature. The pain settled promptly following 300 mg aspirin orally and 800 mcg glyceryl trinitrate (GTN) spray sublingually administered by paramedics in the community. He smoked 20 cigarettes daily (38 pack years) but was not aware of any other cardiovascular risk factors. On examination he appeared comfortable and was able to complete sentences fully. There were no heart murmurs present on cardiac auscultation. Blood pressure was 180/105 mmHg, heart rate was 83 bpm and regular, oxygen saturation was 97%.
What is the most likely diagnosis?
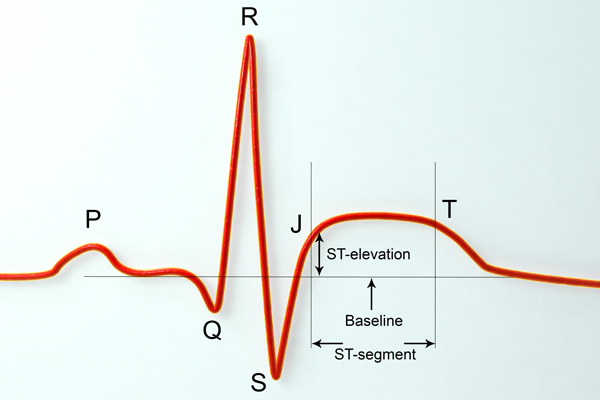
An ECG was requested and is shown in figure 1.
How would you manage the patient? (The patient has already received 300 mg aspirin).
30 minutes later the patient's chest pain returned with greater intensity whilst waiting in the emergency department. Now, he described the pain as though “an elephant is sitting on his chest”. The nurse has already done an ECG by the time you were called to see him. This is shown in figure 2.
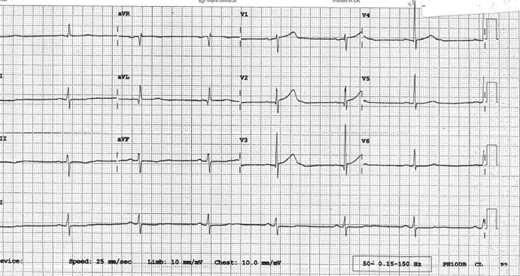
ECG on admission.
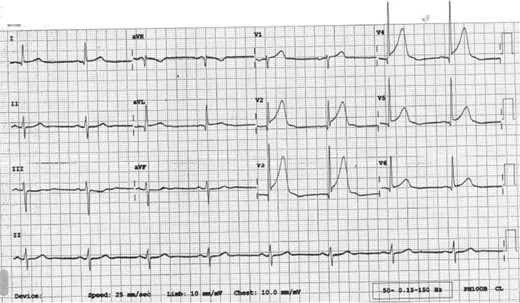
ECG 30 minutes after admission.
What would be the optimal management for this patient?
He was taken to the catheterization lab where the left anterior descending coronary artery (LAD) was shown to be completely occluded. Following successful percutaneous intervention and one drug eluding stent implantation in the LAD normal flow is restored (Thrombosis in myocardial infarction, TIMI = 3). 72 hours later, he is ready to be discharged home. The patient is keen to return to work and asks when he could do so.
When would you advise him that he could return to work?
One week later, he receives a letter informing him that he is required to attend cardiac rehabilitation. The patient is confused as to what cardiac rehabilitation entails, although he does remember a nurse discussing this with him briefly before he was discharged. He phones the hospital in order to get some more information.
Which of the following can be addressed during cardiac rehabilitation?
A - Acute coronary syndrome
Although the presentation could be attributable to any of the above differential diagnoses, the most likely etiology given the clinical picture and risk factors is one of cardiac ischemia. Risk factors include gender, smoking status and age making the diagnosis of acute coronary syndrome the most likely one. The broad differential diagnosis in patients presenting with chest pain has been discussed extensively in the medical literature. An old but relevant review can be found freely available 1 as well as more recent reviews. 2 , 3
C - Atorvastatin 80 mg, Clopidogrel 300 mcg, GTN 500 mcg, Ramipril 2.5 mg,
In patients with ACS, medications can be tailored to the individual patient. Some medications have symptomatic benefit but some also have prognostic benefit. Aspirin 4 , Clopidogrel 5 , Atenolol 6 and Atorvastatin 7 have been found to improve prognosis significantly. ACE inhibitors have also been found to improve left ventricular modeling and function after an MI. 8 , 9 Furthermore, GTN 10 and morphine 11 have been found to be of only significant symptomatic benefit.
Oxygen should only to be used when saturations <95% and at the lowest concentration required to keep saturations >95%. 12
There is no evidence that diltiazem, a calcium channel blocker, is of benefit. 13
His ECG in figure 1 does not fulfil ST elevation myocardial infarction (STEMI) criteria and he should therefore be managed as a Non-STEMI. He would benefit prognostically from beta-blockade however his heart rate is only 42 bpm and therefore this is contraindicated. He should receive a loading dose of clopidogrel (300 mg) followed by daily maintenance dose (75 mg). 14 , 15 He might not require GTN if he is pain-free but out of the available answers 3 is the most correct.
D - Proceed to coronary angiography
The ECG shows ST elevation in leads V2-V6 and confirms an anterolateral STEMI, which suggests a completely occluded LAD. This ECG fulfils the criteria to initiate reperfusion therapy which traditionally require one of the three to be present: According to guidance, if the patient can undergo coronary angiography within 120 minutes from the onset of chest pain, then this represents the optimal management. If it is not possible to undergo coronary angiography and potentially percutaneous intervention within 2 hours, then thrombolysis is considered an acceptable alternative. 12 , 16
≥ 1 mm of ST change in at least two contiguous limb leads (II, III, AVF, I, AVL).
≥ 2 mm of ST change in at least two contiguous chest leads (V1-V6).
New left bundle branch block.
GTN and morphine administration can be considered in parallel but they do not have a prognostic benefit.
E - Not before an exercise test
This patient is a lorry driver and therefore has a professional heavy vehicle driving license. The regulation for driving initiation in a lorry driver following a NSTEMI/ STEMI may be different in various countries and therefore the local regulations should be followed.
In the UK, a lorry driver holds a category 2 driving license. He should therefore refrain from driving a lorry for at least 6 weeks and can only return to driving if he completes successfully an exercise evaluation. An exercise evaluation is performed on a bicycle or treadmill. Drivers should be able to complete 3 stages of the standard Bruce protocol 17 or equivalent (e.g. Myocardial perfusion scan) safely, having refrained from taking anti-anginal medication for 48 hours and should remain free from signs of cardiovascular dysfunction during the test, notably: angina pectoris, syncope, hypotension, sustained ventricular tachycardia, and/or electrocardiographic ST segment shift which is considered as being indicative of myocardial ischemia (usually >2 mm horizontal or down-sloping) during exercise or the recovery period. 18
For a standard car driving license (category 1), driving can resume one week after successful intervention providing that no other revascularization is planned within 4 weeks; left ventricular ejection fraction (LVEF) is at least 40% prior to hospital discharge and there is no other disqualifying condition.
Therefore if this patent was in the UK, he could restart driving a normal car one week later assuming an echocardiogram confirmed an EF > 40%. However, he could only continue lorry driving once he has passed the required tests. 18
E - All of the above
Cardiac rehabilitation bridges the gap between hospitals and patients' homes. The cardiac rehabilitation team consists of various healthcare professions and the programme is started during hospital admission or after diagnosis. Its aim is to educate patients about their cardiac condition in order to help them adopt a healthier lifestyle. This includes educating patients' about their diet, exercise, risk factors associated with their condition such as smoking and alcohol intake and finally, about the medication recommended. There is good evidence that adherence to cardiac rehabilitation programmes improves survival and leads to a reduction in future cardiovascular events. 19 , 20
Oille JA . Differential diagnosis of pain in the chest . Can Med Assoc J . 1937 ; 37 (3) : 209 – 216 . http://www.ncbi.nlm.nih.gov/pmc/articles/PMC536075/ .
Google Scholar
Lee TH , Goldman L . Evaluation of the patient with acute chest pain . N Engl J Med . 2000 ; 342 (16) : 1187 – 1195 . http://www.nejm.org/doi/full/10.1056/NEJM200004203421607 .
Douglas PS , Ginsburg GS . The evaluation of chest pain in women . N Engl J Med . 1996 ; 334 (20) : 1311 – 1315 . http://www.nejm.org/doi/full/10.1056/NEJM199605163342007 .
Baigent C , Collins R , Appleby P , Parish S , Sleight P , Peto R . ISIS-2: 10 year survival among patients with suspected acute myocardial infarction in randomised comparison of intravenous streptokinase, oral aspirin, both, or neither. the ISIS-2 (second international study of infarct survival) collaborative group . BMJ . 1998 ; 316 (7141) : 1337 – 1343 . http://www.ncbi.nlm.nih.gov/pmc/articles/PMC28530/ .
Yusuf S , Zhao F , Mehta S , Chrolavicius S , Tognoni G , Fox K . Clopidogrel in unstable angina to prevent recurrent events trail investigators . effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation . N Engl J Med . 2001 ; 345 (7) : 494 – 502 . http://www.nejm.org/doi/full/10.1056/NEJMoa010746#t=articleTop .
Yusuf S , Peto R , Lewis J , Collins R , Sleight P . Beta blockade during and after myocardial infarction: An overview of the randomized trials . Prog Cardiovasc Dis . 1985 ; 27 (5) : 335 – 371 . http://www.sciencedirect.com/science/article/pii/S0033062085800037 .
Schwartz GG , Olsson AG , Ezekowitz MD et al. . Effects of atorvastatin on early recurrent ischemic events in acute coronary syndromes: The MIRACL study: A randomized controlled trial . JAMA . 2001 ; 285 (13) : 1711 – 1718 . http://jama.jamanetwork.com/article.aspx?articleid=193709 .
Pfeffer MA , Lamas GA , Vaughan DE , Parisi AF , Braunwald E . Effect of captopril on progressive ventricular dilatation after anterior myocardial infarction . N Engl J Med . 1988 ; 319 (2) : 80 – 86 . http://content.onlinejacc.org/article.aspx?articleid=1118054 .
Sharpe N , Smith H , Murphy J , Hannan S . Treatment of patients with symptomless left ventricular dysfunction after myocardial infarction . The Lancet . 1988 ; 331 (8580) : 255 – 259 . http://www.sciencedirect.com/science/article/pii/S0140673688903479 .
Ferreira JC , Mochly-Rosen D . Nitroglycerin use in myocardial infarction patients . Circ J . 2012 ; 76 (1) : 15 – 21 . http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3527093/ .
Herlitz J , Hjalmarson A , Waagstein F . Treatment of pain in acute myocardial infarction . Br Heart J . 1989 ; 61 (1) : 9 – 13 . http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1216614/ .
Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC), Steg PG, James SK, et al . ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation . Eur Heart J . 2012 ; 33 (20) : 2569 – 2619 . http://eurheartj.oxfordjournals.org/content/33/20/2569 .
The effect of diltiazem on mortality and reinfarction after myocardial infarction . the multicenter diltiazem postinfarction trial research group . N Engl J Med . 1988 ; 319 (7) : 385 – 392 . http://www.nejm.org/doi/full/10.1056/NEJM198808183190701 .
Jneid H , Anderson JL , Wright RS et al. . 2012 ACCF/AHA focused update of the guideline for the management of patients with unstable angina/Non–ST-elevation myocardial infarction (updating the 2007 guideline and replacing the 2011 focused update) A report of the american college of cardiology foundation/american heart association task force on practice guidelines . J Am Coll Cardiol . 2012 ; 60 (7) : 645 – 681 . http://circ.ahajournals.org/content/123/18/2022.full .
Hamm CW , Bassand JP , Agewall S et al. . ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The task force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the european society of cardiology (ESC) . Eur Heart J . 2011 ; 32 (23) : 2999 – 3054 . http://eurheartj.oxfordjournals.org/content/32/23/2999.long .
O'Gara PT , Kushner FG , Ascheim DD et al. . 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: Executive summary: A report of the american college of cardiology foundation/american heart association task force on practice guidelines . J Am Coll Cardiol . 2013 ; 61 (4) : 485 – 510 . http://content.onlinejacc.org/article.aspx?articleid=1486115 .
BRUCE RA , LOVEJOY FW Jr . Normal respiratory and circulatory pathways of adaptation in exercise . J Clin Invest . 1949 ; 28 (6 Pt 2) : 1423 – 1430 . http://www.ncbi.nlm.nih.gov/pmc/articles/PMC439698/ .
DVLA . Https://Www.gov.uk/current-medical-guidelines-dvla-guidance-for-professionals-cardiovascular-chapter-appendix .
British Heart Foundation . Http://Www.bhf.org.uk/heart-health/living-with-heart-disease/cardiac-rehabilitation.aspx .
Kwan G , Balady GJ . Cardiac rehabilitation 2012: Advancing the field through emerging science . Circulation . 2012 ; 125 (7) : e369–73. http://circ.ahajournals.org/content/125/7/e369.full .
Author notes
- knowledge acquisition
Email alerts
Citing articles via, affiliations.
- Online ISSN 2053-8855
- Copyright © 2024 Oxford University Press
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- Introduction
- Conclusions
- Article Information
The start of the early coronavirus disease 2019 (COVID-19) period (February 23, 2020) and later COVID-19 period (March 29, 2020), as defined by segmented regression analysis, are indicated by vertical lines. Dotted lines indicate the best-fit regression lines for the 3 periods (including the before COVID-19 period). Projected volumes with 95% CIs are displayed in gray. STEMI indicates ST-segment elevation myocardial infarction.
eTable 1. ICD-10 Codes
eTable 2. MS-DRG Codes Used in Treatment Approaches Analysis
eTable 3. Weekly Case Volumes in 2020
eFigure 1. Weekly Volumes by State
eFigure 2. Treatment Approaches
See More About
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Others Also Liked
- Download PDF
- X Facebook More LinkedIn
Gluckman TJ , Wilson MA , Chiu S, et al. Case Rates, Treatment Approaches, and Outcomes in Acute Myocardial Infarction During the Coronavirus Disease 2019 Pandemic. JAMA Cardiol. 2020;5(12):1419–1424. doi:10.1001/jamacardio.2020.3629
Manage citations:
© 2024
- Permissions
Case Rates, Treatment Approaches, and Outcomes in Acute Myocardial Infarction During the Coronavirus Disease 2019 Pandemic
- 1 Center for Cardiovascular Analytics, Research and Data Science (CARDS), Providence Heart Institute, Providence St Joseph Health, Portland, Oregon
- 2 Clinical Analytics, Providence St Joseph Health, Renton, Washington
- 3 Heart and Vascular Institute, Providence Regional Medical Center Everett, Everett, Washington
- 4 Providence Heart Institute, Providence St Peter Hospital, Olympia, Washington
Question How have case rates, treatment approaches, and in-hospital outcomes changed for patients with acute myocardial infarction (AMI) during the coronavirus disease 2019 (COVID-19) pandemic?
Findings In this cross-sectional study of 15 244 hospitalizations involving 14 724 patients with AMI, case rates began to decrease on February 23, 2020, followed by a modest recovery after 5 weeks. Although no statistically significant difference in treatment approaches was found, the risk-adjusted mortality rate among patients with ST-segment elevation myocardial infarction increased substantially.
Meaning The findings of this study show that changes in AMI hospitalizations and in-hospital outcomes occurred during the COVID-19 pandemic periods analyzed; additional research is warranted to explain the higher mortality rate among patients with ST-segment elevation myocardial infarction.
Importance The coronavirus disease 2019 (COVID-19) pandemic has changed health care delivery worldwide. Although decreases in hospitalization for acute myocardial infarction (AMI) have been reported during the pandemic, the implication for in-hospital outcomes is not well understood.
Objective To define changes in AMI case rates, patient demographics, cardiovascular comorbidities, treatment approaches, and in-hospital outcomes during the pandemic.
Design, Setting, and Participants This cross-sectional study retrospectively analyzed AMI hospitalizations that occurred between December 30, 2018, and May 16, 2020, in 1 of the 49 hospitals in the Providence St Joseph Health system located in 6 states (Alaska, Washington, Montana, Oregon, California, and Texas). The cohort included patients aged 18 years or older who had a principal discharge diagnosis of AMI (ST-segment elevation myocardial infarction [STEMI] or non–ST-segment elevation myocardial infarction [NSTEMI]). Segmented regression analysis was performed to assess changes in weekly case volumes. Cases were grouped into 1 of 3 periods: before COVID-19 (December 30, 2018, to February 22, 2020), early COVID-19 (February 23, 2020, to March 28, 2020), and later COVID-19 (March 29, 2020, to May 16, 2020). In-hospital mortality was risk-adjusted using an observed to expected (O/E) ratio and covariate-adjusted multivariable model.
Exposure Date of hospitalization.
Main Outcomes and Measures The primary outcome was the weekly rate of AMI (STEMI or NSTEMI) hospitalizations. The secondary outcomes were patient characteristics, treatment approaches, and in-hospital outcomes of this patient population.
Results The cohort included 15 244 AMI hospitalizations (of which 4955 were for STEMI [33%] and 10 289 for NSTEMI [67%]) involving 14 724 patients (mean [SD] age of 68 [13] years and 10 019 men [66%]). Beginning February 23, 2020, AMI-associated hospitalizations decreased at a rate of –19.0 (95% CI, –29.0 to –9.0) cases per week for 5 weeks (early COVID-19 period). Thereafter, AMI-associated hospitalizations increased at a rate of +10.5 (95% CI, +4.6 to +16.5) cases per week (later COVID-19 period). No appreciable differences in patient demographics, cardiovascular comorbidities, and treatment approaches were observed across periods. The O/E mortality ratio for AMI increased during the early period (1.27; 95% CI, 1.07-1.48), which was disproportionately associated with patients with STEMI (1.96; 95% CI, 1.22-2.70). Although the O/E mortality ratio for AMI was not statistically different during the later period (1.23; 95% CI, 0.98-1.47), increases in the O/E mortality ratio were noted for patients with STEMI (2.40; 95% CI, 1.65-3.16) and after risk adjustment (odds ratio, 1.52; 95% CI, 1.02-2.26).
Conclusions and Relevance This cross-sectional study found important changes in AMI hospitalization rates and worse outcomes during the early and later COVID-19 periods. Future studies are needed to identify contributors to the increased mortality rate among patients with STEMI.
The coronavirus disease 2019 (COVID-19) pandemic has profoundly changed health care delivery worldwide. Although early attention to COVID-19 was disproportionately focused on efforts to flatten the (pandemic) curve, recent studies have revealed a substantial decrease in hospitalization rates for acute myocardial infarction (AMI). Reports from Austria, 1 Italy, 2 and the US (California) 3 have noted lower admission rates for both ST-segment elevation myocardial infarction (STEMI) and non–ST-segment elevation myocardial infarction (NSTEMI). This decreased hospitalization rate likely reflects multiple factors. Most worrisome among these factors has been the reluctance of patients with AMI to seek medical attention out of fear that they may become infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). 4
We performed a retrospective, cross-sectional study of all AMI hospitalizations in a large multistate health care system. We sought to define changes in AMI case rates, patient demographics, cardiovascular comorbidities, treatment approaches, and in-hospital outcomes during the pandemic.
This study included patients aged 18 years or older with a principal discharge diagnosis of AMI who were admitted between December 30, 2018, and May 16, 2020, into 1 of 49 hospitals in the Providence St Joseph Health (PSJH) system located in 6 states (Alaska, Washington, Montana, Oregon, California, and Texas). We used International Statistical Classification of Diseases and Related Health Problems, Tenth Revision , codes to define the population (eTable 1 in the Supplement ). Individuals who were admitted as an outpatient were excluded. This study was approved by the PSJH Institutional Review Board, which waived the informed consent requirement because of the retrospective nature of the study.
The primary outcome was the weekly rate of AMI (STEMI or NSTEMI) hospitalizations before and after the pandemic onset. The secondary outcomes were patient characteristics, treatment approaches, and in-hospital outcomes (mortality, length of stay, and discharge disposition) of patients with STEMI or NSTEMI. Treatment approaches were defined by Medicare Severity-Diagnosis Related Groups (MS-DRGs) for percutaneous coronary intervention, coronary artery bypass graft surgery, and medical management of AMI (eTable 2 in the Supplement ).
Weekly volumes of AMI hospitalizations (categorized as STEMI or NSTEMI) are presented in the Figure as line graphs. Segmented regression analysis was used to ascertain volume changes over time. Using 2 identified break points (February 23, 2020 and March 29, 2020), we grouped cases into 1 of 3 periods for analysis: before COVID-19 (December 30, 2018, to February 22, 2020), early COVID-19 (February 23, 2020, to March 28, 2020), and later COVID-19 (March 29, 2020, to May 16, 2020). Segmented regression analysis was also used to identify the slope change in weekly hospitalizations during the 3 periods, with consideration of time dependence in the model.
Risk-adjusted in-hospital mortality was examined with 2 models. The first was the PSJH mortality risk model, which was a lookup table consisting of more than 5430 expected mortality rates. Such data were derived from the 3M All Patient Refined DRG, risk of mortality, and severity-of-illness grouper algorithm applied to a large inpatient database in the western US (eMethods in the Supplement ). The second was a multivariable logistic model, which considered all demographic variables listed in Table 1 . Results of the multivariable model were presented as adjusted odds ratio (OR) with 95% CI.
Patient demographics, cardiovascular comorbidities, treatment approaches, and in-hospital outcomes were summarized as descriptive statistics. Categorical data were presented as frequency (percentage). Numeric data were tested for normality and presented as mean (SD) or median (interquartile range [IQR]), as appropriate. Trends among the 3 COVID-19 periods were compared using univariate χ 2 , Fisher exact, or Kruskal-Wallis tests, as appropriate, for each variable. The level of statistical significance varied from P < .05 to P < .008, depending on Bonferroni adjustment for multiple comparisons (eMethods in the Supplement ).
The study cohort comprised 15 244 hospitalizations for AMI (4955 for STEMI [33%] and 10 289 for NSTEMI [67%]) involving 14 724 patients. Of those hospitalized, 5225 were women (34%) and 10 019 were men (66%), with a mean (SD) age of 68 (13) years ( Table 1 ). Before the COVID-19 period, the mean (SD) weekly case rate was 222 (17) patients for AMI, 72 (9) patients for STEMI, and 150 (13) patients for NSTEMI ( Figure and eTable 3 in the Supplement ). Beginning February 23, 2020, AMI hospitalizations decreased at a rate of –19.0 (95% CI, –29.0 to –9.0) cases per week for 5 weeks, marking the early COVID-19 period ( Figure ). Thereafter, AMI hospitalizations increased at a rate of +10.5 (95% CI, +4.6 to +16.5) cases per week, marking the later COVID-19 period. Weekly AMI hospitalization rates had not returned to baseline, however, by the last week evaluated (May 10, 2020; eTable 3 in the Supplement ). Similar trends in hospitalization for AMI, STEMI, and NSTEMI were observed in the PSJH system in all 6 states (eFigure 1 in the Supplement ).
Patients hospitalized for AMI in the early and later COVID-19 periods vs the before period were slightly younger (mean [SD] age, 67 [13] years vs 68 [13] years; P < .001) and more likely to be Asian (50 [6%] and 62 [6%] vs 667 [5%]; P = .01) or Native American individuals (20 [2%] and 21 [2%] vs 151 [1%]; P = .01) ( Table 1 ). Treatment approaches for patients with STEMI or NSTEMI were not statistically different across periods (eFigure 2 in the Supplement ). Median (IQR) length of stay for patients with AMI was shorter in the early COVID-19 period by 7 hours and in the later COVID-19 period by 6 hours compared with the before period (56 [41-115] hours and 57 [41-116] hours vs 63 [43-122] hours, respectively; P < .001) ( Table 2 ). Similar trends were observed for both types of AMI. A greater number of patients with AMI were discharged to home in the early and later COVID-19 periods vs the before COVID-19 period, with consistent findings among those with STEMI (235 [83%] and 284 [81%] vs 3402 [79%]; P = .02) and NSTEMI (465 [81%] and 587 [83%] vs 6976 [77%]; P = .006).
The observed (crude) in-hospital mortality rate was similar between periods for all groups ( Table 2 ). Compared with the before COVID-19 period, however, patients with STEMI had a statistically greater risk of mortality during the later COVID-19 period after adjusting for patient demographic characteristics and comorbidities (OR, 1.52; 95% CI, 1.02-2.26). Using the PSJH model, the observed to expected (O/E) hospital mortality ratio for patients with AMI was statistically increased in the early COVID-19 period (O/E ratio, 1.27; 95% CI, 1.07-1.48), with consistent findings in the later period as well (O/E ratio, 1.23; 95% CI, 0.98-1.47). These findings, however, were different for patients with STEMI vs those with NSTEMI. For patients with STEMI, the O/E mortality ratio was substantially higher in all 3 COVID-19 periods. These patients had a stepwise increase in the O/E mortality ratio from the before period (O/E ratio, 1.48; 95% CI, 1.34-1.62) to the early (O/E ratio, 1.96; 95% CI, 1.22-2.70) and later (O/E ratio, 2.40; 95% CI, 1.65-3.16) periods. The O/E mortality ratio for STEMI in the later period was statistically greater than the before period. In contrast, patients with NSTEMI had a consistently lower O/E mortality ratio for all 3 periods (before: O/E ratio, 0.80 [95% CI, 0.71-0.88]; early: O/E ratio, 0.91 [95% CI, 0.46-1.36]; later: O/E ratio, 0.71 [95% CI, 0.49-0.93]).
Consistent with previous reports, this study found a substantial decrease in AMI hospitalization rates in the early COVID-19 period. Beginning March 29, 2020, however, hospitalizations for AMI began to increase, albeit at a slower rate. Among the many factors likely associated with this rebound in cases was encouragement of patients with symptoms or signs of AMI to seek immediate medical attention, even amid the pandemic. 5 , 6
Although patient demographics and treatment approaches were fairly consistent across periods, patients with AMI hospitalized during the COVID-19 period were 1 to 3 years younger, had a shorter length of stay, and were more likely to be discharged to home. Possible explanations for these findings were greater reluctance by older patients to seek medical attention, hospital efforts to maintain bed availability, patient preference for early discharge, and concern about risk of contracting SARS-CoV-2 in post–acute care facilities.
Notable differences in risk-adjusted mortality were observed over the periods analyzed. Patients hospitalized for AMI during the early COVID-19 period had an increased O/E mortality ratio, associated disproportionately with patients with STEMI. In this population, the O/E ratio and risk-adjusted mortality rates were even greater during the later COVID-19 period. Given the time-sensitive nature of STEMI, any delay by patients, emergency medical services, the emergency department, or cardiac catheterization laboratory may have played a role. 7 , 8 Additional complications from delayed reperfusion (eg, conduction disturbances, heart failure, cardiogenic shock, and mechanical complications) 9 may have occurred in some patients. Further research is needed to identify factors associated with the higher mortality rate in patients with STEMI.
In the weeks and months to come, clinicians may see greater numbers of patients with more severe manifestations of AMI. With the uncertainty on timing of a COVID-19 vaccine, this study reinforces the need to address important care processes for patients with AMI to help mitigate further risk.
This study has several limitations. First, because the cohort was defined by coding data, it is possible that the primary reason for hospitalization was misclassified as an AMI. Second, the treatment analysis excluded outpatients and those with other MS-DRG codes. Although this group represented a small percentage of the total patient cohort (8% [1165]), treatment shifts may have been underappreciated. Third, the data set did not allow us to evaluate potential timing-related factors that may have contributed to higher in-hospital mortality (eg, time of symptom onset, first medical contact, and hospital arrival). Fourth, although the PSJH mortality risk model is not AMI-specific, we found consistent results with a multivariable model adjusted for patient demographic characteristics and comorbidities. Fifth, the COVID-19 status of patients included in the analysis was not available. As such, the higher observed rate of AMI mortality during the COVID-19 period could have been associated with concurrent SARS-CoV-2 infection.
Results of this cross-sectional study appear to validate previous concerns that large numbers of patients with AMI initially avoided hospitalization during the COVID-19 pandemic, likely out of fear of contracting SARS-CoV-2. Hospitalization rates for AMI have begun to increase but so has the risk of in-hospital mortality. Further research into factors associated with an increase in the STEMI mortality rate is warranted.
Accepted for Publication: July 10, 2020.
Corresponding Author: Ty J. Gluckman, MD, Center for Cardiovascular Analytics, Research and Data Science (CARDS), Providence Heart Institute, Providence St Joseph Health, 9427 SW Barnes Rd, Ste 594, Portland, OR 97225 ( [email protected] ).
Published Online: August 7, 2020. doi:10.1001/jamacardio.2020.3629
Author Contributions: Drs Gluckman and Chiu had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Gluckman, Chiu, Penny, Spinelli.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Gluckman, Chiu, Spinelli.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Chiu.
Administrative, technical, or material support: Gluckman, Wilson, Penny, Chepuri, Waggoner, Spinelli.
Supervision: Gluckman, Spinelli.
Conflict of Interest Disclosures: None reported.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Myocardial Infarction (MI) Case Study (45 min)
Watch More! Unlock the full videos with a FREE trial
Included In This Lesson
Study tools.
Access More! View the full outline and transcript with a FREE trial
Definition of Myocardial Infarction (MI)
Myocardial infarction, commonly known as a heart attack, is a critical medical event that occurs when the blood supply to the heart muscle is severely reduced or completely blocked. It is a leading cause of death worldwide and a significant public health concern.
Introduction to Myocardial Infarction (MI)
This nursing case study aims to provide a comprehensive understanding of myocardial infarction by delving into its various aspects, including its pathophysiology, risk factors, clinical presentation, diagnostic methods, and management strategies. Through the exploration of a fictional patient’s journey, we will shed light on the intricate nature of this life-threatening condition and highlight the importance of early recognition and intervention.
Background and Significance of Myocardial Infarction
Myocardial infarction is a sudden and often catastrophic event that can have profound consequences on an individual’s health and well-being. Understanding its underlying mechanisms and risk factors is essential for healthcare professionals, as timely intervention can be life-saving. This case study not only serves as a learning tool but also emphasizes the critical role of medical practitioners in identifying and managing myocardial infarctions promptly.
Pathophysiology of Myocardial Infarction
A crucial aspect of comprehending myocardial infarction is exploring its pathophysiology. We will delve into the intricate details of how atherosclerosis, the buildup of plaque in coronary arteries, leads to the formation of blood clots and the subsequent interruption of blood flow to the heart muscle. This disruption in blood supply triggers a cascade of events, ultimately resulting in the death of cardiac cells.
Risk Factors of Myocardial Infarction
Understanding the risk factors associated with myocardial infarction is vital for prevention and early detection. This case study will examine both modifiable and non-modifiable risk factors, including age, gender, family history, smoking, high blood pressure, diabetes, and high cholesterol levels. Recognizing these risk factors is instrumental in developing effective strategies for prevention and risk reduction.
Clinical Presentation Myocardial Infarction
Recognizing the signs and symptoms of myocardial infarction is crucial for timely intervention. We will present a fictional patient’s experience, illustrating the typical clinical presentation, which often includes chest pain or discomfort, shortness of breath, nausea, lightheadedness, and diaphoresis. Through this patient’s journey, we will highlight the importance of accurate symptom assessment and prompt medical attention.
Diagnostic Methods for Myocardial Infarction
Modern medicine offers various diagnostic tools to confirm a myocardial infarction swiftly and accurately. This case study will explore these diagnostic methods, such as electrocardiography (ECG), cardiac biomarkers, and imaging techniques like coronary angiography. By understanding these diagnostic modalities, healthcare professionals can make informed decisions and initiate appropriate treatments promptly.
Management Strategies for Myocardial Infarction
The management of myocardial infarction involves a multidisciplinary approach, including medication, revascularization procedures, and lifestyle modifications. We will discuss the fictional patient’s treatment plan, emphasizing the importance of reestablishing blood flow to the affected heart muscle and preventing further complications.
Nursing Case Study for Myocardial Infarction (MI)
Having established a foundational understanding of myocardial infarction, we will now delve deeper into Mr. Salazar’s case, tracing his journey through diagnosis, treatment, and recovery. This in-depth examination will shed light on the real-world application of the principles discussed in the introduction, providing valuable insights into the clinical management of myocardial infarction and its impact on patient outcomes.
Mr. Salazar, a 57-year-old male, arrives at the Emergency Department (ED) with complaints of chest pain that began approximately one hour after dinner while he was working. He characterizes the discomfort as an intense “crushing pressure” located centrally in his chest, extending down his left arm and towards his back. He rates the pain’s severity as 4/10. Upon examination, Mr. Salazar exhibits diaphoresis and pallor, accompanied by shortness of breath (SOB).
What further nursing assessments need to be performed for Mr. Salazar?
- Heart Rate (HR): The number of heartbeats per minute.
- Blood Pressure (BP): The force of blood against the walls of the arteries, typically measured as systolic (during heartbeats) and diastolic (between heartbeats) pressure.
- Respiratory Rate (RR): The number of breaths a patient takes per minute.
- Body Temperature (Temp): The measurement of a patient’s internal body heat.
- Oxygen Saturation (SpO2): The percentage of oxygen in the blood.
- S1: The first heart sound, often described as “lub,” is caused by the closure of the mitral and tricuspid valves.
- S2: The second heart sound, known as “dub,” results from the closure of the aortic and pulmonic valves.
- These sounds provide important diagnostic information about the condition of the heart.
- Clear: Normal, healthy lung sounds with no added sounds.
- Crackles (Rales): Discontinuous, often high-pitched sounds are heard with conditions like pneumonia or heart failure.
- Wheezes: Whistling, musical sounds often associated with conditions like asthma or chronic obstructive pulmonary disease (COPD).
- Pulses refer to the rhythmic expansion and contraction of arteries with each heartbeat. Common pulse points for assessment include the radial artery (wrist), carotid artery (neck), and femoral artery (groin). Evaluating pulses helps assess the strength, regularity, and rate of blood flow.
- Edema is the abnormal accumulation of fluid in body tissues, leading to swelling. It can occur in various body parts and may indicate underlying conditions such as heart failure, kidney disease, or localized injury. Edema assessment involves evaluating the degree of swelling and its location.
- Skin condition (temperature, color, etc.)
What interventions do you anticipate being ordered by the provider?
- Oxygen therapy involves administering oxygen to a patient to increase the level of oxygen in their blood. It is used to treat conditions such as respiratory distress, and hypoxia (low oxygen levels), and to support patients with breathing difficulties.
- Nitroglycerin is a medication used to treat angina (chest pain) and to relieve symptoms of heart-related conditions. It works by relaxing and widening blood vessels, which improves blood flow to the heart, reducing chest pain.
- Aspirin is a common over-the-counter medication and antiplatelet drug. In the context of myocardial infarction (heart attack), it is often administered to reduce blood clot formation, potentially preventing further blockage in coronary arteries.
- A 12-lead EKG is a diagnostic test that records the electrical activity of the heart from 12 different angles. It provides information about the heart’s rhythm, rate, and any abnormalities, helping diagnose conditions like arrhythmias, heart attacks, and ischemia.
- Cardiac enzymes are proteins released into the bloodstream when heart muscle cells are damaged or die, typically during a heart attack. Measuring these enzymes, such as troponin and creatine kinase-MB (CK-MB), helps confirm a heart attack diagnosis and assess its severity.
- A chest X-ray is a diagnostic imaging procedure that creates images of the chest and its internal structures, including the heart and lungs. It is used to identify issues like lung infections, heart enlargement, fluid accumulation, or fractures in the chest area.
- Possibly an Echocardiogram
Upon conducting a comprehensive assessment, it was observed that the patient exhibited no signs of jugular vein distention (JVD) or edema. Auscultation revealed normal heart sounds with both S1 and S2 present, while the lungs remained clear, albeit with scattered wheezes. The patient’s vital signs were recorded as follows:
- BP 140/90 mmHg SpO 2 90% on Room Air
- HR 92 bpm and regular Ht 173 cm
- RR 32 bpm Wt 104 kg
- Temp 36.9°C
The 12-lead EKG repor t indicated the presence of “Normal sinus rhythm (NSR) with frequent premature ventricular contractions (PVCs) and three- to four-beat runs of ventricular tachycardia (VT).” Additionally, there was ST-segment elevation in leads I, aVL, and V2 through V6 (3-4mm), accompanied by ST-segment depression in leads III and aVF.
Cardiac enzyme levels were collected but were awaiting results at the time of assessment. A chest x-ray was also ordered to provide further diagnostic insights.
In response to the patient’s condition, the healthcare provider prescribed the following interventions:
- Aspirin: 324 mg administered orally once.
- Nitroglycerin: 0.4 mg administered sublingually (SL), with the option of repeating the dose every five minutes for a maximum of three doses.
- Morphine: 4 mg to be administered intravenously (IVP) as needed for unrelieved chest pain.
- Oxygen: To maintain oxygen saturation (SpO2) levels above 92%.
These interventions were implemented to address the patient’s myocardial infarction (heart attack) and alleviate associated symptoms, with a focus on relieving chest pain, improving oxygenation, and closely monitoring vital signs pending further diagnostic results.
What intervention should you, as the nurse, perform right away? Why?
- Apply oxygen – this can be done quickly and easily and can help to prevent further complications from low oxygenation.
- Oxygen helps to improve oxygenation as well as to decrease myocardial oxygen demands.
- Often it takes a few minutes or more for medications to be available from the pharmacy, so it makes sense to take care of this intervention first.
- ABC’s – breathing/O 2 .
What medication should be the first one administered to this patient? Why? How often?
- Nitroglycerin 0.4mg SL – it is a vasodilator and works on the coronary arteries. The goal is to increase blood flow to the myocardium. If this is effective, the patient merely has angina. However, if it is not effective, the patient may have a myocardial infarction.
- Aspirin should also be given, but it is to decrease platelet aggregation and reduce mortality. While it can somewhat help prevent the worsening of the blockage, it does little for the current pain experienced by the patient.
- Morphine should only be given if the nitroglycerin and aspirin do not relieve the patient’s chest pain.
What is the significance of the ST-segment changes on Mr. Salazar's 12-lead EKG?
- ST-segment changes on a 12-lead EKG indicate ischemia (lack of oxygen/blood flow) or infarction (death of the muscle tissue) of the myocardium (heart muscle).
- This indicates an emergent situation. The patient’s coronary arteries are blocked and need to be reopened by pharmacological (thrombolytic) or surgical (PCI) intervention.
- Time is tissue – the longer the coronary arteries stay blocked, the more of the patient’s myocardium that will die. Dead heart tissue doesn’t beat.
Mr. Salazar’s chest pain was unrelieved after three (3) doses of sublingual nitroglycerin (NTG). Morphine 5 mg intravenous push (IVP) was administered, as well as 324 mg chewable baby aspirin. His pain was still unrelieved at this point
Mr. Salazar’s cardiac enzyme results were as follows:
Troponin I 3.5 ng/mL
Based on the results of Mr. Salazar's labs and his response to medications, what is the next intervention you anticipate? Why?
- Mr. Salazar needs intervention. He will either receive thrombolytics or a heart catheterization (PCI).
- Based on the EKG changes, elevated Troponin level, and the fact that his symptoms are not subsiding, it’s possible the patient has a significant blockage in one or more of his coronary arteries.
- It seems as though it may be an Anterior-Lateral MI because ST elevation is occurring in I, aVL, and V 2 -V 6 .
Mr. Salazar was taken immediately to the cath lab for a Percutaneous Coronary Intervention (PCI). The cardiologist found a 90% blockage in his left anterior descending (LAD) artery. A stent was inserted to keep the vessel open.
What is the purpose of Percutaneous Coronary Intervention (PCI), also known as a heart catheterization?
- A PCI serves to open up any coronary arteries that are blocked. First, they use contrast dye to determine where the blockage is, then they use a special balloon catheter to open the blocked vessels.
- If that doesn’t work, they will place a cardiac stent in the vessel to keep it open.[ /faq]
[faq lesson="true" blooms="Application" question="What is the expected outcome of a PCI? What do you expect to see in your patient after they receive a heart catheterization?"]
- Blood flow will be restored to the myocardium with minimal residual damage.
- The patient should have baseline vital signs, relief of chest pain, normal oxygenation status, and absence of heart failure symptoms (above baseline).
- The patient should be able to ambulate without significant chest pain or SOB.
- The patient should be free from bleeding or hematoma at the site of catheterization (often femoral, but can also be radial or (rarely) carotid.
Mr. Salazar tolerated the PCI well and was admitted to the cardiac telemetry unit for observation overnight. Four (4) hours after the procedure, Mr. Salazar reports no chest pain. His vital signs are now as follows:
- BP 128/82 mmHg SpO 2 96% on 2L NC
- HR 76 bpm and regular RR 18 bpm
- Temp 37.1°C
Mr. Salazar will be discharged home 24 hours after his arrival to the ED and will follow up with his cardiologist next week.
What patient education topics would need to be covered with Mr. Salazar?
- He should be taught any dietary and lifestyle changes that should be made.
- Diet – low sodium, low cholesterol, avoid sugar/soda, avoid fried/processed foods.
- Exercise – 30-45 minutes of moderate activity 5-7 days a week, u nless instructed otherwise by a cardiologist. This will be determined by the patient’s activity tolerance – how much can they do and still be able to breathe and be pain-free?
- Stop smoking and avoid caffeine and alcohol.
- Medication Instructions
- Nitroglycerin – take one SL tab at the onset of chest pain. If the pain does not subside after 5 minutes, call 911 and take a second dose. You can take a 3rd dose 5 minutes after the second if the pain does not subside. Do NOT take if you have taken Viagra in the last 24 hours.
- Aspirin – take 81 mg of baby aspirin daily
- Anticoagulant – the patient may be prescribed an anticoagulant if they had a stent placed. They should be taught about bleeding risks.
- When to call the provider – CP unrelieved by nitroglycerin after 5 minutes. Syncope. Evidence of bleeding in stool or urine (if on anticoagulant). Palpitations, shortness of breath, or difficulty tolerating activities of daily living.
Linchpins for Myocardial Infarction Nursing Case Study
In summary, Mr. Salazar’s case highlights the urgency of recognizing and responding to myocardial infarction promptly. The application of vital signs, EKG, cardiac enzymes, and medications like aspirin, nitroglycerin, and morphine played a pivotal role in his care. Diagnostic tools like echocardiography and chest X-rays contributed to a comprehensive evaluation.
Nurses must remain vigilant and compassionate in such emergencies. This case study emphasizes the importance of adhering to best practices in the assessment, diagnosis, and management of myocardial infarction, with the ultimate goal of achieving favorable patient outcomes.
View the FULL Outline
When you start a FREE trial you gain access to the full outline as well as:
- SIMCLEX (NCLEX Simulator)
- 6,500+ Practice NCLEX Questions
- 2,000+ HD Videos
- 300+ Nursing Cheatsheets
“Would suggest to all nursing students . . . Guaranteed to ease the stress!”
Nursing Case Studies

This nursing case study course is designed to help nursing students build critical thinking. Each case study was written by experienced nurses with first hand knowledge of the “real-world” disease process. To help you increase your nursing clinical judgement (critical thinking), each unfolding nursing case study includes answers laid out by Blooms Taxonomy to help you see that you are progressing to clinical analysis.We encourage you to read the case study and really through the “critical thinking checks” as this is where the real learning occurs. If you get tripped up by a specific question, no worries, just dig into an associated lesson on the topic and reinforce your understanding. In the end, that is what nursing case studies are all about – growing in your clinical judgement.
Nursing Case Studies Introduction
Cardiac nursing case studies.
- 6 Questions
- 7 Questions
- 5 Questions
- 4 Questions
GI/GU Nursing Case Studies
- 2 Questions
- 8 Questions
Obstetrics Nursing Case Studies
Respiratory nursing case studies.
- 10 Questions
Pediatrics Nursing Case Studies
- 3 Questions
- 12 Questions
Neuro Nursing Case Studies
Mental health nursing case studies.
- 9 Questions
Metabolic/Endocrine Nursing Case Studies
Other nursing case studies.
- Campus Directory
- Current Students
- Faculty & Staff

Acute Myocardial Infarction Case Study
Myocardial infarction (heart attack) is the leading cause of death in the United States. It is estimated that one in every five deaths in the US is due to a heart attack. Approximately one million patients are admitted to hospitals each year due to heart attacks. 200,000 to 300,000 individuals die from heart attacks before ever receiving medical care. In Case #2 we’ll join 48-year-old Jason Dixon as he experiences a life-threatening heart attack.
Module 7: Acute Myocardial Infarction
48 year old Jason Dixon had not been feeling well all day and around 10:00 p.m he went to bed...
AMI - Page 1
Before we progress further into this relatively complex case, please review module 6 in the...
AMI - Page 2
Case continued: Enroute to the ER, the patient's acute symptoms had been relieved...
AMI - Page 3
This is a critical decision point for the cardiologist. There are several algorithms...
AMI - Page 4
Case Summary
Summary of the Case
AMI - Summary

Answers to Case Questions
AMI - Answers

Professionals
Health Professionals Introduced in Case
AMI - Professionals
Additional Links
Optional Links to Explore Further
AMI - Links
- Publications
- Conferences & Events
- Professional Learning
- Science Standards
- Awards & Competitions
- Daily Do Lesson Plans
- Free Resources
- American Rescue Plan
- For Preservice Teachers
- NCCSTS Case Collection
- Partner Jobs in Education
- Interactive eBooks+
- Digital Catalog
- Regional Product Representatives
- e-Newsletters
- Bestselling Books
- Latest Books
- Popular Book Series
- Prospective Authors
- Web Seminars
- Exhibits & Sponsorship
- Conference Reviewers
- National Conference • Denver 24
- Leaders Institute 2024
- National Conference • New Orleans 24
- Submit a Proposal
- Latest Resources
- Professional Learning Units & Courses
- For Districts
- Online Course Providers
- Schools & Districts
- College Professors & Students
- The Standards
- Teachers and Admin
- eCYBERMISSION
- Toshiba/NSTA ExploraVision
- Junior Science & Humanities Symposium
- Teaching Awards
- Climate Change
- Earth & Space Science
- New Science Teachers
- Early Childhood
- Middle School
- High School
- Postsecondary
- Informal Education
- Journal Articles
- Lesson Plans
- e-newsletters
- Science & Children
- Science Scope
- The Science Teacher
- Journal of College Sci. Teaching
- Connected Science Learning
- NSTA Reports
- Next-Gen Navigator
- Science Update
- Teacher Tip Tuesday
- Trans. Sci. Learning

MyNSTA Community
- My Collections
The Heart of the Problem
From Heart Attack to Kidney Failure
By Kristine A. Garner, Brandy C. Ree
Share Start a Discussion

This interrupted case study was developed for an undergraduate class in human cardiac physiology. The story follows a patient whose heart attack damaged a papillary muscle in the left ventricle of the heart. This caused valve dysfunction and mitral valve regurgitation resulting in left-sided heart failure, which in turn led to systemic problems including pulmonary edema and kidney failure. This case study was designed to follow a chapter or unit covering the heart and/or the cardiovascular system, and would be appropriate for any undergraduate human anatomy and physiology course or for nursing students. Before beginning the activity, students should know the anatomy of the heart, understand the function of the heart valves and blood flow through the heart, be able to calculate cardiac output, and understand the implications of blood pressure on capillary filtration. This case study was written specifically for students who have not yet covered the respiratory system or the urinary system.
Download Case
Date Posted
- Describe the structure and function of the heart.
- Describe the direction of blood flow in the heart.
- State the function of heart valves.
- Relate cardiac output to blood pressure.
- Link pressure dynamics to blood flow in the body.
- Explain how blood pressure is related to capillary filtration.
- Correlate the functions of the cardiovascular system to the pulmonary and urinary systems.
Heart failure; mitral valve prolapse; blood pressure; blood flow; cardiac output; capillary filtration;
Subject Headings
EDUCATIONAL LEVEL
Undergraduate lower division, Clinical education
TOPICAL AREAS
TYPE/METHODS
Teaching Notes & Answer Key
Teaching notes.
Case teaching notes are protected and access to them is limited to paid subscribed instructors. To become a paid subscriber, purchase a subscription here .
Teaching notes are intended to help teachers select and adopt a case. They typically include a summary of the case, teaching objectives, information about the intended audience, details about how the case may be taught, and a list of references and resources.
Download Notes
Answer Keys are protected and access to them is limited to paid subscribed instructors. To become a paid subscriber, purchase a subscription here .
Download Answer Key
Materials & Media
Supplemental materials.
The supplemental material below is recommended for use with this case study.

You may also like
Web Seminar
Join us on Thursday, June 13, 2024, from 7:00 PM to 8:00 PM ET, to learn about the science and technology of firefighting. Wildfires have become an e...
Join us on Thursday, October 10, 2024, from 7:00 to 8:00 PM ET, for a Science Update web seminar presented by NOAA about climate science and marine sa...

New heart disease calculator could save lives by identifying high-risk patients missed by current tools
Collaborative research, led from the University of Oxford and published today in Nature Medicine , has developed a new tool called QR4 that more accurately predicts an individual's 10-year risk of cardiovascular diseases, like heart disease and stroke, particularly identifying high-risk patients that current prediction tools miss.
Cardiovascular disease is a leading cause of death globally. The new tool, QR4 can be thought of as a type of calculator that lets doctors use an individual’s health data, such as blood pressure, age and medical history, to estimate their likelihood of developing a cardiovascular disease over the next 10 years, allowing them to intervene early to prevent illness.
QR4 includes seven new risk factors applicable to all adults: chronic obstructive pulmonary disease (COPD), learning disabilities, Down syndrome and four cancer types (blood, lung, oral and brain), highlighting how other significant diseases impact on heart health.
QR4 also identified factors specific to women's health that were predictive of future heart disease risk, such as complications from high blood pressure during pregnancy, and postnatal depression.
'While traditional cardiovascular risk factors such as smoking and high cholesterol are well-recognised, our latest research identifies less obvious, yet crucial risk indicators,' said Professor Julia Hippisley-Cox , lead author, Professor of Clinical Epidemiology and General Practice, at the University of Oxford’s Nuffield Department of Primary Care Health Sciences . 'For instance, conditions like postnatal depression and Down’s syndrome significantly contribute to cardiovascular risk, underscoring the complex interplay between mental health, genetic factors, and heart health. QR4 also helps to address inequalities in health, particularly around learning disabilities, which often coincide with barriers to effective health management and access, leading to an increased risk.
'We believe that these findings are important to both patients and policy makers,' said P rofessor Hippisley-Cox . 'They indicate that more groups of people are at increased risk for heart and circulatory diseases than previously recognised. These people could and should now benefit from treatments and other preventive measures to reduce their risk.'
'Our findings also reveal that women with COPD are at a higher risk of cardiovascular diseases than previously understood,' said Professor Mona Bafadhel , co-author, Chair of Respiratory Medicine, King’s College, London and Asthma + Lung UK Professor. 'This underscores the critical need for targeted cardiovascular monitoring and interventions in these patients, which begins with an early diagnosis.'
As part of a comprehensive evaluation, the QR4 algorithm was rigorously tested against some of the most well-established cardiovascular risk assessment tools currently used in both the United States and Europe. It outperformed the most widely used heart disease risk calculators, including QRISK3 recommended by the National Institute for Health and Care Excellence (NICE) in the UK, accurately identifying more high-risk patients.
'This important update to the QRISK tool will allow clinicians to build the clearest picture yet of individuals’ risk of developing heart and circulatory diseases,' said Professor Bryan Williams , Chief Scientific and Medical Officer at the British Heart Foundation . 'Informed by large amounts of data from diverse populations, the new and improved algorithm takes vital steps towards improving risk assessment in populations where cardiovascular risk may often go under-detected. The QR4 tool will offer a much-needed, renewed focus on better identifying people at risk and improving the prevention of cardiovascular diseases.'
'Cardiovascular risk has been under-recognised in some populations, which through QR4 we can now better address,' said Professor Keith Channon , BHF Professor of Cardiovascular Medicine at the University of Oxford. 'The new findings will help identify more diverse groups of people who have high cardiovascular risk, enabling them to access interventions and treatments to reduce their risk.'
'The QR4 model potentially sets a new standard in cardiovascular risk assessment,' said Dr Carol Coupland , senior researcher at the University of Oxford and Professor of Medical Statistics in Primary Care at the University of Nottingham and co-author of the study. 'Our head-to-head comparisons with established models show that QR4 provides a more detailed risk profile for each individual, allowing for earlier and more precise intervention strategies. This is crucial in a field where early detection can save lives and could significantly impact how we approach prevention on a global scale.'
This new algorithm builds on almost two decades of work and global leadership in the field of risk algorithms, and cardiovascular risk algorithms in particular. QR4’s predecessor, QRISK is widely used in the NHS to assess over 5 million patients a year, often as part of NHS Health Checks.
The researchers hope that clinicians, advisory bodies, regulators, and health and care policymakers consider the implications of QR4's advanced predictive capabilities on national health guidelines and support its adoption in clinical settings to improve cardiovascular health outcomes.
The study ' Development and validation of a new algorithm for improved cardiovascular risk prediction ' is published in Nature Medicine .
DISCOVER MORE
- Support Oxford's research
- Partner with Oxford on research
- Study at Oxford
- Research jobs at Oxford
You can view all news or browse by category
Find cars that meet your safety needs with AARP Auto Buying Program powered by TrueCar. Learn more.
Popular Searches
AARP daily Crossword Puzzle
Hotels with AARP discounts
Life Insurance
AARP Dental Insurance Plans
Suggested Links
AARP MEMBERSHIP — $12 FOR YOUR FIRST YEAR WHEN YOU SIGN UP FOR AUTOMATIC RENEWAL
Get instant access to members-only products and hundreds of discounts, a free second membership, and a subscription to AARP the Magazine.
- right_container
Work & Jobs
Social Security
AARP en Español
- Membership & Benefits
AARP Rewards
- AARP Rewards %{points}%
Conditions & Treatments
Drugs & Supplements
Health Care & Coverage
Health Benefits

Staying Fit
Your Personalized Guide to Fitness

AARP Hearing Center
Ways To Improve Your Hearing

Brain Health Resources
Tools and Explainers on Brain Health

A Retreat For Those Struggling
Scams & Fraud
Personal Finance
Money Benefits

View and Report Scams in Your Area

AARP Foundation Tax-Aide
Free Tax Preparation Assistance

AARP Money Map
Get Your Finances Back on Track

How to Protect What You Collect
Small Business
Age Discrimination

Flexible Work
Freelance Jobs You Can Do From Home

AARP Skills Builder
Online Courses to Boost Your Career

31 Great Ways to Boost Your Career

ON-DEMAND WEBINARS
Tips to Enhance Your Job Search

Get More out of Your Benefits

When to Start Taking Social Security

10 Top Social Security FAQs

Social Security Benefits Calculator

Medicare Made Easy
Original vs. Medicare Advantage

Enrollment Guide
Step-by-Step Tool for First-Timers

Prescription Drugs
9 Biggest Changes Under New Rx Law

Medicare FAQs
Quick Answers to Your Top Questions
Care at Home
Financial & Legal
Life Balance

LONG-TERM CARE
Understanding Basics of LTC Insurance

State Guides
Assistance and Services in Your Area

Prepare to Care Guides
How to Develop a Caregiving Plan

End of Life
How to Cope With Grief, Loss
Recently Played
Word & Trivia
Atari® & Retro
Members Only
Staying Sharp
Mobile Apps
More About Games

Right Again! Trivia

Right Again! Trivia – Sports

Atari® Video Games

Throwback Thursday Crossword
Travel Tips
Vacation Ideas
Destinations
Travel Benefits

Beach vacation ideas
Vacations for Sun and Fun

Plan Ahead for Tourist Taxes

AARP City Guide
Discover Seattle

25 Ways to Save on Your Vacation
Entertainment & Style
Family & Relationships
Personal Tech
Home & Living
Celebrities
Beauty & Style

TV for Grownups
Best Reality TV Shows for Grownups

Robert De Niro Reflects on His Life

Looking Back
50 World Changers Turning 50

Sex & Dating
Spice Up Your Love Life

Navigate All Kinds of Connections

Life & Home
Couple Creates Their Forever Home

Store Medical Records on Your Phone?

Maximize the Life of Your Phone Battery

Virtual Community Center
Join Free Tech Help Events

Create a Hygge Haven

Soups to Comfort Your Soul

Your Ultimate Guide to Mulching
Driver Safety
Maintenance & Safety
Trends & Technology

AARP Smart Guide
How to Keep Your Car Running

We Need To Talk
Assess Your Loved One's Driving Skills

AARP Smart Driver Course

Building Resilience in Difficult Times

Tips for Finding Your Calm

Weight Loss After 50 Challenge

Cautionary Tales of Today's Biggest Scams

7 Top Podcasts for Armchair Travelers

Jean Chatzky: ‘Closing the Savings Gap’

Quick Digest of Today's Top News

AARP Top Tips for Navigating Life

Get Moving With Our Workout Series
You are now leaving AARP.org and going to a website that is not operated by AARP. A different privacy policy and terms of service will apply.
Go to Series Main Page
Heart Attack vs. Cardiac Arrest: What’s the Difference?
The two are often mistaken for one another, but causes, warnings signs and treatments can differ.
Rachel Nania,

When Nicole Smith went to visit her 83-year-old father in the hospital last fall, she never imaged she’d become a patient, too. But that’s exactly what happened to the Fort Lauderdale, Florida, resident after she suddenly collapsed in the cafeteria.
“I woke up and I was in the intensive care unit,” says Smith, 53. The diagnosis: sudden cardiac arrest. With no known heart risks or warning signs, she never saw it coming. “This was the furthest thing from my mind that something like this could happen,” she said.

AARP Membership — $12 for your first year when you sign up for Automatic Renewal
While often confused with a heart attack, cardiac arrest is a completely different health emergency — and it’s one that requires prompt recognition and response.
Here’s what you need to know about each of the two conditions and what to do if you suspect someone is experiencing a serious heart event.
Cardiac arrest
What is cardiac arrest? Cardiac arrest is when the heart suddenly stop pumping, depriving the body and brain of oxygen-rich blood.
The impact is immediate: Breathing stops and the person loses consciousness. “If somebody has a cardiac arrest, it’s not subtle. They are on the ground, and they are not responding to you,” says Gregory Katz, M.D., a cardiologist at NYU Langone and an assistant professor in the Department of Medicine at NYU Grossman School of Medicine.
What causes cardiac arrest? Cardiac arrest is caused by irregular heart rhythms, called arrhythmias, that cause the heart to stop working properly, says the National Heart, Lung and Blood Institute (NHLBI).
Many health conditions that are common among older adults can disrupt the heart’s rhythm and increase the risk of cardiac arrest, including coronary heart disease , a prior heart attack, atrial fibrillation , heart inflammation, cardiomyopathy (an enlarged heart), and leaky or narrow heart valves. Still, the NHLBI says about half of cardiac arrests happen to people who did not know they had a heart problem, as was the case with Smith.
Most Popular

AARP NEWSLETTERS

%{ newsLetterPromoText }%
%{ description }%
Privacy Policy
ARTICLE CONTINUES AFTER ADVERTISEMENT
Sometimes heavy alcohol use or drug use can trigger cardiac arrest. So can severe stress , a blow to the chest (this is what recently happened to NFL player Damar Hamlin) and respiratory arrest, or when a person stops breathing.
Are there warning signs and symptoms of cardiac arrest? Unlike many other health issues, there aren’t usually any signs or symptoms to warn an individual that cardiac arrest is imminent, though some people may experience chest pain, nausea, vomiting or shortness of breath before losing consciousness. “People may get no warning whatsoever,” Katz says.
AARP® Vision Plans from VSP™
Exclusive vision insurance plans designed for members and their families
What should you do? If you see someone in cardiac arrest, “the immediate thing that you do is you start chest compressions, and you call 9-1-1,” Katz says. Starting CPR — which helps keep blood flow active until emergency responders arrive — “really is the difference between somebody having a good outcome versus a tragic outcome,” he says. About 350,000 people die from cardiac arrest every year in the U.S., and less than half of people who experience cardiac arrest outside the hospital receive the right care from bystanders.
The American Heart Association says anyone can perform CPR with hands-only chest compressions (no need for mouth-to-mouth unless you’re trained and feel comfortable doing it). Push hard and fast in the center of the chest to the beat of “Stayin’ Alive” by the Bee Gees or another song that is equivalent to about 100 to 120 beats per minute. And if an automated external defibrillator (AED) is available, use it. These portable devices that can often be found in public places such as airports and malls can stimulate the heart to resume beating.
Heart Attack vs. Cardiac Arrest
A quick way to remember the difference:
Cardiac arrest is an “electrical” problem
- If you see someone going into cardiac arrest, call 911 and start CPR right away.
Heart attack is a “circulation” problem
- If someone is having a heart attack, call 911.
Source: American Heart Association
Smith considers herself fortunate that her cardiac arrest — which her doctor says was possibly caused by a ventricular fibrillation, or an irregular heartbeat, and may have been brought on by stress — occurred inside a hospital. She now has a small device known as an implantable cardioverter-defibrillator in her chest to detect and correct any irregular heartbeats that could cause this to happen again.
Heart attack
What is a heart attack? Unlike with cardiac arrest, the heart is still pumping when a person has a heart attack; it’s just that the heart is under stress, says Mistyann-Blue Miller, M.D., a cardiologist with Cleveland Clinic in Vero Beach, Florida. And that’s because blood flow to the heart is being blocked. If this blood flow is not restored quickly, the oxygen-starved heart muscle will start to die.
What causes a heart attack? Most heart attacks are caused by coronary artery disease, according to the NHLBI, or plaque buildup along the walls of the arteries that supply blood to the heart. Cholesterol and other fatty substances can lead to this buildup.
A number of modifiable factors can increase your risk for coronary artery disease, including physical inactivity, unhealthy eating, smoking and being overweight , according to the Centers for Disease Control and Prevention. Other risk factors include a family history of heart disease.

Join AARP today for $16 per year. Get instant access to members-only products and hundreds of discounts, a free second membership, and a subscription to AARP The Magazine.
Are there warning signs or symptoms of a heart attack? Also different from cardiac arrest is that many people who have a heart attack experience symptoms. For some, they can start slowly and be mild. For others, symptoms can come on suddenly and be severe.
“I describe it to patients that it can be anything weird between your chin and your belly button,” Katz says. And those odd or uncomfortable feelings typically gets worse with physical activity. “The idea that everyone has an elephant sitting on their chest as their heart attack symptom is just not borne out in the real world,” he adds.
Heart attack symptoms can include:
- Chest pain or discomfort
- Pain or discomfort in the arms, back, shoulders, neck, jaw and stomach (above the belly button)
- Shortness of breath
- Nausea and vomiting
- Lightheadedness or dizziness
- Rapid or irregular heartbeat
Women tend to have more “nonspecific” heart attack symptoms that are easier to attribute to other things , such as stress, Miller says. “That can be a dull, achy feeling between the shoulder blades, maybe fatigue, decreased exercise tolerance,” she explains. “If something doesn’t feel right, definitely report that to your doctor.”
Katz says older adults are also less likely to experience the classic heart attack symptoms.
What should you do? If you suspect a heart attack, call 9-1-1 right away. CPR isn’t necessary unless the person isn’t breathing or you can’t find a pulse. “You really need to go to an emergency room,” Katz says, where doctors can quickly locate and address the blockage. The longer the heart goes without oxygen, the more likely a person is to experience permanent damage, even death.
Rachel Nania is an award-winning health editor and writer at AARP.org, who covers a range of topics including diseases and treatments.
Discover AARP Members Only Access
Already a Member? Login

More From AARP
Heart Health: News, Tips and Healthy Habits
Information and tips on exercise, diet, and other lifestyle habits to keep your heart healthy

8 Major Health Risks for People 50 and Older
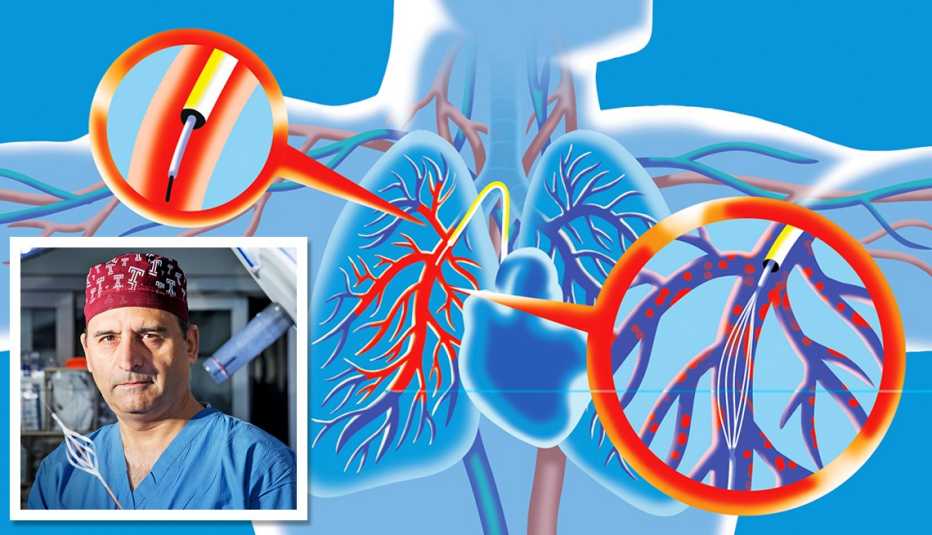
Medical Advancements in Cardiovascular Disease
New research is changing the future for older Americans' heart health

Rare Heart Condition Offers Few Clues
A common symptom was the only warning sign for a fast and fatal disease
Recommended for You
AARP Value & Member Benefits

Learn, earn and redeem points for rewards with our free loyalty program

AARP® Dental Insurance Plan administered by Delta Dental Insurance Company
Dental insurance plans for members and their families

The National Hearing Test
Members can take a free hearing test by phone

AARP® Staying Sharp®
Activities, recipes, challenges and more with full access to AARP Staying Sharp®
SAVE MONEY WITH THESE LIMITED-TIME OFFERS
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Arq Bras Cardiol
- v.105(4); 2015 Oct

Case 4 – A 79-Year-Old Man with Congestive Heart Failure Due to Restrictive Cardiomyopathy
Sumaia mustafa.
1 Instituto do Coração (InCor) HC-FMUSP, São Paulo, SP – Brasil
Alice Tatsuko Yamada
Fabio mitsuo lima.
2 Grupo Fleury Medicina e Saúde, São Paulo, SP – Brasil
Valdemir Melechco Carvalho
Vera demarchi aiello, jussara bianchi castelli.
JAP, a 79-year-old male and retired metalworker, born in Várzea Alegre (Ceará, Brazil) and residing in São Paulo was admitted to the hospital in October 2013 due to decompensated heart failure.
The patient was referred 1 year before to InCor with a history of progressive dyspnea triggered by less than ordinary activities, lower-extremity edema, and abdominal enlargement. He sought medical care due to the abdominal enlargement, which was diagnosed as an ascites. He denied chest pain, hospitalization due to myocardial infarction or stroke, hypertension, dyslipidemia, and diabetes.
The patient was a previous smoker and had stopped smoking at the age of 37 years. He was also an alcoholic and reported drinking alcohol for the last time 1 year before.
He was referred to InCor for treatment of heart failure.
An echocardiogram revealed an increased thickness in the septum (17 mm) and free left ventricular wall (15 mm), and a left ventricular ejection fraction of 26%.
The patient reported daily use of enalapril 10 mg, spironolactone 25 mg, furosemide 80 mg, omeprazole 40 mg, and ferrous sulfate (40 mg Fe) three tablets.
On March 12, 2013, his physical examination showed a weight of 55 kg, height of 1.75 m, body mass index (BMI) of 18 kg/m 2 , heart rate of 60 bpm, blood pressure of 90 X 50 mm Hg, and the presence of a hepatojugular reflux. There were no signs of jugular venous hypertension, and the pulmonary and cardiac auscultations were normal. He had ascites, and his liver was palpable 5 cm below the right costal margin. Peripheral pulses were palpable, and a ++/4+ edema was observed.
An ECG (February 23, 2012) had shown a sinus rhythm, heart rate of 52 bpm, PR interval of 192 ms, QRS duration of 106 ms, indirect signs of right atrial overload (wide variability in QRS amplitude between V1 and V2), and left atrial overload (prolonged and notched P waves), low QRS voltage in the frontal plane with an indeterminate axis, an electrically inactive area in the anteroseptal region and secondary changes in ventricular repolarization ( Figure 1 ).

ECG: sinus bradycardia, low-voltage QRS complexes in the frontal plane, indirect signs of right atrial overload (small QRS complexes in V1 and wide QRS complexes in V2), left atrial overload, electrically inactive area in the anteroseptal region.
A chest x-ray showed cardiomegaly.
Laboratory tests performed on April 20, 2012, had shown the following results: hemoglobin 13.1 g/dL, hematocrit 40%, mean corpuscular volume (MCV) 87 fL, leukocytes 9,230/mm 3 (banded neutrophils 1%, segmented neutrophils 35%, eosinophils 20%, basophils 1%, lymphocytes 33%, and monocytes 10%), platelets 222,000 /mm 3 , cholesterol 207 mg/dL, HDL-cholesterol 54 mg/dL, LDL-cholesterol 138 mg/dL, triglycerides 77 mg/dL, creatine phosphokinase (CPK) 77 U/L, blood glucose 88 mg/dL, urea 80 mg/dL, creatinine 1.2 mg/dL (glomerular filtration rate ≥ 60 mL/min/1.73 m 2 ), sodium 131 mEq/L, potassium 6.3 mEq/L, aspartate aminotransferase (AST) 22 U/L, alanine aminotransferase (ALT) 34 U/L, uric acid 6.3 mg/dL, TSH 1.24 µUI/mL, free T4 1.36 ng/dL, prostate-specific antigen (PSA) 1.24 ng/mL. On urinalysis, urine specific gravity was 1.007, pH 5.5, the sediment was normal, and there were no abnormal elements.
A new echocardiographic assessment on April 20, 2012, had shown an aortic diameter of 32 mm, left atrium of 52 mm, septal and posterior left ventricular wall thickness of 15 mm, diastolic/systolic left ventricular diameters of 46/40 mm, and left ventricular ejection fraction of 28%. Both ventricles had diffuse and marked hypokinesia. The valves were normal and the pulmonary artery systolic pressure was estimated at 32 mmHg ( Figure 2 ).

Echocardiogram - a) Four-chamber view: marked enlargement of the left and right atria; b) parasternal long-axis view: enlarged left atrium, left ventricular wall thickening, normal cavity.
A 24-hour electrocardiographic (Holter) monitoring on April 19, 2012, showed a baseline sinus rhythm with a lowest rate of 46 bpm and greatest rate of 97 bpm; 48 isolated, polymorphic, and paired ventricular extrasystoles; 137 atrial extrasystoles; and an episode of atrial tachycardia over three beats with a frequency of 98 bpm. There were no atrioventricular or intraventricular blocks interfering with the conduction of the stimulus.
The patient was transferred from the pacemaker clinic to the general cardiopathy clinic.
During a clinic appointment on January 22, 2013, the patient was asymptomatic and reported the use of enalapril 10 mg, spironolactone 25 mg, furosemide 60 mg, and carvedilol 12.5 mg. His physical examination was normal.
The main diagnostic hypotheses were hypertrophic or restrictive cardiomyopathy.
A testicular ultrasound (September 09, 2013) was normal, except for cystic formations in the right inguinal canal. An abdominal ultrasonography (September 10, 2013) showed substantial ascites and hepatic cysts with internal septations, and no signs of portal hypertension.
After presenting an increase in dyspnea with the development of paroxysmal nocturnal dyspnea, worsening ascites and lower-extremity edema, and paresthesia on hands and feet, the patient was admitted to the hospital.
On physical examination (October 19, 2013) he was oriented and eupneic, with a heart rate of 69 bpm, blood pressure of 80 X 60 mmHg, a normal pulmonary auscultation, cardiac auscultation with arrhythmia and no murmurs, substantial ascites, and edema and hyperemia of the lower extremities.
A chest x-ray (October 21, 2013) showed cardiomegaly and interstitial lung infiltrates; the lateral incidence showed the right ventricle markedly enlarged ( Figures 3 and and4 4 ).

Chest x-ray (October 21, 2013), posteroanterior (PA) view: pulmonary interstitial infiltrates and cardiomegaly.

Chest x-ray (October 21, 2013) in lateral view: right ventricle markedly enlarged.
On ECG, the patient presented atrial flutter with variable atrioventricular block, indirect signs of right atrial overload (Peñaloza-Tranchesi sign), heart rate of 61 bpm, low QRS voltage in the frontal plane, intraventricular conduction impairment, left ventricular overload, and secondary changes in ventricular repolarization ( Figure 5 ).

ECG: Atrial flutter, impaired intraventricular conduction, left ventricular overload.
Laboratory tests on October 19, 2013, showed the following results: hemoglobin 13.5 g/dL, hematocrit 42%, leukocytes 7,230/mm 3 (neutrophils 66%, eosinophils 12%, lymphocytes 13%, monocytes 9%), platelets 232,000 /mm 3 , urea 193 mg/dL, creatinine 2.03 m/dL (glomerular filtration rate of 34 mL/min/1,73 m 2 ), sodium 133 mEq/L, potassium 3.9 mEq/L, C-reactive protein (CRP) 18.1 mg/L, vitamin B12 360 pg/mL, folic acid 8.35 ng/mL, total bilirubin 0.75 mg/dL, direct bilirubin 0.37 mg/dL, AST 24 U/L, ALT 16 U/L, gamma-glutamyl transferase (gamma GT) 241 U/L, alkaline phosphatase 166 U/L, iron 71 µg/dL, ferritin 62.9 ng/mL, prothrombin time (PT, INR) 0.95, activated partial thromboplastin time (aPTT, rel) 0.95, ionic calcium 1.09 mmol/L, chloride 89 mEq/L, and arterial lactate 15 mg/dL. Urinalysis showed urine specific gravity of 1.020, pH 5.5, proteinuria 0.25 g/L, epithelial cells 4,000/mL, leukocytes 2,000/mL, erythrocytes 3,000/mL, and hyaline casts 27,250/mL.
Another echocardiogram performed on October 21, 2013, showed a left atrial diameter of 56 mm, septal thickness of 18 mm, posterior wall thickness of 13 mm, left ventricle (diastole/systole) with 46/40 mm, left ventricular ejection fraction of 28%, pulmonary artery systolic pressure estimated at 45 mmHg, marked left ventricular and moderate right ventricular dysfunction, and moderate tricuspid insufficiency.
An ultrasound of the kidneys and urinary tract (October 24, 2013) showed that the left kidney measured 9.6 cm, and the right kidney measured 9 cm and had simple cortical cysts.
Serum protein electrophoresis was normal, and a urinary electrophoresis did not detect proteins. Measurement of serum beta 2-microglobulin was 7 mg/mL (limit for individuals above the age of 60 years = 2.6 mg/mL).
A biopsy of the cheek mucosa (October 23, 2013) showed deposits of amyloid substance in the deep chorion and in the adjacent adipose tissue.
Stool microscopy (October 25, 2013) was positive for Blastocystis hominis and Entamoeba coli .
A paracentesis drained 3,500 mL of a yellowish fluid with normal cellularity.
During hospitalization, the patient received daily intravenous furosemide 60 mg, carvedilol 25 mg, hydrochlorothiazide 100 mg, hydralazine 75 mg, isosorbide 80 mg, aspirin 100 mg, spironolactone 25 mg, and enoxaparin 40 mg. The patient also received oxacillin 2 g/day for 7 days initially, and later vancomycin, meropenem and teicoplanin, and piperacillin/tazobactam.
A new chest x-ray (November 08, 2013) showed cardiomegaly and an interstitial pulmonary infiltrate suggestive of pulmonary congestion ( Figure 6 ).

Chest x-ray (November 08, 2013): pulmonary interstitial infiltrates suggestive of pulmonary congestion and cardiomegaly.
During a new paracentesis (November 11, 2013), the aspirated fluid was bloody, and the patient presented hypotension and decreased consciousness, progressing to cardiac arrest with pulseless electrical activity, which was reverted. This was followed by ventricular tachycardia, cardioverted with 200 J.
New tests (November 11, 2013 - morning) showed the following results: hemoglobin 11.9 g/dL, hematocrit 36%, leukocytes 7,780/mm 3 (neutrophils 83%, eosinophils 2%, lymphocytes 9%, and monocytes 6%), platelets 188,000 /mm 3 , urea 301 mg/dL, creatinine 4.14 mg/dL, sodium 125 mEq/L, potassium 4.4 mEq/L, CRP 97.06 mg/L. On venous blood gas analysis, pH was 7.33, bicarbonate 19.9 mmol/L, and base excess (-) 5.4 mmol/L. Additional tests performed on the same day (November 11, 2013 – 5:44 pm) showed hemoglobin of 6.3 g/dL, sodium of 123 mEq/L, potassium of 5.4 mEq/L, venous lactate of 93 mg/dL, PT (INR) of 3.2 and aPTT (rel) of 1.98.
Later during the day, the patient progressed with shock refractory to high doses of dobutamine (20 µg/kg/min ) and norepinephrine (1.2 µg/kg/min), followed by cardiac arrest with pulseless electrical activity that recovered but was followed by a new irreversible cardiac arrest with pulseless electrical activity during intra-aortic balloon placement (November 11, 2013 – 6:30 pm).
Clinical Aspects
The patient JAB, a 79-year-old previous smoker and alcoholic man residing in São Paulo, attended an outpatient clinic at InCor due to heart failure which worsened progressively since 2012, requiring hospitalization for treatment.
Heart failure is a systemic and complex clinical syndrome, defined as a cardiac dysfunction that causes the blood supply to be insufficient to meet tissular metabolic demands, in the presence of a normal venous return, or which only meets the demands with high filling pressure 1 .
Prevalence studies estimate that 23 million individuals worldwide have heart failure and that 2 million new cases are diagnosed annually. According to DATASUS information, Brazil has about 2 million individuals with heart failure and 240,000 new cases diagnosed annually 2 .
The main causes of heart failure are hypertension, coronary artery disease, Chagas disease, cardiomyopathies, endocrinopathies, toxins, and drugs, among others 1 . The cardinal manifestations of heart failure are dyspnea and fatigue, and may include exercise intolerance, fluid retention, and pulmonary and systemic congestion 3 . The patient in this case presented with progressive dyspnea triggered by less than ordinary activities, lower-extremity edema, and ascites, which characterized him as class III according to the New York Heart Association (NYHA) classification.
On complementary tests, the echocardiogram showed marked left ventricular hypertrophy with some degree of asymmetry, and reduced ejection fraction. Cardiac hypertrophy is often associated with hypertension or hypertrophic cardiomyopathy, but both present with normal or increased ECG voltage. Therefore, the findings of ventricular hypertrophy associated with decreased ECG voltage in the absence of pericardial effusion are exclusive of infiltrative cardiomyopathies, a group of cardiac disorders within the restrictive cardiomyopathies 4 .
Restrictive cardiomyopathy may occur with a wide variety of systemic diseases. Some restrictive cardiomyopathies are rare in clinical practice and may present initially with heart failure. This type of cardiomyopathy is characterized by filling restriction, with reduced diastolic volume in one or both ventricles, normal or close to normal systolic function, and ventricular wall thickening. It may be idiopathic or associated with other diseases, such as amyloidosis, endomyocardial disease with or without eosinophilia, sarcoidosis, and hemochromatosis, among others 5 . In this case, the presence of amyloid deposits in the cheek mucosa biopsy indicated a diagnosis of amyloidosis, and the increase in serum beta-2 microglobulin reflected a worse prognosis 5 .
Amyloidosis is characterized by deposits of amyloid protein in different organs and tissues. These deposits may be responsible for different types of clinical presentation, with a spectrum that ranges from lack of symptoms to sequential organic dysfunction culminating with death 6 .
Cardiac amyloidosis is caused by amyloid deposits around cardiac fibers, and can be identified by a left ventricular wall thickening exceeding 12 mm in the absence of hypertension with at least one of the following characteristics: conduction disorder and low voltage complexes on the ECG, restrictive cardiomyopathy, low cardiac output, isolate atrial involvement (as commonly seen in elderly individuals) or diffuse involvement affecting the ventricles. In the latter situation, it can cause heart failure with a poor prognosis 4 , 7 .
Our patient, who was not hypertensive, presented low voltage complexes on the ECG, which were more prominent in the frontal plane, an electrically inactive area in the anteroseptal region, and diffuse changes in ventricular repolarization. This pattern can be found in some diseases in addition to infiltrative cardiomyopathies, such as decompensated hypothyroidism, pericardial effusion, chronic obstructive pulmonary disease, and obesity. Other electrocardiographic information, such as the pattern of infarction, can be found with or without obstructive coronary atherosclerotic disease by deposition of substances in the microcirculation and small intramyocardial arteries 8 .
Amyloidosis may be classified as primary, secondary, or hereditary. Primary amyloidosis, in which AL is the primarily involved protein, may be further subdivided into idiopathic (localized forms) or associated with multiple myeloma or other plasma cell dyscrasias (systemic forms) 9 .
Multiple myeloma is a neoplastic disorder of plasma cells that affects individuals with an average age of 70 years at diagnosis. Some characteristics of the patient in this case could suggest multiple myeloma: age, male gender, renal failure, and cylindruria. However, other important clinical parameters were absent, such as hypercalcemia, anemia, and bone disease. Also, the Bence-Jones protein, which is present in up to 75% of the cases, was not detected on urinary electrophoresis 10 .
The secondary type of amyloidosis results from deposits of AA protein and frequently arises as a complication of infectious or inflammatory processes, such as rheumatoid arthritis (the most common cause), tuberculosis, systemic lupus erythematosus, inflammatory bowel disease, syphilis, or even neoplastic diseases. Pro-inflammatory cytokines, which are present in these disorders, stimulate the hepatic production of serum A amyloid 11 .
Finally, the hereditary type of the disease has an autosomal dominant transmission and may involve several types of amyloid proteins, such as the AA protein in some groups of patients with familial Mediterranean fever, and the ATTR protein (derived from the transthyretin or prealbumin) in familial amyloid polyneuropathy 12 .
As for the treatment, measures to control symptoms related to diastolic heart failure, such as volume control, should be implemented. Diuretics and vasodilators should be administered with caution since the cardiac output in these patients is greatly dependent on increased venous pressures. Specific treatment should be directed to the etiology of the amyloidosis 13 .
After an evaluation in the clinic on January, 2013, the patient received medications that are proven to modify the rates of hospitalization and mortality in heart failure with reduced ejection fraction (beta-blockers, angiotensin-converting enzyme inhibitors, aldosterone antagonist), and symptom-relieving agents (diuretics) 14 . The patient was receiving enalapril 10 mg, spironolactone 25 mg, furosemide 60 mg, and carvedilol 12.5 mg.
After 8 months, due to the decompensated heart failure and hypotension, the patient returned to the emergency room and required hospitalization. The use of conventional therapy for heart failure often worsens the progression of amyloidosis. Therefore, cardiac amyloidosis should be suspected when the patient’s clinical condition worsens in response to conventional treatment, particularly in individuals older than 50 years. The therapy is exclusively symptomatic and should not include digitalis, beta-blockers, angiotensin-converting enzyme inhibitors, or calcium channel antagonists, since some studies have shown an increased sensitivity to these drugs which can lead to hypotension and intensification of conduction disorders 15 .
Therefore, the decompensation of the patient’s heart failure with deterioration of the ascites culminated in two paracenteses, with the last paracentesis probably accompanied by a puncture accident due to the appearance of bloody fluid, decrease in red blood count, and hypovolemic shock associated with cardiogenic shock, culminating in a mixed refractory shock and cardiac arrest with pulseless electrical activity (Dr. Sumaia Mustafa, Dr. Alice Tatsuko Yamada).
Diagnostic hypotheses:
- Heart failure due to restrictive cardiomyopathy (probably cardiac amyloidosis associated with multiple myeloma);
- Decompensated heart failure;
- Cause of death: mixed shock (hypovolemic + cardiogenic) with cardiac arrest with pulseless electrical activity (Dr. Sumaia Mustafa, Dr. Alice Tatsuko Yamada) .
The heart weighed 680 g and was increased in volume due to moderate cavity dilation and wall thickening in all four chambers ( Figure 7 ). The myocardium had an increased consistency. The endocardium of the atria, in particular, was finely granular and brown-yellowish in appearance. There were no significant changes in the valves, and the coronary arteries were armed without significant obstruction of their lumen.

Gross Section of the heart base showing biatrial enlargement and thickening of the cardiac walls. Note the granular aspect of the right atrial endocardium (area demarcated with an ellipse).
Histological examination of the myocardium showed extracellular deposits of amorphous and eosinophilic material promoting atrophy of the contractile cells. These deposits stained positive with Congo red when observed under polarized light ( Figures 8 and and9). 9 ). This same material was present in the interstitium of the cheek mucosa evaluated by biopsy ( Figure 10 ) according to data from the clinical history. Deposits were also observed in the tunica media of muscular arteries in both lungs ( Figure 11 ) and in the renal hilum.

Photomicrography of the ventricular myocardium showing atrophic cardiomyocytes due to deposits of amorphous eosinophilic material in the interstitium. Hematoxylin and eosin staining (20x objective magnification).

Photomicrography of myocardial tissue obtained under polarized light. Note the greenish material that corresponds to amyloid substance stained by Congo red (5x objective magnification).

Biopsy of the cheek mucosa performed approximately 1 month before death. Note that the mucosal chorion reacts positively to Congo red (photomicrography obtained under conventional microscopy with a 10x objective magnification).

Photomicrography of a peripheral muscular pulmonary artery showing areas of positivity for deposits of amyloid in the arterial wall (Congo red staining photographed under conventional microscopy, 5x objective magnification).
Bone marrow histological examination showed hypercellularity of moderate degree for the patient's age, and no signs of monoclonal proliferation. Immunohistochemical reactions for immunoglobulin kappa and lambda light chains were inconclusive, and CD138 labeling showed no proliferation of plasma cells.
Autopsy findings included a 4-cm hepatic cyst in the right lobe lined with flat cells without atypia, and retention cysts in the right kidney. The right adrenal weighed 44 g and was increased in volume and completely calcified. The histological examination showed only calcification and was inconclusive for the possibility of prior malignancy.
There was a voluminous serosanguinous ascites and a serous pericardial effusion. We found no visceral or abdominal vessel injury resulting from the paracentesis and the amount of bloody material in the ascitic fluid was small.
Histologically, there were signs of congestive heart failure in the lungs and liver (Dr. Vera Demarchi Aiello) .
Diagnoses: Cardiovascular amyloidosis;
Congestive heart failure;
Calcified nodule in the right adrenal gland (Dr. Vera Demarchi Aiello).
Mass spectrometry
Mass spectrometry gathers all qualities to establish an unequivocal diagnosis of amyloidosis since it has a high sensitivity and ability to identify the proteins through sequencing 16 . Therefore, we adopted an approach based on shotgun proteomics to identify the amyloid deposits in the sample.
Sections of heart tissue containing amyloid deposits (confirmed by staining with Congo red) fixed in formalin and embedded in paraffin were dissected and the proteins were then extracted with Liquid Tissue® MS Protein Prep Kit (Expression Pathology) according to the manufacturer's protocol. After digestion with trypsin, the resulting peptides were analyzed by high-resolution liquid chromatography-mass spectrometry using the mass spectrometer Q-Exactive (Thermo Fisher Scientific). The acquisitions of spectral data were carried out using the DDA (date dependent analysis) mode with a selection of the 10 most abundant ions for sequencing by HCD (Higher-energy collisional dissociation). The data were processed with the software MaxQuant. The proteomic analysis was performed in triplicate.
The processed data generated lists of proteins representing the protein content of the sample. In total, 25 possible amyloid proteins were investigated in these lists in order to determine the identity of the deposited substance. There were 15 peptides belonging to transthyretin that together covered 76.2% of the full sequence of the protein.
To confirm the result, we also evaluated the abundance of different peptides present in the sample. Among the 25 most abundant peptides, three belonged to transthyretin (ALGISPFHEHAEVVFTANDSGPR, TSESGELHGLTTEEEFVEGIYK, and GSPAINVAVHVFR). The others were assigned to actin, myosin, desmin, and myoglobin, confirming the identity of the amyloid protein (Dr. Fabio Mitsuo Lima and Dr. Valdemir Melechco Carvalho- Fleury Group).
Cardiovascular amyloidosis due to deposition of transthyretin (Dr. Vera Demarchi Aiello, Dr. Jussara Bianchi Castelli, Dr. Fabio Mitsuo Lima and Dr. Valdemir Melechco Carvalho) .
This case demonstrates how important it is in amyloidosis to investigate the deposited substance. Amyloidosis is a generic name to describe a group of diseases characterized by extracellular deposits of different substances in different organs. These substances are fibrillar proteins that become insoluble with changes in their spatial conformation. More than 20 types of proteins have been described in these deposits 16 . From an anatomopathological perspective, the deposits can be characterized by immunohistochemical reactions, but with some restrictions as described below. The cardiovascular system is most often affected by the AL protein (deposits of light-chain immunoglobulin), senile, and familial forms 17 , 18 .
The pathologist may identify neoplastic proliferation of plasmocytes producing the deposited immunoglobulins by bone marrow examination labeled for these cells. In tissue preparations, the pathologist may demonstrate by immunohistochemistry if the deposited substance is one of these immunoglobulins. Some authors recommend a biopsy of other organs before the endomyocardial biopsy to confirm the diagnosis and identify the type of amyloid 19 . In this case, immunohistochemical labeling was not helpful in establishing the diagnosis, because it was inconclusive to the type of protein deposited.
Although there are reports in the literature of identification of transthyretin in tissues by immunohistochemical reactions, this was not possible in this case. However, with mass spectrometry analysis, we identified that the deposited protein was transthyretin, which is usually present in senile and familial forms of amyloidosis. In this patient, the familial form was less likely due to the exclusive involvement of heart and blood vessels. However, only a genetic research and evaluation of other members of the family could exclude it completely.
Another point that deserves discussion in this case is the laboratory report of high levels of immunoglobulin E. We could assume that this referred to the deposited protein, but the diagnostic methods performed to complement the autopsy revealed that this was not the case.
Dr. Vera Demarchi Aiello and Dr. Jussara Bianchi Castelli (Pathology Laboratory, InCor, FMUSP).
Heart Failure; Cardiomyopathy, Restrictive; Ascites; Cardiomegaly; Heart Arrest.
Editor da Seção: Alfredo José Mansur ( rb.psu.rocni@rusnamja )
Editores Associados: Desidério Favarato ( rb.psu.rocni@otaravaflcd )
Vera Demarchi Aiello ( rb.psu.rocni@arevpna )

Create Free Account or
- Acute Coronary Syndromes
- Anticoagulation Management
- Arrhythmias and Clinical EP
- Cardiac Surgery
- Cardio-Oncology
- Cardiovascular Care Team
- Congenital Heart Disease and Pediatric Cardiology
- COVID-19 Hub
- Diabetes and Cardiometabolic Disease
- Dyslipidemia
- Geriatric Cardiology
- Heart Failure and Cardiomyopathies
- Invasive Cardiovascular Angiography and Intervention
- Noninvasive Imaging
- Pericardial Disease
- Pulmonary Hypertension and Venous Thromboembolism
- Sports and Exercise Cardiology
- Stable Ischemic Heart Disease
- Valvular Heart Disease
- Vascular Medicine
- Clinical Updates & Discoveries
- Advocacy & Policy
- Perspectives & Analysis
- Meeting Coverage
- ACC Member Publications
- ACC Podcasts
- View All Cardiology Updates
- Earn Credit
- View the Education Catalog
- ACC Anywhere: The Cardiology Video Library
- CardioSource Plus for Institutions and Practices
- ECG Drill and Practice
- Heart Songs
- Nuclear Cardiology
- Online Courses
- Collaborative Maintenance Pathway (CMP)
- Understanding MOC
- Image and Slide Gallery
- Annual Scientific Session and Related Events
- Chapter Meetings
- Live Meetings
- Live Meetings - International
- Webinars - Live
- Webinars - OnDemand
- Certificates and Certifications
- ACC Accreditation Services
- ACC Quality Improvement for Institutions Program
- CardioSmart
- National Cardiovascular Data Registry (NCDR)
- Advocacy at the ACC
- Cardiology as a Career Path
- Cardiology Careers
- Cardiovascular Buyers Guide
- Clinical Solutions
- Clinician Well-Being Portal
- Diversity and Inclusion
- Infographics
- Innovation Program
- Mobile and Web Apps
Beta Blockers May Not Benefit Many Heart Attack Survivors
Study suggests routine use is likely unnecessary for those with normal ejection fraction.
Apr 07, 2024
Contact: Nicole Napoli , [email protected], 202-669-1465
ATLANTA (Apr 07, 2024) -
Taking beta blockers after a heart attack did not significantly reduce the risk of death or a second heart attack among people with normal heart pumping ability, as indicated by an ejection fraction of 50% or higher, according to a study presented at the American College of Cardiology’s Annual Scientific Session.
The findings call into question the routine use of beta blockers for all patients following a heart attack, which have stood as a mainstay of care for decades. Approximately 50% of heart attack survivors do not experience heart failure. Among such patients, the study found no difference in the composite primary endpoint of death from any cause or new non-fatal heart attack between those who were prescribed beta blockers and those who were not.
“I think that, following this study, many doctors will not find an indication to routinely treat all their patients with beta blockers following a heart attack,” said Troels Yndigegn, MD, interventional cardiologist at Lund University in Sweden and the study’s lead author. “We believe that the evidence still supports beta blockers for patients with a large myocardial infarction that experience heart failure, but for patients with no signs of heart failure and a normal ejection fraction, this trial establishes that there’s no indication that routine use of beta blockers is beneficial.”
Heart failure occurs when the heart muscle becomes too weak or stiff to pump blood effectively. It is primarily assessed in terms of left ventricle ejection fraction, which is the proportion of blood pushed out of the heart’s left ventricle with each heartbeat. An ejection fraction above 40%–50% is considered normal.
Beta blockers lower blood pressure by inhibiting certain hormones, such as adrenaline, that speed up the heart. Many clinicians prescribe beta blockers to all patients following a heart attack, typically for at least a year or often for the rest of the patient’s life, based on evidence that they can help to prevent a second heart attack. However, researchers said that the clinical trials that led to this routine use of beta blockers were conducted before the advent of many newer procedures that are now widely used to open blocked arteries.
“At that time, the damage to the heart muscle was greater than we see today, and we didn’t have the possibility to revascularize patients with percutaneous coronary intervention and stents like we do today,” Yndigegn said. “What we see today is more myocardial infarctions that are smaller and that do not damage the heart muscle to the same extent.”
To elucidate the potential benefits of beta blockers considering this changed landscape, the REDUCE-AMI study enrolled 5,020 patients treated for an acute heart attack at 45 centers in Sweden, Estonia and New Zealand who participated in the SWEDEHEART Registry. All patients had an ejection fraction of 50% or higher as assessed with an echocardiogram performed within one week of their heart attack. Half were randomly assigned to receive long-term beta blocker medications and the rest did not take beta blockers.
Over a median follow-up period of 3.5 years, there were no significant differences between groups in the rate of the composite primary endpoint or in secondary clinical endpoints such as heart failure, atrial fibrillation or symptoms like chest pain and shortness of breath. There were also no differences in safety endpoints such as stroke, abnormally low blood pressure or fainting.
Researchers said that the lack of benefits associated with beta blockers observed in this patient group could potentially free many patients from the burdens of taking these medications, allowing them to avoid side effects such as mood disorders, fatigue and sexual dysfunction.
“Many patients report side effects or suspected side effects with these medications, so I think this finding will have an impact for thousands of patients,” Yndigegn said.
The study did not involve a placebo control and participants knew which group they were assigned. While this unblinded approach could potentially introduce bias, researchers said that this was not likely to have an effect on outcomes such as death and heart attacks. Yndigegn said the results should be generalizable beyond the population in which the study was conducted and added that other observational studies are underway that can help shed light on the routine use of beta blockers across diverse populations.
The researchers plan to separately analyze outcomes related to quality of life and sexual health.
The study was funded by the Swedish Research Council, Swedish Heart Lung Foundation and Stockholm County Council.
This study was simultaneously published online in the New England Journal of Medicine at the time of presentation.
Yndigegn will be available to the media in a press conference on Sunday, April 7, 2024, at 11:15 a.m. ET / 15:15 UTC in Room B203.
Yndigegn will present the study, “Long-term Beta-blocker Treatment after Acute Myocardial Infarction and Preserved Left Ventricular Ejection Fraction – The REDUCE-AMI Trial,” on Sunday, Apr il 7 , 2024 , at 9:45 a.m. ET / 13:45 UTC in the Hall B-1 Main Tent.
ACC.24 will take place April 6-8, 2024, in Atlanta, bringing together cardiologists and cardiovascular specialists from around the world to share the newest discoveries in treatment and prevention. Follow @ACCinTouch , @ACCMediaCenter and #ACC24 for the latest news from the meeting.
The American College of Cardiology (ACC) is the global leader in transforming cardiovascular care and improving heart health for all. As the preeminent source of professional medical education for the entire cardiovascular care team since 1949, ACC credentials cardiovascular professionals in over 140 countries who meet stringent qualifications and leads in the formation of health policy, standards and guidelines. Through its world-renowned family of JACC Journals, NCDR registries, ACC Accreditation Services, global network of Member Sections, CardioSmart patient resources and more, the College is committed to ensuring a world where science, knowledge and innovation optimize patient care and outcomes. Learn more at ACC.org .
< Back to Listings
You must be logged in to save to your library.
Jacc journals on acc.org.
- JACC: Advances
- JACC: Basic to Translational Science
- JACC: CardioOncology
- JACC: Cardiovascular Imaging
- JACC: Cardiovascular Interventions
- JACC: Case Reports
- JACC: Clinical Electrophysiology
- JACC: Heart Failure
- Current Members
- Campaign for the Future
- Become a Member
- Renew Your Membership
- Member Benefits and Resources
- Member Sections
- ACC Member Directory
- ACC Innovation Program
- Our Strategic Direction
- Our History
- Our Bylaws and Code of Ethics
- Leadership and Governance
- Annual Report
- Industry Relations
- Support the ACC
- Jobs at the ACC
- Press Releases
- Social Media
- Book Our Conference Center
Clinical Topics
- Chronic Angina
- Congenital Heart Disease and Pediatric Cardiology
- Diabetes and Cardiometabolic Disease
- Hypertriglyceridemia
- Invasive Cardiovascular Angiography and Intervention
- Pulmonary Hypertension and Venous Thromboembolism
Latest in Cardiology
Education and meetings.
- Online Learning Catalog
- Products and Resources
- Annual Scientific Session
Tools and Practice Support
- Quality Improvement for Institutions
- Accreditation Services
- Practice Solutions
Heart House
- 2400 N St. NW
- Washington , DC 20037
- Email: [email protected]
- Phone: 1-202-375-6000
- Toll Free: 1-800-253-4636
- Fax: 1-202-375-6842
- Media Center
- ACC.org Quick Start Guide
- Advertising & Sponsorship Policy
- Clinical Content Disclaimer
- Editorial Board
- Privacy Policy
- Registered User Agreement
- Terms of Service
- Cookie Policy
© 2024 American College of Cardiology Foundation. All rights reserved.
Evidence Review of the Adverse Effects of COVID-19 Vaccination and Intramuscular Vaccine Administration
Vaccines are a public health success story, as they have prevented or lessened the effects of many infectious diseases. To address concerns around potential vaccine injuries, the Health Resources and Services Administration (HRSA) administers the Vaccine Injury Compensation Program (VICP) and the Countermeasures Injury Compensation Program (CICP), which provide compensation to those who assert that they were injured by routine vaccines or medical countermeasures, respectively. The National Academies of Sciences, Engineering, and Medicine have contributed to the scientific basis for VICP compensation decisions for decades.
HRSA asked the National Academies to convene an expert committee to review the epidemiological, clinical, and biological evidence about the relationship between COVID-19 vaccines and specific adverse events, as well as intramuscular administration of vaccines and shoulder injuries. This report outlines the committee findings and conclusions.
Read Full Description
- Digital Resource: Evidence Review of the Adverse Effects of COVID-19 Vaccination
- Digital Resource: Evidence Review of Shoulder Injuries from Intramuscular Administration of Vaccines
- Press Release
Recent News
The Challenge of Predicting Climate Migration
Celebrating Earth Day with the National Academies
Rohr Named U.S. Winner of Frontiers Planet Prize
NAS Launches Science and Innovation Fund for Ukraine
- Load More...

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Heart-Healthy Living
- High Blood Pressure
- Sickle Cell Disease
- Sleep Apnea
- Information & Resources on COVID-19
- The Heart Truth®
- Learn More Breathe Better®
- Blood Diseases and Disorders Education Program
- Publications and Resources
- Blood Disorders and Blood Safety
- Sleep Science and Sleep Disorders
- Lung Diseases
- Health Disparities and Inequities
- Heart and Vascular Diseases
- Precision Medicine Activities
- Obesity, Nutrition, and Physical Activity
- Population and Epidemiology Studies
- Women’s Health
- Research Topics
- Clinical Trials
- All Science A-Z
- Grants and Training Home
- Policies and Guidelines
- Funding Opportunities and Contacts
- Training and Career Development
- Email Alerts
- NHLBI in the Press
- Research Features
- Past Events
- Upcoming Events
- Mission and Strategic Vision
- Divisions, Offices and Centers
- Advisory Committees
- Budget and Legislative Information
- Jobs and Working at the NHLBI
- Contact and FAQs
- NIH Sleep Research Plan
- News and Events
- < Back To All News
Protecting Navajo children with asthma: A case study

Joncita Todechine, a mother of four who lives on the Navajo Nation, knows all too well what can trigger asthma symptoms in her daughter Ashley. But she didn’t always. She recalls a time in 2013, living in Phoenix and attending medical assistant school, when she rushed her then-three-year-old to the Indian Medical Center.
“She was really sick,” Todechine said. “She was fevering, coughing, and had shortness of breath. We had no idea what was wrong.”
Ashley was admitted to the hospital and stayed for an entire week before the doctors could make a diagnosis of asthma. Now a thriving 13-year-old, Ashley loves gaming, social media, and riding on her hoverboard. These days she lives on the Navajo reservation with her family, who moved there shortly after her mother finished school. For the most part, she keeps her asthma under control by taking medication and doing her best to avoid her asthma triggers.
But that can be challenging.
On the Navajo Nation, there are many asthma triggers. The semi-arid environment is plagued by drought, so on windy days, the gusts kick up ever-present dust and sand into the air. Shuttered coal-fired powerplants dot the landscape and, though they are closed, residual soot still dirties the air. Uranium and other heavy metals contaminate the landscape, and people breathe diesel fumes from the buses that take children to and from school every day. The many dogs and livestock roaming the reservation carry other allergens.
“And that’s just the outdoor pollution,” said Bruce Bender, Ph.D., professor in the pediatrics department at National Jewish Health in Denver, Colorado. “Seventy percent of households heat with indoor stoves that burn wood or charcoal and can leak a lot of smoke into the air.”
Bender would know. He’s co-project leader of an NHLBI-funded project focused on reducing health disparities in children living on the Navajo Nation, and he’s studied some of the factors that make those disparities worse. He’s also looked at the health data overall and found that while Native adults suffer from higher rates of chronic conditions like cardiovascular diseases and diabetes, it’s asthma that remains one of the most common chronic diseases in children. Some 18% of children on the Navajo reservation have it, compared to 10.2% of children nationwide.
“Asthma can be incredibly scary for children and their families, especially those who cannot get emergency care easily or quickly,” said Michelle Freemer, M.D., M.P.H., director of the asthma program in NHLBI’s Division of Lung Diseases.
The Navajo Nation extends across more than 27,000 square miles, making it the largest Native land area in the U.S. "For families of children with asthma, the distances and travel conditions on the reservation may add challenges,” said Freemer. “The investigators partnered with the community to find solutions that work where they live, not simply provide asthma care that has been shown to work in other places."
A local solution
Bender and his colleague, Lynn B. Gerald, Ph.D., M.S.P.H., assistant vice chancellor for population health at the University of Illinois-Chicago, started a large-scale effort to teach educators, children, their families, and local medical providers on the Navajo Nation how to identify an asthma attack and what to do in an emergency. (Gerald had worked previously at the University of Arizona and had gained a wealth of knowledge from the university's Native collaborators.) The program rolled out in three Arizona communities on the reservation: Tuba City, Chinle, and Fort Defiance. Combined, these towns represent 43% of the Navajo Nation population and are home to more than 8,000 children with asthma.
But before they began, the investigators knew they needed to build relationships with the Navajo people – who refer to themselves as Diné – as the community’s prior experiences with non-Native researchers had left them skeptical. The research team began by ensuring the program was tailored to the needs and wishes of the community itself.
“The Navajo Nation human research review board is very careful and thorough,” Bender said. “They’re protecting their population. We had to earn their trust.”
Once the investigators got approval, they hit the ground running, starting in Tuba City. In the hospitals, the research team provided tools for medical professionals, using self-directed online learning and in-person workshops, to increase their use of practices that have been shown to be important in asthma care.
In the schools, the investigators provided education using the American Lung Association’s Asthma Basics and Open Airways for Schools® training, to teach school staff about asthma, its triggers, and what to do when a child is having an attack and to teach Diné children how to manage their asthma.
Using a “train-the-trainer” model, school staff, community health workers, respiratory therapists, and pharmacists became students and then instructors. This made it possible for the Diné participants to teach additional staff, ensuring the community can sustain the program after the research funding ends.
Still, there was another urgent need that Bender and Gerald realized had not been addressed. “Less than 15% of children with asthma actually have an inhaler at school when they need it,” Gerald said. In response, the team helped start a program in two of the three communities that provided stock inhalers to schools for children who need them.
A global threat
After starting the program in Tuba City as planned and spending a year there, the research team moved their focus to Chinle. The goal was to be able to compare how well the program worked in each of the three communities. But a global pandemic had other plans.
“The COVID-19 pandemic hit right in the middle of our time in Chinle,” Bender said. “After that, we weren’t allowed on the reservation for two years.”
While the pandemic changed life for all Americans, it devastated many Native communities. Schools closed and medical clinics focused on emergencies. The research team pivoted: they continued some training virtually and were able to keep learning from families about their needs, especially using the Diné members of the research team who were on the reservation.
Taking stock
Today, despite the challenges of the pandemic, all three communities have completed the original program, and 439 Diné members have been trained to identify asthma and its triggers. Yet the work is far from over. The investigators are analyzing the data they collected. “Particularly important is returning the results to the community,” Gerald said. As soon as they are ready, she said, they will be meeting with the school boards and health boards and joining community meetings to share them.
Freemer said that all the materials the researchers developed through their NHLBI funding are available to the community and have also been shared with those at the Indian Health Service leading the Asthma Control in Tribal Communities program.
“The researchers also took the opportunity to build research capacity,” she said. They developed an agreement with Diné College, the only four-year college on the reservation, to provide training through their Summer Research Experience Program. “In that program, students learned about research and were able to readily reach the families who appreciated the interactions with Diné research team members.”
Todechine said knowing that her child will be cared for if the worst happens has given her peace of mind. “Now the school systems have their own asthma alert systems that the employees and even the bus drivers take part in,” she said. “For me, I feel safer for her to be at school without me.”
Resources:
Learn more about Asthma in Our Communities with specific resources for American Indians.
Related Health Topics
Brazilian Government Forced Censorship on X: New Report Reveals
- Two copies each of 28 orders, in Portuguese and in English translation, issued by Justice Alexandre de Moraes to X Corp.;
- An additional 23 orders issued by Justice Alexandre de Moraes for which X Corp. does not have an English translation; and
- 37 orders issued by the Superior Electoral Court of Brazil.
- Jair Messias Bolsonaro, 38th President of Brazil
- Marcos do Val, Current Member of the Federal Senate in Brazil
- Paulo Figueiredo Filho, Brazilian journalist

What a Terror Attack in Israel Might Reveal About Psychedelics and Trauma
Thousands of Israelis were using mind-altering substances when Hamas-led fighters attacked a desert festival on Oct. 7. Now, scientists are studying the ravers to determine the effects of such drugs at a moment of extreme trauma.
This photo of Yuval Tapuhi was taken at the Tribe of Nova festival on Oct. 7, before the Hamas-led terrorist attack. Credit... Avishag Shaar-Yashuv for The New York Times
Supported by
- Share full article
By Natan Odenheimer , Aaron Boxerman and Gal Koplewitz
- April 11, 2024
One Israeli said that being high on LSD during the Hamas-led attack on Oct. 7 prompted a spiritual revelation that helped him escape the carnage at a desert rave. Another is certain the drug MDMA made him more decisive and gave him the strength to carry his girlfriend as they fled the scene. A third said that experiencing the assault during a psychedelic trip has helped him more fully process the trauma.
Listen to this article with reporter commentary
Some 4,000 revelers gathered on the night of Oct. 6 at a field in southern Israel, mere miles from the Gaza border, for the Tribe of Nova music festival. At dawn, thousands of Hamas-led terrorists stormed Israel’s defenses under the cover of a rocket barrage.
About 1,200 people were killed that day, the deadliest in Israeli history according to the Israeli authorities, including 360 at the rave alone. Many of the ravers were under the influence of mind-altering substances like LSD, MDMA and ketamine as they witnessed the carnage or fled for their lives.
For a group of Israeli researchers at the University of Haifa, the attack has created a rare opportunity to study the intersection of trauma and psychedelics, a field that has drawn increased interest from scientists in recent years.
The survivors of the Nova festival present a case study that would be impossible to replicate in a lab: a large group of people who endured trauma while under the influence of substances that render the brain more receptive and malleable.
Illegal in most countries, including Israel, these substances are now on the cusp of entering the psychiatric mainstream. Recent research suggests that careful doses of drugs like MDMA and psilocybin , the active ingredient in “magic mushrooms,” might be useful in treating post-traumatic stress disorder.
The festival participants were under the influence during their trauma, not in a controlled clinical setting, but researchers say studying them could help scientists better understand how psychedelics might be used to treat patients after a traumatic event.
The researchers surveyed more than 650 Nova survivors. Roughly 23 percent said they took hallucinogens like LSD, also known as acid, and about 27 percent used MDMA, a stimulant and psychedelic commonly called molly or ecstasy. Many attendees used more than one substance.

Participants in the survey described a variety of experiences while using drugs on Oct. 7, ranging from hallucinations to extreme clarity, from panic to resolve and from paralysis to action.
“Even though people were dropping on the ground screaming next to me, I felt a growing sense of confidence, that I was invincible,” said Yarin Reichenthal, 26, a judo coach who experienced the attack while on LSD. “I felt enlightened. I felt no fear at all.”
In many instances, according to preliminary results of the researchers’ survey, even festivalgoers using the same drugs experienced the attack in different ways — variances that might have meant the difference between life and death.
The scientists cautioned that the study was not a comprehensive review of how every participant at the rave fared because so many were killed.
“We only hear the stories of those who made it out alive,” said Roy Salomon, a cognitive science professor at the University of Haifa and a co-author of the study. “So our understanding is influenced by survivors’ bias.”
Witnesses said that for many attendees, drug use appeared to hamper their ability to flee for safety. Some ravers were too zoned out on psychedelics to realize what was happening and escape. The researchers said that those experiences were also important to their findings.
“There are two main questions,” said Roee Admon, a University of Haifa psychology professor and a co-author of the study. “How is the traumatic event experienced under different psychedelics, and what might the long-term clinical impact be?”
Professor Admon and Professor Salomon, who are leading the survey, are studying the survivors in the hopes of gleaning information about how drug use affected their experience of trauma. They are also studying how the attendees appear to be recovering and coping. A graduate student, Ophir Netzer, also helped write the study.
Of those who made it out alive, some survivors appeared to be recovering well and others reported feeling numb and detached. Some said they had increased their drug use since the attack to cope.
“We were all in such a heightened emotional state, which made us all the more vulnerable when the attack began,” said Tal Avneri, 18, who said he stayed relatively lucid on Oct. 7 after taking MDMA. “And when you’re hurt at your most fragile, you can later become numb.”
For devotees of Israel’s trance scene, a festival like Nova is more than just a way to let loose. Many view the raves — often held in forests and deserts, with pounding electronic beats and mind-altering substances — as spiritual journeys amid a like-minded community.
“The love I felt on the dance floor, the raves, the psychedelics — they helped me cope with my mother’s death,” said Yuval Tapuhi, a 27-year-old Nova survivor from Tel Aviv.
Around 6:30 a.m. on Oct. 7, as the sky turned pink and many revelers were beginning the most intense part of their trips, rockets from Gaza suddenly streaked through the sky. Air-raid sirens and loud explosions cut through the music.
Some people fell to the ground and burst out crying, multiple survivors said. Some attendees scrambled to evade the terrorists by hiding in bushes, behind trees or in riverbeds. Others sprinted through open fields, running for hours before reaching safety.
Still others fled in their cars, creating a huge traffic jam at the rave’s main exit, where they became easy targets for Palestinian gunmen swarming across the border.
Amid the gunfire and rocket barrage, Mr. Reichenthal, the judo coach, had what he describes as a transcendent experience, which he credits with his survival. The LSD trip, he said, made it feel as if his fear had been stripped away, and he murmured Bible verses as he ran to safety.
Many survivors described their initial panic being replaced with a coolheaded resolve — a function, one expert said, of stress counteracting the effects of the drugs.
Sebastian Podzamczer, 28, attributed his survival, at least in part, to a huge rush of energy and clarity he experienced while using MDMA. The drug’s influence, he said, gave him what he believes was the strength to carry his girlfriend, who had been paralyzed by fear.
Mr. Podzamczer, a former combat medic in the Israeli military, had PTSD after his service. Taking psychedelics recreationally, he said, helped him unravel some of that pain, allowing him to speak about his military service without shaking and panicking.
“But I always thought that if I was caught in an extreme situation like that, I’d be paralyzed by panic from my PTSD,” Mr. Podzamczer said. Instead, he found that the MDMA he took at the rave “helped me stay afloat, to act more quickly and decisively.”
High levels of stress can almost “overwhelm” the effects of a drug and jolt people back to reality, said Rick Doblin, the founder of the Multidisciplinary Association for Psychedelic Studies, a nonprofit organization in California that finances scientific research but is not involved in the Nova survivor study.
Almog Arad, 28, said that her acid trip kicked in after the attack began but that the circumstances quickly “minimized” the drug’s effects. While she continued to see intense colors and patterns as she fled, her decision-making remained relatively sound, she said.
“Adrenaline was the strongest drug I took that day,” she said.
The University of Haifa researchers plan to follow the survivors for years, tracking their neural activity with functional magnetic resonance imaging, or fMRI.
They have presented their preliminary findings in a preprint paper , a scientific manuscript undergoing peer review.
Compared with survivors who used other substances, attendees who used MDMA are recovering better and showing less severe symptoms of PTSD, according to the study’s preliminary conclusions.
Many MDMA users in particular, the researchers said, believe that using the drug helped them survive. That perception, the scientists added, could have influenced their ability to cope with their trauma.
“The way in which we remember the trauma has a great impact on how we process it,” Professor Admon said. “So even if a victim’s perception is subjective, it will still have a great impact on their recovery.”
The researchers said it was difficult to assess the exact doses that the festivalgoers used, making it hard to analyze how different quantities of drugs affected people.
Mr. Reichental said he witnessed one man at the rave who appeared to be so out of it that as gunfire sounded and another raver tried to help him escape, the man instead began to flirt with her. “How lucky it is that destiny brought us together,” Mr. Reichenthal recalled the man saying. He does not believe the man survived the attack.
Psychologists and survivors said those ravers who took ketamine, a psychedelic with an intense tranquilizing and dissociative effect, appeared to be one of the groups hit hardest.
Immediately after the Nova massacre, a group of therapists and experts established a volunteer relief network for survivors, known as Safe Heart, that provided psychological support for more than 2,200 people. The group has collaborated with the University of Haifa researchers as well as with a separate , qualitative study led by Guy Simon, a psychotherapist and doctoral candidate at Bar-Ilan University.
“Most people who undergo a traumatic experience do not develop PTSD,” Professor Admon said. “Identifying those who do and treating them as early as possible is critical to their healing.”
Read by Natan Odenheimer
Audio produced by Adrienne Hurst .
Aaron Boxerman is a Times reporting fellow with a focus on international news. More about Aaron Boxerman
Our Coverage of the Israel-Hamas War
News and Analysis
Israel has not provided evidence to support its accusations that many employees of the main U.N. agency for Palestinian refugees are members of terrorist organizations, according to an independent review commissioned by the United Nations.
The United Nations says famine is likely to set in by May in Gaza. For those living under Israel’s attacks and a crippling blockade, every day is a race against time. Here’s how two Palestinian families try to keep their children alive.
Israel has failed to achieve its two primary goals of the war, while the suffering of Palestinians erodes support even among its allies. Here’s a look inside the stark reality of Israel’s fight in Gaza.
The United States is considering imposing sanctions on one or more Israeli battalions accused of human rights violations during operations in the occupied West Bank , according to a person familiar with the deliberations.
PEN America’s Fallout: The free expression group PEN America has canceled its 2024 literary awards ceremony following months of escalating protests over the organization’s response to the war in Gaza , which has been criticized as overly sympathetic to Israel.
Fears Over Iran Buoy Netanyahu: The Israeli prime minister lost considerable support after the Hamas-led Oct. 7 attacks on Israel. Tensions with Iran have helped him claw some of it back.
A Surprising Rift: The Israel-Hamas war, which has roiled cultural and political institutions far beyond the Middle East, is causing divisions in a prominent Japanese American group .
Mobilizing the American Left: As the death toll in Gaza climbed, the pro-Palestinian movement grew into a powerful, if disjointed, political force in the United States . Democrats are feeling the pressure.
Advertisement

IMAGES
VIDEO
COMMENTS
A 57 year-old male lorry driver, presented to his local emergency department with a 20-minute episode of diaphoresis and chest pain. The chest pain was central, radiating to the left arm and crushing in nature. The pain settled promptly following 300 mg aspirin orally and 800 mcg glyceryl trinitrate (GTN) spray sublingually administered by ...
On examination, the temperature was 36.4°C, the heart rate 103 beats per minute, the blood pressure 79/51 mm Hg, the respiratory rate 30 breaths per minute, and the oxygen saturation 99% while ...
This is the case report of a 66-year-old man with systemic hypertension and a chronic smoker that presented with acute severe chest pain. After medical assessment, he was diagnosed with acute myocardial infarction and the patient underwent coronary angiography, which disclosed proximal occlusion of the left anterior descending artery with ...
Presentation of Case. Dr. Jacqueline B. Henson (Medicine): A 54-year-old man was evaluated at this hospital after cardiac arrest associated with ventricular fibrillation. The patient had been in ...
A 67-year-old woman sought emergency medical care due to prolonged chest pain. In April 2009 the patient had prolonged chest pain and at that time she sought medical care. She was admitted at the hospital and diagnosed with myocardial infarction. The patient had hypertension, diabetes mellitus, dyslipidemia and was a smoker.
Key Points. Question How have case rates, treatment approaches, and in-hospital outcomes changed for patients with acute myocardial infarction (AMI) during the coronavirus disease 2019 (COVID-19) pandemic?. Findings In this cross-sectional study of 15 244 hospitalizations involving 14 724 patients with AMI, case rates began to decrease on February 23, 2020, followed by a modest recovery after ...
Historically, studies regarding CVD use 40-45 years old as the lower limit defining a "young" patient with CVD. These studies have found that 5-10% of patients experiencing an MI are younger than 40. 1. When a patient presents to the ED with chest pain, the HEART score is often used to assess the risk of an acute coronary syndrome (ACS).
Myocardial infarction, commonly known as a heart attack, is a critical medical event that occurs when the blood supply to the heart muscle is severely reduced or completely blocked. ... This case study will examine both modifiable and non-modifiable risk factors, including age, gender, family history, smoking, high blood pressure, diabetes, and ...
Acute Myocardial Infarction Case Study. Myocardial infarction (heart attack) is the leading cause of death in the United States. It is estimated that one in every five deaths in the US is due to a heart attack. Approximately one million patients are admitted to hospitals each year due to heart attacks. 200,000 to 300,000 individuals die from ...
Heart Attack Research. The NHLBI leads and supports basic research, clinical trials, and large long-term studies related to heart attacks. Our research has helped scientists and doctors better understand the causes of heart attacks and has led to improved treatment options for this condition. We continue to fund research to help find ways to ...
In one study of 515 women, patients. Symptoms of Myocardial Infarction. 2, 5, 6. Symptoms experienced by both men and women: •. chest pressure or pain • pain or discomfort in one or both arms •. sweating • lightheadedness Symptoms more likely to be experienced by women: • shortness of breath •.
Myocardial infarction (MI), colloquially known as "heart attack," is caused by decreased or complete cessation of blood flow to a portion of the myocardium. Myocardial infarction may be "silent" and go undetected, or it could be a catastrophic event leading to hemodynamic deterioration and sudden death.[1] Most myocardial infarctions are due to underlying coronary artery disease, the ...
Dr. Amy A. Sarma: A 54-year-old man was evaluated at this hospital because of new heart failure. One month before this evaluation, a nonproductive cough developed after the patient took a business ...
ED treatment. Internal STEMI Code paged at 22:55 Patient arrived at 22:57 Interventions Chest X‐Ray Assessment Repeat 12 Lead EKG. 5,000 Units IV Heparin. ED treatment. 22:05 (8 minutes after arrival) Compressions started Defibrillated at 150 J. ED treatment. 18 minutes in ED. Interventions Continued 180 mg ticagrelor Patient undressed ...
after a heart attack - clinical case study. Journal of Education, Health and Sport. 2019;9(11):194-199. eISSN 2391-8306. ... Almost 25% of US deaths are caused by a heart attack. In Poland,
Abstract. This interrupted case study was developed for an undergraduate class in human cardiac physiology. The story follows a patient whose heart attack damaged a papillary muscle in the left ventricle of the heart. This caused valve dysfunction and mitral valve regurgitation resulting in left-sided heart failure, which in turn led to ...
Collaborative research, led from the University of Oxford and published today in Nature Medicine, has developed a new tool called QR4 that more accurately predicts an individual's 10-year risk of cardiovascular diseases, like heart disease and stroke, particularly identifying high-risk patients that current prediction tools miss.
New mom Naiya Atkins had a heart attack, then went into cardiac arrest. A year later, she got a heart transplant in time for her son's first birthday. ... accuracy and reliability of studies published in American Heart Association scientific journals or presented at American Heart Association scientific meetings are solely those of the study ...
Heart Attack vs. Cardiac Arrest. A quick way to remember the difference: Cardiac arrest is an "electrical" problem. If you see someone going into cardiac arrest, call 911 and start CPR right away. Heart attack is a "circulation" problem. If someone is having a heart attack, call 911. Source: American Heart Association.
This article provides a comprehensive review of the current evidence and guidelines for the management of chronic heart failure, with a focus on pharmacological and non-pharmacological therapies, device implantation, and surgical options. It also presents two clinical cases that illustrate the challenges and controversies in the diagnosis and treatment of chronic heart failure.
Angeline Alexandre Professor Bizzarro Advanced adult health May 22, 2020 Heart Attack case study. Part I. Which of Mr. Helms' vital signs and lab values were abnormal? BP- 90/ HR -120, irregular R - 33, labored O2 - 89%; 2 additional medical tests would you order for Mr. Helms? In other words, what other information would be useful?
Results from previous studies that used laboratory-confirmed influenza infection were inconsistent, 15-18 but a case-control study from ... Secular trends in ischemic heart disease and stroke ...
ATLANTA (Apr 07, 2024) -. Taking beta blockers after a heart attack did not significantly reduce the risk of death or a second heart attack among people with normal heart pumping ability, as indicated by an ejection fraction of 50% or higher, according to a study presented at the American College of Cardiology's Annual Scientific Session.
Not only is AFib more common under 65 years of age than previously thought but it also increases the risk for hospitalization from heart attack, heart failure, and all-cause stroke, a new study finds.
WASHINGTON — A new report from the National Academies of Sciences, Engineering, and Medicine reviews evidence for 19 potential harms of the COVID-19 vaccines, and for nine potential shoulder injuries from intramuscular administration of vaccines more broadly. The committee that conducted the review identified sufficient evidence to draw 20 conclusions about whether these vaccines could cause ...
April 23, 2024. Joncita Todechine, a mother of four who lives on the Navajo Nation, knows all too well what can trigger asthma symptoms in her daughter Ashley. But she didn't always. She recalls a time in 2013, living in Phoenix and attending medical assistant school, when she rushed her then-three-year-old to the Indian Medical Center.
WASHINGTON, D.C. - Today, the House Judiciary Committee released an interim staff report titled, "The Attack on Free Speech Abroad and the Biden Administration's Silence: The Case of Brazil."The report exposes Brazil's censorship campaign and presents a startling case study of how a government can justify censorship in the name of stopping so-called "hate" speech and the "subversion" of "order."
Any level of marijuana use raises the risk of stroke by 42% and heart attack by 25%, ... Studies show overuse of marijuana by youth with mood disorders leads to a rise in self-harm, ...
current issue. current issue; browse recently published; browse full issue index; learning/cme
April 11, 2024. One Israeli said that being high on LSD during the Hamas-led attack on Oct. 7 prompted a spiritual revelation that helped him escape the carnage at a desert rave. Another is ...