Appointments at Mayo Clinic
- Pregnancy week by week
- Fetal presentation before birth
The way a baby is positioned in the uterus just before birth can have a big effect on labor and delivery. This positioning is called fetal presentation.
Babies twist, stretch and tumble quite a bit during pregnancy. Before labor starts, however, they usually come to rest in a way that allows them to be delivered through the birth canal headfirst. This position is called cephalic presentation. But there are other ways a baby may settle just before labor begins.
Following are some of the possible ways a baby may be positioned at the end of pregnancy.

Head down, face down
When a baby is head down, face down, the medical term for it is the cephalic occiput anterior position. This the most common position for a baby to be born in. With the face down and turned slightly to the side, the smallest part of the baby's head leads the way through the birth canal. It is the easiest way for a baby to be born.

Head down, face up
When a baby is head down, face up, the medical term for it is the cephalic occiput posterior position. In this position, it might be harder for a baby's head to go under the pubic bone during delivery. That can make labor take longer.
Most babies who begin labor in this position eventually turn to be face down. If that doesn't happen, and the second stage of labor is taking a long time, a member of the health care team may reach through the vagina to help the baby turn. This is called manual rotation.
In some cases, a baby can be born in the head-down, face-up position. Use of forceps or a vacuum device to help with delivery is more common when a baby is in this position than in the head-down, face-down position. In some cases, a C-section delivery may be needed.

Frank breech
When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head. This is the most common type of breech presentation.
If you are more than 36 weeks into your pregnancy and your baby is in a frank breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Most babies in a frank breech position are born by planned C-section.

Complete and incomplete breech
A complete breech presentation, as shown below, is when the baby has both knees bent and both legs pulled close to the body. In an incomplete breech, one or both of the legs are not pulled close to the body, and one or both of the feet or knees are below the baby's buttocks. If a baby is in either of these positions, you might feel kicking in the lower part of your belly.
If you are more than 36 weeks into your pregnancy and your baby is in a complete or incomplete breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Many babies in a complete or incomplete breech position are born by planned C-section.

When a baby is sideways — lying horizontal across the uterus, rather than vertical — it's called a transverse lie. In this position, the baby's back might be:
- Down, with the back facing the birth canal.
- Sideways, with one shoulder pointing toward the birth canal.
- Up, with the hands and feet facing the birth canal.
Although many babies are sideways early in pregnancy, few stay this way when labor begins.
If your baby is in a transverse lie during week 37 of your pregnancy, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of your health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a transverse lie, talk with a member of your health care team about the choices you have for delivery. Many babies who are in a transverse lie are born by C-section.

If you're pregnant with twins and only the twin that's lower in the uterus is head down, as shown below, your health care provider may first deliver that baby vaginally.
Then, in some cases, your health care team may suggest delivering the second twin in the breech position. Or they may try to move the second twin into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
Your health care team may suggest delivery by C-section for the second twin if:
- An attempt to deliver the baby in the breech position is not successful.
- You do not want to try to have the baby delivered vaginally in the breech position.
- An attempt to move the baby into a head-down position is not successful.
- You do not want to try to move the baby to a head-down position.
In some cases, your health care team may advise that you have both twins delivered by C-section. That might happen if the lower twin is not head down, the second twin has low or high birth weight as compared to the first twin, or if preterm labor starts.

- Landon MB, et al., eds. Normal labor and delivery. In: Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed May 19, 2023.
- Holcroft Argani C, et al. Occiput posterior position. https://www.updtodate.com/contents/search. Accessed May 19, 2023.
- Frequently asked questions: If your baby is breech. American College of Obstetricians and Gynecologists https://www.acog.org/womens-health/faqs/if-your-baby-is-breech. Accessed May 22, 2023.
- Hofmeyr GJ. Overview of breech presentation. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Strauss RA, et al. Transverse fetal lie. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Chasen ST, et al. Twin pregnancy: Labor and delivery. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Cohen R, et al. Is vaginal delivery of a breech second twin safe? A comparison between delivery of vertex and non-vertex second twins. The Journal of Maternal-Fetal & Neonatal Medicine. 2021; doi:10.1080/14767058.2021.2005569.
- Marnach ML (expert opinion). Mayo Clinic. May 31, 2023.
Products and Services
- A Book: Obstetricks
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- 3rd trimester pregnancy
- Fetal development: The 3rd trimester
- Overdue pregnancy
- Pregnancy due date calculator
- Prenatal care: 3rd trimester
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
Make twice the impact
Your gift can go twice as far to advance cancer research and care!
Fetal Presentation, Position, and Lie (Including Breech Presentation)
- Variations in Fetal Position and Presentation |
During pregnancy, the fetus can be positioned in many different ways inside the mother's uterus. The fetus may be head up or down or facing the mother's back or front. At first, the fetus can move around easily or shift position as the mother moves. Toward the end of the pregnancy the fetus is larger, has less room to move, and stays in one position. How the fetus is positioned has an important effect on delivery and, for certain positions, a cesarean delivery is necessary. There are medical terms that describe precisely how the fetus is positioned, and identifying the fetal position helps doctors to anticipate potential difficulties during labor and delivery.
Presentation refers to the part of the fetus’s body that leads the way out through the birth canal (called the presenting part). Usually, the head leads the way, but sometimes the buttocks (breech presentation), shoulder, or face leads the way.
Position refers to whether the fetus is facing backward (occiput anterior) or forward (occiput posterior). The occiput is a bone at the back of the baby's head. Therefore, facing backward is called occiput anterior (facing the mother’s back and facing down when the mother lies on her back). Facing forward is called occiput posterior (facing toward the mother's pubic bone and facing up when the mother lies on her back).
Lie refers to the angle of the fetus in relation to the mother and the uterus. Up-and-down (with the baby's spine parallel to mother's spine, called longitudinal) is normal, but sometimes the lie is sideways (transverse) or at an angle (oblique).
For these aspects of fetal positioning, the combination that is the most common, safest, and easiest for the mother to deliver is the following:
Head first (called vertex or cephalic presentation)
Facing backward (occiput anterior position)
Spine parallel to mother's spine (longitudinal lie)
Neck bent forward with chin tucked
Arms folded across the chest
If the fetus is in a different position, lie, or presentation, labor may be more difficult, and a normal vaginal delivery may not be possible.
Variations in fetal presentation, position, or lie may occur when
The fetus is too large for the mother's pelvis (fetopelvic disproportion).
The uterus is abnormally shaped or contains growths such as fibroids .
The fetus has a birth defect .
There is more than one fetus (multiple gestation).

Position and Presentation of the Fetus
Variations in fetal position and presentation.
Some variations in position and presentation that make delivery difficult occur frequently.
Occiput posterior position
In occiput posterior position (sometimes called sunny-side up), the fetus is head first (vertex presentation) but is facing forward (toward the mother's pubic bone—that is, facing up when the mother lies on her back). This is a very common position that is not abnormal, but it makes delivery more difficult than when the fetus is in the occiput anterior position (facing toward the mother's spine—that is facing down when the mother lies on her back).
When a fetus faces up, the neck is often straightened rather than bent,which requires more room for the head to pass through the birth canal. Delivery assisted by a vacuum device or forceps or cesarean delivery may be necessary.
Breech presentation
In breech presentation, the baby's buttocks or sometimes the feet are positioned to deliver first (before the head).
When delivered vaginally, babies that present buttocks first are more at risk of injury or even death than those that present head first.
The reason for the risks to babies in breech presentation is that the baby's hips and buttocks are not as wide as the head. Therefore, when the hips and buttocks pass through the cervix first, the passageway may not be wide enough for the head to pass through. In addition, when the head follows the buttocks, the neck may be bent slightly backwards. The neck being bent backward increases the width required for delivery as compared to when the head is angled forward with the chin tucked, which is the position that is easiest for delivery. Thus, the baby’s body may be delivered and then the head may get caught and not be able to pass through the birth canal. When the baby’s head is caught, this puts pressure on the umbilical cord in the birth canal, so that very little oxygen can reach the baby. Brain damage due to lack of oxygen is more common among breech babies than among those presenting head first.
In a first delivery, these problems may occur more frequently because a woman’s tissues have not been stretched by previous deliveries. Because of risk of injury or even death to the baby, cesarean delivery is preferred when the fetus is in breech presentation, unless the doctor is very experienced with and skilled at delivering breech babies or there is not an adequate facility or equipment to safely perform a cesarean delivery.
Breech presentation is more likely to occur in the following circumstances:
Labor starts too soon (preterm labor).
The uterus is abnormally shaped or contains abnormal growths such as fibroids .
Other presentations
In face presentation, the baby's neck arches back so that the face presents first rather than the top of the head.
In brow presentation, the neck is moderately arched so that the brow presents first.
Usually, fetuses do not stay in a face or brow presentation. These presentations often change to a vertex (top of the head) presentation before or during labor. If they do not, a cesarean delivery is usually recommended.
In transverse lie, the fetus lies horizontally across the birth canal and presents shoulder first. A cesarean delivery is done, unless the fetus is the second in a set of twins. In such a case, the fetus may be turned to be delivered through the vagina.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
Unknown Error
This content is only available to UpToDate ® subscribers. Please sign in to gain access.

Cephalic presentation
October 14, 2016
A cephalic presentation or head presentation or head-first presentation is a situation at childbirth where the fetus is in a longitudinal lie and the head enters the pelvis first; the most common form of cephalic presentation is the vertex presentation where the occiput is the leading part (the part that first enters the birth canal). All other presentations are abnormal (malpresentations) which are either more difficult to deliver or not deliverable by natural means.
The movement of the fetus to cephalic presentation is called head engagement. It occurs in the third trimester. In head engagement, the fetal head descends into the pelvic cavity so that only a small part (or none) of it can be felt abdominally. The perineum and cervix are further flattened and the head may be felt vaginally. Head engagement is known colloquially as the baby drop, and in natural medicine as the lightening because of the release of pressure on the upper abdomen and renewed ease in breathing. However, it severely reduces bladder capacity, increases pressure on the pelvic floor and the rectum, and the mother may experience the perpetual sensation that the fetus will “fall out” at any moment.
The vertex is the area of the vault bounded anteriorly by the anterior fontanelle and the coronal suture, posteriorly by the posterior fontanelle and the lambdoid suture and laterally by 2 lines passing through the parietal eminences.
In the vertex presentation the occiput typically is anterior and thus in an optimal position to negotiate the pelvic curve by extending the head. In an occiput posterior position, labor becomes prolonged and more operative interventions are deemed necessary. The prevalence of the persistent occiput posterior is given as 4.7 %
The vertex presentations are further classified according to the position of the occiput, it being right, left, or transverse, and anterior or posterior:
Left Occipito-Anterior (LOA), Left Occipito-Posterior (LOP), Left Occipito-Transverse (LOT); Right Occipito-Anterior (ROA), Right Occipito-Posterior (ROP), Right Occipito-Transverse (ROT);
By Mikael Häggström – Own work, Public Domain
Cephalic presentation. (2016, September 17). In Wikipedia, The Free Encyclopedia . Retrieved 05:18, September 17, 2016, from https://en.wikipedia.org/w/index.php?title=Cephalic_presentation&oldid=739815165
Insert/edit link
Enter the destination URL
Or link to existing content
- Getting Pregnant
- Registry Builder
- Baby Products
- Birth Clubs
- See all in Community
- Ovulation Calculator
- How To Get Pregnant
- How To Get Pregnant Fast
- Ovulation Discharge
- Implantation Bleeding
- Ovulation Symptoms
- Pregnancy Symptoms
- Am I Pregnant?
- Pregnancy Tests
- See all in Getting Pregnant
- Due Date Calculator
- Pregnancy Week by Week
- Pregnant Sex
- Weight Gain Tracker
- Signs of Labor
- Morning Sickness
- COVID Vaccine and Pregnancy
- Fetal Weight Chart
- Fetal Development
- Pregnancy Discharge
- Find Out Baby Gender
- Chinese Gender Predictor
- See all in Pregnancy
- Baby Name Generator
- Top Baby Names 2023
- Top Baby Names 2024
- How to Pick a Baby Name
- Most Popular Baby Names
- Baby Names by Letter
- Gender Neutral Names
- Unique Boy Names
- Unique Girl Names
- Top baby names by year
- See all in Baby Names
- Baby Development
- Baby Feeding Guide
- Newborn Sleep
- When Babies Roll Over
- First-Year Baby Costs Calculator
- Postpartum Health
- Baby Poop Chart
- See all in Baby
- Average Weight & Height
- Autism Signs
- Child Growth Chart
- Night Terrors
- Moving from Crib to Bed
- Toddler Feeding Guide
- Potty Training
- Bathing and Grooming
- See all in Toddler
- Height Predictor
- Potty Training: Boys
- Potty training: Girls
- How Much Sleep? (Ages 3+)
- Ready for Preschool?
- Thumb-Sucking
- Gross Motor Skills
- Napping (Ages 2 to 3)
- See all in Child
- Photos: Rashes & Skin Conditions
- Symptom Checker
- Vaccine Scheduler
- Reducing a Fever
- Acetaminophen Dosage Chart
- Constipation in Babies
- Ear Infection Symptoms
- Head Lice 101
- See all in Health
- Second Pregnancy
- Daycare Costs
- Family Finance
- Stay-At-Home Parents
- Breastfeeding Positions
- See all in Family
- Baby Sleep Training
- Preparing For Baby
- My Custom Checklist
- My Registries
- Take the Quiz
- Best Baby Products
- Best Breast Pump
- Best Convertible Car Seat
- Best Infant Car Seat
- Best Baby Bottle
- Best Baby Monitor
- Best Stroller
- Best Diapers
- Best Baby Carrier
- Best Diaper Bag
- Best Highchair
- See all in Baby Products
- Why Pregnant Belly Feels Tight
- Early Signs of Twins
- Teas During Pregnancy
- Baby Head Circumference Chart
- How Many Months Pregnant Am I
- What is a Rainbow Baby
- Braxton Hicks Contractions
- HCG Levels By Week
- When to Take a Pregnancy Test
- Am I Pregnant
- Why is Poop Green
- Can Pregnant Women Eat Shrimp
- Insemination
- UTI During Pregnancy
- Vitamin D Drops
- Best Baby Forumla
- Postpartum Depression
- Low Progesterone During Pregnancy
- Baby Shower
- Baby Shower Games
Breech, posterior, transverse lie: What position is my baby in?

Fetal presentation, or how your baby is situated in your womb at birth, is determined by the body part that's positioned to come out first, and it can affect the way you deliver. At the time of delivery, 97 percent of babies are head-down (cephalic presentation). But there are several other possibilities, including feet or bottom first (breech) as well as sideways (transverse lie) and diagonal (oblique lie).
Fetal presentation and position
During the last trimester of your pregnancy, your provider will check your baby's presentation by feeling your belly to locate the head, bottom, and back. If it's unclear, your provider may do an ultrasound or an internal exam to feel what part of the baby is in your pelvis.
Fetal position refers to whether the baby is facing your spine (anterior position) or facing your belly (posterior position). Fetal position can change often: Your baby may be face up at the beginning of labor and face down at delivery.
Here are the many possibilities for fetal presentation and position in the womb.
Medical illustrations by Jonathan Dimes
Head down, facing down (anterior position)
A baby who is head down and facing your spine is in the anterior position. This is the most common fetal presentation and the easiest position for a vaginal delivery.
This position is also known as "occiput anterior" because the back of your baby's skull (occipital bone) is in the front (anterior) of your pelvis.
Head down, facing up (posterior position)
In the posterior position , your baby is head down and facing your belly. You may also hear it called "sunny-side up" because babies who stay in this position are born facing up. But many babies who are facing up during labor rotate to the easier face down (anterior) position before birth.
Posterior position is formally known as "occiput posterior" because the back of your baby's skull (occipital bone) is in the back (posterior) of your pelvis.
Frank breech
In the frank breech presentation, both the baby's legs are extended so that the feet are up near the face. This is the most common type of breech presentation. Breech babies are difficult to deliver vaginally, so most arrive by c-section .
Some providers will attempt to turn your baby manually to the head down position by applying pressure to your belly. This is called an external cephalic version , and it has a 58 percent success rate for turning breech babies. For more information, see our article on breech birth .
Complete breech
A complete breech is when your baby is bottom down with hips and knees bent in a tuck or cross-legged position. If your baby is in a complete breech, you may feel kicking in your lower abdomen.
Incomplete breech
In an incomplete breech, one of the baby's knees is bent so that the foot is tucked next to the bottom with the other leg extended, positioning that foot closer to the face.
Single footling breech
In the single footling breech presentation, one of the baby's feet is pointed toward your cervix.
Double footling breech
In the double footling breech presentation, both of the baby's feet are pointed toward your cervix.
Transverse lie
In a transverse lie, the baby is lying horizontally in your uterus and may be facing up toward your head or down toward your feet. Babies settle this way less than 1 percent of the time, but it happens more commonly if you're carrying multiples or deliver before your due date.
If your baby stays in a transverse lie until the end of your pregnancy, it can be dangerous for delivery. Your provider will likely schedule a c-section or attempt an external cephalic version , which is highly successful for turning babies in this position.
Oblique lie
In rare cases, your baby may lie diagonally in your uterus, with his rump facing the side of your body at an angle.
Like the transverse lie, this position is more common earlier in pregnancy, and it's likely your provider will intervene if your baby is still in the oblique lie at the end of your third trimester.
Was this article helpful?
What to know if your baby is breech

What's a sunny-side up baby?

What happens to your baby right after birth

How your twins’ fetal positions affect labor and delivery

BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies .
Ahmad A et al. 2014. Association of fetal position at onset of labor and mode of delivery: A prospective cohort study. Ultrasound in obstetrics & gynecology 43(2):176-182. https://www.ncbi.nlm.nih.gov/pubmed/23929533 Opens a new window [Accessed September 2021]
Gray CJ and Shanahan MM. 2019. Breech presentation. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK448063/ Opens a new window [Accessed September 2021]
Hankins GD. 1990. Transverse lie. American Journal of Perinatology 7(1):66-70. https://www.ncbi.nlm.nih.gov/pubmed/2131781 Opens a new window [Accessed September 2021]
Medline Plus. 2020. Your baby in the birth canal. U.S. National Library of Medicine. https://medlineplus.gov/ency/article/002060.htm Opens a new window [Accessed September 2021]

Where to go next

We have a new app!
Take the Access library with you wherever you go—easy access to books, videos, images, podcasts, personalized features, and more.
Download the Access App here: iOS and Android . Learn more here!
- Remote Access
- Save figures into PowerPoint
- Download tables as PDFs

Chapter 10: Normal Mechanisms of Labor
- Download Chapter PDF
Disclaimer: These citations have been automatically generated based on the information we have and it may not be 100% accurate. Please consult the latest official manual style if you have any questions regarding the format accuracy.
Download citation file:
- Search Book
Jump to a Section
Left occiput anterior: loa.
- BIRTH OF THE PLACENTA
- CLINICAL COURSE OF LABOR: LOA
- RIGHT OCCIPUT ANTERIOR: ROA
- Full Chapter
- Supplementary Content
LOA is a common longitudinal cephalic presentation ( Fig. 10-1 ). Two-thirds of occiput anterior positions are in the LOA position. The attitude is flexion, the presenting part is the posterior part of the vertex and the posterior fontanelle, and the denominator is the occiput (O).
FIGURE 10-1.
Left occiput anterior.

Diagnosis of Position: LOA
Abdominal examination.
The lie is longitudinal. The long axis of the fetus is parallel to the long axis of the mother
The head is at or in the pelvis
The back is on the left and anterior and is palpated easily except in obese women
The small parts are on the right and are not felt clearly
The breech is in the fundus of the uterus
The cephalic prominence (in this case the forehead) is on the right. When the attitude is flexion, the cephalic prominence and the back are on opposite sides. The reverse is true in attitudes of extension
Fetal Heart
The fetal heart is heard loudest in the left lower quadrant of the mother's abdomen. In attitudes of flexion, the fetal heart rate is transmitted through the baby's back. The point of maximum intensity varies with the degree of rotation. As the child's back approaches the midline of the maternal abdomen, so does the point where the fetal heart is heard most strongly. Therefore, in a left anterior position, it is heard below the umbilicus and somewhere to the left of the midline, depending on the exact situation of the back.
Vaginal Examination
The station of the head is noted—whether it is above, at, or below the ischial spines
If the cervix is dilated, the suture lines and the fontanelles of the baby's head can be felt. In the LOA position, the sagittal suture is in the right oblique diameter of the pelvis
The small posterior fontanelle is anterior and to the mother's left
The bregma is posterior and to the right
Since the head is probably flexed, the occiput is a littler lower than the brow
Normal Mechanism of Labor: LOA
The mechanism of labor as we know it today was described first by William Smellie during the 18th century. It is the way the baby adapts itself to and passes through the maternal pelvis. There are six movements, with considerable overlapping:
Internal rotation
Restitution
External rotation
The following description is for left anterior positions of the occiput.
Pop-up div Successfully Displayed
This div only appears when the trigger link is hovered over. Otherwise it is hidden from view.
Please Wait
- Normal Normal and Abnormal First Trimester Exam Normal Fetal Ultrasound Biometry Fetal Heart Ultrasound Determining Fetal Situs Fetal Urinary System Umbilical Cord CNS Critical Anatomy CNS Embryology and Early Development CNS Later Development CNS Ultrasound Brain Anatomy
- Fetal Anomalies Fetal Heart Fetal Chest Fetal Colon Fetal Central Nervous System Facial Clefts Skeletal Dysplasia Genetic Markers
- Doppler Editorial Board Fetal Doppler Middle Cerebral Artery Doppler
- Fetal/Maternal Conditions Transvaginal Ultrasound Fetal Anemia Interventions Preterm Labor Placenta and Umbilical Cord
- Twins Key Views Twins: Videos Diamniotic Dichorionic and Diamniotic Monochorionic Twins Monochorionic Monoamniotic Twins Twin to Twin Transfusion Syndrome Fetal Growth Restriction Twin Reversed Arterial Perfusion Conjoined Twins
- Video Topics
- Access CMEs
- Other Links Topics A-Z Links CME Videos Upload Your Case Editorial Board
- Take A Free Tour
- Free Videos
- Editorial Board

Determining Normal Fetal Situs (Situs Solitus)
One of the first steps in obtaining cardiac views is to determine how the fetus is oriented within the uterus and to determine the right and left side of the abdominal contents versus the right and left side of the heart and thoracic contents. This is not as easy as it might seem since the fetal left side can be on the maternal right and the opposite can be true.
In summary, situs refers to the right and left orientation of fetal organs. For example situs solitus is the normal left to right axis arrangement in the fetus with the stomach and spleen on the left side of the body, and the liver and gallbladder on the right side.

Visual Summary of Normal Fetal Situs
Below are steps required to determine situs related to cephalic or breech presentation, and whether the spine or back is up (anterior) or down (posterior).
1. Determine the lie of the fetus:
A. Is the fetus head first with the head in front of the ultrasound screen? This could also be termed cephalic or vertex presentation. B. Is the fetal feet or bottom first with the head behind the screen? This could also be termed footling or breech presentation. C. Determine whether the spine or back is anterior (back up) or posterior (back down).
2. Obtain a transverse cut of the thorax to demonstrate a 4-chamber view. The left atrium is nearest the spine and the cardiac axis points to the left.
Detailed Method to Determine Fetal Situs
1. Define within the uterus the presentation of the fetus (generally vertex or breech; less often the presentation is oblique or transverse.).
2. Determine whether the fetal spine is parallel or transverse to the maternal spine. In sagittal view, if the fetal and maternal spine are parallel, the fetus is in longitudinal lie. When the fetal spine is perpendicular to the maternal spine, the fetus is in a transverse lie.
3. Determine the position of the fetal left side. The fetal left side will be as follows: A. With respect to the maternal abdomen, the fetal left side is anterior and near to the ultrasound transducer. B. With respect to the posterior uterine wall, the fetal left side is posterior and farthest from the transducer. C. With respect to the right uterine wall, the fetal left side will be on the maternal right. D. With respect to the left uterine wall, the fetal left side will be on the maternal left.
4. Obtain a transverse view of the abdomen and define the fetal stomach which is positioned in the left side of the fetal abdomen.
5. Obtain a 4-chamber view of the heart by obtaining a transverse view of the thorax. The left atrium and descending aorta are nearest to the spine and the cardiac axis points to the left.
6. Finally, ascertain if the stomach and heart are in their correct respective locations, i.e., the stomach is on the left side and the cardiac axis points to the left.
7. Place a transverse image of the fetal abdomen and heart side by side and validate that the left side of the fetal abdomen (stomach near to the spine) is concordant with the left side of the fetal heart (left atrium and descending aorta near to the spine). This is done by displaying a side by side comparison of a transverse view through the fetal stomach and a 4-chamber cardiac view.

Above. Normal ultrasound orientation for situs solitus.
Right Hand Rule of Thumb: Introduction
In their article “Sonographic definition of the fetal situs,” Bronshtein, Gover, and Zimmer [ 1 ] describe a “right hand rule of thumb” to define fetal situs during transabdominal scanning, and a “left hand rule of thumb” for transvaginal scanning.

Right Hand Rule of Thumb: Cephalic, supine, back down

Left. The sonographer’s right hand represents the fetus with the thumb pointing to the fetal left. The palm of the hand is anterior, or represents the ventral or face surface of the fetus. The fetus is therefore face up, back down, and the thumb points to the fetal left.
Right. Again, the imaginary fetus is back down with the stomach and cardiac axis pointing to the left. (Ignore color scheme of fetal heart and vessels.)

Right Hand Rule of Thumb: Cephalic, prone, back up
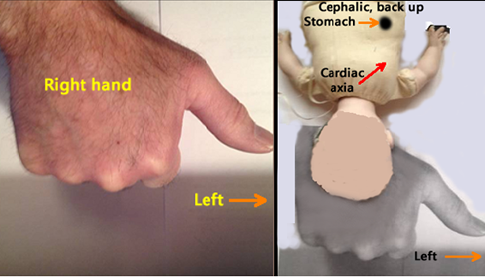
Left. The sonographer’s right hand represents the fetus with the thumb pointing to the fetal left. The top of the hand (dorsal surface or prone position) represents back up.
Right. The imaginary fetus is back up with the stomach and cardiac axis pointing to the fetal left.

Right Hand Rule of Thumb: Breech, supine, back down
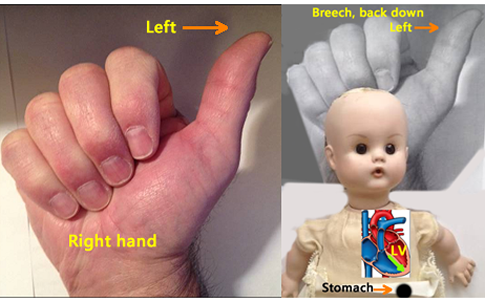
Left. The sonographer’s right hand represents the fetus with the thumb pointing to the fetal left. The palm of the sonographer’s hand is anterior, or represents the ventral surface of the fetus. The fetus is therefore face up, back down, and the thumb points to the fetal left.
Right . The imaginary fetus is back down with the stomach and cardiac axis pointing to the left. (Ignore color scheme of fetal heart and vessels).

Right Hand Rule of Thumb: Breech, prone, back up

Right . The imaginary fetus is back up with the stomach and cardiac axis pointing to the fetal left side.

- Normal CNS Anatomy
- Fetal Situs
- Normal Fetal Ultrasound Biometry
All are web-based courses. Subscribe Today!
- Literature Reviews
- Terms of Use
Procedure by Kate Leonard, MD, and Will Stone, MD, Walter Reed National Military Medical Center Residency in Obstetrics and Gynecology; and Shad Deering, COL, MD, Chair, Department of Obstetrics and Gynecology, Uniformed Services University. Assisted by Elizabeth N. Weissbrod, MA, CMI, Eric Wilson, 2LT, and Jamie Bradshaw at the Val G. Hemming Simulation Center at the Uniformed Services University.
- Fetal Presentation, Position, and Lie (Including Breech Presentation)
Fastest Obstetric, Gynecology and Pediatric Insight Engine
- Abdominal Key
- Anesthesia Key
- Basicmedical Key
- Otolaryngology & Ophthalmology
- Musculoskeletal Key
- Obstetric, Gynecology and Pediatric
- Oncology & Hematology
- Plastic Surgery & Dermatology
- Clinical Dentistry
- Radiology Key
- Thoracic Key
- Veterinary Medicine
- Gold Membership
Fetal Situs
● INTRODUCTION The first step in the ultrasonographic evaluation of the fetus is the assessment of fetal visceral situs as some organs are arranged symmetrically and others, such as the abdominal and thoracic organs, are arranged asymmetrically ( 1 ). A clear definition of left and right sidedness in the body is noted since early embryogenesis. A good understanding of fetal situs is important during ultrasound examinations, as some fetal anomalies are associated with abnormal laterality of abdominal and/or thoracic organs. Evaluating the orientation and position of the fetal heart in the thorax and the anatomic relationship of the abdominal organs is part of the targeted fetal cardiac examination. Knowledge of the anatomic landmarks in the chest and abdomen can facilitate the routine cardiac screening examination and provide clues to the presence of cardiac abnormality ( 1 , 2 ). This chapter will focus on the fetal situs, including the anatomic orientation of the organs in the chest and upper abdomen. ● SEQUENTIAL SEGMENTAL ANALYSIS In evaluating fetal cardiac anatomy, a sequential segmental approach helps in the description of cardiac abnormalities in a clear and simple approach. For many years, pathologists and pediatric cardiologists have been using this approach to describe normal and abnormal hearts ( 1 , 3 , 4 ). In the sequential segmental approach, the cardiovascular system is divided into segments, and for each segment, the anatomy, the position, and the connection with the next segment are described. This sequential segmental analysis involves three anatomic regions: the atria, the ventricles, and the arterial trunks. Each anatomic region is also partitioned into a right- and left-sided component. Atrioventricular valves separate the atria from the ventricles, and the semilunar valves separate the ventricles from the arterial trunks. A fourth anatomic segment, systemic and pulmonary venous connections, should also be evaluated. The cardiac chambers are therefore recognized by their morphologic structures rather than their anatomic locations. The direction of blood flow also helps assess the atrioventricular and ventriculoarterial connections. Assessment of visceral situs and cardiac position, which is described in detail in this chapter, should be part of this sequential segmental approach ( 1 , 3 , 4 ). Table 6.1 presents the steps for the sequential segmental analysis in fetal cardiac evaluation. Detailed anatomic evaluation of cardiac chambers, valvular structures, arterial trunks, and venous systems will be presented in the following chapters. TABLE 6.1 Steps for Sequential Segmental Analysis in the Fetus 1. Identify visceral situs 2. Identify atrial arrangement (morphologic right and left atrium) 3. Identify atrioventricular (AV) connections (AV valves) 4. Identify ventricular arrangement (morphologic right and left ventricle) 5. Identify ventriculoarterial connections (semilunar valves) 6. Identify arterial trunk arrangement (aorta and pulmonary artery) 7. Identify systemic and pulmonary venous connections ● FETAL VISCERAL SITUS Assessment of the fetal thoracic and visceral situs is the initial approach to the sequential segmental analysis of the fetal heart by ultrasound ( 5 ). Heterotaxy syndrome commonly involves cardiac and abdominal anomalies, and thus focusing on the fetal heart without an evaluation of the upper abdomen often results in an incomplete diagnosis. Although the current method for the determination of fetal situs relies on the position of the stomach and heart in the abdomen and chest, respectively, careful attention should also be paid to the position of the aorta and inferior vena cava below the diaphragm ( 4 , 5 ) ( Fig. 6.1 ), the orientation of the umbilical vein with the portal sinus, the presence and position of the gallbladder, and when feasible the presence and location of the spleen. It is generally agreed that the positions of the aorta and inferior vena cava below the diaphragm are more reliable criteria for the determination of right or left isomerism than the location of the stomach in the abdomen. Technique 1. Locate the fetal head within the uterus and determine the presenting part (e.g., cephalic, breech) ( Fig. 6.2 ). 2. Determine the fetal lie within the uterus by obtaining a sagittal view of the fetal spine. (Longitudinal lie: when the fetal spine is parallel to the maternal spine; transverse lie: when the fetal spine is perpendicular to the maternal spine; oblique lie: when the fetal spine is oblique to the maternal spine.) 3. After establishing the exact position of the fetus with steps 1 and 2, determine the location of the fetal left side with regard to the maternal abdomen (fetal left side is anterior [closer to the transducer], posterior [closer to the posterior uterine wall], right lateral [closer to the maternal right uterine wall], left lateral [closer to the maternal left uterine wall]) ( Fig. 6.2 ). 4. Obtain a transverse view of the fetal abdomen by rotating the transducer 90 degrees from the sagittal view of the lower thoracic spine. The fetal stomach is imaged in the left side of the abdomen, the descending aorta is posterior to the left, and the inferior vena cava is anterior to the right ( Figs. 6.1 and 6.3 ). In addition, the intrahepatic part of the umbilical vein is seen connecting with the left portal vein and portal sinus with an L-shape to the right ( Figs. 6.1 and 6.3 ). By sliding the transducer toward the fetal chest, a four-chamber view of the heart is imaged. Note that the apex of the heart is pointing toward the left side of the fetal chest ( Figs. 6.2 and 6.4 ). Determining that the stomach, descending aorta, and cardiac apex are located on the fetal left side and the inferior vena cava is located on the right side establishes normal visceral situs ( Figs. 6.1 and 6.3 ). Figure 6.1: Schematic drawing of a cross section of the upper abdomen for the assessment of the abdominal situs. The vertical line divides this plane into right and left. The right-sided structures include the gallbladder, the portal sinus, a large part of the liver, and inferior vena cava (IVC). The left-sided structures include the descending aorta, the stomach, and the spleen. Figure 6.3 is the corresponding ultrasound plane. Figure 6.2: Determining fetal situs in longitudinal lie: In A , the fetus is in a cephalic presentation with the fetal spine close to the left uterine wall, resulting in the right side being anterior and left side posterior. In B , the fetus is in a cephalic presentation with the fetal spine close to the right uterine wall, resulting in the left side being anterior and right side posterior. In C , the fetus is in a breech presentation with the fetal spine close to the left uterine wall, resulting in the left side being anterior and right side posterior. In D , the fetus is in a breech presentation with the fetal spine close to the right uterine wall, resulting in the right side being anterior and left side posterior. Note the corresponding transverse ultrasound planes of the chest and abdomen. Blue arrows point to fetal stomach, red arrows to the apex of the heart, and yellow arrows to the descending aorta. See text for details. Several methods for determining fetal situs during the ultrasound examination have been described. Cordes et al. ( 6 ) described a technique that involves orienting the transducer in a standardized way so that the fetal head is on the right side of the screen in a fetal sagittal plane as a starting point and then rotating the transducer 90 degrees in clockwise to obtain the caudocranial transverse views. Another method reported by Bronshtein et al. ( 7 ) is referred to as the right-hand rule for abdominal scanning and the left-hand rule for transvaginal scanning ( Fig. 6.5 ). The palm of the hand corresponds to the face of the fetus, and the examiner holds the hand according to the side of the fetal face; the fetal heart and stomach are shown by the examiner’s thumb. Figure 6.3: Axial view of the fetal abdomen in a fetus with situs solitus. Note the location of the liver, portal sinus (PS), and inferior vena cava (IVC) in right side (R); and the stomach (St) and descending aorta (Ao) in left side (L). The umbilical vein (UV) is located in the midline. Compare with Figure 6.1 . Figure 6.4: Schematic drawing of a cross section of the thorax at the level of the four-chamber view in a fetus with situs solitus. Note the position of the heart in the left chest with a normal cardiac axis of 45 degrees. See text for details. LA, left atrium; RA, right atrium; LV, left ventricle; RV, right ventricle; Ao, Aorta; L, left; R, right. Situs Solitus, Situs Inversus, and Situs Ambiguous Three types of visceral situs exist: situs solitus, situs inversus, and situs ambiguous ( Table 6.2 ). a.) Situs solitus refers to the normal arrangement of vessels and organs within the body ( Fig. 6.1 ). b.) Situs inversus, with an incidence of about 0.01% of the population, refers to a mirror-image arrangement of organs and vessels to situs solitus. Situs inversus is associated with a slight increase in the incidence of complex congenital heart disease (CHD), in the order of 0.3% to 5% ( 8 ), and with the presence of Kartagener syndrome in about 20% of the cases ( 9 ). Kartagener syndrome, with an autosomal recessive transmission, primarily involves ciliary dysfunction with recurrent respiratory infection and reduced fertility. c.) Situs ambiguous (heterotaxy), which refers to visceral malpositions and malformations different from situs solitus or inversus, is commonly associated with complex CHD, abnormalities in venous drainage, bowel malrotations and obstruction, and splenic, biliary, and bronchial tree abnormalities. The incidence of situs ambiguous has been estimated around 1 per 10,000 infants ( 10 ). Two types of heterotaxy exist: right isomerism and left isomerism. In right isomerism, also referred to as asplenia, both sides of the body show the right morphology; in left isomerism, also referred to as polysplenia, both sides of the body show the left morphology. Chapter 30 presents a detailed overview of heterotaxy and isomerism in the fetus. Figure 6.5: Determining fetal situs: A diagram of the fetus is presented in back posterior ( 1 and 3 ) and back anterior ( 2 and 4 ) positions. In transabdominal scanning, the ultrasound beam (S) is directed from top to bottom. The palm of the right hand represents the face of the fetus, and the fetal heart and stomach are on the same side of the examiner’s thumb. (Modified from Bronshtein M, Gover A, Zimmer EZ. Sonographic definition of the fetal situs. Obstet Gynecol. 2002;99( 6 ):1129–1130, with permission.)
Share this:
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)
Related posts:
- Fetal Cardiac Measurements and Reference Ranges
- Color Doppler in Fetal Echocardiography
- The Three-Vessel-Trachea View and Upper Mediastinum
- Three- and Four-Dimensional Ultrasound of the Fetal Heart
Stay updated, free articles. Join our Telegram channel
Comments are closed for this page.

Full access? Get Clinical Tree


An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

- Health Topics
- Drugs & Supplements
- Medical Tests
- Medical Encyclopedia
- About MedlinePlus
- Customer Support
Your baby in the birth canal
During labor and delivery, your baby must pass through your pelvic bones to reach the vaginal opening. The goal is to find the easiest way out. Certain body positions give the baby a smaller shape, which makes it easier for your baby to get through this tight passage.
The best position for the baby to pass through the pelvis is with the head down and the body facing toward the mother's back. This position is called occiput anterior.
Information
Certain terms are used to describe your baby's position and movement through the birth canal.
FETAL STATION
Fetal station refers to where the presenting part is in your pelvis.
- The presenting part. The presenting part is the part of the baby that leads the way through the birth canal. Most often, it is the baby's head, but it can be a shoulder, the buttocks, or the feet.
- Ischial spines. These are bone points on the mother's pelvis. Normally the ischial spines are the narrowest part of the pelvis.
- 0 station. This is when the baby's head is even with the ischial spines. The baby is said to be "engaged" when the largest part of the head has entered the pelvis.
- If the presenting part lies above the ischial spines, the station is reported as a negative number from -1 to -5.
In first-time moms, the baby's head may engage by 36 weeks into the pregnancy. However, engagement may happen later in the pregnancy, or even during labor.
This refers to how the baby's spine lines up with the mother's spine. Your baby's spine is between their head and tailbone.
Your baby will most often settle into a position in the pelvis before labor begins.
- If your baby's spine runs in the same direction (parallel) as your spine, the baby is said to be in a longitudinal lie. Nearly all babies are in a longitudinal lie.
- If the baby is sideways (at a 90-degree angle to your spine), the baby is said to be in a transverse lie.
FETAL ATTITUDE
The fetal attitude describes the position of the parts of your baby's body.
The normal fetal attitude is commonly called the fetal position.
- The head is tucked down to the chest.
- The arms and legs are drawn in towards the center of the chest.
Abnormal fetal attitudes include a head that is tilted back, so the brow or the face presents first. Other body parts may be positioned behind the back. When this happens, the presenting part will be larger as it passes through the pelvis. This makes delivery more difficult.
DELIVERY PRESENTATION
Delivery presentation describes the way the baby is positioned to come down the birth canal for delivery.
The best position for your baby inside your uterus at the time of delivery is head down. This is called cephalic presentation.
- This position makes it easier and safer for your baby to pass through the birth canal. Cephalic presentation occurs in about 97% of deliveries.
- There are different types of cephalic presentation, which depend on the position of the baby's limbs and head (fetal attitude).
If your baby is in any position other than head down, your doctor may recommend a cesarean delivery.
Breech presentation is when the baby's bottom is down. Breech presentation occurs about 3% of the time. There are a few types of breech:
- A complete breech is when the buttocks present first and both the hips and knees are flexed.
- A frank breech is when the hips are flexed so the legs are straight and completely drawn up toward the chest.
- Other breech positions occur when either the feet or knees present first.
The shoulder, arm, or trunk may present first if the fetus is in a transverse lie. This type of presentation occurs less than 1% of the time. Transverse lie is more common when you deliver before your due date, or have twins or triplets.
CARDINAL MOVEMENTS OF LABOR
As your baby passes through the birth canal, the baby's head will change positions. These changes are needed for your baby to fit and move through your pelvis. These movements of your baby's head are called cardinal movements of labor.
- This is when the widest part of your baby's head has entered the pelvis.
- Engagement tells your health care provider that your pelvis is large enough to allow the baby's head to move down (descend).
- This is when your baby's head moves down (descends) further through your pelvis.
- Most often, descent occurs during labor, either as the cervix dilates or after you begin pushing.
- During descent, the baby's head is flexed down so that the chin touches the chest.
- With the chin tucked, it is easier for the baby's head to pass through the pelvis.
Internal Rotation
- As your baby's head descends further, the head will most often rotate so the back of the head is just below your pubic bone. This helps the head fit the shape of your pelvis.
- Usually, the baby will be face down toward your spine.
- Sometimes, the baby will rotate so it faces up toward the pubic bone.
- As your baby's head rotates, extends, or flexes during labor, the body will stay in position with one shoulder down toward your spine and one shoulder up toward your belly.
- As your baby reaches the opening of the vagina, usually the back of the head is in contact with your pubic bone.
- At this point, the birth canal curves upward, and the baby's head must extend back. It rotates under and around the pubic bone.
External Rotation
- As the baby's head is delivered, it will rotate a quarter turn to be in line with the body.
- After the head is delivered, the top shoulder is delivered under the pubic bone.
- After the shoulder, the rest of the body is usually delivered without a problem.
Alternative Names
Shoulder presentation; Malpresentations; Breech birth; Cephalic presentation; Fetal lie; Fetal attitude; Fetal descent; Fetal station; Cardinal movements; Labor-birth canal; Delivery-birth canal

Barth WH. Malpresentations and malposition. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies . 8th ed. Philadelphia, PA: Elsevier; 2021:chap 17.
Kilpatrick SJ, Garrison E, Fairbrother E. Normal labor and delivery. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies . 8th ed. Philadelphia, PA: Elsevier; 2021:chap 11.
Review Date 11/10/2022
Updated by: John D. Jacobson, MD, Department of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Related MedlinePlus Health Topics
- Childbirth Problems
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
- Management of breech presentation
Evidence review M
NICE Guideline, No. 201
National Guideline Alliance (UK) .
- Copyright and Permissions
Review question
What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy?
Introduction
Breech presentation of the fetus in late pregnancy may result in prolonged or obstructed labour with resulting risks to both woman and fetus. Interventions to correct breech presentation (to cephalic) before labour and birth are important for the woman’s and the baby’s health. The aim of this review is to determine the most effective way of managing a breech presentation in late pregnancy.
Summary of the protocol
Please see Table 1 for a summary of the Population, Intervention, Comparison and Outcome (PICO) characteristics of this review.
Summary of the protocol (PICO table).
For further details see the review protocol in appendix A .
Methods and process
This evidence review was developed using the methods and process described in Developing NICE guidelines: the manual 2014 . Methods specific to this review question are described in the review protocol in appendix A .
Declarations of interest were recorded according to NICE’s conflicts of interest policy .
Clinical evidence
Included studies.
Thirty-six randomised controlled trials (RCTs) were identified for this review.
The included studies are summarised in Table 2 .
Three studies reported on external cephalic version (ECV) versus no intervention ( Dafallah 2004 , Hofmeyr 1983 , Rita 2011 ). One study reported on a 4-arm trial comparing acupuncture, sweeping of fetal membranes, acupuncture plus sweeping, and no intervention ( Andersen 2013 ). Two studies reported on postural management versus no intervention ( Chenia 1987 , Smith 1999 ).
Seven studies reported on ECV plus anaesthesia ( Chalifoux 2017 , Dugoff 1999 , Khaw 2015 , Mancuso 2000 , Schorr 1997 , Sullivan 2009 , Weiniger 2010 ). Of these studies, 1 study compared ECV plus anaesthesia to ECV plus other dosages of the same anaesthetic ( Chalifoux 2017 ); 4 studies compared ECV plus anaesthesia to ECV only ( Dugoff 1999 , Mancuso 2000 , Schorr 1997 , Weiniger 2010 ); and 2 studies compared ECV plus anaesthesia to ECV plus a different anaesthetic ( Khaw 2015 , Sullivan 2009 ).
Ten studies reported ECV plus a β2 receptor agonist ( Brocks 1984 , Fernandez 1997 , Hindawi 2005 , Impey 2005 , Mahomed 1991 , Marquette 1996 , Nor Azlin 2005 , Robertson 1987 , Van Dorsten 1981 , Vani 2009 ). Of these studies, 5 studies compared ECV plus a β2 receptor agonist to ECV plus placebo ( Fernandez 1997 , Impey 2005 , Marquette 1996 , Nor Azlin 2005 , Vani 2009 ); 1 study compared ECV plus a β2 receptor agonist to ECV alone ( Robertson 1987 ); and 4 studies compared ECV plus a β2 receptor agonist to no intervention ( Brocks 1984 , Hindawi 2005 , Mahomed 1991 , Van Dorsten 1981 ).
One study reported on ECV plus Ca 2+ channel blocker versus ECV plus placebo ( Kok 2008 ). Two studies reported on ECV plus β2 receptor agonist versus ECV plus Ca 2+ channel blocker ( Collaris 2009 , Mohamed Ismail 2008 ). Four studies reported on ECV plus a µ-receptor agonist ( Burgos 2016 , Liu 2016 , Munoz 2014 , Wang 2017 ), of which 3 compared against ECV plus placebo ( Liu 2016 , Munoz 2014 , Wang 2017 ) and 1 compared to ECV plus nitrous oxide ( Burgos 2016 ).
Four studies reported on ECV plus nitroglycerin ( Bujold 2003a , Bujold 2003b , El-Sayed 2004 , Hilton 2009 ), of which 2 compared it to ECV plus β2 receptor agonist ( Bujold 2003b , El-Sayed 2004 ) and compared it to ECV plus placebo ( Bujold 2003a , Hilton 2009 ). One study compared ECV plus amnioinfusion versus ECV alone ( Diguisto 2018 ) and 1 study compared ECV plus talcum powder to ECV plus gel ( Vallikkannu 2014 ).
One study was conducted in Australia ( Smith 1999 ); 4 studies in Canada ( Bujold 2003a , Bujold 2003b , Hilton 2009 , Marquette 1996 ); 2 studies in China ( Liu 2016 , Wang 2017 ); 2 studies in Denmark ( Andersen 2013 , Brocks 1984 ); 1 study in France ( Diguisto 2018 ); 1 study in Hong Kong ( Khaw 2015 ); 1 study in India ( Rita 2011 ); 1 study in Israel ( Weiniger 2010 ); 1 study in Jordan ( Hindawi 2005 ); 5 studies in Malaysia ( Collaris 2009 , Mohamed Ismail 2008 , Nor Azlin 2005 , Vallikkannu 2014 , Vani 2009 ); 1 study in South Africa ( Hofmeyr 1983 ); 2 studies in Spain ( Burgos 2016 , Munoz 2014 ); 1 study in Sudan ( Dafallah 2004 ); 1 study in The Netherlands ( Kok 2008 ); 2 studies in the UK ( Impey 2005 , Chenia 1987 ); 9 studies in US ( Chalifoux 2017 , Dugoff 1999 , El-Sayed 2004 , Fernandez 1997 , Mancuso 2000 , Robertson 1987 , Schorr 1997 , Sullivan 2009 , Van Dorsten 1981 ); and 1 study in Zimbabwe ( Mahomed 1991 ).
The majority of studies were 2-arm trials, but there was one 3-arm trial ( Khaw 2015 ) and two 4-arm trials ( Andersen 2013 , Chalifoux 2017 ). All studies were conducted in a hospital or an outpatient ward connected to a hospital.
See the literature search strategy in appendix B and study selection flow chart in appendix C .
Excluded studies
Studies not included in this review with reasons for their exclusions are provided in appendix K .

Summary of clinical studies included in the evidence review
Summaries of the studies that were included in this review are presented in Table 2 .
Summary of included studies.
See the full evidence tables in appendix D and the forest plots in appendix E .
Quality assessment of clinical outcomes included in the evidence review
See the evidence profiles in appendix F .
Economic evidence
A systematic review of the economic literature was conducted but no economic studies were identified which were applicable to this review question.
A single economic search was undertaken for all topics included in the scope of this guideline. See supplementary material 2 for details.
Economic studies not included in this review are listed, and reasons for their exclusion are provided in appendix K .
Summary of studies included in the economic evidence review
No economic studies were identified which were applicable to this review question.
Economic model
No economic modelling was undertaken for this review because the committee agreed that other topics were higher priorities for economic evaluation.
Evidence statements
Clinical evidence statements, comparison 1. complementary therapy versus control (no intervention), critical outcomes, cephalic presentation in labour.
No evidence was identified to inform this outcome.
Method of birth
Caesarean section.
- Very low quality evidence from 1 RCT (N=204) showed that there is no clinically important difference between acupuncture and control (no intervention) on the number of caesarean sections in pregnant women with breech presentation: RR 0.74 (95% CI 0.38 to 1.43).
- Very low quality evidence from 1 RCT (N=200) showed that there is no clinically important difference between acupuncture plus membrane sweeping and control (no intervention) on the number of caesarean sections in pregnant women with breech presentation: RR 1.29 (95% CI 0.73 to 2.29).
Admission to SCBU/NICU
- Very low quality evidence from 1 RCT (N=204) showed that there is no clinically important difference between acupuncture and control (no intervention) on admission to SCBU/NICU in pregnant women with breech presentation: RR 0.19 (95% CI 0.02 to 1.62).
- Very low quality evidence from 1 RCT (N=200) showed that there is no clinically important difference between acupuncture plus membrane sweeping and control (no intervention) on admission to SCBU/NICU in pregnant women with breech presentation: RR 0.40 (0.08 to 2.01).
Fetal death after 36 +0 weeks gestation
Infant death up to 4 weeks chronological age, important outcomes, apgar score <7 at 5 minutes.
- Very low quality evidence from 1 RCT (N=204) showed that there is no clinically important difference between acupuncture and control (no intervention) on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RR 0.32 (95% CI 0.01 to 7.78).
- Very low quality evidence from 1 RCT (N=200) showed that there is no clinically important difference between acupuncture plus membrane sweeping and control (no intervention) on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RR 0.33 (0.01 to 8.09).
Birth before 39 +0 weeks of gestation
Comparison 2. complementary therapy versus other treatment.
- Low quality evidence from 1 RCT (N=207) showed that there is no clinically important difference between acupuncture and membrane sweeping on the number of caesarean sections in pregnant women with breech presentation: RR 0.64 (95% CI 0.34 to 1.22).
- Low quality evidence from 1 RCT (N=204) showed that there is no clinically important difference between acupuncture and acupuncture plus membrane sweeping on the number of caesarean sections in pregnant women with breech presentation: RR 0.57 (95% CI 0.30 to 1.07).
- Very low quality evidence from 1 RCT (N=203) showed that there is no clinically important difference between acupuncture plus membrane sweeping and membrane sweeping on the number of caesarean sections in pregnant women with breech presentation: RR 1.13 (95% CI 0.66 to 1.94).
- Very low quality evidence from 1 RCT (N=207) showed that there is no clinically important difference between acupuncture and membrane sweeping on admission to SCBU/NICU in pregnant women with breech presentation: RR 0.33 (95% CI 0.03 to 3.12).
- Very low quality evidence from 1 RCT (N=204) showed that there is no clinically important difference between acupuncture and acupuncture plus membrane sweeping on admission to SCBU/NICU in pregnant women with breech presentation: RR 0.48 (95% CI 0.04 to 5.22).
- Very low quality evidence from 1 RCT (N=203) showed that there is no clinically important difference between acupuncture plus membrane sweeping and membrane sweeping on admission to SCBU/NICU in pregnant women with breech presentation: RR 0.69 (95% CI 0.12 to 4.02).
- Low quality evidence from 1 RCT (N=207) showed that there is no clinically important difference between acupuncture and membrane sweeping on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.02 to 0.02).
- Low quality evidence from 1 RCT (N=204) showed that there is no clinically important difference between acupuncture and acupuncture plus membrane sweeping on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.02 to 0.02).
- Low quality evidence from 1 RCT (N=203) showed that there is no clinically important difference between acupuncture plus membrane sweeping and membrane sweeping on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.02 to 0.02).
Comparison 3. ECV versus no ECV
- Moderate quality evidence from 2 RCTs (N=680) showed that there is clinically important difference favouring ECV over no ECV on cephalic presentation in labour in pregnant women with breech presentation: RR 1.83 (95% CI 1.53 to 2.18).
Cephalic vaginal birth
- Very low quality evidence from 3 RCTs (N=740) showed that there is a clinically important difference favouring ECV over no ECV on cephalic vaginal birth in pregnant women with breech presentation: RR 1.67 (95% CI 1.20 to 2.31).
Breech vaginal birth
- Very low quality evidence from 2 RCTs (N=680) showed that there is no clinically important difference between ECV and no ECV on breech vaginal birth in pregnant women with breech presentation: RR 0.29 (95% CI 0.03 to 2.84).
- Very low quality evidence from 3 RCTs (N=740) showed that there is no clinically important difference between ECV and no ECV on the number of caesarean sections in pregnant women with breech presentation: RR 0.52 (95% CI 0.23 to 1.20).
- Very low quality evidence from 1 RCT (N=60) showed that there is no clinically important difference between ECV and no ECV on admission to SCBU//NICU in pregnant women with breech presentation: RR 0.50 (95% CI 0.14 to 1.82).
- Very low evidence from 3 RCTs (N=740) showed that there is no statistically significant difference between ECV and no ECV on fetal death after 36 +0 weeks gestation in pregnant women with breech presentation: Peto OR 0.29 (95% CI 0.05 to 1.73) p=0.18.
- Very low quality evidence from 2 RCTs (N=120) showed that there is no clinically important difference between ECV and no ECV on Apgar score <7 at 5 minutes in pregnant women with breech presentation: Peto OR 0.28 (95% CI 0.04 to 1.70).
Comparison 4. ECV + Amnioinfusion versus ECV only
- Very low quality evidence from 1 RCT (N=109) showed that there is no clinically important difference between ECV plus amnioinfusion and ECV alone on cephalic presentation in labour in pregnant women with breech presentation: RR 1.74 (95% CI 0.74 to 4.12).
- Low quality evidence from 1 RCT (N=109) showed that there is no clinically important difference between ECV plus amnioinfusion and ECV alone on the number of caesarean sections in pregnant women with breech presentation: RR 0.95 (95% CI 0.75 to 1.19).
Comparison 5. ECV + Anaesthesia versus ECV only
- Very low quality evidence from 2 RCTs (N=210) showed that there is no clinically important difference between ECV plus anaesthesia and ECV alone on cephalic presentation in labour in pregnant women with breech presentation: RR 1.16 (95% CI 0.56 to 2.41).
- Very low quality evidence from 5 RCTs (N=435) showed that there is no clinically important difference between ECV plus anaesthesia and ECV alone on cephalic vaginal birth in pregnant women with breech presentation: RR 1.16 (95% CI 0.77 to 1.74).
- Very low quality evidence from 1 RCT (N=108) showed that there is no clinically important difference between ECV plus anaesthesia and ECV alone on breech vaginal birth in pregnant women with breech presentation: RR 0.33 (95% CI 0.04 to 3.10).
- Very low quality evidence from 3 RCTs (N=263) showed that there is no clinically important difference between ECV plus anaesthesia and ECV alone on the number of caesarean sections in pregnant women with breech presentation: RR 0.76 (95% CI 0.42 to 1.38).
- Moderate quality evidence from 1 RCT (N=69) showed that there is a clinically important difference favouring ECV plus anaesthesia over ECV alone on admission to SCBU/NICU in pregnant women with breech presentation: MD −1.80 (95% CI −2.53 to −1.07).
- Low quality evidence from 1 RCT (N=126) showed that there is no clinically important difference between ECV plus anaesthesia and ECV alone on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.03 to 0.03).
Comparison 6. ECV + Anaesthesia versus ECV + Anaesthesia
- Very low quality evidence from 1 RCT (N=120) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 5mg Bupivacaine plus 0.015mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 1.13 (95% CI 0.73 to 1.74).
- Low quality evidence from 1 RCT (N=119) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 7.5mg Bupivacaine plus 0.015mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 0.81 (95% CI 0.53 to 1.23).
- Very low quality evidence from 1 RCT (N=120) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 10mg Bupivacaine plus 0.015mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 0.96 (95% CI 0.61 to 1.50).
- Very low quality evidence from 1 RCT (N=95) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 0.05mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 0.69 (95% CI 0.37 to 1.28).
- Low quality evidence from 1 RCT (N=119) showed that there is no clinically important difference between ECV plus 5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 7.5mg Bupivacaine plus 0.015mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 0.81 (95% CI 0.53 to 1.23).
- Very low quality evidence from 1 RCT (N=120) showed that there is no clinically important difference between ECV plus 5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 10mg Bupivacaine plus 0.015mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 0.96 (95% CI 0.61 to 1.50).
- Very low evidence from 1 RCT (N=119) showed that there is no clinically important difference between ECV plus 7.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 10mg Bupivacaine plus 0.015mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 1.19 (95% CI 0.79 to 1.79).
- Low quality evidence from 1 RCT (N=120) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 5mg Bupivacaine plus 0.015mg Fentanyl on the number of caesarean sections in pregnant women with breech presentation: RR 0.92 (95% CI 0.68 to 1.24).
- Very low evidence from 1 RCT (N=119) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 7.5mg Bupivacaine plus 0.015mg Fentanyl on the number of caesarean sections in pregnant women with breech presentation: RR 1.08 (95% CI 0.78 to 1.50).
- Very low evidence from 1 RCT (N=120) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 10mg Bupivacaine plus 0.015mg Fentanyl on the number of caesarean sections in pregnant women with breech presentation: RR 0.94 (95% CI 0.70 to 1.28).
- Low quality evidence from 1 RCT (N=119) showed that there is no clinically important difference between ECV plus 5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 7.5mg Bupivacaine plus 0.015mg Fentanyl on the number of caesarean sections in pregnant women with breech presentation: RR 1.17 (95% CI 0.86 to 1.61).
- Very low quality evidence from 1 RCT (N=120) showed that there is no clinically important difference between ECV plus 5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 10mg Bupivacaine plus 0.015mg Fentanyl on the number of caesarean sections in pregnant women with breech presentation: RR 1.03 (95% CI 0.77 to 1.37).
- Low quality evidence from 1 RCT (N=119) showed that there is no clinically important difference between ECV plus 7.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 10mg Bupivacaine plus 0.015mg Fentanyl on the number of caesarean sections in pregnant women with breech presentation: RR 0.88 (95% CI 0.64 to 1.20).
Comparison 7. ECV + β2 agonist versus Control (no intervention)
- Moderate quality evidence from 2 RCTs (N=256) showed that there is a clinically important difference favouring ECV plus β2 agonist over control (no intervention) on cephalic presentation in labour in pregnant women with breech presentation: RR 4.83 (95% CI 3.27 to 7.11).
- Very low quality evidence from 3 RCTs (N=265) showed that there no clinically important difference between ECV plus β2 agonist and control (no intervention) on cephalic vaginal birth in pregnant women with breech presentation: RR 2.03 (95% CI 0.22 to 19.01).
- Very low quality evidence from 4 RCTs (N=513) showed that there is a clinically important difference favouring ECV plus β2 agonist over control (no intervention) on breech vaginal birth in pregnant women with breech presentation: RR 0.38 (95% CI 0.20 to 0.69).
- Low quality evidence from 4 RCTs (N=513) showed that there is a clinically important difference favouring ECV plus β2 agonist over control (no intervention) on the number of caesarean sections in pregnant women with breech presentation: RR 0.53 (95% CI 0.41 to 0.67).
- Very low quality evidence from 1 RCT (N=48) showed that there is no clinically important difference between ECV plus β2 agonist and control (no intervention) on admission to SCBU/NICU in pregnant women with breech presentation: RD 0.00 (95% CI −0.08 to 0.08).
- Very low quality evidence from 3 RCTs (N=208) showed that there is no statistically significant difference between ECV plus β2 agonist and control (no intervention) on fetal death after 36 +0 weeks gestation in pregnant women with breech presentation: RD −0.01 (95% CI −0.03 to 0.01) p=0.66.
- Very low quality evidence from 2 RCTs (N=208) showed that there is no clinically important difference between ECV plus β2 agonist and control (no intervention) on Apgar score <7 at 5 minutes in pregnant women with breech presentation: Peto OR 0.80 (95% CI 0.31 to 2.10).
Comparison 8. ECV + β2 agonist versus ECV only
- Very low quality evidence from 2 RCTs (N=172) showed that there is no clinically important difference between ECV plus β2 agonist and ECV only on cephalic vaginal birth in pregnant women with breech presentation: RR 1.32 (95% CI 0.67 to 2.62).
- Very low quality evidence from 1 RCT (N=58) showed that there is no clinically important difference between ECV plus β2 agonist and ECV only on breech vaginal birth in pregnant women with breech presentation: RR 0.75 (95% CI 0.22 to 2.50).
- Very low quality evidence from 2 RCTs (N=172) showed that there is no clinically important difference between ECV plus β2 agonist and ECV only on the number of caesarean sections in pregnant women with breech presentation: RR 0.79 (95% CI 0.27 to 2.28).
- Very low quality evidence from 1 RCT (N=114) showed that there is no clinically important difference between ECV plus β2 agonist and ECV only on admission to SCBU/NICU in pregnant women with breech presentation: RR 1.00 (95% CI 0.21 to 4.75).
Comparison 9. ECV + β2 agonist versus ECV + Placebo
- Very low quality evidence from 2 RCTs (N=146) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus placebo on cephalic presentation in labour in pregnant women with breech presentation: RR 1.54 (95% CI 0.24 to 9.76).
- Very low quality evidence from 2 RCTs (N=125) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus placebo on cephalic vaginal birth in pregnant women with breech presentation: RR 1.27 (95% CI 0.41 to 3.89).
- Very low quality evidence from 2 RCTs (N=227) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus placebo on breech vaginal birth in pregnant women with breech presentation: RR 1.00 (95% CI 0.33 to 2.97).
- Low quality evidence from 4 RCTs (N=532) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus placebo on the number of caesarean sections in pregnant women with breech presentation: RR 0.81 (95% CI 0.72 to 0.92)
- Very low quality evidence from 2 RCTs (N=146) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus placebo on admission to SCBU/NICU in pregnant women with breech presentation: RR 0.78 (95% CI 0.17 to 3.63).
- Very low quality evidence from 1 RCT (N=124) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus placebo on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.03 to 0.03).
Comparison 10. ECV + Ca 2+ channel blocker versus ECV + Placebo
- Moderate quality evidence from 1 RCT (N=310) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus placebo on cephalic presentation in labour in pregnant women with breech presentation: RR 1.13 (95% CI 0.87 to 1.48).
- Moderate quality evidence from 1 RCT (N=310) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus placebo on cephalic vaginal birth in pregnant women with breech presentation: RR 0.90 (95% CI 0.73 to 1.12).
- Moderate quality evidence from 1 RCT (N=310) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus placebo on the number of caesarean sections in pregnant women with breech presentation: RR 1.11 (95% CI 0.88 to 1.40).
- High quality evidence from 1 RCT (N=310) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus placebo on admission to SCBU/NICU in pregnant women with breech presentation: MD −0.20 (95% CI −0.70 to 0.30).
- Moderate quality evidence from 1 RCT (N=310) showed that there is no statistically significant difference between ECV plus Ca 2+ channel blocker and ECV plus placebo on fetal death after 36 +0 weeks gestation in pregnant women with breech presentation: RD 0.00 (95% CI −0.01 to 0.01) p=1.00.
- Low quality evidence from 1 RCT (N=310) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus placebo on Apgar score <7 at 5 minutes in pregnant women with breech presentation: Peto OR 0.52 (95% 0.05 to 5.02).
Comparison 11. ECV + Ca2+ channel blocker versus ECV + β2 agonist
- Low quality evidence from 1 RCT (N=90) showed that there is a clinically important difference favouring ECV plus β2 agonist over ECV plus Ca 2+ channel blocker on cephalic presentation in labour in pregnant women with breech presentation: RR 0.62 (95% CI 0.39 to 0.98).
- Very low quality evidence from 2 RCTs (N=126) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus β2 agonist on cephalic vaginal birth in pregnant women with breech presentation: RR 1.26 (95% CI 0.55 to 2.89).
- Very low quality evidence from 2 RCTs (N=132) showed that there is a clinically important difference favouring ECV plus β2 agonist over ECV plus Ca 2+ channel blocker on the number of caesarean sections in pregnant women with breech presentation: RR 1.42 (95% CI 1.06 to 1.91).
- Very low quality evidence from 2 RCTs (N=176) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus β2 agonist on admission to SCBU/NICU in pregnant women with breech presentation: Peto OR 0.53 (95% CI 0.05 to 5.22).
- Very low quality evidence from 2 RCTs (N=176) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus β2 agonist on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.03 to 0.03).
Comparison 12. ECV + µ-receptor agonist versus ECV only
- High quality evidence from 1 RCT (N=80) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV alone on cephalic vaginal birth in pregnant women with breech presentation: RR 1.00 (95% CI 0.80 to 1.24).
- Low quality evidence from 1 RCT (N=80) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV alone on the number of caesarean sections in pregnant women with breech presentation: RR 1.00 (95% CI 0.42 to 2.40).
- Low quality evidence from 1 RCT (N=126) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV alone on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.03 to 0.03).
Comparison 13. ECV + µ-receptor agonist versus ECV + Placebo
Cephalic vaginal birth after successful ecv.
- High quality evidence from 2 RCTs (N=98) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus placebo on cephalic vaginal birth after successful ECV in pregnant women with breech presentation: RR 1.00 (95% CI 0.86 to 1.17).
Caesarean section after successful ECV
- Low quality evidence from 2 RCTs (N=98) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus placebo on caesarean section after successful ECV in pregnant women with breech presentation: RR 0.97 (95% CI 0.33 to 2.84).
Breech vaginal birth after unsuccessful ECV
- High quality evidence from 3 RCTs (N=186) showed that there is a clinically important difference favouring ECV plus µ-receptor agonist over ECV plus placebo on breech vaginal birth after unsuccessful ECV in pregnant women with breech presentation: RR 0.10 (95% CI 0.02 to 0.53).
Caesarean section after unsuccessful ECV
- Moderate quality evidence from 3 RCTs (N=186) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus placebo on caesarean section after unsuccessful ECV in pregnant women with breech presentation: RR 1.19 (95% CI 1.09 to 1.31).
- Low quality evidence from 1 RCT (N=137) showed that there is no statistically significant difference between ECV plus µ-receptor agonist and ECV plus placebo on fetal death after 36 +0 weeks gestation in pregnant women with breech presentation: RD 0.00 (95% CI −0.03 to 0.03) p=1.00.
Comparison 14. ECV + µ-receptor agonist versus ECV + Anaesthesia
- Moderate quality evidence from 1 RCT (N=92) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus anaesthesia on cephalic vaginal birth in pregnant women with breech presentation: RR 1.04 (95% CI 0.84 to 1.29).
- Very low quality evidence from 2 RCTs (N=212) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus anaesthesia on the number of caesarean sections in pregnant women with breech presentation: RR 0.90 (95% CI 0.61 to 1.34).
- Very low quality evidence from 1 RCT (N=129) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus anaesthesia on admission to SCBU/NICU in pregnant women with breech presentation: RR 2.30 (95% CI 0.21 to 24.74).
- Low quality evidence from 2 RCTs (N=255) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus anaesthesia on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.02 to 0.02).
Comparison 15. ECV + Nitric oxide donor versus ECV + Placebo
- Very low quality evidence from 3 RCTs (N=224) showed that there is no clinically important difference between ECV plus nitric oxide donor and ECV plus placebo on cephalic presentation in labour in pregnant women with breech presentation: RR 1.13 (95% CI 0.59 to 2.16).
- Low quality evidence from 1 RCT (N=99) showed that there is no clinically important difference between ECV plus nitric oxide donor and ECV plus placebo on cephalic vaginal birth in pregnant women with breech presentation: RR 0.78 (95% CI 0.49 to 1.22).
- Low quality evidence from 2 RCTs (N=125) showed that there is no clinically important difference between ECV plus nitric oxide donor and ECV plus placebo on the number of caesarean sections in pregnant women with breech presentation: RR 0.83 (95% CI 0.68 to 1.01).
Comparison 16. ECV + Nitric oxide donor versus ECV + β2 agonist
- Low quality evidence from 1 RCT (N=74) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus nitric oxide donor on cephalic presentation in labour in pregnant women with breech presentation: RR 0.56 (95% CI 0.29 to 1.09).
- Very low quality evidence from 2 RCTs (N=97) showed that there is no clinically important difference between ECV plus nitric oxide donor and ECV plus β2 agonist on cephalic vaginal birth in pregnant women with breech presentation: RR 0.98 (95% CI 0.47 to 2.05).
- Very low quality evidence from 1 RCT (N=59) showed that there is no clinically important difference between ECV plus nitric oxide donor and ECV plus β2 agonist on the number of caesarean sections in pregnant women with breech presentation: RR 1.07 (95% CI 0.73 to 1.57).
Comparison 17. ECV + Talcum powder versus ECV + Gel
- Low quality evidence from 1 RCT (N=95) showed that there is no clinically important difference between ECV plus talcum powder and ECV plus gel on cephalic presentation in labour in pregnant women with breech presentation: RR 1.02 (95% CI 0.68 to 1.53).
- Low quality evidence from 1 RCT (N=95) showed that there is no clinically important difference between ECV plus talcum powder and ECV plus gel on cephalic vaginal birth in pregnant women with breech presentation: RR 1.08 (95% CI 0.67 to 1.74).
- Low quality evidence from 1 RCT (N=95) showed that there is no clinically important difference between ECV plus talcum powder and ECV plus gel on the number of caesarean sections in pregnant women with breech presentation: RR 0.94 (95% CI 0.67 to 1.33).
- Low quality evidence from 1 RCT (N=95) showed that there is no clinically important difference between ECV plus talcum powder and ECV plus gel on admission to SCBU/NICU in pregnant women with breech presentation: RR 1.96 (95% CI 0.38 to 10.19).
Comparison 18. Postural management versus No postural management
- Low quality evidence from 1 RCT (N=76) showed that there is no clinically important difference between postural management and no postural management on cephalic presentation in labour in pregnant women with breech presentation: RR 1.26 (95% CI 0.70 to 2.30).
- Low quality evidence from 1 RCT (N=76) showed that there is no clinically important difference between postural management and no postural management on cephalic vaginal birth in pregnant women with breech presentation: RR 1.11 (95% CI 0.59 to 2.07).
Breech vaginal delivery
- Low quality evidence from 1 RCT (N=76) showed that there is no clinically important difference between postural management and no postural management on breech vaginal delivery in pregnant women with breech presentation: RR 1.15 (95% CI 0.67 to 1.99).
- Low quality evidence from 1 RCT (N=76) showed that there is no clinically important difference between postural management and no postural management on the number of caesarean sections in pregnant women with breech presentation: RR 0.69 (95% CI 0.31 to 1.52).
- Low quality evidence from 1 RCT (N=76) showed that there is no clinically important difference between postural management and no postural management on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RR 0.24 (95% CI 0.03 to 2.03).
Comparison 19. Postural management + ECV versus ECV only
- Moderate quality evidence from 1 RCT (N=100) showed that there is no clinically important difference between postural management plus ECV and ECV only on the number of caesarean sections in pregnant women with breech presentation: RR 1.05 (95% CI 0.80 to 1.38).
- Low quality evidence from 1 RCT (N=100) showed that there is no clinically important difference between postural management plus ECV and ECV only on Apgar score <7 at 5 minutes in pregnant women with breech presentation: Peto OR 0.13 (95% CI 0.00 to 6.55).
Economic evidence statements
No economic evidence was identified which was applicable to this review question.
The committee’s discussion of the evidence
Interpreting the evidence, the outcomes that matter most.
Provision of antenatal care is important for the health and wellbeing of both mother and baby with the aim of avoiding adverse pregnancy outcomes and enhancing maternal satisfaction and wellbeing. Breech presentation in labour may be associated with adverse outcomes for the fetus, which has contributed to an increased likelihood of caesarean birth. The committee therefore agreed that cephalic presentation in labour and method of birth were critical outcomes for the woman, and admission to SCBU/NICU, fetal death after 36 +0 weeks gestation, and infant death up to 4 weeks chronological age were critical outcomes for the baby. Apgar score <7 at 5 minutes and birth before 39 +0 weeks of gestation were important outcomes for the baby.
The quality of the evidence
The quality of the evidence for interventions for managing a longitudinal lie fetal malpresentation (that is breech presentation) in late pregnancy ranged from very low to high, with most of the evidence being of a very low or low quality.
This was predominately due to serious overall risk of bias in some outcomes; imprecision around the effect estimate in some outcomes; indirect population in some outcomes; and the presence of serious heterogeneity in some outcomes, which was unresolved by subgroup analysis. The majority of included studies had a small sample size, which contributed to imprecision around the effect estimate.
No evidence was identified to inform the outcomes of infant death up to 4 weeks chronological age and birth before 39 +0 weeks of gestation.
There was no publication bias identified in the evidence. However, the committee noted the influence pharmacological developers may have in these trials as funders, and took this into account in their decision making.
Benefits and harms
The committee discussed that in the case of breech presentation, a discussion with the woman about the different options and their potential benefits, harms and implications is needed to ensure an informed decision. The committee discussed that some women may prefer a breech vaginal birth or choose an elective caesarean birth, and that her preferences should be supported, in line with shared decision making.
The committee discussed that external cephalic version is standard practice for managing breech presentation in uncomplicated singleton pregnancies at or after 36+0 weeks. The committee discussed that there could be variation in the success rates of ECV based on the experience of the healthcare professional providing the ECV. There was some evidence supporting the use of ECV for managing a breech presentation in late pregnancy. The evidence showed ECV had a clinically important benefit in terms of cephalic presentations in labour and cephalic vaginal deliveries, when compared to no intervention. The committee noted that the evidence suggested that ECV was not harmful to the baby, although the effect estimate was imprecise relating to the relative rarity of the fetal death as an outcome.
Cephalic (head-down) vaginal birth is preferred by many women and the evidence suggests that external cephalic version is an effective way to achieve this. The evidence suggested ECV increased the chance for a cephalic vaginal birth and the committee agreed that it was important to explain this to the woman during her consultation.
The committee discussed the optimum timing for ECV. Timing of ECV must take into account the likelihood of the baby turning naturally before a woman commences labour and the possibility of the baby turning back to a breech presentation after ECV if it is done too early. The committee noted that in their experience, current practice was to perform ECV at 37 gestational weeks. The majority of the evidence demonstrating a benefit of ECV in this review involved ECV performed around 37 gestational weeks, although the review did not look for studies directly comparing different timings of ECV and their relative success rates.
The evidence in this review excluded women with previous complicated pregnancies, such as those with previous caesarean section or uterine surgery. The committee discussed that a previous caesarean section indicates a complicated pregnancy and that this population of women are not the focus of this guideline, which concentrates on women with uncomplicated pregnancies.
The committee’s recommendations align with other NICE guidance and cross references to the NICE guideline on caesarean birth and the section on breech presenting in labour in the NICE guideline on intrapartum care for women with existing medical conditions or obstetric complications and their babies were made.
ECV combined with pharmacological agents
There were some small studies comparing a variety of pharmacological agents (including β2 agonists, Ca 2+ channel blockers, µ-receptor agonists and nitric oxide donors) given alongside ECV. Overall the evidence typically showed no clinically important benefit of adding any pharmacological agent to ECV except in comparisons with a control arm with no ECV where it was not possible to isolate the effect of the ECV versus the pharmacological agent. The evidence tended toward benefit most for β2 agonists and µ-receptor agonists however there was no consistent or high quality evidence of benefit even for these agents. The committee agreed that although these pharmacological agents are used in practice, there was insufficient evidence to make a recommendation supporting or refuting their use or on which pharmacological agent should be used.
The committee discussed that the evidence suggesting µ-receptor agonist, remifentanil, had a clinically important benefit in terms reducing breech vaginal births after unsuccessful ECV was biologically implausible. The committee noted that this pharmacological agent has strong sedative effects, depending on the dosage, and therefore studies comparing it to a placebo had possible design flaws as it would be obvious to all parties whether placebo or active drug had been received. The committee discussed that the risks associated with using remifentanil such as respiratory depression, likely outweigh any potential added benefit it may have on managing breech presentation.
There was some evidence comparing different anaesthetics together with ECV. Although there was little consistent evidence of benefit overall, one small study of low quality showed a combination of 2% lidocaine and epinephrine via epidural catheter (anaesthesia) with ECV showed a clinically important benefit in terms of cephalic presentations in labour and the method of birth. The committee discussed the evidence and agreed the use of anaesthesia via epidural catheter during ECV was uncommon practice in the UK and could be expensive, overall they agreed the strength of the evidence available was insufficient to support a change in practice.
Postural management
There was limited evidence on postural management as an intervention for managing breech presentation in late pregnancy, which showed no difference in effectiveness. Postural management was defined as ‘knee-chest position for 15 minutes, 3 times a day’. The committee agreed that in their experience women valued trying interventions at home first which might make postural management an attractive option for some women, however, there was no evidence that postural management was beneficial. The committee also noted that in their experience postural management can cause notable discomfort so it is not an intervention without disadvantages.
Cost effectiveness and resource use
A systematic review of the economic literature was conducted but no relevant studies were identified which were applicable to this review question.
The committee’s recommendations to offer external cephalic version reinforces current practice. The committee noted that, compared to no intervention, external cephalic version results in clinically important benefits and that there would also be overall downstream cost savings from lower adverse events. It was therefore the committee’s view that offering external cephalic version is cost effective and would not entail any resource impact.
Andersen 2013
Brocks 1984
Bujold 2003
Burgos 2016
Chalifoux 2017
Chenia 1987
Collaris 2009
Dafallah 2004
Diguisto 2018
Dugoff 1999
El-Sayed 2004
Fernandez 1997
Hindawi 2005
Hilton 2009
Hofmeyr 1983
Mahomed 1991
Mancuso 2000
Marquette 1996
Mohamed Ismail 2008
NorAzlin 2005
Robertson 1987
Schorr 1997
Sullivan 2009
VanDorsten 1981
Vallikkannu 2014
Weiniger 2010
Appendix A. Review protocols
Review protocol for review question: What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy? (PDF, 260K)
Appendix B. Literature search strategies
Literature search strategies for review question: What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy? (PDF, 281K)
Appendix C. Clinical evidence study selection
Clinical study selection for: What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy? (PDF, 113K)
Appendix D. Clinical evidence tables
Clinical evidence tables for review question: What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy? (PDF, 1.2M)
Appendix E. Forest plots
Forest plots for review question: What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy? (PDF, 678K)
Appendix F. GRADE tables
GRADE tables for review question: What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy? (PDF, 1.0M)
Appendix G. Economic evidence study selection
Economic evidence study selection for review question: what is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy, appendix h. economic evidence tables, economic evidence tables for review question: what is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy, appendix i. economic evidence profiles, economic evidence profiles for review question: what is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy, appendix j. economic analysis, economic evidence analysis for review question: what is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy.
No economic analysis was conducted for this review question.
Appendix K. Excluded studies
Excluded clinical and economic studies for review question: what is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy, clinical studies, table 24 excluded studies.
View in own window
Economic studies
No economic evidence was identified for this review.
Appendix L. Research recommendations
Research recommendations for review question: what is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy.
No research recommendations were made for this review question.
Evidence reviews underpinning recommendation 1.2.38
These evidence reviews were developed by the National Guideline Alliance, which is a part of the Royal College of Obstetricians and Gynaecologists
Disclaimer : The recommendations in this guideline represent the view of NICE, arrived at after careful consideration of the evidence available. When exercising their judgement, professionals are expected to take this guideline fully into account, alongside the individual needs, preferences and values of their patients or service users. The recommendations in this guideline are not mandatory and the guideline does not override the responsibility of healthcare professionals to make decisions appropriate to the circumstances of the individual patient, in consultation with the patient and/or their carer or guardian.
Local commissioners and/or providers have a responsibility to enable the guideline to be applied when individual health professionals and their patients or service users wish to use it. They should do so in the context of local and national priorities for funding and developing services, and in light of their duties to have due regard to the need to eliminate unlawful discrimination, to advance equality of opportunity and to reduce health inequalities. Nothing in this guideline should be interpreted in a way that would be inconsistent with compliance with those duties.
NICE guidelines cover health and care in England. Decisions on how they apply in other UK countries are made by ministers in the Welsh Government , Scottish Government , and Northern Ireland Executive . All NICE guidance is subject to regular review and may be updated or withdrawn.
- Cite this Page National Guideline Alliance (UK). Management of breech presentation: Antenatal care: Evidence review M. London: National Institute for Health and Care Excellence (NICE); 2021 Aug. (NICE Guideline, No. 201.)
- PDF version of this title (2.2M)
In this Page
Other titles in this collection.
- NICE Evidence Reviews Collection
Related NICE guidance and evidence
- NICE Guideline 201: Antenatal care
Supplemental NICE documents
- Supplement 1: Methods (PDF)
- Supplement 2: Health economics (PDF)
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Review Identification of breech presentation: Antenatal care: Evidence review L [ 2021] Review Identification of breech presentation: Antenatal care: Evidence review L National Guideline Alliance (UK). 2021 Aug
- Vaginal delivery of breech presentation. [J Obstet Gynaecol Can. 2009] Vaginal delivery of breech presentation. Kotaska A, Menticoglou S, Gagnon R, MATERNAL FETAL MEDICINE COMMITTEE. J Obstet Gynaecol Can. 2009 Jun; 31(6):557-566.
- Review Cephalic version by moxibustion for breech presentation. [Cochrane Database Syst Rev. 2005] Review Cephalic version by moxibustion for breech presentation. Coyle ME, Smith CA, Peat B. Cochrane Database Syst Rev. 2005 Apr 18; (2):CD003928. Epub 2005 Apr 18.
- [Fetal expulsion: Which interventions for perineal prevention? CNGOF Perineal Prevention and Protection in Obstetrics Guidelines]. [Gynecol Obstet Fertil Senol. 2...] [Fetal expulsion: Which interventions for perineal prevention? CNGOF Perineal Prevention and Protection in Obstetrics Guidelines]. Riethmuller D, Ramanah R, Mottet N. Gynecol Obstet Fertil Senol. 2018 Dec; 46(12):937-947. Epub 2018 Oct 28.
- Foetal weight, presentaion and the progress of labour. II. Breech and occipito-posterior presentation related to the baby's weight and the length of the first stage of labour. [J Obstet Gynaecol Br Emp. 1961] Foetal weight, presentaion and the progress of labour. II. Breech and occipito-posterior presentation related to the baby's weight and the length of the first stage of labour. BAINBRIDGE MN, NIXON WC, SMYTH CN. J Obstet Gynaecol Br Emp. 1961 Oct; 68:748-54.
Recent Activity
- Management of breech presentation Management of breech presentation
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Face Presentation
- First Online: 02 August 2023
Cite this chapter

- Shubhra Agarwal 2 &
- Suchitra Pandit 3
475 Accesses
Face presentation is defined as a cephalic presentation in which the presenting part is face and it occurs due to factors that lead to extension of of fetal head. It is a rare obstetric presentation and may not be encountered even in the entire carrier of an obstetrician.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Durable hardcover edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Shaffer BL. Face presentation: predictors and delivery route. Am J Obstet Gynecol. 2006;194:e10–2.
Article PubMed Google Scholar
Schwartz Z, Dgani R, Lancet M, Kessler I. Face presentation. Aust N Z J Obstet Gynaecol. 1986;26:172–6.
Article CAS PubMed Google Scholar
Westgren M, et al. Face presentation in modern obstetrics-a study with special reference to fetal long term morbidity. Z Geburtshilfe Perinatol. 1984;188(2):87–9.
CAS PubMed Google Scholar
Download references
Author information
Authors and affiliations.
Department of Obstetrics and Gynaecology, TMMC&RC, Moradabad, India
Shubhra Agarwal
Department of Obstetrics and Gynaecology, Surya Hospital, Mumbai, India
Suchitra Pandit
You can also search for this author in PubMed Google Scholar
Editor information
Editors and affiliations.
Department of Obstetrics and Gynecology, Sarojini Naidu Medical College, Agra, Uttar Pradesh, India
Ruchika Garg
Rights and permissions
Reprints and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Agarwal, S., Pandit, S. (2023). Face Presentation. In: Garg, R. (eds) Labour and Delivery. Springer, Singapore. https://doi.org/10.1007/978-981-19-6145-8_6
Download citation
DOI : https://doi.org/10.1007/978-981-19-6145-8_6
Published : 02 August 2023
Publisher Name : Springer, Singapore
Print ISBN : 978-981-19-6144-1
Online ISBN : 978-981-19-6145-8
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research

IMAGES
VIDEO
COMMENTS
Frank breech. When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head.
In breech presentation, the presenting part is a poor dilating wedge, which can cause the head to be trapped during delivery, often compressing the umbilical cord. For breech presentation, usually do cesarean delivery at 39 weeks or during labor, but external cephalic version is sometimes successful before labor, usually at 37 or 38 weeks.
Head first (called vertex or cephalic presentation) Facing backward (occiput anterior position) Spine parallel to mother's spine (longitudinal lie) Neck bent forward with chin tucked. Arms folded across the chest . If the fetus is in a different position, lie, or presentation, labor may be more difficult, and a normal vaginal delivery may not ...
The term presentation describes the leading part of the fetus or the anatomical structure closest to the maternal pelvic inlet during labor. The presentation can roughly be divided into the following classifications: cephalic, breech, shoulder, and compound. Cephalic presentation is the most common and can be further subclassified as vertex, sinciput, brow, face, and chin.
Head Down, Facing Down (Cephalic Presentation) This is the most common position for babies in-utero. In the cephalic presentation, the baby is head down, chin tucked to chest, facing their mother's back. This position typically allows for the smoothest delivery, as baby's head can easily move down the birth canal and under the pubic bone ...
Occiput or cephalic anterior: This is the best fetal position for childbirth. It means the fetus is head down, facing the birth parent's spine (facing backward). Its chin is tucked towards its chest. The fetus will also be slightly off-center, with the back of its head facing the right or left. This is called left occiput anterior or right ...
Cephalic presentation occurs in about 97% of deliveries. There are different types of cephalic presentation, which depend on the position of the baby's limbs and head (fetal attitude). If your baby is in any position other than head down, your doctor may recommend a cesarean delivery. Breech presentation is when the baby's bottom is down ...
External cephalic version, or "ECV," is a procedure to try to turn a baby around while they are still in the uterus. Before birth, babies lie in the uterus in different positions. They can lie with their head, shoulders, legs, or buttocks closest to the vagina. Doctors call it "breech" when a baby's feet or buttocks are closest to the vagina ...
A cephalic presentation or head presentation or head-first presentation is a situation at childbirth where the fetus is in a longitudinal lie and the head enters the pelvis first; the most common form of cephalic presentation is the vertex presentation, where the occiput is the leading part (the part that first enters the birth canal). All other presentations are abnormal (malpresentations ...
A cephalic presentation or head presentation or head-first presentation is a situation at childbirth where the fetus is in a longitudinal lie and the head enters the pelvis first; the most common form of cephalic presentation is the vertex presentation where the occiput is the leading part (the part that first enters the birth canal). All other presentations are abnormal (malpresentations ...
Fetal presentation, or how your baby is situated in your womb at birth, is determined by the body part that's positioned to come out first, and it can affect the way you deliver. ... This is called an external cephalic version, and it has a 58 percent success rate for turning breech babies. For more information, ...
Vertex Presentation. A vertex presentation is the ideal position for a fetus to be in for a vaginal delivery. It means the fetus is head down, headfirst and facing your spine with its chin tucked to its chest. Vertex presentation describes a fetus being head-first or head down in the birth canal.
The long axis of the fetus is parallel to the long axis of the mother. The head is at or in the pelvis. The back is on the left and anterior and is palpated easily except in obese women. The small parts are on the right and are not felt clearly. The breech is in the fundus of the uterus. The cephalic prominence (in this case the forehead) is on ...
Detailed Method to Determine Fetal Situs. 1. Define within the uterus the presentation of the fetus (generally vertex or breech; less often the presentation is oblique or transverse.). 2. Determine whether the fetal spine is parallel or transverse to the maternal spine. In sagittal view, if the fetal and maternal spine are parallel, the fetus ...
The global cesarean section rate has increased from approximately 23% to 34% in the past decade. Fetal malpresentation is now the third-most common indication for cesarean delivery, encompassing nearly 17% of cases. Almost one-fourth of all fetuses are in a breech presentation at 28 weeks gestational age; this number decreases to between 3% and 4% at term. In current clinical practice, most ...
How To Do External Cephalic Version. Procedure by Kate Leonard, MD, and Will Stone, MD, Walter Reed National Military Medical Center Residency in Obstetrics and Gynecology; and Shad Deering, COL, MD, Chair, Department of Obstetrics and Gynecology, Uniformed Services University. Assisted by Elizabeth N. Weissbrod, MA, CMI, Eric Wilson, 2LT, and ...
Figure 6.2: Determining fetal situs in longitudinal lie: In A, the fetus is in a cephalic presentation with the fetal spine close to the left uterine wall, resulting in the right side being anterior and left side posterior. ... Figure 6.5: Determining fetal situs: A diagram of the fetus is presented in back posterior (1 and 3) ...
Cephalic presentation occurs in about 97% of deliveries. There are different types of cephalic presentation, which depend on the position of the baby's limbs and head (fetal attitude). If your baby is in any position other than head down, your doctor may recommend a cesarean delivery. Breech presentation is when the baby's bottom is down ...
ment, but reference values and norms are lacking for infants, especially in the first year after birth. Discussion Key publications were reviewed by the authors to provide a narrative review of the 1) origin of the cephalic index (CI), 2) adaptations of the measure over time, 3) anatomical landmarks and alignments used, 4) clinical tools, 5) necessary considerations for different ethnic, sex ...
Introduction. Breech presentation of the fetus in late pregnancy may result in prolonged or obstructed labour with resulting risks to both woman and fetus. Interventions to correct breech presentation (to cephalic) before labour and birth are important for the woman's and the baby's health. The aim of this review is to determine the most ...
A type of cephalic presentation in which the presenting part is the face, the area between chin and glabella. The incidence varies from 1 in 500 to 1 in 1000 deliveries. Primary face presentation is rare. Secondary face presentation caused by extension of head during labor is common. Thus, the diagnosis is usually made during active phase of ...
Following the term breech trial (TBT), the incidence of Caesarean section secondary to breech presentations increased, from 76.9 % to 89.7 %. External Cephalic Version (ECV) is a safe effective method to reduce non-cephalic presentation at time of delivery.