Ethical care for research animals

WHY ANIMAL RESEARCH?
The use of animals in some forms of biomedical research remains essential to the discovery of the causes, diagnoses, and treatment of disease and suffering in humans and in animals., stanford shares the public's concern for laboratory research animals..
Many people have questions about animal testing ethics and the animal testing debate. We take our responsibility for the ethical treatment of animals in medical research very seriously. At Stanford, we emphasize that the humane care of laboratory animals is essential, both ethically and scientifically. Poor animal care is not good science. If animals are not well-treated, the science and knowledge they produce is not trustworthy and cannot be replicated, an important hallmark of the scientific method .
There are several reasons why the use of animals is critical for biomedical research:
• Animals are biologically very similar to humans. In fact, mice share more than 98% DNA with us!
• Animals are susceptible to many of the same health problems as humans – cancer, diabetes, heart disease, etc.
• With a shorter life cycle than humans, animal models can be studied throughout their whole life span and across several generations, a critical element in understanding how a disease processes and how it interacts with a whole, living biological system.
The ethics of animal experimentation
Nothing so far has been discovered that can be a substitute for the complex functions of a living, breathing, whole-organ system with pulmonary and circulatory structures like those in humans. Until such a discovery, animals must continue to play a critical role in helping researchers test potential new drugs and medical treatments for effectiveness and safety, and in identifying any undesired or dangerous side effects, such as infertility, birth defects, liver damage, toxicity, or cancer-causing potential.
U.S. federal laws require that non-human animal research occur to show the safety and efficacy of new treatments before any human research will be allowed to be conducted. Not only do we humans benefit from this research and testing, but hundreds of drugs and treatments developed for human use are now routinely used in veterinary clinics as well, helping animals live longer, healthier lives.
It is important to stress that 95% of all animals necessary for biomedical research in the United States are rodents – rats and mice especially bred for laboratory use – and that animals are only one part of the larger process of biomedical research.
Our researchers are strong supporters of animal welfare and view their work with animals in biomedical research as a privilege.
Stanford researchers are obligated to ensure the well-being of all animals in their care..
Stanford researchers are obligated to ensure the well-being of animals in their care, in strict adherence to the highest standards, and in accordance with federal and state laws, regulatory guidelines, and humane principles. They are also obligated to continuously update their animal-care practices based on the newest information and findings in the fields of laboratory animal care and husbandry.
Researchers requesting use of animal models at Stanford must have their research proposals reviewed by a federally mandated committee that includes two independent community members. It is only with this committee’s approval that research can begin. We at Stanford are dedicated to refining, reducing, and replacing animals in research whenever possible, and to using alternative methods (cell and tissue cultures, computer simulations, etc.) instead of or before animal studies are ever conducted.

Organizations and Resources
There are many outreach and advocacy organizations in the field of biomedical research.
- Learn more about outreach and advocacy organizations

Stanford Discoveries
What are the benefits of using animals in research? Stanford researchers have made many important human and animal life-saving discoveries through their work.
- Learn more about research discoveries at Stanford

Research using animals: an overview
Around half the diseases in the world have no treatment. Understanding how the body works and how diseases progress, and finding cures, vaccines or treatments, can take many years of painstaking work using a wide range of research techniques. There is overwhelming scientific consensus worldwide that some research using animals is still essential for medical progress.
Animal research in the UK is strictly regulated. For more details on the regulations governing research using animals, go to the UK regulations page .

Why is animal research necessary?
There is overwhelming scientific consensus worldwide that some animals are still needed in order to make medical progress.
Where animals are used in research projects, they are used as part of a range of scientific techniques. These might include human trials, computer modelling, cell culture, statistical techniques, and others. Animals are only used for parts of research where no other techniques can deliver the answer.
A living body is an extraordinarily complex system. You cannot reproduce a beating heart in a test tube or a stroke on a computer. While we know a lot about how a living body works, there is an enormous amount we simply don’t know: the interaction between all the different parts of a living system, from molecules to cells to systems like respiration and circulation, is incredibly complex. Even if we knew how every element worked and interacted with every other element, which we are a long way from understanding, a computer hasn’t been invented that has the power to reproduce all of those complex interactions - while clearly you cannot reproduce them all in a test tube.
While humans are used extensively in Oxford research, there are some things which it is ethically unacceptable to use humans for. There are also variables which you can control in a mouse (like diet, housing, clean air, humidity, temperature, and genetic makeup) that you could not control in human subjects.
Is it morally right to use animals for research?
Most people believe that in order to achieve medical progress that will save and improve lives, perhaps millions of lives, limited and very strictly regulated animal use is justified. That belief is reflected in the law, which allows for animal research only under specific circumstances, and which sets out strict regulations on the use and care of animals. It is right that this continues to be something society discusses and debates, but there has to be an understanding that without animals we can only make very limited progress against diseases like cancer, heart attack, stroke, diabetes, and HIV.
It’s worth noting that animal research benefits animals too: more than half the drugs used by vets were developed originally for human medicine.
Aren’t animals too different from humans to tell us anything useful?
No. Just by being very complex living, moving organisms they share a huge amount of similarities with humans. Humans and other animals have much more in common than they have differences. Mice share over 90% of their genes with humans. A mouse has the same organs as a human, in the same places, doing the same things. Most of their basic chemistry, cell structure and bodily organisation are the same as ours. Fish and tadpoles share enough characteristics with humans to make them very useful in research. Even flies and worms are used in research extensively and have led to research breakthroughs (though these species are not regulated by the Home Office and are not in the Biomedical Sciences Building).
What does research using animals actually involve?
The sorts of procedures research animals undergo vary, depending on the research. Breeding a genetically modified mouse counts as a procedure and this represents a large proportion of all procedures carried out. So does having an MRI (magnetic resonance imaging) scan, something which is painless and which humans undergo for health checks. In some circumstances, being trained to go through a maze or being trained at a computer game also counts as a procedure. Taking blood or receiving medication are minor procedures that many species of animal can be trained to do voluntarily for a food reward. Surgery accounts for only a small minority of procedures. All of these are examples of procedures that go on in Oxford's Biomedical Sciences Building.

How many animals are used?
Figures for 2023 show numbers of animals that completed procedures, as declared to the Home Office using their five categories for the severity of the procedure.
# NHPs - Non Human Primates
Oxford also maintains breeding colonies to provide animals for use in experiments, reducing the need for unnecessary transportation of animals.
Figures for 2017 show numbers of animals bred for procedures that were killed or died without being used in procedures:
Why must primates be used?
Primates account for under half of one per cent (0.5%) of all animals housed in the Biomedical Sciences Building. They are only used where no other species can deliver the research answer, and we continually seek ways to replace primates with lower orders of animal, to reduce numbers used, and to refine their housing conditions and research procedures to maximise welfare.
However, there are elements of research that can only be carried out using primates because their brains are closer to human brains than mice or rats. They are used at Oxford in vital research into brain diseases like Alzheimer’s and Parkinson’s. Some are used in studies to develop vaccines for HIV and other major infections.

What is done to primates?
The primates at Oxford spend most of their time in their housing. They are housed in groups with access to play areas where they can groom, forage for food, climb and swing.
Primates at Oxford involved in neuroscience studies would typically spend a couple of hours a day doing behavioural work. This is sitting in front of a computer screen doing learning and memory games for food rewards. No suffering is involved and indeed many of the primates appear to find the games stimulating. They come into the transport cage that takes them to the computer room entirely voluntarily.
After some time (a period of months) demonstrating normal learning and memory through the games, a primate would have surgery to remove a very small amount of brain tissue under anaesthetic. A full course of painkillers is given under veterinary guidance in the same way as any human surgical procedure, and the animals are up and about again within hours, and back with their group within a day. The brain damage is minor and unnoticeable in normal behaviour: the animal interacts normally with its group and exhibits the usual natural behaviours. In order to find out about how a disease affects the brain it is not necessary to induce the equivalent of full-blown disease. Indeed, the more specific and minor the brain area affected, the more focussed and valuable the research findings are.
The primate goes back to behavioural testing with the computers and differences in performance, which become apparent through these carefully designed games, are monitored.
At the end of its life the animal is humanely killed and its brain is studied and compared directly with the brains of deceased human patients.
Primates at Oxford involved in vaccine studies would simply have a vaccination and then have monthly blood samples taken.

How many primates does Oxford hold?
* From 2014 the Home Office changed the way in which animals/ procedures were counted. Figures up to and including 2013 were recorded when procedures began. Figures from 2014 are recorded when procedures end.
What’s the difference between ‘total held’ and ‘on procedure’?
Primates (macaques) at Oxford would typically spend a couple of hours a day doing behavioural work, sitting in front of a computer screen doing learning and memory games for food rewards. This is non-invasive and done voluntarily for food rewards and does not count as a procedure. After some time (a period of months) demonstrating normal learning and memory through the games, a primate would have surgery under anaesthetic to remove a very small amount of brain tissue. The primate quickly returns to behavioural testing with the computers, and differences in performance, which become apparent through these carefully designed puzzles, are monitored. A primate which has had this surgery is counted as ‘on procedure’. Both stages are essential for research into understanding brain function which is necessary to develop treatments for conditions including Alzheimer’s, Parkinson’s and schizophrenia.
Why has the overall number held gone down?
Numbers vary year on year depending on the research that is currently undertaken. In general, the University is committed to reducing, replacing and refining animal research.
You say primates account for under 0.5% of animals, so that means you have at least 16,000 animals in the Biomedical Sciences Building in total - is that right?
Numbers change daily so we cannot give a fixed figure, but it is in that order.
Aren’t there alternative research methods?
There are very many non-animal research methods, all of which are used at the University of Oxford and many of which were pioneered here. These include research using humans; computer models and simulations; cell cultures and other in vitro work; statistical modelling; and large-scale epidemiology. Every research project which uses animals will also use other research methods in addition. Wherever possible non-animal research methods are used. For many projects, of course, this will mean no animals are needed at all. For others, there will be an element of the research which is essential for medical progress and for which there is no alternative means of getting the relevant information.
How have humans benefited from research using animals?
As the Department of Health states, research on animals has contributed to almost every medical advance of the last century.
Without animal research, medicine as we know it today wouldn't exist. It has enabled us to find treatments for cancer, antibiotics for infections (which were developed in Oxford laboratories), vaccines to prevent some of the most deadly and debilitating viruses, and surgery for injuries, illnesses and deformities.
Life expectancy in this country has increased, on average, by almost three months for every year of the past century. Within the living memory of many people diseases such as polio, tuberculosis, leukaemia and diphtheria killed or crippled thousands every year. But now, doctors are able to prevent or treat many more diseases or carry out life-saving operations - all thanks to research which at some stage involved animals.
Each year, millions of people in the UK benefit from treatments that have been developed and tested on animals. Animals have been used for the development of blood transfusions, insulin for diabetes, anaesthetics, anticoagulants, antibiotics, heart and lung machines for open heart surgery, hip replacement surgery, transplantation, high blood pressure medication, replacement heart valves, chemotherapy for leukaemia and life support systems for premature babies. More than 50 million prescriptions are written annually for antibiotics.
We may have used animals in the past to develop medical treatments, but are they really needed in the 21st century?
Yes. While we are committed to reducing, replacing and refining animal research as new techniques make it possible to reduce the number of animals needed, there is overwhelming scientific consensus worldwide that some research using animals is still essential for medical progress. It only forms one element of a whole research programme which will use a range of other techniques to find out whatever possible without animals. Animals would be used for a specific element of the research that cannot be conducted in any alternative way.
How will humans benefit in future?
The development of drugs and medical technologies that help to reduce suffering among humans and animals depends on the carefully regulated use of animals for research. In the 21st century scientists are continuing to work on treatments for cancer, stroke, heart disease, HIV, malaria, tuberculosis, diabetes, neurodegenerative diseases like Alzheimer's and Parkinson’s, and very many more diseases that cause suffering and death. Genetically modified mice play a crucial role in future medical progress as understanding of how genes are involved in illness is constantly increasing.
Email Subscription
Have Any Questions?
Copyright © 2016 - 2022 Foundation for Biomedical Research
ADDRESS THE NHP CRISIS TODAY!
Immediate action needed.
DRUG DEVELOPMENT PIPELINE AT RISK
Advocating SOUND PUBLIC POLICY
in support of ethical and essential animal research.
PROTECTING VITAL ROLE ANIMALS PLAY
in biomedical research
FACILITATING DIALOGUE BETWEEN
our members and their congressional delegations on animal research issues
PRESERVING BIOMEDICAL RESEARCHERS'
abilities to use animals in ethical and responsible research
SUPPORTING HUMANE CARE & TREATMENT OF LABORATORY ANIMALS
in biomedical research, training, and education
PROVIDING OUR MEMBERS
with information and consultation on state and local issues
CREATING A FORUM FOR THE BIOMEDICAL COMMUNITY
to develop common positions on legislative and regulatory issues
PROTECTING THE ABILITY TO STUDY WHOLE LIVING ORGANISMS
in support of biomedical research
Founded in 1979, the National Association for Biomedical Research (NABR) is a 501(c)(6) non-profit association dedicated to sound public policy for the humane use of animals in biomedical research, education, and testing. NABR provides a unified voice for the scientific community on legislative, regulatory and legal matters affecting the responsible, humane, and ethical use of laboratory animals. Members include more than 340 universities, medical and veterinary schools, teaching hospitals, pharmaceutical and biotechnology companies, patient groups, and academic and professional societies who rely on humane and responsible animal research to advance global human and animal health. For more than 40 years, and as the only national, non-profit organization solely dedicated to advocating sound public policy for ethical and essential animal research, NABR has worked to safeguard the future of biomedical research.
NABR Files Formal Petition Challenging the Listing of Long-Tailed Macaque by the IUCN
Working with recognized, independent scientists, the National Association for Biomedical Research (NABR) filed an initial petition on June 15, 2023 with the International Union for Conservation of Nature (IUCN) challenging the recent designation of the long-tailed macaque ( Macaca fascicularis ) as endangered under IUCN listing criteria. This designation is a result of improperly used data that do not support the endangered species listing. NABR called for an immediate review. Read more by clicking here .
After several weeks of discussions between NABR and the IUCN, on September 11, 2023, NABR filed a formal petition with the IUCN challenging its decision to uplist the status of the long-tailed macaque from “vulnerable” to “endangered.” Read NABR’s formal IUCN petition and the addendum here. Read NABR’s press release here .
In October 2023, the IUCN formally accepted NABR’s petition. Read the press release here .
On February 1, 2024, NABR submitted an expanded petition to the IUCN concerning the long-tailed macaque status. The expanded petition can be found here and the press release about the expanded petition can be found here .
Read NABR’s February 2024 response to the authors of the study the IUCN relied on to uplist the status of long-tailed macaques to “endangered.”
NABR's IUCN Petition: Noteworthy Articles
Read the August 1, 2023 article in the journal Science by Shanghai correspondent Dennis Normile about NABR’s IUCN petition. Normile also discusses a recent study in Biological Reviews according to which long-tailed macaques are hyperabundant in formerly wild environments where humans have started settling. He highlights the inherent contradiction between the IUCN’s “endangered” listing of long-tailed macaques on the one hand, and the scientific data presented in the Biological Reviews study and NABR’s petition on the other hand.
Read the NABR press release announcing the December 21, 2023 American Journal of Primatology article that disputes information used to determine a faulty conservation status of long-tailed macaques the IUCN issued. You can also read the AJP article directly here .
YOUR HELP NEEDED
The U.S. Fish and Wildlife Service is denying permits related to Cambodian origin nonhuman primates (NHPs) and samples. Roughly 60% of the preclinical animal models of the drug development process are Cambodian origin NHPs. This action has put the development of new drugs to treat thousands of diseases for which there is no treatment or cure at significant risk. Our message is simple: We are calling on the U.S. government to work with, not against, the biomedical research sector, to find solutions to remedy the disruption in the biomedical research supply chain. Thank you for helping us do that.
Institutional Sign-on Letter
NABR is organizing an institutional sign-on letter to be sent to key members of Congress. The sign-on letter is here , and we are asking as many organizations as possible to add their names. Some organizations have asked whether the U.S. Fish and Wildlife Service has issued any public notice regarding the denial of permits affecting Cambodian origin NHPs and samples. Unfortunately, there has been no public statement or public notice regarding this decision, which is one impetus for our correspondence to the government. At least 60% of the NHPs in the drug development pipeline are of Cambodian origin, which underscores the impact this decision has on the creation of new medications for thousands of diseases for which there is no treatment or cure.
If you would like to sign-on, please email [email protected] .
Individual Letters
NABR members have submitted more than 2,000 letters to Congress regarding the NHP crisis, so let’s keep the momentum going! Please broadly circulate the link [ speak4.app/lp/24d1d8/ ] and encourage others at your organization to do the same. Alternately, you can click the "Take Action" bubble at the bottom right of your screen. The process is fast and easy, and it does make a difference. NABR is hearing from Capitol Hill staff who have taken an interest in this critical issue.
NHP Shortage News
December 26, 2023 The South Florida Sun Sentinel: https://www.sun-sentinel.com/2023/12/26/international-organizations-monkey-business-will-slow-medical-research-opinion/
September 4, 2023 The Washington Times : www.washingtontimes.com/news/2023/sep/4/activists-are-trying-to-slow-down-lifesaving-medic/
August 4, 2023 BioSpace.com: www.biospace.com/article/scientists-veterinarians-and-conservationists-offer-recommendations-to-address-the-shortage-of-long-tailed-macaques-required-for-continued-health-advancements-/
August 3, 2023 ScienMag.com: www.scienmag.com/scientists-veterinarians-and-conservationists-offer-recommendations-to-address-shortage-of-long-tailed-macaques-required-for-continued-health-advancements/
June 27, 2023 The San Joaquin Valley Sun : www.sjvsun.com/u-s/advocates-peta-pressuring-feds-to-bar-on-primate-use-for-dug-research/
June 15, 2023 The San Joaquin Valley Sun : www.sjvsun.com/business/report-false-designation-for-primate-could-block-ability-to-test-groundbreaking-drugs/
June 15, 2023 E&E News : www.subscriber.politicopro.com/article/eenews/2023/06/15/researchers-challenge-endangered-status-of-lab-primate-00102155
May 22, 2023 The Salina, Kansas Post : www.salinapost.com/posts/a5f331c8-afd1-49e0-b32c-f6e4ad0b2092
May 4, 2023 STAT+ : www.statnews.com/pharmalot/2023/05/04/nih-primates-macaques-research-biomedical-animals-organs/
May 4, 2023 NABR press release: https://www.nabr.org/about-nabr/news/nas-report-affirms-necessity-nhp-models-and-highlights-shortage-crisis
May 4, 2023 The Wall Street Journal : The U.S. Is Running Out of Research Monkeys
May 4, 2023 STAT+: NIH systems for non-human primate research fall short, threatening biomedical research
May 4, 2023 AP News Research monkey shortage undermines US readiness, panel says
March 27, 2023 www.openaccessgovernment.org : https://www.openaccessgovernment.org/article/fostering-nonhuman-primate-nhp-brain-research-without-animal-sacrifice/155741/
March 20, 2023 UK Guardian : Fate of 1,000 trafficked lab monkeys at center of US investigation in limbo
March 6, 2023 Endpoints News : Pharma industry lobbies Congress for solution to primate shortage after indictments for alleged smuggling
March 3, 2023 ScienceDirect: Is biomedical research demand driving a monkey business?
March 3, 2023 STAT+: As a U.S. agency denies permits to import monkeys for research, industry starts pushing back
March 3, 2023 The Wall Street Journal : Monkey Business Threatens U.S. Drug Discovery
March 1, 2023 Washington Post : How a Cambodian monkey-smuggling ring could worsen U.S. lab shortages
January 20, 2023 The Dispatch: America's Primate Problem
June 23, 2022 Mother Jones : A Plane of Monkeys, a Pandemic, and a Botched Deal: Inside the Science Crisis You’ve Never Heard Of
September 28, 2022 Bloomberg News: Lab Monkeys Are the Latest Covid Shortage
August 31, 2020 The Atlantic: America Is Running Low on a Crucial Resource for COVID-19 Vaccines
FAQs on the FDA Modernization Act
Does the fda modernization act 2.0 end animal testing.
No. The FDA Modernization Act 2.0 does not eliminate animal testing nor does it state or imply that animal testing is unnecessary. It simply clarifies the definition under the Food, Drug and Cosmetic Act of a nonclinical test or study to include adjunct and complementary testing methods like organs-on-a-chip, micro-physiological systems and computer simulations. Animal models continue to be highly relevant to test the safety and efficacy of a drug as part of the approval process. NABR supports the use of alternative models to animal testing when scientifically feasible and when scientifically validated, and remains confident in the ability of FDA scientific reviewers to determine the best data that should be submitted in new drug applications.
The FDA states that many procedures intended to reduce animal tests are still in various stages of development[1,2]. Adjunct and complementary tests have a purpose, but ultimately testing must progress to a whole intact, living system, including a rodent and non-rodent species during preclinical drug trials[3,4,5]. Not conducting animal tests, when necessary, would likely subject humans and other animals to unreasonable risks.
What is the FDA Modernization Act 2.0?
The FDA Modernization Act 2.0, passed as part of the Omnibus appropriations legislation in December of 2022, amends the Federal Food, Drug, and Cosmetic Act (21 U.S.C. 355) to clarify methods manufacturers and sponsors can use to investigate the safety and efficacy of a drug by inserting language on “nonclinical tests,” where “nonclinical tests” are defined broadly as follows [6] :
- · A test or study that is most likely to predict human response based on scientific evidence and occurs before or during the clinical trial phase of the investigation of the safety and effectiveness of a drug. Such test or study may include the following:
- o Cell-based assays
- o Organ chips and microphysiological systems
- o Sophisticated computer modeling
- o Other human biology-based test methods
- o Animal tests
It is important to note that the FDA previously had the authority to allow non-animal data to be considered during safety and efficacy reviews of new drugs and previously issued guidance regarding such. Ultimately, the FDA Modernization Act 2.0 may not materially change the current drug approval process at the FDA. In fact, a spokesperson for the FDA stated on the record that the new law does not change the regulatory process for drugs [7].
Why is animal testing important as part of the drug approval process?
The Food, Drug and Cosmetic Act was enacted in 1938 after the drug sulfanilamide, marketed for strep throat in the U.S. without human or animal research data establishing its safety or its efficacy, killed and sickened hundreds of people due to toxic levels of antifreeze it contained[8]. Additional animal research safety and efficacy data became required under the Act in 1963 to prevent incidents like the thalidomide incident in Europe and other parts of the world [9].
Animal testing followed by human clinical trials currently remains the best way to examine complex physiological, neuroanatomical, reproductive, developmental and cognitive effects of drugs to determine if they are safe and effective for market approval.
The overwhelming majority of drugs on the market today relied on safety and efficacy data from multiple animal models before being allowed to move to human clinical trials as demonstrated by the Foundation for Biomedical Research's Top 25 Drugs and Animal Model study [10].
NABR’s press statement on the FDA Modernization Act 2.0

NABR Files Expanded Petition Challenging the Listing of Long-Tailed Macaques by the IUCN

NABR April Webinar: “One Health and Animal Research: The Good, the Bad, and the Ugly”

NABR Press Release: LTM Conservation Status

The FY 2023 USDA Oversight Process
Nabr insights.
NABR contributes a great deal of time and resources towards developing and compiling industry relevant reports, webinars, and other informative documents for the benefit of its members. Please click the links below to access a variety of valuable resources and information in the Member's Only section.
Crisis Management Guide
Available for all NABR members. Download
Legal Resources for Managing Security at Private Residences

2022 NABR USDA Inspection Management Guide

Available for all NABR members. Explore
FOIA/Open Records
Available for all NABR members.
Legislation

Regulatory Comments
FY22 Appropriation Items

NABR Position Statement on Retirement/Adoption
DOT Secretary Pete Buttigieg on NABR’s complaint

Outgoing NIH Director Francis Collins Discusses Animal Research Ethics in Popular Podcast
FASEB Joins Partners to Support Biomedical Animal Research

Why Animal Research?
Animal research is a major contributor to almost all advances in human and animal health. The similarity in biological makeup between humans and some animals provides insight into diseases such as COVID-19, Diabetes, Cancer and many more. Animal testing also allows scientists to control factors such as temperature, lighting and diet, which is rather difficult and sometimes unethical during human trials.
FAQ on Animal Research
Why is animal research necessary.
Modern medical research, including research using animals, is necessary to understanding disease and creating medicines to improve human and animal lives and reduce suffering. Every known medical breakthrough known has a basis in animal research and all of the top 25 most prescribed drugs were developed with the assistance of animal models. To learn more about the indispensable role of animal research, watch a brief PSA by the Foundation for Biomedical Research (FBR) by clicking here .
Why is it even necessary to move animals?
Biomedical research is conducted in universities and commercial laboratories across the globe. Important breakthroughs are typically dependent on collaborative efforts from different laboratories in many states and countries.
Successful research depends on a reliable source of healthy laboratory animals. The best way of achieving this is through a global supply and transportation chain. Animals obtained from the same source have consistent genetics allowing scientists to better interpret data from animal studies. Professional breeders with highly controlled environments produce disease free animals with special characteristics important in studying human disease.
A shared source of genetically defined and healthy animals dramatically reduces the total number of animals required for a research program. A striking benefit of collaboration is the refinement of animal use. By including collaborators with the highest expertise and the best modern methodology to conduct animal studies, better data is produced.
Without the ability to transport laboratory animals from licensed commercial breeders and between research facilities, each research site would have to breed its own animals. This would be costly and would unnecessarily increase the number of animals for research.
How are animals transported?
Experienced and licensed professional transport companies are used to safely move laboratory animals. Animals are transported in vehicles equipped with temperature and humidity monitors and controls. Travel routes are designed to take the shortest time reasonable to reduce travel stress. To keep the journey as brief as possible, animals are frequently transported via airplane.
During transport, animals are provided with food, water and appropriate temperatures and conditions. Shipping containers are designed for proper ventilation and to protection animals from escape or injury. Bedding materials are provided for comfort and are specific to the needs of each species. Veterinarians specializing in the care of laboratory animals coordinate the shipping process, working with trained staff who monitor animals throughout the shipping process.

Why do we need to import nonhuman primates?
It is often in the best interests of an animal to be born and raised in areas with a climate well suited to the welfare of their species and where year-round outdoor housing is available. Nonhuman primates most commonly used in research are native to tropical and subtropical regions, and breeding facilities in those regions can provide captive animals with a suitable environment. These captive bred animals are reared to young adulthood before being moved to research facilities around the world.
Where do we get research animals?
The preferred source for research animals is a professional breeder. These producers are dedicated to supplying healthy, high quality animals to the research community. Animals are obtained from licensed, inspected and accredited facilities that employ experienced handlers, caretakers, and veterinarians. The research community demands high quality standards for food, water, sanitation and welfare for research animals, creating conditions that often exceed those of typical house pets.
Is it safe for animals?
The regulated transportation of laboratory animals is very safe. Industry statistics show there is an error rate of less than 1% for either land or air transportation of animals. Most of these errors do not impact the health or welfare of the shipment, so the actual impact on animal safety is even lower.
What would happen if we couldn’t transport animals in the future?
Without the ability to transport laboratory animals, research would be restricted to fewer locations and would lose the contributions of many talented scientists. Further, scientists would not always be able to use the most appropriate model to study a disease or response to a medication, delaying or stopping much needed medical advances.
The development of new medicines would slow, or even stop, denying cures and treatments to the people who need them. Research institutions would have to divert precious funding, manpower and laboratory space to breeding animals, taking resources away from important research.
Scientific collaboration across the world would be hampered by inconsistency in their research animals and difficulty interpreting data. Without the ability to transport laboratory animals by air, the research community would be unable to provide the best possible conditions for shipping animals quickly and safely. Without air transportation options, animals would often be subject to longer and more stressful transportation by land or sea.
Crisis Management
Read more about NABR's Crisis Management Guide.
Click to Open
Become part of a unified voice for the scientific community.
Congressional and Legislative Action
Learn more about NABR's advocacy efforts, like the passage of the AETA.
Medical breakthroughs underpinned by animal research
The use of animals in biomedical research helps researchers better understand the biological processes that are central to our health. This is essential for developing safe and effective ways of preventing or treating disease.
For over a century, research using animals has advanced the scientific understanding of human health, and the impact of this research is so vast that it can be difficult to measure. However, some key recent examples of lifesaving treatments that were developed thanks to animal research are worth highlighting.
COVID-19 vaccine trials
Professor Sarah Gilbert and her team at the University of Oxford spearheaded a vaccine trial in which they used a safe version of an adenovirus. An adenovirus is a virus that can cause a common cold-like illness.
Previous work funded by the Medical Research Council (MRC) through the UK Vaccine Network used this adenovirus (known as ChAdOx1) by Professor Gilbert in the production of vaccines against the Middle East Respiratory Syndrome coronavirus.
Engineering a spike protein
The team engineered ChAdOx1 to make a specific coronavirus protein, known as the spike protein, from the SARS-CoV-2 virus. As a result, our immune system should in theory be able to recognise the spike protein as ‘foreign’ and form antibodies against it. And then attack the SARS-CoV-2 virus and stop it from causing an infection.
It is hoped that long lasting immunity can be provided through vaccination by ‘bluffing’ the body in this way, and by slipping in parts of the virus that do not harm, but induce the release of antibodies.
The vaccine testing involved animal trials in ferrets and non-human primates at the Public Health England (PHE) laboratories. The team also collaborated with researchers at the BBSRC-funded Pirbright Institute to study the effect of this vaccine in pigs.
Vaccinating millions of people worldwide
Under normal circumstances, animal work must be completed before human trials can start. But because similar vaccines have worked safely in trials for other diseases, the work was accelerated and happened in parallel. It led to the approval by the Medical and Healthcare products Regulatory Agency on 30 December 2020.
This vaccine, commonly known as the Oxford AstraZeneca vaccine, has now been administered to millions of people worldwide.
Professor Alain Townsend’s team at the MRC Human Immunology Unit worked in collaboration with:
- MRC Weatherall Institute of Molecular Medicine
- Radcliffe Department of Medicine
- University of Oxford
- the Biotechnology and Biological Sciences Research Council’s (BBSRC) Pirbright Institute.
Further vaccine development
They have shown that a new potential vaccine against COVID-19, named RBD-SpyVLP, produces a strong antibody response in mice and pigs. It provides vital information for the further development of the vaccine.
Investing in the research and development of the second generation of COVID-19 vaccines is important because they will help fill gaps in efficacy against novel variants. It also addresses issues around production and distribution such as the requirement for cold chain supply logistics.
Find out more about the Oxford-produced RBD-SpyVLP vaccine candidate .
Llama antibody has ‘significant potential’ as COVID-19 treatment
A unique antibody produced by llamas could be developed as a new frontline treatment against COVID-19 and could be taken by patients as a simple nasal spray.
The laboratory research is led by scientists at the Rosalind Franklin Institute. The research was funded by:
- Engineering and Physical Sciences Research Council (EPSRC)
- EPA Cephalosporin Fund
The research has shown that nanobodies (a smaller, simple form of antibody generated by llamas and camels) can effectively target the SARS-CoV-2 virus that causes COVID-19. It is the first step towards developing a new type of treatment against COVID-19.
Preparing for human clinical studies
The scientists are hoping to progress this work from the animal setting to prepare for clinical studies in humans.
Human antibodies have been an important treatment for serious cases during the pandemic, but typically need to be administered by infusion through a needle in hospital.
However, nanobodies have several potential advantages over human antibodies:
- they are cheaper to produce
- it is possible to deliver them directly to the airways through a nebuliser or nasal spray, so they could be self-administered at home rather than needing an injection.
This could have benefits in terms of ease of use by patients, but it also gets the treatment directly to the site of infection in the respiratory tract.
Gene therapy treatment for treating blindness
Inherited eye conditions are currently untreatable because they are caused by mutations in our DNA, which form defective copies of key genes required for normal vision. Gene therapy aims to deliver healthy copies of these defective genes directly to the retina, to correct these genetic mistakes.
MRC has been funding research into gene therapy for inherited eye diseases since 2004. Animal research in mice and dogs has been vital for establishing the necessary proof-of-concept for ocular gene therapy.
Developing a new, efficient technique
In 2011, with MRC funding, a team of scientists at the UCL Institute of Ophthalmology developed a new technique for improving the efficiency of this gene therapy. The results of which were confirmed in mouse models, a special strain of mice to study a particular human disease or condition.
Once the safety and efficacy of this approach was established in mice, the work rapidly progressed to two clinical trials. The first patients receiving this ground-breaking treatment have benefited from significant vision restoration, with more patients now in clinical trials. As well as the benefit to patients, this work is now widely regarded as a landmark for the entire gene therapy field.
Last updated: 17 August 2023
This is the website for UKRI: our seven research councils, Research England and Innovate UK. Let us know if you have feedback or would like to help improve our online products and services .
Bainbridge site offers opportunity to advance medical research
There has been much discussion in recent weeks about plans by Safer Human Medicine to build a facility in southern Georgia aimed at addressing the critical shortage of nonhuman primates, animals which are crucial to medical research in the United States.However, I also know that animal-based research can often be misunderstood and I’m certain residents in southern Georgia and northern Florida have plenty of questions. That’s why, after many years of work caring for research animals, I have dedicated my career to helping people better understand the crucial importance of animal studies. Simply put, nonhuman primate research saves lives. Without it, countless medicines and therapies would not be possible.
If you’ve received a flu vaccine, or given your child cold medicine, you have directly benefited from animal research. If you’ve taken insulin for diabetes, received the polio vaccine, undergone chemotherapy, underwent coronary bypass surgery, had kidney dialysis, or taken medications for psychiatric illnesses, research in nonhuman primates played a big part in those treatments.Critics often argue that computer models or organs-on-a-chip can replace animal research. And while these technologies help reduce the number of animals that need to be studied, they are still in their infancy and cannot fully replicate the intricate workings of the human body. Moreover, the FDA requires that drugs and other candidate therapies that are in development be safety tested before human trials begin. In almost every case, this assurance requires animal studies, because no other alternative exists. Primates are frequently involved in these final steps of the pre-clinical (pre-human) research process, providing critical data that cannot be ethically or safely obtained in human studies.Despite overwhelming scientific consensus that animal studies remain necessary, opposition groups seek to achieve their goals and mislead the public by injecting distrust and fear. To be clear, ethical discussions are at the forefront of every animal research endeavor. Institutions conducting such research are bound by strict regulations and oversight, including the laws within the Animal Welfare Act and strict guidelines required by the National Institutes of Health. These measures help ensure humane treatment and care for research animals. The contribution of nonhuman primates to medical research cannot be overstated. As we look to emerging health challenges, the need for a readily available domestic supply of these animals for research remains as critical as ever. I hope residents throughout southern Georgia and northern Florida recognize the unique opportunity they must play a critical role in supporting the medical research we so desperately need for the life-saving medicines of tomorrow.
Paula Clifford is executive director of Americans for Medical Progress, which is based in Washington, DC.
JOIN THE CONVERSATION
Send letters to the editor (up to 200 words) or Your Turn columns (about 500 words) to [email protected] . Please include your address for verification purposes only, and if you send a Your Turn, also include a photo and 1-2 line bio of yourself. You can also submit anonymous Zing!s at Tallahassee.com/Zing. Submissions are published on a space-available basis. All submissions may be edited for content, clarity and length, and may also be published by any part of the USA TODAY NETWORK.
- Skip to main content
- Skip to FDA Search
- Skip to in this section menu
- Skip to footer links

The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
U.S. Food and Drug Administration
- Search
- Menu
- For Consumers
- Consumer Updates
Ivermectin and COVID-19
One of the U.S. Food and Drug Administration’s jobs is to carefully evaluate the scientific data on a drug to be sure that it is both safe and effective for a particular use.
There continues to be interest in a drug called ivermectin for the prevention or treatment of COVID-19 in humans. The FDA has not authorized or approved ivermectin for use in preventing or treating COVID-19 in humans or animals.
For humans, ivermectin tablets are approved at specific doses to treat some parasitic worms, and there are topical (on the skin) formulations for head lice and skin conditions like rosacea. For animals, certain pour-on, injectable, paste, chewable, and “drench” ivermectin products are approved in the U.S. to treat or prevent parasites in animals.
The FDA has received multiple reports of patients who have required medical attention, including hospitalization, after self-medicating with ivermectin intended for animals.
Here’s What You Need to Know
- The FDA has not authorized or approved ivermectin for use in preventing or treating COVID-19 in humans or animals.
- The FDA has determined that currently available clinical trial data do not demonstrate that ivermectin is effective against COVID 19 in humans.
- Animal ivermectin products are different formulations than those approved for humans. Due to the lack of testing of these formulations in humans, the safety of these products in humans is not known. Never use medications intended for animals on yourself or other people.
- Taking large doses of ivermectin can be dangerous.
- From the FDA’s perspective, with few exceptions, health care professionals may choose to prescribe or use an approved human drug for an unapproved use when they judge that the unapproved use is medically appropriate for an individual patient. If your health care provider writes you an ivermectin prescription, fill it through a legitimate source such as a pharmacy.
How is Ivermectin Used?
Ivermectin tablets are approved by the FDA to treat people with intestinal strongyloidiasis and onchocerciasis, two conditions caused by parasitic worms. In addition, some topical forms of ivermectin are approved to treat external parasites like head lice and for skin conditions such as rosacea.
Some forms of animal ivermectin are approved to prevent heartworm disease and treat certain internal and external parasites in animals. It’s important to note that these products are different from the ones for people, and safe only when used in animals as labeled or as prescribed.
The FDA has not authorized or approved ivermectin for the treatment or prevention of COVID-19 in people or animals. The FDA has not determined that ivermectin is safe or effective for these indications (uses).
When Can Taking Ivermectin Be Unsafe?
You may have heard that it’s okay to take large doses of ivermectin. Taking large doses of ivermectin can be dangerous.
Even doses of ivermectin for approved human uses can interact with other medications, like blood-thinners. You can also overdose on ivermectin, which can cause nausea, vomiting, diarrhea, hypotension (low blood pressure), allergic reactions (itching and hives), dizziness, ataxia (problems with balance), seizures, coma and even death.
Lowering Your Risk from COVID-19
Current CDC guidance provides practical recommendations and information to help people lower risk from a range of common respiratory viral illnesses, including COVID-19.
Talk to your health care provider about available COVID-19 vaccines and treatment options. Your provider can help determine the best option for you, based on your health history.
Consumer Update Email
Subscribe to receive FDA Consumer Update email notifications
Stop COVID Cohort: An Observational Study of 3480 Patients Admitted to the Sechenov University Hospital Network in Moscow City for Suspected Coronavirus Disease 2019 (COVID-19) Infection
Collaborators.
- Sechenov StopCOVID Research Team : Anna Berbenyuk , Polina Bobkova , Semyon Bordyugov , Aleksandra Borisenko , Ekaterina Bugaiskaya , Olesya Druzhkova , Dmitry Eliseev , Yasmin El-Taravi , Natalia Gorbova , Elizaveta Gribaleva , Rina Grigoryan , Shabnam Ibragimova , Khadizhat Kabieva , Alena Khrapkova , Natalia Kogut , Karina Kovygina , Margaret Kvaratskheliya , Maria Lobova , Anna Lunicheva , Anastasia Maystrenko , Daria Nikolaeva , Anna Pavlenko , Olga Perekosova , Olga Romanova , Olga Sokova , Veronika Solovieva , Olga Spasskaya , Ekaterina Spiridonova , Olga Sukhodolskaya , Shakir Suleimanov , Nailya Urmantaeva , Olga Usalka , Margarita Zaikina , Anastasia Zorina , Nadezhda Khitrina
Affiliations
- 1 Department of Pediatrics and Pediatric Infectious Diseases, Institute of Child's Health, Sechenov First Moscow State Medical University (Sechenov University), Moscow, Russia.
- 2 Inflammation, Repair, and Development Section, National Heart and Lung Institute, Faculty of Medicine, Imperial College London, London, United Kingdom.
- 3 Soloviev Research and Clinical Center for Neuropsychiatry, Moscow, Russia.
- 4 School of Physics, Astronomy, and Mathematics, University of Hertfordshire, Hatfield, United Kingdom.
- 5 Biobank, Institute for Regenerative Medicine, Sechenov First Moscow State Medical University (Sechenov University), Moscow, Russia.
- 6 Institute for Regenerative Medicine, Sechenov First Moscow State Medical University (Sechenov University), Moscow, Russia.
- 7 Chemistry Department, Lomonosov Moscow State University, Moscow, Russia.
- 8 Department of Polymers and Composites, N. N. Semenov Institute of Chemical Physics, Moscow, Russia.
- 9 Department of Clinical and Experimental Medicine, Section of Pediatrics, University of Pisa, Pisa, Italy.
- 10 Institute of Social Medicine and Health Systems Research, Faculty of Medicine, Otto von Guericke University Magdeburg, Magdeburg, Germany.
- 11 Institute for Urology and Reproductive Health, Sechenov First Moscow State Medical University (Sechenov University), Moscow, Russia.
- 12 Department of Intensive Care, Sechenov First Moscow State Medical University (Sechenov University), Moscow, Russia.
- 13 Clinic of Pulmonology, Sechenov First Moscow State Medical University (Sechenov University), Moscow, Russia.
- 14 Department of Internal Medicine No. 1, Institute of Clinical Medicine, Sechenov First Moscow State Medical University (Sechenov University), Moscow, Russia.
- 15 Department of Forensic Medicine, Sechenov First Moscow State Medical University (Sechenov University), Moscow, Russia.
- 16 Department of Statistics, University of Oxford, Oxford, United Kingdom.
- 17 Medical Research Council Population Health Research Unit, Nuffield Department of Population Health, University of Oxford, Oxford, United Kingdom.
- 18 Centre for Tropical Medicine and Global Health, Nuffield Department of Medicine, University of Oxford, Oxford, United Kingdom.
- 19 Oxford University Hospitals NHS Foundation Trust, John Radcliffe Hospital, Oxford, United Kingdom.
- 20 Sechenov First Moscow State Medical University (Sechenov University), Moscow, Russia.
- PMID: 33035307
- PMCID: PMC7665333
- DOI: 10.1093/cid/ciaa1535
Background: The epidemiology, clinical course, and outcomes of patients with coronavirus disease 2019 (COVID-19) in the Russian population are unknown. Information on the differences between laboratory-confirmed and clinically diagnosed COVID-19 in real-life settings is lacking.
Methods: We extracted data from the medical records of adult patients who were consecutively admitted for suspected COVID-19 infection in Moscow between 8 April and 28 May 2020.
Results: Of the 4261 patients hospitalized for suspected COVID-19, outcomes were available for 3480 patients (median age, 56 years; interquartile range, 45-66). The most common comorbidities were hypertension, obesity, chronic cardiovascular disease, and diabetes. Half of the patients (n = 1728) had a positive reverse transcriptase-polymerase chain reaction (RT-PCR), while 1748 had a negative RT-PCR but had clinical symptoms and characteristic computed tomography signs suggestive of COVID-19. No significant differences in frequency of symptoms, laboratory test results, and risk factors for in-hospital mortality were found between those exclusively clinically diagnosed or with positive severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) RT-PCR. In a multivariable logistic regression model the following were associated with in-hospital mortality: older age (per 1-year increase; odds ratio, 1.05; 95% confidence interval, 1.03-1.06), male sex (1.71; 1.24-2.37), chronic kidney disease (2.99; 1.89-4.64), diabetes (2.1; 1.46-2.99), chronic cardiovascular disease (1.78; 1.24-2.57), and dementia (2.73; 1.34-5.47).
Conclusions: Age, male sex, and chronic comorbidities were risk factors for in-hospital mortality. The combination of clinical features was sufficient to diagnose COVID-19 infection, indicating that laboratory testing is not critical in real-life clinical practice.
Keywords: COVID-19; Russia; SARS-CoV-2; cohort; mortality risk factors.
© The Author(s) 2020. Published by Oxford University Press for the Infectious Diseases Society of America. All rights reserved. For permissions, e-mail: [email protected].
Publication types
- Observational Study
- Research Support, Non-U.S. Gov't
- Hospitalization
- Middle Aged
Grants and funding
- 20-04-60063/Russian Foundation for Basic Research

Research Animal Veterinary Technician
- Madison, Wisconsin
- VC FOR RESEARCH AND GRADUATE EDUCATION/RESEARCH ANIMAL RESOURCES & COMPLIANCE
- Animal Care Services
- Staff-Full Time
- Opening at: Apr 15 2024 at 15:25 CDT
- Closing at: Apr 29 2024 at 23:55 CDT
Job Summary:
Are you looking for a challenging new position? Do you have experience as a Veterinary Technician? This position provides veterinary care to research animals in the UW-Madison research animal program. The research animal veterinary technician assists veterinarians in restraint, examination, and medical and surgical treatment of sick and injured animals. Veterinary technicians observe the health and welfare of research animals and document observations and treatments in appropriate records. The veterinary technician will use multiple electronic methods of communicating with laboratory and veterinary staff and documenting treatments. They will also prepare and administer oral, topical and injectable medications (including anesthetic agents) as directed by the veterinarians. This position may assist or initiate preparation of animals for medical, surgical, diagnostic and research procedures, monitor animals during anesthesia, and provide post-operative care. The veterinary technician performs multiple methods of euthanasia on multiple species. This position may also train lab staff in the management of chronic medical conditions of genetically modified mice, such as dermatitis and dental problems, by teaching them to do certain treatments to improve the welfare of the animals. This position is considered essential personnel and is 100% onsite.
Responsibilities:
- 45% Assists veterinarians and researchers in animal care, diagnostic, preventative, research, anesthesia, surgery, post-operative care, euthanasia and radiology procedures under minimal supervision. May perform minor surgical procedures or other minor invasive procedures
- 10% Prepares, completes, monitors, and documents complex technical animal care procedures and work unit activities, assessments, and medication administration according to established care plans and medical necessity
- 5% Keeps records of all controlled substances and inventory records
- 5% Maintains surgical support facilities in sanitized, well-stocked, and in orderly manner; and ensures that preventative maintenance of equipment is performed
- 5% Schedules and performs routine testing and vaccinations on United States Department of Agriculture (USDA) regulated animals
- 5% Assists in training new veterinary and/or animal care technicians and supervises work as appropriate
- 5% May assist in data collection or reporting for designated aspects of research, animal care programs, or colony management
- 20% Maintains records regarding animal treatments, medications, diagnostic procedures, and illness
Institutional Statement on Diversity:
Diversity is a source of strength, creativity, and innovation for UW-Madison. We value the contributions of each person and respect the profound ways their identity, culture, background, experience, status, abilities, and opinion enrich the university community. We commit ourselves to the pursuit of excellence in teaching, research, outreach, and diversity as inextricably linked goals. The University of Wisconsin-Madison fulfills its public mission by creating a welcoming and inclusive community for people from every background - people who as students, faculty, and staff serve Wisconsin and the world. For more information on diversity and inclusion on campus, please visit: Diversity and Inclusion
Preferred Associate's Degree
Qualifications:
Experience with research animals preferred. Certification of Wisconsin Veterinary Technician or eligibility to obtain preferred or experience equivalent.
License/Certification:
Preferred CVT - Certified Veterinary Technician
Work Schedule:
Flexible work schedule between 7:00 am and 6:00 pm. 1-2 holidays per year and 1 weekend flexible sign up required every 2 months.
Full Time: 100% It is anticipated this position requires work be performed in-person, onsite, at a designated campus work location.
Appointment Type, Duration:
Ongoing/Renewable
Minimum $22.00 HOURLY Depending on Qualifications Employees in this position can expect to receive benefits such as 3.5 weeks vacation and paid holidays, sick pay, competitive insurance (health, dental, life) and flexible savings accounts, as well as many retirement benefits.
Additional Information:
A successful applicant will be responsible for ensuring eligibility for employment in the United Stateson or before the effective date of the appointment. University sponsorship is not available for this position. The Veterinary Technician must be able to comply with entry requirements for specialized animal facilities including, but not limited to health screening, periodic tuberculosis testing, vaccinations, and have the ability to wear appropriate personal protective equipment (PPE) (e.g. mask, respirator, etc.) as required by SOPs or policies.
How to Apply:
To apply for this position, please click the "Apply Now" button. You will be asked to submit a resume and cover letter that describes your qualifications as they relate to the position.
Tambrey Dinges [email protected] 608-263-9057 Relay Access (WTRS): 7-1-1. See RELAY_SERVICE for further information.
Official Title:
Veterinary Technician III(AN004)
Department(s):
A34-OVCR/RARC/VET CARE UNIT
Employment Class:
University Staff-Ongoing
Job Number:
The university of wisconsin-madison is an equal opportunity and affirmative action employer..
You will be redirected to the application to launch your career momentarily. Thank you!
Frequently Asked Questions
Applicant Tutorial
Disability Accommodations
Pay Transparency Policy Statement
Refer a Friend
You've sent this job to a friend!
Website feedback, questions or accessibility issues: [email protected] .
Learn more about accessibility at UW–Madison .
© 2016–2024 Board of Regents of the University of Wisconsin System • Privacy Statement
Office of the Vice President for Research
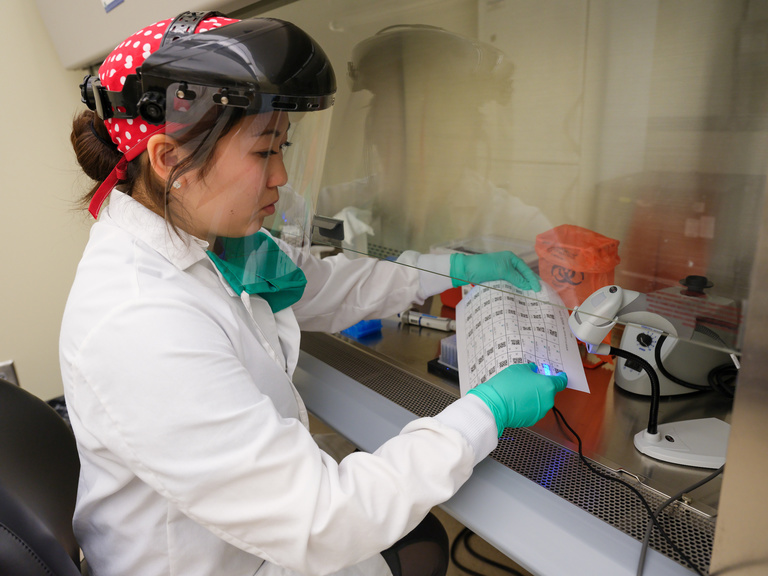
Lab week 2024: celebrating medical laboratory professionals.
April 14 - 20, 2024, is Medical Laboratory Professionals Week, an annual celebration to highlight and show appreciation for laboratory professionals, including those at the State Hygienic Laboratory (SHL) at the University of Iowa.
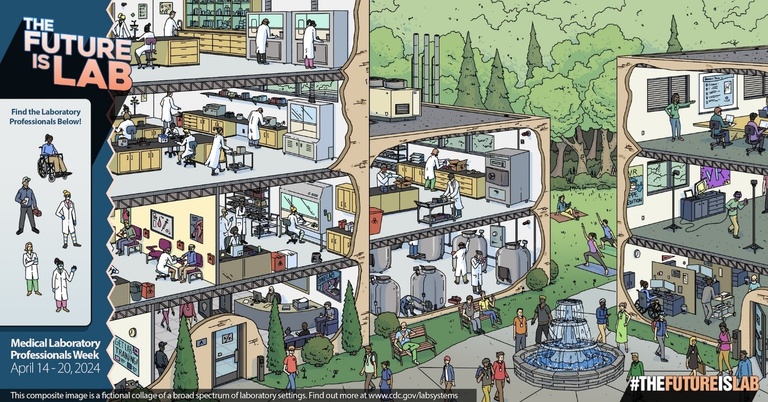
Lab Week is sponsored by the American Society for Clinical Laboratory Science and coordinated by 17 national clinical laboratory organizations.
“At the State Hygienic Laboratory, our teams have demonstrated again and again that we are prepared to skillfully respond to evolving emerging public health threats, adapting to meet the changing needs of laboratory medicine and the evolution of diagnostic testing,” said Michael Pentella, SHL director.
Established in 1904, the SHL works closely with local, state, and federal partners to fulfill its mission in the Iowa Code to investigate and evaluate any issues that are in the interest of environmental quality and public health in the state. The lab serves all of Iowa’s 99 counties through disease detection, environmental monitoring, and newborn and maternal screening. Today, the SHL also quickly responds to infectious disease threats, including mpox, SARS-CoV-2, whooping cough, and much more.
“Our teams are continually forward-thinking in terms of taking continuing education classes to prepare us for the future challenges of laboratory medicine,” said Pentella. “We are proud of our role to help ensure that Iowa communities are healthy places to live, work, and play.”
- Medical Tourism
Best Hospitals In Russia | Top 10 Hospitals in Russia

In the vast and diverse landscape of Russia, a nation renowned for its historical splendor, cultural richness, and scientific prowess, healthcare services have continued to evolve, keeping pace with global advancements. Among the vast network of hospitals, certain institutions have distinguished themselves by consistently delivering excellence in healthcare. These facilities are not only recognized for their state-of-the-art technology, top-notch medical professionals, and comprehensive services, but also for their unwavering commitment to patient care and safety. Welcome to our curated list of the top 10 hospitals in Russia, where we explore these exceptional institutions and the key attributes that set them apart in Russia's healthcare ecosystem.
List of Top 10 Hospitals in Russia
Pirogov national medical and surgical center - moscow, sklifosovsky institute of emergency care - moscow, moscow clinical scientific center (mcc) - moscow, city clinical hospital no. 31 - saint petersburg, almazov national medical research centre - saint petersburg, academician i.p. pavlov first saint petersburg state medical university hospital - saint petersburg, federal center for cardiovascular surgery - astrakhan, federal research and clinical center of physical-chemical medicine - moscow, n.n. blokhin national medical research center of oncology - moscow, city hospital no. 1 - novosibirsk.
- About Hospital: Pirogov National Medical and Surgical Center, located in Moscow, is renowned for its comprehensive medical services. With a legacy dating back to 1802, it combines rich traditions with cutting-edge technology, providing top-notch healthcare to patients.
- Team and Specialties: Pirogov Center boasts a highly skilled team of medical professionals specializing in various fields, including cardiology, neurology, orthopedics, and oncology. Their expertise ensures precise diagnoses and effective treatments for patients.
- Infrastructure: The hospital features state-of-the-art facilities equipped with modern medical equipment. From advanced operating theaters to diagnostic imaging units, the infrastructure supports accurate diagnostics and innovative medical interventions.
- Location: Moscow, Russia
- Hospital Address: Pirogovskaya Embankment, 1, Moscow, 105203, Russia
Facilities:
- Intensive care units with advanced life-support systems
- Specialized departments for organ transplants
- Advanced diagnostic imaging facilities (MRI, CT scans)
- Rehabilitation centers offering comprehensive therapies
- Well-equipped emergency department for prompt medical attention
- Dedicated research and development center for medical advancements
- Modernized laboratory facilities for accurate diagnostics
- Comfortable patient rooms with essential amenities
- Pharmacy providing a wide range of medications
- Cafeteria and parking facilities for the convenience of patients and visitors
Hospital Awards:
- National Healthcare Excellence Award for Outstanding Patient Care
- Recognition for Innovative Research in Medical Sciences
- Best Hospital for Cardiac Care in Moscow
- Accreditation by the Joint Commission International (JCI)
- National Recognition for Excellence in Surgical Services
Available Specialties:
- Orthopedics
- Gastroenterology
- Obstetrics and Gynecology
- Ophthalmology
- Dermatology
- About Hospital: The Sklifosovsky Institute of Emergency Care, located in Moscow, is a renowned medical institution specializing in emergency and trauma care. With a legacy spanning over a century, it has become a symbol of excellence in emergency medicine in Russia.
- Team and Specialties: Sklifosovsky Institute boasts a highly skilled team of emergency care specialists, including trauma surgeons, anesthesiologists, and critical care physicians. The hospital is equipped to handle a wide range of medical emergencies, from severe injuries to life-threatening conditions.
- Infrastructure: The hospital is equipped with state-of-the-art emergency rooms, operating theaters, and intensive care units to provide immediate and critical care services. It also houses specialized units for cardiac emergencies, neurosurgery, and burns.
- Hospital Address: Bolshaya Sukharevskaya Square, 3, Moscow, 129090, Russia
- Emergency department with round-the-clock services
- Specialized trauma units equipped for complex surgeries
- Advanced imaging technology for rapid diagnostics
- Helicopter landing pad for quick transfer of critically ill patients
- Rehabilitation center offering comprehensive post-trauma care
- Advanced life support systems in ambulances for safe patient transportation
- Research and training facilities for emergency medicine advancements
- Well-designed waiting areas and patient rooms for comfort
- Pharmacy providing necessary medications
- Cafeteria and parking facilities for convenience
- National Award for Excellence in Emergency Care
- Recognition for Outstanding Trauma Services
- Best Emergency Care Hospital in Moscow
- National Recognition for Research and Innovation in Emergency Medicine
- Trauma Care
- Cardiac Emergencies
- Neurosurgery
- Burns and Plastic Surgery
- Critical Care Medicine
- Pediatric Emergencies
- Respiratory Emergencies
- Obstetric Emergencies
- Gastrointestinal Emergencies
- About Hospital: Moscow Clinical Scientific Center is a leading multidisciplinary medical institution in Moscow. It combines clinical practice, education, and scientific research to provide comprehensive healthcare services. The hospital is known for its commitment to evidence-based medicine and patient-centered care.
- Team and Specialties: MCC boasts a team of highly experienced physicians, surgeons, and researchers specializing in various medical fields. The hospital offers a wide range of specialties, including cardiology, oncology, neurology, gastroenterology, and endocrinology.
- Infrastructure: The hospital features modern infrastructure and advanced medical technologies. It houses well-equipped operating rooms, diagnostic imaging facilities, and specialized units for various medical disciplines. The infrastructure supports efficient and accurate diagnostics, minimally invasive procedures, and advanced surgical interventions.
- Hospital Address: Stromynka St, 7, Moscow, 107076, Russia
- Comprehensive diagnostic services, including MRI, CT scans, and laboratory tests
- Specialized clinics for outpatient care
- Advanced surgical units for complex procedures
- Intensive care units with cutting-edge monitoring and life support systems
- Rehabilitation center offering physical therapy and rehabilitation programs
- Well-designed patient rooms ensuring comfort and privacy
- Research and innovation center promoting scientific advancements
- Emergency services available 24/7
- National Recognition for Excellence in Patient Safety
- Award for Outstanding Contributions to Medical Research
- Best Multidisciplinary Hospital in Moscow
- National Award for Innovation in Healthcare Services
- Endocrinology
- Pulmonology
- Rheumatology
- Otolaryngology (ENT)
- About Hospital: City Clinical Hospital No. 31, located in Saint Petersburg, is a prominent healthcare institution providing comprehensive medical services. With a focus on patient care and advanced treatment approaches, the hospital has gained recognition for its excellence in healthcare delivery.
- Team and Specialties: The hospital is home to a skilled team of medical professionals, including specialists in internal medicine, surgery, pediatrics, and more. The hospital's departments cover a wide range of medical specialties, ensuring personalized and specialized care for patients.
- Infrastructure: City Clinical Hospital No. 31 features modern infrastructure with well-equipped operating rooms, advanced diagnostic facilities, and specialized units. The hospital utilizes state-of-the-art technology and medical equipment to deliver accurate diagnoses and effective treatments.
- Location: Saint Petersburg, Russia
- Hospital Address: Marshala Tukhachevskogo St., 28, Saint Petersburg, 195067, Russia
- Specialized clinics for various medical specialties
- Advanced diagnostic imaging services (MRI, CT scans, X-rays)
- Operating theaters equipped with modern surgical instruments
- Intensive care units providing critical care support
- Rehabilitation center offering comprehensive therapy programs
- Well-designed patient rooms with modern amenities
- Emergency department for immediate medical attention
- Laboratory facilities for accurate diagnostic testing
- Convenient parking and cafeteria facilities
- Excellence in Patient Care Award
- National Recognition for Medical Innovation
- Best Hospital for Pediatric Care in Saint Petersburg
- Award for Outstanding Surgical Services
- Internal Medicine
- Surgery (General, Orthopedic, Neurosurgery, etc.)
- Gynecology and Obstetrics
- About Hospital: Almazov National Medical Research Centre is a leading medical institution located in Saint Petersburg. It is a renowned center for medical research, education, and patient care. The hospital focuses on delivering advanced treatments and improving healthcare through scientific innovation.
- Team and Specialties: Almazov Centre boasts a multidisciplinary team of highly skilled healthcare professionals, including physicians, surgeons, researchers, and support staff. The hospital offers specialized care in areas such as cardiology, cardiovascular surgery, genetics, and endocrinology.
- Infrastructure: The hospital features state-of-the-art infrastructure with advanced medical equipment and facilities. It houses cutting-edge diagnostic imaging centers, hybrid operating rooms, and specialized units for research and clinical trials. The infrastructure supports the delivery of precise diagnostics, minimally invasive procedures, and complex surgeries.
- Hospital Address: Akkuratova St., 2, Saint Petersburg, 197341, Russia
- Advanced cardiovascular imaging services (MRI, CT scans, angiography)
- Hybrid operating rooms for minimally invasive surgeries
- Specialized clinics for cardiology, endocrinology, genetics, and more
- Intensive care units equipped with advanced monitoring systems
- Rehabilitation center offering comprehensive recovery programs
- Well-appointed patient rooms ensuring comfort and privacy
- Cafeteria, garden, and parking facilities for convenience
- National Award for Excellence in Cardiology Services
- Recognition for Research and Innovation in Medical Sciences
- Best Hospital for Cardiovascular Care in Saint Petersburg
- National Award for Advancements in Genetic Medicine
- Cardiovascular Surgery
- About Hospital: The Academician I.P. Pavlov First Saint Petersburg State Medical University Hospital, affiliated with the esteemed medical university, is a leading medical institution in Saint Petersburg. It combines academic excellence with clinical expertise to provide high-quality healthcare services.
- Team and Specialties: The hospital is staffed by a dedicated team of medical professionals, including renowned professors, experienced physicians, and specialists across various medical fields. The hospital offers comprehensive care in specialties such as cardiology, neurology, oncology, and pediatrics.
- Infrastructure: The hospital is equipped with modern infrastructure, including state-of-the-art diagnostic facilities, advanced operating theaters, and specialized treatment units. The infrastructure supports accurate diagnostics, advanced surgical interventions, and innovative treatment approaches.
- Hospital Address: L'va Tolstogo St., 6-8, Saint Petersburg, 197022, Russia
- Comprehensive diagnostic services, including imaging, laboratory, and pathology
- Advanced operating theaters with cutting-edge surgical equipment
- Intensive care units providing specialized critical care support
- Rehabilitation center offering a range of therapies for recovery
- Research and innovation center fostering scientific advancements
- Training facilities for medical education and research
- National Recognition for Excellence in Medical Education
- Award for Outstanding Research Contributions
- Best Hospital for Academic Medicine in Saint Petersburg
- National Award for Pediatric Care
- About Hospital: The Federal Center for Cardiovascular Surgery, located in Astrakhan, is a renowned institution specializing in cardiac care. It is dedicated to providing comprehensive cardiovascular services, including diagnosis, treatment, and rehabilitation, to patients with heart conditions.
- Team and Specialties: The hospital houses a team of highly skilled cardiologists, cardiac surgeons, and specialized healthcare professionals. They have extensive expertise in various areas of cardiovascular medicine, such as interventional cardiology, electrophysiology, and cardiac surgery.
- Infrastructure: The hospital is equipped with state-of-the-art infrastructure and cutting-edge technology specific to cardiovascular care. It features advanced cardiac catheterization laboratories, hybrid operating rooms, and specialized units for cardiac rehabilitation. The infrastructure supports precision diagnostics and advanced interventions for optimal patient outcomes.
- Location: Astrakhan, Russia
- Hospital Address: 20th Building Line, 26, Astrakhan, 414011, Russia
- Advanced cardiac diagnostic services, including angiography and echocardiography
- Hybrid operating rooms for minimally invasive and complex cardiac surgeries
- Intensive care units specialized in cardiac critical care
- Rehabilitation center with tailored programs for cardiac patients
- Well-appointed patient rooms ensuring comfort and recovery
- Research and education center for advancements in cardiovascular medicine
- Pharmacy providing specialized cardiac medications
- Emergency services for immediate cardiac care
- Laboratory facilities for comprehensive cardiac testing
- National Recognition for Excellence in Cardiovascular Services
- Award for Innovation in Cardiac Procedures
- Best Cardiovascular Hospital in Astrakhan
- National Award for Cardiac Rehabilitation Services
- Interventional Cardiology
- Cardiac Surgery
- Electrophysiology
- Heart Failure Management
- Cardiovascular Imaging
- Pediatric Cardiology
- Cardiac Rehabilitation
- Vascular Surgery
- Hypertension Management
- Cardiac Genetics
- About Hospital: The Federal Research and Clinical Center of Physical-Chemical Medicine, located in Moscow, is a leading medical institution specializing in physical-chemical medicine and advanced therapies. It is dedicated to research, innovation, and personalized treatments for various diseases.
- Team and Specialties: The hospital boasts a multidisciplinary team of experts, including physicians, researchers, and scientists. The center focuses on integrating physical-chemical medicine into clinical practice, offering specialized care in areas such as regenerative medicine, personalized therapy, and targeted drug delivery.
- Infrastructure: The hospital features state-of-the-art infrastructure with advanced laboratories, research facilities, and specialized treatment units. It utilizes cutting-edge technologies and techniques to develop innovative treatments and personalized medicine approaches.
- Hospital Address: Kashirskoye Shosse, 46, Moscow, 115522, Russia
- Advanced laboratories for research and development
- Specialized treatment units for regenerative medicine and targeted therapy
- Advanced diagnostic imaging services (MRI, CT scans, etc.)
- Rehabilitation center offering tailored programs for patients
- Well-equipped patient rooms ensuring comfort and recovery
- Pharmacy providing specialized medications
- National Recognition for Excellence in Research and Innovation
- Award for Advancements in Personalized Medicine
- Best Hospital for Physical-Chemical Medicine in Moscow
- National Award for Regenerative Medicine
- Regenerative Medicine
- Targeted Therapy
- Personalized Medicine
- Nanomedicine
- Drug Delivery Systems
- Biomaterials and Tissue Engineering
- Genetic Medicine
- Radiopharmaceuticals
- Molecular Diagnostics
- Theranostics
- About Hospital: The N.N. Blokhin National Medical Research Center of Oncology, located in Moscow, is a prestigious medical institution specializing in cancer care and research. It is dedicated to the diagnosis, treatment, and prevention of various types of cancers.
- Team and Specialties: The hospital boasts a highly skilled team of oncologists, surgeons, radiation therapists, and researchers. They specialize in various areas of oncology, including medical oncology, surgical oncology, radiation oncology, and pediatric oncology.
- Infrastructure: The hospital features advanced infrastructure and cutting-edge technologies for cancer diagnosis and treatment. It has state-of-the-art radiation therapy units, specialized surgical theaters, and multidisciplinary clinics. The infrastructure supports precise cancer diagnostics, minimally invasive procedures, and comprehensive treatment plans.
- Hospital Address: Kashirskoye Shosse, 24, Moscow, 115478, Russia
- Advanced diagnostic services, including PET-CT scans and molecular diagnostics
- Radiation therapy units equipped with modern linear accelerators
- Specialized surgical theaters for oncologic surgeries
- Multidisciplinary clinics for comprehensive cancer care
- Pediatric oncology department with child-friendly facilities
- Rehabilitation center offering supportive care programs
- Research and innovation center for advancements in cancer treatment
- Pharmacy providing specialized oncology medications
- Emergency services for immediate oncologic care
- National Recognition for Excellence in Cancer Care
- Award for Innovations in Oncology Treatment
- Best Oncology Center in Moscow
- National Award for Pediatric Oncology Services
- Medical Oncology
- Surgical Oncology
- Radiation Oncology
- Pediatric Oncology
- Palliative Care
- Genetic Counseling
- Clinical Trials
- Supportive Care
- Cancer Prevention and Screening
- About Hospital: City Hospital No. 1, located in Novosibirsk, is a prominent healthcare institution providing comprehensive medical services to the community. It is recognized for its commitment to patient care, advanced treatments, and medical education.
- Team and Specialties: The hospital boasts a team of highly skilled physicians, specialists, and support staff dedicated to delivering quality healthcare. It offers a wide range of medical specialties, including internal medicine, surgery, pediatrics, and gynecology.
- Infrastructure: City Hospital No. 1 features modern infrastructure with well-equipped departments, diagnostic facilities, and treatment units. It utilizes advanced medical technologies to ensure accurate diagnostics, efficient treatments, and excellent patient outcomes.
- Location: Novosibirsk, Russia
- Hospital Address: Ulitsa Timiryazeva, 2, Novosibirsk, 630099, Russia
- Outpatient clinics providing primary and specialized care
- Advanced diagnostic imaging services, including X-rays and ultrasound
- Well-equipped operating theaters for various surgical procedures
- Intensive care units offering critical care support
- Rehabilitation center with comprehensive therapy programs
- National Recognition for Excellence in Patient Care
- Award for Best Hospital in Novosibirsk
- Recognition for Contributions to Medical Education
- National Award for Quality Improvement in Healthcare Services
- General Surgery
In conclusion, Russia is home to a diverse range of exceptional hospitals that are at the forefront of healthcare delivery, research, and innovation. The top 10 hospitals mentioned in this blog represent a selection of these outstanding institutions, each offering specialized medical services and demonstrating a commitment to patient care.
From the Pirogov National Medical and Surgical Center in Moscow to the City Hospital No. 1 in Novosibirsk, these hospitals showcase the highest standards of healthcare delivery in Russia. They feature advanced infrastructure, cutting-edge technology, and highly skilled medical professionals who specialize in various fields, ensuring comprehensive and personalized care for patients.
These hospitals have received recognition and awards for their excellence in medical services, patient satisfaction, research contributions, and innovations in healthcare. Their commitment to advancing medical knowledge, embracing technological advancements, and providing patient-centered care sets them apart as leaders in the healthcare industry.
When it comes to seeking medical care, these top hospitals in Russia are reliable choices for individuals looking for the best treatment options and outcomes. They are committed to improving the health and well-being of their patients, emphasizing the importance of quality healthcare in enhancing lives.
As healthcare continues to evolve, these hospitals will undoubtedly remain at the forefront of medical advancements, driving innovation and delivering exceptional care to the people of Russia. When faced with medical challenges, individuals can confidently rely on these hospitals to provide the highest level of medical expertise, state-of-the-art facilities, and compassionate patient care.
PLEASE NOTE: The medical/health information on our website is for information purposes and not a substitute for medical advice.
--- published by sunil kumar, latest medical tourism.

Best Hospitals For Cancer Treatment In Telangana | Top 10 H...

Best Hospitals For Cancer Treatment In Rajasthan | Top 10 H...

Best Hospitals For Cancer Treatment In Gujarat | Top 10 Hosp...

Best Hospitals For Liver Transplant In Assam | Top 10 Hospit...

Best Hospitals For Liver Transplant In Odisha | Top 10 Hospi...

Change Password

Please Enter Valid Email Id!
Invalid captcha.
Destinations
- International
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Cambridge Open

The Flaws and Human Harms of Animal Experimentation
Nonhuman animal (“animal”) experimentation is typically defended by arguments that it is reliable, that animals provide sufficiently good models of human biology and diseases to yield relevant information, and that, consequently, its use provides major human health benefits. I demonstrate that a growing body of scientific literature critically assessing the validity of animal experimentation generally (and animal modeling specifically) raises important concerns about its reliability and predictive value for human outcomes and for understanding human physiology. The unreliability of animal experimentation across a wide range of areas undermines scientific arguments in favor of the practice. Additionally, I show how animal experimentation often significantly harms humans through misleading safety studies, potential abandonment of effective therapeutics, and direction of resources away from more effective testing methods. The resulting evidence suggests that the collective harms and costs to humans from animal experimentation outweigh potential benefits and that resources would be better invested in developing human-based testing methods.
Introduction
Annually, more than 115 million animals are used worldwide in experimentation or to supply the biomedical industry. 1 Nonhuman animal (hereafter “animal”) experimentation falls under two categories: basic (i.e., investigation of basic biology and human disease) and applied (i.e., drug research and development and toxicity and safety testing). Regardless of its categorization, animal experimentation is intended to inform human biology and health sciences and to promote the safety and efficacy of potential treatments. Despite its use of immense resources, the animal suffering involved, and its impact on human health, the question of animal experimentation’s efficacy has been subjected to little systematic scrutiny. 2
Although it is widely accepted that medicine should be evidence based , animal experimentation as a means of informing human health has generally not been held, in practice, to this standard. This fact makes it surprising that animal experimentation is typically viewed as the default and gold standard of preclinical testing and is generally supported without critical examination of its validity. A survey published in 2008 of anecdotal cases and statements given in support of animal experimentation demonstrates how it has not and could not be validated as a necessary step in biomedical research, and the survey casts doubt on its predictive value. 3 I show that animal experimentation is poorly predictive of human outcomes, 4 that it is unreliable across a wide category of disease areas, 5 and that existing literature demonstrates the unreliability of animal experimentation, thereby undermining scientific arguments in its favor. I further show that the collective harms that result from an unreliable practice tip the ethical scale of harms and benefits against continuation in much, if not all, of experimentation involving animals. 6
Problems of Successful Translation to Humans of Data from Animal Experimentation
Although the unreliability and limitations of animal experimentation have increasingly been acknowledged, there remains a general confidence within much of the biomedical community that they can be overcome. 7 However, three major conditions undermine this confidence and explain why animal experimentation, regardless of the disease category studied, fails to reliably inform human health: (1) the effects of the laboratory environment and other variables on study outcomes, (2) disparities between animal models of disease and human diseases, and (3) species differences in physiology and genetics. I argue for the critical importance of each of these conditions.
The Influence of Laboratory Procedures and Environments on Experimental Results
Laboratory procedures and conditions exert influences on animals’ physiology and behaviors that are difficult to control and that can ultimately impact research outcomes. Animals in laboratories are involuntarily placed in artificial environments, usually in windowless rooms, for the duration of their lives. Captivity and the common features of biomedical laboratories—such as artificial lighting, human-produced noises, and restricted housing environments—can prevent species-typical behaviors, causing distress and abnormal behaviors among animals. 8 Among the types of laboratory-generated distress is the phenomenon of contagious anxiety. 9 Cortisone levels rise in monkeys watching other monkeys being restrained for blood collection. 10 Blood pressure and heart rates elevate in rats watching other rats being decapitated. 11 Routine laboratory procedures, such as catching an animal and removing him or her from the cage, in addition to the experimental procedures, cause significant and prolonged elevations in animals’ stress markers. 12 These stress-related changes in physiological parameters caused by the laboratory procedures and environments can have significant effects on test results. 13 Stressed rats, for example, develop chronic inflammatory conditions and intestinal leakage, which add variables that can confound data. 14
A variety of conditions in the laboratory cause changes in neurochemistry, genetic expression, and nerve regeneration. 15 In one study, for example, mice were genetically altered to develop aortic defects. Yet, when the mice were housed in larger cages, those defects almost completely disappeared. 16 Providing further examples, typical noise levels in laboratories can damage blood vessels in animals, and even the type of flooring on which animals are tested in spinal cord injury experiments can affect whether a drug shows a benefit. 17
In order to control for potential confounders, some investigators have called for standardization of laboratory settings and procedures. 18 One notable effort was made by Crabbe et al. in their investigation of the potential confounding influences of the laboratory environment on six mouse behaviors that are commonly studied in neurobehavioral experiments. Despite their “extraordinary lengths to equate test apparatus, testing protocols, and all possible features of animal husbandry” across three laboratories, there were systematic differences in test results in these labs. 19 Additionally, different mouse strains varied markedly in all behavioral tests, and for some tests the magnitude of genetic differences depended on the specific testing laboratory. The results suggest that there are important influences of environmental conditions and procedures specific to individual laboratories that can be difficult—perhaps even impossible—to eliminate. These influences can confound research results and impede extrapolation to humans.
The Discordance between Human Diseases and Animal Models of Diseases
The lack of sufficient congruence between animal models and human diseases is another significant obstacle to translational reliability. Human diseases are typically artificially induced in animals, but the enormous difficulty of reproducing anything approaching the complexity of human diseases in animal models limits their usefulness. 20 Even if the design and conduct of an animal experiment are sound and standardized, the translation of its results to the clinic may fail because of disparities between the animal experimental model and the human condition. 21
Stroke research presents one salient example of the difficulties in modeling human diseases in animals. Stroke is relatively well understood in its underlying pathology. Yet accurately modeling the disease in animals has proven to be an exercise in futility. To address the inability to replicate human stroke in animals, many assert the need to use more standardized animal study design protocols. This includes the use of animals who represent both genders and wide age ranges, who have comorbidities and preexisting conditions that occur naturally in humans, and who are consequently given medications that are indicated for human patients. 22 In fact, a set of guidelines, named STAIR, was implemented by a stroke roundtable in 1999 (and updated in 2009) to standardize protocols, limit the discrepancies, and improve the applicability of animal stroke experiments to humans. 23 One of the most promising stroke treatments later to emerge was NXY-059, which proved effective in animal experiments. However, the drug failed in clinical trials, despite the fact that the set of animal experiments on this drug was considered the poster child for the new experimental standards. 24 Despite such vigorous efforts, the development of STAIR and other criteria has yet to make a recognizable impact in clinical translation. 25
Under closer scrutiny, it is not difficult to surmise why animal stroke experiments fail to successfully translate to humans even with new guidelines. Standard stroke medications will likely affect different species differently. There is little evidence to suggest that a female rat, dog, or monkey sufficiently reproduces the physiology of a human female. Perhaps most importantly, reproducing the preexisting conditions of stroke in animals proves just as difficult as reproducing stroke pathology and outcomes. For example, most animals don’t naturally develop significant atherosclerosis, a leading contributor to ischemic stroke. In order to reproduce the effects of atherosclerosis in animals, researchers clamp their blood vessels or artificially insert blood clots. These interventions, however, do not replicate the elaborate pathology of atherosclerosis and its underlying causes. Reproducing human diseases in animals requires reproducing the predisposing diseases, also a formidable challenge. The inability to reproduce the disease in animals so that it is congruent in relevant respects with human stroke has contributed to a high failure rate in drug development. More than 114 potential therapies initially tested in animals failed in human trials. 26
Further examples of repeated failures based on animal models include drug development in cancer, amyotrophic lateral sclerosis (ALS), traumatic brain injury (TBI), Alzheimer’s disease (AD), and inflammatory conditions. Animal cancer models in which tumors are artificially induced have been the basic translational model used to study key physiological and biochemical properties in cancer onset and propagation and to evaluate novel treatments. Nevertheless, significant limitations exist in the models’ ability to faithfully mirror the complex process of human carcinogenesis. 27 These limitations are evidenced by the high (among the highest of any disease category) clinical failure rate of cancer drugs. 28 Analyses of common mice ALS models demonstrate significant differences from human ALS. 29 The inability of animal ALS models to predict beneficial effects in humans with ALS is recognized. 30 More than twenty drugs have failed in clinical trials, and the only U.S. Food and Drug Administration (FDA)–approved drug to treat ALS is Riluzole, which shows notably marginal benefit on patient survival. 31 Animal models have also been unable to reproduce the complexities of human TBI. 32 In 2010, Maas et al. reported on 27 large Phase 3 clinical trials and 6 unpublished trials in TBI that all failed to show human benefit after showing benefit in animals. 33 Additionally, even after success in animals, around 172 and 150 drug development failures have been identified in the treatment of human AD 34 and inflammatory diseases, 35 respectively.
The high clinical failure rate in drug development across all disease categories is based, at least in part, on the inability to adequately model human diseases in animals and the poor predictability of animal models. 36 A notable systematic review, published in 2007, compared animal experimentation results with clinical trial findings across interventions aimed at the treatment of head injury, respiratory distress syndrome, osteoporosis, stroke, and hemorrhage. 37 The study found that the human and animal results were in accordance only half of the time. In other words, the animal experiments were no more likely than a flip of the coin to predict whether those interventions would benefit humans.
In 2004, the FDA estimated that 92 percent of drugs that pass preclinical tests, including “pivotal” animal tests, fail to proceed to the market. 38 More recent analysis suggests that, despite efforts to improve the predictability of animal testing, the failure rate has actually increased and is now closer to 96 percent. 39 The main causes of failure are lack of effectiveness and safety problems that were not predicted by animal tests. 40
Usually, when an animal model is found wanting, various reasons are proffered to explain what went wrong—poor methodology, publication bias, lack of preexisting disease and medications, wrong gender or age, and so on. These factors certainly require consideration, and recognition of each potential difference between the animal model and the human disease motivates renewed efforts to eliminate these differences. As a result, scientific progress is sometimes made by such efforts. However, the high failure rate in drug testing and development, despite attempts to improve animal testing, suggests that these efforts remain insufficient to overcome the obstacles to successful translation that are inherent to the use of animals. Too often ignored is the well-substantiated idea that these models are, for reasons summarized here, intrinsically lacking in relevance to, and thus highly unlikely to yield useful information about, human diseases. 41
Interspecies Differences in Physiology and Genetics
Ultimately, even if considerable congruence were shown between an animal model and its corresponding human disease, interspecies differences in physiology, behavior, pharmacokinetics, and genetics would significantly limit the reliability of animal studies, even after a substantial investment to improve such studies. In spinal cord injury, for example, drug testing results vary according to which species and even which strain within a species is used, because of numerous interspecies and interstrain differences in neurophysiology, anatomy, and behavior. 42 The micropathology of spinal cord injury, injury repair mechanisms, and recovery from injury varies greatly among different strains of rats and mice. A systematic review found that even among the most standardized and methodologically superior animal experiments, testing results assessing the effectiveness of methylprednisolone for spinal cord injury treatment varied considerably among species. 43 This suggests that factors inherent to the use of animals account for some of the major differences in results.
Even rats from the same strain but purchased from different suppliers produce different test results. 44 In one study, responses to 12 different behavioral measures of pain sensitivity, which are important markers of spinal cord injury, varied among 11 strains of mice, with no clear-cut patterns that allowed prediction of how each strain would respond. 45 These differences influenced how the animals responded to the injury and to experimental therapies. A drug might be shown to help one strain of mice recover but not another. Despite decades of using animal models, not a single neuroprotective agent that ameliorated spinal cord injury in animal tests has proven efficacious in clinical trials to date. 46
Further exemplifying the importance of physiological differences among species, a 2013 study reported that the mouse models used extensively to study human inflammatory diseases (in sepsis, burns, infection, and trauma) have been misleading. The study found that mice differ greatly from humans in their responses to inflammatory conditions. Mice differed from humans in what genes were turned on and off and in the timing and duration of gene expression. The mouse models even differed from one another in their responses. The investigators concluded that “our study supports higher priority to focus on the more complex human conditions rather than relying on mouse models to study human inflammatory disease.” 47 The different genetic responses between mice and humans are likely responsible, at least in part, for the high drug failure rate. The authors stated that every one of almost 150 clinical trials that tested candidate agents’ ability to block inflammatory responses in critically ill patients failed.
Wide differences have also become apparent in the regulation of the same genes, a point that is readily seen when observing differences between human and mouse livers. 48 Consistent phenotypes (observable physical or biochemical characteristics) are rarely obtained by modification of the same gene, even among different strains of mice. 49 Gene regulation can substantially differ among species and may be as important as the presence or absence of a specific gene. Despite the high degree of genome conservation, there are critical differences in the order and function of genes among species. To use an analogy: as pianos have the same keys, humans and other animals share (largely) the same genes. Where we mostly differ is in the way the genes or keys are expressed. For example, if we play the keys in a certain order, we hear Chopin; in a different order, we hear Ray Charles; and in yet a different order, it’s Jerry Lee Lewis. In other words, the same keys or genes are expressed, but their different orders result in markedly different outcomes.
Recognizing the inherent genetic differences among species as a barrier to translation, researches have expressed considerable enthusiasm for genetically modified (GM) animals, including transgenic mice models, wherein human genes are inserted into the mouse genome. However, if a human gene is expressed in mice, it will likely function differently from the way it functions in humans, being affected by physiological mechanisms that are unique in mice. For example, a crucial protein that controls blood sugar in humans is missing in mice. 50 When the human gene that makes this protein was expressed in genetically altered mice, it had the opposite effect from that in humans: it caused loss of blood sugar control in mice. Use of GM mice has failed to successfully model human diseases and to translate into clinical benefit across many disease categories. 51 Perhaps the primary reason why GM animals are unlikely to be much more successful than other animal models in translational medicine is the fact that the “humanized” or altered genes are still in nonhuman animals.
In many instances, nonhuman primates (NHPs) are used instead of mice or other animals, with the expectation that NHPs will better mimic human results. However, there have been sufficient failures in translation to undermine this optimism. For example, NHP models have failed to reproduce key features of Parkinson’s disease, both in function and in pathology. 52 Several therapies that appeared promising in both NHPs and rat models of Parkinson’s disease showed disappointing results in humans. 53 The campaign to prescribe hormone replacement therapy (HRT) in millions of women to prevent cardiovascular disease was based in large part on experiments on NHPs. HRT is now known to increase the risk of these diseases in women. 54
HIV/AIDS vaccine research using NHPs represents one of the most notable failures in animal experimentation translation. Immense resources and decades of time have been devoted to creating NHP (including chimpanzee) models of HIV. Yet all of about 90 HIV vaccines that succeeded in animals failed in humans. 55 After HIV vaccine gp120 failed in clinical trials, despite positive outcomes in chimpanzees, a BMJ article commented that important differences between NHPs and humans with HIV misled researchers, taking them down unproductive experimental paths. 56 Gp120 failed to neutralize HIV grown and tested in cell culture. However, because the serum protected chimpanzees from HIV infection, two Phase 3 clinical trials were undertaken 57 —a clear example of how expectations that NHP data are more predictive than data from other (in this case, cell culture) testing methods are unproductive and harmful. Despite the repeated failures, NHPs (though not chimpanzees or other great apes) remain widely used for HIV research.
The implicit assumption that NHP (and indeed any animal) data are reliable has also led to significant and unjustifiable human suffering. For example, clinical trial volunteers for gp120 were placed at unnecessary risk of harm because of unfounded confidence in NHP experiments. Two landmark studies involving thousands of menopausal women being treated with HRT were terminated early because of increased stroke and breast cancer risk. 58 In 2003, Elan Pharmaceuticals was forced to prematurely terminate a Phase 2 clinical trial when an investigational AD vaccine was found to cause brain swelling in human subjects. No significant adverse effects were detected in GM mice or NHPs. 59
In another example of human suffering resulting from animal experimentation, six human volunteers were injected with an immunomodulatory drug, TGN 1412, in 2006. 60 Within minutes of receiving the experimental drug, all volunteers suffered a severe adverse reaction resulting from a life-threatening cytokine storm that led to catastrophic systemic organ failure. The compound was designed to dampen the immune system, but it had the opposite effect in humans. Prior to this first human trial, TGN 1412 was tested in mice, rabbits, rats, and NHPs with no ill effects. NHPs also underwent repeat-dose toxicity studies and were given 500 times the human dose for at least four consecutive weeks. 61 None of the NHPs manifested the ill effects that humans showed almost immediately after receiving minute amounts of the test drug. Cynomolgus and rhesus monkeys were specifically chosen because their CD28 receptors demonstrated similar affinity to TGN 1412 as human CD28 receptors. Based on such data as these, it was confidently concluded that results obtained from these NHPs would most reliably predict drug responses in humans—a conclusion that proved devastatingly wrong.
As exemplified by the study of HIV/AIDS, TGN 1412, and other experiences, 62 experiments with NHPs are not necessarily any more predictive of human responses than experiments with other animals. The repeated failures in translation from studies with NHPs belie arguments favoring use of any nonhuman species to study human physiology and diseases and to test potential treatments. If experimentation using chimpanzees and other NHPs, our closest genetic cousins, are unreliable, how can we expect research using other animals to be reliable? The bottom line is that animal experiments, no matter the species used or the type of disease research undertaken, are highly unreliable—and they have too little predictive value to justify the resultant risks of harms for humans, for reasons I now explain.
The Collective Harms That Result from Misleading Animal Experiments
As medical research has explored the complexities and subtle nuances of biological systems, problems have arisen because the differences among species along these subtler biological dimensions far outweigh the similarities , as a growing body of evidence attests. These profoundly important—and often undetected—differences are likely one of the main reasons human clinical trials fail. 63
“Appreciation of differences” and “caution” about extrapolating results from animals to humans are now almost universally recommended. But, in practice, how does one take into account differences in drug metabolism, genetics, expression of diseases, anatomy, influences of laboratory environments, and species- and strain-specific physiologic mechanisms—and, in view of these differences, discern what is applicable to humans and what is not? If we cannot determine which physiological mechanisms in which species and strains of species are applicable to humans (even setting aside the complicating factors of different caging systems and types of flooring), the usefulness of the experiments must be questioned.
It has been argued that some information obtained from animal experiments is better than no information. 64 This thesis neglects how misleading information can be worse than no information from animal tests. The use of nonpredictive animal experiments can cause human suffering in at least two ways: (1) by producing misleading safety and efficacy data and (2) by causing potential abandonment of useful medical treatments and misdirecting resources away from more effective testing methods.
Humans are harmed because of misleading animal testing results. Imprecise results from animal experiments may result in clinical trials of biologically faulty or even harmful substances, thereby exposing patients to unnecessary risk and wasting scarce research resources. 65 Animal toxicity studies are poor predictors of toxic effects of drugs in humans. 66 As seen in some of the preceding examples (in particular, stroke, HRT, and TGN1412), humans have been significantly harmed because investigators were misled by the safety and efficacy profile of a new drug based on animal experiments. 67 Clinical trial volunteers are thus provided with raised hopes and a false sense of security because of a misguided confidence in efficacy and safety testing using animals.
An equal if indirect source of human suffering is the opportunity cost of abandoning promising drugs because of misleading animal tests. 68 As candidate drugs generally proceed down the development pipeline and to human testing based largely on successful results in animals 69 (i.e., positive efficacy and negative adverse effects), drugs are sometimes not further developed due to unsuccessful results in animals (i.e., negative efficacy and/or positive adverse effects). Because much pharmaceutical company preclinical data are proprietary and thus publicly unavailable, it is difficult to know the number of missed opportunities due to misleading animal experiments. However, of every 5,000–10,000 potential drugs investigated, only about 5 proceed to Phase 1 clinical trials. 70 Potential therapeutics may be abandoned because of results in animal tests that do not apply to humans. 71 Treatments that fail to work or show some adverse effect in animals because of species-specific influences may be abandoned in preclinical testing even if they may have proved effective and safe in humans if allowed to continue through the drug development pipeline.
An editorial in Nature Reviews Drug Discovery describes cases involving two drugs in which animal test results from species-specific influences could have derailed their development. In particular, it describes how tamoxifen, one of the most effective drugs for certain types of breast cancer, “would most certainly have been withdrawn from the pipeline” if its propensity to cause liver tumor in rats had been discovered in preclinical testing rather than after the drug had been on the market for years. 72 Gleevec provides another example of effective drugs that could have been abandoned based on misleading animal tests: this drug, which is used to treat chronic myelogenous leukemia (CML), showed serious adverse effects in at least five species tested, including severe liver damage in dogs. However, liver toxicity was not detected in human cell assays, and clinical trials proceeded, which confirmed the absence of significant liver toxicity in humans. 73 Fortunately for CML patients, Gleevec is a success story of predictive human-based testing. Many useful drugs that have safely been used by humans for decades, such as aspirin and penicillin, may not have been available today if the current animal testing regulatory requirements were in practice during their development. 74
A further example of near-missed opportunities is provided by experiments on animals that delayed the acceptance of cyclosporine, a drug widely and successfully used to treat autoimmune disorders and prevent organ transplant rejection. 75 Its immunosuppressive effects differed so markedly among species that researchers judged that the animal results limited any direct inferences that could be made to humans. Providing further examples, PharmaInformatic released a report describing how several blockbuster drugs, including aripiprazole (Abilify) and esomeprazole (Nexium), showed low oral bioavailability in animals. They would likely not be available on the market today if animal tests were solely relied on. Understanding the implications of its findings for drug development in general, PharmaInformatic asked, “Which other blockbuster drugs would be on the market today, if animal trials would have not been used to preselect compounds and drug-candidates for further development?” 76 These near-missed opportunities and the overall 96 percent failure rate in clinical drug testing strongly suggest the unsoundness of animal testing as a precondition of human clinical trials and provide powerful evidence for the need for a new, human-based paradigm in medical research and drug development.
In addition to potentially causing abandonment of useful treatments, use of an invalid animal disease model can lead researchers and the industry in the wrong research direction, wasting time and significant investment. 77 Repeatedly, researchers have been lured down the wrong line of investigation because of information gleaned from animal experiments that later proved to be inaccurate, irrelevant, or discordant with human biology. Some claim that we do not know which benefits animal experiments, particularly in basic research, may provide down the road. Yet human lives remain in the balance, waiting for effective therapies. Funding must be strategically invested in the research areas that offer the most promise.
The opportunity costs of continuing to fund unreliable animal tests may impede development of more accurate testing methods. Human organs grown in the lab, human organs on a chip, cognitive computing technologies, 3D printing of human living tissues, and the Human Toxome Project are examples of new human-based technologies that are garnering widespread enthusiasm. The benefit of using these testing methods in the preclinical setting over animal experiments is that they are based on human biology. Thus their use eliminates much of the guesswork required when attempting to extrapolate physiological data from other species to humans. Additionally, these tests offer whole-systems biology, in contrast to traditional in vitro techniques. Although they are gaining momentum, these human-based tests are still in their relative infancy, and funding must be prioritized for their further development. The recent advancements made in the development of more predictive, human-based systems and biological approaches in chemical toxicological testing are an example of how newer and improved tests have been developed because of a shift in prioritization. 78 Apart from toxicology, though, financial investment in the development of human-based technologies generally falls far short of investment in animal experimentation. 79
The unreliability of applying animal experimental results to human biology and diseases is increasingly recognized. Animals are in many respects biologically and psychologically similar to humans, perhaps most notably in the shared characteristics of pain, fear, and suffering. 80 In contrast, evidence demonstrates that critically important physiological and genetic differences between humans and other animals can invalidate the use of animals to study human diseases, treatments, pharmaceuticals, and the like. In significant measure, animal models specifically, and animal experimentation generally, are inadequate bases for predicting clinical outcomes in human beings in the great bulk of biomedical science. As a result, humans can be subject to significant and avoidable harm.
The data showing the unreliability of animal experimentation and the resultant harms to humans (and nonhumans) undermine long-standing claims that animal experimentation is necessary to enhance human health and therefore ethically justified. Rather, they demonstrate that animal experimentation poses significant costs and harms to human beings. It is possible—as I have argued elsewhere—that animal research is more costly and harmful, on the whole, than it is beneficial to human health. 81 When considering the ethical justifiability of animal experiments, we should ask if it is ethically acceptable to deprive humans of resources, opportunity, hope, and even their lives by seeking answers in what may be the wrong place. In my view, it would be better to direct resources away from animal experimentation and into developing more accurate, human-based technologies.
Aysha Akhtar , M.D., M.P.H., is a neurologist and preventive medicine specialist and Fellow at the Oxford Centre for Animal Ethics, Oxford, United Kingdom.
1. Taylor K, Gordon N, Langley G, Higgins W. Estimates for worldwide laboratory animal use in 2005 . Alternatives to Laboratory Animals 2008; 36 :327–42. [ PubMed ] [ Google Scholar ]
2. Systematic reviews that have been conducted generally reveal the unreliability and poor predictability of animal tests. See Perel P, Roberts I, Sena E, Wheble P, Briscoe C, Sandercock P, et al. Comparison of treatment effects between animal experiments and clinical trials: Systematic review. BMJ 2007;334:197. See also Pound P, Bracken MB. Is animal research sufficiently evidence based to be a cornerstone of biomedical research? BMJ 2014;348:g3387. See Godlee F. How predictive and productive is animal research? BMJ 2014;348:g3719. See Benatar M. Lost in translation: Treatment trials in the SOD 1 mouse and in human ALS. Neurobiology Disease 2007; 26 :1–13 [ PubMed ] [ Google Scholar ] . And see Akhtar AZ, Pippin JJ, Sandusky CB. Animal studies in spinal cord injury: A systematic review of methylprednisolone . Alternatives to Laboratory Animals 2009; 37 :43–62. [ PubMed ] [ Google Scholar ]
3. Mathews RAJ. Medical progress depends on animal models—doesn’t it? Journal of the Royal Society of Medicine 2008; 101 :95–8. [ PMC free article ] [ PubMed ] [ Google Scholar ]
4. See Shanks N, Greek R, Greek J. Are animal models predictive for humans? Philosophy, Ethics, and Humanities in Medicine 2009; 4 :2 [ PMC free article ] [ PubMed ] [ Google Scholar ] . See also Wall RJ, Shani M. Are animal models as good as we think? Theriogenology 2008; 69 :2–9. [ PubMed ] [ Google Scholar ]
5. See note 3, Mathews 2008. See also Hartung T, Zurlo J. Food for thought… alternative approaches for medical countermeasures to biological and chemical terrorism and warfare . ALTEX 2012; 29 :251–60 [ PubMed ] [ Google Scholar ] . See Leist M, Hartung T. Inflammatory findings on species extrapolations: Humans are definitely no 70-kg mice . Archives in Toxicology 2013; 87 :563–7 [ PMC free article ] [ PubMed ] [ Google Scholar ] . See Mak IWY, Evaniew N, Ghert M. Lost in translation: Animal models and clinical trials in cancer treatment . American Journal in Translational Research 2014; 6 :114–18 [ PMC free article ] [ PubMed ] [ Google Scholar ] . And see Pippin J. Animal research in medical sciences: Seeking a convergence of science, medicine, and animal law . South Texas Law Review 2013; 54 :469–511. [ Google Scholar ]
6. For an overview of the harms-versus-benefits argument, see LaFollette H. Animal experimentation in biomedical research In: Beauchamp TL, Frey RG, eds. The Oxford Handbook of Animal Ethics . Oxford: Oxford University Press; 2011:812–18. [ Google Scholar ]
7. See Jucker M. The benefits and limitations of animal models for translational research in neurodegenerative diseases . Nature Medicine 2010; 16 :1210–14 [ PubMed ] [ Google Scholar ] . See Institute of Medicine. Improving the Utility and Translation of Animal Models for Nervous System Disorders: Workshop Summary. Washington, DC: The National Academies Press; 2013. And see Degryse AL, Lawson WE. Progress towards improving animal models for IPF . American Journal of Medical Science 2011; 341 :444–9. [ PMC free article ] [ PubMed ] [ Google Scholar ]
8. See Morgan KN, Tromborg CT. Sources of stress in captivity . Applied Animal Behaviour Science 2007; 102 :262–302 [ Google Scholar ] . See Hart PC, Bergner CL, Dufour BD, Smolinsky AN, Egan RJ, LaPorte L, et al. Analysis of abnormal repetitive behaviors in experimental animal models In Warrick JE, Kauleff AV, eds. Translational Neuroscience and Its Advancement of Animal Research Ethics . New York: Nova Science; 2009:71–82 [ Google Scholar ] . See Lutz C, Well A, Novak M. Stereotypic and self-injurious behavior in rhesus macaques: A survey and retrospective analysis of environment and early experience . American Journal of Primatology 2003; 60 :1–15 [ PubMed ] [ Google Scholar ] . And see Balcombe JP, Barnard ND, Sandusky C. Laboratory routines cause animal stress . Contemporary Topics in Laboratory Animal Science 2004; 43 :42–51. [ PubMed ] [ Google Scholar ]
9. Suckow MA, Weisbroth SH, Franklin CL. The Laboratory Rat . 2nd ed. Burlington, MA: Elsevier Academic Press; 2006, at 323.
10. Flow BL, Jaques JT. Effect of room arrangement and blood sample collection sequence on serum thyroid hormone and cortisol concentrations in cynomolgus macaques ( Macaca fascicularis ). Contemporary Topics in Laboratory Animal Science 1997;36:65–8.
11. See note 8, Balcombe et al. 2004.
12. See note 8, Balcombe et al. 2004.
13. Baldwin A, Bekoff M. Too stressed to work. New Scientist 2007;194:24.
14. See note 13, Baldwin, Bekoff 2007.
15. Akhtar A, Pippin JJ, Sandusky CB. Animal models in spinal cord injury: A review . Reviews in the Neurosciences 2008; 19 :47–60. [ PubMed ] [ Google Scholar ]
16. See note 13, Baldwin, Bekoff 2007.
17. See note 15, Akhtar et al. 2008.
18. See Macleod MR, O’Collins T, Howells DW, Donnan GA. Pooling of animal experimental data reveals influence of study design and publication bias . Stroke 2004; 35 :1203–8 [ PubMed ] [ Google Scholar ] . See also O’ Neil BJ, Kline JA, Burkhart K, Younger J. Research fundamentals: V. The use of laboratory animal models in research. Academic Emergency Medicine 1999;6:75–82.
19. Crabbe JC, Wahlsten D, Dudek BC. Genetics of mouse behavior: Interactions with laboratory environment . Science 1999; 284 :1670–2, at 1670. [ PubMed ] [ Google Scholar ]
20. See Curry SH. Why have so many drugs with stellar results in laboratory stroke models failed in clinical trials? A theory based on allometric relationships. Annals of the New York Academy of Sciences 2003;993:69–74. See also Dirnagl U. Bench to bedside: The quest for quality in experimental stroke research . Journal of Cerebral Blood Flow & Metabolism 2006; 26 :1465–78 [ PubMed ] [ Google Scholar ] .
21. van der Worp HB, Howells DW, Sena ES, Poritt MJ, Rewell S, O’Collins V, et al. Can animal models of disease reliably inform human studies? PLoS Medicine 2010; 7 :e1000245. [ PMC free article ] [ PubMed ] [ Google Scholar ] .
22. See note 20, Dirnagl 2006. See also Sena E, van der Worp B, Howells D, Macleod M. How can we improve the pre-clinical development of drugs for stroke? Trends in Neurosciences 2007; 30 :433–9. [ PubMed ] [ Google Scholar ]
23. See Gawrylewski A. The trouble with animal models: Why did human trials fail? The Scientist 2007;21:44. See also Fisher M, Feuerstein G, Howells DW, Hurn PD, Kent TA, Savitz SI, et al. Update of the stroke therapy academic industry roundtable preclinical recommendations . Stroke 2009; 40 :2244–50. [ PMC free article ] [ PubMed ] [ Google Scholar ]
24. See note 23, Gawrylewski 2007. There is some dispute as to how vigorously investigators adhered to the suggested criteria. Nevertheless, NXY-059 animal studies were considered an example of preclinical studies that most faithfully adhered to the STAIR criteria. For further discussion see also Wang MM, Guohua X, Keep RF. Should the STAIR criteria be modified for preconditioning studies? Translational Stroke Research 2013; 4 :3–14 [ PMC free article ] [ PubMed ] [ Google Scholar ] .
25. See note 24, Wang et al. 2013.
26. O’Collins VE, Macleod MR, Donnan GA, Horky LL, van der Worp BH, Howells DW. 1,026 experimental treatments in acute stroke . Annals of Neurology 2006; 59 :467–7 [ PubMed ] [ Google Scholar ] .
27. See note 5, Mak et al. 2014.
28. See note 5, Mak et al. 2014.
29. See Perrin S. Preclinical research: Make mouse studies work . Nature 2014; 507 :423–5 [ PubMed ] [ Google Scholar ] . See also, generally, Wilkins HM, Bouchard RJ, Lorenzon NM, Linseman DA. Poor correlation between drug efficacies in the mutant SOD1 mouse mode versus clinical trials of ALS necessitates the development of novel animal models for sporadic motor neuron disease. In: Costa A, Villalba E, eds. Horizons in Neuroscience Research. Vol. 5. Hauppauge, NY: Nova Science; 2011:1–39.
30. Traynor BJ, Bruijn L, Conwit R, Beal F, O’Neill G, Fagan SC, et al. Neuroprotective agents for clinical trials in ALS: A systematic assessment . Neurology 2006; 67 :20–7 [ PubMed ] [ Google Scholar ] .
31. Sinha G. Another blow for ALS . Nature Biotechnology 2013; 31 :185 [ Google Scholar ] . See also note 30, Traynor et al. 2006.
32. See Morales DM, Marklund N, Lebold D, Thompson HJ, Pitkanen A, Maxwell WL, et al. Experimental models of traumatic brain injury: Do we really need a better mousetrap? Neuroscience 2005; 136 :971–89 [ PubMed ] [ Google Scholar ] . See also Xiong YE, Mahmood A, Chopp M. Animal models of traumatic brain injury . Nature Reviews Neuroscience 2013; 14 :128–42 [ PMC free article ] [ PubMed ] [ Google Scholar ] . And see commentary by Farber: Farber N. Drug development in brain injury. International Brain Injury Association ; available at http://www.internationalbrain.org/articles/drug-development-in-traumatic-brain-injury/ (last accessed 7 Dec 2014).
33. Maas AI, Roozenbeek B, Manley GT. Clinical trials in traumatic brain injury: Past experience and current developments . Neurotherapeutics 2010; 7 :115–26. [ PMC free article ] [ PubMed ] [ Google Scholar ]
34. Schneider LS, Mangialasche F, Andreasen N, Feldman H, Giacobini E, Jones R, et al. Clinical trials and late-stage drug development in Alzheimer’s disease: An appraisal from 1984 to 2014 . Journal of Internal Medicine 2014; 275 :251–83 [ PMC free article ] [ PubMed ] [ Google Scholar ] .
35. Seok J, Warren HS, Cuenca AG, Mindrinos MN, Baker HV, Xu W, et al. Genomic responses in mouse models poorly mimic human inflammatory diseases . Proceedings of the National Academy of Sciences USA 2013; 110 :3507–12. [ PMC free article ] [ PubMed ] [ Google Scholar ]
36. Palfreyman MG, Charles V, Blander J. The importance of using human-based models in gene and drug discovery . Drug Discovery World 2002. Fall:33–40 [ Google Scholar ] .
37. See note 2, Perel et al. 2007.
38. Harding A. More compounds failing phase I. The Scientist 2004 Sept 13; available at http://www.the-scientist.com/?articles.view/articleNo/23003/title/More-compounds-failing-Phase-I/ (last accessed 2 June 2014).
39. See note 5, Pippin 2013.
40. See note 5, Hartung, Zurlo 2012.
41. Wiebers DO, Adams HP, Whisnant JP. Animal models of stroke: Are they relevant to human disease? Stroke 1990; 21 :1–3. [ PubMed ] [ Google Scholar ]
42. See note 15, Akhtar et al. 2008.
43. See note 2, Akhtar et al. 2009.
44. Lonjon N, Prieto M, Haton H, Brøchner CB, Bauchet L, Costalat V, et al. Minimum information about animal experiments: Supplier is also important . Journal of Neuroscience Research 2009; 87 :403–7. [ PubMed ] [ Google Scholar ]
45. Mogil JS, Wilson SG, Bon K, Lee SE, Chung K, Raber P, et al. Heritability of nociception I: Responses of 11 inbred mouse strains on 12 measures of nociception . Pain 1999; 80 :67–82. [ PubMed ] [ Google Scholar ]
46. Tator H, Hashimoto R, Raich A, Norvell D, Fehling MG, Harrop JS, et al. Translational potential of preclinical trials of neuroprotection through pharmacotherapy for spinal cord injury . Journal of Neurosurgery: Spine 2012; 17 :157–229. [ PubMed ] [ Google Scholar ]
47. See note 35, Seok et al. 2013, at 3507.
48. Odom DT, Dowell RD, Jacobsen ES, Gordon W, Danford TW, MacIsaac KD, et al. Tissue-specific transcriptional regulation has diverged significantly between human and mouse . Nature Genetics 2007; 39 :730–2 [ PMC free article ] [ PubMed ] [ Google Scholar ] .
49. Horrobin DF. Modern biomedical research: An internally self-consistent universe with little contact with medical reality? Nature Reviews Drug Discovery 2003; 2 :151–4. [ PubMed ] [ Google Scholar ]
50. Vassilopoulous S, Esk C, Hoshino S, Funke BH, Chen CY, Plocik AM, et al. A role for the CHC22 clathrin heavy-chain isoform in human glucose metabolism . Science 2009; 324 :1192–6. [ PMC free article ] [ PubMed ] [ Google Scholar ]
51. See Guttman-Yassky E, Krueger JG. Psoriasis: Evolution of pathogenic concepts and new therapies through phases of translational research . British Journal of Dermatology 2007; 157 :1103–15 [ PubMed ] [ Google Scholar ] . See also The mouse model: Less than perfect, still invaluable. Johns Hopkins Medicine ; available at http://www.hopkinsmedicine.org/institute_basic_biomedical_sciences/news_events/articles_and_stories/model_organisms/201010_mouse_model.html (last accessed 10 Dec 2014). See note 23, Gawrylewski 2007. See note 2, Benatar 2007. See note 29, Perrin 2014 and Wilkins et al. 2011. See Cavanaugh S, Pippin J, Barnard N. Animal models of Alzheimer disease: Historical pitfalls and a path forward. ALTEX online first; 2014 Apr 10. And see Woodroofe A, Coleman RA. ServiceNote: Human tissue research for drug discovery . Genetic Engineering and Biotechnology News 2007; 27 :18 [ Google Scholar ] .
52. Lane E, Dunnett S. Animal models of Parkinson’s disease and L-dopa induced dyskinesia: How close are we to the clinic? Psychopharmacology 2008; 199 :303–12. [ PubMed ] [ Google Scholar ]
53. See note 52, Lane, Dunnett 2008.
54. See note 5, Pippin 2013.
55. Bailey J. An assessment of the role of chimpanzees in AIDS vaccine research . Alternatives to Laboratory Animals 2008; 36 :381–428. [ PubMed ] [ Google Scholar ]
56. Tonks A. The quest for the AIDs vaccine . BMJ 2007; 334 :1346–8 [ PMC free article ] [ PubMed ] [ Google Scholar ] .
57. Johnston MI, Fauci AS. An HIV vaccine—evolving concepts . New England Journal of Medicine 2007; 356 :2073–81. [ PubMed ] [ Google Scholar ]
58. See Rossouw JE, Andersen GL, Prentice RL, LaCroix AZ, Kooperberf C, Stefanick ML, et al. Risks and benefits of estrogen plus progestin in healthy menopausal women: Principle results from the Women’s Health Initiative randomized controlled trial . JAMA 2002; 288 :321–33 [ PubMed ] [ Google Scholar ] . See also Andersen GL, Limacher A, Assaf AR, Bassford T, Beresford SA, Black H, et al. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: The Women’s Health Initiative randomized controlled trial . JAMA 2004; 291 :1701–12 [ PubMed ] [ Google Scholar ] .
59. Lemere CA. Developing novel immunogens for a safe and effective Alzheimer’s disease vaccine . Progress in Brain Research 2009; 175 :83. [ PMC free article ] [ PubMed ] [ Google Scholar ] .
60. Allen A. Of mice and men: The problems with animal testing. Slate 2006 June 1; available at http://www.slate.com/articles/health_and_science/medical_examiner/2006/06/of_mice_or_men.html (last accessed 10 Dec 2014).
61. Attarwala H. TGN1412: From discovery to disaster . Journal of Young Pharmacists 2010; 2 :332–6 [ PMC free article ] [ PubMed ] [ Google Scholar ] .
62. See Hogan RJ. Are nonhuman primates good models for SARS? PLoS Medicine 2006; 3 :1656–7 [ PMC free article ] [ PubMed ] [ Google Scholar ] . See also Bailey J. Non-human primates in medical research and drug development: A critical review . Biogenic Amines 2005; 19 :235–55. [ Google Scholar ]
63. See note 4, Wall, Shani 2008.
64. Lemon R, Dunnett SB. Surveying the literature from animal experiments: Critical reviews may be helpful—not systematic ones . BMJ 2005; 330 :977–8. [ PMC free article ] [ PubMed ] [ Google Scholar ]
65. Roberts I, Kwan I, Evans P, Haig S. Does animal experimentation inform human health care? Observations from a systematic review of international animal experiments on fluid resuscitation . BMJ 2002; 324 :474–6 [ PMC free article ] [ PubMed ] [ Google Scholar ] .
66. See note 60,Allen 2006. See also Heywood R. Target organ toxicity . Toxicology Letters 1981; 8 :349–58 [ PubMed ] [ Google Scholar ] . See Fletcher AP. Drug safety tests and subsequent clinical experience . Journal of the Royal Society of Medicine 1978; 71 :693–6. [ PMC free article ] [ PubMed ] [ Google Scholar ]
67. See note 60, Allen 2006. See note 5, Pippin 2013. See also Greek R, Greek J. Animal research and human disease . JAMA 2000; 283 :743–4 [ PubMed ] [ Google Scholar ] .
68. See note 60, Allen 2006. See also note 5, Leist, Hartung 2013.
69. Food and Drug Administration. Development & approval process (drugs); available at http://www.fda.gov/Drugs/DevelopmentApprovalProcess/ (last accessed 7 Dec 2014). See also http://www.fda.gov/drugs/resourcesforyou/consumers/ucm143534.htm (last accessed 7 Dec 2014).
70. Drug discovery pipeline. IRSF; available at http://www.rettsyndrome.org/research-programs/programmatic-overview/drug-discovery-pipeline (last accessed 24 Sept 2014).
71. See note 60, Allen 2006.
72. Follow the yellow brick road. Nature Reviews Drug Discovery 2003;2:167, at 167.
73. See note 5, Pippin 2013.
74. For data on aspirin, see Hartung T. Per aspirin as astra … Alternatives to Laboratory Animals 2009; 37 (Suppl 2 ):45–7 [ PubMed ] [ Google Scholar ] . See also note 5, Pippin 2013. For data on penicillin, see Koppanyi T, Avery MA. Species differences and the clinical trial of new drugs: A review . Clinical Pharmacology and Therapeutics 1966; 7 :250–70 [ PubMed ] [ Google Scholar ] . See also Schneierson SS, Perlman E. Toxicity of penicillin for the Syrian hamster . Proceedings of the Society for Experimental Biology and Medicine 1956; 91 :229–30. [ PubMed ] [ Google Scholar ]
75. See note 67, Greek, Greek 2000.
76. Oral bioavailability of blockbuster drugs in humans and animals. PharmaInformatic . available at http://www.pharmainformatic.com/html/blockbuster_drugs.html (last accessed 19 Sept 2014).
77. Sams-Dodd F. Strategies to optimize the validity of disease models in the drug discovery process . Drug Discovery Today 2006; 11 :355–63 [ PubMed ] [ Google Scholar ] .
78. Zurlo J. No animals harmed: Toward a paradigm shift in toxicity testing . Hastings Center Report 2012;42. Suppl:s23–6 [ PubMed ] [ Google Scholar ] .
79. There is no direct analysis of the amount of money spent on animal testing versus alternatives across all categories; however, in 2008 the Chronicle of Higher Education reported that funding of research involving animals (under basic research) of the National Institute of Health (NIH) remained steady at about 42 percent since 1990. See Monastersky R. Protesters fail to slow animal research. Chronicle of Higher Education 2008:54. In 2012, NIH director Francis Collins noted that the NIH’s support for basic research has held steady at 54 percent of the agency’s budget for decades. The remainder of the NIH’s budget is heavily funded toward clinical research, suggesting that preclinical human-based testing methods are much less funded. See also Wadman M. NIH director grilled over translational research centre. Nature News Blog 2012 Mar 20. Available at http://blogs.nature.com/news/2012/03/nih-director-grilled-over-translational-research-center.html (last accessed 5 Mar 2015). There is no data that suggests that the NIH’s funding of animal experimentation has decreased. A 2010 analysis estimates that at least 50 percent of the NIH’s extramural funding is directed into animal research; see Greek R, Greek J. Is the use of sentient animals in basic research justifiable? Philosophy, Ethics, and Humanities in Medicine 2010; 5 :14 [ PMC free article ] [ PubMed ] [ Google Scholar ] .
80. For a helpful discussion on animal pain, fear, and suffering, see DeGrazia D. Taking Animals Seriously: Mental Lives and Moral Status . New York: Cambridge University Press; 1996:116–23. [ Google Scholar ]
81. See Akhtar A. Animals and Public Health: Why Treating Animals Better Is Critical to Human Welfare . Hampshire, UK: Palgrave Macmillan; 2012:chap. 5.

IMAGES
VIDEO
COMMENTS
Many people have questions about animal testing ethics and the animal testing debate. We take our responsibility for the ethical treatment of animals in medical research very seriously. At Stanford, we emphasize that the humane care of laboratory animals is essential, both ethically and scientifically. Poor animal care is not good science.
Medical Progress and Biomedical Research The Nobel Laureates. Every Nobel Prize in Medicine awarded in the last three decades was dependent on data from animal models. Overall, 83% of the Nobel Prizes awarded for outstanding contributions to medicine have involved animal research since the program was founded in 1901, more than 100 years ago.
There is overwhelming scientific consensus worldwide that some animals are still needed in order to make medical progress. Where animals are used in research projects, they are used as part of a range of scientific techniques. These might include human trials, computer modelling, cell culture, statistical techniques, and others.
Animal Testing and Medicine. "The greatness of a nation and its moral progress can be judged by the way its animals are treated.". - Mahatma Gandhi. Animals have been used repeatedly throughout the history of biomedical research. Early Greek physician-scientists, such as Aristotle, (384 - 322 BC) and Erasistratus, (304 - 258 BC ...
Keywords: animal research, animal testing, alternative methods, animal replacement, New Approach Methodologies (NAMs) 1. Introduction. We believe that there is an urgent need to modernize medical research. We use this term to refer to the process of replacing animal experiments with techniques that have greater direct relevance to human ...
Abstract. The use of non-human animals in biomedical research has given important contributions to the medical progress achieved in our day, but it has also been a cause of heated public, scientific and philosophical discussion for hundreds of years. This review, with a mainly European outlook, addresses the history of animal use in biomedical ...
Nearly every medicine, medical device, surgical procedure or therapy we have today has depended on animal testing and research.
Animal testing, science, medicine, animal welfare, animal rights, ethics. Animal testing, also known as animal experimentation, animal research, and in vivo testing, is the use of non-human animals in experiments that seek to control the variables that affect the behavior or biological system under study. This approach can be contrasted with ...
Animal testing followed by human clinical trials currently remains the best way to examine complex physiological, neuroanatomical, reproductive, developmental and cognitive effects of drugs to determine if they are safe and effective for market approval. ... Modern medical research, including research using animals, is necessary to ...
Gene therapy aims to deliver healthy copies of these defective genes directly to the retina, to correct these genetic mistakes. MRC has been funding research into gene therapy for inherited eye diseases since 2004. Animal research in mice and dogs has been vital for establishing the necessary proof-of-concept for ocular gene therapy.
The phrase "animal testing" refers to the range of experiments performed on living animals for the purpose of studying diseases and biology, the effectiveness of newly developed pharmaceuticals and medications, and the safety of consumer products like cosmetics, cleaners, and food additives. In the context of biomedical research, animal ...
January 24, 2023 - While several different approaches are used during clinical research, traditional biomedical research involving animal testing to develop new treatments and drugs may be a strategy of the past after the FDA Modernization Act 2.0 was signed in December 2022. This act allows organizations to use scientifically rigorous, proven, non-animal testing methods, such as cell-based ...
History of Animal Testing. Animals are used to develop medical treatments, determine the toxicity of medications, check the safety of products destined for human use, and other biomedical, commercial, and health care uses. Research on living animals has been practiced since at least 500 BC. Descriptions of the dissection of live animals have ...
The main concept of animal testing is using animals in research and experiments for several purposes, including the safety and efficacy of drugs, advancing medical knowledge, and studying diseases. The aspects of the concept of animal testing are as follows: - Safety assessment. - Drug development. - Biomedical research.
If you've received a flu vaccine, or given your child cold medicine, you have directly benefited from animal research. If you've taken insulin for diabetes, received the polio vaccine ...
Ethical Considerations and Advances in the Understanding of Animal Cognition. Apprehension around burgeoning medical research in the late 1800s and the first half of the 20 th century sparked concerns over the use of humans and animals in research , .Suspicions around the use of humans were deepened with the revelation of several exploitive research projects, including a series of medical ...
The American Association of Laboratory Animal Science (AALAS) Foundation is a 501(c)(3) non-profit organization dedicated to the mission of informing the public about the caring professionals working in the field of biomedical research and the vital role of animals in that research. We understand the challenges and uncertainties that may accompany public outreach efforts in the field of ...
For animals, certain pour-on, injectable, paste, chewable, and "drench" ivermectin products are approved in the U.S. to treat or prevent parasites in animals.
The combination of clinical features was sufficient to diagnose COVID-19 infection, indicating that laboratory testing is not critical in real-life clinical practice. Age, male sex, and chronic comorbidities were risk factors for in-hospital mortality. ... 17 Medical Research Council Population Health Research Unit, Nuffield Department of ...
The research animal veterinary technician assists veterinarians in restraint, examination, and medical and surgical treatment of sick and injured animals. ... This position may assist or initiate preparation of animals for medical, surgical, diagnostic and research procedures, monitor animals during anesthesia, and provide post-operative care ...
International Regulations for Animal Exports (IRegs) IRegs provides exporters with our best understanding of importing countries' requirements for live animals, including hatching eggs and germplasm. Please select the country of destination from the drop-down menu below, and then click "View Requirements."
Discussion. The outcome portrays the essentiality of using animals to determine materials that would help the population to live healthily ().However, in the past few decades, the number of animals used for testing drugs has been steadily decreasing ().The data indicates that most of the medical research processes involving animal testing emanate from genetically oriented studies, which ...
The International Medical Cluster regularly hosts training seminars for doctors, nurses and hospital managers. Their main feature is the participation of foreign experts from clinics represented in the cluster. In 2021, our own educational center was opened. In February 2021, the International Medical Cluster hosted an educational center.
April 14 - 20, 2024, is Medical Laboratory Professionals Week, an annual celebration to highlight and show appreciation for laboratory professionals, including those at the State Hygienic Laboratory (SHL) at the University of Iowa. Lab Week is sponsored by the American Society for Clinical
Introduction. Animal model-based research has been performed for a very long time. Ever since the 5 th century B.C., reports of experiments involving animals have been documented, but an increase in the frequency of their utilization has been observed since the 19 th century [].Most institutions for medical research around the world use non-human animals as experimental subjects [].
Students can undergo a mandatory annual medical examination at the polyclinic. Diagnostic Medical Center №1, located at ul. Miklouho-Maclay 29 bldg. 2, provides round-the-clock emergency medical care for students living in University dormitory. Emergency phone number: + 7-495-330-80-65 (around the clock).
Pirogov National Medical and Surgical Center - Moscow. About Hospital: Pirogov National Medical and Surgical Center, located in Moscow, is renowned for its comprehensive medical services. With a legacy dating back to 1802, it combines rich traditions with cutting-edge technology, providing top-notch healthcare to patients.
Introduction. Annually, more than 115 million animals are used worldwide in experimentation or to supply the biomedical industry. 1 Nonhuman animal (hereafter "animal") experimentation falls under two categories: basic (i.e., investigation of basic biology and human disease) and applied (i.e., drug research and development and toxicity and safety testing).