- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board

Medicare Assignment: Everything You Need to Know
Medicare assignment.
- Providers Accepting Assignment
- Providers Who Do Not
- Billing Options
- Assignment of Benefits
- How to Choose
Frequently Asked Questions
Medicare assignment is an agreement between Medicare and medical providers (doctors, hospitals, medical equipment suppliers, etc.) in which the provider agrees to accept Medicare’s fee schedule as payment in full when Medicare patients are treated.
This article will explain how Medicare assignment works, and what you need to know in order to ensure that you won’t receive unexpected bills.
fizkes / Getty Images
There are 35 million Americans who have Original Medicare. Medicare is a federal program and most medical providers throughout the country accept assignment with Medicare. As a result, these enrollees have a lot more options for medical providers than most of the rest of the population.
They can see any provider who accepts assignment, anywhere in the country. They can be assured that they will only have to pay their expected Medicare cost-sharing (deductible and coinsurance, some or all of which may be paid by a Medigap plan , Medicaid, or supplemental coverage provided by an employer or former employer).
It’s important to note here that the rules are different for the 29 million Americans who have Medicare Advantage plans. These beneficiaries cannot simply use any medical provider who accepts Medicare assignment.
Instead, each Medicare Advantage plan has its own network of providers —much like the health insurance plans that many Americans are accustomed to obtaining from employers or purchasing in the exchange/marketplace .
A provider who accepts assignment with Medicare may or may not be in-network with some or all of the Medicare Advantage plans that offer coverage in a given area. Some Medicare Advantage plans— health maintenance organizations (HMOs) , in particular—will only cover an enrollee’s claims if they use providers who are in the plan's network.
Other Medicare Advantage plans— preferred provider organizations (PPOs) , in particular—will cover out-of-network care but the enrollee will pay more than they would have paid had they seen an in-network provider.
Original Medicare
The bottom line is that Medicare assignment only determines provider accessibility and costs for people who have Original Medicare. People with Medicare Advantage need to understand their own plan’s provider network and coverage rules.
When discussing Medicare assignment and access to providers in this article, keep in mind that it is referring to people who have Original Medicare.
How to Make Sure Your Provider Accepts Assignment
Most doctors, hospitals, and other medical providers in the United States do accept Medicare assignment.
Provider Participation Stats
According to the Centers for Medicare and Medicaid Services, 98% of providers participate in Medicare, which means they accept assignment.
You can ask the provider directly about their participation with Medicare. But Medicare also has a tool that you can use to find participating doctors, hospitals, home health care services, and other providers.
There’s a filter on that tool labeled “Medicare-approved payment.” If you turn on that filter, you will only see providers who accept Medicare assignment. Under each provider’s information, it will say “Charges the Medicare-approved amount (so you pay less out-of-pocket).”
What If Your Provider Doesn’t Accept Assignment?
If your medical provider or equipment supplier doesn’t accept assignment, it means they haven’t agreed to accept Medicare’s approved amounts as payment in full for all of the services.
These providers can still choose to accept assignment on a case-by-case basis. But because they haven’t agreed to accept Medicare assignment for all services, they are considered nonparticipating providers.
Note that "nonparticipating" does not mean that a provider has opted out of Medicare altogether. Medicare will still pay claims for services received from a nonparticipating provider (i.e., one who does not accept Medicare assignment), whereas Medicare does not cover any of the cost of services obtained from a provider who has officially opted out of Medicare.
If a Medicare beneficiary uses a provider who has opted out of Medicare, that person will pay the provider directly and Medicare will not be involved in any way.
Physicians Who Have Opted Out
Only about 1% of all non-pediatric physicians have opted out of Medicare.
For providers who have not opted out of Medicare but who also don’t accept assignment, Medicare will still pay nearly as much as it would have paid if you had used a provider who accepts assignment. Here’s how it works:
- Medicare will pay the provider 95% of the amount they would pay if the provider accepted assignment.
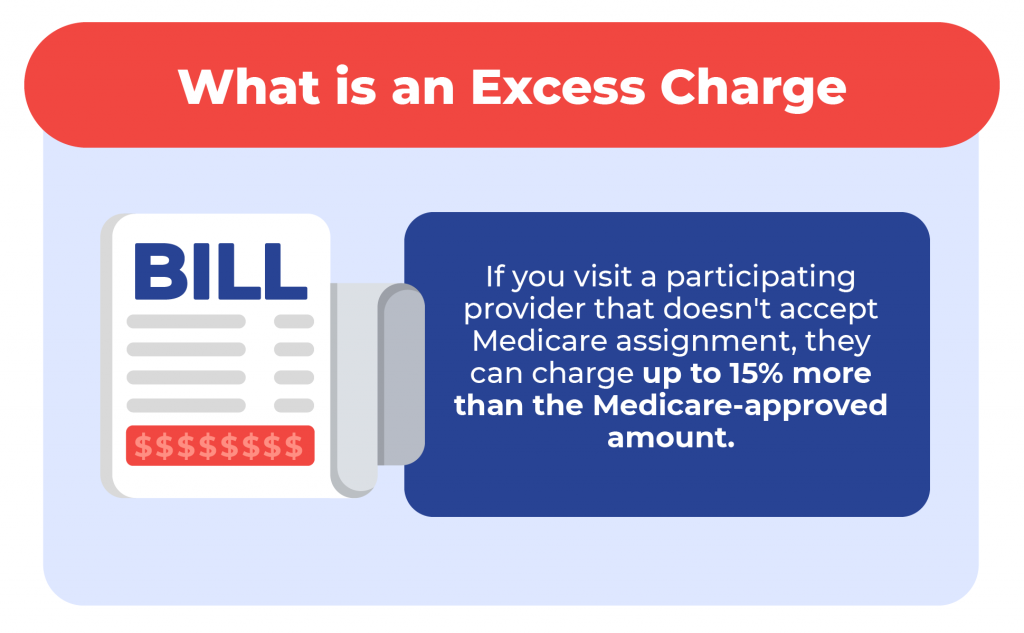
- The provider can charge the person receiving care more than the Medicare-approved amount, but only up to 15% more (some states limit this further). This extra amount, which the patient has to pay out-of-pocket, is known as the limiting charge . But the 15% cap does not apply to medical equipment suppliers; if they do not accept assignment with Medicare, there is no limit on how much they can charge the person receiving care. This is why it’s particularly important to make sure that the supplier accepts Medicare assignment if you need medical equipment.
- The nonparticipating provider may require the person receiving care to pay the entire bill up front and seek reimbursement from Medicare (using Form CMS 1490-S ). Alternatively, they may submit a claim to Medicare on behalf of the person receiving care (using Form CMS-1500 ).
- A nonparticipating provider can choose to accept assignment on a case-by-case basis. They can indicate this on Form CMS-1500 in box 27. The vast majority of nonparticipating providers who bill Medicare choose to accept assignment for the claim being billed.
- Nonparticipating providers do not have to bill your Medigap plan on your behalf.
Billing Options for Providers Who Accept Medicare
When a medical provider accepts assignment with Medicare, part of the agreement is that they will submit bills to Medicare on behalf of the person receiving care. So if you only see providers who accept assignment, you will never need to submit your own bills to Medicare for reimbursement.
If you have a Medigap plan that supplements your Original Medicare coverage, you should present the Medigap coverage information to the provider at the time of service. Medicare will forward the claim information to your Medigap insurer, reducing administrative work on your part.
Depending on the Medigap plan you have, the services that you receive, and the amount you’ve already spent in out-of-pocket costs, the Medigap plan may pay some or all of the out-of-pocket costs that you would otherwise have after Medicare pays its share.
(Note that if you have a type of Medigap plan called Medicare SELECT, you will have to stay within the plan’s network of providers in order to receive benefits. But this is not the case with other Medigap plans.)
After the claim is processed, you’ll be able to see details in your MyMedicare.gov account . Medicare will also send you a Medicare Summary Notice. This is Medicare’s version of an explanation of benefits (EOB) , which is sent out every three months.
If you have a Medigap plan, it should also send you an EOB or something similar, explaining the claim and whether the policy paid any part of it.
What Is Medicare Assignment of Benefits?
For Medicare beneficiaries, assignment of benefits means that the person receiving care agrees to allow a nonparticipating provider to bill Medicare directly (as opposed to having the person receiving care pay the bill up front and seek reimbursement from Medicare). Assignment of benefits is authorized by the person receiving care in Box 13 of Form CMS-1500 .
If the person receiving care refuses to assign benefits, Medicare can only reimburse the person receiving care instead of paying the nonparticipating provider directly.
Things to Consider Before Choosing a Provider
If you’re enrolled in Original Medicare, you have a wide range of options in terms of the providers you can use—far more than most other Americans. In most cases, your preferred doctor and other medical providers will accept assignment with Medicare, keeping your out-of-pocket costs lower than they would otherwise be, and reducing administrative hassle.
There may be circumstances, however, when the best option is a nonparticipating provider or even a provider who has opted out of Medicare altogether. If you choose one of these options, be sure you discuss the details with the provider before proceeding with the treatment.
You’ll want to understand how much is going to be billed and whether the provider will bill Medicare on your behalf if you agree to assign benefits (note that this is not possible if the provider has opted out of Medicare).
If you have supplemental coverage, you’ll also want to check with that plan to see whether it will still pick up some of the cost and, if so, how much you should expect to pay out of your own pocket.
A medical provider who accepts Medicare assignment is considered a participating provider. These providers have agreed to accept Medicare’s fee schedule as payment in full for services they provide to Medicare beneficiaries. Most doctors, hospitals, and other medical providers do accept Medicare assignment.
Nonparticipating providers are those who have not signed an agreement with Medicare to accept Medicare’s rates as payment in full. However, they can agree to accept assignment on a case-by-case basis, as long as they haven’t opted out of Medicare altogether. If they do not accept assignment, they can bill the patient up to 15% more than the Medicare-approved rate.
Providers who opt out of Medicare cannot bill Medicare and Medicare will not pay them or reimburse beneficiaries for their services. But there is no limit on how much they can bill for their services.
A Word From Verywell
It’s in your best interest to choose a provider who accepts Medicare assignment. This will keep your costs as low as possible, streamline the billing and claims process, and ensure that your Medigap plan picks up its share of the costs.
If you feel like you need help navigating the provider options or seeking care from a provider who doesn’t accept assignment, the Medicare State Health Insurance Assistance Program (SHIP) in your state may be able to help.
A doctor who does not accept Medicare assignment has not agreed to accept Medicare’s fee schedule as payment in full for their services. These doctors are considered nonparticipating with Medicare and can bill Medicare beneficiaries up to 15% more than the Medicare-approved amount.
They also have the option to accept assignment (i.e., accept Medicare’s rate as payment in full) on a case-by-case basis.
There are certain circumstances in which a provider is required by law to accept assignment. This includes situations in which the person receiving care has both Medicare and Medicaid. And it also applies to certain medical services, including lab tests, ambulance services, and drugs that are covered under Medicare Part B (as opposed to Part D).
In 2021, 98% of American physicians had participation agreements with Medicare, leaving only about 2% who did not accept assignment (either as a nonparticipating provider, or a provider who had opted out of Medicare altogether).
Accepting assignment is something that the medical provider does, whereas assignment of benefits is something that the patient (the Medicare beneficiary) does. To accept assignment means that the medical provider has agreed to accept Medicare’s approved fee as payment in full for services they provide.
Assignment of benefits means that the person receiving care agrees to allow a medical provider to bill Medicare directly, as opposed to having the person receiving care pay the provider and then seek reimbursement from Medicare.
Centers for Medicare and Medicaid Services. Medicare monthly enrollment .
Centers for Medicare and Medicaid Services. Annual Medicare participation announcement .
Centers for Medicare and Medicaid Services. Lower costs with assignment .
Centers for Medicare and Medicaid Services. Find providers who have opted out of Medicare .
Kaiser Family Foundation. How many physicians have opted-out of the Medicare program ?
Center for Medicare Advocacy. Durable medical equipment, prosthetics, orthotics, and supplies (DMEPOS) updates .
Centers for Medicare and Medicaid Services. Check the status of a claim .
Centers for Medicare and Medicaid Services. Medicare claims processing manual. Chapter 26 - completing and processing form CMS-1500 data set .
Centers for Medicare and Medicaid Services. Ambulance fee schedule .
Centers for Medicare and Medicaid Services. Prescription drugs (outpatient) .
By Louise Norris Norris is a licensed health insurance agent, book author, and freelance writer. She graduated magna cum laude from Colorado State University.
How long do Medicare enrollees wait for care? Learn about this and more in our Medicare resource center.
Popular Searches
AARP daily Crossword Puzzle
Hotels with AARP discounts
Life Insurance
AARP Dental Insurance Plans
Suggested Links
AARP MEMBERSHIP — $12 FOR YOUR FIRST YEAR WHEN YOU SIGN UP FOR AUTOMATIC RENEWAL
Get instant access to members-only products and hundreds of discounts, a free second membership, and a subscription to AARP the Magazine.
- right_container
Work & Jobs
Social Security
AARP en Español
- Membership & Benefits
AARP Rewards
- AARP Rewards %{points}%
Conditions & Treatments
Drugs & Supplements
Health Care & Coverage
Health Benefits

Staying Fit
Your Personalized Guide to Fitness

AARP Hearing Center
Ways To Improve Your Hearing

Brain Health Resources
Tools and Explainers on Brain Health

A Retreat For Those Struggling
Scams & Fraud
Personal Finance
Money Benefits

View and Report Scams in Your Area

AARP Foundation Tax-Aide
Free Tax Preparation Assistance

AARP Money Map
Get Your Finances Back on Track

How to Protect What You Collect
Small Business
Age Discrimination

Flexible Work
Freelance Jobs You Can Do From Home

AARP Skills Builder
Online Courses to Boost Your Career

31 Great Ways to Boost Your Career

ON-DEMAND WEBINARS
Tips to Enhance Your Job Search

Get More out of Your Benefits

When to Start Taking Social Security

10 Top Social Security FAQs

Social Security Benefits Calculator

Medicare Made Easy
Original vs. Medicare Advantage

Enrollment Guide
Step-by-Step Tool for First-Timers

Prescription Drugs
9 Biggest Changes Under New Rx Law

Medicare FAQs
Quick Answers to Your Top Questions
Care at Home
Financial & Legal
Life Balance

LONG-TERM CARE
Understanding Basics of LTC Insurance

State Guides
Assistance and Services in Your Area

Prepare to Care Guides
How to Develop a Caregiving Plan

End of Life
How to Cope With Grief, Loss
Recently Played
Word & Trivia
Atari® & Retro
Members Only
Staying Sharp
Mobile Apps
More About Games

Right Again! Trivia

Right Again! Trivia – Sports

Atari® Video Games

Throwback Thursday Crossword
Travel Tips
Vacation Ideas
Destinations
Travel Benefits

Beach vacation ideas
Vacations for Sun and Fun

Plan Ahead for Tourist Taxes

AARP City Guide
Discover Seattle

25 Ways to Save on Your Vacation
Entertainment & Style
Family & Relationships
Personal Tech
Home & Living
Celebrities
Beauty & Style

TV for Grownups
Best Reality TV Shows for Grownups

Robert De Niro Reflects on His Life

Looking Back
50 World Changers Turning 50

Sex & Dating
Spice Up Your Love Life

Navigate All Kinds of Connections

Life & Home
Couple Creates Their Forever Home

Store Medical Records on Your Phone?

Maximize the Life of Your Phone Battery

Virtual Community Center
Join Free Tech Help Events

Create a Hygge Haven

Soups to Comfort Your Soul

Your Ultimate Guide to Mulching
Driver Safety
Maintenance & Safety
Trends & Technology

AARP Smart Guide
How to Keep Your Car Running

We Need To Talk
Assess Your Loved One's Driving Skills

AARP Smart Driver Course

Building Resilience in Difficult Times

Tips for Finding Your Calm

Weight Loss After 50 Challenge

Cautionary Tales of Today's Biggest Scams

7 Top Podcasts for Armchair Travelers

Jean Chatzky: ‘Closing the Savings Gap’

Quick Digest of Today's Top News

AARP Top Tips for Navigating Life

Get Moving With Our Workout Series
You are now leaving AARP.org and going to a website that is not operated by AARP. A different privacy policy and terms of service will apply.
Go to Series Main Page
What is Medicare assignment and how does it work?
Kimberly Lankford,
Because Medicare decides how much to pay providers for covered services, if the provider agrees to the Medicare-approved amount, even if it is less than they usually charge, they’re accepting assignment.
A doctor who accepts assignment agrees to charge you no more than the amount Medicare has approved for that service. By comparison, a doctor who participates in Medicare but doesn’t accept assignment can potentially charge you up to 15 percent more than the Medicare-approved amount.
That’s why it’s important to ask if a provider accepts assignment before you receive care, even if they accept Medicare patients. If a doctor doesn’t accept assignment, you will pay more for that physician’s services compared with one who does.

AARP Membership — $12 for your first year when you sign up for Automatic Renewal
How much do I pay if my doctor accepts assignment?
If your doctor accepts assignment, you will usually pay 20 percent of the Medicare-approved amount for the service, called coinsurance, after you’ve paid the annual deductible. Because Medicare Part B covers doctor and outpatient services, your $240 deductible for Part B in 2024 applies before most coverage begins.
All providers who accept assignment must submit claims directly to Medicare, which pays 80 percent of the approved cost for the service and will bill you the remaining 20 percent. You can get some preventive services and screenings, such as mammograms and colonoscopies , without paying a deductible or coinsurance if the provider accepts assignment.
What if my doctor doesn’t accept assignment?
A doctor who takes Medicare but doesn’t accept assignment can still treat Medicare patients but won’t always accept the Medicare-approved amount as payment in full.
This means they can charge you up to a maximum of 15 percent more than Medicare pays for the service you receive, called “balance billing.” In this case, you’re responsible for the additional charge, plus the regular 20 percent coinsurance, as your share of the cost.
How to cover the extra cost? If you have a Medicare supplement policy , better known as Medigap, it may cover the extra 15 percent, called Medicare Part B excess charges.
All Medigap policies cover Part B’s 20 percent coinsurance in full or in part. The F and G policies cover the 15 percent excess charges from doctors who don’t accept assignment, but Plan F is no longer available to new enrollees, only those eligible for Medicare before Jan. 1, 2020, even if they haven’t enrolled in Medicare yet. However, anyone who is enrolled in original Medicare can apply for Plan G.
Remember that Medigap policies only cover excess charges for doctors who accept Medicare but don’t accept assignment, and they won’t cover costs for doctors who opt out of Medicare entirely.
Good to know. A few states limit the amount of excess fees a doctor can charge Medicare patients. For example, Massachusetts and Ohio prohibit balance billing, requiring doctors who accept Medicare to take the Medicare-approved amount. New York limits excess charges to 5 percent over the Medicare-approved amount for most services, rather than 15 percent.

AARP NEWSLETTERS

%{ newsLetterPromoText }%
%{ description }%
Privacy Policy
ARTICLE CONTINUES AFTER ADVERTISEMENT
How do I find doctors who accept assignment?
Before you start working with a new doctor, ask whether he or she accepts assignment. About 98 percent of providers billing Medicare are participating providers, which means they accept assignment on all Medicare claims, according to KFF.
You can get help finding doctors and other providers in your area who accept assignment by zip code using Medicare’s Physician Compare tool .
Those who accept assignment have this note under the name: “Charges the Medicare-approved amount (so you pay less out of pocket).” However, not all doctors who accept assignment are accepting new Medicare patients.
AARP® Vision Plans from VSP™
Exclusive vision insurance plans designed for members and their families
What does it mean if a doctor opts out of Medicare?
Doctors who opt out of Medicare can’t bill Medicare for services you receive. They also aren’t bound by Medicare’s limitations on charges.
In this case, you enter into a private contract with the provider and agree to pay the full bill. Be aware that neither Medicare nor your Medigap plan will reimburse you for these charges.
In 2023, only 1 percent of physicians who aren’t pediatricians opted out of the Medicare program, according to KFF. The percentage is larger for some specialties — 7.7 percent of psychiatrists and 4.2 percent of plastic and reconstructive surgeons have opted out of Medicare.
Keep in mind
These rules apply to original Medicare. Other factors determine costs if you choose to get coverage through a private Medicare Advantage plan . Most Medicare Advantage plans have provider networks, and they may charge more or not cover services from out-of-network providers.
Before choosing a Medicare Advantage plan, find out whether your chosen doctor or provider is covered and identify how much you’ll pay. You can use the Medicare Plan Finder to compare the Medicare Advantage plans and their out-of-pocket costs in your area.
Return to Medicare Q&A main page
Kimberly Lankford is a contributing writer who covers Medicare and personal finance. She wrote about insurance, Medicare, retirement and taxes for more than 20 years at Kiplinger’s Personal Finance and has written for The Washington Post and Boston Globe . She received the personal finance Best in Business award from the Society of American Business Editors and Writers and the New York State Society of CPAs’ excellence in financial journalism award for her guide to Medicare.
Discover AARP Members Only Access
Already a Member? Login

More on Medicare

How Do I Create a Personal Online Medicare Account?
You can do a lot when you decide to look electronically

I Got a Medicare Summary Notice in the Mail. What Is It?
This statement shows what was billed, paid in past 3 months
Understanding Medicare’s Options: Parts A, B, C and D
Making sense of the alphabet soup of health care choices
Recommended for You
AARP Value & Member Benefits

Learn, earn and redeem points for rewards with our free loyalty program

AARP® Dental Insurance Plan administered by Delta Dental Insurance Company
Dental insurance plans for members and their families

The National Hearing Test
Members can take a free hearing test by phone

AARP® Staying Sharp®
Activities, recipes, challenges and more with full access to AARP Staying Sharp®
SAVE MONEY WITH THESE LIMITED-TIME OFFERS
Medicare Assignment: Understanding How It Works

Medicare assignment is a term used to describe how a healthcare provider agrees to accept the Medicare-approved amount. Depending on how you get your Medicare coverage, it could be essential to understand what it means and how it can affect you.
What is Medicare assignment?
Medicare sets a fixed cost to pay for every benefit they cover. This amount is called Medicare assignment.
You have the largest healthcare provider network with over 800,000 providers nationwide on Original Medicare . You can see any doctor nationwide that accepts Medicare.
Understanding the differences between your cost and the difference between accepting Medicare and accepting Medicare assignment could be worth thousands of dollars.
Doctors that accept Medicare
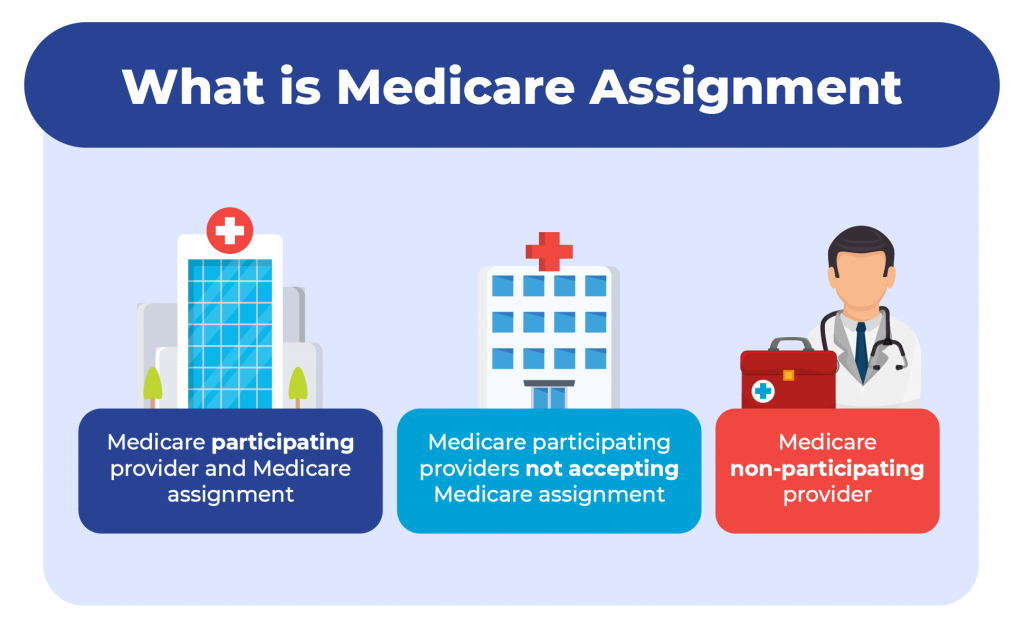
Your healthcare provider can fall into one of three categories:
Medicare participating provider and Medicare assignment
Medicare participating providers not accepting medicare assignment, medicare non-participating provider.
More than 97% of healthcare providers nationwide accept Medicare. Because of this, you can see almost any provider throughout the United States without needing referrals.
Let’s discuss the three categories the healthcare providers fall into.
Participating providers are doctors or healthcare providers who accept assignment. This means they will never charge more than the Medicare-approved amount.
Some non-participating providers accept Medicare but not Medicare assignment. This means you can see them the same way a provider accepts assignment.
You need to understand that since they don’t take the assigned amount, they can charge up to 15% more than the Medicare-approved amount.
Since Medicare will only pay the Medicare-approved amount, you’ll be responsible for these charges. The 15% overcharge is called an excess charge. A few states don’t allow or limit the amount or services of the excess charges. Only about 5% of providers charge excess charges.
Opt-out providers don’t accept Original Medicare, and these healthcare providers are in the minority in the United States. If healthcare providers don’t accept Medicare, they won’t be paid by Medicare.
This means choosing to see a provider that doesn’t accept Medicare will leave you responsible for 100% of what they charge you. These providers may be in-network for a Medicare Advantage plan in some cases.
Avoiding excess charges
Excess charges could be large or small depending on the service and the Medicare-approved amount. Avoiding these is easy. The simplest way is to ask your provider if they accept assignment before service.
If they say yes, they don’t issue excess charges. Or, on Medicare.gov , a provider search tool will allow you to look up your healthcare provider and show if they accept Medicare assignment or not.
Medicare Supplement and Medicare assignment
Medigap plans are additional insurance that helps cover your Medicare cost-share . If you are on specific plans, they’ll pay any extra costs from healthcare providers that accept Medicare but not Medicare assigned amount. Most Medicare Supplement plans don’t cover the excess charges.
The top three Medicare Supplement plans cover excess charges if you use a provider that accepts Medicare but not Medicare assignment.
Medicare Advantage and Medicare assignment
Medicare assignment does not affect Medicare Advantage plans since Medicare Advantage is just another way to receive your Medicare benefits. Since your Medicare Advantage plan handles your healthcare benefits, they set the terms.
Most Medicare Advantage plans require you to use network providers. If you go out of the network, you may pay more. If you’re on an HMO, you’d be responsible for the entire charge of the provider not being in the network.
Do all doctors accept Medicare Supplement plans?
All doctors that accept Original Medicare accept Medicare Supplement plans. Some doctors don’t accept Medicare. In this case, those doctors won’t accept Medicare Supplements.
Where can I find doctors who accept Medicare assignment?
Medicare has a physician finder tool that will show if a healthcare provider participates in Medicare and accepts Medicare assignments. Most doctors nationwide do accept assignment and therefore don’t charge the Part B excess charges.
Why do some doctors not accept Medicare?
Some doctors are called concierge doctors. These doctors don’t accept any insurance and require cash payments.
What is a Medicare assignment?
Accepting Medicare assignment means that the healthcare provider has agreed only to charge the approved amount for procedures and services.
What does it mean if a doctor does not accept Medicare assignment?
The doctor can change more than the Medicare-approved amount for procedures and services. You could be responsible for up to a 15% excess charge.
How many doctors accept Medicare assignment?
About 97% of doctors agree to accept assignment nationwide.
Is accepting Medicare the same as accepting Medicare assignment?
No. If a doctor accepts Medicare and accepts Medicare assigned amount, they’ll take what Medicare approves as payment in full.
If they accept Medicare but not Medicare assignment, they can charge an excess charge of up to 15% above the Medicare-approved amount. You could be responsible for this excess charge.
What is the Medicare-approved amount?
The Medicare-approved amount is Medicare’s charge as the maximum for any given medical service or procedure. Medicare has set forth an approved amount for every covered item or service.
Can doctors balance bill patients?
Yes, if that doctor is a Medicare participating provider not accepting Medicare assigned amount. The provider may bill up to 15% more than the Medicare-approved amount.
What happens if a doctor does not accept Medicare?
Doctors that don’t accept Medicare will require you to pay their full cost when using their services. Since these providers are non-participating, Medicare will not pay or reimburse for any services rendered.
Get help avoiding Medicare Part B excess charges
Whether it’s Medicare assignment, or anything related to Medicare, we have licensed agents that specialize in this field standing by to assist.
Give us a call, or fill out our online request form . We are happy to help answer questions, review options, and guide you through the process.
Related Articles
- What are Medicare Part B Excess Charges?
- How to File a Medicare Reimbursement Claim?
- Medicare Defined Coinsurance: How it Works?
- Welcome to Medicare Visit
- Guide to the Medicare Program

CALL NOW (833) 972-1339
What Medicare Assignment Is and How It Impacts You

If a doctor or other healthcare provider accepts a Medicare assignment for a particular service, a patient covered by Medicare will likely have to pay less out of pocket for that service. Accepting Medicare assignment means the healthcare provider has agreed to charge no more than the amount Medicare approved for that service. It also means the doctor agreed to bill Medicare rather than charging you directly. Providers who don’t accept assignments can charge 15% more and require immediate payment from the patient. A financial advisor can help you develop a financial strategy to pay for your healthcare.
Medicare Assignment Basics
Medicare is the government-sponsored national healthcare plan for about 63 million Americans over age 65. Original Medicare is the fee-for-service plan that includes Medicare Part A , which covers hospital costs. And it also includes Medicare Part B , which pays for other healthcare services, including doctor’s office visits.
Almost all doctors accept patients covered by Medicare. And almost all doctors who take Medicare patients accept Medicare assignments. Doctors who accept Medicare assignments are also known as assignment providers, participating providers and Medicare-enrolled providers.
A Medicare assignment provider agrees to charge no more than the Medicare-approved price for a specific service. The doctor or other provider also agrees to bill Medicare directly, rather than charging the patient on the day of service. This means that if you go to a Medicare-participating provider, you won’t usually have to pay anything at the time of service. And you will likely pay less out-of-pocket when all is said and done.
While Medicare assignment is relevant to people covered by Original Medicare, it doesn’t affect people covered by Medicare Advantage plans. These plans have their own rules.
How Medicare Assignment Affects Your Cost

Doctors and other providers who don’t accept Medicare may charge as much as 15% more than the Medicare-approved amount. The exact percentage varies by state. If you go to a non-accepting provider, you may have to pay the extra over the Medicare-approved amount, plus the 20% share of the cost Medicare passes on to all Medicare-insured patients.
For example, consider a visit to an occupational therapist who charges $120 for a treatment session. The Medicare-approved cost of the service is $100.
If the therapist accepts the Medicare assignment, they will charge you $100 and bill Medicare. After Medicare pays $100, you’ll owe 20%, or $20 for coinsurance. That’s if you have already met your Part B deductible. If not, Medicare may not pay anything, up to the amount of the deductible, and you may be responsible for the entire bill.
If the therapist does not accept Medicare assignment, they may charge 15% more than the Medicare-approved amount, or $115. Plus they may ask you to pay the entire amount . If that happens, you have to file with Medicare to get reimbursement.
Whether you or the provider sends the invoice to Medicare, Medicare will pay only 80% of the approved amount, or $80. Your out-of-pocket costs in this case will be $120 minus $80, or $35 instead of $20.
Finding Medicare Assignment Providers
Nearly all healthcare providers accept Medicare assignments. One way to check is to use Medicare’s online tool . You can filter these searches for, among other things, whether the provider accepts Medicare assignments.
You can also ask the provider whether they accept Medicare when you visit. In addition, you may also request information in advance detailing how much they’ll bill Medicare for the service and how much you’ll be expected to pay at the time of the visit.
Bottom Line

Medicare assignment means a doctor or other healthcare provider will charge no more than the Medicare-approved amount for a particular service. This usually means lower out-of-pocket costs for patients who are covered by Medicare. It also means the provider will bill Medicare rather than expecting the patient to pay the full amount at the time of service. Nearly all doctors accept Medicare assignments. But to be sure, you can check Medicare’s provider search tool for more information or ask before your next doctor’s visit.
Healthcare Tips
- Consider discussing how you plan to pay for your healthcare with a financial advisor. Finding such an expert doesn’t have to be hard. SmartAsset’s free tool matches you with up to three vetted financial advisors who serve your area. And you can interview your advisor matches at no cost to decide which one is right for you. If you’re ready to find an advisor who can help you achieve your financial goals, get started now .
- Healthcare costs can be a significant issue for retirees. How big an issue? Median out-of-pocket retiree healthcare costs for 2018 came to $4,311, according to one study. That means after Medicare or other insurance paid everything it would pay, the retiree had to come up with that much in cash to pay for healthcare in that one year alone. That’s why having a plan to pay for healthcare is an important part of retirement planning.
Photo credit: ©iStock.com/shapecharge, ©iStock.com/dragana991, ©iStock.com/Asawin_Klabma
What Does It Mean for a Doctor to Accept Medicare Assignment?
Written by: Malini Ghoshal, RPh, MS
Reviewed by: Malinda Cannon, Licensed Insurance Agent
Key Takeaways
Doctors who accept Medicare assignment are paid agreed-upon rates for services.
It’s important to verify that your doctor accepts assignment before receiving services to avoid high out-of-pocket costs.
A doctor or clinician may be “non-participating” but can still agree to accept Medicare assignment for some services.
If you visit a doctor or clinician who has opted out (doesn’t accept Medicare), you may have to pay for your entire visit cost unless it’s a medical emergency.
Medigap Supplemental insurance (Medigap) plans won’t pay for service costs from doctors who don’t accept assignment.
One of the things that Original Medicare beneficiaries often enjoy about their coverage is that they can use it anywhere in the country. Unlike plans with provider networks, they can visit doctors either at home or on the road; both are covered the same.
But do all doctors accept Medicare patients?
Truth is, this wide-ranging coverage area only applies to doctors who accept Medicare assignment. Fortunately, most do. If you’re eligible for Medicare, it’s important to visit doctors and clinicians who accept Medicare assignment. This will help keep your out-of-pocket costs within your control. Doctors who agree to accept Medicare assignment sign an agreement that they’re willing to accept payment from Medicare for their services.
If you’re a current beneficiary or nearing enrollment, you may have other questions. Do all doctors accept Medicare Advantage plans? What about Medicare Supplement insurance (Medigap)? Read on to learn how to find doctors that accept Medicare assignment and how this keeps your healthcare costs down.
Your Ideal Medicare Plan is out there.
What Is Medicare Assignment of Benefits?
When you’re eligible for Medicare, you have the option to visit doctors and clinicians who accept assignment. This means they are Medicare-approved providers who agree to receive Medicare reimbursement rates for covered services. This helps save you money.
If you have Original Medicare (Part A and B), your doctor visits are covered by your Part B plan. Inpatient services such as hospital stays and some skilled nursing care are covered by Part A .
In order for a participating doctor (or facility) to bill Medicare and be reimbursed, you must authorize Medicare to reimburse your doctor directly for your covered services. This is called the Medicare assignment of benefits. You transfer your right to receive Medicare payment for a covered service to your doctor or other provider.
Note: If you have a Medicare Supplement insurance ( Medigap ) plan to pay for out-of-pocket costs, you may also need to sign a separate assignment of benefits form for Medigap reimbursement. More on Medigap below.
How Can I Find Doctors Near Me That Accept Medicare?
There are several ways to find doctors and other clinicians who accept Medicare assignment close to you.
First, let’s take a look at the different types of Medicare providers.
They include:
Participating providers: Medicare-participating doctors and providers sign a participation agreement stating they will accept Medicare reimbursement rates for their services.
Non-participating providers: Doctors or providers who are non-participating providers are eligible to accept Medicare assignment but haven’t signed a Medicare agreement. They may choose to accept assignment on a case-by-case basis. If you visit a non-participating provider, make sure to ask if they accept assignment for your particular service. Also get a copy of their fees. They will need to select “yes” on Centers for Medicare & Medicaid Services CMS Form 1500 to accept assignment for the service.
Opt-out providers: Some doctors and other providers choose not to accept Medicare. If they choose to opt out, the period is two years (based on Medicare guidelines). The opt-out automatically renews if the provider doesn’t request a change in their status. You would be responsible for paying all costs for services received from an opt-out provider. You cannot bill Medicare for reimbursement unless the service was an urgent or emergency medical need. According to a report from KFF , roughly 1% of non-pediatric physicians opted out of Medicare in 2023.
Visiting a doctor who doesn’t accept assignment may cost you more. These providers can charge you up to 15% more than the Medicare-approved rate for a given service. This 15% charge is called the limiting charge. Some states limit this extra charge to a certain percent. This may also be called the Part B excess charge.
Here are some tips for finding doctors and providers who accept Medicare assignment:
- The easiest way to find a doctor who accepts Medicare assignment is to contact their office and ask them directly.
- If you’re looking for a new doctor, you can use the Medicare search tool to find clinicians and doctors that accept Medicare assignment.
- You can also ask a state health insurance assistance program (SHIP) representative for help in locating a doctor that accepts Medicare assignment.
- Don’t assume that having a longstanding relationship with your doctor means nothing will ever change. Check in with them to make sure they still accept Medicare assignment and whether they’re planning to opt out.
Note: Your doctor can choose to become a non-participating provider or opt out of participating in Medicare. It’s important to verify they accept Medicare assignment before receiving any services.
Looking for dental, vision and hearing coverage?
Do Doctors Who Accept Medicare Have to Accept Supplement Plans?
If your doctor accepts Medicare assignment and you have Original Medicare (Medicare Part A and Part B) with a Medicare Supplement (Medigap) plan, they will accept the supplemental insurance. Depending on your Medigap plan coverage , it may pay all or part of your out-of-pocket costs such as deductibles, copayments and coinsurance.
However, if you have a Medicare Advantage plan (Part C), you may have a network of covered doctors under the plan. If you visit an out-of-network doctor, you may need to pay all or part of the cost for your services.
Keep in mind that you can’t have a Medigap supplemental plan if you have a Medicare Advantage plan.
If you have questions or want to learn more about different Medicare plans like Original Medicare with Medigap versus Medicare Advantage, GoHealth has licensed insurance agents ready to help. They can shop your different options and offer impartial guidance where you need it.
Do Most Doctors Accept Medicare Advantage Plans?
Many doctors accept Medicare Advantage (Part C) plans, but these plans often use provider networks. These networks are groups of doctors and providers in an area that have agreed to treat an insurance company’s customers. If you have a Part C plan, you may be required to see in-network doctors with few exceptions. However, these types of plans are popular options for all-in-one coverage for your health needs. Plans must offer Part A and B coverage, plus a majority also include Part D , or prescription drug coverage. But whether a doctor accepts a Medicare Advantage plan may depend on where you live and the type of Medicare Advantage plan you have.
There are several types of Medicare Advantage plans including:
- Health Maintenance Organization (HMO): These plans have a network of covered providers, as well as a primary care physician to manage your care. If you visit a doctor outside your plan network, you may have to pay the full cost of your visit.
- Preferred Provider Organization (PPO): You’ll probably still have a primary care physician, but these are more flexible plans that allow you to go out of network in some cases. But you may have to pay more.
- Private Fee for Service (PFFS): You may be able to visit any doctor or provider with these plans, but your costs may be higher.
- Special Needs Plan (SNP): This type of plan is only for certain qualified individuals who either have a specific health condition ( C-SNP ) or who qualify for both Medicaid and Medicare insurance ( D-SNP ).
Start your Medicare PlanFit CheckUp today.
What Are Medicare Assignment Codes?
Medicare assignment codes help Medicare pay for covered services. If your doctor or other provider accepts assignment and is a participating provider, they will file for reimbursement for services with a CMS-1500 form and the code will be “assigned.”
But non-participating providers can select “not assigned.” This means they are not accepting Medicare-assigned rates for a given service. They can charge up to 15% over the full Medicare rate for the service.
If you go to a doctor or provider who accepts assignment, you don’t need to file your own claim. Your doctor’s office will directly file with Medicare. Always check to make sure your doctor accepts assignment to avoid excess charges from your visit.
Health Insurance Claim Form . CMS.gov.
Lower costs with assignment . Medicare.gov.
How Many Physicians Have Opted-Out of the Medicare Program? KFF.org.
Joining a plan . Medicare.gov.
This website is operated by GoHealth, LLC., a licensed health insurance company. The website and its contents are for informational and educational purposes; helping people understand Medicare in a simple way. The purpose of this website is the solicitation of insurance. Contact will be made by a licensed insurance agent/producer or insurance company. Medicare Supplement insurance plans are not connected with or endorsed by the U.S. government or the federal Medicare program. Our mission is to help every American get better health insurance and save money. Any information we provide is limited to those plans we do offer in your area. Please contact Medicare.gov or 1-800-MEDICARE to get information on all of your options.
Let's see if you're missing out on Medicare savings.
We just need a few details.
Related Articles

What Is Medicare IRMAA?
What Is an IRMAA in Medicare?

How to Report Medicare Fraud
Medicare Fraud Examples & How to Report Abuse

How to Change Your Address with Medicare
Reporting a Change of Address to Medicare

Can I Get Medicare if I’ve Never Worked?
Can You Get Medicare if You've Never Worked?

Why Are Some Medicare Advantage Plans Free?
Why Are Some Medicare Advantage Plans Free? $0 Premium Plans Explained

What Is Medicare Assignment?

Am I Enrolled in Medicare?

When and How Do I Enroll?
When and How Do I Enroll in Medicare?

Medicare Frequently Asked Questions
Let’s see if you qualify for Medicare savings today!
Everything PTs Need to Know About Accepting Medicare Assignment
There's no one-size-fits-all answer as to whether or not a PT should accept Medicare assignment, but you can better understand your options.
There's no one-size-fits-all all answer as to whether or not a PT should accept Medicare assignment, but you can better understand your options.

Get the latest news and tips directly in your inbox by subscribing to our monthly newsletter
Discuss any topic within rehab therapy, and chances are that Medicare will come up at some point. Whether it’s talking about Medicare and direct access or Medicare supervision requirements , it’s hard to avoid discussing the ins and outs of the program, given its prominence in healthcare at large. However, there’s one question that probably doesn't get asked enough: do providers have to participate in Medicare? We’re going to dive into the specifics of what rehab therapists can and can’t do when it comes to accepting Medicare assignment, and the pros and cons of each.
What it means to “accept Medicare assignment”
In short, accepting Medicare assignment means signing a contract to accept whatever Medicare pays for a covered service as full payment. Participating and non-participating status only applies to Medicare Part B; Medicare Advantage plans operate with contracts similar to commercial insurance with in-network and out-of-network providers.
Participating Providers
If you’re accepting Medicare assignment for all covered services, you are considered to be a participating provider under Medicare and may not charge patients above and beyond what Medicare agrees to pay. In this case, you can charge 100% of the Medicare Physician Fee Schedule (MPFS) and are paid at 80% of that rate, minus the Multiple Procedure Payment Reduction (MPPR) and the 2% sequestration adjustment.
You may, however, collect patient deductibles and coinsurances—although, as explained in the Medicare payer guide , these providers typically ask Medicare to pay its share before collecting anything from the patient. Per the same resource, these providers are required to submit claims directly to Medicare for reimbursement and cannot charge patients for the claim submission. As Dr. Jarod Carter, PT, DPT, MTC, writes in Medicare and Cash-Pay PT Services , “This is the most common and best-understood relationship that physical therapists have with Medicare.”
Because Medicare beneficiaries often pay less out-of-pocket costs when receiving care from a provider who accepts assignment, patients may be more willing to work with these providers. Thus, if you accept assignment, you may have access to not only more Medicare patients but also more potential referral partners who only work with assignment-accepting providers.
You must accept whatever Medicare deems appropriate compensation, and as we know, that’s below market value more often than not. Given the recently announced cuts to assistant-provided services and the 8% cut to all physical therapy services , accepting assignment may be increasingly less appealing to physical therapists. That said, if you serve a large Medicare population, the volume of patients you see may make it financially beneficial for you to continue playing by Medicare’s rules.
If you don’t want to accept Medicare assignment, what are your other options?
Non-participating providers.
As Meredith Castin explains in 4 Things to Know About Billing for Cash-Pay PT , Medicare also allows physical therapists to be non-participating providers (a.k.a. non-enrolled providers), which simply means that, while they are still in a contractual relationship with Medicare (and thus, are eligible to provide covered services to Medicare beneficiaries), they have not agreed to accept assignment across the board.
If a non-participating provider opts to accept assignment for a case, they can charge 95%.
If they do not accept assignment but still treat the patient, these providers may charge up to what Medicare calls “the limiting charge” for a service—which is 15% above the Medicare allowed amount. Non-participating providers may choose to accept assignment for some services, but not others —or no services at all. For services that are not under assignment, the provider may collect payment directly from the patient; however, he or she must still bill Medicare, so that Medicare may reimburse the patient.
Non-participating providers are still eligible to serve Medicare beneficiaries, but they maintain some degree of freedom when it comes to pricing their services. In other words, if you are a non-participating provider, you are less beholden to what Medicare deems as appropriate payment than you are as a participating provider.
That said, you do still have to charge within Medicare’s limit, which means your freedom is far from total. Additionally, because patients may have to pay more out of pocket for your services and/or pay and wait for reimbursement from Medicare, you may have to work harder to convince them that you’re worth the financial investment. With the right data and marketing , it’s definitely doable; it may just require more effort.
No Relationship with Medicare
Physicians are eligible to “opt-out” of Medicare, which means that even if they are neither participating nor non-participating providers, they can still see Medicare beneficiaries on a cash-pay basis. Physical therapists do not enjoy the same privilege. So, if you decide not to be a Medicare participating provider or non-participating provider, then you effectively have no relationship with Medicare. Thus, you are not able to provide Medicare-covered services to Medicare beneficiaries.
That said, all physical therapists, regardless of their relationship with Medicare, may provide never-covered services to Medicare beneficiaries, including wellness services. According to Castin, though, providers who go down that route, “need to be very clear about Medicare’s definition of ‘wellness services’ versus ‘physical therapy services.’” According to cash-pay PT Jarod Carter , it’s imperative for your documentation to clearly support that the services were indeed wellness as opposed to therapy.
As a provider with no relationship with Medicare, you’re not required to play by Medicare’s rules when it comes to reporting requirements or (lowball) payments. You’re also not at all affected by Medicare’s most recent cuts, which, quite frankly, is a big bonus.
However, as of 2007 , 15% of the US population was enrolled in Medicare; that’s 44 million people—most of whom could benefit from seeing a physical therapist to improve function and mobility and decrease pain. And that number is projected to grow to 79 million people by 2030. As such, choosing not to play ball with Medicare means you’re walking away from a very large market of patients who need your services.
It’s your decision.
Deciding on accepting Medicare assignment—and what type of relationship you’d like to have with Medicare—is not an easy decision to make, and there are a lot of factors to take into consideration before getting involved or breaking it off with this substantial federal payer. That said, it is important to know that you have options. Have more questions about what it means to accept assignment as a PT? Ask them below, and we’ll do our best to find you an answer.
Related posts

Are Treatment Plans Overburdening Older Patients?


Four Things You Need to Know About OT Salary

Founder Letter: What We Can Learn from Change Healthcare

Medicare and Cash-Pay PT Services, Part 1: The Must-Know Concepts to Avoid Legal Issues and Capitalize on Opportunities

Medicare and Direct Access

The Medicare Maintenance Care Myth

Learn how WebPT’s PXM platform can catapult your practice to new heights.

Medicare Interactive Medicare answers at your fingertips -->
Participating, non-participating, and opt-out providers, outpatient provider services.
You must be logged in to bookmark pages.
Email Address * Required
Password * Required
Lost your password?
If you have Original Medicare , your Part B costs once you have met your deductible can vary depending on the type of provider you see. For cost purposes, there are three types of provider, meaning three different relationships a provider can have with Medicare . A provider’s type determines how much you will pay for Part B -covered services.
- These providers are required to submit a bill (file a claim ) to Medicare for care you receive. Medicare will process the bill and pay your provider directly for your care. If your provider does not file a claim for your care, there are troubleshooting steps to help resolve the problem .
- If you see a participating provider , you are responsible for paying a 20% coinsurance for Medicare-covered services.
- Certain providers, such as clinical social workers and physician assistants, must always take assignment if they accept Medicare.
- Non-participating providers can charge up to 15% more than Medicare’s approved amount for the cost of services you receive (known as the limiting charge ). This means you are responsible for up to 35% (20% coinsurance + 15% limiting charge) of Medicare’s approved amount for covered services.
- Some states may restrict the limiting charge when you see non-participating providers. For example, New York State’s limiting charge is set at 5%, instead of 15%, for most services. For more information, contact your State Health Insurance Assistance Program (SHIP) .
- If you pay the full cost of your care up front, your provider should still submit a bill to Medicare. Afterward, you should receive from Medicare a Medicare Summary Notice (MSN) and reimbursement for 80% of the Medicare-approved amount .
- The limiting charge rules do not apply to durable medical equipment (DME) suppliers . Be sure to learn about the different rules that apply when receiving services from a DME supplier .
- Medicare will not pay for care you receive from an opt-out provider (except in emergencies). You are responsible for the entire cost of your care.
- The provider must give you a private contract describing their charges and confirming that you understand you are responsible for the full cost of your care and that Medicare will not reimburse you.
- Opt-out providers do not bill Medicare for services you receive.
- Many psychiatrists opt out of Medicare.
Providers who take assignment should submit a bill to a Medicare Administrative Contractor (MAC) within one calendar year of the date you received care. If your provider misses the filing deadline, they cannot bill Medicare for the care they provided to you. However, they can still charge you a 20% coinsurance and any applicable deductible amount.
Be sure to ask your provider if they are participating, non-participating, or opt-out. You can also check by using Medicare’s Physician Compare tool .
Update your browser to view this website correctly. Update my browser now
Medicare Options
To help ensure that physicians are making informed decisions about their contractual relationships with the Medicare program, the AMA has developed a “Medicare Participation Kit”(www.ama-assn.org) that explains the various participation options that are available to physicians. A summary of those options is presented below. The AAFP is not advising or recommending any of the options. The purpose of sharing this information is merely to ensure that physician decisions about Medicare participation are made with complete information about the available options. Please note that the summary below does not account for any payment adjustments that a participating or non-participating physician may incur through one of the Medicare initiatives, such as the Physician Quality Reporting System. Physicians wishing to change their Medicare participation or non-participation status for a given year are usually required to do so by December 31 of the prior year (e.g., December 31, 2015 for 2016). Participation decisions are effective January 1 of the year in question and are binding for the entire year.
The Three Options
There are basically three Medicare contractual options for physicians. Physicians may sign a participating (PAR) agreement and accept Medicare's allowed charge as payment in full for all of their Medicare patients. They may elect to be a non-PAR physician, which permits them to make assignment decisions on a case-by-case basis and to bill patients for more than the Medicare allowance for unassigned claims. Or they may become a private contracting physician, agreeing to bill patients directly and forego any payments from Medicare to their patients or themselves. Physicians who wish to change their status from PAR to non-PAR or vice versa may do so annually. Once made, the decision is generally binding until the next annual contracting cycle except where the physician's practice situation has changed significantly, such as relocation to a different geographic area or a different group practice. To become a private contractor, physicians must give 30 days notice before the first day of the quarter the contract takes effect. Those considering a change in status should first determine that they are not bound by any contractual arrangements with hospitals, health plans or other entities that require them to be PAR physicians. In addition, some states have enacted laws that prohibit physicians from balance billing their patients.
Participation
PAR physicians agree to take assignment on all Medicare claims, which means that they must accept Medicare's approved amount (which is the 80% that Medicare pays plus the 20% patient copayment) as payment in full for all covered services for the duration of the calendar year. The patient or the patient's secondary insurer is still responsible for the 20% copayment but the physician cannot bill the patient for amounts in excess of the Medicare allowance. While PAR physicians must accept assignment on all Medicare claims, however, Medicare participation agreements do not require physician practices to accept every Medicare patient who seeks treatment from them.
Medicare provides a number of incentives for physicians to participate:
- The Medicare payment amount for PAR physicians is 5% higher than the rate for non-PAR physicians.
- Directories of PAR physicians are provided to senior citizen groups and individuals who request them.
- Medicare administrative contractors (MAC) provide toll-free claims processing lines to PAR physicians and process their claims more quickly.
Non-Participation
Medicare approved amounts for services provided by non-PAR physicians (including the 80% from Medicare plus the 20% copayment) are set at 95% of Medicare approved amounts for PAR physicians, although non-PAR physicians can charge more than the Medicare approved amount.
Limiting charges for non-PAR physicians are set at 115% of the Medicare approved amount for non-PAR physicians. However, because Medicare approved amounts for non-PAR physicians are 95% of the rates for PAR physicians, the 15% limiting charge is effectively only 9.25% above the PAR approved amounts for the services. Therefore, when considering whether to be non-PAR, physicians must determine whether their total revenues from Medicare, patient copayments and balance billing would exceed their total revenues as PAR physicians, particularly in light of collection costs, bad debts and claims for which they do accept assignment. The 95% payment rate is not based on whether physicians accept assignment on the claim, but whether they are PAR physicians; when non-PAR physicians accept assignment for their low-income or other patients, their Medicare approved amounts are still only 95% of the approved amounts paid to PAR physicians for the same service. Non-PAR physicians would need to collect the full limiting charge amount roughly 35% of the time they provided a given service in order for the revenues from the service to equal those of PAR physicians for the same service. If they collect the full limiting charge for more than 35% of the services that they provide, their Medicare revenues will exceed those of PAR physicians.
Assignment acceptance, for either PAR or non-PAR physicians, also means that the MAC pays the physician the 80% Medicare payment. For unassigned claims, even though the physician is required to submit the claim to Medicare, the program pays the patient, and the physician must then collect the entire amount for the service from the patient.
Example: A service for which Medicare fee schedule amount is $100
Private contracting.
Provisions in the Balanced Budget Act of 1997 give physicians and their Medicare patients the freedom to privately contract to provide health care services outside the Medicare system. Private contracting decisions may not be made on a case-by-case or patient-by-patient basis, however. Once physicians have opted out of Medicare, they cannot submit claims to Medicare for any of their patients for a two-year period.
A physician who has not been excluded under sections 1128, 1156 or 1892 of the Social Security Act may, however, order, certify the need for, or refer a beneficiary for Medicare-covered items and services, provided the physician is not paid, directly or indirectly, for such services (except for emergency and urgent care services). For example, if a physician who has opted out of Medicare refers a beneficiary for medically necessary services, such as laboratory, DMEPOS or inpatient hospitalization, those services would be covered by Medicare.
To privately contract with a Medicare beneficiary, a physician must enter into a private contract that meets specific requirements, as set forth in the sample private contract below. In addition to the private contract, the physician must also file an affidavit that meets certain requirements, as contained in the sample affidavit below. To opt out, a physician must file an affidavit that meets the necessary criteria and is received by the MAC at least 30 days before the first day of the next calendar quarter. There is a 90-day period after the effective date of the first opt-out affidavit during which physicians may revoke the opt-out and return to Medicare as if they had never opted out.
Emergency and Urgent Care Services Furnished During the "Opt-Out" Period
Physicians who have opted-out of Medicare under the Medicare private contract provisions may furnish emergency care services or urgent care services to a Medicare beneficiary with whom the physician has previously entered into a private contract so long as the physician and beneficiary entered into the private contract before the onset of the emergency medical condition or urgent medical condition. These services would be furnished under the terms of the private contract.
Physicians who have opted-out of Medicare under the Medicare private contract provisions may continue to furnish emergency or urgent care services to a Medicare beneficiary with whom the physician has not previously entered into a private contract, provided the physician:
- Submits a claim to Medicare in accordance with both 42 CFR part 424 (relating to conditions for Medicare payment) and Medicare instructions (including but not limited to complying with proper coding of emergency or urgent care services furnished by physicians and qualified health care professionals who have opted-out of Medicare).
- Collects no more than the Medicare limiting charge, in the case of a physician (or the deductible and coinsurance, in the case of a qualified health care professional).
Note that a physician who has been excluded from Medicare must comply with Medicare regulations relating to scope and effect of the exclusion (42 C.F.R. § 1001.1901) when the physician furnishes emergency services to beneficiaries, and the physician may not bill and be paid for urgent care services.
Sample Medicare Private Contract and Affidavit
The sample private contract and affidavit below contain the provisions that Medicare requires (unless otherwise noted) to be included in these documents.
Private contracts must meet specific requirements:
- The physician must sign and file an affidavit agreeing to forgo receiving any payment from Medicare for items or services provided to any Medicare beneficiary for the following 2-year period (either directly, on a capitated basis or from an organization that received Medicare reimbursement directly or on a capitated basis).
- Medicare does not pay for the services provided or contracted for. The contract must be in writing and must be signed by the beneficiary before any item or service is provided.
- The contract cannot be entered into at a time when the beneficiary is facing an emergency or an urgent health situation.
In addition, the contract must state unambiguously that by signing the private contract, the beneficiary:
- gives up all Medicare payment for services furnished by the "opt out" physician;
- agrees not to bill Medicare or ask the physician to bill Medicare;
- is liable for all of the physician's charges, without any Medicare balance billing limits;
- acknowledges that Medigap or any other supplemental insurance will not pay toward the services; and acknowledges that he or she has the right to receive services from physicians for whom Medicare coverage and payment would be available.
If you determine that you want to "opt out" of Medicare under a private contract, we recommend that you consult with your attorney to develop a valid contract containing other standard non-Medicare required provisions that generally are included in any standard contract.
Download sample contracts:
- Sample Medicare Private Contract
- Sample Medicare Private Contracts "Opt-Out" Affidavit
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
- Alzheimer's & Dementia
- Asthma & Allergies
- Atopic Dermatitis
- Breast Cancer
- Cardiovascular Health
- Environment & Sustainability
- Exercise & Fitness
- Headache & Migraine
- Health Equity
- HIV & AIDS
- Human Biology
- Men's Health
- Mental Health
- Multiple Sclerosis (MS)
- Parkinson's Disease
- Psoriatic Arthritis
- Sexual Health
- Ulcerative Colitis
- Women's Health
- Nutrition & Fitness
- Vitamins & Supplements
- At-Home Testing
- Men’s Health
- Women’s Health
- Latest News
- Medical Myths
- Honest Nutrition
- Through My Eyes
- New Normal Health
- 2023 in medicine
- Why exercise is key to living a long and healthy life
- What do we know about the gut microbiome in IBD?
- My podcast changed me
- Can 'biological race' explain disparities in health?
- Why Parkinson's research is zooming in on the gut
- Health Hubs
- Find a Doctor
- BMI Calculators and Charts
- Blood Pressure Chart: Ranges and Guide
- Breast Cancer: Self-Examination Guide
- Sleep Calculator
- RA Myths vs Facts
- Type 2 Diabetes: Managing Blood Sugar
- Ankylosing Spondylitis Pain: Fact or Fiction
- Our Editorial Process
- Content Integrity
- Conscious Language
- Health Conditions
- Health Products
Do most doctors accept Medicare?

Many doctors do accept people with Medicare, but there may be some out-of-pocket costs to consider.
Medicare is very well established and has built an extensive network of healthcare providers since its inception.
In 2017, the American Academy of Family Physicians surveyed members about their participation in the Medicare program, and 83% of physicians reported that they accept new Medicare patients.
Today, most doctors do accept Medicare patients, and there are many ways to check if a healthcare provider is participating.
In this article, we look at finding a doctor and treatment costs, and for Medicare Advantage members, we look at information about in-network and out-of-network providers.
We may use a few terms in this piece that can be helpful to understand when selecting the best insurance plan: Deductible: This is an annual amount that a person must spend out of pocket within a certain time period before an insurer starts to fund their treatments. Coinsurance: This is a percentage of a treatment cost that a person will need to self-fund. For Medicare Part B, this comes to 20%. Copayment: This is a fixed dollar amount that an insured person pays when receiving certain treatments. For Medicare, this usually applies to prescription drugs.
When a doctor accepts assignment

Assignment means that a doctor agrees to accept the Medicare-approved amount as full payment for covered health services and supplies.
The majority of doctors accept assignment. Participating health providers have an agreement with Medicare to accept assignment for all Medicare-covered services.
If the doctor accepts assignment:
- out-of-pocket costs may be less
- the doctor agrees to charge only the Medicare coinsurance and deductible, and the doctor will usually wait for Medicare to pay its share before billing an individual
- the doctor is required to submit the claim directly to Medicare, and the doctor cannot charge a person to file the claim
If a doctor accepts assignment, Medicare determines the amount the doctor will be paid for health services and supplies.
What if the doctor does not accept assignment?
A doctor who does not have an agreement with Medicare to accept assignment is considered a non-participating provider.
It may be important for a person to note, however, that even though a provider may be non-participating, they may choose to accept assignment for some types of services.
What happens when a doctor is a non-participating provider?
If a healthcare provider does not have an agreement with Medicare, a person may be required to pay the entire bill at the time of service.
If the doctor is willing, they can submit a claim to Medicare directly for any Medicare-covered services they provide, but they cannot charge a person for submitting a claim.
Individuals may have to pay for a service and submit a claim themselves, using Form CMS-1490S for reimbursement.
Excess charges
Sometimes, a doctor can charge a person more than the Medicare-approved amount, creating an excess. The excess is any amount over the Medicare-approved cost.
In these cases, Medicare will not cover the excess, but some Medigap plans may help with these expenses.
Limiting charge
There is a limit to the amount a doctor can bill for a service, called a limiting charge. This means that doctors can charge up to a maximum of 15% more than the amount Medicare will cover.
The limiting charge applies to doctors who have chosen to accept Medicare for some services only. The charge does not apply to providers who are fully non-participating.
Finding participating providers
To find a doctor that accepts Medicare, a person can visit the Medicare Physician Compare site and search by location, and by entering either:
- the last name of the healthcare professional
- the group practice name
- medical specialty
- medical condition
The search results will then provide a list of participating professionals in the location specified.
Medicare Advantage providers
Private medical insurance companies administer Medicare Advantage plans, also known as Medicare Part C . These are bundled health plans that offer an alternative to original Medicare.
Each Medicare Advantage plan has different rules for how a person may receive services, like whether a person needs a referral to see a specialist, and whether visiting an in-network healthcare provider must be used.
What is a provider network?
A provider network is a group of doctors, healthcare providers, and hospitals that a plan has a contract with, making them in-network.
A healthcare provider who has no contract with a plan is an out-of-network provider.
A private insurance company that offers Medicare Advantage policies may have different networks for different plans, so when a person searches for a healthcare provider online, it may be beneficial to ensure the correct plan is selected.
In-network providers can also be located by calling the insurer.
Seeing a specialist
Some Medicare Advantage plans have different rules for when a visit to a specialist is needed, such as:
Health Maintenance Organization (HMO) plans : Usually, a person is required to obtain a referral from their primary care physician to see a specialist under an HMO. Some services do not require a referral, such as a yearly mammogram screening.
Preferred Provider Organization (PPO) plans : A person does not normally need a referral to see a specialist under a PPO. If a person uses an in-network specialist, their costs for covered services may be lower than if they use an out-of-network provider.
Most doctors accept Medicare, and if they do not, they may still accept Medicare for certain services.
If a doctor accepts assignment, it means they have a formal agreement with Medicare to accept the Medicare-approved amount as full payment for all covered services.
A provider network is a group of healthcare providers who have contracted with a particular health plan to provide cost-effective care to its members, making them in-network.
To find a doctor that accepts Medicare, a person can visit the Medicare Physician Compare page.
Last medically reviewed on August 11, 2020
- Health Insurance / Medical Insurance
- Medicare / Medicaid / SCHIP
- Primary Care
How we reviewed this article:
- AAFP member survey provides valuable perspective. (2020). https://www.aafp.org/news/blogs/inthetrenches/entry/20170801ITT_Survey.html
- CMS 1490S. (n.d.) https://www.cms.gov/Medicare/CMS-Forms/CMS-Forms/CMS-Forms-Items/CMS012949
- Find Medicare physicians and other clinicians. (n.d.) https://www.medicare.gov/physiciancompare/
- Lower costs with assignment. (n.d.). https://www.medicare.gov/your-medicare-costs/part-a-costs/lower-costs-with-assignment
- Specialists and referrals in Medicare Advantage plans. (n.d.). https://www.medicare.gov/sign-up-change-plans/types-of-medicare-health-plans/specialists-referrals-in-medicare-advantage-plans
- What you should know about provider networks. (2017). https://marketplace.cms.gov/outreach-and-education/what-you-should-know-provider-networks.pdf
Share this article
Latest news
- Newly identified genetic variant may protect against Alzheimer’s
- Exercise may help reverse aging by reducing fat buildup in tissues
- How menopause symptoms may increase the risk of cardiovascular disease
- Exercise may reduce heart disease risk by changing how the brain reacts to stress
- Plant-based, low-sugar diet linked to lower heart failure risk in large study
Related Coverage
Medicare Part A covers inpatient care, skilled nursing services, some home health and rehabilitation costs, and hospice care for people aged 65 years…
Medicare Part B covers medical expenses and outpatient care. Many services have a 20% coinsurance, and the 2020 deductible is $198. Read more here.
Medicare Part C, or Medicare Advantage, bundles together coverage for hospital costs, medical visits, and drug prescriptions. Read more here.
Medigap supplement insurance plans are designed to supplement a person's original Medicare benefits, while Medicare Advantage plans offer all-in-one…
Xarelto is a brand name for the drug rivaroxaban. Parts of Medicare cover the cost of prescription medication, including Part A, Part D, and Advantage…
How Medicare beneficiaries with Part D plans can help ensure their medications are covered

If you have a Medicare Part D prescription drug plan and take one or more brand-name medications—especially, expensive ones—there’s a very good chance you’ll run into trouble getting it covered.
Even worse, according to two recent studies, the possibility of being told by the plan that you either can’t get an expensive brand-name drug because it’s not on its “formulary” list or will need prior authorization has grown significantly.
And that can be bad for your health, considering that people with Medicare Part D plans take an average of four or five prescription drugs a month.
Branded medications often have Medicare restrictions
“When you’re talking about branded products, almost seven out of 10 have either some restriction or they’re excluded. That’s pretty high,” says Geoffrey Joyce, director of health policy at the USC Schaeffer Center, citing data from the March 2024 Health Affairs article he coauthored, “ Medicare Part D Plans Greatly Increased Utilization Restrictions on Prescription Drugs, 2011–20 .”
Joyce and his colleagues found that restrictions in Part D plans (what plans call “utilization management”) grew dramatically between 2011 and 2020 for both traditional Medicare and private insurers’ Medicare Advantage plans. In 2011, 21% of medications they reviewed had restrictions. In 2020, 44% did.
Sometimes, the plan’s list of covered medications (known as its formulary) didn’t include certain prescriptions. That was truer for traditional Medicare Part D plans than for Medicare Advantage Part D plans.
The three biggest pharmacy benefit managers excluded 1,356 medications for at least a year from 2019 to 2022, according to a Pembroke Consulting study.
Prior authorization, step therapy, and exclusions
Other times, beneficiaries needed to take a prescription similar to the one they wanted before they could get the one that they and their physicians preferred, a practice known as step therapy.
In many instances, people needed prior authorization: Their doctors had to prove to the Part D plan that the drug was medically necessary for them to get it covered.
Health insurers want to “steer patients and doctors toward what they think are lower-cost, more cost-effective therapies,” says Joyce. “So, in theory, it’s not necessarily bad.”
Formulary exclusions prevent “all but the few who successfully appeal or can afford to pay out-of-pocket from getting a restricted medication if it is prescribed by their physician,” the Health Affairs article said.
Zarek Brot-Goldberg, a University of Chicago public policy professor, says a 2023 National Bureau of Economic Research (NBER) study he and Harvard Medical School researchers conducted found that between one-fifth and one-quarter of all prescription drug spending from 2007 to 2015 required prior authorization.
Jumping through hoops
“If you take a really expensive drug, you’re going to have to go through prior authorization,” says Brot-Goldberg. “You would never want prior authorization for things like statins and beta blockers that are cheap and everyone should be getting. Those don’t have prior authorization that often.”
But some people do need expensive medications and “we’re making them jump through hoops,” he noted.
In Brot-Goldberg’s study, all the Part D plans had some degree of prior authorization, but each plan targeted different drugs.
More than 60% of primary care physicians surveyed by the Commonwealth Fund health research group said the amount of time they spend getting patients needed medications or treatments because of coverage restrictions is a “major” problem.
“You talk to doctors and they say, ‘I want the whole range’” of related medications to be available for my patients, says Joyce. “If drug A doesn’t work, I want to switch them to B and then C. But I’m not able to do that in a lot of these plans.”
Things could get worse in 2025
Leigh Purvis, the prescription drug policy principal at AARP, believes Medicare’s $2,000 annual out-of-pocket cap on prescriptions taking effect in 2025 could lead to more Part D plan prior authorization restrictions.
“I do think there’s a possibility that we could see plans changing their formularies and potentially becoming less generous because of the cost they’re facing” from the $2,000 cap, she says.
Already, many prescription drugs advertised on television—like Eliquis, Xarelto, Trulicity, and Enbrel—can cost Medicare beneficiaries thousands of dollars.
Prices for some of those medications have soared far more than the inflation rate.
A 2023 AARP Public Policy Institute report found that list prices for the top Medicare Part D drugs increased in price by an average of 226% since entering the market. The median price of new prescription drugs approved by the Food and Drug Administration tops $200,000.
The problem for low-income Medicare beneficiaries
The NBER paper found another Part D prior authorization problem among people eligible for Medicare’s low-income subsidy .
When those beneficiaries hadn’t signed up for a Part D plan and Medicare randomly assigned them a free version, the researchers discovered, half were required to get a different but related drug, and half were turned down for the prescription altogether.
But many low-income Medicare beneficiaries who learned at the pharmacy that they’d need prior authorization to get the similar drug never took steps to do so and wound up not taking any medication for their medical issue.
An inefficient system
“Prior authorization is not administered in what I would call the most efficient way,” says Brot-Goldberg. “What should happen is the patient should go back to their doctor and get them to submit a prior authorization request.”
Instead, he noted, they sometimes get discouraged and don’t bother.
“It’s puzzling because you’d think that many of these people have chronic diseases that doctors should be following up on,” Brot-Goldberg added. “Where are the doctors in all this, getting patients onto these drugs?”
Harm to Medicare patients
Exactly how much harm Part D prior authorization delays cause Medicare beneficiaries is hard to say, because data is scarce. “I don’t think we really have an idea of how bad this is,” says Brot-Goldberg.
In a 2022 American Medical Association survey , though, roughly a third of the 1,011 doctors polled said prior authorization led to a serious adverse event for a patient.
Joyce says that when he and his colleagues looked at people with Part D plans who were told they needed to take the generic blood thinner warfarin for Medicare coverage instead of pricier brand-name alternatives, “we showed some higher rates of stroke.”
Joyce’s research team is now studying whether patients with MS are facing health problems because they’re unable to get the drugs their doctors prescribed.
An October 2023 American Medical Association journal study found that roughly 15% of patients with cancer whose medication required prior authorization saw treatment delays of more than four weeks as a result; nearly 40% waited one to four weeks.
“Dealing with prior authorization issues adds an extra layer of stress, which is known to increase anxiety and can worsen treatment-related and disease-related symptoms and adverse effects,” the study authors wrote.
Frequent formulary changes
Part D prescription drug plans can, and do, change their formularies and prior authorization rules at any time. So, just because your Part D plan covers your expensive medication now doesn’t mean it will in the future.
“There are absolutely a lot of changes that take place from year to year,” says Purvis. That frustrates Medicare beneficiaries, Joyce noted.
The Biden administration has begun cracking down on prior authorization in Medicare Advantage plans , setting time limits on the delays. A few states have passed prior authorization laws exempting certain doctors in Medicare Advantage networks, too. Some large health insurers say they’re working to reduce prior authorization for Medicare beneficiaries.
In a small number of states, prescription drug affordability boards have tried to limit costs of certain medications, though pharmaceutical companies have challenged them.
Advice to avoid Part D prescription snags
So, what can people with Medicare Part D plans or those looking to enroll do to help ensure that the medications their doctors want them to take are covered?
Start by diving into Medicare’s online Plan Finder tool, which lets you see how each Part D plan works and compare alternatives.
“During Medicare Open Enrollment [generally Oct. 15 to Dec. 7], you really need to look at the Part D plans available to you and figure out whether the drugs you’re taking are subject to utilization management,” says Purvis. (People eligible for Medicare’s low-income subsidy can switch Part D plans anytime.)
Even if you have a Part D plan, study its latest documents online since the rules for what’s covered could be different than when you signed up.
When using Plan Finder, you’ll likely need to spend time unearthing the prior authorization rules and seeing which medications are on the plan’s formulary.
Brot-Goldberg did this last year for his father when he enrolled in Medicare for the first time.
“I avoided my dad facing prior authorization on one of his drugs,” says Brot-Goldberg.
But, he adds, doing the research for this was hard. “And I’m an expert.” He’ll go through the process again for his mother next month.
You might also call your State Health Insurance Assistance Program , known as a SHIP. Here, knowledgeable staffers and volunteers can answer your Medicare questions and guide you through the Part D puzzle.
The Part D appeals process
If your Part D plan denies you coverage for a medication, you can try to appeal .
The process can be cumbersome and exhausting, but it could lead to a reversal.
“They string you along and make it hard,” says Joyce. You need to make a stronger medical case than just saying your doctor wanted you to take the drug, he notes.
Most Popular

The independent source for health policy research, polling, and news.
Medicare Part D in 2024: A First Look at Prescription Drug Plan Availability, Premiums, and Cost Sharing
Juliette Cubanski and Anthony Damico Published: Nov 08, 2023
During the Medicare open enrollment period from October 15 to December 7 each year, people with Medicare can enroll in a plan that provides Part D prescription drug coverage , either a stand-alone prescription drug plan (PDP) for people in traditional Medicare, or a Medicare Advantage plan that covers all Medicare benefits, including prescription drugs (MA-PD). In 2023, 50.5 million of the 66 million people covered by Medicare are enrolled in Part D plans, with more than half (56%) enrolled in MA-PDs and 44% in PDPs. This issue brief provides an overview of Part D plan availability and premiums in 2024 and key trends over time. (An overview of the 2024 Medicare Advantage market is also available.) ( See Methods box for details on the analysis).
Part D Highlights for 2024
- The average Medicare beneficiary has a choice of close to 60 Medicare plans with Part D drug coverage in 2024 , including 21 Medicare stand-alone drug plans and 36 Medicare Advantage drug plans. While the market for Part D coverage overall remains robust, the number of PDP options for 2024 is lower and the number of MA-PD options is higher than in any other year since Part D started. The total number of PDPs (709) and firms offering these plans (11) have decreased from 2023 .
- Medicare beneficiaries who receive Part D Low-Income Subsidies (LIS) will have access to fewer so-called “benchmark” PDPs in 2024 than in any year since Part D started, with three benchmark plans available out of the average 21 PDPs available overall for 2024. Benchmark plans are PDPs available to LIS enrollees for no monthly premium. The reduction in the number of benchmark plans for 2024 is largely the result of PDPs offered by Cigna, Humana, and CVS Health qualifying as benchmark plans in far fewer regions in 2024 compared to 2023. An estimated 2.4 million LIS enrollees – half of all LIS enrollees in PDPs – need to switch plans during the 2023 open enrollment period if they want to be enrolled in a benchmark plan in 2024.
- Although the Inflation Reduction Act included a premium stabilization provision that capped annual growth in the Part D base beneficiary premium at 6%, the law did not apply this 6% cap to individual plan premiums that enrollees pay. The Part D base beneficiary premium of $34.70 for 2024 is based on standardized bids submitted by PDPs and MA-PDs to cover basic Part D benefits in 2024, while actual Part D plan premiums vary across plans and may be higher or lower than the base beneficiary premium, depending on several factors. The estimated average enrollment-weighted monthly premium for Medicare Part D stand-alone drug plans is projected to be $48 in 2024, based on current enrollment, up 21% from $40 in 2023 . This increase is driven by higher expected plan costs to provide the Part D benefit in 2024, including a new cap on enrollees’ out-of-pocket spending above the catastrophic threshold rather than requiring them to pay 5% coinsurance, as in prior years. After accounting for enrollment choices by new enrollees and plan changes by current enrollees, the actual average weighted PDP premium for 2024 is likely to be lower than the estimated weighted average of $48.
- Monthly premiums for drug coverage are substantially higher for PDPs compared to MA-PDs – five times higher, on average, in 2024 (based on unweighted amounts). While the average premium is projected to increase between 2023 and 2024 for PDPs, it is expected to remain stable (and low, or even zero) for MA-PDs. MA-PD sponsors can use rebate dollars from Medicare payments to lower or eliminate their Part D premiums , but there is no equivalent rebate system for PDPs.
- Average monthly premiums for the 14 national PDPs are projected to range from under $1 to $108 in 2024 . Premium variation across plans is in part related to whether plans offer basic or enhanced benefits and the value of benefits offered, as well as variation in the underlying costs that plans incur for their enrollees. Among the national PDPs, average monthly premiums are increasing for 12 PDPs, including 4 PDPs with increases greater than $20 and 3 with increases between $10 and $20.
- Most PDP enrollees will face much higher cost sharing for brands than for generic drugs in 2024, as in prior years, including coinsurance for non-preferred drugs of 50% (the maximum coinsurance rate allowed for the non-preferred drug tier) in 6 of the 14 national PDPs . PDP enrollees in 9 of the 14 national PDPs will also face coinsurance, rather than copays, for preferred brands, ranging from 15% to 25%, and coinsurance for specialty tier drugs ranging from 25% in 7 of the national PDPs to 33% in 2 national PDPs. Coinsurance can mean less predictable out-of-pocket costs than copayments. In a change from prior years, however, beneficiaries in 2024 will no longer be required to pay 5% coinsurance once they qualify for catastrophic coverage, due to a provision in the Inflation Reduction Act that eliminated this cost-sharing requirement.
Part D Plan Availability
For 2024, the average medicare beneficiary has fewer stand-alone drug plan options than in prior years but more medicare advantage drug plan options.
The Part D market for 2024 offers the average Medicare beneficiary fewer choices for drug coverage from stand-alone prescription drug plans than in prior years but more choices for coverage from Medicare Advantage drug plans. The average Medicare beneficiary has a choice of close to 60 options for Part D coverage in 2024, including 21 PDPs and 36 MA-PDs (Figure 1). Since 2020, the number of PDPs available to the average beneficiary has decreased by 25% while the number of MA-PDs has increased by 57%.
Of the 21 PDPs available to the average beneficiary in 2024, 14 are national PDPs – that is, available in all 34 PDP regions nationwide ( Appendix Table 1). This is a reduction of two national PDPs from 2023, the result of one plan sponsor (Elixir Insurance) pulling out of the Part D market entirely and an AARP-branded PDP sponsored by UnitedHealthcare no longer being offered in all 34 regions in 2024. The 270,000 enrollees in Elixir’s PDPs (as of March 2023) will need to select a new Part D plan from a different plan sponsor during the 2023 open enrollment period if they want their Part D coverage to continue in 2024.
A Total of 709 Medicare Part D Stand-Alone Prescription Drug Plans Will Be Offered by 11 Firms in 2024, the Lowest Number of PDPs and Firms Offering These Plans Since Part D Started
In 2024, a total of 709 PDPs will be offered by 11 firms in the 34 PDP regions (plus another 10 PDPs in the territories), a decrease of 92 PDPs (-11%) from 2023, and the lowest number of PDPs available in any year since Part D started in 2006 (Figure 2). The number of firms sponsoring stand-alone drug plans is decreasing from 15 firms in 2023 to 11 firms in 2024, the smallest number since the Medicare benefit was launched in 2006.
Despite the reduction in PDP availability overall, beneficiaries in each state will have a choice of multiple PDPs, ranging from 15 PDPs in New York to 24 PDPs in Alabama and Tennessee, plus multiple MA-PDs offered at the local level (Figure 3, Appendix Table 2).
Although the Inflation Reduction Act included a premium stabilization provision that capped annual growth in the Part D base beneficiary premium at 6% beginning in 2024, the base beneficiary premium is not the same as the amount that Part D enrollees pay for coverage, and the law did not cap the growth in individual plan premiums to 6%. The Part D base beneficiary premium of $34.70 for 2024 is based on standardized bids submitted by PDPs and MA-PDs to cover basic Part D benefits in 2024. (Absent the premium stabilization provision, the 2024 base beneficiary premium would have increased by 20% to $39.35, reflecting a higher average plan bid for offering Part D coverage in 2024 compared to 2023 .) Actual Part D plan premiums for 2024 vary across plans, may be higher or lower than the base beneficiary premium, and may be increasing by more or less than 6% (or even decreasing).
The estimated national average monthly PDP premium is projected to be $48 in 2024, a 21% increase from $40 in 2023, weighted by June 2023 enrollment. This higher average projected premium is driven by higher expected plan costs to provide the Part D benefit in 2024, including a new cap on enrollees’ out-of-pocket spending above the catastrophic threshold rather than requiring them to pay 5% coinsurance, as in prior years. This change is based on a provision in the Inflation Reduction Act.
Comparing monthly premiums for Part D coverage between stand-alone PDPs and MA-PDs shows the competitive advantage that MA-PDs have over PDPs when it comes to the premiums that enrollees pay for drug coverage. On an unweighted basis, monthly premiums for drug coverage are substantially higher for PDPs compared to MA-PDs – five times higher, on average in 2024 ($60 vs. $12) (Figure 4). Moreover, between 2023 and 2024, the unweighted average premium is increasing for PDPs, while remaining stable for MA-PDs. MA-PD sponsors can use rebate dollars from Medicare payments to lower or eliminate their Part D premiums and/or offer other extra benefits, but there is no equivalent rebate system for PDPs. According to MedPAC, Medicare Advantage monthly rebates per enrollee have more than doubled over the last five years, from $95 in 2018 to $196 in 2023 .
It is likely that, after accounting for enrollment choices by new enrollees and plan changes by current enrollees, the actual average weighted PDP premium for 2024 will be lower than the estimated weighted average of $48 but well above the average MA-PD premium. In 2023, the enrollment-weighted average monthly portion of the premium for drug coverage in MA-PDs is $10, compared to $40 for PDPs.
Average Monthly Premiums for the 14 National PDPs Are Projected to Range from Less Than $1 to $108 in 2024
PDP premiums will vary widely across plans in 2024, as in previous years. Among the 14 national PDPs, there is a difference of more than $1,200 in average annual premiums between the highest-premium PDP and the lowest-premium PDP. At the high end, the monthly premium for Humana Premier Rx Plan (the 10 th largest plan by overall enrollment) will be $108, totaling nearly $1,300 annually. At the low end, the monthly premium for Wellcare Value Script (the second largest plan) will average $0.40, or $5 annually (Figure 5). In addition to Humana Premier Rx Plan, two other national PDPs will charge monthly premiums of more than $100 in 2024: AARP Medicare Rx Preferred, the fourth largest plan ($106), and CVS Health’s SilverScript Plus, the 12 th largest plan ($103).
Two-Thirds of Part D Stand-alone Drug Plan Enrollees Without Low-income Subsidies Will Pay Higher Premiums in 2024 If They Stay in Their Current Plan
Two-thirds of Part D stand-alone plan enrollees (66%) – 8.6 million of the 12.9 million Part D PDP enrollees who are responsible for paying the entire premium (which excludes Low-Income Subsidy (LIS) recipients) – will see their monthly premium increase in 2024 if they stay in their current plan, while 4.4 million (34%) will see a premium reduction if they stay in their current plan (Figure 6).
Compared to 2023, more Medicare Part D stand-alone drug plan enrollees will see their monthly premium either increase or decrease by $10 or more if they stay in their same plan in 2024 (Figure 7). For 2024, 4.8 million non-LIS PDP enrollees (37%) will see a premium increase of $10 or more per month – or at least $120 more annually if they remain in their current plan – compared to 2.1 million enrollees (16%) in 2023.
Among the 14 national PDPs, average monthly premiums are increasing for 12 PDPs, including 7 PDPs (having a combined 3.9 million non-LIS enrollees) with increases exceeding $10:
- AARP Medicare Rx Walgreens (+$30, from $30 to $60)
- SilverScript Plus (+$29, from $74 to $103)
- Humana Premier Rx (+$25, from $83 to $108)
- Cigna Extra Rx (+$22, from $63 to $85)
- SilverScript Choice (+$16, from $33 to $49)
- Cigna Secure Rx (+$14, from $33 to $47)
- Humana Basic Rx Plan (+$14, from $37 to $51)
Another 1.6 million non-LIS PDP enrollees (12%) will see a monthly premium reduction of $10 or more for 2024, compared to under 150,000 (1%) for 2023. This largely reflects a premium reduction for the second largest PDP, Wellcare Value Script, where the average monthly premium will decrease by $9, from $10 in 2023 to less than $1 in 2024. These amounts are averaged over the 34 PDP regions; enrollees in this plan in 16 of the 34 regions will see a premium reduction of $10 or more.
Over half (56%) of non-LIS enrollees (7.3 million) are projected to pay monthly premiums of at least $40 if they stay in their current plans, or nearly $500 annually, including 2.1 million (16% of non-LIS enrollees) projected to pay monthly premiums of at least $100, or at least $1,200 annually. These estimates are higher than the comparable estimates for 2023, when 40% of non-LIS PDP enrollees (5.3 million) were projected to pay at least $40 per month, including 1.6 million paying $100 or more, if they stayed in their plans.
- Cost Sharing
Part D Enrollees Pay Much Higher Cost Sharing for Brands and Non-preferred Drugs Than for Generic-Tier Drugs, and a Mix of Copays and Coinsurance for Different Formulary Tiers
In 2024, as in prior years, Part D enrollees will face much higher cost-sharing amounts for brands and non-preferred drugs (which can include both brands and generics) than for drugs on a generic tier, and a mix of copayments and coinsurance for different formulary tiers. The typical five-tier formulary design in Part D includes tiers for preferred generics, generics, preferred brands, non-preferred drugs, and specialty drugs.
Among all PDPs, median standard cost sharing in 2024 for different types of drugs is (Figure 8):
- Generics : $0 for preferred generics and $5 for other generics
- Preferred brands : a copayment of $47 or coinsurance of 21% for preferred brands (up from $44/17% in 2023)
- Non-preferred drugs : 46% coinsurance for non-preferred drugs, which can include both brands and generics (an increase from 45% in 2023; the maximum allowed is 50%)
- Specialty drugs : 25% coinsurance for specialty drugs (the same as in 2023; the maximum allowed is 33%)
Among the 14 national PDPs, 9 PDPs will charge $0 for preferred generics in 2024, but copays of $40 to $47 or coinsurance of 16% to 25% for preferred brands, and coinsurance ranging from 39% to 50% for non-preferred drugs; 6 out of the 14 national PDPs are charging the maximum 50% coinsurance for non-preferred drugs. Coinsurance for specialty tier drugs ranges from 25% to 33% in these plans, with 7 of the 14 national PDPs charging 25% and 2 charging 33%. (Plans that charge the full deductible amount cannot charge more than 25% for specialty tier drugs.)
Low-Income Subsidy Plan Availability
In 2024, a smaller number of part d stand-alone drug plans will be premium-free to enrollees receiving the low-income subsidy than in any year since part d started.
Through the Part D LIS program, enrollees with low incomes and modest assets are eligible for assistance with Part D plan premiums and cost sharing. More than 13 million Part D enrollees are receiving LIS, including 8.3 million (62%) in MA-PDs and 5.2 million (38%) in PDPs.
In 2024, a smaller number of PDPs will be premium-free benchmark plans – that is, PDPs available for no monthly premium to Medicare Part D enrollees receiving the Low-Income Subsidy (LIS) – than in any year since Part D started, with 126 premium-free benchmark plans, or less than 20% of all PDPs in 2024 (Figure 9). The number of benchmark plans available in 2024 will vary by region, from two to seven ( Appendix Table 2).
PDPs offering basic benefits qualify to be benchmark plans if they have premiums below the benchmark amount in a given region. The benchmark is calculated as a weighted average of the beneficiary premiums for basic drug coverage offered by both PDPs and MA-PDs in a given region (calculated before taking MA rebates into account). (MA-PD premiums are included in this calculation even though MA-PDs do not qualify as benchmark plans.)
The reduction in the number of benchmark plans for 2024 is largely the result of PDPs offered by Cigna, Humana, and CVS Health qualifying as benchmark plans in far fewer regions in 2024 compared to 2023: Cigna Secure Rx (from 34 down to 16 regions); Humana Basic Rx Plan (from 27 down to 11 regions); and CVS Health’s SilverScript Choice (from 34 down to 11 regions).
On average (weighted by 2023 Medicare enrollment), LIS beneficiaries have three benchmark plans available to them out of the average 21 PDPs available overall for 2024 – the lowest average number of benchmark plan options in any year since Part D started. All LIS enrollees can select any plan offered in their area, but if they enroll in a non-benchmark plan, they must pay some portion of their chosen plan’s monthly premium.
In 2024, half (49%) of all LIS PDP enrollees who are eligible for premium-free Part D coverage (2.4 million LIS enrollees) will pay Part D premiums averaging $15 per month unless they switch or are reassigned by CMS to premium-free plans. Among this group are the 1.9 million LIS enrollees in Cigna Secure Rx, Humana Basic Rx Plan, or CVS Health’s SilverScript Choice in the regions where these PDPs will no longer qualify as benchmark plans. These enrollees will need to switch plans for 2024 if they want to remain in a benchmark (premium-free) plan.
The overall market for Part D coverage remains robust based on the overall number of plan options, but recent years have seen a growing divide in the Part D plan market between stand-alone PDPs, where the number of plans has generally been trending downward over time in conjunction with a reduction in PDP enrollment, and MA-PDs, where plan availability and enrollment have experienced steady growth.
The average weighted monthly premium for PDPs in 2024 will increase substantially over the 2023 amount (based on current enrollment), while premiums for drug coverage offered by MA-PDs are likely to remain stable (and low or zero). Provisions in the Inflation Reduction Act to make the Part D benefit more generous – such as the elimination of the 5% coinsurance requirement for catastrophic coverage taking effect in 2024 – will help lower out-of-pocket costs for enrollees, but with these changes, it could become harder for some Part D plan sponsors to offer low-priced coverage, particularly sponsors of stand-alone drug plans. MA-PD sponsors have a competitive advantage in this regard because they can use rebate dollars from Medicare payments to lower or eliminate their Part D premiums . The premium imbalance between PDPs and MA-PDs could be exacerbated as plans assume greater liability for high drug costs above the catastrophic threshold in 2025 with a $2,000 cap on out-of-pocket spending. To keep Part D premiums low in the face of rising costs for the basic Part D benefit, Medicare Advantage plans may end up using more of their rebate dollars to buy down the Part D premium. This could mean less rebate money available for other benefit enhancements or lower profits, depending on the amount of rebates plans receive in the future.
The increasing availability of low- or zero-premium MA-PDs, combined with the aggressive marketing of Medicare Advantage plans and the appeal of other features of these plans, such as supplemental benefits, could tilt enrollment even more towards Medicare Advantage plans in the future. Monitoring trends in Part D plan availability and enrollment could inform policymakers in considering whether or how to ensure continued availability of competitively priced stand-alone Part D drug plans for the millions of Medicare beneficiaries in traditional Medicare.
Juliette Cubanski is with KFF. Anthony Damico is an independent contractor.
Appendix Tables
- Medicare Part D
- Medicare Advantage
- Prescription Drugs
news release
- With Medicare Open Enrollment Underway, Beneficiaries Typically Will Have a Choice of 43 Medicare Advantage Plans for 2024, Consistent with 2023 But More than Double The Number From 2018
Also of Interest
- An Overview of the Medicare Part D Prescription Drug Benefit
- Changes to Medicare Part D in 2024 and 2025 Under the Inflation Reduction Act and How Enrollees Will Benefit
- Key Facts About Medicare Part D Enrollment and Costs in 2023
- Medicare Advantage in 2023: Enrollment Update and Key Trends

Sign up for the Health News Florida newsletter
Ahca selects 5 health plans for medicaid managed-care program.

The contracts will involve tens of billions of dollars in the coming years, with about 3.45 million people receiving health care through the managed-care system as of February
The state Agency for Health Care Administration on Friday announced plans to award contracts to five health plans to take part in the Medicaid managed-care program.
The contracts will involve tens of billions of dollars in the coming years, with about 3.45 million people receiving health care through the managed-care system as of February, according to data posted on the agency’s website.
The five health plans are Florida Community Care, Humana Medical Plan, Simply Healthcare Plans, Sunshine State Health Plan and South Florida Community Care Network, which does business as Community Care Plan.
A document posted on the agency website indicated Humana, Simply Healthcare and Sunshine State Health Plan would receive statewide contracts, while the other two would receive contracts in regions of the state.
The contracting process has taken the past year, and 11 plans responded to what is known as an “invitation to negotiate” to try to get contracts, information on the website said.
Plans that do not receive contracts can file challenges. The agency is required to go through a procurement process for the contracts every six years.

Opinion | Biden Shrinks Medicare Advantage
P resident Biden keeps accusing Republicans of trying to gut Medicare. No doubt he hopes seniors don’t notice that his Administration recently cut payments to Medicare Advantage plans, which will lead to higher patient costs and reduced benefits.
About half of seniors are enrolled in Medicare Advantage plans, which are administered by private insurers with government funding. These plans have been increasing in popularity, especially among lower-income Americans, because they offer additional benefits such as dental and vision care. Out-of-pocket costs tend to be lower than in traditional fee-for-service Medicare.
Critics of Medicare Advantage say insurers sometimes put up bureaucratic hurdles to covering needed treatments and procedures, which is true. But they also prevent unnecessary care, which is rife in traditional Medicare. Insurers also do a better job of coordinating care and keeping patients out of the hospital. If seniors disliked the program, it wouldn’t be growing.
Enter the Biden Administration, which is trying to limit the program’s growth by squeezing insurers. Progressives oppose Medicare Advantage because they dislike private market competition and want the government to control all of healthcare. The Administration last year restricted plan marketing and cut payments to insurers on average by 1.1%.
Now the Centers for Medicare and Medicaid Services is clipping insurer base payments by another 0.16%, which will take effect next year. The cut comes as insurers report increasing utilization among seniors owing to delayed pandemic care. Providers are also seeking higher reimbursements from insurers to offset rising overhead and labor costs.
Berkeley Research Group projects Medicare Advantage medical costs will climb by 4% to 6% next year. In response to last year’s payment cut, many plans increased patient co-pays and premiums, reduced benefits like vision and dental care, and tightened provider networks. More will have to do so next year.
Shares of insurers tumbled after CMS’s announcement, especially those with large Medicare businesses such as Humana (-10%), UnitedHealthcare (-8%) and CVS Health (-6%). Investors also fear the cuts will reduce enrollment. This may be why Cigna in January sold its Medicare business to Health Care Service Corporation.
Medicare Advantage plans send notices of annual plan changes in the autumn—a few weeks before the November election. Seniors may be in for a rude cost and benefit shock when they try to renew. If seniors like their doctor, they might not be able to keep her.
Perhaps election considerations explain why a bipartisan group of 61 Senators, including Majority Leader Chuck Schumer, urged CMS in a January letter to “ensure payment and policy stability for the Medicare Advantage program,” adding that seniors must “have stable access to the extra benefits and out-of-pocket protections only available in Medicare Advantage.”
Will Mr. Schumer now protest the Administration’s cut to drive more seniors out of private plans? By the way, CMS is also cutting physician payments in traditional Medicare to control its ballooning costs. The predictable result will be more provider consolidation, less healthcare competition, and a shift in costs to privately insured Americans.
If only Republicans had nominated a presidential standard-bearer who could explain all this to Americans.
An official website of the United States government
Here's how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
CMS Newsroom
Search cms.gov.
- Physician Fee Schedule
- Local Coverage Determination
- Medically Unlikely Edits
Provider Assignment
On this page:, provider nomination and the geographic assignment rule.
- Part A and Part B (A/B) and Home Health and Hospice (HH+H)
- Durable Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS)
- Specialty Providers and Demonstrations
- Railroad Retirement Beneficiaries Entitled to Medicare
- Qualified Chains
- Out-of-Jurisdiction Providers (OJP)
Section 911(b) of the Medicare Prescription Drug, Improvement, and Modernization Act of 2003 (MMA), Public Law 108-173 , repealed the provider nomination provisions formerly found in Section 1816 of the Title XVIII of the Social Security Act and replaced it with the Geographic Assignment Rule. Generally, a provider or supplier will be assigned to the Medicare Administrative Contractor (MAC) that covers the state where the provider or supplier is located. The Center for Medicare & Medicaid Services’ (CMS) has defined the following approach for assigning providers, physicians, and suppliers to MACs.
return to top
Part A/Part B (A/B) and Home Health and Hospice (HH+H) Rule
All A/B and HH+H providers will be assigned to the MAC contracted by CMS to administer A/B and HH+H claims for the geographic locale in which the provider is physically located. Learn more about the current A/B MAC jurisdictions and HH+H areas and view the corresponding maps at Who are the MACs.
Durable Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS) Rule
Each DMEPOS supplier submits claims to the DME MAC contracted by CMS to administer DMEPOS claims for the geographic locale in which the beneficiary resides permanently. Learn more about the current DME MAC jurisdictions and view the corresponding map at Who are the MACs.
Specialty Providers and Demonstrations Rule
Specialty providers and providers involved with certain demonstrations will submit claims to a specific MAC designated by CMS. Learn more about a specific A/B MAC or DME MAC and view the corresponding maps at Who are the MACs .
Railroad Retirement Beneficiaries Entitled to Medicare Rule
Physicians and other suppliers (except for DMEPOS suppliers) will continue to enroll with and bill the contractor designated by the Railroad Retirement Board for Part B services furnished to their beneficiaries. Each DMEPOS supplier will submit claims to the DME MAC contracted by CMS to administer DMEPOS claims for the geographic locale in which the beneficiary resides permanently. Learn more about the current DME MAC jurisdictions and view the corresponding map at W ho are the MACs.
Qualified Chains Rule
The Geographic Assignment Rule states that generally, a provider or supplier will be assigned to the MAC that covers the state where the provider or supplier is located. However, it does provide an exception for qualified chains. A qualified chain home office may request that its hospitals and skilled nursing facilities be serviced by the A/B MAC that covers the state where the home office is located. A qualified chain home office may send an inquiry to: CMS [email protected]
Out-of-Jurisdiction Providers (OJP) Rule
An OJP is a provider that is not currently assigned to an A/B MAC in accordance with the geographic assignment rule and the qualified chain exception. For example, a hospital not part of a qualified chain located in Maine, but currently assigned to the A/B MAC in Jurisdiction F would be an OJP.
Each A/B MAC will initially service some OJPs until CMS undertakes the final reassignment of all OJPs to their destination MACs based on the geographic assignment rule and its exceptions.
CMS has not set a timetable for moving OJP’s.
- Election 2024
- Entertainment
- Newsletters
- Photography
- Personal Finance
- AP Investigations
- AP Buyline Personal Finance
- Press Releases
- Israel-Hamas War
- Russia-Ukraine War
- Global elections
- Asia Pacific
- Latin America
- Middle East
- Election Results
- Delegate Tracker
- AP & Elections
- March Madness
- AP Top 25 Poll
- Movie reviews
- Book reviews
- Personal finance
- Financial Markets
- Business Highlights
- Financial wellness
- Artificial Intelligence
- Social Media
Court says judge had no authority to halt Medicare Advantage plan for Delaware government retirees
- Copy Link copied
DOVER, Del. (AP) — Delaware’s Supreme Court has overturned a lower court ruling that prevented officials from moving state government retirees from a Medicare supplement plan to a Medicare Advantage plan.
The justices ruled Friday that a Superior Court judge had no jurisdiction to enter the stay because he wrongly determined that the state panel that approved the Medicare Advantage plan had violated the state’s Administrative Procedures Act. The selection of a particular Medicare plan is not a regulation subject to APA notice and public hearing requirements, and the judge therefore had no jurisdiction under the APA to halt the plan, the court said.
Justice Abigail LeGrow, writing for a three-judge panel, said a regulation under the APA is a statement of law, procedure or policy that is used as a rule or standard to guide, regulate, or act as a model for future action. The choice of a Medicare plan does not fall within the plain meaning of those terms, she said.
“Accordingly, the Superior Court did not have jurisdiction to enter the challenged stay, and we reverse the decision on appeal,” LeGrow wrote. “The important policy considerations that attend the selection of healthcare coverage for state retirees are questions appropriately addressed to the legislative and executive branches.”
The court rejected an appeal by plan opponents seeking to force the state to pay their attorney fees because of the state’s “reprehensible conduct.” Fee shifting, available only against a losing party, was mooted by the reversal of the lower court decision, LeGrow noted.
Democratic Gov. John Carney’s office released a statement praising the ruling.
“We are pleased with the result at the Supreme Court, which reaffirms the role of the executive branch in making important decisions around procurement of health care and other services,” the statement reads. “This ruling will protect taxpayers in the long run.”
In February 2022, the State Employee Benefits Committee unanimously agreed to replace a Medicare part A and B supplemental plan with a new Part C Medicare Advantage plan, effective Jan. 1, 2023. The move set off a firestorm of opposition from state retirees and, in turn, prompted lawmakers to introduce legislation eliminating the option of providing state pensioners with a Medicare Advantage plan.
Opponents, including former Democratic state Sen. Karen Peterson, were particularly unhappy with the prospect of having fewer medical providers to choose from and needing prior authorization for many medical procedures.
In October 2022, Superior Court Judge Calvin Scott Jr. halted implementation of the Medicare Advantage plan, saying it amounted to a new regulation under the APA. He rejected the administration’s argument that the State Employee Benefits Committee was authorized by law to change retiree healthcare plans without following formal APA requirements.
In the wake of the lawsuit, the State Employee Benefits Committee and Highmark Blue Cross Blue Shield agreed last year to terminate the Medicare Advantage contract. The State Employee Benefits Committee also voted to solicit bids for a new Medicare supplement plan.
Meanwhile, lawmakers introduced a bill to add a state retiree and an additional representative of organized labor to the State Employee Benefits Committee, and to establish a Retiree Healthcare Benefits Advisory Subcommittee. Carney signed the bill into law last year just two weeks after it was introduced.
A separate bill eliminating the option of providing state pensioners with a Medicare Advantage plan was introduced this year. It was amended last month to allow a Medicare Advantage plan as an option for eligible pensioners hired on or after Jan. 1, 2025, but only if the plan is adopted by the State Employee Benefits Committee as a regulation under the APA. The bill passed the House unanimously last month and is awaiting consideration by a Senate committee.

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- What's New
- News Releases & Articles
- Media Materials
Examining How Improper Payments Cost Taxpayers Billions and Weaken Medicare and Medicaid
U.s. house committee on energy and commerce, subcommittee on oversight and investigations testimony on examining how improper payments cost taxpayers billions and weaken medicare and medicaid.
Christi A. Grimm, Inspector General, Office of Inspector General, U.S. Department of Health and Human Services

Watch the Testimony

IMAGES
VIDEO
COMMENTS
Here's how it works: Medicare will pay the provider 95% of the amount they would pay if the provider accepted assignment. The provider can charge the person receiving care more than the Medicare-approved amount, but only up to 15% more (some states limit this further). This extra amount, which the patient has to pay out-of-pocket, is known as ...
All providers who accept assignment must submit claims directly to Medicare, which pays 80 percent of the approved cost for the service and will bill you the remaining 20 percent. You can get some preventive services and screenings, such as mammograms and colonoscopies, without paying a deductible or coinsurance if the provider accepts assignment.
Medicare assignment is a fee schedule agreement between the federal government's Medicare program and a doctor or facility. When Medicare assignment is accepted, it means your doctor agrees to the payment terms of Medicare. Doctors that accept Medicare assignment fall under one of three designations: a participating doctor, a non ...
This is called "accepting assignment." If a provider accepts assignment, it's for all Medicare-covered Part A and Part B services. Using a provider that accepts assignment. Most doctors, providers, and suppliers accept assignment, but always check to make sure that yours do. ... or set up a payment plan with the provider through a private ...
Summary: Medicare Assignment is an agreement between healthcare providers and Medicare, where providers accept the Medicare-approved amount as full payment, preventing them from charging beneficiaries extra. This benefits Medicare beneficiaries by controlling their costs and ensuring they only pay deductibles and copayments.
Medicare Supplement and Medicare assignment. Medigap plans are additional insurance that helps cover your Medicare cost-share. If you are on specific plans, they'll pay any extra costs from healthcare providers that accept Medicare but not Medicare assigned amount. Most Medicare Supplement plans don't cover the excess charges.
Bottom Line. Medicare assignment means a doctor or other healthcare provider will charge no more than the Medicare-approved amount for a particular service. This usually means lower out-of-pocket costs for patients who are covered by Medicare. It also means the provider will bill Medicare rather than expecting the patient to pay the full amount ...
A medical provider that accepts Medicare assignment must submit claims directly to Medicare on your behalf. They will be paid the agreed upon amount by Medicare, and you will pay any copayments or deductibles dictated by your plan. If your doctor is non-participating, they may accept Medicare assignment for some services but not others.
1. Participating providers, or those who accept Medicare assignment. These providers have an agreement with Medicare to accept the Medicare-approved amount as full payment for their services. You don't have to pay anything other than a copay or coinsurance (depending on your plan) at the time of your visit.
When a provider accepts Medicare assignment, they accept the Medicare-approved amount as the full cost for a covered service. Learn more about assignment here. Speak with a Licensed Insurance Agent (888) 335-8996; Medicare 101. ... We do not offer every plan available in your area. Currently we represent 26 organizations which offer 3,740 ...
The Medicare accept assignment definition pertains to physicians, medical suppliers and medical providers that agree to accept Medicare-approved charges as total and full payment for all covered services without adding extra charges. These providers also agree to charge only the allowed Medicare deductible and coinsurance charges to patients.
According to the Medicare website: Assignment means that your doctor, provider, or supplier agrees (or is required by law) to accept the Medicare-approved amount as full payment for covered services. This means that for Medicare to cover the entire cost of a covered service, you'll need to go to a service provider who accepts assignment.
Medicare "participation" means you agree to accept claims assignment for all Medicare-covered services to your patients. By accepting assignment, you agree to accept Medicare-allowed amounts as payment in full. You may not collect more from the patient than the Medicare deductible and coinsurance or copayment. Participating Provider or ...
Medicare assignment codes help Medicare pay for covered services. If your doctor or other provider accepts assignment and is a participating provider, they will file for reimbursement for services with a CMS-1500 form and the code will be "assigned.". But non-participating providers can select "not assigned.".
What it means to "accept Medicare assignment". In short, accepting Medicare assignment means signing a contract to accept whatever Medicare pays for a covered service as full payment. Participating and non-participating status only applies to Medicare Part B; Medicare Advantage plans operate with contracts similar to commercial insurance ...
Many psychiatrists opt out of Medicare. Providers who take assignment should submit a bill to a Medicare Administrative Contractor (MAC) within one calendar year of the date you received care. If your provider misses the filing deadline, they cannot bill Medicare for the care they provided to you. However, they can still charge you a 20% ...
Nonassignment of Benefits. The second reimbursement method a physician/supplier has is choosing to not accept assignment of benefits. Under this method, a non-participating provider is the only provider that can file a claim as non-assigned. When the provider does not accept assignment, the Medicare payment will be made directly to the beneficiary.
PAR physicians agree to take assignment on all Medicare claims, which means that they must accept Medicare's approved amount (which is the 80% that Medicare pays plus the 20% patient copayment) as ...
The standard monthly Part B premium in 2024 is $174.70, an increase of $9.80 from the $164.90 beneficiaries paid in 2023. Be aware that your premium may increase depending on your income. Premiums ...
The majority of doctors accept assignment. Participating health providers have an agreement with Medicare to accept assignment for all Medicare-covered services. If the doctor accepts assignment ...
The official U.S. government website for Medicare, a health insurance program for people age 65 or older and younger people with disabilities. ... Find health & drug plans Find & compare plans in your area. Find Plans Now. Find care providers Compare hospitals, nursing homes, & more. Find Providers Near Me ...
• Original Medicare includes Medicare Part A (Hospital Insurance) and Part B (Medical Insurance). • You can join a separate Medicare drug plan to get Medicare drug coverage (Part D). • You can use any doctor or hospital that takes Medicare, anywhere in the U.S. • To help pay your out-of-pocket costs in Original Medicare (like your 20%
Joyce and his colleagues found that restrictions in Part D plans (what plans call "utilization management") grew dramatically between 2011 and 2020 for both traditional Medicare and private ...
The average Medicare beneficiary has a choice of close to 60 Medicare plans with Part D drug coverage in 2024, including 21 Medicare stand-alone drug plans and 36 Medicare Advantage drug plans ...
Medicare Advantage plans can use these rebate dollars to advertise a wide array of supplemental benefits, including special supplemental benefits for chronically ill enrollees. In 2022, over 99% of Medicare Advantage plans offered at least one supplemental benefit. The median was 23 supplemental benefits, and the most frequently offered ...
The contracts will involve tens of billions of dollars in the coming years, with about 3.45 million people receiving health care through the managed-care system as of February, according to data posted on the agency's website. The five health plans are Florida Community Care, Humana Medical Plan, Simply Healthcare Plans, Sunshine State Health ...
Medicare Advantage plans send notices of annual plan changes in the autumn—a few weeks before the November election. Seniors may be in for a rude cost and benefit shock when they try to renew. ...
Provider Nomination and the Geographic Assignment Rule. Section 911(b) of the Medicare Prescription Drug, Improvement, and Modernization Act of 2003 (MMA), Public Law 108-173, repealed the provider nomination provisions formerly found in Section 1816 of the Title XVIII of the Social Security Act and replaced it with the Geographic Assignment ...
The selection of a particular Medicare plan is not a regulation subject to APA notice and public hearing requirements, and the judge therefore had no jurisdiction under the APA to halt the plan, the court said. Justice Abigail LeGrow, writing for a three-judge panel, said a regulation under the APA is a statement of law, procedure or policy ...
U.S. House Committee on Energy and Commerce, Subcommittee on Oversight and Investigations Testimony on Examining How Improper Payments Cost Taxpayers Billions and Weaken Medicare and Medicaid April 16, 2024, 10:30 a.m. Christi A. Grimm, Inspector General, Office of Inspector General, U.S. Department of Health and Human Services