Handwashing in Communities: Clean Hands Save Lives

Regular handwashing is one of the best ways to remove germs, avoid getting sick, and prevent the spread of germs to others. Whether you are at home, at work, traveling, or out in the community, find out how handwashing with soap and water can protect you and your family.

Keeping hands clean can prevent 1 in 3 diarrheal illnesses and 1 in 5 respiratory infections, such as a cold or the flu.

School-based programs promoting hand hygiene can result in less illness and fewer missed school days.

When your family is healthy, you don’t have to worry about missing school, work, or other activities.

See CDC’s recommendations and resources for hand hygiene in healthcare settings.
Learn about key times to wash, the five steps, and more information.
See the data behind handwashing and using hand sanitizer.
Learn ways to promote hand hygiene in your home and community.
Learn information about when and how to use hand sanitizer.
Use resources to promote handwashing and prevent illness.
Find information on key hand hygiene topics.
Each year on October 15, this observance highlights the importance of handwashing.
Find links to information on trainings and educational resources.

Use CDC materials to raise awareness of hand hygiene in your community:
- Fact Sheets
- Social media library
To receive email updates about this topic, enter your email address:

Get answers to frequently asked questions about washing your hands and using hand sanitizer in community settings.
- Hand Hygiene at Work
- Handwashing: A Healthy Habit in the Kitchen
- Show Me the Science – How to Wash Your Hands
- Show Me the Science – When & How to Use Hand Sanitizer in Community Settings

Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.

Yes, washing our hands really can help curb the spread of coronavirus
Professor and Programme Director, SA MRC Centre for Health Economics and Decision Science - PRICELESS SA (Priority Cost Effective Lessons in Systems Strengthening South Africa), University of the Witwatersrand
Associate Professor in the SAMRC Centre for Health Economics and Decision Science - PRICELESS SA (Priority Cost Effective Lessons in Systems Strengthening South Africa), University of the Witwatersrand
Disclosure statement
Karen Hofman currently receives research funding from the IDRC (Canada), UK Wellcome Trust, UK National Institutes for Health Research, Bloomberg Philanthropies and the South African Medical Research Council. In the past, she has also received funding from the Bill and Melinda Gates Foundation, WHO and UNFPA.
Susan Goldstein is Associate Professor at the SA MRC Centre for Health Economics and Decision Science - PRICELESS SA (Priority Cost Effective Lessons in Systems Strengthening South Africa), School of Public Health, University of the Witwatersrand.
University of the Witwatersrand provides support as a hosting partner of The Conversation AFRICA.
View all partners
Much of the media discussion about coronavirus revolves around diagnosis and management of suspected cases. But the first piece of advice that is essential for anyone worried about contracting the coronavirus is something your grandparents might have suggested: wash your hands. It’s at the top of the list of many of the players trying to prevent the spread of the disease. This includes the World Health Organisation (WHO), the US Centers for Disease Control and Prevention and other health authorities around the world.
But, ask the cynics, could preventing the spread of disease really be as simple as washing my hands?
The answer is yes. Because the science says so.
Hand washing is a tried and true, scientifically proven preventive strategy that reduces the likelihood of transmitting both viral and bacterial borne diseases. It has been shown to decrease both respiratory and diarrhoeal diseases in countries across the world. One review found that hand washing reduced diarrhoea cases by 30%. This is because it prevented bacteria being transmitted from faeces to the mouth.
It may seem like a low-cost – and incredibly simple – intervention. But not emphasising it would be a huge missed opportunity.
Read more: Why hand-washing really is as important as doctors say
The American Centers for Disease Control and Prevention recommends the following five‑step approach:
1) Wet your hands and turn off the tap (to save water),
3) Rub your hands together for at least 20 seconds (possibly while singing Happy Birthday twice),
4) Rinse, and
Do this multiple times a day, especially before eating. Using hand sanitiser is another option, as long as it is composed of 60% or more alcohol.
The benefits of hand washing over other preventive measures are clear: soap is easy to access. Both soap and an alcohol-based products for cleaning hands are cost effective interventions.
But millions of us don’t wash our hands as often and as well as we should. A study done in South Korea indicated that 93.2% of 2,800 survey respondents did not wash their hands after coughing or sneezing.
The history
The current outbreak of the new coronavirus disease (COVID-19) was first reported on 31 December 2019 in Wuhan, China. By early March 2020 more than 90,000 people from 71 countries had been infected. More than 3,000 people have died so far. It is not clear what the fatality rate is and this may not be known until the outbreak is over – but it has been quoted as around 2.5% by the WHO.
Other diseases carry much higher fatalities. For example, tuberculosis claims the lives of 4,100 people worldwide every day. And the Ebola virus fatality rate is 50% .
Nevertheless, the spread of the new virus has set off alarm bells, with China famously building two hospitals in 10 days , cruise ships being quarantined and cities effectively being shut down .
The reason for the panic is that Corona-19 (more correctly named SARS-CoV-2) is a newly discovered virus. We don’t know exactly how infectious it is or who is at risk and why. As the WHO director-general said: we are entering uncharted territory .
Apart from hand washing it’s important to try not to touch one’s face and not shake hands. Face masks are really only useful for those who already have the virus or are caring with someone known to have the virus. Proper use of face masks is explained by the WHO.
Consideration should also be given to the fact that a run on medical masks could cause a shortage for public health-care workers who need them for protection against other diseases such as drug-resistant TB. This is particularly true in South Africa.
What the science says about hand washing
Research shows that hand washing isn’t just effective in preventing transmission of coronavirus. MIT recently conducted a study to identify the most effective mitigation strategy for hand hygiene that could contribute most to the reduction of global epidemic risk. Researchers used modelling and data‐driven simulations.
The study found that if 60% of travellers moving through airports worldwide had clean hands, global disease spread could be curbed by almost 70%. And if this rate could be maintained in only 10 of the busiest airports internationally, an astounding 37% of infections could be prevented.
Research has also shown that hand washing can prevent about 30% of diarrhoea-related sicknesses and about 20% of respiratory infections . Some scientists go as far as to argue that 80% of diseases can be prevented by proper hand washing.
Not everyone is convinced. Hand washing has been treated with scepticism as a significant disease prevention and eradication measure by some who favour “hard science interventions”.
This is not without precedent.
A Hungarian-born physician in the mid-19th century, Ignaz Semmelweis , was ostracised and shunned by his colleagues because he was so bold as to make a link between decreased maternal mortality and hand washing for doctors who went directly from the dissection halls to deliver babies.
Despite the growing body of research showing its effectiveness, hand washing habits are inadequate.
The MIT study assumes that 30% of people do not wash their hands at all after using a bathroom, and that correct hand washing is practised at such low rates that only 20% of people in airports actually have clean hands.
In South Africa, a national hand hygiene behaviour strategy estimated that only 20% of South Africans washed their hands with soap at critical times such as before, during and after preparing food, after going to the toilet, after sneezing or coughing, after touching animals, after changing nappies of babies, and after caring for an ill person.
Hand washing is simple and should already be part of everyone’s daily routine. If it became a habit for everyone in the world, it would not just prevent mortality and illness from coronavirus. It could be the start of a more viable strategy to prevent death from other bacterial and viral diseases.
While the full implications of this global pandemic are still unfolding, and a vaccine has yet to be developed, we need to act without delay using the one tool we already have.
- Public health
- Infectious diseases
- Coronavirus
- Hand hygiene
- Hand washing
- Disease prevention

Project Offier - Diversity & Inclusion

Senior Lecturer - Earth System Science

Sydney Horizon Educators (Identified)

Deputy Social Media Producer

Associate Professor, Occupational Therapy
Healthdirect Free Australian health advice you can count on.
Medical problem? Call 1800 022 222. If you need urgent medical help, call triple zero immediately
healthdirect Australia is a free service where you can talk to a nurse or doctor who can help you know what to do.
Hand washing
6-minute read
Share via email
There is a total of 5 error s on this form, details are below.
- Please enter your name
- Please enter your email
- Your email is invalid. Please check and try again
- Please enter recipient's email
- Recipient's email is invalid. Please check and try again
- Agree to Terms required
Error: This is required
Error: Not a valid value
- Hand washing is important because it helps to prevent the spread of infections such as COVID-19, colds, the flu and gastroenteritis.
- You should wash your hands before touching anything that needs to stay clean, and after touching anything that might contaminate your hands.
- Warm, soapy water is the best option for washing your hands when they are visibly dirty.
- Hand sanitiser is only effective if your hands have no visible dirt on them.
Why is good hand hygiene important?
Germs collect on your hands as you go about everyday life. When you touch your eyes, nose or mouth, the germs can spread to these vulnerable areas. So one of the best ways to avoid getting sick and spreading illness is to frequently wash your hands.
Hand washing helps prevent the spread of infections such as common colds, flu, COVID-19 and gastroenteritis . This is important, especially if you care for babies, older people or sick people who are more vulnerable to these illnesses.
Babies and children need to wash their hands too. They’re more vulnerable to getting infections because their immune systems aren’t yet mature.
If your child is too young to stand at a hand basin, you can wash their hands with disposable wipes or a wet, soapy cloth. Always make sure all soap is rinsed off and their hands thoroughly dried.
Teaching children good hand hygiene sets up lifelong habits to stop the spread of infection.
Hand washing is also one of the most important ways to prevent the spread of infection among people in hospital. People’s immune systems are often weakened after illness or surgery, so infections are easy to catch and can be hard to treat. They may then become life-threatening.
When should I wash my hands?
You should wash your hands before touching anything that needs to stay clean. You should also wash your hands after touching anything that might contaminate your hands or make them dirty.
Examples of times when you should wash your hands include:
- when your hands are visibly dirty
- after going to the toilet
- after helping a child go to the toilet, or changing a nappy
- after handling rubbish, household or garden chemicals, or anything that could be contaminated
- before you prepare or eat food
- after touching raw meat
- after blowing your nose or sneezing, or wiping a child’s nose
- after patting an animal
- after cleaning up blood, vomit or other body fluids
- after cleaning the bathroom
- before and after you visit a sick person in hospital
- before and after touching a wound, cut or rash
- before breastfeeding or feeding a child
- before handling medicine or applying ointment
- when holding a sick child
What is the best way to wash my hands?
Warm, soapy water is the best option for washing your hands when they are visibly dirty. Follow these simple tips on good hand hygiene.
To wash your hands:
- Wet hands with running water (preferably warm).
- Apply soap or liquid soap — enough to cover all of your hands. Normal soap is just as good as antibacterial soap.
- Rub your hands together for at least 20 seconds.
- Make sure you cover all surfaces, including the backs of your hands and in between your fingers.
- Rinse hands, making sure you remove all soap, and turn off the tap using the towel or paper towel.
- Dry your hands thoroughly with a paper towel, a clean hand towel or an air dryer if you are in a public toilet.

When should I use waterless hand sanitiser?
An alcohol-based hand rub (hand sanitiser) is a good way to clean your hands if you don't have access to soap and water. Hand sanitiser is only effective if your hands have no visible dirt on them.
To use hand sanitiser:
- Put about half a teaspoon of the product in the palm of your hand, rub your hands together, covering all the surfaces of your hand, including between your fingers.
- Keep rubbing until your hands are dry (about 20 to 30 seconds).
Alcohol-based hand sanitiser can be poisonous if swallowed. Follow these tips to keep kids safe around hand sanitiser.

Other tips for good hand hygiene
- Carry some hand sanitiser with you and use it whenever you want to decontaminate your hands, for example, after using public transport.
- Cough or sneeze into a tissue or your elbow, instead of into your hands.
- Wear disposable gloves before handling dirty nappies or cleaning up blood or any other body fluid.
- Be a good role model and encourage children to wash their hands properly and frequently.
- When using cloth towels to dry your hands, hang the towel up to dry after each use, and launder the towels regularly.
Learn more here about the development and quality assurance of healthdirect content .
Last reviewed: December 2023
Search our site for
- Food Hygiene
- Respiratory Hygiene
Need more information?
These trusted information partners have more on this topic.
Top results
How to hand wash correctly
Read more on St John Ambulance Australia website

Hand washing for hygiene | Health and wellbeing | Queensland Government
How to protect yourself from flu, e-coli, measles and other diseases by washing your hands.
Read more on Queensland Health website

Hand Hygiene | SA Health
Hand hygiene refers to any method which effectively removes soil and any harmful germs.
Read more on SA Health website

Handwashing - Why it's important - Better Health Channel
Washing your hands with soap and warm water can help stop the spread of infectious diseases.
Read more on Better Health Channel website

Patients and Carers - Sepsis Australia
Centers for Disease Control and Prevention (CDC) (USA) Global Sepsis Alliance Hand Hygiene Australia Infection Prevention & Healthcare Facilities – Australasian College for Infection Prevention and Control Limbs for Life Amputee Peer Support National Institute of General Medical Sciences (NIGMS) Sepsis Factsheet Sepsis Alliance website Information on Treatment When a…
Read more on Sepsis Australia website

Hand Washing - Miracle Babies
Most illnesses are transmitted to infants by the hands; therefore regular hand washing is essential and is the single best way to avoid the spread of disease
Read more on Miracle Babies Foundation website

Hand washing | National Centre for Farmer Health
Washing your hands is one of the simplest, yet most effective, things you can do to protect your health and the health of others. Farmers come in contact with many potential sources of disease and illness. Read more...
Read more on National Centre for Farmer Health website

No Germs on Me | NT.GOV.AU
No Germs on Me campaign to promote hand washing in your community.
Read more on NT Health website

Childhood infections: minimising the spread - MyDr.com.au
The 3 most effective ways of stopping the spread of childhood infections are: getting your children vaccinated; keeping them at home when they are sick; and careful hand washing.
Read more on myDr website

Personal hygiene for children: in pictures | Raising Children Network
Our illustrated guide to personal hygiene for children covers hand-washing, bathing, toileting, cleaning teeth, blowing noses and more. Download or print.
Read more on raisingchildren.net.au website

Hand Hygiene | Ausmed
Thousands of people around the world die every day from infections caught while in care, and appropriate and adequate hand hygiene is a crucial prevention technique we can all utilise to reduce the spread of harmful infections and diseases.
Read more on Ausmed Education website

Compulsions | CRUfAD
CONTACT US URGENT CARE About Us Our Research For Patients For Clinicians Select Page Compulsions OCD Pages 271-276 from the Management of Mental Disorders, published by World Health Organization, Sydney
Read more on CRUfAD – Clinical Research Unit for Anxiety and Depression website

Superbugs Explained | Ausmed
Resistance to an antibiotic occurs when a microorganism grows in the presence of an antibiotic which would usually be sufficient to inhibit or kill organisms of the same species. The severity of a superbug depends on the number of different antibiotics the microorganism is resistant to.
Stool culture | Pathology Tests Explained
The stool culture is a test that detects and identifies bacteria that cause infections of the lower digestive tract. The test distinguishes between the types
Read more on Pathology Tests Explained website

Mycoplasma | Pathology Tests Explained
Mycoplasma testing is used to determine whether someone currently has or recently had a mycoplasma infection. It is a group of tests that either measure anti
Gastroenteritis Symptoms, Spread and Prevention | Ausmed
Gastroenteritis is an infection and inflammation of the stomach and intestines. It is a common illness with a variety of causes including viruses, bacteria, parasites, toxins, chemicals and drugs. There are many kinds of gastroenteritis, most of them contagious.
Cytomegalovirus | Pathology Tests Explained
Cytomegalovirus (CMV) is a common virus that occurs widely but rarely causes symptoms. In Australia, by the age of 20 years, around 50% of adults have been i
Respiratory syncytial virus (RSV) | Pathology Tests Explained
RSV testing is used to detect respiratory syncytial virus, the most common cause of lower respiratory tract infections in infants around the world. RSV tends
Healthdirect Australia is not responsible for the content and advertising on the external website you are now entering.
Healthdirect 24hr 7 days a week hotline
24 hour health advice you can count on
1800 022 222
Government Accredited with over 140 information partners
We are a government-funded service, providing quality, approved health information and advice
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
© 2024 Healthdirect Australia Limited
Support for this browser is being discontinued
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.

- Publications
- Amplify! Blog
How handy is your handwashing policy?
Handwashing and drying might sound trivial to the uninitiated, but getting it right is a major action for reducing the spread of infectious diseases and staying healthy when working with children.
By CELA on 24 Sep, 2018
Handwashing and drying might sound trivial to the uninitiated, but getting it right is a major action for reducing the spread of infectious diseases and staying healthy when working with children. This story is by CELA Writers Margaret Paton and Bec Lloyd
Along with curriculum and ethics, work safety and inclusion, there’s another core topic most professional educators learn: how to wash and dry their hands correctly and how to teach children to do the same.
Gastrointestinal (gastro) and respiratory infections (colds and flu) of children attending early learning or OSHC are frustratingly common.
Wherever human beings gather together, there’s a risk of contagion. When you add in a high level of physical contact (including toileting) and lower immunity among young children who haven’t yet been exposed to every common germ, you can expect to see an even higher rate of transmission.
Dangers to children
While far less common in developed countries with ready access to clean water, the Centre for Disease Control estimates:
About 1.8 million children under the age of 5 die each year from diarrheal diseases and pneumonia, the top two killers of young children around the world 8 .
- Handwashing with soap could protect about 1 out of every 3 young children who get sick with diarrhea 2 , 3 and almost 1 out of 5 young children with respiratory infections like pneumonia 3 , 5 .
- Although people around the world clean their hands with water, very few use soap to wash their hands. Washing hands with soap removes germs much more effectively 9 .
- Handwashing education and access to soap in schools can help improve attendance 10 , 11 , 12 .
- Good handwashing early in life may help improve child development in some settings 13 .
- Estimated global rates of handwashing after using the toilet are only 19% 6 .
In Australia, new parents are often warned by friends and family to expect a couple of years of ‘catching everything’ when their baby or toddler commences long day care, with the consolation that many families see fewer missed school days later on because of increased immunity built up through earlier illnesses.
As one of the ‘bibles’ of this sector, Staying Healthy , explains, good handwashing practices are the single most important thing you can do to reduce exposure to many infectious illnesses for yourself, your colleagues, the children and their families.
Handwashing in the NQF
Handwashing is a fundamental means of supporting the aims of the National Quality Framework , particularly Element 2.1.2. You can also read in the need for good handwashing practices in Regulation 88 and Regulation 168(2)(c) of the Education and Care Services National Regulations (last updated 1 July 2018).
In fact, the regulations say that if an approved provider doesn’t take ‘reasonable steps’ to ‘prevent the spread of … infectious disease’ after an outbreak, they face a penalty of $2000, and another penalty of $1000 applies if providers fail to have appropriate policies and procedures in place to prevent infectious diseases – of course, this includes the critical act of washing and drying hands.
Apart from the penalties, there’s an awareness day coming up to remind us all how important this is. With Global Handwashing Day approaching on October 15 this year, it’s a good time to think about how handwashing works in your service or office.
Have you found a balance around the sustainability around water use and drying options, for example? Do you have a song or transition habit for the children’s handwashing that reinforces the practice? Do you make it easy for families to be your partners so that handwashing practices at your service are mirrored at home, too?
How good are Australians at handwashing?
The Hand Hygiene Australia (HHA) organisation collects data nationally – but mostly from hospitals.
Its three-month audit to the end of June this year showed an 85% good handwashing compliance rate. However, HHA is happy with that result, because the National Hand Hygiene Benchmark (which the Australian Health Ministers’ Advisory Council have set) is 80%.
Their site has smartphone apps to enter hand hygiene audit data, and collect data on a mobile. Plus you can learn more about the issue and complete an online training module . There’s even a free annual Hand Hygiene Workshop , which is being held in Brisbane this year on 18 November.
What works?
Dutch researchers who took on this topic in early childhood centres found that explicit instructions and prompts for adults (more so than the children) were best practice. Their research showed when visible, practical interventions were developed to target educators’ compliance with hand washing, they worked.
The interventions included free refills of paper towels, soap, alcohol-based hand sanitiser and hand cream for six months.
The educators were also given more individual training, an information booklet, and team training to work out how they could further improve. The research showed that children’s handwashing habits also improved in the services being studied.
When to wash
There are several credible resources to help you form or update your service’s policy and practices. Apart from Staying Healthy , the Australian Government’s Health Direct website has a good overview for anyone (not just people working with children) on when you need to wash your.
We’ve combined that list with other reputable sources to create this summary:
- on arriving and leaving your service
- when your hands are visibly dirty
- after going to the toilet
- after helping a child go to the toilet, or changing a nappy
- after handling rubbish, household or garden chemicals, or anything that could be contaminated
- before you prepare or eat food or handle a baby’s bottle
- after touching raw meat
- after wiping/blowing your nose or sneezing
- after patting an animal
- after cleaning up or touching sores, a wound/cut, blood, vomit or other body fluids or faeces
- after removing gloves
- before and after giving medication
- after playing outside
How to wash
Here’s the National Health and Medical Research Council’s six steps in a downloadable poster .
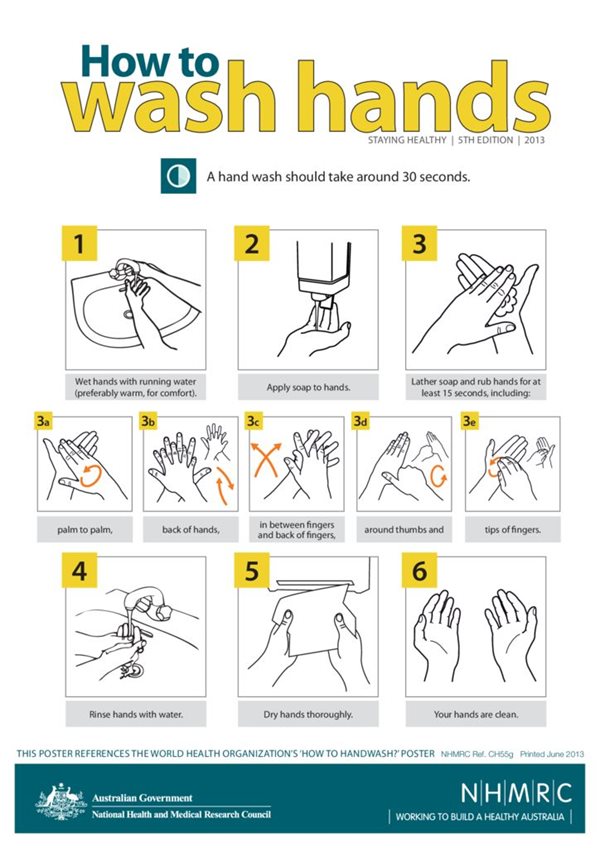
The key to good handwashing is time – around 30 seconds is the current recommendation, which is about the time it takes to sing two rounds of the Happy Birthday To You song.
The kinds of soap you use might vary according to special needs in your service for skin sensitivities or for the physical set up in your bathrooms and kitchens.
Be aware, though, that hand sanitiser is not recommended as a substitute for handwashing. Bacteria are clever at avoiding death-by-disinfectant and hand sanitisers are reportedly losing their effectiveness against some germs.
Read this recent NPR report for the story of how hand sanitisers in Australian hospitals may have actually increased the spread of some diseases.
A handwashing song ( If you’re happy and you know it tune)
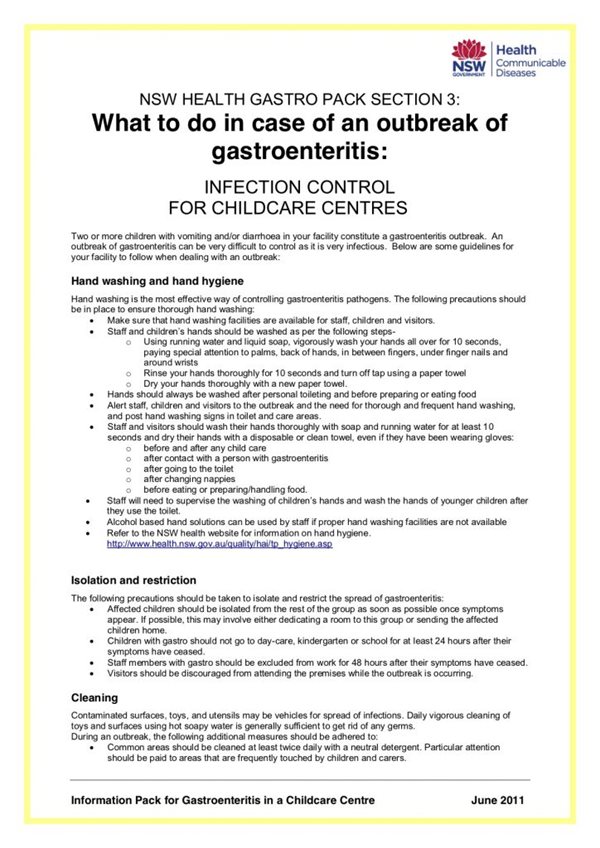
As for hand drying, paper towels are favoured by most of the sources we consulted. Take a look at NSW Health’s Gastro Pack advice about controlling infections in the early learning sector. We’ve included an extract below.
But it’s not all clear cut. A study in the international Infection, Disease & Health journal found children who dried their hands with a retractable cloth towel and a warm air dryer significantly reduced “bacterial numbers translocating to skin, food or a toy”.
Meanwhile, WorkSafe Western Australia’s Guidance Note on Reducing the Risk of Infectious Disease in Child Care Workplaces suggests using a paper towel or dryer. And a study from the Mayo Clinic in the USA comes out strongly recommending paper towels ‘in locations where hygiene is paramount, such as in hospitals and clinics’. That’s also endorsed by this researcher from the United Kingdom who completed a peer-reviewed study.
Sustainability balancing act
However, paper towels kill trees! So when handwashing appears in a service’s sustainability policy , it’s not unusual to see something like this approach we are quoting from Goolwa Children’s Centre in South Australia:
…where relevant, review policies and procedures within the service to find more sustainable outcomes, eg using hand dryers or washers instead of paper towel to dry hands.
It can be tricky to find a balance for two important outcomes – sanitation and sustainability – and like many other aspects of your professional procedures, where there is evidence backing a number of possible approaches you may just have to choose which is the best ‘fit’ for your service and your community.
And when in doubt, you can always turn to the Wiggles! The is a resource sheet here , and a UNICEF promoted video here.
Share your handwashing and drying habits with us in the comments – how are you doing it differently than in the past?
Related articles and resources
- Examples of a service’s hand washing policy and another one here
- ACECQA – Occasional Paper 2: Quality Area 2: Children’s health and safety
- Wash Your Hands song – Pinkfong Songs for Children on YouTube
- Myriam Sidibe’s TED talk on The Simple Power of Hand-washing
- Global Handwashing Day – October 15
- Downloads from Staying Healthy: Preventing infectious diseases in early childhood education and care services (5th Edition)
- Staying Healthy: Preventing infectious diseases in early childhood education and care services (5th Edition) (PDF, 3.3MB)
- The chain of infection – Poster (PDF, 211KB)
- Changing a nappy without spreading germs – Poster (PDF, 847KB)
- How to use alcohol-based hand rub – Poster (PDF, 552KB)
- How to wash hands – Poster (PDF, 771KB)
- Recommended minimum exclusion periods – Poster (856KB)
- The role of hands in the spread of infection – Poster (PDF, 325KB)
- Exclusion periods explained – Information for families (PDF, 1MB)
- Breaking the chain of infection – Information for families (PDF, 1.3MB)
- What causes infections – Information for families (PDF, 917KB)
- regulations
- sustainability
- The Wiggles

Community Early Learning Australia is a not for profit organisation with a focus on amplifying the value of early learning for every child across Australia - representing our members and uniting our sector as a force for quality education and care.
Your email address will not be published. Required fields are marked *
Guild Insurance
CELA’s insurer of choice. Protecting Australian businesses and individuals with tailored insurance products and caring personal service.
Thank you for requesting a new password.
If your email address is registered with CELA, you will receive a link to reset your password from us shortly. Please check your inbox and spam folder. If you need help, please call us on 1800 157 818.
Warm regards, The CELA team
Guest checkout
Join CELA to access discounts and member benefits.
Don't forget to log in to save!
Log in to access discounts and member benefits
Member Login
Forgot your password?
Don't have an account yet? Become a member today to access great free resources and discounted prices!
Become a member and save!
We launched our refreshed website on Friday 23 July. If you are logging in for the first time since the launch, you will need to request a new password using the 'forgot your password?' link below the 'confirm membership' box. Please check your spam inbox if you can’t find the new password, or call us on 1800 157 818 .
- Open access
- Published: 18 April 2024
Research ethics and artificial intelligence for global health: perspectives from the global forum on bioethics in research
- James Shaw 1 , 13 ,
- Joseph Ali 2 , 3 ,
- Caesar A. Atuire 4 , 5 ,
- Phaik Yeong Cheah 6 ,
- Armando Guio Español 7 ,
- Judy Wawira Gichoya 8 ,
- Adrienne Hunt 9 ,
- Daudi Jjingo 10 ,
- Katherine Littler 9 ,
- Daniela Paolotti 11 &
- Effy Vayena 12
BMC Medical Ethics volume 25 , Article number: 46 ( 2024 ) Cite this article
641 Accesses
5 Altmetric
Metrics details
The ethical governance of Artificial Intelligence (AI) in health care and public health continues to be an urgent issue for attention in policy, research, and practice. In this paper we report on central themes related to challenges and strategies for promoting ethics in research involving AI in global health, arising from the Global Forum on Bioethics in Research (GFBR), held in Cape Town, South Africa in November 2022.
The GFBR is an annual meeting organized by the World Health Organization and supported by the Wellcome Trust, the US National Institutes of Health, the UK Medical Research Council (MRC) and the South African MRC. The forum aims to bring together ethicists, researchers, policymakers, research ethics committee members and other actors to engage with challenges and opportunities specifically related to research ethics. In 2022 the focus of the GFBR was “Ethics of AI in Global Health Research”. The forum consisted of 6 case study presentations, 16 governance presentations, and a series of small group and large group discussions. A total of 87 participants attended the forum from 31 countries around the world, representing disciplines of bioethics, AI, health policy, health professional practice, research funding, and bioinformatics. In this paper, we highlight central insights arising from GFBR 2022.
We describe the significance of four thematic insights arising from the forum: (1) Appropriateness of building AI, (2) Transferability of AI systems, (3) Accountability for AI decision-making and outcomes, and (4) Individual consent. We then describe eight recommendations for governance leaders to enhance the ethical governance of AI in global health research, addressing issues such as AI impact assessments, environmental values, and fair partnerships.
Conclusions
The 2022 Global Forum on Bioethics in Research illustrated several innovations in ethical governance of AI for global health research, as well as several areas in need of urgent attention internationally. This summary is intended to inform international and domestic efforts to strengthen research ethics and support the evolution of governance leadership to meet the demands of AI in global health research.
Peer Review reports
Introduction
The ethical governance of Artificial Intelligence (AI) in health care and public health continues to be an urgent issue for attention in policy, research, and practice [ 1 , 2 , 3 ]. Beyond the growing number of AI applications being implemented in health care, capabilities of AI models such as Large Language Models (LLMs) expand the potential reach and significance of AI technologies across health-related fields [ 4 , 5 ]. Discussion about effective, ethical governance of AI technologies has spanned a range of governance approaches, including government regulation, organizational decision-making, professional self-regulation, and research ethics review [ 6 , 7 , 8 ]. In this paper, we report on central themes related to challenges and strategies for promoting ethics in research involving AI in global health research, arising from the Global Forum on Bioethics in Research (GFBR), held in Cape Town, South Africa in November 2022. Although applications of AI for research, health care, and public health are diverse and advancing rapidly, the insights generated at the forum remain highly relevant from a global health perspective. After summarizing important context for work in this domain, we highlight categories of ethical issues emphasized at the forum for attention from a research ethics perspective internationally. We then outline strategies proposed for research, innovation, and governance to support more ethical AI for global health.
In this paper, we adopt the definition of AI systems provided by the Organization for Economic Cooperation and Development (OECD) as our starting point. Their definition states that an AI system is “a machine-based system that can, for a given set of human-defined objectives, make predictions, recommendations, or decisions influencing real or virtual environments. AI systems are designed to operate with varying levels of autonomy” [ 9 ]. The conceptualization of an algorithm as helping to constitute an AI system, along with hardware, other elements of software, and a particular context of use, illustrates the wide variety of ways in which AI can be applied. We have found it useful to differentiate applications of AI in research as those classified as “AI systems for discovery” and “AI systems for intervention”. An AI system for discovery is one that is intended to generate new knowledge, for example in drug discovery or public health research in which researchers are seeking potential targets for intervention, innovation, or further research. An AI system for intervention is one that directly contributes to enacting an intervention in a particular context, for example informing decision-making at the point of care or assisting with accuracy in a surgical procedure.
The mandate of the GFBR is to take a broad view of what constitutes research and its regulation in global health, with special attention to bioethics in Low- and Middle- Income Countries. AI as a group of technologies demands such a broad view. AI development for health occurs in a variety of environments, including universities and academic health sciences centers where research ethics review remains an important element of the governance of science and innovation internationally [ 10 , 11 ]. In these settings, research ethics committees (RECs; also known by different names such as Institutional Review Boards or IRBs) make decisions about the ethical appropriateness of projects proposed by researchers and other institutional members, ultimately determining whether a given project is allowed to proceed on ethical grounds [ 12 ].
However, research involving AI for health also takes place in large corporations and smaller scale start-ups, which in some jurisdictions fall outside the scope of research ethics regulation. In the domain of AI, the question of what constitutes research also becomes blurred. For example, is the development of an algorithm itself considered a part of the research process? Or only when that algorithm is tested under the formal constraints of a systematic research methodology? In this paper we take an inclusive view, in which AI development is included in the definition of research activity and within scope for our inquiry, regardless of the setting in which it takes place. This broad perspective characterizes the approach to “research ethics” we take in this paper, extending beyond the work of RECs to include the ethical analysis of the wide range of activities that constitute research as the generation of new knowledge and intervention in the world.
Ethical governance of AI in global health
The ethical governance of AI for global health has been widely discussed in recent years. The World Health Organization (WHO) released its guidelines on ethics and governance of AI for health in 2021, endorsing a set of six ethical principles and exploring the relevance of those principles through a variety of use cases. The WHO guidelines also provided an overview of AI governance, defining governance as covering “a range of steering and rule-making functions of governments and other decision-makers, including international health agencies, for the achievement of national health policy objectives conducive to universal health coverage.” (p. 81) The report usefully provided a series of recommendations related to governance of seven domains pertaining to AI for health: data, benefit sharing, the private sector, the public sector, regulation, policy observatories/model legislation, and global governance. The report acknowledges that much work is yet to be done to advance international cooperation on AI governance, especially related to prioritizing voices from Low- and Middle-Income Countries (LMICs) in global dialogue.
One important point emphasized in the WHO report that reinforces the broader literature on global governance of AI is the distribution of responsibility across a wide range of actors in the AI ecosystem. This is especially important to highlight when focused on research for global health, which is specifically about work that transcends national borders. Alami et al. (2020) discussed the unique risks raised by AI research in global health, ranging from the unavailability of data in many LMICs required to train locally relevant AI models to the capacity of health systems to absorb new AI technologies that demand the use of resources from elsewhere in the system. These observations illustrate the need to identify the unique issues posed by AI research for global health specifically, and the strategies that can be employed by all those implicated in AI governance to promote ethically responsible use of AI in global health research.
RECs and the regulation of research involving AI
RECs represent an important element of the governance of AI for global health research, and thus warrant further commentary as background to our paper. Despite the importance of RECs, foundational questions have been raised about their capabilities to accurately understand and address ethical issues raised by studies involving AI. Rahimzadeh et al. (2023) outlined how RECs in the United States are under-prepared to align with recent federal policy requiring that RECs review data sharing and management plans with attention to the unique ethical issues raised in AI research for health [ 13 ]. Similar research in South Africa identified variability in understanding of existing regulations and ethical issues associated with health-related big data sharing and management among research ethics committee members [ 14 , 15 ]. The effort to address harms accruing to groups or communities as opposed to individuals whose data are included in AI research has also been identified as a unique challenge for RECs [ 16 , 17 ]. Doerr and Meeder (2022) suggested that current regulatory frameworks for research ethics might actually prevent RECs from adequately addressing such issues, as they are deemed out of scope of REC review [ 16 ]. Furthermore, research in the United Kingdom and Canada has suggested that researchers using AI methods for health tend to distinguish between ethical issues and social impact of their research, adopting an overly narrow view of what constitutes ethical issues in their work [ 18 ].
The challenges for RECs in adequately addressing ethical issues in AI research for health care and public health exceed a straightforward survey of ethical considerations. As Ferretti et al. (2021) contend, some capabilities of RECs adequately cover certain issues in AI-based health research, such as the common occurrence of conflicts of interest where researchers who accept funds from commercial technology providers are implicitly incentivized to produce results that align with commercial interests [ 12 ]. However, some features of REC review require reform to adequately meet ethical needs. Ferretti et al. outlined weaknesses of RECs that are longstanding and those that are novel to AI-related projects, proposing a series of directions for development that are regulatory, procedural, and complementary to REC functionality. The work required on a global scale to update the REC function in response to the demands of research involving AI is substantial.
These issues take greater urgency in the context of global health [ 19 ]. Teixeira da Silva (2022) described the global practice of “ethics dumping”, where researchers from high income countries bring ethically contentious practices to RECs in low-income countries as a strategy to gain approval and move projects forward [ 20 ]. Although not yet systematically documented in AI research for health, risk of ethics dumping in AI research is high. Evidence is already emerging of practices of “health data colonialism”, in which AI researchers and developers from large organizations in high-income countries acquire data to build algorithms in LMICs to avoid stricter regulations [ 21 ]. This specific practice is part of a larger collection of practices that characterize health data colonialism, involving the broader exploitation of data and the populations they represent primarily for commercial gain [ 21 , 22 ]. As an additional complication, AI algorithms trained on data from high-income contexts are unlikely to apply in straightforward ways to LMIC settings [ 21 , 23 ]. In the context of global health, there is widespread acknowledgement about the need to not only enhance the knowledge base of REC members about AI-based methods internationally, but to acknowledge the broader shifts required to encourage their capabilities to more fully address these and other ethical issues associated with AI research for health [ 8 ].
Although RECs are an important part of the story of the ethical governance of AI for global health research, they are not the only part. The responsibilities of supra-national entities such as the World Health Organization, national governments, organizational leaders, commercial AI technology providers, health care professionals, and other groups continue to be worked out internationally. In this context of ongoing work, examining issues that demand attention and strategies to address them remains an urgent and valuable task.
The GFBR is an annual meeting organized by the World Health Organization and supported by the Wellcome Trust, the US National Institutes of Health, the UK Medical Research Council (MRC) and the South African MRC. The forum aims to bring together ethicists, researchers, policymakers, REC members and other actors to engage with challenges and opportunities specifically related to research ethics. Each year the GFBR meeting includes a series of case studies and keynotes presented in plenary format to an audience of approximately 100 people who have applied and been competitively selected to attend, along with small-group breakout discussions to advance thinking on related issues. The specific topic of the forum changes each year, with past topics including ethical issues in research with people living with mental health conditions (2021), genome editing (2019), and biobanking/data sharing (2018). The forum is intended to remain grounded in the practical challenges of engaging in research ethics, with special interest in low resource settings from a global health perspective. A post-meeting fellowship scheme is open to all LMIC participants, providing a unique opportunity to apply for funding to further explore and address the ethical challenges that are identified during the meeting.
In 2022, the focus of the GFBR was “Ethics of AI in Global Health Research”. The forum consisted of 6 case study presentations (both short and long form) reporting on specific initiatives related to research ethics and AI for health, and 16 governance presentations (both short and long form) reporting on actual approaches to governing AI in different country settings. A keynote presentation from Professor Effy Vayena addressed the topic of the broader context for AI ethics in a rapidly evolving field. A total of 87 participants attended the forum from 31 countries around the world, representing disciplines of bioethics, AI, health policy, health professional practice, research funding, and bioinformatics. The 2-day forum addressed a wide range of themes. The conference report provides a detailed overview of each of the specific topics addressed while a policy paper outlines the cross-cutting themes (both documents are available at the GFBR website: https://www.gfbr.global/past-meetings/16th-forum-cape-town-south-africa-29-30-november-2022/ ). As opposed to providing a detailed summary in this paper, we aim to briefly highlight central issues raised, solutions proposed, and the challenges facing the research ethics community in the years to come.
In this way, our primary aim in this paper is to present a synthesis of the challenges and opportunities raised at the GFBR meeting and in the planning process, followed by our reflections as a group of authors on their significance for governance leaders in the coming years. We acknowledge that the views represented at the meeting and in our results are a partial representation of the universe of views on this topic; however, the GFBR leadership invested a great deal of resources in convening a deeply diverse and thoughtful group of researchers and practitioners working on themes of bioethics related to AI for global health including those based in LMICs. We contend that it remains rare to convene such a strong group for an extended time and believe that many of the challenges and opportunities raised demand attention for more ethical futures of AI for health. Nonetheless, our results are primarily descriptive and are thus not explicitly grounded in a normative argument. We make effort in the Discussion section to contextualize our results by describing their significance and connecting them to broader efforts to reform global health research and practice.
Uniquely important ethical issues for AI in global health research
Presentations and group dialogue over the course of the forum raised several issues for consideration, and here we describe four overarching themes for the ethical governance of AI in global health research. Brief descriptions of each issue can be found in Table 1 . Reports referred to throughout the paper are available at the GFBR website provided above.
The first overarching thematic issue relates to the appropriateness of building AI technologies in response to health-related challenges in the first place. Case study presentations referred to initiatives where AI technologies were highly appropriate, such as in ear shape biometric identification to more accurately link electronic health care records to individual patients in Zambia (Alinani Simukanga). Although important ethical issues were raised with respect to privacy, trust, and community engagement in this initiative, the AI-based solution was appropriately matched to the challenge of accurately linking electronic records to specific patient identities. In contrast, forum participants raised questions about the appropriateness of an initiative using AI to improve the quality of handwashing practices in an acute care hospital in India (Niyoshi Shah), which led to gaming the algorithm. Overall, participants acknowledged the dangers of techno-solutionism, in which AI researchers and developers treat AI technologies as the most obvious solutions to problems that in actuality demand much more complex strategies to address [ 24 ]. However, forum participants agreed that RECs in different contexts have differing degrees of power to raise issues of the appropriateness of an AI-based intervention.
The second overarching thematic issue related to whether and how AI-based systems transfer from one national health context to another. One central issue raised by a number of case study presentations related to the challenges of validating an algorithm with data collected in a local environment. For example, one case study presentation described a project that would involve the collection of personally identifiable data for sensitive group identities, such as tribe, clan, or religion, in the jurisdictions involved (South Africa, Nigeria, Tanzania, Uganda and the US; Gakii Masunga). Doing so would enable the team to ensure that those groups were adequately represented in the dataset to ensure the resulting algorithm was not biased against specific community groups when deployed in that context. However, some members of these communities might desire to be represented in the dataset, whereas others might not, illustrating the need to balance autonomy and inclusivity. It was also widely recognized that collecting these data is an immense challenge, particularly when historically oppressive practices have led to a low-trust environment for international organizations and the technologies they produce. It is important to note that in some countries such as South Africa and Rwanda, it is illegal to collect information such as race and tribal identities, re-emphasizing the importance for cultural awareness and avoiding “one size fits all” solutions.
The third overarching thematic issue is related to understanding accountabilities for both the impacts of AI technologies and governance decision-making regarding their use. Where global health research involving AI leads to longer-term harms that might fall outside the usual scope of issues considered by a REC, who is to be held accountable, and how? This question was raised as one that requires much further attention, with law being mixed internationally regarding the mechanisms available to hold researchers, innovators, and their institutions accountable over the longer term. However, it was recognized in breakout group discussion that many jurisdictions are developing strong data protection regimes related specifically to international collaboration for research involving health data. For example, Kenya’s Data Protection Act requires that any internationally funded projects have a local principal investigator who will hold accountability for how data are shared and used [ 25 ]. The issue of research partnerships with commercial entities was raised by many participants in the context of accountability, pointing toward the urgent need for clear principles related to strategies for engagement with commercial technology companies in global health research.
The fourth and final overarching thematic issue raised here is that of consent. The issue of consent was framed by the widely shared recognition that models of individual, explicit consent might not produce a supportive environment for AI innovation that relies on the secondary uses of health-related datasets to build AI algorithms. Given this recognition, approaches such as community oversight of health data uses were suggested as a potential solution. However, the details of implementing such community oversight mechanisms require much further attention, particularly given the unique perspectives on health data in different country settings in global health research. Furthermore, some uses of health data do continue to require consent. One case study of South Africa, Nigeria, Kenya, Ethiopia and Uganda suggested that when health data are shared across borders, individual consent remains necessary when data is transferred from certain countries (Nezerith Cengiz). Broader clarity is necessary to support the ethical governance of health data uses for AI in global health research.
Recommendations for ethical governance of AI in global health research
Dialogue at the forum led to a range of suggestions for promoting ethical conduct of AI research for global health, related to the various roles of actors involved in the governance of AI research broadly defined. The strategies are written for actors we refer to as “governance leaders”, those people distributed throughout the AI for global health research ecosystem who are responsible for ensuring the ethical and socially responsible conduct of global health research involving AI (including researchers themselves). These include RECs, government regulators, health care leaders, health professionals, corporate social accountability officers, and others. Enacting these strategies would bolster the ethical governance of AI for global health more generally, enabling multiple actors to fulfill their roles related to governing research and development activities carried out across multiple organizations, including universities, academic health sciences centers, start-ups, and technology corporations. Specific suggestions are summarized in Table 2 .
First, forum participants suggested that governance leaders including RECs, should remain up to date on recent advances in the regulation of AI for health. Regulation of AI for health advances rapidly and takes on different forms in jurisdictions around the world. RECs play an important role in governance, but only a partial role; it was deemed important for RECs to acknowledge how they fit within a broader governance ecosystem in order to more effectively address the issues within their scope. Not only RECs but organizational leaders responsible for procurement, researchers, and commercial actors should all commit to efforts to remain up to date about the relevant approaches to regulating AI for health care and public health in jurisdictions internationally. In this way, governance can more adequately remain up to date with advances in regulation.
Second, forum participants suggested that governance leaders should focus on ethical governance of health data as a basis for ethical global health AI research. Health data are considered the foundation of AI development, being used to train AI algorithms for various uses [ 26 ]. By focusing on ethical governance of health data generation, sharing, and use, multiple actors will help to build an ethical foundation for AI development among global health researchers.
Third, forum participants believed that governance processes should incorporate AI impact assessments where appropriate. An AI impact assessment is the process of evaluating the potential effects, both positive and negative, of implementing an AI algorithm on individuals, society, and various stakeholders, generally over time frames specified in advance of implementation [ 27 ]. Although not all types of AI research in global health would warrant an AI impact assessment, this is especially relevant for those studies aiming to implement an AI system for intervention into health care or public health. Organizations such as RECs can use AI impact assessments to boost understanding of potential harms at the outset of a research project, encouraging researchers to more deeply consider potential harms in the development of their study.
Fourth, forum participants suggested that governance decisions should incorporate the use of environmental impact assessments, or at least the incorporation of environment values when assessing the potential impact of an AI system. An environmental impact assessment involves evaluating and anticipating the potential environmental effects of a proposed project to inform ethical decision-making that supports sustainability [ 28 ]. Although a relatively new consideration in research ethics conversations [ 29 ], the environmental impact of building technologies is a crucial consideration for the public health commitment to environmental sustainability. Governance leaders can use environmental impact assessments to boost understanding of potential environmental harms linked to AI research projects in global health over both the shorter and longer terms.
Fifth, forum participants suggested that governance leaders should require stronger transparency in the development of AI algorithms in global health research. Transparency was considered essential in the design and development of AI algorithms for global health to ensure ethical and accountable decision-making throughout the process. Furthermore, whether and how researchers have considered the unique contexts into which such algorithms may be deployed can be surfaced through stronger transparency, for example in describing what primary considerations were made at the outset of the project and which stakeholders were consulted along the way. Sharing information about data provenance and methods used in AI development will also enhance the trustworthiness of the AI-based research process.
Sixth, forum participants suggested that governance leaders can encourage or require community engagement at various points throughout an AI project. It was considered that engaging patients and communities is crucial in AI algorithm development to ensure that the technology aligns with community needs and values. However, participants acknowledged that this is not a straightforward process. Effective community engagement requires lengthy commitments to meeting with and hearing from diverse communities in a given setting, and demands a particular set of skills in communication and dialogue that are not possessed by all researchers. Encouraging AI researchers to begin this process early and build long-term partnerships with community members is a promising strategy to deepen community engagement in AI research for global health. One notable recommendation was that research funders have an opportunity to incentivize and enable community engagement with funds dedicated to these activities in AI research in global health.
Seventh, forum participants suggested that governance leaders can encourage researchers to build strong, fair partnerships between institutions and individuals across country settings. In a context of longstanding imbalances in geopolitical and economic power, fair partnerships in global health demand a priori commitments to share benefits related to advances in medical technologies, knowledge, and financial gains. Although enforcement of this point might be beyond the remit of RECs, commentary will encourage researchers to consider stronger, fairer partnerships in global health in the longer term.
Eighth, it became evident that it is necessary to explore new forms of regulatory experimentation given the complexity of regulating a technology of this nature. In addition, the health sector has a series of particularities that make it especially complicated to generate rules that have not been previously tested. Several participants highlighted the desire to promote spaces for experimentation such as regulatory sandboxes or innovation hubs in health. These spaces can have several benefits for addressing issues surrounding the regulation of AI in the health sector, such as: (i) increasing the capacities and knowledge of health authorities about this technology; (ii) identifying the major problems surrounding AI regulation in the health sector; (iii) establishing possibilities for exchange and learning with other authorities; (iv) promoting innovation and entrepreneurship in AI in health; and (vi) identifying the need to regulate AI in this sector and update other existing regulations.
Ninth and finally, forum participants believed that the capabilities of governance leaders need to evolve to better incorporate expertise related to AI in ways that make sense within a given jurisdiction. With respect to RECs, for example, it might not make sense for every REC to recruit a member with expertise in AI methods. Rather, it will make more sense in some jurisdictions to consult with members of the scientific community with expertise in AI when research protocols are submitted that demand such expertise. Furthermore, RECs and other approaches to research governance in jurisdictions around the world will need to evolve in order to adopt the suggestions outlined above, developing processes that apply specifically to the ethical governance of research using AI methods in global health.
Research involving the development and implementation of AI technologies continues to grow in global health, posing important challenges for ethical governance of AI in global health research around the world. In this paper we have summarized insights from the 2022 GFBR, focused specifically on issues in research ethics related to AI for global health research. We summarized four thematic challenges for governance related to AI in global health research and nine suggestions arising from presentations and dialogue at the forum. In this brief discussion section, we present an overarching observation about power imbalances that frames efforts to evolve the role of governance in global health research, and then outline two important opportunity areas as the field develops to meet the challenges of AI in global health research.
Dialogue about power is not unfamiliar in global health, especially given recent contributions exploring what it would mean to de-colonize global health research, funding, and practice [ 30 , 31 ]. Discussions of research ethics applied to AI research in global health contexts are deeply infused with power imbalances. The existing context of global health is one in which high-income countries primarily located in the “Global North” charitably invest in projects taking place primarily in the “Global South” while recouping knowledge, financial, and reputational benefits [ 32 ]. With respect to AI development in particular, recent examples of digital colonialism frame dialogue about global partnerships, raising attention to the role of large commercial entities and global financial capitalism in global health research [ 21 , 22 ]. Furthermore, the power of governance organizations such as RECs to intervene in the process of AI research in global health varies widely around the world, depending on the authorities assigned to them by domestic research governance policies. These observations frame the challenges outlined in our paper, highlighting the difficulties associated with making meaningful change in this field.
Despite these overarching challenges of the global health research context, there are clear strategies for progress in this domain. Firstly, AI innovation is rapidly evolving, which means approaches to the governance of AI for health are rapidly evolving too. Such rapid evolution presents an important opportunity for governance leaders to clarify their vision and influence over AI innovation in global health research, boosting the expertise, structure, and functionality required to meet the demands of research involving AI. Secondly, the research ethics community has strong international ties, linked to a global scholarly community that is committed to sharing insights and best practices around the world. This global community can be leveraged to coordinate efforts to produce advances in the capabilities and authorities of governance leaders to meaningfully govern AI research for global health given the challenges summarized in our paper.
Limitations
Our paper includes two specific limitations that we address explicitly here. First, it is still early in the lifetime of the development of applications of AI for use in global health, and as such, the global community has had limited opportunity to learn from experience. For example, there were many fewer case studies, which detail experiences with the actual implementation of an AI technology, submitted to GFBR 2022 for consideration than was expected. In contrast, there were many more governance reports submitted, which detail the processes and outputs of governance processes that anticipate the development and dissemination of AI technologies. This observation represents both a success and a challenge. It is a success that so many groups are engaging in anticipatory governance of AI technologies, exploring evidence of their likely impacts and governing technologies in novel and well-designed ways. It is a challenge that there is little experience to build upon of the successful implementation of AI technologies in ways that have limited harms while promoting innovation. Further experience with AI technologies in global health will contribute to revising and enhancing the challenges and recommendations we have outlined in our paper.
Second, global trends in the politics and economics of AI technologies are evolving rapidly. Although some nations are advancing detailed policy approaches to regulating AI more generally, including for uses in health care and public health, the impacts of corporate investments in AI and political responses related to governance remain to be seen. The excitement around large language models (LLMs) and large multimodal models (LMMs) has drawn deeper attention to the challenges of regulating AI in any general sense, opening dialogue about health sector-specific regulations. The direction of this global dialogue, strongly linked to high-profile corporate actors and multi-national governance institutions, will strongly influence the development of boundaries around what is possible for the ethical governance of AI for global health. We have written this paper at a point when these developments are proceeding rapidly, and as such, we acknowledge that our recommendations will need updating as the broader field evolves.
Ultimately, coordination and collaboration between many stakeholders in the research ethics ecosystem will be necessary to strengthen the ethical governance of AI in global health research. The 2022 GFBR illustrated several innovations in ethical governance of AI for global health research, as well as several areas in need of urgent attention internationally. This summary is intended to inform international and domestic efforts to strengthen research ethics and support the evolution of governance leadership to meet the demands of AI in global health research.
Data availability
All data and materials analyzed to produce this paper are available on the GFBR website: https://www.gfbr.global/past-meetings/16th-forum-cape-town-south-africa-29-30-november-2022/ .
Clark P, Kim J, Aphinyanaphongs Y, Marketing, Food US. Drug Administration Clearance of Artificial Intelligence and Machine Learning Enabled Software in and as Medical devices: a systematic review. JAMA Netw Open. 2023;6(7):e2321792–2321792.
Article Google Scholar
Potnis KC, Ross JS, Aneja S, Gross CP, Richman IB. Artificial intelligence in breast cancer screening: evaluation of FDA device regulation and future recommendations. JAMA Intern Med. 2022;182(12):1306–12.
Siala H, Wang Y. SHIFTing artificial intelligence to be responsible in healthcare: a systematic review. Soc Sci Med. 2022;296:114782.
Yang X, Chen A, PourNejatian N, Shin HC, Smith KE, Parisien C, et al. A large language model for electronic health records. NPJ Digit Med. 2022;5(1):194.
Meskó B, Topol EJ. The imperative for regulatory oversight of large language models (or generative AI) in healthcare. NPJ Digit Med. 2023;6(1):120.
Jobin A, Ienca M, Vayena E. The global landscape of AI ethics guidelines. Nat Mach Intell. 2019;1(9):389–99.
Minssen T, Vayena E, Cohen IG. The challenges for Regulating Medical Use of ChatGPT and other large Language models. JAMA. 2023.
Ho CWL, Malpani R. Scaling up the research ethics framework for healthcare machine learning as global health ethics and governance. Am J Bioeth. 2022;22(5):36–8.
Yeung K. Recommendation of the council on artificial intelligence (OECD). Int Leg Mater. 2020;59(1):27–34.
Maddox TM, Rumsfeld JS, Payne PR. Questions for artificial intelligence in health care. JAMA. 2019;321(1):31–2.
Dzau VJ, Balatbat CA, Ellaissi WF. Revisiting academic health sciences systems a decade later: discovery to health to population to society. Lancet. 2021;398(10318):2300–4.
Ferretti A, Ienca M, Sheehan M, Blasimme A, Dove ES, Farsides B, et al. Ethics review of big data research: what should stay and what should be reformed? BMC Med Ethics. 2021;22(1):1–13.
Rahimzadeh V, Serpico K, Gelinas L. Institutional review boards need new skills to review data sharing and management plans. Nat Med. 2023;1–3.
Kling S, Singh S, Burgess TL, Nair G. The role of an ethics advisory committee in data science research in sub-saharan Africa. South Afr J Sci. 2023;119(5–6):1–3.
Google Scholar
Cengiz N, Kabanda SM, Esterhuizen TM, Moodley K. Exploring perspectives of research ethics committee members on the governance of big data in sub-saharan Africa. South Afr J Sci. 2023;119(5–6):1–9.
Doerr M, Meeder S. Big health data research and group harm: the scope of IRB review. Ethics Hum Res. 2022;44(4):34–8.
Ballantyne A, Stewart C. Big data and public-private partnerships in healthcare and research: the application of an ethics framework for big data in health and research. Asian Bioeth Rev. 2019;11(3):315–26.
Samuel G, Chubb J, Derrick G. Boundaries between research ethics and ethical research use in artificial intelligence health research. J Empir Res Hum Res Ethics. 2021;16(3):325–37.
Murphy K, Di Ruggiero E, Upshur R, Willison DJ, Malhotra N, Cai JC, et al. Artificial intelligence for good health: a scoping review of the ethics literature. BMC Med Ethics. 2021;22(1):1–17.
Teixeira da Silva JA. Handling ethics dumping and neo-colonial research: from the laboratory to the academic literature. J Bioethical Inq. 2022;19(3):433–43.
Ferryman K. The dangers of data colonialism in precision public health. Glob Policy. 2021;12:90–2.
Couldry N, Mejias UA. Data colonialism: rethinking big data’s relation to the contemporary subject. Telev New Media. 2019;20(4):336–49.
Organization WH. Ethics and governance of artificial intelligence for health: WHO guidance. 2021.
Metcalf J, Moss E. Owning ethics: corporate logics, silicon valley, and the institutionalization of ethics. Soc Res Int Q. 2019;86(2):449–76.
Data Protection Act - OFFICE OF THE DATA PROTECTION COMMISSIONER KENYA [Internet]. 2021 [cited 2023 Sep 30]. https://www.odpc.go.ke/dpa-act/ .
Sharon T, Lucivero F. Introduction to the special theme: the expansion of the health data ecosystem–rethinking data ethics and governance. Big Data & Society. Volume 6. London, England: SAGE Publications Sage UK; 2019. p. 2053951719852969.
Reisman D, Schultz J, Crawford K, Whittaker M. Algorithmic impact assessments: a practical Framework for Public Agency. AI Now. 2018.
Morgan RK. Environmental impact assessment: the state of the art. Impact Assess Proj Apprais. 2012;30(1):5–14.
Samuel G, Richie C. Reimagining research ethics to include environmental sustainability: a principled approach, including a case study of data-driven health research. J Med Ethics. 2023;49(6):428–33.
Kwete X, Tang K, Chen L, Ren R, Chen Q, Wu Z, et al. Decolonizing global health: what should be the target of this movement and where does it lead us? Glob Health Res Policy. 2022;7(1):3.
Abimbola S, Asthana S, Montenegro C, Guinto RR, Jumbam DT, Louskieter L, et al. Addressing power asymmetries in global health: imperatives in the wake of the COVID-19 pandemic. PLoS Med. 2021;18(4):e1003604.
Benatar S. Politics, power, poverty and global health: systems and frames. Int J Health Policy Manag. 2016;5(10):599.
Download references
Acknowledgements
We would like to acknowledge the outstanding contributions of the attendees of GFBR 2022 in Cape Town, South Africa. This paper is authored by members of the GFBR 2022 Planning Committee. We would like to acknowledge additional members Tamra Lysaght, National University of Singapore, and Niresh Bhagwandin, South African Medical Research Council, for their input during the planning stages and as reviewers of the applications to attend the Forum.
This work was supported by Wellcome [222525/Z/21/Z], the US National Institutes of Health, the UK Medical Research Council (part of UK Research and Innovation), and the South African Medical Research Council through funding to the Global Forum on Bioethics in Research.
Author information
Authors and affiliations.
Department of Physical Therapy, Temerty Faculty of Medicine, University of Toronto, Toronto, Canada
Berman Institute of Bioethics, Johns Hopkins University, Baltimore, MD, USA
Bloomberg School of Public Health, Johns Hopkins University, Baltimore, MD, USA
Department of Philosophy and Classics, University of Ghana, Legon-Accra, Ghana
Caesar A. Atuire
Centre for Tropical Medicine and Global Health, Nuffield Department of Medicine, University of Oxford, Oxford, UK
Mahidol Oxford Tropical Medicine Research Unit, Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand
Phaik Yeong Cheah
Berkman Klein Center, Harvard University, Bogotá, Colombia
Armando Guio Español
Department of Radiology and Informatics, Emory University School of Medicine, Atlanta, GA, USA
Judy Wawira Gichoya
Health Ethics & Governance Unit, Research for Health Department, Science Division, World Health Organization, Geneva, Switzerland
Adrienne Hunt & Katherine Littler
African Center of Excellence in Bioinformatics and Data Intensive Science, Infectious Diseases Institute, Makerere University, Kampala, Uganda
Daudi Jjingo
ISI Foundation, Turin, Italy
Daniela Paolotti
Department of Health Sciences and Technology, ETH Zurich, Zürich, Switzerland
Effy Vayena
Joint Centre for Bioethics, Dalla Lana School of Public Health, University of Toronto, Toronto, Canada
You can also search for this author in PubMed Google Scholar
Contributions
JS led the writing, contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. JA contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. CA contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. PYC contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. AE contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. JWG contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. AH contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. DJ contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. KL contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. DP contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper. EV contributed to conceptualization and analysis, critically reviewed and provided feedback on drafts of this paper, and provided final approval of the paper.
Corresponding author
Correspondence to James Shaw .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions

About this article
Cite this article.
Shaw, J., Ali, J., Atuire, C.A. et al. Research ethics and artificial intelligence for global health: perspectives from the global forum on bioethics in research. BMC Med Ethics 25 , 46 (2024). https://doi.org/10.1186/s12910-024-01044-w
Download citation
Received : 31 October 2023
Accepted : 01 April 2024
Published : 18 April 2024
DOI : https://doi.org/10.1186/s12910-024-01044-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Artificial intelligence
- Machine learning
- Research ethics
- Global health
BMC Medical Ethics
ISSN: 1472-6939
- General enquiries: [email protected]

Turn Your Curiosity Into Discovery
Latest facts.
11 Facts About National Love Your Produce Manager Day April 2nd
10 Facts About National Clean Out Your Medicine Cabinet Day April 19th
40 facts about elektrostal.
Written by Lanette Mayes
Modified & Updated: 02 Mar 2024
Reviewed by Jessica Corbett

Elektrostal is a vibrant city located in the Moscow Oblast region of Russia. With a rich history, stunning architecture, and a thriving community, Elektrostal is a city that has much to offer. Whether you are a history buff, nature enthusiast, or simply curious about different cultures, Elektrostal is sure to captivate you.
This article will provide you with 40 fascinating facts about Elektrostal, giving you a better understanding of why this city is worth exploring. From its origins as an industrial hub to its modern-day charm, we will delve into the various aspects that make Elektrostal a unique and must-visit destination.
So, join us as we uncover the hidden treasures of Elektrostal and discover what makes this city a true gem in the heart of Russia.
Key Takeaways:
- Elektrostal, known as the “Motor City of Russia,” is a vibrant and growing city with a rich industrial history, offering diverse cultural experiences and a strong commitment to environmental sustainability.
- With its convenient location near Moscow, Elektrostal provides a picturesque landscape, vibrant nightlife, and a range of recreational activities, making it an ideal destination for residents and visitors alike.
Known as the “Motor City of Russia.”
Elektrostal, a city located in the Moscow Oblast region of Russia, earned the nickname “Motor City” due to its significant involvement in the automotive industry.
Home to the Elektrostal Metallurgical Plant.
Elektrostal is renowned for its metallurgical plant, which has been producing high-quality steel and alloys since its establishment in 1916.
Boasts a rich industrial heritage.
Elektrostal has a long history of industrial development, contributing to the growth and progress of the region.
Founded in 1916.
The city of Elektrostal was founded in 1916 as a result of the construction of the Elektrostal Metallurgical Plant.
Located approximately 50 kilometers east of Moscow.
Elektrostal is situated in close proximity to the Russian capital, making it easily accessible for both residents and visitors.
Known for its vibrant cultural scene.
Elektrostal is home to several cultural institutions, including museums, theaters, and art galleries that showcase the city’s rich artistic heritage.
A popular destination for nature lovers.
Surrounded by picturesque landscapes and forests, Elektrostal offers ample opportunities for outdoor activities such as hiking, camping, and birdwatching.
Hosts the annual Elektrostal City Day celebrations.
Every year, Elektrostal organizes festive events and activities to celebrate its founding, bringing together residents and visitors in a spirit of unity and joy.
Has a population of approximately 160,000 people.
Elektrostal is home to a diverse and vibrant community of around 160,000 residents, contributing to its dynamic atmosphere.
Boasts excellent education facilities.
The city is known for its well-established educational institutions, providing quality education to students of all ages.
A center for scientific research and innovation.
Elektrostal serves as an important hub for scientific research, particularly in the fields of metallurgy, materials science, and engineering.
Surrounded by picturesque lakes.
The city is blessed with numerous beautiful lakes, offering scenic views and recreational opportunities for locals and visitors alike.
Well-connected transportation system.
Elektrostal benefits from an efficient transportation network, including highways, railways, and public transportation options, ensuring convenient travel within and beyond the city.
Famous for its traditional Russian cuisine.
Food enthusiasts can indulge in authentic Russian dishes at numerous restaurants and cafes scattered throughout Elektrostal.
Home to notable architectural landmarks.
Elektrostal boasts impressive architecture, including the Church of the Transfiguration of the Lord and the Elektrostal Palace of Culture.
Offers a wide range of recreational facilities.
Residents and visitors can enjoy various recreational activities, such as sports complexes, swimming pools, and fitness centers, enhancing the overall quality of life.
Provides a high standard of healthcare.
Elektrostal is equipped with modern medical facilities, ensuring residents have access to quality healthcare services.
Home to the Elektrostal History Museum.
The Elektrostal History Museum showcases the city’s fascinating past through exhibitions and displays.
A hub for sports enthusiasts.
Elektrostal is passionate about sports, with numerous stadiums, arenas, and sports clubs offering opportunities for athletes and spectators.
Celebrates diverse cultural festivals.
Throughout the year, Elektrostal hosts a variety of cultural festivals, celebrating different ethnicities, traditions, and art forms.
Electric power played a significant role in its early development.
Elektrostal owes its name and initial growth to the establishment of electric power stations and the utilization of electricity in the industrial sector.
Boasts a thriving economy.
The city’s strong industrial base, coupled with its strategic location near Moscow, has contributed to Elektrostal’s prosperous economic status.
Houses the Elektrostal Drama Theater.
The Elektrostal Drama Theater is a cultural centerpiece, attracting theater enthusiasts from far and wide.
Popular destination for winter sports.
Elektrostal’s proximity to ski resorts and winter sport facilities makes it a favorite destination for skiing, snowboarding, and other winter activities.
Promotes environmental sustainability.
Elektrostal prioritizes environmental protection and sustainability, implementing initiatives to reduce pollution and preserve natural resources.
Home to renowned educational institutions.
Elektrostal is known for its prestigious schools and universities, offering a wide range of academic programs to students.
Committed to cultural preservation.
The city values its cultural heritage and takes active steps to preserve and promote traditional customs, crafts, and arts.
Hosts an annual International Film Festival.
The Elektrostal International Film Festival attracts filmmakers and cinema enthusiasts from around the world, showcasing a diverse range of films.
Encourages entrepreneurship and innovation.
Elektrostal supports aspiring entrepreneurs and fosters a culture of innovation, providing opportunities for startups and business development.
Offers a range of housing options.
Elektrostal provides diverse housing options, including apartments, houses, and residential complexes, catering to different lifestyles and budgets.
Home to notable sports teams.
Elektrostal is proud of its sports legacy, with several successful sports teams competing at regional and national levels.
Boasts a vibrant nightlife scene.
Residents and visitors can enjoy a lively nightlife in Elektrostal, with numerous bars, clubs, and entertainment venues.
Promotes cultural exchange and international relations.
Elektrostal actively engages in international partnerships, cultural exchanges, and diplomatic collaborations to foster global connections.
Surrounded by beautiful nature reserves.
Nearby nature reserves, such as the Barybino Forest and Luchinskoye Lake, offer opportunities for nature enthusiasts to explore and appreciate the region’s biodiversity.
Commemorates historical events.
The city pays tribute to significant historical events through memorials, monuments, and exhibitions, ensuring the preservation of collective memory.
Promotes sports and youth development.
Elektrostal invests in sports infrastructure and programs to encourage youth participation, health, and physical fitness.
Hosts annual cultural and artistic festivals.
Throughout the year, Elektrostal celebrates its cultural diversity through festivals dedicated to music, dance, art, and theater.
Provides a picturesque landscape for photography enthusiasts.
The city’s scenic beauty, architectural landmarks, and natural surroundings make it a paradise for photographers.
Connects to Moscow via a direct train line.
The convenient train connection between Elektrostal and Moscow makes commuting between the two cities effortless.
A city with a bright future.
Elektrostal continues to grow and develop, aiming to become a model city in terms of infrastructure, sustainability, and quality of life for its residents.
In conclusion, Elektrostal is a fascinating city with a rich history and a vibrant present. From its origins as a center of steel production to its modern-day status as a hub for education and industry, Elektrostal has plenty to offer both residents and visitors. With its beautiful parks, cultural attractions, and proximity to Moscow, there is no shortage of things to see and do in this dynamic city. Whether you’re interested in exploring its historical landmarks, enjoying outdoor activities, or immersing yourself in the local culture, Elektrostal has something for everyone. So, next time you find yourself in the Moscow region, don’t miss the opportunity to discover the hidden gems of Elektrostal.
Q: What is the population of Elektrostal?
A: As of the latest data, the population of Elektrostal is approximately XXXX.
Q: How far is Elektrostal from Moscow?
A: Elektrostal is located approximately XX kilometers away from Moscow.
Q: Are there any famous landmarks in Elektrostal?
A: Yes, Elektrostal is home to several notable landmarks, including XXXX and XXXX.
Q: What industries are prominent in Elektrostal?
A: Elektrostal is known for its steel production industry and is also a center for engineering and manufacturing.
Q: Are there any universities or educational institutions in Elektrostal?
A: Yes, Elektrostal is home to XXXX University and several other educational institutions.
Q: What are some popular outdoor activities in Elektrostal?
A: Elektrostal offers several outdoor activities, such as hiking, cycling, and picnicking in its beautiful parks.
Q: Is Elektrostal well-connected in terms of transportation?
A: Yes, Elektrostal has good transportation links, including trains and buses, making it easily accessible from nearby cities.
Q: Are there any annual events or festivals in Elektrostal?
A: Yes, Elektrostal hosts various events and festivals throughout the year, including XXXX and XXXX.
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
Share this Fact:
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Indian J Med Res
- v.134(5); 2011 Nov
Hand hygiene: Back to the basics of infection control
Purva mathur.
Department of Laboratory Medicine, Jai Prakash Narain Apex Trauma Centre, All India Institute of Medical Sciences, New Delhi, India
Health care associated infections are drawing increasing attention from patients, insurers, governments and regulatory bodies. This is not only because of the magnitude of the problem in terms of the associated morbidity, mortality and cost of treatment, but also due to the growing recognition that most of these are preventable. The medical community is witnessing in tandem unprecedented advancements in the understanding of pathophysiology of infectious diseases and the global spread of multi-drug resistant infections in health care set-ups. These factors, compounded by the paucity of availability of new antimicrobials have necessitated a re-look into the role of basic practices of infection prevention in modern day health care. There is now undisputed evidence that strict adherence to hand hygiene reduces the risk of cross-transmission of infections. With “Clean Care is Safer Care” as a prime agenda of the global initiative of WHO on patient safety programmes, it is time for developing countries to formulate the much-needed policies for implementation of basic infection prevention practices in health care set-ups. This review focuses on one of the simplest, low cost but least accepted from infection prevention: hand hygiene.
Introduction
Hand hygiene is now regarded as one of the most important element of infection control activities. In the wake of the growing burden of health care associated infections (HCAIs), the increasing severity of illness and complexity of treatment, superimposed by multi-drug resistant (MDR) pathogen infections, health care practitioners (HCPs) are reversing back to the basics of infection preventions by simple measures like hand hygiene. This is because enough scientific evidence supports the observation that if properly implemented, hand hygiene alone can significantly reduce the risk of cross-transmission of infection in healthcare facilities (HCFs) 1 – 5 .
Historical background
The significance of hand washing in patient care was conceptualized in the early 19 th century 6 – 8 . Labarraque 6 provided the first evidence that hand decontamination can markedly reduce the incidence of puerperal fever and maternal mortality. Semmelweis 7 worked in the Great hospital in Vienna in the 1840s. There were two maternity clinics in the hospital, with alternate day admission policy. The first clinic was attended by medical students, who moved straight from autopsy rooms to the delivery suite and had an average maternal mortality rate due to puerperal fever of about 10 per cent. The second clinic, attended by midwives had a maternal mortality of only 2 per cent. The puzzled Semmelweis got a breakthrough in 1847, following the death of colleague Jokob Kolletschka, who had been accidentally got a cut by a student's scalpel while performing an autopsy. His autopsy showed a pathological condition similar to that of women drying from puerperal fever. Semmelweis concluded that some “unknown cadaverous material” caused puerperal fever. He instituted a policy of washing hands with chlorinted lime for those leaving the autopsy room, following which the rate of maternal mortality dropped ten-folds, comparable to the second clinic. Thus, he almost conducted a controlled trial, in an era when microbes were yet to be discovered and the germ theory of disease was not defined 6 – 8 . In another landmark study in the wake of Staphylococcal epidemics in 1950s, Mortimer et al 9 showed that direct contact was the main mode of transmission of S. aureus in nurseries. They also demonstrated that hand washing by patients’ contacts reduced the level of S. aureus acquisition by babies.
In 1975 and 1985, the CDC published guidelines on hand washing practices in hospitals, primarily advocating hand washing with non antimicrobial soaps; washing with antimicrobial soap was advised before and after performing invasive procedures or during care for high risk patients. Alcohol-based solutions were recommended only in situations where sinks were not available 10 , 11 . In 1995, the Hospital Infection Control Practices Advisory Committee (HICPAC) advocated the use of antimicrobial soap or a waterless antiseptic agent for cleaning hands upon leaving the rooms of patients infected with multidrug-resistant pathogens 12 . In 2002, the CDC published revised guidelines for hand hygiene 3 . A major change in these guidelines was the recommendation to use alcohol based hand rubs for decontamination of hands between each patient contact (of non-soiling type) and the use of liquid soap and water for cleaning visibly contaminated or soiled hands. A systematic review of handwashing by the Thames Valley University as part of the evaluation of processes and indicators in infection control (EPIC) study 13 , concluded that there was a good evidence that direct patient contact resulted in hand contamination by pathogens. The EPIC study also showed the superiority of 70 per cent alcohol/ alcohol based antiseptic hand rubs 13 , 14 .
With the growing burden of HAIs, limited options of effective antimicrobials evidence supporting the role of hand hygiene in reduction of HAIs, the WHO has launched a global hand hygiene campaign. In 2005, it introduced the first Global Patient Safety Challenge “Clean Care is Safer Care (CCiSC)”, as part of its world alliance for patient safety 15 , 16 . In 2006, advanced draft guidelines on "Hand Hygiene in Health Care" were published and a suite of implementation tools were developed and tested 17 . The first Global Handwashing Day was observed on October 15, 2008. A WHO Patient Safety 2009 initiative has been established to catalyse this progress. This is the next phase of the ‘First Challenge's work on CCiSC′ 15 – 18 . This initiative has, as of April 2009, seen a total of 3,863 health care facilities registering their commitment, effectively equating to a staff of over 3.6 million people, globally. On May 5, 2009, the WHO highlighted the importance of hand hygiene and launched guidelines and tools on hand hygiene, based on the next phase of patient safety work programme “SAVE LIVES: Clean Your Hands” 1 , 2 , 15 – 18 .
Normal flora of hands
There are two types of microbes colonizing hands: the resident flora, which consists of microorganisms residing under the superficial cells of the stratum corneum and the transient flora, which colonizes the superficial layers of the skin, and is more amenable to removal by routine hand hygiene. Transient microorganisms survive, but do not usually multiply on the skin. They are often acquired by health care workers (HCWs) during direct contact with patients or their nearby contaminated environmental surfaces and are the organisms most frequently associated with HCAIs 1 – 3 .
Colonization of hands with pathogens and their role in transmission
The hands of HCWs are commonly colonized with pathogens like methicillin resistant S. aureus (MRSA), vancomycin resistant Enterococcus (VRE), MDR-Gram Negative bacteria (GNBs), Candida spp. and Clostridium difficle , which can survive for as long as 150 h. Approximately 10 6 skin epithelial cells containing viable microorganisms are shed daily from the normal skin 2 , 19 , which can contaminate the gowns, bed linen, bedside furniture, and other objects in the patient's immediate environment. Hand carriage of resistant pathogens has repeatedly been shown to be associated with nosocomial infections 1 – 3 . The highest rates of hand contamination are reported from critical care areas, which also report most cases of cross-transmission. The hands may become contaminated by merely touching the patent's intact skin or inanimate objects in patients’ rooms or during the “clean” procedures like recording blood pressure 1 – 3 .
Importance of hand hygiene
Proper hand hygiene is the single most important, simplest, and least expensive means of reducing the prevalence of HAIs and the spread of antimicrobial resistance 1 – 3 , 20 – 23 . Several studies have demonstrated that handwashing virtally eradicates the carriage of MRSA which invariably occurs on the hands of HCPs working in ICUs 24 , 25 . An increase in handwashing compliance has been found to be accompanied by a fall in MRSA rates 26 . The hand hygiene liason group identified nine controlled studies, all of which showed significant reductions in infection related outcomes, even in settings with a high infection rates in critically ill patients 14 , 27 , 28 . Transmission of Health-care-associated Klebsiella sp. has also been documented to reduce with improvement in hand hygiene 2 , 3 , 23 . The evidence suggests that adherence to hand hygiene practices has significantly reduced the rates of acquisition of pathogens on hands and has ultimately reduced the rates of HAIs in a hospital 22 , 23 , 26 , 29 – 31 .
Indications for hand hygiene during patient care
Wash hands with soap and water when ( i ) visibly dirty or contaminated with proteinaceous material, blood, or other body fluids and if exposure to Bacillus anthracis is suspected or proven (since the physical action of washing and rinsing hands in such circumstances is recommended because alcohols, chlorhexidine, iodophors, and other antiseptic agents have poor activity against spores); ( ii ) After using a restroom, wash hands with a non-antimicrobial soap and water or with an antimicrobial soap and water; and ( iii ) before and after having food 1 – 3 , 21 – 23 , 32 .
In all other clinical situations described below, when hands are not visibly soiled, an alcohol-based hand rub should be used routinely for decontaminating hands 1 – 3 , 21 – 23 , 32 . ( i ) Before having direct contact with patients. ( ii ) Before donning sterile gloves when inserting a central intravascular catheter. ( iii ) Before inserting indwelling urinary catheters, peripheral vascular catheters, or other invasive devices that do not require a surgical procedure. ( iv ) After contact with a patient's intact skin ( e.g ., when taking a pulse or blood pressure or lifting a patient). ( v ) After contact with body fluids or excretions, mucous membranes, nonintact skin, and wound dressings if hands are not visibly soiled. ( vi ) After contact with inanimate objects (including medical equipment) in the immediate vicinity of the patient. ( vii ) After removing gloves. ( viii ) If moving from a contaminated body site to a clean body site during patient care.
The WHO “SAVE LIVES: Clean Your Hands” programme 1 , 2 reinforces the “My 5 Moments for Hand Hygiene” approach as key to protect the patients, HCWs and the health-care environment against the spread of pathogens and thus reduce HAIs. This approach encourages HCWs to clean their hands: before touching a patient, before clean/aseptic procedures, after body fluid exposure/risk, after touching a patient and after touching patient surroundings 1 , 2 .
Other precautions in relation to hand sanitation
Avoid unnecessary touching of surfaces in close proximity to the patient. In 2002, the CDC/HICPAC recommended that artificial fingernails and extenders not to be worn by HCPs who have contact with high-risk patients, due to their association with outbreaks of Gram-negative bacillary and candidal infections 12 . Although rings harbour a high count of pathogens, they have not been found to be associated with transmission of infections 12 .
Method of hand washing 1 , 2 , 21
For handwashing, remove the jewelry and rinse hands under running water (preferably warm). Lather with soap and using friction, cover all surfaces of hands and fingers. Wash thoroughly under running water. Turn off faucet with wrist/elbow. Dry hands with a single use towel or by using forced air drying. Pat skin rather than rubbing to avoid cracking. If disposable towels are used, throw in trash immediately. Skin excoriation may lead to bacteria colonizing the skin and the possible spread of blood borne viruses as well as other microorganisms. Sore hands may also lead to decreased compliance with hand washing protocols 1 , 2 , 21 . If using antiseptic rub, take an adequate amount and rub on all surfaces for the recommended time. Let the antiseptic dry on its own.
Agents used for hand hygiene
Table I lists the properties, advantages and disadvantages of the commonly used agents for hand hygiene 1 – 4 , 21 , 33 .
Properties of hand hygiene products

Selecting hand hygiene products for health set-ups
The major determinants for product selection are antimicrobial profile, user acceptance, and cost 2 , 4 , 21 . Post-contamination hand hygiene products must have at least bactericidal, fungicidal (yeasts), and virucidal (coated viruses) activity. Since hands of HCWs are frequently contaminated with blood during routine patient care, activity against coated viruses should be included in the minimum spectrum of activity of an agent for hand hygiene 4 . Additional activity against fungi (including molds), mycobacteria, and bacterial spores may be relevant in high risk wards or during outbreaks. Pre-operative hand hygiene should be at least bactericidal and fungicidal (yeasts), since the hands of most HCWs carry yeasts and surgical- site infections have also been associated with hand carriage of yeasts during an outbreak 4 .
Hospital administrators should also take into account the acceptability of product (smell, feel, skin irritation) by the users and its allergenic potential 1 – 4 , 21 . When comparing the cost of hand hygiene products, it has been found that the excess hospital cost associated with only 4-5 HAIs of average severity may equal the entire annual budget for hand hygiene products used for in-patient care areas 3 , 34 .
One of the key elements in improving hand hygiene practice is the use of an alcohol based hand rub instead of washing with soap and water. An alcohol-based hand rub requires less time, is microbiologically more effective and is less irritating to skin than traditional hand washing with soap and water 2 , 3 , 35 . In the ICUs, switching to alcohol hand disinfection would decrease the time necessary for hand hygiene from 1.3 h (or 17% of total nursing time) to 0.3 h (or 4% of total nursing time) 35 , 36 .
Reasons for poor hand hygiene practices
In most health care institutions, adherence to recommended hand-washing practices remains unacceptably low, rarely exceeding 40 per cent of situations in which hand hygiene is indicated 35 , 37 . Hand hygiene reflects attitudes, behaviours and beliefs. Some of the observed/self reported factors found to be affecting hand hygiene behaviours are enlisted in Table II 2 , 3 , 38 – 41 .
Factors affecting compliance to hand hygiene

Methods used to improve hand hygiene compliance
Multimodal strategies have been shown to be more successful in improving rates of adherence with hand hygiene in HCWs than single interventions 16 . Targeted, multi-faceted approaches focusing on system change, administrative support, motivation, availability of alcohol-based hand rubs, training and intensive education of HCWs and reminders in the workplace have been recommended for improvement in hand hygiene 16 .
Recent studies support the fact that interactive educational programmes combined with free availability of hand disinfectants significantly increased the hand hygiene compliance 42 , 43 . A single lecture on basic hand hygiene protocols had a significant and sustained effect in enhancing hand hygiene compliance in a Swedish hospital 42 . The four member States of the European Union, which implemented National Hand Hygiene Campaigns found the following strategies to be extremely useful in their countries: Governmental support, the use of indicators for hand hygiene benchmarking, developing national surveillance systems for auditing alcohol based hand rub consumption and auditing hand hygiene compliance 44 . Trampuz et al 35 advocated simple training sessions for HCWs to be held in each ward to introduce the advantage of alcohol hand rubs over hand washing.
Other factors like positive role modeling (hand hygiene behaviour of senior practitioners) and the use of performance indicators also remarkably improve adherence to hand hygiene 40 , 41 . There should be adequate supply of hand hygiene products, lotions and creams, disposable towels and facilities for hand washing, where necessary 2 – 4 , 35 , 40 , 41 . Alcohol hand rubs should be available at the point of care in sufficient quantities. It needs to be emphasized that wearing gloves does not replace the need for hand hygiene and that contamination may occur during glove removal. Studies by Pitet 26 , 45 showed a remarkable and long lasting improvement in hand hygiene compliance using a multimodal strategy, which has been adopted by the first Global Patient Safety Challenge of WHO to develop hand hygiene strategies. The availability of individual, pocket carried bottles also increased compliance 38 – 40 , 46 – 48 .
Apart from this, all hospitals should have a dynamic infection control team, robust surveillance system, adequate staff to disseminate evidence-based knowledge in an easily comprehensible way to all cadres of staff. At a more local or regional level, there is a need for institutional frameworks or programmes to deal with HAIs 49 . The Institute for Healthcare Improvement ( www.ihi.org ) offers elaborate training modules on various aspects of patient care. The guide for implementation of WHO's CCiSC and a range of tools to facilitate hand hygiene is available 50 .
Research and education
To develop successful interventions, more research into behavioural determinants is needed, in particular, how these determinants can be applied to improve hand hygiene 51 , 52 . Process indicators are vital and an understanding of why some interventions succeed and others fail is needed. Since hand hygiene is more of a behavioural practice, the first step towards the development of interventions should be to identify the prevalence of risk behaviours ( i.e . non compliance) and the difference in risk behaviours. Since the reasons for non-compliance vary among countries, large scale systematic studies are needed to identify the reasons thereof and plan remedial strategies.
An expert panel has recommended that measuring hand hygiene compliance is essential to understand the current situation, facilitate change and to measure the impact of interventions 53 . This can be done by direct observation, automated electronic monitoring, product consumption and self reporting by HCW 54 .
The important aspect of role models for students, whose adherence is strongly influenced by their mentor's attitude at bed side should be exploited in moulding the behaviour of young medical students. A few lectures in the undergraduate curriculum may prime the medical students to this basic necessity. The Hand Hygiene Liason Group strongly advocates teaching of elementary hygiene practices at medical schools 55 . In an elaborate study focusing on MBBS students, it was noted that assessing the knowledge, attitude and practices of final year MBBS students and providing a positive role modeling at undergraduate level is a good initiative 56 .
Indian scenario
In India, the quality of healthcare is governed by various factors, the principal amongst these being whether the health care organization is government or private-sector run. There is also an economic and regional disparity throughout the country. About 75 per cent of health infrastructure, medical manpower and other health resources are concentrated in urban areas, where 27 per cent of the population lives 57 . There is a lack of availability of clean water for drinking and washing. Like in other developing countries, the priority given to prevention and control of HCAI is minimal. This is primarily due to lack of infrastructure, trained manpower, surveillance systems, poor sanitation, overcrowding and understaffing of hospitals, unfavourable social background of population, lack of legislations mandating accreditation of hospitals and a general attitude of non-compliance amongst health care providers towards even basic procedures of infection control. In India, although hand hygiene is imbibed as a custom and promoted at school and community levels to reduce the burden of diarrhoea, there is a paucity of information on activities to promote hand hygiene in HCFs. Sporadic reports document the role of hands in spreading infection and isolated efforts at improving hand hygiene across the country 54 , 58 – 60 .
The practice of compulsory training on standard precautions, safe hospital practices and infection control for all postgraduates upon course-induction, as is being done in a few Delhi medical colleges seems very promising for our country. Such an exercise may be made mandatory across all medical and nursing colleges of India, especially since the “patient safety” is increasingly being prioritized by the Government of India and the country being one of the 120 signatories pledging support to the WHO launched world alliance (available at http://www.who.int/patientsafery/events/06/statememts/India_pledge.pdf ).
Challenges ahead
Although evidence based guidelines are increasingly being implemented in the developed countries, the developing countries still lack basic health care facilities, surveillance networks and resources to curtail HAIs 61 – 63 . Lack of hand washing facilities ( e.g ., sinks, running water and sewage systems) are major deterrents for implementation of hand hygiene 61 . The use of WHO advocated alcohol based hand rubs is a practical solution to overcome these constraints, because these can be distributed individually to staff for pocket carriage and placed at the point of care. The major advantage is that its use is well applicable to situations typical of developing countries, such as two patients sharing the same bed, or patient's relatives being requested to help in care provision. Several hospitals are now reporting increased compliance after implementation of CCiSC 64 . Several countries have also initiated nationally co-ordinated activities ( http://www.who.int/gpsc/national-campaigns/en/ ) to promote hand hygiene 54 . However, global Healthcare Infection Prevention programmes can only be successful, if these populous developing nations are able to control the menace by formulation of national or local policies and strictly implementing the guidelines.
Hand washing should become an educational priority. Educational interventions for medical students should provide clear evidence that HCWs hands become grossly contaminated with pathogens upon patient contact and that alcohol hand rubs are the easiest and most effective means of decontaminating hands and thereby reducing the rates of HAIs. Increasing the emphasis on infection control, giving the charge of infection control to senior organizational members, changing the paradigm of surveillance to continuous monitoring and effective data feedback are some of the important measures which need to be initiated in Indian hospitals.
One of the reasons microbes have survived in nature is probably their simplicity: a simple genomic framework with genetic encryptation of basic survival strategies. To tackle these microbes, human beings will have to follow basic and simple protocols of infection prevention. The health care practitioners in our country need to brace themselves to inculcate the simple, basic and effective practice of hand hygiene in their daily patient care activities and serve as a role model for future generations of doctors, nurses and paramedical personnels.
Quick links
- Find funding
- Find publications
- News centre
- Outcomes of funding rounds
- Sapphire Login
- Publications
Australian Guidelines for the Prevention and Control of Infection in Healthcare (2019)
The guidelines are produced by the National Health and Medical Research Council (NHMRC) in collaboration with the Australian Commission on Safety and Quality in Healthcare, and are published on the MAGICapp platform .
Publication Data
Table of contents.
For information relevant to COVID-19 please refer to: For health and other care settings - the advice from the Infection Control Expert Group . For all other settings – the Department of Health COVID-19 webpage . Your local state and territory health departments. The Australian Commission on Safety and Quality in Healthcare has recently released COVID-19 specific resources regarding PPE and the application of transmission-based precautions to complement Commonwealth and state and territory resources. The Australian Guidelines for the Prevention and Control of Infection in Healthcare have been developed for use in all healthcare settings, including office-based practices. They contain guidance on personal protective equipment (PPE), standard and transmission-based precautions and outbreak management in section 3 . For advice on infection control in community and other settings please go to the Department of Health website .
About the guidelines
There are over 165,000 healthcare associated infections in Australian acute healthcare facilities every year. This makes healthcare associated infections the most common complication affecting patients in hospital. But this problem does not just affect patients and workers in hospitals — healthcare associated infections can occur in any healthcare setting, including office-based practices (e.g. general practice clinics, dental clinics, community health facilities), the settings in which paramedics work and in long-term care facilities.
Effective infection prevention and control is central to providing high quality healthcare for patients and a safe working environment for those who work in healthcare settings. The guidelines provide evidence-based recommendations that outline the critical aspects of infection prevention and control, focusing on core principles and priority areas for action.
The guidelines have been developed to specifically support improved infection prevention and control in acute health settings. While some of the principles and recommendations described in the guidelines may be applicable to other health settings, all healthcare facilities should consider the risk of transmission of infection in their setting and implement the guidelines and its recommendations according to their specific setting and circumstances.
The guidelines are for use by all working in healthcare – including healthcare workers, management and support staff. They provide a risk-management framework to ensure that the basic principles of infection prevention and control can be applied to a wide range of healthcare settings. The level of risk may differ in different types of healthcare facilities; risk assessments are encouraged as part of the decision making and use of guideline recommendations.
Accessing and using the guidelines
The Australian Guidelines for the Prevention and Control of Infection in Healthcare are published on MAGICapp allowing for ‘point of care’ use where the guidelines can be viewed on any tablet, phone or computer.
You can access the most recent version, at any time, on MAGICapp .
Additionally, an up-to-date PDF version can be generated directly from the guidelines by clicking on the PDF button on MAGICapp:

IMAGES
COMMENTS
A hand wash should take around 30 seconds. 1 Wet hands with running water (preferably warm, for comfort). palm to palm, back of hands, in between fingers and back of fingers, around thumbs and tips of fingers. 2 Apply soap to hands. 4 Rinse hands with water. 6 Your hands are clean. 5 Dry hands thoroughly. 3 Lather soap and rub hands for at
Handwashing practices in the patient care setting began in the early 19th century. The practice evolved over the years with evidential proof of its vast importance and coupled with other hand-hygienic practices, decreased pathogens responsible for nosocomial or hospital-acquired infections (HAI). [1][2][3]
Introduction. The expanding global outbreak of Coronavirus Disease 2019 (COVID-19) demands an evidence-based public health response. Seasonal human coronavirus strains and COVID-19 appear to be transmitted via droplets, direct and indirect contact with infected secretions and, to an unknown extent by aerosol 1- 4.Hand hygiene measures are recommended by health authorities and public health ...
Two studies [37, 39] focused on both, the duration of hand washing (for at least 20 seconds) and hand washing or ABHR use at specific times, including after contact with high-risk or symptomatic individuals, washing hands when hands are visibly dirty, before eating, before or after handling food, after using toilet, after outdoor activity ...
Staying Healthy public consultation draft, National Health and Medical Research Council, July 2023 . Breaking the chain of infection . R. ... • Perform hand hygiene. When changing a nappy, it is very important to wash your hands or use hand sanitiser before you put on gloves. This is so that when you have finished changing the child, you can ...
Celebrate Global Handwashing Day. Regular handwashing is one of the best ways to remove germs, avoid getting sick, and prevent the spread of germs to others. Whether you are at home, at work, traveling, or out in the community, find out how handwashing with soap and water can protect you and your family.
AHRQ Research Summit on Learning Health Systems; National Advisory Council Meetings; AHRQ Research Conferences; About. About AHRQ. AHRQ's 35th Anniversary; ... This CDC webpage shares information on hand hygiene in healthcare settings. ... Agency for Healthcare Research and Quality. 5600 Fishers Lane Rockville, MD 20857 Telephone: (301) 427 ...
1) Wet your hands and turn off the tap (to save water), 2) Lather, 3) Rub your hands together for at least 20 seconds (possibly while singing Happy Birthday twice), 4) Rinse, and. 5) Dry. Do this ...
To wash your hands: Wet hands with running water (preferably warm). Apply soap or liquid soap — enough to cover all of your hands. Normal soap is just as good as antibacterial soap. Rub your hands together for at least 20 seconds. Make sure you cover all surfaces, including the backs of your hands and in between your fingers.
The implementation of health education to promote hand hygiene can effectively support children, medical staff, and patients to improve their hand washing frequency and technique (55-60). At the same time, improvements in hand washing facilities can also increase the frequency of hand washing, such as the availability of soap or hand sanitizer ...
Washing hands with soap removes germs much more effectively 9. Handwashing education and access to soap in schools can help improve attendance 10,11,12. Good handwashing early in life may help improve child development in some settings 13. Estimated global rates of handwashing after using the toilet are only 19% 6.
Published by the Australian Commission on Safety and Quality in Health Care. Level 5, 255 Elizabeth Street, Sydney NSW 2000 Phone: (02) 9126 3600 Email: [email protected] Website: www.safetyandquality.gov.au. ISBN: 978-1-922880-39-. Australian Commission on Safety and Quality in Health Care 2023.
Saint-Petersburg Research Institute of Radiation Hygiene after Professor P.V. Ramzaev, Federal Service for Surveillance on Consumer Rights Protection and Human W ell-Being, Saint-Petersburg, Russia
In 1954, Elemash began to produce fuel assemblies, including for the first nuclear power plant in the world, located in Obninsk. In 1959, the facility produced the fuel for the Soviet Union's first icebreaker. Its fuel assembly production became serial in 1965 and automated in 1982. 1. Today, Elemash is one of the largest TVEL nuclear fuel ...
The ethical governance of Artificial Intelligence (AI) in health care and public health continues to be an urgent issue for attention in policy, research, and practice. In this paper we report on central themes related to challenges and strategies for promoting ethics in research involving AI in global health, arising from the Global Forum on Bioethics in Research (GFBR), held in Cape Town ...
40 Facts About Elektrostal. Elektrostal is a vibrant city located in the Moscow Oblast region of Russia. With a rich history, stunning architecture, and a thriving community, Elektrostal is a city that has much to offer. Whether you are a history buff, nature enthusiast, or simply curious about different cultures, Elektrostal is sure to ...
Introduction. Hand hygiene is now regarded as one of the most important element of infection control activities. In the wake of the growing burden of health care associated infections (HCAIs), the increasing severity of illness and complexity of treatment, superimposed by multi-drug resistant (MDR) pathogen infections, health care practitioners (HCPs) are reversing back to the basics of ...
The guidelines are produced by the National Health and Medical Research Council (NHMRC) in collaboration with the Australian Commission on Safety and Quality in Healthcare, and are published on the MAGICapp platform. Publication Data. Reference number. CD34. ISBN. 978-1-86496-028-. 2019.
See other industries within the Health Care and Social Assistance sector: Child Care Services , Community Food and Housing, and Emergency and Other Relief Services , Continuing Care Retirement Communities and Assisted Living Facilities for the Elderly , General Medical and Surgical Hospitals , Home Health Care Services , Individual and Family Services , Medical and Diagnostic Laboratories ...