Appointments at Mayo Clinic
- Pregnancy week by week
- Fetal presentation before birth
The way a baby is positioned in the uterus just before birth can have a big effect on labor and delivery. This positioning is called fetal presentation.
Babies twist, stretch and tumble quite a bit during pregnancy. Before labor starts, however, they usually come to rest in a way that allows them to be delivered through the birth canal headfirst. This position is called cephalic presentation. But there are other ways a baby may settle just before labor begins.
Following are some of the possible ways a baby may be positioned at the end of pregnancy.

Head down, face down
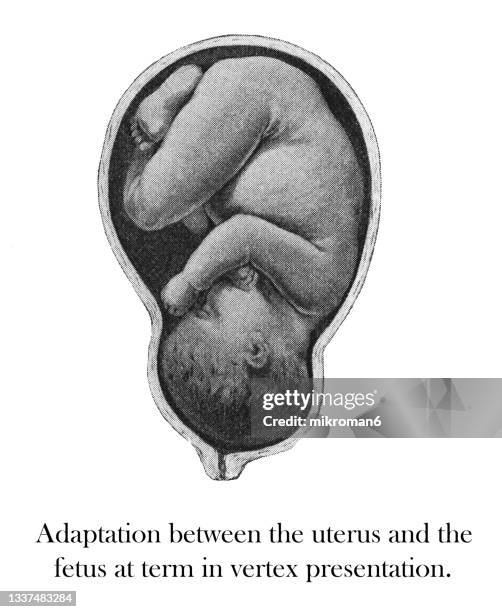
When a baby is head down, face down, the medical term for it is the cephalic occiput anterior position. This the most common position for a baby to be born in. With the face down and turned slightly to the side, the smallest part of the baby's head leads the way through the birth canal. It is the easiest way for a baby to be born.

Head down, face up
When a baby is head down, face up, the medical term for it is the cephalic occiput posterior position. In this position, it might be harder for a baby's head to go under the pubic bone during delivery. That can make labor take longer.
Most babies who begin labor in this position eventually turn to be face down. If that doesn't happen, and the second stage of labor is taking a long time, a member of the health care team may reach through the vagina to help the baby turn. This is called manual rotation.
In some cases, a baby can be born in the head-down, face-up position. Use of forceps or a vacuum device to help with delivery is more common when a baby is in this position than in the head-down, face-down position. In some cases, a C-section delivery may be needed.

Frank breech
When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head. This is the most common type of breech presentation.
If you are more than 36 weeks into your pregnancy and your baby is in a frank breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Most babies in a frank breech position are born by planned C-section.

Complete and incomplete breech
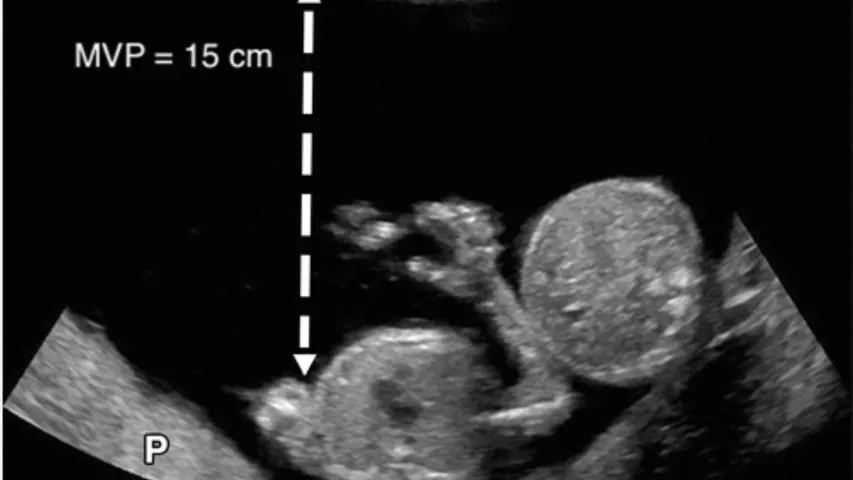
A complete breech presentation, as shown below, is when the baby has both knees bent and both legs pulled close to the body. In an incomplete breech, one or both of the legs are not pulled close to the body, and one or both of the feet or knees are below the baby's buttocks. If a baby is in either of these positions, you might feel kicking in the lower part of your belly.
If you are more than 36 weeks into your pregnancy and your baby is in a complete or incomplete breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Many babies in a complete or incomplete breech position are born by planned C-section.

When a baby is sideways — lying horizontal across the uterus, rather than vertical — it's called a transverse lie. In this position, the baby's back might be:
- Down, with the back facing the birth canal.
- Sideways, with one shoulder pointing toward the birth canal.
- Up, with the hands and feet facing the birth canal.
Although many babies are sideways early in pregnancy, few stay this way when labor begins.
If your baby is in a transverse lie during week 37 of your pregnancy, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of your health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a transverse lie, talk with a member of your health care team about the choices you have for delivery. Many babies who are in a transverse lie are born by C-section.

If you're pregnant with twins and only the twin that's lower in the uterus is head down, as shown below, your health care provider may first deliver that baby vaginally.
Then, in some cases, your health care team may suggest delivering the second twin in the breech position. Or they may try to move the second twin into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
Your health care team may suggest delivery by C-section for the second twin if:
- An attempt to deliver the baby in the breech position is not successful.
- You do not want to try to have the baby delivered vaginally in the breech position.
- An attempt to move the baby into a head-down position is not successful.
- You do not want to try to move the baby to a head-down position.
In some cases, your health care team may advise that you have both twins delivered by C-section. That might happen if the lower twin is not head down, the second twin has low or high birth weight as compared to the first twin, or if preterm labor starts.

- Landon MB, et al., eds. Normal labor and delivery. In: Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed May 19, 2023.
- Holcroft Argani C, et al. Occiput posterior position. https://www.updtodate.com/contents/search. Accessed May 19, 2023.
- Frequently asked questions: If your baby is breech. American College of Obstetricians and Gynecologists https://www.acog.org/womens-health/faqs/if-your-baby-is-breech. Accessed May 22, 2023.
- Hofmeyr GJ. Overview of breech presentation. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Strauss RA, et al. Transverse fetal lie. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Chasen ST, et al. Twin pregnancy: Labor and delivery. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Cohen R, et al. Is vaginal delivery of a breech second twin safe? A comparison between delivery of vertex and non-vertex second twins. The Journal of Maternal-Fetal & Neonatal Medicine. 2021; doi:10.1080/14767058.2021.2005569.
- Marnach ML (expert opinion). Mayo Clinic. May 31, 2023.
Products and Services
- A Book: Obstetricks
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- 3rd trimester pregnancy
- Fetal development: The 3rd trimester
- Overdue pregnancy
- Pregnancy due date calculator
- Prenatal care: 3rd trimester
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
Let’s celebrate our doctors!
Join us in celebrating and honoring Mayo Clinic physicians on March 30th for National Doctor’s Day.
- AI Generator
64 Fetal Presentation Stock Photos & High-Res Pictures
Browse 64 fetal presentation photos and images available, or start a new search to explore more photos and images..
Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
- Find in topic
RELATED TOPICS
INTRODUCTION
PATHOGENESIS AND RISK FACTORS
● The fetus does not fully occupy the pelvis, thus allowing a fetal extremity room to prolapse. Predisposing factors include early gestational age, multiple gestation, polyhydramnios, or a large maternal pelvis relative to fetal size [ 2,3 ].
● Membrane rupture occurs when the presenting part is still high, which allows flow of amniotic fluid to carry a fetal extremity, umbilical cord, or both toward the birth canal.
Medical Information

Delivery, Face Presentation, and Brow Presentation: Understanding Fetal Positions and Birth Scenarios
Introduction:.
During childbirth, the position of the baby plays a significant role in the delivery process. While the most common fetal presentation is the head-down position (vertex presentation), variations can occur, such as face presentation and brow presentation. This comprehensive article aims to provide a thorough understanding of delivery, face presentation, and brow presentation, including their definitions, causes, complications, and management approaches.
Delivery Process:
- Normal Vertex Presentation: In a typical delivery, the baby is positioned head-down, with the back of the head (occiput) leading the way through the birth canal.
- Engagement and Descent: Prior to delivery, the baby's head engages in the pelvis and gradually descends, preparing for birth.
- Cardinal Movements: The baby undergoes a series of cardinal movements, including flexion, internal rotation, extension, external rotation, and restitution, which facilitate the passage through the birth canal.
Face Presentation:
- Definition: Face presentation occurs when the baby's face is positioned to lead the way through the birth canal instead of the vertex (head).
- Causes: Face presentation can occur due to factors such as abnormal fetal positioning, multiple pregnancies, uterine abnormalities, or maternal pelvic anatomy.
- Complications: Face presentation is associated with an increased risk of prolonged labor, difficulties in delivery, increased fetal malposition, birth injuries, and the need for instrumental delivery.
- Management: The management of face presentation depends on several factors, including the progression of labor, the size of the baby, and the expertise of the healthcare provider. Options may include closely monitoring the progress of labor, attempting a vaginal delivery with careful maneuvers, or considering a cesarean section if complications arise.
Brow Presentation:
- Definition: Brow presentation occurs when the baby's head is partially extended, causing the brow (forehead) to lead the way through the birth canal.
- Causes: Brow presentation may result from abnormal fetal positioning, poor engagement of the fetal head, or other factors that prevent full flexion or extension.
- Complications: Brow presentation is associated with a higher risk of prolonged labor, difficulty in descent, increased chances of fetal head entrapment, birth injuries, and the potential need for instrumental delivery or cesarean section.
- Management: The management of brow presentation depends on various factors, such as cervical dilation, progress of labor, fetal size, and the presence of complications. Close monitoring, expert assessment, and a multidisciplinary approach may be necessary to determine the safest delivery method, which can include vaginal delivery with careful maneuvers, instrumental assistance, or cesarean section if warranted.
Delivery Techniques and Intervention:
- Obstetric Maneuvers: In certain situations, skilled healthcare providers may use obstetric maneuvers, such as manual rotation or the use of forceps or vacuum extraction, to facilitate delivery, reposition the baby, or prevent complications.
- Cesarean Section: In cases where vaginal delivery is not possible or poses risks to the mother or baby, a cesarean section may be performed to ensure a safe delivery.
Conclusion:
Delivery, face presentation, and brow presentation are important aspects of childbirth that require careful management and consideration. Understanding the definitions, causes, complications, and appropriate management approaches associated with these fetal positions can help healthcare providers ensure safe and successful deliveries. Individualized care, close monitoring, and multidisciplinary collaboration are crucial in optimizing maternal and fetal outcomes during these unique delivery scenarios.
Hashtags: #Delivery #FacePresentation #BrowPresentation #Childbirth #ObstetricDelivery
On the Article

Krish Tangella MD, MBA

Alexander Enabnit

Alexandra Warren
Please log in to post a comment.
Related Articles
Test your knowledge, asked by users, related centers, related specialties, related physicians, related procedures, related resources, join dovehubs.
and connect with fellow professionals
Related Directories
At DoveMed, our utmost priority is your well-being. We are an online medical resource dedicated to providing you with accurate and up-to-date information on a wide range of medical topics. But we're more than just an information hub - we genuinely care about your health journey. That's why we offer a variety of products tailored for both healthcare consumers and professionals, because we believe in empowering everyone involved in the care process. Our mission is to create a user-friendly healthcare technology portal that helps you make better decisions about your overall health and well-being. We understand that navigating the complexities of healthcare can be overwhelming, so we strive to be a reliable and compassionate companion on your path to wellness. As an impartial and trusted online resource, we connect healthcare seekers, physicians, and hospitals in a marketplace that promotes a higher quality, easy-to-use healthcare experience. You can trust that our content is unbiased and impartial, as it is trusted by physicians, researchers, and university professors around the globe. Importantly, we are not influenced or owned by any pharmaceutical, medical, or media companies. At DoveMed, we are a group of passionate individuals who deeply care about improving health and wellness for people everywhere. Your well-being is at the heart of everything we do.
For Patients
For professionals, for partners.
Enter search terms to find related medical topics, multimedia and more.
Advanced Search:
- Use “ “ for exact phrases.
- For example: “pediatric abdominal pain”
- Use – to remove results with certain keywords.
- For example: abdominal pain -pediatric
- Use OR to account for alternate keywords.
- For example: teenager OR adolescent
Toward the end of pregnancy, the fetus moves into position for delivery. Normally, the presentation is vertex (head first), and the position is occiput anterior (facing toward the pregnant person's spine) and with the face and body angled to one side and the neck flexed.
Variations in fetal presentations include face, brow, breech, and shoulder. Occiput posterior position (facing forward, toward the mother's pubic bone) is less common than occiput anterior position (facing backward, toward the mother's spine).
- IN THIS TOPIC
- Normal Normal and Abnormal First Trimester Exam Normal Fetal Ultrasound Biometry Fetal Heart Ultrasound Determining Fetal Situs Fetal Urinary System Umbilical Cord CNS Critical Anatomy CNS Embryology and Early Development CNS Later Development CNS Ultrasound Brain Anatomy
- Fetal Anomalies Fetal Heart Fetal Chest Fetal Colon Fetal Central Nervous System Facial Clefts Skeletal Dysplasia Genetic Markers
- Doppler Editorial Board Fetal Doppler Middle Cerebral Artery Doppler
- Fetal/Maternal Conditions Transvaginal Ultrasound Fetal Anemia Interventions Preterm Labor Placenta and Umbilical Cord
- Twins Key Views Twins: Videos Diamniotic Dichorionic and Diamniotic Monochorionic Twins Monochorionic Monoamniotic Twins Twin to Twin Transfusion Syndrome Fetal Growth Restriction Twin Reversed Arterial Perfusion Conjoined Twins
- Video Topics
- Access CMEs
- Other Links Topics A-Z Links CME Videos Upload Your Case Editorial Board
- Take A Free Tour
- Free Videos
- Editorial Board

Determining Normal Fetal Situs (Situs Solitus)
One of the first steps in obtaining cardiac views is to determine how the fetus is oriented within the uterus and to determine the right and left side of the abdominal contents versus the right and left side of the heart and thoracic contents. This is not as easy as it might seem since the fetal left side can be on the maternal right and the opposite can be true.
In summary, situs refers to the right and left orientation of fetal organs. For example situs solitus is the normal left to right axis arrangement in the fetus with the stomach and spleen on the left side of the body, and the liver and gallbladder on the right side.

Visual Summary of Normal Fetal Situs
Below are steps required to determine situs related to cephalic or breech presentation, and whether the spine or back is up (anterior) or down (posterior).
1. Determine the lie of the fetus:
A. Is the fetus head first with the head in front of the ultrasound screen? This could also be termed cephalic or vertex presentation. B. Is the fetal feet or bottom first with the head behind the screen? This could also be termed footling or breech presentation. C. Determine whether the spine or back is anterior (back up) or posterior (back down).
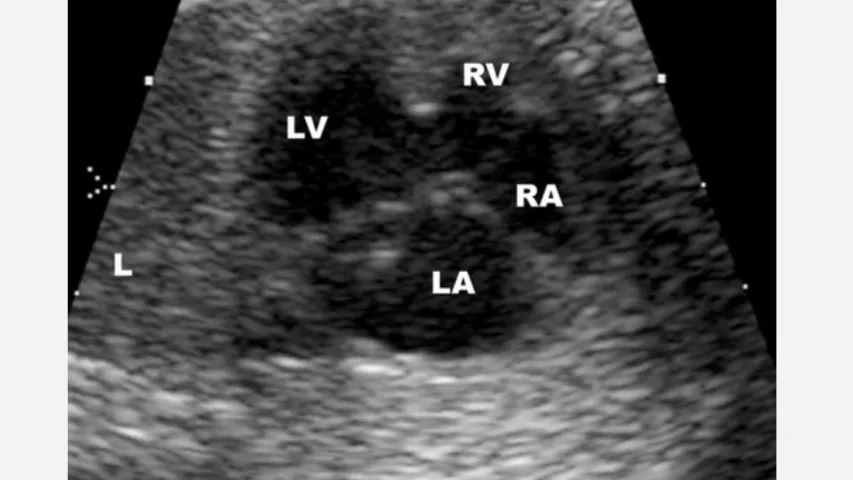
2. Obtain a transverse cut of the thorax to demonstrate a 4-chamber view. The left atrium is nearest the spine and the cardiac axis points to the left.
Detailed Method to Determine Fetal Situs
1. Define within the uterus the presentation of the fetus (generally vertex or breech; less often the presentation is oblique or transverse.).
2. Determine whether the fetal spine is parallel or transverse to the maternal spine. In sagittal view, if the fetal and maternal spine are parallel, the fetus is in longitudinal lie. When the fetal spine is perpendicular to the maternal spine, the fetus is in a transverse lie.
3. Determine the position of the fetal left side. The fetal left side will be as follows: A. With respect to the maternal abdomen, the fetal left side is anterior and near to the ultrasound transducer. B. With respect to the posterior uterine wall, the fetal left side is posterior and farthest from the transducer. C. With respect to the right uterine wall, the fetal left side will be on the maternal right. D. With respect to the left uterine wall, the fetal left side will be on the maternal left.
4. Obtain a transverse view of the abdomen and define the fetal stomach which is positioned in the left side of the fetal abdomen.
5. Obtain a 4-chamber view of the heart by obtaining a transverse view of the thorax. The left atrium and descending aorta are nearest to the spine and the cardiac axis points to the left.
6. Finally, ascertain if the stomach and heart are in their correct respective locations, i.e., the stomach is on the left side and the cardiac axis points to the left.
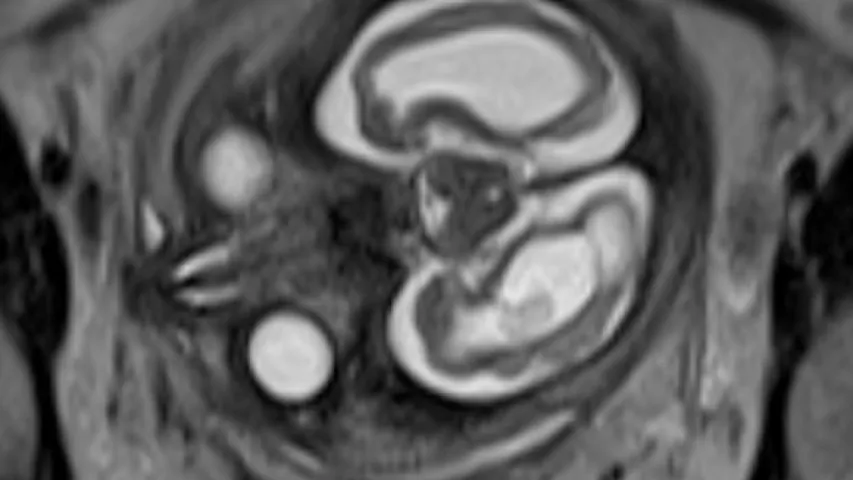
7. Place a transverse image of the fetal abdomen and heart side by side and validate that the left side of the fetal abdomen (stomach near to the spine) is concordant with the left side of the fetal heart (left atrium and descending aorta near to the spine). This is done by displaying a side by side comparison of a transverse view through the fetal stomach and a 4-chamber cardiac view.

Above. Normal ultrasound orientation for situs solitus.
Right Hand Rule of Thumb: Introduction
In their article “Sonographic definition of the fetal situs,” Bronshtein, Gover, and Zimmer [ 1 ] describe a “right hand rule of thumb” to define fetal situs during transabdominal scanning, and a “left hand rule of thumb” for transvaginal scanning.

Right Hand Rule of Thumb: Cephalic, supine, back down

Left. The sonographer’s right hand represents the fetus with the thumb pointing to the fetal left. The palm of the hand is anterior, or represents the ventral or face surface of the fetus. The fetus is therefore face up, back down, and the thumb points to the fetal left.
Right. Again, the imaginary fetus is back down with the stomach and cardiac axis pointing to the left. (Ignore color scheme of fetal heart and vessels.)

Right Hand Rule of Thumb: Cephalic, prone, back up
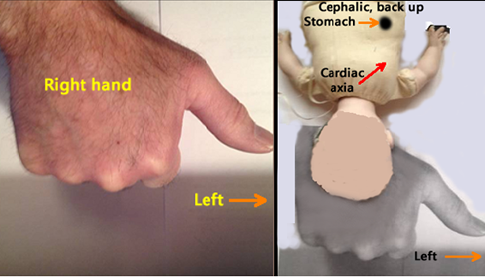
Left. The sonographer’s right hand represents the fetus with the thumb pointing to the fetal left. The top of the hand (dorsal surface or prone position) represents back up.
Right. The imaginary fetus is back up with the stomach and cardiac axis pointing to the fetal left.

Right Hand Rule of Thumb: Breech, supine, back down
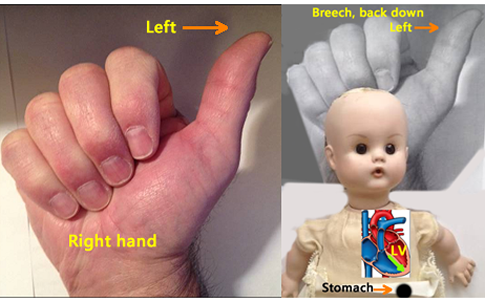
Left. The sonographer’s right hand represents the fetus with the thumb pointing to the fetal left. The palm of the sonographer’s hand is anterior, or represents the ventral surface of the fetus. The fetus is therefore face up, back down, and the thumb points to the fetal left.
Right . The imaginary fetus is back down with the stomach and cardiac axis pointing to the left. (Ignore color scheme of fetal heart and vessels).

Right Hand Rule of Thumb: Breech, prone, back up

Right . The imaginary fetus is back up with the stomach and cardiac axis pointing to the fetal left side.

- Normal CNS Anatomy
- Fetal Situs
- Normal Fetal Ultrasound Biometry
All are web-based courses. Subscribe Today!
- Literature Reviews
- Terms of Use

- Mammary Glands
- Fallopian Tubes
- Supporting Ligaments
- Reproductive System
- Gametogenesis
- Placental Development
- Maternal Adaptations
- Menstrual Cycle
- Antenatal Care
- Small for Gestational Age
- Large for Gestational Age
- RBC Isoimmunisation
- Prematurity
- Prolonged Pregnancy
- Multiple Pregnancy
- Miscarriage
- Recurrent Miscarriage
- Ectopic Pregnancy
- Hyperemesis Gravidarum
- Gestational Trophoblastic Disease
- Breech Presentation
- Abnormal lie, Malpresentation and Malposition
- Oligohydramnios
- Polyhydramnios
- Placenta Praevia
- Placental Abruption
- Pre-Eclampsia
- Gestational Diabetes
- Headaches in Pregnancy
- Haematological
- Obstetric Cholestasis
- Thyroid Disease in Pregnancy
- Epilepsy in Pregnancy
- Induction of Labour
- Operative Vaginal Delivery
- Prelabour Rupture of Membranes
- Caesarean Section
- Shoulder Dystocia
- Cord Prolapse
- Uterine Rupture
- Amniotic Fluid Embolism
- Primary PPH
- Secondary PPH
- Psychiatric Disease
- Postpartum Contraception
- Breastfeeding Problems
- Primary Dysmenorrhoea
- Amenorrhoea and Oligomenorrhoea
- Heavy Menstrual Bleeding
- Endometriosis
- Endometrial Cancer
- Adenomyosis
- Cervical Polyps
- Cervical Ectropion
- Cervical Intraepithelial Neoplasia + Cervical Screening
- Cervical Cancer
- Polycystic Ovary Syndrome (PCOS)
- Ovarian Cysts & Tumours
- Urinary Incontinence
- Genitourinary Prolapses
- Bartholin's Cyst
- Lichen Sclerosus
- Vulval Carcinoma
- Introduction to Infertility
- Female Factor Infertility
- Male Factor Infertility
- Female Genital Mutilation
- Barrier Contraception
- Combined Hormonal
- Progesterone Only Hormonal
- Intrauterine System & Device
- Emergency Contraception
- Pelvic Inflammatory Disease
- Genital Warts
- Genital Herpes
- Trichomonas Vaginalis
- Bacterial Vaginosis
- Vulvovaginal Candidiasis
- Obstetric History
- Gynaecological History
- Sexual History
- Obstetric Examination
- Speculum Examination
- Bimanual Examination
- Amniocentesis
- Chorionic Villus Sampling
- Hysterectomy
- Endometrial Ablation
- Tension-Free Vaginal Tape
- Contraceptive Implant
- Fitting an IUS or IUD
Abnormal Fetal lie, Malpresentation and Malposition
Original Author(s): Anna Mcclune Last updated: 1st December 2018 Revisions: 12
- 1 Definitions
- 2 Risk Factors
- 3.2 Presentation
- 3.3 Position
- 4 Investigations
- 5.1 Abnormal Fetal Lie
- 5.2 Malpresentation
- 5.3 Malposition
The lie, presentation and position of a fetus are important during labour and delivery.
In this article, we will look at the risk factors, examination and management of abnormal fetal lie, malpresentation and malposition.
Definitions
- Longitudinal, transverse or oblique
- Cephalic vertex presentation is the most common and is considered the safest
- Other presentations include breech, shoulder, face and brow
- Usually the fetal head engages in the occipito-anterior position (the fetal occiput facing anteriorly) – this is ideal for birth
- Other positions include occipito-posterior and occipito-transverse.
Note: Breech presentation is the most common malpresentation, and is covered in detail here .
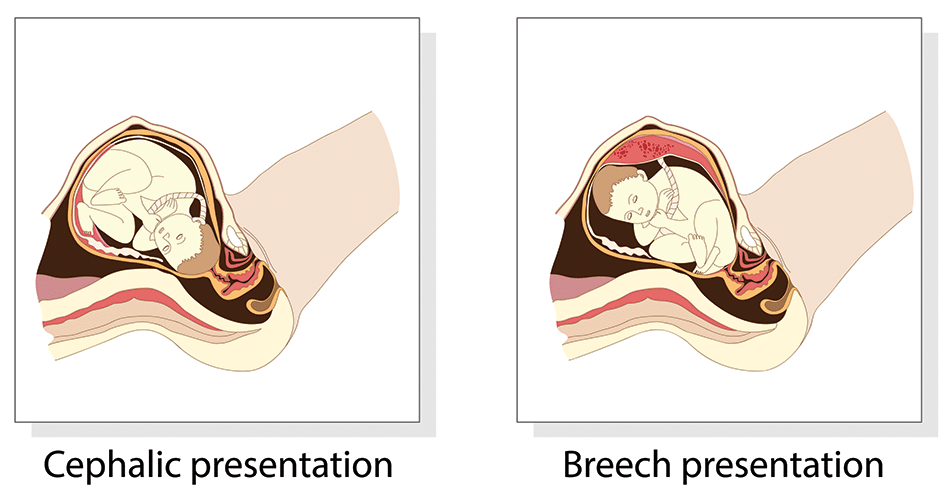
Fig 1 – The two most common fetal presentations: cephalic and breech.
Risk Factors
The risk factors for abnormal fetal lie, malpresentation and malposition include:
- Multiple pregnancy
- Uterine abnormalities (e.g fibroids, partial septate uterus)
- Fetal abnormalities
- Placenta praevia
- Primiparity
Identifying Fetal Lie, Presentation and Position
The fetal lie and presentation can usually be identified via abdominal examination. The fetal position is ascertained by vaginal examination.
For more information on the obstetric examination, see here .
- Face the patient’s head
- Place your hands on either side of the uterus and gently apply pressure; one side will feel fuller and firmer – this is the back, and fetal limbs may feel ‘knobbly’ on the opposite side
Presentation
- Palpate the lower uterus (above the symphysis pubis) with the fingers of both hands; the head feels hard and round (cephalic) and the bottom feels soft and triangular (breech)
- You may be able to gently push the fetal head from side to side
The fetal lie and presentation may not be possible to identify if the mother has a high BMI, if she has not emptied her bladder, if the fetus is small or if there is polyhydramnios .
During labour, vaginal examination is used to assess the position of the fetal head (in a cephalic vertex presentation). The landmarks of the fetal head, including the anterior and posterior fontanelles, indicate the position.
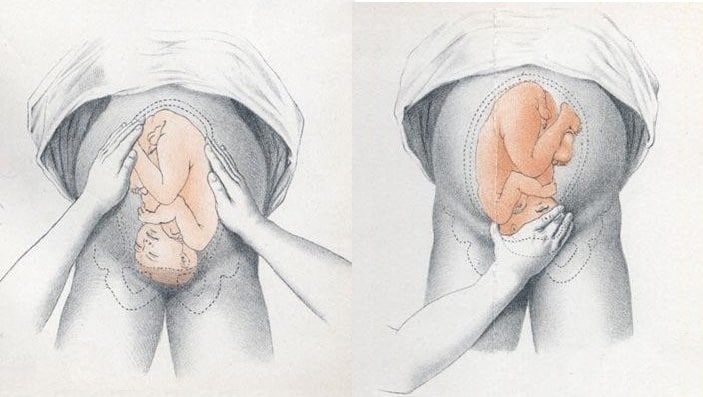
Fig 2 – Assessing fetal lie and presentation.
Investigations
Any suspected abnormal fetal lie or malpresentation should be confirmed by an ultrasound scan . This could also demonstrate predisposing uterine or fetal abnormalities.
Abnormal Fetal Lie
If the fetal lie is abnormal, an external cephalic version (ECV) can be attempted – ideally between 36 and 38 weeks gestation.
ECV is the manipulation of the fetus to a cephalic presentation through the maternal abdomen.
It has an approximate success rate of 50% in primiparous women and 60% in multiparous women. Only 8% of breech presentations will spontaneously revert to cephalic in primiparous women over 36 weeks gestation.
Complications of ECV are rare but include fetal distress , premature rupture of membranes, antepartum haemorrhage (APH) and placental abruption. The risk of an emergency caesarean section (C-section) within 24 hours is around 1 in 200.
ECV is contraindicated in women with a recent APH, ruptured membranes, uterine abnormalities or a previous C-section .
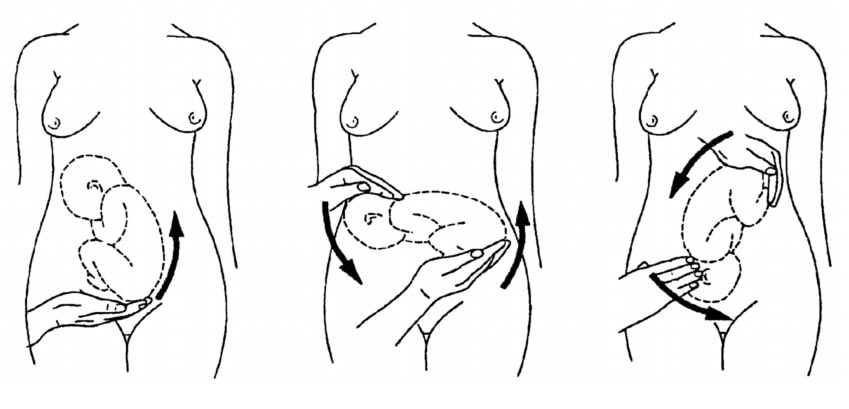
Fig 3 – External cephalic version.

Malpresentation
The management of malpresentation is dependent on the presentation.
- Breech – attempt ECV before labour, vaginal breech delivery or C-section
- Brow – a C-section is necessary
- If the chin is anterior (mento-anterior) a normal labour is possible; however, it is likely to be prolonged and there is an increased risk of a C-section being required
- If the chin is posterior (mento-posterior) then a C-section is necessary
- Shoulder – a C-section is necessary
Malposition
90% of malpositions spontaneously rotate to occipito-anterior as labour progresses. If the fetal head does not rotate, rotation and operative vaginal delivery can be attempted. Alternatively a C-section can be performed.
- Usually the fetal head engages in the occipito-anterior position (the fetal occiput facing anteriorly) - this is ideal for birth
If the fetal lie is abnormal, an external cephalic version (ECV) can be attempted - ideally between 36 and 38 weeks gestation.
- Breech - attempt ECV before labour, vaginal breech delivery or C-section
Found an error? Is our article missing some key information? Make the changes yourself here!
Once you've finished editing, click 'Submit for Review', and your changes will be reviewed by our team before publishing on the site.
We use cookies to improve your experience on our site and to show you relevant advertising. To find out more, read our privacy policy .
Privacy Overview
Enter search terms to find related medical topics, multimedia and more.
Advanced Search:
- Use “ “ for exact phrases.
- For example: “pediatric abdominal pain”
- Use – to remove results with certain keywords.
- For example: abdominal pain -pediatric
- Use OR to account for alternate keywords.
- For example: teenager OR adolescent
Position and Presentation of the Fetus
- IN THIS TOPIC
- AI Generator
63 Fetal Presentation Stock Photos and High-res Pictures
Browse 63 fetal presentation photos and images available, or start a new search to explore more photos and images..
- AI Generator
Search form

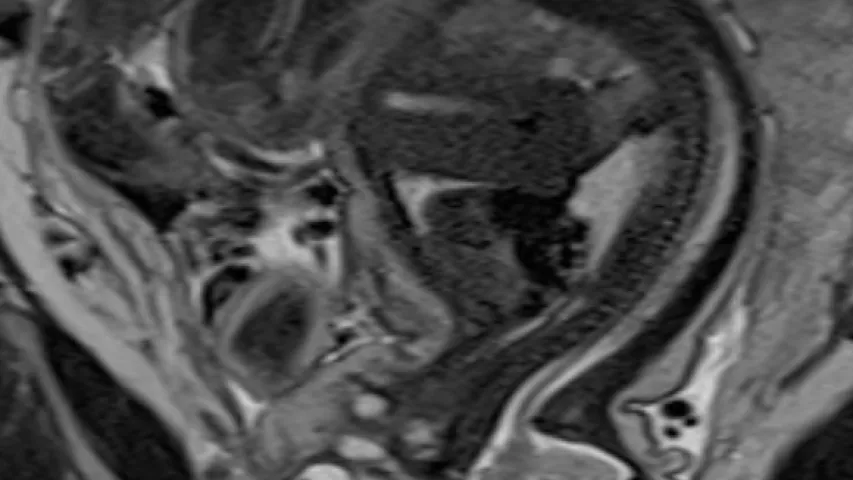
An MRI of a fetus inside the mother. The freakish appearance of the eyes and the face are normal for MRI fetal imaging. Image courtesy of RSNA
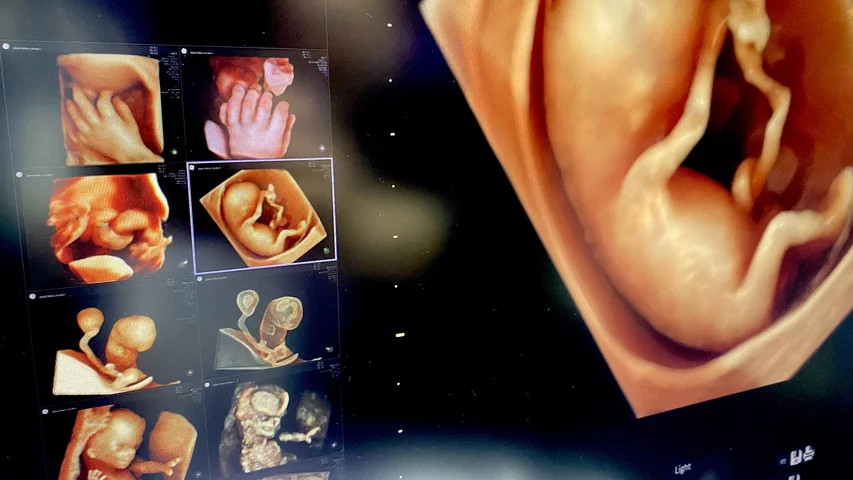
This is a clinical photo gallery of fetal imaging that explains what all can be seen on medical imaging, including baby ultrasound imaging, how to determine the sex of a fetus, fetal echocardiograms, how fetal ultrasound measurements are used to track the development of a baby, and how potential issues with a baby can be diagnosed before birth. It includes examples of fetal ultrasound, the primary imaging modality used during gestation, magnetic resonance imaging (MRI) and some rare images of fetal computed tomography (CT).
Hover over images to see the captions. You also can click on images to enlarge them.

A 3D ultrasound fetal image showing the umbilical cord inside the amniotic sac. Image courtesy of Alpinion.
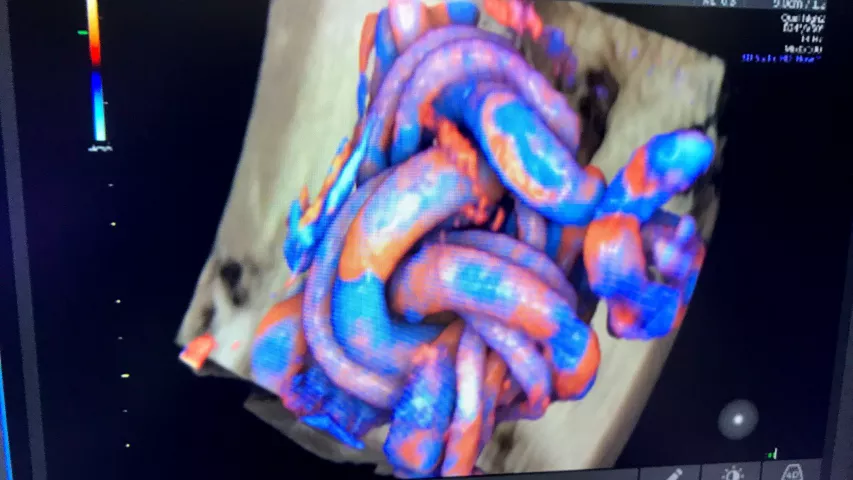
Umbilical cord tied into a knot from fetal movement seen on a 3D/4D ultrasound. The color coding shows the blood flow, which can help determine if the fetus is getting enough oxygen from the mother's blood supply.
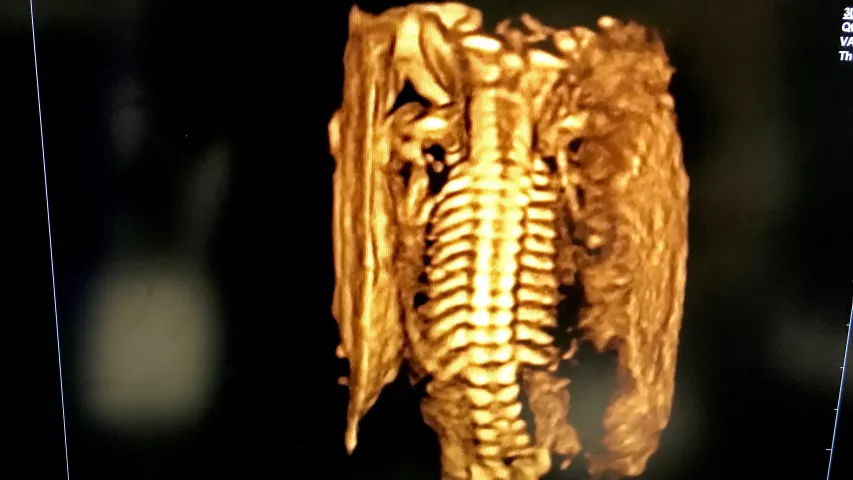
Fetal spine on 3D ultrasound. Image from Alpinion at RSNA 2022.
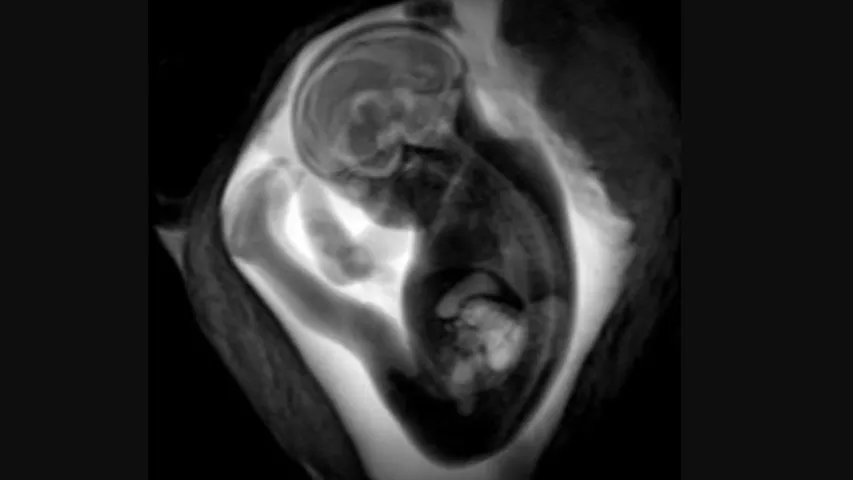
MRI of a fetus inside the mother. Image courtesy of RSNA.

A standard view of a 3D fetal ultrasound exam, where 2D images are shown in the three standard imaging planes, each showing the same anatomy from a different angle, and a rendered 3D volume image. Sonographers and radiologists use the 2D images to make diagnoses and to take measurements. Image courtesy of Konica-Minolta.

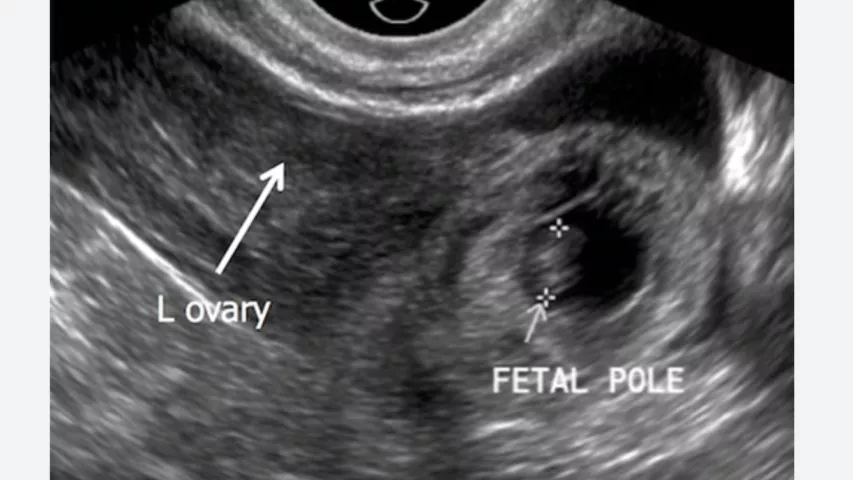
Transvaginal ultrasound of a fetus in early development during the first trimester. Image courtesy of RSNA

A patient undergoing a fetal ultrasound exam.

Fetal 3D ultrasound face shown by the vendor Alpinion. The company also OEMs its technology to some of the bigger vendors on the floor at the large RSNA radiology conference.
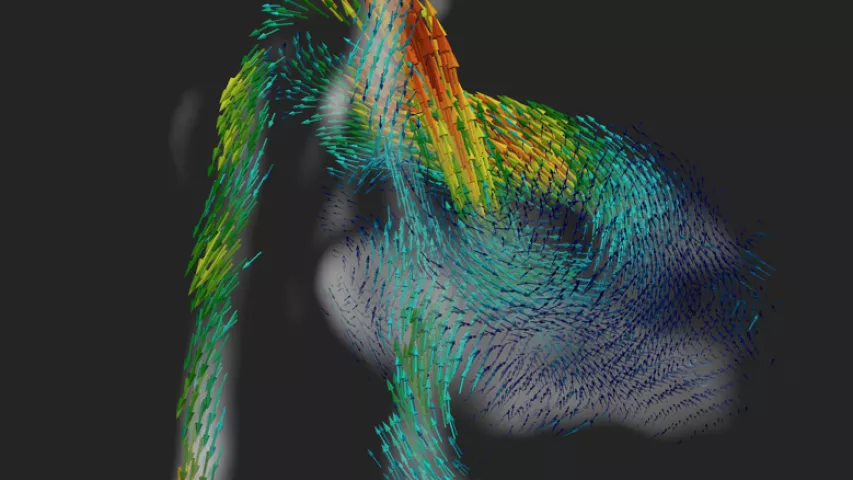
A 4D fetal heart MRI showing the major vessels and blood flow circulation being developed by the School of Biomedical Engineering and Imaging Sciences, Kings College London. With further development, the method could become a new tool for aiding diagnosis of congenital heart disease where conventional methods like ultrasound might fail. Fetal hearts are so small and beat so fast, it is very difficult to capture details. Rather than just getting a snapshot of the heart, a series of images is taken, allowing cardiologists to see the heart contracting and beating. Image courtesy of King’s College London. Read more
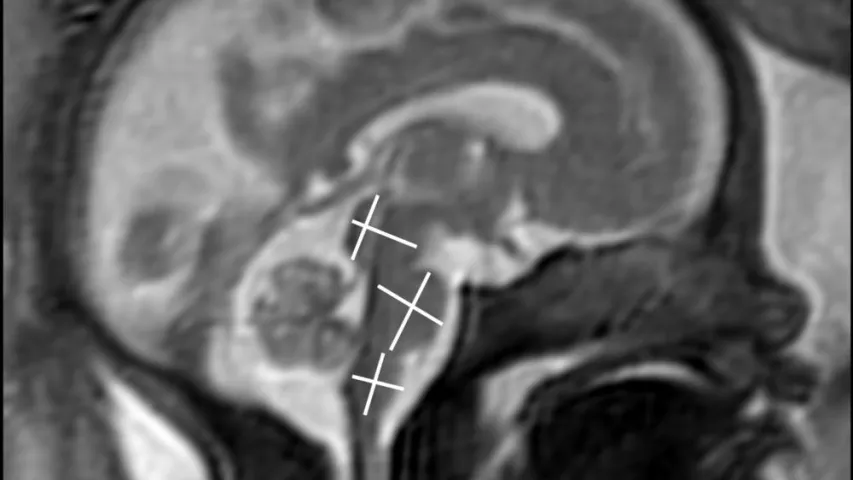
MRI image to assess fetal brain development. Image courtesy of RSNA

Assessment of the left ventricular outflow tract (LVOT) of the heart and aorta to look for congenital heart defect anomalies. A demo image from GE Healthcare at RSNA 2022.
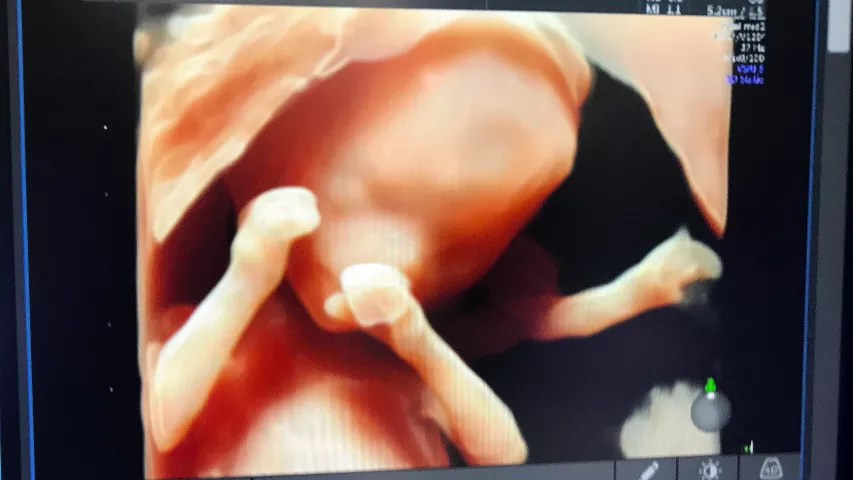
Example of 3D photo-realistic ultrasound technology at RSNA 2022. The simulated lighting source can be moved around to change the locations of the shadows. This makes for great portrait shots for the parents, but also allows physicians to better understand the relationship of anatomical structures if needed during fetal assessments. This is the HDlive rendering technology on the GE Voluson E10 system.

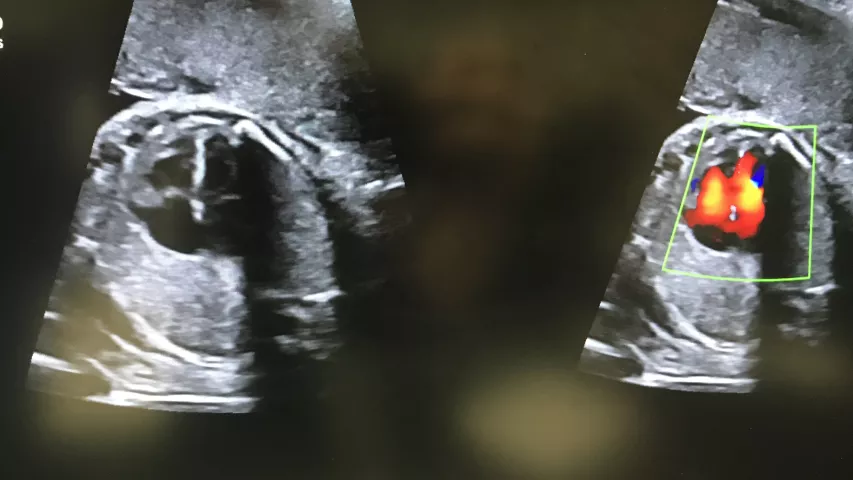
Fetal heart blood flow seen in a Doppler flow 2D ultrasound, showing a regurgitant jet of blood (area of bright yellow) flowing back into a heart chamber due to an issue with a heart valve not sealing properly during systole. This type of assessment can help determine if there are issues with the heart, including congenital heart detects, that will need to be addressed with early surgical interventions after birth. Image courtesy of Alpinion
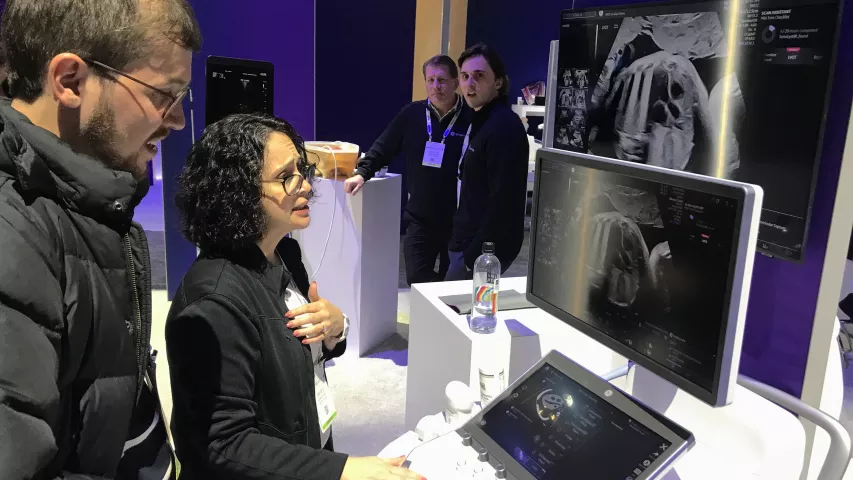
Questions by the sonograpger or radiologist often come up during an exam, especially when there are atypical findings, which often requires a consult with another physician. This is a demonstration at the RSNA 2022 conference for GE Healthcare's Digital Expert technology, showing how users have the ability to interact with peers at various locations to get support before, after, or even during an exam using the GE software. The demo shows a fetal heart and great vessel assessment.

Fetal arm, showing the ulna and radius bones and elbow. Image courtesy of Alpinion
Middle cerebral artery blood flow assessment in the fetal brain. This is used to assess blood flow and fetal hypoxemia. The white oval outline in the images is the fetal skull. Image courtesy of Alpinion.
Example of a fetal head profile on 2D ultrasound. This is a common image shown to the mother during exams because it is easy for most people to identify it as a baby, and it shows the outline of the fetal face with the chin and nose. The top of the screen shows the layers of skin, fat and muscle tissue closest to the ultrasound transducer. The gray layer below is the wall of the uterus. The black areas around the face are the amniotic fluid. The white lines that outline the head is the skull and bone starting to form in the bones that make up the skull under the face. The dark shadows that radiate down below the chin and face are acoustic shadows caused by the sound waves not penetrating the areas of bone. Image from Alpinion.

3D ultrasound of a fetus early in development. Image courtesy of Alpinion.

Example of one of the four standard views used in prenatal ultrasound assessment of the head, imaged from the top of the skull looking down into the brain. This is the posterior fossa or transcerebellar view. It is an axial image of a fetus at about 18 weeks gestation at the level of the thalamus or midbrain.
MRI of a fetus infected with zika virus microcephaly, which causes a smaller head circumference measurement than what is normal and the top of the head looks as if it were pushed down. Image from a zika patient in Brazil, which was the epicenter of the mosquito-borne zika virus outbreak. Image courtesy of RSNA.
MRI of a fetus infected with zika virus microcephaly, which causes a smaller head circumference measurement than what is normal. Image from a zika patient in Brazil, which was at the epicenter of the mosquito-borne zika virus outbreak. Image courtesy of RSNA
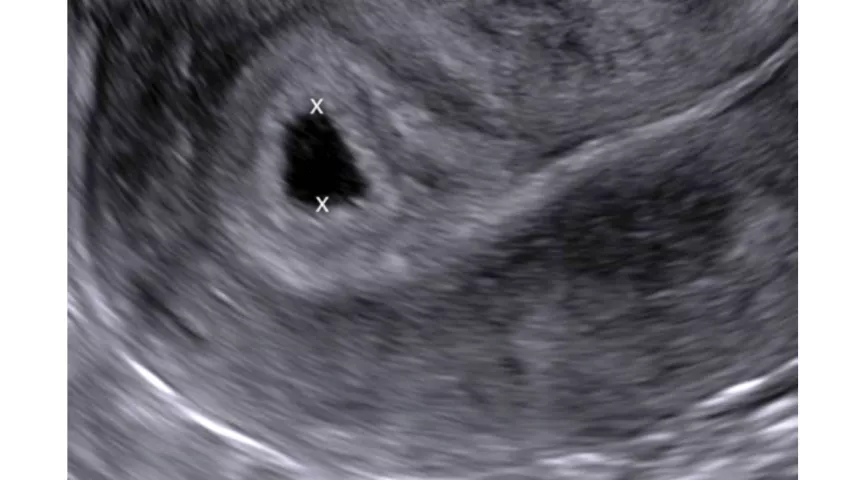
Early first trimester ultrasound measurements are used to calculate the gestational age of the pregnancy. This is the average of orthogonal diameters of the gestational sac, measured from inner border to inner border. An intrauterine sac–like structure without a yolk sac or embryo, as seen in this example, is described as a probable intrauterine pregnancy. Follow-up ultrasound is performed at 14 days, at which time a live embryo should be visible. Images courtesy of RSNA
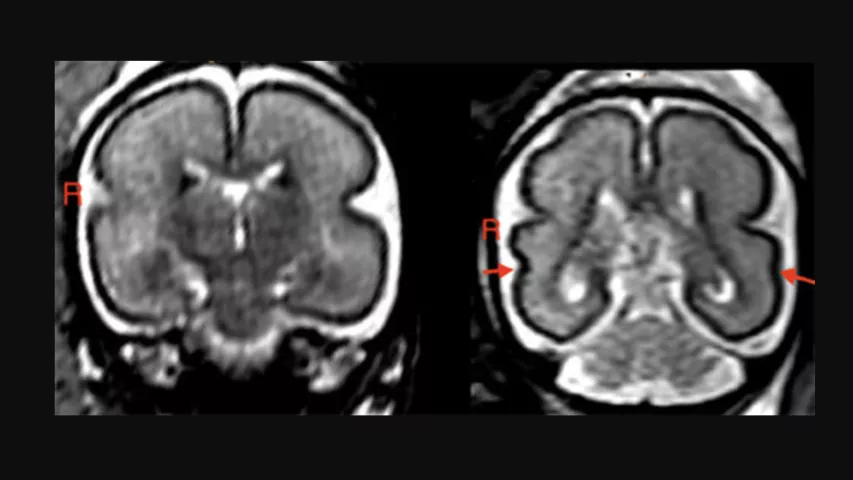
Alcohol consumption during pregnancy can change the unborn baby’s brain structure and delay brain development. Left: Fetal brain post-intrauterine alcohol exposure in fetus between 25 and 29 gestational weeks. Note the smooth cortex in the frontoparietal and temporal lobes. Right: Brain of matched healthy control case in fetus between 25 and 28 gestational weeks. The superior temporal sulcus is already bilaterally formed (red arrows) and appears deeper on the right hemisphere than on the left. Read more about this study.

Fetal hand in a 3D ultrasound. Image courtesy of Hitachi.
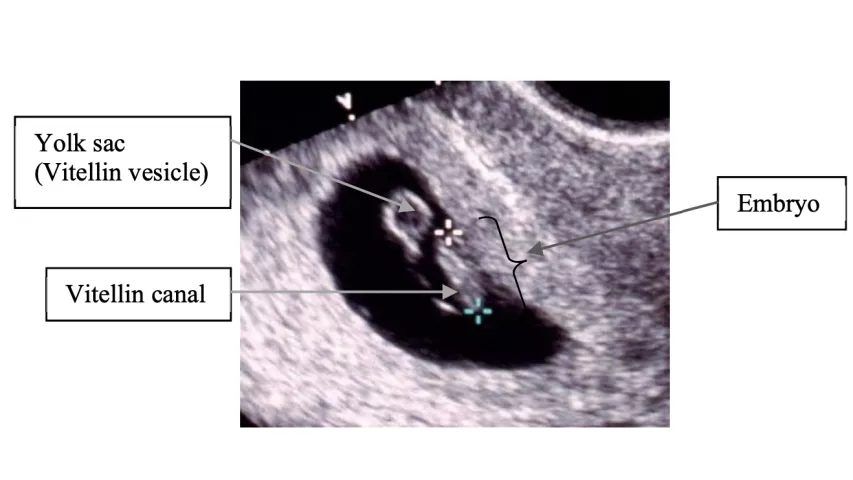
An example of a first trimester transvaginal ultrasound showing the sac and the embryo embedded on the edge of the uterine wall. I mage courtesy of the Department of Global Health, University of Washington .

Third trimester fetal face and cerebral blood flow images with a Hitachi Prosound F37 ultrasound system. Ultrasound of pericallose artery in fetal brain with highly sensitive color mode (DFI). Image courtesy of Hitachi.

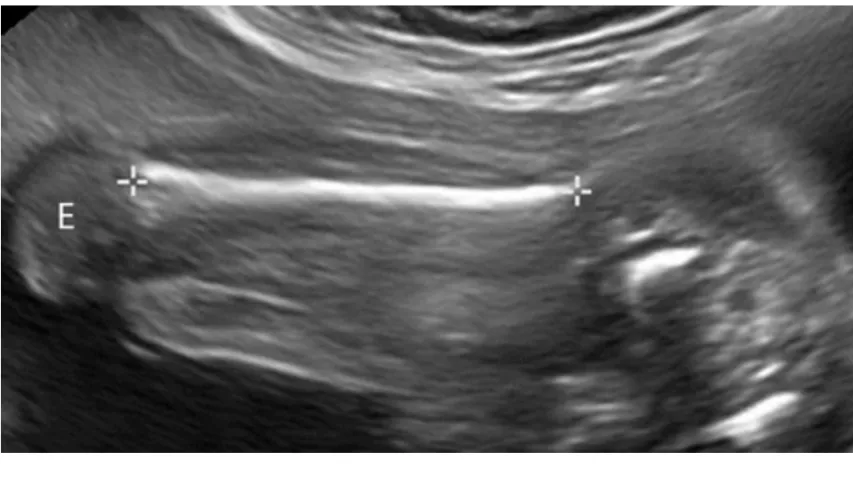
As a pregnancy advances, the embryo is easier to see, and accurate measurements can be obtained with transabdominal ultrasound. This ultrasound shows a crown-rump length (CRL) measurement with calipers. CRL is the average of discrete fetal measurements from the tip of the head end to the tip of the rump end in the midsagittal plane of the embryo. This is highly accurate for pregnancy dating in the first trimester. Images courtesy of RSNA .

Ultrasound scan shows the fetus at the end of the first trimester, by which time the fetus has a recognizable human appearance. The maximal length in the craniocaudal direction is measured in a straight line between the calipers to make a crown-rump length (CRL) measurement. This is highly accurate for pregnancy dating in the first trimester, but other measures are used to assess gentational age later during the pregnancy. Images courtesy of RSNA .
Ultrasound of a femur length measurement in a fetus at 24 weeks gestation. It shows the the epiphysis (E), the end part of the bone that initially grows separately from the shaft, without internal calcification. Bones in the fetus and babies ossifies into solid bone over time, allowing the bones to grow more rapidly. Image courtesy of RSNA .

Ultrasound measurement of kidney length in a 23 week-old fetus. Renal measurements are one of several fetal anatomic structures that demonstrate consistent growth throughout the latter half of gestation, and measurements of these structures reliably correlate with gestational age (GA). This can be important in the second trimester and beyond as a more accurate measure of GA than body length. Image courtesy of RSNA .

Measurement of the fetal head to determine biparietal diameter (BPD), the cross-sectional diameter of the skull, which is also known as the fetal head circumference. Using a BPD index, it is possible to know the growth, weight and size of the fetus before birth. This needs to be measured between 13th and 20th week of pregnancy, because from the 20th week onwards, the index gradually loses its accuracy. Image courtesy of the Department of Global Health, University of Washington .
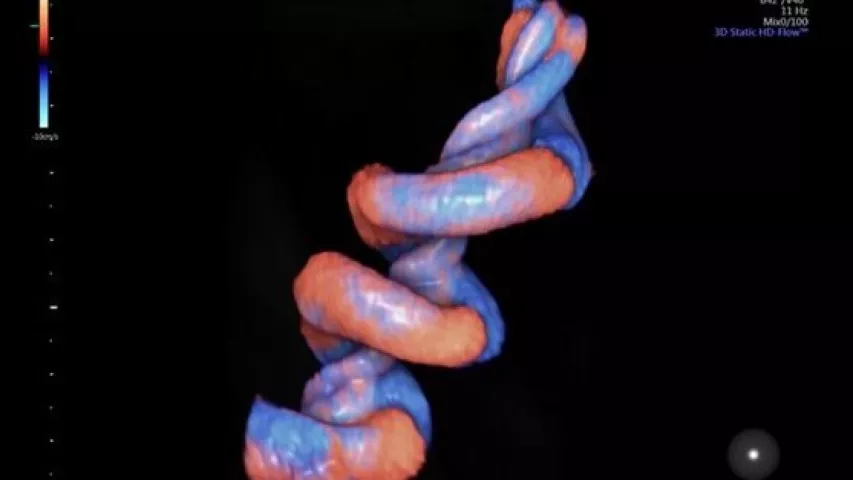
Very detailed view of the umbilical cord in a 3D/4D fetal ultrasound using the GE Healthcare HDlive Flow technology. The color code of the Doppler ultrasound shows blood flowing toward and away from the transducer to enable blood flow assessments.

Twin pregnancy, where the head of the second fetus can be seen on the right side and the rest of its body outside the imaging plane. Image courtesy of the Department of Global Health, University of Washington .
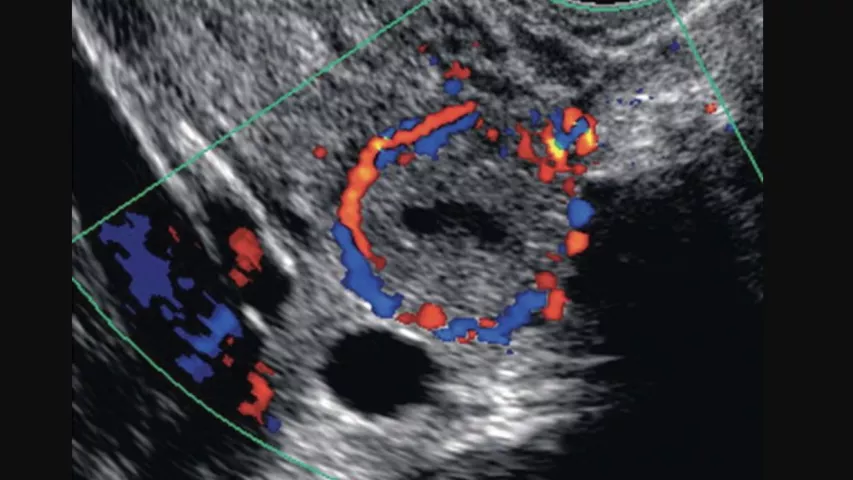
Ectopic pregnancy confirmed by Doppler ultrasound that shows a "ring of fire" sign caused by increased blood flow in a region. Ectopic pregnancy occurs when an embryo begins to develop outside of the uterus and can be dangerous for the mother. Ectopic pregnancies can occur in the fallopian tubes, ovaries and in the peritoneal space of the abdomen. Image courtesy of RSNA .
Ectopic pregnancy in a fallopian tube where the developing embryo can be seen inside the tube on ultrasound. Ectopic pregnancy occurs when an embryo begins to develop outside of the uterus and can be dangerous for the mother. Ectopic pregnancies can occur in the fallopian tubes, ovaries and in the peritoneal space of the abdomen. Image courtesy of RSNA .

A standard four-chamber view of a fetal heart on ultrasound. The heart is examined to look for congenital heart disease (CHD), such as transposed vessels, connections between the chambers and defective heart valves. Image courtesy of RSNA .
A congenital heart defect seen on a fetal ultrasound. The connection between the right and left ventricles has a ventricular septal defect (VSD), which can cause unoxygenated blood to be recirculated through the body. Image courtesy of RSNA .
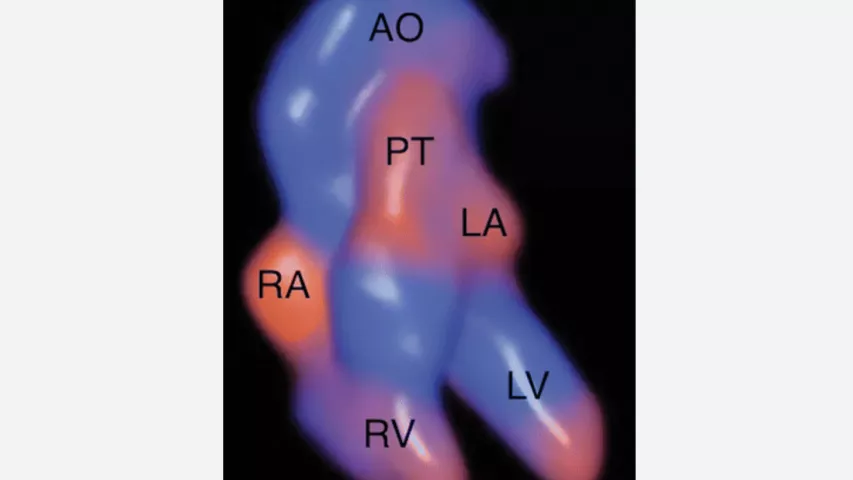
Four-dimensional “Glassbody” rendered image obtained in the Doppler cardiac spatio-temporal image correlation mode, showing the fetal cardiac anatomy at 16 weeks gestation. Retrograde flow is in red, and antegrade flow is in blue. This type of view may help earlier diagnosis of congenital heart disease in fetal imaging. AO = aorta, LA = left atrium, LV = left ventricle, PT = pulmonary trunk, RA = right atrium, RV = right ventricle. Image courtesy of RSNA .

Twins seen in 3D fetal ultrasound. Image from GE Healthcare.
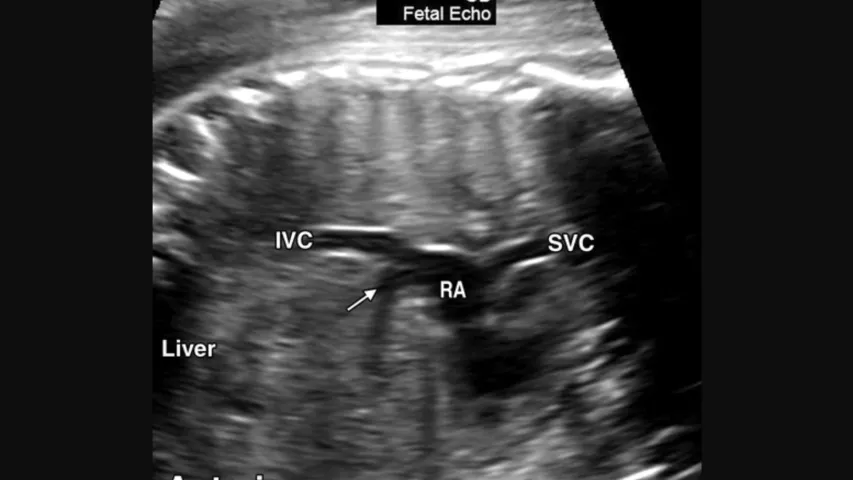
Fetal ultrasound evaluation of the vena cava connection into the right atrium of the heart to check for congenital heart abnormalities that merit referral for further evaluation. A similar evaluation will be performed on the aortic outflow tract of the heart to ensure there is normal anatomy. Image courtesy of RSNA .

Example of a fetal heart contractility assessment ultrasound on the GE Voluson system. It divides fetal ventricles into 24 segments to simultaneously examine the size, shape and contractility of the fetal heart to help diagnose heart issues and congenital heart disease earlier in fetal development. Congenital heart defects affect 1 in 110 babies born around the world. Image from GE Healthcare.
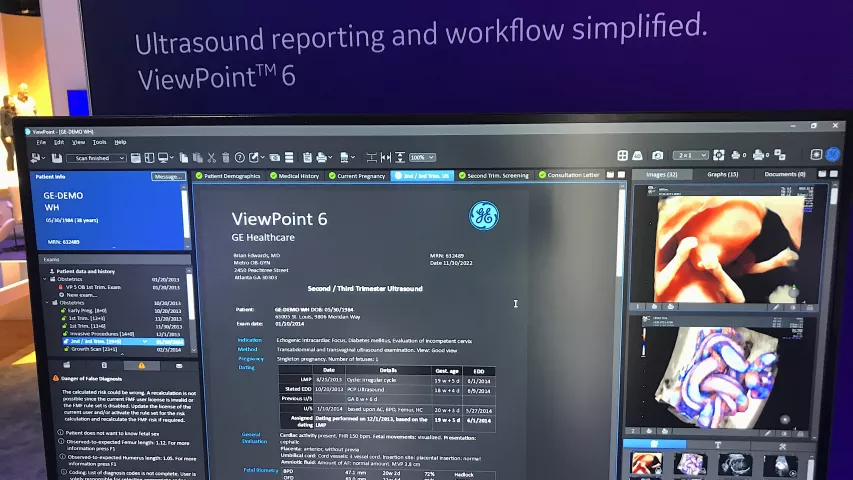
Example of a fetal ultrasound radiology report and the screen the physician sees. It shows the final report, notes in the patient's chart and images from the exam. Image from the GE Healthcare booth at RSNA 2022.

Example of a cleft lip detected deformity on 3D fetal ultrasound. Image courtesy of RSNA .
Twins on fetal ultrasound. Visible are the two heads and one of them has their arm outstretched. Image courtesy of RSNA .

Twins on fetal ultrasound in first trimester. Visible are the separate amniotic sacs, each with an embryo inside. Image courtesy of RSNA .
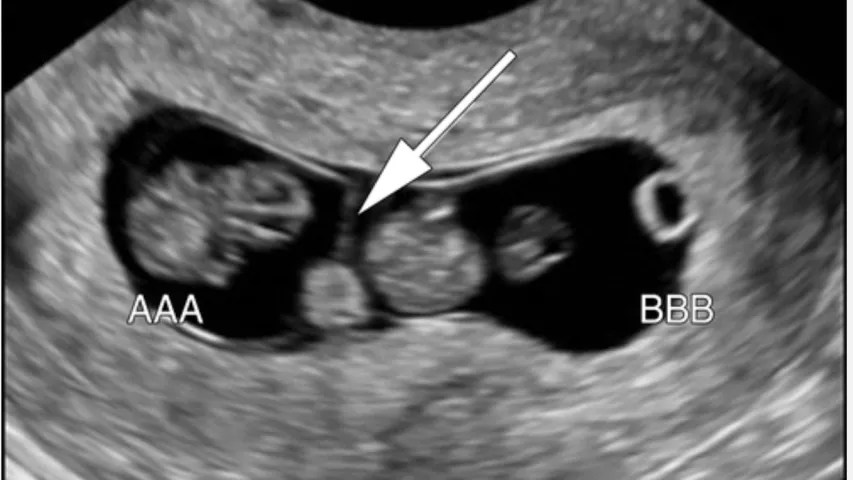
Twins on fetal ultrasound. The arrow points to the line showing the separate of the amniotic sacs. Image courtesy of RSNA .

An MRI of a fetus inside the mother. The freakish appearance of the eyes and the face are normal for MRI fetal exams. Image courtesy of RSNA .

High definition 3D ultrasound of baby face. Image courtesy of Hitachi.

As a fetus develops, sonographers can identify the sex on ultrasound. This is an an example of a female and the "hamburger" sign of the vagina, which looks like the two buns of a hamburger or an equal sign. Males are identified by the "turtle" sign, where the genitalia look like a small turtle, or a turtle's head poking out.
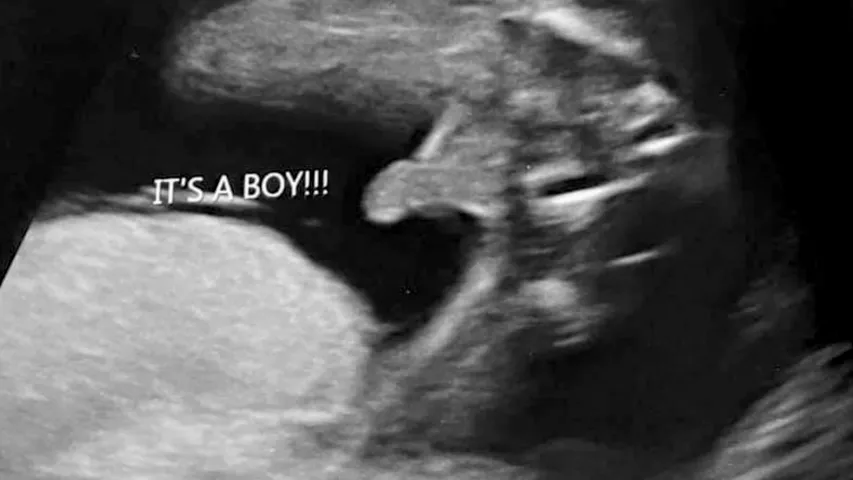
As a fetus develops, sonographers can identify the sex on ultrasound. This is an an example of the "turtle" sign, where the genitalia looks like a small turtle, or a turtle's head poking out. Females can be identifed by the "hamburger" sign of the vagina, which looks like the two buns of a hamburger or an equal sign.

Sagittal computed tomography (CT) of a fetus inside the mother. CT is generally not used on pregnant women unless deemed necessary or in emergencies because of concerns about ionizing radiation dose to the developing fetus. For this reason, CT scans of fetuses are not common and there are usually protocols in place concerning when to image pregnant women with CT. Image courtesy of RSNA .

Axial computed tomography (CT) image of a third-trimester fetus. The patient was referred for CT by the emergency department because of right lower quadrant abdominal pain. Later-term pregnant patients often exceed the display field of view (arrows). The image shows a portion of the mother's hips and bottom of the spine (sacrum) and part of the baby's head and arm. CT is generally not used unless necessary on pregnant women because of concerns about ionizing radiation dose to the developing fetus. Image courtesy of RSNA .
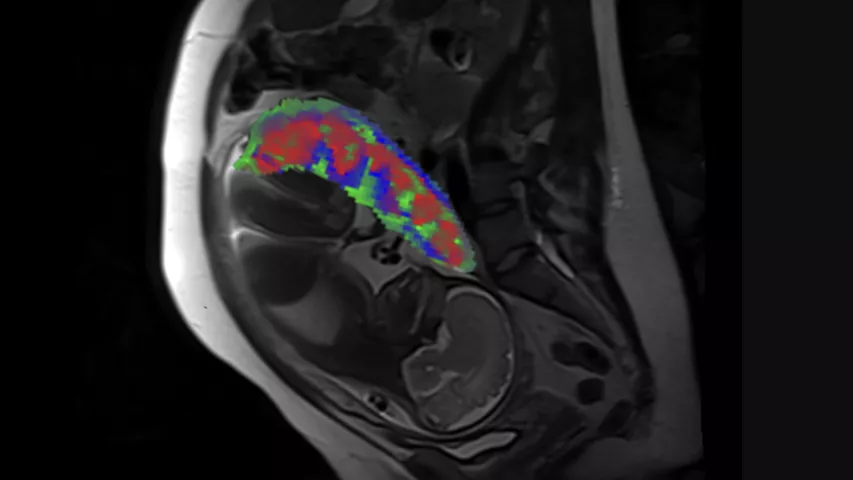
MRI scan showing the fetus and placental compartments—intervillous space (red), placental vessels (green), and placental tissue (blue). Researchers funded by the National Institutes of Health have developed a new method to process MRI scans to reveal the distinct compartments of the placenta, take measurements of oxygen levels in each region and determine if there are malformations in blood vessels (i.e., placental lesions). Obtaining this level of detail is currently not possible using standard MRI analysis methods. Image courtesy Wang Lab, Washington University in St. Louis
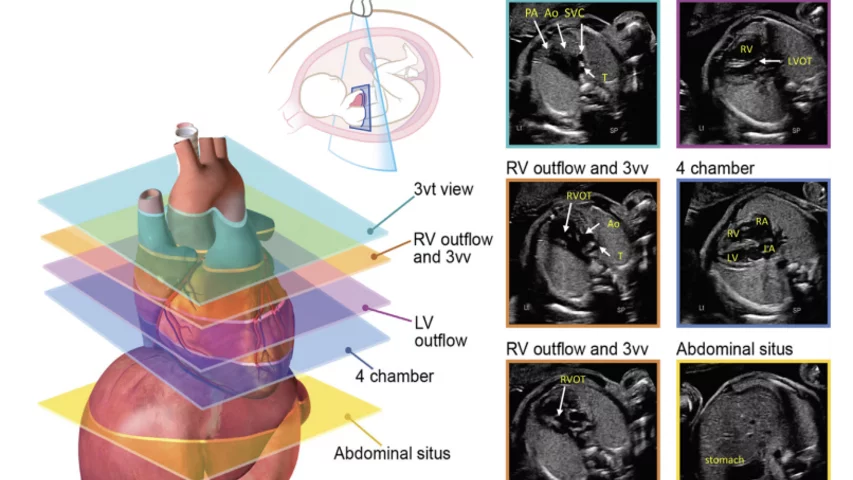
Axial imaging planes are suggested in the 2023 fetal echo guidelines for screening the fetal heart at the time of the obstetric anatomic survey and as an initial series obtained during fetal echocardiography. Read more
3D fetal ultrasound image of a 4-week old fetus images with a GE Voluson Expert 22 system, displayed at RSNA 2023.

Same image as the previous, but with an artificial lighting source that can be moved around the 3D ultrasound this 4-week old fetus images to give a life-like view, using an GE Voluson Expert 22 system. Rotation of the lighting source allows changes in contrast to help physicians better interpret the images.

Fetal umbilical cord hernia. Prenatal diagnosis is important to prevent inadvertent injury to the bowel during cord clamping at the time of delivery. This type of hernia can include a bulging of the intestines outside of the abdomen, but it is covered by the umbilical cord so may not be seen during delivery. This is a rare but important finding on prenatal ultrasounds, so a safe distance to clamp can be determined from the imaging and palpation of the cord during the time of delivery. Imaged using a GE Voluson Expert 22 ultrasound system.

3D ultrasound images of first trimester fetal twins, scanned using a Canon Aplio 500.

A preserved 14-week-old fetus inside the uterus on display as part of a permanent exhibit on the stages of fetal development at the Chicago Museum of Science and Industry. Link to museum's virtual tour. This image helps show correlation with fetal medical imaging. Photo by Dave Fornell.
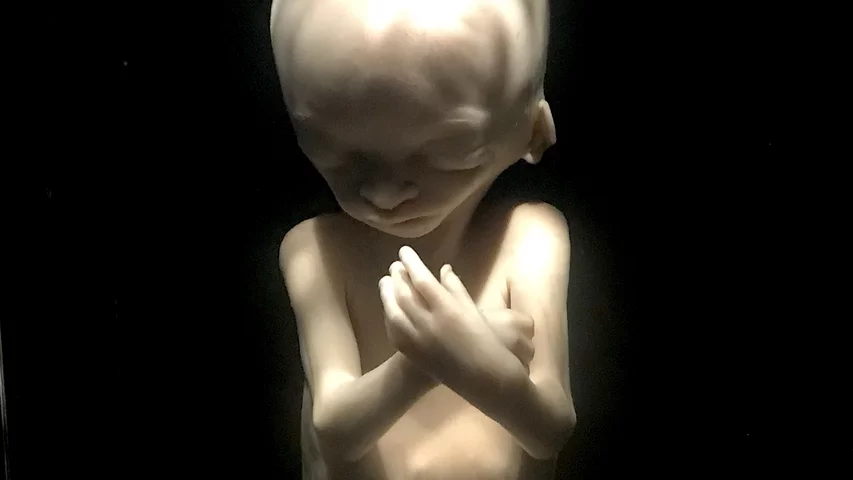
A preserved 18-week-old fetus on display as part of a permanent exhibit on the stages of fetal development at the Chicago Museum of Science and Industry. Link to virtual tour of the exhibit. This image helps show correlation with fetal medical imaging. Photo by Dave Fornell.
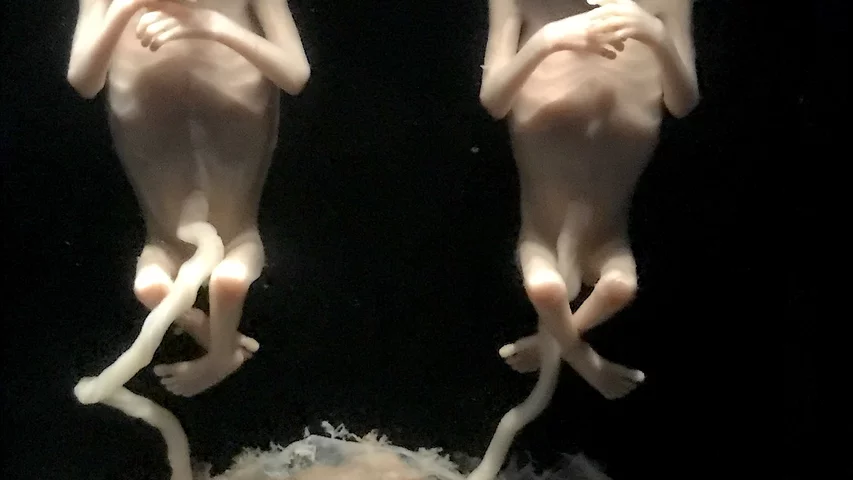
Preserved 13-week-old twin fetuses on display as part of a permanent exhibit on the stages of fetal development at the Chicago Museum of Science and Industry. These two fetuses developed when a single fertilized egg split, but both share the same genes and are identical twins. Link to virtual tour of the exhibit. This image helps show correlation with fetal medical imaging. Photo by Dave Fornell.

Dave Fornell has covered healthcare for more than 17 years, with a focus in cardiology and radiology. Fornell is a 5-time winner of a Jesse H. Neal Award, the most prestigious editorial honors in the field of specialized journalism. The wins included best technical content, best use of social media and best COVID-19 coverage. Fornell was also a three-time Neal finalist for best range of work by a single author. He produces more than 100 editorial videos each year, most of them interviews with key opinion leaders in medicine. He also writes technical articles, covers key trends, conducts video hospital site visits, and is very involved with social media. E-mail: [email protected]
Related Content
- Help & Feedback
- About epocrates
Breech presentation
Highlights & basics, diagnostic approach, risk factors, history & exam, differential diagnosis.
- Tx Approach
Emerging Tx
Complications.
PATIENT RESOURCES
Patient Instructions
Breech presentation refers to the baby presenting for delivery with the buttocks or feet first rather than head.
Associated with increased morbidity and mortality for the mother in terms of emergency cesarean section and placenta previa; and for the baby in terms of preterm birth, small fetal size, congenital anomalies, and perinatal mortality.
Incidence decreases as pregnancy progresses and by term occurs in 3% to 4% of singleton term pregnancies.
Treatment options include external cephalic version to increase the likelihood of vaginal birth or a planned cesarean section, the optimal gestation being 37 and 39 weeks, respectively.
Planned cesarean section is considered the safest form of delivery for infants with a persisting breech presentation at term.
Quick Reference
Key Factors
buttocks or feet as the presenting part
Fetal head under costal margin, fetal heartbeat above the maternal umbilicus.
Other Factors
subcostal tenderness
Pelvic or bladder pain.
Diagnostics Tests
1st Tests to Order
transabdominal/transvaginal ultrasound
Treatment options.
presumptive
<37 weeks' gestation
specialist evaluation
corticosteroid
magnesium sulfate
≥37 weeks' gestation not in labor
unsuccessful ECV with persistent breech
Classifications
Types of breech presentation
Baby's buttocks lead the way into the birth canal
Hips are flexed, knees are extended, and the feet are in close proximity to the head
65% to 70% of breech babies are in this position.
Baby presents with buttocks first
Both the hips and the knees are flexed; the baby may be sitting cross-legged.
One or both of the baby's feet lie below the breech so that the foot or knee is lowermost in the birth canal
This is rare at term but relatively common with premature fetuses.
Common Vignette
Other Presentations
Epidemiology
33% of births less than 28 weeks' gestation
14% of births at 29 to 32 weeks' gestation
9% of births at 33 to 36 weeks' gestation
6% of births at 37 to 40 weeks' gestation.
Pathophysiology
- Natasha Nassar, PhD
- Christine L. Roberts, MBBS, FAFPHM, DrPH
- Jonathan Morris, MBChB, FRANZCOG, PhD
- John W. Bachman, MD
- Rhona Hughes, MBChB
- Brian Peat, MD
- Lelia Duley, MBChB
- Justus Hofmeyr, MD

Clinical exam
Palpation of the abdomen to determine the position of the baby's head
Palpation of the abdomen to confirm the position of the fetal spine on one side and fetal extremities on the other
Palpation of the area above the symphysis pubis to locate the fetal presenting part
Palpation of the presenting part to confirm presentation, to determine how far the fetus has descended and whether the fetus is engaged.
Ultrasound examination
Premature fetus.
Prematurity is consistently associated with breech presentation. [ 6 ] [ 9 ] This may be due to the smaller size of preterm infants, who are more likely to change their in utero position.
Increasing duration of pregnancy may allow breech-presenting fetuses time to grow, turn spontaneously or by external cephalic version, and remain cephalic-presenting.
Larger fetuses may be forced into a cephalic presentation in late pregnancy due to space or alignment constraints within the uterus.
small for gestational age fetus
Low birth-weight is a risk factor for breech presentation. [ 9 ] [ 11 ] [ 12 ] [ 13 ] [ 14 ] Term breech births are associated with a smaller fetal size for gestational age, highlighting the association with low birth-weight rather than prematurity. [ 6 ]
nulliparity
Women having a first birth have increased rates of breech presentation, probably due to the increased likelihood of smaller fetal size. [ 6 ] [ 9 ]
Relaxation of the uterine wall in multiparous women may reduce the odds of breech birth and contribute to a higher spontaneous or external cephalic version rate. [ 10 ]
fetal congenital anomalies
Congenital anomalies in the fetus may result in a small fetal size or inappropriate fetal growth. [ 9 ] [ 12 ] [ 14 ] [ 15 ]
Anencephaly, hydrocephaly, Down syndrome, and fetal neuromuscular dysfunction are associated with breech presentation, the latter due to its effect on the quality of fetal movements. [ 9 ] [ 14 ]
previous breech delivery
The risk of recurrent breech delivery is 8%, the risk increasing from 4% after one breech delivery to 28% after three. [ 16 ]
The effects of recurrence may be due to recurring specific causal factors, either genetic or environmental in origin.
uterine abnormalities
Women with uterine abnormalities have a high incidence of breech presentation. [ 14 ] [ 17 ] [ 18 ] [ 19 ]
female fetus
Fifty-four percent of breech-presenting fetuses are female. [ 14 ]
abnormal amniotic fluid volume
Both oligohydramnios and polyhydramnios are associated with breech presentation. [ 1 ] [ 12 ] [ 14 ]
Low amniotic fluid volume decreases the likelihood of a fetus turning to a cephalic position; an increased amniotic fluid volume may facilitate frequent change in position.
placental abnormalities
An association between placental implantation in the cornual-fundal region and breech presentation has been reported, although some studies have not found it a risk factor. [ 8 ] [ 20 ] [ 21 ] [ 22 ] [ 10 ] [ 14 ]
The association with placenta previa is also inconsistent. [ 8 ] [ 9 ] [ 22 ] Placenta previa is associated with preterm birth and may be an indirect risk factor.
Pelvic or vaginal examination reveals the buttocks and/or feet, felt as a yielding, irregular mass, as the presenting part. [ 26 ] In cephalic presentation, a hard, round, regular fetal head can be palpated. [ 26 ]
The Leopold maneuver on examination suggests breech position by palpation of the fetal head under the costal margin. [ 26 ]
The baby's heartbeat should be auscultated using a Pinard stethoscope or a hand-held Doppler to indicate the position of the fetus. The fetal heartbeat lies above the maternal umbilicus in breech presentation. [ 1 ]
Tenderness under one or other costal margin as a result of pressure by the harder fetal head.
Pain due to fetal kicks in the maternal pelvis or bladder.
breech position
Visualizes the fetus and reveals its position.
Used to confirm a clinically suspected breech presentation. [ 28 ]
Should be performed by practitioners with appropriate skills in obstetric ultrasound.
Establishes the type of breech presentation by imaging the fetal femurs and their relationship to the distal bones.
Transverse lie
Differentiating Signs/Symptoms
Fetus lies horizontally across the uterus with the shoulder as the presenting part.
Similar predisposing factors such as placenta previa, abnormal amniotic fluid volume, and uterine anomalies, although more common in multiparity. [ 1 ] [ 2 ] [ 29 ]
Differentiating Tests
Clinical examination and fetal auscultation may be indicative.
Ultrasound confirms presentation.
Treatment Approach
Breech presentation <37 weeks' gestation.
The UK Royal College of Obstetricians and Gynaecologists (RCOG) recommends that corticosteroids should be offered to women between 24 and 34+6 weeks' gestation, in whom imminent preterm birth is anticipated. Corticosteroids should only be considered after discussion of risks/benefits at 35 to 36+6 weeks. Given within 7 days of preterm birth, corticosteroids may reduce perinatal and neonatal death and respiratory distress syndrome. [ 32 ] The American College of Obstetricians and Gynecologists (ACOG) recommends a single course of corticosteroids for pregnant women between 24 and 33+6 weeks' gestation who are at risk of preterm delivery within 7 days, including those with ruptured membranes and multiple gestations. It may also be considered for pregnant women starting at 23 weeks' gestation who are at risk of preterm delivery within 7 days. A single course of betamethasone is recommended for pregnant women between 34 and 36+6 weeks' gestation at risk of preterm birth within 7 days, and who have not received a previous course of prenatal corticosteroids. Regularly scheduled repeat courses or serial courses (more than two) are not currently recommended. A single repeat course of prenatal corticosteroids should be considered in women who are less than 34 weeks' gestation, who are at risk of preterm delivery within 7 days, and whose prior course of prenatal corticosteroids was administered more than 14 days previously. Rescue course corticosteroids could be provided as early as 7 days from the prior dose, if indicated by the clinical scenario. [ 33 ]
Magnesium sulfate given before anticipated early preterm birth reduces the risk of cerebral palsy in surviving infants. Physicians electing to use magnesium sulfate for fetal neuroprotection should develop specific guidelines regarding inclusion criteria, treatment regimens, and concurrent tocolysis. [ 34 ]
Breech presentation from 37 weeks' gestation, before labor
ECV is the initial treatment for a breech presentation at term when the patient is not in labor. It involves turning a fetus presenting by the breech to a cephalic (head-down) presentation to increase the likelihood of vaginal birth. [ 35 ] [ 36 ] Where available, it should be offered to all women in late pregnancy, by an experienced clinician, in hospitals with facilities for emergency delivery, and no contraindications to the procedure. [ 35 ] There is no upper time limit on the appropriate gestation for ECV, with success reported at 42 weeks.
There is no general consensus on contraindications to ECV. Contraindications include multiple pregnancy (except after delivery of a first twin), ruptured membranes, current or recent (<1 week) vaginal bleeding, rhesus isoimmunization, other indications for cesarean section (e.g., placenta previa or uterine malformation), or abnormal electronic fetal monitoring. [ 35 ] One systematic review of relative contraindications for ECV highlighted that most contraindications do not have clear empirical evidence. Exceptions include placental abruption, severe preeclampsia/HELLP syndrome, or signs of fetal distress (abnormal cardiotocography and/or Doppler flow). [ 36 ]
The procedure involves applying external pressure and firmly pushing or palpating the mother's abdomen to coerce the fetus to somersault (either forward or backward) into a cephalic position. [ 37 ]
The overall ECV success rate varies but, in a large series, 47% of women following an ECV attempt had a cephalic presentation at birth. [ 35 ] [ 38 ] Various factors influence the success rate. One systematic review found ECV success rates to be 68% overall, with the rate significantly higher for women from African countries (89%) compared with women from non-African countries (62%), and higher among multiparous (78%) than nulliparous women (48%). [ 39 ] Overall, the ECV success rates for nulliparous and multiparous non-African women were 43% and 73%, respectively, while for nulliparous and multiparous African women rates were 79% and 91%, respectively. Another study reported no difference in success rate or rate of cesarean section among women with previous cesarean section undergoing ECV compared with women with previous vaginal birth. However, numbers were small and further studies in this regard are required. [ 40 ]
Women's preference for vaginal delivery is a major contributing factor in their decision for ECV. However, studies suggest women with a breech presentation at term may not receive complete and/or evidence-based information about the benefits and risks of ECV. [ 41 ] [ 42 ] Although up to 60% of women reported ECV to be painful, the majority highlighted the benefits outweigh the risks (71%) and would recommend ECV to their friends or be willing to repeat for themselves (84%). [ 41 ] [ 42 ]
Cardiotocography and ultrasound should be performed before and after the procedure. Tocolysis should be used to facilitate the maneuver, and Rho(D) immune globulin should be administered to women who are Rhesus negative. [ 35 ] Tocolytic agents include adrenergic beta-2 receptor stimulants such as albuterol, terbutaline, or ritodrine (widely used with ECV in some countries, but not yet available in the US). One Cochrane review of tocolytic beta stimulants demonstrates that these are less likely to be associated with failed ECV, and are effective in increasing cephalic presentation and reducing cesarean section. [ 43 ] There is no current evidence to recommend one beta-2 adrenergic receptor agonist over another. Until these data are available, adherence to a local protocol for tocolysis is recommended. The Food and Drug Administration has issued a warning against using injectable terbutaline beyond 48 to 72 hours, or acute or prolonged treatment with oral terbutaline, in pregnant women for the prevention or prolonged treatment of preterm labor, due to potential serious maternal cardiac adverse effects and death. [ 44 ] Whether this warning applies to the subcutaneous administration of terbutaline in ECV is still unclear; however, studies currently support this use. The European Medicines Agency (EMA) recommends that injectable beta agonists should be used for up to 48 hours between the 22nd and 37th week of pregnancy only. They should be used under specialist supervision with continuous monitoring of the mother and unborn baby owing to the risk of adverse cardiovascular effects in both the mother and baby. The EMA no longer recommends oral or rectal formulations for obstetric indications. [ 45 ]
If ECV is successful, pregnancy care should continue as usual for any cephalic presentation. One systematic review assessing the mode of delivery after a successful ECV found that these women were at increased risk for cesarean section and instrumental vaginal delivery compared with women with spontaneous cephalic pregnancies. However, they still had a lower rate of cesarean section following ECV (i.e., 47%) compared with the cesarean section rate for those with a persisting breech (i.e., 85%). With a number needed to treat of three, ECV is still considered to be an effective means of preventing the need for cesarean section. [ 46 ]
Planned cesarean section should be offered as the safest mode of delivery for the baby, even though it carries a small increase in serious immediate maternal complications compared with vaginal birth. [ 24 ] [ 25 ] [ 31 ] In the US, most unsuccessful ECV with persistent breech will be delivered via cesarean section.
A vaginal mode of delivery may be considered by some clinicians as an option, particularly when maternal request is provided, senior and experienced staff are available, there is no absolute contraindication to vaginal birth (e.g., placenta previa, compromised fetal condition), and with optimal fetal growth (estimated weight above the tenth centile and up to 3800 g). Other factors that make planned vaginal birth higher risk include hyperextended neck on ultrasound and footling presentation. [ 24 ]
Breech presentation from 37 weeks' gestation, during labor
The first option should be a planned cesarean section.
There is a small increase in the risk of serious immediate maternal complications compared with vaginal birth (RR 1.29, 95% CI 1.03 to 1.61), including pulmonary embolism, infection, bleeding, damage to the bladder and bowel, slower recovery from the delivery, longer hospitalization, and delayed bonding and breast-feeding. [ 23 ] [ 31 ] [ 47 ] [ 48 ] [ 49 ] [ 50 ] [ 51 ] [ 52 ] [ 53 ] [ 54 ] [ 55 ] [ 56 ] [ 57 ] [ 58 ] Consider using antimicrobial triclosan-coated sutures for wound closure to reduce the risk of surgical site infection. [ 59 ]
The long-term risks include potential compromise of future obstetric performance, increased risk of repeat cesarean section, infertility, uterine rupture, placenta accreta, placental abruption, and emergency hysterectomy. [ 60 ] [ 61 ] [ 62 ] [ 63 ]
Planned cesarean section is safer for babies, but is associated with increased neonatal respiratory distress. The risk is reduced when the section is performed at 39 weeks' gestation. [ 64 ] [ 65 ] [ 66 ] For women undergoing a planned cesarean section, RCOG recommends an informed discussion about the potential risks and benefits of a course of prenatal corticosteroids between 37 and 38+6 weeks' gestation. Although prenatal corticosteroids may reduce admission to the neonatal unit for respiratory morbidity, it is uncertain if there is any reduction in respiratory distress syndrome, transient tachypnea of the newborn, or neonatal unit admission overall. In addition, prenatal corticosteroids may result in harm to the neonate, including hypoglycemia and potential developmental delay. [ 32 ] ACOG does not recommend corticosteroids in women >37 weeks' gestation. [ 33 ]
Undiagnosed breech in labor generally results in cesarean section after the onset of labor, higher rates of emergency cesarean section associated with the least favorable maternal outcomes, a greater likelihood of cord prolapse, and other poor infant outcomes. [ 23 ] [ 67 ] [ 49 ] [ 68 ] [ 69 ] [ 70 ] [ 71 ]
This mode of delivery may be considered by some clinicians as an option for women who are in labor, particularly when delivery is imminent. Vaginal breech delivery may also be considered, where suitable, when delivery is not imminent, maternal request is provided, senior and experienced staff are available, there is no absolute contraindication to vaginal birth (e.g., placenta previa, compromised fetal condition), and with optimal fetal growth (estimated weight above the tenth centile and up to 3800 g). Other factors that make planned vaginal birth higher risk include hyperextended neck on ultrasound and footling presentation. [ 24 ]
Findings from one systematic review of 27 observational studies revealed that the absolute risks of perinatal mortality, fetal neurologic morbidity, birth trauma, 5-minute Apgar score <7, and neonatal asphyxia in the planned vaginal delivery group were low at 0.3%, 0.7%, 0.7%, 2.4%, and 3.3%, respectively. However, the relative risks of perinatal mortality and morbidity were 2- to 5-fold higher in the planned vaginal than in the planned cesarean delivery group. Authors recommend ongoing judicious decision-making for vaginal breech delivery for selected singleton, term breech babies. [ 72 ]
ECV may also be considered an option for women with breech presentation in early labor, when delivery is not imminent, provided that the membranes are intact.
A woman presenting with a breech presentation <37 weeks is an area of clinical controversy. Optimal mode of delivery for preterm breech has not been fully evaluated in clinical trials, and the relative risks for the preterm infant and mother remain unclear. In the absence of good evidence, if diagnosis of breech presentation prior to 37 weeks' gestation is made, prematurity and clinical circumstances should determine management and mode of delivery.
Primary Options
12 mg intramuscularly every 24 hours for 2 doses
6 mg intramuscularly every 12 hours for 4 doses
The UK Royal College of Obstetricians and Gynaecologists recommends that corticosteroids should be offered to women between 24 and 34+6 weeks' gestation, in whom imminent preterm birth is anticipated. Corticosteroids should only be considered after discussion of risks/benefits at 35 to 36+6 weeks. Given within 7 days of preterm birth, corticosteroids may reduce perinatal and neonatal death and respiratory distress syndrome. [ 32 ]
The American College of Obstetricians and Gynecologists recommends a single course of corticosteroids for pregnant women between 24 and 33+6 weeks' gestation who are at risk of preterm delivery within 7 days, including those with ruptured membranes and multiple gestations. It may also be considered for pregnant women starting at 23 weeks' gestation who are at risk of preterm delivery within 7 days. A single course of betamethasone is recommended for pregnant women between 34 and 36+6 weeks' gestation at risk of preterm birth within 7 days, and who have not received a previous course of prenatal corticosteroids. Regularly scheduled repeat courses or serial courses (more than two) are not currently recommended. A single repeat course of prenatal corticosteroids should be considered in women who are less than 34 weeks' gestation, who are at risk of preterm delivery within 7 days, and whose prior course of prenatal corticosteroids was administered more than 14 days previously. Rescue course corticosteroids could be provided as early as 7 days from the prior dose, if indicated by the clinical scenario. [ 33 ]
consult specialist for guidance on dose
external cephalic version (ECV)
There is no upper time limit on the appropriate gestation for ECV; it should be offered to all women in late pregnancy by an experienced clinician in hospitals with facilities for emergency delivery and no contraindications to the procedure. [ 35 ] [ 36 ]
ECV involves applying external pressure and firmly pushing or palpating the mother's abdomen to coerce the fetus to somersault (either forward or backward) into a cephalic position. [ 37 ]
There is no general consensus on contraindications to ECV. Contraindications include multiple pregnancy (except after delivery of a first twin), ruptured membranes, current or recent (<1 week) vaginal bleeding, rhesus isoimmunization, other indications for cesarean section (e.g., placenta previa or uterine malformation), or abnormal electronic fetal monitoring. [ 35 ] One systematic review of relative contraindications for ECV highlighted that most contraindications do not have clear empirical evidence. Exceptions include placental abruption, severe preeclampsia/HELLP syndrome, or signs of fetal distress (abnormal cardiotocography and/or Doppler flow). [ 36 ]
Cardiotocography and ultrasound should be performed before and after the procedure.
If ECV is successful, pregnancy care should continue as usual for any cephalic presentation. A systematic review assessing the mode of delivery after a successful ECV found that these women were at increased risk for cesarean section and instrumental vaginal delivery compared with women with spontaneous cephalic pregnancies. However, they still had a lower rate of cesarean section following ECV (i.e., 47%) compared with the cesarean section rate for those with a persisting breech (i.e., 85%). With a number needed to treat of 3, ECV is still considered to be an effective means of preventing the need for cesarean section. [ 46 ]
tocolytic agents
see local specialist protocol for dosing guidelines
Tocolytic agents include adrenergic beta-2 receptor stimulants such as albuterol, terbutaline, or ritodrine (widely used with external cephalic version [ECV] in some countries, but not yet available in the US). They are used to delay or inhibit labor and increase the success rate of ECV. There is no current evidence to recommend one beta-2 adrenergic receptor agonist over another. Until these data are available, adherence to a local protocol for tocolysis is recommended.
The Food and Drug Administration has issued a warning against using injectable terbutaline beyond 48-72 hours, or acute or prolonged treatment with oral terbutaline, in pregnant women for the prevention or prolonged treatment of preterm labor, due to potential serious maternal cardiac adverse effects and death. [ 44 ] Whether this warning applies to the subcutaneous administration of terbutaline in ECV is still unclear; however, studies currently support this use. The European Medicines Agency (EMA) recommends that injectable beta agonists should be used for up to 48 hours between the 22nd and 37th week of pregnancy only. They should be used under specialist supervision with continuous monitoring of the mother and unborn baby owing to the risk of adverse cardiovascular effects in both the mother and baby. The EMA no longer recommends oral or rectal formulations for obstetric indications. [ 45 ]
A systematic review found there was no evidence to support the use of nifedipine for tocolysis. [ 73 ]
There is insufficient evidence to evaluate other interventions to help ECV, such as fetal acoustic stimulation in midline fetal spine positions, or epidural or spinal analgesia. [ 43 ]
Rho(D) immune globulin
300 micrograms intramuscularly as a single dose
Nonsensitized Rh-negative women should receive Rho(D) immune globulin. [ 35 ]
The indication for its administration is to prevent rhesus isoimmunization, which may affect subsequent pregnancy outcomes.
Rho(D) immune globulin needs to be given at the time of external cephalic version and should be given again postpartum to those women who give birth to an Rh-positive baby. [ 74 ]
It is best administered as soon as possible after the procedure, usually within 72 hours.
Dose depends on brand used. Dose given below pertains to most commonly used brands. Consult specialist for further guidance on dose.
elective cesarean section/vaginal breech delivery
Mode of delivery (cesarean section or vaginal breech delivery) should be based on the experience of the attending clinician, hospital policies, maternal request, and the presence or absence of complicating factors. In the US, most unsuccessful external cephalic version (ECV) with persistent breech will be delivered via cesarean section.
Cesarean section, at 39 weeks or greater, has been shown to significantly reduce perinatal mortality and neonatal morbidity compared with vaginal breech delivery (RR 0.33, 95% CI 0.19 to 0.56). [ 31 ] Although safer for these babies, there is a small increase in serious immediate maternal complications compared with vaginal birth (RR 1.29, 95% CI 1.03 to 1.61), as well as long-term risks for future pregnancies, including pulmonary embolism, bleeding, infection, damage to the bladder and bowel, slower recovery from the delivery, longer hospitalization, and delayed bonding and breast-feeding. [ 23 ] [ 31 ] [ 47 ] [ 48 ] [ 49 ] [ 50 ] [ 51 ] [ 52 ] [ 53 ] [ 54 ] [ 55 ] [ 56 ] [ 57 ] [ 58 ] Consider using antimicrobial triclosan-coated sutures for wound closure to reduce the risk of surgical site infection. [ 59 ]
Vaginal delivery may be considered by some clinicians as an option, particularly when maternal request is provided, when senior and experienced staff are available, when there is no absolute contraindication to vaginal birth (e.g., placenta previa, compromised fetal condition), and with optimal fetal growth (estimated weight above the tenth centile and up to 3800 g). Other factors that make planned vaginal birth higher risk include hyperextended neck on ultrasound and footling presentation. [ 24 ]
For women undergoing a planned cesarean section, the UK Royal College of Obstetricians and Gynaecologists recommends an informed discussion about the potential risks and benefits of a course of prenatal corticosteroids between 37 and 38+6 weeks' gestation. Although prenatal corticosteroids may reduce admission to the neonatal unit for respiratory morbidity, it is uncertain if there is any reduction in respiratory distress syndrome, transient tachypnea of the newborn, or neonatal unit admission overall. In addition, prenatal corticosteroids may result in harm to the neonate, including hypoglycemia and potential developmental delay. [ 32 ] The American College of Obstetricians and Gynecologists does not recommend corticosteroids in women >37 weeks' gestation. [ 33 ]
It is best administered as soon as possible after delivery, usually within 72 hours.
Administration of postpartum Rho (D) immune globulin should not be affected by previous routine prenatal prophylaxis or previous administration for a potentially sensitizing event. [ 74 ]
≥37 weeks' gestation in labor: no imminent delivery
planned cesarean section
For women with breech presentation in labor, planned cesarean section at 39 weeks or greater has been shown to significantly reduce perinatal mortality and neonatal morbidity compared with vaginal breech delivery (RR 0.33, 95% CI 0.19 to 0.56). [ 31 ]
Although safer for these babies, there is a small increase in serious immediate maternal complications compared with vaginal birth (RR 1.29, 95% CI 1.03 to 1.61), as well as long-term risks for future pregnancies, including pulmonary embolism, infection, bleeding, damage to the bladder and bowel, slower recovery from the delivery, longer hospitalization, and delayed bonding and breast-feeding. [ 23 ] [ 31 ] [ 47 ] [ 48 ] [ 49 ] [ 50 ] [ 51 ] [ 52 ] [ 53 ] [ 54 ] [ 55 ] [ 56 ] [ 57 ] [ 58 ] Consider using antimicrobial triclosan-coated sutures for wound closure to reduce the risk of surgical site infection. [ 59 ]
Continuous cardiotocography monitoring should continue until delivery. [ 24 ] [ 25 ]
vaginal breech delivery
Mode of delivery (cesarean section or vaginal breech delivery) should be based on the experience of the attending clinician, hospital policies, maternal request, and the presence or absence of complicating factors.
This mode of delivery may be considered by some clinicians as an option, particularly when maternal request is provided, when senior and experienced staff are available, when there is no absolute contraindication to vaginal birth (e.g., placenta previa, compromised fetal condition), and with optimal fetal growth (estimated weight above the tenth centile and up to 3800 g). Other factors that make planned vaginal birth higher risk include hyperextended neck on ultrasound and footling presentation. [ 24 ]
For women with persisting breech presentation, planned cesarean section has, however, been shown to significantly reduce perinatal mortality and neonatal morbidity compared with vaginal breech delivery (RR 0.33, 95% CI 0.19 to 0.56). [ 31 ]
ECV may also be considered an option for women with breech presentation in early labor, provided that the membranes are intact.
There is no upper time limit on the appropriate gestation for ECV. [ 35 ]
Involves applying external pressure and firmly pushing or palpating the mother's abdomen to coerce the fetus to somersault (either forward or backward) into a cephalic position. [ 37 ]
Relative contraindications include placental abruption, severe preeclampsia/HELLP syndrome, and signs of fetal distress (abnormal cardiotocography and/or abnormal Doppler flow). [ 35 ] [ 36 ]
Rho(D) immune globulin needs to be given at the time of ECV and should be given again postpartum to those women who give birth to an Rh-positive baby. [ 74 ]
≥37 weeks' gestation in labor: imminent delivery
cesarean section
For women with persistent breech presentation, planned cesarean section has been shown to significantly reduce perinatal mortality and neonatal morbidity compared with vaginal breech delivery (RR 0.33, 95% CI 0.19 to 0.56). [ 31 ] Although safer for these babies, there is a small increase in serious immediate maternal complications compared with vaginal birth (RR 1.29, 95% CI 1.03 to 1.61), as well as long-term risks for future pregnancies, including pulmonary embolism, infection, bleeding, damage to the bladder and bowel, slower recovery from the delivery, longer hospitalization, and delayed bonding and breast-feeding. [ 23 ] [ 31 ] [ 47 ] [ 48 ] [ 49 ] [ 50 ] [ 51 ] [ 52 ] [ 53 ] [ 54 ] [ 55 ] [ 56 ] [ 57 ] [ 58 ] Consider using antimicrobial triclosan-coated sutures for wound closure to reduce the risk of surgical site infection. [ 59 ]
This mode of delivery may be considered by some clinicians as an option, particularly when delivery is imminent, maternal request is provided, when senior and experienced staff are available, when there is no absolute contraindication to vaginal birth (e.g., placenta previa, compromised fetal condition), and with optimal fetal growth (estimated weight above the tenth centile and up to 3800 g). Other factors that make planned vaginal birth higher risk include hyperextended neck on ultrasound and footling presentation. [ 24 ]
It is best administered as soon as possible after the delivery, usually within 72 hours.
External cephalic version before term
Moxibustion, postural management, follow-up overview, perinatal complications.
Compared with cephalic presentation, persistent breech presentation has increased frequency of cord prolapse, abruptio placentae, prelabor rupture of membranes, perinatal mortality, fetal distress (heart rate <100 bpm), preterm delivery, lower fetal weight. [ 10 ] [ 11 ] [ 67 ]
complications of cesarean section
There is a small increase in the risk of serious immediate maternal complications compared with vaginal birth (RR 1.29, 95% CI 1.03 to 1.61), including pulmonary embolism, infection, bleeding, damage to the bladder and bowel, slower recovery from the delivery, longer hospitalization, and delayed bonding and breast-feeding. [ 23 ] [ 31 ] [ 47 ] [ 48 ] [ 49 ] [ 50 ] [ 51 ] [ 52 ] [ 53 ] [ 54 ] [ 55 ] [ 56 ] [ 57 ] [ 58 ]
The long-term risks include potential compromise of future obstetric performance, increased risk of repeat cesarean section, infertility, uterine rupture, placenta accreta, placental abruption, and emergency hysterectomy. [ 60 ] [ 61 ] [ 62 ] [ 63 ] The evidence suggests that using sutures, rather than staples, for wound closure after cesarean section reduces the incidence of wound dehiscence. [ 59 ]
Emergency cesarean section, compared with planned cesarean section, has demonstrated a higher risk of severe obstetric morbidity, intra-operative complications, postoperative complications, infection, blood loss >1500 mL, fever, pain, tiredness, and breast-feeding problems. [ 23 ] [ 48 ] [ 50 ] [ 70 ] [ 81 ]
Key Articles
Impey LWM, Murphy DJ, Griffiths M, et al; Royal College of Obstetricians and Gynaecologists. Management of breech presentation: green-top guideline no. 20b. BJOG. 2017 Jun;124(7):e151-77. [Full Text]
Hofmeyr GJ, Hannah M, Lawrie TA. Planned caesarean section for term breech delivery. Cochrane Database Syst Rev. 2015 Jul 21;(7):CD000166. [Abstract] [Full Text]
Royal College of Obstetricians and Gynaecologists. External cephalic version and reducing the incidence of term breech presentation. March 2017 [internet publication]. [Full Text]
Cluver C, Gyte GM, Sinclair M, et al. Interventions for helping to turn term breech babies to head first presentation when using external cephalic version. Cochrane Database Syst Rev. 2015 Feb 9;(2):CD000184. [Abstract] [Full Text]
de Hundt M, Velzel J, de Groot CJ, et al. Mode of delivery after successful external cephalic version: a systematic review and meta-analysis. Obstet Gynecol. 2014 Jun;123(6):1327-34. [Abstract]
Referenced Articles
1. Cunningham F, Gant N, Leveno K, et al. Williams obstetrics. 21st ed. New York: McGraw-Hill; 1997.
2. Kish K, Collea JV. Malpresentation and cord prolapse. In: DeCherney AH, Nathan L, eds. Current obstetric and gynecologic diagnosis and treatment. New York: McGraw-Hill Professional; 2002.
3. Scheer K, Nubar J. Variation of fetal presentation with gestational age. Am J Obstet Gynecol. 1976 May 15;125(2):269-70. [Abstract]
4. Nassar N, Roberts CL, Cameron CA, et al. Diagnostic accuracy of clinical examination for detection of non-cephalic presentation in late pregnancy: cross sectional analytic study. BMJ. 2006 Sep 16;333(7568):578-80. [Abstract] [Full Text]
5. Roberts CL, Peat B, Algert CS, et al. Term breech birth in New South Wales, 1990-1997. Aust N Z J Obstet Gynaecol. 2000 Feb;40(1):23-9. [Abstract]
6. Roberts CL, Algert CS, Peat B, et al. Small fetal size: a risk factor for breech birth at term. Int J Gynaecol Obstet. 1999 Oct;67(1):1-8. [Abstract]
7. Brar HS, Platt LD, DeVore GR, et al. Fetal umbilical velocimetry for the surveillance of pregnancies complicated by placenta previa. J Reprod Med. 1988 Sep;33(9):741-4. [Abstract]
8. Kian L. The role of the placental site in the aetiology of breech presentation. J Obstet Gynaecol Br Commonw. 1963 Oct;70:795-7. [Abstract]
9. Rayl J, Gibson PJ, Hickok DE. A population-based case-control study of risk factors for breech presentation. Am J Obstet Gynecol. 1996 Jan;174(1 Pt 1):28-32. [Abstract]
10. Westgren M, Edvall H, Nordstrom L, et al. Spontaneous cephalic version of breech presentation in the last trimester. Br J Obstet Gynaecol. 1985 Jan;92(1):19-22. [Abstract]
11. Brenner WE, Bruce RD, Hendricks CH. The characteristics and perils of breech presentation. Am J Obstet Gynecol. 1974 Mar 1;118(5):700-12. [Abstract]
12. Hall JE, Kohl S. Breech presentation. Am J Obstet Gynecol. 1956 Nov;72(5):977-90. [Abstract]
13. Morgan HS, Kane SH. An analysis of 16,327 breech births. JAMA. 1964 Jan 25;187:262-4. [Abstract]
14. Luterkort M, Persson P, Weldner B. Maternal and fetal factors in breech presentation. Obstet Gynecol. 1984 Jul;64(1):55-9. [Abstract]
15. Braun FH, Jones KL, Smith DW. Breech presentation as an indicator of fetal abnormality. J Pediatr. 1975 Mar;86(3):419-21. [Abstract]
16. Albrechtsen S, Rasmussen S, Dalaker K, et al. Reproductive career after breech presentation: subsequent pregnancy rates, interpregnancy interval, and recurrence. Obstet Gynecol. 1998 Sep;92(3):345-50. [Abstract]
17. Zlopasa G, Skrablin S, Kalafatić D, et al. Uterine anomalies and pregnancy outcome following resectoscope metroplasty. Int J Gynaecol Obstet. 2007 Aug;98(2):129-33. [Abstract]
18. Acién P. Breech presentation in Spain, 1992: a collaborative study. Eur J Obstet Gynecol Reprod Biol. 1995 Sep;62(1):19-24. [Abstract]
19. Michalas SP. Outcome of pregnancy in women with uterine malformation: evaluation of 62 cases. Int J Gynaecol Obstet. 1991 Jul;35(3):215-9. [Abstract]
20. Fianu S, Vaclavinkova V. The site of placental attachment as a factor in the aetiology of breech presentation. Acta Obstet Gynecol Scand. 1978;57(4):371-2. [Abstract]
21. Haruyama Y. Placental implantation as the cause of breech presentation [in Japanese]. Nihon Sanka Fujinka Gakkai Zasshi. 1987 Jan;39(1):92-8. [Abstract]
22. Filipov E, Borisov I, Kolarov G. Placental location and its influence on the position of the fetus in the uterus [in Bulgarian]. Akush Ginekol (Sofiia). 2000;40(4):11-2. [Abstract]
23. Waterstone M, Bewley S, Wolfe C. Incidence and predictors of severe obstetric morbidity: case-control study. BMJ. 2001 May 5;322(7294):1089-93. [Abstract] [Full Text]
24. Impey LWM, Murphy DJ, Griffiths M, et al; Royal College of Obstetricians and Gynaecologists. Management of breech presentation: green-top guideline no. 20b. BJOG. 2017 Jun;124(7):e151-77. [Full Text]
25. American College of Obstetricians and Gynecologists Committee on Obstetric Practice. ACOG committee opinion no. 745: mode of term singleton breech delivery. Obstet Gynecol. 2018 Aug;132(2):e60-3. [Abstract] [Full Text]
26. Beischer NA, Mackay EV, Colditz P, eds. Obstetrics and the newborn: an illustrated textbook. 3rd ed. London: W.B. Saunders; 1997.
27. Royal College of Obstetricians and Gynaecologists. Antepartum haemorrhage: green-top guideline no. 63. November 2011 [internet publication]. [Full Text]
28. American College of Obstetricians and Gynecologists. Practice bulletin no. 175: ultrasound in pregnancy. Obstet Gynecol. 2016 Dec;128(6):e241-56. [Abstract]
29. Enkin M, Keirse MJNC, Neilson J, et al. Guide to effective care in pregnancy and childbirth. 3rd ed. Oxford: Oxford University Press; 2000.
30. Hofmeyr GJ, Kulier R, West HM. External cephalic version for breech presentation at term. Cochrane Database Syst Rev. 2012 Oct 17;(10):CD000083. [Abstract] [Full Text]
31. Hofmeyr GJ, Hannah M, Lawrie TA. Planned caesarean section for term breech delivery. Cochrane Database Syst Rev. 2015 Jul 21;(7):CD000166. [Abstract] [Full Text]
32. Stock SJ, Thomson AJ, Papworth S, et al. Antenatal corticosteroids to reduce neonatal morbidity and mortality: Green-top Guideline No. 74. BJOG. 2022 Jul;129(8):e35-60. [Abstract] [Full Text]
33. American College of Obstetricians and Gynaecologists Committee on Obstetric Practice. Committee opinion no. 713: antenatal corticosteroid therapy for fetal maturation. August 2017 (reaffirmed 2020) [internet publication]. [Full Text]
34. American College of Obstetricians and Gynecologists Committee on Obstetric Practice. Committee opinion no. 455: magnesium sulfate before anticipated preterm birth for neuroprotection. March 2010 (reaffirmed 2020) [internet publication]. [Full Text]
35. Royal College of Obstetricians and Gynaecologists. External cephalic version and reducing the incidence of term breech presentation. March 2017 [internet publication]. [Full Text]
36. Rosman AN, Guijt A, Vlemmix F, et al. Contraindications for external cephalic version in breech position at term: a systematic review. Acta Obstet Gynecol Scand. 2013 Feb;92(2):137-42. [Abstract]
37. Hofmeyr GJ. Effect of external cephalic version in late pregnancy on breech presentation and caesarean section rate: a controlled trial. Br J Obstet Gynaecol. 1983 May;90(5):392-9. [Abstract]
38. Beuckens A, Rijnders M, Verburgt-Doeleman GH, et al. An observational study of the success and complications of 2546 external cephalic versions in low-risk pregnant women performed by trained midwives. BJOG. 2016 Feb;123(3):415-23. [Abstract]
39. Nassar N, Roberts CL, Barratt A, et al. Systematic review of adverse outcomes of external cephalic version and persisting breech presentation at term. Paediatr Perinat Epidemiol. 2006 Mar;20(2):163-71. [Abstract]
40. Sela HY, Fiegenberg T, Ben-Meir A, et al. Safety and efficacy of external cephalic version for women with a previous cesarean delivery. Eur J Obstet Gynecol Reprod Biol. 2009 Feb;142(2):111-4. [Abstract]
41. Pichon M, Guittier MJ, Irion O, et al. External cephalic version in case of persisting breech presentation at term: motivations and women's experience of the intervention [in French]. Gynecol Obstet Fertil. 2013 Jul-Aug;41(7-8):427-32. [Abstract]
42. Nassar N, Roberts CL, Raynes-Greenow CH, et al. Evaluation of a decision aid for women with breech presentation at term: a randomised controlled trial [ISRCTN14570598]. BJOG. 2007 Mar;114(3):325-33. [Abstract] [Full Text]
43. Cluver C, Gyte GM, Sinclair M, et al. Interventions for helping to turn term breech babies to head first presentation when using external cephalic version. Cochrane Database Syst Rev. 2015 Feb 9;(2):CD000184. [Abstract] [Full Text]
44. US Food & Drug Administration. FDA Drug Safety Communication: new warnings against use of terbutaline to treat preterm labor. Feb 2011 [internet publication]. [Full Text]
45. European Medicines Agency. Restrictions on use of short-acting beta-agonists in obstetric indications - CMDh endorses PRAC recommendations. October 2013 [internet publication]. [Full Text]
46. de Hundt M, Velzel J, de Groot CJ, et al. Mode of delivery after successful external cephalic version: a systematic review and meta-analysis. Obstet Gynecol. 2014 Jun;123(6):1327-34. [Abstract]
47. Lydon-Rochelle M, Holt VL, Martin DP, et al. Association between method of delivery and maternal rehospitalisation. JAMA. 2000 May 10;283(18):2411-6. [Abstract]
48. Yokoe DS, Christiansen CL, Johnson R, et al. Epidemiology of and surveillance for postpartum infections. Emerg Infect Dis. 2001 Sep-Oct;7(5):837-41. [Abstract]
49. van Ham MA, van Dongen PW, Mulder J. Maternal consequences of caesarean section. A retrospective study of intra-operative and postoperative maternal complications of caesarean section during a 10-year period. Eur J Obstet Gynecol Reprod Biol. 1997 Jul;74(1):1-6. [Abstract]
50. Murphy DJ, Liebling RE, Verity L, et al. Early maternal and neonatal morbidity associated with operative delivery in second stage of labour: a cohort study. Lancet. 2001 Oct 13;358(9289):1203-7. [Abstract]
51. Lydon-Rochelle MT, Holt VL, Martin DP. Delivery method and self-reported postpartum general health status among primiparous women. Paediatr Perinat Epidemiol. 2001 Jul;15(3):232-40. [Abstract]
52. Wilson PD, Herbison RM, Herbison GP. Obstetric practice and the prevalence of urinary incontinence three months after delivery. Br J Obstet Gynaecol. 1996 Feb;103(2):154-61. [Abstract]
53. Persson J, Wolner-Hanssen P, Rydhstroem H. Obstetric risk factors for stress urinary incontinence: a population-based study. Obstet Gynecol. 2000 Sep;96(3):440-5. [Abstract]
54. MacLennan AH, Taylor AW, Wilson DH, et al. The prevalence of pelvic disorders and their relationship to gender, age, parity and mode of delivery. BJOG. 2000 Dec;107(12):1460-70. [Abstract]
55. Thompson JF, Roberts CL, Currie M, et al. Prevalence and persistence of health problems after childbirth: associations with parity and method of birth. Birth. 2002 Jun;29(2):83-94. [Abstract]
56. Australian Institute of Health and Welfare. Australia's mothers and babies 2015 - in brief. October 2017 [internet publication]. [Full Text]
57. Mutryn CS. Psychosocial impact of cesarean section on the family: a literature review. Soc Sci Med. 1993 Nov;37(10):1271-81. [Abstract]
58. DiMatteo MR, Morton SC, Lepper HS, et al. Cesarean childbirth and psychosocial outcomes: a meta-analysis. Health Psychol. 1996 Jul;15(4):303-14. [Abstract]
59. National Institute for Health and Care Excellence. Caesarean birth. Mar 2021 [internet publication]. [Full Text]
60. Greene R, Gardeit F, Turner MJ. Long-term implications of cesarean section. Am J Obstet Gynecol. 1997 Jan;176(1 Pt 1):254-5. [Abstract]
61. Coughlan C, Kearney R, Turner MJ. What are the implications for the next delivery in primigravidae who have an elective caesarean section for breech presentation? BJOG. 2002 Jun;109(6):624-6. [Abstract]
62. Hemminki E, Merilainen J. Long-term effects of cesarean sections: ectopic pregnancies and placental problems. Am J Obstet Gynecol. 1996 May;174(5):1569-74. [Abstract]
63. Gilliam M, Rosenberg D, Davis F. The likelihood of placenta previa with greater number of cesarean deliveries and higher parity. Obstet Gynecol. 2002 Jun;99(6):976-80. [Abstract]
64. Morrison JJ, Rennie JM, Milton PJ. Neonatal respiratory morbidity and mode of delivery at term: influence of timing of elective caesarean section. Br J Obstet Gynaecol. 1995 Feb;102(2):101-6. [Abstract]
65. Annibale DJ, Hulsey TC, Wagner CL, et al. Comparative neonatal morbidity of abdominal and vaginal deliveries after uncomplicated pregnancies. Arch Pediatr Adolesc Med. 1995 Aug;149(8):862-7. [Abstract]
66. Hook B, Kiwi R, Amini SB, et al. Neonatal morbidity after elective repeat cesarean section and trial of labor. Pediatrics. 1997 Sep;100(3 Pt 1):348-53. [Abstract]
67. Nassar N, Roberts CL, Cameron CA, et al. Outcomes of external cephalic version and breech presentation at term: an audit of deliveries at a Sydney tertiary obstetric hospital, 1997-2004. Acta Obstet Gynecol Scand. 2006;85(10):1231-8. [Abstract]
68. Nwosu EC, Walkinshaw S, Chia P, et al. Undiagnosed breech. Br J Obstet Gynaecol. 1993 Jun;100(6):531-5. [Abstract]
69. Flamm BL, Ruffini RM. Undetected breech presentation: impact on external version and cesarean rates. Am J Perinatol. 1998 May;15(5):287-9. [Abstract]
70. Cockburn J, Foong C, Cockburn P. Undiagnosed breech. Br J Obstet Gynaecol. 1994 Jul;101(7):648-9. [Abstract]
71. Leung WC, Pun TC, Wong WM. Undiagnosed breech revisited. Br J Obstet Gynaecol. 1999 Jul;106(7):638-41. [Abstract]
72. Berhan Y, Haileamlak A. The risks of planned vaginal breech delivery versus planned caesarean section for term breech birth: a meta-analysis including observational studies. BJOG. 2016 Jan;123(1):49-57. [Abstract] [Full Text]
73. Wilcox C, Nassar N, Roberts C. Effectiveness of nifedipine tocolysis to facilitate external cephalic version: a systematic review. BJOG. 2011 Mar;118(4):423-8. [Abstract]
74. Qureshi H, Massey E, Kirwan D, et al. BCSH guideline for the use of anti-D immunoglobulin for the prevention of haemolytic disease of the fetus and newborn. Transfus Med. 2014 Feb;24(1):8-20. [Abstract] [Full Text]
75. Hutton EK, Hofmeyr GJ, Dowswell T. External cephalic version for breech presentation before term. Cochrane Database Syst Rev. 2015 Jul 29;(7):CD000084. [Abstract] [Full Text]
76. Coyle ME, Smith CA, Peat B. Cephalic version by moxibustion for breech presentation. Cochrane Database Syst Rev. 2012 May 16;(5):CD003928. [Abstract] [Full Text]
77. Hofmeyr GJ, Kulier R. Cephalic version by postural management for breech presentation. Cochrane Database Syst Rev. 2012 Oct 17;(10):CD000051. [Abstract] [Full Text]
78. Hannah ME, Whyte H, Hannah WJ, et al. Maternal outcomes at 2 years after planned cesarean section versus planned vaginal birth for breech presentation at term: the International Randomized Term Breech Trial. Am J Obstet Gynecol. 2004 Sep;191(3):917-27. [Abstract]
79. Eide MG, Oyen N, Skjaerven R, et al. Breech delivery and Intelligence: a population-based study of 8,738 breech infants. Obstet Gynecol. 2005 Jan;105(1):4-11. [Abstract]
80. Whyte H, Hannah ME, Saigal S, et al. Outcomes of children at 2 years after planned cesarean birth versus planned vaginal birth for breech presentation at term: the International Randomized Term Breech Trial. Am J Obstet Gynecol. 2004 Sep;191(3):864-71. [Abstract]
81. Brown S, Lumley J. Maternal health after childbirth: results of an Australian population based survey. Br J Obstet Gynaecol. 1998 Feb;105(2):156-61. [Abstract]
Published by
American College of Obstetricians and Gynecologists
2016 (reaffirmed 2022)
Royal College of Obstetricians and Gynaecologists (UK)
National Institute for Health and Care Excellence (UK)
Topic last updated: 2024-03-05
Natasha Nassar , PhD
Associate Professor
Menzies Centre for Health Policy
Sydney School of Public Health
University of Sydney
Christine L. Roberts , MBBS, FAFPHM, DrPH
Research Director
Clinical and Population Health Division
Perinatal Medicine Group
Kolling Institute of Medical Research
Jonathan Morris , MBChB, FRANZCOG, PhD
Professor of Obstetrics and Gynaecology and Head of Department
Peer Reviewers
John W. Bachman , MD
Consultant in Family Medicine
Department of Family Medicine
Mayo Clinic
Rhona Hughes , MBChB
Lead Obstetrician
Lothian Simpson Centre for Reproductive Health
The Royal Infirmary
Brian Peat , MD
Director of Obstetrics
Women's and Children's Hospital
North Adelaide
South Australia
Lelia Duley , MBChB
Professor of Obstetric Epidemiology
University of Leeds
Bradford Institute of Health Research
Temple Bank House
Bradford Royal Infirmary
Justus Hofmeyr , MD
Head of the Department of Obstetrics and Gynaecology
East London Private Hospital
East London
South Africa
We’re sorry, but Freepik doesn’t work properly without JavaScript enabled. FAQ Contact
- Notifications
- Go back Remove
- No notifications to show yet You’ll see useful information here soon. Stay tuned!
- Downloads 0/60 What is this?
- My collections
- My subscription
Find out what’s new on Freepik and get notified about the latest content updates and feature releases.
Fetal Presentation Photos

- Add to collection
- Save to Pinterest
- couple home
- romantic couple

- pregnancy test
- pregnant test

- pregnant woman

- pregnant doctor
- pregnancy doctor

- baby accessories

- pregnant couple

- baby nursery
- nursery room

- pregnancy woman

- computer networking
- application

- lesbian couple
- family care

- pregnant belly
- touch screen

- dry clothes

- baby clothes

- pregnancy announcement

- doctor desk
- doctor office

- gynaecologist
- gynaecology

- pregnant mom

- stethoscope
- doctor stethoscope

- family together

- pregnant lady

- pregnant mother

- flat lay background

- baby in womb

- male female

- light purple

- mother father
- people talking


IMAGES
VIDEO
COMMENTS
Frank breech. When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head.
Possible fetal positions can include: Occiput or cephalic anterior: This is the best fetal position for childbirth. It means the fetus is head down, facing the birth parent's spine (facing backward). Its chin is tucked towards its chest. The fetus will also be slightly off-center, with the back of its head facing the right or left.
Maternal Fetal Care International and Babytalk Magazine Present the Lullaby Ball. of 2. United States. Browse Getty Images' premium collection of high-quality, authentic Fetal Presentation stock photos, royalty-free images, and pictures. Fetal Presentation stock photos are available in a variety of sizes and formats to fit your needs.
Fetal presentation, or how your baby is situated in your womb at birth, is determined by the body part that's positioned to come out first, and it can affect the way you deliver. At the time of delivery, 97 percent of babies are head-down (cephalic presentation). But there are several other possibilities, including feet or bottom first (breech ...
Development at 8 Weeks. 4 /13. The embryo is now a little over half an inch in size. Eyelids and ears are forming, and you can see the tip of the nose. The arms and legs are well formed. The ...
When a fetus faces up, the neck is often straightened rather than bent,which requires more room for the head to pass through the birth canal. Delivery assisted by a vacuum device or forceps Operative Vaginal Delivery Operative vaginal delivery is delivery using a vacuum extractor or forceps. A vacuum extractor consists of a small cup made of a rubberlike material that is connected to a vacuum.
During routine prenatal care, clinicians assess fetal lie and presentation with physical examination in the late third trimester. Ultrasonography can also be done. If breech presentation is detected, external cephalic version can sometimes move the fetus to vertex presentation before labor, usually at 37 or 38 weeks.
Compound presentation is a fetal presentation in which an extremity presents alongside the part of the fetus closest to the birth canal. The majority of compound presentations consist of a fetal hand or arm presenting with the head [ 1 ]. This topic will review the pathogenesis, clinical manifestations, diagnosis, and management of this ...
Causes: Brow presentation may result from abnormal fetal positioning, poor engagement of the fetal head, or other factors that prevent full flexion or extension. Complications: Brow presentation is associated with a higher risk of prolonged labor, difficulty in descent, increased chances of fetal head entrapment, birth injuries, and the ...
The fetus undergoes a series of changes in position, attitude, and presentation during labor. This process is essential for the accomplishment of a vaginal delivery. The presence of a fetal malpresentation or an abnormality of the maternal pelvis can significantly impede the likelihood of a vaginal delivery. The contractile aspect of the uterus ...
Normally, the presentation is vertex (head first), and the position is occiput anterior (facing toward the pregnant person's spine) and with the face and body angled to one side and the neck flexed. Variations in fetal presentations include face, brow, breech, and shoulder.
Detailed Method to Determine Fetal Situs. 1. Define within the uterus the presentation of the fetus (generally vertex or breech; less often the presentation is oblique or transverse.). 2. Determine whether the fetal spine is parallel or transverse to the maternal spine. In sagittal view, if the fetal and maternal spine are parallel, the fetus ...
Abnormal Fetal Lie. If the fetal lie is abnormal, an external cephalic version (ECV) can be attempted - ideally between 36 and 38 weeks gestation. ECV is the manipulation of the fetus to a cephalic presentation through the maternal abdomen. It has an approximate success rate of 50% in primiparous women and 60% in multiparous women.
Position and Presentation of the Fetus. Toward the end of pregnancy, the fetus moves into position for delivery. Normally, the position of a fetus is facing rearward (toward the woman's back) with the face and body angled to one side and the neck flexed, and presentation is head first. An abnormal position is facing forward, and abnormal ...
Browse 63 fetal presentation photos and images available, or start a new search to explore more photos and images. old engraved illustration of adaptation between the uterus and the fetus at term in vertex presentation - fetal presentation stock pictures, royalty-free photos & images.
Find Fetal Presentation stock photos and editorial news pictures from Getty Images. Select from premium Fetal Presentation of the highest quality.
Browse 30+ fetal presentation stock photos and images available, or start a new search to explore more stock photos and images. Sort by: Most popular. Position of the fetus in the womb. Pregnancy. Position of the fetus in the womb. Pregnancy illustration for your design. The development of the embryo.
Previous123456Next. Download and use 9,000+ Fetal Presentation stock photos for free. Thousands of new images every day Completely Free to Use High-quality videos and images from Pexels.
The white oval outline in the images is the fetal skull. Image courtesy of Alpinion. Example of a fetal head profile on 2D ultrasound. This is a common image shown to the mother during exams because it is easy for most people to identify it as a baby, and it shows the outline of the fetal face with the chin and nose.
Knowledge of the fetal presentation is important at the time of delivery (regardless of gestation) and prior to delivery as the pregnancy approaches term because this is when external cephalic version becomes an option. Diagnosis after the onset of labor is associated with increased maternal and infant morbidity and mortality.
Find & Download the most popular Fetal Presentation Photos on Freepik Free for commercial use High Quality Images Over 51 Million Stock Photos. #freepik #photo