- Open access
- Published: 21 September 2023

A systematic review on gender dysphoria in adolescents and young adults: focus on suicidal and self-harming ideation and behaviours
- Elisa Marconi ORCID: orcid.org/0000-0001-6722-8390 1 na1 ,
- Laura Monti ORCID: orcid.org/0000-0001-8339-265X 1 na1 ,
- Angelica Marfoli ORCID: orcid.org/0009-0007-7324-577X 2 ,
- Georgios D. Kotzalidis ORCID: orcid.org/0000-0002-0281-6324 3 , 4 , 7 ,
- Delfina Janiri ORCID: orcid.org/0000-0003-2485-6121 4 , 7 ,
- Cecilia Cianfriglia ORCID: orcid.org/0009-0000-6777-7007 2 ,
- Federica Moriconi ORCID: orcid.org/0000-0003-1593-0043 1 ,
- Stefano Costa ORCID: orcid.org/0000-0002-0137-2370 5 ,
- Chiara Veredice ORCID: orcid.org/0000-0003-2267-8077 6 ,
- Gabriele Sani ORCID: orcid.org/0000-0002-9767-8752 4 , 7 &
- Daniela Pia Rosaria Chieffo ORCID: orcid.org/0000-0002-0130-6584 1 , 8
Child and Adolescent Psychiatry and Mental Health volume 17 , Article number: 110 ( 2023 ) Cite this article
4448 Accesses
1 Citations
17 Altmetric
Metrics details
Introduction
Gender dysphoria (GD) is characterized by the incongruence between one’s experienced and expressed gender and assigned-sex-at-birth; it is associated with clinically significant distress. In recent years, the number of young patients diagnosed with GD has increased considerably. Recent studies reported that GD adolescents present behavioural and emotional problems and internalizing problems. Furthermore, this population shows a prevalence of psychiatric symptoms, like depression and anxiety. Several studies showed high rates of suicidal and non-suicidal self-injurious thoughts and behaviour in GD adolescents. To increase understanding of overall mental health status and potential risks of young people with GD, this systematic review focused on risk of suicide and self-harm gestures.
We followed the PRISMA 2020 statement, collecting empirical studies from four electronic databases, i.e., PubMed, Scopus, PsycINFO, and Web of Science.
Twenty-one studies on GD and gender nonconforming identity, suicidality, and self-harm in adolescents and young adults met inclusion criteria. Results showed that GD adolescents have more suicidal ideation, life-threatening behaviour, self-injurious thoughts or self-harm than their cisgender peers. Assessment methods were heterogeneous.
A standardised assessment is needed. Understanding the mental health status of transgender young people could help develop and provide effective clinical pathways and interventions.
Gender dysphoria (GD) is a condition characterized by a marked incongruence between one’s experienced and expressed gender and the one assigned at birth and is often associated with clinically significant distress or impairment in social, occupational, or other important areas of functioning, especially when reported early [ 1 ]. In recent years, the number of young patients diagnosed with GD or and gender-diverse identity—including nonbinary and questioning sexual identities—has considerably increased [ 2 , 3 , 4 , 5 ]. Current studies document that this population may be exposed to a higher risk of adverse events affecting health status and well-being [ 6 , 7 ]. This further impacted this vulnerable population, with the most negative consequences for those who experience a gender not congruent with the one they were assigned at birth [ 8 , 9 , 10 ]. Indeed, children and adolescents with GD and transgender or transgender and gender nonconforming (TGNC) are described as a psychologically and socially vulnerable population, facing a wide range of physical and mental health concerns that could benefit from early intervention [ 11 , 12 , 13 ]. GD during adolescence develops in individuals whose brain is still developing to reach full maturity only some years later, hence the need to dedicate special attention to this population.
As a population perceiving gender minority stress [ 14 ], adolescents with GD are likely to lack social acceptance and suffer stigma laid upon them by others [ 15 ], but also tend to internalisation [ 16 ]. A corollary may be that several studies found adolescents with GD, compared to their age-matched cisgender peers, to show more often behavioural and emotional problems and higher levels of individual distress-generating internalising problems, rather than environment-perturbing externalising problems [ 17 , 18 , 19 ]. Consequently, adolescents with GD show a higher prevalence of psychiatric issues, such as depression and anxiety disorders [ 17 , 20 , 21 ], likely due to social stigma.
Adolescents and young adults with GD and gender-diverse identity report higher suicidal thinking, planning, and attempts as well as non-suicidal self-harming thoughts and behaviours (NSSI) than the general population [ 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 ]. Suicidality is an umbrella term including suicidal ideation, suicidal behaviours, and suicide attempts and plans which are correlated to the desire to die [ 33 ]; we will use suicidality sparingly in this paper and focus instead upon the above-mentioned specific terms, when possible. Non-suicidal self-harming behaviours and thoughts, however, refer to self-injurious acts without intending to end one’s own life, but involve self-punishment or negative emotion regulation [ 34 ]. In both cases, early age at onset has been identified as an important vulnerability factor, with onset during childhood and adolescence being associated with a poorer prognosis [ 17 ], based on different surveys of high-school students [ 31 ]. For example, in New Zealand, 20% of students with GD reported attempting suicide in the past 12 months, compared to 4% of all students [ 35 ]. Similarly, in the United States, 15% of students with GD reported a suicide attempt requiring medical treatment in the last 12 months, compared to 3% of all students [ 36 , 37 , 38 ]. In another American survey, 41% of students with GD reported having attempted suicide during their lifetime, compared to 14% of all students [ 39 ]. Moreover, Surace and her colleagues [ 40 ] found a mean prevalence of 28.2% for NSSI, 28.0% for suicidal ideation, and 14.8% for suicide attempts in young TGNC clinical populations up to 25 years old.
Besides aspects of GD like body dysmorphic disorder, feeling uncomfortable in one’s own body, and hopelessness about obtaining gender-affirming medical procedures, a possible contribution to elevated suicidal risk and behaviours in the GD population might lie within the social stigma experienced by TGNC adolescents, such as discrimination, prejudice, social stress, and ostracism within the peer group and/or family [ 41 ]. Suicidal ideation and self-injurious behaviours generally relate to significant emotional problems, such as depressive and anxiety symptoms, which in turn trigger psychosocial and biological imbalance, could increase the wish to die [ 42 , 43 , 44 , 45 ], thus adding to the above.
In summary, several studies have shown higher rates of suicidal and non-suicidal self-harming thoughts and behaviours in adolescents and young adults with GD and gender-diverse identity—such as nonbinary and questioning sexual identity—compared to their male and female cisgender peers. However, the evidence heretofore is piecemeal, probably due to social stigma currently associated with GD and the concern of stigmatising individuals suffering from this condition. To better understand the mental state of adolescents and young adults with TGNC, we conducted a systematic review focusing on the risk for suicide and self-harming gestures in the GD population. The aim of this review was to estimate the frequency of suicidal and self-harm behaviour in adolescents and young adults with GD, comparing them with cisgender adolescents where possible.
We performed a systematic review in compliance with the 2020 PRISMA guidelines for systematic reviews and meta-analyses [ 46 ] to increase comprehensiveness and transparency of reporting.
Information sources and database search
To systematically collect empirical studies on the possible relation between suicidality/self-harming and GD in adolescents and young adults, several keywords were used to search for appropriate publications in four electronic databases, i.e., PubMed, Scopus, PsycINFO, and Web of Science since their inception and no date or language restriction.
Authors conducted the search separately in each database using the following agreed upon search strategy for PubMed and adapting the search for the other databases: (suicid* OR self-injur* OR self-harm* OR self-inflict* OR self-lesion*) AND (gender dysphori* OR transgender) AND (child* OR adolesc* OR "young adult*" OR youth* OR "school age"). Since the terms GD and transgender are used by many people as synonymous, in our searches we used both terms to identify possible eligible articles.
Eligibility criteria
Inclusion criteria were a study published in a peer-reviewed journal, reporting data on suicide and related behaviours (thinking, planning, and attempts) and/or non-suicidal self-harming thoughts and acts (using methods that reliably obtain the desired result) in adolescent and young adult (14–27 years old) samples with GD/transgender status/gender diverse identity.
Exclusion criteria were studies conducted on children or adult samples and those with mixed populations not providing data for adolescents and young adults separately. Also, opinion papers, such as editorials, letters to the editor, and hypotheses without providing data were excluded, as well as case reports or series, reviews/meta-analyses, animal studies, studies with inadequate/poor methodology and inadequate reporting of data, unfocused, or unrelated to the subject matter. All inter- and intra-database duplicates were removed, as well as abstracts, meeting presentations and studies presenting incomplete data.
Although reviews and meta-analyses were not included, their reference lists were screened to identify additional eligible publications. Eligibility for each study was decided with Delphi rounds among all authors until complete consensus was reached.
Data extraction
The analysis was conducted by all authors, who applied the eligibility criteria on each database. Each author conducted the selection process separately from others; at a final step, all authors compared their results in Delphi rounds (either in-person or remotely) aimed at obtaining full consensus.
Data collection and risk of bias assessment
Data collected for each study included country of origin, number of paediatric patients, demographic information (age and biological sex), presence/absence of GD and if present, type of GD, and clinical symptoms focused on self-harm (suicide behaviour, suicidal ideation, suicidal intent and planning, non-suicidal self-harm, and other self-injurious behaviour).
The evaluation of the risk of bias was conducted by a quality index derived from the Qualsyst’ Tool [ 47 ]. The quality of selected studies was assessed independently by all investigators and disagreements were resolved by consensus (results of risk-of-bias for all studies in the Additional file 1 ).
Identified studies
On February 7, 2023, we located 1416 articles (Fig. 1 , PRISMA flowchart) [ 39 ], of which 128 articles were assessed for eligibility. Of these papers, 107 articles were excluded according to eligibility criteria; 21 dealing with the relationship between GD and gender non-conforming identity, and suicidality and self-harm in adolescents and young adults met inclusion criteria.
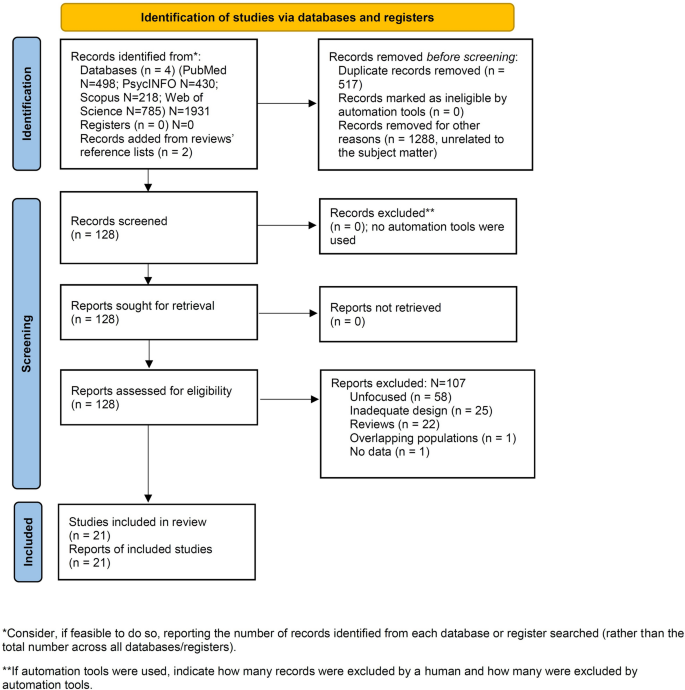
PRISMA2020 flow diagram for new systematic reviews: Search findings and selection with detailed reasons for exclusion
For the purpose of this systematic review, we have focused our analyses on these 21 studies. Figure 1 provides a PRISMA flow diagram showing search results.
Due to the breadth of the topic and the variety of variables included in this systematic review, the subject matter was organized according to the categories of psychopathological symptoms of interest in the study (Tables 1 and 2 ) and a final mixed category (Table 3 ). Of 21 studies meeting the inclusion criteria, there were 2 studies where self-harming behaviours and thoughts was the outcome in TGNC adolescents (Table 1 ), 6 studies where suicide was the outcome (Table 2 ), and 13 studies where the outcome was committing suicide combined to self-injurious attitudes (Table 3 ).
The 21 studies were mainly from the United States, the United Kingdom and Europe. Included studies were also conducted in China, Iran, Turkey, Canada and Australia. Studies were non-interventional and observational, with 17 being cross-sectional or retrospective and 4 longitudinal.
GD and non-suicidal self-harming ideation and behaviours were investigated by two studies [ 48 , 49 ], GD and suicidality by six studies [ 6 , 17 , 24 , 29 , 39 , 51 ], and GD and both suicidality and non-suicidal self-harm by 13 [ 11 , 21 , 22 , 25 , 30 , 50 , 52 , 53 , 54 , 55 , 56 , 57 , 58 ]; of these studies, four [ 11 , 21 , 55 , 58 ] detected the presence of internalizing problems (depressive and anxiety disorders) in GD adolescents and young adults. Detailed results are provided in the Additional file 1 .
Summary results
Detailed results of each study are shown in Tables 1 – 3 and in the Additional file 1 . We will here summarise results in GD and transgender populations regarding studies of (1) non-suicidal self-harm, (2) suicidal ideation and attempts, and (3) non-suicidal self-harm, suicidal ideation, and suicide attempts combined.
- Non-suicidal self-harming was explored in two studies [ 48 , 49 ]; transgender adolescents showed higher tendency toward self-harm ideation than cisgender adolescents, while non-suicidal self-inflicted behaviours were more common in cisgender males and females than among transgender adolescents [ 49 ]. AFAB adolescents showed nominally more lifetime and current NSSI than AMAB, but this did not reach statistical significance [ 48 ] (Table 1 ).
- Suicidal thinking and attempts only were examined in six studies [ 6 , 17 , 24 , 29 , 39 , 51 ] and generally identified a high prevalence in GD/transgender populations of suicide behaviours and attempts, ranging from 14.3% of severe suicidal ideation in Heino et al. [ 29 ] to a cumulative “high risk” of 80.9% in Alizadeh Mohajer et al. [ 6 ]; however, studies used different assessment instruments, so it becomes difficult to draw conclusions as to the real extent of suicidality in our target population. Gender-diverse adolescents displayed high suicidal ideation (Table 2 ). Transgender/GD adolescents displayed more suicidal behaviour than cisgender adolescents, either males or females [ 39 ]. Suicidality did not differ between AMAB and AFAB transgender adolescents/younger adults [ 51 ].
- Suicidality and non-suicidal self-harm combined were explored in thirteen studies [ 11 , 21 , 22 , 25 , 30 , 50 , 52 , 53 , 54 , 55 , 56 , 57 , 58 ]. Both NSSI and suicidality were higher in transgender/GD youths than in cisgender participants. AMAB and AFAB showed higher NSSI and suicidality rates than cisgender boys and girls [ 11 ] (Table 3 ).
Additional considerations will be detailed further on.
The last decade has seen an increase in cases of GD in adolescents worldwide and our knowledge of the epidemiological and clinical features continues to evolve [ 59 ]. An adequate understanding of the phenomenon and any related symptoms is important for the early management and possible prevention of distress. Indeed, the literature has highlighted the existence of a high association of psychological and psychiatric symptoms in adolescents with GD.
Several studies used different methods to investigate whether transgender identity and clinical outcomes in the general adolescent population are related [ 6 , 17 , 21 , 22 , 24 , 25 , 29 , 30 , 39 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 ]. The present review focused particularly on high-severity psychological symptoms in young people, such as self-harm and suicidal symptomatology. Indeed, the results of the studies underline a statistically significant correlation between youth TGNC—including gender dysphoric, non-binary and questioning adolescents—and prevalence of suicidal thinking and plans/attempts and self-harming thoughts and behaviours compared to cisgender populations [ 20 , 29 , 60 , 61 , 62 , 63 , 64 , 65 ]. Currently, there is a dearth of results from population-based samples, hence generalizing current findings is still very premature [ 59 ]. Despite progress and availability of resilience factors to face stigma and discrimination in some societies and social groups, there are considerable anti-LGBT attitudes in some countries and other social groups, ensuing in GD adolescents showing more mental symptoms and distress compared to cisgender peers [ 52 , 66 , 67 ]. Gender dysphoric adolescents show higher rates of depression leading to suicidal risk and engage in more self-injurious behaviours than their cisgender peers, confirming that a significant proportion of this population experience severe suicidal ideation and almost one third attempt suicide [ 4 ]. Other studies highlight that half of transgender youths are diagnosed with depression and anxiety disorders as well as poorer overall health and sleep quality [ 11 , 66 , 68 ]. Furthermore, puberty appears to exacerbate mental health problems in people with GD [ 30 ].
The main theoretical models, such as the gender minority stress model [ 69 ], identify potential risk factors among transgender individuals, link exposure to stigma, discrimination, and lack of social support. Previous research identified sexual minority status as a fundamental risk factor for own life-threatening behaviours [ 70 ]. In fact, adolescents diagnosed with GD experience victimization from their peers, negative parental reactions to their gender-nonconforming expression and identity, and family violence. These exogenous factors often lead transgender individuals to experience personal distress and isolation, which might elicit higher rates of own-life-threatening behaviours, such as suicidal attempts and ideation and self-harm thoughts than their heterosexual peers [ 70 , 71 , 72 , 73 ].
Overall, results of the studies included in this systematic review confirmed that, compared to cisgender adolescents, TGNC adolescents reported a significantly higher frequency of suicidal attempts, suicidal thoughts, making suicide plans, self-harm ideation and deliberately participating in self-harm acts. Higher depressive and anxiety symptoms and lower overall physical health were also positively associated with GD [ 11 , 55 , 57 , 58 , 74 ].
However, results were heterogeneous. Specifically, Wang and colleagues [ 11 ] indicated that among the gender minority groups transgender girls had the greater risk of planning and attempting suicide, transgender boys had the highest risk of performing deliberate self-harm, and questioning youth AFAB had the highest risk of suicidal ideation. Similar results were obtained in another study [ 24 ], with the risk ratios analysis highlighting the greater rate of suicidality among birth-assigned females. This pattern is consistent with many other studies showing that suicidality is more common among AFAB adolescents than it is among AMAB youth [ 75 ]. Some studies found possible gender differences between AFAB and AMAB and possible consequences for their mental health, suggesting that although AMAB might experience more stigmatization and preconceptions, AFAB youth seem to cope differently with distress [ 17 , 25 , 48 ]. Nevertheless, this outcome was different from Toomey and colleagues’ work [ 39 ], which found that transgender boys had a higher rate of attempted suicide than transgender girls.
At any rate, despite these within-group discrepancies, general findings emerging from quantitative studies provide evidence that a large proportion of adolescents referred for GD and other transgender youth, whether “AFAB” or “AMAB”, have a substantial co-occurring history of psychosocial and psychological vulnerability, causing a higher risk for suicidal ideation and life-threatening behaviours, such as self-harm thoughts and self-injurious gestures [ 70 , 76 ].
Since society is becoming increasingly liquid according to Zygmunt Bauman [ 77 ], more cases of transgender states and GD are anticipated to occur; this will mean that we will have more of the general population at enhanced risk for self-harming acts, suicidal thinking, and suicidal behaviour. Under this perspective, it should be important to develop a comprehensive psychological assessment aimed at identifying people at risk of the above behaviours so to enforce preventive programmes [ 78 , 79 , 80 ].
For this reason, results provided by this systematic review may enhance the knowledge of health professionals about adolescents referred for GD. Furthermore, a better understanding of the mental health status of transgender youth and the associated risks could help to develop and provide effective interventions. The need for more knowledge and tools is also a key aspect of supporting each individual properly [ 30 , 81 ]. Finally, increasing social awareness and scientific knowledge can also help target support programs for parents. Indeed, parents could benefit from interventions dedicated to understanding the impact of attitudes, behaviours and decisions, as well as assisting them in the therapeutic paths they take with their children with GD [ 70 ].
Limitations . This review contains heterogeneous data that could not be subjected to a meta-analysis. Heterogeneity regarded the instruments used to assess the populations included and the variables examined. To add to the high heterogeneity, the population under study belonged to multiple categories, such as cisgender males, cisgender females, individuals assigned female at birth whose experienced gender was male (so-called female-to-male transgender), individuals assigned male at birth whose experienced gender was female (so-called male-to-female transgender), and nonbinary. Often studies did not differentiate possible transgender from nonbinary identities. We attempted at focusing on GD only, but had to deal also with other populations as well, since the literature treats these populations as they were one and the same, which of course is not the case. Furthermore, a distinction between self-harm and suicide attempts was not always possible. Moreover, the social stigma laid upon gender diverse populations and current cultural trends may have directly or indirectly affected the writing of this review and its final results and conclusions.
Conclusions
In conclusion, the overall findings emerging from this review provide evidence that a large proportion of adolescents with GD have a substantial concomitant history of psychosocial and psychological vulnerability, with a higher risk of suicidal ideation, life-threatening behaviour, and self-injurious thoughts or self-harm. Understanding the mental health status of transgender young people could help developing and providing effective clinical pathways and interventions. The relatively new issue of suicide in adolescent/young adult populations currently suffers from poor assessment standardization. There is a need for standardized assessment, culturally adapted research, and destigmatisation of this socially vulnerable population to address the issue of increased suicidal thinking and attempts.
Availability of data and materials
American Psychiatric Association. diagnostic and statistical manual of mental disorders, 5th edition, text revision (DSM-5-TR). Washington, D.C.: American Psychiatric Publishing Inc.; 2022. https://doi.org/10.1176/appi.books.9780890425596 .
Book Google Scholar
Zucker KJ. Epidemiology of gender dysphoria and transgender identity. Sex Health. 2017;14(5):404–11. https://doi.org/10.1071/SH17067 .
Article PubMed Google Scholar
Indremo M, White R, Frisell T, Cnattingius S, Skalkidou A, Isaksson J, Papadopoulos FC. Validity of the gender dysphoria diagnosis and incidence trends in Sweden: a nationwide register study. Sci Rep. 2021;11(1):16168. https://doi.org/10.1038/s41598-021-95421-9.4 .
Article CAS PubMed PubMed Central Google Scholar
Thompson L, Sarovic D, Wilson P, Sämfjord A, Gillberg C. A PRISMA systematic review of adolescent gender dysphoria literature: 1) epidemiology. PLOS Glob Publ Health. 2022;2(3):e0000245. https://doi.org/10.1371/journal.pgph.0000426 .
Article Google Scholar
Oshima Y, Matsumoto Y, Terada S, Yamada N. Prevalence of gender dysphoria by gender and age in japan: a population-based internet survey using the utrecht gender dysphoria scale. J Sex Med. 2022;19(7):1185–95. https://doi.org/10.1016/j.jsxm.2022.03.605 .
Alizadeh Mohajer M, Adibi A, Mozafari AA, Sahebi A, Bakhtiyari A. Suicidal ideation in patients with gender identity disorder in western Iran from March 2019 to March 2020. Int J Med Toxicol Forensic Med. 2020;10(4):31353. https://doi.org/10.32598/ijAMABm.v10i4.31353 .
Shin KE, Baroni A, Gerson RS, Bell KA, Pollak OH, Tezanos K, Spirito A, Cha CB. Using behavioral measures to assess suicide risk in the psychiatric emergency department for youth. Child Psychiatr Hum Dev. 2023. https://doi.org/10.1007/s10578-023-01507-y .
Perl L, Oren A, Klein Z, Shechner T. Effects of the COVID19 pandemic on transgender and gender non-conforming adolescents’ mental health. Psychiatr Res. 2021;302:114042. https://doi.org/10.1016/j.psychres.2021.114042 .
Article CAS Google Scholar
Hawke LD, Hayes E, Darnay K, Henderson J. Mental health among transgender and gender diverse youth: an exploration of effects during the COVID-19 pandemic. Psychol Sex Orientat Gend Divers. 2021;8(2):180–7. https://doi.org/10.1037/sgd0000467 .
Mitchell KJ, Ybarra ML, Banyard V, Goodman KL, Jones LM. Impact of the COVID-19 pandemic on perceptions of health and well-being among sexual and gender minority adolescents and emerging adults. LGBT Health. 2022;9(1):34–42. https://doi.org/10.1089/lgbt.2021.0238 .
Article PubMed PubMed Central Google Scholar
Wang Y, Yu H, Yang Y, Drescher J, Li R, Yin W, Yu R, Wang S, Deng W, Jia Q, Zucker KJ, Chen R. Mental health status of cisgender and gender-diverse secondary school students in China. JAMA Network Open. 2020;3(10):e2022796. https://doi.org/10.1001/jamanetworkopen.2020.22796 .
Andresen JB, Graugaard C, Andersson M, Bahnsen MK, Frisch M. Adverse childhood experiences and mental health problems in a nationally representative study of heterosexual, homosexual and bisexual danes. World Psychiatr. 2022;21(3):427–35. https://doi.org/10.1002/wps.21008 .
Sun S, Xu S, Guy A, Guigayoma J, Zhang Y, Wang Y, Operaio D, Chen R. Analysis of psychiatric symptoms and suicide risk among younger adults in china by gender identity and sexual orientation. JAMA Netw Open. 2023;6(3):e232294. https://doi.org/10.1001/jamanetworkopen.2023.2294 .
Hunter J, Butler C, Cooper K. Gender minority stress in trans and gender diverse adolescents and young people. Clin Child Psychol Psychiatry. 2021;26(4):1182–95. https://doi.org/10.1177/13591045211033187 .
Joseph AA, Kulshreshtha B, Shabir I, Marumudi E, George TS, Sagar R, Mehta M, Ammini AC. Gender issues and related social stigma affecting patients with a disorder of sex development in India. Arch Sex Behav. 2017;46(2):361–7. https://doi.org/10.1007/s10508-016-0841-0 .
Jackman KB, Dolezal C, Bockting WO. Generational differences in internalized transnegativity and psychological distress among feminine spectrum transgender people. LGBT Health. 2018;5(1):54–60. https://doi.org/10.1089/lgbt.2017.0034 .
Fisher AD, Ristori J, Castellini G, Sensi C, Cassioli E, Prunas A, Mosconi M, Vitelli R, Dèttore D, Ricca V, Maggi M. Psychological characteristics of Italian gender dysphoric adolescents: a case-control study. J Endocrinol Invest. 2017;40(9):953–65. https://doi.org/10.1007/s40618-017-0647-5 .
Article CAS PubMed Google Scholar
de Vries AL, Doreleijers TA, Steensma TD, Cohen-Kettenis PT. Psychiatric comorbidity in gender dysphoric adolescents. J Child Psychol Psychiatry. 2011;52(11):1195–202. https://doi.org/10.1111/j.1469-7610.2011.02426.x .
Zucker KJ, Wood H, Singh D, Bradley SJ. A developmental, biopsychosocial model for the treatment of children with gender identity disorder. J Homosex. 2012;59(3):369–97. https://doi.org/10.1080/00918369.2012.653309 .
Dhejne C, Van Vlerken R, Heylens G, Arcelus J. Mental health and gender dysphoria: a review of the literature. Int Rev Psychiatry. 2016;28(1):44–57. https://doi.org/10.3109/09540261.2015.1115753 .
Kozlowska K, McClure G, Chudleigh C, Maguire AM, Gessler D, Scher S, Ambler GR. Australian children and adolescents with gender dysphoria: clinical presentations and challenges experienced by a multidisciplinary team and gender service. Hum Syst Ther, Cult Attach. 2021;1(1):70–95. https://doi.org/10.1177/26344041211010777 .
Skagerberg E, Parkinson R, Carmichael P. Self-harming thoughts and behaviors in a group of children and adolescents with gender dysphoria. Int J Transgenderism. 2013;14(2):86–92. https://doi.org/10.1080/15532739.2013.817321 .
Aitken M, VanderLaan DP, Wasserman L, Stojanovski S, Zucker KJ. Self-Harm and suicidality in children referred for gender dysphoria. J Am Acad Child Adolesc Psychiatry. 2016;55(6):513–20. https://doi.org/10.1016/j.jaac.2016.04.001 .
de Graaf NM, Steensma TD, Carmichael P, VanderLaan DP, Aitken M, Cohen-Kettenis PT, de Vries ALC, Kreukels BPC, Wasserman L, Wood H, Zucker KJ. Suicidality in clinic-referred transgender adolescents. Eur Child Adolesc Psychiatry. 2022;31(1):67–83. https://doi.org/10.1007/s00787-020-01663-9 .
Thoma BC, Salk RH, Choukas-Bradley S, Goldstein TR, Levine MD, Marshal MP. Suicidality disparities between transgender and cisgender adolescents. Pediatrics. 2019;144(5):e20191183. https://doi.org/10.1542/peds.2019-1183 .
Mann GE, Taylor A, Wren B, de Graaf N. Review of the literature on self-injurious thoughts and behaviours in gender-diverse children and young people in the United Kingdom. Clin Child Psychol Psychiatry. 2019;24(2):304–21. https://doi.org/10.1177/1359104518812724 .
Dickey LM, Budge SL. Suicide and the transgender experience: a public health crisis. Am Psychol. 2020;75(3):380–90. https://doi.org/10.1037/amp0000619 .
Hatchel T, Polanin JR, Espelage DL. Suicidal thoughts and behaviors among LGBTQ youth: meta-analyses and a systematic review. Arch Suicide Res. 2021;25(1):1–37. https://doi.org/10.1080/13811118.2019.1663329 .
Heino E, Fröjd S, Marttunen M, Kaltiala R. Transgender identity is associated with severe suicidal ideation among finnish adolescents. Int J Adolesc Med Health. 2021. https://doi.org/10.1515/ijamh-2021-0018 .
Hartig A, Voss C, Herrmann L, Fahrenkrug S, Bindt C, Becker-Hebly I. Suicidal and nonsuicidal self-harming thoughts and behaviors in clinically referred children and adolescents with gender dysphoria. Clin Child Psychol Psychiatry. 2022;27(3):716–29. https://doi.org/10.1177/13591045211073941 .
Biggs M. Suicide by clinic-referred transgender adolescents in the United Kingdom. Arch Sex Behav. 2022;51(2):685–90. https://doi.org/10.1007/s10508-022-02287-7 .
Faruki F, Patel A, Jaka S, Kaur M, Sejdiu A, Bajwa A, Patel RS. Gender dysphoria in pediatric and transitional-aged youth hospitalized for suicidal behaviors: a cross-national inpatient study. Prim Care Companion CNS Disord. 2023;25(2):46284. https://doi.org/10.4088/PCC.22m03352 .
O’Connor RC, Nock MK. The psychology of suicidal behaviour. Lancet Psychiatry. 2014;1(1):73–85. https://doi.org/10.1016/S2215-0366(14)70222-6 .
Claes L, Vandereycken W. Self-injurious behavior: differential diagnosis and functional differentiation. Compr Psychiatry. 2007;48(2):137–44. https://doi.org/10.1016/j.comppsych.2006.10.009 .
Clark TC, Lucassen MF, Bullen P, Denny SJ, Fleming TM, Robinson EM, Rossen FV. The health and well-being of transgender high school students: results from the New Zealand adolescent health survey (Youth’12). J Adolesc Health. 2014;55(1):93–9. https://doi.org/10.1016/j.jadohealth.2013.11.008 .
Kann L, McManus T, Harris WA, Shanklin SL, Flint KH, Queen B, Lowry R, Chyen D, Whittle L, Thornton J, Lim C, Bradford D, Yamakawa Y, Leon M, Brener N, Ethier KA. Youth risk behavior surveillance—United States 2017. MMWR Morb Mortal Wkly Rep Surveill Summ. 2018;67(8):1–114. https://doi.org/10.15585/mmwr.ss6708a1 .
Johns MM, Lowry R, Andrzejewski J, Barrios LC, Demissie Z, McManus T, Rasberry CN, Robin L, Underwood JM. Transgender identity and experiences of violence victimization, substance use, suicide risk, and sexual risk behaviors among high school students—19 states and large urban school districts 2017. MMWR Morb Mortal Wkly Rep. 2019;68(3):67–71. https://doi.org/10.15585/mmwr.mm6803a3 .
Jackman KB, Caceres BA, Kreuze EJ, Bockting WO. Suicidality among gender minority youth: analysis of 2017 youth risk behavior survey data. Arch Suicide Res. 2021;25(2):208–23. https://doi.org/10.1080/13811118.2019.1678539 .
Toomey RB, Syvertsen AK, Shramko M. Transgender adolescent suicide behavior. Pediatrics. 2018;142(4):e20174218. https://doi.org/10.1542/peds.2017-4218 .
Surace T, Fusar-Poli L, Vozza L, Cavone V, Arcidiacono C, Mammano R, Basile L, Rodolico A, Bisicchia P, Caponnetto P, Signorelli MS, Aguglia E. Lifetime prevalence of suicidal ideation and suicidal behaviors in gender non-conforming youths: a meta-analysis. Eur Child Adolesc Psychiatry. 2021;30(8):1147–61. https://doi.org/10.1007/s00787-020-01508-5 .
Arnold JC, McNamara M. Transgender and gender-diverse youth: an update on standard medical treatments for gender dysphoria and the sociopolitical climate. Curr Opin Pediatr. 2023. https://doi.org/10.1097/MOP.0000000000001256 .
Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674–97. https://doi.org/10.1037/0033-2909.129.5.674 .
Hendricks ML, Testa RJ. A conceptual framework for clinical work with transgender and gender nonconforming clients: an adaptation of the minority stress model. Prof Psychol Res Pract. 2012;43(5):460–7. https://doi.org/10.1037/a0029597 .
de Graaf NM, Cohen-Kettenis PT, Carmichael P, de Vries ALC, Dhondt K, Laridaen J, Pauli D, Ball J, Steensma TD. Psychological functioning in adolescents referred to specialist gender identity clinics across Europe: a clinical comparison study between four clinics. Eur Child Adolesc Psychiatry. 2018;27(7):909–19. https://doi.org/10.1007/s00787-017-1098-4 .
Rotondi NK, Bauer GR, Scanlon K, Kaay M, Travers R, Travers A. Prevalence of and risk and protective factors for depression in female-to-male transgender ontarians: results from the trans PULSE project. Can J Commun Ment Health. 2011;30(2):135–55. https://doi.org/10.7870/cjcmh-2011-0021 .
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Br Med J. 2021;372:n71. https://doi.org/10.1136/bmj.n71 .
Kmet LM, Lee RC, Cook LS. Standard quality assessment criteria for evaluating primary research papers from a variety of fields. HTA Initiative # 13. Edmonton: Alberta Herit Found Med Res. 2004
Arcelus J, Claes L, Witcomb GL, Marshall E, Bouman WP. Risk factors for non-suicidal self-injury among trans youth. J Sex Med. 2016;13(3):402–12. https://doi.org/10.1016/j.jsxm.2016.01.003 .
Butler C, Joiner R, Bradley R, Bowles M, Bowes A, Russell C, Roberts V. Self-harm prevalence and ideation in a community sample of cis, trans and other youth. Int J Transgenderism. 2019;20(4):447–58. https://doi.org/10.1080/15532739.2019.1614130 .
Mak J, Shires DA, Zhang Q, Prieto LR, Ahmedani BK, Kattari L, Becerra-Culqui TA, Bradlyn A, Flanders WD, Getahun D, Giammattei SV, Hunkeler EM, Lash TL, Nash R, Quinn VP, Robinson B, Roblin D, Silverberg MJ, Slovis J, Tangpricha V, Vupputuri S, Goodman M. Suicide attempts among a cohort of transgender and gender diverse people. Am J Prev Med. 2020;59(4):570–7. https://doi.org/10.1016/j.amepre.2020.03.026 .
Yüksel Ş, Aslantaş Ertekin B, Öztürk M, Bikmaz PS, Oğlağu Z. A Clinically neglected topic: risk of suicide in transgender individuals. Noro Psikiyatri Arsivi. 2017;54(1):28–32. https://doi.org/10.5152/npa.2016.10075 .
Veale JF, Watson RJ, Peter T, Saewyc EM. Mental health disparities among canadian transgender youth. J Adolesc Health. 2017;60(1):44–9. https://doi.org/10.1016/j.jadohealth.2016.09.014 .
Becerra-Culqui TA, Liu Y, Nash R, Cromwell L, Flanders WD, Getahun D, Giammattei SV, Hunkeler EM, Lash TL, Millman A, Quinn VP, Robinson B, Roblin D, Sandberg DE, Silverberg MJ, Tangpricha V, Goodman M. Mental health of transgender and gender nonconforming youth compared with their peers. Pediatrics. 2018;141(5):e20173845. https://doi.org/10.1542/peds.2017-3845 .
Bechard M, VanderLaan DP, Wood H, Wasserman L, Zucker KJ. Psychosocial and psychological vulnerability in adolescents with gender dysphoria: a “proof of principle” study. J Sex Marital Ther. 2017;43(7):678–88. https://doi.org/10.1080/0092623X.2016.1232325 .
Peterson CM, Matthews A, Copps-Smith E, Conard LA. Suicidality, self-harm, and body dissatisfaction in transgender adolescents and emerging adults with gender dysphoria. Suicide Life-Threat Behav. 2017;47(4):475–82. https://doi.org/10.1111/sltb.12289 .
Mitchell HK, Keim G, Apple DE, Lett E, Zisk A, Dowshen NL, Yehya N. Prevalence of gender dysphoria and suicidality and self-harm in a national database of paediatric inpatients in the USA: a population-based, serial cross-sectional study. Lancet Child Adolesc Health. 2022;6(12):876–84. https://doi.org/10.1016/S2352-4642(22)00280-2 .
Karvonen M, Karukivi M, Kronström K, Kaltiala R. The nature of co-morbid psychopathology in adolescents with gender dysphoria. Psychiatry Res. 2022;317:114896. https://doi.org/10.1016/j.psychres.2022.114896 .
Tordoff DM, Wanta JW, Collin A, Stepney C, Inwards-Breland DJ, Ahrens K. Mental health outcomes in transgender and nonbinary youths receiving gender-affirming care. JAMA Netw Open. 2022;5(2):e220978–e220978. https://doi.org/10.1001/jamanetworkopen.2022.0978 .
Kaltiala-Heino R, Bergman H, Työläjärvi M, Frisén L. Gender dysphoria in adolescence: current perspectives. Adolesc Health Med Ther. 2018;9:31–41. https://doi.org/10.2147/AHMT.S135432 .
Connolly MD, Zervos MJ, Barone CJ II, Johnson CC, Joseph CL. The mental health of transgender youth: advances in understanding. J Adolesc Health. 2016;59(5):489–95. https://doi.org/10.1016/j.jadohealth.2016.06.012 .
Bränström R, van der Star A, Pachankis JE. Untethered lives: barriers to societal integration as predictors of the sexual orientation disparity in suicidality. Soc Psychiatry Psychiatr Epidemiol. 2020;55(1):89–99. https://doi.org/10.1007/s00127-019-01742-6 .
Garthe RC, Blackburn AM, Kaur A, Sarol JN Jr, Goffnett J, Rieger A, Reinhart C, Smith DC. Suicidal ideation among transgender and gender expansive youth: mechanisms of risk. Transgender Health. 2022;7(5):416–22. https://doi.org/10.1089/trgh.2021.0055 .
Clark KA, Hatzenbuehler ML, Bränström R, Pachankis JE. Sexual orientation-related patterns of 12-month course and severity of suicidality in a longitudinal, population-based cohort of young adults in Sweden. Soc Psychiatry Psychiatr Epidemiol. 2022;57(9):1931–4. https://doi.org/10.1007/s00127-022-02326-7 .
Bränström R, Stormbom I, Bergendal M, Pachankis JE. Transgender-based disparities in suicidality: a population-based study of key predictions from four theoretical models. Suicide Life-Threat Behav. 2022;52(3):401–12. https://doi.org/10.1111/sltb.12830 .
Chang CJ, Feinstein BA, Fulginiti A, Dyar C, Selby EA, Goldbach JT. A longitudinal examination of the interpersonal theory of suicide for predicting suicidal ideation among LGBTQ+ youth who utilize crisis services: the moderating effect of gender. Suicide Life-Threat Behav. 2021;51(5):1015–25. https://doi.org/10.1111/sltb.12787 .
Mezzalira S, Scandurra C, Mezza F, Miscioscia M, Innamorati M, Bochicchio V. Gender felt pressure, affective domains, and mental health outcomes among transgender and gender diverse (TGD) children and adolescents: a systematic review with developmental and clinical implications. Int J Environ Res Publ Health. 2022;20(1):785. https://doi.org/10.3390/ijerph20010785 .
Wolford-Clevenger C, Flores LY, Stuart GL. Proximal correlates of suicidal ideation among transgender and gender diverse people: a preliminary test of the three-step theory. Suicide Life-Threat Behav. 2021;51(6):1077–85. https://doi.org/10.1111/sltb.12790 .
Lehavot K, Simpson TL, Shipherd JC. Factors associated with suicidality among a national sample of transgender veterans. Suicide Life-Threat Behav. 2016;46(5):507–24. https://doi.org/10.1111/sltb.12233 .
Reisner SL, Vetters R, Leclerc M, Zaslow S, Wolfrum S, Shumer D, Mimiaga MJ. Mental health of transgender youth in care at an adolescent urban community health center: a matched retrospective cohort study. J Adolesc Health. 2015;56(3):274–9. https://doi.org/10.1016/j.jadohealth.2014.10.264 .
Grossman AH, D’Augelli AR. Transgender youth and life-threatening behaviors. Suicide Life-Threat Behav. 2007;37(5):527–37. https://doi.org/10.1521/suli.2007.37.5.527 .
D’Augelli AR, Grossman AH, Salter NP, Vasey JJ, Starks MT, Sinclair KO. Predicting the suicide attempts of lesbian, gay, and bisexual youth. Suicide Life-Threat Behav. 2005;35(6):646–60. https://doi.org/10.1521/suli.2005.35.6.646 .
Grossman AH, D’Augelli AR, Howell TJ, Hubbard S. Parent’reactions to transgender youth’gender nonconforming expression and identity. J Gay Lesbian Soc Serv. 2005;18(1):3–16. https://doi.org/10.1300/J041v18n01_02 .
Grossman AH, D’augelli AR, Salter NP. Male-to-female transgender youth: gender expression milestones, gender atypicality, victimization, and parents’ responses. J GLBT Fam Stud. 2006;2(1):71–92. https://doi.org/10.1300/J461v02n01_04 .
Randall AB, van der Star A, Pennesi JL, Siegel JA, Blashill AJ. Gender identity-based disparities in self-injurious thoughts and behaviors among pre-teens in the United States. Suicide Life-Threat Behav. 2022. https://doi.org/10.1111/sltb.12937 .
Miranda-Mendizabal A, Castellví P, Parés-Badell O, Alayo I, Almenara J, Alonso I, Alonso J. Gender differences in suicidal behavior in adolescents and young adults: systematic review and meta-analysis of longitudinal studies. Int J Public Health. 2019;64:265–83. https://doi.org/10.1007/s00038-018-1196-1 .
Horwitz AG, Berona J, Busby DR, Eisenberg D, Zheng K, Pistorello J, Albucher R, Coryell W, Favorite T, Walloch JC, King CA. Variation in suicide risk among subgroups of sexual and gender minority college students. Suicide Life-Threat Behav. 2020;50(5):1041–53. https://doi.org/10.1111/sltb.12637 .
Bauman Z. Liquid modernity. 2nd ed. Cambridge: Polity Press; 2012.
Google Scholar
Adelson SL. & American academy of child and adolescent psychiatry (AACAP) committee on quality issues (CQI): practice parameter on gay, lesbian, or bisexual sexual orientation, gender nonconformity, and gender discordance in children and adolescents. J Am Acad Child Adolesc Psychiatry. 2012;51:957–74. https://doi.org/10.1016/j.jaac.2012.07.004 .
Byne W, Bradley SJ, Coleman E, Eyler AE, Green R, Menvielle EJ, Meyer-Bahlburg HFL, Pleak RR, Tompkins DA. Report of the American psychiatric pssociation task force on treatment of gender identity disorder. Arch Sex Behav. 2012;41(4):759–96. https://doi.org/10.1007/s10508-012-9975-x .
Olson-Kennedy J, Cohen-Kettenis PT, Kreukels BPC, Meyer-Bahlburg HFL, Garofalo R, Meyer W, Rosenthal SM. Research priorities for gender nonconforming/transgender youth: gender identity development and biopsychosocial outcomes. Curr Opin Endocrinol Diabetes Obes. 2016;23:172–9. https://doi.org/10.1097/MED.0000000000000236 .
Dunlop BJ, Coleman SE, Hartley S, Carter LA, Taylor PJ. Self-injury in young bisexual people: a microlongitudinal investigation (SIBL) of thwarted belongingness and self-esteem on non-suicidal self-injury. Suicide Life-Threat Behav. 2022;52(2):317–28. https://doi.org/10.1111/sltb.12823 .
Download references
Acknowledgements
We greatly appreciate the help Drs. Alessio Simonetti and Evelina Bernardi provided in statistical issues.
This work has received no funding.
Author information
Elisa Marconi and Laura Monti are first authors as they equally contributed to the manuscript.
Authors and Affiliations
Clinical Psychology Unit, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Largo Agostino Gemelli 1, 00168, Rome, Italy
Elisa Marconi, Laura Monti, Federica Moriconi & Daniela Pia Rosaria Chieffo
Catholic University of the Sacred Heart—Rome, Largo Francesco Vito 1, 00168, Rome, Italy
Angelica Marfoli & Cecilia Cianfriglia
NESMOS Department (Neurosciences, Mental Health, and Sensory Organs), University of Rome “La Sapienza”, Via Di Grottarossa1035-1039, 00198, Rome, Italy
Georgios D. Kotzalidis
Department of Psychiatry, Department of Neuroscience, Head, Neck and Thorax, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Largo Agostino Gemelli 1, 00168, Rome, Italy
Georgios D. Kotzalidis, Delfina Janiri & Gabriele Sani
UOSD Operative Unit Psychiatry and Psychotherapy for Adolescents, Azienda USL Di Bologna, Ospedale MaggioreLargo Bartolo Nigrisoli, 2, 40133, Bologna, Italy
Stefano Costa
Pediatric Neuropsychiatry Unit, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, 00168, Rome, Italy
Chiara Veredice
Institute of Psychiatry, Department of Neuroscience, Catholic University of the Sacred Heart—Rome, Largo Francesco Vito 1, 00168, Rome, Italy
Departement of Life Sciences and Public Health Department, Catholic University of Sacred Heart, 00168, Rome, Italy
Daniela Pia Rosaria Chieffo
You can also search for this author in PubMed Google Scholar
Contributions
EM, LM, AM, CC, and DPRC. conceived the review. EM, LM, AM, CC, and GDK. organized and collected the material and wrote the first draft of the manuscript. AM, EM, GDK, DJ, FM, and SC. performed literature searches. EM, LM, AM, CC and GDK. wrote the Methods and decided eligibility criteria. DPRC, GDK. and GS. supervised the writing of the manuscript. DPRC, CV, AM, GDK. and GS. revised the final version of the manuscript. All authors contributed to the writing of the manuscript, read, and approved the submitted version.
Corresponding author
Correspondence to Elisa Marconi .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
All authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Supplement to Marconi et al. (2023)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Marconi, E., Monti, L., Marfoli, A. et al. A systematic review on gender dysphoria in adolescents and young adults: focus on suicidal and self-harming ideation and behaviours. Child Adolesc Psychiatry Ment Health 17 , 110 (2023). https://doi.org/10.1186/s13034-023-00654-3
Download citation
Received : 04 April 2023
Accepted : 30 August 2023
Published : 21 September 2023
DOI : https://doi.org/10.1186/s13034-023-00654-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Gender dysphoria
- Transgender
- Suicidal thinking
- Suicidal attempts
- Non-suicidal self-harm
Child and Adolescent Psychiatry and Mental Health
ISSN: 1753-2000
- Submission enquiries: [email protected]

Practical Clinical Andrology pp 263–272 Cite as
Gender Dysphoria: Overview and Psychological Interventions
- Elisabetta Lavorato 5 ,
- Antonio Rampino 6 &
- Valentina Giorgelli 6
- Open Access
- First Online: 15 October 2022
8446 Accesses
1 Citations
4 Altmetric
In the DSM V, the condition known as “Gender Identity Disorder” becomes “Gender Dysphoria” in order to avoid the stigma of being labeled as carriers of psychopathology. Gender Dysphoria (GD) refers to mental discomfort deriving by incongruence between the expressed gender and the assigned one. The term Transgender refers to identities or gender expressions that differ from social expectations typically based on the birth assigned sex. Not all people living “Gender Variance” express psychological or physic discomfort. The personal gender identity develops influenced by emotionally significant relationships and by socialeducational environment, based on predisposing biological characteristics. Most of clinical and psycho-social studies agree on multifactorial nature of this process, focusing on the combined action of biological, psychological, social and cultural factors. The first symptoms of gender dysphoria may appear from first years of life and then they may persist in puberty and adulthood. The causes of Gender Dysphoria are still unclear.
Both psychosocial and biological factors have been called into question to explain the onset. The Gender Dysphoria Treatment aims to reduce, or to remove, suffering of person with GD and it is based on teamwork of psychologists, psychiatrists, endocrinologists and surgeons. The cure is, firstly, psychological and is provided by mental health experts. Hormone therapy can be prescribed to all people with persistent and well documented Gender Dysphoria if there are no medical contraindications; lastly, sex reassignment surgery. The formation and definition of transgender and transsexual identity obviously represents a specific complexity, to which is added an environmental, cultural and consequently individual and conditioning stigmatization.
You have full access to this open access chapter, Download chapter PDF
20.1 Introduction
The nosography of Gender Dysphoria (GD) has recently been object of an important change. In the Statistical and Diagnostic Manual of Mental Disorders, DSM V [ 1 ], this diagnosis was separated from paraphilias and sexual disorders, becoming an independent category. The most important innovative aspect introduced by the DSM V concerns the condition known as “Gender Identity Disorder”, which is now referred to as “Gender Dysphoria”. The new nomenclature emphasizes the salient aspect of distress overcoming the stigmatizing definition of “disorder”, previously used.
Literature reports that Gender Dysphoria (GD)—defined as marked incongruence between one’s expressed gender and her/his assigned gender [ 2 ] (APA 2014)—is associated with psychological suffering characterized by anxiety, depression, impaired relationships, and suicidal ideation. The difference between one’s expressed gender and her/his physical sexual characteristics is expressed by the desire to get rid of them and/or to have the primary and secondary sexual characteristics of the opposite gender. The peculiarity of this disorder is the coexistence of medical aspects (biological sex) and psychological aspects (subjective experience). Previous studies highlight that psychological risk does not derive from the gender inconsistency, but from childhood traumatic experiences in different contexts, such as family, school, and because of non-recognition of psychological and sexual identity [ 3 ]. The community non-acceptance persists in adulthood, magnified by cultural stereotypes.
Therefore, Gender Dysphoria (GD) represents the condition of partial or complete discordance between assigned sex, based on external genitalia, and the gender recognized by the brain. So, it is characterized by suffering, malaise, and stress. This existential state has an intrinsic complexity that deserves as much attention and management as the medical issues related. Therefore, in a service dedicated to GD, it is necessary to create a multidisciplinary team dealing with all aspects of the transition process. Accordingly, an elective modality of “cure” has been proposed: on the one hand, the person carrying GD is supported from a psychological point of view; on the other hand, s/he is allowed to choose how to transform his/her morphological characteristics according to his/her subjective experience of identity, through endocrinological and surgical treatments. Of note, Law number 164 on 14th April 1982 (“ Rules on the rectification of gender attribution ”) establishes the possibility of carrying out a Surgical Sex Reassignment (SSR) and/or a change of sex at registry office even without SSR. In any case, it is permitted only after a clear diagnosis of GD has been formulated by a psychiatrist.
In Italy, the Observatory on Gender Identity (ONIG) has identified the centres able to take care of these cases throughout the national territory. Such centres must meet the criteria of Standards of Care (SOC) of the World Professional Association for Transgender Health [ 4 ], as defined by the Harry Benjamin International Gender Dysphoria Association. In fact, in all countries of the world, this Association reunited and supported people who, despite different skills, desire to develop the best possible practices and the most useful support to improve the quality of life of this population.
As a general expectation, people born with male sex identify themselves as men, while those born with female sex as women. Nonetheless, this is not what real experience teaches us and can be prejudicial if not detached from reality. In fact, a person, who experiences a so-called “Gender Variance”, does not recognize him/herself in this binary system occurring at birth. He/she does not perceive the gender identity as corresponding to birth assigned sex.
In fact, while there is biological sex depending on differences in chromosome numbers and genital conformation, gender identity is a more intimate feeling of belonging to the male or female gender, or to some combination of them. Therefore, Gender Identity allows people to say: “I am a man”, “I am a woman”, “I am a genderqueer”, regardless of the birth assigned sex.
The term Transgender refers to identities or gender expressions that differ from social expectations typically based on the birth assigned sex. Transgender people can have a binary gender identity (identifying themselves as women if at birth they were men or as men if at birth they were women) or non-binary (identifying themselves with subjective combination of genres). Not all people living “Gender Variance” express psychological or physical discomfort. Most of them find balance between the perception of oneself and the subjective model of relationships. On the other hand, if there is a psychological or physical distress, the so-called Gender Dysphoria, the person could feel the need to adapt the external reality (anatomical and personal data) to his or her emotional inner world. This is possible thanks to different interventions, including intake of feminizing or masculinizing hormones, surgical interventions, and/or modification of personal data. There are currently no data indicating a prevalence of people with gender variance. Nevertheless, there are data on the prevalence of Gender Dysphoria based on people entering specialized centres. Specifically, the World Professional Association for Transgender Health Standards of Care reported a prevalence of 1 in 11,900–45,000 for people assigned at birth to the male gender and 1 in 30,400–200,000 for people assigned at birth to the female gender.
The personal gender identity develops influenced by emotionally significant relationships and by social-educational environment, based on predisposing biological characteristics. Most of clinical and psycho-social studies agree on multifactorial nature of this process, focusing on the combined action of biological, psychological, social, and cultural factors.
20.2 Basic Concepts: Sexual and Gender Identity
To understand the experiences of Transgender people, we refer to behavioural and phenomenological markers of psychosexual development. Most of scholars refer to a tripartite model based on gender identity, gender role, and sexual orientation . Some authors also consider a further construct: gender expression . These components drive and guide the development of sexual identity . There are different definitions of gender identity ; first, it is not a stable construct because it is acquired step by step in the entire existence and it is influenced by different experiences. The sexual identity consists of biological sex (male or female according to certain biological parameters), gender identity (feeling male or female), gender role (adherence to the expectations of social context related to both biological sex and one’s own gender identity experience), and then sexual orientation (the gender towards which the individual feels sexual attraction).
The biological sex is the set of all biological characteristics of being female or male (biological sex): the sex chromosomes (XY for males and XX for females), the gonads (testes for males and ovaries for females), external genitalia, and secondary sexual characteristics (development of breasts, presence of face hair, tone of the voice, etc.) which appear during the sexual development (puberty).
Gender is a more complex construct and refers to characteristics depending on cultural, social, and psychological factors that define typical behaviours for men and women. For most people, biological sex and gender identity match. The term transgender identifies people with gender identity other than biological sex: for example, a person born as male, but feeling female (or vice versa). The condition that gender identity differs from biological sex is known as gender incongruence. The gender incongruence is not a disorder. In the last edition of International statistical classification of diseases and related health problems (ICD-11), gender incongruence was declassified from the chapter of mental health and included in the chapter of sexual health . If psychological discomfort of gender incongruence is structured in persistent and specific symptoms with an associated alteration of the global functioning, that is Gender Dysphoria.
Epidemiological data : as previously reported, prevalence data of Gender Dysphoria in adults (>18 years) are collected by specialized centres. Such data are most probably underestimated because not all people with gender incongruence develop Gender Dysphoria, then not all people affected by Gender Dysphoria come to a specialized centre. The estimated prevalence of GD is 0.005–0.014% of people with biological male sex and 0.002–0.003% of people with biological female sex [ 5 ]. Therefore, gender dysphoria is more common in the MtF form with a male/female ratio of approximately 3:1. In children under 12, the male/female ratio ranges from 3:1 to 2:1; while in teenagers, over 12 years, the male/female ratio is about 1:1.7 [ 5 ]. We highlight Gender Dysphoria is independent from sexual preference, which indicates sexual and emotional attraction for a person of the same sex (homosexuality), of opposite sex (heterosexuality), or of both genders (bisexuality). Transgender people can have any sexual and sentimental orientation, for example, they can be heterosexual or lesbian, gay or bisexual.
20.3 Symptoms
Gender Dysphoria appears as malaise and discomfort towards one’s body, felt as a stranger; the same sense of strangeness is experienced towards behaviours and attitudes that are typical of one’s sex, within which the person does not recognize her/himself.
The first symptoms of gender dysphoria may appear from the very early years of life, 2–3 years. In studies on childhood, it was seen gender dysphoria remains until adulthood for 6–23% among males and 12–27% among females. In other words, less than a third of children, in whom gender dysphoria has been diagnosed, will maintain this condition even during adolescence. However, when gender dysphoria persists in the early stage of sexual development (puberty), it rarely disappears over time, and nearly all adolescents with gender dysphoria maintain this condition well into adulthood.
20.3.1 Children
Characteristic behaviours of gender dysphoria among children may include:
Desire to wear clothes, use toys or take part to games typically associated to the other gender, preferring to play with children of opposite biological sex.
Refusal to urinate as other children of the same biological sex do (standing for boys or sitting for girls).
Desire to get rid of their genitals and want to have genitals of the opposite biological sex (for example a boy may say he wants to get rid of his penis and a girl may wish to have a penis).
Extreme discomfort with the changes in the body that occur during puberty.
These behaviours in gender dysphoria are associated with deep suffering and distress at school and in relationships. Rather consistently, in children with gender dysphoria, anxiety and depression are common.
20.3.2 Teenagers and Adults
In teenagers and adults, symptoms may include:
Certainty that one’s true gender is not aligned with one’s body.
Disgust towards one’s own genitals.
Strong desire to get rid of one’s genitals and other characteristics of one’s biological sex.
It is very difficult to have or suppress these feelings, and as a result, people with gender dysphoria may present with anxiety, depression, engage in self-harm, and have suicidal thoughts.
In the Diagnostic and Statistical Manual of Mental disorders, fifth edition (DSM-5—American Psychiatric Association) details about the diagnostic criteria for gender dysphoria according to age (children, adolescents, and adults) are reported.
20.3.3 DSM 5
20.3.3.1 gender dysphoria criteria in adults.
A marked incongruence between one’s experienced/expressed gender and their assigned gender, lasting at least 6 months , as manifested by at least two of the following:
A marked incongruence between one’s experienced/expressed gender and primary and/or secondary sex characteristics (or in young adolescents, the anticipated secondary sex characteristics).
A strong desire to get rid of one’s primary and/or secondary sex characteristics because of a marked incongruence with one’s experienced/expressed gender (or in young adolescents, a desire to prevent the development of the anticipated secondary sex characteristics).
A strong desire for the primary and/or secondary sex characteristics of the other gender.
A strong desire to be of the other gender (or some alternative gender different from one’s assigned gender).
A strong desire to be treated as the other gender (or some alternative gender different from one’s assigned gender).
A strong conviction that one has the typical feelings and reactions of the other gender (or some alternative gender different from one’s assigned gender).
The condition must also be associated with clinically significant distress or impairment in social, occupational, or other important areas of functioning .
20.3.3.2 Gender Dysphoria Criteria in Children
A marked incongruence between one’s experienced/expressed gender and their assigned gender, lasting at least 6 months, as manifested by at least two of the following (one of which must be the first criterion):
A strong desire to be of the other gender or an insistence that one is the other gender (or some alternative gender different from one’s assigned gender).
In boys (assigned gender), a strong preference for cross-dressing or simulating female attire; or in girls (assigned gender), a strong preference for wearing only typical masculine clothing and a strong resistance to the wearing of typical feminine clothing.
A strong preference for cross-gender roles in make-believe play or fantasy play.
A strong preference for the toys, games, or activities stereotypically used or engaged in by the other gender.
A strong preference for playmates of the other gender.
In boys (assigned gender), a strong rejection of typically masculine toys, games, and activities and a strong avoidance of rough-and-tumble play; or in girls (assigned gender), a strong rejection of typically feminine toys, games, and activities.
A strong dislike of one’s sexual anatomy.
A strong desire for the physical sex characteristics that match one’s experienced gender.
The condition must be associated with clinically significant distress or impairment in social, occupational, or other important areas of functioning.
Specify whether a Sexual Development Disorder is present.
20.3.3.3 Gender Dysphoria Criteria in Adolescents
A marked incongruence between one’s experienced/expressed gender and their assigned gender, lasting at least 6 months, as manifested by at least two of the following:
After confirming the diagnosis, the person affected by Gender Dysphoria must be informed about all strategies of treatments, as well as about the associated risks and the irreversibility of some of them. The symptoms described above explain the need to provide adequate responses to specific needs, bearing in mind, as we are about to clarify, the multifactorial nature of the condition of gender incongruence and of Gender Dysphoria.
20.4 Causes: Etiological Theories
The causes of Gender Dysphoria are still unclear and both psychosocial and biological factors have been implicated. Currently, the most accepted hypothesis is that both factors contribute to its development [ 6 , 7 ]. Even if social factors, such as education, environment, and events of life, are of great importance in emergence of gender dysphoria, there is still no experimental evidence to support this theory.
Studies carried out on twin populations have shown that in monozygotic twins (i.e. generated by the same egg-cell and, therefore, with the same genetic makeup) the possibility of gender dysphoria occurring in both twins is higher than in heterozygous twins (generated by two distinct egg cells and therefore with 50% of the same genetic makeup). This suggests genetic factors are important in gender dysphoria. There are also numerous theories that consider the influence of sex hormones on the onset of gender dysphoria. As established by animal model experiments, the process of sexual differentiation is not limited to the development of the genitals, but it involves the structures of the central nervous system that regulate sexual behaviours. Since the differentiation of the genitals occurs in the first 2 months of intrauterine life, while that of the central nervous system begins in the second half of pregnancy and becomes manifest in adult life, it has been hypothesized that in subjects with gender dysphoria these two processes occur in a disharmonic way. In this regard, the importance of prenatal male sex hormones, particularly testosterones, in development of male sexual identity was suggested. Indeed, some studies highlighted that low levels of testosterone in male foetuses can be associated with an increased incidence of Gender Dysphoria. Furthermore, a reduced sensitivity to testosterone and, therefore, a defective functioning of this hormone has been evidenced in MtF people.
Other studies focused on brain area differences between male and female population and suggested that cerebral architecture of individuals with Gender Dysphoria resembles the one of individuals with the same gender identity rather than those with the same biological sex, thus suggesting that non-biological factors may play a predominant role in GD genesis. The diagnosis of Gender Dysphoria requires evaluation by a mental health expert (psychologist or psychiatrist). In general, a psychologist or a psychiatrist assesses whether Gender Dysphoria criteria are satisfied, with a focus on the way feelings and behaviours develop over time, and on the family and social context (if it is present and supportive). The team also assesses all condition for differential diagnosis, i.e. a non-compliance to stereotyped gender role behaviours, or a strong desire to belong to another gender than the one assigned and the degree and pervasiveness of activities and interests that vary with respect to gender for reasons inherent to the gender role rather than identity. GD must be distinguished from Transvestic Disorder, a cross-dressing behaviour that generates sexual arousal and causes suffering and/or impairment without questioning one’s primary gender. GD differs from Body Dysmorphism; the focus is on the alteration or removal of a specific part of the body as it is perceived as abnormal and not because it is representative of an assigned gender that is repudiated. It should also be distinguished from psychotic mental disorders, in which gender inconsistency can be underlying a delusional construct.
20.5 Treatment
Treatment of Gender Dysphoria aims to reduce, or remove, suffering based on teamwork of psychologists, psychiatrists, endocrinologists, and surgeons. There are standards of care proposed by the World Professional Association of Transgender Health (WPATH, [ 8 ]) and international guidelines [ 9 ] which health workers refer to. Some people with Gender Dysphoria decide to modify their body to make it more alike to how they feel, through a “ path of affirmation of gender ” that proceeds in successive phases and can include hormonal and/or surgical treatment. Treatments are not always necessary and the treatment process is not the same for all people. Indeed, the procedure is different according to real needs of the individual.
20.5.1 Treatment for Children and Adolescents
First line treatment of GD in children and adolescents is psychological intervention that must be provided by mental health experts (child psychologists and neuropsychiatrists), especially if specialized in issues related to developmental age. Psychological support allows to face current problems and provides help to reduce emotional suffering sometimes allowing for more drastic treatment avoidance.
Non-medical intervention is planned. So far, there is no consensus about the best intervention with children with GD, because the studies on the effectiveness of the different psychological approaches are poor and inconclusive. However, there is expert convergence on the opinion that the aim of a clinical intervention in children with GD must be to reduce discomfort and—if present—the associated emotional difficulties. The goal is the psychological well-being of the child. The better described approach is the so-called watchful waiting , which has the aim to encourage people with GD to explore their gender identity for it to develop in a natural and spontaneous way, while the individual maintains a neutral attitude towards any development outcome. The aim of the clinician (psychologist and/or psychotherapist) is to inform and to train the family about GD and to support it in making decisions following a careful evaluation of costs and benefits. Major associations dealing with developmental age or transgender health, such as the World Professional Association for Transgender Health (WPATH) and the American Academy of Child and Adolescent Psychiatry, condemned all interventions aimed at identity gender modification as unethical or attempts at prevention of a future non-heterosexual orientation.
The approach to Gender Dysphoria in adolescence requires careful evaluation, with particular care in making differential diagnoses with other conditions in order to define individualized paths. For example, it is important to distinguish Gender Dysphoria from internalized homophobia that occurs in some adolescents who, failing to accept their homosexual orientation, may require a medical gender reassignment (GR). Depending on the cultural context, their belief system, or even stereotyped views of social arrangements, some homosexual adolescents may mistake their sexual orientation for gender identity, due to a history of borderline behaviours and cross-gender interests in childhood. First, differential diagnosis needs to exclude the “Transvestic Disorder”. Transvestism mostly characterizes male adolescents who occasionally wear female clothes without a connected sexual motivation; in fact, in adolescence this behavioural manifestation can represent a phase of experimentation. Transvestic Disorder in DSM-5 is among the Paraphilic Disorders and generally occurs in males of hetero- or bisexual orientation who experience sexual arousal in wearing women’s clothing associated with emotional distress. Transvestism disorder is distinguished from Gender Dysphoria because in the first case, gender identity is not in question. Gender Dysphoria must also be distinguished from “Body Dysmorphic Disorder” characterized by pervasive concern for presumed physical defects or imperfections, which are associated with repetitive behaviours in response to worries about such defects. In these cases, the modification or removal of a specific part of the body is required because it is perceived as abnormal or deformed, and not because it is attributable to the gender assigned at birth.
It is important to point out that Gender Dysphoria in adolescence is often accompanied by concomitant psychopathologies. Adolescents with Gender Dysphoria report higher levels of suicidal risk, depression, anxiety, social isolation, and bodily dissatisfaction.
The persistence of Gender Dysphoria in adolescence and the frequency of other associated psychopathologies—reactively to the condition of Gender Dysphoria—supports the importance of early intervention, including medical intervention. The guidelines of the Endocrine Society and the WPATH Standards of Care, together with the recommendations of the main national scientific societies, suggest to interrupt pubertal development with GnRH analogues (GnRHa) in adolescents with GD who meet specific criteria, i.e. an early onset of DG whose symptoms intensified during the early stages of puberty; the absence of psychosocial issues that may have interfered with diagnosis or treatment; a good understanding for the consequences of GR (Gender Reassignment) in one’s existence. In addition to psychological support, the administration of GnRHa is indicated to postpone puberty when Tanner stage 2 has been reached. GnRH analogues, which are prescribed by the endocrinologist, work by suppressing the production of sex hormones, therefore they block the physical changes induced by puberty. Therefore, they allow adolescents for a longer exploration of their gender identity and the mental health experts to observe adolescents’ gender identity while relieving the suffering that can come from contact with a body that develops in an unwanted direction. The effects of therapy with GnRH analogues are completely reversible: if the treatment is interrupted, pubertal development immediately begins in the direction of biological sex. If GD persists and if specific eligibility criteria are met, it is possible to start a first hormonal GR, from 16 years onwards with the intake of cross-sex hormones (CHT). Surgery is also allowed as an extreme strategy, but better after age of 18.
20.5.2 Treatment for Adults
Psychological support if necessary.
Feminizing or masculinizing hormone treatment (cross-sex therapy).
Sex reassignment surgery.
In this section, we will deal with the psychological support provided to people with Gender Dysphoria, mentioning hormone therapy only in relation to the involvement of mental health professionals. The prerequisite for any psychotherapeutic approach can be summarized in some fundamental requirements that health professionals must apply always and in every area such as: the respect due to users with Gender Dysphoria without pathologizing the differences related to gender identities and expressions; the ability to provide adequate information about the services that transsexual, transgender and gender non-conforming people can benefit from the National Health System and, in particular, on the benefits and risks of the treatment; to guarantee personalized psychotherapeutic approaches, which are shaped on the individual needs; to facilitate the access to the most appropriate cures based on the condition of the individual. Taking charge of user with Gender Dysphoria provides for multiple paths and possibilities that the psychologist and/or psychotherapist are required to know. Indeed, some people do not feel the need to modify the somatic characteristics of their body—through medical-surgical paths of virilization or feminization—especially if capable of integrating their trans- or cross-gender experience in the gender assigned at birth. Alternatively, people may consider only a few changes in gender role or gender expression or wish to make a transition even physical in line with the change in their gender role, requiring hormonal therapies but not surgery. Finally, people may wish surgery to complete the transition process and thus alleviate dysphoria but not other non-surgical strategies. It is therefore essential for health professionals, and especially for psychologists and psychotherapists, to make an effort to deeply understand the individual’s life history and support him/her in an individualized way.
In fact, treatment of gender dysphoria should always explore the different possibilities of expression of identity. Psychotherapy (individual, couple, family, or group) therefore aims: to explore gender identity, role, and expression; to alleviate the stressful impact of Gender Dysphoria and social stigma on mental health; to reduce internalized transphobia; to provide tools for the user to enhance their social network and peers; to improve their body image; and ultimately to promote resilience.
Hormone therapy can be prescribed to all people with persistent and well-documented Gender Dysphoria; who are of age (if minors it is necessary to refer to guidelines for adolescents with gender dysphoria); they must be able to make a fully informed decision and to agree with the treatment and, finally, that they do not present medical or psychological problems.
In order to start hormone therapy, no minimum time for evaluation, psychological support, or social transition is required. However, the physician prescribing sex hormones (usually an endocrinologist) has the responsibility of making sure that hormone therapy is the best way to meet the user’s needs and reduce their suffering, without inducing health problems. Therefore, it is considered appropriate to provide multidisciplinary care, so that different professional skills are continuously integrated. An accurate assessment of the psychological and existential status of the person, as well as their psychosocial context of reference, is necessary.
It is good to proceed to:
Analysis and evaluation of the psychological motivations that led the subject to undertake his/her treatment path;
Analysis of awareness of achievable goals and hypothesized emotional reactions related to the realistic change of the body according to the desired identity, to any sex reassignment surgery procedures, to the functionality of the genital system;
Assessment of the users’ ability to share with their family and social context with respect to their transition process and assessment of the resources of the family and social context to welcome and support the user.
Such a general assessment is necessary in order to have a snapshot of the personal and relational situation of the user with Gender Dysphoria and make psychotherapeutic management personalized.
However, it is important to underline WPATH recognizes that health does not depend only on clinical care, but also on a social and political climate that guarantees social tolerance, equality, respect, and the full right of citizenship. Health is guaranteed with public policies and legal reforms that promote tolerance and fairness towards all gender differences and aimed to eliminate prejudice, discrimination, and stigmatization.
A significant part of transgender people’s suffering originates precisely from the stigmatization deriving from a stereotyped vision of the concept of gender along with all additional stressors, connected to the stigma of gender non-conformity, and that may negatively affect the psycho-physical health of the individual. This phenomenon, known as Minority Stress, affects people belonging to social categories stigmatized and subjected to excessively high levels of stress, such as those derived from violence, discrimination, and stigmatization. Stigma can certainly be defined as a social process that negatively connotes a member or a community based on its characteristics to which inferior qualities are arbitrarily attributed. Stigma can be experienced on at least three levels: structural, interpersonal, and individual. Structural stigma refers to the level of social institutions and it constitutes a barrier to access to fundamentals, such as work or care; the interpersonal stigma is a particular behavioural structure which manifests itself through verbal abuse, physical or sexual violence, or threats; the individual stigma instead refers to the feelings and emotions that the stigmatized person feels or what he believes that others think of himself. All three types of stigma are widely represented among transgender people and connected with the adverse psycho-physical health outcomes. It is evident that psychotherapy work must focus on the individual’s resources to promote resilience, while being aware that structural and interpersonal aspects of the stigma cannot be eradicated with psychotherapeutic work alone.
20.6 Conclusions
The formation and definition of transgender and transsexual identity have a high specific complexity, to which environmental and cultural stigmatizations add further complexity. However, it is essential to recognize that the transgender and transsexual evolutionary path preserves the typical dynamics of any identity construction process. Therefore, in clinical work with these people, it is important to consider both the identity structure of the person and the universal evolutionary processes. Approaching transsexual people with the prejudice of an absolute diversity in the formation of the self and identity can compromise the understanding of psychological processes behind while preventing from a fully empathic relationship, that is needed in order to establish a good therapeutic alliance.
American Psychiatric Association (APA). Diagnostic and statistical manual of mental disorders: fifth edition (DSM-5). Washington DC: American Psychiatric Association; 2013.
Book Google Scholar
American Psychiatric Association (APA). Diagnostic and statistical manual of mental disorders: 5fth edition (DSM-5). Washington DC: American Psychiatric Association. 2013.
Google Scholar
Lingiardi V, Giovanardi G, Fortunato A, Nassisi V, Speranza AM. Personality and Attachment in Transsexual Adults. Arch Sex Behav. 2017 Jul;46(5):1313-1323. https://doi.org/10.1007/s10508-017-0946-0 . Epub 2017 Feb 16. PMID: 28210932.
WPATH 2012” World Professional Association for Transgender Health. Standards of Care for the Health of Transsexual, Transgender, and Gender Nonconforming People [7th Version]. (2012). https://www.wpath.org/publications/soc .
Zucker KJ. Epidemiology of gender dysphoria and transgender identity [Sintesi]. Sex Health. 2017;14(5):404–11.
Article Google Scholar
Chipkin SR, Kim F. Ten Most important things to know about caring for transgender patients. Am J Med. 2017;130:1238–45.
Winter S, et al. Transgender people: health at the margins of society [Sintesi]. Lancet. 2016;388:390–400.
Coleman E, et al. Standards of Care for the Health of transsexual, transgender, and gender-nonconforming people, version 7 [Sintesi]. Int J Transgend. 2012;13(4):165–232.
Hembree WC, et al. Endocrine treatment of gender-dysphoric/gender-incongruent persons: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2017;102:3869–903.
Link to Further Information
ICD-11. Gender incongruence of adolescence or adulthood: https://www.who.int/standards/classifications/frequently-asked-questions/gender-incongruence-and-transgender-health-in-the-icd .
Infotrans: https://www.infotrans.it/ .
Mayo Clinic. Gender Dysphoria: https://www.mayoclinic.org/diseases-conditions/gender-dysphoria/symptoms-causes/syc-20475255 .
NHS Choices. Gender Dysphoria: https://www.nhs.uk/conditions/gender-dysphoria/ .
ONIG: https://www.onig.it/drupal8/ .
World Professional Association for Transgender Health. Standards of care: https://www.wpath.org/soc8 .
Download references
Author information
Authors and affiliations.
“Azienda Ospedaliera Universitaria Policlinico di Bari”—Psychiatry Unit, Bari, Italy
Elisabetta Lavorato
Group of Psychiatric Neuroscience, Department of Basic Medical Sciences, Neuroscience and Sense Organs, University of Bari Aldo Moro, Bari, Italy
Antonio Rampino & Valentina Giorgelli
You can also search for this author in PubMed Google Scholar
Editor information
Editors and affiliations.
Andrology and Male Genitalia Reconstructive Surgery Unit, University of Foggia, Policlinico “Riuniti” Foggia, Foggia, Italy
Carlo Bettocchi
Department of Urology, University of Foggia, Policlinico “Riuniti” Foggia, Foggia, Italy
Gian Maria Busetto
Giuseppe Carrieri
Department of Urology and Andrology, University of Foggia, “L. Bonomo” Teaching Hospital Andria, Andria, Italy
Luigi Cormio
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Reprints and permissions
Copyright information
© 2023 The Author(s)
About this chapter
Cite this chapter.
Lavorato, E., Rampino, A., Giorgelli, V. (2023). Gender Dysphoria: Overview and Psychological Interventions. In: Bettocchi, C., Busetto, G.M., Carrieri, G., Cormio, L. (eds) Practical Clinical Andrology. Springer, Cham. https://doi.org/10.1007/978-3-031-11701-5_20
Download citation
DOI : https://doi.org/10.1007/978-3-031-11701-5_20
Published : 15 October 2022
Publisher Name : Springer, Cham
Print ISBN : 978-3-031-11700-8
Online ISBN : 978-3-031-11701-5
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
- Open access
- Published: 02 January 2024
Physical and psychosocial challenges of people with gender dysphoria: a content analysis study
- Zahra Ghiasi 1 ,
- Fatemeh Khazaei 2 ,
- Mohsen Khosravi 3 &
- Nasrin Rezaee 4
BMC Public Health volume 24 , Article number: 16 ( 2024 ) Cite this article
1292 Accesses
Metrics details
The mismatch between the gender experienced by a person and the gender attributed to him/her leads to gender dysphoria. It seems that people’s perception of gender dysphoria is affected by individual, cultural, and sociological factors and these factors affect different aspects of their biological, psychological, and social health. To this end, this qualitative study aimed to identify the physical, psychological, and social challenges of people with gender dysphoria referring to the Department of forensic medicine in Iran.
This qualitative study was conducted using conventional content analysis on 9 individuals who were selected through purposive sampling. A total of 16 interviews were conducted with 9 participants. Each interview lasted 60–90 min. The participants’ gender dysphoria was confirmed by the Department of forensic medicine. The data were collected through face-to-face semi-structured interviews with the participants.
The data revealed 3 main categories and 10 subcategories. The main categories were living in agony, confusion, and social concerns. The subcategories were annoying physical characteristics, mental suffering, disturbing sexual changes, concerns about public reaction, helplessness, surrender, the final solution, retreating to isolation, stressful family conditions, and lack of public recognition.
The findings showed that people with gender dysphoria suffer from some problems including living in agony, confusion, and social concerns. Each of these problems is associated with several challenges. It seems that most of the challenges faced by people with gender dysphoria are caused by unawareness of their conditions by the family and the public, which in turn is caused by the failure of related organizations and experts in this field to provide adequate information about the conditions of these people. Thus, the findings of the present study can have some implications for resolving the challenges faced by people with gender dysphoria.
Peer Review reports
Gender dysphoria (GD) refers to a person’s dissatisfaction with the sex assigned at birth. According to the diagnostic criteria, gender dysphoria refers to cases such as the mismatch between the gender experienced and the secondary or primary sexual characteristics of the person, a strong preference to get rid of the secondary or primary sexual characteristics, and a strong desire to have another gender [ 1 ]. Gender dysphoria is often associated with a person’s dissatisfaction with their physical appearance. An unfavorable physical appearance may lead to an unclear perception of gender identity. The mismatch between the gender experienced by an individual and the gender attributed to them in the community leads to the individual’s dissatisfaction [ 2 ]. Gender identity affects all aspects of people’s lives. People with gender dysphoria experience some degree of discrimination due to gender experiences that are not in line with the normal values of society [ 3 ]. Some of the people who cannot stand public judgments suffer many traumatic experiences in their daily life and as a result, they may hide their feelings about their gender identity to the extent that they even prefer to live in a different place and hide their past after sex reassignment surgery [ 4 ].
Gender dysphoria usually develops in early childhood and can remain stable for years until gender changes. Early diagnosis and measures during childhood and adolescence can reduce the probability of comorbidities and improve the quality of life of the affected person [ 5 ]. Studies conducted in Turkey, the Netherlands, and Iran show that gender reassignment surgery has a positive effect on the quality of life, family support, and interpersonal relationships of people with gender dysphoria [ 4 , 6 , 7 ]. A review study showed that people with gender dysphoria have a high risk of suffering from mental illnesses [ 8 ]. A majority of people with gender dysphoria may undergo stressful conditions due to gender identity conflict and discomfort with their biological gender [ 9 ]. A study in the United States showed that depression, anxiety, and suicidal thoughts are more prevalent among GD sufferers than in the general population [ 8 ]. Another study in the United States showed that gender reassignment improves the health, self-confidence, and quality of life of people with GD [ 9 ]. A study by Yıldızhan et al. (2018) in Turkey compared the lifestyle, social relationships, and quality of life of people with GD who had or had not performed gender reassignment surgery. The results showed people who had performed gender reassignment surgery had reduced anxiety related to gender discrimination, but increased anxiety related to disclosure of their past compared to the group who did not perform this surgery [ 4 ].
It seems that people’s perception of gender dysphoria is affected by individual, cultural, and sociological factors, and these factors affect various aspects of their biological, psychological, and social health. In Iran, gender reassignment and surgery are simply not possible for GD patients. In Iran, changing one’s legal gender can be a difficult and complex process. This is because the country’s legal system is based on Islamic law, which has specific rules and regulations regarding gender and related issues. Additionally, certain cultural and social attitudes toward gender can make it challenging for individuals to change their gender identity [ 10 ]. Thus, to better understand the challenges faced by these people, it is necessary to analyze their experiences and statements in a real context. Qualitative research helps the researcher to identify the challenges ahead by entering the inner world of these people and exploring their perspectives.
Sistan and Baluchistan province is located in the southeast of Iran. In this province, due to religious and cultural beliefs, it is difficult to talk about gender dissatisfaction, because it is Guilt and taboo. In addition, no institution provide support for GD individuals. However, no qualitative study has addressed the physical, psychological, and social challenges faced by people with gender dysphoria in the cultural and social context of Sistan and Baluchistan Province. Research findings in this field will help therapists to provide effective solutions for people with gender dysphoria to improve their health.
This study sought to identify the physical, psychological, and social challenges faced by people with gender dysphoria referring to the department of forensic medicine in Zahedan, Iran.
Study design and setting
This qualitative study was conducted using conventional content analysis to explore the physical, psychological, and social challenges faced by people with gender dysphoria referring to the Department of forensic medicine in Zahedan. The conventional content analysis approach is a flexible method for analyzing textual data. This approach is used when there is not enough knowledge about a phenomenon. Using an inductive approach, conventional content analysis focuses on the creation and development of categories and the interpretation of written or spoken content [ 11 ].
Participants
The participants in this study were selected through purposive sampling from people whose gender dysphoria was confirmed by the Department of forensic medicine and who were willing to participate in the study.
Data collection
The data in this study were collected through face-to-face semi-structured interviews from June to late November 2022. The transcripts of the interviews were analyzed using conventional content analysis. A total of 16 interviews were conducted with 9 participants. Each interview lasted 60–90 min. The interviews were conducted in the forensic medicine department in a private room where the participants feel comfortable. Examples of the questions asked in the interview were as follows; How do/did you feel about your gender? How did you deal with it? How did you talk about it with your parents? How did your parents react to it? (Could you describe your memories?) Could you talk about your situation in the community (outside home/school/sports/extracurricular activities/workplace)? (Could you give some examples and describe your memories?) What irregular experience did you experience in the community? How do you interact with the people around you (family members, friends) and vice versa? How is their relationship with you? And what solutions do you think will help you to reduce your problems? Moreover, probing questions (e.g., what do you mean? Could you please give an example) were asked for further clarification. The interviews continued until data saturation i.e., when no new information was obtained from additional interviews. The participants’ interviews were recorded using a voice recorder and then transcribed into an MS Word file for subsequent analysis.
Data analysis
Data analysis was done at the same time as data collection.To analyze the data, the texts of the interviews were read several times and then the primary codes were extracted. The extracted codes with similar meanings merged into more general clusters. The extracted clusters were revised and placed into some categories and subcategories around a core category [ 12 ].
In qualitative research, the rigor of the data is established through four criteria of dependability, credibility, transferability, and confirmability [ 13 ]. In this study, the researcher was engaged with the research procedure for 2 years. The rigor of the data was established through continuous reviews of the data i.e., transcribing the interviews, reviewing the data to extract the main categories, and revising the data through the member and peer checking. The dependability of the data was confirmed through the prolonged engagement with the data in all stages of the study.
Table 1 shows the participants’ demographic characteristics. The analysis of the data revealed 3 main categories and 10 subcategories. The main categories were living in agony, confusion, and social concerns. The subcategories were annoying physical characteristics, mental suffering, disturbing sexual changes, concerns about public reaction, helplessness, surrender, the final solution, retreating to isolation, stressful family conditions, and lack of public recognition as shown in Table 2 .
A. Living in agony
One of the challenges pointed out by the participants in this study was living in agony due to annoying physical characteristics and mental suffering (Table 2 ).
Annoying physical characteristics
The participants stated that they had to live in agony due to annoying physical features. Thus, they suffered from female appearance, hid and disliked their feminine characteristics, and hated their feminine appearance. Accordingly, one of the participants stated:
“ I usually try not to look at myself in the mirror from the neck down. It bothers me to see this feminine look. I try not to be seen in any way. Sometimes I have to wear a chador ” (Participant #2).
Another participant narrated her childhood memories:
“ I remember the first day of primary school when I was sent to a girls’ school. I was crying about why my parents didn’t send me to a school for boys. Even my mother told me when I was 4 years old, I cried a lot when they asked me to wear female dresses and earrings while going to a relative’s wedding and I told them I was a boy and why should I wear them ” (Participant #4).
Mental suffering
The participants stated that they had a lot of mental suffering because of distress, unforgivable sin, endless abuse, guilt, living in a cage, extreme humiliation, and being the black sheep of the family. One of the participants stated:
“ Despite my religious beliefs, I had a lot of mental suffering that turned my life into a real hell. Even if God said you shouldn’t do this, I couldn’t accept it ” (Participant #6).
Another participant described the deprivation from gender identity:
“It bothers me a lot that I cannot be a perfect man even by undergoing gender reassignment surgery. I have told God many times why, despite all the efforts I have made to be a good person and not commit any sin, I have to suffer a lot for being deprived of the simplest blessing, which is having a body that matches my identity ” (Participant #1).
Disturbing sexual changes
The participants reported concerns about their sexual changes including concerns about impotence, their appearance after gender reassignment surgery, marriage after the surgery, their sexual partners, and fertility after the surgery. One of the participants said:
“ One of my concerns is that after surgery and hormone therapy, I will not have the feminine look and physique I desire ” (Participant #3).
Another participant stated: “ I think a lot about my marriage after the surgery. I wonder if there will be someone who will accept me with these conditions ” (Participant #4).
Concerns about public reaction
The participants reported that they were afraid of other people’s reaction to their new sexual identity and they were worried about the parents’ reaction, the family’s behavior, not being accepted after the surgery, people’s curiosity about their previous sexual identity, and the lack of public recognition of their new identity. One of the participants stated: “ I am worried that I will not be recognized as male by the people around me even after the gender reassignment surgery ” (Participant #1).
Another participant was worried that others would find out about his former sexual identity: “ I am worried that after the surgery, people will find out about my past and my previous gender identity ” (Participant #8).
B. Confusion
One of the challenges reported by the people with gender dysphoria was confusion that led to their helplessness, surrender, and the final solution (Table 2 ):

Helplessness
The participants stated that they felt helpless due to the lack of family support in choosing the type of clothing, confusion about their sexual identity, other people’s confusion about their identity, and complaints about God. One of the participants stated:
“ Once my sister and I went to a bank to open a bank account. We were wearing male clothes. The bank clerk refused to open a bank account and said that our identity documents belong to two girls, but you are boys ” (Participant #1).
Another participant stated:
“ My parents were confused from the very beginning. They realized that I was different from the others, but they didn’t know exactly that I had gender dysphoria. They only knew that I had girlish behaviors. Even my mother told me that when I was 4, I used to play with the girl next door and I preferred to play with dolls ” (Participant #5).
A third participant reported:
“ At first, I didn’t know exactly what condition I was suffering from and I only knew that I was different from other children of my age and this was a secret that I had to keep with me and I really felt helpless ” (Participant #6).
The participants reported that they had to surrender to the challenges faced by them such as wearing clothes according to local norms, other people’s surprise at their identity, family conflict, and futile attempts to keep their identity. One of the participants said:
“ I have to wear girl’s clothes outdoor in public places; otherwise, I will face other people’s surprise or their judgmental behavior ” (Participant #4).
“ Although I had a boyish appearance at school, my friends and school staff said that I behaved like a girl, and I was teased many times by my classmates and teachers. At first, it was very painful for me, but I got used to it little by little ” (Participant #5).
The final solution
The participants stated that they had to make a final decision to overcome their challenges such as insistence, preparing for independence or being rejected after the gender reassignment surgery, leaving school due to clothing not fitting their gender, committing suicide when feeling helpless, migration, and deciding to have a specific gender identity. One of the participants stated:
“ If I conclude that there is no way out of this situation, I will think of committing suicide ” (Participant #4).
However, another participant stated:
“ Finally, I will do a gender reassignment surgery, but probably I will be rejected by my family, or my current partner will break her relationship with me. In any case, true identity is important to me ” (Participant #3).
C. Social concerns
The participants in this study talked about their social concerns and stated that retreating to isolation, stressful family conditions, and lack of public recognition were their main social concerns and challenges (Table 2 ).
Retreating to isolation
The participants reported that they preferred to retreat to isolation due to their annoying clothing, feeling safe in isolation, fear of the disclosure of their true identity, low self-confidence, and disillusionment with their current identity. One of the participants stated:
“ We had a female classmate with a lot of extra hair on her body due to hormonal problems. The students rumored that she was bisexual. This rumor spread quickly in the university, and unfortunately, it had a bad psychological effect on that girl so she had to continue her studies at another university. This caused a lot of anxiety for me and I was very afraid of the students finding out about my problem. Thus, I had to not communicate with anyone ” (Participant #8).
“ I don’t go out much, but sometimes when I go to a coffee shop or restaurant with my partner, especially in men’s clothes, people look at us with surprise, and some even point at us mockingly and say that we are gay. Things get worse and they make fun of me when I start talking. Well, I don’t come out anymore ” (Participant #3).
Stressful family conditions
The participants reported stressful family conditions as one of their social concerns caused by the tense psychological atmosphere in the family, forced and disgusting marriage, the sense of being the black sheep of the family, the persuasion of the parents, and religious bias. One of the participants stated:
“ On the street and in places where I feel that someone might recognize me, I wear girl’s clothes or appear less frequently because no one except my family members knows about this. The reputation of my family is very important to me and I am afraid of people’s reaction ” (Participant #4).
“ My father forced me to get engaged to a girl. We didn’t have any kind of emotional relationship, and even when she sat next to me, she gave me a disgusting feeling. There was a lot of tension in the family because of my resistance to getting married, but in the end, I decided to break up with her ” (Participant #3).
Lack of public recognition
Another social concern of the participants was the lack of public recognition including non-acceptance of appearance characteristics, futile attempts to convince others, public unawareness, non-acceptance of gender identity by others, worry about police threats, people surprise, obstacles to finding a job, public judgment, and interrogation in public and governmental departments and offices. A participant stated:
“ When I went to the court to get an introduction letter to the forensic medicine department, the judge reacted badly and said that there was no such thing, as a person can be either a man or a woman, and all these were my illusions. Upon hearing this answer, I had a terrible feeling ” (Participant #9).
Another participant reported:
“ I was busy painting a building. I heard from one of my friends that somebody told the owner of the house that the guy who was painting the house was bisexual and he wants this money for the gender reassignment surgery. He had convinced the owner that he would commit a great sin if he allowed me to paint the house and he would be disgraced. Thus, the owner dismissed me ” (Participant #6).
“ I can never go to public places with peace of mind because I hate other people’s judgments about me. For example, they say I’m bisexual or how ugly it is for a girl to act like a boy or other things that they may say about me ” (Participant #4).
This study sought to examine the physical, psychological, and social challenges faced by people with gender dysphoria. The data analysis showed that living in agony, confusion, and social concerns were the main challenges faced by people with gender dysphoria. The participants stated that they were living in agony due to their annoying physical characteristics and they hated and tried to hide feminine features. In their study from 2007 to 2012 in Amsterdam, van de Grift et al. showed that having a physical appearance inconsistent with gender identity may lead to more difficult psychological adaptation and exposure to discrimination and stigma [ 2 ]. Moreover, in their study in England, Coleman-Smith et al. (2020) showed that all the participants reported distress and suffering as a result of the mismatch between their gender identity and the gender they were born with [ 14 ]. A study by Campbell et al. (2018) in Africa showed that many people with gender dysphoria have a strong desire to have the opposite gender due to their suffering caused by their different physical characteristics [ 15 ]. It seems that the participants’ suffering due to their physical characteristics is caused by the mismatch between their true gender identity and their biological gender, and this mismatch can be the source of a lot of psychological harm in these people.
Another challenge reported by the participants with gender dysphoria was their concerns about sexual changes due to the development of secondary sexual characteristics, as well as functional impairment and the inability to have sex after the gender reassignment surgery, and concerns about the public reaction after realizing their conditions and their previous gender identity. In their study in Turkey, Yıldızhan et al. (2018) showed people who had performed gender reassignment surgery had reduced anxiety related to gender discrimination, but increased anxiety related to disclosure of their past compared to the group who did not perform this surgery [ 4 ]. Another study by Holt et al. (2016) in England showed that the level of anxiety and worry in people with gender dysphoria increases when reaching puberty, so a significant percentage of these people experienced suicidal thoughts, low mood, and depression [ 16 ]. Another study conducted by Ross and Need (1989) in the United States showed that people with gender dysphoria have concerns about sex reassignment, including erectile dysfunction, lack of social support, family reactions, urinary incontinence, and the need for more surgeries [ 17 ]. Following these findings, people with gender dysphoria develop concerns about the occurrence of changes caused by secondary sexual characteristics and the intensification of the conflict between their true sexual identity and their physical appearance. Besides, the sexual changes developed after gender reassignment may not be efficient in creating a proper sexual relationship. In addition, public unawareness of the conditions of these people and the conflict between their bodies and gender identity before the surgery can make other people mistreat people with gender dysphoria. However, after the surgery, people’s awareness of their past conditions and the lack of public recognition may create concerns in these people.
The patients with gender dysphoria in this study also reported that sometimes they felt confused and helpless and thus they decided to commit suicide. Some of the participants stated that if for any reason they could not undergo gender reassignment surgery, they would inevitably surrender to it and would live in distress caused by the conflict between their true gender identity and their body for the rest of their lives. A study by Ghazanfari et al. (2018) in Iran showed that due to the stigma caused by gender dysphoria, a large number of people with this condition never go to a psychiatrist, some emigrate and some spend the rest of their lives in distress, and confusion caused by the conflict between body and soul [ 18 ]. Another study by Mantashloo et al. (2019) in Iran showed that psychological pain, feelings of helplessness, withdrawal from life events, isolation, and suppression of emotions are more common in people with gender dysphoria [ 19 ]. In their study in Canada, Aitken et al. (2016) found that one of the possible reasons for the presence of suicidal thoughts and self-harm behaviors in people with gender dysphoria is that gender dysphoria itself inherently causes distress and confusion in these people [ 20 ]. Moreover, a study by Peterson et al. (2017) in the United States showed that the prevalence of suicide attempts and self-harm was higher in people who tended to have a male gender than those who tended to have a female gender [ 8 ]. It seems that a feeling of helplessness and confusion in these people is caused by psychological distress due to gender dysphoria that they have experienced. Besides, one of the reasons why these people surrender to the special conditions they experience and do not perform gender reassignment surgery can be the stigma caused by gender dysphoria in Iran. Under the influence of cultural and religious norms, people consider gender reassignment surgery as a sin, making the performance of this surgery more difficult for people with gender dysphoria, and this can intensify the feeling of helplessness and confusion in these people and force them to surrender to the status quo.
The participants in this study talked about their social concerns and stated that retreating to isolation, stressful family conditions, and lack of public recognition were their main social concerns and challenges. However, Wong and Drake (2017) evaluated the experiences of parents who allowed their children with GD to change social roles at an early age in Canada and showed that these children had better social relations and more effective interactions with their parents [ 21 ]. Javaherian and Koochakian (2006) showed that although gender reassignment surgery is allowed in Iran’s legal system, people with gender dysphoria face many social and cultural problems in private and public areas [ 22 ]. Furthermore, in their study in Iran, Rahimi Ahmadabadi et al. (2016) showed that people with gender dysphoria scored higher than the control group in terms of stress, anxiety, depression, and gender role disorder. They also found that raising parents’ awareness cannot solve the problems associated with gender dysphoria because it has cultural, social, and reputational aspects [ 23 ]. In another study in Iran, Heidari et al. (2020) indicated that the reaction of the family members of people with gender dysphoria to their situation follows a wide spectrum and families do their best to avoid shame and embarrassment in the community [ 24 ]. Previous studies have also reported that people with gender dysphoria may be rejected by their families, especially after they reveal their true gender identity. They may also lose support from their families and friends. These studies show that people with gender dysphoria who sought treatment did not have the desire to find new friends until they completed gender reassignment procedures, and all these cases lead to the isolation of these people [ 25 , 26 ].
It seems that most of the challenges faced by people with gender dysphoria are caused by unawareness of their conditions by the family and the public, which in turn is caused by the failure of related organizations and experts to provide adequate information about the conditions of these people. Thus, psychological and culture-based interventions may be effective in solving these challenges.
One of the limitations of the present study was the unavailability of people with gender dysphoria. Thus, to collect adequate data, additional interviews were conducted with the participants to address all aspects of the issue in question.
The findings of the present study show the numerous personal and social challenges of people suffering from gender dysphoria, which appeared in the classes of “living in agony”, “confusion” and “social concerns”. The findings indicate that the challenges of these people are caused by the lack of understanding of their conditions by the family and society, and it is a sign of the lack of awareness of families and communities about their conditions and poor information from the responsible institutions, so the results of this study can be By recognizing the challenges, it can be the solution to the problems of these people. It is suggested to conduct a qualitative study on the experiences of these people’s families.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available to protect the privacy of study participants but are available from the corresponding author upon reasonable request.
Butler G, De Graaf N, Wren B, Carmichael P. Assessment and support of children and adolescents with gender dysphoria. Arch Dis Child. 2018;103(7):631–6. https://doi.org/10.1136/archdischild-2018-314992 .
Article PubMed Google Scholar
van de Grift TC, Cohen-Kettenis PT, Steensma TD, De Cuypere G, Richter-Appelt H, Haraldsen IR, Dikmans RE, Cerwenka SC, Kreukels BP. Body satisfaction and physical appearance in gender dysphoria. Arch Sex Behav. 2016;45(3):575–85. https://doi.org/10.1007/s10508-015-0614-1 . Epub 2015 Oct 16. PMID: 26474976.
Cooper K, Russell A, Mandy W, Butler C. The phenomenology of gender dysphoria in adults: a systematic review and meta-synthesis. Clin Psychol Rev. 2020;80:101875. https://doi.org/10.1016/j.cpr.2020.101875 . Epub 2020 Jun 11. PMID: 32629301; PMCID: PMC7441311.
Article PubMed PubMed Central Google Scholar
Özata Yıldızhan B, Yüksel Ş, Avayu M, Noyan H, Yıldızhan E. Effects of gender reassignment on Quality of Life and Mental Health in people with gender dysphoria. Turk Psikiyatri Derg. 2018;29(1):11–21. PMID: 29730870.
PubMed Google Scholar
Zaliznyak M, Bresee C, Garcia MM. Age at First experience of gender Dysphoria among Transgender adults seeking gender-affirming Surgery. JAMA Netw Open. 2020;3(3):e201236. https://doi.org/10.1001/jamanetworkopen.2020.1236 .
van de Grift TC, Elaut E, Cerwenka SC, Cohen-Kettenis PT, Kreukels BPC, Surgical Satisfaction. Quality of life, and their association after gender-affirming Surgery: a follow-up study. J Sex Marital Ther. 2018;44(2):138–48. https://doi.org/10.1080/0092623X.2017.1326190 .
Simbar M, Nazarpour S, Mirzababaie M, Emam Hadi MA, Ramezani Tehrani F, Alavi Majd H. Quality of life and body image of individuals with gender dysphoria. J Sex Marital Ther. 2018;44(6):523–32. https://doi.org/10.1080/0092623X.2017.1419392 .
Peterson CM, Matthews A, Copps-Smith E, Conard LA, Suicidality. Self-Harm, and body dissatisfaction in Transgender adolescents and emerging adults with gender dysphoria. Suicide Life Threat Behav. 2017;47(4):475–82. https://doi.org/10.1111/sltb.12289 .
White Hughto JM, Reisner SL. A systematic review of the effects of hormone therapy on psychological functioning and quality of life in Transgender individuals. Transgender Health. 2016;1(1):21–31. https://doi.org/10.1089/trgh.2015.0008 .
Pirnia B, Pirnia K. Sex reassignment Surgery in Iran, Re-birth or Human Rights Violations against Transgender people? Iran J Public Health. 2022;51(11):2632–3. https://doi.org/10.18502/ijph.v51i11.11183 . PMID: 36561249; PMCID: PMC9745420.
Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures, and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(2):105–12. https://doi.org/10.1016/j.nedt.2003.10.001 .
Article CAS PubMed Google Scholar
Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs. 2008;62(1):107–15. https://doi.org/10.1111/j.1365-2648.2007.04569.x .
Lincoln YS, Guba EG. (1985) Naturalistic Inquiry. 1985:SAGE, Thousand Oaks, 289–331. https://doi.org/10.1016/0147-1767(85)90062-8 .
Coleman-Smith RS, Smith R, Milne E, Thompson AR. Conflict versus congruence’: a qualitative study exploring the experience of gender dysphoria for adults with Autism Spectrum Disorder. J Autism Dev Disord. 2020;50(8):2643–57. https://doi.org/10.1007/s10803-019-04296-3 .
Campbell MM, Fresán A, Addinall RM, Böhmke W, Grobler GP, Marais A, Wilson D, Stein DJ, Reed GM, Robles R. Experiences of gender incongruence and the relationship between social exclusion, psychological distress, and dysfunction among South African transgender adults: a field-study for ICD-11. Ann Clin Psychiatry. 2018;30(3):168–74. PMID: 30028890.
Holt V, Skagerberg E, Dunsford M. Young people with features of gender dysphoria: demographics and associated difficulties. Clin Child Psychol Psychiatry. 2016;21(1):108–18. https://doi.org/10.1177/1359104514558431 .
Ross MW, Need JA. Effects of the adequacy of gender reassignment Surgery on psychological adjustment: a follow-up of fourteen male-to-female patients. Arch Sex Behav. 1989;18(2):145–53. https://doi.org/10.1007/BF01543120 .
Ghazanfari F, Khodarahimi S. Gender dysphoria disorder: diagnosis, theory, and intervention. Rooyesh. 2018;6(4):9–28. http://frooyesh.ir/article-1-981-en.html .
Google Scholar
Mantashloo S, Shairi M, Heydarinasab L. Comparison of personality characteristics between people with gender dysphoria disorder and healthy subjects. Health Res J. 2019;4(2):96–103.
Article Google Scholar
Aitken M, VanderLaan DP, Wasserman L, Stojanovski S, Zucker KJ. Self-harm and suicidality in children referred for gender dysphoria. J Am Acad Child Adolesc Psychiatry. 2016;55(6):513–20. https://doi.org/10.1016/j.jaac.2016.04.001 .
Wong W, Drake S. A qualitative study of transgender children with early social transition: parent perspectives and clinical implications. pijss [Internet]. 2017 Nov. 1 [cited 2023 Feb. 4];3(2):1970-85. Available from: https://grdspublishing.org/index.php/people/article/view/1128 .
Javaherian F, Koochakian Z. Gender identity disorders and its social aspects: the Case Study on Trans sexuality in Iran. Refahj. 2006;5(21):265–92. http://Refahj.uswr.ac.ir/article-1-2054-en.html .
Rahimi Ahmadabadi S, Hejazi A, Attaran H, Rahimi A, Kohestani L, Karashki H, et al. Comparison of stress, anxiety, Depression & sexual role in subjects involved gender dysphoria with normal subjects. Iran J Forensic Med. 2016;22(1):67–75. http://sjfm.ir/article-1-783-en.html .
Heidari N, Abdullahzadeh M, Naji AL, LIVED EXPERIENCES OF TRANSGENDER INDIVIDUALS REGARDING THE FAMILY’S REACTION, TO GENDER DYSPHORIA: A PHENOMENOLOGICAL STUDY. Nursing and Midwifery Journal. 2020; 18 (7):519–531. URL: http://unmf.umsu.ac.ir/article-1-4176-en.html .
Koken JA, Bimbi DS, Parsons JT. Experiences of familial acceptance-rejection among transwomen of color. J Fam Psychol. 2009;23(6):853–60. https://doi.org/10.1037/a0017198 .
Bryan Tully. Aspects of interpersonal relationships for people with gender dysphoria and associated paraphilias, sexual and marital therapy. 1993(8)2: 137–45. https://doi.org/10.1080/02674659308408189 .
Download references
Acknowledgements
The authors are grateful to all the participants.
This study received no specific grant from any funding agency, commercial or not-for-profit sectors.
Author information
Authors and affiliations.
School of Medicine, Zahedan University of Medical Sciences, Zahedan, Iran
Zahra Ghiasi
Zahedan University of Medical Sciences, Zahedan, Iran
Fatemeh Khazaei
Department of Psychiatry, Zahedan University of Medical Sciences, Zahedan, Iran
Mohsen Khosravi
Community Nursing Research Center, Zahedan University of Medical Sciences, Zahedan, Iran
Nasrin Rezaee
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to this project and article equally. All authors read and approved the final version of the manuscript.
Corresponding author
Correspondence to Nasrin Rezaee .
Ethics declarations
Ethics approval and consent to participate.
All participants in this study gave full informed consent to participate. The study adhered to the principles of the Declaration of Helsinki and has ethics approval from the ethics committee of Zahedan University of Medical Sciences with the code IR.ZAUMS.REC.1400.388. To collect the data, the researcher went to the Department of forensic medicine in Zahedan and conducted interviews with the participants in a private room where participants feel comfortable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ghiasi, Z., Khazaei, F., Khosravi, M. et al. Physical and psychosocial challenges of people with gender dysphoria: a content analysis study. BMC Public Health 24 , 16 (2024). https://doi.org/10.1186/s12889-023-17537-z
Download citation
Received : 20 February 2023
Accepted : 19 December 2023
Published : 02 January 2024
DOI : https://doi.org/10.1186/s12889-023-17537-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Psychosocial challenges
- Gender dysphoria
- Qualitative study
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Adolesc Health Med Ther
Gender dysphoria in adolescence: current perspectives
Riittakerttu kaltiala-heino.
1 Faculty of Medicine and Life Sciences, University of Tampere, Tampere, Finland
2 Department of Adolescent Psychiatry, Tampere University Hospital, Tampere, Finland
3 Vanha Vaasa Hospital, Vaasa, Finland
Hannah Bergman
4 Department of Clinical Neuroscience, Karolinska Institutet, Stockholm, Sweden
Marja Työläjärvi
Louise frisén.
Increasing numbers of adolescents are seeking treatment at gender identity services in Western countries. An increasingly accepted treatment model that includes puberty suppression with gonadotropin-releasing hormone analogs starting during the early stages of puberty, cross-sex hormonal treatment starting at ~16 years of age and possibly surgical treatments in legal adulthood, is often indicated for adolescents with childhood gender dysphoria (GD) that intensifies during puberty. However, virtually nothing is known regarding adolescent-onset GD, its progression and factors that influence the completion of the developmental tasks of adolescence among young people with GD and/or transgender identity. Consolidation of identity development is a central developmental goal of adolescence, but we still do not know enough about how gender identity and gender variance actually evolve. Treatment-seeking adolescents with GD present with considerable psychiatric comorbidity. There is little research on how GD and/or transgender identity are associated with completion of developmental tasks of adolescence.
Gender dysphoria and related concepts
The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) 1 defines gender dysphoria (GD) as a condition in which a person has marked incongruence between the expressed or experienced gender and the biological sex at birth. This causes clinically significant distress or impairment in social, occupational or other important areas of functioning. Individuals with GD experience a strong desire to be treated as the other gender (or some alternative gender different from their assigned gender) and/or to be rid of their sex characteristics, and/or the strong conviction of having feelings and reactions typical of the other gender (or some alternative gender). The previous diagnostic term, gender identity disorder, was rejected in the DSM-5 to avoid pathologizing identity.
According to the International Classification of Diseases (ICD)-10, 2 transsexualism is defined as a desire to live and be accepted as a member of the opposite sex, usually accompanied by a sense of discomfort with or the inappropriateness of one’s anatomical sex and a wish to undergo surgery and hormonal treatment to make the body as congruent as possible with the individual’s preferred sex. The forthcoming ICD-11 will reconceptualize gender identity-related diagnoses using gender incongruence as the main term. 3
In addition to the DSM-5 diagnostic term, gender dysphoria can also refer to anxiety and distress about gender features at large. Gender nonconformity refers to behaviors and an appearance that are considered atypical of an individual’s assigned gender. Gender variance refers to a spectrum of gender experience, in contrast to the dichotomized conception of gender. The term “transgender” is used as an umbrella term to refer to wider variation of gender identities. Not all who identify as transgender or display gender nonconformity or gender variance suffer from dysphoria.
In this article, we use the DSM-5 and ICD-10 terms “gender dysphoria (GD)” and “transsexualism/transsexual”, respectively, when referring to diagnosed clinical samples, and also when referring to the literature published when earlier versions of the DSM classification were in use. We use “transgender” to refer to self-identified population samples and “gender dysphoria” to refer to those who present clinical symptoms.
How common are GD and transgender identity among adults and adolescents?
The number of people who seek treatment suggest that male-to-female transsexualism has a prevalence of 6.8/100,000 and female-to-male transsexualism has a prevalence of 2.6/100,000 among adults. 4 , 5 In the Netherlands, 0.6% of men and 0.2% of women (aged 15–70 years) reported incongruent gender identity and a desire to undergo sex reassignment (SR). 6 Population surveys have suggested that about 0.5% of adults in the general population identify as transgender. 5 , 7
The number of adolescents contacting specialized gender identity services has risen considerably over the past decade across Europe and North America. 8 , 9 No conclusions regarding the prevalence of GD in general or of GD/transsexualism specifically can be drawn based on these increases. Studies using short (one to three item) self-reports of gender identity and its variance suggest that 0.17%–1.3% of adolescents and young adults identify as transgender. 5 , 10 A school-based survey eliciting gender experiences with scales commonly used at gender identity services suggested that 1.3% of 16–19 year olds had potentially clinically significant gender dysphoria. 11
Gender identity
Identity is the way one understands, describes and expresses oneself and the reflection of those entities to others. Identity consists of many integrated aspects such as gender, nationality, language, academic and occupational endeavors, and religious and political convictions. It is affected by interpersonal relationships, society and different events throughout the life course. 12 Adolescence is an important period of identity formation and integration. 12 , 13 Adolescents and young adults establish their identity by actively exploring identity-related choices and making identity commitments in their chosen directions. 12 , 13
Gender identity concerns the individual’s core sense of being “female”, “male” or another gender. The development of gender identity is a complex process affected by multiple factors. 14 , 15 In the research tradition of gender identity, the broad focus has been on the theme “sex differences”, and two major topics have received the most attention: the description and measurement of sex differences and the etiology of these differences. 16 Several theories have been proposed. According to early psychodynamic theories, gender variant behavior was hypothesized to derive from parent–infant interpersonal issues or trauma (see Gray et al 15 ). However, these theories have not undergone adequate scientific testing. Gender identity development has mostly been described from the viewpoint of cognitive and social learning theories, which argue that human beings are active constructors of cognitive schemas, including gender, in continuous interaction with the environment. 14 Other theories on processes of gender typing have focused on proximal and distal biological influences, genetic and epigenetic or hormonal and neural mechanisms as well as brain anatomy differences in the etiology of gendered behavior and gender variance. 17 – 19 There are structural and functional sex differences in the brain, some of them observable across the life span and others only during specific developmental phases. Sex differences in the brain are largely determined by steroid hormone exposure during a perinatal sensitive period that alters subsequent hormonal and non-hormonal responses throughout the lifespan, but they also depend on genes on sex chromosomes. Moreover, there is continuous interaction between genes and experiences, “epigenetics”, which changes the expression of genes without any change in the underlying DNA sequence. Research suggests that, for example, early social experiences may act as such epigenetic influence that they ultimately shape lasting sex differences in brain and behavior, 20 – 22 but a lot more research is needed in this field to obtain solid knowledge relevant for understanding GD.
While the theories proposed in the past have generally been either essentialist or social cognitive/constructivist in nature, researchers today are expanding the focus to include the bio-psycho-social processes that probably occur across development. 14 , 15 , 23
Childhood GD and puberty development
GD in childhood (GDC) 1 describes a feeling of incongruence between the experienced (psychological) gender and the sex assigned at birth. A corresponding diagnosis is included in the ICD-10. 2 Healthy children vary considerably in their gendered behaviors. 15 The diagnosis of GD in prepubescent children has been widely discussed throughout the history of gender identity research, mainly in terms of weighing the risk of stigmatization against diagnosis as a means of access to publicly funded or insurance-covered health care. 3 , 24 The prevalence of GDC is not known. 5
Adolescence is a crucial time for identity and psychosexual development in young people with gender identity concerns. 25 The outcomes of GDC have been discussed in terms of its persistence and desistence. For most children with GDC, whether GD will persist or desist will probably be determined between the ages of 10 and 13 years, 26 although some may need more time. 27 Evidence from the 10 available prospective follow-up studies from childhood to adolescence (reviewed in the study by Ristori and Steensma 28 ) indicates that for ~80% of children who meet the criteria for GDC, the GD recedes with puberty. Instead, many of these adolescents will identify as non-heterosexual. 17 , 29 Steensma et al 26 interviewed adolescents with different outcomes of GDC (persistence or desistance). The adolescents mentioned social environment, the anticipated results of bodily changes and first romantic and/or sexual experiences as central factors in the desistance or persistence of GD.
Treatment of GD intensifying in puberty: the Dutch model
The most commonly used guidelines for the treatment of GD in children and adolescents are those of The Endocrine Society 30 and the Standard of Care from the World Professional Association for Transgender Health, 31 which are based on the so-called Dutch Model protocols published and practiced at the Amsterdam Gender Clinic in the Netherlands. 32
The Dutch protocol recommends medical treatment if GD intensifies in puberty, while the care for children with GD and their families consists of providing information, psychological support, parental or/and family counseling. In adolescents, medical treatment is recommended at age 12 years and older for those who are in or beyond the early stages (Tanner II–III) of puberty and are still experiencing persistent GD. Puberty suppression with gonadotropin-releasing hormone analogs is part of the protocol for these patients. The purpose of puberty suppression is to relieve the psychological suffering caused by the development of secondary sex characteristics, to give the adolescent time to make a balanced decision regarding whether to undergo actual medical gender-confirming treatment (with cross-sex hormones and surgery) and to make social “passing” in the experienced gender easier. Cross-sex hormones are used for adolescents aged 16 years and older who continue to experience persistent GD. People aged 18 years and older with a diagnosis of GD may undergo SR surgery. 32
Outcome of and ethical debates around medical interventions for GD in adolescence
The Dutch protocol is largely used, but it has its critics. 33 – 35 Controversy regarding the use of drugs for puberty touches on fundamental ethical concepts in pediatrics: the best interests of the minor, autonomy and the role of social context. Professionals recognize the distress of young people with GD and feel an urge to treat them. At the same time, most of these professionals have doubts because of the lack of data regarding long-term physical and psychological outcomes. 36 , 37
Reports of the outcomes of puberty suppression treatment in adolescents have shown reasonable safety and good outcomes regarding patient satisfaction and psychosocial functioning, but research is still scarce. Nevertheless, puberty suppression is not indicated in a considerable proportion of gender dysphoric minors because of several reasons, for example, severe psychiatric comorbidity, considerable instability of psychosocial support or onset of GD later during puberty and diagnostic uncertainty; 38 – 40 nevertheless, more follow-up data even from patients who are fulfilling the criteria for “the Dutch model” are still needed. 37
Psychiatric disorders among adolescents with GD
Descriptive studies of adolescents referred to specialized gender identity services at different centers in Europe and North America have mainly suggested that ~40%–45% of these young people present with clinically significant psychopathology. 38 , 39 , 41 – 50 The lowest figures for psychiatric comorbidity (one-third of the presenting population) were reported in the Netherlands, 41 and the highest (up to three quarters) was reported in Finland and Canada. 39 , 50 Gender-referred adolescents actually appear to display clinically significant psychopathology to the same extent as adolescents referred to mental health services due to other reasons. 48 , 50 The most commonly reported disorders are depression and anxiety disorders. Self-harm and suicidal ideation/behavior are also common, whereas conduct disorder and antisocial development do not appear central in this population.
Likewise, community-level information suggests that transgender-identifying youth present four to six times more often with depression and three to four times more often with self-harm and/or suicidal behavior compared with cisgender adolescents. 10 , 51 Clinical and population data, though scarce, also suggest an overrepresentation of eating pathology among adolescents with GD or transgender identity. 46 , 52
An increased prevalence of autism spectrum disorders (ASDs), varying from ~6% to over 20%, has been reported among samples of adolescents referred to gender identity services. 39 , 42 , 46 , 53 This vastly exceeds the estimated prevalence of 0.6%–0.7% 54 in the general population. In comparison, among children and early adolescents with ASDs, gender variance is >7-fold more common than among non-referred controls. 53 , 55
Hypotheses to explain this are manifold. The theory of the extreme male brain suggests that individuals with ASD demonstrate an extreme of the typical male pattern of behaviors and cognitions originating from high levels of fetal testosterone. High fetal levels could likewise contribute to GD in natal girls, explaining their male identity and behavior. However, this theory cannot explain the association between ASD and GD in natal boys. Social factors-related hypotheses propose that the social perception and communication difficulties typical of autism could make a child more likely to miss social cues regarding how to conform to gender norms or to identify with the opposite sex when he/she faces difficulties joining the peer group of her/his own sex. Hypotheses focusing on individual psychological characteristics suggest, firstly, that gender could be among the preoccupations or obsessions often seen in ASDs. On the other hand, the development of atypical gender identity in autism could relate to the developmental rigidity typical of autism. Individuals with ASD might not reach normative flexibility in gender development necessary to deal with gender variant feelings, which might lead to the overrepresentation of ASD in GD. 53 , 56 The suggested causes, however, remain speculative. In a recent study, both boys and girls with GD displayed elevated levels of autistic symptomatology in all subdomains of autism, which did not exclusively support any of the suggested hypotheses. 56 Nevertheless, ASDs pose particular challenges for the diagnosis and treatment of GD in adolescents.
GD and the developmental tasks of adolescence
“Developmental tasks” refer to the normative developmental milestones that should be reached during a given developmental stage. 57 , 58 They arise from interactions among physical development, personal attributes and societal expectations. Favorable completion of the developmental tasks of a given stage is a prerequisite for success in the subsequent stages. The developmental tasks of adolescence were first formulated by Havighurst 57 and comprise accepting one’s body, adopting a masculine or feminine social role, achieving emotional independence from parents, developing close relationships with peers of the same and opposite genders, preparing for an occupation, preparing for marriage and family life, establishing a personal value or an ethical system and achieving socially responsible behavior. Although puberty now occurs earlier and the transition to adulthood occurs later than they did when these developmental tasks were initially proposed, they remain relevant. 58 The relationship with one’s own body and the acquisition of a gendered social role – not necessarily binary – are by definition challenging for adolescents with GD. In the following sections, we discuss the available information on GD/transgender identity and the other developmental tasks of adolescence.
GD in adolescence and relationships with parents
Parents of adolescents with GD and/or transgender identity may face special challenges that are shaped by a variety of factors, such as ethnicity, religious background, social class and the prevailing attitudes in their community and society. 59 , 60 These challenges likely shape the support that a nonconforming adolescent can receive. Adverse parental reactions toward an adolescent’s gender nonconformity have been noted as a special risk, 61 but parents of sexual- and gender-minority offspring have also reported particular positive aspects of being a parent in this situation, such as personal growth, unconditional love, activism, social connection and closer relationships. 62 However, few studies have empirically explored the parental reactions and support among youth with GD and/or transgender identity.
In a Canadian community study of transgender-identifying youth, 63 of those who had disclosed their gender identity to their parents, 34% considered their parents “very” supportive and 25% considered their parents “somewhat” supportive. Forty-two percent reported that their parents were “not very” or “not at all” supportive. However, the study was based on a nonrandom sample and solely adolescent self-reports, so findings need to be interpreted with caution and causalities cannot be concluded. Strong perceived parental support was, nevertheless, associated with many positive mental health outcomes. Lack of parental support was associated with inadequate housing and homelessness in addition to negative psychological outcomes. Better parental support has also been associated with fewer risk-taking sexual behaviors among transgender youth. 64
In a community study of trans female adolescents and young adults, 65 more than half of the participants reported that their parents supported their gender identity, showed their support in many ways and believed the respondent could have a happy future as a trans adult. However, approximately two in five respondents had not experienced parental acceptance. Parental acceptance was associated with perceiving parents as the primary source of social support.
In a school-based survey 51 transgender-identifying adolescents felt less often (odds Ratio 0.3) than their cis-gender peers that at least one parent cared for them.
Studies of clinically referred gender dysphoric youth have rarely addressed parent-related issues. Simons et al 66 reported that in a clinical sample of adolescents with GD, parental support was significantly associated with higher life satisfaction, lower perceived burden of being transgender and fewer depressive symptoms. In a Finnish study comparing childhood gender identity in community and clinical samples, a smaller proportion of adolescents with GD than of non-referred adolescents in the population agreed with the statement ”I always felt that my parents cared fore me.” 11 It was also noticed that the clinically referred adolescents with GD less commonly lived with both their parents than the adolescents in the normal population (48% vs. 78%). 67 In British and Spanish samples of gender-referred adolescents, parental divorce was observed in the background of approximately three in five participants, but the authors did not compare this finding with a corresponding rate in the general population. 46 , 49
Gender nonconformance and peer relationships in adolescence
During adolescence, peer relationships are critical for psychological well-being. 68 , 69 Peer relationships also shape development, including aspects of gender identity consolidation. 70 Loneliness and social isolation from peer relationships is associated with developmental difficulties and impaired mental health. 71 , 72 An important peer network-related risk factor is bullying. 73
Observations in referred samples of adolescents with GD suggest considerable peer relationship difficulties. In both the UK 46 and in Finland, 39 approximately half of adolescents who presented at a specialized gender identity service reported significant experiences of being bullied. In the Finland study, 45% of the referred adolescents also had a history of marked periods of social isolation in childhood and/or adolescence. In the Netherlands and in Canada, self-, parent and teacher ratings indicated poorer peer relationships among adolescents referred for GD than in the same-aged population 47 , 48 and poor peer relationships were an important correlate of mental health problems in this group. Similarly, in another Canadian comparison among gender-referred, mental health-referred and general population adolescents bullying was reported by the GD group more commonly than by population controls, and to the same extent as by those referred due to mental health issues. Gender-related bullying was most common among the GD group. 74
On the population level, Clark et al 51 found that trans-gender-identifying adolescents had 4.5-fold increased odds of being bullied and were approximately twice as likely to report being afraid for their personal safety, having been in a serious physical fight and having been hit or otherwise harmed by others, compared with their cisgender-identifying peers. They also less commonly felt that their friends cared about them and that school was okay.
Gender-nonconforming behavior is characteristic of both sexual- and gender-minority youth and has been associated with an increased likelihood of experiencing bullying and harassment in peer groups. 75 , 76 Adolescents with GD likely represent the extreme end of gender nonconformity, and this may strongly contribute to their experiences of being bullied. Bullying and stigmatization have also been suggested to (partially) mediate the association between gender nonconformity and lower mental well-being across adolescence. 74 , 77 – 79
However, not all the difficulties the gender dysphoric adolescents face in peer relationships can be explained by gender expression-related victimization or discrimination. In the Finnish clinical sample, of the gender identity-referred adolescents who had experienced severe bullying at school, three quarters had been bullied before they ever questioned their gender. Likewise, three-quarters of them reported that the bullying had not been related to gender expression or sexual identity, but to other factors such as not being slim, being successful at school or having unfashionable hobbies and interests. 39 Bullying is a severe problem regardless of the reported reasons for it, but it is important to acknowledge that adolescents who develop GD also have unrelated difficulties that may need attention.
GD, transgender identity and sexuality in adolescence
Sexual orientation and gender identity are different entities, and transgender people present with a variety of sexual orientations. Nevertheless, sexual orientation has long been used to subtype GD/transsexualism. 80 During adolescence, the different facets of sexual orientation – attraction, behavior and identity – may still be developing. It may be more important to determine whether adolescents with GD or transgender identity display developmentally appropriate and favorable involvement in romantic and erotic relationships.
In adolescence, sexual development accelerates. Young people’s experiences of a maturing and changing body, sexuality and their developing gender identity affect intrapersonal, interpersonal and societal interactions. 81 In Western countries, between one-tenth and one-third of adolescents first experience sexual intercourse by the age of 15, and the vast majority experience it by age 20. 82 , 83 Various practices of kissing and petting typically precede first sexual intercourse by several years. Early sexual activity has been viewed as a problem behavior associated with risky sexual behaviors, psychosocial difficulties and emotional and behavioral disorders. 82 , 83 In contrast, in the late stages of adolescent development, a lack of experiences might suggest developmental difficulties.
GD and/or transgender identification could be expected to be associated with delayed sexual development, given that it is the sexual body, in particular, that is the source of distress in GD and that differing from the mainstream may increase the adolescent’s risk of problems in social relationships, including dating, and sexual encounters. Sexual- and gender-minority adolescents may also have a reduced availability of potential partners and increased challenges in finding potential partners than their heterosexual peers. 84 However, developmental challenges have also been associated with premature and risky sexual behavior. 82 , 85 Adolescents with GD and/or transgender identification could engage in risky sexual behaviors due to identity experiments or because associated mental health problems could increase their search for comfort in intimacy or decrease their self-protection skills.
To the best of our knowledge, the only study focusing on the sexual experiences of treatment-seeking adolescents with GD is that of Bungener et al 86 from the Netherlands. They compared the sexual experiences of 137 transsexual adolescents (mean [SD] age 14.69 [2.2] years) with those of a same-aged adolescent population. Transsexual adolescents had fewer sexual experiences than the same-aged population in all areas measured (falling in love, romantic relationships, kissing, petting, intercourse). However, a majority of the transsexual adolescents had fallen in love and approximately half had been involved in romantic relationships. One quarter had experienced petting while undressed, and 5% had experienced sexual intercourse. Fewer transsexual adolescents than the adolescents in the same-aged population (24% vs. 48%) valued sex as important. In a descriptive study of clinically presenting adolescents with GD in the USA, 45 nearly half of the respondents (mean [SD] age 19.2 [2.9] years) reported being sexually active.
Some population studies provide information regarding transgender identity in adolescence and aspects of sexual development. Korchmaros et al 84 compared the romantic relationships of lesbian, gay, bisexual, transgender and questioning (LGBTQ) adolescents and those of adolescents with mainstream sexual and gender identities. Contrary to expectations, the LGBTQ adolescents were more experienced with romantic relationships and more active in initiating relationships both online and offline. Results were not reported separately for the transgender group. Robinson and Espel-age 87 reported that LGBTQ adolescents were more likely to display risky sexual behaviors than same-aged non-LGBTQ youth. However, in more detailed analyses, the risk was associated with homosexual/bisexual orientation and not with transgender identity. Veale et al 88 set out to study pregnancy involvement among transgender youth and the health correlates of this involvement. In a large (n=923) sample of transgender-identifying youth, 540 responded to the pregnancy involvement item. Almost 5% of Canadian transgender adolescents had ever been pregnant or impregnated a partner; approximately the same proportion as their same-aged peers. Those with a history of pregnancy involvement were also more likely to have a history of sexually transmitted disease, but they did not differ from the rest of the transgender youth in terms of hormone use, living in the felt gender, self-reported mental health and level of social support.
Sexual harassment is a common problem among adolescent populations. 89 Transgender-identifying adolescents appear to be at the greatest risk of sexual harassment and to experience the greatest distress due to it. 89 Sexual harassment is suggested to function to maintain heteronormativity, which transgender adolescents likely challenge. Their perception of sexual harassment as more distressing compared with other adolescents could be due to harsher harassment, increased vulnerability due to uncertainty about self, or fear. 89
Similarly, in a large school-based survey study on teen dating violence, 90 the few transgender-identifying youth in the sample reported the highest victimization rates for physical dating violence, psychological dating abuse, cyber dating abuse and sexual coercion. Differences from cisgender adolescents varied from 2- to 7-fold for the different forms of violence. However, the transgender-identifying youth also reported the highest rates of perpetrating dating violence. Minority stress theory 91 posits that the chronic stressors that minorities experience (e.g., gender-based discrimination) shape their coping mechanisms (such as substance use, aggression) and lead to adverse psychosocial and health outcomes. The particular vulnerability to perpetrating dating violence observed among transgender adolescents by Dank et al 90 could be understood through minority stress theory, but more research is needed.
Transgender adolescents and young adults, particularly trans females, are at a disproportionately high risk of contracting human immunodeficiency virus and other sexually transmitted diseases. 79 , 92 The risk of unprotected sex in this population has been associated with sex work and drug use, which are further associated with rejection, stigma and discrimination. 79 , 92 Of the studies of referred samples, only one addressed sex work. 45 In that sample, 6% of the referred adolescents reported engaging in the trading of sex.
Sexual education is an important way to promote positive and responsible sexual behaviors in youth. The planned curricula and practical applications likely vary widely across countries and schools. Sexual- and gender-minority youth were found to desire minority-inclusive sexual education in a study by Gowen and Wingez-Yanez. 93 The sexual- and gender-minority youth felt that the sexual education that was offered isolated them by silencing them, adopting a heterocentric perspective and pathologizing minorities. Reflecting on the available sexual education in light of these findings is appropriate for all educators.
Preparing for occupation: academic performance and socioeconomic status
To the best of our knowledge, research has not specifically focused on academic performance and the progression to work life among adolescents with GD, but given the burden of psychiatric comorbidities among gender-referred youth, special needs regarding education are likely to exist.
Aspects of social relationships are relevant to well-being in school, school performance and pathways to occupation. Transgender youth have been reported to experience bullying and discrimination in schools, not only by peers but even by teachers; consequently, they perceive schools as unsafe places, which again increases the risk of non-attendance and poorer results. 75 , 94 Gender- and sexuality-related victimization may impair academic performance through, for example, decreased motivation, concentration and self-efficacy and the resulting school avoidance and harmful coping strategies. 94 , 95 Nevertheless, being “out” at school improves self-esteem among gender- and sexual-minority youth and increases their well-being, which can have a positive impact on academic performance. 94
School dropout is strongly linked to social exclusion. School dropout was associated with high masculinity in girls and low masculinity combined with high femininity in boys in a study of late-adolescent school dropouts and attenders in the Netherlands. 96 The authors suggested that such deviation from gender norms increases the risk of unpopularity among peers, which again predisposes individuals toward school dropout. However, school dropout was also associated with very masculine attitudes and self-evaluations among boys. The role of gendered behaviors, attitudes and experiences in school adjustment and academic performance deserves further research.
In Clark et al’s 51 school-based survey, adolescents reporting non-cisgender identity came disproportionately often from families with high socioeconomic deprivation and less often felt that their family got along. Any explanation for this remains unknown; however, young people are likely to stay in the same socioeconomic position as their parents. 97 Jacob and Cox 98 also pinpointed transgender people’s greater risk of having a disadvantaged socioeconomic status (in the USA), associating this with increased unemployment, and employment in low-paid jobs, because of stigmatization.
Why the increase in referrals?
Zucker et al 99 observed an increase in the number of adolescents presenting at gender identity services in the early 2000s. Since then, several gender identity services for minors from across Western countries have reported increases. 8 , 9 , 42 , 49 Simultaneously, the earlier overrepresentation of natal boys has equaled or turned to overrepresentation of natal girls. 9 Natal girls now comprise from half 49 to ~90% 39 of clinical adolescent samples. The reasons for these changes are not known. The increase in referrals could be attributable to enhanced provision of services, or the threshold for seeking help may now be lower due to increased knowledge and improved societal acceptance. Aitken et al, 9 however, did not find evidence supporting a lowered threshold to gender identity services. Sociocultural features related to what kind of identities are available for whom, and sex-related differences of pressure to conform may play a role.
Research regarding the clinical treatment of adolescents with GD has mainly focused on childhood-onset GD that intensifies during puberty, and the Dutch treatment protocol is also tailored for this group. There is little empirical knowledge regarding young people who experience their first signs of GD in adolescence, well after the onset of puberty, especially regarding biological girls. 50 , 100 Among a treatment-seeking sample in the UK, 18% experienced their first feelings of GD in adolescence 46 compared with approximately two-thirds of the Finnish sample, 39 and for the majority of adolescent-onset cases, GD presented in the context of severe mental disorders and general identity confusion. In such situations, appropriate treatment for psychiatric comorbidities may be warranted before conclusions regarding gender identity can be drawn. Gender-referred adolescents actually display psychopathology to the same extent as mental health–referred youth. 48 , 50 In a nationwide long-term follow-up study of adult cases, psychiatric morbidity, suicide attempts and suicide mortality persisted as elevated after juridical and medical SR. 101
Emerging discussions raise concern for post-pubertally abruptly emerging cross-gender identification (“rapid onset”), particularly among biological girls, suggesting a role for intensive media influences and generous group validation as shaping the understanding of, and giving new meanings to, the body discomfort common among female adolescents at large. 100 The persistence of increasing adolescent-onset transgender identification is not known. 5 , 100
More empirical research is needed regarding virtually all aspects of GD in adolescence to create treatment approaches that optimize these young people’s future psychosocial health and well-being. It seems unlikely that all the psychopathology observed in the referred samples is secondary to gender identity issues and would resolve with hormonal and later surgical treatments. There is still no clear consensus regarding hormonal treatment for adolescents because long-term data are unavailable; 36 actually, only one long-term follow up has been carried out, with a highly selected intervention group and an at baseline non-comparable comparison group. 102
An affirmative approach 103 is increasingly implemented in the health care of gender nonconforming children. This includes, based on a comprehensive psychological and psychosocial assessment, work with the children and their families and schools to support the gender-nonconforming minors to express themselves in a way that feels most comfortable for them. With the starting point that gender presentations are fluid and changing over time, gender variant children need to be allowed to freely explore a range of gender identities and expressions. A debate concerns whether or not a prepubertal child should be allowed to completely transition to live in other than birth gender. Concerns include that childhood transition may be forcing adolescents to proceed to biomedical interventions, as stepping back may be psychologically troublesome, even though identity development has taken a new direction. 28 , 104
The etiology of gender incongruence remains unknown. Gender identity differentiation does not occur in a psychosocial vacuum; instead, research in the field suggests that the developmental course is influenced by numerous psychosocial factors, likely in continuous interaction with biological factors. 23 , 105 Gray et al 15 noted that the general narrative in the research literature concerning gender variation among children focuses on gender “atypical” behavior and deviation from “normative patterns”, thus viewing gender in a binary way instead of as a wider spectrum of (healthy) identities, personalities and behaviors among children. This is surely relevant for adolescents as well. These authors also requested a shift in research paradigms away from the study of outcomes of sexuality and gender identity and the child/adolescent in isolation toward outcomes of adjustment and the child/adolescent in contexts that affect adjustment. Along with further discussions of the best treatment interventions, it is relevant to attempt to contribute to societal attitudes that enable children and adolescents with gender variance to express themselves and successfully complete the developmental tasks common to all, independent of gender.
The authors report no conflicts of interest in this work.
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- Gender dysphoria in...
Gender dysphoria in young people is rising—and so is professional disagreement
Linked feature.
Gender identity services in the UK are on pause as evidence comes under scrutiny
- Related content
- Peer review
- Jennifer Block , investigations reporter
- jblock{at}bmj.com
More children and adolescents are identifying as transgender and are being offered medical treatment, especially in the US—but some providers and European authorities are urging caution because of a lack of strong evidence. Jennifer Block reports
Last October the American Academy of Pediatrics (AAP) gathered inside the Anaheim Convention Center in California for its annual conference. Outside, several dozen people rallied to hear speakers including Abigail Martinez, a mother whose child began hormone treatment at age 16 and died by suicide at age 19. Supporters chanted the teen’s given name, Yaeli; counter protesters chanted, “Protect trans youth!” For viewers on a livestream, the feed was interrupted as the two groups fought for the camera.
The AAP conference is one of many flashpoints in the contentious debate in the United States over if, when, and how children and adolescents with gender dysphoria should be medically or surgically treated. US medical professional groups are aligned in support of “gender affirming care” for gender dysphoria, which may include gonadotrophin releasing hormone analogues (GnRHa) to suppress puberty; oestrogen or testosterone to promote secondary sex characteristics; and surgical removal or augmentation of breasts, genitals, or other physical features. At the same time, however, several European countries have issued guidance to limit medical intervention in minors, prioritising psychological care.
The discourse is polarised in the US. Conservative politicians, pundits, and social media influencers accuse providers of pushing “gender ideology” and even “child abuse,” lobbying for laws banning medical transition for minors. Progressives argue that denying access to care is a transphobic violation of human rights. There’s little dispute within the medical community that children in distress need care, but concerns about the rapid widespread adoption of interventions and calls for rigorous scientific review are coming from across the ideological spectrum. 1
The surge in treatment of minors
More adolescents with no history of gender dysphoria—predominantly birth registered females 2 —are presenting at gender clinics. A recent analysis of insurance claims by Komodo Health found that nearly 18 000 US minors began taking puberty blockers or hormones from 2017 to 2021, the number rising each year. 3 4 Surveys aiming to measure prevalence have found that about 2% of high school aged teens identify as “transgender.” 5 These young people are also more likely than their cisgender peers to have concurrent mental health and neurodiverse conditions including depression, anxiety, attention deficit disorders, and autism. 6 In the US, although Medicaid coverage varies by state and by treatment, the Biden administration has warned states that not covering care is in violation of federal law prohibiting discrimination. 7 Meanwhile, the number of private clinics that focus on providing hormones and surgeries has grown from just a few a decade ago to more than 100 today. 4
As the number of young people receiving medical transition treatments rises, so have the voices of those who call themselves “detransitioners” or “retransitioners,” some of whom claim that early treatment caused preventable harm. 8 Large scale, long term research is lacking, 9 and researchers disagree about how to measure the phenomenon, but two recent studies suggest that as many as 20-30% of patients may discontinue hormone treatment within a few years. 10 11 The World Professional Association for Transgender Health (WPATH) asserts that detransition is “rare.” 12
Chloe Cole, now aged 18, had a double mastectomy at age 15 and spoke at the AAP rally. “Many of us were young teenagers when we decided, on the direction of medical experts, to pursue irreversible hormone treatments and surgeries,” she read from her tablet at the rally, which had by this time moved indoors to avoid confrontation. “This is not informed consent but a decision forced under extreme duress.”
Scott Hadland, chief of adolescent medicine at Massachusetts General Hospital and Harvard Medical School, dismissed the “handful of cruel protesters” outside the AAP meeting in a tweet that morning. He wrote, “Inside 10 000 pediatricians stand in solidarity for trans & gender diverse kids & their families to receive evidence-based, lifesaving, individualized care.” 13
Same evidence, divergent recommendations
Three organisations have had a major role in shaping the US’s approach to gender dysphoria care: WPATH, the AAP, and the Endocrine Society (see box). On 15 September 2022 WPATH published the eighth edition of its Standards of Care for the Health of Transgender and Gender Diverse People, with new chapters on children and adolescents and no minimum age requirements for hormonal and surgical treatments. 2 12 GnRHa treatment, says WPATH, can be initiated to arrest puberty at its earliest stage, known as Tanner stage 2.
The Endocrine Society also supports hormonal and surgical intervention in adolescents who meet criteria in clinical practice guidelines published in 2009 and updated in 2017. 14 And the AAP’s 2018 policy statement, Ensuring Comprehensive Care and Support for Transgender and Gender-Diverse Children and Adolescents , says that “various interventions may be considered to better align” a young person’s “gender expression with their underlying identity.” 15 Among the components of “gender affirmation” the AAP names social transition, puberty blockers, sex hormones, and surgeries. Other prominent professional organisations, such as the American Medical Association, have issued policy statements in opposition to legislation that would curtail access to medical treatment for minors. 16 17 18 19
These documents are often cited to suggest that medical treatment is both uncontroversial and backed by rigorous science. “All of those medical societies find such care to be evidence-based and medically necessary,” stated a recent article on transgender healthcare for children published in Scientific American . 20 “Transition related healthcare is not controversial in the medical field,” wrote Gillian Branstetter, a frequent spokesperson on transgender issues currently with the American Civil Liberties Union, in a 2019 guide for reporters. 21 Two physicians and an attorney from Yale recently opined in the Los Angeles Times that “gender-affirming care is standard medical care, supported by major medical organizations . . . Years of study and scientific scrutiny have established safe, evidence-based guidelines for delivery of lifesaving, gender-affirming care.” 22 Rachel Levine, the US assistant secretary for health, told National Public Radio last year regarding such treatment, “There is no argument among medical professionals.” 23
Internationally, however, governing bodies have come to different conclusions regarding the safety and efficacy of medically treating gender dysphoria. Sweden’s National Board of Health and Welfare, which sets guidelines for care, determined last year that the risks of puberty blockers and treatment with hormones “currently outweigh the possible benefits” for minors. 24 Finland’s Council for Choices in Health Care, a monitoring agency for the country’s public health services, issued similar guidelines, calling for psychosocial support as the first line treatment. 25 (Both countries restrict surgery to adults.)
Medical societies in France, Australia, and New Zealand have also leant away from early medicalisation. 26 27 And NHS England, which is in the midst of an independent review of gender identity services, recently said that there was “scarce and inconclusive evidence to support clinical decision making” 28 for minors with gender dysphoria 29 and that for most who present before puberty it will be a “transient phase,” requiring clinicians to focus on psychological support and to be “mindful” even of the risks of social transition. 30
The origins of paediatric gender medicine in the United States
The World Professional Association for Transgender Health (WPATH) began as a US based advocacy group and issued the first edition of the Standards of Care in 1979, when it was serving a small population of mostly adult male-to-female transsexuals. “WPATH became the standard because there was nobody else doing it,” says Erica Anderson, a California based clinical psychologist and former WPATH board member. The professional US organisations that lined up in support “looked heavily to WPATH and the Endocrine Society for their guidance,” she told The BMJ .
The Endocrine Society’s guidance for adolescents grew out of clinicians’ research in the Netherlands in the late 1990s and early 2000s. Peggy Cohen-Kettenis, a Utrecht gender clinic psychologist, collaborated with endocrinologists in Amsterdam, one of whom had experience of prescribing gonadotrophin releasing hormone analogues, relatively new at the time. Back then, gender dysphoric teens had to wait until the age of majority for sex hormones, but the team proposed that earlier intervention could benefit carefully selected minors. 40
The clinic treated one natal female patient with triptorelin, published a case study and feasibility proposal, and began treating a small number of children at the turn of the millennium. The Dutch Protocol was published in 2006, referring to 54 children whose puberty was being suppressed and reporting preliminary results on the first 21. 41 The researchers received funding from Ferring Pharmaceuticals, the manufacturer of triptorelin.
In 2007 the endocrinologist Norman Spack began using the protocol at Boston Children’s Hospital and joined Cohen-Kettenis and her Dutch colleagues in writing the Endocrine Society’s first clinical practice guideline. 42 When that was published in 2009, puberty had been suppressed in just over 100 gender dysphoric young people. 40
American Academy of Pediatrics (AAP) committee members began discussing the need for a statement in 2014, four years before publication, says Jason Rafferty, assistant professor of paediatrics and psychiatry at Brown University, Rhode Island, and the statement’s lead author. “The AAP recognised that it had a responsibility to provide some clinical guidance, but more importantly to come out with a statement that said we need research, we need to integrate the principles of gender affirmative care into medical education and into child health,” he says. “What our policy statement is not meant to be is a protocol or guidelines in and of themselves.”
“Don’t call them evidence based”
“The brief history of guidelines is that, going back more than 30 years ago, experts would write articles and so on about what people should do. But formal guidelines as we think of them now were seldom or non-existent,” says Gordon Guyatt, distinguished professor in the Department of Health Research Methods, Evidence, and Impact at McMaster University, Ontario.
That led to the movement towards developing criteria for what makes a “trustworthy guideline,” of which Guyatt was a part. 31 One pillar of this, he told The BMJ , is that they “are based on systematic review of the relevant evidence,” for which there are also now standards, as opposed to a traditional narrative literature review in which “a bunch of experts write whatever they felt like using no particular standards and no particular structure.”
Mark Helfand, professor of medical informatics and clinical epidemiology at Oregon Health and Science University, says, “An evidence based recommendation requires two steps.” First, “an unbiased, thorough, critical systematic review of all the relevant evidence.” Second, “some commitment to link the strength of the recommendations to the quality of the evidence.”
The Endocrine Society commissioned two systematic reviews for its clinical practice guideline, Endocrine Treatment of Gender-Dysphoric/Gender-Incongruent Persons : one on the effects of sex steroids on lipids and cardiovascular outcomes, the other on their effects on bone health. 32 33 To indicate the quality of evidence underpinning its various guidelines, the Endocrine Society employed the GRADE system (grading of recommendations assessment, development, and evaluation) and judged the quality of evidence for all recommendations on adolescents as “low” or “very low.”
Guyatt, who co-developed GRADE, found “serious problems” with the Endocrine Society guidelines, noting that the systematic reviews didn’t look at the effect of the interventions on gender dysphoria itself, arguably “the most important outcome.” He also noted that the Endocrine Society had at times paired strong recommendations—phrased as “we recommend”—with weak evidence. In the adolescent section, the weaker phrasing “we suggest” is used for pubertal hormone suppression when children “first exhibit physical changes of puberty”; however, the stronger phrasing is used to “recommend” GnRHa treatment.
“GRADE discourages strong recommendations with low or very low quality evidence except under very specific circumstances,” Guyatt told The BMJ . Those exceptions are “very few and far between,” and when used in guidance, their rationale should be made explicit, Guyatt said. In an emailed response, the Endocrine Society referenced the GRADE system’s five exceptions, but did not specify which it was applying.
Helfand examined the recently updated WPATH Standards of Care and noted that it “incorporated elements of an evidence based guideline.” For one, WPATH commissioned a team at Johns Hopkins University in Maryland to conduct systematic reviews. 34 35 However, WPATH’s recommendations lack a grading system to indicate the quality of the evidence—one of several deficiencies. Both Guyatt and Helfand noted that a trustworthy guideline would be transparent about all commissioned systematic reviews: how many were done and what the results were. But Helfand remarked that neither was made clear in the WPATH guidelines and also noted several instances in which the strength of evidence presented to justify a recommendation was “at odds with what their own systematic reviewers found.”
For example, one of the commissioned systematic reviews found that the strength of evidence for the conclusions that hormonal treatment “may improve” quality of life, depression, and anxiety among transgender people was “low,” and it emphasised the need for more research, “especially among adolescents.” 35 The reviewers also concluded that “it was impossible to draw conclusions about the effects of hormone therapy” on death by suicide.
Despite this, WPATH recommends that young people have access to treatments after comprehensive assessment, stating that the “emerging evidence base indicates a general improvement in the lives of transgender adolescents.” 12 And more globally, WPATH asserts, “There is strong evidence demonstrating the benefits in quality of life and well-being of gender-affirming treatments, including endocrine and surgical procedures,” procedures that “are based on decades of clinical experience and research; therefore, they are not considered experimental, cosmetic, or for the mere convenience of a patient. They are safe and effective at reducing gender incongruence and gender dysphoria.” 12
Those two statements are each followed by more than 20 references, among them the commissioned systematic review. This stood out to Helfand as obscuring which conclusions were based on evidence versus opinion. He says, “It’s a very strange thing to feel that they had to cite some of the studies that would have been in the systematic review or purposefully weren’t included in the review, because that’s what the review is for.”
For minors, WPATH contends that the evidence is so limited that “a systematic review regarding outcomes of treatment in adolescents is not possible.” But Guyatt counters that “systematic reviews are always possible,” even if few or no studies meet the eligibility criteria. If an entity has made a recommendation without one, he says, “they’d be violating standards of trustworthy guidelines.” Jason Rafferty, assistant professor of paediatrics and psychiatry at Brown University, Rhode Island, and lead author of the AAP statement, remarks that the AAP’s process “doesn’t quite fit the definition of systematic review, but it is very comprehensive.”
Sweden conducted systematic reviews in 2015 and 2022 and found the evidence on hormonal treatment in adolescents “insufficient and inconclusive.” 24 Its new guidelines note the importance of factoring the possibility that young people will detransition, in which case “gender confirming treatment thus may lead to a deteriorating of health and quality of life (i.e., harm).”
Cochrane, an international organisation that has built its reputation on delivering independent evidence reviews, has yet to publish a systematic review of gender treatments in minors. But The BMJ has learnt that in 2020 Cochrane accepted a proposal to review puberty blockers and that it worked with a team of researchers through 2021 in developing a protocol, but it ultimately rejected it after peer review. A spokesperson for Cochrane told The BMJ that its editors have to consider whether a review “would add value to the existing evidence base,” highlighting the work of the UK’s National Institute for Health and Care Excellence, which looked at puberty blockers and hormones for adolescents in 2021. “That review found the evidence to be inconclusive, and there have been no significant primary studies published since.”
In 2022 the state of Florida’s Agency for Health Care Administration commissioned an overview of systematic reviews looking at outcomes “important to patients” with gender dysphoria, including mental health, quality of life, and complications. Two health research methodologists at McMaster University carried out the work, analysing 61 systematic reviews and concluding that “there is great uncertainty about the effects of puberty blockers, cross-sex hormones, and surgeries in young people.” The body of evidence, they said, was “not sufficient” to support treatment decisions.
Calling a treatment recommendation “evidence based” should mean that a treatment has not just been systematically studied, says Helfand, but that there was also a finding of high quality evidence supporting its use. Weak evidence “doesn’t just mean something esoteric about study design, it means there’s uncertainty about whether the long term benefits outweigh the harms,” Helfand adds.
“Evidence itself never tells you what to do,” says Guyatt. That’s why guidelines must make explicit the values and preferences that underlie the recommendation.
The Endocrine Society acknowledges in its recommendations on early puberty suppression that it is placing “a high value on avoiding an unsatisfactory physical outcome when secondary sex characteristics have become manifest and irreversible, a higher value on psychological well-being, and a lower value on avoiding potential harm.” 14
WPATH acknowledges that while its latest guidelines are “based upon a more rigorous and methodological evidence-based approach than previous versions,” the evidence “is not only based on the published literature (direct as well as background evidence) but also on consensus-based expert opinion.” In the absence of high quality evidence and the presence of a patient population in need—who are willing to take on more personal risk—consensus based guidelines are not unwarranted, says Helfand. “But don’t call them evidence based.”
An evidence base under construction
In 2015 the US National Institutes of Health awarded a $5.7m (£4.7m; €5.3m) grant to study “the impact of early medical treatment in transgender youth.” 36 The abstract submitted by applicants said that the study was “the first in the US to evaluate longitudinal outcomes of medical treatment for transgender youth and will provide essential evidence-based data on the physiological and psychosocial effects and safety” of current treatments. Researchers are following two groups, one of participants who began receiving GnRHa in early puberty and another group who began cross sex hormone treatment in adolescence. The study doesn’t include a concurrent no-treatment control group.
Robert Garofalo, chief of adolescent medicine at the Lurie Children’s Hospital in Chicago and one of four principal investigators, told a podcast interviewer in May 2022 that the evidence base remained “a challenge . . . it is a discipline where the evidence base is now being assembled” and that “it’s truly lagging behind [clinical practice], I think, in some ways.” That care, he explained, was “being done safely. But only now, I think, are we really beginning to do the type of research where we’re looking at short, medium, and long term outcomes of the care that we are providing in a way that I think hopefully will be either reassuring to institutions and families and patients or also will shed a light on things that we can be doing better.” 37
While Garofalo was doing the research he served as “contributor” on the AAP’s widely cited 2018 policy statement, which recommends that children and adolescents “have access to comprehensive, gender-affirming, and developmentally appropriate health care,” including puberty blockers, sex hormones, and, on a case-by-case basis, surgeries. 15
Garofalo said in the May interview, “There is universal support for gender affirming care from every mainstream US based medical society that I can think of: the AMA, the APA, the AAP. I mean, these organisations never agree with one another.” Garofalo declined an interview and did not respond to The BMJ ’s requests for comment.
The rush to affirm
Sarah Palmer, a paediatrician in private practice in Indiana, is one of five coauthors of a 2022 resolution submitted to the AAP’s leadership conference asking that it revisit the policy after “a rigorous systematic review of available evidence regarding the safety, efficacy, and risks of childhood social transition, puberty blockers, cross sex hormones and surgery.” In practice, Palmer told The BMJ , clinicians define “gender affirming” care so broadly that “it’s been taken by many people to mean go ahead and do anything that affirms. One of the main things I’ve seen it used for is masculinising chest surgery, also known as mastectomy in teenage patients.” The AAP has told The BMJ that all policy statements are reviewed after five years and so a “revision is under way,” based on its experts’ own “robust evidence review.”
Palmer says, “I’ve seen a quick evolution, from kids with a very rare case of gender dysphoria who were treated with a long course of counselling and exploration before hormones were started,” to treatment progressing “very quickly—even at the first visit to gender clinic—and there’s no psychologist involved anymore.”
Laura Edwards-Leeper, a clinical psychologist who worked with the endocrinologist Norman Spack in Boston and coauthored the WPATH guidelines for adolescents, has observed a similar trend. “More providers do not value the mental health component,” she says, so in some clinics families come in and their child is “pretty much fast tracked to medical intervention.” In a study of teens at Seattle Children’s Hospital’s gender clinic, two thirds were taking hormones within 12 months of the initial visit. 38
The British paediatrician Hilary Cass, in her interim report of a UK review into services for young people with gender identity issues, noted that some NHS staff reported feeling “under pressure to adopt an unquestioning affirmative approach and that this is at odds with the standard process of clinical assessment and diagnosis that they have been trained to undertake in all other clinical encounters.”
Eli Coleman, lead author of WPATH’s Standards of Care and former director of the Institute for Sexual and Gender Health at the University of Minnesota, told The BMJ that the new guidelines emphasised “careful assessment prior to any of these interventions” by clinicians who have appropriate training and competence to assure that minors have “the emotional and cognitive maturity to understand the risks and benefits.” He adds, “What we know and what we don’t know has to be explained to youth and their parents or caregivers in a balanced way which really details that this is the evidence that we have, that we obviously would like to have more evidence, and that this is a risk-benefit scenario that you have to consider.”
Joshua Safer, director of the Center for Transgender Medicine and Surgery at Mount Sinai Hospital in New York and coauthor of the Endocrine Society guidelines, told The BMJ that assessment is standard practice at the programme he leads. “We start with a mental health evaluation for anybody under the age of 18,” he says. “There’s a lot of talking going on—that’s a substantial element of things.” Safer has heard stories of adolescents leaving a first or second appointment with a prescription in hand but says that these are overblown. “We really do screen these kids pretty well, and the overwhelming majority of kids who get into these programmes do go on to other interventions,” he says.
Without an objective diagnostic test, however, others remain concerned. The demand for services has led to a “perfunctory informed consent process,” wrote two clinicians and a researcher in a recent issue of the Journal of Sex and Marital Therapy , 39 in spite of two key uncertainties: the long term impacts of treatment and whether a young person will persist in their gender identity. And the widespread impression of medical consensus doesn’t help. “Unfortunately, gender specialists are frequently unfamiliar with, or discount the significance of, the research in support of these two concepts,” they wrote. “As a result, the informed consent process rarely adequately discloses this information to patients and their families.”
For Guyatt, claims of certainty represent both the success and failure of the evidence based medicine movement. “Everybody now has to claim to be evidence based” in order to be taken seriously, he says—that’s the success. But people “don’t particularly adhere to the standard of what is evidence based medicine—that’s the failure.” When there’s been a rigorous systematic review of the evidence and the bottom line is that “we don’t know,’” he says, then “anybody who then claims they do know is not being evidence based.”
This feature has been funded by the BMJ Investigations Unit. For details see bmj.com/investigations .
Competing interests: I have read and understood BMJ policy on declaration of interests and have no relevant interests to declare.
Provenance: commissioned; externally peer reviewed.
- ↵ Parker K, Horowitz JM, Brown A. Americans’ complex views on gender identity and transgender issues. Pew Research Center’s Social & Demographic Trends Project. 2022. https://www.pewresearch.org/social-trends/2022/06/28/americans-complex-views-on-gender-identity-and-transgender-issues/
- ↵ Respaut R, Terhune C. Number of transgender children seeking treatment surges in US. Reuters 2022 Oct 6. https://www.reuters.com/investigates/special-report/usa-transyouth-data/
- ↵ Terhune C, Respaut R, Conlin M. As children line up at gender clinics, families confront many unknowns. Reuters 2022 Oct 6. https://www.reuters.com/investigates/special-report/usa-transyouth-care/
- Andrzejewski J ,
- Becerra-Culqui TA ,
- ↵ Gomez I, Ranji U, Salganicoff A, et al. Update on Medicaid coverage of gender-affirming health services. KFF. 2022 https://www.kff.org/womens-health-policy/issue-brief/update-on-medicaid-coverage-of-gender-affirming-health-services/
- ↵ Respaut R, Terhune C, Conlin M. Why detransitioners are crucial to the science of gender care. Reuters 2022 Dec 22. https://www.reuters.com/investigates/special-report/usa-transyouth-outcomes/
- Hackett T ,
- Roberts CM ,
- Adirim TA ,
- Schvey NA ,
- Hisle-Gorman E
- Coleman E ,
- Bouman WP ,
- ↵ Hadland S. A handful of cruel protesters outside the #AAP2022 meeting, but inside 10 000 pediatricians stand in solidarity for trans & gender-diverse kids & their families to receive evidence based, lifesaving, individualized care between patients, parents & their doctor. @AmerAcadPeds: pic.twitter.com/b2K2JdRnX9 . Twitter. 2022. https://twitter.com/DrScottHadland/status/1578815082590400512
- Hembree WC ,
- Cohen-Kettenis PT ,
- Rafferty J ,
- Committee on Psychosocial Aspects of Child and Family Health ,
- Committee on Adolescence ,
- Section on Lesbian, Gay, Bisexual, and Transgender Health and Wellness
- ↵ American Academy of Child and Adolescent Psychiatry. AACAP statement responding to efforts to ban evidence-based care for transgender and gender diverse. https://www.aacap.org/AACAP/Latest_News/AACAP_Statement_Responding_to_Efforts-to_ban_Evidence-Based_Care_for_Transgender_and_Gender_Diverse.aspx
- ↵ American Medical Association. March 26, 2021: State advocacy update. 2021. https://www.ama-assn.org/health-care-advocacy/advocacy-update/march-26-2021-state-advocacy-update
- ↵ American Psychological Association. Resolution on supporting sexual/gender diverse children and adolescents in schools. 2020. https://www.apa.org/pi/lgbt/resources/policy/gender-diverse-children
- ↵ American Psychiatric Association. Position statement on treatment of transgender (trans) and gender diverse youth. 2020. https://www.psychiatry.org/File%20Library/About-APA/Organization-Documents-Policies/Policies/Position-Transgender-Gender-Diverse-Youth.pdf
- ↵ Boerner H. What the science on gender-affirming care for transgender kids really shows. Sci Am 2022 (published online 12 May). https://www.scientificamerican.com/article/what-the-science-on-gender-affirming-care-for-transgender-kids-really-shows/
- ↵ Branstetter G. Transgender youth & health care: a guide for reporters. Medium 2019. https://gillbranstetter.medium.com/transgender-youth-health-care-a-guide-for-reporters-820f8fbaff21
- ↵ Olezeski C, McNamara M, Alstott A. Op-ed: Denying trans youth gender-affirming care is an affront to science and medical ethics. Los Angeles Times 2022. https://www.latimes.com/opinion/story/2022-06-13/trans-youth-healthcare-state-bans
- ↵ Simmons-Duffin S. Rachel Levine calls state anti-LGBTQ bills disturbing and dangerous to trans youth. NPR 2022 Apr 29. https://www.npr.org/sections/health-shots/2022/04/29/1095227346/rachel-levine-calls-state-anti-lgbtq-bills-disturbing-and-dangerous-to-trans-you
- ↵ Socialstyrelsen: National Board of Health and Welfare. Care of children and adolescents with gender dysphoria. Report 2022-3-7799. 2022. https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/kunskapsstod/2022-3-7799.pdf
- ↵ Palveluvalikoima (Council for Choices in Health Care in Finland). Medical treatment methods for gender dysphoria in non-binary adults—recommendation. Jun 2020. https://palveluvalikoima.fi/documents/1237350/22895623/Summary_non-binary_en.pdf/8e5f9035-6c98-40d9-6acd-7459516d6f92/Summary_non-binary_en.pdf?t=1592318035000
- ↵ Académie Nationale de Médecine. La médecine face à la transidentité de genre chez les enfants et les adolescents [Medicine and gender transidentity in children and adolescents. 25 Feb 2022. https://www.academie-medecine.fr/la-medecine-face-a-la-transidentite-de-genre-chez-les-enfants-et-les-adolescents/?lang=en (In French and English)
- ↵ Royal Australian and New Zealand College of Psychiatrists. Recognising and addressing the mental health needs of people experiencing gender dysphoria/gender incongruence. 2021. https://www.ranzcp.org/news-policy/policy-and-advocacy/position-statements/gender-dysphoria
- ↵ NHS England. Implementing advice from the Cass review. https://www.england.nhs.uk/commissioning/spec-services/npc-crg/gender-dysphoria-clinical-programme/implementing-advice-from-the-cass-review/
- ↵ Cass Review. NICE evidence reviews. 2021. https://cass.independent-review.uk/nice-evidence-reviews/
- ↵ NHS England. Interim service specification: specialist service for children and young people with gender dysphoria (phase 1 providers). Oct 2022. https://www.engage.england.nhs.uk/specialised-commissioning/gender-dysphoria-services/user_uploads/b1937-ii-specialist-service-for-children-and-young-people-with-gender-dysphoria-1.pdf
- Institute of Medicine ,
- Board on Health Care Services ,
- Committee on Standards for Developing Trustworthy Clinical Practice Guidelines
- Singh Ospina N ,
- Rodriguez-Gutierrez R ,
- Singh-Ospina N ,
- Wilson LM ,
- Dukhanin V ,
- McArthur K ,
- Robinson KA
- ↵ Baker KE, Wilson LM, Sharma R, Dukhanin V, McArthur K, Robinson KA. Hormone therapy, mental health, and quality of life among transgender people: a systematic review. J Endocr Soc 2021;5:bvab011.
- ↵ National Institutes of Health. The impact of early medical treatment in transgender youth. NIH Reporter. https://reporter.nih.gov/project-details/8965408
- ↵ Northwestern University Feinberg School of Medicine. Evidence-based gender-affirming care for young adults with Robert Garofalo, MD, MPH. 20 May 2022. https://www.feinberg.northwestern.edu/research/news/podcast/2022/evidence-based-gender-affirming%20-care-for-young-adults-with-robert-Garofalo-md-mph.html
- Tordoff DM ,
- Stepney C ,
- Inwards-Breland DJ ,
- Levine SB ,
- Abbruzzese E ,
- Delemarre-van de Waal HA ,
- Cohen-Kettenis PT
- Cohen-Kettenis P ,
- Endocrine Society

- KI Open Archive Home
- Avhandlingar / Theses
- Doktorsavhandlingar / Doctoral Theses
On gender dysphoria
Collections.
- Doktorsavhandlingar / Doctoral Theses - K8 (CNS)
- Doktorsavhandlingar / Doctoral Theses - SwePub
Total Visits
Total visits per month, file visits, top country views, top cities views, general information.

- Sexuality / Gender
Gender Dysphoria in Children Thesis
Pages: 17 (5712 words) · Style: APA · Bibliography Sources: 10 · File: .docx · Level: College Senior · Topic: Women's Issues - Sexuality
TOPIC: Thesis on Gender Dysphoria in Children Assignment
Two Ordering Options:
- To download this paper immediately , it takes only 2 minutes to subscribe. You can individually download any of our 2,000,000+ private & exclusive papers, 24/7! You'll also receive a permanent, 10% discount on custom writing. (After you pay and log-in, the "Download Full Paper" link will instantly download any paper(s) that you wish!)
- One of our highly experienced experts will write a brand new, 100% unique paper matching the exact specifications and topic that you provide! You'll be the only person on the planet to receive the one-of-a-kind paper that we write for you! Use code "Save10" to save 10% on your 1st order!
Download the perfectly formatted MS Word file!
We'll follow your exact instructions! Chat with the writer 24/7.
Related Thesis Papers:
Gender Identity Disorder Term Paper …
GID Gender Identity disorder has received a great deal of attention in recent years. The purpose of this discussion is to emphasize current treatment strategies for clients affected by Gender…
Pages: 10 (3105 words) · Type: Term Paper · Style: APA · Bibliography Sources: 15
Gender Identity Disorder The objective of this work is to research and report the diagnostic criteria and typical course of gender identity disorder including the theories of this disorder and…
Pages: 6 (1507 words) · Type: Term Paper · Style: APA · Bibliography Sources: 5
Homosexuality Demedicalization of the Gender Identity Disorder Essay …
Homosexuality Demedicalization of the Gender Identity Disorder Gender identity is a highly controversial subject. The notion that one's gender is a significant determination of personality traits, behavioral characteristics, social tendencies,…
Pages: 6 (1703 words) · Type: Essay · Bibliography Sources: 1
Gid the Changing Discourse Term Paper …
GID The Changing Discourse on GID The public discourse on homosexuality and gender-orientation differences is one that is in state of steady of evolution. Once treated strictly as anathema and…
Pages: 4 (1143 words) · Type: Term Paper · Bibliography Sources: 3
Identity Crisis Understanding Their Stance Chapter …
Transgender Identity Crisis A person's gender identity (i.e. inner concept of one's gender) is a multilayered, intricate construct. A majority of individuals have their gender identity and their anatomy in…
Pages: 4 (1505 words) · Type: Chapter · Bibliography Sources: 4
View other related papers >>
View 200+ other related papers >>
How to Cite "Gender Dysphoria in Children" Thesis in a Bibliography:
Chicago Style
Wed, Apr 17, 2024
- 5-Day Trial for $8.97
- Write a Paper for Me!
- Download 175K Essays
- Paper Topics
- Paper Editing Service
- Writing Samples
- Essay Writing Tutorials
- Info / FAQ / Guarantee
- Beware of Copycats!
- Listen to our radio ad!
- 1-866-7O7-27З7
- Text (super fast):
- 1-65O-585-OOO5
EssayTown.com © and ™ 2001–2024. All Rights Reserved. Terms & Privacy
- TEXT: 1-65O-585-OOO5
- Avoid Copycats!
- Listen to our radio music ad

Does Our Approach to Gender Dysphoria Need an Overhaul?
A new review concludes that many gender-related treatments lack strong evidence..
Posted April 15, 2024 | Reviewed by Devon Frye
- The treatment of gender distress is highly politicized, but scientific evidence is lacking.
- A new review concludes that hormone treatment may not reduce the risk of suicide in gender dysphoric youth.
- The review also finds no clear evidence that social transition in childhood has any effects on mental health.
- Blocking puberty may not induce changes in gender dysphoria or body satisfaction.
"Gender incongruence" is the term used to describe a marked and persistent incongruence between an individual’s experienced gender and their assigned gender or biological sex. " Gender dysphoria ," which commonly arises after the onset of puberty, happens when gender incongruence is associated with clinically significant distress or functional impairment. Many of those who experience gender dysphoria will end up identifying as transgender (or trans, for short), an umbrella term for people whose gender identity is different from the gender they were assigned at birth.
How should children and adolescents who experience gender incongruence and gender dysphoria be treated?
Persistent emotional distress—gender-related or otherwise—is, to an important degree, a health (and healthcare) matter. Yet gender distress has in recent years become politicized, and the lives and health of gender-troubled children and adolescents have become fodder for the political and ideological culture wars. As American politics and ideology often go, this complex and nuanced issue has thus been shoved into a tired, dichotomous formula.
For the progressives, the issue is one of minority rights. Gender dysphoric children and adolescents should thus be supported in their struggle to live as they wish, free of prejudice and discrimination . Early intervention to align the children’s body and appearance with their preferred gender must be encouraged. Those who question this view are typically accused of transphobia.
For conservatives, gender dysphoria is at best a passing individual fancy or troubling societal trend to be mocked and at worst a disease to be cured. Those who want to honor and affirm children’s gender struggles are seen as hopelessly "woke" social justice warriors pushing a radical agenda.
As culture wars go, this one, too, has been generating much heat in recent years, but very little light. Thus, the clinical healthcare services provided to children and adolescents who struggle with gender dysphoria have not been based on a solid foundation of high-quality research evidence.
A move forward from this abysmal state may have just happened, in the form of The Independent Review of Gender Identity Services for Children and Young People, commissioned by NHS England in 2019, with the goal of making evidence-based recommendations on the questions relating to the provision of these services. The final report of what is known as the Cass report (for Hilary Cass, the pediatrician who chaired the review team) just dropped in April 2024. It is consequential.

For one, the report is a good example of how such tasks should be approached and executed: a thorough, detailed, evenhanded, and levelheaded examination that puts child welfare front and center and follows the available empirical evidence wherever it leads, while acknowledging—but not succumbing to—the various ideological, political, and societal forces at play.
The review examined the existing formal research as well as receiving input from “people with relevant lived experience,” organizations working with LGBTQ+ children and young people, and medical and mental health professionals who provide care and support to children and young people struggling with gender identity.
Writes Cass: “The aim of this Review is to make recommendations that ensure that children and young people who are questioning their gender identity or experiencing gender dysphoria receive a high standard of care. Care that meets their needs, is safe, holistic, and effective. “
The findings of the review are quite eye-opening.
Cass first attempts to explain the dramatic recent increase in the number of gender dysphoric cases, as well as the recent shift in the gender dysphoric population from male to female majority. She argues that the increased social acceptance of trans phenomena is not a sufficient explanation. “The exponential change in referrals over a particularly short five-year timeframe is very much faster than would be expected for normal evolution of acceptance of a minority group. This also does not adequately explain the switch from birth-registered males to birth-registered females, which is unlike trans presentations in any prior historical period.”

Cass notes that these gender dysphoria trends are immersed in the broader context of increased rates of mental health problems in children and adolescents (particularly females) in the last decade, and a corresponding increase in the number of young people “presenting with other bodily manifestations of distress; for example, eating disorders, tics and body dysmorphic disorder.” Gender identity and expression are determined by a difficult-to-disentangle mix of biological, neurological, psychological, and societal factors. Ostensible gender identity problems may thus be symptomatic of other, underlying and unresolved issues, Cass argues. Gender dysphoria, in other words, is not always about gender, just as germ phobia is not always about germs.
Cass then discusses the role and impact of social transitioning, defined here as “social changes to live as a different gender such as altering hair or clothing, name change, and/or use of different pronouns.” She notes that such transitioning is not a one-size-fits-all phenomenon. “There is a spectrum from young people who make relatively limited gender non-conforming changes in appearance to those who may have fully socially transitioned from an early age and may be living in stealth.”
She notes that a key difference between children and adolescents is that “parental attitudes and beliefs will have an impact on whether the child socially transitions. For adolescents, exploration is a normal process, and rigid binary gender stereotypes can be unhelpful.”
The debate over the benefits and harms of social transitioning is a flashpoint in the culture wars. Cass, however, found “no clear evidence that social transition in childhood has any positive or negative mental health outcomes, and relatively weak evidence for any effect in adolescence . However, those who had socially transitioned at an earlier age and/or prior to being seen in clinic were more likely to proceed to a medical pathway.”
“Although it is not possible to know from these studies whether earlier social transition was causative in this outcome, lessons from studies of children with differences in sexual development (DSD) show that a complex interplay between prenatal androgen levels, external genitalia, sex of rearing and sociocultural environment all play a part in eventual gender identity… Therefore, sex of rearing seems to have some influence on eventual gender outcome, and it is possible that social transition in childhood may change the trajectory of gender identity development for children with early gender incongruence.”
She concludes: “Avoiding premature decisions and considering partial rather than full transitioning can be a way of ensuring flexibility and keeping options open until the developmental trajectory becomes clearer.”
Cass then turns to inquire about the evidence regarding medical transitioning (a part of transition in which a transgender person undergoes medical treatments so that their physical and sex characteristics better match their gender identity).
She first addresses the common use of puberty blockers with gender dysphoric children. “The original rationale for the use of puberty blockers,” Cass notes, “was that this would buy ‘time to think’ by delaying the onset of puberty and also improve the ability to ‘pass’ in later life. Subsequently, it was suggested that they may also improve body image and psychological well-being.” The evidence, however, shows that blocking induces “no changes in gender dysphoria or body satisfaction,” she writes.
Evidence as to the effects of puberty suppression on psychological or psychosocial wellbeing, cognitive development, cardio-metabolic risk, and fertility is found to be “insufficient” and “inconsistent.” Moreover, the fact that a vast majority of young people who are started on puberty blockers proceed to masculinising/feminising hormones suggests that puberty blockers do not in fact “buy time to think” and may rather “change the trajectory of psychosexual and gender identity development.”
Cass thus proposes that “because puberty blockers only have clearly defined benefits in quite narrow circumstances, and because of the potential risks to neurocognitive development, psychosexual development, and longer-term bone health, they should only be offered under a research protocol.”
The evidence about hormone treatment is examined next. “It has been suggested that hormone treatment reduces the elevated risk of death by suicide in this population,” Cass notes, “but the evidence found did not support this conclusion.” Cass notes the lack of high-quality outcome research—short- and long-term—of hormone interventions in adolescents with gender dysphoria or incongruence.
Thus, she writes, “No conclusions can be drawn about the effect on gender dysphoria, body satisfaction, psychosocial health, cognitive development, or fertility. Uncertainty remains about the outcomes for height/growth, cardiometabolic, and bone health. There is suggestive evidence from mainly pre-post studies that hormone treatment may improve psychological health, although robust research with long-term follow-up is needed.”
Cass notes that while a diagnosis of gender dysphoria is often considered a prerequisite for hormone treatment, such diagnosis “is not reliably predictive of whether that young person will have longstanding gender incongruence in the future, or whether medical intervention will be the best option for them.” Therefore, Cass recommends “an extremely cautious clinical approach and a strong clinical rationale for providing hormones before the age of 18. This would keep options open during this important developmental window, allowing time for management of any co-occurring conditions, building of resilience , and fertility preservation, if required.”
Cass notes the overall dearth of quality long-term outcome data on both medical and non-medical interventions, which means that “young people and their families have to make decisions without an adequate picture of the potential impacts and outcomes.”
In sum, youngsters' gender concerns should not be mocked or denied. Gender curiosity and exploration are common, particularly in adolescence, and should not be unduly pathologized. At the same time, young children should not be hustled onto a path toward gender transition. However well-intentioned, the Cass review suggests that current official guidelines, such as those of The American Academy of Pediatrics, are not rooted in solid evidence.
Likewise, the popular, medicalized approach known as “ gender-affirming care ," which is based on the notion that children’s early declarations of identity must be accepted at face value and their transition aggressively assisted, may not be justified by the evidence. Gender dysphoria may be transitory; it may at times be a symptom of underlying stress unrelated to gender identity. Changing one’s gender affiliation and appearance are often insufficient to resolve the underlying psychological dysfunction and alleviate distress.
Yet for some youngsters, transition is a solution. “Being gender-questioning or having a trans identity means different things to different people. Among those being referred to children and young people’s gender services, some may benefit from medical intervention and some may not. The clinical approach must reflect this.”
Finally, the healthcare we provide to youngsters who are struggling with gender distress should be a means to an end of helping them, rather than a means of winning a battle in the culture wars. Focusing on gender needs to be supplanted by a focus on the person. The care we provide youngsters who struggle with gender distress needs to be based in empirical facts, not merely good intentions or ideological and political theories.

Noam Shpancer, Ph.D., is a professor of psychology at Otterbein University and a practicing clinical psychologist in Columbus, Ohio.
- Find a Therapist
- Find a Treatment Center
- Find a Support Group
- International
- New Zealand
- South Africa
- Switzerland
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience
- Share full article
Advertisement
Supported by
Transgender Veterans Sue V.A. Over Gender-Affirming Surgeries

By Aishvarya Kavi
Reporting from Washington
An advocacy group for transgender veterans has filed a lawsuit over the failure of the Department of Veterans Affairs to provide or pay for gender-affirming surgeries.
The federal lawsuit , filed on Monday by the Transgender American Veterans Association , said the decision “amounts to discrimination on the basis of sex and transgender status” and threatens the health of veterans. It also accused the V.A. of letting the issue “languish” in the three years since the department’s secretary, Denis McDonough, said the administration would work to provide the surgeries.
In response to a request for comment, the department said it was unable to discuss the pending litigation.

Why It Matters
The Department of Veterans Affairs offers the majority of medical procedures known as gender-affirming care, including hormone therapy, prosthetics and hair removal. But veterans must seek surgeries outside of V.A. hospitals, where they have to rely on private health insurance coverage or pay the costs out of pocket.
Josie Caballero, the association’s acting president, said the cost could force veterans to settle for lower-quality care or delay care, heightening distress.
The National Center for Transgender Equality estimates there are more than 134,000 transgender veterans. In a V.A. survey of transgender and gender-nonconforming veterans conducted in 2022 and 2023, 78 percent of 6,600 respondents said they wanted gender-affirming surgeries. More than half said they had delayed or gone without treatment, and the majority cited cost as the reason.
V.A. doctors already perform procedures that would be considered gender-reaffirming surgeries. For example, a mastectomy would be covered in order to treat or prevent breast cancer, but the same procedure is not covered for a veteran experiencing gender dysphoria. An exception is made when revising or treating complications from surgeries that were done outside the V.A. system.
“That is a deep frustration that a lot of veterans have,” Ms. Caballero said. “The surgeons are there. They just need the permission to do it.”
Soon after President Biden took office in 2021, Mr. McDonough announced that the administration would offer the surgeries. At the time, it was estimated that changing the health care benefits for transgender veterans could take years.
The advocacy group took the delay to court in January. Mr. McDonough responded with a letter denying the proposed policy change, saying the department was not ready “at this time.”
In a news conference days later, Mr. McDonough suggested that the availability of gender-affirming surgeries would be delayed until Dr. Shereef Elnahal, the department’s under secretary for health, completed a review of the 2022 PACT Act, a law that expanded benefits for veterans .
“We’ve given him several months to do that,” Mr. McDonough said in February. He added, “V.A. remains committed to providing care to transgender vets, but we’re not ready at this point to initiate rule-making addressing the specific regulatory changes proposed in the petition.”
What Happens Next
Lindsey Cormack , an associate professor at the Stevens Institute of Technology who studies veterans policies, said the administration was probably in the middle of the bureaucratic rule-making process, trying to clear a legal path to make sure that expanding health care provisions to include gender-affirming surgeries is allowed under the PACT Act.
Ms. Cormack pointed out there had been other health care treatments that the Department of Veterans Affairs did not offer, such as ketamine therapy or psychedelic drugs .
It is unclear how soon the policy can be changed to make gender-affirming surgeries available at V.A. hospitals. The department has only recently expanded other medical treatments to all veterans, like offering in vitro fertilization to unmarried veterans and those in same-sex marriages.
The Transgender American Veterans Association is represented in this lawsuit by the Veterans Legal Services Clinic at Yale Law School, which successfully sued the department to make those fertility treatments more widely available.
“The veterans administration itself, it moves slow,” Ms. Cormack said. “It’s not a fast, expedient, changing thing.”
Aishvarya Kavi is based in the Washington bureau. More about Aishvarya Kavi

IMAGES
VIDEO
COMMENTS
The DSM-III (3rd ed.; DSM-III; American Psychiatric Association, 1980) was the first edition of the DSM to include a gender-related diagnosis, called Transsexualism located within the "psychosexual disorders" category.The adult diagnosis of transsexualism referred to "discomfort and inappropriateness" of one's biological sex alongside the wish to be rid of one's genitals and live in ...
For the purpose of this thesis, I will use the term "transgender" to refer to individuals who do not identify with their assigned gender at birth, but rather with the opposite binary ... gender dysphoria, Schneider et al. (2016) discuss the rapidly changing definition of gender
Gender dysphoria (GD) is a condition characterized by a marked incongruence between one's experienced and expressed gender and the one assigned at birth and is often associated with clinically significant distress or impairment in social, occupational, or other important areas of functioning, especially when reported early [].In recent years, the number of young patients diagnosed with GD or ...
gender dysphoria as the result of a sociological process rooted in power imbalances. In the. process of gender dysphoria we see gender euphoric desires for affirmation filtered through ...
Introduction. Gender dysphoria is a psychological condition in which a person's subjectively felt identity and gender are not congruent with their biological sex, often causing clinically significant impairment in social and other areas of functioning (American Psychiatric Association, Citation 2013; Smith & Matthews, Citation 2015; De Vries et al., Citation 2011).
On Gender Dysphoria THESIS FOR DOCTORAL DEGREE (Ph.D.) at Karolinska Institutet, to be publicly defended in lecture hall Nanna Svartz, ... Gender dysphoria refers to the discomfort or distress that gender incongruence may cause. If the distress is clinically significant, the individual may need gender-affirming treatment. The literature is ...
Bourgeois, Beau, "IMPLICATIONS OF GENDER DYSPHORIA ON GENDER SCHEMA AND SOCIAL COGNITIVE THEORIES OF GENDER DEVELOPMENT" (2022). Electronic Theses and Dissertations. 2200. https://egrove.olemiss.edu/etd/2200 This Thesis is brought to you for free and open access by the Graduate School at eGrove. It has been accepted for
Gender dysphoria (GD) is the extreme distress experienced by an individual because of a mismatch between their gender identity and the sex assigned at birth. GD has been an ambiguous category in psychiatry, initially termed as "gender identity disorder" till Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition ( DSM-5 ...
The nosography of Gender Dysphoria (GD) has recently been object of an important change. In the Statistical and Diagnostic Manual of Mental Disorders, DSM V [], this diagnosis was separated from paraphilias and sexual disorders, becoming an independent category.The most important innovative aspect introduced by the DSM V concerns the condition known as "Gender Identity Disorder", which is ...
Gender Identity, Trauma, Adverse Childhood Experience (ACE). ABSTRACT . It has been established that individuals with transgender* identities experience abuse and trauma at higher frequencies than individuals with non-transgender identities (Mascis, 2011). Gender dysphoria currently exists as a mental health diagnosis, perpetuating stigma as ...
medical interventions for adolescents might prolong gender dysphoria and contribute to an appearance that could provoke abuse and stigmatization."6 Of note, when it comes to chest surgery, another gender affirming irreversible surgery, the specific age of majority requirement in the SOC criteria is not present. According to WPATH SOC:
Gender dysphoria (GD) refers to a person's dissatisfaction with the sex assigned at birth. According to the diagnostic criteria, gender dysphoria refers to cases such as the mismatch between the gender experienced and the secondary or primary sexual characteristics of the person, a strong preference to get rid of the secondary or primary sexual characteristics, and a strong desire to have ...
Gender dysphoria and related concepts. The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5)1 defines gender dysphoria (GD) as a condition in which a person has marked incongruence between the expressed or experienced gender and the biological sex at birth. This causes clinically significant distress or impairment in social, occupational or other important ...
The surge in treatment of minors. More adolescents with no history of gender dysphoria—predominantly birth registered females2—are presenting at gender clinics. A recent analysis of insurance claims by Komodo Health found that nearly 18 000 US minors began taking puberty blockers or hormones from 2017 to 2021, the number rising each year.3 4 Surveys aiming to measure prevalence have found ...
Gender dysphoria and related concepts. The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) Citation 1 defines gender dysphoria (GD) as a condition in which a person has marked incongruence between the expressed or experienced gender and the biological sex at birth. This causes clinically significant distress or impairment in social, occupational or other ...
of the content discussed in this thesis. Chapter 4 explores the history of gender dysphoria and the statistics of those diagnosed with this condition. It also provides definitions of terms that will be used throughout the paper. Chapter 5 provides two approaches to treating gender dysphoria in
Gender dysphoria refers to the discomfort or distress that gender incongruence may cause. If the distress is clinically significant, the individual may need gender-affirming treatment. The literature is sparse with respect to the etiology, prevalence, and long-term outcomes. The overall aim of this thesis is to further our understanding of ...
Gender dysphoria and related concepts. The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) 1 defines gender dysphoria (GD) as a condition in which a person has marked incongruence between the expressed or experienced gender and the biological sex at birth. This causes clinically significant distress or impairment in social, occupational or other important ...
TOPIC: Thesis on Gender Dysphoria in Children Assignment Most social researchers would likely agree that human experience their worlds in unique ways, but almost everyone is influenced by both nature and nurture as they develop over the life course. When some young people experience a gender identity that is at odds with their anatomical sex ...
The evidence, however, shows that blocking induces "no changes in gender dysphoria or body satisfaction," she writes. Evidence as to the effects of puberty suppression on psychological or ...
In a V.A. survey of transgender and gender-nonconforming veterans conducted in 2022 and 2023, 78 percent of 6,600 respondents said they wanted gender-affirming surgeries.