
ESSAY SAUCE
FOR STUDENTS : ALL THE INGREDIENTS OF A GOOD ESSAY

Essay: Cardiovascular disease (CVD)
Essay details and download:.
- Subject area(s): Health essays
- Reading time: 2 minutes
- Price: Free download
- Published: 22 October 2015*
- File format: Text
- Words: 293 (approx)
- Number of pages: 2 (approx)
Text preview of this essay:
This page of the essay has 293 words. Download the full version above.
Cardiovascular disease (CVD) is the leading cause of non-communicable disease deaths worldwide (World Health Organization, 2014). The World Health Organization predicts that the number of deaths caused by CVD will reach 23.3 million by 2030. CVD is an umbrella term that encompasses a group of disorders of the heart and blood vessels. These diseases include hypertension, coronary heart disease, stroke, heart failure, and cardiomyopathies to name a few. One of the risk factors for CVD is overweight or obesity and sedentary behavior. Obesity is an excessive accumulation of adipose tissue. Overweight and obesity are defined by the International Obesity Task Force as a Body Mass Index (BMI) between 25.0 and 29.9 kg/m^2 and a BMI ‘30.0 kg/m^2 respectively (Low et al., 2009). The worldwide prevalence of overweight and obesity has increased exponentially in the last decade and is highest in the Americas with 61% overweight or obese (World Health Organization, 2014). This has had large impacts on the health care system, with the current estimated cost of overweight and obesity at over 100 billion U.S. dollars per year (Meckling et al., 2004). There as been an increased focus on reducing the ‘obesity epidemic’ and preventing the increased risks of CVD. It is estimated that 45% of American women and 30% of American men diet to lose weight, largely as a result of increased awareness regarding both obesity and CVD, and because it is an effective and cost efficient weight loss strategy. There is comprehensive research on the effects of diets on weight and body composition however their effects on cardiovascular health are largely unknown and require further research (Phillips, 2008). This study will focus on two of the more commonly used weight loss diets, low-fat diet and low-carbohydrate diet. There are several forms of both diets, however low-fat diets are most commonly defined as <30% of daily energy intake from total fat and <7% saturated fat (Bazzano et al., 2014). Several definitions of low-carbohydrate diets include 30-130g of carbohydrate per day, <30% of daily energy intake from carbohydrates, or very low-carbohydrate diets consisting of <30 g of carbohydrates per day. The Dr. Atkin's New Diet Revolution is one of the most popular low-carbohydrate diets and has been modeled in several studies. It consists of 12 weeks of <20 g/day of carbohydrates followed by a 5g/day per week increase (Foster et al., 2010). This study aims to research the effects of a low-fat diet vs. a low-carbohydrate diet on weight loss in overweight and obese individuals and on CVD risk factors linked to obesity. Based on a review of the literature this proposal predicts that both diets will achieve similar results in weight loss reduction and body composition factors among individuals of obese status. This proposal also predicts to observe divergent effects on CVD risk factors by each diet, more specifically a greater reduction in several markers of CVD in participants assigned the low-fat diet. When consuming a low-carbohydrate diet there is an increased proportion of dietary intake from fat. This has several implications on endothelial health as a result of increased low-density lipoprotein cholesterol and fat (Bazzano et al., 2014 & Phillips et al., 2008). This research is extremely relevant within contemporary society due to both the prevalence of overweight and obesity worldwide as well as CVD, resulting in increased mortality rates yearly. Knowing the effects of a low-fat and low-carbohydrate diet on CVD markers will also assist health professionals in their practices when recommending or administering diets to their patients.
...(download the rest of the essay above)
About this essay:
If you use part of this page in your own work, you need to provide a citation, as follows:
Essay Sauce, Cardiovascular disease (CVD) . Available from:<https://www.essaysauce.com/health-essays/essay-cardiovascular-disease-cvd/> [Accessed 01-04-24].
These Health essays have been submitted to us by students in order to help you with your studies.
* This essay may have been previously published on Essay.uk.com at an earlier date.
Essay Categories:
- Accounting essays
- Architecture essays
- Business essays
- Computer science essays
- Criminology essays
- Economics essays
- Education essays
- Engineering essays
- English language essays
- Environmental studies essays
- Essay examples
- Finance essays
- Geography essays
- Health essays
- History essays
- Hospitality and tourism essays
- Human rights essays
- Information technology essays
- International relations
- Leadership essays
- Linguistics essays
- Literature essays
- Management essays
- Marketing essays
- Mathematics essays
- Media essays
- Medicine essays
- Military essays
- Miscellaneous essays
- Music Essays
- Nursing essays
- Philosophy essays
- Photography and arts essays
- Politics essays
- Project management essays
- Psychology essays
- Religious studies and theology essays
- Sample essays
- Science essays
- Social work essays
- Sociology essays
- Sports essays
- Types of essay
- Zoology essays
Home — Essay Samples — Nursing & Health — Cardiovascular System — Cardiovascular disease: Risk Factors
Cardiovascular Disease: Risk Factors.
- Categories: Cardiovascular System Heart
About this sample

Words: 477 |
Published: Dec 18, 2018
Words: 477 | Page: 1 | 3 min read

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Prof. Kifaru
Verified writer
- Expert in: Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
2 pages / 858 words
2 pages / 1178 words
1 pages / 668 words
3 pages / 1304 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Cardiovascular System
The cardiovascular system is a major part of the body and is not appreciated as much as it should be. The movement of the blood is known as the cardiovascular system. The main components of the system are the heart, the blood [...]
NCDs, also known as chronic diseases, are not passed from person to person. They are of long duration and generally progress slowly. The four main types of NCDs are cardiovascular diseases (myocardial infarction, stroke), [...]
Hemostasis is the process that occurs when a blood vessel ruptures and large amounts of plasma and formed elements may escape (Bostwick and Wingerd, 2013). It can be divided into primary and secondary hemostasis. Primary [...]
In Godric, Frederick Buechner uses multiple characters who are at once medieval and modern to not only tell the uncommon tale of a flawed saint, but to depict through medieval text and setting his modern comments, [...]
Abstract This paper includes the studies of techniques used to prevent, treat and nutritional or surgical therapies used for Coronary artery disease. This paper also outlines some of the causes and possible threats of having [...]
Throughout history, the discovery of anatomy through the process of dissection has always elicited curiosity in numerous scholars scattered through the empires of the world. Of interest is how dissection was incorporated in the [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Springer Nature - PMC COVID-19 Collection

Cardiovascular Disease: An Introduction
Marc thiriet.
INRIA project team REO, Université Pierre et Marie Curie, Laboratoire Jacques-Louis Lions, Paris, France
Cardiovascular disease (CVD) is a collective term designating all types of affliction affecting the blood circulatory system, including the heart and vasculature, which, respectively, displaces and conveys the blood.
Cardiovascular disease (CVD) is a collective term designating all types of affliction affecting the blood circulatory system, including the heart and vasculature, which, respectively, displaces and conveys the blood. This multifactorial disorder encompasses numerous congenital and acquired maladies. CVD represents the leading noncommunicable cause of death in Europe (∼50% of all deaths; ∼30% of all deaths worldwide) [ 29 ]. In 2008, nine million people died of noncommunicable diseases prematurely before the age of 60 years; approximately eight million of these premature deaths occurred in low- and middle-income countries [ 30 ].
Cardiovascular disease encompasses atherosclerosis with its subtypes (coronary [CoAD], cerebral [CeAD], and peripheral artery disease [PAD]) with two major complications, myocardial infarction and ischemic stroke (more common than hemorrhagic stroke; Sect. 1.1.5 and Vol. 13, Chap. 5. Atherosclerosis), heart failure (HF), cardiac valvulopathies and arrhythmias, rheumatic heart disease (damage of the myocardium and cardiac valves caused by streptococci bacteria), congenital heart disease, and deep vein thrombosis with its own complication, pulmonary embolism.
Rare cardiovascular maladies are classified into [ 31 ]:
- Rare afflictions of the systemic (class I ) and pulmonary circulation (class II )
- Rare cardiomyopathies (class III )
- Rare congenital cardiovascular disorders (class IV )
- Rare cardiac arrhythmias (class V )
- Cardiac tumors and cardiovascular affections related to cancer (class V I )
- Cardiovascular sickness in pregnancy (class V II )
- Other types of rare cardiovascular illness (class V III )
Etiology 1 of a given malady refers to the cause, set of causes, or manner of causation of a disease. CVD is multicausal, with clinical (dyslipoproteinemia and hypertension) and behavioral factors (sedentarity, overnutrition, smoking, and a stressful life). Deficiency or excess of trace elements in soil may contribute to CVD [ 32 ]. A major cause of CVD is atherosclerosis.
Diagnosis 2 of many diseases, in addition to assessment of prognosis, is facilitated by the utilization of specific markers that can be proteins and nucleic acids, such as short microRNAs and long a priori nonprotein-coding RNA implicated in the regulation of metabolism, control of blood circulation, and inflammation.
Epidemiological studies are aimed at extracting individual, 3 environmental (indoor and outdoor air pollution, second-hand smoke), and societal risk factors, ranking them to the determined predominant factors according to their impact, morbidity, and mortality rate. These studies also aimed to propose strategies to reduce CVD burden and for the prevention of early adverse events. In a health system that brings research into practice, the aim is to reduce risk factors and determine appropriate treatments [ 33 ].
Vasculopathies and Vasculitides
Vasculopathy corresponds to any disease affecting the blood vessels that can be caused by degenerative, metabolic (e.g., diabetic vasculopathy), and inflammatory disorders in addition to thromboembolic maladies.
Vasculitis , or angiitis , is more specific, as it is defined by a focal or widespread inflammation of the vascular wall, whatever the blood vessel type (i.e., arteries, arterioles, capillaries, venules, and veins), size (i.e., large, medium, or small), number, and location.
Ethnicity and gender can affect vascular physiological and pathophysiological mechanisms. Data obtained in a general population, such as correlation between a risk factor and a given disease or complication associated with a given gene mutation, may not be representative of features of a homogeneous subpopulation. Sex differences in incidence, prevalence, morbidity, and mortality from CVD, which include sex-specific disorders and sex-dependent symptom presentation and evolution of pathophysiological processes common to both genders (e.g., hypertension and atherosclerosis), represent a source of health disparity [ 34 ]. Sex and racial differences in pharmacodynamics and -kinetics affect therapy efficiency [ 35 ].
Ethnic Differences
Ethnicity is a source of health inequalities. People from certain ethnicities suffer from premature CVD. In particular, ethnic heritage influences the occurrence rates of hypertension and diabetes.
According to the American Heart Association and National Institute of Health, 40% of African American men and women have a coronary disease (versus 30 and 24% of European-American men and women, respectively) due to genetic differences between ethnic groups rather than by life conditions and diet. Moreover, African American women with coronary disease are at a twofold higher risk for myocardial infarction than European American women. In the USA:
- African Americans are at a higher risk for hypertension.
- North American Latinos have higher rates of obesity and diabetes.
- The coronary artery disease rate is highest in the South Asian population.
- The stroke rate is the highest in individuals of African-Caribbean descent, the prevalence of diabetes in these two ethnic groups being much higher than in the White population.
In the UK [ 36 ]:
- The incidence of myocardial infarction is higher in South Asians than in non-South Asians for both sexes.
- The incidence of stroke in black people is higher than in White people, whatever the sex.
- The prevalence of CoAD is highest in Indian and Pakistani men.
- The revascularization rate is higher in the White ethnic group than in the black and Asian ethnic groups.
- Individuals from different ethnic groups tend to store fat in different regions of the body.
- The prevalence of overweight and obesity in young children is highest in the Black ethnic group.
- The prevalence of diabetes is much higher in Black Caribbean, Indian, Pakistani, and Bangladeshi men.
However, these inequalities can be related not only to genetic differences but also to distinct cultural and social practices. The influence of ethnicity can be difficult to distinguish from that of the socioeconomic status. Moreover, a genetic diversity can exist within racial and ethnic groups.
Gender Influence
Hormonal in addition to genetic and environmental factors contribute to sex differences in CVD. The organism environment influences hormonal secretion, which, in turn, affects the brain function, hormones acting on the genome of neural cells that contain their cognate receptors. For example, the ventromedial and ventrolateral and arcuate nuclei contain estrogen-sensitive neurons, the ventromedial nucleus responding more rapidly than the arcuate nucleus [ 37 ].
In addition, hormonal secretion by the adrenal gland and gonads (testis and ovary) is controlled not only by temperature (heat or cold), threat, and sexual excitement, which prime adaptive responses, but also by circadian oscillators entrained by environmental signals (light and dark).
Repeated psychosocial stress can provoke neuronal loss in the hippocampus, which receives heavy input from the dentate gyrus mossy fiber system [ 37 ]. Adrenal steroids, which protect in the short term, operate in conjunction with neural excitatory amino acids, causing damage and allostatic load in the long term, when the adaptive response is not managed efficiently and persists. Gonadal hormones can also produce both protection and damage according to their concentration and duration of exposure.
Sex is mainly determined by the X and Y chromosomes, which create a sex-specific expression pattern. Men possess a single copy of each type (XY genotype) and women two copies of the X chromosome (XX genotype), one of the X chromosome being silenced during embryogenesis (X-chromosome inactivation).
In general, premenopausal women are at a lower CVD risk than men of a similar age. Men develop hypertension at younger ages than women. The sex-determining region Y (SRY locus) of the Y chromosome regulates the transcription of tyrosine hydroxylase (TH; or Tyr 3-monooxygenase), the rate-limiting enzyme in the synthesis of catecholamines such as noradrenaline, and yields a gender-dependent difference in sympathetic activity, predisposing men to hypertension to a greater extent than women [ 34 ].
The Y chromosome also includes genes involved in inflammation and innate immunity linked to macrophage activation [ 34 ]. On the other hand, the X chromosome affects expression of genes associated with apoptosis, lipid oxidation, and generation of reactive oxygen species (ROS) by the mitochondrion.
In individuals from European countries, some chromosomal loci related to lipid metabolism exhibit sex-specific effects, in particular the HMGCR and NCAN genes encoding 3-hydroxy 3-methylglutaryl coenzyme-A reductase and neurocan (or chondroitin sulfate proteoglycan CSPG3), respectively [ 34 ].
A sex-specific single-nucleotide polymorphism in the locus of the CPS1 gene encoding mitochondrial carbamoyl–phosphate synthase-1, which is involved in hepatic nitrogen urea metabolism and synthesis of arginine, a precursor of nitric oxide (NO), has a greater effect in women than in men [ 34 ].
The gene encoding the androgen receptor resides on the X chromosome and displays a polymorphism linked to a highly variable number of CAG repeats. Variants in this gene have a greater impact in men than in women [ 34 ]. Genetic variants also affect enzymes involved in synthesis, conversion, and degradation of sex steroids.
Estrogens (e.g., estradiol [E 2 ]) and androgens (e.g., testosterone and dihydrotestosterone [DHT; or androstanolone]) govern multiple processes in both women and men [ 38 ].
Estrogen Signaling
Estradiol is synthesized primarily in the granulosa cells of ovaries and Sertoli cells in males. It tethers to various types of cytosolic ERα and ERβ (i.e., ligand-activated transcription factors NR3a1–NR3a2) in cardiomyocytes (CMCs) and vascular smooth muscle (vSMCs) and endothelial cells (ECs) in addition to plasmalemmal estrogen receptor GPER1 (or GPR30) in vascular endotheliocytes and smooth myocytes, renal intercalated and tubular cells, and cells of the hypothalamic–pituitary–adrenal axis [ 38 ].
Membrane-initiated rapid (nongenomic) signaling launched by sex steroid hormones produced by the adrenal cortex, ovary, and testis involves estrogen receptors in the plasma membrane. In addition to the membrane estrogen receptor GPER1, sex steroid receptors such as NR3a1 and NR3a2 can localize to the plasma membrane; NR3a1 can be identified in caveolae associated with proteic complexes), its palmitoylation (Cys447) being required for its translocation to the plasma membrane [ 39 ]. NR3a1 and NR3a2 are necessary and sufficient for rapid estrogen-triggered signaling. At the plasma membrane, caveolin-1 serves as a scaffold for other signaling molecules (e.g., trimeric G protein, Src, PI3K, GFR, and MNAR) 4 that are activated by the E 2 –NR3a1 couple in caveolae, which facilitates the fast generation of early signals (e.g., Ca 2+ influx). 5 Other NR3a1 move to the nucleus chaperoned by heat shock protein HSP90 owing to a nuclear localization sequence or to mitochondria. Nuclear NR3a1 is mandatory for the development of the female reproductive tract and mammary gland.
NR3a2 prevents adverse cardiac remodeling (hypertrophy and fibrosis). The E 2 –NR3a2 couple stimulates PI3K and primes transcription of the RCAN gene that encodes the regulator of calcineurin (PP3) [ 39 ]. 6 In addition, the E 2 –NR3a2 couple launches synthesis of the natriuretic peptides ANP and BNP, which hampers adverse cardiac hypertrophy via ERK kinases in the CMC. On the other hand, atherogenic 27-hydroxycholesterol serves as an endogenous selective estrogen receptor modulator (SERM), which abounds in the diseased arterial wall. It competitively precludes E 2 –NR3a binding and hence both the rapid (i.e., NO-mediated vasodilation) and delayed transcriptional E 2 actions [ 39 ].
Estrogens are also synthesized in the central nervous system from cholesterol or converted from aromatizable androgens in presynaptic terminals [ 38 ]. Estrogens can then diffuse. Both NR3a1 and NR3a2 are produced in nuclei in the forebrain and brainstem that regulate cardiac frequency and blood pressure (solitary tract [NTS] and parabrachial nuclei [PBN] and rostral ventrolateral medulla [RVLM]), enhancing sympathetic nervous system-mediated baroreflex. They regulate the local renin–angiotensin axis (RAA), these brain nuclei possessing renin, angiotensinogen, angiotensin convertases ACE1 and ACE2, and angiotensin Agt2 receptors (e.g., AT 1 and AT 2 ). Angiotensin-2 and aldosterone stimulate ROS production in the brain by NAD(P)H oxidase, thereby raising sympathetic nerve activity. In the subfornical organ (SFO), estrogens via NR3a1 and NR3a2 prevent intracellular ROS formation. Estradiol reduces both Agt2- and aldosterone-induced hypertension in male and ovariectomized female rodents [ 38 ].
However, NR3a1 and NR3a2 regulate blood pressure differently. In male rats, injection of E 2 into the paraventricular nucleus (PVN) does not affect cardiac frequency and blood pressure. In female mice, activated CNS NR3a1 protects against Agt2-induced hypertension, whereas PVN NR3a2 and RVLM NR3a2 protect against aldosterone-induced hypertension. In female and male mice, activated CNS NR3a2 preserves resting blood pressure via RVLM Ca V channels [ 38 ]. Therefore, at least in female and male rodents, specific NR3a subtypes mediate E 2 -mediated protection in different nuclei.
Nitric oxide synthase NOS1 is produced to a greater extent in the SFO and PVN of female mice than in these nuclei in male mice [ 38 ]. In addition, estrogens rapidly stimulate NO production by NOS3 via NR3a1 in the vascular endothelium, whatever the gender.
Estrogens signal to the kidney when salt sensitivity increases in menopausal women, likely because estrogens support NO action and lower the AT 1 / AT 2 ratio, hence preserving renal Na + handling [ 38 ]. In premenopausal women, salt loading during estrogen peaks alleviates filtration fraction and causes a sustained renal vasodilation. In postmenopausal women, salt loading raises the filtration fraction. In addition, NR3a1 mediates regulation of the renal ACE1/ACE2 ratio by estrogens, ACE2 converting vasoconstrictive, prohypertrophic, and proproliferative angiotensin-2 into Agt (1–7) .
GPER1 on arterial and venous endotheliocytes and smooth myocytes counters endothelin-1– and prostanoid-primed vasoconstriction and lessens superoxide production, hence protecting against hypertension [ 38 ]. Furthermore, GPER1 activates NOS3 in the vascular endothelium. It also attenuates vascular smooth muscle cell (vSMC) proliferation and vascular inflammation.
Estrogens operate on low-density lipoproteins (LDLs) and the LDL receptor (LDLR) to improve lipidemia. Estradiol upregulates LDLR production and stimulates sterol 27-hydroxylase CyP27a1 activity, which hampers LDL formation. In addition, estrogens promote synthesis of the apolipoprotein ApoA1 in the liver and of ApoE [ 38 ]. They also boost ABCa1 production, facilitating reverse cholesterol transport, but hinder ScaRb1 expression, hence prolonging the duration of circulating high-density lipoproteins (HDLs).
Many leukocytes infiltrating atherosclerotic plaques, such as macrophages, B and T lymphocytes, and mastocytes possess sex hormone receptors; estrogens can thus influence inflammation [ 38 ]. Estrogens exert the anti-inflammatory M2 phenotype in macrophages; reduce LDL oxidation, endothelial activation, and adhesion of neutrophils and monocytes to the endothelium; and impede NOx activity and hence ROS production.
Estradiol that dampens inflammation can reduce formation of tumor-necrosis factor superfamily member TNFSF1 and prevent its secretion [ 38 ]. Moreover, it activates NR3a2 and subsequently Iκ Bα which represses NFκB-boosted inflammation.
Estrogen supports angiogenesis in PAD owing to NOS3 [ 38 ]. Proangiogenic estrogens favor mobilization of endothelial progenitor cells and incorporation into neovascularization sites owing to NOS3 stimulation and MMP9 activity in the bone marrow.
Relatively high concentrations of circulating female sex hormones protect against abdominal aortic aneurysm (AAA) development, as these hormones reduce inflammation and matrix metallopeptidase activity in the aortic wall [ 38 ]. In female animals, a higher concentration of plasminogen activator inhibitor PAI1, which precludes MMP2 and MMP9 production, protects against AAA development. Estrogens also lower MMP2 and MMP9 concentrations in addition to immunocyte infiltration in AAA and hence slow dilation rate with respect to ovariectomized rodents. In addition, NO production stimulated by estrogens protect against AAA. Aortas from female mice contain larger NR3a1 amounts and lower matrix metalloproteinase (MMP) activity.
On the other hand, in humans, AAA samples contain larger concentrations of 3-hydroxyanthranilic acid (3HAA), indoleamine (2,3)-dioxygenase (IDO), and kynureninase than adjacent aortic segments. Indoleamine dioxygenase is the first and rate-limiting enzyme in the kynurenine pathway of tryptophan metabolism that creates 3HAA. Acute infusion of angiotensin-2 favors abdominal aortic aneurysm development in APOE −∕− mice, but not in APOE −∕− and Ido −∕− mice, in which elastic lamina degradation and aortic expansion decay [ 40 ]. Angiotensin-2 activates interferon-γ which launches expression of IDO and kynureninase, thereby raising production in medial smooth myocytes and subsequently its concentration in the aortic wall and plasma of 3HAA, which upregulates synthesis of MMP2 via NFκB.
The risk of cerebral aneurysms is augmented in postmenopausal women, whereas estrogen replacement protects against intracranial aneurysms, protection ensured by estrogens being mediated by NR3a2 and cerebral vascular NO production [ 38 ]. 7
Androgen Signaling
Testosterone is synthesized in testicular Leydig cells and ovarian theca cells. It is converted to the more potent 5α-DHT by 5α-reductase.
Both androgen types connect to another ligand-activated transcription factor, androgen receptor (AR or NR3c4), which is detected in endotheliocytes and smooth myocytes, platelets, and macrophages. Two variants (ARa–ARb) lodge in most organs with varying expression levels according to the tissue type [ 38 ]. Testosterone is also converted to E 2 by aromatase, in particular in the brain.
Androgen signaling is linked to metabolism, cell proliferation, differentiation, and apoptosis, and protein secretion, whatever the gender. Androgens can trigger alternative rapid (nongenomic) signaling after binding to membrane-associated or cytosolic AR that releases intracellular Ca 2+ and activates kinases (e.g., MAPK, PKA, PKB, and PKC) [ 38 ]. Membrane-associated ARs in aortic endotheliocytes interact with Src and caveolin-1.
Postmenopausal women experience more rapid age-related hypertension than age-matched men [ 38 ]. Hypoandrogenism may be linked to hypertension in older men, suggesting that a normal androgen concentration is antihypertensive. Testosterone rapidly activates NOS3 in vascular endotheliocytes via the PI3K–PKB pathway. On the other hand, in young, obese, hypoandrogenic male rats, 10-week testosterone supplementation improves body weight and lipid profiles but increases blood pressure. Androgens can elevate blood pressure via ruptured abdominal aortic aneurysm (RAAA) constituents in the kidney. They can contribute to Agt2-induced hypertension in male animals via renal inflammation, renal lymphocyte infiltration being greater in male than in female mice [ 38 ].
Although NR3a diminishes the formation of adhesion molecules in endotheliocytes exposed to atherogenic factors, NR3c4 stimulates vcam1 production in male-derived endotheliocytes due to a higher NR3c4 concentration (not in cells of female origin).
In men, androgen deficiency is linked to endothelial dysfunction. On the other hand, in women, hyperandrogenemia favors atherogenesis and arterial calcification [ 38 ].
In both sexes experiencing hypoxia caused by occlusive peripheral artery disease, androgens promote angiogenesis via NR3c4, the upregulated formation of vascular endothelial growth factor (VEGF) and its receptors in endotheliocytes, and VEGF-primed phosphorylation of PKB and NOS3 [ 38 ]. Administration of DHT augments male-derived (but not female) endotheliocyte migration, proliferation, and tubulogenesis.
In male animals, relatively high concentrations of androgens, which upregulate expression of RAAA components, favor macrophage recruitment and extracellular matrix degradation via MMPs, and hence AAA formation, the castration of male mice limiting Agt2-induced AAA genesis and expansion to levels observed in intact female mice [ 38 ]. Male rodents can also be predisposed to AAA by androgens via elevated MMP activity.
Enzymes of Steroid Hormone Metabolism
Steroids are lipophilic, low-molecular-weight compounds derived from cholesterol. In fluids, they are usually found in either a conjugated form (i.e., linked to a hydrophilic moiety, such as sulfate or glucuronide derivatives) or bound to proteins. In the plasma, unconjugated steroids are mainly bound to carrier proteins, albumin (20–50%), serpin-A6 (or corticosteroid-binding globulin [CBG]), and sex hormone-binding globulin (SHBG) [ 42 ].
Mitochondria of steroidogenic cells of the adrenal gland, gonads, placenta during gestation, and brain are essential sites for steroid hormone synthesis. The adrenal gland synthesizes androgens and corticosteroids (mineralo- and glucocorticoids), ovary estrogens and progestins, and testis (mainly androgens). In men, the adipose tissue contains aromatase, a source of androgen-derived estrogens.
Once they are released into the bloodstream, these endocrine messengers act on target cells, including those of the central nervous system. The latter also form neurosteroids with auto- and paracrine effects. They diffuse easily through the plasma membrane. Circulating steroids are processed in target cells, which can form active metabolites.
Removal of part of the cholesterol side chain generates C21-steroids of the pregnane series (progestins and corticosteroids), total removal of C19-steroids of the androstane series (e.g., androgens), and loss of the 19-methyl group the estrane series (e.g., estrogens) [ 42 ].
Steroids are characterized by the presence or absence of functional groups (mainly hydroxy, keto(oxo), and aldehyde) at certain positions of the carbon skeleton (particularly at positions 3, 5, 11, 17, 18, 20, and 21) [ 42 ]. These functional groups characterized by their type, number, position, and orientation engender a large number of stereoisomers (i.e., molecules having the same chemical formula but distinct three-dimensional conformation).
Enzymes involved in steroid synthesis include (Tables 1.1 and 1.2 ) [ 42 ]:
- Mitochondrial desmolases (or lyases), which remove parts of the cholesterol side chain via sequential hydroxylation of adjacent carbon atoms using molecular oxygen, reduced nicotinamide adenine dinucleotide phosphate (NADPH), and cytochrome P450
- Membrane-bound mitochondrial or microsomal hydroxylases , which also require cytochrome-P450, O 2 , and NADPH
- Cytosolic and microsomal hydroxysteroid dehydrogenase , these oxidoreductases depending on NADP(H) or NAD(H)
- Membrane-bound aromatase that involves a sequence of hydroxylation and loss of the C19 methyl group, its substrate being 4-androstenedione or testosterone
Enzymes of steroid synthesis ( Part 1 ; CyP i X j : cytochrome-P450 family i , subfamily x, polypeptide j [i, j: integers, x: letter])
Androstenediol and androstenedione are weak androgen and estrogen steroid hormones and intermediates in the synthesis of estrone and testosterone. Androstenedione is converted to testosterone and estrone by the 17β-hydroxysteroid dehydrogenases (HSDH17β1–HSDH17β3 and HSDH17β7) and aromatase, respectively. Androstenediol is processed by the 3β-hydroxysteroid dehydrogenases HSDH3β1 and HSDH3β2 into testosterone. The three estrogens, estrone (E 1 ), a weakly active E 2 precursor, which is also named the estrogen of the menopause; estradiol (E 2 ), the most active estrogen; and estriol (E 3 ), a weakly active E 2 metabolite, which is also called the estrogen of pregnancy, are produced by aromatase. Both estriol and estrone can interact with the estrogen receptor and thus antagonize estradiol action
Enzymes of steroid synthesis ( Part 2 ; AKR aldo–keto reductase)
Mitochondria contain the cholesterol desmolase CyP11a1, which catalyzes cholesterol side-chain cleavage to yield pregnenolone, a C21 compound, in addition to its electron transfer partners, ferredoxin and ferredoxin reductase [ 43 ].
Pregnenolone can be converted either to progesterone, which leads to glucocorticoids, androgens, and estrogens, or to 17α-hydroxypregnenolone, which also forms androgens and estrogens. In the adrenal gland, androgen formation is limited to dehydroepiandrosterone and androstenedione, whereas in Leydig cells of the testis, 17β-hydroxysteroid dehydrogenase (17HSDH) produces testosterone [ 43 ]. In granulosa cells of the ovary, estrogen synthesis requires the aromatase complex that uses the substrate androstenedione and testosterone to create estrone and estradiol, respectively.
Hydroxylation of progesterone at carbon 21 yields 11-deoxycorticosterone (DOC) and additional hydroxylation at carbon 11 corticosterone , a major glucocorticoid in mammalian species that do not produce cortisol. The main glucocorticoid secreted by human adrenal glands, cortisol , is formed of 17α-hydroxyprogesterone via the intermediate 11-deoxycortisol.
Further hydroxylation and redox at carbon 18 give rise to aldosterone.
Several other steroidogenic enzymes, such as 3β-hydroxysteroid dehydrogenase, 11β-hydroxylase, and aldosterone synthase, also reside in mitochondria.
Cholesterol ingress into the mitochondrion is regulated by the steroidogenic acute regulatory protein, StAR, the action of which requires the machinery of the outer mitochondrial membrane, which comprises translocator protein (Tspo), 8 voltage-dependent anion channel VDAC1, Tspo-associated acylCoA-binding domain-containing protein ACBD3, and protein kinase-A regulatory subunit PKA r1 α [ 43 ].
The main site of catabolism is the liver. It involves various reaction types:
- Reduction of a double bond at C4 and a reduction of an oxo(keto) group at C3 to a secondary alcoholic group
- Reduction of an oxo group at C20 to a secondary alcoholic group
- Oxidation of a 17β-hydroxyl group
- Further hydroxylations at various positions
- Conjugation of a sulfate group (SO 4 2 − ) 9 and/or glucuronosyl groups (glucuronidation), which yields steroid sulfates and glucuronides, by Mg 2+ -dependent steroid sulfokinases and glucuronyl transferase, respectively, thereby forming hydrophilic molecules that can be more easily excreted by the kidney
Corticosteroid 11β-dehydrogenase HSD11β2 converts cortisol into its inactive metabolite cortisone.
Four human aldo–keto reductases (AKR1c1–AKR1c4), also named hydroxysteroid (HSDHs) and dihydrodiol dehydrogenases (DHDHs), are involved in the metabolism of steroids in addition to drugs. These enzymes catalyze the conversion of aldehydes and ketones into their corresponding alcohols using NADH and/or NADPH as cofactors (Table 1.3 ) [ 45 ]. In humans, the aldo–keto reductase superfamily also includes aldehyde (AKR1a1) and aldose reductase (AKR1b1) and aldose reductase-like proteins AKR1b10 of the small intestine and AKR1b15, δ(4–3)-ketosteroid 5β-reductase AKR1d1, aldo–keto reductase-1C-like proteins AKR1cL1 and AKR1cL2 (or testis-specific AKR1e2), and aflatoxin aldehyde reductases AKR7a2 and AKR7a3 [ 46 ].
Aldo–keto reductases (AKRs) in steroid hormone metabolism (Source: [ 47 ])
Enzymes of the AKR set are soluble, monomeric, NAD(P)(H)-dependent oxidoreductases that interconvert carbonyl groups with alcohols. In humans, 13 isoforms exist, among which AKR1c1 to AKR1c4 and AKR1d1 regulate the local concentration of steroid hormones. The members of the AKR1C subset (AKR1c1–AKR1c4) reduce ketosteroids to hydroxysteroids
AKR1c1 converts progesterone to inactive 20α-dihydroxyprogesterone, AKR1c2, and liver-specific AKR1c4 dihydrotestosterone to less active 3α-diol, and AKR1c3 catalyzes reduction of prostaglandins PGd 2 and PGh 2 , and oxidation of (9α, 11β)PGf 2 to PGd 2 in addition to preferentially transforming androstenedione to testosterone [ 45 ]. AKR1c1, AKR1c2, and AKR1c3 reduce cytotoxic aldehydes derived from lipid peroxidation into less toxic metabolites.
The liver is the primary site of metabolism of steroid hormones containing a Δ 4 -3 functionality, such as testosterone and progesterone, which are converted into tetrahydrosteroids that are then eliminated. Steroid hormones are conjugated in two-phase reactions, reduction by 5α- or 5β-steroid reductases to form the respective dihydrosteroids, and, in the subsequent step, the 3-oxo group of dihydrosteroids is reduced by ketosteroid reductases to form tetrahydrosteroids. In humans, the four members of the AKR1C subset (AKR1c1–AKR1c4) reduce 5α- and 5β-dihydrosteroids [ 48 ].
The AKR1C isozymes are thus involved in the metabolism of testosterone and progesterone. They are pluripotent, but with a cell-specific expression pattern and distinct substrate preference. All four isozymes are produced in the liver. AKR1c1 to AKR1c3 are highly expressed in the mammary gland and prostate but distinctly expressed in the lung, mammary gland, prostate, and testis, whereas AKR1c4 is specific to the liver [ 48 ].
In particular, AKR1c3 is detected in stromal, endothelial, and uroepithelial cells, in addition to adenocarcinoma cells in the prostate [ 47 ]. Prostate epitheliocytes produce higher concentrations of AKR1c1 to AKR1c3 than stromal cells, the synthesis rate augmenting in prostate cancers. In the mammary gland, AKR1c3 creates a pro-estrogenic state, as it converts androstenedione to testosterone, which, upon aromatization by CyP19 aromatase, yields 17β-estradiol, and transforms active progesterone to inactive 20α-hydroxyprogesterone, thereby altering the estrogen/progesterone ratio [ 47 ].
The AKR1C enzymes catalyze ketosteroid reduction at the 3-, 17-, or 20-position to varying degrees according to the substrate. The 5β-pathway is linked to 5β-steroid reductase AKR1d1. 5β-Pregnane (3,20)-dione is a potent ligand for the pregnane X receptor (PXR or NR1i2) and constitutive androstane receptor (CAR or NR1i3). Activated hepatic NR1i3 stimulates cytochrome-P450 CyP3a4, which processes approximately 50% of consumed drugs [ 48 ].
In addition, 5β-reduced pregnanes are neuroactive steroids (synthesized in the brain) that are implicated in vasodilation [ 49 ]. They are implicated not only in the regulation of steroid receptors, exerting their action on gene expression via nuclear steroid hormone receptors, but also of ligand-gated ion channels, thereby influencing neuronal excitability. They inhibit or stimulate neurotransmission, as they act as allosteric modulators of the GABA A receptor.
Unsaturated fatty acids (FAs) are potent competitive inhibitors of the AKR enzymes. The sensitivity of AKRs for FAs varies, and the most potent inhibitors for AKR1c1, AKR1c2, and AKR1c4 are docosahexaenoic, palmitoleic, and linoleic acid, respectively [ 45 ]. FAs have the strongest inhibitory potency for 3α-hydroxysteroid dehydrogenase AKR1c3.
Sulfate conjugation is involved in the transformation of steroid and thyroid hormones, catecholamines, cholesterol, and bile acids, in addition to the detoxification of dietary and environmental xenobiotics. Cytosolic sulfotransferases (SulTs) transfer the sulfonate group from phosphoadenosine phosphosulfate (PAPS) to acceptor substrates. In humans, 13 SulT isoforms constitute four subsets [ 50 ]. The SULT1 subfamily encompasses SulT1a1 to SulT1a3, SulT1b1, SulT1c2 to SulT1c4, and SulT1e1, and the SULT2 subfamily SulT2a1, SulT2b1a, and SulT2b1b, whereas other subfamilies contain a single element, SulT4a1 and SulT6b1, respectively.
Splice variants encode distinct SulT1c3 isoforms (SulT1c3a, SulT1c3c, and SulT1C3d) [ 50 ]. Although SulT1c3a has a weaker activity and is specific for hydroxyl-chlorinated biphenyls, SulT1c3d has a broader substrate specificity, sulfating bile acids, thyroid hormones, pyrenes, and hydroxyl biphenyls.
Vasculitis (Angiitis)
Vasculitides are defined by the presence of inflammatory leukocytes in vascular walls caused by various immunological processes and possibly triggered by infectious agents. Vasculitis targets arterial and venous walls of any size in any organ, but frequently in the skin.
Vasculitides can be classified according to the size of blood vessels or histological examination (e.g., lymphocytic, leukocytoclastic, and granulomatous [nodular]).
Giant cell (GGA) and young women (Takayasu [TA]) arteritis 10 and autoinflammatory Behçet disease (BD) 11 affect large vessels. Complications include inflammatory obstructions and aneurysms.
Livedoid vasculitis , also named segmental hyalinizing vasculopathy and livedo reticularis, most commonly affects women with thromboses and ulcerations of the lower extremities.
Eosinophilic granulomatosis with polyangiitis (EGPA), previously called Churg–Strauss syndrome, mainly affects small and medium-sized blood vessels of men and women between 30 and 45 years of age. It commonly targets the lung and skin but also the heart, kidney, bowel, and nerves.
Granulomatosis with polyangiitis , previously named Wegener’s granulomatosis, mainly affects blood vessels in the nose, sinuses, ears, lungs, and kidneys of middle-aged or elderly individuals.
Vascular Wall Disorders
Wall disorders in large arteries and veins appear not only in the presence of risk factors, such as smoking, long periods without bodily motion, hypertension (Chap. 10.1007/978-3-319-89315-0_3), diabetes (Chap. 10.1007/978-3-319-89315-0_4), 12 obesity (Chap. 10.1007/978-3-319-89315-0_5 ), and a family history of vasculopathies, but also most often in a context that encompasses aging (Vol. 9, Chap. 3. Aging), one of the most important cardiovascular event predictors, injury, ciliopathies (Vol. 9, Chap. 1. Ciliopathies), replication stress, air pollution, and sleep disorders (Vol. 9, Chap. 4. Anomalies of the Respiratory Tract), among other factors.
Hemostasis and Thrombosis
The intact and healthy vascular endothelium maintains an anticoagulant surface. Thrombomodulin is an integral membrane protein on the wetted surface of endotheliocytes that serves as a cofactor for thrombin. Once it is bound to thrombin, the anticoagulant serine peptidase protein-C is rapidly activated [ 52 ]. Activation of protein-C by the thrombin–thrombomodulin complex depends on Ca 2+ ion. This complex also prevents thrombin activation of the clotting factor- V . Thrombomodulin thus has two distinct anticoagulant functions: (1) to impede the ability of thrombin to clot fibrinogen and to activate F V and (2) to accelerate activation of the anticoagulant protein-C [ 52 ]. Heparan sulfate proteoglycans on the endotheliocyte surface stimulate activation of the serine peptidase inhibitor antithrombin, or serpin-C1, which inactivates thrombin and factor- X a [ 53 ].
In addition, the endothelium produces the antiplatelet aggregation factors prostacyclin and nitric oxide. Some types of activated platelets also generate NO, thereby stimulating the sGC–PKG axis and limiting their own adhesion and aggregation [ 54 ]. PKG phosphorylates vasodilator-stimulated phosphoprotein (VASP), preventing integrin-α 2B β 3 activation, which stabilizes initial platelet rolling, adhesion, and recruitment to the site of the injury. PKG also represses integrin-α 2B β 3 activation via IP 3 R-associated cyclic guanosine monophosphate (cGMP) kinase substrate (IRAG) and inhibition of thromboxane receptor activation.
When any segment of the vasculature is damaged, the subendothelial matrix is exposed to blood. Matrix components launch hemostasis, initiating formation of a blood clot composed primarily of platelets and fibrin within seconds. Hemostasis stops bleeding from a damaged blood vessel, thereby avoiding hemorrhage, a normal blood flow being maintained elsewhere in the circulatory circuit. This first stage of wound healing involves blood coagulation, blood, a suspension of cells in plasma, in which molecules are suspended, changing from a liquid to gel, that is, by the local formation of a hemostatic plug.
Primary hemostasis refers to aggregation of activated platelets, which are small anuclear cell fragments derived from megakaryocytes, and subsequent platelet plug production.
In humans, platelets form subpopulations according to the presence and absence of NOS3, which produces NO, an endogenous platelet inhibitor [ 54 ]. Approximately 20% of platelets lack NOS3 and thus fail to produce NO and have defective sGC–PKG signaling. NOS3− platelets primarily initiate adhesion to collagen or von Willebrand factor; activate integrin-α 2B β 3 , which elicits between-platelet aggregation; and secrete MMP2, which elicits recruitment of NOS3+ platelets to the forming aggregate. Conversely, platelets with intact NOS3–sGC–PKG signaling form the bulk of the aggregate (thrombus) owing to their higher PGhS1 (COx1) content and greater thromboxane-A 2 generation, the platelet aggregate being amplified by thromboxane-A 2 synthesis, and ultimately limit the aggregate size via NO.
Secondary hemostasis designates the simultaneous deposition of insoluble fibrin generated by the proteolytic coagulation cascade that forms a meshwork into and around the platelet plug, which strengthens and stabilizes the blood clot.
Hemostasis relies on the balance between procoagulant (platelets and coagulation cascade components) and anticoagulant elements (protein-C and -S, fibrinolysis, serpins).
As a blood clot in hemostasis, a pathological thrombus is the final product of blood coagulation in the absence of vascular contusion (but not intrinsic vascular injury). An elevated ratio of NOS3+ / NOS3− platelets may contribute to thrombosis.
Thromboembolism results from thrombus breakage and shedding followed by embolus carriage in the bloodstream, and subsequent obstruction of a distal vessel.
- Venous walls can be injured and lose their strength, thereby being the source of thrombi that are shorn and generate emboli (Vols. 12, Chap. 4. Thrombosis and Lymphedema, and 13, Chap. 8. Venous Pathologies). Venous thrombus consists mostly of fibrin with entrapped red blood capsules. Venous thrombi can cause pulmonary embolism. Venous thromboembolism (VTE) is a collective name incorporating deep vein thrombosis (DVT) and pulmonary embolism.
- Arterial thrombus subjected to a higher flow rate and shear is mainly composed of aggregated platelets. Arterial emboli most often provoke ischemia and infarction of the heart, brain (stroke), gastrointestinal tract, kidney, or leg.
Obesity and dyslipidemia are risk factors for both arterial and venous thrombosis. The classical acquired risk factors for venous thrombosis include cancer, immobilization, surgery, fractures, and pregnancy.
Neutrophils contribute to host defense, not only as they process pathogens via phagocytosis and produce toxic chemicals to kill intruders directly but also as dying neutrophils mix their DNA with toxic components from their cytosolic granules and release them in the form of neutrophil extracellular traps (NETs) that trap and neutralize microbes. Neutrophil extracellular traps are lattices of processed chromatin (i.e., neutrophil DNA and histones) linked to secreted and cytoplasmic proteins released by neutrophils during inflammation. However, inappropriate NETosis is harmful, favoring sustained and excessive inflammation and thrombosis. NETs released into the vasculature can cause platelet adhesion and activation of the extrinsic and intrinsic coagulation cascade. They also damage pulmonary epithelia and endothelia. On the other hand, two deoxyribonucleases, Dnase1 and Dnase1L3, degrade extracellular (cell-free) nuclear and mitochondrial DNA, hence circulating NETs in a partly redundant manner [ 55 ]. However, Dnase1 disrupts NETs, but does not dissolve them.
The receptor tumor necrosis factor receptor superfamily (TNFRSF)-interacting protein kinase RIPK3 is involved not only in inflammation in addition to apoptosis and necroptosis but also in hemostasis, as it amplifies platelet activation. Upon vessel injury, platelets are recruited by adenosine diphosphate (ADP), thrombin, and thromboxane-A 2 , which connect to their cognate G-protein-coupled receptors and activate integrin inside–out signaling mediated by extracellular signal-related kinases (ERKs) and launch granule secretion. RIPK3 produced in platelets interacting with G13 activates PKB and supports platelet aggregation and spreading on fibrinogen via PKB1 or PKB2 in addition to the second wave of dense granule content secretion in response to thrombin, thromboxane-A 2 , and clot retraction [ 56 ]. The G13 subtype selectively enables thrombin- and TxA 2 -induced platelet aggregation, but does not influence ADP-primed aggregation. RIPK3 operates independently of its substrate used in cell necrosis and clearance, mixed lineage kinase domain-like pseudokinase (MLKL). Therefore, RIPK3 favors arterial thrombus formation.
On the other hand, heparin, a sulfated polysaccharide, prevents blood coagulation, as it connects to antithrombin (serpin-C1) and then accelerates the interaction of antithrombin with thrombin (F II a), and activated clotting factors F V II a and F IX a to F XII a, thereby preventing completion of the coagulation cascade.
Inflammation and Angiogenesis
Inflammation of the vascular wall is initiated in response to injury, infection, and lipid peroxidation. Moreover, hypertension (Chap. 10.1007/978-3-319-89315-0_3), obesity (Sect. 10.1007/978-3-319-89315-0_5#Sec44 ), and diabetes (Chap. 10.1007/978-3-319-89315-0_4) are associated with chronic inflammation. Elevated concentrations of inflammatory markers predict future cardiovascular events [ 57 ].
Hypertension is linked to both macro- and microvascular disease. It alters endothelial integrity and hence vascular permeability, facilitating inflammatory leukocyte recruitment.
In addition to vasoconstriction, angiotensin-2 causes redox stress, inflammation, endothelial dysfunction, and vascular remodeling with fibrosis. It provokes accumulation of PTPRc+ leukocytes in aortic perivascular adipose tissue and upregulates MMP2 expression in these leukocytes, MMP2 favoring Agt2-primed vascular inflammation and injury [ 58 ]. Agt2 augments the generation of ROS in the aortic media and perivascular medium and of vcam1 and CCL2, thereby eliciting perivascular infiltration of monocytes, macrophages, and T lymphocytes. It also increases the density of monocytes and activated CD4+ helper and CD8+ cytotoxic T cells in the spleen in the presence of MMP2. MMP2 is synthesized in higher amounts in CD4+ effector T H1 cells than in T H2 or naive T H0 cells. In addition, T H1 cells can stimulate MMP2 synthesis in macrophages. Within the cell, Agt2 promotes phosphorylation of EGFR in addition to ERK1 and ERK2 via heparin-binding epidermal growth factor (HBEGF) shedding in vascular smooth myocytes [ 58 ].
Matrix metallopeptidases synthesized in vascular smooth muscle and endothelial cells not only modify and remodel the extracellular matrix, degrading matrix constituents (e.g., collagen, elastin, and fibronectin), but also shed growth factors (e.g., HBEGF and matrix-bound latent transforming growth factor-β), cytokines, and chemokines, hence favoring inflammation, in addition to autacoids (e.g., big endothelin-1 and other vasoactive peptides) [ 58 ]. In particular, MMP2 cleaves (activates) CCL7 and CXCL12 and processes S100 [ 59 ].
The MMPs are regulated by tissue inhibitors of metallopeptidases (TIMPs), which impede their activity, as they bind to their catalytic site. Among the four TIMPs (TIMP1–TIMP4), TIMP2 can inhibit or activate MMPs; TIMP2 is required with MMP14 for proMMP2 activation [ 58 ]. In addition to MMP2, other MMP types may participate in Agt2 action.
On the other hand, MMP2 deficiency reduces Agt2-induced redox stress, inflammation, endothelial dysfunction, medial hypertrophy, and vascular stiffness, but not SBP elevation [ 58 ]. Both vascular and immune cell-derived MMP2 contribute to impaired vascular relaxation to acetylcholine and endothelial dysfunction. Immunocytes contribute to Agt2-induced hypertension, as Mmp2 deletion in immunocytes reduces BP [ 58 ].
Atherosclerosis (Sect. 1.1.5 and Vol. 13, Chap. 5. Atherosclerosis—Biological Aspects) can be considered as a diffuse inflammatory disease of the vasculature. Inflammation is indeed observed at all stages of atherogenesis, from initial lesions to fatty streaks, evolved plaques, and end-stage complications, that is, thromboembolism after unstable plaque rupture linked to an excess inflammatory episode [ 60 ]. Atherosclerosis is triggered by oxidized LDLs conveying cholesterol. Activated endotheliocytes express adhesion molecules for the diapedesis of circulating leukocytes, activated macrophages, lymphocytes, and smooth myocytes releasing cytokines and chemokines. The procoagulant cytokine increases the synthesis and secretion of fibrinogen, plasminogen activator inhibitor PAI1 (serpin-E1), and acute phase proteins such as C-reactive protein (CRP), thereby amplifying the inflammatory and procoagulant response [ 61 ]. Inflammatory cytokines (e.g., IL1, TNFSF1, and CRP) induce the formation of adhesion molecules, provoking a vicious cycle. C-reactive protein supports the production of tissue factor by monocytes and represses that of NO, hence contributing to the creation of a proinflammatory and prothrombotic milieu. Anti-inflammatory drugs can reduce cardiovascular risk [ 62 ].
Furthermore, systemic autoimmune rheumatic diseases (SARDs), 13 that is, a group of disorders that share chronic inflammation causing connective tissue and organ damage (rheumatoid arthritis [RA], systemic lupus erythematosus [SLE], ankylosing spondylitis, gout, psoriatic arthritis, systemic sclerosis [SSc; or scleroderma], polymyositis [PM], dermatomyositis [DM], Sjögren’s syndrome [SjS], 14 mixed connective tissue disease [MCTD], 15 and systemic vasculitis), can be associated with medium- and large-vessel vasculitides (granulomatous and microscopic polyangiitis, eosinophilic granulomatosis with polyangiitis, and giant cell arteritis) and an increased risk of premature cardiovascular disease, in particular coronary arteritis and premature atherosclerosis [ 63 ].
Angiogenesis is not only involved in organogenesis and repair but also in inflammatory diseases (at least in RA, SLE, SSc, and vasculitides) [ 64 ]. This programmed cascade of events relies on cellular (monocytes, macrophages, and endotheliocytes) and molecular mediators and inhibitors (angiostatin, endostatin, osteonectin [SPARC], thrombospondin, and, under some circumstances, TGFβ; cytokines IL1, IL4, IL6, Ifnα, and Ifnβ; and chemokines CXCL4, CXCL9, and CXCL10).
Angiogenic factors, such as growth factors (EGF, FGF1, FGF2, HGF, IGF1, PDGF, TGFβ, and VEGF), cytokines (TNFSF1, IL1, IL6, IL13, IL15, and IL18), chemokines (CCL2, CXCL1, CXCL5, CXCL7, CXCL8, CXCL12, and CX 3 CL1), cell adhesion molecules (endoglin, integrins, selectins, pecam1, and vcam1), matrix components (collagen-1, fibronectin, laminin, and heparan sulfate proteoglycans), and other factors (angiogenin, platelet-activating factor, substance-P, prostaglandin-E 2 , and prolactin]) activate endotheliocytes.
Endotheliocytes then produce matrix metallopeptidases and plasminogen activators to degrade their basement membrane and the perivascular extracellular matrix. These cells proliferate and migrate, forming a sprout that grows, tubulates, matures, and anchors onto another vessel or builds a capillary network, the endotheliocytes producing further generations of sprouts from the primary sprout.
Mastocytes are involved in innate and acquired immunity, inflammation, allergy, and autoimmunity. They release histamine, tumor-necrosis factor TNFSF1, interleukins IL1β and IL6, chemokine CXCL8, and VEGF. Proinflammatory substance-P and IL33, two major agents of diseases, cooperate to enhance TNFSF1 synthesis and secretion from mastocytes via activation of the tachykinin (neurokinin/substance-P) receptor TacR1 (NK1R or SPR) and IL1RL1 (IL33R) [ 65 ]. Owing to this mutual excitation, IL33 potentiates SP-primed TNFSF1 production more than 100-fold in mastocytes. Mastocyte-derived tryptase can cleave extracellular IL33 into its mature active form, which then activates mastocytes, which, in turn, can release soluble IL1RL1 that modulates the effects of IL33. Substance-P also stimulates histamine secretion from mastocytes. Moreover, IL33 and SP upregulate synthesis of both TacR1 and IL1RL1 receptors. In addition, IL3 enhances SP-triggered VEGF release by mastocytes [ 66 ]. IL33 also augments the frequency and magnitude of mastocyte degranulation and chemokine production, worsening chronic inflammation, even at low concentrations. The receptors TacR1 and IL1RL1 interfere; TacR1 complexes with IL1RL1 and its coreceptor IL1RAP (IL1R accessory protein); IL33 may participate in complexing TacR1 and IL1RL1 [ 65 ]. The stem cell factor receptor (SCFR) also complexes with IL1RL1 and IL1RAP in mastocytes for cross-activation. The natural flavonoid tetramethoxyluteolin inhibits mastocytes stimulated by IL33, SP, or their combination, thereby reducing chronic inflammation.
Oxidative and Nitrosative Stresses
Accrual amounts of ROS, which are toxic by-products of aerobic metabolism, cause redox stress and alleviate the fitness level and ability to maintain homeostasis. The term oxidative stress was coined by H. Sies as “a disturbance in the prooxidant–antioxidant balance in favor of the former.” The rate of ROS production increases with aging, ROS being responsible for the accumulation of cellular and tissular deterioration over time in the postreproductive phase of life [ 67 ].
Injurious oxidative stress is characterized by a shift in the oxidative–reductive balance to a more oxidative state because of augmented ROS production by prooxidant enzymes and reduced antioxidant defense mechanisms that scavenge excess ROS.
Deleterious reductive stress is characterized by an aberrant increase in reducing equivalents, such as reduced glutathione and reduced NADPH, increased activation of antioxidant enzymes, and reduced prooxidant capacity, shifting the redox balance from an oxidative to a reduced state.
Exercise is an oxidant stimulus used in redox biology studies; free radicals produced during exercise modulated muscular and systemic adaptation to physical activity. However, exercise induces oxidative or reductive stress according to the individual [ 68 ]. Using redox markers (e.g., glutathione, F2-isoprostanes, and protein carbonyls) in plasma, red blood capsules, and urine samples before and 2 days after exercise, concentrations of the oxidant markers, F2-isoprostanes and protein carbonyls, increase or decrease, whereas the amount of glutathione amount declines or rises, respectively. 16
The term redox stress , which is associated with the oxidation–reduction reaction disorder, combines oxidative and reductive stress. Both contribute to the pathogenesis of CVD; hence, redox stress is the preferred term.
Loss of function of glutathione peroxidase GPOx1 causes both oxidative and reductive stress. Reductive stress provokes S glutathionylation of the cytoplasmic protein Tyr phosphatase PTPn1 (SHP2) and vascular remodeling [ 69 ].
Reactive Oxygen and Nitrogen Species
All layers of the vascular wall produce ROS and reactive nitrogen species (RNS; Vol. 11, Chap. 7. Reactive Oxygen and Nitrogen Species) that include superoxide anion radical (O 2 • − ), hydrogen peroxide (H 2 O 2 ), hydroxyl radical (OH • ), nitric oxide (NO • ), and peroxynitrite (ONOO − ).
Superoxide can be converted by superoxide dismutase (SOD) into hydrogen peroxide. Hydroxyl radical is formed from oxidation of glutathione, ascorbic acid, NADPH, hydroquinone, catechol, and riboflavin by hydrogen peroxide and H 2 O 2 catalysis [ 70 ]; glutathione can scavenge it [ 71 ]. Oxy- and methemoglobin can generate hydroxyl radicals from hydrogen peroxide [ 72 ].
Superoxide reacts rapidly with anti-inflammatory, anticoagulant, and vasodilatory NO, forming the oxidant peroxynitrite. The latter oxidizes tetrahydrobiopterin, a NOS cofactor, lowering NO availability and provoking endothelial dysfunction.
Among ROS and RNS, hydroxyl radical and peroxynitrite are not considered signaling molecules; these highly reactive agents contribute to redox stress and tissular damage.
ROS and RNS Sources
The main sources of vascular ROS comprise:
- NAD(P)H oxidases (NOx1–NOx2 and NOx4–NOx5)
- Mitochondrial electron transport chain (ETC) involved in oxidative phosphorylation, mainly ETC complex- I and - III (i.e., NADH–ubiquinone and ubiquinone–cytochrome-C reductase)
- Uncoupled nitric oxide synthase and to a lesser extent
- Xanthine oxidase
- Prostaglandin-G/H synthases (cyclooxygenases)
Lipoxygenases
- The endothelial cytochrome-P450 epoxygenase CyP2c9, which produces vasodilatory epoxyeicosatrienoic acids (11,12)EETs [ 73 ]
- Myeloperoxidase 17
Mitochondrial Electron Transport Chain
In the heart, ROS are produced primarily by mitochondrial ETC and mitochondrial and extramitochondrial enzymes, such as NOxs. Superoxide produced in the mitochondrial matrix is rapidly dismutated by SOD2 to hydrogen peroxide, which diffuses out of the mitochondrion.
NAD(P)H Oxidases
Enzymes of the NOX set synthesize O 2 • − , except NOx4, which predominantly produces H 2 O 2 . They localize to caveolae and membrane rafts, endoplasmic reticulum, endosomes, and mitochondria.
Constitutively active canonical NOx1 in addition to NOx2 function in a complex formed by their regulators and binding partners:
- NOx1: P22PhOx–NoxO1–NoxA1–Rac1/2
- NOx2: P22PhOx–NOxO2–NOxA2–P40PhOx–Rac1/2
NOx4 remains constitutively active in the presence of oxygen. Calcium-dependent NOx5 is regulated by cytosolic calcium concentration. Although NOx2 and NOx4 produce ROS in CMCs and fibroblasts, NOx1, NOx4, and NOx5 operate in the vascular smooth myocytes [ 71 ].
The NOx complexes produce O 2 • − on the extracytoplasmic face of cellular membranes, that is, plasma membrane-bound NOxs outside the cell and intracellular NOxs in the lumen of organelles [ 74 ].
The NOx4 subtypes in the outer mitochondrial membrane and mitochondrial ETC are major ROS sources in diabetes. NOx4 is involved in migration and differentiation of vascular smooth myocytes, cardiac cells, fibroblasts, and stem cells. Upon TGFβ exposure, NOx4 oxidizes (inhibits) the phosphatase DUSP1 (MAPK phosphatase MKP1), inactivating P38MAPK, which phosphorylates SRF, which binds to MRTF, activating smooth muscle α-actin (Actα2) and promoting vSMC differentiation [ 71 ]. In addition, NOx4 activates RhoA.
Xanthine Oxidoreductase (Dehydrogenase/Oxidase)
Xanthine dehydrogenase (XDH) and oxidase (XOx) are interconvertible forms encoded by a single gene, the XDH (XOR) gene. Whereas XOx uses hypoxanthine or xanthine as substrate and O 2 as cofactor (electron acceptor) to produce superoxide and uric acid, XDH acts on the same substrates but utilizes NAD + as cofactor (electron receptor) to produce NADH [ 75 ]. Hypoxia, inflammation, apoptosis, and ROS generation from other sources cause XDH conversion into XOx [ 71 ].
Xanthine oxidase participates in the cellular redox status. It is a source of oxygen radicals in granulocytes and endothelial, epithelial, and connective tissue cells. It is involved in detoxification of aldehydes. It serves as a messenger in the activation of neutrophils and T lymphocytes and the triggering of defense mechanisms rather than as a free radical generator. However, it can be implicated in cytotoxicity and tissue injury, especially in inflammation and ischemia.
Arachidonate lipoxygenases ALOx5, ALOx12, and ALOx15 are implicated in CVD genesis. Arachidonic acid (AA) is oxidized by ALOxs into hydroperoxides, which are further reduced into hydroxides and leukotrienes. Each ALOx subtype generates different metabolites according to the target AA carbons.
Arachidonate lipoxygenases mediate Agt2-primed NOx activity in vSMCs. Synthesis of ALOx5 is upregulated by redox stress following excess ROS formation by NOx or mitochondrial ETC. It generates 5HETE and LTa 4 from AA, which serves as a substrate for several enzymes producing proinflammatory molecules LTb 4 , LTc 4 , LTd 4 , and LTe 4 , which activate endotheliocytes, macrophages, neutrophils, mastocytes, T lymphocytes, in addition to foam cells [ 71 ].
Both ALOx12 and ALOx15 are involved in inflammation and redox stress. Generated AA metabolites 12HPETE and 15HPETE and their reduced 12HETE and 15HETE are pro- and anti-inflammatory. They oxidize LDLs [ 71 ]. The metabolite 15HETE favors ROS creation by mitochondrial ETC and NOx4. Under hypoxia, 15HETE provokes endotheliocyte migration and pulmonary arterial smooth myocyte proliferation via P38MAPK activation, hence favoring pulmonary vascular remodeling and pulmonary hypertension. NOx4 is associated with ALOx12 and ALOx15 activity in diabetic hearts.
Myeloperoxidase
Myeloperoxidase (MPOx), encoded by the MPO gene, which produces a single-chain precursor, subsequently cleaved into a light and heavy chain that tetramerize. It is stored in large quantities in neutrophils, constituting a major component of neutrophil azurophilic granules, and, to a lesser extent, in monocytes and macrophages. This heme protein is synthesized during myeloid differentiation. This microbicide is an element of the host immune defense. It also influences endothelial function.
Myeloperoxidase catalyzes H 2 O 2 and halide or semihalide ions reactions that produce hypohalous acids, 18 such as hypochlorous acid (HOCl − ) and hypothiocyanous acid (HOSCN), a potent microbicide [ 71 ]. HOCl − reacts mainly with nitrogen and sulfur atoms in cysteine residues, especially glutathione, Cys oxidation inactivating or activating cellular molecules.
Myeloperoxidase is involved in redox stress and inflammation; it can serve as a marker of atherosclerotic plaque instability [ 76 ]. Glutathione sulfonamide, the product of G SH oxidation primarily by HOCL − , can serve as a marker of MPOx damage. Smoking engenders high amounts of thiocyanate (SCN − ), 19 a small ubiquitous acidic pseudohalide thiolate that reduces H 2 O 2 by MPOx and increases quantities of hypothiocyanous acid [ 71 ]. The POx–SCN–H 2 O 2 axis is an element of host defense.
Thiocyanate can act as an antioxidant, as it interacts with peroxidases and can protect cells against injurious redox damage via hypohalous acids such as HOCl and HOBr [ 77 ]. It ablates toxicity yielded by the MPOx–Cl − –H 2 O 2 axis at concentrations of 100–400 μmol/l in the nervous system and lungs, among other organs, in addition to endotheliocytes. It also detoxifies H 2 O 2 formed by the LPOx–SCN–glucose oxidase (GluOx) axis [ 77 ]. On the other hand, SCN can play a cytotoxic role. However, diseases associated with increased SCN and HOSCN amounts are also related to exposure to other toxic agents (e.g., cyanide, tobacco smoke, and cyanogenic glucosides), which can contribute to pathogenesis.
Hypothiocyanous acid reacts with thiols, oxidizing Trp and damaging protein Tyr phosphatases, causing a hyperphosphorylation state within the cell, altering MAPK signaling, and launching apoptosis. It can also oxidize LDLs and HDLs, in addition to NO [ 71 ].
Cytochrome-P450
Enzymes of the cytochrome-P450 superfamily are involved in the oxidative metabolism of various xenobiotics using molecular oxygen and electrons supplied by CyP450 oxidoreductase (POR), also called NADPH–CyP450 reductase (CPR) [ 78 ]. 20 They insert an oxygen atom into a substrate. Processing by CyP450 enzymes is inefficient as the oxidation of substrates is associated with the production of varying proportions of superoxide and/or hydrogen peroxide.
Three types of NADPH-dependent oxidations by microsomal CyP450 monooxygenases comprise [ 79 , 80 ]:
- Regio- and stereo-selective olefin epoxidation of arachidonic acid (epoxygenase reaction), which produces (5,6)-, (8,9)-, (11,12)-, and (14,15)-EETs by the cytochrome-P450 epoxygenases (HETEs) 21
- Arachidonic acid allylic oxidation (lipoxygenase-like reaction), which generates 5-, 8-, 9-, 11-, 12-, 15-hydroxyeicosatetraenoic acids (HETEs)
- ω- and (ω-1)-Hydroxylation (at or near the terminal carbons [C16–C20]), which forms 16- (ω-4) to 20HETEs (ω) by AA ω- and (ω-1)-hydroxylases CyP1a1, CyP1a2, CyP4a11, and CyP4a22
Four EET regioisomers, (5,6)-, (8,9)-, (11,12)-, and (14,15)-EETs, operate as auto- and paracrine messengers. The prime vasodilation of EETs is via smooth myocytic large-conductance Ca 2+ -activated K + channel (big potassium [BK]) [ 81 ]. 22 Activation by EETs of endothelial TRP channels and resulting Ca 2+ influx is an alternative endothelial-derived hyperpolarizing factor. They also have an anti-inflammatory effect on blood vessels and promote angiogenesis via an EPHb4-coupled PI3K–PKB pathway or sphingosine kinase SphK1 [ 81 ]. They convert eicosapentaenoic acid into vasoactive epoxy derivatives and endocannabinoids, whereas soluble epoxide hydrolase (sEH) transforms EETs to dihydroxyeicosatrienoic acids (DHETs), attenuating many EET effects.
Heme Oxygenases
Membrane-bound heme oxygenases HOx1 and HOx2 catalyze the rate-limiting step of heme catabolism using molecular oxygen and electrons supplied by CyP450 oxidoreductase, converting heme to CO, biliverdin, and ferrous iron. Heme is a potent hydrophobic prooxidant that intercalates in membranes and mediates peroxidation of membrane phospholipids [ 78 ].
The HOx1 subtype is constitutively expressed in the liver, spleen, and bone marrow and is inducible in most organs by redox stress, heat shock, nutrient depletion, disrupted intracellular calcium homeostasis, exposure to cytotoxins, and proinflammatory stimuli [ 78 ]. It synthesizes the second messenger CO, a gaseous vasodilator, thereby protecting hepatic microcirculation subjected to redox stress, among other vascular beds. The HOx2 isoform resides in the brain, liver, spleen, and testis.
Heme oxygenase HOx1 protects against redox stress, as it competes with CyP450 for binding to their common redox partner, CyP450 oxidoreductase, diminishing CyP450 action and associated ROS production [ 78 ]. Induction of HOx1 slows down the microsomal production rate by CyP1a2 of hydrogen peroxide and hydroxyl radical. In addition, oxidative injury caused by CyP2e1 is partly prevented by HOx1.
Crosstalk exists among ROS sources. Hydrogen peroxide can activate NOx and induce xanthine dehydrogenase transformation into xanthine oxidase. Peroxynitrite induces superoxide production [ 71 ]. In addition, mitochondrial ETC and NOx can interact for mutual induction, elaborating an oxidative cycle. Hyperglycemia favors this interference.
Production of ROS partners depends on vessel location. Vascular smooth muscle and endothelial, immune, and other hematopoietic types of cells have different expression patterns for ROS-related proteins.
Redox Signaling
At low concentrations, certain ROS, such as superoxide and hydrogen peroxide, are signaling mediators involved in redox signaling (or redox control).
Intracellular signaling effectors stimulated by ROS encompass the MAPK module with ERK1, ERK2, and ERK4, protein Tyr kinases Src and Syk, and different redox-sensitive isoenzymes of the PKC set in addition to redox-sensitive transcription factors, such as AP1, ETS, HIF1, NFκB, and P53 [ 74 , 83 ].
Hydrogen peroxide has a longer half-life than superoxide, and unlike superoxide, it can cross lipidic membranes by diffusion or transfer through aquaporins to initiate intracellular signaling [ 89 ]. Superoxide penetrates the cell through anion chloride channel ClC3 [ 74 ].
Superoxide and hydrogen peroxide can provoke cell growth, proliferation, and via oxidative activation of signaling molecules (e.g., PKB, Src, PLC, and MAPK) or inactivation of protein Tyr phosphatases [ 74 ].
At low concentrations, ROS regulate vascular smooth myocyte proliferation in addition to its contraction–relaxation state [ 84 ].
Antioxidant Defense
Organisms use enzymatic and non-enzymatic antioxidant defense to prevent overload of highly reactive very short half-life free radicals. Redox-sensitive proteins are confined to signaling nanodomains in cells of the cardiovascular apparatus. Antioxidant protection consists of four sequential levels: preventive, chain-breaking, repairing, and adaptive [ 83 ]. (1) The first level of antioxidant defense involves enzymes, such as superoxide dismutases (SOD1–SOD3), glutathione peroxidases (GPOx1–GPOx8), and catalase. Extracellular SOD is produced by vSMCs (but not ECs). (2) The second level of defense, which involves vitamins C and E and probably carotenoids, prevents accumulation of secondary radicals produced in chain reactions such as lipid peroxidation. (3) The third level of defense corresponds to enzymatic prevention of the formation and removal of secondary radicals.
Adaptation to stress relies on stress response linked to protein cysteine reduction–oxidation and launched by the transcription factors NFκB NFE2L2. ROS upregulate the formation of NFE2L2, which increases synthesis of numerous antioxidant enzymes.
Upon redox stress, MAP3K5 operates in a ROS-induced cellular response. ROS mediate angiotensin-2-induced MAP3K5 activation. In unstressed cells, MAP3K5 homo-oligomerizes and forms the inactive MAP3K5–TRdx signalosome. Upon ROS stimulation, this signalosome liberates its inhibitor TRdx and forms a fully activated complex with TRAF2 and TRAF6 [ 85 ].
Antioxidants include superoxide dismutases, catalase, glutathione peroxidases (GPOxs), and the thioredoxin–thioredoxin reductase couple, which counterbalance ROS production (Table 1.4 ). Glutathione peroxidase, catalase, and peroxiredoxins catabolize hydrogen peroxide.
Catabolism of reaction oxygen species (ROS) (Source: [ 71 ]; Cat catalase [encoded by the CAT gene], GPOxi type- i glutathione peroxidase [encoded by the GPX1–GPX8 genes], GsR glutathione reductase [encoded by the GSR gene], PRdxi type- i peroxiredoxin [encoded by the PRDX1–PRDX6 genes], TRdxRdi type- i thioredoxin reductase [encoded by the TXNRD1–TXNRD3 genes])
Disulfide bridge characterizes the oxidized form (SS or S 2 )
Removal of hydrogen peroxide prevents formation of the highly reactive hydroxyl radical, which can be formed by the reaction of hydrogen peroxide with Fe 2+ (Fenton’s reaction). In various intracellular antioxidant reactions such as H 2 O 2 removal, the reduced form of glutathione (G SH ) is oxidized into glutathione disulfide (G SS G), which can then be excreted from cells or reconverted to G SH by NADPH-dependent glutathione disulfide reductase.
Superoxide Dismutases
Extracellular (SOD3), cytosolic copper- and zinc-(SOD1), and mitochondrial manganese-containing superoxide dismutase (SOD2) process O 2 • − into the messenger hydrogen peroxide and molecular oxygen, thereby preventing peroxynitrite formation (Table 1.5 ). Dismutation of O 2 • − into H 2 O 2 by SOD involves the reduction and re-oxidation of a redox active transition catalytic metallic ion, such as copper (SOD with its oxidized [SOD MI ox ] and reduced metal ion [SOD MI red ]: SOD Cu 2 + and SOD Cu + , respectively) and manganese (SOD Mn 3 + and SOD Mn 2 + ) [ 74 ]. 23
Superoxide dismutases in vascular walls (Source: [ 74 ]; Atox copper chaperone antioxidant, ATP7 α copper-transporting ATPase-7α, CCS copper carrier and chaperone for superoxide dismutase, IMS intermembrane space of the mitochondrial envelope)
The SOD3 isozyme is anchored in the extracellular matrix via heparan sulfate proteoglycans, collagen, and fibulin-5
Catalase lodges principally in peroxisomes, H 2 O 2 being generated by peroxisomal β-oxidation of long-chain FAs. Heme-containing homotetrameric catalase does not usually lodge in mitochondria, except in the heart, where it resides in the mitochondrial matrix. Red blood capsules, in addition to the liver and kidney, have the highest catalase activity, the brain, heart, and skeletal muscle having a low catalase activity.
It neutralizes hydrogen peroxide, thereby preventing accumulation of hydroxyl radicals. Catalase degrades H 2 O 2 using two different mechanisms [ 86 ]. In dismutation, the oxyferryl heme is reduced back to the ferric form by another H 2 O 2 molecule, H 2 O 2 being both oxidant and reductant ( catalatic reaction ). Alternatively, catalase can use other electron donors ( peroxidatic mechanism ).
Peroxiredoxins
Ubiquitous homodimeric peroxiredoxins are nonheme peroxidases that detoxify low- and high-molecular-mass peroxides (ROOH, where R can be a hydrogen atom or a complex phospholipid). Most PRdxs use thioredoxin as a donor of reducing equivalents (of hydrogen), although PRdx6 functions as a reduced glutathione-dependent peroxidase. Glutaredoxins and cyclophilins are additional electron donors for peroxiredoxins.
Peroxiredoxins lodge in different subcellular compartments, such as the mitochondrion (e.g., PRdx3 and PRdx5) and cytosol (e.g., PRdx1, PRdx2, and PRdx6), PRdx4 residing predominantly in the endoplasmic reticulum and PRdx5 also in the cytosol and peroxisomes [ 87 ].
Peroxiredoxins are regulated by phosphorylation in response to extracellular signals, redox state, and oligomerization. They contain one or a pair of active cysteines sensitive to oxidation by H 2 O 2 , which reacts with the thiolate deprotonated form of cysteine. Peroxiredoxins are classified into three sets: typical (PRdx1–PRdx4) and atypical 2-Cys (PRdx5) and 1-Cys forms (PRdx6). They also reduce ONOO − and lipid peroxides.
Antioxidant sestrins can regenerate oxidized peroxiredoxins, scavenge ROS, and hamper expression of NOx4, especially in glomerular mesangiocytes, and TORC1-induced ROS [ 88 ].
Glutathione Peroxidases
Glutathione peroxidase GPOx1 is one of the most abundant members of the GPOX family, which includes epithelial GPOx2, highly expressed in the intestine, and secreted GPOx3, among other subtypes. GPOx1 lodges in the cytosol, mitochondrion, and peroxisome.
The intracellular antioxidant selenocysteine-containing enzyme GPOx1 reduces hydrogen peroxide to water, thereby limiting its accumulation and subsequent harmful oxidative effect on nucleic acids, proteins, and membrane lipids and preventing carcinogenesis and the development of cardiovascular disease [ 89 ].
GPOx1 can also reduce lipid hydroperoxides and other soluble hydroperoxides after their release from membrane lipids [ 89 ]. It also reduces phospholipid and monoacylglycerol hydroperoxides, such as linoleoyl lysophosphatidylcholine hydroperoxide, but not tri- or diacylglycerol hydroperoxides. These other types of membrane-associated phospholipids are reduced by GPOx4 [ 89 ]. GPOx1 may also act as a peroxynitrite reductase.
Expression of GPOx1 is regulated by transcriptional, post-transcriptional, translational, and post-translational mechanisms [ 89 ]. Estradiol and ROS contribute to GPOx1 transcription control. Selenium stabilizes mRNA, avoiding nonsense-mediated decay. Translation involves Sec insertion sequence (SecIS)-binding proteins such as SBP2. At the post-translational level, GPOx1 can be oxidatively inactivated by excess ROS or NO, whereas the kinase Abl phosphorylates (activates) GPOx1.
Redox Stress
At excessive and sustained concentrations, ROS have deleterious effects. Reversible and irreversible oxidations of cellular proteins, lipids, carbohydrates, RNA, and DNA have an impact on cellular functions. Mitochondrial DNA is particularly vulnerable to ROS and RNS. Generalized oxidation causes cell dysfunction, apoptosis, or necrosis [ 90 ].
Reactive oxygen species operate in inflammation. In particular, macrophages release glutathionated peroxiredoxin-2, which acts as an alarmin (or damage-associated molecular pattern molecules [DAMPs]), which triggers innate immune response and production of TNFSF1 [ 91 ].
Reactive oxygen species function in the initiation and progression of CVD. They are involved in proinflammatory signaling within vascular endothelial cells (vECs) and vSMCs, which then synthesize cell adhesion molecules and chemokines. They also activate MMPs.
Major vascular risk factors (hypertension, dyslipidemia, diabetes, and smoking) are associated with augmented vascular ROS production. A chronic metabolic disturbance favors inflammation and redox stress, an imbalance between pro- and antioxidants and their sources and sinks. Obese sedentary individuals have greater NOx activity in skeletal muscles and blood ROS concentrations than lean active subjects [ 92 ]. Adequate diet that attenuates redox stress prevents obesity-associated disorders [ 84 ].
Mitochondrial superoxide production corresponds to 1–2% of the molecular oxygen consumed. However, excess mitochondrial O 2 • − influences the perivascular neutrophil niche [ 92 ]. Lysophosphatidylcholine is implicated in mitochondrial ROS production and in endotheliocyte activation likely because of electron leakage across the mitochondrial membrane. Hydrogen peroxide derived from mitochondrial O 2 • − alters the caliber of the coronary resistance artery.
Chronic production of inflammatory and vasoconstrictive prostaglandins exacerbates hypertension via both inflammation and vasoconstriction.
Oxidation and glycation of LDLs engender proinflammatory and proatherogenic adducts. On the other hand, high-density lipoproteins lessen lipoprotein oxidation and hence generation of oxidized LDLs (oxLDLs), the antioxidant effect relying on HDL-associated paraoxonase [ 90 ].
In atherosclerotic lesions, ROS stabilize HIF1α, which is produced in hypoxic regions of plaques and favors M1 macrophage phenotype and hence atherogenesis [ 92 ].
Migration of macrophages primed by oxLDLs depends on FAK, PTPN11, NOx, ROS, and ScaRb3 [ 92 ]. On the other hand, ScaRb3 activation by ROS in extracellular vesicles precludes the migration of endotheliocytes.
Growth factors (e.g., platelet-derived growth factor [PDGF] and TGFβ), cytokines (e.g., TNFSF1 and IL1β), and hemodynamic stress (shear and stretch) regulate expression and/or activity of vascular NOxs [ 83 ]. The autacoids angiotensin-2, endothelin-1, and thrombin activate NOx. Agt2 not only stimulates NOx but also upregulates expression of its subunits, provoking ROS generation by ECs, vSMCs, and adventitial fibroblasts via its AT 1 receptor. Thrombin, in addition to PDGF, TGFβ, and TNFSF1, also activates NOx in vSMCs. Endothelin-1 increases NOx activity in ECs via its ET A receptor.
Angiotensin-2 causes mitochondrial dysfunction via endothelial NOx, PKC, and ONOO − , elevates mitochondrial H 2 O 2 production, and reduces endothelial NO availability [ 93 ]. On the other hand, the amount of mitochondrial ROS is lowered by manganese-containing superoxide dismutase SOD2, and/or peroxiredoxins PRdx3, and/or PRdx5, which protects against mitochondrial oxidative damage. In vascular smooth myocytes and endotheliocytes, the mitochondrial ATP-sensitive potassium channel is implicated in Agt2-induced mitochondrial ROS production, as it increases K + influx and alkalinizes the mitochondrial matrix. Mitochondrial permeability transition pore-opening also contributes to Agt2-mediated ROS production.
In some diseases, NOx1 expression is upregulated in vascular endotheliocytes and smooth myocytes. Interaction between thrombospondin-1 with neurophilin (CD47) activates NOx1 [ 92 ]. Cyclic stretch applied on vessels induces formation of myocyte-enhancing factor MEF2b, which launches NOx1 production and vSMC phenotype switching to a proliferative state. Both NOx1 and NOx4 syntheses are upregulated by hyperglycemia, leading to ROS-induced PKC-dependent downregulation of PKG production and hence repression of the NO–sGC–cGMP–PKG signaling.
Inducible NOx2, which is produced to a greater extent in fibroblasts and immunocytes, participates in recruiting macrophages to inflammation sites to remove infectious pathogens. However, NOx2 overexpression in the endothelium favors sustained leukocyte infiltration in the vasculature and thrombosis.
Hydrogen peroxide (H 2 O 2 ) formed by constitutively active brown adipocytic NOx4 protects the vasculature via PKG [ 92 ]. In addition, adipocytic NOx4 slows obesity-linked inflammation in addition to T2DM progression. On the other hand, endoplasmic reticular stress stimulates NOx4, which produces both superoxide and hydrogen peroxide. Intermedin 1−−53 , a N-terminal fragment of adrenomedullin-2, reduces NOx4 production.
Reactive nitrogen species, that is, NO • , an endothelial function marker, and its derivatives, participate in vasculopathies. In healthy vessels, NO prevents circulating leukocyte adhesion to the wetted endothelial surface and triggers vasodilation. In addition to endotheliocytes, circulating hematopoietic cells are important sources of NO in blood [ 92 ]. Excess NO production, often due to the hyperactivity of NOS2, has harmful effects on the vasculature. In obese mice, the perivascular adipose tissue causes NOS3 uncoupling, converting it from NO producer to O 2 • − generator, which exacerbates the underlying pathological condition.
In endothelial and smooth muscle cells, the oxidation state (ferric versus ferrous) of hemoproteins modulates NO signaling. In particular, the redox state of hemoglobin Hbα at the myoendothelial junction regulates NO activity. In the ferric state, Hbα has a reduced binding affinity for NO, which then diffuses between endotheliocytes and smooth myocytes [ 92 ]. In the reduced ferrous Hbα state, NO is sequestered, and the NO–sGC–cGMP–PKG axis and subsequent vasodilation of resistance arteries in both the systemic and pulmonary circulation are repressed. The flavoprotein methemoglobin reductase 24 also inhibits NO signaling via the myoendothelial junction. On the other hand, in vSMCs, methemoglobin reductase reduces soluble guanylate cyclase (sGC) heme iron from the ferric to the ferrous state, thereby enabling NO sensing and subsequent arterial dilation. In addition, cGMP is not only degraded by phosphodiesterases PDE3 and PDE5 but is also exported from the cell [ 92 ].
Receptor for Advanced Glycation End Products
Proinflammatory multiligand receptor for advanced glycation end products (RAGE) generates ROS via NOx activation and mitochondrial production amplification and thus operates via redox stress [ 94 ].
The RAGE resides on diverse cell types (e.g., endothelial progenitor cells, cardiac endotheliocytes, vascular smooth myocytes, cells of the nervous system, pancreatic β cells, renal mesangiocytes, osteoblasts, and inflammatory leukocytes). Its cytoplasmic domain binds to the formin diaphanous-1 that activates Rac1 and NOx in aortic smooth myocytes exposed to the RAGE ligand S100b.
The RAGE connects to proinflammatory members of the S100–calgranulin set (S100a8, S100a9, and S100a12 [calgranulin-A–calgranulin-C]), which are predominantly expressed by neutrophils, monocytes, and activated macrophages, S100a8 being a potent antioxidant, in addition to high-mobility group box-containing protein HMGB1, amyloid β-peptide and β-sheet fibrils, lysophosphatidic acid, α M β 2 -integrin (CR3), and complement component C1q [ 94 ].
Advanced glycation end products (AGEs) are products of non-enzymatic glycation and oxidation of proteins and lipids formed in vascular cells, CMCs, neurons of the central and peripheral nervous systems, alveolar pneumocytes, podocytes, and inflammatory leukocytes, among other cell types [ 94 ]. In the heart, the detoxifier glyoxalase-1 of glycation precursors such as 3-deoxyglucosone of the AGE N𝜖1-carboxymethyllysine prevents diabetes-induced redox damage, inflammation, fibrosis, and diabetic cardiomyopathy [ 95 ].
Lipid Peroxidation
Lipids, with their reactive double bonds, are targets of oxidation. Lipid peroxidation generates isoprostanes and malondialdehyde (MDA; Table 1.6 ).
Lipid peroxidation (Source: [ 71 ])
Isoprostanes are stable prostaglandin-like compounds engendered from arachidonic acid peroxidation and subsequently released from cellular membranes into the bloodstream by phospholipases. Isoprostane concentrations in plasma and urine samples correlate with cigarette smoking, hypercholesterolemia, obesity, T2DM, and hyperhomocysteinemia [ 90 ].
Malondialdehyde is formed from peroxidation of polyunsaturated FAs. It interacts with proteins, particularly with lysine residues, building Lys–Lys crosslinks, such as in ApoB of oxLDLs [ 90 ].
Protein Tyrosine Nitration
Proteins are also oxidized and then associated with pathophysiological processes in addition to aging. Protein tyrosine nitration, which consists of adding a nitro group (–NO 2 ), is mediated by RNS such as peroxynitrite (ONOO − ) and nitrogen dioxide (NO 2 • ). This reaction involves two steps: the oxidation of the phenolic ring of tyrosine to tyrosyl radical (Tyr • ) and the addition of NO 2 • to the Tyr by a nitrating agent. Myeloperoxidase, with its transition metal center, can react with ONOO − and hence facilitate nitration [ 90 ]. Nitrotyrosine formation on enzymes, such as sarcoplasmic reticulum Ca 2+ ATPase (serca2a), manganese-containing superoxide dismutase ( Mn SOD or SOD2), prostacyclin synthase, tyrosine hydroxylase, and aldolase-A, inhibits their activity. On the other hand, nitrotyrosine in fibrinogen raises its activity and accelerates clot formation.
Protein Glutathionation
S Glutathionation, that is, formation of a disulfide bridge between a reactive cysteine residue and the tripeptide glutathione, mediates redox regulation of numerous cellular proteins (e.g., NOS3, ryanodine receptor, SERCA, and Na + –K + ATPase, thereby affecting their function and intracellular Na + and Ca 2+ handling [ 90 ]). S Glutathionation of hemoglobin can serve as a marker of redox stress.
Aging is associated with declining organ functioning and metabolism. It is related to chronic inflammation, the so-called inflammaging , redox stress, and arterial stiffening. Arterial redox stress contributes to arterial stiffening, as it favors elastin degradation and collagen overproduction, in addition to inflammation.
Many lipids are synthesized from precursors within the body, but some essential FAs must be ingested with food intake. For example, fish contains the essential long-chain ω3 FAs eicosapentaenoic (EPA) and docosahexaenoic acid (DHA). Vegans do not eat animal products and vegetarians neither meat nor fish; semi-vegetarians consume fish, seafood, and sometimes even poultry; lacto-vegetarians add dairy products and lacto-ovo-vegetarians eggs to their diet.
Lipids can be divided into eight categories: FAs, glycerolipids, glycerophospholipids, sphingolipids, sterol and prenol lipids, saccharolipids, and polyketides). Their concentration ranges from the attomolar to the micromolar level. Lipidomics is aimed at investigating lipid fate and signaling in addition to the effects of nutritional supplementation and its role in immune and inflammatory responses and cardiovascular and pulmonary diseases. Signaling lipids include oxylipins, especially the initiation and termination of inflammation.
Oxylipins are lipophilic messengers generated by oxygenation by cyclooxygenases (COxs; or prostaglandin-G/H synthases [PGhS]), cytochrome-P450 enzymes (CyPs), and lipoxygenases (LOxs), in addition to the non-enzymatic auto-oxidation of polyunsaturated fatty acids (PUFAs), such as the ω6-fatty acids arachidonic (AA) and linoleic acid (LA) in addition to ω3-fatty acid α-linolenic acid (α LA), the plasmatic concentrations of which change not only with diet but also during aging [ 96 ].
Oxylipins are involved in immunity and hence inflammation in addition to vasomotor tone and blood coagulation. They can also be bactericides.
Eicosanoids are oxylipins derived from AA, a component of cellular membrane phospholipids. Cyclooxygenases generate class- II (2 double bonds) prostaglandins (PGs) and thromboxanes (Txs) from arachidonic acid. Class- I and- III PGs and Txs are formed from dihomo-γ-linolenic acid (DGLA) and EPA, respectively.
Lipoxygenase products encompass:
- HETEs from AA, which mediate neutrophil chemotaxis and degranulation
- Hydroxyoctadecadienoic acids (HODEs) from LA
- Hydroxyeicosapentaenoic acids (HEPEs) from EPA
Lipoxygenase LOx5 synthesizes leukotrienes and other metabolites, such as proinflammatory 5HETE, 5oxoETE, and LTb 4 , from AA, and 9HODE and trihydroxyoctadecenoic acids (triHOMEs) from LA. ALOx12 and ALOx15 produce 12HETE, 12oxoHETE, and proinflammatory 9HETE from AA.
The CyP enzymes generate epoxides, such as EETs from AA and epoxyoctadecamonoenic acids (EOMEs) from LA, which dilate arteries. These products are converted to dihydroxyoctadecenoic (diHOMEs) and DHETs by soluble epoxide hydrolase (sEH).
Aging, Inflammation, and Redox Stress
Inflammaging partly results from increased concentrations of alarmins, which activate pattern recognition receptors (PRRs). Toll-like (TLRs) and nucleotide-binding oligomerization domain-like receptors (NLRs) are expressed not only on or in innate immunocytes but also on or in cells of the neurovascular unit and blood–brain barrier [ 97 ]. Among these PRRs, TLR2, TLR4, NLRP1, and NLRP3 are activated during aging in neurons, astrocytes, microgliocytes, and possibly endotheliocytes and pericytes.
Cardiovascular disease is linked to chronic obstructive pulmonary disorder (COPD) via chronic inflammation and aging with reduced sirtuin activity and exposure to cigarette smoke [ 98 ].
Desmosine and isodesmosine are involved in elastin crosslinking and can serve as indicators of elevated elastin fiber turnover and degradation, such as in COPD and atherosclerosis complications.
Sirtuins (SIRT1–SIRT7) are NAD + -dependent protein (histone) deacetylases implicated in lifespan and health regulation. Sirtuin-1 regulates endothelial function as it deacetylates NOS3 [ 98 ]. In addition, it counters senescence, as it deacetylates P53 and STK11 (LKB1), and angiogenesis, as it deacetylates FoxO1 and notch-1 [ 98 ]. It also activates liver X receptor (NR1h2/3), which is involved in reverse cholesterol transport, hence promoting cholesterol efflux. It has an antioxidant effect. Furthermore, it inhibits NFκB [ 98 ]. On the other hand, sirtuin-1 precludes vascular smooth myocyte proliferation and atherothrombosis, as it downregulates endothelial formation of tissue factor and upregulates that of tissue inhibitor of metallopeptidase TIMP3 [ 98 ]. Prolonged moderate exercise training enhances FoxO3a expression, reduces redox stress, and raises SIRT1 activity in the heart and adipose tissue of aged rats.
Sirtuin-3 hampers cardiac hypertrophy as it controls ROS concentrations. Sirtuin-6 in endotheliocytes protects against telomere and gene damage, and Sirtuin-7 interacts with P53 and protects CMCs against apoptosis and redox and genotoxic stresses [ 98 ].
Reactive oxygen species participate in aging. However, dietary antioxidants, such as vitamins C and E, do not slow aging [ 99 ].
Mitochondria are a major ROS source and thus mediate adverse processes in aging. Supplementation with the orally active mitochondrial antioxidant MitoQ ([dimethoxy methyl dioxo-cyclohexadien decyl] triphenyl methanesulfonate), a derivative of the potent antioxidant ubiquinone conjugated to triphenylphosphonium, which accumulates within mitochondria, prevents mitochondrial redox damage. It thus attenuates the production of proliferative, proinflammatory, and profibrogenic mediators (e.g., tumor growth factor [TGFβ], connective tissue growth factor [CTGF], and PDGF) by neighboring and infiltrating cells in the liver (i.e., activated hepatic stellate cells, which form a collagen-rich matrix, Kupffer cells, and cholangiocytes, in addition to injured hepatocytes, platelets, and leukocytes), and hence redox stress, hepatocyte death, and hepatic inflammation, together with liver fibrosis and cirrhosis in mice [ 100 ]. Its administration for 4 weeks limits the reduction of elastin content and decreases aortic stiffness in 27-month-old mice, affects neither young mice nor age-related collagen synthesis and deposition, and increases proinflammatory cytokine formation [ 101 ].
Aging and Altered Proteostasis
Aging and age-related diseases are associated with disturbed balance of protein production, folding, and degradation, in addition to subsequent accumulation of misfolded proteins and proteic aggregates. In CMCs, altered proteostasis can participate in the development of cardiac hypertrophy, cardiomyopathies, and heart failure.
Hydrotropes are small molecules, typically amphiphilic agents, that solubilize hydrophobic molecules in aqueous solutions. The canonical energy carrier and autacoid, adenosine triphosphate (ATP), an energy source for chemical reactions at micromolar concentrations, including muscular contraction, possesses at physiological millimolar concentrations (5–10 mmol/l) the properties of a hydrotrope, as it maintains protein solubility and prevents molecular aggregation [ 102 ]. At relatively high concentrations, ATP enhances the solubility of solutes, such as nonpolar lipophilic proteins (unlike polar hydrophilic proteins) and organic substances, which are nearly insoluble in the usual aqueous solutions. Amphiphilic hydrotrope molecules have shorter hydrophobic regions and therefore do not spontaneously self-aggregate in the aqueous phase [ 103 ]. Adenosine triphosphate precludes not only formation of protein aggregates, hampering aggregation of prion and amyloid fibers from amyloid-β4 protein, but also contributes to dissolving a previously formed agglutinated mass, as it can dissolve liquid–liquid phase-separated droplets, keeping the RNA-binding protein fused in sarcoma (FUS) in a water-soluble state and preventing its accumulation into separate liquid drops [ 102 ].
For most ATP users such as ATP-dependent enzymes, the Michaelis–Menten constant of cardiac actin-based nanomotor myosin evolves in the micromolar range (β-myosin encoded by the MYH7 gene [cardiac myosin heavy chain-7]: 40 ± 6μmol/l), whereas the nucleotide ATP is typically present in millimolar concentrations in the cytoplasm of CMCs [ 103 ]. Therefore, the discrepancy between ATP concentration needed by ATP-consuming enzymes and its intracellular level can be explained, at least partly, by its hydrotrope function.
The intracellular ATP amount declines with aging in addition to impaired mitochondrial oxidative phosphorylation.
Variant proteins containing expansions of glutamine repeats (polyQ repeats), that is, with increased polyglutamine motif length, which is encoded by the DNA nucleotide sequence CAG, can misfold and form aggregates, which can sequester proteins. Expansion of polyQ domains in huntingtin and the deubiquitinase ataxin-3 causes Huntington’s disease characterized by loss of striatal neurons and hence changes in mood and personality, defective motor coordination, and involuntary movements and type-3 spinocerebellar ataxia (SCA3), a form of neurodegeneration in the striatum and cerebellum, respectively [ 104 ]. PolyQ expansions in addition to soluble N-terminal huntingtin fragment comprising exon 1 are toxic. Autophagy that is aimed at attenuating protein toxicity removes polyQ-expanded proteins, such as abnormal huntingtin and ataxin-3.
On the other hand, some polyQ-containing proteins regulate degradation of misfolded proteins and autophagy. Ataxin-3 deubiquitinates beclin-1 that then escapes proteasomal destruction and triggers starvation-induced autophagy. Short polyQ domain enables interaction between ataxin-3 and beclin-1 [ 105 ]. On the other hand, a mutated form of huntingtin that contains an expanded polyQ region competes with ataxin-3 for beclin-1 binding, thereby increasing beclin-1 degradation and dysregulating autophagy. Huntingtin also participates in stress-activated autophagy, as it competes for binding to another autophagic regulator.
Expansion of the polyglutamine stretch in ataxin-1 (Atxn1) causes the hereditary neurodegenerative disease type-1 spinocerebellar ataxia (SCA1), hence its other alias SCA1. The ATXN family includes proteins characterized by the presence of an AXH domain implicated in protein–protein interactions. 25
The deubiquitinase Atxn3L targets the zinc finger-containing transcription factor KLF5, which promotes cell survival and proliferation in addition to tumoral growth, partly as it upregulates synthesis of fibroblast growth factor-binding protein FGFBP1 26 and microsomal prostaglandin-E synthase PtgES1 [ 106 ]. It belongs to the DUB subset of Machado–Joseph disease (MJD) proteic domain-containing peptidases with Atxn3 (a.k.a. MJD1 and SCA3), encoded by the gene mutated in MJD, also termed type-3 spinocerebellar ataxia (SCA3), and Josephin domain-containing DUbs JosD1 and JosD2 (Table 1.7 ). 27
Ataxins (Atxns; Source: [ 107 , 108 ]; boat brother of ataxin-1, MJDL Machado–Joseph disease protein-like protein)
Expansion of the polyglutamine sequence in ataxins provokes spinocerebellar ataxia (SCA)
Aggregates formed by polyglutamine-expanded ataxin-7 sequester ubiquitin-specific peptidase USP22 that cannot then fulfill its deubiquitinating function in the SAGA complex, causing cytotoxicity and neurodegeneration [ 109 ].
Sleep Disorders
Sleep disorders and short sleep duration (≤ 5 h/night) alter neurohormonal regulation and the circadian rhythm of blood pressure with its nocturnal decrease, blunting nocturnal surge in melatonin secretion and favoring hypertension. Sleep deprivation is related not only to hypertension but also diabetes mellitus and coronary artery disease [ 110 ].
Cardiovascular and metabolic disease (i.e., hypertension, atherosclerosis, heart failure, cardiac arrhythmias, obesity, and metabolic syndrome) are linked to sleep anomalies (sleep curtailment, shift work, and sleep-disordered breathing) [ 111 ]. Sleep affects the autonomic nervous system, hemodynamics, endothelial and myocardial function, and blood coagulation.
Central sleep apnea (CSA) is caused by a lack of neural input for breathing. Breathing effort is attenuated or absent during airflow cessation, typically for 10–30 s, either intermittently or in cycles.
Breathing is controlled by central and peripheral chemoreceptors. Medullary neurons respond to CO 2 content via shifts in H + concentration and chemoreceptors of the carotid body to arterial blood O 2 and CO 2 content. Elevated chemoresponsiveness along with blunted chemosensitivity can destabilize the breathing pattern. In addition, several other homeostatic feedback mechanisms regulate breathing amplitude and frequency to maintain gas exchange, such as afferent input from Golgi tendon organs and muscle spindles from respiratory muscles [ 112 ]. Ventilatory response to hypoxia and hypercapnia and respiratory load compensation are reduced during sleep, particularly during the rapid eye movement stage.
Several CSA manifestations encompass high-altitude-induced periodic breathing, idiopathic CSA, narcotic-induced central apnea, obesity hypoventilation syndrome, and Cheyne–Stokes breathing [ 112 ]. Nighttime breathing disturbances increase the risk for adverse cardiovascular outcomes.
Obstructive sleep apnea (OSA) with breathing pauses 5–30 times per hour during sleep because of upper airway hindrance is associated with respiratory efforts. It can be linked to hypertension, arrhythmia, stroke, and heart failure. Obstructive sleep apnea is associated with obesity; the resulting sleep deprivation can favor obesity, forming a vicious cycle.
Vascular Tumors and Malformations
Vascular anomalies encompass tumors and malformations (direct connections between arteries and veins), in addition to infection, trauma, and adverse remodeling.
- Vascular congenital tumors comprise infantile congenital hemangioma, especially in girls, which is usually solitary, but can be multiple, along with tufted angioma, infantile fibrosarcoma, myofibromatosis, and kaposiform hemangioepithelioma.
- Vascular malformations that bypass the capillary bed generally result from embryogenic errors. However, most arteriovenous malformations are idiopathic. They arise spontaneously. They differ from those engendered by gene mutations by their location and evolution.
A classification of vascular anomalies was proposed by the International Society for the Study of Vascular Anomalies (ISSVA) that categorizes benign vascular lesions into two groups according to the predominant type of vascular channel affected and flow magnitude: (1) vascular tumors , the most common form being infantile hemangioma, and (2) vascular malformations, which are created by errors of vasculo- and angiogenesis [ 113 ]. Vascular malformations usually develop gradually, but their growth is faster than that of the body, with peak growth occurring during puberty.
Birth defects can be independent of genetic cause but rely on environmental factors. For example, cardiac and craniofacial birth defects can result from maternal fever during the first trimester of pregnancy. Neural crest cells are precursors of cells forming tissues of the heart and head (face). Hyperthermia-activated TRPV1 and TRPV4 channels 28 in neural crest cells of chick embryos provoke cardiac and craniofacial birth defects [ 114 ].
Vascular tumors encompass non-involuting (NICH) and rapidly involuting congenital (RICH) and infantile hemangiomas, tufted angiomas, kaposiform, spindle cell, and other rare hemangioendotheliomas, in addition to dermatologically acquired vascular tumors (e.g., pyogenic granuloma, targetoid, glomeruloid, and microvenular hemangioma).
Slow-flow vascular malformations include venous (e.g., blue rubber bleb nevus syndrome, familial cutaneous and mucosal venous malformation, glomuvenous malformation), capillary (e.g., telangiectasia and angiokeratoma), and lymphatic malformations (primary lymphedema, and micro- and macrocystic lymphatic malformations in addition to combined vascular malformations [capillary (C), venous (V), and/or lymphatic (L) malformations (M), that is, CVMs, CLMs, LVMs, and CLVMs]).
Telangiectasias 29 are small, permanently dilated blood vessels that engender small cutaneous red dots or linear or stellate lesions. They often progress to form papules, particularly on the face [ 113 ].
Angiokeratomas constitute a heterogeneous group of red–violaceous to black papules due to vascular dilation in the papillary dermis with epidermal hyperplasia and hyperkeratosis [ 113 ].
Angiokeratoma corporis diffusum represents a diffuse form of angiokeratoma. They are associated with deficiencies in:
- Lysosomal α N acetylgalactosaminidase (NAGα), which is encoded by the NAGA gene, mutations of which causes aspartylglucosaminuria and type- I (infantile) and - II (adulthood) Schindler disease
- Lysosomal α-galactosidase-A (Glα), mutations in the GLA gene engendering Fabry disease
- α-Fucosidase (Fucα), mutations in the FUCA1 (or FUCA) gene causing severe infantile type- I and milder type- II fucosidosis
- β-Galactosidase (Glβ) and neuraminidase (Neu1–Neu4 or sialidase-1 to -4), which provokes early and late infantile and juvenile/adult galactosialidosis , which results from mutations in the CTSA gene that encodes lysosomal cathepsin-A, which cooperates and complexes with neuraminidase-1 and β-galactosidase (hence the other CtsA name, protective protein for β-galactosidase [PPGβ])
- Lysosomal β-mannosidase (Manβ), mutations in the MANBA gene causing β-mannosidosis (mutations in the MAN2B1 gene that encodes lysosomal acid α-mannosidase class 2B member 1 provoking α-mannosidosis)
- Lysosomal monosialotetrahexosylganglioside GM1, mutations in the GLB1 gene that encodes acid galactosidase-β1 (Glβ1), generating GM1 gangliosidosis, GM1 ganglioside that cannot be catabolized accumulating to toxic levels
- Lysosomal sialidase-1, or neuraminidase Neu1, mutations in the NEU1 gene engendering type- I (partial Neu1 deficiency) and more severe type- II sialidosis (severe reduction or even elimination of Neu1 activity)
Verrucous hemangioma is a separate entity with respect to angiokeratoma. These generally deep lesions are often linked to hyperkeratosis [ 113 ].
Fast-flow vascular malformations comprise arterial and arteriovenous malformations, arteriovenous fistulas (AVFs), and combined vascular malformations (e.g., arterial [A], venous, and lymphatic (AVMLMs) and CMAVMs).
Ectopic Vascular Calcification
Arteries are not only sites of abnormal caliber changes, either narrowing ( stenosis ; Vol. 13, Chap. 7. Arterial Stenosis—Mechanical and Clinical Aspects) or enlarging ( aneurysm ; Vol. 13, Chaps. 3. Aortopathies and 4. Aneurysms), but also of ectopic calcifications.
Vascular calcification (Vol. 10, Chap. 3. Adverse Wall Remodeling) relies on bone morphogenetic proteins (BMPs; Sect. 1.4.5.6 ), the Wnt pathway (Sect. 1.4.5.2 ), tumor-necrosis factor superfamily member TNFSF11, and receptors TNFRSF11a and TNFRSF11b, in addition to various other calcification regulators, such as inflammatory factors and oxidized lipids.
Lipoprotein-A (LPa) carries proinflammatory and procalcific phosphocholine-containing oxidized phospholipids (OxPLs) [ 115 ]. In fact, various lipoproteins contribute to the progression from sclerosis to stenosis, although LPa is the preferential OxPL carrier.
Atherosclerosis
Atherosclerotic cardiovascular disease (ASCVD), or simply atherosclerosis, 30 is characterized by the subendothelial retention of modified lipoproteins, immunocyte infiltration, maladaptive chronic inflammation of the arterial wall, and vSMC-mediated fibrous cap formation. Atherosclerosis progression is linked to cell death, fibrous cap thinning, plaque rupture, and thrombosis.
Accumulated intracellular cholesterol can be removed using the reverse cholesterol transport that begins from cholesterol egress from cells and subsequent elimination from the body, thereby protecting against the development and progression of atherosclerosis.
On the other hand, an imbalance between the uptake of cholesterol from oxidized or aggregated LDLs through scavenger receptors and the efflux of cholesterol to apolipoprotein-A and HDLs through ABC transporters leads to atherogenesis.
Low-density lipoproteins can be oxidized, glycated, acetylated, ethylated, and methylated. Oxidized and glycated LDLs in arterial walls initiate atherogenesis. Modifications target LDL components such as their surface protein ApoB, which mediates LDL binding to its receptor. The early stage of atherogenesis is linked to oxidized LDLs that accumulate in the subendothelial space, where they activate endotheliocytes, which then produce adhesion molecules and chemokines, recruiting inflammatory leukocytes. Attracted monocytes differentiate into macrophages that internalize oxLDLs and release cytokines and ROS, further oxidizing LDLs and attracting medial smooth myocytes into the intima. These smooth myocytes contribute to atherogenesis via apoptosis and foam cell formation. Non-enzymatic glycation of lysine residues of ApoB diminishes LDL affinity for its receptor, thereby augmenting its plasmatic lifetime and uptake of glycated LDLs (glLDLs) by vascular cells and macrophages. Furthermore, LDL glycation renders them more susceptible to oxidation (gl–oxLDLs). Upon uptake of modified LDLs via scavenger receptors and pinocytosis, macrophages in the arterial intima differentiate into foam cells.
Mitochondria produce ATP and are involved in ion transfer, ROS generation, and apoptotic signaling. Mitochondrial DNA contains 37 genes that encode subunits of ETC complex- I , - III , and - IV and ATP synthase (i.e., ETC complex- V ), in addition to corresponding ribosomal and transfer RNAs.
Mitochondrial ROS damage mitochondrial DNA, a circular molecule linked to the inner mitochondrial membrane; mitochondrial dysfunction and subsequent mitophagy precede lesion development [ 116 ]. Mitochondrial DNA damage lessens mitochondrial oxidative phosphorylation. Decreased mitochondrial oxidative phosphorylation causes thinning of the fibrous cap via vascular smooth myocyte dysfunction and apoptosis, and increased necrotic core formation due to macrophage activation.
Mitochondrial DNA is replicated by the Mt DNA replisome, which comprises the twinkle helicase, Mt DNA polymerase, and mitochondrial single-stranded DNA-binding protein.
Reduced Mt DNA number and oxidative phosphorylation increase mitophagy in plaque vSMCs, whereas overexpression of the mitochondrial DNA helicase twinkle reduces Mt DNA damage but does not affect Mt DNA copy number [ 117 ]. Twinkle protects vascular smooth myocytes and macrophages against redox stress-primed apoptosis. In macrophages, overexpression of twinkle increases Mt DNA copy number without affecting Mt DNA damage. In both cell types, possibly via increased ETC subunit synthesis, twinkle overexpression enhances oxidative phosphorylation, thickening the fibrous cap via increased vSMC proliferation and reduced apoptosis and attenuating necrotic core formation via macrophage inactivation.
Atherosclerosis is a chronic disease of the arterial wall that involves both innate and adaptive immunity, inflammation being implicated at all stages of the disease. This inflammatory disease involves accumulation of lipids in the arterial intima, infiltration and proliferation of monocytes, and their differentiation into macrophages, among other leukocytes, recruitment of medial smooth myocytes, and production and degradation of the extracellular matrix. It is characterized by hardened arterial segments with narrowed or enlarged lumens (i.e., stenoses and fusiform aneurysms).
Arteriosclerosis , the hardening (or stiffening) of normally distensible arteries was described by the German-born French pathologist J.G.C.F.M. Lobstein (1777–1835). It encompasses atherosclerosis, medial thickening, and medial and intimal calcifications (e.g., Mönckeberg medial sclerosis, the most common form of medial calcifications in the arteries of the extremities) [ 118 ].
In 2013, atherosclerosis, particularly angina pectoris and myocardial and cerebral infarction ( stroke), and other types of cardiovascular affections (e.g., arrhythmias, heart failure, and cardiac valvulopathies) caused 51% and 42% of deaths among women and men, respectively [ 29 ]. In many countries, they provoke more than twice the number of deaths as cancer. However, in at least ten countries (Belgium, Denmark, France, Israel, Luxembourg, Netherlands, Portugal, Slovenia, Spain, and San Marino), cancer engenders more deaths than CVD among men and in one country (Denmark), among women [ 29 ].
Coronary atherosclerosis , also currently named coronary artery and heart disease and ischemic heart disease, 31 and cerebrovascular disease (another collective term standing for all diseases of arteries irrigating the brain), which are the first and second leading contributors to CVD burden, account for 20 and 12% of all deaths in Europe annually, respectively [ 29 ]. Inequalities exist among countries (e.g., Russia and Ukraine versus France). Approximately 63% of ischemic and 80% of hemorrhagic strokes now occur in low- and mid-income countries [ 121 ].
Acute coronary syndrome is a collective term incorporating unstable angina, ST-elevation myocardial infarction, and non-ST-elevation myocardial infarction due to atherosclerotic plaque erosion that can evolve into rupture. The resulting intraluminal thrombosis engenders sustained myocardial ischemia and infarction owing to local partial or complete vascular occlusion or, most often, embolization and subsequent obstruction of downstream arterial segments upon shedding of platelet aggregates.
Ischemia causes simultaneous massive cell death, releasing alarmins that activate NFκB, thereby producing proinflammatory cytokines. Debris from dead cells are taken up by macrophages, which then launch inflammation, relying on interferon regulatory factor IRF3 and type- I interferons, which protect against infection and cancer, IRF3 initiating a specific gene expression program. However, excessive IRF3 activation and type- I Ifn production are deleterious. Myocardial infarction stimulates IRF3 in a distinct population of interferon-inducible cardiac macrophages [ 122 ]. Secreted type- I interferons target the IfnAR receptor in an auto- and paracrine manner. In mice, deficiency in the cytosolic DNA sensor cyclic GMP–AMP synthase (cGAS), its adaptor, STING, the cGAS–STING axis activating IRF3 via TBK1, IRF3, type- I Ifns, or IfnAR, improves cell survival. In Irf3 −∕− mice, myocardial infarction-induced type- I Ifn response is nearly completely abrogated. Therefore, a transient inhibition of the interferon-dependent innate immune response in ischemia can reduce inflammation and limit the adverse ventricular remodeling.
Limbs subjected to brief periods of ischemia protect multiple organs, in particular the lung, from ischemia–reperfusion damage. Limb remote ischemic preconditioning results from the release into the bloodstream of irisin, a myokine derived from the extracellular portion of fibronectin domain-containing protein FnDC5 in skeletal muscle, which targets mitochondria and prevents some of the deleterious effects of redox stress [ 123 ]. Interaction between irisin and mitochondrial uncoupling protein UCP2 hampers ischemia–reperfusion event-induced redox stress and preserves mitochondrial function.
Vasculopathies and Cardiac Dysfunction
Heart failure , a complication of coronary atherosclerosis, hypertension, cardiomyopathies, myocarditis, heart defects, and valvular heart disease (or heart valve disease), has an estimated prevalence in North America and Europe of up to 2%. Eighty percent of new cases occur in people older than 65 years, contributing to about 11% of deaths [ 121 ].
Rheumatic heart disease (RHD), which is most frequently detected in low-income countries (Oceania; Central, South, and Southeast Asia; sub-Saharan Africa; the Caribbean; and Middle East [e.g., Yemen]), is the fifth and sixth leading cause of CVD-related mortality and disability, respectively [ 121 ].
Cardiomyopathies are categorized into various disease spectra according to their etiology and natural history, and these determine their medical management (Sect. 10.1007/978-3-319-89315-0_7#Sec1). They can result from (1) left ventricular stiffening associated with adverse wall remodeling, (2) impaired sensitivity to β-agonists and insulin, (3) depressed autonomic function with altered myocardial catecholamine concentrations, (4) endothelial dysfunction, (5) abnormal ionic currents, and (6) disturbed flow in the coronary macro- and microcirculation. The most common forms are dilated and ischemic cardiomyopathies.
Dilated cardiomyopathy (DCM) is currently defined by left ventricular or biventricular dilation and systolic dysfunction (i.e., abnormal ejection fraction) in the absence of abnormal loading conditions (e.g., hypertension and valvulopathies) or coronary atherosclerosis. It comprises a set of time-varying electrochemical and functional anomalies and can be engendered by genetic and acquired disorders. Genetic predisposition can be combined with environmental factors [ 124 ].
Inherited DCM can be transmitted by an autosomal dominant or recessive, X-linked, or matrilinear mode. The main genes implicated in DCM encompass BAG3 (BCL2-associated athanogene-3), LMNA (lamin-A/C), MYBPC3 (cardiac myosin-binding protein-C), MYH7 (myosin heavy chain), MYPN (myopalladin), PLN (phospholamban), RBM20 (RNA-binding motif protein-20), SCN5A (voltage-gated sodium channel α subunit Na V 1.5), TNNT2 (troponin-T), and TTN (titin). DCM can also have a genetic origin within the framework of neuromuscular disorders, such as Becker and Duchenne muscular dystrophy and myotonic dystrophy, may be linked to mitochondrial diseases and tafazzin [ 124 ].
On the other hand, DCM can derive from viral, bacterial, fungal, and parasitic infections in addition to systemic diseases (e.g., polymyositis, sarcoidosis, and systemic lupus erythematosus) [ 124 ]. It can arise as a complication of acromegaly, diabetes mellitus, hyper- and hypothyroidism, Addison and Cushing disease, 32 and pheochromocytoma. Dilated cardiomyopathy can be induced by excess alcohol consumption and chemotherapeutic and psychiatric drugs and by electrolyte disturbances (hypocalcemia and hypophosphatemia), overload (iron) or deficiency (carnitine, copper, selenium, thiamine, and zinc), anti-heart antibodies, and toxics (e.g., arsenic and cobalt). Peri- and postpartum cardiomyopathy (PPCM) is caused by autoimmunity, fetal microchimerism, viral infection, stress-activated cytokines, and toxic cleavage product of prolactin [ 124 ].
Hypokinetic nondilated cardiomyopathy (HNDC) is defined by left ventricular or biventricular systolic dysfunction (ejection fraction< 45%) without dilation [ 124 ].
Ischemic cardiomyopathy results from altered flow in large epicardial coronary arteries that are stenosed and/or parietal microcirculation associated with chronic inflammation. Rheumatoid arthritis, systemic lupus erythematosus, and systemic sclerosis yield an important risk background for myocardial ischemia.
Hypertrophic cardiomyopathy (HCM) is another form with abnormal and often asymmetric myocardial thickening, preserved left ventricular function, phenotypic heterogeneity, and incomplete penetrance. This autosomal dominant inherited disease can be caused by mutations of genes (> 50 genes, mainly those encoding sarcomeric constituents [e.g., MYL2]). The presence of additional risk factors, especially hypertension, exacerbates the disease penetrance and severity, as MYL2 E22K mutation does not exhibit clinical symptoms in most carriers [ 125 ].
Diabetic cardiomyopathy is characterized by reduced diastolic function and left ventricular hypertrophy. Its clinical management relies on appropriate glucose and HbA1c monitoring. However, in individuals of African ancestry, a specific variant that shortens the lifespan of red blood capsules reduces HbA1c concentration [ 126 ].
Diabetic cardiomyopathy is mainly linked to a shift to exclusive FAs as an energetic substrate for CMCs, instead of the usual sources (amino acids, carbohydrates, FAs, ketones, and lactate), due to AMPK at an early stage and then NR1c1 (PPARα) [ 127 ]. 33 On the other hand, endotheliocytes use preferentially glucose (∼85%) for ATP synthesis, the faster rate of glycolysis compensating for the greater amounts of ATP per mole of glucose yielded by mitochondrial oxidative phosphorylation and sparing oxygen for CMCs [ 127 ]. However, diabetic endotheliocytes have an aberrant metabolism. Production of GluT1 is not sensitive to hyperglycemia, and glucose egress to the CMC is not adequate. Moreover, high intracellular glucose concentration creates ROS and prevents glycolysis, glycolytic intermediates accumulating and being processed by the polyol, hexosamine, and methylglyoxal pathways, which form ROS and RNS and AGEs.
Arrhythmogenic cardiomyopathy is mainly caused by mutations in genes encoding desmosomal elements. It is characterized by progressive fibroadipose replacement of the myocardium, arrhythmias, and sudden death. Cardiac mesenchymal stromal cells have a lower expression of plakophilin, contain more lipid droplets, and differentiate into adipocytes, contributing to the adipogenic substitution in arrhythmogenic cardiomyopathy.
Arrhythmogenic atrial fibrosis characterized by excess extracellular matrix deposition and fibroblast proliferation and differentiation into collagen-secreting myofibroblasts favors atrial fibrillation (AF), the most common persistent arrhythmia. This cardiac rhythm disorder is the sixth and eighth leading cause of CVD-related mortality and disability among other CVD causes, respectively, the highest prevalence being observed in North America and lowest in the Asia-Pacific region [ 121 ]. Excess collagen can disrupt atriomyocyte bundle continuity, lessen intercellular coupling, and engender longitudinal anisotropy. Moreover, fibroblasts and myofibroblasts are electrochemically connected to CMCs, thereby modulating their electrical activity and promoting re-entry [ 128 ]. Persistent AF is maintained by re-entrant drivers (or rotors) related to extensive atrial remodeling, slowing action potential propagation, reducing cell excitability, and causing unidirectional block [ 129 ]. These rotors are confined in regions characterized with high fibrosis density.
Cardiac Wall Remodeling
Cardiac walls remodel after pressure and volume overload or myocardial injury. This can result in heart failure.
Heart failure is associated with impaired signaling and pathological cardiac (or ventricular) wall remodeling (Vol. 7, Chap. 3. Adverse Cardiac Remodeling). Maladaptive cardiac remodeling is characterized by structural changes in dimensions, mass, and shape and metabolic remodeling with functional alterations due to molecular, cellular, and interstitial changes in response to abnormal hemodynamic load and/or damage linked to neurohormonal activation.
Congestive heart failure is marked by atrial and ventricular wall enlargement and reduced cardiac contractility and adrenergic responsiveness. The sympathetic nervous system and renin–angiotensin–aldosterone axis are activated to compensate for reduced cardiac output but further favor heart failure progression via maladaptive wall remodeling.
Cardiac modifications comprise cell death, redox stress, inflammation, hypertrophy and/or atrophy, fibrosis, and occurrence of arrhythmias. In particular, cardiac fibrosis causes electrical and mechanical dysfunction.
Ion carriers (channels, pumps, and transporters), such as plasmalemmal (sarcolemmal) Na V 1.5 and Ca V 1.2 channels, Na + –Ca 2+ and Na + –H + exchangers, K ATP channel, sarco(endo)plasmic reticulum ryanodine-sensitive Ca 2+ channel, and SERCA pump, in addition to their regulators, in particular kinases and phosphatases, are implicated in heart failure [ 130 ]. In heart failure, regulation of intracellular sodium and activity of K + channels and Ca 2+ cycling are defective.

Cardiac Wall Hypertrophy
Adverse left ventricular and arterial and arteriolar wall hypertrophy, along with associated stiffness, results from sustained hypertension (Vol. 7, Chap. 3. “Adverse Cardiac Remodeling”). However, hypertension-induced arterial wall hypertrophy of large- and medium-caliber arteries is not necessarily associated with a decreased arterial distensibility [ 131 ]. On the other hand, aging alters distensibility independently of blood pressure.
Na + –K + ATPase (Na + pump) is a plasmalemmal αβ dimer [ 132 ]. The catalytic ouabain-resistant α1 isoform is expressed in all cell types; most cells produce a second α isoform (ouabain-sensitive α2–α3, α4 being detected in the sperm). The catalytic α subunit contains the Na + , K + , ATP, and cardiotonic steroid-binding sites. Sodium ATPase β subunit exists in three isoforms (β1–β3) that support catalytic activity of chaperoned α subunit. β1 Subunit is the most important isoform in cardiac and vascular smooth muscle cells, where it forms both α1β1 and α2β1 protomers. 34 Arterial smooth myocytes also manufacture α2 isoform, which localizes to endoplasmic reticulum–plasma membrane contact sites, the so-called plasmerosomes, and controls myogenic tone. On the other hand, α1 subunit is more uniformly distributed.
Sodium pumps are regulated by multiple factors, such as hormones (e.g., aldosterone, insulin, and catecholamines) and protein phosphorylation [ 132 ]. The cardiotonic steroids, ouabain, digoxin, and bufalin, block cation transport by Na + pump.
Both Na + and K + affinities are modulated by the transmembrane regulator phospholemman (Plm) encoded by the FXYD1 gene (FXYD domain-containing ion transport regulator-1), which also regulates activity of Na + –Ca 2+ exchanger NCX1 [ 132 ]. Unphosphorylated Plm binds to the α2β dimer and reduces affinity of α2 subunit for intracellular Na + and extracellular K + ion. Phosphorylation of cardiac and arterial Plm by PKA or PKC relieves Na + ATPase inhibition and restores high Na + affinity.
Hence, in arterial smooth myocytes, Na + pump α2 subunit is structurally and functionally linked to NCX1. This crosstalk may be influenced by other adjacent channels, pumps, and transporters, such as TRPC6 and serca2 [ 132 ].
Activation of the renin–angiotensin–aldosterone axis stimulates ROS generation, causing glutathionation of β1 subunit and Na + pump inhibition. On the other hand, Plm promotes Na + pump deglutathionation and protects against oxidation (inhibition) of Na + pump in arteries and the heart [ 132 ].
Reduced expression of smooth muscle-specific Na + pump α2-subunit elevates blood pressure and sensitivity to angiotensin-2 and dietary salt, whereas its overexpression lowers basal BP and Agt2 and NaCl sensitivity [ 132 ]. Chronic salt retention augments endogenous ouabain-like compound (EOLC), a cardio- and vasotonic steroid synthesized and secreted by the adrenal cortex and Na + pump inhibitor, thereby causing salt-dependent hypertension mediated by Na + –Ca 2+ exchanger.
Ouabain triggers signaling that relies on various effectors, such as ERK1, ERK2, PI3K c1 α , PKB, and Src, in addition to NFκB [ 132 ].
In addition, another cardiotonic steroid, marinobufagenin, can be detected in human plasma and urine [ 132 ]. Prolonged exposure to ouabain or marinobufagenin causes hypertension in normal rats (but neither digoxin nor digitoxin).
Sodium ion and water retention raises blood volume and subsequently plasmatic EOLC concentration, thereby inhibiting Na + pump. Resulting elevated cytosolic Na + concentration elevates cytosolic Ca 2+ concentration due to Ca 2+ entry through NCX, hence increasing myogenic tone and total peripheral systemic vascular resistance to blood flow.
Transaortic constriction-induced hypertrophy in mice is impeded by immunoneutralizing circulating endogenous ouabain [ 133 ]. Endogenous ouabain and its receptor, Na + pump α2-subunit, are involved in hypertension-induced cardiac hypertrophy.
In many forms of hypertension, the brain RAAA is activated via circumventricular organs such as the subfornical organ, increasing arterial sympathetic nerve activity by the central nervous system and α-adrenoceptor-mediated arterial constriction [ 132 ]. The hypothalamic component of this neurohumoral pathway involves local aldosterone production, mineralocorticoid receptor, ENaCs, local endogenous ouabain release, and Na + pump.
The cardioprotective deacetylase sirtuin-2 operates via STK11 (LKb1) and AMPK in aging-related and angiotensin-2-induced adverse cardiac hypertrophy [ 134 ]. Sirtuin-2 deacetylates STK11 (Lys48), thereby eliciting STK11 phosphorylation and subsequently launching the STK11–AMPK axis. In Sirt2 −∕− aged (24-month-old) mice and Agt2-treated mice, cardiac hypertrophy and fibrosis are magnified. Conversely, cardiac-specific SIRT2 overexpression protects against Agt2-primed cardiac hypertrophy and fibrosis and rescues cardiac function.
Cardiac Wall Fibrosis
Fibrosis is a complication of chronic inflammatory diseases. Initiation of fibrogenesis involves activation of monocytes and differentiation into profibrotic macrophages. On the other hand, TGFβ provokes proliferation of myofibroblasts.
Fibrosis is assessed by its regulators and markers MMP1–MMP3 and MMP7–MMP28 and TIMP1–TIMP4. In particular, TIMP1 inhibits MMP9 [ 135 ]. TIMP1 can be a strong predictor of death from CVD, at least in some populations, such as Iceland.
Fibroblasts transdifferentiate into activated myofibroblasts, which synthesize α-smooth muscle actin (Actα2) and secrete matrix constituents such as type- I α1-procollagen (encoded by the COL1A1 gene). Persistent myofibroblast activation distinguishes pathological fibrosis from wound healing. Myofibroblasts integrate a feedback loop that perpetuates fibrosis and extracellular matrix stiffening. Fibroblast-to-myofibroblast differentiation driven by matrix stiffness provokes mitochondrial priming in activated myofibroblasts (but not in quiescent fibroblasts). Activity of proapoptotic proteins such as BCL2L11 thus increases in myofibroblasts that become particularly susceptible to apoptosis; these agents can reverse fibrosis [ 136 ]. On the other hand, myofibroblasts depend on antiapoptotic proteins such as BCL2L1 to prevent their death.
Cardiac fibrosis is characterized by an uncontrolled accumulation of extracellular matrix by cardiofibroblasts in the interstitial and perivascular spaces.
Transcription of typical fibrosis genes, such as Comp and NOX4, which encode cartilage oligomeric matrix protein and NADPH oxidase subtype NOx4, respectively, is upregulated.
Hepatic fibrosis is characterized by the accumulation of matrix proteins, mainly fibrillar collagen-1, which confers mechanical stability. Cartilage oligomeric matrix protein (COMP), 35 or thrombospondin-5, provokes collagen-1 formation via ScaRb3 and MAP2K1/2–ERK1/2 pathway, in addition to its deposition. Also, COMP supports matrix metallopeptidases MMP2, MMP9, and MMP13, but does not prevent collagen-1 cleavage by MMP1 [ 137 ].
Cartilage oligomeric matrix protein binds with high affinity to collagen-1 and to collagen-12 at the surface of collagen-1 fibrils [ 138 ]. In fact, it tethers to the fibril-forming collagens Col1 and Col2, the nonfibrillar fibril-associated collagens with interrupted triple helices (FACIT) collagens (Col9, Col12, and Col14), along with other types of matrix proteins, such as fibronectin and matrilins, and proteoglycans. It also assists secretion of collagens [ 138 ]. Therefore, in the extracellular matrix, COMP helps the organization of a collagen fibril meshwork that yields the organ rheology, whereas within the cell, COMP enables efficient secretion of collagens into the extracellular space.
This fibrillar collagen assembly regulator is implicated in fibrosis in various organs and can thus serve as a fibrosis marker [ 139 , 140 ]. Cartilage oligomeric matrix protein is indeed synthesized in fibrotic regions, where it colocalizes with vimentin around SMAD3+ cells. Stimulation of fibroblasts with TGFβ1 increases COMP production.
Reactive oxygen species produced by NADPH oxidases regulate cell differentiation. The isozyme NOx4 is implicated in cardiac and pulmonary myofibroblast differentiation. For example, in idiopathic pulmonary fibrosis, NOx4 expression rises in fibrogenic lung fibroblasts, which contain high concentrations of the hyaluronan receptor, epican variant containing exon 6 (CD44v6), thereby mediating TGFβ1-induced fibroblast differentiation into myofibroblasts [ 141 ]. Synthesis of hyaluronan and epican is augmented in numerous fibrotic organs. The TGFβ1–CD44v6 pathway is implicated in collagen-1 and Actα synthesis in pulmonary myofibroblasts [ 142 ]. It raises early growth response EGR1 formation. Production of CD44v6 is triggered by TGFβ1 via EGR1 and activator protein AP1. The ERK–EGR1 axis promotes CD44v6 splicing. Conversely, CD44v6 sustains ERK signaling, which supports AP1 activity in pulmonary fibroblasts. Hyaluronan produced by hyaluronan synthase HAS2 is required for colocalization of CD44v6 and Tβ R1 and subsequent TGFβ1–CD44v6–ERK1–EGR1 signaling, which constitutes a positive feedback loop that links TGFβ1 to the myofibroblast phenotype [ 142 ].
Transforming growth factor (TGFβ1), a major profibrotic factor, upregulates synthesis of IL11, which serves as its profibrotic effector. Interleukin-11 produced by activated fibroblasts does indeed cause cardiac fibrosis [ 143 ]. Its receptor IL11Rα is expressed at its highest concentration in fibroblasts. In these cells, the IL11–IL11Rα couple launches alternative ERK-dependent autocrine signaling used in fibrogenic protein synthesis. Production of IL11 is also upregulated in fibroblasts from patients with idiopathic pulmonary fibrosis (100-fold).
After an acute myocardial injury, cardiofibroblasts release proinflammatory cytokines that trigger their proliferation (feedforward loop) and differentiation into myofibroblasts, which secrete high amounts of proinflammatory and fibrotic agents and matrix constituents. Adaptive collagen-based fibrotic scarring preserves myocardial structure, but prolonged activation of cardiofibroblasts causes fibrosis (Vol. 10, Chap. 3. Adverse Wall Remodeling).
Fibroblasts extend filopodia into the T-tubular lumen. Heterotrimeric collagen-6 (Col6α1–Col6α2–Col6α3 with other possible chains homologous to Col6α3 [Col6α4–Col6α6]) tetramerizes and, once it is secreted, forms microfibrils. Into T-tubules, collagen colocalizes with the dystrophin complex, which links the extracellular matrix to actin microfilaments and microtubules of the cytoskeleton, and transmits stress and strain between these two compartments [ 144 ]. Dystrophin localizes to the T-tubule periphery and serves as a mechanosensor at the Z disc. Deposition of fibrillar Col1 and Col3 stiffen, T-tubule membranes, whereas nonfibrillar Col4 and Col6 may anchor fibrillar collagens to the basement membrane of CMCs [ 145 ].
The endothelium-controlled paracrine couple constituted by neuregulin-1 and receptor protein Tyr kinase human epidermal growth factor receptor (HER) modulates cardiac performance and adaptation [ 146 ]. Neuregulin-1 operates on cardiofibroblasts and has an antifibrotic effect in the left ventricle. It attenuates myocardial hypertrophy and fibrosis in a mouse model of angiotensin-2-induced myocardial remodeling in addition to pulmonary fibrosis. Moreover, the Nrg1–HER axis also regulates the function of macrophages. Neuregulin-1 at least partly inhibits macrophages, alleviates myocardial macrophage infiltration and cytokine expression, and improves ventricular stiffness. On the other hand, in mice with myeloid cell-specific deletion of the Her4 gene, myocardial fibrosis in response to Agt2 increases. Neuregulin-1 activates HER4 on macrophages and inhibits the PI3K–PKB pathway in addition to STAT3, lessening inflammatory cytokine release.
Myofibroblasts, which are derived from the differentiation of fibroblasts, fibrocytes, and epitheliocytes, are the principal effectors of fibrosis. Establishment and maintenance of myofibroblasts rely on TGFβ1-primed promotion of a hyaluronan-rich pericellular matrix, the hyaluronan coat [ 147 ].
The heparan sulfate proteoglycan epican (CD44) is a receptor for the extracellular matrix constituent hyaluronan, which mediates cell–cell and cell–matrix interactions. It is encoded by the Cd44 gene, which consists of 19 exons. Its other ligands include collagens, osteopontin (or secreted phosphoprotein SPP1), soluble galactoside-binding lectin LGalS9, and matrix metallopeptidases. Hyaluronan has various isoforms due to a variable pattern of N- and O-linked glycosylation and the existence of multiple splice variants. Exons 1 to 5, 15 to 17, and 19, which encode the extracellular N-terminus, transmembrane domain, and the cytoplasmic region, are present in all alternatively spliced Cd44 mRNA species [ 147 ]. The presence of exons 6 to 14 varies between isoforms. Exon 18 is removed before translation in most isoforms owing to an early stop codon. In mice, exons v4 to v6 in splice variants (CD44v4, CD44v5, and CD44v6) facilitate migration of Langerhans cells (dendrocytes of the skin and mucosa) to lymph nodes [ 148 ]. In rats, exons v3 and v6 are involved in FGF-mediated mesenchymal cell proliferation during limb bud development. The standard epican isoform enhances myofibroblast differentiation, thereby favoring fibrosis [ 147 ]. On the other hand, its alternatively spliced isoform containing variant exons v7–v8, CD44v7v8, prevents myofibroblast differentiation.
Hyaluronan is degraded by hyaluronoglucosaminidases or hyaluronidases, encoded by the HYAL1 to HYAL4 genes, Hyal1 and Hyal2 being the most abundant species. Hyaluronidase-2 supports CD44v7/8 production [ 147 ]. Hyaluronidase-2 lodges in lysosomes, the acidic milieu being optimal for Hyal activity. However, Hyal2 is also a plasma membrane-anchored protein with weak enzymatic activity. Hyaluronidase-2 can be enzymatically inactive. It plays a non-enzymatic role, as it participates in regulating epican splicing, promoting CD44v7v8 production.
On the other hand, when pulmonary fibroblasts are stimulated by BMP7, which prevents or reverses differentiation of cells into myofibroblasts, Hyal2 translocates to the nucleus, where it displaces components of the splicing machinery from the spliceosome, enabling Hyal2, the spliceosomal components U1 and U2 small nuclear ribonucleoproteins, and Cd44 pre-mRNA to complex, whereas arginine- and serine-rich (RS) proteins, which mediate exon exclusion, promote profibrotic standard CD44 synthesis. Both SRSF2 and SRSF5 control Cd44 pre-mRNA splicing relevant to fibrosis. 36 Splicing regulators, argonaute-mediated histone modifications, KHDRBS1, 37 and RS-rich splicing factor SFRS10 regulate Cd44 splicing [ 147 ]. Hyal2 facilitates the inclusion of Cd44 exons 11 and 12, which support expression of the antifibrotic CD44v7v8 isoform at the cell surface [ 147 ].
Cardiomyocyte Remodeling
Markers of cardiac remodeling have either an increased expression, such as α-myosin heavy chain isoform (MyH6), GluT1, α-actin (ActC1), natriuretic peptide, galectin, caveolin, nitric oxide synthase (NOS1), angiotensin convertase or decreased production, such as β-MHC (MyH7), GluT4, and serca2a [ 149 ].
Energy Metabolism
Cardiac energetics is impaired because of mitochondrial dysfunction in addition to calcium handling, disturbing myocardial contractility.
In the heart, the rates of ATP production and turnover are very high owing to contraction–relaxation cycles. Under normoxia, more than 95% of ATP generated in the heart is created by oxidative phosphorylation in mitochondria and the remaining mainly from glycolysis and, to a lesser extent, from the tricarboxylic acid cycle (TCAC; also named citric acid and Krebs cycle) [ 150 ]. Approximately 70–90% of cardiac ATP is produced by fatty acid oxidation and the remaining from the oxidation of glucose and lactate, small amounts deriving from ketone bodies and certain types of amino acids. About two-thirds of the ATP generated is used by the sarcomere and the remaining by ion pumps such as endoplasmic reticulum Ca 2+ ATPase (SERCA), which determines lusitropy.
Substrates are transported across the plasma membrane into the cytosol, where they are metabolized. In oxidative pathways, the metabolic intermediates, such as pyruvate or acylCoA from glycolysis and β-oxidation, are transported across the inner mitochondrial membrane by specific carriers. Inside the mitochondrial matrix, these substrates are oxidized or carboxylated (anaplerosis) and enter the TCAC, thereby generating reducing equivalents, such as FADH 2 and NADH, which are used by the ETC to generate a proton gradient, which, in turn, is used for ATP production. The energy generated is immediately used or stored in the form of phosphocreatine.
Metabolic intermediates regulate many pathways in addition to ATP production, serving as messengers (Table 1.8 ).
Metabolic intermediates regulators (Source: [ 150 ]; AMPK AMP-activated protein kinase, BCAA branched-chain amino acids, CoA coenzyme-A, ER endoplasmic reticulum, PGC peroxisome proliferator-activated receptor PPATγ coactivator, PKC protein kinase-C, PP protein phosphatase, ROS reactive oxygen species, TOR target of rapamycin)
O-GlcNAcylation is the O-linked attachment of monosaccharide β N acetylglucosamine ( O Glc N Ac )
The myocardial energy pool includes ATP and phosphocreatine (PCr), the latter being an ATP transporter and buffer. In the mitochondrion, the high-energy phosphate bond in ATP can be transferred to creatine by creatine kinase to form PCr, which can easily diffuse through the mitochondrial membrane into the cytosol, where it can generate ATP from ADP using cytosolic creatine kinase [ 150 ].
Glucose metabolism comprises glycolysis and accessory pathways, that is, glycogen synthesis and pentose phosphate (PPP) and hexosamine synthetic pathway (HSP). The PPP, which relies on glucose 6-phosphate dehydrogenase (G6PDH), is an NADPH source used in lipid synthesis and anaplerosis (i.e., replenishment of the TCAC intermediate pool through pathways independent of acetylCoA, as these intermediates are constantly removed from the TCAC for synthesis of amino and nucleic acids and thus need to be replaced), in addition to redox stress. The hexosamine synthetic pathway (HSP), which forms UDP N acetylglucosamine (GlcNAc), a monosaccharide donor for the O-GlcNAcylation of proteins, requires glucose together with acetylCoA and glutamine. These accessory pathways can play a greater role in heart disease genesis.
Fatty acid oxidation is impaired in cardiac hypertrophy and failure, leading to reduced ATP production. Glucose oxidation can remain unchanged in compensated hypertrophy but can decrease in heart failure [ 150 ]. Non-ATP-generating pathways of glucose metabolism (HSP, PPP, and anaplerosis) are boosted. Metabolic remodeling in HF is characterized by a declined energy production linked to progressive impaired substrate use and mitochondrial genesis and function.
Ion Carriers
Cardiomyocytic T tubules contribute to regulating ion fluxes. Bridging integrator BIn1 (or amphiphysin Amph2) is a T-tubule protein residing in the inner membrane folds that is linked to calcium motion. The cardiac-specific splice variant BIn1v13v17 (including exons 3 and 17) promotes actin polymerization. It then generates and stabilizes dense T-tubule membrane folds that create a diffusion barrier to extracellular ions [ 151 ]. Its expression is downregulated in heart failure.
Cardiofibroblasts influence myocardial function by their chemical, electrical, and mechanical interactions with CMCs. Multiple ion channels regulate their fate and activity (e.g., Ca V 1, Ca V 3, BK, SOCE, TRPA1, TRPC1, TRPC6, TRPM7, Na V 1.5, K V 4.3, K IR 2.1, and volume-sensitive [Cl vol ] and Ca 2+ -gated Cl − channel [Cl Ca or anoctamin-1]) [ 152 ]. They participate in myofibroblast differentiation.
Defective ion handling by Ca 2+ , K + , and Na + channels, pumps, and transporters in addition to connexins and nonselective channels causes cardiac arrhythmias.
Defective Calcium Handling
In the membrane of the endoplasmic (sarcoplasmic) reticulum, ryanodine-sensitive Ca 2+ channel and SERCA pump enable Ca 2+ release from and reuptake within this organelle. Released Ca 2+ binds to the actin-connected troponin-C and allows actin–myosin interaction.
Homotetrameric ryanodine receptor at junctions between the endoplasmic reticulum and transverse tubule is an essential component of excitation–contraction coupling via Ca 2+ -induced Ca 2+ release (CICR). 38 It is linked to regulators, such as FK506-binding protein FKBP1b, a member of the immunophilin family of cis-trans peptidyl prolyl isomerases, cAMP-dependent protein kinase PKA and its anchoring protein, AKAP6, and protein phosphatases, PP1 and PP2 [ 130 ]. Muscle-selective AKAP6 coordinates a cAMP-sensitive negative feedback loop that comprises PKA and the cAMP-selective phosphodiesterase PDE4d3, PKA phosphorylating PDE4D3 and increasing its affinity for AKAP6, enhancing recruitment of PDE4D3 and hence faster signal termination [ 155 ].
Upon depletion of ER Ca 2+ content and arrest of Ca V 1.2 gating, that is, at the end of the systole, diastole begins, RyRs are inactivated and Ca 2+ is pumped back into the ER by serca2a regulated by phospholamban and out of the cell by sarcolemmal NCX, which governs lusitropy.
Stimulation by β-adrenoceptor increases inotropy. Calcium flux regulators are phosphorylated (activated) by PKA and CamK2, both targeting Ca V 1.2 and RyR in addition to phospholamban, the latter facilitating the process.
Failing ventriculomyocytes have an impaired contractility. The Ca 2+ transient amplitude lessens, excitation–contraction coupling declines, and the rate of diastolic Ca 2+ transient decay slows down. The SR Ca 2+ content drops, serca2a activity is diminishing, and Ca 2+ extrusion is caused by NCX rising. Neurohormonal stimulation causes RyR hyperphosphorylation by PKA and RyR dephosphorylation decays due to defective association of PP1 and PP2 and presence of PDE4d3 in the RyR complex [ 130 ]. In addition, increased RyR2 phosphorylation (Ser2808) favors its dissociation from its regulator FKBP1b, which increases Ca 2+ sensitivity and reduced RyR closing, and hence diastolic ER Ca 2+ leak.
Dephosphorylation of phospholamban by PP1 inhibits serca2a; this inhibition is relieved upon its phosphorylation by PKA (Ser16) and CamK2 (Thr17). In heart failure, expression of both serca2a and Pln is altered [ 130 ]. In addition, Pln phosphorylation is reduced, repressing serca2a activity.
Altered Sodium Control
In heart failure, intracellular Na + concentration rises, in particular because of the late Na + influx, a fraction of Na V 1.5 channels failing to enter an inactivated state [ 130 ].
Cardiac-specific sodium–hydrogen exchanger SLC9a1 (NHE1) electroneutrally exchanges intracellular H + for extracellular Na + to regulate intracellular H + and intracellular Na + concentrations, the inward gradient produced by the Na + –K + ATPase providing a driving force for SLC9a1-mediated H + extrusion and Na + influx [ 130 ]. Its activity increases upon exposure to ROS, intracellular acidosis, angiotensin-2, endothelin, and α1-adrenoceptor. Increased SLC9a1 activity causes Ca 2+ overload through Na + –Ca 2+ exchanger.
The Na + –K + ATPase 39 actively transports Na + out and K + into the CMC. Phospholemman regulates the function of this enzyme. It is also the receptor of cardiac glycosides (e.g., digoxin and ouabain) and exerts a positive inotropic effect, as they inhibit pump activity, thereby decreasing the driving force for Na + –Ca 2+ exchange and increasing cellular content and release of Ca 2+ during depolarization [ 156 ].
Impaired Potassium Control
The transient outward current ( i K,to ) through K V 4.2 and K V 4.3 is involved in early repolarization. It decays in heart failure, extending action potential duration [ 130 ].
Mitochondrial K ATP channel (K IR 6.2) serves as a metabolic sensor, adjusting membrane excitability to match cellular energetic demand. It opens in response to ischemia, physical exercise, and stress hormone exposure, shortening the action potential. It can protect the heart against hypertension.
Transverse Tubules
In heart failure, loss and defects of transverse tubules (T-tubules), that is, adverse reorganization of the T-tubular structure (e.g., dilation of the tubular lumen and the occurrence of sheet-like structures), affect Ca 2+ signaling [ 145 ]. In ventriculomyocytes, excitation–contraction coupling depends on these deep invaginations of the plasma membrane at Z-line levels, where apposed cellular structures and proteic complexes reside, aimed at synchronizing Ca 2+ release from the endoplasmic reticulum and hence contraction. Disrupted Ca 2+ release reduces contractility in heart failure. Enlargement of the T-tubular lumen augments the diffusion space of extracellular ions, in particular Ca 2+ and K + , thereby favoring arrhythmia. In addition, loss of the T-tubular anchor junctophilin-2 decreases T-tubule density. Moreover, several collagen isoforms (Col1, Col3–Col4, and Col6) are involved in T-tubule expansion, whereas modest amounts of collagen normally exist within the interior of T-tubules [ 144 ].
Mitochondrion
Integral outer mitochondrial membrane FUN14 domain-containing protein FunDC1 provokes hypoxia-induced mitophagy. It interacts with kinesin light chain KLC1 (but with neither the motor subunit of kinesin-1 KIF5b nor the motor subunit of kinesin-2 KIF3a) [ 158 ]. In addition, FunDC1 binds to endoplasmic reticulum-resident inositol trisphosphate receptor IP 3 R2 and localizes to mitochondrion-associated endoplasmic reticulum membranes, which participate in apoptosis and autophagy, hence promoting communication between mitochondria and the endoplasmic reticulum, modulating Ca 2+ release, and maintaining MAERMs and mitochondrial morphology and function [ 159 ]. Overexpression of FunDC1 increases mitochondrial concentrations of IP 3 R2 and Ca 2+ ion. Ablation of the FUNDC1 gene reduces intracellular Ca 2+ concentration and suppresses formation of mitochondrial fission protein Fis1 and hence mitochondrial fission, as it impedes the binding of CREB to the Fis1 promoter. The FunDC1–CREB–Fis1 axis is repressed in patients with heart failure.
Altered Signaling
In normal conditions, CMCs and endotheliocytes interfere and mutually control their metabolism.
Proper functioning of the cardiovascular system relies at least partly on interactions between CMCs and endotheliocytes of the cardiac capillaries and endocardium, dysregulated communication between these two cell types being implicated in the development of cardiac structural and functional anomalies and disturbed endothelium-related signaling based on NO and neuregulin being involved in heart failure [ 160 ].
Endothelial cardioactive factors encompass angiopoietins, angiotensin-2, apelin, dickkopf-3, endothelin-1, follistatin, neuregulin-1, NO, periostin, prostaglandins such as prostacyclin, thrombospondin-1, connective tissue, fibroblast, vascular endothelial growth factor, and endothelial microRNAs (Table 1.9 ) [ 160 ]. They operate briefly or have a sustained action, and they can cooperate.
Endothelial modulators of CMC activity (Source: [ 160 ]; cGMP cyclic guanosine monophosphate, CTGF connective tissue growth factor, Dkk dickkopf, ET endothelin, Fst follistatin, FstL follistatin-like protein, HER human epidermal growth factor receptor, miR microRNA, Nrg neuregulin, NO nitric oxide, PGi 2 prostacyclin, PtgIR prostacyclin receptor, sGC soluble guanylate cyclase, TGF transforming growth factor, Tsp thrombospondin)
Nitric oxide and natriuretic peptides launch the synthesis of cyclic guanosine monophosphate using different effectors, sGC and particulate guanylate cyclase (pGC), respectively, and spatially distinct pools, sGC and pGC lodging in the cytosol and cortex, and hence different responses. Among phosphodiesterases hydrolyzing cGMP, PDE2 limits the subsarcolemmal cGMP pool and PDE5 the cytosolic cGMP pool [ 160 ]. Whereas cGMP produced by pGC and sGC has a positive lusitropic effect, cGMP produced by sGC blunts myocardial response to β-adrenoceptor.
At low NO concentrations, the NO–sGC–cGMP axis can have a positive inotropic effect via activation of PKG and PKA, which increases Ca 2+ concentration [ 160 ]. Higher NO amounts have a negative inotropic effect due to the blockage of sarcolemmal Ca 2+ channels and reduction in the sensitivity of troponin-C to Ca 2+ ion. Moreover, NO has a positive lusitropic effect. Phosphorylation of troponin-I reduces sarcomeric sensitivity to Ca 2+ and promotes cross-bridge detachment. Phosphorylation of titin by PKA and/or PKG also improves lusitropy. Furthermore, NO provokes vasodilation and hence reduces afterload.
The chronotropic effect of NO depends on its site of action, being positive upon stimulation by cGMP of a hyperpolarization-activated pacemaker current and negative at the postsynaptic level [ 160 ].
Nitric oxide is synthesized by nitric oxide synthases (NOSs), constitutive NOS1 and NOS3 binding their cofactors (FAD, FMN, and BH 4 ), dimerizing, and being stimulated by Ca 2+ –calmodulin (Table 1.10 ) [ 161 ]. NOS3 also requires proper localization to caveolae using HSP90 and caveolin and phosphorylation. In addition to constitutive NOS1 and NOS3 and inducible NOS2, constitutively active Mt NOS localizes to the inner mitochondrial membrane, where it participates in modulating the transmembrane potential.
Features of NOS isozymes (Source: [ 161 ])
Nitric oxide mediates parasympathetic endothelium-dependent vasodilation in the vasculature in addition to parasympathetic control of cardiac function, guanylate cyclase supporting muscarinic agonists on the cardiac frequency, atrioventricular conduction, and myocardial contractility.
Endotheliocytes secrete nitric oxide, which not only relaxes vascular smooth myocytes and prevents platelet aggregation, leukocyte–endotheliocyte adhesion, and vascular smooth myocyte proliferation but also influences CMC contractility via β-adrenergic and muscarinic acetylcholine receptors and control cardiac substrate utilization, NOS3 concentration being much higher in endotheliocytes than CMCs [ 127 ]. 40
The chronotropic and inotropic response to β-adrenergic and muscarinic agonists is preserved in isolated cardiac tissue preparations from Nos3 −∕− mice in addition to β-adrenergic stimulation and muscarinic inhibition of Ca V 1.2a current [ 163 ]. However, NO formed in CMCs attenuates inotropic and lusitropic response to stimulation in addition to basal conditions [ 161 ]. In CMCs, NOS3 links to caveolin-3 at the plasma membrane, where it can interact with Ca V 1.2a and β AR, thereby blunting inotropic response to isoproterenol stimulation. On the other hand, NO produced by NOS1 at the CMC endoplasmic reticulum nitrosylates (activates) the ryanodine receptor [ 161 ]. In addition, NOS1 associated with NOS1-activating protein (NOS1AP) regulates cardiac frequency.
In young Nos3 −∕− and Nos3 +∕+ mice, cardiac contractibility does not differ [ 164 ]. However, CMCs from old Nos3 −∕− mice exhibit a reduced inotropic response to isoproterenol with respect to age-matched Nos3 +∕+ mice. On the other hand, CMCs of Nos1 −∕− mice display a greater contraction and slower relaxation. Therefore, constitutive NOS3 in murine ventriculomyocytes does not markedly affect the muscarinic-mediated inhibition of β-adrenergic signaling and controls neither basal nor β-adrenoceptor stimulated CMC contraction. The myocardial constitutive NOS1 isozyme is responsible for the NO-mediated autocrine regulation of myocardial inotropy and lusitropy [ 164 ].
In addition, NO contributes to the metabolism regulation. It inhibits the ETC complex- I , - II , and - IV of the mitochondrial electron transport chain [ 165 ]. Acute NOS inhibition reversibly affects cardiac substrate utilization. Cardiac uptake of lactate and glucose increases whereas that of free fatty acids decreases owing to a shift to carbohydrate oxidation, acute administration of a NO donor canceling cardiac metabolic changes [ 165 ]. Hence, NO hinders glucose uptake and supports free fatty acid consumption.
Neuregulin-1, a member of the EGF superfamily, 41 operates in the cardiovascular apparatus genesis and in the postnatal heart to regulate cardiac adaptation to stress. Nrg1 is released by the endocardial and microvascular endothelia. It binds to the receptor protein Tyr kinases HER3 and HER4 receptors, which are expressed in ventriculomyocytes [ 166 ], HER4 being the most important in the heart [ 160 ]. Nrg1 activates ERK1 and ERK2 (sarcomeric organization and protein synthesis), the Src–FAK couple (focal adhesion formation), NOS (cardiac function), and the PI3K–PKB axis (CMC survival), thereby attenuating adrenergic stimulation and hence its positive inotropic effect and enhancing lusitropy [ 160 ]. The Nrg1–HER couple also influences myocardial metabolism, provoking glucose uptake via PI3K by CMCs, and excess saturated fatty acid exposure causing Nrg resistance [ 127 , 166 ].
In response to hyperglycemia and subsequent notch activation, ECs secrete inactive latent and lysosomal-stored active forms of heparanase using ATP, both heparanase forms liberating VEGFa and VEGFb bound to heparan sulfate proteoglycans (HSPG) of the CMC surface, which represent a rapidly accessible auxiliary reservoir, to facilitate fatty acid transfer by FABP4 (Sect. 10.1007/978-3-319-89315-0_2#Sec50 ) 42 and FATPs 43 in addition to angiogenesis [ 127 ]. On the other hand, angiogenesis is impeded the hexosamine synthesis pathway. Heparanase also interacts with LPL (or lipase-D).
Reciprocally, CMCs produce the majority of LPL, which matures owing to the lipase maturation factor LMF1 and is subsequently secreted owing to AMPK and P38MAPK that phosphorylates HSP25 [ 127 ]. Afterward, LPL momentarily attaches to syndecan-1 at the CMC surface and is then detached by heparinase, transported to the luminal endothelial surface, where it tethers to HSPGs and GPIHBP1, 44 and metabolizes the triglyceride core of lipoproteins to FAs, which are transferred to CMCs [ 127 ].
Activity of FoxO increases upon insulinemia decrease. Increased activity of cardiomyocytic FoxO1 augments plasmalemmal ScaRb3 concentration via actin cytoskeleton rearrangement[ 127 ]. Endothelial FoxO1 also restricts vascular expansion.
Chronic heart failure is associated with altered β-adrenoceptor signaling and subsequent reduced cAMP formation. Long-term sympathetic stimulation desensitizes β-adrenoceptors, reduces expression of β1AR, and upregulates that of inhibitory G-protein-coupled receptor kinases (GRKs). In addition, expression of the Gi subunit increases up to about 30% in end-stage heart failure (ESHF), shifting Gs-primed adenylate cyclase stimulation to Gi-mediated inhibition of AC via β2AR [ 171 ].
Reduced ventriculomyocytic cAMP concentration and the subsequent fall in PKA activity, coupled with augmented phosphatase activity, lower the phosphorylation of key cardiac Ca 2+ -handling proteins and subsequently Ca 2+ transient amplitude and CMC contraction efficiency (negative inotropic effect).
Among GRKs, GRK5 abounds in the myocardium; its synthesis is upregulated in heart failure [ 172 ]. This regulator of cardiac GPCRs has alternative activity in the nucleus after stress, particularly during adverse hypertrophy. On the other hand, IGF1, a mediator of adaptive cardiac hypertrophy does not induce GRK5 nuclear translocation in CMCs.
Nucleoside diphosphate kinases (NDPKs) abound at the plasma membrane of CMCs in ESHF patients. Group- I NDPKs (NDPKa–NDPKd) are enzymes. NDPKb, but not NDPKa, complexes with the Gβγ dimer and can activate cardiac G proteins independently of GPCRs [ 171 ]. NDPKc can heterohexamerize with NDPKa and NDPKb. Among isozymes, synthesis of NDPKc, which enables formation of the NDPKb–NDPKc complex and interaction between NDPK isozymes and G proteins, is upregulated in ESHF patients and in rats after long-term stimulation with isoprenaline, which elicits translocation of NDPKc to the plasma membrane [ 171 ]. In CMCs, overexpressed NDPKc raises cAMP concentration and sensitizes CMCs to isoprenaline, which augments contractility. In NDPKB −∕− mice, NDPKc production remains normal, but long-term isoprenaline exposure causes contractile dysfunction and adverse cardiac remodeling. In ESHF patients, the amount of the NDPKb–NDPKc complex rises, whereas the NDPKc–Gs interaction decays, switching G-protein activation from Gs to Gi2 and contributing to a decrease in the cAMP level. Moderate changes in the Gs/ Gi ratio can determine the G-protein subunit subtypes that tether to NDPKc [ 171 ].
Upon injury and stressor exposure, various fetal signaling pathways such as the canonical Wnt–β Ctnn signaling cascade are reactivated, priming transcription of genes implicated in cardiac fibrosis, a consequence of maladaptive hypertrophy and a major cause of HF.
The plasmalemmal receptor CDO, 45 which predominantly localizes to intercalated discs, 46 controls connexin-43 location and function. CDO counters Wnt signaling, as it interacts with the LRP6 coreceptor, preventing abnormal myocardial structure and action potential propagation [ 173 ]. Abnormal Wnt signaling is linked to Cx43 upregulated expression and mislocalization to CMC lateral sides.
Interrelation Between the Heart and Kidney
The cardiovascular apparatus and kidney are closely interconnected, under both normal and pathological conditions. Maintenance of the vasomotor tone and blood volume depends on interactions between blood circulation and the kidney.
Chronic kidney disease (CKD) often accelerates the evolution of CVD; conversely, cardiac dysfunction causes renal dysfunction, which is a common complication of CVD.
Renal dysfunction is an independent strong cardiovascular risk factor. The prevalence of CVD in the elderly (age≥66 yr) with CKD (∼70%) is twice that of non-CKD patients (∼35%); it is associated with a poor survival rate [ 174 ]. 47
Acute or chronic dysfunction has a bidirectional nature, each dysfunctional organ (heart and kidney) sustaining disease in the other organ. This mutual adverse interaction engenders cardiorenal syndrome (CRS), which is characterized by endothelial and vSMC dysfunction and resistance to natriuretic peptides and diuretics.
Defective renal perfusion and exacerbated vasoconstriction are associated with a persistent neurohormonal activation due to overactivity of arterial baroreceptors and intrarenal sensors and hence of the sympathetic nervous system, sympathoadrenal and renin–angiotensin–aldosterone axes, adenosine, and vasopressin, dysregulated hydroelectrolytic and calcium–phosphate balance, anemia, inflammation, and redox stress.
Furthermore, protein-bound uremic toxins (PBUTs), such as indoxyl (IS) and p-cresyl sulfate (pCS), which derive from dietary amino acid metabolites by colonic microorganisms, accumulate when renal excretion declines, form large complexes with albumin, and yield renal and cardiovascular toxicity [ 174 , 177 ]. These toxins affect the proliferation, migration, and senescence of vSMCs and ECs and provoke inflammation, calcification, and redox stress.
Calcific uremic arteriolopathy (CUA), also named calcific obliterative arteriolopathy and calciphylaxis, is typically observed in CKD patients, especially women of Caucasian ethnicity and individuals at end-stage renal disease. 48 Risk factors encompass malnutrition, insulin resistance, obesity, diabetes mellitus, alcoholic steatohepatitis, secondary hyperparathyroidism (elevated parathyroid hormone concentration), deficiency in protein-C and/or -S, and elevated activity of alkaline phosphatase, in addition to some therapies [ 179 ].
The uremic milieu predisposes to metabolic toxicity, redox stress linked to elevated concentrations of ROS, inflammation via activation of the transcription factor NFκB and the TNFSF11–TNFRSF11a axis, and vasoconstriction by increased activity of endothelin-1 [ 179 ].
The resulting arteriolopathy is associated with endothelial dysfunction, a prothrombotic state, intimal hyperplasia, fibrosis, and vascular smooth myocyte apoptosis and differentiation into osteoblast-like cells that provoke medial calcification [ 179 ].
Ectopic Calcification
Soft-tissue calcification (Vol. 10, Chap. 3. Adverse Wall Remodeling) results from a combination of tissue injury; exposure to sensitizing factors, such as parathyroid hormone and vitamin D; and a diet rich in calcium and phosphorus. It is triggered in a context combining hypercalcemia, hyperphosphatemia, and hyperparathyroidism, whereas activity of calcification inhibitors, such as matrix γ-carboxyglutamate acid (Gla)-containing protein (MGP) and fetuin-A, decays [ 179 ]. Hyperglycemia, hyperhomocysteinemia, hyperbeta2microglobulinemia, 49 elevated levels of oxidized low-density lipoprotein–cholesterol (LDL CS ), and low levels of high-density lipoprotein–cholesterol (HDL CS ) are additional factors that can raise ROS formation and contribute to vascular calcification.
Calcific aortic valve disease (CAVD), which evolves from mild focal valve thickening without blood flow obstruction (aortic sclerosis), thickening of the valve leaflets, and formation of calcium nodules, to end-stage calcification with impaired leaflet motion (aortic stenosis), 50 is the most common indication for surgical or transcutaneous valve therapy in the world [ 185 ].
Mutations in the genes encoding notch, LDLR, and LP A , an OxPL carrier, are linked to the risk for calcification.
Oxidized phospholipids are involved in the progression of CAVD. They are carried by apolipoprotein-B100 (ApoB100 OxPL ) and apolipoprotein A (i.e., lipoprotein-A [Apo A OxPL ]). An increased Lpa concentration is also a CoAD risk factor. It is heritable; two variants (rs10455872 and rs3798220) in the LP A gene-linked 6q26-27 locus are strongly associated with increased Lpa concentration [ 186 ]. Both ApoB100 OxPL ) and Apo A OxPL are causal CAVD risk factors [ 115 ].
Autoimmune Disorders
Giant cell arteritis (GCA; or granulomatous arteritis) is an autoimmune vasculitis, which particularly targets the temporal arteries (hence its other name temporal arteritis ). Many altered genes predispose to GCA, such as those encoding class- I and - II human leukocyte antigens, which form a gene cluster on chromosome 6, and PTPN22, NLRP1, IL17A, IL33, and LRRC32 genes; familial GCA cases exist [ 187 ].
In GCA, immunocytes, especially CD4+ effector helper T cells (T H1 and T H17 ), invade large arterial walls. Adventitial microvascular endotheliocytes control access of inflammatory leukocytes to the media and intima. In GCA patients, circulating CD4+ T cells have left the quiescent state, their activation resulting from the notch–TORC1 pathway, and differentiate into vasculitogenic T H1 and T H17 cells.
In GCA patients, expression of the notch ligand jagged-1 is upregulated in these endotheliocytes owing to increased circulating concentration of VEGF (augmented vegfemia) [ 188 ]. T lymphocytes endowed with notch-1 receive aberrant activating signals from jagged-1+ adventitial endotheliocytes.
Vessel walls are involved in inflammatory (autoimmune) disorders, such as systemic rheumatoid arthritis, disseminated lupus erythematosus, and scleroderma.
- Systemic rheumatoid vasculitis results from an autoimmune inflammation of small and medium-sized vessels, which is associated with inflammation of joints.
- Systemic lupus erythematosus is a connective tissue autoimmune disease that affects the skin, joints, brain, kidney, and lung, among other organs, vasculopathy being a typical element.
- Scleroderma , or systemic sclerosis , is a connective tissue autoimmune disease characterized by fibrosis and vasculopathy in multiple organs. Many clinical complications arise from dysfunctional microvascular beds that cause tissue ischemia in addition to medium-sized vessels that can provoke endothelial dysfunction and pulmonary arterial hypertension, among other symptoms. Raynaud’s syndrome is a form of limited systemic sclerosis.
Raynaud’s syndrome corresponds to a transient cessation of blood flow in the fingers and toes due to a vasospasm of the digital arteries in the hands and feet. It can be triggered by either cold or emotion. This vasculopathy is linked to myofibroblast proliferation and matrix deposition in the subendothelial layer, leading to obliterative thickening of the vessel walls in addition to mononuclear infiltrates. It is characterized by cyanosis and pain due to ischemia of the sensory nerves and is more common in women. The pathophysiological process underlying abnormal vascular reactivity involves the hyperactive adrenergic nervous system, α2-adrenoceptors, central stress response, serotonin, endothelin, depressed vasodilatory response to NO, prostaglandin-G/H synthase (cyclooxygenase), the cGMP–PKG signaling cascade, and redox stress [ 189 ].
Congenital Vascular Malformations
Vascular malformations are localized defects of vascular development that usually affect a limited number of vessels in a restricted area of the body. Most malformations, which are present at birth and grow proportionately with age during childhood, result from gene mutations. Inherited new lesions can appear, but they remain small. They are either sporadic with a single lesion or characterized by multifocality in familial forms [ 190 ]. Familial vascular malformations follow a paradominant inheritance. Sporadic forms are caused by somatic mutations in the same genes (Tables 1.11 and 1.12 ). Major mediators involved in anomalies of blood and lymph vessels and their pathways are given in Table 1.13 .
Chromosomal loci and genes involved in vascular malformations ( Part 1 ; Sources: [ 190 – 194 ]; ACDMPV alveolar capillary dysplasia with misalignment of pulmonary veins, AT ataxia–telangiectasia [Louis–Bar syndrome], BRBNS blue rubber bleb nevus syndrome, CCM cerebral cavernous (or capillary) malformation, CMAVM capillary malformation–arteriovenous malformation, CMVM cutaneomucosal venous malformation, GVM glomuvenous malformation, ATMK ataxia telangiectasia mutated kinase, FoxF1 [or ACDMPV] forkhead box-containing transcription factor-F1, KrIT1 ankyrin repeat-containing Krev [Kirsten sarcoma virus Ras-revertant] interaction trapped protein-1 [angiogenesis inhibitor that binds Rap1 (or Krev1)], PdCD10 programmed cell death protein-10 [CCM3 protein], RasA1 [or CMAVM] Ras GTPase-activating protein [RasGAP], TIE protein Tyr kinase with Ig and EGF homology domains [angiopoietin receptor])
Chromosomal loci and genes involved in vascular malformations ( Part 2 ; Sources: [ 190 – 194 ]; HCD hemangiomatosis chondrodystrophica, HHT hereditary hemorrhagic telangiectasia, HLTS hypotrichosis–lymphedema–telangiectasia syndrome, JHHT juvenile polyposis–HHT syndrome, KTWS Klippel–Trenaunay–Weber syndrome, LCS lymphedema–cholestasis syndrome [Aagenaes syndrome], LDS lymphedema–distichiasis syndrome, OLEDAID osteoporosis, lymphedema, and anhydrotic ectodermal dysplasia with immunodeficiency, PCL primary congenital lymphedema [Milroy disease], PHTS PTEN hamartoma tumor syndrome, PPCM progressive patchy capillary malformation [angioma serpiginosum], ALK1 activin-A type- I receptor-like kinase-1 [AcvRL1], IDH1 soluble cytosolic NADP + -dependent isocitrate dehydrogenase-1, IDH2 mitochondrial NADP + -dependent isocitrate dehydrogenase-2, I κ BK γ [ IKK γ] inhibitor of NFκB kinase subunit-γ, PI3K phosphatidylinositol 3-kinase, PTen phosphatase and tensin homolog deleted on chromosome ten [phosphatidylinositol 3-phosphatase], SMAD son of mothers against decapentaplegia homolog, Sox sex-determining region Y [SRY]-related high mobility group [HMG] homeobox-derived [DNA-binding domain]-containing transcription factor)
Examples of mediators and pathways involved in congenital vascular anomalies (Source: [ 190 ]; BEC blood endotheliocyte, LEC lymph endotheliocyte, vSMC vascular smooth myocyte)
Classification of Congenital Vascular Malformations
Congenital vascular malformations (CVMs) are categorized by the Mulliken classification into high- and low-flow lesions. The Hamburg classification distinguishes vascular malformations according to their predominant histological components (lymphatic, arterial, and/or venous). Arterial and venous CVMs are composed entirely of arteries and veins, respectively. Arterial defect is related to the absence of development of an arterial segment, which is thus missing, the irrigated organ being perfused by a collateral artery, which does not wither. Venous defects form thin-walled venous lakes or grape-like clusters of lakes.
Congenital vascular malformations are also formed when arteriovenous shunts persist. They include a single pair of vessels ( arteriovenous fistulas [AVFs]), or a cluster of vessels ( arteriovenous malformations [AVMs]). Truncular lesions arise from disturbances in late embryonic angiogenesis from the normal vasculature, whereas extratruncular lesions derive from the early development stage without direct connection with the normal vasculature.
Cerebral (CeAVMs) and peripheral arteriovenous malformations (PAVM) are congenital localized defects caused by altered embryonic angiogenesis that can affect the arterial, venous, and lymphatic circuits. Most AVMs are localized. Multiple AVMs are very rare lesions but can cause numerous hemorrhagic episodes. Multifocal AVMs can be observed in autosomal dominant disorders, such as hereditary hemorrhagic telangiectasia , that is, dilation of the microvasculature (microaneurysms, or telangiectasia) with bleedings in the skin and mucosae, and capillary malformation–arteriovenous malformation syndrome (CMAVM). CMAVM is characterized by small round spots of enlarged capillaries in the dermis, most often on the face, arms, and legs.
Capillary malformations can be associated with arteriovenous malformations and fistulas. Type- I CMAVM is caused by mutations in the RASA1 gene, which encodes the RasGAP RasA1. Type- II multifocal CMAVM is engendered by mutations in the EPHB4 gene that encodes the receptor protein Tyr kinase ephrin type-B receptor EPHb4, which is involved in contact-dependent bidirectional signaling between apposed cells [ 195 ]. It is implicated in cardio- and angiogenesis and in postnatal angiogenesis and vascular remodeling. Therefore, the EPHb4–Ras–ERK pathway is a major axis for AVMs.
Ephrin binds to the erythropoietin-producing hepatocyte (EPH) receptors on the surface of the apposed cell and triggers EPH aggregation, fostering EPH transphosphorylation (transactivation). Polymerization of the receptor is first carried out by assembling monomers (6–8) into active oligomers (activation phase) that then condensate into large clusters (hundreds of monomers), which dampens signaling (inactivation phase), thereby creating a fast and transient response [ 196 ]. The polymerization–condensation model states that the coalescence of oligomers into large aggregates reduces the recruitment of free monomers, as it accelerates formation of large-scale, slowly diffusing clusters and subsequent primes receptor endocytosis and signaling termination.
Arteriovenous malformations are characterized by a reduced flow resistance. These shunts connect high- to low-pressure vascular compartment, bypassing the capillary bed. Resulting arterial steal and venous hypertension depends on the lesion type and architecture.
- Cirsoid AVM , the most common type (size> 1 cm), consists of multiple dilated feeding arteries and draining veins, which have a tortuous shape, hence with multiple arteriovenous connections [ 197 ]. It is adjacent to the collecting circuit.
- Angiomatous AVM (size< 1 cm) is composed of a single artery feeding multiple interconnecting distal branches and draining veins.
- Aneurysmal AVM consists of a single feeding artery and a single draining vein with dilation (diameter> 1 cm), which resembles an acquired fistula.
Yakes’ AVM classification defines:
- Type- I anomalies, which connect a single artery to a single vein without a vascular nidus
- Type- II lesions, which link many arteries directly to veins and indirectly via arterioles and venules, which form a relatively simple network
- Type- III malformations, which associate many arteries via arterioles to a dilated segment, which gives birth to a single or many veins
- Type- IV anomalies that connect arteries and veins via a complicated arteriolovenular network [ 198 ]
Coronary arteries can communicate with the cardiac chambers (coronary–cameral fistulas) or veins (coronary arteriovenous malformations).
An arteriovenous fistula is an abnormal single direct passage from artery to vein. In addition to congenital fistulas, those acquired after birth are caused by infections, degeneration, trauma, or iatrogenic interventions (e.g., during angiography, biopsy, bypass grafting, and pacemaker implantation). Congenital arteriovenous malformation and acquired AVFs are rare causes of secondary hypertension.
Venous Malformations
Venous malformations (VMs) includes sporadic and cutaneomucosal (or mucocutaneous) VMs (CMVMs), and glomuvenous malformations (GVM) [ 190 ]. Multiple inherited venous lesions are identified in venous, glomuvenous, and cerebral cavernous malformations.
Sporadic venous malformations are bluish or violaceous, solitary or multiple, localized or diffuse, superficial or deep lesions most often on the head and neck [ 113 ]. Venous malformations evolve slowly and progressively in the absence of bleeding. Thrombi and calcifications ( phleboliths ) can occur in tortuous veins. Venous nevus , or nevus venosus, is a variant of sporadic venous malformations.
Blue rubber bleb nevus 51 is a sporadic syndrome (BRBNS; also called Bean syndrome) 52 characterized by cutaneous and gastrointestinal VMs of various numbers, sizes, and locations. It can be caused by mutations in the TEK ( Tie2) gene. Nevi in the intestine can bleed spontaneously, provoking anemia. Families follow autosomal dominant inheritance but in fact have other multifocal venous malformations.
Hemangiomatosis chondrodystrophica , also termed dyschondrodysplasia with hemangiomas, enchondromatosis with multiple cavernous hemangiomas, and Maffucci syndrome, primarily affects the bone and skin. It is characterized by multiple enchondromas (cartilage enlargements), bone deformities, and hemangiomas (tangles of abnormal blood vessels [benign tumors]). IDH is caused by mutations in the Idh1 or Idh2 gene, which encode NADP + -dependent IDH1 and IDH2, respectively.
Klippel–Trenaunay–Weber syndrome (KTWS) is a disorder pertaining to the PIK3CA gene-related overgrowth spectrum (PROS), which also includes megalencephaly capillary malformation and polymicrogyria syndrome (MCAP) and congenital lipomatous overgrowth, vascular malformations, epidermal nevi, and skeletal/spinal abnormalities (CLOVES) syndrome, hemimegalencephaly, fibroadipose hyperplasia, and epidermal nevus. It affects the development of blood vessels, engendering varicose veins and malformations of deep veins in the limbs, and causes overgrowth of soft tissues and bones. It results from mutations in the PIK3CA gene, which encodes PI3K c1 α .
Cutaneomucosal Venous Malformations
Cutaneomucosal venous malformations (in the skin and mucosae) commonly infiltrate underlying muscle and joints [ 190 ]. Although mostly sporadic (∼98% cases), CMVMs obey autosomal dominant inheritance.
They are caused by mutations in the TEK gene located in the VMCM1 locus on chromosomal locus 9p21.22 (e.g., single-nucleotide polymorphisms R849W and Y897S), which encodes the endothelial-specific receptor protein Tyr kinase TIE2 [ 190 ]. 53 These gain-of-function (GOF) mutations (e.g., C2545T in exon 15, A2690G, G2744A, C2752T, G2755T, and G2773T in exon 17, and G3300C in exon 22 [ 201 ]) increase ligand-independent autophosphorylation of TIE2 without launching endotheliocyte proliferation.
Three TIE2 ligands include angiopoietins AngPt1, AngPt2, and AngPt4 (the latter corresponding to mouse AngPt3). AngPt1 has a stronger effect than competitive AngPt2, which is considered to be a AngPt1 inhibitor. Once it is liganded, TIE2 dimerizes and cross-phosphorylates, triggering mainly the MAPK module and PI3K pathway, which activates PKB and inhibits apoptosis.
Glomuvenous Malformations
Glomuvenous malformations are usually nodular multifocal lesions located on the extremities that involve the skin and subcutis, occasionally the mucosa [ 190 ]. They are characterized by abnormally differentiated vSMCs (glomus cells) in the walls of distended veins.
These autosomal dominant disorders are caused by loss-of-function (LOF) mutations in the GLMN gene on chromosomal locus 1p21-22, which encodes glomulin , an essential protein for vasculature development. Glomulin is a ligand of the immunophilins FKBP1a and FKBP4, hence its other name, FKBP-associated protein. Glomulin synthesis is restricted to vSMCs; it is involved in their differentiation [ 190 ].
Differentiation of vSMCs also depends on TGFβ, which competes with glomulin to bind Tβ R1; glomulin thus precludes TGFβ signaling. Conversely, lack of glomulin provokes TGFβ hyperactivity.
Glomulin also interacts with HGFR; upon HGF binding, glomulin is phosphorylated and released and triggers phosphorylation of S6K, thereby influencing protein synthesis.
As it also interacts with Cul7, glomulin can also control protein degradation via ubiquitination by the CRL7 complex.
Capillary Malformations
Capillary malformations (CapMs) form cutaneous lesions most frequently located in the head and neck. These slow-flow vascular malformations can comprise arterioles and postcapillary venules. Except for birthmarks, capillary malformations do not have a predilection for gender [ 113 ]. They are generally sporadic, but familial cases can be observed.
Megalencephaly capillary malformation syndrome , or macrocephaly (megalocephaly) cutis marmorata telangiectatica congenita, a rare, sporadic congenital capillary malformation, associates overgrowth of organs (megalencephaly) and cutaneous capillary malformations. These malformations are most often unilateral on the lower limbs. Enlarged capillaries augment blood flow near the skin surface. They can disappear spontaneously after several months or years, but they occasionally persist throughout life. This disorder is caused by mutations in the PIK3CA gene on chromosomal locus 3q26.
PTEN hamartoma tumor syndrome (PHTS) refers to a spectrum of disorders characterized by multiple hamartomas, 54 which are often intramuscular, multifocal, and associated with ectopic lipid depots. This spectrum includes (1) Cowden and Cowden-like syndrome involving mutations in the PTEN, SDHB, SDHD, and KLLN genes, which encode PTen, succinate dehydrogenase subunits B and D, and killin, respectively; (2) Bannayan–Riley–Ruvalcaba syndrome , characterized by macrocephaly and hamartomas of the intestine (hamartomatous intestinal polyps) resulting from mutations in the PTEN gene or partial or complete deletion of this gene; and (3) Proteus and Proteus-like syndrome , 55 which is characterized by usually asymmetrical overgrowth of the bones, skin, and other organs and results from a mutation in the AKT1 (Pkb1) gene on chromosomal locus 14q32.3.
Familial multiple nevi flammei is caused by mutations in the GNAQ gene, which encodes guanine nucleotide-binding (G) protein subunit Gα q . Nevi flammei (nevus flammeus neonatorum) correspond to birthmarks. These non-elevated, sharply circumscribed patches fade progressively.
Salmon patches on the forehead, eyelids, and neck, in addition to the back, legs, and arms, also termed angel kisses , when erythematous macules typically affect the glabella, but also eyelids, nose, upper lip, and sacral region, and stork bites , when observed in the back of the neck, are picturesque names that depict very common birthmarks. A port wine stain (nevus flammeus) is a cutaneous firemark due to an abnormal aggregation of capillaries, the color of which (pink to purple macules) resembles port wine, the most common location being the face.
Nevus comedonicus is a rare type of epidermal nevus with predilection for the face and neck caused by mutations in the NEK9 gene 56 on chromosomal locus 14q24.
Nevus anemicus is a nonhereditary congenital disorder characterized by irregular hypopigmented macules that coalesce to form plaques, which are generally present at birth or develop in the first postpartum days. They localize especially on the chest. This disorder results from sustained vasoconstriction due to vascular hypersensitivity to catecholamines and not to partial aplasia of dermal blood vessels [ 113 ].
Nevus roseus is characterized by a pale red or even pink color; hence, its other name “rosé wine stain.” It remains unchanged during life [ 113 ].
Phacomatosis pigmentovascularis associates a vascular nevus and extensive pigmentary nevus. It is categorized into five groups according to the pigmentary anomaly [ 113 ]: type I corresponds to nevus flammeus and pigmented linear epidermal nevi; type II to nevus flammeus, Mongolian spots, and/or nevus anemicus; type III to nevus flammeus and spilus and/or anemicus; type- IV to nevus flammeus, Mongolian spots, and nevus spilus and/or anemicus; and type V to cutis marmorata telangiectatica congenita and Mongolian spots. This classification was later simplified into phacomatosis cesioflammea (i.e., nevus cesius [blue spot] and flammeus) and spilorosea (i.e., nevus spilus and roseus).
Capillary malformation–arteriovenous malformation syndrome (CMAVM) results from mutations in the RASA1 gene, which encodes the Ras GTPase-activating protein (RasGAP) RasA1 (also aliased as CMAVM) [ 190 ].
Sporadic and autosomal dominant angioma serpiginosum (AS) is a benign cutaneous disease characterized by a progressive dilation of the subepidermal vessels manifesting as clusters of punctate erythematous lesions, usually on the lower limbs. It can be considered a type of capillary nevus. It occurs almost exclusively in women. It results from mutations in the chromosomal locus Xp11.3–Xq12.
Lymphatic Malformations
Two categories of lymphatic malformations (LMs) affect the skin: lymphedema and congenital, superficial or deep, solitary or multiple lymphatic malformations. Lymphatic malformations are localized dilated lymphatic channels or pseudo-vesicles (lymphangiectasias) that are not connected to the lymphatic circuit.
Cystic lesions are macro- (formerly called cystic hygromas) or microcystic, or mixed. Microcystic lymphatic malformations are also termed lymphangioma, lymphangioma circumscriptum or simplex, verrucous hemangioma, and angiokeratoma circumscriptum [ 113 ]. Macrocystic lymphatic malformations lodge in the neck, axillas, or lateral edges of the trunk. They can be solitary or multiple, and can be interconnected.
Lymphedema , that is, chronic swelling in the body, usually in the lower extremities, due to abnormal lymphatic vessels, can be primary or secondary. Primary lymphedema comprises various types (Lmph1A–Lmph1D), which are linked to the chromosomal region 5q35, 6q16.2–q22.1, 1q42, and 4q34 [ 194 ].
Type- I A hereditary lymphedema (Lmph1A), also named primary congenital lymphedema (PCL) and Milroy disease, most commonly affects the inferior limbs, from the feet up to the knees. This autosomal dominant disorder is caused by missense mutations in the FLT4 gene, which encodes VEGFR3 [ 190 ].
Type- I B hereditary lymphedema (Lmph1B) is caused by anatomical or functional defects in the lymphatic circuit. It usually appears at birth or in early childhood but can occur later [ 194 ].
Type- I C hereditary lymphedema (Lmph1C) can be governed by autosomal dominant inheritance of heterozygous mutations in the GJC2 gene that encodes gap junction protein-γ2, or connexin Cx46.6 or Cx47 [ 194 ].
Type- I D hereditary lymphedema (Lmph1D) is engendered by heterozygous mutations in the VEGFC gene, the transmission pattern being consistent with autosomal dominant inheritance [ 194 ].
Type- II late-onset lymphedema (Lmph2), also called Meige’s disease and lymphedema praecox, develops around puberty. It involves the upper and lower limbs, face, and larynx and can provoke a persistent pleural effusion. It can result from truncating and some missense mutations in the FOXC2 gene situated in the chromosomal locus 16q24.3 [ 190 ].
Hypotrichosis–lymphedema–telangiectasia syndrome (HLTS) is characterized by lymphedema and cutaneous telangiectasias. Both autosomal dominant and recessive inheritance can be observed [ 190 ]. Dominant and recessive forms are caused by mutations in the SOX18 gene, which encodes the transcription factor Sox18, an early marker of lymphatic differentiation. Sox18 interacts with MEF2c and regulates synthesis of vcam1.
Osteoporosis lymphedema anhydrotic ectodermal dysplasia with immunodeficiency syndrome (OLEDAID) is engendered by mutations (e.g., X420W) in the IKBKG gene that encodes Iκ BKγ, which reduces NFκB activation [ 190 ]. 57
Lymphedema–cholestasis syndrome (LCS), also termed Aagenaes syndrome, is most often an autosomal recessive disorder, although an autosomal dominant mutation may be involved [ 190 ].
Endothelial Signaling in Vasculo- and Angiogenesis
Vasculo- (i.e., de novo blood vessel formation involving differentiation and migration of endothelial precursors), angio- (i.e., development of new blood vessels by capillary sprouting from preexisting vessels), and lymphangiogenesis construct (1) the vascular closed circuit, which is formed from arteries downstream from the heart, capillaries perfusing the body’s tissues, and veins upstream from the heart and (2) vascular walls, which are composed of vECs and mural cells (vMCs). The proper structure of blood and lymph vessels consists of a single layer of endotheliocytes surrounded by pericytes or a variable number of layers of vascular smooth myocytes separated by elastic laminae in the micro- (i.e., capillaries and upstream lymphatics) and macrovasculature, respectively. Correct organization of the vascular circuit requires the controlled activities of multiple types of messengers that regulate vessel formation, vascular branching, elongation and pruning, capillary fusion, vascular stability and anastomosis, and arterial and venous differentiation of endotheliocytes, which segregates arteries from veins.
Vascular development and maintenance are controlled by a transcriptional program that integrates both extra- and intracellular signals in endotheliocytes.
Vasculo- and angiogenesis are controlled by numerous signaling cascades in addition to hemodynamic stress. The initiation and formation of new blood vessels, that is, sprouting angiogenesis, is mainly regulated by the messengers VEGFa and notch.
Angiogenesis is orchestrated by endothelial tip cells that form the vascular front and are followed by proliferating stalk cells. Tip cells sense multiple extracellular pro- and antiangiogenic signals and migrate toward the hypoxic region.
In mice and cardiac organ culture, coronary vessels arise from angiogenic sprouts of the sinus venosus, that is, the vein returning blood to the embryonic heart [ 202 ]. Sprouting venous endotheliocytes thus dedifferentiate as they migrate over and invade the myocardium. Intramyocardial ECs then redifferentiate into arterial and capillary cells, whereas epicardial ECs redifferentiate into venous cells.
Endotheliocyte differentiation into arterial and venous cells is genetically controlled for both vessel types. It precedes the onset of blood circulation. Arterial and venous angioblasts segregate from the beginning of vasculogenesis [ 203 ]. Acquisition of arterial identity is governed by a set of messengers (e.g., notch [Sect. 1.4.5.1 ], SHh [Sect. 1.4.5.3 ], and VEGF [Sect. 1.4.5.4 ]). Acquisition of venous phenotype relies on the nuclear receptor NR2f2 that suppresses notch signaling [ 203 ]. Ephrins and their receptors (e.g., the transmembrane ligand ephrin-B2 and its cognate receptor EPHb4 [Sect. 1.4.5.5 ]) are also involved in the establishment of arterial and venous identity.
Susceptibility to certain vasculopathies differs between arteries and veins. The intracellular receptor NR2f2 is involved in regulating pathophysiological processes in adult blood vessels [ 204 ]. It acts as an antiatherogenic and -osteogenic agent that downregulates formation of inflammatory factors, upregulates that of antithrombotic agents, and represses osteogenic transcriptional program and endothelial-to-mesenchymal transition. It also regulates the TGFβ pathway, as it controls production of TGFβ2 and BMP4, which support conversion of endotheliocytes into mesenchymal stem cell-like cells and undergo osteogenic differentiation.
Notch, FoxC, SoxF, and NR2f2
The notch receptor (notch-1–notch-4) binds one of its ligands, jagged proteins (Jag1–Jag2) and delta-like ligands (DLL1–DLL3). In mouse early embryo at least, Jag1, Jag2, and DLL4 are specifically expressed in arterial endotheliocytes.
Notch cleavage releases the notch intracellular domain (notch ICD ) into the cytosol. Notch ICD associates with RBPJκ, 58 a DNA-binding protein and transcriptional repressor in the absence of notch signaling, and Mastermind (Mam), a transcriptional coactivator. Notch ICD translocates to the nucleus, where it interacts with RBPJκ and converts it to a transcriptional activator, priming synthesis of basic helix–loop–helix (bHLH) transcription factors HESs 59 and HRTs. 60 In zebrafish at least, notch signaling acts downstream of the SHh and VEGF pathways in arterial specification.
Notch-1 and notch-4 are essential for maintaining vessel identity. Notch signaling overcomes activin receptor-like kinase (ALK1) loss, as it restores EfnB2 expression in endotheliocytes. Notch signaling is also implicated in tip-to-stalk cell conversion (Vol. 5, Chap. 10. Vasculature Growth, and Vol. 10, Chap. 2. Vascular Growth and Remodeling).
In endotheliocytes of mouse and zebrafish embryos, SOXF 61 proteins act in synergy with RBPJκ [ 207 ]. They function upstream from notch signaling. Sox17 activates notch signaling, as it tethers to promoters of multiple genes involved in the notch pathway.
Three SOXF genes, SOX7, SOX17, and SOX18, encode transcription factors of the SOXF group, which are expressed in vascular endotheliocytes during blood circulation development, whereas only Sox18 is involved in lymphangiogenesis [ 208 ]. Sox7 and Sox18 cooperate in the specification of arterial and venous identity.
Single nucleotide polymorphisms at the SOX17 chromosomal locus can engender intracranial aneurysms.
High concentrations of VEGF stimulate production of delta-like ligand DLL4 by tip cells, which activates notch on adjacent endotheliocytes to confer stalk cell identity. In adult venous endotheliocytes, VEGFa inhibits formation of EPHb4, a venous marker, and stimulates that of DLL4, an arterial marker.
Whereas DLL4 is involved in initiating the arterial program, DLL1 is required for the maintenance of arterial identity. In mouse embryos, DLL1 formation is restricted to arterial endotheliocytes after embryonic day 13 [ 208 ]. VEGF controls notch signaling, which is activated by DLL1, notch regulating neuropilin-1 (Nrp1) synthesis.
Among transcription factors of the forkhead box group implicated in cardiovascular system development, members of the FOXC subgroup, FoxC1 and FoxC2, which are expressed in both arteries and veins of the mouse embryo, play an overlapping role. They contribute to regulating the formation of arterial-specific genes (e.g., Dll4 and Hrt2) and vascular remodeling of primitive blood vessels. They directly activate the Dll4 gene transcription using a FoxC-binding element (FBE), upstream of notch signaling [ 208 ].
In FOXC1 +∕− and FOXC2 −∕− mice, AVMs form and their endotheliocytes fail to express DLL4, and expression of other arterial markers (notch-1, notch-4, Jag1, HRT2, and EfnB2) declines [ 209 ]. Although FoxC1 and FoxC2 are required for DLL4 synthesis, deletion of the forkhead-binding element on the Dll4 promoter does not attenuate Dll4 gene transcription by the FoxC factors, notch1 ICD and notch4 ICD using the RBPJ-binding site. As FoxC2 and notch ICD act synergistically on the Hrt2 gene promoter, FoxC and notch ICD may also cooperate on the Dll4 gene promoter [ 209 ].
In endotheliocytes, FoxC1 and FoxC2 control expression of HRT2, the Hrt2 promoter containing two FBEs [ 208 ]. In addition, Foxc2, but not FoxC1, binds to the RBPJ (or Csl) gene promoter. Foxc2 complexes with CSL and notch ICD to launch HRT2 synthesis. Production of DLL4 and HRT2 by FoxC is enhanced by VEGF in endotheliocytes.
The genetic determinant of venous specification, NR2f2, is specifically expressed in venous endotheliocytes and acts upstream from EPHb4 in mice, impeding Nrp1 and notch formation. However, it cooperates with other factors for venous cell fate determination [ 208 ]. Furthermore, it interacts with Prox1 to launch lymphatic gene expression.
Notch regulates responsiveness of endotheliocytes to BMP2 and BMP6 via inhibitory SMAD6, which is involved in neovessel branching formation [ 210 ].
The notch- and ALK1-mediated signaling cascades interact and can partly compensate for each other. Sequestration of BMP9 and BMP10 and subsequent ALK1 inhibition and notch blockage engender a hyperfused and hypersprouting vascular plexus in a neonatal mouse retina model [ 209 ]. SMAD1/5/8 binding sites exist in the regulatory region of many notch-targeted genes (e.g., HES1 and HRT1–HRT2).
Wnt and Sox
Wnt signaling regulates multiple biological processes, such as angiogenesis, inflammation, and tumorigenesis. Wnt morphogens are secreted by cysteine-rich palmitoylated glycoproteins that play an essential role in cell fate determination, tissue homeostasis, and embryo- and fetogenesis.
Canonical Wnt signaling elicits vascular invasion into the central nervous system [ 207 ]. Messengers Wnt and norrin target the receptor frizzled, coreceptors LRP5 and LRP6, coactivators tetraspanin-12 and GPR124, and effector β-catenin. In the absence of any of these Wnt signaling mediators, vascular cerebral network formation aborts, despite the high VEGF concentration produced by the hypoxic organ.
Norrin (or Norrie disease protein), a homodimeric secreted cysteine-rich and cystine knot-like 62 growth factor produced from a precursor encoded by the NDP gene, is an atypical Wnt ligand. It activates the canonical Wnt signaling pathway via Fzd4 and LRP5, acting in cooperation with TSpan12 to activate Fzd4, independently of Wnt [ 207 ]. Norrin mimics Wnt, as it can tether and activate frizzled via assembly of a molecular platform consisting of Fzd4, its LRP5–LRP6 coreceptor complex, auxiliary TSpan12, and associated HSPG [ 211 , 212 ]. It then launches the Ctnnβ1—LEF/TCF axis. Norrin maintains the blood–retina and blood–brain barriers and regulates angiogenesis in the eye, ear (cochlea), brain, and female reproductive organs (uterus) [ 211 ]. In addition, norrin connects to secreted frizzled-related proteins (sFRPs).
In retinal arterioles, capillaries, and veins, Sox17 production depends on frizzled-4 and norrin [ 207 ]. Members of the SOXF group participate in regulating the development of the blood and lymph vasculature in addition to arterial and venous identity (i.e., vascular differentiation), remodeling, and maintenance in a functionally redundant fashion (strong, but partial redundancy), compensating for defective activity of any SOXF factor. Each SOXF factor exhibits a distinct pattern of production among the different classes of retinal blood vessels [ 207 ]. Sox7 and Sox18 have a similar temporal expression pattern. They are mainly produced in endothelia at the very early stages of endothelial differentiation, but their synthesis is differently regulated [ 203 ]. They also localize to distinct vessels in zebrafishes [ 213 ].
Both Sox7 and Sox18 are dispensable for the initial specification and positioning of the major trunk vessels. On the other hand, Sox17 is mainly formed during gastrulation [ 203 ]. All three SOXF group members are coexpressed in vascular endotheliocytes. Members of the SOXF group are reciprocally regulated in the developing blood vasculature.
In mice, Sox17 and Sox18 act redundantly in postnatal angiogenesis; Sox7 and Sox18 present an overlapping expression pattern [ 213 ]. Sox7, Sox17, and Sox18 are functionally redundant in the developing mouse retinal vasculature (cell differentiation and vessel growth) and maintenance of the mature vasculature [ 207 ]. Vascular endothelial-specific deletion of a single SOXF member gene has little or no effect on vascular architecture or differentiation because of the overlapping function of Sox7 and Sox17 and the reciprocal regulation of gene expression. Combined deletion of Sox7, Sox17, and Sox18 at the onset of retinal angiogenesis leads to a dense capillary plexus, with a nearly complete loss of radial arteries and veins, whereas the presence of a single Sox17 allele largely restores arterial identity with vSMC coverage. Indeed, Sox17 plays a major role in vSMC coverage of radial retinal arteries. In the developing retina, expression of all three SOXF genes is reduced in the absence of canonical Wnt signaling mediated by norrin and frizzled-4 but remains unaffected by reduced VEGF signaling after deletion of the NRP1 gene. In adulthood, Sox7, Sox17, and Sox18 also have redundant functions in blood vessel maintenance. At adulthood onset, vascular endothelial-specific deletion of all three SOXF genes causes massive edema, despite nearly normal vascular architecture.
The production of the endothelial adhesion G-protein-coupled receptor GPR124, also named tumor endothelial marker TEM5, 63 is upregulated in endotheliocytes during physiological and tumoral angiogenesis. Its synthesis is induced by Rac during capillary network formation [ 214 ], and it prevents endotheliocyte proliferation.
Secreted sonic hedgehog signals via the transmembrane receptor patched (Ptc) and G-protein-coupled receptor smoothened (Smo) on recipient cells. It can induce arterial cell fate in zebrafish angioblasts. Zebrafish embryos lacking SHh lose arterial expression of ephrin-B2, as it generates formation of VEGF, which, in turn, activates notch [ 208 ].
In mice, defective Shh signaling does not cause severe vascular defects, although vascularization is attenuated in the developing lung and formation of the dorsal aorta and remodeling of the yolk sac vasculature are altered. Murine SHh signaling may be dispensable for arterial and venous specification.
Vascular Endothelial Growth Factor
In angiogenesis, the specification of tip and stalk cells relies on VEGF. Relatively high VEGF concentrations provoke DLL4 synthesis in tip cells, which activates notch signaling on adjacent endotheliocytes, thereby conferring stalk cell identity (Vol. 10, Chap. 2. Vascular Growth and Remodeling).
In mice, lower-molecular-weight isoforms, diffusible VEGFa 120 and intermediate VEGFa 164 are required for arterial development in the retina, rather than VEGFa 188 [ 208 ].
Neuropilin-1, a VEGFa 164 coreceptor, cooperates with VEGFR2 to trigger signaling. In mice, when Nrp1 activity is defective, arterial differentiation is impaired.
Vascular endothelial growth factor triggers the PI3K pathway and induces synthesis of notch-1 and DLL4, the VEGF–DLL4–notch–HRT2 cascade promoting arterial cell determination [ 208 ]. It modulates FoxC activity, and this modulation depends on the balance between PI3K and ERK activity. Relatively high VEGF concentrations (∼50 ng/ml) induce arterial marker genes, whereas lower VEGF concentrations (≤10 ng/ml) upregulate expression of the venous marker NR2f2; according to its level, VEGF signaling may preferentially activate either the PI3K or ERK pathway [ 208 ].
The protein Tyr phosphatase receptor, PTPRJ, is involved in arterial specification. It interacts with VEGFR2-primed signaling in endotheliocytes [ 208 ].
The calcitonin receptor-like receptor (CalRLR) is a G-protein-coupled receptor for adrenomedullin, which is coordinated with the VEGF and notch pathways in arterial differentiation in mouse embryos. CalRLR is expressed in the somite and arterial progenitors of zebrafish upon VEGF exposure, VEGF activity being regulated by SHh [ 208 ]. CalRLR supports arterial gene expression such as ephrin-B2 and notch-5.
Neuropilin-2 is expressed in venous and lymphatic endotheliocytes [ 208 ]. VEGFR3, which is initially detected in blood vessels of the early embryo, later becomes restricted to venous and then lymphatic endotheliocytes.
The VEGFR3 ligand, VEGFc, is mainly expressed in mesenchymal cells surrounding embryonic veins [ 208 ]. Prox1+ VEFR3+ lymphatic endothelial progenitors subsequently bud and migrate from veins using paracrine VEGFc–VEGFR3 signaling, initiating developmental lymphangiogenesis.
Hence, a subpopulation of venous endotheliocytes progressively synthesize the transcription factors Sox18 and Prox1 and acquire a lymphatic endothelial phenotype. Sox18 is first detected in a subpopulation of the cardinal vein and precedes the onset of Prox1 synthesis [ 208 ]. Sox18 induces Prox1 expression using two Sox18-binding sites on the Prox1 promoter. Sox18 is indispensable for induction of lymphatic differentiation but dispensable for lymphatic phenotype maintenance. Prox1 is a master regulator of lymphatic endothelial identity that elicits expression of lymphatic markers, such as VEGFR3 and lymphatic vessel endothelial hyaluronan receptor LyVE1. Moreover, Prox1 controls migration of lymphatic endotheliocytes triggered by VEGFc, as it cooperates with NR2f2 to prime synthesis of FGFR3, VEGFR3, and integrin-α 9 [ 208 ].
FoxC1 and FoxC2 may contribute to regulating lymphatic vessel development, pericyte recruitment to lymphatic vessels, and lymphatic valve formation in a paracrine manner [ 208 ].
Ephrin-B2 and Its EPHb4 Receptor
The protein Tyr kinase receptor EPHb4 and its primary transmembrane ligand ephrin-B2 (EfnB2) are exclusively expressed on venous and arterial endotheliocytes, respectively (Table 1.14 ). They support but are not mandatory for arterial and venous specification.
Regulators of arterial, venous, and lymphatic specification (Source: [ 208 ]; CalCRL calcitonin receptor-like receptor, Efn ephrin [EPH receptor interactor], EPH erythropoietin-producing hepatocyte receptor kinase, Fox forkhead box-containing transcription factor, NR nuclear receptor [transcription factor], Nrp neuropilin [VEGFR coreceptor], Prox Prospero homeodomain-containing transcription factor, PTPRJ protein Tyr phosphatase receptor type J, SHh sonic hedgehog, Sox sex determining region-Y box (SOX) homeodomain-containing transcription factor, VEGF vascular endothelial growth factor)
Expression of EfnB2 and EPHb4 is distinctively detected in the primary vascular plexus before the onset of circulation in the developing embryo [ 208 ]. Arterial–venous identity is genetically predetermined, although it is influenced by hemodynamic forces that enable remodeling and EC phenotype change.
Bidirectional signals mediated by both proteins play an important role in vascular development. EfnB2 and EPHb4 are differentially expressed in arterial and venous endotheliocytes of the mouse embryo and thus considered to be markers of arterial and venous identity during embryogenesis. EfnB2 forward signaling via EPHb4 (EfnB2–EPHb4 axis) prevents cell adhesion and migration and suppresses cell proliferation, whereas EPHb4 reverse signaling via EfnB2 (EPHB4–EfnB2 axis) elicits cell attachment and migration [ 215 ].
The EfnB2–EPHb4 is involved in embryonic vascular circuit development, vascular remodeling, in addition to neovascularization, arteriovenous differentiation, and tumoral angiogenesis in adults. In hemorrhagic (hCeAVMs) and nonhemorrhagic cerebral arteriovenous malformations (nhCeAVMs), veins and arteries are coated by EPHb4+ and EfnB2+ endotheliocytes, respectively, EPHb4 and EfnB2 content being larger in hCeAVMs than in nhCeAVMs, whereas endotheliocytes of the normal superficial temporal artery express neither EPHb4 nor EfnB2 [ 216 ].
Arterial specification relies on VEGF that induces expression of notch and DLL4, the transcription factors FoxC1 and FoxC2 regulating DLL4 synthesis [ 208 ]. Notch stimulates HRT1 and HRT2, promoting arterial differentiation.
On the other hand, the nuclear receptor NR2f2 is a determinant for venous specification, as it hampers expression of arterial specification genes, such as Nrp1 and notch [ 208 ].
A subpopulation of venous endotheliocytes progressively express the transcription factors Sox18 and Prox1, thereby acquiring lymphatic fate and differentiating into lymphatic endotheliocytes [ 208 ].
A mutual coordination of size between developing arteries and veins establishes a functional vasculature. The size of the developing dorsal aorta and cardinal vein is reciprocally balanced in mouse embryos. Gain-of-function notch mutations engender enlarged aortas and small cardinal veins, whereas LOF mutations show small aortas and large cardinal veins [ 217 ].
The dorsal aorta emerges before the cardinal vein via the assembly of endotheliocytes into the dorsal aorta primordium, a transient capillary plexus. Remodeling of this primitive structure generates the dorsal aorta. The cardinal vein appears slightly later, at a stage during which transient capillaries develop between the dorsal aorta and cardinal vein. Ephrin-B2 is specifically expressed in arterial endotheliocytes before the onset of blood circulation, but does not determine arterial specification of endotheliocytes [ 217 ]. Notch controls the proportion of endotheliocytes in the dorsal aorta and cardinal vein, as it promotes arterial specification and regulates both artery and vein size. Interdependence between arterial and venous size relies on a balanced allocation of endotheliocytes between these vessel types. Notch regulates endotheliocyte allocation, because it determines arterial specification and hence the ratio of arterial to venous endotheliocytes.
Loss of EfnB2 or EPHb4 also leads to enlarged aortas and small cardinal veins. However, endotheliocytes with venous identity mislocalize in the aorta. EfnB2–EPHb4 signaling may operate distinctly from notch, sorting arterial and venous endotheliocytes into their respective vessels.
Arterioles and venules are covered by EPHb4+ endotheliocytes. EPHb4+ capillaries of sprouts contain a significantly higher EphB4 amount than capillaries connecting arterioles and venules [ 218 ]. Hence, EPHb4 is not an arterial- or venous-specific marker in adult rat microvasculature but rather an indicator of capillary sprouting.
Transforming Growth Factor- β Group
Members of the transforming growth factor-β superfamily and among them, bone morphogenetic proteins, play an essential role in embryo- and fetogenesis and in the maintenance of organ function. Altered signaling in endotheliocytes by members of the TGFβ and BMP group causes diffuse malformations. Aortic aneurysms also arise from deregulated TGFβ/ BMP signaling.
The TGFβ signaling cascades involve:
- Numerous messengers, three TGFβ subtypes (TGFβ1–TGFβ3), BMPs, growth differentiation factors (GDFs), activins, nodal, and inhibins.
- 7 type- I receptors ( ALK1–ALK7), ALK5 corresponding to Tβ R1, ALK3 and ALK6 to BMPR1a and BMPR1b, and ALK2, ALK4, ALK7, and ALK1 64 to AcvR1a to AcvR1c and AcvRL1, respectively.
- 5 type- II receptors (Tβ R2, BMPR2, AcvR2a–AcvR2b, and AMHR2).
- Coreceptors, endoglin, which resides predominantly on endotheliocytes, cryptic, and β-glycan (Tβ R3); they modulate the activity of type- I and - II receptors.
Numerous ligand–receptor combinations trigger distinct TGFβ/ BMP signaling. For example, ALK2, which primarily propagates BMP6 signal, can also function as a BMP9 receptor. Heterotetrameric receptors made up from type- I and - II receptors, which, according to targeted type- I receptor type in the endothelium, predominantly endothelial ALK1 and ubiquitous ALK5, stimulate a given SMAD signaling cascade; ALK1 signals via SMAD1, SMAD5, and SMAD8 and ALK5 via SMAD2 and SMAD3.
The transmembrane receptor ALK1 is activated by BMP9 (GDF2) and BMP10 and by TGFβ1, but weakly. Once ALK1 is liganded, cytosolic SMAD1, SMAD5, and SMAD8 are phosphorylated by the ALK1–Eng–Tβ R2 complex.
Intracellular ALK1 signaling is implicated in diseases. Endothelium-specific ALK1 promotes arterial endothelial maturation and quiescence. In mice, deletion of genes encoding ALK1, endoglin, and MAP3K7 causes embryonic lethality associated with altered morphogenesis of the vascular circuit resulting from impaired arterial endothelium differentiation [ 219 ].
Phosphorylated SMADs complex with common SMAD4 and translocates to the nucleus, where they activate or repress transcription of specific target genes. Inhibitory SMADs, Smad6 and Smad7, are linked to ALK1 and ALK5, respectively (self-regulatory loop). They compete for type- I receptor binding or recruitment of specific ubiquitin ligases or phosphatases for proteasomal degradation or dephosphorylation of receptors.
In the early stages of blood vessel formation, proangiogenic BMP2 and BMP6 prevail; they signal via ALK2 or ALK3 [ 210 ]. On the other hand, antiangiogenic BMP9 and BMP10, two major ALK1 ligands, signal via ALK1 predominantly during vascular remodeling and maturation. Both BMP9 and BMP10 impede EC proliferation and migration. Endoglin and ALK1 are active in sites of vasculo- and angiogenesis during embryogenesis. During mouse postnatal development, except in the lung endothelium, ALK1 synthesis decreases, but at a high enough concentration to keep the adult vasculature quiescent via BMP9–ALK1 signaling. In wound healing and during tumorigenesis, ALK1 production linked to angiogenesis increases.
On the one hand, the BMP9–ALK1 couple upregulates the formation of notch-related mediators, HES1 (bHLHb39), HRT1 (bHLHb31), HRT2 (bHLHb32), and Jag1, in addition to endoglin, ephrin-B2, transmembrane protein TMem100, and endothelin-1 [ 210 ]. On the other hand, it downregulates the formation of E-selectin, CXCR4, and apelin.
Intracellular transmembrane protein TMem100, which localized mainly to the endoplasmic reticulum (but not to the plasma membrane), is an embryonic endothelium-enriched protein, synthesis of which is activated by BMP9 and BMP10 via the ALK1 receptor [ 219 ]. TMem100 may assist in post-translational protein modification or intracellular sorting.
In neurons, TMem100 controls the interaction between ankyrin-like and vanilloid TRP channels TRPA1 and TRPV1, disconnecting them and promoting Ca 2+ influx [ 209 ]. Both TRPA1 and TRPV1 reside on endotheliocytes; TRPV1 contributes to regulating the vasomotor tone, whereas TRPV4 facilitates arteriogenesis.
Calcium signaling upstream from NFATc1 is defective in TMEM100 −∕− embryos [ 209 ]. In Bmp10 −∕− mice, cardiac growth is impaired without defects of angiogenesis [ 219 ]. Among ALK1 targets, ablation of TMEM100 gives rise to a phenotype similar to Alk1 mutants (but not identical) [ 209 ]. Both Alk1 −∕− and TMEM100 −∕− mice have heart defects, failed vascular remodeling, and abnormal dilation and narrowing of the dorsal aorta, in addition to detachment of the endo- and mesodermal layers in the yolk sac. When TMEM100 is ablated postnatally, AVMs form in the lung and intestine, but not injury-induced cutaneous AVMs, as in Alk1 −∕− mice.
Both TMEM100 −∕− and EC TMEM100 −∕− mice die in utero because signaling from ALK1, notch, and PKB decays or is even suppressed and hence differentiation of arterial endothelium and vascular morphogenesis are defective [ 219 ].
The notch heterodimer forms owing to calcium; hence, the transplasmalemmal gradient in Ca 2+ concentration participates in notch activation in endotheliocytes [ 209 ]. When extracellular calcium concentration is low, notch subunits dissociate, promoting its cleavage.
Notch and its ligands abound in arterial (but not venous) endothelium of mouse embryos. Notch-1, notch-4, DLL4, CSL 65 (or RBPJκ), HRT1, and HRT2 elicit arterial cell fate [ 219 ]. Altered signaling from ALK1, notch, and TMem100 affects vascular smooth myocyte recruitment or differentiation during arterial maturation. In addition, activity of PKB and presenilin-1, which interacts with the notch pathway, are repressed in TMEM100 −∕− and Alk1 −∕− mouse embryos. The PKB kinase enhances PS1-mediated notch cleavage. Reciprocally, the PS1 peptidase provokes PKB activation. Altered presenilin-1 causes apoptosis via impaired PKB activity.
Synthesis of ALK1 depends on blood flow, which promotes the association of endoglin with ALK1, thus sensitizing endotheliocytes to low BMP9 concentrations [ 210 ]. In ALK1-deficient mice, arteriovenous malformation, enlarged veins, and hyperbranching of the capillary plexus in the retina are observed. Retinal arteriovenous malformations occur predominantly in regions of higher blood flow. In addition, endotheliocytes have a migratory phenotype. Although the pericyte coverage is normal at the migration front of the retina, there is less pericyte coverage in capillaries in the central region of the capillary plexus. Endotheliocytes of AVMs express the venous marker EPHb4, but loss of the arterial marker Jag1.
Endoglin-defective endotheliocytes are unable to sense and adapt to applied wall shear stress. This homodimeric glycoprotein of the vascular endothelium binds TGFβ1 with high affinity. It contributes to the regulation of angiogenesis, which involves tip cell selection, endotheliocyte proliferation and migration, mural cell recruitment, lumen formation, anastomosis, neovessel growth, and pruning.
Endoglin is linked to Tβ R3 encoded by the TGFBR3 gene that retains TGFβ for presentation to the signaling receptors. It acts as a TGFβ coreceptor, which is particularly implicated in BMP9 signaling in endotheliocytes.
Endoglin participates in the regulation of VEGFR2 signaling. Endoglin and VEGFR2 colocalize in intracellular vesicles. Endoglin affects VEGFR2 transfer and recycling and hence the balance between endotheliocyte proliferation and migration after VEGFa stimulation, favoring PKB activation. Furthermore, PKB phosphorylation promotes venous differentiation at the expense of arteriogenesis.
Hereditary hemorrhagic telangiectasia (HHT; or Osler–Weber–Rendu syndrome) and cerebral cavernous malformation (CCM) result from lowered and elevated signaling from the TGFβ/ BMP receptor complexes and sensitivity to messengers, respectively [ 210 ].
Endoglin cooperates with the component of the CCM pathway, which inhibits angiogenesis KRIT1 66 (or CCM1), and ALK1 (or HHT2). The CCM complex includes CCM1 (KRIT1), CCM2 (aka OSM 67 and malcavernin), and CCM3 (or PdCD10). 68
Loss-of-function mutations in the ENG and ACVRL1 genes provoke a defective regulation of processes involved in angiogenesis. Although LOF ENG mutations are linked to a mild hyperbranching phenotype, LOF ACVRL1 mutations favor tip cell potential and branching. Cells with LOF ENG mutations fail to adequately respond to migratory signals provided by the direction of blood flow [ 220 ].
Hereditary Hemorrhagic Telangiectasia
Hereditary hemorrhagic telangiectasia is an autosomal dominant disorder characterized by AVMs, capillary overgrowth, and fragile vessels in less than 2 in 10,000 individuals.
In AVMs, flow bypasses capillaries; blood flows directly from some arteries directly to veins; the latter then undergo higher stress and strain and thus enlarge (enlarged shunts).
Near the skin, they form telangiectasias , that is, focal dilations of postcapillary venules with excessive layers of vSMCs. Cutaneomucosal telangiectasias cause bleeding (epistaxis). AVMs occur in the lung, liver, and brain [ 190 ].
Several forms of HHT are distinguished mainly by their genetic cause rather than by differences in symptoms. Patients with type- I (HHT1) have symptoms earlier than those with type- II (HHT2) and more frequently present vascular malformations in the brain and lung. The prevalence of pulmonary AVMs is greater in HHT1 than in HHT2 [ 209 ].
Juvenile polyposis combined with HHT, that is, a syndrome characterized by both AVMs, which grow and regress during life, and polyps in the gastrointestinal tract, is caused by mutations in the Smad4 gene [ 190 ]. Two additional chromosomal loci, 5q31 and 7p14, are linked to other types, HHT3 and HHT4 [ 190 ].
Heterozygous LOF autosomal dominant mutations in the ENG 69 and Alk1 genes, which encodes two receptors of the TGFβ pathway that predominantly lodge on endotheliocytes, engender HHT1 and HHT2, respectively. Arteriovenous malformations are observed in the brain, spinal cord, lung, gastrointestinal tract, and liver.
In endotheliocytes, LOF mutations of the ENG gene, which encodes endoglin cause type-1 HHT (HHT1) favored by VEGFa, and arteriolar endotheliocytes acquire venous characteristics. Endotheliocytes overexpressing endoglin serve as tip cells, preferentially in the arterial compartment [ 220 ]. Deletion of the ENG gene alters VEGFa–VEGFR2 signaling but primes the PI3K–PKB axis.
Mutations in the ACVRL1 gene that encodes ALK1 are responsible for HHT2. Arterial endotheliocytes produce EfnB2, which participates in vascular development. Its concentration decreases in ACVRL1 −∕− mice. The ALK1 ligand BMP9 induces EfnB2 production in endotheliocytes via ALK1 and its coreceptors BMPR2 and AcvR2 [ 221 ].
BMP9 activates inhibitors of DNA binding ID1 and ID3 (bHLHb24–bHLHb25), both being required for EfnB2 formation [ 221 ]. Inhibitors of DNA binding heterodimerize with other ubiquitous or cell type-specific bHLH transcription factors, especially the class-1 bHLH transcriptional activators, E-proteins (TcFE2α [E2A or bHLHb21], TcF4 [E2-2 or bHLHb19], and TcF12 [HEB or bHLHb20]), but also effectors of ALK1 and notch signaling, HES1 (bHLHb39) and HRT1 (bHLHb31), thereby inhibiting their DNA binding. 70 Both ID1 and ID3 repress cell differentiation, but support cell proliferation [ 209 ]. In addition, IDs downstream from SMAD1 and SMAD5 promote stalk cell phenotype during angiogenesis, avoiding excessive tip cell formation.
Loss of ALK1 or EfnB2, which targets EPHb4 receptor involved in venous specification, causes arteriovenous anastomosis, whereas loss of ALK1 (but not EfnB2) upregulates VEGFR2 production and capillary sprouting. Conversely, BMP9 blocks endothelial sprouting via the ALK1–BMPR2–AcvR2 receptor complex in addition to ID1 and ID3 [ 221 ].
Several HHT markers encompass VEGF, TGFβ, soluble endoglin, angiopoietin-2, clotting factor F V III , and von Willebrand factor, in addition to microRNAs, such as miR27a, a proangiogenic microRNA, miR205, which reduces EC proliferation, migration, and tubulogenesis and inhibits SMAD1 and SMAD4, and miR210 [ 210 ].
The GJA5 gene that encodes the gap junction protein connexin-40 is targeted by the BMP9–ALK1 pathway in human aortic endotheliocytes and can explain heterogeneity and the severity of HHT2 [ 222 ]. In ACVRL1 +∕− mice that develop AVMs similar to those in HHT2 patients, GJA5 haploinsufficiency causes arterial vasodilation and rarefaction of the capillary bed. Reduced Cx40 concentration also provokes ROS production and hence vessel remodeling. Capillaries form transient arteriovenous shunts that can develop into large malformations upon stressor exposure.
Although some idiopathic AVMs are linked to elevated notch signaling (notch-1 and notch-4 in addition to Jag1 and DLL4), in HHT notch activity declines [ 209 ]. Both GOF and LOF notch signaling cause abnormal arterial and venous specification and hence fusion of arteries and veins. In adult mice, constitutively active notch-4 causes AVMs in the brain, liver, skin, and uterus, which can shrink upon removal of constitutively active notch-4. Endotheliocyte-specific constitutively active notch-1 also provokes AVMs.
In HHT patients, AVMs grow because of endotheliocyte proliferation, which enlarges the arteriovenous shunt, whereas idiopathic AVMs result from endotheliocyte hypertrophy [ 209 ]. A decayed notch signaling increases endotheliocyte proliferation and may at least partly explain vascular enlargement in HHT-related AVMs.
Cerebral Cavernous Malformations
Cerebral cavernous (or capillary venous) malformations consist of dilated capillary-like vessels ( cavernomas ) mixed with large saccular vessels with thickened walls in the cerebral parenchyma. Endotheliocytes lack tight junctions and are thus separated by gaps [ 190 ].
These disorders occur in a sporadic and familiar form with, in general, single and multiple lesions, respectively. They obey autosomal dominant inheritance; four chromosomal loci are implicated: (1) 7q11.22 with mutations in KRIT1 gene (Ccm1; ∼40% cases), (2) 7p13 with mutations in the Ccm2 gene (encoding malcavernin, a stabilizer of endotheliocyte junctions, also abbreviated CCM2), (3) 3q26.1 with mutations in the PDCD10 gene (Ccm3), and (4) 3q26.3–27.2 [ 190 ].
These disorders are pseudodominant diseases. Although patients are heterozygous for mutation in the Ccm genes, biallelic mutation of the Ccm genes is observed locally in lesions [ 210 ]. Biallelic Ccm mutation is also observed in lesions of patients with sporadic CCM.
Loss-of-function mutations of the KRIT1 gene, which encodes KrIT1 produced in neurons, astrocytes, various types of epitheliocytes, and in capillary and arteriolar endotheliocytes, engender hyperkeratotic cutaneous capillary venous malformations in addition to CCMs [ 190 ]. KrIT1 links to microtubules and interacts with integrin-β 1 -binding protein Itgβ1BP1, which participates in regulating cell adhesion and migration, thereby controlling EC fate. Conversely, Itgβ1BP1 can sequester KrIT1 in the nucleus. Malcavernin is able to sequester KrIT1 in the cytoplasm. PdCD10 may also be involved in the same pathway [ 190 ].
Gain-of-function mutations in any of the CCM genes exacerbate TGFβ/ BMP signaling, endothelial-to-mesenchymal transition, and ultimately cerebral cavernomas. Sustained exposure to TGFβ and subsequent KLF4-induced augmented formation of BMP2 and BMP6 dismantle cellular junctions, increase vascular permeability, and provoke hyperproliferation and acquisition of mesenchymal markers, creating AVMs and multilumen cavernomas [ 210 ].
The transcription factor KLF4 enables endothelial-to-mesenchymal transition. Both KLF2 and KLF4 are overexpressed early after ablation of any Ccm genes. Stimulation by BMPs in cultured human umbilical vein ECs upregulates KLF4 synthesis [ 210 ]. However, KLF4 can also be activated by the MAP3K3–MAP2K5–ERK5 pathway, which also stimulates the transcription factors MEF2a and MEF2c, upregulating KLF4 production. In addition, KLF4 can launch BMP6 formation, thereby establishing a positive feedback loop.
1 αιτιoλoγ𝜖ω: inquire into causes, reason, account for; αιτιoλoγια: giving the cause.
2 διαγιγνoσκω: know one from the other, distinguish, discern.
3 For example, abdominal obesity, diabetes mellitus, hypertension, smoking, unhealthy diet, regular alcohol consumption, lack of physical activity, and psychosocial factors, in addition to biological indices such as concentrations of total cholesterol and low-density lipoproteins, total cholesterol/high-density lipoprotein, and apolipoprotein ApoB/ApoA1 ratios.
4 GFR: growth factor receptor; MNAR: modulator of nongenomic action of the estrogen receptor. The coactivator of estrogen receptor-mediated transcription and corepressor of other nuclear hormone receptors (transcription factors) that facilitates NR3a1 nongenomic signaling via Src and PI3K is also called proline-, glutamate-, and leucine-rich protein PELP1. The plasmalemmal NR3a signalosome comprises G-protein subunits, receptor and nonreceptor protein Tyr kinases (e.g., Src), protein Ser/Thr kinases (PKB), lipid kinases (PI3K and PDK1), and scaffold proteins (MNAR, SHC, striatin) [ 39 ]. It interacts with several growth factor signaling components (e.g., EGFR and HGF-regulated protein Tyr kinase substrate (HRS)). It interacts with androgen (AR or NR3c4) and glucocorticoid receptor (GR or NR3c1) and thus influences nuclear receptor (NR) signaling.
5 Both NR3a1 and NR3a2 can activate Gα and Gβγ. Plasmalemmal NR3a monomers in the absence of sex steroids rapidly homodimerize upon estrogen exposure. These dimers can then associate with Gα and Gβγ subunits. Estradiol rapidly stimulates calcium entry via the TRPV6 channel [ 39 ].
6 Regulators of calcineurin RCan1, RCan2, and RCan3 are also termed calcipressin-1 to -3 in addition to modulatory (or myocyte-enriched) calcineurin-interacting proteins MCIP1 to MCIP3. The RCan protein binds to protein phosphatase PP3 in the cytoplasm, blocking its activity triggered by angiotensin-2 and other hypertrophic factors. Indeed, it prevents dephosphorylation of transcription factors of the NFAT family, sequestering them in the cytoplasm and impeding their nuclear translocation [ 39 ].
7 Connexin-37 forms gap junctions in myoendothelial communication between microvascular endothelial and smooth muscle cells. Its phosphorylated Tyr332 controls the gap junction-dependent spread of calcium signals. Nitric oxide precludes Tyr332 dephosphorylation by PTPn11 and hence Ca 2+ transfer induced by mechanical stimulation of endotheliocytes, but enhances Ca 2+ spreading within the endothelium, thereby boosting endothelium-dependent vasodilation in response to acetylcholine, even despite inhibition of soluble guanylate cyclase [ 41 ].
Translocator protein interacts with voltage-dependent anion channel (VDAC) and the adenine nucleotide translocase (ANT), comprising the mitochondrial permeability transition pore (MPTP), which lodges at contact sites between the OMM and the inner mitochondrial membrane (IMM) [ 44 ]. Tspo thus participates in mitochondrial cholesterol and protein import, cell proliferation, and apoptosis.
Translocator protein clusters owing to ATP and the cytosolic chaperone HSP90 and is imported as 66-kDa heteropolymers with metaxin-1, VDAC1, and nonspecific lipid-transfer protein [ 44 ]. At the OMM–IMM interface, Tspo forms 800-kDa mitochondrial complexes with VDAC1, VDAC3, ANT, ApoA1, ApoA2, fatty acid synthase, annexin-A2, and mitofilin.
The transduceosome is composed of the cytosolic proteins star, PKA, and acylCoA-binding domain-containing protein ACBD3 (Golgi complex-associated protein GoCAP11, Golgi body-resident protein GCP60, or peripheral benzodiazepine receptor [PBR]- and PKA-associated protein PAP7), and OMM proteins Tspo and VDAC1.
9 A sulfonate group (sulfur trioxide moiety [SO 3 − ]) can be transferred rather than a sulfate group (sulfation). Sulfation means that esters or salts of sulfuric acid (sulfates) are formed. Sulfonation refers to attachment of the sulfonic acid group (–SO 3 H) to a carbon in an organic compound by sulfotransferases using phosphoadenosine phosphosulfate as donor. However, sulfation is also defined either by the replacement of a hydrogen atom of an organic compound with a sulfate group (–OSO 2 OH) and sulfonation by the replacement of a hydrogen atom of an organic compound with a sulfonic acid group (–SO 3 H).
10 Takayasu arteritis affects arteries exiting from the heart and their main branches.
11 Behçet disease is characterized by ulcers of the mouth and genital organs, skin lesions, and ocular anomalies.
- In type-1 diabetes mellitus (T1DM), the body lacks pancreatic insulin-producing β cells. Patients with T1DM have a three- to five-fold elevated CVD risk [ 51 ].
- In type-2 diabetes mellitus (T2DM), which is more common and often develops later in life, cells fail to respond to insulin.
Diabetes insipidus is characterized by an impaired secretion of or response to vasopressin.
13 In autoimmune diseases, immunological tolerance of the body’s cells is lost and hence the immune system, which is aimed at identifying and destroying foreign invaders attacking target cells. A genetic susceptibility predisposes the immune system to defective immunological tolerance. The genetic marker HLAdr4 increases the risk for developing rheumatoid arthritis. An environmental trigger (e.g., viruses, smoking) initiates the disease. Angiogenesis participates in the genesis of rheumatoid arthritis and other inflammatory diseases.
14 Sjögren’s syndrome affects the lachrymal and salivary glands, thereby drying the mouth and eyes.
15 A rheumatic overlap syndrome with anti-RNP antibodies (i.e., abnormally high concentrations of antibodies against U1 small nuclear ribonucleoprotein) and characterized by arthritis and often myositis, pulmonary hypertension, and interstitial lung disease.
16 The reduced (G SH ) and oxidized glutathione (glutathione disulfide [G SS G]) redox couple is the traditional marker of oxidative stress. F2-isoprostanes serve as the reference marker of oxidative damage.
17 Myeloperoxidase abounds in granules of activated neutrophils, monocytes, and macrophages. It converts hydrogen peroxide to hydroxyl radical (OH • OH), peroxynitrite, hypochlorous acid (HOCl), and nitrogen dioxide (NO 2 • ).
18 Hypohalous acids are oxoacids of halogens (e.g., bromine [Br], chlorine [Cl], fluorine [F], and iodine [I]), such as hypobromous, hypochlorous, hypofluorous, and hypoiodous acid (general formula HOX, where X is the halogen atom). Hypohalites are any salts of hypohalous acids (general formula M(OX) N ).
19 Many types of peroxidases utilize sodium voltage-gated channels (SCNs), such as eosinophil (EPOx), gastric (GaPOx), salivary (SPOx; or secreted lactoperoxidase [LPOx]), and thyroid peroxidase (TPOx), in addition to MPOx. These enzymes generate HOSCN via a two-electron halogenation. Thiocyanate is detected at various concentrations (0.01–3 mmol/l) in extracellular fluids (plasma, saliva, airway surface fluid, milk, tears, and gastric juice) [ 77 ]. Airway SCN is concentrated from the plasma pool via its active transport through the basolateral sodium–iodide symporter (SLC5a5 or NIS) and apical anion channels, such as the cystic fibrosis transmembrane conductance regulator (CFTR) in addition to cytokine-regulated channels SLC26a4 (pendrin), an electroneutral halide exchanger, and anoctamin-1 (transmembrane protein TMem16a), a Ca 2+ -dependent Cl − channel and halide transporter [ 77 ]. The SCN originates primarily from the diet, especially from glucosidic cyanogen-rich plants (e.g., cassava, linseed, maize, sorghum, sugar cane, and yam). It is also a product of glucosinolate metabolism in addition to N-conjugated thiocyanates and structurally related isothiocyanates (e.g., sulforaphane) [ 77 ].
20 Catalytic turnover requires electron transfer from NADPH to the P450 heme iron, a reaction catalyzed by the membrane-bound flavoprotein, POR.
21 In particular, membrane-bound, heme-containing cytochrome-P450 epoxygenases metabolize polyunsaturated FAs such as arachidonic acid to epoxide products such as (14,15)EET.
22 Endothelial cytochrome-P450 monooxygenases, such as CyP1a, CyP2b6, CyP2c, and CyP2j, oxidize arachidonic acid, enzymatic cleavage of molecular oxygen being followed by insertion of a single atom of oxygen into the substrate, whereas the remainder is released as water. These enzymes regulate the vasomotor tone via produced epoxy FAs such as vasodilatory (11,12)EET [ 82 ].
23 Oxidation and reduction correspond to a loss and gain of electrons, respectively.
24 Also known as NADH cytochrome-B5 reductase-3.
25 The alias AXH stands for Ataxin-1 and HBP1 (HBP1: high-mobility–group box transcriptional repressor-1).
26 Also known as 17-kDa heparin-binding growth factor-binding protein HBP17.
27 Deubiquitinases can be categorized into six subsets: ubiquitin-specific peptidases (USPs); ubiquitin carboxy-terminal hydrolases (UCHs); ovarian tumor peptidases (OTus); MJD peptidases; JAMM/MPN domain-associated metallopeptidases (JAMMs); and monocyte chemotactic protein-induced protein (MCPIP).
28 TRP: transient receptor potential.
29 Also telangiectasis (plural telangiectases). From Greek τ𝜖λιωμα: completion; τ𝜖λo ς : end, term, achievement; αγγ𝜖ιoν: (hollow) vessel, vein; 𝜖κτασι ς : extension, dilation.
30 αθηρωμα: tumor full of gruel-like matter; σκληρo: hard. The Swiss scientist A. von Haller (1708–1777) described atherosclerosis in his book “Opuscula Pathologica” published in 1755. The German physician F. Marchand (1846–1928) introduced the term atherosclerosis in 1904.
Plaques with lipid-rich necrotic cores are one of the main causes of myocardial infarction. Low-density noncalcified plaque is the most relevant feature associated with ischemia in arteries with 30–69% stenoses [ 120 ]. Contrast density difference, which is defined as the maximum percentage difference in contrast attenuation between the stenosed lumen and proximal normal reference segment is used to predict ischemia, is the most relevant plaque feature associated with ischemia in stenoses equal to or larger than 70%.
Cushing disease results from benign ACTH-producing tumors of the pituitary gland that augments ACTH concentration, subsequently causing hypercortisolism. Surgical removal of ACTH-producing tumors of the pituitary gland engenders secondary adrenal insufficiency.
Adaptive activation of AMPK ensures adequate cardiac energy supply, as it raises fatty acid delivery via its activation of lipoprotein lipase (LPL), repositioning of the fatty acid transporter ScaRb3 to the plasma membrane, and inactivating phosphorylation of acetylCoA carboxylase, inhibiting carnitine palmitoyltransferase CPT1, which carries fatty acylCoA into the mitochondrion.
Activated cardiac NR1c1 elicits transcription of genes involved in various steps of fatty acid oxidation.
34 Astrocytes synthesize α1 and α2 subunits and most neurons α1 and α3 subunits.
35 Cartilage oligomeric matrix protein is an abundant component in the extracellular matrix of load-bearing organs, such as tendons, cartilage, and pericartilage tissues. It interacts with other matrix proteins, such as collagens and fibronectin, thereby stabilizing the matrix.
36 SRSF5 binds to intronic splicing sites within introns 10 and 11 of Cd44 pre-mRNA and recruits small nuclear ribonucleoproteins, forming mature spliceosomes (binary U1–U2 and ternary U4–U5–U6 complexes), which prime variant exon exclusion via double-exon skipping alternative splicing [ 147 ]. SRSF2 does not bind to the intron-10 and -11 region of Cd44 pre-mRNA but connects to the U1–U2 snRNP complex, promoting U1–U2 splicing initiation and mature trisnRNP U4–U5–U6 complex binding, thereby promoting the synthesis of standard Cd44 transcripts, which are translated into CD44s protein [ 147 ]. In the nucleus, Hyal2 counteracts SRSF5 action, displacing it from the early U1–U2 spliceosome and precluding the SRSF5-mediated formation of mature spliceosome and SRSF5 binding to intron 12 of the Cd44 pre-mRNA. In addition, Hyal2 may inhibit SRSF2 production and its interaction with Cd44 pre-mRNA.
37 KH domain-containing, RNA-binding, signal transduction-associated protein-1 is also termed 68-kDa Src-associated in mitosis protein (SAM68). It is activated by Ras and its effectors ERK1 and ERK2 [ 147 ], and favors profibrotic CD44v5 expression.
Calsequestrin is a major Ca 2+ buffer in the ER lumen that oligomerizes and interacts with the membrane-associated proteins junctin and triadin to control RyR activity [ 153 ].
Calmodulin associates with RyR at its cytoplasmic face; at high Ca 2+ concentrations, it inhibits both RyR1 and RyR2; at low Ca 2+ concentrations, it activates RyR1 but inhibits RyR2 [ 153 ]. According to [ 154 ], at nanomolar free Ca 2+ concentrations, although apoCam inhibits RyR2, it potentiates RyR1 and RyR3 activity; at micromolar ones, Ca 2+ –Cam inhibits all RyR isoforms. apoCam and Ca 2+ –CaM inhibit RyR2.
The adaptor homer-1C can activate RyR1 and inhibit RyR2 [ 153 ]. In addition, RyR is inhibited by Mg 2+ and activated by ATP, cytosolic dimeric Ca 2+ -binding S100a1, and NO, thereby potentiating Ca 2+ release.
39 This heteromeric pump consists of α and β subunits. Several cell-specific isoforms of these subunits exist (α1–α4 and β1–β3). In the human heart, α1 to α3 are expressed together with β1 and, to a lesser extent, β2 in a region-specific manner [ 156 ]. The α1 isoform is ubiquitous and participates in pumping and signaling and in cell survival, ROS generation, and cardiac hypertrophy and fibrosis [ 157 ]. The α2 isoform contributes to regulating intracellular Ca 2+ signaling and contractility in addition to adverse hypertrophy. The α3 isoform may be involved in cardiac hypertrophy. The expression of the α subunit is often altered in cardiac hypertrophy and failure.
On the other hand, NO reduces contractile response to adrenergic stimulation in heart failure, limits post-infarction remodeling, and protects against ischemia, at least partly via the NO–AC–cGMP–PKG–K ATP pathway [ 162 ].
41 Four related genes encode neuregulins (NRG1–NRG4), NRg1 being the most abundant member in the cardiovascular system. Alternative splicing at the C-terminus of the EGF domain of NRG1 leads to Nrg1α and Nrg1β variants, with distinct receptor affinity. Neuregulin-1 can be further subdivided into three types. Type- I Nrg1 is a type- I transmembrane protein, its active form being released after cleavage by adam17, adam19, or memapsin; type- II Nrg1 is also cleaved, generating an active ligand on secretion; and type- III Nrg1 is almost exclusively produced in neurons and binds to membranes.
Fatty acid-binding proteins facilitate FA transport in the cell for lipid oxidation in the mitochondrion or peroxisome, transcriptional regulation in the nucleus, membrane synthesis and trafficking in the endoplasmic reticulum, regulation of enzyme activity, and storage as lipid droplets in the cytoplasm [ 167 ].
The plasmalemmal PM FABP belongs to a distinct family of fatty acid-handling proteins. It is detected on the extracellular surface of cardiac and skeletal myocytes, hepatocytes, adipocytes, and endotheliocytes [ 168 ]. It also lodges in the mitochondrial membrane, acting as the glutamate oxaloacetate transaminase-2 (GOT2) and aspartate aminotransferase (AspAT).
Fatty acid-binding protein FABP4, both a nuclear and cytoplasmic protein, contributes to maintaining glucose and lipid homeostasis. FABP4 is not only produced in adipocytes and macrophages but also in endotheliocytes, in which VEGFa via VEGFR2 (but not VEGFR1) and FGF2 upregulate its synthesis [ 169 ]. Inhibition of FABP4 blocks most of the VEGFa effects [ 170 ]. the DLL4–notch couple triggers FABP4 synthesis using the transcription factor FoxO1, independently of VEGFa [ 170 ]. Hence, FoxO1 is needed for the basal expression of FABP4, whereas its upregulated proangiogenic formation relies on VEGFa or notch.
In fact, three FABPs are expressed in endotheliocytes (FABP3–FABP5). FABP3 is also synthesized in CMCs, renal epitheliocytes, and neurons of the brain; FABP4 in adipocytes and macrophages; and FABP5 in the heart, skeletal muscle, lung, and skin [ 168 ]. Adipocytic, macrophagic, and dendrocytic FABPs include FABP4 and FABP5 [ 167 ].
In adipocytes, FABP4 is a carrier protein for the transport of FAs generated by lipolysis from lipid droplets. β AR–AC–PKA and NPRa/GC–PKG pathways activate (trigger phosphorylation) of hormone-sensitive lipase (HSL or lipase-E), thereby priming lipolysis; FABP4 interacts with HSL [ 167 ]. In addition, FABP4 is secreted in association with lipolysis. Its plasmatic concentration decays after a meal with a high fat content, when the insulin concentration rises [ 167 ]. Insulin-induced antilipolytic signaling does indeed suppress FABP4 secretion. Furthermore, FABP4 serves as an adipokine that promotes hepatic glucose production, reduces CMC contraction in addition to NOS3 activity in vascular endotheliocytes, and supports the proliferation and migration of vascular smooth myocytes in addition to glucose-stimulated insulin secretion in pancreatic β cells.
In endotheliocytes, FABP4 promotes angiogenesis. Intermittent hypoxia increases FABP4 formation in endotheliocytes [ 167 ]. Conversely, angiopoietin-1 impedes FoxO1-mediated FABP4 synthesis. On the other hand, FABP4 and FABP5 may be involved in endotheliocyte senescence.
In the kidney, FABP4 is expressed in endotheliocytes of the peritubular capillaries and veins in both the cortex and medulla, but not in glomerular or arterial endotheliocytes [ 167 ]. Ectopic FABP4 expression in the glomerulus is associated with renal dysfunction.
In the lung, FABP4 is detected in endotheliocytes of peribronchial blood vessels and a subset of macrophages [ 167 ]. Interleukins IL4 and IL13 raise FABP4 production in bronchial epitheliocytes, whereas interferon-γ hampers it.
Fatty acids are then carried through the vascular endothelium to be used by cells. Three sets of proteins are implicated in lcFA ingress: (1) fatty acid transporter proteins (FATP1–FATP6) of the SLC27A group, which enable cellular lcFA uptake, (2) the scavenger receptor ScaRb3 (or fatty acid translocase), and (3) intracellular fatty acid-binding proteins (FABPs) Vascular endotheliocytes are endowed with FATP3 (SLC27a3), FATP4 (SLC27a4), ScaRb3, and FABP3 to FABP5, in addition to PM FABP, whereas FATP1 (SLC27a1) is produced in the heart, muscle, brown and white adipose tissue, kidney, and brain; FATP2 (SLC27a2) in the kidney, brown adipose tissue, and liver; FATP4 also in CMCs, adipocytes, hepatocytes, and keratinocytes; FATP5 (SLC27a5) in the liver; and FATP6 (SLC27a6) in the heart [ 168 ]. They are predominately located in the plasma membrane, Golgi body, and endoplasmic reticulum.
Vascular endothelia growth factor b (VEGFb), which binds specifically to VEGFR1 and neuropilin-1, regulates this transfer, as it controls the synthesis of endothelial FATPs [ 168 ]. In particular, paracrine signaling by VEGFb from cells to endotheliocytes triggers formation of the FATP3 and FATP4 subtypes.
Adipocytes store large quantities of lipids. On the other hand, excess lipid amount in other cell types causes metabolic dysfunction, intracellular FA accumulation impairing insulin signaling and glucose uptake, causing insulin resistance.
During fasting periods, FFAs are generated by lipolysis in the white adipose tissue and carried in the bloodstream bound to albumin.
44 GPIHBP1: glycosylphosphatidylinositol-anchored high-density lipoprotein-binding protein-1.
45 CDO: cell adhesion molecule-related/downregulated by oncogenes. It belongs to the set of immunoglobulin-like cell adhesion molecules. This suppressor of Wnt signaling promotes neuronal differentiation and development of the skeletal muscle via sonic hedgehog and cell adhesion signaling [ 173 ]. Upon CDO depletion, expression of axin-2, connexin-43, and collagen-1A is upregulated.
46 Intercalated discs of CMCs enable their synchronous contraction and support the mechanical load, as they anchor actin and intermediate filaments. They contain gap junctions that provide electrical coupling between adjacent CMCs, which are composed of connexin-43 (Cx43).
47 African–Americans are at a higher risk for CKD and hypertension than Americans without African ancestry, independently of socioeconomic and traditional clinical risk factors, owing to mutations in the APOL1 gene that encodes apolipoprotein-L1, a component of dense HDL3 [ 175 ]. Circulating ApoL1 can destroy the sub-Saharan African parasite Trypanosoma brucei, which is transmitted by the tsetse fly. However, Trypanosoma brucei gambiense and rhodesiense become resistant, as they produce a protein that neutralizes ApoL1. Nevertheless, 2 APOL1 gene variants (G1–G2) engender ApoL1 with a reduced affinity for the trypanosomal protein, thereby struggling against the parasite. Although African-Americans who are homozygous for either APOL1 variant and heterozygous are protected against African trypanosomiasis (or sleeping sickness), they are at an increased risk for renal disease. In any case, individuals with APOL1 risk variants do not carry a higher risk of CVD [ 176 ].
48 Thiosulfate, a sulfide donor, is one of the products formed during oxidative H 2 S metabolism that is used to treat CUA patients on dialysis. Thiosulfate modulates H 2 S metabolite levels and signaling. Under hypoxia, concentrations of reduced (G SH ) and oxidized glutathione (G SS G), and of free H 2 S and acid-labile sulfide, decrease in endotheliocytes [ 178 ]. Exogenous thiosulfate significantly diminishes the G SH / G SS ratio after short episodes of hypoxia but markedly raises this ratio after sustained hypoxia. Under both normoxia and hypoxia, thiosulfate represses VEGF-primed cystathionase expression, EC proliferation, and angiogenesis.
In humans, two types of MHC molecules, MHC I and MHC II , reside on the surface of cells, where they present peptides. Peptide binding in the endoplasmic reticulum is mediated by the chaperones tapasin and TAP-binding protein-related protein (TAPBPR) [ 180 , 181 ]. When these MHC-loaded peptides on antigen-presenting cells are antigenic, the resulting MHC I –peptide complexes, such as those on infected and cancerous cells, are recognized by effector cytotoxic CD8+ T lymphocytes, whereas MHC II –peptide complexes are detected by CD4+ T lymphocytes.
β2-Microglobulin serves as a marker for the activation of the cellular immunity, increased cell turnover, hematological cancers linked to the B-lymphocyte lineage, in addition to adverse cardiovascular outcomes in patients with carotid atherosclerosis [ 182 ]. Its concentration in blood also rises in chronic inflammation, hepatic and renal dysfunction, and some acute viral infections. After long-term dialysis, retention of this uremic toxin produces deposition of amyloid-like fibrils (dialysis-related amyloidosis).
50 Calcific aortic stenosis is characterized by large nodular calcific masses within the aortic cusps that protrude through the outflow surfaces into the sinuses of Valsalva, impeding normal leaflet opening [ 183 ]. Hemodynamic stress can activate latent transforming growth factor TGFβ1, a profibrotic agent that can induce calcification [ 184 ]. Signaling from Wnt and increased calcium concentration via the kallikrein–kinin axis are also involved in CAVD. The Wnt proteins interact with LDL receptors; β-catenins mediate osteoblastic transformation of valvular interstitial cells. Bone morphogenetic proteins BMP2 and BMP4 are produced by myofibroblasts and preosteoblasts adjacent to T-cell infiltrates, which form upon endothelial injury. Mutations in the transcriptional regulator notch-1 cause severe calcification owing to impaired repression of the transcription factor Runx2, an osteoblast stimulator.
51 A nevus is an abnormal benign tissular patch caused by a cellular overgrowth.
52 In 1958, W. B. Bean coined the term blue rubber nevus syndrome for its color and consistency [ 199 ], although nevi of the viscera were discovered in 1860 by M. Gascoyen [ 200 ].
53 TIE: protein Tyr kinase with immunoglobulin and epidermal growth factor homology domains.
54 αμαρτα ς : error; αμαρτημα and αμαρτια: failure, fault; the suffix “-oma” from -ωμα in medical terms meaning morbid growth, tumor (καρκινωμκ: cancer, chancre, sore, ulcer). A hamartoma is commonly a benign, focal malformation linked to disorganized tissular growth, which is made up of an abnormal mixture of cells normally found in the organ where it resides. For example, in the lung, hamartomas are composed of adipose, epithelial, and fibrous tissue and cartilage; pulmonary hamartomas are the most common benign tumors of the lung detected as solitary pulmonary nodules on medical images.
55 Π ρωτ𝜖υ ς : Proteus, the old God of the sea, Poseidon’s eldest son; πρωτιoν: chief rank, first place; πρωτιo ς : of the first quality. The Greek god Proteus, the ancient polymorphous creature, who can change his shape at will via manifold transformations. Proteus syndrome is an extremely variable condition involving atypical growth of the skin and skull observed in unrelated children.
56 NeK: never in mitosis gene-A (NIMA)-related kinase.
57 Iκ BKγ: inhibitor of NFκB (nuclear factor κ light chain enhancer of activated B cells) subunit-γ. The Iκ B kinase (IKK) complex is composed of three subunits IKKα, IKKβ, and IKKγ, which are encoded by conserved helix–loop–helix ubiquitous kinase (CHUK; also abbreviated as IKK1, IKKA, and IKBKA), IKBKB, and IKBKG gene, respectively.
58 RBPJκ: recombination signal-binding protein for immunoglobulin-κ J region, that is, suppressor of hairless (SuH) homolog. It is also called C promoter-binding factor CBF1, SuH, and LAG1 and is abbreviated CSL.
59 HES: hairy and enhancer of split (HES1–HES7 [bHLHb37–bHLHb43]).
60 HRT: HES-related transcription factor (HRT1–HRT3 [bHLHb31–bHLHb33]).
In humans, 20 SOX genes are categorized into several groups: SOXA (SRY); SOXB1 (Sox1–Sox3); SOXB2 (Sox14 and Sox21); SOXC (Sox4 and Sox11–Sox12); SOXD (Sox5–Sox6 and Sox13); SOXE (Sox8–Sox10); SOXF (Sox7 and Sox17–Sox18); SOXG (Sox15); and SOXH (Sox30) [ 205 , 206 ]. They are expressed by multiple types of progenitor and stem cells.
62 The cystine knot structural motif is contained in various types of peptides and proteins, such as ion channel blockers, hemolytic agents, and antiviral and antibacterial molecules. Three types of cystine knots exist: the growth factor cystine knot (GFCK), inhibitor cystine knot (ICK), and cyclic cystine knot (CCK). Norrin belongs to the GFCK category.
63 Transmembrane tumor endothelial markers TEM1, TEM5, TEM7, and TEM8 abound in tumoral vessels.
64 Type-1 activin receptor-like kinase ALK1 is also abbreviated AcvRL1 and HHT2, as LOF mutations in the ACVRL1 gene cause type-2 hereditary hemorrhagic telangiectasia.
65 CSL: C promoter-binding factor CBF1, suppressor of Hairless [SuH], and LAG1.
66 KRIT1: Kirsten sarcoma virus Ras-revertant [KRev]-interaction trapped protein-1 [Krev1 being Rap1a].
67 OSM: osmosensing scaffold for MAP3K3.
68 PdCD10: programmed cell death protein-10.
69 Eng: endoglin. The ENG gene resides in chromosomal locus 9q34.
70 HES1 binds to its own promoter, thereby preventing its synthesis and enabling proper loss of arterial identity in endotheliocytes. On the other hand, IDs preclude HES1 autoinhibition, but do not affect regulation of other HES1 target genes [ 209 ].
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 13 March 2024
The prevalence of cardiovascular disease risk factors among adults living in extreme poverty
- Pascal Geldsetzer ORCID: orcid.org/0000-0002-8878-5505 1 , 2 na1 ,
- Rebecca L. Tisdale ORCID: orcid.org/0000-0003-2749-6889 3 , 4 na1 ,
- Lisa Stehr ORCID: orcid.org/0009-0009-4445-6150 5 ,
- Felix Michalik ORCID: orcid.org/0000-0001-5589-5700 1 , 5 ,
- Julia Lemp ORCID: orcid.org/0000-0002-1524-3641 5 ,
- Krishna K. Aryal ORCID: orcid.org/0000-0003-0801-0775 6 ,
- Albertino Damasceno ORCID: orcid.org/0000-0003-0925-494X 7 ,
- Corine Houehanou 8 ,
- Jutta Mari Adelin Jørgensen 9 ,
- Nuno Lunet ORCID: orcid.org/0000-0003-1870-1430 7 ,
- Mary Mayige ORCID: orcid.org/0000-0003-4861-7870 10 ,
- Sahar Saeedi Moghaddam 11 ,
- Kibachio Joseph Mwangi ORCID: orcid.org/0000-0003-3725-1762 12 ,
- Christian Bommer 5 , 13 ,
- Maja-Emilia Marcus ORCID: orcid.org/0000-0003-4904-2087 13 , 14 ,
- Michaela Theilmann ORCID: orcid.org/0000-0003-3413-232X 5 ,
- Cara Ebert ORCID: orcid.org/0000-0002-5542-8712 15 ,
- Rifat Atun ORCID: orcid.org/0000-0002-1531-5983 16 , 17 ,
- Justine Ina Davies ORCID: orcid.org/0000-0001-6834-1838 18 , 19 , 20 ,
- David Flood 21 ,
- Jennifer Manne-Goehler 22 , 23 ,
- Jacqueline Seiglie 24 , 25 ,
- Till Bärnighausen 5 , 26 na2 &
- Sebastian Vollmer ORCID: orcid.org/0000-0002-7863-0462 13 , 14 na2
Nature Human Behaviour ( 2024 ) Cite this article
277 Accesses
151 Altmetric
Metrics details
- Cardiovascular diseases
- Development studies
- Human behaviour
- Risk factors
Evidence on cardiovascular disease (CVD) risk factor prevalence among adults living below the World Bank’s international line for extreme poverty (those with income <$1.90 per day) globally is sparse. Here we pooled individual-level data from 105 nationally representative household surveys across 78 countries, representing 85% of people living in extreme poverty globally, and sorted individuals by country-specific measures of household income or wealth to identify those in extreme poverty. CVD risk factors (hypertension, diabetes, smoking, obesity and dyslipidaemia) were present among 17.5% (95% confidence interval (CI) 16.7–18.3%), 4.0% (95% CI 3.6–4.5%), 10.6% (95% CI 9.0–12.3%), 3.1% (95% CI 2.8–3.3%) and 1.4% (95% CI 0.9–1.9%) of adults in extreme poverty, respectively. Most were not treated for CVD-related conditions (for example, among those with hypertension earning <$1.90 per day, 15.2% (95% CI 13.3–17.1%) reported taking blood pressure-lowering medication). The main limitation of the study is likely measurement error of poverty level and CVD risk factors that could have led to an overestimation of CVD risk factor prevalence among adults in extreme poverty. Nonetheless, our results could inform equity discussions for resource allocation and design of effective interventions.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
111,21 € per year
only 9,27 € per issue
Rent or buy this article
Prices vary by article type
Prices may be subject to local taxes which are calculated during checkout
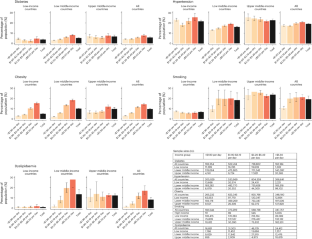
Similar content being viewed by others
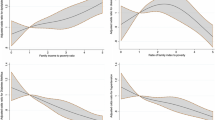
Family income and cardiovascular disease risk in American adults
Abdul Mannan Khan Minhas, Vardhmaan Jain, … Anurag Mehta
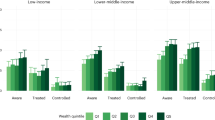
Hypertension care cascades and reducing inequities in cardiovascular disease in low- and middle-income countries
Dorit Talia Stein, Marissa B. Reitsma, … Stéphane Verguet

Disparities in absolute cardiovascular risk, metabolic syndrome, hypertension, and other risk factors by income within racial/ethnic groups among middle-aged and older US people
Gulam Muhammed Al Kibria, Reese Crispen, … Christina Stennett
Data availability
This study includes individual-level data from 105 surveys. Data are publicly available for 102 of these surveys. For data that are not publicly accessible and for which we have arranged specific data-use agreements, we are unable to share these data given the terms of our agreements.
Code availability
All data management and analysis code have been posted in a public repository available at https://github.com/LisaStehr/CVD-risk-factors-among-bottom-billion/tree/main . We calculated average marginal effects of Poisson regression models using R (v.4.1.3) margins package using complex survey design, with documentation available at https://cran.r-project.org/web/packages/margins/vignettes/Introduction.html .
Zuccala, E. & Horton, R. Reframing the NCD agenda: a matter of justice and equity. Lancet 396 , 939–940 (2020).
Article CAS PubMed PubMed Central Google Scholar
Yach, D., Hawkes, C., Gould, C. L. & Hofman, K. J. The global burden of chronic diseases: overcoming impediments to prevention and control. J. Am. Med. Assoc. 291 , 2616–2622 (2004).
Article CAS Google Scholar
Banerjee, A. V. & Duflo, E. The economic lives of the poor. J. Econ. Perspect. 21 , 141–168 (2007).
Article PubMed PubMed Central Google Scholar
Subramanian, S. & Deaton, A. The demand for food and calories. J. Political Econ. 104 , 133–162 (1996).
Article Google Scholar
Akhter, U. A. et al. The World’s Most Deprived: Characteristics and Causes of Extreme Poverty and Hunger (International Food Policy Research Institute, 2007).
Hickel, J. The true extent of global poverty and hunger: questioning the good news narrative of the Millennium Development Goals. Third World Q. 37 , 749–767 (2016).
Svedberg, P. Poverty and Undernutrition: Theory, Measurement and Policy (Oxford Univ. Press, 2000).
Wanyama, R. N. Food security and dietary patterns among the urban poor in Africa . PhD thesis, Georg-August-University Göttingen (2019); https://doi.org/10.53846/goediss-7447
Hassen, I. W., Dereje, M., Minten, B. & Hirvonen, K. Diet Transformation in Africa: The Case of Ethiopia (International Food Policy Research Institute, 2016).
Daily meat consumption per person (Our World in Data, accessed 14 July 2022); https://ourworldindata.org/grapher/daily-meat-consumption-per-person
Share of energy from cereals, roots and tubers vs. GDP per capita (Our World in Data, accessed 14 July 2022); https://ourworldindata.org/grapher/share-of-energy-from-cereals-roots-and-tubers-vs-gdp-per-capita
Gindling, T. H. & Newhouse, D. Self-employment in the developing world. World Dev. 56 , 313–331 (2014).
Collins, D., Morduch, J., Rutherford, S. & Ruthven, O. Portfolios of the Poor: How the World’s Poor Live on $2 a Day (Princeton Univ. Press, 2009); https://doi.org/10.1515/9781400829965
Roth, G. A. et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J. Am. Coll. Cardiol. 76 , 2982–3021 (2020).
Allen, L. et al. Socioeconomic status and non-communicable disease behavioural risk factors in low-income and lower-middle-income countries: a systematic review. Lancet Glob. Health 5 , e277–e289 (2017).
Williams, J. et al. A systematic review of associations between non-communicable diseases and socioeconomic status within low- and lower-middle-income countries. J. Glob. Health 8 , 020409 (2018).
Article ADS PubMed PubMed Central Google Scholar
Rosengren, A. et al. Socioeconomic status and risk of cardiovascular disease in 20 low-income, middle-income and high-income countries: the Prospective Urban Rural Epidemiologic (PURE) study. Lancet Glob. Health 7 , e748–e760 (2019).
Article PubMed Google Scholar
Gupta, R. et al. Socioeconomic factors and use of secondary preventive therapies for cardiovascular diseases in South Asia: the PURE study. Eur. J. Prev. Cardiol. 22 , 1261–1271 (2015).
Steinert, J. I., Cluver, L. D., Melendez-Torres, G. J. & Vollmer, S. One size fits all? The validity of a composite poverty index across urban and rural households in South Africa. Soc. Indic. Res. 136 , 51–72 (2018).
Poverty and Shared Prosperity 2018: Piecing Together the Poverty Puzzle (World Bank, 2018); http://elibrary.worldbank.org/doi/epdf/10.1596/978-1-4648-1330-6
Goyal, A. et al. Attained educational level and incident atherothrombotic events in low- and middle-income compared with high-income countries. Circulation 122 , 1167–1175 (2010).
Yu, Z. Changes in cardiovascular risk factors in different socioeconomic groups: seven year trends in a Chinese urban population. J. Epidemiol. Community Health 54 , 692–696 (2000).
Reddy, K. S. et al. Educational status and cardiovascular risk profile in Indians. Proc. Natl Acad. Sci. USA 104 , 16263–16268 (2007).
Article CAS ADS PubMed PubMed Central Google Scholar
Shavers, V. L. Measurement of socioeconomic status in health disparities research. J. Natl Med. Assoc. 99 , 1013–1023 (2007).
PubMed PubMed Central Google Scholar
Fomba, B. K., Talla, D. N. D. F. & Ningaye, P. Institutional quality and education quality in developing countries: effects and transmission channels. J. Knowl. Econ . 14 , 86–115 (2022).
Altinok, N., Angrist, N. & Patrinos, H. A. Global Data Set on Education Quality (1965–2015) (World Bank, 2018); https://doi.org/10.1596/1813-9450-8314
Poverty Headcount Ratio at $1.90 a Day (2011 PPP) (% of Population) (World Bank, accessed 10 May 2022); https://data.worldbank.org/indicator/SI.POV.DDAY
Population, Total (World Bank, accessed 10 May 2022); https://data.worldbank.org/indicator/SP.POP.TOTL
Bukhman, G. et al. The Lancet NCDI Poverty Commission: bridging a gap in universal health coverage for the poorest billion. Lancet 396 , 991–1044 (2020).
Member HDSSs. INDEPTH Network http://www.indepth-network.org/member-centres
Bukhman, G., Mocumbi, A. O. & Horton, R. Reframing NCDs and injuries for the poorest billion: a Lancet Commission. Lancet 386 , 1221–1222 (2015).
Chomistek, A. K. et al. Healthy lifestyle in the primordial prevention of cardiovascular disease among young women. J. Am. Coll. Cardiol. 65 , 43–51 (2015).
Heath, L., Jebb, S. A., Aveyard, P. & Piernas, C. Obesity, metabolic risk and adherence to healthy lifestyle behaviours: prospective cohort study in the UK Biobank. BMC Med. 20 , 65 (2022).
Di Cesare, M. et al. Inequalities in non-communicable diseases and effective responses. Lancet 381 , 585–597 (2013).
Kruk, M. E. et al. High-quality health systems in the Sustainable Development Goals era: time for a revolution. Lancet Glob. Health 6 , e1196–e1252 (2018).
Srinivas, A., Jalota, S., Mahajan, A. & Miller, G. Illness and wage loss: longitudinal evidence from India (and Implications for the Universal Health Coverage Agenda). Preprint at medRxiv https://doi.org/10.1101/2021.11.04.21265892 (2021).
Yusuf, S. et al. Cardiovascular risk and events in 17 low-, middle- and high-income countries. N. Engl. J. Med. 371 , 818–827 (2014).
Article CAS PubMed Google Scholar
Dieleman, J. L. et al. Sources and focus of health development assistance, 1990–2014. J. Am. Med. Assoc. 313 , 2359–2368 (2015).
Chang, A. Y. et al. Past, present and future of global health financing: a review of development assistance, government, out-of-pocket and other private spending on health for 195 countries, 1995–2050. Lancet 393 , 2233–2260 (2019).
World Population Prospects 2022 (United Nations Department of Economic and Social Affairs, 2022); https://population.un.org/wpp/Download/Standard/Population/
Howe, L. D. et al. Measuring socio-economic position for epidemiological studies in low- and middle-income countries: a methods of measurement in epidemiology paper. Int. J. Epidemiol. 41 , 871–886 (2012).
Alkire, S., Kanagaratnam, U., & Suppa, N. Global Multidimensional Poverty Index 2021: Unmasking Disparities by Ethnicity, Caste and Gender (OPHI & UNDP, 2021); https://ora.ox.ac.uk/objects/uuid:ce6a7338-9c0f-46e6-bbbd-2743e95563cb/files/s5q47rp795
Whelton, P. K. et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation and management of high blood pressure in adults: a report of the American College of Cardiology/American heart association task force on clinical practice guidelines. Hypertension 71 , 1269–1324 (2018).
American Diabetes Association. Professional Practice Committee. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes—2022. Diabetes Care 45 , S17–S38 (2021).
World Bank Country and Lending Groups—World Bank Data Help Desk (World Bank, accessed 6 May 2022); https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups
Unger, T. et al. International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension 75 , 1334–1357 (2020).
Sacks, D. B. et al. Guidelines and recommendations for laboratory analysis in the diagnosis and management of diabetes mellitus. Clin. Chem. 57 , e1–e47 (2011).
Definition and Diagnosis of Diabetes Mellitus and Intermediate Hyperglycaemia: Report of a WHO/IDF Consultation (World Health Organization & International Diabetes Federation, 2006).
Obesity: Preventing and Managing the Global Epidemic: Report of a WHO Consultation (WHO, 2000).
Friedewald, W. T., Levy, R. I. & Fredrickson, D. S. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin. Chem. 18 , 499–502 (1972).
National Cholesterol Education Program E. Detection, Evaluation and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III)—Final Report (National Institutes of Health, 2001); https://www.nhlbi.nih.gov/files/docs/resources/heart/atp-3-cholesterol-full-report.pdf
Ahmad, O. B., Boschi-pinto, C., Lopez, A. D., Lozano, R. & Inoue, M. Age Standardization of Rates: A New WHO Standard (WHO, 2009).
WHO Package of Essential Noncommunicable (PEN) Disease Interventions for Primary Health Care (WHO, 2020); https://www.who.int/publications/i/item/9789240009226
The WHO CVD Risk Chart Working Group. World Health Organization cardiovascular disease risk charts: revised models to estimate risk in 21 global regions. Lancet Glob. Health 7 , e1332–e1345 (2019).
Poverty Headcount Ratio at $3.20 a day (2011 PPP) (% of population) (World Bank, accessed 19 July 2022); https://data.worldbank.org/indicator/SI.POV.LMIC
Poverty Headcount Ratio at $5.50 a day (2011 PPP) (% of population) (World Bank, accessed 19 July 2022); https://data.worldbank.org/indicator/SI.POV.UMIC
World Development Indicators. GDP per capita, PPP (constant 2011 international $) (World Bank, accessed 19 May 2022); https://data.worldbank.org/indicator/NY.GDP.PCAP.PP.KD
Poverty Gap at $1.90 a Day (2011 PPP) (%) (World Bank, accessed 18 July 2022); https://data.worldbank.org/indicator/SI.POV.GAPS
Download references
Acknowledgements
We would like to thank all participants in the household surveys that have been harmonized and analysed in this study. The authors received no specific funding for this work.
Author information
These authors contributed equally: Pascal Geldsetzer, Rebecca L. Tisdale.
These authors jointly supervised this work: Till Bärnighausen, Sebastian Vollmer.
Authors and Affiliations
Department of Medicine, Division of Primary Care and Population Health, Stanford University School of Medicine, Stanford, CA, USA
Pascal Geldsetzer & Felix Michalik
Chan Zuckerberg Biohub – San Francisco, San Francisco, CA, USA
Pascal Geldsetzer
Veterans Affairs Palo Alto Health Care System, Palo Alto, CA, USA
Rebecca L. Tisdale
Department of Medicine, Stanford University School of Medicine, Stanford, CA, USA
Heidelberg Institute of Global Health, Faculty of Medicine and University Hospital, Heidelberg University, Heidelberg, Germany
Lisa Stehr, Felix Michalik, Julia Lemp, Christian Bommer, Michaela Theilmann & Till Bärnighausen
Department for International Development/Nepal Health Sector Programme 3/Monitoring Evaluation and Operational Research, Abt Associates, Kathmandu, Nepal
Krishna K. Aryal
Department of Public and Forensic Health Sciences and Medical Education, Faculty of Medicine, University of Porto, Porto, Portugal
Albertino Damasceno & Nuno Lunet
Laboratory of Epidemiology of Chronic and Neurological Diseases, Faculty of Health Sciences, University of Abomey-Calavi, Cotonou, Benin
Corine Houehanou
Institute of Global Health, Dept of Public Health and Epidemiology, Copenhagen University, Copenhagen, Denmark
Jutta Mari Adelin Jørgensen
National Institute for Medical Research, Dar es Salaam, Tanzania
Mary Mayige
Non-Communicable Diseases Research Center, Endocrinology and Metabolism Population Sciences Institute, Tehran University of Medical Sciences, Tehran, Iran
Sahar Saeedi Moghaddam
Division of Non-Communicable Diseases, Ministry of Health, Nairobi, Kenya
Kibachio Joseph Mwangi
Centre for Modern Indian Studies, University of Goettingen, Göttingen, Germany
Christian Bommer, Maja-Emilia Marcus & Sebastian Vollmer
Department of Economics, University of Goettingen, Göttingen, Germany
Maja-Emilia Marcus & Sebastian Vollmer
RWI-Leibniz Institute for Economic Research, Essen (Berlin Office), Berlin, Germany
Department of Global Health and Population, Harvard T. H. Chan School of Public Health, Boston, MA, USA
Department of Global Health and Social Medicine, Harvard Medical School, Harvard University, Boston, MA, USA
Institute of Applied Health Research, University of Birmingham, Birmingham, UK
Justine Ina Davies
MRC/Wits Rural Public Health and Health Transitions Research Unit, School of Public Health, University of the Witwatersrand, Johannesburg, South Africa
Centre for Global Surgery, Department of Global Health, Stellenbosch University, Cape Town, South Africa
Division of Hospital Medicine, Department of Medicine, University of Michigan, Ann Arbor, MI, USA
David Flood
Division of Infectious Diseases, Brigham and Women’s Hospital, Boston, MA, USA
Jennifer Manne-Goehler
Medical Practice Evaluation Center, Massachusetts General Hospital, Harvard Medical School, Boston, MA, USA
Diabetes Unit, Massachusetts General Hospital, Boston, MA, USA
Jacqueline Seiglie
Department of Medicine, Harvard Medical School, Boston, MA, USA
Harvard Center for Population and Development Studies, Cambridge, MA, USA
Till Bärnighausen
You can also search for this author in PubMed Google Scholar
Contributions
P.G., R.L.T., R.A., T.B. and S.V. conceived this work. P.G., L.S., F.M., J.L., K.K.A., A.D., C.H., J.M.A.J., N.L., M.M., S.S.M., K.J.M., C.B., M.E.M., M.T., C.E., J.I.D., D.F., J.M.G., J.S., T.B. and S.V. were involved in data curation. P.G., L.S., F.M. and J.L. undertook formal analysis. P.G., L.S., F.M., J.L., M.E.M., T.B. and S.V. developed the methodology. P.G., L.S. and F.M. undertook visualization. P.G., R.L.T. and L.S. wrote the original draft. P.G., R.L.T., L.S., F.M., J.L., K.K.A., A.D., C.H., J.M.A.J., N.L., M.M., S.S.M., K.J.M., C.B., M.E.M., M.T., R.A., J.I.D., D.F., J.M.G., J.S., T.B. and S.V. were involved in reviewing and editing the final paper.
Corresponding author
Correspondence to Pascal Geldsetzer .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Peer review
Peer review information.
Nature Human Behaviour thanks Anthony Etyang, Rajeev Gupta, Aditya Khetan, Vahé Nafilyan and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Peer reviewer reports are available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information.
Supplementary Figs. 1–28, Methods 1–5, Tables 1–54 and References.
Reporting Summary
Peer review file, rights and permissions.
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cite this article.
Geldsetzer, P., Tisdale, R.L., Stehr, L. et al. The prevalence of cardiovascular disease risk factors among adults living in extreme poverty. Nat Hum Behav (2024). https://doi.org/10.1038/s41562-024-01840-9
Download citation
Received : 03 November 2022
Accepted : 24 January 2024
Published : 13 March 2024
DOI : https://doi.org/10.1038/s41562-024-01840-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

IMAGES
VIDEO
COMMENTS
A cardiovascular disease (CVD) is defined as any illness that attacks the heart, brain, kidney or peripheral arteries of the cardiovascular system (Cooper et al, 2000). In all types of cardiovascular diseases, there is the involvement of the blood vessels. The blood vessels in the circulatory system include the arteries, capillaries and veins.
Published: Nov 16, 2018. A group of diseases that affects the heart, blood flow and circulatory system are defined as cardiovascular diseases (CVD). The common types of CVD are: Coronary heart disease, Stroke, Heart failure, high blood pressure. Cardiovascular health is affected by extensive smoking, leading sedentary lifestyle, malnutrition ...
Cardiovascular Disease essay example for your inspiration. ️ 1115 words. Read and download unique samples from our free paper database. ... circulations of blood and the heart. Examples of cardiovascular diseases include heart attack, angina, stroke, coronary heart disease, and congenital heart disease. ...
Cardiovascular Disease in Middle Aged Individuals in a Worksite Setting. Cardio-vascular disease (CVD) is the leading cause of death and leads the statistics for emergency room (ER) cases. This literature review combines two primary causative agents in CVD: (1) Stress in the workplace, and (2) Middle Age.
Cardiovascular disease is defined as a group of disorders damaging the heart and blood vessels, usually involving the blockage of vessels, which in turn harm the heart (WHO, 2015). A 2011 American Heart Association statement predicted that without intervention, 40% of United States adults will have at least one form of Cardiovascular disease.
Cardiovascular disease (CVD) is the leading cause of non-communicable disease deaths worldwide (World Health Organization, 2014). The World Health Organization predicts that the number of deaths caused by CVD will reach 23.3 million by 2030. CVD is an umbrella term that encompasses a group of disorders of the heart and blood vessels.
Heart disease, also known as cardiovascular disease, is a condition in which the blood vessels can become either narrowed or blocked (BHL Center, 2015). Some examples of cardiovascular diseases are: stroke, heart attack, high blood pressure, and heart failure. Cardiovascular disease is
The Importance of Heart Diseases. Heart disease is a prevalent and serious health issue that affects millions of people worldwide. It is one of the leading causes of death globally, and its impact on individuals, families, and societies is significant. In this essay, we will explore the importance of heart diseases, including their prevalence ...
The Coronary Heart Disease National Service Framework. By the mid 1980s, it had been generally accepted by most clinicians that there was strong evidence to support the existence of a linear relationship between cholesterol levels and cardiac mortality (Shaper et al. 1985, Stamler et al. 1986), and that therefore lowering total cholesterol levels would reduce the risk of individuals developing ...
Essay Sample: Through cohort study designs and other evidence-based management studies, identify the major causes of CVD, and analyze the key steps, including current ... The understanding of the pathophysiology of many cardiovascular diseases is evolving rapidly, especially atherosclerosis, hypertension, myocardial, ischemia, and congestive ...
What causes cardiovascular disease? The causes of cardiovascular disease can vary depending on the specific type. For example, atherosclerosis (plaque buildup in your arteries) causes coronary artery disease and peripheral artery disease. Coronary artery disease, scarring of your heart muscle, genetic problems or medications can cause arrhythmias.
Get original essay. However, there are modifiable risks factors that patients are able to control. For instance tobacco use, physical inactivity, stress, obesity, stress, high blood pressure and high cholesterol. Smoking cigarettes play a significant role in the development of CVD, according to the CDC smoking cigarettes increases the chances ...
Heart Disease - Free Essay Examples and Topic Ideas. Heart disease refers to a range of conditions that affect the heart's ability to function properly. These conditions may include issues with the heart's blood vessels, valves, or rhythm. Heart disease is a leading cause of death worldwide, and common risk factors include a poor diet, lack ...
Cardiovascular disease (CVD) is a collective term designating all types of affliction affecting the blood circulatory system, including the heart and vasculature, which, respectively, displaces and conveys the blood. This multifactorial disorder encompasses numerous congenital and acquired maladies. CVD represents the leading noncommunicable cause of death in Europe (∼50% of all deaths; ∼ ...
Cardiovascular Disease. The term "heart disease" is often used interchangeably with the term "cardiovascular disease." Cardiovascular disease generally refers to conditions that involve narrowed or blocked blood vessels that can lead to a heart attack, chest pain (angina) or stroke. Other heart conditions, such as those that affect your heart ...
6 percent are reported to have coronary heart disease. (Statistical Fact Sheet - Populations, 2003) Cardiovascular disease is actually a process, comprising of a number of factors, the continuity of which eventually lead to its incidence. Among several, a few are: high blood pressure, tobacco consumption, physical inactivity, and overweight ...
Evidence on cardiovascular disease (CVD) risk factor prevalence among adults living below the World Bank's international line for extreme poverty (those with income <$1.90 per day) globally is ...
In basic terms, a person with a BMI of above 30 is considered obese. According to the National heart, Lung, and Blood Institute (2019), "the higher your BMI, the higher your risk for certain disease such as heart disease, high blood pressure, type 2 diabetes.". Also, in as far as waist circumference is concerned, the patient's waist size ...