- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board

What to Know About Metoidioplasty (Bottom Surgery)
- Who Qualifies?
- Surgical Techniques
- Neophallus Function
- Surgery Follow-Up
- Where to Have Surgery
Metoidioplasty , or "bottom surgery," is a gender-affirming surgical procedure that involves creating a neophallus (new penis) from a hormonally enlarged clitoris . Transgender men and transmasculine people assigned female at birth (AFAB) may elect for a metoidioplasty if they want their genital appearance to align with their gender identity.
In contrast to the more complex phalloplasty that involves several surgeries, metoidioplasty offers a more straightforward phallic reconstruction in one procedure.
During a metoidioplasty, a surgeon cuts the ligaments that connect the clitoris to the pubic bone to release the clitoris and create a penis with erogenous (sexual) sensations. It may also include additional steps, such as urethral lengthening and scrotoplasty (forming a scrotum), to enhance the appearance and functionality of the neophallus.
This article explores metoidioplasty surgical techniques, the recovery process, and what to expect post-surgery.
CarlosDavid.org / Getty Images
Who Qualifies for Metoidioplasty Surgery?
Metoidioplasty is a gender-affirming (sex-reassignment) surgery for transgender men assigned female at birth. According to the 2015 U.S. Transgender Survey, about 4% of trans men have undergone the procedure, while another 53% expressed a desire to undergo metoidioplasty in the future.
The World Professional Association for Transgender Health (WPATH) developed the criteria for gender reaffirmation surgeries to ensure optimal physical and psychological outcomes for those pursuing bottom (genital) surgeries. The eligibility criteria for metoidioplasty include the following:
- Ongoing and well-documented gender dysphoria
- The ability to make informed decisions and provide consent for treatment
- Being 18 years of age or older
- Medical or mental health concerns are well-managed (if applicable)
- At least 12 consecutive months of gender-affirming testosterone therapy
- Living as a male or masculine-presenting person for at least one year in all settings (e.g., work, school, with family members and community)
Though it is not required, regular visits with a mental health or other medical professional are highly recommended before undergoing a metoidioplasty.
Metoidioplasty Surgical Techniques
People can choose a few different metoidioplasty surgical techniques depending on their preferences. Other procedures can occur simultaneously (e.g., hysterectomy) if desired.
Simple Release Metoidioplasty
In the simple release procedure, ligaments attached to the pubic bone are cut and released, and the clitoris is separated from surrounding tissue to enhance the position and visibility of the clitoris. The labia minora are wrapped around the clitoris to create the glans (head) of the newly formed penis.
Ring Metoidioplasty
Similar to the simple release, this technique involves releasing the clitoral ligaments to lengthen the clitoris. This procedure also involves lengthening the urethra using a flap of tissue from the vaginal wall and labia minora. This procedure gives trans men a micropenis with more girth and the ability to stand while urinating.
Belgrade (Full) Metoidioplasty
The Belgrade technique, or full metoidioplasty, involves the removal of the vagina (vaginectomy) and releasing the clitoris to lengthen and straighten the clitoris. The urethra is lengthened using vaginal tissue and buccal mucosa (inner cheek) skin grafts. The penis is reconstructed with the remaining clitoral and labial skin to give it more girth.
Then, the labia minor flaps are joined to create a scrotum (scrotoplasty), and testicular implants may be inserted into the newly created scrotum. A penile pump or vacuum is recommended three weeks post-surgery to lengthen the neophallus and prevent retraction.
Simultaneous Procedures
In addition to metoidioplasty, some trans men may opt for additional procedures performed at the same time to achieve their desired outcomes. These procedures may include:
- Hysterectomy : Removal of the uterus
- Bilateral salpingo-oophorectomy : Removal of the ovaries and fallopian tubes
- Vaginectomy : Removal of the vagina and surrounding tissues
- Scrotoplasty : Forms a new scrotum; testicular implants may be placed to give the appearance of natural testicles
- Erectile implant : A device is placed inside the neophallus to help achieve erections
Metoidioplasty vs. Phalloplasty
Metoidioplasty and phalloplasty are surgical options for transgender men seeking gender-affirming genital reconstruction. Metoidioplasty involves using existing genital tissue, such as the hormonally enlarged clitoris, to create a neophallus. It usually results in a smaller but functional neophallus.
Phalloplasty involves constructing a neophallus using various techniques, including grafting tissue from other body parts. This procedure can provide a larger and more visually realistic phallus but is more complex and may require multiple stages. The choice between metoidioplasty and phalloplasty depends on individual preferences, desired outcomes, and considerations such as surgical risk, recovery time, and aesthetic goals.
Risks to Understand Before Metoidioplasty
While metoidioplasty is generally considered safe, like any surgical intervention, it carries certain risks. Before undergoing metoidioplasty, discuss the risks with a healthcare provider to gain a comprehensive understanding and make an informed decision.
Potential risks include:
- Urethral stricture or stenosis : Narrowing of the urethral passage, leading to difficulty with urination and potential obstruction of urine flow. Sometimes, urine flow may be blocked entirely, requiring surgery to correct the problem.
- Urethral fistula : An abnormal connection or passageway between the urethra and the skin or surrounding tissues. This can result in urine leakage or an abnormal opening along the neophallus.
- Sensation changes : The newly formed penis may have decreased or loss of sensation or feel hypersensitive and tender.
Function of Neophallus Post-Bottom Surgery
Trans men who have undergone metoidioplasty report high levels of satisfaction with the procedure's results, both in appearance and function.
While a neophallus created through metoidioplasty is usually considered a micropenis (1–4 inches), erections and orgasms are achieved by nearly all who have undergone the procedure. Penetrative sex may or may not be possible. Urinating while standing is possible for most men after metoidioplasty.
Metoidioplasty Recovery Period
The recovery period following metoidioplasty depends on the specific surgical technique and can vary from person to person. Most people can expect one week of bed rest immediately following the procedure and gradually resume their activities within about six weeks.
Initially, there will be discomfort, swelling, and bleeding in the genital region, which will gradually subside over time. You may also experience:
- Bruising in the genital area that spreads from the belly down to the legs
- Itching and short, sharp, shooting sensations as the area heals
- Numbness at or near the incision sites, which can persist for months
- Scarring on the genitals that will first appear red or pink and fade over time
Metoidioplasty Follow-Up (and Asking for Help)
You will need assistance and support during the follow-up period after metoidioplasty, as the recovery process can involve discomfort, limited mobility, and restricted activity. You will need a caretaker for at least a week or two after the procedure—someone who can help with daily tasks such as meal preparation, household chores, and running errands.
Your surgeon may restrict certain activities, such as driving, sex, and heavy lifting. You may need help with transportation to follow-up appointments for about six weeks. Most people can resume their normal activities within six weeks post-surgery. Still, getting the OK from a healthcare provider is important to ensure you are properly healed and to lower the risk of complications.
Where to Have Metoidioplasty Surgery
Specialized surgeons with experience in transgender healthcare often perform metoidioplasty surgery. The procedure is usually carried out in a hospital or surgical center with the necessary tools and equipment for the surgery. It is essential to choose a reputable medical facility that is experienced in transgender surgeries and maintains a supportive and inclusive environment.
When considering where to have metoidioplasty surgery, start by asking a mental health professional or another healthcare provider for referrals and recommendations of surgeons who specialize in the procedure. They can provide information and guidance on the options available to you.
Researching and gathering information about the surgeon's qualifications, experience, and success rates, as well as reading reviews or testimonials from other people who have undergone metoidioplasty at the facility, can also help you select the most suitable location for the surgery. Open communication with healthcare providers can ensure that all your questions and concerns are addressed before deciding where to have metoidioplasty surgery.
Metoidioplasty is a gender-affirming surgery for trans-male people assigned female at birth (AFAB). The procedure involves releasing the clitoral ligaments and utilizing the hormonally enlarged clitoris to create a neophallus (new penis).
There are a few different metoidioplasty techniques. Sometimes, people undergo simultaneous procedures, such as hysterectomy and vaginectomy. Metoidioplasty is considered a safe, effective procedure that results in a 1–4 inch functional penis that gives trans men the opportunity to align their physical characteristics with their gender identity.
Djordjevic ML, Stojanovic B, Bizic M. Metoidioplasty: Techniques and outcomes . Transl Androl Urol . 2019;8(3):248-253. doi:10.21037/tau.2019.06.12
Kjölhede A, Cornelius F, Huss F, Kratz G. Metoidioplasty and groin flap phalloplasty as two surgical methods for the creation of a neophallus in female-to-male gender-confirming surgery: A retrospective study comprising 123 operated patients . JPRAS Open . 2019;22:1-8. doi:10.1016/j.jpra.2019.07.003
Stojanovic B, Bencic M, Bizic M, Djordjevic ML. Metoidioplasty in gender affirmation: A review . Indian J Plast Surg . 2022;55(2):156-161. doi:10.1055/s-0041-1740081
National Center for Transgender Equality. Injustice at every turn: a report of the national transgender discrimination survey .
The World Professional Association for Transgender Health. Standards of care for the health of transsexual, transgender, and gender nonconforming people .
Heston AL, Esmonde NO, Dugi DD 3rd, Berli JU. Phalloplasty: techniques and outcomes . Transl Androl Urol . 2019;8(3):254-265. doi:10.21037/tau.2019.05.05
Alberta Medical Association. Metoidioplasty .
Bordas N, Stojanovic B, Bizic M, et al. Metoidioplasty: Surgical options and outcomes in 813 cases . Front Endocrinol (Lausanne) . 2021;12:760284. doi:10.3389/fendo.2021.760284
TransCare BC. Provincial Health Services Authority. Metoidioplasty .
Michigan Medicine: University of Michigan. What to expect: Metoidioplasty at Michigan Medicine .
TransHealthCare. Metoidioplasty - list of surgeons in the USA .
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 16 May 2017
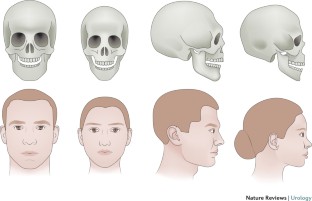
An overview of female-to-male gender-confirming surgery
- Shane D. Morrison 1 ,
- Mang L. Chen 2 &
- Curtis N. Crane 2
Nature Reviews Urology volume 14 , pages 486–500 ( 2017 ) Cite this article
2646 Accesses
60 Citations
13 Altmetric
Metrics details
- Reconstruction
- Sexual behaviour
Gender-confirming surgery is becoming a more frequently encountered procedure for urologists, plastic surgeons, and gynaecologists
Female-to-male gender-confirming surgery consists of facial masculinization, chest masculinization, body contouring, and genital surgery
Metoidioplasty (hypertrophy with systemic hormones and mobilization of the clitoris with urethroplasty) can produce a sensate microphallus
Phalloplasty can produce an aesthetic and sensate phallus with ability to micturate in a standing position and engage in penetrative sexual intercourse if proper nerve coaptation and prosthetic insertion are performed
Urethral complications following genital surgery in transmen are generally higher than 30% and include urethral fistulas and strictures; revisional urethroplasty can address most urethral complications following genital surgery
Advances in basic sciences, transgender-specific prostheses, and patient-reported outcomes will continue to offer options for improvements in gender-confirming surgery
Gender dysphoria is estimated to occur in approximately 25 million people worldwide, and can have severe psychosocial sequelae. Medical and surgical gender transition can substantially improve quality-of-life outcomes for individuals with gender dysphoria. Individuals seeking to undergo female-to-male (FtM) transition have various surgical options available for gender confirmation, including facial and chest masculinization, body contouring, and genital surgery. The World Professional Association for Transgender Health guidelines should be met before the patient undergoes surgery, to ensure that gender-confirming surgery is appropriate and indicated. Chest masculinization and metoidioplasty or phalloplasty are the most common procedures pursued, and both generally result in high levels of patient satisfaction. Phalloplasty, with a resultant aesthetic and sensate phallus along with implantable prosthetic, can take upwards of a year to accomplish, and is associated with a considerable risk of complications. Urethral complications are most frequent, and can be addressed with revision procedures. A number of scaffolds, implants, and prostheses are now in development to improve outcomes in FtM patients.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
195,33 € per year
only 16,28 € per issue
Rent or buy this article
Prices vary by article type
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others

Male-to-female gender affirmation surgery: breast reconstruction with Ergonomix round prostheses
Fien Decuypere, Edward De Wolf, … Marlon Buncamper

Overview on metoidioplasty: variants of the technique
Marta Bizic, Borko Stojanovic, … Miroslav Djordjevic

Masculinizing genital gender-affirming surgery: metoidioplasty and urethral lengthening
Ervin Kocjancic, Omer Acar, … Loren Schechter
World Professional Association for Transgender Health. Standards of Care for the Health of Transsexual, Transgender, and Gender Nonconforming People. 7th Version (World Professional Association for Transgender Health, 2011). Standards of care for transgender and gender nonconforming patients to assist all providers caring for patients within this population.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders 5th edn (American Psychiatric Association, 2013).
Benjamin, H. The Transsexual Phenomenon (Julian Press, 1966).
Google Scholar
Byne, W. et al . Report of the American Psychiatric Association task force on treatment of gender identity disorder. Arch. Sex. Behav. 41 , 759–796 (2012).
Article PubMed Google Scholar
Dhejne, C. et al . Long-term follow-up of transsexual persons undergoing sex reassignment surgery: cohort study in Sweden. PLoS ONE 6 , e16885 (2011).
Article CAS PubMed PubMed Central Google Scholar
Dhejne, C., Oberg, K., Arver, S. & Landen, M. An analysis of all applications for sex reassignment surgery in Sweden, 1960-2010: prevalence, incidence, and regrets. Arch. Sex. Behav. 43 , 1535–1545 (2014).
Lawrence, A. A. Gender assignment dysphoria in the DSM-5. Arch. Sex. Behav. 43 , 1263–1266 (2014).
Leiter, E., Futterweit, W. & Brown, G. R. in Reconstructive Urology Vol. 2 (eds Webster, G., Kirby, R., King, L. & Goldwasser, B.) 921–932 (Blackwell Scientific Publications, 1993).
Winter, S. et al . Transgender people: health at the margins of society. Lancet 388 , 390–400 (2016). Evaluation of the difficulties experienced by transgender patients in seeking healthcare.
Wylie, K. et al . Serving transgender people: clinical care considerations and service delivery models in transgender health. Lancet 388 , 401–411 (2016).
Gooren, L. J. Clinical practice. Care of transsexual persons. N. Engl. J. Med. 364 , 1251–1257 (2011).
Article CAS PubMed Google Scholar
Deutsch, M. B. et al . Electronic medical records and the transgender patient: recommendations from the World Professional Association for Transgender Health EMR Working Group. J. Am. Med. Inform. Assoc. 20 , 700–703 (2013).
Article PubMed PubMed Central Google Scholar
Morrison, S. D. The care transition in plastic surgery. Plast. Reconstr. Surg. 136 , 861e–862e (2015).
Morrison, S. D. & Swanson, J. W. Surgical justice. Plast. Reconstr. Surg. 136 , 291e–292e (2015).
De Cuypere, G., Elaut, E. & Heylens, G. Long-term follow-up: psychosocial outcome of Belgian transsexuals after sex reassignment surgery. Sexologies 15 , 126–133 (2006).
Article Google Scholar
De Cuypere, G. et al . Sexual and physical health after sex reassignment surgery. Arch. Sex. Behav. 34 , 679–690 (2005).
Hage, J. J. & Karim, R. B. Ought GIDNOS get nought? Treatment options for nontranssexual gender dysphoria. Plast. Reconstr. Surg. 105 , 1222–1227 (2000).
Lawrence, A. A. Sexuality before and after male-to-female sex reassignment surgery. Arch. Sex. Behav. 34 , 147–166 (2005).
Wierckx, K. et al . Sexual desire in female-to-male transsexual persons: exploration of the role of testosterone administration. Eur. J. Endocrinol. 165 , 331–337 (2011).
Wierckx, K. et al . Sexual desire in trans persons: associations with sex reassignment treatment. J. Sex. Med. 11 , 107–118 (2014). Evaluation of the sexual desires experienced by transgender patients after gender-confirming surgery.
Wierckx, K. et al . Long-term evaluation of cross-sex hormone treatment in transsexual persons. J. Sex. Med. 9 , 2641–2651 (2012).
Wierckx, K. et al . Quality of life and sexual health after sex reassignment surgery in transsexual men. J. Sex. Med. 8 , 3379–3388 (2011).
Zaker-Shahrak, A., Chio, L. W., Isaac, R. & Tescher, J. Economic impact assessment: Gender nondiscrimination in health insurance. (ed. Department of Insurance) (State of California, 2012).
Monstrey, S. et al . Surgical therapy in transsexual patients: a multi-disciplinary approach. Acta Chir. Belg. 101 , 200–209 (2001).
CAS PubMed Google Scholar
Selvaggi, G., Dhejne, C., Landen, M. & Elander, A. The 2011 WPATH standards of care and penile reconstruction in female-to-male transsexual individuals. Adv. Urol. 2012 , 581712 (2012).
Gooren, L. J. Management of female-to-male transgender persons: medical and surgical management, life expectancy. Curr. Opin. Endocrinol. Diabetes Obes. 21 , 233–238 (2014).
Davis, S. R. et al . Testosterone for low libido in postmenopausal women not taking estrogen. N. Engl. J. Med. 359 , 2005–2017 (2008).
Gooren, L. J. & Giltay, E. J. Review of studies of androgen treatment of female-to-male transsexuals: effects and risks of administration of androgens to females. J. Sex. Med. 5 , 765–776 (2008).
Gooren, L. J., Giltay, E. J. & Bunck, M. C. Long-term treatment of transsexuals with cross-sex hormones: extensive personal experience. J. Clin. Endocrinol. Metab. 93 , 19–25 (2008).
Mueller, A. & Gooren, L. Hormone-related tumors in transsexuals receiving treatment with cross-sex hormones. Eur. J. Endocrinol. 159 , 197–202 (2008).
Van Caenegem, E. et al . Bone mass, bone geometry, and body composition in female-to-male transsexual persons after long-term cross-sex hormonal therapy. J. Clin. Endocrinol. Metab. 97 , 2503–2511 (2012).
Monstrey, S. J., Ceulemans, P. & Hoebeke, P. Sex reassignment surgery in the female-to-male transsexual. Semin. Plast. Surg. 25 , 229–244 (2011).
Morrison, S. D., Perez, M. G., Carter, C. K. & Crane, C. N. Pre- and post-operative care with associated intra-operative techniques for phalloplasty in female-to-male patients. Urol. Nurs. 35 , 134–138 (2015).
Morrison, S. D., Perez, M. G., Nedelman, M. & Crane, C. N. Current state of female-to-male gender confirming surgery. Curr. Sex. Health Rep. 7 , 38–48 (2015).
Selvaggi, G. & Bellringer, J. Gender reassignment surgery: an overview. Nat. Rev. Urol. 8 , 274–282 (2011).
Morrison, S. D. et al . Educational exposure to transgender patient care in plastic surgery training. Plast. Reconstr. Surg. 138 , 944–953 (2016). Evaluation of resident exposure to transgender patient care in plastic surgery.
Obedin-Maliver, J. et al . Lesbian, gay, bisexual, and transgender-related content in undergraduate medical education. JAMA 306 , 971–977 (2011).
Dy, G. W. et al . Exposure to and attitudes regarding transgender education among urology residents. J. Sex. Med. 13 , 1466–1472 (2016). Evaluation of resident exposure to transgender patient care in urology.
Morrison, S. D. et al . Facial feminization: systematic review of the literature. Plast. Reconstr. Surg. 137 , 1759–1770 (2016).
Ousterhout, D. K. Dr. Paul Tessier and facial skeletal masculinization. Ann. Plast. Surg. 67 , S10–S15 (2011).
Deschamps-Braly, J. C., Sacher, C. L., Fick, J. & Ousterhout, D. K. First female-to-male facial confirmation surgery with description of a new procedure for masculinization of the thyroid cartilage (Adam's apple). Plast. Reconstr. Surg. 139 , 883e–887e (2017). First report of facial masculinization in transmen.
Monstrey, S. et al . Chest-wall contouring surgery in female-to-male transsexuals: a new algorithm. Plast. Reconstr. Surg. 121 , 849–859 (2008). Algorithmic approach to chest wall masculinization.
Richards, C. & Barrett, J. The case for bilateral mastectomy and male chest contouring for the female-to-male transsexual. Ann. R. Coll. Surg. Engl. 95 , 93–95 (2013).
Berry, M. G., Curtis, R. & Davies, D. Female-to-male transgender chest reconstruction: a large consecutive, single-surgeon experience. J. Plast. Reconstr. Aesthet. Surg. 65 , 711–719 (2012).
Colic, M. M. & Colic, M. M. Circumareolar mastectomy in female-to-male transsexuals and large gynecomastias: a personal approach. Aesthetic Plast. Surg. 24 , 450–454 (2000).
Nelson, L., Whallett, E. J. & McGregor, J. C. Transgender patient satisfaction following reduction mammaplasty. J. Plast. Reconstr. Aesthet. Surg. 62 , 331–334 (2009).
Vukadinovic, V., Stojanovic, B., Majstorovic, M. & Milosevic, A. The role of clitoral anatomy in female to male sex reassignment surgery. ScientificWorldJournal 2014 , 437378 (2014).
Weyers, S. et al . Gynaecological aspects of the treatment and follow-up of transsexual men and women. Facts Views Vis. Obgyn. 2 , 35–54 (2010).
CAS PubMed PubMed Central Google Scholar
Ergeneli, M. H., Duran, E. H., Ozcan, G. & Erdogan, M. Vaginectomy and laparoscopically assisted vaginal hysterectomy as adjunctive surgery for female-to-male transsexual reassignment: preliminary report. Eur. J. Obstet. Gynecol. Reprod. Biol. 87 , 35–37 (1999).
Weyers, S., Selvaggi, G. & Monstrey, S. Two-stage versus one-stage sex reassignment surgery in female-to-male transsexual individuals. Gynecol. Surg. 3 , 190–194 (2006).
Morrison, S. D. et al . Phalloplasty: a review of techniques and outcomes. Plast. Reconstr. Surg. 138 , 594–615 (2016). Contemporary evaluation of techniques and outcomes of phalloplasty.
Perrone, A. M. et al . Hysterectomy and bilateral salpingoovariectomy in a transsexual subject without visible scaring. Diagn. Ther. Endosc. 2010 , 845029 (2010).
Chen, Y. J. et al . Single-port compared with conventional laparoscopic-assisted vaginal hysterectomy: a randomized controlled trial. Obstet. Gynecol. 117 , 906–912 (2011).
Bogliolo, S. et al . Robotic single-site surgery for female-to-male transsexuals: preliminary experience. ScientificWorldJournal 2014 , 674579 (2014).
Obedin-Maliver, J., Light, A., Dehaan, G., Steinauer, J. & Jackson, R. Vaginal hysterectomy as a viable option for female-to-male transgender men. Obstet. Gynecol. 123 (Suppl. 1), 126S–127S (2014).
Djordjevic, M. L. et al . Urethral lengthening in metoidioplasty (female-to-male sex reassignment surgery) by combined buccal mucosa graft and labia minora flap. Urology 74 , 349–353 (2009).
Djordjevic, M. L. & Bizic, M. R. Comparison of two different methods for urethral lengthening in female to male (metoidioplasty) surgery. J. Sex. Med. 10 , 1431–1438 (2013). Assessment of outcomes of urethral lengthening following metoidioplasty.
Zhang, Y. F. et al . Is vaginal mucosal graft the excellent substitute material for urethral reconstruction in female-to-male transsexuals? World J. Urol. 33 , 2115–2123 (2015).
Hage, J. J. & Bloem, J. J. Review of the literature on construction of a neourethra in female-to-male transsexuals. Ann. Plast. Surg. 30 , 278–286 (1993).
Hage, J. J., Bouman, F. G. & Bloem, J. J. Construction of the fixed part of the neourethra in female-to-male transsexuals: experience in 53 patients. Plast. Reconstr. Surg. 91 , 904–910 (1993).
Rohrmann, D. & Jakse, G. Urethroplasty in female-to-male transsexuals. Eur. Urol. 44 , 611–614 (2003).
Selvaggi, G. & Elander, A. Penile reconstruction/formation. Curr. Opin. Urol. 18 , 589–597 (2008).
Salgado, C. J., Chim, H., Tang, J. C., Monstrey, S. J. & Mardini, S. Penile reconstruction. Semin. Plast. Surg. 25 , 221–228 (2011).
Hage, J. J. & De Graaf, F. H. Addressing the ideal requirements by free flap phalloplasty: some reflections on refinements of technique. Microsurgery 14 , 592–598 (1993).
Monstrey, S. et al . Penile reconstruction: is the radial forearm flap really the standard technique? Plast. Reconstr. Surg. 124 , 510–518 (2009). Largest evaluation of outcomes of RFFF phalloplasty.
Zhang, W. R., Garrett, G. L., Arron, S. T. & Garcia, M. M. Laser hair removal for genital gender affirming surgery. Transl Androl. Urol. 5 , 381–387 (2016).
Durfee, R. & Rowland, W. in Proceedings of the Second Interdisciplinary Symposium on Gender Dysphoria Syndrome (eds Laub, D. R. & Gandy, P.) 181–183 (Stanford Univ. Press, 1973).
Lebovic, G. S. & Laub, D. R. in Reconstructive and Plastic Surgery of the External Genitalia (eds Ehrlich, R. M. & Alter, G. J.) 355–360 (WB Saunders, 1999).
Hage, J. J. Metaidoioplasty: an alternative phalloplasty technique in transsexuals. Plast. Reconstr. Surg. 97 , 161–167 (1996).
Hage, J. J. & van Turnhout, A. A. Long-term outcome of metaidoioplasty in 70 female-to-male transsexuals. Ann. Plast. Surg. 57 , 312–316 (2006).
Oakley, S. H. et al . Innervation and histology of the clitoral-urethal complex: a cross-sectional cadaver study. J. Sex. Med. 10 , 2211–2218 (2013).
Djordjevic, M. L. et al . Metoidioplasty as a single stage sex reassignment surgery in female transsexuals: Belgrade experience. J. Sex. Med. 6 , 1306–1313 (2009).
Perovic, S. V. & Djordjevic, M. L. Metoidioplasty: a variant of phalloplasty in female transsexuals. BJU Int. 92 , 981–985 (2003).
Takamatsu, A. & Harashina, T. Labial ring flap: a new flap for metaidoioplasty in female-to-male transsexuals. J. Plast. Reconstr. Aesthet. Surg. 62 , 318–325 (2009).
Bogoras, N. Über die volle plastische Wiederherstellung eines zum Koitus fähigen Penis (Peniplastica totalis) [German]. Zentralbl. Chir. 63 , 1271–1276 (1936).
Gillies, H. & Millard, R. The Principles and Art of Plastic Surgery Vol. II 369–388 (Little, Brown and Company, 1957).
Kaplan, I. A rapid method for constructing a functional sensitive penis. Br. J. Plast. Surg. 24 , 342–344 (1971).
Puckett, C. L., Reinisch, J. F. & Montie, J. E. Free flap phalloplasty. J. Urol. 128 , 294–297 (1982).
Hu, W. et al . A preliminary report of penile transplantation: part 2. Eur. Urol. 50 , 1115–1116 (2006).
Hu, W. et al . A preliminary report of penile transplantation. Eur. Urol. 50 , 851–853 (2006).
Morrison, S. D. et al . Penile replantation: a retrospective analysis of outcomes and complications. J. Reconstr. Microsurg. 33 , 227–232 (2017).
Monstrey, S. et al . Radial forearm phalloplasty: a review of 81 cases. Eur. J. Plast. Surg. 28 , 206–212 (2005).
Bettocchi, C., Ralph, D. J. & Pryor, J. P. Pedicled pubic phalloplasty in females with gender dysphoria. BJU Int. 95 , 120–124 (2005).
Shaeer, O. & El-Sebaie, A. Construction of neoglans penis: a new sculpturing technique from rectus abdominis myofascial flap. J. Sex. Med. 2 , 259–265 (2005).
Terrier, J. E., Courtois, F., Ruffion, A. & Morel Journel, N. Surgical outcomes and patients' satisfaction with suprapubic phalloplasty. J. Sex. Med. 11 , 288–298 (2014).
Alanis, S. Z. An innovation in total penis reconstruction. Plast. Reconstr. Surg. 43 , 418–422 (1969).
Davies, D. Phalloplasty. S. Afr. Med. J. 31 , 990–991 (1957).
Davies, D. M. & Matti, B. A. A method of phalloplasty using the deep inferior epigastric flap. Br. J. Plast. Surg. 41 , 165–168 (1988).
Dubin, B. J., Sato, R. M. & Laub, D. R. Results of phalloplasty. Plast. Reconstr. Surg. 64 , 163–170 (1979).
Santi, P. et al . Immediate reconstruction of the penis using an inferiorly based rectus abdominis myocutaneous flap. Plast. Reconstr. Surg. 81 , 961–964 (1988).
Zhang, Y., Lu, L., Zhang, W., Jiang, H. & Zhu, X. A simple and effective method for phalloplasty in female-to-male transsexuals. Plast. Reconstr. Surg. 126 , 264e–265e (2010).
Lumen, N., Hoebeke, P. & Oosterlinck, W. Urethroplasty for urethral strictures: quality assessment of an in-home algorithm. Int. J. Urol. 17 , 167–174 (2010).
Krauss, E. M., Tung, T. H. & Moore, A. M. Free functional muscle transfers to restore upper extremity function. Hand Clin. 32 , 243–256 (2016).
Ranno, R. et al . Neo-phalloplasty with re-innervated latissimus dorsi free flap: a functional study of a novel technique. Acta Chir. Plast. 49 , 3–7 (2007).
Ranno, R., Hyza, P., Vesely, J., Dessy, L. A. & Kadanka, Z. An objective evaluation of contraction power of neo-phallus reconstructed with free re-innervated LD in female-to-male transsexuals. Acta Chir. Plast. 49 , 8–12 (2007).
Mori, R. L. & Angermeier, K. W. Staged urethroplasty in the management of complex anterior urethral stricture disease. Transl Androl. Urol. 4 , 29–34 (2015).
PubMed PubMed Central Google Scholar
Djordjevic, M. L., Bumbasirevic, M. Z., Vukovic, P. M., Sansalone, S. & Perovic, S. V. Musculocutaneous latissimus dorsi free transfer flap for total phalloplasty in children. J. Pediatr. Urol. 2 , 333–339 (2006).
Lin, C. T. & Chen, L. W. Using a free thoracodorsal artery perforator flap for phallic reconstruction — a report of surgical technique. J. Plast. Reconstr. Aesthet. Surg. 62 , 402–408 (2009).
Perovic, S. V., Djinovic, R., Bumbasirevic, M., Djordjevic, M. & Vukovic, P. Total phalloplasty using a musculocutaneous latissimus dorsi flap. BJU Int. 100 , 899–905 (2007).
Vesely, J. et al . New technique of total phalloplasty with reinnervated latissimus dorsi myocutaneous free flap in female-to-male transsexuals. Ann. Plast. Surg. 58 , 544–550 (2007).
Kessler, T. M. et al . Long-term results of surgery for urethral stricture: a statistical analysis. J. Urol. 170 , 840–844 (2003).
Mathur, R. K. et al . Single-stage preputial skin flap urethroplasty for long-segment urethral strictures: evaluation and determinants of success. BJU Int. 113 , 120–126 (2014).
Taguchi, H., Saito, K. & Yamada, T. A simple method of total reconstruction of the penis. Case reports. Plast. Reconstr. Surg. 60 , 454–456 (1977).
Hage, J. J., Winters, H. A. & Van Lieshout, J. Fibula free flap phalloplasty: modifications and recommendations. Microsurgery 17 , 358–365 (1996).
Sadove, R. C., Sengezer, M., McRoberts, J. W. & Wells, M. D. One-stage total penile reconstruction with a free sensate osteocutaneous fibula flap. Plast. Reconstr. Surg. 92 , 1314–1323 (1993).
McRoberts, J. W. & Sadove, R. C. Penile reconstruction with a free sensate osteocutaneous fibula flap in the surgical management of the intersex patient. Adv. Exp. Med. Biol. 511 , 283–287 (2002).
Sengezer, M., Ozturk, S., Deveci, M. & Odabasi, Z. Long-term follow-up of total penile reconstruction with sensate osteocutaneous free fibula flap in 18 biological male patients. Plast. Reconstr. Surg. 114 , 439–450 (2004).
Dabernig, J., Chan, L. K. & Schaff, J. Phalloplasty with free (septocutaneous) fibular flap sine fibula. J. Urol. 176 , 2085–2088 (2006).
Papadopulos, N. A., Schaff, J. & Biemer, E. The use of free prelaminated and sensate osteofasciocutaneous fibular flap in phalloplasty. Injury 39 (Suppl. 3), S62–S67 (2008).
Salgado, C. J., Rampazzo, A., Xu, E. & Chen, H. C. Treatment of dyspareunia by creation of a pseudojoint in rigid bone following total penile reconstruction with fibular osteocutaneous flap. J. Sex. Med. 5 , 2947–2950 (2008).
Sun, G. C. & Huang, J. J. One-stage reconstruction of the penis with composite iliac crest and lateral groin skin flap. Ann. Plast. Surg. 15 , 519–528 (1985).
Cutting, C. B. & McCarthy, J. G. Comparison of residual osseous mass between vascularized and nonvascularized onlay bone transfers. Plast. Reconstr. Surg. 72 , 672–675 (1983).
Weiland, A. J., Phillips, T. W. & Randolph, M. A. Bone grafts: a radiologic, histologic, and biomechanical model comparing autografts, allografts, and free vascularized bone grafts. Plast. Reconstr. Surg. 74 , 368–379 (1984).
Zielinski, T. Phalloplasty using a lateral groin flap in female-to-male transsexuals. Acta Chir. Plast. 41 , 15–19 (1999).
Akoz, T., Erdogan, B., Gorgu, M., Kapucu, M. R. & Kargi, E. Penile reconstruction in children using a double vascular pedicle composite groin flap. Scand. J. Urol. Nephrol. 32 , 225–230 (1998).
Akoz, T. & Kargi, E. Phalloplasty in a female-to-male transsexual using a double-pedicle composite groin flap. Ann. Plast. Surg. 48 , 423–427 (2002).
Puckett, C. L. & Montie, J. E. Construction of male genitalia in the transsexual, using a tubed groin flap for the penis and a hydraulic inflation device. Plast. Reconstr. Surg. 61 , 523–530 (1978).
Felici, N. & Felici, A. A new phalloplasty technique: the free anterolateral thigh flap phalloplasty. J. Plast. Reconstr. Aesthet. Surg. 59 , 153–157 (2006).
Lee, G. K., Lim, A. F. & Bird, E. T. A novel single-flap technique for total penile reconstruction: the pedicled anterolateral thigh flap. Plast. Reconstr. Surg. 124 , 163–166 (2009).
Hasegawa, K., Namba, Y. & Kimata, Y. Phalloplasty with an innervated island pedicled anterolateral thigh flap in a female-to-male transsexual. Acta Med. Okayama 67 , 325–331 (2013).
PubMed Google Scholar
Morrison, S. D. et al . Modification of the tube-in-tube pedicled anterolateral thigh flap for total phalloplasty: the mushroom flap. Ann. Plast. Surg. 72 (Suppl. 1), S22–S26 (2014).
Mutaf, M. A new surgical procedure for phallic reconstruction: Istanbul flap. Plast. Reconstr. Surg. 105 , 1361–1370 (2000).
Hoebeke, P. B. et al . Erectile implants in female-to-male transsexuals: our experience in 129 patients. Eur. Urol. 57 , 334–340 (2010).
Lumen, N. et al . Erectile implants in female-to-male transsexuals: our experience in 130 patients [abstract]. Eur. Urol. Suppl. 7 , 117 (2008).
Neuville, P. et al . Surgical outcomes of erectile implants after phalloplasty: retrospective analysis of 95 procedures. J. Sex. Med. 13 , 1758–1764 (2016). Recent evaluation of outcomes of prosthetics in phalloplasty.
Gurjala, A. N., Nazerali, R. S., Salim, A. & Lee, G. K. World's first baby born through natural insemination by father with total phalloplasty reconstruction. Ann. Plast. Surg. 76 (Suppl. 3), S179–S183 (2016).
Sinove, Y. et al . Preoperative planning of a pedicled anterolateral thigh (ALT) flap for penile reconstruction with the multidetector CT scan. Handchir. Mikrochir. Plast. Chir. 45 , 217–222 (2013).
Liu, C. Y., Wei, Z. R., Jiang, H., Zhao, Y. Z. & Zhang, Y. F. Preconstruction of the pars pendulans urethrae for phalloplasty with digestive mucosa using a prefabricated anterolateral thigh flap in a one-arm patient. Plast. Reconstr. Surg. Glob. Open 1 , e53 (2013).
Rubino, C. et al . Innervated island pedicled anterolateral thigh flap for neo-phallic reconstruction in female-to-male transsexuals. J. Plast. Reconstr. Aesthet. Surg. 62 , e45–e49 (2009).
Chang, T. S. & Hwang, W. Y. Forearm flap in one-stage reconstruction of the penis. Plast. Reconstr. Surg. 74 , 251–258 (1984).
Monstrey, S. et al . Radial Forearm Phalloplasty: a Review of 91 Cases. ANIR-ANHP 6 , 193–199 (2004).
Selvaggi, G. et al . Genital sensitivity after sex reassignment surgery in transsexual patients. Ann. Plast. Surg. 58 , 427–433 (2007). Evaluation of genital sensitivity following phalloplasty for transmen.
Fang, R. H., Kao, Y. S., Ma, S. & Lin, J. T. Phalloplasty in female-to-male transsexuals using free radial osteocutaneous flap: a series of 22 cases. Br. J. Plast. Surg. 52 , 217–222 (1999).
Kim, S. K. et al . The etiology and treatment of the softened phallus after the radial forearm osteocutaneous free flap phalloplasty. Arch. Plast. Surg. 39 , 390–396 (2012).
Trost, L., Wanzek, P. & Bailey, G. A practical overview of considerations for penile prosthesis placement. Nat. Rev. Urol. 13 , 33–46 (2016).
Biemer, E. Penile construction by the radial arm flap. Clin. Plast. Surg. 15 , 425–430 (1988).
Doornaert, M. et al . Penile reconstruction with the radial forearm flap: an update. Handchir. Mikrochir. Plast. Chir. 43 , 208–214 (2011).
Matti, B. A., Matthews, R. N. & Davies, D. M. Phalloplasty using the free radial forearm flap. Br. J. Plast. Surg. 41 , 160–164 (1988).
Salgado, C. J. et al . Immediate pedicled gracilis flap in radial forearm flap phalloplasty for transgender male patients to reduce urinary fistula. J. Plast. Reconstr. Aesthet. Surg. 69 , 1551–1557 (2016).
Selvaggi, G. et al . Donor-site morbidity of the radial forearm free flap after 125 phalloplasties in gender identity disorder. Plast. Reconstr. Surg. 118 , 1171–1177 (2006).
Bardsley, A. F., Soutar, D. S., Elliot, D. & Batchelor, A. G. Reducing morbidity in the radial forearm flap donor site. Plast. Reconstr. Surg. 86 , 287–292 (1990).
Boorman, J. G., Brown, J. A. & Sykes, P. J. Morbidity in the forearm flap donor arm. Br. J. Plast. Surg. 40 , 207–212 (1987).
Richardson, D., Fisher, S. E., Vaughan, E. D. & Brown, J. S. Radial forearm flap donor-site complications and morbidity: a prospective study. Plast. Reconstr. Surg. 99 , 109–115 (1997).
Van Caenegem, E. et al . Long-term evaluation of donor-site morbidity after radial forearm flap phalloplasty for transsexual men. J. Sex. Med. 10 , 1644–1651 (2013).
Rieger, U. M. et al . Comparative study of the free microvascular groin flap: optimizing the donor site after free radial forearm flap phalloplasty. Urology 95 , 192–196 (2016).
Fang, R. H., Lin, J. T. & Ma, S. Phalloplasty for female transsexuals with sensate free forearm flap. Microsurgery 15 , 349–352 (1994).
Gottlieb, L. J. & Levine, L. A. A new design for the radial forearm free-flap phallic construction. Plast. Reconstr. Surg. 92 , 276–283 (1993).
Hage, J. J., Bouman, F. G., de Graaf, F. H. & Bloem, J. J. Construction of the neophallus in female-to-male transsexuals: the Amsterdam experience. J. Urol. 149 , 1463–1468 (1993).
Kim, S. K., Lee, K. C., Kwon, Y. S. & Cha, B. H. Phalloplasty using radial forearm osteocutaneous free flaps in female-to-male transsexuals. J. Plast. Reconstr. Aesthet. Surg. 62 , 309–317 (2009).
Koshima, I., Tai, T. & Yamasaki, M. One-stage reconstruction of the penis using an innervated radial forearm osteocutaneous flap. J. Reconstr. Microsurg. 3 , 19–26 (1986).
Leriche, A. et al . Long-term outcome of forearm flee-flap phalloplasty in the treatment of transsexualism. BJU Int. 101 , 1297–1300 (2008).
Ma, S., Cheng, K. & Liu, Y. Sensibility following innervated free radial forearm flap for penile reconstruction. Plast. Reconstr. Surg. 127 , 235–241 (2011).
Ma, S., Liu, Y., Chang, T. & Cheng, K. Long-term follow-up of sensation recovery of the penis reconstructed by Cheng's method. Plast. Reconstr. Surg. 127 , 1546–1552 (2011).
Papadopulos, N. A., Schaff, J. & Biemer, E. Usefulness of free sensate osteofasciocutaneous forearm and fibula flaps for neophallus construction. J. Reconstr. Microsurg. 17 , 407–412 (2001).
Sasaki, K., Nozaki, M., Morioka, K. & Huang, T. T. Penile reconstruction: combined use of an innervated forearm osteocutaneous flap and big toe pulp. Plast. Reconstr. Surg. 104 , 1054–1058 (1999).
Song, C., Wong, M., Wong, C. H. & Ong, Y. S. Modifications of the radial forearm flap phalloplasty for female-to-male gender reassignment. J. Reconstr. Microsurg. 27 , 115–120 (2011).
Vriens, J. P., Acosta, R., Soutar, D. S. & Webster, M. H. Recovery of sensation in the radial forearm free flap in oral reconstruction. Plast. Reconstr. Surg. 98 , 649–656 (1996).
Waits, C. A., Toby, E. B., Girod, D. A. & Tsue, T. T. Osteocutaneous radial forearm free flap: long-term radiographic evaluation of donor site morbidity after prophylactic plating of radius. J. Reconstr. Microsurg. 23 , 367–372 (2007).
Ma, S., Cheng, K., Liu, Y. & Chen, F. A new surgical procedure for penile reconstruction by combined free radial forearm flap and dorsalis pedis flap. Urology 97 , 232–237 (2016).
Hoebeke, P., de Cuypere, G., Ceulemans, P. & Monstrey, S. Obtaining rigidity in total phalloplasty: experience with 35 patients. J. Urol. 169 , 221–223 (2003).
Selvaggi, G. et al . Scrotal reconstruction in female-to-male transsexuals: a novel scrotoplasty. Plast. Reconstr. Surg. 123 , 1710–1718 (2009). Presentation of the novel technique for transman scrotoplasty.
Hage, J. J., Bouman, F. G. & Bloem, J. J. Constructing a scrotum in female-to-male transsexuals. Plast. Reconstr. Surg. 91 , 914–921 (1993).
Millard, D. R. Jr. Scrotal construction and reconstruction. Plast. Reconstr. Surg. 38 , 10–15 (1966).
Reid, C. F. & Wright, J. H. Jr. Scrotal reconstruction following an avulsion injury. J. Urol. 133 , 681–682 (1985).
Sengezer, M. & Sadove, R. C. Scrotal construction by expansion of labia majora in biological female transsexuals. Ann. Plast. Surg. 31 , 372–376 (1993).
Still, E. F. II & Goodman, R. C. Total reconstruction of a two-compartment scrotum by tissue expansion. Plast. Reconstr. Surg. 85 , 805–807 (1990).
Lumen, N., Monstrey, S., Goessaert, A. S., Oosterlinck, W. & Hoebeke, P. Urethroplasty for strictures after phallic reconstruction: a single-institution experience. Eur. Urol. 60 , 150–158 (2011). Analysis of outcomes and techniques for urethral fistula and stricture repair in phalloplasty.
Wilson, S. C. et al . Fasciocutaneous flap reinforcement of ventral onlay buccal mucosa grafts enables neophallus revision urethroplasty. Ther. Adv. Urol. 8 , 331–337 (2016).
Dabernig, J., Shelley, O. P., Cuccia, G. & Schaff, J. Urethral reconstruction using the radial forearm free flap: experience in oncologic cases and gender reassignment. Eur. Urol. 52 , 547–553 (2007).
Garaffa, G., Ralph, D. J. & Christopher, N. Total urethral construction with the radial artery-based forearm free flap in the transsexual. BJU Int. 106 , 1206–1210 (2010).
Kim, S. K., Moon, J. B., Heo, J., Kwon, Y. S. & Lee, K. C. A new method of urethroplasty for prevention of fistula in female-to-male gender reassignment surgery. Ann. Plast. Surg. 64 , 759–764 (2010).
Bayramicli, M. & Akdeniz, Z. D. Urethra reconstruction with lateral pectoral flap in female-to-male transsexual patients. J. Plast. Reconstr. Aesthet. Surg. 69 , 1558–1560 (2016).
De Filippo, R. E., Yoo, J. J. & Atala, A. Urethral replacement using cell seeded tubularized collagen matrices. J. Urol. 168 , 1789–1792 (2002).
Chen, K. L., Eberli, D., Yoo, J. J. & Atala, A. Bioengineered corporal tissue for structural and functional restoration of the penis. Proc. Natl Acad. Sci. USA 107 , 3346–3350 (2010).
Joo, K. J. et al . Porcine vesical acellular matrix graft of tunica albuginea for penile reconstruction. Asian J. Androl. 8 , 543–548 (2006).
Kwon, T. G., Yoo, J. J. & Atala, A. Autologous penile corpora cavernosa replacement using tissue engineering techniques. J. Urol. 168 , 1754–1758 (2002).
Kropp, B. P. et al . Use of small intestinal submucosa for corporal body grafting in cases of severe penile curvature. J. Urol. 168 , 1742–1745 (2002).
Raya-Rivera, A. M. et al . Tissue-engineered autologous vaginal organs in patients: a pilot cohort study. Lancet 384 , 329–336 (2014).
Sopko, N. A. et al . Ex vivo model of human penile transplantation and rejection: implications for erectile tissue physiology. Eur. Urol. 71 , 584–593 (2017).
Tuffaha, S. H. et al . Using the dorsal, cavernosal, and external pudendal arteries for penile transplantation: technical considerations and perfusion territories. Plast. Reconstr. Surg. 134 , 111e–119e (2014).
Selvaggi, G., Branemark, R., Elander, A., Liden, M. & Stalfors, J. Titanium-bone-anchored penile epithesis: preoperative planning and immediate postoperative results. J. Plast. Surg. Hand. Surg. 49 , 40–44 (2015).
Selvaggi, G., Elander, A. & Branemark, R. Penile epithesis: preliminary study. Plast. Reconstr. Surg. 126 , 265e–266e (2010).
Massie, J. P., Morrison, S. D., Smith, J. R., Wilson, S. C. & Satterwhite, T. Letter to the editor regarding “Surgical outcome after penile inversion vaginoplasty: a retrospective study of 475 transgender women” by Buncamper et al . Plast. Reconstr. Surg. http://dx.doi.org/10.1097/PRS.0000000000003479 (2017).
Berli, J. U. et al . What surgeons need to know about gender confirmation surgery when providing care for transgender individuals: a review. JAMA Surg. 152 , 394–400 (2017).
Download references
Author information
Authors and affiliations.
Division of Plastic and Reconstructive Surgery, Department of Surgery, University of Washington School of Medicine, 1959 NE Pacific Street, Seattle, 98195, WA, USA
Shane D. Morrison
Brownstein & Crane Surgical Services, 575 Sir Francis Drake Blvd, Ste 1, Greenbrae, 94904, CA, USA
Mang L. Chen & Curtis N. Crane
You can also search for this author in PubMed Google Scholar
Contributions
S.D.M., C.N.C and M.C. researched data for article, made substantial contributions to discussions of content, and reviewed and edited the manuscript before submission. S.D.M. and M.C. wrote the article.
Corresponding author
Correspondence to Curtis N. Crane .
Ethics declarations
Competing interests.
The authors declare no competing financial interests.
PowerPoint slides
Powerpoint slide for fig. 1, powerpoint slide for fig. 2, powerpoint slide for fig. 3, powerpoint slide for fig. 4, powerpoint slide for fig. 5, powerpoint slide for fig. 6, powerpoint slide for fig. 7, powerpoint slide for table 1.
Inherent discordance of a patient's gender expression and their anatomy leading to distress
Tissue forming the nipple and surrounding areola on the breast or chest
A physical examination test to determine the patency of the palmar or plantar arches as a correlate for the dominant inflow vessel to the hand or foot. Most commonly it is used in the hand where the radial and ulnar arteries are both occluded with pressure from the examiners hand and each is released sequentially while maintaining the pressure on the other artery. The perfusion of the hand is monitored to ensure both vessels can perfuse the hand.
A person born as a male and whose gender identity is male.
Urological procedure for urethral strictures, in which the ventral aspect of the phallus is opened through the urethra. The urethra is secured to the skin and urine is diverted. A second stage completed months later is used to repair the urethra with grafted tissue over a catheter.
Flaps containing multiple tissue types (skin, bone, mucosa.) based on a single angiosome used for complex reconstruction.
Local flap used for advancing tissue generally to cover a wound, but can be used in other procedures. An incision shaped like a V is made through the subcutaneous tissue, advanced into its new position relying on subcutaneous perfusion, and closed in a Y pattern.
Closure of a urethral stricture with a longitudinal incision followed by a transverse closure.
A person born with female sexual organs, but whose gender identity is male
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Morrison, S., Chen, M. & Crane, C. An overview of female-to-male gender-confirming surgery. Nat Rev Urol 14 , 486–500 (2017). https://doi.org/10.1038/nrurol.2017.64
Download citation
Published : 16 May 2017
Issue Date : August 2017
DOI : https://doi.org/10.1038/nrurol.2017.64
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Geschlechtsinkongruenz – definition, diagnosestellung und transitionsoptionen.
- Antje Feicke
- Barbara Mijuskovic
Urologie in der Praxis (2023)
(De-)centralized health care delivery, surgical outcome, and psychosocial health of transgender and gender-diverse people undergoing vaginoplasty: results of a retrospective, single-center study
- Andreas Koehler
- Bernhard Strauß
- Timo O. Nieder
World Journal of Urology (2023)
Gender Affirmation Surgery for the Transmasculine Patient
- Michael Callegari
- Gaetan Pettigrew
- Shubham Gupta
Current Obstetrics and Gynecology Reports (2022)
Urethral complications after gender reassignment surgery: a systematic review
- L. R. Doumanian
International Journal of Impotence Research (2021)
Suprapubic phalloplasty in transmen: surgical results and critical review
- Manon Terrier
- Nicolas Morel-Journel
- Paul Neuville
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Patient Care & Health Information
- Tests & Procedures
- Feminizing surgery
Feminizing surgery, also called gender-affirming surgery or gender-confirmation surgery, involves procedures that help better align the body with a person's gender identity. Feminizing surgery includes several options, such as top surgery to increase the size of the breasts. That procedure also is called breast augmentation. Bottom surgery can involve removal of the testicles, or removal of the testicles and penis and the creation of a vagina, labia and clitoris. Facial procedures or body-contouring procedures can be used as well.
Not everybody chooses to have feminizing surgery. These surgeries can be expensive, carry risks and complications, and involve follow-up medical care and procedures. Certain surgeries change fertility and sexual sensations. They also may change how you feel about your body.
Your health care team can talk with you about your options and help you weigh the risks and benefits.
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Available Sexual Health Solutions at Mayo Clinic Store
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
Many people seek feminizing surgery as a step in the process of treating discomfort or distress because their gender identity differs from their sex assigned at birth. The medical term for this is gender dysphoria.
For some people, having feminizing surgery feels like a natural step. It's important to their sense of self. Others choose not to have surgery. All people relate to their bodies differently and should make individual choices that best suit their needs.
Feminizing surgery may include:
- Removal of the testicles alone. This is called orchiectomy.
- Removal of the penis, called penectomy.
- Removal of the testicles.
- Creation of a vagina, called vaginoplasty.
- Creation of a clitoris, called clitoroplasty.
- Creation of labia, called labioplasty.
- Breast surgery. Surgery to increase breast size is called top surgery or breast augmentation. It can be done through implants, the placement of tissue expanders under breast tissue, or the transplantation of fat from other parts of the body into the breast.
- Plastic surgery on the face. This is called facial feminization surgery. It involves plastic surgery techniques in which the jaw, chin, cheeks, forehead, nose, and areas surrounding the eyes, ears or lips are changed to create a more feminine appearance.
- Tummy tuck, called abdominoplasty.
- Buttock lift, called gluteal augmentation.
- Liposuction, a surgical procedure that uses a suction technique to remove fat from specific areas of the body.
- Voice feminizing therapy and surgery. These are techniques used to raise voice pitch.
- Tracheal shave. This surgery reduces the thyroid cartilage, also called the Adam's apple.
- Scalp hair transplant. This procedure removes hair follicles from the back and side of the head and transplants them to balding areas.
- Hair removal. A laser can be used to remove unwanted hair. Another option is electrolysis, a procedure that involves inserting a tiny needle into each hair follicle. The needle emits a pulse of electric current that damages and eventually destroys the follicle.
Your health care provider might advise against these surgeries if you have:
- Significant medical conditions that haven't been addressed.
- Behavioral health conditions that haven't been addressed.
- Any condition that limits your ability to give your informed consent.
Like any other type of major surgery, many types of feminizing surgery pose a risk of bleeding, infection and a reaction to anesthesia. Other complications might include:
- Delayed wound healing
- Fluid buildup beneath the skin, called seroma
- Bruising, also called hematoma
- Changes in skin sensation such as pain that doesn't go away, tingling, reduced sensation or numbness
- Damaged or dead body tissue — a condition known as tissue necrosis — such as in the vagina or labia
- A blood clot in a deep vein, called deep vein thrombosis, or a blood clot in the lung, called pulmonary embolism
- Development of an irregular connection between two body parts, called a fistula, such as between the bladder or bowel into the vagina
- Urinary problems, such as incontinence
- Pelvic floor problems
- Permanent scarring
- Loss of sexual pleasure or function
- Worsening of a behavioral health problem
Certain types of feminizing surgery may limit or end fertility. If you want to have biological children and you're having surgery that involves your reproductive organs, talk to your health care provider before surgery. You may be able to freeze sperm with a technique called sperm cryopreservation.
How you prepare
Before surgery, you meet with your surgeon. Work with a surgeon who is board certified and experienced in the procedures you want. Your surgeon talks with you about your options and the potential results. The surgeon also may provide information on details such as the type of anesthesia that will be used during surgery and the kind of follow-up care that you may need.
Follow your health care team's directions on preparing for your procedures. This may include guidelines on eating and drinking. You may need to make changes in the medicine you take and stop using nicotine, including vaping, smoking and chewing tobacco.
Because feminizing surgery might cause physical changes that cannot be reversed, you must give informed consent after thoroughly discussing:
- Risks and benefits
- Alternatives to surgery
- Expectations and goals
- Social and legal implications
- Potential complications
- Impact on sexual function and fertility
Evaluation for surgery
Before surgery, a health care provider evaluates your health to address any medical conditions that might prevent you from having surgery or that could affect the procedure. This evaluation may be done by a provider with expertise in transgender medicine. The evaluation might include:
- A review of your personal and family medical history
- A physical exam
- A review of your vaccinations
- Screening tests for some conditions and diseases
- Identification and management, if needed, of tobacco use, drug use, alcohol use disorder, HIV or other sexually transmitted infections
- Discussion about birth control, fertility and sexual function
You also may have a behavioral health evaluation by a health care provider with expertise in transgender health. That evaluation might assess:
- Gender identity
- Gender dysphoria
- Mental health concerns
- Sexual health concerns
- The impact of gender identity at work, at school, at home and in social settings
- The role of social transitioning and hormone therapy before surgery
- Risky behaviors, such as substance use or use of unapproved hormone therapy or supplements
- Support from family, friends and caregivers
- Your goals and expectations of treatment
- Care planning and follow-up after surgery
Other considerations
Health insurance coverage for feminizing surgery varies widely. Before you have surgery, check with your insurance provider to see what will be covered.
Before surgery, you might consider talking to others who have had feminizing surgery. If you don't know someone, ask your health care provider about support groups in your area or online resources you can trust. People who have gone through the process may be able to help you set your expectations and offer a point of comparison for your own goals of the surgery.
What you can expect
Facial feminization surgery.
Facial feminization surgery may involve a range of procedures to change facial features, including:
- Moving the hairline to create a smaller forehead
- Enlarging the lips and cheekbones with implants
- Reshaping the jaw and chin
- Undergoing skin-tightening surgery after bone reduction
These surgeries are typically done on an outpatient basis, requiring no hospital stay. Recovery time for most of them is several weeks. Recovering from jaw procedures takes longer.
Tracheal shave
A tracheal shave minimizes the thyroid cartilage, also called the Adam's apple. During this procedure, a small cut is made under the chin, in the shadow of the neck or in a skin fold to conceal the scar. The surgeon then reduces and reshapes the cartilage. This is typically an outpatient procedure, requiring no hospital stay.
Top surgery
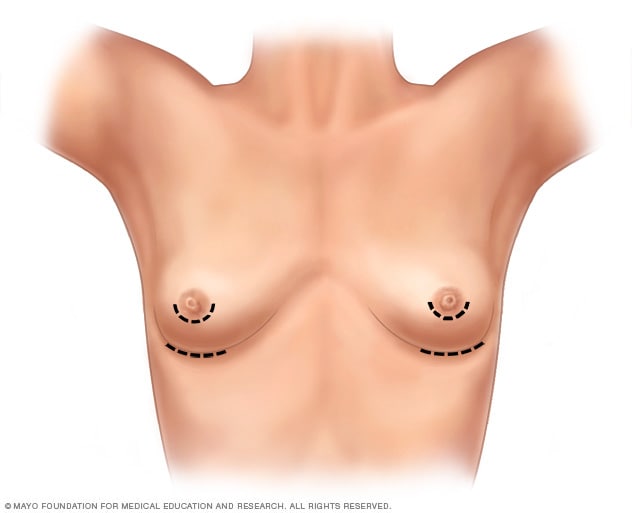
- Breast augmentation incisions
As part of top surgery, the surgeon makes cuts around the areola, near the armpit or in the crease under the breast.
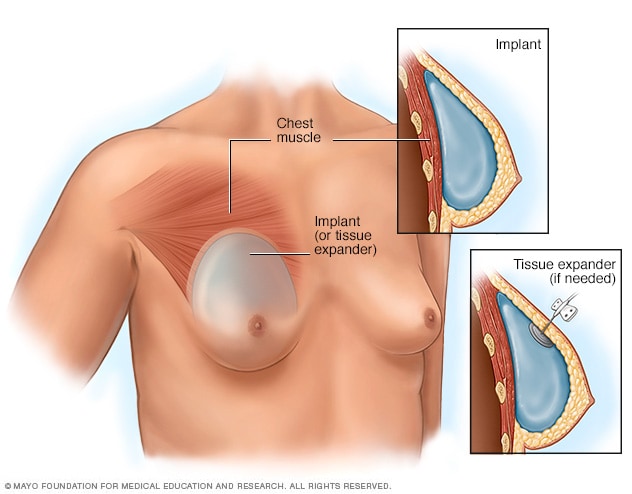
- Placement of breast implants or tissue expanders
During top surgery, the surgeon places the implants under the breast tissue. If feminizing hormones haven't made the breasts large enough, an initial surgery might be needed to have devices called tissue expanders placed in front of the chest muscles.
Hormone therapy with estrogen stimulates breast growth, but many people aren't satisfied with that growth alone. Top surgery is a surgical procedure to increase breast size that may involve implants, fat grafting or both.
During this surgery, a surgeon makes cuts around the areola, near the armpit or in the crease under the breast. Next, silicone or saline implants are placed under the breast tissue. Another option is to transplant fat, muscles or tissue from other parts of the body into the breasts.
If feminizing hormones haven't made the breasts large enough for top surgery, an initial surgery may be needed to place devices called tissue expanders in front of the chest muscles. After that surgery, visits to a health care provider are needed every few weeks to have a small amount of saline injected into the tissue expanders. This slowly stretches the chest skin and other tissues to make room for the implants. When the skin has been stretched enough, another surgery is done to remove the expanders and place the implants.
Genital surgery
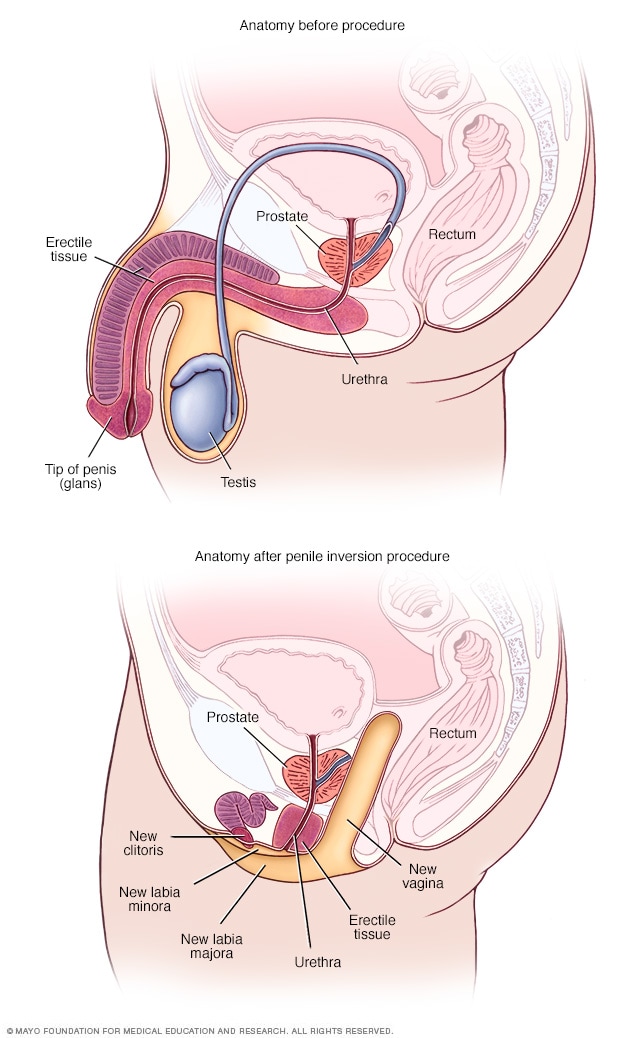
- Anatomy before and after penile inversion
During penile inversion, the surgeon makes a cut in the area between the rectum and the urethra and prostate. This forms a tunnel that becomes the new vagina. The surgeon lines the inside of the tunnel with skin from the scrotum, the penis or both. If there's not enough penile or scrotal skin, the surgeon might take skin from another area of the body and use it for the new vagina as well.
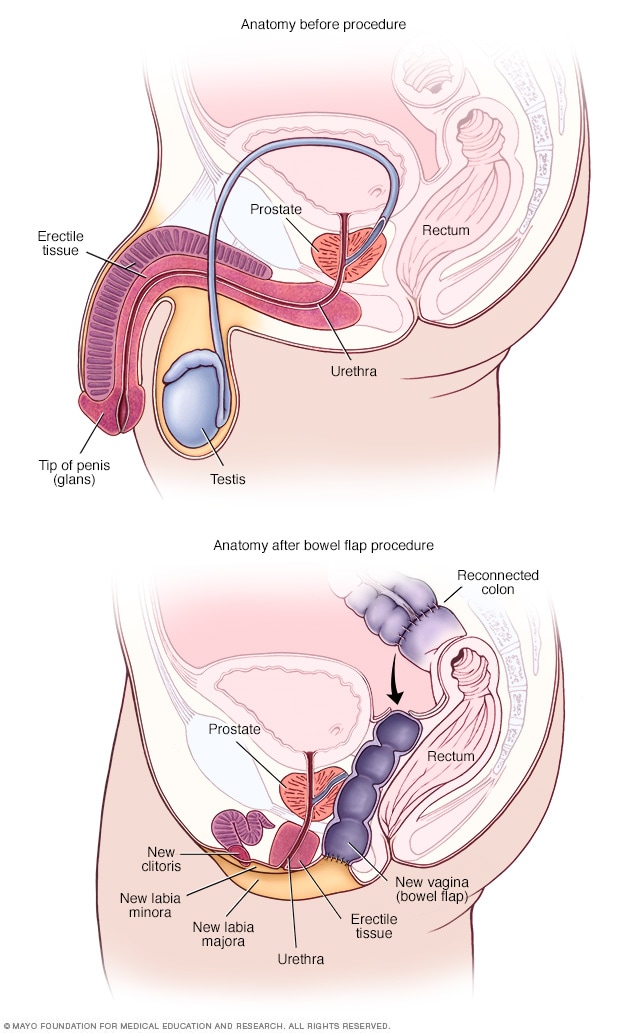
- Anatomy before and after bowel flap procedure
A bowel flap procedure might be done if there's not enough tissue or skin in the penis or scrotum. The surgeon moves a segment of the colon or small bowel to form a new vagina. That segment is called a bowel flap or conduit. The surgeon reconnects the remaining parts of the colon.
Orchiectomy
Orchiectomy is a surgery to remove the testicles. Because testicles produce sperm and the hormone testosterone, an orchiectomy might eliminate the need to use testosterone blockers. It also may lower the amount of estrogen needed to achieve and maintain the appearance you want.
This type of surgery is typically done on an outpatient basis. A local anesthetic may be used, so only the testicular area is numbed. Or the surgery may be done using general anesthesia. This means you are in a sleep-like state during the procedure.
To remove the testicles, a surgeon makes a cut in the scrotum and removes the testicles through the opening. Orchiectomy is typically done as part of the surgery for vaginoplasty. But some people prefer to have it done alone without other genital surgery.
Vaginoplasty
Vaginoplasty is the surgical creation of a vagina. During vaginoplasty, skin from the shaft of the penis and the scrotum is used to create a vaginal canal. This surgical approach is called penile inversion. In some techniques, the skin also is used to create the labia. That procedure is called labiaplasty. To surgically create a clitoris, the tip of the penis and the nerves that supply it are used. This procedure is called a clitoroplasty. In some cases, skin can be taken from another area of the body or tissue from the colon may be used to create the vagina. This approach is called a bowel flap procedure. During vaginoplasty, the testicles are removed if that has not been done previously.
Some surgeons use a technique that requires laser hair removal in the area of the penis and scrotum to provide hair-free tissue for the procedure. That process can take several months. Other techniques don't require hair removal prior to surgery because the hair follicles are destroyed during the procedure.
After vaginoplasty, a tube called a catheter is placed in the urethra to collect urine for several days. You need to be closely watched for about a week after surgery. Recovery can take up to two months. Your health care provider gives you instructions about when you may begin sexual activity with your new vagina.
After surgery, you're given a set of vaginal dilators of increasing sizes. You insert the dilators in your vagina to maintain, lengthen and stretch it. Follow your health care provider's directions on how often to use the dilators. To keep the vagina open, dilation needs to continue long term.
Because the prostate gland isn't removed during surgery, you need to follow age-appropriate recommendations for prostate cancer screening. Following surgery, it is possible to develop urinary symptoms from enlargement of the prostate.
Dilation after gender-affirming surgery
This material is for your education and information only. This content does not replace medical advice, diagnosis and treatment. If you have questions about a medical condition, always talk with your health care provider.
Narrator: Vaginal dilation is important to your recovery and ongoing care. You have to dilate to maintain the size and shape of your vaginal canal and to keep it open.
Jessi: I think for many trans women, including myself, but especially myself, I looked forward to one day having surgery for a long time. So that meant looking up on the internet what the routines would be, what the surgery entailed. So I knew going into it that dilation was going to be a very big part of my routine post-op, but just going forward, permanently.
Narrator: Vaginal dilation is part of your self-care. You will need to do vaginal dilation for the rest of your life.
Alissa (nurse): If you do not do dilation, your vagina may shrink or close. If that happens, these changes might not be able to be reversed.
Narrator: For the first year after surgery, you will dilate many times a day. After the first year, you may only need to dilate once a week. Most people dilate for the rest of their life.
Jessi: The dilation became easier mostly because I healed the scars, the stitches held up a little bit better, and I knew how to do it better. Each transgender woman's vagina is going to be a little bit different based on anatomy, and I grew to learn mine. I understand, you know, what position I needed to put the dilator in, how much force I needed to use, and once I learned how far I needed to put it in and I didn't force it and I didn't worry so much on oh, did I put it in too far, am I not putting it in far enough, and I have all these worries and then I stress out and then my body tenses up. Once I stopped having those thoughts, I relaxed more and it was a lot easier.
Narrator: You will have dilators of different sizes. Your health care provider will determine which sizes are best for you. Dilation will most likely be painful at first. It's important to dilate even if you have pain.
Alissa (nurse): Learning how to relax the muscles and breathe as you dilate will help. If you wish, you can take the pain medication recommended by your health care team before you dilate.
Narrator: Dilation requires time and privacy. Plan ahead so you have a private area at home or at work. Be sure to have your dilators, a mirror, water-based lubricant and towels available. Wash your hands and the dilators with warm soapy water, rinse well and dry on a clean towel. Use a water-based lubricant to moisten the rounded end of the dilators. Water-based lubricants are available over-the-counter. Do not use oil-based lubricants, such as petroleum jelly or baby oil. These can irritate the vagina. Find a comfortable position in bed or elsewhere. Use pillows to support your back and thighs as you lean back to a 45-degree angle. Start your dilation session with the smallest dilator. Hold a mirror in one hand. Use the other hand to find the opening of your vagina. Separate the skin. Relax through your hips, abdomen and pelvic floor. Take slow, deep breaths. Position the rounded end of the dilator with the lubricant at the opening to your vaginal canal. The rounded end should point toward your back. Insert the dilator. Go slowly and gently. Think of its path as a gentle curving swoop. The dilator doesn't go straight in. It follows the natural curve of the vaginal canal. Keep gentle down and inward pressure on the dilator as you insert it. Stop when the dilator's rounded end reaches the end of your vaginal canal. The dilators have dots or markers that measure depth. Hold the dilator in place in your vaginal canal. Use gentle but constant inward pressure for the correct amount of time at the right depth for you. If you're feeling pain, breathe and relax the muscles. When time is up, slowly remove the dilator, then repeat with the other dilators you need to use. Wash the dilators and your hands. If you have increased discharge following dilation, you may want to wear a pad to protect your clothing.
Jessi: I mean, it's such a strange, unfamiliar feeling to dilate and to have a dilator, you know to insert a dilator into your own vagina. Because it's not a pleasurable experience, and it's quite painful at first when you start to dilate. It feels much like a foreign body entering and it doesn't feel familiar and your body kind of wants to get it out of there. It's really tough at the beginning, but if you can get through the first month, couple months, it's going to be a lot easier and it's not going to be so much of an emotional and uncomfortable experience.
Narrator: You need to stay on schedule even when traveling. Bring your dilators with you. If your schedule at work creates challenges, ask your health care team if some of your dilation sessions can be done overnight.
Alissa (nurse): You can't skip days now and do more dilation later. You must do dilation on schedule to keep vaginal depth and width. It is important to dilate even if you have pain. Dilation should cause less pain over time.
Jessi: I hear that from a lot of other women that it's an overwhelming experience. There's lots of emotions that are coming through all at once. But at the end of the day for me, it was a very happy experience. I was glad to have the opportunity because that meant that while I have a vagina now, at the end of the day I had a vagina. Yes, it hurts, and it's not pleasant to dilate, but I have the vagina and it's worth it. It's a long process and it's not going to be easy. But you can do it.
Narrator: If you feel dilation may not be working or you have any questions about dilation, please talk with a member of your health care team.
Research has found that that gender-affirming surgery can have a positive impact on well-being and sexual function. It's important to follow your health care provider's advice for long-term care and follow-up after surgery. Continued care after surgery is associated with good outcomes for long-term health.
Before you have surgery, talk to members of your health care team about what to expect after surgery and the ongoing care you may need.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Feminizing surgery care at Mayo Clinic
- Tangpricha V, et al. Transgender women: Evaluation and management. https://www.uptodate.com/ contents/search. Accessed Aug. 16, 2022.
- Erickson-Schroth L, ed. Surgical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Aug. 17, 2022.
- Coleman E, et al. Standards of care for the health of transgender and gender diverse people, version 8. International Journal of Transgender Health. 2022; doi:10.1080/26895269.2022.2100644.
- AskMayoExpert. Gender-affirming procedures (adult). Mayo Clinic; 2022.
- Nahabedian, M. Implant-based breast reconstruction and augmentation. https://www.uptodate.com/contents/search. Accessed Aug. 17, 2022.
- Erickson-Schroth L, ed. Medical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Aug. 17, 2022.
- Ferrando C, et al. Gender-affirming surgery: Male to female. https://www.uptodate.com/contents/search. Accessed Aug. 17, 2022.
- Doctors & Departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Let’s celebrate our doctors!
Join us in celebrating and honoring Mayo Clinic physicians on March 30th for National Doctor’s Day.
- Introduction
- Conclusions
- Article Information
Error bars represent 95% CIs. GAS indicates gender-affirming surgery.
Percentages are based on the number of procedures divided by number of patients; thus, as some patients underwent multiple procedures the total may be greater than 100%. Error bars represent 95% CIs.
eTable. ICD-10 and CPT Codes of Gender-Affirming Surgery
eFigure. Percentage of Patients With Codes for Gender Identity Disorder Who Underwent GAS
Data Sharing Statement
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Wright JD , Chen L , Suzuki Y , Matsuo K , Hershman DL. National Estimates of Gender-Affirming Surgery in the US. JAMA Netw Open. 2023;6(8):e2330348. doi:10.1001/jamanetworkopen.2023.30348
Manage citations:
© 2024
- Permissions
National Estimates of Gender-Affirming Surgery in the US
- 1 Department of Obstetrics and Gynecology, Columbia University College of Physicians and Surgeons, New York, New York
- 2 Department of Obstetrics and Gynecology, University of Southern California, Los Angeles
Question What are the temporal trends in gender-affirming surgery (GAS) in the US?
Findings In this cohort study of 48 019 patients, GAS increased significantly, nearly tripling from 2016 to 2019. Breast and chest surgery was the most common class of procedures performed overall; genital reconstructive procedures were more common among older individuals.
Meaning These findings suggest that there will be a greater need for clinicians knowledgeable in the care of transgender individuals with the requisite expertise to perform gender-affirming procedures.
Importance While changes in federal and state laws mandating coverage of gender-affirming surgery (GAS) may have led to an increase in the number of annual cases, comprehensive data describing trends in both inpatient and outpatient procedures are limited.
Objective To examine trends in inpatient and outpatient GAS procedures in the US and to explore the temporal trends in the types of GAS performed across age groups.
Design, Setting, and Participants This cohort study includes data from 2016 to 2020 in the Nationwide Ambulatory Surgery Sample and the National Inpatient Sample. Patients with diagnosis codes for gender identity disorder, transsexualism, or a personal history of sex reassignment were identified, and the performance of GAS, including breast and chest procedures, genital reconstructive procedures, and other facial and cosmetic surgical procedures, were identified.
Main Outcome Measures Weighted estimates of the annual number of inpatient and outpatient procedures performed and the distribution of each class of procedure overall and by age were analyzed.
Results A total of 48 019 patients who underwent GAS were identified, including 25 099 (52.3%) who were aged 19 to 30 years. The most common procedures were breast and chest procedures, which occurred in 27 187 patients (56.6%), followed by genital reconstruction (16 872 [35.1%]) and other facial and cosmetic procedures (6669 [13.9%]). The absolute number of GAS procedures rose from 4552 in 2016 to a peak of 13 011 in 2019 and then declined slightly to 12 818 in 2020. Overall, 25 099 patients (52.3%) were aged 19 to 30 years, 10 476 (21.8%) were aged 31 to 40, and 3678 (7.7%) were aged12 to 18 years. When stratified by the type of procedure performed, breast and chest procedures made up a greater percentage of the surgical interventions in younger patients, while genital surgical procedures were greater in older patients.
Conclusions and Relevance Performance of GAS has increased substantially in the US. Breast and chest surgery was the most common group of procedures performed. The number of genital surgical procedures performed increased with increasing age.
Gender dysphoria is characterized as an incongruence between an individual’s experienced or expressed gender and the gender that was assigned at birth. 1 Transgender individuals may pursue multiple treatments, including behavioral therapy, hormonal therapy, and gender-affirming surgery (GAS). 2 GAS encompasses a variety of procedures that align an individual patient’s gender identity with their physical appearance. 2 - 4
While numerous surgical interventions can be considered GAS, the procedures have been broadly classified as breast and chest surgical procedures, facial and cosmetic interventions, and genital reconstructive surgery. 2 , 4 Prior studies 2 - 7 have shown that GAS is associated with improved quality of life, high rates of satisfaction, and a reduction in gender dysphoria. Furthermore, some studies have reported that GAS is associated with decreased depression and anxiety. 8 Lastly, the procedures appear to be associated with acceptable morbidity and reasonable rates of perioperative complications. 2 , 4
Given the benefits of GAS, the performance of GAS in the US has increased over time. 9 The increase in GAS is likely due in part to federal and state laws requiring coverage of transition-related care, although actual insurance coverage of specific procedures is variable. 10 , 11 While prior work has shown that the use of inpatient GAS has increased, national estimates of inpatient and outpatient GAS are lacking. 9 This is important as many GAS procedures occur in ambulatory settings. We performed a population-based analysis to examine trends in GAS in the US and explored the temporal trends in the types of GAS performed across age groups.
To capture both inpatient and outpatient surgical procedures, we used data from the Nationwide Ambulatory Surgery Sample (NASS) and the National Inpatient Sample (NIS). NASS is an ambulatory surgery database and captures major ambulatory surgical procedures at nearly 2800 hospital-owned facilities from up to 35 states, approximating a 63% to 67% stratified sample of hospital-owned facilities. NIS comprehensively captures approximately 20% of inpatient hospital encounters from all community hospitals across 48 states participating in the Healthcare Cost and Utilization Project (HCUP), covering more than 97% of the US population. Both NIS and NASS contain weights that can be used to produce US population estimates. 12 , 13 Informed consent was waived because data sources contain deidentified data, and the study was deemed exempt by the Columbia University institutional review board. This cohort study followed the Strengthening the Reporting of Observational Studies in Epidemiology ( STROBE ) reporting guideline.
We selected patients of all ages with an International Statistical Classification of Diseases and Related Health Problems, Tenth Revision ( ICD-10 ) diagnosis codes for gender identity disorder or transsexualism ( ICD-10 F64) or a personal history of sex reassignment ( ICD-10 Z87.890) from 2016 to 2020 (eTable in Supplement 1 ). We first examined all hospital (NIS) and ambulatory surgical (NASS) encounters for patients with these codes and then analyzed encounters for GAS within this cohort. GAS was identified using ICD-10 procedure codes and Common Procedural Terminology codes and classified as breast and chest procedures, genital reconstructive procedures, and other facial and cosmetic surgical procedures. 2 , 4 Breast and chest surgical procedures encompassed breast reconstruction, mammoplasty and mastopexy, or nipple reconstruction. Genital reconstructive procedures included any surgical intervention of the male or female genital tract. Other facial and cosmetic procedures included cosmetic facial procedures and other cosmetic procedures including hair removal or transplantation, liposuction, and collagen injections (eTable in Supplement 1 ). Patients might have undergone procedures from multiple different surgical groups. We measured the total number of procedures and the distribution of procedures within each procedural group.
Within the data sets, sex was based on patient self-report. The sex of patients in NIS who underwent inpatient surgery was classified as either male, female, missing, or inconsistent. The inconsistent classification denoted patients who underwent a procedure that was not consistent with the sex recorded on their medical record. Similar to prior analyses, patients in NIS with a sex variable not compatible with the procedure performed were classified as having undergone genital reconstructive surgery (GAS not otherwise specified). 9
Clinical variables in the analysis included patient clinical and demographic factors and hospital characteristics. Demographic characteristics included age at the time of surgery (12 to 18 years, 19 to 30 years, 31 to 40 years, 41 to 50 years, 51 to 60 years, 61 to 70 years, and older than 70 years), year of the procedure (2016-2020), and primary insurance coverage (private, Medicare, Medicaid, self-pay, and other). Race and ethnicity were only reported in NIS and were classified as White, Black, Hispanic and other. Race and ethnicity were considered in this study because prior studies have shown an association between race and GAS. The income status captured national quartiles of median household income based of a patient’s zip code and was recorded as less than 25% (low), 26% to 50% (medium-low), 51% to 75% (medium-high), and 76% or more (high). The Elixhauser Comorbidity Index was estimated for each patient based on the codes for common medical comorbidities and weighted for a final score. 14 Patients were classified as 0, 1, 2, or 3 or more. We separately reported coding for HIV and AIDS; substance abuse, including alcohol and drug abuse; and recorded mental health diagnoses, including depression and psychoses. Hospital characteristics included a composite of teaching status and location (rural, urban teaching, and urban nonteaching) and hospital region (Northeast, Midwest, South, and West). Hospital bed sizes were classified as small, medium, and large. The cutoffs were less than 100 (small), 100 to 299 (medium), and 300 or more (large) short-term acute care beds of the facilities from NASS and were varied based on region, urban-rural designation, and teaching status of the hospital from NIS. 8 Patients with missing data were classified as the unknown group and were included in the analysis.
National estimates of the number of GAS procedures among all hospital encounters for patients with gender identity disorder were derived using discharge or encounter weight provided by the databases. 15 The clinical and demographic characteristics of the patients undergoing GAS were reported descriptively. The number of encounters for gender identity disorder, the percentage of GAS procedures among those encounters, and the absolute number of each procedure performed over time were estimated. The difference by age group was examined and tested using Rao-Scott χ 2 test. All hypothesis tests were 2-sided, and P < .05 was considered statistically significant. All analyses were conducted using SAS version 9.4 (SAS Institute Inc).
A total of 48 019 patients who underwent GAS were identified ( Table 1 ). Overall, 25 099 patients (52.3%) were aged 19 to 30 years, 10 476 (21.8%) were aged 31 to 40, and 3678 (7.7%) were aged 12 to 18 years. Private insurance coverage was most common in 29 064 patients (60.5%), while 12 127 (25.3%) were Medicaid recipients. Depression was reported in 7192 patients (15.0%). Most patients (42 467 [88.4%]) were treated at urban, teaching hospitals, and there was a disproportionate number of patients in the West (22 037 [45.9%]) and Northeast (12 396 [25.8%]). Within the cohort, 31 668 patients (65.9%) underwent 1 procedure while 13 415 (27.9%) underwent 2 procedures, and the remainder underwent multiple procedures concurrently ( Table 1 ).
The overall number of health system encounters for gender identity disorder rose from 13 855 in 2016 to 38 470 in 2020. Among encounters with a billing code for gender identity disorder, there was a consistent rise in the percentage that were for GAS from 4552 (32.9%) in 2016 to 13 011 (37.1%) in 2019, followed by a decline to 12 818 (33.3%) in 2020 ( Figure 1 and eFigure in Supplement 1 ). Among patients undergoing ambulatory surgical procedures, 37 394 (80.3%) of the surgical procedures included gender-affirming surgical procedures. For those with hospital admissions with gender identity disorder, 10 625 (11.8%) of admissions were for GAS.
Breast and chest procedures were most common and were performed for 27 187 patients (56.6%). Genital reconstruction was performed for 16 872 patients (35.1%), and other facial and cosmetic procedures for 6669 patients (13.9%) ( Table 2 ). The most common individual procedure was breast reconstruction in 21 244 (44.2%), while the most common genital reconstructive procedure was hysterectomy (4489 [9.3%]), followed by orchiectomy (3425 [7.1%]), and vaginoplasty (3381 [7.0%]). Among patients who underwent other facial and cosmetic procedures, liposuction (2945 [6.1%]) was most common, followed by rhinoplasty (2446 [5.1%]) and facial feminizing surgery and chin augmentation (1874 [3.9%]).
The absolute number of GAS procedures rose from 4552 in 2016 to a peak of 13 011 in 2019 and then declined slightly to 12 818 in 2020 ( Figure 1 ). Similar trends were noted for breast and chest surgical procedures as well as genital surgery, while the rate of other facial and cosmetic procedures increased consistently from 2016 to 2020. The distribution of the individual procedures performed in each class were largely similar across the years of analysis ( Table 3 ).
When stratified by age, patients 19 to 30 years had the greatest number of procedures, 25 099 ( Figure 2 ). There were 10 476 procedures performed in those aged 31 to 40 years and 4359 in those aged 41 to 50 years. Among patients younger than 19 years, 3678 GAS procedures were performed. GAS was less common in those cohorts older than 50 years. Overall, the greatest number of breast and chest surgical procedures, genital surgical procedures, and facial and other cosmetic surgical procedures were performed in patients aged 19 to 30 years.
When stratified by the type of procedure performed, breast and chest procedures made up the greatest percentage of the surgical interventions in younger patients while genital surgical procedures were greater in older patients ( Figure 2 ). Additionally, 3215 patients (87.4%) aged 12 to 18 years underwent GAS and had breast or chest procedures. This decreased to 16 067 patients (64.0%) in those aged 19 to 30 years, 4918 (46.9%) in those aged 31 to 40 years, and 1650 (37.9%) in patients aged 41 to 50 years ( P < .001). In contrast, 405 patients (11.0%) aged 12 to 18 years underwent genital surgery. The percentage of patients who underwent genital surgery rose sequentially to 4423 (42.2%) in those aged 31 to 40 years, 1546 (52.3%) in those aged 51 to 60 years, and 742 (58.4%) in those aged 61 to 70 years ( P < .001). The percentage of patients who underwent facial and other cosmetic surgical procedures rose with age from 9.5% in those aged 12 to 18 years to 20.6% in those aged 51 to 60 years, then gradually declined ( P < .001). Figure 2 displays the absolute number of procedure classes performed by year stratified by age. The greatest magnitude of the decline in 2020 was in younger patients and for breast and chest procedures.
These findings suggest that the number of GAS procedures performed in the US has increased dramatically, nearly tripling from 2016 to 2019. Breast and chest surgery is the most common class of procedure performed while patients are most likely to undergo surgery between the ages of 19 and 30 years. The number of genital surgical procedures performed increased with increasing age.
Consistent with prior studies, we identified a remarkable increase in the number of GAS procedures performed over time. 9 , 16 A prior study examining national estimates of inpatient GAS procedures noted that the absolute number of procedures performed nearly doubled between 2000 to 2005 and from 2006 to 2011. In our analysis, the number of GAS procedures nearly tripled from 2016 to 2020. 9 , 17 Not unexpectedly, a large number of the procedures we captured were performed in the ambulatory setting, highlighting the need to capture both inpatient and outpatient procedures when analyzing data on trends. Like many prior studies, we noted a decrease in the number of procedures performed in 2020, likely reflective of the COVID-19 pandemic. 18 However, the decline in the number of procedures performed between 2019 and 2020 was relatively modest, particularly as these procedures are largely elective.
Analysis of procedure-specific trends by age revealed a number of important findings. First, GAS procedures were most common in patients aged 19 to 30 years. This is in line with prior work that demonstrated that most patients first experience gender dysphoria at a young age, with approximately three-quarters of patients reporting gender dysphoria by age 7 years. These patients subsequently lived for a mean of 23 years for transgender men and 27 years for transgender women before beginning gender transition treatments. 19 Our findings were also notable that GAS procedures were relatively uncommon in patients aged 18 years or younger. In our cohort, fewer than 1200 patients in this age group underwent GAS, even in the highest volume years. GAS in adolescents has been the focus of intense debate and led to legislative initiatives to limit access to these procedures in adolescents in several states. 20 , 21
Second, there was a marked difference in the distribution of procedures in the different age groups. Breast and chest procedures were more common in younger patients, while genital surgery was more frequent in older individuals. In our cohort of individuals aged 19 to 30 years, breast and chest procedures were twice as common as genital procedures. Genital surgery gradually increased with advancing age, and these procedures became the most common in patients older than 40 years. A prior study of patients with commercial insurance who underwent GAS noted that the mean age for mastectomy was 28 years, significantly lower than for hysterectomy at age 31 years, vaginoplasty at age 40 years, and orchiectomy at age 37 years. 16 These trends likely reflect the increased complexity of genital surgery compared with breast and chest surgery as well as the definitive nature of removal of the reproductive organs.
This study has limitations. First, there may be under-capture of both transgender individuals and GAS procedures. In both data sets analyzed, gender is based on self-report. NIS specifically makes notation of procedures that are considered inconsistent with a patient’s reported gender (eg, a male patient who underwent oophorectomy). Similar to prior work, we assumed that patients with a code for gender identity disorder or transsexualism along with a surgical procedure classified as inconsistent underwent GAS. 9 Second, we captured procedures commonly reported as GAS procedures; however, it is possible that some of these procedures were performed for other underlying indications or diseases rather than solely for gender affirmation. Third, our trends showed a significant increase in procedures through 2019, with a decline in 2020. The decline in services in 2020 is likely related to COVID-19 service alterations. Additionally, while we comprehensively captured inpatient and ambulatory surgical procedures in large, nationwide data sets, undoubtedly, a small number of procedures were performed in other settings; thus, our estimates may underrepresent the actual number of procedures performed each year in the US.
These data have important implications in providing an understanding of the use of services that can help inform care for transgender populations. The rapid rise in the performance of GAS suggests that there will be a greater need for clinicians knowledgeable in the care of transgender individuals and with the requisite expertise to perform GAS procedures. However, numerous reports have described the political considerations and challenges in the delivery of transgender care. 22 Despite many medical societies recognizing the necessity of gender-affirming care, several states have enacted legislation or policies that restrict gender-affirming care and services, particularly in adolescence. 20 , 21 These regulations are barriers for patients who seek gender-affirming care and provide legal and ethical challenges for clinicians. As the use of GAS increases, delivering equitable gender-affirming care in this complex landscape will remain a public health challenge.
Accepted for Publication: July 15, 2023.
Published: August 23, 2023. doi:10.1001/jamanetworkopen.2023.30348
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2023 Wright JD et al. JAMA Network Open .
Corresponding Author: Jason D. Wright, MD, Division of Gynecologic Oncology, Department of Obstetrics and Gynecology, Columbia University College of Physicians and Surgeons, 161 Fort Washington Ave, 4th Floor, New York, NY 10032 ( [email protected] ).
Author Contributions: Dr Wright had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Wright, Chen.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Wright.
Critical review of the manuscript for important intellectual content: All authors.
Statistical analysis: Wright, Chen.
Administrative, technical, or material support: Wright, Suzuki.
Conflict of Interest Disclosures: Dr Wright reported receiving grants from Merck and personal fees from UpToDate outside the submitted work. No other disclosures were reported.
Data Sharing Statement: See Supplement 2 .
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- BOOK CONSULTATION
- The Surgical Journey
- Where do I start?
- Am I eligible for surgery?
- Preparing for Surgery
- General Recovery Info
- Risks & Safety
- Top Surgery
- Top Surgery Techniques
- Techniques Beyond the Binary
- Top Surgery Videos
- Breast Augmentation
- Facial Surgery
- Techniques & Incisions
- Body Contouring
- Body Feminization
- Body Masculinization
- Non-Binary Body Contouring
- Bottom Surgery
- “Feminizing” Techniques & Recovery
- “Masculinizing” Techniques & Recovery
- Our Services
- Currently Offered
- Outside Services
- Transition 101
- Introduction to Transitioning
- Support Services: Helpful Links
- Transitioning Later In Life
- Legal Name & Gender Change
- Transmasculine & Pregnancy
- Transgender Healthcare
- Mental Health
- Hormone Therapy
Trans Youth & Adolescents
- Mental Health Support
- Common Questions About Your Child’s Transition
- For Caregivers
- Explaining Your Child’s Identity
- Talking With Schools About Your Child
- Puberty Blockers
- Challenging Topics
- Detransition
- Adolescents
- Gatekeeping vs Empowerment
- Rapid Onset Gender Dysphoria
- Double Incision
- Periareolar
- Inverted T / Aggressive Breast Reduction
- Gynecomastia
- Facial Feminization
- Facial Masculinization
- Labiaplasty
- Vaginoplasty
- Fees & Financing
- Insurance Approval
- Insurance Denial
- Insurance Accepted
- Referral Letters
- Advocacy Team
- Make a Payment Now
- Our Philosophy
- Meet Our Team
- Office & Facilities
- Testimonials
- Get in Touch
- For Current Patients
- For Providers
Consultation request
- Interpretation Services
- Privacy Policy

slide toggle Demystifying and Navigating Your Options: Gender Reassignment Surgery
Do you have any questions? Check our F.A.Q. section or contact us directly!
Demystifying and Navigating Your Options: Gender Reassignment Surgery
Medically reviewed by Paul Gonzales on March 25, 2024.

Previously, the term gender reassignment surgery (GRS) referred to genital reconstruction bottom surgeries like vaginoplasty, vulvoplasty, phalloplasty, or metoidioplasty. Individuals who look up this term on a search engine do so looking for information on gender-affirming procedures generally for transgender, non-binary and gender non-conforming people. This detailed guide breaks down everything you need to know about these procedures, their costs, their eligibility requirements, the potential benefits and risks and more. If you are interested in undergoing any gender-affirming or “gender reassignment” surgery, you can schedule a free, virtual consultation with one of our surgeons.
At the Gender Confirmation Center (GCC), we generally avoid using terminology like GRS in a clinical setting out of the recognition that for the vast majority of our patients, surgeries do not “reassign” anyone’s gender. Rather, surgery can help individuals experience greater alignment with their bodies and greater gender euphoria as a result.
Types of Gender “Reassignment” Surgeries: “Female to Male (FTM)”
Female to Male (FTM) is outdated terminology that the GCC does not use in our clinical practice. This abbreviation leaves out the experiences of many trans masculine and non-binary patients who do not identify with being labeled as a “woman becoming a man.”
In the past, “FTM gender confirmation surgery” was used to describe surgical procedures that reverse the effects of an initial estrogenic puberty or procedures that reconstruct a patient’s genitals. We still receive various inquiries about which “FTM” procedures we offer, so below you can find a list of surgeries that have typically been placed under this label.
Please note that patients can seek out any of these procedures regardless of their gender identity. The goal of our practice is not to make our patients “into men,” but to help them feel more comfortable, affirmed, and/or aligned with their bodies.
Chest Surgery or Top Surgery
“FTM” top surgery is an antiquated term that refers to gender-affirming chest reconstruction and/or breast reduction. Practices who use this acronym sometimes have limited experience meeting the unique needs of non-binary patients seeking top surgery . Patients who would like to remove their chest tissue to have a flatter chest can choose from a variety of incision options to reach their desired results around chest tightness, contour and/or scar shape.
Not all patients who pursue top surgery want flat chests. Whether you would like to opt for a breast reduction or a chest reconstruction with some volume left behind, the button buttonhole incision is the most commonly pursued type.
Top surgery patients who would like to maintain an erotic or a high level of sensation in their nipples can ask their surgeon about nerve-preservation techniques . Inversely, many patients who get top surgery choose to have their nipples removed .
Genital Reconstruction or Bottom Surgery
While the following bottom surgery procedures are traditionally put under the “FTM” category, we recognize that not all patients who pursue these procedures identify as men nor are they looking to “masculinize” their genitals.
Two procedures can be used to reconstruct a penis or “neophallus”: metoidioplasty and phalloplasty. Metoidioplasty or “meta” releases the ligaments around the erectile tissue (called a clitoris or penis) to extend it to about 2-4 inches in length. A phalloplasty uses a donor flap (usually from the forearm or thigh) to construct a penis of 4 inches in length or more (depending on availability of tissue). Both procedures can be specialized to allow a patient to maintain erotic sensation in their genitals (nerve preservation) and/or urinate standing up (urethroplasty).
Associated procedures include the removal of the uterus (hysterectomy), the removal of the vaginal canal (vaginectomy), the construction of a scrotum (scrotoplasty), the insertion of penile/testicular implants, and more.
Body Masculinization Surgery (BMS)
Body Masculinization Surgery (BMS) refers to a series of body contouring procedures. Most often, BMS involves liposuction of one or more of the following areas: abdomen, flanks, hips, thighs, buttocks, or arms. BMS can also involve removing unwanted, excess skin from fat loss or liposuction. Occasionally, some patients may opt for silicone pectoral implants alongside or after their top surgery results.
Facial Masculinization Surgery (FMS)
Facial Masculinization Surgery (FMS) refers to a series of procedures that patients can choose from to give their face a more angular, conventionally masculine appearance. In the bottom third of the face, the chin, jaw, or laryngeal prominence (aka Adam’s apple) can be augmented or increased in size. In the middle third of the face, the appearance of the nose and/or cheeks can be altered. In the top third of the face, the hairline’s position can be changed and the forehead can be augmented.

Types of Gender “Reassignment” Surgeries: “Male to Female (MTF)”
Male to Female (MTF) is outdated terminology that we do not use in our clinical practice. This abbreviation leaves out the experiences of many trans feminine and non-binary patients who do not identify with being labeled as a “man becoming a woman.”
In the past, “MTF gender confirmation surgery” was used to describe surgical procedures that reverse the effects of an initial androgenic (testosterone-dominant) puberty and/or reconstruct a patient’s genitals. As a practice, we still get asked by prospective patients about the “MTF” procedures we offer, which is why we have compiled a guide of surgeries that have typically been placed under this category.
Please note that patients can seek out any of these procedures regardless of their gender identity. The goal of our practice is not to make our patients turn “into women,” but to help them feel greater gender congruence with their bodies.
Breast Augmentation or “MTF” Top Surgery
Typically, for trans feminine and non-binary patients who prefer to have more volume on their chest, breast augmentation with saline or silicone implants allows for greater success in their desired outcomes. Fat grafting procedures limit the amount of volume transferred to the chest based on available body fat that can be safely removed.
Genital Reconstruction or Bottom Surgeries
The most common surgeries that are placed under this category are vaginoplasty and vulvoplasty (also called zero-depth vaginoplasty) procedures. The most common vaginoplasty uses a penile-inversion technique to reconstruct a vaginal canal. However, a penile-preserving vaginoplasty is also another option for patients. Lifelong dilation after this procedure is necessary to maintain the depth of the canal so that it can be used for penetrative sex. Labiaplasty revisions are sometimes sought out by patients wishing to adjust the size, shape and symmetry of their labia and/or clitoral hood.
Before a vaginoplasty, patients may opt to remove the testicles ( orchiectomy ). Patients of varying gender identities undergo orchiectomies for many reasons, such as chronic pain or to simplify their hormone therapy. For patients who plan to have a vaginoplasty in the future, it’s best to consider the timing of an orchiectomy procedure since scrotal tissue can be used to construct the labia.
Facial Feminization Surgery (FFS)
FFS refers to a series of procedures that a patient can choose from to give their face a softer, more conventionally feminine appearance. In the bottom third of the face, the laryngeal prominence (or Adam’s apple), chin, or jaw can be reduced in size. In the middle third of the face, the appearance of the nose and/or cheeks can be altered. In the top third of the face, the hairline’s position can be changed and the forehead can be reduced.
Body Feminization Surgery (BFS)
BFS encompasses a series of body contouring procedures. Most often, BFS involves removal of fat through liposuction of one or more of the following areas: the thighs, the abdomen/waist, or the arms. The fat removed from these areas of the body can be transferred to the buttocks and/or hip areas and is commonly referred to as a Brazilian butt lift (BBL). BFS can also involve removing unwanted excess skin from fat loss or liposuction, a procedure often referred to as a tummy tuck or abdominoplasty.
Evaluating Candidacy for Gender Affirmation Surgery
Strict guidelines evaluate patient readiness for life-altering GRS procedures.
Informed consent
The GCC follows an informed consent model for surgery because it gives patients autonomy over their health. Under this model, adults can consent to procedures if they have received adequate education about their risks, advantages, and potential effects on their health given their unique medical history. Historically, TGD people have had a difficult time accessing quality gender-affirming health care in part because of gatekeeping and discrimination based on requirements set by insurance companies. For example, letters from medical and mental health providers are a part of these requirements. We recognize that therapists and other healthcare providers are invaluable sources of support for patients undergoing a medical gender transition.
Health factors
We recommend our patients get medical clearance from their primary care provider (PCP) before surgery. If you have medical conditions that may affect your surgery, we can work with your PCP or specialist to ensure a safe recovery. Patients should inform their surgeons of any cardiovascular or respiratory issues, history of anorexia, diabetes, or use of immunosuppressant medications.
Different surgeons may consider a patient’s Body Mass Index (BMI) as part of their eligibility for surgery. You can read more about our requirements and recommendations around BMI here .
We require all our patients to stop smoking or consuming any form of nicotine for at least 3 weeks before and 3 weeks after surgery, as this can lead to significant problems with delayed wound healing. Please do not drink alcohol for at least 1 week before and 1 week after surgery or until prescription pain medications are discontinued.
Insurance requirements
Patients who wish to have their insurance cover their gender affirming surgery need to fulfill certain requirements. You will need to get a letter of support from a mental health professional to confirm that the procedure is medically necessary. If the surgeon is outside of your insurance’s in-network providers, you will need to get a referral letter from your primary care provider (PCP). Additionally, some insurance companies may require that a patient undergo gender-affirming hormone therapy to cover surgery.
Hormone Therapy Considerations
At GCC, we do not require our patients to undergo hormone therapy to access medically necessary, gender-affirming surgeries. That said, undergoing hormones before surgery can help some patients improve the appearance of post-op results.
- Facial surgery: It may take up to 1.5 years on hormone therapy before soft tissue changes can appear on the face so patients should consider waiting to undergo facial surgery until these changes have settled.
- Bottom surgery: Maximal bottom growth may take up to 2 years for patients on a standard dose of testosterone so patients should consider undergoing metoidioplasty until maximal growth is achieved for optimal outcomes.
- Breast augmentation: Maximal breast growth may take up to 1.5 to 2 years for patients on a standard dose of estrogen so patients should consider undergoing breast augmentation until maximal growth is achieved.
- Body contouring: It may take up to 1.5 years on hormone therapy before the fat redistribution process settles so patients should consider waiting until then before undergoing liposuction or fat grafting procedures.
When it comes to age and eligibility for surgery, we are typically asked about 2 populations: adolescents and seniors. The World Professional Association for Transgender Health (WPATH) has outlined in their Standards of Care (SOC), Version 8 , the need for the involvement of caregivers/parents and mental health professionals in the informed consent process for adolescents. If these protocols are followed, the only type of gender-affirming surgery that an adolescent can undergo is top surgery.
As long they are in good health and cleared for surgery, senior patients are eligible for surgery regardless of their age and can achieve good aesthetic outcomes. It’s important to consider what accommodations are necessary to support post-op recovery. You can read more about our eligibility standards here .
Weighing GRS Benefits Against Complications
The decision to undergo “gender reassignment surgery” is a highly personal one. Understanding both the pros and cons provides critical insight.
How GRS Can Transform Lives
The WPATH’s SOC 8 reviews the medical research literature around the long-term effects of gender-affirming surgery on trans and non-binary patients. Gender-affirming procedures report greater satisfaction and lower regret rates compared to similar cosmetic and reconstructive procedures performed in cisgender patients.
- Improved mental health
- Improved body-image, etc.
- Enhanced quality of life
Rates of anxiety, depression, and suicide risk all tend to decrease substantially following surgery for those who need it, which is why these procedures are considered medically necessary for many patients.
Risk Factors and Long-Term Effects
All surgeries carry risks of complications. Generally speaking, patients who optimize their health prior to surgery (e.g., do not smoke tobacco) and manage any pre-existing medical conditions can greatly reduce their risk for complications. Undergoing surgery with a board-certified surgeon who has hospital access privileges can help ensure the integrity of your surgical process. If you have specific questions about surgical complications and how to prevent them, you can consult our content library on this question.
Navigating Emotions
Surgery not only takes a physical, but also an emotional toll on the body. Experiencing pain, inflammation, discomfort and limitations on physical activity occasionally mat result in temporary postoperative depression. Likewise, having to wait weeks or months to have a sense of what your final results from surgery will look like can give some patients temporary feelings of regret during recovery. For this reason, we highly encourage patients to tap into their support networks of friends, (chosen) family and/or mental health professionals during this time. To learn more about the emotional recovery process, click here .
Conclusion: Is Gender Reassignment Surgery the Right Choice?
While gender-affirming surgery has been proven to be positively life-changing for many trans and non-binary individuals. Whether you seek surgery or not, we remain dedicated to your health, empowerment, and right to be your authentic self.
More Articles
Understanding the cost of double incision top surgery: a comprehensive guide, gatekeeping vs. empowerment: accessing gender affirming care, treating gender dysphoria in adolescents, sign up for instructions to get a virtual consultation.
The virtual consultation will be billed to your insurance company. We will accept the insurance reimbursement as payment in full.
Dr. Scott Mosser Suite 1010, 450 Sutter St San Francisco, CA 94108 Phone: (415) 780-1515 Fax: ( 628) 867-6510
Gender Journey Resources
- Trans Youth & Adolescents
Before & After
- Top surgery
- Virtual Consultations
Board Certification & Memberships

- Terms of Use
Copyright © 2023 Gender Confirmation Center. All Rights Reserved.
How Gender Reassignment Surgery Works (Infographic)
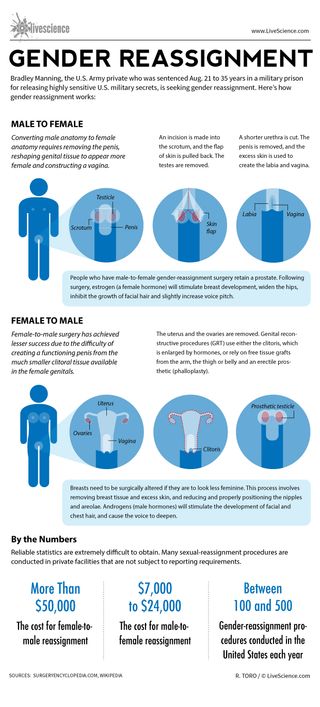
Bradley Manning, the U.S. Army private who was sentenced Aug. 21 to 35 years in a military prison for releasing highly sensitive U.S. military secrets, is seeking gender reassignment. Here’s how gender reassignment works:
Converting male anatomy to female anatomy requires removing the penis, reshaping genital tissue to appear more female and constructing a vagina.
An incision is made into the scrotum, and the flap of skin is pulled back. The testes are removed.
A shorter urethra is cut. The penis is removed, and the excess skin is used to create the labia and vagina.
People who have male-to-female gender-reassignment surgery retain a prostate. Following surgery, estrogen (a female hormone) will stimulate breast development, widen the hips, inhibit the growth of facial hair and slightly increase voice pitch.
Female-to-male surgery has achieved lesser success due to the difficulty of creating a functioning penis from the much smaller clitoral tissue available in the female genitals.
The uterus and the ovaries are removed. Genital reconstructive procedures (GRT) use either the clitoris, which is enlarged by hormones, or rely on free tissue grafts from the arm, the thigh or belly and an erectile prosthetic (phalloplasty).
Breasts need to be surgically altered if they are to look less feminine. This process involves removing breast tissue and excess skin, and reducing and properly positioning the nipples and areolae. Androgens (male hormones) will stimulate the development of facial and chest hair, and cause the voice to deepen.
Reliable statistics are extremely difficult to obtain. Many sexual-reassignment procedures are conducted in private facilities that are not subject to reporting requirements.
The cost for female-to-male reassignment can be more than $50,000. The cost for male-to-female reassignment can be $7,000 to $24,000.
Between 100 to 500 gender-reassignment procedures are conducted in the United States each year.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Man's years of premature ejaculation had a rare cause
Viagra alternatives? Study of mouse erections hints at new ways to treat erectile dysfunction
Space photo of the week: James Webb telescope reveals surprising starburst in ancient galaxy
Most Popular
By Anna Gora December 27, 2023
By Anna Gora December 26, 2023
By Anna Gora December 25, 2023
By Emily Cooke December 23, 2023
By Victoria Atkinson December 22, 2023
By Anna Gora December 16, 2023
By Anna Gora December 15, 2023
By Anna Gora November 09, 2023
By Donavyn Coffey November 06, 2023
By Anna Gora October 31, 2023
By Anna Gora October 26, 2023
- 2 James Webb telescope confirms there is something seriously wrong with our understanding of the universe
- 3 'You could almost see and smell their world': Remnants of 'Britain's Pompeii' reveal details of life in Bronze Age village
- 4 Amazfit Balance review
- 5 9,000-year-old rock art discovered among dinosaur footprints in Brazil
- 2 How much does Earth weigh?
- 3 Tardigrade proteins could slow aging in humans, small cell study finds
- 4 'Novel' swine flu virus sickens Pennsylvania child in 1st case of the year
latest in US News

Trailer of Bibles intentionally set on fire in front of Tennessee...

Israeli tech entrepreneur and wife killed in Calif. plane crash...

Heavy spring snow in Northeast, New England this week could mean...

Florida car chase in 2020 may be linked to Havana syndrome: report

Migrants arrested in southern border 'riot' released by El Paso...

Denver official suggests migrants go to NYC, warning they would...

1 dead, 4 wounded in shooting at Nashville restaurant during...

Woman, 75, stabbed multiple times in head by parolee who followed...
Trans-identifying male in women’s prison found having sex with female inmate: report.
Thanks for contacting us. We've received your submission.
A transgender-identifying male was discovered having sex with a female inmate at a Washington state women’s prison earlier this month, according to an incident report of the event.
A corrections officer at the Washington Corrections Center for Women (WCCW) discovered 35-year-old Bryan Kim, who murdered his parents and now goes by Amber FayeFox Kim, having sex with 25-year-old Sincer-A Marie Nerton on March 14 during a routine check at the medium security unit (MSU), National Review reported.
The incident resulted in an infraction, but a hearing is expected to follow.
According to the report, “This is against MSU rules and policy. WAC-504-Engaging in a sex act with another person within the facility that is not otherwise included in these rules, except in an approved extended family visit.”
Before Kim was transferred to the women’s prison in February 2021 under the state Department of Correction’s (DOC) gender-inclusion policy, Kim was incarcerated at a men’s facility in the state.
An anonymous Washington DOC employee told National Review that there is “technically” no consensual sex among incarcerated individuals, but that “Washington has been mitigating the sanctions on offenders involved” if both parties claim the intercourse is consensual, resulting in “less trouble” for the offenders.
Under the Prison Rape Elimination Act (PREA), a federal law enacted in 2003, the Washington DOC states “consensual, non-coerced sexual activity between individuals” is prohibited, but is not a violation of PREA.

WCCW told Fox News Digital that it “takes the safety of all individuals in our care and custody seriously,” adding, “There has not been a reported case of rape against an individual during this timeframe” and if there was, it would be reported to law enforcement, likely resulting in a criminal case.
The DOC would not confirm the report, only indicating a rape did not occur, then provided information regarding its policies on transgender-identifying incarcerated individuals, which “establishes procedures to ensure equitable treatment of transgender, intersex and/or gender non-binary people during intake screening and determining housing, classification, programming and supervision.”
Keep up with today's most important news
Stay up on the very latest with Evening Update.
Thanks for signing up!
Please provide a valid email address.
By clicking above you agree to the Terms of Use and Privacy Policy .
Never miss a story.
All people under the DOC’s care and custody are assessed upon intake and, “if they self-identify as transgender, intersex and/or gender non-binary, the policy provides detailed guidance on placement and programming,” the DOC told Fox News Digital.
“DOC has developed this comprehensive housing assignment process to determine where an incarcerated individual is housed considering objective criteria that includes their gender identity,” the statement added. “If a person identifies as transgender or non-binary, they participate in a thorough mental health assessment, healthcare assessment and facility evaluation.”
The DOC also said their health plan provides services in accordance with the Washington state Health Care Authority Apple Health Transhealth program.

The Transhealth program offers primary care, behavioral health services, speech therapy, including voice training and hormone therapy, including puberty blockers.
“Several multidisciplinary teams must review all requests for transfer for a final placement determination,” the DOC statement added. “Each situation is considered on a case-by-case basis, with a focus on safety both for the individual and those who are housed at the facility.”
Share this article:
- Reference Manager
- Simple TEXT file
People also looked at
Original research article, male-to-female gender-affirming surgery: 20-year review of technique and surgical results.

- 1 Serviço de Urologia, Hospital de Clínicas de Porto Alegre, Porto Alegre, Brazil
- 2 Serviço de Psiquiatria, Hospital de Clínicas de Porto Alegre, Porto Alegre, Brazil
- 3 Serviço de Psiquiatria, Pontifical Catholic University of Rio Grande do Sul, Porto Alegre, Brazil
Purpose: Gender dysphoria (GD) is an incompatibility between biological sex and personal gender identity; individuals harbor an unalterable conviction that they were born in the wrong body, which causes personal suffering. In this context, surgery is imperative to achieve a successful gender transition and plays a key role in alleviating the associated psychological discomfort. In the current study, a retrospective cohort, we report the 20-years outcomes of the gender-affirming surgery performed at a single Brazilian university center, examining demographic data, intra and postoperative complications. During this period, 214 patients underwent penile inversion vaginoplasty.
Results: Results demonstrate that the average age at the time of surgery was 32.2 years (range, 18–61 years); the average of operative time was 3.3 h (range 2–5 h); the average duration of hormone therapy before surgery was 12 years (range 1–39). The most commons minor postoperative complications were granulation tissue (20.5 percent) and introital stricture of the neovagina (15.4 percent) and the major complications included urethral meatus stenosis (20.5 percent) and hematoma/excessive bleeding (8.9 percent). A total of 36 patients (16.8 percent) underwent some form of reoperation. One hundred eighty-one (85 percent) patients in our series were able to have regular sexual intercourse, and no individual regretted having undergone GAS.
Conclusions: Findings confirm that it is a safety procedure, with a low incidence of serious complications. Otherwise, in our series, there were a high level of functionality of the neovagina, as well as subjective personal satisfaction.
Introduction
Transsexualism (ICD-10) or Gender Dysphoria (GD) (DSM-5) is characterized by intense and persistent cross-gender identification which influences several aspects of behavior ( 1 ). The terms describe a situation where an individual's gender identity differs from external sexual anatomy at birth ( 1 ). Gender identity-affirming care, for those who desire, can include hormone therapy and affirming surgeries, as well as other procedures such as hair removal or speech therapy ( 1 ).
Since 1998, the Gender Identity Program (PROTIG) of the Hospital de Clínicas de Porto Alegre (HCPA), Universidade Federal do Rio Grande do Sul, Brazil has provided public assistance to transsexual people, is the first one in Brazil and one of the pioneers in South America. Our program offers psychosocial support, health care, and guidance to families, and refers individuals for gender-affirming surgery (GAS) when indicated. To be eligible for this surgery, transsexual individuals must have been adherent to multidisciplinary follow-up for at least 2 years, have a minimum age of 21 years (required for surgical procedures of this nature), have a positive psychiatric or psychological report, and have a diagnosis of GD.
Gender-affirming surgery (GAS) is increasingly recognized as a therapeutic intervention and a medical necessity, with growing societal acceptance ( 2 ). At our institution, we perform the classic penile inversion vaginoplasty (PIV), with an inverted penis skin flap used as the lining for the neovagina. Studies have demonstrated that GAS for the management of GD can promote improvements in mental health and social relationships for these patients ( 2 – 5 ). It is therefore imperative to understand and establish best practice techniques for this patient population ( 2 ). Although there are several studies reporting the safety and efficacy of gender-affirming surgery by penile inversion vaginoplasty, we present the largest South-American cohort to date, examining demographic data, intra and postoperative complications.
Patients and Methods
Subjects and study setup.
This is a retrospective cohort study of Brazilian transgender women who underwent penile inversion vaginoplasty between January of 2000 and March of 2020 at the Hospital de Clínicas de Porto Alegre, Porto Alegre, Brazil. The study was approved by our institutional medical and research ethics committee.
At our institution, gender-affirming surgery is indicated for transgender women who are under assistance by our program for transsexual individuals. All transsexual women included in this study had at least 2 years of experience as a woman and met WPATH standards for GAS ( 1 ). Patients were submitted to biweekly group meetings and monthly individual therapy.
Between January of 2000 and March of 2020, a total of 214 patients underwent penile inversion vaginoplasty. The surgical procedures were performed by two separate staff members, mostly assisted by residents. A retrospective chart review was conducted recording patient demographics, intraoperative and postoperative complications, reoperations, and secondary surgical procedures. Informed consent was obtained from all individual participants included in the study.
Hormonal Therapy
The goal of feminizing hormone therapy is the development of female secondary sex characteristics, and suppression/minimization of male secondary sex characteristics.
Our general therapy approach is to combine an estrogen with an androgen blocker. The usual estrogen is the oral preparation of estradiol (17-beta estradiol), starting at a dose of 2 mg/day until the maximum dosage of 8 mg/day. The preferred androgen blocker is spironolactone at a dose of 200 mg twice a day.
Operative Technique
At our institution, we perform the classic penile inversion vaginoplasty, with an inverted penis skin flap used as the lining for the neovagina. For more details, we have previously published our technique with a step-by-step procedure video ( 6 ). All individuals underwent intestinal cleansing the evening before the surgery. A first-generation cephalosporin was used as preoperative prophylaxis. The procedure was performed with the patient in a dorsal lithotomy position. A Foley catheter was placed for bladder catheterization. A inverted-V incision was made 4 cm above the anus and a flap was created. A neovaginal cavity was created between the prostate and the rectum with blunt dissection, in the Denonvilliers space, until the peritoneal fold, usually measuring 12 cm in extension and 6 cm in width. The incision was then extended vertically to expose the testicles and the spermatic cords, which were removed at the level of the external inguinal rings. A circumferential subcoronal incision was made ( Figure 1 ), the penis was de-gloved and a skin flap was created, with the de-gloved penis being passed through the scrotal opening ( Figure 2 ). The dorsal part of the glans and its neurovascular bundle were bluntly dissected away from the penile shaft ( Figure 3 ) as well as the urethra, which included a portion of the bulbospongious muscle ( Figure 4 ). The corpora cavernosa was excised up to their attachments at the symphysis pubis and ligated. The neoclitoris was shaped and positioned in the midline at the level of the symphysis pubis and sutured using interrupted 5-0 absorbable suture. The corpus spongiosum was reduced and the urethra was shortened, spatulated, and placed 1 cm below the neoclitoris in the midline and sutured using interrupted 4-0 absorbable suture. The penile skin flap was inverted and pulled into the neovaginal cavity to become its walls ( Figure 5 ). The excess of skin was then removed, and the subcutaneous tissue and the skin were closed using continuous 3-0 non-absorbable suture ( Figure 6 ). A neo mons pubis was created using a 0 absorbable suture between the skin and the pubic bone. The skin flap was fixed to the pubic bone using a 0 absorbable suture. A gauze impregnated with Vaseline and antibiotic ointment was left inside the neovagina, and a customized compressive bandage was applied ( Figure 7 —shows the final appearance after the completion of the procedures).

Figure 1 . The initial circumferential subcoronal incision.

Figure 2 . The de-gloved penis being passed through the scrotal opening.

Figure 3 . The dorsal part of the glans and its neurovascular bundle dissected away from the penile shaft.
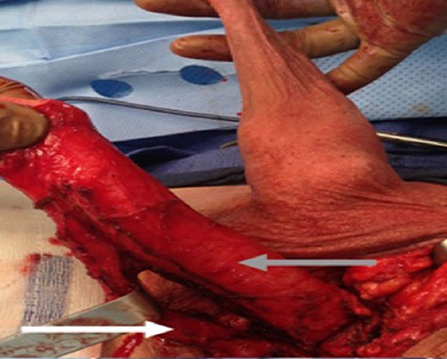
Figure 4 . The urethra dissected including a portion of the bulbospongious muscle. The grey arrow shows the penile shaft and the white arrow shows the dissected urethra.

Figure 5 . The inverted penile skin flap.
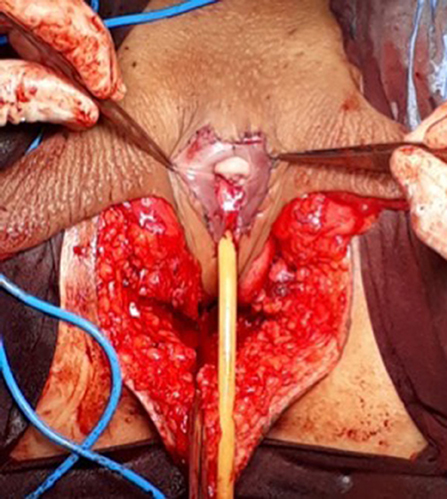
Figure 6 . The neoclitoris and the urethra sutured in the midline and the neovaginal cavity.
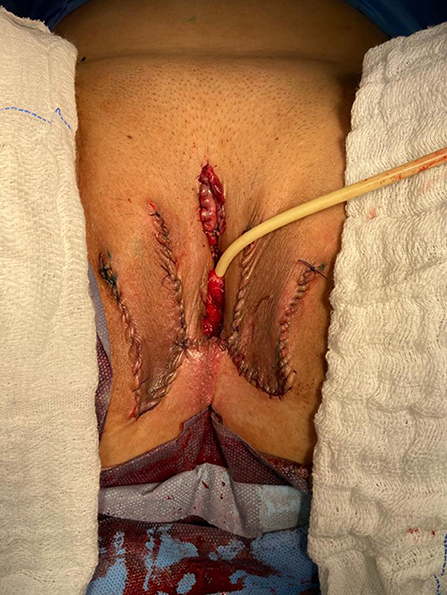
Figure 7 . The final appearance after the completion of the procedures.
Postoperative Care and Follow-Up
The patients were usually discharged within 2 days after surgery with the Foley catheter and vaginal gauze packing in place, which were removed after 7 days in an ambulatorial attendance.
Our vaginal dilation protocol starts seven days after surgery: a kit of 6 silicone dilators with progressive diameter (1.1–4 cm) and length (6.5–14.5 cm) is used; dilation is done progressively from the smallest dilator; each size should be kept in place for 5 min until the largest possible size, which is kept for 3 h during the day and during the night (sleep), if possible. The process is performed daily for the first 3 months and continued until the patient has regular sexual intercourse.
The follow-up visits were performed 7 days, 1, 2, 3, 6, and 12 months after surgery ( Figure 8 ), and included physical examination and a quality-of-life questionnaire.

Figure 8 . Appearance after 1 month of the procedure.
Statistical Analysis
The statistical analysis was conducted using Statistical Product and Service Solutions Version 18.0 (SPSS). Outcome measures were intra-operative and postoperative complications, re-operations. Descriptive statistics were used to evaluate the study outcomes. Mean values and standard deviations or median values and ranges are presented as continuous variables. Frequencies and percentages are reported for dichotomous and ordinal variables.
Patient Demographics
During the period of the study, 214 patients underwent penile inversion vaginoplasty, performed by two staff surgeons, mostly assisted by residents ( Table 1 ). The average age at the time of surgery was 32.2 years (range 18–61 years). There was no significant increase or decrease in the ages of patients who underwent SRS over the study period (Fisher's exact test: P = 0.065; chi-square test: X 2 = 5.15; GL = 6; P = 0.525). The average of operative time was 3.3 h (range 2–5 h). The average duration of hormone therapy before surgery was 12 years (range 1–39). The majority of patients were white (88.3 percent). The most prevalent patient comorbidities were history of tobacco use (15 percent), human immunodeficiency virus infection (13 percent) and hypertension (10.7 percent). Other comorbidities are listed in Table 1 .
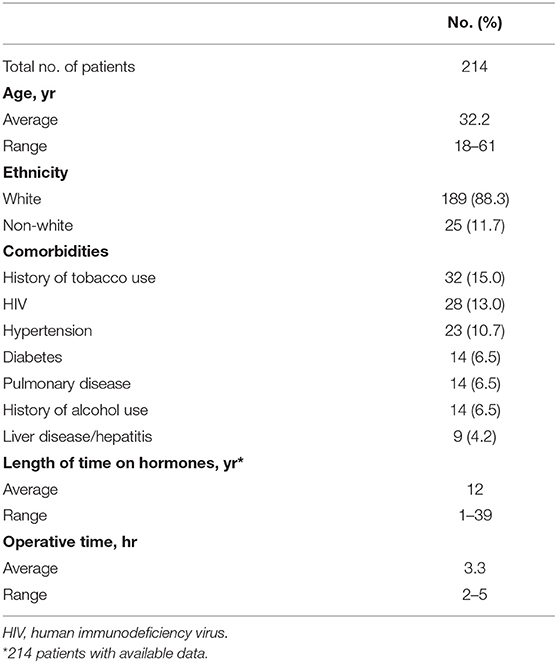
Table 1 . Patient demographics.
Multidisciplinary follow-up was comprised of 93.45% of patients following up with a urologist and 59.06% of patients continuing psychiatric follow-up, median follow-up time of 16 and 9.3 months after surgery, respectively.
Postoperative Results
The complications were classified according to the Clavien-Dindo score ( Table 2 ). The most common minor postoperative complications (Grade I) were granulation tissue (20.5 percent), introital stricture of the neovagina (15.4 percent) and wound dehiscence (12.6 percent). The major complications (Grade III-IV) included urethral stenosis (20.5 percent), urethral fistula (1.9 percent), intraoperative rectal injury (1.9 percent), necrosis (primarily along the wound edges) (1.4 percent), and rectovaginal fistula (0.9 percent). A total of 17 patients required blood transfusion (7.9 percent).
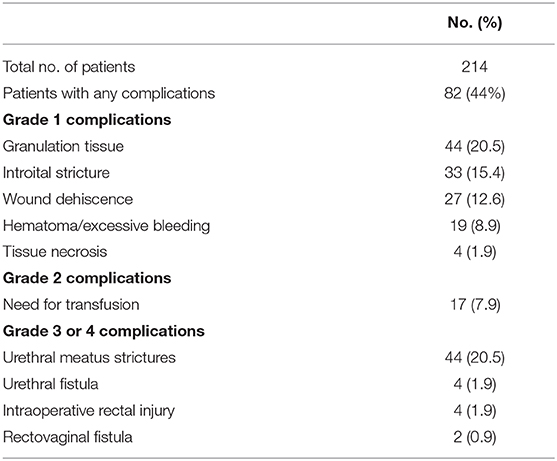
Table 2 . Complications after penile inversion vaginoplasty.
A total of 36 patients (16.8 percent) underwent some form of reoperation.
One hundred eighty-one (85 percent) patients in our series were able to have regular sexual vaginal intercourse, and no individual regretted having undergone GAS.
Penile inversion vaginoplasty is the gold-standard in gender-affirming surgery. It has good functional outcomes, and studies have demonstrated adequate vaginal depths ( 3 ). It is recognized not only as a cosmetic procedure, but as a therapeutic intervention and a medical necessity ( 2 ). We present the largest South-American cohort to date, examining demographic data, intra and postoperative complications.
The mean age of transsexual women who underwent GAS in our study was 32.2 years (range 18–61 years), which is lower than the mean age of patients in studies found in the literature. Two studies indicated that the mean ages of patients at time of GAS were 36.7 years and 41 years, respectively ( 4 , 5 ). Another study reported a mean age at time of GAS of 36 years and found there was a significant decrease in age at the time of GAS from 41 years in 1994 to 35 years in 2015 ( 7 ). According to the authors, this decrease in age is associated with greater tolerance and societal approval regarding individuals with GD ( 7 ).
There was no grade IV or grade V complications. Excessive bleeding noticed postoperatively occurred in 19 patients (8.9 percent) and blood transfusion was required in 17 cases (7.9 percent); all patients who required blood transfusions were operated until July 2011, and the reason for this rate of blood transfusion was not identified.
The most common intraoperative complication was rectal injury, occurring in 4 patients (1.9 percent); in all patients the lesion was promptly identified and corrected in 2 layers absorbable sutures. In 2 of these patients, a rectovaginal fistula became evident, requiring fistulectomy and colonic transit deviation. This is consistent with current literature, in which rectal injury is reported in 0.4–4.5 percent of patients ( 4 , 5 , 8 – 13 ). Goddard et al. suggested carefully checking for enterotomy after prostate and bladder mobilization by digital rectal examination ( 4 ). Gaither et al. ( 14 ) commented that careful dissection that closely follows the urethra along its track from the central tendon of the perineum up through the lower pole of the prostate is critical and only blunt dissection is encouraged after Denonvilliers' fascia is reached. Alternatively, a robotic-assisted approach to penile inversion vaginoplasty may aid in minimizing these complications. The proposed advantages of a robotic-assisted vaginoplasty include safer dissection to minimize the risk of rectal injury and better proximal vaginal fixation. Dy et al. ( 15 ) has had no rectal injuries or fistulae to date in his series of 15 patients, with a mean follow-up of 12 months.
In our series, we observed 44 cases (20.5 percent) of urethral meatus strictures. We credit this complication to the technique used in the initial 5 years of our experience, in which the urethra was shortened and sutured in a circular fashion without spatulation. All cases were treated with meatal dilatation and 11 patients required surgical correction, being performed a Y-V plastic reconstruction of the urethral meatus. In the literature, meatal strictures are relatively rare in male-to-female (MtF) GAS due to the spatulation of the urethra and a simple anastomosis to the external genitalia. Recent systematic reviews show an incidence of five percent in this complication ( 16 , 17 ). Other studies report a wide incidence of meatal stenosis ranging from 1.1 to 39.8 percent ( 4 , 8 , 11 ).
Neovagina introital stricture was observed in 33 patients (15.4 percent) in our study and impedes the possibility of neovaginal penetration and/or adversely affects sexual life quality. In the literature, the reported incidence of introital stenosis range from 6.7 to 14.5 percent ( 4 , 5 , 8 , 9 , 11 – 13 ). According to Hadj-Moussa et al. ( 18 ) a regimen of postoperative prophylactic dilation is crucial to minimize the development of this outcome. At our institution, our protocol for vaginal dilation started seven days after surgery and was performed three to four times a day during the first 3 months and was continued until the individual had regular sexual intercourse. We treated stenosis initially with dilation. In case of no response, we propose a surgical revision with diamond-shaped introitoplasty with relaxing incisions. In recalcitrant cases, we proposed to the patient a secondary vaginoplasty using a full-thickness skin graft of the lower abdomen.
One hundred eighty-one (85 percent) patients were classified as having a “functional vagina,” characterized as the capacity to maintain satisfactory sexual vaginal intercourse, since the mean neovaginal depth was not measured. In a review article, the mean neovaginal depth ranged from 10 to 13.5 cm, with the shallowest neovagina depth at 2.5 cm and the deepest at 18 cm ( 17 ). According to Salim et al. ( 19 ), in terms of postoperative functional outcomes after penile inversion vaginoplasty, a mean percentage of 75 percent (range from 33 to 87 percent) patients were having vaginal intercourse. Hess et al. found that 91.4% of patients who responded to a questionnaire were very satisfied (34.4%), satisfied (37.6%), or mostly satisfied (19.4%) with their sexual function after penile inversion vaginoplasty ( 20 ).
Poor cosmetic appearance of the vulva is common. Amend et al. reported that the most common reason for reoperation was cosmetic correction in the form of mons pubis and mucosa reduction in 50% of patients ( 16 ). We had no patient regrets about performing GAS, although 36 patients (16.8 percent) were reoperated due to cosmetic issues. Gaither et al. propose in order to minimize scarring to use a one-stage surgical approach and the lateralization of surgical scars to the groin ( 14 ). Frequently, cosmetic issues outcomes are often patient driven and preoperative patient education is necessary ( 14 ).
Analyzing the quality of life, in 2016, our health care group (PROTIG) published a study assessing quality of life before and after gender-affirming surgery in 47 patients using the diagnostic tool 100-item WHO Quality of Life Assessment (WHOQOL-100) ( 21 ). The authors found that GAS promotes the improvement of psychological aspects and social relations. However, even 1 year after GAS, MtF persons continue to report problems in physical and difficulty in recovering their independence. In a systematic review and meta-analysis of QOL and psychosocial outcomes in transsexual people, researchers verified that sex reassignment with hormonal interventions more likely corrects gender dysphoria, psychological functioning and comorbidities, sexual function, and overall QOL compared with sex reassignment without hormonal interventions, although there is a low level of evidence for this ( 22 ). Recently, Castellano et al. assessed QOL in 60 Italian transsexuals (46 transwomen and 14 transmen) at least 2 years after SRS using the WHOQOL-100 (general QOL score and quality of sexual life and quality of body image scores) to focus on the effects of hormonal therapy. Overall satisfaction improved after SRS, and QOL was similar to the controls ( 23 ). Bartolucci et al. evaluated the perception of quality of sexual life using four questions evaluating the sexual facet in individuals with gender dysphoria before SRS and the possible factors associated with this perception. The study showed that approximately half the subjects with gender dysphoria perceived their sexual life as “poor/dissatisfied” or “very poor/very dissatisfied” before SRS ( 24 ).
Our study has some limitations. The total number of operated patients is restricted within the long follow-up period. This is due to a limitation in our health system, which allows only 1 sexual reassignment surgery to be performed per month at our institution. Neovagin depth measurement was not performed routinely in the follow-up of operated patients.
Conclusions
The definitive treatment for patients with gender dysphoria is gender-affirming surgery. Our series demonstrates that GAS is a feasible surgery with low rates of serious complications. We emphasize the high level of functionality of the vagina after the procedure, as well as subjective personal satisfaction. Complications, especially minor ones, are probably underestimated due to the nature of the study, and since this is a surgical population, the results may not be generalizable for all transgender MTF individuals.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Hospital de Clínicas de Porto Alegre. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
GM: conception and design, data acquisition, data analysis, interpretation, drafting the manuscript, review of the literature, critical revision of the manuscript and factual content, and statistical analysis. ML and TR: conception and design, data interpretation, drafting the manuscript, critical revision of the manuscript and factual content, and statistical analysis. DS, KS, AF, AC, PT, AG, and RC: conception and design, data acquisition and data analysis, interpretation, drafting the manuscript, and review of the literature. All authors contributed to the article and approved the submitted version.
This study was supported by the Fundo de Incentivo à Pesquisa e Eventos (FIPE - Fundo de Incentivo à Pesquisa e Eventos) of Hospital de Clínicas de Porto Alegre.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Coleman E, Bockting W, Botzer M, Cohen-Kettenis P, DeCuypere G, Feldman J, et al. Standards of care for the health of transsexual, transgender, and gender-non-conforming people, version 7. Int J Transgend. (2012) 13:165–232. doi: 10.1080/15532739.2011.700873
CrossRef Full Text | Google Scholar
2. Massie JP, Morrison SD, Maasdam JV, Satterwhite T. Predictors of patient satisfaction and postoperative complications in penile inversion vaginoplasty. Plast Reconstruct Surg. (2018) 141:911–921. doi: 10.1097/PRS.0000000000004427
PubMed Abstract | CrossRef Full Text | Google Scholar
3. Pan S, Honig SC. Gender-affirming surgery: current concepts. Curr Urol Rep . (2018) 19:62. doi: 10.1007/s11934-018-0809-9
4. Goddard JC, Vickery RM, Qureshi A, Summerton DJ, Khoosal D, Terry TR. Feminizing genitoplasty in adult transsexuals: early and long-term surgical results. BJU Int . (2007) 100:607–13. doi: 10.1111/j.1464-410X.2007.07017.x
5. Rossi NR, Hintz F, Krege S, Rübben H, Vom DF, Hess J. Gender reassignment surgery – a 13 year review of surgical outcomes. Eur Urol Suppl . (2013) 12:e559. doi: 10.1016/S1569-9056(13)61042-8
6. Silva RUM, Abreu FJS, Silva GMV, Santos JVQV, Batezini NSS, Silva Neto B, et al. Step by step male to female transsexual surgery. Int Braz J Urol. (2018) 44:407–8. doi: 10.1590/s1677-5538.ibju.2017.0044
7. Aydin D, Buk LJ, Partoft S, Bonde C, Thomsen MV, Tos T. Transgender surgery in Denmark from 1994 to 2015: 20-year follow-up study. J Sex Med. (2016) 13:720–5. doi: 10.1016/j.jsxm.2016.01.012
8. Perovic SV, Stanojevic DS, Djordjevic MLJ. Vaginoplasty in male transsexuals using penile skin and a urethral flap. BJU Int. (2001) 86:843–50. doi: 10.1046/j.1464-410x.2000.00934.x
9. Krege S, Bex A, Lümmen G, Rübben H. Male-to-female transsexualism: a technique, results and long-term follow-up in 66 patients. BJU Int. (2001) 88:396–402. doi: 10.1046/j.1464-410X.2001.02323.x
10. Wagner S, Greco F, Hoda MR, Inferrera A, Lupo A, Hamza A, et al. Male-to-female transsexualism: technique, results and 3-year follow-up in 50 patients. Urol International. (2010) 84:330–3. doi: 10.1159/000288238
11. Reed H. Aesthetic and functional male to female genital and perineal surgery: feminizing vaginoplasty. Semin PlasticSurg. (2011) 25:163–74. doi: 10.1055/s-0031-1281486
12. Raigosa M, Avvedimento S, Yoon TS, Cruz-Gimeno J, Rodriguez G, Fontdevila J. Male-to-female genital reassignment surgery: a retrospective review of surgical technique and complications in 60 patients. J Sex Med. (2015) 12:1837–45. doi: 10.1111/jsm.12936
13. Sigurjonsson H, Rinder J, Möllermark C, Farnebo F, Lundgren TK. Male to female gender reassignment surgery: surgical outcomes of consecutive patients during 14 years. JPRAS Open. (2015) 6:69–73. doi: 10.1016/j.jpra.2015.09.003
14. Gaither TW, Awad MA, Osterberg EC, Murphy GP, Romero A, Bowers ML, et al. Postoperative complications following primary penile inversion vaginoplasty among 330 male-to-female transgender patients. J Urol. (2018) 199:760–5. doi: 10.1016/j.juro.2017.10.013
15. Dy GW, Sun J, Granieri MA, Zhao LC. Reconstructive management pearls for the transgender patient. Curr. Urol. Rep. (2018) 19:36. doi: 10.1007/s11934-018-0795-y
16. Amend B, Seibold J, Toomey P, Stenzl A, Sievert KD. Surgical reconstruction for male-to-female sex reassignment. Eur Urol. (2013) 64:141–9. doi: 10.1016/j.eururo.2012.12.030
17. Horbach SER, Bouman MB, Smit JM, Özer M, Buncamper ME, Mullender MG. Outcome of vaginoplasty in male-to-female transgenders: a systematic review of surgical techniques. J Sex Med . (2015) 12:1499–512. doi: 10.1111/jsm.12868
18. Hadj-Moussa M, Ohl DA, Kuzon WM. Feminizing genital gender-confirmation surgery. Sex Med Rev. (2018) 6:457–68.e2. doi: 10.1016/j.sxmr.2017.11.005
19. Salim A, Poh M. Gender-affirming penile inversion vaginoplasty. Clin Plast Surg. (2018) 45:343–50. doi: 10.1016/j.cps.2018.04.001
20. Hess J, Rossi NR, Panic L, Rubben H, Senf W. Satisfaction with male-to-female gender reassignment surgery. DtschArztebl Int. (2014) 111:795–801. doi: 10.3238/arztebl.2014.0795
21. Silva DC, Schwarz K, Fontanari AMV, Costa AB, Massuda R, Henriques AA, et al. WHOQOL-100 before and after sex reassignment surgery in brazilian male-to-female transsexual individuals. J Sex Med. (2016) 13:988–93. doi: 10.1016/j.jsxm.2016.03.370
22. Murad MH, Elamin MB, Garcia MZ, Mullan RJ, Murad A, Erwin PJ, et al. Hormonal therapy and sex reassignment: a systematic review and meta-analysis of quality of life and psychosocial outcomes. Clin Endocrinol . (2010) 72:214–31. doi: 10.1111/j.1365-2265.2009.03625.x
23. Castellano E, Crespi C, Dell'Aquila C, Rosato R, Catalano C, Mineccia V, et al. Quality of life and hormones after sex reassignment surgery. J Endocrinol Invest . (2015) 38:1373–81. doi: 10.1007/s40618-015-0398-0
24. Bartolucci C, Gómez-Gil E, Salamero M, Esteva I, Guillamón A, Zubiaurre L, et al. Sexual quality of life in gender-dysphoric adults before genital sex reassignment surgery. J Sex Med . (2015) 12:180–8. doi: 10.1111/jsm.12758
Keywords: transsexualism, gender dysphoria, gender-affirming genital surgery, penile inversion vaginoplasty, surgical outcome
Citation: Moisés da Silva GV, Lobato MIR, Silva DC, Schwarz K, Fontanari AMV, Costa AB, Tavares PM, Gorgen ARH, Cabral RD and Rosito TE (2021) Male-to-Female Gender-Affirming Surgery: 20-Year Review of Technique and Surgical Results. Front. Surg. 8:639430. doi: 10.3389/fsurg.2021.639430
Received: 17 December 2020; Accepted: 22 March 2021; Published: 05 May 2021.
Reviewed by:
Copyright © 2021 Moisés da Silva, Lobato, Silva, Schwarz, Fontanari, Costa, Tavares, Gorgen, Cabral and Rosito. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gabriel Veber Moisés da Silva, veber.gabriel@gmail.com
This article is part of the Research Topic
Gender Dysphoria: Diagnostic Issues, Clinical Aspects and Health Promotion
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Can Urol Assoc J
- v.15(10); 2021 Oct
Adult transgender care: A review for urologists
Kate anderson.
1 Department of Urology, Dalhousie University, Halifax, NS, Canada
Yonah Krakowsky
2 Department of Surgery, University of Toronto, Toronto, ON, Canada
Emery Potter
Jill hudson, ashley r. cox, introduction.
Current population studies estimate that 0.4–1.1% of adults self-identify as transgender. 1 Transgender non-binary (TGNB) patients seek urological consultations for a variety of reasons, including: surgical procedures related to their gender, postoperative complications, sexual health concerns, or for general urological issues. Despite the likelihood that urologists will have clinical encounters with TGNB patients, a Canadian study found that minimal education in residency is focused on this topic. 2
The World Professional Association for Transgender Health (WPATH) is an international, multidisciplinary professional association. They put forth a set of evidence and expert opinion-based standards of care (SOC), which are viewed as the prevailing clinical guidelines worldwide. 3 The Endocrine Society (ES) also has published guidelines on the treatment of gender-dysphoric/gender-incongruent persons. 4 The recommendations and guidelines discussed in this article are based on the SOC set forth by WPATH, in addition to those from ES.
The purpose of this narrative review is to act as a reference for urologists to help understand and provide quality urological care for TGNB patients. We aim to provide pertinent information related to the transition process, hormonal therapies, surgical interventions, and urological issues facing the TGNB population.
Terminology
TGNB individuals have genders that are not aligned with the sex assigned to them at birth. Cisgender refers to individuals whose gender identity matches their sex assigned at birth. For the purposes of simplifying the language used in this review ( Table 1 ), we will be referring to people whose birth-assigned sex was female but identify as male as “transgender men.” People assigned male at birth but who identify as female will be referred to as “transgender women.” It is important for a healthcare provider to inquire what pronouns patients use to ensure the appropriate language is used and to establish trust. Pronouns can include “she/her,” “he/him,” “they/them,” and others. Terminology is ever-changing. Staying current on trans-competent language may lead to improved patient care.
The transition process
Gender dysphoria/incongruence is defined as distress that may accompany the incongruence between one’s gender identity and one’s assigned sex at birth. 5 Transition is a term used to describe the process one might take to express their felt gender identity. Transition may involve social, medical, or surgical elements. Social transition can include aspects such dressing in clothing that reflects their gender identity, name/pronoun change, and changing government identification. Social transitioning alone may alleviate distress from gender dysphoria with improved quality of life and well-being. 6 Medical transition generally refers to starting hormone therapies. Surgical transition can include many possible surgeries to alter one’s primary and secondary sex characteristics. There is not one way that a TGNB individual transitions. The process is individualized. For many TGNB patients, social, medical, and surgical transition can greatly improve gender dysphoria. 7
In Ontario, the TransPULSE study surveyed 433 participants regarding the transition process. 8 Of those surveyed, 30% had not undertaken any steps in the transition process, while 23% were living in their felt gender but without any medical intervention. Forty-six percent of transgender women and 39% of transgender men were currently using hormones for a medical transition. Twenty-three percent reported having completely transitioned, which was self-defined and could include medical or surgical measures. Of surgical interventions, orchiectomy was most common, reported by 21% of transgender women. Vaginoplasty was reported in 15% of transgender women. In contrast, only 0.4% of transgender men had undergone phalloplasty. The study confirmed this population represents a heterogeneous group in terms of accessing different aspects of transition. This study also suggested that we may be at the “tip of the iceberg” in terms of the numbers of patients going through this process.
Hormonal and medical therapies
Many patients choose to pursue medical treatments to address their gender dysphoria. Hormonal therapy is generally overseen by the patient’s primary care provider or endocrinologist. Hormonal modulation has quality of life benefits for transgender patients. 9 , 10 Criteria for the prescription of hormone therapy includes: gender incongruence, capacity to make informed decisions, and reasonable control of associated mental health conditions. 11
For transgender men, masculinizing hormonal treatment is primarily exogenous testosterone therapy. Transdermal, subcutaneous, and intramuscular (IM) formulations are most commonly used. 4 Target testosterone levels are the same as for cisgender males of the same age. Patients should be screened for contraindications to testosterone therapy, including pregnancy, unstable coronary artery disease, and untreated polycythemia. 12 Patients with a history of estrogen-sensitive malignancy may require a referral to oncology due to the potential for testosterone to be converted to estrogen through aromatization. In addition, patients with underlying polycystic ovary syndrome (PCOS) may need further evaluation due to an elevated risk of side effects with testosterone. Transgender men at risk of becoming pregnant also require effective birth control measures due to the potential teratogenicity of testosterone.
Masculinizing changes on testosterone therapy include increased facial/body hair growth, voice deepening, increased muscle mass, reduced fertility, atrophy of breast tissue, cessation of menses, weight gain, increased libido, possible clitoral virilization, and vaginal atrophy. Hormonal changes occur over variable time frames and to varying degrees. Like any medical therapy, there are potential risks associated with the use of masculinizing hormone therapy ( Table 2 ).
Medical therapies commonly used during the transition process
CAD: coronary artery disease; CVD: cardiovascular disease; DVT: deep venous thrombosis; GnRH: gonadotropin-releasing hormone; PE: pulmonary embolism.
For transgender women, feminizing hormonal therapy requires both estrogen for feminization and an anti-androgen to suppress testosterone levels. 4 Exogenous estrogen works via a central feedback mechanism to reduce androgen production. It may be delivered through a transdermal patch, orally, and intramuscularly. Oral and intramuscular estrogen therapy, as well as higher estrogen doses, may lead to a higher risk of venous thromboembolic events (VTE). 4 Ethinyl estrodiol oral therapy carries a high risk of VTE and should not be used. Transdermal estrogen is preferable due to its side effect profile but is costly.
The goals of feminizing hormonal therapy include reducing growth of facial hair, skin softening, inducing breast development and promoting fat and muscle redistribution. 11 Erectile dysfunction, testicular atrophy, and infertility may occur. Hormonal therapy is guided by the normal physiological range of cisgender women and may take 6–18 months. Patients must be screened for contraindications to estrogen therapy, including previous VTE related to a hypercoagulable state, previous hormone-sensitive neoplasm, or end-stage chronic liver disease.
Due to the potential for side effects and to potentiate the effects of estrogen, estrogen is typically used in combination with anti-androgens to minimize the required amount of estrogen to achieve feminizing effects. Gonadotropin-releasing hormone (GnRH) agonists are thought to be as effective as other anti-androgens with possibly lower side effects, but cost is prohibitive. 13 , 14 In Canada, spironolactone and cyproterone acetate (Androcur ® ) are commonly used. Spironolactone works via blockage of the androgen receptor and decreases testosterone levels, while cyproterone acetate works by both central and peripheral inhibition. Spironolactone is often prescribed at much higher doses than what is used for hypertension and patients must be monitored for hyperkalemia. Cyproterone acetate carries concerns regarding hepatotoxicity. 15 5-alpha reductase inhibitors, such as finasteride and dutasteride, are typically not necessary, as the testosterone levels are almost fully suppressed with estrogen and an anti-estrogen.
Patients on hormonal therapy require ongoing followup, including physical examination and laboratory investigations to assess for hormonal effects and potential complications of treatment. Goals of hormonal manipulation should be to maintain the physiological level required to meet the patient’s desired gender expression.
Transition-related genitourinary surgery
Gender-affirming surgical therapies are summarized in Table 3 . Surgery can be a crucial step in alleviating gender dysphoria. There is an accumulation of data that outcomes are overtly positive for improving gender dysphoria, as well as quality of life. 16
Gender-affirming surgery
Modified from WPATH. 1
The WPATH SOC has several criteria for patients seeking any genital surgery. Patients undergoing reproductive organ surgery (orchiectomy, hysterectomy, oophorectomy) must have two referral letters to the surgeon and have completed at least one year of hormonal therapy. In general, the writer of the referral letter must be a medical doctor, nurse practitioner, or Masters-level social worker with an interest or prior training in providing transgender healthcare. Provinces may vary in terms of specific requirements for who is eligible to write the referral. The required content of the referral letter is described in Table 4 . The same is recommended before undergoing genital surgery, such as metoidioplasty, phalloplasty, or vaginoplasty. However, it is also recommended that these patients demonstrate 12 continuous months of living in a gender role that is congruent with their gender identity prior to surgery.
Recommended content of the referral letters for gender-affirming surgery
Orchiectomy
The benefits of bilateral orchiectomy for transgender women include the ability to discontinue anti-androgen medication and its associated costs, occasional reduction in estrogen dose, increased ability to “tuck,” and increased ease of wearing gender-congruent clothing. Surgery generally involves a single, median raphe incision and removal of both testicles. 17 If vaginoplasty is intended, preservation of the paragonadal fat pad, dartos fascia, and scrotal skin is important for future reconstruction. Patients should be informed of the potential risks of bleeding/hematoma, infection, permanent infertility, worsening erectile dysfunction, poor cosmesis, and palpable cord stump. Patients may opt for an inguinal or subinguinal approach to remove more of the spermatic cord, which if left, may be bothersome. As a dose reduction in hormone therapy may be required postoperatively, communication with the healthcare provider prescribing hormones is important.
Vaginoplasty
Penile inversion vaginoplasty (PIV) is the most common technique performed. 18 In brief, the penile skin and prepuce are used to create a neovaginal cavity. A neovagina is created between the rectum and the urethra. Following scrotectomy and orchiectomy, the remaining skin is used to create labial folds, while the glans penis is reconstructed to form the neoclitoris. The corporal cavernosal tissue is removed as proximally as possible. In order to minimize complications, the prostate is not removed ( Fig. 1 ). 19 More involved operations may include intestinal or peritoneal vaginoplasty, which allow for the creation of a self-lubricating neovagina. Permanent hair removal (laser/electrolysis) to the scrotum and penile shaft is encouraged to prevent hair growth in the vaginal canal postoperatively. Some patients may also choose to pursue zero-depth vaginoplasty/vulvoplasty. This obviates the need to dilate and avoids the risk of fistula. Vulvoplasty refers to the creation of a clitoris, clitoral hooding, and labia minora and majora.

Penile inversion vaginoplasty. Copyright© 2019 Massachusetts Medical Society. Reprinted with permission from Massachusetts Medical Society. 11
There are many potential long-term issues following vaginoplasty, as shown in Table 5 . 20 There is a large range of complication rates reported in the literature. Neovaginal stenosis (1.2–43%) and wound dehiscence appear to be the most common complications (12–33%) 20 following penile inversion therapy. As this surgery is only offered in few centers in Canada, long-term postoperative followup is challenging.
Potential urological complications related to gender-affirming surgery
STI: sexually transmitted infection.
Metoidioplasty and phalloplasty
There are several goals to consider when approaching genital surgery for transgender men. Functional goals include gaining the ability to stand to void, consolidation of sexual sensation to the neophallus, and ability to achieve an erection satisfactory for penetrative intercourse.
Metoidioplasty uses the virilized clitoral body to create a small phallus, in order to masculinize the phallus while avoiding the morbidity associated with a phalloplasty. Vaginectomy may be performed. During the procedure, the clitoris is degloved and the suspensory ligament divided. The urethra is lengthened using a combination of labia minora and anterior vaginal wall flaps in addition to buccal mucosa. Patients may gain the ability to stand to void via the phallus. The labia majora may be used to create a neoscrotum. 21 Testicular implants may also be placed.
Advantages of metoidioplasty include decreased average number of procedures required, good erogenous sensation consolidation to the neophallus, and lower rates of complications compared to phalloplasty. 22 Common urological complaints following metoidioplasty are described in Table 5 . Urethrocutaneous fistula occurs in 5–23% of cases, 23 with approximately 50% of these requiring surgical repair. Since the neophallus length is usually only 5–7 cm, penetrative intercourse may be unachievable following metoidioplasty. 24
Phalloplasty is a complicated, often multistage operation where a flap (usually free flap), is raised to create a neophallus and provide urethral lengthening. There are many different techniques employed based on individual patient needs. 25 One well-studied example is the radial artery forearm free flap ( Fig. 2 ). 26 This technique employs a tube-within-a-tube design for formation of the neo-urethra and a neo-phallus large enough to accommodate an erectile prosthesis during a subsequent surgery. The overall complication rate for phalloplasty is high, estimated to be 40–70%. 27 Common complications are described in Table 5 . Complications requiring further surgical reconstruction occurs in approximately 25% of patients following phalloplasty. 28 Urethrocutaneous fistulas frequently occur (18–78%) and more than half require surgical revision. 22 Prosthetic erectile implants carry a higher complication rate than in cisgender men, with a 12% infection rate reported in one large study. 29 As well, the flap donor site deformity is an unavoidable downside for this surgery. Phalloplasty (with penile prosthesis) offers a higher likelihood of successful penetrative intercourse and the capacity to stand to void postoperatively. Advantages must be weighed against the longer cumulative surgery and recovery time, and the potential complications. Scrotoplasty with staged placement of testicular implants typically accompanies both metoidioplasty and phalloplasty in transgender men.

Phalloplasty. Copyright© 2019 Massachusetts Medical Society. Reprinted with permission from Massachusetts Medical Society. 11
Despite the need for multiple surgeries, risk of postoperative complications and potential costs, patients seldom report regret following gender-affirming surgery. 30
Urological issues in transgender patients
Urological malignancy.
Little is known about reproductive malignancies in the transgender population. 31 A retrospective analysis of the North American Association of Central Cancer Registries (NAACR) database from 1995–2013 assessed gender minority cancer patients. Nash et al found a lower proportional incidence ratio of prostate and testicular malignancies for transgender females compared to similar-aged cisgender men. 32 A large retrospective study of 2306 transgender females reported a prostate cancer prevalence of only 0.04%. 33 Transgender women have castrate levels of testosterone and prostate-specific antigen (PSA) values need to be interpreted with that in mind. Overall, there is a lack of literature regarding the diagnosis, management, and followup of prostate cancer in transgender women.
As the transgender patient population increases, prostate cancer in this population will become a more common urological scenario. Experts recommend following the same screening protocols as for cisgender men. 34 It is unclear how prolonged estrogen and anti-androgen therapy affects prostate cancer risk. In addition, previous gender-affirming surgery may impact the ability to examine the prostate, which may need to be done via examination of the anterior wall of the neovagina.
Testicular cancer is a rare malignancy. Review of the literature found only three case reports of testicular cancer in transgender women on hormonal therapy. 35 – 37 As with cis-gendered men, self-examination should be encouraged, and imaging requested if there are any worrisome lesions, especially prior to gender-affirming surgery, as the presence of a testicular mass will alter one’s approach to orchiectomy. It is important for urologists to be aware of several barriers to care in this complex patient population to ensure the diagnosis of urological malignancies are not missed. 33
Hormonal and surgical therapies for gender dysphoria have obvious deleterious effects on fertility. Yet, many individuals desire to have genetically related children. Reproductive options should be discussed prior to initiating the transition process. 38 It is imperative that both transgender men and women are counselled on fertility options prior to commencing hormonal or surgical therapies.
For transgender men, options include oocyte or embryo freezing prior to hormonal therapy or surgery. Ideally, this would be completed prior to starting masculinizing hormones. However, there is evidence that ovarian function may recover after exposure to testosterone. 39 The success of this is likely dependent on patient age and length of time on testosterone. In addition, successful pregnancies using assisted reproductive techniques (ART) are possible following cessation of hormone therapies. 40 Some transgender men may want to become pregnant even after having transitioned socially or medically. 41 Literature is emerging on the outcomes of ART for transgender men.
It is important to note that although testosterone may alter ovarian function in transgender men, it is not a form of contraception. Patients who do not want to conceive should be counselled on the importance of contraception. 41
Transgender women should be counselled on the role of sperm banking prior to starting hormone therapy. Some evidence suggests that even prior to hormonal therapy, some transgender women have abnormal semen parameters in comparison to fertile cisgender men. 42 Certainly, following hormonal therapy, decreased spermatogenesis and fertility occurs. However, cessation of hormone therapy (mean discontinuation period 4.4 months) may allow for recovery of semen parameters comparable to hormone-naive transgender women. 43 One post-orchiectomy study on 135 transgender women who had been treated with hormonal therapy found that nearly 80% had negligible spermatogenesis. 44 Patients must be counselled regarding the irreversibility of infertility following orchiectomy. Little data exists reporting outcomes of ART for transgender women who have chosen sperm cryopreservation.
Prior to transitioning medically or surgically, patients should be advised on the costs associated with sperm/oocyte cryopreservation and made aware that ART is costly and may not be widely available.
Urinary function
Transgender patients may present to urology due to lower urinary tract symptoms for multiple reasons, including complications of gender-affirming surgery. Following gender-affirming surgery, transgender females may develop storage or voiding symptoms related to meatal stenosis or urethral strictures. 28 Incontinence may be a result of urinary retention, stress incontinence, urgency incontinence, or potentially fistula formation. During vaginoplasty, dissection between the rectum and bladder may impact the autonomous nerve supply to the bladder, leading to lower urinary tract dysfunction. 20 Transgender patients may also experience urinary tract infections following reconstructive surgery.
Following phalloplasty in transgender men, the rate of urethral strictures is high, ranging from 25–58%. 45 The most common site of stricture formation is the anastomosis between the native and neourethra, as well as the meatus. Postvoid dribbling may occur due to a lack of bulbospongiosus muscle and corpora spongiosum surrounding the neourethra. 46 Urinary tract infections may also occur following genitourinary reconstruction in transgender men.
A full surgical history should be obtained to narrow the differential diagnosis based on associated common complications. Physical exam and measurement of postvoid residual volumes should be completed. If indicated, cystoscopy may need to be performed with sedation or general anesthetic in some patients with gender dysphoria. Caution should be used when navigating the urethra due the high rate of urethral complications in both transgender men and women following gender-affirming surgery. In the case of acute urinary retention, placement of a Foley catheter or suprapubic catheter, if necessary, is appropriate. Contacting the patient’s surgeon to seek direction for further care may be required. If need be, patients should be referred back to the surgeon who performed the GAS, or to a reconstructive urologist comfortable with complex anatomy.
Conclusions
The TGNB population represents a growing, heterogeneous group of patients. The transition process may or may not include social changes, hormonal therapy, and/or surgery to alter primary and secondary sex characteristics. Transgender patients may be referred to urologists for reasons such as surgical procedures related to their gender transition, postoperative complications, sexual health concerns, or for other general urological issues. Despite a deficiency in formalized training during residency and lack of specialized surgical centers in Canada, urologists must be well-versed in transgender healthcare when it comes to urological issues. Urologists have a responsibility to accept patient referrals and provide support. This will allow optimal urological care of this patient population.
Competing interests: The authors do not report any competing personal or financial interests related to this work.
This paper has been peer-reviewed.
To answer the multiple-choice questions associated with this article, go to: www.cuasection3credits.org/cuajoctober2021 . This program is an Accredited Self-Assessment Program (Section 3) as defined by the Maintenance of Certification Program of The Royal College of Physicians & Surgeons of Canada, and approved by the Canadian Urological Association. Remember to visit MAINPORT ( www.mainport.org/mainport/ ) to record your learning and outcomes. You may claim a maximum of 1 hour of credit.

IMAGES
VIDEO
COMMENTS
Gender-affirming surgery for female-to-male transgender people includes a variety of surgical procedures that alter anatomical traits to provide physical traits more comfortable to the trans man's male identity and functioning. Often used to refer to phalloplasty, metoidoplasty, or vaginectomy, sex reassignment surgery can also more broadly ...
Female-to-male surgery is a type of gender-affirmation or gender-affirming surgery. There are multiple forms of gender-affirming surgery, including altering the genital region, known as "bottom ...
The authors provide a state-of-the-art overview of the different gender reassignment surgery procedures that can be performed in a female-to-male transsexual. ... Selvaggi G, Monstrey S, et al. Two-stage versus one-stage sex reassignment surgery in female-to-male transsexual individuals. Gynecol Surg. 2006; 3:190-194. [Google Scholar ...
Breast augmentation is often performed as an outpatient procedure but some patients may require one night stay in the hospital. 1 of 7. See before and after photos of patients who have undergone gender-affirming surgeries at Cleveland Clinic, including breast augmentations, facial feminizations, mastectomies and vaginoplasty.
Featured Expert: Fan Liang, M.D. Phalloplasty is surgery for masculinizing gender affirmation. Phalloplasty is a multistaged process that may include a variety of procedures, including: Creating the penis. Lengthening the urethra so you are able to stand to urinate. Creating the tip (glans) of the penis. Creating the scrotum.
Unlike sex assigned at birth (either male or female), gender identity is the way you understand your body and present yourself to others. ... Gender reassignment is an outdated term for gender affirmation surgery. The new language, "gender affirmation," is more accurate in terms of what the surgery does (and doesn't) do. ...
The cost of transitioning can often exceed $100,000 in the United States, depending upon the procedures needed. A typical genitoplasty alone averages about $18,000. Rhinoplasty, or a nose job, averaged $5,409 in 2019. Insurance Coverage for Sex Reassignment Surgery.
Gender affirming surgery can be used to create a vulva and vagina. It involves removing the penis, testicles and scrotum. During a vaginoplasty procedure, tissue in the genital area is rearranged to create a vaginal canal (or opening) and vulva (external genitalia), including the labia. A version of vaginoplasty called vulvoplasty can create a ...
Today, many transgender people prefer to use the term "gender confirmation surgery," because when we say something like gender "reassignment" or "sex change," it implies that a person ...
Abstract. The current management of female to male (FTM) gender confirmation surgery is based on the advances in neo phalloplasty, perioperative care and the knowledge of the female genital anatomy, as well as the changes that occur to this anatomy with preoperative hormonal changes in transgender population. Reconstruction of the neophallus is ...
Metoidioplasty is a gender-affirming (sex-reassignment) surgery for transgender men assigned female at birth. According to the 2015 U.S. Transgender Survey, about 4% of trans men have undergone the procedure, while another 53% expressed a desire to undergo metoidioplasty in the future.
Gender-affirming surgery is a surgical procedure, or series of procedures, that alters a person's physical appearance and sexual characteristics to resemble those associated with their identified gender.The phrase is most often associated with transgender health care and intersex medical interventions, although many such treatments are also pursued by cisgender and non-intersex individuals.
Gender transition can substantially improve quality-of-life in individuals with gender dysphoria, and various surgical options are available for female-to-male (FtM) transition, including facial ...
Introduction. Transsexualism (ICD-10) or Gender Dysphoria (GD) (DSM-5) is characterized by intense and persistent cross-gender identification which influences several aspects of behavior ().The terms describe a situation where an individual's gender identity differs from external sexual anatomy at birth ().Gender identity-affirming care, for those who desire, can include hormone therapy and ...
Overview. Feminizing surgery, also called gender-affirming surgery or gender-confirmation surgery, involves procedures that help better align the body with a person's gender identity. Feminizing surgery includes several options, such as top surgery to increase the size of the breasts. That procedure also is called breast augmentation.
Papadopulos NA, Zavlin D, Lellé JD, et al. Male-to-female sex reassignment surgery using the combined technique leads to increased quality of life in a prospective study. Plast Reconstr Surg . 2017;140(2):286-294. doi: 10.1097/PRS.0000000000003529 PubMed Google Scholar Crossref
Miroslav Djordjevic, MD, PhD, an internationally renowned surgeon and a leading authority on surgery for transgender individuals, is developing a procedure to match two patients undergoing transgender surgery—one male-to-female, the other female-to-male—and transfer the genitalia between these live donors in a one-stage procedure instead of discarding them as is done now.
Types of Gender "Reassignment" Surgeries: "Female to Male (FTM)" Female to Male (FTM) is outdated terminology that the GCC does not use in our clinical practice. This abbreviation leaves out the experiences of many trans masculine and non-binary patients who do not identify with being labeled as a "woman becoming a man."
Gender-affirming surgery for male-to-female transgender women or transfeminine non-binary people describes a variety of surgical procedures that alter the body to provide physical traits more comfortable and affirming to an individual's gender identity and overall functioning.. Often used to refer to vaginoplasty, sex reassignment surgery can also more broadly refer to other gender-affirming ...
The cost for female-to-male reassignment can be more than $50,000. The cost for male-to-female reassignment can be $7,000 to $24,000. Between 100 to 500 gender-reassignment procedures are ...
Summary. Transgender men may choose to have gender-affirming surgery, such as metoidioplasty or phalloplasty. These may provide sensations and functions including erections and urinating standing ...
Rachlin K, Hansbury G, Pardo ST. Hysterectomy and oophorectomy experiences of female-to-male transgender individuals. Int J Transgenderism. 2010 Oct 12;12(3):155-66. Obedin-Maliver J, Light A, DeHaan G, Steinauer J, Jackson R. Vaginal hysterectomy as a viable option for female-to-male transgender men: Obstet Gynecol. 2014 May;123:126S - 127S.
A transgender-identifying male was discovered having sex with a female inmate at a Washington state women's prison earlier this month, according to an incident report of the event.
Purpose: Gender dysphoria (GD) is an incompatibility between biological sex and personal gender identity; individuals harbor an unalterable conviction that they were born in the wrong body, which causes personal suffering. In this context, surgery is imperative to achieve a successful gender transition and plays a key role in alleviating the associated psychological discomfort. In the current ...
Current population studies estimate that 0.4-1.1% of adults self-identify as transgender. 1 Transgender non-binary (TGNB) patients seek urological consultations for a variety of reasons, including: surgical procedures related to their gender, postoperative complications, sexual health concerns, or for general urological issues.
Female dogs tend to be calmer than males. While there haven't been any scientific studies on the subject, female dogs are often said to be calmer than males. Maybe raising pups requires a degree ...
Welcome to the website for Wyoming Governor Mark Gordon, an official State of Wyoming website.