- Open access
- Published: 22 March 2021

Patient safety from the perspective of quality management frameworks: a review
- Amrita Shenoy ORCID: orcid.org/0000-0001-8355-7792 1
Patient Safety in Surgery volume 15 , Article number: 12 ( 2021 ) Cite this article
21k Accesses
3 Citations
1 Altmetric
Metrics details
Patient safety is one of the overarching goals of patient care and quality management. Of the many quality management frameworks, Beauchamp and Childress’s four principles of biomedical ethics presents aspects of patient centeredness in clinical care. The Institute of Medicine’s six aims for improvement encapsulates elements of high-quality patient care. The Institute of Healthcare Improvement’s Triple Aim focuses on three aspects of care, cost, and health. Given the above frameworks, the present review was designed to emphasize the initiatives the system has taken to address various efforts of improving quality and patient safety. We, hereby, present a contemplative review of the concepts of informed consent, informed refusal, healthcare laws, policy programs, and regulations. The present review, furthermore, outlines measures and policies that management and administration implement and enforce, respectively, to ensure patient centered care. We, conclusively, explore prototype policies such as the Delivery System Reform Incentive Payment Program that imbues the elements of quality management frameworks, Hospital-Acquired Conditions Reduction Program that supports patient safety, and Hospital Readmissions Reduction Program that focuses on curbing readmissions.
The logistics of patient care and healthcare management revolve around many aspects of optimized high-quality care. The Joint Commission (TJC), Malcolm Baldrige National Quality Award (MBNQA), and The Magnet Recognition Program signify healthcare accreditation, performance excellence, and nursing excellence, respectively [ 1 , 2 , 3 ]. TJC is the recognized global leader of healthcare accreditation [ 4 ]. It is an independent not-for-profit organization that offers an unbiased assessment of quality achievement in patient care and safety [ 4 ]. MBNQA is the nation’s highest presidential honor for performance excellence [ 5 ]. The Magnet Recognition Program designates organizations worldwide where nursing leaders successfully align their nursing strategic goals to improve the organization’s patient outcomes [ 6 ]. In addition to the above healthcare recognition, the Institute of Medicine (IOM) categorizes aspects of care delivery with its six aims for improvement [ 7 ]. The Institute of Healthcare Improvement’s (IHI's) Triple Aim comprises of three aspects: improving the experience of care, improving the health of populations, and reducing per capita costs of healthcare.
We, hereby, present a synthesis of how the perspectives of biomedical ethics, six aims for improvement, and the Triple Aim converge into a focal point of preserving patient safety and promoting improvement in care delivery. The present review elaborates and explains the clinical and managerial roles inherent in the logistics of patient safety in emergencies and non-emergencies. The impetus here is to exemplify existing policies supporting patient centeredness while preserving the parameters that improve patient care, preserve quality, and promote patient safety.
As one of the cornerstones of high-quality healthcare, patient safety is intrinsic to all healthcare professionals. Clinicians are involved in direct patient care. However, does that imply that policymakers, leadership, and managers are separate and distinct components not involved in patient safety? The answer to the above question is not likely because these entities devise and enforce policies to preserve and augment patient safety in communities, institutions, and departments. At the macro-level, policymakers devise and recommend healthcare policies that at the micro-level, leadership, management, and clinicians enforce, adopt, and practice, respectively, at the point of patient care.
Research questions and objectives
Past literature establishes quality management frameworks such as Beauchamp and Childress’s Principles of Biomedical Ethics, six aims for improvement and the Triple Aim. The above frameworks, broadly, capture the patient’s needs/preferences while aligning with improvement in care delivery. However, there are instances in which patients when presented in an unconscious or inebriated state cannot communicate their treatment preferences. Given the above case, the first research question is: what are some recourses that providers can choose to adopt as safe harbors while treating such patients? The second research question is: what are the practices that clinicians could potentially adhere when the patient consents or refuses to consent? As a close follow-up, the third research question is: what is the role of administration in implementing policies that fall outside the purview of already enforced laws? The objective of the present review is threefold. First, we aim to propose answers to the dos and don’ts that clinicians could potentially adopt in emergency and non-emergency cases, given the concepts of informed consent and informed refusal. Second, we attempt to explain how hospital leadership can best facilitate patient safety and manage risk while facilitating high-quality patient care. Finally, we explore prototype policies such as the Delivery System Reform Incentive Payment program, Quadruple Aim, Hospital-Acquired Conditions Reduction Program, and Hospital Readmissions Reduction Program which have been implemented more recently as systemic initiatives to preserve patient safety and promote measures in care delivery.
Literature review
Quality management frameworks preserving patient safety: an overview of three established frameworks, beauchamp and childress’s principles of biomedical ethics.
Faculty in medicine and surgery have a substantial role in ethically creating a culture of safety via medical and surgical treatments for patients. In this context, four principles of biomedical ethics come into the picture. Those principles are autonomy, non-maleficence, beneficence, and justice [ 9 ]. The above four principles are the four pillars of medical ethics and form the basis of ethical practice in medicine and surgery. Some more aspects of biomedical ethics stemming from the above four principles are considered in ethical medical and surgical decision making [ 10 ]. A list of those additional aspects are as follows: [ 10 ].
Truthfulness, Full Disclosure, and Confidentiality: On the one hand, truthfulness is not distorting facts while presenting information to the patient; full disclosure is accurately and completely informing the details of the patient’s medical condition. On the other hand, confidentiality is the principle of not revealing information about the patient’s medical condition to third parties [ 10 ].
Autonomy and Freedom: Autonomy is the principle of providing the patient discretion, freedom, and independence to choose treatment preferences. This concept particularly comes into the spotlight in end-of-life hospice treatments and medical terminations of pregnancies [ 10 ].
Beneficence is the principle of doing good and inflicting the least harm to the patient.
The Institute of medicine’s six aims for improvement model
The Agency for Healthcare Research and Quality (AHRQ) Patient Safety Network expands upon the definition of prevention of harm as, “freedom from accidental or preventable injuries produced by medical care” [ 11 ]. Furthermore, the IOM introduced six aims for improvement in healthcare to meet the patient’s healthcare needs and preserve patient safety. Those six aims are as follows: [ 7 ].
Safe: avoiding injuries to patients from the care that is intended to help them. Patient safety can be a system-wide approach when patients see measures adopted and practiced that create a safe environment [ 7 ].
Efficient: avoiding waste including waste from equipment, supplies, ideas, and energy. Healthcare wastes are also in the form of defensive medicine, malpractice litigation, systemic complexities, and administrative fraud and abuse. Cost-effective care potentially supports efficiency in healthcare [ 7 ].
Effective: providing services based on scientific knowledge to all those who could benefit. In this context, Evidence Based Medicine is incorporating scientific knowledge into treatment and procedure options [ 7 ].
Patient-centered: providing care that is respectful of and responsive to the patient’s needs, preferences, and values. Delivery of care is considered to be patient-centered when the patient can choose certain aspects of care. This approach towards patient care prospectively ingrains elements of cooperation and collaboration [ 7 ].
Timely: reducing waiting times and detrimental delays for both, recipients and providers of care. Waits and harmful delays potentially produce life threatening illnesses worsening quality outcomes throughout the continuum of a patient care [ 7 ].
Equitable: providing care that is consistent and does not vary in quality based on personal aspects such as gender, ethnicity, geographic location, and socioeconomic status, etc. [ 7 ].
As per the IOM’s six aims for improvement, first, healthcare processes need to be safe which implies the provider makes an active attempt to ensure patient safety. Second, patient care prospectively needs to be aligned with recent developments to be potentially effective. Third, patient-centered care takes into consideration the patient’s culture, dietary and personal preferences incorporated into care delivery methods. The above concept plays an important role in end-of-life or hospice care provided to the elderly. Fourth, timeliness is providing and receiving care in a manner that reduces waiting times and delays. On the one hand, unforeseen wait periods may delay care and result in serious unintended harm to patients. On the other hand, the provision of timely care is essential to patient safety. Fifth, focusing on eliminating wastes and redundant processes could potentially help conserving resources and making care more affordable. Finally, providing equitable care is that which does not vary in terms of race, ethnicity, socioeconomic status, and income [ 7 ].
The Institute of healthcare improvement’s triple aim model
The Institute of Healthcare Improvement’s (IHI’s) Triple Aim model synthesizes and incorporates aspects of care, cost, and health [ 8 ]. The IHI’s Triple Aim model involves the following three components: [ 8 ].
Improving the experience of care: Implementing Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) and Consumer Assessment of Healthcare Providers and Systems (CAHPS) surveys are few of the many ways of recording patient experience of care [ 12 , 13 ]. The National Practitioner Data Bank (NPDB), additionally, assists in promoting quality health care and deterring fraud and abuse within health care delivery systems [ 14 ].
Reducing per capita costs of care: Cost of care could be reduced with the help of using generic drugs instead of brand name drugs for prescriptions, as an example [ 8 ].
Improving the health of populations [ 8 ].
The IHI's Triple Aim is a framework that describes an approach with a threefold purpose. First, improving the experience of care regarding healthcare quality, second, decreasing per capita costs of care that aims at reducing wastes and variation in healthcare, and third, improving the health of populations. The IHI’s Triple Aim model has universal applications that cover medical treatment, surgical care, therefore, opening avenues to solve administrative complexities for preserving health and wellness in populations.
The first component of the Triple Aim, improving the experience of care applies to advances in medical technology making a positive impact in the patient experience of care [ 8 ]. The second component of the Triple Aim, reducing per capita costs of care, applies to implementing telemedicine and telehealth projects, as an example. Telemedicine brings to fruition, efficient and timely care when physicians may not be in the vicinity of the patient [ 8 ]. On the one hand, one of pros of telemedicine is the potential to enhance access to care. On the other hand, it introduces this concept to some practitioners and patients who have little to no experience with e-health. The third component of the Triple Aim, improving the overall health of the population applies to facilitating a combination of the above two aims. The IHI’s Triple Aim model, therefore, is a three-pointed framework in which the first two aims are intrinsic to the third aim, improving population health [ 8 ].
The roles of clinical faculty and administration in patient safety: adoption and implementation of best practices in emergency and non-emergency cases
Emergency Medical Treatment and Active Labor Act (EMTALA) is a federal law that requires anyone coming to an emergency department to be stabilized and treated, regardless of their insurance status or ability to pay [ 15 ]. As per EMTALA, the patient has a right to be treated and clinicians are bound to provide treatment [ 15 ]. In this context, let us consider an example of an unconscious patient in the emergency department that does not culturally prefer receiving blood transfusions. In the above case, hypothetically, if the treating provider is not knowledgeable of the cultural preference of the unconscious patient and proceeds to revive the patient via a blood transfusion, then, was patient centered care provided? The answer likely lies in the provider’s assessment in the context of EMTALA. The assessment, first and foremost, relates to the binding duty of the clinician to provide care to every patient, especially in times of emergencies.
The dynamics of the above hypothetical scenario entirely changes in non-emergency situations in which patients can choose a provider to treat them; and reciprocally, even providers can choose whom to treat. The rationale behind this is the physician-patient relationship that specifies the terms and conditions of a physician-patient contract [ 16 ]. This legal relationship is based on contract principles because the physician agrees to provide treatment in return for payment in the presence of the contract [ 16 ]. The law usually imposes no duty on the physician to treat the patient in the absence of a physician-patient contract [ 16 ].
In the process of providing treatment, obtaining informed consent is the concept in which the clinician explains the proposed line of treatment, duration, benefits, risks of opting in as well as opting out of the treatment, alternatives to the proposed treatment with an opportunity to answer patient questions [ 17 ]. In 1914, an American judge Benjamin Cardozo composed the foundational principle of informed consent as, “Every human being of adult years and sound mind has a right to determine what shall be done with his own body; and a surgeon who performs an operation without his patient’s consent commits an assault for which he is liable in damages” [ 18 ]. An interesting aspect of treatment in non-emergency cases is when the patient does not agree to informed consent which brings forth the concept of “Informed Refusal” [ 19 , 20 ]. A living will is an example of an informed refusal document in which the patient states his or her end of life preferences [ 21 ]. In the above case, the provider honors the patient’s end of life preferences and/or withholds treatment for the patient as specified in the living will.
The role of leadership is to enforce EMTALA and help clinicians' awareness of informed consent and informed refusal processes in organizations. Moreover, they ensure that providers implement the above policies regarding patient preferences. In medical cases that fall outside the purview of the already enforced laws, leadership can prospectively make rules but with caution that those rules are not against public policy.
Macro-level healthcare programs focusing on patient safety: prototype policies
Delivery system reform incentive payment program: focusing on alignment with quality management frameworks.
The Delivery System Reform Incentive Payment (DSRIP) program is one prototype policy that incorporates six aims for improvement and the Triple Aim model. DSRIP has multiple healthcare projects that improve health statuses incorporating numerous metrics and milestones in primary care, specialty care, chronic care, navigation and case management, disease prevention and wellness, and general categories [ 23 , 24 ]. These projects are reimbursed by the State Department of Health in a systematic manner when adopted by healthcare institutions [ 22 , 23 , 24 , 25 , 26 ].
DSRIP’s framework involves four components: (1) Infrastructure Development, (2) Program Innovation and Redesign, (3) Quality Improvement, and (4) Improvement in Population Health in states where its projects are implemented [ 22 , 23 , 24 , 25 , 26 ]. In its third year of implementation, the Texas DSRIP program in the southeastern county region had about 172 projects in eight cohorts those being, primary care, emergency care, chronic care, navigation/case management, disease prevention and wellness, behavioral health/substance abuse prevention, and general.[ 22 , 23 , 25 ] Each cohort had a set number of projects that involve meeting patient care milestones and metrics, simultaneously incorporating IOM’s six patient care aims of medical care being safe, efficient, effective, patient centered, timely, and equitable [ 22 , 23 , 24 , 25 ].
DSRIP, with all its projects implemented in the adopted regions and counties has been measured to improve population health [ 25 ]. A metric of measuring improvement in population health within the DSRIP program was preventable hospitalization rate [ 24 ]. The decrease in preventable hospitalization rates may have been attributed to the inherent design and dynamics of the DSRIP policy [ 23 , 24 ]. Those dynamics comprised of factors such as physician-administrator collaboration, mechanisms of incentive payments, types of measures for reporting outcomes in quality, and interplaying healthcare externalities [ 24 ]. In the adopted regions and counties, a statistically significant decrease in preventable hospitalization rates was observed when tested with an interrupted time series method [ 25 ].
There were two phases of the Texas DSRIP program, DSRIP 1.0 and 2.0. It was in DSRIP 2.0 that comprehensive Diabetes Care: eye exam metric improved by 16 % while Influenza immunization improved by 12 % in the latter [ 27 ]. Researchers Revere et al. have identified that in DSRIP 2.0, the metrics for Central Line Associated Bloodstream Infection (CLABSI) rates, Catheter Associated Urinary Tract Infections (CAUTI), and Surgical Site Infection (SSI) rates improved by 26 %, 10 %, and 9 %, respectively [ 27 ].
Quadruple aim framework: focusing on the evolution of the triple aim
The Triple Aim, formulated in 2008, drew focus on three aims which were based on care, cost, and health. Sikka and colleagues, in 2015, constructed a fourth aim, improving the experience of providing care. This was made to acknowledge the importance of physicians, nurses, and all employees in “finding joy and meaning in their work and in doing so improving the experience of providing care” [ 28 ]. At the core of the fourth aim is the experience of joy and meaning in providing care making it synonymous with acquiring accomplishment and meaning in their contributions. The Quadruple Aim has broad implications in theory and practice factoring inclusiveness in terms of all members in the healthcare workforce [ 28 ].
Hospital-Acquired conditions reduction program: focusing on patient safety
The Hospital-Acquired Conditions Reduction Program (HACRP) is a Medicare pay-for-performance program that supports the CMS’ long-standing effort to link Medicare payments to healthcare quality in the inpatient hospital setting [ 29 ]. HACRP focuses on specific conditions that the Centers for Disease Control and Prevention (CDC) National Healthcare Safety Network (NHSN) healthcare- associated infection (HAI) measures which are: [ 30 ] (1) Central Line Associated Blood Stream Infection (CLABSI), (2) Catheter Associated Urinary Tract Infection (CAUTI), (3) Surgical Site Infection (SSI) for colon and hysterectomy, (4) Methicillin-Resistant Staphylococcus Aureus (MRSA) bacteremia, (5) Clostridium Difficile Infection (CDI).
Additionally, eight Patient Safety Indicators (PSIs) included in the program comprise of: [ 31 ] (1) PSI 03 - Pressure Ulcer Rate, (2) PSI 06 - Iatrogenic Pneumothorax Rate (3) PSI 07 - Central Venous Catheter-Related Bloodstream Infection Rate, (4) PSI 08 - Postoperative Hip Fracture Rate, (5) PSI 12 - Perioperative Pulmonary Embolism or Deep Vein Thrombosis Rate, (6) PSI 13 - Postoperative Sepsis Rate, (7) PSI 14 - Postoperative Wound Dehiscence Rate, (8) PSI 15 - Accidental Puncture or Laceration Rate.
Hospital readmissions reduction program: focusing on patient safety
The Hospital Readmissions Reduction Program (HRRP) is a Medicare value-based purchasing program that reduces payments to hospitals with excess readmissions. The program supports the national goal of improving healthcare by linking payment to the quality of hospital care [ 32 ]. HRRP has a specific focus on the following conditions to reduce readmissions that in turn improve patient safety [ 32 ]. Those conditions are as follows: [ 32 ] (1) Acute Myocardial Infarction (AMI), (2) Chronic Obstructive Pulmonary Disease (COPD), (3) Heart Failure (HF), (4) Pneumonia (5) Coronary Artery Bypass Graft (CABG) surgery, and (6) Elective Primary Total Hip Arthroplasty and/or Total Knee Arthroplasty (THA/TKA) [ 32 ].
The purpose of the present review was to analyze patient safety through the lens of the above quality management frameworks. We, specifically, illuminated policies and laws such as EMTALA, informed consent, informed refusal, and living will as examples. In emergency cases, the rules of EMTALA apply whereas in non-emergency cases, the same applies to obtaining informed consent from the patient. In the event the patient refuses treatment, documenting the informed refusal would be ideal. We underscored selective new prototype policies percolating from national policymaking to institutional levels with a focus on the initiatives the system has actively taken to preserve patient safety and promote improvement in care delivery.
Facts about The Joint Commission. Retrieved from https://www.jointcommission.org/about_us/about_the_joint_commission_main.aspx . Accessed 16 Feb 2021
Malcolm Baldrige Award. Retrieved from https://baldrigefoundation.org/ . Accessed 16 Feb 2021
Magnet Recognition Criteria. Retrieved from https://www.mghpcs.org/PCS/Magnet/Documents/Education_Toolbox/01_Intro-Ovrvw/Magnet-Overview-2017.pdf . Accessed 16 Feb 2021.
The Joint Commission is the recognized global leader of healthcare accreditation and offers an unbiased assessment of quality achievement in patient care and safety Retrieved from: https://www.jointcommission.org/accreditation-and-certification/why-the-joint-commission/ . Accessed 16 Feb 2021
The Malcolm Baldrige National Quality Award being the nation's highest presidential honor for performance excellence. Retrieved from: https://asq.org/quality-resources/malcolm-baldrige-national-quality-award . Accessed 16 Feb 2021
The Magnet Recognition Program’s alignment of nursing strategic goals to improve the organization’s patient outcomes. Retrieved from: https://www.nursingworld.org/organizational-programs/magnet/ . Accessed 16 Feb 2021
The Institute of Medicine Committee on Quality of Health Care in America. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academies Press (US); 2001.
Google Scholar
Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff. 2008;27(3):759–69.
Article Google Scholar
Page K. The four principles: Can they be measured and do they predict ethical decision making? BMC Med Ethics. 2012;13(1):10.
Landau R, Osmo R. Professional and personal hierarchies of ethical principles. Int J Soc Welfare. 2003;12(1):42–9.
Mitchell PH. Defining patient safety and quality care. In: Hughes RG, editor Patient safety and quality: An evidence-based handbook for nurses. Rockville: Agency for Healthcare Research and Quality (US); 2008. Chapter 1. NBK2681.
Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) Survey of Patient Perspectives. Retrieved from https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/HospitalHCAHPS . Accessed 16 Feb 2021.
Consumer Assessment of Healthcare Providers and Systems (CAHPS) Survey assessing patient experience. Retrieved from https://www.ahrq.gov/cahps/about-cahps/cahps-program/index.html . Accessed 16 Feb 2021
National Practitioner Data Bank Web site. Retrieved from: https://www.npdb.hrsa.gov/topNavigation/aboutUs.jsp . Accessed 16 Feb 2021.
Emergency Medical Treatment and Labor Act (EMTALA). Retrieved from https://www.acep.org/life-as-a-physician/ethics--legal/emtala/emtala-fact-sheet/ . Accessed 16 Feb 2021.
Showalter JS. The Law of Healthcare Administration. Eighth Edition. Chicago, Washington, DC: Health Administration Press; 2017.
Boland GL. The doctrines of lack of consent and lack of informed consent in medical procedures in Louisiana. La L Rev. 1984;45:1.
Alexis O, Caldwell J. Administration of medicines–the nurse’s role in ensuring patient safety. Brit J Nurs. 2013;22(1):32–5.
Wagner RF Jr, Torres A, Proper S. Informed consent and informed refusal. Dermatol Surg. 1995;21(6):555–9.
Ridley DT. Informed consent, informed refusal, informed choice–what is it that makes a patient’s medical treatment decisions informed? Med Law. 2001;20(2):205–14.
CAS PubMed Google Scholar
Emanuel L. Living wills can help doctors and patients talk about dying. West J Med. 2000;173(6):368–9. https://doi.org/10.1136/ewjm.173.6.368 .
Article CAS PubMed PubMed Central Google Scholar
Shenoy A, Revere L, Begley C, Linder S, Daiger S. The Texas DSRIP program: An exploratory evaluation of its alignment with quality assessment models in healthcare. Int J Healthcare Manage. 2017;12(2):165–72. https://doi.org/10.1080/20479700.2017.1397339 .
Begley C, Hall J, Shenoy A, Hanke J, Wells R, Revere L, Lievsay N. Design and implementation of the Texas Medicaid DSRIP program. Popul Health Manag. 2017;20(2):139–45.
Shenoy A, Begley C, Revere L, Linder S, Daiger SP. Delivery system innovation and collaboration: A case study on influencers of preventable hospitalizations. Int J Healthcare Manage. 2017:1–8. DOI: https://doi.org/10.1080/20479700.2017.14057772017.1405777
Shenoy AG, Begley CE, Revere L, Linder SH, Daiger SP. Innovating patient care delivery: DSRIP’s interrupted time series analysis paradigm. Healthcare. 2019;7(1):44–50. https://doi.org/10.1016/j.hjdsi.2017.11.004 .
Article PubMed Google Scholar
Shenoy AG. DSRIP’s innovation and collaboration in population health management: A cross-sectional segmented time series model. Health Serv Manage Res. 2020;33(1):2–12. https://doi.org/10.1177/0951484819868679 .
Revere L, Kavarthapu N, Hall J, Begley C. Achieving triple aim outcomes: An evaluation of the Texas medicaid waiver. Inquiry. 2020;57:46958020923547. https://doi.org/10.1177/0046958020923547 .
Sikka R, Morath JM, Leape L. The Quadruple aim: care, health, cost and meaning in work. BMJ Qual Safety. 2015;24:608–10.
Hospital Acquired Conditions Reduction Program. Retrieved from https://www.cms.gov/Medicare/Medicare-Fee-for-ServicePayment/AcuteInpatientPPS/HAC-Reduction-Program . Accessed 16 Feb 2021.
HACRP List of Conditions. Retrieved from https://qualitynet.cms.gov/inpatient/hac Accessed 16 Feb 2021.
List of PSI 90. Retrieved from https://www.qualityindicators.ahrq.gov/Modules/PSI_TechSpec_ICD10_v2020.aspx . Accessed 16 Feb 2021
Hospital Readmissions Reduction Program. Retrieved from https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program . Accessed 16 Feb 2021
Download references
Acknowledgements
Not applicable.
Conflict of interest and financial disclosure statement
The authors collectively declare that there is no conflict of interest and have no financial interests with any sponsoring organization, for-profit or not-for-profit.
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and affiliations.
College of Public Affairs, School of Health and Human Services, Healthcare Administration Program, University of Baltimore, 1420 N. Charles Street, MD, 21201, Baltimore, USA
Amrita Shenoy
You can also search for this author in PubMed Google Scholar
Contributions
The author read and approved the final manuscript. AS conducted the literature search and review, drafted the manuscript and responded the reviewer's comments.
Authors' information
Dr. Amrita Shenoy is an Assistant Professor of Healthcare Admin-istration at the University of Baltimore and the Winner of the 2011 McGraw-Hill/Irwin Distinguished Paper Award. She leverageseconometrics to quantify policy impact and qualitatively exploreshealthcare laws and policies for a deeper comprehension of its ana-lytical spectra. Dr. Shenoy received her PhD from the University ofTexas Health Science Center at Houston School of Public Health,MHA/MBA from the University of Houston — Clear Lake and MScfrom Nottingham Trent University, United Kingdom. Her researchareas spotlight topics in healthcare law, policy, and quality with abroad emphasis on public health and healthcare management.
Corresponding author
Correspondence to Amrita Shenoy .
Ethics declarations
Ethics approval and consent to participate.
Ethics approval and consent to participate on data involving the use of any animal/human tissue Not applicable
Consent for publication
Not applicable
Competing interests
The authors have no competing interests to declare.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Shenoy, A. Patient safety from the perspective of quality management frameworks: a review. Patient Saf Surg 15 , 12 (2021). https://doi.org/10.1186/s13037-021-00286-6
Download citation
Received : 04 January 2021
Accepted : 23 February 2021
Published : 22 March 2021
DOI : https://doi.org/10.1186/s13037-021-00286-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Quality management frameworks
- IOM’s six aims for improvement
- IHI’s Triple Aim
- Patient safety
- Patient centeredness
- High‐quality clinical care
Patient Safety in Surgery
ISSN: 1754-9493
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Service quality in the healthcare sector: a systematic review and meta-analysis
LBS Journal of Management & Research
ISSN : 0972-8031
Article publication date: 16 January 2023
Issue publication date: 4 September 2023
The purpose of this study is to summarize the available pool of literature on service quality to identify different dimensions of service quality in the healthcare industry and understand how it is measured. The study attempts to explore the research gaps in the literature about different service quality dimensions and patient satisfaction.
Design/methodology/approach
A systematic literature review process was followed to achieve the objectives of the study. Various inclusion and exclusion criteria were used to select relevant research articles from 2000–2020 for the study, and a total of 100 research articles were selected.
The study identified 41 different dimensions of healthcare service quality measurement and classified these dimensions into four categories, namely servicescape, personnel, hospital administration and patients. It can be concluded that SERVQUAL is the most widely used service quality measurement tool.
Originality/value
The study identified that a majority of the researchers deduced a positive relationship between SERVQUAL dimensions and the quality of healthcare services. The findings of study will assist hospital executives in formulating effective strategies to ensure that patients receive superior quality healthcare services.
- Healthcare sector
- Service quality
- Systematic review
Darzi, M.A. , Islam, S.B. , Khursheed, S.O. and Bhat, S.A. (2023), "Service quality in the healthcare sector: a systematic review and meta-analysis", LBS Journal of Management & Research , Vol. 21 No. 1, pp. 13-29. https://doi.org/10.1108/LBSJMR-06-2022-0025
Emerald Publishing Limited
Copyright © 2022, Mushtaq Ahmad Darzi, Sheikh Basharul Islam, Syed Owais Khursheed and Suhail Ahmad Bhat
Published in LBS Journal of Management & Research . Published by Emerald Publishing Limited. This article is published under the Creative Commons Attribution (CC BY 4.0) licence. Anyone may reproduce, distribute, translate and create derivative works of this article (for both commercial and no commercial purposes), subject to full attribution to the original publication and authors. The full terms of this licence may be seen at http://creativecommons.org/licences/by/4.0/legalcode
Introduction
The quality of healthcare services has long been a subject of concern for both private and public healthcare service providers across the globe. According to Senic and Marinkovic (2013) , integrity and competitiveness of a nation's healthcare structure are gauged by the quality of healthcare services rendered. Indian National Health Policy 2017 envisions that everyone should have access to high-quality healthcare without facing financial suffering ( MoHFW, 2017 ). Adherence to quality standards and improved quality design results in a better-perceived value, which leads to better prices, better income and greater profitability ( Zeithaml, 2000 ). Customers of the healthcare industry in developing countries are becoming more and more aware of their right to quality healthcare. Consequently, delivering high-quality service by healthcare service providers is gaining momentum ( Abuosi & Atinga, 2013 ). According to Yee, Yeung, and Cheng (2010) , healthcare service providers need to provide high-quality services to sustain the trustworthiness of patients. Demand for superior service quality is growing due to an increase in the per capita income of customers and increased aspirations of the customer ( Singh & Prasher, 2019 ). Also, as a result of competition from private healthcare service providers, public care providers are facing pressing demand for delivering high-quality services ( Zarei, Arab, Froushani, Rashidian, & Ghazi-Tabatabaei, 2012 ).
Mosadeghrad (2014, p. 78) defined healthcare quality as “ consistently delighting the patient by providing efficacious, effective and efficient healthcare services according to the latest clinical guidelines and standards, which meet the patient ' s needs and satisfies providers ”. Ovretveit (2009, p. 4) defines quality care as the “ p rovision of care that exceeds patient expectations and achieves the highest possible clinical outcomes with the resources available ”. Parasuraman, Zeithaml and Berry (1985) described service quality as the gap between a customer's expectations of service and the customer's perception of service after the service is rendered. When perception exceeds expectations, the customer will be satisfied ( Kalaja, Myshketa, & Scalera, 2016 ). Several studies have confirmed that customer expectations of service are much higher than the customer perception of services rendered by both public and private sector institutions ( Andaleeb, Siddiqui, & Khandakar, 2007 ; Zarei et al. , 2012 ; Manulik, Rosińczuk, & Karniej, 2016 ). A firm provides quality service when its services at least meet or exceed the expectations of the customer ( Owusu-Frimpong, Nwankwo, & Dason, 2010 ). Service quality evaluation varies from the service provider's and service receiver's point of view. Service delivery professionals evaluate service based on delivery and design aspects, while receivers of service evaluate it based on their overall perception after consuming the service ( Brown & Swartz, 1989 ). Traditionally healthcare quality was judged based on some objective criteria such as mortality rate, morbidity rate, infant mortality rate, etc. However, as time passes, the structure of the industry changed, and the role of patients in deciding quality has been given more and more consideration ( Dagger, Sweeney, & Johnson, 2007 ). To survive in the modern competitive markets, it has become of utmost importance for service providers to understand the needs and expectations of customers. They must deliver what the customer is expected instead of what they feel is important for a customer to maintain the business demand ( Singh & Prasher, 2019 ). Kotler and Keller (2006) suggest that in the consumer-oriented healthcare market where healthcare delivery is commodified and patient-led, the patient should be the judge of service quality. Hence, to provide better quality services, healthcare service providers need to identify the main dimensions of service quality in healthcare and focus on those dimensions rated more important by the patients ( Singh & Prasher, 2019 ).
Studies on healthcare service quality have been conducted in a variety of settings worldwide, namely Albania ( Kalaja et al. , 2016 ), Australia ( Copnell et al. , 2009 ; Dagger et al. , 2007 ; Levesque & Sutherland, 2020 ), Bangladesh ( Andaleeb et al. , 2007 ), China ( Li et al. , 2015 ; Wu, Li, & Li, 2016 ), Denmark ( Engelbrecht, 2005 ; Groene, Skau, & Frølich, 2008 ), Ghana ( Abuosi & Atinga, 2013 ; Agyapong, Afi, & Kwateng, 2018 ), India ( Chahal, 2008 ; Aagja & Garg, 2010 ; Chahal & Kumari, 2010 ; Gupta & Rokade, 2016 ; Singh & Prasher, 2019 ; Upadhyai, Jain, Roy, & Pant, 2019 ; Jog et al. , 2020 ), Iran ( Goshtasebi et al. , 2009 ; Mohammadkarim, Jamil, Pejman, Seyyed, & Mostafa, 2011 ; Mosadeghrad, 2014 ), Malaysia ( Ahmad & Sungip, 2008 ; Hasan, Ilias, Rahman, & Razak, 2009 ), Pakistan ( Irfan & Ijaz, 2011 ; Shabbir, Malik, & Malik, 2016 ; Fatima, Malik, & Shabbir, 2018 ; Dhahri, Iqbal, & Khan, 2020 ), Turkey ( Beyan & Baykal, 2012 ) and USA ( Lee, 2003 ; Hegji & Self, 2009 ; Mustafa, Yang, Mortezavi, Vadamalai, & Ramsey, 2020 ; Thompson, Shen, & Lee, 2020 ). The purpose of this paper is to investigate and summarize the available literature on healthcare service quality to understand what constitutes healthcare service quality and its principal dimensions and also to highlight the prominent research gaps that will provide direction for future research.
Methodology
The study followed a systematic review process to obtain research articles relevant to the research problem understudy. The systematic review process is a structured way of identifying, evaluating and interpreting the available literature related to any particular area ( Kamboj & Rahman, 2015 ). A systematic literature review is a two-step process. First, defining the criteria for inclusion of articles and second, identifying databases and research studies ( McLean & Antony, 2014 ).
Inclusion criteria
Papers published during 2000–2020 were considered for the study. This was done by applying a custom range filter. The reason for selecting the above mention time frame is the most recent two decades were selected for article search.
Research articles related to healthcare service quality were included in the review process. The criterion was adopted in line with the primary objective of the review process.
Empirical and review articles published in peer-reviewed journals were considered.
Only papers in the English language were included.
Database and article selection
The literature search was conducted in the autumn of 2021. The databases selected for the literature search included Emerald, Elsevier, Sage, Taylor and Francis and Google Scholar. Filters such as custom range and sort by relevance were applied to restrict the search results to keywords. The systematic review process is presented in Figure 1 . In stage 1 of the review process, the literature was searched using the keywords such as healthcare, healthcare services, service quality and SERVQUAL. The search obtained 209 research articles. The research papers were selected based on relevance to the topic understudy and the popularity of the articles. Researchers such as Beaulieu (2015) argued that the popularity of journal articles with above 10 citations are considered in top 24% of the highest cited articles, and articles that receive 100 citations are considered among 1.8% of the most popular articles across the globe, which makes the current study a worth addition to the existing body of literature. In stage 2, the screening of articles was then conducted first based on title and abstract and then based on inclusion criteria. Screening of articles based on the title and abstract resulted in the exclusion of 63 research articles, and 146 articles were moved to the next level of screening.
Then articles were screened by applying inclusion criteria to exclude articles that do not fulfill the above-stated criteria ( Kamboj & Rahman, 2015 ). This screening obtained 100 research articles that were finally considered for review, and the rest of the articles (46) were excluded from the study. Finally, in stage 3 of the review process, the study provides a summary (publication trend, journal-wise distribution, methodology that includes sampling method and data analysis tools used and key findings) of the 100 articles included in the review.
Common characteristics of reviewed articles
Classification of articles by research type and hospital setting
Table 1 displays the classification of research articles based on research type and hospital setting. The research type describes the nature of the research and yields that a maximum number of articles were quantitative studies (62 articles) followed by qualitative studies (15 articles) and only 07 studies that were both qualitative and quantitative. A few review articles (14 articles) were also considered during the process. The results of the review substantiate that there is a need of conducting qualitative research that can provide an in-depth understanding of how various service quality dimensions affect the perceived quality of care among patients and the treatment satisfaction level. Qualitative studies can also provide insights into the priorities of patients while receiving medical services.
The classification based on hospital setting yields more than 77 articles that have purposively chosen a specific hospital setting and the rest have collected data from respondents in general. Out of 77 articles, 49% of research studies were conducted in a public hospital setting, and 25% were conducted in a private hospital setting. Around 26% of research were conducted in both public and private hospital settings. The direct comparison of healthcare services and perceived service quality among patients was observed as the main motivator in choosing both hospital settings ( Ovretveit, 2000 ; Mostafa, 2005 ; Taner & Antony, 2006 ; Andaleeb et al. , 2007 ; Owusu-Frimpong et al. , 2010 ; Manulik et al. , 2016 ; Dhahri et al. , 2020 ).
Data analysis tool
Figure 2 presents the frequency of various data analysis tools used by researchers to obtain meaningful results. The examination of articles selected for review revealed that 15 different data analysis techniques have been utilized in the past two decades. Descriptive statistics (29 articles) including mean and standard deviation has been the most frequently applied technique in healthcare service quality research followed by t -test (18 articles). It was also found that both techniques have been applied in combination because service quality can be obtained by ascertaining the difference between service perception and service expectation of patients using the SERVQUAL model ( Ahmad & Sungip, 2008 ; Irfan & Ijaz, 2011 ; Zarei, Daneshkohan, Khabiri, & Arab, 2015 ; Torabipour, Sayaf, Salehi, & Ghasemzadeh, 2016 ). Other major techniques preferred by researchers include correlation (17 articles), regression (17 articles), systematic literature review (12 articles) and ANOVA (11 articles). However, only 20 articles in total have applied structural equation modeling (SEM), MANOVA, content analysis, chi-square test, Shapiro–Wilk test, Mann–Whitney U-test, Kruskal–Wallis tests and Wilcoxon test, making them among the least preferred techniques in healthcare service quality research.
Sampling method
Articles selected for review depict that both nonprobability and probability sampling have been applied to study healthcare service quality and patient satisfaction. The articles have adopted 08 different sampling methods in addition to the complete enumeration (Census), which was employed for 03 articles. From nonprobability sampling techniques, convenience sampling (18 articles) is the most widely used sampling technique, and simple random sampling (19 articles) is the most frequently applied sampling method from the probability sampling group. Cluster sampling was found to be the least applied sampling technique among probability sampling methods because most of the studies were focused on specific regions with a limited geographical area. Targeting a smaller geographical area or specific site increases the feasibility of reaching out to sampling units because of the limited population spread. Therefore, when further segregation based on the geographical area seems impossible, the applicability of cluster sampling becomes impractical ( Cameron & Miller, 2015 ).
Findings and discussion
The systematic review of 100 articles has fetched several important findings in terms of measures of healthcare service quality and the theories applied in examining healthcare service quality.
Measures of healthcare service quality
Healthcare service quality, because of its intangible character and subjective nature, is difficult to define and measure. The comprehensive study of research articles about healthcare service quality illustrated that service quality in healthcare is examined by using different measures primarily related to servicescape, personnel, hospital administration and patients. The study has identified 41 distinctive measures of healthcare service quality ( Table 2 ). The factors commonly used to measure the quality of servicescape are identified as physical environmental quality, diagnostic aspect of care, resources and capacity, tangibility, financial and physical access to care and access ( Herstein & Gamliel, 2006 ; Ahmad & Sungip, 2008 ; Sharma & Narang, 2011 ; Simou, Pliatsika, Koutsogeorgou, & Roumeliotou, 2014 ; Marzban, Najafi, Etedal, Moradi, & Rajaee, 2015 ). Among the mentioned dimensions of servicescape, utilization has been less studied in the past. Future researchers can explore these areas because often in healthcare centers, the infrastructure capacity is overutilized or underutilized, which hinders the delivery of healthcare services. The determinants mostly employed to determine the quality of human resources (personnel) include healthcare personnel conduct, efficacy, efficiency, empathy, interaction quality, physician and staff performance, provider competency/performance, reliability, responsiveness, timeliness and trustworthiness ( Chahal & Kumari, 2012 ; Manulik et al. , 2016 ; Singh & Prasher, 2019 ). Some of the fewer studied factors under personnel characteristics include quality of patient-staff communication, outcome quality, professional quality, provider motivation and satisfaction encounters. These factors can influence the service quality of healthcare centers but are less researched in the past. The factors concerning quality aspects of hospital management/administration include admission, assurance, healthcare delivery system, infection rate, standard operating procedures, leadership and management and medical service ( Ovretveit, 2000 ; Herstein & Gamliel, 2006 ; Taner & Antony, 2006 ; Aagja & Garg, 2010 ; Irfan & Ijaz, 2011 ; Gupta & Rokade, 2016 ; Torabipour et al. , 2016 ). Among the determinants of hospital administration availability of doctors and paramedical staff, discharge mechanism of patients, documentation procedure in the hospital, social responsibility consciousness among the staff, management quality and drug availability in the hospital are some of the key factors that influence the service encounters between staff and patients. These determinants are less studied in the literature. Future researchers can build their research on these less studied variables. Lastly, the factors affecting service quality in terms of patient characteristics include patient satisfaction, the average length of stay, patient cooperation, patient quality/illness and patient socio-demographic variables ( Ovretveit, 2000 ; Mosadeghrad, 2014 ; Gupta & Rokade, 2016 ). It was observed that most of the service quality determinants identified can be summarized under the major 05 SERVQUAL determinants.
Theories applied to healthcare service quality
The list of popular theories that have been applied to examine healthcare service quality across the globe is presented in Figure 3 . A total of 11 different theories were identified during the review process. Less than 50% of papers identified for review have adopted one or the other service quality measurement framework and around 70% (32 research articles) among them have applied the SERVQUAL framework by Parasuraman, Zeithaml, and Berry (1988) . This makes SERVQUAL the mostly widely applied service quality framework. The other theories that have been utilized in the recent decade to examine the service quality of healthcare system include total quality management, fuzzy analytical hierarchy process, service performance model and health monitoring indicators system: health map ( Chahal & Kumari, 2012 ; Ramez, 2012 ; Zarei et al. , 2015 ; Amole, Oyatoye, & Adebiyi, 2015 ; Singh & Prasher, 2019 ; Zaid, Arqawi, Mwais, Al Shobaki, & Abu-Naser, 2020 ). The elements used to measure the perceived service quality of hospitals under different theories other than the SERVQUAL model can largely be classified under five SERVQUAL dimensions. However, outcome quality, process quality, administrative/management quality, utilization, technical quality and trustworthiness are identified as additional new dimensions being used to examine the service quality of hospitals ( Ovretveit, 2000 ; Chahal & Kumari, 2010 ; Simou et al. , 2014 ; Singh & Prasher, 2019 ; Zaid et al. , 2020 ).
Limitations and future research directions
The current study has some shortcomings which open up opportunities for future research. The present study followed a systematic review process to obtain research articles from different databases, like Emerald, Elsevier, Sage, Taylor and Francis and Google Scholar. Several inclusion criteria were applied, and only those full-text articles that are available in the English language were selected for the review. Therefore, there is the possibility of excluding some articles that are not available in these databases or are available in some other languages. Further, most of the studies selected for review were from developed nations. There is a lot of difference between the healthcare system of developed and developing nations. Thus, the findings of the present study cannot be generalized to developing nations without additional validation ( Kamboj & Rahman, 2015 ). Therefore, there is a need of carrying out empirical research in developing nations in this area.
The review of available literature has revealed that there are a large number of measurement tools available for the assessment of service quality in healthcare. However, the majority of these measurement instruments developed by the researchers assess quality from patients' perspectives and do not take into consideration service providers' perspectives. The technical aspect of service quality cannot be assessed by patients alone ( Upadhyai et al. , 2019 ). For a better understanding of service quality evaluation and satisfaction of service encounters, both service providers' and receivers' perspectives should be taken into consideration ( Brown & Swartz, 1989 ). Therefore, future researchers need to explore the knowledge gap (gap 1) of the SERVQUAL gap given proposed by Parasuraman et al. (1985) .
Practical implications
The study has attempted to identify and describe all dimensions and measurement tools relevant to healthcare service quality in light of the available literature. The study provides a thorough description of a vast number of investigations and reflects their outcomes. This research could help understand the diverse conceptualizations of service quality in healthcare compared to other types of services. The study also identified various gaps in the available literature that could be answered by future research.
The results of this study will help hospital executives in understanding the various constituents of quality and their impact on patient satisfaction. This will help hospital managers in formulating strategies that will improve patient satisfaction and ultimately improving the overall performance of hospitals. The study also highlighted the factors in which patients weigh more, thereby helping hospital managers to set priorities and help in proper resource utilization.
The current study presents an in-depth review of the literature concerning service quality and patient satisfaction in the healthcare industry. Service quality is a subjective measure and hence tends to vary from place to place and from patient to patient based on preference. The study has identified different measures that have been utilized to date to examine service quality or quality gaps in various hospital settings. Most of the studies selected for review have employed SERVQUAL dimensions of quality as service quality parameters. Service quality in the majority of the studies was established based on a difference between perceived and expected scores of service quality determinants, and the t -test was identified as the widely used statistical measure for testing its significance. In addition to this, various measures to determine patient satisfaction were identified and classified based on extra 3Ps of services marketing, namely physical evidence, people and process. The maximum number and most weighted factors affecting patient satisfaction are related to human resources actively engaged in providing medical services. It was observed that SERVQUAL determinants are popularly being used as a tool to determine the level of satisfaction among patients. All SERVQUAL determinants were found to have a significant positive relationship with patient satisfaction. Finally, 11 popular theories were identified among which SERVQUAL is widely applied.
Systematic literature review process
Theories applied in healthcare service quality
Aagja , J. P. , & Garg , R. ( 2010 ). Measuring perceived service quality for public hospitals (PubHosQual) in the Indian context . International Journal of Pharmaceutical and Healthcare Marketing , 4 ( 1 ), 60 – 83 .
Abu-Kharmeh , S. S. ( 2012 ). Evaluating the quality of health care services in the Hashemite Kingdom of Jordan . International Journal of Business and Management , 7 ( 4 ), 195 – 205 .
Abuosi , A. A. , & Atinga , R. A. ( 2013 ). Service quality in healthcare institutions: Establishing the gaps for policy action . International Journal of Health Care Quality Assurance , 26 ( 5 ), 481 – 492 .
Adebayo , E. T. , Adesina , B. A. , Ahaji , L. E. , & Hussein , N. A. ( 2014 ). Patient assessment of the quality of dental care services in a Nigerian hospital . Journal of Hospital Administration , 3 ( 6 ), 20 – 28 .
Aghamolaei , T. , Eftekhaari , T. E. , Rafati , S. , Kahnouji , K. , Ahangari , S. , Shahrzad , M. E. , & Hoseini , S. H. ( 2014 ). Service quality assessment of a referral hospital in southern Iran with SERVQUAL technique: Patients' perspective . BMC Health Services Research , 14 ( 1 ), 1 – 5 .
Agyapong , A. , Afi , J. D. , & Kwateng , K. O. ( 2018 ). Examining the effect of perceived service quality of health care delivery in Ghana on behavioural intentions of patients: The mediating role of customer satisfaction . International Journal of Healthcare Management , 11 ( 4 ), 276 – 288 .
Ahmad , A. , & Sungip , Z. ( 2008 ). An assessment on service quality in Malaysia insurance industry . Communications of the IBIMA , 1 , 13 – 26 . Available from: https://www.airitilibrary.com/Publication/alDetailedMesh?docid=19437765-200802-201406040030-201406040030-13-26
Ahmed , R. , & Samreen , H. ( 2011 ). Assessing the Service quality of some selected hospitals in Karachi based on the SERVQUAL model . Pakistan Business Review , 32 ( 5 ), 266 – 314 .
Al Fraihi , K. J. , Famco , D. , & Latif , S. A. ( 2016 ). Evaluation of outpatient service quality in Eastern Saudi Arabia: Patient's expectations and perceptions . Saudi Medical Journal , 37 ( 4 ), 420 – 428 .
Amole , B. B. , Oyatoye , E. O. , & Adebiyi , S. O. ( 2015 ). Prioritization of service quality influences on patients satisfaction using analytic hierarchy process: The Nigeria experience . Economics and Applied Informatics , 3 , 25 – 35 . Available from: https://www.ceeol.com/search/article-detail?id=530660
Andaleeb , S. S. , Siddiqui , N. , & Khandakar , S. ( 2007 ). Patient satisfaction with health services in Bangladesh . Health Policy and Planning , 22 ( 4 ), 263 – 273 .
Andrews , M. A. , Areekal , B. , Rajesh , K. R. , Krishnan , J. , Suryakala , R. , Krishnan , B. , & Santhosh , P. V. ( 2020 ). First confirmed case of COVID-19 infection in India: A case report . The Indian Journal of Medical Research , 151 ( 5 ), 490 – 492 .
Bahadori , M. , Raadabadi , M. , Jamebozorgi , M. H. , Salesi , M. , & Ravangard , R. ( 2014 ). Measuring the quality of provided services for patients with chronic kidney disease . Nephro-urology Monthly , 6 ( 5 ), e21810 .
Beaulieu , L. ( 2015 ). How many citations are actually a lot of citations? . Available from: https://lucbeaulieu.com/2015/11/19/how-many-citations-are-actually-a-lot-of-citations/ (accessed on: 11 December 2021) .
Beyan , O. D. , & Baykal , N. ( 2012 ). A knowledge-based search tool for performance measures in health care systems . Journal of Medical Systems , 36 ( 1 ), 201 – 221 .
Boshoff , C. , & Gray , B. ( 2004 ). The relationship between service quality, customer satisfaction and buying intentions in the private hospital industry . South African Journal of Business Management , 35 ( 4 ), 27 – 37 .
Brady , M. K. , & Cronin , J. J. ( 2001 ). Some new thoughts on conceptualizing perceived service quality: A hierarchical approach . Journal of Marketing , 65 , 34 – 49 .
Brown , S. W. , & Swartz , T. A. ( 1989 ). A gap analysis of professional service quality . The Journal of Marketing , 53 ( 2 ), 92 – 98 .
Cameron , A. C. , & Miller , D. L. ( 2015 ). A practitioner’s guide to cluster-robust inference . Journal of Human Resources , 50 ( 2 ), 317 – 372 .
Carini , E. , Gabutti , I. , Frisicale , E. M. , Di Pilla , A. , Pezzullo , A. M. , de Waure , C. , & Specchia , M. L. ( 2020 ). Assessing hospital performance indicators. What dimensions? Evidence from an umbrella review . BMC Health Services Research , 20 ( 1 ), 1 – 13 .
Chahal , H. ( 2008 ). Predicting patient loyalty and service quality relationship: A case study of civil hospital, Ahmedabad, India . Vision , 12 ( 4 ), 45 – 55 .
Chahal , H. , & Kumari , N. ( 2010 ). Development of multidimensional scale for healthcare service quality (HCSQ) in Indian context . Journal of Indian Business Research , 2 ( 4 ), 230 – 255 .
Chahal , H. , & Kumari , N. ( 2012 ). Service quality and performance in the public health-care sector . Health Marketing Quarterly , 29 ( 3 ), 181 – 205 .
Chahal , H. , & Mehta , S. ( 2013 ). Modeling patient satisfaction construct in the Indian health care context . International Journal of Pharmaceutical and Healthcare Marketing , 7 ( 1 ), 75 – 92 .
Chakravarty , A. ( 2011 ). Evaluation of service quality of hospital outpatient department services . Medical Journal Armed Forces India , 67 ( 3 ), 221 – 224 .
Chaudhury , N. , Hammer , J. , Knemer , M. , Muralidharan , K. , & Rogers , F. H. ( 2006 ). Missing in action: Teacher and health worker absence in developing countries . Journal of Economic Perspectives , 20 ( 1 ), 91 – 116 .
Choi , K.-S. , Lee , H. , Kim , C. , & Lee , S. ( 2005 ). The service quality dimensions and patient satisfaction relationships in South Korea: Across gender, age and type of service . Journal of Service Marketing , 19 ( 3 ), 140 – 149 .
Conly , J. , Seto , W. H. , Pittet , D. , Holmes , A. , Chu , M. , & Hunter , P. R. ( 2020 ). Use of medical face masks versus particulate respirators as a component of personal protective equipment for health care workers in the context of the COVID-19 pandemic . Antimicrobial Resistance and Infection Control , 9 ( 1 ), 1 – 7 .
Copnell , B. , Hagger , V. , Wilson , S. G. , Evans , S. M. , Sprivulis , P. C. , & Cameron , P. A. ( 2009 ). Measuring the quality of hospital care: An inventory of indicators . Internal Medicine Journal , 39 ( 6 ), 352 – 360 .
Dagger , T. S. , Sweeney , J. C. , & Johnson , L. W. ( 2007 ). A hierarchical model of health service quality: Scale development and investigation of an integrated model . Journal of Service Research , 10 ( 2 ), 123 – 142 .
De los Santos , J. A. A. , & Labrague , L. J. ( 2021 ). The impact of fear of COVID-19 on job stress, and turnover intentions of frontline nurses in the community: A cross-sectional study in the Philippines . Traumatology , 27 ( 1 ), 52 – 59 .
Dhahri , A. A. , Iqbal , M. R. , & Khan , A. F. A. ( 2020 ). A cross-sectional survey on availability of facilities to healthcare workers in Pakistan during the COVID-19 pandemic . Annals of Medicine and Surgery , 59 , 127 – 130 .
D'Souza , S. C. , & Sequeira , A. H. ( 2011 ). Application of MBNQA for service quality management and performance in healthcare organizations . International Journal of Engineering, Science and Technology , 3 ( 7 ), 73 – 88 .
Engelbrecht , S. ( 2005 ). Motivation and burnout in human service work: The case of midwifery in Denmark: Roskilde university, faculty of psychology . Philosophy and Science Studies .
Fatima , T. , Malik , S. A. , & Shabbir , A. ( 2018 ). Hospital healthcare service quality, patient satisfaction and loyalty: An investigation in context of private healthcare systems . International Journal of Quality and Reliability Management , 35 ( 6 ), 1195 – 1214 .
Gandjour , A. , Kleinschmit , F. , Littmann , V. , & Lauterbach , K. W. ( 2002 ). An evidence-based evaluation of quality and efficiency indicators . Quality Management in Healthcare , 10 ( 4 ), 41 – 52 .
Goshtasebi , A. , Vahdaninia , M. , Gorgipour , R. , Samanpour , A. , Maftoon , F. , Farzadi , F. , & Ahmadi , F. ( 2009 ). Assessing hospital performance by the pabon Lasso model . Iranian Journal of Public Health , 38 ( 2 ), 119 – 124 .
Groene , O. , Skau , J. K. , & Frølich , A. ( 2008 ). An international review of projects on hospital performance assessment . International Journal for Quality in Health Care , 20 ( 3 ), 162 – 171 .
Gupta , K. S. , & Rokade , V. ( 2016 ). Importance of quality in health care sector: A review . Journal of Health Management , 18 ( 1 ), 84 – 94 .
Gustafsson , A. , Johnson , M. D. , & Roos , I. ( 2005 ). The effects of customer satisfaction, relationship commitment dimensions, and triggers on customer retention . Journal of Marketing , 69 ( 4 ), 210 – 218 .
Haque , A. , Sarwar , A. A. I.-M. , Yasmin , F. , & Nuruzzaman , A. A. ( 2012 ). The impact of customer perceived service quality on customer satisfaction for private health centre in Malaysia: A structural equation modeling approach . Information Management and Business Review , 4 ( 5 ), 257 – 267 .
Hasan , H. F. A. , Ilias , A. , Rahman , R. A. , & Razak , M. Z. A. ( 2009 ). Service quality and student satisfaction: A case study at private higher education institutions . International Business Research , 1 ( 3 ), 163 – 175 .
Hegji , C. E. , & Self , D. R. ( 2009 ). The impact of hospital quality on profits, volume, and length of stay . Health Marketing Quarterly , 26 , 209 – 223 .
Herstein , R. , & Gamliel , E. ( 2006 ). The role of private branding in improving service quality . Managing Service Quality , 16 ( 4 ), 306 – 319 .
Herzlinger , R. E. ( 2003 ). Consumer-driven health care: Implications for providers, payers, and policy-makers . Healthplan , 44 ( 6 ), 26 – 29 .
Irfan , S. M. , & Ijaz , A. ( 2011 ). Comparison of service quality between private and public hospitals: Empirical evidences from Pakistan . Journal of Quality and Technology Management , 7 ( 1 ), 1 – 22 .
Israr , M. , Awan , N. , Jan , D. , Ahmad , N. , & Ahmad , S. ( 2016 ). Patients' perception, views and satisfaction with community health center services at mardan district of Khyber Pakhtunkhwa . American Journal of Public Health Research , 4 ( 3 ), 79 – 87 .
Iyengar , S. , & Dholakia , R. H. ( 2012 ). Access of the rural poor to primary healthcare in India . Review of Market Integration , 4 ( 1 ), 71 – 109 .
Jog , S. , Kelkar , D. , Bhat , M. , Patwardhan , S. , Godavarthy , P. , Dhundi , U. , & Bhavsar , R. ( 2020 ). Preparedness of acute care facility and a hospital for COVID-19 pandemic: What we did! . Indian Journal of Critical Care Medicine: Peer-Reviewed, Official Publication of Indian Society of Critical Care Medicine , 24 ( 6 ), 385 .
Kalaja , R. , Myshketa , R. , & Scalera , F. ( 2016 ). Service quality assessment in health care sector: The case of Durres public hospital . Procedia-Social and Behavioral Sciences , 235 , 557 – 565 .
Kamboj , S. , & Rahman , Z. ( 2015 ). Marketing capabilities and firm performance: Literature review and future research agenda . International Journal of Productivity and Performance Management , 64 ( 8 ), 1041 – 1067 .
Karydis , A. , Komboli‐Kodovazeniti , M. , Hatzigeorgiou , D. , & Panis , V. ( 2001 ). Expectations and perceptions of Greek patients regarding the quality of dental health care . International Journal for Quality in Health Care , 13 ( 5 ), 409 – 416 .
Kazemi , N. , Ehsani , P. , Abdi , F. , & Bighami , M. ( 2013 ). Measuring hospital service quality and its influence on patient satisfaction: An empirical study using structural equation modelling . Management Science Letters , 3 ( 7 ), 2125 – 2136 .
Kotler , P. , & Keller , K. ( 2006 ). Marketing management ( 12th ed. ). London : Pearson Education .
Lee , F. ( 2003 ). To build loyalty, hospitals need to exceed customer's expectation . Marketing Health Service , ( Summer ), 33 – 37 .
Levesque , J. F. , & Sutherland , K. ( 2017 ). What role does performance information play in securing improvement in healthcare? A conceptual framework for levers of change . BMJ Open , 7 ( 8 ), 1 – 9 , e014825 .
Levesque , J. F. , & Sutherland , K. ( 2020 ). Combining patient, clinical and system perspectives in assessing performance in healthcare: An integrated measurement framework . BMC Health Services Research , 20 ( 1 ), 1 – 14 .
Li , M. , Lowrie , D. B. , Huang , C. Y. , Lu , X. C. , Zhu , Y. C. , Wu , X. H. … Lu , H. Z. ( 2015 ). Evaluating patients' perception of service quality at hospitals in nine Chinese cities by use of the ServQual scale . Asian Pacific Journal of Tropical Biomedicine , 5 ( 6 ), 497 – 504 .
Lim , J. , Lim , K. , Heinrichs , J. , Al-Aali , K. , Aamir , A. , & Qureshi , M. ( 2018 ). The role of hospital service quality in developing the satisfaction of the patients and hospital performance . Management Science Letters , 8 ( 12 ), 1353 – 1362 .
Liu , J. W. , Lu , S. N. , Chen , S. S. , Yang , K. D. , Lin , M. C. , Wu , C. C. … Chen , C. L. ( 2006 ). Epidemiologic study and containment of a nosocomial outbreak of severe acute respiratory syndrome in a medical center in Kaohsiung, Taiwan . Infection Control and Hospital Epidemiology , 27 ( 5 ), 466 – 472 .
Loiacono , E. T. , Watson , R. T. , & Goodhue , D. L. ( 2007 ). WebQual: An instrument for consumer evaluation of web sites . International Journal of Electronic Commerce , 11 ( 3 ), 51 – 87 .
Mahajan , N. N. , Pednekar , R. , Patil , S. R. , Subramanyam , A. A. , Rathi , S. , Malik , S. … Srivastava , S.A. ( 2020 ). Preparedness, administrative challenges for establishing obstetric services, and experience of delivering over 400 women at a tertiary care COVID‐19 hospital in India . International Journal of Gynecology and Obstetrics , 151 ( 2 ), 188 – 196 .
Manulik , S. , Rosińczuk , J. , & Karniej , P. ( 2016 ). Evaluation of health care service quality in Poland with the use of SERVQUAL method at the specialist ambulatory health care center . Patient Preference and Adherence , 10 , 1435 – 1442 .
Marzban , S. , Najafi , M. , Etedal , M. G. , Moradi , S. , & Rajaee , R. ( 2015 ). The evaluation of outpatient quality services in physiotherapy in the teaching health centers of Shahid Beheshti University based on SERVQUAL tools . European Journal of Biology and Medical Science Research , 3 ( 3 ), 46 – 53 .
McLean , R. , & Antony , J. ( 2014 ). Why continuous improvement initiatives fail in manufacturing environments? A systematic review of the evidence . International Journal of Productivity and Performance Management , 63 ( 3 ), 370 – 376 .
Ministry of Health and Family Welfare (MoHFW) ( 2017 ). National health policy 2017 . Available from: https://main.mohfw.gov.in/documents/policy ( accessed 15 January 2022 ).
Mohammadkarim , B. , Jamil , S. , Pejman , H. , Seyyed , M. H. , & Mostafa , N. ( 2011 ). Combining multiple indicators to assess hospital performance in Iran using the Pabon Lasso Model . The Australasian Medical Journal , 4 ( 4 ), 175 – 179 .
Mosadeghrad , A. M. ( 2014 ). Factors influencing healthcare service quality . International Journal of Health Policy and Management , 3 ( 2 ), 77 – 89 .
Mostafa , M. M. ( 2005 ). An empirical study of patient's expectations and satisfactions in Egyptian hospitals . International Journal of Health Care Quality Assurance , 18 ( 7 ), 516 – 532 .
Murti , A. , Deshpande , A. , & Srivastava , N. ( 2013 ). Service quality, customer (patient) satisfaction and behavioural intention in health care services: Exploring the Indian perspective . Journal of Health Management , 15 ( 1 ), 29 – 44 .
Mustafa , S. S. , Yang , L. , Mortezavi , M. , Vadamalai , K. , & Ramsey , A. ( 2020 ). Patient satisfaction with telemedicine encounters in an allergy and immunology practice during the coronavirus disease 2019 pandemic . Annals of Allergy, Asthma and Immunology , 125 ( 4 ), 478 – 479 .
Nasiripour , A. A. , Kazemi , M. A. A. , & Izadi , A. ( 2012 ). Designing a hospital performance assessment model based on balanced scorecard . HealthMED , 6 ( 9 ), 2983 – 2989 .
Ovretveit , J. ( 2000 ). Total quality management in European healthcare . International Journal of Health Care Quality Assurance , 13 ( 2 ), 74 – 80 .
Ovretveit , J. ( 2009 ). Does improving quality save money? . In A Review of Evidence of Which Improvements to Quality Reduce Costs to Health Service Providers , London : The Health Foundation .
Owusu-Frimpong , N. , Nwankwo , S. , & Dason , B. ( 2010 ). Measuring service quality and patient satisfaction with access to public and private healthcare delivery . International Journal of Public Sector Management , 23 ( 3 ), 203 – 220 .
Pandey , N. , Kaushal , V. , Puri , G. D. , Taneja , S. , Biswal , M. , Mahajan , P. , … Agarwal , R. ( 2020 ). Transforming a general hospital to an infectious disease hospital for COVID-19 over 2 weeks . Frontiers in Public Health , 8 , 1 – 8 .
Parasuraman , A. , Zeithaml , V. A. , & Berry , L. L. ( 1985 ). A conceptual model of service quality and its implications for future study . Journal of Marketing , 49 ( 10 ), 41 – 50 .
Parasuraman , A. , Zeithaml , V. A. , & Berry , L. ( 1988 ). Servqual: A multiple-item scale for measuring consumer perceptions of service quality . Journal of Retailing , 64 ( 1 ), 12 – 40 .
Prajoko , Y. W. , & Supit , T. ( 2020 ). Cancer patient satisfaction and perception of chemotherapy services during COVID-19 pandemic in central Java, Indonesia . Asian Pacific Journal of Cancer Care , 5 ( 1 ), 43 – 50 .
Rameshan , P. , & Singh , S. ( 2004 ). Quality of service of primary health centres: Insights from a field study . Vikalpa , 29 ( 3 ), 71 – 82 .
Ramez , W. S. ( 2012 ). Patients' perception of health care quality, satisfaction and behavioral intention: An empirical study in Bahrain . International Journal of Business and Social Science , 3 ( 18 ), 131 – 141 .
Robb , C. E. , de Jager , C. A. , Ahmadi-Abhari , S. , Giannakopoulou , P. , Udeh-Momoh , C. , McKeand , J. , & Middleton , L. ( 2020 ). Associations of social isolation with anxiety and depression during the early COVID-19 pandemic: A survey of older adults in London, UK . Frontiers in Psychiatry , 11 , 1 – 12 .
Saleh , S. , Alameddine , M. , Mourad , Y. , & Natafgi , N. ( 2015 ). Quality of care in primary health care setting in the eastern mediterranean region: A systematic review of the literature . International Journal for Quality in Health Care , 27 ( 2 ), 79 – 88 .
Senic , V. , & Marinkovic , V. ( 2013 ). Patient care, satisfaction and service quality in health care . International Journal of Consumer Studies , 37 ( 3 ), 312 – 319 .
Shabbir , A. , Malik , S. A. , & Malik , S. A. ( 2016 ). Measuring patients' healthcare service quality perceptions, satisfaction, and loyalty in public and private sector hospitals in Pakistan . International Journal of Quality and Reliability Management , 33 ( 5 ), 538 – 557 .
Sharma , J. K. , & Narang , R. ( 2011 ). Quality of healthcare services in rural India: The user perspective . Vikalpa , 36 ( 1 ), 51 – 60 .
Sharma , A. , Prinja , S. , & Aggarwal , A. K. ( 2019 ). Comprehensive measurement of health system performance at district level in India: Generation of a composite index . The International Journal of Health Planning and Management , 34 ( 4 ), e1783 – e1799 .
Simou , E. , Pliatsika , P. , Koutsogeorgou , E. , & Roumeliotou , A. ( 2014 ). Developing a national framework of quality indicators for public hospitals . The International Journal of Health Planning and Management , 29 ( 3 ), e187 – e206 .
Singh , A. , & Prasher , A. ( 2019 ). Measuring healthcare service quality from patients' perspective: Using fuzzy AHP application . Total Quality Management and Business Excellence , 30 ( 3-4 ), 284 – 300 .
Sohail , M. S. ( 2003 ). Service quality in hospitals: More favourable than you might think . Managing Service Quality , 13 ( 3 ), 197 – 206 .
Taner , T. , & Antony , J. ( 2006 ). Comparing public and private hospital care service quality in Turkey . Leadership in Health Services , 19 ( 2 ), 1 – 10 .
Taqi , M. , Bidhuri , S. , Sarkar , S. , Ahmad , W. S. , & Wangchok , P. ( 2017 ). Rural healthcare infrastructural disparities in India: A critical analysis of availability and accessibility . Journal of Multidisciplinary Research in Healthcare , 3 ( 2 ), 125 – 149 .
Tashobya , C. K. , da Silveira , V. C. , Ssengooba , F. , Nabyonga-Orem , J. , Macq , J. , & Criel , B. ( 2014 ). Health systems performance assessment in low-income countries: Learning from international experiences . Globalization and Health , 10 ( 1 ), 1 – 19 .
Taylor , G. ( 2012 ). Readability of OHS documents–A comparison of surface characteristics of OHS text between some languages . Safety Science , 50 ( 7 ), 1627 – 1635 .
Thompson , C. C. , Shen , L. , & Lee , L. S. ( 2020 ). COVID-19 in endoscopy: Time to do more? Gastrointestinal Endoscopy , 92 ( 2 ), 435 – 439 .
Torabipour , A. , Sayaf , R. , Salehi , R. , & Ghasemzadeh , R. ( 2016 ). Analyzing the quality Gapsin the services of rehabilitation centers using the SERVQUAL technique in Ahvaz, Iran . Jundishapur Journal of Health Sciences , 8 ( 1 ), 25 – 30 .
Tucker , J. L. III. , & Adams , S. R. ( 2001 ). Incorporating patient's assessment of satisfaction and quality: An integrative model of patient's evaluations of their care . Managing Service Quality , 11 ( 4 ), 272 – 286 .
Upadhyai , R. , Jain , A. K. , Roy , H. , & Pant , V. ( 2019 ). A review of healthcare service quality dimensions and their measurement . Journal of Health Management , 21 ( 1 ), 102 – 127 .
Wiesniewski , M. , & Wiesniewski , H. ( 2005 ). Measuring service in a hospital colposcopy clinic . International Journal of Health Care Quality Assurance , 18 ( 3 ), 217 – 228 .
Wu , H. Y. , Lin , Y. K. , & Chang , C. H. ( 2011 ). Performance evaluation of extension education centres in universities based on the balanced scorecard . Evaluation and Program Planning , 34 ( 1 ), 37 – 50 .
Wu , H. C. , Li , T. , & Li , M. Y. ( 2016 ). A study of behavioral intentions, patient satisfaction, perceived value, patient trust and experiential quality for medical tourists . Journal of Quality Assurance in Hospitality and Tourism , 17 ( 2 ), 114 – 150 .
Wu , B. , Xiao , H. , Dong , X. , Wang , M. , & Xue , L. ( 2012 ). Tourism knowledge domains: A keyword analysis . Asia Pacific Journal of Tourism Research , 17 ( 4 ), 355 – 380 .
Yee , R. W. , Yeung , A. C. , & Cheng , T. E. ( 2010 ). An empirical study of employee loyalty, service quality and firm performance in the service industry . International Journal of Production Economics , 124 ( 1 ), 109 – 120 .
Yeşilada , F. , & Direktör , E. ( 2010 ). Health care service quality: A comparison of public and private hospitals . African Journal of Business Management , 4 ( 6 ), 962 – 971 .
Zaid , A. A. , Arqawi , S. M. , Mwais , R. M. A. , Al Shobaki , M. J. , & Abu-Naser , S. S. ( 2020 ). The impact of total quality management and perceived service quality on patient satisfaction and behavior intention in Palestinian healthcare organizations . Technology Reports of Kansai University , 62 ( 03 ), 221 – 232 .
Zarei , A. , Arab , M. , Froushani , A. R. , Rashidian , A. , & Ghazi-Tabatabaei , S. M. ( 2012 ). Service quality of private hospitals: The Iranian Patients' perspective . BMC Health Services Research , 12 ( 31 ), 66 – 76 .
Zarei , E. , Daneshkohan , A. , Khabiri , R. , & Arab , M. ( 2015 ). The effect of hospital service quality on patient's trust . Iranian Red Crescent Medical Journal , 17 ( 1 ), 1 – 5 .
Zeithaml , V. A. ( 2000 ). Service quality, profitability, and the economic worth of customers: what we know and what we need to learn . Journal of the Academy of Marketing Science , 28 ( 1 ), 67 – 85 .
Zineldin , M. ( 2006 ). The quality of health care and patient satisfaction: An exploratory investigation of the 5Qs model at some Egyptian and Jordanian medical clinics . International Journal of Health Care Quality Assurance , 19 , 60 – 92 .
Corresponding author
About the authors.
Related articles
We’re listening — tell us what you think, something didn’t work….
Report bugs here
All feedback is valuable
Please share your general feedback
Join us on our journey
Platform update page.
Visit emeraldpublishing.com/platformupdate to discover the latest news and updates
Questions & More Information
Answers to the most commonly asked questions here
Best practices in implementing and sustaining quality of care. A review of the quality improvement literature
Affiliation.
- 1 Arkansas Foundation for Medical Care Quality, and University of Arkansas for Medical Sciences, 4301 West Markham, Little Rock, AR 72205, USA. [email protected]
- PMID: 20077965
- DOI: 10.3928/19404921-20080701-07
A literature review was undertaken to explore both published and unpublished quality improvement studies, projects, and initiatives that strove to develop more efficient systems to support an infrastructure for nursing home quality of care. The review included a search of all available, full-text published literature from 1997 to 2007 available from PubMed, CINAHL, and MEDLINE. The methods used by the researchers were varied, and this article identified several primary findings: the use of a specific, measurable mission or goal statement; the use of multidepartmental and multidisciplinary involvement; the need for further education and resource materials; the use of a reward/incentive program; the need for internal and external stakeholders to be identified along with a project champion; and the process of feedback and outcome measurement. This article summarizes the findings from the review and offers key recommendations that are supported for improving quality of care and sustaining quality gains.
Copyright 2009, SLACK Incorporated.
Publication types
- Research Support, Non-U.S. Gov't
- Benchmarking / organization & administration*
- Nursing Administration Research
- Nursing Homes / organization & administration*
- Organizational Objectives
- Outcome and Process Assessment, Health Care
- Patient Care Team
- Quality of Health Care / organization & administration*
- Total Quality Management / organization & administration*
- United States
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Emerg Med

Clinical care review systems in healthcare: a systematic review
Laura e. walker.
1 Department of Emergency Medicine and Health Sciences Research, Mayo Clinic, 200 First St. SW, Rochester, MN 55905 USA
David M. Nestler
Torrey a. laack, casey m. clements, patricia j. erwin.
2 Mayo Clinic Libraries and Health Sciences Research, Mayo Clinic, Rochester, MN USA
Lori Scanlan-Hanson
M. fernanda bellolio, associated data.
Clinical care review is the process of retrospectively examining potential errors or gaps in medical care, aiming for future practice improvement. The objective of our systematic review is to identify the current state of care review reported in peer-reviewed publications and to identify domains that contribute to successful systems of care review.
A librarian designed and conducted a comprehensive literature search of eight electronic databases. We evaluated publications from January 1, 2000, through May 31, 2016, and identified common domains for care review. Sixteen domains were identified for further abstraction.
We found that there were few publications that described a comprehensive care review system and more focus on individual pathways within the overall systems. There is inconsistent inclusion of the identified domains of care review.
While guidelines for some aspects of care review exist and have gained traction, there is no comprehensive standardized process for care review with widespread implementation.
Electronic supplementary material
The online version of this article (10.1186/s12245-018-0166-y) contains supplementary material, which is available to authorized users.
Clinical care review is the process of retrospectively examining potential errors or gaps in medical care, with a goal of future practice improvement. This goes by many different names, sometimes with different audiences or case types, including peer review, adverse event review, sentinel event review, and root cause analysis. The concept of care review is widely accepted and encouraged among safety and quality healthcare leaders. However, a paucity of literature exists discussing and describing the current state of clinical care review.
The challenges and risks of contemporary medical care are well described. Medical error and its resulting outcomes have been defined and measured in many different ways, leading to varying quantifications of the effects [ 1 ]. The Institute of Medicine’s (IOM) 1999 report entitled “To Err is Human” [ 2 ] estimated that as many as 44,000 to 98,000 deaths annually in the USA occur as a result of medical error. Publication of “To Err is Human” was a landmark event in the recognition of the role of adverse events in medical care in the USA. This represents a shift in the focus on adverse events to look toward systems issues as a cause or error and a call to identify and act to prevent medical error. The National Quality Foundation estimates that, in 2010, medical errors affected 15.5% of Medicare beneficiaries, with nearly half of these errors considered preventable [ 3 ]. More recently, Makary and Daniel estimated that as many as 250,000 deaths per year in the USA are due to medical error, making it the third leading cause of death by their estimation [ 1 ]. Review of adverse events allows for investigation into, and classification of the causes of, the event and presents an opportunity to modify systems and behaviors to prevent future similar errors. As a part of the strategic approach for increasing safety, the IOM’s “To Err is Human” recommended “Identifying and learning from errors by ... encouraging health care organizations and practitioners to develop and participate in voluntary reporting systems.” They went on to say “Such systems can focus on a much broader set of errors, mainly those that do no or minimal harm, and help detect system weaknesses that can be fixed before the occurrence of serious harm, thereby providing rich information to health care organizations in support of their quality improvement efforts” [ 1 ].
Given the long standing call for clinical care review, with limited literature to inform care review systems, we conducted a qualitative systematic review to identify characteristics discussed in existing models for care review. The objectives are to (1) describe the current state of care review and (2) identify elements from published care review systems that contribute to their success. This systematic review will allow for a more complete evaluation of the current state of clinical care review and will identify areas for future scholarly activity.
This is a qualitative systematic review of studies describing and evaluating care review systems. This study was exempt from our IRB review. This report adheres to the recommendations made in the preferred reporting items for systematic reviews (PRISMA) statement [ 4 ]. A protocol was written before the beginning of the investigation.
We included original research studies with any methodological design including cohort studies, case controls, and randomized trials, as well as commentaries, narrative reviews, letters to the editor, and abstracts in peer-reviewed journals that reported models for care review. Search results were limited to publications after January 1, 2000, to focus on publications since the release of “To Err is Human” [ 1 ]—a turning point in the way adverse events are analyzed and regarded. In choosing relevant publications, some articles described their process as the main purpose of the article, while others incidentally described a care review process, while instead focusing on a specific intervention or aspect of their mechanism for review. Either was acceptable, as they both shed light on a review system for analysis.
All types of patients and hospital settings were included, as well as recommendations from professional organizations and companies. This study’s investigators are physicians with involvement in quality improvement, adverse event identification and management, patient safety, and leadership of committees for clinical care review.
A senior expert librarian (P.E.) designed and conducted a comprehensive search of eight electronic databases, including Ovid MEDLINE, Ovid EMBASE, EBSCO CINAHL, Ovid CENTRAL, Ovid Cochrane Database of Systematic Reviews, Web of Science, and Scopus. Our search was done on June 10, 2016, and includes publications from January 1, 2000, through May 31, 2016. We included published conference abstracts in our search. There was no language restriction to the search strategy. Bibliography and reference lists of the articles obtained through database search were reviewed to identify additional publications for inclusion. The search strategy can be found in the Additional file 1 .
Qualitative assessment and data abstraction process
Two investigators (L.W. and D.N.) identified common domains in the initial literature review to determine which data to abstract, and included additional variables determined to be clinically important based on their experience in the clinical care review process and practice improvement. Domains included were description of systems improvement, educational output and feedback, description of a standardized process and referral mechanism, consideration of the case outcome, deliverables of the review system including non-punitive process and recognition of excellence, multidisciplinary involvement, dedicated process leadership, reviewer training, case blinding/anonymity, and implementation of improvement recommendations by the investigating group. These are further described in Table 1 .
Descriptions of the 16 domains of care review
In phase I of the review, one investigator (L.W.) independently screened all titles yielded by the initial search strategy for possible inclusion. After identifying appropriateness for possible inclusion, phase II consisted of two reviewers (L.W. and D.N.) independently evaluating the abstracts of publications identified in phase I. The publications from phase II were then retrieved in full text and assessed for inclusion of domain abstraction in phase III by two independent reviewers. The agreed-upon articles were assessed by independent reviewers in duplicate, to abstract the identified domains of care review in phase III.
In phase II, disagreement between reviewers was reconciled by discussion and consensus. The investigators were not blinded to the authors, journals, or results of studies. In phase III, disagreements on the data abstraction were resolved by a third independent reviewer who assessed the article and determined if the theme was included in the care review process. Descriptions of the 16 domains were supplied to all reviewers prior to data abstraction for reference.
Critical appraisal is the process of systematically examining research evidence to assess its validity, results, and relevance before using it to inform a decision. Instruments developed to support quality appraisal usually share some basic criteria for the assessment of qualitative research. These include the need for research to have been conducted ethically, the consideration of relevance to inform practice or policy, the use of appropriate and rigorous methods, and the clarity, coherence of reporting, address of reliability, validity, and objectivity [ 5 ].
In considering the most appropriate instruments to use for critical appraisal, we considered using the Cochrane Collaboration Bias Appraisal Tool [ 6 ] and a modified Newcastle-Ottawa Scale tool [ 7 ]. The nature of our qualitative data abstraction precluded the use of these tools. While the studies we evaluated may have included randomized controlled trials and been at risk for bias, the results of the publications evaluated were not typically relevant to our goal of qualitative domain abstraction. Many publications we evaluated were narrative in nature—describing a process without presentation of data, either qualitative or quantitative. For those publications that did present data relevant to our domains, the effect of bias within the study was felt to be unlikely to impact our qualitative data collection because the abstracted domains—descriptions of processes—were not affected by the results of the studies. We reviewed the items described in the Standards for Reporting Qualitative Research (SRQR) [ 8 ] and the Enhancing Transparency in Reporting the Synthesis of Qualitative Research (ENTREQ) [ 9 ] statement. The SRQR and ENTREQ aim to improve the transparency of all aspects of qualitative research by providing clear standards for reporting qualitative research. When assessing the risk of bias, we decided not to exclude articles based on their quality assessment. All potentially valuable insights were included. From each study, we extracted the domains relevant to care review processes. We tabulated the results and created graphics based on frequencies. No quantitative data was appropriate for abstraction, so we did not perform a meta-analysis.
The initial library search strategy identified 1318 titles for review. In phase I, 440 abstracts were reviewed, 76 of which were selected for full-text review in phase II. Fifteen articles from outside sources and bibliography review were also identified and reviewed. In total, 91 full-text articles were assessed, and after reconciliation between two independent reviewers, 47 articles were initially found to be appropriate for inclusion in our analysis of the domains of care review. One article was removed in the abstraction process, as both reviewers independently determined that it did not meet inclusion criteria [ 10 ] leading to 46 unique articles reviewed.
Domains were abstracted by two independent reviewers for each of the 46 articles in phase III. Articles that described a care review process from the same institution were consolidated to reflect the most complete view of that process possible, as aspects may have been reported differently in multiple articles/abstracts. Figure 1 shows the study selection process. Ultimately, we evaluated the care review systems from 35 unique institutions.

Study selection process
Study characteristics
Among the 46 studies, 35 represented unique institutions and 11 were same authors/institutions describing different aspects of the process or domains. The types of articles identified included 14 descriptive [ 11 – 24 ], three editorials [ 25 – 27 ] 15 prospective [ 28 – 42 ], seven quality improvement projects [ 12 , 43 – 48 ], and ten retrospective [ 11 , 30 , 49 – 56 ]. The 16 domains of successful care review that were identified for abstraction are presented and defined in Table 1 .
The percentage of frequency of each component is shown in Fig. 2 . The most commonly identified component of a care review process was utilizing an analysis of systems issues contributing to the case (32 institutions, 91.4%), followed by utilizing a standardized process for case review (30 institutions, 85.7%) and use of a structured case classification system (28 institutions, 80.0%). The least common components identified were recognition of excellence and use of case blinding/anonymity in reviews (5 institutions, 14.3%). Some articles were consistent with more than one article type and were classified as both.

Frequency of domain identification
Table 2 shows the distribution of all components in the full-text articles reviewed, with consolidation of same-institutions. No article/institution identified all 16 items evaluated by reviewers. Two institutions identified 14 of 16 items: Lehigh Valley and Johns Hopkins.
Distribution of care review domains
Our systematic review shows that, in the first two decades since the IOM report calling for improved safety systems, there have been few articles outlining a comprehensive clinical care review process. Additionally, most articles discuss their care review systems in the context of describing an aspect of their process, or corresponding improvement initiative.
Systems analysis—defined as the assessment of the effects of external forces such as policies, workflows, and software such as the electronic medical record on the critical event—was the most commonly identified care review process characteristic. Many identified articles describe the importance of evaluating how a person works within a system, rather than in isolation, to identify improvement opportunities. Assuming individuals are properly motivated with benign intent, looking at the system surrounding, the care avoids an antagonistic approach and supports the IOM’s underlying reasons for calling for care review processes—to prevent future errors.
Similarly, standardized processes and structured case classification were frequently discussed in the literature. To meet the IOM’s recommendations for creating care review “systems,” having a standardized process that uses structured classification is likely necessary. Without standardization, reviews would likely be sporadic, inefficient, and challenging to implement and subsequently inform future practice. Without structured classification, one could assume that conclusions would also be difficult to interpret.
Although some of these characteristics were common among reported care review systems, others are only rarely reported. Recognition of excellence and blinding of cases were reported in just five (14%) of the reports. Institutions that recognize excellence while performing care reviews were supportive of the practice, and one can understand why this would support the culture needed to have an effective care review system, and perhaps designers of future care review systems may wish to consider implementing this component. Similarly, anonymous review, or blinding, is intended to reduce bias and may allow a more objective review of each case. However, its infrequent mention may be indicative of unpublished prior experiences that may have supported avoiding this practice. From our experience, these are controversial topics, and future work is needed to understand the effects of specific characteristics on the overall care review process.
One additional characteristic that review processes must be supported by a functioning organizational system should receive particular attention. Although this was specifically identified by only 19 organizations, the downstream benefit to reviewing an episode of care and making recommendations for change in a non-functional system is likely lost. Key stakeholders in the process (physicians, nurse practitioners, physician assistants, nursing staff, support staff, etc.) are seemingly necessary for the care review process, and the administrative and leadership structure must be supportive of recommendations for change after care review is completed. This combination is strongly conducive to a process that engenders trust from the care team, which in turn bolsters the system as cases are referred for review, and staff engage in further problem solving.
Limitations
The articles evaluated come from a variety of settings—from consulting firms to in situ care review systems. Some authors strove to describe a comprehensive local practice, while others focused primarily on a particular component of a larger system. This heterogeneity limits the generalizability as the variability from one system to another may indicate institution- or system-specific adaptations to facilitate the process. A solution for one setting may not represent a good solution for another. We included articles from institutions and consulting firms describing or self-reporting care review systems, and it is not possible to know the true effectiveness of the processes described when removed from clinical context. It may be that there is an over-emphasis on some areas of care review believed to be ideal that are not practiced as described, and also possible that not all aspects of a process are represented. Particularly in the articles that discuss the care review process as the context for a specific project, it is possible that not all the details on the over-arching system of care review in place are described resulting in abstraction of domains in what is an incomplete description.
The domains we used during abstraction were determined by screening the included articles and supplemented by expert opinion. It is possible that there are additional variables that are more important, but less common, and were not included in our analysis. It is possible that a care review process we reviewed may include some of the 16 characteristics but did not specifically mention them in the articles reviewed. Additionally, the qualitative nature of the abstraction and interpretation of each item definitions are complex and may lead to less reliable results.
In an effort to reduce the effects of bias and definition complexity, all articles were reviewed in duplicate—both for inclusion in the study as well as abstraction of data. Disagreements were resolved by discussion and consensus for article inclusion and adjudicated by a third reviewer for the domain abstraction.
Despite increased discussion among institutions such as IOM and the National Patient Safety Foundation, in the last 16 years, there have been relatively few publications describing clinical care review processes and no clear evidence of a cultural shift to embrace clinical care review in an organized fashion. We have identified 16 domains of focus in a care review process and found that the approach to care review is highly variable as represented in the literature.
Future research
The effects of different aspects of care review processes have not been well studied. This presents an opportunity to evaluate processes that are present in many hospitals and health systems and identify truly effective, rather than simply common, practices, as identified within.
Additional file
Search strategy. (DOCX 14 kb)
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Authors’ contributions
All the authors have contributed substantially to this manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Laura E. Walker, Email: [email protected] .
David M. Nestler, Email: [email protected] .
Torrey A. Laack, Email: [email protected] .
Casey M. Clements, Email: [email protected] .
Patricia J. Erwin, Email: [email protected] .
Lori Scanlan-Hanson, Email: [email protected] .
M. Fernanda Bellolio, Phone: 507-775-5607, Email: [email protected] .
- Open access
- Published: 03 September 2021
A literature-based study of patient-centered care and communication in nurse-patient interactions: barriers, facilitators, and the way forward
- Abukari Kwame 1 &
- Pammla M. Petrucka 2
BMC Nursing volume 20 , Article number: 158 ( 2021 ) Cite this article
317k Accesses
143 Citations
96 Altmetric
Metrics details
Providing healthcare services that respect and meet patients’ and caregivers’ needs are essential in promoting positive care outcomes and perceptions of quality of care, thereby fulfilling a significant aspect of patient-centered care requirement. Effective communication between patients and healthcare providers is crucial for the provision of patient care and recovery. Hence, patient-centered communication is fundamental to ensuring optimal health outcomes, reflecting long-held nursing values that care must be individualized and responsive to patient health concerns, beliefs, and contextual variables. Achieving patient-centered care and communication in nurse-patient clinical interactions is complex as there are always institutional, communication, environmental, and personal/behavioural related barriers. To promote patient-centered care, healthcare professionals must identify these barriers and facitators of both patient-centered care and communication, given their interconnections in clinical interactions. A person-centered care and communication continuum (PC4 Model) is thus proposed to orient healthcare professionals to care practices, discourse contexts, and communication contents and forms that can enhance or impede the acheivement of patient-centered care in clinical practice.
Peer Review reports
Providing healthcare services that respect and meet patients’ and their caregivers’ needs are essential in promoting positive care outcomes and perceptions of quality of care, thus constituting patient-centered care. Care is “a feeling of concern for, or an interest in, a person or object which necessitates looking after them/it” [ 1 ]. The Institute of Medicine (IOM) noted that to provide patient-centered care means respecting and responding to individual patient’s care needs, preferences, and values in all clinical decisions [ 2 ]. In nursing care, patient-centered care or person-centered care must acknowledge patients’ experiences, stories, and knowledge and provide care that focuses on and respects patients’ values, preferences, and needs by engaging the patient more in the care process [ 3 ]. Healthcare providers and professionals are thus required to fully engage patients and their families in the care process in meaningful ways. The IOM, in its 2003 report on Health Professions Education , recognized the values of patient-centered care and emphasized that providing patient-centered care is the first core competency that health professionals’ education must focus on [ 4 ]. This emphasis underscored the value of delivering healthcare services according to patients’ needs and preferences.
Research has shown that effective communication between patients and healthcare providers is essential for the provision of patient care and recovery [ 5 , 6 , 7 , 8 ]. Madula et al. [ 6 ], in a study on maternal care in Malawi, noted that patients reported being happy when the nurses and midwives communicated well and treated them with warmth, empathy, and respect. However, other patients said poor communication by nurses and midwives, including verbal abuse, disrespect, or denial from asking questions, affected their perceptions of the services offered [ 6 ]. Similarly, Joolaee et al. [ 9 ] explored patients’ experiences of caring relationships in an Iranian hospital where they found that good communication between nurses and patients was regarded as “more significant than physical care” among patients.
According to Boykins [ 10 ], effective communication is a two-way dialogue between patients and care providers. In that dialogue, both parties speak and are listened to without interrupting; they ask questions for clarity, express their opinions, exchange information, and grasp entirely and understand what the others mean. Also, Henly [ 11 ] argued that effective communication is imperative in clinical interactions. He observed that health and illness affect the quality of life, thereby making health communication critical and that the “intimate and sometimes overwhelming nature of health concerns can make communicating with nurses and other healthcare providers very challenging” [ 11 ]. Furthermore, Henly [ 11 ] added that patient-centered communication is fundamental to ensuring optimal health outcomes, reflecting long-held nursing values that care must be individualized and responsive to patient health concerns. Given the prevalence of face-to-face and device-mediated communications and interactions in healthcare settings, we must explore and clarify who, what, where, when, why, and how interactions with individuals, families, and communities are receiving care and health services [ 11 ].
The value of effective communication in nurse-patient clinical interactions cannot be overemphasized, as “research has shown that communication processes are essential to more accurate patient reporting and disclosure” [ 12 ]. Respectful communication between nurses and patients can reduce uncertainty, enhance greater patient engagement in decision making, improve patient adherence to medication and treatment plans, increase social support, safety, and patient satisfaction in care [ 12 , 13 ]. Thus, effective nurse-patient clinical communication is essential to enhancing patient-centered care and positive care outcomes.
Patient-centered communication, also known as person-centered communication or client-centered communication, is defined as a process that invites and encourages patients and their families to actively participate and negotiate in decision-making about their care needs, as cited in [ 7 ]. Patient-centered communication is crucial in promoting patient-centered care and requires that patients and their caregivers engage in the care process. As McLean [ 14 ] observed, patient-centered care can be enhanced through patient-centered communication by valuing patients’ dignity and rights. Through open communication and collaboration, where information and care plans are shared among care providers, patients, and their families, care provision becomes patient-centered [ 14 ].
Given the interconnected nature of patient-centered care and communication, we must identify the barriers and enablers of patient-centered care and communication and proposed efficient ways to enhance that because patient-centered communication is essential in achieving patient-centered care. Our aim in this paper is to identify the barriers and facilitators of patient-centered care and communication and propose and present a patient-centered care and communication continuum (PC4) Model to explain how patient-centered care can be enhanced in nurse-patient clinical interactions. As Grant and Booth argued, critical reviews are often used to present, analyse, and synthesized research evidence from diverse sources, the outcome of which is a hypothesis or a model as an interpretation of existing data to enhance evidence-based practice [ 15 ]. Thus, this critical literature review study explores the questions: what are the barriers and facilitators of patient-centered care and how can patient-centered care be enhanced through effective clinical communication?
An earlier version of this study was submitted as part of author AK’s doctoral comprehensive exams in February 2021. An interdisciplinary doctoral committee recommended many of the included literature and the questions explored in this study based on the current discourse of patient-centered care advocated for in many healthcare facilities and in recognition of the universal healthcare access objective of the health sustainable development goal. Additional searches for literature were conducted between September and November 2020 using keywords such as barriers and facilitators of nurse-patient interaction, patient-centered care, patient-centered communication , and nurse-patient communication . Databases searched included CINAHL, PubMed, Medline, and Google Scholar. Included studies in this critical review were empirical research on nurse-patient interactions in different care settings published in English and open access. All relevant articles were read, and their main findings relevant to our review questions were identified and organized into themes and subthemes discussed in this paper. Other published studies were read, and together with those that addressed the review question, a model was developed regarding how to enhance patient-centered care through effective communication.
Barriers to Patient-Centered Care and Communication
Nurses constitute a significant workforce of care providers whose practices can severely impact care outcomes (both positive and negative). Nurses spend much time with patients and their caregivers. As a result, positive nurse-patient and caregiver relationships are therapeutic and constitute a core component of care [ 9 , 13 ]. In many instances, nurses serve as translators or patients’ advocates, in addition to performing their primary care duties. Although good nurse-patient relationships positively impact nurse-patient communication and interaction, studies have shown that several factors impede these relationships with significant consequences on care outcomes and quality [ 6 , 16 , 17 ]. Thus, these barriers limit nurses’ and other care providers’ efforts to provide healthcare that meets patients’ and caregivers’ needs. We categorize the barriers to patient-centered care and communication into four kinds: institutional and healthcare system-related, communication-related, environment-related, and personal and behaviour-related barriers. Although these barriers are discussed in separate subheadings, they are interlinked in complex ways during clinical practice.
Institutional and Healthcare System Related Barriers
Many barriers to providing patient-centered care and communication during nurse-patient interactions emanate from healthcare institutional practices or the healthcare system itself. Some of these factors are implicated in healthcare policy or through management styles and strategies.
Shortage of nursing staff, high workload, burnout, and limited-time constituted one complex institutional and healthcare system-level barrier to effective care delivery [ 18 , 19 ]. For instance, Loghmani et al. [ 20 ] found that staffing shortages prevented nurses from having adequate time with patients and their caregivers in an Iranian intensive care unit. Limitations in nursing staff, coupled with a high workload, led to fewer interactions between nurses, patients, and caregivers. Similarly, Anoosheh et al. [ 16 ] found that heavy nursing workload was ranked highest as a limiting factor to therapeutic communication in nurse-patient interactions in Iran.
In a study on communication barriers in two hospitals affiliated with Alborz University of Medical Sciences, Norouzinia et al. [ 21 ] found that shortage of nurses, work overload, and insufficient time to interact with patients were significant barriers to effective nurse-patient interactions. Similar factors are identified as barriers to nurse-patient communication and interactions in other studies [ 13 , 16 , 18 ]. For instance, Amoah et al. [ 16 ] reported that nursing staff shortage and high workload were barriers to patient-centered care and therapeutic communication among Ghanaian nurses and patients. Amoah and colleagues reported a patient’s statement that:
[B]ecause there are few nurses at the ward, sometimes you would want a nurse to attend to you, but he or she might be working on another patient, so in such case, the nurse cannot divide him or herself into two to attend to you both [ 16 ].
Nurses and patients and their caregivers have noted that limited time affects nurse-patient interactions, communication, and care quality. Besides, Yoo et al. [ 22 ] reported that limited visiting hours affected communications between caregivers and nurses in a tertiary hospital in Seoul, Korea. Since the caregivers had limited time to spend with patients, they had little knowledge about the intensive care unit and distrusted the nurses.
Although nursing staff shortage is a significant barrier to patient-centered care and communication that healthcare institutions and managers must know, some healthcare scholars have critique nurses’ complaints of time limitation. For instance, McCabe [ 7 ] argued that the quality of nurse-patient interactions is what matters and not the quantity of time spent with patients and their caregivers. McCabe maintained that “spending long periods with patients does not always result in positive nurse-patient relationships” [ 7 ]. He argued that implementing patient-centered care does not require additional time; hence, nurses’ perceptions of being too busy cannot excuse poor therapeutic communication during clinical interactions. Instead, nurses are encouraged to develop self-awareness, self-reflection, and a commitment to ensuring that patients receive the needed care.
Another institution-related barrier to patient-centered care and communication is the healthcare system’s emphasis on task-centered care. Care providers are more focused on completing care procedures than satisfying patients’ and caregivers’ needs and preferences. This barrier to patient-centered care and communication is acknowledged in several studies [ 7 , 14 , 20 , 22 , 23 ]. For example, McLean [ 14 ] studied dementia care in nursing homes in the United States. She found that patient-centered care and communication in one nursing home (Snow I) were severely affected when nurses, physicians, and care managers focused on completing tasks or observing care and institutional routines to the detriment of satisfying patients’ care needs. However, in the other care home (Snow II), patient-centered care was enhanced as nurses, physicians, and the care home managers focused on addressing patients’ needs and values rather than completing care routines and tasks.
Similarly, Yoo and colleagues [ 22 ] observed that nurse-patient communication was affected when the ICU nurses placed urgency on completing tasks linked directly to patients’ health (e.g., stabilizing vital signs) than communicating to addressed patients’ specific needs. This evidence shows that when nurses are more task-focused, patients and caregivers are treated as bodies and objects, on which medical and care practices must be performed to restore health. Research has shown that when nurses focus on task-oriented care, it becomes hard to provide holistic care to patients or teach and communicate with patients even when nurses are less busy [ 20 ].
Nursing managers and their management styles can affect patient-centered care and communication. Studies have revealed that the management styles that nursing managers implement can either facilitate or impede patient-centered care [ 14 , 22 ]. When nurse managers orient their nursing staff towards task-centered care practices, it affects nurse-patient interaction and communication. Moreover, when nurse managers fail to address their staff’s mental health needs and personal challenges, it influences how nurses attend to patients’ care needs. For example, nurses have indicated that nurse-patient communication is affected when nurse managers are unsupportive or unresponsive to their needs [ 20 ].
In a study exploring nursing and midwifery managers’ perspectives on obstacles to compassion giving and therapeutic care across 17 countries, Papadopoulos et al. [ 24 ] discovered that nurses and midwifery managers’ characteristics and experiences could facilitate or impede compassion and therapeutic interactions in nursing care. Negative personal attitudes, including selfishness, arrogance, self-centeredness, rudeness, lack of leadership skills, the desire for power, and feelings of superiority among nurses and midwifery managers, were obstacles to compassion building. The study further showed that managers who emphasize rules, tasks, and results do not prioritize relationship-building and see their staff as workers rather than team members [ 24 ]. Therefore, nurse managers and care administrators must monitor nurse-patient interaction and communication to address nurses’ concerns and support them, especially in resource-constrained and high patient turnover contexts [ 25 , 26 ].
Communication-Related Barriers
Effective communication is essential to providing patient-centered care. Studies have shown that poor communication between care providers and patients and their caregivers affects care outcomes and perceptions of care quality [ 7 , 16 , 27 , 28 ]. A consistent communication-related barrier in nurse-patient interaction is miscommunication, which often leads to misunderstandings between nurses, patients, and their families [ 20 ]. Other communication-related barriers include language differences between patients and healthcare providers [ 6 , 16 , 27 ], poor communication skills, and patients’ inability to communicate due to their health state, especially in ICU, dementia, or end-of-life care contexts [ 13 , 22 ]. For instance, in their maternity care study, Madula et al. [ 6 ] noted that language barriers significantly affected effective communication between nurses/midwives and expectant mothers. A patient in their study indicated that although many nurses were polite and communicated well, some nurses had challenges communicating with patients in the Chitumbuka language, which affected those nurses’ ability to interact effectively with patients [ 6 ].
Furthermore, Norouzinia et al. [ 21 ] asserted that effective communication could not be established when nurses and patients have a language difference. Moreover, the meanings of certain non-verbal communication acts (e.g., head nodding, eye gaze, touch) can invoke different interpretations across different cultures, which could impede the interactions between patients and nurses. Even in healthcare contexts where nurses and patients speak the same language, “differences in vocabulary, rate of speaking, age, background, familiarity with medical technology, education, physical capability, and experience can create a huge cultural and communication chasm” between nurses and patients [ 12 ]. In ICU and other similar care settings, nurses find it difficult to effectively communicate with patients because the mechanical ventilators made it hard for patients to talk [ 22 ].
To overcome the communication-related barriers, healthcare institutions must make it a responsibility to engage translators and interpreters to facilitate nurse-patient interactions where a language barrier exists. Moreover, nurses working in ICU and other similar settings should learn and employ alternative forms of communication to interact with patients.
Environment-Related Barriers
The environment of the care setting can impact nurse-patient communication and the resulting care. Thus, “good health care experiences start with a welcoming environment” [ 29 ]. Mastors believed that even though good medicine and the hands working to provide care and healing to the sick and wounded are essential, we must not “forget the small things: a warm smile, an ice chip, a warm blanket, a cool washcloth. A pillow flipped to the other side and a boost in bed” [ 29 ]. The environment-related barriers are obstacles within the care setting that inhibit nurse-patient interaction and communication and may include a noisy surrounding, unkept wards, and beds, difficulties in locating places, and navigating care services. Noisy surroundings, lack of privacy, improper ventilation, heating, cooling, and lighting in specific healthcare units can affect nurse-patient communication. These can prevent patients from genuinely expressing their healthcare needs to nurses, which can subsequently affect patient disclosure or make nursing diagnoses less accurate [ 13 , 18 , 21 ]. For instance, Amoah et al. [ 16 ] revealed that an unconducive care environment, including noisy surroundings and poor ward conditions, affected patients’ psychological states, impeding nurse-patient relationships and communication. Moreover, when care services are not well-coordinated, new patients and their caregivers find it hard to navigate the care system (e.g., locating offices for medical tests and consultations), which can constrain patient-centered care and communication.
Reducing the environment-related barriers will require making the care setting tidy/clean, less noisy, and coordinating care services in ways that make it easy for patients and caregivers to access. Coordinating and integrating care services, making care services accessible, and promoting physical comfort are crucial in promoting patient-centered care, according to Picker’s Eight Principles of Patient-Centered Care [ 30 ].
Personal and Behaviour Related Barriers
The kind of nurse-patient relationships established between nurses and patients and their caregivers will affect how they communicate. Since nurses and patients may have different demographic characteristics, cultural and linguistic backgrounds, beliefs, and worldviews about health and illnesses, nurses’, patients’, and caregivers’ attitudes can affect nurse-patient communication and care outcomes. For instance, differences in nurses’ and patients’ cultural backgrounds and belief systems have been identified as barriers to therapeutic communication and care [ 12 , 13 , 21 ]. Research shows that patients’ beliefs and cultural backgrounds affected their communication with nurses in Ghana [ 16 ]. These scholars found that some patients refused a blood transfusion, and Muslim patients refused female nurses to attend to them because of their religious beliefs [ 16 ]. Further, when nurses, patients, or their caregivers have misconceptions about one another due to past experiences, dissatisfaction about the care provided, or patients’ relatives and caregivers unduly interfere in the care process, nurse-patient communication and patient-centered care were affected [ 16 , 21 ].
Similarly, nurse-patient communication was affected when patients or caregivers failed to observe nurses’ recommendations or abuse nurses due to misunderstanding [ 20 ], while patients’ bad attitudes or disrespectful behaviours towards nurses can inhibit nurses’ ability to provide person-centered care [ 31 ]. The above-reviewed studies provided evidence on how patients’ and caregivers’ behaviours can affect nurses’ ability to communicate and deliver patient-centered care.
On the other hand, nurses’ behaviours can also profoundly affect communication and care outcomes in the nurse-patient dyad. When nurses disrespect, verbally abuse (e.g., shouting at or scolding), and discriminate against patients based on their social status, it affects nurse-patient communication, care outcomes, and patient disclosure [ 6 , 32 ]. For instance, Al-Kalaldeh et al. [ 18 ] believe that nurse-patient communication is challenged when nurses become reluctant to hear patients’ feelings and expressions of anxiety. When nurses ignore patients’ rights to share ideas and participate in their care planning, such denials may induce stress, discomfort, lack of trust in nurses, thereby leading to less satisfaction of care [ 18 ].
Furthermore, when nurses fail to listen to patients’ and caregivers’ concerns, coerce patients to obey their rules and instructions [ 16 , 17 , 20 ], or fail to provide patients with the needed information, nurse-patient communication and patient-centered care practices suffer. To illustrate, in Ddumba-Nyanzia et al.‘s study on communication between HIV care providers and patients, a patient remarked that: “I realized no matter how much I talked to the counselor, she was not listening. She was only hearing her point of view and nothing else, [and] I was very upset” [ 17 ]. This quote indicates how care provider attitudes can constrain care outcomes. Due to high workload, limited time, poor remunerations, and shortage of personnel, some nurses can develop feelings of despair, emotional detachment, and apathy towards their job, which can lead to low self-esteem or poor self-image, with negative consequences on nurse-patient interactions [ 13 , 18 ].
Given the significance of effective communication on care, overcoming the above personal and behaviour related barriers to patient-centered care and communication is crucial. Nurses, patients, and caregivers need to reflect on the consequences of their behaviours on the care process. Thus, overcoming these barriers begins with embracing the facilitators of patient-centered care and communication, which we turn to in the next section.
Facilitators of patient-centered care and communication
Patient-centered care and communication can be facilitated in several ways, including building solid nurse-patient relationships.
First, an essential facilitator of patient-centered care and communication is overcoming practical communication barriers in the nurse-patient dyad. Given the importance of communication in healthcare delivery, nurses, patients, caregivers, nursing managers, and healthcare administrators need to ensure that effective therapeutic communication is realized in the care process and becomes part of the care itself. Studies have shown that active listening among care providers is essential to addressing many barriers to patient-centered care and communication [ 7 , 13 ]. Although handling medical tasks promptly in the care process is crucial, the power of active listening is critical, meaningful, and therapeutic [ 22 ]. By listening to patients’ concerns, nurses can identify patients’ care needs and preferences and address their fears and frustrations.
Another facilitator of patient-centered care is by understanding patients and their unique needs [ 25 ], showing empathy and attending attitudes [ 7 , 13 ], expressing warmth and respect [ 22 ], and treating patients and caregivers with dignity and compassion as humans. For instance, McCabe [ 7 ] noted that attending, which obligates nurses to demonstrate that they are accessible and ready to listen to patients, is a patient-centered care process; a fundamental requirement for nurses to show genuineness and empathy, despite the high workload. Showing empathy, active listening, respect, and treating patients with dignity are core to nursing and care, and recognized in the Code of Ethics for Nurses [ 33 ], and further emphasized in the ongoing revision of the Code of Ethics for nurses [ 34 ].
Besides, engaging patients and caregivers in the care process through sharing information, inviting their opinion, and collaborating with them constitutes another facilitator of patient-centered care and communication. When patients and caregivers are engaged in the care process, misunderstandings and misconceptions are minimized. When information is shared, patients and caregivers learn more about their health conditions and the care needed. As McLean [ 14 ] argued, ensuring open communication between care providers and patients and their families is essential to enhancing patient-centered care. Conflicts ensue when patients or their families are denied information or involvement in the care process. As a result, the Harvard Medical School [ 30 ] identified patient engagement, information sharing, and nurse-patient collaboration during care as essential patient-centered care principles.
Finally, health policy must be oriented towards healthcare practices and management to facilitate patient-centered care and communication. These policies, at a minimum, can involve changes in management styles within healthcare institutions, where nurse managers and healthcare administrators reflect on nursing and care practices to ensure that the Code of Ethics of Nurses and patients’ rights are fully implemented. Resource constraints, staff shortages, and ethical dilemmas mainly affect care practices and decision-making. Nonetheless, if patients are placed at the center of care and treated with dignity and respect, most of the challenges and barriers of patient-centered care will diminish. Empowering practicing nurses, equipping them with interpersonal communication skills through regular in-service training, supporting them to overcome their emotional challenges, and setting boundaries during nurse-patient interactions will enhance patient-centered care practices.
In line with the above discussion, Camara et al. [ 25 ] identify three core dimensions that nurses, patients, and caregivers must observe to enhance patient-centered care: treating the patient as a person and seeing the care provider as a person and a confidant. Regarding the first dimension, care providers must welcome patients, listen to them, share information with them, seek their consent, and show them respect when providing care. The second dimension requires that the healthcare provider be seen and respected as a person, and negative perceptions about care providers must be demystified. According to Camara et al. [ 25 ], care providers must not overemphasize their identities as experts but rather establish good relationships with patients to understand patients’ personal needs and problems. Lastly, patients and caregivers must regard care providers as confidants who build and maintain patients’ trust and encourage patients’ participation in care conversations. With this dimension, patients and caregivers must know that nurses and other care providers have the patient at heart and work to meet their care needs and recovery process.
Camara et al.‘s [ 25 ] three dimensions are essential and position patients, their caregivers, and nurses as partners who must engage in dialogic communication to promote patient-centered care. As a result, effective communication, education, and increased health literacy among patients and caregivers will be crucial in that direction.
Enhancing Patient-Centered Care and Communication: A Proposed Model
Nursing care practices that promote patient-centered communication will directly enhance patient-centered care, as patients and their caregivers will actively engage in the care process. To enhance patient-centered communication, we propose person-centered care and communication continuum (PC4) as a guiding model to understand patient-centered communication, its pathways, and what communication and care practices healthcare professionals must implement to achieve person-centered care. In this PC4 Model, we emphasize the person instead of the patient because they are a person before becoming a patient. Moreover, the PC4 Model is supposed to apply to all persons associated with patient care; thus, respect for the dignity of their personhood is crucial.
Although much is written about patient-centered communication in the healthcare literature, there is a gap regarding its trajectory and what communication content enhances patient-centered communication. Also, little is known about how different clinical discourse spaces influence communication and its content during nurse-patient clinical interactions. Using evidence from Johnsson et al. [ 3 ], Murira et al. [ 23 ], and Liu et al. [ 35 ], among other studies, we outline the components of the PC4 Model and how different discourse spaces in the clinical setting and the content of communication impact patient-centered care and communication.
The proposed PC4 Model in this paper has three unbounded components based on the purpose of and how communication is performed among care providers, patients, and their caregivers. Figure 1 illustrates the PC4 Model, its features, and trajectory.
A Person-Centered Care and Communication Continuum (PC4 Model)
Task-Centered Communication
At the lowest end of the PC4 Model is task-centered communication. Here, the care provider’s role is to complete medical tasks as fast as possible with little or no communication with the patient and their caregivers. Patients and caregivers are treated as bodies or objects whose disease symptoms need to be studied, identified, recorded, treated, or cured. As Johnsson et al. [ 3 ] observed, communication content at this stage is mainly biomedically oriented, where nurses and other healthcare professionals focus on the precise medical information (e.g., history taking, medical examination, test results, medication, etc.) about the patient. With a task-centered orientation, nurses make journal entries about their patients’ disease state and ensure that treatment plans, diagnostic tests, and medical prescriptions are completed. Communication at this stage is often impersonal or rigid (see [ 23 ] for details). Care providers may address patients and their caregivers by using informal attributes (e.g., bed 12, the woman in the red shirt, card 8, etc.), thereby ignoring patients’ and caregivers’ personal and unique identities. Patients’ and caregivers’ nonverbal communication signs are mostly overlooked.
Motivations for task-centered communication can be attributed to time limitation, high workload, and staff shortage, thereby pushing nurses and other care providers to reach as many patients as possible. Moreover, the healthcare system’s orientation towards and preference for biomedically-focused care seems to favour task-centered communication [ 7 , 14 ].
Depending on the clinical discourse space under which patient-provider interactions occur, different forms of communication are employed. Clinical discourse spaces can be public (e.g., in the ward, patient bedside), private (e.g., consulting rooms, medical test labs, nurse staff station, etc.), or semi-private (e.g., along the corridor) [ 35 ]. In these clinical discourse spaces, nurse-patient communication can be uninformed (patients or caregivers are not informed about patients’ care conditions or why specific data and routines are performed). It can be non-private (others can hear what the nurse and patient are talking about) or authoritative (care providers demonstrate power and control and position themselves as experts) [ 23 ]. Finally, in task-centered communication, healthcare providers often use medical jargon or terminologies [ 3 ] since the goal of communication is not to engage the patient in the process. Usually, patients or their caregivers are not allowed to ask questions, or their questions get ignored or receive superficial, incomprehensible responses.
Process-Centered Communication
Process-centered communication is an intermediate stage on the continuum, which could slip back into the task-centered or leap forward into person-centered communication. Through process-centered communication, care providers make an effort to know patients and their caregivers as they perform care routines. Care providers ask patients or their caregivers questions to understand the care conditions but may not encourage patients or caregivers to express their thoughts about their care needs. Patients and caregivers are recognized as persons with uniques care needs but may not have the agency to influence the care process. Care providers may chit-chat with patients or their caregivers to pass the time as they record patients’ medical records or provide care. Unlike task-centered communication, there is informative and less authoritative communication between nurses and patients and their caregivers. The goal of process-centered communication could be a mixture of instrumental and relational, with less display of power and control by nurses.
Person-Centered Communication
This is the highest point of the PC4 Model, where patient-centered care is actualized. At this stage of the communication continuum, patients and caregivers are treated as unique persons with specific care needs and are seen as collaborators in the care process. As McLean [ 14 ] observed, caregiving becomes a transactional relationship between the care provider and receiver at the person-centered stage of the continuum. The care itself becomes intersubjective, a mutual relational practice, and an ongoing negotiation for care providers and receivers [ 14 ].
The content of communication at this stage of the continuum is both “personal” and “explanatory” [ 3 ]. Nurses and other healthcare providers create meaningful relationships with patients and their caregivers, understand patients’ concerns, needs, and problems, use open-ended questions to encourage patients or caregivers to express their thoughts and feelings about the care situation. Nurses and other healthcare professionals explain care routines, patients’ health conditions, and management plans in lay language to patients and caregivers through person-centered communication. Accomplishing this level includes employing alternative forms of communication to meet the needs of intensive care unit patients, deaf patients, and ventilated and intubated patients. For instance, it has been shown that “deaf people […] frequently do not have access to clear and efficient communication in the healthcare system, which deprives them of critical health information and qualified health care” [ 36 ]. Empathetic communication practices, including active listening, showing genuine interest in patients’ care, and respect and warmth, become a significant part of nursing care [ 3 , 7 , 14 , 22 ].
Different communication strategies are employed based on the care situation and context. Chit-chatting, as a form of personal communication [ 3 ], use of humor as a communication strategy [ 7 , 8 ], and even maintaining silence [ 28 ] are essential in enhancing person-centered care and communication. Both care providers and patients or their caregivers use relationship-building and -protecting humor (see [ 28 ] for details) to address difficult situations in the care process.
Implications of the PC4 Model for Nursing Practice
Given the values of effective communication in nurse-patient interactions and care outcomes, nurses and other healthcare providers must ensure that they develop therapeutic relationships with patients, their families, and caregivers to promote person-centered care and communication. Achieving that begins with knowing and reflecting on the barriers of therapeutic communication and ways to minimize them. The PC4 Model draws nurses and all healthcare providers’ attention to patient-centered care pathways and how effective communication is necessary. Healthcare professionals, including nurses, must be aware of how their communication orientation–––either oriented toward completing tasks, following care processes or toward addressing patients’ and their caregivers’ needs––can impact patient-centered care. Healthcare providers must observe the care context, patients’ unique situations, their non-verbal language and action, and whether they belong to historically marginalized groups or cultures.
Mastors [ 29 ] has offered healthcare providers some guidance to reflect on as they communicate and interact with patients and caregivers. Thus, (a) instead of asking patients, “What’s the matter?“ care providers must consider asking them, “What’s important to you?“ With this question, the patient is given a voice and empowered to contribute to their own care needs. Care providers should (b) check with patients in the waiting room to update patients whose waiting time has been longer than usual, based on the care context. They should also (c) try to remember their conversations with patients to build on them during subsequent interactions. This continuity can be enhanced by nurse managers reexamining how they deploy care providers to patients. The same nurse can be assigned to the same patients for the duration of the patient’s stay to help patients feel valued and visible [ 29 ].
Knowledge of cultural competence, sensitivity, humility, and interpersonal communication skills will help achieve and implement the PC4 Model. As Cuellar [ 37 ] argues, “[h]umility is about understanding and caring for all people [and] being empathetic.“ Cultural competence is a “dynamic process of acquiring the ability to provide effective, safe, and quality care to the patients through considering their different cultural aspects” [ 38 ]. The concept of cultural competence entails “cultural openness, awareness, desire, knowledge and sensitivity” during care [ 39 ]. It demands that care providers respect and tailor care to align with patients’ and caregivers’ values, needs, practices, and expectations, based on care and moral ethics and understanding [ 39 ]. Active listening and showing compassion as therapeutic relationship-building skills are essential, and continuous education and mentorship will be crucial to developing these skills among healthcare providers.
We invite qualitative and quantitative studies, especially on language use and communication strategies, to explore and evaluate the PC4 Model. Providing in-depth and experiential data on ways to increase its effectiveness as a tool to guide healthcare providers is highly desired. More knowledge can support healthcare providers in offering evidence-based patient-centered care in different healthcare settings and units.
Conclusions
Effective communication is an essential factor in nurse-patient interactions and a core component of nursing care. When communication in the nurse-patient dyad is patient-centered, it becomes therapeutic. It allows for trust and mutual respect in the care process, thereby promoting care practices that address patients’ and caregivers’ needs, concerns, and preferences. We have identified the barriers and facilitators of patient-centered care and communication and proposed a person-centered care and communication continuum (PC4 Model) to demonstrate how patient-centered communication intersects with patient-centered care.
Availability of data and materials
Not applicable.
Abbreviations
Intensive Care Unit
Institution of Medicine
Person-Centered Care and Communication Continuum
Etheredge HR. “Hey sister! Where’s my kidney?“ Exploring ethics and communication in organ transplantation in Gauteng, South Africa, Ph.D. dissertation, Johannesburg. University of the Witwatersrand; 2015.
Institute of Medicine. Crossing the quality chasm: A new health system for the 21st century. National Academy Press; 2001.
Johnsson A, Wagman P, Boman A, Pennbrant S. What are they talking about? Content of the communication exchanges between nurses, patients and relatives in a department of medicine for older people: An ethnographic study. J Clin Nurs. 2018 Apr;27(7–9):e1651-9. doi: https://doi.org/10.1111/jocn.14315 .
Long KA. The Institute of Medicine report on health professions education: A bridge to quality. Policy Polit Nurs Pract. 2003 Nov;4(4):259–62. doi: https://doi.org/10.1177/1527154403258304 .
Crawford T, Candlin S, Roger P. (2017). New perspectives on understanding cultural diversity in nurse-patient communication. Collegian, 2017 Feb 1;24(1):63 – 9. https://doi.org/10.1016/j.colegn.2015.09.001 .
Madula P, Kalembo WF, Yu H, Kaminga CA. Healthcare provider-patient communication: A qualitative study of women’s perceptions during childbirth. Reprod Health. 2018 Dec;15(135):1–10. https://doi.org/10.1186/s12978-018-0580-x .
McCabe C. Nurse-patient communication: An exploration of patients’ experiences. J Clin Nurs. 2004 Jan;13(1):41–9.
Schöpf AC, Martin GS, Keating MA. Humor as a communication strategy in provider-patient communication in a chronic care setting. Qual Health Res. 2017 Feb;27(3):374–90. doi: https://doi.org/10.1177/1049732315620773 .
Joolaee S, Joolaei A, Tschudin V, Bahrani N, Nikbakht NA. Caring relationship: the core component of patients’ rights practice as experienced by patients and their companions. J Med Ethics Hist Med. 2010;3(4):1–7.
Google Scholar
Boykins AD. Core communication competences in patient-centered care. The ABNF J. 2014 Apr 1;25(2):40 – 5.
Henly SJ. Health communication research for nursing science and practice. Nurs Res [Editorial] 2016:257–8. doi: https://doi.org/10.1097/NNR.0000000000000171 .
Ruben BD. Communication theory and health communication practice: The more things change, the more they stay the same. Health Commun. 2016 Jan 2;31(1):1–11. doi: https://doi.org/10.1080/10410236.2014.923086 .
Bello P. Effective communication in nursing practice: A literature review. BSc Nursing Thesis. Arcada; 2017. Available at https://core.ac.uk/download/pdf/84798372.pdf Accessed 20 Jan 2021.
McLean A. The person in dementia: A study of nursing home care in the US. Toronto, University of Toronto Press; 2007.
Grant MJ, Booth A. A typology of reviews: An analysis of 14 review types and associated methodologies. Health Info Libraries J. 2009;26:91–108. Doi: https://doi.org/10.1111/j.1471-1842.2009.00848.x .
Article Google Scholar
Amoah KMV, Anokye R, Boakye SD, Acheampong E, Budu-Ainooson A, Okyere E, Kumi-Boateng G, Yeboah C, Afriyie OJ. A qualitative assessment of perceived barriers to effective therapeutic communication among nurses and patients. BMC Nurs. 2019 Dec;18(4)1–8. https://doi.org/10.1186/s12912-019-0328-0 .
Ddumba-Nyanzia I, Kaawa-Mafigiria D, Johannessen H. Barriers to communication between HIV care providers (HCPs) and women living with HIV about childbearing: A qualitative study. Patient Educ Couns. 2016 May 1:99(5):754–9. https://doi.org/10.1016/j.pec.2015.11.023 .
Al-Kalaldeh M, Amro N, Qtait M. Barriers to effective nurse-patient communication in the emergency department. Emerg Nurse. 2021 Mar 2;29(2). doi: https://doi.org/10.7748/en.2020.e1969 .
Sethi D, Rani MK. Communication barrier in health care setting as perceived by nurses and patient. Int J Nurs Educ 2017 Oct. 2016;9(4):30. doi: https://doi.org/10.5958/j.2320-8651.2.1.001 .
Loghmani L, Borhani F, Abbaszadeh A. Factors affecting the nurse-patients’ family communication in intensive care unit of Kerman: A qualitative study. J Caring Sci. 2014 Mar;3(1):67–2. doi: https://doi.org/10.5681/jcs.2014.008 .
Norouzinia R, Aghabarari M, Shiri M, Karimi M, Samami E. Communication barriers perceived by nurses and patients. Glob J Health Sci. 2016 Jun;8(6):65–4. https://doi.org/10.5539/gjhs.v8n6p65 .
Yoo HJ, Lim OB, Shim JL. Critical care nurses’ communication experiences with patients and families in an intensive care unit: A qualitative study. PLoS One. 2020 Jul 9;15(7):e0235694. https://doi.org/10.1371/journal.pone.0235694 .
Murira N, Lützen K, Lindmark G, Christensson K. Communication patterns between healthcare providers and their clients at an antenatal clinic in Zimbabwe. Health Care Women Int. 2003 Feb 1;24(2):83 – 2. https://doi.org/10.1080/07399330390170060 .
Papadopoulos I, Lazzarino R, Koulouglioti C, Aagard M, Akman O, Alpers L-M, Apostolara P, Araneda Bernal J, Biglete-Pangilinan S, Eldar-Regev O, Gonzalez-Gil MT, Kouta C, Zorba A. Obstacles to compassion-giving among nursing and midwifery managers: An international study. Int Nurs Rev. 2020 Aug;11:1–13.
Camara BS, Belaid L, Manet H, Kolie D, Guilard E, Bigirimana T, Delamou A. What do we know about patient-provider interactions in sub-Saharan Africa? A scoping review. Pan Afr Med J. 2020;88(88):1–13. doi: https://doi.org/10.11604/pamj.2020.37.88.24009 .
Kwame A, Petrucka PM. Communication in nurse-patient interaction in healthcare settings in sub-Saharan Africa: A scoping review. Int J Afr Nurs Sci. 2020 Jan 1;12:100198. https://doi.org/10.1016/j.ijans.2020.100198 .
Anoosheh M, Zarkhah S, Faghihzadeh S, Vaismoradi M. Nurse-patient communication barriers in Iranian nursing. Int Nurs Rev. 2009 Jun;56(2):243–9.
Vuković M, Gvozdenović BS, Stamatović-Gajić B, Ilić M, Gajić T. Development and evaluation of the nurse quality of communication with patient questionnaire. Srp Arh Celok Lek. 2010;138(1–2):79–4. doi: https://doi.org/10.2298/SARH1002079V .
Article PubMed Google Scholar
Mastors P. (2018). What do patients want, need, and have the right to expect? Nurs Adm Q. 2018 Jul 1;42(3):192-8. doi: https://doi.org/10.1097/NAQ.0000000000000297 .
Harvard Medical School. The Eight Principles of Patient Centered Care; 2015 Nov 18. Available from OneView: https://www.oneviewhealthcare.com/the-eight-principles-of-patient-centered-care/ Accessed 28 Dec 2020.
White J, Phakoe M, Rispel LC. ‘Practice what you preach’: Nurses’ perspectives on the Code of Ethics and Service Pledge in five South African hospitals. Glob Health Action. 2015 Dec 1;8(1):26341. https://doi.org/10.3402/gha.v8.26341 .
Kruger L-M, Schoombee C. The other side of caring: abuse in a South African maternity ward. J Reprod Infant Psychol. 2010 Feb 1;28(1):84–101. doi: https://doi.org/10.1080/02646830903294979 .
International Council of Nurses. ICN Code of Ethics for Nurses; 2012. Available from www.icn.ch/images/stories/documents/about/icncode_english.pdf . Accessed 20 Dec 2020.
Stievano A, Tschudin V. The ICN code of ethics for nurses: A time for revision. Nurs Health Policy Perspect. 2019 Jun;66(2):154–6.
Liu W, Manias E, Gerdtz M. Medication communication during ward rounds on medical wards: Power relations and spatial practices. Health 2012 Mar. 2012;17(2):113–34. doi: https://doi.org/10.1177/1363459312447257 .
Hoglind TA. Healthcare language barriers affect deaf people, too. 2018 Oct 11. Retrieved from Boston University [BU] School of Public Health: Available from https://www.bu.edu/sph/news/articles/2018/healthcare-language-barriers-affect-deaf-people-too/ Accessed 15 Jan 2021.
Cuellar NG. Humility. A concept in cultural sensitivity. JTranscult Nurs [Editorial]. 2018 Apr 26; 29(4):317. https://doi.org/10.1177/1043659618772384 .
Sharifi N, Adib-Hajbaghery M, Najafi M. Cultural competence in nursing: A concept analysis. Int J Nurs Stud. 2019 Nov 1;99(103386):1–8. https://doi.org/10.1016/j.ijnurstu.2019.103386 .
Henderson S, Horne M, Hills R, Kendall E. Cultural competence in healthcare in the community: A concept analysis. Health Soc Care Community. 2018 Jul;26(4):590–603. doi: https://doi.org/10.1111/hsc.12556 .
Download references
Acknowledgments
We express our gratitude to the first author’s doctoral committee members for their valuable comments, suggestions, and critique of an earlier version of this paper. We are also grateful to the anonymous reviewers for the insightful comments and suggestions that have helped us improve the study’s quality.
Authors' information
Abukari Kwame is a Ph.D. candidate in Interdisciplinary Studies in the College of Graduate and Postdoctoral Studies, University of Saskatchewan, interested in patients' rights in nurse-patient clinical communications and interactions in the hospital setting. He holds two Master of Philosophy degrees in Indigenous Studies and English Linguistics. Abukari's research interests include language use in social interaction, health communication, First/Second language acquisition, African traditional medical knowledge, and Indigenous and qualitative research methodologies.
Pammla M. Petrucka is a professor in Nursing and has international research experience with many of her graduate students from Africa, Asia, and the Caribbean. Pammla has published extensively in the field of nursing. Her research interests are vast, including child and maternal health, Indigenous peoples' health, global health, and vulnerable populations, with extensive experiences in qualitative research and indigenous research methodologies. Pammla is co-editor of the BMC Nursing journal and a reviewer for many other academic journals.
The authors have not received any funding for the conduct, preparation, and publication of this paper.
Author information
Authors and affiliations.
College of Graduate and Postdoctoral Studies, University of Saskatchewan, Saskatoon, Canada
Abukari Kwame
College of Nursing, University of Saskatchewan, Regina Campus, Regina, Canada
Pammla M. Petrucka
You can also search for this author in PubMed Google Scholar
Contributions
Both authors conceived the topic. PMP recommended the literature, AK searched and added more sources, and drafted the paper. PMP reviewed the paper for intellectual content. Both AK and PMP read and approved the final version.
Corresponding author
Correspondence to Abukari Kwame .
Ethics declarations
Ethics approval and consent to participate.
Not Applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Kwame, A., Petrucka, P.M. A literature-based study of patient-centered care and communication in nurse-patient interactions: barriers, facilitators, and the way forward. BMC Nurs 20 , 158 (2021). https://doi.org/10.1186/s12912-021-00684-2
Download citation
Received : 05 May 2021
Accepted : 18 August 2021
Published : 03 September 2021
DOI : https://doi.org/10.1186/s12912-021-00684-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Patient-centered care
- Therapeutic communication
- Nurse-patient interactions
- Clinical discourse space
- Patient-centered care and communication continuum
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
- Open access
- Published: 06 December 2022
What improves access to primary healthcare services in rural communities? A systematic review
- Zemichael Gizaw 1 ,
- Tigist Astale 2 &
- Getnet Mitike Kassie 2
BMC Primary Care volume 23 , Article number: 313 ( 2022 ) Cite this article
13k Accesses
9 Citations
1 Altmetric
Metrics details
To compile key strategies from the international experiences to improve access to primary healthcare (PHC) services in rural communities. Different innovative approaches have been practiced in different parts of the world to improve access to essential healthcare services in rural communities. Systematically collecting and combining best experiences all over the world is important to suggest effective strategies to improve access to healthcare in developing countries. Accordingly, this systematic review of literature was undertaken to identify key approaches from international experiences to enhance access to PHC services in rural communities.
All published and unpublished qualitative and/or mixed method studies conducted to improvement access to PHC services were searched from MEDLINE, Scopus, Web of Science, WHO Global Health Library, and Google Scholar. Articles published other than English language, citations with no abstracts and/or full texts, and duplicate studies were excluded. We included all articles available in different electronic databases regardless of their publication years. We assessed the methodological quality of the included studies using mixed methods appraisal tool (MMAT) version 2018 to minimize the risk of bias. Data were extracted using JBI mixed methods data extraction form. Data were qualitatively analyzed using emergent thematic analysis approach to identify key concepts and coded them into related non-mutually exclusive themes.
Our analysis of 110 full-text articles resulted in ten key strategies to improve access to PHC services. Community health programs or community-directed interventions, school-based healthcare services, student-led healthcare services, outreach services or mobile clinics, family health program, empanelment, community health funding schemes, telemedicine, working with traditional healers, working with non-profit private sectors and non-governmental organizations including faith-based organizations are the key strategies identified from international experiences.
This review identified key strategies from international experiences to improve access to PHC services in rural communities. These strategies can play roles in achieving universal health coverage and reducing disparities in health outcomes among rural communities and enabling them to get healthcare when and where they want.
Peer Review reports
Introduction
Universal health coverage (UHC) is used to provide expanding services to eliminate access barriers. Universal health coverage is defined by the world health organization (WHO) as access to key promotional, preventive, curative and rehabilitative health services for all at an affordable rate and ensuring equity in access. The term universal has been described as the State's legal obligation to provide healthcare to all its citizens, with particular attention to ensuring that all poor and excluded groups are included [ 1 , 2 , 3 ].
Strengthening primary healthcare (PHC) is the most comprehensive, reliable and productive approach to improving people's physical and mental wellbeing and social well-being, and that PHC is a pillar of a sustainable health system for UHC and health-related sustainable development goals [ 4 , 5 ]. Despite tremendous progress over the last decades, there are still unaddressed health needs of people in all parts of the world [ 6 , 7 ]. Many people, particularly the poor and people living in rural areas and those who are in vulnerable circumstances, face challenges to remain healthy [ 8 ].
Geographical and financial inaccessibility, inadequate funding, inconsistent medication supply and equipment and personnel shortages have left the reach, availability and effect of PHC services in many countries disappointingly limited [ 9 , 10 ]. A recent Astana Declaration recognized those aspects of PHC need to be changed to adapt adequately to current and emerging threats to the healthcare system. This declaration discussed that implementation of a need-based, comprehensive, cost-effective, accessible, efficient and sustainable healthcare system is needed for disadvantaged and rural populations in more local and convenient settings to provide care when and where they want it [ 8 ].
Different innovative approaches have been practiced in different parts of the world to improve access to essential healthcare services in rural communities. Systematically collecting and combining best experiences all over the world is important to suggest effective strategies to improve access to healthcare in developing countries. Accordingly, this systematic review of literature was undertaken to identify key approaches from international experiences to enhance access to PHC services in rural communities. The findings of this systematic literature review can be used by healthcare professionals, researchers and policy makers to improve healthcare service delivery in rural communities.
Methodology
Research question.
What improves access to PHC services in rural communities? We used the PICO (population, issue/intervention, comparison/contrast, and outcome) construct to develop the search question [ 11 ]. The population is rural communities or remote communities in developing countries who have limited access to healthcare services. Moreover, we extended the population to developed countries to capture experiences of both developing and developed countries. The issue/intervention is implementation of different community-based health interventions to access to essential healthcare services. In this systematic review, we focused on PHC health services, mainly essential or basic healthcare services, community or public health services, and health promotion or health education. Primary healthcare is “a health care system that addressed social, economic, and political causes of poor health promotes health though health services at the primary care level enhances health of the community” [ 12 ]. Comparison/contrast is not appropriate for this review. The outcome is improved access to essential healthcare services.
Outcome measures
The outcome of this review is access to PHC services, such as preventive, promotive, curative, rehabilitative, and palliative health services which are affordable, convenient or acceptable, and available to all who need care.
Criteria for considering studies for this review
All published and unpublished qualitative and/or mixed method studies conducted to improve access to PHC services were included. Government and international or national organizations reports were also included. Different organizations whose primary mission is health or promotion of community health were selected. We included articles based on these eligibility criteria: context or scope of studies (access to PHC services), article type (primary studies), and publication language (English). Articles published other than English language, citations with no abstracts and/or full texts, reviews, and duplicate studies were excluded. We included all articles available in different electronic databases regardless of their publication years. We didn’t use time of publication for screening.
Information sources and search strategy
We searched relevant articles from MEDLINE, Scopus, Web of Science, WHO Global Health Library, and Google Scholar to access all forms of evidence. An initial search of MEDLINE was undertaken followed by analysis of the text words contained in the title and abstract, and of the index terms used to describe articles. We used the aforementioned performance indicators of PHC delivery and the PICO as we described above to choose keywords. A second search using all identified keywords and index terms was undertaken across all included databases. Thirdly, references of all identified articles were searched to get additional studies. The full electronic search strategy for MEDLINE, a major database we used for this review is included as a supplementary file (Additional file 1 : Appendix 1).
Study selection and assessment of methodological quality
Search results from different electronic databases were exported to Endnote reference manager version 7 to remove duplication. Two independent reviewers (ZG and BA) screened out records. An initial screening of titles and abstracts was done based on the PICO criteria and language of publication. Secondary screening of full-text papers was done for studies we included at the initial screening phase. We further investigated and assessed records included in the full-text articles against the inclusion and exclusion criteria. We sat together and discussed the eligibility assessment. The interrater agreement was 90%. We resolved disagreements by consensus for points we had different rating. We used the PRISMA flow diagram to summarize the study selection processes.
Methodological quality of the included studies was assessed using mixed methods appraisal tool (MMAT) version 2018 [ 13 ]. As it is clearly indicated in the user guide of the MMAT tool, it is discouraged to calculate an overall score from the ratings of each criterion. Instead, it is advised to provide a more detailed presentation of the ratings of each criterion to better inform quality of the included studies. The rating of each criterion was, therefore, done as per the detail explanations included in the guideline. Almost all the included full text articles fulfilled the criteria and all the included full text articles were found to be better quality.
Data extraction
We independently extracted data from papers included in the review using JBI mixed methods data extraction form. This form is only used for reviews that follow a convergent integrated approach, i.e. integration of qualitative data and qualitative data [ 14 ]. The data extraction form was piloted on randomly selected papers and modified accordingly. One reviewer extracted the data from the included studies and the second reviewer checked the extracted data. Disagreements were resolved by discussion between the two reviewers. Information was extracted from each included study on: list of authors, year of publication, study area, population of interest, study type, methods, focus of the studies, main findings, authors’ conclusion, and limitations of the study.
Synthesis of findings
The included full-text articles were qualitatively analyzed using emergent thematic analysis approach to identify key concepts and coded them into related non-mutually exclusive themes. Themes are strategies mentioned or discussed in the included records to improve access to PHC services. Themes were identified manually by reading the included records again and again. We then synthesized each theme by comparing the discussion and conclusion of the included articles.
Systematic review registration number
The protocol of this review is registered in PROSPERO (the registration number is: CRD42019132592) to avoid unplanned duplication and to enable comparison of reported review methods with what was planned in the protocol. It is available at https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42019132592 .
Schematic of the systematic review and reporting of the search
We used PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) 2009 checklist [ 15 ] for reporting of this systematic review.
Study selection
The search strategy identified 1148 titles and abstracts [914 from PubMed (Table 1 ) and 234 from other sources] as of 10 March 2022. We obtained 900 after we removed duplicated articles. Following assessment by title and abstract, 485 records were excluded because these records did not meet the criteria as mentioned in the method section. Additional 256 records were discarded because the records did not discuss the outcome of interest well and some records were systematic reviews. The full text of the remaining 159 records was examined in more detail. It appeared that 49 studies did not meet the inclusion criteria as described in the method section. One hundred ten records met the inclusion criteria and were included in the systematic review or synthesis (Fig. 1 ).
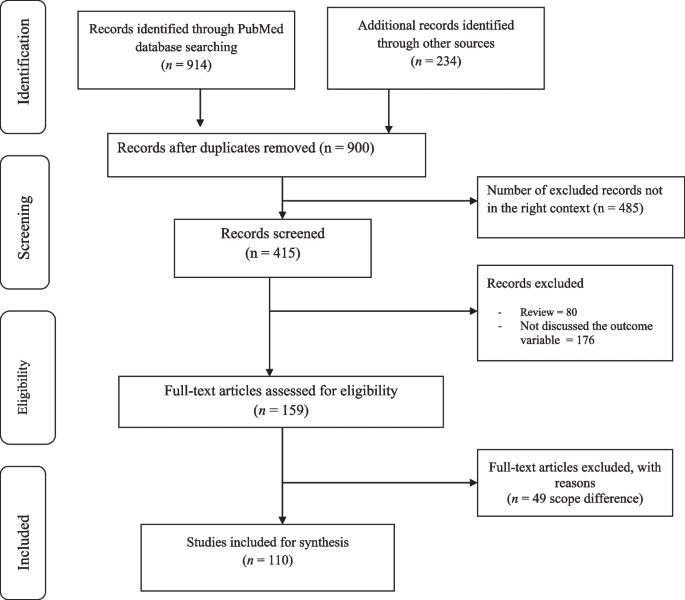
Study selection flow diagram
Of 900 articles resulting from the search term, 110 (12.2%) met the inclusion criteria. The included full-text articles were published between 1993 and 2021. Ninety-two (83.6%) of the included full-text articles were research articles, 5(4.5%) were technical reports, 3 (2.7%) were perspective, 4 (3.6%) was discussion paper, 3(2.7%) were dissertation or thesis, 2 (1.8%) were commentary, and 1 (0.9) was a book. Thirty-six (33%) and 29 (26%) of the included full-text articles were conducted in Africa and North America, respectively (Fig. 2 ).
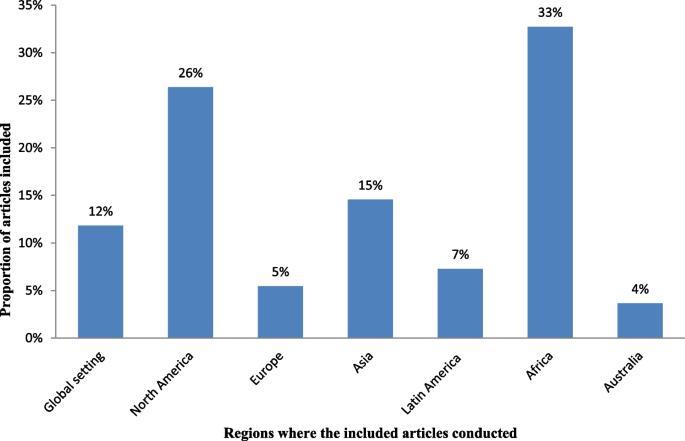
Regions where the included full-test articles conducted
Key strategies identified
The analysis of 110 full-text articles resulted in 10 themes. The themes are key strategies to improve access to PHC services in rural communities. The key strategies identified are community health programs or community-directed healthcare interventions, school-based healthcare services, student-led healthcare services, outreach services or mobile clinics, family health program, empanelment, community health funding schemes, telemedicine, promoting the role of traditional medicine, working with non-profit private sectors and non-governmental organizations (NGOs) including faith-based organizations (Table 2 ).
Description of strategies
a. Community health programs or community-directed healthcare interventions
Twenty-four (21.8%) of the full-text articles included in this review discussed that community health programs (CHPs) or community-directed healthcare interventions are best strategies to provide basic health and medical care close to the community to increase access and coverage of essential health services. Community health programs are locally based health promotion, disease prevention, and treatment programs available typically to communities in need and community-directed intervention strategy is an approach in which communities themselves direct the planning and implementation of intervention delivery. Rural communities, especially, in developing countries have no access to healthcare facilities in the near distance and have less chance to receive healthcare from doctors, health officers, nurses or midwives. In response to this critical problems, many countries have been investing heavily in community based primary health care to bring services to rural and remote areas where most of the population lives. Community health programs include construction of health posts or community health centers close to the community and deployment of community health workers (CHWs), such as health extension workers, to reach-out every village, who play a prominent role as the gatekeepers of healthcare in rural communities. Community-directed healthcare intervention is an approach in which communities themselves direct the planning and implementation of healthcare interventions. Community participation remains crucial in the identification of health problems, planning or designing of health interventions and implementation of the interventions, which enhances need-based and demand-driven provision of health services while promoting sustainability and ownership (Additional file 2 : Appendix 2, Table A1).
b. School-based primary healthcare
In this review, 9 of 110 (8.2%) of the included full-text articles pointed out that school-based healthcare services can be effective to improve access to PHC services. School-based health services are health programs that offer health care to children and youth either in a school or on school grounds and usually staffed according to school community needs and resources. School-based health services provide a variety of healthcare services to underserved children, youth and vulnerable populations in a convenient and accessible environment. Access to comprehensive health services via schools leads to improved access to healthcare (Additional file 3 : Appendix 3, Table A2).
c. Student-led healthcare services
In this review, 5 of 110 (4.5%) of the full-text articles discussed that the use of medical and health science students as healthcare service providers can minimize problems related with shortage of health professionals in rural healthcare system and can play appreciable roles to minimize healthcare service access problems in rural communities. Student-led healthcare services are developed through consultation between universities and local health providers and are purposefully designed clinical placements with a focus on clinical educational activities for pre-registration students. Student-led clinics link students, healthcare professionals, community-based organizations, universities, and communities. In this approach, students can gain practical experience in an interdisciplinary setting and through exposure to a community with unique and severe needs (Additional file 4 : Appendix 4, Table A3).
d. Outreach services or mobile clinics
In this systematic literature review, 18 of 110 (16.4%) of the included studies discussed that outreach services or mobile clinics in primary care and rural hospital settings can improve access to PHC services in rural communities. Mobile outreach service is defined as healthcare services provided by a mobile team of trained providers, from a higher-level health facility to a lower-level health facilities or locally available community facilities that are not used for clinical services, such as schools, health posts, or other community structures. Outreach services improve access to specialists and hospital-based services, strengthen connections between specialists and PHC providers, and give the benefits of consultations in primary care settings. Specialist outreach services have the potential to overcome access barriers faced by disadvantaged rural and remote communities. Furthermore, a community-based mobile clinics can be effective in uncovering illness and in directing patients to a healthcare home (Additional file 5 : Appendix 5, Table A4).
e. Family health program
Four (3.6%) of the included full-text articles discussed that family health program (FHP) is highly cost-effective tool for improving access to healthcare services for deprived areas (such as rural communities). Family health program means the program is a program designed to provide primary care as well as the prevention and early treatment of communicable and non-communicable diseases in defined populations by deploying interdisciplinary healthcare teams include physicians, nurses, nurse assistants, and full-time community health agents. It has evolved into a robust approach to providing primary care for defined populations by deploying interdisciplinary healthcare teams. The nucleus of each team includes a physician, a nurse, a nurse assistant, and full-time community health agents. This approach is effective on improving access to healthcare and eliminating health disparities (Additional file 6 : Appendix 6, Table A5).
f. Empanelment
This systematic review of literature identified that empanelment (also known as rostering) is a best strategy to proactively provide coordinated primary healthcare towards achieving universal health coverage. Empanelment is a continuous, iterative set of processes that identify and assign populations to facilities, care teams, or primary care providers who have a responsibility to know their assigned population. It enables health systems to improve health outcomes and to reduce costs. Empanelment establishes a point of care for individuals and simultaneously holds primary healthcare providers and care teams accountable for actively managing care for a specific group of individuals (Additional file 7 : Appendix 7, Table A6).
g. Community health funding schemes
In this systematic review of literature, 11 (10%) of the included articles discussed that community health funding schemes such as community-based health insurance (CBHI) increases access to healthcare services in low-income rural communities. Community-based health insurance schemes are usually voluntary and characterized by community members pooling funds to offset the cost of healthcare. Moreover, this approach is effective to mobilize domestic resources for health at low income levels. For low-income countries, community health financing has modest ability to increase the total amount of funds for healthcare. Properly structured community health financing system can significantly improve efficiency, reduce the cost of healthcare, improve quality and health outcomes, and pool risks. Community-financing schemes could improve preventive services and reduce the incidence of diseases. It could also improve people’s access to healthcare and the quality of services, thus improving their health status. Community health financing could also improve risk pooling and reduce health-induced impoverishment. Community health insurance has potential positive impacts on health and social security (Additional file 8 : Appendix 8, Table A7).
h. Telemedicine
In this review, 13 of 110 (11.8%) articles discussed that telemedicine is one of the solutions for rural subspecialty healthcare delivery. Telemedicine can be defined as the use of technology (computers, video, phone, messaging) by a medical professional to diagnose and treat patients in a remote location. The provision of subspecialty services using telemedicine to a remote and medically underserved population provides improved access to subspecialty care. Telemedicine brings sustainable healthcare to rural populations. Use of information and communication technologies in support of health and health-related fields, including healthcare services, health surveillance, health education, and health research has the potential to greatly improve health service efficiency, expand or scale up treatment delivery to thousands of patients in the rural populations (Additional file 9 : Appendix 9, Table A8).
i. Promoting the role of traditional medicine
Seven (6.4%) of the included articles showed that incorporating traditional healers into public health system addresses healthcare needs of people with limited access to allopathic medicine. Traditional medicine is the sum total of the knowledge, skill, and practices based on the theories, beliefs, and experiences indigenous to different cultures, whether explicable or not, used in the maintenance of health as well as in the prevention, diagnosis, improvement or treatment of physical and mental illness. Knowledge about traditional medicine has a catalyzing effect in meeting health sector development objectives. Integrating traditional medicine into national health systems in combination with national policy and regulation for products, practices and providers can enhance access to PHC services in remote populations (Additional file 10 : Appendix 10, Table A9).
j. Working with non-profit private sectors and non-governmental organizations
In this systematic review, 15 of 110 (13.6%) of the included articles revealed that working with non-profit private sectors and NGOs strengthens the healthcare system. Involving the non-profit private sectors, faith-based organizations (FBOs), and NGOs for health system strengthening eventually contributes to create a healthcare system reflecting an increased efficiency, more equity and good governance in health. International and local NGOs have endeavored to fill the gaps in access to healthcare services, research and advocacy. Non-profit private sectors and NGOs have a key role in improving health in low- and middle-income countries. With networks that reach even the most remote communities, many FBOs are well positioned to promote demand and access for healthcare services. Partnership among FBOs is critical in increasing access to healthcare services, and ensuring sustainability by influencing behaviors at the community, family and individual level. Faith-based organizations play an integral role in the healthcare system by increasing health seeking behaviors and delivering supportive services that address common access and cultural barriers (Additional file 11 : Appendix 11, Table A10).
This systematic literature review found that community health programs or community-directed healthcare interventions, school-based healthcare services, student-led healthcare services, outreach services or mobile clinics, family health program, empanelment, community health funding schemes, telehealth, integrative medicine, and working with non-profit private sectors and NGOs are key strategies to improve access to PHC services in rural communities. The identified strategies address the four major pillars of primary healthcare (i.e., community participation, inter-sectoral coordination, appropriate technology, and support mechanism made available) [ 126 ]. Moreover, the identified strategies are effective to improve access to healthcare services to rural communities. Moreover, the identified strategies are effective to solve shortage of manpower and to build knowledge and skill of the local health workforces in rural healthcare system. The ability of a healthcare system to meet health needs of the population depends largely on the knowledge, skills, motivation and deployment of the people responsible for organizing and delivering health services. The results of this review can strengthen the health information system, which are core elements of the healthcare system that ensure community engagement through dissemination and use of timely and reliable health information to rural populations. This review also suggests strategies to narrow down the health disparities among rural populations, which is wide in most Least and Middle Income Countries (LMICs). Healthcare services are usually disproportionately concentrated in major urban areas. As a result, rural communities face growing health disparities, largely attributed to weak policies, inefficiencies, poor leadership, and governance in healthcare system.
This review identified that community health programs or community-directed healthcare interventions address health disparities by ensuring equitable access to health resources in communities where health equity is limited by socioeconomic and geographical factors. Community health programs include identifying and prioritizing public health problems in a specific geographic area; designing and implementing public health interventions (such as establishing community health centers, mobile clinics, and outreach programs); providing services (such as health education, screenings, social support, and counseling), and deploying community health workers to promote healthy behaviors; advocating for improved care for populations at risk; and working with stakeholders to address community healthcare needs [ 16 , 17 , 18 , 127 , 128 , 129 , 130 ]. The community-oriented PHC model which is socially responsive medicine makes a healthcare system more rational, accountable, appropriate, and socially relevant to the public. Consequently, this model serves as a paradigm for reforming healthcare systems. Community-directed interventions can be considered as a realistic means to increase accessibility of interventions at community-level in rural areas [ 32 , 33 , 34 , 35 , 36 , 37 , 38 ]. This approach is best in situations where there are cultural barriers to implement interventions because this strategy is effective to develop ownership in the community. In-service and on-the-job training for community health workers, close supervision and government support, and program evaluation is very important to strengthen the community health program [ 131 , 132 , 133 ].
This review identified that school-based PHC services are effective strategies to improve access to PHC services. School-based health services provide a variety of healthcare services to children, youth and vulnerable populations in a convenient and accessible environment which indirectly improve leadership and governance. Science teachers and home room teachers play important roles to implement this strategy. It impacts on delivering preventive care such as immunizations, managing chronic illnesses and providing reproductive health services for adolescents. Comprehensive health services via schools improve access to healthcare information [ 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 ]. Access to school around the world increased drastically in the last century [ 134 ]. This high schooling rate is a good opportunity to provide healthcare services to school learners in accessible places and to disseminate health messages to families. Prior researches suggest that school-based healthcare services increase access to healthcare by increasing utilization of primary care, prevention services, and health maintenance visits [ 135 , 136 ]. Including science teachers, home room teachers, school principals, students, communities, community health workers, and other interested parties in the school-based healthcare system as main actors or promoters must be considered to sustain the impact. Health and education sectors should work in collaboration with the above-mentioned actors to plan, implement and monitor the progress. School-based healthcare services are preferable in situations when there is high schooling rate and limited access to healthcare institutions. This strategy is also an alternative way in areas where the health seeking behavior of the community is low.
The use of medical and health science students in rural healthcare system was identified as a key strategy to minimize health inequalities in rural communities due to shortages in health workforce and distribution of healthcare resources [ 49 , 50 , 51 , 52 , 53 ]. Student-led health intervention is an alternative approach to provide essential healthcare services to the community where there is shortage of healthcare workers [ 137 , 138 ]. Students will have opportunities to learn professional skills and competencies while they are providing healthcare services to the community. Moreover, benefits for student learning include increased communication, collaboration, and leadership skills [ 53 , 139 ]. Student-led health intervention also enables increased access to services, more time for assessments and treatments, increased depth of health teaching, holistic and integrated healthcare, and free health supports [ 140 , 141 , 142 , 143 ]. However, the use of medical and health science students in the rural healthcare system may have ethical and competency issues. Supporting strategies such as close supervision, preparing clear protocols, and including senior experts in the team should be considered.
This systematic review of literature found that outreach services or mobile clinics can improve access to PHC service delivery in rural populations [ 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 ]. In developing countries, the highest proportion of people lives in rural areas where doctor services are not available. Rural communities travel to major cities to get specialist services. This reflects a desire for closer integration between primary and secondary care. Specialist outreach services or mobile clinics have become one of the effective solution to solve health disparities, to improve access to healthcare services, and to build capacity of local healthcare workforces. This strategy is preferable in situations when there are high loads in tertiary or referral level hospitals and when there is high patient leakage in the referral system [ 63 , 64 , 65 , 66 , 67 , 68 , 69 ]. However, the implementation may not be easy. It needs well established healthcare system and budget. Moreover, the efficiency of care may be lower compared with hospital-based cares and the effect on patients’ health outcomes might be small [ 56 , 57 , 61 ] . Irregular specialist visits in rural areas may not have real impacts unless the services are sustainable with a strong commitment at national and local levels. Outreach activities should be included in health policies with strong leadership, healthcare financing, and private initiatives must be encouraged to maintain the activities over time.
This review revealed that FHP is highly effective tool for improving health for rural communities. The FHP has provided a new, more robust model of primary healthcare services designed to provide accessible, first contact, comprehensive, and whole person care that is coordinated with other healthcare services. It has positive results to improved availability, access to, and use of health services, and improved health indicators, such as reduced infant mortality, improved detection of cases of neglected diseases, and reduced health disparities [ 73 , 144 , 145 , 146 ]. The FHP deploys interdisciplinary healthcare teams. The team includes a physician, a nurse, a nurse assistant, and full-time community health agents. Family health teams are organized geographically. The teams are responsible for delivering public health interventions [ 72 , 74 ]. Family health program is an alternative strategy in rural healthcare system in situations when there are inequities in access to care; when there is high hospitalization rate; when there is low health seeking behavior in the community; and when there is poor case detecting and reporting system. Despite these remarkable achievements, the FHP has some challenges include difficulties in the recruitment and retention of doctors trained appropriately to deliver primary healthcare, large variations in quality of local care, patchy integration of primary care services with existing secondary and tertiary care, and slow adoption of FHP in large population [ 147 ].
In this review, empanelment has been identified as a best strategy to deliver coordinated primary healthcare towards achieving universal health coverage [ 76 , 77 , 78 , 79 ]. The goal of empanelment is provide people-centered healthcare services based on their needs to ensure that every established patient receives optimal care, whether he/she regularly visits healthcare centers. Major activities in this approach include assignment of all patients to a healthcare provider panel; update panel assignments on a regular basis; and use panel data to educate, and track patients [ 79 ]. Empanelment enables healthcare systems to improve patient experiences, reduce costs, and improve health outcomes. Empanelment is an effective strategy to deliver four key functions: first-contact accessibility, continuity, comprehensiveness, and coordination [ 148 ]. Effective empanelment requires responsibility for the health of a target population, including providing healthcare services based on their health status, which is an important step in moving towards people-centered integrated healthcare [ 79 ].
This review identified that community health funding schemes such as community-based health insurance (CBHI) increases access to healthcare in low-income rural communities. Moreover, this approach is effective to mobilize domestic resources for health at low income levels [ 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 ]. Community-based health insurance is an emerging strategy to provide financial protection against the cost of illness. It is an effective strategy to improve access to quality health services for low-income rural households [ 149 ]. Existence of social capital in the community is a determinant factor for the effectiveness of CBHI as social capital has a positive effect on the community's demand for insurance [ 150 , 151 ]. Moreover, solidarity and trust between the members are the key principles for the good functioning of a CBHI. Solidarity and trust stir-up members who are susceptible to risk to put together their resources for common use [ 149 , 152 , 153 ]. Affordability of premiums or contributions, technical arrangements made by the scheme management, timing of collecting the contributions, trust in the integrity and competence of the managers of the CBHI, The quality of care offered through the CBHI, accessible across different population groups are some of the determinant factors to be considered to increase people’s decision to join the CBHI schemes [ 154 , 155 ].
In this review, telemedicine has been identified as one of the many possible solutions for rural subspecialty healthcare delivery. Telemedicine is a vital technological tool to increase healthcare access, improve care delivery systems, engage in culturally competent outreach, health workforce development, and health information system [ 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 ]. Telemedicine can be a great alternative to the traditional healthcare system in situations like diagnoses of common medical problems; inquiries about various medical issues for home treatments; post-treatment check-ins or follow-up for chronic care; holidays, weekends, late night or any other situation when regular medical care is not possible; patient inability to leave the house; patients who lack regular access to relevant medical expertise in their geographic area ; and etc. However, technological issues are challenges when dealing with telemedicine, especially in developing countries. General problems of Internet connectivity and access to infrastructure can minimize benefits of this strategy. Costs associated with technology can also be a barrier. Furthermore, health technology requires human capacity to use it. Therefore, strengthening the information communication technologies (ICT) and human capacity building on ICT are important to address the health needs of the rural communities.
This systematic review of literature identified that promoting the role of TM solves problems of access to allopathic medicine. Integration of TM in health system will result in increased coverage and access to healthcare services. The role of complementary and alternative medicine for health is undisputed particularly in light of its role in health promotion and well-being. It also supports local health workforces [ 104 , 105 , 106 , 107 , 108 , 109 ]. Incorporating traditional healers into the public health system addresses healthcare needs [ 156 , 157 ]. However, integrating TM to the public healthcare system is challenging. It is a general belief that TM defies scientific procedures in terms of objectivity, measurement, codification and classification [ 157 ]. If integrated, who provides training to medical doctors on the ontology, epistemology and the efficacies of TM in modern medicine [ 157 ]. Due to these, some scholars suggest that both TM and modern medicine be allowed to operate and develop independent of one another [ 158 , 159 ]. Another fundamental challenge to TM is the widespread reported cases of fake healers and healings [ 157 ]. Generally, this strategy is more of feasible in areas where formal trainings on integrative medicine are available. Even though the integration is challenging, the health sector can use traditional healers as health educators or health promoters by providing training and continuous support. It can be also possible to use traditional healers as facilitators in the community-directed approaches. In general TM can be used in the primary healthcare system where no access to allopathic medicine and when conventional medicine is ineffective in treatment of disease [ 160 ].
Working with non-profit private sectors and NGOs has been identified as effective strategies to strengthen the healthcare system in developing countries [ 111 , 112 , 113 , 114 , 115 , 116 , 117 , 118 ]. Since governments in developing countries are challenged to meet the health needs of their populations because of financial constraints, limited human resources, and weak health infrastructure; the private sector (especially the non-profit private sectors) and non-governmental organizations can help expand access to healthcare services through its resources, expertise, and infrastructure. However, the presence of an NGO in the operation, may contribute to unrealistic expectations of health services, affecting perceptions of the latter negatively [ 113 ]. Moreover, reports have it that besides other issues in many instances NGOs allocated funds only to disease specific projects (vertical programming) rather than to broad based investments (horizontal programming) [ 161 ]. There are also concerns that donor expenditures in developing countries are not only unsustainable but may be considered as inadequate considering the enormous healthcare burden [ 161 , 162 , 163 , 164 ]. To avoid unrealistic expectations and dissatisfaction, and to increase and sustain the population’s trust in the organization, NGOs should operate in a manner that is as integrated as possible within the existing structure and should work close to the population it serves, with services anchored in the community. Moreover, faith-based organizations contribute in health such as disease prevention, health education or promotion, and community health development beyond psychological and spiritual care [ 119 , 120 , 121 , 122 , 123 , 124 ]. Religious organizations can reach all segments of rural populations. Therefore, integrating PHC services, especially health education and promotion, diseases prevention and community health development with religious organizations intensifies delivery of healthcare services. Working with FBOs is a best way in situations where cultural and faith-based barriers are common and in areas, where access problems are often related to lack of providers. However, religious organizations need intensive training on health promotion and health system to enable them to respond to local contexts within the framework of national policies. Moreover, there should be strong partnership with government agenesis to sustain the effort [ 165 , 166 , 167 , 168 ].
Contribution of this review
Various studies reported one or more strategies to improve access to primary healthcare services. However, the strategies reported by individual studies are not compiled together and there is lack of pooled evidence on effective strategies to improve access to healthcare system. This systematic literature review was, therefore, conducted to compile effective strategies to improve access to healthcare services in rural communities. The review suggests key strategies to improve access to PHC services in rural communities. These suggested strategies are implementable in countries that suffer from shortage of health workers and healthcare financing because all the strategies used locally available opportunities. The local healthcare system needs, therefore, scan the available opportunities in the locality for implementing the suggested strategies and needs to integrate the strategies in the healthcare system to sustain the impacts. Healthcare providers, researchers and policy makers could use the results of this systematic literature review to increase access to healthcare services in hard-to-reach areas. As the strategies are compiled from experiences of different countries (developed and least developed countries), there might be contextual differences like socio-economic, cultural, institutional, and geographical challenges to adopt the identified strategies. Moreover, some of the experiences only come from one or two countries. Therefore, strategy developers and implementers need to consider these contextual challenges or variation during adopting and implementing different strategies.
Strengths and limitations of the study
As a strength, this systematic review explores international (both developed and developing countries) best experiences on primary healthcare service delivery and identified ten key approaches to improve access to PHC services in rural communities. We also searched relevant published or unpublished articles, dissertations or theses, discussion papers, and perspectives from a wide range of sources, such as MEDLINE, Scopus, Web of Science, WHO Global Health Library, and Google Scholar.
As a limitation, we entirely relied on electronic databases to search relevant articles. We didn’t include locally available printed out records. We also applied limits for language. We excluded articles published other than English language. We believed we could get more relevant articles if we had access to records available in prints and if we include articles published other than English language. Furthermore, since the strategies are compiled from experiences of different countries (developed and least developed countries), there might be contextual differences like socio-economic, cultural, institutional and geographical challenges to adopt the identified strategies. There was also limited evidence for some articles, especially reports to rate their methodological quality. Readers should also note that our review might missed some important work in improving access to PHC services and the identified strategies are not the only strategies to improve access to PHC services. There might be other effective strategies which are not included in this review. In addition generalizability might be affected since some of the experiences only come from one or two countries. Moreover, this review focuses on access not quality of care delivered.
This review identified key strategies from international experiences to improve access to PHC services in rural communities. These strategies are effective to improve access to healthcare services in rural or remote communities. They can also play roles in achieving UHC and reducing disparities in health outcomes and increase access to rural communities to get healthcare when and where they want. Therefore, incorporating these key strategies suggested by this review in to the healthcare system is useful to enhance PHC services and to minimize impacts of health disparity in rural communities. However, the identified strategies may not be easy to implement. Increasing number and capacity of human resource for health; strengthening the healthcare financing system; improving medicine and supplies; working in different partners and communities; establishing monitoring and evaluation system; strong and committed leadership; and encouraging private initiatives must be considered to implement and maintain these strategies over time. Moreover, policy makers, program planners and implementers who want to utilize findings of this review should be aware that these are not the only effective strategies to improve access to primary healthcare services.
Availability of data and materials
All the extracted data are included in the manuscript.
Abbreviations
Community-based health insurance
Faith-based organizations
Family health program
Information communication technologies
Mixed methods appraisal tool
Non-governmental organizations
- Primary healthcare
Primary Health Care Performance Initiative
Population, phenomena of interest and context)
Traditional medicine
Universal health coverage
Hampton MB, Kettle AJ, Winterbourn CC. Inside the neutrophil phagosome: oxidants, myeloperoxidase, and bacterial killing. Blood. 1998;92(9):3007–17.
Article CAS Google Scholar
Kirby M. The right to health fifty years on: Still skeptical? Health Hum Rights. 1999;4(1):6–25.
O’Connell T, Rasanathan K, Chopra M. What does universal health coverage mean? The Lancet. 2014;383(9913):277–9.
White F. Primary health care and public health: foundations of universal health systems. Med Princ Pract. 2015;24(2):103–16.
Article Google Scholar
Sanders D, Nandi S, Labonté R, Vance C, Van Damme W. From primary health care to universal health coverage—one step forward and two steps back. The Lancet. 2019;394(10199):619–21.
Brezzi M, Luongo P. Regional Disparities In Access To Health Care. 2016.
Google Scholar
Hartley D. Rural health disparities, population health, and rural culture. Am J Public Health. 2004;94(10):1675–8.
Walraven G. The 2018 Astana declaration on primary health care, is it useful? J Glob Health. 2019;9(1).
Gillam S. Is the declaration of Alma Ata still relevant to primary health care? BMJ (Clinical research ed). 2008;336(7643):536–8.
Tollman S, Doherty J, Mulligan JA. General Primary Care. In: Jamison DT, Breman JG, Measham AR, Alleyne G, Claeson M, Evans DB, Jha P, Mills A, Musgrove P, editors. Disease Control Priorities in Developing Countries. Washington: World Bank The International Bank for Reconstruction and Development/The World Bank Group; 2006. Available at https://www.ncbi.nlm.nih.gov/books/NBK11789/pdf/Bookshelf_NBK11789.pdf .
Stern C, Jordan Z, McArthur A. Developing the review question and inclusion criteria. AJN The Am J Nurs. 2014;114(4):53–6.
World Health Organization. losing the gap in a generation. Commission on Social Determinants of Health FINAL REPORT. 2008. Available at https://www.who.int/social_determinants/final_report/csdh_finalreport_2008.pdf . Accessed on 22 March 2022.
Hong QN, Pluye P, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, GagnonM-P GF, Nicolau B, O’Cathain A. Mixed methods appraisal tool (MMAT), version 2018. Canada: IC Canadian Intellectual Property Office, Industry; 2018. Available at https://mixedmethodsappraisaltoolpublicpbworks.com/w/file/fetch/127916259/MMAT_2018_criteria-manual_2018-08-01_ENG.pdf .
JBI Manual for Evidence Synthesis. Appendix 8.1 JBI Mixed Methods Data Extraction Form following a Convergent Integrated Approach. Available at https://jbi-global-wiki.refined.site/space/MANUAL/3318284375/Appendix+8.1+JBI+Mixed+Methods+Data+Extraction+Form+following+a+Convergent+Integrated+Approach . Accessed on 12 August 2021.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Assefa Y, Gelaw YA, Hill PS, Taye BW, Van Damme W. Community health extension program of Ethiopia, 2003–2018: successes and challenges toward universal coverage for primary healthcare services. Glob Health. 2019;15(1):1–11.
Admassie A, Abebaw D, Woldemichael AD. Impact evaluation of the Ethiopian health services extension programme. J Dev Eff. 2009;1(4):430–49.
Yitayal M, Berhane Y, Worku A, Kebede Y. The community-based Health extension Program significantly improved contraceptive utilization in West gojjam Zone, ethiopia. J Multidiscip Healthc. 2014;7:201.
Croke K, Mengistu AT, O’Connell SD, Tafere K. The impact of a health facility construction campaign on health service utilisation and outcomes: analysis of spatially linked survey and facility location data in Ethiopia. BMJ Glob Health. 2020;5(8):e002430.
Arwal S. Health Posts in Afghanistan. J Gen Practice. 2015;3(213):2.
Negussie A, Girma G. Is the role of Health Extension Workers in the delivery of maternal and child health care services a significant attribute? The case of Dale district, southern Ethiopia. BMC Health Serv Res. 2017;17(1):1–8.
Than KK, Mohamed Y, Oliver V, Myint T, La T, Beeson JG, Luchters S. Prevention of postpartum haemorrhage by community-based auxiliary midwives in hard-to-reach areas of Myanmar: a qualitative inquiry into acceptability and feasibility of task shifting. BMC Pregnancy Childbirth. 2017;17(1):1–10.
Medhanyie A, Spigt M, Kifle Y, Schaay N, Sanders D, Blanco R, GeertJan D, Berhane Y. The role of health extension workers in improving utilization of maternal health services in rural areas in Ethiopia: a cross sectional study. BMC Health Serv Res. 2012;12(1):1–9.
Sakeah E, McCloskey L, Bernstein J, Yeboah-Antwi K, Mills S, Doctor HV. Can community health officer-midwives effectively integrate skilled birth attendance in the community-based health planning and services program in rural Ghana? Reprod Health. 2014;11(1):1–13.
Sarmento DR. Traditional birth attendance (TBA) in a health system: what are the roles, benefits and challenges: a case study of incorporated TBA in Timor-Leste. Asia Pac Fam Med. 2014;13(1):1–9.
Rahmawati R, Bajorek B. Peer Reviewed: A Community Health Worker-Based Program for Elderly People with Hypertension in Indonesia: A Qualitative Study, 2013. Prev Chronic Dis. 2015;12:E175.
Feltner FJ, Ely GE, Whitler ET, Gross D, Dignan M. Effectiveness of community health workers in providing outreach and education for colorectal cancer screening in Appalachian Kentucky. Soc Work Health Care. 2012;51(5):430–40.
Hughes MM, Yang E, Ramanathan D, Benjamins MR. Community-based diabetes community health worker intervention in an underserved Chicago population. J Community Health. 2016;41(6):1249–56.
Panday S, Bissell P, Van Teijlingen E, Simkhada P. The contribution of female community health volunteers (FCHVs) to maternity care in Nepal: a qualitative study. BMC Health Serv Res. 2017;17(1):1–11.
Datiko DG, Lindtjørn B. Health extension workers improve tuberculosis case detection and treatment success in southern Ethiopia: a community randomized trial. PLoS ONE. 2009;4(5):e5443.
le Roux KW, Almirol E, Rezvan PH, Le Roux IM, Mbewu N, Dippenaar E, Stansert-Katzen L, Baker V, Tomlinson M, Rotheram-Borus M. Community health workers impact on maternal and child health outcomes in rural South Africa–a non-randomized two-group comparison study. BMC Public Health. 2020;20(1):1–14.
Witmer A, Seifer SD, Finocchio L, Leslie J, O’Neil EH. Community health workers: integral members of the health care work force. Am J Public Health. 1995;85(8 Pt 1):1055–8.
Wright RA. Community-oriented primary care. The cornerstone of health care reform. Jama. 1993;269(19):2544–7.
Makaula P, Bloch P, Banda HT, Mbera GB, Mangani C, de Sousa A, Nkhono E, Jemu S, Muula AS. Primary Health Care in rural Malawi - a qualitative assessment exploring the relevance of the community-directed interventions approach. BMC Health Serv Res. 2012;12:328.
Katabarwa MN, Habomugisha P, Richards FO Jr, Hopkins D. Community-directed interventions strategy enhances efficient and effective integration of health care delivery and development activities in rural disadvantaged communities of Uganda. Trop Med Int Health : TM & IH. 2005;10(4):312–21.
Madon S, Malecela MN, Mashoto K, Donohue R, Mubyazi G, Michael E. The role of community participation for sustainable integrated neglected tropical diseases and water, sanitation and hygiene intervention programs: A pilot project in Tanzania. Soc Sci Med. 1982;2018(202):28–37.
Okeibunor JC, Orji BC, Brieger W, Ishola G, Otolorin E, Rawlins B, Ndekhedehe EU, Onyeneho N, Fink G. Preventing malaria in pregnancy through community-directed interventions: evidence from Akwa Ibom State, Nigeria. Malaria J. 2011;10:227.
Brieger WR, Sommerfeld JU, Amazigo UV. The Potential for Community-Directed Interventions: Reaching Underserved Populations in Africa. Int Q Community Health Educ. 2015;35(4):295–316.
Braimah JA, Sano Y, Atuoye KN, Luginaah I. Access to primary health care among women: the role of Ghana’s community-based health planning and services policy. Prim Health Care Res Dev. 2019;20:e82.
Kaplan DW, Brindis CD, Phibbs SL, Melinkovich P, Naylor K, Ahlstrand K. A comparison study of an elementary school–based health center: effects on health care access and use. Arch Pediatr Adolesc Med. 1999;153(3):235–43.
Allison MA, Crane LA, Beaty BL, Davidson AJ, Melinkovich P, Kempe A. School-based health centers: improving access and quality of care for low-income adolescents. Pediatrics. 2007;120(4):e887–94.
Keeton V, Soleimanpour S, Brindis CD. School-based health centers in an era of health care reform: Building on history. Curr Probl Pediatr Adolesc Health Care. 2012;42(6):132–56.
Brindis CD, Klein J, Schlitt J, Santelli J, Juszczak L, Nystrom RJ. School-based health centers: Accessibility and accountability. J Adolesc Health. 2003;32(6):98–107.
Hutchinson P, Carton TW, Broussard M, Brown L, Chrestman S. Improving adolescent health through school-based health centers in post-Katrina New Orleans. Child Youth Serv Rev. 2012;34(2):360–8.
Paschall MJ, Bersamin M. School-based health centers, depression, and suicide risk among adolescents. Am J Prev Med. 2018;54(1):44–50.
Minguez M, Santelli JS, Gibson E, Orr M, Samant S. Reproductive health impact of a school health center. J Adolesc Health. 2015;56(3):338–44.
Gibson EJ, Santelli JS, Minguez M, Lord A, Schuyler AC. Measuring school health center impact on access to and quality of primary care. J Adolesc Health. 2013;53(6):699–705.
Bozigar M. A Cross-Sectional Survey to Evaluate Potential for Partnering With School Nurses to Promote Human Papillomavirus Vaccination. Prev Chronic Dis. 2020;17:E111.
Suen J, Attrill S, Thomas JM, Smale M, Delaney CL, Miller MD. Effect of student-led health interventions on patient outcomes for those with cardiovascular disease or cardiovascular disease risk factors: a systematic review. BMC Cardiovasc Disord. 2020;20(1):1–10.
Atuyambe LM, Baingana RK, Kibira SP, Katahoire A, Okello E, Mafigiri DK, Ayebare F, Oboke H, Acio C, Muggaga K. Undergraduate students’ contributions to health service delivery through communitybased education. BMC Med Educ. 2016;16:123.
Stuhlmiller CM, Tolchard B. Developing a student-led health and wellbeing clinic in an underserved community: collaborative learning, health outcomes and cost savings. BMC Nurs. 2015;14(1):1–8.
Campbell DJ, Gibson K, O’Neill BG, Thurston WE. The role of a student-run clinic in providing primary care for Calgary’s homeless populations: a qualitative study. BMC Health Serv Res. 2013;13(1):1–6.
Simpson SA, Long JA. Medical student-run health clinics: important contributors to patient care and medical education. J Gen Intern Med. 2007;22(3):352–6.
Gruen RL, O’Rourke IC, Bailie RS, d’Abbs PH, O’Brien MM, Verma N. Improving access to specialist care for remote Aboriginal communities: evaluation of a specialist outreach service. Med J Aust. 2001;174(10):507–11.
Gruen RL, Weeramanthri T, Bailie R. Outreach and improved access to specialist services for indigenous people in remote Australia: the requirements for sustainability. J Epidemiol Community Health. 2002;56(7):517–21.
Gruen RL, Bailie RS, Wang Z, Heard S, O’Rourke IC. Specialist outreach to isolated and disadvantaged communities: a population-based study. The Lancet. 2006;368(9530):130–8.
Bond M, Bowling A, Abery A, McClay M, Dickinson E. Evaluation of outreach clinics held by specialists in general practice in England. J Epidemiol Community Health. 2000;54(2):149–56.
Irani M, Dixon M, Dean JD. Care closer to home: past mistakes, future opportunities. J R Soc Med. 2007;100(2):75–7.
Bailey JJ, Black ME, Wilkin D. Specialist outreach clinics in general practice. BMJ (Clinical research ed). 1994;308(6936):1083–6.
De Roodenbeke E, Lucas S, Rouzaut A, Bana F. Outreach services as a strategy to increase access to health workers in remote and rural areas. Geneva: WHO; 2011.
Bowling A, Stramer K, Dickinson E, Windsor J, Bond M. Evaluation of specialists’ outreach clinics in general practice in England: process and acceptability to patients, specialists, and general practitioners. J Epidemiol Community Health. 1997;51(1):52–61.
Spencer N. Consultant paediatric outreach clinics–a practical step in integration. Arch Dis Child. 1993;68(4):496–500.
Aljasir B, Alghamdi MS. Patient satisfaction with mobile clinic services in a remote rural area of Saudi Arabia. East Mediterr Health J. 2010;16(10):1085–90.
Lee EJ, O’Neal S. A mobile clinic experience: nurse practitioners providing care to a rural population. J Pediatr Health Care. 1994;8(1):12–7.
Cone PH, Haley JM. Mobile clinics in Haiti, part 1: Preparing for service-learning. Nurse Educ Pract. 2016;21:1–8.
Diaz-Perez Mde J, Farley T, Cabanis CM. A program to improve access to health care among Mexican immigrants in rural Colorado. J Rural Health. 2004;20(3):258–64.
Hill C, Zurakowski D, Bennet J, Walker-White R, Osman JL, Quarles A, Oriol N. Knowledgeable Neighbors: a mobile clinic model for disease prevention and screening in underserved communities. Am J Public Health. 2012;102(3):406–10.
Edgerley LP, El-Sayed YY, Druzin ML, Kiernan M, Daniels KI. Use of a community mobile health van to increase early access to prenatal care. Matern Child Health J. 2007;11(3):235–9.
Peters G, Doctor H, Afenyadu G, Findley S, Ager A. Mobile clinic services to serve rural populations in Katsina State, Nigeria: perceptions of services and patterns of utilization. Health Policy Plan. 2014;29(5):642–9.
Neke NM, Gadau G, Wasem J. Policy makers’ perspective on the provision of maternal health services via mobile health clinics in Tanzania—Findings from key informant interviews. PLoS ONE. 2018;13(9):e0203588.
Padmadas SS, Johnson FA, Leone T, Dahal GP. Do mobile family planning clinics facilitate vasectomy use in Nepal? Contraception. 2014;89(6):557–63.
Macinko J, Harris MJ. Brazil’s family health strategy—delivering community-based primary care in a universal health system. N Engl J Med. 2015;372(23):2177–81.
Macinko J, Lima Costa MF. Access to, use of and satisfaction with health services among adults enrolled in Brazil’s Family Health Strategy: evidence from the 2008 National Household Survey. Tropical Med Int Health. 2012;17(1):36–42.
Dourado I, Oliveira VB, Aquino R, Bonolo P, Lima-Costa MF, Medina MG, Mota E, Turci MA, Macinko J. Trends in primary health care-sensitive conditions in Brazil: the role of the Family Health Program (Project ICSAP-Brazil). Medical care. 2011;49:577–84.
Aquino R, De Oliveira NF, Barreto ML. Impact of the family health program on infant mortality in Brazilian municipalities. Am J Public Health. 2009;99(1):87–93.
Chong P-N, Tang WE. Transforming primary care—the way forward with the TEAMS2 approach. Fam Pract. 2019;36(3):369–70.
Primary Health Care Performance Initiatives (phcpi). Improvement strategies model: Population health management: Empanelment. Available at https://improvingphc.org/sites/default/files/Empanelment%20-%20v1.2%20-%20last%20updated%2012.13.2019.pdf . Accessed on 18 March 2022.
McGough P, Chaudhari V, El-Attar S, Yung P. A health system’s journey toward better population health through empanelment and panel management. Healthcare. 2018;6(66):1–9.
Bearden T, Ratcliffe HL, Sugarman JR, Bitton A, Anaman LA, Buckle G, Cham M, Quan DCW, Ismail F, Jargalsaikhan B. Empanelment: A foundational component of primary health care. Gates Open Res. 2019;3:1654.
Hsiao WC. Unmet health needs of two billion: is community financing a solution? 2001.
Wang W, Temsah G, Mallick L. The impact of health insurance on maternal health care utilization: evidence from Ghana, Indonesia and Rwanda. Health Policy Plan. 2017;32(3):366–75.
Atnafu DD, Tilahun H, Alemu YM. Community-based health insurance and healthcare service utilisation, North-West, Ethiopia: a comparative, cross-sectional study. BMJ Open. 2018;8(8):e019613.
USAID. Ethiopia’s Community-based Health Insurance: A Step on the Road to Universal Health Coverage. Available at https://www.hfgproject.org/ethiopias-community-based-health-insurance-step-road-universal-health-coverage/ . Accessed on 18 March 2022.
Blanchet NJ, Fink G, Osei-Akoto I. The effect of Ghana’s National Health Insurance Scheme on health care utilisation. Ghana Med J. 2012;46(2):76–84.
CAS Google Scholar
Nshakira-Rukundo E, Mussa EC, Nshakira N, Gerber N, von Braun J. Impact of community-based health insurance on utilisation of preventive health services in rural Uganda: a propensity score matching approach. Int J Health Econ Manag. 2021;21(2):203–27.
Mwaura JW, Pongpanich S. Access to health care: the role of a community based health insurance in Kenya. Pan Afr Med J. 2012;12(1):35.
Jutting JP. The Impact Of Health Insurance On The Access To Health Care And Financial Protection In Rural Developing Countries: The Example of Senegal. HNP discussion paper series;. World Bank, Washington, DC. © World Bank. 2011. https://openknowledge.worldbank.org/handle/10986/13774 . License: CC BY 3.0 IGO.
Balamiento NC. The impact of social health insurance on healthcare utilization outcomes: evidence from the indigent program of the Philippine National Health Insurance. International Institute of Social Studies. 2018. Available at https://thesis.eur.nl/pub/46445/Balamiento,%20Neeanne_MA_2017_18%20_ECD.pdf . Accessed 30 Nov 2022.
Farrell CM, Gottlieb A. The effect of health insurance on health care utilization in the justice-involved population: United States, 2014–2016. Am J Public Health. 2020;110(S1):S78–84.
Thuong NTT. Impact of health insurance on healthcare utilisation patterns in Vietnam: a survey-based analysis with propensity score matching method. BMJ Open. 2020;10(10):e040062.
Custodio R, Gard AM, Graham G. Health information technology: addressing health disparity by improving quality, increasing access, and developing workforce. J Health Care Poor Underserved. 2009;20(2):301–7.
Meier CA, Fitzgerald MC, Smith JM. eHealth: extending, enhancing, and evolving health care. Annu Rev Biomed Eng. 2013;15:359–82.
Anstey Watkins JOT, Goudge J, Gomez-Olive FX, Griffiths F. Mobile phone use among patients and health workers to enhance primary healthcare: A qualitative study in rural South Africa. Soc Sci Med. 1982;2018(198):139–47.
Kuntalp M, Akar O. A simple and low-cost Internet-based teleconsultation system that could effectively solve the health care access problems in underserved areas of developing countries. Comput Methods Programs Biomed. 2004;75(2):117–26.
Price M, Yuen EK, Goetter EM, Herbert JD, Forman EM, Acierno R, Ruggiero KJ. mHealth: a mechanism to deliver more accessible, more effective mental health care. Clin Psychol Psychother. 2014;21(5):427–36.
Bashshur RL, Shannon GW, Krupinski EA, Grigsby J, Kvedar JC, Weinstein RS, Sanders JH, Rheuban KS, Nesbitt TS, Alverson DC, et al. National telemedicine initiatives: essential to healthcare reform. Telemed J E Health. 2009;15(6):600–10.
Norton SA, Burdick AE, Phillips CM, Berman B. Teledermatology and underserved populations. Arch Dermatol. 1997;133(2):197–200.
Raza T, Joshi M, Schapira RM, Agha Z. Pulmonary telemedicine–a model to access the subspecialist services in underserved rural areas. Int J Med Informatics. 2009;78(1):53–9.
Shouneez YH. Smartphone hearing screening in mHealth assisted community-based primary care. UPSpace Institutional Repository, Department of Liberary Service. Dissertation (MCommPath)--University of Pretoria. 2016. Available at http://hdl.handle.net/2263/53477 . Accessed 17 Mar 2022.
Marcin JP, Ellis J, Mawis R, Nagrampa E, Nesbitt TS, Dimand RJ. Using telemedicine to provide pediatric subspecialty care to children with special health care needs in an underserved rural community. Pediatrics. 2004;113(1 Pt 1):1–6.
Olu O, Muneene D, Bataringaya JE, Nahimana M-R, Ba H, Turgeon Y, Karamagi HC, Dovlo D. How can digital health technologies contribute to sustainable attainment of universal health coverage in Africa? A perspective. Front Public Health. 2019;7:341.
Ryan MH, Yoder J, Flores SK, Soh J, Vanderbilt AA. Using health information technology to reach patients in underserved communities: A pilot study to help close the gap with health disparities. Global J Health Sci. 2016;8(6):86.
Buckwalter KC, Davis LL, Wakefield BJ, Kienzle MG, Murray MA. Telehealth for elders and their caregivers in rural communities. Fam Community Health. 2002;25(3):31–40.
WHO Regional Committee for Africa. Promoting the role of traditional medicine in health systems: a strategy for the African Region. World Health Organization. Regional Office for Africa. Available at http://www.who.int/iris/handle/10665/95467. .
Mishra SR, Neupane D, Kallestrup P. Integrating complementary and alternative medicine into conventional health care system in developing countries: an example of Amchi. J Evid-Based Complementary Altern Med. 2015;20(1):76–9.
Mbwambo ZH, Mahunnah RL, Kayombo EJ. Traditional health practitioner and the scientist: bridging the gap in contemporary health research in Tanzania. Tanzan Health Res Bull. 2007;9(2):115–20.
Poudyal AK, Jimba M, Murakami I, Silwal RC, Wakai S, Kuratsuji T. A traditional healers’ training model in rural Nepal: strengthening their roles in community health. Trop Med Int Health : TM & IH. 2003;8(10):956–60.
Payyappallimana U. Role of Traditional Medicine in Primary Health Care: An Overview of Perspectives and Challenges. Yokohama J Social Sciences. 2009;14(6):723–43.
Kange’ethe SM. Traditional healers as caregivers to HIV/AIDS clients and other terminally challenged persons in Kanye community home-based care programme (CHBC), Botswana. SAHARA J. 2009;6(2):83–91.
Habtom GK. Integrating traditional medical practice with primary healthcare system in Eritrea. J Complement Integr Med. 2015;12(1):71–87.
Ejaz I, Shaikh BT, Rizvi N. NGOs and government partnership for health systems strengthening: a qualitative study presenting viewpoints of government, NGOs and donors in Pakistan. BMC Health Serv Res. 2011;11(1):1–7.
Wu FS. International non-governmental actors in HIV/AIDS prevention in China. Cell Res. 2005;15(11):919–22.
Biermann O, Eckhardt M, Carlfjord S, Falk M, Forsberg BC. Collaboration between non-governmental organizations and public services in health–a qualitative case study from rural Ecuador. Glob Health Action. 2016;9(1):32237.
Mercer A, Khan MH, Daulatuzzaman M, Reid J. Effectiveness of an NGO primary health care programme in rural Bangladesh: evidence from the management information system. Health Policy Plan. 2004;19(4):187–98.
Baqui AH, Rosecrans AM, Williams EK, Agrawal PK, Ahmed S, Darmstadt GL, Kumar V, Kiran U, Panwar D, Ahuja RC. NGO facilitation of a government community-based maternal and neonatal health programme in rural India: improvements in equity. Health Policy Plan. 2008;23(4):234–43.
Ricca J, Kureshy N, LeBan K, Prosnitz D, Ryan L. Community-based intervention packages facilitated by NGOs demonstrate plausible evidence for child mortality impact. Health Policy Plan. 2014;29(2):204–16.
Ahmed N, DeRoeck D, Sadr-Azodi N. Private sector engagement and contributions to immunisation service delivery and coverage in Sudan. BMJ Glob Health. 2019;4(2):e001414.
Edimond BJ. The Contribution of Non-Governmental Organizations in Delivery of Basic Health Services in Partnership with Local Government. Doctoral Dissertation, Uganda Martyrs University. 2014.
Chand S, Patterson J: Faith-Based Models for Improving Maternal and Newborn Health. IMA World Health and ActionAid International USA, 2007 Available at https://imaworldhealthorg/wp-content/uploads/2014/06/faith_based_models_for_improving_maternal_and_newborn_health.pdf
Magezi V. Churchdriven primary health care: Models for an integrated church and community primary health care in Africa (a case study of the Salvation Army in East Africa). HTS Teologiese Studies/ Theological Studies. 2018;74(2):4365.
Villatoro AP, Dixon E, Mays VM. Faith-based organizations and the Affordable Care Act: Reducing Latino mental health care disparities. Psychol Serv. 2016;13(1):92–104.
Levin J. Faith-based initiatives in health promotion: history, challenges, and current partnerships. American journal of health promotion : AJHP. 2014;28(3):139–41.
Green A, Shaw J, Dimmock F, Conn C. A shared mission? Changing relationships between government and church health services in Africa. Int J Health Plann Manage. 2002;17(4):333–53.
Bandy G, Crouch A. Building from common foundations : the World Health Organization and faith-based organizations in primary healthcare. World Health Organization; 2008. Available at https://apps.who.int/iris/handle/10665/43884 . Accessed 16 Mar 2022.
Zahnd WE, Jenkins WD, Shackelford J, Lobb R, Sanders J, Bailey A. Rural cancer screening and faith community nursing in the era of the Affordable Care Act. J Health Care Poor Underserved. 2018;29(1):71–80.
Wagle K. Primary Health Care (PHC): History, Principles, Pillars, Elements & Challenges. Global Health, 2020. Available at https://www.publichealthnotes.com/primary-health-care-phc-history-principles-pillars-elements-challenges/ . Accessed 4 June 2022.
Bhatt J, Bathija P. Ensuring access to quality health care in vulnerable communities. Acad Med. 2018;93(9):1271.
Arvey SR, Fernandez ME. Identifying the core elements of effective community health worker programs: a research agenda. Am J Public Health. 2012;102(9):1633–7.
Pennel CL, McLeroy KR, Burdine JN, Matarrita-Cascante D, Wang J. Community health needs assessment: potential for population health improvement. Popul Health Manag. 2016;19(3):178–86.
Chudgar RB, Shirey LA, Sznycer-Taub M, Read R, Pearson RL, Erwin PC. Local health department and academic institution linkages for community health assessment and improvement processes: a national overview and local case study. J Public Health Manag Pract. 2014;20(3):349–55.
Desta FA, Shifa GT, Dagoye DW, Carr C, Van Roosmalen J, Stekelenburg J, Nedi AB, Kols A, Kim YM. Identifying gaps in the practices of rural health extension workers in Ethiopia: a task analysis study. BMC Health Serv Res. 2017;17(1):1–9.
Lehmann U, Sanders D. Community health workers: what do we know about them. The state of the evidence on programmes, activities, costs and impact on health outcomes of using community health workers Geneva: World Health Organization; 2007. Available at https://www.hrhresourcecenter.org/node/1587.html . Accessed 17 Mar 2022.
Chen N, Raghavan M, Albert J, McDaniel A, Otiso L, Kintu R, West M, Jacobstein D. The community health systems reform cycle: strengthening the integration of community health worker programs through an institutional reform perspective. Global Health: Sci Practice. 2021;9(Supplement 1):S32–46.
Roser M, Ortiz-Ospina E: Global rise of education. Our World in Data 2017. Available at https://ourworldindata.org/global-rise-of-education . Accessed on 29 May 2019.
Santelli J, Morreale M, Wigton A, Grason H. School health centers and primary care for adolescents: a review of the literature. J Adolesc Health. 1996;18(5):357–66.
Wade TJ, Mansour ME, Guo JJ, Huentelman T, Line K, Keller KN. Access and utilization patterns of school-based health centers at urban and rural elementary and middle schools. Public Health Reports. 2008;123(6):739–50.
Johnson I, Hunter L, Chestnutt IG. Undergraduate students’ experiences of outreach placements in dental secondary care settings. Eur J Dent Educ. 2012;16(4):213–7.
Ndira S, Ssebadduka D, Niyonzima N, Sewankambo N, Royall J. Tackling malaria, village by village: a report on a concerted information intervention by medical students and the community in Mifumi Eastern Uganda. Afr Health Sci. 2014;14(4):882–8.
Frakes K-a, Brownie S, Davies L, Thomas JB, Miller M-E, Tyack Z. Capricornia Allied Health Partnership (CAHP): a case study of an innovative model of care addressing chronic disease through a regional student-assisted clinic. Aust Health Rev. 2014;38(5):483–6.
Frakes KA, Brownie S, Davies L, Thomas J, Miller ME, Tyack Z. The sociodemographic and health-related characteristics of a regional population with chronic disease at an interprofessional student-assisted clinic in Q ueensland C apricornia A llied H ealth P artnership. Aust J Rural Health. 2013;21(2):97–104.
Frakes K-A, Tyzack Z, Miller M, Davies L, Swanston A, Brownie S. The Capricornia Project: Developing and implementing an interprofessional student-assisted allied health clinic. 2011.
Frakes K-A, Brownie S, Davies L, Thomas J, Miller M-E, Tyack Z. Experiences from an interprofessional student-assisted chronic disease clinic. J Interprof Care. 2014;28(6):573–5.
Schutte T, Tichelaar J, Dekker RS, van Agtmael MA, de Vries TP, Richir MC. Learning in student-run clinics: A systematic review. Med Educ. 2015;49(3):249–63.
Paim J, Travassos C, Almeida C, Bahia L, Macinko J. The Brazilian health system: history, advances, and challenges. The Lancet. 2011;377(9779):1778–97.
Rocha R, Soares RR. Evaluating the impact of community-based health interventions: evidence from Brazil’s Family Health Program. Health Econ. 2010;19(S1):126–58.
Rasella D, Harhay MO, Pamponet ML, Aquino R, Barreto ML. Impact of primary health care on mortality from heart and cerebrovascular diseases in Brazil: a nationwide analysis of longitudinal data. BMJ (Clinical research ed). 2014;349:g4014.
Harris M. Brazil’s Family Health Programme: A cost effective success that higher income countries could learn from. BMJ: Br Med J. 2010;341(7784):1171–2.
Starfield B. Is primary care essential? The lancet. 1994;344(8930):1129–33.
Donfouet HPP, Mahieu P-A. Community-based health insurance and social capital: a review. Heal Econ Rev. 2012;2(1):1–5.
Zhang L, Wang H, Wang L, Hsiao W. Social capital and farmer’s willingness-to-join a newly established community-based health insurance in rural China. Health Policy. 2006;76(2):233–42.
Donfouet HPP. Essombè J-RE, Mahieu P-A, Malin E: Social capital and willingness-to-pay for community-based health insurance in rural Cameroon. Global J Health Sci. 2011;3(1):142.
Grunau J. Exploring people’s motivation to join or not to join the community-based health insurance’Sina Passenang’in Sotouboua, Togo. 2013.
Gitahi JW. Innovative Healthcare Financing and Equity through Community Based Health Insurance Schemes (CBHHIS) In Kenya. United States International University-Africa Digital Repository. Available at http://erepo.usiu.ac.ke/11732/3654 . Accessed 18 May 2022.
Carrin G, Waelkens MP, Criel B. Community-based health insurance in developing countries: a study of its contribution to the performance of health financing systems. Tropical Med Int Health. 2005;10(8):799–811.
Umeh CA, Feeley FG. Inequitable access to health care by the poor in community-based health insurance programs: a review of studies from low-and middle-income countries. Global Health: Science And Practice. 2017;5(2):299–314.
Odebiyi AI. Western trained nurses’ assessment of the different categories of traditional healers in southwestern Nigeria. Int J Nurs Stud. 1990;27(4):333–42.
Abdullahi AA. Trends and challenges of traditional medicine in Africa. Afr J Tradit Complement Altern Med : AJTCAM. 2011;8(5 Suppl):115–23.
Taye OR. Yoruba Traditional Medicine and the Challenge of Integration. The J Pan Afr Studies. 2009;3(3):73–90.
Konadu K. Medicine and Anthropology in Twentieth Century Africa: Akan Medicine and Encounters with (Medical) Anthropology. African Studies Quarterly. 2008;10(2 & 3).
Benzie IF, Wachtel-Galor S: Herbal medicine: biomolecular and clinical aspects. 2nd Ed. 2011. Available at https://www.crcpress.com/Herbal-Medicine-Biomolecular-and-Clinical-Aspects-Second-Edition/Benzie-Wachtel-Galor/p/book/9781439807132 . Accessed 21 May 2022.
Ejughemre U. Donor support and the impacts on health system strengthening in sub-saharan africa: assessing the evidence through a review of the literature. Am J Public Health Res. 2013;1(7):146–51.
Seppey M, Ridde V, Touré L, Coulibaly A. Donor-funded project’s sustainability assessment: a qualitative case study of a results-based financing pilot in Koulikoro region. Mali Globalization and health. 2017;13(1):1–15.
Shaw RP, Wang H, Kress D, Hovig D. Donor and domestic financing of primary health care in low income countries. Health Systems & Reform. 2015;1(1):72–88.
Gotsadze G, Chikovani I, Sulaberidze L, Gotsadze T, Goguadze K, Tavanxhi N. The challenges of transition from donor-funded programs: results from a theory-driven multi-country comparative case study of programs in Eastern Europe and Central Asia supported by the Global Fund. Global Health: Science and Practice. 2019;7(2):258–72.
Ascroft J, Sweeney R, Samei M, Semos I, Morgan C. Strengthening church and government partnerships for primary health care delivery in Papua New Guinea: Lessons from the international experience. Health policy and health finance knowledge hub Working paper series. 2011(16).
Campbell MK, Hudson MA, Resnicow K, Blakeney N, Paxton A, Baskin M. Church-based health promotion interventions: evidence and lessons learned. Annu Rev Public Health. 2007;28:213–34.
Olivier J, Wodon Q. The role of faith-inspired health care providers in Sub-Saharan Africa and public private partnerships: Strengthening the Evidence for faith-inspired health engagement in Africa, Volume 1. Health, Nutrition and Population (HNP) Discussion Paper Series 76223v1. Available at https://documents1.worldbank.org/curated/en/851911468203673017 . Accessed 20 May 2022.
Schumann C, Stroppa A, Moreira-Almeida A. The contribution of faith-based health organisations to public health. Int Psychiatry. 2011;8(3):62–4.
Download references
Acknowledgements
The author would like to thank IPHC- E for funding this review.
This review was funded by International Institute for Primary Health Care- Ethiopia (IPHC- E).
Author information
Authors and affiliations.
Department of Environmental and Occupational Health and Safety, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Zemichael Gizaw
International Institute for Primary Health Care- Ethiopia, Ethiopian Public Health Institute, Addis Ababa, Ethiopia
Tigist Astale & Getnet Mitike Kassie
You can also search for this author in PubMed Google Scholar
Contributions
ZG prepared the manuscript. TA and GMK critically reviewed the protocol and manuscript. All the authors read and approved the final manuscript.
Corresponding author
Correspondence to Zemichael Gizaw .
Ethics declarations
Ethics approval and consent to participate.
Systematic review does not required ethics approval.
Consent for publication
This manuscript does not contain any individual person’s data.
Competing interests
The authors declared that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: .
Searchstrategy. MEDLINE (PubMed).
Additional file 2: Appendix 2: Table A1.
Description of full-text articles which discussed community health programs or community-directed interventions as a strategy to improve PHC service delivery in ruralcommunities.
Additional file 3:
Appendix 3: Table A2. Description of full-text articles which discussed school-based healthcareservices as a strategy to improve PHCservice delivery in rural communities.
Additional file 4:
Appendix 4: Table A3. Description of full-text articles which discussed student-led healthcareservices as a strategy to improve PHC service delivery in ruralcommunities.
Additional file 5: Appendix 5: Table A4
. Descriptionof full-text articles which discussed outreach services or mobile clinics as astrategy to improve PHC service delivery in ruralcommunities.
Additional file 6:
Appendix 6: Table A5. Description of full-text articles which discussed family health program as astrategy to improve PHC service delivery in rural,communities.
Additional file 7:
Appendix 7: Table A6. Description of full-text articles whichdiscussed empanelment as a strategy to improve PHC service delivery in ruralcommunities.

Additional file 8:
Appendix 9: Table A8. Description of full-text articles which discussed telemedicine or mobile healthas a strategy to improve PHC service delivery in ruralcommunities.
Additional file 9:
Appendix 8: Table A7. Description of full-text articles which discussed community health funding schemes as a strategy to improve PHC service delivery in ruralcommunities.
Additional file 10:
Appendix 10: Table A9. Description of full-text articles which discussed promoting the role of workingwith traditional healers as a strategy toimprove PHC service delivery in rural communities.
Additional file 11:
Appendix 11: Table A10. Description of full-text articles which discussed working with non-profitprivate sectors and non-governmental organizations as a strategy to improve PHC service delivery in rural communities.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Gizaw, Z., Astale, T. & Kassie, G.M. What improves access to primary healthcare services in rural communities? A systematic review. BMC Prim. Care 23 , 313 (2022). https://doi.org/10.1186/s12875-022-01919-0
Download citation
Received : 09 August 2022
Accepted : 18 November 2022
Published : 06 December 2022
DOI : https://doi.org/10.1186/s12875-022-01919-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Access to PHC services
- Rural communities
- Key strategies to improve access to PHC services
BMC Primary Care
ISSN: 2731-4553
- General enquiries: [email protected]
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Study Protocol
The role of advanced practice nurses in improving healthcare outcomes for patients with chronic kidney disease: A scoping review protocol
Roles Conceptualization, Data curation, Investigation, Methodology, Project administration, Writing – original draft
* E-mail: [email protected]
Affiliation Department of Nursing, Yamagata Tokushukai Hospital, Yamagata, Yamagata, Japan
Roles Conceptualization, Formal analysis, Investigation, Methodology, Writing – original draft
Affiliation Graduate School of Medicine, Nagoya University, Nagoya, Aichi, Japan
Roles Conceptualization, Supervision, Writing – review & editing
Affiliation Graduate School of Health and Environment Sciences, Tohoku Bunka Gakuen University, Sendai, Miyagi, Japan
Contributed equally to this work with: Tomoko Araki, Hidetaka Sato, Takao Watanabe
Roles Supervision, Writing – review & editing
Affiliation Department of Urology, Yamagata Tokushukai Hospital, Yamagata, Yamagata, Japan
- Hanako Nozu,
- Haruka Tamura,
- Takemi Kudo,
- Tomoko Araki,
- Hidetaka Sato,
- Takao Watanabe,
- Isoji Sasagawa

- Published: April 4, 2024
- https://doi.org/10.1371/journal.pone.0301676
- Reader Comments
Introduction
The number of patients with chronic kidney disease is increasing worldwide; previous studies have suggested that advanced practice nurses, including nurse practitioners and clinical nurse specialists, with expert practice skills can provide high-quality care and solve complex healthcare problems. In general, nurse practitioners are generalist nurses who work as autonomous clinicians with whole personal care. Clinical nurse specialists, in contrast, are nurses with advanced nursing knowledge and skills for individuals or specific populations. Their roles are independent and different; however, similarities exist in their role in potentially improving healthcare outcomes. Although two previous studies described the role of nephrology nurse practitioners, they were systematic reviews, and their outcomes were limited. To clarify the overall aspect of advanced practice nurses’ role, it is necessary to extract the studies illustrating advanced practice nurses’ practices for patients with chronic kidney disease.
This study aims to map the literature describing the role of advanced practice nurses in improving healthcare outcomes for patients with chronic kidney disease.
Materials and methods
This scoping review will be conducted using the Joanna Briggs Institute methodology for scoping review. Online databases will be searched across MEDLINE (PubMed), CINAHL (EBSCOhost), Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials, and Web of Science. Only studies published in English will be included, and no date limit will be set. Chronic kidney disease, renal replacement therapy, and advanced practice nurses as keywords and related search terms will be used. Two independent reviewers will screen the title and abstract/full-text; in case of discrepancy, a third reviewer will make the final decision. The results will be extracted and presented following the review question concerning the study characteristics, patients’ characteristics, condition of chronic kidney disease, and role of advanced practice nurses.
Citation: Nozu H, Tamura H, Kudo T, Araki T, Sato H, Watanabe T, et al. (2024) The role of advanced practice nurses in improving healthcare outcomes for patients with chronic kidney disease: A scoping review protocol. PLoS ONE 19(4): e0301676. https://doi.org/10.1371/journal.pone.0301676
Editor: Udoka Okpalauwaekwe, University of Saskatchewan, CANADA
Received: June 9, 2023; Accepted: March 15, 2024; Published: April 4, 2024
Copyright: © 2024 Nozu et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: Data sharing not applicable as no datasets generated and/or analyzed for this protocol.
Funding: The funders did not and will not have a role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: The authors have declared that no competing interests exist.
The prevalence of all stages of chronic kidney disease (CKD) in the general population is 9–15% [ 1 , 2 ]. According to the report of the Global Burden of Disease, the global prevalence of CKD at all ages has increased by 29.3% (95% UI 26.4 to 32.6) from 1990 to 2017 [ 1 ]. CKD is a progressive chronic disease; if patients have multiple comorbidities that progress to renal dysfunction, the status of the kidney progresses more rapidly [ 3 , 4 ]. When the kidneys function inefficiently, waste products and extra fluid accumulate in the body, resulting in a myriad of health problems, including cardiac disease and hypertension [ 5 ]. The incidence rate of treated end-stage renal disease (ESRD) is relatively stable, has decreased or increased slightly in some high-income countries, but has increased substantially in others, with a global trend [ 6 ]. ESRD negatively affects patients’ quality of life [ 7 , 8 ], leading to increased hospitalization and mortality [ 9 ]. It is important that patients with CKD, which is a chronic disease, maintain their daily life and quality of life while controlling complications and receiving necessary treatment; however, to accomplish these tasks, high-quality care is required.
Advanced practice nurses (APNs) are expected to provide a high level of care and be able to cope with the complexity of the problem. APNs, such as nurse practitioners (NPs) and clinical nurse specialists (CNSs), are the most common. The International Council of Nursing describes APNs as “a generalist or specialized nurse who has acquired, through additional graduate education (at least a master’s degree), the expert knowledge base, complex decision-making skills, and clinical competencies for advanced nursing practice [ 10 ]. NPs have provided primary, acute, and specialty healthcare to a diverse group of patients of all ages for nearly half a century [ 11 ]. The NP education program was established at the University of Colorado in 1965 to increase the primary care workforce and integrate the content into a nursing master’s program [ 12 ]. Conversely, the pioneer CNS program was developed in 1956 by Hildegard Peplau in the United States [ 13 – 15 ]. CNSs are expert clinicians focused on a specialist area and provide high-quality care with clinical excellence in multiple healthcare settings [ 10 , 14 ]. NPs and CNSs have autonomy and perform different functions, but they share the core of advanced practice competencies and provide high-quality care [ 16 , 17 ]. Both have overlapping roles in the clinical setting and contribute to solving complex patient problems as APNs [ 18 – 20 ]. In recent years, APNs have spread and developed worldwide [ 21 ].
In the nephrology setting, APNs have also provided high-level care for patients with CKD. In the United States, the presence of nephrology APNs in dialysis units was first reported in 1976 [ 22 ]. In the early 2000s, some literature described the role of nephrology APNs and showed their practice [ 23 – 25 ]. Nowadays, nephrology APNs have contributed to improving the healthcare outcomes of patients with all CKD stages who are not yet on dialysis [ 26 – 28 ], are on dialysis [ 29 , 30 ], or are pre- or post-kidney transplant [ 31 , 32 ]. We believe it is worthwhile to identify and present such cumulative practice of nephrology APNs. This is because nephrology APNs may have the opportunity to access and share knowledge regarding their roles that they may not be aware of. Of these roles, improving healthcare outcomes for patients with CKD is directly linked to promoting their well-being.
We have identified two systematic reviews that have been done on similar topics [ 33 , 34 ]. Xu et al. compared nurse- and physician-led care for patients with CKD. This meta-analysis showed that a nurse-coordinated care model reduced the risks of composite outcomes, including death, the occurrence rate of end-stage renal disease, and doubled serum creatinine [ 33 ]. McCrory et al. reported the outcomes of patients with CKD stages 2–4, where NPs were the primary workforce. The results of this review reported that NPs provided care equal to or superior to that of physicians in terms of blood pressure control, low-density lipoprotein, phosphate, and parathormone levels, as well as glycemic control [ 34 ]. NPs did do additional roles under the indirect supervision of a nephrologist in these studies. However, there are a few limitations to these studies. First, because the systematic review was intended to integrate previous research and specific conditions with strict eligibility criteria, the role of APNs for patients on peritoneal dialysis and pre- or post- kidney transplant was excluded. Second, only the NP-level nursing care providers were included in the studies. Then, we cannot view the practice of CNS-level nursing. We consider that there are some gaps in these reviews to describe the role of APNs in improving the healthcare outcomes for CKD. As such, we considered a scoping review to be an appropriate method to research this topic, as it deals with a wide range of subjects and allows better identification of gaps in the current literature. In addition, the results of this scoping review will help APNs access the literature describing their role in nephrology.
Review question
What is the role of APNs that could improve healthcare outcomes for patients with CKD, and what are their outcomes?
This study aims to map the literature describing the role of APNs in improving healthcare outcomes of patients with CKD. This scoping review will be conducted by the Joanna Briggs Institute (JBI) methodology for scoping reviews [ 35 ]. The eligibility criteria for study selection are described in terms of participants, concept, context (PCC) framework, and type of sources following JBI methods. The study protocol is reported in accordance with Preferred Reporting Items for Systematic Review and Meta-analysis Protocols (PRISMA-P) ( S1 Checklist ) [ 36 ]. In addition, we will use the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) ( S2 Checklist ) [ 37 , 38 ] to ensure that this scoping review complies with the scoping review guidelines.
Eligibility criteria
Participants..
The review will consider all literature that includes patients aged >18 years with all stages of CKD and describe improved healthcare outcomes after receiving some care from APNs. We will include patients with ESRD receiving any type of renal replacement therapy and include studies of conservative therapy for ESRD, if available. Renal transplantation therapy will be also included in this scoping review.
APNs are “a generalist or specialized nurse who has acquired, through additional graduate education (at least a master’s degree), the expert knowledge base, complex decision-making skills, and clinical competencies for advanced nursing practice.” Globally, the most common APNs are NPs and CNSs [ 10 ]. The title of APNs, including NPs/CNSs, differs from each country: advanced practice registered nurse, specialist nurse, nurse clinician, etc [ 18 , 21 ]. Additionally, the definition of APNs varies from country to country, but generally, the education is at the master’s level or higher [ 18 , 21 ]. In this study, we used education at the master’s level or higher as the basis for APNs. For these reasons, the definition of APNs in this study emphasizes concepts rather than titles.
The review will include literature wherein patients received care from APNs in collaboration with specialists in other disciplines.
Our review will provide an overview of the role of nephrology APNs in improving healthcare outcomes for CKD. The role of APNs includes direct care and indirect care; ordering, performing, supervising, and interpreting diagnostic and laboratory tests; making diagnoses; initiating and managing treatment, including prescribing medication and non-pharmacologic treatments; coordinating care; counseling; and educating patients, but not limited to [ 10 , 11 ]. It could also include demonstrating leadership and establishing health care services [ 10 ]. We assume that some of the studies that will be screened in our review will not have improved healthcare outcomes significantly. However, it is considered the studies that have not improved healthcare outcomes also have very important findings for APNs. Therefore, we will exclude these studies but will summarize them as appendixes.
The review will consider studies conducted in any facility and country. We will consider studies conducted in institutional and non-institutional settings, including hospitals, public or private community clinics, long-term care facilities, and home care.
Types of sources
This scoping review will consider experimental and quasi-experimental study designs, including randomized controlled trials, non-randomized controlled trials, before and after studies, and interrupted time-series studies. Additionally, analytical observational studies, including prospective and retrospective cohort, case-control, and analytical cross-sectional studies, will be considered for inclusion. Finally, this review will consider descriptive observational study designs, including case series, individual case reports, and descriptive cross-sectional studies but not limited to. Qualitative studies will also be considered if they focus on data including, but not limited to, designs, such as phenomenology, grounded theory, ethnography, qualitative description, and action research. Systematic reviews, meta-analysis, and trial protocols will be excluded. However, references cited in systematic reviews will be deemed suitable for inclusion.
Gray literature and unpublished studies will also be included. However, text and opinion papers will not be considered for inclusion in this scoping review.
Search strategy
To provide a comprehensive and up-to-date search, a preliminary search of existing systematic reviews about this topic was conducted using the MEDLINE, CINAHL, and Cochrane Database of Systematic Reviews databases on February 20, 2024.
The search strategy will aim to locate both published and unpublished studies. A three-step search will be utilized for each component of this review [ 35 ].
An initial limited search of MEDLINE (via PubMed) and CINAHL (via EBSCOhost) will be performed to identify articles on the topic. Thereafter, the words in the titles and abstracts of the relevant articles and the index terms used to describe the articles will be used to develop a complete search strategy. This search strategy will be adapted for each information source, including all the identified keywords and index terms.
A second search using all identified keywords and index terms will be performed across all included databases. An example of a search strategy conducted by MEDLINE (via PubMed) on February 26, 2024, is shown in S1 Table . The databases to be searched will include MEDLINE (via PubMed) and CINAHL (via EBSCOhost), Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials (CENTRAL; via EBSCOhost), and Web of Science. Databases of gray literature include ProQuest and the first 300 hits on Google Scholar because our initial search results indicate that approximately 300 papers will be suitable for the present study [ 39 ]. We will deal with unpublished studies as well; ongoing studies or completed but unpublished studies. The Cochrane Handbook for Systematic Reviews of Interventions recommends using the Trial Registry database as a search strategy for these unpublished studies. Therefore, ClinicalTrials gov. and the International Clinical Trials Registry Platform will be used as our search strategy for unpublished studies.
Third, the reference lists of all the identified reports and articles selected for this scoping review will be screened for additional studies.
Only articles published in English will be included because of the lack of translation services.
When noting missing data or poorly reported items, we aim to contact the author by e-mail, which is considered the most efficient tool [ 40 , 41 ], upon checking the contact information listed in the eligible study or most recent study. Depending on the case, we may consider contacting the authors’ affiliation. We will continue to contact the authors until the completion of the analysis of our scoping review [ 40 , 41 ].
Study/Source of evidence selection
Following the search, all identified citations will be collated and uploaded into Mendeley V1.19.8 (Mendeley Ltd., Elsevier, Netherlands), and duplicates will be removed. Following a pilot test, titles and abstracts will be screened by two or more independent reviewers to assess whether they meet the inclusion criteria for the review. Potentially relevant sources will be retrieved, and their citation details will be imported into the JBI System for the Unified Management, Assessment, and Review of Information (JBI SUMARI; JBI, Adelaide, Australia). The full texts of the selected citations will be assessed in detail against the inclusion criteria by two independent reviewers. This scoping review will record and report reasons for excluding sources of evidence that do not meet the inclusion criteria in the full text. Any disagreements that arise between the reviewers at each stage of the selection process will be resolved through discussion; if there is a difference in opinion, the decision of a third reviewer will be final.
The search results and study inclusion process will be reported in full in the final scoping review and presented in a PRISMA-ScR flow diagram [ 37 ].
Data extraction
Data will be extracted from the papers included in the review using a charting table aligned by two independent reviewers to the objective and question of this research S2 Table , as indicated by the methodology for scoping reviews developed by JBI [ 35 ]. We will extract data about; study characteristics (author, publication year, country, study design, main result), patients’ characteristics (sample size, age, location of patient), condition of CKD (CKD stages of patient, Renal Replacement Therapy type), the role of APNs (title of APNs, types of healthcare provider, characteristics of APNs roles. The draft data extraction tool will be modified and revised as necessary while extracting data from the included sources. The modifications are detailed in this scoping review. Any reviewer disagreements will be resolved through discussion or by a third reviewer.
Data analysis and presentation
The overview of the reviewed material, where possible and appropriate, will be presented in tabular form along with a narrative summary that aligns with the objectives and scope of this review. A descriptive summary will accompany the tabulated and charted results and describe how the results relate to the review’s objectives and questions. A summary of each article will include the author(s) name, year of publication, country of origin, population, sample size, methodology, concepts of interest, and key findings related to the scoping review question.
CKD is a common chronic disease, and healthcare providers must provide appropriate care. It is expected that advanced practice nursing will solve complex matters for CKD. APNs have provided high-quality care and accumulated evidence by researching and reporting their own practices. We suggest extracting the literature on the role of nephrology APNs in improving healthcare outcomes for all stages of CKD. The results of this scoping review will help nephrology APNs develop their role and identify new gaps in unreported areas.
There is no common understanding of the role of APNs because their scope of practice differs in different countries [ 42 – 44 ]. It is difficult to synthesize these differences in this scoping review. However, we believe that to map this heterogeneous literature, a scoping review is the best method. The methods used in this scoping review protocol are based on the JBI methodology for scoping reviews. In addition, PRISMA-P and PRISMA-ScR were used to ensure that this Scoping review is in accordance with these guidelines. We consider this a methodological limitation because the search strategy may not fully cover all publications and is limited by language and databases. Additionally, the scope of APNs practice in each country is different; hence, the results we are trying to show in this study may not be directly applicable.
Supporting information
S1 checklist. prisma-p 2015 checklist..
https://doi.org/10.1371/journal.pone.0301676.s001
S2 Checklist. PRISMA-ScR 2018 checklist.
https://doi.org/10.1371/journal.pone.0301676.s002
S1 Table. Search strategies.
https://doi.org/10.1371/journal.pone.0301676.s003
S2 Table. Data extraction.
https://doi.org/10.1371/journal.pone.0301676.s004
Acknowledgments
We thank Editage ( www.editage.jp ) for English-language editing.
- View Article
- PubMed/NCBI
- Google Scholar
- 10. International Council of Nurses. Guidelines on advanced practice nursing 2020. 2020. https://npac-aiipc.org/wp-content/uploads/2020/07/ICN_APN-Report-EN.pdf .
- 11. American Association of Nurse Practitioners. All About NPs. https://www.aanp.org/about/all-about-nps .
- 38. Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D et al. PRISMA-ScR CHECKLIST ITEMS. 2019;11–12. http://www.prisma-statement.org/documents/PRISMA-ScR Fillable Checklist.pdf .
- 41. Cochrane Handbook for Systematic Reviews of Interventions Version 6.4, 2023 [Internet]. https://training.cochrane.org/handbook/current .
- Open access
- Published: 01 December 2023
Compassion fatigue in healthcare providers: a scoping review
- Anna Garnett 1 ,
- Lucy Hui 2 ,
- Christina Oleynikov 1 &
- Sheila Boamah 3
BMC Health Services Research volume 23 , Article number: 1336 ( 2023 ) Cite this article
2539 Accesses
2 Altmetric
Metrics details
The detrimental impacts of COVID-19 on healthcare providers’ psychological health and well-being continue to affect their professional roles and activities, leading to compassion fatigue. The purpose of this review was to identify and summarize published literature on compassion fatigue among healthcare providers and its impact on patient care. Six databases were searched: MEDLINE (Ovid), PsycINFO (Ovid), Embase (Ovid), CINAHL, Scopus, Web of Science, for studies on compassion fatigue in healthcare providers, published in English from the peak of the pandemic in 2020 to 2023. To expand the search, reference lists of included studies were hand searched to locate additional relevant studies. The studies primarily focused on nurses, physicians, and other allied health professionals. This scoping review was registered on Open Science Framework (OSF), using the Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) extension to scoping review. From 11,715 search results, 24 met the inclusion criteria. Findings are presented using four themes: prevalence of compassion fatigue; antecedents of compassion fatigue; consequences of compassion fatigue; and interventions to address compassion fatigue. The potential antecedents of compassion fatigue are grouped under individual-, organization-, and systems-level factors. Our findings suggest that healthcare providers differ in risk for developing compassion fatigue in a country-dependent manner. Interventions such as increasing available personnel helped to minimize the occurrence of compassion fatigue. This scoping review offers important insight on the common causes and potential risks for compassion fatigue among healthcare providers and identifies potential strategies to support healthcare providers’ psychological health and well-being.
• What do we already know about this topic? The elevated and persistent mental stress associated with the COVID-19 pandemic predisposed healthcare providers (HCP) to various psychological conditions such as compassion fatigue. Declines in health providers’ mental health has been observed to negatively impact their professional performance and the quality of patient care.
• How does your research contribute to the field? This review provides an overview of the prevalence of compassion fatigue among HCPs across the globe during the COVID-19 pandemic. The main risk factors for compassion fatigue include younger age, female sex, being either a physician or a nurse, high workload, extensive work hours, and limited access to personal protective equipment (PPE). Negative behavioral intention towards patients has been identified to be a consequence of compassion fatigue. Interventions such as the provision of emotional support, increased monitoring for conditions such as stress and burnout, and increasing available personnel helped to minimize the occurrence of compassion fatigue.
• What are your research’s implications towards theory, practice, or policy? While the public health emergency associated with the COVID-19 pandemic has ended, the impact on human health resources persists. The findings of this review can inform policy decisions and implementation of evidence-based strategies to prevent, manage, and lessen the negative effects of compassion fatigue on HCPs and its subsequent impacts on patient care.
Peer Review reports
Introduction
The 2019-novel coronavirus disease (COVID-19) outbreak spread rapidly and by January 30 th , 2022 was formally proclaimed a global health emergency despite being first identified just over a month prior [ 1 ]. Although there have been five other global health emergencies associated with disease outbreaks since 2009, none has matched the scale and scope of the COVID-19 pandemic [ 2 ]. In the short-term the rapid increase in patients requiring acute care services presented unprecedented challenges for health systems. Care provision and infection control strategies were hampered by capacity limitations, staffing shortfalls and supply chain challenges [ 3 ]. As a result, healthcare providers (HCPs) encountered mounting levels of strain which have continued with little reprieve for the duration of and beyond the global COVID-19 pandemic. Limited access to personal protective equipment (PPEs) exacerbated transmission of the virus, compounding healthcare providers’ fears of contracting and spreading COVID-19 among their peers, patients and families [ 4 , 5 , 6 , 7 ]. HCPs also contracted COVID-19, became seriously ill and died with global estimates of HCP death between January 2020 and May 2021 being over 100,000. With time, the number of absences, extended sick leaves and staff turnovers increased [ 7 , 8 ]. The combination of short staffing, frequent changes to workflow and continuous care provision to patients who were gravely ill and had high mortality amplified the toll on health care providers [ 8 , 9 ]. While no longer a global health emergency, there continue to be COVID-19 cases and deaths. As of July 14, 2023 there were 767,972,961 COVID-19 cases and 6,950,655 deaths globally [ 10 ].
HCPs around the globe who treated severe COVID-19 cases, a process which necessitated in-depth compassionate engagement, became vulnerable to developing compassion fatigue as a result of their continued and in-depth involvement in the care of these severely ill patients and their families [ 11 ]. Compassion fatigue is defined as a composite of two measurements: burnout (sustained employment-related stress that compromises an individual’s desire to work) and secondary trauma (the development of traumatic symptoms resulting from the protracted exposure to the suffering of others) [ 12 , 13 ]. An individual experiencing compassion fatigue has a reduced ability for showing compassion to others, resulting from the prolonged exposure to witnessing the suffering of others without being able to relieve one’s anguish despite having the desire to do so [ 9 ]. Individuals experiencing compassion fatigue may express a range of behaviors such as increased work absences or declines in the ability to engage in work-related tasks such as decision-making. Burnout and secondary trauma are suggested to be mediated by compassion satisfaction—the pleasure that comes from helping behavior [ 11 , 12 ].
As the pandemic shifts from being a global health emergency to an endemic disease, there continues to be concern for HCP health and well-being [ 14 , 15 , 16 ]. The increased and chronic nature of the stress experienced during and beyond the COVID-19 pandemic has heightened HCPs risk for a range of negative psychological impacts such as depression, fearfulness, grief and post-traumatic stress disorder (PTSD) [ 17 ]. Prior infectious disease outbreaks (SARS-CoV-1, H1N1, MERS-CoV, Ebola) are also associated with an increased prevalence of declining mental health in HCPs [ 18 ]. A growing body of research on the COVID-19 pandemic highlights the range of psychological symptoms HCPs developed following their sustained exposure to COVID-19 including burnout, feelings of isolation, insomnia, grief, emotional exhaustion, depression, post-traumatic stress and depersonalization, some of which have persisted over time [ 14 , 17 , 19 , 20 , 21 , 22 ]. The consequences of HCPs’ declining psychological health and well-being has had impacts on the quality of patient care and indirectly on patient outcomes through inadequate staffing [ 18 ]. Compromises in HCPs’ ability to provide optimal clinical care can have serious consequences, including the worsening of patient conditions and the increased transmission of the infection from patients to others in the hospital [ 18 ]. In addition, compassion fatigue may be exacerbated by the COVID-19 pandemic, potentially leading to moral injury, decreased productivity, increased turnover, and reduced quality of care [ 23 ]. Moreover, a growing body of literature suggests that challenges across health systems will persist although COVID-19 is no longer a global health emergency [ 24 , 25 ]. As such, it is important to have a fulsome understanding of COVID-19’s toll on HCPs and tailor health system strategies accordingly.
As health care systems continue to experience a health human resources crisis, it is important to identify and understand the prevalence of compassion fatigue, identify contributing factors, and increase understanding of the consequences and actions that can be taken to address compassion fatigue among HCPs. While there has been in an increase in the body of published literature on the health and well-being of HCPs since the onset of the COVID-19 pandemic, there continues to be a knowledge gap mapping the incidence of compassion fatigue, its resultant impact on HCP well-being, and its potential influence on patient care provision [ 11 , 17 ]. A comprehensive review of the literature on compassion fatigue among HCPs can inform policy and practice initiatives to improve the current health human resources crisis experienced by many health systems. It may also aid in identifying prospective research foci.
The purpose of this scoping review was to synthesize and provide a synopsis of the literature on compassion fatigue among HCPs during the COVID-19 pandemic and to understand its broader impact. The review was guided by the following question: What is the current state of knowledge on compassion fatigue among HCPs over the course of COVID-19?
Project registration
This scoping review was registered under Open Science Framework. A project outline was submitted including the study hypotheses, design, and data collection procedures. The DOI for the registered project is as follows: https://doi.org/10.17605/OSF.IO/F4T7N . In addition, a scoping review protocol for this review has been published in a peer-reviewed journal ( https://doi.org/10.1136/bmjopen-2022-069843 ).
Study design
A systematic scoping review strategy was chosen to explore the existing body of literature pertaining to the research topic. The objective of a scoping review is to identify relevant literature on a given topic, without focusing on evaluating research quality or conducting a thorough analysis of selected studies, as systematic reviews typically do. Current gaps in research and directions for future research can be identified by means of summarizing emerging literature on compassion fatigue in HCPs.
The current scoping review used two methodological tools, namely the Arksey and O’Mally scoping review framework as well as the Joanna Briggs Institute Critical Appraisal Tools. The Arksey and O’Malley framework comprises five stages, which include: (1) formulating the research question; (2) identifying relevant studies; (3) selecting studies for inclusion; (4) extracting and organizing the data; and (5) collating, summarizing, and reporting the findings [ 26 ]. While scoping reviews typically do not require article appraisal, all articles were evaluated by one author (CO) using the methodology established by the Joanna Briggs Institute (JBI) to enhance the overall quality of the review [ 27 ]. No articles were excluded based on their quality, in accord with the Arksey and O’Malley framework [ 26 ].
Stage I: Identifying the research question(s)
The research objective and question were drafted by the authors (AG, LH, CO, SB) and can be found in the previous section under “Research aim”.
Stage II: Identifying relevant studies
As outlined by the JBI methodology, a three-step approach was used to identify relevant studies. These steps include: (1) conducting a preliminary search of at least two suitable databases; (2) identifying relevant keywords and index terms to perform a secondary search across all chosen databases; and (3) manually examining the reference lists of the included articles to discover additional relevant studies [ 28 ] (p11) .
Preliminary literature search
To establish the criteria for inclusion and exclusion, an initial and restricted search was conducted on the subject of interest. The preliminary literature exploration encompassed three scholarly electronic databases: MEDLINE (Ovid), Scopus, and Web of Science. The search employed the keywords “compassion fatigue” and incorporated the timeframe March 1, 2020, to June 15, 2022, so that the most impactful waves of the COVID-19 pandemic were represented in the included literature, resulting in 1519, 2489, and 2246 studies, from the respective databases. These three databases were selected due to their likelihood of yielding results relevant to the research topic. To construct a comprehensive search strategy, a collection of keywords and index terms were identified from the titles and abstracts of relevant articles. The search strategy was further refined in collaboration with a social science librarian.
Structured search strategy
A systematic search was conducted across six scholarly electronic databases: MEDLINE (Ovid), Embase (Ovid), CINAHL, Scopus, and Web of Science. These databases were deliberately chosen to encompass a broad range of relevant findings within the current knowledge landscape regarding the research topic. The systematic search of the literature commenced once the scoping review was peer reviewed and revisions were addressed by the authors. Using the selected vocabulary and Boolean connectors as shown in Table 1 , a string of relevant search terms was developed. The search strategy was adapted accordingly for each individual database (e.g., Medical Subject Headings [MeSH] terms for MEDLINE [Ovid]). In the final stage of the search strategy, the reference lists of all included studies were manually examined to identify additional relevant studies.
Inclusion criteria
The inclusion criteria for this review was formulated using the PCC (Population, Concept, Context) mnemonic developed by JBI (Table 1 ). The participants included in this review were HCPs who were employed across healthcare systems during the COVID-19 pandemic (e.g., physicians, registered nurses, nurse practitioners, physician assistants, and licensed clinical social workers). The concept explored in this review focused on compassion fatigue among HCPs working in healthcare systems during the COVID-19 pandemic. The context of the study encompassed various care settings where HCPs carry out their professional activities across different clinical specialties (e.g., surgery, critical care, palliative care), as well as clinical settings (e.g., inpatient and outpatient). For the purposes of this scoping review, formal healthcare settings were broadly classified as those that provided health services and were situated within and administered by healthcare institutions.
This scoping review only included articles published in English. A time filter was applied to encompass studies conducted between 2020 to 2023, spanning the period from the onset of the COVID-19 pandemic to the present. A range of study designs were included in the review (i.e., experiments, quasi-experimental studies, analytical observational studies, descriptive observational studies, mixed-methods studies, and qualitative studies).
Exclusion criteria
Through the past two decades, compassion fatigue has been defined in different ways, sometimes being considered synonymous with burnout and secondary traumatic stress, or as an outcome resulting from both components [ 12 , 13 ]. Yet recently, it has been suggested that compassion fatigue is a focal concept related to the management of traumatic situations whereas burnout is a general concept that may have multiple contributors [ 26 ]. Due to the conceptual ambiguity surrounding compassion fatigue, articles that solely examine the components of compassion fatigue, such as burnout and secondary trauma, without directly addressing compassion fatigue itself, were excluded from consideration.
Studies that failed to meet the inclusion criteria or lacked full-text availability were excluded from the review. Additionally, editorials, letters to the editor, commentaries, and reviews were also excluded as they did not offer sufficient information for addressing the research questions.
Stage III: Study selection
After the full database searches were conducted, all identified citations were compiled and uploaded into Covidence. Any duplicate citations were automatically excluded.
Three reviewers (LH, CO, AG) independently screened the titles and abstracts of the identified studies to assess their eligibility according to the pre-established inclusion and exclusion criteria. Subsequently, the full texts of 736 selected studies were evaluated to arrive at the final list of articles for data extraction. The reasons for excluding specific studies were documented. Throughout the process, any disagreements that arose at each stage of study selection were resolved through discussions with a third reviewer (AG, SB).
The outcomes of the study selection process were presented in a flow diagram adhering to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for scoping reviews (PRISMA-ScR) guidelines (Fig. 1 ) [ 29 ]. Additionally, all the included studies underwent an assessment of their risk of bias (quality) using established critical appraisal tools from the Joanna Briggs Institute (JBI) for Evidence Synthesis [ 30 ]. Although not mandatory for scoping reviews, appraisals of study quality will contribute to the subsequent implications and future steps stemming from this scoping review [ 31 ]. The JBI provides critical appraisal checklists for various study designs, encompassing experimental, quasi-experimental, randomized controlled trials, observational, and qualitative study designs. One reviewer (CO) conducted the assessments of all the included studies, and a second reviewer (AG) verified the evaluations. Any discrepancies that arose were discussed and resolved in consultation with both reviewers. In line with the methodology of scoping reviews, no studies were excluded based on their quality assessments, ensuring a comprehensive understanding of the current state of the literature on compassion fatigue among HCPs during the COVID-19 pandemic. A summary of the quality assessments were presented in the results section of the review, while the full appraisals can be found in Additional file 1 .
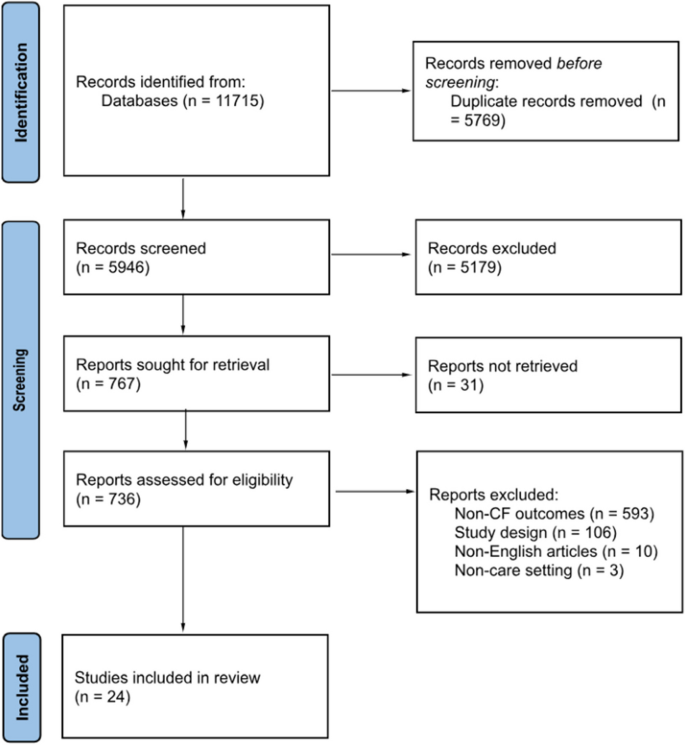
PRISMA flow chart [ 28 ]
Stage IV: Data extraction
To facilitate data extraction aligned with the research objectives, a data-extraction template was developed by one reviewer (LH). This template encompassed various aspects of the included studies (i.e., authors, publication year, study populations, country, study design, aims, sample size, assessment instruments, risk factors, protective factors, consequences of compassion fatigue, and measures to prevent/manage/reduce compassion fatigue). Utilizing Covidence, two independent reviewers (LH, CO) extracted the relevant data from the studies included in the final list of citations.
Stage V: Risk of bias
Standardized tools developed by the Joanna Briggs Institute for respective study types were used to assess risk of bias (quality) for all studies included in the review [ 27 ]. The study appraisals were conducted by one reviewer (CO) and reviewed by another reviewer (AG). Any discrepancies were discussed and resolved together. While no studies were excluded based on the appraisal scores to ensure a comprehensive presentation of the available literature on compassion fatigue among healthcare providers, the findings for the risk of bias assessments are summarized in the results section and the full appraisals are presented in Additional file 1 .
Stage VI: Collating, summarizing, and reporting the results
To summarize and synthesize the findings, the study followed a three-step approach proposed by Levac et al. [ 32 ]: (1) collating and analyzing the collected data; (2) reporting the results and outcomes to address the study objectives; and (3) discussing the potential implications that findings hold for future research and policy considerations [ 31 ]. The review process adhered to the PRISMA Extension for Scoping Reviews checklist, which provided guidance for conducting the review and reporting the findings [ 26 ].
Search results
Figure 1 displays the PRISMA-ScR flowchart of the scoping review search strategy. The search and reference list initially yielded 11,715 studies. Of these, 5769 were excluded as duplicates. Following the title and abstract screening of the remaining studies, 5179 studies were excluded as they met the exclusion criteria. Finally, the full-texts of the remaining 736 studies were screened, and 712 were excluded as they did not meet the inclusion criteria. In total, 24 eligible studies were included in the review for further analysis.
Risk of bias of included studies
The complete assessment of risk of bias of all 24 included studies is available in Additional file 1 . Within the two mixed-methods studies risk of bias primarily stemmed from the quantitative strand of the studies with a lack of clarity provided about study inclusion criteria, study setting, and identification of confounding factors [ 29 ]. Other sources of bias in other quantitative studies were vagueness around the criteria used for outcome measurement [ 30 ] and only one study identified potential cofounding factors along with strategies to manage them [ 31 ]. Further shortcomings related to the failure to provide transparency around the use of valid and reliable outcome measures [ 23 , 31 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 ]. Within qualitative studies not all provided information about the researchers’ theoretical stance [ 29 , 41 , 43 ] and two studies did not provide documentation of ethics approval for the conducted research [ 43 , 44 ]. One included case report met most assessment criteria for risk of bias although more description of assessment, post-assessment condition and adverse events were warranted [ 45 ].
Characteristics of studies
Study characteristics are presented in Table 2 . Of the 24 eligible studies, 18 studies used quantitative methods [ 23 , 30 , 31 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 46 , 47 , 48 , 49 , 50 , 51 ], 3 studies used qualitative methods [ 43 , 44 , 45 ], and the remaining studies used mixed-methods approaches [ 29 , 41 , 52 ]. Additionally, 13 studies focused on the antecedents of compassion fatigue [ 23 , 29 , 33 , 34 , 35 , 36 , 40 , 41 , 42 , 45 , 46 , 47 , 48 ] and 5 studies examined the consequences of compassion fatigue [ 30 , 37 , 43 , 44 , 49 ]. Six studies were conducted in the United States, with the others being conducted in a range of countries including Ecuador, Spain, United Kingdom, Italy, Greece, Turkey, Iran, Uganda, Taiwan, Japan, Philippines, China, and India. These studies primarily focused on nurses, physicians, and other allied health professionals. The study samples included both male and female HCPs. Only one study focused exclusively on female HCPs [ 43 ].
A variety of assessment tools were used to measure compassion fatigue across included studies. Common tools included Compassion Fatigue Short Scale (CFSS) [ 33 , 47 , 48 ], Compassion Fatigue Scale (CFS) [ 30 , 49 ], Professional Quality of Life Scale Version 5 (ProQoL 5) [ 23 , 29 , 29 , 31 , 35 , 36 , 38 , 39 , 40 , 41 , 42 , 50 , 51 ], Work-Related Quality of Life Scale (WRQoL) [ 46 ], and Compassion Fatigue and Satisfaction Self-Test (CFST) [ 37 , 52 ] (Table 3 ).
The time period of the study period shows that most of the studies were conducted in the first six months of 2020, coinciding with the World Health Organization’s declaration of the COVID-19 outbreak as a pandemic [ 54 ]. No studies included in the review were conducted between March 2021 and May 2023 (Fig. 2 ).
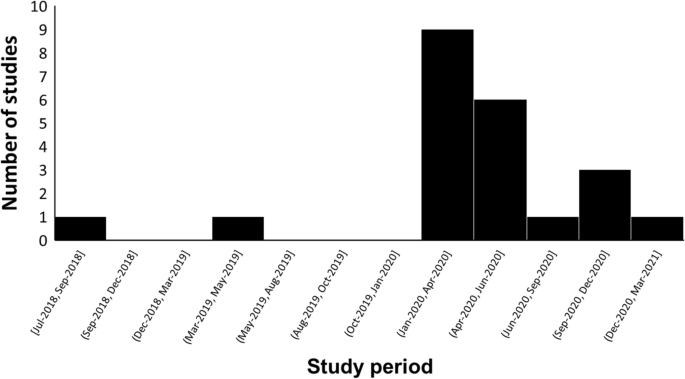
The time trend of study periods on compassion fatigue in HCPs during the COVID-19 pandemic
Findings were synthesized and presented using the following 4 themes: (1) prevalence of compassion fatigue, (2) antecedents of compassion fatigue (individual-Level, organizational-Level, and systems-level factors), (3) consequences of compassion fatigue, and (4) interventions for compassion fatigue.
Theme 1: Prevalence of compassion fatigue
Of the studies reviewed, five measured the prevalence of compassion fatigue among HCPs during the COVID-19 pandemic [ 23 , 30 , 31 , 36 , 41 ]. In a study conducted in Spain, 306 out of 506 (60.4%) HCPs reported high levels of compassion fatigue while 170 (33.6%) showed moderate levels of compassion fatigue (ProQoL 5: M = 19.9, SD = 7.6) [ 36 ]. In a sample composed of 395 Ugandan frontline nurses, 49.11% of the nurses reported high levels of compassion fatigue, while 29.6% experienced moderate levels of compassion fatigue [ 23 ]. Over half of the nurses in the study (54.94%) reported direct exposure to COVID-19 cases. A study conducted in Greece found that in a sample of 105 nurses, the majority of nurses (51.4%) experienced moderate levels of compassion fatigue (ProQoL 5: M = 22.26, SD = 6.76) [ 41 ]. In a Taiwanese study of 503 HCPs, the majority of the participants (63.2%) experienced low levels of compassion fatigue (ProQoL 5: M = 20.9, SD = 7.6) [ 31 ]. Finally, in a Filipino sample composed of 270 frontline nurses, 61.4% of the nurses reported low levels of compassion fatigue (CFS: M = 2.213, SD = 0.979) [ 30 ].
Theme 2: Antecedents of compassion fatigue
Individual-level factors.
Age and sex were key factors associated with compassion fatigue among participant HCPs. Younger HCPs with less experience were more likely to experience mental health issues and conflicting feelings with regards to providing care to COVID-19 patients [ 23 , 29 , 44 , 46 ]. Seven studies included in the review determined that female HCPs were more likely than male HCPs to experience compassion fatigue [ 23 , 35 , 36 , 38 , 40 , 50 , 52 ]. Physicians were also reported to have higher levels of compassion fatigue compared to nurses in three studies [ 36 , 38 , 39 ]. While nursing assistants had higher levels of compassion fatigue when compared to nurses in one study (ProQol 5: Nursing assistants = 29.15 ± 6.94; Nurse = 25.68 ± 5.87) [ 29 ]. Furthermore, the risk was higher in permanent workers compared to temporary workers (ProQoL 5: Permanent = 2.48 ± 1.29; Temporary = 2.11 ± 1.15; P -value < 0.05) [ 35 ]. One included study determined that marital status and education levels were not correlated with compassion fatigue [ 23 ]. Psychiatric comorbidities such as past trauma, burnout, stress, anxiety, and depression exacerbated HCPs’ psychological well-being across a number of included studies [ 31 , 33 , 36 , 38 , 39 , 41 , 49 , 50 ]. Other psychological factors such as excessive empathetic engagement, sensitive sensory processes, and overidentification from frequent witnessing of patient suffering and deaths were found to aggravate the development of compassion fatigue [ 34 , 39 , 45 ]. The inability to cope with the rapidly evolving landscape of healthcare provision and a lack of self-care contributed to increased burden and blurring of role boundaries between professional and private lives [ 29 , 41 , 43 , 44 , 51 , 52 ]. One study that used Compassion Fatigue and Satisfaction Self-Tests and a questionnaire of personal and professional characteristics found that feelings of underappreciation, insufficient compensations, and social isolation incurred psychological burden on pediatric sub-specialists [ 52 ]. Additionally, a decrease in occupational hardiness, as measured by the Occupational Hardiness Questionnaire, increased the risk of compassion fatigue among HCPs in two studies [ 42 , 50 ]. Negative outcomes to the HCPs’ families and concerns revolving around their patients’ families also predicted higher risk of experiencing compassion fatigue [ 45 , 48 , 52 ]. Finally, HCPs’ fear of COVID-19 with regards to infection and transmission was identified as a predictor of compassion fatigue [ 29 , 40 , 43 , 44 , 47 ].
Two studies identified social support from family, friends, peers, and hospital leadership as a crucial protective factor for compassion fatigue [ 43 , 52 ]. Coping mechanisms such as venting and exercising were found to help alleviate stress among HCPs [ 44 ]. Psychological qualities such as compassion satisfaction, professional satisfaction, resilience, vigor, and hardiness were found to help protect the psychological health of HCPs as well as reducing turnover intention and increasing perceived quality of care [ 30 , 34 , 36 , 37 , 39 , 40 , 42 , 46 , 50 ]. Self-care, self-awareness of limitations, and self-regulation of emotions were crucial for reducing risk of compassion fatigue in two studies comprised of physicians and nurses [ 44 , 50 ]. Lastly, spirituality, religiosity, and meditation also served as protective factors in three studies on compassion fatigue in HCPs [ 41 , 44 , 51 ].
Organizational-level factors
In five of the articles reviewed, increased workload [ 23 , 29 , 44 , 45 ], long working hours [ 23 , 29 , 44 , 45 ], and increased number of patients [ 50 ] were identified as common predictors of compassion fatigue. Furthermore, providing direct care to COVID-19 patients, which were often emotionally challenging cases, exacerbated the psychological risks to HCPs [ 23 , 36 , 46 , 48 , 50 ]. Chronic exposure to a dynamic work environment also increased the risk of compassion fatigue among HCPs [ 29 ]. Lack of access to suitable PPEs and lack of foresight from management and human resources teams regarding infection control guidelines contributed to HCPs’ distress [ 29 ]. Adjusting to the discomfort caused by wearing PPEs presented as a challenge to maintaining the efficiency of work activities [ 29 ]. Lastly, in two studies, HCPs identified that while there were plenty of wellness resources provided by healthcare organizations to support mindfulness, there was a lack of practical and pragmatic resources for social and emotional support, work-life balance, and remuneration [ 23 , 43 ].
Positive work conditions, such as a visible presence and engagement by leadership and management, as well as a positive work culture allowing HCPs to seek help without fear of judgment was found to be important protective factors against the development of compassion fatigue [ 44 ]. The social aspects of teamwork facilitated the sharing of feelings of trauma which in turn contributed to resilience and improved psychological well-being among HCPs in three studies [ 41 , 43 , 44 ]. One study observed that workplace wellness activities and a sense of feeling valued can prevent high levels of compassion fatigue [ 52 ]. Words of appreciation from supervisors boosted morale for some HCPs [ 44 ]. Attention to workplace safety in the form of PPEs and early access to vaccines alleviated the fear of infection [ 44 ]. Finally, two studies determined that adequate preparation and education to handle COVID-19 cases and increased autonomy decreased the risk of compassion fatigue and increased professional fulfillment [ 42 , 44 ].
Systems-level factors
Significant and frequently changing public health measures over the course of the pandemic presented a challenge as they were disruptive to workflow and resulted in uncertainty, feelings of inadequacy, and distress among HCPs across a range of geographical contexts [ 29 , 41 , 43 , 49 ]. Increases in the incidence of COVID-19 cases also contributed to a rise in the number of hospital admissions, aggravating HCPs’ workload [ 35 ]. Social-distancing policies precluded informal team interactions, such as sharing meals together, which posed a risk to HCPs’ psychological well-being by decreasing social support [ 43 , 52 ]. Transitions to tele-health also increased social isolation [ 43 ]. A theme that emerged was the negative impact of stigma on HCPs, with their proximity to contagion, as a possible risk factor [ 35 , 41 ]. Aggressive behaviors and verbal abuse from patients were sources of emotional stress for some HCPs [ 44 ]. Finally, negative peer pressure was identified as a barrier to HCPs engaging in self-care as they felt pressure to conform to sociocultural norms of an expected level of dedication [ 44 ]. In contrast to the impacts of stigma, a positive perception of one’s own profession is related to increased commitment and decreased compassion fatigue [ 46 ].
Theme 3: Consequences of compassion fatigue
The findings of one study suggested that compassion fatigue associated with HCP’s professional practice impacted their private lives, predicting greater parental burnout ( r = 0.542), child abuse ( r = 0.468), child neglect ( r = 0.493), spouse conflict ( r = 0.340), and substance abuse ( r = 0.298) [ 48 ]. This study identified factors such as direct care of COVID-19 patients ( r = 0.255), exposure to patient death and suffering due to COVID-19 ( r = 0.281), and family income loss due to COVID-19 ( r = 0.366) as risk factors for compassion fatigue [ 48 ]. Additionally, at an organizational-level, two studies conducted in 2020 and 2021 observed that Turkish and Filipino HCPs who reported compassion fatigue also reported lower job satisfaction and reduced professional commitment [ 30 , 46 ]. Consequently, elevated compassion fatigue also increased organizational turnover intent among Filipino HCPs (β = 0.301, P -value = 0.001) [ 30 ]. A study conducted in China found that compassion fatigue predicted negative behavioral intentions towards treating COVID-19 patients, as measured by the Attitude, Subjective Norms, and Behavioral Intention of Nurses toward Mechanically Ventilated Patients (ASIMP) questionnaire [ 33 ]. This suggests that quality of care may be adversely impacted [ 33 ]. Finally, an American study observed that compassion fatigue among HCPs was associated with deteriorating workplace culture [ 52 ].
- Patient care
The provision of care during the pandemic was impacted by the general lack of preparation for handling novel tasks experienced by many HCPs [ 23 ]. Findings from one study found that many HCPs (73%) experienced a shift in their clinical practice setting, for example, from in-personal care to virtual telehealth consults as a result of the pandemic [ 43 ]. HCPs also experienced an increase in the need to provide palliative care as a result of the negative health impacts of COVID-19, something they may have had limited prior experience with [ 43 ]. In a case study conducted in Japan, the physician reported feeling inexperienced with handling the psychological impact of the pandemic experienced by not only the patients but also the patients’ family [ 45 ]. The consequences of not being able to provide optimal care was found to exacerbate feelings of guilt, powerlessness, and frustration in HCPs [ 41 , 43 ]. In turn, study findings suggest that worsening compassion fatigue may reduce the quality of care provided by HCPs because it has been found to be a significant predictor of negative behavioral intention [ 30 , 33 , 40 , 52 ].
Theme 4: Interventions for compassion fatigue
Two studies in Japan and Uganda investigated potential interventions to support HCPs experiencing COVID-19 related compassion fatigue. On an individual-level, regularly engaging in self-care activities such as expressions of gratitude as well as learning how to recognize signs and symptoms of compassion fatigue were identified as crucial first steps in its management [ 45 , 52 ]. Emotional support from colleagues and mental health specialists was found to be effective in improving the mental health of a Japanese physician experiencing compassion fatigue [ 45 ]. Findings of two studies identified the need for a systematic approach to monitor the progression of psychological symptoms and providing tailored resources in a timely manner to HCPs to help ameliorate compassion fatigue and its consequences [ 29 , 45 ]. Suggested strategies included: facilitating regular consultations with each department [ 45 , 52 ], increasing the staffing number of HCPs in busy departments [ 23 , 45 ], and providing PPEs and vaccines in a timely manner [ 23 , 52 ]. Lastly, findings from two studies in Uganda and the United States suggested that increased remuneration may prevent or minimize compassion fatigue [ 23 , 52 ].
Key findings
This scoping review sought to provide a comprehensive summary of the literature published between January 2020 and May 2023 on the impact of the COVID-19 pandemic on compassion fatigue among HCPs and its subsequent impact on patient care. Most of the included studies were conducted in 2020 and used cross-sectional study designs. Given that the COVID-19 outbreak was declared a global health emergency in early 2020 [ 1 ], cross-sectional study designs were well-placed to provide prompt and important insights on compassion fatigue across the HCP population. Review findings were presented using four themes addressing the prevalence, antecedents, consequences, and consequences of compassion fatigue in HCPs. The prevalence of compassion fatigue was observed to vary across countries. The negative psychological outcomes reported by included studies were precipitated by individual-level factors such as age and occupational role; organizational-factors such as lack of access to PPE; and systems-level factors such as loss of social engagement and stigma. The consequences of compassion fatigue impacted HCPs’ personal and professional roles. Findings suggest an urgent need for policy makers, health managers, and team leaders to develop and implement strategies that target the potential root causes of compassion fatigue in HCPs.
Prevalence of compassion fatigue
Among the five studies that measured prevalence of compassion fatigue, results were highly variable across countries [ 23 , 30 , 31 , 36 , 41 ]. This may be attributed to differences in preparedness for infection containment and variability among health systems’ preparation and ability to respond to supply chain issues [ 53 ]. Taiwan provides an example of how digital technologies were adopted to improve disease surveillance and monitor medical supply chains [ 55 ]. Using the stringent Identify-Isolate-Inform model in conjunction with public mask-wearing and physical distancing, the spread of the disease was effectively contained in Taiwan [ 53 ]. Consequently, despite not enforcing lockdowns, Taiwan blocked the first wave of cases and slowed down subsequent outbreaks, which may contribute to the observed low prevalence of compassion fatigue among HCPs [ 56 ]. In the Philippines, responses to disease outbreaks varied across different municipalities and provinces [ 57 ]. Effective containment measures such as strict border control and early lockdowns in addition to plentiful medical supplies and personnel allowed certain regions to mount a strong response to this public health emergency, subsequently resulting in the observed low prevalence of compassion fatigue among HCPs [ 57 ]. In Uganda, there were generally low levels of preparedness with regards to the infection identification, PPE supply, access to hand-washing facilities, and establishment of isolation facilities [ 58 ]. This may have contributed to an overwhelmed healthcare system and overworked HCPs as the surge of cases was exacerbated by the shortage of disease containment resources [ 58 ]. In April 2020, Spain experienced the second highest infection incidence in the world [ 59 ]. The Spanish health system was overwhelmed by the abundance of patients due to lack of HCPs [ 60 ], hospital capacity, and material supplies [ 59 ]. An increase in compassion fatigue among HCPs was also observed in recent studies from Italy and Canada [ 61 , 62 ]. Overall, the various strategies used to address the resultant COVID-19-related public health crisis presented distinctive challenges to HCPs in different countries. Caution must be taken when interpreting the study findings given the contextual differences across various healthcare systems. The psychological burden and prevalence of compassion fatigue subsequently varied depending on the context.
Antecedents of compassion fatigue
The findings of this review suggest that individual characteristics such as age and occupational role are significant contributing factors to the development of compassion fatigue during COVID-19 [ 63 ]. Specifically, older HCPs were less likely to experience compassion fatigue than younger HCPs according to regression analyses [ 23 , 29 , 44 , 46 ]. This observation may be attributed to their increased work experience. Resilience was also positively linearly related to age [ 64 ]. Factors identified as potential contributors to the observed age-related advantage in wellbeing were access to job resources, better job security, work-life balance, and coping skills [ 64 ]. The compounding of stressors such as an increase in workload during the COVID-19 pandemic could have exacerbated the psychological health of younger HCPs. In the context of telework, older employees tended to create clear boundaries between work and non-work responsibilities [ 64 ]. The rise in telework among HCPs was mostly a consequence of the COVID-19 pandemic which may have increased the psychological burden on younger HCPs [ 65 ]. In addition, a study examining demographic predictors of resilience in nurses reported that younger nurses had less exposure to stress, and thus have fewer opportunities to develop skills in stress management [ 66 ]. As a result of these factors, the younger HCPs were at high risk for compassion fatigue during the COVID-19 pandemic. Interestingly, three of the included studies in this review also observed that physicians were at a higher risk of compassion fatigue compared to nurses [ 36 , 38 , 39 ]. This difference may be attributed to the burden of responsibility in relation to breaking bad news, a task that is often the physicians’ responsibility [ 67 ]. A study examining compassion fatigue in HCPs determined that conflict arising during patient interactions placed HCPs at a risk for compassion fatigue [ 68 ]. Delivery of bad or uncertain news also predicted a greater mental health burden in HCPs [ 68 ].
At the organizational level, findings from the studies included in this review identified that a lack of access to PPE was a contributor to compassion fatigue in HCPs during COVID-19 [ 29 , 52 ]. Specifically, one study reported that the fear of infection and transmission to patients, family, and friends added to the concern of HCPs working in high-risk environments [ 69 ]. This finding can potentially be explained by the increased vulnerability that HCPs experience following a lag in the provision of PPE. Several organizational factors were determined as potential barriers to the distribution of PPE; the unprecedented nature of the pandemic presented challenges for maintaining domestic inventories [ 70 ]. Disruptions to the PPE global supply chain also amplified the equipment shortage [ 70 ]. This finding highlights the importance of monitoring and ensuring that domestic health supplies are adequately stocked.
At the system level, loss of social engagement [ 43 , 52 ] and stigma [ 35 , 41 ] were identified in the studies included in the review as antecedents to compassion fatigue. Public policies such as social-distancing and occupancy capacity limits negatively impact social interactions which may explain the loss of social engagement in addition to worsening mental health well-being in HCPs [ 71 ]. As certain practices transition to telehealth, other studies have found increased mental fatigue and difficulty with maintaining empathetic rapport, which has important implications on patient care [ 72 , 73 ]. In addition, other studies have found that given the proximity of their role to contagion, stigma towards HCPs from patients increased during COVID-19 [ 74 , 75 ]. Consequently, the combinatorial experience of being socially isolated and stigmatized may worsen mental health outcomes [ 76 ]. This points to a need for increased access to support services for HCPs such as virtual communities.
Consequences of compassion fatigue
Review findings suggest that compassion fatigue impacted the private and professional lives of HCPs. The risk for parental burnout has increased across many occupations during the pandemic [ 77 ]. Factors related to low levels of social support, lack of leisure time, and greater parental responsibilities in face of education disruptions adds to the psychological burden of parents [ 77 ]. HCPs were placed in a unique position having to work in highly stressful environments while also balancing household responsibilities and increased challenges related to childcare [ 48 , 78 ]. This finding highlights a need for the provision of child support services for HCPs or a reduction in workload to alleviate the burden of parental and homecare responsibilities particularly in times of public health crises.
Beyond their private lives, this review has found that decreases in HCPs’ professional commitment due to compassion fatigue, may endanger the quality of patient care delivered [ 79 ]. In particular, this may be attributed to the surge in palliative care cases during the pandemic in conjunction with an unprepared workforce, creating psychological stress for HCPs [ 80 ]. In a study examining palliative care preparedness during the pandemic, a lack of core palliative care training and expertise among frontline HCPs [ 81 ] meant many felt emotionally unprepared to address cases with seriously ill patients [ 45 ]. An increased frequency of breaking bad news to patients’ families was associated with negative psychological outcomes [ 82 ]. Providing training on relevant communication skills may protect HCPs from compassion fatigue [ 83 , 84 ].
Implications
The findings of this review highlight the urgency to provide support for HCPs who may be at risk for compassion fatigue which could have subsequent impacts on the provision of patient care [ 85 ]. To address the antecedents of compassion fatigue, this scoping review has identified a need for increased staffing, recruitment, and retention efforts on the part of hospital human resources departments [ 23 , 45 ]. Interventions suggested by studies included in the review encompass the monitoring of psychological well-being among HCPs to inform timely provision of resources [ 29 , 45 ]. Specifically, structured debriefing, training on self-care routine, reduced workload, and normalization of trauma-related therapy are essential interventions [ 86 ]. Additionally, a study identified that fostering collaborative workplace culture encourages social and emotional support among staff [ 45 ]. Certain hospitals have adopted “wobble rooms” as a private unwinding and venting space for employees [ 87 ]. Studies have observed that interventions aimed at improving the well-being of HCPs resulted in enhanced quality and safety of care being delivered [ 75 ].
Strengths and limitations
There are both strengths and limitations in this review. Although some literature reviews focused on the psychological health status of HCPs (e.g., burnout, anxiety, depression), very few studies have specifically explored compassion fatigue. Reviews that considered the impact of the COVID-19 pandemic on HCPs were even more limited. It is known that compassion is a cornerstone of quality health care improvement and increases successful medical outcomes [ 88 , 89 , 90 ]. Nevertheless, prolonged exposure to distressing events by HCPs, such as patient death and suffering, results in the absorption of negative emotional responses and leads to the development of compassion fatigue [ 91 ]. This scoping review presents an extensive exploration of the current body of literature on compassion fatigue among HCPs during the COVID-19 pandemic. Another strength in this study lies in the transparency and reproducibility of the methodology. The scoping review protocol has been published in a peer-reviewed journal to establish high methodological standards for the final scoping review [ 92 ]. Additionally, the study plan was pre-registered with Open Science Framework to ensure commitment to the methodology. Double extraction was performed to ensure that a comprehensive descriptive summary of the studies was achieved.
Some limitations include the short time frame chosen for the included studies that were published since the COVID-19, which may have constrained the breadth and quality of the studies. Longitudinal studies may not be captured in the review as this study methodology requires a prolonged period of time to yield meaningful observations. More data is needed to support conclusions on the impact of compassion fatigue on patient care. Additionally, none of the studies included in the review were conducted between March 2021 and May 2023, which may miss out on meaningful trends in levels of compassion fatigue in HCPs. This scoping review only included literature published in English so studies published in other languages were not assessed. Additionally, no comparisons of compassion fatigue were made among the HCP groups in spite of potentially relevant differences such as patient exposure. There was also a lack of allied health profession representation, with the majority of the study population being nurses or physicians. Lastly, grey literature was not included in this scoping review which may delimitate the information included in the scoping review.
There were recurring themes related to limitations in the included research studies. Several studies identified sampling issues including small sample sizes, restricted sample frame, low response rate, and selection error [ 23 , 29 , 31 , 38 , 39 , 40 , 41 , 42 , 43 , 47 , 50 , 51 , 83 ]. Other studies have called for investigations into how different sociodemographic factors, other psychiatric diseases, health care settings, and workplace environment impact compassion fatigue in HCPs [ 38 , 39 , 47 , 48 , 83 ]. One study observed a lack of homogeneity in the sample due to an overrepresentation of female HCPs in the sample [ 38 ]. Lastly, many studies employed a cross-sectional study design which limits the interpretation of the data in terms of causality [ 23 , 30 , 31 , 34 , 42 , 47 , 48 , 50 ]. While there are limitations to the study, a comprehensive summary of existing literature may be useful to inform future research and policies.
Future research is needed to examine the longitudinal impacts of COVID-19 on compassion fatigue in HCPs. Moreover, research in this area could be strengthened by including a consultation phase with external experts on compassion fatigue to improve the robustness of the scoping review.
Conclusions
The COVID-19 pandemic presented a unique set of challenges to healthcare systems across the globe. This scoping review indicated that the prevalence of compassion fatigue was inconsistent across countries and may reflect the variability of pandemic preparedness among the individual countries. Primary risk factors for the development of compassion fatigue included being younger, female, a physician or nurse, and having limited access to PPE in conjunction with an excessive workload and prolonged work hours. The negative impacts of compassion fatigue were experienced at the individual and organizational level. The findings suggest there is a systemic need to assess, monitor and support health professionals’ well-being particularly during conditions of protracted health crises such as a pandemic. In addition, many health systems and sectors are facing a profound health human resources crisis and therefore ongoing efforts must be made to improve workplace environments and increase recruitment and retention efforts. Lastly, pandemic planning must include provisions to support health providers’ ability to safely do their jobs while also minimizing negative impacts to their health and well-being.
Availability of data and materials
All the material presented in the manuscript is owned by the authors and/or no permissions are required.
Coronavirus disease (COVID-19) pandemic. Accessed 16 Jan 2023. https://www.who.int/europe/emergencies/situations/covid-19
Wilder-Smith A, Osman S. Public health emergencies of international concern: a historic overview. J Travel Med. 2020;27(8):taaa227. https://doi.org/10.1093/jtm/taaa227 .
Article PubMed Google Scholar
Gristina GR, Piccinni M. COVID-19 pandemic in ICU. limited resources for many patients: approaches and criteria for triaging. Minerva Anestesiol. 2021;87(12):1367–79. https://doi.org/10.23736/S0375-9393.21.15736-0 .
Chaka EE, Mekuria M, Melesie G. Access to Essential personal safety, availability of personal protective equipment and perception of healthcare workers during the COVID-19 in public hospital in West Shoa. Infect Drug Resist. 2022;15:2315–23. https://doi.org/10.2147/IDR.S344763 .
Article PubMed PubMed Central Google Scholar
Gholami M, Fawad I, Shadan S, et al. COVID-19 and healthcare workers: a systematic review and meta-analysis. Int J Infect Dis. 2021;104:335–46. https://doi.org/10.1016/j.ijid.2021.01.013 .
Article CAS PubMed PubMed Central Google Scholar
Schug C, Geiser F, Hiebel N, et al. Sick Leave and Intention to Quit the Job among Nursing Staff in German Hospitals during the COVID-19 Pandemic. Int J Environ Res Public Health. 2022;19(4):1947. https://doi.org/10.3390/ijerph19041947 .
Lancet T. COVID-19: protecting health-care workers. Lancet Lond Engl. 2020;395(10228):922. https://doi.org/10.1016/S0140-6736(20)30644-9 .
Article Google Scholar
Beck E, Daniels J. Intolerance of uncertainty, fear of contamination and perceived social support as predictors of psychological distress in NHS healthcare workers during the COVID-19 pandemic. Psychol Health Med. Published online July 6, 2022:1–13. https://doi.org/10.1080/13548506.2022.2092762.
Nikeghbal K, Kouhnavard B, Shabani A, Zamanian Z. Covid-19 effects on the mental workload and quality of work life in Iranian nurses. Ann Glob Health. 2021;87(1):79. https://doi.org/10.5334/aogh.3386.
WHO Coronavirus (COVID-19) Dashboard. Accessed 16 Jan 2023. https://covid19.who.int
Lluch C, Galiana L, Doménech P, Sansó N. The Impact of the COVID-19 pandemic on burnout, compassion fatigue, and compassion satisfaction in healthcare personnel: a systematic review of the literature published during the first year of the pandemic. Healthcare. 2022;10(2):364. https://doi.org/10.3390/healthcare10020364 .
Salmond E, Salmond S, Ames M, Kamienski M, Holly C. Experiences of compassion fatigue in direct care nurses: a qualitative systematic review. JBI Evid Synth. 2019;17(5):682. https://doi.org/10.11124/JBISRIR-2017-003818 .
Sinclair S, Raffin-Bouchal S, Venturato L, Mijovic-Kondejewski J, Smith-MacDonald L. Compassion fatigue: A meta-narrative review of the healthcare literature. Int J Nurs Stud. 2017;69:9–24. https://doi.org/10.1016/j.ijnurstu.2017.01.003 .
Majid U, Hussain SAS, Zahid A, Haider MH, Arora R. Mental health outcomes in health care providers during the COVID-19 pandemic: an umbrella review. Health Promot Int. 2023;38(2):daad025. https://doi.org/10.1093/heapro/daad025 .
Rahmani F, Hosseinzadeh M, Gholizadeh L. Complicated grief and related factors among nursing staff during the Covid-19 pandemic: a cross-sectional study. BMC Psychiatry. 2023;23(1):73. https://doi.org/10.1186/s12888-023-04562-w .
Statement on the fifteenth meeting of the IHR (2005) Emergency Committee on the COVID-19 pandemic. Accessed July 6, 2023. https://www.who.int/news/item/05-05-2023-statement-on-the-fifteenth-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-coronavirus-disease-(covid-19)-pandemic
Ghahramani S, Kasraei H, Hayati R, Tabrizi R, Marzaleh MA. Health care workers’ mental health in the face of COVID-19: a systematic review and meta-analysis. Int J Psychiatry Clin Pract. 2022;0(0):1–10. https://doi.org/10.1080/13651501.2022.2101927 .
Article CAS Google Scholar
Nie A, Su X, Zhang S, Guan W, Li J. Psychological impact of COVID-19 outbreak on frontline nurses: a cross-sectional survey study. J Clin Nurs. 2020;29(21–22):4217–26. https://doi.org/10.1111/jocn.15454 .
Jalili M, Niroomand M, Hadavand F, Zeinali K, Fotouhi A. Burnout among healthcare professionals during COVID-19 pandemic: a cross-sectional study. Int Arch Occup Environ Health. 2021;94(6):1345–52. https://doi.org/10.1007/s00420-021-01695-x .
Iddrisu M, Poku CA, Mensah E, Attafuah PYA, Dzansi G, Adjorlolo S. Work-related psychosocial challenges and coping strategies among nursing workforce during the COVID-19 pandemic: a scoping review. BMC Nurs. 2023;22(1):210. https://doi.org/10.1186/s12912-023-01368-9 .
Yang BJ, Yen CW, Lin SJ, et al. Emergency nurses’ burnout levels as the mediator of the relationship between stress and posttraumatic stress disorder symptoms during COVID-19 pandemic. J Adv Nurs. 2022;78(9):2861–71. https://doi.org/10.1111/jan.15214 .
Fukushima H, Imai H, Miyakoshi C, Naito A, Otani K, Matsuishi K. The sustained psychological impact of coronavirus disease 2019 pandemic on hospital workers 2 years after the outbreak: a repeated cross-sectional study in Kobe. BMC Psychiatry. 2023;23(1):313. https://doi.org/10.1186/s12888-023-04788-8 .
Amir K, Okalo P. Frontline nurses’ compassion fatigue and associated predictive factors during the second wave of COVID-19 in Kampala. Uganda Nurs Open. 2022;9(5):2390–6. https://doi.org/10.1002/nop2.1253 .
Calkins K, Guttormson J, McAndrew NS, et al. The early impact of COVID-19 on intensive care nurses’ personal and professional well-being: a qualitative study. Intensive Crit Care Nurs. 2023;76:103388. https://doi.org/10.1016/j.iccn.2023.103388 .
Sexton JB, Adair KC, Proulx J, et al. Emotional exhaustion among US health care workers before and during the COVID-19 Pandemic, 2019–2021. JAMA Netw Open. 2022;5(9):e2232748. https://doi.org/10.1001/jamanetworkopen.2022.32748 .
Slatten LA, David Carson K, Carson PP. Compassion fatigue and burnout what managers should know. Health Care Manag. 2011;30(4):325–33. https://doi.org/10.1097/HCM.0b013e31823511f7 .
Martin J. © Joanna Briggs Institute 2017 Critical Appraisal Checklist for Systematic Reviews and Research Syntheses. Published online 2017.
PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation | Annals of Internal Medicine. Accessed 16 Jan 16 2023. https://www.acpjournals.org/doi/full/ https://doi.org/10.7326/M18-0850?rfr_dat=cr_pub++0pubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org
Moreno-Mulet C, Sansó N, Carrero-Planells A, et al. The Impact of the COVID-19 Pandemic on ICU healthcare professionals: a mixed methods study. Int J Environ Res Public Health. 2021;18(17):9243. https://doi.org/10.3390/ijerph18179243 .
Labrague LJ, de los Santos JAA. Resilience as a mediator between compassion fatigue, nurses’ work outcomes, and quality of care during the COVID-19 pandemic. Appl Nurs Res. 2021;61:151476.
Su PA, Lo MC, Wang CL, et al. The correlation between professional quality of life and mental health outcomes among hospital personnel during the Covid-19 pandemic in Taiwan. J Multidiscip Healthc. 2021;14:3485–95. https://doi.org/10.2147/JMDH.S330533 .
Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implementation Sci. 2010;5:69. https://doi.org/10.1186/1748-5908-5-69 .
Cheng J, Cui J, Yu W, Kang H, Tian Y, Jiang X. Factors influencing nurses’ behavioral intention toward caring for COVID-19 patients on mechanical ventilation: a cross-sectional study. PLoS ONE. 2021;16(11):e0259658. https://doi.org/10.1371/journal.pone.0259658 .
Pérez-Chacón M, Chacón A, Borda-Mas M, Avargues-Navarro ML. Sensory processing sensitivity and compassion satisfaction as risk/protective factors from burnout and compassion fatigue in healthcare and education professionals. Int J Environ Res Public Health. 2021;18(2):611. https://doi.org/10.3390/ijerph18020611 .
Ramaci T, Barattucci M, Ledda C, Rapisarda V. Social Stigma during COVID-19 and its Impact on HCWs Outcomes. Sustainability. 2020;12(9):3834. https://doi.org/10.3390/su12093834 .
Ruiz-Fernández MD, Ramos-Pichardo JD, Ibáñez-Masero O, Cabrera-Troya J, Carmona-Rega MI, Ortega-Galán ÁM. Compassion fatigue, burnout, compassion satisfaction and perceived stress in healthcare professionals during the COVID-19 health crisis in Spain. J Clin Nurs. 2020;29(21–22):4321–30. https://doi.org/10.1111/jocn.15469 .
Kase SM, Gribben JL, Guttmann KF, Waldman ED, Weintraub AS. Compassion fatigue, burnout, and compassion satisfaction in pediatric subspecialists during the SARS-CoV-2 pandemic. Pediatr Res. 2022;91(1):143–8. https://doi.org/10.1038/s41390-021-01635-y .
Article CAS PubMed Google Scholar
Carmassi C, Dell’Oste V, Bertelloni CA, et al. Gender and occupational role differences in work-related post-traumatic stress symptoms, burnout and global functioning in emergency healthcare workers. Intensive Crit Care Nurs. 2022;69:103154. https://doi.org/10.1016/j.iccn.2021.103154 .
Ruiz-Fernández MD, Ramos-Pichardo JD, Ibáñez-Masero O, Carmona-Rega MI, Sánchez-Ruiz MJ, Ortega-Galán ÁM. Professional quality of life, self-compassion, resilience, and empathy in healthcare professionals during COVID-19 crisis in Spain. Res Nurs Health. 2021;44(4):620–32. https://doi.org/10.1002/nur.22158 .
Yılmaz A, Bay F, Erdem Ö, Özkalp B. The professional quality of life for healthcare workers during the COVID-19 Pandemic in Turkey and the influencing factors. Bezmialem Sci. 2022;10(3):361–9. https://doi.org/10.14235/bas.galenos.2021.5837 .
Missouridou E, Mangoulia P, Pavlou V, et al. Wounded healers during the COVID-19 syndemic: Compassion fatigue and compassion satisfaction among nursing care providers in Greece. Perspect Psychiatr Care. 2022;58(4):1421–32. https://doi.org/10.1111/ppc.12946 . Published online September 10, 2021.
Zakeri MA, Rahiminezhad E, Salehi F, Ganjeh H, Dehghan M. compassion satisfaction, compassion fatigue and hardiness among nurses: a comparison before and during the COVID-19 Outbreak. Front Psychol. 2022;12:815180. https://doi.org/10.3389/fpsyg.2021.815180 .
Austin EJ, Blacker A, Kalia I. “Watching the tsunami come”: a case study of female healthcare provider experiences during the COVID-19 pandemic. Appl Psychol Health Well-Being. 2021;13(4):781–97. https://doi.org/10.1111/aphw.12269 .
Kong KYC, Ganapathy S. Are we in control of our demons?: understanding compassion satisfaction, compassion fatigue and burnout in an asian pediatric emergency department in a pandemic. Pediatr Emerg Care. 2022;38(3):e1058. https://doi.org/10.1097/PEC.0000000000002656 .
Nishihara T, Ohashi A, Nakashima Y, Yamashita T, Hiyama K, Kuroiwa M. Compassion fatigue in a health care worker treating COVID-19 patients: a case report. Biopsychosoc Med. 2022;16(1):10. https://doi.org/10.1186/s13030-022-00239-0 .
Kaya ŞD, Mehmet N, Şafak K. Professional commitment, satisfaction and quality of life of nurses during the COVID-19 Pandemic in Konya. Turkey Ethiop J Health Sci. 2022;32(2):393–404. https://doi.org/10.4314/ejhs.v32i2.20 .
Kottoor AS, Chacko N. Role of entrapment in relation between fear of Covid-19 and compassion fatigue among nurses. Int J Behav Sci. 2022;15(4):250–5. https://doi.org/10.30491/ijbs.2022.288846.1573 .
Stevenson MC, Schaefer CT, Ravipati VM. COVID-19 patient care predicts nurses’ parental burnout and child abuse: Mediating effects of compassion fatigue. Child Abuse Negl. 2022;130:105458. https://doi.org/10.1016/j.chiabu.2021.105458 .
Hochwarter W, Jordan S, Kiewitz C, et al. Losing compassion for patients? The implications of COVID-19 on compassion fatigue and event-related post-traumatic stress disorder in nurses. J Manag Psychol. 2022;37(3):206–23. https://doi.org/10.1108/JMP-01-2021-0037 .
Cuartero-Castañer ME, Hidalgo-Andrade P, Cañas-Lerma AJ. professional quality of life, engagement, and self-care in healthcare professionals in Ecuador during the COVID-19 Pandemic. Healthcare. 2021;9(5):515. https://doi.org/10.3390/healthcare9050515 .
Spiridigliozzi S. Exploring the relationship between faith and the experience of burnout, compassion fatigue, and compassion satisfaction for hospice workers during a global pandemic: a multidisciplinary study. Dr Diss Proj. Published online April 1, 2022. https://digitalcommons.liberty.edu/doctoral/3572
Gribben JL, Kase SM, Guttmann KF, Waldman ED, Weintraub AS. Impact of the SARS-CoV-2 pandemic on pediatric subspecialists’ well-being and perception of workplace value. Pediatr Res. Published online January 20, 2023:1–7. https://doi.org/10.1038/s41390-023-02474-9.
Chien LC, Beÿ CK, Koenig KL. Taiwan’s Successful COVID-19 mitigation and containment strategy: achieving quasi population immunity. Disaster Med Public Health Prep.:1–4. https://doi.org/10.1017/dmp.2020.357.
Cucinotta D, Vanelli M. WHO Declares COVID-19 a Pandemic. Acta Bio-Medica Atenei Parm. 2020;91(1):157–60. https://doi.org/10.23750/abm.v91i1.9397 .
Kuo S, Ou HT, Wang CJ. Managing medication supply chains: Lessons learned from Taiwan during the COVID-19 pandemic and preparedness planning for the future. J Am Pharm Assoc. 2021;61(1):e12–5. https://doi.org/10.1016/j.japh.2020.08.029 .
Cheng HY, Liu DP. Early Prompt Response to COVID-19 in Taiwan: Comprehensive surveillance, decisive border control, and information technology support. J Formos Med Assoc. Published online November 11, 2022. https://doi.org/10.1016/j.jfma.2022.11.002.
S. Talabis DA, Babierra AL, H. Buhat CA, Lutero DS, Quindala KM, Rabajante JF. Local government responses for COVID-19 management in the Philippines. BMC Public Health. 2021;21:1711. https://doi.org/10.1186/s12889-021-11746-0 .
Rashid N, Nazziwa A, Nanyeenya N, Madinah N, Lwere K. Preparedness, identification and care of COVID-19 cases by front line health workers in selected health facilities in mbale district uganda: a cross-sectional study. East Afr Health Res J. 2021;5(2):144–50. https://doi.org/10.24248/eahrj.v5i2.665 .
Alfonso Viguria U, Casamitjana N. Early Interventions and Impact of COVID-19 in Spain. Int J Environ Res Public Health. 2021;18(8):4026. https://doi.org/10.3390/ijerph18084026 .
Rodríguez-Almagro J, Hernández-Martínez A, Romero-Blanco C, Martínez-Arce A, Prado-Laguna MD, García-Sanchez FJ. Experiences and Perceptions of Nursing Students during the COVID-19 Crisis in Spain. Int J Environ Res Public Health. 2021;18(19):10459.
Dodek PM, Cheung EO, Burns KEA, et al. Moral distress and other wellness measures in Canadian critical care physicians. Ann Am Thorac Soc. 2021;18(8):1343–51. https://doi.org/10.1513/AnnalsATS.202009-1118OC .
Franza F, Basta R, Pellegrino F, Solomita B, Fasano V. The role of fatigue of compassion, burnout and hopelessness in healthcare: experience in the time of covid-19 outbreak. Psychiatr Danub. 32.
Coşkun Şimşek D, Günay U. Experiences of nurses who have children when caring for COVID-19 patients. Int Nurs Rev. 2021;68(2):219–27. https://doi.org/10.1111/inr.12651 .
Scheibe S, De Bloom J, Modderman T. Resilience during crisis and the role of age: involuntary telework during the COVID-19 Pandemic. Int J Environ Res Public Health. 2022;19(3):1762. https://doi.org/10.3390/ijerph19031762 .
Mann DM, Chen J, Chunara R, Testa PA, Nov O. COVID-19 transforms health care through telemedicine: Evidence from the field. J Am Med Inform Assoc JAMIA. 2020;27(7):1132–5. https://doi.org/10.1093/jamia/ocaa072 .
Afshari D, Nourollahi-darabad M, Chinisaz N. Demographic predictors of resilience among nurses during the COVID-19 pandemic. Work. 2021;68(2):297–303. https://doi.org/10.3233/WOR-203376 .
Monden KR, Gentry L, Cox TR. Delivering bad news to patients. Proc Bayl Univ Med Cent. 2016;29(1):101–2.
Sorenson C, Bolick B, Wright K, Hamilton R. Understanding compassion fatigue in healthcare providers: a review of current literature. J Nurs Scholarsh. 2016;48(5):456–65. https://doi.org/10.1111/jnu.12229 .
Alharbi J, Jackson D, Usher K. The potential for COVID-19 to contribute to compassion fatigue in critical care nurses. J Clin Nurs. 2020;29(15–16):2762–4. https://doi.org/10.1111/jocn.15314 .
Cohen J, van der Meulen Rodgers Y. Contributing factors to personal protective equipment shortages during the COVID-19 pandemic. Prev Med. 2020;141:106263.
Institute of Professional Psychology, Bahria University Karachi Campus, Karachi, Pakistan, Waris Nawaz M, Imtiaz S, Quaid-i-Azam University Islamabad, Islamabad, Pakistan, Kausar E, Institute of Professional Psychology, Bahria University Karachi Campus, Karachi, Pakistan. self-care of frontline health care workers: during covid-19 pandemic. Psychiatr Danub. 2020;32(3–4):557–62. https://doi.org/10.24869/psyd.2020.557 .
Mano MS, Morgan G. Telehealth, social media, patient empowerment, and physician burnout: seeking middle ground. Am Soc Clin Oncol Educ Book Am Soc Clin Oncol Annu Meet. 2022;42:1–10. https://doi.org/10.1200/EDBK_100030 .
Myronuk L. Effect of telemedicine via videoconference on provider fatigue and empathy: Implications for the Quadruple Aim. Healthc Manage Forum. 2022;35(3):174–8. https://doi.org/10.1177/08404704211059944 .
Abuhammad S, Alzoubi KH, Al‐Azzam S, et al. Stigma toward healthcare providers from patients during COVID‐19 era in Jordan. Public Health Nurs Boston Mass. Published online March 25, 2022: https://doi.org/10.1111/phn.13071
Nashwan AJ, Valdez GFD, AL-Fayyadh S, et al. Stigma towards health care providers taking care of COVID-19 patients: a multi-country study. Heliyon. 2022;8(4):e09300. https://doi.org/10.1016/j.heliyon.2022.e09300 .
Shiu C, Chen WT, Hung CC, Huang EPC, Lee TSH. COVID-19 stigma associates with burnout among healthcare providers: evidence from Taiwanese physicians and nurses. J Formos Med Assoc Taiwan Yi Zhi. 2022;121(8):1384–91. https://doi.org/10.1016/j.jfma.2021.09.022 .
Griffith AK. Parental burnout and child maltreatment during the COVID-19 Pandemic. J Fam Violence. 2022;37(5):725–31. https://doi.org/10.1007/s10896-020-00172-2 .
Çakmak G, Öztürk ZA. Being both a parent and a healthcare worker in the pandemic: who could be exhausted more? Healthcare. 2021;9(5):564. https://doi.org/10.3390/healthcare9050564 .
Cavanagh N, Cockett G, Heinrich C, et al. Compassion fatigue in healthcare providers: a systematic review and meta-analysis. Nurs Ethics. 2020;27(3):639–65. https://doi.org/10.1177/0969733019889400 .
Boufkhed S, Harding R, Kutluk T, Husseini A, Pourghazian N, Shamieh O. What is the preparedness and capacity of palliative care services in Middle-Eastern and North African Countries to Respond to COVID-19? a rapid survey. J Pain Symptom Manage. 2021;61(2):e13–50. https://doi.org/10.1016/j.jpainsymman.2020.10.025 .
Gelfman LP, Morrison RS, Moreno J, Chai E. Palliative care as essential to a hospital system’s pandemic preparedness planning: how to get ready for the next wave. J Palliat Med. 2021;24(5):656–8. https://doi.org/10.1089/jpm.2020.0670 .
Messerotti A, Banchelli F, Ferrari S, et al. Investigating the association between physicians self-efficacy regarding communication skills and risk of “burnout.” Health Qual Life Outcomes. 2020;18:271. https://doi.org/10.1186/s12955-020-01504-y .
Gribben JL, Kase SM, Waldman ED, Weintraub AS. A cross-sectional analysis of compassion fatigue, burnout, and compassion satisfaction in pediatric critical care physicians in the United States. Pediatr Crit Care Med J Soc Crit Care Med World Fed Pediatr Intensive Crit Care Soc. 2019;20(3):213–22. https://doi.org/10.1097/PCC.0000000000001803 .
Sengupta M, Roy A, Gupta S, Chakrabarti S, Mukhopadhyay I. Art of breaking bad news: a qualitative study in Indian healthcare perspective. Indian J Psychiatry. 2022;64(1):25–37. https://doi.org/10.4103/indianjpsychiatry.indianjpsychiatry_346_21 .
Cross LA. Compassion fatigue in palliative care nursing: a concept analysis. J Hosp Palliat Nurs. 2019;21(1):21. https://doi.org/10.1097/NJH.0000000000000477 .
Paiva-Salisbury ML, Schwanz KA. Building compassion fatigue resilience: awareness, prevention, and intervention for pre-professionals and current practitioners. J Health Serv Psychol. 2022;48(1):39–46. https://doi.org/10.1007/s42843-022-00054-9 .
Jun 8, information 2020 | For more, Corpuz-Bosshart contact L. ‘Wobble room’ provides time-out for COVID-19 frontliners. UBC News. Published June 8, 2020. Accessed 17 Jan 2023. https://news.ubc.ca/2020/06/08/making-a-difference-wobble-room-provides-time-out-for-covid-19-frontliners/
Gupta N, Dhamija S, Patil J, Chaudhari B. Impact of COVID-19 pandemic on healthcare workers. Ind Psychiatry J. 2021;30(Suppl 1):S282–4. https://doi.org/10.4103/0972-6748.328830 .
Menon GR, Yadav J, Aggarwal S, et al. Psychological distress and burnout among healthcare worker during COVID-19 pandemic in India—a cross-sectional study. PLoS ONE. 2022;17(3):e0264956. https://doi.org/10.1371/journal.pone.0264956 .
Nishimura Y, Miyoshi T, Sato A, et al. Burnout of healthcare workers amid the COVID-19 Pandemic: a follow-up study. Int J Environ Res Public Health. 2021;18(21):11581. https://doi.org/10.3390/ijerph182111581 .
Jemal K, Hailu D, Mekonnen M, Tesfa B, Bekele K, Kinati T. The importance of compassion and respectful care for the health workforce: a mixed-methods study. J Public Health. 2023;31(2):167–78. https://doi.org/10.1007/s10389-021-01495-0 .
Hui L, Garnett A, Oleyniov C, Boamah S. Compassion fatigue in health providers during the COVID-19 pandemic: A scoping review protocol. BMJ Open. 2023;13:e069843. https://doi.org/10.1136/bmjopen-2022-069843 .
Download references
Acknowledgements
I declare that the authors have no competing interests as defined by BMC, or other interests that might be perceived to influence the results and/or discussion reported in this paper.
Author information
Authors and affiliations.
Arthur Labatt Family School of Nursing, Western University, London, ON, Canada
Anna Garnett & Christina Oleynikov
Medical Sciences, Western University, London, ON, Canada
School of Nursing, McMaster University, Hamilton, ON, Canada
Sheila Boamah
You can also search for this author in PubMed Google Scholar
Contributions
AG is responsible for conception and design of the review. AG, LH, CO & SB contributed to the acquisition and analysis of the data. AG, LH & SB interpreted the data. LH drafted the manuscript and AG was a major contributor to the final version of the manuscript. AG, LH, CO & SB read, provided feedback and approved the final manuscript
Corresponding author
Correspondence to Anna Garnett .
Ethics declarations
Ethics approval and consent to participate.
Ethics approval was not required because this manuscript is a review of published literature.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Critical appraisals of included articles.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Garnett, A., Hui, L., Oleynikov, C. et al. Compassion fatigue in healthcare providers: a scoping review. BMC Health Serv Res 23 , 1336 (2023). https://doi.org/10.1186/s12913-023-10356-3
Download citation
Received : 07 August 2023
Accepted : 20 November 2023
Published : 01 December 2023
DOI : https://doi.org/10.1186/s12913-023-10356-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Compassion fatigue
- Healthcare provider
- Psychological health
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
- Open access
- Published: 06 April 2024
Delayed discharge in inpatient psychiatric care: a systematic review
- Ashley-Louise Teale ORCID: orcid.org/0000-0002-1756-7711 1 ,
- Ceri Morgan ORCID: orcid.org/0000-0002-2417-8677 1 ,
- Tom A. Jenkins ORCID: orcid.org/0000-0001-7875-4417 1 &
- Pamela Jacobsen ORCID: orcid.org/0000-0001-8847-7775 1
International Journal of Mental Health Systems volume 18 , Article number: 14 ( 2024 ) Cite this article
Metrics details
Delayed discharge is problematic. It is financially costly and can create barriers to delivering best patient care, by preventing return to usual functioning and delaying admissions of others in need. This systematic review aimed to collate existing evidence on delayed discharge in psychiatric inpatient settings and to develop understanding of factors and outcomes of delays in these services.
A search of relevant literature published between 2002 and 2022 was conducted on Pubmed, PsycInfo and Embase. Studies of any design, which published data on delayed discharge from psychiatric inpatient care in high income countries were included. Studies examining child and adolescent, general medical or forensic settings were excluded. A narrative synthesis method was utilised. Quality of research was appraised using the Mixed Methods Appraisal Tool (MMAT).
Eighteen studies from England, Canada, Australia, Ireland, and Norway met the inclusion criteria. Six main reasons for delayed discharge were identified: (1) accommodation needs, (2) challenges securing community or rehabilitation support, (3) funding difficulties, (4) family/carer factors, (5) forensic considerations and (6) person being out of area. Some demographic and clinical factors were also found to relate to delays, such as having a diagnosis of schizophrenia or other psychotic disorder, cognitive impairment, and increased service input prior to admission. Being unemployed and socially isolated were also linked to delays. Only one study commented on consequences of delays for patients, finding they experienced feelings of lack of choice and control. Four studies examined consequences on services, identifying high financial costs.
Overall, the findings suggest there are multiple interlinked factors relevant in delayed discharge that should be considered in practice and policy. Suggestions for future research are discussed, including investigating delayed discharge in other high-income countries, examining delayed discharge from child and forensic psychiatric settings, and exploring consequences of delays on patients and staff. We suggest that future research be consistent in terms used to define delayed discharge, to enhance the clarity of the evidence base.
Review registration number on PROSPERO
Date of registration.
9th December 2021.
Delayed discharge, also termed ‘bed blocking’ and ‘delayed transfer of care,’ refers to when patients remain in hospital beyond the time they are determined to be clinically fit to leave [ 1 , 2 ]. It is an international challenge, costly to individuals, health services and governments [ 3 , 4 ], impacting physical health settings, and also psychiatric inpatient services [ 5 ].
Psychiatric inpatient stays are one of the most expensive forms of treatment for mental health conditions, particularly when compared to care delivered in community settings [ 6 ]. Prolonged stays in mental health hospitals likely increase resource use and as such financial expenditure. This is particularly concerning in instances of delayed discharge when stays are determined to not be of clinical benefit. Delayed discharge also could prevent admission of new patients, contributing to bed crises, where there are not enough beds for all who require admission [ 7 ]. This can have consequences on the course of recovery for newly referred patients, either delaying admission, contributing to inappropriate placements, or leading to individuals being placed out of area [ 7 , 8 ]. Extended hospital stay could also detrimentally impact the delayed patient themselves, preventing their return to usual day-to-day functioning and make returning to the community increasingly difficult [ 9 , 10 ].
Existing reviews have examined predictors of longer stays in psychiatric inpatient settings, finding substance use and being employed are associated with shorter length of stay; while being female, having a diagnoses of mood or psychotic disorders and use of Electroconvulsive Therapy are associated with longer stay [ 11 ]. However, there is not to our knowledge a systematic review collating evidence examining delayed discharge in psychiatric settings. As delayed discharge is a unique experience, distinct from long stay driven by clinical need, it requires separate focus to further understand this specific experience.
Furthermore, a large body of evidence has examined delayed discharge in physical health settings with several systematic reviews, examining causes and outcomes. Such reviews have found that delayed discharges were linked to problems in discharge planning, transfer of care difficulties and patient age [ 12 , 13 ]. Outcomes for services included overcrowding and financial costs, whereas outcomes for patients included infections, depression, reduction in activities and mortality. There may be both overlapping and non-overlapping factors associated with delayed discharge between physical and psychiatric inpatient settings. For example, inpatient psychiatric services may differ in organisational structure, daily workings, and treatment focus from general medical services. The clinical population might also differ in psychiatric and physical health settings, for example in age, socio-economic status, and other demographic, plus clinical factors. As such, it is vital that separate attention be given to the area of psychiatric care.
This systematic review aims to fill the current research gap and synthesise existing literature on psychiatric delayed discharges. We aimed to synthesise the available international data from high-income countries, as the prevalence and underlying reasons for delayed discharge are likely to be highly sensitive to context and heterogeneous across countries. This is due to factors such as different models of healthcare funding, and the varying social role of the family in providing care, for example. Developing in-depth understanding of the causes and consequences of delays in a psychiatric inpatient context is important in informing practice and policies at a service, organisational, societal, and government level. This could help develop ways to reduce occurrence of delays and mitigate any negative impacts.
The aim of this review was to increase understanding of what is known about factors influencing delayed discharge in adult psychiatric inpatient settings. Secondary aims were to examine outcomes of delayed discharge for patients and compare findings across different psychiatric settings and age groups.
The systematic review protocol was pre-registered on PROSPERO before the review was started and the searches were run (PROSPERO: 292515). The review is reported in line with PRISMA guidelines [ 14 , 15 ]. The primary research question of this review is: What is known about factors associated with delayed discharge from inpatient psychiatric care settings?
Secondary research questions were:
What are the outcomes for those who have experienced delayed discharge from inpatient psychiatric settings, for example, in mental health outcomes, health outcomes, readmissions and quality of life?
What are the outcomes on services in terms of resources and costs from delayed psychiatric inpatient discharge?
What are the experiences of staff and patients of delayed discharge from inpatient mental health wards?
Are there differences between types of inpatient services, including acute, rehabilitation or specialist inpatient wards, in factors and costs, are there differences between working age adults and older adults, in experiences of delayed discharge, search strategy.
Initial searches were conducted on the 15th of January 2022, and updated on the 5th of August 2022. Pubmed, PsycInfo and Embase were searched.
Search terms (Appendix B in supplementary materials) were developed through examining key words of published studies on the topic, reviewing the terms used in comparative reviews based in physical health settings and thesaurus mapping. Terms included: “delayed discharge,” “bed blocking” and “long stays.” Search terms were piloted on each database prior to running the final search.
The search included studies published from 2002. A 20-year search timeframe was selected, as psychiatric inpatient care has adapted in response to changing need and updated knowledge over time. As such, studies published before 2002 are likely to be less relevant to current practice.
Following database searches, reference lists of included papers were examined, to identify any relevant studies missed in the search. A forward citation search was also conducted, to identify any relevant studies that were cited in the included papers.
Inclusion and exclusion criteria
Studies were included if they reported data related to delayed discharge or associated outcomes, in adult psychiatric inpatient wards. Specialist and rehabilitation psychiatric inpatient settings were included. Studies of any design were included, providing they were published in a peer-reviewed journal. Both quantitative and qualitative studies were included.
Studies exploring delayed discharge in child or adolescent units and/or forensic units were excluded. This was because the causes and outcomes of delays in such settings are likely unique, given the specialist context. For example, there is likely different systemic involvement from families and different governing legislation in these contexts. As such, it was determined that such settings were too disparate, and synthesising studies from these settings together with adult psychiatric settings could lead to inaccurate conclusions. Physical health settings were also excluded, given the different processes, procedures and treatment focus involved in such settings. In addition, reviews have already been conducted examining delayed discharge from such settings. Studies not conducted in high-income countries were also excluded. In this review, we included high-income countries as defined by World Bank criteria, accessed in January 2022 [ 16 ] (see Appendix C in supplementary material for the list of included countries). Globally, countries differ in the conceptualisation of mental health and provisions offered, therefore, limiting this review to only high-income countries would enable comparisons to be made.
Study selection and data extraction
Screening was conducted using Covidence Systematic Review Software [ 17 ]. All records were independently double-screened by two reviewers at both title/abstract and full-text stage. Conflicts were resolved by discussion to reach consensus, with referral to the senior author (PJ) when needed.
A standardised template was used for data extraction, with all included studies being independently double extracted by two reviewers, with consensus achieved by discussion where needed.
A narrative synthesis method was used. For data examining reasons for delayed discharge, a deductive approach was taken initially. Authors identified possible reasons for delays based on existing literature and organised data under these categories/themes. Any data that did not fit into the pre-defined categories was pooled as ‘other’. All categories were then reviewed, with particular attention placed on the ‘other’ categories, to determine if additional categories need to be added or existing categories adapted. Sub-categories were identified when appropriate through coding. Once categories were established, the number of papers which reported each reason/factor were tabulated and data was reviewed to examine relationships, exploring both links and disparities within and between studies. The final synthesis was checked by three authors (AT, TJ, and CM), to achieve final agreement.
Data relating to outcomes/consequences of delayed discharge was synthesised in a similar way, with data initially organised into three categories: (1) consequences for patients, (2) consequences for service, (3) consequences for staff. Categories were reviewed by the authors following synthesis. Financial costs were converted to US dollars by the authors to support comparison.
Quality assessment of the included studies formed part of the synthesis with the appraisal of quality considered in the interpretation of results.
Quality Assessment
Quality assessment of studies was completed during the synthesis stage. In the protocol, we initially outlined that the Quality Assessment Tool for Studies of Diverse Designs (QATSDD) would be utilised [ 18 ]. However, following a trial of this tool with the included papers, we noted disparities in interpretations between authors. Therefore, the Mixed Methods Appraisal Tool (MMAT) was established to be a more suitable appraisal of quality for the included studies. The MMAT was developed for assessing and comparing the quality of studies using quantitative, qualitative and mixed-methods design, in one tool [ 19 ]. This tool was selected as studies of different designs were included in the review and this tool allows for quality appraisal across five different study types, distinguishing between methodology.
Two initial screening questions were answered to determine appropriateness of using the MMAT to assess quality of the study (are there clear research questions and do the collected data address the research questions). If screening questions are not passed, this tool is deemed inappropriate. Providing the screening questions were passed, quality was assessed on five questions within one of five categories. The category in which questions were answered was determined by study design. The MMAT discourages from scoring and assigning qualitative labels to describe quality, instead advises a more detailed evaluation of quality [ 19 ]. This approach has therefore been taken in this paper.
To achieve reliable and accurate quality ratings, every study was quality rated by two members of the research team and conflicts were discussed to reach consensus.
Identification of studies
Figure 1 (PRISMA flowchart) shows the study selection process. After removing duplicates, a total of 4891 papers were identified for screening. 4397 papers were excluded at title and abstract stage. Full texts were then obtained for 492 papers. Two full texts could not be obtained via the library service and the authors did not respond to a request for the paper. There were four papers obtained that were erratum’s, all of which related to excluded studies that were not examining delayed discharge and as such, were not linked to the included studies. Following full text screening 18 papers were eligible for inclusion. Each paper represented a different study.
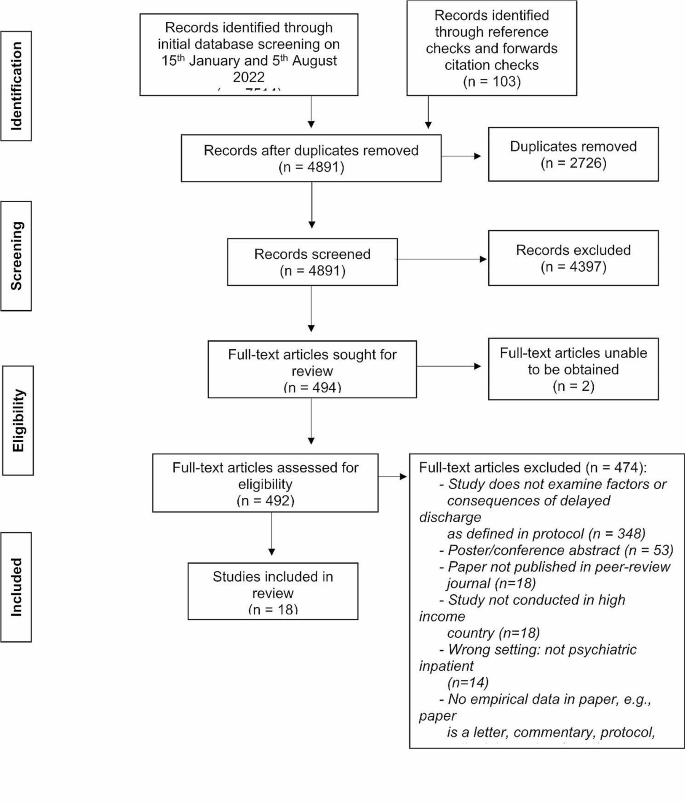
Preferred reporting items for systematic reviews and meta-analyses (PRISMA) flowchart
Study characteristics
Table 1 shows the characteristics of the 18 included studies. Twelve of these studies examined delayed discharge as a primary outcome, with three of these studies specifically examining Housing Related Delayed Discharge (HRDD). HRDD is defined as instances where delayed discharge is attributed to housing issues. The remaining studies ( n = 6) reported delayed discharge as secondary outcomes. Fifteen studies were of quantitative observational design, two studies used mixed methodologies and one was qualitative.
In the included studies, there was a range of psychiatric inpatient settings: psychiatric/general mental health units ( n = 11), Psychiatric Intensive Care Units (PICUs) ( n = 2), older adult psychiatric units ( n = 3) and Mental Health Trusts ( n = 1). One study looked across three inpatient settings: acute psychiatric, PICU and older adult. Studies were conducted in five high income countries (England = 10, Ireland = 1, Australia = 3, Canada = 3, and Norway = 1). There were no studies from any other high-income countries, identified in the search.
The MMAT quality scores are shown (Table 2 ). One included study [ 20 ] did not meet initial criteria to be assessed using this tool, as the research questions were unclear.
All studies were of fairly good quality, with all studies meeting at least three out of five of the quality assessment criteria. Quality was highest in Australian and Canadian studies, with included papers in these countries meeting all five quality assessment criteria [ 21 , 22 , 23 , 24 , 25 , 26 ]. Quality assessment ratings indicate that three quantitative descriptive studies included, did not clearly report use of a representative sample or appropriate measures. Ratings per question are shown in Table two.
Research Q1
What is known about factors associated with delayed discharge.
Thirteen studies identified reasons for delayed discharge (Table 1 ). The results showed that there are many complex reasons for delays with often overlapping contributing factors. We categorised reasons for delay into six categories: (1) accommodation needs, (2) difficulty securing rehabilitation or community support, (3) finance/funding challenges, (4) family/carer factors, (5) forensic factors, (6) patient being out of area.
The most common reason for delays was due to accommodation and placement factors. This was identified as a contributing reason for delay in twelve studies and a further two studies assessed Housing-Related Delayed Discharge (HRDD), suggesting accommodation factors contributing to delay in these cases. Accommodation/placement factors included limited availability of placements ( n = 7), difficulty finding appropriate placements ( n = 5), awaiting or undergoing placement assessment ( n = 3), challenges in person returning to accommodation ( n = 3), e.g., awaiting repairs or adaptations to their home, individuals being rejected from placement ( n = 2), patients/family rejecting placement ( n = 2) and awaiting transfer ( n = 1). It should be noted that one of the studies which examined specific accommodation factors was unable to be quality assessed due to not having clear research questions and therefore did not meet the screening criteria for assessment with the MMAT [ 20 ], and two studies only met three of the five quality assessment criteria, with queries regarding the quality of measures used and analysis technique for one study [ 27 ], and some difficulties integrating and meeting the full quality criteria for the mixed methods approaches used in the second [ 28 ]. The second reason identified for delays was difficulty sourcing support for the person to enable discharge, such as community, rehabilitation, and homecare support. This contributed to delays in twelve studies. Eight of these studies met four to five of the quality assessment criteria, one was not able to be assessed [ 20 ], and three only met three of the five quality assessment criteria [ 27 , 28 , 29 ]. A third reason for delay was finance/funding challenges identified in nine studies. These included challenges obtaining funding, patients/families’ refusal to pay for placements and funding applications being rejected. Six studies identified family/carers factors in creating delays, such as family conflict, family not wanting the person to live with them and ongoing family discussion. The quality of two of the studies identifying family and finance factors should be considered, as one of these studies was unable to be quality assessed due to a lack of clear research questions [ 20 ] and a second met only three of the five quality assessment criteria [ 28 ]. The fifth reason identified in this review as contributing to delay was forensic factors, which accounted for delays in three studies, all of good methodological quality. Forensic delays incorporated delay by Ministry of Justice and awaiting forensic assessment. Person being out of area was highlighted as a reason for delay in only one study and it was not possible to quality assess this study due to no specific research questions identified [ 20 ], suggesting limited exploration or evidence for out of areas contributing to delays.
Fourteen studies included in this review examined the demographic and clinical factors relevant in delays, with eight conducting significance testing to establish associations. Significant associations with delay were having a diagnosis of schizophrenia or other psychotic disorder ( n = 4), cognitive impairment ( n = 3) and type/amount of service input prior to admission ( n = 3). All studies reporting these significant results were of a good methodological quality, achieving at least four of the five MMAT quality criteria. Results were mainly consistent across those studies which examined significance, however, there was one study of good quality that did not find significant association with schizophrenia diagnosis [ 22 ]. The impact of physical health differed between Australia and England, where in one English study having fair-excellent health was more associated with delays [ 30 ], though two Australian studies found poorer physical health linked to delays [ 24 , 25 ]. Findings related to demographic characteristics, including gender, age, ethnicity, socio-economic status, were inconsistent across studies. The only consistent finding was that a smaller proportion of the delayed group were employed ( n = 3). One of these studies found significant association between being unemployed and delayed discharge. The two other studies found only one member of the delayed group was employed, less than non-delayed groups, though this was not significance tested. There was some indication that being not being married and lacking a support network, was higher in delayed groups. One study found significant relationships to being unmarried and another finding that the delayed group were visited significantly less often by relatives. The other studies did not conduct significance testing. However, there was no significant relationship related to marriage between delayed and non-delayed groups in two studies [ 22 , 31 ]. One of these studies only clearly met three of the quality assessment criteria [ 31 ], though the other met all five quality assessment criteria. Being male was significantly associated with delays in two Canadian studies [ 21 , 22 ]. No significant association with gender was found in other studies.
The supplementary materials provide additional analysis of results for research question one, further describing each study’s findings. Additional materials also include tables showing tabulation of which study examined each variable.
Research Q2
What are the outcomes for those who have experienced delayed discharge from inpatient psychiatric settings for example, in mental health outcomes, health outcomes, readmissions and quality of life.
Only one study examined individual outcomes of delayed discharge for patients [ 26 ]. As such, there is limited data to draw conclusions to answer this research question. The study that evaluated patient outcomes was of qualitative design and good quality. The study explored Housing-Related Delayed Discharge (HRDD) in Australia for 10 patients using semi-structured interviews. They found consequences of lack of choice and control for patients, which impacted mental wellbeing, physical health and created a sense of anticipation for transition to community. Some participants highlighted a positive outcome of delayed discharge in preventing homelessness.
Research Q3
What is the outcome on services in terms of resources and costs from delayed psychiatric inpatient discharge.
Four studies assessed financial costs of delayed discharge for services, providing limited evidence in terms of financial outcomes. Each study focused on a different country. At an old age psychiatry unit in England, delayed discharges were estimated to cost over $855,820 for the year [ 20 ]. Notably, this study was not quality assessed due to the omission of research questions. In a high-quality paper from Australia, HRDD cost the health district $2,828,174 over one year [ 25 ]. While both papers present yearly costs, there is disparity in area covered, contributing to difficulty making comparisons regarding financial expenditure. Two studies calculated financial expenditure and did not present the cost per year. In a Canadian study, using the median number of delayed days ( M = 17), it was calculated that the average cost incurred by one episode of delayed days was approximately $5,746 [ 21 ]. Furthermore, in Norway, $491,406 was allocated to delays on the acute ward included in the study, though methodological quality might be queried, due to lack of clarity on whether the sample was representative and the appropriateness of measures utilised [ 29 ]. The information necessary to calculate costs per year or costs per delayed day, to enable comparisons to be made across studies, has not included in the studies.
Aside from financial costs, no other type of outcome for services were assessed.
Research Q4
None of the included studies explored specific experiences of delayed discharge for staff. Some information on experiences for patients is detailed in question two.
Research Q5
This systematic review identified studies in acute psychiatric, older adult and Psychiatric Intensive Care Unit (PICU) settings. Only one study included Learning Disability inpatient care settings [ 28 ]. This study was of mixed-method design and met three quality assessment criteria. No studies reported data from rehabilitation units. There were few differences identified between types of setting. Prevalence of delayed discharge was highest in older adult settings (56.9%) [ 30 ] and PICU settings (51.1%) [ 32 ], compared to working age adult settings (18–32%) [ 31 , 33 ]. However, the highest proportion of delayed days was found in acute psychiatric settings in Norway acute psychiatric units (54.8%) [ 29 ]. More information on prevalence is provided in supplementary materials.
Reasons for delay did not vary much across type of setting. There is a potential service difference in the impact of physical health in delays, as having fair-excellent health was more associated with delays in an English older adult study [ 30 ], while in a working age adult sample in Australian studies [ 24 , 25 ], having poor health was more associated with delays. However, this could represent a disparity in country. There were some other differences across countries found. Forensic reasons for delay were only found in the UK ( n = 2), as was due to patient being out of area ( n = 1). In UK settings, there was no significant difference found in gender between those delayed and those not [ 30 , 34 ], though there was in Canada [ 21 ]. England and Australia were the only countries identifying funding issues as contributing to delay. Each country will have its own respective funding system, which could impact delays. For example, two Australian studies identified difficulties with their own National Disability Insurance Scheme [ 24 , 25 ].
Research Q6
Only five of the included studies looked specifically at older adult settings, all of which were in the UK. A further five studies, from the UK and Canada, included older adults within their sample, despite not examining a specific older adult setting.
The highest proportion of inpatients experiencing delayed discharge were from older adult settings, with one study identifying 56.9% [ 30 ] of inpatients experiencing delays. There were lower rates of delayed patients in working age adult psychiatric inpatient settings in comparison, with 3.5% [ 21 , 25 ] to 39.1% [ 29 ] of patients experiencing delay. Similarly, two studies in Canada identified that a higher proportion of older adults made up the delayed group compared to the non-delayed group, suggesting that older adult inpatients are more likely to experience delay [ 21 , 22 ]. However, two English studies found delayed discharge was not associated with age [ 31 , 35 ]. One of these studies met only three quality assessment criteria, with lack of clarity regarding the quality of sampling and representativeness of the sample [ 31 ].
In terms of reasons for delay, no clear differences were found across age groups. Although when limiting comparisons to studies conducted in the UK, family/carer factors was identified as a reason for delay more frequently in older adult samples ( n = 3) compared to studies looking at working age adults ( n = 1). To support this finding, one study in England found that eight older adult trusts identified patient/carer exercising choice as a reason for delay, whereas the same was true for only four working age adult trusts [ 28 ]. However, this finding cannot be generalised across all countries. There is also some indication that cognitive impairment/dementia might increase likelihood of delay in older adult samples, as two studies identified the role of dementia and greater cognitive impairment in the delayed older adult groups [ 20 , 30 ]. A further two studies examined the impact of cognitive impairment, finding association with delay [ 21 , 22 ]. However, these studies included working age samples, so it is unclear who in the sample this impacted. In addition, physical health status could cause delays differently in older adult populations. In an older adult UK sample having fair-excellent health was more associated with delays [ 30 ], whereas two Australian studies in working age adult inpatient settings found poorer physical health increased delays [ 24 , 25 ]. This difference could however be attributed to country or setting. Funding was identified as a reason for delay in all studies in older adult settings ( n = 5), but the same was not true for the other setting types. Forensic factors were not found to be a reason for delay in any of the studies with older adult inpatients, conversely patient being out of area was only identified as a reason for delay in an older adult sample [ 20 ].
This systematic review aimed to fill a research gap and examine factors contributing to delayed discharge in adult psychiatric inpatient settings and explore associated consequences. This adds a unique contribution to the evidence base, which predominantly has focused on delayed discharge from physical health settings. Eighteen studies were included for synthesis.
The findings suggest that there are varying inter-related reasons for delay, including accommodation or placement needs, difficulties securing the required support services, funding and finance challenges, family/carer factors, forensic factors and the person being out of area. There were mixed findings regarding demographic and clinical characteristics associated with delays. However, this review showed that delays could be associated with the person having diagnosis of schizophrenia or other psychotic disorder, cognitive impairment, being unemployed and receiving increased service input prior to admission.
There were only a few studies that commented on outcomes of delays. Only one study examined outcomes for patients, identifying feelings of lack of choice and control, while four studies looked at financial outcomes for services, finding large costs associated with delays. This points to a lack of evidence examining the outcomes and experiences of psychiatric delayed discharge, and therefore requires further attention in research.
This review adds to and expands on existing findings, identifying similarities and differences between longer stay generally. For example, one review [ 11 ] found that long stay was associated with mood and psychotic disorders, use of Electroconvulsive Therapy, and being female. Being married, employed, and using substances were associated with a shorter stay [ 11 ]. Our review found that psychiatric delayed discharge was also associated with diagnosis of schizophrenia or other psychotic disorder and being unemployed. However, we found delayed discharge to be associated with cognitive impairment and increased service input prior to admission, but not gender or treatment. This could suggest some important differences in those at risk of delays or those requiring longer inpatient treatment. It is important to note however, the review by Gopalakrishina and colleagues did not distinguish between those patients with long stay clinically warranted and delayed discharge patients [ 11 ]. It would be of benefit for future research on long stay patients to better define their sample based on those who clinically needed treatment or longer stay patients in the context of delayed discharge, allowing similarities and differences to be better explored. This will support policy makers and service managers to better identify those at risk of delays that are not clinically necessary, and those who might need additional clinical input. The findings in this review provide some suggestion that there could be benefit in considering a person’s social context when they are admitted to psychiatric inpatient care, including their living situation at admission, employment status and cognitive functioning. Identifying patients at higher risk of delays earlier in admission might be useful, to ensure more time be given to organise and find appropriate accommodations, placements and service support and facilitate discharge. Wider policy and structural changes are needed, such as improving the availability of appropriate accommodation placements.
It is important to highlight that there were discrepancies across studies in language used to term delayed discharge, e.g., ‘alternate level of care,’ ‘waiting days’ and ‘prolonged stay.’ Due to such discrepancies in definitions and terminology, during the screening process it was at times difficult to determine if studies were focused on delayed discharge or longer lengths of stay clinically required. In this review, studies were excluded if the focus was unclear to prevent incorrect conclusions being drawn related to the unique experience of delayed discharge. However, this means other relevant findings might have been missed. It would therefore be useful for future research on psychiatric inpatient care to ensure clarity in the terminology and definitions used in reports. There were also discrepancies in the way financial costs related to delays were reported, i.e., whether reported as cost per day, cost per year. This made comparing the costs across countries challenging and prevented clear conclusions being drawn. Future research should therefore aim to ensure clarity when reporting financial expenditure, for example, by calculating the daily cost of delays. It is important to highlight that only eighteen studies were identified over the 20-year search period, suggesting this area has not yet been subject to much research focus. All high-income countries met inclusion, but the final sample included studies from only five countries. It might have been expected that studies in other high-income countries be identified, particularly given the expensive nature of inpatient stays and as such delayed discharge. It might be beneficial for future research to further examine delayed discharge in psychiatric settings across other countries, particularly in the USA and EU. For the purposes of this review, studies not conducted in high-income countries were excluded. This was because lower-income countries might experience different factors contributing to delays due to differences in healthcare funding and social factors. As such, separate attention should be given to these settings, to understand similarities or differences in reasons for delays across low- and mid- income countries. Studies on forensic psychiatric settings and child and adolescent settings were also excluded in this instance, so again, there might be benefit in future research examining these areas.
Furthermore, future research could look not only at factors creating delays, but those causing longer delays. Some of the studies in this review began examining this, but more research in this area could be of interest. Finally, while the quality of included studies was relatively high, the studies were primarily of quantitative audit design and infrequently conducted significance testing. As such, further exploration of associations using significance testing would strengthen the evidence base.
In conclusion, 18 studies identified reasons for delayed discharge, including accommodation and placement related factors, challenges securing appropriate support, funding difficulties, family/carer factors, forensic factors and person being out of area. Delay was associated with having a diagnosis of schizophrenia or other psychotic disorder, cognitive impairment, increased service involvement prior to admission, and being unemployed. Service, societal and policy changes might be indicated, to improve accommodation and care provisions following discharge. Future research should continue to examine prolonged inpatient psychiatric stays, ensuring to distinguish between long stays and delayed discharge and improve clarity in terminology used.
Data availability
The data on which this review is based will be made publicly available on publication. A link to data for anonymous peer-review is here: https://osf.io/j4kng/?view_only=1fbf2558d9d044bbb1778fccd5fd6f51 .
Bryan K. Policies for reducing delayed discharge from hospital. Br Med Bull. 2010;95(1):33–46.
Article PubMed Google Scholar
NHS England. Monthly delayed transfers of care situation reports: definitions and guidance. London: NHS England; 2015.
Google Scholar
House of Commons Health Committee. Delayed Discharges (third report). In: Committee H, editor. 2002.
Rojas-García A, Turner S, Pizzo E, Hudson E, Thomas J, Raine R. Impact and experiences of delayed discharge: a mixed‐studies systematic review. Health Expect. 2018;21(1):41–56.
Christ W. Factors delaying discharge of psychiatric patients. Health Soc Work. 1984;9(3):178–87.
Article CAS Google Scholar
Department of Health. NHS reference costs 2013 to 2014. Department of Health London; 2013.
Glasby J, Lester H. Delayed hospital discharge and mental health: the policy implications of recent research. Social Policy Adm. 2004;38(7):744–57.
Article Google Scholar
National Institute of Health and Care Excellence [NICE]. Transition between inpatient mental health settings and community or care home settings. National Institue for Health and Care Excellence; 2016.
Katsakou C, Rose D, Amos T, Bowers L, McCabe R, Oliver D, et al. Psychiatric patients’ views on why their involuntary hospitalisation was right or wrong: a qualitative study. Soc Psychiatry Psychiatr Epidemiol. 2012;47:1169–79.
Csipke E, Williams P, Rose D, Koeser L, McCrone P, Wykes T, et al. Following the Francis report: investigating patient experience of mental health in-patient care. Br J Psychiatry. 2016;209(1):35–9.
Article CAS PubMed PubMed Central Google Scholar
Gopalakrishna G, Ithman M, Malwitz K. Predictors of length of stay in a psychiatric hospital. Int J Psychiatry Clin Pract. 2015;19(4):238–44.
Micallef A, Buttigieg SC, Tomaselli G, Garg L. Defining delayed discharges of inpatients and their impact in acute hospital care: a scoping review. Int J Health Policy Manage. 2022;11(2):103.
Cadel L, Guilcher SJ, Kokorelias KM, Sutherland J, Glasby J, Kiran T, et al. Initiatives for improving delayed discharge from a hospital setting: a scoping review. BMJ open. 2021;11(2):e044291.
Article PubMed PubMed Central Google Scholar
Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group* t. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–9.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. Updating guidance for reporting systematic reviews: development of the PRISMA 2020 statement. J Clin Epidemiol. 2021;134:103–12.
World Bank. World Bank Country and Lending Groups 2022 [ https://datahelpdesk.worldbank.org/knowledgebase/articles/906519.]
Covidence systematic review software. Veritas health innovation Melbourne, Australia. 2020. Available at: www.covidence.org.
Sirriyeh R, Lawton R, Gardner P, Armitage G. Reviewing studies with diverse designs: the development and evaluation of a new tool. J Eval Clin Pract. 2012;18(4):746–52.
Hong QN, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, et al. The mixed methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Educ Inform. 2018;34(4):285–91.
Hanif I, Rathod B. Delays in discharging elderly psychiatric in-patients. Psychiatr Bull. 2008;32(6):211–3.
Little J, Hirdes JP, Daniel I, editors. ALC status in in-patient mental health settings: evidence based on the Ontario Mental Health Reporting System. Healthcare Management Forum. Los Angeles, CA: SAGE Publications Sage CA; 2015.
Little J, Hirdes JP, Perlman CM, Meyer SB. Clinical predictors of delayed discharges in inpatient mental health settings across Ontario. Adm Policy Mental Health Mental Health Serv Res. 2019;46:105–14.
Aflalo M, Soucy N, Xue X, Colacone A, Jourdenais E, Boivin J-F. Characteristics and needs of psychiatric patients with prolonged hospital stay. Can J Psychiatry. 2015;60(4):181–8.
Honey A, Arblaster K, Nguyen J, Heard R. Predicting Housing Related delayed discharge from Mental Health Inpatient units: a Case Control Study. Adm Policy Mental Health Mental Health Serv Res. 2022;49(6):962–72.
Nguyen J, Honey A, Arblaster K, Heard R. Housing-related delayed discharge from inpatient mental health units: Magnitude and contributors in a metropolitan mental health service. Australian J Social Issues. 2022;57(1):144–63.
Chuah CPT, Honey A, Arblaster K. I’m institutionalised… there’s not much I can do’: lived experience of housing related delayed discharge. Aust Occup Ther J. 2022;69(5):574–84.
Cowman J, Whitty P. Prevalence of housing needs among inpatients: a 1 year audit of housing needs in the acute mental health unit in Tallaght Hospital. Ir J Psychol Med. 2016;33(3):159–64.
Article CAS PubMed Google Scholar
Lewis R, Glasby J. Delayed discharge from mental health hospitals: results of an English postal survey. Health Soc Care Commun. 2006;14(3):225–30.
Berg JE, Restan A. Duration of bed occupancy as calculated at a random chosen day in an acute care ward. Implications for the use of scarce resources in psychiatric care. Ann Gen Psychiatry. 2005;4(1):1–6.
Tucker S, Hargreaves C, Wilberforce M, Brand C, Challis D. What becomes of people admitted to acute old age psychiatry wards? An exploration of factors affecting length of stay, delayed discharge and discharge destination. Int J Geriatr Psychiatry. 2017;32(9):1027–36.
Tyrer P, Suryanarayan G, Rao B, Cicchetti D, Fulop N, Roberts F, et al. The bed requirement inventory: a simple measure to estimate the need for a psychiatric bed. Int J Soc Psychiatry. 2006;52(3):267–77.
Onyon R, Khan S, George M. Delayed discharges from a psychiatric intensive care unit–are we detaining patients unlawfully? J Psychiatric Intensive Care. 2006;2(2):59–64.
Impey M, Milner E. Delayed discharge from mental health inpatient care in the UK. Mental Health Pract. 2013;16(9).
Haw C, Otuwehinmi O, Kotterbova E. Out of area admissions to two independent sector PICUs: patient characteristics, length of stay and delayed discharges. J Psychiatric Intensive Care. 2017;13(1):27–36.
Poole R, Pearsall A, Ryan T. Delayed discharges in an urban in-patient mental health service in England. Psychiatric Bull. 2014;38(2):66–70.
Commander M, Rooprai D. Survey of long-stay patients on acute psychiatric wards. Psychiatr Bull. 2008;32(10):380–3.
Paton JM, Fahy MA, Livingston GA. Delayed discharge—a solvable problem? The place of intermediate care in mental health care of older people. Aging Ment Health. 2004;8(1):34–9.
Download references
No funding to declare.
Author information
Authors and affiliations.
Department of Psychology, University of Bath, Bath, BA2 7AY, UK
Ashley-Louise Teale, Ceri Morgan, Tom A. Jenkins & Pamela Jacobsen
You can also search for this author in PubMed Google Scholar
Contributions
AT and PJ formulated the initial research questions and developed the systematic review protocol. AT ran the searches on databases. AT, CM and TJ conducted the screening, data extraction and quality assessment. PJ acted as senior reviewer to resolve any conflicts. AT synthesised the results. All authors contributed to data synthesis and interpretation. AT wrote the paper. All authors read and approved the final version of manuscript for submission.
Corresponding author
Correspondence to Ashley-Louise Teale .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Teale, AL., Morgan, C., Jenkins, T.A. et al. Delayed discharge in inpatient psychiatric care: a systematic review. Int J Ment Health Syst 18 , 14 (2024). https://doi.org/10.1186/s13033-024-00635-9
Download citation
Received : 28 July 2023
Accepted : 25 March 2024
Published : 06 April 2024
DOI : https://doi.org/10.1186/s13033-024-00635-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Delayed discharge
- Bed blocking
- Delayed transfer
- Psychiatric inpatient
- Inpatient treatment
- Prolonged stays
- Length of stay
International Journal of Mental Health Systems
ISSN: 1752-4458
- Submission enquiries: [email protected]

The use and impact of surveillance-based technology initiatives in inpatient and acute mental health settings: A systematic review
- Find this author on Google Scholar
- Find this author on PubMed
- Search for this author on this site
- ORCID record for Jessica L. Griffiths
- For correspondence: [email protected]
- ORCID record for Katherine R. K. Saunders
- ORCID record for Una Foye
- ORCID record for Anna Greenburgh
- ORCID record for Antonio Rojas-Garcia
- ORCID record for Brynmor Lloyd-Evans
- ORCID record for Sonia Johnson
- ORCID record for Alan Simpson
- Info/History
- Supplementary material
- Preview PDF
Background: The use of surveillance technologies is becoming increasingly common in inpatient mental health settings, commonly justified as efforts to improve safety and cost-effectiveness. However, the use of these technologies has been questioned in light of limited research conducted and the sensitivities, ethical concerns and potential harms of surveillance. This systematic review aims to: 1) map how surveillance technologies have been employed in inpatient mental health settings, 2) identify any best practice guidance, 3) explore how they are experienced by patients, staff and carers, and 4) examine evidence regarding their impact. Methods: We searched five academic databases (Embase, MEDLINE, PsycInfo, PubMed and Scopus), one grey literature database (HMIC) and two pre-print servers (medRxiv and PsyArXiv) to identify relevant papers published up to 18/09/2023. We also conducted backwards and forwards citation tracking and contacted experts to identify relevant literature. Quality was assessed using the Mixed Methods Appraisal Tool. Data were synthesised using a narrative approach. Results: A total of 27 studies were identified as meeting the inclusion criteria. Included studies reported on CCTV/video monitoring (n = 13), Vision-Based Patient Monitoring and Management (VBPMM) (n = 6), Body Worn Cameras (BWCs) (n = 4), GPS electronic monitoring (n = 2) and wearable sensors (n = 2). Twelve papers (44.4%) were rated as low quality, five (18.5%) medium quality, and ten (37.0%) high quality. Five studies (18.5%) declared a conflict of interest. We identified minimal best practice guidance. Qualitative findings indicate that patient, staff and carer perceptions and experiences of surveillance technologies are mixed and complex. Quantitative findings regarding the impact of surveillance on outcomes such as self-harm, violence, aggression, care quality and cost-effectiveness were inconsistent or weak. Discussion: There is currently insufficient evidence to suggest that surveillance technologies in inpatient mental health settings are achieving the outcomes they are employed to achieve, such as improving safety and reducing costs. The studies were generally of low methodological quality, lacked lived experience involvement, and a substantial proportion (18.5%) declared conflicts of interest. Further independent coproduced research is needed to more comprehensively evaluate the impact of surveillance technologies in inpatient settings, including harms and benefits. If surveillance technologies are to be implemented, it will be important to engage all key stakeholders in the development of policies, procedures and best practice guidance to regulate their use, with a particular emphasis on prioritising the perspectives of patients.
Competing Interest Statement
AS and UF have undertaken and published research on BWCs. We have received no financial support from BWC or any other surveillance technology companies. All other authors declare no competing interests.
Clinical Protocols
https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=463993
Funding Statement
This study is funded by the National Institute for Health and Care Research (NIHR) Policy Research Programme (grant no. PR-PRU-0916-22003). The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. ARG was supported by the Ramon y Cajal programme (RYC2022-038556-I), funded by the Spanish Ministry of Science, Innovation and Universities.
Author Declarations
I confirm all relevant ethical guidelines have been followed, and any necessary IRB and/or ethics committee approvals have been obtained.
I confirm that all necessary patient/participant consent has been obtained and the appropriate institutional forms have been archived, and that any patient/participant/sample identifiers included were not known to anyone (e.g., hospital staff, patients or participants themselves) outside the research group so cannot be used to identify individuals.
I understand that all clinical trials and any other prospective interventional studies must be registered with an ICMJE-approved registry, such as ClinicalTrials.gov. I confirm that any such study reported in the manuscript has been registered and the trial registration ID is provided (note: if posting a prospective study registered retrospectively, please provide a statement in the trial ID field explaining why the study was not registered in advance).
I have followed all appropriate research reporting guidelines, such as any relevant EQUATOR Network research reporting checklist(s) and other pertinent material, if applicable.
Data Availability
The template data extraction form is available in Supplementary 1. MMAT quality appraisal ratings for each included study are available in Supplementary 2. All data used is publicly available in the published papers included in this review.
View the discussion thread.
Supplementary Material
Thank you for your interest in spreading the word about medRxiv.
NOTE: Your email address is requested solely to identify you as the sender of this article.

Citation Manager Formats
- EndNote (tagged)
- EndNote 8 (xml)
- RefWorks Tagged
- Ref Manager
- Tweet Widget
- Facebook Like
- Google Plus One
- Addiction Medicine (316)
- Allergy and Immunology (617)
- Anesthesia (159)
- Cardiovascular Medicine (2277)
- Dentistry and Oral Medicine (279)
- Dermatology (201)
- Emergency Medicine (370)
- Endocrinology (including Diabetes Mellitus and Metabolic Disease) (798)
- Epidemiology (11578)
- Forensic Medicine (10)
- Gastroenterology (678)
- Genetic and Genomic Medicine (3577)
- Geriatric Medicine (336)
- Health Economics (616)
- Health Informatics (2305)
- Health Policy (913)
- Health Systems and Quality Improvement (864)
- Hematology (335)
- HIV/AIDS (752)
- Infectious Diseases (except HIV/AIDS) (13154)
- Intensive Care and Critical Care Medicine (757)
- Medical Education (359)
- Medical Ethics (100)
- Nephrology (389)
- Neurology (3348)
- Nursing (191)
- Nutrition (507)
- Obstetrics and Gynecology (651)
- Occupational and Environmental Health (645)
- Oncology (1756)
- Ophthalmology (524)
- Orthopedics (209)
- Otolaryngology (284)
- Pain Medicine (223)
- Palliative Medicine (66)
- Pathology (438)
- Pediatrics (1002)
- Pharmacology and Therapeutics (422)
- Primary Care Research (406)
- Psychiatry and Clinical Psychology (3062)
- Public and Global Health (5989)
- Radiology and Imaging (1221)
- Rehabilitation Medicine and Physical Therapy (714)
- Respiratory Medicine (811)
- Rheumatology (367)
- Sexual and Reproductive Health (352)
- Sports Medicine (316)
- Surgery (386)
- Toxicology (50)
- Transplantation (170)
- Urology (142)
Developing a procedure for the repeated heat treatment (resintering) of UO 2 fuel pellets
- Theory and Processes of Formation and Sintering of Powdered Materials
- Published: 08 September 2009
- Volume 50 , pages 404–407, ( 2009 )
Cite this article
- V. V. Basov 1
45 Accesses
Explore all metrics
The basic parameters of testing the fuel pellets produced by powder metallurgy for resintering, which should be provided by repeated heat treatment, are stated. The expressions for calculating the pellet resintering level and describing the procedure developed at OAO Mashinostroitel’nii zavod (Elektrostal’) for evaluating the resintering of various types of fuel pellets are presented.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others

Investigation of (U, Th)O2 Fuel
I. S. Kurina, V. N. Rumyantsev & S. G. Samoilov*

Consolidation of commercial-size UO2 fuel pellets using spark plasma sintering and microstructure/microchemical analysis
Bowen Gong, Tiankai Yao, … Jie Lian
Changing the rules of the game: used fuel studies outside of a remote handling facility
Jon M. Schwantes, Michele Conroy, … Richard A. Clark
An Acceptable Model and Related Statistical Methods for the Analysis of Fuel Densification , US Nuclear Regulatory Commission, Regulatory Guide 1.126.
Moisio, I., Literature References and Resintering Test: Short Review , Finland: Power Station Department, 1987.
Google Scholar
Freshley, M.D., Brite, D.M., Daniel, I.L., and Hart, P.E., J. Nucl. Mater. , 1976, vol. 62, no. 2, p. 138.
Article ADS CAS Google Scholar
Brite, D.W., Daniel, I.L., Davis, N.C., et al., Report 131 , Power Research Institute, 1975.
Guidebook on Quality Control of Water Reactor Fuel: Techn. Rep. Ser. 221 , Vienna: International Atomic Energy Agency, 1983.
Meyer, R.O., The Analysis of Fuel Densification , US Nuclear Regulatory Commission, 1976.
Assmann, H. and Stehle, H., J. Nucl. Mater. , 1979, vol. 81, pp. 19–30.
Henke, M., Kernenergie , 1981, vol. 24, p. 142.
Radford, K. and Pope, I., J. Nucl. Mater. , 1977, vol. 64, p. 289.
Radford, K. and Pope, I., Mat. Res. Bull. , 1976, vol. 11, p. 585.
Article Google Scholar
US Patent 4430276, 1984.
Basov, V.V., Opredelenie kharakteristik termicheskoi stabil’nosti toplivnykh tabletok tipov R, R-E, V: Metodika (tekhnologicheskaya instruktsiya) (Determination of Characteristics of Thermal Stability of Fuel Pellets of Types R, R-E, and V: Procedure (Technological Manual), Elektrostal’: OAO Mashinostroitel’nyi zavod, 1999.
Download references
Author information
Authors and affiliations.
OAO Mashinostroitel’nii zavod, ul. K. Marksa 12, Elektrostal’, Moscow oblast, 144001, Russia
V. V. Basov
You can also search for this author in PubMed Google Scholar
Additional information
Original Russian Text © V.V. Basov, 2009, published in Izvestiya VUZ. Poroshkovaya Metallurgiya i Funktsional’nye Pokrytiya, 2009, No. 1, pp. 25–28.
About this article
Basov, V.V. Developing a procedure for the repeated heat treatment (resintering) of UO 2 fuel pellets. Russ. J. Non-ferrous Metals 50 , 404–407 (2009). https://doi.org/10.3103/S1067821209040191
Download citation
Published : 08 September 2009
Issue Date : August 2009
DOI : https://doi.org/10.3103/S1067821209040191
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- powder metallurgy
- fuel pellets
- fuel behavior forecasting
- out-of-pile and in-pile tests
- resintering
- resinterability
- microstructure
- evaluation procedure of resintering
- temperature-time diagram
- Find a journal
- Publish with us
- Track your research
- Popular Professionals
- Design & Planning
- Construction & Renovation
- Finishes & Fixtures
- Landscaping & Outdoor
- Systems & Appliances
- Interior Designers & Decorators
- Architects & Building Designers
- Design-Build Firms
- Kitchen & Bathroom Designers
- General Contractors
- Kitchen & Bathroom Remodelers
- Home Builders
- Roofing & Gutters
- Cabinets & Cabinetry
- Tile & Stone
- Hardwood Flooring Dealers
- Landscape Contractors
- Landscape Architects & Landscape Designers
- Home Stagers
- Swimming Pool Builders
- Lighting Designers and Suppliers
- 3D Rendering
- Sustainable Design
- Basement Design
- Architectural Design
- Universal Design
- Energy-Efficient Homes
- Multigenerational Homes
- House Plans
- Home Remodeling
- Home Additions
- Green Building
- Garage Building
- New Home Construction
- Basement Remodeling
- Stair & Railing Contractors
- Cabinetry & Cabinet Makers
- Roofing & Gutter Contractors
- Window Contractors
- Exterior & Siding Contractors
- Carpet Contractors
- Carpet Installation
- Flooring Contractors
- Wood Floor Refinishing
- Tile Installation
- Custom Countertops
- Quartz Countertops
- Cabinet Refinishing
- Custom Bathroom Vanities
- Finish Carpentry
- Cabinet Repair
- Custom Windows
- Window Treatment Services
- Window Repair
- Fireplace Contractors
- Paint & Wall Covering Dealers
- Door Contractors
- Glass & Shower Door Contractors
- Landscape Construction
- Land Clearing
- Garden & Landscape Supplies
- Deck & Patio Builders
- Deck Repair
- Patio Design
- Stone, Pavers, & Concrete
- Paver Installation
- Driveway & Paving Contractors
- Driveway Repair
- Asphalt Paving
- Garage Door Repair
- Fence Contractors
- Fence Installation
- Gate Repair
- Pergola Construction
- Spa & Pool Maintenance
- Swimming Pool Contractors
- Hot Tub Installation
- HVAC Contractors
- Electricians
- Appliance Services
- Solar Energy Contractors
- Outdoor Lighting Installation
- Landscape Lighting Installation
- Outdoor Lighting & Audio/Visual Specialists
- Home Theater & Home Automation Services
- Handyman Services
- Closet Designers
- Professional Organizers
- Furniture & Accessories Retailers
- Furniture Repair & Upholstery Services
- Specialty Contractors
- Color Consulting
- Wine Cellar Designers & Builders
- Home Inspection
- Custom Artists
- Columbus, OH Painters
- New York City, NY Landscapers
- San Diego, CA Bathroom Remodelers
- Minneapolis, MN Architects
- Portland, OR Tile Installers
- Kansas City, MO Flooring Contractors
- Denver, CO Countertop Installers
- San Francisco, CA New Home Builders
- Rugs & Decor
- Home Improvement
- Kitchen & Tabletop
- Bathroom Vanities
- Bathroom Vanity Lighting
- Bathroom Mirrors
- Bathroom Fixtures
- Nightstands & Bedside Tables
- Kitchen & Dining
- Bar Stools & Counter Stools
- Dining Chairs
- Dining Tables
- Buffets and Sideboards
- Kitchen Fixtures
- Wall Mirrors
- Living Room
- Armchairs & Accent Chairs
- Coffee & Accent Tables
- Sofas & Sectionals
- Media Storage
- Patio & Outdoor Furniture
- Outdoor Lighting
- Ceiling Lighting
- Chandeliers
- Pendant Lighting
- Wall Sconces
- Desks & Hutches
- Office Chairs
- View All Products
- Designer Picks
- Side & End Tables
- Console Tables
- Living Room Sets
- Chaise Lounges
- Ottomans & Poufs
- Bedroom Furniture
- Nightstands
- Bedroom Sets
- Dining Room Sets
- Sideboards & Buffets
- File Cabinets
- Room Dividers
- Furniture Sale
- Trending in Furniture
- View All Furniture
- Bath Vanities
- Single Vanities
- Double Vanities
- Small Vanities
- Transitional Vanities
- Modern Vanities
- Houzz Curated Vanities
- Best Selling Vanities
- Bathroom Vanity Mirrors
- Medicine Cabinets
- Bathroom Faucets
- Bathroom Sinks
- Shower Doors
- Showerheads & Body Sprays
- Bathroom Accessories
- Bathroom Storage
- Trending in Bath
- View All Bath
- Houzz x Jennifer Kizzee
- Houzz x Motivo Home
- How to Choose a Bathroom Vanity

- Patio Furniture
- Outdoor Dining Furniture
- Outdoor Lounge Furniture
- Outdoor Chairs
- Adirondack Chairs
- Outdoor Bar Furniture
- Outdoor Benches
- Wall Lights & Sconces
- Outdoor Flush-Mounts
- Landscape Lighting
- Outdoor Flood & Spot Lights
- Outdoor Decor
- Outdoor Rugs
- Outdoor Cushions & Pillows
- Patio Umbrellas
- Lawn & Garden
- Garden Statues & Yard Art
- Planters & Pots
- Outdoor Sale
- Trending in Outdoor
- View All Outdoor
- 8 x 10 Rugs
- 9 x 12 Rugs
- Hall & Stair Runners
- Home Decor & Accents
- Pillows & Throws
- Decorative Storage
- Faux Florals
- Wall Panels
- Window Treatments
- Curtain Rods
- Blackout Curtains
- Blinds & Shades
- Rugs & Decor Sale
- Trending in Rugs & Decor
- View All Rugs & Decor
- Pendant Lights
- Flush-Mounts
- Ceiling Fans
- Track Lighting
- Wall Lighting
- Swing Arm Wall Lights
- Display Lighting
- Table Lamps
- Floor Lamps
- Lamp Shades
- Lighting Sale
- Trending in Lighting
- View All Lighting
- Bathroom Remodel
- Kitchen Remodel
- Kitchen Faucets
- Kitchen Sinks
- Major Kitchen Appliances
- Cabinet Hardware
- Backsplash Tile
- Mosaic Tile
- Wall & Floor Tile
- Accent, Trim & Border Tile
- Whole House Remodel
- Heating & Cooling
- Building Materials
- Front Doors
- Interior Doors
- Home Improvement Sale
- Trending in Home Improvement
- View All Home Improvement
- Cups & Glassware
- Kitchen & Table Linens
- Kitchen Storage and Org
- Kitchen Islands & Carts
- Food Containers & Canisters
- Pantry & Cabinet Organizers
- Kitchen Appliances
- Gas & Electric Ranges
- Range Hoods & Vents
- Beer & Wine Refrigerators
- Small Kitchen Appliances
- Cookware & Bakeware
- Tools & Gadgets
- Kitchen & Tabletop Sale
- Trending in Kitchen & Tabletop
- View All Kitchen & Tabletop
- Storage & Organization
- Baby & Kids

- View all photos
- Dining Room
- Breakfast Nook
- Family Room
- Bed & Bath
- Powder Room
- Storage & Closet
- Outdoor Kitchen
- Bar & Wine
- Wine Cellar
- Home Office
- Popular Design Ideas
- Kitchen Backsplash
- Deck Railing
- Privacy Fence
- Small Closet
- Stories and Guides
- Popular Stories
- Renovation Cost Guides
- Fence Installation Cost Guide
- Window Installation Cost Guide
- Discussions
- Design Dilemmas
- Before & After
- Houzz Research
- View all pros
- View all services
- View all products
- View all sales
- Living Room Chairs
- Dining Room Furniture
- Coffee Tables
- Home Office Furniture
- Join as a Pro
- Interior Design Software
- Project Management
- Custom Website
- Lead Generation
- Invoicing & Billing
- Landscape Contractor Software
- General Contractor Software
- Remodeler Software
- Builder Software
- Roofer Software
- Architect Software
- Takeoff Software
- Lumber & Framing Takeoffs
- Steel Takeoffs
- Concrete Takeoffs
- Drywall Takeoffs
- Insulation Takeoffs
- Stories & Guides
- LATEST FROM HOUZZ
- HOUZZ DISCUSSIONS
- SHOP KITCHEN & DINING
- Kitchen & Dining Furniture
- Sinks & Faucets
- Kitchen Cabinets & Storage
- Knobs & Pulls
- Kitchen Knives
- KITCHEN PHOTOS
- FIND KITCHEN PROS
- Bath Accessories
- Bath Linens
- BATH PHOTOS
- FIND BATH PROS
- SHOP BEDROOM
- Beds & Headboards
- Bedroom Decor
- Closet Storage
- Bedroom Vanities
- BEDROOM PHOTOS
- Kids' Room
- FIND DESIGN PROS
- SHOP LIVING
- Fireplaces & Accessories
- LIVING PHOTOS
- SHOP OUTDOOR
- Pool & Spa
- Backyard Play
- OUTDOOR PHOTOS
- FIND LANDSCAPING PROS
- SHOP LIGHTING
- Bathroom & Vanity
- Flush Mounts
- Kitchen & Cabinet
- Outdoor Wall Lights
- Outdoor Hanging Lights
- Kids' Lighting
- Decorative Accents
- Artificial Flowers & Plants
- Decorative Objects
- Screens & Room Dividers
- Wall Shelves
- About Houzz
- Houzz Credit Cards
- Privacy & Notice
- Cookie Policy
- Your Privacy Choices
- Mobile Apps
- Copyright & Trademark
- For Professionals
- Houzz vs. Houzz Pro
- Houzz Pro vs. Ivy
- Houzz Pro Advertising Reviews
- Houzz Pro 3D Floor Planner Reviews
- Trade Program
- Buttons & Badges
- Your Orders
- Shipping & Delivery
- Return Policy
- Houzz Canada
- Review Professionals
- Suggested Professionals
- Accessibility
- Houzz Support
- COUNTRY COUNTRY
Gardeners & Lawn Care Companies in Elektrostal'
Location (1).
- Use My Current Location
Popular Locations
- Albuquerque
- Cedar Rapids
- Grand Rapids
- Indianapolis
- Jacksonville
- Kansas City
- Little Rock
- Los Angeles
- Minneapolis
- New Orleans
- Oklahoma City
- Orange County
- Philadelphia
- Portland Maine
- Salt Lake City
- San Francisco
- San Luis Obispo
- Santa Barbara
- Washington D.C.
- Elektrostal', Moscow Oblast, Russia
Professional Category (1)
- Accessory Dwelling Units (ADU)
Featured Reviews for Gardeners & Lawn Care Companies in Elektrostal'
What types of services do gardeners and lawn care companies provide, questions to ask a prospective gardener or lawn care service:, business services, connect with us.
Yakor Hotel

View prices for your travel dates
- Excellent 1
- Very Good 2
- All languages ( 6 )
- Russian ( 6 )
- English ( 0 )
Own or manage this property? Claim your listing for free to respond to reviews, update your profile and much more.
YAKOR HOTEL - Reviews (Elektrostal, Russia)

IMAGES
VIDEO
COMMENTS
Surveying the literature on the assessment of quality of care from the patient's perspective, the concept has often been operationalized as patient satisfaction. Patient satisfaction has been a widely investigated subject in health care research, and dozens of measuring instruments were developed during the past decade.
The Patient Perspective of Quality Care: A Literature Review. January 2019. The George Washington University Undergraduate Review 2 (Spring 2019) DOI: 10.4079/2578-9201.2 (2019).10. Authors ...
This literature review included peer-reviewed studies in English, and excluded grey literature as well as foreign language journals. Furthermore, the results show a very limited number of studies on the relationship between benchmarking and quality improvement, despite the growing interest and research on this topic at the international level.
Quality of care is one of the most frequently quoted principles of health policy, and it is currently high up on the agenda of policy-makers at national, European and international levels (EC, 2016; OECD, 2017; WHO, 2018; WHO/OECD/World Bank, 2018). At the national level, addressing the issue of healthcare quality may be motivated by various reasons - ranging from a general commitment to ...
Quality care continues to be a prominent "true north" indicator of the healthcare system. The quality of the healthcare system is a lumping parameter that reflects patient safety and satisfaction, service delivery efficiency, cost competitiveness, and aspects of sustainability ().Therefore, measurement of quality care is an important practice in the healthcare system to ensure the ...
Systematic reviews that summarize the available information on a topic are an important part of evidence-based health care. There are both research and non-research reasons for undertaking a literature review. It is important to systematically review the literature when one would like to justify the need for a study, to update personal ...
The logistics of patient care and healthcare management revolve around many aspects of optimized high-quality care. The Joint Commission (TJC), Malcolm Baldrige National Quality Award (MBNQA), and The Magnet Recognition Program signify healthcare accreditation, performance excellence, and nursing excellence, respectively [1,2,3].TJC is the recognized global leader of healthcare accreditation [].
Method. By performing a literature review via PubMed, the author identified and surveyed 23 studies that compared the quality of care in teaching hospitals with that in nonteaching hospitals. The studies were published from 1989-2004 and in all but one case dealt exclusively with U.S. hospitals.
homes will be required to implement a program to improve quality of care (Mills et.al., 2018). With the growing need of LTC services and the lack of quality care in these facilities, the purpose of this systematic literature review is to identify the current quality initiatives for nursing homes in the United States.
Quality of care in primary health care setting in the eastern mediterranean region: A systematic review of the literature. International Journal for Quality in Health Care , 27 ( 2 ), 79 - 88 . Senic , V. , & Marinkovic , V. ( 2013 ).
The review concludes that the methodology and instruments used to evaluate the patient perspective depend heavily upon specific intentions driving the evaluation. Furthermore, as global health systems become more patient-centric, organizations are implored to review their internal resources and values to determine why and if a patient-centric ...
Quality Nursing Care: a Selective Review of the Literature of Patients' and Nurses' Interpretations. January 2009; ... • Quality nursing care is a context specific term, meaning that many ...
A finding in the current study that has not been well articulated in the previous literature is participants' recognition of their responsibilities in healthcare quality that extend beyond the provision of competent, person-centred, safe care, to care that is aligned with best evidence and clinical standards (Evidence Based Practice domain ...
A literature review was undertaken to explore both published and unpublished quality improvement studies, projects, and initiatives that strove to develop more efficient systems to support an infrastructure for nursing home quality of care. The review included a search of all available, full-text published literature from 1997 to 2007 available ...
To understand better how to achieve a good quality literature review, it is helpful to look at the specific processes of the archetypes of literature reviews introduced in Section 2.5; they can also be found in Fig. 3.1, which presents a further classification of the protocol-driven approaches to literature reviews.Even though different archetypes serve different purposes, there are similar ...
Given the long standing call for clinical care review, with limited literature to inform care review systems, we conducted a qualitative systematic review to identify characteristics discussed in existing models for care review. ... Edwards MT. A longitudinal study of clinical peer review's impact on quality and safety in US hospitals. J ...
Providing healthcare services that respect and meet patients' and caregivers' needs are essential in promoting positive care outcomes and perceptions of quality of care, thereby fulfilling a significant aspect of patient-centered care requirement. Effective communication between patients and healthcare providers is crucial for the provision of patient care and recovery. Hence, patient ...
In this systematic literature review, 18 of 110 (16.4%) of the included studies discussed that outreach services or mobile clinics in primary care and rural hospital settings can improve access to PHC services in rural communities.
The review will include literature wherein patients received care from APNs in collaboration with specialists in other disciplines. Concept. ... APNs have provided high-quality care and accumulated evidence by researching and reporting their own practices. We suggest extracting the literature on the role of nephrology APNs in improving ...
The detrimental impacts of COVID-19 on healthcare providers' psychological health and well-being continue to affect their professional roles and activities, leading to compassion fatigue. The purpose of this review was to identify and summarize published literature on compassion fatigue among healthcare providers and its impact on patient care. Six databases were searched: MEDLINE (Ovid ...
Delayed discharge is problematic. It is financially costly and can create barriers to delivering best patient care, by preventing return to usual functioning and delaying admissions of others in need. This systematic review aimed to collate existing evidence on delayed discharge in psychiatric inpatient settings and to develop understanding of factors and outcomes of delays in these services.
Background: The use of surveillance technologies is becoming increasingly common in inpatient mental health settings, commonly justified as efforts to improve safety and cost-effectiveness. However, the use of these technologies has been questioned in light of limited research conducted and the sensitivities, ethical concerns and potential harms of surveillance. This systematic review aims to ...
The basic parameters of testing the fuel pellets produced by powder metallurgy for resintering, which should be provided by repeated heat treatment, are stated. The expressions for calculating the pellet resintering level and describing the procedure developed at OAO Mashinostroitel'nii zavod (Elektrostal') for evaluating the resintering of various types of fuel pellets are presented.
Search 14 Elektrostal' gardeners & lawn care companies to find the best gardener or lawn care service for your project. See the top reviewed local gardeners & lawn care services in Elektrostal', Moscow Oblast, Russia on Houzz.
Elektrostal, city, Moscow oblast (province), western Russia.It lies 36 miles (58 km) east of Moscow city. The name, meaning "electric steel," derives from the high-quality-steel industry established there soon after the October Revolution in 1917. During World War II, parts of the heavy-machine-building industry were relocated there from Ukraine, and Elektrostal is now a centre for the ...
Yakor Hotel, Elektrostal: See 6 traveler reviews, candid photos, and great deals for Yakor Hotel, ranked #3 of 7 hotels in Elektrostal and rated 3.5 of 5 at Tripadvisor.