Ohio State nav bar
The Ohio State University
- BuckeyeLink
- Find People
- Search Ohio State

Patient Case Presentation
Patient presentation.
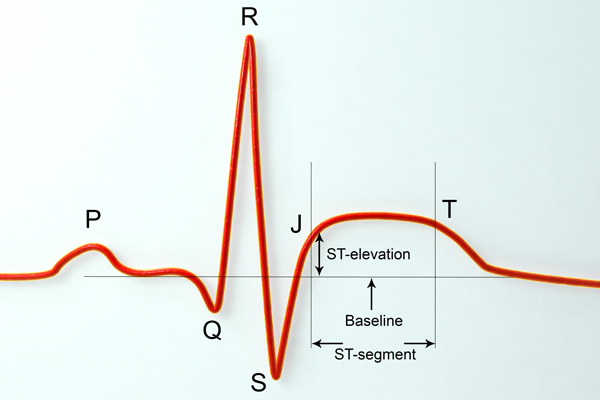
Mr. Smith is a 60-year-old Caucasian male, who presents with 8/10 chest pain after working out. He just quit smoking and started a new workout and diet program after recently retiring. He has noticed some chest and shoulder discomfort with working out that usually resolves with rest, but decided to come to the emergency department because this episode was unrelenting and more severe. Mr. Smith describes his current pain as severe and sharp, and also complains of nausea and shortness of breath. Vital signs are HR: 110 BP: 150/90 RR: 30 Temp 97.6 O2 Sat: 92% on 2L nasal cannula, EKG shows ST segment elevation in leads II, III and AVf. Labs were drawn, including an elevated troponin (4.23 ng/ml), and slightly elevated white blood cell count (13.6 × 10 9 /L) .
Past Medical History
Type II diabetes (age 47), dyslipidemia (age 33), atherosclerosis (age 52), hypertension (age 49), obesity (age 33), viral pneumonia (age 29), hiatal hernia (age 28), peptic ulcer disease (age 41)
Family Medical History
Mother (deceased) – atrial fibrillation (diagnosed at age 45), died of MI (age 65)
Father (83) – obesity, type II diabetes (diagnosed at 50), COPD (diagnosed at 55)
Social History
Smoker (20 pack years), worked in an office sitting at a desk his whole career (35 years), recently began working out at his local gym since retiring this year.
Myocardial Infarction (MI) Case Study (45 min)
Watch More! Unlock the full videos with a FREE trial
Included In This Lesson
Study tools.
Access More! View the full outline and transcript with a FREE trial
Definition of Myocardial Infarction (MI)
Myocardial infarction, commonly known as a heart attack, is a critical medical event that occurs when the blood supply to the heart muscle is severely reduced or completely blocked. It is a leading cause of death worldwide and a significant public health concern.
Introduction to Myocardial Infarction (MI)
This nursing case study aims to provide a comprehensive understanding of myocardial infarction by delving into its various aspects, including its pathophysiology, risk factors, clinical presentation, diagnostic methods, and management strategies. Through the exploration of a fictional patient’s journey, we will shed light on the intricate nature of this life-threatening condition and highlight the importance of early recognition and intervention.
Background and Significance of Myocardial Infarction
Myocardial infarction is a sudden and often catastrophic event that can have profound consequences on an individual’s health and well-being. Understanding its underlying mechanisms and risk factors is essential for healthcare professionals, as timely intervention can be life-saving. This case study not only serves as a learning tool but also emphasizes the critical role of medical practitioners in identifying and managing myocardial infarctions promptly.
Pathophysiology of Myocardial Infarction
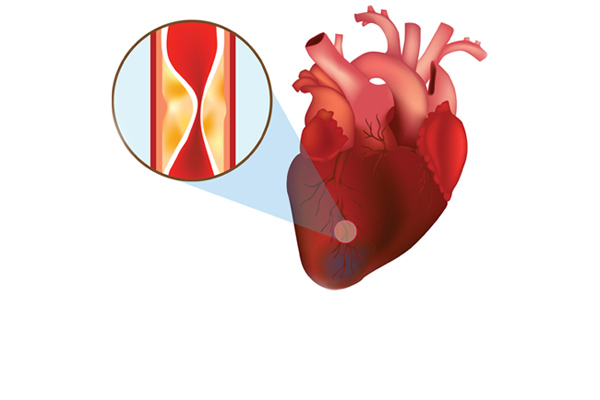
A crucial aspect of comprehending myocardial infarction is exploring its pathophysiology. We will delve into the intricate details of how atherosclerosis, the buildup of plaque in coronary arteries, leads to the formation of blood clots and the subsequent interruption of blood flow to the heart muscle. This disruption in blood supply triggers a cascade of events, ultimately resulting in the death of cardiac cells.
Risk Factors of Myocardial Infarction
Understanding the risk factors associated with myocardial infarction is vital for prevention and early detection. This case study will examine both modifiable and non-modifiable risk factors, including age, gender, family history, smoking, high blood pressure, diabetes, and high cholesterol levels. Recognizing these risk factors is instrumental in developing effective strategies for prevention and risk reduction.
Clinical Presentation Myocardial Infarction
Recognizing the signs and symptoms of myocardial infarction is crucial for timely intervention. We will present a fictional patient’s experience, illustrating the typical clinical presentation, which often includes chest pain or discomfort, shortness of breath, nausea, lightheadedness, and diaphoresis. Through this patient’s journey, we will highlight the importance of accurate symptom assessment and prompt medical attention.
Diagnostic Methods for Myocardial Infarction
Modern medicine offers various diagnostic tools to confirm a myocardial infarction swiftly and accurately. This case study will explore these diagnostic methods, such as electrocardiography (ECG), cardiac biomarkers, and imaging techniques like coronary angiography. By understanding these diagnostic modalities, healthcare professionals can make informed decisions and initiate appropriate treatments promptly.
Management Strategies for Myocardial Infarction
The management of myocardial infarction involves a multidisciplinary approach, including medication, revascularization procedures, and lifestyle modifications. We will discuss the fictional patient’s treatment plan, emphasizing the importance of reestablishing blood flow to the affected heart muscle and preventing further complications.
Nursing Case Study for Myocardial Infarction (MI)
Having established a foundational understanding of myocardial infarction, we will now delve deeper into Mr. Salazar’s case, tracing his journey through diagnosis, treatment, and recovery. This in-depth examination will shed light on the real-world application of the principles discussed in the introduction, providing valuable insights into the clinical management of myocardial infarction and its impact on patient outcomes.
Mr. Salazar, a 57-year-old male, arrives at the Emergency Department (ED) with complaints of chest pain that began approximately one hour after dinner while he was working. He characterizes the discomfort as an intense “crushing pressure” located centrally in his chest, extending down his left arm and towards his back. He rates the pain’s severity as 4/10. Upon examination, Mr. Salazar exhibits diaphoresis and pallor, accompanied by shortness of breath (SOB).
What further nursing assessments need to be performed for Mr. Salazar?
- Heart Rate (HR): The number of heartbeats per minute.
- Blood Pressure (BP): The force of blood against the walls of the arteries, typically measured as systolic (during heartbeats) and diastolic (between heartbeats) pressure.
- Respiratory Rate (RR): The number of breaths a patient takes per minute.
- Body Temperature (Temp): The measurement of a patient’s internal body heat.
- Oxygen Saturation (SpO2): The percentage of oxygen in the blood.
- S1: The first heart sound, often described as “lub,” is caused by the closure of the mitral and tricuspid valves.
- S2: The second heart sound, known as “dub,” results from the closure of the aortic and pulmonic valves.
- These sounds provide important diagnostic information about the condition of the heart.
- Clear: Normal, healthy lung sounds with no added sounds.
- Crackles (Rales): Discontinuous, often high-pitched sounds are heard with conditions like pneumonia or heart failure.
- Wheezes: Whistling, musical sounds often associated with conditions like asthma or chronic obstructive pulmonary disease (COPD).
- Pulses refer to the rhythmic expansion and contraction of arteries with each heartbeat. Common pulse points for assessment include the radial artery (wrist), carotid artery (neck), and femoral artery (groin). Evaluating pulses helps assess the strength, regularity, and rate of blood flow.
- Edema is the abnormal accumulation of fluid in body tissues, leading to swelling. It can occur in various body parts and may indicate underlying conditions such as heart failure, kidney disease, or localized injury. Edema assessment involves evaluating the degree of swelling and its location.
- Skin condition (temperature, color, etc.)
What interventions do you anticipate being ordered by the provider?
- Oxygen therapy involves administering oxygen to a patient to increase the level of oxygen in their blood. It is used to treat conditions such as respiratory distress, and hypoxia (low oxygen levels), and to support patients with breathing difficulties.
- Nitroglycerin is a medication used to treat angina (chest pain) and to relieve symptoms of heart-related conditions. It works by relaxing and widening blood vessels, which improves blood flow to the heart, reducing chest pain.
- Aspirin is a common over-the-counter medication and antiplatelet drug. In the context of myocardial infarction (heart attack), it is often administered to reduce blood clot formation, potentially preventing further blockage in coronary arteries.
- A 12-lead EKG is a diagnostic test that records the electrical activity of the heart from 12 different angles. It provides information about the heart’s rhythm, rate, and any abnormalities, helping diagnose conditions like arrhythmias, heart attacks, and ischemia.
- Cardiac enzymes are proteins released into the bloodstream when heart muscle cells are damaged or die, typically during a heart attack. Measuring these enzymes, such as troponin and creatine kinase-MB (CK-MB), helps confirm a heart attack diagnosis and assess its severity.
- A chest X-ray is a diagnostic imaging procedure that creates images of the chest and its internal structures, including the heart and lungs. It is used to identify issues like lung infections, heart enlargement, fluid accumulation, or fractures in the chest area.
- Possibly an Echocardiogram
Upon conducting a comprehensive assessment, it was observed that the patient exhibited no signs of jugular vein distention (JVD) or edema. Auscultation revealed normal heart sounds with both S1 and S2 present, while the lungs remained clear, albeit with scattered wheezes. The patient’s vital signs were recorded as follows:
- BP 140/90 mmHg SpO 2 90% on Room Air
- HR 92 bpm and regular Ht 173 cm
- RR 32 bpm Wt 104 kg
- Temp 36.9°C
The 12-lead EKG repor t indicated the presence of “Normal sinus rhythm (NSR) with frequent premature ventricular contractions (PVCs) and three- to four-beat runs of ventricular tachycardia (VT).” Additionally, there was ST-segment elevation in leads I, aVL, and V2 through V6 (3-4mm), accompanied by ST-segment depression in leads III and aVF.
Cardiac enzyme levels were collected but were awaiting results at the time of assessment. A chest x-ray was also ordered to provide further diagnostic insights.
In response to the patient’s condition, the healthcare provider prescribed the following interventions:
- Aspirin: 324 mg administered orally once.
- Nitroglycerin: 0.4 mg administered sublingually (SL), with the option of repeating the dose every five minutes for a maximum of three doses.
- Morphine: 4 mg to be administered intravenously (IVP) as needed for unrelieved chest pain.
- Oxygen: To maintain oxygen saturation (SpO2) levels above 92%.
These interventions were implemented to address the patient’s myocardial infarction (heart attack) and alleviate associated symptoms, with a focus on relieving chest pain, improving oxygenation, and closely monitoring vital signs pending further diagnostic results.
What intervention should you, as the nurse, perform right away? Why?
- Apply oxygen – this can be done quickly and easily and can help to prevent further complications from low oxygenation.
- Oxygen helps to improve oxygenation as well as to decrease myocardial oxygen demands.
- Often it takes a few minutes or more for medications to be available from the pharmacy, so it makes sense to take care of this intervention first.
- ABC’s – breathing/O 2 .
What medication should be the first one administered to this patient? Why? How often?
- Nitroglycerin 0.4mg SL – it is a vasodilator and works on the coronary arteries. The goal is to increase blood flow to the myocardium. If this is effective, the patient merely has angina. However, if it is not effective, the patient may have a myocardial infarction.
- Aspirin should also be given, but it is to decrease platelet aggregation and reduce mortality. While it can somewhat help prevent the worsening of the blockage, it does little for the current pain experienced by the patient.
- Morphine should only be given if the nitroglycerin and aspirin do not relieve the patient’s chest pain.
What is the significance of the ST-segment changes on Mr. Salazar's 12-lead EKG?
- ST-segment changes on a 12-lead EKG indicate ischemia (lack of oxygen/blood flow) or infarction (death of the muscle tissue) of the myocardium (heart muscle).
- This indicates an emergent situation. The patient’s coronary arteries are blocked and need to be reopened by pharmacological (thrombolytic) or surgical (PCI) intervention.
- Time is tissue – the longer the coronary arteries stay blocked, the more of the patient’s myocardium that will die. Dead heart tissue doesn’t beat.
Mr. Salazar’s chest pain was unrelieved after three (3) doses of sublingual nitroglycerin (NTG). Morphine 5 mg intravenous push (IVP) was administered, as well as 324 mg chewable baby aspirin. His pain was still unrelieved at this point
Mr. Salazar’s cardiac enzyme results were as follows:
Troponin I 3.5 ng/mL
Based on the results of Mr. Salazar's labs and his response to medications, what is the next intervention you anticipate? Why?
- Mr. Salazar needs intervention. He will either receive thrombolytics or a heart catheterization (PCI).
- Based on the EKG changes, elevated Troponin level, and the fact that his symptoms are not subsiding, it’s possible the patient has a significant blockage in one or more of his coronary arteries.
- It seems as though it may be an Anterior-Lateral MI because ST elevation is occurring in I, aVL, and V 2 -V 6 .
Mr. Salazar was taken immediately to the cath lab for a Percutaneous Coronary Intervention (PCI). The cardiologist found a 90% blockage in his left anterior descending (LAD) artery. A stent was inserted to keep the vessel open.
What is the purpose of Percutaneous Coronary Intervention (PCI), also known as a heart catheterization?
- A PCI serves to open up any coronary arteries that are blocked. First, they use contrast dye to determine where the blockage is, then they use a special balloon catheter to open the blocked vessels.
- If that doesn’t work, they will place a cardiac stent in the vessel to keep it open.[ /faq]
[faq lesson="true" blooms="Application" question="What is the expected outcome of a PCI? What do you expect to see in your patient after they receive a heart catheterization?"]
- Blood flow will be restored to the myocardium with minimal residual damage.
- The patient should have baseline vital signs, relief of chest pain, normal oxygenation status, and absence of heart failure symptoms (above baseline).
- The patient should be able to ambulate without significant chest pain or SOB.
- The patient should be free from bleeding or hematoma at the site of catheterization (often femoral, but can also be radial or (rarely) carotid.
Mr. Salazar tolerated the PCI well and was admitted to the cardiac telemetry unit for observation overnight. Four (4) hours after the procedure, Mr. Salazar reports no chest pain. His vital signs are now as follows:
- BP 128/82 mmHg SpO 2 96% on 2L NC
- HR 76 bpm and regular RR 18 bpm
- Temp 37.1°C
Mr. Salazar will be discharged home 24 hours after his arrival to the ED and will follow up with his cardiologist next week.
What patient education topics would need to be covered with Mr. Salazar?
- He should be taught any dietary and lifestyle changes that should be made.
- Diet – low sodium, low cholesterol, avoid sugar/soda, avoid fried/processed foods.
- Exercise – 30-45 minutes of moderate activity 5-7 days a week, u nless instructed otherwise by a cardiologist. This will be determined by the patient’s activity tolerance – how much can they do and still be able to breathe and be pain-free?
- Stop smoking and avoid caffeine and alcohol.
- Medication Instructions
- Nitroglycerin – take one SL tab at the onset of chest pain. If the pain does not subside after 5 minutes, call 911 and take a second dose. You can take a 3rd dose 5 minutes after the second if the pain does not subside. Do NOT take if you have taken Viagra in the last 24 hours.
- Aspirin – take 81 mg of baby aspirin daily
- Anticoagulant – the patient may be prescribed an anticoagulant if they had a stent placed. They should be taught about bleeding risks.
- When to call the provider – CP unrelieved by nitroglycerin after 5 minutes. Syncope. Evidence of bleeding in stool or urine (if on anticoagulant). Palpitations, shortness of breath, or difficulty tolerating activities of daily living.
Linchpins for Myocardial Infarction Nursing Case Study
In summary, Mr. Salazar’s case highlights the urgency of recognizing and responding to myocardial infarction promptly. The application of vital signs, EKG, cardiac enzymes, and medications like aspirin, nitroglycerin, and morphine played a pivotal role in his care. Diagnostic tools like echocardiography and chest X-rays contributed to a comprehensive evaluation.
Nurses must remain vigilant and compassionate in such emergencies. This case study emphasizes the importance of adhering to best practices in the assessment, diagnosis, and management of myocardial infarction, with the ultimate goal of achieving favorable patient outcomes.
View the FULL Outline
When you start a FREE trial you gain access to the full outline as well as:
- SIMCLEX (NCLEX Simulator)
- 6,500+ Practice NCLEX Questions
- 2,000+ HD Videos
- 300+ Nursing Cheatsheets
“Would suggest to all nursing students . . . Guaranteed to ease the stress!”
Nursing Case Studies

This nursing case study course is designed to help nursing students build critical thinking. Each case study was written by experienced nurses with first hand knowledge of the “real-world” disease process. To help you increase your nursing clinical judgement (critical thinking), each unfolding nursing case study includes answers laid out by Blooms Taxonomy to help you see that you are progressing to clinical analysis.We encourage you to read the case study and really through the “critical thinking checks” as this is where the real learning occurs. If you get tripped up by a specific question, no worries, just dig into an associated lesson on the topic and reinforce your understanding. In the end, that is what nursing case studies are all about – growing in your clinical judgement.
Nursing Case Studies Introduction
Cardiac nursing case studies.
- 6 Questions
- 7 Questions
- 5 Questions
- 4 Questions
GI/GU Nursing Case Studies
- 2 Questions
- 8 Questions
Obstetrics Nursing Case Studies
Respiratory nursing case studies.
- 10 Questions
Pediatrics Nursing Case Studies
- 3 Questions
- 12 Questions
Neuro Nursing Case Studies
Mental health nursing case studies.
- 9 Questions
Metabolic/Endocrine Nursing Case Studies
Other nursing case studies.
Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
Mr. Bob Carlson is a 59 year old male who came to Ventura County Medical Center (VCMC) with nausea, upper back pain he rated 7/10, and diaphoretic. His vital signs were BP 156/92, HR 90, RR 22 SpO2 90%, and temperature 99.5. Physical examination revealed clear lung sounds, mild tachypnea, S1 S2 present, and several ulcerations to the right foot. Ordes were given to obtain a 12-lead ECG and labs (CBC, CMP, Coagulations, Cardiac Enzymes, and Lipid Profile). In addition orders were given to start Mr. Carlson on 2L oxygen via nasal cannula and obtain venous access. A 20 gauge IV was started in his left AC.
Mr. Carlson’s medical history revealed that he is a type II diabetic, has hypertension, hyperlipidemia, and smokes 1/2 pack of cigarettes a day for the past 40 years. His diabetes is poorly managed and Mr.Carlson had a left below the knee amputation 2 years ago due to diabetic ulcers that were gangrenous. In addition, Mr. Carlson has a history of IV drug use but now receives a daily dose (90 mg) of Methadone at a local clinic. He is divorced, no children and is currently living with his 85 year old mother.
Mr. Carlson’s ECG results showed ST-segment elevation in leads II, III, and aVf and in V4, V5 and V6 with ST-segment depression V1, V2, and V3. The provider identified this to be an MI occurring in the inferior portion of the heart, likely affecting his right coronary artery (RCA). Lab results confirmed a ST-segment elevation MI (Troponin-I 12.9, CK 520, and CKMB 25.2). A code STEMI was called and Mr. Carlson was immediately prepared for a Percutaneous coronary intervention (PCI). While waiting for transfer to the Catheterization Lab at Community Memorial Hospital (CMH) Mr. Carlson was given 325 mg of Aspirin, 2 mg Morphine, and was started on a 5000 unit bolus of Heparin. Nitroglycerin was not given due to the profound hypotension associated with nitroglycerin and patients experiencing an inferior myocardial infarction.
Mr. Carlson was transferred to the CMH catheterization lab. His vitals were stable and he was able to give informed consent. The cardiac angiography showed a 95% occlusion to the RCA. A stent was placed, the patient tolerated the procedure well. The patient’s right femoral artery was closed successfully with manual pressure.
Mr. Carlson returned to the cardiac care unit where upon assessment his groin was found to be soft and without hepatoma and with minimal drainage from incision site. His peripheral pulses were present, and distal to the incision his skin was warm with capillary refill less than 2 seconds. Mr. Carlson was transferred back to VCMC the following day were he recovered without further incident.
Before discharge Mr. Carlson’s was educated on his new prescriptions and was educated on the importance of taking his daily aspirin. He met with the diabetes educator, dietician, and social worker before discharge. Mr. Carlson was informed of smoking cessation programs in the area but declined to enroll. Case Management found placement in a skilled nursing facility for 20 days, the amount of days 100% covered by Medi-Cal, where he could start a cardiac rehabilitation program. A home health organization was organized to help provide care for Mr. Carlson when he returned to his home.
- What medications do you anticipate Mr. Carlson being prescribed upon discharge? Aspirin, ACE-I or ARB, beta blocker, and a statin
- What nursing interventions are critical prior to the patient being taken to the cath lab? -Assess the client’s and family’s knowledge and understanding of the procedure. – Provide routine preoperative care as ordered. Signed consent is required and maintain patient NPO. -Assess for hypersensitivity to iodine, radiologic contrast media, or seafood. An iodine-based radiologic contrast dye is typically used for angiogram. Iodine or seafood allergy increases the risk for anaphylaxis and requires an alternative dye or special precautions. -Record baseline assessment data, including vital signs, height, and weight. Mark the locations of peripheral pulses; document their equality and amplitude.
- Which risk factors may have contributed to Mr. Carlson’s myocardial infarction? Hyperlipidemia, uncontrolled diabetes, smoking, inactivity, drug use, and diet.
Nursing Case Studies by and for Student Nurses Copyright © by jaimehannans is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License , except where otherwise noted.
Share This Book
- Campus Directory
- Current Students
- Faculty & Staff

Acute Myocardial Infarction Case Study
Myocardial infarction (heart attack) is the leading cause of death in the United States. It is estimated that one in every five deaths in the US is due to a heart attack. Approximately one million patients are admitted to hospitals each year due to heart attacks. 200,000 to 300,000 individuals die from heart attacks before ever receiving medical care. In Case #2 we’ll join 48-year-old Jason Dixon as he experiences a life-threatening heart attack.
Module 7: Acute Myocardial Infarction
48 year old Jason Dixon had not been feeling well all day and around 10:00 p.m he went to bed...
AMI - Page 1
Before we progress further into this relatively complex case, please review module 6 in the...
AMI - Page 2
Case continued: Enroute to the ER, the patient's acute symptoms had been relieved...
AMI - Page 3
This is a critical decision point for the cardiologist. There are several algorithms...
AMI - Page 4
Case Summary
Summary of the Case
AMI - Summary

Answers to Case Questions
AMI - Answers

Professionals
Health Professionals Introduced in Case
AMI - Professionals
Additional Links
Optional Links to Explore Further
AMI - Links
- Search Menu
- Browse content in Arts and Humanities
- Browse content in Archaeology
- Anglo-Saxon and Medieval Archaeology
- Archaeological Methodology and Techniques
- Archaeology by Region
- Archaeology of Religion
- Archaeology of Trade and Exchange
- Biblical Archaeology
- Contemporary and Public Archaeology
- Environmental Archaeology
- Historical Archaeology
- History and Theory of Archaeology
- Industrial Archaeology
- Landscape Archaeology
- Mortuary Archaeology
- Prehistoric Archaeology
- Underwater Archaeology
- Urban Archaeology
- Zooarchaeology
- Browse content in Architecture
- Architectural Structure and Design
- History of Architecture
- Residential and Domestic Buildings
- Theory of Architecture
- Browse content in Art
- Art Subjects and Themes
- History of Art
- Industrial and Commercial Art
- Theory of Art
- Biographical Studies
- Byzantine Studies
- Browse content in Classical Studies
- Classical History
- Classical Philosophy
- Classical Mythology
- Classical Literature
- Classical Reception
- Classical Art and Architecture
- Classical Oratory and Rhetoric
- Greek and Roman Epigraphy
- Greek and Roman Law
- Greek and Roman Papyrology
- Greek and Roman Archaeology
- Late Antiquity
- Religion in the Ancient World
- Digital Humanities
- Browse content in History
- Colonialism and Imperialism
- Diplomatic History
- Environmental History
- Genealogy, Heraldry, Names, and Honours
- Genocide and Ethnic Cleansing
- Historical Geography
- History by Period
- History of Emotions
- History of Agriculture
- History of Education
- History of Gender and Sexuality
- Industrial History
- Intellectual History
- International History
- Labour History
- Legal and Constitutional History
- Local and Family History
- Maritime History
- Military History
- National Liberation and Post-Colonialism
- Oral History
- Political History
- Public History
- Regional and National History
- Revolutions and Rebellions
- Slavery and Abolition of Slavery
- Social and Cultural History
- Theory, Methods, and Historiography
- Urban History
- World History
- Browse content in Language Teaching and Learning
- Language Learning (Specific Skills)
- Language Teaching Theory and Methods
- Browse content in Linguistics
- Applied Linguistics
- Cognitive Linguistics
- Computational Linguistics
- Forensic Linguistics
- Grammar, Syntax and Morphology
- Historical and Diachronic Linguistics
- History of English
- Language Acquisition
- Language Evolution
- Language Reference
- Language Variation
- Language Families
- Lexicography
- Linguistic Anthropology
- Linguistic Theories
- Linguistic Typology
- Phonetics and Phonology
- Psycholinguistics
- Sociolinguistics
- Translation and Interpretation
- Writing Systems
- Browse content in Literature
- Bibliography
- Children's Literature Studies
- Literary Studies (Asian)
- Literary Studies (European)
- Literary Studies (Eco-criticism)
- Literary Studies (Romanticism)
- Literary Studies (American)
- Literary Studies (Modernism)
- Literary Studies - World
- Literary Studies (1500 to 1800)
- Literary Studies (19th Century)
- Literary Studies (20th Century onwards)
- Literary Studies (African American Literature)
- Literary Studies (British and Irish)
- Literary Studies (Early and Medieval)
- Literary Studies (Fiction, Novelists, and Prose Writers)
- Literary Studies (Gender Studies)
- Literary Studies (Graphic Novels)
- Literary Studies (History of the Book)
- Literary Studies (Plays and Playwrights)
- Literary Studies (Poetry and Poets)
- Literary Studies (Postcolonial Literature)
- Literary Studies (Queer Studies)
- Literary Studies (Science Fiction)
- Literary Studies (Travel Literature)
- Literary Studies (War Literature)
- Literary Studies (Women's Writing)
- Literary Theory and Cultural Studies
- Mythology and Folklore
- Shakespeare Studies and Criticism
- Browse content in Media Studies
- Browse content in Music
- Applied Music
- Dance and Music
- Ethics in Music
- Ethnomusicology
- Gender and Sexuality in Music
- Medicine and Music
- Music Cultures
- Music and Religion
- Music and Media
- Music and Culture
- Music Education and Pedagogy
- Music Theory and Analysis
- Musical Scores, Lyrics, and Libretti
- Musical Structures, Styles, and Techniques
- Musicology and Music History
- Performance Practice and Studies
- Race and Ethnicity in Music
- Sound Studies
- Browse content in Performing Arts
- Browse content in Philosophy
- Aesthetics and Philosophy of Art
- Epistemology
- Feminist Philosophy
- History of Western Philosophy
- Metaphysics
- Moral Philosophy
- Non-Western Philosophy
- Philosophy of Science
- Philosophy of Language
- Philosophy of Mind
- Philosophy of Perception
- Philosophy of Action
- Philosophy of Law
- Philosophy of Religion
- Philosophy of Mathematics and Logic
- Practical Ethics
- Social and Political Philosophy
- Browse content in Religion
- Biblical Studies
- Christianity
- East Asian Religions
- History of Religion
- Judaism and Jewish Studies
- Qumran Studies
- Religion and Education
- Religion and Health
- Religion and Politics
- Religion and Science
- Religion and Law
- Religion and Art, Literature, and Music
- Religious Studies
- Browse content in Society and Culture
- Cookery, Food, and Drink
- Cultural Studies
- Customs and Traditions
- Ethical Issues and Debates
- Hobbies, Games, Arts and Crafts
- Lifestyle, Home, and Garden
- Natural world, Country Life, and Pets
- Popular Beliefs and Controversial Knowledge
- Sports and Outdoor Recreation
- Technology and Society
- Travel and Holiday
- Visual Culture
- Browse content in Law
- Arbitration
- Browse content in Company and Commercial Law
- Commercial Law
- Company Law
- Browse content in Comparative Law
- Systems of Law
- Competition Law
- Browse content in Constitutional and Administrative Law
- Government Powers
- Judicial Review
- Local Government Law
- Military and Defence Law
- Parliamentary and Legislative Practice
- Construction Law
- Contract Law
- Browse content in Criminal Law
- Criminal Procedure
- Criminal Evidence Law
- Sentencing and Punishment
- Employment and Labour Law
- Environment and Energy Law
- Browse content in Financial Law
- Banking Law
- Insolvency Law
- History of Law
- Human Rights and Immigration
- Intellectual Property Law
- Browse content in International Law
- Private International Law and Conflict of Laws
- Public International Law
- IT and Communications Law
- Jurisprudence and Philosophy of Law
- Law and Politics
- Law and Society
- Browse content in Legal System and Practice
- Courts and Procedure
- Legal Skills and Practice
- Primary Sources of Law
- Regulation of Legal Profession
- Medical and Healthcare Law
- Browse content in Policing
- Criminal Investigation and Detection
- Police and Security Services
- Police Procedure and Law
- Police Regional Planning
- Browse content in Property Law
- Personal Property Law
- Study and Revision
- Terrorism and National Security Law
- Browse content in Trusts Law
- Wills and Probate or Succession
- Browse content in Medicine and Health
- Browse content in Allied Health Professions
- Arts Therapies
- Clinical Science
- Dietetics and Nutrition
- Occupational Therapy
- Operating Department Practice
- Physiotherapy
- Radiography
- Speech and Language Therapy
- Browse content in Anaesthetics
- General Anaesthesia
- Neuroanaesthesia
- Browse content in Clinical Medicine
- Acute Medicine
- Cardiovascular Medicine
- Clinical Genetics
- Clinical Pharmacology and Therapeutics
- Dermatology
- Endocrinology and Diabetes
- Gastroenterology
- Genito-urinary Medicine
- Geriatric Medicine
- Infectious Diseases
- Medical Toxicology
- Medical Oncology
- Pain Medicine
- Palliative Medicine
- Rehabilitation Medicine
- Respiratory Medicine and Pulmonology
- Rheumatology
- Sleep Medicine
- Sports and Exercise Medicine
- Clinical Neuroscience
- Community Medical Services
- Critical Care
- Emergency Medicine
- Forensic Medicine
- Haematology
- History of Medicine
- Browse content in Medical Dentistry
- Oral and Maxillofacial Surgery
- Paediatric Dentistry
- Restorative Dentistry and Orthodontics
- Surgical Dentistry
- Browse content in Medical Skills
- Clinical Skills
- Communication Skills
- Nursing Skills
- Surgical Skills
- Medical Ethics
- Medical Statistics and Methodology
- Browse content in Neurology
- Clinical Neurophysiology
- Neuropathology
- Nursing Studies
- Browse content in Obstetrics and Gynaecology
- Gynaecology
- Occupational Medicine
- Ophthalmology
- Otolaryngology (ENT)
- Browse content in Paediatrics
- Neonatology
- Browse content in Pathology
- Chemical Pathology
- Clinical Cytogenetics and Molecular Genetics
- Histopathology
- Medical Microbiology and Virology
- Patient Education and Information
- Browse content in Pharmacology
- Psychopharmacology
- Browse content in Popular Health
- Caring for Others
- Complementary and Alternative Medicine
- Self-help and Personal Development
- Browse content in Preclinical Medicine
- Cell Biology
- Molecular Biology and Genetics
- Reproduction, Growth and Development
- Primary Care
- Professional Development in Medicine
- Browse content in Psychiatry
- Addiction Medicine
- Child and Adolescent Psychiatry
- Forensic Psychiatry
- Learning Disabilities
- Old Age Psychiatry
- Psychotherapy
- Browse content in Public Health and Epidemiology
- Epidemiology
- Public Health
- Browse content in Radiology
- Clinical Radiology
- Interventional Radiology
- Nuclear Medicine
- Radiation Oncology
- Reproductive Medicine
- Browse content in Surgery
- Cardiothoracic Surgery
- Gastro-intestinal and Colorectal Surgery
- General Surgery
- Neurosurgery
- Paediatric Surgery
- Peri-operative Care
- Plastic and Reconstructive Surgery
- Surgical Oncology
- Transplant Surgery
- Trauma and Orthopaedic Surgery
- Vascular Surgery
- Browse content in Science and Mathematics
- Browse content in Biological Sciences
- Aquatic Biology
- Biochemistry
- Bioinformatics and Computational Biology
- Developmental Biology
- Ecology and Conservation
- Evolutionary Biology
- Genetics and Genomics
- Microbiology
- Molecular and Cell Biology
- Natural History
- Plant Sciences and Forestry
- Research Methods in Life Sciences
- Structural Biology
- Systems Biology
- Zoology and Animal Sciences
- Browse content in Chemistry
- Analytical Chemistry
- Computational Chemistry
- Crystallography
- Environmental Chemistry
- Industrial Chemistry
- Inorganic Chemistry
- Materials Chemistry
- Medicinal Chemistry
- Mineralogy and Gems
- Organic Chemistry
- Physical Chemistry
- Polymer Chemistry
- Study and Communication Skills in Chemistry
- Theoretical Chemistry
- Browse content in Computer Science
- Artificial Intelligence
- Computer Architecture and Logic Design
- Game Studies
- Human-Computer Interaction
- Mathematical Theory of Computation
- Programming Languages
- Software Engineering
- Systems Analysis and Design
- Virtual Reality
- Browse content in Computing
- Business Applications
- Computer Security
- Computer Games
- Computer Networking and Communications
- Digital Lifestyle
- Graphical and Digital Media Applications
- Operating Systems
- Browse content in Earth Sciences and Geography
- Atmospheric Sciences
- Environmental Geography
- Geology and the Lithosphere
- Maps and Map-making
- Meteorology and Climatology
- Oceanography and Hydrology
- Palaeontology
- Physical Geography and Topography
- Regional Geography
- Soil Science
- Urban Geography
- Browse content in Engineering and Technology
- Agriculture and Farming
- Biological Engineering
- Civil Engineering, Surveying, and Building
- Electronics and Communications Engineering
- Energy Technology
- Engineering (General)
- Environmental Science, Engineering, and Technology
- History of Engineering and Technology
- Mechanical Engineering and Materials
- Technology of Industrial Chemistry
- Transport Technology and Trades
- Browse content in Environmental Science
- Applied Ecology (Environmental Science)
- Conservation of the Environment (Environmental Science)
- Environmental Sustainability
- Environmentalist Thought and Ideology (Environmental Science)
- Management of Land and Natural Resources (Environmental Science)
- Natural Disasters (Environmental Science)
- Nuclear Issues (Environmental Science)
- Pollution and Threats to the Environment (Environmental Science)
- Social Impact of Environmental Issues (Environmental Science)
- History of Science and Technology
- Browse content in Materials Science
- Ceramics and Glasses
- Composite Materials
- Metals, Alloying, and Corrosion
- Nanotechnology
- Browse content in Mathematics
- Applied Mathematics
- Biomathematics and Statistics
- History of Mathematics
- Mathematical Education
- Mathematical Finance
- Mathematical Analysis
- Numerical and Computational Mathematics
- Probability and Statistics
- Pure Mathematics
- Browse content in Neuroscience
- Cognition and Behavioural Neuroscience
- Development of the Nervous System
- Disorders of the Nervous System
- History of Neuroscience
- Invertebrate Neurobiology
- Molecular and Cellular Systems
- Neuroendocrinology and Autonomic Nervous System
- Neuroscientific Techniques
- Sensory and Motor Systems
- Browse content in Physics
- Astronomy and Astrophysics
- Atomic, Molecular, and Optical Physics
- Biological and Medical Physics
- Classical Mechanics
- Computational Physics
- Condensed Matter Physics
- Electromagnetism, Optics, and Acoustics
- History of Physics
- Mathematical and Statistical Physics
- Measurement Science
- Nuclear Physics
- Particles and Fields
- Plasma Physics
- Quantum Physics
- Relativity and Gravitation
- Semiconductor and Mesoscopic Physics
- Browse content in Psychology
- Affective Sciences
- Clinical Psychology
- Cognitive Psychology
- Cognitive Neuroscience
- Criminal and Forensic Psychology
- Developmental Psychology
- Educational Psychology
- Evolutionary Psychology
- Health Psychology
- History and Systems in Psychology
- Music Psychology
- Neuropsychology
- Organizational Psychology
- Psychological Assessment and Testing
- Psychology of Human-Technology Interaction
- Psychology Professional Development and Training
- Research Methods in Psychology
- Social Psychology
- Browse content in Social Sciences
- Browse content in Anthropology
- Anthropology of Religion
- Human Evolution
- Medical Anthropology
- Physical Anthropology
- Regional Anthropology
- Social and Cultural Anthropology
- Theory and Practice of Anthropology
- Browse content in Business and Management
- Business Strategy
- Business Ethics
- Business History
- Business and Government
- Business and Technology
- Business and the Environment
- Comparative Management
- Corporate Governance
- Corporate Social Responsibility
- Entrepreneurship
- Health Management
- Human Resource Management
- Industrial and Employment Relations
- Industry Studies
- Information and Communication Technologies
- International Business
- Knowledge Management
- Management and Management Techniques
- Operations Management
- Organizational Theory and Behaviour
- Pensions and Pension Management
- Public and Nonprofit Management
- Strategic Management
- Supply Chain Management
- Browse content in Criminology and Criminal Justice
- Criminal Justice
- Criminology
- Forms of Crime
- International and Comparative Criminology
- Youth Violence and Juvenile Justice
- Development Studies
- Browse content in Economics
- Agricultural, Environmental, and Natural Resource Economics
- Asian Economics
- Behavioural Finance
- Behavioural Economics and Neuroeconomics
- Econometrics and Mathematical Economics
- Economic Systems
- Economic History
- Economic Methodology
- Economic Development and Growth
- Financial Markets
- Financial Institutions and Services
- General Economics and Teaching
- Health, Education, and Welfare
- History of Economic Thought
- International Economics
- Labour and Demographic Economics
- Law and Economics
- Macroeconomics and Monetary Economics
- Microeconomics
- Public Economics
- Urban, Rural, and Regional Economics
- Welfare Economics
- Browse content in Education
- Adult Education and Continuous Learning
- Care and Counselling of Students
- Early Childhood and Elementary Education
- Educational Equipment and Technology
- Educational Strategies and Policy
- Higher and Further Education
- Organization and Management of Education
- Philosophy and Theory of Education
- Schools Studies
- Secondary Education
- Teaching of a Specific Subject
- Teaching of Specific Groups and Special Educational Needs
- Teaching Skills and Techniques
- Browse content in Environment
- Applied Ecology (Social Science)
- Climate Change
- Conservation of the Environment (Social Science)
- Environmentalist Thought and Ideology (Social Science)
- Natural Disasters (Environment)
- Social Impact of Environmental Issues (Social Science)
- Browse content in Human Geography
- Cultural Geography
- Economic Geography
- Political Geography
- Browse content in Interdisciplinary Studies
- Communication Studies
- Museums, Libraries, and Information Sciences
- Browse content in Politics
- African Politics
- Asian Politics
- Chinese Politics
- Comparative Politics
- Conflict Politics
- Elections and Electoral Studies
- Environmental Politics
- European Union
- Foreign Policy
- Gender and Politics
- Human Rights and Politics
- Indian Politics
- International Relations
- International Organization (Politics)
- International Political Economy
- Irish Politics
- Latin American Politics
- Middle Eastern Politics
- Political Methodology
- Political Communication
- Political Philosophy
- Political Sociology
- Political Behaviour
- Political Economy
- Political Institutions
- Political Theory
- Politics and Law
- Public Administration
- Public Policy
- Quantitative Political Methodology
- Regional Political Studies
- Russian Politics
- Security Studies
- State and Local Government
- UK Politics
- US Politics
- Browse content in Regional and Area Studies
- African Studies
- Asian Studies
- East Asian Studies
- Japanese Studies
- Latin American Studies
- Middle Eastern Studies
- Native American Studies
- Scottish Studies
- Browse content in Research and Information
- Research Methods
- Browse content in Social Work
- Addictions and Substance Misuse
- Adoption and Fostering
- Care of the Elderly
- Child and Adolescent Social Work
- Couple and Family Social Work
- Developmental and Physical Disabilities Social Work
- Direct Practice and Clinical Social Work
- Emergency Services
- Human Behaviour and the Social Environment
- International and Global Issues in Social Work
- Mental and Behavioural Health
- Social Justice and Human Rights
- Social Policy and Advocacy
- Social Work and Crime and Justice
- Social Work Macro Practice
- Social Work Practice Settings
- Social Work Research and Evidence-based Practice
- Welfare and Benefit Systems
- Browse content in Sociology
- Childhood Studies
- Community Development
- Comparative and Historical Sociology
- Economic Sociology
- Gender and Sexuality
- Gerontology and Ageing
- Health, Illness, and Medicine
- Marriage and the Family
- Migration Studies
- Occupations, Professions, and Work
- Organizations
- Population and Demography
- Race and Ethnicity
- Social Theory
- Social Movements and Social Change
- Social Research and Statistics
- Social Stratification, Inequality, and Mobility
- Sociology of Religion
- Sociology of Education
- Sport and Leisure
- Urban and Rural Studies
- Browse content in Warfare and Defence
- Defence Strategy, Planning, and Research
- Land Forces and Warfare
- Military Administration
- Military Life and Institutions
- Naval Forces and Warfare
- Other Warfare and Defence Issues
- Peace Studies and Conflict Resolution
- Weapons and Equipment

- < Previous chapter
- Next chapter >
21 Myocardial Infarction
- Published: February 2013
- Cite Icon Cite
- Permissions Icon Permissions
Case 21 introduces A 52-year-old insurance adjuster is brought to a small rural community hospital in an ambulance. His wife, who accompanied him, states that they were on vacation in a remote lodge and that during dinner he started to complain of excruciating chest pain in the region of the sternum. The patient indicates that the pain is retrosternal and describes it as “crushing” and “like an elephant is sitting on my chest.” He reports that the pain came on gradually and has gotten progressively more severe, so that it is currently an “11 out of 10.” The pain radiates to the left arm and jaw. The pain does not alter with change in position or worsen with inspiration. These symptoms are accompanied by nausea, one episode of vomiting, and severe shortness of breath.
Signed in as
Institutional accounts.
- GoogleCrawler [DO NOT DELETE]
- Google Scholar Indexing
Personal account
- Sign in with email/username & password
- Get email alerts
- Save searches
- Purchase content
- Activate your purchase/trial code
Institutional access
- Sign in with a library card Sign in with username/password Recommend to your librarian
- Institutional account management
- Get help with access
Access to content on Oxford Academic is often provided through institutional subscriptions and purchases. If you are a member of an institution with an active account, you may be able to access content in one of the following ways:
IP based access
Typically, access is provided across an institutional network to a range of IP addresses. This authentication occurs automatically, and it is not possible to sign out of an IP authenticated account.
Sign in through your institution
Choose this option to get remote access when outside your institution. Shibboleth/Open Athens technology is used to provide single sign-on between your institution’s website and Oxford Academic.
- Click Sign in through your institution.
- Select your institution from the list provided, which will take you to your institution's website to sign in.
- When on the institution site, please use the credentials provided by your institution. Do not use an Oxford Academic personal account.
- Following successful sign in, you will be returned to Oxford Academic.
If your institution is not listed or you cannot sign in to your institution’s website, please contact your librarian or administrator.
Sign in with a library card
Enter your library card number to sign in. If you cannot sign in, please contact your librarian.
Society Members
Society member access to a journal is achieved in one of the following ways:
Sign in through society site
Many societies offer single sign-on between the society website and Oxford Academic. If you see ‘Sign in through society site’ in the sign in pane within a journal:
- Click Sign in through society site.
- When on the society site, please use the credentials provided by that society. Do not use an Oxford Academic personal account.
If you do not have a society account or have forgotten your username or password, please contact your society.
Sign in using a personal account
Some societies use Oxford Academic personal accounts to provide access to their members. See below.
A personal account can be used to get email alerts, save searches, purchase content, and activate subscriptions.
Some societies use Oxford Academic personal accounts to provide access to their members.

Viewing your signed in accounts
Click the account icon in the top right to:
- View your signed in personal account and access account management features.
- View the institutional accounts that are providing access.
Signed in but can't access content
Oxford Academic is home to a wide variety of products. The institutional subscription may not cover the content that you are trying to access. If you believe you should have access to that content, please contact your librarian.
For librarians and administrators, your personal account also provides access to institutional account management. Here you will find options to view and activate subscriptions, manage institutional settings and access options, access usage statistics, and more.
Our books are available by subscription or purchase to libraries and institutions.
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Rights and permissions
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 18 April 2024
The relationship between cardiac oxidative stress, inflammatory cytokine response, cardiac pump function, and prognosis post-myocardial infarction
- Dongpeng Duan 1 ,
- Hongjun Li 2 ,
- Shiyun Chai 3 ,
- Linlin Zhang 4 ,
- Tianfeng Fan 1 ,
- Zhenfeng Hu 5 &
- Yan Feng 6
Scientific Reports volume 14 , Article number: 8985 ( 2024 ) Cite this article
244 Accesses
Metrics details
- Cardiovascular biology
- Risk factors
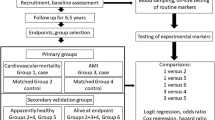
This study delves into the potential connections between cardiac oxidative stress, inflammatory cytokine response, cardiac pump function, and prognosis in individuals following myocardial infarction. A total of 276 patients were categorized into two groups: the control group (n = 130) and the observation group (n = 146), based on the drug intervention strategies. The control group received standard drug treatment, while the observation group received early drug intervention targeting antioxidant and anti-inflammatory treatment in addition to standard treatment. Serum levels of inflammatory factors, including tumor necrosis factor-α (TNF-α), interleukin-1β (IL-1β), and interleukin-9 (IL-6), were assessed using enzyme-linked immuno sorbent assay (ELISA) kits. The Forkhead Box Protein A2 (FOX2) reagent was used to determine the overall oxidation level. Left Ventricular End-Diastolic Diameter (LVEDD), Left Ventricular Ejection Fraction (LVEF), and End-Systolic Diameter (ESD) were measured using Doppler ultrasound. The observation group exhibited significantly reduced serum levels of TNF-α, IL-1β, and IL-6 compared to the control group ( P < 0.05). Moreover, the observation group exerted lower total oxidation levels, OSI, EDD, and ESD compared to the control group ( P < 0.05), while the LVEF and TAS levels in the observation group were higher than those in the control group ( P < 0.05). Remarkably, the observation group experienced a significant reduction in the incidences of reinfarction, heart failure, arrhythmia, and abnormal valve function compared to the control group (P < 0.05). Decreased cardiac pump function and a more unfavorable prognosis were associated with elevated levels of cardiac oxidative stress and inflammatory factors ( P < 0.05). Timely intervention with appropriate medications have a crucial effect in decreasing inflammatory marker levels, mitigating oxidative pressure, and enhancing cardiac pumping capacity and overall prognosis.
Similar content being viewed by others
Increased C reactive protein, cardiac troponin I and GLS are associated with myocardial inflammation in patients with non-ischemic heart failure
Serum biomarkers, including nitric oxide metabolites (NOx), for prognosis of cardiovascular death and acute myocardial infarction in an ESSE-RF case–control cohort with 6.5-year follow up
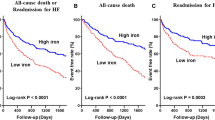
Serum iron: a new predictor of adverse outcomes independently from serum hemoglobin levels in patients with acute decompensated heart failure
Introduction.
Persistent myocardial ischemia and hypoxia resulting from coronary artery occlusion can lead to the development of myocardial infarction 1 . Despite significant advancements in medical technology and treatments in recent decades, myocardial infarction remains a prominent global cause of mortality. The impact of myocardial infarction on cardiac function and prognosis is substantial 2 , 3 . Hence, a comprehensive understanding of the pathophysiological alterations following a heart attack and the impact of associated factors on patients’ quality of life and prognosis is of significant importance. Cardiac function and prognosis are profoundly influeced influenced by two fundamental physiological processes that emerge after a myocardial infarction: cardiac oxidative stress and the inflammatory cytokine response 4 , 5 , 6 . The occurrence of a heart attack triggers an ongoing deficiency of oxygen cardiacmuscle tissue due to the blockage in the coronary artery. This, in turn, causes dysfunction in mitochondrial activity and an excessive generation of free radicals 7 . These reactive oxygen species significantly contribute to oxidative stress by causing damage to cellular membranes, proteins, and nucleic acids, ultimately leading to cellular injury and death. Additionally, oxidative stress holds the ability to initiate diverse cellular signaling pathways, exerting a significant influence on the regulation of both physiological and pathological contexts within cardiac cells 7 , 8 . While the inflammatory reaction serves as a mechanism to maintain tissue homeostasis to a certain extent, an excessive or persistent inflammatory reaction may aggravate heart injury, increase heart stress, and detrimentally impact heart function 9 . Cardiac oxidative stress and the inflammatory cytokine response exhibit a reciprocal relationship. Oxidative stress can stimulate the generation of inflammatory agents, and conversely, inflammatory agents can further escalate oxidative stress 10 , 11 . This interaction exacerbates the pathophysiological alterations of the heart following a heart attack, significantly influencing cardiac function and prognosis. Consequently, investigating the regulatory mechanism of oxidative stress in the heart and the inflammatory cytokine response post-heart attack, along with their correlation to cardiac function and prognosis, holds substantial clinical and scientific significance. The objective of this research is to investigate the correlation between cardiacoxidative stress, inflammatory cytokine response, cardiac pump function, and prognosis in individuals following a heart attack.
Materials and methods
General information.
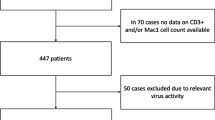
The study included 138 individuals diagnosed with myocardial infarction, admitted to the emergency and cardiothoracic departments of the author’s hospital between February 2021 and November 2022. Participants’ ages ranged from 36 to 70, with a mean age of 62.27 ± 5.46 years. Of the participants, 164 were males and 112 females. Based on prescribed drug intervention protocols, participants were categorized into two groups: the control group (n = 130) and the observation group (n = 146). The control group received standard medication, whereas the observation group underwent early drug intervention targeting anti-oxidation and anti-inflammatory reactions, in addition to the conventional drug treatment provided by the control group. Before being included in the study, all participants were informed about the study procedure and provided their informed consent.
03/08/2023 is the full date of first registration (ChiCTR2300069171).
Inclusion criteria
Participants were required to fall within the age range of 18–70 years and exhibit ST segment elevation or new left bundle branch block in their electrocardiogram. Additionally, an increase in cardiac biomarkers such as troponin T and the presence of typical symptoms like chest pain or angina pectoris were necessary. The onset of myocardial infarction should not have exceeded 72 h, and individuals needed to express voluntary willingness to participate in the study, accompanied by providing informed consent.
Exclusion criteria
Exclusion criteria encompassed the presence of severe underlying cardiovascular conditions, such as severe arrhythmia and heart valve diseases. Diagnosis of severe heart failure, concurrent presence of other malignant tumors, and immune system diseases were also grounds for exclusion.
Ethical information
The research was approved by our hospital’s Ethics Committee, ensuring that all procedures adhered to ethical norms and regulations. Inclusion in the study was contingent upon patients providing written informed consent.
Drug intervention
Upon admission, every patient received immediate comprehensive care, encompassing procedures such as electrocardiogram (ECG) monitoring, blood pressure measurement, blood oxygen saturation assessment, bed rest, and establishment of venous access, among others. All patients were administered either atorvastatin or rosuvastatin for the plaque stabilization before undergoing emergency PCI. For patients in the observation group, an additional oral dose of aspirin (300 mg) was administered, along with vitamins C and E, to provide anti-inflammatory and antioxidant therapy.
Analysis of plasma oxidative stress
Upon admission to the hospital, blood samples were obtained and subsequently separated into plasma and serum components. The FOX2 reagent, as previously described by Harma et al. in 2005, was employed to assess the overall plasma peroxide concentration. The preparation of FOX2 reagent involved dissolving ammonium ferrous sulfate in H 2 SO 4 , followed by the addition of butyl hydroxytoluene (BHT) in methanol to the solution. Subsequent addition of xylenol orange led to the formation of the working solution. Plasma was mixed with FOX2 reagent and allowed to incubate at a temperature of 25 ℃. The liquid above the sediment was gathered, and the measurement of light absorption was taken at a wavelength of 560 nm. The Erelmethod (Ozcan, 2004) was applied to determine the total antioxidantstatus (TAS) of the plasma. The antioxidant content of the sample caused the conversion of the colored ABTS radical intoa colorlessform, which was measured as an absorbance at 740 nm. For determination and calibration purposes, a conventional Trolox equivalent known as the standard antioxidant solution was employed. The oxidative stress index (OSI) was defined as the proportion of overall peroxide to total antioxidant status (TAS). The OSI value, measured in arbitrary units, was calculated by multiplying the total peroxide value by 100 and then dividing it by the TASvalue.
Determination of cytokines
ELISA kit was utilized to measure the levels of serum cytokines TNF-α, IL-1β, and IL-6, following the manufacturer’s instructions.
Heart pump function evaluation
Siemens PRIME ACUSON ES2000 and Philips EPIQ 7C Doppler ultrasound systems were utilized to measure the left ventricular dimensions, including EDD, LVEF, and ESD.
The incidence of security events
The incidence of re-infarction, heart failure, arrhythmia, and abnormal valve function were analyzed.
Statistical analysis
Statistical analysis was conducted using the GraphPad Prism software, based in San Diego, USA. The Shapiro–Wilk test was employed to examine whether the record values in each group followed a normal distribution. Parameter data were analyzed using a one-way ANOVA followed by Tukey test, while non-parametric data were analyzed using a Kruskal–Wallis test followed by Dunn’s multiple comparison test. Correlation among parameters was assesse dusing Pearson and Spearman correlation tests. Significance was considered at p-values equal to or less than 0.05 for all analyses.
Patient demographics statistics
Based on the overall patient data, the control group exhibited a male-to-female ratio of 76:54. The average age in this group was 60.21 ± 4.53 years, accompanied by an average BMI of 23.39 ± 1.88 kg/m 2 . Within this group, 36 individuals had hypertension, 14 had diabetes, 40 were smokers, and 32 were alcohol consumers. On the other hand, the observation group included 88 males and 58 females, with an average age of 67.45 ± 5.28 years and an average BMI of 22.57 ± 2.05 kg/m 2 . This group included 40 individuals with hypertension, 12 with diabetes, 46 who smoked, and 36 who consumed alcohol. The general data showed no significant differences between the two groups ( P > 0.05). (Table 1 ).
Analysis of inflammatory factors in patients
The observation group exhibited markedly decreased serum levels of TNF-α, IL-1β, and IL-6 compared to the control group ( P < 0.05). (Table 2 ).
Analysis of oxidative stress levels
Utilizing the FOX2 reagent, the total oxidation level was determined, and the TAS level was assessed using the Erel method. The observation group exhibited lower total oxidation levels and OSI compared to the control group ( P < 0.05), whereas the TAS level in the observation group was higher than the control group ( P < 0.05), as laid out in Table 3 .
Analysis of patients’ heart pump function
Doppler ultrasound was utilized to measure the EDD, LVEF, and ESD. The observation group exerted lower EDD and ESD compared to the control group (P < 0.05), while the LVEF in the observation group was elevated in comparison ( P < 0.05). (Fig. 1 , Table 4 ).
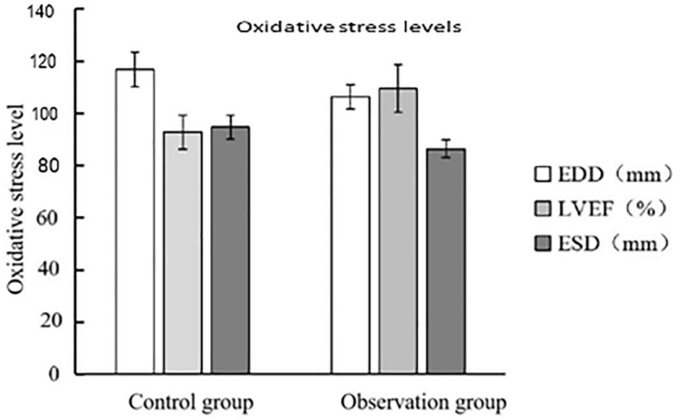
Patient heart pump function.
Analysis of prognosis of patients
In the observation group, occurrences of recurrent heart attacks, cardiac insufficiency, irregular heartbeats, and valve malfunctions were significantly lower compared to the control group ( P < 0.05). (Fig. 2 , Table 5 ).
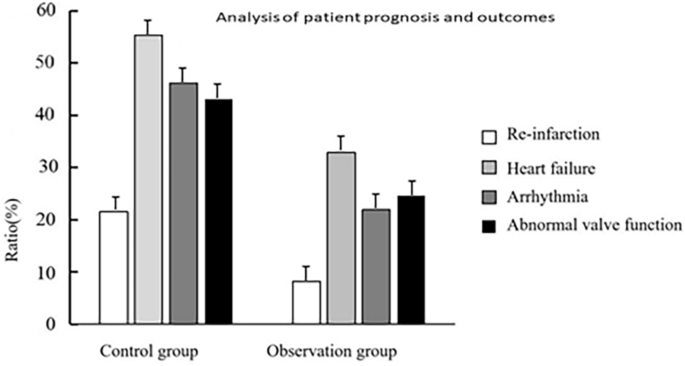
Analysis of prognosis of patients.
Logistic regression and multiple regression analyses
Through the implantation of logistic regression and multiple regression, the impact of cardiac oxidative stress and inflammatory factors on cardiac pump function and prognosis was investigated. The analysis indicated that these factors played a pivotal role in influencing both cardiac pump function and prognosis following myocardial infarction ( P < 0.05). Furthermore, a clear correlation was observed between elevated cardiac oxidative stress and inflammatory markers and the decline in cardiac pump function and prognosis ( P < 0.05). (Table 6 ).
The meaning of “Oxidative stress in the heart” and “Inflammatory factors” has been added.
Myocardial infarction, a severe cardiovascular disease, commonly triggers myocardial ischemia and necrosis due to the occlusion of coronary arteries. The occurrence of ischemia–reperfusion injury initiates a complex cascade of intricate pathophysiological changes, encompassing the onset of oxidative stress and inflammatory reactions 12 , 13 . The recovery of cardiac function and prognosis is highly associated with the alterations in cardiac oxidative stress and inflammatory markers following myocardial infarction 14 . When myocardial infarction occurs, the myocardial tissue confronts hypoxia due to coronary artery occlusion, resulting in an insufficient oxygen supply 15 , 16 . As hypoxia persists, it disrupts the oxidative phosphorylation process within cellular mitochondria, resulting in the excessive production of free oxygen radicals. These oxygen radicals significantly contribute to oxidative stress, posing a threat due to their capacity to damage lipids, proteins, and DNA. In addition, oxidative stress can activate intracellular signaling pathways, possibly triggering inflammatory reaction and apoptosis 17 , 18 . Following a heart attack, tissue damage and necrosis incite an inflammatory response characterized by the release of inflammatory cells and factors 19 , 20 . Of note, prominent inflammatory factors including TNF-α, IL-1β, and IL-6 have the potential to activate myocardial cells and attract inflammatory cells, exacerbating myocardial injury and increasing the burden on the heart, with evident impact on cardiac function 21 . The interplay between cardiac oxidative stress and inflammatory factors is intricate. Signal pathways can be activated, potentially inducing the release of inflammatory agents, possibly due to oxidative stress 22 . On the other hand, the presence of inflammatory agents can exacerbate oxidative stress by stimulating the generation of harmful molecules known as free radicals. This interaction worsens the extent of heart damage following a heart attack and impacts the recovery of heart function and overall prognosis 23 . Understanding the dynamic alterations in cardiac oxidative stress and inflammatory markers following a heart attack is crucial for developing targeted treatment strategies. This approach is significant for minimizing cardiac injury, enhancing cardiac function recovery, decreasing the occurrence of cardiac events, and enhancing patients’ prognosis. As a result, addressing cardiac oxidative stress and inflammatory markers has been focused on in the research and management of heart attacks.
This research was undertaken with the objective of elucidating the correlation between oxidative stress in the heart, the inflammatory cytokine response, and their combined influence on cardiac pump function and prognosis following a heart attack. By analyzing 138 patients with myocardial infarction, the study unveiled the impact of cardiac oxidative stress and inflammatory cytokines on cardiac pump function and prognosis after myocardial infarction. The insight garnered from this study greatly contributes to understanding the significance of early drug intervention in treating myocardial infarction.
According to our findings, the observation group underwent prompt medication intervention, leading to a decrease in serum levels of inflammatory markers, including TNF-α, IL-1β, and IL-6. The presence of these inflammatory markers play a crucial role in the pathophysiology following a heart attack, and changes in their concentrations are strongly linked to the extent of cardiac damage, modification in cardiac performance, and overall prognosis. The implementation of early medication intervention aimed at decreasing the levels of inflammatory factors held significant benefits. This approach serves to curtail the inflammatory response, safeguard myocardial tissue, and ultimately improve cardiac function and prognosis. After aheart attack, the substantial inflammatory factors TNF-α, IL-1β, and IL-6 play a significant regulatory role. In fact, activation of these substances can trigger an inflammatory response, resulting in the infiltration of inflammatory cells and subsequent tissue damage. The secretion of inflammatory substances further stimulates signaling pathways, intensifying oxidative stress, inducing lipid peroxidation of cellular membranes, and causing oxidative damage to proteins. These combined effects ultimately exacerbate myocardial damage 24 . Therefore, reducing the magnitude of these inflammatory agents can mitigate the intensity of the inflammatory response following a heart attack, thereby positively influencing the safeguarding of cardiac tissue. By selecting appropriate drug intervention strategies, it becomes feasible to regulate the progression of the inflammatory response, diminish the damage inflicted oncardiac tissue, and facilitate the restoration of normal myocardial function, thereby promoting the process of myocardial repair. Following timely drug intervention, the observation group exhibited significant changes in cardiac oxidative stress. This was characterized by a reduction in the overall oxidation level, a decline in OSI, and an elevation in TAS. These findings underscores the substantial role of timely medication intervention in managing cardiac oxidative stress, thus contributing to its protection against oxidative damage. Cardiac oxidative stress plays a crucial role in the development process after myocardial infarction, and the results of this experiment are consistent with the research of Hao Y et al. The study depicts that due to coronary artery occlusion, myocardial tissue is subjected to hypoxia and reperfusion injury, producing a large amount of free oxygen radicals, which can react with cell membranes, proteins, and nucleic acids, leading to abnormalities in cell structure and function. Oxidative stress can also activate intracellular signaling pathways, leading to inflammatory responses and cell apoptosis 25 . Therefore, reducing cardiac oxidative stress is crucial for protecting the heart from further damage.
Regarding cardiac pump function, subjects within the observation group exhibited reductions in EDD and ESD, along with an elevated LVEF. These findings suggest that early medication intervention could potentially enhance both systolic and diastolic performance of the heart, thereby optimizing blood ejection efficacy from the heart. Furthermore, the observation group manifested significantly lower occurrences of re-infarction, heart failure, arrhythmia, and valve dysfunction compared to the control group, implying that early medication intervention could positively influence patients’ prognosis. Through the utilization of logistic regression and multiple regression analyses, this research further validated the impact of cardiac oxidative stress and inflammatory markers on cardiac pump function and prognosis. Moreover, it discovered a significant correlation between the escalation of cardiac oxidative stress and inflammatory markers and the deterioration of cardiac pump function and prognosis. These findings highlights the pivotal roles played by oxidative stress and the inflammatory response in the pathological progression following myocardial infarction. Our study paves the way for novel treatment strategies in the management of myocardial infarction. Early intervention, directed towards addressing cardiac oxidative stress and inflammatory factors, emerges as a promising avenue for enhancing cardiac function, decreasing the incidence of adverse cardiac events, and ultimately enhancing patients’ prognosis quality. Nevertheless, it is essential to acknowledge that despite significant advancements in research methods and outcomes, certain constraints exist, including a relatively limited sample size and restricted research duration. To further enrich the understanding of myocardial infarction treatment and prognosis, future studies should consider enlarging the sample size, prolonging the research duration, and investigating additional biological mechanisms.
To conclude, our study highlights the crucial importance of cardiac oxidative stress and the inflammatory cytokine response in influencing cardiac pump function and prognosis following a heart attack. Timely drug intervention emerges as a vital factor in decreasing the levels of inflammatory markers, mitigating oxidative stress, enhancing cardiac pumping function, and improving prognosis. This novel perspective on myocardial infarction treatment has the potential to improve patients’ quality of life and mitigate the likelihood of cardiovascular events.
Data availability
The data and materials used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Butyl hydroxytoluene
Electrocardiogram
Oxidative stress index
Total antioxidantstatus
Lamb, F. S. et al. TNFα and reactive oxygen signaling in vascular smooth muscle cells in hypertension and atherosclerosis. Am. J. Hypertens. 33 , 902–913 (2020).
Article CAS PubMed PubMed Central Google Scholar
Du, J. et al. Glatiramer acetate protects against oxygen-glucose deprivation/reperfusion-induced injury by inhibiting Egr-1 in H9c2 cells. Mol. Immunol. 120 , 61–66 (2020).
Article CAS PubMed Google Scholar
Feng, L. et al. Simvastatin relieves myocardial ischemia/reperfusion injury in rats through hedgehog signaling pathway. Eur. Rev. Med. Pharmacol. Sci. 24 , 6400–6408 (2020).
CAS PubMed Google Scholar
Hsu, W. T. et al. 5-Methoxytryptophan attenuates postinfarct cardiac injury by controlling oxidative stress and immune activation. J. Mol. Cell Cardiol. 158 , 101–114 (2021).
Li, X. et al. Potential biomarkers and therapeutic targets: Inflammation and oxidative stress in left carotid artery stenosis with coronary artery disease. Curr. Pharm. Des. 29 , 966–979 (2023).
Chen, Y. et al. Boeravinone B alleviates gut dysbiosis during myocardial infarction-induced cardiotoxicity in rats. J. Cell Mol. Med. 25 , 6403–6416 (2021).
Cheng, G. et al. Cardioprotective effect of gossypin against myocardial ischemic/reperfusion in rats via alteration of oxidative stress, inflammation and gut microbiota. J. Inflamm. Res. 15 , 1637–1651 (2022).
Iqubal, A. et al. Natural bioactive as a potential therapeutic approach for the management of cyclophosphamide-induced cardiotoxicity. Curr. Top. Med. Chem. 21 , 2647–2670 (2021).
Leung, K. S. et al. Enrichment of alpha-linolenic acid in rodent diet reduced oxidative stress and inflammation during myocardial infarction. Free RadicBiol. Med. 162 , 53–64 (2021).
Article CAS Google Scholar
Maeda, H. et al. TAT-dextran-mediated mitochondrial transfer enhances recovery from models of reperfusion injury in cultured cardiomyocytes. J. Cell Mol. Med. 24 , 5007–5020 (2020).
Lan, Z. et al. CircSLC8A1 exacerbates hypoxia-induced myocardial injury via interacting with MiR-214-5p to upregulate TEAD1 expression. Int. Heart J. 63 , 591–601 (2022).
Sun, W. et al. Aloin antagonizes stimulated ischemia/reperfusion-induced damage and inflammatory response in cardiomyocytes by activating the Nrf2/HO-1 defense pathway. Cell Tissue Res. 384 , 735–744 (2021).
Shahzad, S. et al. Effect of syringic acid and syringaldehyde on oxidative stress and inflammatory status in peripheral blood mononuclear cells from patients of myocardial infarction. NaunynSchmiedebergs Arch. Pharmacol. 393 , 691–704 (2020).
Song, Y. et al. LINC01588 regulates WWP2-mediated cardiomyocyte injury by interacting with HNRNPL. Environ. Toxicol. 37 , 1629–1641 (2022).
Article ADS CAS PubMed Google Scholar
Elseweidy, M. M. et al. Vanillin and pentoxifylline ameliorate isoproterenol-induced myocardial injury in rats via the Akt/HIF-1α/VEGF signaling pathway. Food Funct. 14 , 3067–3082 (2023).
Ramakrishna, K. & Krishnamurthy, S. Indole-3-carbinol ameliorated the isoproterenol-induced myocardial infarction via multimodal mechanisms in Wistarrats. Nat. Prod. Res. 36 , 6044–6049 (2022).
Hedayati-Moghadam, M. et al. The role of chemokines in cardiovascular diseases and the therapeutic effect of curcumin on CXCL8 and CCL2 as pathological chemokines in atherosclerosis. Adv. Exp. Med. Biol. 1328 , 155–170 (2021).
Ma, B. et al. SIRT1 regulates hypoxia-induced oxidative stress in cardiomyocytes via PI3K/MTOR signaling. Cell. Mol. Biol. (Noisy-le-grand) 68 , 48–53 (2022).
Article PubMed Google Scholar
Saad, H. et al. The pathogenic role of oxidative stress, cytokine expression, and impaired hematological indices in diabetic cardiovascular diseases. Inflammation 46 , 146–160 (2023).
Shi, M. et al. Diosmetin alleviates cerebral ischemia-reperfusion injury through Keap1-mediated Nrf2/ARE signaling pathway activation and NLRP3 inflammasome inhibition. Environ. Toxicol. 37 , 1529–1542 (2022).
Cinar, I. et al. In vivo and in vitro cardioprotective effect of gossypin against isoproterenol-induced myocardial infarction injury. Cardiovasc. Toxicol. 22 , 52–62 (2022).
Naseroleslami, M. et al. Nesfatin-1 attenuates injury in a rat model of myocardial infarction by targeting autophagy, inflammation, and apoptosis. Arch. Physiol. Biochem. 129 , 122–130 (2023).
Sun, L. et al. Protective role of poly(lactic-co-glycolic) acid nanoparticle loaded with resveratrol against isoproterenol-induced myocardial infarction. Biofactors 46 , 421–431 (2020).
Li, S., Wang, H. & Zhou, Y. JAK2/STAT3 pathway mediates beneficial effects of pterostilbene on cardiac contractile and electrical function in the setting of myocardial reperfusion injury. Physiol. Res. 71 , 489–499 (2022).
Hao, Y., Xiong, R. & Gong, X. Memantine, NMDA receptor antagonist, attenuates ox-LDL-induced inflammation and oxidative stress via activation of BDNF/TrkB signaling pathway in HUVECs. Inflammation 44 , 659–670 (2021).
Download references
This study was funded by Handan Medical Science Research Project in 2022 (No. 22422083088Z).
Author information
Authors and affiliations.
Department of Emergency, Affiliated Hospital of Hebei Engineering University, Handan, Hebei, China
Dongpeng Duan & Tianfeng Fan
Publicity and Development Department, Affiliated Hospital of Hebei Engineering University, Handan, Hebei, China
Departmentof Renaissance Orthopedics & Otolaryngology Head and Neck Surgery, Affiliated Hospital of Hebei Engineering University, Handan, Hebei, China
Shiyun Chai
Department of Infectious Diseases, Affiliated Hospital of Hebei Engineering University, Handan, Hebei, China
Linlin Zhang
Department of General Suegery, Affiliated Hospital of Hebei Engineering University, Handan, Hebei, China
Zhenfeng Hu
Department of Critical Care Medicine, Affiliated Hospital of Hebei Engineering University, No.81 Congtai Road, Handan, 056000, Hebei, China
You can also search for this author in PubMed Google Scholar
Contributions
Y. F. contributed to the conception and design of the study. D. P. D. organized the database and organized the database. H. J. L., S. Y. C., L. L. Z., T. F. F. and Z. F. Y. interpreted the data and searched the literature. DPD wrote the first draft of the manuscript. Y. F. edited the manuscript. All authors reviewed and approved the final version of the manuscript.
Corresponding author
Correspondence to Yan Feng .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Duan, D., Li, H., Chai, S. et al. The relationship between cardiac oxidative stress, inflammatory cytokine response, cardiac pump function, and prognosis post-myocardial infarction. Sci Rep 14 , 8985 (2024). https://doi.org/10.1038/s41598-024-59344-5
Download citation
Received : 04 December 2023
Accepted : 09 April 2024
Published : 18 April 2024
DOI : https://doi.org/10.1038/s41598-024-59344-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Myocardial infarction
- Oxidative stress
- Inflammatory cells
- Cardiac pump function
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Myocardial Infarction Essay (Critical Writing)
Introduction.
Myocardial Infarction is a disease of the heart that is caused by occlusions in the coronary arteries. The circulation of blood through the ventricles is reduced and the capacity of the heart to absorb oxygen is diminished. Artherosclerosis is mainly implicated with myocardial infarction.
MI is primarily evaluated using the ECG readings in which the ST-segment is usually elevated. By, analyzing the morphology of the ECG inconjuction with other tests, the condition can be correctly evaluated. The coronary occlusions can be dissolved using thrombolytic therapy.
In this case study, the close collaboration between nursing and other interventions illustrates the clinical procedure for handling patients with myocardial infarction in a hospital setting. It also gives insight into the complications of MI that may occur in a patient together with the necessary interventions from the nursing staff. The study questions are answered sequentially as follows;
Mr. Jones gradually developed symptoms of myocardial infarction. He started by experiencing excruciating chest pain that radiated to his jaw and left arm, shortness of breath (dyspnea) and diaphoresis (sweating), which culminated in sudden unconsciousness (syncope). These are the typical signs and symptoms of myocardial infarction.
They do not present immediately but gradually. The classic symptom of myocardial infaction is usually chest pains, which radiate to other parts of the body such as the left and right arms, lower jaw, neck, back, and the epigastrium, which resemble the heartburn.
Often, MIs are caused by accumulation of atherosclerotic plaque, which stimulates the forming of intracoronary thrombus. Intracoronary thrombus results in the occlusion of the coronary artery. This gives rise to insufficient circulation of blood through the ventricles hence myocardial infarction. The level of occlusion determines the severity of MI (Cotran, Kumar & Robbins, 1994).
Many other conditions that are uncommon can cause the coronary artery to block and thereby cause a myocardial infarction. They include rare inflammation of coronary arteries, a blood clot in another place of the body other than the ventricle e.g., in the heart chamber, a wound near the heart through a stab, the spasmal effects of taking cocaine on the coronary artery, and complications arising from heart surgery and/ or another rare heart conditions.
An ECG is performed to compare cardiac activities in the ventricular areas. The ST segment elevation is used to indicate on the ECG. Mr. Jones’ ECG signal indicated that there was an ST-segment elevation in leads II, III, and aVf on the ECG, which is indicative of MI. however, the ECG alone cannot be used to reliably diagnose myocardial infarction. It should be noted that the ECG also evaluates other heart conditions.
Consequently, the morphology and the principal components of the signal may give contradictory diagnosis. For instance, myocardial infarction is evaluated by observing the characteristics of the ST segmement. An elevation of the segment is indicative of possible myocardial infarction. However, the ST segment elevation is also indicative of the inherited type of cardiac arrhythmia called Brugada Syndrome. Consequently, other tests are necessary including laboratory tests, urine and blood sample analysis etc..
Cardiac enzymes are used as biomarkers that are evaluated to determine the heart function. There are particularly useful in evaluation of myocardial infaction although they are essential in assessment of other conditions that may lead to increment in cardiac biomarker level (Rao, Miller, Rosenbaum, & Lakier, 1999).
Cardiac enzymes such as creatine kinase-MB are ordered when the severity of myocardial infarction needs to be determined. The level of cardiac proteins in the blood corresponds to the severity of the myocardial infarction in the patient. Therefore, by determining these enzymes it makes the work of risk stratification of patients with myocardial infarction easier.
Once admitted to the CCU, It is the prerogative of the nurses to measure the blood pressure, changes in the heart and respiratory rates related to the physical examination of the patient. The most common examination performed on patients with suspected myocardial infarction is an ECG, which often indicates the presence of abnormalities in the left ventricle. In addition, laboratory tests of blood proteins related to the heart is performed to indicate if degeneration of myocardial cells is present.
MI results in diminished supply of oxygen to the heart due to the degeneration of cardiac cells. Consequently, the capacity of the heart to extract oxygen from blood may be compromised. The significance of using oxygen to make sure that the red blood cells are saturated maximally to compensate for the heart’s diminished ability to extract the oxygen.
Mr. Jones’ oxygen demands clearly outstripped supply oxygen dosage ameliorated the situation before comprehensive diagnosis and treatment ensued (Cotran, Kumar & Robbins, 1994). Administration of oxygen supplements treatment of patients with MI. Mr. Jones had shortness of breath and an episode of syncope. As treatment ensued, his oxygen supply had to be stabilized through administration of supplemental oxygen.
Myocardial infarction may give rise to other cardiac conditions that may need proper medical attention. Such conditions include the Wenckebach (Type 1) and Type 2 disarrhythmias. Wenckebach or Type I block is an intermittent cardiac conduction failure. In Wenckeback, conduction reduces as conduction velocity progressively reduces until failure of cardiac electrical conduction occurs. The ECG pattern of the condition shows the PR interval getting progressively longer until the non-conducted wave occurs.
Thrombolytic therapy initiates cardiac hemorrhage in patients with myocardial infaction. It is initiated to dissolve the coronary clots thereby easing the flow of blood and supply of oxygen to the heart. However, this therapy is not suitable in certain conditions such as recent surgery, stroke in the recent past, high blood pressure e.t.c.
The thrombolytic drugs are known to cause hemorrhage elsewhere in the body that can be life threatening in scenarios where a patient underwent surgery recently or is hypertension is present. In the case of Mr. Jones, he became unconscious as soon as he arrived at the reception. In addition, he had very high pressure at 130/92, which made it inappropriate to initiate thrombolytic therapy (Marcus, et al, 2007).
Myocardial infarction is associated with complications such as angina, free wall rupture, reinfarction, extension of infarct, heart failure, aneurysms, cardiogenic shock, valve dysfunction, arrhythmias, central nervous system (CNS) or peripheral embolisation, pericarditis, and psychosocial complications. Mr. Jones developed arrhythmias which were corrected by administration of drugs.
The ECG is the common procedure for diagnosis of myocardial infarctions. However, other diagnostic tests can be carried out on Mr. Jones. They include blood and urine tests, swabs, diagnostic and lab tests, and pathology testing. Pathology testing is important as myocardial infarction could have been caused by a certain underlying pathogen. These tests are performed in order to confirm presence of myocardial infarction because an ECG cannot provide a comprehensive assessment of the condition.
Cotran R., Kumar V. & Robbins S. (1994). Robbins Pathologic Basis of Disease. 5th Ed. Philadelphia, PL: WB Saunders Press.
Marcus, et al. (2007). The utility of gestures in patients with chest discomfort American Journal of Medicine , 120(1), 83–9.
Rao P., Miller S., Rosenbaum R., & Lakier J. (1999). Cardiac troponin I and cardiac enzymes after electrophysiologic studies, ablations, and defibrillator implantations. American Journal of Cardiology, 84(4), 470.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2020, July 3). Myocardial Infarction. https://ivypanda.com/essays/myocardial-infarction-case-study/
"Myocardial Infarction." IvyPanda , 3 July 2020, ivypanda.com/essays/myocardial-infarction-case-study/.
IvyPanda . (2020) 'Myocardial Infarction'. 3 July.
IvyPanda . 2020. "Myocardial Infarction." July 3, 2020. https://ivypanda.com/essays/myocardial-infarction-case-study/.
1. IvyPanda . "Myocardial Infarction." July 3, 2020. https://ivypanda.com/essays/myocardial-infarction-case-study/.
Bibliography
IvyPanda . "Myocardial Infarction." July 3, 2020. https://ivypanda.com/essays/myocardial-infarction-case-study/.
- Myocardial Infarction in Australia Analysis
- Myocardial Infarction: Diagnostic and Treatment
- Risk Factors for Acute Myocardial Infarction
- Lobbying for Funds to Implement Telehealth Services
- Core Measures of Acute Myocardial Infarction
- Heart Disease: Cell Death During Myocardial Infarction
- Myocardial Infarction Treatment With Clopidogrel & Plavix
- Myocardial Infarction and Heart Attack
- Myocardial Infarction: Cardiac Shock and Transportation the Patients
- Nursing Care of Myocardial Infarction Patients
- Health Care Conditions in the United States
- Health Care Reforms in G8 Countries and Turkey
- Taking Blood Pressure: Storyboard Concept
- What is Hypertension?
- Giving an Overview of Music Education
Myocardial Infarction
Learn about the nursing care management of patients with myocardial infarction in this nursing study guide .
Table of Contents
- What is Myocardial Infarction?
Pathophysiology
Statistics and epidemiology, clinical manifestations, assessment and diagnostic findings, pharmacologic therapy, emergent percutaneous coronary intervention, nursing assessment, planning & goals, nursing priorities, nursing interventions, discharge and home care guidelines, documentation guidelines, practice quiz: myocardial infarction, what is myocardial infarction.
Myocardial infarction (MI) , is used synonymously with coronary occlusion and heart attack, yet MI is the most preferred term as myocardial ischemia causes acute coronary syndrome (ACS) that can result in myocardial death .
- In an MI, an area of the myocardium is permanently destroyed because plaque rupture and subsequent thrombus formation result in complete occlusion of the artery.
- The spectrum of ACS includes unstable angina , non-ST-segment elevation MI , and ST-segment elevation MI .
In each case of MI, a profound imbalance exists between myocardial oxygen supply and demand.
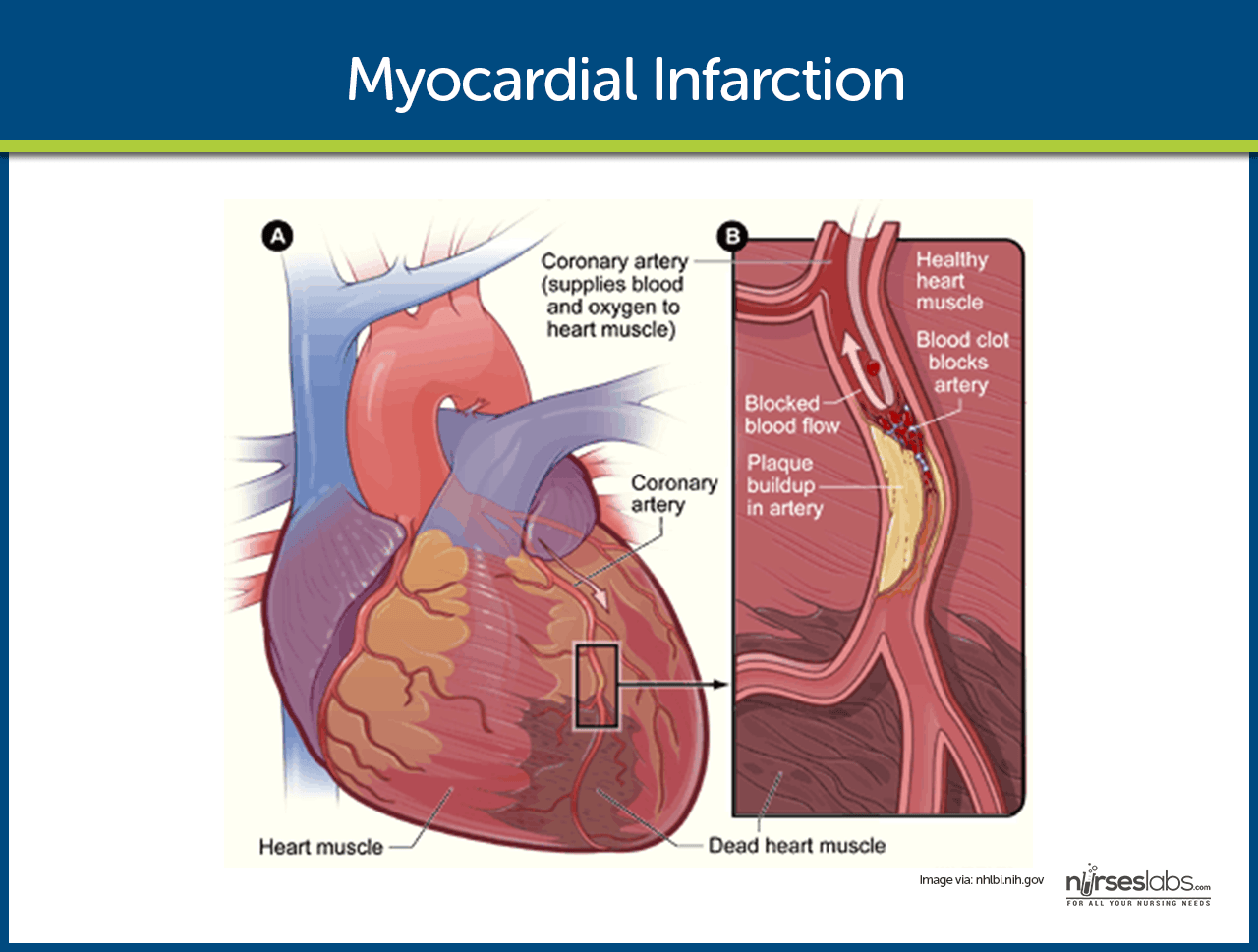
- Unstable angina . There is reduced blood flow in a coronary artery, often due to rupture of an atherosclerotic plaque, but the artery is not completely occluded.
- Development of infarction. As the cells are deprived of oxygen, ischemia develops, cellular injury occurs, and lack of oxygen leads to infarction or death of the cells.
- Schematic Diagram of Myocardial Infarction via Scribd
“Time is muscle ”; this is the reflection of the urgency of appropriate treatments to improve patient outcome.
- Each year in the United States, nearly 1 million people have acute MIs.
- One fourth of the people with the disease die of MI.
- Half of the people who die with acute MI never reach the hospital.
The causes of MI primarily stems from the vascular system.
- Vasospasm. This is the sudden constriction or narrowing of the coronary artery.
- Decreased oxygen supply. The decrease in oxygen supply occurs from acute blood loss , anemia , or low blood pressure .
- Increased demand for oxygen. A rapid heart rate, thyrotoxicosis, or ingestion of cocaine causes an increase in the demand for oxygen.
Some of the patients have prodromal symptoms or a previous diagnosis of CAD, but about half report no previous symptoms.
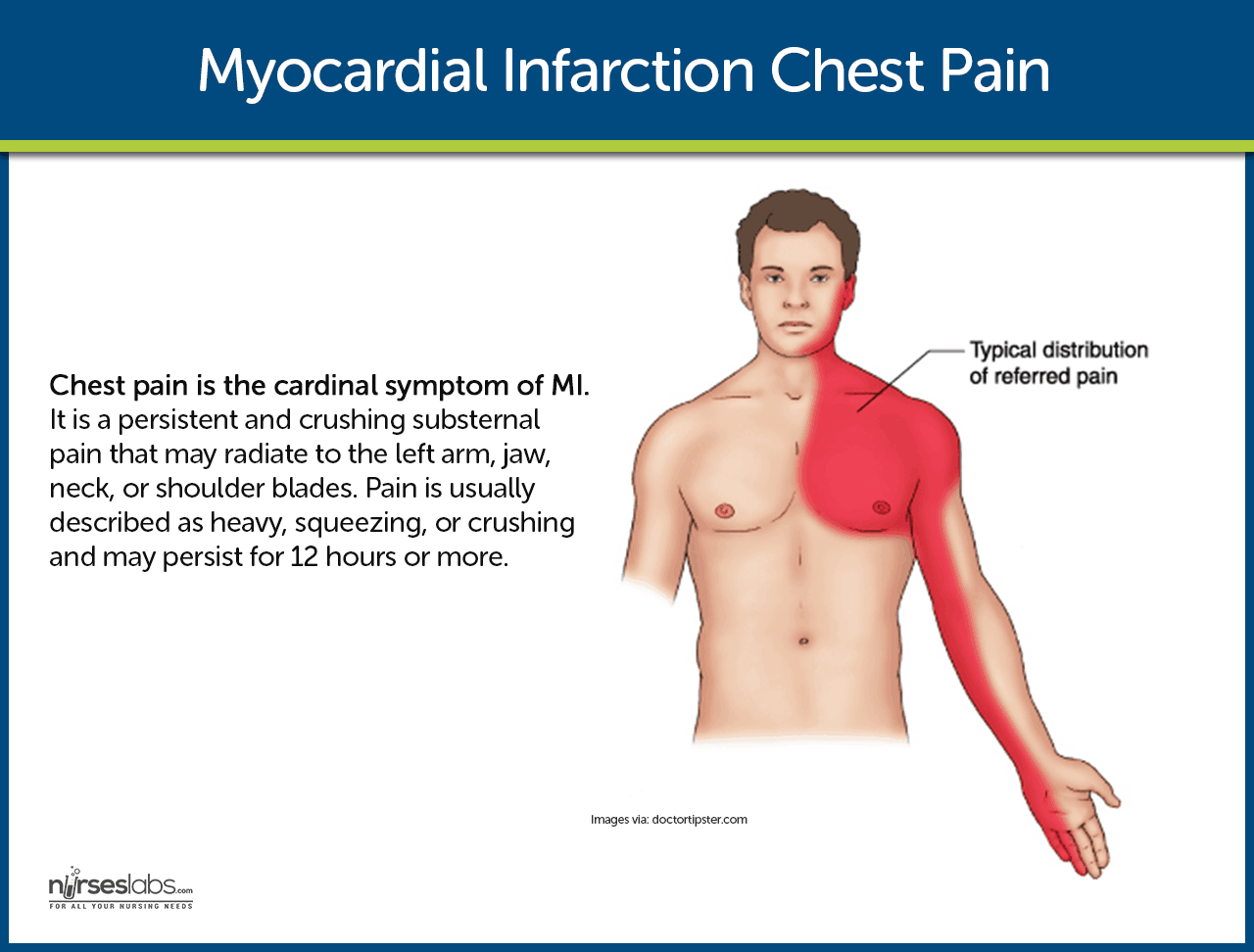
- Chest pain . This is the cardinal symptom of MI. Persistent and crushing substernal pain that may radiate to the left arm, jaw, neck, or shoulder blades. Pain is usually described as heavy, squeezing, or crushing and may persist for 12 hours or more.
- Shortness of breath. Because of increased oxygen demand and a decrease in the supply of oxygen, shortness of breath occurs.
- Indigestion. Indigestion is present as a result of the stimulation of the sympathetic nervous system .
- Tachycardia and tachypnea. To compensate for the decreased oxygen supply, the heart rate and respiratory rate speed up.
- Catecholamine responses. The patient may experience such as coolness in extremities, perspiration, anxiety , and restlessness.
- Fever. Unusually occurs at the onset of MI, but a low-grade temperature elevation may develop during the next few days.
A healthy lifestyle could help prevent the development of MI.
- Exercise. Exercising at least thrice a week could help lower cholesterol levels that cause vasoconstriction of the blood vessels.
- Balanced diet. Fruits, vegetables, meat and fish should be incorporated in the patient’s daily diet to ensure that he or she gets the right amount of nutrients he or she needs.
- Smoking cessation. Nicotine causes vasoconstriction which can increase the pressure of the blood and result in MI.
The diagnosis of MI is generally based on the presenting symptoms.
- Patient history. The patient history includes the description of the presenting symptoms, the history of previous cardiac and other illnesses, and the family history of heart diseases.
- ECG . ST elevation signifying ischemia; peaked upright or inverted T wave indicating injury; development of Q waves signifying prolonged ischemia or necrosis.
- Cardiac enzymes and isoenzymes. CPK-MB (isoenzyme in cardiac muscle): Elevates within 4–8 hr, peaks in 12–20 hr, returns to normal in 48–72 hr.
- LDH. Elevates within 8–24 hr, peaks within 72–144 hr, and may take as long as 14 days to return to normal. An LDH 1 greater than LDH 2 (flipped ratio) helps confirm/diagnose MI if not detected in acute phase.
- Troponins. Troponin I (cTnI) and troponin T (cTnT): Levels are elevated at 4–6 hr, peak at 14–18 hr, and return to baseline over 6–7 days. These enzymes have increased specificity for necrosis and are therefore useful in diagnosing postoperative MI when MB-CPK may be elevated related to skeletal trauma .
- Myoglobin. A heme protein of small molecular weight that is more rapidly released from damaged muscle tissue with elevation within 2 hr after an acute MI, and peak levels occurring in 3–15 hr.
- Electrolytes . Imbalances of sodium and potassium can alter conduction and compromise contractility.
- WBC. Leukocytosis (10,000–20,000) usually appears on the second day after MI because of the inflammatory process.
- ESR. Rises on second or third day after MI, indicating inflammatory response.
- Chemistry profiles. May be abnormal, depending on acute/chronic abnormal organ function/perfusion.
- ABGs / pulse oximetry . May indicate hypoxia or acute/chronic lung disease processes.
- Lipids (total lipids, HDL, LDL, VLDL, total cholesterol, triglycerides, phospholipids). Elevations may reflect arteriosclerosis as a cause for coronary narrowing or spasm.
- Chest x-ray . May be normal or show an enlarged cardiac shadow suggestive of HF or ventricular aneurysm .
- Two-dimensional echocardiogram . May be done to determine dimensions of chambers, septal/ventricular wall motion, ejection fraction (blood flow), and valve configuration/function.
- Nuclear imaging studies: Persantine or Thallium. Evaluates myocardial blood flow and status of myocardial cells, e.g., location/extent of acute/previous MI.
- Cardiac blood imaging/MUGA. Evaluates specific and general ventricular performance, regional wall motion, and ejection fraction.
- Technetium. Accumulates in ischemic cells, outlining necrotic area(s).
- Coronary angiography. Visualizes narrowing/occlusion of coronary arteries and is usually done in conjunction with measurements of chamber pressures and assessment of left ventricular function (ejection fraction). Procedure is not usually done in acute phase of MI unless angioplasty or emergency heart surgery is imminent.
- Digital subtraction angiography (DSA). Technique used to visualize status of arterial bypass grafts and to detect peripheral artery disease.
- Magnetic resonance imaging (MRI). Allows visualization of blood flow, cardiac chambers or intraventricular septum, valves, vascular lesions, plaque formations, areas of necrosis/infarction, and blood clots.
- Exercise stress test. Determines cardiovascular response to activity (often done in conjunction with thallium imaging in the recovery phase).
Medical Management
The goals of medical management are to minimize myocardial damage, preserve myocardial function, and prevent complications.
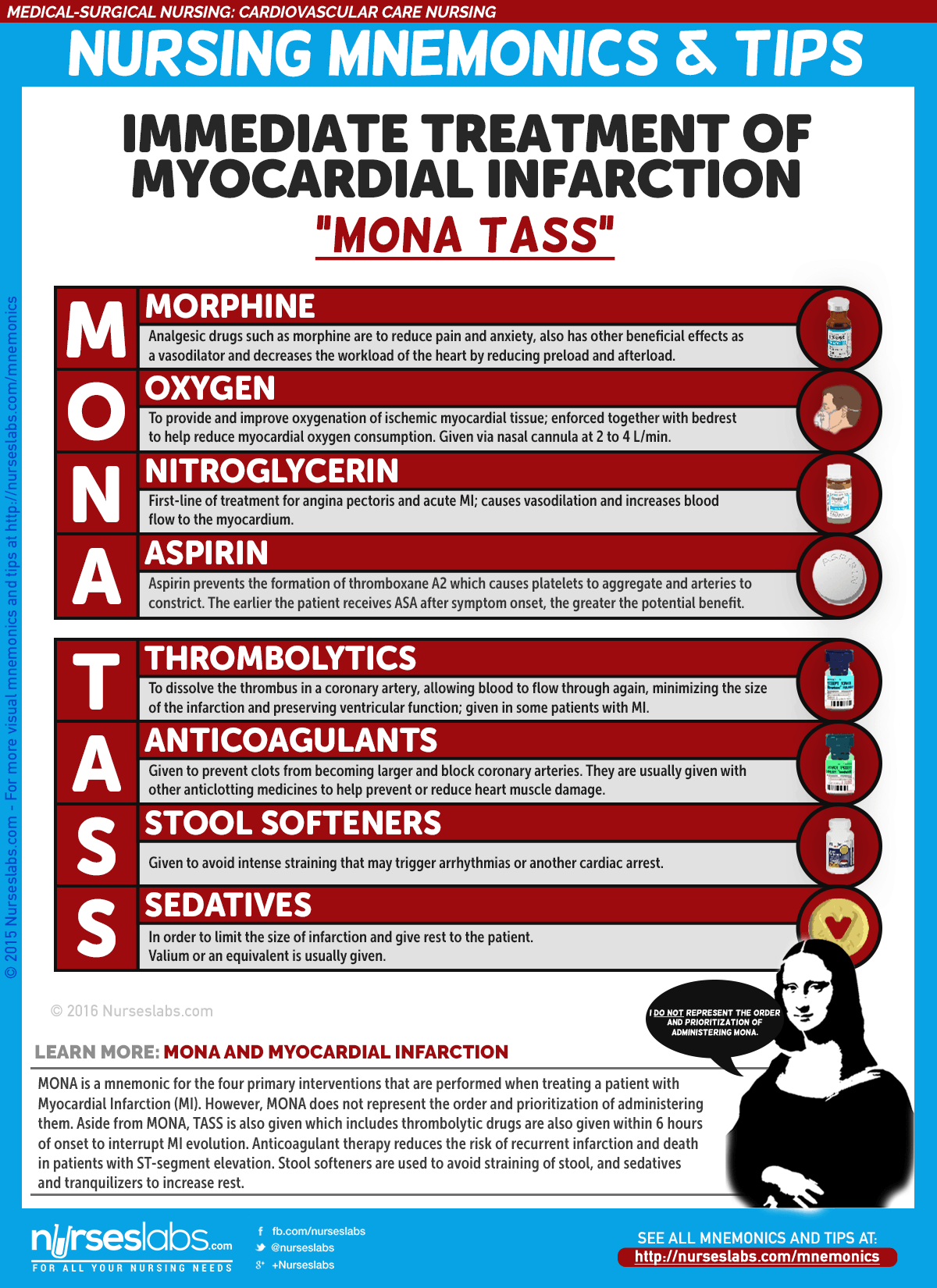
- Morphine administered in IV boluses is used for MI to reduce pain and anxiety.
- ACE Inhibitors . ACE inhibitors prevent the conversion of angiotensin I to angiotensin II to decrease blood pressure and for the kidneys to secrete sodium and fluid, decreasing the oxygen demand of the heart.
- Thrombolytics. Thrombolytics dissolve the thrombus in the coronary artery,allowing blood to flow through the coronary artery again, minimizing the size of the infarction and preserving ventricular function.
- The procedure is used to open the occluded coronary artery and promote reperfusion to the area that has been deprived of oxygen.
- PCI may also be indicated in patients with unstable angina and NSTEMI for patients who are at high risk due to persistent ischemia.
Nursing Management
The nursing management involved in MI is critical and systematic, and efficiency is needed to implement the care for a patient with MI.
One of the most important aspects of care of the patient with MI is the assessment.
- Assess for chest pain not relieved by rest or medications.
- Monitor vital signs, especially the blood pressure and pulse rate.
- Assess for presence of shortness of breath, dyspnea , tachypnea, and crackles.
- Assess for nausea and vomiting .
- Assess for decreased urinary output.
- Assess for the history of illnesses.
- Perform a precise and complete physical assessment to detect complications and changes in the patient’s status.
- Assess IV sites frequently.
Based on the clinical manifestations, history, and diagnostic assessment data, major nursing diagnoses may include.
- Ineffective cardiac tissue perfusion related to reduced coronary blood flow.
- Risk for ineffective peripheral tissue perfusion related to decreased cardiac output from left ventricular dysfunction.
- Deficient knowledge related to post-MI self-care .
Main Article: 7 Myocardial Infarction (Heart Attack) Nursing Care Plans
To establish a plan of care, the focus should be on the following:
- Relief of pain or ischemic signs and symptoms.
- Prevention of myocardial damage.
- Absence of respiratory dysfunction.
- Maintenance or attainment of adequate tissue perfusion.
- Reduced anxiety.
- Absence or early detection of complications.
- Chest pain absent/controlled.
- Heart rate/rhythm sufficient to sustain adequate cardiac output/tissue perfusion.
- Achievement of activity level sufficient for basic self-care.
- Anxiety reduced/managed.
- Disease process, treatment plan, and prognosis understood.
- Plan in place to meet needs after discharge.
- Relieve pain, anxiety.
- Reduce myocardial workload.
- Prevent/detect and assist in treatment of life-threatening dysrhythmias or complications.
- Promote cardiac health, self-care.
Nursing interventions should be anchored on the goals in the nursing care plan .
- Administer oxygen along with medication therapy to assist with relief of symptoms.
- Encourage bed rest with the back rest elevated to help decrease chest discomfort and dyspnea.
- Encourage changing of positions frequently to help keep fluid from pooling in the bases of the lungs .
- Check skin temperature and peripheral pulses frequently to monitor tissue perfusion.
- Provide information in an honest and supportive manner.
- Monitor the patient closely for changes in cardiac rate and rhythm, heart sounds, blood pressure, chest pain, respiratory status, urinary output, changes in skin color, and laboratory values.
After the implementation of the interventions within the time specified, the nurse should check if:
- There is an absence of pain or ischemic signs and symptoms.
- Myocardial damage is prevented.
- Adequate tissue perfusion maintained.
- Anxiety is reduced.
The most effective way to increase the probability that the patient will implement a self-care regimen after discharge is to identify the patient’s priorities.
- Education. This is one of the priorities that the nurse must teach the patient about heart-healthy living.
- Home care. The home care nurse assists the patient with scheduling and keeping up with the follow-up appointments and with adhering to the prescribed cardiac rehabilitation management.
- Follow-up monitoring. The patient may need reminders about follow-up monitoring including periodic laboratory testing and ECGs, as well as general health screening.
- Adherence. The nurse should also monitor the patient’s adherence to dietary restrictions and prescribed medications.
To ensure that every action documented is an action done, documentation must be secured. The following should be documented:
- Individual findings.
- Vital signs, cardiac rhythm , presence of dysrhythmias.
- Plan of care and those involved in planning.
- Teaching plan.
- Response to interventions, teaching, and actions performed.
- Attainment or progress towards desired outcomes.
- Modifications to plan of care.
Let’s reinforce what you’ve learned with this 5-item NCLEX practice quiz about Myocardial Infarction. Please visit our nursing test bank for more NCLEX practice questions .
1. Which of the following is the most common symptom of myocardial infarction (MI)?
A. Chest pain B. Dyspnea C. Edema D. Palpitations
2. An intravenous analgesic frequently administered to relieve chest pain associated with MI is:
A. Meperidine hydrochloride B. Hydromorphone hydrochloride C. Morphine sulfate D. Codeine sulfate
3. The classic ECG changes that occur with an MI include all of the following except:
A. An absent P wave B. An abnormal Q wave C. T-wave inversion D. ST segment elevation
4. Which of the following statements about myocardial infarction pain is incorrect?
A. It is relieved by rest and inactivity. B. It is substernal in location. C. It is sudden in onset and prolonged in duration. D. It is viselike and radiates to the shoulders and arms.
5. Myocardial cell damage can be reflected by high levels of cardiac enzymes. The cardiac-specific isoenzyme is:
A. Alkaline phosphatase B. Creatine kinase (CK-MB) C. Myoglobin D. Troponin
1. Answer: A. Chest pain
- A: The most common symptom of an MI is chest pain, resulting from deprivation of oxygen to the heart.
- B: Dyspnea is the second most common symptom, related to an increase in the metabolic needs of the body during an MI.
- C: Edema is a later sign of heart failure , often seen after an MI.
- D: Palpitations may result from reduced cardiac output, producing arrhythmias.
2. Answer: C. Morphine sulfate
- C: Morphine administered in IV boluses is used for MI to reduce pain and anxiety.
- A: Meperidine hydrochloride is not the analgesic of choice for MI.
- B: Hydromorphone hydrochloride is not the analgesic of choice for MI.
- D: Codeine sulfate is not the analgesic of choice for MI.
3. Answer: A. An absent P wave
- A: An absent P wave is not part of the classic changes seen in an ECG result.
- B: An abnormal Q wave is an indication of MI.
- C: T-wave inversion is a classic ECG change in a patient with MI.
- D: ST segment elevation is an indication of MI.
4. Answer: A. It is relieved by rest and inactivity.
- A: MI pain continues despite rest and medications.
- B: The pain occurs substernally or at the chest area.
- C: MI pain occurs suddenly and is prolonged in duration.
- D: The pain grips the patient like a vise and radiates towards the arms or the shoulders.
5. Answer: B. Creatine kinase (CK-MB)
- B: CK-MB is the isoenzyme for the heart muscle and the cardiac-specific enzyme.
- A: Alkaline phosphatase is not part of the creatine kinase isoenzymes.
- C: Myoglobin is a heme protein that helps transport oxygen.
- D: Troponin regulates the myocardial contractile process.
Posts related to Myocardial Infarction:
- 7 Myocardial Infarction (Heart Attack) Nursing Care Plans
- Myocardial Infarction and Heart Failure NCLEX Practice Quiz (70 Items)
- Heart Failure
- Cardiovascular Care Nursing Mnemonics and Tips
3 thoughts on “Myocardial Infarction”
Good lecture
Very refreshing lecture
Leave a Comment Cancel reply
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Myocardial infarction.
Niranjan Ojha ; Amit S. Dhamoon .
Affiliations
Last Update: August 8, 2023 .
- Continuing Education Activity
Myocardial infarction (MI), colloquially known as "heart attack," is caused by decreased or complete cessation of blood flow to a portion of the myocardium. Myocardial infarction may be"silent," and go undetected, or it could be a catastrophic event leading to hemodynamic deterioration and sudden death. Most myocardial infarctions are due to underlying coronary artery disease, the leading cause of death in the United States. With coronary artery occlusion, the myocardium is deprived of oxygen. Prolonged deprivation of oxygen supply to the myocardium can lead to myocardial cell death and necrosis. Patients can present with chest discomfort or pressure that can radiate to the neck, jaw, shoulder, or arm. In addition to the history and physical exam, myocardial ischemia may be associated with ECG changes and elevated biochemical markers such as cardiac troponins. This activity describes the pathophysiology, evaluation, and management of myocardial infarction and highlights the role of the interprofessional team in improving care for affected patients.
- Review the basic pathophysiology of myocardial infarction.
- Explain the management protocol when presented with acute myocardial infarction, including all necessary laboratory and other diagnostic testing.
- Summarize the long-term management and rehabilitation for a patient post-MI.
- Explain interprofessional team strategies for improving care coordination and communication to advance the prevention and management of myocardial infarction leading to improved outcomes.
- Introduction
Myocardial infarction (MI), colloquially known as “heart attack,” is caused by decreased or complete cessation of blood flow to a portion of the myocardium. Myocardial infarction may be “silent” and go undetected, or it could be a catastrophic event leading to hemodynamic deterioration and sudden death. [1] Most myocardial infarctions are due to underlying coronary artery disease, the leading cause of death in the United States. With coronary artery occlusion, the myocardium is deprived of oxygen. Prolonged deprivation of oxygen supply to the myocardium can lead to myocardial cell death and necrosis. [2] Patients can present with chest discomfort or pressure that can radiate to the neck, jaw, shoulder, or arm. In addition to the history and physical exam, myocardial ischemia may be associated with ECG changes and elevated biochemical markers such as cardiac troponins. [3] [4]
As stated above, myocardial infarction is closely associated with coronary artery disease. INTERHEART is an international multi-center case-control study which delineated the following modifiable risk factors for coronary artery disease: [5] [6]
- Abnormal lipid profile/blood apolipoprotein (raised ApoB/ApoA1)
- Hypertension
- Diabetes mellitus
- Abdominal obesity (waist/hip ratio) (greater than 0.90 for males and greater than 0.85 for females)
- Psychosocial factors such as depression, loss of the locus of control, global stress, financial stress, and life events including marital separation, job loss, and family conflicts
- Lack of daily consumption of fruits or vegetables
- Lack of physical activity
- Alcohol consumption (weaker association, protective)
The INTERHEART study showed that all the above risk factors were significantly associated with acute myocardial infarction except for alcohol consumption, which showed a weaker association. Smoking and abnormal apolipoprotein ratio showed the strongest association with acute myocardial infarction. The increased risk associated with diabetes and hypertension were found to be higher in women, and the protective effect of exercise and alcohol was also found to be higher in women. [5]
Other risk factors include a moderately high level of plasma homocysteine, which is an independent risk factor of MI. Elevated plasma homocysteine is potentially modifiable and can be treated with folic acid, vitamin B6, and vitamin B12. [7]
Some non-modifiable risk factors for myocardial infarction include advanced age, male gender (males tend to have myocardial infarction earlier in life), genetics (there is an increased risk of MI if a first-degree relative has a history of cardiovascular events before the age of 50). [6] [8] The role of genetic loci that increase the risk for MI is under active investigation. [9] [10]
- Epidemiology
The most common cause of death and disability in the western world and worldwide is coronary artery disease. [11] Based on 2015 mortality data from the National Health Interview Survey (NHIS-CDC), MI mortality was 114,023, and MI any-mention mortality (i.e., MI is mentioned as a contributing factor in the death certificate) was 151,863.
As per the National Health and Nutrition Examination Survey (NHANES)-CDC data from 2011 to 2014, an estimated 16.5 million Americans older than 20 years of age have coronary artery disease, and the prevalence was higher in males than females for all ages. As per the NHANES 2011 through 2014, the overall prevalence of MI is 3.0% in US adults older than 20 years of age.
Prevalence of MI in the US Sub-populations
Non-Hispanic Whites
- 4.0% (Male)
- 2.4% (Female)
Non-Hispanic Blacks
- 3.3% (Male)
- 2.2% (Female)
- 2.9% (Male)
- 2.1% (Female)
Non-Hispanic Asians
- 2.6% (Male)
- 0.7% (Female)
Based on the Atherosclerosis Risk in Communities Study (ARIC) performed by National Heart, Lung, and Blood Institute (NHLBI) collected between 2005 and 2014, the estimated annual incidence is 605,000 new MIs and 200,000 recurrent MIs. [12]
The ARIC study also found that the average age at first MI is 65.6 years for males and 72.0 years for females. In the past decades, several studies have shown a declining incidence of MI in the United States. [12]
- Pathophysiology
The acute occlusion of one or multiple large epicardial coronary arteries for more than 20 to 40 minutes can lead to acute myocardial infarction. The occlusion is usually thrombotic and due to the rupture of a plaque formed in the coronary arteries. The occlusion leads to a lack of oxygen in the myocardium, which results in sarcolemmal disruption and myofibril relaxation. [2] These changes are one of the first ultrastructural changes in the process of MI, which are followed by mitochondrial alterations. The prolonged ischemia ultimately results in liquefactive necrosis of myocardial tissue. The necrosis spreads from sub-endocardium to sub-epicardium. The subepicardium is believed to have increased collateral circulation, which delays its death. [2] Depending on the territory affected by the infarction, the cardiac function is compromised. Due to the negligible regeneration capacity of the myocardium, the infarcted area heals by scar formation, and often, the heart is remodeled characterized by dilation, segmental hypertrophy of remaining viable tissue, and cardiac dysfunction. [13]
- History and Physical
The imbalance between oxygen supply and the demand leads to myocardial ischemia and can sometimes lead to myocardial infarction. The patient’s history, electrocardiographic findings, and elevated serum biomarkers help identify ischemic symptoms. Myocardial ischemia can present as chest pain, upper extremity pain, mandibular, or epigastric discomfort that occurs during exertion or at rest. Myocardial ischemia can also present as dyspnea or fatigue, which are known to be ischemic equivalents. [14] The chest pain is usually retrosternal and is sometimes described as the sensation of pressure or heaviness. The pain often radiates to the left shoulder, neck, or arms with no obvious precipitating factors, and it may be intermittent or persistent. The pain usually lasts for more than 20 minutes. [15] It is usually not affected by positional changes or active movement of the region. Additional symptoms, such as sweating, nausea, abdominal pain, dyspnea, and syncope, may also be present. [14] [16] [17] The MI can also present atypically with subtle findings such as palpitations, or more dramatic manifestations, such as cardiac arrest. The MI can sometimes present with no symptoms. [18]
The three components in the evaluation of the MI are clinical features, ECG findings, and cardiac biomarkers.
The resting 12 lead ECG is the first-line diagnostic tool for the diagnosis of acute coronary syndrome (ACS). It should be obtained within 10 minutes of the patient’s arrival in the emergency department. [17] Acute MI is often associated with dynamic changes in the ECG waveform. Serial ECG monitoring can provide important clues to the diagnosis if the initial EKG is non-diagnostic at initial presentation. [14] Serial or continuous ECG recordings may help determine reperfusion or re-occlusion status. A large and prompt reduction in ST-segment elevation is usually seen in reperfusion. [14]
ECG findings suggestive of ongoing coronary artery occlusion (in the absence of left ventricular hypertrophy and bundle branch block): [19]
ST-segment elevation in two contiguous lead (measured at J-point) of
- Greater than 5 mm in men younger than 40 years, greater than 2 mm in men older than 40 years, or greater than 1.5 mm in women in leads V2-V3 and/or
- Greater than 1 mm in all other leads
ST-segment depression and T-wave changes
- New horizontal or down-sloping ST-segment depression greater than 5 mm in 2 contiguous leads and/or T inversion greater than 1 mm in two contiguous leads with prominent R waves or R/S ratio of greater than 1
The hyperacute T-wave amplitude, with prominent symmetrical T waves in two contiguous leads, maybe an early sign of acute MI that may precede the ST-segment elevation. Other ECG findings associated with myocardial ischemia include cardiac arrhythmias, intraventricular blocks, atrioventricular conduction delays, and loss of precordial R-wave amplitude (less specific finding). [14]
ECG findings alone are not sufficient to diagnose acute myocardial ischemia or acute MI as other conditions such as acute pericarditis, left ventricular hypertrophy (LVH), left bundle branch block (LBBB), Brugada syndrome, Takatsubo syndrome (TTS), and early repolarization patterns also present with ST deviation.
ECG changes associated with prior MI (in the absence of left ventricular hypertrophy and left bundle branch block):
- Any Q wave in lead V2-V3 greater than 0.02 s or QS complex in leads V2-V3
- Q wave > 03 s and greater than 1 mm deep or QS complex in leads I, II, aVL, aVF or V4-V6 in any two leads of contiguous lead grouping (I, aVL; V1-V6; II, III, aVF)
- R wave > 0.04 s in V1-V2 and R/S greater than 1 with a concordant positive T wave in the absence of conduction defect.
Biomarker Detection of MI
Cardiac troponins (I and T) are components of the contractile apparatus of myocardial cells and expressed almost exclusively in the heart. Elevated serum levels of cardiac troponin are not specific to the underlying mode of injury (ischemic vs. tension) [14] [20] . The rising and/or falling pattern of cardiac troponins (cTn) values with at least one value above the 99 percentile of upper reference limit (URL) associated with symptoms of myocardial ischemia would indicate an acute MI. Serial testing of cTn values at 0 hours, 3 hours, and 6 hours would give a better perspective on the severity and time course of the myocardial injury. Depending on the baseline cTn value, the rising/falling pattern is interpreted. If the cTn baseline value is markedly elevated, a minimum change of greater than 20% in follow up testing is significant for myocardial ischemia. Creatine kinase MB isoform can also be used in the diagnosis of MI, but it is less sensitive and specific than cTn level. [4] [21]
Different imaging techniques are used to assess myocardial perfusion, myocardial viability, myocardial thickness, thickening and motion, and the effect of myocyte loss on the kinetics of para-magnetic or radio-opaque contrast agents indicating myocardial fibrosis or scars. [14] Some imaging modalities that can be used are echocardiography, radionuclide imaging, and cardiac magnetic resonance imaging (cardiac MRI). Regional wall motion abnormalities induced by ischemia can be detected by echocardiography almost immediately after the onset of ischemia when greater than 20% transmural myocardial thickness is affected. Cardiac MRI provides an accurate assessment of myocardial structure and function. [14]
- Treatment / Management
Acute Management
Reperfusion therapy is indicated in all patients with symptoms of ischemia of less than 12-hours duration and persistent ST-segment elevation. Primary percutaneous coronary intervention (PCI) is preferred to fibrinolysis if the procedure can be performed <120 minutes of ECG diagnosis. If there is no immediate option of PCI (>120 minutes), fibrinolysis should be started within 10 minutes of STEMI after ruling out contraindications. If transfer to a PCI center is possible in 60 to 90 minutes after a bolus of the fibrinolytic agent and patient meets reperfusion criteria, a routine PCI can be done, or a rescue PCI can be planned. [19] [17] If fibrinolysis is planned, it should be carried out with fibrin-specific agents such as tenecteplase, alteplase, or reteplase (class I). [19]
Relief of pain, breathlessness, and anxiety: The chest pain due to myocardial infarction is associated with sympathetic arousal, which causes vasoconstriction and increased workload for the ischemic heart. Intravenous opioids (e.g., morphine) are the analgesics most commonly used for pain relief (Class IIa). [19] The results from CRUSADE quality improvement initiative have shown that the use of morphine may be associated with a higher risk of death and adverse clinical outcomes. [22] The study was done from the CIRCUS (Does Cyclosporine Improve outcome in STEMI patients) database, which showed no significant adverse events associated with morphine use in a case of anterior ST-segment elevation MI. [23] A mild anxiolytic (usually a benzodiazepine) may be considered in very anxious patients (class IIa). Supplemental oxygen is indicated in patients with hypoxemia (SaO2 <90% or PaO2 <60mm Hg) (Class I). [19]
Nitrates: Intravenous nitrates are more effective than sublingual nitrates with regard to symptom relief and regression of ST depression (NSTEMI). The dose is titrated upward until symptoms are relieved, blood pressure is normalized in hypertensive patients, or side effects such as a headache and hypotension are noted. [17]
Beta-blockers: This group of drugs reduces myocardial oxygen consumption by lowering heart rate, blood pressure, and myocardial contractility. They block beta receptors in the body, including the heart, and reduce the effects of circulating catecholamines. Beta-blockers should not be used in suspected coronary vasospasm.
Platelet inhibition: Aspirin is recommended in both STEMI and NSTEMI in an oral loading dose of 150 to 300 mg (non-enteric coated formulation) and a maintenance dose of 75 to 100 mg per day long-term regardless of treatment strategy (class I). [17] Aspirin inhibits thromboxane A2 production throughout the lifespan of the platelet. [24]
Most P2Y12 inhibitors are inactive prodrugs (except for ticagrelor, which is an orally active drug that does not require activation) that require oxidation by hepatic cytochrome P450 system to generate an active metabolite which selectively inhibits P2Y12 receptors irreversibly. Inhibition of P2Y12 receptors leads to inhibition of ATP induced platelet aggregation. The commonly used P2Y12 inhibitors are clopidogrel, prasugrel, and ticagrelor.
The loading dose for clopidogrel is 300 to 600 mg loading dose followed by 75 mg per day.
Prasugrel, 60 mg loading dose, and 10 mg per day of a maintenance dose have a faster onset when compared to clopidogrel. [19]
Patients undergoing PCI should be treated with dual antiplatelet therapy (DAPT) with aspirin + P2Y12 inhibitor and a parenteral anticoagulant. In PCI, the use of prasugrel or ticagrelor is found to be superior to clopidogrel. Aspirin and clopidogrel are also found to decrease the number of ischemic events in NSTEMI and UA. [17]
The anticoagulants used during PCI are unfractionated heparin, enoxaparin, and bivalirudin. The bivalirudin is recommended during primary PCI if the patient has heparin-induced thrombocytopenia. [19]
Long-Term Management
Lipid-lowering treatment: It is recommended to start high-intensity statins that reduce low-density lipoproteins (LDLs) and stabilize atherosclerotic plaques. High-density lipoproteins are found to be protective. [19]
Antithrombotic therapy: Aspirin is recommended lifelong, and the addition of another agent depends on the therapeutic procedure done, such as PCI with stent placement.
ACE inhibitors are recommended in patients with systolic left ventricular dysfunction, or heart failure, hypertension, or diabetes.
Beta-blockers are recommended in patients with LVEF less than 40% if no other contraindications are present.
Antihypertensive therapy can maintain a blood pressure goal of less than 140/90 mm Hg.
Mineralocorticoid receptor antagonist therapy is recommended in a patient with left ventricular dysfunction (LVEF less than 40%).
Glucose lowering therapy in people with diabetes to achieve current blood sugar goals. [19]
Lifestyle Modifications
Smoking cessation is the most cost-effective secondary measure to prevent MI. Smoking has a pro-thrombotic effect, which has a strong association with atherosclerosis and myocardial infarction. [6]
Diet, alcohol, and weight control: A diet low in saturated fat with a focus on whole grain products, vegetables, fruits, and the fish is considered cardioprotective. The target level for bodyweight is body mass index of 20 to 25 kg/m2 and waist circumference of <94 cm for the men and <80 cm for the female. [25]
- Differential Diagnosis
- Angina pectoris
- Non-ST segment elevation myocardial infarction (NSTEMI)
- ST-segment elevation myocardial infarction (STEMI)
- Pulmonary embolism
- Pneumothorax
Despite many advances in treatment, acute MI still carries a mortality rate of 5-30%; the majority of deaths occur prior to arrival to the hospital. In addition, within the first year after an MI, there is an additional mortality rate of 5% to 12%. The overall prognosis depends on the extent of heart muscle damage and ejection fraction. Patients with preserved left ventricular function tend to have good outcomes. Factors that worsen prognosis include:
- Advanced age
- Delayed reperfusion
- Low ejection fraction
- Presence of congestive heart failure
- Elevations in C-reactive protein and B-type natriuretic peptide ( BNP ) levels
- Complications
Type and Manifestation
I: Ischemic
- Reinfarction
- Extension of infarction
II: Arrhythmias
- Supraventricular or ventricular arrhythmia
- Sinus bradycardia and atrioventricular block
III: Mechanical
- Myocardial dysfunction
- Cardiac failure
- Cardiogenic shock
- Cardiac rupture (Free wall rupture, ventricular septal rupture, papillary muscle rupture)
IV: Embolic
- Left ventricular mural thrombus,
- Peripheral embolus
V: Inflammatory
- Pericarditis (infarct associated pericarditis, late pericarditis, or post-cardiac injury pericarditis)
- Pericardial effusion
- Enhancing Healthcare Team Outcomes
The diagnosis and management of patients with ischemic heart disease are best done with an interprofessional team. In most hospitals, there are cardiology teams that are dedicated to the management of these patients.
For patients who present with chest pain, the key to the management of MI is time to treatment. Thus, healthcare professionals, including nurses who work in the emergency department, must be familiar with the symptoms of MI and the importance of rapid triage. A cardiology consult should be made immediately to ensure that the patient gets treated within the time frame recommendations. Because MI can be associated with several serious complications, these patients are best managed in an ICU setting.
There is no cure for ischemic heart disease, and all treatments are symptom-oriented. The key to improving outcomes is to prevent coronary artery disease. The primary care provider and nurse practitioner should educate the patient on the benefits of a healthy diet, the importance of controlling blood pressure and diabetes, exercising regularly, discontinuing smoking, maintaining healthy body weight, and remaining compliant with medications. The pharmacist should educate the patient on types of medication used to treat ischemic heart disease, their benefits, and potential adverse effects.
Only through such a team approach can the morbidity and mortality of myocardial infarction be lowered. [Level 5]
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Myocardial Infarction (Heart Attack) Warning Signs in Women. U.S. Department of Health and Human Services Office on Women's Health
ECG With Pardee Waves Indicating AMI. Pardee waves indicate acute myocardial infarction in the inferior leads II, III, and aVF with reciprocal changes in the anterolateral leads. Wikimedia Commons, Glenlarson
Transesophageal echocardiography, Thrombo embolism, Pulmonary artery, Pulmonary Embolism, Thromboembolic , Right Pulmonary artery, TE, RPA, Acute ECG segment elevation mimicking myocardial infarction in a patient with pulmonary embolism Contribute by (more...)
Ischemic ventricular tachycardia in a patient with an old inferior myocardial infarction Contributed by Alina Negru, MD
Disclosure: Niranjan Ojha declares no relevant financial relationships with ineligible companies.
Disclosure: Amit Dhamoon declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Ojha N, Dhamoon AS. Myocardial Infarction. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Myocardial Infarction (Nursing). [StatPearls. 2024] Myocardial Infarction (Nursing). Ojha N, Dhamoon AS, Chapagain R. StatPearls. 2024 Jan
- Review Context-independent identification of myocardial ischemia in the prehospital ECG of chest pain patients. [J Electrocardiol. 2024] Review Context-independent identification of myocardial ischemia in the prehospital ECG of chest pain patients. Swenne CA, Ter Haar CC. J Electrocardiol. 2024 Jan-Feb; 82:34-41. Epub 2023 Nov 7.
- Enhanced External Counterpulsation (EECP): An Evidence-Based Analysis. [Ont Health Technol Assess Ser....] Enhanced External Counterpulsation (EECP): An Evidence-Based Analysis. Medical Advisory Secretariat. Ont Health Technol Assess Ser. 2006; 6(5):1-70. Epub 2006 Mar 1.
- Association of Silent Myocardial Infarction and Sudden Cardiac Death. [JAMA Cardiol. 2019] Association of Silent Myocardial Infarction and Sudden Cardiac Death. Vähätalo JH, Huikuri HV, Holmström LTA, Kenttä TV, Haukilahti MAE, Pakanen L, Kaikkonen KS, Tikkanen J, Perkiömäki JS, Myerburg RJ, et al. JAMA Cardiol. 2019 Aug 1; 4(8):796-802.
- Review Prevention of ventricular fibrillation, acute myocardial infarction (myocardial necrosis), heart failure, and mortality by bretylium: is ischemic heart disease primarily adrenergic cardiovascular disease? [Am J Ther. 2004] Review Prevention of ventricular fibrillation, acute myocardial infarction (myocardial necrosis), heart failure, and mortality by bretylium: is ischemic heart disease primarily adrenergic cardiovascular disease? Bacaner M, Brietenbucher J, LaBree J. Am J Ther. 2004 Sep-Oct; 11(5):366-411.
Recent Activity
- Myocardial Infarction - StatPearls Myocardial Infarction - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

IMAGES
VIDEO
COMMENTS
A 57 year-old male lorry driver, presented to his local emergency department with a 20-minute episode of diaphoresis and chest pain. The chest pain was central, radiating to the left arm and crushing in nature. The pain settled promptly following 300 mg aspirin orally and 800 mcg glyceryl trinitrate (GTN) spray sublingually administered by ...
Patient Presentation. Mr. Smith is a 60-year-old Caucasian male, who presents with 8/10 chest pain after working out. He just quit smoking and started a new workout and diet program after recently retiring. He has noticed some chest and shoulder discomfort with working out that usually resolves with rest, but decided to come to the emergency ...
Most deaths from myocardial infarction occur in the first hours of disease onset, with 40-65% occurring within the first hour and approximately 80% in the first 24 hours 5,6. The recently implemented therapies for MI treatment have been proven to modify patient evolution and prognosis.
A 44-year-old woman presented with cough, dyspnea, and chest pain. On examination, she had tachycardia and hypotension. Evaluation revealed SARS-CoV-2 RNA in a nasopharyngeal swab, as well as eleva...
A Case Report: Acute Myocardial Infarction in a 29-year-old Male. 2/5/2019 Aaron Tiffee, MD, FACEP , Zariad Saran, DO , Tyler Ingersoll, MS. The HEART score is a go-to tool in assessing the risk of an acute coronary syndrome. But in this case, a score of 3 did not mean the 29-year-old patient was safe. Cardiovascular disease (CVD) is currently ...
Understanding the risk factors associated with myocardial infarction is vital for prevention and early detection. This case study will examine both modifiable and non-modifiable risk factors, including age, gender, family history, smoking, high blood pressure, diabetes, and high cholesterol levels. Recognizing these risk factors is instrumental ...
A 67-year-old woman sought emergency medical care due to prolonged chest pain. In April 2009 the patient had prolonged chest pain and at that time she sought medical care. She was admitted at the hospital and diagnosed with myocardial infarction. The patient had hypertension, diabetes mellitus, dyslipidemia and was a smoker.
Presentation of Case. Dr. Jacqueline B. Henson (Medicine): A 54-year-old man was evaluated at this hospital after cardiac arrest associated with ventricular fibrillation. The patient had been in ...
7. Mr. Bob Carlson is a 59 year old male who came to Ventura County Medical Center (VCMC) with nausea, upper back pain he rated 7/10, and diaphoretic. His vital signs were BP 156/92, HR 90, RR 22 SpO2 90%, and temperature 99.5. Physical examination revealed clear lung sounds, mild tachypnea, S1 S2 present, and several ulcerations to the right foot.
Case 28-2013: A 52-Year-Old Man with Cardiac Arrest after an Acute Myocardial Infarction. Dr. Lisa A. Arvold (Emergency Medicine): A 52-year-old man was brought to the emer-gency department at this hospital because of chest pain and ST-segment elevations on electrocardiography (ECG). The patient had been in his usual health, with hypertension ...
ED treatment. Internal STEMI Code paged at 22:55 Patient arrived at 22:57 Interventions Chest X‐Ray Assessment Repeat 12 Lead EKG. 5,000 Units IV Heparin. ED treatment. 22:05 (8 minutes after arrival) Compressions started Defibrillated at 150 J. ED treatment. 18 minutes in ED. Interventions Continued 180 mg ticagrelor Patient undressed ...
risk for complications. However, constant in the management of the patient with myocardial infarction is the commitment of the nursing to an evidence-based holistic approach. This article applies a case study method to explore the present evidence-based nursing practice (EBNP) that informs the assessment, clinical decision-
Acute Myocardial Infarction Case Study. Myocardial infarction (heart attack) is the leading cause of death in the United States. It is estimated that one in every five deaths in the US is due to a heart attack. Approximately one million patients are admitted to hospitals each year due to heart attacks. 200,000 to 300,000 individuals die from ...
The diagnosis is myocardial infarction with ST segment elevation due to occlusion of a coronary artery. Discussion Ischemic heart disease, or heart disease caused by insufficient blood supply to the heart muscle, is one of the most frequent conditions encountered in patients older than 40 years of age.
Gustafsson, Lampa et al. used proteomics, metabolomics and clinical factors in a case-cohort study to identify biomarkers of imminent myocardial infarction and devise a prediction model for ...
The study included 138 individuals diagnosed with myocardial infarction, admitted to the emergency and cardiothoracic departments of the author's hospital between February 2021 and November 2022 ...
Introduction. Myocardial infarction in the absence of obstructive (>50% stenosis) coronary artery disease (MINOCA) is found in approximately 6% of all patients with acute myocardial infarction (MI) who are referred for coronary angiography. 1, 2 The term MINOCA should be reserved for patients in whom there is an ischaemic basis for their clinical presentation and should be considered a ...
Introduction. Myocardial Infarction is a disease of the heart that is caused by occlusions in the coronary arteries. The circulation of blood through the ventricles is reduced and the capacity of the heart to absorb oxygen is diminished. Artherosclerosis is mainly implicated with myocardial infarction. MI is primarily evaluated using the ECG ...
Myocardial infarction with non-obstructive CAD (MINOCA) is clinically defined as acute myocardial infarction in the absence of (≥50% stenosis) obstructive CAD in any artery . The Women's Ischemic Syndrome Evaluation (WISE) study at 10-year follow-up demonstrated that women with no obstructive CAD were at increased risk of death or nonfatal ...
Practice an example case study like you will see on the the Next Generation NCLEX (NGN) exam. Expert nurse educator Cat, RN, MSN explains each question and a...
Myocardial infarction (MI), is used synonymously with coronary occlusion and heart attack, yet MI is the most preferred term as myocardial ischemia causes acute coronary syndrome (ACS) that can result in myocardial death. ... In each case of MI, a profound imbalance exists between myocardial oxygen supply and demand. Unstable angina ...
The case presented here is a good example of the relevance of late PCI. 1 BACKGROUND. Patients presenting with myocardial infarction and high-grade AV blocks have worse outcomes, while early coronary interventions have shown improved results. ... Studies focusing on outcomes in these situations are limited with complete heart block being a bad ...
The patient was in the initial phase of cardiogenic shock. In order to exclude myocardial infarction of the right ventricle the electrodes were clasped on the right side of the chest. The record did Figure 1. Record ECG. Changes in leads: II and III. Myocardial infarction of interior wall: a case study273.
Myocardial infarction (MI), colloquially known as "heart attack," is caused by decreased or complete cessation of blood flow to a portion of the myocardium. Myocardial infarction may be "silent" and go undetected, or it could be a catastrophic event leading to hemodynamic deterioration and sudden death.[1] Most myocardial infarctions are due to underlying coronary artery disease, the ...
Objectives: Recent reports have highlighted myocardial infarction (MI) patients without standard modifiable risk factors (SMRF), noting them to be surprisingly common and to have a substantial risk of adverse outcomes. The objective of this study was to address the challenge of identifying at-risk patients without SMRF and providing preventive therapy. Methods: Patients presenting between 2001 ...
This case study aims to explain and illustrate how to care for patients with acute myocardial. infarction based on the rationale and nursing practice evidence underlying the holistic approach ...
Objective We sought to validate the clinical performance of a rapid assessment pathway incorporating the Siemens Atellica IM high sensitivity cardiac troponin I (hs-cTnI) assay in patients presenting to the emergency department (ED) with suspected acute myocardial infarction (AMI). Methods This was a multicentre prospective observational study of adult ED patients presenting to five Australian ...
tudy (GWAS), employing the inverse variance-weighted (IVW) method as the primary approach. Comprehensive sensitivity analyses were conducted to validate the robustness of the results. Evaluation of instrumental variables was performed using the F-statistic, and a meta-analysis was employed to assess the average gene-predicted effect between ferritin and MI. The MR study revealed a negative ...