PARANOID INDIVIDUALS WITH SCHIZOPHRENIA SHOW GREATER SOCIAL COGNITIVE BIAS AND WORSE SOCIAL FUNCTIONING THAN NON-PARANOID INDIVIDUALS WITH SCHIZOPHRENIA
Affiliations.
- 1 School of Behavioral and Brain Sciences, The University of Texas at Dallas, Richardson, TX, 75080; Department of Psychiatry, University of Texas Southwestern Medical School, Dallas, TX, 75390.
- 2 Department of Psychiatry and Behavioral Sciences, University of Miami Miller School of Medicine, Miami, FL, 33136; Research Service, Bruce W Carter VA Medical Center, Miami, FL, 33125.
- 3 Department of Psychology, University of North Carolina, Chapel Hill, NC, 27599; Australian Catholic University, Melbourne, VIC 3065.
- PMID: 27990352
- PMCID: PMC5156478
- DOI: 10.1016/j.scog.2015.11.002
Paranoia is a common symptom of schizophrenia that may be related to how individuals process and respond to social stimuli. Previous investigations support a link between increased paranoia and greater social cognitive impairments, but these studies have been limited to single domains of social cognition, and no studies have examined how paranoia may influence functional outcome. Data from 147 individuals with schizophrenia were used to examine whether actively paranoid and non-paranoid individuals with schizophrenia differ in social cognition and functional outcomes. On measures assessing social cognitive bias, paranoid individuals endorsed more hostile and blaming attributions and identified more faces as untrustworthy; however, paranoid and non-paranoid individuals did not differ on emotion recognition and theory of mind tasks assessing social cognitive ability. Likewise, paranoid individuals showed greater impairments in real-world interpersonal relationships and social acceptability as compared to non-paranoid patients, but these differences did not extend to performance based tasks assessing functional capacity and social competence. These findings isolate specific social cognitive disparities between paranoid and non-paranoid subgroups and suggest that paranoia may exacerbate the social dysfunction that is commonly experienced by individuals with schizophrenia.
Keywords: Attributions; Functional Outcome; Social Cognition.

Grants and funding
- R01 MH093432/MH/NIMH NIH HHS/United States
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 24 February 2022
Systematic literature review of schizophrenia clinical practice guidelines on acute and maintenance management with antipsychotics
- Christoph U. Correll ORCID: orcid.org/0000-0002-7254-5646 1 , 2 , 3 ,
- Amber Martin 4 ,
- Charmi Patel 5 ,
- Carmela Benson 5 ,
- Rebecca Goulding 6 ,
- Jennifer Kern-Sliwa 5 ,
- Kruti Joshi 5 ,
- Emma Schiller 4 &
- Edward Kim ORCID: orcid.org/0000-0001-8247-6675 7
Schizophrenia volume 8 , Article number: 5 ( 2022 ) Cite this article
14k Accesses
48 Citations
14 Altmetric
Metrics details
- Schizophrenia
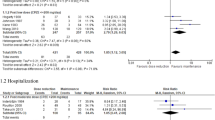
Clinical practice guidelines (CPGs) translate evidence into recommendations to improve patient care and outcomes. To provide an overview of schizophrenia CPGs, we conducted a systematic literature review of English-language CPGs and synthesized current recommendations for the acute and maintenance management with antipsychotics. Searches for schizophrenia CPGs were conducted in MEDLINE/Embase from 1/1/2004–12/19/2019 and in guideline websites until 06/01/2020. Of 19 CPGs, 17 (89.5%) commented on first-episode schizophrenia (FES), with all recommending antipsychotic monotherapy, but without agreement on preferred antipsychotic. Of 18 CPGs commenting on maintenance therapy, 10 (55.6%) made no recommendations on the appropriate maximum duration of maintenance therapy, noting instead individualization of care. Eighteen (94.7%) CPGs commented on long-acting injectable antipsychotics (LAIs), mainly in cases of nonadherence (77.8%), maintenance care (72.2%), or patient preference (66.7%), with 5 (27.8%) CPGs recommending LAIs for FES. For treatment-resistant schizophrenia, 15/15 CPGs recommended clozapine. Only 7/19 (38.8%) CPGs included a treatment algorithm.
Similar content being viewed by others

A meta-analysis of effectiveness of real-world studies of antipsychotics in schizophrenia: Are the results consistent with the findings of randomized controlled trials?
Factors associated with successful antipsychotic dose reduction in schizophrenia: a systematic review of prospective clinical trials and meta-analysis of randomized controlled trials
The efficacy and heterogeneity of antipsychotic response in schizophrenia: A meta-analysis
Introduction.
Schizophrenia is an often debilitating, chronic, and relapsing mental disorder with complex symptomology that manifests as a combination of positive, negative, and/or cognitive features 1 , 2 , 3 . Standard management of schizophrenia includes the use of antipsychotic medications to help control acute psychotic episodes 4 and prevent relapses 5 , 6 , whereas maintenance therapy is used in the long term after patients have been stabilized 7 , 8 , 9 . Two main classes of drugs—first- and second-generation antipsychotics (FGA and SGA)—are used to treat schizophrenia 10 . SGAs are favored due to the lower rates of adverse effects, such as extrapyramidal effects, tardive dyskinesia, and relapse 11 . However, pharmacologic treatment for schizophrenia is complicated because nonadherence is prevalent, and is a major risk factor for relapse 9 and poor overall outcomes 12 . The use of long-acting injectable (LAI) versions of antipsychotics aims to limit nonadherence-related relapses and poor outcomes 13 .
Patient treatment pathways and treatment choices are determined based on illness acuity/severity, past treatment response and tolerability, as well as balancing medication efficacy and adverse effect profiles in the context of patient preferences and adherence patterns 14 , 15 . Clinical practice guidelines (CPG) serve to inform clinicians with recommendations that reflect current evidence from meta-analyses of randomized controlled trials (RCTs), individual RCTs and, less so, epidemiologic studies, as well as clinical experience, with the goal of providing a framework and road-map for treatment decisions that will improve quality of care and achieve better patients outcomes. The use of clinical algorithms or other decision trees in CPGs may improve the ease of implementation of the evidence in clinical practice 16 . While CPGs are an important tool for mental health professionals, they have not been updated on a regular basis like they have been in other areas of medicine, such as in oncology. In the absence of current information, other governing bodies, healthcare systems, and hospitals have developed their own CPGs regarding the treatment of schizophrenia, and many of these have been recently updated 17 , 18 , 19 . As such, it is important to assess the latest guidelines to be aware of the changes resulting from consideration of updated evidence that informed the treatment recommendations. Since CPGs are comprehensive and include the diagnosis as well as the pharmacological and non-pharmacological management of individuals with schizophrenia, a detailed comparative review of all aspects of CPGs for schizophrenia would have been too broad a review topic. Further, despite ongoing efforts to broaden the pharmacologic tools for the treatment of schizophrenia 20 , antipsychotics remain the cornerstone of schizophrenia management 8 , 21 . Therefore, a focused review of guideline recommendations for the management of schizophrenia with antipsychotics would serve to provide clinicians with relevant information for treatment decisions.
To provide an updated overview of United States (US) national and English language international guidelines for the management of schizophrenia, we conducted a systematic literature review (SLR) to identify CPGs and synthesize current recommendations for pharmacological management with antipsychotics in the acute and maintenance phases of schizophrenia.
Systematic searches for the SLR yielded 1253 hits from the electronic literature databases. After removal of duplicate references, 1127 individual articles were screened at the title and abstract level. Of these, 58 publications were deemed eligible for screening at the full-text level, from which 19 were ultimately included in the SLR. Website searches of relevant organizations yielded 10 additional records, and an additional three records were identified by the state-by-state searches. Altogether, this process resulted in 32 records identified for inclusion in the SLR. Of the 32 sources, 19 primary CPGs, published/issued between 2004 and 2020, were selected for extraction, as illustrated in the PRISMA diagram (Fig. 1 ). While the most recent APA guideline was identified and available for download in 2020, the reference to cite in the document indicates a publication date of 2021.
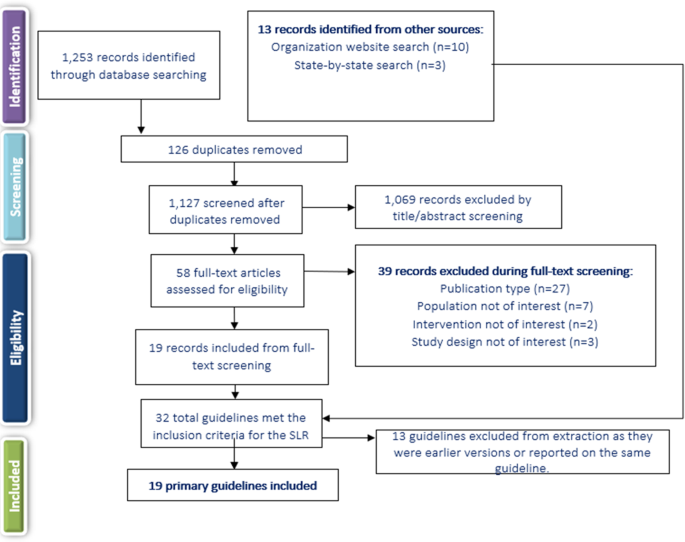
SLR systematic literature review.
Of the 19 included CPGs (Table 1 ), three had an international focus (from the following organizations: International College of Neuropsychopharmacology [CINP] 22 , United Nations High Commissioner for Refugees [UNHCR] 23 , and World Federation of Societies of Biological Psychiatry [WFSBP] 24 , 25 , 26 ); seven originated from the US; 17 , 18 , 19 , 27 , 28 , 29 , 30 , 31 , 32 three were from the United Kingdom (British Association for Psychopharmacology [BAP] 33 , the National Institute for Health and Care Excellence [NICE] 34 , and the Scottish Intercollegiate Guidelines Network [SIGN] 35 ); and one guideline each was from Singapore 36 , the Polish Psychiatric Association (PPA) 37 , 38 , the Canadian Psychiatric Association (CPA) 14 , the Royal Australia/New Zealand College of Psychiatrists (RANZCP) 39 , the Association Française de Psychiatrie Biologique et de Neuropsychopharmacologie (AFPBN) from France 40 , and Italy 41 . Fourteen CPGs (74%) recommended treatment with specific antipsychotics and 18 (95%) included recommendations for the use of LAIs, while just seven included a treatment algorithm Table 2 ). The AGREE II assessment resulted in the highest score across the CPGs domains for NICE 34 followed by the American Psychiatric Association (APA) guidelines 17 . The CPA 14 , BAP 33 , and SIGN 35 CPGs also scored well across domains.
Acute therapy
Seventeen CPGs (89.5%) provided treatment recommendations for patients experiencing a first schizophrenia episode 14 , 17 , 18 , 19 , 22 , 23 , 24 , 28 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 39 , 40 , 41 , but the depth and focus of the information varied greatly (Supplementary Table 1 ). In some CPGs, information on treatment of a first schizophrenia episode was limited or grouped with information on treating any acute episode, such as in the CPGs from CINP 22 , AFPBN 40 , New Jersey Division of Mental Health Services (NJDMHS) 32 , the APA 17 , and the PPA 37 , 38 , while the others provided more detailed information specific to patients experiencing a first schizophrenia episode 14 , 18 , 19 , 23 , 24 , 28 , 33 , 34 , 35 , 36 , 39 , 41 . The American Association of Community Psychiatrists (AACP) Clinical Tips did not provide any information on the treatment of schizophrenia patients with a first episode 29 .
There was little agreement among CPGs regarding the preferred antipsychotic for a first schizophrenia episode. However, there was strong consensus on antipsychotic monotherapy and that lower doses are generally recommended due to better treatment response and greater adverse effect sensitivity. Some guidelines recommended SGAs over FGAs when treating a first-episode schizophrenia patient (RANZCP 39 , Texas Medication Algorithm Project [TMAP] 28 , Oregon Health Authority 19 ), one recommended starting patients on an FGA (UNHCR 23 ), and others stated specifically that there was no evidence of any difference in efficacy between FGAs and SGAs (WFSBP 24 , CPA 14 , SIGN 35 , APA 17 , Singapore guidelines 36 ), or did not make any recommendation (CINP 22 , Italian guidelines 41 , NICE 34 , NJDMHS 32 , Schizophrenia Patient Outcomes Research Team [PORT] 30 , 31 ). The BAP 33 and WFBSP 24 noted that while there was probably no difference between FGAs and SGAs in efficacy, some SGAs (olanzapine, amisulpride, and risperidone) may perform better than some FGAs. The Schizophrenia PORT recommendations noted that while there seemed to be no differences between SGAs and FGAs in short-term studies (≤12 weeks), longer studies (one to two years) suggested that SGAs may provide benefits in terms of longer times to relapse and discontinuation rates 30 , 31 . The AFPBN guidelines 40 and Florida Medicaid Program guidelines 18 , which both focus on use of LAI antipsychotics, both recommended an SGA-LAI for patients experiencing a first schizophrenia episode. A caveat in most CPGs was that physicians and their patients should discuss decisions about the choice of antipsychotic and that the choice should consider individual patient factors/preferences, risk of adverse and metabolic effects, and symptom patterns 17 , 18 , 19 , 22 , 24 , 28 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 39 , 41 .
Most CPGs recommended switching to a different monotherapy if the initial antipsychotic was not effective or not well tolerated after an adequate antipsychotic trial at an appropriate dose 14 , 17 , 18 , 19 , 22 , 23 , 24 , 28 , 32 , 33 , 35 , 36 , 39 . For patients initially treated with an FGA, the UNHCR recommended switching to an SGA (olanzapine or risperidone) 23 . Guidance on response to treatment varied in the measures used but typically required at least a 20% improvement in symptoms (i.e. reduction in Positive and Negative Syndrome Scale or Brief Psychiatric Rating Scale scores) from pre-treatment levels.
Several CPGs contained recommendations on the duration of antipsychotic therapy after a first schizophrenia episode. The NJDMHS guidelines 32 recommended nine to 12 months; CINP 22 recommended at least one year; CPA 14 recommended at least 18 months; WFSBP 25 , the Italian guidelines 41 , and NICE 34 recommended 1 to 2 years; and the RANZCP 39 , BAP 33 , and SIGN 35 recommended at least 2 years. The APA 17 and TMAP 28 recommended continuing antipsychotic treatment after resolution of first-episode symptoms but did not recommend a specific length of therapy.
Twelve guidelines 14 , 18 , 22 , 24 , 28 , 30 , 31 , 33 , 34 , 35 , 36 , 39 , 40 (63.2%) discussed the treatment of subsequent/multiple episodes of schizophrenia (i.e., following relapse). These CPGs noted that the considerations guiding the choice of antipsychotic for subsequent/multiple episodes were similar to those for a first episode, factoring in prior patient treatment response, adverse effect patterns and adherence. The CPGs also noted that response to treatment may be lower and require higher doses to achieve a response than for first-episode schizophrenia, that a different antipsychotic than used to treat the first episode may be needed, and that a switch to an LAI is an option.
Several CPGs provided recommendations for patients with specific clinical features (Supplementary Table 1 ). The most frequently discussed group of clinical features was negative symptoms, with recommendations provided in the CINP 22 , UNHCR 23 , WFSBP 24 , AFPBN 40 , SIGN 35 , BAP 33 , APA 17 , and NJDMHS guidelines; 32 negative symptoms were the sole focus of the guidelines from the PPA 37 , 38 . The guidelines noted that due to limited evidence in patients with predominantly negative symptoms, there was no clear benefit for any strategy, but that options included SGAs (especially amisulpride) rather than FGAs (WFSBP 24 , CINP 22 , AFPBN 40 , SIGN 35 , NJDMHS 32 , PPA 37 , 38 ), and addition of an antidepressant (WFSBP 24 , UNHCR 23 , SIGN 35 , NJDMHS 32 ) or lamotrigine (SIGN 35 ), or switching to another SGA (NJDMHS 32 ) or clozapine (NJDMHS 32 ). The PPA guidelines 37 , 38 stated that the use of clozapine or adding an antidepressant or other medication class was not supported by evidence, but recommended the SGA cariprazine for patients with predominant and persistent negative symptoms, and other SGAs for those with full-spectrum negative symptoms. However, the BAP 33 stated that no recommendations can be made for any of these strategies because of the quality and paucity of the available evidence.
Some of the CPGs also discussed treatment of other clinical features to a limited degree, including depressive symptoms (CINP 22 , UNHCR 23 , CPA 14 , APA 17 , and NJDMHS 32 ), cognitive dysfunction (CINP 22 , UNHCR 23 , WFSBP 24 , AFPBN 40 , SIGN 35 , BAP 33 , and NJDMHS 32 ), persistent aggression (CINP 22 , WFSBP 24 , CPA 14 , AFPBN 40 , NICE 34 , SIGN 35 , BAP 33 , and NJDMHS 32 ), and comorbid psychiatric diagnoses (CINP 22 , RANZCP 39 , BAP 33 , APA 17 , and NJDMHS 32 ).
Fifteen CPGs (78.9%) discussed treatment-resistant schizophrenia (TRS); all defined it as persistent, predominantly positive symptoms after two adequate antipsychotic trials; clozapine was the unanimous first choice 14 , 17 , 18 , 19 , 22 , 23 , 24 , 28 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 39 . However, the UNHCR guidelines 23 , which included recommendations for treatment of refugees, noted that clozapine is only a reasonable choice in regions where white blood cell monitoring and specialist supervision are available, otherwise, risperidone or olanzapine are alternatives if they had not been used in the previous treatment regimen.
There were few options for patients who are resistant to clozapine therapy, and evidence supporting these options was limited. The CPA guidelines 14 therefore stated that no recommendation can be given due to inadequate evidence. Other CPGs discussed options (but noted there was limited supporting evidence), such as switching to olanzapine or risperidone (WFSBP 24 , TMAP 28 ), adding a second antipsychotic to clozapine (CINP 22 , NICE 34 , TMAP 28 , BAP 33 , Florida Medicaid Program 18 , Oregon Health Authority 19 , RANZCP 39 ), adding lamotrigine or topiramate to clozapine (CINP 22 , Florida Medicaid Program 18 ), combination therapy with two non-clozapine antipsychotics (Florida Medicaid Program 18 , NJDMHS 32 ), and high-dose non-clozapine antipsychotic therapy (BAP 33 , SIGN 35 ). Electroconvulsive therapy was noted as a last resort for patients who did not respond to any pharmacologic therapy, including clozapine, by 10 CPGs 17 , 18 , 19 , 22 , 24 , 28 , 32 , 35 , 36 , 39 .
Maintenance therapy
Fifteen CPGs (78.9%) discussed maintenance therapy to various degrees via dedicated sections or statements, while three others referred only to maintenance doses by antipsychotic agent 18 , 23 , 29 without accompanying recommendations (Supplementary Table 2 ). Only the Italian guideline provided no reference or comments on maintenance treatment. The CINP 22 , WFSBP 25 , RANZCP 39 , and Schizophrenia PORT 30 , 31 recommended keeping patients on the same antipsychotic and at the same dose on which they had achieved remission. Several CPGs recommended maintenance therapy at the lowest effective dose (NJDMHS 32 , APA 17 , Singapore guidelines 36 , and TMAP 28 ). The CPA 14 and SIGN 35 defined the lower dose as 300–400 mg chlorpromazine equivalents or 4–6 mg risperidone equivalents, and the Singapore guidelines 36 stated that the lower dose should not be less than half the original dose. TMAP 28 stated that given the relapsing nature of schizophrenia, the maintenance dose should often be close to the original dose. While SIGN 35 recommended that patients remain on the same antipsychotic that provided remission, these guidelines also stated that maintenance with amisulpride, olanzapine, or risperidone was preferred, and that chlorpromazine and other low-potency FGAs were also suitable. The BAP 33 recommended that the current regimen be optimized before any dose reduction or switch to another antipsychotic occurs. Several CPGs recommended LAIs as an option for maintenance therapy (see next section).
Altogether, 10/18 (55.5%) CPGs made no recommendations on the appropriate duration of maintenance therapy, noting instead that each patient should be considered individually. Other CPGs made specific recommendations: Both the Both BAP 33 and SIGN 35 guidelines suggested a minimum of 2 years, the NJDMHS guidelines 32 recommended 2–3 years; the WFSBP 25 recommended 2–5 years for patients who have had one relapse and more than 5 years for those who have had multiple relapses; the RANZCP 39 and the CPA 14 recommended 2–5 years; and the CINP 22 recommended that maintenance therapy last at least 6 years for patients who have had multiple episodes. The TMAP was the only CPG to recommend that maintenance therapy be continued indefinitely 28 .
Recommendations on the use of LAIs
All CPGs except the one from Italy (94.7%) discussed the use of LAIs for patients with schizophrenia to some extent. As shown in Table 3 , among the 18 CPGs, LAIs were primarily recommended in 14 CPGs (77.8%) for patients who are non-adherent to other antipsychotic administration routes (CINP 22 , UNHCR 23 , RANZCP 39 , PPA 37 , 38 , Singapore guidelines 36 , NICE 34 , SIGN 35 , BAP 33 , APA 17 , TMAP 28 , NJDMHS 32 , AACP 29 , Oregon Health Authority 19 , Florida Medicaid Program 18 ). Twelve CPGs (66.7%) also noted that LAIs should be prescribed based on patient preference (RANZCP 39 , CPA 14 , AFPBN 40 , Singapore guidelines 36 , NICE 34 , SIGN 35 , BAP 33 , APA 17 , Schizophrenia PORT 30 , 31 , AACP 29 , Oregon Health Authority 19 , Florida Medicaid Program 18 ).
Thirteen CPGs (72.2%) recommended LAIs as maintenance therapy 18 , 19 , 24 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 39 , 40 . While five CPGs (27.8%), i.e., AFPBN 40 , RANZCP 39 , TMAP 28 , NJDMHS 32 , and the Florida Medicaid Program 18 recommended LAIs specifically for patients experiencing a first episode. While the CPA 14 did not make any recommendations regarding when LAIs should be used, they discussed recent evidence supporting their use earlier in treatment. Five guidelines (27.8%, i.e., Singapore 36 , NICE 34 , SIGN 35 , BAP 33 , and Schizophrenia PORT 30 , 31 ) noted that evidence around LAIs was not sufficient to support recommending their use for first-episode patients. The AFPBN guidelines 40 also stated that LAIs (SGAs as first-line and FGAs as second-line treatment) should be more frequently considered for maintenance treatment of schizophrenia. Four CPGs (22.2%, i.e., CINP 22 , UNHCR 23 , Italian guidelines 41 , PPA guidelines 37 , 38 ) did not specify when LAIs should be used. The AACP guidelines 29 , which evaluated only LAIs, recommended expanding their use beyond treatment for nonadherence, suggesting that LAIs may offer a more convenient mode of administration or potentially address other clinical and social challenges, as well as provide more consistent plasma levels.
Treatment algorithms
Only Seven CPGs (36.8%) included an algorithm as part of the treatment recommendations. These included decision trees or flow diagrams that map out initial therapy, durations for assessing response, and treatment options in cases of non-response. However, none of these guidelines defined how to measure response, a theme that also extended to guidelines that did not include treatment algorithms. Four of the seven guidelines with algorithms recommended specific antipsychotic agents, while the remaining three referred only to the antipsychotic class.
LAIs were not consistently incorporated in treatment algorithms and in six CPGs were treated as a separate category of medicine reserved for patients with adherence issues or a preference for the route of administration. The only exception was the Florida Medicaid Program 18 , which recommended offering LAIs after oral antipsychotic stabilization even to patients who are at that point adherent to oral antipsychotics.
Benefits and harms
The need to balance the efficacy and safety of antipsychotics was mentioned by all CPGs as a basic treatment paradigm.
Ten CPGs provided conclusions on benefits of antipsychotic therapy. The APA 17 and the BAP 33 guidelines stated that antipsychotic treatment can improve the positive and negative symptoms of psychosis and leads to remission of symptoms. These CPGs 17 , 33 as well as those from NICE 34 and CPA 14 stated that these treatment effects can also lead to improvements in quality of life (including quality-adjusted life years), improved functioning, and reduction in disability. The CPA 14 and APA 17 guidelines noted decreases in hospitalizations with antipsychotic therapy, and the APA guidelines 17 stated that long-term antipsychotic treatment can also reduce mortality. The UNHCR 23 and the Italian 41 guidelines noted that early intervention increased positive outcomes. The WFSBP 24 , AFPBN 40 , CPA 14 , BAP 33 , APA 17 , and NJDMHS 32 affirmed that relapse prevention is a benefit of continued/maintenance treatment.
Some CPGs (WFSBP 24 , Italian 41 , CPA 14 , and SIGN 35 ) noted that reduced risk for extrapyramidal adverse effects and treatment discontinuation were potential benefits of SGAs vs. FGAs.
The risk of adverse effects (e.g., extrapyramidal, metabolic, cardiovascular, and hormonal adverse effects, sedation, and neuroleptic malignant syndrome) was noted by all CPGs as the major potential harm of antipsychotic therapy 14 , 17 , 18 , 19 , 22 , 23 , 24 , 28 , 29 , 30 , 31 , 32 , 34 , 35 , 36 , 37 , 39 , 40 , 41 , 42 . These adverse effects are known to limit long-term treatment and adherence 24 .
This SLR of CPGs for the treatment of schizophrenia yielded 19 most updated versions of individual CPGs, published/issued between 2004 and 2020. Structuring our comparative review according to illness phase, antipsychotic type and formulation, response to antipsychotic treatment as well as benefits and harms, several areas of consistent recommendations emerged from this review (e.g., balancing risk and benefits of antipsychotics, preferring antipsychotic monotherapy; using clozapine for treatment-resistant schizophrenia). On the other hand, other recommendations regarding other areas of antipsychotic treatment were mostly consistent (e.g., maintenance antipsychotic treatment for some time), somewhat inconsistent (e.g., differences in the management of first- vs multi-episode patients, type of antipsychotic, dose of antipsychotic maintenance treatment), or even contradictory (e.g., role of LAIs in first-episode schizophrenia patients).
Consistent with RCT evidence 43 , 44 , antipsychotic monotherapy was the treatment of choice for patients with first-episode schizophrenia in all CPGs, and all guidelines stated that a different single antipsychotic should be tried if the first is ineffective or intolerable. Recommendations were similar for multi-episode patients, but factored in prior patient treatment response, adverse effect patterns, and adherence. There was also broad consensus that the side-effect profile of antipsychotics is the most important consideration when making a decision on pharmacologic treatment, also reflecting meta-analytic evidence 4 , 5 , 10 . The risk of extrapyramidal symptoms (especially with FGAs) and metabolic effects (especially with SGAs) were noted as key considerations, which are also reflected in the literature as relevant concerns 4 , 45 , 46 , including for quality of life and treatment nonadherence 47 , 48 , 49 , 50 .
Largely consistent with the comparative meta-analytic evidence regarding the acute 4 , 51 , 52 and maintenance antipsychotic treatment 5 effects of schizophrenia, the majority of CPGs stated there was no difference in efficacy between SGAs and FGAs (WFSBP 24 , CPA 14 , SIGN 35 , APA 17 , and Singapore guidelines 36 ), or did not make any recommendations (CINP 22 , Italian guidelines 41 , NICE 34 , NJDMHS 32 , and Schizophrenia PORT 30 , 31 ); three CPGs (BAP 33 , WFBSP 24 , and Schizophrenia PORT 30 , 31 ) noted that SGAs may perform better than FGAs over the long term, consistent with a meta-analysis on this topic 53 .
The 12 CPGs that discussed treatment of subsequent/multiple episodes generally agreed on the factors guiding the choices of an antipsychotic, including that the decision may be more complicated and response may be lower than with a first episode, as described before 7 , 54 , 55 , 56 .
There was little consensus regarding maintenance therapy. Some CPGs recommended the same antipsychotic and dose that achieved remission (CINP 22 , WFSBP 25 , RANZCP 39 , and Schizophrenia PORT 30 , 31 ) and others recommended the lowest effective dose (NJDMHS 32 , APA 17 , Singapore guidelines 36 , TMAP 28 , CPA 14 , and SIGN 35 ). This inconsistency is likely based on insufficient data as well as conflicting results in existing meta-analyses on this topic 57 , 58 , 59 .
The 15 CPGs that discussed TRS all used the same definition for this condition, consistent with recent commendations 60 , and agreed that clozapine is the primary evidence-based treatment choice 14 , 17 , 18 , 19 , 22 , 23 , 24 , 28 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 39 , reflecting the evidence base 61 , 62 , 63 . These CPGs also agreed that there are few options well supported by evidence for patients who do not respond to clozapine, with a recent meta-analysis of RCTs showing that electroconvulsive therapy augmentation may be the most evidence-based treatment option 64 .
One key gap in the treatment recommendations was how long patients should remain on antipsychotic therapy after a first episode or during maintenance therapy. While nine of the 17 CPGs discussing treatment of a first episode provided a recommended timeframe (varying from 1 to 2 years) 14 , 22 , 24 , 32 , 33 , 34 , 35 , 39 , 41 , the APA 17 and TMAP 28 recommended continuing antipsychotic treatment after resolution of first-episode symptoms but did not recommend a specific length of therapy. Similarly, six of the 18 CPGs discussing maintenance treatment recommended a specific duration of therapy (ranging from two to six years) 14 , 22 , 25 , 32 , 39 , while as many as 10 CPGs did not point to a firm end of the maintenance treatment, instead recommending individualized decisions. The CPGs not stating a definite endpoint or period of maintenance treatment after repeated schizophrenia episodes or even after a first episode of schizophrenia, reflects the different evidence types on which the recommendation is based. The RCT evidence ends after several years of maintenance treatment vs. discontinuation supporting ongoing antipsychotic treatment; however, naturalistic database studies do not indicate any time period after which one can safely discontinue maintenance antipsychotic care, even after a first schizophrenia episode 8 , 65 . In fact, stopping antipsychotics is associated not only with a substantially increased risk of hospitalization but also mortality 65 , 66 , 67 . In this sense, not stating an endpoint for antipsychotic maintenance therapy should not be taken as an implicit statement that antipsychotics should be discontinued at any time; data suggest the contrary.
A further gap exists regarding the most appropriate treatment of negative symptoms, such as anhedonia, amotivation, asociality, affective flattening, and alogia 1 , a long-standing challenge in the management of patients with schizophrenia. Negative symptoms often persist in patients after positive symptoms have resolved, or are the presenting feature in a substantial minority of patients 22 , 35 . Negative symptoms can also be secondary to pharmacotherapy 22 , 68 . Antipsychotics have been most successful in treating positive symptoms, and while eight of the CPGs provided some information on treatment of negative symptoms, the recommendations were generally limited 17 , 22 , 23 , 24 , 32 , 33 , 35 , 40 . Negative symptom management was a focus of the PPA guidelines, but the guidelines acknowledged that supporting evidence was limited, often due to the low number of patients with predominantly negative symptoms in clinical trials 37 , 38 . The Polish guidelines are also one of the more recently developed and included the newer antipsychotic cariprazine as a first-line option, which although being a point of differentiation from the other guidelines, this recommendation was based on RCT data 69 .
Another area in which more direction is needed is on the use of LAIs. While all but one of the 19 CPGs discussed this topic, the extent of information and recommendations for LAI use varied considerably. All CPGs categorized LAIs as an option to improve adherence to therapy or based on patient preference. However, 5/18 CPGs (27.8%) recommended the use of LAI early in treatment (at first episode: AFPBN 40 , RANZCP 39 , TMAP 28 , NJDMHS 32 , and Florida Medicaid Program 18 ) or across the entire illness course, while five others stated there was not sufficient evidence to recommend LAIs for these patients (Singapore 36 , NICE 34 , SIGN 35 , BAP 33 , and Schizophrenia PORT 30 , 31 ). The role of LAIs in first-episode schizophrenia was the only point where opposing recommendations were found across CPGs. This contradictory stance was not due to the incorporation of newer data suggesting benefits of LAIs in first episode and early-phase patients with schizophrenia 70 , 71 , 72 , 73 , 74 in the CPGs recommending LAI use in first-episode patients, as CPGs recommending LAI use were published between 2005 and 2020, while those opposing LAI use were published between 2011 and 2020. Only the Florida Medicaid CPG recommended LAIs as a first step equivalent to oral antipsychotics (OAP) after initial OAP response and tolerability, independent of nonadherence or other clinical variables. This guideline was also the only CPG to fully integrate LAI use in their clinical algorithm. The remaining six CPGs that included decision tress or treatment algorithms regarded LAIs as a separate paradigm of treatment reserved for nonadherence or patients preference rather than a routine treatment option to consider. While some CPGs provided fairly detailed information on the use of LAIs (AFPBN 40 , AACP 29 , Oregon Health Authority 19 , and Florida Medicaid Program 18 ), others mentioned them only in the context of adherence issues or patient preference. Notably, definitions of and means to determine nonadherence were not reported. One reason for this wide range of recommendations regarding the placement of LAIs in the treatment algorithm and clinical situations that prompt LAI use might be due to the fact that CPGs generally favor RCT evidence over evidence from other study designs. In the case of LAIs, there was a notable dissociation between consistent meta-analytic evidence of statistically significant superiority of LAIs vs OAPs in mirror-image 75 and cohort study designs 76 and non-significant advantages in RCTs 77 . Although patients in RCTs comparing LAIs vs OAPs were less severely ill and more adherent to OAPs 77 than in clinical care and although mirror-image and cohort studies arguably have greater external validity than RCTs 78 , CPGs generally disregard evidence from other study designs when RCT evidence exits. This narrow focus can lead to disregarding important additional data. Nevertheless, a most updated meta-analysis of all 3 study designs comparing LAIs with OAPs demonstrated consistent superiority of LAIs vs OAPs for hospitalization or relapse across all 3 designs 79 , which should lead to more uniform recommendations across CPGs in the future.
Only seven CPGs included treatment algorithms or flow charts to guide LAI treatment selection for patients with schizophrenia 17 , 18 , 19 , 24 , 29 , 35 , 40 . However, there was little commonality across algorithms beyond the guidance on LAIs mentioned above, as some listed specific treatments and conditions for antipsychotic switches, while others indicated that medication choice should be based on a patient’s preferences and responses, side effects, and in some cases, cost effectiveness. Since algorithms and flow charts facilitate the reception, adoption and implementation of guidelines, future CPGs should include them as dissemination tools, but they need to reflect the data and detailed text and be sufficiently specific to be actionable.
The systematic nature in the identification, summarization, and assessment of the CPGs is a strength of this review. This process removed any potential bias associated with subjective selection of evidence, which is not reproducible. However, only CPGs published in English were included and regardless of their quality and differing timeframes of development and publication, complicating a direct comparison of consensus and disagreement. Finally, based on the focus of this SLR, we only reviewed pharmacologic management with antipsychotics. Clearly, the assessment, other pharmacologic and, especially, psychosocial interventions are important in the management of individuals with schizophrenia, but these topics that were covered to varying degrees by the evaluated CPGs were outside of the scope of this review.
Numerous guidelines have recently updated their recommendations on the pharmacological treatment of patients with schizophrenia, which we have summarized in this review. Consistent recommendations were observed across CPGs in the areas of balancing risk and benefits of antipsychotics when selecting treatment, a preference for antipsychotic monotherapy, especially for patients with a first episode of schizophrenia, and the use of clozapine for treatment-resistant schizophrenia. By contrast, there were inconsistencies with regards to recommendations on maintenance antipsychotic treatment, with differences existing on type and dose of antipsychotic, as well as the duration of therapy. However, LAIs were consistently recommended, but mainly suggested in cases of nonadherence or patient preference, despite their established efficacy in broader patient populations and clinical scenarios in clinical trials. Guidelines were sometimes contradictory, with some recommending LAI use earlier in the disease course (e.g., first episode) and others suggesting they only be reserved for later in the disease. This inconsistency was not due to lack of evidence on the efficacy of LAIs in first-episode schizophrenia or the timing of the CPG, so that other reasons might be responsible, including possibly bias and stigma associated with this route of treatment administration. Lastly, gaps existed in the guidelines for recommendations on the duration of maintenance treatment, treatment of negative symptoms, and the development/use of treatment algorithms whenever evidence is sufficient to provide a simplified summary of the data and indicate their relevance for clinical decision making, all of which should be considered in future guideline development/revisions.
The SLR followed established best methods used in systematic review research to identify and assess the available CPGs for pharmacologic treatment of schizophrenia with antipsychotics in the acute and maintenance phases 80 , 81 . The SLR was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, including use of a prespecified protocol to outline methods for conducting the review. The protocol for this review was approved by all authors prior to implementation but was not submitted to an external registry.
Data sources and search algorithms
Searches were conducted by two independent investigators in the MEDLINE and Embase databases via OvidSP to identify CPGs published in English. Articles were identified using search algorithms that paired terms for schizophrenia with keywords for CPGs. Articles indexed as case reports, reviews, letters, or news were excluded from the searches. The database search was limited to CPGs published from January 1, 2004, through December 19, 2019, without limit to geographic location. In addition to the database sources, guideline body websites and state-level health departments from the US were also searched for relevant CPGs published through June 2020. A manual check of the references of recent (i.e., published in the past three years), relevant SLRs and relevant practice CPGs was conducted to supplement the above searches and ensure and the most complete CPG retrieval.
This study did not involve human subjects as only published evidence was included in the review; ethical approval from an institution was therefore not required.
Selection of CPGs for inclusion
Each title and abstract identified from the database searches was screened and selected for inclusion or exclusion in the SLR by two independent investigators based on the populations, interventions/comparators, outcomes, study design, time period, language, and geographic criteria shown in Table 4 . During both rounds of the screening process, discrepancies between the two independent reviewers were resolved through discussion, and a third investigator resolved any disagreement. Articles/documents identified by the manual search of organizational websites were screened using the same criteria. All accepted studies were required to meet all inclusion criteria and none of the exclusion criteria. Only the most recent version of organizational CPGs was included for data extraction.
Data extraction and synthesis
Information on the recommendations regarding the antipsychotic management in the acute and maintenance phases of schizophrenia and related benefits and harms was captured from the included CPGs. Each guideline was reviewed and extracted by a single researcher and the data were validated by a senior team member to ensure accuracy and completeness. Additionally, each included CPG was assessed using the Appraisal of Guidelines for Research and Evaluation II (AGREE II) tool. Following extraction and validation, results were qualitatively summarized across CPGs.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
The data that support the findings of the SLR are available from the corresponding author upon request.
Correll, C. U. & Schooler, N. R. Negative symptoms in schizophrenia: a review and clinical guide for recognition, assessment, and treatment. Neuropsychiatr. Dis. Treat. 16 , 519–534 (2020).
Article PubMed PubMed Central Google Scholar
Kahn, R. S. et al. Schizophrenia. Nat. Rev. Dis. Prim. 1 , 15067 (2015).
Article PubMed Google Scholar
Millan, M. J. et al. Altering the course of schizophrenia: progress and perspectives. Nat. Rev. Drug Discov. 15 , 485–515 (2016).
Article CAS PubMed Google Scholar
Huhn, M. et al. Comparative efficacy and tolerability of 32 oral antipsychotics for the acute treatment of adults with multi-episode schizophrenia: a systematic review and network meta-analysis. Lancet 394 , 939–951 (2019).
Article CAS PubMed PubMed Central Google Scholar
Kishimoto, T., Hagi, K., Nitta, M., Kane, J. M. & Correll, C. U. Long-term effectiveness of oral second-generation antipsychotics in patients with schizophrenia and related disorders: a systematic review and meta-analysis of direct head-to-head comparisons. World Psychiatry 18 , 208–224 (2019).
Leucht, S. et al. Antipsychotic drugs versus placebo for relapse prevention in schizophrenia: a systematic review and meta-analysis. Lancet 379 , 2063–2071 (2012).
Carbon, M. & Correll, C. U. Clinical predictors of therapeutic response to antipsychotics in schizophrenia. Dialogues Clin. Neurosci. 16 , 505–524 (2014).
Correll, C. U., Rubio, J. M. & Kane, J. M. What is the risk-benefit ratio of long-term antipsychotic treatment in people with schizophrenia? World Psychiatry 17 , 149–160 (2018).
Emsley, R., Chiliza, B., Asmal, L. & Harvey, B. H. The nature of relapse in schizophrenia. BMC Psychiatry 13 , 50 (2013).
Correll, C. U. & Kane, J. M. Ranking antipsychotics for efficacy and safety in schizophrenia. JAMA Psychiatry 77 , 225–226 (2020).
Kane, J. M. & Correll, C. U. Pharmacologic treatment of schizophrenia. Dialogues Clin. Neurosci. 12 , 345–357 (2010).
Kane, J. M., Kishimoto, T. & Correll, C. U. Non-adherence to medication in patients with psychotic disorders: epidemiology, contributing factors and management strategies. World Psychiatry 12 , 216–226 (2013).
Correll, C. U. et al. The use of long-acting injectable antipsychotics in schizophrenia: evaluating the evidence. J. Clin. Psychiatry 77 , 1–24 (2016).
Remington, G. et al. Guidelines for the pharmacotherapy of schizophrenia in adults. Can. J. Psychiatry 62 , 604–616 (2017).
American Psychiatric Association. Treatment recommendations for patients with schizophrenia. Am. J. Psychiatry 161 , 1–56 (2004).
Institute of Medicine (US) Committee to Advise the Public Health Service on Clinical Practice Guidelines, Field, M. J., & Lohr, K. N. (Eds.). Clinical Practice Guidelines: Directions for a New Program. (National Academies Press (US), 1990).
American Psychiatric Association. Practice Guideline for the Treatment of Patients With Schizophrenia , 3rd edn. (2021). https://doi.org/10.1176/appi.books.9780890424841 .
Florida Medicaid Drug Therapy Management Program. 2019–2020 Florida Best Practice Psychotherapeutic Medication Guidelines for Adults . (2020). Available at: https://floridabhcenter.org/wp-content/uploads/2021/04/2019-Psychotherapeutic-Medication-Guidelines-for-Adults-with-References_06-04-20.pdf .
Mental Health Clinical Advisory Group, Oregon Health Authority. Mental Health Care Guide for Licensed Practitioners and Mental Health Professionals. (2019). Available at: https://sharedsystems.dhsoha.state.or.us/DHSForms/Served/le7548.pdf .
Krogmann, A. et al. Keeping up with the therapeutic advances in schizophrenia: a review of novel and emerging pharmacological entities. CNS Spectr. 24 , 38–69 (2019).
Fountoulakis, K. N. et al. The report of the joint WPA/CINP workgroup on the use and usefulness of antipsychotic medication in the treatment of schizophrenia. CNS Spectr . https://doi.org/10.1017/S1092852920001546 (2020).
Leucht, S. et al. CINP Schizophrenia Guidelines . (CINP, 2013). Available at: https://www.cinp.org/resources/Documents/CINP-schizophrenia-guideline-24.5.2013-A-C-method.pdf .
Ostuzzi, G. et al. Mapping the evidence on pharmacological interventions for non-affective psychosis in humanitarian non-specialised settings: A UNHCR clinical guidance. BMC Med. 15 , 197 (2017).
Hasan, A. et al. World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for Biological Treatment of Schizophrenia, Part 1: Update 2012 on the acute treatment of schizophrenia and the management of treatment resistance. World J. Biol. Psychiatry 13 , 318–378 (2012).
Hasan, A. et al. World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for Biological Treatment of Schizophrenia, Part 2: Update 2012 on the long-term treatment of schizophrenia and management of antipsychotic-induced side effects. World J. Biol. Psychiatry 14 , 2–44 (2013).
Hasan, A. et al. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of schizophrenia - a short version for primary care. Int. J. Psychiatry Clin. Pract. 21 , 82–90 (2017).
Moore, T. A. et al. The Texas Medication Algorithm Project antipsychotic algorithm for schizophrenia: 2006 update. J. Clin. Psychiatry 68 , 1751–1762 (2007).
Texas Medication Algorithm Project (TMAP). Texas Medication Algorithm Project (TMAP) Procedural Manual . (2008). Available at: https://jpshealthnet.org/sites/default/files/inline-files/tmapalgorithmforschizophrenia.pdf .
American Association of Community Psychiatrists (AACP). Clinical Tips Series, Long Acting Antipsychotic Medications. (2017). Accessed at: https://drive.google.com/file/d/1unigjmjFJkqZMbaZ_ftdj8oqog49awZs/view .
Buchanan, R. W. et al. The 2009 schizophrenia PORT psychopharmacological treatment recommendations and summary statements. Schizophr. Bull. 36 , 71–93 (2010).
Kreyenbuhl, J. et al. The Schizophrenia Patient Outcomes Research Team (PORT): updated treatment recommendations 2009. Schizophr. Bull. 36 , 94–103 (2010).
New Jersey Division of Mental Health Services. Pharmacological Practice Guidelines for the Treatment of Schizophrenia . (2005). Available at: https://www.state.nj.us/humanservices/dmhs_delete/consumer/NJDMHS_Pharmacological_Practice_Guidelines762005.pdf .
Barnes, T. R. et al. Evidence-based guidelines for the pharmacological treatment of schizophrenia: updated recommendations from the British Association for Psychopharmacology. J. Psychopharmacol. 34 , 3–78 (2020).
National Institute for Health and Care Excellence (NICE). Psychosis and schizophrenia in adults: prevention and management. (2014). Available at: http://www.nice.org.uk/guidance/cg178 .
Scottish Intercollegiate Guidelines Network (SIGN). Management of Schizophrenia: A National Clinical Guideline . (2013). Available at: https://www.sign.ac.uk/assets/sign131.pdf .
Verma, S. et al. Ministry of Health Clinical Practice Guidelines: Schizophrenia. Singap. Med. J. 52 , 521–526 (2011).
CAS Google Scholar
Szulc, A. et al. Recommendations for the treatment of schizophrenia with negative symptoms. Standards of pharmacotherapy by the Polish Psychiatric Association (Polskie Towarzystwo Psychiatryczne), part 1. Rekomendacje dotyczace leczenia schizofrenii z. objawami negatywnymi. Stand. farmakoterapii Polskiego Tow. Psychiatrycznego, czesc 1. 53 , 497–524 (2019).
Google Scholar
Szulc, A. et al. Recommendations for the treatment of schizophrenia with negative symptoms. Standards of pharmacotherapy by the Polish Psychiatric Association (Polskie Towarzystwo Psychiatryczne), part 2. Rekomendacje dotyczace leczenia schizofrenii z. objawami negatywnymi. Stand. farmakoterapii Polskiego Tow. Psychiatrycznego, czesc 2. 53 , 525–540 (2019).
Galletly, C. et al. Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for the management of schizophrenia and related disorders. Aust. N. Z. J. Psychiatry 50 , 410–472 (2016).
Llorca, P. M. et al. Guidelines for the use and management of long-acting injectable antipsychotics in serious mental illness. BMC Psychiatry 13 , 340 (2013).
De Masi, S. et al. The Italian guidelines for early intervention in schizophrenia: development and conclusions. Early Intervention Psychiatry 2 , 291–302 (2008).
Article Google Scholar
Barnes, T. R. Evidence-based guidelines for the pharmacological treatment of schizophrenia: recommendations from the British Association for Psychopharmacology. J. Psychopharmacol. 25 , 567–620 (2011).
Correll, C. U. et al. Efficacy of 42 pharmacologic cotreatment strategies added to antipsychotic monotherapy in schizophrenia: systematic overview and quality appraisal of the meta-analytic evidence. JAMA Psychiatry 74 , 675–684 (2017).
Galling, B. et al. Antipsychotic augmentation vs. monotherapy in schizophrenia: systematic review, meta-analysis and meta-regression analysis. World Psychiatry 16 , 77–89 (2017).
Pillinger, T. et al. Comparative effects of 18 antipsychotics on metabolic function in patients with schizophrenia, predictors of metabolic dysregulation, and association with psychopathology: a systematic review and network meta-analysis. Lancet Psychiatry 7 , 64–77 (2020).
Rummel-Kluge, C. et al. Second-generation antipsychotic drugs and extrapyramidal side effects: a systematic review and meta-analysis of head-to-head comparisons. Schizophr. Bull. 38 , 167–177 (2012).
Angermeyer, M. C. & Matschinger, H. Attitude of family to neuroleptics. Psychiatr. Prax. 26 , 171–174 (1999).
CAS PubMed Google Scholar
Dibonaventura, M., Gabriel, S., Dupclay, L., Gupta, S. & Kim, E. A patient perspective of the impact of medication side effects on adherence: results of a cross-sectional nationwide survey of patients with schizophrenia. BMC Psychiatry 12 , 20 (2012).
McIntyre, R. S. Understanding needs, interactions, treatment, and expectations among individuals affected by bipolar disorder or schizophrenia: the UNITE global survey. J. Clin. Psychiatry 70 (Suppl 3), 5–11 (2009).
Tandon, R. et al. The impact on functioning of second-generation antipsychotic medication side effects for patients with schizophrenia: a worldwide, cross-sectional, web-based survey. Ann. Gen. Psychiatry 19 , 42 (2020).
Zhang, J. P. et al. Efficacy and safety of individual second-generation vs. first-generation antipsychotics in first-episode psychosis: a systematic review and meta-analysis. Int. J. Neuropsychopharmacol. 16 , 1205–1218 (2013).
Zhu, Y. et al. Antipsychotic drugs for the acute treatment of patients with a first episode of schizophrenia: a systematic review with pairwise and network meta-analyses. Lancet Psychiatry 4 , 694–705 (2017).
Kishimoto, T. et al. Relapse prevention in schizophrenia: a systematic review and meta-analysis of second-generation antipsychotics versus first-generation antipsychotics. Mol. Psychiatry 18 , 53–66 (2013).
Leucht, S. et al. Sixty years of placebo-controlled antipsychotic drug trials in acute schizophrenia: systematic review, Bayesian meta-analysis, and meta-regression of efficacy predictors. Am. J. Psychiatry 174 , 927–942 (2017).
Samara, M. T., Nikolakopoulou, A., Salanti, G. & Leucht, S. How many patients with schizophrenia do not respond to antipsychotic drugs in the short term? An analysis based on individual patient data from randomized controlled trials. Schizophr. Bull. 45 , 639–646 (2019).
Zhu, Y. et al. How well do patients with a first episode of schizophrenia respond to antipsychotics: a systematic review and meta-analysis. Eur. Neuropsychopharmacol. 27 , 835–844 (2017).
Bogers, J. P. A. M., Hambarian, G., Michiels, M., Vermeulen, J. & de Haan, L. Risk factors for psychotic relapse after dose reduction or discontinuation of antipsychotics in patients with chronic schizophrenia. A systematic review and meta-analysis. Schizophr. Bull. Open 46 , Suppl 1 S326 (2020).
Tani, H. et al. Factors associated with successful antipsychotic dose reduction in schizophrenia: a systematic review of prospective clinical trials and meta-analysis of randomized controlled trials. Neuropsychopharmacology 45 , 887–901 (2020).
Uchida, H., Suzuki, T., Takeuchi, H., Arenovich, T. & Mamo, D. C. Low dose vs standard dose of antipsychotics for relapse prevention in schizophrenia: meta-analysis. Schizophr. Bull. 37 , 788–799 (2011).
Howes, O. D. et al. Treatment-resistant schizophrenia: treatment response and resistance in psychosis (TRRIP) working group consensus guidelines on diagnosis and terminology. Am. J. Psychiatry 174 , 216–229 (2017).
Masuda, T., Misawa, F., Takase, M., Kane, J. M. & Correll, C. U. Association with hospitalization and all-cause discontinuation among patients with schizophrenia on clozapine vs other oral second-generation antipsychotics: a systematic review and meta-analysis of cohort studies. JAMA Psychiatry 76 , 1052–1062 (2019).
Siskind, D., McCartney, L., Goldschlager, R. & Kisely, S. Clozapine v. first- and second-generation antipsychotics in treatment-refractory schizophrenia: systematic review and meta-analysis. Br. J. Psychiatry 209 , 385–392 (2016).
Siskind, D., Siskind, V. & Kisely, S. Clozapine response rates among people with treatment-resistant schizophrenia: data from a systematic review and meta-analysis. Can. J. Psychiatry 62 , 772–777 (2017).
Wang, G. et al. ECT augmentation of clozapine for clozapine-resistant schizophrenia: a meta-analysis of randomized controlled trials. J. Psychiatr. Res. 105 , 23–32 (2018).
Tiihonen, J., Tanskanen, A. & Taipale, H. 20-year nationwide follow-up study on discontinuation of antipsychotic treatment in first-episode schizophrenia. Am. J. Psychiatry 175 , 765–773 (2018).
Taipale, H. et al. Antipsychotics and mortality in a nationwide cohort of 29,823 patients with schizophrenia. Schizophr. Res . 197 , 274–280 (2018).
Taipale, H. et al. 20-year follow-up study of physical morbidity and mortality in relationship to antipsychotic treatment in a nationwide cohort of 62,250 patients with schizophrenia (FIN20). World Psychiatry 19 , 61–68 (2020).
Carbon, M. & Correll, C. U. Thinking and acting beyond the positive: the role of the cognitive and negative symptoms in schizophrenia. CNS Spectr. 19 (Suppl 1), 38–52 (2014).
PubMed Google Scholar
Krause, M. et al. Antipsychotic drugs for patients with schizophrenia and predominant or prominent negative symptoms: a systematic review and meta-analysis. Eur. Arch. Psychiatry Clin. Neurosci. 268 , 625–639 (2018).
Kane, J. M. et al. Effect of long-acting injectable antipsychotics vs usual care on time to first hospitalization in early-phase schizophrenia: a randomized clinical trial. JAMA Psychiatry 77 , 1217–1224 (2020).
Schreiner, A. et al. Paliperidone palmitate versus oral antipsychotics in recently diagnosed schizophrenia. Schizophr. Res. 169 , 393–399 (2015).
Subotnik, K. L. et al. Long-acting injectable risperidone for relapse prevention and control of breakthrough symptoms after a recent first episode of schizophrenia. A randomized clinical trial. JAMA Psychiatry 72 , 822–829 (2015).
Tiihonen, J. et al. A nationwide cohort study of oral and depot antipsychotics after first hospitalization for schizophrenia. Am. J. Psychiatry 168 , 603–609 (2011).
Zhang, F. et al. Efficacy, safety, and impact on hospitalizations of paliperidone palmitate in recent-onset schizophrenia. Neuropsychiatr. Dis. Treat. 11 , 657–668 (2015).
Kishimoto, T., Nitta, M., Borenstein, M., Kane, J. M. & Correll, C. U. Long-acting injectable versus oral antipsychotics in schizophrenia: a systematic review and meta-analysis of mirror-image studies. J. Clin. Psychiatry 74 , 957–965 (2013).
Kishimoto, T. et al. Effectiveness of long-acting injectable vs oral antipsychotics in patients with schizophrenia: a meta-analysis of prospective and retrospective cohort studies. Schizophr. Bull. 44 , 603–619 (2018).
Kishimoto, T. et al. Long-acting injectable vs oral antipsychotics for relapse prevention in schizophrenia: a meta-analysis of randomized trials. Schizophr. Bull. 40 , 192–213 (2014).
Kane, J. M., Kishimoto, T. & Correll, C. U. Assessing the comparative effectiveness of long-acting injectable vs. oral antipsychotic medications in the prevention of relapse provides a case study in comparative effectiveness research in psychiatry. J. Clin. Epidemiol. 66 , S37–41 (2013).
Kishimoto, T., Hagi, K., Kurokawa, S., Kane, J. M. & Correll, C. U. Long-acting injectable versus oral antipsychotics for the maintenance treatment of schizophrenia: a systematic review and comparative meta-analysis of randomised, cohort, and pre-post studies. Lancet Psychiatry 8 , 387–404 (2021).
Cook, D. J., Mulrow, C. D. & Haynes, R. B. Systematic reviews: synthesis of best evidence for clinical decisions. Ann. Intern. Med. 126 , 376–380 (1997).
Higgins, J. P. T. & Green, S. Cochrane Collaboration Handbook for Systematic Reviews of Interventions . (The Cochrane Collaboration and John Wiley & Sons, Ltd, 2008).
Download references
Acknowledgements
This study received financial funding from Janssen Scientific Affairs.
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and affiliations.
The Zucker Hillside Hospital, Department of Psychiatry, Northwell Health, Glen Oaks, NY, USA
- Christoph U. Correll
Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Department of Psychiatry and Molecular Medicine, Hempstead, NY, USA
Charité Universitätsmedizin Berlin, Department of Child and Adolescent Psychiatry, Berlin, Germany
Evidera, Waltham, MA, USA
Amber Martin & Emma Schiller
Janssen Scientific Affairs, LLC, Titusville, NJ, USA
Charmi Patel, Carmela Benson, Jennifer Kern-Sliwa & Kruti Joshi
Goulding HEOR Consulting Inc., Vancouver, BC, Canada
Rebecca Goulding
Biohaven Pharmaceuticals, New Haven, CT, USA
You can also search for this author in PubMed Google Scholar
Contributions
C.C., A.M., R.G., C.P., C.B., K.J., J.K.S., E.S. and E.K. contributed to the conception and the design of the study. A.M., R.G. and E.S. conducted the literature review, including screening, and extraction of the included guidelines. All authors contributed to the interpretations of the results for the review; A.M. and C.C. drafted the manuscript and all authors revised it critically for intellectual content. All authors gave their final approval of the completed manuscript.
Corresponding author
Correspondence to Christoph U. Correll .
Ethics declarations
Competing interests.
C.C. has received personal fees from Alkermes plc, Allergan plc, Angelini Pharma, Gedeon Richter, Gerson Lehrman Group, Intra-Cellular Therapies, Inc, Janssen Pharmaceutica/Johnson & Johnson, LB Pharma International BV, H Lundbeck A/S, MedAvante-ProPhase, Medscape, Neurocrine Biosciences, Noven Pharmaceuticals, Inc, Otsuka Pharmaceutical Co, Inc, Pfizer, Inc, Recordati, Rovi, Sumitomo Dainippon Pharma, Sunovion Pharmaceuticals, Inc, Supernus Pharmaceuticals, Inc, Takeda Pharmaceutical Company Limited, Teva Pharmaceuticals, Acadia Pharmaceuticals, Inc, Axsome Therapeutics, Inc, Indivior, Merck & Co, Mylan NV, MedInCell, and Karuna Therapeutics and grants from Janssen Pharmaceutica, Takeda Pharmaceutical Company Limited, Berlin Institute of Health, the National Institute of Mental Health, Patient Centered Outcomes Research Institute, and the Thrasher Foundation outside the submitted work; receiving royalties from UpToDate; and holding stock options in LB Pharma. A.M., R.G., and E.S. were all employees of Evidera at the time the study was conducted on which the manuscript was based. C.P., C.B., K.J., J.K.S., and E.K. were all employees of Janssen Scientific Affairs, who hold stock/shares, at the time the study was conducted.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information, reporting summary, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Correll, C.U., Martin, A., Patel, C. et al. Systematic literature review of schizophrenia clinical practice guidelines on acute and maintenance management with antipsychotics. Schizophr 8 , 5 (2022). https://doi.org/10.1038/s41537-021-00192-x
Download citation
Received : 26 February 2021
Accepted : 02 November 2021
Published : 24 February 2022
DOI : https://doi.org/10.1038/s41537-021-00192-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Psychosis superspectrum ii: neurobiology, treatment, and implications.
- Roman Kotov
- William T. Carpenter
- Katherine G. Jonas
Molecular Psychiatry (2024)
Antipsychotic Discontinuation through the Lens of Epistemic Injustice
- Helene Speyer
- Lene Falgaard Eplov
Community Mental Health Journal (2024)
Delphi panel to obtain clinical consensus about using long-acting injectable antipsychotics to treat first-episode and early-phase schizophrenia: treatment goals and approaches to functional recovery
- Celso Arango
- Andrea Fagiolini
BMC Psychiatry (2023)
Machine learning methods to predict outcomes of pharmacological treatment in psychosis
- Lorenzo Del Fabro
- Elena Bondi
- Paolo Brambilla
Translational Psychiatry (2023)
Comparison of clinical outcomes in patients with schizophrenia following different long-acting injectable event-driven initiation strategies
- Carmela Benson
- Panagiotis Mavros
Schizophrenia (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
The Use of Narrative Therapy on Paranoid Schizophrenia
- Research in progress
- Published: 10 May 2023
- Volume 68 , pages 273–280, ( 2023 )
Cite this article

- Karina Therese G. Fernandez 1 ,
- Anne Therese Marie B. Martin 1 &
- Dana Angelica S. Ledesma 1
961 Accesses
Explore all metrics
Research suggests that a clinical diagnosis of schizophrenia is strongly linked with experiencing negative stereotypes and an inability to recover. In challenging the scientific-logical practice of diagnostic labeling, which totalizes the person’s experience around the illness, Narrative therapy offers a unique approach to treating schizophrenia by putting the spotlight on the client’s values, strengths, and beliefs. This allows the client to discover an alternative life narrative beyond their diagnosis. This study presents a case of a 40-year-old woman with paranoid schizophrenia. She felt that the people in her workplace were out to harm her so she would never work in her field again. At home, she had also begun to question herself as a mother. Narrative therapy techniques such as externalization, thickening the landscape of action and identity, and re-membering were used to aid the client’s recovery and helped her to shift from a problematic view of her identity. The present case focuses on providing steps to guide practitioners in using Narrative therapy for a case where the client has internalized their diagnosis as their identity.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions

Similar content being viewed by others

The Soul of Therapy: The Therapist’s Use of Self in the Therapeutic Relationship

The Biopsychosocial Approach: Towards Holistic, Person-Centred Psychiatric/Mental Health Nursing Practice
Existential approaches and cognitive behavior therapy: challenges and potential, data availability.
The authors have no data or materials to declare that are relevant to the content of this article.
Code Availability
The authors did not use any software application and thus do not have a code.
Abbreviations
Diagnostic and Statistical Manual V
American Psychiatric Association (APA). (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington DC: American Psychiatric Association.
American Psychiatric Association (APA). (2022). Diagnostic and statistical manual of mental disorders (5th ed., text rev.). https://doi.org/10.1176/appi.books.9780890425787
Beaudoin, M. (2005). Agency and choice in the face of trauma: A narrative therapy map. Journal of Systemic Therapies, 24 (4), 32–50. https://doi.org/10.1521/jsyt.2005.24.4.32
Article Google Scholar
Bullimore, P. (2003). Altering the balance of power: Working with voices. International Journal of Narrative Therapy and Community Work, 3 , 22–28.
Google Scholar
Carey, M., & Russell, S. (2002). Externalising: Commonly asked questions. International Journal of Narrative Therapy & Community Work, 2 , 76–84.
Carr, A. (1998). Michael White’s Narrative Therapy. Contemporary Family Therapy, 20 (4), 485–503.
Chae, Y., & Kim, J. (2015). Case study on narrative therapy for schizophrenic adolescents. Procedia—Social and Behavioral Science, 205 , 53–55.
Corrigan, P. W., Watson, A. C., & Barr, L. (2006). The self-stigma of mental illness: Implications for self-esteem and self-efficacy. Journal of Social and Clinical Psychology, 25 (8), 875–884. https://doi.org/10.1521/jscp.2006.25.8.875
Denborough, D. (2014). Retelling the stories of our lives: Everyday narrative therapy to draw inspiration and transform experience . W W Norton & Co.
Fung, K. M. T., Tsang, H. W. H., & Corrigan, P. W. (2008). Self-stigma of people with schizophrenia as predictor of their adherence to psychosocial treatment. Psychiatric Rehabilitation Journal, 32 (2), 95–104. https://doi.org/10.2975/32.2.2008.95.104
Article PubMed Google Scholar
Hasan, A. A. -H., & Musleh, M. (2018). Self-stigma by people diagnosed with schizophrenia, depression and anxiety: Cross-sectional survey design. Perspectives in Psychiatric Care, 54 (2), 142–148. https://doi.org/10.1111/ppc.12213
Kinjo, T., & Morioka, M. (2011). Narrative responsibility and moral dilemma: A case study of a family’s decision about a brain-dead daughter. Theoretical Medicine and Bioethics, 32 (2), 91–99. https://doi.org/10.1007/s11017-010-9160-y
Kondrat, D. C., & Teater, B. (2009). An anti-stigma approach to working with persons with severe mental disability: Seeking real change through narrative change. Journal of Social Work Practice, 23 (1), 35–47. https://doi.org/10.1080/02650530902723308
Lloyd, H., Lloyd, J., Fitzpatrick, R., & Peters, M. (2017). The role of life context and self-defined well-being in the outcomes that matter to people with a diagnosis of schizophrenia. Health Expectations: An International Journal of Public Participation in Health Care and Health Policy, 20 (5), 1061–1072. https://doi.org/10.1111/hex.12548
MacLeod, M. (2019). Using the narrative approach with adolescents at risk for suicide. Canadian Journal of Counselling and Psychotherapy, 53 (1). Retrieved from https://cjc-rcc.ucalgary.ca/article/view/61213
Morgan, A. (2000). What is Narrative Therapy: An Easy to Read Introduction . Dulwich Center Publication.
Ngazimbi, E. E., Lambie, G. W., & Shillingford, M. A. (2008). The use of narrative therapy with clients diagnosed with bipolar disorder. Journal of Creativity in Mental Health, 3 (2), 157–174. https://doi.org/10.1080/15401380802226661
Özçelik, E. K., & Yıldırım, A. (2018). Schizophrenia patients’ family environment, internalized stigma and quality of life. Journal of Psychiatric Nursing / Psikiyatri Hemsireleri Dernegi, 9 (2), 80–87. https://doi.org/10.14744/phd.2017.07088
Sugawara, H., & Mori, C. (2018). The self-concept of person with chronic schizophrenia in Japan. Neuropsychopharmacology Reports, 38 (3), 124–132. https://doi.org/10.1002/npr2.12016
Article PubMed PubMed Central Google Scholar
White, M. (2005). Michael White workshop notes . Dulwich Centre. https://dulwichcentre.com.au/product/michael-whites-workshop-notes-michael-white/
White, M. (2007). Maps of narrative practice . W. W. Norton
White, M. (2011). Narrative practice: Continuing the conversations . (D. Denborough, Ed.). W W Norton & Co.
White, M. (2016). Chapter 1: Deconstruction and therapy. In Narrative Therapy Classics (pp. 11–54). Adelaide: Dulwich Centre Pty Ltd.
White, M., & Epston, D. (1990). Narrative means to therapeutic ends . W. W. Norton, New York
Download references
Acknowledgements
The authors would like to acknowledge the Ateneo Bulatao Center for its constant encouragement and support to advance academic research alongside clinical practice.
The authors did not receive support from any organization for the submitted work.
Author information
Authors and affiliations.
Department of Psychology, Ateneo de Manila University, Katipunan Avenue, 1108, Quezon City, Metro Manila, Philippines
Karina Therese G. Fernandez, Anne Therese Marie B. Martin & Dana Angelica S. Ledesma
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the study. Material preparation, data collection, and analysis were performed by Karina Therese G. Fernandez. The first draft of the manuscript was written by Karina Therese G. Fernandez, Anne Therese Marie B. Martin, and Dana Angelica S. Ledesma. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Karina Therese G. Fernandez .
Ethics declarations
Conflicts of interest.
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethics Approval
This study received ethical approval from the University Research Ethics Office of the Ateneo de Manila University. This research study was conducted retrospectively from data obtained for clinical purposes. A copy of the approval letter has been provided in Appendix A.
Consent to Participate and Publication
In the informed consent given by the Ateneo Bulatao Center for Psychological Services to its therapy clients, there is a very detailed checklist of the extent of how their information can be used. One specific item is “session notes for the purposes of research (paper publications and paper presentations). We have attached a copy of an unsigned informed consent form for reference (see Appendix B).
Informed Consent
By signing an informed consent form, we obtained permission from the client to share her story. Furthermore, her identifying information was changed to ensure confidentiality. Though the informed consent form already covers the consent for data in the therapy sessions to be published, as recommended by informal discussions with members of the University Research Ethics Committee of the Ateneo de Manila University, a second request for informed consent to publish was made after therapy.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Fernandez, K.T.G., Martin, A.T.M.B. & Ledesma, D.A.S. The Use of Narrative Therapy on Paranoid Schizophrenia. Psychol Stud 68 , 273–280 (2023). https://doi.org/10.1007/s12646-022-00709-z
Download citation
Received : 12 July 2021
Accepted : 15 December 2022
Published : 10 May 2023
Issue Date : September 2023
DOI : https://doi.org/10.1007/s12646-022-00709-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Paranoid schizophrenia
- Internalized stigma
- Narrative therapy
- Find a journal
- Publish with us
- Track your research
- Open access
- Published: 08 November 2023

Conceptualizing a less paranoid schizophrenia
- James Long 1 &
- Rachel Hull 2
Philosophy, Ethics, and Humanities in Medicine volume 18 , Article number: 14 ( 2023 ) Cite this article
1886 Accesses
1 Altmetric
Metrics details
Schizophrenia stands as one of the most studied and storied disorders in the history of clinical psychology; however, it remains a nexus of conflicting and competing conceptualizations. Patients endure great stigma, poor treatment outcomes, and condemnatory prognosis. Current conceptualizations suffer from unstable categorical borders, heterogeneity in presentation, outcome and etiology, and holes in etiological models. Taken in aggregate, research and clinical experience indicate that the class of psychopathologies oriented toward schizophrenia are best understood as spectra of phenomenological, cognitive, and behavioral modalities. These apparently taxonomic expressions are rooted in normal human personality traits as described in both psychodynamic and Five Factor personality models, and more accurately represent explicable distress reactions to biopsychosocial stress and trauma. Current categorical approaches are internally hampered by axiomatic bias and systemic inertia rooted in the foundational history of psychological inquiry; however, when such axioms are schematically decentralized, convergent cross-disciplinary evidence outlines a more robust explanatory construct. By reconceptualizing these disorders under a dimensional and cybernetic model, the aforementioned issues of instability and inaccuracy may be resolved, while simultaneously opening avenues for both early detection and intervention, as well as for more targeted and effective treatment approaches.
Schizophrenia is one of the oldest and most studied mental disorders within the history of psychological science. Mental and medical health practices consistently fall short for patients diagnosed with schizophrenia spectrum conditions. Treatment plans are predominantly stereotyped, heavily reliant on second-generation antipsychotics [ 1 , 2 , 3 , 4 ], and rarely include validated psychosocial or psychotherapeutic interventions [ 5 , 6 , 7 ], Verdoux et al., 2010). This pattern persists despite widespread agreement on heterogenous presentation and treatment outcome [ 3 , 8 , 9 , 10 , 11 ], moreover, a tremendous amount of the variability in prognosis, etiology, and even the effectiveness of pharmacotherapy is accounted for by factors overlooked in diagnosis and/or outcomes monitoring [ 10 , 12 , 13 , 14 ]. This poses an ethical issue in that, to the extent that the goal of the mental health field is to alleviate human suffering and to promote human flourishing, past and present approaches miss the mark. This also implies that the currently accepted conceptualization(s) of schizophrenia spectrum disorders is at least partially flawed. Finally, this treatment failure incurs a heavy social and economic cost. The US domestic economic cost of schizophrenia is staggering, estimated at US$60 billion per annum [ 15 ], moreover, accounting for indirect costs, this is likely a conservative estimate.
The reasons for this systemic deficiency are as diverse as the schizotypy spectrum itself, ranging from foundational flaws in the current diagnostic model of mental health to constraints inherent in the contemporary mental health system. The increase in biologization of the field [ 16 ] has encouraged efforts to identify neural correlates in line with a disease model, while the preponderance of evidence indicates that schizotypy, in all of its manifestations, is profoundly moderated by environment. Such emphasis on materialism has not mitigated stigma or improved treatment outcomes and likely contributes to the current and historical plight of the population [ 5 ]. Accounting for the schizotypal population as a whole, it may be appropriate to conceptualize schizophrenia as “the story of the way that poverty, violence, and being on the wrong side of power drive us mad” ([ 17 ], p.197), or perhaps more succinctly, “bad things happen and can drive you crazy” ([ 3 ], p. 145).
Housing the etiological locus solidly within the realm of environment and not genetics is consistent with the Hearing Voices Movement (HVM; [ 18 ], which seeks to reframe psychosis symptoms within culture and context, and refrain from treatment of those experiences as a “biogenetic disease state,” [ 18 ], p. 134) which is not supported by recent data. While the model and perspective proposed in this paper aspire towards a new operational explanation, the body of research necessary and sufficient for such a definition is either nascent or theoretical,nonetheless, there exists precedent for de-stigmatizing and de-pathologizing psychosis (the symptom) and schizotypy (the syndrome).
The heterogeneity of presentation and treatment outcome has lead other researchers to argue that the construct of schizophrenia as a whole needs to be reconceptualized [ 3 , 18 , 19 , 20 , 21 , 22 ]. Inasmuch as disagreement may be attributed to the unknowns inherent in any scientific dispute, the issues around schizophrenia are more pronounced. This is likely due to numerous factors. The foremost being that all issues involving psychosis lie contrary to the unspoken morality of post-enlightenment societies, the overarching dogma of which describes a world which is ultimately without contradiction, and which can only be truly understood through the mechanisms of reason. The second unspoken assumption is that such an understanding is unquestionably good. Given the ubiquity of instrumental rationality as final arbiter of value, the ability to participate in consensus reality becomes a measure of one’s human worth, and one’s divergence from said explanatory consensus is an index of one’s illness. This cultural and methodological axiom thus doubly binds the schizotype, as their phenomenological position is simultaneously given an unspoken moral dimension while providing tools for study and care predisposed to pathologize and dispense with said position as inherently aberrant and symptomatic.
The present article will begin with rationale explicating the historical, philosophical, and conceptual difficulties precipitating myopic approaches to treatment and research within the population. Secondly, it will survey relevant evidence from various disciplines which provide converging evidence toward a more comprehensive view of schizotypy and its manifestations with psychotic features. Finally, the present authors propose a more thorough conceptualization of the schizotypal spectrum, along with a framework to reconceptualize schizotypal diagnoses as identifiable patterns within a dimensional paradigm incorporating both “healthy” and “pathological” members. Finally, clinical implications will be discussed.
Ultimately, it will be argued that a properly developed cybernetic model, rooted in trauma-informed personality theory, best captures the nature and breadth of this human experience. It is the present authors’ hope that with such a reconceptualization, self-stigma in those with schizophrenia will mitigate as well, as self-stigma in individuals on the schizotypal spectrum has been recognized as a “second illness” [ 23 ], as cited in [ 3 , 24 , 25 , 26 , 27 , 28 , 29 ].
Historical and philosophical precedents
Underlying axioms and paradigmatic blind spots.
Although there is room to debate many of his specific points and inferences, Foucault (1965) addressed many of the genealogical ideas that underlie current mental health practice. Salient are the social and moral implications of mental illness in a post-enlightenment age. Reason and empiricism were held up as the means by which humanity would extract itself from the arbitrary and oppressive moral and social systems that characterized the preceding epochs. However, as no human or society can exist without an orienting value system (ought from is) [ 30 ], this revolution merely altered the parameters. Moral punishment became reserved for “healthy” individuals with deviant behavior, while those whose behavior was determined to be medical in origin were to be cured (i.e. brought back to reason and regulated passions). However, in both cases it was deviance from the collectively understood “good” which was targeted. In the former case, deviant behavior was punished or corrected through learning, while in the latter psychological deviance imbued society with a moral duty to treat or cure. Much of our current approach to treatment, such as cognitive-behavioral theory, is predicated on this idea, that it is irrational thoughts that cause distress, based on the underlying assumption that showing the person that their thinking is irrational is itself a kind of cure for their experience.
In a recent review of 30 consecutive court-mandated medication hearings, 29 were approved without a jury, most in cases where serious neurological damage had been caused by medications and at higher doses than would be recommended. All cases of treatment had entirely discounted options such as psychotherapy, despite defendant and family protest, demonstrating that the line between moral capability, medical impairment, and societal responsibility is still quite blurry [ 5 ].
The presenting issues involving psychosis are inherently aberrant against the axioms of the age, giving their expression a numinous quality absent from comparable symptomology. While a “healthy” person can empathize with a depressive or obsessional person (seeing their experience as merely an extreme version of their own), the hallucinations, delusions, disorganized thoughts, and behaviors of psychosis are deeply unsettling. Such a person may be pitied or sympathized with, but how can one empathize with a person who is not participating in consensus reality, let alone take their perspective seriously?
The rational-empirical model Foucault was dissecting had more comprehensive effects as well, establishing the parameters by which reality was defined. Truth was to be determined through careful observation, data collection, and objective analysis of results. One could subsequently remove the confounds of arbitrary values and subjectivity and determine what was and was not “real.” This idea has been one of the most important and useful tools in human history, and its benefits cannot be overstated; however, as with any idea, it rests upon axioms and results in outcomes with predictable constraints.
As much of the unspoken paradigm scaffolding within scientific models can be traced back to the ideas of rationalism and empiricism, and to the extent this paper aims to address axiomatic flaws in those models, it is worth exploring the concepts. Broadly speaking, the rationalists argued that knowledge was attained through logic and reason and that human understanding was founded on innate ideas. In contrast, the empiricists argued that humans were tabula rasa, and that knowledge was gained exclusively through sensory experience. Responding to both, Kant [ 31 ] outlined his synthetic a priori propositions on reason and its recognition of necessary cognitive structures preceding sensory modification. He argued that the only way in which a human being could have knowledge in a functionally infinite sea of data was through categorization. That we contained an innate scaffolding which predisposed us to select and judge our sensory data, and that without such we could not possibly perceive the world in any meaningful way at all. Moreover, as we were goal-oriented creatures, this was an inherently value-laden conceptualization. While this perspective was revolutionary in overall enlightenment thinking, its ultimately phenomenological approach to reality has had little impact on the scientific endeavor to understand that very rationality.
What has been retained is something of the desire which drove Kant’s deductive exploration; namely to arrive at a surety of knowledge without call to a divine authority. His endeavors into synthetic a priori knowledge assumed and ultimately sought to prove that foundational sure knowledge could be found and worked upwards from to arrive at universal and objective truth. The distillation of this is the reductionism which subtly underlies scientific inquiry to this day; the belief that the best way to understand a complex system is to break it into its smallest constituent units and then extrapolate upwards. From this we may identify the roots of the atomism and materialism which will be discussed further in this paper.
Equally important to these methodological axioms however is the subtle implications of a unitary truth when applied to the psyche and its inquires (i.e. that a single correct perspective is attainable and thus deviation therefrom is an error to be corrected). Through this lineage one has dispensed with subjectivity (the valuing ‘ought’ and its many constraints) in favor of objective proxies as a means of study and have thus over time, often with a sense of moral duty, come to see subjectivity as (at best) epiphenomenal. This trend has likely reinforced, if not outright caused, the current preference for biological interventions for subjective experiences while viewing aberrant subjectivities as a problem to be solved. The more strictly empirical approach can likely be attributed to the structural disconnect between verifiable data and subjective experience endemic to objective and materialistic approach to science; however, this inattention has created potential blind-spots in investigative assumptions.
Congruent models and fractal patterns
While Kant arrived at his categorical phenomenological conclusions from deduction and intuition, Jean Piaget [ 32 ] outlined a nearly identical process by observing the developmental construction of schemata in young children. In highlighting the evolution of children’s reports and understandings of reality, Piaget stands as a kind of naturalist of the same process proposed by Kant, in which a rather simple set of structures give rise over time to the operations of intelligence. In both Kant’s concept of understanding and Piaget’s concept of a schema (in a total sense), a person can only conceive of realities congruent with the structure of their framework,that is, they have a subjective perspective. Where Piaget’s observations stand out is in his detailing of the process by which these structures update and organize themselves across time (e.g. the famous cognitive revolution children experience when developing a theory of mind). In light of contemporary evolutionary, genetic, and personality research though, the full scope of potential schematic diversity remains an open question. That is, to what degree do we converge upon a universal perception of reality and to what degree are we perceiving and conceptualizing differently?
Regardless, the implication of the symptom-focused taxonomy of the DSM or ICD is that subjective diversity is either irrelevant or non-existent and thus our scientific study of the mind cannot account for it. Given that our schemata expand and evolve through assimilation and accommodation, and that they are the medium through which we construct our reality, the means by which that dynamic equilibrium is affected by biological predisposition and the specific nature of events experienced during this process must be accounted for if psychology is to succeed as a scientific pursuit. Understanding the forces which led to and maintain such an equilibrated structure carries implications for psychological models of cognition and perception as well as for clinical treatment.
Symmetrical to Piaget’s schemata, Kuhn’s [ 33 ] description of the paradigmatic nature of scientific discovery demonstrates this process at the level of consensus reality and may also indicate the core problem with current models of schizophrenia-spectrum disorders. Much in the same way a developing child in Piaget’s model works pragmatically within a ‘good enough’ schema until sufficient development and anomalous information induces a reorganizational (and thus perceptual) classification, Kuhn noted that scientific paradigms (collective schemata of interpretation and behavior) progress until sufficient anomalous data induces a reorganization of core assumptions, such that previous evidence and anomalous evidence remain, are accounted for, and explained. Much as two individuals with incompatible schemata would find mutual understanding impossible without accommodation on one or both ends, the current paradigms informing much of psychological research (e.g. objectivism, materialism, etc.) cannot account for the symptomatic manifestations of the schizotypal spectrum other than as pathological deviation, and thus remain obtusely focused. Instead, models must account for the biological and environmental impacts on schematic development as a necessary component in any defensible definition of mental health. Currently, models such as the Five-Factor Model of personality (FFM); [ 34 ] offer avenues to begin exploring and discussing this scientifically, however their implications have yet to meaningfully propagate throughout the psychological field.
Outcomes and limitations of unexamined axioms
In a discussion on the theoretical challenges facing psychology today, Slife (as cited in Lambert, 2004) identified numerous constraints on theory and its practical application. Objectivism essentially posits that the logic inherent in the methods and techniques of science and clinical practice can be relatively free of systematic biases and values. This is achieved through the use of logical reasoning (rationalism) and unbiased observation of phenomena (empiricism). This permits a certain unbiased standard of proof that can be verified and agreed upon without appeal to arbitrary authority or preconceived assumptions; however, it also leads to limitations. It bounds what can be studied (and thus proven) to those things which can be observed and replicated. In psychology, this translates to examining the psyche by proxy. As one can have no direct observation of experience, various behaviors are examined instead with the assumption that these act as indicators of internal states and dynamics. Where behaviors cannot be determined, states are operationalized; anxiety becomes the nexus of racing thoughts, restlessness, distractibility, etc. What cannot be captured is the valence, meaning, and experience of anxiety, or the idiosyncratic relationships an individual's anxiety has with their own history, conceptual framework, and day-to-day experience.
For example, within a psychodynamic framework, a clinician would find it important to determine whether a patient’s depression was anaclitic or introjective, thus accounting for the inner subjectivity underlying the overall state. However, most strictly empirical research and certainly most pharmacological research must measure itself by symptom reduction within the DSM criteria of depression, which does not account for personality style. In this way, the methods by which research is conducted systemically deem irrelevant domains of human experience and psychological evolution, becoming blind to them.
A second axiom is materialism, which posits that psychological experiences will eventually be shown to have observable and biological bases. All psychology is simultaneously biology. As with objectivism, this assumption is predominantly benign or beneficial; however, it too creates complications. One is the implicit causal direction; that the core problem is contained within, and thus solvable and explicable through, biology. Indeed, materialism is tightly wedded to objectivism as it is often far easier to study physical systems than social or psychological ones. This belief underlies much of the faith in and reliance on pharmaceuticals as “cures” for psychological disorders. Once a biological correlation is identified, it is treated as the cause despite our knowledge that the relationship is more complicated; moreover, the entire DSM/ICD classification systems assume biologic etiology. This causal direction also promotes an aura of preeminence to biological markers over holistic biopsychosocial assessment. For example, if research finds that serotonin differences act as a biomarker of depression, it is assumed that such differences causally precede the psychological state and so become the target of treatment, despite evidence that such neurotransmitters are themselves greatly influenced by environment and cognitive framing [ 35 , 36 ].
Finally, the axiom of atomism assumes that the qualities of people are contained within the individual, and so treatment should focus on individual cognition, biology, and behavior. As can be seen, atomism dovetails seamlessly with reductionism (the individual is the indivisible member of the collective), materialism (the biological operations of others do not influence those around them), objectivism (it is easiest to observe the components of an individual rather than the network of influences between them and their environment over time) and implicit morality (the locus of choice and thus moral human agency exists within the individual). These assumptions, while almost certainly a necessary heuristic, can lead researchers and practitioners to underestimate or ignore the impact of relationship factors or social context.
These and other axioms inform many more areas of human life than the field of psychology, and in many of them (e.g. particle physics), they may operate more or less perfectly. Inasmuch as psychology is to be the study of the psyche, however, it must at some point include the study of human subjectivity; moreover, it is the experience of suffering that we aim to alleviate, not its proxies. This is decidedly difficult within a framework that goes to great lengths to remove all subjectivity before even beginning its search.
Furthermore, whatever it is one means by the psyche, it is a dynamic and multi-level phenomenon. It is shaped by the past through memories and biological alterations (processes which continue to change throughout the lifetime); simultaneously, how a person conceives of the future continuously alters behaviors, cognitions, and relationships (which in turn recontextualizes memories and alters biology). Each of these is further informed by the idiosyncratic relationships a person has (as well as how he conceives of them) and the environment in which he lives (physical and social). It is in fact this entire set of inter-penetrating and interlocking systems which determine how any particular experience manifests. Within the framework above, those elements which are most difficult to operationalize or which lie perpendicular to accepted rigor are granted a reality significantly less substantial than those which are considered more “evidence-based,” and thus most often lay unaccounted for in final etiology and nosology.
The DSM’s taxonomy, as well as its preeminence in mental health practice, is the distillation of this process. It testifies to the strengths this approach has brought to the field, and simultaneously contains its weaknesses. As has been noted by clinicians throughout its development and subsequent iterations, the DSM’s approach dispenses with, misinterprets, or lies contrary to the bulk of historical and contemporary clinical wisdom [ 37 , 38 , 39 , 40 ].
Without an explicit definition or discussion of mental health, the DSM implies that the removal or reduction in stated symptoms is the goal (empiricism and reductionism). This creates the following three issues: (1) While symptom relief may be desired, no other medical professional would equate symptom reduction with a cure. (2) The DSM can offer no discussion or guidance on important qualia within those symptoms (e.g. recall objectivism—is the depressive experience fundamentally anaclitic or introjective). (3) The DSM offers no insight on the depth of, interactions between, or potential functions of experiences as outlined. One may contend that none of these was meant to be the function of the DSM, which was instead intended to be one tool in an arsenal the clinician would bring to bear. However, whether due to the constraints of time and energy, the demands of insurance companies, the limitations of training, the (above-outlined) biased nature of research, the fact that the DSM is subservient to the ICD, or any combination of these factors, it is often the case that the DSM is used in exactly this manner. In 2013, the National Institute of Mental Health (NIMH) ceased funding DSM-based research citing the model’s overall “lack of validity” (Insel, as cited in [ 41 ], p. 522).
The weight of evidence accrued even within this framework calls its assumptions into question. It has been noted, for example, that in clinical settings, depression is usually paired with anxiety and somatic symptoms, while also manifesting in highly variable ways (aggression, risk-taking behaviors, etc.) [ 39 ]. Simple diagnosis is insufficient for treatment planning [ 42 ] and ultimately leads to stereotyped and imprecise responses; moreover, if disorders were, in fact, distinct categories, one should expect them to have distinct boundaries with matched biological correlations. However, antidepressant medications are used to treat anxiety and other mood disorders, and antipsychotic agents are prescribed for bipolar disorder and various severe personality disorders. Symmetrically on the treatment side, cognitive-behavioral therapy (developed to address internalizing disorders) has since expanded to encompass nearly every class of mental disorder [ 43 ], despite major methodological flaws in the research that supports CBT [ 44 ]. Moreover, longitudinal and epidemiological evidence indicates that etiology, prognosis, and even pharmaceutical effectiveness depend on psychosocial factors disregarded in the current taxonomy. For example, in patients with schizotypy and psychosis, treatment and pharmacological outcomes depend much more on factors such as childhood trauma, social factors, and neurocognition [ 3 , 11 , 45 ].
While the full impact of this dynamic stretches throughout the whole of psychology, select points are particularly relevant. In striving toward the objectivity so highly valued under our society's ruling metanarrative, psychological practice and research has adopted, almost axiomatically, a “disease” model of psychological suffering; we document symptoms and attempt to place them into distinct categories which would have distinct biological/behavioral underpinnings which can be discretely addressed. Thus, the experience of a disorder and its treatment can be generalized and divided into discrete components. It also implies that, as the symptom expressor, the problem lies within the individual and so must be addressed at that level. As was outlined through underlying Enlightenment philosophies earlier, these assumptions are natural outcomes; that the moral locus lies within the individual’s own rationality (their claim to full personhood) and so remains unquestioned within most research models. As Higgs [ 18 ] purported, “the advancement of neoliberal values and policies likewise favors naturalizing inequality through the lens of biology, locating the suffering caused by social problems within individual bodies, which are perceived as self-contained and (ideally) fully independent” (p. 138).
Given that such a model is conducive to research, conforms well to the needs of insurance and pharmaceutical companies, and carries the implied authority of decades of acceptance, the situation is self-reinforcing. Moreover, the taxonomic model implies a baseline human experience, deviation from which constitutes the nature of psychopathology. Given biologization and atomism, the problem is seen as localized within the person, and treatment focuses on the adjustment of biological systems and the resolution of irrational thoughts and behaviors. In so doing, the complexity of human psychology and the entirety of subjectivity is done away with; a serious issue given that the psyche is defined by and experienced through subjectivity. Indeed, “a grisly tradition of ‘biologizing social facts’ exists within psychiatry” [ 18 ], p. 137–138). This divides much of psychology as a body of knowledge from the bulk of clinical wisdom and makes the training, expansion, and transmission of this understanding difficult at best. It limits the field’s understanding of human psychology and our ability to address individuals’ actual experiences. For example, in addition to the model’s inability to discuss characterological differences or dynamic interactions between disorders and psyche, it has nothing to say about the positive side of human experience as a necessary component of health. Finally, while this complex is problematic for any psychological disorder, it becomes more so the more deeply and/or longitudinally it exists within the client, and the further from placidity, conformity, and rationality it takes her. A person experiencing an anxiety attack has a problem, a person with borderline personality disorder needs extensive management, and a person with schizophrenia is beyond the pale.
Philosophical summary and subsequent steps
The broad philosophical assumptions which form the basis for the rational-empirical model informing current scientific inquiry have given primacy to objectivity as the measure of truth as a matter of course. In so doing, it has ultimately directed research and our collective understanding of psychology into a taxonomic and symptom-based structure which will naturally prioritize biological causation and atomistic approaches to treatment. Simultaneously, the same axioms which dictate our current scientific paradigm contain implicit moral assumptions which reflexively pathologize experiences, perspectives, and expressions which are deemed “irrational,” regardless of whether they are themselves the source of distress. This interaction has led to an overall approach to psychological research and treatment which stigmatizes patients (particularly those on the schizotypal spectrum) while concurrently falling short in developing effective treatments and models due to inherent methodological flaws; despite clear evidence that current taxonomies are unstable and that the assumed biological mechanisms underlying them do not align with their framework. Moreover, given the shared genealogy of both these processes, they are self-reinforcing and inherently perpetuated through the systems and approaches they generated. Without a revolution within the paradigm (systemic schema), psychology as a whole will struggle to fully grasp its subject matter (the psyche). Much as in Piagetian models, it is the failure of schemata to account for experience through assimilation that sparks accommodation. Current evidence from within our paradigm indicates a similar process needs to occur to progress. Thus, developing a full conceptualization of schizotypy requires an act of decentralization and a re-examination of the current body of evidence as a whole if the field is to mature.
In contrast to categorical approaches, current evidence suggests that adopting a cybernetic model better captures the complexity of the phenomena, the etiology of pathological development, and ultimately offers insight into the phenomenological bases of and treatment approaches for the schizotypal population. Briefly, cybernetic models seek to map the behavior of complex self-regulating systems. The mathematician Norbert Wiener defined cybernetics as the study of “control and communication in the animal and the machine.” [ 46 ] and noted its applicability to biological systems, computer systems, and broad organizational structures such as governments. What must be understood is that within a cybernetic model, a number of interlocking processes exist within a network of mutually influential relationships. Such systems are reactive and attempt to reach equilibrium through alterations in one or more of their domains. In the case of small disturbances, a cybernetic system may merely make a minor adjustment in one domain to achieve homeostasis; however, in cases where a sufficiently large disruption occurs, the system as a whole may reorganize into an entirely novel point of balance. In such systems, feedback loops between systems are conceptualized; accounting for how over time relatively minor interactions can reinforce and strengthen each other sufficiently to cause such a restructuring. It should be noted the conceptual resonance such a framework has with Piagetian schemata, Kuhnian paradigms, and many psychodynamic conceptualizations of personality development.
With this in mind, the following sections will begin outlining relevant insights gained across a number of disciplines outlining the qualities of the proposed schizotypal population and suggesting the important factors contributing to the development of experiences such as schizophrenia.
The Schizotypal spectrum within categorical models
While schizophrenia spectrum disorders have been recognized categories of pathology for many decades, the debate about whether there is an underlying genotype or phenotype which preceded each disorder is ongoing. Indeed, there are larger limitations in the assessment of schizophrenia spectrum syndromes than any assessment’s individual construct validity. These are understandable, due to the disorder’s complex etiology and overall institutional focus on diagnosis as a starting point. Given the vast number of contributing factors both preceding and subsequent to formal diagnosis, capturing the most salient dimensions of any particular patient’s experience requires a long list of assessments and extensive clinical interviewing. That is, if there were a healthy population out of which schizophrenia spectrum disorders arise, one cannot know their characteristics except perhaps through post-hoc inference as assessments capture only symptoms of the most extreme pole of disorders. Currently, there is no comprehensive assessment covering all or even most of the domains noted through clinical research and experience. As such, developing an informed treatment plan would demand a complex exploratory phase and numerous specific follow-up assessments to achieve reliable effectiveness; however, given the stereotyped nature of current schizophrenia treatment [ 1 , 2 , 3 , 4 ], such a comprehensive assessment would likely be too unwieldy for clinical use, or so broad as to merely perpetuate the problem.
Despite this, the schizotypal spectrum exists implicitly as an entire chapter in the DSM (though syndromes are arbitrarily demarcated) in the temporal evolution from brief psychotic disorder through to formal schizophrenia. In contrast, the autism spectrum exists as a single F-code with level of impairment handwritten in (Levels 1–3). At the present moment, the field appears to be quite confused as to how to understand the schizophrenia spectrum. This factor remarkably complicates assessment. Despite diagnostic confusion, known empirical correlates exist with MMPI3 and Rorschach, for example; however, such correlates exist for personality traits [ 47 ], Mondal & Kumar, 2021), which may be helpful in diagnosing shizoid PD and schizotypal PD, but less helpful for a brief psychotic episode all the way through to formal schizophrenia. One’s transient state greatly impacts presentation, a second complicating factor of assessment. Thirdly, scales on the MMPI such as Scale 8 (entitled “Schizophrenia” on the MMPI2) and Restructured Clinical Scale 8 (RC8; entitled “Bizarre Ideation”) on the MMPI3 do a fine job gathering data on positive symptoms, as does the Achenbach System of Empirically Based Assessment’s “Thought Problems” subscale [ 48 ], however, negative symptoms are easier to overlook and possess a more abstract developmental quality. This is decidedly problematic given the evidence that it is negative symptoms which most influence the etiology and the treatment of schizophrenia spectrum disorders [ 49 , 50 , 51 ].
Toward issues around diagnosis the problem is even more obtuse. As the current diagnostic model requires the presentation of 2 or more serious symptoms such as hallucinations or delusions for a significant period of time and persistence of disturbance for six months [ 8 ], clinicians are caught in an orientation of triage, approaching the problem after the fact. While the DSM-5TR does imply a manner of progression from brief psychotic disorder to schizophreniform disorder and finally schizophrenia, this interpretation also focuses on the presentation of the most extreme symptoms, creates an observational perspective (altering diagnoses as various milestones are reached), and ultimately fails to properly account for the broad heterogeneity of patient presentation and differential reactions to treatment [ 52 , 53 ].
It is an essential theoretical assumption that underlies the current paper that these categories more accurately represent extreme presentations along a spectrum of “schizotypy”; essentially, a spectrum which manifests diversity in presentation. Similar models already exist within psychology [ 54 ], as does the overall diagnostic mindset (e.g. identifying and treating those on the autism spectrum). It is believed that the spectrum framework better accounts for the heterogeneity of presentation and treatment outcome within the population with implications for more accurate prognosis and effective treatment. This also normalizes and contextualizes the variability and range of symptom expression. Said normalization carries not only ethical implications but also suggests dimensions of treatment that offer increased dignity and resilience to those currently experiencing the spectrum’s most distressing presentations while simultaneously opening avenues for pre-morbid interventions to prevent many otherwise healthy schizotypal individuals from experiencing said distress and its accompanying stigma. Indeed, “because the incontrovertibly psychotic diagnosis of schizophrenia fits people at the disturbed end of the schizoid continuum, and because the behavior of schizoid people can be unconventional, eccentric, or even bizarre, non-schizoid others tend to pathologize those with schizoid dynamics” [ 55 ], p. 196). Schizotypes find themselves in a double-bind: those with poor insight often have poor outcomes, and those who possess high insight are frequently besieged with depression, low self-esteem, and suicidality [ 56 ]. Thus, developing a comprehensive and destigmatizing model is an essential element in treating the population.
The presence or absence of psychosis is not an appropriate criterion measure of a distinct schizophrenia spectrum condition, nor is it deviant or divergent. Approximately 7% of the general population will have a psychotic experience within their lifetime. Of those 80% will be transitory, with only 7% going on to develop a psychotic disorder [ 21 ]. Psychotic experiences are also transdiagnostic and thus may be inappropriately conceptualized as unique to schizophrenia. “It is only when high levels of schizotypy are combined with other aetiological risk factors that an individual may be considered at risk for schizophrenia and other psychotic disorders. According to this perspective, unless high schizotypy is combined with other risk factors, it is considered neutral in regards to psychopathology” [ 57 ], as cited in [ 20 ].
The overall focus on psychosis (and, its “irrational” positive symptoms) is an axiomatic bias. However, there is empirical and clinical evidence that a population exists which is predisposed to psychotic experience and more likely to do so for much longer periods of time. If true, two questions must be answered. Firstly, what are the qualities which define this population and how do these qualities relate to psychotic experiences? Secondly, what factors (internally and externally) select some members for pathological expression?
Dimensional models
Spectra of phenomenology.
There is significant evidence supporting a dimensional reframing of psychological disorders [ 3 , 39 , 40 ]. During DSM–5 field trials, 40% of diagnoses did not meet cutoff for acceptable interrater reliability (IRR). Operationalized dimensionally, the same disorders achieved excellent IRR [ 39 ]. A dimension, in this context, is a psychological continuum stretching from the average range to extreme expression. It is the individual’s degree along a dimension and his specific dimensional interactions that ultimately lead to the higher order complexes addressed in psychotherapy.
The Hierarchical Taxonomy of Psychopathology (HiTOP) model, for example, describes ascending levels of complexity beginning with dimensions and rising through components, traits, syndromes, subfactors, spectra, and super-spectra. In such a conceptualization, an individual traditionally diagnosed as having depression, anxiety, and an attentional disorder is understood instead as having an interlocking network of specific and interacting anxiety, avoidant, and/or internalizing dimensions. Ultimately, a dimensional framework addresses many of the problems within categorical models, including heterogenous presentation, comorbidity, diagnostic instability, and unstable boundaries with normal psychological functioning, all while having a much stronger empirical basis [ 39 , 40 ].
In research on schizotypy and psychoticism, strong evidence exists that individuals manifesting these disorders instead represent a small cross-section of a more diverse psychological phenotype within the general population. As was noted, clinically significant psychotic experiences are not uncommon in the general population [ 21 ]. In a six-year general population study, it was found that subclinical positive psychotic experiences themselves were insufficient to predict transition into clinical disorder; alternatively, it was the presence and persistence of environmental factors such as childhood trauma, developmental problems and ethnic minority status, as well as severity of secondary distress due to these experiences that best predicted a disorder status [ 3 , 48 ]. Most individuals with psychotic experiences also carry an additional diagnosis (most often a mood disorder), and the presence of such a disorder is highly predictive of poor prognosis [ 21 ]. This is consistent with epidemiological research indicating that the negative symptom dimension (such as poor emotional expression and avolition) is a strong predictor of outcome measures, including the need for treatment at all [ 58 ].
As any phenomenology is reactive to its environment, it can be understood how stressful and traumatic experiences can begin altering patterns of cognition and behavior along such dimensional lines. While the more extreme presentations along the schizotypal spectrum (catatonia, flat affect, delusional thinking, etc.) may appear entirely unique, they are not inconsistent with trauma research. Those suffering traumatic or sufficiently stressful experiences often display magical thinking, irrational narratives, affectively-driven reactions incongruous with present reality, and behavioral tendencies towards withdrawal, explosive externalization, and somatic behavior [ 59 , 60 ]. Moreover, such experiences also create neurological and biological changes quite consistent with those in schizophrenia [ 61 , 62 , 63 ]. Thus conceived, even the most extreme presentations within the spectrum can be rooted in explicable and often even beneficial human behaviors and predilections, merely pushed beyond their capacity for stress.
Given the above, there is reason to believe that much of the current conceptualization of schizotypal individuals suffers from a kind of survivorship bias. That is, research is conducted and models are created based on those individuals already in sufficient distress to seek help, and in attempting to reverse-engineer an etiology, the most unusual symptoms are given priority. However, while the presence of positive symptoms such as hallucinations or delusions can certainly be distressing on their own, evidence suggests that these symptoms are acute responses to internal suffering and environmental stressors and rarely, if ever, rise to the level of clinical significance outside of prolonged and unresolved stress [ 48 , 64 , 65 , 66 ]. From a dimensional perspective, any psychopathology is understood as a dynamic interaction of symptoms influencing each other over time. Thus, in the earliest stages of an “illness,” symptoms are diffuse. Specific syndromes manifest only after prolonged influence and interaction. The specific expressed disorder depends on the nature of the stressors, the developmental stage in which they appeared, and their duration [ 48 , 66 ]. Equally or more important is the individual’s idiosyncratic response style based on differentiation of dynamics between mental states [ 48 ].
To reframe the problem in terms of the overall philosophical blind spots outlined earlier: In trying to understand the nature of schizophrenia so late in its etiology, those elements which seem most alien to our implicit beliefs about mental health are accepted as descriptive of and central to “the problem.” Consequently, we ignore those elements driving the observed symptoms, and subsequent treatment becomes mere management of those symptoms most distressing to norms and caretakers. This may be necessary when a schizotypal individual’s perceptions and thought patterns create distress, isolation, or additional issues; however, it is insufficient to claim that merely subduing these expressions is equivalent to successful treatment, if the underlying sources of stress, maladaptive defenses, and/or relational/attachment experiences remain.
Personality organization and clinical understandings
In her discussion about schizoid personality structure, McWilliams [ 55 ] limned its key traits from a psychodynamic perspective: (1) schizotypes are easily overstimulated and report the experience of their own and others’ affect as overwhelming (p. 198), (2) often perceive the world as threatening to damage or distort their individuality and security; “A deep ambivalence about attachment pervades their subjective life. They crave closeness yet feel the constant threat of engulfment by others; they seek distance to reassure themselves of their safety and separateness yet may complain of alienation and loneliness” (p. 201). (3) As favoring the defense of withdrawal (e.g. into fantasy or physical isolation) while often lacking many of the more common defenses (though projection, introjection, idealization, devaluation and intellectualization are not unheard of); “Under stress, schizoid individuals may withdraw from their own affect as well as from external stimulation, appearing blunted, flat, or inappropriate, often despite showing evidence of heightened attunement to affective messages coming from other” (p. 200). (4) they often speak and act in eccentric and non-conforming ways and may have a natural reliance on metaphor, symbolism, and creative expression when conveying thoughts and experiences; “Even when they see some expediency in fitting in, they tend to feel awkward and even fraudulent making social chitchat or participating in communal forms, regarding them as essentially contrived and artificial” (p. 204).
Applied under a dimensional framework (not incongruous with psychodynamic concepts such as defense mechanisms) the above qualities lead to a probability field of likely dynamics. For example, a person who instinctually withdraws when distressed, and receives little internal reinforcement for casual social interaction, is less likely to develop robust interpersonal skills while being simultaneously forced to understand and manage their powerful affect without guidance or community. If such a person also speaks and acts in an eccentric or unusual way, while maintaining sensitivity to others’ reactions, it is likely they will develop an “othered” conception of self. It is straightforward enough to see a potential for self-reinforcing patterns of pain, expression, social failure, withdrawal, and isolation. If this combines with a penchant for imagistic/symbolic thinking/representation, an entirely separate phenomenological language could begin to develop.
Germane to the larger point is that none of these components are pathological in and of themselves. Indeed, McWilliams argued that most schizoid-organized individuals are quite functional, some even highly so. Although they may be stigmatized and misunderstood (even, and perhaps especially, within the mental health field) due to an unexamined normativity bias [ 67 ], an effective clinician should explore both the valid content within their unusual expressions as well as the characterological strengths rather than assuming them to be meaningless, aberrant, or dangerous. In fact, she noted that working with such a client may be quite pleasant as they are often well in tune with their own internal dynamics and how those influence their own experiences and broader environment.
Personality research and parallels
A third conceptually parallel line of inquiry has been conducted within the frameworks of Five Factor Model of personality theory (FFM) which offers to blend the phenomenological depth of psychodynamic understanding with the scientific rigor of empirical inquiry along dimensional lines. While debates about the structure, components, evolution, and even the ontological nature of human personality are nearly endless, FFM is notable for several reasons. From a broadly conceptual standpoint, FFM stands out in that its development was nearly atheoretical; that is, rather than being reverse-engineered from an existing psychological or culturally instantiated models of human nature, it was instead derived in a bottom-up fashion based on factor-analysis of patterns with linguistic representations. This lends a certain assurance that the model contains fewer a priori assumptions than many of the other popular models espoused. Furthermore, from a more purely empirical perspective, FFM has shown remarkable performance in research settings.
While the initial model was developed through a lexical analysis of English, subsequent studies have been performed utilizing numerous other languages (e.g. Filipino, German, Czech, Dutch, Korean, Hebrew, etc.), which have reasonably confirmed the same five dimensional structure [ 68 , 69 , 70 , 71 ]. Cross-cultural multivariate behavioral genetic analysis demonstrated that the phenotypic structure of the FFM reflected a universal genetic and environmental structure [ 72 ]. Longitudinal studies have shown temporal stability across lifetime as well as the dimensions’ antecedent impact on later psychopathology [ 73 , 74 ], and FFM research indicates that dimensions such as neuroticism and extraversion are central elements underlying the vast majority of currently designated disorders [ 75 , 76 ]. This level of construct validity is lacking in current DSM-based personality disorders [ 77 ], and as was noted earlier in this paper, is an issue with current disorder constructs categorically.
As with any living model, there are varying ways of dividing and organizing the personality dimensions depending on the area of inquiry. For example, some models explore a construct directly labeled psychoticism, while others do not. Given the modular and hierarchical nature of the model though, it largely avoids the decoherence this diversity might otherwise imply. At core, FFM postulates that personality is composed of an individual’s position along five continuous dimensions: extraversion (sociability or positive affectivity), agreeableness (compassion or cooperation), conscientiousness (diligence or constraint), neuroticism (emotional instability or negative affectivity), and openness (intellect or unconventionality). Depending on the level of analysis, each dimension can be meaningfully decomposed into sub-elements (e.g. conscientiousness may be broken into component parts of orderliness and industriousness) [ 78 ] which can then be differentiated further into even more specific facets, behaviors, and tendencies. It is worth noting that it is at this level where the chirality between FFM and dimensional models such as HiTOP comes into focus; they do not neatly superimpose when reflected over each other; FFM being a bottom-up model beginning with foundational tendencies and investigating upwards and outwards, most other dimensional models may be viewed as top-down, beginning with a psychopathological state and deconstructing it into it constituent elements and antecedents. In the latter case, explorations of experiences such as hallucinations tend to cease at the point where hallucination-like experiences do. If (as this paper postulates) such higher-order expressions are emergent properties of entirely benign faculties, then such top-down explorations will have little insight into this non-pathological domain. Where FFM shows the greatest potential as a framework is in its potential for providing phenomenologically causal explanations for behavior rooted in “normal” personality structures while offering broad avenues for research into biological instantiation.
The schizotypal spectrum has been a robust area of interest within FFM research for a number of years. Most consistently, schizotypal individuals score highly on trait neuroticism and low on trait extraversion [ 79 , 80 , 81 ]. This is unsurprising in light of previously mentioned clinical profiles and the generally accepted symptoms within current taxonomies, as negative affectivity is found to load onto the former, while detachment loads onto the latter [ 82 ]. Additionally, research has indicated that low agreeableness is a factor in positive symptoms [ 81 ] and perhaps in manifestations overall [ 83 ] and some research has implicated low conscientiousness compared to “healthy” controls [ 52 ]. Most contemporary factor research highlights specific subcomponents of each dimension (e.g. the level of trust vs. mistrust within trait agreeableness is often indicated as accounting for much of the variability). However, given the high number and variability of these, a full overview is unwieldy.
Of particular interest within FFM schizotypy research is trait openness. While studies into the personality components of psychopathologies have consistently found meaningful contributions for the first four traits, the data around openness is much more variable. This has led to some speculation that trait openness is functionally dissociable from psychological disorders [ 84 , 85 ],however, it is consistently found to be one of the best personality markers for those on the schizotypal spectrum [ 86 , 87 ]. In parallel, it has been shown to carry greater variance with PID-5 Psychoticism [ 86 ].
The construct of openness provides perhaps the best theoretical basis within FFM for understanding the positive symptoms associated with schizotypy (e.g. hallucinations, delusions, disordered thoughts/behaviors, etc.). Broadly speaking, openness encompasses intelligence and creativity, or one's interest in ideas and one's interest in aesthetics [ 86 ]. It may be meaningfully differentiated into subcomponents such as openness to fantasy, aesthetics, feelings, actions, ideas, and values, and it is tied to scores on measures such as divergent thinking and fantasy-proneness [ 34 , 85 ]. There is an obvious conceptual link between these facets and many of the positive symptoms of interest; however, much of the research looking to tie the trait to specific symptoms has delivered conflicting results [ 86 ]. Some of the conflicting findings may be accounted for by the complex nature of the trait. For example, it has been demonstrated that while interest in aesthetics meaningfully predicts variance in positive symptoms, interest in ideas/intelligence has a negative correlation with the same [ 86 , 88 ]. This finding is supported in neural modeling research demonstrating that psychoticism, openness, and their shared variance were positively related to coherence in the default network (simulation of experience rather than attention to sensory input) and negatively related to coherence in the frontoparietal cortical network (voluntary control of attention), which have each been tied to psychosis and trait intelligence respectively [ 88 ]. Further research has shown that the positive dimension is better captured by measuring the “maladaptive” poles of the traits (i.e. the extreme high and low ends of expression) [ 83 , 87 , 89 , 90 ]. Within a cybernetic model, this predictive extreme is precisely what would be expected as such extremity would require equally extreme adaptation to achieve equilibrium. Moreover, with the context of the trauma work cited earlier, one would expect that highly stressful experiences would themselves push the natural pathways of behavior into radical adaptation.
Schizotypal individuals obtain higher scores in divergent thinking [ 91 ], a trait linked to openness as well as creative performance generally [ 9 , 87 , 92 ]. Fractional anisotropy measurements of white matter integrity have shown “an apparent overlap in specific white matter architecture underlying the normal variance of divergent thinking, openness, and psychotic-spectrum traits, consistent with the idea of a continuum” [ 92 ]. As well, trait openness and creative achievement show a negative correlation with latent inhibition (cognitive shielding from information previously coded as irrelevant), indicating a higher psychological permeability [ 89 ], consistent with the noted sensitivity and eccentricity of schizoid individuals within psychodynamic understandings.
FFM research generally finds openness to ideas and openness to aesthetics to be distinct factors. There is evidence for opposing influences between the two factors and positive psychotic symptoms, and correlational data indicates a relationship between the aesthetic/fantasy-prone dimension and schizophrenia spectrum disorders; therefore, a discussion of the psychological concept of aesthetics is relevant.
While a full interrogation of the science of aesthetics is beyond the scope of this paper, contemporary literature highlights some salient points about component experience. Firstly, that aesthetic appreciation derives neither from simple perception nor from straightforward complexity, but instead arises as a higher-order experience comprised of an evaluative dimension (sensory‐motor), a phenomenological/affective dimension (emotion‐valuation), and semantic (meaning‐knowledge) and their neural correlates [ 93 , 94 ]. Secondly, the appreciation arises from the diversity of sources of information that come into play, and the diversity of ways in which this information can be used, combined, and associated [ 95 ]. Thirdly, the aesthetic response can be reflexive and momentary, or manifest in long-lasting mood shifts [ 95 ]. Notably, this higher-order and emergent experience goes some way toward accounting for some of the difficulty in measuring motivational patterns in openness [ 36 , 96 ], which often seek to measure the value of merely novel information without context. As well, to the extent that schizotypal-spectrum experiences load onto openness and are dopaminergic, it dove-tails cleanly with dopamine models understanding the phenomenological function of the neurotransmitter as coding emotional salience [ 97 , 98 ]. As currently the dopamine hypothesis is one of the leading biological explanations for schizophrenia-spectrum disorders, this begins to offer a more intuitive understanding of such findings.
Comprehensively, this evidence indicates that the aesthetic dimension of openness implicated in schizotypal research is driven by an experience of derived or constructed meaning in complex stimuli. That is, recognizing and associating patterns (across sensory, affective, and cognitive levels) and deriving meaning. This is important as it begins to provide a phenomenological outline with potential neural mechanisms for many of the seemingly more inexplicable traits associated with the spectrum such as delusional thinking, disordered speech, and magical thinking in scientific research, as well as the noted predilection for symbolic and metaphorical understanding and high affective sensitivity in psychodynamic conceptualizations.
Contemporary approaches
Schizophrenia and related disorders occupy a unique place within the social consciousness. While contemporary discourse around mental health has demystified and destigmatized many disorders, experience of psychosis is rarely included in this trend. Even within the mental health field, individuals experiencing psychotic symptoms are differentially received. Clinicians across disciplines stigmatize patients with schizotypal spectrum syndromes more than patients with other diagnoses [ 99 , 100 , 101 ]. “Schizophrenia is one of the most serious and frightening of all mental illnesses. No other disorder arouses as much anxiety in the general public, the media, and doctors” [ 102 ], p. 91).
De-stigmatising psychosis as a symptom both separate from schizophrenia proper and “mad” in it’s own right is a hallmark of the Hearing Voices Movement (HVM), which began in the late 1980’s [ 18 , 103 ]. “Some disability scholars further emphasize the role of ‘madness as testimony’: as Clementine Morrigan explains, so-called symptoms occurring in the wake of trauma may in fact be ‘acts of resistance to violence,’ a means of sounding an alarm that something is very wrong” [ 18 ], p. 138).
More research is needed to establish an evidence-base for Hearing Voices Groups (HVGs); however, such psychosocial interventions hold promise, particularly since isolation is often a hallmark of both schizotypy and psychosis. Such group therapies approach treating the voices (auditory hallucinations) as non-pathological and not necessarily a sign that one is mentally ill. Participants in HVGs have reported a sense of higher self-esteem and social competence [ 104 , 105 ], while those who have learned to form more positive and active relationships with their voices have reported a less negative and sometimes supportive and beneficial relationship with said voices [ 106 , 107 , 108 ] Groups are growing, international, and are usually led by a “voice hearer” and a clinical practitioner. Though CBT interventions appear to be the most promising in terms of change mechanisms, more randomized clinical trials are needed [ 103 ]. Another psychosocial intervention that may hold promise is the concept of the Phone Pal (Into de Costa, 2020) to combat isolation in those experiencing psychosis. Marriage and family therapy is also effective for treating first-episode psychosis and reducing relapse rates [ 109 ].
Read and Dillon [ 3 ] utilized a grounded theory approach to collect qualitative data related to identifying effective psychosocial interventions. Researchers found that in cases of first-episode psychosis after which the patient desired to talk about and explore the experience, assisting the patient in such a discussion was therapeutic. Though it may be theoretically “simple,” perhaps it is in the process of relating to a caring and authentic other that one may find and share one’s own voice and begin to consolidate experiences. Such understanding embodies insight, which then results in a patient who “integrates” rather than “seals over” the psychotic experience. “Sealing over is the tendency to dismiss the experience as having little personal relevance, whereas ‘integration’ reflects a curiosity about the experience and its personal significance” [ 3 ], p. 180).
Within the Open Dialogue (OD) approach, patients within the population required the use of neuroleptics less frequently and for shorter periods [ 19 ]. While more an approach to care than a specific intervention, the hallmark of OD is shared decision- and meaning-making processes, aiming to guarantee both continuity of care and an immediate need-adapted and social network-oriented response. Research into interfamily therapy (which seeks to generate a conversation where experiences can be shared, and emotions can be expressed safely) has indicated lower relapse rates, with fewer psychiatric admissions and of shorter duration among patients during the year of participation [ 109 ], while a meta-analysis of 14 studies showed that family intervention in first psychotic episodes led to a 58% reduction in relapse rates, shorter duration of hospitalizations, less severe psychotic symptoms and improved functionality up to 24 months after the intervention [ 110 ].
In accounting for trauma within psychosis treatment, post-traumatic growth (PTG) was found to be elicited through narrative interaction with themes of meaning in life, coping self-efficacy and core beliefs; mediating the relationship between total PANSS scores and PTG. Notably, emotional experience was noted as the least frequent facilitator of PTG, casting doubt on the symptom -focused approaches of current treatment [ 111 ]. Consistent with this, individuals experiencing psychosis who engaged in poetry as a form of therapy and expression reported greater experiences of integration and acceptance, and overall higher senses of meaning and efficacy, through the practice. It was postulated that such carnivalesque spaces (in which the alternative, transgressive or idiosyncratic are explorable and celebrated) directly supported the wellbeing of the participants [ 112 ].
Taken in aggregate, the successes and implications of these approaches lends strong support to the overall premise of the proposed conceptualization. Namely, that the targeted eccentricities of schizotypal individuals are not themselves the issue within the population, but instead it is underlying stress and distress which drives the formation of states such as schizophrenia; and thus must themselves be the target of effective intervention. Moreover, that in reconnecting such individuals with others, providing a voice to meaningfully express their experiences, utilizing their sense of creativity and divergent thinking, and engaging their inner representational dynamic, the suffering experienced by schizotypal individuals can be mitigated without stigma or permanent pharmaceutical interventions.
“A good metaphor for psychotherapy of psychosis could be that it is a form of prayer: striving to bring order out of chaos, helping patients recover confidence in their humanness, seeking something of a resurrection, returning the patient to emotional life from a position of deadness” [ 3 ], p. 245).
Clinical implications
Taken as converging lines of evidence, the aforementioned paradigm allows for a reconceptualization of the psychopathology currently understood as schizophrenia and its related disorders as emergent properties of a particular spectrum of psychological predispositions under stress. Although a dimensional model, it does not adhere to any currently proposed but instead seeks to harmonize the evidence collected across multiple lines of inquiry. With this in mind, we propose a cybernetic model, which accounts not only for the strengths of dimensional templates but provides a means for elucidating the nature of development within and amongst those dimensions over time; offering means of understanding the emergent properties manifested in extreme poles or interactions. Models such as HiTOP are understood as arriving at their traits and dimensions from a predominantly “top-down” approach, working backwards from observed disorders to identify their constituent parts. Models such as FFM are oriented from a predominantly “bottom-up” perspective, and so can better capture what may be meant by normal personality. In so doing, it is proposed that informed clinicians would better understand how a person's natural interest in aesthetics might predispose them to proto-psychotic equilibrated states (thus aiding prognosis and early intervention) while also indicating how one might utilize this trait in strength-based treatment. As FFM already contains frameworks for understanding its dimensions as motivational frames, the component forces driving the homeostatic tendencies within the psyche (which give rise to the defense mechanisms and idiosyncratic feedback loops schizotypal syndromes would likely display) are explicable. While such a view certainly helps to normalize what might otherwise be seen as inexplicable psychosis, it also offers avenues for more robust and bespoke treatment and early identification of at-risk individuals.
At very early ages these individuals would likely have the heritable biological predispositions toward a specific general profile of FFM personality traits; namely some combination of high openness, low extraversion, high neuroticism, and low agreeableness. Probable attributes include high sensitivity to their external environment [ 55 , 113 ] and relatively socially reserved disposition [ 55 , 114 ]. Attachment theory research has shown how fundamental habits of behavior within mother-infant dyads create characteristic patterns that reinforce over time (Bowlby, as cited in [ 115 ]. Natural inclinations toward introversion and cognitive abstraction are likely to become reinforced by the overall social environment. Additionally, it is feasible that such individuals would be differentially rewarded for information-seeking, complex and conceptual pattern identification, and social interaction. As the individual developed his natural inclinations combined with idiosyncratic environmental patterns, disposition would tend toward the broad personality profiles described in psychodynamic literature, namely introverted, outwardly eccentric, metaphorically and fantasy-oriented, affectively and behaviorally sensitive, and favoring withdrawal when psychologically threatened. They would likely show heightened divergent thinking, be creatively or intellectually motivated, display less regard for social expectations, and show lower levels of trust in others overall.
Where the risk develops is in how these factors can interact under highly stressful and traumatic experiences. A natural tendency to withdraw rather than express leaves a person, particularly a developing child, far more vulnerable to further psychological damage [ 65 , 116 ]. Childhood trauma victims often develop magical or illogical narratives to conceptualize their experiences while maintaining identity integrity and basic trust. Children who do not externalize distress are far less likely to receive direct help or more mature interpretations from adults in their lives, and thus those beliefs are less likely to be revised. Introverted and eccentric children are predisposed to fewer and less frequent social interactions, yielding a slower growth curve in social competence, thus widening the gap and reinforcing natural tendencies to withdraw. Higher natural neuroticism creates a more sensitive threat-detection response, which coupled with natural distrust, high sensitivity to affect and behavior, divergent thinking, and high internal motivation toward complex pattern resolution, creates a network of feedback loops favoring loose, complex, affectively potent interpretive frameworks built on an internal lexicon to some degree tangential to consensus social understandings. As initially small and disparate behaviors and cognitive tools become habit, they begin to interact and create more complex syndromes based on the individuals’ natural tendencies, their specific environment, and their own phenomenological choices. The specific complexes will be in some ways unique; however, they will follow relatively predictable patterns. Based on the severity and specific combination of these, an individual is then ultimately given a categorical diagnosis of schizophrenia, schizoaffective, etc.
What is principal under this view is that while the traits underlying the more unique features of schizotypal psychosis are involved in the etiology of the disorder, none of them are themselves inherently pathological. Instead, they act as “paths of least resistance,” and in some cases, socio-behavioral risk factors when faced with highly stressful or traumatic experiences. In many ways, the symptoms of delusions, hallucinations, and disordered speech/behavior, etc., would then represent the individual’s greatest psychological strengths pushed well outside of their functional equilibrium and ultimately forced into self-reinforcing feedback loops. However, as it is trauma and emotional pain acting as fuel for these specific symptoms, it is here where treatment ought to focus. Certainly, the presence of psychotic symptoms would necessitate approaches specific to their management and interpretation; however, overall approaches would be formulated much more heavily along trauma recovery lines (i.e. establishing safety, building authentic relationships, reconnecting with the social environment, etc.). Indeed, it is likely that robust and prolonged treatment would need to engage constructively with the individual’s natural areas of strength as part of its process as they will represent that individual’s highest yield sources of positive affect, self-esteem, social recognition, etc. For example, to gain the benefits of greater social engagement, the schizotypal individual must be given the skills to utilize their naturally metaphorical style of communication effectively (rather than pushing them to conform to more traditional social expectations) for the interaction to feel authentic and the sense of connection to be meaningful.
Within a cybernetic model of the human psyche, the state of equilibrium is itself endlessly complex; inasmuch as it requires achieving physiological needs, fulfilling interpersonal needs, maintaining needs around identity and meaning, the solutions to which (in each case) impact one’s ability to do each of the others and more. This is further complicated by the fact that humans are dynamic and goal-oriented creatures, and so this state is itself a moving target constantly informed by experiences and shifting patterns of response. For conceptual purposes only, the specifics will be subsumed into the word equilibrium for now; however, by utilizing this lens, clear bridges can be made between the domains of clinical psychodynamics, personality theory, and biological research. What is frequently discussed under names of defense mechanisms, cognitive distortions, and behavioral patterns, etc., are understood as solutions and corrective measures to achieve this equilibrated state, the specifics of which are shaped by the natural inclinations of the individual (e.g. low extraversion) and their idiosyncratic experiences.
For example, an abused child may develop a narrative of nearly magical self-blame, as their ability to solve the problem of their suffering is nearly zero; however, they must find a logical explanation for their experiences to manage their anxiety, confusion, loss, and pain. Less extreme, a socially anxious person may simply stop engaging with people at all to keep anxiety tolerable. Each person’s specific needs will vary based on their makeup (this is roughly what is called “personality” in FFM), and thus there will be characteristic strategies, obstacles, and areas of flourishing individuals will construct along the way. However, as psyches are permeable structures by any measure, that natural equilibrium point can be moved over a lifetime. Each adaptation creates new forces of its own and must be accounted for by the others, thus necessitating new adaptations. A stressor of sufficient duration or intensity may demand such extreme adjustment that the settling point itself is (more or less) permanently moved. Within the dimensional models such as HiTOP, this is roughly the process by which dimensions impact each other and combine to ultimately create symptoms and syndromes.
In the case of schizotypy, we can highlight some tendencies. Naturally high levels of emotional salience beget heightened need for affect management; as they are likely also to score high in neuroticism, much of this heightened affect is likely to be anxiety-related. Tendencies toward introversion mean fewer opportunities to express internal states or experience other’s internal states. Differential motivation and reward systems create interest toward complex and abstract constructs (ideas, aesthetics, literature, etc.) and favors the individual toward inner worldbuilding over outer worldbuilding. During stressful experiences, natural tendencies to withdraw, to use imagination and abstract problem-solving skills, etc. are favored and likely to become habitual parts of identity. As is with any human trait or capacity, these bring their own sets of challenges and advantages; however, they are themselves neither pathological nor particularly unusual. Nonetheless, under extreme or prolonged stress, his natural tendencies can put the schizotypal person at heightened risk. Tendencies to withdraw mean that they are less likely to receive aid from others, and so prolonged isolated suffering is more likely. Heightened emotional salience means that the likelihood of an emotional overload is increased. Natural strengths in divergent thinking, coupled with tendencies toward abstraction, pattern recognition, and problem solving are likely to leave an individual anxiously searching their environment for explanations for and solutions to their unbearable feelings while receiving very little input from others.
Over time and based on the nature of the psyche-environment interaction, the entire structure of psychic equilibrium can begin moving in profound ways as the individual attempts to use the tools available and the conceptions to which they have experiential access, to navigate the world and manage their own phenomenology. Thus, natural abilities like divergent thinking, or tendencies such as withdrawal into fantasy, begin to themselves become overly stressed and utilized and may themselves become sources of stress as the person moves through life. However, while observing such a mind well into this process (e.g. unequivocal schizophrenia), though its entire makeup may appear fundamentally illogical, it is in fact a complex psychological adaptation to challenges and suffering in life. That is, constructs such as schizophrenia are unstable, heterogenous, and contentious because they are emergent properties within a complex and self-correcting system. While certainly accounting for etiology, heterogeneity, as well as currently clinically unaccounted for though empirically verified biopsychosocial factors, this frame also opens up approaches to treatment that account for differential motivational patterns (as established in FFM research), which indicate potentially effective strength-based modalities for the population.
The various models, perspectives, and orientations discussed so far represent a wide cross-section of interest into the phenomenon of psychosis and schizophrenia spectrum disorders, as well as personality and psychological research. It is the stance of this paper that these and others represent converging lines of evidence for a schizotypal population naturally occurring within the larger human population overall. Furthermore, this population would span the range from “normal” and “high-functioning” individuals to those experiencing major and prolonged schizophrenic episodes. This schizotypal population would thus be best conceptualized as a cohort “at-risk” of schizotypal psychosis; depending on the number of relevant traits held, their overall intensity, their interactions with each other, and interactions with the environment. The disorders referred to as schizophrenia, schizoaffective, STPD, etc., represent relatively stable emergent states of consciousness appearing as a result of stressful and traumatic experiences within an otherwise healthy population. While their specific presentations may be particularly disorienting and extreme within foundational rationalistic frameworks, they are, in fact, extensions of natural human adaptations under prolonged and/or extreme duress.
Under the proposed conceptualization, a dimensional model similar to HiTOP views the higher-order symptoms accounted for in the DSM as phenomena emergent from specific combinations of more general and mutually influencing sub-traits and behaviors. Rooted in FFM research, this model can be extended beyond simple decomposition of maladaptive traits and defense mechanisms and thus understand how such extreme outcomes arise out of “normal” human personality features while accounting for heritable and biological substrate noted throughout the literature. Functionally, the model reconceptualizes the biological and phenomenological development of more extreme schizotypal presentations as a cybernetic system, in which the ongoing interactions of multiple elements attempting equilibrium to experiences of trauma and stress (whether acute, periodic, or ongoing) arrive at explicable resting states. Thus, disorders such as schizophrenia can be understood as emergent properties of more fundamental systemic interactions rather than discrete disorders in and of themselves. Such a model would account for the clinically significant distinction between those experiencing psychotic episodes and those diagnosed with a schizophrenia-spectrum disorder, as well as the apparent contradiction between the heterogeneity of presentation and the phenotypic resemblance of said disorders.
To the extent that the above is true, this allows not only for a more accurate and tailored understanding of etiology, but also suggests means of risk factor detection early in life and a theoretically sound strengths-based approach to treatment accounting for the underlying affective and characterological engines behind currently targeted symptoms. In so doing, the heterogeneity of traditionally taxonomic disorders is accounted for while offering conceptual bridges between biological, cognitive-behavioral, and psychodynamic understandings of the population and outlining explanatory frameworks for differences between brief psychotic episodes, ongoing and degenerative schizotypal-spectrum disorders, and those cases of total or periodic remission attested to in more culturally diverse literature.
It is the hope of the authors that the proposed understanding of schizotypy as a spectrum rooted in natural and even beneficial psychological functions, and with explicable trauma-driven manifestations, will assist not only in furthering the field’s knowledge of human functioning and treatment of psychosis, but also begin to remove the stigma and aversion which have grown around the concepts. Grounded assessments for early detection will offer incremental validity to a genuinely biopsychosocial approach to research, treatment, and ongoing patient management.
Availability of data and materials
Not applicable.
Kane JM, Marder SR. Psychopharmacologic treatment of schizophrenia. Schizophr Bull. 1993;19(2):287–302. https://doi.org/10.1093/schbul/19.2.287 .
Article Google Scholar
Patel KR, Cherian J, Gohil K, Atkinson D. Schizophrenia: overview and treatment options. Pharmacy and Therapeutics. 2014;39(9):638.
Google Scholar
Read J, Dillon J. Models of Madness: Psychological, social, and biological approaches to psychosis. Routledge; 2013.
Book Google Scholar
Zipursky RB. Why are the outcomes in patients with schizophrenia so poor? J Clin Psychiatry. 2014;75(suppl 2):22442. https://doi.org/10.4088/JCP.13065su1.05 .
Tasch G, Gøtzsche, P.C. Systematic violations of patients’ rights and safety: forced medication of a cohort of 30 patients in Alaska. Psychosis. 1–10. 2023. https://doi.org/10.1080/17522439.2023.2183428
Bustillo JR, Chen H, Gasparovic C, Mullins P, Caprihan A, Qualls C, et al. Glutamate as a marker of cognitive function in schizophrenia: a proton spectroscopic imaging study at 4 Tesla. Biol Psychiatry. 2011;69(1):19–27.
Leamy M, Bird V, Le Boutillier C, Williams J, Slade M. Conceptual framework for personal recovery in mental health: systematic review and narrative synthesis. Br J Psychiatry. 2011;199(6):445–52.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders (5th Ed. - Text Revision). 2022.
Fink A, Weber B, Koschutnig K, Benedek M, Reishofer G, Ebner F, Papousek I, Weiss EM. Creativity and schizotypy from the neuroscience perspective. Cogn Affect Behav Neurosci. 2014;14(1):378–87. https://doi.org/10.3758/s13415-013-0210-6 .
Jobe TH, Harrow M. Long-term outcome of patients with schizophrenia: a review. The Canadian Journal of Psychiatry. 2005;50(14):892–900.
van Os J, Kenis G, Rutten BPF. The environment and schizophrenia. Nature. 2010;468:203–12. https://doi.org/10.1038/nature09563 .
Brand RM, McEnery C, Rossell S, Bendall S, Thomas N. Do trauma-focussed psychological interventions have an effect on psychotic symptoms? A systematic review and meta-analysis. Schizophr Res. 2018;195:13–22. https://doi.org/10.1016/j.schres.2017.08.037 .
Dominguez MDG, Wichers M, Lieb R, Wittchen HU, van Os J. Evidence that onset of clinical psychosis is an outcome of progressively more persistent subclinical psychotic experiences: an 8-year cohort study. Schizophr Bull. 2011;37(1):84–93.
Thomas S, Höfler M, Schäfer I, Lew-Starowicz M. Childhood maltreatment and treatment outcome in psychotic disorders: A systematic review and meta-analysis. Acta Psychiatry Scandinavica. 2019;140:295–312. https://doi.org/10.1111/acps.13077 .
Chong HY, Teoh SL, Wu DB, Kotirum S, Chiou CF, Chaiyakunapruk N. Global economic burden of schizophrenia: A systematic review. Neuropsychiatr Dis Treat. 2016;16(12):357–73. https://doi.org/10.2147/NDT.S96649 .
Slife BD. Theoretical challenges to therapy practice and research: The constraint of naturalism. In: Lambert M, editor. Handbook of psychotherapy and behavior change. New York: Wiley; 2004. p. 44–83.
Luhrmann, T. M., & Marrow, J. (Eds.). Our most troubling madness: Case studies in schizophrenia across cultures (Vol. 11). Univ of California Press. 2016.
Higgs RN. Reconceptualizing psychosis: the hearing voices movement and social approaches to health. Health Hum Rights. 2020;22(1):133.
Bergström T, Seikkula J, Köngäs-Saviaro P, Taskila JJ, Aaltonen J. Need adapted use of medication in the open dialogue approach for psychosis: A descriptive longitudinal cohort study. Psychosis. 2023;15(2):134–44. https://doi.org/10.1080/17522439.2022.2134444 .
Nelson MT, Seal ML, Pantelis C, Phillips LJ. Evidence of a dimensional relationship between schizotypy and schizophrenia: a systematic review. Neurosci Biobehav Rev. 2013;37(3):317–27. https://doi.org/10.1016/j.neubiorev.2013.01.004 .
van Os J, Reininghaus U. Psychosis as a transdiagnostic and extended phenotype in the general population. World Psychiatry. 2016;15(2):118–24. https://doi.org/10.1002/wps.20310 .
Escher S, Romme M. The hearing voices movement. Hallucinations: Research and practice. 2012. p. 385–393. https://doi.org/10.1007/978-1-4614-0959-5_28 .
Schulze, B., & Angermeyer, M. C. Subjective experiences of stigma. A focus group study of schizophrenic patients, their relatives and mental health professionals. Soc Sci Med. 2003;56(2), 299–312. https://doi.org/10.1016/S0277-9536(02)00028-X
Dickerson FB, Sommerville J, Origoni AE, Ringel NB, Parente F. Experiences of stigma among outpatients with schizophrenia. Schizophr Bull. 2002;28(1):143–55. https://doi.org/10.1093/oxfordjournals.schbul.a006917 .
Henry JD, von Hippel C, Shapiro L. Stereotype threat contributes to social difficulties in people with schizophrenia. Br J Clin Psychol. 2010;49:31–41. https://doi.org/10.1348/014466509X421963 .
Rüsch N, Angermeyer MC, Corrigan PW. Mental illness stigma: Concepts, consequences, and initiatives to reduce stigma. Eur Psychiatry. 2005;20(8):529–39. https://doi.org/10.1016/j.eurpsy.2005.04.004 .
Shaheen S, Amin R. Effects of internalized stigma on symptoms and quality of life in schizophrenic patients; mediated by dysfunctional attitude. International Journal Of Health. 2016;4(2):145. https://doi.org/10.14419/ijh.v4i2.6754 .
Valery KM, Prouteau A. Schizophrenia stigma in mental health professionals and associated factors: A systematic review. Eur Psychiatry. 2022;65(S1):S617.
Wheeler Z. Treatment of schizoid personality: An analytic psychotherapy handbook (Doctoral dissertation, Pepperdine University). 2013.
Hume D. A treatise of human nature. Clarendon Press; 1896.
Kant I. Critique of Pure Reason (The Cambridge Edition of the Works of Immanuel Kant) (P. Guyer & A. Wood, Eds.). Cambridge: Cambridge University Press. 1998. https://doi.org/10.1017/CBO9780511804649
Piaget J. The Psychology of Intelligence. Routledge; 2001.
Kuhn TS. The structure of scientific revolutions. The University of Chicago Press. 1970.
McCrae RR, Costa PT Jr. The five-factor theory of personality. In: John OP, Robins RW, Pervin LA, editors. Handbook of personality: Theory and research. The Guilford Press; 2008. p. 159–81.
Anstrom KK, Miczek KA, Budygin E. Increased phasic dopamine signaling in the mesolimbic pathway during social defeat in rats. Neuroscience. 2009;161(1):3–12. https://doi.org/10.1016//j.neuroscience.2009.03.023 .
Smillie LD, Bennett D, Tan NP, Sutcliffe K, Fayn K, Bode S, Wacker J. Does openness/intellect predict sensitivity to the reward value of information? Cogn Affect Behav Neurosci. 2021;21(5):993–1009. https://doi.org/10.3758/s13415-021-00900-1 .
Kotav R, Krueger RF, Watson D, Achenbach TM, Althoff RR, Bagby RM, Brown TA, Carpenter WT, Caspi A, Clark LA, Eaton NR, Forbes MK, Forbush KT, Goldberg D, Hasin D, Hyman SE, Ivanova MY, Lynam DR, Markon K, Miller JD, Moffitt TE, Morrie LC, Sweatt-Mullins SN, Ormel J, Patrick CJ, Regier DA, Rescorla L, Ruggero CJ, Samuel DB, Selbom M, Simms LJ, Skodol AE, Slade T, South SC, Tackett JL, Waldman ID, Waszczuk MA, Widiger TA, Wright AGC, Zimmerman M. The hierarchical taxonomy of psychopathology (HiTOP): A dimensional alternative to traditional nosologies. J Abnorm Psychol. 2017;126(4):454–77. https://doi.org/10.1037/abn0000258 .
Maj M. Why the clinical utility of diagnostic categories in psychiatry is intrinsically limited and how we can use new approaches to complement them. World Psychiatry. 2018;17(2):121. https://doi.org/10.1002/wps.20512 .
Waszczuk MA, Kotov R, Ruggero C, Gamez W, Watson D. Hierarchical structure of emotional disorders: From individual symptoms to the spectrum. J Abnorm Psychol. 2017;126(5):613. https://doi.org/10.1037/abn0000264 .
Widiger TA, Trull TJ. Plate tectonics in the classification of personality disorder: shifting to a dimensional model. Am Psychol. 2007;62(2):71. https://doi.org/10.1037/0003-066X.62.2.71 .
Pickersgill MD. Debating DSM-5: Diagnosis and the sociology of critique. J Med Ethics. 2014;40(8):521–5. https://doi.org/10.1136/medethics-2013-101762 .
Maj M, van Os J, De Hert M, Gaebel W, Galderisi S, Green MF, Guloksuz S, Harvey PD, Jones PB, Malaspina D, McGorry P, Miettunen J, Murray RM, Nuechterlein KH, Peralta V, Thornicroft G, van Winkel R, Ventura J. The clinical characterization of the patient with primary psychosis aimed at personalization of management. World Psychiatry. 2021;20(1):4–33. https://doi.org/10.1002/wps.20809 .
Cuthbert BN, Insel TR. Toward the future of psychiatric diagnosis: the seven pillars of RDoC. BMC med. 2013;11 B(1), 1–8. https://doi.org/10.1186/1741-7015-11-126
Leichsenring F, Steinert C. Is cognitive behavioral therapy the gold standard for psychotherapy?: The need for plurality in treatment and research. JAMA. 2017;318(14):1323–4. https://doi.org/10.1001/jama.2017.13737 .
van Nierop M, Viechtbauer W, Gunther N, Van Zelst C, De Graaf R, Ten Have M, van Dorsselaer S, Bak M, van Winkel R. Childhood trauma is associated with a specific admixture of affective, anxiety, and psychosis symptoms cutting across traditional diagnostic boundaries. Psychol Med. 2015;45(6):1277–88. https://doi.org/10.1017/S0033291714002372 .
Wiener N. Cybernetics or control and communication in the animal and the machine. MIT press. 2019.
Brown TA, Sellbom M. Associations between MMPI-3 scale scores and the DSM-5 personality styles. J Clin Psychol. 2021;77:2943–64. https://doi.org/10.1002/jclp.23230 .
Wigman J, van Winkel R, Raaijmakers Q, Ormel J, Verhulst SA, Reijneveld J, van Os J, Vollebergh W. Evidence for a persistent, environment-dependent and deteriorating subtype of subclinical psychotic experiences: a 6-year longitudinal general population study. Psychol Med. 2011;41(11):2317–29. https://doi.org/10.1017/S0033291711000304 .
Binbay T, Drukker M, Elbi H, Tanık FA, Özkınay F, Onay H, Zağli N, van Os J, Apterin K. Testing the psychosis continuum: differential impact of genetic and nongenetic risk factors and comorbid psychopathology across the entire spectrum of psychosis. Schizophr Bull. 2012;38(5):992–1002. https://doi.org/10.1093/schbul/sbr003 .
Dominguez MDG, Saka MC, Lieb R, Wittchen HU, van Os J. Early expression of negative/disorganized symptoms predicting psychotic experiences and subsequent clinical psychosis: a 10-year study. Am J Psychiatry. 2010;167(9):1075–82. https://doi.org/10.1176/appi.ajp.2010.09060883 .
Maj M. Beyond diagnosis in psychiatric practice. Ann Gen Psychiatry. 2020;19(1):1–6. https://doi.org/10.1186/s12991-020-00279-2 .
Cicero DC, Jonas KG, Li K, Perlman G, Kotov R. Common taxonomy of traits and symptoms: linking schizophrenia symptoms, schizotypy, and normal personality. Schizophr Bull. 2019;45(6):1336–48. https://doi.org/10.1093/schbul/sbz005 .
Wigman JT, van Os J, Thiery E, Derom C, Collip D, Jacobs N, Wichers M. Psychiatric diagnosis revisited: towards a system of staging and profiling combining nomothetic and idiographic parameters of momentary mental states. PLoS ONE. 2013;8(3): e59559. https://doi.org/10.1371/journal.pone.0059559 .
Barrantes-Vidal N, Grant P, Kwapil TR. The role of schizotypy in the study of the etiology of schizophrenia spectrum disorders. Schizophr Bull. 2015;41(Suppl 2):S408–16. https://doi.org/10.1093/schbul/sbu191 .
McWilliams N. Psychoanalytic diagnosis: Understanding personality structure in the clinical process. Guilford Press. 2011.
Lysaker PH, Vohs J, Hillis JD, Kukla M, Popolo R, Salvatore G, Dimaggio G. Poor insight into schizophrenia: contributing factors, consequences and emerging treatment approaches. Expert Rev Neurother. 2013;13(7):785–93.
Rawlings D, Williams B, Haslam N, Claridge G. Is schizotypy taxonic? Response to Beauchaine, Lenzenweger, and Waller. Personality Individ Differ. 2008;44(8):1663–72. https://doi.org/10.1016/j.paid.2008.01.021 .
Tortorella A. We should improve personalization of management in patients with a diagnosis of schizophrenia. J Clin Med. 2021;11(1):184. https://doi.org/10.3390/jcm11010184 .
Alvarez MJ, Roura P, Osés A, Foguet Q, Solà J, Arrufat FX. Prevalence and clinical impact of childhood trauma in patients with severe mental disorders. J Nerv Ment Dis. 2011;199(3):156–61. https://doi.org/10.1097/NMD.ob013e31820c751c .
Lingiardi, V., & McWilliams, N. (Eds.). The personality diagnostic manual: PDM-2 (2nd ed.). The Guilford Press. 2017.
Buss C, Lord C, Wadiwalla M, Hellhammer DH, Lupien SJ, Meaney MJ, Pruessner JC. Maternal care modulates the relationship between prenatal risk and hippocampal volume in women but not in men. J Neurosci. 2007;27(10):2592–5. https://doi.org/10.1593/JNEUROSCI.3252-06.2007 .
Pollak SD, Nelson CA, Schlaak MF, Roeber BJ, Wewerka SS, Wiik KL, French KA, Logan MM, Gunnar MR. Neurodevelopmental effects of early deprivation in postinstitutionalized children. Child Dev. 2010;81(1):224–36. https://doi.org/10.1111/j.1467-8624.2009.01391.x .
van Harmelen AL, van Tol MJ, van der Wee NJ, Veltman DJ, Aleman A, Spinhoven P, van Buchen MA, Zitman FG, Penninx B, Elzinga BM. Reduced medial prefrontal cortex volume in adults reporting childhood emotional maltreatment. Biol Psychiat. 2010;68(9):832–8. https://doi.org/10.1016/j.biopsych.2010.06.011 .
Cougnard A, Marcelis M, Myin-Germeys I, DeGraaf R, Vollebergh W, Krabbendam L, Lieb R, Wittchen H, Henquet C, Spauwen J, Van Os J. Does normal developmental expression of psychosis combine with environmental risk to cause persistence of psychosis? A psychosis proneness-persistence model. Psychol Med. 2007;37:513–27. https://doi.org/10.1017/S0033291706009731 .
Georgiades, A., Almugrin, A., Rubinic, P., Mouhitzadeh, S., Tognin, S., & Mechelli, A. (2023). Psychosocial stress, interpersonal sensitivity, and social withdrawal in clinical high risk for psychosis: a systematic review. Schizophrenia, 9(38). https://doi.org/10.1038/s41537-023-00362-z
Mackie CJ, Castellanos-Ryan N, Conrod PJ. Developmental trajectories of psychotic-like experiences across adolescence: Impact of victimization and substance use. Psychol Med. 2011;41:47–58. https://doi.org/10.1017/S0033291710000449 .
Pescosolido BA, Martin JK, Lang A, Olafsdottir S. Rethinking theoretical approaches to stigma: A framework integrating normative influences on stigma (FINIS). Soc Sci Med. 2008;67(3):431–40. https://doi.org/10.1016/j.socscimed.2008.03.018 .
Ahmad S, Hussain S. Big five inventory-version 10: A two-minute personality measurement tool in Urdu. J Pak Med Assoc. 2022;72(9):1726–30.
Alansari B, Alali T. Psychometric Properties of the Arabic big five Inventory-2 short form among undergraduates in Kuwait. Eur Psychiatry. 2022;65(S1):S668–S668.
Ashton MC, Lee K. A theoretical basis for the major dimensions of personality. Eur J Pers. 2001;15(5):327–53. https://doi.org/10.1002/per.417 .
Costa Mastrascusa R, de Oliveira Fenili Antunes ML, de Albuquerque NS, Virissimo SL, Foletto Moura M, Vieira Marques Motta B, de Lara Machado W, Moret-Tatay C, Quarti Irigaray T. Evaluating the complete (44-item), short (20-item) and ultra-short (10-item) versions of the Big Five Inventory (BFI) in the Brazilian population. Sci Rep. 2023;13(1):7372.
Yamagata S, Suzuki A, Ando J, Ono Y, Kijima N, Yoshimura K, Ostendorf F, Angleitner A, Riemann R, Spinath FM, Jang KL. Is the genetic structure of human personality universal? A cross-cultural twin study from North America, Europe, and Asia. J Pers Soc Psychol. 2006;90(6):987. https://doi.org/10.1037/0022-3514.90.6.987 .
Mervielde I, De Clercq B, De Fruyt F, Van Leeuwen K. Temperament, personality, and developmental psychopathology as childhood antecedents of personality disorders. J Pers Disord. 2005;19(2):171–201.
Roberts BW, DelVecchio WF. The rank-order consistency of personality traits from childhood to old age: a quantitative review of longitudinal studies. Psychol Bull. 2000;126(1):3. https://doi.org/10.1037/0033-2909.126.1.3 .
Piedmont RL, Ciarrocchi JW. The utility of the revised NEO personality inventory in an outpatient, drug rehabilitation context. Psychol Addict Behav. 1999;13(3):213. https://doi.org/10.1037/0893-164X.13.3.213 .
Widiger, T. A., & Costa Jr, P. T. Personality disorders and the five-factor model of personality: Rationale for the third edition. Am Psychol Assoc. 2013.
Skodol AE, Oldham JM, Bender DS, Dyck IR, Stout RL, Morey LC, Shea MT, Zanarini MC, Sanislow CA, Grilo CM, Gunderson JG. Dimensional representations of DSM-IV personality disorders: Relationships to functional impairment. Am J Psychiatry. 2005;162(10):1919–25. https://doi.org/10.1176/appi.ajp.162.10.1919 .
DeYoung CG, Quilty LC, Peterson JB. Between facets and domains: 10 aspects of the Big Five. J Pers Soc Psychol. 2007;93(5):880. https://doi.org/10.1037/0022-3514.93.5.880 .
Horan WP, Blanchard JJ, Clark LA, Green MF. Affective traits in schizophrenia and schizotypy. Schizophr Bull. 2008;34(5):856–74. https://doi.org/10.1093/schbul/sbn083 .
Kirihara K, Kasai K, Tada M, Nagai T, Kawakubo Y, Yamasaki S, Onitsuka T, Araki T. Neurophysiological impairment in emotional face processing is associated with low extraversion in schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2012;37(2):270–5. https://doi.org/10.1016/j.pnpbp.2012.02.012 .
Lysaker PH, Taylor AC. Personality dimensions in schizophrenia: associations with symptoms and coping concurrently and 12 months later. Psychopathology. 2007;40(5):338–44. https://doi.org/10.1159/000105532 .
Krueger RF, Markon KE. The role of the DSM-5 personality trait model in moving toward a quantitative and empirically based approach to classifying personality and psychopathology. Annu Rev Clin Psychol. 2014;10:477–501. https://doi.org/10.1146/annurev-clinpsy-032813-153732 .
Edmundson, M. (2010). A five-factor measure of schizotypal personality disorder. (Publication No. 57) [Master’s Thesis, University of Kentucky]. UKnowledge. https://doi.org/10.1177/1073191111408228
Connelly BS, Ones DS, Chernyshenko OS. Introducing the special section on openness to experience: Review of openness taxonomies, measurement, and nomological net. J Pers Assess. 2014;96(1):1–16. https://doi.org/10.1080/00223891.2013.830620 .
McCrae RR, Greenberg DM. Openness to experience. The Wiley handbook of genius. 2014. p. 222–43.
Moorman EL, Samuel DB. Representing schizotypal thinking with dimensional traits: A case for the Five Factor Schizotypal Inventory. Psychol Assess. 2018;30(1):19. https://doi.org/10.1037/pas0000497 .
Straub KT, Kerns JG. Positive schizotypy, maladaptive openness, and openness facets. Personal Disord Theory Res Treat. 2021;12(1):51–8. https://doi.org/10.1037/per0000407 .
Blain SD, Grazioplene RG, Ma Y, DeYoung CG. Toward a neural model of the Openness-Psychoticism dimension: Functional connectivity in the default and frontoparietal control networks. Schizophr Bull. 2020;46(3):540–51. https://doi.org/10.1093/schbul/sbz103 .
Käckenmester W, Bott A, Wacker J. Openness to experience predicts dopamine effects on divergent thinking. Personal Neurosci. 2019;2:e3.
Piedmont RL. Personality, spirituality, religiousness, and the personality disorders: Predictive relations and treatment implications. Religion and spirituality in psychiatry. 2009. p. 173–189.
Folley BS, Park S. Verbal creativity and schizotypal personality in relation to prefrontal hemispheric laterality: A behavioral and near-infrared optical imaging study. Schizophr Res. 2005;80(2–3):271–82. https://doi.org/10.1016/j.schres.2005.06.016 .
Jung RE, Grazioplene R, Caprihan A, Chavez RS, Haier RJ. White matter integrity, creativity, and psychopathology: disentangling constructs with diffusion tensor imaging. PLoS ONE. 2010;5(3):e9818. https://doi.org/10.1371/journal.pone.0009818 .
Leder H, Nadal M. Ten years of a model of aesthetic appreciation and aesthetic judgments: The aesthetic episode–Developments and challenges in empirical aesthetics. Br J Psychol. 2014;105(4):443–64. https://doi.org/10.1111/bjop.12084 .
Chatterjee A, Vartanian O. Neuroaesthetics. Trends Cogn Sci. 2014;18(7):370–5.
Chatterjee A. Scientific aesthetics: Three steps forward. Br J Psychol. 2014;105(4):465–7. https://doi.org/10.1111/bjop.12086 .
Jach HK, DeYoung CG, Smillie LD. Why do people seek information? The role of personality traits and situation perception. J Exp Psychol Gen. 2022;151(4):934. https://doi.org/10.1037/xge0001109 .
Cheung C, Yu K, Fung G, Leung M, Wong C, Li Q, McAlonan G. Autistic disorders and schizophrenia: related or remote? An anatomical likelihood estimation. PloS one. 2010;5(8):e12233.
Kapur S. Psychosis as a state of aberrant salience: a framework linking biology, phenomenology, and pharmacology in schizophrenia. Am J Psychiatry. 2003;160(1):13–23.
Valery KM, Pruteau A. Schizophrenia stigma in mental health professionals and associated factors: A systematic review. Psychiatry Res. 2020;290: 113068. https://doi.org/10.1016/j.psychres .
Villares CC, Sartorius N. Challenging the stigma of schizophrenia. Brazilian Journal of Psychiatry. 2003;25:1–2. https://doi.org/10.1590/S1516-44462003000100001 .
Knight MT, Wykes T, Hayward P. 'People don't understand': An investigation of stigma in schizophrenia using Interpretative Phenomenological Analysis (IPA). J Ment Health. 2003;12(3):209–22.
Picchioni MM, Murray RM. Schizophrenia BMJ (Clinical research ed). 2007;335(7610):91–5. https://doi.org/10.1136/bmj.39227.616447.BE .
Riddle M, Buchholz J. Decompensation in a 51-year-old woman with schizophrenia. Curr Psychiatry. 2018;17(3):47.
Abram SV, De Coster L, Roach BJ, Mueller BA, Van Erp TG, Calhoun VD, et al. Oxytocin enhances an amygdala circuit associated with negative symptoms in schizophrenia: a single-dose, placebo-controlled, crossover, randomized control trial. Schizophr Bull. 2020;46(3):661–9.
Longden E, Read J, Dillon J. Assessing the impact and effectiveness of hearing voices network selfhelp groups. Community Ment Health J. 2018;54:184–8.
Serper M, Payne E, Dill C, Portillo C, Taliercio J. Allocating effort and anticipating pleasure in schizophrenia: Relationship with real world functioning. Eur Psychiatry. 2017;46:57–64.
Rácz J, Kaló Z, Kassai S, Kiss M, Pintér JN. The experience of voice hearing and the role of selfhelp group: An interpretative phenomenological analysis. Int J Soc Psychiatry. 2017;63(4):307–13.
Ruddle A, Livingstone S, Huddy V, Johns L, Stahl D, Wykes T. A case series exploring possible predictors and mechanisms of change in hearing voices groups. Psychol Psychother. 2014;87(1):60–79.
Del Castillo IG, García SL, Balaguer AP. Multifamily therapy in first episodes of psychosis: a pilot study. Eur Psychiatry. 2022;65(S1):S783–4. https://doi.org/10.1192/j.europsy.2022.2024 .
Camacho-Gomez M, Castellvi P. Effectiveness of family intervention for preventing relapse in first-episode psychosis until 24 months of follow-up: a systematic review with meta-analysis of randomized controlled trials. Schizophr Bull. 2020;46(1):98–109. https://doi.org/10.1093/schbul/sbz038 .
Ng F, Ibrahim N, Franklin D, Jordan G, Lewandowski F, Fang F, Roe D, Rennick-Egglestone S, Newby C, Hare-Duke L, Llewellyn-Beardsley J, Yeo C, Slade M. Post-traumatic growth in psychosis: a systematic review and narrative synthesis. BMC Psychiatry. 2021;21(1):1–11. https://doi.org/10.1186/s12888-021-03614-3 .
Pearson E, Siskind D, Hubbard R, Gordon E, Coulson E, Arnautovska U, Warren N. Frailty and treatment-resistant schizophrenia: a retrospective cohort study. Community Ment Health J. 2023;59(1):105–9.
Doidge N. Diagnosing The English patient: Schizoid fantasies of being skinless and of being buried alive. J Am Psychoanal Assoc. 2001;49(1):279–309. https://doi.org/10.1177/00030651010490010601 .
McWilliams N. Some thoughts about schizoid dynamics. The Psychoanalytic Review. 2006;93(1):1–24. https://doi.org/10.1521/prev.2006.93.1.1 .
Bretherton I. The origins of attachment theory: John Bowlby and Mary Ainsworth. Dev Psychol. 1992;28(5):759. https://doi.org/10.1037/0012-1649.28.5.759 .
Rubin LH, Carter CS, Bishop JR, Pournajafi-Nazarloo H, Harris MS, Hill SK, et al. Peripheral vasopressin but not oxytocin relates to severity of acute psychosis in women with acutely-ill untreated first-episode psychosis. Schizophr Res. 2013;146(1-3):138–43.
Download references
Acknowledgements
Author information, authors and affiliations.
Department of Psychology, Chestnut Hill College, 7113 Valley Avenue, Philadelphia, PA, 19128, USA
Chestnut Hill College Department of Professional Psychology, 9601 Germantown Avenue, Philadelphia, PA, 19118, USA
Rachel Hull
You can also search for this author in PubMed Google Scholar
Contributions
JL was responsible for the original ideas of the paper, the new conceptual model, and the identification and elucidation of the philosophical and historical precedents. RH contributed to each of JL’s ideas by adding more explanation or attempting to clarify concepts to readers. RH performed most of the editing of the paper. All authors read and approved the final manuscript.
Authors’ information
JL is a philosopher and scientist, whose research interests include schizophrenia spectrum conditions and psychoanalytic theory. RH is a licensed psychologist.
Corresponding author
Correspondence to James Long .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Long, J., Hull, R. Conceptualizing a less paranoid schizophrenia. Philos Ethics Humanit Med 18 , 14 (2023). https://doi.org/10.1186/s13010-023-00142-8
Download citation
Received : 03 April 2023
Accepted : 11 October 2023
Published : 08 November 2023
DOI : https://doi.org/10.1186/s13010-023-00142-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Schizophrenia
- Schizophrenia spectrum disorders
Philosophy, Ethics, and Humanities in Medicine
ISSN: 1747-5341
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- April 01, 2024 | VOL. 181, NO. 4 CURRENT ISSUE pp.255-346
- March 01, 2024 | VOL. 181, NO. 3 pp.171-254
- February 01, 2024 | VOL. 181, NO. 2 pp.83-170
- January 01, 2024 | VOL. 181, NO. 1 pp.1-82
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
On the Origins of Schizophrenia
- René S. Kahn , M.D., Ph.D.
Search for more papers by this author
What have we accomplished for schizophrenia patients since the introduction of chlorpromazine in 1952 ( 1 )? Have we really made a difference in the outcome of schizophrenia? When we examine objective and clinically meaningful “hard” outcomes, the answer appears to be negative. Still only about 10% of schizophrenia patients will find (or hold) gainful employment ( 2 ). Life expectancy in schizophrenia is reduced by almost 15 years, and this has not improved over recent decades ( 3 ). Patients with schizophrenia are rarely able to establish a family, at least when judged by reproductive fitness or fecundity ( 4 ). The reason is not that antipsychotics are ineffective; in fact, they are highly successful in what they were designed to accomplish, which is to reduce psychosis (at least during the initial phase of the illness). Almost two-thirds of first-episode schizophrenia patients reach remission after 4 to 10 weeks of antipsychotic treatment ( 5 ); even after 1 year of treatment, two-thirds are doing well ( 6 ).
So why have these medications not been able to significantly improve the long-term prognosis of schizophrenia patients? One of the reasons is that patients fail to continue treatment. Indeed, when antipsychotics are used uninterruptedly, mortality is reduced ( 7 ) and outcome, expressed as rehospitalization, improves ( 8 ). However, I propose that the principal reason that we have not been able to materially ameliorate the outcome in schizophrenia is that we have been barking up the wrong tree; we have mistakenly focused on psychosis.
Neither Kraepelin nor Bleuler considered psychosis as the core symptom of what we now call schizophrenia; neither defined schizophrenia on the basis of it. Kraepelin delineated the illness on the cognitive decline preceding the onset of psychosis—which he therefore named dementia praecox. Indeed, when Kraepelin first described the disorder, in the 4th edition of his textbook (which has never been translated into English), he starts the narrative with the slow but steady cognitive decline during adolescence ( 9 ). His account of the cognitive (and social) decline precedes the first mention of psychotic symptoms by six pages, indicating the relative priority—both in chronology and in relevance—he attributed to cognition rather than psychosis. Bleuler ( 10 ) viewed delusions and hallucinations as accessory symptoms as well; the basis of the illness was, according to him, determined by disturbance in affect, cognition (associative thinking), social interaction (autism), and volition (ambivalence). So why has research—and drug development—focused so much on that one symptom, or syndrome, in schizophrenia, even to the extent that schizophrenia and psychosis are seen as one and the same? Could the reason be just because our medications are so effective in treating this aspect of schizophrenia? Indeed, it is the treatability of psychosis and, conversely, the stigma associated with the poor outcome of schizophrenia, that is—mistakenly ( 11 )—used as an argument to question the validity of the schizophrenia concept ( 12 ). Focusing on psychosis instead of on the defining phenotype of schizophrenia may well be the reason the field has made little material progress in improving its outcome.
Cognitive Decline in Adolescence: Renewed Focus on a Century-Old Observation
The emphasis on psychosis has permeated our textbooks; consequently our students are still taught that schizophrenia debuts in early adulthood—because that is indeed when the first signs of psychosis usually present themselves to the health care provider. However, several well-designed retrospective and prospective studies show that the first signs of the illness precede the onset of psychosis by a decade or more. Entirely consistent with Kraepelin’s original observations, abundant evidence has accumulated that schizophrenia does not debut with psychosis but with much more subtle deviations from the norm, expressed in motor, social, and cognitive behavior ( 13 , 14 ). The data on cognition are most compelling. Linking cognitive testing results from the Israeli draft board with those of the National Psychiatric Hospitalization Case Registry, Reichenberg et al. ( 15 ) found significant premorbid deficits on intellectual measures during the draft assessment (at ages 16–17) in those who later developed schizophrenia. This was confirmed, using school achievement as an indication of intellectual performance, in a population-wide study relating data from the Swedish National School Register (also acquired at age 16) to the Swedish Hospital Discharge Register ( 16 ). Among psychiatric disorders, lower IQ as a premorbid marker of illness appears to be specific to this disorder; a recent review concluded that individuals who later develop schizophrenia, but not those who develop related psychotic illnesses such as bipolar disorder, exhibit an IQ deficit prior to presentation of the first psychosis ( 17 ). It was estimated, again using data from the Israeli draft board, that poor school performance precedes the onset of the illness by almost a decade ( 18 ). This is consistent with results from our study comparing scholastic aptitude in twins discordant for schizophrenia, where the twin who would go on to develop schizophrenia showed poorer school performance more than a decade before psychosis onset ( 19 ).
Prospective studies assessing participants from birth—and therefore able to identify changes much earlier than the aforementioned retrospective studies—found the first signs of schizophrenia to occur during the early teens, if not earlier. Specifically, studies of birth cohorts from New Zealand and the United Kingdom find poorer cognitive performance at age 13 ( 20 , 21 ) and possibly even at age 4 or age 8 ( 21 ) in those who are later diagnosed with schizophrenia. Also, cognitive function is lower than would be expected on the basis of the educational attainment of their first-degree relatives ( 22 ), suggesting that this underperformance is related to the risk of developing the illness. Thus, there is little doubt that cognitive function starts to decline many years before the first psychotic symptoms manifest themselves in the context of schizophrenia. Equally relevant, this phenomenon is related to the development of schizophrenia and not to psychosis per se.
Lower Cognitive Function Preceding the Onset of Psychosis
The realization that schizophrenia debuts well before patients present with psychosis or are hospitalized has led to the concept of studying individuals who have some psychotic symptoms but do not (yet) fulfill the full criteria for psychosis, let alone schizophrenia. The concept goes by various names and acronyms, such as at-risk mental state (ARMS), ultra high risk (UHR), and, when help seeking, clinical high risk (CHR) ( 23 ). All have in common that the patients are defined by so-called attenuated psychotic symptoms with the outcome defined as “conversion” or “transition” to full psychosis—not necessarily schizophrenia. One of the more problematic, although interesting, issues with the CHR concept is that even in this subsyndromal population, transition to full psychosis is rare: about 15% (e.g., reference 24 ). Moreover, the concept of transition itself is criticized on the basis of the selective sampling of these cohorts and the fact that transition is a binary outcome defined as a higher score on the continuous scale that selected the population in the first place ( 25 )—although recently suggestions have been made for improving sampling strategies ( 26 ). Nevertheless, the exclusive focus on psychosis (both at baseline and as outcome) in the CHR concept may be inherently flawed ( 25 ). Also, it is important to realize that the age range of the subjects included in these studies is usually very wide (from 12 to 35 years), with the upper end far too old to be credibly related to the development of schizophrenia. Nevertheless, the CHR studies have the potential to provide, if indirectly, interesting clues on the risk factors of schizophrenia: in the largest single study to date, including almost 700 CHR patients, cognitive impairment was present in the entire sample but was most pronounced in those who developed full psychosis—although here, as in most CHR studies, schizophrenia as an outcome was not reported ( 27 ). Studies examining the longitudinal course of cognitive development in CHR—essential to reliably draw conclusions on cognitive development in those cohorts—have not been published to date.
Abnormal Brain Maturation Preceding the Onset of Psychosis
The finding that cognitive decline in schizophrenia starts at, if not before, adolescence is consistent with studies examining brain structure in schizophrenia. More than four decades ago, Johnstone et al. ( 28 ) published their seminal paper reporting for the first time reduced brain volume (or, more precisely, increased lateral ventricle volume) in schizophrenia patients on the basis of CT scans. Since this concerned a cross-sectional study in chronic patients, the question remained as to when these changes manifest themselves. Since then, multiple studies in medication-naive patients with first-episode schizophrenia have shown that brain volumes are smaller at the first presentation of psychosis than those of matched control subjects ( 29 ). Consistently, CHR subjects who go on to develop a full psychotic episode exhibit smaller brain volumes before they receive antipsychotic medication ( 24 ). The fact that brain volumes are smaller in schizophrenia before the emergence of the first psychosis suggests that, contrary to what is sometimes suggested ( 30 ), the brain loss cannot be attributed to antipsychotic medication. Although the results from MRI studies in first-episode schizophrenia and CHR subjects suggest that brain loss is present at or before the first psychosis, they do not clarify at what time point the decreases in brain volume first become apparent. However, there is compelling evidence that the process leading to decreased brain volume starts well before the onset of psychosis. This conclusion is based on a simple but often overlooked variable: intracranial volume (ICV), or more simply put, skull size. ICV is a highly reliable measure that is often not assessed, or goes unreported, in neuroimaging studies in schizophrenia. Nevertheless, it is relevant because ICV directly reflects brain growth, as cranial growth is driven by the expansion of the brain. Although the exact age when the brain reaches it maximum size is somewhat variable, it is generally considered to be at the start of puberty ( 31 ). Thus, an ICV that is smaller in schizophrenia patients than in matched healthy control subjects must be due to stunted brain growth (at any point in time) before that age. Since the effect size is small and therefore often, if reported, is not significant in single studies, the results of our meta-analysis in over 18,000 subjects show a small (d=0.2) but highly significant reduction in ICV ( 29 ). These results indicate that some of the brain loss in schizophrenia is developmental in nature and must occur before the early teens—that is, long before there is any indication of psychosis, let alone schizophrenia.
A relatively novel way to study brain development is the so-called brain-age gap—the difference between the “age” of the brain and the chronological age of a person. For instance, a 20-year-old may have a brain that resembles that of a 25-year-old person, in which case the brain-age gap is 5 years. We reported, examining brain age in a longitudinal study across a 50-year age span (16–67 years), that brain age was significantly higher (by 3.6 years) than chronological age in schizophrenia patients ( 32 ). Similarly, when the brain-age gap was studied in a CHR population, albeit in a cross-sectional study, it was found to significantly deviate from the norm in those who transitioned to psychosis ( 33 ). Thus, it appears from the available evidence, which admittedly is still scarce, that abnormal brain maturation starting before the mid-teens is related to the development of schizophrenia. However, large longitudinal studies focusing on young adolescents and using schizophrenia (in contrast to psychosis) as outcome are sorely needed.
Cognitive and Brain Abnormalities and the Genetic Risk for Schizophrenia
Cognitive function is related to brain structure in the healthy population: intelligence positively correlates with global brain volume, explaining a little over 6% of the variance ( 34 ). However, brain volume is not static, nor is IQ. Indeed, in a longitudinal study in 504 healthy subjects, we reported that intelligence is more related to the magnitude and timing of changes in brain structure than to brain structure per se ( 35 ), especially in early adolescence ( 36 ).
In medication-naive first-episode schizophrenia patients, lower IQ was related to smaller brain volumes ( 37 ), with most of the brain volume loss over time confined to the group of patients showing cognitive decline over the first years of illness ( 38 ). Thus, there is growing evidence that changes in IQ are related to (maturational) changes in the cortex, both in healthy subjects and in patients with schizophrenia. Intriguingly, this relationship seems itself age dependent and to present itself predominantly at the onset of puberty. What is more, it appears that genes that increase the risk of developing schizophrenia may drive the changes in both the brain and in cognition.
That schizophrenia is heritable has been suspected since the first days the illness was conceptualized; indeed, it was recently estimated that genetic variation contributes up to 85% of the risk of developing the illness ( 39 ). Brain volume and intelligence are highly heritable as well, with estimates up to 90% for total brain volume ( 40 ) and 80% for IQ ( 41 ). Thus, one may assume that if there is a genetic relationship between risk for schizophrenia and cognition, this risk may also be expressed in brain volume loss. Indeed, on the basis of 1,243 twins, using mathematical models, we concluded that 25% of the total risk variance for schizophrenia is explained by lower IQ, and 4% of this variance is explained by smaller brain volume ( 42 ). Taken together with the early onset of cognitive changes and the smaller intracranial volume found in schizophrenia, these results suggest that part of the genetic risk of developing the illness may be related to an abnormal early development of the brain leading to cognitive deficits. The brain changes appear to be primarily expressed in cortical thickness and white matter integrity ( 43 ). However, it is more likely that the substrate in the brain underlying the cognitive changes in the development of schizophrenia is related to abnormal connectivity rather than gross volume decreases.
Brain Networks and Cognitive Changes in Schizophrenia
Schizophrenia has been conceptualized as a disorder of brain connectivity since the illness was first defined ( 9 , 10 , 44 ), and this idea was revived a century later using more modern techniques ( 45 ). Consistent with these hypotheses, we have shown that white matter connectivity is disrupted in schizophrenia, particularly in those areas that form the hubs for the main connections in the brain ( 46 , 47 ). In view of their rich interconnectedness, these hubs are sometimes collectively called the “rich club” ( 46 ). These networks, also called the “connectome” of the brain ( 48 ), are under genetic control ( 43 , 49 ) and are already being formed in the second trimester of pregnancy ( 50 ). The efficiency of this network—defined as the optimal relationship between functional connectivity and distance between brain areas ( 51 )—is highly related to intelligence ( 52 ), as are the observed changes in this network’s efficiency during adolescence ( 49 ). Not only are brain networks under considerable genetic control, and not only are the abnormalities related to some of the genes conferring increased risk for schizophrenia, but also important changes in these networks crucially occur during early adolescence. In general, the cortex becomes thinner during adolescence (e.g., 53 ), with its connecting white matter fibers increasing in volume ( 54 ). The cortical changes are genetically controlled and are related to cognitive development during adolescence ( 55 ). Crucially, the brain networks become increasingly more efficiently organized during this period ( 49 ), with their efficiency increasing in adolescence between ages 10 and 13 ( 56 ) and the effect leveling off between ages 13 and 18. The connectome’s efficiency itself and the relationship between intelligence and network efficiency are under genetic control (47% and 87%, respectively) ( 54 ). Thus, abnormal development of the brain’s network appears to be a plausible candidate for the neuroanatomical and functional substrate of the cognitive changes that precede the onset of psychosis in schizophrenia. Moreover, in view of the high heritability, abnormalities in the networks’ efficiency could possibly be related to the genetic risk of schizophrenia. Indeed, abnormal network efficiency in the rich club has been found in siblings ( 57 ) and offspring of schizophrenia patients ( 58 ). Interestingly, this effect in the rich club hubs appears to be specific for schizophrenia—it has not been found in patients with bipolar disorder ( 59 ) or their offspring ( 58 ). Since the abnormalities are also observed in medication-naive schizophrenia patients, they cannot be attributed to the use of medication and are most likely present before illness onset ( 60 ). Moreover, connectome organization has been found to be related to functional outcome and decreases in IQ over time in schizophrenia patients ( 61 ). Importantly, the macroscopic hub areas of the brain, as identified with MRI, can also be determined on a cellular, microscopic level, and they are highly related to higher-order cognitive functions, such as IQ ( 62 , 63 ). Moreover, when combining transcriptional profiles of schizophrenia risk genes with data on the decreased hub connectivity, we found that the expression profile of risk genes across cortical regions was significantly correlated with the regional dysconnectivity ( 64 ). In addition, effects were found to be potentially specific to schizophrenia, with transcriptional profiles not related to cortical dysconnectivity in patients with bipolar illness. Especially fascinating is the finding that brain connections present in humans but not in chimpanzees—those predominantly involved in semantic comprehension and language processing—are those affected in schizophrenia and not in other psychiatric disorders, such as autism, obsessive-compulsive disorder, and major depression ( 65 ), suggesting that the same areas that have evolved in humans to acquire higher-order cognitive capabilities, such as language, are those that are particularly vulnerable to being affected in the development of schizophrenia. Another line of evidence suggesting that brain development during adolescence is a crucial factor in the path to schizophrenia is derived from genetic studies.
Brain Networks and The Genetics of Schizophrenia
Currently more than 200 genome-wide significant loci have been associated with the risk of schizophrenia in Caucasian populations ( 66 ). The strongest genetic relationship is that across the major histocompatibility complex (MHC) locus on chromosome 6, which is known for its role in immunity. Sekar et al. ( 67 ) identified alleles of the complement component 4 (C4 genes) in the MHC region as underlying the MHC signal. Also, allelic variation in C4 was related to increased risk for schizophrenia in proportion to its promotion of expression of C4A mRNA. Sekar et al. also found increased levels of C4 mRNA expression in postmortem brain from individuals with schizophrenia compared with matched control subjects. This discovery was recently replicated in a transcriptomic study by the PsychEncode consortium that included 559 schizophrenia case subjects and 936 healthy control subjects ( 68 ). Relevant for the development of schizophrenia during adolescence, Stevens et al. ( 69 ) have shown that proteins of the complement system are involved in activity-dependent synaptic pruning: weak synapses are tagged by these complement proteins and eliminated by microglia. Similar properties were recently found for C4 ( 67 ). In a human in vitro model with induced neurons and microglia, Sellgren et al. ( 70 ) showed that microglia generated from stem cells of schizophrenia patients eliminated more synaptic structures, with both neuronal and microglial factors contributing. These studies have revitalized the hypothesis that schizophrenia may result from abnormalities in brain maturation ( 71 ), specifically abnormalities in the synaptic pruning of prefrontal and temporal cerebral cortex that normally characterizes adolescent brain maturation ( 72 ). Indeed, excessive loss of gray matter and abnormally low numbers of synapses on cortical neurons in these brain regions (i.e., excessive synaptic pruning) are well-replicated pathological findings in schizophrenia ( 73 ). The hypothesis on the role of increased complement activity as a pathogenic mechanism in schizophrenia elegantly links genetic, neuroanatomical, and phenotypical findings ( 74 ). Although it still needs to be properly tested, it provides an inspiring example of how data from various sources can help elucidate the causes of schizophrenia.
Translating Old Findings to New Initiatives
In order to understand schizophrenia, its causes, development, and outcome, and in order to define new subgroups of patients who may be differentially responsive to treatment or, hopefully, prevention interventions, we will need to switch our focus from psychosis to cognition and the related brain development during childhood and early adolescence. It is clear that cognitive decline before the onset of psychosis is an important marker, if not a harbinger, of impending schizophrenia with the possibility, if identified appropriately early, that interventions can be developed to halt this decline and prevent psychosis ( 75 ). Thus, research efforts that target the second decade of life are essential if we are to find mechanisms for intervention and cure. These studies are costly and time-consuming, but there is an example that is rapidly providing some of this information: the UK Biobank, a unique initiative, is an open source of data that is producing the information that will help resolve the issues described above. For instance, in a study using UK Biobank data from more than 2,800 participants from the general population, a relationship was found between the polygenic risk score for schizophrenia and cortical thinning on MRI ( 76 ). These findings confirm—in the general population—the reported association between genetic vulnerability to the disorder and brain pathology in those at increased genetic risk for schizophrenia ( 77 ). Equally important, and showing the need for such large samples, individuals with rare copy number variants (CNVs) were identified in a study of over 400,000 subjects in the UK Biobank reporting a relationship between CNVs that are associated with an increased risk for schizophrenia and lower cognitive performance on neuropsychological tests ( 78 ). Finally, researchers using UK Biobank data were able to identify new loci related to cognitive function ( 79 ) and the related variable of educational attainment ( 80 ) in the general population—information that will be, for reasons outlined here, potentially relevant for the study of schizophrenia. A comparable program in the United States is the Million Veteran Program (MVP), which is expected to be as informative and successful as the UK Biobank; indeed, recently Harvey et al. ( 81 ), using data from the MVP, reported robust associations between greater polygenic loading for schizophrenia risk and poorer cognitive performance.
Clearly, more of such large-scale initiatives will be needed, and they need to longitudinal. Although some cohorts are being followed—the Adolescent Brain and Cognitive Development study comes to mind ( 82 )—their numbers will still be too low to detect causes for relatively rare disorders such as schizophrenia (of the 10,000 subjects included, only 100 are expected to develop schizophrenia).
In addition to these large population-based studies, subjects can be followed who are at greatly increased risk for schizophrenia, which requires, given the large relative risk ratios, much smaller numbers. Schizophrenia risk is probably increased through a combination of many common variants, more of which are being identified as sample sizes are increasing ( 83 ). However, the explained risk is very low for each of these variants, and even these variants in combination. Much larger effects are seen in the people who carry very rare CNVs. Although results obtained from following these subjects will be difficult to interpret in view of their scarcity in the population and less generalizable than results from samples from the general population, they are helpful in studying mechanistic questions. One promising example is the identification of SETD1A as a schizophrenia susceptibility gene ( 84 ). Loss of function in this gene was recently shown to negatively affect the brain connectome in mice, which in turn was related to cognitive deficits in these animals ( 85 ).
The usefulness of examining the role of rare variants has also proven its merit in human studies, such as adolescents with the 22q11.2 deletion syndrome (22q11DS), who have a 25-fold increased risk of developing schizophrenia ( 86 ). When cognitive function was assessed longitudinally in a group of 829 children and adolescents with this syndrome, cognitive performance declined in the entire group of patients, but it was most pronounced in those who went on to develop schizophrenia ( 87 ). Since the 22q11DS is rare—1:4,000 for deletions and 1:1,600 for duplications in the 22q11.2 area ( 88 )—this study could only be successful because all researchers working in this field shared their data. Finally, studying another high-risk group, the offspring of patients with schizophrenia, is a good possibility for enriching samples for the development of schizophrenia. Indeed, long-term follow-up of offspring of patients with bipolar disorder has provided important information on the highly heterogeneous pathways to bipolar illness ( 89 ). Following offspring of schizophrenia patients, although more difficult given the decreased fecundity of schizophrenia patients ( 4 ), would be expected to be as informative.
Conclusions
Despite an enormous expansion in our knowledge on the etiology, pathophysiology, and illness course of schizophrenia, so far we have not been able to materially improve the outcome of this highly incapacitating illness. One of the reasons may be that we have been focusing on psychosis, which is a relatively late-occurring, and nonspecific, symptom of schizophrenia. It has become abundantly clear that schizophrenia debuts with cognitive decline years before the onset of the first psychosis. Cognitive and brain development are highly linked, especially during early adolescence, and both are, independently as well as their interaction, under substantial genetic control. A growing body of evidence suggests that abnormal brain maturation during the early teen years, especially that of the hub areas in the brain, may be causally related to the development of the disorder. These changes can be linked to specific genetic loci that have been found to increase the risk for schizophrenia and can be attributed to abnormal synaptic pruning during this developmental period. Large collaborative longitudinal (population based and high-risk) studies focusing on early adolescence and linking cognition, phenomenology, brain imaging, biomarkers, and genetics may be the path forward to elucidate the causes of schizophrenia. We should then be able to develop the tools to finally improve outcomes for the patients suffering from this devastating disorder.
Dr. Kahn has served as a consultant for Alkermes, Janssen-Cilag, Luye Pharma, Otsuka, and Sunovion.
1 Delay J, Deniker P : Neuroleptic effects of chlorpromazine in therapeutics of neuropsychiatry . J Clin Exp Psychopathol 1955 ; 16:104–112 Medline , Google Scholar
2 Davidson M, Kapara O, Goldberg S, et al. : A nation-wide study on the percentage of schizophrenia and bipolar disorder patients who earn minimum wage or above . Schizophr Bull 2016 ; 42:443–447 Crossref , Medline , Google Scholar
3 Hjorthøj C, Stürup AE, McGrath JJ, et al. : Years of potential life lost and life expectancy in schizophrenia: a systematic review and meta-analysis . Lancet Psychiatry 2017 ; 4:295–301 Crossref , Medline , Google Scholar
4 Haukka J, Suvisaari J, Lönnqvist J : Fertility of patients with schizophrenia, their siblings, and the general population: a cohort study from 1950 to 1959 in Finland . Am J Psychiatry 2003 ; 160:460–463 Link , Google Scholar
5 Kahn RS, Winter van Rossum I, Leucht S, et al. : Amisulpride and olanzapine followed by open-label treatment with clozapine in first-episode schizophrenia and schizophreniform disorder (OPTiMiSE): a three-phase switching study . Lancet Psychiatry 2018 ; 5:797–807 Crossref , Medline , Google Scholar
6 Kahn RS, Fleischhacker WW, Boter H, et al. : Effectiveness of antipsychotic drugs in first-episode schizophrenia and schizophreniform disorder: an open randomised clinical trial . Lancet 2008 ; 371:1085–1097 Crossref , Medline , Google Scholar
7 Tiihonen J, Mittendorfer-Rutz E, Torniainen M, et al. : Mortality and cumulative exposure to antipsychotics, antidepressants, and benzodiazepines in patients with schizophrenia: an observational follow-up study . Am J Psychiatry 2016 ; 173:600–606 Link , Google Scholar
8 Tiihonen J, Mittendorfer-Rutz E, Majak M, et al. : Real-world effectiveness of antipsychotic treatments in a nationwide cohort of 29 823 patients with schizophrenia . JAMA Psychiatry 2017 ; 74:686–693 Crossref , Medline , Google Scholar
9 Kraepelin E: Ein kurzes Lehrbuch für Studirende und Aerzte, 4th ed. Leipzig, Abel, 1893, pp 435–445 Google Scholar
10 Bleuler E : Dementia Praecox oder die Gruppe der Schizophrenien . Leipzig, Deuticke, 1911 Google Scholar
11 Kahn RS : Why the concept of schizophrenia is still alive and kicking . Psychol Med 2018 ; 48:247–248 Crossref , Medline , Google Scholar
12 Guloksuz S, van Os J : The slow death of the concept of schizophrenia and the painful birth of the psychosis spectrum . Psychol Med 2018 ; 48:229–244 Crossref , Medline , Google Scholar
13 Dickson H, Laurens KR, Cullen AE, et al. : Meta-analyses of cognitive and motor function in youth aged 16 years and younger who subsequently develop schizophrenia . Psychol Med 2012 ; 42:743–755 Crossref , Medline , Google Scholar
14 Woodberry KA, Giuliano AJ, Seidman LJ : Premorbid IQ in schizophrenia: a meta-analytic review . Am J Psychiatry 2008 ; 165:579–587 Link , Google Scholar
15 Reichenberg A, Weiser M, Rabinowitz J, et al. : A population-based cohort study of premorbid intellectual, language, and behavioral functioning in patients with schizophrenia, schizoaffective disorder, and nonpsychotic bipolar disorder . Am J Psychiatry 2002 ; 159:2027–2035 Link , Google Scholar
16 Kendler KS, Ohlsson H, Mezuk B, et al. : A Swedish national prospective and co-relative study of school achievement at age 16, and risk for schizophrenia, other nonaffective psychosis, and bipolar illness . Schizophr Bull 2016 ; 42:77–86 Medline , Google Scholar
17 Mollon J, Reichenberg A : Cognitive development prior to onset of psychosis . Psychol Med 2018 ; 48:392–403 Crossref , Medline , Google Scholar
18 Velthorst E, Reichenberg A, Kapra O, et al. : Developmental trajectories of impaired community functioning in schizophrenia . JAMA Psychiatry 2016 ; 73:48–55 Crossref , Medline , Google Scholar
19 van Oel CJ, Sitskoorn MM, Cremer MPM, et al. : School performance as a premorbid marker for schizophrenia: a twin study . Schizophr Bull 2002 ; 28:401–414 Crossref , Medline , Google Scholar
20 Reichenberg A, Caspi A, Harrington H, et al. : Static and dynamic cognitive deficits in childhood preceding adult schizophrenia: a 30-year study . Am J Psychiatry 2010 ; 167:160–169 Link , Google Scholar
21 Mollon J, David AS, Zammit S, et al. : Course of cognitive development from infancy to early adulthood in the psychosis spectrum . JAMA Psychiatry 2018 ; 75:270–279 Crossref , Medline , Google Scholar
22 Keefe RSE, Eesley CE, Poe MP : Defining a cognitive function decrement in schizophrenia . Biol Psychiatry 2005 ; 57:688–691 Crossref , Medline , Google Scholar
23 Fusar-Poli P : The Clinical High-Risk State for Psychosis (CHR-P), Version II . Schizophr Bull 2017 ; 43:44–47 Crossref , Medline , Google Scholar
24 Cannon TD, Chung Y, He G, et al. : Progressive reduction in cortical thickness as psychosis develops: a multisite longitudinal neuroimaging study of youth at elevated clinical risk . Biol Psychiatry 2015 ; 77:147–157 Crossref , Medline , Google Scholar
25 van Os J, Guloksuz S : A critique of the “ultra-high risk” and “transition” paradigm . World Psychiatry 2017 ; 16:200–206 Crossref , Medline , Google Scholar
26 Fusar-Poli P, Sullivan SA, Shah JL, et al. : Improving the detection of individuals at clinical risk for psychosis in the community, primary and secondary care: an integrated evidence-based approach . Front Psychiatry 2019 ; 10:774 Crossref , Medline , Google Scholar
27 Seidman LJ, Shapiro DI, Stone WS, et al. : Association of neurocognition with transition to psychosis: baseline functioning in the second phase of the North American Prodrome Longitudinal Study . JAMA Psychiatry 2016 ; 73:1239–1248 Crossref , Medline , Google Scholar
28 Johnstone EC, Crow TJ, Frith CD, et al. : Cerebral ventricular size and cognitive impairment in chronic schizophrenia . Lancet 1976 ; 2:924–926 Crossref , Medline , Google Scholar
29 Haijma SV, Van Haren N, Cahn W, et al. : Brain volumes in schizophrenia: a meta-analysis in over 18 000 subjects . Schizophr Bull 2013 ; 39:1129–1138 Crossref , Medline , Google Scholar
30 Fusar-Poli P, Smieskova R, Kempton MJ, et al. : Progressive brain changes in schizophrenia related to antipsychotic treatment? A meta-analysis of longitudinal MRI studies . Neurosci Biobehav Rev 2013 ; 37:1680–1691 Crossref , Medline , Google Scholar
31 Libby J, Marghoub A, Johnson D, et al. : Modelling human skull growth: a validated computational model . J R Soc Interface 2017 ; 14: 20170202 Crossref , Medline , Google Scholar
32 Schnack HG, van Haren NEM, Nieuwenhuis M, et al. : Accelerated brain aging in schizophrenia: a longitudinal pattern recognition study . Am J Psychiatry 2016 ; 173:607–616 Link , Google Scholar
33 Chung Y, Addington J, Bearden CE, et al. : Use of machine learning to determine deviance in neuroanatomical maturity associated with future psychosis in youths at clinically high risk . JAMA Psychiatry 2018 ; 75:960–968 Crossref , Medline , Google Scholar
34 Pietschnig J, Penke L, Wicherts JM, et al. : Meta-analysis of associations between human brain volume and intelligence differences: how strong are they and what do they mean? Neurosci Biobehav Rev 2015 ; 57:411–432 Crossref , Medline , Google Scholar
35 Schnack HG, van Haren NEM, Brouwer RM, et al. : Changes in thickness and surface area of the human cortex and their relationship with intelligence . Cereb Cortex 2015 ; 25:1608–1617 Crossref , Medline , Google Scholar
36 Brouwer RM, van Soelen ILC, Swagerman SC, et al. : Genetic associations between intelligence and cortical thickness emerge at the start of puberty . Hum Brain Mapp 2014 ; 35:3760–3773 Crossref , Medline , Google Scholar
37 Rais M, Cahn W, Schnack HG, et al. : Brain volume reductions in medication-naive patients with schizophrenia in relation to intelligence quotient . Psychol Med 2012 ; 42:1847–1856 Crossref , Medline , Google Scholar
38 Kubota M, van Haren NEM, Haijma SV, et al. : Association of IQ changes and progressive brain changes in patients with schizophrenia . JAMA Psychiatry 2015 ; 72:803–812 Crossref , Medline , Google Scholar
39 Kahn RS, Sommer IE, Murray RM, et al. : Schizophrenia . Nat Rev Dis Primers 2015 ; 1:15067 Crossref , Medline , Google Scholar
40 van Haren NEM, Rijsdijk F, Schnack HG, et al. : The genetic and environmental determinants of the association between brain abnormalities and schizophrenia: the Schizophrenia Twins and Relatives Consortium . Biol Psychiatry 2012 ; 71:915–921 Crossref , Medline , Google Scholar
41 Posthuma D, de Geus EJ, Boomsma DI : Perceptual speed and IQ are associated through common genetic factors . Behav Genet 2001 ; 31:593–602 Crossref , Medline , Google Scholar
42 Toulopoulou T, van Haren N, Zhang X, et al. : Reciprocal causation models of cognitive vs volumetric cerebral intermediate phenotypes for schizophrenia in a pan-European twin cohort . Mol Psychiatry 2015 ; 20:1386–1396 Crossref , Medline , Google Scholar
43 Bohlken MM, Mandl RCW, Brouwer RM, et al. : Heritability of structural brain network topology: a DTI study of 156 twins . Hum Brain Mapp 2014 ; 35:5295–5305 Crossref , Medline , Google Scholar
44 Wernicke C : Grundrisse der Psychiatrie . Leipzig, Thieme, 1906 Google Scholar
45 Friston KJ, Frith CD : Schizophrenia: a disconnection syndrome? Clin Neurosci 1995 ; 3:89–97 Medline , Google Scholar
46 van den Heuvel MP, Kahn RS, Goñi J, et al. : High-cost, high-capacity backbone for global brain communication . Proc Natl Acad Sci USA 2012 ; 109:11372–11377 Crossref , Medline , Google Scholar
47 van den Heuvel MP, Sporns O, Collin G, et al. : Abnormal rich club organization and functional brain dynamics in schizophrenia . JAMA Psychiatry 2013 ; 70:783–792 Crossref , Medline , Google Scholar
48 de Reus MA, Saenger VM, Kahn RS, et al. : An edge-centric perspective on the human connectome: link communities in the brain . Philos Trans R Soc Lond B Biol Sci 2014 ; 369: 20130527 Crossref , Medline , Google Scholar
49 Koenis MMG, Brouwer RM, van den Heuvel MP, et al. : Development of the brain’s structural network efficiency in early adolescence: a longitudinal DTI twin study . Hum Brain Mapp 2015 ; 36:4938–4953 Crossref , Medline , Google Scholar
50 Turk E, van den Heuvel MI, Benders MJ, et al. : Functional connectome of the fetal brain . J Neurosci 2019 ; 39:9716–9724 Crossref , Medline , Google Scholar
51 Bullmore E, Sporns O : The economy of brain network organization . Nat Rev Neurosci 2012 ; 13:336–349 Crossref , Medline , Google Scholar
52 van den Heuvel MP, Stam CJ, Kahn RS, et al. : Efficiency of functional brain networks and intellectual performance . J Neurosci 2009 ; 29:7619–7624 Crossref , Medline , Google Scholar
53 Brown TT, Kuperman JM, Chung Y, et al. : Neuroanatomical assessment of biological maturity . Curr Biol 2012 ; 22:1693–1698 Crossref , Medline , Google Scholar
54 Brouwer RM, Mandl RCW, Schnack HG, et al. : White matter development in early puberty: a longitudinal volumetric and diffusion tensor imaging twin study . PLoS One 2012 ; 7: e32316 Crossref , Medline , Google Scholar
55 Teeuw J, Brouwer RM, Koenis MMG, et al. : Genetic influences on the development of cerebral cortical thickness during childhood and adolescence in a Dutch longitudinal twin sample: the Brainscale Study . Cereb Cortex 2019 ; 29:978–993 Crossref , Medline , Google Scholar
56 Koenis MMG, Brouwer RM, Swagerman SC, et al. : Association between structural brain network efficiency and intelligence increases during adolescence . Hum Brain Mapp 2018 ; 39:822–836 Crossref , Medline , Google Scholar
57 Collin G, Kahn RS, de Reus MA, et al. : Impaired rich club connectivity in unaffected siblings of schizophrenia patients . Schizophr Bull 2014 ; 40:438–448 Crossref , Medline , Google Scholar
58 Collin G, Scholtens LH, Kahn RS, et al. : Affected anatomical rich club and structural-functional coupling in young offspring of schizophrenia and bipolar disorder patients . Biol Psychiatry 2017 ; 82:746–755 Crossref , Medline , Google Scholar
59 Collin G, van den Heuvel MP, Abramovic L, et al. : Brain network analysis reveals affected connectome structure in bipolar I disorder . Hum Brain Mapp 2016 ; 37:122–134 Crossref , Medline , Google Scholar
60 Chung Y, Haut KM, He G, et al. : Ventricular enlargement and progressive reduction of cortical gray matter are linked in prodromal youth who develop psychosis . Schizophr Res 2017 ; 189:169–174 Crossref , Medline , Google Scholar
61 Collin G, de Nijs J, Hulshoff Pol HE, et al. : Connectome organization is related to longitudinal changes in general functioning, symptoms, and IQ in chronic schizophrenia . Schizophr Res 2016 ; 173:166–173 Crossref , Medline , Google Scholar
62 Seidlitz J, Váša F, Shinn M, et al. : Morphometric similarity networks detect microscale cortical organization and predict inter-individual cognitive variation . Neuron 2018 ; 97:231–247.e7 Crossref , Medline , Google Scholar
63 van den Heuvel MP, Scholtens LH, de Reus MA, et al. : Associated microscale spine density and macroscale connectivity disruptions in schizophrenia . Biol Psychiatry 2016 ; 80:293–301 Crossref , Medline , Google Scholar
64 Romme IAC, de Reus MA, Ophoff RA, et al. : Connectome disconnectivity and cortical gene expression in patients with schizophrenia . Biol Psychiatry 2017 ; 81:495–502 Crossref , Medline , Google Scholar
65 van den Heuvel MP, Scholtens LH, de Lange SC, et al. : Evolutionary modifications in human brain connectivity associated with schizophrenia . Brain 2019 ; 142:3991–4002 Crossref , Medline , Google Scholar
66 Schizophrenia Working Group of the Psychiatric Genomics Consortium : Biological insights from 108 schizophrenia-associated genetic loci . Nature 2014 ; 511:421–427 Crossref , Medline , Google Scholar
67 Sekar A, Bialas AR, de Rivera H, et al. : Schizophrenia risk from complex variation of complement component 4 . Nature 2016 ; 530:177–183 Crossref , Medline , Google Scholar
68 Gandal MJ, Zhang P, Hadjimichael E, et al. : Transcriptome-wide isoform-level dysregulation in ASD, schizophrenia, and bipolar disorder . Science 2018 ; 362: eaat8127 Crossref , Medline , Google Scholar
69 Stevens B, Allen NJ, Vazquez LE, et al. : The classical complement cascade mediates CNS synapse elimination . Cell 2007 ; 131:1164–1178 Crossref , Medline , Google Scholar
70 Sellgren CM, Gracias J, Watmuff B, et al. : Increased synapse elimination by microglia in schizophrenia patient-derived models of synaptic pruning . Nat Neurosci 2019 ; 22:374–385 Crossref , Medline , Google Scholar
71 Feinberg I : Schizophrenia: caused by a fault in programmed synaptic elimination during adolescence? J Psychiatr Res 1982–1983 ; 17:319–334 Crossref , Medline , Google Scholar
72 McGlashan TH, Hoffman RE : Schizophrenia as a disorder of developmentally reduced synaptic connectivity . Arch Gen Psychiatry 2000 ; 57:637–648 Crossref , Medline , Google Scholar
73 Berdenis van Berlekom A, Muflihah CH, Snijders GJLJ, et al. : Synapse pathology in schizophrenia: a meta-analysis of postsynaptic elements in postmortem brain studies . Schizophr Bull 2019 ; sbz060 Crossref , Google Scholar
74 Johnson MB, Stevens B : Pruning hypothesis comes of age . Nature 2018 ; 554:438–439 Crossref , Google Scholar
75 Keefe RSE, Kahn RS : Cognitive decline and disrupted cognitive trajectory in schizophrenia . JAMA Psychiatry 2017 ; 74:535–536 Crossref , Medline , Google Scholar
76 Neilson E, Shen X, Cox SR, et al. : Impact of polygenic risk for schizophrenia on cortical structure in UK Biobank . Biol Psychiatry 2019 ; 86:536–544 Crossref , Medline , Google Scholar
77 de Zwarte SMC, Brouwer RM, Agartz I, et al. : The association between familial risk and brain abnormalities is disease specific: an ENIGMA-Relatives study of schizophrenia and bipolar disorder . Biol Psychiatry 2019 ; 86:545–556 Crossref , Medline , Google Scholar
78 Kendall KM, Bracher-Smith M, Fitzpatrick H, et al. : Cognitive performance and functional outcomes of carriers of pathogenic copy number variants: analysis of the UK Biobank . Br J Psychiatry 2019 ; 214:297–304 Crossref , Medline , Google Scholar
79 Davies G, Marioni RE, Liewald DC, et al. : Genome-wide association study of cognitive functions and educational attainment in UK Biobank (N=112 151) . Mol Psychiatry 2016 ; 21:758–767 Crossref , Medline , Google Scholar
80 Okbay A, Beauchamp JP, Fontana MA, et al. : Genome-wide association study identifies 74 loci associated with educational attainment . Nature 2016 ; 533:539–542 Crossref , Medline , Google Scholar
81 Harvey PD, Sun N, Bigdeli TB, et al. : Genome-wide association study of cognitive performance in US veterans with schizophrenia or bipolar disorder . Am J Med Genet B Neuropsychiatr Genet (Epub ahead of print, December 24, 2019) Google Scholar
82 Casey BJ, Cannonier T, Conley MI, et al. : The Adolescent Brain Cognitive Development (ABCD) study: imaging acquisition across 21 sites . Dev Cogn Neurosci 2018 ; 32:43–54 Crossref , Medline , Google Scholar
83 Lam M, Chen C-Y, Li Z, et al. : Comparative genetic architectures of schizophrenia in East Asian and European populations . Nat Genet 2019 ; 51:1670–1678 Crossref , Medline , Google Scholar
84 Takata A, Xu B, Ionita-Laza I, et al. : Loss-of-function variants in schizophrenia risk and SETD1A as a candidate susceptibility gene . Neuron 2014 ; 82:773–780 Crossref , Medline , Google Scholar
85 Mukai J, Cannavò E, Crabtree GW, et al. : Recapitulation and reversal of schizophrenia-related phenotypes in Setd1a-deficient mice . Neuron 2019 ; 104:471–487.e12 Crossref , Medline , Google Scholar
86 Tang SX, Gur RE : Longitudinal perspectives on the psychosis spectrum in 22q11.2 deletion syndrome . Am J Med Genet A 2018 ; 176:2192–2202 Crossref , Medline , Google Scholar
87 Vorstman JAS, Breetvelt EJ, Duijff SN, et al. : Cognitive decline preceding the onset of psychosis in patients with 22q11.2 deletion syndrome . JAMA Psychiatry 2015 ; 72:377–385 Crossref , Medline , Google Scholar
88 Olsen L, Sparsø T, Weinsheimer SM, et al. : Prevalence of rearrangements in the 22q11.2 region and population-based risk of neuropsychiatric and developmental disorders in a Danish population: a case-cohort study . Lancet Psychiatry 2018 ; 5:573–580 Crossref , Medline , Google Scholar
89 Mesman E, Nolen WA, Reichart CG, et al. : The Dutch bipolar offspring study: 12-year follow-up . Am J Psychiatry 2013 ; 170:542–549 Link , Google Scholar
- Ned H. Kalin , M.D.
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Paranoid Schizophrenia and the Paradoxical Path to Paraphrenia and Affectivity – a Case Study

International Journal of Research -GRANTHAALAYAH
Motivation: Analyzing a case of paranoid schizophrenia is a challenge to understand the mechanisms underlying the mind of a schizophrenic. The study became captivating because in the patient's delusional cofabulations there were many fingerprints that the communist period of that time left on the woman's psyche, thus observing the repressions following personal failures that probably led to the current state. Objective: Carrying out an analysis of the life history of a patient with paranoid schizophrenia who, although voluntarily presenting at the hospital, does not recognize her diagnosis and treatment. It presents symptoms that include the delusional ideas of persecution or greatness. It has two possible admissions, currently admitted to the psychiatric department in Bucharest. Results: The patient presents disorders regarding perception, memory, affectivity, observing a disorganized discourse that includes a qualitative perceptual disorder, schizophrenia-specific hypopros...
Related Papers
Iulia-Ioana Enache
Introduction: Disorganized schizophrenia is a subtype of schizophrenia which is not recognized in the updated version of DSM. It is found in ICD-10 with the name of hebephrenic schizophrenia. The paper presents a 27-year-old patient with multiple admissions at psychiatry for schizophrenia with an unknown onset, initially considered to be paranoid; the current level of disorganization of the behavioral acts, of the language, of the thinking, having the intensity of hebephrenic schizophrenia. The paper presents a Ganser syndrome in association with alcohol consumption and prohibited substances use. Methods: hospitalization, psychiatric evaluation under antipsychotic treatment with haloperidol and zuclopenthixol, counseling, social assistance. Results: The patient fulfills all the criteria for the classification in hebephrenic schizophrenia, with a reserved prognosis and an involuntary accentuated potential considering the multiple admissions, the early onset, the lack of social and fa...
IOSR Journals
Background: Chronic paranoid schizophrenia involves over time moments of emotional decompensation, in which the person in question, overlaps manic coloring over all the implicit symptoms of positive, negative dimensions and disorganization. Materials and Methods: The methods used were the initial psychological evaluation, the progressive one, the structured and unstructured clinical interview, psychoanalytic psychotherapy cure, periodical psychiatric evaluation and treatment monitoring, psychoanalytic interpretations, analysis of transference and countertransference dynamics, the transgenerational analysis, the analysis of his social functioning, psychological monitoring, as well as the psychiatric treatment. Results: The present case exposes the psychiatric pathology of a 56-year-old patient, in whom the disease started around the age of 20, the one in question being partially treated. It presents a multiple fragmentary delusional ideation based on pseudo-reminiscences gathered from memories of his youth and cryptomnesia, along with fantastic and dreamy conspiracies. The shift to the affective pole of paranoid schizophrenia is felt from the joviality and exaltation both ideational and emotional. Social functioning is severely affected, the patient losing the coherence of her actions and actions. To these is added the social dimension of the case, the one in question has lost its home and no longer has a social support network. As defense mechanisms from the primitive psychotic register are involved: denial, projection and projective identification, the cleavage of the Self and the Self, found in delusional fragments, in the delusional idea of denying filiation and in the emotional inversion towards the family. Conclusion: Suicidal behavior sometimes occurs in response to hallucinatory commands of self-or hetero-aggression. The risk may increase, being higher immediately after discharge or in the period following a psychotic episode.
Open Journal of Social Sciences
Diana Istrate
Alexandra Militaru
Motivation: A psychiatric patient should be looked at in the longitudinal dynamics of their life because it is possible that during youth, mental suffering has a certain tone to it, which is later erased, transformed or moved, through a greater or lesser contact with the ideas or the affect. Objective: We want to present the life history and dynamics of a subject whose first episode of mental illness of a depressive nature was around the age of 20, and to emphasize how over the years, this nature has faded. Currently, there is an absence of connection between the symptoms and the possible causalities. Material and methods: psychiatric and psychoanalytic interviews in dynamics, analysis of the life map, interpretations, the symptom’s evolution under medication, social support, identification of positive and negative prognostic factors, differential diagnoses, performing the diagnostic tree. Results: The patient presented a first depressive episode in youth with a trigger related to a...
Background: Schizophrenia is characterized by symptoms such as delirium, hallucinations, disorganized behavior, which affects the entire personality. All these symptoms are found in a high-intellect patient, but highly suggestable, which makes the disease more complex, especially over such a long period (20 years). Materials and Methods: The present case presents quasi-psychotic episodes. The present paper aims to evaluate a current profile of a schizophrenia and quasi-psychotic episodes in a 40-year-old patient. The methods that were used are the interview (with both the patient and his father), the observation, the administration of psychological tests and psychiatric treatment. The symptoms specific to a schizophrenia filled with quasi-psychotic episodes are well outlined in the light of disorganized ideas, the presence of certain pseudo reminiscences, the internal reality being distorted by the external one. Results: The patient received treatment to stabilize the mental state that led to a decrease in the delirious ideology, but at some point, the medication was interrupted as a result of his father's decision. Conclusion: There are several factors that affects the social functioning of the patient such as medical treatment unauthorized manipulation, the lack of social support, the non-involvement of the relevant authorities.
Angela Enache
International Journal of Research
NAOMI-EVELINA SOARE
Motivation/Background: Historically speaking, the distinction between manic-depressive disorders and schizophrenia finds itself in an unclear and vast spectrum bordered by the two illnesses. In this paper, we will present a case study that raises a question of diagnosis: bipolar disorder or schizoaffective disorder? Following the description of the symptoms and diagnosis criteria of each of the disorders, along with the personal data of the patient (the ones that are available to us), we will attempt analyzing the case as thoroughly as possible. The paper introduces the case of a 40-year-old woman who presents affective/mood related symptoms. Method: psychiatric evaluation, psychiatric interview, psychodynamic interview and psychodynamic interpretation. Results: The subject has a pathology of attachment developed over a structure with homosexual attachment choices. The multiple psychotraumas of childhood and the busy life history overlap with a vulnerability for emotional manifestat...
Procedia - Social and Behavioral Sciences
Ana-Maria Dragut
Yugashini Paramaswaran
Annals of Psychiatry and Treatment
Giulio Perrotta
The psychotic spectrum is the category that groups together a series of disorders linked to symptomatology in which we witness the fragmentation of the plane of reality until it is completely broken. According to the DSM-V nosography, the disorders under examination are schizophrenia, delusional disorder, paranoid disorder, schizoid disorder, schizotypic disorder, schizoaffective disorder, brief psychotic disorder, psychotic break, and catatonia. In this work, theoretical and practical profiles were analyzed, paying attention to neurobiological content and therapeutic profiles, both psychotherapeutic and psychopharmacological. A note of disappointment has been made in the nosographic categorization of dissociative disorders that currently would not be included in the psychotic spectrum disorders, although from the elements that emerged it would be interesting to revise them, precisely because of the clinical nature of the psychopathological category.
RELATED PAPERS
Frontiers in Psychiatry
Laura Orsolini
Comprehensive Psychiatry
T. Manschreck
Thomas Fuchs
Adriana Mavlea
Marcia Brenner
Poorna Rayalu
Psychiatry and Clinical Psychopharmacology
önder küçük
GrigGrog Wainipittapong
Harvard Review of Psychiatry
Ross Baldessarini
Psychopathology
Noura Ahmed
Zeelaf Siraj
Udayan Majumder
Psychiatric Annals
Rajdip Barman
World Journal of Advanced Research and Reviews, 2022, 13(01), 065–071
Gayane Kirakosyan
Beata Borowska-Beszta
Clinical Psychology Review
Nigel Blackwood
Journal of The American Academy of Child and Adolescent Psychiatry
Stephen Setterberg
Silvia Lippi , Célia Lehaire , Laetitia Petit
mohamed Jafferey
Romanian Journal of Psychiatry
Traian Purnichi , Valentin Matei , Ruxandra Moona Matei
Psychiatria Danubina
Katarina Mandic
Cornelia Cosmeanu
The Primary Care Companion to The Journal of Clinical Psychiatry
Muhammed Mehtar
Michelle Arroway
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
Table of Contents - Schizophrenia Biology
- The Most Recent Schizophrenia Biology News
- The Most Recent Schizophrenia Research News and Journal Article Summaries
- The Most Recent Schizophrenia Genetics News
- Schizophrenia Researchers
- Introductory Presentation on the Biology of Schizophrenia
- Reports on Schizophrenia
- Schizophrenia as a Model of Dopamine Dysfunction
- Top Papers, Journals, Researchers and Institutions focused on Schizophrenia
- Other Papers on Genetics and Mental Illness
- Some of the Current Areas of Focus in Schizophrenia Research
- Internet-based Schizophrenia Video Lectures and Presentations
- Recommended Advanced Books on the Biology of Schizophrenia
Recommended Professional Books on Schizophrenia and Psychiatric Drugs
Types of Schizophrenia and Related Illnesses
Schizophrenia Genetics, Research Organizations, and Related Information
- The Most Recent Schizophrenia Research News and Journal Article Summaries See following link for the Archived Full List of Schizophrenia Research News and Journal Article Summaries
- Schizophrenia's Most Zealous Foe
- Interview with Dr. Torrey (1997)
- "BirdBrains" - Dr. E. Fuller Torrey on NIMH Funding Priorities (May 2001)
- Dr. Brain (Princeton Alumni Magazine)
- Brain Storm (Stanford University Magazine)
- Dr. Torry's Biography - (from Treatment Advocacy Center)
- Real Audio Recording: The Mental Illness System: How It Broke and How to Fix It Speaker: Dr. E. Fuller Torrey, President, Treatment Advocacy Center, Bethesda, Maryland, September 2000. Don't have "Real Audio Player" - download a free copy from here .
- Surviving Schizophrenia: A Manual for Families, Consumers, and Providers (4th Edition)
- Surviving Manic Depression: A Manual on Bipolar Disorder for Patients, Families, and Providers
- The Invisible Plague: The Rise of mental Illness from 1750 to the Present
Out of the Shadows : Confronting America's Mental Illness Crisis
- Dr. Michael Flaum on his work with Nancy Andreasen
- Nancy C. Andreasen M,D., Ph.D. Biography
- Ask the Experts: Nancy C. Andreasen M,D., Ph.D.
- Published Books
- Brave New Brain: Conquering Mental Illness in the Era of the Genome
- Introductory Textbook of Psychiatry (3rd Edition)
- The Broken Brain
- Schizophrenia: From Mind to Molecule (American Psychopathological Association)
- Schizophrenia: Positive and Negative Symptoms and Syndromes (Modern Problems of Pharmacopsychiatry, Vol. 24)
- Genetic Research, Icelandic genes offer a wealth of disease clues
- DeCode-ing Schizophrenia
- Gene May Play a Role in Schizophrenia (2nd Study Confirms)
- Interview with Dr. Gottesman (who has been a ever-helpful source of information for schizophrenia.com)
- Psychiatric Genetics and Genomics
- Schizophrenia Genesis: The Origins of Madness
- Can Schizophrenia Be Prevented?
- Focus on proactively treating early-phase schizophrenia in adolescents
- Interview with Dr. Shelton (Harvard University)
- Epidemiology - Genetics Program in Psychiatry
- Zeroing in on Schizophrenia Genes
- Study Shows First Genetic Evidence for Schizophrenia Susceptibility
- Search for Schizophrenia Gene Takes an Unplanned Turn
- New Imaging Research Reveals Dysfunction In The Brain's "Hub" In The Earliest Stages Of Schizophrenia
- 25-minute test distinguishes between different types of schizophrenia
- Schizophrenia test moves closer (BBC)
- Brain images provide a means of screening for schizophrenia (The Scientist)
- In Schizophrenia, Thalamus Is Smaller Than Normal
- Brain Imaging in Schizophrenia: Insights and Applications
- Cognition in Schizophrenia: Impairments, Importance, and Treatment Strategies
- Summary of Greengard lecture , presented at Emory University in April 2005, detailing his work on the dopamine neuron protein DARPP-32
- DARPP-32 may be culprit in schizophrenia symptoms (Psychiatric News, Sept 2002)
- Brain's 'Master Molecule' Produces Same Behavior in Mice From Three Different Psychostimulant Drugs (Science Daily, Nov 2003)
- NARSAD Distinguished Investigator Grant Recipient , 2002
- Recipient of the 1996 Lieber Prize for Outstanding Achievement in Schizophrenia Resesarch
- Interview with Dr. McGuffin
- Interview with Dr. Weinberger
- More Very Good Interviews with Schizophrenia Researchers
- Neurobiological Bases of Psychiatric Disorders
- What do we mean by Disease?
- Inheritability of Disease
- Twin Studies
- Neural Mechanisms Usually Follow Effective Drug Treatment
- Importance of Biogenic Amines
- Schizophrenia - an Overview
- Strong Genetic Component to Schizophrenia
- MRI Images of Brains of People that Have Schizophrenia
- Cellular Disarray in Brains of People that Have Schizophrenia
- Hypofrontality in Schizophrenia
- Chlorpromazine treatment of Schizophrenia
- Dehospitalization Rates After Adoption of Antipsychotic Medications
- Dopamine Hypothesis of Schizophrenia
- Effectiveness of Neuroleptic medications is highly correlated with binding affinity to DA receptors
- How Chlorpromazine Works
- Dopamine is not the Whole Story
- Schizophrenia and Other Psychiatric Disorders (Houghton University)
- Neurobiology of Schizophrenia - by Stephen Rayport, MD, PhD (Columbia University)
- Schizophrenia Presentation
- Schizophrenia Presentation (Audio File) (Real Audio file - Download Free Player here , if you don't have it)
- Schizophrenia Presentation (Transcript)
- Psychotic Disorders (Spring 05, pdf). Source: University of Illinois Dept. of Psych
- Intramuscular Olanzapine - New Drug Application (Lilly)
- Glycine Therapy - A New Direction for Schizophrenia Treatment? (report on the merits of glycine as a possible complementary therapy for schizophrenia, including an interview with researcher Dr. Dan Javitt. Apr 2005. HTML File)
- A Neurological Basis for Poor Insight in Schizophrenia - Review of the Research ( paper for an advanced neuroscience research seminar, Dec 2004. HTML File )
- Recent advances in understanding mental illness and psychotic experiences - Year 2000, 300K PDF File, ( A report by The British Psychological Society, Division of Clinical Psychology)
- Early Psychosis Treatment Guide - Year 2002, University of British Columbia - Note: this is a large (3 MB) PDF file and it may take a few minutes to download if you have a slow internet connection).
- Lecture: Exploring the Mind and Brain in Health and Disease (by Nancy Andreasen)
- Free Access to Schizophrenia Reseach Papers - via Highwire Press at Stanford University
- Distribution of Occurrence
- Genetic Patterns
- Drug Effects and Schizophrenia
- Searching for a Chemical Label
- The DBH Model
- DBH as a rate limiter
- Other Dopamine Models
- Metabolic pathway theories
- Receptor theories
- Endorphin contributions
- Movement Disorders
- The Top 50 Most-Cited Papers in Schizophrenia Research (as of 2001)
- Top Journals on Schizophrenia Research (as of 2001)
- Top Schizophrenia Research Institutions (based on the number of papers published, 2001)
- Top 25 Authors of Schizophrenia Research Papers (2001)
- ScienceWatch - List of High Impact Journals in Psychiatry (2000)
- Best Place to Search for New Research Papers on Schizophrenia: www.pubmed.org
Sample of Papers that are Available On-Line
- An Automated Measurement of Subcortical Brain MR Structures in Schizophrenia (Harvard)
- Finding Genes for Schizophrenia (Source: Swedish PHD Thesis by Carolina Aberg )
- Increased Expression in Dorsolateral Prefrontal Cortex of CAPON in Schizophrenia and Bipolar Disorder
- Decoding Schizophrenia (Scientific American Magazine)
- Scientists identify more gene defects linked to schizophrenia
- Gene May Play a Role in Schizophrenia - Second Major Study Confirms
- Genes clue to schizophrenia - site requires free registration to view
- Israeli Biotech: Schizophrenia Associated With the COMT Gene
- Gene Increases Schizophrenia Risk, Says Study
- SCHIZOPHRENIA: Cause may be interaction of genes and viruses in glia cells
- Hypoglutamatergic hypothesis of schizophrenia: evidence from genetic studies
- Schizophrenia: from dopamine to glutamate and back
- Expression of the ionotropic glutamate receptor subunits and NMDA receptor-associated intracellular proteins in the substantia nigra in schizophrenia
- Targeting metabotropic glutamate receptors for treatment of the cognitive symptoms of schizophrenia
- GABA and schizophrenia: a review of basic science and clinical studies
- The glial growth factors deficiency and synaptic destabilization hypothesis of schizophrenia
- Genes, germs, and schizophrenia: an evolutionary perspective
- Prenatal exposure to influenza as a risk factor for adult schizophrenia
- Smell test 'spots schizophrenia' (early diagnosis opportunities)
- Earlier diagnosis of schizophrenia improves results of treatment (Yale, 2004)
- Eye Movement Studies To Help Diagnose Mental Illness
- Omega 3 and EFA Fatty Acids and Antioxidants Useful for Schizophrenia
- Internet-based Schizophrenia Video Lectures and Presentations are now on their own webpage. Please visit http://www.schizophrenia.com/video/index.htm#biovideo for a complete list
These books cover the science, biology and genetics of schizophrenia. "Nature via Nurture", while not specifically a book about schizophrenia - has an entire chapter (Chapter 4 - The Madness of Causes) on the genetics and environmental influences of schizophrenia. Overall, the book is a well-written and very enjoyable book about the interplay of genes and environment in human development. Dr. Nancy Andreason's and Dr. Irv Gottesman's books are good in-depth college-level books covering schizophrenia by two of the leading researchers that are focused on schizophrenia. Nature Via Nurture : Genes, Experience, and What Makes Us Human by Matt Ridley (Author), Publisher: HarperCollins; (April 29, 2003) ISBN: 0060006781 Psychiatric Genetics and Genomics by Peter McGuffin (Editor), Michael J Owen (Editor), Irving I Gottesman (Editor), Publisher: Oxford University Press; (December 2, 2002), ISBN: 0192631489 Brave New Brain: Conquering Mental Illness in the Era of the Genome by Nancy C. Andreasen, Publisher: Oxford University Press; (April 2001) ISBN: 0195145097 (HARDCOVER) " Excellent introductions to neuroscience, brain imaging, and genetics. Outstanding overviews of what is known about the neuroscience and genetics of the major psychiatric disorders of schizophrenia, mood disorders, dementia, and anxiety disorders. The descriptions of the history and neuroscience of medication are especially good. "--Nature Brave New Brain: Conquering Mental Illness in the Era of the Genome by Nancy C. Andreasen , Publisher: Oxford University Press; (February 2004) , ISBN: 0195167287, (SOFTCOVER) Schizophrenia Genesis: The Origins of Madness by Irving I. Gottesman, Publisher: W H Freeman & Co.; (November 1990) ISBN: 0716721473 The BROKEN BRAIN by Nancy C. Andreasen (Author), Publisher: Perennial; Reprint edition (November 1985) ISBN: 0060912723 (Note: this is an old book -- over 15 years old -- and should only be referenced if the more recent books listed above are not available. Information in the field of genetics is progressing rapidly, and a book that is 15 years old is truly ancient).
Psychiatric Genetics and Genomics by Peter McGuffin (Editor), Michael J Owen (Editor), Irving I Gottesman (Editor), Publisher: Oxford University Press; (December 2, 2002), ISBN: 0192631489 Practice Guidelines for the Treatment of Patients with Schizophrenia by American Psychiatric Association, APA, Publisher: Amer Psychiatric Pr; 1st edition (January 15, 1997) ISBN: 0890423091. Developed by experts on schizophrenia and exhaustively reviewed by APA members, the American Psychiatric Association Practice Guideline for the Treatment of Patients With Schizophrenia provides therapists with a set of patient care strategies that will aid their clinical decision making. Note: This publication is usually available on-line for free at: The American Psychiatric Association website Serious Mental Illness and the Family: The Practitioner's Guide by Diane T. Marsh, Publisher: John Wiley & Sons; 1 edition (October 2, 1998) ISBN: 0471181803 Schizophrenia by Steven R. Hirsch (Editor), Daniel R. Weinberger (Editor), Penny R. Mitchell, Publisher: Blackwell Publishers; 2nd Revision edition (March 2003) ISBN: 0632063882 Comprehensive Care of Schizophrenia by Lieberman, Publisher: Martin Dunitz Ltd; (December 2001) ISBN: 1841841501 Schizophrenia and Mood Disorders: The New Drug Therapies in Clinical Practice By Peter F. Buckley (Editor), John L. Waddington (Editor), Publisher: Edward Arnold; 1st edition (February 15, 2000) ISBN: 0750640960 Insight and Psychosis by Xavier F. Amador (Editor), Anthony S. David (Editor), David Amador, Publisher: Oxford University Press; (January 1998) ISBN: 0195084977 Distinguishing Psychological From Organic Disorders: Screening for Psychological Masquerade by Robert L., Md. Taylor, Publisher: Springer Pub Co; 2nd edition (July 15, 2000) ISBN: 082611329X The Schizophrenias: A Biological Approach to the Schizophrenia Spectrum Disorders (Springer Series on Psychiatry) by Mary Coleman, Christopher Gillberg, Publisher: Springer Pub Co; (September 1996) ASIN: 0826192904 Genetics and Mental Illness: Evolving Issues for Research and Society by Laura Lee Hall (Editor), Publisher: Plenum Pr; (January 1996) ISBN: 0306451662 Treating Schizophrenia (Jossey-Bass Social and Behavioral Science Series) by Werner M. Mendel, Publisher: Jossey-Bass; 1st Edition edition (June 1989) ASIN: 1555421512
- Paranoid schizophrenia - These persons are very suspicious of others and often have grand schemes of persecution at the root of their behavior. Halluciations and delusions are prominent.
- Disorganized schizophrenia (Hebephrenic Schizophrenia) - In this case the person is verbally incoherent and may have moods and emotions that are not appropriate to the situation. Hallucinations are not usually present.
- Catatonic schizophrenia - In this case, the person is extremely withdrawn, negative and isolated, and has marked psychomotor disturbances.
- Residual schizophrenia - In this case the person is not currently suffering from delusions, hallucinations, or disorganized speech and behavior, but lacks motivation and interest in day-to-day living.
- Schizoaffective disorder - These people have symptoms of schizophrenia as well as mood disorder such as major depression, bipolar mania, or mixed mania.
- Undifferentiated Schizophrenia - Conditions meeting the general diagnostic criteria for schizophrenia but not conforming to any of the above subtypes, or exhibiting the features of more than one of them without a clear predominance of a particular set of diagnostic characteristics.
- Schizoid Personality
- Schizophreniform Disorder
- Schizotypal Personality
- Bipolar Disorder (Manic Depression) - frequently misdiagnosed as schizophrenia (and vise versa)
- Database for Schizophrenia candidate genes - "The Database for Schizophrenia candidate genes focusing on Variations(VSD) includes the genes that contains polymorphisms related with schizophrenia. Has also information about the metabolic pathways in an easy-to-use interface."
- U.S. Health Official Puts Schizophrenia Costs At $65 Billion
- 10 Year Goals to be set in Brain Research - Europe
- World Health Organization (WHO) report from 10th International Psychopathology Conference
- The Stanley Foundation Research Programs
- NARSAD - National Alliance for Research on Schizophrenia and Depression
- NIMH Genetics Research Branch
- UCLA Center for Research on Treatment & Rehabilitation of Psychosis
- UC San Diego
- University of Michigan - Meador/Woodruff Laboratory
- Stanford University
- Harvard Schizophrenia Research Project
- Yale - Schizophrenia Research Clinic
- The University of North Carolina at Chapel Hill School of Medicine
- University of Colorado - Schizophrenia Center
- University of Pittsburgh Medical Center’s Western Psychiatric Institute and Clinic (WPIC)
- Toronto - Center for Addiction and Mental Health
- University of British Columbia
- McGill University
- University of Saskatchewan
- University of Alberta
- Research Symposiums and Events
- Archives of General Psychiatry
- Archives of Neurology
- American Journal of Psychiatry
- Behavioral and Brain Sciences
- Biological Psychiatry
- British Medical Journal
- Canadian Medical Association Journal
- International Journal of Psychosocial Rehabilitation
- InterPsych Newsletter
- Journal of Abnormal Psychology
- Journal of the American Medical Association (JAMA)
- Journal of Clinical Psychopharmacology
- Journal of Cognitive Neuroscience
- Journal of Neuroscience
- Journal of Psychiatry & Neuroscience
- Journal of Practical Psychiatry and Behavioral Health (R)
- Journal of the American Academy of Child & Adolescent Psychiatry
- New England Journal of Medicine
- Proceedings of the National Academy of Sciences
- Psychiatry On-line
- Psychological Bulletin
- Psychological Medicine
- Psychosomatic Medicine
- Psychiatry Research
- Schizophrenia Research
- The Journal of Nervous and Mental Disease
- The Neurologist
- American Psychiatric Association (APA)
- American Psychological Society (APS)
- American Psychological Association (APA)
- Society of Biological Psychiatry
- Society for Neuroscience
- American Medical Association (AMA)
- NIMH Genetics Initiative
- Another Company researching Genetics and Schizophrenia
- Canadian Company doing research into genetic causes of Schizophrenia
This site does not provide medical or any other health care or fitness advice, diagnosis, or treatment. The site and its services, including the information above, are for informational purposes only and are not a substitute for professional medical or health advice, examination, diagnosis, or treatment. Always seek the advice of your physician or other qualified health professional before starting any new treatment, making any changes to existing treatment, or altering in any way your current exercise or diet regimen. Do not delay seeking or disregard medical advice based on information on this site. Medical information changes rapidly and while Schizophrenia.com makes efforts to update the content on the site, some information may be out of date. No health information on Schizophrenia.com, including information about herbal therapies and other dietary supplements, is regulated or evaluated by the Food and Drug Administration and therefore the information should not be used to diagnose, treat, cure, or prevent any disease without the supervision of a medical doctor.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Schizophrenia
Prof. michael j owen.
MRC Centre for Neuropsychiatric Genetics and Genomics, Cardiff University, Cardiff, UK
Prof. Akira Sawa
Department of Psychiatry, Johns Hopkins University School of Medicine, USA
Prof. Preben B Mortensen
Department of Economics, School of Business and Social Science, Aarhus University, Denmark
Schizophrenia is a complex, heterogeneous behavioural and cognitive syndrome whose origins appear to lie in genetic and/or environmental disruption of brain development. Dysfunction of dopaminergic neurotransmission appears to contribute to the genesis of psychotic symptoms but the evidence also points to a more widespread and variable involvement of brain areas and circuits. There is emerging evidence that disturbances of synaptic function might underlie abnormalities of neuronal connectivity possibly involving interneurons, but the precise nature, location and timing of these events is uncertain. Current treatment consists largely in the administration of antipsychotic drugs combined with psychological therapies, social support and rehabilitation, but there is a pressing need for more effective treatments and for services to be delivered more effectively. Progress in understanding the disorder has been great in recent years with advances in genomics, epidemiology and neuroscience, and the opportunities for further scientific advance are great: but so are the challenges.
Introduction
Schizophrenia is a severe psychiatric disorder that has a profound impact on the individual and society. While outcomes may not be as uniformly negative as is commonly believed, over 50% of those individuals who receive a diagnosis have intermittent but long-term psychiatric problems and around 20% have chronic symptoms and disability. 1 Unemployment is staggeringly high at 80–90% 2 , 3 and life expectancy is reduced by 10–20 years. 4 In England schizophrenia costs society £11.8 billion per year with around a third of this accounted for by direct expenditure on health and social care, provided both in hospitals and the community. 5 Understanding the aetiology and pathogenesis of schizophrenia and developing new more effective and acceptable treatments remains one of the most formidable challenges facing modern medicine. However, the past decade has seen substantial advances in the application of genomics, epidemiology and neuroscience to schizophrenia; while many challenges remain, the opportunities for progress have never been better.
Clinical presentation, signs and symptoms
Schizophrenia is characterised by diverse psychopathology (Box 1); the core features are positive symptoms (delusions and hallucinations; so-called psychotic symptoms in which there is a loss of contact with reality), negative symptoms (in particular impaired motivation, reduction in spontaneous speech, and social withdrawal) and cognitive impairment (as a group patients with schizophrenia perform more poorly than controls over a wide range of cognitive functions though there is much individual variability). 6 The positive symptoms tend to relapse and remit, though some patients experience residual long-term psychotic symptoms. The negative and cognitive symptoms tend to be chronic and are associated with long-term effects on social function. The first episode of psychosis usually occurs in late adolescence or early adulthood but is frequently preceded by a prodromal phase or “at risk mental state” 7 , 8 and in some instances premorbid impairments in cognition and/or social functioning go back many years. 9 However, in other instances onset is sudden in previously well-functioning individuals.
Diagnosis and differential diagnosis
Diagnosis is made clinically on the basis of history and by examination of the mental state; there are no diagnostic tests or biomarkers. Schizophrenia usually presents with psychosis and the main differential diagnoses, in DSM5 10 , are affective psychoses (bipolar disorder with psychotic features and major depressive disorder with psychotic features), other, closely related, non-affective psychoses (schizoaffective disorder, schizophreniform disorder, delusional disorder, brief psychotic disorder and psychotic disorder not otherwise specified), substance induced psychotic disorders (alcohol induced, other substance induced) and psychotic disorders due to a general medical condition. Differential diagnosis takes into account the duration of illness, the nature and pattern of associated substance abuse, the co-occurrence of depression or mania and the presence of somatic illness.
Schizophrenia, like the majority of psychiatric diagnoses, remains a syndromic concept. The use of operational criteria, such as those embodied in the Diagnostic or Statistical Manual of the American Psychiatric Association (DSM), 11 or the International Classification of Diseases (ICD) of the World Health Organisation 12 has provided a reliable approach to making psychiatric diagnoses in the clinic. However, the assumption that the clinical syndromes defined in this way represent valid disease entities with distinct underlying aetiology and pathogenesis is increasingly seen as having impeded research. 13 – 15 Indeed psychiatric diagnoses have the unusual property of being simultaneously too broad and too narrow. 15 Individuals with a diagnosis of schizophrenia vary greatly in predominant symptoms, response to treatment, course and outcome. However, attempts to resolve this heterogeneity into valid subtypes has repeatedly failed. On the other hand, many psychiatric diagnoses have symptoms in common (Box 1) and the boundaries between schizophrenia and other disorders are indistinct as are the boundaries between disorder and wellness. With regard to the latter there is an increasing realization that psychotic symptoms, such as auditory hallucinations and paranoid thinking, occur in attenuated form in 5–8% of the healthy population. 16 This has led to suggestions that dimensional approaches to diagnosis and classification might replace or enhance current categorical approaches. 15 , 17 , 18
It has long been known on the basis of many genetic epidemiological studies that there is a substantial, but not exclusive, contribution of genetic factors to the aetiology of schizophrenia. 19 , 20 What has changed recently is that, thanks to recent large-scale genomic studies, the contribution of specific variants at the DNA level has begun to emerge and we are beginning to get a clearer picture of how risk alleles (Box 2) of different types contribute to the disorder. We can draw three lessons of general importance from these recent findings.
The first is that schizophrenia is highly polygenic, as predicted many years ago on the basis of genetic epidemiological findings, 21 with hundreds, and possibly thousands, of distinct genetic loci (Box 2) involved at the population level. The findings suggest that alleles with a spectrum of population frequencies contribute to risk ( Fig 1 ). 22 Genome-wide association studies (GWAS, Box 2) have identified over 100 distinct genetic loci containing relatively common alleles of small effect and the en masse effects of many hundreds of such loci. 22 , 23 Genomic studies have also identified 11 rare, but recurrent, copy number variants (CNVs, Box 2) that individually confer relatively high risk of schizophrenia ( Fig 1 ). 24 , 25 Recent studies have also demonstrated a role of newly occurring ( de novo) CNV mutations in schizophrenia. 24 , 26 , 27 Recent whole exome sequencing studies (Box 2) have implicated rare, inherited and de novo single nucleotide and insertion/deletion variants (indels) in schizophrenia, 28 , 29 though the net contribution of mutations of this type is unknown pending much larger sequencing studies. Bearing in mind that schizophrenia is associated with reduced fecundity, 30 the picture that is emerging is one in which alleles that confer high individual risk are rare in the population due to the effects of natural selection, 31 whereas those conferring small effects on individual risk can become common due to genetic drift or balancing selection ( Fig 1 ).

The figure depicts risk alleles for schizophrenia that have been robustly identified by genomic studies. The x -axis is the allele frequency (AF) in controls and the the y -axis is the odds ratio (genotypic relative risk). For clarity, confidence intervals are not shown. Copy number variants associated with schizophrenia are shown as blue diamonds. Single nucleotide polymorphism that are associated with SCZ and are shown as red diamonds. Alleles that confer high individual risk are rare in the population due to the effects of natural selection, whereas those conferring small effects on individual risk can become common due to genetic drift or balancing selection.
The second major lesson from recent genomic studies is that genetic risk appears to be highly pleiotropic (Box 2) and does not map onto current definitions of disease. Pleiotropy has been observed for common variants at the level of individual risk alleles and en masse effects. A recent study found significant sharing of common risk variants between schizophrenia and bipolar disorder, bipolar disorder and major depressive disorder, schizophrenia and major depressive disorder, ADHD and major depressive disorder, and, to a lesser extent, between schizophrenia and ASD 32 . Another study found evidence for overlap between schizophrenia and ADHD. 33 There is also evidence for pleiotropy with regard to the effects of rare variants; CNVs that confer risk to schizophrenia also confer risk to a range of childhood neurodevelopmental disorders such as ASD, intellectual disability (ID), and ADHD as well generalized epilepsy. 24 , 34 , 35 There is also emerging evidence that some rare single nucleotide variants and indels are associated with a similar range of outcomes. 28 Risk alleles that are relatively non-specific to diagnostic group will be easier to detect than those that confer risk to particular diagnoses or sub-groups and indeed recent work is beginning to identify alleles with relatively specific risk profiles. 36 – 38 However the pleiotropic effects observed to date, along with the lack of clear boundaries between disorders in clinical studies, suggest that there are likely to be overlapping mechanisms at work and that current diagnostic categories may not be optimal for stratifying cases for research into aetiology and pathogenesis.
The third point is that, despite the fact that much of the genetic risk for schizophrenia remains unaccounted for at the DNA level, and the complexity of the picture that has already emerged, there are encouraging signs of convergence on to a set of plausible biological processes. Findings from rare mutations, both CNVs and SNVs/indels, implicate genes encoding a variety of synaptic proteins including components of the post-synaptic density (PSD) and members of the voltage-gated calcium channel family of proteins. 39 ( Fig 2 ) Recent large-scale GWAS 23 have also implicated common variation at genes encoding glutamate receptors and the voltage-gated calcium channel family of proteins. Recent GWAS have also implicated common variation at the Dopamine receptor D2 (DRD2) gene, which encodes the principal target of antipsychotic drugs (see below). The relationship between glutamatergic dysfunction and abnormalities of dopamine signalling may provide a clue as to how psychosis and cognitive deficits arise in schizophrenia and related disorders. These are very unlikely to be the only mechanisms involved in the aetiology of schizophrenia, and we can expect more possible processes to emerge as we move into the next phase of genomic studies. It is important to note that the most statistically significant association emerging from GWAS of schizophrenia is with multiple highly correlated variants in the major histocompatibility complex (MHC). This contains many genes not involved with immune function, but preliminary data suggest that variants associated with schizophrenia are also enriched in genomic regions outside the MHC that are potentially involved in acquired immunity. 23 These findings are in accord with epidemiological and clinical studies implicating immune and inflammatory processes in various developmental stages, such as in utero , adolescence, and adulthood, in psychiatric disorders. 40 , 41

Recent advances in human genetics, from both GWAS and large-scale sequencing, have further supported the significance of fine-tuning of glutamatergic neurotransmission in the pathology of schizophrenia. The genes underscored by these studies include those encoding the glutamate receptor, ionotropic, N-methyl D-aspartate 2A (GRIN2A); glutamate receptor ionotropic, AMPA 1 (GRIA1); serine racemase (SRR); calcium channel, voltage-dependent (VDCC), L type, alpha 1C subunit; the ARC complex, and a number of proteins located in, or associated with, the postsynaptic density of glutamatergic synapses. The N-methyl D-aspartate (NMDA)-type glutamate receptors are fine tuned by a co-agonist D-serine, which is synthesized by SRR. The GRIN2A subunit (in dark green) dimerizes with other type of subunit, forming the NMDA receptors, whereas the GRIA1 subunit (in brown) also forms heterodimers for the AMPA receptors. VDCCs (e.g., the protein encoded by the CACNA1C gene) are also likely to be involved in tuning neural excitability and synaptic transmission via intracellular calcium signaling. Proteins associated with postsynaptic scaffold include PSD95, Stargazin, several kinases, Rho/Cdc42/Rac small G-proteins, and ARC complex. In response to activation of glutamate receptors, these proteins convey intracellular signaling that underlies cytoskeletal regulation and receptor trafficking crucial for synaptic plasticity.
The majority of genetic discoveries in schizophrenia do not yet have direct clinical application. The one potential exception is the finding that certain CNVs are associated with risk of schizophrenia and other neurodevelopmental disorders. Testing for CNVs using chromosomal microarray analysis (CMA) is now a routine, first-line diagnostic test for autism and intellectual disability where 10–20% of affected cases have a clinically relevant deletion or duplication. It has been suggested that we should now introduce CMA in schizophrenia, where the prevalence of clinically relevant CNVs is around 5%. 42 A positive test would have implications for genetic counselling and also for medical management since many CNVs are associated with specific patterns of physical morbidities. There are also potential psychological benefits of a genetic diagnosis for individuals with schizophrenia and their families. 42
Epidemiology and environmental risk factors
Schizophrenia occurs worldwide, and for decades it was generally believed to have a uniform lifetime morbid risk of 1% across time, geography, and gender. This implied either that environmental factors are not important in conferring risk or that the relevant exposures are ubiquitous across all populations studied. It was not until relatively recently that this uniform view of risk was efficiently dismantled in a series of meta-analyses by McGrath and colleagues. 43 They provided central estimates of an incidence per 100.000 population per year of approximately 15 in males and 10 in females, a point prevalence of 4.6 per 1000, and a lifetime morbid risk of app 0.7 %. These rates are based upon relatively conservative diagnostic criteria and, when broader criteria including other psychotic disorders such as delusional disorder, brief psychotic disorder and psychosis not otherwise specified are applied, the rates are 2 – 3 fold higher. 44 However, more importantly, McGrath and colleagues documented a large variation across studies, five-fold or more, that could not be ascribed to diagnostic or other methodological differences, but which pointed towards real differences in occurrence and exposure to etiological factors. These findings have revitalized schizophrenia epidemiology and the resulting new wave of studies, together with advances in genetics, have begun to cast light on how the disorder might arise.
The dominant paradigm for understanding the environmental contributions to schizophrenia etiology has for over three decades been the neurodevelopmental hypothesis. 45 This directs attention towards established risk factors for schizophrenia affecting early neurodevelopment during pregnancy. These include maternal stress, 46 maternal infections, 47 , 48 nutritional deficiencies, 47 , 49 intrauterine growth retardation, and pregnancy and birth complications. 50 , 51 However, socio-economic factors, 52 – 54 childhood adversity, 55 and first- and second-generation immigrant background 56 , 57 have also been associated with schizophrenia. There are also consistent reports of higher rates of schizophrenia in individuals born in late winter or early spring, 58 in individuals born and/or raised in cities, 59 and in individuals where the father was relatively old, but also an association with young parents has been found. 60 , 61 The association with advanced paternal age has been ascribed to the increased rate of de novo mutations in their offspring, 62 , 63 but alternative or complementary explanations have been proposed. 64 More recently, evidence has accumulated implicating cannabis use in adolescence, in particular misuse of compounds with high THC content. 65 , 66 Also, several other factors such as head injury, 67 epilepsy, 68 autoimmune diseases 69 , 70 and severe infections 71 – 73 have been associated with increased risk.
It has been pointed out that a number of the environmental exposures associated with schizophrenia, particularly those impacting most directly on early brain development, are also associated with a range of other neurodevelopmental outcomes including ID, autism, ADHD and epilepsy. 74 , 35 This is similar to the range of outcomes associated with large, rare CNVs 24 , 35 , 75 and suggests that schizophrenia might best be conceived as one of a spectrum of clinical outcomes that result from genetically and/or environmentally induced disruption to the developing brain. This points to the need for future epidemiological studies to look more carefully at the range of outcomes associated with particular exposures and not to be constrained by the assumption that current diagnostic approaches delineate disorders with distinct causes and mechanisms.
Many of the associations with environmental risk factors appear robust, and the odds ratios from the cited papers (predominantly the most recent meta-analyses) typically range from 1.5–3.0. However, observational epidemiology suffers from the limitation that is cannot distinguish true causation from association due to confounding, pleiotropy or reverse causation. Thus, at present, caution is required in interpreting these associations and more work is needed before preventive intervention is justified.
Experimental animal studies offer one approach by which evidence can be obtained to support a causative role for environmental risk factors. There is a rapidly growing literature of such studies corroborating epidemiological findings. These include studies of infections, pre-natal maternal inflammation as well as stressors post-natally and onwards, and their impact on behavioural and neurobiological variables that model aspects of schizophrenia. 76 , 77 Interestingly, prenatal factors and pre-pubertal stressors have been found to interact in some of these studies. 78 This points to a more complex model in which the impact of environmental exposures is modified by earlier events and suggests the need for a new generation of more sophisticated longitudinal epidemiological studies integrating prenatal and postnatal factors.
A key challenge for observational epidemiological studies of environmental factors has been the inability to control efficiently for confounding due to differences in genetic liability: in other words, are differences associated with, say, infections, due to a higher rate of infections amongst those more genetically predisposed towards schizophrenia? Until now, epidemiology has, at best, only been able to control for this by taking psychiatric family history into account, and, as only a minority of patients have family members with the disease, this is a highly imprecise measure of liability. This situation is now dramatically changing, with the recent advances in identifying common genetic variants associated with schizophrenia risk. Although of no use as an individual predictor of disease risk, a polygenic risk score summarizing associations with approximately 20,000 variants has been shown to reliably predict 5–10 fold risk differences. 23 This methodology must be expected to develop and improve rapidly over the next few years, providing researchers with an efficient novel tool in the effort to separate nature from nurture in schizophrenia etiology, as well as facilitating studies of how genetic and environmental factors interact (GxE). 79 GxE interactions are very plausibly of substantial importance in schizophrenia as in other complex disorders. The concept of GxE interactions in its broadest sense simply means that the effect of a given environmental factor depends upon single or multiple genetic variants, and vice versa. Although conceptually simple, the study of GxE interactions present a number of challenges, and this emerging literature has taken a number of different approaches. 79 , 80 First, a range of studies has been performed focusing upon a single candidate gene interacting with a specific environmental exposure. These studies have the advantage of a specific prior hypothesis and hence can be performed with a relatively modest sample size. However, as choosing candidate genes must be based upon the existing limited understanding of the genetic architecture of schizophrenia and the likely mechanisms involved in their interactions with the environment, this approach, albeit relevant in its own right, cannot help discover the majority of relevant GxE interactions. However, searching for interactions across the genome in a hypothesis-free manner requires enormous sample sizes. Therefore a number of novel techniques have been developed to perform so-called gene-environment wide interaction studies (GEWIS), and these methods have begun to be applied in schizophrenia research. 81 , 82
Another application of genetic data to enhance the causal interpretation of environmental factors is the Mendelian randomisation design, where genes associated with the level of exposure are used as instrumental variables, 83 and applications of methods to assess the extent to which risk factors are mediated through measures of genetic liability. 84 For example Agerbo et al. 85 showed that a large proportion of the association between a family history of psychosis and schizophrenia risk was mediated through a Polygenic Risk Score, whereas this was not the case as regards socioeconomic risk factors.
In summary, a large body of literature suggests that multiple risk factors, in particular those affecting early neurodevelopment, contribute to the etiology of schizophrenia. There is also emerging evidence that environmental factors, both biological and psychosocial, may impact at later time points ( Fig 3 ). It is certainly possible that the effects on the developing brain of earlier environmental exposures as well as genetic factors increase susceptibility to these later risk factors. However, caution must be observed before inferring causality and there is a need for studies combining measures of both the pre- and post-natal environment with measures of genetic liability. The bringing together of genomics with large-scale epidemiological approaches offers new and exciting ways to better understand the causal role of the environment and this will hopefully lead towards primary prevention.

This shows a schematic view of how multiple genetic and environmental risk factors might impact on long-term neurodevelopmental processes leading to schizophrenia. Schizophrenia typically presents when the first episode of psychosis occurs in late adolescence or early adulthood but is frequently preceded by a prodromal phase and in some instances premorbid impairments in cognition and/or social functioning go back many years. It is proposed that disturbances generated by susceptibility genes (indicated by blue stars) and environmental insults (indicated by pink asterisks) during early development and adolescence disturb postnatal brain maturation. These factors are likely to impair some of the crucial processes in early development, including progenitor cell proliferation, neuronal migration and dendritic arborization and outgrowth. Independent of such initial risks/insults, intrinsic disease-associated factors might also directly affect postnatal brain maturation. Accumulation of such deleterious insults results in overall disturbance of proper postnatal brain maturation, including maturation of interneurons and dopaminergic projections, pruning of glutamate synapses and myelination. Therefore, it is crucial to understand the mechanisms that underlie long-term progression to full disease manifestation in young adulthood to facilitate development of novel therapeutic strategies. This contrasts with classic drug discovery that simply modulates disturbed neurotransmission after full onset of the disease. In this figure, interneuron maturation is plotted as an increase in interneuron response to dopamine D2 agonists in the prefrontal cortex, whereas mesocortical dopaminergic projection is based on levels of tyrosine hydroxylase. The relative levels of glutamatergic synapse density and myelination are depicted. Extensively modified from the original figure appeared in Jaaro-Peled et al, TINS 2009.
Pathophysiology
Many brain imaging and neuropathological studies have attempted to relate the manifestations of schizophrenia to altered structure or function of particular brain regions and circuits. 86 , 87 There has been progress in relating some aspects of the disorder to specific underlying neurobiology and several lines of evidence implicate the involvement of the prefrontal cortex, in particular, in specific cognitive deficits (e.g., working memory and executive control). 88 – 90 However, subtle reductions in grey matter and abnormalities of white matter have been found across many brain regions and circuits. 91 The reduction of grey matter progresses with the duration of illness, especially in the temporal lobe 92 , and seems to be associated with antipsychotic treatment. 93 However, even drug-naïve patients show volume reductions (albeit not as pronounced as treated patients), especially in the caudate nucleus and thalamus. 91 Moreover, despite many hundreds of studies, no circumscribed anatomical or functional abnormalities that are specific to the disorder have been identified. 87 This is likely to reflect the complexity and heterogeneity of the psychopathology and associated cognitive impairments, and the lack of clear boundaries separating schizophrenia from other disorders or wellness.
There is a coherent body of evidence from pharmacological and brain imaging studies implicating dysfunction of dopaminergic neurotransmission in the genesis of psychotic symptoms such as delusions and hallucinations. 94 However, while these occur in the majority of cases of schizophrenia, they are also found in a variety of other psychiatric conditions. 94 Moreover, pharmacological, and other, evidence indicates that dopaminergic dysfunction is unlikely to explain the full range of clinical features of the disorder. Evidence from clinical pharmacology, brain imaging, and clinical physiology has suggested that disturbed glutamatergic function may contribute to the biological processes underlying some clinical features, in particular cognitive dysfunction, in schizophrenia. 88 , 95 , 96 One theory is that glutamatergic dysfunction in schizophrenia is related to dysfunction of parvalbumin-positive interneurons in the cerebral cortex and hippocampus, which are sensitive to alterations in NMDA-type glutamate receptors. 89 These fast spiking neurons synchronize the firing of pyramidal neurons and underlie the generation of gamma oscillations, which is critical to proper cognitive function. 97 Consequently, dysfunction of this population of neurons may lead to the cognitive deficits observed in schizophrenia. [ Fig 4 ] 97

In the cerebral cortex, interneurons (inhibitory neurons) regulate the output of pyramidal neurons (excitatory neurons). Many studies have reported abnormalities of interneurons (in particular parvalbumin-positive interneurons) and deficits of dendritic spines in the pyramidal neurons in the pathology of schizophrenia. Imbalance of excitatory and inhibitory neurons may be a key feature that underlies the pathology. Recent neurobiology indicates that astrocytes and microglia play key a role in maintenance and pruning of the dendritic spines, in association with immune inflammatory response in the brain. Oligodendrocytes create the myelin sheath, which is crucial for signal transmission inside the axon. Abnormalities of these glial cells have also been reported in schizophrenia.
Recent advances in human genetics, from both GWAS (Box 2) and large-scale sequencing, have further supported the significance of fine-tuning of synaptic transmission, in particular at glutamatergic and dopaminergic synapses in the aetiology and pathophysiology of schizophrenia. 23 , 28 , 29 The genes underscored by these studies include those encoding the glutamate and dopamine receptors, and those encoding post-synaptic proteins implicated in receptor-mediated signaling. ( Fig 2 ) 23 , 28 , 29 , 98 , 99
Nonetheless, there is a gap between basic information from genetic and other molecular studies and its application in translational research. While psychiatric genetics now convincingly implicates specific sets of genes involved in synaptic function, it does not provide information about the developmental stages, brain regions and circuitries where the molecules play roles in pathogenesis. This will require further studies of brain imaging, post mortem brains, clinical physiology and animal models to build on genetic findings.
At least two types of molecular pathway may be involved. The development and maintenance of normal synaptic function depends upon a large number of molecular pathways, including the molecules highlighted above ( Fig 2 ), and a number of environmental factors will further impact these as the brain develops. Second, stress-associated signaling cascades, in particular those involving inflammatory processes and oxidative stress, are well known to modulate the development and maintenance of synaptic connectivity ( Fig 4 ). For example, microglia (the glial cells that mediate brain inflammation) are involved in synaptic maintenance and deterioration, in particular synaptic pruning in adolescence, 100 – 102 and the major histocompatibility complex I (MHC class I) and complement system have been implicated in synaptic plasticity. 102 – 108 Furthermore, the fast-spiking parvalbumin-positive interneurons referred to above are particularly vulnerable to oxidative stress 109 , 110 and this can also disrupt proper formation and maintenance of myelination. 110 Evidence for the involvement of these mechanisms has come from recent studies of preclinical models. 111 , 112
In summary, current understanding of the neurobiology of schizophrenia remains largely incomplete. There is strong evidence implicating dysfunction of dopaminergic neurotransmission in the genesis of psychotic symptoms as well as evidence implicating abnormalities of glutamate signaling which might help account for the negative and cognitive symptoms. There is some evidence linking specific brain areas (e.g. prefrontal cortex) to specific cognitive dysfunctions (working memory impairment) but the evidence also points to a widespread and variable involvement of other brain areas and circuits. These findings are consistent with evidence from genetics and epidemiology that, at least in a proportion of cases, the origins of schizophrenia lie in genetic and/or environmental disruption of early brain development. There is emerging evidence from genetics and neurobiology that disturbances of synaptic function might underlie abnormalities of neuronal connectivity possibly involving interneurons, but the precise nature, location and timing of these events is uncertain. There is also evidence that progression towards schizophrenia can be impacted postnatally by further environmental exposures that may be modulated by genetic factors as well as earlier environmental factors. Recent evidence points to the role, in some cases, of oxidative and inflammatory mechanisms that may themselves impact on synaptic function and modulate connectivity at critical developmental stages ( Fig 4 ).
Management and outcome
Since the serendipitous discovery of chlorpromazine over 50 years ago, almost all antipsychotic drugs available in the clinical settings for schizophrenia derive their effectiveness through DRD2 blockade. 113 , 114 Clozapine is the most potent in efficacy, and a group of antipsychotics including clozapine binds and influences not only DRD2 but also other neurotransmitter receptors, such as serotonin receptors 2 (5HT-2R). 115 In the UK Clozapine is only licensed for use in those who have failed to respond to other antispsychotics due to the risk of agranulocytosis and neutropenia (1–3%) requiring ongoing blood monitoring. Antipsychotic drugs are relatively effective in reducing positive symptoms, such as auditory hallucinations and delusions, and remain the mainstay of both acute and long-term pharmacological treatment. However they are not effective for other important clinical features of schizophrenia, such as negative symptoms and cognitive dysfunction, which are more strongly associated with functional impairment than positive symptoms. There is evidence that long-term, maintenance treatment with antipsychotic drugs is effective in preventing relapse of psychotic symptoms, but troublesome side effects such as weight gain, movement disorders and sedation are common and contribute to poor adherence. 116 Moreover, a substantial number of patients show no, or at best partial, response in positive symptoms with current antipsychotic drugs. 117 – 119 Individual response is often idiosyncratic and difficult to predict. Newer, so-called second-generation, antipsychotic drugs can be effective in treating psychotic symptoms with fewer movement disorders, but carry a higher risk of cardio-metabolic side effects. Choice of the optimal antipsychotic is therefore usually pragmatic and balances individual benefits with costs and risks. Clozapine is effective in around 60% of previously treatment refractory cases 127 , but there is evidence that it is underprescribed 5 .
While antipsychotic medication remains the cornerstone of treatment, the effective management of schizophrenia requires pharmacotherapy to be embedded within a framework of strong psychological and social support. These include approaches aimed at improving adherence as well as vocational and educational support, and rehabilitation. This requires a multi-disciplinary approach involving a variety of health-care professionals and agencies delivered in a community-care setting. Specialist early intervention services, which focus on those who are experiencing their first psychotic episode and the following three years, are available in many developed countries, and are popular with service users and carers 5 . These have beneficial effects on outcome in the first few years, but their long-term impact remains uncertain 120 . Psychological treatments have been mandated by current UK NICE guidelines, which recommend that everyone with schizophrenia should be offered cognitive behavioral therapy (CBT) and family intervention as well as antipsychotic medication. A role for CBT is justified by evidence that various potentially mutable psychological mechanisms increase the risk of specific symptoms. 121 However, the degree of efficacy and cost-effectiveness of CBT in schizophrenia is controversial 122 and there is little evidence that it impacts on underlying psychological mechanisms. One possibility is that the efficacy of CBT depends upon non-specific factors such as the quality of the relationship between the therapist and the patient (therapeutic alliance) and there is evidence to support this in regard to schizophrenia. 123 Medical management also focuses upon physical health: in particular preventative measures such as dietary advice, drug abuse, exercise and smoking cessation; and monitoring of cardiovascular and metabolic risk factors. In many countries care is provided by a multidisciplinary team of mental health professionals in primary, secondary and community settings and focuses on both health and social care. 44
In recent years the perception that outcome is necessarily poor has been challenged by results of prospective studies and there is clearly great heterogeneity with relatively good outcome seen in 20–50% of cases. 44 However, while the majority of those with schizophrenia live independently outside hospital, many require continuing support either from services or relatives. Moreover, mortality from all causes of death is substantially increased. 124 , 125 The relative risk for suicide is increased 12-fold with a lifetime risk of approximately 6.5%, 126 but mortality from most natural causes, and in particular cardiovascular disorders, is the strongest contributor to the 10–20 year reduction in life expectancy. The causes of this are believed to include smoking and other life-style factors, and sub-optimal treatment of physical disorders in schizophrenia patients 124 , 127 but also side effects of pharmacological treatment in particular cardio-metabolic. Several trials to reduce the excess mortality are ongoing.
Outstanding research questions
It should be apparent from the forgoing that while progress has been great in the past 5–10 years, we still have much to learn about what causes schizophrenia and how to treat it more effectively. It should also hopefully be clear that the opportunities for progress have never been better.
Genomic studies have begun to reveal the complex genetic architecture of schizophrenia and to converge on some interesting and tractable areas of biology. The focus of genetics for the next few years will be to be to deepen our understanding by identifying more rare as well as common risk alleles. This should allow us to identify other areas of relevant biology and reagents, in the form of more highly penetrant mutations, for animal and cellular studies. Another important question is the extent to which somatic de novo mutations might play a role in schizophrenia. There is evidence that these contribute to some neurodevelopmental disorders 128 but this issue, which requires deep sequencing of brain tissue, has not been addressed yet in schizophrenia. There is also the challenge of how to deepen our insights into the relationships between genetic risk and phenotypic outcome. Genetic studies have undermined our current categorical notions of classification by showing extensive pleiotropy, but the large samples required for robust studies have come at the expense of detailed phenotype data. A major challenge for the future will be to conduct large scale genetic studies with more detailed clinical and endophenotype data. These will be required to understand how genetic risk impacts on brain mechanisms leading to particular clinical outcomes and to develop new approaches to diagnosis and classification that better reflect the underlying disturbances in brain function.
While the recent advances in genetics may have been impressive, epidemiological studies have also been highly productive implicating a number of biological and psychosocial risk factors. However, as noted already, there are limitations to the explanatory power of observational epidemiology and a key challenge for research in the next decade will be to understand the relevance of environmental risk exposures to disease causation. This will benefit from the fact that we can now bring together genomics and epidemiological studies of environmental risk factors and there is a need for longitudinal epidemiological research addressing how environment exposures impacting at different time points interact with each other and with genetic risk to produce clinically relevant outcomes. Such studies will likely benefit from access to routinely collected electronic clinical data though ethical and other challenges remain. This should also allow the identification of protective factors and guide the implementation of public health measures.
What can we expect in the next five to ten years in the biological understanding of schizophrenia? Findings from ongoing and future genetic studies will continue to drive mechanistic studies in patients and model systems. Rare variants conferring high individual risk will be of particular importance, especially for designing cellular and animal models. Bioinformatic analyses of genetic data should also become increasingly informative as study sizes are increasing. However, the further challenge will be to determine how, where and when genetic risk impacts on brain development and function.
Genetically engineered cells obtained directly from patients, such as induced pluripotent stem cells (iPS cells) and induced neuronal cells (iN cells), provide an opportunity to investigate neuronal mechanisms in vitro . 129 It is also possible to introduce risk alleles, and combinations thereof, into human stem cell lines using new genome engineering approaches such as the Clustered Regularly Interspaced Short Palindromic Repeat (CRISPR) system. We can now differentiate cells into many types of central nervous system cells, including different subtypes of neurons (e.g., glutamatergic and dopaminergic neurons) and glial cells, and partially recapitulate neurodevelopmental processes in vitro . 130 It is still unclear whether they capture features of mature neural networks in vivo . Nonetheless, such patient-derived neuronal cells will be useful for addressing cell-autonomous intrinsic susceptibility to the disease. Moreover, if such cellular susceptibility provides valid drug targets, human cell culture may be used for compound screening. 131
The study of animal models, particularly rodents in combination with human brain imaging will be needed to address circuitry mechanisms. The validity of many animal models can be questioned, but the recent advances in genetics allow models of human risk mutations to be developed. The polygenic basis of psychiatric conditions currently limits the utility of genetic rodent models, which often include a single specific mutation, and, at the present time, rare high penetrance alleles offer the best approach to generating models with high construct validity. However, the recently introduced CRISPR system may facilitate the introduction of genetic variations at multiple sites. 132 We need to examine neural circuits in genetic animal models with respect to behavioral changes, with particular attention to the pathological trajectory from early development to full onset of disease in adulthood. Such studies will benefit from recent novel technologies and methodologies to intervene with specific neural cells and circuits. 133 Given that environmental stressors play key roles in the aetiology of schizophrenia, 134 studying gene- environment interactions in cell and animal models will become increasingly important.. Such studies will help us answer important questions such as which biological contexts, cells, and mechanisms are the key sites of convergence of genetic and environmental stressors.
There is a clear need to develop antipsychotic compounds with fewer side effects, in particular those affecting metabolism that result in adverse cardiovascular outcomes. 135 There is also interest in using pharmacogenetics to identify patients at particular risk of specific side-effects. 136 , 137 Furthermore, efforts are being made to develop compounds that show efficacy not only for positive symptoms but also for negative and cognitive symptoms by modulating neurotransmission beyond the dopamine receptor. These efforts include modulation of glutamate and acetylcholine neurotransmission by interfering with glycine transporter 1 and alpha7 nicotinic acetylcholine receptor. 138 – 140 There is also interest in using pharmacogenetics in combination with other biomarkers to identify patients who might respond differentially to drugs with different modes of action 141 and this follows a more general trend to investigate the potential of stratified medicine in which drugs are targeted more efficiently to specific subgroups of patients. It seems likely that the road from recent progress in genetics and biology to the discovery of new treatments will be long one and will depend upon insights from cellular and animal modeling as well as human studies. 142 This work will need to address the key issues of cell type- and circuit-specificity and of the timing of critical events. We will also need advances in high-throughput methodology as well as advances in our ability to model cell circuits in vitro. 142
Recent years have seen burgeoning interest in the possibility of treating those at high risk to prevent the development of full-blown psychosis and to reduce functional impairment. Meta–analyses of randomized controlled trials suggest a positive, if modest, impact despite the wide variety of interventions employed (psychological, pharmacological, nutritional) 140 , 141 , but there is a clear need for further, well-controlled trials 143 , 144 , 145 . As described above, stress-associated signaling cascades are likely to impact upon synaptic pruning and the maturation of neural networks in adolescence. Compounds that can regulate inflammation and oxidative stress are being tested. For example, omega-3 fatty acids displayed beneficial effects in a clinical trial. 146 Preclinical studies have demonstrated that application of antioxidants, including N-acetyl cysteine, ameliorate physiological and behavioral deficits associated with schizophrenia. 111 Encouraged by such preclinical studies, increasing numbers of investigator-initiated clinical trials with antioxidants are ongoing. Future applications of genetic and other biomarkers, together with early neuropsychological, developmental and behavioural risk markers, to identify high risk groups as relevant recipients of preventive interventions, as well as controlled studies of the interventions in high risk children remain high research priorities.
Arguably the greatest challenge facing future research into aetiology, pathogenesis and treatment is the failure of current syndromic definitions to delineate a valid disease entity. If research is to progress, we will need new approaches to patient stratification that recognize the varying degree of overlap between syndromes and which bring modern neuroscience to bear on intermediate phenotypes that index the pathophysiology underlying the various clinical features and impairments. 15 Given the complex and variable clinical features and cognitive impairments associated with the disorder it seems likely that multiple brain systems are impacted to varying extents in different individuals and it would be unwise to expect to implicate dysfunction of a single brain region or circuit that accounts for the full range of features of the disorder and which distinguishes it from other disorders. Rather we should expect that different features of the disorder reflect underlying disturbances of different brain functions and moreover that these will cross current diagnostic boundaries. These considerations also imply that we should expect that novel treatments will target particular symptoms or groups of symptoms sharing common underlying mechanisms and that they will be applicable across diagnostic groups.
Controversies and uncertainties
Schizophrenia has long divided opinion: nature versus nurture, psychosocial versus biological, a myth or an illness, or a sane response to an insane society. It is perhaps a sign of increased knowledge that current controversies are less polarized. But, as should be clear from this seminar, many controversies and uncertainties do remain. For example: How should we diagnose schizophrenia? Should we use categories or dimensions? What clinical features, or combination of features will map best onto underlying neurobiological disturbances? Which environmental risk factors are truly casual and which are secondary to illness or genetic confounding? Is it better viewed a disorder of circumscribed brain regions and circuits, or a disorder of the whole brain? Is there a progressive, neurodegenerative component as well as a neurodevelopmental one? Is it one disorder, several disorders, or part of a continuous landscape of psychopathology analogous to say metabolic syndrome? What is the relationship between schizophrenia and disorders, such as autism and ADHD, with which it shares a number several clinical features and risk factors?
One area, which we have not touched on, which is perhaps of greatest immediate concern, is the poor quality of care for schizophrenia even in developed countries. The Schizophrenia Commission recently reviewed this issue and described current services in the UK as “broken and demoralized” 5 . They not only documented in uncompromising terms the shortcomings of our current approaches to managing schizophrenia but also made a large number of recommendations for improving policy and practice 5 . There seems little doubt that the implementation of these changes would do a great deal to improve the lives of those with schizophrenia and we should all do all that we can to ensure that this happens.
Given the need for an overhaul in the ways in which care is provided, it might seem inappropriate to point out the lack of investment in research in mental disorders relative to burden. 147 It is sometimes argued that this is a consequence rather than a cause of lack of progress and capacity in this area. However, a counterview would be that this is yet another example of the way in which mental disorders fail to achieve parity of esteem with physical illnesses. Whatever the explanation, it is to be hoped that the recent advances and unprecedented opportunities documented in this article will help redress this imbalance.
Acknowledgments
Profs David Linden and Richard Bentall made valuable suggestions. Ruth Sellars, Yukiko Lema, Annette Rand Madsen and Victoria Hirst helped prepare the paper and display items.
Conflicts of Interest
MO receives funding from the MRC, Wellcome Trust, NIMH, EU, and NISCHR. He has been paid a speaker’s fee by Janssen Pharmaceutical Companies. PM receives research funding from the Lundbeck Foundation, the Stanley Medical research Institute, and the ERC. AS receives research funding from NIH, NARSAD/BBRF, Stanley foundation, RUSK foundation, and Maryland Stem Cell Research Funds. Role of the funding sources: None of the funding bodies had any influence on any part of the work on this paper. None of the authors received any payment from any pharmaceutical company or other agency to write this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
Search Strategy and Selection Criteria .
We searched publications in PubMed using the search term “schizophrenia” for reviews and meta-analyses published in the past 5 years. These were assessed for relevance to the topics selected. Further focused searches on PubMed were then done on the selected topics.
Contributor Information
Prof. Michael J Owen, MRC Centre for Neuropsychiatric Genetics and Genomics, Cardiff University, Cardiff, UK.
Prof. Akira Sawa, Department of Psychiatry, Johns Hopkins University School of Medicine, USA.
Prof. Preben B Mortensen, Department of Economics, School of Business and Social Science, Aarhus University, Denmark.

IMAGES
VIDEO
COMMENTS
1. Introduction. Paranoia is the most commonly reported delusion among individuals diagnosed with schizophrenia spectrum illnesses (Bentall et al., 2009) and is evident in almost 50% of individuals seeking initial help for a psychotic disorder (Sartorius et al., 1986, Veling et al., 2007).Despite the high prevalence of this symptom, not all patients experience paranoia, and recent work ...
characterized by symptoms such as: hallucinations, delusions, disorganized communication, poor. planning, reduced motivation, and blunted a ffec t.(3) Genes and environment, and an altered ...
Paranoia is a common symptom of schizophrenia that may be related to how individuals process and respond to social stimuli. ... PARANOID INDIVIDUALS WITH SCHIZOPHRENIA SHOW GREATER SOCIAL COGNITIVE BIAS AND WORSE SOCIAL FUNCTIONING THAN NON-PARANOID INDIVIDUALS WITH SCHIZOPHRENIA ... FL, 33136; Research Service, Bruce W Carter VA Medical Center ...
Schizophrenia is an often debilitating, chronic, and relapsing mental disorder with complex symptomology that manifests as a combination of positive, negative, and/or cognitive features 1,2,3 ...
Research suggests that a clinical diagnosis of schizophrenia is strongly linked with experiencing negative stereotypes and an inability to recover. In challenging the scientific-logical practice of diagnostic labeling, which totalizes the person's experience around the illness, Narrative therapy offers a unique approach to treating schizophrenia by putting the spotlight on the client's ...
Schizophrenia stands as one of the most studied and storied disorders in the history of clinical psychology; however, it remains a nexus of conflicting and competing conceptualizations. Patients endure great stigma, poor treatment outcomes, and condemnatory prognosis. Current conceptualizations suffer from unstable categorical borders, heterogeneity in presentation, outcome and etiology, and ...
The number of published studies in schizophrenia research has been rapidly increasing over the last 25 years and an analysis of medline, a relevant database of international scientific publications, shows that the increase of schizophrenia-related publications since 1990 is much larger than the increase of the total number of all research ...
This paper reports the case of a 27-year-old man with paranoid schizophrenia who was finally stabilized on clozapine medication. After vaccination against severe acute respiratory syndrome ...
Introduction. The goal of this guideline is to improve the quality of care and treatment outcomes for patients with schizophrenia, as defined by the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (American Psychiatric Association 2013).Since publication of the last full practice guideline (American Psychiatric Association 2004) and guideline watch (American Psychiatric ...
The brain changes appear to be primarily expressed in cortical thickness and white matter integrity ( 43 ). However, it is more likely that the substrate in the brain underlying the cognitive changes in the development of schizophrenia is related to abnormal connectivity rather than gross volume decreases.
An International Multidisciplinary Journal of the Schizophrenia International Research Society As official journal of the Schizophrenia International Research Society (SIRS) Schizophrenia Research is THE journal of choice for international researchers and clinicians to share their work with the global schizophrenia research community. More than 6000 institutes have online or print (or both ...
Introduction. Schizophrenia is the major mental illness of our time. It was first described by. Kraepelin (1896) as "dementia praecox" and later given the name "schizophrenia" by. Bleuler ...
View Paranoid Schizophrenia Research Papers on Academia.edu for free. Skip to main content ... To study attitudes towards persons with paranoid schizophrenia of first- and final-year university students taking three different majors, Link's Social Distance Scale, modified to relate to several vignettes presenting different descriptions of a ...
Motivation: Analyzing a case of paranoid schizophrenia is a challenge to understand the mechanisms underlying the mind of a schizophrenic. The study became captivating because in the patient's delusional cofabulations there were many fingerprints that the communist period of that time left on the woman's psyche, thus observing the repressions following personal failures that probably ...
schizophrenia is a mental disorder that is. characterized by delusions, hallucinations, disorganized speech, grossly disorganized or. catatonic behavior, and negative symptoms. including ...
Schizophrenia Introduction, providing overview information Paranoid Schizophrenia, schizophrenia symptoms, schizophrenia causes, etc. ... Top 25 Authors of Schizophrenia Research Papers (2001) ScienceWatch - List of High Impact Journals in Psychiatry (2000) Best Place to Search for New ...
Research on Paranoid Personality Disorder: Th ere is a notable lack of research on paranoid personality disorder (Bateman et al. 2015; Triebwasser et al. 2013). Bernstein and Useda (2007)
Introduction. Schizophrenia is a severe psychiatric disorder that has a profound impact on the individual and society. While outcomes may not be as uniformly negative as is commonly believed, over 50% of those individuals who receive a diagnosis have intermittent but long-term psychiatric problems and around 20% have chronic symptoms and disability. 1 Unemployment is staggeringly high at 80 ...