Loading metrics
Open Access
Peer-reviewed
Research Article

COVID-19 vaccine hesitancy and confidence in the Philippines and Malaysia: A cross-sectional study of sociodemographic factors and digital health literacy
Roles Conceptualization, Data curation, Formal analysis, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation Clinical Informatics Research Unit, Faculty of Medicine, University of Southampton, Southampton, United Kingdom
Roles Data curation, Methodology, Project administration, Resources, Validation, Writing – original draft, Writing – review & editing
Affiliations Department of Community Medicine, International Medical School, Management and Science University, Shah Alam, Malaysia, Department of Community Medicine, Faculty of Medicine, Asia Metropolitan University, Johor Bahru, Malaysia, Global Public Health, Jeffrey Cheah School of Medicine and Health Sciences, Monash University Malaysia, Bandar Sunway, Malaysia
Roles Conceptualization, Data curation, Validation, Writing – original draft, Writing – review & editing
Affiliation Department of Psychiatry, Faculty of Medicine, University of Cyberjaya, Cyberjaya, Malaysia
Roles Conceptualization, Writing – original draft, Writing – review & editing
Affiliation Department: School of Criminal Justice Education, Institution: J.H. Cerilles State College, Caridad, Dumingag, Zamboanga del Sur, Philippines
Roles Conceptualization, Data curation, Supervision, Validation, Writing – original draft, Writing – review & editing
Affiliations Global Public Health, Jeffrey Cheah School of Medicine and Health Sciences, Monash University Malaysia, Bandar Sunway, Malaysia, South East Asia Community Observatory (SEACO), Jeffrey Cheah School of Medicine and Health Sciences, Monash University Malaysia, Bandar Sunway, Malaysia
- Ken Brackstone,
- Roy R. Marzo,
- Rafidah Bahari,
- Michael G. Head,
- Mark E. Patalinghug,

- Published: October 19, 2022
- https://doi.org/10.1371/journal.pgph.0000742
- Peer Review
- Reader Comments
With the emergence of the highly transmissible Omicron variant, large-scale vaccination coverage is crucial to the national and global pandemic response, especially in populous Southeast Asian countries such as the Philippines and Malaysia where new information is often received digitally. The main aims of this research were to determine levels of hesitancy and confidence in COVID-19 vaccines among general adults in the Philippines and Malaysia, and to identify individual, behavioural, or environmental predictors significantly associated with these outcomes. Data from an internet-based cross-sectional survey of 2558 participants from the Philippines ( N = 1002) and Malaysia ( N = 1556) were analysed. Results showed that Filipino (56.6%) participants exhibited higher COVID-19 hesitancy than Malaysians (22.9%; p < 0.001). However, there were no significant differences in ratings of confidence between Filipino (45.9%) and Malaysian (49.2%) participants ( p = 0.105). Predictors associated with vaccine hesitancy among Filipino participants included women (OR, 1.50, 95% CI, 1.03–1.83; p = 0.030) and rural dwellers (OR, 1.44, 95% CI, 1.07–1.94; p = 0.016). Among Malaysian participants, vaccine hesitancy was associated with women (OR, 1.50, 95% CI, 1.14–1.99; p = 0.004), social media use (OR, 11.76, 95% CI, 5.71–24.19; p < 0.001), and online information-seeking behaviours (OR, 2.48, 95% CI, 1.72–3.58; p < 0.001). Predictors associated with vaccine confidence among Filipino participants included subjective social status (OR, 1.13, 95% CI, 1.54–1.22; p < 0.001), whereas vaccine confidence among Malaysian participants was associated with higher education (OR, 1.30, 95% CI, 1.03–1.66; p < 0.028) and negatively associated with rural dwellers (OR, 0.64, 95% CI, 0.47–0.87; p = 0.005) and online information-seeking behaviours (OR, 0.42, 95% CI, 0.31–0.57; p < 0.001). Efforts should focus on creating effective interventions to decrease vaccination hesitancy, increase confidence, and bolster the uptake of COVID-19 vaccination, particularly in light of the Dengvaxia crisis in the Philippines.
Citation: Brackstone K, Marzo RR, Bahari R, Head MG, Patalinghug ME, Su TT (2022) COVID-19 vaccine hesitancy and confidence in the Philippines and Malaysia: A cross-sectional study of sociodemographic factors and digital health literacy. PLOS Glob Public Health 2(10): e0000742. https://doi.org/10.1371/journal.pgph.0000742
Editor: Nnodimele Onuigbo Atulomah, Babcock University, NIGERIA
Received: June 12, 2022; Accepted: September 20, 2022; Published: October 19, 2022
Copyright: © 2022 Brackstone et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: Data are available on the OSF repository: https://osf.io/ncwjq/ .
Funding: The authors received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
Introduction
While many high-income settings have achieved relatively high coverage with their COVID-19 vaccination campaigns, almost 32.1% of the world’s population have not received a single dose of any COVID-19 vaccine as of July 2022 [ 1 ]. The Philippines and Malaysia are among two of the most populous countries in Southeast Asia with an estimated population of 110 million and 32 million people, respectively. To date, Malaysia has seen over 4.6 million cases with a mortality rate of 0.77%, while approximately 3.7 million cases of COVID-19 were detected in the Philippines with a mortality rate of 1.60% [ 2 ]. Malaysia is doing considerably well with their vaccination efforts, with 84.8% of the population currently considered fully vaccinated as of July 2022. However, vaccination campaigns in the Philippines have been more difficult, with 65.6% of the population fully vaccinated [ 3 ]. With the emergence of the highly transmissible Omicron variant across the world [ 4 ], large-scale vaccination coverage remains fundamental to the national and global pandemic response. Regular scientific assessments of factors that may impede the success of COVID-19 vaccination coverage will be critical as vaccination campaigns continue in these nations.
A key factor for the success of vaccination campaigns is people’s willingness to be vaccinated once doses become accessible to them personally. Vaccine hesitancy is defined by the World Health Organization (WHO) as the delay in the acceptance, or blunt refusal of, vaccines. In fact, vaccine hesitancy was described by the WHO as one of the top 10 threats to global health in 2019 [ 5 ]. Conversely, vaccine confidence relates to individuals’ beliefs that vaccines are effective and safe. In general, a loss of trust in health authorities is a key determinant of vaccine confidence, with misconceptions about vaccine safety being among the most common reasons for low confidence in vaccines [ 6 ].
Previously, vaccination in Southeast Asia has been associated with mistrust and fear, particularly in the Philippines, who are still suffering the consequences of the Dengvaxia (dengue) vaccine controversy in 2017 [ 7 ]. Studies suggest that this highly political mainstream event, in which anti-vaccination campaigns linked dengue vaccines with autism spectrum disorder and with corrupt schemes of pharmaceutical companies, continue to erode the population’s trust in vaccines. For example, a survey conducted on over 30,000 Filipinos in early 2021 showed that 41% of respondents would refuse the COVID-19 vaccine once it became available, whereas Malaysia reported 27% hesitancy [ 8 ]. Researchers predict that the controversy surrounding Dengvaxia may have prompted severe medical mistrust and subsequently weakened the public’s attitudes toward vaccines [ 7 , 9 ]. However, there may be many additional factors that weaken confidence in vaccines. For example, incompatibility with religious beliefs is one key driver of weakened confidence in vaccines [ 10 , 11 ], whereas living in urbanised (vs. rural) areas predicts COVID-19 vaccine hesitancy in some countries [ 12 – 14 ], possibly due to being more connected to the internet and social media and being more exposed to COVID-19-related misinformation.
Other predictors of vaccine hesitancy and confidence may include digital health literacy–one’s ability to seek, find, understand, and appraise health information from digital resources–and social media use. Research has shown that beliefs in available information is integral to perceptions of the vaccine safety and effectiveness [ 15 – 17 ]. Previous studies, for example, have associated higher vaccine hesitancy with misinformation about the virus and vaccines, particularly if they relied on social media as a key source of information [ 18 , 19 ]. Social Cognitive Theory (SCT) is a widely accepted theory which may explain individual behaviors, including digital health literacy [ 20 ]. SCT consists of three factors–environmental, personal, and behavioural–and any two of these components interact with each other and influence the third. As such, SCT can assist in establishing a link between one’s behaviour (e.g., information-seeking–one form of digital health literacy) and environmental factors (e.g., availability of information online), which may interact to promote medical mistrust and influence vaccine hesitancy and confidence (personal) [ 21 ]. Thus, health behaviours are often influenced by social systems as well as personal behaviours.
Although vaccine hesitancy and confidence are related concepts (e.g., people who express low confidence in vaccines are more likely to be vaccine-hesitant [ 6 ]), they are also distinct [ 22 ]. Thus, the main aims of this research were to determine levels of hesitancy and confidence in COVID-19 vaccines among general adults in the Philippines and Malaysia, and to identify behavioural or environmental predictors that are significantly associated with both outcomes. Thus, developing a deeper understanding of the factors associated with vaccine hesitancy and confidence will provide insight into how specific population groups may respond to health threats and public health control measures.
Design, subjects, and procedure
This was an internet-based cross-sectional survey conducted from May 2021 to September 2021 in the Philippines and Malaysia. Snowball sampling methods were used for the data collection using social media, including research networks of universities, hospitals, friends, and relatives. Filipino and Malaysian residents aged 18 years or older were invited to take part. The inclusion criteria for participants’ eligibility included 18 years or older, and an understanding of the English language. All invited participants consented to the online survey before completion. Consented participants could only respond to questions once using a single account. The voluntary survey contained a series of questions which assessed sociodemographic variables, social media use, digital literacy skills in health, and attitudes toward the COVID-19 vaccine.
Ethical approval
The study received ethical approval from Asia Metropolitan University’s Medical Research and Ethics Committee (Ref: AMU/FOM/MREC 0320210018). All participants provided informed consent. All study information was written and provided on the first page of the online questionnaire, and participants indicated consent by selecting the agreement box and proceeding to the survey.
Demographics.
Filipino and Malaysian participants indicated their age category (18–24, 25–34, or 35–44), gender (man, woman), community type (rural, urban), educational level (no formal education, primary, secondary, tertiary), employment (unemployed, part-time, full-time), religion (Christian, Buddhism, Muslim, Hinduism, Other, None), income (1 = very insufficient ; 4 = very sufficient ; M = 1.84, SD = 0.81), whether they were permanently impaired by a health problem (no vs. yes), and whether they were social media users (no vs. yes).
Subjective social status.
Participant then rated their own perceived social status using the MacArthur Scale of Subjective Social Status scale [ 23 ]. Participants viewed a drawing of a ladder with 10 rungs, and read that the ladder represented where people stand in society. They read that the top of the ladder consists of people who are best off, have the most money, highest education, and best jobs, and those at the bottom of the ladder consists of people who are worst off, have the least money, lowest education, and worst or no jobs. Using a validated single-item measure, participants placed an ‘X’ on the rung that best represented where they think they stood on the ladder (1 = lowest ; 10 = highest; M = 6.23, SD = 1.86).
Vaccine confidence and hesitancy.
Participants were also asked about their perceived level of confidence in the COVID-19 vaccine (“I am completely confident that the COVID-19 vaccine is safe,” 1 = strongly disagree ; 7 = strongly agree; M = 4.57, SD = 1.48). Then, participants were asked about their level of hesitancy to the COVID-19 vaccine (“I think everyone should be vaccinated according to the national vaccination schedule”; no, I don’t know, yes). These questions were adapted from the World Health Organization, Regional Office for Europe survey [ 24 ]. The tool underwent evaluation by multidisciplinary panel of experts for necessity, clarity, and relevance.
Digital health literacy.
Finally, participants completed the Digital Health Literacy Instrument (DHLI) [ 25 ], which was adapted in the context of the COVID-HL Network. The scale measures one’s ability to seek, find, understand, and appraise health information from digital resources. A total of 12 items (three per each dimension) were asked, and answers were recorded on a four-point Likert scale (1 = very difficult ; 4 = very easy; α = .92; M = 2.15, SD = 0.59). While the original DHLI is comprised of 7 subscales, we used the following four domains, including: (1) information searching or using appropriate strategies to look for information (e.g., “When you search the internet for information on coronavirus virus or related topics, how easy or difficult is it for you to find the exact information you are looking for?”; α = .87; M = 2.15, SD = 0.65), (2) adding self-generated content to online-based platforms (e.g., “When typing a message on a forum or social media such as Facebook or Twitter about the coronavirus a related topic, how easy or difficult is it for you to express your opinion, thought, or feelings in writing?”; α = .74; M = 2.15, SD = 0.65), (3) evaluating reliability of online information (e.g., “When you search the internet for information on the coronavirus or related topics, how easy or difficult is it for you to decide whether the information is reliable or not?”; α = .86; M = 2.20, SD = 0.69), and (4) determining relevance of online information (e.g., “When you search the internet for information on the coronavirus or related topics, how easy or difficult is it for you to use the information you found to make decisions about your health [e.g., protective measures, hygiene regulations, transmission routes, risks and their prevention?”]; α = .87; M = 2.09, SD = 0.68). The reliability statistics for the overall DHL score was 0.92, while the alpha coefficients for the four subscales ranged from 0.74 to 0.87, suggesting acceptable to good internal consistency.
Data analysis
Data were examined for errors, cleaned, and exported into IBM SPSS Statistics 28 for further analysis. All hypotheses were tested at a significance level of 0.05. χ 2 tests were conducted for group differences of categorical variables, and Mann-Whitney tests for continuous variables. Subgroup analyses were performed for Filipino and Malaysian participants.
COVID-19 vaccine hesitancy and confidence were treated as separate dependent variables in a logistic regression model providing the strictest test of potential associations with COVID-19 vaccine hesitancy and confidence among Filipino and Malaysian participants. Low vaccine confidence was operationalised by dichotomising participants’ responses to the statement: “I am completely confident that the COVID-19 vaccine is safe” into those who disagreed or neither agreed nor disagreed (1–4), whereas high vaccine confidence was operationalised by dichotomising participants’ responses into those who agreed to some extent (5–7). Vaccine hesitancy was operationalised by dichotomising responses to the statement: “I think everyone should be vaccinated according to the National vaccination schedule” into those indicating ‘no’ or ‘I don’t know,’ whereas no vaccine hesitancy was operationalized by dichotomising participants’ response into those who indicated ‘yes.’
Independent variables were: age (18–24 vs. 25–34 vs. 35–44 [ref]), gender (women vs. men [ref]), community type (rural vs. urban [ref]), educational level (tertiary vs. secondary or less [ref]), employment (employed to some degree vs. unemployed [ref]), religion (Philippines: Christianity vs. Islam [ref]; Malaysia: Christianity vs. Buddhism vs. Hinduism vs. Islam [ref]), income (low (1–2) vs. high (3–4 [ref])), whether they were permanently impaired by a health problem (yes vs. no [ref]), whether they were social media users [yes vs. no [ref]), their perceived ranking on the MacArthur Scale of Subjective Social Status (continuous variable), and finally the four domains of the DHLI scale (all continuous variables).
A total of 2558 participants completed the online survey. Table 1 shows descriptive statistics of participants from the Philippines ( N = 1002) vs. Malaysia ( N = 1556). Filipino (vs. Malaysian) participants indicated higher rates of education ( p < 0.001), but were more likely to be unemployed ( p < 0.001). Further, Filipino (vs. Malaysian) participants were also more likely to indicate lower income ( p < 0.001) and rate themselves lower on subjective social status ( p < 0.001). Malaysian (vs. Filipino) participants were more likely to live in urban areas ( p < 0.001). Most notably, Filipino participants (56.6%) indicated higher prevalence of COVID-19 vaccine hesitancy compared to Malaysian participants (22.9%; p < 0.001). However, there were no significant differences between Filipino (45.9%) and Malaysian (49.2%) participants in ratings of vaccine confidence ( p = 0.105). Malaysian (vs. Filipino) participants were also more likely to report using social media (96.6 vs. 89.8%; < 0.001).
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
Values are presented as percent (n) or means ± SD.
https://doi.org/10.1371/journal.pgph.0000742.t001
Table 2 shows significant predictors of vaccine hesitancy in both Filipino and Malaysian samples. Among Filipino participants, multivariate logistic regression analyses revealed that factors associated with higher vaccine hesitancy included women (OR, 1.51, 95% CI, 1.14–2.00; p = 0.004), residing in a rural community (OR, 1.45, 95% CI, 1.07–1.95; p = 0.015), and having lower income (OR, 1.62, 95% CI, 1.20–2.19; p = 0.001). Among Malaysian participants, women (OR, 1.51, 95% CI, 1.14–2.00; p = 0.004), being aged 25–34 (vs. 18–24; OR, 1.52, 95% CI, 1.48–2.21; p = 0.027), Christians (OR, 2.45, 95% CI, 1.66–3.62; p < 0.001), completing tertiary education (OR, 2.17, 95% CI, 1.63–2.88; p < 0.001), social media use (OR, 11.59, 95% CI, 5.63–23.84; p < 0.001), and information-seeking behaviours (OR, 2.50, 95% CI, 1.74–3.61; p < 0.001) were predictors of higher vaccine hesitancy, whereas having a health impairment (OR, 0.49, 95% CI, 0.30–0.78; p = 0.003) and higher self-reported ratings on subjective social status (OR, 0.82, 95% CI, 0.75–0.89; p < 0.001) were associated with lower vaccine hesitancy.
https://doi.org/10.1371/journal.pgph.0000742.t002
Table 3 shows significant predictors of vaccine confidence in both Filipino and Malaysian samples. Factors positively associated with higher vaccine confidence among Filipino participants included higher self-reported ratings on subjective social status (OR, 1.16, 95% CI, 1.07–1.25; p < 0.001), whereas factors associated with lower vaccine confidence included women (OR, 0.72, 95% CI, 0.54–0.96; p = 0.026) and information-seeking behaviours (OR, 0.63, 95% CI, 0.49–0.81; p < 0.001). Among Malaysian participants, factors positively associated with higher vaccine confidence included women (OR, 1.27, 95% CI, 1.18–1.60; p = 0.035), completing tertiary education (OR, 1.31, 95% CI, 1.03–1.66; p = 0.026), and higher self-reported ratings on subjective social status (OR, 1.08, 95% CI, 1.00–1.16; p = 0.036). Factors negatively associated with lower vaccine confidence included residing in a rural community (OR, 0.63, 95% CI, 0.47–0.87; p = 0.004), Christians (OR, 0.50, 95% CI, 1.20–2.24; p < 0.001), Buddhists (OR, 0.15., 95% CI, 0.10–0.22; p < 0.001), Hindus (OR, 0.24., 95% CI, 0.17–0.34; p = 0.004), information-seeking behaviours (OR, 0.42, 95% CI, 0.31–0.58; p < 0.001), and determining relevance of online information (OR, 0.68, 95% CI, 0.51–0.92; p = 0.013).
https://doi.org/10.1371/journal.pgph.0000742.t003
Malaysia and the Philippines are among the most populous countries in Southeast Asia. While the economic impact of the COVID-19 pandemic has been permanent in the Philippines, it has been shown thus far to be temporary in Malaysia [ 26 ]. Between January and October 2020, around 30,000 Malaysians had been infected by the virus with a mortality rate of 0.79%, while approximately 380,000 cases of COVID-19 were detected in the Philippines with a mortality rate of 1.9% [ 2 ]. Further, 61.8% of Malaysians had completed their vaccination up until September 2021, while the percentage of completed vaccinations during the same period in the Philippines was only 19.2% [ 27 ]. Vaccine uptake is likely to be a key determining factor in the outcome of a pandemic. Knowledge around factors which predict vaccine hesitancy and confidence is of the utmost important in order to improve vaccination rates. Thus, the core aims of this research were to determine levels of hesitancy and confidence in COVID-19 vaccines among general adults in the Philippines and Malaysia, and to identify behavioural or environmental predictors that are significantly associated with these outcomes.
First, while there were no significant differences in ratings of confidence in the COVID-19 vaccine between Filipino and Malaysian participants, Filipino (compared to Malaysian) participants expressed greater vaccine hesitancy. This may be a consequence of previous vaccine scares in the years leading up to the pandemic, including the Dengvaxia controversy in 2016 [ 7 , 9 ]. Systematic reviews demonstrated that, by the end of 2020, the highest vaccine acceptance was in China, Malaysia, and Indonesia [ 28 , 29 ]. The authors postulated that this elevated awareness was due to being among the first countries affected by the virus, hence resulting in greater confidence in vaccines [ 28 ].
Next, this study shows that women expressed greater vaccine hesitancy in both countries. The evidence base shows mixed findings, with other studies reporting higher hesitancy in women [ 30 ] or in men [ 31 ]. In some countries, the gender gap is not as substantial as others. In a large global study conducted in countries such as Russia and the United States, it was found that there is greater gender gap in vaccine hesitancy among men and women compared to countries such as Nepal and Sierra Leone [ 32 , 33 ]. Unsurprisingly, what drives this hesitancy is the inclusion of pregnant women, where studies have consistently demonstrated that this population is more hesitant toward vaccination due to concerns for their babies [ 34 ]. Hence, after taking all consideration into account, gender differences in vaccine hesitancy cannot be supported with certainty. This also emphasises the need for tailored health promotion towards the key populations at risk.
There are clear differences in predictors of vaccine hesitancy in the Philippines and Malaysia. However, when results for both countries were combined, women, urban dwellers, those of Christian faith, those with higher educational attainment, higher self-reported social class, social media use, and information-seeking tendencies remained as predictors of hesitancy. Urban-dwellers and individuals with more years of education have previously been demonstrated as predictors for vaccine hesitancy [ 35 ], but contradictory results have also previously been shown [ 36 , 37 ]. Urban residents are typically more connected to the internet and social media and, thus, may be more exposed to vaccine-related misinformation than rural inhabitants who have fewer sources of information available to them [ 12 – 14 ]. Nevertheless, reports have shown higher vaccine refusals among those with strong religious beliefs such as the Amish Community in the United States and the Orthodox Protestants in the Netherlands [ 38 ], as well as some Muslim groups in Pakistan [ 18 ].
Frequent social media use is the only strong predictor for vaccine hesitancy in this study, followed by information-seeking behaviours. Research has identified that the safety and effectiveness of the vaccine is the primary concern that people have, including beliefs in available information [ 15 – 17 ]. Unfortunately, high internet literacy is a double-edged sword, since participants in this study preferred to seek information through social media, and thus may have been exposed to inaccurate information regarding COVID-19 vaccine. Previous studies have associated higher vaccine hesitancy with misinformation about the virus and vaccines [ 18 ], particularly if they relied heavily on social media as a key source of vaccine-related information [ 19 ]. A 2022 systematic review discovered that high social media use is the main driver of vaccine hesitancy across all countries around the globe, and is especially prominent in Asia [ 39 ]. Furthermore, vaccine acceptance and uptake improved among those who obtained their information from healthcare providers compared to relatives or the internet [ 40 ].
In terms of vaccine confidence, our findings show that those with higher subjective social status have higher confidence in vaccination, consistent with previous studies describing how those with a higher income had expressed willingness to pay for their COVID-19 vaccination if necessary [ 32 , 41 , 42 ]. Further, those of Christian, Buddhist, and Hindu faiths, as well as those with a tendency to seek out information, were associated with lower vaccine confidence. This is in keeping with the previous findings demonstrating that strong religious convictions are often tied to mistrust of authorities and beliefs about the cause of the COVID-19 pandemic, which is fuelled by social media [ 43 ]. Furthermore, concern on the permissibility of these vaccines in their religion reduces its acceptability [ 10 ]. However, it is interesting to note that, while the majority in Malaysia are Muslims, it did not reduce the rate of vaccine acceptance and confidence in the country.
These findings have important implications for health authorities and governments in areas focusing on improving vaccination uptake. Misinformation about vaccination greatly hampers vaccination efforts. Thus, not only is it important to understand how specific population groups are influenced by digital platforms such as social media, but it is imperative to provide the right information driven by governmental and non-governmental organisations [ 39 ]. This could be achieved by having community-specific public education and role modelling from local health and public officials, which has been shown to increase public trust [ 44 ]. Since the primary reason for hesitancy is concern about the safety of vaccines, it is crucial that education programmes stress the effectiveness and importance of COVID-19 vaccinations [ 45 ]. Participants in this study coped with the pandemic by seeking out new information, but they sought information from social media when information from the authorities was lacking or were viewed as untrustworthy, which may have contained erroneous information. One way to deter this is to empower information-technology companies to monitor vaccine-related materials on social media, remove false information, and create correct and responsible content [ 44 ].
Furthermore, behavioural change techniques have been found to be useful in stressing the consequences of rejecting the vaccine on physical and mental health [ 46 ]. The most effective “nudging” interventions included offering incentives for parents and healthcare workers, providing salient information, and employing trusted figures to deliver this information [ 47 ]. Finally, since religious concerns have been prominent in reducing vaccine confidence and increasing hesitancy in this study, it is important to tailor messages to include information related to religion, and the use of religious leaders to spread these messages [ 48 ]. These are all important factors for increasing uptake of the COVID-19 vaccine, but also may be relevant in acceptability of routine immunisations as countries look to transition towards a post-pandemic delivery of healthcare.
A limitation of this study includes its cross-sectional design and the heterogeneity among participants, which meant that temporal changes in attitudes toward COVID-19 vaccines across time were not captured. Further, the need for internet access among Filipino and Malaysian participants limited the representativeness of the sample population. Thus, certain demographic were under-represented, including Filipino and Malaysian individuals over the age of 45, and people of lower socio-economic status. The surveys were also implemented in English, which may have limited the participation of target participants who were not fluent in English. In addition, due to space limitations, vaccine hesitancy and confidence were each captured using one item, which raises concerns of the items’ validity and reliability. Finally, not all independent variables were accounted for, including medical mistrust [ 49 ], vaccine knowledge [ 50 ], and specific social media platforms used [ 11 ]. We also did not assess whether participants had received any doses of the COVID-19 vaccine previously. Future research should include more important predictors to build a broader picture of vaccine-related hesitancy and confidence in the Philippines and Malaysia, and more items should be utilised to tap into these concepts more comprehensively. Despite these limitations, the core strength of this study relates to its relatively large number of participants from both countries, and its comprehensive analysis of predictors to provide as a starting point going forward.
Conclusions
The main aims of this research were to determine levels of hesitancy and confidence in COVID-19 vaccines among unvaccinated individuals in the Philippines and Malaysia, and to identify predictors significantly associated with these outcomes. Predictors of vaccine hesitancy in this study included the use of social media, information-seeking, and Christianity. Higher socioeconomic status positively predicted vaccine confidence. However, being Christian, Buddhist or Hindu, and the tendency to seek information online, were predictors of hesitancy. Efforts to improve uptake of COVID-19 vaccination must be centred upon providing accurate information to specific communities using local authorities, health services and other locally-trusted voices (such as religious leaders), and for the masses through social media. Further studies should focus on the development of locally-tailored health promotion strategies to improve vaccination confidence and increase the uptake of vaccination–especially in light of the Dengvaxia crisis in the Philippines.
Supporting information
S1 file. inclusivity in global research questionnaire..
https://doi.org/10.1371/journal.pgph.0000742.s001
- 1. Ritchie H, Mathieu E, Rodés-Guirao L, Appel C, Giattino C, Ortiz-Ospina E, et al. Coronavirus pandemic. Published online at OurWorldinData.org. Available from https://ourworldindata.org/covid-vaccinations .
- View Article
- PubMed/NCBI
- Google Scholar
- 3. Ritchie H, Mathieu E, Rodés-Guirao L, Appel C, Giattino C,Ortiz-Ospina E, et al. Philippines: Coronavirus pandemic country profile. Published online at OurWorldinData.org. Available from https://ourworldindata.org/coronavirus/country/philippines .
- 9. Mendoza RU, Valenzuela, S, Dayrit, M. A Crisis of Confidence: The Case of Dengvaxia in the Philippines. SSRN: doi: 10.2139/ssrn.3519736.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 30 March 2022
OCTA as an independent science advice provider for COVID-19 in the Philippines
- Benjamin M. Vallejo Jr 1 &
- Rodrigo Angelo C. Ong 1
Humanities and Social Sciences Communications volume 9 , Article number: 104 ( 2022 ) Cite this article
6010 Accesses
4 Citations
7 Altmetric
Metrics details
- Health humanities
- Science, technology and society
- Social science
We comment on science advice in the political context of the Philippines during the COVID 19 pandemic. We focus on the independent science advisor OCTA Research, whose publicly available epidemiological forecasts have attracted media and government attention. The Philippines government adopted a COVID-19 suppression or “flattening of the curve” policy. As such, it required epidemiological forecasts from science advisors as more scientific information on SARS CoV 2 and COVID 19 became available from April to December 2020. The independent think-tank, OCTA Research has emerged the leading independent science information advisor for the public and government. The factors that made OCTA Research as the dominant science advice source are examined, the diversity of scientific evidence, processes of evidence synthesis and, of evidence brokerage for political decision makers We then describe the dynamics between the government, academic science research and science advisory actors and the problem of science advice role conflation. We then propose approaches for a largely independent government science advisory system for the Philippines given these political dynamics.
Similar content being viewed by others

The Dutch see Red: (in)formal science advisory bodies during the COVID-19 pandemic
Janne Aarts, Eva Gerth, … Phil Macnaghten

An evaluation of North Carolina science advice on COVID-19 pandemic response
Jessica Weinkle
Mobilization of science advice by the Canadian federal government to support the COVID-19 pandemic response
Dominika Bhatia, Sara Allin & Erica Di Ruggiero
Introduction
Pandemic science before COVID 19 presumed “predictable challenges” (Lipsitch et al., 2009 ) that informs government response especially in planning for containment interventions such as lockdowns. The success of government response is in the public perception of a positive outcome and this is reducing the number of infections. The COVID 19 pandemic is a crisis in which the orderly functioning of social and political institutions are placed into disorder and uncertainty (Boin et al., 2016 ). In political institutions this may be a threat to accepted political power arrangements and requires a response which because of their urgency, are occasions for political leaders to demonstrate leadership. However, to do so they will have to rely on actors who provide science, economic and social information and advice. In many cases these actors are within the government bureaucracy itself, as specialized agencies. Academic research institutions also provide advice. Civil society organizations with science and technology advocacies may provide advice. Science advice provided by civil society organizations, citizen science advocacy organizations and non-government think tanks are independent science advice providers. These organizations are a feature of the technical and science advice ecosystems of liberal democracies.
How governments use science advice and decide in a crisis strengthens political legitimacy. In the United Kingdom with its formal structures of government science advice such as the Science Advisory Group for Emergencies (SAGE) a key outcome is lowering SARS CoV 2 transmission (R) rate and the way this can be achieved is to institute a lockdown. SAGE was placed in a high degree of public, media and political scrutiny in its recommendations. While formal science advice structures may work well in countries with a large and well-established science community, in countries with small science communities, independent science advice actors may be more effective than formal science advice actors.
Previous studies on the use of science advice by governments have revealed a dichotomy. Knowledge producers (e.g., academic science community) perceive high uncertainty in scientific results and consequentially become guarded in their science advice or even dispense with it in recognition of their political costs. In contrast knowledge users (e.g. politicians and science advisors in government) perceive less uncertainty in science advice and require assurances in outcomes (MacKenzie, 1993 ). This present challenges for science advice practitioners since differentiating the roles of science knowledge generation and science knowledge users, both of which can be played by academic scientists, can be conflated, and may result in political risks and opportunities.
To remedy this conflation, science advice mechanisms emphasizing independent knowledge brokerage (Gluckman, 2016a ) define a particular role for scientists in listing down science informed options for politicians and policy makers. These roles have their theoretical basis from post-normal science approaches (Funtowicz and Ravetz, 1993 , 1994 ; Ravetz, 1999 ) which place a premium on managing uncertainty in crises through consensus building and identifying of science informed policy options. The science advice “knowledge broker” will not be functioning as part of the knowledge generation constituency but in a purely advisory capacity identifying policy options. This is the model promoted by the International Network for Government Science Advice (INGSA). This also insulates the science advisor from undue political interference.
However, in countries where the science community is small and politically underrepresented, performing these well-defined functions will be difficult due to a lack of experts and the range of scientific expertise they can provide. In small science communities, the problems of role conflation become more apparent and may place the science advisor prone to political pressure. Vallejo and Ong ( 2020 ) reviewed the Philippines government response and science advice for COVID 19 from when the World Health Organization (WHO) advised UN member states of a pandemic health emergency on January 6 to April 30, 2020 when the Philippines government began relaxing quarantine regulations. They noted the roles of various science advice knowledge generation actors such as individual scientists, academe, national science academies and organizations and how these were eventually considered by the Inter Agency Task Force on Emerging Infectious Diseases (IATF-EID) which is the government’s policy recommending body for COVID 19 suppression. Of these advisory actors, the private and independent OCTA Research Group hereafter referred to as OCTA, which consists of a multi-disciplinary team of academics from the medical, social, economic, environmental, and mathematical sciences mostly from the University of the Philippines, became the most prominent source of government science advice with its proactive but unsolicited provision of government science advice.
Because of this engagement, like SAGE in the UK, OCTA became a focus of intense media, public, and political interest and could represent an effective modality for independent science advice especially in newly industrialized countries where the science community is small but gaining a larger base of expertise. While science advice in this context may involve a conflation of science advice roles, we look into this conflation and their political dynamics in pandemic uncertainty and how consensus was formed in COVID 19 policy advice. This paper explores on how independent science advice has proved to be the chief source science advice in a polarized political environment in a Southeast Asian nation from the start of the pandemic in January 2020–October 2021.
The Philippine science advice ecosystem
Science advice in the Philippines takes on formal (with government mandate), informal (without government mandate) solicited and unsolicited modalities. Formal science advice to the President of the Philippines is provided by the National Academy of Science and Technology (NAST) by virtue of Presidential Executive Order Number 812. The government solicits science advice from the NAST which provides advice as position or white papers to cabinet for consideration. The NAST is not a wholly independent body from government. It is attached to the Department of Science and Technology (DOST) for administrative and fiscal purposes.
Other sources of science advice are from the universities such as the University of the Philippines (UP). The UP is designated by charter (Republic Act Number 8500) as the national, research and graduate university. This mandates it to provide science advice to the government. Academics in their individual capacities, as members of think-tanks or civil society organizations provide unsolicited and informal science advice to government through the publication of scientific and position papers as well as technical reports. Academics who are part of non-government science academies such as the Philippine American Academy of Science and Engineering (PAASE) provide similar advice. The science advice system in the Philippines is diverse with each actor having its own political and development advocacy. The system is largely ad hoc and informal, and science advice are largely unsolicited. This dynamic determines its role with the government. Also, when these science advice actors are consulted by the government, they are all primuses inter pares in dealing with political actors in government. Members of the science advisory bodies are mostly active academics. They are all knowledge producers and users at the same time.
There are few studies that directly examine the politics of science advice and uncertainty in the Philippines, and these are in disaster risk reduction management (DRRM). This can serve as a template for analysis for the COVID 19 pandemic in the Philippines which has been construed by government and the public as a global disaster. The strengths and weaknesses of the present science advisory system may be seen in DRRM advice.
DRRM as a framework for government science advice in the Philippines
Disasters which have affected the Philippines in the first decade of the 21st century such as Typhoon Ketsana (Philippine name “Ondoy”) in 2009 which flooded much of the National Capital Region, have resulted in several studies investigating the resilience of urban communities and how science advice is used in crafting urban resilience policies and governance. This disaster was also the major impetus for disaster legislation with enactment of the DRRM law (Republic Act Number 10121). This law institutionalizes and mainstream the development of capacities in disaster management at every level of governance, disaster risk reduction in physical and land-use planning, budget, infrastructure, education, health, environment, housing, and other sectors. The law also institutes the establishment of DRRM councils at each level of government. The councils are composed of members from government departments, the armed forces and police, civil society, humanitarian agencies but most notably, does not include academic research scientists. Science advice is given by CSOs but that is in accordance with their particular advocacies and their political objectives.
A study commissioned by the independent think tank Odi.org and by researchers of De La Salle University in Manila (Pellini et al., 2013 ) concluded that there is a “low uptake of research and analysis” to inform local decision in DRRM. It also identified a reactionary response to disasters rather than a response to disaster risks. Formal and informal science advice is most effective in local government if local executives prioritize risk reduction with consensus building at the local level. In general, formal, and informal science advice is less effective at the national level. The Philippine science advisory ecosystem is focused on formal science advice at the national level and thus the effectiveness of science advice is placed into question. The disaster-prone province of Albay is held as an example where science advice is more effective at a devolved level from the national (Bankoff and Hilhorst, 2009 ; Pellini et al., 2013 ).
At the lower levels of governance, informal science advice is predominant and is provided by science advice actors such as non-government organizations (NGO) or by civil society organizations (CSO). While NGOs, CSOs and, the government communicate using a consensus vocabulary (Funtowicz and Ravetz, 1994 ) in DRRM, differing risk perceptions have resulted in different domains of political engagement (Bankoff and Hilhorst, 2009 ) tied to different interpretations of the risk vocabulary in terms of political costs. And so the dominant paradigm remains disaster reactive with a general trend in “dampening uncertainties” (Pearce, 2020 ) in order to come up with positive political outcomes for the science advisors and the government.
While the present DRRM law institutionalizes consultation and collaboration, the law does not mandate a science or technical advisor to sit on DRRM councils at each level of governance. This is one possible reason for the “low uptake of research and analysis” at higher levels of governance while at lower levels of governance, science advice is provided by CSO and other advocacy organizations in an independent and ad hoc manner as they are more effective in establishing collaborative relationships with local government executives and councils.
IATF-EID and OCTA Research as an independent science advisor
Vallejo and Ong ( 2020 ) review the timeline for the Philippines government COVID 19 response, the formation of the Inter-agency Task Force on Emerging Infectious Diseases (IATF-EID), the science advisory ecosystem, and how the science community began to dispense informal science advice for consideration by IATF-EID. IATF-EID is the government’s policy recommending body for COVID 19 suppression and is composed of members from the cabinet and health agencies of the government. Informal science advice initially came from individual or groups of academics modeling the initial epidemiological trajectory of COVID 19. The IATF-EID is not a science evidence synthesizing or peer review body. It must rely on many science advisory actors as consultants. The University of the Philippines COVID 19 Pandemic Response Team is a major actor as its scientists are well known in the medical and disaster sciences. But it was OCTA which is composed mainly of academics from the University of the Philippines and the University of Santo Tomas. OCTA that has emerged as the leading government science advice actor for COVID 19.
OCTA bills itself as a “polling, research and consultancy firm”(Fig. 1 ). That OCTA has been identified in media reports as the “University of the Philippines OCTA Research group” is to be expected as academic credibility is a premium in the Philippines as like in other countries (Doubleday and Wilsdon, 2012 ). This however can constrain its political relationship with government science advice actors and so OCTA had to publish disclaimers that while it is composed of mostly University of the Philippines academics, it claims to be an independent entity. OCTA’s polling function is separate from its science advice advocacy which is performed by volunteer scientists as testified by OCTA President Ranjit S Rye to the Philippine Congress Committee on Public Accountability on 3 October 2021. The polling function is supported by paid subscribers while the science advice advocacy is supported by unpaid volunteers. Volunteer OCTA epidemiological modelers and policy analysts have provided robust estimates on the COVID 19 reproductive number R0, positivity rates, hospital capacity and attack rates at the national, provincial, and local government levels every fortnight beginning April 27, 2020. It has since issued 76 advisories and updates (Fig. 2 ). Local and provincial governments have used their forecasts in deciding quarantine and lockdown policies in their jurisdictions. OCTA publicly released these forecasts in academic websites, institutional media and social media. This allowed for public vetting and extended peer review with other independent scientists validating its forecast estimates. Some independent scientists contest methodologies and OCTA has appropriately responded to these.
OCTA is a primarily polling organization but has taken on COVID-19 monitoring, forecasting and advice services.
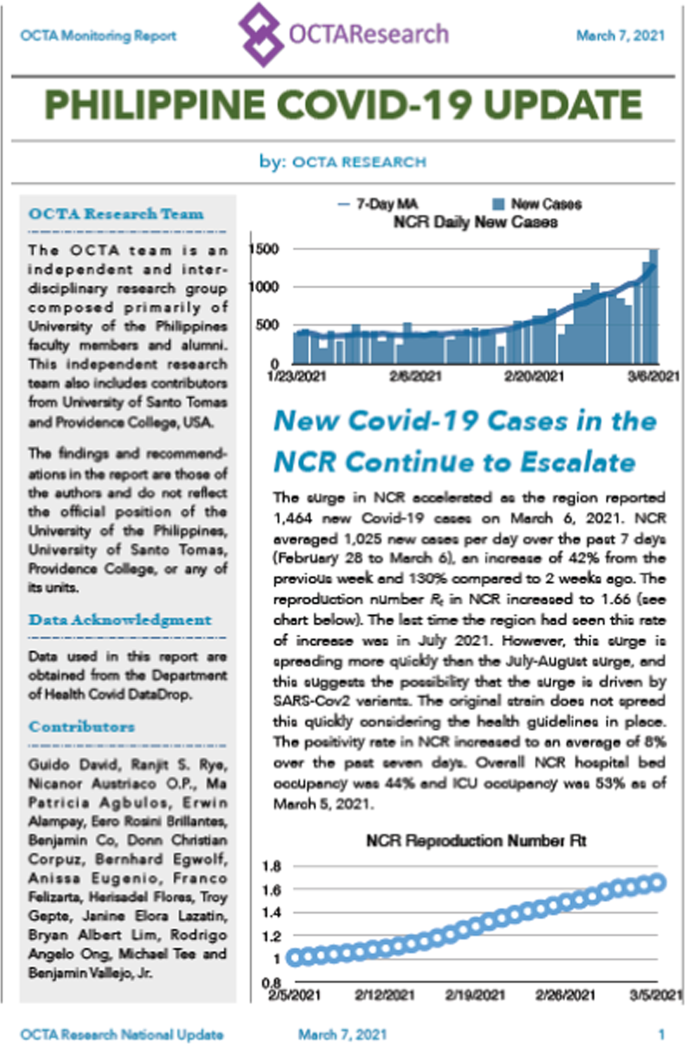
An OCTA COVID-19 forecast update (7 March 2021).
OCTA like other science advice actors, based its epidemiological analyses on the Philippines Department of Health (DOH) Data Drop whose data quality was publicly perceived as poor even though steps have been taken to improve data quality. The DOH in the interest of transparency began Data Drop on April 15, 2020. Data Drop has information on the number of active cases, recovered cases, and hospital admissions. With Data Drop, OCTA was able to issue its first epidemiological forecast.
OCTA does not belong to the formal structures of science advice in the Philippines but is part of the informal science advice community. Its volunteer experts are publicly known. OCTA has emerged as the leading information and science advice provider for the public. How did it become the leading source of science advice and often cited by social and mainstream media and acknowledged by government?
Uncertainty perception in COVID-19 suppression and the political context of role conflation
OCTA became the leading source of science advice when by publishing weekly forecasts on COVID-19 epidemiological trends, it reduced public perception of uncertainty of the pandemic. The bulletins estimated national and regional R0, attack rates, hospital capacity and ICU bed capacity. While most countries worldwide have adopted suppression as the main strategy (Allen et al., 2020 ) a few countries most notably New Zealand, adopting a COVID 19 elimination strategy. The Philippines decided on a suppression policy or a strategy of “flattening the curve” which necessitated lockdowns with the outcome of reducing R0 and COVID-19 hospital admissions.
The most socially and economically disruptive intervention is lockdown with is tied with the uncertainty of lifting quarantine (Caulkins et al., 2020 ). The Philippines instituted a national lockdown beginning 14 March 2020 and instituted a graded system of “community quarantine” which allowed for almost cessation of economic activity and mobility in enhanced community quarantine (ECQ), a modified enhanced community quarantine (MECQ) which allows for the opening of critical services and a limited operation of public transport, to a near open economy and unimpeded local mobility in modified general community quarantine (MGCQ) and a low risk general community quarantine (GCQ) which allows for most economic activities subject to health protocols (Vallejo and Ong, 2020 ) which regulated mobility between quarantine zones.
It is in lockdown policies that uncertainty perception takes on a large political dimension (Gluckman, 2016b ; Pearce, 2020 ). Science advisors have to provide forecasts on the trajectory of R0 for politicians to make a decision on tightening or relaxing of quarantine. In this manner OCTA has provided not only the quarantine grade option but the best option while recognizing that the constraint to lessening the perception of uncertainty lies on data quality itself (Johns, 2020 ). OCTA has raised this concern questions on the accuracy and timeliness of DOH’s Data Drop. In doing so, it has done multiple scenario models to assess the accuracy of data. If the government takes on lockdown as the main strategy for COVID 19 suppression, then it must ensure that science advisory actors are able to deal with the multiple uncertainties that data quality will generate. Science advisory actors can be both knowledge generators and users and this conflation has several consequences such as a tension between knowledge production and use which is called as the “uncertainty monster” (Van der Sluijs, 2005 ).
OCTA it its business model has role conflation. While its polling services are paid for by subscribers, the science advice advocacy function in COVID-19 is volunteer based. This conflation was questioned by members of Congress. Thus, the political context for OCTA is within the problem of role conflation in science in a particular political and academic context which may be the norm in developing countries. The politics of conflation in science advice in the UK was demonstrated when two esteemed epidemiologists belonging to two research groups, Professor Neil Ferguson of the Imperial College London (ICL) and Professor John Edmunds of the London School of Hygiene and Tropical Medicine (LSHTM) released R0 estimates to the public. ICL and LSHTM provided advisories to media and the UK government SAGE, with two different estimates for R0. The ICL estimate (2.0–2.6) were earlier made known to media while the LSHTM estimate (2.7–3.99) underwent peer review and was published in Lancet Public Health (Davies et al., 2020 ). The two estimates became the focus of controversy as the UK Chief Science Advisor Professor Patrick Vallance echoed Edmund’s claim of a case doubling time of 5–6 days. The SAGE consensus was 3–4 days, thus necessitating a sooner rather than later lockdown. The question on when to impose a lockdown is also a political matter. This placed SAGE and its established protocols of keeping experts anonymous under public criticism and scrutiny.
Pearce ( 2020 ) reviews the problem of role conflation of knowledge providers (the modelers) and the knowledge users (government) if they occupy both positions at the same time. Edmunds is a SAGE member (knowledge user) as well as a producer of science information as an academic. This conflation of roles resulted in the “dampening of uncertainties” for political reasons. The government is not acutely aware that this ultimately stems from poor data quality and the resulting scientific uncertainty has great political costs (UP COVID-19 Pandemic Response Team, 2020 ).
Similarly, OCTA has faced questions in its R0 estimates which differs from estimates by other scientists. OCTA’s estimates are higher (2.3) than what government initially used (2.1) in characterizing the surge in cases beginning Feb 2021. With R0 and positivity rates increasing, OCTA recommended an ECQ for the 2021 Easter break which was extended to a MECQ until 30 April 2021 (CNN Philippines, 2021 ). Like in the UK, this will affect policy decision making based on doubling time and the allocation of health resources. But unlike in the UK where there is a formal process of science peer review, in the ad hoc nature of science advice review in the Philippines, much of this “open peer review” by academics was on social media thus giving a polarizing political environment in policy decision.
OCTA has long been aware of the problem of role conflation which is a problem in a country with a small national science community. The national science community is small with only 189 scientists per million people. It thus has sought the expertise of overseas Filipino scientists to expand its advisory bench and to reduce possible role conflation. The overseas scientists are not associated with government health research agencies and so could act more independently. This was a strategy to deal with the possibility of “dampening of evidence”. The Presidential Spokesperson Mr. Harry Roque said that OCTA should cease reporting results to the public and rather send these “privately” to government (Manila Bulletin, 2020 ; Philippine Star, 2020 ). Roque is misconstruing the role of OCTA as a formal government science advisory body when it is not. The statements of the government spokesman may reflect debates in cabinet about the necessity and role of government science advice in and outside of government and their political costs. IATF-EID has its own experts as internal government science advisors. However, their advice must still be subject to peer review and so a mechanism must be found for these experts to compare forecasts with independent advisors such as OCTA. This will minimize public perception that the government silencing OCTA to dampen uncertainties for political outcomes. Public trust in government science advice has always been low if there is no transparency (Dommett and Pearce, 2019 ).
OCTA forecasts have been criticized by government economic planners especially in tourism (Philippine Daily Inquirer, 2020 ) as the forecasts directly affect plans to reopen important economic sectors. Some criticism is apparently political (Manila Times, 2020 ) and implies alienation of OCTA from its academic institutional linkage base. OCTA forecasts have been more and more adopted by the IATF-EID (ABS-CBN, 2021 ) This is a political dynamic for science advice actors sitting in government. Internal science advice actors will have to deal with populist interests in government and their advice may be “written off” (Boin et al., 2016 ). Independent science advice actors do not want their government science advice to be written off and so are likely to take the public route in presenting their synthesis of evidence and options.
Pandemic policy response is all about the management of multiple epidemiological uncertainties. This is when inability of government to manage it became apparent when doctors through the Healthcare Professionals Alliance Against COVID-19 (HPAAC), an organization which is comprised of the component and affiliate societies of the Philippine Medical Association admonished the government to increase quarantine restrictions from General Community Quarantine to Modified Enhanced Community Quarantine for a period of 2 weeks in August to allow the health workers to recover from exhaustion (One News, 2020 ). This is due to the surge in new cases and the overburdening of the healthcare capacity which OCTA earlier forecasted (David et al., 2020 ). The threat of a “doctors strike” would have been politically damaging to the government and the President decided to heed the doctors’ request.
The Philippines response is not very different from response of the majority of 22 countries examined by INGSA’s COVID 19 policy tracker (Allen et al., 2020 ), where these countries embarked on a monitoring and surveillance policy from January to March 2020. The INGSA study also shows that few countries have utilized internal and external formal science advisory bodies in the first 3 months of the pandemic. The Philippines is not one of the countries which INGSA tracked but similarly it started to seek the advice of individual experts by March 2020. Many of these experts posted their unsolicited science advice on social media.
Like most of the 22 INGSA tracked countries, after the 3rd month of the pandemic, the Philippines enacted legislation to deal with the social and economic impact of lockdowns. But this has not yet resulted in legislation passed in the Philippines Congress to deal with developing and improving systems for pandemic response through research and development initiatives although the late Senator Miriam Defensor Santiago filed Senate Bill 1573 “Pandemic and All Hazards Act” in September 2013 (Senate of the Philippines 16th Congress, 2013 ) in response to MERS and Senator Manny Villar in April 2008 filed Senate Bill 2198 “The Pandemic Preparedness Act” (Senate of the Philippines 14th Congress, 2008 ). Both bills institute a Pandemic Emergency Fund and mandates a Pandemic Emergency Council or Task Force, roughly along the lines of the DRRM Law. Defensor-Santiago’s bill was refiled by Senator Grace Poe as Senate Bill 1450 “An Act Strengthening National Preparedness and Response to Public Health Emergencies by Creating a Center for Disease Control” during the first session of the 18th Congress on 27 April 2020 (Senate of the Philippines 18th Congress, 2020 ). Poe’s bill updates Defensor-Santiago’s bill by proposing the creation of Center for Disease Control
These bills have not been enacted into law. The Philippines also did not enact legislation or executive on creating or strengthening science advisory capacity which 12 of the 22 countries INGSA tracked did. However, a senator has recently approached OCTA for policy input in developing formal crisis science advice legislation.
Prospects for independent government science advice in the Philippines
The Philippines government’s COVID 19 suppression policy is based on science informed advice. However, this has been provided informally by individual experts consulted by IATF-EID and this advice is not subjected to formal peer review. This has exposed experts to political criticism and attack as their identities and roles have been spun by media and government media spokespersons as integral to IATF-EID. At least one expert has resigned from providing science advice due to possible conflicts of interests. In this science advice gap, entered OCTA Research in the second quarter of 2020 and continued to 2021 and 2022.
The informal science advice actors more often give their forecasts directly to the media while the formal actors give it to the government agency that commissioned it. The government uses the evidence in determining what quarantine status to implement nationally and regionally through the recommendation of the IATF-EID.
The government’s policy decisions on COVID 19 suppression are chiefly based on a single statistical estimate, R0 but more recently has included positivity rate and hospital capacity. Science advisory bodies must defend R0 and the other estimates to the government and in the public sphere. The estimates will have incorporated all statistical uncertainties in this number. OCTA has done this by publicly reporting low, moderate and high R0 scenarios and the consequent projections for new cases, hospital utilization and attack rates at the national, regional and local government level. The government has used these estimates in its monthly policy responses.
Considering that both use the same DOH Data Drop dataset, dissonance between OCTA and government scientists’ recommendations have been reported in print, broadcast, and social media. This involves largely the differences in interpreting the framework of quarantine status and risks, with government experts tending to question OCTA’s projections with a very conservative precautionary interpretation of evidence. One doctor with the IATF-EID has accuses OCTA of using “erroneous” and “incomplete” data (Kho, 2021 ). This dissonance has led politicians to label OCTA as “alarmist” (David, 2021 ).
OCTA is a knowledge producer in science advice since it constructs DOH epidemiological data into models informed by epidemiological theory. Even if OCTA has decided to remain completely independent as a science advisory body, it is not completely insulated from political attack. Political attack is a result of perceived role conflation in the science advice ecosystem and process which is exacerbated by the nature of uncertainty in science advice leading to accusations of OCTA being “alarmist. OCTA was misconstrued by the government as its own knowledge producer and its critics demanded that it be completely alienated from its academic institutional linkages. OCTA’s weakness and the weakness of the Philippines crisis science advisory system overall, is the lack of external and extended peer review. This is a consequence of a small science community where there are few actors who can perform this role with citizen scientists. In a postnormal science advisory environment, the role of extended peer review is important in validating policy options and creating public consensus.
OCTA has recently partnered with Go Negosyo, a small and medium business entrepreneurship (SME) advocacy, headed by Presidential advisor for entrepreneurship, Joey Concepcion. Mr. Concepcion has a minister’s portfolio. OCTA in this arrangement will provide data analytics services and science advice for SMEs for a business friendly COVID exit policy with a safe reopening of the economy based on vaccination prioritization strategies (Cordero, 2021 ). This move also evidences OCTA’s influence in setting new policy directions in government’s adoption of a new quarantine classification system of Alert Levels, an idea first proposed by OCTA Fellow and medical molecular biologist Rev Dr. Nicanor Austriaco OP and mathematical modeler Dr. Fredegusto Guido David. This is a political move on OCTA’s part to deflect critics in Congress as the business sector has a large political clout in government.
While a pandemic crisis like COVID 19 gives political leaders an advantageous occasion to demonstrate personal leadership, their constituencies will tend to expect a more personalistic crisis management. In this independent science advice plays a crucial political dynamic by building public trust, ensuring reliable statistical estimates reviewed by the academic science community, and managing political advantages and risks. These are all in the context of epidemiological uncertainties. In the Philippines, public criticism of the pandemic response is fierce due to the primarily law and order policing approach which raised concerns on human rights violations (Hapal, 2021 ) as well as those cases began to rise in the first quarter of 2021 (Robles and Robles, 2021 ). The failure to deal with uncertainties in science without effective science advice may entail large political costs. Managing public perception and the use of government scientific and technical advice is a delicate balancing act in liberal democracies. The press and media will report and scrutinize science informed decisions while shaping public opinion of crisis decisions. Academic science and civil society organizations not part of the advisory system provide another level of scrutiny and critique. Social media has extremely broadened the venue for public scrutiny and, open or extended peer review of crisis decisions.
These realities were not faced by political leaders as recently as 30 years ago. However unfair or unrealistic the critique by constituencies and the press, public expectation is real in political terms. And while politicians can “write off” certain social and political sectors in deciding which crisis response is best, this is no longer tenable in democracies in the 21st century.
In these realities emerge new actors of engaged independent academic science advisors such as OCTA. It has certainly played the role of a knowledge generator and to some extent a knowledge broker. And like any science advice actor, OCTA was not immune to political attack, and this would suggest that SAGE with its embeddedness in the administrative and ministerial structures in the UK, largely missing in the Philippines (Berse, 2020 ), will be subject to great political interference which may limit its effectiveness. Political interference may masquerade as technical in nature (Smallman, 2020 ).
The Philippines government response to COVID 19 has been described as “deficient in strategic agility” (Aguilar Jr, 2020 ) partly due to its inability to mobilize scientific expertise and synthesize science informed advice options in governance. Thus, a plausible proposal to strengthen science advice is in reframing the DRRM policy and advisory structures and applying these to crisis in order to strengthen science advice capacity at all levels of governance. As Berse ( 2020 ) suggests “tweaking the National Disaster Risk Reduction and Management Council structure, which has a seat for an academic representative, might do the trick. This national set-up is replicated by law at the provincial, city and municipal levels”.
Berse also suggests that an academic should be appointed to sit at each of these councils. The major constraint is that there are very few academics willing to sit as this will expose them to political criticism and interference. If academics are appointed, then their expertise should not be unduly constrained by political interference. They should be backed by several researchers and citizen scientists coming from multiple disciplines in reviewing science informed policies. More and more citizen scientists have come up with science advice which for consistency of policy should be reviewed in extended consensus by scientists and stakeholders (Funtowicz and Ravetz, 1993 ; Marshall and Picou, 2008 ).
The closed and elitist system of science advice in the Philippines with its handful of actors, mainly appointed by government, are inordinately prone to political pressure. This necessitates the role of independent science advisors. Independent science advisors can act as a “challenge function” to government experts whose recommendation if ignored contributes to further erosion of public trust in government (Dommett and Pearce, 2019 ). Independent science advice when framed in the context of parliamentary democracy can be likened to “shadow cabinets” in this way they provide a check, balance and review of science evidence and is called “shadow science advice” (Pielke, 2020 )
As pandemics and other environmentally related public health emergencies are expected to be more frequent in the 21st century, the public will be less tolerant of social and political instability and demand a clear science informed response from their politicians. However, most politicians do not have enough scientific and technical competency to do so and so will have to rely on science informed advice which has degrees of outcome uncertainty (Gluckman, 2016b ). If science informed options are ignored for political gains, this is not a result of broken science advice and knowledge generation systems but a dysfunctional political and governance system. The huge cost in life and economic opportunity left by the pandemic demands functional government informed by science advice.
Furthermore, any government to cement its legacy must find a COVID 19 crisis exit strategy after the operational aspects such as a mass vaccination strategy have been met and the social, health (Dickens et al., 2020 ), economic and political situation has been stabilized (Gilbert et al., 2020 ). In COVID 19, this is a gradual relaxation of lockdown and quarantine (Leung and Wu, 2020 ) with the roll out of vaccines.
Vaccination is the main COVID-19 exit strategy of the government (Congress of the Philippines, 2021 ) and given the large existing vaccine hesitancy of 46% as OCTA estimated in February 2021 (Tomacruz, 2021 ), there is a need to increase public confidence on vaccines (Vergara et al., 2021 ). Public distrust of vaccines became a major public health concern due to the Dengvaxia vaccine rollout controversy in November 2017 when Sanofi publicly released a warning that vaccination posed a risk if given to people who never had a dengue infection (Larson et al., 2019 ). The political impact was damaging to the Benigno Aquino III presidential administration, which rolled out the vaccine in 2016 before Aquino III’s term ended. The drop in vaccine confidence was significant, from 93% in 2015 to 32% in 2018. The new presidential administration of Rodrigo Duterte placed the blame on Aquino III, and this resulted in social and political polarization, loss of trust in the public health system which have continued in the COVID-19 pandemic. The “blame game” is political risk in any liberal democracy. This can be a long drawn out affair where government will have to establish accountability and the “blame game” is expected with various independent boards and blue ribbon committees setting the narrative (Boin et al., 2016 ). In the Philippines, several hearings in the House and Senate in which Sanofi and previous Department of Health leadership were called to give testimonies, further worsened political and social polarization to vaccination. These independent boards, blue ribbon committees and fact-finding investigations, however, are prone to agency capture by ruling party politics. This is evident in the Philippines. The government exit strategy for COVID-19 is clouded by these polarizations. OCTA will be expected by the public to provide government science advice on vaccination policies, and this will have great political costs for independent science advice. As vaccination in the Philippines has become a political issue more than as a public health issue, other think tanks and academic research institutions which have investigated Dengvaxia, and vaccine compliance have been more guarded as not to attract undue negative political comment. OCTA to its credit, has successfully navigated political risks in its COVID-19 forecasts and in a political move, has allied with a SME advocacy headed by a close Presidential advisor on economic affairs. OCTA can continue to maintain its credibility by periodically issuing forecasts and policy option recommendations and reducing social and political polarizations through consensus building with the public, government, and science community. Here is where the independent science advice actors will have a place, and that is to set the objective bases for science informed policy decisions while recognizing the political dynamic. How independent science advice will result in lasting policy impacts in the Philippines remains to be seen. The government and the public have relied on OCTA forecasts because of OCTA’s increasing presence in broadcast, print, and social media. This is evidence of the effective science communication strategy of the organization. But with the Government increasingly using OCTA’s forecasts and policy recommendations, this is evidence that government science advice has political dividends and risks which may affect politicians’ political standing with the electorate in the 2022 election.
Data availability
COVID-19 open data cited in this paper can be accessed through the Philippines Department of Health Data Drop https://doh.gov.ph/covid19tracker and through OCTA Research https://www.octaresearch.com/ .
ABS-CBN (2021) Metro Manila COVID-19 surge begins ahead of Christmas: OCTA Research. https://news.abs-cbn.com/news/12/22/20/metro-manila-covid-19-surge-begins-ahead-of-christmas-octa-research . Accessed 3 Jan 2021
Aguilar Jr FV (2020) Preparedness, agility, and the Philippine response to the Covid-19 pandemic the early phase in comparative Southeast Asian perspective. Philipp Stud Hist Ethnogr Viewp 68(3):373–421
Article Google Scholar
Allen K, Buklijas T, Chen A, Simon-Kumar N, Cowen L, Wilsdon J, Gluckman P (2020) Tracking global knowledge-to-policy pathways in the coronavirus crisis: a preliminary report from ongoing research. INGSA. https://www.ingsa.org/wp-content/uploads/2020/09/INGSA-Evidence-to-Policy-Tracker_Report-1_FINAL_17Sept.pdf
Bankoff G, Hilhorst D (2009) The politics of risk in the Philippines: comparing state and NGO perceptions of disaster management. Disasters. 33(4):686–704
Berse K (2020) In science we trust? Science advice and the COVID-19 response in the Philippines https://www.ingsa.org/covidtag/covid-19-commentary/berse-philippines/ . Accessed 3 Jan 2021.
Boin A, Stern E, Sundelius B (2016) The politics of crisis management: Public leadership under pressure. Cambridge University Press, Cambridge
Book Google Scholar
Caulkins J, Grass D, Feichtinger G, Hartl R, Kort PM, Prskawetz A, Seidl A, Wrzaczek S (2020) How long should the COVID-19 lockdown continue? PLoS ONE 15(12):e0243413
Article CAS Google Scholar
CNN Philippines (2021) OCTA Research: four-week MECQ to “knock out” COVID-19 case surge. https://cnnphilippines.com/news/2021/3/24/OCTA-Research-4-week-MECQ-knock-out-surge.html . Accessed 16 Apr 2021
Congress of the Philippines (2021) An act establishing the coronavirus disease 2019 (COVID-19) vaccination program expediting the vaccine procurement and administration. Providing Funds Therefor, and for Other Purposes, Manila. https://www.officialgazette.gov.ph/downloads/2021/02feb/20210226-RA-11525-RRD.pdf . Accessed 16 Apr 2021
Cordero T (2021) Go Negosyo, OCTA Research ink partnership on data-sharing, proposals to reopen economy. GMA News Online. https://www.gmanetwork.com/news/money/companies/807569/go-negosyo-octa-research-ink-partnership-on-data-sharing-proposals-to-reopen-economy/story/ . Accessed 25 Oct 2021.
David G, Rye R, Agbulos M, Alampay E, Brillantes E, Lallanam R, Ong R, Vallejo B, Tee M (2020) COVID-19 forecasts in the Philippines: NCR, Cebu and COVID-19 hotspots as of June 25, 2020. OCTA Research, Quezon City, Philippines
Google Scholar
David R (2021) Probing OCTA. Philippine Daily Inquirer https://opinion.inquirer.net/142869/probing-octa . Accessed 25 Oct 2021.
Davies NG, Kucharski AJ, Eggo RM, Gimma A, Edmunds WJ, Jombart T, O’Reilly K, Endo A, Hellewell J, Nightingale ES et al. (2020) Effects of non-pharmaceutical interventions on COVID-19 cases, deaths, and demand for hospital services in the UK: a modelling study. Lancet Public Health 5(7):e375–e385. https://doi.org/10.1016/S2468-2667(20)30133-X
Article PubMed PubMed Central Google Scholar
Dickens BL, Koo JR, Lim JT, Park M, Quaye S, Sun H, Sun Y, Pung R, Wilder-Smith A, Chai LYA et al. (2020) Modelling lockdown and exit strategies for COVID-19 in Singapore. Lancet Reg Health-West Pac 1:100004. https://doi.org/10.1016/j.lanwpc.2020.100004
Dommett K, Pearce W (2019) What do we know about public attitudes towards experts? Reviewing survey data in the United Kingdom and European Union. Public Underst Sci 28(6):669–678
Doubleday R, Wilsdon J (2012) Beyond the great and good. Nature 485(7398):301–302. https://doi.org/10.1038/485301a
Article ADS CAS PubMed Google Scholar
Funtowicz SO, Ravetz JR (1993) Science for the post-normal age. Futures 25:739–755. https://doi.org/10.1016/0016-3287(93)90022-L
Funtowicz SO, Ravetz JR (1994) Uncertainty, complexity, and post‐normal science. Environ Toxicol Chem Int J 13(12):1881–1885
Gilbert M, Dewatripont M, Muraille E, Platteau J-P, Goldman M (2020) Preparing for a responsible lockdown exit strategy. Nat Med 26(5):643–644. https://doi.org/10.1038/s41591-020-0871-y
Article CAS PubMed PubMed Central Google Scholar
Gluckman P (2016a) The science–policy interface. Science 353(6303):969. https://doi.org/10.1126/science.aai8837
Gluckman P (2016b) Making decisions in the face of uncertainty: understanding risk Auckland. Office of the Prime Minister’s Chief Science Advisor, Auckland, New Zealand
Hapal K (2021). The Philippines’ COVID-19 response: securitising the pandemic and disciplining the pasaway. J Curr Southeast Asian Aff. https://doi.org/10.1177/1868103421994261
Kho R (2021) House inquiry sought on OCTA Research group. Businessworld https://www.bworldonline.com/house-inquiry-sought-on-octa-research-group/ . Accessed 25 Oct 2021.
Larson HJ, Hartigan-Go K, de Figueiredo A (2019) Vaccine confidence plummets in the Philippines following dengue vaccine scare: why it matters to pandemic preparedness. Hum Vaccines Immunother 15(3):625–627. https://doi.org/10.1080/21645515.2018.1522468
Leung K, Wu JT (2020) The gradual release exit strategy after lockdown against COVID-19. Lancet Reg Health–West Pac 1. https://doi.org/10.1016/j.lanwpc.2020.100008 . Accessed 4 Jan 2021
Lipsitch M, Riley S, Cauchemez S, Ghani AC, Ferguson NM (2009) Managing and reducing uncertainty in an emerging influenza pandemic. N Engl J Med 361(2):112–115. https://doi.org/10.1056/NEJMp0904380
MacKenzie DA (1993) Inventing accuracy: a historical sociology of nuclear missile guidance. MIT press, Cambridge, MA
Manila Bulletin (2020) OCTA Research reporting continues. https://mb.com.ph/2020/10/15/octa-research-reporting-continues/ . Accessed 3 Jan 2021.
Manila Times (2020) Time for UP OCTA research team to account for its Covid forecasting. https://www.manilatimes.net/2020/07/20/opinion/editorial/time-for-up-octa-research-team-to-account-for-its-covid-forecasting/743476/ . Accessed 3 Jan 2021.
Marshall BK, Picou JS (2008) Postnormal science, precautionary principle, and worst cases: the challenge of twenty‐first century catastrophes. Sociol Inq 78(2):230–247
UP COVID-19 Pandemic Response Team (2020) Prevailing data issues in the time of COVID-19 and the need for open data. University of Philippines. https://www.up.edu.ph/prevailing-data-issues-in-the-time-of-covid-19-and-the-need-for-open-data/ . Accessed 4 Jan 2021
Johns S (2020) Neil Ferguson talks modelling, lockdown and scientific advice with MPs. Imperial News. Imperial College London https://www.imperial.ac.uk/news/198155/neil-ferguson-talks-modelling-lockdown-scientific/ . Accessed 2 Jan 2021.
One News.ph (2020) NO REVOLUTION: medical frontliners tell Duterte they had to go public as distress calls went unanswered. https://www.onenews.ph/no-revolution-medical-frontliners-tell-duterte-they-had-to-go-public-as-distress-calls-went-unanswered . Accessed 4 Jan 2021.
Pearce W (2020) Trouble in the trough: how uncertainties were downplayed in the UK’s science advice on Covid-19. Humanit Soc Sci Commun 7(1):1–6. https://doi.org/10.1057/s41599-020-00612-w
Article MathSciNet Google Scholar
Pellini A, Jabar M, Era M, Erasga D (2013) Towards policy-relevant science and scientifically informed policy: political economy of the use of knowledge and research evidence. ODI, Manila
Philippine Daily Inquirer (2020). Baguio tourism industry objects to OCTA ‘high risk’ tag. INQUIRER.net https://newsinfo.inquirer.net/1364601/baguio-tourism-industry-objects-to-octa-high-risk-tag . Accessed 3 Jan 2021.
Philippine Star (2020) Palace tells UP, UST experts to stop publicizing quarantine status recommendations. Oct 10th, 2013. https://www.philstar.com/headlines/2020/10/13/2049279/palace-tells-experts-stop-publicizing-quarantine-status-recommendations . Accessed 3 Jan 2021.
Pielke RJ (2020) On shadow science advice https://youtu.be/PktWL5xNanc . Accessed 24 March 2021
Ravetz IR (1999) What is post-normal science. Futur-J Forecast Plan Policy 31(7):647–654
Robles A, Robles R. 2021. Where did the Philippines’ pandemic response go wrong? South China Morning Post. https://www.scmp.com/week-asia/health-environment/article/3122257/late-and-slow-motion-where-philippines-pandemic . Accessed Apr 16 2021.
Senate of the Philippines 14th Congress (2008) An act establishing a pandemic preparedness plan and for other purposes therefor. 14th Congress first regular session https://legacy.senate.gov.ph/lis/bill_res.aspx?congress=14&q=SBN-2198 . Accessed 15 Jan 2021
Senate of the Philippines 16th Congress (2013) An act strengthening national preparedness and response to public health emergencies. 16th Congress first regular session https://legacy.senate.gov.ph/lis/bill_res.aspx?congress=16&q=SBN-1573 . Accessed 15 Jan 2021
Senate of the Philippines 18th Congress (2020) An Act Strengthening National Preparedness and Response to Public Health Emergencies by Creating a Center for Disease Control 18th Congress. First regular session http://legacy.senate.gov.ph/lisdata/3260429469!.pdf . Accessed 15 Jan 2021
Smallman M (2020) ‘Independent Sage’ group is an oxymoron. Res Prof News. https://www.researchprofessionalnews.com/rr-news-political-science-blog-2020-5-independent-sage-group-is-an-oxymoron/ . Accessed 4 Jan 2021.
Tomacruz S (2021) 46% of adult Filipinos still unwilling to get vaccinated vs. COVID-19. Rappler https://www.rappler.com/nation/octa-research-filipinos-covid-19-vaccine-willingness-february-2021 . Accessed 15 Apr 2021
Vallejo BM, Ong RAC (2020) Policy responses and government science advice for the COVID 19 pandemic in the Philippines: January to April 2020. Prog Disaster Sci 7:100115. https://doi.org/10.1016/j.pdisas.2020.100115
Van der Sluijs J (2005) Uncertainty as a monster in the science–policy interface: Four coping strategies. Water Sci Technol 52(6):87–92
Vergara RJD, Sarmiento PJD, Lagman JDN (2021) Building public trust: a response to COVID-19 vaccine hesitancy predicament. J Public Health Oxf Engl 43(2):e291–e292. https://doi.org/10.1093/pubmed/fdaa282
Download references
Acknowledgements
The authors thank the University of the Philippines Bayanihan Research Grants for COVID-19 for funding support. We also thank Assistant Professor Ranjit Singh and Dr. Fredegusto Guido David of OCTA Research for providing OCTA COVID-19 forecasts and epidemiological model and Mr. Fil Elefante for proofreading. Many thanks also to Prof. Roger Pielke at the University of Colorado at Boulder and EsCAPE ( www.escapecovid19.org ) for encouraging the publication of this paper.
Author information
Authors and affiliations.
University of the Philippines Diliman, Quezon City, Philippines
Benjamin M. Vallejo Jr & Rodrigo Angelo C. Ong
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Benjamin M. Vallejo Jr .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors. Ethics review is not required.
Informed consent
All statements attributed to specific individuals used in this study are in the public record and no informed consent from individuals is required.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Vallejo, B.M., Ong, R.A.C. OCTA as an independent science advice provider for COVID-19 in the Philippines. Humanit Soc Sci Commun 9 , 104 (2022). https://doi.org/10.1057/s41599-022-01112-9
Download citation
Received : 17 June 2021
Accepted : 23 February 2022
Published : 30 March 2022
DOI : https://doi.org/10.1057/s41599-022-01112-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Open access
- Published: 10 May 2023
Determinants of COVID-19 vaccination decision among Filipino adults
- Lourdes Marie Sequerra Tejero 1 ,
- Rosemary Ruiz Seva 2 ,
- Bettina Joyce Petelo Ilagan 3 &
- Kattleea Lorezca Almajose 4
BMC Public Health volume 23 , Article number: 851 ( 2023 ) Cite this article
5313 Accesses
3 Citations
1 Altmetric
Metrics details
With a number of vaccines against COVID-19 now widely available globally, it is opportune to determine what tips the decision to get vaccinated. In most countries like the Philippines where the government provides these vaccines for free to all its citizens, their COVID-19 vaccine awareness and COVID-19 information sources as well as their socio-demographic profile were considered as primary factors that could possibly affect vaccination decisions. Participants’ income level was considered as a possible financial consideration that can affect vaccination decision as transport to vaccination sites might entail costs to them.
This study used a cross sectional survey design wherein participants came from all regions of the Philippines. An online questionnaire was voluntarily answered by Filipinos aged 18–80 years of age.
A total of 2,268 participated in the survey with 1,462 having complete responses which were included in the analysis. Those who are younger, with higher educational attainment, with public health insurance, with employers requiring vaccination, high awareness about COVID-19 vaccination, and high vaccine confidence are more likely to get vaccinated. On the other hand, those with long-standing illness and those residing outside the national capital region are less likely to get vaccinated.
Vaccination decisions among Filipinos are determined by their age, educational attainment, health insurance, employer requirement, high awareness of the disease, and a high level of vaccine confidence.
Peer Review reports
Introduction
On March 11, 2020, the World Health Organization (WHO), in a media briefing opening remarks by its director-general, characterized COVID-19 as a pandemic. While the development of vaccines is deemed as one of the most important responses to curb this global health crisis, WHO emphasized that it is vaccination per se, and not the vaccines that will put an end to this pandemic. However, WHO also acknowledged that there are challenges to ensure that people around the world get vaccinated.
In January 2021, the Department of Health of the Philippines issued an interim plan for the deployment of COVID-19 vaccines [ 1 ]. The strategy was that of a whole-of-society approach with the government leading the deployment of vaccines and implementation of the vaccination program. Of the 110 million population, about 70 million were considered eligible for the vaccines for 2021, based on pre-identified groupings.
Sallam [ 2 ] found out that vaccine hesitancy, or the “delay in acceptance or refusal of vaccination despite availability of vaccination services”[ 3 ], is considered as a common phenomenon globally. He furthers that, in his review of COVID-19 vaccine acceptance rates worldwide, vaccine hesitancy can be the major hindrance of the control efforts to lessen the negative consequences of COVID-19 pandemic, at least in certain countries/regions.
In the Philippines, decisions to get vaccinated, particularly of the COVID-19 vaccine, are driven by Filipinos’ concerns about having more information about the various vaccines available to them [ 4 ]. United Nations Development Programme (UNDP) Philippines, in August 2021 reported that the facilitating factors for vaccination included concern for family and loved ones, COVID-19 risk perception, approval of an endorsement by either the Food and Drug Administration (FDA) or the Department of Health (DOH), and work-related reasons; while barriers to vaccination included concerns about side-effects, medical reasons, news about vaccines, and vaccine effectiveness and efficacy [ 5 ]. It was mentioned in this same report that COVID-19 vaccination in the Philippines started in March 2021 and that by August 15, 2021, around 40.4 to 44.1% of the adult population have received at least one COVID-19 vaccine shot. The Philippine government’s initial target was 70% of the population by the end of 2021.
Despite these findings, however, several factors affecting decisions to get vaccinated against COVID-19, given the multifaceted nature of vaccine hesitancy [ 2 ] and the history of vaccine uptake in the Philippines marked by critical challenges [ 6 ] required further studies.
Hence, this quantitative, correlational research on the determinants of COVID-19 vaccination decision among Filipino adults. As transport to vaccination sites might entail costs for people, participants’ income level was considered as a financial factor that can affect their vaccination decision. Non-financial factors considered were socio-demographic characteristics; COVID-19 information sources, awareness, and worry; and vaccine confidence and functional health literacy. The study examined if both these financial and non-financial factors could determine participants’ vaccination decision.
Research design
This is a cross sectional survey design wherein participants from all the 17 administrative regions of the Philippines were included in the sample. Following the formula provided by Bujang, et al. [ 7 ], the required number of participants is 850.
Data collection was conducted in the first quarter of 2022, the time when a recent surge of cases was declining early in that quarter [ 8 ], and when the Philippine government is nearing its target of vaccinating 70% of its population against COVID-19 [ 9 ]. It was opportune at this time to investigate the drivers for actual vaccination. Participants of the study were Filipinos aged 18–80 years old, currently residing in the country, were qualified to take the COVID-19 vaccine, could read, and understand Filipino and/or English, and could answer the questionnaire online.
Two questionnaires were developed in two languages: English and Filipino. The English questionnaire was translated from English to Filipino by a qualified translator. The English questionnaire was piloted first to 25 individuals to ensure the clarity of questions. Corrections were made on the format of the questionnaire and order of questions. After translation, the Filipino questionnaire was piloted to another 25 people. The Filipino version was revised to simplify the difficult Filipino terms used in the first version.
The survey was administered online using two methods: first is self-administered (91%) and the second was by a trained research assistant interviewer (9%) for those who were in remote areas and had difficulty accessing the Internet. The main survey questionnaire administration was conducted between March to April of 2022. Participation in the study was voluntary. Recruitment was done through social media platforms and through email. Participants were given an online survey link and they had the option to answer either a questionnaire in English or a questionnaire in Filipino. Answering the questionnaire and subsequently submitting it, constituted participant’s consent in the study. Those who requested reimbursement for the internet services incurred in answering the online questionnaire were reimbursed accordingly. The responses to the questionnaire remained anonymous since the request for reimbursement came in separately from the questionnaire. All the questions in the questionnaire were mandatory.
A questionnaire was designed ad hoc to collect the data for this research. The sociodemographic data included age, sex, educational attainment, employment status, income level, health insurance, health status, and region of residence.
Employer requirement for vaccination and advice by a health care provider to vaccinate against the disease are binary variables in the model where a yes answer was coded as 1. Information sources included three items that identify a person’s social context - family and friends, co-workers, and healthcare workers. Nine items that describe their information environment - government agencies, TV, newspaper, radio, Facebook, Instagram, Twitter, TikTok, and YouTube. The frequency of access followed a five-point Likert scale measured as (1) never, (2) rarely, (3) sometimes, (4) often, and (5) always. For COVID-19 vaccination awareness, participants were asked to answer a 9-item quiz-type survey with statements formulated based on information presented on the websites of the Philippines’ Department of Health and the United States of America’s Center for Disease Control and Prevention. The three levels of awareness were given scores as follows: 1 (correct information), 0 (unaware of the information), and − 1 (wrong information) in the model.
COVID-19-related worry was determined using a three-item scale taken from Head et al., [ 10 ] to measure participants’ personal worry about COVID-19. A 5-point Likert-type scale was used where 1 = strongly disagree to 5 = strongly agree.
Participants’ vaccine-related profiles included information on functional health literacy (FHL) and vaccine confidence. All four items to measure FHL were taken from Biasio et al., [ 11 ]. As for vaccine confidence , five items were adapted from the 8-item Vaccine Confidence Scale by Gilkey et al., [ 12 ] measured using a 10-point sliding scale from 0-strongly disagree to 10-strongly agree because of their relevance to study objectives. The 5 items included were: (1) Vaccines are necessary to protect health, (2) Vaccines do a good job in preventing the diseases they are intended to prevent, (3) Vaccines are safe, (4) If I get vaccinated there can be serious side effects and, (5) In general, medical professionals in charge of vaccinations have my best interest at heart. Item 4 was reverse coded.
Participants’ vaccination status is a binary variable where one refers to getting the full dose of the vaccine or at least one shot of a two-dose vaccine. Their vaccination status equated to their vaccination decision, considered as the dependent variable in the model.
Data analysis
Aside from age, all sociodemographic data were considered categorical variables in the model. Coded data was processed using MS Excel and scored. Responses with scores were summed and used in calculating the total scores of vaccination awareness, COVID-19-related worry, FHL, and vaccine confidence. Sociodemographic data were summarized using a frequency table. Quantitative data were presented as mean and standard deviation. Binary logistic regression (BLR) was performed to determine predictors of COVID-19 vaccine decision. The BLR model was constructed by including all 15 covariates at the same time. A full model was constructed that included all the variables in the analysis. This approach was used to prevent bias in the selection of variables to be included in the model.
Data were analyzed using SPSS 21.0 (IBM Corp.: Armonk, NY, USA). Significance level considered was 0.05.
Ethics statement
All methods were carried out in accordance with relevant guidelines and regulations. Since all participants were 18 years old and above, the consent of a guardian was not required. The introductory letter to participants in the survey questionnaire contained relevant information about the research including objectives, benefits to the participant, anonymity, expected time for their participation, utilization of data gathered, contact information of the researchers, etc. It also indicated that participation was voluntary and continuing to answer the survey was an expression of consent. The study protocol, survey questionnaire, including ‘waiver of informed consent documentation’ were reviewed and approved by the University of the Philippines Manila’s Review Ethics Board, with code UPMREB 2021-0673-01.
A total of 2,268 participated in the survey from which 1,462 complete survey responses were recorded and analyzed. Incomplete responses were not included in the data analysis. A response is considered incomplete if the respondent failed to finish the survey.
Participants’ sociodemographic characteristics
Table 1 summarizes the sociodemographic characteristics of the 1,462 participants in the study. When data gathering was conducted, around 70% of the Philippine population had already been vaccinated. Participants came from all the regions in the Philippines but the distribution of the sample did not follow the actual geographical distribution. 61% (61%) of the participants came from densely populated areas in the Philippines, such as CALABARZON (25%), National Capital Region (20%), and Central Visayas (16%). Participants aged 21–30 comprised the highest percentage of the sample (36%), followed by those younger than 21 (20%). People older than 60 comprised 6% (6%) of the sample only. 69% (69%) of the sample were female. Approximately two-thirds (66%) were college graduates, and 54% were employed. More than half (52%) belong to the poor and low-income group, and 47% have no health insurance. Eighty one percent (81%) do not have a long-standing illness.
Participants’ COVID-19-related Profile
Most (86%) of the participants were either partially or fully vaccinated. Seventy one percent (71%) received a recommendation from a healthcare professional to get a COVID-19 vaccine. Of the 785 employed participants, 83% were required by their employers to get vaccinated against the disease.
As can be seen in Table 2 , the average awareness score is 2.81 indicating that participants know at least 3 correct COVID-19 vaccine information. Details of the COVID-19 Awareness data were included in Annex 2. Majority (93%) are aware that the vaccines are free, that they come in different brands (89%) and they are effective in helping protect against severe disease and death (83%). However, around 96% are not aware that vaccines have side effects that are normal and believe that it contains microchips that can alter DNA (89%).
The mean FHL score indicates a general difficulty understanding published information about COVID-19 vaccines. The participants are highly worried about getting infected by the virus but have high levels of confidence in the vaccine.
Table 3 summarizes the sources and frequency of access to COVID-19 vaccination information. The top three most often accessed sources of information on COVID-19 vaccination are Facebook, TV, and family and friends.
Sociodemographics, COVID-19-related Profile, and vaccine-related Profile Associated with Vaccination decision
The results of the binomial logistic model of the sociodemographic, COVID-19-related profile and information sources are presented in Table 4 . Logistic regression analysis was performed to explore the influencing factors associated with the decision to get vaccinated against the COVID-19 virus. Younger age (aOR = 0.94, 95% CI = 0.92–0.96), higher educational attainment (aOR = 5.25, 95% CI = 2.75–10.03; aOR = 6.22, 95% CI = 2.14–18.13), those with public health insurance (aOR = 2.47, 95% CI = 1.23–4.96), those with employers requiring vaccination (aOR = 4.28, 95% CI = 2.18–8.43), high awareness about COVID-19 vaccination (aOR = 1.22, 95% CI = 1.11–1.34), and high vaccine confidence (aOR = 1.15, 95% CI = 1.12–1.19) are more likely to get vaccinated. Those with long-standing illness tend not to get vaccinated (aOR = 0.38, 95% CI = 0.19–0.76). As for the region of residence, those regions outside the national capital region (NCR) are less likely to get vaccinated.
Several socio-demographic variables significantly affect the vaccination decision of participants in the sample. Results suggest that young participants are more likely to take the vaccine as the proportion of unvaccinated individuals increases with age. This is consistent with previous findings that young people are less hesitant to receive the COVID19 vaccine [ 13 , 14 ]. During the survey, health authorities in the Philippines struggled to vaccinate its elderly population because they do not turn up at the vaccination sites, meeting only 5% of the target during a three-day vaccination drive [ 15 ]. One of the reasons cited by health authorities is the belief of older adults that they do not have many years to live, making the vaccine unnecessary[ 16 ]. Some elderly people are also difficult to reach, especially those living in rural areas [ 16 ].
Higher education levels such as college and postgraduate degrees, largely determine vaccination decisions in this study. A closer look at the data showed vaccine awareness and functional literacy levels are lower for those without college degrees. Literature on vaccine determinants worldwide consistently showed that fewer years of education decreases the chance of COVID19 vaccine uptake [ 17 , 18 ]. People with higher education have heightened awareness of the risks and benefits of the vaccine because they have more knowledge about the vaccine and the vaccination process. Similarly, high vaccine acceptance rates among college students in China were associated with high knowledge [ 19 ].
Sex, employment status, and family income were unrelated to the study’s vaccination decision, probably because the Philippine government made COVID-19 vaccines free for all its citizens; thus, financial incapacity and unemployment did not deter anyone from getting vaccinated. Men and women received the vaccines to comply with institutional requirements. Our study showed that employers requiring COVID-19 vaccination increased Filipinos’ likelihood of vaccinating. The Presidential announcement requiring vaccination for employees working onsite [ 20 ] strongly influenced the people’s decision to get the shots. For the unvaccinated, their options were to work from home or undergo regular RT-PCR testing as prescribed by the Philippine Department of Labor and employment [ 21 ]. With the high costs of tests, employees generally opted to get vaccinated.
Geographic location has a strong association with vaccination uptake since the Philippines is an archipelago consisting of more than 7,000 islands. Delivering the vaccines to far-flung areas from the National Capital Region (NCR) is a logistical challenge that contributes to the difference in vaccination rates across areas. During the time of the vaccine rollout, local government units (LGUs) interviewed from Luzon, Visayas, and Mindanao expressed concerns about vaccine handling, especially the need for cold storage facilities and vehicles to transport the vaccines [ 22 ]. Aside from logistical problems, the Geographically Isolated and Disadvantaged Areas (GIDA) in the Philippines are also affected by the pandemic response due to communist terrorist groups in the area [ 23 ].
The participants came from all the regions of the country although the distribution of the sample did not reflect the actual geographical distribution. The participants lived mainly in highly urbanized areas whereas the Philippines has more rural communities. NCR is the center of the country’s economic activity and the largest of all metropolitan areas. The likelihood of getting vaccinated decreases as the region gets further away from the NCR as urbanization significantly determines the vaccine acceptance rate [ 24 ]. In Canada, more people were vaccinated in large metropolitan areas, just like the NCR [ 24 ]. Moreover, population density is generally higher in urban areas, especially in the NCR, making the people more concerned about disease transmission.
Vaccine awareness of participants in this study is generally high as most lived in urban areas. There was high awareness in NCR and Luzon. People who live far from the capital and/or urban areas may have less access to information materials and modalities, hence the lower vaccination uptake in these areas. Two common mistakes emerged from our results about COVID19 vaccines. Most participants believed that they do not have to take the full dose of the vaccine and that vaccines can alter or change their DNA, turning them into genetically modified human beings. The false information about DNA modification lowered vaccine acceptance and was found to be one of the most common themes in a study of 52 countries about vaccine rumors and conspiracy theories [ 25 ]. Taking only the first of a 2-dose COVID-19 vaccine gives protection for a limited period. The second dose prolongs the duration of this protection by activating the helper T cells of the immune system [ 26 ].
Participants who know about vaccine brands, compositions, and doses, as well as vaccination effectiveness and side effects after vaccination being considered normal, have a higher tendency to decide to get vaccinated than those with little or no knowledge of these things. Nomura et al. [ 27 ] also found that people’s perceptions of the risks and benefits of a COVID-19 vaccine were significantly associated with their vaccination intention. These findings imply that for vaccination intention and eventually vaccination decision to increase, people should be made aware of the benefits of availing the COVID-19 vaccine.
Having misconceptions about the vaccine strongly correlated with the study participants’ not getting vaccinated. This is corollary of their most frequently cited source of information which was Facebook where fake news abound [ 28 ]. Moreover, the moderate level of functional health literacy of the participants reflects the difficulties they may have in discerning false from true information. Thus, more effective and targeted information dissemination schemes are needed to address this situation.
People with long standing illness were not likely to get vaccinated against COVID 19. Vaccine hesitancy remains to be an issue among those with health problems. Reluctance is due to lack of understanding, fear of adverse effects, and negative COVID-19 Vaccination information [ 16 ]. In the Philippines, more than a quarter of those aged 35–59 years have been diagnosed with illnesses that predispose them to serious effects of COVID-19 [ 29 ]. With the community quarantine focusing more on these high-risk groups, they are more susceptible to such fear and reluctance.
The level of vaccine confidence among the participants is high. Those who indicated that the COVID-19 vaccines are safe and needed to protect one’s health were more likely to get vaccinated. The lowest confidence rating was related to the vaccine’s side effects, followed by doubt about its safety. Findings of similar studies in Japan and South Korea showed that the most cited reasons for low vaccine confidence were side effects and that vaccines had not been sufficiently tested [ 30 ]. The decline in the COVID19 vaccine confidence in the Philippines may have been influenced by the Dengvaxia vaccine fiasco in 2017. The controversy caused the vaccine confidence of Filipinos to decline from 93% to 2015 to 32% in 2018 [ 31 ]. Traumatic experiences concerning previous vaccination and information obtained from traditional, social media, and neighbors further contribute to delay and refusal of vaccination [ 32 ].
Those who have public health insurance are more likely to get vaccinated. Since the COVID-19 vaccination program for the whole Philippines is government-funded and controlled, those with public health insurance may be more familiar with the public health system and may be able to access the COVID-19 vaccination program.
The results of this study have implications for the public health approach to increasing COVID-19 vaccinations. Since the younger ones are more inclined to get vaccinated, they may serve as the conduit to reach the older ones, especially the hesitant people with chronic illnesses, as they are more at risk of contracting COVID-19. The government can increase the vaccination rate of older people by offering packages to incentivize young people taking their older parents for vaccination. Since the lines for vaccination are usually long, a young person together with a person aged more than 50 years old may be in the priority lane.
Results also indicate that the educated and those with higher awareness levels of COVID-19 are more likely to get vaccinated. This is consistent with the findings of previous studies [ 33 , 34 ]. Since the community quarantine is easing up and people can go out of their homes, information, education, and communication (IEC) materials should be designed for the less educated people and be situated in locations where these people frequent like the streets, bus stops, and the like. Around 72% of Filipinos have access to a smartphone [ 35 ] so the government can possibly tie up with telecommunications companies to spread crucial information through text messages about COVID-19 vaccination and correct false information from social media. This can be especially effective for those in the rural areas where information through the media may be harder to reach. Thus, for rural areas the IEC materials may be placed in locations and settings where people usually congregate, like in the market, plaza, municipal hall, and the like.
Study findings showed that participants actively sought for COVID-19 vaccination information from Facebook, TV, and family and friends almost every week. This result implies that there is a need for concerned officials to fill their Facebook pages and posts with information related to their respective COVID-19 vaccination programs. In this case, individuals who can acquire these pieces of information can share these with family and friends who seek the same from them.
The study should also provide an impetus for the government to provide the infrastructure and equipment for better vaccine deployment for COVID-19 and other potential disease outbreaks in the future. The US Agency for International Development pledged USD 315 million for cold chain facilities and mobile vaccination sites to reach far flung areas in the Philippines [ 36 ]. This is a short-term solution to address current needs; however, the government has to strategically plan and identify supply chain solutions at the national level such as providing roads, bridges, and basic infrastructure especially to underdeveloped areas.
This study’s results are comparable to the findings in countries near the Philippines. In Malaysia where the government also purchased their vaccines against COVID, about two-thirds of the respondents were willing to get vaccinated. They were those from the lower age group, those with higher education, females, and not having chronic disease. Moreover, the strongest drivers for their decision to get vaccinated were vaccine effectiveness and suggestions from their Ministry of Health [ 37 ]. In China on the other hand, those who were older, had a lower education level, lower income, higher trust in the vaccine and higher perceived risk of infection showed a higher probability to vaccinate [ 38 ]. There is a greater proportion of older people in China than in the Philippines or Malaysia which may explain the differing results in terms of age. There are also differences in literacy rate which may account for the different results. What is common among these countries is that the perceived effectiveness of the vaccine is the main driver for people to get vaccinated.
The present study was conducted in the second year after the start of the pandemic when the Philippines had gone through peaks of the COVID-19 infection that claimed thousands of lives. The vaccine seemed to be the only hope to avoid deaths. Moreover, people needed to work for their sustenance. Even those who were previously hesitant to get vaccinated, did so because it was required by their employers [ 20 ]. Thus, the proportion of those who got vaccinated is high. As the threat of COVID-19 waned with the increased herd immunity, there is a decreased uptake of the booster doses of the vaccine [ 39 ]. It is foreseen that there may be an eventual decline in the uptake of the biannual booster shots. Unless there is an effective campaign not only from the medical community but more importantly from the government, people will not take the succeeding doses of the vaccine. This study offers some directions in devising campaign strategies based on the factors influencing decision to vaccinate against COVID-19.
Limitations for this present study include using purposive sampling in recruiting participants instead of probability sampling because of the constraints brought about by the pandemic situation. The link to the survey was sent to contacts and institutions all over the country through electronic means. Researchers ensured that respondents came from all the 17 regions in the country, representing the different categories of the main variables of this study. There were difficulties in finding unvaccinated individuals as the proportion of the vaccinated went over 80% in the NCR. With the collaboration of enumerators from different regions, an adequate number of unvaccinated people were eventually included in the study, approximating the proportions in the regional levels. Potential bias in the collection of data by enumerators from various regions may have happened but this was minimized with the proper orientation of the enumerators.
Online questionnaires naturally are accessible by those with the appropriate gadgets and internet access, thus potentially limiting the inclusion of those with low resources. To mitigate this, the researchers offered to refund the internet fees incurred by respondents. Moreover, the enumerators aided those who were old, illiterate, and without gadgets to record their responses on their own devices. Thus, there were some respondents from these categories who were able to participate in this study.
Based on the findings of the study, it can be concluded that among Filipino adults, COVID-19 vaccination decision is determined by their age, educational attainment, health insurance, and employer requirement. Further, it can be concluded that a high awareness of the disease and a high level of vaccine confidence correlates with the decision to get vaccinated.
Accessing the true information about the disease and vaccine is key in reaching the decision to get vaccinated. It also contributes to high levels of vaccine confidence. Thus, effective information dissemination schemes targeted according to the socio-demographic profile, health literacy and sources of information of the intended audience will result in better vaccine uptake.
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Department of Health. The PhilippineNational Deployment and Vaccination January 2021. https://doh.gov.ph/sites/default/files/basic-page/The%20Philippine%20National%20COVID-19%20Vaccination%20Deployment%20Plan.pdf . Accessed 25 December 2022.
Sallam M. COVID-19 Vaccine Hesitancy Worldwide: a concise systematic review of Vaccine Acceptance Rates. Vaccines. 2021;9(2):160.
Article CAS PubMed PubMed Central Google Scholar
MacDonald NE. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–4.
Article PubMed Google Scholar
Berdida DJE, Grande RAN, Lopez V. Filipinos’ health information-seeking behaviors and their implications for COVID-19 vaccination. Public Health Nurs. 2022;39(3):553–61.
UNDP. Trends in COVID-19 vaccine acceptance in the Philippines and their implications on health communication. Philippines; 2021.
Reyes M, Dee EC, Ho BL. Vaccination in the Philippines: experiences from history and lessons for the future. Hum Vaccin Immunother. 2021;17(6):1873–6.
Bujang MA, Sa’at N, Sidik T, Joo LC. Sample size guidelines for logistic regression from Observational Studies with large Population: emphasis on the Accuracy between Statistics and Parameters based on Real Life Clinical Data. Malays J Med Sci. 2018;25(4):122–30.
PubMed PubMed Central Google Scholar
World Health Organization. Philippines Coronavirus disease (COVID-19) Situation Report #98, 28 March 2022 Apr 4., 2022. https://reliefweb.int/report/philippines/philippines-coronavirus-disease-covid-19-situation-report-98-28-march-2022 . Accessed 21 December 2022.
Department of Health. Vaccines Administered in the Philippines as of March 2., 2022. https://caro.doh.gov.ph/vaccines-administered-in-the-philippines-as-of-march-2-2022/ . Accessed 21 December 2022.
Head KJ, Kasting ML, Sturm LA, Hartsock JA, Zimet GD. A National Survey assessing SARS-CoV-2 vaccination intentions: implications for Future Public Health Communication efforts. Sci Commun. 2020;42(5):698–723.
Article PubMed Central Google Scholar
Biasio LR, Bonaccorsi G, Lorini C, Pecorelli S. Assessing COVID-19 vaccine literacy: a preliminary online survey. Hum Vaccines Immunotherapeutics. 2021;17(5):1304–12.
Article CAS Google Scholar
Gilkey MB, Magnus BE, Reiter PL, McRee A-L, Dempsey AF, Brewer NT. The vaccination confidence scale: a brief measure of parents’ vaccination beliefs. Vaccine. 2014;32(47):6259–65.
Article PubMed PubMed Central Google Scholar
Bermejo-Martins E, Luis EO, Sarrionandia A, Martínez M, Garcés MS, Oliveros EY et al. Different Responses to Stress, Health Practices, and Self-Care during COVID-19 Lockdown: A Stratified Analysis. Int J Environ Res Public Health. 2021;18(5).
Marzo R, Sami W, Alam M, Acharya S, Jermsittiparsert K, Songwathana K, et al. Hesitancy in COVID-19 vaccine uptake and its associated factors among the general adult population: a cross-sectional study in six southeast asian countries. Tropical Medicine and Health; 2022.
Aben E. Philippines struggles to vaccinate elderly as few turn up for COVID-19 jabs. Arab News. 2022. https://www.arabnews.com/node/2041226/world . Accessed 11 June 2022.
Montemayor T. 2.4 M senior citizens still unvaxxed vs. Covid-19: NVOC. Philippine News Agency. 2022. https://www.pna.gov.ph/articles/1168191 . Accessed 11 June 2022.
de Figueiredo A, Simas C, Karafillakis E, Paterson P, Larson HJ. Mapping global trends in vaccine confidence and investigating barriers to vaccine uptake: a large-scale retrospective temporal modelling study. The Lancet. 2020;396(10255):898–908.
Article Google Scholar
Galanis P, Vraka I, Siskou O, Konstantakopoulou O, Katsiroumpa A, Moisoglou I et al. Cross-sectional assessment of predictors for COVID-19 vaccine uptake: an online survey in Greece. Vacunas. 2022.
Jiang N, Gu P, Liu K, Song N, Jiang X. Acceptance of COVID-19 vaccines among college students: a study of the attitudes, knowledge, and willingness of students to vaccinate. Hum Vaccines Immunotherapeutics. 2021;17(12):4914–24.
Lema K, Sanjeev M, editors. Philippines to require vaccination for employees working on-site. [Internet]. 2021. https://www.reuters.com/world/asia-pacific/philippines-require-vaccination-employees-working-on-site-2021-11-12/ . Accessed 1 September 2022.
Patinio F. Work options for unvaxxed workers up to employers: DOLE. Philippine News Agency. 2021. https://www.pna.gov.ph/articles/1160519 . Accessed 10 June 2022.
Nieva J, Romulo F, Robles YR, Benosa C, Aileen C, Faraon A, Rosendo G. Strengthening Provincial Supply Chain Management Capacity for COVID-19 Vaccines. In: Governance DJMRIo, editor. Policy Brief2021.
Kabagani LJ. PH rises above challenges in Covid-19 vax rollout Manila. Philippine News Agency; 2022. https://www.pna.gov.ph/articles/1166135 .
Shareef L, Fawzi Al-Hussainy A, Majeed Hameed S. COVID-19 vaccination hesitancy among Iraqi general population between beliefs and barriers: An observational study [version 2; peer review: 2 approved]. F1000Research. 2022;11(334).
Islam MS, Kamal A-HM, Kabir A, Southern DL, Khan SH, Hasan SMM, et al. COVID-19 vaccine rumors and conspiracy theories: the need for cognitive inoculation against misinformation to improve vaccine adherence. PLoS ONE. 2021;16(5):e0251605.
Wei-Haas M. Why we shouldn’t panic about the millions who missed their second vaccine dose—yet. National Geographic - Science [Internet]. 2021. Available from: https://www.nationalgeographic.com/science/article/why-we-shouldnt-panic-about-the-millions-who-missed-their-second-vaccine-dose-yet . Accessed 18 December 2022.
Nomura S, Eguchi A, Yoneoka D, Kawashima T, Tanoue Y, Murakami M, et al. Reasons for being unsure or unwilling regarding intention to take COVID-19 vaccine among japanese people: a large cross-sectional national survey. Lancet Reg Health - Western Pac. 2021;14:100223.
Guess A, Nagler J, Tucker J. Less than you think: prevalence and predictors of fake news dissemination on Facebook. Sci Adv. 2019;5(1):eaau4586.
Abalos JB. Prevalence of chronic diseases associated with increased risk of severe COVID-19 in the Philippines. N-IUSSP. 2020 November 9, 2020.
Mahase E. Covid-19: UK has highest vaccine confidence and Japan and South Korea the lowest, survey finds. BMJ (Clinical research ed). 2021;373:n1439.
PubMed Google Scholar
Mendoza RU, Dayrit MM, Alfonso CR, Ong MMA. Public trust and the COVID-19 vaccination campaign: lessons from the Philippines as it emerges from the Dengvaxia controversy. Int J Health Plann Manag. 2021;36(6):2048–55.
Landicho-Guevarra J, Reñosa MDC, Wachinger J, Endoma V, Aligato MF, Bravo TA, et al. Scared, powerless, insulted and embarrassed: hesitancy towards vaccines among caregivers in Cavite Province, the Philippines. BMJ Global Health. 2021;6(9):e006529.
Di Giuseppe G, Pelullo CP, Lanzano R, Lombardi C, Nese G, Pavia M. COVID-19 Vaccination Uptake and Related Determinants in Detained Subjects in Italy. Vaccines (Basel). 2022;10(5).
Biswas N, Mustapha T, Khubchandani J, Price JH. The Nature and Extent of COVID-19 vaccination hesitancy in Healthcare Workers. J Community Health. 2021;46(6):1244–51.
Statista. Mobile phone internet user penetration in the Philippines from 2017 to 2025. 2021.
Calonzo A. After supply, logistics emerges as biggest threat to vaccination programs. Business Standard 2022. https://www.business-standard.com/article/current-affairs/after-supply-logistics-emerges-as-biggest-threat-to-vaccination-programs-122011900257_1.html . Accessed 19 December 2022.
Mohamed NA, Solehan HM, Mohd Rani MD, Ithnin M, Che Isahak CI. Knowledge, acceptance and perception on COVID-19 vaccine among Malaysians: a web-based survey. PLoS ONE. 2021;16(8):e0256110.
Leng A, Maitland E, Wang S, Nicholas S, Liu R, Wang J. Individual preferences for COVID-19 vaccination in China. Vaccine. 2021;39(2):247–54.
Article CAS PubMed Google Scholar
Number of coronavirus (COVID. -19) vaccine doses administered in the Philippines as of December 13, 2022. Statistica. 2022. https://www.statista.com/statistics/1236727/philippines-coronavirus-covid19-vaccine-rollout/ Accessed 19 Dec 2022.
Download references
Acknowledgements
The researchers are grateful to all the enumerators from the different regions of the Philippines in effectively collecting data from the respondents.
The publication of this paper is funded by the De La Salle University Manila and the Engineering Research and Development for Technology (ERDT) of the Philippine government. The research was partially funded by Cavite State University.
Author information
Authors and affiliations.
Technology Transfer and Business Development office, University of the Philippines Manila, Manila, Philippines
Lourdes Marie Sequerra Tejero
Industrial and Systems Engineering, De La Salle University, Manila, Philippines
Rosemary Ruiz Seva
College of Arts and Sciences, Cavite State University, Indang, Cavite, Philippines
Bettina Joyce Petelo Ilagan
Lyceum of the Philippines University Manila, Manila, Philippines
Kattleea Lorezca Almajose
You can also search for this author in PubMed Google Scholar
Contributions
LMST, RRS and BJPI conceptualized and wrote the protocol of the research. KLA, BJPI, LMST, RRS collected data. RRS and LMST statistically analyzed the data. LMST, RRS, BJPI, KLA wrote the article, reviewed and edited the final manuscript.
Corresponding author
Correspondence to Lourdes Marie Sequerra Tejero .
Ethics declarations
Ethics approval and consent to participate.
All methods were carried out in accordance with relevant guidelines and regulations. A survey questionnaire was used for data collection, wherein the identity of the respondent remained anonymous. As such, a formal informed consent was not necessary since the act of answering the questionnaire expressed consent from the participant. The study protocol, research tool, including the ‘waiver of informed consent documentation’ were reviewed and approved by the University of the Philippines Manila’s Review Ethics Board, with code UPMREB 2021-0673-01. Since all participants were 18 years old and above, they did not need the consent of a guardian. An introductory letter at the beginning of the questionnaire provided the participant about the necessary information regarding the study like the research objectives, benefits to the participant, anonymity, expected time for their participation, utilization of data gathered, contact information of the researchers, etc. Thus, the privacy and autonomy of the participant were ensured, as well as respect of the rights of the individual. The letter likewise indicated that participation is voluntary and continuing to answer the survey is an expression of consent . (Please see ‘waiver of informed consent documentation’ in #13 under the section ‘ETHICAL GUIDELINES FOR EPIDEMIOLOGIC RESEARCH’ in the National Ethical Guidelines located through this link: http://49.231.15.21/deptw13/upload/files/hercF256312041721022781.pdf ).
Consent for publication
Not applicable.
Competing interest
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Tejero, L.M.S., Seva, R., Petelo Ilagan, B. et al. Determinants of COVID-19 vaccination decision among Filipino adults. BMC Public Health 23 , 851 (2023). https://doi.org/10.1186/s12889-023-15712-w
Download citation
Received : 10 September 2022
Accepted : 19 April 2023
Published : 10 May 2023
DOI : https://doi.org/10.1186/s12889-023-15712-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Vaccination
- Logistic regression
- Vaccine acceptance

BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
ORIGINAL RESEARCH article
Impact of the covid-19 pandemic on physical and mental health in lower and upper middle-income asian countries: a comparison between the philippines and china.

- 1 College of Medicine, University of the Philippines Manila, Manila, Philippines
- 2 Faculty of Education, Institute of Cognitive Neuroscience, Huaibei Normal University, Huaibei, China
- 3 Department of Psychological Medicine, Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore
- 4 Southeast Asia One Health University Network, Chiang Mai, Thailand
- 5 Department of Psychological Medicine, National University Health System, Singapore, Singapore
- 6 Institute of Health Innovation and Technology (iHealthtech), National University of Singapore, Singapore, Singapore
Objective: The differences between the physical and mental health of people living in a lower-middle-income country (LMIC) and upper-middle-income country (UMIC) during the COVID-19 pandemic was unknown. This study aimed to compare the levels of psychological impact and mental health between people from the Philippines (LMIC) and China (UMIC) and correlate mental health parameters with variables relating to physical symptoms and knowledge about COVID-19.
Methods: The survey collected information on demographic data, physical symptoms, contact history, and knowledge about COVID-19. The psychological impact was assessed using the Impact of Event Scale-Revised (IES-R), and mental health status was assessed by the Depression, Anxiety, and Stress Scale (DASS-21).
Findings: The study population included 849 participants from 71 cities in the Philippines and 861 participants from 159 cities in China. Filipino (LMIC) respondents reported significantly higher levels of depression, anxiety, and stress than Chinese (UMIC) during the COVID-19 ( p < 0.01) while only Chinese respondents' IES-R scores were above the cut-off for PTSD symptoms. Filipino respondents were more likely to report physical symptoms resembling COVID-19 infection ( p < 0.05), recent use of but with lower confidence on medical services ( p < 0.01), recent direct and indirect contact with COVID ( p < 0.01), concerns about family members contracting COVID-19 ( p < 0.001), dissatisfaction with health information ( p < 0.001). In contrast, Chinese respondents requested more health information about COVID-19. For the Philippines, student status, low confidence in doctors, dissatisfaction with health information, long daily duration spent on health information, worries about family members contracting COVID-19, ostracization, and unnecessary worries about COVID-19 were associated with adverse mental health. Physical symptoms and poor self-rated health were associated with adverse mental health in both countries ( p < 0.05).
Conclusion: The findings of this study suggest the need for widely available COVID-19 testing in MIC to alleviate the adverse mental health in people who present with symptoms. A health education and literacy campaign is required in the Philippines to enhance the satisfaction of health information.
Introduction
The World Health Organization (WHO) declared coronavirus disease 2019 (COVID-19) to be a Public Health Emergency of International Concern on January 30 ( 1 ) and a pandemic on March 11, 2020 ( 2 ). COVID-19 predominantly presents with respiratory symptoms (cough, sneezing, and sore throat), along with fever, fatigue and myalgia. It is thought to spread through droplets, contaminated surfaces, and asymptomatic individuals ( 3 ). By the end of April, over 3 million people have been infected globally ( 4 ).
The first country to identify the novel virus as the cause of the pandemic was China. The authorities responded with unprecedented restrictions on movement. The response included stopping public transport before Chinese New Year, an annual event that sees workers' mass emigration to their hometowns, and a lockdown of whole cities and regions ( 1 ). Two new hospitals specifically designed for COVID-19 patients were rapidly built in Wuhan. Such measures help slow the transmission of COVID-19 in China. As of May 2, there are 83,959 confirmed cases and 4,637 deaths from the virus in China ( 4 ). The Philippines was also affected early by the current crisis. The first case was suspected on January 22, and the country reported the first death from COVID-19 outside of mainland China ( 5 ). Similar to China, the Philippines implemented lockdowns in Manila. Other measures included the closure of schools and allowing arrests for non-compliance with measures ( 6 ). At the beginning of May, the Philippines recorded 8,772 cases and 579 deaths ( 4 ).
China was one of the more severely affected countries in Asia in the early stage of pandemic ( 7 ) while the Philippines is still experiencing an upward trend in the COVID-19 cases ( 6 ). The gross national income (GNI) per capita of the Philippines and China are USD 3,830 and 9,460, respectively, were classified with lower (LMIC) and upper-middle-income countries (UMIC) by the Worldbank ( 8 ). During the COVID-19 pandemic, five high-income countries (HIC), including the United States, Italy, the United Kingdom, Spain, and France, account for 70% of global deaths ( 9 ). The HIC faced the following challenges: (1) the lack of personal protection equipment (PPE) for healthcare workers; (2) the delay in response strategy; (3) an overstretched healthcare system with the shortage of hospital beds, and (4) a large number of death cases from nursing homes ( 10 ). The COVID-19 crisis threatens to hit lower and middle-income countries due to lockdown excessively and economic recession ( 11 ). A systematic review on mental health in LMIC in Asia and Africa found that LMIC: (1) do not have enough mental health professionals; (2) the negative economic impact led to an exacerbation of mental issues; (3) there was a scarcity of COVID-19 related mental health research in Asian LMIC ( 12 ). This systematic review could not compare participants from different middle-income countries because each study used different questionnaires. During the previous Severe Acute Respiratory Syndrome (SARS) epidemic, the promotion of protective personal health practices to reduce transmission of the SARS virus was found to reduce the anxiety levels in the community ( 13 ).
Before COVID-19, previous studies found that stress might be a modifiable risk factor for depression in LMICs ( 14 ) and UMICs ( 15 – 17 ). Another study involving thirty countries found that unmodifiable risk factors for depression included female gender, and depression became more common in 2004 to 2014 compared to previous periods ( 18 ). Further, there were cultural differences in terms of patient-doctor relationship and attitudes toward healthcare systems before the COVID-19 pandemic. In China, <20% of the general public and medical professionals view the doctor and patient relationship as harmonious ( 19 ). In contrast, Filipino seemed to have more trust and be compliant to doctors' recommendations ( 20 ). Patient satisfaction was more important than hospital quality improvement to maintain patient loyalty to the Chinese healthcare system ( 21 ). For Filipinos, improvement in the quality of healthcare service was found to improve patients' satisfaction ( 22 ).
Based on the above studies, we have the following research questions: (1) whether COVID-19 pandemic could be an important stressor and risk factor for depression for the people living in LMIC and UMIC ( 23 ), (2) Are physical symptoms that resemble COVID-19 infection and other concerns be risk factors for adverse mental health? (3) Are knowledge of COVID-19 and health information protective factors for mental health? (4) Would there be any cultural differences in attitudes toward doctors and healthcare systems during the pandemic between China and the Philippines? We hypothesized that UMIC (China) would have better physical and mental health than LMIC (the Philippines). The aims of this study were (a) to compare the physical and mental health between citizens from an LMIC (the Philippines) and UMIC (China); (b) to correlate psychological impact, depression, anxiety, and stress scores with variables relating to physical symptoms, knowledge, and concerns about COVID-19 in people living in the Philippines (LMIC) and China (UMIC).
Study Design and Study Population
We conducted a cross-cultural and quantitative study to compare Filipinos' physical and mental health with Chinese during the COVID-19 pandemic. The study was conducted from February 28 to March 1 in China and March 28 to April 7, 2020 in the Philippines, when the number of COVID-19 daily reported cases increased in both countries. The Chinese participants were recruited from 159 cities and 27 provinces. The Filipino participants, on the other hand, were recruited from 71 cities and 40 provinces representing the Luzon, Visayas, and Mindanao archipelago. A respondent-driven recruitment strategy was utilized in both countries. The recruitment started with a set of initial respondents who were associated with the Huaibei Normal University of China and the University of the Philippines Manila; who referred other participants by email and social network; these in turn refer other participants across different cities in China and the Philippines.
As both Chinese and Filipino governments recommended that the public minimize face-to-face interaction and isolate themselves during the study period, new respondents were electronically invited by existing study respondents. The respondents completed the questionnaires through an online survey platform (“SurveyStar,” Changsha Ranxing Science and Technology in China and Survey Monkey Online Survey in the Philippines). The Institutional Review Board of the University of Philippines Manila Research Ethics Board (UPMREB 2020-198-01) and Huaibei Normal University (China) approved the research proposal (HBU-IRB-2020-002). All respondents provided informed or implied consent. The collected data were anonymous and treated as confidential.
This study used the National University of Singapore COVID-19 questionnaire, and its psychometric properties had been established in the initial phase of the COVID-19 epidemic ( 24 ). The National University of Singapore COVID-19 questionnaire consisted of questions that covered several areas: (1) demographic data; (2) physical symptoms related to COVID-19 in the past 14 days; (3) contact history with COVID-19 in the past 14 days; and (4) knowledge and concerns about COVID-19.
Demographic data about age, gender, education, household size, marital status, parental status, and residential city in the past 14 days were collected. Physical symptoms related to COVID-19 included breathing difficulty, chills, coryza, cough, dizziness, fever, headache, myalgia, sore throat, nausea, vomiting, and diarrhea. Respondents also rated their physical health status and stated their history of chronic medical illness. In the past 14 days, health service utilization variables included consultation with a doctor in the clinic, being quarantined by the health authority, recent testing for COVID-19 and medical insurance coverage. Knowledge and concerns related to COVID-19 included knowledge about the routes of transmission, level of confidence in diagnosis, source, and level of satisfaction of health information about COVID-19, the likelihood of contracting and surviving COVID-19 and the number of hours spent on viewing information about COVID-19 per day.
The psychological impact of COVID-19 was measured using the Impact of Event Scale-Revised (IES-R). The IES-R is a self-administered questionnaire that has been well-validated in the European and Asian population for determining the extent of psychological impact after exposure to a traumatic event (i.e., the COVID-19 pandemic) within one week of exposure ( 25 , 26 ). This 22-item questionnaire, composed of three subscales, aims to measure the mean avoidance, intrusion, and hyperarousal ( 27 ). The total IES-R score is divided into 0–23 (normal), 24–32 (mild psychological impact), 33–36 (moderate psychological impact) and >37 (severe psychological impact) ( 28 ). The total IES-R score > 24 suggests the presence of post-traumatic stress disorder (PTSD) symptoms ( 29 ).
The respondents' mental health status was measured using the Depression, Anxiety, and Stress Scale (DASS-21) and the calculation of scores was based on a previous Asian study ( 30 ). DASS has been demonstrated to be a reliable and valid measure in assessing mental health in Filipinos ( 31 – 33 ) and Chinese ( 34 , 35 ). IES-R and DASS-21 were previously used in research related to the COVID-19 epidemic ( 26 , 36 – 38 ).
Statistical Analysis
Descriptive statistics were calculated for demographic characteristics, physical symptom, and health service utilization variables, contact history variables, knowledge and concern variables, precautionary measure variables, and additional health information variables. To analyze the differences in the levels of psychological impact, levels of depression, anxiety and stress, the independent sample t -test was used to compare the mean score between the Filipino (LMIC) and Chinese (UMIC) respondents. The chi-squared test was used to analyze the differences in categorical variables between the two samples. We used linear regressions to calculate the univariate associations between independent and dependent variables, including the IES-S score and DASS stress, anxiety, and depression subscale scores for the Filipino and Chinese respondents separately with adjustment for age, marital status, and education levels. All tests were two-tailed, with a significance level of p < 0.05. Statistical analysis was performed on SPSS Statistic 21.0.
Demographic Characteristics and Their Association With Psychological Impact and Adverse Mental Health Status
We received 849 responses from the Philippines and 861 responses from China for 1,710 individual respondents from both countries. The majority of Filipino respondents were women (71.0%), age between 22 and 30 years (26.6%), having a household size of 3–5 people (53.4%), high educational attainment (91.4% with a bachelor or higher degree), and married (68.9%). Similarly, the majority of Chinese respondents were women (75%), having a household size of 3–5 people (80.4%) and high educational attainment (91.4% with a bachelor or higher degree). There was a significantly higher proportion of Chinese respondents who had children younger than 16 years ( p < 0.001) and student status ( p < 0.001; See Table 1 ).
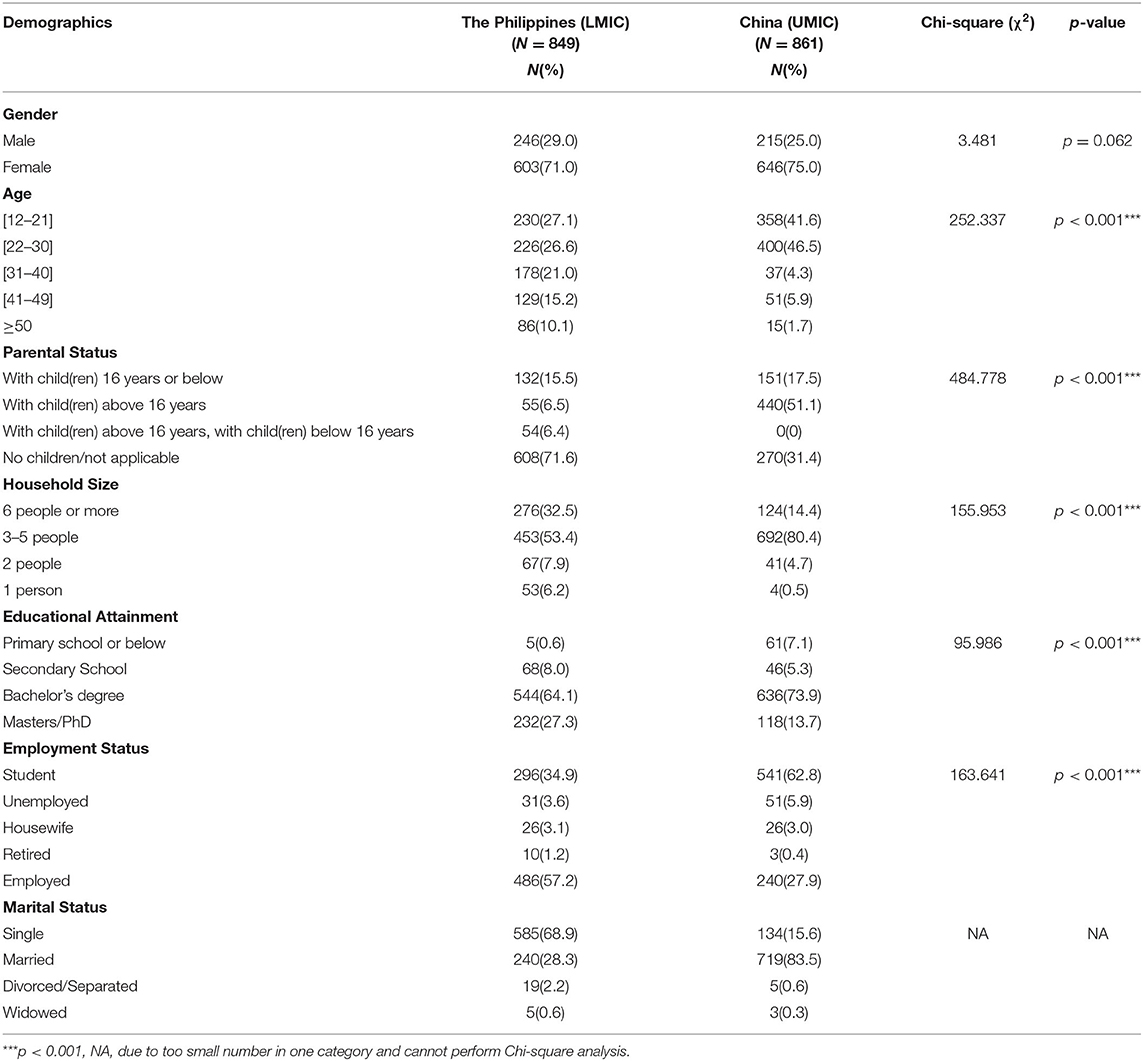
Table 1 . Comparison of demographic characteristics between Filipino (LMIC) and Chinese (UMIC) respondents ( N = 1,710).
For Filipino respondents, the male gender and having a child were protective factors significantly associated with the lower score of IES-R ( p < 0.05) and depression ( p < 0.001), respectively. Single status was significantly associated with depression ( p < 0.05), and student status was associated with higher IES-R, stress and depression scores ( p < 0.01) (see Table 2 ). For Chinese respondents, the male gender was significantly associated with a lower score of IES-R but higher DASS depression scores ( p < 0.01). Notwithstanding, there were other differences between Filipino and China respondents. Chinese respondents who stayed in a household with 3–5 people ( p < 0.05) and more than 6 people ( p < 0.05) were significantly associated with a higher score of IES-R as compared to respondents who stayed alone.
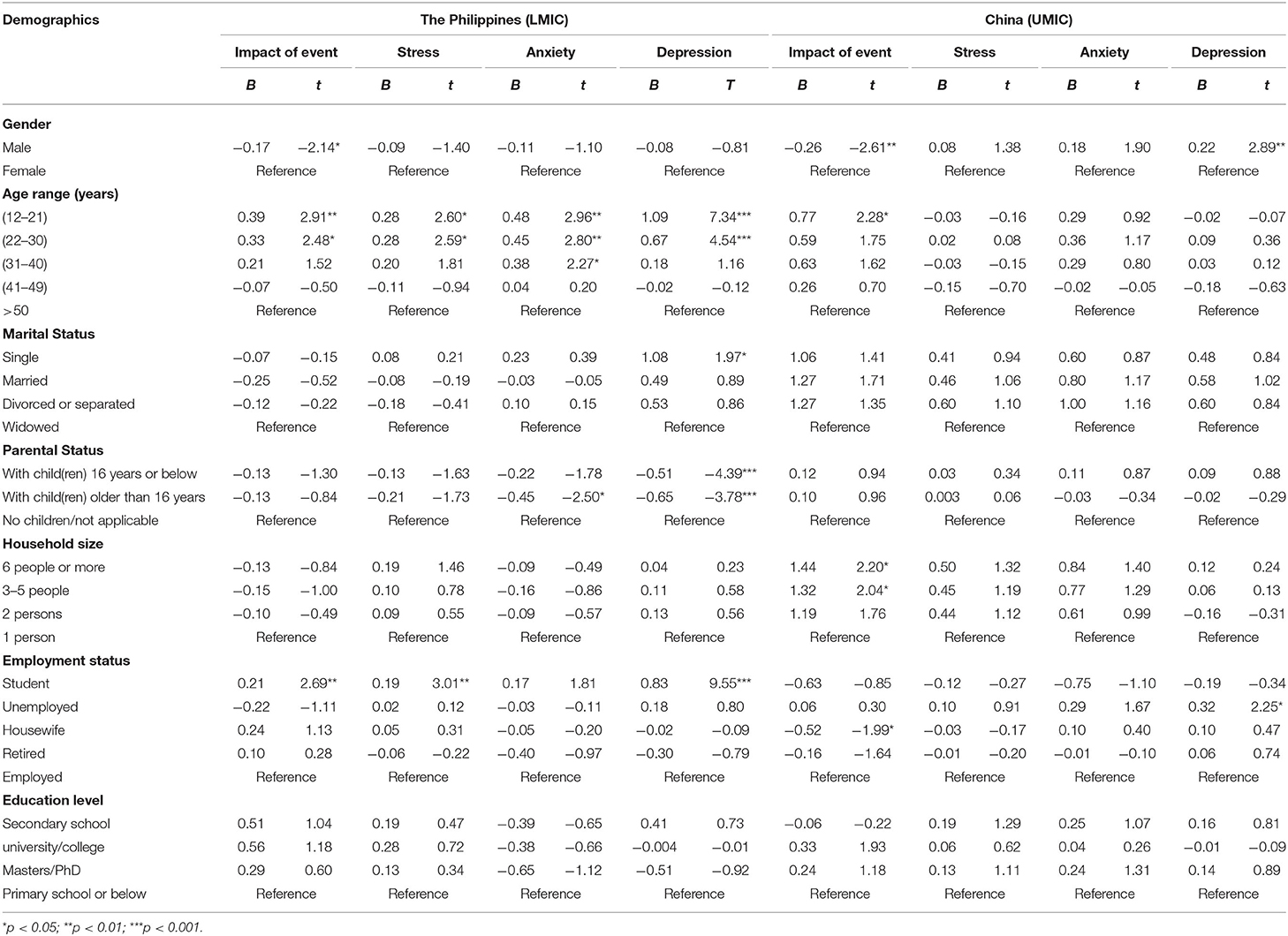
Table 2 . Comparison of the association between demographic variables and the psychological impact as well as adverse mental health status between Filipino (LMIC) and Chinese (UMIC) respondents ( n = 1,710).
Comparison Between the Filipino (LMIC) and Chinese (UMIC) Respondents and Their Mental Health Status
Figure 1 compares the mean scores of DASS-stress, anxiety, and depression subscales and IES-R scores between the Filipino and Chinese respondents. For the DASS-stress subscale, Filipino respondents reported significantly higher stress ( p < 0.001), anxiety ( p < 0.01), and depression ( p < 0.01) than Chinese (UMIC). For IES-R, Filipino (LMIC) had significantly lower scores than Chinese ( p < 0.001). The mean IES-R scores of Chinese were higher than 24 points, indicating the presence of PTSD symptoms in Chinese respondents only.
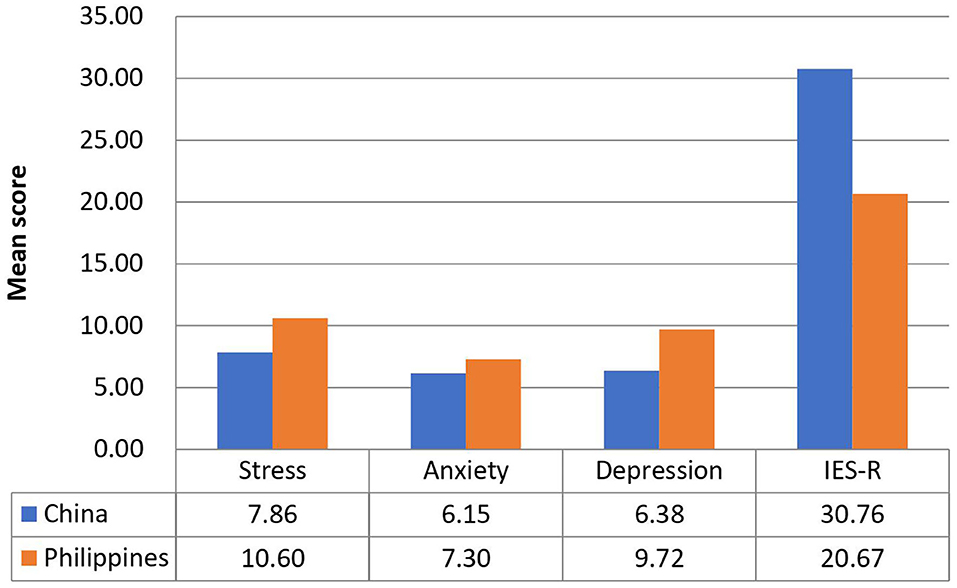
Figure 1 . Comparison of the mean scores of DASS-stress, anxiety and depression subscales, and IES-R scores between Filipino and Chinese respondents.
Physical Symptoms, Health Status, and Its Association With Psychological Impact and Adverse Mental Health Status
There were significant differences between Filipino (LMIC) and Chinese (UMIC) respondents regarding physical symptoms resembling COVID-19 and health status. There was a significantly higher proportion of Filipino respondents who reported headache ( p < 0.001), myalgia ( p < 0.001), cough ( p < 0.001), breathing difficulty ( p < 0.001), dizziness ( p < 0.05), coryza ( p < 0.001), sore throat ( p < 0.001), nausea and vomiting ( p < 0.001), recent consultation with a doctor ( p < 0.01), recent hospitalization ( p < 0.001), chronic illness ( p < 0.001), direct ( p < 0.001), and indirect ( p < 0.001) contact with a confirmed diagnosis of COVID-19 as compared to Chinese (see Supplementary Table 1 ). Significantly more Chinese respondents were under quarantine ( p < 0.001).
Linear regression showed that headache, myalgia, cough, dizziness, coryza as well as poor self-rated physical health were significantly associated with higher IES-R scores, DASS-21 stress, anxiety, and depression subscale scores in both countries after adjustment for confounding factors ( p < 0.05; see Table 3 ). Furthermore, breathing difficulty, sore throat, and gastrointestinal symptoms were significantly associated with higher DASS-21 stress, anxiety and depression subscale scores in both countries ( p < 0.05). Chills were significantly associated with higher DASS-21 stress and depression scores ( p < 0.01) in both countries. Recent quarantine was associated with higher DASS-21 subscale scores in Chinese respondents only ( p < 0.05).
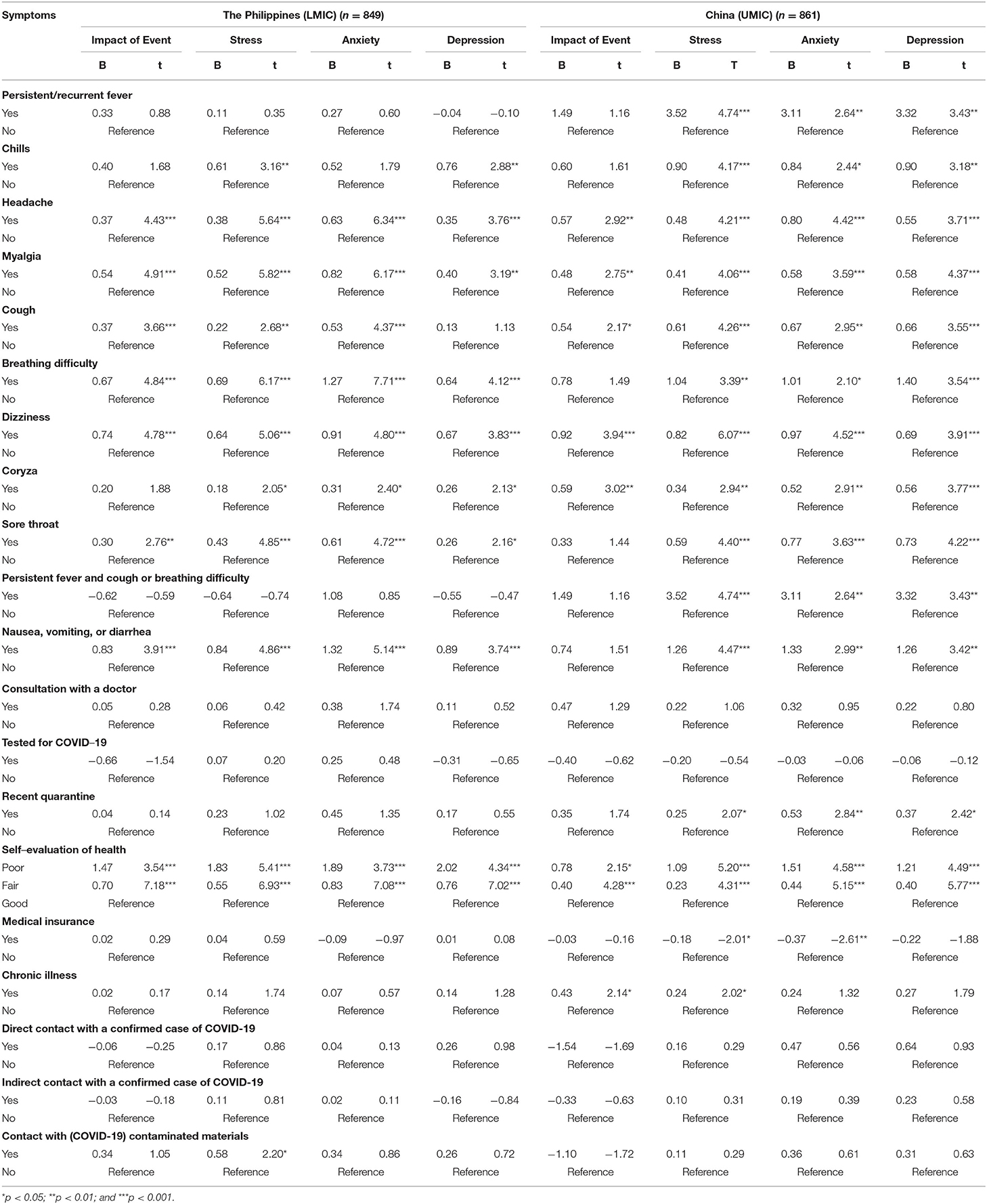
Table 3 . Association between physical health status and contact history and the perceived impact of COVID-19 outbreak as well as adverse mental health status during the epidemic after adjustment for age, gender, and marital status ( n = 1,710).
Perception, Knowledge, and Concerns About COVID-19 and Its Association With Psychological Impact and Adverse Mental Health Status
Filipino (LMIC) and Chinese (UMIC) respondents held significantly different perceptions in terms of knowledge and concerns related to COVID-19 (see Supplementary Table 2 ). For the routes of transmission, there were significantly more Filipino respondents who agreed that droplets transmitted the COVID-19 ( p < 0.001) and contact via contaminated objects ( p < 0.001), but significantly more Chinese agreed with the airborne transmission ( p < 0.001). For the detection and risk of contracting COVID-19, there were significantly more Filipino who were not confident about their doctor's ability to diagnose COVID-19 ( p < 0.001). There were significantly more Filipino respondents who were worried about their family members contracting COVID-19 ( p < 0.001). For health information, there were significantly more Filipino who were unsatisfied with the amount of health information ( p < 0.001) and spent more than three hours per day on the news related to COVID-19 ( p < 0.001). There were significantly more Chinese respondents who felt ostracized by other countries ( p < 0.001).
Linear regression analysis after adjustment of confounding factors showed that the Filipino and Chinese respondents showed different findings (see Table 4 ). Chinese respondents who reported a very low perceived likelihood of contracting COVID-19 were significantly associated with lower DASS depression scores ( p < 0.05). There were similarities between the two countries. Filipino and Chinese respondents who perceived a very high likelihood of survival were significantly associated with lower DASS-21 depression scores ( p < 0.05). Regarding the level of confidence in the doctor's ability to diagnose COVID-19, both Filipino and Chinese respondents who were very confident in their doctors were significantly associated with lower DASS-21 depression scores ( p < 0.01). Filipino and Chinese respondents who were satisfied with health information were significantly associated with lower DASS-21 anxiety and depression scores ( p < 0.01). Chinese and Filipino respondents who were worried about their family members contracting COVID-19 were associated with higher IES-R and DASS-21 subscale scores ( p < 0.05). In contrast, only Filipino respondents who spent <1 h per day monitoring COVID-19 information was significantly associated with lower IES-R and DASS-21 stress and anxiety scores ( p < 0.05). Filipino respondents who felt ostracized were associated with higher IES-R and stress scores ( p < 0.05).
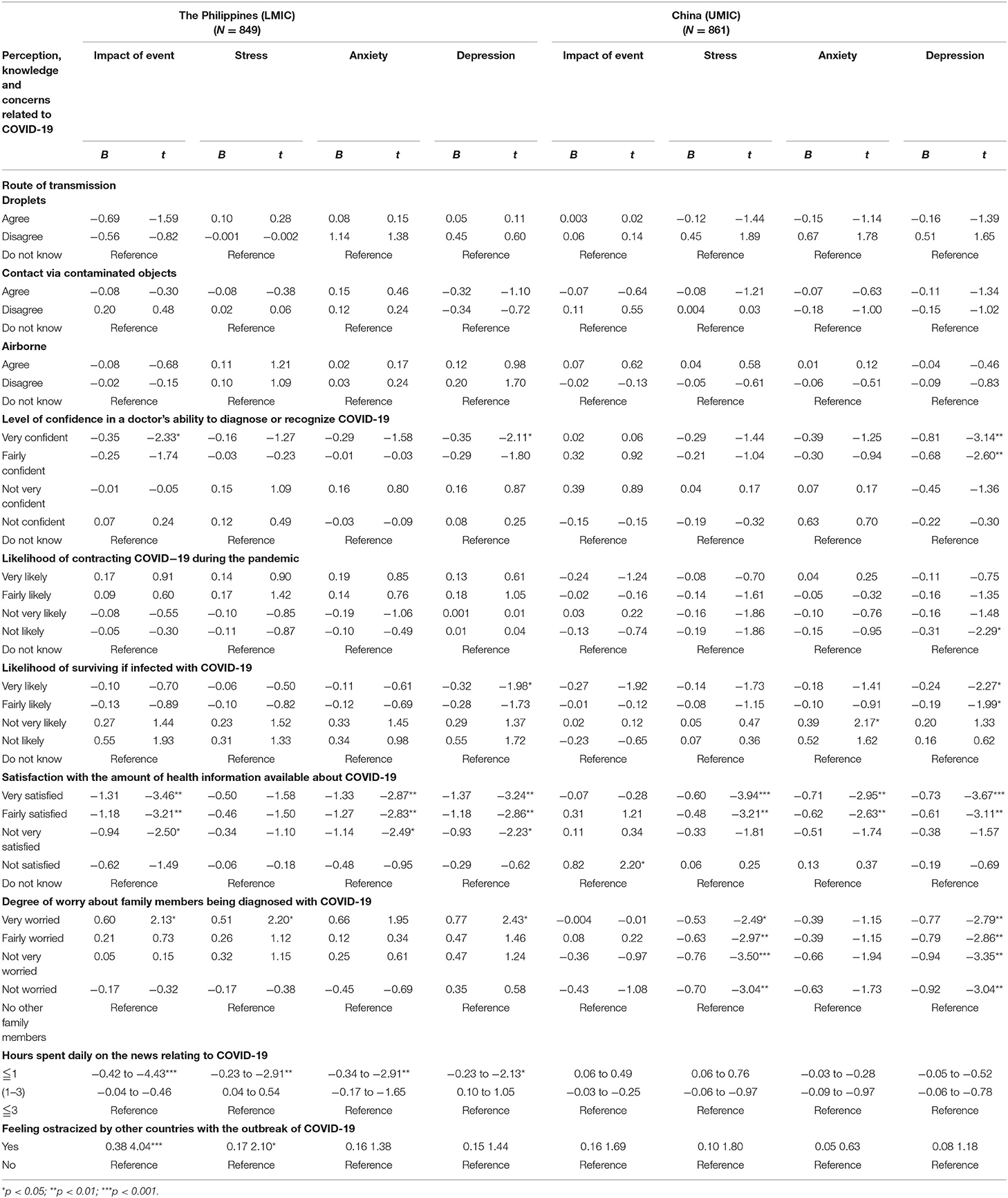
Table 4 . Comparison of association of knowledge and concerns related to COVID-19 with mental health status after adjustment for age, gender, and marital status ( N = 1,710).
Health Information About COVID-19 and Its Association With Psychological Impact and Adverse Mental Health Status
Filipino (LMIC) and Chinese (UMIC) respondents held significantly different views on the information required about COVID-19. There were significantly more Chinese respondents who needed information on the symptoms related to COVID-19, prevention methods, management and treatment methods, regular information updates, more personalized information, the effectiveness of drugs and vaccines, number of infected by geographical locations, travel advice and transmission methods as compared to Filipino ( p < 0.01; See Supplementary Table 3 ). In contrast, there were significantly more Filipino respondents who needed information on other countries' strategies and responses than Chinese ( p < 0.001).
Information on management methods and transmission methods were significantly associated with higher IES-R scores in Chinese respondents ( p < 0.05; see Table 5 ). Travel advice, local transmission data, and other countries' responses were significantly associated with lower DASS-21 stress and depression scores in Chinese respondents only ( p < 0.05). There was only one significant association observed in Filipino respondents; information on transmission methods was significantly associated with lower DASS-21 depression scores ( p < 0.05).
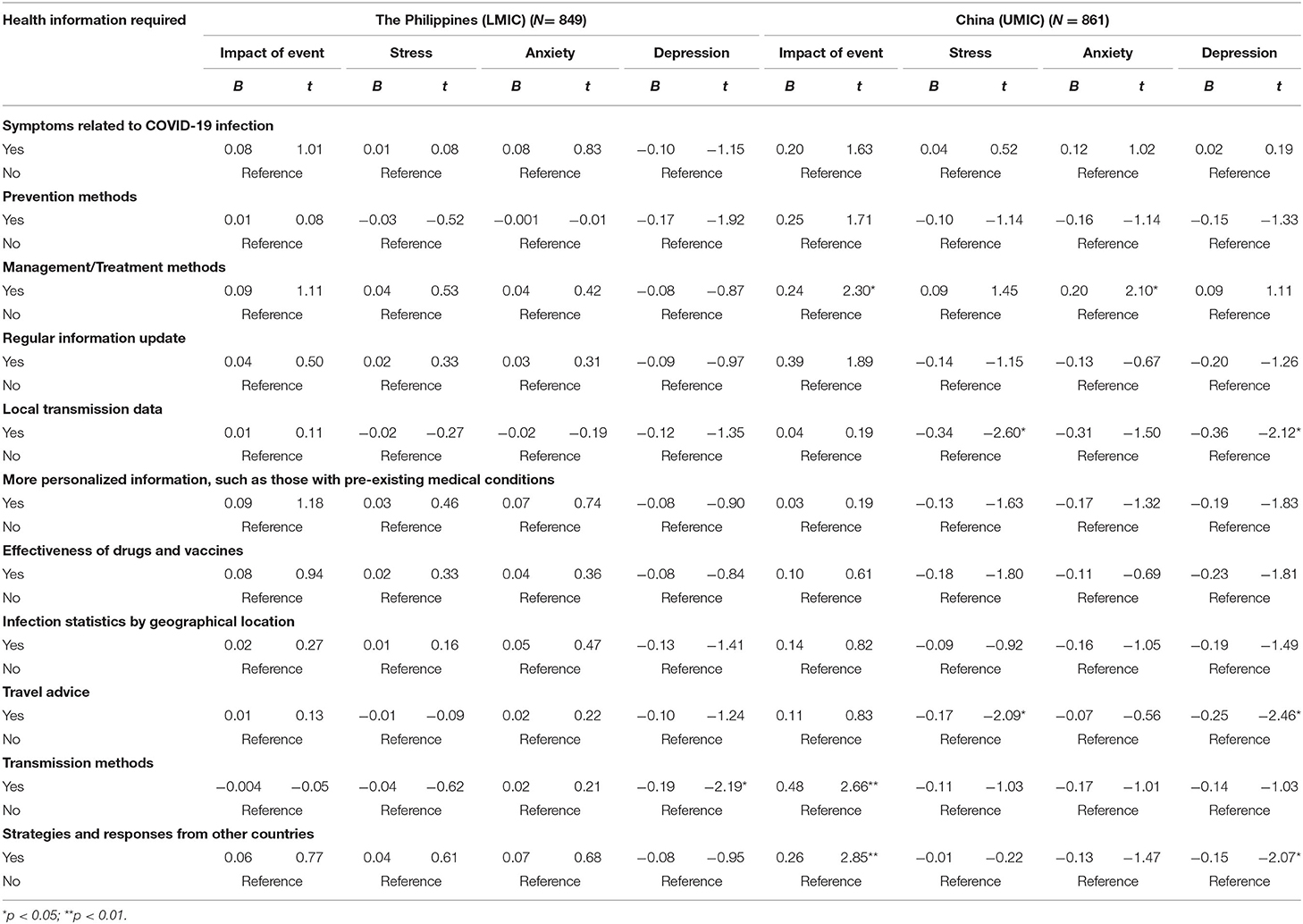
Table 5 . Comparison of the association between information needs about COVID-19 and the psychological impact as well as adverse mental health status between Filipino (LMIC) and Chinese (UMIC) participants after adjustment for age, gender, and marital status ( N = 1,710).
To our best knowledge, this is the first study that compared the physical and mental health as well as knowledge, attitude and belief about COVID-19 between citizens from an LMIC (The Philippines) and UMIC (China). Filipino respondents reported significantly higher levels of depression, anxiety and stress than Chinese during the COVID-19, but only the mean IES-R scores of Chinese respondents were above the cut-off scores for PTSD symptoms. Filipino respondents were more likely to report physical symptoms resembling COVID-19 infection, recent use of medical services with lower confidence, recent direct, and indirect contact with COVID, concerns about family members contracting COVID-19 and dissatisfaction with health information. In contrast, Chinese respondents requested more health information about COVID-19 and were more likely to stay at home for more than 20–24 h per day. For the Filipino, student status, low confidence in doctors, unsatisfaction of health information, long hours spent on health information, worries about family members contracting COVID-19, ostracization, unnecessary worries about COVID-19 were associated with adverse mental health.
The most important implication of the present study is to understand the challenges faced by a sample of people from an LMIC (The Philippines) compared to a sample of people from a UMIC (China) in Asia. As physical symptoms resembling COVID-19 infection (e.g., headache, myalgia, dizziness, and coryza) were associated with adverse mental health in both countries, this association could be due to lack of confidence in healthcare system and lack of testing for coronavirus. Previous research demonstrated that adverse mental health such as depression could affect the immune system and lead to physical symptoms such as malaise and other somatic symptoms ( 39 , 40 ). Based on our findings, the strategic approach to safeguard physical and mental health for middle-income countries would be cost-effective and widely available testing for people present with COVID-19 symptoms, providing a high quality of health information about COVID-19 by health authorities.
Students were afraid that confinement and learning online would hinder their progress in their studies ( 41 ). This may explain why students from the Philippines reported higher levels of IES-R and depression scores. Schools and colleges should evaluate the blended implementation of online and face-to-face learning to optimize educational outcomes when local spread is under control. As a significantly higher proportion of Filipino respondents lack confidence in their doctors, health authorities should ensure adequate training and develop hospital facilities to isolate COVID-19 cases and prevent COVID-19 spread among healthcare workers and patients ( 42 ). Besides, our study found that Filipino respondents were dissatisfied with health information. In contrast, Chinese respondents demanded more health information related to COVID-19. The difference could be due to stronger public health campaign launched by the Chinese government including national health education campaigns, a health QR (Quick Response) code system and community engagement that effectively curtailed the spread of COVID-19 ( 43 ). The high expectation for health information could be explained by high education attainment of participants as about 91.4 and 87.6% of participants from China and the Philippines have a university education.
Furthermore, the governments must employ communication experts to craft information, education, and messaging materials that are target-appropriate to each level of understanding in the community. That the Chinese Government rapidly deployed medical personnel and treated COVID-19 patients at rapidly-built hospitals ( 44 ) is in itself a confidence-building measure. Nevertheless, recent quarantine was associated with higher DASS-21 subscale scores in Chinese respondents only. It could be due to stricter control and monitoring of movements imposed by the Chinese government during the lockdown ( 45 ). Chinese respondents who stayed with more than three family members were associated with higher IES-R scores. The high IES-R scores could be due to worries of the spread of COVID-19 to family members and overcrowded home environment during the lockdown. The Philippines also converted sports arena into quarantine/isolation areas for COVID-19 patients with mild symptoms. These prompt actions helped restore public confidence in the healthcare system ( 46 ). A recent study reported that cultural factors, demand pressure for information, the ease of information dissemination via social networks, marketing incentives, and the poor legal regulation of online contents are the main reasons for misinformation dissemination during the COVID-19 pandemic ( 47 ). Bastani and Bahrami ( 47 ) recommended the engagement of health professionals and authorities on social media during the pandemic and the improvement of public health literacy to counteract misinformation.
Chinese respondents were more likely to feel ostracized and Filipino respondents associated ostracization with adverse mental health. Recently, the editor-in-chief of The Lancet , Richard Horton, expressed concern of discrimination of a country or particular ethnic group, saying that while it is important to understand the origin and inter-species transmission of the coronavirus, it was both unhelpful and unscientific to point to a country as the origin of the Covid-19 pandemic, as such accusation could be highly stigmatizing and discriminatory ( 48 ). The global co-operation involves an exchange of expertise, adopting effective prevention strategies, sharing resources, and technologies among UMIC and LIMC to form a united front on tackling the COVID-19 pandemic remains a work in progress.
Strengths and Limitations
The main strength of this study lay in the fact that we performed in-depth analysis and studied the relationship between physical and mental outcomes and other variables related to COVID-19 in the Philippines and China. However, there are several limitations to be considered when interpreting the results. Although the Philippines is a LMIC and China is a UMIC, the findings cannot be generalized to other LIMCs and UMICs. Another limitation was the potential risk of sampling bias. This bias could be due to the online administration of questionnaires, and the majority of respondents from both countries were respondents with good educational attainment and internet access. We could not reach out to potential respondents without internet access (e.g., those who stayed in the countryside or remote areas). Further, our findings may not be generalizable to other middle-income countries.
During the COVID-19 pandemic, Filipinos (LMIC) respondents reported significantly higher levels of depression, anxiety and stress than Chinese (UMIC). Filipino respondents were more likely to report physical symptoms resembling COVID-19 infection, recent use of medical services with lower confidence, recent direct and indirect contact with COVID, concerns about family members contracting COVID-19 and dissatisfaction with health information than Chinese. For the current COVID-19 and future pandemic, Middle income countries need to adopt the strategic approach to safeguard physical and mental health by establishing cost-effective and widely available testing for people who present with COVID-19 symptoms; provision of high quality and accurate health information about COVID-19 by health authorities. Our findings urge middle income countries to prevent ostracization of a particular ethnic group, learn from each other, and unite to address the challenge of the COVID-19 pandemic and safeguard physical and mental health.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
Ethical review and approval was required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin. The Institutional Review Board of the University of Philippines Manila Research Ethics Board (UPMREB 2020- 198-01) and Huaibei Normal University (China) approved the research proposal (HBU-IRB-2020-002).
Author Contributions
Concept and design: CW, MT, CT, RP, VK, and RH. Acquisition, analysis, and interpretation of data: CW, MT, CT, RP, LX, CHa, XW, YT, and VK. Drafting of the manuscript: CW, MT, CT, RH, and JA. Critical revision of the manuscript: MT, CT, CHo, and JA. Statistical analysis: CW, PR, RP, LX, XW, and YT. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2020.568929/full#supplementary-material
1. Sohrabi C, Alsafi Z, O'Neill N, Khan M, Kerwan A, Al-Jabir A, et al. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19). Int J Surg. (2020) 76:71–6. doi: 10.1016/j.ijsu.2020.02.034
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Mahase E. Covid-19: WHO declares pandemic because of “alarming levels” of spread, severity, and inaction. BMJ. (2020) 368:m1036. doi: 10.1136/bmj.m1036
3. Singhal T. A review of coronavirus disease-2019 (COVID-19). Indian J. Pediatr. (2020) 87:281–6. doi: 10.1007/s12098-020-03263-6
CrossRef Full Text | Google Scholar
4. Oxford. Oxford U of. Coronavirus Disease (COVID-19) - Statistics and Research . (2020). Available online at: https://ourworldindata.org/coronavirus%0D (accessed May 17, 2020).
Google Scholar
5. Edrada EM, Lopez EB, Villarama JB, Salva Villarama EP, Dagoc BF, Smith C, et al. First COVID-19 infections in the Philippines: a case report. Trop Med Health. (2020) 48:21. doi: 10.1186/s41182-020-00218-7
6. CNN. TIMELINE: How the Philippines is Handling COVID-19. (2020). Available online at: https://cnnphilippines.com/news/2020/4/21/interactive-timeline-PH-handling-COVID-19.html (accessed May 17, 2020).
7. Worldmeters. COVID-19 Coronavirus Pandemic. (2020). Available online at: https://www.worldometers.info/coronavirus/ (accessed December 4 2020).
8. WorldBank. World Bank National Accounts Data, and OECD National Accounts Data Files . (2020). Available online at: https://data.worldbank.org/indicator/NY.GNP.PCAP.CD (accessed April 16 2020).
9. Schellekens P, Sourrouille D. The Unreal Dichotomy in COVID-19 Mortality between High-Income and Developing Countries. (2020). Available online at: https://www.brookings.edu/blog/future-development/2020/05/05/the-unreal-dichotomy-in-covid-19-mortality-between-high-income-and-developing-countries/ (accessed May 10 2020).
10. Medicalexpress. ‘Slow Response’: How Britain Became Worst-Hit in Europe by Virus. (2020). Available online at: https://medicalxpress.com/news/2020-05-response-britain-worst-hit-europe-virus.html (accessed May 8 2020).
11. Mamun MA, Ullah I. COVID-19 suicides in Pakistan, dying off not COVID-19 fear but poverty? - The forthcoming economic challenges for a developing country. Brain Behav Immun. (2020) 87:163–6. doi: 10.1016/j.bbi.2020.05.028
12. Kar SK, Oyetunji TP, Prakash AJ, Ogunmola OA, Tripathy S, Lawal MM, et al. Mental health research in the lower-middle-income countries of Africa and Asia during the COVID-19 pandemic: a scoping review. Neurol Psychiatry Brain Res. (2020) 38:54–64. doi: 10.1016/j.npbr.2020.10.003
13. Leung GM, Lam TH, Ho LM, Ho SY, Chan BH, Wong IO, et al. The impact of community psychological responses on outbreak control for severe acute respiratory syndrome in Hong Kong. J Epidemiol Community Health. (2003) 57:857–63. doi: 10.1136/jech.57.11.857
14. Cristóbal-Narváez P, Haro JM, Koyanagi A. Perceived stress and depression in 45 low- and middle-income countries. J Affect Disord. (2020) 274:799–805. doi: 10.1016/j.jad.2020.04.020
15. Vallejo MA, Vallejo-Slocker L, Fernández-Abascal EG, Mañanes G. Determining factors for stress perception assessed with the perceived stress scale (PSS-4) in Spanish and other European samples. Front Psychol. (2018) 9:37. doi: 10.3389/fpsyg.2018.00037
16. Shin C, Kim Y, Park S, Yoon S, Ko YH, Kim YK, et al. Prevalence and associated factors of depression in general population of Korea: results from the Korea National Health and Nutrition Examination Survey, 2014. J Korean Med Sci. (2017) 32:1861–9. doi: 10.3346/jkms.2017.32.11.1861
17. Olsen LR, Mortensen EL, Bech P. Prevalence of major depression and stress indicators in the Danish general population. Acta Psychiatr Scand. (2004) 109:96–103. doi: 10.1046/j.0001-690X.2003.00231.x
18. Lim GY, Tam WW, Lu Y, Ho CS, Zhang MW, Ho RC. Prevalence of depression in the community from 30 countries between 1994 and (2014). Sci Rep. (2018) 8:2861. doi: 10.1038/s41598-018-21243-x
19. Sang T, Zhou H, Li M, Li W, Shi H, Chen H, et al. Investigation of the differences between the medical personnel's and general population's view on the doctor-patient relationship in China by a cross-sectional survey. Global Health. (2020) 16:99. doi: 10.21203/rs.3.rs-41725/v2
20. Ferrer RR, Ramirez M, Beckman LJ, Danao LL, Ashing-Giwa KT. The impact of cultural characteristics on colorectal cancer screening adherence among Filipinos in the United States: a pilot study. Psychooncology. (2011) 20:862–70. doi: 10.1002/pon.1793
21. Lei P, Jolibert A. A three-model comparison of the relationship between quality, satisfaction and loyalty: an empirical study of the Chinese healthcare system. BMC Health Serv Res. (2012) 12:436. doi: 10.1186/1472-6963-12-436
22. Peabody JW, Florentino J, Shimkhada R, Solon O, Quimbo S. Quality variation and its impact on costs and satisfaction: evidence from the QIDS study. Med Care. (2010) 48:25–30. doi: 10.1097/MLR.0b013e3181bd47b2
23. Xiong J, Lipsitz O, Nasri F, Lui LMW, Gill H, Phan L, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. (2020) 277:55–64. doi: 10.1016/j.jad.2020.08.001
24. Wang C, Pan R, Wan X, Tan Y, Xu L, McIntyre RS, et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun. (2020) 87:40–8. doi: 10.1016/j.bbi.2020.04.028
25. Zhang MW, Ho CS, Fang P, Lu Y, Ho RC. Usage of social media and smartphone application in assessment of physical and psychological well-being of individuals in times of a major air pollution crisis. JMIR Mhealth Uhealth. (2014) 2:e16. doi: 10.2196/mhealth.2827
26. Chew NWS, Lee GKH, Tan BYQ, Jing M, Goh Y, Ngiam NJH, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun. (2020) 88:559–65. doi: 10.1016/j.bbi.2020.04.049
27. Zhang MWB, Ho CSH, Fang P, Lu Y, Ho RCM. Methodology of developing a smartphone application for crisis research and its clinical application. Technol Health Care. (2014) 22:547–59. doi: 10.3233/THC-140819
28. Creamer M, Bell R, Failla S. Psychometric properties of the Impact of Event Scale - Revised. Behav Res Ther. (2003) 41:1489–96. doi: 10.1016/j.brat.2003.07.010
29. Lee SM, Kang WS, Cho A-R, Kim T, Park JK. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr Psychiatry. (2018) 87:123–7. doi: 10.1016/j.comppsych.2018.10.003
30. Le TA, Le MQT, Dang AD, Dang AK, Nguyen CT, Pham HQ, et al. Multi-level predictors of psychological problems among methadone maintenance treatment patients in difference types of settings in Vietnam. Subst Abuse Treat Prev Policy. (2019) 14:39. doi: 10.1186/s13011-019-0223-4
31. Cheung JTK, Tsoi VWY, Wong KHK, Chung RY. Abuse and depression among Filipino foreign domestic helpers. A cross-sectional survey in Hong Kong. Public Health. (2019) 166:121–7. doi: 10.1016/j.puhe.2018.09.020
32. Tee ML, Tee CA, Anlacan JP, Aligam KJG, Reyes PWC, Kuruchittham V, et al. Psychological impact of COVID-19 pandemic in the Philippines. J Affect Disord. (2020) 277:379–91. doi: 10.1016/j.jad.2020.08.043
33. Tee CA, Salido EO, Reyes PWC, Ho RC, Tee ML. Psychological State and Associated Factors During the 2019 Coronavirus Disease (COVID-19) pandemic among filipinos with rheumatoid arthritis or systemic lupus erythematosus. Open Access Rheumatol. (2020) 12:215–22. doi: 10.2147/OARRR.S269889
34. Ho CSH, Tan ELY, Ho RCM, Chiu MYL. Relationship of anxiety and depression with respiratory symptoms: comparison between depressed and non-depressed smokers in Singapore. Int J Environ Res Public Health. (2019) 16:163. doi: 10.3390/ijerph16010163
35. Quek TC, Ho CS, Choo CC, Nguyen LH, Tran BX, Ho RC. Misophonia in Singaporean psychiatric patients: a cross-sectional study. Int J Environ Res Public Health. (2018) 15:1410. doi: 10.3390/ijerph15071410
36. Hao F, Tan W, Jiang L, Zhang L, Zhao X, Zou Y, et al. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav Immun. (2020) 87:100–6. doi: 10.1016/j.bbi.2020.04.069
37. Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus Disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. (2020) 17:E1729. doi: 10.3390/ijerph17051729
38. Tan BYQ, Chew NWS, Lee GKH, Jing M, Goh Y, Yeo LLL, et al. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann Intern Med . (2020) 173:317–20. doi: 10.7326/M20-1083
39. Liu Y, Ho RC, Mak A. Interleukin (IL)-6, tumour necrosis factor alpha (TNF-α) and soluble interleukin-2 receptors (sIL-2R) are elevated in patients with major depressive disorder: a meta-analysis and meta-regression. J Affect Disord. (2012) 139:230–9. doi: 10.1016/j.jad.2011.08.003
40. Viljoen M, Panzer A. Proinflammatory cytokines: a common denominator in depression and somatic symptoms? Can J Psychiatry. (2005) 50:128. doi: 10.1177/070674370505000216
41. Li HY, Cao H, Leung DYP, Mak YW. The psychological impacts of a COVID-19 outbreak on college students in China: a longitudinal study. Int J Environ Res Public Health. (2020) 17:3933. doi: 10.3390/ijerph17113933
42. Krishnakumar B, Rana S. COVID 19 in INDIA: strategies to combat from combination threat of life and livelihood. J Microbiol Immunol Infect. (2020) 53:389–91. doi: 10.1016/j.jmii.2020.03.024
43. Huang Y, Wu Q, Wang P, Xu Y, Wang L, Zhao Y, et al. Measures undertaken in China to avoid COVID-19 infection: internet-based, cross-sectional survey study. J Med Internet Res. (2020) 22:e18718. doi: 10.2196/18718
44. Salo J. China Orders 1,400 Military Doctors, Nurses to Treat Coronavirus. (2020). Available online at: https://nypost.com/2020/02/02/china-orders-14000-military-doctors-nurses-to-treat-coronavirus/ (accessed March 22, 2020).
45. Burki T. China's successful control of COVID-19. Lancet Infect Dis. (2020) 20:1240–1. doi: 10.1016/S1473-3099(20)30800-8
46. Esguerra DJ. Philippine Arena to Start Accepting COVID-19 Patients Next Week . (2020). Available online at: https://newsinfo.inquirer.net/1255623/philippine-arena-to-start-accepting-covid-19-patients-next-week (accessed November 18, 2020).
47. Bastani P, Bahrami MA. COVID-19 related misinformation on social media: a qualitative study from Iran. J Med Internet Res. (2020). doi: 10.2196/preprints.18932. [Epub ahead of print].
48. Catherine W. It's Unfair to Blame China for Coronavirus Pandemic, Lancet Editor Tells State Media. (2020). Available online at: https://www.scmp.com/news/china/science/article/3082606/its-unfair-blame-china-coronavirus-pandemic-lancet-editor-tells (accessed May 8, 2020).
Keywords: anxiety, China, COVID-19, depression, middle-income, knowledge, precaution, Philippines
Citation: Tee M, Wang C, Tee C, Pan R, Reyes PW, Wan X, Anlacan J, Tan Y, Xu L, Harijanto C, Kuruchittham V, Ho C and Ho R (2021) Impact of the COVID-19 Pandemic on Physical and Mental Health in Lower and Upper Middle-Income Asian Countries: A Comparison Between the Philippines and China. Front. Psychiatry 11:568929. doi: 10.3389/fpsyt.2020.568929
Received: 02 June 2020; Accepted: 22 December 2020; Published: 09 February 2021.
Reviewed by:
Copyright © 2021 Tee, Wang, Tee, Pan, Reyes, Wan, Anlacan, Tan, Xu, Harijanto, Kuruchittham, Ho and Ho. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Cuiyan Wang, wcy@chnu.edu.cn
† These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Western Pac Surveill Response J
- v.12(1); Jan-Mar 2021
Early response to COVID-19 in the Philippines
Arianna maever l. amit.
a College of Medicine, University of the Philippines Manila, Manila, Philippines.
b School of Medicine and Public Health, Ateneo de Manila University, Pasig City, Philippines.
Veincent Christian F. Pepito
Manuel m. dayrit.
Low- and middle-income countries (LMICs) with weak health systems are especially vulnerable during the COVID-19 pandemic. In this paper, we describe the challenges and early response of the Philippine Government, focusing on travel restrictions, community interventions, risk communication and testing, from 30 January 2020 when the first case was reported, to 21 March 2020. Our narrative provides a better understanding of the specific limitations of the Philippines and other LMICs, which could serve as basis for future action to improve national strategies for current and future public health outbreaks and emergencies.
The Philippine health system and the threat of public health emergencies
Despite improvements during the past decade, the Philippines continues to face challenges in responding to public health emergencies because of poorly distributed resources and capacity. The Philippines has 10 hospital beds and six physicians per 10 000 people. ( 1 , 2 ) and only about 2335 critical care beds nationwide. ( 3 ) The available resources are concentrated in urban areas, and rural areas have only one physician for populations up to 20 000 people and only one bed for a population of 1000. ( 4 ) Disease surveillance capacity is also unevenly distributed among regions and provinces. The primary care system comprises health centres and community health workers, but these are generally ill-equipped and poorly resourced, with limited surge capacity, as evidenced by lack of laboratory testing capacity, limited equipment and medical supplies, and lack of personal protective equipment for health workers in both primary care units and hospitals. ( 5 ) Local government disaster preparedness plans are designed for natural disasters and not for epidemics.
Inadequate, poorly distributed resources and capacity nationally and subnationally have made it difficult to respond adequately to public health emergencies in the past, as in the case of typhoon Haiyan in 2013. ( 6 ) The typhoon affected 13.3 million people, overwhelming the Government’s capacity to mobilize human and financial resources rapidly to affected areas. ( 7 ) Failure to deliver basic needs and health services resulted in disease outbreaks, including a community outbreak of gastroenteritis. ( 8 ) Access to care has improved in recent years due to an increase in the number of private hospital beds; ( 5 ) however, improvements in private sector facilities mainly benefit people who can afford them, in both urban and rural areas.
In this paper, we describe the challenges and early response of the Philippine Government, focusing on travel restrictions, community interventions, risk communication and testing, from 30 January 2020 when the first case was reported, to 21 March 2020.
Early response to COVID-19
Travel restrictions.
Travel restrictions in the Philippines were imposed as early as 28 January, before the first confirmed case was reported on 30 January ( Fig. 1a ). ( 9 ) After the first few COVID-19 cases and deaths, the Government conducted contact tracing and imposed additional travel restrictions, ( 10 ) with arrivals from restricted countries subject to 14-day quarantine and testing. While travel restrictions in the early phase of the COVID-19 response prevented spread of the disease by potentially infected people, travellers from countries not on the list of restricted countries were not subject to the same screening and quarantine protocols. The restrictions were successful in delaying the spread of the disease only briefly, as the number of confirmed cases increased in the weeks that followed. ( 11 ) Fig. 1b shows all interventions, including travel restrictions undertaken before 6 March, when the Government declared the occurrence of community spread, and after 11 March, when WHO declared COVID-19 a pandemic.

New cases of COVID-19 in the Philippines, 30 January–21 March 2020
[ insert Figure 1a ]

Timeline of key events and developments in the Philippines, 30 January–21 March 2020
[ insert Figure 1b ]
Community interventions
The Government declared “enhanced community quarantine” (ECQ) for Metro Manila between 15 March and 14 April ( Fig. 2a ), which was subsequently extended to the whole island of Luzon ( Fig. 2b ). The quarantine consisted of: strict home quarantine in all households, physical distancing, suspension of classes and introduction of work from home, closure of public transport and non-essential business establishments, prohibition of mass gatherings and non-essential public events, regulation of the provision of food and essential health services, curfews and bans on sale of liquor and a heightened presence of uniformed personnel to enforce the quarantine procedures. ( 12 ) ECQ – an unprecedented move in the country’s history – was modelled on the lockdown in Hubei, China, which was reported to have slowed disease transmission. ( 13 ) Region-wide disease control interventions, such as quarantining of the entire Luzon island, were challenging to implement because of their scale and social and economic impacts, but they were deemed necessary to “flatten the curve” so that health systems were not overwhelmed. ( 14 ) While the lockdown implemented by the Government applied only to the island of Luzon, local governments in other parts of the country followed this example and also locked down. The ECQ gave the country the opportunity to mobilize resources and organize its pandemic response, which was especially important in a country with poorly distributed, scarce resources and capacity.

Provinces placed under enhanced community quarantine (ECQ). (2a) The Government declared ECQ in Metro Manila effective 15 March 2020; (2b) The Government declared ECQ on the entire island of Luzon effective 17 March 2020.
[ insert Figure 2 ]
Risk communication
The Government strengthened and implemented national risk communication plans to provide information on the new disease. The Government conducted daily press briefings, sponsored health-related television and Internet advertisements and circulated infographics on social media. Misinformation and conspiracy theories about COVID-19 were nevertheless a challenge for a population that spends more than 10 hours a day on the Internet. ( 15 , 16 ) These spread quickly and became increasingly difficult to correct. Furthermore, the Government’s messages did not reach all households, despite access to health services and information, resulting in limited knowledge of preventive practices, except for hand-washing. ( 17 )
Testing is key to controlling the pandemic but was done on a small scale in the Philippines. As of 19 March, fewer than 1200 individuals had been tested, ( 11 ) as only the Research Institute for Tropical Medicine located in Metro Manila performed tests and assisted subnational reference laboratories in testing. ( 18 ) No positivity rates for RT–PCR tests were reported until early April 2020. Because of the limited capacity for testing at the start of the pandemic, the Department of Health imposed strict protocols to ration testing resources while ramping up testing capacity. Most tests were conducted for individuals in urban areas, where the incidence was highest. ( 19 )
Conclusions
At the start of the COVID-19 pandemic, the country’s initial response lacked organizational preparedness to counter the public health threat. The Philippines’ disease surveillance system could conduct contact tracing, but this was overwhelmed in the early phases of outbreak response. Similarly, in February, only one laboratory could conduct reverse transcriptase polymerase chain reaction (RT–PCR) testing, so the country could not rapidly deploy extensive laboratory testing for infected cases. In addition, the primary care system of the Philippines did not serve as a primary line of defence, as people went straight to hospitals in urban areas, overwhelming critical care capacity in the early stages of the COVID-19 pandemic.
In response to the early phase of the pandemic, the Government of the Philippines implemented travel restrictions, community quarantine, risk communication and testing; however, the slow ramping up of capacities particularly on testing contributed to unbridled disease transmission. By 15 October, the number of confirmed cases had exponentially grown to 340 000 of which 13.8% were deemed active. ( 11 ) The lack of pandemic preparedness had left the country poorly defended against the new virus and its devastating effects. Investing diligently and consistently in pandemic preparedness, surveillance and testing capacity in particular is a lesson that the Philippines and other LMICs should learn from COVID-19.
Acknowledgements
Conflict of interests.
None reported
Not applicable
First COVID-19 infections in the Philippines: a case report
Affiliations.
- 1 San Lazaro Hospital, Manila, Philippines.
- 2 2School of Tropical Medicine and Global Health, Nagasaki University, Nagasaki, Japan.
- 3 3Faculty of Infectious and Tropical Diseases, London School of Hygiene and Tropical Medicine, London, UK.
- 4 4Department of Microbiology, Faculty of Medicine, Oita University, Oita, Japan.
- 5 5Institute of Tropical Medicine, Nagasaki University, Nagasaki, Japan.
- 6 6Research Institute for Tropical Medicine, Alabang, Philippines.
- PMID: 32308532
- PMCID: PMC7154063
- DOI: 10.1186/s41182-020-00203-0
Background: The novel coronavirus (COVID-19) is responsible for more fatalities than the SARS coronavirus, despite being in the initial stage of a global pandemic. The first suspected case in the Philippines was investigated on January 22, 2020, and 633 suspected cases were reported as of March 1. We describe the clinical and epidemiological aspects of the first two confirmed COVID-19 cases in the Philippines, both admitted to the national infectious disease referral hospital in Manila.
Case presentation: Both patients were previously healthy Chinese nationals on vacation in the Philippines travelling as a couple during January 2020. Patient 1, a 39-year-old female, had symptoms of cough and sore throat and was admitted to San Lazaro Hospital in Manila on January 25. Physical examination was unremarkable. Influenza B , human coronavirus 229E, Staphylococcus aureus and Klebsiella pneumoniae were detected by PCR on initial nasopharyngeal/oropharyngeal (NPS/OPS) swabs. On January 30, SARS-CoV-2 viral RNA was reported to be detected by PCR on the initial swabs and she was identified as the first confirmed COVID-19 case in the Philippines. Her symptoms resolved, and she was discharged. Patient 2, a 44-year-old male, had symptoms of fever, cough, and chills. Influenza B and Streptococcus pneumoniae were detected by PCR on initial NPS/OPS swabs. He was treated for community-acquired pneumonia with intravenous antibiotics, but his condition deteriorated and he required intubation. On January 31, SARS-CoV-2 viral RNA was reported to be detected by PCR on the initial swabs, and he was identified as the 2nd confirmed COVID-19 infection in the Philippines. On February 1, the patient's condition deteriorated, and following a cardiac arrest, it was not possible to revive him. He was thus confirmed as the first COVID-19 death outside of China.
Conclusions: This case report highlights several important clinical and public health issues. Despite both patients being young adults with no significant past medical history, they had very different clinical courses, illustrating how COVID-19 can present with a wide spectrum of disease. As of March 1, there have been three confirmed COVID-19 cases in the Philippines. Continued vigilance is required to identify new cases.
Keywords: COVID-19; Case report; Coronavirus; Manila; Philippines; SARS-CoV-2.
© The Author(s) 2020.
Publication types
- Case Reports
Evidence Review of the Adverse Effects of COVID-19 Vaccination and Intramuscular Vaccine Administration
Vaccines are a public health success story, as they have prevented or lessened the effects of many infectious diseases. To address concerns around potential vaccine injuries, the Health Resources and Services Administration (HRSA) administers the Vaccine Injury Compensation Program (VICP) and the Countermeasures Injury Compensation Program (CICP), which provide compensation to those who assert that they were injured by routine vaccines or medical countermeasures, respectively. The National Academies of Sciences, Engineering, and Medicine have contributed to the scientific basis for VICP compensation decisions for decades.
HRSA asked the National Academies to convene an expert committee to review the epidemiological, clinical, and biological evidence about the relationship between COVID-19 vaccines and specific adverse events, as well as intramuscular administration of vaccines and shoulder injuries. This report outlines the committee findings and conclusions.
Read Full Description
- Digital Resource: Evidence Review of the Adverse Effects of COVID-19 Vaccination
- Digital Resource: Evidence Review of Shoulder Injuries from Intramuscular Administration of Vaccines
- Press Release
Recent News
NAS Launches Science and Innovation Fund for Ukraine
Science Academies Issue Statements to Inform G7 Talks
Supporting Family Caregivers in STEMM
A Vision for High-Quality Preschool for All
- Load More...
Skip to Content
‘An epidemic of loneliness’: How the pandemic changed life for aging adults
Stock image of a sign at a park in 2020, calling for social distancing. Four years later, a new study shows many are still keeping to themselves more than they did pre-pandemic.
- Share via Twitter
- Share via Facebook
- Share via LinkedIn
- Share via E-mail
Years after the U.S. began to slowly emerge from mandatory COVID-19 lockdowns, more than half of older adults still spend more time at home and less time socializing in public spaces than they did pre-pandemic, according to new CU Boulder research.
Participants cited fear of infection and “more uncomfortable and hostile” social dynamics as key reasons for their retreat from civic life.
“The pandemic is not over for a lot of folks,” said Jessica Finlay, an assistant professor of geography whose findings are revealed in a series of new papers . “Some people feel left behind.”
The study comes amid what the U.S. Surgeon General recently called an “ epidemic of loneliness ” in which older adults—especially those who are immune compromised or have disabilities—are particularly vulnerable.
“We found that the pandemic fundamentally altered neighborhoods, communities and everyday routines among aging Americans, and these changes have long-term consequences for their physical, mental, social and cognitive health,” said Finlay.
‘I just can’t go back’
As a health geographer and environmental gerontologist, Finlay studies how social and built environments impact health as we age.
In March 2020 as restaurants, gyms, grocery stores and other gathering places shuttered amid shelter-in-place orders, she immediately wondered what the lasting impacts would be. Shortly thereafter, she launched the COVID-19 Coping Study with University of Michigan epidemiologist Lindsay Kobayashi. They began their research with a baseline and monthly survey. Since then, nearly 7,000 people over age 55 from all 50 states have participated.
The researchers check in annually, asking open-ended questions about how neighborhoods and relationships have changed, how people spend their time, opinions and experiences of the COVID-19 pandemic, and their physical and mental health.
By the numbers
How aging adults spend their time
- 59% spend more time at home than before pandemic
- 41% go to the grocery less often
- 75% eat out less often
- 57% exercise indoors less often
- 62% visit an arts or cultural site less often
- 53% attend religious services less often
- 10% exercise outdoors more often
Source: Data from COVID-19 Coping Study survey results from May 2022. A more recent survey found that more than half still had not returned to pre-pandemic social routines.
“We’ve been in the field for some incredibly pivotal moments,” said Finlay, noting that surveys went out shortly after George Floyd was murdered in May 2020 and again after the attack on the U.S. Capitol on Jan. 6, 2021.
Collectively, the results paint a troubling picture in which a substantial portion of the older population remains isolated even after others have moved on.
In one paper published in February in the journal Wellbeing, Space and Society , 60% of respondents said they spend more time in their home while 75% said they dine out less. Some 62% said they visit cultural and arts venues less, and more than half said they attend church or the gym less than before the pandemic.
The most recent survey, taken in spring 2023, showed similar trends, with more than half of respondents still reporting that their socialization and entertainment routines were different than they were pre-pandemic.
In another paper titled “ I just can’t go back ,” 80% of respondents reported there are some places they are reluctant to visit in person anymore.
“The thought of going inside a gym with lots of people breathing heavily and sweating is not something I can see myself ever doing again,” said one 72-year-old male.
Those who said they still go to public places like grocery stores reported that they ducked in and out quickly and skipped casual chitchat.
“It’s been tough,” said one 68-year-old female. “You don’t stop and talk to people anymore.”
Many respondents reported they were afraid of getting infected with a virus or infecting young or immune-compromised loved ones, and said they felt “irresponsible” for being around a lot of people.
Some reported getting dirty looks or rude comments when wearing masks or asking others to keep their distance—interpersonal exchanges that reinforced their inclination to stay home.
Revitalizing human connection

Jessica Finlay, a health geographer and environmental gerontologist, studies how built environments impact aging.
The news is not all bad, stresses Finlay.
At least 10% of older adults report exercising outdoors more frequently since the pandemic. And a small but vocal minority said that their worlds had actually opened up, as more meetings, concerts and classes became available online.
Still, Finlay worries that the loss of spontaneous interactions in what sociologists call “third places” could have serious health consequences.
Previous research shows that a lack of social connection can increase risk of premature death as much as smoking 15 cigarettes a day and exacerbate mental illness and dementia.
“For some older adults who live alone, that brief, unplanned exchange with the butcher or the cashier may be the only friendly smile they see in the day, and they have lost that,” Finlay said.
Societal health is also at risk.
“It is increasingly rare for Americans with differing sociopolitical perspectives to collectively hang out and respectfully converse,” she writes.
Finlay hopes that her work can encourage policymakers to create spaces more amenable to people of all ages who are now more cautious about getting sick—things like outdoor dining spaces, ventilated concert halls or masked or hybrid events.
She also hopes that people will give those still wearing masks or keeping distance some grace.
“It is a privilege to be able to ‘just get over’ the pandemic and many people, for a multitude of reasons, just don’t have that privilege. The world looks different to them now,” she said. “How can we make it easier for them to re-engage?”
News Headlines
Related articles.

Joints that could heal themselves? Researchers could get there in 5 years

How genes work together to shape how much you smoke

You’re (very likely) not going to win, so why play?
- Arts & Humanities
- Business & Entrepreneurship
- Climate & Environment
- Education & Outreach
- Health & Society
- Law & Politics
- Science & Technology
Campus Community
- Administration
- Announcements & Deadlines
- Career Development
- Getting Involved
- Mind & Body
Events & Exhibits
- Arts & Culture
- Conferences
- Lectures & Presentations
- Performances & Concerts
- Sports & Recreation
- Workshops & Seminars
Subscribe to CUBT
Sign up for Alerts
Administrative eMemos
Buff Bulletin Board
Events Calendar
- Top Stories
- Stock Market
- BUYING RATES
- FOREIGN INTEREST RATES
- Philippine Mutual Funds
- Leaders and Laggards
- Stock Quotes
- Stock Markets Summary
- Non-BSP Convertible Currencies
- BSP Convertible Currencies
- US Commodity futures
- Infographics
- B-Side Podcasts
- Agribusiness
- Arts & Leisure
- Special Features
- Special Reports
- BW Launchpad

Philippines in talks with OceanX for marine research

By Kyle Aristophere T. Atienza, Reporter
SINGAPORE — US-based exploration startup OceanX on Wednesday said it is in talks with the Philippine government to conduct marine research in its waters to help harness the potential of its blue economy.
Its f lagship vessel OceanXplorer , which carries four deep sea vehicles and four labs, would probably conduct research and exploration activities in Philippine waters next year, science program director Mattie Rodrigue told BusinessWorld during a media tour of the ship on the sidelines of the Asia Philanthropy Summit here.
“We’ve just started discussions about a collaboration… with the Philippine government to bring OceanXplorer and conduct scientific work in the area,” she said. “We’re hoping that after our mission is completed in Malaysia and our talks progress successfully with the Philippine government, then we’ll be able to get the vessel in as early as next year.”
The global ocean exploration nonprofit in March said it would embark on a series of research expeditions to better understand Southeast Asia’s marine biodiversity. This includes missions in Indonesia and Malaysia, where it will work with government agencies and scientists to study the ocean for better science, policy and economic decisions.
Two of the four vehicles aboard the 87.1-meter OceanXplorer are manned submersibles that can go as deep as 1,000 meters.
The ship, which has Hollywood production capabilities, also has two 6,000-meter remote-operated vehicles. It uses state-of-the-art optical technology to stream ocean exploration in real time.
Ms. Rodrigue said OceanX partners with government agencies and local scientists for the “stewardship of marine resources.” “We do an in-country request for scienti f ic proposals.”
Philippine ocean-based industries grew by 21.1% in 2022, accounting for 3.9% of the country’s economic output, according to the state statistics agency. But local economists have said the country should do more to maximize the bene f its from the ocean.
The Philippine government has included a blue economy bill in its list of priority legislation this year. The measure seeks to create a comprehensive framework and boost multisectoral coordination in managing the country’s marine and coastal resources.
The Southeast Asian nation has been seeking to explore oil and gas within its exclusive economic zone in the South China Sea, one of the world’s most important waterways that China claims almost in its entirety, as its sole indigenous source of natural gas is expected to run dry by 2027.
Reed Bank, which is near a Philippine feature that China had been patrolling in recent months, could hold up to 55.1 trillion cubic feet of natural gas and up to 5.4 billion barrels of oil, according to the United States Energy Information Administration.
President Ferdinand R. Marcos, Jr. has said his government seeks to pursue exploration activities in nonconflict areas of the South China Sea.
The Philippine government has cited the destruction of coral reefs near features it claims in the waterway.
The Center for Strategic and International Studies in February said China had destroyed at least 21,000 acres of coral reefs within the Philippines’ exclusive economic zone.
Another think tank, the Asia Maritime Transparency Initiative, also attributed coral reef destruction in the waterway to Chinese activities such as dredging, island-building and clam harvesting.
‘FULL PICTURE’ OceanX said deep sea research in Southeast Asia and other parts of the world has been underfunded.
“Every country doesn’t necessarily contribute resources to understanding the deep sea,” Ms. Rodrigue said. She added that blue economy goals have been largely centered on coastal ecosystems, often ignoring the potential of the deep sea to contribute to economic growth.
“The entire ocean space and all of these ecosystems are intertwined and connected,” she said. “So often, the understudied areas in these regions are going to be the deep sea. If scientists are able to access technology, that will then allow them to access those deep spaces.”
“That’s really the way to get a full picture of the environment, to drive forward in blue economic progress,” she added.
OceanX said only 25% of the world’s ocean f loors have been mapped, with its f lagship vessel having explored 145,000 square kilometers so far.
“In the proportion of the entire global ocean it’s just a drop in the bucket,” Ms. Rodrigue said. “But we hope when we go to different areas [we can help] develop and support their own mapping programs. There are vessels, ships, cargo ships moving back and forth and all have the ability to at least generate data.”
OceanX is the brainchild of Mark Dalio, a former f ilmmaker at the National Geographic, and his father Ray, the billionaire philanthropist behind the investment firm Bridgewater Associates.
The father-and-son team is behind the Singapore-based Dalio Philanthropies, a founding core member of the Temasek Trust’s Philanthropy Asia Alliance.
OceanX supports the Seabed 2030 project, which aims to map all of the world’s oceans by the end of the decade. OceanXplorer, which f irst sailed in 2020 in the Red Sea, is manned by more than a dozen nationalities including Filipinos.
The philanthropic alliance on Tuesday launched an initiative that seeks to generate funding for sustainable projects involving the blue economy, sustainable land use and inclusive education.
“The so-called Blue Oceans Community under the initiative will focus on the conservation and sustainable use of oceans, seas and marine resources, with a focus on Asia,” according to a statement from the alliance.
“It will look at science and exploration to build our connectivity to, and appreciation of, the importance of oceans and their related marine and coastal ecosystems,” it added.
RELATED ARTICLES MORE FROM AUTHOR
Rate cut delays seen to slow growth
Outages linked to failure to expand power plants’ capacity
PHL education faces increasing challenges from climate change

Nationwide round-up (03/17/21)
Dict targets vaccine management system rollout by q2, house leaders agree to fast-track budget approval after row.

(Un)fit to Nurse: Efficiency and Discipline at the Philippine General Hospital, 1898–1916
Ren Capucao , MSN, RN will speak on Thursday, April 25, 2024 at 2:00 PM ET. This talk will be live-streamed globally, and archived , by NIH VideoCasting and live-streamed on the NLM YouTube Channel . Mr. Capucao is a PhD Candidate at the Bjoring Center for Nursing Historical Inquiry in the School of Nursing at the University of Virginia. Circulating Now interviewed him about his research and upcoming talk .
Circulating Now: Please tell us a little about yourself. Where are you from? What do you do? What is your typical workday like?

The quotidian flow of my “typical workday,” however, is only a recent event. At the start of my doctoral program, I worked as a guest service associate at the Virginia Museum of History and Culture . As coursework went virtual due to the COVID-19 pandemic, I determined this was the best time to undergo my first nursing position. I worked as a pediatric nurse at the Virginia Commonwealth University Health System until I received a Fulbright fellowship to conduct historical and ethnographical research at the University of the Philippines College of Nursing . My ten months abroad required many adjustments, but I learned something new about Philippine culture and myself daily. For example, I formerly feared riding motorcycles, but for the sake of affordability and getting around traffic, I came to enjoy riding motorbike taxis. Overall, I have embraced the chaos surrounding my education and self-growth as a great adventure still unfolding.
CN: What initially sparked your interest in the History of Medicine?
RC: The spark that drew me to the history of medicine ignited during my childhood. I spent a lot of time at the hospital, whether being hospitalized due to my accident-prone nature or just visiting my mother—also a nurse—at work. The fondness I developed in experiencing the healthcare environment intertwined with my favorite school subject, history. History helped me understand the cultural and intergenerational dissonance I experienced growing up under Filipino immigrant parents. I learned about my mother and her career path as a nurse, including its joys and tribulations, so my interest in the history of medicine is deeply personal. My mother’s narrative and mine are interwoven into the broader colonial history of the Filipino nurse diaspora.
My professional interest in the history of medicine took place during my master’s entry program in nursing at the University of Virginia. While learning how to be a nurse, I was also learning how to become a historian of nursing; I wanted to gain broader insight into the uneven life chances and unilateral migration patterns nurses face in the Global South. I was taken under the wing of Dr. Barbra Mann Wall, then director of the Bjoring Center for Nursing Historical Inquiry , who instilled in me a sense of curiosity and confidence to pursue doctoral studies. Since then, I have also become indebted to the mentorship of the current director, Dr. Dominique Tobbell, who has continued to help me grow and refine my scholarship. I also show gratitude to the Filipino communities I have worked alongside who continue to fuel my fervor to drive change toward decolonization and global health equity, such as the Philippine Nurses Association of America, specifically its Virginia chapter , the Filipino Nursing Diaspora Network , and the University of the Philippines College of Nursing.

CN: Your talk, “ (Un)fit to Nurse: Efficiency and Discipline at the Philippine General Hospital, 1898–1916 ,” explores a dramatic event in 1916 at the Philippine General Hospital. What happened?

RC: I myself was surprised by the events that unfolded! So, in mid-August 1916, Florentina Papa, a student nurse with exceptional record at the Philippine General Hospital (PGH), the government hospital serving the entire archipelago, committed suicide after being chastised by the American superintendent of nursing for breaking nursing’s code of conduct. Previously, she had gotten into a heated exchange with a patient on the ward who lambasted her and demeaned the professional status of nursing to servitude. She could not live with the dishonor or disrespect and chose to end her life.
On August 29, up to 150 student nurses walked out of the hospital to protest the disciplinary culture that led to Florentina’s death. Some believe politicians orchestrated the strike in the background, as on the same day the U.S. Congress enacted the Jones Law, which laid out the conditions for Philippine independence. One of these conditions was a stable government, and the strike indicated otherwise. In the student nurse’s petition to the hospital director, the most evident grievances surrounded the mandatory physical training course that began in June earlier that year and the associated punishments for absence and tardiness. On top of coursework and ward duty, all students were required to participate in calisthenics outdoors for forty-five minutes five times a week. The hospital director reasoned the course would overcome the physical weakness of Filipino nurses, whose bodies he deemed inferior to their American counterparts. He also considered the improved fitness of these nurses as a boon to the hospital’s efficiency.

In the aftermath of the two-day strike the director of civil service conducted an investigation. His report exonerated the hospital, which caused a public uproar. Shortly thereafter, the hospital director and nursing superintendent resigned, leading to the Filipinization of nursing services at the hospital. While the chain of events proves interesting, this particular moment in time must be examined within the history of PGH, a modern medical institution constructed under the American colonial government and its “benevolent” project of establishing the fitness of Filipinos for life under liberal modernity. Through this history, we can better understand the emotions, behaviors, and desires of the actors driving the development of professional nursing, the culture of discipline at the hospital, and the abledment of the Filipino nurse.
CN: The event touched many lives. In researching this subject, were you drawn to any particular event or individual’s story?

RC: One particular event that piqued my attention emerged from the investigative report on the strike, which included an analysis of past issues at PGH. One of the thematic problems reported was suicides and the alleged suicide attempts of Filipino nurses within the span of three years. I learned that Florentina was not the first suicide, as another nurse had died two years prior. There were also three cases of alleged suicide attempts. Through a nursing and (dis)ability lens, the pattern of mortality, or heightened risk of death, does not appear accidental but rather intentional. To me, all of the nurses in these cases felt pressured by being unable to live up to the ableist and racialized image of the ideal nurse. The affective labor of these nurses further stimulated my curiosity about the culture of discipline at the hospital and the various subjectivities formed under the pressure of the American model of nursing. These morbid accounts must be recounted with empathy. They provide necessary interventions to rupture the linear narrative of progress lauded by benevolent colonialism, the notion of care and nursing as inherently benign, and the image of the Filipino nurse as an object of care with an unfailing body.
CN: In your research at NLM what materials were most enlightening for you? Was there a particular document that stood out?

RC: For this research project, I found materials pertinent to detailing the institutional history of PGH and its training school, including the History and Description of the Philippine General Hospital: Manila, Philippine Islands, 1900 to 1911 and the 1913 and 1915 school catalogs. Furthermore, the NLM’s extensive collection of The Filipino Nurse , the professional journal of the Filipino Nurses Association (now the Philippine Nurses Association) dating back to 1926, greatly assisted me in exhuming the lived experience of Filipino nurses during the formative years of Philippine nursing. Despite the publishing start date, many of the pioneering nurses at the hospital would become leaders in the professional organization, so biographies and interviews of these nurses can be found dispersed across the journal’s issues.

Beyond this project, one item that caught my attention was the Philippines Nurses’ Directory published by the Filipino Nurses Association. This directory, more or less, compiles a list of all known nurses from 1911 to 1941, with entries including name, alma mater, graduation year, last known address, and current employment. Overall, I’m excited about harnessing the potential of this geospatial dataset through digital mapping.
Watch on YouTube
Ren Capucao’s presentation is part of our NLM History Talks , which promote awareness and use of the National Library of Medicine and other historical collections for research, education, and public service in biomedicine, the social sciences, and the humanities. All talks are live-streamed globally, and subsequently archived, by NIH VideoCasting . Stay informed about the lecture series on Twitter at #NLMHistTalk .
Circulate this:
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to share on Tumblr (Opens in new window)
- Click to share on Reddit (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
- Click to email a link to a friend (Opens in new window)
- Click to print (Opens in new window)
- Click to share on WhatsApp (Opens in new window)
- Click to share on Pocket (Opens in new window)
- Click to share on Telegram (Opens in new window)
Leave a Reply Cancel reply
This site uses Akismet to reduce spam. Learn how your comment data is processed .
Discover more from Circulating Now from the NLM Historical Collections
Subscribe now to keep reading and get access to the full archive.
Type your email…
Continue reading
Computer simulation predicts Australia's COVID-19 vaccine campaign prevented thousands of deaths before Omicron spread
COVID-19 vaccinations may have prevented almost 18,000 deaths among older Australians in NSW during the early Omicron era, new research has suggested.
A computer simulation carried out by researchers found the death rate "in the absence of a vaccination campaign" would have been approximately six times the actual total.
The research team, based out of universities in Melbourne and Tel Aviv, said in their report the campaign prevented 17,760 deaths among over-50s between August 2021 and July 2022.
"The Australian vaccination campaign was successful in reducing mortality over 2022," the report said.
The team attributed the success to "high levels of engagement" by Australians with the vaccination campaign and the achievement of high levels of vaccination just before the 2022 Omicron outbreak.
Their research used modelling of state and federal health department data to show the effect on over-50s in NSW in three scenarios:
- How many deaths could have been averted if complete vaccination had been achieved by July 28, 2021;
- How many deaths were averted by the booster vaccine rollout; and
- How many deaths would have occurred in the absence of vaccination
"Australia was relatively late in mass vaccinating its population … beginning its program on 22 February 2021," the report said.
"Four months later, less than five per cent of the population were fully vaccinated with two doses, making it the second-lowest vaccination coverage of any OECD nation at the time.
"Yet a few months later at the end of 2021, Australia had achieved one of the highest vaccination rates in the world, with more than 85 per cent of its eligible population fully vaccinated with at least two doses.
"Due to the rapid pace of the Australian roll-out [and] the very high public engagement with the program, vaccination coverage was at high levels when Omicron arrived."
The report predicted 440 deaths would have been prevented with earlier vaccination, while 1,860 deaths were prevented by the booster campaign.
In mid-2022, cross-checking of death certificates in NSW revealed the state's COVID-19 death toll was 2,433 as of April of the same year.
"In the [no vaccination campaign] scenario the entire population remains unvaccinated," the report said.
"In the complete absence of vaccination, the model predicts an almost immediate major outbreak of Delta, followed by an even more extreme outbreak in the Omicron period in January 2022.
"The predicted but hypothetical Delta outbreak would have reached a maximum of 15,000 cases and maximum of 500 deaths per week in the NSW 50+ population.
"The real Delta outbreak on the other hand had approximately 75 deaths per week."
Data at the time showed 82 per cent of deaths, around 270 people, occurred after January 2022 — when the Omicron wave was reaching its peak.
University of Melbourne epidemiologist Professor Tony Blakely said the rapid rush of vaccination before the Omicron variant began to spread was "good luck" for Australians.
"Australia was further lucky that when we opened up, Omicron was the circulating virus that was less lethal than [for example] Delta," he said.
"But this paper makes the important point that even Omicron, in an unvaccinated population, would have had a massive death toll.
"The estimated deaths averted in this paper are probably underestimates, as higher vaccination rates would have had positive spill over effects of reducing transmission.
"In future pandemics, we hope that vaccines will be good at both stopping you dying and stopping you transmitting the virus – as this would reduce the health loss even more."
Deakin University's Associate Professor in Epidemiology Hassan Vally said the study formed part of an "important" assessment of the roll-out.
"Whilst it can't be ignored that there were missteps, and there are things that could have been done better, it was a significant achievement that in Australia we were able to achieve one of the highest vaccination coverages globally," he said.
"Importantly, the study authors have been fully transparent about the various limitations of this study and highlight that further work needs to be done when better data becomes available."
The team noted their results "may be under-estimated and conservative" because actual death rates among unvaccinated Australians could have been impacted by herd immunity.
It also said the effects could have been affected by "potentially confounding factors [such] as age and comorbidity" in the over-50s age group.
Professor Paul Griffin, director of Infectious Diseases at Mater Health Services and a professor of medicine at the University of Queensland, said it was important to consider these limitations.
"While a really useful study in my opinion to show just how much benefit was likely obtained from the vaccination rollout in this country ... [it] used data from one state only, NSW," he said.
"It would be great to see a similar study from across the country as the experience with COVID-19 was not the same in all states.
"However there is not a single source of data that makes a larger study easy to do and NSW is the largest state.
"Modelling studies do not necessarily predict perfectly what would have actually happened.
"There are additional confounders that are difficult to take into account and the outcome from modelling is only as strong as the data that is put into the model, however in this case the data and methods seem robust."
The study has been published in peer-reviewed scientific journal PLOS ONE this week.
- X (formerly Twitter)
- Epidemics and Pandemics
- Vaccines and Immunity

IMAGES
COMMENTS
COVID-19 dynamics in the Philippines are driven by age, contact structure, mobility, and MHS adherence. Continued compliance with low-cost MHS should help the Philippines control the epidemic until vaccines are widely distributed, but disease resurgence may be occurring due to a combination of low population immunity and detection rates and new variants of concern.
The Philippines is contending with one of the worst COVID-19 outbreaks in southeast Asia. As of April 18, 2021, there were 926 052 cases of SARS-CoV-2 infection and 15 810 deaths recorded. WHO has warned that the country's health-care system risks being overwhelmed. From March 29, 2021, a new round of lockdown was implemented in Manila and four ...
Introduction The SARS-CoV-2, virus that caused the COVID-19 global pandemic, possesses a neuroinvasive potential. Patients with COVID-19 infection present with neurological signs and symptoms aside from the usual respiratory affectation. Moreover, COVID-19 is associated with several neurological diseases and complications, which may eventually affect clinical outcomes. Objectives The ...
This study was approved by the Research Ethics Board of the University of the Philippines Manila (UPMREB 2020-198-01). 2.3. Statistical analysis ... During the early phase of the COVID-19 pandemic in the Philippines, one-fourth of the respondents reported moderate-to-severe anxiety, one-seventh reported moderate-to-severe stress levels and one ...
The Philippine population of 110 million comprises a relatively young population. On May 22, 2021, the number of confirmed COVID-19 cases reported in the country is 1,171,403 with 55,531 active ...
Introduction. Coronavirus disease 2019 (COVID-19) was declared a global pandemic by the World Health Organization (WHO) on 12 March 2020 [].Current and published epidemiological research on COVID-19 has largely focused on China and other high-income countries such as South Korea, Japan, the USA, Italy and Spain [].Further research on the distribution and burden of COVID-19 in low- and middle ...
100 days of COVID-19 in the Philippines: How WHO supported the Philippine response. 9 May 2020. Exactly 100 days have passed since the first confirmed COVID-19 case was announced in the Philippines on 30 January 2020, with a 38-year old female from Wuhan testing positive for the novel coronavirus. On the same day, on the other side of the world ...
COVID-19 in the Philippines Situation Report 85. 13 September 2021. | Emergency Situational Updates. Download (2.8 MB)
The novel coronavirus disease 2019 (COVID-19, caused by SARS-CoV-2) has spread globally since its first report in Wuhan, China on December 31, 2019. On January 30, the Philippines reported its first two imported cases of COVID-19 in a couple from Wuhan. One of them died on February 1st, becoming the first COVID-19 death outside China.
WHO Philippines situation reports by date. 20 December 2023. COVID-19 in the Philippines Situation Report 142. 27 November 2023. COVID-19 in the Philippines Situation Report 141. 12 November 2023. COVID-19 in the Philippines Situation Report 140. 29 October 2023.
COVID-19 in the Philippines Abstract Lockdowns and policy actions to curtail the transmission of COVID-19 have widespread health system, economic, and societal impacts. ... Over the past year we partnered with research institutions in Kenya, the Philippines, South Africa, and Uganda to document, from a whole-of-health perspective, what we know ...
Responses of subnational government units are crucial in the containment of the spread of pathogens in a country. To mitigate the impact of the COVID-19 pandemic, the Philippine national government through its Inter-Agency Task Force on Emerging Infectious Diseases outlined different quarantine measures wherein each level has a corresponding degree of rigidity from keeping only the essential ...
Background: The 2019 coronavirus disease (COVID-19) pandemic poses a threat to societies' mental health. This study examined the prevalence of psychiatric symptoms and identified the factors contributing to psychological impact in the Philippines. Methods: A total of 1879 completed online surveys were gathered from March 28-April 12, 2020.
The COVID-19 pandemic in the Philippines was a part of the worldwide pandemic of coronavirus disease 2019 caused by severe acute respiratory syndrome ... By the end of January 2020, the Research Institute for Tropical Medicine (RITM) in Muntinlupa, Metro Manila began its testing operations and became the country's first testing ...
With the emergence of the highly transmissible Omicron variant, large-scale vaccination coverage is crucial to the national and global pandemic response, especially in populous Southeast Asian countries such as the Philippines and Malaysia where new information is often received digitally. The main aims of this research were to determine levels of hesitancy and confidence in COVID-19 vaccines ...
We comment on science advice in the political context of the Philippines during the COVID 19 pandemic. We focus on the independent science advisor OCTA Research, whose publicly available ...
Philippines Coronavirus disease (COVID-19) Situation Report #72, 19 March 2021. 19 March 2021. Situation report dated 19 March 2021; Situation summary • Out of a total 648,066 confirmed cases reported in the Philippines as of today, 54% are male, with the most affected age group 20-29 years (26%) followed by the age group 30-39 years (23.6%)
With a number of vaccines against COVID-19 now widely available globally, it is opportune to determine what tips the decision to get vaccinated. In most countries like the Philippines where the government provides these vaccines for free to all its citizens, their COVID-19 vaccine awareness and COVID-19 information sources as well as their socio-demographic profile were considered as primary ...
In contrast, Chinese respondents requested more health information about COVID-19. For the Philippines, student status, low confidence in doctors, dissatisfaction with health information, long daily duration spent on health information, worries about family members contracting COVID-19, ostracization, and unnecessary worries about COVID-19 were ...
Low- and middle-income countries (LMICs) with weak health systems are especially vulnerable during the COVID-19 pandemic. In this paper, we describe the challenges and early response of the Philippine Government, focusing on travel restrictions, community interventions, risk communication and testing, from 30 January 2020 when the first case was reported, to 21 March 2020.
The first suspected case in the Philippines was investigated on January 22, 2020, and 633 suspected cases were reported as of March 1. We describe the clinical and epidemiological aspects of the first two confirmed COVID-19 cases in the Philippines, both admitted to the national infectious disease referral hospital in Manila.
The sudden lockdown and social isolation caused by the COVID-19 pandemic substantially affected the physical and psychological aspects of our lives. This study used a sequential explanatory research design to explore how human-animal interactions (HAI) can reduce stress and improve quality of life (QOL) for employees working from home during the period. A total of 770 respondents took part ...
WASHINGTON — A new report from the National Academies of Sciences, Engineering, and Medicine reviews evidence for 19 potential harms of the COVID-19 vaccines, and for nine potential shoulder injuries from intramuscular administration of vaccines more broadly. The committee that conducted the review identified sufficient evidence to draw 20 conclusions about whether these vaccines could cause ...
Mounting evidence continues to show that COVID-19 may have originated from a lab in Wuhan, China. Dr. Robert Redfield, former director of the U.S. Centers for Disease Control and Prevention (CDC), testified how science indicates COVID-19 infections were likely the result of an accidental lab leak in Wuhan. His conclusion is based on the biology ...
How aging adults spend their time. 59% spend more time at home than before pandemic; 41% go to the grocery less often; 75% eat out less often ; 57% exercise indoors less often; 62% visit an arts or cultural site less often; 53% attend religious services less often; 10% exercise outdoors more often; Source: Data from COVID-19 Coping Study survey results from May 2022. A more recent survey found ...
According to the publisher's analysis, although COVID -19 has had a certain adverse impact on the Philippine fertilizer industry in 2020-2021, in 2022-2023, the Philippine fertilizer industry has ...
Philippine ocean-based industries grew by 21.1% in 2022, accounting for 3.9% of the country's economic output, according to the state statistics agency. But local economists have said the country should do more to maximize the bene f its from the ocean.
As coursework went virtual due to the COVID-19 pandemic, I determined this was the best time to undergo my first nursing position. I worked as a pediatric nurse at the Virginia Commonwealth University Health System until I received a Fulbright fellowship to conduct historical and ethnographical research at the University of the Philippines ...
In short: A new research study suggests the COVID-19 vaccine campaign prevented 17,760 deaths among NSW residents aged 50 years and over. The study used computer modelling to predict the death ...