Login to your account
If you don't remember your password, you can reset it by entering your email address and clicking the Reset Password button. You will then receive an email that contains a secure link for resetting your password
If the address matches a valid account an email will be sent to __email__ with instructions for resetting your password

Current Issue Links
Articles in press.
- Past Issues
Submit Mobile
- Submit article Opens in new window
- Press Releases
- Special Issues Opens in new window
- Submit Article Opens in new window
- Aims and Scope
- For Authors
- Supports Open Access
- NSF Twitter Opens in new window
- Sleep Health Twitter Opens in new window
- NSF Opens in new window
Webinar on Sleep Assessment via actigraphy

Missed our webinar? Watch it today! Opens in new window
Join Dr. Mathias Basner as he discusses this important topic with engaging group of experts on Sleep Assessment via actigraphy.
Trajectories of sleep duration and quality and their association with mild cognitive impairment, frailty, and all-cause mortality
The importance of sleep regularity: a consensus statement of the National Sleep Foundation sleep timing and variability panel
Performance of wearable sleep trackers during nocturnal sleep and periods of simulated real-world smartphone use
A comparison of perceived barriers to optimal child sleep among families with low and high income, sleep health journal article highlights differences between adults reporting sleeping issues to healthcare providers.
Washington, D.C. (October 11, 2023): New research published in the National Sleep Foundation’s (NSF) Sleep Health journal shows differences in sex, race, education, and other factors between adults at high risk of obstructive sleep apnea (OSA) who have and have not reported trouble sleeping to a healthcare provider.
Sleep Health Journal Article Highlights Association Between Bedtime Procrastination and Sleep Health
Washington, D.C. (September 13, 2023): New research published in the National Sleep Foundation’s (NSF) Sleep Health journal shows bedtime procrastination was associated with poorer sleep health.
National Sleep Foundation Reinforces Consistent Sleep Schedules with New Consensus Guideline
Washington, D.C. (September 6, 2023): The National Sleep Foundation (NSF) issued a new guideline emphasizing the benefit of consistent sleep schedules on health and performance.
Sleep Health Journal Article Highlights Association Between Experiencing Discrimination and Poorer Sleep
Washington, D.C. (July 25, 2023) : New research published in the National Sleep Foundation’s (NSF) Sleep Health journal shows experiencing discrimination is associated with poorer sleep. Discrimination is associated with higher anxiety and lower social well-being which are associated with poorer sleep.
More Press Releases
Sleep Health: Journal of the National Sleep Foundation
About the national sleep foundation.

The National Sleep Foundation (NSF) is dedicated to improving health and well-being through sleep education and advocacy. Founded in 1990, NSF is committed to advancing excellence in sleep health theory, research and practice. theNSF.org Opens in new window SleepHealthJournal.org Opens in new window .
Free access to Volume 6 / Issue 4 of Sleep Health. The latest issue of the National Sleep Foundation’s Sleep Health Journal features a collection of new research studies that add to the evidence base for racial, ethnic, and socioeconomic disparities in sleep health. Read & Download the articles here .
- More Journal Metrics Opens in new window
- Submit a Manuscript Opens in new window
- Top Social Media Articles
- Time to Online Publication

About the Cover Art

Sleep Health Webinars
Sleep, Emotions and Physical Activity Opens in new window
Sleep and the Family System Opens in new window
Sleep Health During COVID-19 Pandemic Webinar Opens in new window

Position Statement
Read NSF’s Sleep Health Equity Position Statement Opens in new window
Development of the Couples' Sleep Conflict Scale: A new tool to assess conflict around sleep in romantic relationships
Self-reported neighborhood stressors and sleep quality among puerto rican young adults.
Which adolescents are more likely to complete home-based sleep manipulation trials?
Most read (last 30 days).
National Sleep Foundation’s sleep time duration recommendations: methodology and results summary
The national sleep foundation's sleep health index.
Associations of time spent on homework or studying with nocturnal sleep behavior and depression symptoms in adolescents from Singapore
Is there an association between daytime napping, cognitive function, and brain volume? A Mendelian randomization study in the UK Biobank
Adolescent use of social media and associations with sleep patterns across 18 European and North American countries
Most cited (previous 3 years).
- Access for Developing Countries
- Articles & Issues
- Articles In Press
- Current Issue
- List of Issues
- Special Issues
- Supplements
- Author Information
- Download Conflict of Interest Form
- Researcher Academy
- Submit a Manuscript
- Style Guidelines for In Memoriam
- Download Online Journal CME Program Application
- NSF CME Mission Statement
- Professional Practice Gaps in Sleep Health
- Journal Info
- About the Journal
- Activate Online Access
- Information for Advertisers
- Career Opportunities
- Editorial Board
- New Content Alerts
- More Periodicals
- Find a Periodical
- Go to Product Catalog
The content on this site is intended for healthcare professionals.
- Privacy Policy
- Terms and Conditions
- Accessibility
- Help & Contact

- Search by keyword
- Search by citation
Page 1 of 2
Sex-specific prevalence and correlates of possible undiagnosed obstructive sleep apnea in rural Canada
Obstructive Sleep Apnea (OSA) has been under-investigated in rural communities, particularly through a sex/gender lens. The purpose of this study was to examine the prevalence and correlates of OSA risk among ...
- View Full Text
A preliminary study of factors influencing the occurrence of post-arousal hypersynchrony
Post-arousal hypersynchrony (PAH) is a continuous delta wave occurring after arousal. We hypothesized that PAH would decrease with age because PAH is affected by sleep pressure, which decreases with age.
Evaluation of psychometric properties of sleep quality questionnaire among medical students of Guilan University of Medical Sciences
Since evaluating sleep quality among students is of great importance and is one of the challenges facing the health field regarding this group, we were determined to conduct this study to evaluate the psychome...
Didge you sleep: a feasibility study of didgeridoo training for obstructive sleep apnea
Intolerance of positive airway pressure therapy for obstructive sleep apnea is common. Upper airway muscle therapies show promise as alternative treatments. The didgeridoo, which is a musical instrument, can b...
Synthesizing the risk of morbidities and lifestyle factors on insomnia symptoms among middle-aged and older adult persons in India
Most of the time increasing age and improper lifestyle enhance the burgeoning health challenge for middle-aged and older adult persons. In this way, the present study seeks to know the association of morbidity...
Associations between circadian, sleep, and mood disturbances in Uruguayan dance students
Current evidence supports associations between circadian, sleep, and mood disturbances. However, it is still debated to what extent different chronobiological and mood variables act independently or in synergy...
Anthropometric screening approach for obstructive sleep apnea in Japanese men: development and validation of the ABC scale
The existing screening tools for the detection of moderate and severe obstructive sleep apnea (OSA) are tailored to Western individuals. The aim of this study was to formulate and validate a simple anthropomet...
Comparison of the clinical and electrophysiological characteristics between type 1 and type 2 narcolepsy: a cross-sectional study
Narcolepsy is a chronic brain disease characterized by excessive sleepiness and classified into two types based on the presence of cataplexy or reduced level of cerebrospinal fluid orexin-A (hypocretine-1): na...
The effect of nutrition and physical activity on sleep quality among adults: a scoping review
Sleep quality and its effects have become a public concern over the last few years. While the prevalence of sleep disorders was increasing, several studies have linked diet and physical activity as a cause of ...
Understanding daytime functioning in insomnia: responder and correlation analyses in patients treated with daridorexant
Improving daytime functioning is a key treatment goal for patients with insomnia disorder. In a phase 3 study, using the Insomnia Daytime Symptoms and Impacts Questionnaire (IDSIQ), daridorexant 50 mg signific...
Hyperactivity in patients with narcolepsy and idiopathic hypersomnia: an exploratory study
Patients with either Idiopathic Hypersomnia or Narcolepsy demonstrate excessive daytime somnolence (EDS) with resultant inattention mimicking Attention Deficit Hyperactivity Disorder (ADHD). Patients with ADHD...
Gender differences in obstructive sleep apnea with comorbid treatment-resistant depression
A bidirectional relationship between major depression and obstructive sleep apnea (OSA) has been established, suggesting the possibility of overlapping and compounding disease processes. Depression, however, w...
Impairment in sleep health in young adults with chronic pain: a modifiable risk factor
Impairments in sleep health are associated with the development or worsening of chronic pain. Further, chronic pain can cause sleep health disruption by impacting sleep onset, sleep maintenance, sleep quality,...
Sleep as a vital sign
Sleep is causally linked to the maintenance of every major physiological body system and disturbed sleep contributes to myriad diseases. The problem is, however, is that patients do not consistently, nor spont...
Clinical application of headache impact test (HIT)-6 and epworth sleepiness scale (ESS) for sleep apnea headache
Sleep apnea headache is a major symptom accompanying obstructive sleep apnea (OSA), but relatively little evidence has been reported on the magnitude of its negative effects on patients or the evaluation of th...
From good sleep to health and to quality of life – a path analysis of determinants of sleep quality of working adults in Abu Dhabi
Sleep quality has significant impacts on many aspects of quality of life. Therefore, identifying the association of sleep quality with that quality of life domains could lead to deeper insights for social poli...
Lingering impacts on sleep following the Daylight Savings Time transition in the Project Baseline Health Study
The “spring forward” change to Daylight Savings Time (DST) has been epidemiologically linked with numerous health and safety risks in the days following the transition, but direct measures of sleep are infrequ...
The relationship between perinatal circadian rhythm and postnatal depression: an overview, hypothesis, and recommendations for practice
Postnatal depression (PND) is an important public health problem with far-reaching consequences for mothers, families, and society. Current treatment approaches tend to focus on the depressive symptoms of the ...
Sleep quality and associated factors among type 2 Dm patients and non-Dm individuals in Bahir Dar governmental hospitals: comparative cross-sectional study
Multiple factors may contribute to sleep disruption among individuals with type 2 diabetes mellites. Sleep disruption among individuals with type 2 diabetes mellites is frequently associated with long-term dam...
Prevalence and associated factors of sleep deprivation among Haramaya University students, Ethiopia, 2021: cross-sectional study
Sleep deprivation is the lack of sleep that is associated with an increased risk of cardiovascular illness, diabetes, obesity, cognitive impairment, vehicle accidents, and workplace accidents, as well as being...
Chinese translation and validation of the adolescent sleep wake scale
Inadequate sleep is a problem for teens world-wide. Identifying the biological and cultural factors that underlie this phenomenon is dependent on tools that can accurately query sleep-related behaviors. While ...
Poor sleep quality and associated factors among pregnant women on antenatal care follow up at Nekemte Referral Hospital and Wollega University Hospital, Nekemte, Ethiopia, 2019: a cross-sectional study
Sleep disturbances are common in women, especially during pregnancy. This can result in emotional and psychological consequences for pregnant women, and it could lead to some serious complications for both mot...
Correction: Measurement properties of the minimal insomnia symptom scale (MISS) in adolescents
The original article was published in Sleep Science and Practice 2022 6 :5
The prevalence of obstructive sleep apnea in patients with type 2 diabetes: a systematic review and meta-analysis
Obstructive Sleep Apnea (OSA) is one of the diseases related to diabetes. Considering the varying prevalence of OSA in patients with type 2 diabetes in different parts of the world, in order to aggregate the r...
Measurement properties of the minimal insomnia symptom scale (MISS) in adolescents
The Minimal Insomnia Symptom Scale (MISS) is a three-item screening instrument that has been found to be psychometrically sound and capable of screening for insomnia among adults and older people. This study a...
The Correction to this article has been published in Sleep Science and Practice 2022 6 :8
In-office communication about excessive daytime sleepiness associated with treated obstructive sleep apnea: insights from an ethnographic study of physician-patient visits
Excessive daytime sleepiness (EDS), a primary symptom of obstructive sleep apnea (OSA), negatively affects functioning and quality of life (QoL). EDS can persist despite primary airway therapy, and often remai...
Effects of mattress support on sleeping position and low-back pain
To determine the efficacy of decreasing spinal curvature – when sleeping laterally – in reducing low-back pain (LBP) and improving sleep quality in people with chronic LBP. Secondly, to investigate whether sle...
Quantitative effects of head rotation angle on apnea hypopnea index in positional obstructive sleep apnea – a preliminary case series
Quantify the effects of head rotation and head incline on obstructive sleep apnea (OSA) severity.
Objectively-measured sleep patterns and cardiometabolic health in a rural South African setting: a cross sectional analysis
To investigate the relationship between objectively-measured, free-living sleep patterns, and cardiometabolic health, in a rural South African health and demographic surveillance site.
Obstructive sleep apnea and associated factors among hypertensive patients attending a tertiary cardiac center in Tanzania: a comparative cross-sectional study
There is mounting evidence for a reciprocal yet bidirectional association between sleep-disordered breathing and hypertension. Obstructive sleep apnea (OSA), a common cause of systemic hypertension is an indep...
Correlations between sleep disturbance and brain cortical morphometry in healthy children
While the importance of adequate sleep duration to normal brain development is well known, more studies are needed to characterize how undiagnosed sleep disturbance other than suboptimal sleep duration may imp...
Sleep apnea and unilateral upper and lower extremity allodynia as a result of a large thoracic disc herniation: a case report
Clinically significant disc herniations in the thoracic spine are rare accounting for approximately 1% of all disc herniations. In patients with significant spinal cord compression, presenting symptoms typical...
Human blood serum proteome changes after 6 hours of sleep deprivation at night
The aim of this study was to discover significantly changed proteins in human blood serum after loss of 6 h sleep at night. Furthermore, to reveal affected biological process- and molecular function categories...
Palmitoylethanolamide for sleep disturbance. A double-blind, randomised, placebo-controlled interventional study
Sleep is essential for wellbeing, yet sleep disturbance is a common problem linked to a wide range of health conditions. Palmitoylethanolamide (PEA) is an endogenous fatty acid amide proposed to promote better...
Sleep during infancy, inhibitory control and working memory in toddlers: findings from the FinnBrain cohort study
Sleep difficulties are associated with impaired executive functions (EFs) in school-aged children. However, much less is known about how sleep during infancy relates to EF in infants and toddlers. The aim of t...
Revisiting level II sleep studies in the era of COVID-19: a theoretical economic decision model in patients with suspected obstructive sleep apnea
The recent pandemic has made it more challenging to assess patients with suspected obstructive sleep apnea (OSA) with in laboratory polysomnography (PSG) due to concerns of patient and staff safety. The purpos...
Case report: fast reversal of malignant obesity hypoventilation syndrome after noninvasive ventilation and pulmonary rehabilitation
Malignant obesity hypoventilation syndrome (MOHS) is described as a subtype condition of OHS, characterized by extreme obesity, obese-related hypoventilation, and multiorgan dysfunction. Because of low awarene...
Energy cost of walking and functional aerobic capacity during moderate intensity exercise in adults with obstructive sleep apnea: a cross-sectional study
Autonomic dysregulation associated with obstructive sleep apnea (OSA) may limit cardiopulmonary responses to exercise, which, in turn, may impair functional aerobic capacity (FAC) and walking economy. We aimed...
Self-administered electroencephalography-based sleep assessment: compliance and perceived feasibility in children and adults
Sleep is a crucial part of our lives and insufficient sleep has been linked to several health disorders in both children and adults. However, most studies are based on single night laboratory polysomnography, ...
Magnitude and correlates of sleep quality among undergraduate medical students in Ethiopia: cross –sectional study
Poor quality of sleep has a negative effect on academic performance of medical students. Quantity and quality of sleep in addition to average sleep time are strongly linked with students’ learning abilities, p...
Correction to: Transcranial magnetic stimulation therapeutic applications on sleep and insomnia: a review
An amendment to this paper has been published and can be accessed via the original article.
The original article was published in Sleep Science and Practice 2021 5 :3
Transcranial magnetic stimulation therapeutic applications on sleep and insomnia: a review
Repetitive transcranial magnetic stimulation (rTMS) is a neuromodulatory technique approved by the US Food and Drug Administration for use in treatment-resistant major depressive disorder. It works by generati...
The Correction to this article has been published in Sleep Science and Practice 2021 5 :6
Changes in insomnia as a risk factor for the incidence and persistence of anxiety and depression: a longitudinal community study
The aim of this investigation was to examine the longitudinal association between change in insomnia status and the development of anxiety and depression in the general population.
Association between cardiometabolic health and objectively-measured, free-living sleep parameters: a pilot study in a rural African setting
To investigate the relationship between objectively-measured, free-living sleep quantity and quality, and cardiometabolic health, in a rural African setting in 139 adults (≥40 years, female: n = 99, male: n = 40)...
Quality of sleep and associated factors among people living with HIV/AIDS on follow up at Ethiopian Zewditu memorial hospital, 2018
Sleep disturbance is a common complaint in people living with HIV/AIDS. Despite the influence of sleep disturbance on treatment adherence, quality of life, work productivity, risk of chronic illness, it remain...
Cardiac function and cognitive function in patients with obstructive sleep apnea
This study was designed to evaluate echocardiographic findings in patients with obstructive sleep apnea (OSA) with cognitive impairment and compare it with the control group.
An automatic estimation of the rest-interval for MotionWatch8© using uniaxial movement and lux data
Poor sleep is linked with chronic conditions common in older adults, including diabetes, heart disease, and dementia. Valid and reliable field methods to objectively measure sleep are thus greatly needed to ex...
Prevalence of high risk obstructive sleep apnoea by Berlin questionnaire in patients with hypertension: study from a tertiary care hospital
Obstructive Sleep Apnoea (OSA), a condition characterized by a complete or partial cessation of airflow during sleep, can cause various cardiovascular disorders including hypertension. The aim of the study was...
The anti-snoring bed - a pilot study
Avoiding supine position can reduce snoring in most habitual snorers. However, devices that restrict the sleeping position cause discomfort or disrupt sleep resulting in low compliance. Therefore, mechanisms, ...
Sensory stimulation in the treatment of children with sleep-related rhythmic movement disorder: a feasibility and acceptability study
Sleep-related rhythmic movement disorder is characterized by repetitive gross-motor movements at sleep onset or during sleep, which result in clinical consequences such as impact on daytime functioning and inj...
- Editorial Board
- Manuscript editing services
- Instructions for Editors
- Sign up for article alerts and news from this journal
Annual Journal Metrics
2023 Speed 23 days submission to first editorial decision for all manuscripts (Median) 135 days submission to accept (Median)
2023 Usage 195,913 downloads 89 Altmetric mentions
Sleep Science and Practice
ISSN: 2398-2683
- General enquiries: [email protected]
- Search Menu
- Advance Articles
- Supplements
- Editor's Choice
- Virtual Issues
- Virtual Roundtables
- Abstract Supplements
- Basic Science
- Circadian Disorders
- Cognitive, Affective and Behavioral Neuroscience of Sleep
- Neurological Disorders
- Sleep Across the Lifespan
- Sleep and Metabolism
- Sleep Disordered Breathing
- Sleep Health and Safety
- Author Guidelines
- Instructions for Reviewers
- Submission Site
- Open Access Options
- Additional Resources
- Self-Archiving Policy
- About SLEEP
- Editorial Board
- Dispatch Dates
- Permissions
- Advertising & Corporate Services
- Journals Career Network
- Reprints and ePrints
- Sponsored Supplements
- Journals on Oxford Academic
- Books on Oxford Academic

Advance articles
Is sleep the new treatment for pain two issues need resolving before deciding.
- View article
REM sleep is reduced in late middle-aged and older APOE4 allele carriers
- Supplementary data
Association between Longitudinal Change of Sleep Patterns and the Risk of Cardiovascular Diseases
The nfκb dif is required for behavioral and molecular correlates of sleep homeostasis in drosophila, effect of dynamic binaural beats on sleep quality: a proof-of-concept study with questionnaire and biosignals, clinical efficacy and safety of intravenous ferric carboxymaltose for treatment of restless legs syndrome: a multicenter, randomized, placebo-controlled clinical trial, pathogenesis of sleep disordered breathing in the setting of opioid use: a multiple mediation analysis using physiology, the dynamic responses of mood and sleep physiology to chronic sleep restriction and subsequent recovery sleep, longer sleep duration in alzheimer’s disease progression: a compensatory response, insomnia gone in one week, without medication: too good to be true, daily associations between salivary cortisol and eeg-assessed sleep: a 15-day intensive longitudinal study, effects of a work schedule with abated quick returns on insomnia, sleepiness and work-related fatigue: results from a large-scale cluster randomized controlled trial, perturbation of the insomnia wdr90 gwas locus pinpoints rs3752495 as a causal variant influencing distal expression of neighboring gene, pig-q, sphyncs: feasibility of long-term monitoring with fitbit smartwatches in central disorders of hypersomnolence and extraction of digital biomarkers in narcolepsy, correction to: sleepmat: a new behavioral analysis software program for sleep and circadian rhythms, heart rate variability analysis in obstructive sleep apnoea patients with daytime sleepiness, longer sleep duration and neuroinflammation in at-risk elderly with a parental history of alzheimer's disease, electroencephalography connectome changes in chronic insomnia disorder are correlated with neurochemical signatures, thermoneutral temperature exposure enhances slow wave sleep with a correlated improvement in amyloid pathology in a triple-transgenic mouse model of alzheimer’s disease, increased flow limitation during sleep is associated with decreased psychomotor vigilance task performance in individuals with suspected obstructive sleep apnea: a multi-cohort study, cognitive behavioral therapy for insomnia works: but do we have product-market fit, the unique vulnerabilities of nighttime smartphone use: a commentary on “tracked and self-reported nighttime smartphone use, general health, and healthcare utilization: results from the smartsleep study” by drews et al., correction to: the effect of total sleep deprivation on working memory: evidence from diffusion model, the role of actigraphy in detecting and characterizing the early phases of alzheimer’s disease, eeg rhythmic and arrhythmic spectral components and functional connectivity at resting state may predict the development of synucleinopathies in idiopathic rem sleep behavior disorder, electroencephalographic spectro-spatial covariance patterns related to phenoconversion in isolated rapid eye movement sleep behavior disorder and their longitudinal trajectories in α-synucleinopathies, spindle-slow wave coupling and problem-solving skills: impact of age, the wake intrusion index: a new approach to arousals, a new perspective on insomnia, con: can comparing adherent to non-adherent patients provide useful estimates of the effect of continuous positive airway pressure, pro: comparing adherent to non-adherent patients can provide useful estimates of the effect of continuous positive airway pressure on cardiovascular outcomes, not there yet; the challenge of treating sleep-disordered breathing in people living with spinal cord injury/disease, sleep-slow oscillation-spindle coupling precedes spindle-ripple coupling during development, narcolepsy type 2: phenotype is fundamental, most dynorphin neurons in the zona incerta-perifornical area are active in waking relative to non-rapid-eye movement and rapid-eye movement sleep, circadian photoentrainment varies by season and depressed state: associations between light sensitivity and sleep and circadian timing, actigraphic sleep dimensions and associations with academic functioning among adolescents.

Is neurotrauma-related rapid eye movement behavior disorder a harbinger of synucleinopathy?
An online behavioral self-help intervention rapidly improves acute insomnia severity and subjective mood during the coronavirus disease-2019 pandemic: a stratified randomized controlled trial, insomnia medications for children, adolescents, and young adults: shedding light in the darkness, psychiatric comorbidities and prescribing tendencies of sleep medications and related medications in young people with insomnia: a united states commercial claims-based analysis, is napping in older adults problematic or productive the answer may lie in the reason they nap., intensive support does not improve positive-airway pressure use in spinal cord injury/disease: a randomized clinical trial.

When shall we intervene to prevent insomnia development among minoritized youth?: the earlier, the better
Changes in electroencephalographic microstates between evening and morning are associated with overnight sleep slow waves in healthy individuals, electroencephalographic slowing during rem sleep in older adults with subjective cognitive impairment and mild cognitive impairment, evaluating a novel 24-hour rest/activity rhythm marker of preclinical β-amyloid deposition, data-driven, generalizable prediction of adolescent sleep disturbances in the multisite adolescent brain cognitive development study, keeping the balance: the benefits of catch-up sleep versus the risks of sleep irregularity, tracked and self-reported nighttime smartphone use, general health, and healthcare utilization: results from the smartsleep study, medication-induced central sleep apnea: a unifying concept, wake intrusions in the electroencephalogram: a novel application of the odds ratio product in identifying subthreshold arousals, eeg-based machine learning models for the prediction of phenoconversion time and subtype in isolated rapid eye movement sleep behavior disorder, daily light exposure profiles and the association with objective sleep quality in patients with parkinson’s disease: the phase study, a patient-enriched meis1 coding variant causes a restless legs syndrome-like phenotype in mice.

Latency To N3 Interruption In Arousal Disorders
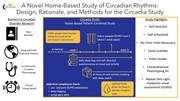
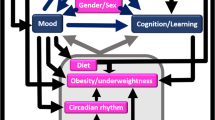
Sleep as a prognostic factor in low back pain: a systematic review of prospective cohort studies and secondary analyses of randomized controlled trials, racial/ethnic disparities in the trajectories of insomnia symptoms from childhood to young adulthood, efficacy of intravenous iron for restless legs syndrome—moving beyond monotherapy and into the “real world”, white matter integrity in narcolepsy: the structural blueprint for functional complaints, waking up to sleep extension for cardiometabolic health, narcolepsy severity scale-2 and idiopathic hypersomnia severity scale to better quantify symptoms severity and consequences in narcolepsy type 2, comorbid neurotrauma increases neurodegenerative-relevant cognitive, motor, and autonomic dysfunction in patients with rapid eye movement sleep behavior disorder: a substudy of the north american prodromal synucleinopathy consortium, disrupted topological properties of structural brain networks present a glutamatergic neuropathophysiology in people with narcolepsy, a mouse model of meis1-associated restless legs syndrome: insights and challenges, sleep and insulin sensitivity in adolescents at risk of type 2 diabetes: the sleep manipulation in adolescents at risk of type 2 diabetes randomized crossover study, napping and circadian sleep–wake regulation during healthy aging, the organization of sleep–wake patterns around daily schedules in college students, what is cataplexy, hypoxia not ahi in adults with sleep apnea midlife markedly increases risk of late-onset epilepsy—carosella cm et al sleep apnea, hypoxia, and late-onset epilepsy: the atherosclerosis risk in communities study sleep-2023-0175.r1, phenomenology and psychiatric correlates of pseudocataplexy, sleep apnea, hypoxia, and late-onset epilepsy: the atherosclerosis risk in communities study, a novel home-based study of circadian rhythms: design, rationale, and methods for the circadia study.
Restless Legs Syndrome in Patients with Epilepsy: Risk analysis, Polysomnography, and Quality of Life evaluation

PRO: Home Sleep Studies in Children – Are We There Yet?
Con: home sleep studies in children – are we there yet, sleep is a fire with smoke: time to incorporate sleep as a fundamental component in cancer treatment protocols, the effect of adenotonsillectomy and rapid maxillary expansion on the upper airway in pediatric obstructive sleep apnea: a randomized crossover-controlled trial, use of a blinded hypnotic tapering strategy to promote hypnotic discontinuation, email alerts.
- Recommend to Your Librarian
- Advertising and Corporate Services
Affiliations
- Online ISSN 1550-9109
- Print ISSN 0161-8105
- Copyright © 2024 Sleep Research Society
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 01 October 2019
Sleep quality, duration, and consistency are associated with better academic performance in college students
- Kana Okano 1 ,
- Jakub R. Kaczmarzyk 1 ,
- Neha Dave 2 ,
- John D. E. Gabrieli 1 &
- Jeffrey C. Grossman ORCID: orcid.org/0000-0003-1281-2359 3
npj Science of Learning volume 4 , Article number: 16 ( 2019 ) Cite this article
426k Accesses
119 Citations
1717 Altmetric
Metrics details
Although numerous survey studies have reported connections between sleep and cognitive function, there remains a lack of quantitative data using objective measures to directly assess the association between sleep and academic performance. In this study, wearable activity trackers were distributed to 100 students in an introductory college chemistry class (88 of whom completed the study), allowing for multiple sleep measures to be correlated with in-class performance on quizzes and midterm examinations. Overall, better quality, longer duration, and greater consistency of sleep correlated with better grades. However, there was no relation between sleep measures on the single night before a test and test performance; instead, sleep duration and quality for the month and the week before a test correlated with better grades. Sleep measures accounted for nearly 25% of the variance in academic performance. These findings provide quantitative, objective evidence that better quality, longer duration, and greater consistency of sleep are strongly associated with better academic performance in college. Gender differences are discussed.
Similar content being viewed by others
Effect of sleep and mood on academic performance—at interface of physiology, psychology, and education
Kosha J. Mehta
A 4-year longitudinal study investigating the relationship between flexible school starts and grades
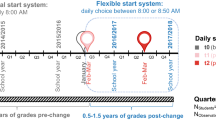
Anna M. Biller, Carmen Molenda, … Eva C. Winnebeck

Macro and micro sleep architecture and cognitive performance in older adults
Ina Djonlagic, Sara Mariani, … Shaun M. Purcell
Introduction
The relationship between sleep and cognitive function has been a topic of interest for over a century. Well-controlled sleep studies conducted with healthy adults have shown that better sleep is associated with a myriad of superior cognitive functions, 1 , 2 , 3 , 4 , 5 , 6 including better learning and memory. 7 , 8 These effects have been found to extend beyond the laboratory setting such that self-reported sleep measures from students in the comfort of their own homes have also been found to be associated with academic performance. 9 , 10 , 11 , 12 , 13
Sleep is thought to play a crucial and specific role in memory consolidation. Although the exact mechanisms behind the relationship between sleep, memory, and neuro-plasticity are yet unknown, the general understanding is that specific synaptic connections that were active during awake-periods are strengthened during sleep, allowing for the consolidation of memory, and synaptic connections that were inactive are weakened. 5 , 14 , 15 Thus, sleep provides an essential function for memory consolidation (allowing us to remember what has been studied), which in turn is critical for successful academic performance.
Beyond the effects of sleep on memory consolidation, lack of sleep has been linked to poor attention and cognition. Well-controlled sleep deprivation studies have shown that lack of sleep not only increases fatigue and sleepiness but also worsens cognitive performance. 2 , 3 , 16 , 17 In fact, the cognitive performance of an individual who has been awake for 17 h is equivalent to that exhibited by one who has a blood alcohol concentration of 0.05%. 1 Outside of a laboratory setting, studies examining sleep in the comfort of peoples’ own homes via self-report surveys have found that persistently poor sleepers experience significantly more daytime difficulties in regards to fatigue, sleepiness, and poor cognition compared with persistently good sleepers. 18
Generally, sleep is associated with academic performance in school. Sleep deficit has been associated with lack of concentration and attention during class. 19 While a few studies report null effects, 20 , 21 most studies looking at the effects of sleep quality and duration on academic performance have linked longer and better-quality sleep with better academic performance such as school grades and study effort. 4 , 6 , 9 , 10 , 11 , 12 , 13 , 22 , 23 , 24 , 25 , 26 , 27 Similarly, sleep inconsistency plays a part in academic performance. Sleep inconsistency (sometimes called “social jet lag”) is defined by inconsistency in sleep schedule and/or duration from day to day. It is typically seen in the form of sleep debt during weekdays followed by oversleep on weekends. Sleep inconsistency tends to be greatest in adolescents and young adults who stay up late but are constrained by strict morning schedules. Adolescents who experience greater sleep inconsistency perform worse in school. 28 , 29 , 30 , 31
Although numerous studies have investigated the relationship between sleep and students’ academic performance, these studies utilized subjective measures of sleep duration and/or quality, typically in the form of self-report surveys; very few to date have used objective measures to quantify sleep duration and quality in students. One exception is a pair of linked studies that examined short-term benefits of sleep on academic performance in college. Students were incentivized with offers of extra credit if they averaged eight or more hours of sleep during final exams week in a psychology class 32 or five days leading up to the completion of a graphics studio final assignment. 33 Students who averaged eight or more hours of sleep, as measured by a wearable activity tracker, performed significantly better on their final psychology exams than students who chose not to participate or who slept less than eight hours. In contrast, for the graphics studio final assignments no difference was found in performance between students who averaged eight or more hours of sleep and those who did not get as much sleep, although sleep consistency in that case was found to be a factor.
Our aim in this study was to explore how sleep affects university students’ academic performance by objectively and ecologically tracking their sleep throughout an entire semester using Fitbit—a wearable activity tracker. Fitbit uses a combination of the wearer’s movement and heart-rate patterns to estimate the duration and quality of sleep. For instance, to determine sleep duration, the device measures the time in which the wearer has not moved, in combination with signature sleep movements such as rolling over. To determine sleep quality, the Fitbit device measures the wearer’s heart-rate variability which fluctuates during transitions between different stages of sleep. Although the specific algorithms that calculate these values are proprietary to Fitbit, they have been found to accurately estimate sleep duration and quality in normal adult sleepers without the use of research-grade sleep staging equipment. 34 By collecting quantitative sleep data over the course of the semester on nearly 100 students, we aimed to relate objective measures of sleep duration, quality, and consistency to academic performance from test to test and overall in the context of a real, large university college course.
A secondary aim was to understand gender differences in sleep and academic performance. Women outperform men in collegiate academic performance in most subjects 35 , 36 , 37 , 38 and even in online college courses. 39 Most of the research conducted to understand this female advantage in school grades has examined gender differences in self-discipline, 40 , 41 , 42 and none to date have considered gender differences in sleep as a mediating factor on school grades. There are inconsistencies in the literature on gender differences in sleep in young adults. While some studies report that females get more quantity 43 but worse quality sleep compared with males, 43 , 44 other studies report that females get better quality sleep. 45 , 46 In the current study, we aim to see whether we would observe a female advantage in grades and clarify how sleep contributes to gender differences.
Bedtime and wake-up times
On average, students went to bed at 1:54 a.m. (Median = 1:47 a.m., Standard Deviation (SD) of all bedtime samples = 2 h 11 min, SD of mean bedtime per participant = 1 h) and woke up at 9:17 a.m. (Median = 9:12 a.m., SD of all wake-up time samples = 2 h 2 min; SD of mean wake-up time per participant = 54 min). The data were confirmed to have Gaussian distribution using the Shapiro–Wilks normality test. We conducted an ANOVA with the overall score (sum of all grade-relevant quizzes and exams—see “Procedure”) as the dependent variable and bedtime (before or after median) and wake-up time (before or after median) as the independent variables. We found a main effect of bedtime ( F (1, 82) = 6.45, p = 0.01), such that participants who went to bed before median bedtime had significantly higher overall score ( X = 77.25%, SD = 13.71%) compared with participants who went to bed after median bedtime ( X = 70.68%, SD = 11.01%). We also found a main effect of wake-up time ( F (1, 82) = 6.43, p = 0.01), such that participants who woke up before median wake-up time had significantly higher overall score ( X = 78.28%, SD = 9.33%) compared with participants who woke up after median wake-up time ( X = 69.63%, SD = 14.38%), but found no interaction between bedtime and wake-up time ( F (1, 82) = 0.66, p = 0.42).
A Pearson’s product-moment correlation between average bedtime and overall score revealed a significant and negative correlation ( r (86) = −0.45, p < 0.0001), such that earlier average bedtime was associated with a higher overall score. There was a significant and negative correlation between average wake-up time and overall score ( r (86) = −0.35, p < 0.001), such that earlier average wake-up time was associated with a higher overall score. There was also a significant and positive correlation between average bedtime and average wake-up time (r (86) = 0.68, p < 0.0001), such that students who went to bed earlier tended to also wake up earlier.
Sleep duration, quality, and consistency in relation to academic performance
Overall, the mean duration of sleep for participants throughout the entire semester was 7 h 8 min (SD of all sleep samples = 1 h 48 min, SD of mean sleep duration per participant = 41 min). There was a significant positive correlation between mean sleep duration throughout the semester (sleep duration) and overall score ( r (86) = 0.38, p < 0.0005), indicating that a greater amount of sleep was associated with a higher overall score (Fig. 1a ). Similarly, there was a significant positive correlation between mean sleep quality throughout the semester (Sleep Quality) and Overall Score ( r (86) = 0.44, p < 0.00005). Sleep inconsistency was defined for each participant as the standard deviation of the participant’s daily sleep duration in minutes so that a larger standard deviation indicated greater sleep inconsistency. There was a significant negative correlation between sleep inconsistency and overall score ( r (86) = −0.36, p < 0.001), indicating that the greater inconsistency in sleep duration was associated with a lower overall score (Fig. 1b ).
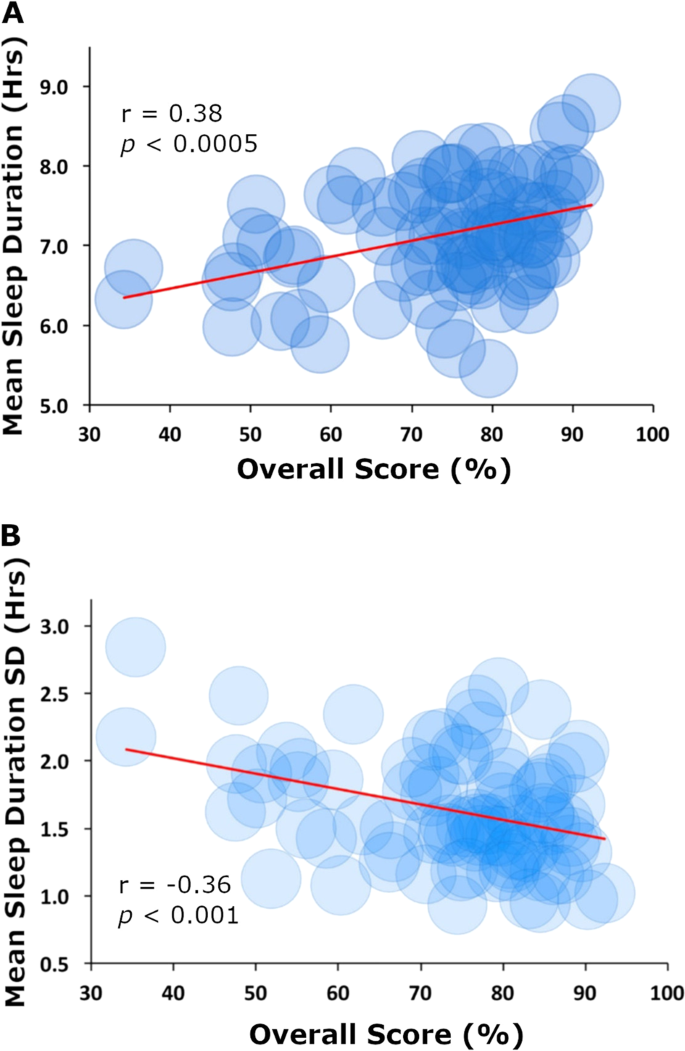
Correlations between sleep measures and overall score. a Average daily hours slept (sleep duration) vs. overall score for the semester. b Standard deviation of average daily hours of sleep (sleep inconsistency) vs. overall score in class
Timing of sleep and its relation to academic performance
To understand sleep and its potential role in memory consolidation, we examined the timing of sleep as it related to specific assessments. All Pearson correlations with three or more comparisons were corrected for multiple comparisons using false discovery rate. 47
Night before assessments
We conducted a correlation between sleep quality the night before a midterm and respective midterm scores as well as sleep duration the night before a midterm and respective scores. There were no significant correlations with sleep duration or sleep quality for all three midterms (all r s < 0.20, all p s > 0.05). Similar analyses for sleep duration and sleep quality the night before respective quizzes revealed no correlations ( r s from 0.01 to 0.26, all p s > 0.05).
Week and month leading up to assessments
To understand the effect of sleep across the time period while course content was learned for an assessment, we examined average sleep measures during the 1 month leading up to the midterms. We found a significant positive correlation between average sleep duration over the month leading up to scores on each midterm ( r s from 0.25 to 0.34, all p s < 0.02). Similar analyses for average sleep duration over one week leading up to respective quizzes were largely consistent with those of midterms, with significant correlations on 3 of 8 quizzes (rs from 0.3 to 0.4, all p s < 0.05) and marginal correlations on an additional 3 quizzes (rs from 0.25 to 0.27, all p s < 0.08).
There was a significant and positive correlation between sleep quality scores averaged over the month leading up to each midterm for all three midterms ( r s from 0.21 to 0.38, all p s < 0.05). Similar analyses for average Sleep Quality over one week leading up to respective quizzes revealed a significant correlation on 1 of 8 quizzes ( r (86) = 0.42, p < 0.005) and marginal correlations on 3 quizzes ( r s from 0.25 to 0.27, all p s < 0.08).
Variance of assessment performance accounted for by sleep measures
In order to calculate how much of the variance on assessment performance was accounted for by the sleep measures, we conducted a stepwise regression on overall score using three regressors: sleep duration, sleep quality, and sleep inconsistency. The relative importance of each variable was calculated using the relaimpo package in R 48 to understand individual regressor’s contribution to the model, which is not always clear from the breakdown of model R 2 when regressors are correlated. We found a significant regression ( F (3,84) = 8.95, p = .00003), with an R 2 of 0.24. Students’ predicted overall score was equal to 77.48 + 0.21 (sleep duration) + 19.59 (Sleep Quality) – 0.45 (sleep inconsistency). While sleep inconsistency was the only significant individual predictor of overall score ( p = 0.03) in this analysis, we found that 24.44% of variance was explained by the three regressors. The relative importance of these metrics were 7.16% sleep duration, 9.68% sleep quality, and 7.6% sleep inconsistency.
Gender differences
Females had better Sleep Quality ( t (88) = 2.63, p = 0.01), and less sleep inconsistency ( t (88) = 2.18, p = 0.03) throughout the semester compared with males, but the two groups experienced no significant difference in sleep duration ( t (88) = 1.03, p = 0.3). Sleep duration and sleep quality were significantly correlated in both males ( r (41) = 0.85, p < 0.00001) and females ( r (43) = 0.64, p < 0.00001), but this correlation was stronger in males ( Z = −2.25, p = 0.02) suggesting that it may be more important for males to get a long-duration sleep in order to get good quality sleep. In addition, sleep inconsistency and sleep quality were significantly negatively correlated in males ( r (41) = −0.51, p = 0.0005) but not in females ( r (43) = 0.29, p > 0.05), suggesting that it may be more important for males to stick to a regular daily sleep schedule in order to get good quality sleep.
Females scored higher on overall score compared with males ( t (88) = −2.48, p = 0.01), but a one-way analysis of covariance (ANCOVA) revealed that females and males did not perform significantly different on overall score when controlling for Sleep Quality, F (1, 85) = 2.22, p = 0.14. Sleep inconsistency and overall score were negatively correlated in males ( r (41) = −0.44, p = 0.003) but not in females ( r (43) = −0.13, p = 0.39), suggesting that it is important for males to stick to a regular sleep schedule in order to perform well in academic performance but less so for females. No other gender differences were detected between other sleep measures and overall score.
This study found that longer sleep duration, better sleep quality, and greater sleep consistency were associated with better academic performance. A multiple linear regression revealed that these three sleep measures accounted for 24.44% of the variance in overall grade performance. Thus, there was a substantial association between sleep and academic performance. The present results correlating overall sleep quality and duration with academic performance are well aligned with previous studies 6 , 11 , 12 , 24 , 25 on the role of sleep on cognitive performance. Similarly, this study compliments the two linked studies that found longer sleep duration during the week before final exams 47 and consistent sleep duration five days prior to a final assignment 48 enhanced students’ performance. The present study, however, significantly extends our understanding of the relation between sleep and academic performance by use of multiple objective measures of sleep throughout an entire semester and academic assessments completed along the way.
The present study also provides new insights about the timing of the relation between sleep and academic performance. Unlike a prior study, 23 we did not find that sleep duration the night before an exam was associated with better test performance. Instead we found that both longer sleep duration and better sleep quality over the full month before a midterm were more associated with better test performance. Rather than the night before a quiz or exam, it may be more important to sleep well for the duration of the time when the topics tested were taught. The implications of these findings are that, at least in the context of an academic assessment, the role of sleep is crucial during the time the content itself is learned, and simply getting good sleep the night before may not be as helpful. The outcome that better “content-relevant sleep” leads to improved performance is supported by previous controlled studies on the role of sleep in memory consolidation. 14 , 15
Consistent with some previous research 45 , 46 female students tended to experience better quality sleep and with more consistency than male students. In addition, we found that males required a longer and more regular daily sleep schedule in order to get good quality sleep. This female advantage in academic performance was eliminated once sleep patterns were statistically equated, suggesting that it may be especially important to encourage better sleep habits in male students (although such habits may be helpful for all students).
Several limitations of the present study may be noted. First, the sleep quality measures were made with proprietary algorithms. There is an evidence that the use of cardiac, respiratory, and movement information from Fitbit devices can accurately estimate sleep stages, 32 but there is no published evidence that Fitbit’s 1~10 sleep quality scores represent a valid assessment of sleep quality. Second, the relation between sleep and academic performance may be moderated by factors that can affect sleep, such as stress, anxiety, motivation, personality traits, and gender roles. Establishing a causal relation between sleep and academic performance will require experimental manipulations in randomized controlled trials, but these will be challenging to conduct in the context of real education in which students care about their grades. Third, these findings occurred for a particular student population at MIT enrolled in a particular course, and future studies will need to examine the generalizability of these findings to other types of student populations and other kinds of classes.
In sum, this study provides evidence for a strong relation between sleep and academic performance using a quantifiable and objective measures of sleep quality, duration, and consistency in the ecological context of a live classroom. Sleep quality, duration, and consistency together accounted for a substantial amount (about a quarter) of the overall variance in academic performance.
Participants
One hundred volunteers (47 females) were selected from a subset of students who volunteered among 370 students enrolled in Introduction to Solid State Chemistry at the Massachusetts Institute of Technology to participate in the study. Participants were informed of the study and gave written consent obtained in accordance with the guidelines of and approved by the MIT Committee on the Use of Humans as Experimental Subjects. Due to limitations in funding, we only had access to 100 Fitbit devices and could not enroll all students who volunteered; consequently, the first 100 participants to volunteer were selected. All participants were gifted a wearable activity tracker at the completion of the study in exchange for their participation. Seven participants were excluded from analysis because they failed to wear their activity tracker for more than 80% of the semester, three participants were excluded because they lost their wearable activity tracker, and another two participants were excluded because they completed less than 75% of the assessments in the class. Of the 88 participants who completed the study (45 females), 85 were freshmen, one was a junior and two were seniors (mean age = 18.19 years).
The Solid State Chemistry class is a single-semester class offered in the fall semester and geared toward freshmen students to satisfy MIT’s general chemistry requirement. The class consisted of weekly lectures by the professor and two weekly recitations led by 12 different teaching assistants (TAs). Each student was assigned to a specific recitation section that fit their schedule and was not allowed to attend other sections; therefore, each student had the same TA throughout the semester. Students took (1) weekly quizzes that tested knowledge on the content covered the week leading up to the quiz date, (2) three midterms that tested knowledge on the content covered in the 3–4 weeks leading up to the exam date, and (3) a final exam that tested content covered throughout the semester. Based on a one-way between subjects’ analysis of variance (ANOVA) to compare the effect of teaching assistants (TAs) on overall grade, we found no significant differences in overall grade across the TAs (F (10, 77) = 1.82, p = 0.07. (One TA was removed from the analysis because he only had one student who was participating in this study).
Participants were asked to wear an activity tracker for the entire duration of the semester without going below 80% usage each week. If 80% or more usage was not maintained, warning emails were sent at the end of that respective week. Participants were asked to return the device if they dipped below 80% usage more than three out of the 14 weeks of the semester. The average usage rate at the end of the semester for the 88 participants who completed the study was 89.4% (SD = 5.5%). The missing data appeared to be at random and were deleted prior to data analysis. As part of a separate research question, 22 of the 88 participants joined an intense cardiovascular exercise class for which they received separate physical education credit. These students performed similarly to the other 67 participants in terms of final class grade ( t (88) = 1.57, p = 0.12), exercise amount (total amount of moderately and very active minutes on the wearable device) (t (88) = 0.59, p = 0.56), sleep amount ( t (88) = 0.3, p = 0.77), and sleep quality ( t (88) = 0.14, p = 0.9), so they were included in all of the analyses.
Participants’ activities were tracked using a Fitbit Charge HR. Data from the device were recorded as follows: heart rate every 5 min; steps taken, distance traveled, floors climbed, calories burned and activity level measurements every 15 min; resting heart rate daily; and sleep duration and quality for every instance of sleep throughout the day. Sleep quality was determined using Fitbit’s proprietary algorithm that produces a value from 0 (poor quality) to 10 (good quality).
Assessments
Nine quizzes, three midterm examinations, and one final examination were administered throughout the 14-week class to assess the students’ academic achievement. The students’ cumulative class grade was made up of 25% for all nine quizzes (lowest quiz grade was dropped from the average), 15% for each midterm exam, and 30% for the final exam for a total of 100%.
At MIT, freshmen are graded on a Pass or No Record basis in all classes taken during their first semester. Therefore, all freshmen in this class needed a C- level or better (≥50%, no grading on a curve) to pass the class. A failing grade (a D or F grade) did not go on their academic record. All upperclassmen were given letter grades; A (≥85%), B (70–84%), C (50–69%), D (45–49%), F (≤44%). Because a large portion of the class had already effectively “passed” the class before taking Quiz 9 and the final exam, we excluded these two assessments from our analyses due to concerns about students’ motivation to perform their best. We calculated for each student an overall score defined as the sum of the eight quizzes and three midterms to summarize academic performance in the course.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Code availability
No custom codes were used in the analysis of this study
Dawson, D. & Reid, K. Fatigue, alcohol and performance impairment. Nature 388 , 540–545 (1997).
Article Google Scholar
Lim, J. & Dinges, D. F. A meta-analysis of the impact of short-term sleep deprivation on cognitive variables. Psychol. Bull. 136 , 375–389 (2010).
Harrison, Y. & Horne, J. A. The impact of sleep deprivation on decision making: a review. J. Exp. Psychol. Appl. 6 , 236–249 (2000).
Article CAS Google Scholar
Wagner, U., Gais, S., Haider, H., Verleger, R. & Born, J. Sleep inspires insight. Nature 427 , 352–355 (2004).
Walker, M. P. & Stickgold, R. Sleep, memory, and plasticity. Annu. Rev. Psychol. 57 , 139–166 (2006).
Wong, M. L. et al. The interplay between sleep and mood in predicting academic functioning, physical health and psychological health: a longitudinal study. J. Psychosom. Res. 74 , 271–277 (2013).
Diekelmann, S., Wilhelm, I. & Born, J. The whats and whens of sleep-dependent memory consolidation. Sleep. Med. Rev. 13 , 309–321 (2009).
Fogel, S. M., Smith, C. T. & Cote, K. A. Dissociable learning-dependent changes in REM and non-REM sleep in declarative and procedural memory systems. Behav. Brain Res. 180 , 48–61 (2007).
Eliasson, A. H. & Lettieri, C. J. Early to bed, early to rise! Sleep habits and academic performance in college students. Sleep. Breath. 14 , 71–75 (2010).
Gaultney, J. F. The prevalence of sleep disorders in college students: Impact on academic performance. J. Am. Coll. Health 59 , 91–97 (2010).
Gilbert, S. P. & Weaver, C. C. Sleep quality and academic performance in university students: A wake-up call for college psychologists. J. Coll. Stud. Psychother. 24 , 295–306 (2010).
Gomes, A. A., Tavares, J. & de Azevedo, M. H. P. Sleep and academic performance in undergraduates: A multi-measure, multi-predictor approach. Chronobiol. Int. 28 , 786–801 (2011).
Lemma, S., Berhane, Y., Worku, A., Gelaye, B. & Williams, M. A. Good quality sleep is associated with better academic performance among university students in Ethiopia. Sleep. Breath. 18 , 257–263 (2014).
Gilestro, G. F., Tononi, G. & Cirelli, C. Widespread changes in synaptic markers as a function of sleep and wakefulness in drosophila. Science 324 , 109–112 (2009).
Rasch, B. & Born, J. About sleep’s role in memory. Physiol. Rev. 93 , 681–766 (2013).
Alhola, P. & Polo-Kantola, P. Sleep deprivation: Impact on cognitive performance. Neuropsychiatr. Dis. Treat. 3 , 553–567 (2007).
PubMed PubMed Central Google Scholar
Durmer, J. S. & Dinges, D. F. Neurocognitive consequences of sleep deprivation. Semin. Neurol. 25 , 117–129 (2005).
Alapin, I. et al. How is good and poor sleep in older adults and college students related to daytime sleepiness, fatigue, and ability to concentrate? J. Psychosom. Res. 49 , 381–390 (2000).
Orzech, K. M., Salafsky, D. B. & Hamilton, L. A. The state of sleep among college students at a large public university. J. Am. Coll. Health 59 , 612–619 (2011).
Eliasson, A., Eliasson, A., King, J., Gould, B. & Eliasson, A. Association of sleep and academic performance. Sleep. Breath. 6 , 45–48 (2002).
Johns, M. W., Dudley, H. A. & Masterton, J. P. The sleep habits, personality and academic performance of medical students. Med. Educ. 10 , 158–162 (1976).
Merikanto, I., Lahti, T., Puusniekka, R. & Partonen, T. Late bedtimes weaken school performance and predispose adolescents to health hazards. Sleep. Med. 14 , 1105–1111 (2013).
Zeek, M. L. et al. Sleep duration and academic performance among student pharmacists. Am. J. Pharm. Educ. 79 , 5–12 (2015).
Hartmann, M. E. & Prichard, J. R. Calculating the contribution of sleep problems to undergraduates’ academic success. Sleep. Health 4 , 463–471 (2018).
Mirghani, H. O., Mohammed, O. S., Almurtadha, Y. M. & Ahmed, M. S. Good sleep quality is associated with better academic performance among Sudanese medical students. BMC Res. Notes 8 , 706 (2015).
Onyper, S. V., Thacher, P. V., Gilbert, J. W. & Gradess, S. G. Class start times, Sleep, and academic performance in college: a path analysis. Chronobiol. Int. 29 , 318–335 (2012).
Ming, X. et al. Sleep insufficiency, sleep health problems and performance in high school students. Clin. Med. Insights Circ. Respir. Pulm. Med. 5 , 71–79 (2011).
Lee, Y. J., Park, J., Soohyun, K., Seong-jin, C. & Seog Ju, K. Academic performance among adolescents with behaviorally. J. Clin. Sleep. Med. 11 , 61–68 (2015).
Díaz-Morales, J. F. & Escribano, C. Social jetlag, academic achievement and cognitive performance: Understanding gender/sex differences. Chronobiol. Int. 32 , 822–831 (2015).
Raley, H., Naber, J., Cross, S. & Perlow, M. The impact of duration of sleep on academic performance in University students. Madr. J. Nurs. 1 , 11–18 (2016).
Haraszti, R. Á., Ella, K., Gyöngyösi, N., Roenneberg, T. & Káldi, K. Social jetlag negatively correlates with academic performance in undergraduates. Chronobiol. Int. 31 , 603–612 (2014).
Scullin, M. K. The eight hour sleep challenge during final exams week. Teach. Psychol. 46 , 55–63 (2018).
King, E., Mobley, C. & Scullin, M. K. The 8‐hour challenge: incentivizing sleep during end‐of‐term assessments. J. Inter. Des. 44 , 85–99 (2018).
PubMed Google Scholar
Beattie, Z. et al. Estimation of sleep stages using cardiac and accelerometer data from a wrist-worn device. Sleep 40 , A26–A26 (2017).
Clark, M. J. & Grandy, J. Sex differences in the academic performance of scholastic aptitude test takers. ETS Res. Rep. Ser. 2 , 1-27 (1984).
Google Scholar
Kimball, M. M. A new perspective on women’s math achievement. Psychol. Bull. 105 , 198–214 (1989).
Mau, W.-C. & Lynn, R. Gender differences on the scholastic aptitude test, the American college test and college grades. Educ. Psychol. 21 , 133–136 (2001).
Willingham, W. W. & Cole, N. S. Gender and fair assessment . (Mahwah, NJ, US, Lawrence Erlbaum Associates, 1997).
Volchok, E. Differences in the performance of male and female students in partially online courses at a community college. Community Coll . J . Res . Pract . 1–17, https://doi.org/10.1080/10668926.2018.1556134 (2018).
Duckworth, A. L. et al. Will not want: self-control rather than motivation explains the female advantage in report card grades. Learn. Individ. Differ. 39 , 13–23 (2015).
Carvalho, R. G. G. Gender differences in academic achievement: The mediating role of personality. Pers. Individ. Differ. 94 , 54–58 (2016).
Duckworth, A. L. & Seligman, M. E. P. Self-discipline gives girls the edge: gender in self-discipline, grades, and achievement test scores. J. Educ. Psychol. 98 , 198–208 (2006).
Tsai, L. L. & Li, S. P. Sleep patterns in college students: Gender and grade differences. J. Psychosom. Res. 56 , 231–237 (2004).
Becker, S. P. et al. Sleep in a large, multi-university sample of college students: sleep problem prevalence, sex differences, and mental health correlates. Sleep Health 4 , 174–181 (2018).
Bixler, E. O. et al. Women sleep objectively better than men and the sleep of young women is more resilient to external stressors: effects of age and menopause. J. Sleep. Res. 18 , 221–228 (2009).
Mallampalli, M. P. & Carter, C. L. Exploring sex and gender differences in sleep health: a Society for Women’s Health Research Report. J. Women’s. Health 23 , 553–562 (2014).
Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. J. R. Stat. Soc. Ser. B (Methodol.) 57 , 289–300 (1995).
Grömping, U. Relative importance for linear regression in R: The package relaimpo. J. Stat. Softw. 17 , 1–27 (2015).
Download references

Acknowledgements
This research was supported by a grant from the Horace A. Lubin Fund in the MIT Department of Materials Science and Engineering to J.C.G. and funding from MIT Integrated Learning Initiative to K.O. and J.R.K. The authors are grateful for many useful discussions with Carrie Moore and Matthew Breen at the Department of Athletics, Physical Education, and Recreation at MIT.
Author information
Authors and affiliations.
MIT Integrated Learning Initiative, Department of Brain and Cognitive Sciences, and McGovern Institute for Brain Research, Massachusetts Institute of Technology, Cambridge, MA, 02139, USA
Kana Okano, Jakub R. Kaczmarzyk & John D. E. Gabrieli
Harvard Business School, Boston, MA, 02163, USA
Department of Materials Science and Engineering Massachusetts Institute of Technology, Cambridge, MA, 02139, USA
Jeffrey C. Grossman
You can also search for this author in PubMed Google Scholar
Contributions
K.O. and J.C.G. conceived, designed, supervised, and analyzed the project. J.K. and N.D. helped analyze the data. The manuscript was written by K.O., J.D.E.G., and J.C.G.
Corresponding author
Correspondence to Jeffrey C. Grossman .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Reporting summary, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Okano, K., Kaczmarzyk, J.R., Dave, N. et al. Sleep quality, duration, and consistency are associated with better academic performance in college students. npj Sci. Learn. 4 , 16 (2019). https://doi.org/10.1038/s41539-019-0055-z
Download citation
Received : 20 March 2019
Accepted : 17 July 2019
Published : 01 October 2019
DOI : https://doi.org/10.1038/s41539-019-0055-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Social isolation consequences: lessons from covid-19 pandemic in a context of dynamic lock-down in chile.
- Alessandra Patrono
- Stefano Renzetti
- Roberto G. Lucchini
BMC Public Health (2024)
From good sleep to health and to quality of life – a path analysis of determinants of sleep quality of working adults in Abu Dhabi
- Masood Badri
- Mugheer Alkhaili
- Asma Alrashdi
Sleep Science and Practice (2023)
The association between academic performance indicators and lifestyle behaviors among Kuwaiti college students
- Ahmad R. Al-Haifi
- Balqees A. Al-Awadhi
- Hazzaa M. Al-Hazzaa
Journal of Health, Population and Nutrition (2023)
Screen time and sleep among medical students in Germany
- Lukas Liebig
- Antje Bergmann
- Henna Riemenschneider
Scientific Reports (2023)
Ontogeny and social context regulate the circadian activity patterns of Lake Malawi cichlids
- Aakriti Rastogi
- Alex C. Keene
Journal of Comparative Physiology B (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Advertisement
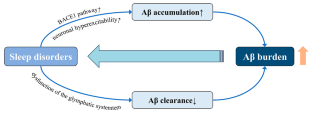
Relationship of Sleep Disorder with Neurodegenerative and Psychiatric Diseases: An Updated Review
- Published: 18 December 2023
- Volume 49 , pages 568–582, ( 2024 )
Cite this article
- Xiao Xiao 1 , 2 na1 ,
- Yimin Rui 1 , 2 na1 ,
- Yu Jin 2 &
- Ming Chen 2
644 Accesses
2 Citations
10 Altmetric
Explore all metrics
Sleep disorders affect many people worldwide and can accompany neurodegenerative and psychiatric diseases. Sleep may be altered before the clinical manifestations of some of these diseases appear. Moreover, some sleep disorders affect the physiological organization and function of the brain by influencing gene expression, accelerating the accumulation of abnormal proteins, interfering with the clearance of abnormal proteins, or altering the levels of related hormones and neurotransmitters, which can cause or may be associated with the development of neurodegenerative and psychiatric diseases. However, the detailed mechanisms of these effects are unclear. This review mainly focuses on the relationship between and mechanisms of action of sleep in Alzheimer’s disease, depression, and anxiety, as well as the relationships between sleep and Parkinson’s disease, Huntington’s disease, and amyotrophic lateral sclerosis. This summary of current research hotspots may provide researchers with better clues and ideas to develop treatment solutions for neurodegenerative and psychiatric diseases associated with sleep disorders.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others
The missing link between sleep disorders and age-related dementia: recent evidence and plausible mechanisms.
Feng Zhang, Rujia Zhong, … Weidong Le

Sleep as a Therapeutic Target in the Aging Brain
Thierno M. Bah, James Goodman & Jeffrey J. Iliff
Sleep in Neurodegenerative Disorders
Roneil Malkani & Hrayr Attarian
Abbreviations
Amyloid β-protein
Alzheimer’s disease
Amyotrophic lateral sclerosis
Amyloid precursor protein
Aquaporin 4
Acute sleep deprivation
Β-site APP cleaving enzyme 1
Brain-derived neurotrophic factor
Brain and muscle arnt-like protein-1
Chronic sleep deprivation
Cerebrospinal fluid
Chronic sleep restriction
Huntington’s disease
Hypothalamic-pituitary-adrenal
Interleukin
Interstitial fluid
Kelch-like ECH-associated protein 1
Low-density lipoprotein receptor-related protein 1
Mild cognitive impairment
Normal cognition
Non-rapid eye movement
Nuclear factor erythroid 2-related factor
Obstructive sleep apnea
Parkinson’s disease
Receptor of advanced glycation end products
Rapid eye movement sleep-behavior disorder
Rapid eye movement
Sleep deprivation
Sleep-disordered breathing
Slow-wave activity
Slow wave sleep
43-kDa TAR DNA-binding protein
Total sleep deprivation
Grandner MA, Fernandez FX (2021) The translational neuroscience of sleep: a contextual framework. Science 374:568–573
Article CAS PubMed PubMed Central ADS Google Scholar
Voysey Z, Fazal SV, Lazar AS, Barker RA (2021) The sleep and circadian problems of Huntington’s Disease: when, why and their importance. J Neurol 268:2275–2283
Article CAS PubMed Google Scholar
Joiner WJ (2018) The neurobiological basis of Sleep and Sleep disorders. Physiol (Bethesda) 33:317–327
CAS Google Scholar
Léger D, Bayon V (2010) Societal costs of insomnia. Sleep Med Rev 14:379–389
Article PubMed Google Scholar
Hillman DR, Lack LC (2013) Public health implications of sleep loss: the community burden. Med J Aust 199:S7–10
Latreille MKP V (2019) Sleep disorders. Am J Med 132:292–299
Liew SC, Aung T (2021) Sleep deprivation and its association with diseases- a review. Sleep Med 77:192–204
Banks S, Dinges DF (2007) Behavioral and physiological consequences of sleep restriction. J Clin Sleep Med 3:519–528
Article PubMed PubMed Central Google Scholar
Umemura GS, Furtado F, Dos Santos FC, Gonçalves B, Forner-Cordero A (2022) Is Balance Control affected by Sleep Deprivation? A systematic review of the impact of Sleep on the control of balance. Front Neurosci 16:779086
Pires GN, Bezerra AG, Tufik S, Andersen ML (2016) Effects of acute sleep deprivation on state anxiety levels: a systematic review and meta-analysis. Sleep Med 24:109–118
Colwell CS (2021) Defining circadian disruption in neurodegenerative disorders. J Clin Invest 131
Fang H, Tu S, Sheng J, Shao A (2019) Depression in sleep disturbance: a review on a bidirectional relationship, mechanisms and treatment. J Cell Mol Med 23:2324–2332
Wang YQ, Li R, Zhang MQ, Zhang Z, Qu WM, Huang ZL (2015) The neurobiological mechanisms and treatments of REM sleep disturbances in Depression. Curr Neuropharmacol 13:543–553
Article CAS PubMed PubMed Central Google Scholar
Guo B, Zhang M, Hao W, Wang Y, Zhang T, Liu C (2023) Neuroinflammation mechanisms of neuromodulation therapies for anxiety and depression. Transl Psychiatry 13:5
Gauthier S, Webster C, Servaes S, Morais JA, Rosa-Neto P (2022) World Alzheimer Report 2022: Life after diagnosis: Navigating treatment, care and support. In. Alzheimer’s Disease International, London, England
Okuda S, Tetsuka J, Takahashi K, Toda Y, Kubo T, Tokita S (2019) Association between sleep disturbance in Alzheimer’s Disease patients and burden on and health status of their caregivers. J Neurol 266:1490–1500
Kastanenka KV, Hou SS, Shakerdge N, Logan R, Feng D, Wegmann S, Chopra V, Hawkes JM, Chen X, Bacskai BJ (2017) Optogenetic restoration of disrupted slow oscillations halts amyloid deposition and restores Calcium Homeostasis in an animal model of Alzheimer’s Disease. PLoS ONE 12:e0170275
Suh SW, Han JW, Lee JR, Byun S, Kwon SJ, Oh SH, Lee KH, Han G, Hong JW, Kwak KP, Kim BJ, Kim SG, Kim JL, Kim TH, Ryu SH, Moon SW, Park JH, Seo J, Youn JC, Lee DY, Lee DW, Lee SB, Lee JJ, Jhoo JH, Kim KW (2018) Sleep and cognitive decline: a prospective nondemented elderly cohort study. Ann Neurol 83:472–482
Lucey BP, Wisch J, Boerwinkle AH, Landsness EC, Toedebusch CD, McLeland JS, Butt OH, Hassenstab J, Morris JC, Ances BM, Holtzman DM (2021) Sleep and longitudinal cognitive performance in preclinical and early symptomatic Alzheimer’s Disease. Brain 144:2852–2862
Maestri M, Carnicelli L, Tognoni G, Di Coscio E, Giorgi FS, Volpi L, Economou NT, Ktonas P, Ferri R, Bonuccelli U, Bonanni E (2015) Non-rapid eye movement sleep instability in mild cognitive impairment: a pilot study. Sleep Med 16:1139–1145
Pase MP, Himali JJ, Grima NA, Beiser AS, Satizabal CL, Aparicio HJ, Thomas RJ, Gottlieb DJ, Auerbach SH, Seshadri S (2017) Sleep architecture and the risk of incident Dementia in the community. NEUROLOGY 89:1244–1250
Lucey BP, McCullough A, Landsness EC, Toedebusch CD, McLeland JS, Zaza AM, Fagan AM, McCue L, Xiong C, Morris JC, Benzinger TLS, Holtzman DM (2019) Reduced non-rapid eye movement sleep is associated with tau pathology in early Alzheimer’s disease. Sci Transl Med 11
Liu S, Meng Y, Wang N, Lei Q, He L, Hong X, Li Z (2023) Disturbance of REM sleep exacerbates microglial activation in APP/PS1 mice. Neurobiol Learn Mem 200:107737
Chylinski D, Van Egroo M, Narbutas J, Muto V, Bahri MA, Berthomier C, Salmon E, Bastin C, Phillips C, Collette F, Maquet P, Carrier J, Lina JM, Vandewalle G (2022) Timely coupling of sleep spindles and slow waves linked to early amyloid-β burden and predicts memory decline. eLife 11
Chylinski DO, Van Egroo M, Narbutas J, Grignard M, Koshmanova E, Berthomier C, Berthomier P, Brandewinder M, Salmon E, Bahri MA, Bastin C, Collette F, Phillips C, Maquet P, Muto V, Vandewalle G (2021) Heterogeneity in the links between sleep arousals, amyloid-β, and cognition. JCI Insight 6
Winer JR, Deters KD, Kennedy G, Jin M, Goldstein-Piekarski A, Poston KL, Mormino EC (2021) Association of short and long sleep duration with Amyloid-β Burden and Cognition in Aging. JAMA Neurol 78:1187–1196
Fan L, Xu W, Cai Y, Hu Y, Wu C (2019) Sleep duration and the risk of Dementia: a systematic review and Meta-analysis of prospective cohort studies. J Am Med Dir Assoc 20:1480–1487e1485
Leng Y, Ackley SF, Glymour MM, Yaffe K, Brenowitz WD (2021) Genetic risk of Alzheimer’s Disease and Sleep Duration in Non-demented elders. Ann Neurol 89:177–181
Xu W, Tan L, Su BJ, Yu H, Bi YL, Yue XF, Dong Q, Yu JT (2020) Sleep characteristics and cerebrospinal fluid biomarkers of Alzheimer’s Disease pathology in cognitively intact older adults: the CABLE study. Alzheimers Dement 16:1146–1152
Cavaillès C, Berr C, Helmer C, Gabelle A, Jaussent I, Dauvilliers Y (2022) Complaints of daytime sleepiness, insomnia, hypnotic use, and risk of Dementia: a prospective cohort study in the elderly. Alzheimers Res Ther 14:12
Anderson EL, Richmond RC, Jones SE, Hemani G, Wade KH, Dashti HS, Lane JM, Wang H, Saxena R, Brumpton B, Korologou-Linden R, Nielsen JB, Åsvold BO, Abecasis G, Coulthard E, Kyle SD, Beaumont RN, Tyrrell J, Frayling TM, Munafò MR, Wood AR, Ben-Shlomo Y, Howe LD, Lawlor DA, Weedon MN, Davey Smith G (2021) Is disrupted sleep a risk factor for Alzheimer’s Disease? Evidence from a two-sample mendelian randomization analysis. Int J Epidemiol 50:817–828
André C, Rehel S, Kuhn E, Landeau B, Moulinet I, Touron E, Ourry V, Le Du G, Mézenge F, Tomadesso C, de Flores R, Bejanin A, Sherif S, Delcroix N, Manrique A, Abbas A, Marchant NL, Lutz A, Klimecki OM, Collette F, Arenaza-Urquijo EM, Poisnel G, Vivien D, Bertran F, de la Sayette V, Chételat G, Rauchs G (2020) Association of Sleep-Disordered Breathing with Alzheimer Disease biomarkers in Community-Dwelling older adults: a secondary analysis of a Randomized Clinical Trial. JAMA Neurol 77:716–724
Lee JE, Yang SW, Ju YJ, Ki SK, Chun KH (2019) Sleep-disordered breathing and Alzheimer’s Disease: a nationwide cohort study. Psychiatry Res 273:624–630
Liguori C, Maestri M, Spanetta M, Placidi F, Bonanni E, Mercuri NB, Guarnieri B (2021) Sleep-disordered breathing and the risk of Alzheimer’s Disease. Sleep Med Rev 55:101375
Bubu OM, Andrade AG, Umasabor-Bubu OQ, Hogan MM, Turner AD, de Leon MJ, Ogedegbe G, Ayappa I, Jean-Louis GG, Jackson ML, Varga AW, Osorio RS (2020) Obstructive sleep apnea, cognition and Alzheimer’s Disease: a systematic review integrating three decades of multidisciplinary research. Sleep Med Rev 50:101250
Sharma RA, Varga AW, Bubu OM, Pirraglia E, Kam K, Parekh A, Wohlleber M, Miller MD, Andrade A, Lewis C, Tweardy S, Buj M, Yau PL, Sadda R, Mosconi L, Li Y, Butler T, Glodzik L, Fieremans E, Babb JS, Blennow K, Zetterberg H, Lu SE, Badia SG, Romero S, Rosenzweig I, Gosselin N, Jean-Louis G, Rapoport DM, de Leon MJ, Ayappa I, Osorio RS (2018) Obstructive sleep apnea severity affects amyloid Burden in Cognitively Normal Elderly. A longitudinal study. Am J Respir Crit Care Med 197:933–943
Punjabi NM (2008) The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc 5:136–143
Ooms S, Overeem S, Besse K, Rikkert MO, Verbeek M, Claassen JA (2014) Effect of 1 night of total sleep deprivation on cerebrospinal fluid β-amyloid 42 in healthy middle-aged men: a randomized clinical trial. JAMA Neurol 71:971–977
Lucey BP, Hicks TJ, McLeland JS, Toedebusch CD, Boyd J, Elbert DL, Patterson BW, Baty J, Morris JC, Ovod V, Mawuenyega KG, Bateman RJ (2018) Effect of sleep on overnight cerebrospinal fluid amyloid β kinetics. Ann Neurol 83:197–204
Benedict C, Blennow K, Zetterberg H, Cedernaes J (2020) Effects of acute sleep loss on diurnal plasma dynamics of CNS health biomarkers in young men. NEUROLOGY 94:e1181–e1189
Wei M, Zhao B, Huo K, Deng Y, Shang S, Liu J, Li Y, Ma L, Jiang Y, Dang L, Chen C, Wei S, Zhang J, Yang H, Gao F, Qu Q (2017) Sleep Deprivation Induced plasma Amyloid-β transport disturbance in healthy young adults. J Alzheimers Dis 57:899–906
Ju Y-ES, Ooms SJ, Sutphen C, Macauley SL, Zangrilli MA, Jerome G, Fagan AM, Mignot E, Zempel JM, Claassen JAHR, Holtzman DM (2017) Slow wave sleep disruption increases cerebrospinal fluid amyloid-β levels. Brain 140:2104–2111
Qiu H, Zhong R, Liu H, Zhang F, Li S, Le W (2016) Chronic sleep deprivation exacerbates Learning-Memory disability and Alzheimer’s Disease-Like pathologies in AβPP(swe)/PS1(∆E9) mice. J Alzheimers Dis 50:669–685
Zhao HY, Wu HJ, He JL, Zhuang JH, Liu ZY, Huang LQ, Zhao ZX (2017) Chronic sleep restriction induces cognitive deficits and cortical Beta-amyloid deposition in mice via BACE1-Antisense activation. CNS Neurosci Ther 23:233–240
Zhao B, Liu P, Wei M, Li Y, Liu J, Ma L, Shang S, Jiang Y, Huo K, Wang J, Qu Q (2019) Chronic sleep restriction induces Aβ Accumulation by disrupting the balance of Aβ production and clearance in rats. Neurochem Res 44:859–873
Xie Y, Ba L, Wang M, Deng SY, Chen SM, Huang LF, Zhang M, Wang W, Ding FF (2020) Chronic sleep fragmentation shares similar pathogenesis with neurodegenerative Diseases: Endosome-autophagosome-lysosome pathway dysfunction and microglia-mediated neuroinflammation. CNS Neurosci Ther 26:215–227
Vasciaveo V, Iadarola A, Casile A, Dante D, Morello G, Minotta L, Tamagno E, Cicolin A, Guglielmotto M (2023) Sleep fragmentation affects glymphatic system through the different expression of AQP4 in wild type and 5xFAD mouse models. Acta Neuropathol Commun 11:16
Nick H, Fenik P, Zhu Y, Veasey S (2022) Hypocretin/orexin influences chronic sleep disruption injury in the hippocampus. Front Aging Neurosci 14:1025402
Kent BA, Feldman HH, Nygaard HB (2021) Sleep and its regulation: an emerging pathogenic and treatment frontier in Alzheimer’s Disease. Prog Neurobiol 197:101902
Tabuchi M, Lone SR, Liu S, Liu Q, Zhang J, Spira AP, Wu MN (2015) Sleep interacts with aβ to modulate intrinsic neuronal excitability. Curr Biol 25:702–712
Ba L, Huang L, He Z, Deng S, Xie Y, Zhang M, Jacob C, Antonecchia E, Liu Y, Xiao W, Xie Q, Huang Z, Yi C, D’Ascenzo N, Ding F (2021) Does chronic sleep fragmentation lead to Alzheimer’s Disease in Young Wild-Type mice? Front Aging Neurosci 13:759983
Owen JE, Zhu Y, Fenik P, Zhan G, Bell P, Liu C, Veasey S (2021) Late-in-life neurodegeneration after chronic sleep loss in young adult mice. Sleep 44
Zhang F, Niu L, Zhong R, Li S, Le W (2023) Chronic sleep disturbances alters Sleep structure and tau phosphorylation in AβPP/PS1 AD mice and their wild-type littermates. J Alzheimers Dis 92:1341–1355
Zhu Y, Zhan G, Fenik P, Brandes M, Bell P, Francois N, Shulman K, Veasey S (2018) Chronic sleep disruption advances the temporal progression of Tauopathy in P301S Mutant mice. J Neurosci 38:10255–10270
Niu L, Zhang F, Xu X, Yang Y, Li S, Liu H, Le W (2022) Chronic sleep deprivation altered the expression of circadian clock genes and aggravated Alzheimer’s Disease neuropathology. Brain Pathol 32:e13028
Lucey BP (2020) It’s complicated: the relationship between sleep and Alzheimer’s Disease in humans. Neurobiol Dis 144:105031
Sato C, Barthélemy NR, Mawuenyega KG, Patterson BW, Gordon BA, Jockel-Balsarotti J, Sullivan M, Crisp MJ, Kasten T, Kirmess KM, Kanaan NM, Yarasheski KE, Baker-Nigh A, Benzinger TLS, Miller TM, Karch CM, Bateman RJ (2018) Tau kinetics in neurons and the Human Central Nervous System. Neuron 98:861–864
Yanamandra K, Patel TK, Jiang H, Schindler S, Ulrich JD, Boxer AL, Miller BL, Kerwin DR, Gallardo G, Stewart F, Finn MB, Cairns NJ, Verghese PB, Fogelman I, West T, Braunstein J, Robinson G, Keyser J, Roh J, Knapik SS, Hu Y, Holtzman DM (2017) Anti-tau antibody administration increases plasma tau in transgenic mice and patients with tauopathy. Sci Transl Med 9
Yamada K, Holth JK, Liao F, Stewart FR, Mahan TE, Jiang H, Cirrito JR, Patel TK, Hochgräfe K, Mandelkow EM, Holtzman DM (2014) Neuronal activity regulates extracellular tau in vivo. J Exp Med 211:387–393
Holth JK, Fritschi SK, Wang C, Pedersen NP, Cirrito JR, Mahan TE, Finn MB, Manis M, Geerling JC, Fuller PM, Lucey BP, Holtzman DM (2019) The sleep-wake cycle regulates brain interstitial fluid tau in mice and CSF tau in humans. Sci (New York NY) 363:880–884
Article CAS ADS Google Scholar
Irwin MR, Vitiello MV (2019) Implications of sleep disturbance and inflammation for Alzheimer’s Disease Dementia. Lancet Neurol 18:296–306
Wu R, Tripathy S, Menon V, Yu L, Buchman AS, Bennett DA, De Jager PL, Lim ASP (2022) Fragmentation of rest periods, astrocyte activation, and cognitive decline in older adults with and without Alzheimer’s disease. Alzheimers Dement
Kaneshwaran K, Olah M, Tasaki S, Yu L, Bradshaw EM, Schneider JA, Buchman AS, Bennett DA, De Jager PL, Lim ASP (2019) Sleep fragmentation, microglial aging, and cognitive impairment in adults with and without Alzheimer’s Dementia. Sci Adv 5:eaax7331
Bellesi M, de Vivo L, Chini M, Gilli F, Tononi G, Cirelli C (2017) Sleep loss promotes astrocytic phagocytosis and microglial activation in mouse cerebral cortex. J Neurosci 37:5263–5273
Kincheski GC, Valentim IS, Clarke JR, Cozachenco D, Castelo-Branco MTL, Ramos-Lobo AM, Rumjanek V, Donato J Jr., De Felice FG, Ferreira ST (2017) Chronic sleep restriction promotes Brain Inflammation and synapse loss, and potentiates memory impairment induced by amyloid-β oligomers in mice. Brain Behav Immun 64:140–151
Liu P, Zhao B, Wei M, Li Y, Liu J, Ma L, Shang S, Huo K, Wang J, Li R, Qu Q (2020) Activation of inflammation is Associated with Amyloid-β Accumulation Induced by Chronic Sleep restriction in rats. J Alzheimers Dis 74:759–773
Berk M, Williams LJ, Jacka FN, O’Neil A, Pasco JA, Moylan S, Allen NB, Stuart AL, Hayley AC, Byrne ML, Maes M (2013) So depression is an inflammatory Disease, but where does the inflammation come from? BMC Med 11:200
Siegel JM (2005) Clues to the functions of mammalian sleep. Nature 437:1264–1271
Wulff K, Gatti S, Wettstein JG, Foster RG (2010) Sleep and circadian rhythm disruption in psychiatric and neurodegenerative Disease. Nat Rev Neurosci 11:589–599
Mendoza J (2019) Circadian insights into the biology of depression: symptoms, treatments and animal models. Behav Brain Res 376:112186
Chellappa SL, Aeschbach D (2022) Sleep and anxiety: from mechanisms to interventions. Sleep Med Rev 61:101583
Mirchandaney R, Barete R, Asarnow LD (2022) Moderators of cognitive behavioral treatment for Insomnia on Depression and anxiety outcomes. Curr Psychiatry Rep 24:121–128
Soehner AM, Kaplan KA, Harvey AG (2014) Prevalence and clinical correlates of co-occurring insomnia and hypersomnia symptoms in depression. J Affect Disord 167:93–97
Zhou F, Li S, Xu H (2022) Insomnia, sleep duration, and risk of anxiety: a two-sample mendelian randomization study. J Psychiatr Res 155:219–225
Bean CAL, Ciesla JA (2021) Naturalistic partial sleep deprivation leads to Greater Next-Day anxiety: the moderating role of baseline anxiety and depression. Behav Ther 52:861–873
Palmer CA, Alfano CA (2020) Anxiety modifies the emotional effects of sleep loss. Curr Opin Psychol 34:100–104
Zhou L, Zhang H, Luo Z, Liu X, Yang L, Hu H, Wang Y, Wang C, Wang F (2020) Abnormal night sleep duration and inappropriate sleep initiation time are associated with elevated anxiety symptoms in Chinese rural adults: the Henan Rural Cohort. Psychiatry Res 291:113232
Riemann D (2007) Insomnia and comorbid psychiatric disorders. Sleep Med 8(Suppl 4):S15–20
Lopez R, Barateau L, Evangelista E, Dauvilliers Y (2017) Depression and Hypersomnia: a Complex Association. Sleep Med Clin 12:395–405
Luik AI, Zuurbier LA, Direk N, Hofman A, Van Someren EJ, Tiemeier H (2015) 24-HOUR ACTIVITY RHYTHM AND SLEEP DISTURBANCES IN DEPRESSION AND ANXIETY: A POPULATION-BASED STUDY OF MIDDLE-AGED AND OLDER PERSONS. Depress Anxiety 32:684–692
Bouwmans ME, Conradi HJ, Bos EH, Oldehinkel AJ, de Jonge P (2017) Bidirectionality between sleep symptoms and core depressive symptoms and their long-term course in Major Depression. Psychosom Med 79:336–344
Casement MD, Keenan KE, Hipwell AE, Guyer AE, Forbes EE (2016) Neural reward Processing mediates the relationship between insomnia symptoms and Depression in Adolescence. Sleep 39:439–447
Coles ME, Schubert JR, Nota JA (2015) Sleep, circadian rhythms, and anxious traits. Curr Psychiatry Rep 17:73
Horváth A, Montana X, Lanquart JP, Hubain P, Szűcs A, Linkowski P, Loas G (2016) Effects of state and trait anxiety on sleep structure: a polysomnographic study in 1083 subjects. Psychiatry Res 244:279–283
Short MA, Louca M (2015) Sleep deprivation leads to mood deficits in healthy adolescents. Sleep Med 16:987–993
Taraku B, Zavaliangos-Petropulu A, Loureiro JR, Al-Sharif NB, Kubicki A, Joshi SH, Woods RP, Espinoza R, Narr KL, Sahib AK (2023) White matter microstructural perturbations after total sleep deprivation in depression. Front Psychiatry 14:1195763
Hu B, Liu C, Mou T, Luo F, Lv T, Qian C, Zhang J, Ye M, Liu Z (2021) Meta-analysis of Sleep Deprivation effects on patients with Depression. Front Psychiatry 12:783091
Dong L, Xie Y, Zou X (2022) Association between sleep duration and depression in US adults: a cross-sectional study. J Affect Disord 296:183–188
Tartar JL, Ward CP, Cordeira JW, Legare SL, Blanchette AJ, McCarley RW, Strecker RE (2009) Experimental sleep fragmentation and sleep deprivation in rats increases exploration in an open field test of anxiety while increasing plasma corticosterone levels. Behav Brain Res 197:450–453
Pires GN, Bezerra AG, Tufik S, Andersen ML (2016) Effects of experimental sleep deprivation on anxiety-like behavior in animal research: systematic review and meta-analysis. Neurosci Biobehav Rev 68:575–589
Finan PH, Quartana PJ, Smith MT (2015) The effects of Sleep Continuity disruption on positive Mood and Sleep Architecture in healthy adults. Sleep 38:1735–1742
Meerlo P, Mistlberger RE, Jacobs BL, Heller HC, McGinty D (2009) New neurons in the adult brain: the role of sleep and consequences of sleep loss. Sleep Med Rev 13:187–194
Clasadonte J, McIver SR, Schmitt LI, Halassa MM, Haydon PG (2014) Chronic sleep restriction disrupts sleep homeostasis and behavioral sensitivity to alcohol by reducing the extracellular accumulation of adenosine. J Neurosci 34:1879–1891
Arvin P, Ghafouri S, Bavarsad K, Hajipour S, Khoshnam SE, Sarkaki A, Farbood Y (2023) Administration of growth hormone ameliorates adverse effects of total sleep deprivation. Metab Brain Dis 38:1671–1681
Klumpers UM, Veltman DJ, van Tol MJ, Kloet RW, Boellaard R, Lammertsma AA, Hoogendijk WJ (2015) Neurophysiological effects of sleep deprivation in healthy adults, a pilot study. PLoS ONE 10:e0116906
Jordan W, Tumani H, Cohrs S, Eggert S, Rodenbeck A, Brunner E, Rüther E, Hajak G (2004) Prostaglandin D synthase (beta-trace) in healthy human sleep. Sleep 27:867–874
Zhang Y, Dai C, Shao Y, Peng J, Yang Y, Hou Y (2021) Decreased functional connectivity in the reward network and its relationship with negative emotional experience after total sleep deprivation. Front Neurol 12:641810
Bosch OG, Rihm JS, Scheidegger M, Landolt HP, Stämpfli P, Brakowski J, Esposito F, Rasch B, Seifritz E (2013) Sleep deprivation increases dorsal nexus connectivity to the dorsolateral prefrontal cortex in humans. Proc Natl Acad Sci U S A 110:19597–19602
Lopez-Rodriguez F, Wilson CL, Maidment NT, Poland RE, Engel J (2003) Total sleep deprivation increases extracellular serotonin in the rat hippocampus. Neuroscience 121:523–530
Wu JC, Gillin JC, Buchsbaum MS, Schachat C, Darnall LA, Keator DB, Fallon JH, Bunney WE (2008) Sleep deprivation PET correlations of Hamilton symptom improvement ratings with changes in relative glucose metabolism in patients with depression. J Affect Disord 107:181–186
Grassi Zucconi G, Cipriani S, Balgkouranidou I, Scattoni R (2006) One night’ sleep deprivation stimulates hippocampal neurogenesis. Brain Res Bull 69:375–381
Tartar JL, Ward CP, McKenna JT, Thakkar M, Arrigoni E, McCarley RW, Brown RE, Strecker RE (2006) Hippocampal synaptic plasticity and spatial learning are impaired in a rat model of sleep fragmentation. Eur J Neurosci 23:2739–2748
Grubac Z, Sutulovic N, Ademovic A, Velimirovic M, Rasic-Markovic A, Macut D, Petronijevic N, Stanojlovic O, Hrncic D (2019) Short-term sleep fragmentation enhances anxiety-related behavior: the role of hormonal alterations. PLoS ONE 14:e0218920
Nair D, Zhang SX, Ramesh V, Hakim F, Kaushal N, Wang Y, Gozal D (2011) Sleep fragmentation induces cognitive deficits via nicotinamide adenine dinucleotide phosphate oxidase-dependent pathways in mouse. Am J Respir Crit Care Med 184:1305–1312
Stepnowsky CJ, Palau JJ, Zamora T, Ancoli-Israel S, Loredo JS (2011) Fatigue in sleep apnea: the role of depressive symptoms and self-reported sleep quality. Sleep Med 12:832–837
Gong L, Liao T, Liu D, Luo Q, Xu R, Huang Q, Zhang B, Feng F, Zhang C (2019) Amygdala Changes in Chronic Insomnia and Their Association with sleep and anxiety symptoms: insight from shape analysis. Neural Plast 2019:8549237
Gong L, Shi M, Wang J, Xu R, Yu S, Liu D, Ding X, Zhang B, Zhang X, Xi C (2021) The abnormal functional connectivity in the Locus Coeruleus-Norepinephrine System Associated with anxiety Symptom in Chronic Insomnia Disorder. Front Neurosci 15:678465
Xu M, Wang Q, Li B, Qian S, Wang S, Wang Y, Chen C, Liu Z, Ji Y, Liu K, Xin K, Niu Y (2023) Cerebellum and hippocampus abnormalities in patients with insomnia comorbid depression: a study on cerebral blood perfusion and functional connectivity. Front Neurosci 17:1202514
Motomura Y, Katsunuma R, Ayabe N, Oba K, Terasawa Y, Kitamura S, Moriguchi Y, Hida A, Kamei Y, Mishima K (2021) Decreased activity in the reward network of chronic insomnia patients. Sci Rep 11:3600
Gong L, Yu S, Xu R, Liu D, Dai X, Wang Z, Hu Y, Yan B, Kui Y, Zhang B, Feng F (2021) The abnormal reward network associated with insomnia severity and depression in chronic insomnia disorder. Brain Imaging Behav 15:1033–1042
Rahmani M, Rahmani F, Rezaei N (2020) The brain-derived neurotrophic factor: missing Link between Sleep Deprivation, Insomnia, and Depression. Neurochem Res 45:221–231
Schmitt K, Holsboer-Trachsler E, Eckert A (2016) BDNF in sleep, insomnia, and sleep deprivation. Ann Med 48:42–51
Konakanchi S, Raavi V, Ml HK, Shankar Ms V (2022) Effect of chronic sleep deprivation and sleep recovery on hippocampal CA3 neurons, spatial memory and anxiety-like behavior in rats. Neurobiol Learn Mem 187:107559
Xia M, Li Z, Li S, Liang S, Li X, Chen B, Zhang M, Dong C, Verkhratsky A, Guan D, Li B (2020) Sleep Deprivation Selectively Down-Regulates Astrocytic 5-HT(2B) Receptors and Triggers Depressive-Like Behaviors via Stimulating P2X(7) Receptors in Mice. Neurosci Bull 36:1259–1270
Manchanda S, Singh H, Kaur T, Kaur G (2018) Low-grade neuroinflammation due to chronic sleep deprivation results in anxiety and learning and memory impairments. Mol Cell Biochem 449:63–72
Kiecolt-Glaser JK, Derry HM, Fagundes CP (2015) Inflammation: depression fans the flames and feasts on the heat. Am J Psychiatry 172:1075–1091
Liu H, Huang X, Li Y, Xi K, Han Y, Mao H, Ren K, Wang W, Wu Z (2022) TNF signaling pathway-mediated microglial activation in the PFC underlies acute paradoxical sleep deprivation-induced anxiety-like behaviors in mice. Brain Behav Immun 100:254–266
Merikanto I, Partonen T (2021) Eveningness increases risks for depressive and anxiety symptoms and hospital treatments mediated by insufficient sleep in a population-based study of 18,039 adults. Depress Anxiety 38:1066–1077
Stahl ST, Smagula SF, Rodakowski J, Dew MA, Karp JF, Albert SM, Butters M, Gildengers A, Reynolds CF 3rd (2021) Subjective Sleep Quality and trajectories of Interleukin-6 in older adults. Am J Geriatr Psychiatry 29:204–208
Selvi Y, Boysan M, Kandeger A, Uygur OF, Sayin AA, Akbaba N, Koc B (2018) Heterogeneity of sleep quality in relation to circadian preferences and depressive symptomatology among major depressive patients. J Affect Disord 235:242–249
Taylor BJ, Hasler BP (2018) Chronotype and Mental Health: recent advances. Curr Psychiatry Rep 20:59
Merikanto I, Kronholm E, Peltonen M, Laatikainen T, Vartiainen E, Partonen T (2015) Circadian preference links to depression in general adult population. J Affect Disord 188:143–148
Schapira AHV, Chaudhuri KR, Jenner P (2017) Non-motor features of Parkinson Disease. Nat Rev Neurosci 18:435–450
Stefani A, Högl B (2020) Sleep in Parkinson’s Disease. NEUROPSYCHOPHARMACOLOGY 45:121–128
Morawska MM, Moreira CG, Ginde VR, Valko PO, Weiss T, Büchele F, Imbach LL, Masneuf S, Kollarik S, Prymaczok N, Gerez JA, Riek R, Baumann CR, Noain D (2021) Slow-wave sleep affects synucleinopathy and regulates proteostatic processes in mouse models of Parkinson’s Disease. Sci Transl Med 13:eabe7099
Zuzuárregui JRP, During EH (2020) Sleep issues in Parkinson’s Disease and their management. Neurotherapeutics 17:1480–1494
Hermanowicz N, Jones SA, Hauser RA (2019) Impact of non-motor symptoms in Parkinson’s Disease: a PMDAlliance survey. Neuropsychiatr Dis Treat 15:2205–2212
Kay DB, Tanner JJ, Bowers D (2018) Sleep disturbances and depression severity in patients with Parkinson’s Disease. Brain Behav 8:e00967
Latif S, Jahangeer M, Maknoon Razia D, Ashiq M, Ghaffar A, Akram M, El Allam A, Bouyahya A, Garipova L, Ali Shariati M, Thiruvengadam M, Azam Ansari M (2021) Dopamine in Parkinson’s Disease. Clin Chim Acta 522:114–126
Dauvilliers Y, Schenck CH, Postuma RB, Iranzo A, Luppi PH, Plazzi G, Montplaisir J, Boeve B (2018) REM sleep behaviour disorder. Nat Rev Dis Primers 4:19
Miglis MG, Adler CH, Antelmi E, Arnaldi D, Baldelli L, Boeve BF, Cesari M, Dall’Antonia I, Diederich NJ, Doppler K, Dušek P, Ferri R, Gagnon JF, Gan-Or Z, Hermann W, Högl B, Hu MT, Iranzo A, Janzen A, Kuzkina A, Lee JY, Leenders KL, Lewis SJG, Liguori C, Liu J, Lo C, Ehgoetz Martens KA, Nepozitek J, Plazzi G, Provini F, Puligheddu M, Rolinski M, Rusz J, Stefani A, Summers RLS, Yoo D, Zitser J, Oertel WH (2021) Biomarkers of conversion to α-synucleinopathy in isolated rapid-eye-movement sleep behaviour disorder. Lancet Neurol 20:671–684
Si XL, Gu LY, Song Z, Zhou C, Fang Y, Jin CY, Wu JJ, Gao T, Guo T, Guan XJ, Xu XJ, Yin XZ, Yan YP, Zhang MM, Pu JL (2020) Different Perivascular Space burdens in Idiopathic Rapid Eye Movement Sleep Behavior Disorder and Parkinson’s Disease. Front Aging Neurosci 12:580853
Maggi G, Trojano L, Barone P, Santangelo G (2021) Sleep disorders and cognitive dysfunctions in Parkinson’s Disease: a Meta-Analytic Study. Neuropsychol Rev 31:643–682
Lin YQ, Chen SD (2018) RBD: a red flag for cognitive impairment in Parkinson’s Disease? Sleep Med 44:38–44
Lazar AS, Panin F, Goodman AO, Lazic SE, Lazar ZI, Mason SL, Rogers L, Murgatroyd PR, Watson LP, Singh P, Borowsky B, Shneerson JM, Barker RA (2015) Sleep deficits but no metabolic deficits in Premanifest Huntington’s Disease. Ann Neurol 78:630–648
Vas S, Nicol AU, Kalmar L, Miles J, Morton AJ (2021) Abnormal patterns of sleep and EEG power distribution during non-rapid eye movement sleep in the sheep model of Huntington’s Disease. Neurobiol Dis 155:105367
Cabanas M, Pistono C, Puygrenier L, Rakesh D, Jeantet Y, Garret M, Cho YH (2019) Neurophysiological and behavioral effects of anti-orexinergic treatments in a mouse model of Huntington’s Disease. Neurotherapeutics: The Journal of the American Society for Experimental NeuroTherapeutics 16:784–796
Hulisz D (2018) Amyotrophic Lateral Sclerosis: Disease state overview. Am J Manag Care 24:S320–s326
PubMed Google Scholar
Liu S, Ren Q, Gong G, Sun Y, Zhao B, Ma X, Zhang N, Zhong S, Lin Y, Wang W, Zheng R, Yu X, Yun Y, Zhang D, Shao K, Lin P, Yuan Y, Dai T, Zhang Y, Li L, Li W, Zhao Y, Shan P, Meng X, Yan C (2022) Hypothalamic subregion abnormalities are related to body mass index in patients with sporadic Amyotrophic Lateral Sclerosis. J Neurol 269:2980–2988
Gnoni V, Zoccolella S, Giugno A, Urso D, Tamburrino L, Filardi M, Logroscino G (2023) Hypothalamus and Amyotrophic Lateral Sclerosis: potential implications in sleep disorders. Front Aging Neurosci 15:1193483
Lo Martire V, Caruso D, Palagini L, Zoccoli G, Bastianini S (2020) Stress & sleep: a relationship lasting a lifetime. Neurosci Biobehav Rev 117:65–77
Basta M, Vgontzas AN, Fernandez-Mendoza J, Antypa D, Li Y, Zaganas I, Panagiotakis S, Karagkouni E, Simos P (2022) Basal cortisol levels are increased in patients with mild cognitive impairment: role of Insomnia and short sleep duration. J Alzheimers Dis 87:933–944
Gabery S, Ahmed RM, Caga J, Kiernan MC, Halliday GM, Petersén Å (2021) Loss of the metabolism and sleep regulating neuronal populations expressing orexin and oxytocin in the hypothalamus in Amyotrophic Lateral Sclerosis. Neuropathol Appl Neurobiol 47:979–989
Boentert M (2019) Sleep disturbances in patients with Amyotrophic Lateral Sclerosis: current perspectives. Nat Sci Sleep 11:97–111
Download references
Acknowledgements
We would like to thank Editage ( www.editage.cn ) for English language editing.
This study was supported by grants from the National Natural Science Foundation of China (No. 82371541), the project for the improvement of research skill in Anhui Medical University (No.2021xkjT003), Talent Training Program from the School of Basic Medical Sciences of Anhui Medical University (No. 2022YPJH201), Research Fund of Anhui Institute of translational medicine (No. 2022zhyx-C11) and National Training Project of Innovation and Entrepreneurship for Undergraduates of China (No. 202310366060 & No. 202310366037).
Author information
Xiao Xiao and Yimin Rui contributed equally to this work.
Authors and Affiliations
School of Mental Health and Psychological Sciences, Anhui Medical University, Hefei, Anhui, China
Xiao Xiao & Yimin Rui
Department of Pharmacology, School of Basic Medical Sciences, Anhui Medical University, Hefei, Anhui, China
Xiao Xiao, Yimin Rui, Yu Jin & Ming Chen
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the manuscript. X.X. had the idea for the article. X.X., Y.M.R. and Y. J. performed the literature search, drafted the manuscript and created the figures. M.C. revised critically the manuscript. All authors read and approved the manuscript.
Corresponding author
Correspondence to Ming Chen .
Ethics declarations
Competing interests.
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Xiao, X., Rui, Y., Jin, Y. et al. Relationship of Sleep Disorder with Neurodegenerative and Psychiatric Diseases: An Updated Review. Neurochem Res 49 , 568–582 (2024). https://doi.org/10.1007/s11064-023-04086-5
Download citation
Received : 22 September 2023
Revised : 08 December 2023
Accepted : 09 December 2023
Published : 18 December 2023
Issue Date : March 2024
DOI : https://doi.org/10.1007/s11064-023-04086-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Sleep Disorder
- Alzheimer’s Disease
- Parkinson’s Disease
- Find a journal
- Publish with us
- Track your research
Our websites may use cookies to personalize and enhance your experience. By continuing without changing your cookie settings, you agree to this collection. For more information, please see our University Websites Privacy Notice .
UConn Today
- School and College News
- Arts & Culture
- Community Impact
- Entrepreneurship
- Health & Well-Being
- Research & Discovery
- UConn Health
- University Life
- UConn Voices
- University News
April 17, 2024 | Kim Krieger - UConn Communications
Researchers Look at Sleep Quality in Black and Hispanic Women of Childbearing Age
The research will serve as the foundation for future health promotion programs to address sleep quality

(Adobe Stock)
Not getting enough sleep is bad for your health. And while many of us don’t get enough, Black and Hispanic women report particularly poor quality sleep. Now a team of researchers in Connecticut is working with urban communities in the state to figure out how Black and Hispanic women can get more rest.
The National Institutes of Health National Center on Sleep Disorders Research has awarded $3.5 million to a team of researchers led by Nancy S. Redeker, senior associate dean for research and scholarship in the School of Nursing. The grant will fund research looking at how behaviors and social factors affect sleep quality among Black and Hispanic women of childbearing age. The research is designed to be the foundation for future health promotion programs to address sleep quality and its negative effects, including pregnancy outcomes and lifelong heart problems.
Other researchers on the team include UConn’s Natalie Shook and Eileen Condon from the School of Nursing, and geographer Chuanrong Zhang, as well as colleagues from Yale University, including certified nurse-midwife Heather Reynolds who will lead the community advisory board. The board will also include members of the Black and Hispanic communities in New Haven, Hartford, and Waterbury, where the researchers will recruit participants for the study.
The researchers will ask women questions about their health and their sleep, including how long they sleep, how regular their sleep is, and what affects their sleep. Women will use a wrist worn device to measure daily sleep and wear a device to determine whether they have sleep apnea. The data will provide information about sleep quality and health in Black and Hispanic women of childbearing age before they get pregnant. The researchers hope to extend this work in the future to develop and test programs to promote sleep health.
“If you sleep well before you’re pregnant, it’s more likely we can support your sleep while you’re pregnant,” Redeker says. Eventually, the researchers hope the studies will reveal ways in which women can increase their odds of a healthy pregnancy and birth, and possibly improve their lifelong health by adjusting their sleep patterns.
Recent Articles

April 18, 2024
Dana Parrott ’24, College of Liberal Arts and Sciences
Read the article

UConn Gives: Countless Reasons to Get Involved
School of Nursing Sees 32% Increase in Undergraduate Applications Since the Last Year Amidst a National Nursing Shortage
Only 26% of Americans Say They Get at Least Eight Hours of Sleep, New Gallup Poll Says
It seems Americans don't think they're particularly well-rested

Wilfredo Lee
FILE - A traveler takes a nap as he waits for a ride outside Miami International Airport, Friday, July 1, 2022, in Miami. The Gallup survey, released Monday, April 15, 2024, says that a majority of Americans say they would feel better if they could have more sleep. But in the U.S., where the ethos of grinding and pulling yourself up by your own bootstraps is ubiquitous, getting enough sleep can seem like a dream. (AP Photo/Wilfredo Lee, File)
NEW YORK (AP) — If you're feeling — YAWN — sleepy or tired while you read this and wish you could get some more shut-eye, you're not alone. A majority of Americans say they would feel better if they could have more sleep, according to a new poll.
But in the U.S., the ethos of grinding and pulling yourself up by your own bootstraps is ubiquitous, both in the country's beginnings and our current environment of always-on technology and work hours. And getting enough sleep can seem like a dream.
The Gallup poll , released Monday, found 57% of Americans say they would feel better if they could get more sleep, while only 42% say they are getting as much sleep as they need. That’s a first in Gallup polling since 2001; in 2013, when Americans were last asked, it was just about the reverse — 56% saying they got the needed sleep and 43% saying they didn’t.
Younger women, under the age of 50, were especially likely to report they aren't getting enough rest.
The poll also asked respondents to report how many hours of sleep they usually get per night: Only 26% said they got eight or more hours, which is around the amount that sleep experts say is recommended for health and mental well-being. Just over half, 53%, reported getting six to seven hours. And 20% said they got five hours or less, a jump from the 14% who reported getting the least amount of sleep in 2013.
(And just to make you feel even more tired, in 1942, the vast majority of Americans were sleeping more. Some 59% said they slept eight or more hours, while 33% said they slept six to seven hours. What even IS that?)
Photos You Should See - April 2024

THE REASONS AREN'T EXACTLY CLEAR
The poll doesn't get into reasons WHY Americans aren't getting the sleep they need, and since Gallup last asked the question in 2013, there's no data breaking down the particular impact of the last four years and the pandemic era.
But what's notable, says Sarah Fioroni, senior researcher at Gallup, is the shift in the last decade toward more Americans thinking they would benefit from more sleep and particularly the jump in the number of those saying they get five or less hours.
“That five hours or less category ... was almost not really heard of in 1942,” Fioroni said. “There’s almost nobody that said they slept five hours or less.”
In modern American life, there also has been “this pervasive belief about how sleep was unnecessary — that it was this period of inactivity where little to nothing was actually happening and that took up time that could have been better used,” said Joseph Dzierzewski, vice president for research and scientific affairs at the National Sleep Foundation.
It’s only relatively recently that the importance of sleep to physical, mental and emotional health has started to percolate more in the general population, he said.
And there’s still a long way to go. For some Americans, like Justine Broughal, 31, a self-employed event planner with two small children, there simply aren't enough hours in the day. So even though she recognizes the importance of sleep, it often comes in below other priorities like her 4-month-old son, who still wakes up throughout the night, or her 3-year-old daughter.
“I really treasure being able to spend time with (my children),” Broughal says. “Part of the benefit of being self-employed is that I get a more flexible schedule, but it’s definitely often at the expense of my own care.”
THERE'S A CULTURAL BACKDROP TO ALL THIS, TOO
So why are we awake all the time? One likely reason for Americans' sleeplessness is cultural — a longstanding emphasis on industriousness and productivity.
Some of the context is much older than the shift documented in the poll. It includes the Protestants from European countries who colonized the country, said Claude Fischer, a professor of sociology at the graduate school of the University of California, Berkeley. Their belief system included the idea that working hard and being rewarded with success was evidence of divine favor.
“It has been a core part of American culture for centuries,” he said. “You could make the argument that it ... in the secularized form over the centuries becomes just a general principle that the morally correct person is somebody who doesn’t waste their time.”
Jennifer Sherman has seen that in action. In her research in rural American communities over the years, the sociology professor at Washington State University says a common theme among people she interviewed was the importance of having a solid work ethic. That applied not only to paid labor but unpaid labor as well, like making sure the house was clean.
A through line of American cultural mythology is the idea of being “individually responsible for creating our own destinies," she said. “And that does suggest that if you’re wasting too much of your time ... that you are responsible for your own failure.”
“The other side of the coin is a massive amount of disdain for people considered lazy," she added.
Broughal says she thinks that as parents, her generation is able to let go of some of those expectations. “I prioritize ... spending time with my kids, over keeping my house pristine,” she said.
But with two little ones to care for, she said, making peace with a messier house doesn't mean more time to rest: “We’re spending family time until, you know, (my 3-year-old) goes to bed at eight and then we’re resetting the house, right?”
THE TRADEOFFS OF MORE SLEEP
While the poll only shows a broad shift over the past decade, living through the COVID-19 pandemic may have affected people's sleep patterns. Also discussed in post-COVID life is “revenge bedtime procrastination,” in which people put off sleeping and instead scroll on social media or binge a show as a way of trying to handle stress.
Liz Meshel is familiar with that. The 30-year-old American is temporarily living in Bulgaria on a research grant, but also works a part-time job on U.S. hours to make ends meet.
On the nights when her work schedule stretches to 10 p.m., Meshel finds herself in a “revenge procrastination” cycle. She wants some time to herself to decompress before going to sleep and ends up sacrificing sleeping hours to make it happen.
“That applies to bedtime as well, where I’m like, ’Well, I didn’t have any me time during the day, and it is now 10 p.m., so I am going to feel totally fine and justified watching X number of episodes of TV, spending this much time on Instagram, as my way to decompress,” she said. “Which obviously will always make the problem worse.”
Sanders reported from Washington, D.C.
Copyright 2024 The Associated Press . All rights reserved. This material may not be published, broadcast, rewritten or redistributed.
Join the Conversation
Tags: Associated Press , children , health
America 2024

Health News Bulletin
Stay informed on the latest news on health and COVID-19 from the editors at U.S. News & World Report.
Sign in to manage your newsletters »
Sign up to receive the latest updates from U.S News & World Report and our trusted partners and sponsors. By clicking submit, you are agreeing to our Terms and Conditions & Privacy Policy .
You May Also Like
The 10 worst presidents.
U.S. News Staff Feb. 23, 2024

Cartoons on President Donald Trump
Feb. 1, 2017, at 1:24 p.m.

Photos: Obama Behind the Scenes
April 8, 2022

Photos: Who Supports Joe Biden?
March 11, 2020

Democrats Split on Helping Johnson
Aneeta Mathur-Ashton April 18, 2024

Interest Rates, Inflation Hamper Economy
Tim Smart April 18, 2024

Boeing Called Out for ‘Defective’ Planes
Laura Mannweiler April 17, 2024

Senate Kills Mayorkas Impeachment
Aneeta Mathur-Ashton April 17, 2024

Fed: Strong Economy Stalling Rate Cuts
Tim Smart April 17, 2024

The Implications of Trump Legal Wins
Lauren Camera April 16, 2024

Articles on New research, Australia New Zealand
Displaying 1 - 20 of 48 articles.

Falls, fractures and self-harm : 4 charts on how kids’ injury risk changes over time and differs for boys and girls
Lisa Nicole Sharwood , UNSW Sydney ; Rebecca Ivers , UNSW Sydney , and Warwick Teague , Royal Children's Hospital

First evidence of ancient human occupation found in giant lava tube cave in Saudi Arabia
Mathew Stewart , Griffith University ; Huw Groucutt , University of Malta , and Michael Petraglia , Griffith University

Could not getting enough sleep increase your risk of type 2 diabetes?
Giuliana Murfet , University of Technology Sydney and ShanShan Lin , University of Technology Sydney

For 600 years the Voynich manuscript has remained a mystery. Now we think it’s partly about sex
Keagan Brewer , Macquarie University

We found three new species of extinct giant kangaroo – and we don’t know why they died out when their cousins survived
Isaac A. R. Kerr , Flinders University

Rogue waves in the ocean are much more common than anyone suspected, says new study
Alessandro Toffoli , The University of Melbourne

Trillions of tonnes of carbon locked in soil has been left out of environmental models – and it’s on the move
Yuanyuan Huang , Chinese Academy of Sciences ; Pep Canadell , CSIRO , and Yingping Wang , CSIRO
Friday essay: ‘too many Aboriginal babies’ – Australia’s secret history of Aboriginal population control in the 1960s
Laura Rademaker , Australian National University ; Jakelin Troy , University of Sydney , and Julia Hurst , The University of Melbourne

Roads of destruction: we found vast numbers of illegal ‘ghost roads’ used to crack open pristine rainforest
Bill Laurance , James Cook University

Aboriginal people made pottery and sailed to distant offshore islands thousands of years before Europeans arrived
Sean Ulm , James Cook University ; Ian J. McNiven , Monash University , and Kenneth McLean , Indigenous Knowledge

Flash droughts are becoming more common in Australia. What’s causing them?
Milton Speer , University of Technology Sydney and Lance M Leslie , University of Technology Sydney

Heat from El Niño can warm oceans off West Antarctica – and melt floating ice shelves from below
Maurice Huguenin , UNSW Sydney ; Matthew England , UNSW Sydney , and Paul Spence , University of Tasmania
We saw one of the most powerful magnets in the Universe come to life – and our theories can’t quite explain it
Marcus Lower , CSIRO ; Gregory Desvignes , Max Planck Institute for Radio Astronomy , and Patrick Weltevrede , University of Manchester

Australians are open to self-driving vehicles, but want humans to retain ultimate control
Hussein Dia , Swinburne University of Technology and Ali Matin , Swinburne University of Technology

Daylight saving has 80% support in Australia and a majority in every state
Thomas Sigler , The University of Queensland

Australian writers have been envisioning AI for a century. Here are 5 stories to read as we grapple with rapid change
Leah Henrickson , The University of Queensland ; Catriona Mills , The University of Queensland ; David Tang , The University of Queensland , and Maggie Nolan , The University of Queensland

Australian ‘bush glass’ bears the fingerprints of a cosmic collision with an iron meteorite
Aaron J. Cavosie , Curtin University

After 10 years of work, landmark study reveals new ‘tree of life’ for all birds living today
Jacqueline Nguyen , Flinders University and Simon Ho , University of Sydney
Quantum computing just got hotter: 1 degree above absolute zero
Andrew Dzurak , UNSW Sydney and Andre Luiz Saraiva De Oliveira , UNSW Sydney
A cosmic ‘speed camera’ just revealed the staggering speed of neutron star jets in a world first
James Miller-Jones , Curtin University
Related Topics
- Better Cities
- Climate change
- Environment
- Extreme heat
- Friday essay
- Global warming
- Greenhouse gas emissions (GHG)
- New research

Deputy Social Media Producer

Research Fellow /Senior Research Fellow – Implementation Science

Associate Professor, Occupational Therapy

GRAINS RESEARCH AND DEVELOPMENT CORPORATION CHAIRPERSON

Faculty of Law - Academic Appointment Opportunities
Top contributors.
Associate Professor of Human Geography, The University of Queensland
Adjunct Professor, School of Civil and Environmental Engineering, University of Technology Sydney
Casual Academic, Faculty of Health, University of Technology Sydney
Director of Aboriginal & Torres Strait Islander Research Office, University of Sydney
Research Fellow, Department of Media, Communications, Creative Arts, Language, and Literature, Macquarie University
Lecturer in Clinical Psychology, La Trobe University
Research Fellow, Australian Research Centre for Human Evolution, Griffith University
Associate Professor in Clinical Psychology, Griffith University
Lecturer in Mediterranean Prehistory, University of Malta
Associate Professor, Department of Psychology, Simon Fraser University
Director, Australian Research Centre for Human Evolution, Griffith University
Professor of Psychology, University of Toronto
Professor, School of Design, University of Technology Sydney
Research Fellow, Centre for Childhood Nutrition Research, Queensland University of Technology
Faculty of Arts Indigenous Postdoctoral Fellow, Indigenous and Settler Relations Collaboration, The University of Melbourne
- X (Twitter)
- Unfollow topic Follow topic
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection

Important advances in sleep research in 2021
Leslie c west.
a Division of Sleep Medicine, Department of Psychiatry and Behavioral Sciences, Stanford University School of Medicine, Palo Alto, CA 94305, USA
Clete A Kushida
Advances in sleep research in 2021 have brought about clinical developments for the next decade. Additionally, sleep telemedicine services have expanded rapidly, driven by the COVID-19 pandemic, to best serve patients with sleep disorders. 1 Here, we will explore some of the most impactful clinical studies from this field in 2021.
Progress has been made in evaluating the relationship between obstructive sleep apnoea and incidence of Alzheimer's disease. In a large cohort study of 53 321 patients with obstructive sleep apnoea, patients treated with continuous positive airway pressure (CPAP) were compared with those who were not. In adjusted models, those who were treated had a significantly lower odds of incident diagnosis of Alzheimer's disease or dementia (odds ratio 0·78, 95% CI 0·69–0·89). 2 This finding adds population-based evidence to suggest a temporal association between obstructive sleep apnoea treatment and dementia risk. In a study that analysed autopsy brains from 34 Icelandic patients with clinically verified obstructive sleep apnoea, Owen and colleagues 3 found that, as the severity of obstructive sleep apnoea increased, the burden of amyloid β in the hippocampus increased too, even after controlling for age, sex, body-mass index, and CPAP use. These findings, although in a small sample size, provide further neuropathological evidence for an association between Alzheimer's disease and obstructive sleep apnoea.
Throughout the COVID-19 pandemic, there have been reports of more frequent sleep disturbances. Morin and colleagues 4 conducted a multicentre survey of 22 330 adults from 13 countries and found that more than 35% of respondents reported insomnia symptoms, with about 17% meeting criteria for a probable insomnia disorder during the first months of the pandemic. These data provide an indication of the need for programmes to tackle insomnia during a global crisis. Arnedt and colleagues 5 reported findings of a placebo-controlled randomised trial of 65 adults assigned to telemedicine or in-person delivery of cognitive behavioural therapy for insomnia. They showed that cognitive behaviour therapy delivered via telemedicine was non-inferior to therapy done in-person, according to the reduction in insomnia severity index score.
Dual orexin receptor antagonists have been evaluated in clinical research as an additional treatment option for insomnia. 12-month results from the phase 3 analysis of the Study of the Efficacy and Safety of Lemborexant in Subjects 55 and Older with Insomnia Disorder (SUNRISE 2) were published in 2021. 6 This international, multicentre, randomised, double-blind, placebo-controlled, parallel-group study compared two doses of lemborexant (5 mg and 10 mg) with placebo, and enrolled 949 participants, including 318 who received placebo. Patients randomly assigned to treatment showed a benefit, with shorter sleep onset latency, increased subjective total sleep time, and decreased subjective wake after sleep onset, at 12-month follow-up.
Dauvilliers and colleagues 7 conducted a phase 3 randomised controlled trial of lower-sodium oxybate for the treatment of patients with idiopathic hypersomnia. They found a significant change in the Epworth Sleepiness Scale compared with placebo (difference of –6·5, 95% CI –8·0 to –5·0), indicating a clinically meaningful effect on excessive daytime sleepiness. Overall idiopathic hypersomnia symptom severity showed significant improvement in patients randomly assigned to lower-sodium oxybate compared with placebo.
Gaspar and colleagues 8 examined the effect of obstructive sleep apnoea on disruption of circadian rhythms. Their study was the first to compare the effect of CPAP in the short term (4 months) and long term (2 years) on circadian characteristics in a case-control study of 34 male patients with obstructive sleep apnoea and seven age-matched and sex-matched healthy controls. The investigators found that long-term, but not short-term, CPAP treatment was able to re-establish levels of major clock circadian outputs, including plasma melatonin, cortisol, and body temperature. The authors found that CPAP does not fully re-establish the expression profile of clock genes, but leads to evident improvements.
Regarding public health policy, further evidence was published from the Changing Start Times: Longitudinal Effects Study (CaSTLES) evaluating school start times at or after 0830 h for middle-school and high-school students. 9 The findings showed that, when start times were 40–70 min later, middle-school students obtained an extra 2·4 h of sleep per week and high-school students an extra 3·8 h of sleep per week, with maintenance of this effect over 2 years.
In basic sleep science research, Konkoly and colleagues 10 provided proof-of-concept evidence that individuals can be interviewed about their dreams while they are dreaming. In four independent laboratories in France, Germany, the Netherlands, and the USA, healthy participants and one patient with narcolepsy provided evidence for real-time communication during rapid eye movement (REM) sleep. This example of bidirectional communication during REM sleep showed the use of working memory, with yet-to-be explored potential clinical applications for cognitive improvement, learning, and beyond.
In conclusion, the advances during this year have included a broad landscape of investigations, while researchers and clinical teams adapted to the challenge of conducting studies during a pandemic, and provided far-reaching new insights for sleep medicine.
CAK reports personal fees related to consultancies or participation in medical advisory boards from XW Pharma, Idorsia, Merck, Jazz Pharmaceuticals, Avadel Pharmaceuticals, Cerebra, and VIVOS; grants or contracts with the National Institutes of Health, Avadel Pharmaceuticals, AmCad BioMed Corporation, Jazz Pharmaceuticals, Merck Sharp & Dohme, Parexel International Corporation, Asate, Inspire Medical Systems, and Respironics; lecture honoraria from ResMed Asia and Itamar Medical; and stock or stock options from M3 Public Benefit Corporation, Restful Robotics, VIVOS, and Koko. LCW declares no competing interests.
An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Entire Site
- Research & Funding
- Health Information
- About NIDDK
- Diabetes Overview
Healthy Living with Diabetes
- Español
On this page:
How can I plan what to eat or drink when I have diabetes?
How can physical activity help manage my diabetes, what can i do to reach or maintain a healthy weight, should i quit smoking, how can i take care of my mental health, clinical trials for healthy living with diabetes.
Healthy living is a way to manage diabetes . To have a healthy lifestyle, take steps now to plan healthy meals and snacks, do physical activities, get enough sleep, and quit smoking or using tobacco products.
Healthy living may help keep your body’s blood pressure , cholesterol , and blood glucose level, also called blood sugar level, in the range your primary health care professional recommends. Your primary health care professional may be a doctor, a physician assistant, or a nurse practitioner. Healthy living may also help prevent or delay health problems from diabetes that can affect your heart, kidneys, eyes, brain, and other parts of your body.
Making lifestyle changes can be hard, but starting with small changes and building from there may benefit your health. You may want to get help from family, loved ones, friends, and other trusted people in your community. You can also get information from your health care professionals.
What you choose to eat, how much you eat, and when you eat are parts of a meal plan. Having healthy foods and drinks can help keep your blood glucose, blood pressure, and cholesterol levels in the ranges your health care professional recommends. If you have overweight or obesity, a healthy meal plan—along with regular physical activity, getting enough sleep, and other healthy behaviors—may help you reach and maintain a healthy weight. In some cases, health care professionals may also recommend diabetes medicines that may help you lose weight, or weight-loss surgery, also called metabolic and bariatric surgery.
Choose healthy foods and drinks
There is no right or wrong way to choose healthy foods and drinks that may help manage your diabetes. Healthy meal plans for people who have diabetes may include
- dairy or plant-based dairy products
- nonstarchy vegetables
- protein foods
- whole grains
Try to choose foods that include nutrients such as vitamins, calcium , fiber , and healthy fats . Also try to choose drinks with little or no added sugar , such as tap or bottled water, low-fat or non-fat milk, and unsweetened tea, coffee, or sparkling water.
Try to plan meals and snacks that have fewer
- foods high in saturated fat
- foods high in sodium, a mineral found in salt
- sugary foods , such as cookies and cakes, and sweet drinks, such as soda, juice, flavored coffee, and sports drinks
Your body turns carbohydrates , or carbs, from food into glucose, which can raise your blood glucose level. Some fruits, beans, and starchy vegetables—such as potatoes and corn—have more carbs than other foods. Keep carbs in mind when planning your meals.
You should also limit how much alcohol you drink. If you take insulin or certain diabetes medicines , drinking alcohol can make your blood glucose level drop too low, which is called hypoglycemia . If you do drink alcohol, be sure to eat food when you drink and remember to check your blood glucose level after drinking. Talk with your health care team about your alcohol-drinking habits.

Find the best times to eat or drink
Talk with your health care professional or health care team about when you should eat or drink. The best time to have meals and snacks may depend on
- what medicines you take for diabetes
- what your level of physical activity or your work schedule is
- whether you have other health conditions or diseases
Ask your health care team if you should eat before, during, or after physical activity. Some diabetes medicines, such as sulfonylureas or insulin, may make your blood glucose level drop too low during exercise or if you skip or delay a meal.
Plan how much to eat or drink
You may worry that having diabetes means giving up foods and drinks you enjoy. The good news is you can still have your favorite foods and drinks, but you might need to have them in smaller portions or enjoy them less often.
For people who have diabetes, carb counting and the plate method are two common ways to plan how much to eat or drink. Talk with your health care professional or health care team to find a method that works for you.
Carb counting
Carbohydrate counting , or carb counting, means planning and keeping track of the amount of carbs you eat and drink in each meal or snack. Not all people with diabetes need to count carbs. However, if you take insulin, counting carbs can help you know how much insulin to take.
Plate method
The plate method helps you control portion sizes without counting and measuring. This method divides a 9-inch plate into the following three sections to help you choose the types and amounts of foods to eat for each meal.
- Nonstarchy vegetables—such as leafy greens, peppers, carrots, or green beans—should make up half of your plate.
- Carb foods that are high in fiber—such as brown rice, whole grains, beans, or fruits—should make up one-quarter of your plate.
- Protein foods—such as lean meats, fish, dairy, or tofu or other soy products—should make up one quarter of your plate.
If you are not taking insulin, you may not need to count carbs when using the plate method.

Work with your health care team to create a meal plan that works for you. You may want to have a diabetes educator or a registered dietitian on your team. A registered dietitian can provide medical nutrition therapy , which includes counseling to help you create and follow a meal plan. Your health care team may be able to recommend other resources, such as a healthy lifestyle coach, to help you with making changes. Ask your health care team or your insurance company if your benefits include medical nutrition therapy or other diabetes care resources.
Talk with your health care professional before taking dietary supplements
There is no clear proof that specific foods, herbs, spices, or dietary supplements —such as vitamins or minerals—can help manage diabetes. Your health care professional may ask you to take vitamins or minerals if you can’t get enough from foods. Talk with your health care professional before you take any supplements, because some may cause side effects or affect how well your diabetes medicines work.
Research shows that regular physical activity helps people manage their diabetes and stay healthy. Benefits of physical activity may include
- lower blood glucose, blood pressure, and cholesterol levels
- better heart health
- healthier weight
- better mood and sleep
- better balance and memory
Talk with your health care professional before starting a new physical activity or changing how much physical activity you do. They may suggest types of activities based on your ability, schedule, meal plan, interests, and diabetes medicines. Your health care professional may also tell you the best times of day to be active or what to do if your blood glucose level goes out of the range recommended for you.

Do different types of physical activity
People with diabetes can be active, even if they take insulin or use technology such as insulin pumps .
Try to do different kinds of activities . While being more active may have more health benefits, any physical activity is better than none. Start slowly with activities you enjoy. You may be able to change your level of effort and try other activities over time. Having a friend or family member join you may help you stick to your routine.
The physical activities you do may need to be different if you are age 65 or older , are pregnant , or have a disability or health condition . Physical activities may also need to be different for children and teens . Ask your health care professional or health care team about activities that are safe for you.
Aerobic activities
Aerobic activities make you breathe harder and make your heart beat faster. You can try walking, dancing, wheelchair rolling, or swimming. Most adults should try to get at least 150 minutes of moderate-intensity physical activity each week. Aim to do 30 minutes a day on most days of the week. You don’t have to do all 30 minutes at one time. You can break up physical activity into small amounts during your day and still get the benefit. 1
Strength training or resistance training
Strength training or resistance training may make your muscles and bones stronger. You can try lifting weights or doing other exercises such as wall pushups or arm raises. Try to do this kind of training two times a week. 1
Balance and stretching activities
Balance and stretching activities may help you move better and have stronger muscles and bones. You may want to try standing on one leg or stretching your legs when sitting on the floor. Try to do these kinds of activities two or three times a week. 1
Some activities that need balance may be unsafe for people with nerve damage or vision problems caused by diabetes. Ask your health care professional or health care team about activities that are safe for you.

Stay safe during physical activity
Staying safe during physical activity is important. Here are some tips to keep in mind.
Drink liquids
Drinking liquids helps prevent dehydration , or the loss of too much water in your body. Drinking water is a way to stay hydrated. Sports drinks often have a lot of sugar and calories , and you don’t need them for most moderate physical activities.
Avoid low blood glucose
Check your blood glucose level before, during, and right after physical activity. Physical activity often lowers the level of glucose in your blood. Low blood glucose levels may last for hours or days after physical activity. You are most likely to have low blood glucose if you take insulin or some other diabetes medicines, such as sulfonylureas.
Ask your health care professional if you should take less insulin or eat carbs before, during, or after physical activity. Low blood glucose can be a serious medical emergency that must be treated right away. Take steps to protect yourself. You can learn how to treat low blood glucose , let other people know what to do if you need help, and use a medical alert bracelet.
Avoid high blood glucose and ketoacidosis
Taking less insulin before physical activity may help prevent low blood glucose, but it may also make you more likely to have high blood glucose. If your body does not have enough insulin, it can’t use glucose as a source of energy and will use fat instead. When your body uses fat for energy, your body makes chemicals called ketones .
High levels of ketones in your blood can lead to a condition called diabetic ketoacidosis (DKA) . DKA is a medical emergency that should be treated right away. DKA is most common in people with type 1 diabetes . Occasionally, DKA may affect people with type 2 diabetes who have lost their ability to produce insulin. Ask your health care professional how much insulin you should take before physical activity, whether you need to test your urine for ketones, and what level of ketones is dangerous for you.
Take care of your feet
People with diabetes may have problems with their feet because high blood glucose levels can damage blood vessels and nerves. To help prevent foot problems, wear comfortable and supportive shoes and take care of your feet before, during, and after physical activity.

If you have diabetes, managing your weight may bring you several health benefits. Ask your health care professional or health care team if you are at a healthy weight or if you should try to lose weight.
If you are an adult with overweight or obesity, work with your health care team to create a weight-loss plan. Losing 5% to 7% of your current weight may help you prevent or improve some health problems and manage your blood glucose, cholesterol, and blood pressure levels. 2 If you are worried about your child’s weight and they have diabetes, talk with their health care professional before your child starts a new weight-loss plan.
You may be able to reach and maintain a healthy weight by
- following a healthy meal plan
- consuming fewer calories
- being physically active
- getting 7 to 8 hours of sleep each night 3
If you have type 2 diabetes, your health care professional may recommend diabetes medicines that may help you lose weight.
Online tools such as the Body Weight Planner may help you create eating and physical activity plans. You may want to talk with your health care professional about other options for managing your weight, including joining a weight-loss program that can provide helpful information, support, and behavioral or lifestyle counseling. These options may have a cost, so make sure to check the details of the programs.
Your health care professional may recommend weight-loss surgery if you aren’t able to reach a healthy weight with meal planning, physical activity, and taking diabetes medicines that help with weight loss.
If you are pregnant , trying to lose weight may not be healthy. However, you should ask your health care professional whether it makes sense to monitor or limit your weight gain during pregnancy.
Both diabetes and smoking —including using tobacco products and e-cigarettes—cause your blood vessels to narrow. Both diabetes and smoking increase your risk of having a heart attack or stroke , nerve damage , kidney disease , eye disease , or amputation . Secondhand smoke can also affect the health of your family or others who live with you.
If you smoke or use other tobacco products, stop. Ask for help . You don’t have to do it alone.
Feeling stressed, sad, or angry can be common for people with diabetes. Managing diabetes or learning to cope with new information about your health can be hard. People with chronic illnesses such as diabetes may develop anxiety or other mental health conditions .
Learn healthy ways to lower your stress , and ask for help from your health care team or a mental health professional. While it may be uncomfortable to talk about your feelings, finding a health care professional whom you trust and want to talk with may help you
- lower your feelings of stress, depression, or anxiety
- manage problems sleeping or remembering things
- see how diabetes affects your family, school, work, or financial situation
Ask your health care team for mental health resources for people with diabetes.
Sleeping too much or too little may raise your blood glucose levels. Your sleep habits may also affect your mental health and vice versa. People with diabetes and overweight or obesity can also have other health conditions that affect sleep, such as sleep apnea , which can raise your blood pressure and risk of heart disease.

NIDDK conducts and supports clinical trials in many diseases and conditions, including diabetes. The trials look to find new ways to prevent, detect, or treat disease and improve quality of life.
What are clinical trials for healthy living with diabetes?
Clinical trials—and other types of clinical studies —are part of medical research and involve people like you. When you volunteer to take part in a clinical study, you help health care professionals and researchers learn more about disease and improve health care for people in the future.
Researchers are studying many aspects of healthy living for people with diabetes, such as
- how changing when you eat may affect body weight and metabolism
- how less access to healthy foods may affect diabetes management, other health problems, and risk of dying
- whether low-carbohydrate meal plans can help lower blood glucose levels
- which diabetes medicines are more likely to help people lose weight
Find out if clinical trials are right for you .
Watch a video of NIDDK Director Dr. Griffin P. Rodgers explaining the importance of participating in clinical trials.
What clinical trials for healthy living with diabetes are looking for participants?
You can view a filtered list of clinical studies on healthy living with diabetes that are federally funded, open, and recruiting at www.ClinicalTrials.gov . You can expand or narrow the list to include clinical studies from industry, universities, and individuals; however, the National Institutes of Health does not review these studies and cannot ensure they are safe for you. Always talk with your primary health care professional before you participate in a clinical study.
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts.
NIDDK would like to thank: Elizabeth M. Venditti, Ph.D., University of Pittsburgh School of Medicine.
Sleep Deprivation and Neurological Disorders
Affiliations.
- 1 Department of Pharmacology, JSS College of Pharmacy, JSS Academy of Higher Education & Research, Mysuru, India.
- 2 Department of Food Science and Nutrition, CAMS, Sultan Qaboos University, Muscat, Oman.
- 3 Ageing and Dementia Research Group, Sultan Qaboos University, Muscat, Oman.
- 4 Department of Medical Bioscience, Faculty of Natural Science, University of the Western Cape, Robert Sobukwe Road, Bellville 7535, South Africa.
- 5 School of Anatomical Sciences, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, York Road, Parktown, 2193 Johannesburg, South Africa.
- 6 Department of Biochemistry, Saveetha Dental College, Saveetha Institute of Medical and Technical Sciences, Saveetha University, 600 077, Chennai, India.
- 7 Department of Biochemistry, Panimalar Medical College Hospital & Research Institute, Varadharajapuram, Poonamallee, 600123, Chennai, India.
- 8 Department of Biological Sciences and Institute of Neuroimmune Pharmacology, Seton Hall University, 400 South Orange Ave South Orange, NJ 07079, USA.
- 9 College of Pharmacy and Nutrition, University of Saskatchewan, 107, Wiggins Road, Saskatoon, SK, Canada S7N 5C9.
- 10 Neuroinflammation Group, Faculty of Medicine and Health Sciences, Macquarie University, NSW 2109, Australia.
- 11 Research & Policy Department, World Innovation Summit for Health (WISH), Qatar Foundation, P.O. Box 5825, Doha, Qatar.
- 12 Department of Biological Sciences, University of the Pacific, Arthur Dugoni School of Dentistry, San Francisco, CA, USA.
- PMID: 33381558
- PMCID: PMC7755475
- DOI: 10.1155/2020/5764017
Sleep plays an important role in maintaining neuronal circuitry, signalling and helps maintain overall health and wellbeing. Sleep deprivation (SD) disturbs the circadian physiology and exerts a negative impact on brain and behavioural functions. SD impairs the cellular clearance of misfolded neurotoxin proteins like α -synuclein, amyloid- β , and tau which are involved in major neurodegenerative diseases like Alzheimer's disease and Parkinson's disease. In addition, SD is also shown to affect the glymphatic system, a glial-dependent metabolic waste clearance pathway, causing accumulation of misfolded faulty proteins in synaptic compartments resulting in cognitive decline. Also, SD affects the immunological and redox system resulting in neuroinflammation and oxidative stress. Hence, it is important to understand the molecular and biochemical alterations that are the causative factors leading to these pathophysiological effects on the neuronal system. This review is an attempt in this direction. It provides up-to-date information on the alterations in the key processes, pathways, and proteins that are negatively affected by SD and become reasons for neurological disorders over a prolonged period of time, if left unattended.
Copyright © 2020 Muhammed Bishir et al.
Publication types
- Alzheimer Disease / complications
- Brain Mapping
- Epilepsy / complications
- Gene Expression Profiling
- Gene Expression Regulation
- Glymphatic System / metabolism
- Huntington Disease / complications
- Immune System
- Multiple Sclerosis / complications
- Nervous System Diseases / complications*
- Neurons / metabolism*
- Oxidation-Reduction
- Oxidative Stress
- Parkinson Disease / complications
- Sleep / physiology*
- Sleep Deprivation / complications*

IMAGES
VIDEO
COMMENTS
INTRODUCTION. Sleep is vital for health and well-being in children, adolescents, and adults. 1-3 Healthy sleep is important for cognitive functioning, mood, mental health, and cardiovascular, cerebrovascular, and metabolic health. 4 Adequate quantity and quality of sleep also play a role in reducing the risk of accidents and injuries caused by sleepiness and fatigue, including workplace ...
Sleep is a crucial biological process, and has long been recognised as an essential determinant of human health and performance. Whilst not all of sleep's functions are fully understood, it is ...
Article 16 November 2020. ... The role of sleep in cognitive performance has gained increasing attention in neuroscience and sleep research in recent decades 8,9. Numerous experimental methods ...
A total of 41 articles, including 92 340 unique participants from 14 countries, met inclusion criteria. Sleep was assessed objectively in 37% of studies and subjectively in 63% of studies. Findings suggest that later sleep timing and greater sleep variability were generally associated with adverse health outcomes.
NREM includes stage 1 (N1), stage 2 (N2), and stage 3 (N3). Sleep progresses from light sleep to deeper sleep across these three stages as the ease of arousability decreases. N3 (formerly divided into N3 and N4) is also termed slow-wave sleep due to the high-amplitude slow waves (0.5-4 Hz) observed in the EEG.
Below are two lists that highlight noteworthy studies published in 2020 in the Journal of Clinical Sleep Medicine. The first list includes the 10 articles with the highest Altmetric scores. Altmetric scores are calculated by adding the number of times the study is reported on in the news and shared on social media.
Sleep articles from across Nature Portfolio. Sleep is a state characterized by a reduced responsiveness to sensory stimuli, suppressed locomotor activity and rapid reversibility to wakefulness. It ...
Join the SRS Virtual Seminar Series as trainees and early career investigators deliver professional talks to an audience of peers and colleagues. SLEEP is the official journal of the Sleep Research Society (SRS). Publishes content on sleep, sleep medicine and circadian research.
The Journal of Sleep Research, owned by the European Sleep Research Society, is an international journal dedicated to basic and clinical sleep research. reflecting the progress in this rapidly expanding field, promoting the exchange of ideas between scientists at a global level. Detailed Author Guidelines with valued input and quick decision ...
Sleep research in 2020: COVID-19-related sleep disorders. 2020 has been an unprecedented year because a modified coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), spread rapidly from China to all continents, leading to the COVID-19 pandemic. The first studies of COVID-19-associated sleep disorders were reported in China.
Sleep Health Journal Article Highlights Association Between Experiencing Discrimination and Poorer Sleep . Washington, D.C. (July 25, 2023): New research published in the National Sleep Foundation's (NSF) Sleep Health journal shows experiencing discrimination is associated with poorer sleep. Discrimination is associated with higher anxiety ...
Sleep research in 2020: COVID-19-related sleep disorders. Repurposed drugs for ALS are also of increasing interest, as evidenced by promising results from a phase 2 double-blind placebo-controlled study of AMX0035.10 This com-bination of sodium phenylbutyrate and taurur sodiol was designed to prevent neuronal death by simul-taneously mitigating ...
This study was designed to evaluate echocardiographic findings in patients with obstructive sleep apnea (OSA) with cognitive impairment and compare it with the control group. Ensieh Vahedi, Arezoo Khosravi, Rahman Alizadian and Taleb Badri. Sleep Science and Practice 2021 5 :1.
Research Article 31 December 2021. The effect of adenotonsillectomy and rapid maxillary expansion on the upper airway in pediatric obstructive sleep apnea: a randomized crossover-controlled trial ... Pathogenesis of sleep disordered breathing in the setting of opioid use: A multiple mediation analysis using physiology
We conducted a systematic review of all studies examining the relationships between continuous white noise or similar broadband noise and sleep (PROSPERO 2020: CRD42020148736). Animal studies and studies using intermittent white noise to disrupt sleep or enhance slow wave activity were excluded. Two reviewers independently screened titles and ...
Decades of research have linked chronic sleep deprivation to an increased risk for obesity, heart disease, Type 2 diabetes, and problems with immune function (" Sleep and Sleep Disorders ," Centers for Disease Control and Prevention). Sleeping more or less than recommended—typically 7 to 9 hours a night—is a significant predictor of ...
In the inaugural issue of the Journal of Clinical Sleep Medicine (2005), a feature article 1 traced early milestones in the developing field of sleep medicine, which slowly emerged from the older field of sleep research during the 1970s and 1980s. Sleep medicine, the article noted, was closely linked with and made possible by the discovery of electrical activity in the brain.
Importance: Obstructive sleep apnea (OSA) affects 17% of women and 34% of men in the US and has a similar prevalence in other countries. This review provides an update on the diagnosis and treatment of OSA. Observations: The most common presenting symptom of OSA is excessive sleepiness, although this symptom is reported by as few as 15% to 50% of people with OSA in the general population.
2020 has been an unprecedented year because a modified coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), spread rapidly from China to all continents, leading to the COVID-19 pandemic. The first studies of COVID-19-associated sleep disorders were reported in China. Huang and Zhao1 collected information from a survey of 7236 volunteers (mean age 35·3 years [SD 5·6]).
Sleep quality and the circadian rhythm both have strong effects on metabolism, with previous research showing a link between circadian rhythm disruption and higher risk of metabolic diseases, such ...
Article 16 November 2020. ... they have been found to accurately estimate sleep duration and quality in normal adult sleepers without the use of research-grade sleep staging equipment. 34 By ...
AD is a common neurodegenerative disorder. The World Health Organization reported that the number of people living with dementia is expected to increase from 55 million in 2019 to 139 million by 2050 [].Sleep disorders are a prevalent clinical symptom of AD, causing physical and psychological burdens on patients and resulting in poorer health status of their caregivers [].
WASHINGTON, D.C. -- For the first time in Gallup polling since 2001, a majority of U.S. adults, 57%, say they would feel better if they got more sleep, while 42% say they get as much sleep as they need. This is nearly a reversal of the figures last measured in 2013, when 56% of Americans got the sleep they needed and 43% did not.
The grant will fund research looking at how behaviors and social factors affect sleep quality among Black and Hispanic women of childbearing age. The research is designed to be the foundation for future health promotion programs to address sleep quality and its negative effects, including pregnancy outcomes and lifelong heart problems. Other ...
Wilfredo Lee. FILE - A traveler takes a nap as he waits for a ride outside Miami International Airport, Friday, July 1, 2022, in Miami. The Gallup survey, released Monday, April 15, 2024, says ...
Mathew Stewart, Griffith University; Huw Groucutt, University of Malta, and Michael Petraglia, Griffith University. New research reveals signs of ancient human habitation in a vast cave beneath ...
Advances in sleep research in 2021 have brought about clinical developments for the next decade. Additionally, sleep telemedicine services have expanded rapidly, driven by the COVID-19 pandemic, to best serve patients with sleep disorders. 1 Here, we will explore some of the most impactful clinical studies from this field in 2021. Progress has been made in evaluating the relationship between ...
Healthy living is a way to manage diabetes. To have a healthy lifestyle, take steps now to plan healthy meals and snacks, do physical activities, get enough sleep, and quit smoking or using tobacco products. Healthy living may help keep your body's blood pressure, cholesterol, and blood glucose level, also called blood sugar level, in the ...
Sleep plays an important role in maintaining neuronal circuitry, signalling and helps maintain overall health and wellbeing. Sleep deprivation (SD) disturbs the circadian physiology and exerts a negative impact on brain and behavioural functions. SD impairs the cellular clearance of misfolded neurotoxin proteins like α -synuclein, amyloid- β ...
The Santa Barbara Sense of Direction Scale is widely used in navigation research. Studies suggest that people are fairly accurate at evaluating their own sense of direction. Personality, too, appears to play a role in developing navigational ability. "To get good at navigating, you have to be willing to explore," says Uttal.