
- Clinical Pharmacy and Pharmacology
Explore the latest in clinical pharmacy and pharmacology, including topics in drug safety, development, pharmacogenetics, and pharmacoeconomics.

Publication
Article type.
This cross-sectional study investigates the scope and breadth of artificial intelligence use in drug development.
This randomized clinical trial examines the efficacy of ivonescimab plus chemotherapy vs chemotherapy alone for patients with advanced or metastatic non–small cell lung cancer with the epidermal growth factor receptor ( EGFR ) variant.
This narrative review discusses psychological, attitudinal, and educational factors among both health care professionals and payers that may play a role in slowing biosimilar uptake.
This economic evaluation compares the cost-effectiveness of durvalumab for maintenance treatment of stage III non–small cell lung cancer (NSCLC) across the US, Brazil, Singapore, and Spain.
This economic evaluation assesses potential Medicare Part D savings on ophthalmic generic drugs if discount coupon prices are used.
This cluster randomized clinical trial investigates whether a government-led, mailed, direct-to-consumer educational brochure reduces prescription opioid use among community-dwelling adults with long-term opioid prescriptions.
This case series study examines clinical outcomes of isotretinoin among transgender and gender-diverse individuals receiving gender-affirming hormonal therapy.
This post hoc analysis of the ELAN randomized clinical trial investigates whether infarct size modifies the safety and efficacy of early vs late direct oral anticoagulation initiation after ischemic stroke in individuals with atrial fibrillation.
This randomized clinical trial investigates the safety and effectiveness of immediate- vs delayed-intensive statin in patients with acute cerebral ischemia from atherosclerosis.
This cross-sectional study examines the levels of lead in household drinking water of individuals with kidney failure.
This cohort study investigates whether antenatal magnesium sulfate (MgSO 4 ) administration prior to early preterm birth is associated with changes in functional connectivity in the neonatal brain in a cohort of neonates who participated in a multicenter randomized clinical trial.
This randomized clinical trial investigates the magnitude of the effect of maternal progesterone therapy on neurodevelopment for fetuses with congenital heart defects (CHDs).
This cohort study examines the prevalence of and factors associated with glucagon-like peptide 1 agonist discontinuation among new users.
This cohort study examines the implications of physician-pharmacy integration for the use of, cost of, and adherence to anticancer drugs among patients with late-stage cancer.
This nonrandomized controlled trial assessed the benefits and toxic effects of intensity-modulated reirradiation therapy with nivolumab in the treatment of patients with recurrent or second primary head and neck squamous cell carcinoma.
A 70-year-old woman with hypertension and dyslipidemia presented with slow communication and difficulty walking 90 days after 6 courses of postoperative chemotherapy following right breast cancer surgery. What is your diagnosis?
This cohort study evaluates the risk for pregnancy onset during valproic acid treatment across indications and assesses the use of contraception during treatment among US women of childbearing age.
This cohort study examines patterns of melatonin use among participants in the Adolescent Brain Cognitive Development (ABCD) Study and characterizes factors associated with use.
This cohort study investigates whether a β-blocker prescription at hospital discharge is associated with mortality or adverse cardiopulmonary events among patients with chronic obstructive pulmonary disease hospitalized for acute myocardial infarction.
This cross-sectional study evaluates the association between Medicare coverage and patient out-of-pocket costs for cardiovascular-kidney-metabolic medications.
Select Your Interests
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Top five research articles of 2020

Despite the significant challenges this year has posed, The Pharmaceutical Journal has continued to publish high-quality peer-reviewed research.
Our researchers have made a range of investigations — from evaluating pharmacist interventions using the Simpler tool in Malaysia , to a pharmacist-led virtual thiopurine clinic to support people with inflammatory bowel disease and auto-immune hepatitis, here in the UK.
We have some exciting research coming up in 2021, but in case you missed them the first time around, here are the top five most popular research articles of 2020:
5. Misuse of prescription and over-the-counter drugs to obtain illicit highs: how pharmacists can prevent abuse
Use of prescription and over-the-counter drugs for recreational purposes is increasing, and this perspective article collates the existing literature to provide an in-depth overview of the misuse and diversion of a range of drugs with psychoactive potential, including gabapentinoids, antihistamine drugs and loperamide.
4. Effective detection and management of hypertension through community pharmacy in England
Community pharmacists can play a big role in managing hypertension — from the identification of medication-related problems, to providing lifestyle advice. Despite this, they are not routinely involved in structured hypertension management or screening programmes. So, this review summarises the evidence to recommend the roll-out of a community pharmacy-led hypertension management service.
3. Recent advances in the oral delivery of biologics
Oral administration of medicines is often preferred by patients for its convenience, but, for biologics, the gastrointestinal tract poses challenges for administering in this way. This review discusses the advantages and limitations of several novel drug delivery strategies, and highlights the work to be done to put this technology into clinical practice.
2. Immuno-oncology agents for cancer therapy
Immuno-oncology is a novel treatment that works by conditioning the body’s immune cells to recognise and kill cancer cells — combining this treatment with conventional therapies has led to promising improvements in patient outcomes. This review looks at the range of immuno-oncology agents, and how problems such as their toxicity and high cost can be overcome.
1. Investigational treatments for COVID-19
The emergence of COVID-19 resulted in a global research effort to find effective treatment options to relieve healthcare burdens and, ultimately, save lives. In June 2020, this rapid review summarised the clinical trials and treatment evidence at the time.
Check out The Pharmaceutical Journal’ s ‘Everything you should know about the coronavirus outbreak’ for the latest on this continually evolving situation.
Find the full catalogue of articles in our research section .
Call for submissions
In 2021, The Pharmaceutical Journal will keep adding to the evidence base with review, perspective and research articles. If you have undertaken research into innovations and initiatives that can improve pharmacy services and administration, the pharmacological management of disease, or advances in drug development, please submit your article for consideration by email to: [email protected]
You may also be interested in
Artificial intelligence: act or be acted upon — staying relevant in the ai era, equality, diversity and inclusion: why true allyship must shift words into action, pharmacy needs to be at the forefront of shaping digital health — but how do we get there.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
Pharmacology articles from across Nature Portfolio
Pharmacology is a branch of biomedical science, encompassing clinical pharmacology, that is concerned with the effects of drugs/pharmaceuticals and other xenobiotics on living systems, as well as their development and chemical properties.
Related Subjects
- Clinical pharmacology
- Pharmacodynamics
- Pharmacogenetics
- Pharmacokinetics
- Receptor pharmacology
Latest Research and Reviews

Integrated PBPK-EO modeling of osimertinib to predict plasma concentrations and intracranial EGFR engagement in patients with brain metastases
- Yimei Zhang
- Xiaoling Zhang

Repeated caffeine intake suppresses cerebral grey matter responses to chronic sleep restriction in an A 1 adenosine receptor-dependent manner: a double-blind randomized controlled study with PET-MRI
- Yu-Shiuan Lin
- Denise Lange
- David Elmenhorst
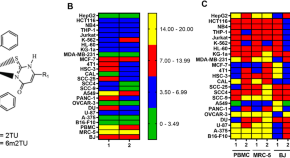
Ru(II)-based complexes containing 2-thiouracil derivatives suppress liver cancer stem cells by targeting NF-κB and Akt/mTOR signaling
- Larissa M. Bomfim
- Sara P. Neves
- Daniel P. Bezerra

Highly biased agonism for GPCR ligands via nanobody tethering
Activated GPCRs signal through multiple pathways. Ligands that signal through a single pathway are highly valued. The authors demonstrate that tethering ligands to receptors via conjugation with binding nanobodies enables pathway-specific signaling.
- Shivani Sachdev
- Brendan A. Creemer
- Ross W. Cheloha
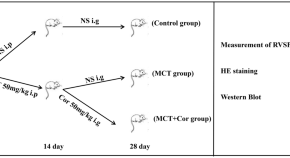
Mechanisms of cordycepin in the treatment of pulmonary arterial hypertension in rats based on metabonomics and transcriptomics
- Jiangpeng Lin
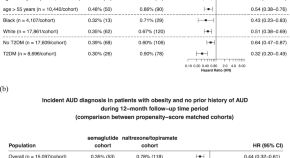
Associations of semaglutide with incidence and recurrence of alcohol use disorder in real-world population
Anecdotal reports from patients prescribed semaglutide describe a reduced desire to drink. Here, the authors show that semaglutide is associated with a 50%-56% reduced risk for both the incidence and recurrence of alcohol use disorder in real-world populations.
- William Wang
- Nora D. Volkow
News and Comment
Beyond traditional pharmacology: evaluating phosphodiesterase inhibitors in autism spectrum disorder.
- Fernando E. Padovan-Neto
- Ana Júlia de Oliveira Cerveira
- Danilo Leandro Ribeiro
Biosimilar ranibizumab in India- overview of phase 3 clinical trial designs
- Ashish Sharma
- Nilesh Kumar
- Baruch D. Kuppermann
Given the fraught history of fluorine, Michelle Francl wonders what made medicinal chemists consider fluorine derivatives?
- Michelle Francl
Comment on: “History of testosterone therapy through the ages”
- Diederik F. Janssen
Aflibercept biosimilars – update on the development progress
- Anat Loewenstein
Comment on: Effects of selective dopamine D3 receptor partial agonist/antagonists on oxycodone self-administration and antinociception in monkeys
- Samantha Chong
- Sandra D. Comer
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Can Pharm J (Ott)
- v.149(4); 2016 Jul
Pharmacy Practice Research Abstracts
Table of contents.
This year, the Canadian Pharmacists Association (CPhA) and the Alberta Pharmacists’ Association (RxA) partnered to deliver four days of exciting educational sessions, exceptional keynote speakers, social events and networking opportunities at the annual Canadian Pharmacists Conference.
The Canadian Pharmacists Conference is an excellent opportunity for pharmacists from across Canada to network with colleagues and to share new and exciting ideas, research and innovation. Our oral and poster pharmacy practice research presentations provide an opportunity for members of the pharmacy community to engage in sessions that promote evidence-based practice and decision-making.
To help promote and disseminate pharmacy practice research, CPhA publishes the abstracts of the research presented at the conference in this special supplement of the Canadian Pharmacists Journal .
PHARMACY PRACTICE AND CARDIOVASCULAR HEALTH
S1 ECG screening in community pharmacy: An innovative pilot program to improve detection of cardiac arrhythmias in high-risk patients
S2 Impact of the Community Pharmacists Assisting Total Cardiovascular Health (CPATCH) strategy for improving medication adherence from community pharmacies – A cluster-randomized trial
S3 The Alberta Vascular Risk Reduction Community Pharmacy Project: RxEACH
SUCCESSFUL PHARMACISTS: POINT OF CARE AND MORE
S4 Implementation of a standardized HbA1c clinic worksheet to improve detection of drug therapy problems: Results from a multi-pharmacy pilot program
S5 Community pharmacist bone density point-of-care screening with osteoporosis and fracture risk estimation
S6 Defining characteristics of successful pharmacists
THE ELDERLY IN PHARMACY
S7 Development and implementation of a pharmacist intervention for frail elderly patients in an interdisciplinary primary care team: A qualitative analysis
S8 Identifying drug-related problems in retirement home residents following community pharmacist administered flu vaccinations
S9 Deprescribing guidelines for the elderly: Overview of findings from a 3-year program of research
MEDICATION ASSESSMENT AND MODELS OF CARE
S10 Community pharmacist standardized home medication consultation program by referral: Structured approach to identifying drug-related problems in the home-bound population
S11 The Medication Assessment Centre: A novel student training and patient care program
S12 Collaborative care model involving eHealth to improve treatment adherence and health outcomes of patients with gout
HOT TOPICS IN PHARMACY PRACTICE RESEARCH
S13 Effectiveness of community-based pharmacist interventions in chronic non-cancer pain: A systematic review
S14 The consideration of sex/gender and vulnerable populations in pharmacy practice research
POSTER ABSTRACTS
S15 Introducing a unit-based clinical pharmacist: A pilot study
S16 Patient-centered renovations
S17 Medication reconciliation practices on discharge into primary care homes in Prince George, British Columbia
S18 Stakeholder perspectives on economic analyses of billable pharmacy services in Ontario
S19 Opportunity and cost: Self-monitoring of blood glucose in Manitoba, 2000-2013
S20 Ibuprofen provides superior antipyretic efficacy vs. acetaminophen in childhood fever: Pooled analysis of 2 randomized trials
S21 Development of a hormonal contraception decision support tool for pharmacists
S22 The pharmacy services framework: Communicating the shift to clinical pharmacy services in Alberta
S23 Provider and patient perspectives regarding a community pharmacist-based case finding and intervention program — Alberta Vascular Risk Reduction Community Pharmacy project: RxEACH
S24 An audit of 8 centres’ use of anticoagulant therapies when discharging patients from hospital with acute venous thromboembolism
S25 An audit of 8 centres’ use of anticoagulant therapies when discharging patients from the emergency department
S26 Enhancing depression outcomes with better use of antidepressants: Evaluation of a pharmacy benefit manager–sponsored depression disease state management program
S27 Pharmacist intervention for a frail elderly population in primary care
S28 Impact of pharmacist assessment on classes of high-risk medications in a geriatric outpatient clinic
S29 Description of medication management problems and supports used in community-dwelling seniors
S30 Effectiveness of the peer-to-peer mentoring model for transitioning from classroom to professional practice
S31 Community pharmacy reports of potential QTc-prolonging drug interactions involving fluoroquinolones or macrolides: A multi-incident analysis
S32 Medication incidents involving insulin: A multi-incident analysis
S33 Potentially inappropriate medication use in older adults: A multi-incident analysis
S34 Patient counseling: An overarching method to mitigate medication errors and ensure continuity of care
S35 Older people’s attitudes towards deprescribing: A community study in Quebec
S36 The effect of health media reporting on self-medication use
S37 Documentation of functional medication management in older adults within an acute care hospital
S38 Global citizenship framework — Application to pharmacy student experience
S39 How does pharmacist prescribing fit with family physicians’ practice in Alberta? Developing a knowledge translation strategy
S40 Medication incidents involving smoking cessation therapies
S41 Medication incidents involving immunosuppressive agents
S42 Medication incidents that could have been prevented at the prescribing stage
S43 Direct oral anticoagulant medication incidents
S44 Drug allergy incidents in community pharmacies
S45 Medication incidents associated with hospital discharge
S46 Successful pharmacists: A qualitative study to understand pharmacists’ definitions of successful pharmacy practices
ECG screening in community pharmacy: An innovative pilot program to improve detection of cardiac arrhythmias in high-risk patients
John Papastergiou, BScPhm; Larissa Boychuk, BSc, PharmD candidate
Objectives:
Undiagnosed arrhythmias such as atrial fibrillation and torsades de pointes can have serious health consequences. Atrial fibrillation causes 1/3 of strokes and 1.4% of these patients are undiagnosed. Over 150 medications are known to prolong QT intervals. The purpose of this study is to assess point-of-care ECG screening in identifying undiagnosed abnormalities in high-risk patients in a community pharmacy setting.
High-risk patients were invited to participate in ECG screening at two community pharmacies in Toronto, Ontario. Patients met eligibility requirements if they were at risk of QT prolongation or atrial fibrillation secondary to medication therapy or a CHADS2 score of >2, respectively. Using the HeartCheckPenTM handheld device, a 30 second lead II screening test was performed. Data was uploaded to an ECG reading service where results were interpreted by a qualified professional. Results were forwarded to the pharmacy for follow-up. Pharmacists referred all patients with abnormal readings to their primary care physician for further investigation.
Thirty-five patients participated in the program. Eleven were identified at risk for atrial fibrillation and 18 for QT prolongation — 5 patients met both criteria. Screening identified 10 (28.6%) patients with one or more abnormal rhythms. These included premature atrial contraction (n=3), wide QRS (n=4), sinus arrhythmia (n=1), sinus tachycardia (n=3) and QT prolongation (n=1). Pharmacists referred all patients and, in the case of QT prolongation, intervened to alter therapy.
Conclusions:
Our experience demonstrates that point-of-care ECG testing can be successfully integrated into pharmacy workflow. The results illustrate the prevalence of abnormal rhythms in high-risk patients. They highlight a significant opportunity for pharmacists to use point-of-care screening as a tool to detect abnormal rhythms, intervene when warranted, and improve medication safety.
Impact of the Community Pharmacists Assisting Total Cardiovascular Health (CPATCH) strategy for improving medication adherence from community pharmacies – A cluster-randomized trial
David Blackburn, PharmD; Charity Evans, PhD; Jeff Taylor, PhD; Kerry Mansell, PharmD; Derek Jorgenson, PharmD; Yvonne Shevchuk, PharmD; Alfred Rémillard, PharmD; Dean Eurich, PhD; Bill Semchuk, PharmD; Anne Champagne, BSP
The highest risk for non-adherence occurs during the first year after starting a new chronic medication. Community pharmacists are well positioned to identify problems and provide support during this critical time.
Thirty community pharmacies in Saskatchewan, Canada, were randomized to deliver a brief adherence intervention or usual care to new users of HMG-CoA reductase inhibitors (statins). The intervention consisted of screening for new statin users, assessment for adherence barriers, and individualized follow-up when appropriate. The primary endpoint was mean statin adherence measured by the proportion of days covered (PDC). During follow-up, intervention pharmacies performed monthly assessments to estimate compliance with the study protocol.
A total of 1,906 new statin users were followed for six to twelve months following their first statin dispensation. No significant differences between intervention and control pharmacies were observed for mean adherence (72% (SD 33) vs 71% (SD 33); p=0.64), median adherence (89% versus 88%; p=0.84), or the percentage of subjects achieving optimal adherence (i.e., PDC ≥80%: 57.3% (520/907) versus 55.8% (558/999); p=0.51). However, several intervention stores reported poor compliance to the study protocol. In post-hoc analyses, mean adherence among pharmacies reporting good compliance with the study protocol was substantially higher than stores with poor compliance (76% versus 66%; p<0.01), and the percentage of patients achieving optimal adherence was 63% vs 52% (p<0.01) respectively.
The CPATCH strategy was not effective for improving statin adherence compared to usual care in community pharmacies. However, post-hoc analyses suggested that successful implementation might be the key to achieving important benefits.
The Alberta Vascular Risk Reduction Community Pharmacy Project: RxEACH
Yazid Al-Hamarneh, BS(Pharm), PhD; Ross T. Tsuyuki, BSc(Pharm), PharmD, MSc; Charlotte A. Jones, MD, PhD; Brenda R. Hemmelgarn MD, PhD
Despite the risk associated with hypertension, diabetes, dyslipidemia, and smoking, these cardiovascular disease (CVD) risk factors remain poorly identified and controlled. To evaluate the effect of a community pharmacy-based case finding and intervention program on estimated cardiovascular risk.
Design: Randomized controlled trial. Setting: 56 community pharmacies across Alberta. Population: Adults at high risk for CVD events, including those with diabetes, chronic kidney disease, vascular disease and/or Framingham score > 20% who have at least one uncontrolled risk factor (hypertension, LDL-cholesterol (LDL-c), HbA1c, or current smoking). Randomization: Participants were randomized (1:1 basis) into advanced or usual care groups. Advanced care: Pharmacists provided participants with: Physical and laboratory assessments; Individualized CVD risk assessment and education; Pharmacists prescribed where appropriate to achieve treatment targets; Regular monthly follow-ups for 3 months. Usual care: Usual pharmacist care with no specific intervention for 3 months. Primary outcome: The difference in change in estimated CVD risk between advanced and usual care groups, calculated using a relevant risk calculator based on participants’ co- morbidities (Framingham, International, or UKPDS).
We enrolled 723 patients. Median age was 62 years (interquartile range 54-69), 57% were male and 27% were smokers. After adjusting for baseline values, the difference in change in CVD risk was 21% (p<0.001): a change of 0.2 mmol/L in LDL-c (p<0.001), 9.4 mmHg in systolic blood pressure (p<0.001), 0.92% in HbA1c (p<0.001), and 20.2% in smoking cessation (p=0.002) between advanced and usual care groupsaccess (96% and 91%).
This is the first large randomized trial of CVD risk reduction in community pharmacy settings. Patients in the advanced care group were 21% less likely to have a heart attack, stroke, or peripheral artery disease when compared to those in the usual care group. RxEACH provides evidence for the benefit of pharmacist care on both global CVD risk and individual risk factors
Implementation of a standardized HbA1c clinic worksheet to improve detection of drug therapy problems: Results from a multi-pharmacy pilot program
John Papastergiou, BScPhm; Bryan Gray, BScPharm, RPh, CDE
Point-of-care HbA1c screening devices are a valuable tool that community pharmacists can use to monitor patients with diabetes and improve their overall management. Here, we report data from a multi-pharmacy pilot program where a standardized worksheet was used by pharmacists offering HbA1c clinics in order to standardize the structure of the patient interviews and improve detection of drug therapy problems.
Thirteen community pharmacies from across Ontario interested in offering HbA1c screening as part of their professional programmes participated in the pilot program. Pharmacists received training on the use of the standardized worksheet and were provided with all the tools required to hold a clinic. HbA1c analysis was performed using the Roxon A1c Now®. Data collection took place over a period of 4 months beginning August 2015.
Eighty-eight patient attended the clinics. The mean HbA1c of the population was 7.76. Overall, 36% of patients had optimal glycaemic control (A1c <7.0%), 45% were hyperglycaemic (A1c >7 and <9%) and 19% of patients had marked hyperglycaemia (A1c >9.0). A total of 204 interventions were performed by pharmacists. An average of 2.32 interventions were performed per patient, and we observed a trend towards increased numbers of interventions in patients with poorer glycemic control. Interestingly, 23% and 15% of patients met the CDA guideline requirements for therapy with a statin and an ACE/ARB, respectively, but were identified by pharmacists as not receiving the appropriate therapy.
These results illustrate the prevalence of suboptimal glycaemic control among patients with diabetes in the community. They highlight a significant opportunity for pharmacists to use point-of-care screening in combination with a standardized worksheet to more readily detect drug therapy problems and intervene to improve disease management when warranted.
Community pharmacist bone density point-of-care screening with osteoporosis and fracture risk estimation
Bryan Gray, BScPharm, RPh, CDE
Point-of-care bone density screening is a valuable tool that community pharmacists can use to identify and educate patients at risk for osteoporosis and fractures. Here, we report data from screening 66 patients (12 male) at structured bone density clinics held at a community pharmacy in Thunder Bay, ON.
Bone density analysis was performed using the Omnisense 8000. Fracture risk factors and the point of care T-scores were interpreted with both the Canadian CAROC estimator and the WHO FRAX risk estimator to provide a 10-year fracture risk assessment. Recruitment involved in-pharmacy promotion to all patients. Data collection took place over a period of 3 months.
Testing successfully identified patients potentially at risk for osteoporosis and fracture. The CAROC found 5, 7, and 54 patients at high, moderate, low risk, respectively, for developing fracture over a 10-year period. The WHO FRAX calculator found a similar distribution with ten patients receiving a major fracture risk estimate 10% or greater, and five patients with a hip fracture risk estimate 5% or greater. The average patient age was 61, and the average BMI was overweight at 29. A total of 273 recommendations were provided by the pharmacist — average 4.13 per patient.
These results illustrate the prevalence of potentially undiagnosed osteoporosis for patients in the community. Our intervention data suggests that a structured bone density consultation by a community pharmacist can identify patients at risk for fractures. Patients at low risk were given evidence based and practical recommendations to maintain their bone health and reduce the risk of developing osteoporosis. Continued expansion in scope of pharmacy practice may contribute to increased osteoporosis identification and reduction in fracture risk.
Defining characteristics of successful pharmacists
Jay Mutch, BScPharm (student); Lydia Cheung, BScPharm (student); Theresa Charrois, BScPharm, ACPR, MSc; Jill Hall, BScPharm, ACPR, PharmD; Meagen Rosenthal, PhD; Ken Cor, PhD
Our primary objective was to identify the self-described characteristics of pharmacists that contribute to their success. Our working definition of success in pharmacy is based on the premise that successful pharmacists practice to the full extent of their knowledge and skills. The definition was derived from a literature review as well as the Blueprint for Pharmacy.
Semi-structured individual interviews were conducted with selected pharmacists. The interview tool was developed using previous research on success in health care professions and was modified based on trial interviews with faculty and practitioners. Potential candidates were nominated by prominent pharmacists in the field, using our definition of success. Lists from the nominators were compared and 10 pharmacists who appeared on more than one list were invited to participate.
A total of 8 out of 10 interviews have been analyzed to date. All 8 pharmacists had additional prescribing authorization (APA), with 4 of those pharmacists being early adopters (receiving APA prior to remuneration model implementation). In terms of factors contributing to success, participants noted strong communication skills and developing relationships as important. When asked what success meant to them, participants believed that self-development played a large role. Participants also felt a focus on emotional intelligence would help ensure the success of pharmacist practice in the future.
A clearly delineated definition of success was developed and used to frame interviews with practitioners viewed as successful by their peers. Communication skills were the most prominent factor that contributed to success. This data will help individual pharmacists become aware of what characteristics they may want to foster in themselves in order to have success in practice.
Development and implementation of a pharmacist intervention for frail elderly patients in an interdisciplinary primary care team: A qualitative analysis
Tejal Patel, PharmD; Lindsay Donaldson, BA; Linda Lee, MD; Jillian Bauer, BScPharm; Cathy Schill, BScPharm
There is a paucity of published literature describing activities involved in the implementation of an intervention in an interdisciplinary primary care environment. The objective of this research is to describe the development and implementation of the pharmacist intervention (PI) for frail elderly patients in an interdisciplinary primary care team.
This study is a deductive qualitative analysis of emails and meeting minutes pertaining to the PI for frail patients. Classical content analysis was conducted to quantify previously established codes and themes pertaining to: 1. Goal of the PI (e.g. codes: literature review, objectives of PI, etc); 2. Delivery of the PI (e.g. codes: care provision, follow-up, tracking outcomes, etc); 3. Work Environment (e.g. codes: roles and responsibilities, availability of staff, workflow processes, etc) and 4. Sustainability of PI (e.g. codes: scheduling, etc).
Of the 2,830 email items and minutes of 4 meetings between pharmacists, physicians, nurses, receptionists and administrators that were reviewed, 172 emails and 4 meeting minutes were eligible for classical content analysis. Of the resulting 718 coded items, 40% were related to Work Environment, 36% to the Delivery of the PI, 12%, each, to the Goal and Sustainability of the PI. The number of items coded for Goal of PI decreased from a high of 50 items in the period of 6 months pre-initiation to 2 items at the end of 24 months post initiation of PI. The number of items pertaining to the codes, “tracking” and “follow-up” of patients increased from 4 and 0 at 6 months pre-initiation to 19 and 39 at 24 months post-initiation of PI, respectively.
The impact and importance of the different aspects, such as the goal, delivery of the program, working environment and relationships changed with time. This analysis may be used to improve planning of other interventions in primary care in the future.
Identifying drug-related problems in retirement home residents following community pharmacist administered flu vaccinations
Community pharmacist administered flu vaccinations serve as an opportunity to screen patient’s medication profiles for drug-related problems. Here, we report data from medication consultations of 58 patients (16 male) from three retirement homes in Thunder Bay, ON.
Consenting retirement home residents were scheduled for a flu vaccination and a subsequent medication consultation. Following intramuscular vaccine administration, resident’s medication regimens and health status were screened for potential drug-related problems. Following consultation, the community pharmacist communicated potential drug-related problems to the resident’s primary care provider. Data collection took place over a period of 1 month.
Following vaccination, standardized medication consultations identified a total of 579 potential drug-related problems — an average of 9.98 interventions per patient. Very few of the patients were aware of their overall vaccination status (291 recommendations). Many patients were receiving inappropriate cardiovascular disease medications (over treating hypertension or lipids (76 recommendations). Consolidation of the medication regimen was very well received by residents (46 recommendations). The average patient age was 87 years old, with 9.5 medications per patient (average), with an average number of dosing intervals of 3.6 per day. Recommendations to improve adherence could reduce dosing intervals to 1.9 per day. Patients were appreciative to have their medication regimen and health status reviewed by the pharmacist instead of waiting independently for the 15 minutes post vaccination time period to pass.
In addition to the benefits provided by vaccination, subsequent medication consultations successfully identified potential drug-related problems.This data suggests that retirement home residents may be at risk for drug-related problems which may be mitigated by pharmacist intervention.
Deprescribing guidelines for the elderly: Overview of findings from a 3-year program of research
Barbara Farrell, BScPhm, PharmD, FCSHP; Lalitha Raman-Wilms, BScPhm, PharmD, FCSHP; James Conklin, PhD; Lisa McCarthy, BScPhm, PharmD, MSc; Kevin Pottie; MD MCISc; Carlos Rojas-Fernandez, BSc(Pharm), PharmD; Lise Bjerre, MD, PhD, MCFP; Hannah Irving, MA
Class-specific deprescribing guidelines are a potential solution to address the problem of polypharmacy. Optimal approaches to developing and implementing such guidelines with practitioners have yet to be identified. The purpose of the study was to understand factors associated with successful deprescribing guideline development, implementation and uptake and whether self-efficacy for deprescribing was affected.
Deprescribing guidelines were developed using AGREE-II (Appraisal of Guidelines for Research and Evaluation), and GRADE (Grading of Recommendations Assessment, Development, and Evaluation) to rate certainty of evidence and strength of recommendations. Developmental evaluation was performed using ethnographic methods: observations and interviews with guideline development and site implementation teams, and facilitated feedback sessions to discuss and agree on process improvements. Self-efficacy surveys were completed. Setting and participants included guideline development team members; members of three Family Health Teams and three Long-Term Care sites in Ottawa, Canada; and study team members.
Three evidence-based deprescribing guidelines were developed (proton pump inhibitors, benzodiazepine receptor agonists and antipsychotics). Process components and resulting decision-aid algorithms will be presented. Factors that facilitate successful development include team members’ expertise in content/ methods, access to additional expertise/resources through professional networks, and staff support. Development processes were modified for the 2nd and 3rd guidelines to ensure clarity in scope and responsibilities. Site implementation experience suggests practitioners are more interested in how to implement deprescribing approaches versus existing evidence to support stopping medications, that practice site priorities and processes shape ability to incorporate recommendations and that aligning guidelines with existing processes is critical to implementation success. Self-efficacy increased among 9 consistent respondents across all guidelines. Examples of how site experiences influence development of deprescribing guidelines will be provided.
Optimizing a deprescribing guideline development and implementation process aims to facilitate clinicians’ ability to address polypharmacy. Developmental evaluation contributes to the improvement of processes used to develop and implement such guidelines.
Community pharmacist standardized home medication consultation program by referral: Structured approach to identifying drug-related problems in the home-bound population
Bryan Gray, BScPharm, RPh, CDE; Laura Bron, BScPharm, RPh, CDE
Perform home medication consultation to identify drug-related problems and communicate concerns to the primary prescriber. Secondary objectives: Identify trends across the different intervention categories, identify drug-related problem trends by disease states and project the anticipated cost savings from avoided hospital admissions.
A referring agency in Thunder Bay, ON, sent requests for Home Medication Consultations for 33 patients (11 male) over a 3 month period. Pharmacists screened the patient’s medication regimen and health status for potential drug-related problems. Following consultation, the community pharmacist communicated potential drug-related problems to the resident’s primary care provider.
A total of 223 interventions (average of 6.76 per patient) were provided to 23 different prescribers. Average age was 76 years. Twelve were immediately accepted, 8 were immediately declined, and the remaining 203 would be discussed at the patient’s next visit Secondary outcome: Pharmaceutical Opinion Classification Trends — The majority of recommendations were related to: requiring additional drug therapy, adherence, and sub-optimal response to current therapy. Secondary outcome: Disease State DRP Trends — Based upon disease state and medical conditions, immunization/vaccination status was the most common DRP, followed by adherence (opportunity to reduce dosing frequency, merge drugs to combination therapy, and adherence packaging), and mental health (8 DRPs related to sleep/insomnia, 14 DRPs related to depression/mood/anxiety, and 2 DRPs related to smoking). Secondary outcome: Projected Case Cost Forecasted Savings — This totals $12,062.19 cost savings for avoided hospital admissions with 2 avoided hospital admissions.
A standardized and structured approach to performing home medication consultations successfully identified potential drug-related problems.
The Medication Assessment Centre: A novel student training and patient care program
Derek Jorgenson, BSP, PharmD, FCSHP; Eric Landry, BSP, ACPR; Katherine Lysak, BSP, MSc candidate
The Medication Assessment Centre (MAC) was launched in 2011 by the College of Pharmacy and Nutrition (University of Saskatchewan), with the dual purposes of: (1) providing access to pharmacist-led comprehensive medication assessments for highly complex patients who cannot access the service elsewhere; and, (2) creating a novel faculty supervised experiential training program for pharmacy students, located on campus. The objective of this project was perform an evaluation of this program from the perspective of patients and physicians.
A retrospective chart review was performed on all patients who attended at least one MAC appointment between March 2014 and July 2015 to measure: number/ description of patients; referral sources; and numbers/severity of drug therapy problems (DTPs). An experience/satisfaction survey was mailed to patients and their physicians who utilized MAC between April and October 2015.
A total of 173 patients were included in the chart review. Patients were referred from both health professionals (65.9%) and self-referrals (34.1%). Patient mean age was 64.8, with a mean of 6.5 diagnoses and 13.8 different chronic medications each. Pharmacists identified 6.2 DTPs per patient (31.1% moderate severity using Schneider criteria). Surveys were mailed to 121 patients and 81 physicians (response rates 66.9% and 43.2%, respectively). Almost 95% of both groups described their experience as very satisfied/satisfied and reported that they would refer MAC to their friends/family/colleagues; 59.2% of patients and 88.6% of physicians felt MAC improved patient outcomes; 98.8% of patients felt they were treated with dignity/ respect and that the pharmacist listened to their concerns; and 97.5% of patients felt they were involved in decisions about their health.
MAC is meeting its objective of providing access to medication assessments for highly complex patients. Physician and patient experience has been very positive and highly supportive of the program.
Collaborative care model involving eHealth to improve treatment adherence and health outcomes of patients with gout
Nicole Tsao, BSc, BScPharm, MScPharm; Kam Shojania, MD; Alison Kydd, MD, PhD; Jessica Galo, BSc; Alyssa Howren, BSc; Carlo Marra, BScPharm, PharmD, PhD; Mary De Vera, PhD
The prevalence of gout is increasing and despite availability of efficacious therapies, sub-optimal clinical outcomes persist due largely to medication non adherence. Pharmacists may have a role in supporting patients to improve their gout management. The objective of this study is to pilot the feasibility of an interdisciplinary care model involving rheumatology, pharmacy, and dietetics using shared electronic medical records (EMRs) to provide gout care.
This is a proof-of-concept study that employs a pharmacist-driven protocol whereby they are responsible for providing medication management, adherence counselling, interpretation of lab tests, and corresponding titration of urate-lowering therapies. Eligible patients are adults age ≥19 who have been diagnosed with gout by a rheumatologist for ≥1 year, ≥1 flare in the past year, and serum uric acid (SUA) >360 µmol/L within past 2 months. Remotely located health team members use shared EMRs to exchange patient information and communicate on care plans. Study outcomes include the impact of the care model on patients’: SUA levels (target <360 µmol/L); medication adherence (Compliance Questionnaire for Rheumatology 5-items); functional status (HAQ); and quality of life (EQ-5D); assessed at 0, 3, 6, and 12 months. Target enrollment is 50 patients.
Preliminary results on 21 patients enrolled from 3 rheumatology clinics since Feb. 2015 include 85% males, mean age 56 years (SD 15). All patients were prescribed allopurinol. At 6 months, adherence rate was 50%, and average SUA was 350 µmol/L versus 445 µmol/L at baseline. To date, pharmacy has provided 71 consultations and dietetics 12 consults. Anecdotal pharmacist interventions also included drug dose increases, discontinuation of unnecessary medications, and prescription continuations.
A virtual interdisciplinary clinic for gout management with expanded pharmacists’ role appears feasible with preliminary data showing improvement in SUA.
Effectiveness of community-based pharmacist interventions in chronic non-cancer pain: A systematic review
Feng Chang, BScPhm, PharmD; Mo Chen, BSc, MSc candidate; Tejal Patel, BScPhm, PharmD
Chronic pain is a common condition that has significant impact on patients’ physical and psychological well-being. Pharmacists have a key role in providing patient-centred care to optimize drug therapy used in the management of chronic pain. To evaluate the effectiveness of interventions by pharmacists providing care in community settings for ambulatory patients with chronic non-cancer pain.
Six electronic databases (PubMed, Cumulative Index to Nursing and Allied Health Literature, COCHRANE, PsychInfo, EMBASE and International Pharmaceutical Abstract) were searched for randomized controlled trials (RCT) and non-randomized studies (NRS) published in the English language involving pharmacists providing direct care in the management of chronic non-cancer pain. Team based approaches were included if a pharmacist was involved. Manual bibliography searches with retrieved articles were conducted. Risk of bias was assessed for all included studies.
The search strategy identified 17 full-text articles from 14 studies. Six of the studies were based on pharmacist-only interventions and the other 8 involved pharmacists working as part of an interprofessional team. The most frequently used pharmacist intervention was consultation involving medication review, recommendations, follow-up, and patient education. There was variation across pain measures and other self-reported measures in the included studies, but most studies showed positive results. Pharmacist interventions significantly decreased pain scores, improved quality of life and patient satisfaction, and reduced medication-related side effects and cost. Pain intensity reduction achieved ranged 8%-21%.
Pharmacist interventions were positive in several domains studied. However, the clinical significance remains debatable due to heterogeneity in relation to intervention, outcome measures, clinical setting, sample size, and study duration.
The consideration of sex/gender and vulnerable populations in pharmacy practice research
Nancy Waite, PharmD; Martin Cooke, PhD; Katie Cook, MA; Emily Milne, PhD; Feng Chang, PhD; Lisa McCarthy, PharmD; Beth Sproule, PharmD
Funders often now require that sex and gender are main considerations in research programs, but provide little guidance about how this can be accomplished. The Ontario Pharmacy Research Collaboration (OPEN), a multi-institutional and multidisciplinary research program, adopted a sex/gender and vulnerable population (GVP) model within the collaboration to promote incorporation of sex, gender and other dimensions of vulnerability across OPEN’s research projects. This presentation (1) addresses why the consideration of GVPs matter to pharmacy practice and (2) describes the GVP model’s mandate, activities and experiences.
This mixed method study incorporates: (1) literature search of published work on this topic; (2) critical reflection of co-leads of the GVP team with regards to the creation and implementation of the model; and (3) surveys (n=37) and interviews (n=23) conducted with OPEN members about their knowledge of GVP issues and engagement with GVP services.
The consideration of sex/gender and vulnerable populations within pharmacy practice research is necessary, but lacking. Within OPEN, a GVP team was established to support research projects in their incorporation of sex/gender and various dimensions of vulnerability into research design, analysis and interpretation. According to OPEN members, knowledge pertaining to GVP issues in research increased through OPEN involvement. The GVP model “surfaced” domains traditionally neglected in the field but important to ensuring quality pharmacist practice. OPEN members have been receptive and engaged with the GVP model and mandate. However, more work needs to be done in order to fully translate this awareness into research practices.
There is a need for increased awareness and consideration of sex/gender and vulnerable populations in pharmacy practice research. The experience of OPEN suggests that a cross-project structure can help integrate these considerations into a large and complex research project. We encourage practitioners to consider GVP focused initiatives, tools, and models within their work.
Introducing a unit-based clinical pharmacist: A pilot study
Vinita Arora, RPh, BScPhm, ACPR, MEd, PharmD; Heather Parker, RPh, BScPhm; Alexandra Hernandez, PhD; Karyn Li, BSc candidate; Mehrdad Alizadeh, RPh, PharmD
A pharmacist was stationed on a forensic mental health unit to more fully participate in the interprofessional team. Since clinical pharmacy services were previously centralized, we evaluated the impact of this change on staff and patients of a forensic wing.
We administered anonymous surveys at three time periods, post 1, post 2, and post 3, at 1, 5, and 12 months, respectively (72 beds; nstaff 25, 27, 28; npatients 21, 21, 18) to examine themes of accessibility, education, and medication therapy management (MTM). Non-parametric chi-square analyses were used to examine differences in overall satisfaction (Strongly Agree and Agree responses combined) scores over the time periods. We also compared percentages of satisfaction in these themes and qualitative changes over time.
The average change in staff satisfaction from post 1 to post 3 was 8% for the Accessibility theme, 9.5% for the Education theme (2 to 17%) and 11% for the MTM theme (1 to 30%), with the increase in MTM satisfaction approaching significance (x2=5.911, p=0.052). The average change in patient satisfaction from post 1 to post 3 for questions in the Education theme was -12.5% (-5 to -24%) and -28% for questions in the Accessibility theme, however the decreases were not statistically significant. Qualitatively, there were positive changes stated by staff in all themes, most notably, accessibility; while patients expressed desire for increased services in all themes.
Being situated on a forensic mental health unit enhances involvement of the clinical pharmacist in the interprofessional team. Accessibility may be a precursor to provision of increased MTM and education. Limitations surrounding patient satisfaction need further consideration.
Patient-centered renovations
Joan Cochrane, BSP
My object was to renovate my pharmacy to make it easy for my pharmacists to provide better patient care.
We have designed our pharmacy so that the pharmacist is the first point of contact for the patient. The pharmacist is situated in a semi-private area at the front of the store. Our design has 2 of these “pharmacist interaction stations” to decrease wait time. The patient comes to the pharmacy, gives their prescription, refill or new, to the pharmacist and sits down across from the pharmacist. The pharmacist station has a computer with Internet access, a phone, a scanner and a computerized blood pressure monitoring system. This allows the pharmacist to handle the prescription in a single efficient interaction with the patient. If there are no problems to solve, the pharmacist can fill the prescription, the label prints at the island in the main dispensary area, if in the robot, it is automatically counted, if not, the technician assembles the medication and then brings it over to the pharmacist, who can hand it out. The pharmacist has been talking to the patient about the prescription and giving the appropriate information. Then the prescription is handed to the patient who is directed to the cash station. If there are problems, drug interactions, 3rd party coverage issues, etc., they can be taken care of right away.
Our staff and patients are very happy with the layout. We are doing more prescriptions every month and yet have found that we have more time than we used to. Our patients feel that when it is their turn with the pharmacist they have their undivided attention. They like that both they and the pharmacist are sitting down.
It is much easier to provide meaningful patient care if you have a pharmacy that is designed primarily with this function in mind. This new design with pharmacist stations and a work island for the techs replacing the long counter has proven to be very effective.
Medication reconciliation practices on discharge into primary care homes in Prince George, British Columbia
Robert Pammett, BSc, BSP, MSc
Medication reconciliation is an integral part of safe medication practices, and should occur at all stages of hospital transition, including discharge to the primary care home (PCH). Ensuring that the PCH has an up to date list of patient medications after discharge can help avoid medication misadventures. The objectives of this study were: (1) to determine the proportion of patients who had a discharge medication list communicated to the primary care home which contained discrepancies from the hospital medication list, and (2) to categorize discrepancies as prescription medication, non-prescription medication, or medication dose.
Two PCHs were recruited to participate in the retrospective chart review. Records of 50 patients who received a hospital discharge from June 1 2014 to May 31 2015 were identified at each PCH. The list of hospital medications at discharge was compared to the medication list that was communicated to the PCH at discharge. Discrepancies between these lists were identified and categorized, as was the medium in which the medication list was communicated to the PCH.
Seventy-eight cases were included in the final data analysis. Mean age of patients was 46.7 years, 59% being female. The mean number of medications taken was 6.3 per case. Four cases had no medication use. All discharge medication information was communicated via a dictated discharge summary. The total number of discrepancies identified was 280, a mean of 3.6 per case. The majority of discrepancies were prescription medication omissions or errors (69%). The remaining discrepancies were non-prescription medication omissions or errors (18%) and medication dose discrepancies (13%).
A large number of discrepancies were present between the hospital chart and the discharge summary that was sent to the PCH. Improving communication of the medication list at discharge should be encouraged to reduce potential medication errors.
Stakeholder perspectives on economic analyses of billable pharmacy services in Ontario
Sherilyn Houle, BSP, PhD; Jilan Yang, MD, MSc, PhD
A number of pharmacy services in Ontario are government-funded; however, little is known about the costs and benefits of these services. This study solicited stakeholder perspectives on the most valuable economic analysis designs, the priority services, and concerns related to the conduct of the research or dissemination of results.
Semi-structured telephone interviews were conducted with 16 stakeholders from government, academia, pharmacy industry/associations/regulators, and insurers in March and April 2015. Interviews were audiotaped, transcribed verbatim, and coded both manually and using NVivo. Data analysis employed the constant comparison approach to identify emerging themes and patterns.
There was consensus among stakeholders that high-quality economic evaluations of pharmacy services are needed. While evaluation of MedsCheck reviews was considered highest priority, influenza vaccination was widely identified as a suitable starting point given data availability and clear patient outcome measurement. A broad perspective including those of government/payers, the pharmacy profession, and patients is encouraged, with patient outcomes identified as more valuable than financial outcomes. However, accurate and complete patient outcome data collection was identified as a key challenge. Stakeholders reported a desire to be actively involved in economic evaluations and knowledge dissemination.
Researchers considering economic evaluations of pharmacy services are encouraged by stakeholders to incorporate broad perspectives beyond solely the interests of the profession. While patient health outcomes are valued above financial outcomes, care should be taken to ensure this outcome data is accurate and complete to minimize the impact of assumptions on the validity of the results. Stakeholder engagement at all stages of the research can help ensure the relevance and uptake of economic analyses conducted.
Opportunity and cost: Self-monitoring of blood glucose in Manitoba, 2000-2013
Olena Serwylo, BSc(Pharm), PharmD candidate; Kevin Friesen, BSc(Pharm), MSc candidate; Jamie Falk, BSc(Pharm), PharmD; Shawn Bugden, BSc(Pharm), MSc, PharmD
Given the limited evidence of benefit of frequent self-monitoring of blood glucose (SMBG) by non-insulin using patients with diabetes, new guidelines and test strip limit policies have been suggested and implemented in various Canadian jurisdictions. The objective of this study was to assess the overall utilization and cost associated with blood glucose test strips (BGTS) and lancets for SMBG in Manitoba from 2000 to 2013 and to assess potential implications of such a policy.
A cohort of all patients with diabetes in Manitoba from 2000-2013 was established. Test strip and lancet utilization and cost were assessed for the overall cohort and for subgroups based on the type of diabetes treatment. The potential opportunity for a more selective practice of SMBG was assessed.
In the year 2000, 8 million BGTS were dispensed in Manitoba, and this increased by 270% to 21.7 million by 2013. Insulin users accounted for the majority of test strip use. However, it was estimated that test strip use could be reduced by 16 million test strips over 5 years by taking a guideline based approach to monitoring, with 95% of the potential reduction occurring in groups not using insulin. Over the next 5 years, a guideline based approach is projected to save $12.35 million, including $7.3 million in government spending.
Some provinces have placed therapy-linked limits on BGTS use. Whether or not a test strip limit policy is in place there is an important opportunity for pharmacists to help guide patients with diabetes to determine optimal frequency of SMBG. Expenditures above guideline recommendations represent an opportunity cost, money which could be redirected to programs and more useful interventions for the growing population of patients with diabetes in Manitoba.
Ibuprofen provides superior antipyretic efficacy vs. acetaminophen in childhood fever: Pooled analysis of 2 randomized trials
David Kellstein, PhD; Shyamalie Jayawardena, PhD
Compare antipyretic efficacy and safety of ibuprofen (IBU) vs acetaminophen (APAP) in children with fever from a pooled analysis of 2 studies.
Two IRB-approved, randomized, double-blind studies enrolled children 0.5 - 11 y, 13 - 95 lb with fever (101.5 - 104.9°F, rectally, ages 0.5 - 3 y; 101.0 - 103.9°F, orally, ages 4 - 11 y) for ≥2-h duration to single-dose IBU suspension (Children’s Advil® Suspension 7.5 mg/kg) or APAP suspension (Children’s Tylenol® Suspension 10 – 15 mg/kg) based on labelled dose/age. Temperatures (temperature; average of 2 readings) were assessed at baseline (predose) and after single dose of study medication at 15, 30 and 45 min and hourly from 1 - 8 h thereafter. Primary efficacy: time-weighted sum of temp difference from baseline over 8 h evaluated via analysis of variance. Secondary efficacy endpoints included time to onset and duration of temp control (temp: <100°F orally or <101°F rectally) via Cox proportional hazards; percentage with temperature control (Cochran-Mantel-Haenszel); safety was monitored throughout.
In total, 319 children (144 male, 175 female; 94% white; mean age 4.6 y; mean weight 42 lb) were evaluable for efficacy; 333 comprised the safety set. On primary efficacy, IBU 7.5 mg/kg was significantly better in terms of time-weighted sum of temperature differences vs APAP 10 – 15 mg/kg: mean (SD) -11.1 (8.5) vs -7.6 (8.0); p<0.001. Onset of temperature control occurred significantly earlier (median: 94.5 vs 111.6 min; p<0.001), lasted significantly longer (median: 191.3 vs 122.7 min; p=0.042) and occurred in a significantly higher percentage of children (89.6 vs 66.7%; p<0.001) with IBU suspension vs APAP suspension. Fifteen AEs occurred in each group; none severe. Most common AE was vomiting (4.6%: IBU; 6.3%: APAP; p>0.05).
IBU paediatric suspension (7.5mg/kg) is superior to APAP suspension (10 - 15mg/ kg) in treating paediatric fever, with better temperature reduction that was faster and of longer duration compared with APAP. Both products were well tolerated.
Development of a hormonal contraception decision support tool for pharmacists
Nese Yuksel, BScPharm, PharmD, FCSHP, NCMP; Humirah Sultani; Tasneem Siyam, BScPharm, MSc
Hormonal contraception continues to be a popular and effective method of contraception among women. With the expanded scope of practice in Alberta, pharmacists are perfectly positioned to manage the hormonal contraceptive needs of women, including initiating and adjusting hormonal contraceptives. The objective of this project is to develop a decision support tool to help pharmacists manage hormonal contraceptives in the community.
Development of the decision support tool involved a panel of local pharmacists with expertise in women’s health. Content of the tool was informed by current contraception guidelines, published literature and research team experience. The developed prototype was then reviewed by experts in the field including a pharmacist and nurse specialized in contraception, an obstetrician-gynecologist and a family physician with interest in women’s health. The modified prototype was alpha tested in a small cohort of community pharmacists (n=10) for acceptability and usability.
The tool includes 4 sections: (1) Patient Assessment — includes screening for indications, contraindications and risk factors, (2) Initiating Hormonal Contraceptives — includes guidance in choosing among different products, (3) Patient Education — provides an educational overview for shared decision making, and (4) Managing Ongoing Therapy — includes monitoring recommendations, approaches to dealing with side effects and adjusting therapy. An appendix with available Canadian Hormonal Contraceptives is also provided.
An evidence based clinical decision support tool may be a useful tool for pharmacists managing hormonal contraception in the community. Future plans are to evaluate the feasibility and applicability of the tool in the community setting.
The pharmacy services framework: Communicating the shift to clinical pharmacy services in Alberta
Theresa J. Schindel, BSP, MCE; Christine A. Hughes, BScPharm, PharmD; René Breault, BScPharm, PharmD; Deborah Hicks, MA, MLIS
To gain insight into communication of the Compensation Plan for Pharmacy Services, known as the Pharmacy Services Framework (PSF), by interpreting information described in news media articles, policies, government reports, and communications about the PSF.
Publicly available documents published 2012 - 2015 were obtained from websites such as the Government of Alberta, Alberta Blue Cross, the Alberta College of Pharmacists, the Alberta Pharmacists’ Association, and the Blueprint for Pharmacy. Searches using the Canadian Newsstand database and Google identified additional documents. Search terms included “Pharmacy Services Framework,” “Compensation Plan for Pharmacy Services,” pharm*, compensat*, reimburse*, and Alberta. One research team member completed initial analysis of documents using a grounded theory approach and the entire team reviewed emerging thematic categories. During the analysis, attention was paid to how the PSF was presented to pharmacists and other audiences.
Preliminary analysis of documents written for practicing pharmacists consisting of government policies, newsletters, and other communications identified four main themes: reimbursing patient care services, legitimizing pharmacists’ professionalism, shifting focus to patient care role, and collaborating with health care team members. The PSF was framed as payment for professional services and as offering external validation and legitimization for pharmacists’ changing professional service roles. Further analysis of news media and communications directed to other audiences is underway.
Preliminary findings provide insight into how the PSF was communicated to pharmacists and other audiences. Researchers need to consider political and societal contexts that influence provision and reimbursement of clinical services. The results of this study will provide a foundation for future research on how clinical services reimbursed by the PSF are implemented.
Provider and patient perspectives regarding a community pharmacist-based case finding and intervention program — Alberta Vascular Risk Reduction Community Pharmacy project: RxEACH
Maoliosa Donald, BSc, MSc; Kathryn King-Shier, PhD; Ross T. Tsuyuki, BSc(Pharm), PharmD, MSc; Yazid Al Hamarneh, PhD; Charlotte Jones, MD; Braden Manns, MSc, MD; Marcello Tonelli, SM, MD; Brenda Hemmelgarn, PhD, MD
To gain firsthand knowledge of pharmacists’ and patients’ experiences with pharmacist-based management of adults at risk for cardiovascular events.
Design: Qualitative descriptive — one on one telephone interviews. Setting: Community — Alberta. Population: Community pharmacists and patients. Data analysis: Multi-step process using conventional qualitative content analysis.
We completed 35 telephone interviews — 21 pharmacists and 14 patients, where we had 14 dyads (pharmacist and patient relationship). The majority of pharmacists were female (57%) between the ages of 36-45, and worked in an urban setting (57%) with 10 or less years of practice. Pharmacists reported a variety of factors that affected their ability to manage patients’ cardiovascular risk. These included features of their workplace (i.e., work autonomy, resources and physical space); their personal outlook and perspective (i.e., expanded professional role and professional development); collaborative physician/pharmacist relationship; and patient uptake. Common themes identified by patients included their trust of the pharmacist, ease of access to pharmacist services and presumed health care cost.
Understanding the provider and patient perspectives are key to maximizing the impact and sustainability of a pharmacy-based program to manage patients at high cardiovascular risk. Generally, patients were pleased with the clinical services provided by the pharmacist and pharmacists embraced the expanded clinical role.
An audit of 8 centres’ use of anticoagulant therapies when discharging patients from hospital with acute venous thromboembolism
Tammy Bungard, BSP, PharmD; Bruce Ritchie, MD; Cindy Jones, BScPharm; Jennifer Bolt, BScPharm, ACPR, PharmD; William Semchuk, MSc, PharmD, FCSHP
To report anticoagulant (AC) therapies patients receive for acute venous thromboembolism (VTE) upon hospital discharge.
This retrospective chart review from April 2014 to March 2015 included 4 urban Edmonton hospitals, 2 urban Regina hospitals and 3 rural Alberta hospitals. Patients > 18 years of age who were discharged with a diagnosis of VTE (DVT or PE) that lacked another indication for anticoagulant therapy and had an anticipated lifespan > 3 months were included. We primarily sought to assess the anticoagulant regimen prescribed for patients at hospital discharge and with whom follow-up care was to occur. Moreover, we sought to compare differences among the urban and rural centres.
After screening 1,047 patients, 692 (66.1%) were included. The majority of patients discharged from hospital had a PE (Edmonton 84.4%, Regina 81.2%, rural Alberta 63.3%). Novel oral anticoagulants (NOACS) were the most common discharge therapy in rural Alberta (50.0%), followed by warfarin (+/- a parenteral AC) (30.0%). In rural Alberta follow-up most commonly occurred with the GP (66.7%). In Regina, the most common therapy at discharge was warfarin (+/- a parenteral AC (59.0%) followed by a NOAC (23.9%), and a parenteral AC alone (16.2%). In Regina, the majority of follow-up was with the GP (52.1%) or specialist (52.1%). In Edmonton, 40.5% were discharged on warfarin (+/- a parenteral AC), 29.2% a parenteral agent alone, and 28.4% on a NOAC. Follow-up most commonly was with the general practitioner [GP] (29.9%) or VTE clinic (29.1%) in Edmonton.
The majority discharged after VTE-related hospitalizations have PEs, and NOACs are used more commonly in rural Alberta (50%) compared to urban centres (~25%). Depending on the centre, follow-up is either done via the family doctor or through specialists / VTE clinic.
An audit of 8 centres’ use of anticoagulant therapies when discharging patients from the emergency department
To report anticoagulant (AC) therapies patients receive for acute venous thromboembolism (VTE) upon discharge from the emergency department (ED).
This retrospective chart review included patients discharged from the ED with a diagnosis of VTE (DVT or PE) between April 2014 and March 2015. Two urban Edmonton hospitals having VTE clinics (Edm-VTE), 2 without VTE clinics (Edm), 2 urban Regina hospitals and 3 rural Alberta hospitals were included. We primarily sought to assess the AC regimen at ED discharge to the community and with whom follow-up care was to occur. Moreover, we compared differences among the urban and rural centres.
After screening 1,734 patients, 418 (24.1%) were included. The majority were discharged with DVT as compared to PE/PE plus DVT (Edm-VTE 54.5%, Edm 59.0%, Regina 91.7%, rural Alberta 80.0%). For Edm-VTE, discharge therapy with a parenteral AC alone (60.1%) or novel oral anticoagulant (NOAC) (20.0%) with follow up in the VTE clinic (80.6%) was most common. The majority for Edm were prescribed a parenteral AC (41.0%) or NOAC (40.3%) with either general practitioner [GP] (28.1%) or VTE clinic (33.8%) follow-up. In Regina, the majority (75.0%) were discharged on a parenteral AC with warfarin, with 11.9% each on a parenteral AC or NOAC, with GP follow-up (56.0%). Rural Alberta sites most commonly used NOACs (43.3%) or a parenteral AC with warfarin (26.7%), with GP follow up (53.3%).
Urban Alberta sites discharge more patients with PE (43.4%) from ED compared with Regina or rural Alberta sites. Traditional therapy with a parenteral AC (+/- warfarin) is still most commonly used at discharge, with anywhere from 12-43%receiving a NOAC across the sites assessed. NOAC use was most common (~40%) in rural Alberta and at the Edmonton site not having a VTE clinic. Variation in practice is evident.
Enhancing depression outcomes with better use of antidepressants: Evaluation of a pharmacy benefit manager– sponsored depression disease state management program
Katherine Giannoulis, BScPharm, CGP; Leanne McFarlane, BScPharm; Heather Creighton, BScPharm; Moira Reiley, BScPharm, CGP
Non-adherence to antidepressants is associated with poor health outcomes and is common in people with depression. Studies using medication possession ratio (MPR) or proportion of days covered (PDC) to calculate adherence found 34-56% of patients were adherent to therapy. Persistence to antidepressants at 1, 3 and 6 months is estimated to be 70-75%, 56-60% and 40-43% respectively. To improve adherence and patient depression outcomes MHCSI developed and funded a two-year pharmacist Depression Disease State Management (DSM) pilot program for plan members.
Pharmacists within MHCSI’s Preferred Provider Network were encouraged to have multiple consultations with each patient in-program over a one-two year period. Pharmacists received equal compensation for each consultation. Adherence was calculated at program completion based on drug claims data using the PDC method. Patients were considered adherent if the PDC was >80%. Persistence was calculated for patients new to antidepressant therapy. Pharmacists completed a Patient Outcome Survey for each patient.
There were 59 patients in the Depression DSM program. Patients had an average of three consults. The percentage of patients considered adherent to antidepressant therapy was 70%. The average proportion of days covered for participants was 81%. Persistence to 1, 3 and 6 months was 100%, 89% and 61%. Patient Outcome Surveys were completed for 57 of the 59 patients with 81% of respondents reporting that the patient had a better understanding of condition/treatment, 65% of the patients reported “feeling better” and 54% reported productivity gains.
This suggests a pharmacist longitudinal follow-up model may improve adherence to antidepressant medication with the goal of improving patient health outcomes.
Pharmacist intervention for a frail elderly population in primary care
Tejal Patel, PharmD; Jillian Bauer, BScPharm; Linda Lee, MD; Cathy Schill, BScPharm
In 2013, the Centre for Family Medicine Family Health Team initiated a new program called the “Case-Finding for Complex Chronic Conditions in seniors 75+ (C5-75)” to systematically screen for frailty among all persons aged 75 years and older to address medical conditions appropriately and to avert crises. As a component of this program, a pharmacist intervention was developed to address medication-related problems (MRPs). The objectives of this study are to describe the medication use in the population referred and activities performed by pharmacists in this program.
This was a retrospective medical records review of frail elderly patients seen by pharmacists in the C5-75 program from April 2013 to August 2015. Data pertaining to patient demographics, medical conditions, and medication history as well as activities performed and recommendations made by pharmacists were abstracted.
Of 142 patients (54 males and 88 females, mean age 85 years [range: 75-98]) identified as frail, 54 patients accepted the offer of a medication review with a pharmacist in the C5-75 program. At initial visit with the pharmacist, the means for number of total medications was 11.60 (range: 5-23), for prescribed medications, 7.67 (range: 3-20), and for over-the-counter medications, 3.93 (0-15). Polypharmacy and high-risk medication use was highly prevalent (83% and 93%, respectively). A total of 218 MRPs were identified among the 41 patients with at least one follow-up visit with the pharmacist. Pharmacists made a total of 222 recommendations. Of the 138 that were measurable, physicians had accepted 70% and 50% were implemented at most recent follow-up.
Polypharmacy, high-risk medication use and MRPs are highly prevalent in the frail elderly in primary care. Pharmacists were able to address these problems with recommendations, many of which were accepted and implemented.
Impact of pharmacist assessment on classes of high-risk medications in a geriatric outpatient clinic
Sharon Ong, BPharm, PharmD; Alexandra Marin, MD, CCFP, Dip. COR; Imran Hassan, MSc; Ross T. Tsuyuki, BSc(Pharm), PharmD, MSc, FCSHP, FACC; Cheryl Sadowski, BSc(Pharm), PharmD, FCSHP
Seniors often take multiple medications because of a high burden of chronic diseases. This complex population is vulnerable to medication-related problems. Pharmacists can improve suboptimal prescribing in older adults, however, the evidence base for this is weak. Our objective was to determine if pharmacist assessment is effective in reducing classes of high-risk medications in seniors at a geriatric clinic.
We reviewed the medical charts of 245 patients aged 65 and over who were referred to our outpatient geriatric clinic and assessed using comprehensive geriatric assessment (CGA). The CGA team consisted of a geriatrician, medical trainee (student, resident or fellow), pharmacist (available part-time), and nurse. Since the pharmacist was only in the clinic on certain days, we conducted a non-randomized comparison of medication use in those seen by a pharmacist versus those who were not. Number of medications was compared using t-test and exact McNemar’s test was performed to assess medication changes.
The mean number of medications of patients assessed by pharmacist (n=99) vs not assessed by pharmacist (n=89) was 10.5 (SD 5.5) vs 9.4 (SD 4.7) with a mean difference of 1.07 (95% CI, -0.41 to 2.55), p=0.157. The proportions of patients taking acetylcholinesterase inhibitor in both pharmacist and non-pharmacist groups increased, respectively, from 20% to 37%, p<0.001 and 14% to 28%, p=0.001. Other classes of medication with statistical significant changes were exclusively in the pharmacist group, such as selective serotonin reuptake inhibitor from 20% to 27%, p=0.007; over-the-counter analgesic e.g. acetaminophen from 30% to 41%, p=0.002; non-steroidal anti-inflammatory drug from 22% to 16%, p=0.013; and antihistamine or other anticholinergic (not for overactive bladder) from 7% to 2%, p=0.016.
Pharmacist assessment as part of an interprofessional geriatric clinic team led to an improvement in medication use.
Description of medication management problems and supports used in community-dwelling seniors
Objective(s).
Seniors commonly have problems managing their medications due to extensive medication use, medication regimen complexity, and functional or cognitive limitations. With an aging population, it is important to identify these problems so that resources can be directed to meet their health care needs. The purpose of our study was to describe the medication management problems of seniors living in the community.
A retrospective chart review of patients aged 65 years and over who were referred to our geriatric clinic and assessed using comprehensive geriatric assessment (CGA). The CGA team consisted of a geriatrician, medical trainee (student, resident or fellow), pharmacist and nurse. Data were analyzed descriptively and McNemar’s test was used for changes in calendar packaging.
The mean age was 80.6 (SD 7.2) years, 41% lived alone and 46% lived with spouse/ partner. On admission, the mean number of medications (n=236) per patient was 9.8 (SD 4.8), and 46% had medications administered via a non-oral route. Medication-related problems were non-adherence (43%), difficulty managing medication (40%) and dependence with medication use (49%). The dependent patients obtained assistance from spouse or partner (37%), family member/living separately (25%), family member/living with (18%), formal home care cueing/ administration (11%) or monitoring (8%), and caregiver (9%). Calendar packaging from 55% to 70%, p<0.001, and community care services from 27% to 42%, following assessment.
Conclusion(s)
About half the seniors seen at the geriatric outpatient clinic had complex medication regimens, were non-adherent, had difficulty managing medications and were dependent with medication use. There appeared to be a high dependency on their spouse and family members in medication management. As such, assessing seniors for medication management and inquiring about supports for medication assistance are important roles for pharmacists in a geriatric practice.
Effectiveness of the peer-to-peer mentoring model for transitioning from classroom to professional practice
Thomas Huang, PharmD (student); Annie Lee, MSc(T), ACPR; Certina Ho, RPh, BScPhm, MISt, MEd; Edric Paw Cho Sing, PharmD; Michael Vinh, PharmD
To better prepare pharmacy students for practice by implementing a peer-to-peer mentoring model of student-led pharmacotherapy sessions (SLPS) in the PharmD program. The learning impact and the utility of the model for student preparedness for Advanced Pharmacy Practice Experiences and the licensing exam were examined.
Fourth-year students delivered SLPS on Cardiology, Infectious Diseases, and Patient Self-Care online and live to both third- and fourth-year students. Retrospective self-assessment surveys were administered after each SLPS. Five knowledge domains (etiology, clinical presentation, pharmacotherapy, monitoring/follow-up, and overall knowledge) were assessed. A paired t-test was utilized to evaluate the survey data. Thematic analysis was applied to the qualitative comments on the survey.
Eighty-one students (59% third-years; 41% fourth-years) responded to the survey. Prior to the SLPS, 46.8% of students rated their knowledge “Average” (3 of 5), while 33.1% rated their knowledge “Above Average” (4 of 5) in all knowledge domains. After the SLPS, 53.6% of students rated their knowledge to be “Above Average” (4 of 5), while 27.5% rated their knowledge “Excellent” (5 of 5) in all knowledge domains. Statistically significant increase (p<0.001) was shown in all five knowledge domains post-SLPS for both third- and fourth-year students. Students stated that cases, drug charts and therapeutic overview were the most useful. Suggestions for improvement included increased interactions, counselling points, and providing practice examples.
The peer-to-peer mentoring model was an effective model for student learning. Students perceived a therapeutic knowledge increase after attending the SLPS. Student presenters developed public speaking skills and built confidence while consolidating knowledge. This model has proven to be effective in developing skills and knowledge for students transitioning into professional practice.
Community pharmacy reports of potential QTc-prolonging drug interactions involving fluoroquinolones or macrolides: A multi-incident analysis
Roshan Tahavori, RPh, BScPhm, PharmD; Certina Ho, RPh, BScPhm, MISt, MEd
Significantly prolonged QTc may lead to torsades de pointes (TdP) in at-risk patients. Fluoroquinolones (FQs) and macrolides have the potential to prolong the QTc, and given their widespread use, are implicated in relatively high number of significant QTc-prolongation events. The purpose of this project was to analyze incidents of potential QTc-prolonging drug interactions involving FQs and macrolides, in order to fill in patient-safety gaps.
We searched the Community Pharmacy Incident Reporting program for QTc-related incidents involving FQs and macrolides between April 2010 and January 2015. Using a qualitative, multi-incident analysis approach, we analyzed 56 incidents, identified themes, potential contributing factors, and provided recommendations.
Most incidents were pharmacy-intercepted drug interactions (i.e., near misses) involving moxifloxacin, ciprofloxacin, clarithromycin, and azithromycin. Commonly reported classes of interacting drugs were antidepressants, antiarrhythmics, and antipsychotics. The following themes and possible contributing factors were captured: 1) Prescriber-triggered potential for QTc-prolongation due to absence of drug-interaction assessment, 2) Potentially inappropriate pharmacist-intervention due to absence of patient risk-assessment, and 3) Patient-potentiated risk for harm due to polydoctoring and polypharmacy practices while failing to disclose complete medication lists to the providers.
Prescribers should seek patients’ complete medication list and medical history, and make TdP risk-assessment when prescribing drugs with QTc-liability. Pharmacists should assess patients’ risk factors for QTc-prolongation before intervening on drug-interactions. We developed a QTc-Prolongation Risk Factors Checklist to facilitate these assessments. Patients should regularly be provided with a comprehensive medication list and educated on safe medication use by pharmacists.
Medication incidents involving insulin: A multi-incident analysis
Carolyn Kasprzak, RPh, PharmD; Certina Ho, RPh, BScPhm, MISt, MEd
Insulin is a life-saving pharmacological therapy for many diabetic patients. However, insulin has been identified as a high alert medication as it has the potential to cause detrimental patient harm when used in error; particularly, an excessive dose can lead to life-threatening hypoglycemia. The objective of this multi-incident analysis was to examine insulin-related medication incidents and determine potential system-based improvements that may be customized in pharmacy practice to enhance medication safety.
Reports of medication incidents involving insulin were extracted from a national incident reporting database between January and December 2014. After a review of 226 incidents, 81 were included in this qualitative, multi-incident analysis. The incidents were then analyzed and categorized into main themes and subthemes.
The four main themes identified were: (1) product selection (related to unique insulin properties), with prescribing, order entry and dispensing as subthemes; (2) therapeutic regimen change; (3) dosage calculations; and (4) storage requirements. Potential solutions for prevention of insulin-related incidents included the use of standardized pre-printed order forms, integrating warning flags into pharmacy software, incorporation of independent double checks throughout the entire pharmacy workflow, and conducting comprehensive diabetes-focused medication reviews with patients.
Medication incidents involving insulin in pharmacy practice are common and have the potential to cause serious patient harm. Findings from this analysis are intended to educate health care professionals on the vulnerabilities in the medication-use process that may contribute to insulin-specific medication incidents and offer recommendations to prevent such events from recurring.
Potentially inappropriate medication use in older adults: A multi-incident analysis
Kelly Ng, BSc, PharmD candidate; Certina Ho, RPh, BScPhm, MISt, MEd; Roger Cheng, RPh, BScPhm, PharmD
Potentially inappropriate medication use in older adults can lead to preventable adverse events, which may account for a significant portion of emergency room visits and hospitalization. This multi-incident analysis identifies points of intervention in the community setting in order to prevent medication incidents that may compromise patient safety.
A qualitative, multi-incident analysis was conducted on medication incidents reported to the Community Pharmacy Incident Reporting (CPhIR) program. Reports of medication incidents involving drug therapy problems, contraindications, and duplications in patients over 65 years of age were extracted between 2010 and 2015. In total, 184 incidents met the inclusion criteria of this multi-incident analysis.
Two main themes were identified: (1) patient-specific factors and (2) drug interactions. Patient specific factors include incidents where the medication was not best suited for the patient due to their intolerances or allergies, medical conditions, and inappropriate dosing/prescribing for older adults over 65 years old. Medication incidents involving drug interactions include antibiotic and chronic medication interactions, interactions between different therapeutic classes, and drug duplications of the same therapeutic class. Comprehensive medication reviews (such as MedsChecks in Ontario) help to ensure patients are safely and appropriately using medication therapies and reduce potential adverse drug events when transitioning between points of care.
Although the use of multiple medications may be appropriate in older adults, the complexity of these medication regimens increases the risk of errors and adverse effects. Implementing system-based strategies in the pharmacy workflow can help pharmacists improve patient safety and mitigate the risks of potentially inappropriate medication use in older adults.
Patient counseling: An overarching method to mitigate medication errors and ensure continuity of care
Tracy He, PharmD candidate; Certina Ho, RPh, BScPhm, MISt, MEd
To explore the methods and behavioural tools in which community pharmacists utilize patient counselling to prevent medication incidents. The findings of this qualitative, multi-incident analysis will substantiate the strongholds in which pharmacists mitigate errors and the role of patient education in encouraging health literacy and continuity of care.
A multi-incident analysis was performed on medication incidents reported to the Community Pharmacy Incident Reporting Program (CPhIR) developed by the Institute for Safe Medication Practices Canada. The keywords in the incident description included patient-counselling terminology, such as “identified,” “counsel,” “explain,” and “teach.” The incidents included in this analysis spanned from September 2014 to August 2015. They were then stratified thematically based on their modes of identification.
Of the 115 incidents that met the inclusion criteria, two emergent themes were identified: pharmacist-led and patient-led identification of medication incidents. The themes gave rise to further subthemes respectively, focussing on prescription reconciliation, therapy evaluation and clarification, storage education, patient identifier verification, and product demonstration. Reinforcement of safe medication use at the stage of patient counselling can also gear pharmacists towards patient-focused care and effective medication therapy management.
Community pharmacy practitioners can effectively identify near misses and medication incidents at the stage of patient counselling. Having a dialogue with patients at the point of care will not solely be helpful for the mitigation of errors, but also serve as a quality assurance of continuity of care.
Older people’s attitudes towards deprescribing: A community study in Quebec
Caroline Sirois, BPharm, PhD; Nicole Ouellet, PhD; Marie-Eve Gagnon, BInf; Joanie Renaud; Lyndia Huard
Polypharmacy is very common among older individuals and has been associated with adverse outcomes. Reducing the number of medications (deprescribing) might be a valuable option to reduce the risks. However, little is known about older individuals’ attitudes towards deprescribing.
We ran a pilot study to evaluate the feasibility of using a self-administered questionnaire among community-dwelling older individuals to address their perceptions towards deprescribing. We used a French version of the Australian Patient’s Attitudes Towards Deprescribing Questionnaire. The questionnaires were distributed in ten community pharmacies and two community centers in the province of Quebec. The participants (n=129) completed the questionnaire containing 10 Likert type questions about polypharmacy/deprescribing and 5 multiple-choice questions. We used descriptive statistics to summarize the participants’ characteristics. We performed chi-square tests to compare the proportions of agreement, and evaluated correlations with Spearman’s Rho (alpha=0.05).
The participants were mostly women (63%) with a median age of 76 years (IQR:7180). The median number of daily medication was 6 (IQR: 3-8). Half of the participants considered they were taking a lot of medications, but 80% judged these medications were necessary and felt comfortable with the number they were taking. More than 80% would agree to take more medications for their health condition if required. Nonetheless, 50% of the participants mentioned they would like to reduce the number of medications they were taking. If their doctor said it would be possible, 71% would be willing to reduce the number of medications used. Those who thought they were taking a lot of medications were more willing to have their number reduced (p<0.001).
The results show that older individuals in the community are eager to undertake deprescribing, conditional on their doctor’s approval.
The effect of health media reporting on self-medication use
I fan Kuo, BSc (Pharm), ACPR, MSc, PharmD; Amanda Church, BSc (Pharm) candidate; Christopher Louizos, BSc (Pharm), PharmD; Brenna Shearer, PhD
The news media serves the crucial role of conveying complex scientific findings and health issues to the general public. The main objectives of this study are (1) to describe the public’s perception of health-related content in the news media and their dependence on the media in decision-making surrounding self-medication use, and (2) to examine potential factors, both individual and media-related, that influence self-medication behaviour.
Twenty-Nine adult volunteers participated in five focus group interviews that were conducted at the College of Pharmacy, University of Manitoba in Winnipeg. Each 90 minute interview was moderated by a study coordinator, audio-recorded, and transcribed. Two study team members independently analyzed the transcripts.
The general public expressed varying degrees of uncertainty towards the reliability of health reporting in news media. Most felt overwhelmed and frustrated by the excess sources of information, and the often mixed and transient messages in health news reports. A trusting relationship with a pharmacist or physician was identified as the most important factor in self-medication decision, but not all individuals had access to health care providers, due to a variety of reasons. Other influences on over-the-counter product use include education background, previous experience, upbringing, credentials of the sources, and the individual’s social circle.
Decision-making surrounding the use of over-the-counter products is a complex process, often implicitly influenced by health news reporting in the media. Trusting interaction with health care providers, especially pharmacists is an important component in choosing non-prescription product use, but one that is not always readily accessible. Pharmacists are yet to maximize the opportunity in filling this health care gap.

Documentation of functional medication management in older adults within an acute care hospital
Monika Bolina, BScPharm, ACPR; Allyson Jones, PhD; Sheri Koshman, BScPharm, PharmD, ACPR; Erin Heintz, BScPharm, ACPR; Ronald Lehmann, BScPharm, ACPR; Cheryl Sadowski, BSc(Pharm), PharmD, FCSHP
To describe the documentation of functional medication management (FMM) in adults, age 65 years and older, on medicine wards, during their hospital stay. The secondary objective was to describe the characteristics of the health care providers (HCP) documenting on FMM.
This study was a retrospective chart review of a random selection of 140 patients admitted at the University of Alberta Hospital from January 2013 to October 2014. FMM was defined as the process of taking medications (including ordering, picking up, organizing, preparing, monitoring, and administering medications). This ability requires assessing factors such as physical function (including vision, dexterity, and swallowing ability) related to medications and cognitive function.
A total of 140 patient charts were reviewed. The average age was 78.9 (SD 8.4) years, 68 (48%) male, and mean 8 (SD 3.1) scheduled oral medications taken. Commonly documented components of FMM included administration of medications (52%), organizing of medication (33%), assessments of physical function including vision (25%), swallowing ability of medications (18%), and cognitive function (21%). Documention of these activities was most frequently done by physicians (39%), occupational therapists (34%), and pharmacists (17%).
Clinicians occasionally document FMM. Given the complexity of medication regimens and the functional demands of handling these, there is a need to incorporate these assessments when evaluating patients.
Global citizenship framework — Application to pharmacy student experience
Cheryl Sadowski, BSc(Pharm), PharmD, FCSHP; Lynette Shultz, PhD, Marlene Gukert, BScPharm, ACPR; Cheryl Cox, BSP, MBA
The role of pharmacists as citizens is important in terms of community engagement, public health, and advocacy. Student exposure to global citizenship is important in order to develop a view of citizenship in their future role as pharmacists. The purpose of our research was to apply a framework for global citizenship to student experiences in an international course taught in Italy.
This was an exploratory qualitative study. Students at the University of Alberta enrolled in Pharm 453 (Intercultural Exploration of Pharmacy & Health) between 2011 and 2013 were invited to participate after completing the course. Students who consented individually participated in a semi-structured interview regarding their experience. We applied a published framework and the data was transcribed and analyzed by content analysis methods.
The framework included 4 main components, with examples of application in practice. The components were politics/ideology, social/collective, self/ subjectivity, and praxis/engagement. Examples of each component include: (1) politics — awareness of food insecurity, injustices; (2) social — appreciation of interconnectedness, inclusion of those with different values; (3) self — being aware of one’s own perspectives, concern for social justice; (4) praxis — ethical action and active participation in society.
Applying a framework in describing student experiences with global citizenship through an international course was valuable, and demonstrated that students can be engaged with important citizenship issues.
How does pharmacist prescribing fit with family physicians’ practice in Alberta? Developing a knowledge translation strategy
Chowdhury Faruquee, BPharm, MPharm, MBA; Amandeep Khera, MD, CCFP, MPH; Lisa Guirguis, BSc Pharm, PhD
Alberta family physicians are seeing patients with an increasing number of chronic diseases and complex medication regimens. Pharmacists are medication experts with prescribing authority who can help both physicians and patients to manage medications. However, literature and anecdotes suggest physicians have low level of understanding and speculative beliefs about pharmacist prescribing. Our objective is to develop a knowledge translation strategy to address family physicians’ gap in understanding of pharmacist prescribing.
Qualitative interviews were used to explore Alberta family physicians’ understanding and experience with pharmacist prescribing. We used purposeful sampling method with semi structured face to face or telephone interviews. We planned to interview 12 to 15 Alberta family physicians having experience of pharmacist prescribing in their practice as well as pharmacists who are working with these physicians. Gaps in physicians’ understanding were identified and will be used to develop infographics to communicate pharmacists’ roles in prescribing medications
To date we have interviewed 11 physicians and one pharmacist. Often, family physicians first learned of pharmacist prescribing after receiving notification that a patient received this service or from the pharmacists they work with on teams. Preliminary themes include interprofessional hierarchy, assorted acceptability, building trust, and shared goals. Gaps include knowledge about pharmacist expertise and pharmacist prescribing authority, and communication strategies to foster collaboration. We will create infographics as educational tools, addressing the gaps. We will develop a usability testing survey to test its usability and will refine the educational tools using feedback. We will disseminate our infographics to both physicians and pharmacists through Alberta PCN leads, professional associations, and encourage pharmacists to use it with individual physicians.
We confirmed that some Alberta family physicians have limited understanding of pharmacist prescribing, resulting in lack of trust. Future research should evaluate the effectiveness of this knowledge translation strategy in the Alberta context.
Medication incidents involving smoking cessation therapies
Phillip Yang, PharmD; Certina Ho, RPh, BScPhm, MISt, MEd
Ontario pharmacists have been granted the authority to prescribe medications for smoking cessation in their expanded scope of practice. To help pharmacists minimize errors when prescribing for smoking cessation, medication incidents involving varenicline and bupropion must be examined. The objective of this project was to identify areas of vulnerability when prescribing and dispensing smoking cessation therapies.
A qualitative, multi-incident analysis was conducted using anonymous incident reports submitted to the Institute for Safe Medication Practices Canada Community Pharmacy Incident Reporting Program. Medication incidents involving varenicline and bupropion were included in the analysis.
A total of 360 incidents were analyzed. Our findings were divided into two main themes according to the medication therapies: (1) varenicline and (2) bupropion. The main themes were then further divided into subthemes, comprising prescription instructions, quantity of tablets, and drug formulation. Safety interventions include separation of instructions for starter pack and continuation packs, implementation of preprinted order forms and independent double checks in the pharmacy workflow, and verification of the medication with patients during patient counselling.
As more patients access smoking cessation therapies, there are more opportunities for pharmacist-patient interactions. With pharmacists’ expanded scope of practice, there is also a new potential for near misses and incidents involving prescribing errors in the pharmacy. Through shared learning of existing smoking cessation medication incidents from this project, pharmacists will be more prepared and aware of safe medication use when executing their expanded scopes.
Medication incidents involving immunosuppressive agents
Melody Truong, RPh, BScPhm, PharmD; Amanda Chen, RPh, BSc, BScPhm, ACPR, PharmD; Jim Kong, BSc, PharmD; Certina Ho, RPh, BScPhm, MISt, MEd
Immunosuppressants are potent, immune-modulating medications that can cause significant harm to patients if used incorrectly. The objective of this multi-incident analysis is to assess the challenges of managing immunosuppressive therapy in the community setting and identifying system-based vulnerabilities.
Oral immunosuppressive agents of interest, such as azathioprine and cyclosporine, were retrieved from the American Hospital Formulary Service classification system. Intravenous agents were excluded due to a lack of presence in the community setting. Relevant medication incidents were gathered from ISMP Canada’s Community Pharmacy Incident Reporting (CPhIR) Program between January 2010 and May 2015. From an initial collection of 61 cases, a total of 47 medication incidents met inclusion criteria and were analyzed and reviewed by two analysts independently.
Quantitative analysis found that of the initial 61 medication incidents, 59% (36) were near-misses, 18% (11) resulted in no harm, and 3% (2) resulted in mild harm to the patient. The remaining 20% (12) were excluded due to insufficient narrative information provided by the reporter. Qualitative analysis uncovered three major themes that ran prevalent throughout all 47 incidents: (1) indication, (2) effectiveness, and (3) safety. Indication referred to incidents where an incorrect drug was being prescribed or dispensed due to look-alike/sound-alike names and/ or formulation oversight. Effectiveness primarily focused on medication errors arising from sub-therapeutic dosing that resulted in therapy failure, while safety referred to incidents that resulted in toxicity due to either supra-therapeutic dosing or drug interactions. System-based vulnerabilities included factors such as confirmation bias, practitioner’s knowledge gap, and lack of independent double checks in pharmacy workflow.
Immunosuppressive agents are commonly used by all patient populations within the community. Analysis of medication incidents provides an opportunity for health care practitioners to learn from errors and advance safe medication practices for quality patient care.
Medication incidents that could have been prevented at the prescribing stage
Kacy Park, BSc, PharmD candidate; Jim Kong, BSc, PharmD; Certina Ho, RPh, BScPhm, MISt, MEd
As the initial step in the medication-use process, prescribing errors can lead to a cascade effect that ultimately places the patient at risk for harm. The goal of this multi-incident analysis was to identify and prevent the occurrence of these systematic errors to mitigate patient harm.
Data were gathered from the Community Pharmacy Incident Reporting (CPhIR) Program between January 2010 and April 2015. Search criteria excluded incidents that did not occur during the “Prescribing” stage and/or resulted in “No Error.” A total of 111 incidents met the initial search criteria with 50 incidents being excluded due to insufficient narrative descriptions. The remaining 61 incidents were then analyzed.
Of the 61 medication incidents analyzed, quantitative analysis showed that 84% (51) resulted in mild harm and 16% (10) resulted in moderate harm. No incidents resulted in patient death. Qualitatively, two main themes were extrapolated from these incidents: (1) Therapeutic Plan Error and (2) Therapeutic Plan Execution Error. Therapeutic Plan Error consisted of incidents that occurred due to incorrect dose, medication discrepancy, drug allergies or drug-drug interactions. Underlying contributing factors included a lack of reliable Computerized Decision Support Systems to help capture potential drug therapy problems, and limited communication networks between health care professionals within the patient’s circle of care. Therapeutic Plan Execution Error included incidents that occurred due to incomplete prescriptions, illegible writing, or wrong patients. Potential contributing factors included a lack of system-based or forcing functions to support prescribers when prescribing and documenting medication therapies.
The prescribing stage represents a key step in the patient’s encounter with the medication-use process. Both physicians and pharmacists can improve patient safety by developing system-based strategies to prevent medication incidents at this crucial stage of patient care.
Direct oral anticoagulant medication incidents
Nusrat Amin, PharmD; Jim Kong, BSc, PharmD; Certina Ho, RPh, BScPhm, MISt, MEd
Direct oral anticoagulation utilizing apixaban, dabigatran and rivaroxaban has become highly prevalent due to their ease of use and convenient monitoring parameters. Though their unique pharmacologic properties make them a popular choice among health care professionals, increasing use has also led to an increase in medication incidents involving these medications. This multi-incident analysis serves to explore themes that contribute to incidents involving direct oral anticoagulation medications in the community setting.
Incidents were extracted from the Community Pharmacy Incident Reporting (CPhIR) Program between January 2010 and April 2015. A total of 145 incidents met the initial search criteria with 36 being excluded due to insufficient narrative descriptions. The remaining 109 incidents were then analyzed.
Qualitative, multi-incident analysis found a total of five major themes underlying all medication incidents involving direct oral anticoagulants. These included look-alike/ sound-alike medications, drug-drug interactions, transition of care, intricacies of anticoagulant dosing/frequency, and pharmacy operation. Although the primary focus of the analysis was on medication incidents in the community, transition of care presented a unique challenge as it referred to medication incidents that occurred when patients were transitioning from a different health care setting into the community setting. Numerous contributing factors such as confirmation bias, a lack of reliable Computerized Decision Support Systems, and knowledge deficit of health care practitioners all played a role in facilitating these medication incidents.
The expanding role of direct oral anticoagulants in conventional chronic drug therapy requires increased vigilance from health care professionals. In the community setting, long-term use of direct oral anticoagulants can place the patient at risk of harm if not managed and monitored appropriately. By developing safe medication practices, pharmacists can help educate patients and prevent anticoagulant medication incidents.
Drug allergy incidents in community pharmacies
Leo Kim, RPh, PharmD; Jim Kong, BSc, PharmD; Certina Ho, RPh, BScPhm, MISt, MEd
Drug-induced allergic reactions are frequent, unpredictable events of medication usage in the community setting. The lack of homogeneity in their presentation and severity can range from mild, localized discomfort to systemic, life-threatening anaphylaxis, which presents a challenge for community pharmacists to manage. The objective of this multi-incident analysis was to identify common themes underlying drug allergy medication incidents, involving patients with documented allergies, and offer recommendations to help prevent future incidents in the community setting.
Incidents were extracted from the Community Pharmacy Incident Reporting (CPhIR) Program utilizing the inclusion criteria of “Drug Therapy Problem Documented allergy” for the type of medication incident, and generalized signs and symptoms of anaphylaxis as key words in the narrative description. A total of 273 medication incidents were captured and reviewed in this multi-incident analysis.
The three major themes identified were: (1) missing documentation, (2) computer detection incapacity, and (3) alert bypass. Missing documentation involved medication incidents that stemmed from both prescriber and pharmacy-related databases, while computer detection incapacity and alert bypass incidents only involved pharmacy-related dispensing systems. Recommendations primarily focused on the proper usage/maintenance of computer databases and communication strategies with patients. System-based strategies such as various enhancements to existing pharmacy databases, along with other continuous quality improvement programs, provide further solutions to prevent patient harm.
Drug-induced allergies can be easily screened and documented given the right tools and appropriate resources. Although unpredictable in nature, the presence of an existing drug allergy should prompt health care professionals to be mindful and cautious when prescribing and/or dispensing medications.
Medication incidents associated with hospital discharge
John Cao, PharmD; Kelly Ng, BSc, PharmD candidate; Jim Kong, BSc, PharmD; Certina Ho, RPh, BScPhm, MISt, MEd
Hospital discharge is a form of transitional patient care that involves multistep processes with multiple health care professionals at different levels of care. Due to its innate complexity, this process places patients at high risk for medication errors and potential subsequent hospital readmissions. This project examines common themes that are prevalent in medication incidents associated with hospital discharge, and provides insight into system-based recommendations for advancing safe medication practices.
Incidents were extracted from ISMP Canada’s Community Pharmacy Incident Reporting (CPhIR) Program between April 2010 and December 2014. A total of 83 incidents met the inclusion criteria. These incidents were analyzed and reviewed by two analysts independently.
A qualitative, multi-incident analysis revealed three main themes underlying these medication incidents: (1) error on the discharge prescription, (2) communication issues, and (3) community integration. Error on the discharge prescription involved preparation errors in the hospital such as inappropriate medications being ordered, inadvertent omission of medications, dosing errors, and wrong patient name on discharge prescriptions. Communication issues referred to miscommunication incidents between the hospital and community that involved illegible writing/ print on faxed and written discharge prescriptions, as well as complex medication orders. Finally, community integration explored the lack of continuity between hospital and community care that facilitated medication errors. This included issues such as duplication in medication therapy, different preparations used in the hospital compared to community, and interruptions/additions to multi-medication compliance aids. Medication reconciliation is an effective strategy that can empower community pharmacists to mitigate patient harm and enhance transitional care during hospital discharge.
Patients discharged from hospitals will continue to experience harm from medication incidents if system-based vulnerabilities are not addressed properly. The results of this multi-incident analysis, along with further investigations, will help develop or improve seamless and comprehensive transitional care practices.
Successful pharmacists: A qualitative study to understand pharmacists’ definitions of successful pharmacy practices
Meagen Rosenthal, PhD; Joseph A Dikun, PharmD; Ashley S Crumby, PharmD AAHIVP; Jill Hall, BScPharm, ACPR, PharmD; Theresa L. Charrois; BScPharm, ACPR, MSc
Efforts to improve uptake of advanced pharmacy practice services by various pharmacy professional organizations have included the development of definitions of pharmacists’ role in patient care, meant to transmit what is a successful pharmacy practice. However, there is little evidence of how these messages are reaching practicing pharmacists. The objective of this study is to understand success in pharmacy practice from the perspective of pharmacy practitioners in various settings.
In-depth semi-structured interviews were undertaken. Pharmacist participants were identified through reviews of national professional organization awardee lists and contact with state professional organizations in Mississippi, USA. The interview guide was developed from a scoping review by the authors. Interviews continued until saturation had been achieved. Qualitative content analysis was completed on all transcribed interviews.
A total of 14 interviews were conducted. There was an even split between participants practicing in community and hospital/ambulatory care settings. Two major themes emerged in the analysis. First, success was the development of meaningful relationships with patients, which led to the perceived improved uptake by patients of pharmacists’ recommendations. Second, success was achieving job satisfaction. Job satisfaction was often described as knowing they were making a difference in lives of patients. Participants also identified factors contributing to success, which included communication skills, self-confidence, and a supportive work environment.
The number, or kind, of advanced pharmacy services being provided to patients was not part of the definition of practice success offered. This implies a gap between the objectives of pharmacy professional organizations and practicing pharmacists. This study provides insight into the definition of success by practitioners, and direction for how professional organizations can improve communications with practitioners.
- Research topics related to
51 Research topics related to Pharmacy

- November 26, 2022
- No comments
Looking for research topics related to Pharmacy? this page might help you come up with ideas. Research topics are subjects or issues researchers are interested in when conducting research. A well-defined research topic is the starting point of every successful research project. Choosing a topic is an ongoing process by which researchers explore, define, and refine their ideas.
There are many research topics related to Pharmacy , depending on your specializations and interests. The topics below are only for guides. We do not encourage writing on any of them because thousands of people visit this page to also get an idea of what topics to write on.
Pharmacy is the science and practice of discovering, producing, preparing, dispensing, reviewing and monitoring medications, aiming to ensure the safe, effective, and affordable use of medicines The main purposes of research topics related to Pharmacy are to inform action, gather evidence for theories, and solutions to problems, and contribute to developing knowledge.
- A Pharmaceutical Equivalence Study Of The Selected Azithromycin Mg Brands On The [Country] Market
- A Study Of Treatment And Management Procedures Of Peptic Ulcers In Hospitals In [Country]
- Assessment On Analysis Of Water Pollution By Phosphate
- Availability And Storage Of Vaccines In Community Pharmacies
- Antibiotic Sensitivity Patterns Of Staphylococcus Aureus To Methillicin In Clinical Samples At…
- Antihyperlipidemic And Antioxidant Effects Of Phaseolus Vulgaris In [Country]
- Antimicrobial Activity Of Methanol Extract And Fractions Of Moringa Oleifera Lam.
- Assessing Undergraduate Students’ Motivation To Study Pharmacy, Attitudes And Future Career Professional Choices In Universities Of …..
- Assessment Of Knowledge, Attitudes And Practices Of Pharmacovigll, Ance Among Health Care Practitioners At The ….. Hospital
- Assessment Of Quality Of Metronidazole Tablet Brands Sold In Pharmacies In [Location].
- Assessment On Analysis Of Water Pollution By Phisphate In The [Location]
- Assessment Of Effective Use Of Anti-Epileptic Drug Therapy Among Patients At [Location]
- Assessment Of Health Workers’ Adherence To Standard Treatment Guidelines In the Management Of Typhoid Fever At [Location]
- Assessment Of The Chemical Composition And Pesticide Properties Of Cassia Didymobotrya Ash On Myzus Persicae Affecting Tomato Crops In [Location]
- Assessment Of The Quality And Dissolution Profiles Of Branded Fixed Dose Artemetherilumefantrine Tablets Sold At Pharmacies In [Location]
- Availability And Storage Of Vaccines In Community Pharmacies In Some Selected Communities In [Location]
- Determination Of The Microbial Contamination Of Disinfectant And Antiseptic Produced In [Location]
- Determining The Recreational Health Practices By Pregnant Women In Selected Antenatal Clinics
- Development And Validation Of Spectrophotometric Methods For The Determination Of Risperidone In Pure And Tablet Dosage Forms
- Drugs Use Practices In Fako Division: A Case Study Of [Location]
- Estimation Of The Effect Of Cisampelous Owanrensis Benzene Fraction On Glucose Absorption Across The Intestinal Epithelium Of Wister Rats On Aloxan-Induced Diabetes
- Evaluation Of Antibreast And Antiprostate Cancer Activities Of Selected Medicinal Plants From Some Parts Of [Location]
- Factors Affecting Prevalence Of Self Medication Of Antibiotics Among Adult Population In [Location]
- Hypoglycemic Effects Of Sonchus Oleraceus (Moleta) In Normal Albino Rats
- Investigating The Presence Of Staphylococcus Aureus And Escherichia Coli In Dairy Products
- Investigation Of The Social And Economic Impact And Consequences Of Chronic Diseases On Low Income-Earning Family
- Isolation Of Microorganism Associated With Deterioration Of Bananas Fruits
- Inorganic Pollutants In Drinking Water In Mamfe Municipality: Implications On Water Safety And Cancer Risks For The Inhabitants
- Isolation And Identification Of Bacteria Associated With Wound Sepsis
- Isolation Of Microorganisms Associated With Deterioration Of Bananas Fruits In Buea Municipality
- Pharmacoeconomic Analysis Of Hiv/Aids Management Pharmacy
- Pharmacy Project Topics And Materials
- Phytochemical And Antimicrobial Analysis Of Mystetoe Leaves
- Preliminary Phytochemical And Antimicrobial Screening Of Flower And Stalk Of Mangifera Indica (Opioro Mango)
- Preliminary Phytochemical And Antimicrobial Screening Of Seed And Coat Of Citrus Sinensis
- Production Of Mosquitoes Repellants Insecticides (Mosquito Coil) Using Orange Peels (Cestrum)
- Profile Of Antibiotic Use At The Health Centre
- Pharmacoeconomic Analysis Of Hiv/Aids Management Pharmacy In Limbe Municipality
- Prevalence, Treatment, And Gametocyte Carriage In Children With Malaria At [Location]
- Profile Of Antibiotics Use At [Location]
- Recycling Waste Polyethylene Materials To Useful Products Via Pyrolysis
- Reviewing The Nutritional And Pharmacological Importance In Common Vegetables In [Location]
- The Causes And Effects Of Cholera Among Children
- The Effect Of Cisampelous Owarensis Benzene Fraction On Glucose Absorption Across The Intestinal Epithelium Of Wister Rats On Aloxan-Induced Diabetes
- The Use Of Quality Control Parameters In The Evaluation Of Vegetable Crude Drugs
- Working Capital Management And Profitability Of Listed Pharmaceutical Firms In [Location]
- Wound Healing And Anti-Inflammatory Activities Of Ceiba Pentendra (L.) Gaertn In Guinea Pigs
Related Choice
Leave a reply cancel reply.
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
You May Also Like
Research topics related to social media.
- January 5, 2023
63 Research topics related to International Business
100+ research topics related to medical surgical nursing, 160 research topics related to medicine.
- November 29, 2022
70 Research topics related to Media
100 research topics related to mass communication.

FDA Advisory Panel Rejects MDMA-Assisted Therapy for PTSD
The panelists expressed concerns about clinical trial data and concluded that the benefits do not outweigh the risks, but the FDA does not have to follow their recommendation.

As Accessible Providers, Pharmacists Address Inequities in Multiple Sclerosis Care
In addition to racial inequities in access to care, socioeconomic challenges are very common for the specialty medications necessary in MS.

Pharmacy Technician Immunizers Can Provide The Much Needed Shot In The Arm For Community Pharmacies
The immunizing technicians stated they had greater job satisfaction and had a greater sense of being valuable pharmacy members

mRNA-4157 (V940) Plus Pembrolizumab Shows Sustained Improvements in RFS and DMFS in Patients With High-Risk Melanoma
Compared with pembrolizumab alone, the combination treatment showed stronger recurrence-free survival and distant metastasis-free survival in patients with resected high-risk stage III or IV melanoma.

Study Finds No Association Between Physical Activity, Coronary Artery Calcium Progression
In prior studies, higher levels of physical activity were associated with higher prevalence of coronary artery calcium.

Sustained MRD-Negativity With Sc Daratumumab in Newly Diagnosed Multiple Myeloma
Data from the PERSEUS trial supports use of daratumumab in combination with bortezomib, lenalidomide, and dexamethasone followed by daratumumab and lenalidomide maintenance as a new standard of care for patients with newly diagnosed multiple myeloma.

Study Finds Adults Who Use ENDS Have Increased Risk of Asthma Incidence at Earlier Ages
Adults who did not report past 3-day electronic nicotine delivery system use did not have an increased risk of asthma incidence.

Pediatric Weight is Crucial to Perfecting the Dose
Evidence indicates that up to 25% of all prescriptions for children could be dosed inappropriately, making it the most common type of medication administration error.

Enhanced Front Line Therapy for NDMM: Promising Results from the MajesTEC-7 Trial
Results from the initial safety run-in of MajesTEC-7 indicate that the combination of teclistamab, daratumumab, and lenalidomide in newly diagnosed multiple myeloma (NDMM) shows a manageable safety profile with early signs of efficacy.

Phase 3 DREAMM-8 Trial Data Show Superior Efficacy of BPd vs PVd in Relapsed/Refractory Multiple Myeloma
The study showed that belantamab mafodotin plus pomalidomide and dexamethasone (BPd) significantly improved progression-free survival compared to pomalidomide plus bortezomib and dexamethasone (PVd).

Expert: PALOMA-3 Trial Results, Benefits of Subcutaneous Amivantamab for Lung Cancer Treatment
The PALOMA-3 trial showed subcutaneous amivantamab was better than IV for lung cancer patients.

Asciminib Shows Superior Efficacy, Favorable Safety in Patients With Newly Diagnosed Chronic Myeloid Leukemia
Asciminib demonstrated stronger efficacy, safety, and tolerability, as well as less adverse events in patients compared with those who received investigator-selected standard-of-care tyrosine kinase inhibitors.

Daratumumab Treatment Advancements in Newly Diagnosed Multiple Myeloma
Daratumumab in combination with standard treatment regimens shows benefit in multiple myeloma.

American Heart Association Says Obesity Care Depends on Addressing Gaps, Reducing Stigma
Providers, the community, health systems, and health policies can all play a part in addressing various challenges in care for obesity.

Patients With SCD Who Experience Longer Delays Transitioning Between Care More Likely to Be Hospitalized
Patients with sickle cell disease with more than a 6-month delay transitioning from pediatric to adult care were about twice as likely to be hospitalized.

Optimizing a Health System’s Access to Novel Therapies, Payor Networks Can Keep Drug Costs Down

Association Found Between OTC Male Enhancement Supplementation and Liver Injuries
Promises of sexual improvement may ensnare unsuspecting patients with potentially dangerous adverse effects from untested OTC remedies.

An Informatics Approach to Preventing Diversion of Controlled Substances
Data analysis can help hospitals address waste of controlled substances that fuels diversion and increased costs.

T-DXd New Standard of Care Following ET in HER2-Low, -Ultralow HR+ Metastatic Breast Cancer
Data presented at ASCO 2024 show fam-trastuzumab deruxtecan-nxki (T-DXd) delayed cancer growth in patients with hormone receptor-positive (HR+), HER2-low or -ultralow disease that progressed following endocrine therapy (ET).

Osimertinib New Standard of Care for Stage 3, EGFRm NSCLC
The phase 3 LAURA trial data presented at ASCO 2024 showed osimertinib (Tagrisso; AstraZeneca) reduced risk of disease progression or death in patients with stage 3 EGFR-mutated (EGFRm) non–small cell lung cancer (NSCLC) by 84%.

REACH PC Trial: Early Palliative Care Via Telehealth Has Equivalent Efficacy to On-Site Visits for Patients With Advanced NSCLC
Results from the trial provide evidence bolstering ASCO’s clinical practice guideline supporting the integration of early palliative care into standard oncology practice.

Advancing Targets: Latest FDA Approvals, Strategies in NSCLC Treatment Unveiled at ASCO 2024
Matthew A. Gubens, MD, MS, FASCO, highlights the importance of identifying genetic targets in metastatic non–small cell lung cancer (NSCLC), emphasizing the latest updates and strategies.

Addressing Medication Adherence is Crucial in Multiple Sclerosis
Understanding patients’ specific experiences and challenges is crucial to helping them improve medication adherence.

Research Finds In Utero Exposure to Ocrelizumab Not Associated With Increased Adverse Pregnancy, Infant Outcomes for Women With MS
This is the largest dataset of pregnancy outcomes for an anti-CD20 therapy in MS, enabling a more comprehensive understanding of ocrelizumab’s safety.
NATALEE Data Show Ribociclib Reduces Risk of Recurrence for High-Risk Node-Negative Early Breast Cancer
The addition of ribociclib (Kisqali; Novartis) to endocrine therapy demonstrated a 28% risk reduction in invasive disease-free survival.

Pharmacists Play Crucial Role in Helping Patients Navigate Complexities of MS Treatment
In addition to medication management, pharmacists are educating patients and helping them navigate the complex medical system.

FDA Grants Inavolisib Priority Review for Treatment of PIK3CA-Mutated Breast Cancer
The priority review of inavolisib is for treatment of patients with advanced hormone receptor-positive, HER2-negative breast cancer with a PIK3CA mutation.

Cannabis Use Can Exacerbate Cognitive Declines in Patients With Multiple Sclerosis
Although this data seems to overwhelmingly suggest that cannabis use has negative impacts for individuals with multiple sclerosis (MS), listening to patients’ reasoning for using it is crucial.

Receiving Epidural Analgesia During Labor May Reduce Serious Maternal Complications
Women who received epidural analgesia during labor were less likely to experience severe maternal morbidity complications, such as heart attack or heart failure and sepsis.

FDA Approves mRNA-1345 for Protection Against Lower Respiratory Tract Disease Caused by RSV
This is Moderna's second mRNA vaccine approval and the first mRNA vaccine approved for an indication other than COVID-19.
2 Commerce Drive Cranbury, NJ 08512
609-716-7777

Conducting Research Projects
These resources are intended to help residents and students understand the basic steps and principles of conducting practice-based research projects. Pharmacists who want to conduct practice-based projects can also benefit from the information presented. These presentations start with generating the project topic and proceed through planning, design, funding and sharing project results. Knowing how to manage complex projects from start to finish is critical whether you pursue a clinical, managerial, or academic career track. By sharing the results of your project with the health care community, you can contribute important information that helps advance pharmacy practice.
Keep two important considerations in mind as you move along the continuum of developing, implementing, and evaluating a project. You must:
- Understand the limitations of your project and recognize how it does or does not compare with the "ideal" research project.
- Actively develop your project management skills to ensure that the project is as sound and effective as possible.
Selecting Your Project
Perhaps the hardest step in your project is figuring out where to start. Once you've determined your focus and worked up a timeline, however, you have a road map to help you move forward productively. This presentation gives you concrete suggestions for identifying valuable project ideas.
Selecting Your Project Recording
Selecting Your Project Slides
Designing and Planning Your Project
This presentation explains the three categories most residency projects fall into, discusses important aspects of research studies and walks you through the process of creating a project plan.
Designing and Planning Your Project Recording
Designing and Planning Your Project Slides
Procuring Funding for Your Project
Determining your project's needs and identifying resources to meet those needs are critical for success. This presentation will discuss ways to obtain monetary resources for your project or research. It reviews common and no-so-common sources of grant funding as well as tips for soliciting funds.
Procuring Funding for Your Project Recording
Procuring Funding for Your Project Slides
Avoiding Pitfalls in Implementing Your Project
One of the most gratifying things you can do is to completing a project that leads to improved patient care or documents the professional role of the pharmacist. With careful preparation, contingency plans, and a good attitude, problems can often be avoided or overcome. This presentation discusses how to avoid pitfalls and minimize problems as you implement your project, allowing you to complete it on time and create a product you are proud of.
Avoiding Pitfalls in Implementing Your Project Recording
Avoiding Pitfalls in Implementing Your Project Slides
Evaluating Your Project's Impact: Important Considerations
You selected the right project. You struggled with the design, data collection, and analysis. You are poised to write your abstract and present the project to colleagues at an upcoming professional meeting. Isn't that enough? Actually, no. Focusing on project evaluation before you write your abstract and project report is time well spent. This presentation will focus on reviewing your project's impact, communicating the "so what?" of your project effectively and exploring next steps.
Evaluating Your Project's Impact: Important Considerations Recording
Evaluating Your Project's Impact: Important Considerations Slides
Presenting and Publishing Your Project
Making presentations about your project and seeking to publish your findings help you practice essential skills. These activities also get the word out to colleagues about new information, procedures, and evidence, and they give you the opportunity to network with other professionals and receive feedback.
Presenting and Publishing Your Project Recording
Presenting and Publishing Your Project Slides
Acknowledgement
APhA would like to thank Cortney M. Mospan, PharmD, BCACP, BCGP, Assistant Professor of Pharmacy, Wingate University School of Pharmacy, for the development and presentation of these valuable tools.

[100+] Pharmacy Research Topics For College Students With Free [Thesis Pdf] 2023
Are You Searching Research Topics For Pharmacy , Topics For Pharmacy Research Paper, Pharmacy Research Topics For Students, Research Topics Ideas For Pharmacy, Pharmacy Research Topics For Phd, Pharmacy Phd Topics. So You are at right place. At this website you can get lots of Pharmacy Research Topics for College Students, Phd, Mphil, Dissertations, Thesis, Project, Presentation, Seminar or Workshop.
In this article we provide you latest research topics for Pharmacy with full Phd thesis. By these research topics for Pharmacy you can get idea for your research work. Check the suggestions below that can help you choose the right research topics for Pharmacy : You can also Free Download Cyber Crime Research Phd Thesis in Pdf by given link.
Now Check 50+ Pharmacy Research Topics List
Table of Contents
Research Topic For Pharmacy 2023
Pharmacy research topics for dissertation, research topics ideas for pharmacy, pharmacy research topics ideas for college students, topics for pharmacy research paper, pharmacy research topics for thesis, pharmacy research topics for students, pharmacy research topics for undergraduate students, pharmacy research topics for university students, pharmacy research topics for phd, research topics for phd in pharmacy, research topics for mphil pharmacy, pharmacy phd topics, research paper topics for pharmacy, pharmacy research paper topics, phd thesis topic for pharmacy, research topics for pharmacy subject, pharmacy research topics for fisheries, research topics for pharmacy, pharmacy research topics examples.
Note: All Research Work Idea on this website is inspired by Shodhganga: a reservoir of Indian Theses. We provide you mostly research work under Creative Commons Licence. Credit goes to https://shodhganga.inflibnet.ac.in/
If you find any copyright content on this website and you have any objection than plz immediately connect us on [email protected]. We Will remove that content as soon as.
This Post is also helpful for: Pharmacy Thesis Pdf, Pharmacy Thesis Topics, Pharmacy Dissertation Topics, Pharmacy Thesis, Catchy Title For Pharmacy, Phd Thesis Topic for Pharmacy, Pharmacy Research Paper Topics, Pharmacy Phd Topics, Pharmacy Research Topics, Pharmacy Research Topics For College Students
Leave a Comment Cancel reply
Save my name, email, and website in this browser for the next time I comment.
- Potential Research Projects
Research projects for Higher Degree by Research (HDR) students are available within the following School of Pharmacy research areas and research centre.
Please email our academic staff to discuss potential HDR projects and ask if they are available as an advisor for your proposed HDR program.
Clinical Pharmacy and Pharmacometrics
Title: Implementing Pharmacogenomics into Community Pharmacy Practice to Personalise the Treatment of Depression Contact: Associate Professor Chris Freeman
Title: Developing pharmacokinetic models for immunosuppressants in solid organ transplant patients Contact: Dr Christine Staatz
Title: Improving the use of immunosuppressant agents in solid organ transplant patients Contact: Dr Christine Staatz
Medication Use, Safety and Health Services Research
Title: The ethics of pharmacogenomic testing in community pharmacy Contact: Doctor Adam La Caze
Title: Pharmacy ethics and the opioid crisis Contact: Doctor Adam La Caze
Title: Improving the use of immunosuppressant agents in solid organ transplant patients Contact: Dr Christine Staatz
Title: Establishing pharmacokinetic and pharmacodynamic models for antibiotics used in special paediatric populations Contact: Dr Christine Staatz
Title: Queensland Family Cohort (QFC) : Characterising medication usage within the perinatal-postnatal family environment Contact: Dr Meng-Wong Taing
Title: Pharmacy and oral healthcare Contact: Dr Meng-Wong Taing
Pharmacoepidemiology, Pharmacovigilance and Pharmacoeconomics
No projects currently available.
Biotherapeutic Delivery and Diagnostic Solutions
Title: Computer-aided design, synthesis and evaluation of targeted drug delivery systems Contact: Dr Ben Ross
Title: Engineering peptides and proteins as therapeutics Contact: Dr Peter Moyle
Title: Improving the delivery characteristics of protein / peptide drugs Contact: Dr Peter Moyle
Title: Deciphering the roles of post-translational modifications Contact: Dr Peter Moyle
Title: Recombinant, semisynthetic and synthetic vaccines Contact: Dr Peter Moyle
Title: Targeted delivery systems for RNAi and DNA delivery Contact: Dr Peter Moyle
Title: Enhancing the activity of antimicrobial agents Contact: Dr Peter Moyle
Title: Engineering nanostructures and nanomedicines using supercritical fluid technology Contact: Dr James Falconer
Title: Improving delivery of challenging to formulate bioactives using advanced delivery systems Contact: Dr James Falconer
Title: Discovery of new drugs from indigenous Australian plants using supercritical fluids Contact: Dr James Falconer
Title: Design, construction, and development of supercritical fluid technology Contact: Dr James Falconer
Title: Characterisation of high pressure spray behaviour and bioactive Contact: Dr James Falconer
Title: Delivery of therapeutics to the posterior eye Contact: Dr Harendra Parekh
Title: Development of bioresponsive drug/gene carrier systems Contact: Dr Harendra Parekh , Dr Karnaker Tupally
Title: Bioresponsive porous silicon-polymer composite nano- and micro-particles for oral protein delivery Contact: Dr Amirali Popat
Title: Mesoproous silica nanoparticles synthesis and application in drug delivery, diagnosis and therapeutic protein delivery Contact: Dr Amirali Popat
Title: Inorganic nanoparticles for targeting bacterial biofilms Contact: Dr Amirali Popat
Pharmaceutical Biology
Title: Calcium homeostasis in cancer: identification and characterisation of novel drug targets Contact: Professor Greg Monteith and Professor Sarah Roberts-Thomson
Title: Identification and characterization of novel ion and drug transporters and the design of novel high throughput screening assays for new pharmaceuticals Contact: Professor Greg Monteith
Title: Physiological regulation and the role of calcium transporters Contact: Professor Greg Monteith
Title: Morphine and metastasis Contact: Associate Professor Marie-Odile Parat
Title: Role of caveolar proteins in glioblastoma Contact: Associate Professor Marie-Odile Parat
Title: Effect of perioperative pharmacotherapy of cancer patients on tumour Biology Contact: Associate Professor Marie-Odile Parat , Dr Ben Ross and Professor Nick Shaw
Biomedicinal Discovery and Development
Title: Design, synthesis and evaluation of novel molecules for the treatment of Alzheimer's disease Contact: Dr Ben Ross
Title: Computer-aided design, synthesis and evaluation of new drugs for cancer, pain and neurodegenerative diseases Contact: Dr Ben Ross
Pharmacy Education Research Centre
No current projects available.
Alan Grant-Taylor Memorial Scholarship: Community Pharmacy Practice
Find out more about the Alan Grant-Taylor Memorial Scholarship
UQ Summer and Winter Research Programs
Coordinated by the UQ Student Employability Centre, these programs provide an opportunity for scholars to work with a researcher in a formal research environment in their area of interest.
By participating in a program students will gain valuable academic and professional opportunities, develop analytical, critical thinking, and communication skills, and have an opportunity to cultivate links with industry and academic contacts.
It is also a chance to ‘test drive’ research before embarking on further research studies or higher degree research projects. Participation is open to undergraduate students and Masters by coursework students.
All students participating in the summer and winter programs will receive a scholarship. General information on the program, including how to apply, is available from the UQ Student Employability Centre’s program website .
Please see our Summer and Winter Research Program page for a full list of the available programs.
- Research Areas
- Higher Degrees by Research
- Optimising Medicine Information Handover After Discharge (OPTMED-D)
- Safe and Effective Medication Collaborative
- Seminar Series
- Open access
- Published: 24 May 2024
For the rural curious: mixed methods evaluation of a rural pharmacy practice elective
- Timothy P. Stratton 1
BMC Medical Education volume 24 , Article number: 573 ( 2024 ) Cite this article
155 Accesses
Metrics details
As of 2020, 20% of people residing in the United States of America (U.S.) lived in rural communities. Despite rural residents tending to be older, poorer, and having greater disease burden than their urban counterparts, the number of rural primary care providers continues to decline. Nearly 66% of U.S. Primary Care Health Professional Shortage Areas are designated as rural. Pharmacists can help address this shortage of rural primary care providers, often serving as providers of first-contact care; however, only 12% of U.S. pharmacists practice in rural communities. To help address this gap, in 2022 an elective Rural Pharmacy course was created at the University of Minnesota College of Pharmacy by a faculty member who has rural practice experience.
The course combines formal lectures, guest presentations by rural pharmacists and student interviews with additional rural pharmacists. For the 42 students enrolled in the course in 2022 and 2023, non-parametric statistics were used to compare the percentage of students who were raised in rural communities or who otherwise had extensive exposure to rural, and compare student interest ratings (1 to 7) about practicing/living rural at the beginning and end of the course. Students also wrote end-of-course reflection papers, commenting on the course and their interviews with rural pharmacists.
Across both years, 45% of the enrolled students had previous experience in rural communities. The net change in Rural Interest scores among students completing both questionnaires was + 5 in 2022 and + 2 in 2023, both non-significant differences. The largest shifts in student interest were from “Not Sure” at the start of the course to “Interested” or “Not Interested” at the end of the course, and from “Interested” to “Very Interested.” In their reflection papers nearly 60% of students reported being most impressed by their interviews with rural pharmacists.
Conclusions
A course addressing the benefits and challenges of practicing pharmacy in rural communities was well-received by pharmacy students. Even students who have little interest in living in a rural community can benefit from being introduced to rural culture, enabling them to provide more culturally-responsive care for patients from rural communities.
Peer Review reports
Introduction
The Unites States (U.S.) Census Bureau redefined “rural” for the 2020 census as communities with populations of fewer than 5,000 people (fewer than 2,000 housing units) and located more than 1.5 miles (2.4 km) from a high-density urban area. Based on this revised definition, 20% of the U.S. population in 2020 lived in rural communities [ 1 ]. The percentage of rural residents varied greatly by region, with only 11% of people in the West Region residing in rural areas, followed by 16% in the Northeast Region, 24% in the South Region and 26% in the Midwest Region [ 2 ]. At the extremes, fewer than 6% of people in California lived in rural areas, while nearly 65% of Vermont residents lived in rural areas [ 1 ]. In contrast, as of 2021 the U.S. Bureau of Labor Statistics reported that only 12% of the nation’s pharmacists practiced in nonmetro (rural) communities [ 3 ].
On average, rural residents tend to be older [ 4 ], poorer [ 5 ], experience greater disease burden [ 6 ] and lack health insurance or be underinsured [ 7 ] than residents of urban communities. The average age and disease burden among rural residents is increasing due to outmigration of young adults from rural to urban communities and the in-migration of older adults to rural communities following retirement [ 4 ]. Yet as the proportion of older residents in rural communities continues to increase, the availability of primary care providers in rural communities continues to decrease. Nearly 66% of Primary Care Health Professional Shortage Areas in 2023 are designated as rural [ 8 ]. Pharmacists can be part of the solution to address the existing and anticipated shortage of primary care providers in rural communities [ 9 ]. Rural pharmacists often serve as “providers of first-contact care” for patients who are seeking to self-treat a health condition [ 10 ]. Where self-treatment is inappropriate, the pharmacist is in a position to refer the patient to appropriate professional care.
This paper describes a new course taught in the Doctor of Pharmacy (PharmD) program in the University of Minnesota College of Pharmacy that introduces students to the unique benefits and challenges of practicing pharmacy in rural communities.
One college, two campuses
The University of Minnesota (UMN) is a public, research-intensive (Carnegie R1) institution. The UMN College of Pharmacy opened on the Minneapolis campus in 1892 [ 11 ]. Prior to 2003, the College of Pharmacy included four departments: Experimental & Clinical Pharmacology, Medicinal Chemistry, Pharmaceutics, and Pharmacy Care & Health Systems. However, to address a shortage of pharmacists in Greater Minnesota – counties outside of the seven-county Minneapolis-St. Paul Twin Cities Metro Area [ 12 ] – in 2003 the College of Pharmacy expanded its program 150 miles (241 km) north to Duluth on the University of Minnesota Duluth campus, adding a fifth department to the College, Pharmacy Practice and Pharmaceutical Sciences (PPPS).
The specific multi-campus model used by the UMN College of Pharmacy is somewhat unique among multi-campus pharmacy programs in the U.S. The PPPS department includes faculty representing Biochemistry and each of the major Pharmacy disciplines (Clinical Pharmacy, Medicinal Chemistry, Pharmaceutics, Pharmacology, Pharmacy Practice, and Social & Administrative Pharmacy). Didactic courses within the College are taught using videoconferencing technology, with classroom presentations/lectures originating from either Minneapolis or Duluth and being broadcast to the other campus.
The mission of the PPPS department includes preparing pharmacists to provide patient care in rural and Indigenous communities [ 13 ]. PPPS faculty embody this mission in all four areas of an academic health professions program, highlighting the unique health needs of rural residents in their teaching, addressing these needs through community-based participatory research [ 14 ], conducting service activities in rural communities, and providing clinical services. Until 2022, however, no single course in the College of Pharmacy’s curriculum was devoted specifically to rural health.
Rural pharmacy elective-course description and structure
To help address this gap in the College of Pharmacy curriculum, the author – a pharmacist who has practiced hospital, community and long-term care pharmacy in frontier/Indigenous communities in Alaska [ 10 ], Eastern Montana and Minnesota – created a two-credit elective course (two hours per week for 15 weeks) in Rural Pharmacy to introduce students to the benefits and challenges of living and practicing in rural communities. Development of the course was guided by the author’s teaching philosophy; to paraphrase Confucian philosopher Xun Kuang [ 15 ]: “Tell me and I will forget. Show me and I will remember. Involve me and I will understand.”
The Rural Pharmacy course was designed as a HyFlex course [ 16 ] that allows the learner to choose by which content delivery method they would like to learn. Learners in a Hyflex course may elect to attend a live class session in person in a classroom, may attend a live class session remotely via videoconference, or may learn online anytime. Each live class session is recorded to accommodate students who prefer to learn online during a given week, or throughout the entire course.
The Rural Pharmacy elective is a “modified” HyFlex design in that no in-person option is available. University of Minnesota College of Pharmacy faculty and students are accustomed to videoconferencing as a course delivery method, the college having used videoconference technology since 2003 to conduct live, in-person sessions for learners on campuses located 2.5 h apart from one other. Required and elective didactic courses delivered by videoconference are always recorded, enabling learners to view the recording at a more convenient time if they are unable to attend the live class session. Another reason that an in-person option for the Rural Pharmacy elective is not offered is that live course sessions are conducted in the evening to accommodate students from different years in the pharmacy program (P2 and P3) whose other courses are all on different schedules, and Minnesota’s frequent snowy and icy winter conditions are not always conducive to safe travel to and from campus, especially at night.
At the time of this writing, during the first three pre-clinical years University of Minnesota College of Pharmacy students are required to complete 15 credits of elective courses above and beyond their required courses. The Rural Pharmacy elective is open to students in the final two pre-clinical years of the PharmD program (P2 and P3), but enrollment is capped by the instructor at 25 students per offering. Live class sessions are conducted once weekly for two hours in the early evening by videoconference for all students, whether based in Duluth or in the Minneapolis-St. Paul Twin Cities area. The early evening hours avoid conflicts with students’ other courses, which are on different schedules between 8:00 am and 5:30 pm for both of the two years. Students are encouraged to attend as many live videoconference sessions as possible, especially when a guest presenter is scheduled; however, as noted above all class sessions are recorded for viewing or reviewing at a more convenient time. The recordings accommodate students who may be working in a pharmacy as a Pharmacy Intern or Pharmacy Technician at the time class is scheduled, or students who desire to review one or more recorded class sessions prior to the written midterm examination.
A University of Minnesota Post-Graduate Year 1 (PGY1) Rural Pharmacy Resident [ 17 ] serves as the Teaching Assistant for the course each year, participating in the live class sessions via videoconference. The Pharmacy Resident is based out of a rural community in central Minnesota, traveling to two other rural communities and providing comprehensive medication management services [ 18 ] to residents of all three communities. While maintaining patient confidentiality, the Resident shares with students their experiences caring for patients in rural communities, some stories being only a few hours old. In addition to regularly participating in live class sessions, the TA prepares and leads a class session on their own, and conducts the live session interviews with guest rural pharmacists as described below.
About half of the class sessions feature guest pharmacists who currently practice in rural communities, guests joining the live class sessions via videoconference. When a guest pharmacist is invited to participate in the course, the instructor provides the pharmacist with a list of potential interview questions that they would be asked to address during the class session. On rare occasions the visits with pharmacist(s) are pre-recorded either to better accommodate the pharmacist’s work schedule or because of time zone differences between Minnesota and the states where the pharmacists live/work. Pre-recorded interviews are played during the live class session, and students submit questions they would have asked the pharmacist had the pharmacist been able to join the class session in real time. Those questions are then summarized by the instructor and forwarded to the guest pharmacist to respond to as the pharmacist’s time allows. Pharmacists living and practicing in rural and Indigenous communities from throughout Minnesota and from as far away as Alaska have participated in the live sessions, either pre-recorded or in real time. In addition to rural pharmacists, guest presenters have included Advance Practice Nurses [ 19 ] from rural communities, and a Biologist who works with an Indigenous community on the impacts of climate change on the health of the community.
A variety of assessments are utilized in the course including reflection papers, an online multiple-choice/true–false/short answer midterm exam, written participation in online discussions, in-class student presentations and written summaries of interviews with pharmacists practicing in rural communities. The course is graded on a A,B,C,D,F letter grade scale. A total of 300 points are available across nine activities in the course, ranging in value from 5–50 points. The grading scale used in the course is the professional scale used in all of the college’s courses, an A grade being attained by students who earn at least 93% of the available points while students earning fewer than 60% of available points do not receive a passing grade. The possible number of points available on individual assignments are assigned by the instructor based on the amount of time and effort students are expected to expend on the assignment as well as the quality of each assignment’s deliverable.
At the start of the course students complete a brief 7-point Likert-type questionnaire regarding their familiarity with rural communities and interest in possibly practicing in a rural community. The questionnaires are confidential rather than anonymous as students complete the same questionnaire again at the end of the course. The course director uses student names to match start-of-course and end-of-course questionnaires to measure changes in student attitudes. Students also write a brief paper describing their experiences with rural communities and the reason for their interest in learning (or learning more) about living and practicing in rural communities. The instructor uses this information to tailor presentations in the course for the entire class based on the students’ familiarity with rural communities. This information also familiarizes the instructor with students’ backgrounds, enabling the instructor to invite specific students to share their rural experiences as relevant opportunities arise during live class sessions. The initial questionnaire and interest paper collectively constitute 8.37% of the course grade.
The online midterm examination is based on material provided in the textbook [ 20 ] or during instructor or Resident presentations. Students are tested on their knowledge about what constitutes “rural” as defined by several different U.S. government agencies, rural culture, challenges in rural public health, and opportunities and challenges related to practicing pharmacy in rural communities. The midterm exam score constitutes 16.7% of the course grade.
As mentioned previously, the HyFlex nature of the course accommodates students who are unable to attend the live videoconference sessions. All students, however, participate in weekly written online discussions based on the live videoconference session from that week. Live sessions are recorded so that any student may view and listen to the session at their leisure. In the online discussion, students are asked to respond to an instructor-generated question based on that week’s live class session. Students are asked to post their response first, then comment on the response of at least one other classmate. The Canvas learning management system [ 21 ] facilitates this learning approach, providing the instructor the option to require a student to post their response before reading the responses of classmates. Students who post their responses by the weekly deadline receive full participation credit for the week, rather than being graded on the length of their response or on the number of responses they make to classmates’ postings. As a HyFlex course, students are not awarded extra points for attending the live videoconference session, nor are they penalized for not participating in the live videoconference session. Participation constitutes 16.7% of the course grade.
Indigenous people began living in what today is referred to as Minnesota some 13,000 years ago. Among the earliest identifiable tribes in Minnesota were the Dakota (Sioux) circa 1000 CE and the Anishinaabe (Chippewa, Ojibwe) who arrived in the mid-1700s [ 22 ]. Today, Minnesota is home to four Dakota and seven Anishibaabe reservations [ 23 ], most of these communities being located in rural or frontier Minnesota counties. In contrast to these early inhabitants whose ancestors have lived in Minnesota for hundreds of years, today foreign immigrants are arriving in Minnesota in increasing numbers [ 24 ]. Many of these new arrivals settle in communities outside of the Twin Cities Metro Area [ 25 ]. This spectrum of diversity underlies the importance for healthcare providers to learn to provide culturally-responsive care [ 26 ]; therefore, students in the course learn about Indigenous people or foreign-born immigrants they might encounter if practicing in rural Minnesota. Each student is assigned a particular culture (not their own), and through readings about and/or interviews with members from that culture prepares a brief presentation they share with the class during a live videoconference session. Again, because this is a HyFlex course a student who knows in advance that they will be unable to attend class when they are scheduled to present are able to pre-record their presentation. Pre-recorded student presentations are played during the live course session. This exercise constitutes 16.7% of the course grade.
As students in this course are training to become pharmacists, they interview pharmacists who currently practice in rural communities (or who have practiced in a rural community in the recent past). These interviews supplement the rural pharmacy practice stories provided by the instructor, the Resident, and the pharmacists who present during class videoconference sessions. Most, but not all, of the pharmacists who participate in the course are the instructor’s former students from the UMN College of Pharmacy, Duluth. In addition to pharmacists with practice experience in rural Minnesota, pharmacists in the instructor’s circle of contacts from rural Alaska, Wisconsin and Michigan have participated in the course, as have pharmacists from four different rural Indian Health Service [ 27 ] /Tribal Health Clinics. Potential pharmacist participants are contacted by the course instructor before the course begins to gauge their interest and willingness to participate in a live class session or be interviewed by the students, and are provided with the list of interview questions that will be asked. Characteristics and practice settings of the pharmacists who participated during the first two offerings of the course are presented in Table 1 .
The instructor assigns the students to interview teams of two to three students who conduct structured interviews with the rural pharmacists who practice in community, critical access hospital [ 28 ], health system hospital or Indian Health Service/Tribal Health settings. Each student is assigned to one team to interview a community pharmacist, and then to a different team to interview the health system pharmacist. Where possible, teams are structured to reflect gender diversity and include students from different years in the pharmacy program. Each student team contacts their assigned pharmacist and schedules a telephone or videoconference interview. Interviews are intended to last no more than 30 min, but oftentimes go longer as the conversations between the students and the pharmacist range far beyond the structured questions provided by the instructor.
Each student submits written summaries of their two interviews. Each interview team provides informal presentations about their interviews to the class during a live videoconference class session. Each interview assignment constitutes 16.7% of the course grade.
At the end of the course, students once again complete the 7-point Likert-type questionnaire regarding their interest in possibly practicing in a rural community. The numerical results from this questionnaire are compared to the numerical results of the interest questionnaire that the student completed at the start of the course. Each student also writes a brief reflection paper regarding what they learned in the course about practicing pharmacy in a rural community, and what aspect of the course they found most interesting/helpful in their learning. As with the similar assignments at the beginning of the course, the final questionnaire and final reflection paper constitutes 8.37% of the course grade.
Rural pharmacy elective-topics
Topics presented in the course are listed in Table 2 . Topics for didactic sessions early in the course are based on selected chapters from the textbook required for the course, Foundations of Rural Public Health in America (2022), by Joseph N. Inungu and Mark J. Minelli [ 20 ]. The course also features interdisciplinary and interprofessional components. As noted earlier, one guest presenter is a PhD Biologist employed by one of Minnesota’s American Indian tribes. That individual addresses Climate Justice, explaining the impact of climate change on rural Indigenous communities. Also as noted earlier, a group of rural Advanced Practice Nurses in different subspecialties present a panel session addressing the challenges faced by the communities they serve, and describe how they interact with rural pharmacists in their communities.
Assessing course outcomes
The percentages of students enrolled in the course on each campus who reported growing up in a rural community or having spent considerable time visiting relatives who lived in rural communities were compared using Fisher’s exact test [ 29 ]. For students completing rural interest questionnaires both at the beginning and the end of the course, rating scores from both years and both campuses were combined and paired. Given the ordinal nature of the data, beginning/end of course ratings were evaluated using the Wilcoxon signed-rank test [ 30 ]. A two-tailed alpha value of 0.05 was selected as the criterion to indicate significance in all numerical comparisons.
For the first offering of the course in Spring, 2022 a total of 25 students completed the course. Spring 2023 had 17 students in the course. The demographics of the students in these two cohorts are summarized in Table 3 .
Between the first two offerings of this course, 25 students on the Minneapolis campus enrolled in the course. Of these 25, 10 (40%) reported growing up in a rural community or having spent considerable time visiting relatives who lived in rural communities. Among the 17 Duluth students enrolled in the course between the two years, nine (53%) reported having grown up or otherwise spent considerable time in rural areas. This difference was not statistically significant.
At the beginning and end of the course, students rated their interest in living/practicing in rural community using a 7-point Likert-type scale ranging from “1-No interest” to “7-When can I start?!” The results from the 36 students who completed both the pre and post questionnaires are presented in Fig. 1 .
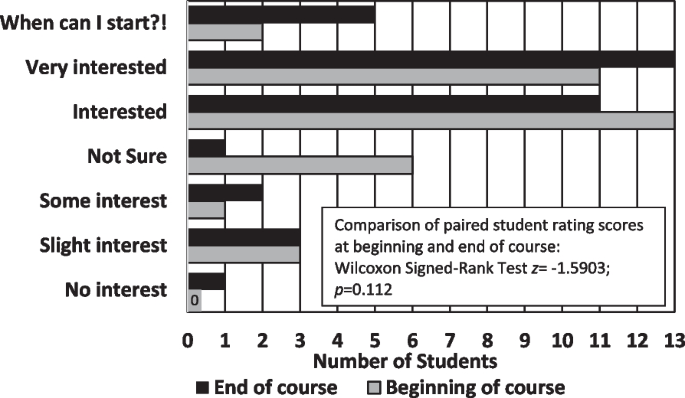
Interest in Practicing Pharmacy in Rural Communities ( n = 36)
The total net change in Rural Interest scores across all students completing both questionnaires was + 5 in 2022 and + 2 in 2023, some student scores increasing, others decreasing, and still others remaining the same. Results of the Wilcoxon Signed-Ranks Test were non-significant ( z = -1.5903; p = 0.112).
The largest change in scores occurred in the “Not sure” category (middle choice), with only one student remaining unsure of their interest in practicing in a rural community at the end of the course compared to six students at the beginning of the course. Four students who selected “Not sure” at the start of the course expressed lower interest in practicing in a rural community at the end of the course, one of these students moving down three levels from “Not sure” to “No interest.” One student who had selected “Interested” at the beginning of the course also dropped three levels at the end of the course to “Slight interest.” In contrast, several students who had selected “Interested” at the start of the course moved up to “Very Interested” or “When can I start?!”.
At the end of the course, students were asked to reflect on the impact of the course on their interest in practicing pharmacy in a rural community. Among the 42 students enrolled in the course during the first two years, 25 students in their reflection papers explicitly expressed appreciation for being able to interview pharmacists currently practicing in rural communities, while 20 explicitly expressed appreciation for having rural pharmacists and other professionals as guest speakers during class sessions. Two word clouds were generated from students’ reflection papers, one based on student perceptions of the benefits of living/practicing in a rural community (Fig. 2 ), and the other based on student perceptions of the challenges of living/practicing in a rural community (Fig. 3 ).
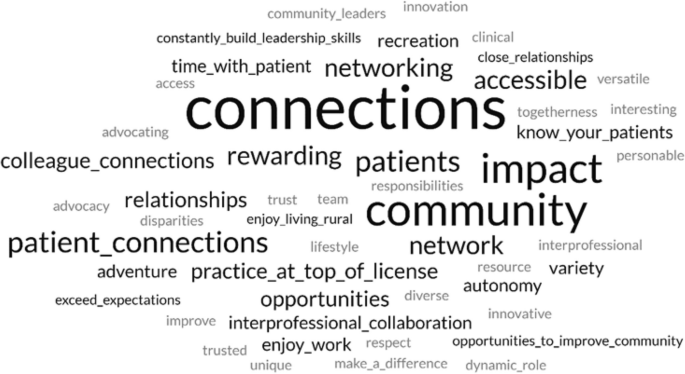
Word cloud featuring perceived benefits of living and practicing pharmacy mentioned in Rural Pharmacy students’ end-of-course reflection papers. “Courtesy of FreeWordCloudGenerator.com”
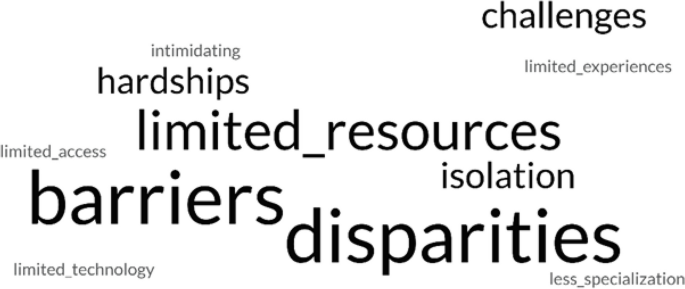
Word cloud featuring perceived challenges of living and practicing pharmacy mentioned in Rural Pharmacy students’ end-of-course reflection papers. “Courtesy of FreeWordCloudGenerator.com”
Representative student comments excerpted from their reflection papers regarding what they had heard from rural pharmacists who participated in the course are provided below. Each student’s comment is followed by that student’s final rating of their interest in practicing pharmacy in a rural community (1 = No interest, 7 = When can I start?!):
Before this course I had no interest in practicing rural before but now I’d at least entertain the idea after speaking and interviewing pharmacists that did or currently practice there. (Student selected ratings of 1 and 2) Hearing so many amazing stories, pharmacists are truly more than just “pill counting” because a single pharmacy can connect them with other rural health professionals, expanding the capabilities of rural pharmacists…. (2) If you can dream it you can do it in rural pharmacy. (5) It was great to have [the pharmacist I interviewed] in my network, as [they] said I can contact [them] anytime with questions outside… [of] my interview. I learned that having many contacts in your network, especially in rural areas, is so important…. (6) This class stimulated a future career interest that I already had, but was not sure exactly how to get started and who to ask if I had any questions. I feel like I now have many resources to reach out to when it comes to my future career, which makes me incredibly happy and comfortable. (7)
Students also expressed appreciation for other aspects of the course, whether the students were interested in practicing in a rural community at the end of the course or not. Again, each student’s comment is followed by that student’s final rating of their interest in practicing pharmacy in a rural community (1 = No interest, 7 = When can I start?!):
Even if I do not practice as a rural pharmacist, I will value the exposure and learning that has come from the topics covered in this course. (3) To be frank, I never even entertained the idea of practicing as a rural pharmacist. I’ve always wanted to work in an urban ambulatory care setting…. I did not expect the class to be as eye opening as it truly was…. I’m much more open to serving in a rural community and may consider it strongly . (3) It would be a huge adjustment to move to a rural area since I have grown up in [an urban community] my whole life. I want to work in a rural community since it is rewarding, but it is difficult to leave family behind and essentially start a new life with new people. (4) This is a rural pharmacy class, but it did not feel biased towards only working rural…. I came into this class knowing that I had an interest in rural pharmacy, but I did not expect to come out of this class even more interested in what rural areas have to offer. (6) Before starting this course, I knew that I wanted to practice pharmacy in a rural community…. Many times during this course we stated, “When you’ve seen one rural community, you’ve seen one rural community.” I did not know how true this statement was before this course…. Despite their vast differences, one common underlying theme is the health disparities seen in rural areas. (7)
It is important that health professions students be introduced to rural culture, even if they are “never” going to live/practice in a rural community themselves. With 5–64% of states’ populations living in rural communities [ 1 ], the odds are good that at some point in their careers, health professionals living in large urban centers are going to care for patients who have come from rural communities to receive more specialized care than is available locally [ 31 ]. Being introduced to rural culture can help students provide more culturally responsive care [ 32 ] to patients from rural communities during their careers.
The purpose of this course was to introduce pharmacy students to the advantages and challenges of practicing and living in rural communities. The course was not intended to “change hearts and minds” of students regarding their possible interest in practicing in a rural setting, and as can be seen from the results, students’ “interest in rural” ratings collectively neither significantly increased nor decreased between the beginning and the end of the course. Regardless, from comments in their reflection papers students generally appreciated the course, finding the interviews with rural pharmacists to be particularly valuable. This finding was heartening to the instructor who was initially concerned about the amount of out-of-class work being asked of the students.
Likewise, guest presenters who participated in the live class sessions and pharmacists interviewed by the students informally expressed their satisfaction with participating in the course, and expressed gratitude that this course was being offered. One pharmacist who previously practiced in a remote Alaska community but had recently moved to a major urban center in the “Lower 48” (Alaskan reference to states in the contiguous United States south of the 49th Parallel) expressed how much they enjoyed sharing their stories with the Rural Pharmacy students. The students with which this pharmacist currently works all desire to practice in large urban centers and are not particularly interested in hearing about the pharmacist’s experiences practicing in small, isolated communities. Another pharmacist noted that they really appreciated joining the students virtually in the live classroom, and was going to recommend this approach to other pharmacy schools with which they work as a way to generate interest in rural pharmacy in general, as well as interest in their particular pharmacy as a clinical rotation site.
A few changes were made in the roster of pharmacists participating in the course from year to year; however, most of the guest speakers and pharmacists who were interviewed by the students participated in the course both years. Another change being considered for the next offering of the course is to add a live videoconference session with a Minnesota Department of Agriculture “Farm Counselor” (a Licensed Professional Counselor) who makes in-person “farm calls” to address farm families’ mental health needs within the unique context of farm culture [ 33 ] (MN Dept of Ag, 2023).
A course specifically addressing the benefits and challenges of practicing pharmacy in rural communities was well-received by pharmacy students enrolled in the course, and by the rural guest presenters and rural pharmacists who were interviewed by the students. Even students who have little interest in living or practicing in a rural community can benefit from being introduced to rural culture, helping all students provide more culturally-responsive care for patients from rural communities.
Availability of data and materials
The data analyzed during the current study are not publicly available due to stipulations in the U.S. Family Educational Rights and Privacy Act (FERPA), but are available in de-identified form from the corresponding author on reasonable request.
Abbreviations
Students enrolled in years 1, 2 or 3 of the Doctor of Pharmacy (PharmD) program
Post-Graduate Year 1
Doctor of Pharmacy
Doctor of Philosophy
Pharmacy Practice and Pharmaceutical Sciences
Teaching Assistant
University of Minnesota
United States of America
United States Census Bureau. Nation’s urban and rural populations shift following 2020 Census. Press Release Number CB22-CN.25. Suitland (MD): U.S. Census Bureau; 2022. Available from: https://www.census.gov/newsroom/press-releases/2022/urban-rural-populations.html . Cited 2023 Aug 29.
United States National Center for Health Statistics. Health, United States, 2020-2021. Hyattsville (MD): U.S. Centers for Disease Control and Prevention; 2023. Available from: https://www.cdc.gov/nchs/hus/sources-definitions/geographic-region.htm . Cited 2024 Jan 22.
RHIhub. Rural Pharmacy and Prescription Drugs. [Internet]. Rural Health Information Hub. Available from: https://www.ruralhealthinfo.org/topics/pharmacy-and-prescription-drugs . Updated 2023 Jan 26; cited 2023 Aug 29.
Davis JC, Rupasingha A, Cromartie J, Sanders A. Rural America at a glance. Washington, DC: U.S: Department of Agriculture, Economic Research Service; 2022. Available from: Rural America at a Glance: 2022 Edition (usda.gov) . Cited 2023 Aug 29.
Google Scholar
United States Department of Agriculture Economic Research Service. Rural poverty & well-being. Washington, DC: U.S. Department of Agriculture; [updated 2022 Nov 29. Available from: USDA ERS - Rural Poverty & Well-Being . Cited 2023 Aug 29.
United States Centers for Disease Control and Prevention. About rural health. [Internet]. Atlanta (GA): Centers for Disease Control and Prevention. Available from: About Rural Health | CSELS | Rural Health | CDC . Updated 2023 May 09; cited 2023 Aug 29.
Turrini G, Branham DK, Chen L, Conmy AB, Chappel AR, De Lew N, Sommers BD. Access to Affordable Care in Rural America: Current Trends and Key Challenges. Washington, DC: United State Department of Health & Human Services, Assistant Secretary for Planning and Evaluation. Available from: https://aspe.hhs.gov/sites/default/files/2021-07/rural-health-rr.pdf . 2021 July 09; Cited 23 Aug 29.
United States. Department of Health & Human Services, Health Resources and Services Administration, Bureau of Health Workforce. Designated health professional shortage areas statistics. Washington, DC: U.S. Department of Health & Human Services. Available from: BCD_HPSA_SCR50_Qtr_Smry.pdf . Updated, 2023 Mar 31; cited 2023 Aug 29. https://data.hrsa.gov/Default/GenerateHPSAQuarterlyReport .
Council on Graduate Medical Education. Rural health policy brief 1. Special needs in rural America: Implications for healthcare workforce education, training and practice. Washington, DC: Health Resources & Services Administration. Available from: COGME Rural Health Policy Brief 1 (hrsa.gov) . Updated 2020 July 17; cited 2023 Aug 29.
Stratton TP. The economic realities of rural pharmacy practice. J Rural Health. 2001;17(2):77–81. https://doi.org/10.1111/j.1748-0361.2001.tb00261.x .
Article Google Scholar
Speedie MK, Ruhrold LN. A history of the University of Minnesota College of Pharmacy, 1892–2017. Research Triangle (NC): Lulu Press, Inc.; 2021. p. 285.
Nagel P, Yuan F. High-resolution land cover and impervious surface classifications in the twin cities metropolitan area with NAIP imagery. Photogrammet Eng Remote Sensing. 2016;82(1):63–71. Available from: https://www.researchgate.net/publication/288684001_High-resolution_Land_Cover_and_Impervious_Surface_Classifications_in_the_Twin_Cities_Metropolitan_Area_with_NAIP_Imagery .
University of Minnesota, College of Pharmacy, Department of Pharmacy Practice and Pharmaceutical Sciences. Minneapolis (MN): University of Minnesota College of Pharmacy; c2023. Available from: https://www.pharmacy.umn.edu/pharmacy-practice-pharmaceutical-sciences . Cited 2023 Aug 29.
United States Department of Health & Human Services, National Institute on Minority Health and Health Disparities. Community-Based Participatory Research Program (CBPR). NIH Guide No. RFA-MD-15-010. [Internet]. Bethesda (MD): National Institutes of Health. Available from: https://www.nimhd.nih.gov/programs/extramural/community-based-participatory.html . Updated 2018 Oct 02; cited 2023 Aug 29.
O’Toole, G. Quote Investigator. Xun Kuang. 2023. Available from: https://www.goodreads.com/quotes/7565817-tell-me-and-i-forget-teach-me-and-i-may . Cited 2023 Aug 29.
Beatty BJ. Hybrid-flexible course design: Implementing student-directed hybrid classes. 2019. Available from: https://edtechbooks.org/hyflex . Cited 2023 Aug 29.
University of Minnesota College of Pharmacy. Residency Sites & Emphasis Areas. Minneapolis (MN): University of Minnesota College of Pharmacy; c2023. Available from: https://www.pharmacy.umn.edu/degrees-programs/postgraduate-pharmacy-residency-program/residency-sites-emphasis-areas-2 . Cited 2023 Aug 29.
GTMRx Institute. c2019. Available from: https://gtmr.org/what-is-the-comprehensive-medication-management-process/ . Cited 2023 Aug 29.
American Nurses Association. Advanced practice registered nurse (APRN). [Internet]. Silver Spring (MD): American Nurses Association. Available from: https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/aprn/ .
Ingunu JN, Minelli MJ. Foundations of rural public health in America. Burlington: Jones & Bartlett Learning; 2022. p. 491.
Canvas LMS. Salt Lake City (UT): Instructure. c2008-2023. Available from: https://www.instructure.com/canvas . Cited 2023 Aug 29.
Furst R. Which Indigenous tribes first called Minnesota home? Star Tribune [Internet] (Minneapolis, Minnesota). 2021. Available from: https://www.startribune.com/native-american-dakota-ojibwe-history/600097050/#:~:text=The%20earliest%20identifiable%20tribe%20in,Ojibwe%20in%20the%20mid%2D1700s . Cited 2023 Aug 29.
State of Minnesota. Minnesota Indian Tribes. St. Paul (MN): State of Minnesota. Available from: https://mn.gov/portal/government/tribal/mn-indian-tribes/#:~:text=In%20Minnesota%2C%20there%20are%20seven,links%20to%20other%20valuable%20resources.&text=What%20does%20the%20term%20Federally%20Recognized%20mean%3F . Cited 2023 Aug 29.
American Immigration Council. Immigrants in Minnesota. Washington, DC: American Immigration Council. c2023. Available from: https://map.americanimmigrationcouncil.org/locations/minnesota/?_gl=1*5ervbb*_ga*MTYyMDYyNjcyNy4xNjkyMjExNzI4*_ga_W0MSMD2GPV*MTY5MjIxMTcyOC4xLjEuMTY5MjIxMTk3Mi4wLjAuMA . Cited 2023 Aug 29.
Minnesota Chamber of Commerce. Economic contributions by region. St. Paul (MN): Minnesota Chamber of Commerce. 2021 Mar 23. Available from: https://www.mnchamber.com/blog/economic-contributions-region . Cited 2023 Aug 29.
Prasad SJ, Nari P, Gadhvi, K, Barai I, Danish H, Philip AB. Cultural humility: treating the patient, not the illness. Med Educ Online. 2016 Feb 3;216;21: 10.3402/meo.v21.30908. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4742464/ . Cited 2023 Aug 29.
U.S. Department of Health and Human Services, Indian Health Service. Rockville (MD): U.S. Department of Health & Human Services. Available from: https://www.ihs.gov/ .
Centers for Medicare and Medicaid Services. Critical Access Hospitals. Woodlawn (MD): Centers for Medicare and Medicaid Services; [updated 2021 Dec 12. Available from: https://www.cms.gov/medicare/provider-enrollment-and-certification/certificationandcomplianc/cahs . Cited 2023 Aug 29.
Siegel S. Fisher’s exact test. Nonparametric statistics for the behavioral sciences. New York: McGraw-Hill. 1956. pp 96–104.
Siegel S. Wilcoxon signed-rank test. Nonparametric statistics for the behavioral sciences. New York: McGraw-Hill; 1956. pp. 75–83.
Casey M, McCullough J, Kreiger R. Which Medicare patients are transferred from rural emergency departments? [Internet]. Minneapolis (MN): University of Minnesota Rural Health Research Center. 2014. p. 19. Available from: https://rhrc.umn.edu/wp-content/uploads/2017/11/whichmedicarepatientsaretransferred.pdf . Cited 2023 Aug 29.
Minnesota Department of Health. Culturally responsive care. St. Paul (MN): Minnesota Department of Health. 2019 May 01. Available from: https://www.health.state.mn.us/docs/communities/titlev/cultresponsive.pdf . Cited 2023 Aug 29.
Minnesota Department of Agriculture. Stress&Crisis: Get Help Now. St. Paul (MN): Minnesota Department of Agriculture. c2023. Available from: https://www.mda.state.mn.us/about/mnfarmerstress/copingstress . Cited 2023 Aug 29.
Download references
Acknowledgements
Not applicable.
No funding was received for this project.
Author information
Authors and affiliations.
University of Minnesota College of Pharmacy, Duluth, MN, USA
Timothy P. Stratton
You can also search for this author in PubMed Google Scholar
Contributions
T.P.S. solely conceived and undertook all aspects of this project and preparation of this manuscript.
Author’s information
TPS is Professor of Pharmacy Practice in the University of Minnesota College of Pharmacy, Duluth. He has practiced community, hospital and long-term care pharmacy in frontier communities in Southeast Alaska, and at Indian Health Service/Tribal Health clinics in frontier Alaska and eastern Montana, and in rural Minnesota. He is a member of the Rural Pharmacy Consortium , a Past Chair of the Small and Rural Hospital Section Advisory Group for the American Society of Health-System Pharmacists, and a Past President of the Minnesota Rural Health Association.
Corresponding author
Correspondence to Timothy P. Stratton .
Ethics declarations
Ethics approval and consent to participate.
Approval - The Institutional Review Board (IRB) of the University of Minnesota determined that this project constituted Exempt Research.
Informed consent - The Institutional Review Board (IRB) of the University of Minnesota waived the need for informed consent in this project.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Stratton, T.P. For the rural curious: mixed methods evaluation of a rural pharmacy practice elective. BMC Med Educ 24 , 573 (2024). https://doi.org/10.1186/s12909-024-05539-3
Download citation
Received : 18 September 2023
Accepted : 08 May 2024
Published : 24 May 2024
DOI : https://doi.org/10.1186/s12909-024-05539-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Rural pharmacy
- Pharmacists
- Rural health
- Pharmacy education
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Pharmacy’s new era—in the home
Customers of the $460 billion retail pharmacy sector are increasingly demanding a pharmacy experience that mirrors the rest of their retail experiences—omnichannel, convenient, and with home delivery at the center. 1 Adam J. Fein, “The 2021 economic report on U.S. pharmacies and pharmacy benefit managers,” Drug Channels Institute, March 2021, drugchannels.net; Victor Fabius, Sajal Kohli, Björn Timelin, and Sofia Moulvad Veranen, “ Meet the next-normal consumer ,” August 17, 2020, McKinsey.com; “The Update: How Walgreens’ customer-focused marketing is driving business growth,” Google, September 2020, thinkwithgoogle.com. While interests vary meaningfully across customer archetypes and can be segmented by various factors (for example, complexity of medical condition, digital experience preferences, and proximity to stores), our pharmacy market research has indicated that there are two key patient archetypes across the spectrum of experience. Making the experience right for these two groups will prepare pharmacies for a broader spectrum of customers.
Patients in one archetype, focused on convenience, are beginning to experiment with new, digital-first pharmacy entrants that facilitate in-home pharmacy experiences, especially during reflections on the COVID-19 crisis. 2 “The Update: How Walgreens’ customer-focused marketing is driving business growth,” Google, September 2020, thinkwithgoogle.com.
Customers in the other archetype—those with multiple chronic conditions—are seeking higher-touch clinical support models in the home and digitally, as well as wanting guidance from a trusted pharmacist in managing multiple medications. 3 Madison Como et al., “Pharmacist-led chronic care management for medically underserved rural populations in Florida during the COVID-19 pandemic,” Preventing Chronic Disease , July 30, 2020, Volume 17, cdc.gov. These developments put pressure on both pharmacy incumbents and new players attempting to define their future pharmacy value propositions. At the same time, these systemic changes present new focus areas for stakeholders across the value chain, giving players a chance to move quickly.
Would you like to learn more about our Healthcare Systems & Services Practice ?
High-value patient archetypes.
Two patient archetypes should be top priority for stakeholders: one that is primarily concerned with convenience, and one that desires an ongoing relationship with their pharmacist to support their chronic conditions and medication needs.
Convenience, convenience, convenience
The thought driving this archetype can be summed up as follows: “I want to spend as little time and energy as possible interacting with my pharmacy.” This tends to be the primary goal of young professionals, busy parents, active retirees, and others. Convenient, direct-to-consumer new pharmacy entrants are working to meet this need and, based on recent venture-funding rounds that value these players in the billions, are achieving early market traction. 4 Katie Jennings, “Digital health startup Ro raised $500 million at $5 billion valuation,” Forbes, March 22, 2021, forbes.com. A physician can prescribe a new prescription virtually, the customer pays online, and the prescription shows up a day later. In addition to providing convenience, delivery and medication synchronization (such as pharmacist coordination of refills) may improve medication adherence in certain use cases. 5 Alexis A. Krumme et al., “Medication synchronization programs improve adherence to cardiovascular medications and health care use,” Health Affairs , January 2018, Volume 37, Number 1, pp. 125–33, healthaffairs.org.
Clinical support for chronic conditions
Patients in the second archetype, in contrast, are looking for much-needed support from their pharmacy (and pharmacist) in managing and adhering to multiple medications. Their driving thought is “I have multiple medications, and I need support from a pharmacist I know and trust.” Polychronic and complex chronic homebound patients taking multiple medications often have adherence challenges and could benefit from a high-touch pharmacist model that includes, for example, adherence counseling and medication reconciliation. 6 Reyan Ghany et al., “High-touch care leads to better outcomes and lower costs in a senior population,” American Journal of Managed Care , August 28, 2018, Volume 24, Number 9, ajmc.com. In addition, complex chronic homebound patients are at a greater risk for high medical costs, including complications of chronic diseases. 7 Katherine A. Ornstein et al., “Epidemiology of the homebound population in the United States,” JAMA Internal Medicine , July 2015, Volume 175, Number 7, pp. 1180–6, pubmed.ncbi.nlm.nih.gov.
Why stakeholders may welcome the shift to home
The who, what, when, where, and how of pharmacy-care delivery is rapidly evolving: from traditional models to tech-enabled models, from in-person pickup to delivery, and from outpatient hospitals and clinics to the home. This shift may be welcomed by many stakeholders because e-commerce penetration in retail pharmacy is low relative to most other retail categories (exhibit).
A number of factors are driving the shift to in-home pharmacy care for convenience seekers:
- Demand tailwinds: The market has experienced a meaningful increase in consumer preference for home options during the COVID-19 crisis, with likely stickiness as normal activity resumes. 8 Victor Fabius, Sajal Kohli, Björn Timelin, and Sofia Moulvad Veranen, “ Meet the next-normal consumer ,” August 17, 2020, McKinsey.com.
- Tech-driven innovation: There has been substantial growth in tech-driven product and service-delivery models (for example, digital pharmacy and direct-to-consumer virtual care clinics) that are penetrating traditional channels and supporting the shift to home. 9 Heather Landi, “In a competitive digital health market, startups move to add new medication delivery services,” Fierce Healthcare , March 8, 2021, fiercehealthcare.com.
In addition to demand tailwinds, several major factors are driving the shift for those needing clinical support for their chronic conditions:
- Growth in homebound populations: The market has seen material growth in homebound populations, including those eligible for Medicare and those with intellectual and developmental disabilities (IDD), as well as an expansion of managed Medicaid and managed dual-eligible patients. 10 Katherine A. Ornstein et al., “Estimation of the incident homebound population in the US among older Medicare beneficiaries, 2012 to 2018,” JAMA Internal Medicine , May 26, 2020, Volume 180, Number 7, pp. 1022–1025, jamanetwork.com.
- Payer actions: Finally, there has been a rise in new medical-necessity and reimbursement policies and innovative programs from payers (for example, the Centers for Medicare & Medicaid Services’ Acute Hospital Care at Home) that have shifted care from hospitals, facility-based settings (for example, long-term acute care hospitals and skilled nursing facilities), and doctor’s offices and clinics to the home. 11 “Acute Hospital Care at Home Program: Approved list of hospitals as of 4/5/2021,” Centers for Medicare & Medicaid Services (CMS), April 5, 2021, cms.gov.
The future of healthcare: Value creation through next-generation business models
The challenges of moving the pharmacy into the home.
Several challenges of serving the pharmacy market have delayed this move into the home:
- Pharmacy is more than drug fulfillment and delivery. New entrants have quickly shown they can offer drug fulfillment and two-day delivery. However, many patients rely on clinical support from their pharmacists. This can manifest as medication review and reconciliation, as adherence counseling, as limited prescribing, and, even more broadly, as disease management. 12 Patti G. Manolakis and Jann B. Skelton, “Pharmacists’ contributions to primary care in the United States collaborating to address unmet patient care needs: The emerging role for pharmacists to address the shortage of primary care providers,” American Journal of Pharmaceutical Education , December 15, 2010, Volume 74, Number 10, ncbi.nlm.nih.gov. To offer these services at home requires a fleet of pharmacists who can meet patients where they are, telepharmacy systems, or both.
- The unit economics of this sector are challenging. 13 Elizabeth Seeley and Surya Singh, “Competition, consolidation, and evolution in the pharmacy market: Implications for efforts to contain drug prices and spending,” Commonwealth Fund, August 12, 2021, commonwealthfund.org. Competitive cost of goods sold (COGS) and reimbursement rates often come with scale, and it can take new entrants meaningful time to establish themselves.
- Today’s in-home offerings from digital disrupters can be limited depending on the prescription need. For example, offerings may not include Schedule 2 narcotics, may only focus on one- or two-day delivery (for example, exclude difficult-to-deliver but immediately needed acute scripts), and may not always offer both traditional and specialty (low-volume but high-value) drugs simultaneously.
Implications for pharmacy incumbents and new entrants
The recent systemic changes in the market present risks for players across the pharmacy value chain. The new, consumer-focused digital disrupters have strong advantages given the newness of their systems, their speed and agility, and their customer-centric foundation. 14 Heather Landi, “NowRx, Medly Pharmacy land new funding as demand for digital pharmacies grows,” Fierce Healthcare , July 17, 2020, fiercehealthcare.com. However, incumbents are also well positioned given their existing platforms, high volumes, and large customer bases in a business that depends heavily on volume. Yet these same incumbents will likely need to do more to stay ahead of the competition. While national retail pharmacy chains have begun to offer home delivery (for example, free one- or two-day delivery with same-day delivery for an additional fee), it is not yet clear whether they will keep up with the delivery speed and experience of new e-commerce players. 15 “CVS Pharmacy prescription delivery now available from all locations nationwide,” CVS Health, June 19, 2018, cvshealth.com. To be successful in this market, incumbents will likely need to fundamentally rethink their existing processes, workflows, technologies, and systems so that they can engage the various customer archetypes in the settings and locations most important to them.
Potential actions in the next normal
Payers have an opportunity to build partnerships across the physical and virtual continuum to create a more coordinated healthcare ecosystem, to improve patient experience, and to drive down the cost of care. Partnerships with a direct-to-consumer pharmacy—likely an attractive offering for the highly convenience-oriented customer archetype—could create a differentiated experience that drives growth and retention. Payers also have an opportunity to improve ratings by partnering with digital pharmacies to close care gaps, improve adherence, and manage multiple medications.
Finally, payers have the opportunity to bundle intensive clinical-care models with mail-order pharmacy capabilities, meeting the needs of patients with chronic conditions. Payers are increasingly focused on chronic care and disease management—driven in part by the shift toward risk-bearing and integrated-care-delivery models—and are often willing to reimburse for in-home clinical services. 16 Christian Worstell, “Does Medicare cover home health care?,” MedicareAdvantage.com, February 23, 2021, medicareadvantage.com.
Success in this space will likely require core pharmacy assets (for example, the ability to sort and repackage medication, to deliver directly to patients at home, and to provide on-demand pharmacist consultations) coupled with direct-to-home assets and access to home health agencies and providers, for example.
Systemic changes have fueled new types of services for key patient archetypes and focus areas for stakeholders across the pharmacy value chain. While near-term pressures may exist for both incumbents and new entrants, those that move quickly will be able to make substantial progress in these focus areas.
Adam Apfel is a partner in McKinsey’s Boston office; Sarah Lorenzana is an associate partner in the Washington, DC, office; Alec McLeod is an associate partner in the Miami office; and BJ Tevelow is a senior partner in the Miami office.
This article was edited by Elizabeth Newman, an executive editor in the Chicago office.
Explore a career with us
Related articles.

The role of personalization in the care journey: An example of patient engagement to reduce readmissions

IMAGES
VIDEO
COMMENTS
Explore the latest in clinical pharmacy and pharmacology, including topics in drug safety, development, pharmacogenetics, and pharmacoeconomics. This randomized clinical trial examines the efficacy of ivonescimab plus chemotherapy vs chemotherapy alone for patients with advanced or metastatic non-small cell lung cancer with the epidermal ...
Hot Topics in Pharmaceutical Research. In this virtual issue, we highlight some of the most impactful recent articles in the journal as reflected by citations in 2022. Highly cited articles provide insight into which research topics are attracting the most attention and reflect innovative new discoveries, or timely reviews and perspectives on ...
Call for submissions. In 2021, The Pharmaceutical Journal will keep adding to the evidence base with review, perspective and research articles. If you have undertaken research into innovations and initiatives that can improve pharmacy services and administration, the pharmacological management of disease, or advances in drug development, please submit your article for consideration by email to ...
Below are suggested topics for submission. Feel free to submit on a topic not listed below. ASHP is also soliciting proposals addressing ASHP's Practice Advancement Initiative 2030*, which includes 59 recommendations to promote optimal, safe, effective medication use; expand pharmacist and technician roles; and implement the latest technologies.
Pharmaceutics is the scientific discipline concerned with the process of creating the dosage form (such as a pill for oral administration or a powder for intravenous injection) of a therapeutic ...
The journal offers practicing pharmacists in-depth useful reviews, research trials, surveys of new drugs and novel therapeutic approaches, pharmacotherapy reviews and controversies, pharmacokinetics, drug interactions, drug administration, adverse drug events, medication safety, pharmacy education, and other pharmacy practice topics.
The use of qualitative research methodology is becoming increasingly common across diverse health-related disciplines, including pharmacy practice. ... 2016a, Hadi and Closs, 2016b argued that quality in qualitative research topic has not been discussed widely in the literature, and therefore Hadi and Closs, 2016a, Hadi and Closs, ...
Pharmacology is a branch of biomedical science, encompassing clinical pharmacology, that is concerned with the effects of drugs/pharmaceuticals and other xenobiotics on living systems, as well as ...
The most cited pharmacology and pharmacy journal advances access to pharmacological discoveries to prevent and treat human disease. ... Research Topics. Submission open Interplay of Radiation Therapy and Tumor Immunology: Unraveling Mechanisms, Biomarkers, Combined Strategies, and Clinical Applications ...
Explore the latest full-text research PDFs, articles, conference papers, preprints and more on CLINICAL PHARMACY. Find methods information, sources, references or conduct a literature review on ...
The final themes summarized participants' views of the benefits of employing qualitative research in pharmacy education. Three benefits surfaced from the interviews. First, the participants discussed how the exploratory nature of qualitative research affords an opportunity to investigate a variety of topics in which little to no research exists.
HOT TOPICS IN PHARMACY PRACTICE RESEARCH. ... Missing documentation involved medication incidents that stemmed from both prescriber and pharmacy-related databases, while computer detection incapacity and alert bypass incidents only involved pharmacy-related dispensing systems. Recommendations primarily focused on the proper usage/maintenance of ...
Drug development and formulation. | Explore the latest full-text research PDFs, articles, conference papers, preprints and more on PHARMACEUTICS. Find methods information, sources, references or ...
Pharmacy Research Topics. Pharmacy research ideas encompasses a variety of topics dealing with drugs and pharmaceuticals. Some broad areas of pharmaceutical research relate to drug delivery, pharmaceutical cell biology, medicinal chemistry and medicine management. Faculty and graduate students at pharmaceutical colleges typically engage in such ...
Journal of Clinical Pharmacy and Therapeutics provides a forum for clinicians, pharmacists and pharmacologists to explore and report on issues of common interest. Its scope embraces all aspects of clinical drug development and therapeutics. ... Research Article. free access. ... Bodyweight and combination with SSRIs are related to bleeding ...
Bariatric Surgery. Barrett's Esophagus. Bioterrorism/Disaster Medicine. Bipolar Disorder. Bladder Cancer. Bone and Mineral Disorders. Benign Prostatic Hyperplasia (BPH) Brain Cancer. Breast Cancer.
Looking for research topics related to Pharmacy? this page might help you come up with ideas. Research topics are subjects or issues researchers are interested in when conducting research. A well-defined research topic is the starting point of every successful research project. Choosing a topic is an ongoing process by which researchers explore ...
Research Areas. The UCSF Pharmaceutical Sciences and Pharmacogenomics Graduate Program offers six areas of research emphasis: 1. Pharmacogenomics and functional genomics. Pharmacogenomics and functional genomics are increasingly recognized scientific areas that are critical to precision medicine.
Research in the Department of Clinical Pharmacy focuses on the precise, personalized relationship between patients and their medications. It also examines broader relationships between patients and the health care and public policy environments that influence factors such as medication cost and access, health disparities, and pharmacy practice models.
Welcome to Hot Topics in Pharmacy Practice which features a variety of episodes covering emerging trends, key topics and areas across medicine. ... Related Links . COVID-19: So What's New? April 26, 2024. Listen Here. Link the whole card. Compliance with USP Chapter . 797> in Small and Rural ... Research that Moves Pharmacy Forward ...
Pharmacy Times offers the latest news and insights for the pharmacy professional and solutions that impact the everyday practice of pharmacy. ... Research Finds In Utero Exposure to Ocrelizumab Not Associated With Increased Adverse Pregnancy, Infant Outcomes for Women With MS. Aislinn Antrim, Assistant Managing Editor ...
These resources are intended to help residents and students understand the basic steps and principles of conducting practice-based research projects. Pharmacists who want to conduct practice-based projects can also benefit from the information presented. These presentations start with generating the project topic and proceed through planning ...
Research Topics For Phd in Pharmacy. Sr. No. Research Topic. Check Thesis. 1. Contribution of alterations in pulative susceptibility genes and genomic imbalances in the occurrence of breast cancer in Northeast Indian population. Click Here. 2. Design and Synthesis of Multifunctional Leads for the Treatment of Neuropathic Pain.
Potential Research Projects. Research. Research projects for Higher Degree by Research (HDR) students are available within the following School of Pharmacy research areas and research centre. Please email our academic staff to discuss potential HDR projects and ask if they are available as an advisor for your proposed HDR program.
Rural pharmacy elective-topics. Topics presented in the course are listed in Table 2. Topics for didactic sessions early in the course are based on selected chapters from the textbook required for the course, Foundations of Rural Public Health in America (2022), by Joseph N. Inungu and Mark J. Minelli . The course also features ...
A number of factors are driving the shift to in-home pharmacy care for convenience seekers: Demand tailwinds: The market has experienced a meaningful increase in consumer preference for home options during the COVID-19 crisis, with likely stickiness as normal activity resumes. 8 Victor Fabius, Sajal Kohli, Björn Timelin, and Sofia Moulvad Veranen, "Meet the next-normal consumer," August ...