- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board

An Overview of the Vaccine Debate
Looking at Both Sides of the Argument
There is a wealth of research demonstrating the efficacy and safety of vaccines —including how some have virtually eradicated infectious diseases that once killed millions. However, this has done little to sway those who believe that untold harms are being hidden from the American public.
The vaccine debate—including the argument as to whether vaccines are safe, effective, or could cause conditions like autism —has received a lot of attention from the media in recent years. With so much conflicting information being publicized, it can be a challenge to discern what is true and what is not. Therefore, it is important to learn the facts before making health decisions.
Claims and Controversy
Those who are part of the anti-vaccination movement include not only non-medical professionals but several scientists and healthcare providers who hold alternative views about vaccines and vaccination in general.
Some notable examples include:
- British healthcare provider Andrew Wakefield, who in 1998 published research linking the MMR vaccine and autism . That study has since been retracted, and he was later removed from the medical registry in the United Kingdom for falsifying scientific data.
- Pediatrician Bob Sears, who wrote the bestseller "The Vaccine Book: Making the Right Decision for your Child ," which suggested that many essential childhood vaccines were "optional." However, he was subsequently put on probation by the Medical Review Board of California in 2018 for alleged medical negligence and the inappropriate writing of medical exemptions for vaccinations.
- Dr. Jane M. Orient, director of the Association of American Healthcare Providers and Surgeons, who was among the leading opponents of the COVID-19 vaccine and one of the leading proponents of using hydroxychloroquine to treat COVID-19 during the pandemic.
These opposing views and claims, along with other information promoted by the news and social media, have led some people to question whether they know everything they need to know about vaccines.
Common Concerns Regarding Vaccines
The arguments made against vaccines are not new and have been made well before the first vaccine was developed for smallpox back in the 18th century.
The following are some of the common arguments against vaccines:
- Vaccines contain "toxic" ingredients that can lead to an assortment of chronic health conditions such as autism.
- Vaccines are a tool of "Big Pharma," in which manufacturers are willing to profit off of harm to children.
- Governments are "pharma shills," meaning they are bought off by pharmaceutical companies to hide cures or approve drugs that are not safe.
- A child’s immune system is too immature to handle vaccines , leading the immune system to become overwhelmed and trigger an array of abnormal health conditions.
- Natural immunity is best , suggesting that a natural infection that causes disease is "better" than receiving a vaccine that may cause mild side effects.
- Vaccines are not tested properly , suggesting a (highly unethical) approach in which one group of people is given a vaccine, another group is not, and both are intentionally inoculated with the same virus or bacteria.
- Infectious diseases have declined due in part to improved hygiene and sanitation , suggesting that hand-washing and other sanitary interventions are all that are needed to prevent epidemics.
- Vaccines cause the body to "shed" virus , a claim that is medically true, although the amount of shed virus is rarely enough to cause infection.
The impact of anti-vaccination claims has been profound. For example, it has led to a resurgence of measles in the United States and Europe, despite the fact that the disease was declared eliminated in the U.S. back in 2000.
Studies have suggested that the anti-vaccination movement has cast doubt on the importance of childhood vaccinations among large sectors of the population. The added burden of the COVID-19 pandemic has led to further declines in vaccination rates.
There is also concern that the same repercussions may affect COVID-19 vaccination rates—both domestically and abroad. Ultimately, vaccine rates must be high for herd immunity to be effective.
According to a study from the Centers for Disease Control and Prevention (CDC), the rate of complete recommended vaccination among babies age 5 months has declined from 66.6% in 2016 to 49.7% by May 2020. Declines in vaccination coverage were seen in other age groups as well.
Benefits of Vaccination
Of the vaccines recommended by the CDC, the benefits of immunization are seen to overwhelmingly outweigh the potential risks. While there are some people who may need to avoid certain vaccines due to underlying health conditions, the vast majority can do so safely.
According to the U.S. Department of Health and Human Services, there are five important reasons why your child should get the recommended vaccines:
- Immunizations can save your child’s life . Consider that polio once killed up to 30% of those who developed paralytic symptoms. Due to polio vaccination, the disease is no longer a public health concern in the United States.
- Vaccination is very safe and effective . Injection site pain and mild, flu-like symptoms may occur with vaccine shots. However, serious side effects , such as a severe allergic reaction, are very rare.
- Immunization protects others . Because respiratory viruses can spread easily among children, getting your child vaccinated not only protects your child but prevents the further spread of disease.
- Immunizations can save you time and money . According to the non-profit Borgen Project, the average cost of a measles vaccination around the world is roughly $1.76, whereas the average cost of treating measles is $307. In the end, the cost of prevention is invariably smaller than the cost of treatment.
- Immunization protects future generations . Smallpox vaccinations have led to the eradication of smallpox . Rubella (German measles) vaccinations have helped eliminate birth defects caused by infection of pregnant mothers in the developed world. With persistence and increased community uptake, measles could one day be declared eliminated (again) as well.
A Word From Verywell
If you have any questions or concerns about vaccinations, do not hesitate to speak with your healthcare provider or your child's pediatrician.
If a vaccine on the immunization schedule has been missed, speak to a healthcare provider before seeking the vaccination on your own (such as at a pharmacy or clinic). In some cases, additional doses may be needed.
Vaccines Healthcare Provider Discussion Guide
Get our printable guide for your next healthcare provider's appointment to help you ask the right questions.
Sign up for our Health Tip of the Day newsletter, and receive daily tips that will help you live your healthiest life.
Thank you, {{form.email}}, for signing up.
There was an error. Please try again.
Eggerton L. Lancet retracts 12-year-old article linking autism to MMR vaccines . CMAJ . 2010 Mar 9; 182(4):e199-200. doi:10.1503/cmaj.109-3179
Park A. Doctor behind vaccine-autism link loses license . Time .
Offit PA, Moser CA. The problem with Dr Bob's alternative vaccine schedule . Pediatrics. 2009 Jan;123 (1):e164-e169. doi:10.1542/peds.2008-2189
Before the Medical Board of California, Department of Consumer Affairs, State of California. In the Matter of the Accusation Against Robert William Sears, M.D., Case No. 800-2015-012268 .
Stolberg SG. Anti-vaccine doctor has been invited to testify before Senate committee . The New York Times.
Wolfe RM, Sharp LK. Anti-vaccinationists past and present . BMJ. 2002;325(7361):430-2. doi:10.1136/bmj.325.7361.430
Agley J, Xiao Y. Misinformation about COVID-19: Evidence for differential latent profiles and a strong association with trust in science . BMC Public Health. 2021;21:89. doi:10.1186/s12889-020-10103-x
Centers for Disease Control and Prevention. Measles history .
Hussain A, Ali S, Ahmed M, Hussain S. The anti-vaccination movement: a regression in modern medicine . Cureus . 2018;10(7): e2919. doi:10.7759/cureus.2919
Bramer CA, Kimmins LM, Swanson R, et al. Decline in child vaccination coverage during the COVID-19 pandemic — Michigan Care Improvement Registry, May 2016–May 2020 . MMWR. 2020 May;69(20):630-1. doi:10.15585/mmwr.mm6920e1
Centers for Disease Control and Prevention. Why vaccinate .
Centers for Disease Control and Prevention. Poliomyelitis .
Centers for Disease Control and Prevention. Making the vaccine decision .
Borgen Project. What is the cost of measles in the developed world? .
By Vincent Iannelli, MD Vincent Iannelli, MD, is a board-certified pediatrician and fellow of the American Academy of Pediatrics. Dr. Iannelli has cared for children for more than 20 years.
Should COVID-19 vaccines be mandatory? Two experts discuss
Senior Research Fellow, Oxford Uehiro Centre for Practical Ethics, University of Oxford
NIHR Academic Clinical Fellow in Public Health Medicine, UCL
Disclosure statement
Alberto Giubilini receives funding from the Arts and Humanities Research Council/UK Research and Innovation (AHRC/UKRI) and has previously received funding from the Wellcome Trust.
Vageesh Jain is affiliated with Public Health England under an honorary contract as a speciality registrar.
University College London provides funding as a founding partner of The Conversation UK.
University of Oxford provides funding as a member of The Conversation UK.
View all partners

To be properly protective, COVID-19 vaccines need to be given to most people worldwide. Only through widespread vaccination will we reach herd immunity – where enough people are immune to stop the disease from spreading freely. To achieve this, some have suggested vaccines should be made compulsory , though the UK government has ruled this out . But with high rates of COVID-19 vaccine hesitancy in the UK and elsewhere , is this the right call? Here, two experts to make the case for and against mandatory COVID-19 vaccines.
Alberto Giubilini, Senior Research Fellow, Oxford Uehiro Centre for Practical Ethics, University of Oxford
COVID-19 vaccination should be mandatory – at least for certain groups. This means there would be penalties for failure to vaccinate, such as fines or limitations on freedom of movement.
The less burdensome it is for an individual to do something that prevents harm to others, and the greater the harm prevented, the stronger the ethical reason for mandating it.
Being vaccinated dramatically reduces the risk of seriously harming or killing others. Vaccines such as the Pfizer , AstraZeneca or Moderna ones with 90-95% efficacy at preventing people from getting sick are also likely to be effective at stopping the virus from spreading, though possibly to a lower degree. Such benefits would come at a very minimal cost to individuals.
Lockdown is mandatory. Exactly like mandatory vaccination, it protects vulnerable people from COVID-19. But, as I have argued in detail elsewhere, unlike mandatory vaccination, lockdown entails very large individual and societal costs. It is inconsistent to accept mandatory lockdown but reject mandatory vaccination. The latter can achieve a much greater good at a much smaller cost.
Also, mandatory vaccination ensures that the risks and burdens of reaching herd immunity are distributed evenly across the population. Because herd immunity benefits society collectively, it’s only fair that the responsibility of reaching it is shared evenly among society’s individual members.
Of course, we might achieve herd immunity through less restrictive alternatives than making vaccination mandatory – such as information campaigns to encourage people to be vaccinated. But even if we reach herd immunity, the higher the uptake of vaccines, the lower the risk of falling below the herd immunity threshold at a later time. We should do everything we can to prevent that emergency from happening – especially when the cost of doing so is low.
Fostering trust and driving uptake by making people more informed is a nice narrative, but it’s risky. Merely giving people information on vaccines does not always result in increased willingness to vaccinate and might actually lower confidence in vaccines. On the other hand, we’ve seen mandatory vaccination policies in Italy recently successfully boost vaccine uptake for other diseases.
Mandatory seatbelt policies have proven very successful in reducing deaths from car accidents, and are now widely endorsed despite the (very small) risks that seatbelts entail. We should see vaccines as seatbelts against COVID-19. In fact, as very special seatbelts, which protect ourselves and protect others.

Vageesh Jain, NIHR Academic Clinical Fellow in Public Health Medicine, UCL
Mandatory vaccination does not automatically increase vaccine uptake. An EU-funded project on epidemics and pandemics, which took place several years before COVID-19, found no evidence to support this notion. Looking at Baltic and Scandinavian countries, the project’s report noted that countries “where a vaccination is mandatory do not usually reach better coverage than neighbour or similar countries where there is no legal obligation”.
According to the Nuffield Council of Bioethics, mandatory vaccination may be justified for highly contagious and serious diseases. But although contagious, Public Health England does not classify COVID-19 as a high-consequence infectious disease due to its relatively low case fatality rate.
COVID-19 severity is strongly linked with age, dividing individual perceptions of vulnerability within populations. The death rate is estimated at 7.8% in people aged over 80, but at just 0.0016% in children aged nine and under. In a liberal democracy, forcing the vaccination of millions of young and healthy citizens who perceive themselves to be at an acceptably low risk from COVID-19 will be ethically disputed and is politically risky.
Public apprehensions for a novel vaccine produced at breakneck speed are wholly legitimate. A UK survey of 70,000 people found 49% were “very likely” to get a COVID-19 vaccine once available. US surveys are similar . This is not because the majority are anti-vaxxers.
Despite promising headlines, the trials and pharmaceutical processes surrounding them have not yet been scrutinised. With the first trials only beginning in April , there is limited data on long-term safety and efficacy. We don’t know how long immunity lasts for. None of the trials were designed to tell us if the vaccine prevents serious disease or virus transmission.
To disregard these ubiquitous concerns would be counterproductive. As a tool for combating anti-vaxxers – estimated at around 58 million globally and making up a small minority of those not getting vaccinated – mandatory vaccines are also problematic. The forces driving scientific and political populism are the same . Anti-vaxxers do not trust experts, industry and especially not the government. A government mandate will not just be met with unshakeable defiance, but will also be weaponised to recruit others to the anti-vaxxer cause.
In the early 1990s, polio was endemic in India , with between 500 and 1,000 children getting paralysed daily. By 2011, the virus was eliminated. This was not achieved through legislation. It was down to a consolidated effort to involve communities, target high-need groups, understand concerns, inform, educate, remove barriers, invest in local delivery systems and link with political and religious leaders.
Mandatory vaccination is rarely justified. The successful roll-out of novel COVID-19 vaccines will require time, communication and trust. We have come too far, too fast, to lose our nerve now.
- Mandatory vaccination
- Coronavirus
- Vaccine hesitancy
- Coronavirus insights

School of Social Sciences – Public Policy and International Relations opportunities

Partner, Senior Talent Acquisition

Deputy Editor - Technology

Sydney Horizon Educators (Identified)

Deputy Vice-Chancellor (Academic and Student Life)
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection
Persuasive messaging to increase COVID-19 vaccine uptake intentions
Erin k. james.
a Yale Institute for Global Health, New Haven, CT, USA
b Department of Internal Medicine, Section of Infectious Diseases, Yale School of Medicine, New Haven, CT, USA
Scott E. Bokemper
c Institution for Social and Policy Studies, Yale University, New Haven, CT, USA
d Center for the Study of American Politics, Yale University, New Haven, CT, USA
Alan S. Gerber
e Department of Political Science, Yale University, New Haven, CT, USA
Saad B. Omer
f Department of Epidemiology of Microbial Diseases, Yale School of Public Health, New Haven, CT, USA
g Yale School of Nursing, West Haven, CT, USA
Gregory A. Huber
Associated data.
Widespread vaccination remains the best option for controlling the spread of COVID-19 and ending the pandemic. Despite the considerable disruption the virus has caused to people’s lives, many people are still hesitant to receive a vaccine. Without high rates of uptake, however, the pandemic is likely to be prolonged. Here we use two survey experiments to study how persuasive messaging affects COVID-19 vaccine uptake intentions. In the first experiment, we test a large number of treatment messages. One subgroup of messages draws on the idea that mass vaccination is a collective action problem and highlighting the prosocial benefit of vaccination or the reputational costs that one might incur if one chooses not to vaccinate. Another subgroup of messages built on contemporary concerns about the pandemic, like issues of restricting personal freedom or economic security. We find that persuasive messaging that invokes prosocial vaccination and social image concerns is effective at increasing intended uptake and also the willingness to persuade others and judgments of non-vaccinators. We replicate this result on a nationally representative sample of Americans and observe that prosocial messaging is robust across subgroups, including those who are most hesitant about vaccines generally. The experiments demonstrate how persuasive messaging can induce individuals to be more likely to vaccinate and also create spillover effects to persuade others to do so as well.
The first experiment in this study was registered at clinicaltrials.gov and can be found under the ID number {"type":"clinical-trial","attrs":{"text":"NCT04460703","term_id":"NCT04460703"}} NCT04460703 . This study was registered at Open Science Framework (OSF) at: https://osf.io/qu8nb/?view_only=82f06ecad77f4e54b02e8581a65047d7.
1. Introduction
The global spread of COVID-19 created an urgent need for safe and effective vaccines against the disease. However, even though several successful vaccines have become available, vaccine hesitancy in the general population has the potential to limit the efficacy of vaccines as a tool for ending the pandemic. For instance, in the United States, the public’s willingness to receive a vaccine has declined from 72 % saying they would be likely to get a COVID-19 vaccine in May 2020 to 60 % of people reporting that they would receive a vaccine as of November 2020 [ 1 ]. Given the considerable amount of skepticism about the safety and efficacy of a COVID-19 vaccine, it has become increasingly important to understand how public health communication can play a role in increasing COVID-19 vaccine uptake.
Vaccination is both a self-interested and a prosocial action [ [2] , [3] , [4] , [5] , [6] , [7] , [8] , [9] ]. By getting vaccinated, people protect themselves from a disease, but they also reduce the chance that they become a vector through which the disease spreads to others. If enough people receive a vaccine, the population gains protection through herd immunity, but this also creates an incentive for an individual to not get vaccinated because they can forgo vaccination and receive protection from others who do vaccinate. Recent research on vaccination in general has demonstrated that people view vaccination as a social contract and are less willing to cooperate with those who choose not to get inoculated [ 10 ]. This work also implies that highlighting the reputational costs of choosing not to vaccinate could be an effective strategy for increasing uptake. Further, appeals to herd immunity and the prosocial aspect of vaccination have been shown to increase uptake intentions [ [11] , [12] , [13] ], but emphasizing the possibility of free riding on other’s immunity reduces the willingness to get vaccinated [ 14 ].
Focusing specifically on vaccination against COVID-19, recent studies have found that messages that explain herd immunity increase willingness to receive a vaccine [ 15 ] and reduces the time that people would wait to get vaccinated when a vaccine becomes available to them [ 16 ]. However, other work has found that prosocial appeals did not increase average COVID-19 vaccination intentions [ 17 ] and the effect of prosocial concerns was present in sparsely populated places, but absent in more densely populated ones [ 18 ]. Given the current state of evidence, it is unclear whether appealing to getting a COVID-19 vaccine as a way to protect others will increase willingness to vaccinate.
Viewing vaccination through the lens of a collective action problem suggests that in addition to increasing individuals’ intentions to receive a vaccine, effective public health messages would also increase people’s willingness to encourage those close to them to vaccinate and to hold negative judgments of those who do not vaccinate. By encouraging those close to them to vaccinate, people are both promoting compliance with social norms and increasing their own level of protection against the disease. Also, by judging those who do not vaccinate more negatively, they apply social pressure to others to promote cooperative behavior. This would be consistent with theories of cooperation, like indirect reciprocity or partner choice, that rely on free riders being punished or ostracized for their past actions to encourage prosocial outcomes [ [19] , [20] , [21] , [22] , [23] ]. Thus, effective messaging could have outsized effects on promoting vaccination if it both causes people to vaccinate themselves and to encourage those around them to do so.
We conducted two pre-registered experiments to study how different persuasive messages affect intentions to receive a COVID-19 vaccine, willingness to persuade friends and relatives to receive one, and negative judgments of people who choose not to vaccinate. In the first experiment, we tested the efficacy of a large number of messages against an untreated control condition (see Table 1 for full text of messages). A subgroup of the messages in Experiment 1 drew on this collective action framework of vaccination and emphasized who benefits from vaccination or how choosing not to vaccinate hurts one’s social image. A second subgroup drew on contemporary arguments about restrictions on liberty and economic activity during the COVID-19 pandemic. In Experiment 2, we retested the most effective messages from Experiment 1 on a nationally representative sample of American adults. By utilizing this test and re-test design, we guard against false positive results that are observed by chance among the large number of messages tested in Experiment 1. In our analysis of both experiments, we examined whether specific messages were more effective among certain subgroups of the population.
Experimental treatment messages for Experiment 1 and Experiment 2. All messages add the prose in the table to the content of the Baseline informational control. All of the messages in the table were tested in Experiment 1. The messages that are bolded were retested in Experiment 2.
Experiment 1 was fielded in early July 2020. Participants were randomly assigned to either a placebo control condition in which they read a story about the effectiveness of bird feeders or one of eleven treatment messages. The first message is a Baseline informational control condition that describes how it is important to receive a vaccine to reduce your risk of contracting COVID-19 or spreading it to others. Informational messages have been shown to be effective at increasing COVID-19 vaccine uptake intentions [ 24 ]. This message also emphasized that vaccines are safe and estimated to save millions of lives per year. The other messages add additional content to this baseline message.
The subgroup of messages that emphasized collective action varied who would benefit from vaccination or what other people might think of someone who chooses to be a free rider by not vaccinating. Focusing on who benefits from vaccination, the second message invoked Self Interest and reinforced the idea that vaccination is a self-protecting action (“Remember, getting vaccinated against COVID-19 is the single best way to protect yourself from getting sick.”). The third message, Community Interest, instead argued that vaccination is a cooperative action to protect other people (“Stopping COVID-19 is important because it reduces the risk that members of your family and community could get sick and die.”). This message also invoked reciprocity by emphasizing the importance of every-one working together to protect others.
The fourth, fifth, and sixth messages added an invocation of an emotion, Guilt, Embarrassment, or Anger, to the Community Interest message. These messages prompted people to think about how they would feel if they chose not to get vaccinated and spread COVID-19 to someone else in the future. Emotions are thought to play a role in cooperation, either by motivating an individual to take an action because of a feeling that they experience or restraining them from taking an action because of the emotional response it would provoke in others [ [25] , [26] , [27] ]. Further, anticipated emotional states have been shown to promote various health behaviors, like vaccination [ [28] , [29] ].
The seventh and eighth messages evoked concerns about one’s reputation and social image, which influences their attractiveness as a cooperative partner to others. The seventh, a Not Bravery message, reframed the idea that being unafraid of the virus is not a brave action, but instead selfish, and that the way to demonstrate bravery is by getting vaccinated because it shows strength and concern for others (“To show strength get the vaccine so you don’t get sick and take resources from other people who need them more”). The eighth message was a Trust in Science message that highlights that scientists believe a vaccine will be an effective way of limiting the spread of COVID-19. This message suggests that those who do not get vaccinated do not understand science and signal this ignorance to others (“Not getting vaccinated will show people that you are probably the sort of person who doesn’t understand how infection spreads and who ignores or are confused about science.”).
The final three messages drew on concerns about restrictions on freedom and economic activity that were widespread during the COVID-19 pandemic. A pair of messages focused on how vaccination would allow for a restoration of Personal Freedom (“Government policies to prevent the spread of COVID-19 limit our freedom of association and movement”) or Economic Freedom (“Government policies to prevent the spread of COVID-19 have stopped businesses from opening up”). These messages take a value that is commonly invoked in individuals’ decision to not vaccinate [ [30] , [31] ] and reframed vaccination as something that would actually restore freedoms that had been taken away. The final message, Community Economic Benefit, argues that a vaccine will help return people’s financial security and strengthen the economy This message is similar to the Community Interest messages that are described above, but instead focuses on cooperating to restore the economy (“We can all end this outbreak and strengthen the national economy by working together and getting vaccinated”).
2.1. Experiment 1 results
Panel A of Fig. 1 plots the effect of each vaccine message relative to the untreated control group on intention to vaccinate. The intention to vaccinate measure was formed by combining responses to a question about the likelihood of getting a COVID-19 vaccine within the first 3 months that one is available with a question about getting a vaccine within the first year that one is available. Specifically, for respondents who did not answer that they were very likely to vaccinate within the first three months that a vaccine is available to them, we asked how likely they would be to vaccinate within a year. This measure coded those who are very likely in the first three months at the highest value on the scale followed by very likely within a year descending down to very unlikely within the first year. Analyzing the vaccination item separately does not substantively change the results. All outcome variables were scored 0 to 1, with higher values indicating greater willingness to endorse the pro-vaccine action or belief (Underlying regressions appear in Table S1 and unless otherwise noted, all analyses were pre-registered).

Experiment 1. Messages that frame vaccination as a cooperative action to protect others or emphasize how non-vaccination might negatively affect one’s social image increase reported willingness to advise a friend, and judgment of non-vaccinators. Panel A displays treatment effects for the combined measure of intention to vaccinate, Panel B displays the advise a friend outcome, and Panel C displays the judging a non-vaccinator outcome. Treatment effects for both panels were estimated using OLS regression that included covariates. The effects displayed are a comparison against the placebo control baseline and are presented with 95% confidence intervals. The dashed vertical line is the effect of the Baseline informational control for each outcome.
Compared to the untreated control, the Baseline informational message was associated with modest increases in intention to vaccinate by 0.034 units (95 % CI:0.002, 0.065; p < .05). This effect represents an increase of approximately 6 % in the scale score compared to the outcome in the control condition.
By comparison, the Community Interest, Community Interest + Guilt, Embarrassment, or Anger, Not Bravery, Trust in Science and Personal Freedom messages all produce larger effects, at least qualitatively, than the Baseline informational message on the intention to vaccinate outcome. Effects for the Self-Interest, Economic Freedom, and Community Economic benefit messages were not consistently distinguishable from the untreated control group outcomes, and their effects were indistinguishable from the effects of the Baseline informational message.
The most promising messages were the Not Bravery, Community Interest, and Community Interest + Embarrassment messages. These messages were associated with effects that were statistically distinguishable from the untreated control group (Not Bravery: 0.077 units, 95 % CI: 0.035, 0.119; p < .01, Community Interest: 0.090 units, 95 % CI: 0.050, 0.129; p < .01, Community Interest + Embarrassment: 0.094 units, 95 % CI: 0.054, 0.134; p < .01) at p < .01. Moreover, their effects were always more than twice as large as the Baseline informational treatment and these differences were significant at p < .05 (two-tailed tests). The effects of the Trust in Science message and the Personal Freedom message were not statistically significant when compared to the Baseline informational message.
To put the magnitudes of the effects into context, we re-estimated our analysis after dichotomizing the intended vaccine uptake measure such that those who report they were “somewhat” or “very” likely to get the vaccine, either with three months or a year, are coded as 1 and those who do not are coded 0 (this analysis was not pre-registered). This produced a predicted rate of intended vaccination in the control group of 58.2 %. Respondents who read the Baseline informational message were 7.4 percentage points (95 % CI: 2.9 pp, 12.0 pp; p < .01) more likely to receive a vaccine. Among those assigned to the Not Bravery or Community Interest messages it was predicted to increase by 10.4 percentage points and 12.7 percentage points (Not Bravery: 95 % CI: 4.3 pp, 16.4 pp; p < .01, Community Interest: 95 % CI: 6.7 pp, 18.7 pp; p < .01) respectively, while among those assigned to the Community Interest + Embarrassment message it was predicted to increases by 15.9 percentage points (95 % CI: 10.2 pp, 21.6 pp; p < .01). This last difference was substantively large, representing a proportional increase of 27 % (0.159/0.582) compared to the control condition and a 13 % increase compared to the Baseline informational condition (0.159-0.074)/(0.582 + 0.074).
Turning to the other regarding outcomes that focused on spurring action by others, Panel B plots the effects of each vaccine message relative to the untreated control for advising a friend to receive a vaccine and Panel C plots the effects for negatively judging someone who refuses to receive one. Here, the effect of the Baseline informational intervention was modest and statistically insignificant. However, the Not Bravery, Trust in Science, Personal Freedom, Community Interest, Community Interest + Guilt, and Community Interest + Embarrassment messages had larger effects on both outcomes that were statistically distinguishable from the control outcome.
The most promising message was the Community Interest + Embarrassment message for the advise a friend outcome, which was associated with a 0.09 unit increase in the scale outcome (95 % CI: 0.049, 0.132; p < .01 two-tailed test), an effect that represents an increase of 27 % compared to the mean scale score in the control group. The effect was 0.067 units compared to the Baseline informational message (95 % CI: 0.027, 0.105; p = .001, two-tailed test). We conducted a similar exercise to the one describe above to gauge the relative magnitude of these treatment effects. For the Community Interest + Embarrassment message we estimated a 15 percentage point increase (95 % CI: 0.088, 0.209; p < .01, two tailed test,) in a binary intention to advise others to vaccinate outcome, a proportional increase of 27 % compared to the control group baseline of 53 % (0.15/0.53). This effect was also 6 percentage points larger than the effect of the baseline message (95 % CI: 0.008, 0.121; p = .03, two-tailed test).
The most promising outcome for the negative judgment of non-vaccinators was the Not Bravery message, which had an effect of 0.09 scale points (95 % CI: 0.052, 0.126; p < .01, two-tailed test) compared to the untreated control and 0.072 scale points versus the Baseline information (95 % CI: 0.037, 0.106; p < .01 Baseline message, two-tailed tests). This corresponded to a 21 % increase compared to the scale outcome in the control group (0.09/0.43). These are both substantively and statistically meaningful effects. The Community Interest, Community Interest + Guilt, Community Interest + Embarrassment, Trust in Science, and Personal Freedom messages all produced effects that were statistically distinguishable from the control condition.
We also investigated the robustness of these findings to sample restrictions and whether certain subgroups were more responsive to specific treatment messages (reported in Figures S2-S12 ). Results were generally robust to restricting the sample to those who were over the 10th percentile and under the 90th percentile for completion time. For subgroup analyses, those scoring low in liberty endorsement appeared more responsive to the Baseline treatment and to the Not Bravery message than are those who scored high in liberty endorsement. Those who report being less likely to take risks appeared robustly more responsive to the Not Bravery message than those who were high in risk taking. Those who were high in risk taking appear more responsive to the Personal Freedom message with regard to their own behavioral intentions. Certain groups appeared generically easier to persuade (Democrats rather than Republicans, an important divide that has emerged during the pandemic [ 32 ], and Women rather than Men), but there were no clear differences in which treatments appeared most effective across these groups. We explored the robustness of these subgroup differences in Experiment 2.
Taken together, the most successful messages in Experiment 1 were those that were theoretically motivated by viewing vaccination as a collective action problem. Consistent with previous work that demonstrates that prosocial appeals are effective in promoting vaccination, the Community Interest message and Community Interest + Guilt, Embarrassment, or Anger messages increased COVID-19 vaccine uptake intentions. Moving beyond who benefits from vaccination, the Not Bravery and Trust in Science messages that invoked concerns about one’s social image if they choose not to vaccinate also increased uptake intentions. All of the collective action oriented messages increased intentions to advise a friend to vaccinate and negative judgments of those who do not, potentially creating spillover effects that induce others to vaccinate. In addition to this subgroup of messages, we found that reframing vaccination as a way to restore freedom was also effective, though the other messages motivated by contemporary debates about the pandemic were generally no more effective than the Baseline condition.
2.2. Experiment 2 results
Experiment 2 tested the subset of the best performing messages from Experiment 1 on a nationally representative sample in September 2020. Notably, in the several month period between Experiment 1 and Experiment 2, the public had grown increasingly skeptical of a potential COVID-19 vaccine [ 1 ]. Panel A of Fig. 2 plots the effect of each vaccine message, relative to the untreated control group, on the same measure of intention to vaccinate used in Experiment 1. (The model specifications shown in the figure were from our pre-registered specifications, underlying regression appear in Table S2.). Given that we observed the messages from Experiment 1 were effective at increasing vaccine uptake, we pre-registered directional hypotheses for Experiment 2 that tested whether the effects could be replicated on a nationally representative sample. Accordingly, we report one-tailed hypothesis tests and 90 % confidence intervals in the results presented below. Results largely confirmed the patterns observed in Experiment 1.

Experiment 2. The Not Bravery, Community Interest, and Community Interest + Embarrassment messages increase both intentions to vaccinate and other-regarding outcomes. Panel A displays treatment effects for intentions to vaccinate, Panel B displays the advise a friend, and Panel C displays the judging a non-vaccinator outcomes. Treatment effects for both panels were estimated using OLS regression that included covariates. The effects displayed are a comparison against the placebo control baseline and are presented with 90 % confidence intervals. The dashed vertical line is the effect of the Baseline informational control for each outcome.
The Baseline informational treatment was associated with a modest increase, 0.029 units, in intention to vaccinate (90 % CI: 0.011, 0.046; p < .01, one-tailed test). This effect was a 6 % increase of the observed scale outcome in the untreated control group.
The Community Interest and Community Interest + Embarrassment messages were associated with qualitatively larger effects on intended vaccine uptake. These messages were associated with increases of 0.045 units (90 % CI: 0.021, 0.070; p < .01, one-tailed test) and 0.043 units (90 % CI: 0.019, 0.067; p < .01, one-tailed test), respectively. As with Experiment 1, we recoded those who stated they were “somewhat” or “very” likely to receive the vaccine as 1 and those who did not report that they were likely to receive it as 0 (this analysis was not pre-registered: for consistency we report 90 % confidence intervals). This binary measure produced a predicted rate of intended vaccination in the control group of 51.4 %. Intended uptake was 3.3 percentage points higher in the Baseline information condition (90 % CI: 0.5 pp, 6.0 pp; p < .05, one-tailed test), 3.5 percentage points higher in the Community Interest + Embarrassment condition (90 % CI: −0.1 pp, 7.0 pp; p = .06, one-tailed test), and 5 percentage points higher in the Community Interest condition (90 % CI: 1.3 pp, 0.8.7 pp; p < .05, one-tailed test). The latter effect was proportionally large—10 % compared to the baseline predict rate in the control group (0.050/0.514).
On average, the Not Bravery, Trust in Science, and Personal Freedom messages were approximately as effective as the informational content to which they were added in increasing intention to vaccinate, which differs from Experiment 1 where they modestly outperformed the Baseline informational condition.
Turning to other regarding outcomes, Panel B of Fig. 2 plots effects for advice given to others and Panel C does so for negative judgments of non-vaccinators. The Baseline informational treatment was again associated with statistically significant increases in each outcome. For these outcomes, the Not Bravery, Trust in Science, and both Community Interest messages produced effects that were at least descriptively larger than the Baseline treatment. The effects for the Personal Freedom message were smaller than the Baseline informational treatment, a result that again diverged from Experiment 1.
In terms of advising others to vaccinate, the most effective message was the Community Interest + Embarrassment message, which was also the most effective message in Experiment 1. This effect was 0.07 scale points (90 % CI: 0.043, 0.095; p < .01, one-tailed test), an increase of 14 % compared to the control group average scale score of 0.51 (0.07/0.51). This effect was also statistically distinguishable from the effect of the Baseline informational treatment (difference = 0.045; 90 % CI: 0.020, 0.069; p < .01, one-tailed test). When dichotomizing the advise a friend outcome to better describe the magnitude of the effect, we estimated that the Community interest + Embarrassment message was associated with a 10 percentage point increase (90 % CI: 0.064, 0.140; p < .01, one-tailed test) in intention to advise others to vaccinate compared to the control group, a proportional increase of 27 % compared to the control group baseline of 38 % (0.10/0.38). This effect was approximately 6 points larger than the effect of the Baseline message (90 % CI: 0.026, 0.099; p < .01, one-tailed test).
In terms of judging non-vaccinators, the largest effects were for the Not Bravery and Trust in Science messages, with each effect also statistically distinguishable from the Baseline message. Notably, in this sample the Trust in Science message had large effects on beliefs and actions toward others but appeared ineffective in changing an individual’s own intended vaccination behavior. The Not Bravery message was also the most effective message in this regard in Experiment 1.
We examined three pre-registered differences in subgroup treatment effects to test the patterns observed in Experiment 1. First, confirming Experiment 1 we found that those who did not endorse liberty values were more responsive to the Not Bravery message (compared to the baseline message) than those who endorsed liberty values for the three outcome measures. Second, we did not confirm either preregistered prediction with regard to differences in treatment effects by risk taking that were observed in Experiment 1.
The remaining subgroup comparisons were not pre-registered. Beginning with gender, in comparison to the untreated control, women responded more to the Trust in Science and Community Interest + Embarrassment message than did men (all five outcomes), while men responded more to the Not Bravery and Community Interest (without embarrassment) messages. Democrats were more responsive than Republicans across the board to the different treatment messages, while Republicans appeared to react only to the Community Interest and Community Interest + Embarrassment messages (magnitudes similar to those of Democrats). We observed a similar pattern for differences by baseline vaccine confidence, measured pre-treatment with a multi-item battery of questions [ 33 ]. Those high in vaccine confidence responded to all messages, while those low in confidence responded reliably only to the Community Interest messages.
3. Discussion
Overall, the results point both to a set of effective messages and the potential efficacy of specific messages for some particular subgroups. On average, a simple informational intervention is effective, but it is even more effective to add language framing vaccine uptake as protecting others and as a cooperative action. Not only does emphasizing that vaccination is a prosocial action increase uptake, but it also increases people’s willingness to pressure others to do so, both by direct persuasion and negative judgment of non-vaccinators. The latter social pressure effects may be enhanced by highlighting how embarrassing it would be to infect someone else after failing to vaccinate. The Not Bravery and Trust in Science messages had substantial effects on other regarding outcomes and for some subgroups, but do not appear to be as effective as the Community Interest messages in promoting own vaccination behavior. Importantly, in distinct samples fielded several months apart, the Community Interest, Community Interest + Embarrassment, and the Not Bravery messages produced substantively meaningful increases for all outcomes measures relative to the untreated control, and in some instances did so in comparison to the Baseline information condition.
Our findings are consistent with the idea that vaccination is often treated as a social contract in which people are expected to vaccinate and those who do not are sanctioned [ 10 ]. In addition to messages emphasizing the prosocial element of vaccination, we observed that messages that invoked reputational concerns were successful at altering judgment of those who would free ride on the contributions of others. This work could also help explain why social norm effects appear to overwhelm the incentive to free ride when vaccination rates are higher [ [34] , [35] ]. That is, messages that increased intentions to vaccinate also increased the moralization of non-vaccinators suggesting that they are fundamentally linked to one another. These messages will need to be adapted in specific cultural contexts with relevant partners, such as community leaders.
The robust effect of the Community Interest message advances our current understanding of whether public health messaging that deploys prosocial concerns could be effective at increasing COVID-19 vaccine uptake. The results of both experiments presented here support prior work that demonstrated the effectiveness of communication that explains herd immunity on promoting vaccination [ [15] , [16] ]. It also suggests that a detailed explanation of herd immunity may not be necessary to induce prosocial behavior.
Beyond the theoretical contribution, the results have practical implications for vaccine communication strategies for increasing COVID-19 vaccine acceptance. We identified multiple effective messages that provide several evidence-based options to immunization programs as they develop their vaccine communication strategies. Importantly, the insights into differential effectiveness of various messages by subgroup (e.g. men vs women) could inform messaging targeted to specific groups. Understanding heterogeneous treatment effects and the mechanisms that cause differential responses to persuasive messaging strategies requires additional testing and theoretical development. We view this as a promising avenue for future work.
The experiments presented here are not without limitations. First, we measured intentions to vaccinate at a time when a vaccine was not currently available and the effectiveness and side effects of potential vaccines were not known. This also meant that we could not observe actual vaccination behavior, which is ultimately the outcome of interest. While intentions predict behavior in many contexts [ [36] , [37] ] including vaccination [ [38] , [39] , [40] ], past research examining the effect of behavioral nudges on COVID-19 vaccine uptake has produced divergent evidence when testing the effect of the same treatments in the field on behavior and in a survey experiment on a behavioral intention [ 41 ]. This observation highlights the need for field testing messages that have shown to be successful on increasing uptake intentions in survey experiments to ascertain whether they also increase vaccine uptake. It may be that field tests reveal certain messages are particularly less effective than in the survey context, or that messages are uniformly less effective. Second, given the rapidly evolving nature of the COVID-19 pandemic, attitudes about vaccines may have changed since the experiments were fielded which could also change the efficacy of the messages that we tested. Third, we cannot be sure whether, or how long, the effects we observe here persist. Finally, we only tested text-based messages, but public health messaging is delivered through many mediums, like public service announcements, videos, and images. Future work can adapt the successful messaging strategies found here and test their efficacy when delivered in alternative formats.
Efforts to vaccinate individuals against COVID-19 are currently underway in the United States and it remains important to convince the mass public of the safety and efficacy of COVID-19 vaccines to ensure that the threshold for herd immunity is reached. Our experiments provide robust evidence that appealing to protecting others has effects on intentions to get vaccinated and to apply social pressure to others to do so as well.
4. Materials and methods
4.1. ethics statement.
The experiments reported here were fielded under an exemption granted by the Yale University IRB. Informed consent was obtained from participants and they were informed that they could stop the study at any time. Data was collected anonymously and contained no personally identifiable information.
4.2. Experiment 1
Participants and Procedure. Participants were recruited by the vendor Luc.id to take a survey. Of those who were recruited, 4,361 participants completed the survey. An examination of attrition during the survey reveals that attrition was balanced across groups which minimizes concerns that the treatment effects estimated in the main manuscript are affected by attrition. The survey was programmed using the survey software Qualtrics. The survey was fielded between July 3, 2020 and July 8, 2020.
Experimental Design. Participants first completed basic demographic and pre-treatment attitudinal questions and were asked about their experience with COVID-19. After this, participants read a treatment message. They were required to spend at least 20 s on the survey page that contained the message to given them an adequate amount of time to read it. We allocated 2/15 of the sample to the untreated control condition and 1/5 of the sample to the Information baseline condition due to the number of comparisons that would utilize these conditions. Each of the remaining conditions received 1/15 of the sample. The design and analysis were pre-registered at ClinicalTrials.gov (protocol ID: 2000027983).
Outcome Measures. For COVID-19 vaccine uptake intentions, participants were asked “How likely are you to get a COVID-19 vaccine within the first 3 months that it is available to you?” and “How likely are you to get a COVID-19 vaccine in the first year that it is available to you?” Respondents answered this question on a five-point scale with end points of “Extremely unlikely” and “Extremely likely.” The main text describes how these items were combined for analysis. Turning to the likelihood of advising someone to vaccinate, respondents were asked “How likely are you to advise a close friend or relative to get vaccinated against COVID-19 once a vaccine becomes available?” Respondents also answered this question on a five-point scale with end points of “Extremely unlikely” and “Extremely likely.” Finally, for judging someone who chooses not to vaccinate, respondents read “we would like you to think about a friend or relative who chose not to receive a COVID-19 vaccine when it is available. What would you think about this person? Are they…”. This prompt was followed by four traits: trustworthy, selfish, likeable, and competent. The response options were “not at all”, “slightly”, “somewhat”, “mostly”, and “very.”
Analysis. We used OLS regression with robust Huber-White standard errors and indicators for assigned treatment to estimate treatment effects. We use robust standard errors to address the heteroscedasticity observed when estimating our primary analysis models without them. We included covariates as described in the Supplementary Materials . Comparisons across treatments are from linear combination of coefficients tests. For the subgroup analyses, we restricted the sample to the stated criteria and estimate the model specified here on the subsample. For liberty endorsement and risk taking, we determined who was high and low by splitting the sample at the mean.
4.3. Experiment 2
Participants and Procedure. Participants ( n = 5,014) were recruited by the vendor YouGov/Polimetrix. YouGov provides subjects using a sampling procedure that is designed to match a number of Census demographics. To determine the sample size, we conducted a power analysis to detect effects that were 80 % as large as those observed in Experiment 1. The experiment was fielded between September 9, 2020 and September 22, 2020.
Experimental Design. Participants first completed basic demographic and pre-treatment attitudinal questions and were asked about their experience with COVID-19. Participants were randomly assigned to one of seven conditions: the untreated control, the Information baseline control, Community Interest, Community Interest + Anticipated Embarrassment, Not Bravery, Trust in Science, or Personal Freedom. As in Experiment 1, more participants were assigned to the untreated control condition and the Baseline information control condition, 1/5 and 3/10 of the sample respectively. The remaining five conditions each received 1/10 of the sample. Participants were required to spend at least 30 s on the survey page that had the treatment message. The design and analysis were pre-registered at Open Science Framework.
Outcome Measures. The outcome measurement was the same as described in Experiment 1 with the exception of intelligent being added to the judgment of a non-vaccinator scale.
Analysis. We used the same modeling approach described above to produce the results displayed in Fig. 2 . We included covariates as described in the Supplementary Materials . For subgroup analyses, we estimated OLS regression models with an indicator variable if a person was a member of a subgroup (e.g. high endorsement of liberty) and zero otherwise.
CRediT authorship contribution statement
Erin K. James: Conceptualization, Writing- original draft, Writing- review and editing. Scott E. Bokemper: Conceptualization, Data curation, Formal analyses. Alan S. Gerber: Conceptualization, Writing- review and editing. Saad B. Omer: Conceptualization, Writing- review and editing. Gregory A. Huber: Conceptualization, Data curation, Formal analyses, Writing- original draft, Writing- review and editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
The authors would like to acknowledge support for the Tobin Center for Economic Policy at Yale University. EKJ and SBO were supported by the Yale Institute for Global Health.
SEB, ASG, and GAH received support from the Institution for Social and Policy Studies and the Center for the Study of American Politics at Yale University.
Appendix A Supplementary data to this article can be found online at https://doi.org/10.1016/j.vaccine.2021.10.039 .
Appendix A. Supplementary material
The following are the Supplementary data to this article:
- Open access
- Published: 09 November 2023
To vaccinate or not to vaccinate? The interplay between pro- and against- vaccination reasons
- Marta Caserotti 1 ,
- Paolo Girardi 2 ,
- Roberta Sellaro 1 ,
- Enrico Rubaltelli 1 ,
- Alessandra Tasso 3 ,
- Lorella Lotto 1 &
- Teresa Gavaruzzi 4
BMC Public Health volume 23 , Article number: 2207 ( 2023 ) Cite this article
1842 Accesses
1 Altmetric
Metrics details
By mid 2023, European countries reached 75% of vaccine coverage for COVID-19 and although vaccination rates are quite high, many people are still hesitant. A plethora of studies have investigated factors associated with COVID-19 vaccine hesitancy, however, insufficient attention has been paid to the reasons why people get vaccinated against COVID-19. Our work aims to investigate the role of reasons in the decision to get vaccinated against COVID-19 in a representative sample of 1,689 adult Italians (March–April 2021) balanced in terms of age, gender, educational level and area of residence.
Through an online questionnaire, we asked participants to freely report up to three reasons for and against COVID-19 vaccination, and the weight each had in the decision to get vaccinated. We first investigated the role of emotional competence and COVID-19 risk perception in the generation of both reasons using regression models. Next, we studied the role that the different reasons had in the vaccination decision, considering both the intention to vaccinate (using a beta regression model) and the decision made by the participants who already had the opportunity to get vaccinated (using a logistic regression model). Finally, two different classification tree analyses were carried out to characterize profiles with a low or high willingness to get vaccinated or with a low or high probability to accept/book the vaccine.
High emotional competence positively influences the generation of both reasons (ORs > 1.5), whereas high risk perception increases the generation of positive reasons (ORs > 1.4) while decreasing reasons against vaccination (OR = 0.64). As pro-reasons increase, vaccination acceptance increases, while the opposite happens as against-reasons increase (all p < 0.001). One strong reason in favor of vaccines is enough to unbalance the decision toward acceptance of vaccination, even when reasons against it are also present ( p < 0.001). Protection and absence of distrust are the reasons that mostly drive willingness to be vaccinated and acceptance of an offered vaccine.
Conclusions
Knowing the reasons that drive people’s decision about such an important choice can suggest new communication insights to reduce possible negative reactions toward vaccination and people's hesitancy. Results are discussed considering results of other national and international studies.
Peer Review reports
Introduction
By mid 2023 the European Union reached nearly 75% vaccine coverage for the primary vaccine cycle against COVID-19, with countries such as Croatia, Slovakia, and Poland falling short of 60% and others such as France, Portugal, and Italy close to 90% [ 1 ]. Although vaccination rates are, on average, quite high, many people are still hesitant. Vaccine hesitancy indicates the delay or refusal of a vaccine despite availability in vaccine services [ 2 , 3 ] and is a multidimensional construct, resulting from the interaction between individual, social, and community aspects [ 4 ]. In the last two years, a plethora of studies have investigated factors associated with COVID-19 vaccine hesitancy showing, for example, that vaccine hesitancy is higher in women [ 5 , 6 ], in young people [ 5 , 7 , 8 ], in people with low education [ 8 , 9 ], low trust in authorities [ 10 , 11 ], and strong conspiracy beliefs [ 5 , 12 , 13 ]. However, to the best of our knowledge no one has investigated the interplay that pro- and against- vaccination reasons may play in the choice to get vaccinated, namely what happens when a person has both pro- and against-vaccine considerations. Trying to fill this gap in the literature, our work aims to investigate how different reasons and the importance people place on them are likely to influence the decision to get vaccinated against COVID-19.
In line with the vaccine hesitancy continuum defined by SAGE [ 2 ], while extremely pro-vax people are likely to express only reasons pro-vaccination and extremely no-vax people are likely to express only reasons against vaccination, individuals who fall between the two extreme end-points are likely to feel some doubts. This large number of people offer us the unique opportunity to assess which category of reasons (pro- vs. against- vaccination) is more impactful in driving people's vaccination decisions. As it is reasonable to imagine, among the reasons for choosing to get (or not) vaccinated some reasons are more rational, while others are more related to affect. For example, there are people who rationally recognize the importance of vaccines but at the same time are frightened by the side effects. Thus, the decision to get (or not) vaccinated is the result of a complex process, in which costs and benefits are weighed more or less rationally. Indeed, while several studies have pointed out that the decision to vaccinate is due to cognitive rather than emotional processes [ 14 , 15 , 16 , 17 ], others have highlighted the role of affect and risk perception in the vaccination decision [ 18 , 19 , 20 ]. Thus, the intention to accept the vaccine is driven by emotional and affective feelings as much as by cognitive and rational judgments. Particular attention to what people feel and think about vaccine-preventable diseases and vaccination in general is paid in the model developed by the “Measuring Behavioral and Social Drivers of Vaccination” (BeSD), a global group of experts established by the World Health Organization [ 21 ]. This model encompasses two groups of proximal antecedents of vaccination, namely, what people think and feel (e.g., perceived risk, worry, confidence, trust and safety concerns) and social processes (e.g., provider recommendation, social norms and rumors). Antecedents affect vaccination motivation (i.e., vaccination readiness, willingness, intention, hesitancy), which can then be strengthened or weakened by practical issues (such as vaccine availability, convenience and cost but also requirements and incentives), resulting in acceptance, delay or refusal of vaccination (vaccination behavior).
Although some studies have considered whether the cognitive or affective component has greater weight in determining the intention to vaccinate, no one, to the best of our knowledge, has studied the interplay between pro- and against- vaccination reasons, nor the weight these have in the choice to vaccinate. In addition to the drivers already studied in the literature [ 5 , 6 , 7 , 8 , 11 , 12 ], we believe that the focus on this interaction may be relevant to better understand the complex phenomena related to vaccine hesitancy. Few recent studies have attempted to investigate the complexity of vaccination choice by studying the reasons why people choose to get (or not) vaccinated against COVID-19. Fieselmann and colleagues [ 22 ] highlighted that among the reasons that reduce adherence to vaccination are a low perception of its benefits, a low perception of the risk of contracting COVID-19, health concerns, lack of information, distrust of the system, and spiritual or religious reasons. Another study, instead, shed light on the reasons that encourage hesitant people to consider vaccination, such as protecting themselves, their family, friends and community from COVID-19, and being able to return to normal life [ 23 ].
In the present study we asked the participants to spontaneously come up with their own reasons to get (or not) vaccinated, without limiting or influencing them with a set of predefined options to choose from, thus aiming to obtain more genuine answers that may better capture the intuitive aspect of people’s opinions (for a similar reasoning see [ 24 ]). The procedure we used has been implemented by Moore et al. [ 23 ], the only study, as far as we know, that asked for reasons with an open-ended question. Critically, in their study, participants were asked to report only reasons in favor of vaccination (e.g., "What are your reasons for getting the COVID-19 vaccine?"), excluding reasons against. By contrast, we asked participants to freely report up to three reasons in favor and up to three reasons against COVID-19 vaccination and to rate on a 5-point Likert scale their weight in the decision about getting (or not) vaccinated.
From a theoretical point of view, the reasons pro- and against vaccination may be seen within the framework of prospect theory [ 25 , 26 ] which suggests that people evaluate the outcome of a choice based on a reference point, against which losses and gains are determined: the former below this point, the latter above this point. Importantly, especially in this specific context, losses and negative consequences are weighted more than gains and benefits, making us hypothesize that if a person has one reason for and one reason against the vaccine, which are of equal importance, they will more likely lean toward choosing not to vaccinate. Consistently, it is known that negative experiences have a greater impact than neutral or positive ones (i.e., the negativity bias [ 27 ]).
Besides delving into the reasons that may influence the choice to get (or not) vaccinated, it would be interesting to also look at the individual differences that may determine the reporting of pro- and against- vaccination reasons and their valence. In this regard, the literature suggests that risk perception and emotion regulation can both have a great impact in the decision to get vaccinated. For instance, studies conducted during H1N1 influenza have shown that perception of disease-related risk is one of the strongest predictors of vaccine adherence [ 28 , 29 ]. Additional insights have been provided by more recent studies investigating the role of COVID-19 risk perception in the decision to get vaccinated against COVID-19. Viswanath and colleagues [ 30 ] showed that people are more willing to vaccinate themselves and those under their care to the extent to which they feel more vulnerable to COVID-19 and rate the consequences of a possible infection as severe. Such a relationship between COVID-19 risk perception and intention to vaccinate was confirmed by another study using a cross-sectional design, which focused on the early months of the pandemic [ 31 ]. This study also examined how risk perception changed during the pandemic phases and showed that during the lockdown, compared to the pre-lockdown phase, also those who reported some hesitancy were more likely to get vaccinated when they perceived a strong COVID-19 risk.
With regard to emotion regulation, the literature suggests that people react differently to affective stimuli [ 32 ] and that their decisions are influenced by their abilities to regulate emotions [ 33 , 34 ]. Recent works investigating the relationship between hesitancy in pediatric vaccinations and the emotional load associated with vaccinations, have shown that a negative affective reaction is one of the factors leading to lower vaccine uptake [ 35 , 36 ]. Specifically, Gavaruzzi and colleagues [ 36 ] showed that concerns about vaccine safety and extreme views against vaccines are associated with vaccine refusal. Interestingly, they also showed that parents' intrapersonal emotional competences, i.e., their ability to manage, identify, and recognize their own emotions, is critical to vaccine acceptance for their children. Therefore, in our study we measured people's risk perception and emotional competencies to assess their possible role in the production of reasons in favor and against vaccination.
As described in Fig. 1 , the relationship between different domains of interest can be hierarchically structured, using a directed acyclic graph, starting from the risk perception and emotion regulation, to the generation of pro- and against- vaccination reasons and their valence, and finally to the vaccination willingness/adherence. With respect to the mentioned structure, we are interested to investigate the following research hypotheses:
The number and weight associated with reasons pro- and against-vaccination should be influenced by individual differences in the ability to regulate emotions;
The number and weight associated with pro-vaccination reasons should be influenced by individual differences in COVID-19 risk perception;
A higher number of strong (i.e., with high weight) reasons pro- (vs. against-) vaccination should correspond to a more (vs. less) likelihood to accept the vaccination.
Generating an equal number of reasons in favor and against vaccination should lead to a weaker likelihood to accept the vaccination.
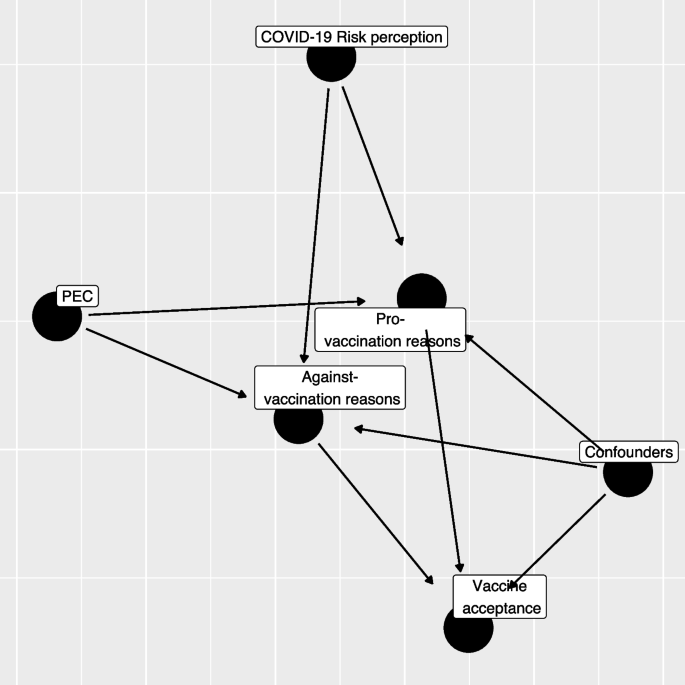
Directed Acyclic Graph (DAG) between variables considered in the study (PEC: Short Profile of Emotional Competence scale)
As we conducted the study between March and April 2021, a time when vaccinations were being progressively rolled out, we decided to consider the role of personal reasons on both the intention to get vaccinated (for those who had not yet had the opportunity to get vaccinated) and the choice already made (e.g., vaccine received or booked vs. refused).
Finally, through a non-parametric classification analysis, we will explore how specific pro- and against-vaccination reasons impact the decision to get (or not) vaccinated. Specifically, we will investigate the role that different categories of reasons play in the choice to vaccinate.
Participants
Data collection was commissioned to a survey and market research agency (Demetra Opinions.net), with the aim of securing a representative sample of the adult (+ 18) Italian population, estimated at 49.8 million [ 37 ]. The sample was balanced in terms of age, gender, educational level (middle school or lower, high school, degree or higher), and area of residence (North, Center, South, and Islands). The agency distributed via email the survey link to its panelists, who freely decided whether to participate in the study in exchange for financial compensation. Out of 1,833 participants who started the questionnaire, 77 (4%) were excluded because they did not complete the survey and 16 (0.9%) were excluded since they reported offensive content in open-ended questions. Finally, 124 (6.8%) participants were excluded because of missing information. Thus, the final sample consisted of 1,689 participants. The project was approved by the ethical committee for Psychology Research of the University of Padova (Italy), with protocol number 3911/2020 and informed consent was obtained for all participants.
We developed an ad-hoc questionnaire including a series of open-ended and closed questions (see Additional file 1 : Appendix 2 for the full material). We first investigated the vaccination status of the participants, asking whether they already had received at least the first dose, whether they had booked it or were still ineligible, and finally whether they had refused the vaccination. Those not yet eligible were asked to rate how likely they would be to get vaccinated at the time they responded (0 = Not at all likely , 100 = Extremely likely ). Then, we asked participants to report a maximum of three reasons both in favor of the COVID-19 vaccine and against it (in counterbalanced order) and to rate how much each of the reported reasons weighed in their choice to vaccinate or not, on a 5-point likert scale (1 = Not at all , 5 = Extremely ). Due to the sparsity on the rate and the number of provided reasons we re-coded the provided information into two semi-quantitative variables, one for pro- and one for against- vaccination reasons, as following: missing/invalid reasons, low average rating (answers 1–3 on the Likert scale) and 1–3 reasons, high rating (answers 4–5 points on the Likert scale) and 1 reason, and high average rating (answer 4–5 points on the Likert scale) and 2–3 reasons.
The questionnaire also included the 20-item Short Profile of Emotional Competence scale (S-PEC; [ 38 ]) to measure intra- and inter-personal emotional competences separately. The intra-personal scale (10 items) refers to emotional competences related to oneself and it includes items such as "In my life I never make decisions based on my emotions'' or "I don't always understand why I react in a certain way". The inter-personal scale (10 items) refers to emotional competences related to other people and it includes items such as “If I wanted, I could easily make someone feel uneasy” or “Most of the time, I understand why the people feel the way they do”. All items are answered on a 7-point likert scale (1 = Not at all agree , 7 = Completely agree ). The internal consistency of the S-PEC scale, measured by means of Cronbach’s α, was adequate (α = 0.81). Further, we measured participants' risk perception of COVID-19 by asking them to indicate how scared they felt of the virus, how serious they think the disease is, how likely they think they are to get sick, and how worried they feel about the various mutations [ 10 , 31 ]. We then asked participants to report their age, gender, educational level, their occupation (health workers, white-collar workers, entrepreneurs, other non-health-related contract forms, and the unemployed), whether they already had COVID-19 (No or don't know, Yes asymptomatic, Yes with few symptoms, and Yes with severe symptoms). The questionnaire was pilot tested by 30 participants who filled the questionnaire first then were asked to discuss and comment on the comprehension of the wording of questions and answer options. Two questions were slightly reworded to improve clarity.
Scoring of reasons
In the first instance, a bottom-up process from reasons to categories was followed by reading a sample of both types of reasons, with the aim of constructing initial categorizing patterns. Examples of pro-vaccination reasons include protection of personal and public health, return to normality, and civic duty; while reasons against vaccination include fears for one's health, sociopolitical perplexity, and distrust of science and institutions (see Additional file 1 : Appendix 1). At this stage, response information was added to the categorizations indicating whether the responses were valid or missing/invalid. Specifically, valid responses had both a reason and the respective weight; missing/invalid responses were those where reason, weight or both were missing or with utterly unrelated concepts or meaningless strings or letters. Finally, by applying a top-down process, we constructed macro categories by merging specific conceptually assimilated categories, so as to avoid the dispersion of data into too many ramifications (see Table S 5 ).
Statistical analysis
Descriptive analysis.
All the analyses were performed only on respondents with no missing observations on the variables of interest (1,681, 92%) excluding also a limited number of those with a non-valid set of pro- or against-vaccination reasons (Table S 1 ; 0.9%). The study variables were summarized in frequency tables and figures (frequency for categorical variables, median and Interquartile Range (IQR) for continuous variables). Kruskal–Wallis tests were computed to compare the distribution of continuous variables across the categories of vaccine status. Categorical variables were compared using chi-squared or Fisher's exact test where expected frequencies in any combination were less than 10. Statistical significance was assumed at the 5% level.
COVID-19 Perceived risk—exploratory factor analysis
An Exploratory Factorial Analysis (EFA) was performed on groups of variables related to COVID-19 perceived risk: scare, severity, contagiousness, and the likelihood of mutation. Since the presence of limited support (0–100 scale) and non-normal marginal distribution, the EFA was performed using a weighted least square mean and variance adjusted (WLSMV) estimator. We extracted from the EFA only the first factor, which explained the highest percentage of variance (Table S 2 ; 61%). The estimated loadings were then used to calculate the regression factor scores. The number and the name of items included, their internal consistency (Cronbach’s α), the estimated loadings, and the proportion of deviance explained are reported in Table S 2 .
Propensity score weighting
At the time of data collection (March–April 2021), the vaccine offer was not opened to the entire population. To adjust the estimates of the following regression models for the propensity to receive the vaccine, we estimated a logistic regression model in which the dependent variable was the response to the question about a previous vaccination offer (Yes/No), while all the factors that can influence the vaccine proposal served as independent variables: age-class (young ≤ 25, young adult 26–45, adult 46–65, elderly 66–84), gender (male, female), occupational status (health worker, not at work, not health worker-employer, not health worker-entrepreneur, not health worker-other), educational level (low = middle school or lower, medium = high school, high = degree or higher), key worker status (yes, no, I don’t know), past COVID-19 contagion (no, yes asymptomatic, yes low symptoms, yes severe symptoms), and familiar status (single/in a relation, married/cohabitant, divorced/separated/other). The predicted probability was used to estimate the weights for the following regression models using a framework based on an inverse probability of treatment weighting (IPTW; for further details, see [ 39 ]).
Regression models
Our research questions can be summarized by trying to describe the relationship exploited by the directed acyclic graph in Fig. 1 . The first step regression model aims to assess how S-PEC scores (inter- and intra-personal) and COVID-19 risk perception influenced the reasons pro- and against-vaccination produced by participants while considering the presence of a set of confounders (age-class, gender, occupational status, educational level, key worker status, and familial status).
Since both the pro- and against-vaccination reasons are formed by a categorical variable with 4 levels (missing/invalid, low 1/2/3 reasons, high 1 reason, high 2/3 reasons), we evaluated whether S-PEC and COVID-19 risk perception scores influenced the distribution of pro- and against-vaccination reasons employing two different multinomial regression models including all the previously mentioned variables (S-PEC, COVID-19 risk perception, and confounders). The overall significance of a variable in the model was tested using an analysis of the variance (ANOVA).
The second step in the analyses was taken to investigate whether the generation of pro- and/or against-vaccination reasons affected the willingness to be vaccinated or the vaccine acceptance. Each participant reported their willingness to get vaccinated on a 0–100 scale or, in case a COVID-19 vaccine had been already offered, their vaccination status (done, booked, or refused). For respondents who had not yet been contacted for booking/getting the vaccination, we evaluated whether pro- and/or against vaccination reasons influenced the willingness to be vaccinated by employing a beta regression model in which the respondent variable scale (0–100) was rescaled to be a relative frequency [ 40 ]. The full models included the semi-quantitative pro- and against-vaccination reasons variables and, even if non-statistically significant, all the confounders in order to adjust for age class, gender, educational level, occupational status, familial status, and key worker status. Beta regression coefficients were estimated using a maximum likelihood estimator (MLE). Results were presented in terms of Odds Ratios (ORs) by exponentiating the estimated coefficients and producing a relative 95% Confidence Interval (95% CI).
A further regression analysis was conducted through a logistic regression model to explain which factors influenced vaccine acceptance (done/booked vs. refused) among those who already received the vaccine offers. The full model included the same variables considered in the previous beta regression model, after recoding the variables related to pro- and against-vaccination reasons into a binary form (missing/invalid vs. presence of at least one valid reason) due to low sample size and the sparsity of the response variable. As a consequence, we tested a simplified version of Hypothesis 3, considering the presence (vs. missing/invalid) of pro- or against-vaccination reasons in order to test their influence on the probability of having accepted/booked the vaccination.
Results were reported employing ORs and relative 95% Confidence Interval (95% CI).
Both the beta regression and logistic regression were weighed using an IPTW scheme to take into account the presence of a different probability of a vaccine offer among respondents.
The presence of an interaction between pro- and against-vaccination reasons was tested by means of a likelihood ratio test. The regression models were estimated through the R 4.0 program (R Core Team, 2021), and for the beta regression we employed the betareg package [ 41 ].
Classification tree analysis
Two different classification tree analyses were carried out to characterize profiles with a low or high willingness to get vaccinated (respondents who had not yet been offered a vaccine) or with a low or high probability to accept/book the vaccine (respondents who had already received a vaccine offer).
Although the dependent variables were non-normally distributed (scale 0–100 or binary 0/1), we considered them continuously distributed adopting a splitting criterion based on the analysis of the variance (ANOVA). We tested the inclusion in the model considering the type of pro- or against-vaccination reasons. A tree pruning strategy was adopted to reduce classification tree overfitting considering the overall determination coefficient (R 2 ) as an indicator and fixing that at each classification step in the tree if the R 2 did not increase by 0.5% the tree should be stopped. Classification tree analysis was performed using the rpart package [ 42 ] on R environment [ 43 ].
The main characteristics of the respondents by vaccination status (received, booked, not yet, and refused) were reported in Table 1 . Among respondents, 23.3% were offered the vaccination and, among them, 13.8% refused it (Fig. S 1 ). Among those not yet eligible, willingness to be vaccinated showed a median value of 80 points (average: 68.7). The distribution of gender was almost equal (51% females, 49% male), and the median age was 47 years old (IQR: 34–57 years). Educational level was low in 41% of the sample, while the most represented employment status was not at work (39%) followed by employed (37%), and entrepreneur (9.8%). A quarter (26%) of respondents classified themselves as key workers during the COVID-19 pandemic. The predominance of respondents (63%) were married or living with a partner, while only 9% had had a COVID-19 infection.
COVID-19 risk perception and the S-PEC score (intra- and inter-personal) were categorized into three categories according to empirical tertiles (low:1 st tertile, medium: 2 nd tertile, high: 3 rd tertile). The level of COVID-19 risk perception differed across vaccination status ( p < 0.001). The reasons pro- and against-vaccination have a different distribution according to COVID-19 vaccination status (Table 2 ). The highest frequency of pro-vaccination reasons was reported by those who received the COVID-19 vaccination; conversely the lowest frequency of pro-vaccination reasons was generated by those who refused the vaccine, whereas, intermediate frequencies were shown by people who were not yet offered the vaccination and those who had booked the vaccine, who reported a comparable distribution of the number of pro-vaccination reasons. A reverse pattern was exhibited for against-vaccination reasons, which were generated with the highest percentage by respondents who refused the vaccine (in particular high and multiple reasons). Conversely those who have booked/done the COVID-19 vaccine showed the lowest frequency of reasons against vaccination, while respondents without a vaccine offer reported an intermediate frequency of reasons against vaccination.
The estimated results of the propensity score model for the vaccine offer are shown in Table S 3 . Respondents older than 65 years exhibited a nearly four-fold increase in the probability to be contacted for the vaccination with respect to the reference age-class (≤ 25 years). All non-health employees showed a high drop in the probability of having received the vaccination offer, while the probability increased as the educational level increased. Being a key worker during pandemic resulted in an increased probability of having received the vaccination proposal while no statistical significant influence was observed for the past COVID-19 contagion or for familial status. The distribution of the propensity score by vaccine status obtained by the model is reported in Fig. S 1 , in which it is shown that the distribution is different by vaccine offer, but the two density functions partially overlap. The discriminant power of the propensity score estimated was only discrete (ROC analysis, AUC: 71.8%).
The results of the multinomial regression models which investigated the effect of emotional competences and risk perception on the generation and the predictors of pro- and against-vaccination reasons with respect to missing/invalid level and the reference categories are presented in Table 3 (see also Fig. 1 ). Compared to the reference category (missing/invalid), high values of S-PEC-self were associated with a higher probability to report pro- and against-vaccination reasons (all ORs > 1.5), while high values of S-PEC-others were associated with a mild probability to report multiple pro-vaccination reasons (all ORs > 1.42). A high (vs. low) COVID-19 risk perception increased the frequency of one strong pro-vaccination reason while it had a null or low decremental effect on the frequency of against weak vaccination reasons. Further, medium (vs. low) COVID-19 risk perception only increased the strong pro-vaccination. Compared to the reference age-class (young), adults and elderly showed a higher probability to generate a strong unique pro-vaccination reason (adults vs. young OR: 1.72, 95%CI: 1.07–2.77); elderly vs. young OR: 2.24, 95%CI: 1.26–4.00), while lower probability to generate against vaccination reasons was observed for elderly compared to young respondents (OR: 0.48, 95%CI: 0.26–0.90). Female participants generated fewer strong pro-vaccination reasons (ORs < 0.73), and also fewer multiple weak against-vaccination reasons (OR: 0.68, 95%CI: 0.51–0.91) compared to male participants. Overall, the occupational status did not affect the generation of pro- and against-vaccination reasons (ANOVA test p > 0.05); however an increased frequency of low 1/2/3 against-vaccination reasons emerged among the category “Other—not health workers” compared to the reference group represented by health workers (OR: 2.52, 95%CI:1.09–5.86). Pro-vaccination reasons are more frequent as the educational level becomes higher, while the relation of the educational level with against- vaccination reasons appears weaker and significantly increased only for the presence of multiple weak reasons against vaccination (High vs. Low educational level, OR: 2.10, 95%CI: 1.45–3.03). Not being a key worker is related to a higher frequency of multiple strong both pro- and against vaccination reasons. The familiar status did not seem to be related to the frequency or the strength of the reasons, except for the status of divorced/separate/other that, with respect to the reference category single/in a relation, showed a twofold increase in the frequency of a strong unique against vaccination reason.
Through a beta regression model we investigated the predictors of willingness to be vaccinated for the participants who had not yet received the vaccination offer. As shown in Table 4 , the generation of pro- and against-vaccination reasons strongly influences the willingness to be vaccinated. The predicted probability from the combination of pro- and against-vaccination reasons is shown in Fig. 2 (and Table S 4 ): respondents who did not report any reasons had an average predicted probability above 60%, while the presence of at least one reason against vaccination decreased the willingness to be vaccinated, in particular in the case of strong multiple against vaccination reasons. On the other hand, the presence of at least one pro-vaccination reason strongly increased the probability. In the end, the presence of both strong multiple pro and against vaccination reasons resulted in a high probability of getting the vaccine. Regression models adjusted by propensity score weighting allowed us to comment the influence of potential confounders: males reported an increased willingness to be vaccinated (vs. females; OR: 1.26, 95%CI: 1.11–1.42), and so did those with a high educational level (vs. low; OR: 1.22, 95%CI: 1.04–1.44) while the opposite was true among no key workers (vs. key workers; OR: 0.85, 95%CI: 0.72–0.99).
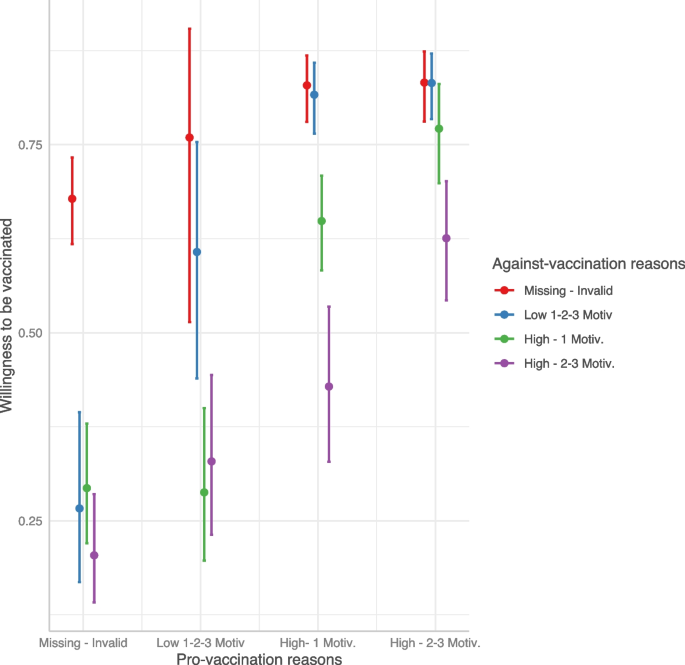
Predicted willingness to get vaccinated by interaction between pro- and against-vaccination reasons
Finally, with a logistic model we investigated the predictors of vaccine acceptance\booking. As shown in Table 5 , people who accepted or booked the COVID-19 vaccine were more likely to show pro-vaccination reasons and less likely to show against-vaccination reasons. Interestingly, when both kinds of reasons were provided, the probability of getting/booking the vaccine remained nevertheless very high (Fig. 3 ). Compared to the age class [46-65], younger age classes reported a strong reduction in the probability to have accepted/booked the vaccine. Male participants (OR: 1.53, 95%CI: 1.10–2.12) and those with a high educational level (OR: 2.65, 95%CI: 1.60–4.54) showed an increased probability of vaccine acceptance/booking when compared to females and participants with medium educational level, respectively. Being a health worker had a strong and positive influence on the probability of getting/booking the vaccine with respect to those employed as no health workers (OR: 6.61, 95%CI: 2.10–30.9).
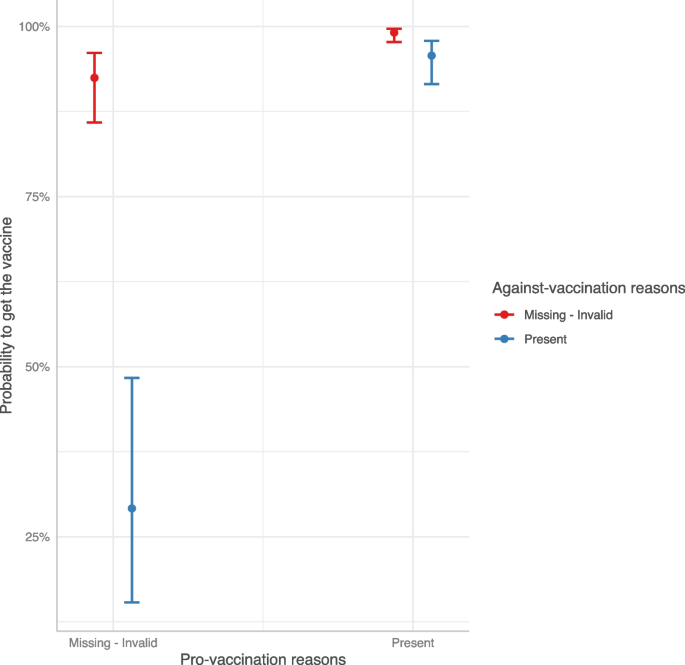
Predicted COVID-19 vaccine acceptance/booking probability by interaction between pro- and against-vaccination reasons
Two regression tree models were estimated separately on the willingness to be vaccinated for those who had not yet received the vaccine offer and on the booking/acceptance of the vaccination in case of vaccine offer. Results are shown in Fig. 4 . Considering the willingness to be vaccinated, the presence of distrust in the vaccination was the most discriminant variable; this latter in conjunction with reasons related to protection, herd immunity, and the absence of no clinical trials guided the willingness to be vaccinated. In particular, the combination of the absence of reasons related to distrust and the presence of protection reasons showed the highest values on the intention to get vaccinated (average value = 83 points, 22% of the sample). On the other side, the presence of at least one reason related to distrust without any positive reasons concerning protection, herd immunity, and trust predicted the lowest willingness to be vaccinated (average value = 29 points, 6% of the sample).
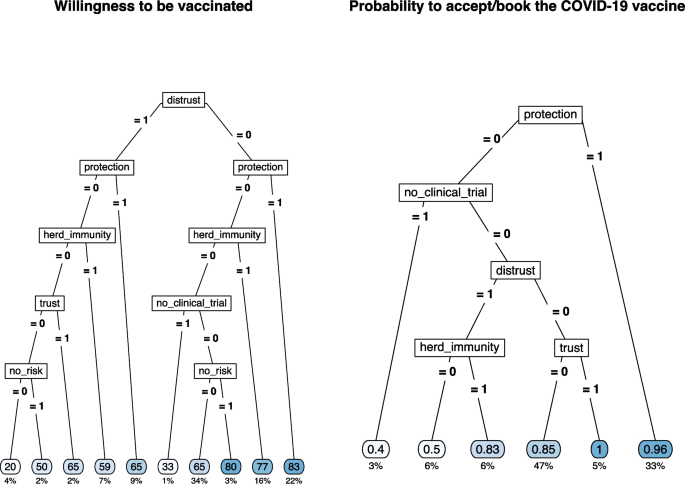
Regression tree for the willingness to be vaccinated (left) and for COVID-19 vaccine acceptance/booking (right) by selected type of pro- and against-vaccination reasons
The sense of protection given by the vaccine or the trust in the vaccination was the main reason for vaccination acceptance/booking (average probability = 0.96 and 1.00, 33% and 5% of the sample, respectively). The combination of the absence of protective reasons and the presence of doubts about the lack of clinical studies results in the lowest likelihood of accepting/booking the vaccination (average probability = 0.40, 3% of the sample). The presence of distrust and the belief in herd immunity were the other discriminant reasons with intermediate results in terms of the probability to accept/book the vaccination.
The frequency of each category of pro- and against-vaccination reasons by COVID-19 vaccine status is shown in Table S 5 .
In the present study we aimed to investigate the reasons behind the decision to get (or not) vaccinated against COVID-19 by asking participants to report up to three reasons in favor and three reasons against the COVID-19 vaccination and to indicate the weight these reasons had in their decision. Although some researchers discourage categorization, the sparsity of the responses related to the number of reasons and their weight implies a semi-quantitative solution since a simple variable multiplication between rating and frequency (recoding to zero in case of zero reasons) is not feasible. In this case, this approach was not satisfactory as such coding would not allow differences underlying identical scores to emerge. For example, only 1 strong motivation (rating 5) would be coded in the same way as three motivations with weights 1, 2, and 2. Instead, we decided to categorize the combination of frequency-weight reasons as categorical variables (missing/invalid, low 1/2/3 reasons, high 1 reason, high 2/3 reasons) in which rating and number of reasons are combined into a single variable. This categorization allows us not only to study the weight that different categories have on the decision to get vaccinated but also to overcome the risk of imputing a specific value for missing responses.
As shown in Fig. 1 , analyses were run in two steps. The first step aimed to assess how emotional competences and risk perception impacted the generation of reasons pro- and against-vaccination (Hypotheses 1A and 1B), whereas the second step investigated how different reasons affected the intention to get vaccinated (Hypotheses 2 and 3). The results support the hypotheses that emotional competences and risk perception play a significant role. Regarding emotional competence as measured by the S-PEC, the results show that high intra-personal emotional competence positively influences the production of stronger and more numerous pro-vaccination and against-vaccination reasons (confirming Hypothesis 1A). This result suggests that greater awareness of one's emotions and of what one is feeling promotes higher fluency in the production of reasons about the vaccination. Research has shown that people can be ambivalent about vaccines and hold both positive and negative reasons [ 2 , 44 ]. It is reasonable to assume that, compared to people with low intra-personal emotional competences, those with high intra-personal emotional competences are more likely to have higher awareness of these contrasting attitudes and to embrace them without suppressing one of the two stances. Furthermore, the results showed that only high inter-personal emotional competences influence the generation of multiple strong reasons in favor of vaccination, and this appears to be related to the perception of vaccines as a public good and a tool to protect others. As for risk perception, a moderate to high perception of risk associated with COVID-19 influences the generation of strong pro-vaccination reasons (confirming Hypothesis 1B). These results are in line with the literature showing that a high perception of risk associated with COVID-19 positively influences the decision to get vaccinated [ 30 , 31 , 45 , 46 , 47 ]. In particular, perceiving a medium/high risk leads to generating a high number of reasons strongly in favor of vaccination, while reducing the number and weight of the reasons against the vaccine. The main premise of the psychological literature examining the relationship between risk perception and affect is that one’s behaviors are affected by rapid and intuitive evaluations, either positive or negative, people make while assessing things happening around them [ 48 , 49 ]. Thus, an event is evaluated not only on the basis of objective information, but also on the basis of the experienced feelings. Emotional competence, which is clearly related to affect, also modulates how we perceive and process the emotional component underlying our judgments [ 36 ].
The results also show that, compared with younger people, those over 45 more frequently produce reasons in favor of vaccines while those over 65 produce fewer reasons against vaccination. These results are in line with the fact that younger people are at lower risk of severe consequences than older people [ 50 ], but can also be explained by considering that age was particularly salient during the period of the data collection, as the vaccination campaign was phased out by age groups, starting from the elderly. As for gender, women produced less strong pro-vaccine and weak-against vaccine reasons than men. These results are congruent with the general findings in the literature on vaccine hesitancy showing that females are more hesitant than males [ 5 , 51 , 52 ]. Furthermore, medium and high educational levels favored the production of both pro- and against-vaccination reasons, whereas not being in a relationship or being divorced/separated increased the generation of a strong reason against vaccination. Consistent with previous work [ 53 ], we confirmed that non-health professionals participants or non-key workers categories showed a lower intention to get vaccinated and a higher likelihood of having refused the vaccine compared to health care and key workers.
Once the role of demographics aspects and individual differences on the generation of reasons pro and/or against vaccination had been established, we ran two additional models to assess the role that those reasons have on the decision to accept the vaccination (see Fig. 1 ). More specifically, we tested the hypothesis that a higher number of pro- (vs. against-) vaccination reasons, connoted by a higher weight, corresponded to a stronger (vs. weaker) acceptance of vaccination (Hypothesis 2). Since data collection took place between March and April 2021, when the vaccination campaign had already started in Italy, we developed two different regression models, with the first investigating the willingness to be vaccinated in participants who were not yet offered the vaccine and the second investigating the likelihood of accepting/booking or refusing the vaccine in those who already received the offer. In particular, thanks to the propensity score weighting technique, we managed to reduce the estimates bias, especially for those factors (age, occupational status, and educational level) that influenced the vaccine offer the most [ 54 ]. The results of the two models are very similar, as the intention to get vaccinated and the likelihood of having accepted/booked the vaccine are predicted by the same factors. Specifically, the production of strong positive reasons increases either the intention to get vaccinated or having accepted/booked the vaccination. In contrast, generating strong negative reasons reduces vaccination intention and predicts the refusal of the vaccination. Hypothesis 2 is thus confirmed.
Results on the interactions between reasons, pro- and against-vaccination, and vaccination intention or vaccination choice are particularly worthy of attention. The third hypothesis was derived from the literature on prospect theory [ 25 , 26 ], suggesting that at equal intensity subjective losses are more important in determining a decision than subjective gains. We therefore expected that negative reasons would count more than positive reasons in deciding whether to get vaccinated or to accept the vaccine. However, in contrast to our hypothesis, the results showed that just the generation of a single positive reason with a strong weight was enough to shift behavior and attitude in favor of the vaccination, regardless of the number and weight of negative reasons. In other words, vaccine refusal is predicted by the absence of any positive strong reasons, while when people generate both positive and negative reasons, the positive ones seem to yield a particularly important role when having a strong weight. According to prospect theory, people evaluate their goals depending on the reference point they focus on. During the pandemic, the vaccination offered an opportunity to be safer, reduced the risk of infection, and more generally appeared as the best way to re-open and get back to life as it was before COVID-19. After a year of pandemic characterized by periods of lockdown and some re-opening attempts, people were likely feeling in a state of loss (e.g., the lost freedom to go out and meet with friends and family, the lost freedom of traveling) and were looking forward to whatever chance available to recover and return to their previous lifestyle and habits. Just as those who gamble are willing to do anything to make up for a loss, so probably those who were not entirely certain about the vaccine were more willing to take risks to recover the loss in quality of life. It follows that the pandemic emergency made people forgo some of their doubts about the vaccine when, at the same time, they had reasons to get their shot. In addition, several studies [ 19 , 55 , 56 ] have highlighted the relationship between anticipated regret and vaccination, showing that anticipated regret is associated with an increased likelihood of adhering, or having one's children adhere, to vaccine offerings. Trusting that the vaccine would work, focusing less on its potential side effects, made sense for people who were looking forward to recovering what was perceived (and was indeed) a loss of quality of life and freedom, because they desired to be back doing the things had ever enjoyed doing (e.g., going to restaurants, movies, etc.). This finding is also interesting from a communicative perspective: providing positive reasons that resonate well with people and have therefore a strong weight for them could offset their doubts, yielding to a greater acceptance of COVID-19 vaccination.
Therefore, it is crucial to consider what kind of reasons drive the decision toward or against vaccination. Allowing participants to openly report their reasons pro- or against- vaccination can facilitate a freer exploration of the concerns and reservations of the most hesitant individuals [ 24 ], thus providing valuable insights for shaping future vaccine-related communications. In fact, thanks to the regression tree on vaccination intention, it emerges that positive attitudes toward vaccines are strongly determined by "Protection" and "Community Protection" reasons. The fact that the sense of individual and collective protection is among the principal determinants of the decision with respect to COVID-19 vaccines suggests that in general vaccination is seen as a means of avoiding nefarious clinical consequences. The effect of the sense of communal protection as the reason favoring vaccination and of other-oriented S-PEC in determining the generation of multiple pro-vaccine motivations confirms previous results suggesting that people often are more willing to get vaccinated primarily to protect their loved ones [ 57 , 58 , 59 ], especially when they have a good understanding of how community immunity works [ 60 , 61 ]. However, it is worth mentioning that, at the time the study was conducted (March–April 2021), there was still uncertainty about whether COVID-19 vaccines could provide sterilizing immunity (i.e., could prevent the transmission of the infection) in addition to protecting the individual. To foster people's willingness to get vaccinated, it is crucial from a public health perspective that people understand that even when vaccines do not yield sterilizing immunity, vaccination can still increase protection of others by reducing the circulation of the virus.
The reasons that influenced the willingness to be vaccinated or the vaccination acceptance/booking were generally in line with the existing literature, although they differed depending on whether respondents had already been offered a vaccine or not: among those who did not received a vaccination offer, the main reasons promoting vaccination acceptance were protection against COVID-19 for oneself, one's family, friends, and community [ 23 ], while among the main reasons that reduced vaccination adherence for those who got the vaccine offer we found the lack of clinical trials [ 62 , 63 ], as well as the distrust of institutions and science [ 22 ]. This latter emerged as the most reported negative reason by those who have refused the vaccine and those who have not yet received the vaccine offer. Thus, effective communication aimed at defusing the perception of risk regarding vaccines themselves should focus on enhancing trust in the scientific process and experimental rigor. Indeed, these reasons were deemed as very important not only by those who refused the vaccination, but also by those who had not yet been offered the vaccine, and even by those who held mixed feelings but eventually chose to get vaccinated. While it is unlikely that individuals firmly against vaccination will be persuaded by simple interventions [ 64 ], we should keep in mind that vaccine hesitancy is a dynamic process. As such, reducing hesitancy or enhancing ambivalence, for example through motivational interviewing (e.g., [ 65 , 66 ]), could potentially lead to small shifts towards greater vaccine acceptance.
Our findings are also in line with the results of other international studies that have used a qualitative approach to examine reasons for and against vaccinations. For example, Hamilton and colleagues [ 67 ] employed a qualitative content analysis to extract the main motivations for and concerns about COVID-19 vaccination from medical records obtained by 102 consults in Australia. The study was conducted in June 2021, and revealed that most consults were driven by doubts about the vaccine available and recommended at that time (i.e., ChAdOx1-S, also known as Vaxzevria), followed by need for further information regarding vaccines and vaccination, also considering specific comorbidities. Notwithstanding the peculiarity of the Australian context in which a very low number of COVID-19 infections was observed, the analysis performed by Hamilton et al. [ 67 ] revealed a set of themes that largely overlaps with the reasons identified in our study. Indeed, among the reason to get vaccinated, 5 themes emerged: a) Protection, b) Occupational or facility responsibility or requirement, c) Trust in primary healthcare physician, d) Autonomy, and e) Civic duty, likewise, concerns about vaccination were mainly in terms of: a) Perceived vaccine risks, b) Perceived vaccine performance, c) Uncertainty, d) Autonomy, and e) Fairness in access. An aspect worth noting is that after the consultation, 81% of participants received the vaccination, 19% did not. Consistent results were observed in another study by Purvis and colleagues [ 68 ] conducted in the USA, which focused specifically on “hesitant adopters”, i.e. those who accepted vaccination but showed some level of hesitancy. To note that in this study the focus was on factors influencing the decision to get the COVID-19 vaccine, not on reasons against it. The authors interviewed 49 participants as a follow up of a larger study ( N = 2022) conducted from mid-September 2021 through mid-October 2021, to explore factors that influenced their decision-making process about COVID-19 vaccination [ 68 ]. Two main themes emerged, each with four subthemes: 1) sociocultural context (political, cultural, health professionals, employment, and media environment) and 2) individual and group influences (attitudes and beliefs related to vaccines, family and social networks, free to return to normal, and COVID-19 outcomes).
As for the Italian context, to the best of our knowledge, only one study (i.e., [ 69 ]) attempted to provide a qualitative examination of the concept associated with vaccination in general, through open-ended and closed questions. Notably, this study was conducted a year later than our own study (April–May 2022) and was administered to a non-representative sample of Italians. The authors used a combination of closed and open-ended questions to assess concepts associated with vaccination in general. Consistent with our findings, Boragno et al. reported that participants who had been vaccinated against COVID-19 (92% of the sample) frequently mentioned concepts related to protection and salvation, whereas those who were not vaccinated frequently mentioned mistrust and ambivalence as concepts associated with vaccination [ 69 ].
This study has some limitations. First, COVID-19 perceived risk score was obtained only with respect to the disease and a similar score should be of interest for the COVID-19 vaccine. Second, data were collected during a vaccine offer limited to a well-defined slice of the population and the investigation on the vaccine acceptance/booking has, as a consequence, a limited sample size. Finally, the lack of a longitudinal perspective does not allow us to evaluate how strong the association is between the willingness to get vaccinated, vaccine acceptance and potential changes in risk perception. Thus, we cannot generalize our results beyond the period of data collection and to other countries or health systems. Since the dynamics have now changed, results may not apply to the decision to get a booster shot or not or an annual shot, however it might be interesting to study what motivations are most relevant now. Likewise, it remains to be established whether our results are generalisable to other populations.
Future studies could consider how the interaction between perceived risk associated with the disease and perceived risk associated with the vaccine influences the choice to get the shot. Furthermore, it would be important to explore how we can harness the reasons that most hold back vaccination in a specific communication strategy for the most hesitant people. Moreover, at the time of data collection, the vaccination campaign was still at an early stage, and only a small portion of the population had already received their shot. Therefore, we believe that it might be of particular interest to know more in detail, with a larger sample, what are the reasons that to date, almost 2 years after the release of the vaccine, still make some people reject the vaccine. Only by knowing these reasons will it be possible to develop appropriate vaccination campaigns.
In conclusion, our work examined pro- and against-vaccination reasons and how these, and their interaction, influence the decision to get vaccinated or not. Specifically, high emotional competence and risk perception influence the generation of pro- and against-vaccination reasons and that the presence of a strong pro-vaccination reason shifts intention toward vaccination. We also highlighted the category of reasons that influence intention to vaccinate. That said, given that the discussion about the next doses is still open and that in any case the next pandemic is a matter of when and not if [ 70 ], it is of paramount importance to know the best way to counteract vaccine hesitancy, fostering more effective communication strategies.
Availability of data and materials
Raw data are available on https://osf.io/dpn2q/?view_only=af05427467634411b471af7a8475ffab .
European Centre for Disease Prevention and Control. Cumulative uptake (%) of the primary course among adults (+18) in EU/EEA countries as of 2023–09–07. https://vaccinetracker.ecdc.europa.eu/public/extensions/COVID-19/vaccine-tracker.html#uptake-tab . Accessed 12 Sept 2023.
MacDonald NE. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015; https://doi.org/10.1016/j.vaccine.2015.04.036.
Bedford H, Attwell K, Danchin M, Marshall H, Corben P, Leask J. Vaccine hesitancy, refusal and access barriers: the need for clarity in terminology. Vaccine. 2018; https://doi.org/10.1016/j.vaccine.2017.08.004.
Paul KT, Zimmermann BM, Corsico P, Fiske A, Geiger S, Johnson S, Kuiper JM, Lievevrouw E, Marelli L, Prainsack B, Spahl W. Anticipating hopes, fears and expectations towards COVID-19 vaccines: a qualitative interview study in seven European countries. SSM-Qual Res Health. 2022; https://doi.org/10.1016/j.ssmqr.2021.100035.
Murphy J, Vallières F, Bentall RP, Shevlin M, McBride O, Hartman TK, McKay R, Bennett K, Mason L, Gibson-Miller J, Levita L. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat Commun. 2021; https://doi.org/10.1038/s41467-020-20226-9.
Soares P, Rocha JV, Moniz M, Gama A, Laires PA, Pedro AR, Dias S, Leite A, Nunes C. Factors associated with COVID-19 vaccine hesitancy. Vaccines. 2021; https://doi.org/10.3390/vaccines9030300.
Fisher KA, Bloomstone SJ, Walder J, Crawford S, Fouayzi H, Mazor KM. Attitudes toward a potential SARS-CoV-2 vaccine: a survey of US adults. Ann Internal Med. 2020; https://doi.org/10.7326/M20-3569.
Robertson E, Reeve KS, Niedzwiedz CL, Moore J, Blake M, Green M, Katikireddi SV, Benzeval MJ. Predictors of COVID-19 vaccine hesitancy in the UK household longitudinal study. Brain Behav Immun. 2021; https://doi.org/10.1016/j.bbi.2021.03.008.
Caserotti M, Gavaruzzi T, Girardi P, Tasso A, Buizza C, Candini V, Zarbo C, Chiarotti F, Brescianini S, Calamandrei G, Starace F. Who is likely to vacillate in their COVID-19 vaccination decision? Free-riding intention and post-positive reluctance. Prev Med. 2022; https://doi.org/10.1016/j.ypmed.2021.106885.
Caserotti M, Girardi P, Tasso A, Rubaltelli E, Lotto L, Gavaruzzi T. Joint analysis of the intention to vaccinate and to use contact tracing app during the COVID-19 pandemic. Sci Rep. 2022; https://doi.org/10.1038/s41598-021-04765-9 .
Pereira B, Fehl AG, Finkelstein SR, Jiga‐Boy GM, Caserotti M. Scarcity in COVID‐19 vaccine supplies reduces perceived vaccination priority and increases vaccine hesitancy. Psychol Mark. 2022; https://doi.org/10.1002/mar.21629 .
Đorđević JM, Mari S, Vdović M, Milošević A. Links between conspiracy beliefs, vaccine knowledge, and trust: Anti-vaccine behavior of Serbian adults. Soc Sci Med. 2021; https://doi.org/10.1016/j.socscimed.2021.113930 .
Candini V, Brescianini S, Chiarotti F, Zarbo C, Zamparini M, Caserotti M, Gavaruzzi T, Girardi P, Lotto L, Tasso A, Starace F. Conspiracy mentality and health-related behaviour during the COVID-19 pandemic: a multi-wave survey in Italy. Public Health. 2023, https://doi.org/10.1016/j.puhe.2022.11.005 .
Asch DA, Baron J, Hershey JC, Kunreuther H, Meszaros J, Ritov I, Spranca M. Omission bias and pertussis vaccination. Medic Decis Mak. 1994; https://doi.org/10.1177/0272989X9401400204 .
Meszaros JR, Asch DA, Baron J, Hershey JC, Kunreuther H, Schwartz-Buzaglo J. Cognitive processes and the decisions of some parents to forego pertussis vaccination for their children. J Clin Epidemiol. 1996; https://doi.org/10.1016/0895-4356(96)00007-8 .
Bell RA, McGlone MS, Dragojevic M. Vicious viruses and vigilant vaccines: Effects of linguistic agency assignment in health policy advocacy. J Health Commun. 2014; https://doi.org/10.1080/10810730.2013.81133 .
Nan X, Madden K. HPV vaccine information in the blogosphere: how positive and negative blogs influence vaccine-related risk perceptions, attitudes, and behavioral intentions. Health Commun. 2012; https://doi.org/10.1080/10410236.2012.661348 .
Christy SM, Winger JG, Raffanello EW, Halpern LF, Danoff-Burg S, Mosher CE. The role of anticipated regret and health beliefs in HPV vaccination intentions among young adults. J Behav Med. 2016; https://doi.org/10.1007/s10865-016-9716-z .
Chapman GB, Coups EJ. Emotions and preventive health behavior: worry, regret, and influenza vaccination. Health Psychol. 2006; https://doi.org/10.1037/0278-6133.25.1.82 .
Klasko-Foster LB, Przybyla S, Orom H, Gage-Bouchard E, Kiviniemi MT. The influence of affect on HPV vaccine decision making in an HPV vaccine naïve college student population. Prev Med Rep. 2020; https://doi.org/10.1016/j.pmedr.2020.101195.
World Health Organization = Organisation mondiale de la Santé. Understanding the behavioural and social drivers of vaccine uptake WHO position paper – May 2022 – Comprendre les facteurs comportementaux et sociaux de l’adoption des vaccins Note de synthèse de l’OMS – mai 2022. Weekly Epidemiological Record = Relevé épidémiologique hebdomadaire, 97 (20), 209 - 224. World Health Organization = Organisation mondiale de la Santé. 2022; https://apps.who.int/iris/handle/10665/354460 .
Fieselmann J, Annac K, Erdsiek F, Yilmaz-Aslan Y, Brzoska P. What are the reasons for refusing a COVID-19 vaccine? A qualitative analysis of social media in Germany. BMC Public Health. 2022; https://doi.org/10.1186/s12889-022-13265-y .
Moore R, Purvis RS, Hallgren E, Willis DE, Hall S, Reece S, CarlLee S, Judkins H, McElfish PA. Motivations to vaccinate among hesitant adopters of the COVID-19 vaccine. J Commun Health. 2022; https://doi.org/10.1007/s10900-021-01037-5 .
Cassels TG, Birch SA. Comparisons of an open-ended vs. forced-choice ‘mind reading’task: Implications for measuring perspective-taking and emotion recognition. PLoS One. 2014; https://doi.org/10.1371/journal.pone.0093653 .
Kahneman D, & Tversky A. On the interpretation of intuitive probability: A reply to Jonathan Cohen. 1979; https://doi.org/10.1016/0010-0277(79)90024-6 .
Tversky A, Kahneman D. Advances in prospect theory: Cumulative representation of uncertainty. J Risk Uncertain. 1992; https://doi.org/10.1007/BF00122574 .
Baumeister RF, Bratslavsky E, Finkenauer C, Vohs KD. Bad is stronger than good. Review of general psychology. 2001; https://doi.org/10.1037/1089-2680.5.4.323 .
Chor JS, Ngai KL, Goggins WB, Wong MC, Wong SY, Lee N, Leung TF, Rainer TH, Griffiths S, Chan PK. Willingness of Hong Kong healthcare workers to accept pre-pandemic influenza vaccination at different WHO alert levels: two questionnaire surveys. BMJ. 2009; https://doi.org/10.1136/bmj.b3391 .
Pareek M, Clark T, Dillon H, Kumar R, Stephenson I. Willingness of healthcare workers to accept voluntary stockpiled H5N1 vaccine in advance of pandemic activity. Vaccine. 2009; https://doi.org/10.1016/j.vaccine.2008.12.006 .
Viswanath K, Bekalu M, Dhawan D, Pinnamaneni R, Lang J, McLoud R. Individual and social determinants of COVID-19 vaccine uptake. BMC Public Health. 2021; https://doi.org/10.1186/s12889-021-10862-1 .
Caserotti M, Girardi P, Rubaltelli E, Tasso A, Lotto L, Gavaruzzi T. Associations of COVID-19 risk perception with vaccine hesitancy over time for Italian residents. Soc Sci Med. 2021; https://doi.org/10.1016/j.socscimed.2021.113688 .
Finucane ML, Peters E, & Slovic P. (2003). Judgment and decision making: The dance of affect and reason. In: S. L. Schneider & J. Shanteau, editors. Emerging Perspectives on Judgment and Decision Research Cambridge. University Press; 2003. 327–364. https://doi.org/10.1017/CBO9780511609978.012 .
Pittarello A, Conte B, Caserotti M, Scrimin S, Rubaltelli E. Emotional intelligence buffers the effect of physiological arousal on dishonesty. Psychonomic Bull Rev. 2018; https://doi.org/10.3758/s13423-017-1285-9 .
Scrimin S, Rubaltelli E. Dehumanization after terrorism: the role of psychophysiological emotion regulation and trait emotional intelligence. Curr Psychol. 2021; https://doi.org/10.1007/s12144‐019‐00189‐x .
Tomljenovic H, Bubic A, Erceg N. It just doesn’t feel right–the relevance of emotions and intuition for parental vaccine conspiracy beliefs and vaccination uptake. Psychol Health. 2020; https://doi.org/10.1080/08870446.2019.1673894 .
Gavaruzzi T, Caserotti M, Leo I, Tasso A, Speri L, Ferro A, Fretti E, Sannino A, Rubaltelli E, Lotto L. The role of emotional competences in parents’ vaccine hesitancy. Vaccines. 2021; https://doi.org/10.3390/vaccines9030298 .
ISTAT. Resident population on 1st January: By age. http://dati.istat.it/?lang=en&SubSessionId=d7024c9e-239b-455d-924b-df19345a27b2 . Accessed Sept 25, 2023.
Mikolajczak M., Brasseur S, & Fantini-Hauwel C. Measuring intrapersonal and interpersonal EQ: The short profile of emotional competence (S-PEC). Pers Individ Differ. 2014; https://doi.org/10.1016/j.paid.2014.01.023 .
Olmos A, Govindasamy P. A practical guide for using propensity score weighting in R. Pract Assess Res Eval. 2015; https://doi.org/10.7275/jjtm-r398 .
Smithson M, Verkuilen J. A better lemon squeezer? Maximum-likelihood regression with beta-distributed dependent variables. Psychological methods. 2006; https://doi.org/10.1037/1082-989X.11.1.54 .
Ferrari S, Cribari-Neto F. Beta regression for modelling rates and proportions. Journal of applied statistics. 2004; https://doi.org/10.1080/0266476042000214501 .
Thernau T, Atkinson B, Ripley B. Rpart: Recursive Partitioning. R Package 4.1–0. http://CRAN.R-project.org/package=rpart .
RC Team. R Core Team R: A language and environment for statistical computing. R. . Foundation for Statistical Computing. 2014. https://www.r-project.org .
Freeman D, Loe BS, Chadwick A, Vaccari C, Waite F, Rosebrock L, ... & Lambe S. COVID-19 vaccine hesitancy in the UK: the Oxford coronavirus explanations, attitudes, and narratives survey (Oceans) II. Psychol Med. 2022; https://doi.org/10.1017/S0033291720005188 .
Caserotti M, Gavaruzzi T, Girardi P, Sellaro R, Rubaltelli E, Tasso A, Lotto L. People’s perspectives about COVID-19 vaccination certificate: Findings from a representative Italian sample. Vaccine. 2022; https://doi.org/10.1016/j.vaccine.2022.08.016 .
MacDonald NE, Comeau J, Dubé È, Graham J, Greenwood M, Harmon S, McElhaney J, Meghan McMurtry C, Middleton A, Steenbeek A, Taddio A. Royal society of Canada COVID-19 report: Enhancing COVID-19 vaccine acceptance in Canada. Facets. 2021; https://doi.org/10.1139/facets-2021-0037 .
Schwarzinger M, Watson V, Arwidson P, Alla F, Luchini S. COVID-19 vaccine hesitancy in a representative working-age population in France: a survey experiment based on vaccine characteristics. Lancet Public Health. 2021; https://doi.org/10.1016/S2468-2667(21)00012-8 .
Slovic P, Finucane M, Peters E, MacGregor DG. Rational actors or rational fools: Implications of the affect heuristic for behavioral economics. J Socio-Econ. 2002; https://doi.org/10.1016/S1053-5357(02)00174-9 .
Slovic P, Finucane ML, Peters E, MacGregor DG. Risk as analysis and risk as feelings: Some thoughts about affect, reason, risk and rationality. In The feeling of risk 2013 Mar 7 (pp. 21–36). Routledge.
Bhopal SS, Bagaria J, Olabi B, Bhopal R. Children and young people remain at low risk of COVID-19 mortality. Lancet Child Adolesc Health. 2021; https://doi.org/10.1016/S2352-4642(21)00066-3 .
Lazarus JV, Wyka K, Rauh L, Rabin K, Ratzan S, Gostin LO, Larson HJ, El-Mohandes A. Hesitant or not? The association of age, gender, and education with potential acceptance of a COVID-19 vaccine: a country-level analysis. J Health Commun. 2020; https://doi.org/10.1080/10810730.2020.1868630 .
Seale H, Heywood AE, Leask J, Sheel M, Durrheim DN, Bolsewicz K, Kaur R. Examining Australian public perceptions and behaviors towards a future COVID-19 vaccine. BMC Infect Dis. 2021; https://doi.org/10.1186/s12879-021-05 .
Butter S, McGlinchey E, Berry E, Armour C. Psychological, social, and situational factors associated with COVID‐19 vaccination intentions: A study of UK key workers and non‐key workers. Br J Health Psychol. 2022; https://doi.org/10.1111/bjhp.12530 .
Freedman DA, Berk RA. Weighting regressions by propensity scores. Eval Rev. 2008; https://doi.org/10.1177/0193841X08317586 .
Lagoe C, Farrar KM. Are you willing to risk it? The relationship between risk, regret, and vaccination intent. Psychol Health Med. 2015; https://doi.org/10.1080/13548506.2014.911923 .
Ziarnowski KL, Brewer NT, Weber B. Present choices, future outcomes: anticipated regret and HPV vaccination. Prev Med. 2009; https://doi.org/10.1016/j.ypmed.2008.10.006 .
Betsch C, Böhm R, Korn L, Holtmann C. On the benefits of explaining herd immunity in vaccine advocacy. Nat Hum Behav. 2017; https://doi.org/10.1038/s41562-017-0056 .
Loomba S, de Figueiredo A, Piatek SJ, de Graaf K, Larson HJ. Measuring the impact of COVID-19 vaccine misinformation on vaccination intent in the UK and USA. Nat Hum Behav. 2021; https://doi.org/10.1038/s41562-021-01056-1 .
Pfattheicher S, Petersen MB, Böhm R. Information about herd immunity through vaccination and empathy promote COVID-19 vaccination intentions. Health Psychol. 2022;41(2):85.
Article PubMed Google Scholar
Hakim H, Provencher T, Chambers CT, Driedger SM, Dube E, Gavaruzzi T, ... & Witteman HO. Interventions to help people understand community immunity: a systematic review. Vaccine. 2019; https://doi.org/10.1016/j.vaccine.2018.11.016 .
Hakim H, Bettinger JA, Chambers CT, Driedger SM, Dubé E, Gavaruzzi T, Giguere AMC, Kavanagh É, Leask J, MacDonald SE, Orji R, Parent E, Paquette J, Roberge J, Sander B, Scherer AM, Tremblay-Breault M, Wilson K, Reinharz D, Witteman HO. A Web Application About Herd Immunity Using Personalized Avatars: Development Study. Journal of medical Internet research. 2020; https://doi.org/10.2196/20113 .
Callaghan T, Moghtaderi A, Lueck JA, Hotez P, Strych U, Dor A, Fowler EF, Motta M. Correlates and disparities of intention to vaccinate against COVID-19. Soc Sci Med (1982). 2021; https://doi.org/10.1016/j.socscimed.2020.113638 .
Griffith J, Marani H, Monkman H. COVID-19 vaccine hesitancy in Canada: Content analysis of tweets using the theoretical domains framework. Journal of medical Internet research. 2021; https://doi.org/10.2196/26874 .
Attwell K, Lake J, Sneddon J, Gerrans P, Blyth C, & Lee J. Converting the maybes: Crucial for a successful COVID-19 vaccination strategy. PLoS One. 2021; https://doi.org/10.1371/journal.pone.0245907 .
Breckenridge LA, Burns D, & Nye C. The use of motivational interviewing to overcome COVID‐19 vaccine hesitancy in primary care settings. Public Health Nurs. 2022; https://doi.org/10.1111/phn.13003 .
Gabarda A, & Butterworth SW. Using best practices to address COVID-19 vaccine hesitancy: The case for the motivational interviewing approach. Health Promot Pract, 2021; https://doi.org/10.1177/152483992110164 .
Hamilton EM, Oversby S, Ratsch A, & Kitchener S.COVID-19 vaccination: An exploratory study of the motivations and concerns detailed in the medical records of a regional Australian population. Vaccines. 2022; https://doi.org/10.3390/vaccines10050657 .
Purvis RS, Moore R, Willis DE, Hallgren E, & McElfish PA. Factors influencing COVID-19 vaccine decision-making among hesitant adopters in the United States. Human Vaccines Immunother. 2022; https://doi.org/10.1080/21645515.2022.2114701 .
Boragno P, Fiabane E, Taino I, Maffoni M, Sommovigo V, Setti I, Gabanelli P. Perceptions of COVID-19 Vaccines: Protective Shields or Threatening Risks? A Descriptive Exploratory Study among the Italian Population. Vaccines. 2023; https://doi.org/10.3390/vaccines11030642 .
Centers for Disease Control and Prevention. Why it matters: The pandemic threat. Retrieved December. 2020;1:2020.
Download references
Acknowledgements
Not applicable.
Open access funding provided by Università degli Studi di Padova. The project was developed thanks to institutional research funding of TG and AT.
Author information
Authors and affiliations.
Department of Developmental Psychology and Socialization, University of Padova, Padua, Italy
Marta Caserotti, Roberta Sellaro, Enrico Rubaltelli & Lorella Lotto
Department of Environmental Sciences, Informatics and Statistics, Ca’ Foscari University of Venezia, Venice, Italy
Paolo Girardi
Department of Humanities, University of Ferrara, Ferrara, Italy
Alessandra Tasso
Department of Medical and Surgical Sciences, University of Bologna, Bologna, Italy
Teresa Gavaruzzi
You can also search for this author in PubMed Google Scholar
Contributions
MC: Conceptualization, Formal analysis, Visualization, Writing—original draft and Writing—review & editing. PG: Conceptualization, Formal analysis, Visualization, Writing—original draft. RS: Conceptualization, Writing—review & editing. ER: Conceptualization, Writing—review & editing. AT: Conceptualization, Writing—review & editing. LL: Conceptualization, Writing—review & editing. TG: Conceptualization, Visualization, Writing—review & editing.
Corresponding author
Correspondence to Marta Caserotti .
Ethics declarations
Ethics approval and consent to participate.
The project was approved by the ethical committee for Psychology Research of the University of Padova (Italy), with protocol number 3911/2020, and informed consent was obtained for all participants.

Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: appendix 1..
Scoring for pro- and against-vaccination reasons. Appendix 2. Structure of the questionnaire. Table S1. Selection criteria. Table S2. Number of items, internal consistency (Cronbach’s α), name of the items and their estimated loadings, total deviance explained by the loadings and proportion of variance explained by EFA for COVID-19 perceived risk. Table S3. Odds ratios (ORs) estimated by the logistic model for the propensity score weighting for the COVID-19 vaccine offer. Table S4 . Predicted willingness to get vaccinated by combination of pro- and against-vaccination reasons by category of reference. Table S5. Frequency of reported categories of pro- and against-vaccination reasons overall, and by COVID-19 vaccine status. Figure S1. Distribution of the propensity scores by vaccine offer.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Caserotti, M., Girardi, P., Sellaro, R. et al. To vaccinate or not to vaccinate? The interplay between pro- and against- vaccination reasons. BMC Public Health 23 , 2207 (2023). https://doi.org/10.1186/s12889-023-17112-6
Download citation
Received : 12 December 2022
Accepted : 30 October 2023
Published : 09 November 2023
DOI : https://doi.org/10.1186/s12889-023-17112-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Pro-and against-reasons
- Vaccination intention
- Risk perception
- Emotional competences
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Persuasive Essay Guide
Persuasive Essay About Covid19
How to Write a Persuasive Essay About Covid19 | Examples & Tips
11 min read

People also read
A Comprehensive Guide to Writing an Effective Persuasive Essay
200+ Persuasive Essay Topics to Help You Out
Learn How to Create a Persuasive Essay Outline
30+ Free Persuasive Essay Examples To Get You Started
Read Excellent Examples of Persuasive Essay About Gun Control
Crafting a Convincing Persuasive Essay About Abortion
Learn to Write Persuasive Essay About Business With Examples and Tips
Check Out 12 Persuasive Essay About Online Education Examples
Persuasive Essay About Smoking - Making a Powerful Argument with Examples
Are you looking to write a persuasive essay about the Covid-19 pandemic?
Writing a compelling and informative essay about this global crisis can be challenging. It requires researching the latest information, understanding the facts, and presenting your argument persuasively.
But don’t worry! with some guidance from experts, you’ll be able to write an effective and persuasive essay about Covid-19.
In this blog post, we’ll outline the basics of writing a persuasive essay . We’ll provide clear examples, helpful tips, and essential information for crafting your own persuasive piece on Covid-19.
Read on to get started on your essay.
- 1. Steps to Write a Persuasive Essay About Covid-19
- 2. Examples of Persuasive Essay About Covid19
- 3. Examples of Persuasive Essay About Covid-19 Vaccine
- 4. Examples of Persuasive Essay About Covid-19 Integration
- 5. Examples of Argumentative Essay About Covid 19
- 6. Examples of Persuasive Speeches About Covid-19
- 7. Tips to Write a Persuasive Essay About Covid-19
- 8. Common Topics for a Persuasive Essay on COVID-19
Steps to Write a Persuasive Essay About Covid-19
Here are the steps to help you write a persuasive essay on this topic, along with an example essay:
Step 1: Choose a Specific Thesis Statement
Your thesis statement should clearly state your position on a specific aspect of COVID-19. It should be debatable and clear. For example:
Step 2: Research and Gather Information
Collect reliable and up-to-date information from reputable sources to support your thesis statement. This may include statistics, expert opinions, and scientific studies. For instance:
- COVID-19 vaccination effectiveness data
- Information on vaccine mandates in different countries
- Expert statements from health organizations like the WHO or CDC
Step 3: Outline Your Essay
Create a clear and organized outline to structure your essay. A persuasive essay typically follows this structure:
- Introduction
- Background Information
- Body Paragraphs (with supporting evidence)
- Counterarguments (addressing opposing views)
Step 4: Write the Introduction
In the introduction, grab your reader's attention and present your thesis statement. For example:
Step 5: Provide Background Information
Offer context and background information to help your readers understand the issue better. For instance:
Step 6: Develop Body Paragraphs
Each body paragraph should present a single point or piece of evidence that supports your thesis statement. Use clear topic sentences, evidence, and analysis. Here's an example:
Step 7: Address Counterarguments
Acknowledge opposing viewpoints and refute them with strong counterarguments. This demonstrates that you've considered different perspectives. For example:
Step 8: Write the Conclusion
Summarize your main points and restate your thesis statement in the conclusion. End with a strong call to action or thought-provoking statement. For instance:
Step 9: Revise and Proofread
Edit your essay for clarity, coherence, grammar, and spelling errors. Ensure that your argument flows logically.
Step 10: Cite Your Sources
Include proper citations and a bibliography page to give credit to your sources.
Remember to adjust your approach and arguments based on your target audience and the specific angle you want to take in your persuasive essay about COVID-19.
Paper Due? Why Suffer? That's our Job!
Examples of Persuasive Essay About Covid19
When writing a persuasive essay about the Covid-19 pandemic, it’s important to consider how you want to present your argument. To help you get started, here are some example essays for you to read:
Check out some more PDF examples below:
Persuasive Essay About Covid-19 Pandemic
Sample Of Persuasive Essay About Covid-19
Persuasive Essay About Covid-19 In The Philippines - Example
If you're in search of a compelling persuasive essay on business, don't miss out on our “ persuasive essay about business ” blog!
Examples of Persuasive Essay About Covid-19 Vaccine
Covid19 vaccines are one of the ways to prevent the spread of Covid-19, but they have been a source of controversy. Different sides argue about the benefits or dangers of the new vaccines. Whatever your point of view is, writing a persuasive essay about it is a good way of organizing your thoughts and persuading others.
A persuasive essay about the Covid-19 vaccine could consider the benefits of getting vaccinated as well as the potential side effects.
Below are some examples of persuasive essays on getting vaccinated for Covid-19.
Covid19 Vaccine Persuasive Essay
Persuasive Essay on Covid Vaccines
Interested in thought-provoking discussions on abortion? Read our persuasive essay about abortion blog to eplore arguments!
Examples of Persuasive Essay About Covid-19 Integration
Covid19 has drastically changed the way people interact in schools, markets, and workplaces. In short, it has affected all aspects of life. However, people have started to learn to live with Covid19.
Writing a persuasive essay about it shouldn't be stressful. Read the sample essay below to get idea for your own essay about Covid19 integration.
Persuasive Essay About Working From Home During Covid19
Searching for the topic of Online Education? Our persuasive essay about online education is a must-read.
Examples of Argumentative Essay About Covid 19
Covid-19 has been an ever-evolving issue, with new developments and discoveries being made on a daily basis.
Writing an argumentative essay about such an issue is both interesting and challenging. It allows you to evaluate different aspects of the pandemic, as well as consider potential solutions.
Here are some examples of argumentative essays on Covid19.
Argumentative Essay About Covid19 Sample
Argumentative Essay About Covid19 With Introduction Body and Conclusion
Looking for a persuasive take on the topic of smoking? You'll find it all related arguments in out Persuasive Essay About Smoking blog!
Examples of Persuasive Speeches About Covid-19
Do you need to prepare a speech about Covid19 and need examples? We have them for you!
Persuasive speeches about Covid-19 can provide the audience with valuable insights on how to best handle the pandemic. They can be used to advocate for specific changes in policies or simply raise awareness about the virus.
Check out some examples of persuasive speeches on Covid-19:
Persuasive Speech About Covid-19 Example
Persuasive Speech About Vaccine For Covid-19
You can also read persuasive essay examples on other topics to master your persuasive techniques!
Tips to Write a Persuasive Essay About Covid-19
Writing a persuasive essay about COVID-19 requires a thoughtful approach to present your arguments effectively.
Here are some tips to help you craft a compelling persuasive essay on this topic:
Choose a Specific Angle
Start by narrowing down your focus. COVID-19 is a broad topic, so selecting a specific aspect or issue related to it will make your essay more persuasive and manageable. For example, you could focus on vaccination, public health measures, the economic impact, or misinformation.
Provide Credible Sources
Support your arguments with credible sources such as scientific studies, government reports, and reputable news outlets. Reliable sources enhance the credibility of your essay.
Use Persuasive Language
Employ persuasive techniques, such as ethos (establishing credibility), pathos (appealing to emotions), and logos (using logic and evidence). Use vivid examples and anecdotes to make your points relatable.
Organize Your Essay
Structure your essay involves creating a persuasive essay outline and establishing a logical flow from one point to the next. Each paragraph should focus on a single point, and transitions between paragraphs should be smooth and logical.
Emphasize Benefits
Highlight the benefits of your proposed actions or viewpoints. Explain how your suggestions can improve public health, safety, or well-being. Make it clear why your audience should support your position.
Use Visuals -H3
Incorporate graphs, charts, and statistics when applicable. Visual aids can reinforce your arguments and make complex data more accessible to your readers.
Call to Action
End your essay with a strong call to action. Encourage your readers to take a specific step or consider your viewpoint. Make it clear what you want them to do or think after reading your essay.
Revise and Edit
Proofread your essay for grammar, spelling, and clarity. Make sure your arguments are well-structured and that your writing flows smoothly.
Seek Feedback
Have someone else read your essay to get feedback. They may offer valuable insights and help you identify areas where your persuasive techniques can be improved.
Tough Essay Due? Hire Tough Writers!
Common Topics for a Persuasive Essay on COVID-19
Here are some persuasive essay topics on COVID-19:
- The Importance of Vaccination Mandates for COVID-19 Control
- Balancing Public Health and Personal Freedom During a Pandemic
- The Economic Impact of Lockdowns vs. Public Health Benefits
- The Role of Misinformation in Fueling Vaccine Hesitancy
- Remote Learning vs. In-Person Education: What's Best for Students?
- The Ethics of Vaccine Distribution: Prioritizing Vulnerable Populations
- The Mental Health Crisis Amidst the COVID-19 Pandemic
- The Long-Term Effects of COVID-19 on Healthcare Systems
- Global Cooperation vs. Vaccine Nationalism in Fighting the Pandemic
- The Future of Telemedicine: Expanding Healthcare Access Post-COVID-19
In search of more inspiring topics for your next persuasive essay? Our persuasive essay topics blog has plenty of ideas!
To sum it up,
You have read good sample essays and got some helpful tips. You now have the tools you needed to write a persuasive essay about Covid-19. So don't let the doubts stop you, start writing!
If you need professional writing help, don't worry! We've got that for you as well.
MyPerfectWords.com is a professional essay writing service that can help you craft an excellent persuasive essay on Covid-19. Our experienced essay writer will create a well-structured, insightful paper in no time!
So don't hesitate and get in touch with our persuasive essay writing service today!
Frequently Asked Questions
Are there any ethical considerations when writing a persuasive essay about covid-19.
Yes, there are ethical considerations when writing a persuasive essay about COVID-19. It's essential to ensure the information is accurate, not contribute to misinformation, and be sensitive to the pandemic's impact on individuals and communities. Additionally, respecting diverse viewpoints and emphasizing public health benefits can promote ethical communication.
What impact does COVID-19 have on society?
The impact of COVID-19 on society is far-reaching. It has led to job and economic losses, an increase in stress and mental health disorders, and changes in education systems. It has also had a negative effect on social interactions, as people have been asked to limit their contact with others.

Caleb S. has been providing writing services for over five years and has a Masters degree from Oxford University. He is an expert in his craft and takes great pride in helping students achieve their academic goals. Caleb is a dedicated professional who always puts his clients first.

Paper Due? Why Suffer? That’s our Job!
Keep reading
How the anti-vaccine movement pits parental rights against public health

Gayle Borne of Springfield, Tennessee, has fostered more than 300 children. In January, she took a foster baby, born extremely premature at just over 2 pounds, to her first doctor’s appointment. But the health providers said that without the consent of the child’s mother, they couldn’t vaccinate the newborn against diseases like pneumonia, hepatitis B and polio.
It’s due to a law Tennessee passed last year that requires the direct consent of birth parents or legal guardians for every routine childhood vaccination. Foster parents and social workers cannot provide permission. Nor can grandparents and other caregivers who take children to routine appointments when parents can’t.
The foster baby’s mother hasn’t been located, so a social worker is now seeking a court order to permit the immunizations. “We are just waiting,” Borne said. “Our hands are tied.”
The Tennessee law claims to “give parents back the right to make medical decisions for their children.” Framed in the rhetoric of choice and consent, it is one of more than a dozen recent and pending pieces of legislation nationwide that pit parental freedom against community and children’s health.
In actuality, these laws create obstacles to vaccination, the foundation of pediatric care. And they have a second effect: seeding yet more doubt about vaccine safety in a climate rife with medical misinformation, where politicians and influencers make false claims about risks, despite studies showing otherwise.
Childhood vaccine rates are already at their lowest in a decade.
Dorit Reiss, a vaccine policy researcher at the University of California Law–San Francisco, fears the revived parental rights movement may eventually abolish routine immunizations to attend school. At a recent campaign rally , presumptive Republican presidential nominee Donald Trump said, “I will not give one penny to any school that has a vaccine mandate.”
Seven in 10 U.S. adults said public schools should require vaccination against measles, mumps and rubella in a 2023 Pew Research Center poll . But numbers have been dropping.
“People who promote parental rights on vaccines tend to downplay the rights of children,” Reiss said.
When lawmakers silence experts
In Tennessee, anti-vaccine activists and libertarian-leaning organizations railed against the state’s health department in 2021 when it recommended COVID-19 vaccines to minors, following CDC guidance. Then the state’s immunization director reminded doctors that a Tennessee law called the Mature Minor Doctrine didn’t require parental permission to vaccinate consenting adolescents 14 or older.
Backlash ensued. State legislators threatened to defund the health department and pressured it into scaling back COVID-19 vaccine promotion, as revealed by The Tennessean , part of the USA TODAY Network. The immunization director was fired. By mid-2022, Tennessee’s COVID-19 death rate climbed to one of the nation’s highest .
When lawmakers introduced a bill to reverse the Mature Minor Doctrine, the health and children’s services departments were silent.
“Children belong to their families, not the state,” Republican Rep. John Ragan said as he presented the bill in April 2023.
Democratic Rep. Justin Pearson did speak out, saying the bill “doesn’t take into account people and children who are neglected.”
Rather than address the concern, Ragan referenced a 2000 Supreme Court ruling in favor of parental rights, where justices determined that a mother had legal authority to decide who could visit her daughters. Yet the Supreme Court has also done the opposite . For instance, it sided against a legal guardian who removed her child from school to proselytize for the Jehovah’s Witnesses.
The bill swiftly became law.
Deborah Lowen, then deputy commissioner of child health at the Tennessee Department of Children’s Services, was flooded with calls from doctors who now face jail time and fines for vaccinating minors without adequate consent. “I was and remain very disheartened,” she said.
Jason Yaun, a Memphis pediatrician and past president of the Tennessee chapter of the American Academy of Pediatrics, had to decline to administer a first series of vaccines to an infant accompanied by a social worker. The experience shook him, he said.
“That child is going into a situation where they are around other children and adults,” he said, “where they could be exposed to something we failed to protect them from.”
“We have had numerous angry grandparents in our waiting room who take kids to appointments because the parents are at work or down on their luck,” said Hunter Butler, a pediatrician in Springfield, Tennessee.
He has called a rehab facility to request verbal consent from a mother to vaccinate her baby. “And it’s unclear if that was OK,” he said.
A right to health
Unvaccinated people put others at risk, including babies too young to be vaccinated and people with weakened immune systems.
“There’s a freedom piece on the other side of this argument,” said Caitlin Gilmet, communications director at the vaccine advocacy group SAFE Communities Coalition and Action Fund. “You should have the right to protect your family from preventable diseases.”
In January, Gilmet and other child health advocates offered free fried chicken biscuits at the Tennessee Statehouse, handing out flyers as legislators and aides drifted in to eat. One pamphlet enumerated the toll of a 2018-19 measles outbreak in Washington state that sickened 72 people, most of whom were unvaccinated: $76,000 in medical care, $2.3 million for the public health response and an estimated $1 million in economic losses due to illness, quarantine and caregiving.
Barb Dentz, an advocate with Tennessee Families for Vaccines, repeated that most of the state’s constituents support strong policies in favor of immunizations.
“Protecting kids should be such a no-brainer,” Dentz told Republican Rep. Sam Whitson later that morning in his office. Whitson agreed.
“Dr. Google and Facebook have been such a challenge,” he said. “Fighting ignorance has become a full-time job.”
Whitson was among a minority of Republicans who voted against Tennessee’s vaccine bill last year. “The parental rights thing has really taken hold,” he said, “and it can be used for and against us.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF – an independent source of health policy research, polling and journalism.
- Newsletters
- Account Activating this button will toggle the display of additional content Account Sign out
Even the Supreme Court’s Conservatives Are Fed Up With the Garbage Coming Out of the 5th Circuit
What happens when a lawless judge and a terrible appeals court embrace the dopiest First Amendment claim you’ve ever heard out of pure spite toward a Democratic president? That would be Murthy v. Missouri , a brain-meltingly dumb case that the Supreme Court was unfortunate enough to hear oral arguments in on Monday. Murthy poses a question so asinine that to ask it is to answer it: Can government officials encourage social media companies to moderate certain content that they deem harmful—most importantly, disinformation about COVID-19 in the middle of the pandemic?
Yes, of course they can: The First Amendment does not gag public officials from urging Facebook or the Washington Post or anyone else to publish or not publish certain information, especially when it contains dangerous lies about a once-in-a-century pandemic that could exacerbate the crisis. The First Amendment bars government censorship, not government persuasion, and the Biden administration planted itself on the latter side of that bright line. At least six justices grasped this basic constitutional principle on Monday. Several of them used arguments to highlight how this inane case illustrates so much of what’s wrong with the judiciary today, and hinted at the dangers it could pose to American democracy in the future. That we should pay attention to. The rest was an unfortunate sideshow.
Like so many Supreme Court cases these days, Murthy is built atop a heap of fake facts. The case began when Missouri and Louisiana sued agencies and officials across the Biden administration, falsely accusing them of coercing social media companies into censoring their residents’ free speech. (These states later added a handful of fringe anti-vaxxers to the suit.) They filed their complaint in the Monroe Division of the Western District of Louisiana, where—surprise!—they were guaranteed to draw a Trump appointee, Terry Doughty, the one judge hearing cases in that division. Judge Doughty has a record of issuing nationwide injunctions against the Biden administration on the basis of dubious legal and factual analysis. Most notably, he issued a nationwide bar against Biden’s vaccine mandate for health care workers in an opinion riddled with anti-vax nonsense (which the Supreme Court reversed ).
Doughty, in other words, was certain to rule against Biden in the social media case. Even still, the opinion he handed down on July 4, 2023, was a humiliating mess of contradictions, fabrications , and (ironically) misinformation . Doughty adopted the plaintiffs’ theory that the administration “coerced” social media companies into removing “conservative” speech about COVID, including posts promoting hydroxychloroquine and rejecting the efficacy of vaccines. He accused government officials of launching a “coordinated campaign” to silence conservatives by forcing private companies to take down anti-vax content, as well as false claims about election fraud. And he issued one of the most sweeping injunctions in the history of the American legal system, prohibiting any employee—including Homeland Security, the State Department, the Department of Justice, and the FBI—from “engaging in any communication of any kind with social-media companies” encouraging content moderation.
Doughty, it turns out, grievously butchered the record to reach his conclusion. An exhaustive analysis by Mike Masnick proves that Doughty consistently misrepresented testimony and other evidence in the record to construct a conspiracy theory with zero basis in reality. He distorted emails and other exchanges to make them look coercive when they were nothing of the sort, cherry-picking and rearranging quotations to put them in a censorious light. Yet the hard-right U.S. Court of Appeals for the 5 th Circuit, where law goes to die , affirmed Doughty’s conclusions and upheld much of his injunction (while narrowing it in part). That move sent the administration racing to the Supreme Court for an emergency stay, which it granted in October, over the dissents of Justices Samuel Alito, Neil Gorsuch, and Clarence Thomas. Monday’s arguments confirmed that a majority is prepared to side with Biden on the merits.
The justices did not sound happy to have the case before them. Justice Sonia Sotomayor scolded Louisiana Solicitor General Benjamin Aguiñaga (a former Alito clerk) for his lack of candor. “I have such a problem with your brief,” she told him. “You omit information that changes the context of some of your claims. You attribute things to people who it didn’t happen to.” Aguiñaga was unable to defend Doughty’s more extreme deceptions. So he had to fall back on what Justice Elena Kagan called an “extremely expansive” argument: the notion that “encouraging people to suppress their own speech” violates the First Amendment, even if it isn’t coercive. Kagan drew upon her past work in the executive branch to explain that, actually, government officials do this all the time . “I’ve had some experience encouraging press to suppress their own speech,” Kagan told Aguiñaga. Example: “You just wrote a bad editorial. Here are the five reasons you shouldn’t write another one.” Is that really unconstitutional?
Justice Brett Kavanaugh, a former White House staff secretary, also provided a real-world perspective after Alito fumed that officials had been too mean to the platforms and would never treat the traditional press so sharply. Kavanaugh gave Alito a reality check: “I’d assumed, thought, [and] experienced government press people throughout the federal government who regularly call up the media and berate them,” he told Deputy Solicitor General Brian Fletcher, who defended the administration. “You said the anger was unusual. I wasn’t entirely clear on that from my own experience.” Translation: Government employees yell at members of the media all the time. The media can accept or reject their requests. That is how it works .
But did Biden officials berate social media employees? Only on a few rare occasions. Here’s what really happened: The platforms in question, most prominently Facebook and Twitter, invited the government to help them identify and remove the most toxic disinformation. At the time, as Fletcher explained, these companies were eager to present themselves as “partners” with the administration in its push for COVID vaccination. Officials could “flag” questionable content, but the platforms made their own judgment calls, without any demonstrable fear of retaliation. Everyone agrees that the government violates free speech when it explicitly coerces companies into censoring expression under the threat of punishment. But, Fletcher persuasively argued, no such thing happened here.
That left Aguiñaga to lean on the theory that the government contravenes the First Amendment when it merely “encourages” specific content moderation. Justice Amy Coney Barrett, a stickler for legible rules, sounded borderline aghast at this baggy, boundless standard; she lobbed a series of hypotheticals at Aguiñaga that showed he was pushing a meaningless and impracticable test. Chief Justice John Roberts tried to help Aguiñaga understand that multiple agencies with competing agendas may pressure platforms in contradictory directions; doesn’t that “dilute the concept of coercion significantly?” (Aguiñaga just sounded confused.) Kavanaugh pointed out that the plaintiffs’ position could prevent officials from urging the press to safeguard national security by, for instance, asserting that a forthcoming article might imperil the troops.
Even Gorsuch, who started out sympathetic to Aguiñaga, was exasperated by the end, complaining that Doughty’s “universal injunction” was part of the “epidemic” that had to be stopped. Only Alito and Thomas sounded like surefire votes for the plaintiffs after nearly two hours of arguments, and Thomas’ heart was not fully in it. Alito stood alone in his increasingly uncontrolled and seething aggrievement .
The pandemic may be over, but Murthy remains a hugely relevant case. Perhaps most obviously, it is a cautionary tale about the extremism of Trump judges like Doughty, who keep issuing these lawless injunctions at the behest of red-state politicians, and the 5 th Circuit, which keeps upholding them. A disproportionate number of the Supreme Court’s cases this term emerge from the 5 th Circuit, which keeps appeasing the Trump-appointed zealots attempting to seize unimaginable amounts of power from the democratic branches. The chief justice is attempting to crack down on the kind of judge-shopping that occurred here, but the fight is just beginning. The evident frustration of Roberts, Kavanaugh, Barrett, and even Gorsuch on Monday suggests that a majority of the court is fed up with this political manipulation of the judiciary by rogue judges with undisguised partisan loyalties.
So, yes, SCOTUS is likely to reach the right result in Murthy . Alarmingly, though, so much damage has already been done. In light of Doughty’s injunction, the federal government shut down all of its efforts to combat disinformation, fearful of judicial sanctions. Bad actors have exploited this development to flood the internet with lies about the upcoming 2024 election. If foreign entities attempt to interfere with the election via social media, the Biden administration will have few tools left to fight them. It is just too late to revive the various task forces that worked with platforms before Doughty disbanded them last year. For the Murthy plaintiffs, then, a Supreme Court defeat may not matter much. They have already done immense damage to truth and transparency on the internet. And at this late date, the worst of it cannot be undone.
Advertisement
Supported by
What’s Next for the Coronavirus?
Scientists studying the virus’s continuing evolution, and the body’s immune responses, hope to head off a resurgence and to better understand long Covid.
- Share full article

By Apoorva Mandavilli
Apoorva Mandavilli has been reporting on Covid since the start of the pandemic.
Rat droppings from New York City. Poop from dog parks in Wisconsin. Human waste from a Missouri hospital. These are some of the materials that are readying us for the next chapter of the coronavirus saga.
More than four years into the pandemic, the virus has loosened its hold on most people’s bodies and minds. But a new variant better able to dodge our immune defenses may yet appear, derailing a hard-won return to normalcy.
Scientists around the country are watching for the first signs.
“We’re not in the acute phases of a pandemic anymore, and I think it’s understandable and probably a good thing” that most people, including scientists, have returned to their prepandemic lives, said Jesse Bloom, an evolutionary biologist at the Fred Hutchinson Cancer Center in Seattle.
“That said, the virus is still evolving, it’s still infecting large numbers of people,” he added. “We need to keep tracking this.”
Dr. Bloom and other researchers are trying to understand how the coronavirus behaves and evolves as populations amass immunity. Other teams are probing the body’s response to the infection, including the complex syndrome called long Covid.
And some scientists have taken on an increasingly difficult task: estimating vaccine effectiveness in a crowded respiratory milieu.
“Intellectually, this virus, to me at least, is only becoming more interesting,” said Sarah Cobey, an evolutionary biologist at the University of Chicago.
“In some ways, SARS-CoV-2 has been a fabulous reminder of some of the deepest questions in the field, and also how far we have to go in answering a lot of them.”
Closely analyzing new variants appearing in wastewater may help predict what additional forms may surface, said Marc Johnson, a virologist at the University of Missouri, who has hunted for iterations of the coronavirus in stool samples from rodents and humans.
“They help inform the evolution of this virus and what’s likely to happen next, and possibly could even inform how to make a better vaccine,” Dr. Johnson said.
The ‘Black Swan Event’
Evolutionary biology was once an esoteric pursuit involving humdrum hours staring at a computer screen. The work’s implications for public health were often tenuous.
The pandemic changed that. Vaccines can now be made more easily and much faster than before, so “really understanding how viruses evolve has more and more practical utility,” Dr. Bloom said.
Many evolutionary biologists who now study the coronavirus, including Dr. Bloom, were experts in influenza, which evolves into a new variant every two to eight years from its most immediate predecessor.
The scientists expected the coronavirus to behave similarly. But Omicron arrived with dozens of new mutations — a shocking “black swan event,” Dr. Bloom said. Then came BA.2.86, another huge jump in evolution, signaling that the virus remained unpredictable.
The iterations of a virus that thrive throughout a population have some sort of advantage — an ability to sidestep the immune system, perhaps, or extreme contagiousness. In an individual, “there is no such evolutionary pressure,” said Katia Koelle, an evolutionary biologist at Emory University.
The result is that a chronic infection — usually in an immunocompromised person — offers the virus an opportunity to experiment with new formats, allowing it to hit the evolutionary equivalent of a fast-forward button. (Viral persistence in the body is also thought to play a role in long Covid.)
Chronic infections with the coronavirus are rare, even among immunocompromised people. But the Alpha variant of late 2020, the Omicron variant in late 2021 and BA.2.86, first detected last summer — all are now thought to have emerged from immunocompromised people.
Some mutations acquired as the virus evolves may offer no benefit at all, or may even hinder it, Dr. Koelle said. Not all of the virus versions pose a widespread threat to the population — BA.2.86 ultimately did not, for example.
But these genetic alterations may nevertheless foreshadow the future.
After BA.2.86 emerged, close analysis of its genome revealed one spot where the virus remained sensitive to the body’s immune defenses. Dr. Johnson guessed that the virus’s next move would be to acquire a mutation in that very spot.
“And sure enough, it just appeared,” he said, referring to JN.1 , the variant that now accounts for a vast majority of infections.
“The more we see these lineages like BA.2.86, which appear to be from chronic infections, the more we have an argument like, Hey, this really is something we should be paying attention to,” he added.
Analyzing more than 20,000 samples of wastewater from across the country, Dr. Johnson has found fewer than 60 viral genetic sequences that are likely to be from immunocompromised people.
Such sequences turn up only when a “super shedder” — an individual who sheds huge amounts of virus in their feces — happens to live in an area with wastewater surveillance. “I’m sure there are a ton more out there,” Dr. Johnson said. “I just don’t know how many more.”
Spotty Surveillance
Scientists looking for signs of renewed danger are constrained by the limited surveillance for coronavirus variants in the United States and elsewhere.
Many countries, including the United States, ramped up tracking efforts at the height of the pandemic. But they have since been cut back, leaving scientists to guess the scale of respiratory virus infections. Wastewater and hospitalizations can provide clues, but neither is a sensitive measure.
“We never have had especially systematic surveillance for respiratory pathogens in the United States, but it’s even less systematic now,” Dr. Cobey said. “Our understanding of the burden of these pathogens, much less their evolution, has been really compromised.”
Not tracking viruses closely has another consequence: With multiple respiratory viruses to combat each year, it is now extremely challenging to gauge how effective the vaccines are.
Before Covid, scientists estimated the effectiveness of the influenza vaccine by comparing the vaccination status of those who tested positive for flu with those who did not.
But now, with vaccines for Covid and respiratory syncytial virus in the mix, the calculations are no longer simple. Patients turn up at clinics and hospitals with similar symptoms, and each vaccine prevents those symptoms to a different degree.
“It becomes this much more complex network of prevention that’s happening,” said Emily Martin, an epidemiologist at the University of Michigan. “It does funny things to the numbers.”
An accurate estimate of effectiveness will be crucial for designing each season’s vaccine, and for preparing doctors and patients to face a rough respiratory season.
In 2021, for example, the University of Michigan experienced an outbreak of influenza. When the researchers worked out that the season’s vaccine didn’t protect against that strain, they were able to warn other college campuses to prepare for clusters in their dorms, and hospitals to stock up on antiviral drugs.
Solving the problem may itself pose complications, because different divisions at the Centers for Disease Control and Prevention work on influenza, Covid and other respiratory diseases.
“It requires problem-solving across these sort of artificial lines of different departments,” Dr. Martin said.
Immunity and Long Covid
As coronavirus variant after variant materialized, it became clear that while the vaccines provided a powerful bulwark against severe illness and death, they were much less effective at stopping viral spread.
For a vaccine to prevent infections, it must induce antibodies not just in the blood, but at sites where the virus invades the body.
“Ideally, you’d want them across mucosal sites — so, in your nose, in your lungs,” said Marion Pepper, an immunologist at the University of Washington in Seattle.
Scientists discovered about 15 years ago that a large part of the body’s defenses comes not just from the cells and organs of the immune system, but from these other tissues.
“One of the things that we’ve been really focused on is trying to understand immune responses in the tissues better than we did before,” Dr. Pepper said.
In a small set of people, the virus itself may also persist in various parts of the body, and may be one of the causes of long Covid. Vaccination and antiviral drugs alleviate some of the symptoms, lending credence to this idea.
At Yale University, Akiko Iwasaki and her colleagues are testing whether a 15-day course of the antiviral drug Paxlovid can eliminate a slowly replicating reservoir of virus in the body.
“We’re hoping to get to the root cause if that’s what’s causing people’s illness,” Dr. Iwasaki said.
She and her colleagues began studying immune responses to the coronavirus almost as soon as the virus appeared. As the pandemic progressed, the collaborations grew larger and more international.
And it became obvious that in many people, the coronavirus leaves a lasting legacy of immune-related problems.
Two years ago, Dr. Iwasaki proposed a new center to study the myriad questions that have arisen. Infections with many other viruses, bacteria and parasites also set off long-term complications , including autoimmunity.
The new virtual institute, started last summer, is dedicated to studying post-infection syndromes and strategies to prevent and treat them.
Before the pandemic, Dr. Iwasaki was already busy studying viral infections with a big lab and multiple projects. But it doesn’t begin to compare with her life now, she said.
“Scientists tend to be obsessed about things that they work on, but not with this level of urgency,” she said. “I’m pretty much working every waking hour.”
A photo caption in an earlier version of this article referred incorrectly to a center at the University of Missouri. It is the Bond Life Sciences Center, not the Lab Science Center.
How we handle corrections
Apoorva Mandavilli is a reporter focused on science and global health. She was a part of the team that won the 2021 Pulitzer Prize for Public Service for coverage of the pandemic. More about Apoorva Mandavilli

IMAGES
COMMENTS
A. Vaccines save lives and they can save money too. It's cheaper to prevent a disease than to treat it. The routine childhood immunization in one child saves $13.6 billion in direct cost. Every dollar spent on childhood vaccinations has saved $18.40 (Colorado Children's Immunization Coalition, 2019).
Caroline Gutman for The New York Times. 2. Hearing pro-vaccine messages from doctors, friends and relatives. For many people who got vaccinated, messages from politicians, national experts and the ...
The vaccine debate—including the argument as to whether vaccines are safe, effective, or could cause conditions like autism —has received a lot of attention from the media in recent years. With so much conflicting information being publicized, it can be a challenge to discern what is true and what is not.
An additional aspect of vaccines many parents are troubled with is the increase in suggested vaccines for young children. "Today, the CDC recommends that children receive vaccines for 10 diseases — plus the flu vaccine — by age 6, which can mean up to 37 separate shots. That compares to five vaccines for the same age group in 1995 ...
Debate on mandatory COVID-19 vaccination: a commentary from the perspective of public health ethics. This article, published in the journal BMC Medical Ethics, explores the ethical arguments for and against imposing mandatory vaccination for COVID-19, considering the principles of beneficence, non-maleficence, autonomy, and justice. The authors also discuss the practical challenges and ...
Guest Essay. Vaccine Mandates Are Coming. Good. June 28, 2021. Smallpox vaccinations in the 1960s. ... The mRNA vaccines, made by Moderna and Pfizer-BioNTech, will likely get full approval for use ...
jane coaston. Today on "The Argument" — do vaccine mandates maybe make things worse? [MUSIC PLAYING] archived recording. You will soon have to show proof of full vaccination if you want to ...
The straightforward ethical argument, then, says: Getting vaccinated isn't just about you. Yes, you have the right to take risks with your own safety. But as the British philosopher John Stuart ...
Alberto Giubilini, Senior Research Fellow, Oxford Uehiro Centre for Practical Ethics, University of Oxford. COVID-19 vaccination should be mandatory - at least for certain groups. This means ...
Here we use two survey experiments to study how persuasive messaging affects COVID-19 vaccine uptake intentions. In the first experiment, we test a large number of treatment messages. One subgroup of messages draws on the idea that mass vaccination is a collective action problem and highlighting the prosocial benefit of vaccination or the ...
Please use one of the following formats to cite this article in your essay, paper or report: APA. Moore, Sarah. (2022, January 17). The Importance of Global COVID-19 Vaccination.
The benefits of vaccinations far outweigh the risks and vaccines do and have eradicated many diseases. The side effects of vaccines are occasionally serious, but are so rare that parents should follow the vaccination schedule to prevent widespread outbreaks. II.Vaccinating children have reduced death rates significantly and the risk of not ...
Persuasive Essay Vaccines "A vaccination is the administration of antigenic material to stimulate an individual immune system to develop adaptive immunity to a pathogen. "(wiki) A vaccination is also taking a small dose of a disease or sickness and injecting it into the human body. Do this causes the human body to fight against the disease ...
Covid vaccine mandates will almost certainly encounter legal trouble, whatever form they take. That's because the Food and Drug Administration has authorized them for only emergency use. Under ...
Background By mid 2023, European countries reached 75% of vaccine coverage for COVID-19 and although vaccination rates are quite high, many people are still hesitant. A plethora of studies have investigated factors associated with COVID-19 vaccine hesitancy, however, insufficient attention has been paid to the reasons why people get vaccinated against COVID-19. Our work aims to investigate the ...
Whatever your point of view is, writing a persuasive essay about it is a good way of organizing your thoughts and persuading others. A persuasive essay about the Covid-19 vaccine could consider the benefits of getting vaccinated as well as the potential side effects. Below are some examples of persuasive essays on getting vaccinated for Covid-19.
Argumentative Essay On Vaccinations For Children. One could say a total nightmare for one's new born child would be having the baby infected with a harmful disease. Today, children and adults of different races and generations are becoming victims of communicable diseases. Fortunately, an English doctor named Edward Jenner developed the first ...
Dorit Reiss, a vaccine policy researcher at the University of California Law-San Francisco, fears the revived parental rights movement may eventually abolish routine immunizations to attend school.
The rest was an unfortunate sideshow. Like so many Supreme Court cases these days, Murthy is built atop a heap of fake facts. The case began when Missouri and Louisiana sued agencies and officials ...
These are some of the materials that are readying us for the next chapter of the coronavirus saga. More than four years into the pandemic, the virus has loosened its hold on most people's bodies ...