Mental health benefits associated with gender-affirming surgery
Gender-affirming surgeries are associated with numerous positive health benefits, including lower rates of psychological distress and suicidal ideation, as well as lower rates of smoking , according to new research led by Harvard T.H. Chan School of Public Health.
The study examined data from the 2015 U.S. Transgender Survey, which included nearly 20,000 participants, 38.8% of whom identified as transgender women, 32.5% of whom identified as transgender men, and 26.6% of whom identified as nonbinary. Of the respondents, 12.8% had undergone gender-affirming surgery at least two years prior and 59.2% wanted to undergo surgery but had not done so yet.
Gender-affirming surgeries were associated with a 42% reduction in psychological distress and a 44% reduction in suicidal ideation when compared with transgender and gender-diverse people who had not had gender-affirming surgery but wanted it, according to the findings. The study also found a 35% reduction in tobacco smoking among people who had gender-affirming surgeries.
“Going into this study, we certainly did believe that the gender-affirming surgeries would be protective against adverse mental health outcomes,” lead author Anthony Almazan, an MPH candidate at Harvard Chan School, said in an April 28, 2021, HealthDay article. “I think we were pleasantly surprised by the strength of the magnitudes of these associations, which really are very impressive and, in our opinion, speaks to the importance of gender-affirming surgery as medically necessary treatment for transgender and gender diverse people who are seeking out this kind of affirmation.”
Read the HealthDay article: Gender-Affirming Surgeries Improve Mental Health in Young, Study Says

Sex-reassignment surgery yields long-term mental health benefits, study finds
When transgender people undergo sex-reassignment surgery, the beneficial effect on their mental health is still evident — and increasing — years later, a Swedish study suggests.
Overall, people in the study with gender incongruence — that is, their biological gender doesn’t match the gender with which they identify — were six times more likely than people in the general population to visit a doctor for mood and anxiety disorders. They were also three times more likely to be prescribed antidepressants, and six times more likely to be hospitalized after a suicide attempt, researchers found.
But among trans people who had undergone gender-affirming surgery, the longer ago their surgery, the less likely they were to suffer anxiety, depression or suicidal behavior during the study period, researchers reported in The American Journal of Psychiatry.

NBC OUT Baylor professor apologizes after guest speaker promotes conversion therapy
Surgery to modify a person’s sex characteristics “is often the last and the most considered step in the treatment process for gender dysphoria,” according to the World Professional Association for Transgender Health.
Many transgender and gender-nonconforming individuals "find comfort with their gender identity, role, and expression without surgery," but for others, "surgery is essential and medically necessary to alleviate their gender dysphoria," according to the organization.
While the new study confirms that transgender individuals are more likely to use mental health treatments, it also shows that gender-affirming therapy might reduce this risk, coauthor Richard Branstrom of the Karolinska Institutet in Stockholm told Reuters Health by email.

NBC OUT Protests, arrests and injuries as Georgians protest gay film's debut
Branstrom and colleague John Pachankis of the Yale School of Public Health in New Haven, Connecticut found that as of 2015, 2,679 people in Sweden had a diagnosis of gender incongruence, out of the total population of 9.7 million.
That year, 9.3 percent of people with gender incongruence visited a doctor for mood disorders, 7.4 percent saw a doctor for anxiety disorders and 29 percent were on antidepressants. In the general population, those percentages were 1 percent, 0.6 percent and 9.4 percent, respectively.
Just over 70 percent of people with gender incongruence were receiving feminizing or masculinizing hormones to modify outward sexual features such as breasts, body fat distribution and facial hair, and 48 percent had undergone gender-affirming surgery. Nearly all of those who had surgery also received hormone therapy.
The benefit of hormone treatment did not increase with time. But “increased time since last gender-affirming surgery was associated with fewer mental health treatments,” the authors report.
In fact, they note, “The likelihood of being treated for a mood or anxiety disorder was reduced by 8 percent for each year since the last gender-affirming surgery,” for up to 10 years.

NBC OUT LGBTQ advocates applaud judges' rejections of Trump health care rule
Transgender individuals’ use of mental health care still exceeded that of the general Swedish population, which the research team suggests is due at least partly to stigma, economic inequality and victimization.
“We need greater visibility and knowledge about challenges people are confronted with while breaking gender and identity norms,” Branstrom said.
Dr. Joshua Safer, executive director at Mount Sinai Center for Transgender Medicine and Surgery in New York City, told Reuters Health by email, “If anything, the study likely under-reports mental health benefits of medical and surgical care for transgender individuals.”
Safer, who was not involved in the study, said the fact that mental health continued to improve for years after surgery “suggests (surgery provides) extended and ongoing benefit to patients living according to gender identity.”
Follow NBC Out on Twitter , Facebook & Instagram
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Preparation and Procedures Involved in Gender Affirmation Surgeries
If you or a loved one are considering gender affirmation surgery , you are probably wondering what steps you must go through before the surgery can be done. Let's look at what is required to be a candidate for these surgeries, the potential positive effects and side effects of hormonal therapy, and the types of surgeries that are available.
Gender affirmation surgery, also known as gender confirmation surgery, is performed to align or transition individuals with gender dysphoria to their true gender.
A transgender woman, man, or non-binary person may choose to undergo gender affirmation surgery.
The term "transexual" was previously used by the medical community to describe people who undergo gender affirmation surgery. The term is no longer accepted by many members of the trans community as it is often weaponized as a slur. While some trans people do identify as "transexual", it is best to use the term "transgender" to describe members of this community.
Transitioning
Transitioning may involve:
- Social transitioning : going by different pronouns, changing one’s style, adopting a new name, etc., to affirm one’s gender
- Medical transitioning : taking hormones and/or surgically removing or modifying genitals and reproductive organs
Transgender individuals do not need to undergo medical intervention to have valid identities.
Reasons for Undergoing Surgery
Many transgender people experience a marked incongruence between their gender and their assigned sex at birth. The American Psychiatric Association (APA) has identified this as gender dysphoria.
Gender dysphoria is the distress some trans people feel when their appearance does not reflect their gender. Dysphoria can be the cause of poor mental health or trigger mental illness in transgender people.
For these individuals, social transitioning, hormone therapy, and gender confirmation surgery permit their outside appearance to match their true gender.
Steps Required Before Surgery
In addition to a comprehensive understanding of the procedures, hormones, and other risks involved in gender-affirming surgery, there are other steps that must be accomplished before surgery is performed. These steps are one way the medical community and insurance companies limit access to gender affirmative procedures.
Steps may include:
- Mental health evaluation : A mental health evaluation is required to look for any mental health concerns that could influence an individual’s mental state, and to assess a person’s readiness to undergo the physical and emotional stresses of the transition.
- Clear and consistent documentation of gender dysphoria
- A "real life" test : The individual must take on the role of their gender in everyday activities, both socially and professionally (known as “real-life experience” or “real-life test”).
Firstly, not all transgender experience physical body dysphoria. The “real life” test is also very dangerous to execute, as trans people have to make themselves vulnerable in public to be considered for affirmative procedures. When a trans person does not pass (easily identified as their gender), they can be clocked (found out to be transgender), putting them at risk for violence and discrimination.
Requiring trans people to conduct a “real-life” test despite the ongoing violence out transgender people face is extremely dangerous, especially because some transgender people only want surgery to lower their risk of experiencing transphobic violence.
Hormone Therapy & Transitioning
Hormone therapy involves taking progesterone, estrogen, or testosterone. An individual has to have undergone hormone therapy for a year before having gender affirmation surgery.
The purpose of hormone therapy is to change the physical appearance to reflect gender identity.
Effects of Testosterone
When a trans person begins taking testosterone , changes include both a reduction in assigned female sexual characteristics and an increase in assigned male sexual characteristics.
Bodily changes can include:
- Beard and mustache growth
- Deepening of the voice
- Enlargement of the clitoris
- Increased growth of body hair
- Increased muscle mass and strength
- Increase in the number of red blood cells
- Redistribution of fat from the breasts, hips, and thighs to the abdominal area
- Development of acne, similar to male puberty
- Baldness or localized hair loss, especially at the temples and crown of the head
- Atrophy of the uterus and ovaries, resulting in an inability to have children
Behavioral changes include:
- Aggression
- Increased sex drive
Effects of Estrogen
When a trans person begins taking estrogen , changes include both a reduction in assigned male sexual characteristics and an increase in assigned female characteristics.
Changes to the body can include:
- Breast development
- Loss of erection
- Shrinkage of testicles
- Decreased acne
- Decreased facial and body hair
- Decreased muscle mass and strength
- Softer and smoother skin
- Slowing of balding
- Redistribution of fat from abdomen to the hips, thighs, and buttocks
- Decreased sex drive
- Mood swings
When Are the Hormonal Therapy Effects Noticed?
The feminizing effects of estrogen and the masculinizing effects of testosterone may appear after the first couple of doses, although it may be several years before a person is satisfied with their transition. This is especially true for breast development.
Timeline of Surgical Process
Surgery is delayed until at least one year after the start of hormone therapy and at least two years after a mental health evaluation. Once the surgical procedures begin, the amount of time until completion is variable depending on the number of procedures desired, recovery time, and more.
Transfeminine Surgeries
Transfeminine is an umbrella term inclusive of trans women and non-binary trans people who were assigned male at birth.
Most often, surgeries involved in gender affirmation surgery are broken down into those that occur above the belt (top surgery) and those below the belt (bottom surgery). Not everyone undergoes all of these surgeries, but procedures that may be considered for transfeminine individuals are listed below.
Top surgery includes:
- Breast augmentation
- Facial feminization
- Nose surgery: Rhinoplasty may be done to narrow the nose and refine the tip.
- Eyebrows: A brow lift may be done to feminize the curvature and position of the eyebrows.
- Jaw surgery: The jaw bone may be shaved down.
- Chin reduction: Chin reduction may be performed to soften the chin's angles.
- Cheekbones: Cheekbones may be enhanced, often via collagen injections as well as other plastic surgery techniques.
- Lips: A lip lift may be done.
- Alteration to hairline
- Male pattern hair removal
- Reduction of Adam’s apple
- Voice change surgery
Bottom surgery includes:
- Removal of the penis (penectomy) and scrotum (orchiectomy)
- Creation of a vagina and labia
Transmasculine Surgeries
Transmasculine is an umbrella term inclusive of trans men and non-binary trans people who were assigned female at birth.
Surgery for this group involves top surgery and bottom surgery as well.
Top surgery includes :
- Subcutaneous mastectomy/breast reduction surgery.
- Removal of the uterus and ovaries
- Creation of a penis and scrotum either through metoidioplasty and/or phalloplasty
Complications and Side Effects
Surgery is not without potential risks and complications. Estrogen therapy has been associated with an elevated risk of blood clots ( deep vein thrombosis and pulmonary emboli ) for transfeminine people. There is also the potential of increased risk of breast cancer (even without hormones, breast cancer may develop).
Testosterone use in transmasculine people has been associated with an increase in blood pressure, insulin resistance, and lipid abnormalities, though it's not certain exactly what role these changes play in the development of heart disease.
With surgery, there are surgical risks such as bleeding and infection, as well as side effects of anesthesia . Those who are considering these treatments should have a careful discussion with their doctor about potential risks related to hormone therapy as well as the surgeries.
Cost of Gender Confirmation Surgery
Surgery can be prohibitively expensive for many transgender individuals. Costs including counseling, hormones, electrolysis, and operations can amount to well over $100,000. Transfeminine procedures tend to be more expensive than transmasculine ones. Health insurance sometimes covers a portion of the expenses.
Quality of Life After Surgery
Quality of life appears to improve after gender-affirming surgery for all trans people who medically transition. One 2017 study found that surgical satisfaction ranged from 94% to 100%.
Since there are many steps and sometimes uncomfortable surgeries involved, this number supports the benefits of surgery for those who feel it is their best choice.
A Word From Verywell
Gender affirmation surgery is a lengthy process that begins with counseling and a mental health evaluation to determine if a person can be diagnosed with gender dysphoria.
After this is complete, hormonal treatment is begun with testosterone for transmasculine individuals and estrogen for transfeminine people. Some of the physical and behavioral changes associated with hormonal treatment are listed above.
After hormone therapy has been continued for at least one year, a number of surgical procedures may be considered. These are broken down into "top" procedures and "bottom" procedures.
Surgery is costly, but precise estimates are difficult due to many variables. Finding a surgeon who focuses solely on gender confirmation surgery and has performed many of these procedures is a plus. Speaking to a surgeon's past patients can be a helpful way to gain insight on the physician's practices as well.
For those who follow through with these preparation steps, hormone treatment, and surgeries, studies show quality of life appears to improve. Many people who undergo these procedures express satisfaction with their results.
Bizic MR, Jeftovic M, Pusica S, et al. Gender dysphoria: Bioethical aspects of medical treatment . Biomed Res Int . 2018;2018:9652305. doi:10.1155/2018/9652305
American Psychiatric Association. What is gender dysphoria? . 2016.
The World Professional Association for Transgender Health. Standards of care for the health of transsexual, transgender, and gender-nonconforming people . 2012.
Tomlins L. Prescribing for transgender patients . Aust Prescr . 2019;42(1): 10–13. doi:10.18773/austprescr.2019.003
T'sjoen G, Arcelus J, Gooren L, Klink DT, Tangpricha V. Endocrinology of transgender medicine . Endocr Rev . 2019;40(1):97-117. doi:10.1210/er.2018-00011
Unger CA. Hormone therapy for transgender patients . Transl Androl Urol . 2016;5(6):877-884. doi:10.21037/tau.2016.09.04
Seal LJ. A review of the physical and metabolic effects of cross-sex hormonal therapy in the treatment of gender dysphoria . Ann Clin Biochem . 2016;53(Pt 1):10-20. doi:10.1177/0004563215587763
Schechter LS. Gender confirmation surgery: An update for the primary care provider . Transgend Health . 2016;1(1):32-40. doi:10.1089/trgh.2015.0006
Altman K. Facial feminization surgery: current state of the art . Int J Oral Maxillofac Surg . 2012;41(8):885-94. doi:10.1016/j.ijom.2012.04.024
Therattil PJ, Hazim NY, Cohen WA, Keith JD. Esthetic reduction of the thyroid cartilage: A systematic review of chondrolaryngoplasty . JPRAS Open. 2019;22:27-32. doi:10.1016/j.jpra.2019.07.002
Top H, Balta S. Transsexual mastectomy: Selection of appropriate technique according to breast characteristics . Balkan Med J . 2017;34(2):147-155. doi:10.4274/balkanmedj.2016.0093
Chan W, Drummond A, Kelly M. Deep vein thrombosis in a transgender woman . CMAJ . 2017;189(13):E502-E504. doi:10.1503/cmaj.160408
Streed CG, Harfouch O, Marvel F, Blumenthal RS, Martin SS, Mukherjee M. Cardiovascular disease among transgender adults receiving hormone therapy: A narrative review . Ann Intern Med . 2017;167(4):256-267. doi:10.7326/M17-0577
Hashemi L, Weinreb J, Weimer AK, Weiss RL. Transgender care in the primary care setting: A review of guidelines and literature . Fed Pract . 2018;35(7):30-37.
Van de grift TC, Elaut E, Cerwenka SC, Cohen-kettenis PT, Kreukels BPC. Surgical satisfaction, quality of life, and their association after gender-affirming aurgery: A follow-up atudy . J Sex Marital Ther . 2018;44(2):138-148. doi:10.1080/0092623X.2017.1326190
American Society of Plastic Surgeons. Gender confirmation surgeries .
American Psychological Association. Transgender people, gender identity, and gender expression .
Colebunders B, Brondeel S, D'Arpa S, Hoebeke P, Monstrey S. An update on the surgical treatment for transgender patients . Sex Med Rev . 2017 Jan;5(1):103-109. doi:10.1016/j.sxmr.2016.08.001
- Accessibility Tools
- Skip to main content
Life After Gender Affirming Surgery: Five Benefits
- Life After Gender Affirming Surgery Five Benefits

Gender affirming surgery includes a wide variety of surgeries for those transitioning from male to female or female to male to help with gender dysphoria. There are many different types of surgeries that can be considered gender affirming surgery but they all have the goal of helping the patient affirm the gender they identify as and are transitioning to. These different surgeries help the patient look and feel more masculine or feminine and are greatly beneficial to the patient and their overall journey.
Different surgery options include, but are not limited to:
- Body contouring
- Rhinoplasty
- Breast augmentation
- Buttock/hip enhancement
- Rib reduction
- Vaginoplasty
- Phalloplasty
- Masculinizing chest surgery
- Facial feminization surgery
- Voice surgery
- Tracheal shave
- Facial masculinization surgery
Knowing the benefits of surgery beforehand can greatly help patients make the right decision about whether to move forward with their desired surgery with peace of mind.
Below we’ll discuss five benefits of gender affirming surgeries and what patients can look forward to with life after.
Long-Term Mental Health Benefits
Research shows that one of the main benefits of gender affirming surgery is the wide array of long-term mental health benefits patients experience. Some studies report that patients who underwent gender affirming surgeries experienced lower rates of psychological distress and suicidal ideation. Another study found that a person’s odds for needing mental health treatment declined by 8% each year after gender affirming surgery.
More and more studies showing the large number of mental health benefits patients are experiencing post-surgery confirm the importance of gender procedures as medically necessary treatments for transgender people.
Higher Quality of Life
Many transgender patients before undergoing gender affirming procedures are looking to have a higher quality of life living as their identifying gender and believe that gender affirming procedures will help provide that. As you might imagine, a higher quality of life is a benefit many patients experience after undergoing surgery. While hormone therapy can make a big difference in one’s transition journey, gender affirming procedures are essential for helping transgender people truly look and feel like themselves.
One study measuring transgender patients’ overall quality of life post-surgery found that three-quarters of patients who underwent a gender affirming surgery have a better quality of life now.
Improved Sexuality
One main concern for transgender people is how their sexuality and experience will change throughout their transition journey. This is especially true for patients who desire to undergo any type of bottom surgery. Common concerns brought up by patients are their ability to experience sexual satisfaction after surgery. Fortunately, many studies have found that transgender patients have reported that they experienced higher levels of sexual satisfaction after gender surgery.
One study shows that over 75% of patients were able to achieve orgasm after surgery. Transgender patients have reported being able to reach orgasm more easily and experience more frequent sexual satisfaction than they had before surgery.
Better Self Image
A number of pre-surgery transgender patients struggle with low self-image, self-esteem, and with positive body image because they don’t look and feel masculine or feminine enough. One of the benefits many patients hope to experience from surgery is feeling more confident in themselves and their gender. One study of transgender men showed that participants had lower self-esteem than cis-gender men and that a mastectomy improved their body image, self-esteem, and self-worth.
Improved Social Affirmation
While transgender people can make a lot of nonsurgical changes to more closely identify with their gender for themselves and to signal others, it can feel challenging for many to affirm their gender socially and feel accepted pre-gender affirming surgery. For some people, changing their pronouns, name, and clothing doesn’t feel like enough to fit in.
Gender affirming surgery allows a trans patient’s physical attributes to align more closely with their self-identified gender and appear as their self-identified gender to others as well. Not only do gender affirming surgeries help trans patients feel more socially accepted, but they also help patients feel more confident overall in public and social settings.
The Bottom Line
As gender affirming surgeries are being studied more and more, the known benefits of life after surgery continue to grow. It’s clear that gender affirming surgeries are a necessity for overall quality of life for transgender people. While many patients have concerns before going through these big, life-changing procedures, knowing the benefits that lie ahead can be comforting.
In addition to knowing the benefits, it’s also essential to undergo a consultation with a surgeon before making any final decisions. This ensures that you’re a good candidate for surgery and that you choose the best procedures to reach your desired outcome.
Ready to get started on your gender affirming surgery journey? Leif Rogers, MD, is an Ivy League-educated, board-certified plastic surgeon and a standing member of the American Society of Plastic Surgeons. To schedule a consultation, get in touch with our team today.
Your Path to Perfection begin your radiant transformation
A Systematic Review of the Psychological Benefits of Gender-Affirming Surgery
Affiliations.
- 1 Department of Child and Adolescent Psychiatry, Hassenfeld Children's Hospital at NYU Langone, 1 Park Avenue, 7th Floor, New York, NY 10016, USA. Electronic address: [email protected].
- 2 Department of Child and Adolescent Psychiatry, Hassenfeld Children's Hospital at NYU Langone, 1 Park Avenue, 7th Floor, New York, NY 10016, USA.
- 3 NYU Langone, Health Sciences Library, New York, NY, USA.
- 4 Ann and Robert H. Lurie Children's Hospital of Chicago, Department of Psychiatry, 225 E Chicago Avenue, Chicago, IL 60611, USA.
- PMID: 31582022
- DOI: 10.1016/j.ucl.2019.07.002
For individuals with gender dysphoria, gender-affirming surgeries (GAS) are one means of reducing the significant distress associated with primary and secondary sex characteristics misaligned with their gender identity. This article uses a systematic review to examine the existing literature on the psychological benefits of GAS. Findings from this review indicate that GAS can lead to multiple, significant improvements in psychological functioning. Methodological differences in the literature demonstrate the need for additional research to draw more definitive conclusions about the psychological benefits of GAS.
Keywords: Gender dysphoria; Gender-affirming surgery; Mental health; Transgender health; Well-being.
Copyright © 2019 Elsevier Inc. All rights reserved.
Publication types
- Systematic Review
- Gender Dysphoria / psychology*
- Gender Dysphoria / surgery*
- Sex Reassignment Surgery / psychology*
- Reconstructive Procedures
Gender Confirmation Surgeries Transgender-Specific Facial, Top and Bottom Procedures
What surgical options are available to transgender and gender non-conforming patients? Gender confirmation surgeries, also known as gender affirmation surgeries, are performed by a multispecialty team that typically includes board-certified plastic surgeons. The goal is to give transgender individuals the physical appearance and functional abilities of the gender they know themselves to be. Listed below are many of the available procedures for transwomen (MTF) and transmen (FTM) to aid in their journey.
Facial Feminization Surgery
Transfeminine top surgery, transfeminine bottom surgery, facial masculinization surgery, transmasculine top surgery, transmasculine bottom surgery, on the blog.

Facial feminization surgery is a combination of procedures designed to soften the facial features and feminize the face. There are many procedures that are available to feminize the face.
- Facial feminization surgery improves gender dysphoria in trans women Josef Hadeed, MD, FACS
- The impact of COVID-19 on gender dysphoria patients Cristiane Ueno, MD
On The Vlog

Facial feminization surgery is always tailored to the individual, but as ASPS member Justine Lee, MD, PhD, explains there are general characteristics such as hairline, brow bones, cheeks and jawline that many patients note and plastic surgeons plan for.
- Gender Affirmation Top Surgery with Dr. Julie Hansen
Find Your Surgeon
Patient care center, before & after photos.

Video Gallery
3d animations, patient safety.
Featured Topics
Featured series.
A series of random questions answered by Harvard experts.
Explore the Gazette
Read the latest.

‘I was frustrated, infuriated, because women are just as capable’

How do you read organization’s silence over rise of Nazism?

When the circus called, she took the leap
Mental health benefits associated with gender-affirming surgery.

Various pride flags are displayed at the Harvard T.H. Chan School of Public Health. Kris Snibbe/Harvard file photo
Gender-affirming surgeries are associated with numerous positive health benefits, including lower rates of psychological distress and suicidal ideation, as well as lower rates of smoking, according to new research led by Harvard T.H. Chan School of Public Health.
The study examined data from the 2015 U.S. Transgender Survey, which included nearly 20,000 participants, 38.8 percent of whom identified as transgender women, 32.5 percent of whom identified as transgender men, and 26.6 percent of whom identified as nonbinary. Of the respondents, 12.8 percent had undergone gender-affirming surgery at least two years prior and 59.2 percent wanted to undergo surgery but had not done so yet.
Gender-affirming surgeries were associated with a 42 percent reduction in psychological distress and a 44 percent reduction in suicidal ideation when compared with transgender and gender-diverse people who had not had gender-affirming surgery but wanted it, according to the findings. The study also found a 35 percent reduction in tobacco smoking among people who had gender-affirming surgeries.
“Going into this study, we certainly did believe that the gender-affirming surgeries would be protective against adverse mental health outcomes,” lead author Anthony Almazan, an M.P.H. candidate at Harvard Chan School, said in an April 28, 2021, HealthDay article. “I think we were pleasantly surprised by the strength of the magnitudes of these associations, which really are very impressive and, in our opinion, speaks to the importance of gender-affirming surgery as medically necessary treatment for transgender and gender diverse people who are seeking out this kind of affirmation.”
Share this article
You might like.
Experiences in Uganda and U.S. fuel Ananda Birungi’s passion for empowering others, especially women and girls

Medical historians look to cultural context, work of peer publications in wrestling with case of New England Journal of Medicine

Extension School allowed trapeze artist Izzy Patrowicz to pursue big top dreams alongside bachelor’s degree
Epic science inside a cubic millimeter of brain
Researchers publish largest-ever dataset of neural connections
Excited about new diet drug? This procedure seems better choice.
Study finds minimally invasive treatment more cost-effective over time, brings greater weight loss
How far has COVID set back students?
An economist, a policy expert, and a teacher explain why learning losses are worse than many parents realize
- Introduction
- Conclusions
- Article Information
Includes 2015 US Transgender Survey respondents who indicated they desired and either had or had not undergone at least 1 type of gender-affirming surgery. Respondents were presented with 1 of 2 lists of gender-affirming surgeries based on their self-reported sex assigned at birth.
- Legislation to Criminalize Gender-Affirming Medical Care for Transgender Youth JAMA Viewpoint June 8, 2021 This Viewpoint describes legislation aiming to criminalize medical care for transgender youth and explains why these bills are harmful and potentially unlawful. Jack L. Turban, MD, MHS; Katherine L. Kraschel, JD; I. Glenn Cohen, JD
- Gender-Affirming Surgeries and Improved Psychosocial Health Outcomes JAMA Surgery Invited Commentary July 1, 2021 Andrew A. Marano, MD; Matthew R. Louis, MD; Devin Coon, MD, MSE
See More About
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Others Also Liked
- Download PDF
- X Facebook More LinkedIn
- CME & MOC
Almazan AN , Keuroghlian AS. Association Between Gender-Affirming Surgeries and Mental Health Outcomes. JAMA Surg. 2021;156(7):611–618. doi:10.1001/jamasurg.2021.0952
Manage citations:
© 2024
- Permissions
Association Between Gender-Affirming Surgeries and Mental Health Outcomes
- 1 Harvard Medical School, Boston, Massachusetts
- 2 Harvard T. H. Chan School of Public Health, Boston, Massachusetts
- 3 The Fenway Institute, Fenway Health, Boston, Massachusetts
- 4 Department of Psychiatry, Massachusetts General Hospital, Boston
- Invited Commentary Gender-Affirming Surgeries and Improved Psychosocial Health Outcomes Andrew A. Marano, MD; Matthew R. Louis, MD; Devin Coon, MD, MSE JAMA Surgery
- Viewpoint Legislation to Criminalize Gender-Affirming Medical Care for Transgender Youth Jack L. Turban, MD, MHS; Katherine L. Kraschel, JD; I. Glenn Cohen, JD JAMA
Question Are gender-affirming surgeries associated with better mental health outcomes among transgender and gender diverse (TGD) people?
Findings In this secondary analysis of the 2015 US Transgender Survey (n = 27 715), TGD people with a history of gender-affirming surgery had significantly lower odds of past-month psychological distress, past-year tobacco smoking, and past-year suicidal ideation compared with TGD people with no history of gender-affirming surgery.
Meaning These findings support the provision of gender-affirming surgeries for TGD people who seek them.
Importance Requests for gender-affirming surgeries are rapidly increasing among transgender and gender diverse (TGD) people. However, there is limited evidence regarding the mental health benefits of these surgeries.
Objective To evaluate associations between gender-affirming surgeries and mental health outcomes, including psychological distress, substance use, and suicide risk.
Design, Setting, and Participants In this study, we performed a secondary analysis of data from the 2015 US Transgender Survey, the largest existing data set containing comprehensive information on the surgical and mental health experiences of TGD people. The survey was conducted across 50 states, Washington, DC, US territories, and US military bases abroad . A total of 27 715 TGD adults took the US Transgender Survey, which was disseminated by community-based outreach from August 19, 2015, to September 21, 2015. Data were analyzed between November 1, 2020, and January 3, 2021.
Exposures The exposure group included respondents who endorsed undergoing 1 or more types of gender-affirming surgery at least 2 years prior to submitting survey responses. The comparison group included respondents who endorsed a desire for 1 or more types of gender-affirming surgery but denied undergoing any gender-affirming surgeries.
Main Outcomes and Measures Endorsement of past-month severe psychological distress (score of ≥13 on Kessler Psychological Distress Scale), past-month binge alcohol use, past-year tobacco smoking, and past-year suicidal ideation or suicide attempt.
Results Of the 27 715 respondents, 3559 (12.8%) endorsed undergoing 1 or more types of gender-affirming surgery at least 2 years prior to submitting survey responses, while 16 401 (59.2%) endorsed a desire to undergo 1 or more types of gender-affirming surgery but denied undergoing any of these. Of the respondents in this study sample, 16 182 (81.1%) were between the ages of 18 and 44 years, 16 386 (82.1%) identified as White, 7751 (38.8%) identified as transgender women, 6489 (32.5%) identified as transgender men, and 5300 (26.6%) identified as nonbinary. After adjustment for sociodemographic factors and exposure to other types of gender-affirming care, undergoing 1 or more types of gender-affirming surgery was associated with lower past-month psychological distress (adjusted odds ratio [aOR], 0.58; 95% CI, 0.50-0.67; P < .001), past-year smoking (aOR, 0.65; 95% CI, 0.57-0.75; P < .001), and past-year suicidal ideation (aOR, 0.56; 95% CI, 0.50-0.64; P < .001).
Conclusions and Relevance This study demonstrates an association between gender-affirming surgery and improved mental health outcomes. These results contribute new evidence to support the provision of gender-affirming surgical care for TGD people.
Transgender and gender diverse (TGD) people experience a disproportionate burden of mental health problems compared with the general population. 1 , 2 Prior studies of mental health among TGD people have demonstrated a 41% lifetime prevalence of suicide attempts, 2 7% to 61% lifetime prevalence of binge drinking, 3 and a 33% prevalence of tobacco use. 4 Increased adverse mental health outcomes among TGD people are likely attributable to stigma, discrimination, pathologization, economic marginalization, violence, and dysphoria associated with an incongruence between gender identity and societal expectations based on one’s sex assigned at birth. 5
According to Standards of Care published by the World Professional Association for Transgender Health, gender-affirming surgery is a medically necessary treatment to alleviate psychological distress for many TGD people. 6 The term gender-affirming surgery refers to any surgical procedures offered to affirm the gender identities of TGD people. The process of surgical gender affirmation is individually tailored because not all TGD people desire or access these procedures. 7 In the largest survey of the TGD community to our knowledge to date, 25% of respondents reported undergoing some type of gender-affirming surgery. 8
As a result of professional recommendations, insurance nondiscrimination laws, and expansion of dedicated transgender health practices, demand for gender-affirming surgery is steadily rising. 9 In the United States, incidence of gender-affirming surgeries has increased annually since 2000. 10 Despite growing demand for and access to gender-affirming surgery, there is a paucity of high-quality evidence regarding its effects on mental health outcomes among TGD people.
Existing evidence on the association between gender-affirming surgeries and mental health outcomes is largely derived from small-sample, cross-sectional, and uncontrolled studies. 1 , 11 , 12 A seminal 1998 review of the experiences of more than 2000 TGD people from 79 predominantly uncontrolled follow-up studies demonstrated qualitative improvement in psychosocial outcomes following gender-affirming surgery. 11 Attempts since then to empirically demonstrate mental health benefits from gender-affirming surgery have generated mixed results. A meta-analysis of 1833 TGD people across 28 studies concluded that studies offered “low-quality evidence” for positive mental health benefits from surgical gender affirmation. 12 The largest existing study on this subject to our knowledge, 13 a total population study including 2679 people diagnosed as having gender incongruence in Sweden, demonstrated a longitudinal association between gender-affirming surgery and reduced mental health treatment utilization. 13 However, a 2020 published correction of this study 14 demonstrated no mental health benefit from gender-affirming surgery after comparison with a control group of TGD people who had not yet undergone surgery. Mental health effects of gender-affirming surgery thus remain controversial.
Given the increasing incidence of surgical gender affirmation among TGD people, there is a significant need for clarification of the mental health benefits of gender-affirming surgery. In this article, we present the largest study to our knowledge to date on the association between gender-affirming surgeries and mental health outcomes. Using the 2015 US Transgender Survey, the largest existing data set on surgical and mental health experiences of TGD people, we investigate the hypothesis that gender-affirming surgeries are associated with improved mental health outcomes, including psychological distress, substance use, and suicidality.
In this study, we performed a secondary analysis of the 2015 US Transgender Survey (USTS). 8 This investigation is reported using Strengthening the Reporting of Observational Studies in Epidemiology ( STROBE ) reporting guidelines.
Quiz Ref ID The 2015 USTS was a cross-sectional, nonprobability sample of responses from 27 715 TGD adults from 50 US states, Washington, DC, US territories, and US military bases abroad. The survey was developed by researchers, advocates, people with lived experience, and subject experts over the course of a year. The final survey contained 324 possible questions with 32 domains addressing subjects including health and health care access. It was disseminated by community-based outreach and administered online from August 19, 2015, to September 21, 2015. The USTS protocol was approved by the University of California, Los Angeles institutional review board. 8 The protocol for the present study was reviewed by the Fenway Institute institutional review board and did not meet criteria for human subjects research. For this reason, consent was not obtained.
Quiz Ref ID Five binary mental health outcomes were examined, including endorsement or denial of the following: (1) past-month severe psychological distress (score on the Kessler Psychological Distress Scale meeting the previously validated threshold of ≥13), 15 (2) past-month binge alcohol use (≥5 alcoholic drinks on one occasion), (3) past-year tobacco smoking, (4) past-year suicidal ideation, and (5) past-year suicide attempt.
The exposure group included respondents who endorsed a history of gender-affirming surgery, defined as undergoing 1 or more types of gender-affirming surgery at least 2 years prior to submitting responses to the USTS. Respondents were asked about their experiences with gender-affirming surgeries through the question, “Have you had or do you want any of the health care listed below for gender transition?” Respondents were presented with 1 of 2 lists of gender-affirming surgeries based on their self-reported sex assigned at birth. For each surgery, respondents were able to indicate one of the following answers: “Have had it,” “Want it some day,” “Not sure if I want this,” or “Do not want this.” Respondents were included in the exposure group if they answered “Have had it” to 1 or more of the following types of gender-affirming procedures: breast augmentation, orchiectomy, vaginoplasty/labiaplasty, trachea shave, facial feminization surgery, or voice surgery. Respondents were also included in the exposure group if they answered “Have had it” to one or more of the following types of gender-affirming procedures: chest surgery, hysterectomy, clitoral release/metoidioplasty/centurion procedure, or phalloplasty.
In this study, outcomes of interest included mental health symptoms in the year prior to taking the USTS. To ensure that exposure to gender-affirming surgeries temporally preceded all outcomes of interest, respondents were included in the exposure group if they had received their first gender-affirming surgery at least 2 years prior to submitting responses to the USTS. For each respondent with a history of gender-affirming surgery, the number of years since their first surgery was calculated by subtracting age at first surgery from current age.
The control group included respondents who desired gender-affirming surgeries but had not yet received any. Respondents were included in this group if they answered “Want it some day” for at least 1 of the aforementioned gender-affirming procedures but did not answer “Have had it” for any of them. We excluded participants who did not report desire for any gender-affirming surgeries.
The following sociodemographic covariates were examined: age (18-44 years, 45-64 years, and ≥65 years), education level (less than high school or high school graduate up to associate degree, bachelor degree, or higher), employment status (employed, unemployed, or out of labor force), gender identity (transgender woman, transgender man, nonbinary, or cross-dresser), health insurance status (uninsured or insured), household income (<$25 000, $25 000-$99 999, or ≥$100 000), race (Alaska Native/American Indian, Asian/Pacific Islander, Black/African American, Latinx/Hispanic, other/biracial/multiracial, or White), sex assigned at birth (female or male), and sexual orientation (asexual, lesbian/gay/bisexual, or heterosexual).
Family rejection was included as a covariate and was defined by the USTS as history of any of the following experiences with a family member owing to the respondent’s gender identity: ending the relationship, physical violence, being forced out of their home, being prevented from wearing desired gender-concordant clothing, and exposure to gender identity conversion efforts. Lifetime exposures to other types of gender-affirming care were also examined, including gender-affirming counseling, pubertal suppression, and hormone therapy. Given the possibility that any of these covariates could confound the relationship between gender-affirming surgeries and mental health outcomes, all covariates were included in the final multivariable models.
All analyses were conducted using Stata, version 16.1 (StataCorp). Unweighted descriptive statistics for exposure and control groups were calculated and are presented as frequencies and percentages.
Multivariable logistic regression models adjusted for all covariates were generated to examine whether undergoing gender-affirming surgery is associated with each of the examined mental health outcomes. 16 , 17 To account for the survey’s nonprobability sampling, all models incorporated survey weights to correct sampling biases related to age and race/ethnicity. Adjusted odds ratios (aORs), 95% CIs, and 2-sided P values are reported.
We performed a post hoc analysis to determine whether associations between gender-affirming surgeries and mental health outcomes differ based on the degree of surgical affirmation. The exposure variable was recoded as 3 categories: those who received all desired surgeries, some desired surgeries, and no desired surgeries. Because the USTS did not collect information on timing of each respondent’s last surgery, respondents for this post hoc analysis could not be excluded to ensure that all exposures temporally preceded mental health outcomes. The recoded 3-category exposure variable was substituted into 5 additional multivariable logistic regression models, adjusted for all aforementioned covariates.
Owing to concerns that baseline mental health status may confound associations between gender-affirming surgery and mental health outcomes, we conducted an additional post hoc analysis to determine whether lifetime mental health measures were associated with exposure to gender-affirming surgeries. We did not incorporate these measures into the primary models due to collinearity. Four separate post hoc models, adjusted for all aforementioned covariates, regressed exposure to gender-affirming surgeries against lifetime suicidal ideation, lifetime suicide attempts, lifetime alcohol use, and lifetime smoking.
To account for multiple hypothesis testing, a Bonferroni correction was applied to adjust for 19 total tests. A P value of less than .002 was used as the corrected threshold for statistical significance.
Less than 2% of the study sample had missing data for exposure and outcome variables, and less than 9% of the study sample had missing data for any covariates. Given that these are acceptably low levels of missingness, 18 respondents with missing data were excluded without compensatory methods.
Of the 27 715 respondents, 3559 (12.8%) endorsed undergoing 1 or more types of gender-affirming surgery at least 2 years prior to submitting survey responses, while 16 401 respondents (59.2%) endorsed a desire to undergo 1 or more types of gender-affirming surgery but denied undergoing any of these.
Compared with the control group, the exposure group had higher percentages of respondents who were older, employed, more educated, endorsed family rejection, reported having health insurance, and reported higher household income. Respondents in the exposure group were more likely to endorse a history of gender-affirming counseling, pubertal suppression, and hormone therapy ( Table 1 ).
For each surgical procedure, the percentage of people who desired it was higher than the percentage of people who endorsed undergoing it ( Figure 1 ). For every adverse mental health outcome, the percentage of respondents who endorsed it was lower in the exposure group than in the control group ( Figure 2 ).
Quiz Ref ID After adjustment for sociodemographic factors and exposure to other types of gender-affirming care, undergoing 1 or more types of gender-affirming surgery was associated with lower past-month psychological distress (aOR, 0.58; 95% CI, 0.50-0.67; P < .001), past-year smoking (aOR, 0.65; 95% CI, 0.57-0.75; P < .001), and past-year suicidal ideation (aOR, 0.56; 95% CI, 0.50-0.64; P < .001). After Bonferroni correction, there was no statistically significant association between gender-affirming surgeries and past-month binge alcohol use or past-year suicide attempts ( Table 2 ).
Quiz Ref ID In the post hoc analysis stratifying by degree of surgical affirmation, 16 401 respondents were in the reference group who received no desired surgeries. Respondents who had undergone all desired surgeries (n = 2448) had significant reductions in the odds of each adverse mental health outcome, and these reductions were more profound than those among respondents who had received only some desired surgeries (n = 3311) ( Table 3 ) .
Quiz Ref ID Measures of lifetime mental health were not associated with exposure to gender-affirming surgeries. After adjustment for all aforementioned covariates, undergoing gender-affirming surgery was not associated with lifetime suicidal ideation (aOR, 1.00; 95% CI, 0.85-1.20; P = .92), lifetime suicide attempts (aOR, 1.16; 95% CI, 1.01-1.34; P = .04), lifetime alcohol use (aOR, 1.00; 95% CI, 0.99-1.01; P = .96), or lifetime smoking (aOR, 1.00; 95% CI, 1.00-1.01; P = .34).
To our knowledge, this is the first large-scale, controlled study to demonstrate an association between gender-affirming surgery and improved mental health outcomes. In this study, we demonstrate that undergoing gender-affirming surgery is associated with decreased odds of past-month severe psychological distress, past-year smoking, and past-year suicidal ideation. The post hoc analysis stratifying by degree of surgical affirmation demonstrates that TGD people who underwent all desired surgeries had significantly lower odds of all adverse mental health outcomes, and these benefits were stronger than among TGD people who only received some desired surgeries.
The observed associations between gender-affirming surgery, psychological distress, and suicide risk reinforce previous small-sample studies suggesting that gender-affirming surgery improves mental health and quality of life among TGD people. 1 , 12 Our findings also reflect evidence from qualitative studies indicating perceived mental health benefits of gender-affirming surgeries among TGD people. 19 - 21 In our primary analysis, although gender-affirming surgery was associated with lower odds of past-year suicidal ideation, there was no statistically significant association between gender-affirming surgeries and past-year suicide attempts. However, in a post hoc analysis respondents who underwent all desired gender-affirming surgeries had significantly lower odds of past-year suicide attempts.
The association observed between gender-affirming surgeries and reduction in substance use behaviors is consistent with previous studies involving small community samples that demonstrated associations between gender-affirming medical care and lower odds of high-risk substance use. 22 , 23 In the primary analysis, undergoing gender-affirming surgery was not significantly associated with past-month binge alcohol use. This may be consistent with evidence that after adjustment for sociodemographic factors, gender minority identity itself does not predict high-risk alcohol use. 24 However, in a post hoc analysis, respondents who underwent all desired gender-affirming surgeries had significantly lower odds of past-month binge alcohol use.
This investigation offers evidence to support the clinical practice of gender-affirming surgery. Guidelines for provision of gender-affirming medical and surgical care have historically been challenged based on a limited evidence base. The American Psychiatric Association has previously concluded that the quality of evidence for treatment of gender dysphoria is low, and consequently, recommendations regarding gender-affirming care have been driven by clinical consensus where empirical evidence is lacking. 25 This study offers new data that substantiate the current clinical consensus by expanding the evidence base in support of gender-affirming surgical care.
The observed mental health benefits of gender-affirming surgeries in this study highlight the importance of policies that facilitate access to surgical gender affirmation. In the present study, the percentages of people who had undergone each gender-affirming surgical procedure were substantially lower than the percentages of people who desired them, suggesting significant barriers to accessing gender-affirming surgeries. State-level prohibitions against insurance exclusions for gender-affirming care have been associated with more extensive coverage of gender-affirming surgical procedures. 26 In light of this study’s results, such policies may be of even greater public health interest. US federal policies related to gender-affirming care have included a recent reversal of Affordable Care Act insurance protections for gender affirmation and the continued prohibition of Veterans Affairs funding allocation for gender-affirming surgeries. 27 , 28 Formulation of evidence-based policies for the financing of gender-affirming surgery will be crucial for advancing the health and well-being of TGD communities.
This study’s strengths include aspects of its design that address prior limitations in the existing literature on this subject. Multiple meta-analyses of studies examining the association between gender-affirming surgeries and mental health outcomes have demonstrated that much of the existing literature consists of evidence derived with small sample sizes, lack of control groups, and lack of adjustment for other kinds of gender-affirming care. 12 , 29 Our study is responsive to these methodologic concerns.
First, we used the largest existing data set containing information on the surgical and mental health experiences of TGD people. Second, this is, to our knowledge, the first large-scale study on this subject to use the ideal control group to examine associations between gender-affirming surgeries and mental health outcomes: individuals who desire gender-affirming surgery but have not yet received it. Experts have cautioned against using comparison groups that conflate TGD people who did not undergo gender-affirming surgery because they were waiting for it with TGD people not seeking it in the first place. Inability to differentiate these 2 groups likely contributed to the lack of significant mental health benefit observed in the 2019 large-scale study on this subject. 13 , 30
Third, although this survey-based investigation uses a cross-sectional study design, we constructed an exposure group that includes only individuals exposed to their first gender-affirming surgery prior to the window of assessment for any adverse mental health outcomes. Thus, we ensured that our exposure temporally preceded our outcomes, allowing us to better understand the direction of observed associations. These exclusions could not be performed in our post hoc analysis stratifying by degree of surgical affirmation, and that analysis should therefore be interpreted with caution.
Fourth, our data set allowed us to control for previous experiences of gender-affirming counseling, pubertal suppression, and hormone therapy. Consequently, this study is, to our knowledge, the first large-scale investigation to ascertain the mental health benefits of gender-affirming surgeries independent of other common forms of gender-affirming health care.
Our study has several limitations. The nonprobability sampling of the USTS may limit generalizability. All measures are self-reported and may be subject to response bias. Furthermore, the USTS only offers data on experiences with 10 specific types of gender-affirming surgeries and does not capture the full range of procedures that constitute gender-affirming surgery. Lastly, because this is an observational study, it may be subject to unmeasured confounding. Much of the literature on mental health benefits of gender-affirming surgery has been complicated by inability to adjust for a key confounder: baseline mental health status. Our post hoc analysis demonstrates that lifetime suicidality and substance use behaviors are not associated with the exposure variable in this sample. Therefore, prior mental health factors do not appear to confound associations between gender-affirming surgery and subsequent mental health outcomes in our study. There may nevertheless be other types of mental health problems not captured in the USTS that confound these associations. These limitations highlight the need for larger probability-based surveys with TGD communities, more consistent gender identity data collection across health care systems, and more comprehensive baseline health data collection with TGD populations.
In this article, we present the largest study to our knowledge to date on associations between gender-affirming surgeries and mental health outcomes. Our results demonstrate that undergoing gender-affirming surgery is associated with improved past-month severe psychological distress, past-year smoking, and past-year suicidal ideation. Our findings offer empirical evidence to support provision of gender-affirming surgical care for TGD people who seek it. Furthermore, this study provides evidence to support policies that expand and protect access to gender-affirming surgical care for TGD communities.
Corresponding Author: Anthony N. Almazan, BA, Harvard Medical School, 25 Shattuck St, Boston, MA 02215 ( [email protected] ).
Accepted for Publication: February 5, 2021.
Published Online: April 28, 2021. doi:10.1001/jamasurg.2021.0952
Author Contributions: Mr Almazan had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: All authors.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: All authors.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Almazan.
Obtained funding: Keuroghlian.
Administrative, technical, or material support: Keuroghlian.
Supervision: Keuroghlian.
Conflict of Interest Disclosures: Dr Keuroghlian reported grants from Patient-Centered Outcomes Research Institute Contract AD-2017C1-6569 (PI: Sari L. Reisner) during the conduct of the study; in addition, Dr Keuroghlian stands to receive future royalties as editor of a forthcoming McGraw-Hill Education textbook on transgender and gender diverse care. No other disclosures were reported.
Funding/Support: This work was supported by contract AD-2017C1-6569 from the Patient-Centered Outcomes Research Institute (PI: Dr Sari L. Reisner).
Role of the Funder/Sponsor: The funding source had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Additional Contributions: We thank the National Center for Transgender Equality for granting us access to the data from the 2015 US Transgender Survey.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
An official website of the United States government
Here's how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
Transgender health care
A transgender person’s assigned sex at birth doesn’t match their gender identity, expression, or behavior.
Refer to glossary for more details.
Applying for Marketplace coverage
Sex-specific preventive services.
A fixed amount ($20, for example) you pay for a covered health care service after you've paid your deductible.
The percentage of costs of a covered health care service you pay (20%, for example) after you've paid your deductible.
The amount you pay for covered health care services before your insurance plan starts to pay. With a $2,000 deductible, for example, you pay the first $2,000 of covered services yourself.
Plans with transgender exclusions
An easy-to-read summary that lets you make apples-to-apples comparisons of costs and coverage between health plans. You can compare options based on price, benefits, and other features that may be important to you. You'll get the "Summary of Benefits and Coverage" (SBC) when you shop for coverage on your own or through your job, renew or change coverage, or request an SBC from the health insurance company.
Medindia » Articles » Procedure » FAQs on Gender-Reassignment Surgery: Everything You Need to Know
Gender-Reassignment Surgery: Everything You Need to Know
- Indications
- Non-Surgical Procedures
- Surgical Procedures
- Risks in Non-Surgical and Surgical Procedures
- Whom to consult?
- Pre-Op Considerations
- Post-Op Considerations
- Impact on Mental Health
- Cost of the Surgery
FAQs on Gender-Reassignment Surgery: Everything You Need to Know
Html.Raw(Model.contents.ToString())
Please use one of the following formats to cite this article in your essay, paper or report:
Dr. Preethi Balasubramanian. (2024, May 08). Gender-Reassignment Surgery: Everything You Need to Know . Medindia. Retrieved on May 15, 2024 from https://www.medindia.net/health/procedure/gender-reassignment-surgery-everything-you-need-to-know-faqs.htm.
Dr. Preethi Balasubramanian. "Gender-Reassignment Surgery: Everything You Need to Know". Medindia . May 15, 2024. <https://www.medindia.net/health/procedure/gender-reassignment-surgery-everything-you-need-to-know-faqs.htm>.
Dr. Preethi Balasubramanian. "Gender-Reassignment Surgery: Everything You Need to Know". Medindia. https://www.medindia.net/health/procedure/gender-reassignment-surgery-everything-you-need-to-know-faqs.htm. (accessed May 15, 2024).
Dr. Preethi Balasubramanian. 2024. Gender-Reassignment Surgery: Everything You Need to Know . Medindia, viewed May 15, 2024, https://www.medindia.net/health/procedure/gender-reassignment-surgery-everything-you-need-to-know-faqs.htm.

ASK A DOCTOR ONLINE

What's New on Medindia

Follow @MedIndia
Gender-Reassignment Surgery: Everything You Need to Know - Related News
- Addressing Mental Health Needs in the Transgender Community
- A Global Comparison: Best Countries for Gender Reassignment Surgery
- Transgender Healthcare Disparities Highlighted
- Why is Thyroid Cancer More Common Among Transgender Female Veterans?
- Is Gender Reassignment Surgery Against Nature?
- Consult Online Doctor
- Take Telemedicine course
- Health Centers
- Health Tools
- Health info by Speciality
- Know Your Body
- Health and Wellness
- Web Stories
- Health Tips
- Nutrition Facts
- Lifestyle & Wellness
- Beauty Tips
- Diet & Nutrition
- Home Remedies
- Obesity & Weight Loss
- Complementary Medicine
- Special Reports
- Press Releases
- Health Guide
- Health articles
- Health Quiz
- Health Facts
- Travel Health
- Medicine and Movies
- Symptom Articles
- Diabetes Tools
- Pediatric Calculators
- Men's Health
- Women's Health
- Height Weight Tools
- Cardiac Tools
- Pharma Tools
- Wellness Interactive Tools
- Drug Information
- Drugs by Condition
- Drug Price List - Brand Names
- Drug Interaction with Food
- Drug Price List - Generic Names
- Drugs - Side Effects
- Drug Videos
- Drug Database
- Doctor Directory
- Diagnostic Lab Directory
- Hospital Directory
- Pharmacy or Chemist
- Medical Equipment Suppliers
- Pharma Directory
- Emergency Services
- PG Education
- Family Medicine
- Other Resources
- Medical Aphorism
- Health Acts in India
- Health Quotations
- Medical Conference
- Amazing Body Facts
- Health poll

- Editorial Team
- Exclusive Interviews
- In the News
- Partners & Affiliates
- Advertise With Us
- हिन्दी
- français
- Español
- 中文
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.82(4); November, 2015
Transsexual attractions and sexual reassignment surgery: Risks and potential risks
Transsexual issues and sexual reassignment surgery (SRS) are receiving a great deal of attention and support in the media, schools, and government. Given the early age at which youth seek treatment for transsexual attractions (TSA) and gender dysphoria and given the serious risks associated with such treatment, it is essential that family and youth be advised about these risks and alternative treatment options. Physicians and mental-health professionals have a professional responsibility to know and communicate the serious risks, in particular risk of suicide, that are associated with SRS; the spontaneous resolution of TSA in youth; the psychological conflicts that have been identified in such patients and in their parents; the successful treatment of conflicts associated TSA and the regrets of those who have been through SRS. SRS and gender theory are also viewed from the faith perspective of Pope Francis and Pope Emeritus Benedict XVI.
Lay summary : Transsexuals and sex-change operations are receiving a great deal of attention. Young people may seek treatment for transsexual attractions at an early age even though these attractions may go away on their own. Psychological conflicts have been identified in these patients and their parents and may be successfully treated. There are serious risks associated with sex change. They include the risk of depressive illness and suicide. Physicians and mental-health professionals should know these risks and the regrets of those who have been through sex-change operations. These patients and their families also should be informed of other treatment options.
Transsexual issues and sexual reassignment surgery are receiving a great deal of attention and support in the media, schools, government and in health professionals today.
Dr. Paul McHugh, former chairperson of the Department of Psychiatry at Johns Hopkins Hospital, has written that,
The idea that one's sex is fluid and a matter open to choice runs unquestioned through our culture and is reflected everywhere in the media, the theater, the classroom, and in many medical clinics. It has taken on cult-like features: its own special lingo, Internet chat rooms providing slick answers to new recruits, and clubs for easy access to dresses and styles supporting the sex change. It is doing much damage to families, adolescents, and children and should be confronted as an opinion without biological foundation wherever it emerges. ( McHugh 2015 )
Transsexual issues are creating a new controversy in our elementary and high schools today as a result of youth and their parents asserting a right to identify the sex of their child without regard to the biological and genetic realities. The parents and child may insist that the child's name be changed to one of the opposite sex and that the child be allowed to wear clothing of the opposite sex and use opposite-sex bathrooms.
These families are often preparing their children for sexual reassignment surgery (SRS) without being given the knowledge of the serious, documented risks associated with such surgery or other treatment options for gender dysphoria, referred to in the past as gender identity disorder (GID). Endocrinologists who are giving hormones to these youth, mental-health professionals who are affirming SRS surgery, and surgeons have a professional responsibility to understand these grave risks; and these patients also should be apprised of these risks.
An early study of these risks included one hundred patients seeking SRS, sixty-six of whom had surgery and 34 of whom did not ( Meyer and Reter 1979 ). The operated-upon groups were followed from the time of surgery, the unoperated-upon group from the time of initial interview at the Gender Identity Clinic at Johns Hopkins. Of those operated on, twenty-one had a trial period (taking hormones and working in the opposite-gender role) while the other thirteen had been well-established in the cross-gender role at the time of surgery but did not have a formal trial period. Follow-up was successful in fifty-two patients, of whom fifty consented to have their data published. Follow-up interviews covered three main areas: adaptation; family relationships and adaptational patterns at major life intervals; and fantasy, dreams, and sexual activity. 73–80 percent of the patients were male. Average follow-up for operated-upon patients was sixty-two months and twenty-five months for the unoperated-upon group.
Residential instability was similar in the groups (average of twenty months between moves in the operated-upon group pre-surgery, eighteen months post-surgery, and twelve months pre-contact and ten months post-contact in the unoperated-upon group). Job levels indicated a slight upward trend in both groups. Changes in psychiatric contacts were also similar in the two groups.
A third group was found that went elsewhere for surgery when this was not performed at Hopkins. Adjustment scores were improved in the surgery and unoperated-upon group to a similar extent, with no significant difference between the groups, but the group that sought surgery elsewhere did less well (although there was no statistical significance to the difference).
As stated by the authors, “At the most simple level, these data suggest that significant change in adjustment scores may be achieved either through surgery or through the passage of time in association with some contact and acceptance into an organized evaluation program” ( Meyer and Reter 1979 ). The conclusion was that SRS was not successful in treating this condition and led to the discontinuation of SRS at Johns Hopkins.
In spite of these early findings, and lack of contravening evidence that SRS conveyed any benefits compared with any unoperated-upon control groups, the practice of SRS has continued and has been extended into younger age groups. In a 2015, Boston study of 180 transsexual youth who had undergone SRS (106 female-to-male; 74 male-to-female), these youth had a twofold to threefold increased risk of psychiatric disorders, including depression, anxiety disorder, suicidal ideation, suicide attempt, self-harm without lethal intent, and both inpatient and outpatient mental health treatment compared to a control group of youth ( Reisner et al. 2015 ).
(An important research study would be that of determining how many of these youth, and their parents or guardians, were informed about the psychiatric risks associated with the surgery which is described in the mental health literature and which should be known by the treating health professionals. Since the mean age at which youth presented for consideration for SRS surgery in the Boston study was age 9, providing this information in a way that the children would understand would be challenging but nonetheless could be done in regard to discussing suicide risks and successful alternative treatments for gender dysphoria. The primary childhood psychological conflicts that interfere with the appreciation of the goodness of a child's masculinity or femininity should be given.)
The largest study to date of the long-term psychological state of post-SRS persons was an analysis of over three hundred people who had undergone SRS in Sweden over the past thirty years. This 2011 study demonstrated that persons after sex reassignment, have considerably higher risks for mortality, suicidal behavior, and psychiatric morbidity than the general population ( Dhejne et al. 2011 ).
In 2014, Dr. Paul McHugh wrote in The Wall Street Journal about this research, “Most shockingly, their suicide mortality rose almost 20-fold above the comparable non-transgender population. This disturbing result has as yet no explanation but probably reflects the growing sense of isolation reported by the aging transgendered after surgery. The high suicide rate certainly challenges the surgery prescription” ( McHugh 2014 ).
In the same article, Dr. McHugh has also described his study of people with gender confusion over the past forty years, twenty-six of which he spent as the psychiatrist in chief of Johns Hopkins Hospital. He wrote, “In fact, gender dysphoria—the official psychiatric term for feeling oneself to be of the opposite sex—belongs in the family of similarly disordered assumptions about the body, such as anorexia nervosa and body dysmorphic disorder. Its treatment should not be directed at the body as with surgery and hormones any more than one treats obesity-fearing anorexic patients with liposuction.” He went on, “The treatment should strive to correct the false, problematic nature of the assumption and to resolve the psychological conflicts provoking it. With youngsters, this is best done in family therapy” ( McHugh 2014 ).
Important medical and psychological issues need to be considered before the educational, medical, political, and judicial systems rush headlong into a process of affirming in youth and in their parents a fixed, false belief that a person can be a sex that is not consistent with their biological and genetic identity and that such individuals have the right to transsexual surgery. Fixed, false beliefs are identified in the mental-health field as manifestations of a serious thinking disorder, specifically a delusion. Health professionals should not be supporting this delusional belief in these youth and their parents.
An understanding of what motivates youth to identify with the opposite sex is essential as well as the reasons why parents would encourage or support transsexual attraction. Dale O'Leary, the author of the important book The Gender Agenda , has co-authored an important 2015 research paper, “Understanding and Responding to the Transgender Movement” ( O'Leary and Sprigg 2015 ). Parents, youth and adults with TSA and health professionals would benefit from reviewing this important research paper.
GID/Gender Dysphoria: The Most Common Precursor to Transsexual Conflicts
Many youths who identify as persons of the opposite sex meet the earlier DSM criteria for GID. GID is a childhood psychiatric disorder (DSM IV TR) in which there is a strong and persistent cross-gender identification with at least four of the following preferences:
- • repeated stated desire to be of the opposite sex,
- • in boys, a preference for cross-dressing or simulating female attire and, in girls, wearing stereotypical masculine clothing and a rejection of feminine clothing such as skirts,
- • a strong and persistent preference for cross-sex role in play,
- • a strong preference for playmates of the opposite sex, and
- • an intense desire to participate in games and pastimes typical of the opposite sex.
The DSM 5 has replaced the diagnosis GID with a new diagnosis, gender dysphoria. It also describes the symptoms that arise from the failure to identify with one's biological sex.
Children who seek SRS should be evaluated for psychological conflicts but regularly are not. A Dutch researcher and clinician, who specializes in treating such youth, Dr. Peggy T. Cohen-Kettenis has written in this regard:
The percentage of children coming to our clinic with GID as adolescents wanting sex reassignment is much higher than the reported percentages in the literature … We believe (psychological) treatment should be available for all children with GID, regardless of their eventual sexual orientation. ( Cohen-Kettenis 2001 )
A Study of Youth from a Gender Identity Center
A 2013 study from a gender identity service in Toronto, that consisted of a sample of 577 children (ages 3–12) and 253 adolescents (ages 13–20), reported a number of findings and comments. These included:
- • A sharp increase in adolescent referrals starting with the 2004–2007 cohort and this increased even more so in the last cohort, 2008–2011.
- • For the first six cohorts (1976–1999), the percentage of boys always exceeded 75 percent, with the sex ratio ranging from a low of 4.61:1 (1988–1991) to a high of 12:1 of boys to girls (1992–1995), but for the last three cohorts (2000–2011) hovered around 75 percent, with the sex ratio ranging from 2.77:1 (2000–2003) to 3.41:1 (2008–2011) of boys to girls.
- • The adolescent sex ratios were closer to parity. Of note, there were two cohorts (1988–1991 and 2008–2011) in which the number of girls exceeded the number of boys.
- • The adolescent cases increased even more from the 2004 to 2007 cohort; and in the 2008 to 2011 cohort, the number of adolescent cases exceeded the number of child cases for the first time since the inception of their clinic in the mid-1970s.
- • For the adolescents, data on sexual orientation were available for 248 patients. The percentage of girls classified as homosexual was greater than the percentage of boys classified as homosexual (76.0% vs. 56.7%).
For the children, 66.4 percent were in two-parent families at the time of assessment compared with 45.8 percent of the adolescents ( Wood et al. 2013 ). Another parameter that struck them as clinically important was that a number of youth commented that, in some ways, it was easier to be transsexual than to be gay or lesbian.
Along similar lines, they have also wondered whether, in some ways, identifying as transsexual has come to occupy a more valued social status than identifying as gay or lesbian in some youth subcultures. Perhaps this social force explains, at least partially, the particularly dramatic increase in female adolescent cases in the 2008–2011 cohort.
Another factor that impressed them in accounting for the increase in adolescent referrals pertained to youth with gender identify disorder who also had an autism spectrum disorder which has been reported by others ( de Varies et al. 2010 ). A center in the Netherlands reported the co-occurrence of GID and autism spectrum disorders (ASD) in a study of children and adolescents (115 boys and 89 girls, mean age 10.8). The incidence of ASD was 7.8 percent. The authors recommended acquiring a greater awareness “of co-occurring ASD and GID and the challenges it generates in clinical management.”
Family Conflicts in Youth with Gender Identity Confusion/Gender Dysphoria
Drs. Zucker and Bradley in Toronto have been recognized as leaders in the study of GID. They have identified a number of conflicts in the families of children with GID that included:
A composite measure of maternal psychopathology correlated quite strongly with Child Behavior Checklist indices of behavior problems in boys with GID.
The rate of maternal psychopathology is high by any standard and includes depression and bipolar disorder.
The boy, who is highly sensitive to maternal signals, perceives the mother's feelings of depression and anger. Because of his own insecurity, he is all the more threatened by his mother's anger or hostility, which he perceives as directed at him. His worry about the loss of his mother intensifies his conflict over his own anger, resulting in high levels of arousal or anxiety. The father's own difficulty with affect regulation and inner sense of inadequacy usually produces withdrawal rather than approach.
The parents have difficulty resolving the conflicts they experience in their own marital relations, and fail to provide support to each other. This produces an intensified sense of conflict and hostility.
In this situation, the boy becomes increasingly unsure about his own self-value because of the mother's withdrawal or anger and the father's failure to intercede. This anxiety and insecurity intensify, as does his anger.
These men (fathers) are often easily threatened and feel inadequate themselves. These qualities appear to make it very difficult for them to connect with sons who display non-masculine behavior.” Withdrawing from their feminine sons, “they often deal with their conflicts by overwork or distancing themselves from their families. The fathers’ difficulty expressing feelings, and their inner sense of inadequacy are the roots of this emotional withdrawal.
Fathers demonstrate depression and substance abuse disorder.
Parental psychopathology among the parents of children with GID deserves thoughtful consideration. ( Zucker et al. 2003 )
Also, Dr. Bradley has described additional maternal conflicts in these youth,
boys with GID appear to believe that they will be more valued by their families or that they will get in less trouble as girls than as boys. These beliefs are related to parents’ experiences within their families of origin especially tendencies on the part of mothers to be frightened by male aggression or to be in need of nurturing, which they perceive as a female characteristic. ( Bradley 2003 , 201–202)
Zucker et al. (2012 ) also found that GID youth had high rates of general behavior problems and poor peer relations.
It should be noted that these observations are not derived from controlled studies. As such, there is no comparison to the prevalence of such conflicts among control groups. Thus the specificity of these conflicts (or their prevalence in children with gender dysphoria) is not clear. There is no conclusive evidence of the role of such conflicts in the development of gender dysphoria or whether treatment aimed at correcting these leads to improvement. However, the comments of Zucker and Bradley do seem relevant to understanding the development of GID.
Additional conflicts that we have seen in engaging in the family therapy recommended by Dr. Paul McHugh include:
In females’ relationships with their fathers, observed conflicts may include:
- 1. Excessive fear of the father's anger or his controlling behaviors, leading to a fear of being hurt due to being a woman, coupled with a belief that being a male would help them feel stronger and safer;
- 2. Severe mistrust of the father because of his insensitive and angry treatment of the mother, because of his harming the family by abandonment or because of his emotional, personality, or behavioral conflicts;
- 3. The father's failure to affirm his daughter's feminine goodness and gifts, to critique and protect her from gender theory errors, and to communicate that fulfillment and happiness can be found in being a psychologically healthy female.
In males’ relationships with their mothers, observed conflicts may include:
- 1. The mother's mistrust of and anxiety with males as a result of growing up with a harsh, angry, distant, or addicted father (the child's grandfather);
- 2. Her desire that her son had been a daughter, leading to initiating or supporting cross dressing and cross-sexual identification;
- 3. A boy's fears that he does not please his mother as a male, together with his unconscious belief that he might receive more love and acceptance from his mother if he identified with femininity;
- 4. A mother's failure to support and encourage her son to have same-sex friendships;
- 5. A failure to critique and protect him from gender theory errors;
- 6. A failure to communicate that fulfillment and happiness can be found in being a psychologically healthy male.
In males’ relationships with their fathers, observed conflicts may include:
- 1. Failure to develop a secure father–son relationship because of a father's emotionally distant behaviors or severe male insecurity;
- 2. A father's excessive anger or rejecting behaviors that undermine a son's ability to model after his father or that create a negative view of masculinity;
- 3. A father's failure to support a son's strong creative and artistic gifts;
- 4. A failure to protect the son from abusive behaviors by siblings or by same-sex peers that contribute to a son's failure to identify with the goodness of masculinity;
- 5. A failure to support same-sex friendships in childhood and adolescence;
- 6. A failure to critique and protect youth from gender theory errors;
- 7. A failure to communicate that fulfillment and happiness can be found in being a psychologically healthy male.
In females’ relationships with their mothers, observed conflicts may include:
- 1. An emotionally distant, angry, selfish, depressed, or critical mother who failed to bond closely with her daughter for any number of reasons, including unresolved anger with the maternal grandmother that was misdirected at the daughter;
- 2. The failure to affirm the daughter's goodness and female gifts;
- 3. A failure to support and encourage same sex friendships;
- 4. A failure to critique and protect her daughter from gender theory errors;
- 5. A failure to communicate that fulfillment and happiness can be found in being a psychologically healthy female.
Other factors and conflicts observed in males may include:
- 1. A keen appreciation and love for beauty that is often associated more with femininity than masculinity and a desire to be what one loves;
- 2. A poor body image and the belief that one would be more attractive if he were of the opposite sex;
- 3. Severe childhood rejection by same-sex peers, creating a sense of not fitting in with them, which results in intense fears of rejection and an unconscious belief that one would feel safer if he were of the opposite sex;
- 4. Repeated failures in relationships with women, associated with a severe loss of self-esteem;
- 5. A sense of pleasure in rejecting the values and moral code of his parents;
- 6. The belief that his sex is not a gift, but a constraint that must be overcome;
- 7. Pressure from a significant other to cross dress, take hormones, and move toward SRS;
- 8. Severe narcissism and acceptance of gender theory with a delusional belief that he can create himself as he wants.
Other factors and conflicts observed in females may include:
- 1. The absence of close female friendships and a sense of not fitting in, along with a belief that she would be less lonely and happier if she were a male;
- 2. In strong, young females, a love for what is perceived as male strength and preferential treatment for males, together with the desire to become what she loves;
- 3. Poor body image and a belief that she would be more attractive if she were of the opposite sex;
- 4. In very athletic and strong young females an intense bonding and identification with young males through athletic activities;
- 5. A sense of failure as a female and a delusional belief that she would feel more confident and happy being a member of the opposite sex;
- 6. Repeated failures in relationships with males with severe loss of self-esteem;
- 8. A sense of pleasure in rejecting the values and moral code of her parents;
- 9. The view that her sex is not a gift but as a constraint that must be overcome;
- 10. Acceptance of gender theory, along with a delusional belief that she can create herself as she wants.
The exposure of youth to gender theory in college can result in their embrace of postmodern philosophies focused on freedom as an end in and of itself. Such ideas come from various sources, including the writings of Friedrich Nietzsche and Jean-Paul Sartre. If freedom (some would call it license) is the greatest good in the world, then why should anyone be constrained by biology? One's sex as male and female is seen not as a gift but as a constraint that must be overcome. So if technology can alter one's body, then so be it.
PC Medicine
Some medical centers fail to or refuse to diagnose the psychological difficulties youth have in accepting and appreciating their biological sex. They neglect to provide proper counseling about treatment and the risks of sexual-reassignment surgery. Instead, they support the beliefs of the youths and their parents and initiate hormone treatments in preparation for eventual body-mutilating surgery.
A pediatric specialist at Boston has a program for boys who feel like girls and girls who want to be boys. He offers his patients—some as young as seven years old—counseling about the “naturalness” of their feelings and hormones to delay the onset of puberty. These drugs stop the natural process of sexual development that would make it more surgically difficult to have a sex alteration later in life.
This physician alleges that those whom he labels as transsexual children are deeply troubled by a lack of understanding of their feelings and have a high level of suicide attempts. While this physician is accurate in his interpretation of the literature—that children with GID and transsexual ideation are deeply troubled—his claims of a high level of suicide attempts in children with GID is not substantially supported by the medical literature. In fact, the literature demonstrates a shocking increase in suicide and in psychiatric illness after sexual reassignment surgery ( Dhejne et al. 2011 ).
In his 2014 Wall Street Journal article, Dr. McHugh wrote that “misguided doctors at medical centers including Boston's Children's Hospital have begun trying to treat” transgenderism in youths “even though the drugs stunt the children's growth and risk causing sterility.” He recommends “a better way to help these children: with devoted parenting” ( McHugh 2014 ).
The Treatment of Youth with Transsexual Confusion
According to Drs. Zucker and Bradley:
The fantasy solution provides relief but at a cost. They are unhappy children who are using their cross-gender behaviors to deal with their distress.
Treatment goal is to develop same-sex skills and friendships.
In general, we concur with those who believe that the earlier treatment begins, the better … It has been our experience that a sizable number of children and their families can achieve a great deal of change.
In these cases, the gender identity disorder resolves fully, and nothing in the children's behavior or fantasy suggest that gender identity issues remain problematic … All things considered, however, we take the position that in such cases clinicians should be optimistic, not nihilistic, about the possibility of helping the children to become more secure in their gender identity. ( Zucker and Bradley 1995 , 281–282)
Zucker and Bradley have been providing sensitive treatment to children with the precursor of transsexual conflicts. They have written that the goal of treatment is to develop skills associated with children of their own biological sex and friendships with such children. We have found a similar treatment approach to be beneficial in treating such children ( Fitzgibbons 2015 ). While data from controlled clinical studies are not available to measure the effectiveness of these therapies, it seems reasonable to follow the recommendations of those with extensive clinical experience until such time as controlled trials are performed.
Also, Dr. McHugh has written that transsexual attractions are often fluid and can change. “When children who reported transsexual feelings were tracked without medical or surgical treatment at both Vanderbilt University and London's Portman Clinic, 70 to 80 percent of them spontaneously lost those feelings” ( McHugh 2014 ). Dr. McHugh has described also his research experiences at Johns Hopkins:
As for the adults who came to us claiming to have discovered their true sexual identity and to have heard about sex-change operations, we psychiatrists have been distracted from studying the causes and natures of their mental misdirections by preparing them for surgery and for a life in the other sex. We have wasted scientific and technical resources and damaged our professional credibility by collaborating with madness rather than trying to study, cure, and ultimately prevent it.
One might expect that those who claim that sexual identity has no biological or physical basis would bring forth more evidence to persuade others. But as I've learned, there is a prejudice in favor of the idea that nature is totally malleable.
A practice that appears to give people what they want turns out to be difficult to combat with ordinary professional experience and wisdom. Even controlled trials or careful follow-up studies to ensure that the practice itself is not damaging are often resisted and the results rejected. ( McHugh 2004 )
Sexual Reassignment Surgery
SRS violates basic medical and ethical principles and is therefore not ethically or medically appropriate.
- 1 SRS mutilates a healthy, non-diseased body. To perform surgery on a healthy body involves unnecessary risks; therefore, SRS violates the principle primum non nocere , “first, do no harm.”
- 2 Candidates for SRS may believe that they are trapped in the bodies of the wrong sex and therefore desire or, more accurately, demand SRS; however, this belief is generated by a disordered perception of self. Such a fixed, irrational belief is appropriately described as a delusion.
- 3 SRS, therefore, is a “category mistake”—it offers a surgical solution for psychological problems, such as a failure to accept the goodness of one's masculinity or femininity, lack of secure attachment relationships in childhood with same-sex peers or a parent, self-rejection, untreated GID, addiction to masturbation and fantasy, poor body image, excessive anger and rebelliousness, and severe psychopathology in a parent.
- 4 SRS does not accomplish what it claims to accomplish. It does not change a person's sex; therefore, it provides no true benefit.
- 5 SRS is a “permanent,” effectively unchangeable, and often unsatisfying surgical attempt to change what may be only a temporary (i.e., psychotherapeutically changeable) psychological/psychiatric condition. ( Fitzgibbons, Sutton, and O'Leary 2009 )
Regrets over SRS
Dr. Renee Richards, a former professional tennis player, has written that her transition failed to meet even her own expectations. She wrote,
I wish that there could have been an alternative way, but there wasn't in 1975. If there was a drug that I could have taken that would have reduced the pressure, I would have been better off staying the way I was—a totally intact person. I know deep down that I'm a second-class woman. I get a lot of inquiries from would-be transsexuals, but I don't want anyone to hold me out as an example to follow. Today there are better choices, including medication, for dealing with the compulsion to cross-dress and the depression that comes from gender confusion. As far as being fulfilled as a woman, I'm not as fulfilled as I dreamed of being. I get a lot of letters from people who are considering having this operation … and I discourage them all. ( Richards 1999 )
Walt Heyer, who went through SRS, also exposes the origins of the practice and its often tragic results in his article ( Heyer 2015 ).
Youth, their parents, and adults who are considering SRS should be informed by their doctors and psychologists about the serious regrets many people have who underwent SRS. This information should also be communicated in schools where SRS is being taught as a healthy step to seeking greater happiness and fulfillment in life.
Parental Responses to Youth with Transsexual Attractions
As the protectors of their children, the first step parents can take is to understand possible reasons why their child is identifying with the opposite sex and has difficulty in embracing the goodness of his masculinity or her femininity. Then parents should learn about the serious health risks associated with SRS. Next, it is essential to do what most health professionals, educators, and the media fail to do, warn their children of the serious psychiatric dangers associated with SRS, especially the risk of suicide.
Many parents report the benefits of limiting time on the Internet for their children with this conflict. They believe that communication with those who are supporting and encouraging SRS reinforces the false belief that their thinking can determine their sex, that they have no emotional conflicts, and that SRS is a path they should pursue.
The leading experts in GID, Zucker and Bradley, have written, “parental ambivalence is, in most cases part of the problem.” Parents, particularly mothers, who might rationalize that it is “cute” to have a boy wear female clothing, often ignore or excuse obvious appearances of effeminacy in males. These psychologists encourage early intervention to prevent the suffering of isolation, unhappiness, and low self-esteem in children who fail to appreciate their goodness as boys or girls.
Children are born with a drive to seek love and acceptance from each parent, as well as siblings and peers. If this need is met, children develop a positive identification with their masculinity or femininity. When this developmental task is successfully completed, the child is free to choose gender-atypical activities. Boys and girls with gender-identity problems are not freely experimenting with gender-atypical activities. They are constrained by deep insecurities and fears and are reacting against the reality of their own sexual identity, often as a result of failing to experience secure attachment relationships with the parents, siblings, or same-sex peers.
Mistakes parents make with children who have transsexual attractions (TSA) may include:
- • failing to identify a child's weakness in embracing the goodness of his masculinity or her femininity;
- • allowing a child unsupervised time on the Internet, especially in the evenings, during which the delusional belief that one can change one's sex can be communicated and affirmed;
- • failing to help understand the causes of their conflicts;
- • failing to warn about the severe dangers of SRS;
- • enabling the delusional thinking that one can change one's sex;
- • depending too much on acceptance by a child;
- • allowing a child to see a health professional who fails to provide adequate information and who fails to explore possible psychological origins of the failure to embrace the goodness of masculinity or femininity;
- • failing to get a professional opinion about the origins of transsexual attractions and the serious risks associated with sexual reassignment surgery;
- • supporting the controlling behavior of the child who insists upon being called by a name of the opposite sex at home and at school;
- • enabling communication with peers and others who encourage SRS.
Children can also learn to correct their cognitive distortions in regard to their natural goodness and beauty as a male or female. The responses could include thinking:
“I can grow to appreciate the goodness of my body and masculinity and femininity.”
“I can be thankful for my special masculinity or femininity.”
“I can grow to feel more comfortable and confident in being who I am.”
While there are no controlled clinical data to support specific interventions in treating children with transsexual conflicts, the following recommendations could be helpful if incorporated into a family therapy treatment program. For boys with transsexual conflicts:
- • increasing quality time for bonding with the father;
- • increasing affirmation of the son's masculine gifts by the father;
- • bonding with the son in his artistic or creative activities;
- • participating in and support for the son's creative efforts by the father;
- • encouraging same-sex friendships and diminishing time with opposite-sex friends;
- • slowly diminishing play with opposite-sex toys;
- • encouraging the boy to be thankful for his special male gifts;
- • working at forgiving boys who may have hurt him;
- • communicating with other parents whose children have been treated successfully for GID and who have come to appreciate and to embrace the goodness of their masculinity and femininity;
- • addressing the emotional conflicts in a mother who wants her son to be a girl;
- • in those with faith, encouraging thankfulness for one's special, God-given masculine gifts.
For girls with transsexual conflicts:
- • encouraging the daughter to appreciate the goodness and beauty of her femininity, including her body;
- • encouraging same-sex friendships and activities;
- • increasing the mother–child quality time;
- • praising their daughter's special goodness and gifts;
- • working with the daughter to forgive peers who have hurt her;
- • encouraging pursuit of a balance in athletic activities;
- • addressing conflicts in a parent who may want her to be a boy;
- • in those with faith, encouraging thankfulness for one's special, God-given femininity.

Transsexual Indoctrination in Schools
Some school districts have been attempting to incorporate transsexual education into the required health programs in junior and senior high schools. In the Fairfax County, Virginia, School District, parents’ groups strongly objected to this attempt; and the program was left in the family life section which is not required for students. In an important article, “Gender Free Children: The newest fad in public education,” the British Columbia Teachers Federation handbook on gender education was cited. It stated that “gender is a product of the mind … Being transgender or gender non-conforming is normal and healthy.”
Author Lee Duigon wrote,
Coming soon, to a public school near you: the teaching that “gender is a spectrum,’ and ‘gender identity” a state of mind, a social construct—and it's all part of a top-down campaign to convince your children that they can be “whoever they want to be.” Boys can be girls and girls can be boys. ( Duigon 2011 )
The author noted that the Redwood Heights Elementary School in Oakland, California, has already installed a “gender coach” in the classroom to teach very young children that “you can be a boy or a girl, or both.” The “coach” was provided by an organization called Gender Spectrum (http:// www.genderspectrum.org ) which presumably would not exist if it did not perceive a demand for its services.
In addition, school principals are placing children at risk and are creating confusion in the minds of many children by giving in to the requests of parents to allow young children to change their names to those of the opposite sex, cross dress, and be accepted as being of the sex opposite of their biological sex. These school administrators either do not know or ignore medical and psychological science and research on transsexual issues and SRS. They are participating in a false belief that the children are not of their biological sex. Such a fixed, false belief is identified in the mental health field as a delusion.
Faith and Transsexual Issues
While he has not specifically addressed the issue of transsexualism, Pope Francis has repeatedly criticized gender theory indoctrination of youth. On January 19, 2015, in an in-flight interview returning from Manila, he described the forcing of gender ideology onto students in schools as a form of “ideological colonization” comparable to Hitler youth indoctrination ( Westen 2015 ). Pope Francis commented on April 15, 2015, at his weekly general audience: “if so-called gender theory is not an expression of frustration and resignation, that aims to cancel out sexual difference as it is no longer able to face it. Yes, we run the risk of taking a step backwards. Indeed, the removal of difference is the problem, not the solution” ( White 2015 ). On June 8, 2015, he stated that so-called gender ideology is challenging the complementarity between a man and a woman under the guise of seeking a more just society. He related, “Let me draw your attention to the value and beauty of marriage. The differences between men and women are not of the order of opposition or subordination, but rather communion and generation, always as the image and semblance of God” ( Montagna 2015 ).
Similarly, Pope Benedict XVI strongly criticized gender theory in his Christmas address to the Roman Curia, December 22, 2008. He stated,
She [the Church] has a responsibility towards creation, and must also publicly assert this responsibility. In so doing, she must not only defend earth, water and air as gifts of creation belonging to all. She must also protect man from self-destruction … .
What is often expressed and understood by the term “gender” ultimately ends up being man's attempt at self-emancipation from creation and the Creator. Man wants to be his own master, and alone—always and exclusively—to determine everything that concerns him. Yet in this way he lives in opposition to the truth, in opposition to the Creator Spirit.
Rain forests deserve indeed to be protected, but no less so does man, as a creature having an innate “message” which does not contradict our freedom, but is instead its very premise. ( Benedict XVI 2008 )
Youth have the right to be provided, by physicians, mental health professionals, school nurses, and the media, with accurate information about gender confusion, the serious medical and psychiatric associated with SRS, and the excellent prognosis associated with an alternative proven treatment described in the medical literature.
Parents, family members, educators, politicians, and clergy have a moral responsibility to be familiar with medical science and to provide prudent counsel to youth that will protect and not harm them.
Biographical Note
Richard Fitzgibbons, M.D., has practiced psychiatry for forty years. He trained at the Hospital of the University of Pennsylvania and the Philadelphia Child Guidance Center. He has worked extensively with marital and family conflicts.
- Benedict Pope., XVI 2008. Address “To the members of the Roman Curia for the traditional exchange of Christmas greetings.” December 22. http://w2.vatican.va/content/benedict-xvi/en/speeches/2008/december/documents/hf_ben-xvi_spe_20081222_curia-romana.html .
- Bradley Susan. 2003. Affect regulation and the development of psychopathology . New York: Guilford Press. [ Google Scholar ]
- Cohen-Kettenis Peggy. 2001. Gender identity disorder in the DSM? Journal of the American Academy of Child and Adolescent Psychiatry 40 : 391. [ PubMed ] [ Google Scholar ]
- de Varies Annelou L., Noens Ilse L.J., Cohen-Kettenis Peggy T., van Berckelaer-Onnes Ina A., and Doreleijers Theo A.. 2010. Autism spectrum disorders in gender dysphoric children and adolescents . Journal of Autism and Developmental Disorders 40 : 930–936. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Dhejne Cecilia, Lichtenstein Paul, Boman Marcus, Johansson Anna L. V., Långström Niklas, and Landén Mikael. 2011. Long-term follow-up of transsexual persons undergoing sex reassignment surgery: Cohort study in Sweden . PLoS ONE 6 : e16885. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Duigon Lee. 2011. Gender free children: The newest fad in public education. ghalcedon. http://chalcedon.edu/research/articles/gender-free-children-the-newest-fad-in-public-education/ .
- Fitzgibbons Richard. 2015. Gender dysphoria, gender identity disorder and informed consent. http://www.childhealing.com/articles/genderidentitydisorder.php .
- Fitzgibbons Richard, Philip M.Sutton, and O'Leary Dale. 2009. The psychopathology of “sex reassignment” surgery: Assessing its medical, psychological, and ethical appropriateness . National Catholic Bioethics Quarterly 9.1 : 109–37. [ Google Scholar ]
- Heyer Walt. 2015. Sex change surgery: What Bruce Jenner, Diane Sawyer and you should know. April 27. http://www.thepublicdiscourse.com/2015/04/14905 .
- McHugh Paul. 2004. Surgical sex . First Things 147 ( November ): 34–38. [ Google Scholar ]
- McHugh Paul. 2014. Transgender surgery isn't the solution. The Wall Street Journal . June 12. http://www.wsj.com/articles/paul-mchugh-transgender-surgery-isnt-the-solution-1402615120 .
- McHugh Paul. 2015. Transgenderism: A pathogenic meme. Public Discourse . June 10. http://www.thepublicdiscourse.com/2015/06/15145 .
- Meyer Jon K., and Reter Donna J.. 1979. Sex reassignment. Follow-up . Archives of General Psychiatry 36 : 1010–5. [ PubMed ] [ Google Scholar ]
- Montagna Diane. 2015. Pope Francis: Gender theory is a threat to society. Aleteia.org . June 9. http://aleteia.org/2015/06/09/pope-francis-gender-theory-is-a-threat-to-society/ .
- O'Leary Dale, and Sprigg Peter. 2015. Understanding and responding to the transgender movement. Family Research Council. http://downloads.frc.org/EF/EF15F45.pdf .
- Reisner Sari, Vetters Ralph, Leclerc M., Zaslow Shayne, Wolfrum Sarah, Shumer Daniel, and Mimiaga Matthew J.. 2015. Mental health of transgender youth in care at an adolescent urban community health center: A matched retrospective cohort study . Journal of Adolescent Health 56 : 274–79. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Richards Renee. 1999. The Liaison Legacy. Tennis Magazine . March.
- Westen John-Henry. 2015. Pope Francis condemns gender theory a third time: “The family is under attack.” Lifesitenews.com . March 23. https://www.lifesitenews.com/news/pope-francis-condemns-gender-theory-a-third-time-the-family-is-under-attack .
- White Hilary. 2015. Pope Francis blasts “gender theory” again: rejecting sexual difference is “a step backwards.” Lifesitenews.com . April 15. http://www.lifesitenews.com/news/pope-francis-blasts-gender-theory-again-rejecting-sexual-difference-is-a-st .
- Wood Hayley, Sasakia Shoko, Bradleya Susan J., Singha Devita, Fantusa Sophia, Owen-Andersona Allison, Di Giacomoa Alexander, Bainb Jerald, and Zucker Kenneth J.. 2013. Patterns of referral to a gender identity service for children and adolescents (1976–2011) age, sex ratio, and sexual orientation . Journal of Sex & Marital Therapy 39 : 1–6. [ PubMed ] [ Google Scholar ]
- Zucker Kenneth, and Bradley Susan. 1995. Gender identity disorder and psychosexual problems in children and adolescents . New York: Guilford Publications. [ PubMed ] [ Google Scholar ]
- Zucker Kenneth, Bradleya Susan J., Owen-Andersona Allison, Kibblewhitea Sarah J., Wooda Hayley, Singha Devita, and Choia Kathryn. 2012. Demographics, behavior problems, and psychosexual characteristics of adolescents with gender identity disorder or transvestic fetishism . Journal of Sex & Marital Therapy 38 : 151–89. [ PubMed ] [ Google Scholar ]
- Zucker Kenneth, Bradley Susan J., Ben-Dat Dahlia N., Ho Caroline, Johnson Laurel, and Owen Allison. 2003. Psychopathology in the parents of boys with gender identity disorder . Journal of the American Academy of Child and Adolescent Psychiatry 42 : 2–4. [ PubMed ] [ Google Scholar ]
- Update Preferences
- Give Online
- Give by Mail or Phone
- Give through Donor Advised Fund
- Donate your Vehicle
- Estate Planning
- Campaign 2024
- Trump Trials
- Biden Impeachment
- Israel-Hamas War
- International
- Election Center 2024
- WORLD Opinions
- SIGN UP FOR NEWSLETTER
The 4th Circuit chooses willful ignorance
Judges push to make states pay for transgender surgery.
The U.S. 4th Circuit Court of Appeals Courthouse on Main Street in Richmond, Va. Associated Press/Photo by Steve Helber

Full access isn’t far.
We can’t release more of our sound journalism without a subscription, but we can make it easy for you to come aboard.
Get started for as low as $3.99 per month.
Current WORLD subscribers can log in to access content. Just go to "SIGN IN" at the top right.
Already a member? Sign in.
In an historic decision, the 4th U.S. Circuit Court of Appeals became the first appellate court to say states must pay for so-called transgender health care including sex “reassignment” surgeries and hormones. The case was a consolidation of two lawsuits, one from West Virginia and another from North Carolina. The 4th Circuit was once considered a more conservative court, but now has a majority eight justices appointed by Democratic presidents. Those eight justices joined to form the majority opinion in the case.
A central question involved the efficacy of cross-sex hormones and plastic surgery. North Carolina argued their decision not to fund these interventions was due, at least in part, to the fact they do not solve the mental distress patients cite as complaint. That argument is hardly on the fringe these days and is arguably becoming a consensus globally.
Just weeks ago, the National Health Service in the United Kingdom announced it would no longer prescribe puberty blockers as a way of treating gender dysphoria. It made the decision after commissioning a study that found “gaps in evidence” around the benefits of the drugs. Now puberty blockers in the United Kingdom can only be used in studies to find out if they are helpful, not under the assumption that they are. A year ago, Sweden, the first country to legalize gender reassignment surgery, also restricted so-called gender reassignment hormone treatments on minors, citing a lack of evidence the treatments benefit patients.
In light of these relatively recent developments, it is almost disorienting to see the majority in the 4th Circuit say : “Without evidence to show that gender-dysphoria treatments are ineffective, the North Carolina Appellants cannot show that the coverage exclusion is narrowly tailored to serve the state’s substantial interest in not covering medically ineffective treatment.” Without evidence? The whole world is talking about the lack of evidence to show these medical interventions are helpful, and much of the world is acting on it.
Having chosen ignorance, the court therefore concluded the state’s decision to provide mastectomies for women with breast cancer but not for women who want to look more like men is illegal, class-based discrimination. In a world where “I want it” is the only justification we require for anything, we see no difference between removing a body part infected with cancer and removing a healthy body part. Reason has been replaced by desire.
But there’s something else going on as well. This case is part of a pattern that has developed over the past 20 years to involve everyone around you in your personal pursuit of happiness, whether they like it or not. People don’t merely believe they have a right to an abortion, they believe they have a right to a taxpayer-funded abortion. And if you’re a doctor, they believe they have a right to make you perform the abortion. They don’t merely believe they have a right to a same-sex wedding, they believe they have a right to make you decorate it. They don’t merely believe they have the right to have children, they believe you should pay the costs of in vitro fertilization and surrogacy if they’re in a relationship incapable of producing children. Now, they don’t merely believe they have the right to cut off the genitals of children and put children on a lifetime supply of hormones, they intend you to pay for it. Their rights, your problem.
This case is certain to be appealed to the U.S. Supreme Court, and there’s reason to believe the outcome will change. Still, we need to understand the state of mind we’re being governed by. Much of the ruling class believes “the science” is settled about nearly everything. They are convinced there is nothing left to learn, so there is no need to think critically or deliberate, and they definitely do not want to know what you think. There’s no time for any of that because a revolution is on. All they want is your submission—and your money.
If you enjoyed this article and would like to support WORLD's brand of Biblically sound journalism, click here .

Joseph Backholm is senior fellow for Biblical worldview and strategic engagement at the Family Research Council. Previously, he served as a legislative attorney and spent 10 years as the president and general counsel of the Family Policy Institute of Washington. He also served as legal counsel and director of What Would You Say? at the Colson Center for Christian Worldview where he developed and launched a YouTube channel of the same name. His YouTube life began when he identified as a 6-foot-5 Chinese woman in a series of YouTube videos exploring the logic of gender identity. He and his wife Brook have four children.
These daily articles have become part of my steady diet. —Barbara
Read the Latest from WORLD Opinions
Andrew T. Walker | Twenty years later, you still cannot redefine marriage

Nathanael Blake | A digital device is a poor memento mori

Anne Kennedy | Modern design reflects moral rebellion

Marc LiVecche | His threat to withhold weapons from Israel makes a lasting peace less likely

Please wait while we load the latest comments...
Please register, subscribe, or log in to comment on this article.
Related Articles
- Newsletters
- Instapundit
- News & Politics
Appeals Court Finds a Constitutional Right to Gender Reassignment Surgery

The 14th Amendment to the Constitution is truly a magical amendment. It was used to justify attempts to kick Donald Trump off the 2024 ballot. Through the decades, judges who want to play at social engineering have used it frequently to justify questionable law.
It's even been invoked to bypass Congress to raise the debt limit.
Now, the Fourth Circuit Court of Appeals has decided that the amendment's "equal protection" clause means that state Medicaid programs have to cover gender reassignment surgeries.
The appeals court ruled that West Virginia's Medicaid rules on mastectomies are unconstitutional because they violate the "equal protection standard" by not covering mastectomies for gender dysphoria.
Yes, really.
The ruling also includes a North Carolina Medicaid case that the state government won't cover "sex changes." The Fourth Circuit nullified the state ban on gender change surgeries, citing the 14th Amendment’s guarantee of “equal protection of the laws.”
This was a court looking for an excuse to make law.
Judge Roger Gregory who wrote the majority opinion in Kadel v. Folwell (8-6) asked, “Is removing a patient’s breasts to treat cancer the same procedure as removing a patient’s breasts to treat gender dysphoria?” He continued, “There is no case law to ground this discussion nor obvious first principles.”
Wall Street Journal:
He is undeterred, and he concludes that gender dysphoria and transgender status are intertwined, so that such insurance exclusions are nothing more than a proxy for discriminating against gender identity. Then he goes further, finding that West Virginia’s and North Carolina’s policies also unconstitutionally discriminate based on sex. How so? Imagine, Judge Gregory says, an unidentified patient seeking a vaginoplasty. Is this a biological female with a rare birth defect? Is it a transgender patient? “By virtue of the fact that they are seeking a vaginoplasty, we know that they were born without a vagina,” he writes. “But we do not know what sex they were assigned at birth. Without that information, we cannot say whether the Plan or Program will cover the surgery.” Ergo, sex discrimination.
Gregory gets even nuttier.
The differences in coverage "is rooted in a gender stereotype: the assumption that people who have been assigned female at birth are supposed to have breasts, and that people assigned male at birth are not."
It's not a "gender stereotype." It's a biological fact.
"No doubt, the majority of those assigned female at birth have breasts, and the majority of those assigned male at birth do not. But we cannot mistake what is for what must be.”
Not just a "majority." It's a universal biological fact with a tiny number of exceptions.
Treating different things differently doesn’t violate the 14th Amendment’s Equal Protection Clause, and jurists aren’t supposed to ignore the obvious. Writing in dissent at the Fourth Circuit, Judge Julius Richardson struggles to contain his exasperation. “The states,” he says, “have chosen to cover alterations of a person’s breasts or genitalia only if the person experiences physical injury, disease, or (in West Virginia) congenital absence of genitalia.” That determination does not turn on the patient’s sex or gender. “Christopher Fain—one of the plaintiffs below—received coverage for a hysterectomy based on a diagnosis unrelated to Fain’s transgender status,” the dissent says. Likewise, males with gynecomastia qualify for surgery coverage in West Virginia only “if they have physical symptoms, like breast pain,” meaning that isn’t a procedure done merely “to affirm a patient’s biological sex.”
The ruling that opened this can of worms was Bostock v. Clayton County, a case that "held that Title VII of the Civil Rights Act of 1964 protects employees against discrimination because of sexuality or gender identity." Now, as a dissenting judge in Kadel v. Folwell, Judge J. Harvie Wilkinson III is saying that this ruling could be a Roe v Wade ruling for the transgender community.
“This is imperial judging at its least defensible,” he says, “What plaintiffs propose is nothing less than to use the Constitution to establish a nationwide mandate that States pay for emerging gender dysphoria treatments.”
He's not wrong. But getting the ruling past this Supreme Court would be a stretch.

Rick Moran has been writing for PJ Media for 18 years. His work has appeared in dozens of media outlets including the Washington Times and ABC News. He was an editor at American Thinker for 14 years. His own blog is Right Wing Nut House . For media inquiries, please contact [email protected] .
Recommended

Trending on PJ Media Videos
- Cohen Made Huge Admission in NYC Trump Case and Now the Tumblers Begin to Fall in Place
- Why Has Biden Betrayed Israel? Look at His New Special Counsel
- Snopes Admits Ashley Biden’s Diary Is Genuine, So Let’s Talk About What It Says
- Advocate Newsletter
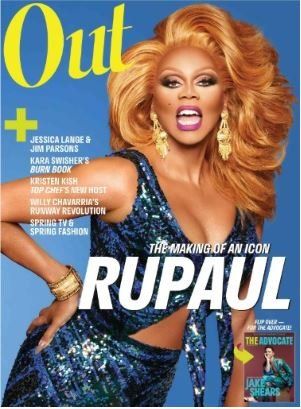
Search form
By continuing to use our site, you agree to our Private Policy and Terms of Use .
Denying gender-affirming care coverage violates federal law, says appeals court

The 11th Circuit made the ruling in the case of Houston County, Ga., sheriff's deputy Anna Lange.
A federal appeals court has upheld a lower court’s ruling that the Houston County, Ga. , Sheriff’s Office violated antidiscrimination law by denying transition-related health care to a deputy.
Anna Lange sued in 2019 because she had been repeatedly denied insurance coverage for gender-affirming care under the county’s employee health plan. A U.S. district court in Georgia ruled in 2022 that the denial violated federal civil rights law, and Monday a three-judge panel of the U.S. Court of Appeals for the 11 Circuit affirmed that ruling.
It is only the second decision by a federal appellate court affirming that it is unlawful for an employer to discriminate against transgender people in an employee health plan, the first being a recent decision on North Carolina's plan for state employees. It is immediately binding on employers in Georgia, Florida, and Alabama, the states covered by the 11th Circuit, notes a press release from the Transgender Legal Defense and Education Fund, which is representing Lange along with a private law firm.
In his ruling for the 2-1 majority, Judge Charles Wilson cited the Supreme Court’s 2020 decision in Bostock v. Clayton County, in which the high court ruled that job discrimination based on sexual orientation and gender identity constitutes sex discrimination, banned by Title VII of the Civil Rights Act of 1964.
“Applying Bostock ’s reasoning to the facts in this case, we conclude that the district court was correct in finding that the Exclusion violated Title VII,” he wrote. “There is no genuine dispute of fact or law as to whether the Exclusion unlawfully discriminates against Lange and other transgender persons. The Exclusion is a blanket denial of coverage for gender-affirming surgery. Health Plan participants who are transgender are the only participants who would seek gender-affirming surgery. Because transgender persons are the only plan participants who qualify for gender-affirming surgery, the plan denies health care coverage based on transgender status.”
“Today’s victory is a win not just for me, but for all transgender Southerners who deserve equal access to life-saving transition-related care,” Lange said in the TLDEF press release. “I have proudly served my community for decades and it has been deeply painful to have the county fight tooth and nail, redirecting valuable resources toward denying me basic health care — health care that the courts and a jury of my peers have already agreed I deserve. I’m pleased to see that yet another court has deemed those efforts to be unfair and illegal.”
Lange has spent 26 years in law enforcement, 17 of them with Houston County. She came out as trans in 2017.
“Today, the 11th Circuit upheld the well-reasoned ruling of the U.S. District Court that treating Sgt. Anna Lange differently because she is transgender is discriminatory,” TLDEF Co-Interim Legal Director Gabriel Arkles said in the release “Houston County and Sheriff [Cullen] Talton have once again lost in court, after spending some $2 million on lawyers to try to deprive Sgt. Lange of medically necessary care that costs orders of magnitude less solely to discriminate against transgender people.”
“We are pleased that the 11th Circuit Court came to the same conclusion as the lower courts that denying health care coverage to transgender individuals is wrong and illegal, and affirmed the lower court ruling in Sgt. Lange’s favor,” added Wesley Powell, partner at Willkie Farr & Gallagher LLP, who serves as co-counsel.
- North Carolina and West Virginia can't deny trans health care: federal appeals court ›
- SCOTUS Lets Trans Woman's Discrimination Suit in Virginia Go Forward ›
- Anti-Trans Workplace Discrimination Is OK in Texas, Judge Rules ›
- Trans Woman Wins Employment Discrimination Suit Using Civil Rights Act ›
- Biden Calls Transgender Discrimination Civil Rights Issue of Our Time ›
Want more breaking equality news & trending entertainment stories?
Check out our NEW 24/7 streaming service: the Advocate Channel!
Download the Advocate Channel App for your mobile phone and your favorite streaming device!
APPLE STORE - GOOGLE PLAY
ROKU - APPLE TV - FIRE TV - GOOGLE TV
From our Sponsors
Most popular, meet all 37 of the queer women in this season's wnba.
17 Celebs Who Are Out & Proud of Their Trans & Nonbinary Kids
Which state is the queerest these are the states with the most lgbtq+ people, these 27 senate hearing room gay sex jokes are truly exquisite, 10 cheeky and homoerotic photos from bob mizer's nude films, here are the 15 gayest travel destinations in the world: report, 13 lgbtq+ british royals in history, black transgender woman starr brown shot to death in memphis. her coworker has confessed to the killing, these are the 5 states with the smallest percentage of lgbtq+ people, 25 pics of hot, shirtless celebs just to remind us of warmer weather, latest stories, harrison butker’s ‘inaccurate, ill-informed and woefully out of step' sexist speech is fact-checked by glaad, maria bello and dominique crenn tie the knot in 'stunning' mexico ceremony, ‘rupaul’s drag race’ winner nymphia wind performs for taiwan’s outgoing president, when laws fail to protect trans people, harmful medicalized norms creep in, dominate vacation prep shopping with the pride store’s summer travel essentials, most black women don't have access to abortion, and they're going to impact the elections, behind the lens & the drag with ‘queen of new york’ director emma fidel (exclusive), biden challenges trump to debate: ' i hear you’re free on wednesdays', from player to broadcaster, meet the queer black soccer pro breaking down the washington spirit, kristin chenoweth defends the lgbtq+ community: 'god loves us all the same', mike johnson shows up outside the courtroom of trump’s hush money trial because the democrats let it happen, months after election, gay house candidate evan low will be on november ballot. here's what happened, kansas city chiefs kicker harrison butker goes on transphobic, sexist rant during graduation speech, don't be 'weak and gay,' missouri republican candidate says in campaign video, moms for liberty joins in suing biden administration over title ix protections for trans students, 'heartstopper' creator alice oseman raising funds for kids in gaza, meet the gay man who will be tennessee's first out lgbtq+ school board member, transgender 18-year-old jazlynn johnson shot to death in las vegas, jonathan groff thought coming out would make fame 'impossible.' here's why he did anyway, mississippi governor signs transgender bathroom ban, trending stories.

All 6 rogue Mississippi cops got long prison sentences in 'Goon Squad' torture of 2 Black men

10 thirsty pics celebrating DJ Dani Brasil’s Capital Pride debut

‘Bridgerton’ stars Nicola Coughlan & Luke Newton on getting OUT of the friendzone

10 last-minute travel destinations and hotels perfect for Pride 2024

‘Ozempic babies’: Reports of surprise pregnancies raise new questions about weight loss drugs

France becomes world’s first country to enshrine abortion rights in constitution
Elon Musk uses burner accounts on X, doesn’t fact-check: report

5 of Jonathan Groff's best (and most iconic) gay roles

'Red, White & Royal Blue' sequel is really happening & we're SCREAMING

Out and About with Joel Kim Booster

How climate disasters hurt mental health in young people

The Talk: Starting your journey with HIV

30 steamy pics of Matteo Lane that got us all hot & bothered

Mixed reviews for airlines in the latest J.D. Powers passenger rankings

Hulu's 'Black Twitter' producers on trailer backlash: 'You got to welcome the smoke'

25 pics of Jonathan Groff that prove why we'll always love him

Marvel's 'Agatha' finally has a REAL title — can you guess what it is? (Updated)

Walmart to close all of its health care clinics
Exclusive: ‘Queen of the North’ Brooke Lynn Hytes makes her South Beach Palace Bar debut

Justice Dept plans to reschedule marijuana as a lower-risk drug

'Looking' cast: Where are they now?

Jonathan Groff is fine not fitting in: 'Being gay has allowed me to forge my own path'

Why is a mother’s mental health so important? A doctor explains

Joe Biden has tied the record for most LGBTQ+ judges confirmed in federal courts
Most recent.

Jennifer Lawrence’s BRUTAL and HILARIOUS takedown of Mike Pence is making our whole week

16 Republican AGs threaten Maine over protections for trans care and abortion

Here's why 'Drag Race's Kim Chi & Eureka are fighting on social media

The brand new 'Wicked' poster has us BEYOND hyped

The Talk: Finding balance with HIV

The Talk: Thriving with HIV

'Drag Race's Kim Chi & Eureka are FOR REAL beefing online — here's why

Yes, RuPaul actually competed on 'Drag Race'—and won!

The menthol diaries: Taking back pride from tobacco

Carrie Underwood solidifies herself as a can't-miss entertainer in Las Vegas

First look at Ellie & Dina's Sapphic love story in The 'Last of Us' season 2

Discover endless fun at The Pride Store: Games & electronics for all ages

Federal judge grants Casa Ruby founder Ruby Corado pre-trial release from D.C. jail

Savor vibrant bites as the best traveling queer food festival continues its journey east
How The Stonewall Gives Back Initiative empowers equality with its impactful legacy
Before AIDS, gay artist Rex drew hot men on the prowl — then he disappeared

Joe Biden launches ‘Out for Biden-Harris’ campaign initiative to engage & woo LGBTQ+ voters (exclusive)

'Drag Race's Jaremi cosplays as drag version of Patrick Star and we're gagging

Charlotte LGBTQ+ travel: Discover pride in North Carolina

The Talk: What HIV isn’t

Was Bad Bunny really spotted cozying up to a man at a gay bar?

Giselle Byrd is taking center stage — and helping others do the same

Election season got you down? This crisis line is soothing LGBTQ+ mental health
Manu Rios' new shirtless Lacoste campaign has us seriously sweating
Andrew Scott and Paul Mescal just had an 'All of Us Strangers' reunion & we wish we were invited
Recommended stories for you.

IMAGES
VIDEO
COMMENTS
Research consistently shows that people who choose gender affirmation surgery experience reduced gender incongruence and improved quality of life. Depending on the procedure, 94% to 100% of people report satisfaction with their surgery results. Gender-affirming surgery provides long-term mental health benefits, too.
Gender-affirming surgeries are associated with numerous positive health benefits, including lower rates of psychological distress and suicidal ideation, as well as lower rates of smoking, according to new research led by Harvard T.H. Chan School of Public Health.. The study examined data from the 2015 U.S. Transgender Survey, which included nearly 20,000 participants, 38.8% of whom identified ...
When transgender people undergo sex-reassignment surgery, the beneficial effect on their mental health is still evident — and increasing — years later, a Swedish study suggests. Overall ...
Much of the literature on mental health benefits of gender-affirming surgery has been complicated by inability to adjust for a key confounder: baseline mental health status. ... Lauri Korajlija A, Jurin T. Psychosocial adjustment to sex reassignment surgery: a qualitative examination and personal experiences of six transsexual persons in ...
Washington - For transgender individuals, gender-affirming surgery can lead to long-term mental health benefits, according to new research published online today in The American Journal of Psychiatry. The study found that among transgender individuals with gender incongruence, undergoing gender-affirming surgery was significantly associated ...
Gender surgery improves quality of life. Dr. Hess and colleagues surveyed 156 people who had all had gender reassignment surgery 6.61 years prior to the study, on average. The survey included open ...
Overview. Gender affirmation surgery, also known as gender confirmation surgery, is performed to align or transition individuals with gender dysphoria to their true gender. A transgender woman, man, or non-binary person may choose to undergo gender affirmation surgery. The term "transexual" was previously used by the medical community to ...
Research shows that one of the main benefits of gender affirming surgery is the wide array of long-term mental health benefits patients experience. Some studies report that patients who underwent gender affirming surgeries experienced lower rates of psychological distress and suicidal ideation. Another study found that a person's odds for ...
Given the benefits of GAS, ... The overall number of health system encounters for gender identity disorder rose from 13 855 in 2016 to 38 470 in 2020. ... Zavlin D, Lellé JD, et al. Male-to-female sex reassignment surgery using the combined technique leads to increased quality of life in a prospective study.
Long-term overall body congruency score was 89.6. Improved mental health outcomes persisted following surgery with significantly reduced suicidal ideation and reported resolution of any mental health comorbidity secondary to gender dysphoria. Conclusion: Gender-affirming surgery is a durable treatment that improves overall patient well-being ...
Gender-affirmation surgery is a rapidly growing field in plastic surgery, urologic surgery, and gynecologic surgery. These procedures offer significant benefit to patients in reducing gender dysphoria and improving well-being. However, the details of gender-affirmation surgery are less well-known to other surgical subspecialties and other medical subspecialties.
Abstract. For individuals with gender dysphoria, gender-affirming surgeries (GAS) are one means of reducing the significant distress associated with primary and secondary sex characteristics misaligned with their gender identity. This article uses a systematic review to examine the existing literature on the psychological benefits of GAS.
Regret after GAS may result from the ongoing discrimination that afflicts the TGNB population, affecting their freely expression of gender identity and, consequently feeling regretful from having had surgery. 15 Poor social and group support, late-onset gender transition, poor sexual functioning, and mental health problems are factors ...
Multiple procedures are typically included as part of gender-affirmation surgery, including facial procedures, top surgery (above the waist) and bottom surgery (below the waist). Call 913-588-6200 to request a consultation. For more information, email our nurse coordinators at [email protected].
Results from studies imply that sex reassignment surgery on the one hand has positive effects in terms of partial aspects of quality of life, such as mental health, sexuality, and life satisfaction, and, on the other hand, on quality of life overall. Because of the studies' high dropout rates (12-77%; median 56%), the results should be ...
Gender confirmation surgeries, also known as gender affirmation surgeries, are performed by a multispecialty team that typically includes board-certified plastic surgeons. The goal is to give transgender individuals the physical appearance and functional abilities of the gender they know themselves to be. Listed below are many of the available ...
Gender-affirming surgeries are associated with numerous positive health benefits, including lower rates of psychological distress and suicidal ideation, as well as lower rates of smoking, according to new research led by Harvard T.H. Chan School of Public Health. The study examined data from the 2015 U.S. Transgender Survey, which included ...
Much of the literature on mental health benefits of gender-affirming surgery has been complicated by inability to adjust for a key confounder: baseline mental health status. ... Jurin T. Psychosocial adjustment to sex reassignment surgery: a qualitative examination and personal experiences of six transsexual persons in croatia ...
Many health plans are still using exclusions such as "services related to sex change" or "sex reassignment surgery" to deny coverage to transgender people for certain health care services. Coverage varies by state. Before you enroll in a plan, you should always look at the complete terms of coverage that are included in the "Evidence ...
Masculinizing Procedures. "Mansculpture". Some trans men feel a sense of dysphoria about their hips, thighs, stomach, or other areas and wish to get liposuction to create a more masculine body contour. Complications are similar to any other liposuction treatment, and include bruising, pain, bleeding, and infection. Hysterectomy.
Tate, who has been with Starbucks for 15 years and now manages a store in Austin, Texas, is one of a growing number of Starbucks partners who have used the company's leading-edge benefits for transgender partners. Starbucks health insurance plans include not only gender reassignment surgery (which had been covered since 2012), but now also a ...
Objective: Despite professional recommendations to consider gender-affirming hormone and surgical interventions for transgender individuals experiencing gender incongruence, the long-term effect of such interventions on mental health is largely unknown. The aim of this study was to ascertain the prevalence of mood and anxiety disorder health care visits and antidepressant and anxiolytic ...
It's essential to carefully consider all options and potential outcomes before undergoing surgery. 5. How long does it take to complete gender reassignment surgery? The duration of surgery varies ...
Abstract. Transsexual issues and sexual reassignment surgery (SRS) are receiving a great deal of attention and support in the media, schools, and government. Given the early age at which youth seek treatment for transsexual attractions (TSA) and gender dysphoria and given the serious risks associated with such treatment, it is essential that ...
In an historic decision, the Fourth Circuit of the U.S. Court of Appeals became the first appellate court to say states must pay for so-called transgender health care including sex "reassignment" surgeries and hormones. The case was a consolidation of two lawsuits, one from West Virginia and another from North Carolina.
Now, the Fourth Circuit Court of Appeals has decided that the amendment's "equal protection" clause means that state Medicaid programs have to cover gender reassignment surgeries. The appeals ...
The Exclusion is a blanket denial of coverage for gender-affirming surgery. Health Plan participants who are transgender are the only participants who would seek gender-affirming surgery. Because ...
Section 3701-59-06 - Hospital quality standards for gender reassignment surgery and genital gender reassigment surgery for minors (A) As used in this rule: (1) "Biological sex," "Birth sex," and "sex" mean the biological indication of male and female, including sex chromosomes, naturally occurring sex hormones, gonads, and nonambiguous internal and external genitalia present at birth, without ...
Section 3701-83-60 - Health care facility quality standards for gender reassignment surgery and genital gender reassignment surgery for minors (A) As used in this rule: (1) "Biological sex," "birth sex," and "sex" mean the biological indication of male and female, including sex chromosomes, naturally occurring sex hormones, gonads, and nonambiguous internal and external genitalia present at ...