Hon’ble Chancellor Vice Chancellor Registrar Principal Vice Principal Medical Superintendent
Anaesthesiology Anatomy Biochemistry Cardiac Anaesthesia Cardiology Cardio vascular & Thoracic Surgery Community Medicine Dermatology (Skin & VD) Emergency Medicine Endocrinology ENT, Head & Neck Surgery Forensic Medicine Gastroenterology
General Medicine General Surgery Interventional Radiology Medical Oncology Microbiology Nephrology Neonatology Neurology Neurosurgery Nuclear Medicine Obstetrics & Gynecology Ophthalmology Orthopedics Pathology
Public Health Research Unit Medical Education MCI Nodal Center Hospital Administration
Pediatrics Pediatric Neurology Pediatric Surgery Pharmacology Physical Medicine & Rehabilitation Physiology Plastic & Reconstructive surgery Psychiatry Radiation Oncology Radiology/Radio-diagnosis Respiratory/Pulmonary Medicine Surgical Oncology Urology

Under Graduate
Post graduate.
Post Doctoral Diploma Courses Public Health Ph.D Hospital Administration Fellowship Courses Allied Courses
Feedback Analysis 2015-20 Feedback Analysis 2021
Syllabus of Courses offered
Under Graduate Post Graduate Post Doctoral Fellowship Courses Ph.D Allied Courses
- KLE Advanced Simulation Centre & Clinical Skills Lab
- Cadaveric Skill Lab
- NIRF Prescribed Format
- JNMC NIRF 2018
- JNMC NIRF 2019
- JNMC NIRF 2020
- JNMC NIRF 2021
- JNMC NIRF 2022
- JNMC NIRF 2023
- JNMC NIRF 2024
- KLE Dr. PBK Hospital & MRC
- KLE Dr.PBK Hospital
- JNMC Women’s & Children’s Health Research Unit
- KLE Society
- Sports Complex
- Convention Center
- Musical Garden
- Shivalaya Temple
- Ganesh Temple
- Attendance Dashboard
- Scientific Society
- Student Association
- Kannada Balaga
- Institutional Ethics Committee
- Internal Complaint Committee
- Anti-Ragging
- Para Medical Course
- Capability Enhancement
- Faculty Login
- Student/Parent Login
- Dissertations
- M.B.B.S Phase III – Part-II
M.S General Surgery Dissertation
Dissertation Topics Completed (KLE Academic of Higher Education and Research, Belagavi):
Dissertation Topics Ongoing (KLE Academic of Higher Education and Research, Belagavi):
Request a Quote
- Hon’ble Chancellor
- Vice Chancellor
- Vice Principal
- Medical Superintendent
- Biochemistry
- Forensic Medicine
- Microbiology
- Pharmacology
- Community Medicine
- Ophthalmology
- Obst & Gynecology
- Orthopaedics
- Skin & VD
- Pulmnonary Medicine
- Anaesthesiology
- Post Doctoral
- Endocrinology
- Department Public Health
- Research Unit
- Medical Education
- MCI Nodal Center
- Diploma Courses
- Department of Public Health
- Hospital Administration
- Govt-Approval
- KLE Dr. PBK Hospital & MRC
- KLE Dr.PBK Charitable Hospital
- PHC & UHC
- Reference Manager
- Simple TEXT file
People also looked at
Original research article, patient views around their hernia surgery: a worldwide online survey promoted through social media.

- 1 Department of General Surgery, Royal Infirmary of Edinburgh, Edinburgh, United Kingdom
- 2 3 rd Department of Surgery, Motol University Hospital, Prague, Czechia
- 3 Patient Representative, London, United Kingdom
- 4 Patient Representative, Glasgow, United Kingdom
- 5 Patient Representative, Liverpool, United Kingdom
- 6 Hernia Istanbul®, Hernia Surgery Center, Istanbul, Turkey
- 7 DISC (Department of Surgical Sciences), University of Genoa, Genoa, Italy
Introduction: Hernias are one of the most common surgical diagnoses, and general surgical operations are performed. The involvement of patients in the decision making can be limited. The aim of this study was to explore the perspectives of patients around their hernia and its management, to aid future planning of hernia services to maximise patient experience, and good outcomes for the patient.
Methods: A SurveyMonkey questionnaire was developed by patient advocates with some advice from surgeons. It was promoted on Twitter and Facebook, such as all found “hernia help” groups on these platforms over a 6-week period during the summer of 2020. Demographics, the reasons for seeking a hernia repair, decision making around the choice of surgeon, hospital, mesh type, pre-habilitation, complications, and participation in a hernia registry were collected.
Results: In total, 397 questionnaires were completed in the study period. The majority of cases were from English speaking countries. There was a strong request for hernia specialists to perform the surgery, to have detailed knowledge about all aspects of hernia disease and its management, such as no operation and non-mesh options. Chronic pain was the most feared complication. The desire for knowledge about the effect of the hernia and surgery on the sexual function in all age groups was a notable finding. Pre-habilitation and a hernia registry participation were well-supported.
Conclusions: Hernia repair is a quality of life surgery. Whether awaiting surgery or having had surgery with a good or bad outcome, patients want information about their condition and treatment, such as the effect on aspects of life, such as sex, and they wish greater involvement in their management decisions. Patients want their surgery by surgeons who can also manage complications of such surgery or recommend further treatment. A large group of “hernia surgery injured” patients feel abandoned by their general surgeon when complications ensue.
Introduction
Hernias are a common affliction worldwide. The main treatment option is surgical repair of the hernia. Much of the research related to hernia surgery focusses on the short- and longer-term outcomes, such as recurrence and more recently chronic pain. Patient reported outcome measures (PROMs) have gained popularity, but PROMs still only ask questions to patients that the doctor wants to be answered ( 1 ). Such questions may not reflect the priorities of the patient, or indeed address elements of the patient experience or barriers to their treatment or what best leads to satisfying outcomes. Such failures in seeking patient focussed data are not unique to hernia surgery ( 2 ). However, patient focussed priorities are a key part of the GRADE approach in writing the clinical guidelines ( 3 ). It dictates: “ to make sensible recommendations guideline panels must consider all outcomes that are important or critical to patients for decision making” . However, there is a lack of research or knowledge about what is important or critical to our patients? Two recent studies exploring some of these issues in ventral hernia repair recruited only 22 and 30 patients, respectively, in single centres, making their generalisability less clear cut ( 4 , 5 ).
An additional area of concern in hernia surgery is the steady growth in mesh related litigation and the increasing number of patient support groups focused on problems possibly related to their mesh. There is a clear need to open discussion with such groups to understand better and thus heal this surgeon—patient relationship. Despite that, some surgeons are reluctant to accept responsibility over implants they use or have insufficient knowledge about their properties or do not inform their patients well about all the risks and benefits of mesh or indeed non-mesh options. Not unsurprisingly, a growing body of patients are losing trust in the surgical industry. Online surveys are good tools to utilise in such situations when large numbers of patients need to be involved ( 6 ).
The aim of this study was to explore and gain insights into the perspectives of patients related to their hernia and its management through an online based survey, promoted through social media.
The research group consisted of eight people. An initial meeting was held online and consisted of the principal researcher, another three surgeons with a major hernia interest, two patient representatives regularly attending hernia meetings, and two more patient representatives, one of which has re-trained as a nurse and the other with expertise in facilitating the patient groups.
At the initial meeting, the investigators agreed on the main aims of the survey—to investigate expectations of patients from hernia surgery focussing on their priorities throughout the process of hernia surgery—initial motivation for repair, preoperative consultation, operative and follow-up preferences, along with their views about mesh use. The study questions were composed and over a period of 4 weeks, the questions were refined in terms of readability in the English language, using the SurveyMonkey platform.
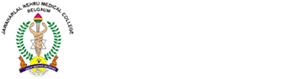
The 42-questions questionnaire was launched on social media. Posts using Twitter on the personal profiles of the investigators and on @EuroHerniaS and @ColostomyUK with a link to the survey were retweeted regularly. Posts on Facebook using similar profiles were undertaken. In addition, all the patient support groups that contained the word “hernia” or “mesh” were approached with a request to share the link to the survey with their members. The groups are listed in Table 1 comprising a total of 29,697 members. A number of groups refused to either accept the principal investigator and/or share the link to the survey and these are listed in the Table 2 . The survey was promoted over a 6-week period during June and July 2020. Link to the survey was promoted by all the authors through their Twitter social media feed, with regular retweets. The survey questions can be viewed at http://www.surveymonkey.com/r/WhatDoPatientsWantFromHerniaOperation .
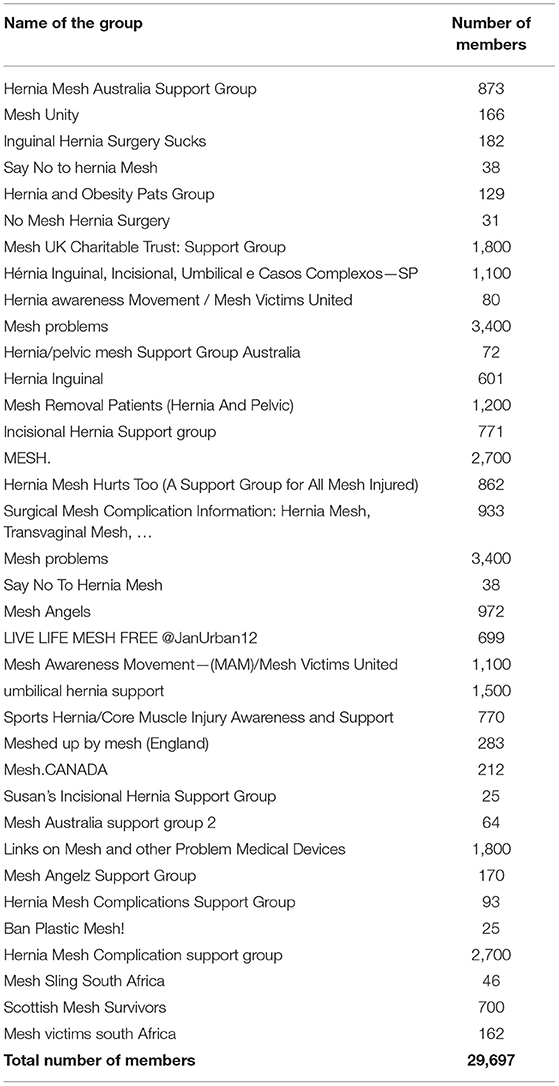
Table 1 . Facebook groups approached who were willing to disseminate the survey with membership number in each group.
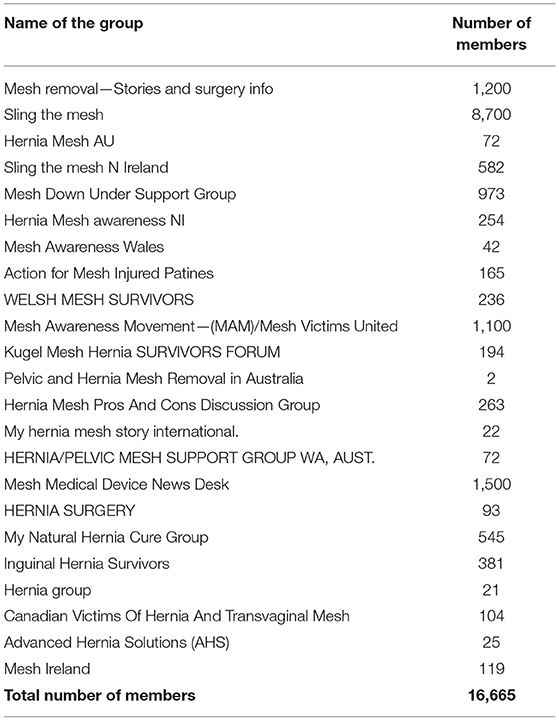
Table 2 . Facebook groups approached who were NOT willing to disseminate the survey with membership number in each group.
It was anticipated that the findings of the survey would be presented as descriptive data, and no statistical analysis was planned.
In total, 397 people who have or have had hernia surgery completed the survey. The age, sex, country/region of residence, type of hernia, and the number of previous repairs where applicable are given in Table 3 . On reviewing the responses, three groups of patients were identified, those who had a hernia repair and were happy with the outcome n = 112 (Group A), those who have had surgery but were unhappy with their outcome n = 176 (Group B), and those with a hernia awaiting surgery n = 105 (Group C). Four patients did not express whether they were happy or unhappy with the procedure they have undergone. The age, sex, average number of hernia repairs, presence of recurrence, and ongoing complication between Groups A and B are given in Table 4 . Of note, patients who are unhappy following hernia surgery are more likely to have a recurrence of their hernia and/or have an ongoing complication of their hernia surgery and were more likely to be women.
Table 3 . Basic demographics of the respondents.
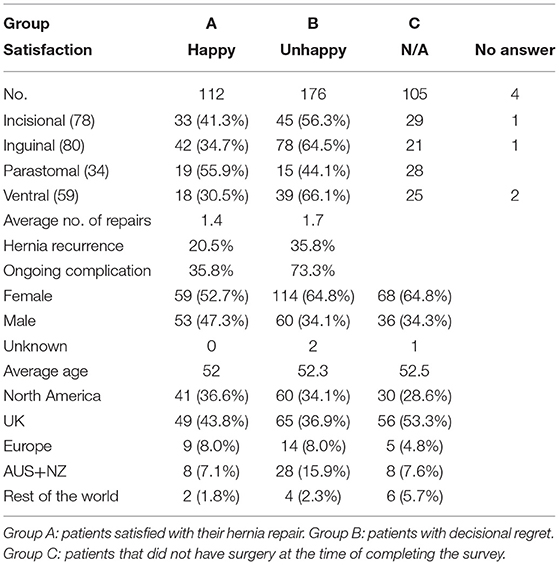
Table 4 . Basic demographics of Groups A, B, and C.
The reasons why patients seek medical help with their hernias are shown in Table 5 . Pain, a bulge, and limitation during sports and other activities are the commonest reasons.
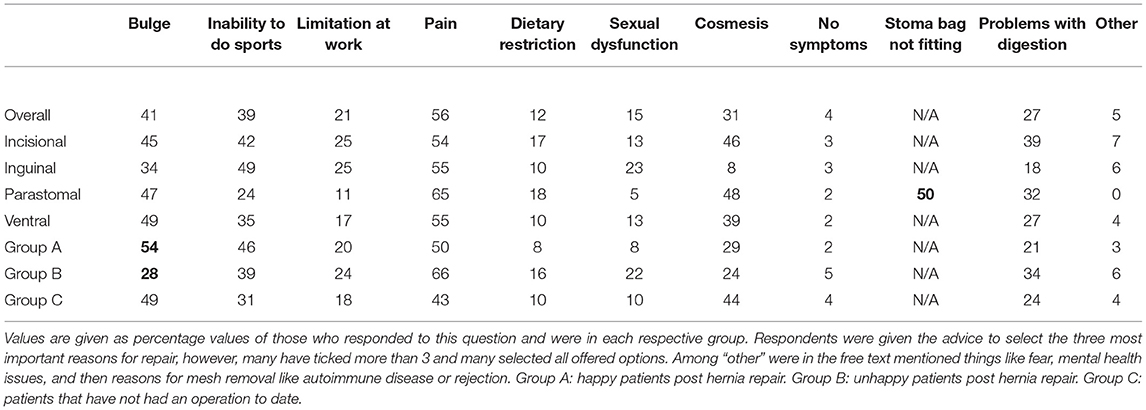
Table 5 . Reason to have a hernia operation by hernia type and by the patient group.
The ability to choose the medical facility was not applicable to 27% (105/393) of the respondents. Out of the remaining 289 patients, 27% would go to their local hospital, 27% to a hernia centre, 25% to a private facility, and 14% to a large university hospital. The remaining patients would either follow their preferred surgeon, recommendation of other patients, or find a facility that provides solely non-mesh repairs.
The ability to choose their surgeon was not applicable to 30% (121/397) of the respondents, and 22% (88/397) did not share their preferences ( Table 6 ). Only 1.3% (5/308) of respondents saw it as an advantage for their surgeon to be involved in hernia research. About 60% of patients would like to be operated by a hernia specialist irrespective of the number of repairs they have undergone, type of repair they would prefer, total complication rate, or satisfaction with previous hernia operation. However, in the group that would prefer a hernia specialist, there were more patients with an ongoing complication than in the other group. In the group of patients that would prefer a non-mesh repair, there were less patients that were happy with previous repairs in comparison with the group that would be willing to receive a mesh.
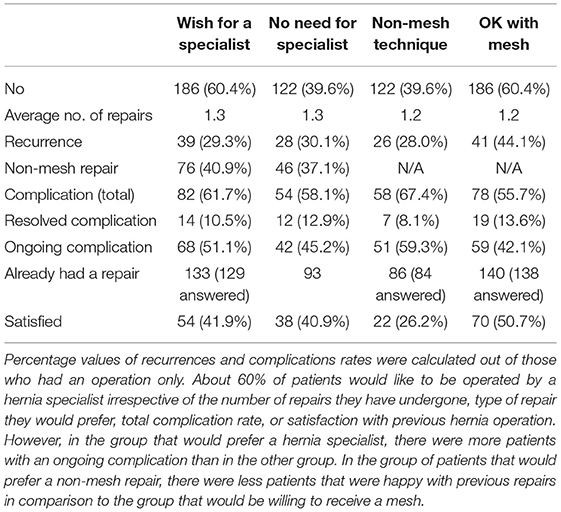
Table 6 . The choice of patients about their surgeon.
Prior to any hernia surgery, there is a strong desire for a detailed explanation around how any operation was going to impact their quality of life (98%), to be told everything about potential complications (99%), such as any impact on their sexual function (84%), to be able to discuss all options with the surgeon and become part of a joint decision process (97%), and to be told what happens if they chose no operation at all (98%). Approximately 97% wanted to be operated by the same person as whom they have seen at the initial appointment. About 85% would appreciate a patient information booklet to be able to educate themselves on their diagnosis, 67% were keen to be involved in a patient support group and being spoken to in a language they understand was important to 98%. However, when asked in a separate question, 9% of respondents agree with the statement that they do not need to be told anything and will fully trust their surgeon which is conflicting with their previous replies.
The choice of operation was also important to the respondents. About 71% of patients would rather have a more complex or difficult operation that minimised the risk of recurrence while 2.5% were happy for a “quick easy operation” that might only last a few years. The rest reported that the choice of operation depends on many factors, and they needed to know more or mention their request for a mesh not to be used.
The preferred type of operation by the three study groups is given in Table 7 . In addition to surgical options, the mesh used was also questioned. About 92% of respondents expect their surgeon to explain to them the pros and cons of various types of the mesh before their operation. When asked about their “ideal” mesh, 41% answered that they would prefer a non-mesh option, 26% would like to select one based on an interview with the surgeon, and only 20% are happy for their surgeon to select one for them. The remaining 14% were split between those who would accept a standard mesh, would like a “new, modern” mesh, biodegradable, biological, resistant to infection, or visible on a CT scan mesh. Only 5/394 respondents mentioned the word “safe.” In the group of parastomal patients who have already had a repair ( n = 34), only 6% would prefer a non-mesh option. And overall, only 8% of respondents are either not interested in knowing about or do not want to be told about non-mesh options.
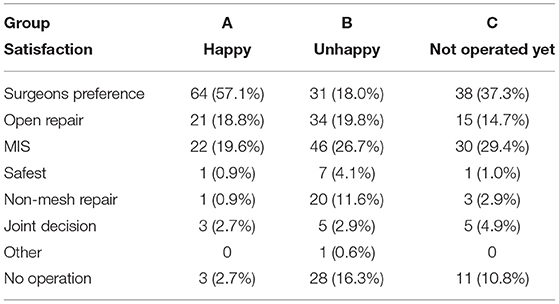
Table 7 . Choice of operative approach by group (MIS—minimally invasive approach).
The majority of respondents would like to be offered a pre-habilitation programme (78%) and 76% would be willing to change their lifestyle prior to the operation had they been told it could improve their outcomes ( Table 8 ). In total, 395 people answered both questions about satisfaction with their hernia repair and the possibility to change their lifestyle. It was found that 292 of those had already undergone a hernia repair. About 50% of those who had a repair and were not going to change their lifestyle are happy with their previous repair. In the group willing to change their lifestyle to improve outcomes, only 37% are happy with the results of the previous surgery ( Table 9 ).
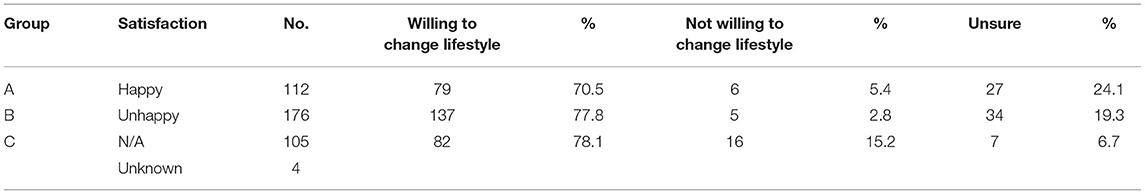
Table 8 . The willingness of patients to change their lifestyle prior to their operation, and take part in pre-habilitation.
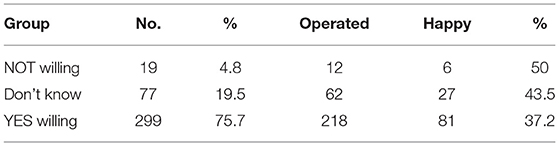
Table 9 . The willingness of patients to change their lifestyle and take part in pre-habilitation vs. reported happiness with their surgical outcome in those who had already undergone one or more operations to repair their hernia.
The complications of hernia surgery that were most feared by the respondents are given in Table 10 by the study group.
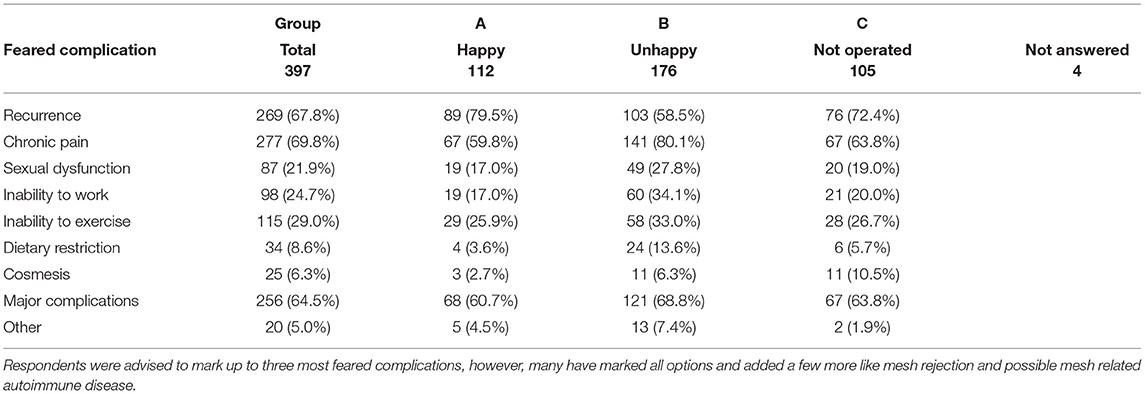
Table 10 . Complications most feared after hernia surgery.
Seeing their surgeon again on the morning of surgery was important to 90% of respondents. In terms of anaesthesia, 7% of respondents would prefer to be awake during the operation, the others either prefer general anaesthesia or will follow the recommendation of the surgeon and/or anaesthetist. Following surgery, 97% of respondents wanted to speak to the surgeon and be able to discuss with them the details of their repair. The majority of respondents (302/390) (77%) are prepared to stay in hospital or be at home as long as it takes to maximise the success of surgery. However, for some patients, return to normal activities (13%), sports (6%), or work (6%) is a priority. Information on how to minimise their risk of hernia recurrence was important to 96%, while 27% would be willing to accept a small recurrence if it did not hurt or enlarge.
Patients with no decisional regret about the operation have reported higher satisfaction with the behaviour of surgeon to the group B. About 93% of respondents would like to be part of a hernia registry and 62% of patients would feel better if they had a planned follow-up for at least 2 years.
This worldwide, online survey of people with a hernia, some of whom have already had at least one hernia repair, has identified several important reminders for surgeons involved in the management of hernias. Patients are looking for their surgeon to be an expert in hernia surgery, and able to spend time to explain their options—which is a discussion of the benefits, risks, and alternatives, such as operation vs. no operation, open vs. laparoscopic, mesh vs. non-mesh repair, and when mesh used, the various mesh options. Linked to all of this was the biggest fear after surgery of chronic pain. Communication with their surgeon during their time in hospital was seen as important by nearly every respondent irrespective of age, sex, nationality, type of hernia, or type of preferred repair. While the idea of a registry was supported by nearly all the respondents, a smaller proportion were willing to return for routine follow up.
The survey was heavily promoted on social media by the investigators with support from the European Hernia Society social media channels. We acknowledge that the majority of respondents are from English speaking countries and were obviously active on Twitter, leading to some bias in our study group. Furthermore, the principal investigator (BE) contacted as many hernias help and mesh help groups that we could identify ( Tables 1 , 2 ). While there was some concern that responses from these groups might skew the data, it was considered that those with a problem may be more motivated to reply to the survey to help improve the situation for others. Nevertheless, there was a strong consensus in the responses to the questions between those who had a hernia repair vs. those who had not, and those who already had surgery with a good outcome compared with a poor outcome. Several hernias help groups refused to have any communication with us. Others were more receptive but had elements within them that replied on social media with quite disturbing messages. There was a high level of mistrust expressed and the principal investigator was often subjected to offensive comments especially when surgical mesh was discussed. In most groups, there were well-educated and articulate patient representatives that have been very helpful through the process of distributing the survey, allaying fears, and encouraging followers to take part. Despite these groups having tens of thousands of members, only 397 responded to the survey in the study period, even when communication had taken place about the reasons for this patient focussed study that leaves us to a question how many of those are actually active. Nevertheless, one of the respondents has summarised it well and has agreed to have their quote and name published. “I would say they want to be fixed and not suffer a far more serious fate because of what was used to repair their hernia. Get some more bloody specialists and get hernia repair out of the hands of a general surgeon.” (Gary McCollom – Canada). While the evidence for hernia specialisation for primary inguinal and ventral hernia is not strong ( 7 ), nor is evidence for a hernia volume related improved outcomes ( 8 ), the feedback was more about the handling of the situation when something went wrong, in particular chronic pain. The general surgeon seemed to have nothing to offer and discharged the patient who still had their problem and did not know where to go for help. Indeed, this was one of the main take home messages for the investigators which came from the free text answers left by 123 respondents. The second main message was the lack of knowledge about hernias in the medical profession. Several respondents mentioned that they had been told to not work, or lift, or exercise with a hernia by their doctor, often in contradiction to recommended practise ( 9 ). Additionally, one patient claimed to have been told while she was pregnant that her umbilical hernia required urgent repair despite no symptoms.
It is clear that patients want knowledge about their condition, their options, and the likely outcomes. It is this knowledge that leads to informed consent. While there are legal implications around the need for informed consent, the primary aim of such interaction is to help the patient choose the right option for them and inform them of all materials used ( 10 ). Other research groups have focused on the communication between medical professionals and patients pointing out the need to improve the process of informed consent prior to hernia surgery. One audit of informed consent documents in patients undergoing inguinal hernia repair noted that only 66% of them contained all the common or serious complications ( 11 ). There are challenges to informed consent, although we understand more about the process including the requirements when producing written information ( 12 ). The present study strongly reiterates the need for detailed patient-surgeon discussion ( 13 ). Keeping in mind that the recollection and understanding of patient of the information given during the consent process can be variable ( 14 ), it is clear that there needs to be more effort spent on giving information and documenting what was given ( 15 ). In our survey, we had many comments from the respondents about not being told that mesh was involved in the repair, or not having other surgical options mentioned, but we have no way how to validate these statements. However, it was mentioned by many patients that general surgeons are no longer trained in non-mesh repairs, in particular for inguinal hernias. There are serious issues for training the hernia surgeons for the future ( 8 ), and the need to be able to offer non-mesh options in certain patient and hernia types ( 16 ).
Pre-habilitation, especially for more complex abdominal wall repair is another area of study. In this survey, two-thirds of respondents were willing to make some lifestyle changes prior to their operation. We acknowledge that this proportion was only a theoretical agreement in an anonymous survey, and the real-world commitment to pre-habilitation may be not so high. Varying literacy amongst patients with hernias may lead to many having unrealistic expectations ( 7 ). It is estimated that in the United States, about 80% of patients have modifiable risk factors prior to ventral hernia repair. Due to low health literacy, 20% have wrong self-assessment and believe they are in a better condition than they really are and only one-third see no barriers in joining pre-habilitation programme ( 17 ). Another study used a small focus group of 22 patients to explore their motivation for surgery and expectations after recovery ( 4 ).
There was a very strong consensus that patients wished to be operated on by the same surgeon they had met during their appointment and it was also important to them that this surgeon knew what they were doing—a hernia specialist. Only 4% did not mind being operated by someone else. This is an important point for healthcare organisers and should be taken into consideration when organising the surgical practise.
When asking patients actively to report adverse outcomes, the reported incidence of such events can increase significantly ( 18 ). A study looked at patient satisfaction after groin hernia repair in 373 adult patients with a special focus on pain and follow-up ( 19 ). For patients who were well, there was a reluctance to attend follow-up. We have observed similar views in our survey. While the idea of a registry was supported by nearly all the respondents, a smaller portion was willing to return for routine follow-up. However, other methods can be used to gain follow-up patient information, smart phone Apps, and online reporting tools. The involvement of patients in what to measure is also important. The type of outcomes perceived as negative by surgeons' changes from strictly defined items like recurrence to much broader ones like quality of life. Hubbard et al. have addressed the lack of patient-led research priorities, and this was confirmed by Alawadi et al. demonstrating the importance of understanding the perspective of patients and addressing their specific needs prior surgery also ( 7 , 20 ). The outcomes that surgeons have measured in the past, are not as important to respondents while other outcomes can have greater weight to them. In this survey, sexual function post hernia repair was mentioned by the majority of our respondents in all the age groups (81% in the group above 65 years of age).
Many patients see “mesh” as the cause of all their problems. For some, this may be the case, but many of the issues described to us, surgical error, lack of pre-optimisation for the surgery, poor communication about complications, and lack of follow-up or care for a complication caused by the operation was more the problem. Mesh-injured is a misnomer, and perhaps should be replaced with “hernia surgery injured.” Many of the people in these support groups are upset with the whole medical industry, often left with debilitating pain and other complications with no one to reach for help, repeatedly rejected by multiple specialists, and often in significant financial difficulties due to the medical state they got in. One gentleman in South Africa who had a laparoscopic IPOM for a small umbilical hernia resulting in multiple bowel obstructions and numerous attempts at mesh removal claimed to have racked up a 400,000 USD debt to his surgeon and has not been able to work ever since. We do not know why all the remedial operations had to be done robotically and the technical standard of the procedure, but “the mesh” was blamed, perhaps not correctly.
It is easy to assume that the increasing number of recurrences and complications leads to an unhappy patient. While there is some truth to this, the stoma patient group in this study actually demonstrated the opposite. This group as a whole had the highest number of complications and yet contained the highest number of patients that were satisfied. Further research to unravel the reasons for this is needed. About 6% of those with a parastomal hernia said they would “prefer no mesh” vs. 52% for inguinal. Communication and trust in their surgeon may be a factor in this study. Detailed analysis by hernia type was not undertaken as such data dredging with increasing smaller numbers (as noted in Table 4 ) was considered scientifically unsound.
Having undertaken this work, we are left with a clear view that while the collection of surgical outcome data by every hernia surgeon is important, the collection of quality of life outcome data, reported by patients is even more important. There is a need to engage further with our patients, and refine quality of life measurements that measure what our patients want us to measure as important to them. The face-to-face patient focus groups, social media campaigns, with appropriate sociology validation of the quality of life tools will all be important in this regard. In addition, hernia registries that include patients undergoing watch and wait, with life-long follow-ups, such as data from patients, other healthcare professionals, utilising smart phone Apps, and emerging machine reading and artificial intelligence of healthcare medical records technology, will add to the knowledge of what management pathway is the best option for each individual patient with a hernia.
Within the bias of our patient population recruited via Twitter, we have found a desire for patients to be looked after by hernia specialists where possible. Elements around quality of life after surgery is their main outcome measure. And if something goes wrong after surgery, they demand to be listened to and have services in place to manage them. Mesh-injured should be replaced by hernia-surgery-injured in the future for clearer communication. Greater patient involvement is needed to help develop hernia services.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
BE: study concept, literature review, survey questionnaire preparation, analysis of data, manuscript writing, revision of the manuscript, and final approval of the manuscript. SH, ND, SB, and LL: survey question preparation and analysis of data. HG and CS: survey questionnaire preparation, analysis of data, and manuscript writing. AB: literature review, survey questionnaire preparation, analysis of data, manuscript writing, revision of the manuscript, and final approval of the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors wish to thank all the patients worldwide that contributed to our project. This manuscript is in honour to them.
1. Muysoms FE, Vanlander A, Ceulemans R, Kyle-Leinhase I, Michiels M, Jacobs I, et al. A prospective, multicenter, observational study on quality of life after laparoscopic inguinal hernia repair with ProGrip laparoscopic, self-fixating mesh according to the European Registry for Abdominal Wall Hernias Quality of Life Instrument. Surgery. (2016) 160:1344–57. doi: 10.1016/j.surg.2016.04.026
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Simons M, Rapport F, Zurynski Y, Cullis J, Davidson A. What are the links between evidence-based medicine and shared decision-making in training programs for junior doctors? A scoping review protocol. BMJ Open. (2020) 10:e037225. doi: 10.1136/bmjopen-2020-037225
3. The GRADE Handbook. Available online at: https://gdt.gradepro.org/app/handbook/handbook.html (accessed July 31, 2020).
4. Lee THJ, Ulisney KL, Choudhuri AK, Swiger JL, Gibeily GJ. Understanding the patient perspective after ventral hernia repair. Hernia. (2019) 23:995–1001. doi: 10.1007/s10029-019-02015-6
5. Alawadi ZA, Leal IM, Flores JR, Holihan JL, Henchcliffe BE, Mitchell TO, et al. Underserved patients seeking care for ventral hernias at a safety net hospital: impact on quality of life and expectations of treatment. J Am Col Surg . (2017) 224:26–34.e2. doi: 10.1016/j.jamcollsurg.2016.09.017
6. Ng D, McMurray J, Wallace J, Morita P. What is being used and who is using it: barriers to the adoption of smartphone patient experience surveys. JMIR Form Res. (2019) 3:e9922. doi: 10.2196/formative.9922
7. Pereira JA, Bravo-Salva A, Montcusí B, Pérez-Farre S, Fresno de Prado L, López-Cano M. Incisional hernia recurrence after open elective repair: expertise in abdominal wall surgery matters. BMC Surg. (2019) 19:103. doi: 10.1186/s12893-019-0569-6
8. Köckerling F, Sheen AJ, Berrevoet F, Campanelli G, Cuccurullo D, Fortelny R, et al. The reality of general surgery training and increased complexity of abdominal wall hernia surgery. Hernia. (2019) 23:1081–91. doi: 10.1007/s10029-019-02062-z
9. Russell S. Physical activity and exercise after stoma surgery: overcoming the barriers. Br J Nurs. (2017) 26:S20–6. doi: 10.12968/bjon.2017.26.5.S20
10. Montgomery v Lanarkshire Health Board [2015] UKSC 11 (11 March 2015). [2015] 2 All ER 1031, 2015 SC (UKSC) 63. Available online at: https://www.supremecourt.uk/cases/docs/uksc-2013-0136-judgment.pdf
11. Khan SU, Bowrey DJ, Williams RN, Soh JY, Peleki A, Muhibullah N, et al. Patient's views of the consent process for groin hernia repair: use of consent template improves compliance with best practice. Ann Med Surg. (2018) 35:67–72. doi: 10.1016/j.amsu.2018.09.033
12. Asarbakhsh M, Smith O, Chitsabesan P, MacLeod T, Lim P, Chintapatla S. A multistage process leading to the development of a structured consent form and patient information leaflet for complex abdominal wall reconstruction (CAWR). Hernia. (2020) 25:277–85. doi: 10.1007/s10029-020-02260-0
13. Say R, Murtagh M, Thomson R. Patients' preference for involvement in medical decision making: a narrative review. Patient Educ Couns. (2006) 60:102–14. doi: 10.1016/j.pec.2005.02.003
14. Sherlock A, Brownie S. Patients' recollection and understanding of informed consent: a literature Review. ANZ J Surg. (2014) 84:207–10. doi: 10.1111/ans.12555
15. Uzzaman MM, Sinha S, Shaygi B, Vitish-Sharma P, Loizides S, Myint F. Evaluation of patient's understanding and recall of the consent process after open inguinal hernia repairs. Int J Surg. (2012) 10:5–10. doi: 10.1016/j.ijsu.2011.10.003
16. HerniaSurge Group. International guidelines for groin hernia management. Hernia . (2018) 22:1–165. doi: 10.1007/s10029-017-1668-x
17. Henchcliffe BE, Holihan JL, Flores-Gonzalez JR, Mitchell TO, Ko TC, Kao LS, et al. Barriers to participation in preoperative risk-reduction programs prior to ventral hernia repair: an assessment of underserved patients at a safety-net hospital. JAMA Surg. (2016) 151:488–90. doi: 10.1001/jamasurg.2015.4452
18. Woodfield J, Deo P, Davidson A, Chen TY, van Rij A. Patient reporting of complications after surgery: what impact does documenting postoperative problems from the perspective of the patient using telephone interview and postal questionnaires have on the identification of complications after surgery? BMJ Open. (2019) 9:e028561. doi: 10.1136/bmjopen-2018-028561
19. Adamu-Biu F, Akoh JA. Survey of patients regarding experience following repair of inguinal Hernias. Hernia . (2020) 24:187–95. doi: 10.1007/s10029-019-02061-0
20. Hubbard G, Taylor C, Beeken B, Campbell A, Gracey J, Grimmett C, et al. Research priorities about stoma-related quality of life from the perspective of people with a stoma: a pilot survey. Health Expect. (2017) 20:1421–7. doi: 10.1111/hex.12585
Keywords: hernia, patient information, patient involvement, PROMs, surgical mesh, surgical outcomes, hernia registry
Citation: East B, Hill S, Dames N, Blackwell S, Laidlaw L, Gök H, Stabilini C and de Beaux A (2021) Patient Views Around Their Hernia Surgery: A Worldwide Online Survey Promoted Through Social Media. Front. Surg. 8:769938. doi: 10.3389/fsurg.2021.769938
Received: 02 September 2021; Accepted: 15 November 2021; Published: 24 December 2021.
Reviewed by:
Copyright © 2021 East, Hill, Dames, Blackwell, Laidlaw, Gök, Stabilini and de Beaux. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Andrew de Beaux, adebeaux@doctors.org.uk
This article is part of the Research Topic
Mesh Complications in Hernia Surgery
A comparative prospective study of short-term outcomes of extended view totally extraperitoneal (e-TEP) repair versus laparoscopic intraperitoneal on lay mesh (IPOM) plus repair for ventral hernia
Affiliations.
- 1 GEM Hospital and Research Centre, Coimbatore, India. [email protected].
- 2 GEM Hospital and Research Centre, Coimbatore, India.
- PMID: 32968915
- DOI: 10.1007/s00464-020-07990-x
Background: Currently, minimally invasive approach is preferred for the treatment of ventral hernias. After the introduction of extended view totally extraperitoneal (e-TEP) technique, there has been a constant debate over the choice of better approach. In this study, we compare the short-term outcomes of e-TEP and laparoscopic IPOM Plus repair for ventral hernias.
Methods: This is a comparative, prospective single-center study done at GEM Hospital and research center Coimbatore, India from July 2018 to July 2019. All patients who underwent elective ventral hernia surgery with defect size of 2 to 6 cm were included. Patient demographics, hernia characteristics, operative and perioperative findings, and postoperative complications were systematically recorded and analyzed.
Results: We evaluated 92 cases (n = 92), 46 in each group. Mean age, sex, BMI, location of hernia, primary and incisional hernia, and comorbidity were comparable in both the groups. Mean defect size for IPOM Plus and e-TEP was 4 cm and 3.89 cm, respectively. Operative time was significantly higher for e-TEP, while postoperative pain (VAS), analgesic requirement, and postoperative hospital stay were significantly less as compared to IPOM Plus. However, 2 cases (4.35%) of e-TEP had recurrence but none in IPOM Plus group.
Conclusion: e-TEP is an evolving procedure and comparable to IPOM Plus in terms of postoperative pain, analgesic requirement, cost of mesh, and length of hospital stay. More randomized controlled and multicentric studies are required with longer follow-up to validate our findings.
Keywords: IPOM Plus; Intraperitoneal; Prospective; Retromuscular; Ventral hernia; e-TEP.
© 2020. Springer Science+Business Media, LLC, part of Springer Nature.
- Hernia, Inguinal*
- Hernia, Ventral* / surgery
- Herniorrhaphy
- Laparoscopy*
- Prospective Studies
- Retrospective Studies
- Surgical Mesh
- Treatment Outcome
- tetraethylpyrazine
Laparoscopic Repair of Internal Hernias: a Case Series with Review of Literature
- Surgical Techniques and Innovations
- Published: 13 January 2021
- Volume 83 , pages 1534–1539, ( 2021 )
Cite this article

- Rafique Umer Harvitkar ORCID: orcid.org/0000-0002-0830-6675 1 &
- Abhijit Joshi 1
119 Accesses
Explore all metrics
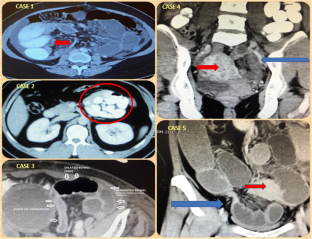
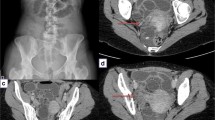
Internal hernias are rare clinical entities. They are potentially life-threatening, yet often neglected and sometimes misdiagnosed surgical conditions. Herein, we report five different cases of internal hernia in adults aged 29–42 years. These include one case each of right and left paraduodenal hernia, two cases of broad ligament hernia and one case of post lower segment caesarean section adhesions related internal hernia. The patients had varied clinical features, presenting with abdominal pain with or without nausea or vomiting and signs of intestinal obstruction. Contrast-enhanced computed tomography of the abdomen accurately diagnosed the two paraduodenal herniae and one of the two broad ligament hernia cases, pre-operatively. It revealed dilated contrast filled small bowel loops with an abrupt transition zone in the left lower abdomen (second broad ligament hernia case) and in the right lower abdomen (adhesion-related internal hernia case). Laparoscopic repair was performed in all five cases, and they were discharged 3–4 days later without any further complication. Clinicians should have a high index of suspicion for internal hernias, especially in those patients who present with chronic, vague, non-specific symptoms, after having ruled out the commoner differential diagnoses. We hope to highlight that even in patients who present with intestinal obstruction, laparoscopy is a viable therapeutic option.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others
Broad Band Ligament Hernias: A Case Report

Management of Amyand’s Hernia: a Case Report
Case report and operative management of gallbladder herniation.
Rahaf S, Huda S, Yazeed B, Haifaa M (2019) Rare case of small bowel obstruction due to para duodenal hernia. Am J Case Rep 20:1581–1586. https://doi.org/10.12659/AJCR.918403
Article Google Scholar
Shadhu K, Ramlagun D, Ping X (2018) Para-duodenal hernia: a report of five cases and review of the literature. BMC Surg 18(1):32. https://doi.org/10.1186/s12893-018-0365-8
Article PubMed PubMed Central Google Scholar
Rae A, Kalyanaraman A, Ward A, Harikrishnanl A et al (2015) An interesting case of retro-caecal internal herniation causing small bowel obstruction. Ann Med Surg View at: https
Edwards HM, Al-Tayar H et al (2013) A trans mesenteric congenital internal hernia presenting in an adult. J Surg Case Rep 2013(12):article rjt099
GGhahremani G, Gore RM, Levine MS (eds) (2000) Abdominal and pelvic hernias Textbook of Gastrointestinal Radiology, 2nd edn. Saunders, Philadelphia, pp 1993–2009
Google Scholar
Meyers MA (1970) Para duodenal hernias: radiologic and arteriographic diagnosis. Radiology 95(1):29–37
Article CAS Google Scholar
Okino Y, Kiyosue H, Mori H et al (2001) Root of the small-bowel mesentery: correlative anatomy and CT features of pathologic conditions. Radio Graphics 21(6):1475–1490
CAS Google Scholar
HizirAkyildiz et al (2009) Internal hernia: complex diagnostic and therapeutic problem. Int J Surg 7(4):334–337. https://doi.org/10.1016/j.ijsu.2009.04.013
Mehra R, Pujahari AK (2016) Right Para duodenal hernia: report of two cases and review of the literature. Gastroenterol Rep (Oxf) 4(2):168–171. https://doi.org/10.1093/gastro/gou076
Shelke B, Joshi A (2020 PRINT ISSN No. 2250 - 1991) Left Para duodenal hernia as a rare cause of intestinal obstruction-Laparoscopic management. Indian J Res 9(8). https://doi.org/10.36106/paripex
Rohatgi Y AbhijitJoshi.Broad ligament hernia: rare cause of intestinal obstruction—laparoscopic management. Indian J Surg, ISSN 0972-2068. https://doi.org/10.1007/s12262-020-02498-z
Palanivelu C, Rangarajan M, Jategaonkar PA et al (2008) Laparoscopic management of Para duodenal hernias: mesh and mesh-less repairs. A report of four cases. Hernia 12(6):649–653
Cilley R, Poterack K, Lemmer J, Dafoe D et al (1986) Defects of the broad ligament of the uterus. Am J Gastroenterol 81:389–391
CAS PubMed Google Scholar
Del Duran A et al (2017) Internal hernia: report of clinical cases. Colomb J Radiol Rev Colomb Radiol 28(4):4797–4804
Takeda M, Ohnuki Y, Uchiyama T, Kubota O, Ohishi K et al (2013) Small intestinal strangulation due to a rare type of primary internal hernia. Int Surg 98(4):409–411
Kleyman S, Ashraf S, Daniel S et al (2013) Peri-cecal hernia: a rare form of internal hernias. J Surg Case Rep (2):rjs021. https://doi.org/10.1093/jscr/rjs021
Imran, Phakula ML, Zimba MT, Koto ZM et al (2016) Small bowel obstruction secondary to para-vesical hernia. Int J Surg Case Rep 26:156–158. https://doi.org/10.1016/j.ijscr.2016.07.021
Lawani I, Yelinhan C, Imorou Y et al Case report: internal hernia strangulated on appendicular tourniquet: a case report of an exceptional anomaly of the appendix revealed by a rare hernia Published: 15 July 2019. Surg Case Rep. https://doi.org/10.1186/s40792-019-0671-0
Olajid TO et al (2020) A rare case of intestinal obstruction from internal hernia through a foramen formed by appendices epiploicae-a case report and review of literature. Maced J Med Sci Open Surg. https://doi.org/10.3889/oamjms.2020.3684
Suwa K, Yamagata T, Hanyu K, Suzuki T et al (2013) Internal hernia through a peritoneal defect in the pouch of Douglas: report of a case. Int J Surg Case Rep 4(1):115–117. https://doi.org/10.1016/j.ijscr.2012.10.015
Article PubMed Google Scholar
Agresta F, Michelet I, Candiotto E, Bedin N (2007) Incarcerated internal hernia of the small intestine through a breach of the broad ligament: two cases and a literature review. JSLS 11(2):255–257
Dritsas ER, Ruiz OR, Kennedy GM, Blackford J, Hasl D (2001) Paraduodenal hernia: a report of two cases. Am Surg 67(8):733–736
Ouedraogo S, Ouedraogo S, Kambire JL, Zida M Occlusion secondary to congenital internal trans mesenteric hernia: 2 cases. Pan Afr Med J 27:131. https://doi.org/10.11604/pamj.2017.27.131.12203
David João Aparício,Carlos Leichsenring, Nuno Pignatelli, Ana Germano, Sérgio Ferreira, Vítor Nunes. Transmesocolic hernia with sigmoid colon strangulation without surgical history: a series of two case reports, J Surg Case Rep, Volume 2019, Issue 3, March 2019, rjz073, https://doi.org/10.1093/jscr/rjz073
Download references
Author information
Authors and affiliations.
Department of Surgery, Dr. L H Hiranandani Hospital, Powai, Mumbai-76, India
Rafique Umer Harvitkar & Abhijit Joshi
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Rafique Umer Harvitkar .
Ethics declarations
Conflict of interest.
The authors declare that they have no conflict of interest.
Ethics Approval and Consent to Participate
Not applicable.
Informed Consent
Written informed consent was obtained from the patient for publication of this study.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Harvitkar, R.U., Joshi, A. Laparoscopic Repair of Internal Hernias: a Case Series with Review of Literature. Indian J Surg 83 , 1534–1539 (2021). https://doi.org/10.1007/s12262-021-02736-y
Download citation
Received : 20 October 2020
Accepted : 07 January 2021
Published : 13 January 2021
Issue Date : December 2021
DOI : https://doi.org/10.1007/s12262-021-02736-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Internal hernia
- Paraduodenal hernia
- Post LSCS adhesions
- Laparoscopic repair
- Broad ligament hernia
- Intestinal obstruction
- Find a journal
- Publish with us
- Track your research
- Open access
- Published: 16 November 2023
Comparative effectiveness of hybrid and laparoscopic techniques for repairing complex incisional ventral hernias: a systematic review and meta-analysis
- Quan Wu 1 ,
- Weijie Ma 2 ,
- Qianqian Wang 3 ,
- Yaqi Liu 1 &
- Yaokai Xu 1
BMC Surgery volume 23 , Article number: 346 ( 2023 ) Cite this article
887 Accesses
2 Altmetric
Metrics details
The recently developed Hybrid Hernia Repair technique (HHR), an adaptation of the laparoscopic method, has been proposed as a potential alternative for the treatment of complex Incisional Ventral Hernias (IVH). While single-arm studies have reported promising outcomes, a comprehensive meta-analysis affirming these benefits is lacking. This meta-analysis aims to compare the clinical outcomes of HHR and Laparoscopic Hernia Repair (LHR) in the management of IVH.
An exhaustive search of the literature was conducted, targeting publications in both English and Chinese that compare HHR and LHR up to March 31, 2023. The primary outcomes examined were operation time, blood loss, and intestinal injury. Secondary outcomes included rates of seroma, wound infection, post-operative acute/chronic pain, recurrence, and mesh bulging. The RevMan 5.0 software facilitated the statistical meta-analysis.
The final analysis incorporated data from 14 studies, encompassing a total of 1158 patients, with 555 undergoing HHR and 603 treated with LHR. Follow-up data, ranging from 12 to 88 months, were available in 12 out of the 14 identified studies. The HHR method was associated with a significantly lower risk of seroma (OR = 0.29, P = 0.0004), but a higher risk of wound infection (OR = 2.10, P = 0.04). No significant differences were observed between the two techniques regarding operation time, blood loss, intestinal injury, intestinal obstruction, post-operative pain, mesh bulging, and recurrence.
Conclusions
The HHR technique did not demonstrate a clear advantage over LHR in reducing surgical complications, apart from a lower incidence of postoperative seroma. Surgeons with substantial expertise may choose to avoid incidental conversion or intentional hybrid procedures. Further research is needed to clarify the optimal surgical approach for IVH.
Peer Review reports
Introduction
Incisional ventral hernias (IVH) are more likely to occur in elderly or obese individuals who have previously undergone abdominal surgery with suboptimal suturing or experienced wound infections. Hernia repair is the only solution to address the abdominal defect, and it can be performed using either an open or minimally invasive IVH repair, including laparoscopic and robotic assisted technique. The laparoscopic approach for hernia repair was first introduced by Le Blanc and Booth in 1993, and it has since gained popularity due to its ability to minimize large subcutaneous flaps, reduce the risk of wound infection, and prevent transfascial suture and mesh bulging, in comparison to the open method [ 1 , 2 , 3 ]. Nonetheless, the laparoscopic approach accounts for an average of 2.4% conversion rate [ 4 ], primarily due to extensive intestinal adhesions. Additionally, this method may predispose patients to postoperative seroma in cases with large orifices when the hernia sac is not excised, or the defect is not closed. The superiority of either technique regarding recurrence rate control remains debatable [ 5 , 6 ]. Circa 2000, a combination of open and laparoscopic techniques was proposed to address the limitations associated with both methods in IVH repair [ 7 ]. This approach has been referred to as a hybrid technique, endoscopically assisted, or limited conversion technique; however, a consensus on its definition has not been reached. The procedure typically involves initial laparoscopic adhesiolysis, or an intention to perform open adhesiolysis followed by conversion to an open approach for sac excision, defect closure, and subsequent mesh placement and fixation under pneumoperitoneum via transfascial sutures and/or metal tacks [ 3 , 8 , 9 , 10 , 11 , 12 ], and this procedure also can be achieved by hybrid robotic-assisted surgery introduced into clinical practice two decades ago, with posterior component separation technique for huge defects if necessary [ 10 ].
While a limited number of double-arm cohort studies [ 13 , 14 , 15 ] in the English literature have reported favorable outcomes with reduced postoperative morbidities, such as lower rates of bowel injury, hematoma, wound infection, and shorter hospital stays, no meta-analysis has comprehensively confirmed these advantages to date. Van den Dop [ 16 ] combined these variables as surgical site occurrences, highlighting the need to further investigate the potential benefits of the Hybrid Hernia Repair (HHR) technique. In this study, we aim to elucidate the clinical outcomes of HHR compared to the Laparoscopic Hernia Repair (LHR) technique for the management of Incisional Ventral Hernias (IVH).
Material and methods
Search strategy and data extraction.
This study was designed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. We conducted a literature search in the following databases: PubMed, Medline, Embase, Web of Science, Cochrane Library, CNKI, and WANFANG. Search terms and MeSH terms included “incisional ventral hernia,” “hybrid technique,” “endoscopically assisted,” “limited conversion,” and “laparoscopy repair.” The publication timeframe was set between 1996 and 31 March, 2023. Additionally, reference lists of identified articles were utilized for supplementary retrieval. The search was limited to articles published in English and Chinese languages.
Following the removal of duplicates, two authors (WQ and MW) independently assessed the eligibility of the studies by reviewing abstracts and full texts. In cases where a consensus could not be reached for a particular study, the final decision was voted by author WQQ. Data pertaining to study characteristics, such as demographics, pertinent surgical details, surgical complications, and prognosis, were extracted by authors LY and XY and recorded in an Excel spreadsheet.
Inclusion and exclusion criteria
Both randomized and non-randomized clinical trials comparing the hybrid repair technique for IVH to the laparoscopic technique were included, while single-arm studies were excluded. In the hybrid operation, mesh placement was limited to either IPOM or IPOM-plus styles, characterized by intraperitoneal mesh placement repair; as such, the Minimally Invasive Less Open Sublay Operation (MILOS) was excluded [ 17 ]. Studies meeting any of the following criteria were also excluded: parastomal hernia, absence of hernia size description, animal studies, letters, reports, and conference abstracts.
Quality assessment
Authors MW and WQQ independently conducted quality assessments. Risk of bias was evaluated using two methods, including the Risk of Bias in Non-Randomized Studies of Interventions (ROBINS-I) [ 18 ] and the Cochrane risk of bias tool [ 19 ]. The former was used to assess the non-randomized studies, and the latter was to evaluate the randomized trials.
Statistical analysis
Data were reported as means ± standard deviation (X ± SD) for continuous variables and as odds ratios (OR) or risk ratios (RR) for dichotomous variables. Meta-analysis was conducted using Review Manager Version 5.0 software (The Cochrane Collaboration, Oxford, UK). Weighted mean difference (WMD) and OR/RR were used to evaluate treatment effects with corresponding 95% confidence intervals (CI) for continuous and categorical variables, respectively. Heterogeneity analysis was assessed by the I 2 value, with an I 2 value > 50% or P < 0.1 considered significant; the fixed-effects or random-effects model was then applied as appropriate. Forest plots were used to display the outcomes of this meta-analyses.
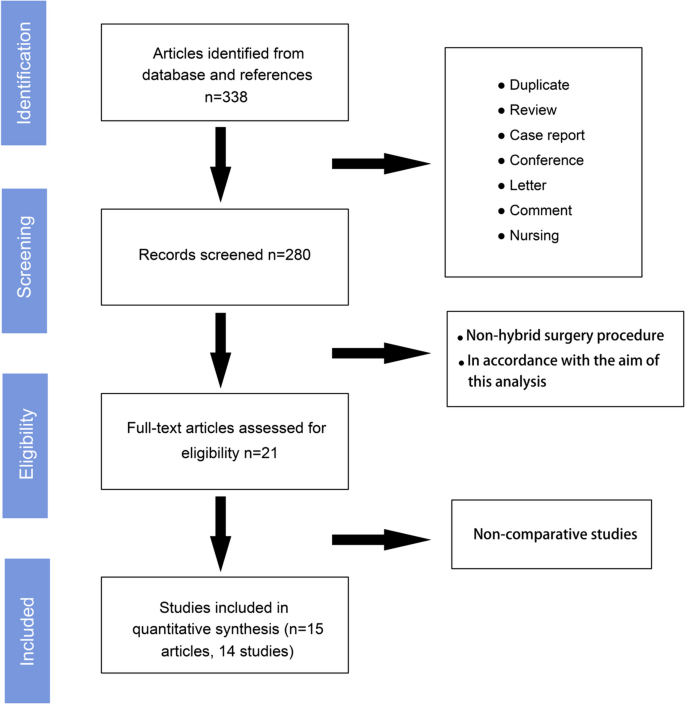
The comprehensive search process is depicted in Fig. 1 . After the elimination of duplicates, case reports, reviews, and articles not directly related to our objective, 21 articles addressing the hybrid technique were identified. Following a thorough full-text review, six non-comparative studies were excluded. Consequently, 15 relevant articles, comprising 14 studies with 555 cases in the HHR group and 603 in the LHR group, were included in the analysis [ 15 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 ].
Among these, 13 were retrospective studies, and one was a randomized controlled trial (RCT), as detailed in Table 1 . Two studies were assessed as low risk of bias, with the remaining exhibiting moderate risk (Table 1 ). The mean diameter of the hernia defects varied from 5.55 cm to 16.8 cm in the LHR group and from 6.34 cm to 21.50 cm in the HHR group (Table 2 ). Eight of the 14 studies documented the “classical” process of the hybrid technique. This process typically begins with laparoscopic exploration and adhesiolysis, followed by open surgery for hernia sac removal, patch placement within the abdominal cavity, and defect closure. The procedure concluded with the laparoscopic fixation of the patch. Three of the 14 studies replaced laparoscopic exploration and adhesiolysis with open surgery, with one suggesting that robotic operation could be a viable substitute for the laparoscopic phase.
Primary outcomes: evaluations of surgical outcomes
Heterogeneity analysis for the comparison of operative time between HHR and LHR was based on 12 studies, as one study lacked standard deviation data [ 23 ]. The I 2 value was 99%, with p < 0.000001. Therefore, the mean difference (MD = 1.99 min) was calculated using the random-effects model, indicating that the operative time for both methods was relatively similar ( p = 0.89) (Fig. 2 a). Intraoperative blood loss in HHR was slightly higher than that in LHR, with an MD of 9.40 ml, 95% CI [−1.81, 20.61], and p = 0.10, as determined from seven studies (Fig. 2 a). Nine studies provided complete data on the incidence of intraoperative intestinal injury, with no heterogeneity observed (I 2 = 40%, p = 0.14). The risk of intestinal injury did not demonstrate a significant preference between HHR and LHR ( p = 0.75) (Fig. 2 b).
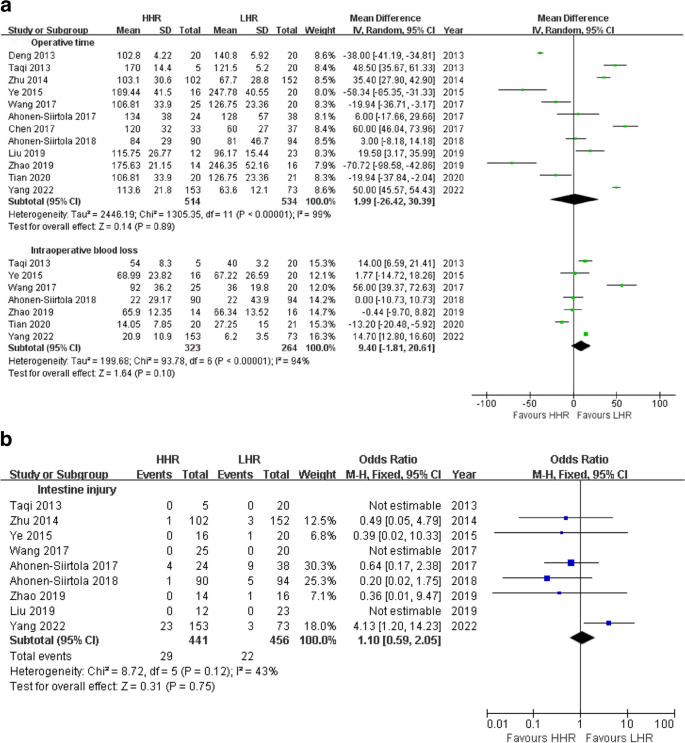
a Meta-analyses of primary outcomes: operative time and blood loss. b Meta-analyses of primary outcome: Intestine injury
Secondary outcomes: assessment of postoperative morbidities
Seroma formation and wound infection.
Subsequently, comparisons of short-term postoperative complications were performed, with a focus on seroma formation and wound infection. Twelve studies provided complete data for seroma formation analysis, revealing significant heterogeneity (I 2 = 53%, p = 0.02) with the risk ratio (RR) effect measure. Upon correcting RR to odds ratio (OR) with the random-effects analysis model, heterogeneity decreased (I 2 = 41%, p = 0.08). The results showed that the risk of seroma formation was significantly lower in HHR compared to LHR (OR = 0.29, 95% CI [0.15, 0.57], p = 0.0004) (Fig. 3 a). A similar outcome (I 2 = 33%, P = 0.14; OR = 0.25, P = 0.0006) was established when excluding one study [ 28 , 31 ] with 1 month of seroma events different from the other included studies.
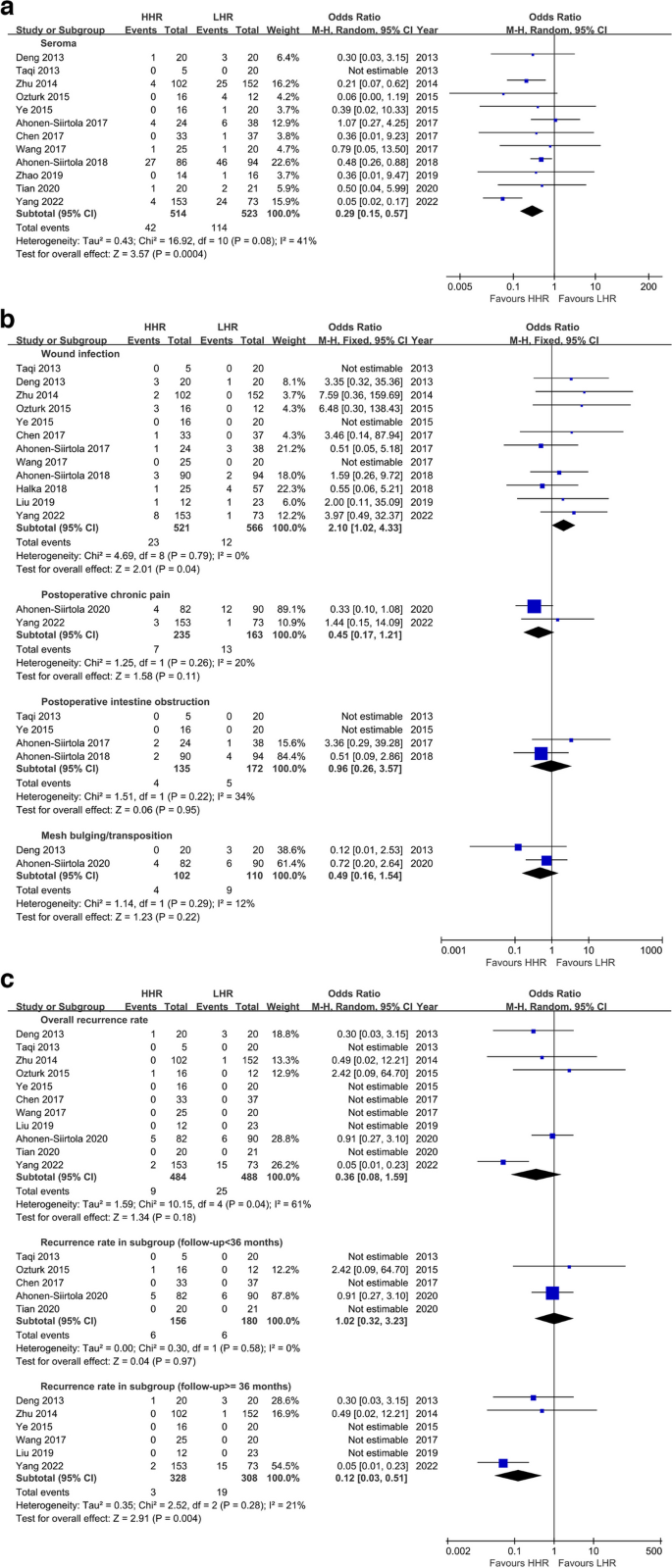
a Meta-analyses of secondary outcome: seroma formation. b Meta-analyses of dichotomous variables in the secondary outcomes. c Meta-analysis of recurrence rate and subgroup analysis
Interestingly, 12 out of 14 studies without heterogeneity (I 2 = 0%, p = 0.79) demonstrated that the risk of wound infection in HHR was 2.1 times higher than in LHR (95% CI [1.02, 4.33], p = 0.04) (Fig. 3 b).
Postoperative pain
Additionally, patients in the HHR group experienced a similar extent of postoperative acute pain (VAS MD = 0.84 scores) compared to the LHR group in an analysis involving four studies with 136 vs. 150 cases ( p = 0.40) (Fig. 4 ). Two studies with 235 vs. 163 cases assessing chronic pain showed a lower incidence rate in HHR compared to LHR, but the difference was not significant (Z = 1.58, p = 0.11) (Fig. 3 b).
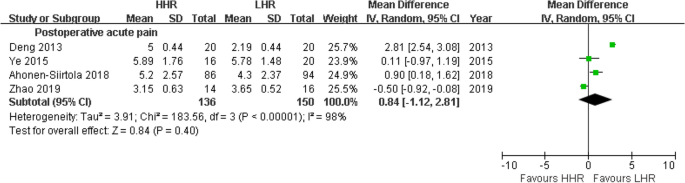
Meta-analyses of secondary outcome:postoperative acute pain
Postoperative intestine obstruction
Four studies analyzed the difference in intestinal obstruction incidence between the two methods, finding no statistically significant difference (OR = 0.96, 95% CI [0.26, 3.57], p = 0.95) (Fig. 3 b).
Mesh bulging and recurrence
Twelve included studies had declared the maximum follow-up periods ranging from 12 to 88 months, with three [ 15 , 25 , 30 ] out of 14 studies that did not indicate the recurrent cases. None of the studies specified 1-year, 3-year, or 5-year data for further stratified analysis except one [ 31 ]. The OR value for overall recurrence rate between HHR and LHR was 0.36 (95% CI [0.08, 1.59], p = 0.18) with heterogeneity (I 2 = 61%, p = 0.04), indicating no statistical difference in recurrence control between the two methods. Further subgroup analysis suggested that the comparison between the two methods in recurrence rates with follow-up less than 36 months did not achieve statistical difference (Z = 0.04, P = 0.97), while in another subgroup analysis with follow-up equal or greater than 36 months, the result indicated HHR had a lower risk of recurrence compared to LHR (OR = 0.12, 95% CI [0.03, 0.51], Z = 2.91, P = 0.004) (Fig. 3 c).
Mesh bulging or transposition, which resembles hernia recurrence in appearance and causes patient dissatisfaction, was reported in only two studies, with no significant difference between HHR and LHR in bulging rates (OR = 0.49, 95% CI [0.16, 1.54], P = 0.22) (Fig. 3 b).
The hybrid technique was proposed around 2000. Stoikes [ 3 ] once described its indications as follows: the anticipation of significant difficulty in adhesiolysis under a fully laparoscopic scenario, recurrent hernia with prior mesh, and avoidance of extensive subcutaneous flap when the hernia preferentially bulges toward one side of the abdomen. In such cases, the hybrid technique was considered a favorable option to decrease surgical complexity. However, unexpectedly, this meta-analysis demonstrated that HHR did not offer advantages in controlling operation time or blood loss compared to LHR. This finding is similar to previous meta-analyses comparing open and laparoscopic procedures, with neither achieving statistical significance, despite both indicating that the laparoscopic procedure took less surgical time than the open procedure (Lap vs. Open, SMD: − 1.83, p = 0.143 and SMD: −0.08, p = 0.97, respectively) [ 6 , 34 ]. We speculate that this may be attributable not only to the more extensive surgical process in HHR compared to LHR, such as additional skin incisions, sac dissection, and closure of the orifice but also to complex morbidities or the extent of adhesion. Furthermore, the incidences of intestinal injury and obstruction between the two methods did not exhibit significant differences in 9 out of 14 studies, suggesting that experienced and proficient surgical performance can minimize potential risks occurring during dense adhesiolysis.
Cassar [ 35 ] summarized numerous studies prior to 2000, reporting that the rates of postoperative seroma formation in open procedures with mesh repair ranged from 1 to 15%, while in laparoscopic procedures, they ranged from 1 to 36%. However, a subsequent meta-analysis [ 34 ] suggested that the risk did not significantly favor patients undergoing laparoscopic repair compared to those undergoing open hernia repair (open vs. lap, OR = 1.54, p = 0.38). In contrast, the results of this meta-analysis supported the notion that HHR yielded a lower incidence of postoperative hematoma or seroma than LHR. Hernia sac excision and subcutaneous suction drainage have long been considered routine processes in hybrid hernia surgery, which may contribute to the reduced risk of postoperative seroma and hematoma formation [ 36 ].
In contrast to seroma and hematoma, which are often asymptomatic and predisposed to self-resolution, wound infection is of greater concern, as it can potentially lead to mesh infection and necessitate mesh removal. In this meta-analysis, the risk of wound infection was found to be more favorable for HHR than LHR, with HHR vs LHR yielding an OR of 2.10 (P = 0.04). This finding aligns with two earlier meta-analyses comparing open and laparoscopic surgeries [ 5 , 34 ]. The higher risk of infection in open or combined open surgeries may be attributed to more extensive subcutaneous mobilization.
Postoperative pain is a common discomfort. In this analysis, four studies assessed pain within 1 week after surgery, referred to here as acute pain. No statistical significance was observed between the two groups in postoperative VAS scores. Sajid [ 6 ] compared the impact of acute pain between laparoscopic and open repair using two RCT trials. The results demonstrated that the laparoscopic approach did not show superiority, lap vs open, VAS SMD = − 0.04, P = 0.84, and similar outcomes were observed in two other later RCT trials [ 37 , 38 ]. In contrast, chronic pain is defined as moderate or severe discomfort persisting for 6 to 8 weeks or even longer than 3 months after the procedure, as reported in various literatures [ 33 , 39 ]. Chronic pain is relatively uncommon in the laparoscopic era. The incidence rate was reported as 1.6% (13/819) by Heniford [ 40 ] and 1.5% (6/389) by Franklin [ 41 ]. A recent systematic review [ 42 ] contributed a pooled incidence rate of 4.49% (0–15.3) for chronic pain in the HHR group, which is nearly as low as that in the LHR group. The causes of chronic pain are associated with skin incision, prosthetic material, and surgical technique, including tension-free procedures, mesh fixation, nerve injury, and nerve entrapment. Since the LHR and HHR methods are relatively similar in surgical procedures, they are expected to have no significant difference in the incidence rate of chronic pain. In this analysis, the risk preference did not show a significant discrepancy between the two techniques, despite the OR of 0.45 indicating the risk more prefer LHR, which appears to confirm the result mentioned above.
This analysis also demonstrated no significant variation in recurrence rates between HHR and LHR method. However, a pronounced heterogeneity was observed. To address this, we designated a minimum follow-up period of 36 months as a benchmark for evaluating hernia recurrence rates [ 4 ], establishing a cutoff point to facilitate subgroup analyses aimed at delineating the source of the heterogeneity. Notably, no heterogeneity was observed within the individual subgroups, indicating that the disparate follow-up durations across the selected trials may have contributed to the significant heterogeneity noted in the overall analysis. Due to the lack of specified data on 1-, 3-, or 5-year recurrence rates, it remains inconclusive whether the risk of recurrence beyond 36 months is more favorable with LHR compared to HHR based on the available trials featuring varied follow-up durations.
Hernia recurrence rates can vary based on the repair methods and materials used. Incisional hernias repaired by suturing have high recurrence rates (12–54%), while mesh repair is associated with recurrence rates ranging from 2 to 36% [ 6 , 43 ]. Al Chalabi [ 5 ] summarized five randomized trials involving 611 IVH patients with follow-up periods ranging from 8 to 35 months, revealing a risk ratio for recurrence rate of 1.29 for laparoscopic versus open repair (95% CI [0.79, 2.11], P = 0.30). Awaiz [ 34 ] also reported a pooled OR of 1.41 for laparoscopic versus open repair (95% CI [0.81, 2.46], P = 0.23) based on six RCT trials consisting of 751 IVH patients with follow-up periods between 2 and 35 months. In the era of mesh repair, the likelihood of encountering high recurrence rates appears to be substantially reduced. Our findings reinforce the reliability of this conclusion, although there were few RCT trials included in this meta-analysis.
Mesh bulging, characterized by uneven protrusions in the area of previous hernia repair, is also referred to as pseudo-recurrence and has been associated with inadequate surgical techniques, particularly when employing the bridging technique without closure of defects [ 44 , 45 ]. In this analysis, two included studies reported no significant differences in mesh bulging occurrence between the two methods. However, neither study specified whether the bridging technique was used in the laparoscopic procedures.
Several limitations are associated with this analysis. First, the inclusion of a large number of non-randomized and retrospective studies potentially increased the risk of selection bias. Second, methodological discrepancies existed among the included studies; for instance, some studies did not report whether defect closure and hernia sac dissection were performed. The HHR method was described as beginning with laparoscopy, transitioning to open, and concluding with laparoscopy; however, some studies reported laparoscopy followed by open, while others did not specify this aspect. Additionally, the evaluation of the extent of abdominal adhesions varied. Lastly, double-arm cohort studies comparing HHR with LHR are scarcely found in English literature. Interestingly, single-arm studies focusing solely on the effect of HHR are more prevalent. To augment the sample size and thus enhance the robustness of our analysis, we incorporated findings from Chinese comparative studies. However, this strategy may potentially increase the risk of language bias. The potential bias will diminish as the literature continues to be enriched with additional randomized controlled trials and comparative studies.
Given the absence of low risk biased Randomized Controlled Trials (RCTs) up until now, considerable caution is required in interpreting the outcomes due to significant heterogeneity in surgical procedures and reporting of postoperative complications. At present, the Hybrid Hernia Repair (HHR) technique does not appear to offer a distinct advantage over the Laparoscopic Hernia Repair (LHR) method in terms of mitigating surgical complications, except for a lower postoperative seroma incidence. Surgeons with significant expertise may avoid incidental conversions or intentional hybrid procedures. Future research should aim to conduct low-risk biased RCTs to clarify these findings and establish the optimal surgical approach for Incisional Ventral Hernias (IVH).
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
LeBlanc KA, Booth WV. Laparoscopic repair of incisional abdominal hernias using expanded polytetrafluoroethylene: preliminary findings. Surg Laparosc Endosc. 1993;3:39–41 PMID: 8258069.
CAS PubMed Google Scholar
LeBlanc KA, Booth WV, Whitaker JM, et al. Laparoscopic incisional and ventral herniorrhaphy in 100 patients. Am J Surg. 2000;180:193–7. https://doi.org/10.1016/s0002-9610(00)00443-8 .
Article CAS PubMed Google Scholar
Stoikes N, Quasebarth M, Brunt LM. Hybrid ventral hernia repair: technique and results. Hernia. 2013;17:627–32. https://doi.org/10.1007/s10029-013-1092-9 .
LeBlanc KA. Incisional hernia repair: laparoscopic techniques. World J Surg. 2005;29:1073–9. https://doi.org/10.1007/s00268-005-7971-1 .
Article PubMed Google Scholar
Al Chalabi H, Larkin J, Mehigan B, et al. A systematic review of laparoscopic versus open abdominal incisional hernia repair, with meta-analysis of randomized controlled trials. Int J Surg. 2015;20:65–74. https://doi.org/10.1016/j.ijsu.2015.05.050 .
Sajid MS, Bokhari SA, Mallick AS, et al. Laparoscopic versus open repair of incisional/ventral hernia: a meta-analysis. Am J Surg. 2009;197:64–72. https://doi.org/10.1016/j.amjsurg.2007.12.051 .
Neff M, Cantor B, Geis WP. Laparoscopic-assisted primary repair of a complicated ventral incisional hernia. JSLS. 2005;9:241–4 PMID: 15984722.
PubMed PubMed Central Google Scholar
Yoshikawa K, Shimada M, Kurita N, et al. Hybrid technique for laparoscopic incisional ventral hernia repair combining laparoscopic primary closure and mesh repair. Asian J Endosc Surg. 2014;7:282–5. https://doi.org/10.1111/ases.12113 .
Meytes V, Lee A, Rivelis Y, et al. Hybrid fascial closure with laparoscopic mesh placement for ventral hernias: a single surgeon experience. Ann Laparosc Endosc. 2017;2(55–60) https://doi.org/10.21037/ales.2017.02.31 .
Kudsi OY, Chang K, Bou-Ayash N, et al. Hybrid robotic hernia repair for incisional hernias: perioperative and patient-reported outcomes. J Laparoendosc Adv Surg Tech A. 2021;31:570–8.
Wasim MD, Muddebihal UM, Rao UV. Hybrid: evolving techniques in laparoscopic ventral hernia mesh repair. J Minim Access Surg. 2020;16:224–8. https://doi.org/10.4103/jmas.JMAS_163_18 .
Article CAS PubMed PubMed Central Google Scholar
Romanowska M, Okniński T, Pawlak J. Hybrid technique for postoperative ventral hernias – own experience. Wideochir Inne Tech Maloinwazyjne. 2016;10:534–40. https://doi.org/10.5114/wiitm.2015.55689 .
Eitan A, Bickel A. Laparoscopically assisted approach for postoperative ventral hernia repair. J Laparoendosc Adv Surg Tech A. 2002;12:309–11. https://doi.org/10.1089/109264202320884036 .
Ji Y, Zhan X, Wang Y, et al. Combined laparoscopic and open technique for the repair of large complicated incisional hernias. Surg Endosc. 2013;27:1778–83. https://doi.org/10.1007/s00464-012-2680-y .
Ahonen-Siirtola M, Rautio T, Biancari F, et al. Laparoscopic versus hybrid approach for treatment of incisional ventral hernia. Dig Surg. 2017;34:502–6. https://doi.org/10.1007/s00464-019-06735-9 .
Van den Dop LM, Smet G, Kleinrensink G, et al. Hybrid operation technique for incisional hernia repair: a systematic review and meta-analysis of intra- and postoperative complications. Hernia. 2021;25:1459–69. https://doi.org/10.1007/s10029-021-02497-3 .
Article PubMed PubMed Central Google Scholar
Reinpold W, Schröder M, Berger C, et al. Mini- or less-open sublay operation (milos): a new minimally invasive technique for the extraperitoneal mesh repair of incisional hernias. Ann Surg. 2019;269:748–55. https://doi.org/10.1097/SLA.0000000000002661 .
Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. https://doi.org/10.1136/bmj.i4919 .
Higgins JPT, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. https://doi.org/10.1136/bmj.d5928 .
Taqi M, Zhong WM, Zhang GY, et al. Laparoscopic tension-free hernioplasty for abdominal wall incisional hernia: a report of 25 cases. J Laparosc Surg. 2013;18:301–4. https://doi.org/10.13499/j.cnki.fqjwkzz.2013.04.014 .
Article Google Scholar
Deng XZ, Wu B, Fan YB, et al. Hybrid repair technique for the treatment of incisional hernia: 40 cases report. J Surg Concepts Pract. 2013;18:232–5. https://doi.org/10.3969/j.issn.1007-9610.2013.03.010 .
Zhu YL, Chen J, Shen YM, et al. Hybrid technique in the treatment of the huge abdominal incisional hernia: an analysis of clinic therapeutic effect. Chin J Pract Surg. 2014;34:432–4. https://doi.org/10.7504/CJPS.ISSN1005-2208.2014.05.18 .
Ozturk G, Malya FU, Ersavas C, et al. A novel reconstruction method for giant incisional hernia: hybrid laparoscopic technique. J Minim Access Surg. 2015;11:267–70. https://doi.org/10.4103/0972-9941.142403 .
Ye JX, Cai X, Ma DD, et al. Comparison of the clinical efficacy between hybrid technique and laparoscopic intraperitoneal onlay mesh for the abdominal incisional hernia repair. J Laparosc Surg. 2015;20:866–9. https://doi.org/10.13499/j.cnki.fqjwkzz.2015.11.866 .
Halka JT, Vasyluk A, DeMare AM, et al. Robotic and hybrid robotic transversus abdominis release may be performed with low length of stay and wound morbidity. Am J Surg. 2018;215:462–5. https://doi.org/10.1016/j.amjsurg.2017.10.053 .
Wang JL, Hua YM, Zhu CY, et al. Skills of laparoscopy or hybrid surgery for large and huge incisional abdominal hernia. Chin J Min Inv Surg. 2017;17:276–8. https://doi.org/10.3969/j.issn.1009-6604.2017.03.024 .
Chen G, Meng YX, Li SJ, et al. Laparoscopic and hybrid technique for the repair of incisional hernia: a report of 70 cases. Chin J Gen Surg. 2017;32:997–9. https://doi.org/10.3760/cma.j.issn.1007-631X.2017.12.004 .
Ahonen-Siirtola M, Nevala T, Vironen J, et al. Laparoscopic versus hybrid approach for treatment of incisional ventral hernia: a prospective randomized multicenter study of 1-month follow-up results. Hernia. 2018;22:1015–22. https://doi.org/10.1007/s10029-018-1784-2 .
Liu ZC, Zhou JP, Gao W, et al. Diagnosis and treatment of abdominal incisional hernia: a report of 79 cases. Med J Liaoning. 2019;33:22–5 https://kns.cnki.net/kcms/detail/detail.aspx?FileName=LNYX201903009&DbName=CJFQ2019 .
Google Scholar
Zhao C, Yao HQ. Clinical study of hybrid surgery and laparoscopic repair in the treatment of incision hernia of abdominal wall. Chin J Hernia Abdominal Wall Surg (Electronic Edition). 2019;13:537–9. https://doi.org/10.3877/cma.j.issn.1674-392X.2019.06.014 .
Ahonen-Siirtola M, Nevala T, Vironen J, et al. Laparoscopic versus hybrid approach for treatment of incisional ventral hernia: a prospective randomised multicentre study, 1-year results. Surg Endosc. 2020;34:88–95. https://doi.org/10.1007/s00464-019-06735-9 .
Tian GJ, Liu P, Yang P, et al. Clinical study of open surgery assisted laparoscopy and complete laparoscopic repair in the treatment of abdominal incisional hernia. Chin J Hernia Abdominal Wall Surg(Electronic Edition). 2020;14:481–4. https://doi.org/10.3877/cma.j.issn.1674-392X.2020.05.004 .
Yang S, Wang M, Nie Y, et al. Outcomes and complications of open, laparoscopic, and hybrid giant ventral hernia repair. World J Clin Cases. 2022;10:51–61. https://doi.org/10.12998/wjcc.v10.i1.51 .
Awaiz A, Rahman F, Hossain MB, et al. Meta-analysis and systematic review of laparoscopic versus open mesh repair for elective incisional hernia. Hernia. 2015;19:449–63. https://doi.org/10.1007/s10029-015-1351-z .
Cassar K, Munro A. Surgical treatment of incisional hernia. Br J Surg. 2002;89:534–45. https://doi.org/10.1046/j.1365-2168.2002.02083.x .
Bittner R, Bain K, Bansal VK, et al. Update of guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (international Endohernia society (IEHS)): part B. Surg Endosc. 2019;33:3511–49. https://doi.org/10.1007/s00464-019-06907-7 .
Misra MC, Bansal VK, Kulkarni MP, et al. Comparison of laparoscopic and open repair of incisional and primary ventral hernia: results of a prospective randomized study. Surg Endosc. 2006;20:1839–45. https://doi.org/10.1007/s00464-006-0118-0 .
Barbaros U, Asoglu O, Seven R, et al. The comparison of laparoscopic and open ventral hernia repairs: a prospective randomized study. Hernia. 2007;11:51–66. https://doi.org/10.1007/s10029-006-0160-9 .
Mathes T, Prediger B, Walgenbach M, et al. Mesh fixation techniques in primary ventral or incisional hernia repair. Cochrane Database Syst Rev. 2021;5:CD011563. https://doi.org/10.1002/14651858.CD011563.pub2 .
Heniford BT, Park A, Ramshaw BJ, et al. Laparoscopic repair of ventral hernias : nine years’ experience with 850 consecutive hernias. Ann Surg. 2003;238:391–9. https://doi.org/10.1097/01.sla.0000086662.49499.ab .
Franklin ME, Gonzalez JJ, Glass JL, et al. Laparoscopic ventral and incisional hernia repair: an 11-year experience. Hernia. 2004;8:23–7. https://doi.org/10.1007/s10029-003-0163-8 .
Sharma A, Sinha C, Baijal M, et al. Hybrid approach for ventral incisional hernias of the abdominal wall: a systematic review of the literature. J Minim Access Surg. 2021;17:7–13. https://doi.org/10.4103/jmas.JMAS_146_19 .
Rudmik LR, Schieman C, Dixon E, et al. Laparoscopic incisional hernia repair: a review of the literature. Hernia. 2006;10:110–9. https://doi.org/10.1007/s10029-006-0066-6 .
Deerenberg EB, Verhelst J, Hovius SER, et al. Mesh expansion as the cause of bulging after abdominal wall hernia repair. Int J Surg Case Rep. 2016;28:200–3. https://doi.org/10.1016/j.ijscr.2016.09.051 .
Suwa K, Okamoto T, Yanaga K. Closure versus non-closure of fascial defects in laparoscopic ventral and incisional hernia repairs: a review of the literature. Surg Today. 2016;46:764–73. https://doi.org/10.1007/s00595-015-1219-y .
Download references
Acknowledgements
Thanks to all participated surgeons, investigators and patients in this study.
Author information
Authors and affiliations.
Department of General Surgery, Beijing Jishuitan Hospital, Capital Medical University, 31 Xinjiekou East Street, Xicheng District, Beijing, 100035, China
Quan Wu, Yaqi Liu & Yaokai Xu
Department of Pathology and Laboratory Medicine, Dartmouth Hitchcock Medical Center, Geisel School of Medicine at Dartmouth, Lebanon, NH, USA
Department of Epidemiology and Biostatistics, Beijing Research Institute of Traumatology and Orthopaedics, Beijing Jishuitan Hospital, Beijing, 100035, China
Qianqian Wang
You can also search for this author in PubMed Google Scholar
Contributions
WQ conceived the study and wrote the paper. MW undertook and refined the searches and co-wrote the paper and prepared Fig. 1 . WQQ undertook the statistical analyses and helped to revise the intellectual content and prepared Figs. 2 – 4 . LY and XY extracted all dada, and they prepared Tables 1 – 2 . All authors read and approved the final manuscript.
Corresponding author
Correspondence to Weijie Ma .
Ethics declarations
Ethics approval and consent to participate.
No ethical approval and patient consent are required because all analyses were based on previous published studies.
Consent for publication
Not applicable.

Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: supplementary table s1..
The Risk of bias domains (ROBINS-I) of included studies. Supplementary Table S2. The Cochrane risk of bias tool for assessing risk of bias in included studies. Supplementary Table S3. Source of the Chinese studies included this analysis
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Wu, Q., Ma, W., Wang, Q. et al. Comparative effectiveness of hybrid and laparoscopic techniques for repairing complex incisional ventral hernias: a systematic review and meta-analysis. BMC Surg 23 , 346 (2023). https://doi.org/10.1186/s12893-023-02254-6
Download citation
Received : 20 May 2023
Accepted : 31 October 2023
Published : 16 November 2023
DOI : https://doi.org/10.1186/s12893-023-02254-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Hybrid hernia repair technique
- Laparoscopic hernia repair technique
- Incisional ventral hernias
- Meta-analysis
BMC Surgery
ISSN: 1471-2482
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Bibliography
- More Referencing guides Blog Automated transliteration Relevant bibliographies by topics
- Automated transliteration
- Relevant bibliographies by topics
- Referencing guides
Dissertations / Theses on the topic 'Hernia. Hernia'
Create a spot-on reference in apa, mla, chicago, harvard, and other styles.
Consult the top 50 dissertations / theses for your research on the topic 'Hernia. Hernia.'
Next to every source in the list of references, there is an 'Add to bibliography' button. Press on it, and we will generate automatically the bibliographic reference to the chosen work in the citation style you need: APA, MLA, Harvard, Chicago, Vancouver, etc.
You can also download the full text of the academic publication as pdf and read online its abstract whenever available in the metadata.
Browse dissertations / theses on a wide variety of disciplines and organise your bibliography correctly.
Bringman, Sven. "Minimally invasive hernia surgery /." Stockholm, 2003. http://diss.kib.ki.se/2003/91-7349-466-6/.
Crispín-Trebejo, Brenda, María Cristina Robles-Cuadros, Edwin Orendo-Velásquez, and Felipe P. Andrade. "Internal abdominal hernia: Intestinal obstruction due to trans-mesenteric hernia containing transverse colon." Elsevier B.V, 2014. http://hdl.handle.net/10757/320534.
Arroyo, Torres Elmer Jesús. "Hernioplastia Lichtenstein en el Centro Médico Naval "CMST". Experiencia de 5 años." Bachelor's thesis, Universidad Nacional Mayor de San Marcos, 2004. https://hdl.handle.net/20.500.12672/1887.
Näsvall, Pia. "Parastomal hernia : investigation and treatment." Doctoral thesis, Umeå universitet, Institutionen för kirurgisk och perioperativ vetenskap, 2015. http://urn.kb.se/resolve?urn=urn:nbn:se:umu:diva-103325.
Beets, Geerard Lucien. "On the repair of inguinal hernia." [Maastricht ; Universiteit Maastricht] ; Maastricht : University Library, Maastricht University [Host], 1997. http://arno.unimaas.nl/show.cgi?fid=5831.
Rajatapiti, Prapapan. "Pulmonary development in congenital diaphragmatic hernia." [S.l.] : Rotterdam : [The Author] ; Erasmus University [Host], 2007. http://hdl.handle.net/1765/10705.
Veen, Ruben Nico van. "New clinical concepts in inguinal hernia." [S.l.] : Rotterdam : [The Author] ; Erasmus University [Host], 2008. http://hdl.handle.net/1765/11998.
Page, Blaithin. "Chronic pain following inguinal hernia repair." Thesis, University of Glasgow, 2009. http://theses.gla.ac.uk/2579/.
Koch, Frisén Angelica. "Audit of Groin Hernia Repair II." Doctoral thesis, Linköpings universitet, Kirurgi, 2010. http://urn.kb.se/resolve?urn=urn:nbn:se:liu:diva-63645.
On the day of the defence date the title of article III was: "Groin hernia repair with Titanium Coated Mesh compared to Prolene Mesh: A Prospective Randomized Controlled Trial".
Kylat, Ranjit I. "Internal Hernia Masquerading As Necrotizing Enterocolitis." FRONTIERS MEDIA SA, 2017. http://hdl.handle.net/10150/626085.
Ahmed, Ahmed Rashid. "Internal hernia following laparoscopic gastric bypass." Thesis, Imperial College London, 2014. http://hdl.handle.net/10044/1/24733.
Delgado, Quispe Johandi. "Comportamiento quirúrgico de las hernias de la región inguinal en el Hospital Nacional Arzobispo Loayza 2009 - 2011." Bachelor's thesis, Universidad Nacional Mayor de San Marcos, 2012. https://hdl.handle.net/20.500.12672/12135.
Pfeiffer, Mark. "Untersuchungen zur Ätiologie der Hernia umbilicalisbeim Ferkel." Diss., lmu, 2006. http://nbn-resolving.de/urn:nbn:de:bvb:19-58977.
Barrientos, Ivan J. Hall. "A tissue-engineered approach to hernia repair." Thesis, University of Strathclyde, 2017. http://digitool.lib.strath.ac.uk:80/R/?func=dbin-jump-full&object_id=30303.
Löfgren, Jenny. "Groin hernias and unmet need for surgery in Uganda : Epidemiology, mosquito nets and cost-effectiveness." Doctoral thesis, Umeå universitet, Kirurgi, 2015. http://urn.kb.se/resolve?urn=urn:nbn:se:umu:diva-107659.
Cantwell, Marie Therese. "An outcomes study: Outpatient versus inpatient hernia repairs." CSUSB ScholarWorks, 1994. https://scholarworks.lib.csusb.edu/etd-project/802.
Jänes, Arthur. "Parastomal hernia : clinical studies on definitions and prevention." Doctoral thesis, Umeå universitet, Kirurgi, 2010. http://urn.kb.se/resolve?urn=urn:nbn:se:umu:diva-36142.
Pfeiffer, Mark. "Untersuchungen zur Ätiologie der Hernia umbilicalis beim Ferkel." [S.l.] : [s.n.], 2006. http://edoc.ub.uni-muenchen.de/archive/00005897.
Fachinelli, Aldo. "Fibras elásticas da parede abdominal anterior em pacientes com hérnia ventral." reponame:Biblioteca Digital de Teses e Dissertações da UFRGS, 2010. http://hdl.handle.net/10183/26918.
Nordin, Pär. "Groin hernia surgery : studies on anaesthesia and surgical technique /." Linköping : Univ, 2003.
Klaassens, Merel. "Genetic factors in the etiology of longenital diaphragmatic hernia." [S.l.] : Rotterdam : [The Author] ; Erasmus University [Host], 2007. http://hdl.handle.net/1765/10297.
Wright, David M. "Clinical studies comparing laparoscopic and open inguinal hernia repair." Thesis, University of Glasgow, 2001. http://theses.gla.ac.uk/5401/.
Magnusson, Niklas. "Postoperative aspects of inguinal hernia surgery : pain and recurrences." Doctoral thesis, Örebro universitet, Institutionen för hälsovetenskap och medicin, 2012. http://urn.kb.se/resolve?urn=urn:nbn:se:oru:diva-26054.
Furtado, Marcelo Lopes. "Análise retrospectiva de casuística de hernioplastia inguinal videolaparoscópica TAPP /." Botucatu, 2015. http://hdl.handle.net/11449/139336.
Furtado, Marcelo Lopes [UNESP]. "Análise retrospectiva de casuística de hernioplastia inguinal videolaparoscópica TAPP." Universidade Estadual Paulista (UNESP), 2015. http://hdl.handle.net/11449/139336.
Lin, Frank C., Jamie S. Lin, Samuel Kim, and Jonathan R. Walker. "A rare diaphragmatic ureteral herniation case report: endoscopic and open reconstructive management." BIOMED CENTRAL LTD, 2017. http://hdl.handle.net/10150/624352.
Russell, Meaghan Kathleen. "Molecular mechanisms of diaphragm development: implications for congenital diaphragmatic hernia." Thesis, Boston University, 2012. https://hdl.handle.net/2144/32051.
Baracho, Ana Sofia Esperança da Palma. "Hérnias diafragmáticas congénitas : revisão bibliográfica a propósito de três casos clínicos." Master's thesis, Universidade Técnica de Lisboa. Faculdade de Medicina Veterinária, 2011. http://hdl.handle.net/10400.5/3773.
Fränneby, Ulf. "Patient-orientated aspects of the postoperative course after hernia surgery /." Stockholm, 2006. http://diss.kib.ki.se/2006/91-7140-810-X/.
Amathieu, Ludivine. "Assessment of a Light-Activated Adhesive for Hernia Mesh Repair." Thesis, KTH, Skolan för kemi, bioteknologi och hälsa (CBH), 2021. http://urn.kb.se/resolve?urn=urn:nbn:se:kth:diva-292214.
Nieri, Tamara Maria. "Modelo experimental para o estudo do comportamento optico da parede abdominal e sua interação com um material protetico por biospeckle : trabalho experimental em ratos." [s.n.], 2005. http://repositorio.unicamp.br/jspui/handle/REPOSIP/310697.
Lau, Hung. "Endoscopic totally extraperitoneal inguinal hernioplasty : techniques and advances for optimal outcome." Click to view the E-thesis via HKUTO, 2006. http://sunzi.lib.hku.hk/hkuto/record/B36425242.
Vassalli, J. Todd Grant Sheila Ann. "Development of electrospun synthetic bioabsorbable fibers for a novel bionanocomposite hernia repair material." Diss., Columbia, Mo. : University of Missouri--Columbia, 2008. http://hdl.handle.net/10355/5631.
Mazzini, Decio Luiz Silva. "Fechamento da parede abdominal com afastamento parcial das bordas da aponeurose utilizando sobreposição com telas de vicryl ou marlex em ratos." [s.n.], 1997. http://repositorio.unicamp.br/jspui/handle/REPOSIP/311250.
Decadt, Bart. "Evidence-based laparoscopic surgery." Thesis, University of East Anglia, 2002. http://ethos.bl.uk/OrderDetails.do?uin=uk.bl.ethos.268504.
Zanchin, Fabiane. "Diagnósticos diferenciais de hérnias umbilicais em Suínos no abate." reponame:Biblioteca Digital de Teses e Dissertações da UFRGS, 2015. http://hdl.handle.net/10183/115189.
Haapaniemi, Staffan. "Quality assessment in groin hernia surgery : the role of a register /." Linköping : Univ, 2001. http://www.bibl.liu.se/liupubl/disp/disp2001/med685s.pdf.
Dahlstrand, Ursula. "Femoral and Inguinal Hernia : How to Minimize Adverse Outcomes Following Repair." Doctoral thesis, Uppsala universitet, Kolorektalkirurgi, 2011. http://urn.kb.se/resolve?urn=urn:nbn:se:uu:diva-162203.
Fortuny, Anguera Gerard. "Dynamical Analysis of Lower Abdominal Wall in the Human Inguinal Hernia." Doctoral thesis, Universitat Politècnica de Catalunya, 2009. http://hdl.handle.net/10803/6697.
Lau, Hung, and 劉雄. "Inguinal hernia repair: the impact of ambulatory and minimal access surgery." Thesis, The University of Hong Kong (Pokfulam, Hong Kong), 2002. http://hub.hku.hk/bib/B25257614.
Lau, Hung. "Inguinal hernia repair : the impact of ambulatory and minimal access surgery." Hong Kong : University of Hong Kong, 2002. http://sunzi.lib.hku.hk/hkuto/record.jsp?B25257614.
Ramakrishnan, Rema. "Ambient Ozone and Cadmium as Risk Factors For Congenital Diaphragmatic Hernia." Scholar Commons, 2017. https://scholarcommons.usf.edu/etd/7439.
Delabaere, Amélie. "Rétinoïdes en intra-trachéal et occlusion de trachée dans le traitement anténatal de la hernie diaphragmatique congénitale sur un modèle lapin." Thesis, Université Clermont Auvergne (2017-2020), 2017. http://www.theses.fr/2017CLFAS024.
Argudo, Aguirre Núria. "Uso de malla profiláctica tras laparotomía en pacientes de riesgo." Doctoral thesis, Universitat Autònoma de Barcelona, 2019. http://hdl.handle.net/10803/667364.
Maciel, Luiz Carlos. "Alterações histopatologicas do ducto deferente de ratos exposto a tela de polipropileno." [s.n.], 2007. http://repositorio.unicamp.br/jspui/handle/REPOSIP/312062.
Fachinelli, Aldo. "Avaliação qualitativa e quantitativa do colágeno total, tipo I e III da linha alba em pacientes portadores de hérnia da parede abdominal anterior." reponame:Biblioteca Digital de Teses e Dissertações da UFRGS, 2005. http://hdl.handle.net/10183/5080.
Lau, Hung, and 劉雄. "Endoscopic totally extraperitoneal inguinal hernioplasty: techniquesand advances for optimal outcome." Thesis, The University of Hong Kong (Pokfulam, Hong Kong), 2006. http://hub.hku.hk/bib/B36425242.
Andriani, Alexandre Ciro. "Estudo histológico do saco herniário de hérnias inguinais indiretas." Florianópolis, SC, 2000. http://repositorio.ufsc.br/xmlui/handle/123456789/78285.
Alcantara, Torres Victor Manuel. "“COMPLICACIONES POSTQUIRURGICAS EN CIRUGIA DE HERNIA INGUINAL, HOSPITAL GENERAL DE IXTLAHUACA, ISEM, 2012”." Tesis de Licenciatura, Medicina-Quimica, 2013. http://hdl.handle.net/20.500.11799/14264.
Eklund, Arne. "Laparoscopic or Open Inguinal Hernia Repair - Which is Best for the Patient?" Doctoral thesis, Uppsala universitet, Centrum för klinisk forskning, Västerås, 2009. http://urn.kb.se/resolve?urn=urn:nbn:se:uu:diva-107630.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Effects of the short-stitch technique for midline abdominal closure: short-term results from the randomised-controlled ESTOIH trial
M. albertsmeier.
1 Department of General, Visceral and Transplantation Surgery, LMU University Hospital, Ludwig-Maximilians-Universität (LMU) Munich, 81377 Munich, Germany
2 Allgemein-, Viszeral- und Tumorchirurgie, Wilhelminenspital, Montleartstr. 37, 1160 Vienna, Austria
3 Department of Medical Scientific Affairs, Aesculap AG, Am Aesculap Platz, 78532 Tuttlingen, Germany
4 Klinik am Eichert, Allgemeinchirurgie, Alb Fils Klinik GmbH, Eichertstr.3, 73035 Göppingen, Germany
C. Reisensohn
J. l. kewer.
5 Klinik für Allgemein-, Viszeral- und Gefäßchirurgie, Klinikum Landkreis Tuttlingen, Zeppelinstr. 21, 78532 Tuttlingen, Germany
J. Hoelderle
A. shamiyeh.
6 Klinik für Allgemein- und Viszeralchirurgie, Kepler Universitätsklinikum GmbH, Krankenhausstr. 9, 4021 Linz, Austria
B. Klugsberger
T. d. maier.
7 Allgemein- und Viszeralchirurgie, Robert-Bosch-Krankenhaus, Auerbachstr. 110, 70376 Stuttgart, Germany
G. Schumacher
8 Chirurgische Klinik, Städtisches Klinikum Braunschweig, Salzdahlumer Str. 90, 38126 Brunswick, Germany
F. Köckerling
9 Klinik für Chirurgie, Viszeral- und Gefäßchirurgie, Vivantes Klinikum Spandau, Neue Bergstr. 6, 13585 Berlin, Germany
10 Zentrum der Chirurgie, Klinik für Allgemein- und Viszeralchirurgie, Universitätsklinikum Frankfurt, Theodor-Stern-Kai, 60590 Frankfurt am Main, Germany
R. H. Fortelny
11 Med. Fakultät, Sigmund Freud Privatuniversität, Freudplatz 3, 1020 Vienna, Austria
Associated Data
Individual de-identified participant data will be made available beginning 6 months after publication and ending after 5 years. Data will be shared with investigators who provide a methodologically sound proposal to the sponsor. Proposals shall be directed to [email protected]. Data requestors will need to sign a data access agreement. Data are available for 5 years at a third party website. The trial protocol has been published with open access in the journal Trials: Fortelny RH, Baumann P, Thasler WE, et al. Effect of suture technique on the occurrence of incisional hernia after elective midline abdominal wall closure: study protocol for a randomised-controlled trial. Trials 2015; 16(1):52.
The short-stitch technique for midline laparotomy closure has been shown to reduce hernia rates, but long stitches remain the standard of care and the effect of the short-stitch technique on short-term results is not well known. The aim of this study was to compare the two techniques, using an ultra-long-term absorbable elastic suture material.
Following elective midline laparotomy, 425 patients in 9 centres were randomised to receive wound closure using the short-stitch (USP 2-0 single thread, n = 215) or long-stitch (USP 1 double loop, n = 210) technique with a poly-4-hydroxybutyrate-based suture material (Monomax ® ). Here, we report short-term surgical outcomes.
At 30 (+10) days postoperatively, 3 (1.40%) of 215 patients in the short-stitch group and 10 (4.76%) of 210 patients in the long-stitch group had developed burst abdomen [OR 0.2830 (0.0768–1.0433), p = 0.0513]. Ruptured suture, seroma and hematoma and other wound healing disorders occurred in small numbers without differences between groups. In a planned Cox proportional hazard model for burst abdomen, the short-stitch group had a significantly lower risk [HR 0.1783 (0.0379–0.6617), p = 0.0115].
Conclusions
Although this trial revealed no significant difference in short-term results between the short-stitch and long-stitch techniques for closure of midline laparotomy, a trend towards a lower rate of burst abdomen in the short-stitch group suggests a possible advantage of the short-stitch technique.
Trial registry
{"type":"clinical-trial","attrs":{"text":"NCT01965249","term_id":"NCT01965249"}} NCT01965249 , registered October 18, 2013.
Introduction
Incisional hernia, which develops in 10–69% of patients, remains a major complication after midline abdominal wall closure [ 1 ]. A low tension of the suture line, sufficient collagen deposition, adequate blood supply and the absence of infection are prerequisites for undisturbed wound healing, while clinical risk factors for the development of incisional hernia include obesity, smoking, steroid therapy and malnutrition [ 1 ].
The first randomised-controlled trial (RCT) comparing large bite and small bite closure techniques published by Millbourn et al. [ 2 ] restarted the discussion regarding the best technique for midline closure. Albeit the INLINE meta-analysis by Diener et al. concluded that a running suture using a long-term absorbable monofilament material should be used for midline closure [ 3 ], specific technical aspects were not highlighted. In several studies, Israelsson had investigated the effects of different suture-to-wound length ratios and detected that a ratio of at least 4–5:1 was associated with fewer wound infections and lower incisional hernia rates even in obese patients [ 4 , 5 ].
In 2015, the European hernia society (EHS) published guidelines on the closure of abdominal wall incisions [ 6 ], which included weak recommendations for the use of small bites, based only on the RCT by Millbourn et al. [ 2 ], and for a suture-to-wound length ratio of at least 4:0. A second RCT comparing small versus large bite was published by Deerenberg et al. [ 7 ] immediately after these guidelines. The results of this study confirmed the superiority of the small bite technique. The surgical site infection (SSI) rate of the STITCH trial was surprisingly high in both groups (21 vs 22%) in comparison to Millbourn (10 vs 5%).
Based on a recently published meta-analysis by Henriksen et al. [ 8 ] including 2 RCTs [ 2 , 7 ], a continuous suture with small bites in combination with a slowly absorbable suture material results in significantly fewer incisional hernias than a large bites technique (9.45 vs 19.30%, OR 0.41, 95% CI 0.19–0.86). These improvements notwithstanding, the surgical site infection rate of 21% and the 1-year incisional hernia rate of 13% in the small bite group of the STITCH study are not satisfactory. Besides stitch length, properties of the suture material such as elasticity, tensile strength and resorption time could significantly influence the results of elective midline closure.
On this account, a multi-centre, international, double-blinded, randomised trial was started to analyse the influence of stitch length on hernia development following elective midline laparotomy closure (ESTOIH study, {"type":"clinical-trial","attrs":{"text":"NCT01965249","term_id":"NCT01965249"}} NCT01965249 ) [ 9 ] using an elastic, extra-long-term absorbable monofilament suture material. Here, we report the short-term results of this trial with a focus on burst abdomen and SSI.
Trial design
This was a multi-centre, double-blinded, controlled, parallel-group study with 1:1 randomisation conducted in Germany and Austria (nine sites). The protocol of this trial has been published previously [ 9 ]. After initiation of the trial, changes have been made to the original trial protocol: originally, a body mass index (BMI) ≥ 30 kg/m 2 had been defined as an exclusion criterion with the intention to keep the study cohort as homogenous as possible. After initiation of the trial, this was found to limit recruitment to the trial. Moreover, Höer et al. had demonstrated that the risk for incisional hernia significantly increases with a BMI > 25 kg/m 2 [ 1 ]. No further difference was seen when the cut-off for BMI was set at 30 kg/m 2 , as most of the high-risk patients are found in the group with BMI < 30 kg/m 2 . Therefore, BMI was dropped from the list of exclusion criteria in an amendment to the study protocol dated 2015-09-23.
Furthermore, the original trial protocol had “pancreatic tumour patients” excluded from the study due to their relatively unfavourable prognosis and the intended 3-year follow-up. In the same amendment, this was changed to “patients undergoing surgery due to a pancreas carcinoma” to allow patients with benign pancreatic tumours to be included in the study.
Participants
Eligible participants were all adults aged ≥ 18 years (American Society of Anaesthesiologists groups I–III) undergoing an elective, primary median laparotomy with an incision length of ≥ 15 cm and an expected survival time longer than 1 year for whom written consent could be obtained.
Exclusion criteria were emergency surgery, BMI ≥ 30 kg/m 2 , pancreatic tumour patients (cf. “Trial Design” for changes to these exclusion criteria), patients operated due to an abdominal aortic aneurysm, peritonitis, coagulopathy, immunosuppressive therapy at the time of surgery (more than 40 mg of a corticoid per day or azathioprine), chemotherapy within the last 2 weeks before operation, radiotherapy of the abdomen within the last 8 weeks before operation, pregnancy, severe neurologic and psychiatric disease and lack of compliance.
Patients were recruited at nine different trials sites in Germany (seven sites) and Austria (two sites) including three university hospitals, three other tertial referral centres and three local and regional hospitals. The trial started with six centres and three centres joined the group after initiation of the trial.
Interventions
The main surgical procedures were carried out according to local standards. The linea alba was prepared to be free from subcutaneous fat and cut in the middle. In both study groups, elastic, extra-long-term absorbable, monofilament sutures manufactured from poly-4-hydroxybutyrate (P4HB) (Monomax ® , B.Braun Surgical, S.A., Rubi, Spain) were used for abdominal wall closure.
In the long-stitch group, a continuous suture with 10 mm stitch intervals and 10 mm distance from the wound edge was performed using a Monomax ® USP 1 150 cm loop with an HR 48 mm needle (suture-to-wound length ratio approx. 4:1). Sutures overlapped in the middle and were knotted separately. In the short stich group, a single continuous suture with 5 mm stitch intervals and 5–8 mm distance from the wound edge was performed using a Monomax ® USP 2/0 single 150 cm thread with an HR 26 mm needle (suture-to-wound length ratio ≥ 5:1). The number of throws per knot was not standardised in the study protocol. In training sessions, at least six throws for the long-stitch technique and a self-fixing knot for the short-stitch technique were recommended.
Surgeon training included study site visits by the principal investigator (R.F.) and training videos. Data related to suture technique were recorded in the case report form, monitored in regular study site visits and trends were discussed in study group meetings.
Outcome measures
This analysis reports short-term results of the ESTOIH trial as defined in the published study protocol [ 9 ]. The main outcome is the frequency of burst abdomen, defined as a clinically evident rupture of the laparotomy wound, at 30 (+10) days postoperatively. Other short-term results include surgical site infections (SSI), the re-operation rate due to burst abdomen, wound healing disorders, seroma and hematoma within 30 (+10) days. Wound infections are classified according to the US centres for disease control and prevention (CDC) as either deep or superficial. We also analysed the length of hospital stay and complications not directly related to wound healing.
The primary endpoint of the ESTOIH trial is the frequency of incisional hernia 1 year postoperatively and will be reported when available.
Sample size calculation and interim analysis
The previously published ISSAAC study had found a 19% risk of developing an incisional hernia within 1 year using a long-stitch technique with P4HB-based suture material for abdominal wall closure following primary elective midline laparotomy [ 10 ]. The aim of the ESTOIH trial is to demonstrate that the short-stitch suture technique decreases the 1-year incisional hernia rate by 50% compared with the long-stitch technique (primary endpoint). Assuming hernia rates of 19% and 9.5% for the respective groups, a sample size of 424 patients (212 per group) was calculated to detect this difference with a power of 80% and an alpha error of 5%. Including a drop-out rate of 10%, we planned to randomise a total of 468 patients. To avoid centre effects, we determined that no more than 200 patients should be recruited per centre. Withdrawn patients were not to be replaced.
Following an interim analysis of the primary outcome, it was decided that recruitment should end when 424 patients had been randomised as planned in the sample size calculation without substituting for patients who had terminated early.
Randomisation
Randomisation was performed intraoperatively briefly before abdominal wall closure. Eligible patients were randomly allocated to receive either the short or the long-stitch suture technique in a 1:1 ratio by opening a sealed opaque randomisation envelope. Envelopes were supplied by the sponsor, according to a randomisation list provided by a statistician using the statistical software SAS 9.1 (SAS Institute Inc., Cary, NC, USA). A separate randomisation list was prepared for each participating trial site to avoid centre-specific effects and to assure a balanced distribution of treatments within centres (stratification). Random blocks of different lengths were used. Randomisation lists were sealed and locked up at the sponsor site.
Randomisation envelopes were assigned to patients in chronological order by a surgeon, according to a consecutive and unique randomisation number. Each envelope contained the suture material pertinent to the indented suture technique as well as a description of the technique to be employed for abdominal wall closure. The study site confirmed the randomisation result by sending a fax to the sponsor.
Outcome assessment was double blinded: the patient and the observer responsible for the evaluation of the clinical outcome were unaware of the stitch length used for closing the midline and the observer had no access to the randomisation list. To document the clinical outcome at each follow-up examination, case report forms were handed to the observer by an independent person (e.g. a study nurse). While surgeons performing the abdominal wall closures could not be blinded, they were not involved in outcome assessment.
Statistical analysis
For this report, data available at the 30 (+10) day follow-up visit were analysed. A planned analysis will be performed after all patients have completed their 1-year follow-up (primary endpoint). Additional analyses will be conducted after completion of the 3- and 5-year follow-up visits. All statistical analyses were done using SAS software version 9.4 (SAS Institute Inc., Cary, NC, USA).
The patient cohort is described as a whole and separately for each treatment group with respect to demographic data and the baseline values of investigated parameters. The secondary endpoints reported here are tabulated as frequencies and rates. Confidence intervals are used when appropriate. The two-sided chi-square test for independent proportions is used to test for independence.
To control for BMI following a protocol amendment that allowed patients with a BMI > 30 kg/m 2 to participate in this study, Cox proportional hazards models were calculated for burst abdomen and wound infection. A stepped backward elimination method was used for model reduction. The stitch group, BMI and factors with p < 0.1 were included in the final model. Statistical significance was defined as a p value < 0.05 for all analyses.
Between March 2014 and December 2019, eligible participants were recruited and randomised to receive either the short-stitch ( n = 215) or long-stitch technique ( n = 210). The trial ended when 425 patients had been randomised; one additional patient had been included due to simultaneous inclusions in this multi-centre trial.
The flow of participants through the study is detailed in Fig. 1 . Participants received clinical visits at the time of enrolment (baseline), 2 days postoperatively, on the day of discharge and at 30 days (±10 days) postoperatively. Follow-up for short-term results ended January 2020 but continues for incisional hernia. Three hundred seventy-three patients (88%) completed short-term follow-up and were included in the present outcome analysis.

CONSORT flow diagram
In the short-stitch group, 23 patients were lost to follow-up until day 30 (+10) due to re-operation ( n = 9), withdrawal of consent ( n = 5), death ( n = 2) and other reasons ( n = 7). In the long-stitch group, 29 patients were lost to follow-up until day 30 (+10) due to re-operation ( n = 22), death ( n = 4) and other reasons ( n = 3).
Study groups were well balanced with respect to baseline clinical and procedure characteristics (Table (Table1). 1 ). More than half of patients had colorectal surgery, followed by upper GI surgery. Procedures were performed by 106 different surgeons.
Baseline demographic and clinical characteristics
Data are n (%) or mean ± standard deviation
At 30 (+10) days postoperatively, 3 (1.40%) of 215 patients in the short-stitch group and 10 (4.76%) of 210 patients in the long-stitch group had developed burst abdomen [OR 0.2830 (0.0768–1.0433), p = 0.0513]. Ruptured sutures occurred in small numbers of patients with no statistically significant differences between groups. Untied knots were not observed. We found superficial incisional SSIs in seven patients (3.26%) from the short-stitch group and 11 patients (5.24%) from the long-stitch group [OR 0.6088 (0.2314–1.6018), p = 0.3440]. Deep incisional SSIs occurred in one patient of each treatment group [0.9766 (0.0607–15.7165), p = 1.0000]. Seroma, hematoma and other wound healing disorders were found in small numbers of patients, and no statistically significant differences between groups were observed.
Anastomotic leakage was less frequent in the short-stitch group (6 of 215, 2.79%) compared to the long-stitch group (15 of 210, 7.14%); [OR 0.3787 (0.1441–0.9958), p = 0.0460]. 1 (0.47%) of 215 participants in the short-stitch group and 4 (1.90%) of 210 participants in the long-stitch group died in the perioperative period [OR 0.2407 (0.0267–2.1711), n.s.]. Patients in the short-stitch group had shorter hospital stays (11.0 ± 5.0 days) compared to patients in the long-stitch group (12.6 ± 7.8 days, p = 0.0204). Outcomes are summarised in Table Table2 2 .
Outcomes: adverse events and length of hospital stay
Bold value indicates p value < 0.05 significant
SSI surgical site infection
Cox proportional hazard models
Cox proportional hazards models were calculated for burst abdomen und wound infection (Table (Table3). 3 ). In the model for burst abdomen, the short-stitch group had a significantly lower risk compared to the long-stitch group [HR 0.1783 (0.0427–0.7435), p = 0.0179]. We observed a trend for a lower risk of burst abdomen with longer fascial closure times. BMI did not increase the risk of burst abdomen. When BMI was removed from the model, the risk of burst abdomen was reduced by 9.7% for every minute that closure of the fascia took longer [HR 1.0965 (1.0094–1.1910), p = 0.0291].
Cox proportional hazard models for burst abdomen and wound infection
In the model for wound infection, both BMI > 30 kg/m 2 [HR 3.0557 (1.0991–8.4947), p = 0.0323] and male gender [HR 3.2958 (1.0926–9.9418), p = 0.0342] were independently associated with a threefold increased risk of developing the complication. Suture technique had no significant influence on wound infections.
In this analysis of short-term results, we show that closing elective midline laparotomies using a short-stitch technique and an elastic suture material is a safe procedure with a low rate of short-term complications. The rate of burst abdomen did not differ significantly between treatment groups in the primary outcome analysis. In multivariate analysis, however, short stitches were associated with a sevenfold decreased risk for developing burst abdomen.
This is the first study showing such a clear trend towards a reduced risk for burst abdomen; previous trials [ 2 , 7 ] had shown no difference between suture techniques. The lack of more unanimous conclusions stems from the fact that the ESTOIH trial was not powered for the analysis of short-term wound complications. The overall rate of burst abdomen (3.1%) lies around the upper limit of the range anticipated from previous studies (e.g. PRIMA: 3.3%, INSECT 2.9%, PROUD: 2.6%, STITCH: 1.1%) [ 7 , 11 – 13 ], probably reflecting the inclusion of many high-risk oncological surgeries in the present trial (Table (Table1). 1 ). In theory, suture material could be an alternative explanation, but this seems unlikely as there were more burst abdomen with the stronger suture. Other outcomes related to wound healing, especially SSIs did not differ between treatment groups. It appears, hence, that if stitch technique did influence healing of the fascia, it did so directly and not primarily via a reduction of wound infections.
Nonetheless, with 4.7% of patients across treatment groups developing an SSI (superficial and deep combined), the rate of wound infections in this trial was low compared to previous trials. In the STITCH trial, e.g. 76 of 560 participants (14.5%) developed superficial or deep SSI [ 7 ]. The reason for the low wound infection rate remains unclear: In the ISSAAC trial, which compared P4HB-based sutures (Monomax ® ) to polydioxanone sutures (Monoplus ® and PDS ® ), no significant difference in the rate of wound infections was found between suture materials [ 10 ]. However, the low rate of wound infections in both treatment groups of the present trial aligns well with results from the MULTIMAC observational cohort study which used P4HB-based suture material in 200 routine patients [ 14 ].
The evidence for the use of a monofilament late absorbable running suture is regarded as robust [ 3 ], as stated in the EHS guidelines [ 6 ] and confirmed in a 2017 Cochrane review [ 15 ]. Nonetheless, the physical properties of P4HB-based and polydioxanone-based monofilament threads—i.e. elasticity, basic strength retention and absorption time—differ substantially: the elasticity (elongation) of P4HB-based suture material has been measured to be 90% compared to 45–50% for polydioxanone-based sutures. Presuming that the fascia, not the suture, constitutes the weakest element of abdominal wall closure, increased elasticity might help to reduce the occurrence of button-hole hernia [ 16 – 18 ] at the wound edges. Furthermore, the degradation time (50% basic strength retention) of P4HB-based suture material is 100 days vs 42 and 35 days for polydioxanone-based sutures, respectively, while the mass absorption time of Monomax ® is 390 days vs 180–210 days for PDS ® and Monoplus ® . The controlled prospective multi-centre ISSAAC trial [ 10 ] showed a non-significant reduction in the combined primary endpoint wound infections and/or burst abdomen in the Monomax ® group compared to polydioxanone-based sutures (7.3 vs 11.3%). The authors concluded that Monomax ® suture material is as safe as PDS ® or Monoplus ® for abdominal wall closure after primary midline laparotomy. In summary, P4HB-based suture material seems to support the healing of the fascia by its high elasticity, high basic strength retention and long-lasting resorption time.
In this context, the use of a triclosan-coated slowly absorbable polydioxanone-based suture material has not been successful in decreasing the risk of SSI. A meta-analysis by Henriksen et al. [ 8 ] concluded that only multifilament triclosan-coated Vicryl ® sutures substantially decrease the risk of SSI following abdominal fascial closure. In the present trial, BMI > 30 kg/m 2 and male gender but not suture technique were risk factors for developing SSI. In sum, it appears that the development of burst abdomen depends on surgical technique and possibly suture material while wound infections are more related to patient factors.
The surgical technique for fascial closure in the ESTOIH trial was highly standardised using study site and video trainings. Adherence to the study protocol is demonstrated by small deviations from the mean stitch length in both treatment groups (Table (Table4). 4 ). The attempted suture-to-wound length ratios were specified based on previous recommendations [ 5 , 6 ] and they were well adhered to in this study (Table (Table4 4 ).
Details of suture technique
Data are mean (SD)
Furthermore, the definition of inclusion and exclusion criteria assured a homogenous patient cohort. Relaparotomy, obesity, abdominal aortic aneurysm, immunosuppression, peritonitis, and emergency surgery had been identified as relevant risk factors for wound healing in previous studies [ 3 , 19 – 22 ] and were, therefore, excluded from the present trial. Following slow recruitment, a protocol amendment was introduced early in the trial allowing obese patients to participate. Participants’ BMI, which is the most prevalent confounder in laparotomy trials, was similar between treatment groups (short stitches: 25.4 kg/m 2 ± 4.2; long stitches: 25.1 kg/m 2 ± 4.1) and comparable to the previously published STITCH trial (median 24 kg/m 2 in both groups) [ 7 ]. On the other hand, open gynaecological procedures are associated with a significantly reduced risk of hernia development [ 23 , 24 ] and were excluded for that reason. Together, these strategies contribute to a high internal validity of results from this study.
External validity of the ESTOIH trial was ensured by the multi-centre setting that included community, regional and university hospitals with a large number of participating surgeons. We chose to perform the study in a general surgical population rather than confining it to an extremely high-risk cohort as in the PRIMA trial [ 22 ] to maintain generalisability. The inclusion of many colorectal procedures (38.8%) ensured an adequate risk profile of our study cohort [ 24 ]. In sum, we believe, that our findings can be generalised to current surgical practice in different situations.
When the short-stitch technique was used, surgeons needed 6 min longer to close abdominal wall, which is acceptable if the procedure proves to be effective. It is an interesting finding of this study, however, that the rate of burst abdomen decreased when the time used for suturing the fascia was longer (independent of stitch technique). This supports the notion that surgical technique is relevant for safe abdominal wall closure.
Admittedly, this trial has some limitations. More patients in the long-stitch group (29 vs 23) dropped out of the study before the visit on day 30, primarily due to re-operations (22 vs 9) which were associated with a greater number of anastomotic leaks (15 vs 6). While it can be excluded that the technique of fascial closure caused these anastomotic leaks or was otherwise the reason for revision surgery except for cases of burst abdomen, the influence of these imbalances on our study results is not clear. The higher drop-out rate in the long-stitch group may have prevented the detection of other complications in these patients.
Furthermore, the longer duration of hospital stays in the long-stitch group may have been caused by the higher frequencies of anastomotic leaks and revision surgery (unrelated to burst abdomen) in this group and not so much by suture technique. Another limitation of this report is the exploratory nature of the secondary outcome analysis for which it was not powered as the predefined primary outcome incisional hernia will be reported when 1-year follow-up has been completed by all patients.
Finally, the long-stitch group was characterised not only by a greater stitch length but also used a double loop suture, which is the current technical standard in many surgical departments. The tissue trauma associated with this technique may be in part a consequence of the double loop with a strong needle and not only stitch length. Using short stitches with a single thread that is a little stronger than USP 2–0 still avoids this kind of tissue trauma and may be a good compromise for those who wish to change their current practice but prefer a more robust suture.
The short-stitch technique for abdominal wall closure potentially reduces the rate of burst abdomen. Furthermore, ultra-long-term absorbable elastic suture material appears to be associated with low wound infection and overall complication rates. Analysis of long-term results of this trial will help clarify the impact of suture technique on hernia development.
Authors contributions
PB and RF designed the trial. MA, PB and RF formed the trial steering committee that took all relevant decisions during the course of the trial. All authors except PB contributed individual patient data. PB performed on-site monitoring visits and data collection. Formal data analysis was performed at Aesculap AG under the supervision of PB and reviewed by MA and RF. MA and RF drafted the manuscript. MW and RF revised the manuscript. All authors have read and approved the final version of the manuscript.
This study was sponsored and funded by B.Braun Surgical SA, Rubi, Spain. The Medical Scientific Affairs department of Aesculap AG was responsible for project management, data management, statistics, study registration and monitoring.
Data and material availability
Declarations.
Participating institutions received case payments from Aesculap AG to cover study costs. P.B. reports personal fees from Aesculap AG during the conduct of the study and outside the submitted work. F.K. reports personal fees from BD Bard outside the submitted work. M.W. received funding from the German Research Association (DFG, 401299842). R.F. reports personal fees from Aesculap AG during the conduct of the study as well as personal fees from Aesculap AG and BD BARD outside the submitted work. The remaining authors declare no other conflicts of interest.
The trial protocol has been approved by institutional review boards (IRBs) at all trial sites. The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
Freely given, informed consent to participate in the study was obtained from all participants before their inclusion in the study.
No personal identifying information is published in this article. Therefore, IRBs did not require explicit consent for publication from individual participants.
No animals were used for this study.
Informed written consent was obtained from all patients before surgery.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
General Surgery

Special Article

Publications

Research Topics
- Biochemistry
- Microbiology
- Pharmacology
- Othopaedics
- Obstetrics and Gynaecology
- Ophthalmology
- Anaesthesia
- Dermatology
- Preventive and Social Medicine

Surgery Thesis Topics for MS /DNB.
Remember Subscribing to the premium thesis topics not only will enable you to browse through premium thesis topics but also you will get access to online guidance about synopsis writing, sample size calculation, inclusion and exclusion criteria and guidance throughout thesis writing. In case you dont subscribe still do not hesitate to contact me for guidance.
Below is the list of 100 free Surgery thesis topics for MD/DNB. You can select any good Surgery thesis topics for MD/DNB from here. For more thesis topics you can avail the service of premium Surgery thesis topics. The premium Surgery thesis topics include list of 2000+ premium and updated Surgery thesis topics as well as recent Surgery topics which has been published in various national and international Surgery journals.
Though Surgery thesis topics can be searched online and for this purpose various Surgery journals can be browsed but its a time consuming process. We have collected all important Surgery thesis topics by painstakingly browsing through past and present issues of Surgery journals. Not only the Surgery journals but also we have compiled the list of all top Surgery thesis topics by physically going through the libraries of various medical colleges.
Needless to say collecting thousands of Surgery thesis topics at one place was a time consuming job. You can browse all these Surgery thesis topics by subscribing to premium Surgery thesis topics. Please share this page with your friends who may be searching for good Surgery thesis topics.
- A study of morbidity associated with temporary loop ileostomy in perforation peritonitis cases
- Investigation of hyperbilirubinemia in amoebic liver abscess patients
- Comparison between ‘Fistulectomy’ and ‘Fistulotomy with marsupialisation’ for treating simple anal fistula: A randomized clinical trial
- Quality of life and rehabilitation requirements of breast cancer survivors
- Assessing lingual mucosal grafts in urethral stricture management
- Correlation between coagulation markers and axillary lymph node metastasis in breast carcinoma
- A clinico-bacteriological examination of post-surgical wound infections
- A controlled examination of risk factors in benign prostatic hyperplasia and prostate carcinoma patients
- Hyperbilirubinemia as a novel diagnostic predictor of gangrenous/perforated appendicitis
- Comparative analysis of elective laparoscopic cholecystectomy with vs. without antibiotic prophylaxis
- Effects of adding levamisole to standard anthracycline-based preoperative chemotherapy on local immune response in invasive breast carcinoma
- Impact of laparoscopic cholecystectomy on gastroesophageal reflux via 24-hour ambulatory esophageal pH monitoring
- The utility of video-assisted thoracoscopic surgery (VATS) in chest trauma patients not improving as expected on tube thoracostomy: A forward-looking clinical trial
- Utility of radioiodine (131 I) uptake and technetium (99m Tc) scans in evaluating thyroid function post-subtotal thyroidectomy for multinodular goitre
- Predicting laparoscopic cholecystectomy challenges using clinical and ultrasonographic criteria
- A prospective, randomized clinical comparison of phytotherapy and potassium citrate in managing mild renal stone disease
- Diagnostic laparoscopy role evaluation in nonspecific abdominal pain patients and its correlation with clinical and imaging findings
- Clinical outcome assessment of laparoscopic anterior partial fundoplication for gastroesophageal reflux disease (GERD)
- Efficacy comparison of ultrasonically activated scalpel (harmonic scalpel)® vs electrocautery in gallbladder removal from the gallbladder bed Role of diagnostic modalities in assessment of Solitary thyroid nodule and management.
- Impact of open tension-free bilateral mesh inguinal hernioplasty on vas deferens functionality
- A comparative study of preservation vs division of ilioinguinal iliohypogastric, and genital nerves during lichenstein hernioplasty.
- A prospective clinical study of acute intestinal obstruction.
- A prospective clinical study of duodenal perforation.
- A prospective clinical study & management of umbilical & para umbilical hernia in adults.
- A prospective clinical study on mass in the right iliac fossa.
- A prospective clinical study of acute appendicitis and evaluation of Alvardo score in the diagnosis”.
- A prospective study on management protocols of lump breast depending on FNAC-excision biopsy and its histopathological correlation.
- A prospective clinical study on gastro intestinal perforation.
- A prospective clinical study on benign thyroid swellings”.
- A prospective clinical study and management of incisional hernia.
- A prospective clinical study of acute peritonitis”.
- A prospective clinical study of benign breast disorders”.
- A prospective clinical study of efficacy of band ligation in the treatment of second-degree haemorrhoids”.
- A prospective clinical study and management of blunt trauma abdomen”.
- A prospective clinical evaluation and management of cholelithiasis”.
- A prospective clinical study and management of varicose veins in the lower limb”.
- Acute intestinal obstruction in adults”
- Comparative study of anatomical repair and lichenstein repair for inguinal hernia.
- Different strategies ( i.v. Lidocaine & gum feeding ) to shorten post surgical ileus — A prospective study.”
- Hyperbilirubinemia and crp as predictors of appendiceal gangrene / perforation — A prospective study
- A clinical study on duodenal perforation”
- A clinical study and different modalities of treatment in ventral hernias.
- Clinico-etio-pathological study of liver abscess.
- Clinical study of acute appendicitis with ference to clinical presentation, treatment and follow up.
- A randomized case control clinical trial to compare antibiotic versus normal saline instillation into the peritoneum in the management of secondary peritonitis.”
- Efficacy of fine needle aspiration cytology in the pathological diagnosis of solitary thyroid nodule.
- Comparative study of laparoscopic and open cholecystectomy for symptomatic stone diseases.
- A prospective study of incidence of malignancy in multi nodular goiters.”
- Evaluation and management of diabetic foot according to wagner’s classification”
- Study on clinical presentation and various modalities of treatment of gall stone disease”
- A clinical study of conventional dressing in diabetic wounds”
- A clinical study of peritonitis
- A clinical study of benign breast disorders”
- A case study of 100 cases of acute abdomen excluding trauma cases with reference to epidemiology and management”
- A clinical study of acute appendicitis and evaluating alvarado score in diagnosis and treatment”.
- Utility of surgical apgar score in predicting post operative morbidity and mortality in general surgical procedures.
- A clinical study of resection and anastomosis of bowel in our surgical practice.
- Role of diagnostic laparoscopy for staging in abdominal malignancies .”
- Clinico pathological study of chronic cervical lymphadenopathy.
- Incidence of SSI in elective abdominal surgery.
- A prospective comparative study of open vs laparoscopic appendicectomy.
- Study of clinical features & management of benign ulcers of the leg & foot.”
- A clinical study of abdominal wound dehiscence.”
- A clinical study of post operative complications of thyroidectomy.”
- A clinical study of hollow viscus perforation. “
- Port site infiltration and intra peritoneal injection of bupivacine vs conventional analgesics in controlling post operative pain following laparoscopic surgeries.”
- Effect of platelet rich plasma on wound healing of leg ulcers. ”
- The study of antibiotic prophylaxis in clean and clean contaminated surgical wounds .”
- Evaluation of upper abdominal pain by upper gastrointestinal endoscopy.”
- Accuracy of ultrasonography in acute and chronic abdominal conditions .”
- Comparative study of topical application of 2% diltiazem and lateral sphincterotomy of chronic fissure in ano. ”
- Clinico pathological study of salivary gland swellings.”
- Role of endoscopic iii ventriculostomy in the comprehensive management of hydrocephalus.”
- A comparative study of clinical findings, ultrasonography and histopathology in benign breast diseases.
- Comparative study between conservative dressings and dressings with papain – urea & silver colloid in case of skin ulcers.
- A case study on post — operative wound infections. “
- A comparative study of open vs laparoscopic hernia repair for umbilical and para umbilical hernia”.
- Evaluation of portsmouth — possum scoring system in assesing the surgical outcome in general surgery patients”.
- A study of uncomplicated inguinal hernia repair as a day care surgery”.
- A clinical study to correlate between cytological and histopathological findings in diagnosis of multinodular goitre”.
- Management of lower limb varicose veins conservatively and surgically based on ceap classification”.
- Comparative study of stainless steel staples closure of skin wound versus 3.0 ethilon closure”.
- Prospective analysis of outcomes in elderly patients undergoing laparotomies for gastro intestinal causes”.
- Clinico pathological study and management of blunt trauma abdomen
- A comparative study of colostrum dressing versus convential dressing in wounds.
- Evaluation of Mannheim’s peritonitis index in patients with peritonitis due to hollow viscus perforation”.
- Comparative study between intermittent & continous suturing in emergency laparotomy”.
- A clinical study comparing pdgf dressing and vac dressing in diabetic ulcer”.
- Clinical study and management of solitary thyroid nodules
- A comparative study of stapler haemorhoidopexy versus open haemorrhoidectomy”.
- Clinical study and management of incisional hernia with mesh repair.
- A clinical study to determine pre-operative predictive factors for difficult laparoscopic cholecystectomy.
- A study of clinical profile and management of non-thyroidal neck swellings.
- A comparative study of serum cholesterol, biiirubin,phospate and calcium in patients with gail stone and normal persons”.
- A clinical study of pancreatitis due to gail stone disease.
- A evaluation of alvarado scoring in diagnosis of acute appendicitis and its correlation with histopathological and operative findings”.
- A clinical study of post operative complications of thyroidectomy.
- A comparative study of percutaneous cathater drainage vs percutaneous needle aspiration in the treatment of liver abscess in teretiary care center.
- A prospective study on factors affecting the outcome in bowel anastamosis in tertiary care center, asram,eluru”.
- An analytical study of clinicopathological and predictive factors in diagnosis, management and outcome in necrotising fascitis”.
- A comparative study of topical phenytoin vs normal saline dressing in the healing of chronic diabetic foot ulcers — a randomized control study”.
- A prospective study comparing the effectiveness of apache ii and mannheim peritonitis index in predecting the outcome in patients with perforative peritonitis”.
- A clinical study of various prognosis factors for better management of diabetic foot.
- Study of breast lumps in females upto 40 years of age.
- A study of patients of HIV presenting with surgical emergencies.
- Clinical study of splenk injury in abdominal trauma and its management.
- A study of abdominal lumps,diagnostic evaluation and operative correlation.
- Study of trauma outcome using the triss method at a tertiary care center.
- Comparison between RTS and GAP scoring systems to predict survival in patients of trauma. (Revised trauma score and Glasgow coma scale- age-pressure)
- A study of the correlation of pre-operative risk factors and complications occuring during and after laparoscopic procedures.
- Study of management of upper gastrointestinal malignancies.
- Clinicopathological study of small bowel and related mesenteric tumours.
- Clinicopathological study and management of breast cancer.
- Role of hyperbaric oxygen therapy in chronic non healing diabetic foot ulcers.
- Neo-adjuvant chemotherapy in locally advanced carcinoma of breast.
- Study of non-Traumatic lower limb amputations.
- A comparative study of three port versus four port techniques in laparoscopic cholecystectomy.
- A prospective study of the common bile duct status during laparoscopic cholecystectomy by using intraoperative cholangiogram.
Disclaimer!
There are many methods of sample size determination. It is one of the first hurdle when someone starts writing a thesis. I have tried to give simplest way of determination of sample size. You need to show the method to your PG teacher before you include this method in your thesis. First confirm from your PG teacher and then only proceed.
- Medical Ebooks
- Health Articles
- Procedure Video

Thesis Topics for MS Surgery ( selected ) AIIMS
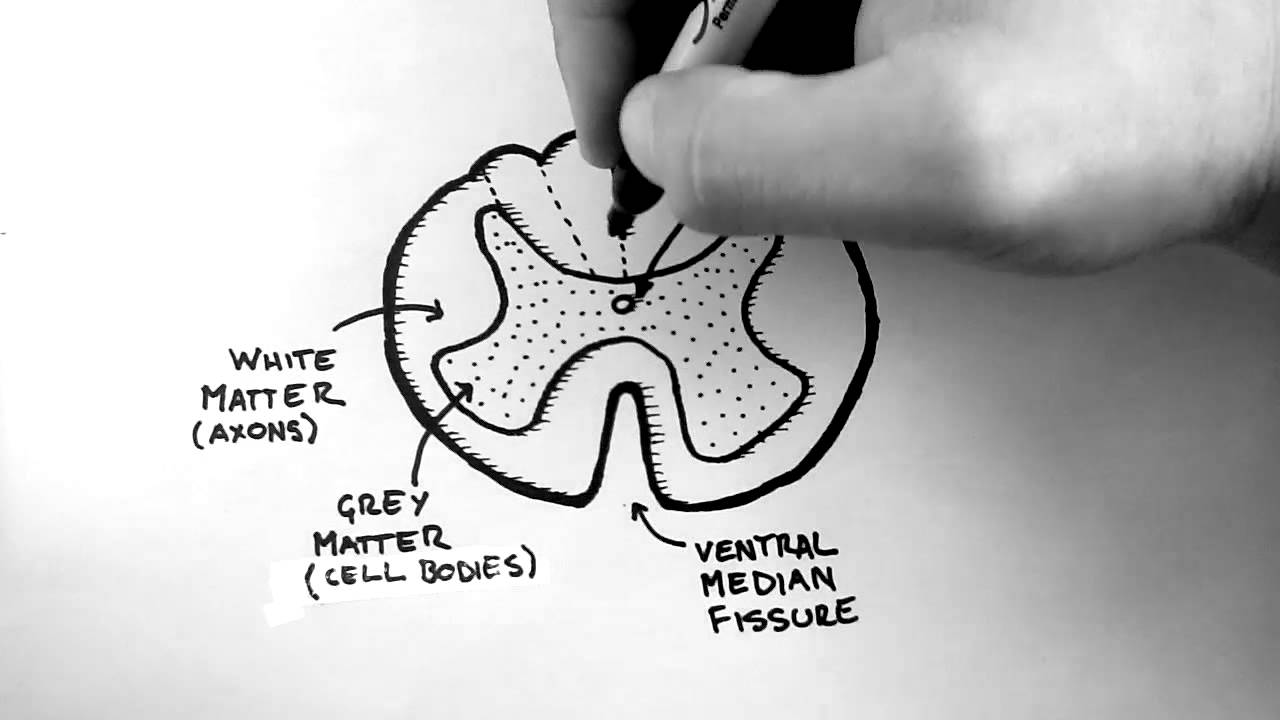
High Yields in Orthopedics |medical study notes
Thesis Topics for MS – Surgery ( selected ) AIIMS
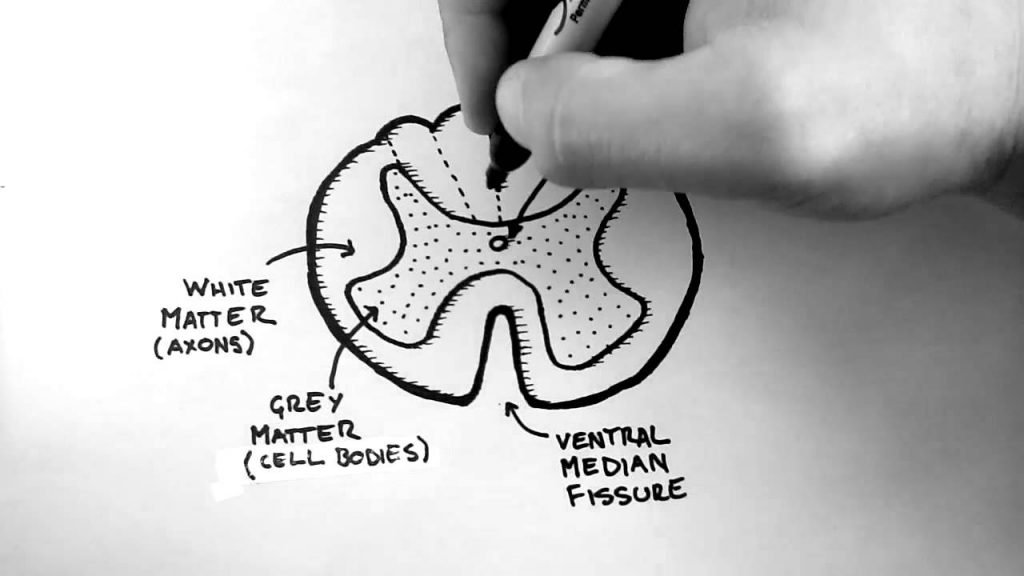
- Accuracy of Sentinel node biopsy in predicting axillary nodal status following neo adjuvant chemotherapy in locally advanced breast cancer. Co -Guide.
- Role of in vitro MR spectroscopy in evaluation of lymph nodes in patients with lymphadenopathy. Co-Guide.
- Effect of bisphosphonates on bone mineral density after renal transplantation as assessed by bone mineral densitometry
- Evaluation of Feasibility and Performance of Minimally invasive Radioguided Parathyroidectomy in Established Cases of Primary Hyperparathyroidism
- Evaluation of the role of Pneumatic Compression Pump in the management of Post-Mastectomy Lymphedema
- Factors affecting incidence of early postoperative complications
- Three port vs. four ports laparoscopic cholecystectomy- A prospective randomized controlled study
- Focused abdominal sonography in trauma (FAST) in patients with blunt trauma abdomen- A prospective study
- Post cholecystectomy symptoms following laparoscopic cholecystectomy
- Ambulatory Laparoscopic hernia repair: A feasibility study
- Evaluation of early outcomes and quality of life after day care conventional inguinal hernia repair
- Role of centchroman in management of mastalgia and fibroadenoma” – a randomized study
- Relationship of Serum TSH with Thyroid Vascularity assessed at operation.
- Advanced Sentinel lymph Node evaluation in breast and head and neck cancers.
- To study the burden of post – operative surgical site infections in clean and clean contaminated operations.
- To evaluate the role of intra – abdominal pressure as a predictor of abdominal wound dehiscence.
- Dyslipidemia and cardiovascular risk factors in renal transplant recipients
- CMV disease in transplantation (Microbiology)
- Total extra peritoneal hernia repair comparison of space creation by direct telescope vs. balloon dissection- A randomized controlled study
- Standardized mesh repair for inguinal hernia- A pilot study
- To study the feasibility of fast track thyroidectomy
- Post operative surgical site infection in clean and clean contaminated operations
- B hCG expression inpatients with benign and malignant breast diseases
- Prospective Study to evaluate the role of Helicobacter pylori in benign and malignant hepatobiliary disease
- “Mammotome guided biopsy for indeterminate breast lesions following fine needle aspiration cytology
- Radical duct excision for nipple discharge (benign breast disease) – its long term follow up.
- Role of Centchroman in regression of Mastalgia and regression of Fibroadenoma and its correlation to histopathology and estrogen and progesterone receptor.
- Safety and efficacy of autologous stem cells in prevention of amputation in patients with chronic critical limb: a randomized multi-centric study.
- Standardized open mesh repair for primary inguinal hernia – A Pilot Study.
- Role of FDG PET-CT in evaluation of axillary lymph node involvement in T1 T2 N0 M0 breast cancer in comparison with Sentinel node Biopsy.
- “Evaluation of neo-adjuvant chemotherapy in locally advanced breast cancer” in collaboration with Department of Radiotherapy, Radiology & Pathology.
- “Sentinel lymph node biopsy for locally advanced breast carcinoma after neoadjuvant chemotherapy” in collaboration with Department of Nuclear Medicine, Pathology, and Radiotherapy.
3. Characterization of thymoma using F18 fluorodeoxyglucose positron emission tomography (FDG PET – CT) and its correlation with histopathology in collaboration with Department of Nuclear Medicine & Pathology. 4. Evaluation of patients with primary mediastinal lymphadenopathy using FDG-PET-CT scan and its correlation with histopathology – A prospective study in collaboration with Medicine, Nuclear Medicine & pathology. 5. Clinical co-relation of ER, PR, HER2 neu expression and BRCA1 gene mutations in Indian breast cancer patients.
Collaborative Research (Ongoing) 1. Quality of life of live related donors ( Nephrology) 2. Molecular typing and detection of Mupirocin and Methicillin Resistant Staph aureus ( Microbiology) 3. Cytokine Gene Polymorphismin Renal Transplant Patients (Transplant Immunology and Immunogenetics) 4. Outcome after laparoscopic cardiomyotomy – early and late” in collaboration with Department of Gastroenterology. 5. Efficacy and feasibility of regional anaesthesia compared to general anaesthesia for totally extraperitoneal laparoscopic inguinal hernia repair in collaboration with Department of Anaesthesiology. 6. “Breast cancer: local tumour staging by MRI and its impact on therapeutic approach” in collaboration with Department of Radiodiagnosis & Pathology. 7. “Evaluation of sentinel lymph nodes in patients with early breast cancer using PET scan in collaboration with Department of Endocrinology, Pathology and Nuclear Medicine 8. Characterization of thymoma using F18 fluorodeoxyglucose positron emission tomography (FDG PET – CT) and its correlation with histopathology in collaboration with Department of Nuclear Medicine & Pathology. 9. Evaluation of patients with primary mediastinal lymphadenopathy using FDG-PET-CT scan and its correlation with histopathology – A prospective study in collaboration with Medicine, Nuclear Medicine & pathology.
Related Post
Breast cancer awareness and early detection, hearing loss. save, surgical site infection prevention a review – dr.rj, oncotype dx – predicts how likely6 cancer comes back or not., related posts.

Early detection of breast cancer aims to reduace mortality and other serious consequences of advanced disease through the early clinical...

Hearing is a gift.hearing is the ability to be able to listen to the external sounds. Hearing loss or hearing...

Anatomy 1 |Usmle step 1 Review Video
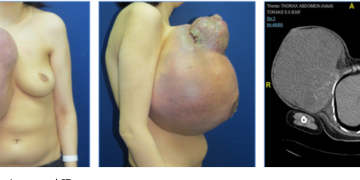
Phyllodes tumors
Phyllodes tumors are rare fibroepithelial lesions that occur in the breast. They are classified as benign, borderline, or malignant. Here’s what...

Fibroadenomas
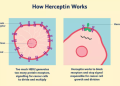
Targeted therapy
Cancer treatment centres in nepal.

Treatment of breast cancer

Bodies in diseases – MBBS Pathology Study Notes
Recent posts.
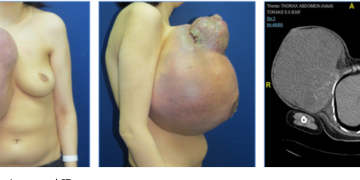
USMLE Step 1 First Aid 2020 30th Edition Free Download
Long cases in general surgery |free ebook download, cardiovascular disorder mcq practice test with answers, special exam patterns – nmc ( nepal medical council ).
© medicospace
Welcome Back!
Login to your account below
Remember Me
Retrieve your password
Please enter your username or email address to reset your password.
- Copyright & Policies
- Privacy Policy

IMAGES
VIDEO
COMMENTS
Dr. Kukreja Barkha Kailashkumar. Dr. Rahul Kenawadekar. "OPEN ANATOMICAL REPAIR V/S LAPAROSCOPIC REPAIR OF UMBILICAL HERNIA USING NO. 1 POLYDIOXANONE SUTURE (PDS), RANDOMIZED CONTROL TRIAL". 2018-2021. Dissertation Topics Ongoing (KLE Academic of Higher Education and Research, Belagavi): Sl No. Name of the PG Student.
Up to one-third of patients with an inguinal hernia have no symptoms from the hernia. Repair of a ventral hernia is a common operation and increasing in frequency. Many operations for hernia are on patients with minimal symptoms but data on outcomes are lacking. The aims of the studies are to: assess the frequency of pain and its effects on
Introduction. Abdominal wall hernia is the most frequently encountered surgical condition that affects all age groups regardless of sex. 1 Globally, the prevalence of abdominal wall hernia was 1.7% for all ages. 2 Abdominal wall hernias are accounting for 15%-18% of all surgical procedures, and annually more than 20 million hernias are operated worldwide. 3-5 Country-specific studies are ...
Introduction: Hernias are one of the most common surgical diagnoses, and general surgical operations are performed. The involvement of patients in the decision making can be limited. The aim of this study was to explore the perspectives of patients around their hernia and its management, to aid future planning of hernia services to maximise patient experience, and good outcomes for the patient ...
important innovation covers the development of tools to improve hernia research. Secondly, prophylactic measures to prevent hernias are an important topic of this thesis. Regarding the performance of hernia research, especially in animals, hardly no guidelines exist.
Obesity is a risk factor for abdominal wall hernia development and hernia recurrence. The management of these two pathologies is complex and often entwined. Bariatric and ventral hernia surgery require careful consideration of physiologic and technical components for optimal outcomes. In this review, a multidisciplinary group of Society of American Gastrointestinal and Endoscopic Surgeons ...
INTRODUCTION. Inguinal hernia is a condition that usually presents as a bulge in the groin due to a protrusion of intra-abdominal content through the abdominal wall [[1], [2], [3]].An inguinal hernia may be asymptomatic but can also be a cause of pain and discomfort, which can significantly worsen quality of life (QoL) [[4], [5], [6]].If symptomatic, an inguinal hernia may be treated by ...
An abdominal wall hernia is an abnormal protrusion of a peritoneal-lined sac through the musculo-aponeurotic covering of the abdomen. 1 The most common variety is groin hernias, of which inguinal hernias (direct and indirect) are far more common than femoral hernias. Hernias of the abdominal wall are quite common, having a prevalence of 1.7% for all ages and 4% for those older than 45 years.
Patient demographics, hernia characteristics, operative and perioperative findings, and postoperative complications were systematically recorded and analyzed. Results: We evaluated 92 cases (n = 92), 46 in each group. Mean age, sex, BMI, location of hernia, primary and incisional hernia, and comorbidity were comparable in both the groups.
Trial 1. Chronic pain persists in most patients who report severe or very severe pain at three months after hernia repair and has a significant effect on patients' daily activities and quality of life. Of those with chronic severe pain at 3 months, 71% did not report severe or very severe pain at 2 ½ years follow up.
The postoperative complication rates of 3.2% for umbilical hernia and 3.5% for epigastric hernia were significantly lower than for incisional hernia, at 9.2% (p < 0.0001).
Internal hernias are rare clinical entities. They are potentially life-threatening, yet often neglected and sometimes misdiagnosed surgical conditions. Herein, we report five different cases of internal hernia in adults aged 29-42 years. These include one case each of right and left paraduodenal hernia, two cases of broad ligament hernia and one case of post lower segment caesarean section ...
Groin hernia repair is one of the most commonly performed surgical procedures. However, the optimal surgical procedure remains controversial [].Moreover, each procedure includes some technical variations: surgical approach [], mesh types [], mesh fixation modalities [], mesh no fixation [], and attitude regarding the hernia sac [].These varieties were developed to reduce postoperative ...
The recently developed Hybrid Hernia Repair technique (HHR), an adaptation of the laparoscopic method, has been proposed as a potential alternative for the treatment of complex Incisional Ventral Hernias (IVH). While single-arm studies have reported promising outcomes, a comprehensive meta-analysis affirming these benefits is lacking. This meta-analysis aims to compare the clinical outcomes of ...
Defect Size Wise Distribution. In our study, the def ect size of incisional hernia in the abdom-. inal wall was calculated b y ultrasonography and was noted. less than 2 cm in 5 patients (12.5% ...
150 cases of ventral hernia 105 (70%) were incisional hernia, 30 (20%) were para-umbilical hernia and 15 (10%) were epigastric hernia. The occurrence of ventral hernia is more common in females (80.2%). Among incisional hernia, out of 105 cases, 101 were females and 4 were males. Among 15 cases of epigastric hernia, 10 cases studied were male
In this thesis, an analysis of the causes of small bowel obstruction after laparoscopic Roux-en-Y gastric bypass (LRYGB) is presented, looking specifically at internal hernia formation. A detailed account of the presentation and radiological findings of internal hernia following laparoscopic gastric bypass is provided.
Data are available for 5 years at a third party website. The trial protocol has been published with open access in the journal Trials: Fortelny RH, Baumann P, Thasler WE, et al. Effect of suture technique on the occurrence of incisional hernia after elective midline abdominal wall closure: study protocol for a randomised-controlled trial.
Thesis Topics on Hernia - Free download as PDF File (.pdf), Text File (.txt) or read online for free.
Join ResearchGate to discover and stay up-to-date with the latest research from leading experts in incisional hernia and many other scientific topics. Join for free. ResearchGate iOS App.
A prospective study of the common bile duct status during laparoscopic cholecystectomy by using intraoperative cholangiogram. A comparative study of three port versus four port techniques in laparoscopic cholecystectomy. List of more than 12000 premium general surgery thesis topics for MS/DNB to choose from.
title (plan of thesis) (session 2016-2019) page 1 of 4 s.no. title (plan of thesis) 1. clinical evaluation of vasculopathy in diabetic foot and its impact on surgical outcomes. 2. critical evaluation of role of usg and ct in guiding surgical management of clinically negative neck (cn0) in carcinoma oral cavity. 3.
9. Evaluation of patients with primary mediastinal lymphadenopathy using FDG-PET-CT scan and its correlation with histopathology - A prospective study in collaboration with Medicine, Nuclear Medicine & pathology. Tags: AIIMS Research Topics general surery topics ms surgery topics research topics surgery thesis Surgery Thesis Titles thesis topics.