Advertisement

Tubercular laryngitis: case series
- Main Article
- Published: 28 January 2009
- Volume 60 , pages 331–334, ( 2008 )
Cite this article

- Rajat Bhatia 1 ,
- Saurabh Varshney 1 ,
- S. S. Bist 1 ,
- Rakesh K. Singh 1 ,
- Nitin Gupta 1 &
- Pratima Gupta 1
50 Accesses
2 Citations
Explore all metrics
Introduction
Tubercular laryngitis is a known entity since a long time but it’s presentation, diagnosis and management has undergone a drastic makeover after the advent of chemotherapy in the form of ATT (Anti tubercular treatment), modernized diagnostic aids and early detection of lesions.
Materials and methods
This prospective study was conducted on 180 patients. Each patient were subjected to detailed history and thorough ENT and head neck examination including laryngeal examination by visualization of the vocal cords, possibly using indirect laryngoscopy,. exible naso-laryngoscopy or rigid laryngoscopy Results Tubercular laryngitis was clinically diagnosed by laryngeal endoscopy and diagnosis con. rmed by laryngeal biopsy.
All patients showed remarkable improvement with anti-tubercular treatment.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others
Primary Laryngeal Tuberculosis: A Series of 15 Cases
Laryngeal Tuberculosis: Current Patterns of Presentation and Management
Association of laryngeal and nasopharyngeal tuberculosis: a case report
Gaelyn GC (1999) Hoarseness. Medical Clinics of North America 83:115–123
Article Google Scholar
Orton HB (1941) Aetiology of hoarseness of voice. Laryngoscope 41:123–175
Google Scholar
Varshney S, Hasan SA (1995) Clinico — Histopathological study of Laryngeal Biopsies. SDMH Journal 19:140–141
Kulkarni N, Gopal GS, Ghaisas SG (2001) Epidemiological considerations and clinical features of ENT Tuberculosis 115:555–558
CAS Google Scholar
Essad M (2001) Laryngeal tuberculosis: Apropos of 15 cases. Rev Laryngol Otol 122:125–128
Gaelyn GC (1999) Hoarseness; Medical Clinics of North America 83:115–123
Kleinsasser O (1982) Pathogenesis of vocal cord polyps. Annals of Otorhinolaryngol 91:378–381
Shin (2000) Changing trends in clinical manifestations of laryngeal tuberculosis. Laryngoscope 110(11):1950–1953
Article PubMed CAS Google Scholar
Farooq A (1994) The Larynx in Pulmonary Kocks. Indian Medical Gazette 361–362
Parikh Nimish P (1991) Aetiological study of 100 cases of hoarseness of voice. Indian Journal of Otolaryngolog 43: 71–73
Rupa V, Bhanu TS (1989) Laryngeal Tuberculosis in the eighties-An Indian Experience. J Laryngol Otol 103: 864–868
PubMed CAS Google Scholar
Galleti F, Freni F, Bucolo S, Spano F, Gambadoro O, Pispica L et al (2000) Laryngeal Tuberculosis: Considerations on the most recent clinical and epidemiological data and presentation of a case report. Acta Otorhinolaryngol Ital 20:196–201
Download references
Author information
Authors and affiliations.
Department of ENT and Microbiology, Himalayan Institute of Medical Sciences, Jolly Grant, Doiwala Dehradun, 248140, Uttarakhand, India
Rajat Bhatia, Saurabh Varshney, S. S. Bist, Rakesh K. Singh, Nitin Gupta & Pratima Gupta
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Saurabh Varshney .
Rights and permissions
Reprints and permissions
About this article
Bhatia, R., Varshney, S., Bist, S.S. et al. Tubercular laryngitis: case series. Indian J Otolaryngol Head Neck S 60 , 331–334 (2008). https://doi.org/10.1007/s12070-008-0111-0
Download citation
Published : 28 January 2009
Issue Date : December 2008
DOI : https://doi.org/10.1007/s12070-008-0111-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Tubercular laryngitis
- Laryngoscopy
- Find a journal
- Publish with us
- Track your research
Laryngitis case study one
Please help WikiDoc by adding content here. It's easy! Click here to learn about editing.
- Needs content
- Inflammations
- Otolaryngologic Disease
- Otolaryngology
- Pulmonology
- Emergency mdicine
- Infectious disease
Navigation menu
We have a new app!
Take the Access library with you wherever you go—easy access to books, videos, images, podcasts, personalized features, and more.
Download the Access App here: iOS and Android . Learn more here!
- Remote Access
- Save figures into PowerPoint
- Download tables as PDFs

4: Pharyngitis
Frank S. Yu; Jonathan C. Cho
- Download Chapter PDF
Disclaimer: These citations have been automatically generated based on the information we have and it may not be 100% accurate. Please consult the latest official manual style if you have any questions regarding the format accuracy.
Download citation file:
- Search Book
Jump to a Section
Patient presentation.
- Full Chapter
- Supplementary Content
Chief Complaint
“Mommy, my throat is on fire!”
History of Present Illness
JT is a 7-year-old Chinese American female, accompanied by her mother, who presents to the community pharmacy with complaints of sore throat and fever, looking for medications to take to relieve her symptoms. She is fussy and describes the pain when she swallows as feeling if her throat is “on fire.” Her symptoms began yesterday morning, and she has only tried drinking a pei pa koa syrup containing medicinal herbs (main active herb is elm bark) and honey to relieve the sore throat. This provided some relief but the pain has been getting worse. She did not have a temperature taken, but her forehead was hot to the touch. She was not given any medications to relieve the fever. She was dressed with additional clothing and blankets to “sweat the fever out,” but the fever still persisted. She reports that there may have been other sick classmates. She denies a prior history of sore throat.
Past Medical History
Attention-deficit disorder, recurrent otitis media (resolved)
Surgical History
Family history.
Non-contributory

Social History
Ear tubes at age 2
Amoxicillin (throat swelling, difficulty breathing)
Home Medications
Methylphenidate ER 18 mg PO daily
Physical Examination
Vital signs.
Temp 101.9°F (oral), Ht 4′4″, Wt 29.55 kg
Appears uncomfortable, tired, grimacing when swallowing
Anterior cervical lymph nodes enlarged and tender; tonsils moist, red, with white exudates
Point-of-Care GAS Rapid Antigen Detection Test
1. What is the most common pathogen responsible for acute bacterial pharyngitis in children?
A. Corynebacterium diphtheriae
B. Neisseria gonorrhoeae
C. Group C streptococcus
D. Group A streptococcus
2. What signs and symptoms in this patient definitely discriminate between GAS pharyngitis rather than viral pharyngitis?
A. Tonsils with white exudates
B. Temperature 101.9°F
C. Pain on swallowing
D. All of the above
3. If GAS is suspected, what age range is typically excluded for testing for GAS?
Sign in or create a free Access profile below to access even more exclusive content.
With an Access profile, you can save and manage favorites from your personal dashboard, complete case quizzes, review Q&A, and take these feature on the go with our Access app.
Pop-up div Successfully Displayed
This div only appears when the trigger link is hovered over. Otherwise it is hidden from view.
Please Wait
Clinical Practice and Cases in Emergency Medicine
A 45-year-old Female with an Atypical Presentation of Pharyngitis
- Schander, Artur ;
- Glickman, Andrew A. ;
- Weber, Nancy ;
- Rodgers, Brian ;
- Carney, Michael B.
Published Web Location
Introduction: Emergency physicians are trained to treat a variety of ailments in the emergency department (ED), some of which are emergent, while others are not. A common complaint seen in the ED is a sore throat. While most sore throats are easily diagnosed and treated, less common causes are often not considered in the differential diagnoses. Therefore, the purpose of this case study was to present an atypical case of sore throat and discuss differential diagnoses.
Case Presentation: The patient was a 45-year-old female who presented to the ED with a three-day history of sore throat that was exacerbated by eating and drinking. The patient was not on any prescription medications, but tried over-the-counter medications for the sore throat without any improvement in symptoms. Review of systems was positive for sore throat, fevers, and chills. Physical examination of her oropharynx revealed mildly dry mucous membranes with confluent plaques and white patchy ulcerative appearance involving the tongue, tonsils, hard palate, and soft palate. Rapid streptococcal antigen, mononucleosis spot test, and KOH test were performed and found to be negative.
Discussion: After initial testing was negative, a follow-up complete blood count with differential and complete metabolic profile were ordered. The patient was found to have decreased lymphocytes and platelets. Based upon those results, a diagnosis was made in the ED, the patient was started on medication, and further laboratory workup was ordered to confirm the diagnosis. ED providers should consider non-infectious as well as infectious causes for a sore throat, as this might lead to a diagnosis of an underlying condition.
Enter the password to open this PDF file:
Advertisement
Supported by
Hot Oceans Worsened Dubai’s Dramatic Flooding, Scientists Say
An international team of researchers found that heavy rains had intensified in the region, though they couldn’t say for sure how much climate change was responsible.
- Share full article

By Raymond Zhong
Scenes of flood-ravaged neighborhoods in one of the planet’s driest regions stunned the world this month. Heavy rains in the United Arab Emirates and Oman submerged cars, clogged highways and killed at least 21 people. Flights out of Dubai’s airport, a major global hub, were severely disrupted.
The downpours weren’t a total surprise — forecasters had anticipated the storms several days earlier and issued warnings. But they were certainly unusual.
Here’s what to know.
Heavy rain there is rare, but not unheard-of.
On average, the Arabian Peninsula receives a scant few inches of rain a year, although scientists have found that a sizable chunk of that precipitation falls in infrequent but severe bursts, not as periodic showers. These rains often come during El Niño conditions like the ones the world is experiencing now.
U.A.E. officials said the 24-hour rain total on April 16 was the country’s largest since records there began in 1949 . And parts of the nation had already experienced an earlier round of thunderstorms in March.
Oman, with its coastline on the Arabian Sea, is also vulnerable to tropical cyclones. Past storms there have brought torrential rain, powerful winds and mudslides, causing extensive damage.
Global warming is projected to intensify downpours.
Stronger storms are a key consequence of human-caused global warming. As the atmosphere gets hotter, it can hold more moisture, which can eventually make its way down to the earth as rain or snow.
But that doesn’t mean rainfall patterns are changing in precisely the same way across every part of the globe.
In their latest assessment of climate research , scientists convened by the United Nations found there wasn’t enough data to have firm conclusions about rainfall trends in the Arabian Peninsula and how climate change was affecting them. The researchers said, however, that if global warming were to be allowed to continue worsening in the coming decades, extreme downpours in the region would quite likely become more intense and more frequent.
Hot oceans are a big factor.
An international team of scientists has made a first attempt at estimating the extent to which climate change may have contributed to April’s storms. The researchers didn’t manage to pin down the connection precisely, though in their analysis, they did highlight one known driver of heavy rain in the region: above-normal ocean temperatures.
Large parts of the Indian, Pacific and Atlantic Oceans have been hotter than usual recently, in part because of El Niño and other natural weather cycles, and in part because of human-induced warming .
When looking only at El Niño years, the scientists estimated that storm events as infrequent as this month’s delivered 10 percent to 40 percent more rain to the region than they would in a world that hadn’t been warmed by human activities. They cautioned, however, that these estimates were highly uncertain.
“Rainfall, in general, is getting more extreme,” said Mansour Almazroui, a climate scientist at King Abdulaziz University in Jeddah, Saudi Arabia, and one of the researchers who contributed to the analysis.
The analysis was conducted by scientists affiliated with World Weather Attribution, a research collaboration that studies extreme weather events shortly after they occur. Their findings about this month’s rains haven’t yet been peer reviewed, but are based on standardized methods .
The role of cloud seeding isn’t clear.
The U.A.E. has for decades worked to increase rainfall and boost water supplies by seeding clouds. Essentially, this involves shooting particles into clouds to encourage the moisture to gather into larger, heavier droplets, ones that are more likely to fall as rain or snow.
Cloud seeding and other rain-enhancement methods have been tried around the world, including in Australia, China, India, Israel, South Africa and the United States. Studies have found that these operations can, at best, affect precipitation modestly — enough to turn a downpour into a bigger downpour, but probably not a drizzle into a deluge.
Still, experts said pinning down how much seeding might have contributed to this month’s storms would require detailed study.
“In general, it is quite a challenge to assess the impact of seeding,” said Luca Delle Monache, a climate scientist at the Scripps Institution of Oceanography in La Jolla, Calif. Dr. Delle Monache has been leading efforts to use artificial intelligence to improve the U.A.E.’s rain-enhancement program.
An official with the U.A.E.’s National Center of Meteorology, Omar Al Yazeedi, told news outlets that the agency didn’t conduct any seeding during the latest storms. His statements didn’t make clear, however, whether that was also true in the hours or days before.
Mr. Al Yazeedi didn’t respond to emailed questions from The New York Times, and Adel Kamal, a spokesman for the center, didn’t have further comment.
Cities in dry places just aren’t designed for floods.
Wherever it happens, flooding isn’t just a matter of how much rain comes down. It’s also about what happens to all that water once it’s on the ground — most critically, in the places people live.
Cities in arid regions often aren’t designed to drain very effectively. In these areas, paved surfaces block rain from seeping into the earth below, forcing it into drainage systems that can easily become overwhelmed.
One recent study of Sharjah , the capital of the third-largest emirate in the U.A.E., found that the city’s rapid growth over the past half-century had made it vulnerable to flooding at far lower levels of rain than before.
Omnia Al Desoukie contributed reporting.
Raymond Zhong reports on climate and environmental issues for The Times. More about Raymond Zhong
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.15(10); 2023 Oct
- PMC10624933

Navigating the Complexities of Laryngeal Tuberculosis: A Comprehensive Case Report and Literature Review
Araya gautam.
1 School of Health Sciences, Teesside University, Middlesbrough, GBR
Harendra Kumar
2 Medicine and Surgery, Dow University of Health Sciences, Karachi, PAK
Abubakar Gapizov
3 General Surgery, American University of Antigua, Coolidge, ATG
Pratik Paudel
4 Neurology, Annapurna Neuro Hospital, Kathmandu, NPL
Rakshya Gautam
5 Internal Medicine, Alka Hospital, Lalitpur, NPL
This case report and literature review presents a detailed exploration of the diagnosis and management of laryngeal tuberculosis, emphasizing the challenges encountered in dealing with rare and multifaceted medical conditions. Through a systematic analysis of the patient's clinical journey and an insightful review of pertinent literature, the study underscores the complexity inherent in diagnosing primary laryngeal tuberculosis and highlights the growing relevance of this rare extrapulmonary manifestation. The case showcases the significance of a comprehensive diagnostic approach, the collaboration of diverse medical specialists, adherence to established treatment guidelines, and the crucial role of continuous patient monitoring. The successful resolution of this intricate case serves as a compelling testament to the power of interdisciplinary coordination and precision medicine, providing valuable insights into navigating the intricate landscape of laryngeal tuberculosis.
Introduction
Laryngeal tuberculosis (TB), a rare and neglected disease, has a misdiagnosis rate of up to 80% due to the lack of specific signs or symptoms [ 1 ]. Nevertheless, it has evolved to become the most prevalent granulomatous condition in endemic countries affecting the larynx, predominantly impacting men aged 40-60 years [ 1 ].
Several risk factors contribute to the likelihood of upper respiratory tract TB infection, including HIV infection, tobacco use, diabetes, recreational drug consumption, malignancies, and immunosuppressive drug utilization. In the realm of laryngeal infection, the disease primarily affects the anterior laryngeal structures, which are the parts of the larynx that are located in the front of the neck. They include the thyroid cartilage, the epiglottis, the vocal cords, and the vestibular folds materializing as hypertrophic, exophytic, or polypoid lesions [ 1 , 2 ]. The prevalence of hypertrophic, exophytic, or polypoid lesions in upper respiratory tract TB infection is not very well documented in the literature. However, some studies have reported the occurrence of these lesions in patients with laryngeal TB, which is a rare form of extrapulmonary TB that affects the anterior laryngeal structures. These lesions can cause symptoms such as hoarseness, dysphonia, dysphagia, odynophagia, and hemoptysis [ 1 , 2 ]
Vocal cords bear the brunt in 50-70% of cases, while false cords are implicated in 40-50% of cases. These critical anatomical regions are vulnerable to inflammation during severe infections, culminating in airway obstruction. The ensuing consequence is rapid respiratory distress, which can escalate to respiratory failure if not promptly identified and managed with appropriate measures [ 2 , 3 ].
The current case demonstrates the complicated diagnostic challenges presented by seemingly disparate symptoms and medical histories. The medical team successfully navigated these problems with a deliberate approach, interdisciplinary collaboration, and a commitment to evidence-based principles.
Case presentation
A 24-year-old Filipino male presented with a chief complaint of difficulty breathing. Past medical history includes bronchial asthma. Family history reveals bronchial asthma in his mother and brother; his mother also had Pott's disease but had been refusing anti-TB treatment. The patient was a driver and egg dealer, residing in a bungalow-type dwelling with his wife, with a history of smoking (nine pack-years) and occasional alcohol consumption (one to two sessions per month). He did not chew betel nuts and used liquefied petroleum gas for cooking at home.
Two years prior to the presentation, he had experienced sudden onset epigastric discomfort with burning pain, which reached an intensity of 5/10 and ascended to his throat. This pain worsened during fasting but was relieved by food intake. He occasionally vomited non-bilious, non-bloody contents after meals. After a visit to a rural health center, he was diagnosed with "hyperacidity" and received unspecified medications that provided temporary relief. Over the following months, he endured persistent epigastric pain but did not seek medical attention. Seven months prior, he developed intermittent, rough, breathy hoarseness that worsened with exertion but improved with voice rest. A private ENT physician diagnosed laryngopharyngeal reflux, and treatment with omeprazole and an unrecalled nasal spray offered temporary relief. As the hoarseness persisted, it led to another ENT consultation, which revealed a suspicious laryngeal mass.
Despite a recommended laryngeal CT scan, the patient's symptoms improved, but he continued to experience hoarseness. Additionally, he began to experience episodes of noisy, wheezy breathing without apparent triggers, requiring salbutamol nebulization at a local hospital. Three weeks prior to presentation, the frequency of hoarseness and breathing difficulties increased, prompting a visit to a district hospital, where he was evaluated as a probable pulmonary (PTB) suspect, with negative direct sputum smear microscopy (DSSM) results and no initiation of anti-TB medications. Shortly before admission, he developed sudden dyspnea, leading to initial evaluation by the Internal Medicine service, which attempted but failed emergency intubation. Subsequently, he was referred to anesthesiology for a challenging intubation and to the ENT service for possible emergency tracheostomy, resulting in his admission.
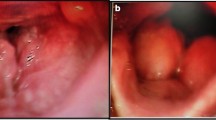
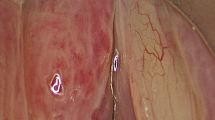
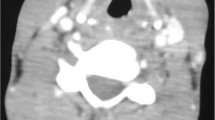
In pursuit of an accurate diagnosis, a systematic approach was adopted. Traumatic causes, inhalation injury, neoplasms, and oropharyngeal obstruction were ruled out through detailed clinical examination and laryngoscopic findings. Table Table1 1 shows the complete blood count and differential count results. The initial chest X-ray as shown in Figure Figure1 1 revealed bilateral hilar lymphadenopathy and normal lung parenchyma. Comprehensive imaging, including chest and neck CT, displayed extensive mediastinal lymphadenopathy encasing the trachea, suggesting impending upper airway obstruction.
MCV: mean corpuscular volume; MCH: mean corpuscular hemoglobin; MCHC: mean corpuscular hemoglobin concentration

Laryngoscopy as shown in Figure Figure2 2 revealed diffuse edema, erythema, ulcers, and immobility of vocal cords, consistent with TB laryngitis, a type of extrapulmonary TB affecting the larynx. The pathophysiology of laryngeal TB was discussed, focusing on Mycobacterium tuberculosis transmission through inhalation and subsequent inflammation causing edema, ulcers, and vocal cord immobility. Mediastinal lymphadenopathy's impact on the recurrent laryngeal nerve and cricoarytenoid joint's implications were emphasized.

Airway security was paramount due to potential complications of laryngeal TB. Immediate measures, including tracheal intubation, were taken to ensure respiratory support in case of airway obstruction. A multidisciplinary team, comprising pulmonologists and infectious disease specialists, collaborated in patient care. Following the National TB Program guidelines for extrapulmonary TB, the patient received a four-drug regimen: isoniazid, rifampicin, pyrazinamide, and ethambutol. Liver function and side effects were closely monitored. During hospitalization, the patient's laryngeal edema and respiratory symptoms improved significantly. After two months of anti-TB treatment, repeat laryngoscopy demonstrated regression of ulcerations and improved vocal cord mobility. The patient completed the six-month anti-TB treatment without adverse effects. Six-month and one-year follow-up appointments post-treatment revealed sustained improvement, and the patient remained asymptomatic throughout this period.
Mycobacterium tuberculosis causes TB, an infectious disease characterized by granulomas [ 1 , 2 , 4 ]. While it mostly affects the lungs, resulting in PTB, it can also affect extrapulmonary areas such as the larynx [ 5 ]. This disease is a significant public health concern in developing countries, particularly in the lungs, which account for 80% of cases [ 4 , 6 ]. Nonetheless, it can cause damage to any part of the body.
Primary laryngeal TB is an uncommon kind of extrapulmonary TB that accounts for fewer than 1% of all TB cases [ 4 , 6 , 7 ]. However, due to a rise in the number of immunocompromised individuals and the prevalence of multidrug-resistant TB, cases of laryngeal TB have become increasingly common [ 7 ]. Extrapulmonary TB accounts for around 30-40% of cases and may affect a variety of organs including eyes, ears, heart, and adrenal glands [ 4 , 6 , 7 ]. TB may affect the larynx, despite the fact that it is seldom addressed. Due to laryngeal inflammation and granulations, laryngeal TB may cause a range of symptoms, from slight voice hoarseness to severe discomfort while swallowing (odynophagia) and difficulty breathing (dyspnea) [ 8 , 9 ]. Given the global resurgence of TB, which is being fueled in part by the spread of HIV, healthcare practitioners and ENT specialists should be aware of the possibility of TB in the larynx [ 9 - 11 ].
While laryngeal TB is rare, it presents a difficult diagnostic challenge due to symptoms that are similar to those of many other respiratory disorders. Early symptoms such as inspiratory stridor, dyspnea, and hoarseness might have been readily attributed to more common illnesses such as vocal cord dysfunction, laryngopharyngeal reflux, or even obstructive sleep apnea [ 7 , 9 , 12 ]. His medical history, however, painted a more convoluted picture, with a history of bronchial asthma, a family history of Pott’s disease, and smoking habits.
The presence of constitutional symptoms such as fatigue, weight loss, and nocturnal sweats complicated the diagnosis even further. A focused technique proved critical in traversing this thick maze of symptoms. After ruling out traumatic causes, inhalation injuries, neoplasms, and oropharyngeal obstructions, the diagnostic range was narrowed to TB-related disease. The presence of bilateral hilar lymphadenopathy on the initial chest X-ray served as a significant clue, shifting the focus of the diagnosis to possible mediastinal involvement. Following extensive imaging, including chest and neck CT scans, substantial mediastinal lymphadenopathy encasing the trachea was seen, raising concerns about imminent upper airway obstruction. Laryngoscopy confirmed the diagnosis, revealing typical TB laryngitis symptoms such as widespread edema, erythema, ulceration, and vocal cord immobility.
With the possibility of an impending airway obstruction, maintaining the patient’s airway security became a top concern. Swift and urgent actions, such as tracheal intubation and standby surgical airway management, were critical in preventing respiratory distress. The collaborative efforts of pulmonologists and infectious disease specialists were critical in developing a comprehensive and effective treatment approach. This regimen, which included isoniazid, rifampicin, pyrazinamide, and ethambutol, not only targeted the causative agent Mycobacterium tuberculosis but also aimed to reduce the development of drug resistance. As the foundation of the treatment plan, rigorous and consistent monitoring of liver function and potential side effects was devised, ensuring patient safety and drug adherence.
Investigating the pathophysiology of laryngeal TB unveils the intricate interplay of the immune system's reactions. Inhaling Mycobacterium tuberculosis causes an inflammatory cascade that results in vocal cord swelling, ulceration, and eventual paralysis [ 3 , 11 , 12 ]. The addition of mediastinal lymphadenopathy adds another layer of complexity, potentially jeopardizing critical structures including the recurrent laryngeal nerve and the cricoarytenoid joint.
The trajectory of the patient's clinical growth throughout the treatment journey attests to the management technique's efficacy. There were noticeable reductions in laryngeal edema and respiratory symptoms two months after starting the anti-TB regimen. A second laryngoscopy revealed ulcer regression and significant improvement in vocal cord mobility, confirming the effectiveness of the chosen treatment approach.
Conclusions
This report provides a comprehensive examination of the diagnosis and treatment of laryngeal TB, shedding insight into the complexities associated with unusual and different medical conditions. The current case exemplifies the difficulties in diagnosing primary laryngeal TB and demonstrates the growing relevance of this uncommon extrapulmonary presentation. It emphasizes the need for a thorough diagnostic approach, collaboration among many medical specialists, adherence to established treatment procedures, and the critical significance of continued patient monitoring. The successful resolution of this tough case is a dramatic testament to the efficacy of multidisciplinary collaboration and precision medicine, providing critical insights for negotiating the complex environment of laryngeal TB. The case highlights the need to take a logical and collaborative approach when dealing with such complex medical concerns, which finally leads to a positive outcome for the patient.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study

IMAGES
VIDEO
COMMENTS
Jun 15, 2020 •. 63 likes • 44,361 views. saheli chakraborty. Laryngitis and nursing management of patient with laryngitis. Health & Medicine. 1 of 40. Download now. Download to read offline. Laryngitis - Download as a PDF or view online for free.
Introduction. Acute infectious laryngitis is one of the most com-mon disorders of the larynx and is often associated with upper respiratory tract infections (URIs), as reported more than a decade ago in a Cochrane re-view.1 Laryngeal inflammation can cause hoarseness, sore throat, and dificulty swallowing.
Patients with laryngitis may also experience odynophonia, dysphagia, odynophagia, dyspnea, rhinorrhea, postnasal discharge, sore throat, congestion, fatigue, and malaise. [ 2] The patient's vocal symptoms usually last 7-10 days. If symptoms persist longer than 3 weeks, a workup for chronic laryngitis should be performed. Next: Physical.
1 of 22. Download Now. Download to read offline. Acute laryngitis. 1 Acute Laryngitis Author: Arvils. 2 Inflammatory process. 3 Etiopathogenesis Caused by »Viral. 4 Loss of. 5 Diagnosis of.
Laryngitis refers to inflammation of the larynx and can present in both acute and chronic forms. [1] Acute Laryngitis is often a mild and self-limiting condition that typically lasts for a period of 3 to 7 days. If this condition lasts for over 3 weeks, then it is termed as chronic laryngitis.
Laryngitis. Oct 7, 2019 • Download as PPTX, PDF •. 3 likes • 5,778 views. Manikandan T. BSC NURSING III YEAR. Health & Medicine. 1 of 5. Download now. Laryngitis - Download as a PDF or view online for free.
A total of 121 patients with acute laryngitis treated in our hospital from January 2016 to December 2018 were selected as subjects. The sex and age distribution of the selected subjects was as; 83 males and 38 females, 36 patients aged. 4 months-1 year, 61 patients aged 1-3 years, 10 patients aged 3-4 years, and only 13 cases were over 4 ...
Although acute laryngitis is common, it is often managed by primary physicians. Therefore, video images documenting its signs are scarce. This series includes 7 professional voice users who previously had undergone baseline strobovideolaryngscopy (SVL) during routine examinations or during evaluations for other complaints and who returned with acute laryngitis.
In a case-control study of 40 adults with hoarseness and symptoms of upper respiratory tract infection, 55% of the patients and 14% of controls had M. catarrhalis isolated from a nasopharyngeal culture. 15 Haemophilus influenzae was the second most frequently recovered bacterial pathogen from patients with laryngitis (8% to 20%), which suggests ...
The thorough knowledge of laryngeal anatomy is key in the understanding pathophysiology of laryngeal disorders. It is very important for physician to have a detailed idea about infectious and inflammatory laryngeal pathologies. Early diagnosis and timely management of those conditions are important to secure voice and a patent airway of patients.
A previously healthy 4-year-old female is seen at a local urgent care with 2 days of fever to 104 °F, fatigue, myalgias, runny nose, cough, hoarse voice, and pain with speaking. A nasopharyngeal swab is positive for influenza A virus. She is diagnosed with influenza infection with associated laryngitis and discharged home with supportive care.
Introduction Tubercular laryngitis is a known entity since a long time but it's presentation, diagnosis and management has undergone a drastic makeover after the advent of chemotherapy in the form of ATT (Anti tubercular treatment), modernized diagnostic aids and early detection of lesions. Materials and methods This prospective study was conducted on 180 patients. Each patient were ...
Nowadays LTB is a rare presentation of TB, ... Articles in which these data were missing have been excluded from the study. Ten case series were included in the analysis, for a total of 308 cases. Results. ... (TB, sarcoidosis, fungal laryngitis and Wegener granulomatosis), the patient was evaluated by a pneumologist who prescribed a sputum ...
Case Studies Case #1. Laryngitis case study one On the Web Most recent articles. Most cited articles. Review articles. CME Programs. Powerpoint slides. Images. American Roentgen Ray Society Images of Laryngitis case study one All Images X-rays Echo & Ultrasound CT Images MRI; Ongoing Trials at Clinical Trials.gov. US National Guidelines ...
there's an urgent need to treat laryngitis — for example, when you need to use your voice to sing or give a speech or oral presentation, or in some cases when a toddler has laryngitis associated with croup. Anatomy & Physiology: Respiratory System decreased pulmonary tissue perfusion associated with decreased cardiac output. Desired ...
Discussion. Laryngeal TB is a rare and often overlooked manifestation of extrapulmonary TB, with its current incidence estimated to be less than 1% of all TB cases [1].In the early 1900s, laryngeal TB had been one of the most common diseases of the larynx [2], but its incidence dropped dramatically after the 1950s with the introduction of anti-TB drugs, improvements in living standards, and ...
Laryngitis. Mar 23, 2013 • Download as PPT, PDF •. 57 likes • 40,706 views. Jay Rami. 1 of 57. Download now. Laryngitis - Download as a PDF or view online for free.
Read chapter 4 of Infectious Diseases: A Case Study Approach online now, exclusively on AccessPharmacy. AccessPharmacy is a subscription-based resource from McGraw Hill that features trusted pharmacy content from the best minds in the field.
Therefore, the purpose of this case study was to present an atypical case of sore throat and discuss differential diagnoses.Case Presentation: The patient was a 45-year-old female who presented to the ED with a three-day history of sore throat that was exacerbated by eating and drinking. The patient was not on any prescription medications, but ...
4 laryngeal disorders. May 5, 2010 • Download as PPT, PDF •. 29 likes • 7,094 views. Sumit Prajapati. Education. 1 of 71. Download now. 4 laryngeal disorders - Download as a PDF or view online for free.
Abstract. Laryngeal tuberculosis (TB) is a rare condition, occurring in less than 1% of patients infected with pulmonary TB. We present a case of a 57-year-old male patient, who presented in extremis with audible stridor, increased work of breathing and cyanosis. In addition, the patient had a complex medical history, including a recent ...
One recent study of Sharjah, the capital of the third-largest emirate in the U.A.E., found that the city's rapid growth over the past half-century had made it vulnerable to flooding at far lower ...
The current case exemplifies the difficulties in diagnosing primary laryngeal TB and demonstrates the growing relevance of this uncommon extrapulmonary presentation. It emphasizes the need for a thorough diagnostic approach, collaboration among many medical specialists, adherence to established treatment procedures, and the critical ...
Pharyngitis - Download as a PDF or view online for free. 4. Causes • environmental exposure to viral agents - adenovirus, influenza virus, Epstein-Barr virus, and herpes simplex virus • Bacterial infection - Ten percent of adults with pharyngitis have group A beta-hemolytic streptococcus (GABHS), which is commonly referred to as group A streptococcus (GAS) or streptococcal pharyngitis.