- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board

Medicare Assignment: Everything You Need to Know
Medicare assignment.
- Providers Accepting Assignment
- Providers Who Do Not
- Billing Options
- Assignment of Benefits
- How to Choose
Frequently Asked Questions
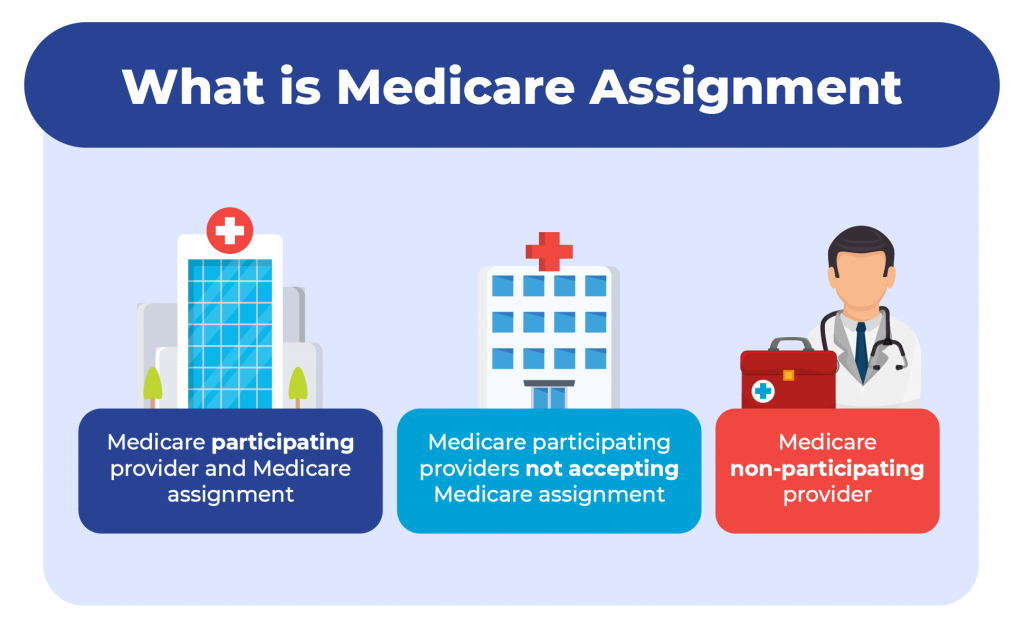
Medicare assignment is an agreement between Medicare and medical providers (doctors, hospitals, medical equipment suppliers, etc.) in which the provider agrees to accept Medicare’s fee schedule as payment in full when Medicare patients are treated.
This article will explain how Medicare assignment works, and what you need to know in order to ensure that you won’t receive unexpected bills.
fizkes / Getty Images
There are 35 million Americans who have Original Medicare. Medicare is a federal program and most medical providers throughout the country accept assignment with Medicare. As a result, these enrollees have a lot more options for medical providers than most of the rest of the population.
They can see any provider who accepts assignment, anywhere in the country. They can be assured that they will only have to pay their expected Medicare cost-sharing (deductible and coinsurance, some or all of which may be paid by a Medigap plan , Medicaid, or supplemental coverage provided by an employer or former employer).
It’s important to note here that the rules are different for the 29 million Americans who have Medicare Advantage plans. These beneficiaries cannot simply use any medical provider who accepts Medicare assignment.
Instead, each Medicare Advantage plan has its own network of providers —much like the health insurance plans that many Americans are accustomed to obtaining from employers or purchasing in the exchange/marketplace .
A provider who accepts assignment with Medicare may or may not be in-network with some or all of the Medicare Advantage plans that offer coverage in a given area. Some Medicare Advantage plans— health maintenance organizations (HMOs) , in particular—will only cover an enrollee’s claims if they use providers who are in the plan's network.
Other Medicare Advantage plans— preferred provider organizations (PPOs) , in particular—will cover out-of-network care but the enrollee will pay more than they would have paid had they seen an in-network provider.
Original Medicare
The bottom line is that Medicare assignment only determines provider accessibility and costs for people who have Original Medicare. People with Medicare Advantage need to understand their own plan’s provider network and coverage rules.
When discussing Medicare assignment and access to providers in this article, keep in mind that it is referring to people who have Original Medicare.
How to Make Sure Your Provider Accepts Assignment
Most doctors, hospitals, and other medical providers in the United States do accept Medicare assignment.
Provider Participation Stats
According to the Centers for Medicare and Medicaid Services, 98% of providers participate in Medicare, which means they accept assignment.
You can ask the provider directly about their participation with Medicare. But Medicare also has a tool that you can use to find participating doctors, hospitals, home health care services, and other providers.
There’s a filter on that tool labeled “Medicare-approved payment.” If you turn on that filter, you will only see providers who accept Medicare assignment. Under each provider’s information, it will say “Charges the Medicare-approved amount (so you pay less out-of-pocket).”
What If Your Provider Doesn’t Accept Assignment?
If your medical provider or equipment supplier doesn’t accept assignment, it means they haven’t agreed to accept Medicare’s approved amounts as payment in full for all of the services.
These providers can still choose to accept assignment on a case-by-case basis. But because they haven’t agreed to accept Medicare assignment for all services, they are considered nonparticipating providers.
Note that "nonparticipating" does not mean that a provider has opted out of Medicare altogether. Medicare will still pay claims for services received from a nonparticipating provider (i.e., one who does not accept Medicare assignment), whereas Medicare does not cover any of the cost of services obtained from a provider who has officially opted out of Medicare.
If a Medicare beneficiary uses a provider who has opted out of Medicare, that person will pay the provider directly and Medicare will not be involved in any way.
Physicians Who Have Opted Out
Only about 1% of all non-pediatric physicians have opted out of Medicare.
For providers who have not opted out of Medicare but who also don’t accept assignment, Medicare will still pay nearly as much as it would have paid if you had used a provider who accepts assignment. Here’s how it works:
- Medicare will pay the provider 95% of the amount they would pay if the provider accepted assignment.
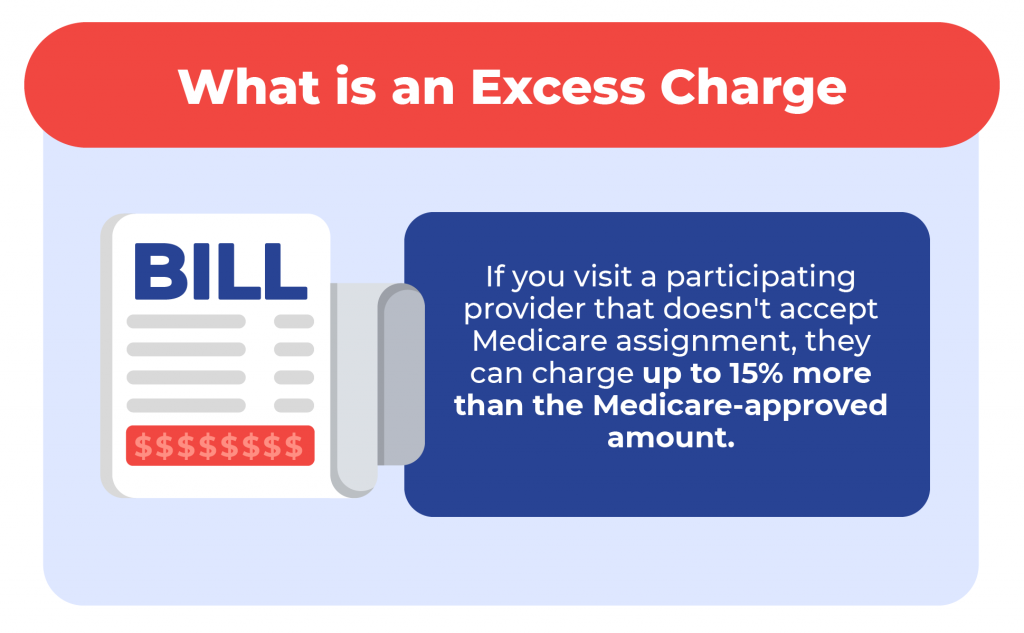
- The provider can charge the person receiving care more than the Medicare-approved amount, but only up to 15% more (some states limit this further). This extra amount, which the patient has to pay out-of-pocket, is known as the limiting charge . But the 15% cap does not apply to medical equipment suppliers; if they do not accept assignment with Medicare, there is no limit on how much they can charge the person receiving care. This is why it’s particularly important to make sure that the supplier accepts Medicare assignment if you need medical equipment.
- The nonparticipating provider may require the person receiving care to pay the entire bill up front and seek reimbursement from Medicare (using Form CMS 1490-S ). Alternatively, they may submit a claim to Medicare on behalf of the person receiving care (using Form CMS-1500 ).
- A nonparticipating provider can choose to accept assignment on a case-by-case basis. They can indicate this on Form CMS-1500 in box 27. The vast majority of nonparticipating providers who bill Medicare choose to accept assignment for the claim being billed.
- Nonparticipating providers do not have to bill your Medigap plan on your behalf.
Billing Options for Providers Who Accept Medicare
When a medical provider accepts assignment with Medicare, part of the agreement is that they will submit bills to Medicare on behalf of the person receiving care. So if you only see providers who accept assignment, you will never need to submit your own bills to Medicare for reimbursement.
If you have a Medigap plan that supplements your Original Medicare coverage, you should present the Medigap coverage information to the provider at the time of service. Medicare will forward the claim information to your Medigap insurer, reducing administrative work on your part.
Depending on the Medigap plan you have, the services that you receive, and the amount you’ve already spent in out-of-pocket costs, the Medigap plan may pay some or all of the out-of-pocket costs that you would otherwise have after Medicare pays its share.
(Note that if you have a type of Medigap plan called Medicare SELECT, you will have to stay within the plan’s network of providers in order to receive benefits. But this is not the case with other Medigap plans.)
After the claim is processed, you’ll be able to see details in your MyMedicare.gov account . Medicare will also send you a Medicare Summary Notice. This is Medicare’s version of an explanation of benefits (EOB) , which is sent out every three months.
If you have a Medigap plan, it should also send you an EOB or something similar, explaining the claim and whether the policy paid any part of it.
What Is Medicare Assignment of Benefits?
For Medicare beneficiaries, assignment of benefits means that the person receiving care agrees to allow a nonparticipating provider to bill Medicare directly (as opposed to having the person receiving care pay the bill up front and seek reimbursement from Medicare). Assignment of benefits is authorized by the person receiving care in Box 13 of Form CMS-1500 .
If the person receiving care refuses to assign benefits, Medicare can only reimburse the person receiving care instead of paying the nonparticipating provider directly.
Things to Consider Before Choosing a Provider
If you’re enrolled in Original Medicare, you have a wide range of options in terms of the providers you can use—far more than most other Americans. In most cases, your preferred doctor and other medical providers will accept assignment with Medicare, keeping your out-of-pocket costs lower than they would otherwise be, and reducing administrative hassle.
There may be circumstances, however, when the best option is a nonparticipating provider or even a provider who has opted out of Medicare altogether. If you choose one of these options, be sure you discuss the details with the provider before proceeding with the treatment.
You’ll want to understand how much is going to be billed and whether the provider will bill Medicare on your behalf if you agree to assign benefits (note that this is not possible if the provider has opted out of Medicare).
If you have supplemental coverage, you’ll also want to check with that plan to see whether it will still pick up some of the cost and, if so, how much you should expect to pay out of your own pocket.
A medical provider who accepts Medicare assignment is considered a participating provider. These providers have agreed to accept Medicare’s fee schedule as payment in full for services they provide to Medicare beneficiaries. Most doctors, hospitals, and other medical providers do accept Medicare assignment.
Nonparticipating providers are those who have not signed an agreement with Medicare to accept Medicare’s rates as payment in full. However, they can agree to accept assignment on a case-by-case basis, as long as they haven’t opted out of Medicare altogether. If they do not accept assignment, they can bill the patient up to 15% more than the Medicare-approved rate.
Providers who opt out of Medicare cannot bill Medicare and Medicare will not pay them or reimburse beneficiaries for their services. But there is no limit on how much they can bill for their services.
A Word From Verywell
It’s in your best interest to choose a provider who accepts Medicare assignment. This will keep your costs as low as possible, streamline the billing and claims process, and ensure that your Medigap plan picks up its share of the costs.
If you feel like you need help navigating the provider options or seeking care from a provider who doesn’t accept assignment, the Medicare State Health Insurance Assistance Program (SHIP) in your state may be able to help.
A doctor who does not accept Medicare assignment has not agreed to accept Medicare’s fee schedule as payment in full for their services. These doctors are considered nonparticipating with Medicare and can bill Medicare beneficiaries up to 15% more than the Medicare-approved amount.
They also have the option to accept assignment (i.e., accept Medicare’s rate as payment in full) on a case-by-case basis.
There are certain circumstances in which a provider is required by law to accept assignment. This includes situations in which the person receiving care has both Medicare and Medicaid. And it also applies to certain medical services, including lab tests, ambulance services, and drugs that are covered under Medicare Part B (as opposed to Part D).
In 2021, 98% of American physicians had participation agreements with Medicare, leaving only about 2% who did not accept assignment (either as a nonparticipating provider, or a provider who had opted out of Medicare altogether).
Accepting assignment is something that the medical provider does, whereas assignment of benefits is something that the patient (the Medicare beneficiary) does. To accept assignment means that the medical provider has agreed to accept Medicare’s approved fee as payment in full for services they provide.
Assignment of benefits means that the person receiving care agrees to allow a medical provider to bill Medicare directly, as opposed to having the person receiving care pay the provider and then seek reimbursement from Medicare.
Centers for Medicare and Medicaid Services. Medicare monthly enrollment .
Centers for Medicare and Medicaid Services. Annual Medicare participation announcement .
Centers for Medicare and Medicaid Services. Lower costs with assignment .
Centers for Medicare and Medicaid Services. Find providers who have opted out of Medicare .
Kaiser Family Foundation. How many physicians have opted-out of the Medicare program ?
Center for Medicare Advocacy. Durable medical equipment, prosthetics, orthotics, and supplies (DMEPOS) updates .
Centers for Medicare and Medicaid Services. Check the status of a claim .
Centers for Medicare and Medicaid Services. Medicare claims processing manual. Chapter 26 - completing and processing form CMS-1500 data set .
Centers for Medicare and Medicaid Services. Ambulance fee schedule .
Centers for Medicare and Medicaid Services. Prescription drugs (outpatient) .
By Louise Norris Norris is a licensed health insurance agent, book author, and freelance writer. She graduated magna cum laude from Colorado State University.
Find cars that meet your safety needs with AARP Auto Buying Program powered by TrueCar. Learn more.
Popular Searches
AARP daily Crossword Puzzle
Hotels with AARP discounts
Life Insurance
AARP Dental Insurance Plans
Suggested Links
AARP MEMBERSHIP — $12 FOR YOUR FIRST YEAR WHEN YOU SIGN UP FOR AUTOMATIC RENEWAL
Get instant access to members-only products and hundreds of discounts, a free second membership, and a subscription to AARP the Magazine.
- right_container
Work & Jobs
Social Security
AARP en Español
- Membership & Benefits
AARP Rewards
- AARP Rewards %{points}%
Conditions & Treatments
Drugs & Supplements
Health Care & Coverage
Health Benefits

Staying Fit
Your Personalized Guide to Fitness

AARP Hearing Center
Ways To Improve Your Hearing

Brain Health Resources
Tools and Explainers on Brain Health
How to Save Your Own Life
Scams & Fraud
Personal Finance
Money Benefits

View and Report Scams in Your Area

AARP Foundation Tax-Aide
Free Tax Preparation Assistance

AARP Money Map
Get Your Finances Back on Track

Budget & Savings
Make Your Appliances Last Longer
Small Business
Age Discrimination

Flexible Work
Freelance Jobs You Can Do From Home

AARP Skills Builder
Online Courses to Boost Your Career

31 Great Ways to Boost Your Career

ON-DEMAND WEBINARS
Tips to Enhance Your Job Search

Get More out of Your Benefits

When to Start Taking Social Security

10 Top Social Security FAQs

Social Security Benefits Calculator

Medicare Made Easy
Original vs. Medicare Advantage

Enrollment Guide
Step-by-Step Tool for First-Timers

Prescription Drugs
9 Biggest Changes Under New Rx Law

Medicare FAQs
Quick Answers to Your Top Questions
Care at Home
Financial & Legal
Life Balance

LONG-TERM CARE
Understanding Basics of LTC Insurance

State Guides
Assistance and Services in Your Area

Prepare to Care Guides
How to Develop a Caregiving Plan

End of Life
How to Cope With Grief, Loss
Recently Played
Word & Trivia
Atari® & Retro
Members Only
Staying Sharp
Mobile Apps
More About Games

Right Again! Trivia

Right Again! Trivia – Sports

Atari® Video Games

Throwback Thursday Crossword
Travel Tips
Vacation Ideas
Destinations
Travel Benefits

Beach vacation ideas
Vacations for Sun and Fun

Plan Ahead for Tourist Taxes

AARP City Guide
Discover Seattle

How to Pick the Right Cruise for You
Entertainment & Style
Family & Relationships
Personal Tech
Home & Living
Celebrities
Beauty & Style

TV for Grownups
Best Reality TV Shows for Grownups

Robert De Niro Reflects on His Life
Free Online Novel
Read 'Chase'

Sex & Dating
Spice Up Your Love Life

Navigate All Kinds of Connections

How to Create a Home Gym

Store Medical Records on Your Phone?

Maximize the Life of Your Phone Battery

Virtual Community Center
Join Free Tech Help Events

Create a Hygge Haven

Soups to Comfort Your Soul

AARP Smart Guide
Spring Clean All of Your Spaces
Driver Safety
Maintenance & Safety
Trends & Technology

How to Keep Your Car Running

We Need To Talk
Assess Your Loved One's Driving Skills

AARP Smart Driver Course

Building Resilience in Difficult Times

Tips for Finding Your Calm

Weight Loss After 50 Challenge

Cautionary Tales of Today's Biggest Scams

7 Top Podcasts for Armchair Travelers

Jean Chatzky: ‘Closing the Savings Gap’

Quick Digest of Today's Top News

AARP Top Tips for Navigating Life

Get Moving With Our Workout Series
You are now leaving AARP.org and going to a website that is not operated by AARP. A different privacy policy and terms of service will apply.
Go to Series Main Page
What is Medicare assignment and how does it work?
Kimberly Lankford,
Because Medicare decides how much to pay providers for covered services, if the provider agrees to the Medicare-approved amount, even if it is less than they usually charge, they’re accepting assignment.
A doctor who accepts assignment agrees to charge you no more than the amount Medicare has approved for that service. By comparison, a doctor who participates in Medicare but doesn’t accept assignment can potentially charge you up to 15 percent more than the Medicare-approved amount.
That’s why it’s important to ask if a provider accepts assignment before you receive care, even if they accept Medicare patients. If a doctor doesn’t accept assignment, you will pay more for that physician’s services compared with one who does.

AARP Membership — $12 for your first year when you sign up for Automatic Renewal
How much do I pay if my doctor accepts assignment?
If your doctor accepts assignment, you will usually pay 20 percent of the Medicare-approved amount for the service, called coinsurance, after you’ve paid the annual deductible. Because Medicare Part B covers doctor and outpatient services, your $240 deductible for Part B in 2024 applies before most coverage begins.
All providers who accept assignment must submit claims directly to Medicare, which pays 80 percent of the approved cost for the service and will bill you the remaining 20 percent. You can get some preventive services and screenings, such as mammograms and colonoscopies , without paying a deductible or coinsurance if the provider accepts assignment.
What if my doctor doesn’t accept assignment?
A doctor who takes Medicare but doesn’t accept assignment can still treat Medicare patients but won’t always accept the Medicare-approved amount as payment in full.
This means they can charge you up to a maximum of 15 percent more than Medicare pays for the service you receive, called “balance billing.” In this case, you’re responsible for the additional charge, plus the regular 20 percent coinsurance, as your share of the cost.
How to cover the extra cost? If you have a Medicare supplement policy , better known as Medigap, it may cover the extra 15 percent, called Medicare Part B excess charges.
All Medigap policies cover Part B’s 20 percent coinsurance in full or in part. The F and G policies cover the 15 percent excess charges from doctors who don’t accept assignment, but Plan F is no longer available to new enrollees, only those eligible for Medicare before Jan. 1, 2020, even if they haven’t enrolled in Medicare yet. However, anyone who is enrolled in original Medicare can apply for Plan G.
Remember that Medigap policies only cover excess charges for doctors who accept Medicare but don’t accept assignment, and they won’t cover costs for doctors who opt out of Medicare entirely.
Good to know. A few states limit the amount of excess fees a doctor can charge Medicare patients. For example, Massachusetts and Ohio prohibit balance billing, requiring doctors who accept Medicare to take the Medicare-approved amount. New York limits excess charges to 5 percent over the Medicare-approved amount for most services, rather than 15 percent.

AARP NEWSLETTERS

%{ newsLetterPromoText }%
%{ description }%
Privacy Policy
ARTICLE CONTINUES AFTER ADVERTISEMENT
How do I find doctors who accept assignment?
Before you start working with a new doctor, ask whether he or she accepts assignment. About 98 percent of providers billing Medicare are participating providers, which means they accept assignment on all Medicare claims, according to KFF.
You can get help finding doctors and other providers in your area who accept assignment by zip code using Medicare’s Physician Compare tool .
Those who accept assignment have this note under the name: “Charges the Medicare-approved amount (so you pay less out of pocket).” However, not all doctors who accept assignment are accepting new Medicare patients.
AARP® Vision Plans from VSP™
Exclusive vision insurance plans designed for members and their families
What does it mean if a doctor opts out of Medicare?
Doctors who opt out of Medicare can’t bill Medicare for services you receive. They also aren’t bound by Medicare’s limitations on charges.
In this case, you enter into a private contract with the provider and agree to pay the full bill. Be aware that neither Medicare nor your Medigap plan will reimburse you for these charges.
In 2023, only 1 percent of physicians who aren’t pediatricians opted out of the Medicare program, according to KFF. The percentage is larger for some specialties — 7.7 percent of psychiatrists and 4.2 percent of plastic and reconstructive surgeons have opted out of Medicare.
Keep in mind
These rules apply to original Medicare. Other factors determine costs if you choose to get coverage through a private Medicare Advantage plan . Most Medicare Advantage plans have provider networks, and they may charge more or not cover services from out-of-network providers.
Before choosing a Medicare Advantage plan, find out whether your chosen doctor or provider is covered and identify how much you’ll pay. You can use the Medicare Plan Finder to compare the Medicare Advantage plans and their out-of-pocket costs in your area.
Return to Medicare Q&A main page
Kimberly Lankford is a contributing writer who covers Medicare and personal finance. She wrote about insurance, Medicare, retirement and taxes for more than 20 years at Kiplinger’s Personal Finance and has written for The Washington Post and Boston Globe . She received the personal finance Best in Business award from the Society of American Business Editors and Writers and the New York State Society of CPAs’ excellence in financial journalism award for her guide to Medicare.
Discover AARP Members Only Access
Already a Member? Login

More on Medicare

How Do I Create a Personal Online Medicare Account?
You can do a lot when you decide to look electronically

I Got a Medicare Summary Notice in the Mail. What Is It?
This statement shows what was billed, paid in past 3 months
Understanding Medicare’s Options: Parts A, B, C and D
Making sense of the alphabet soup of health care choices
Recommended for You
AARP Value & Member Benefits

Learn, earn and redeem points for rewards with our free loyalty program

AARP® Dental Insurance Plan administered by Delta Dental Insurance Company
Dental insurance plans for members and their families

The National Hearing Test
Members can take a free hearing test by phone

AARP® Staying Sharp®
Activities, recipes, challenges and more with full access to AARP Staying Sharp®
SAVE MONEY WITH THESE LIMITED-TIME OFFERS
What Does It Mean for a Doctor to Accept Medicare Assignment?
Written by: Malini Ghoshal, RPh, MS
Reviewed by: Malinda Cannon, Licensed Insurance Agent
Key Takeaways
Doctors who accept Medicare assignment are paid agreed-upon rates for services.
It’s important to verify that your doctor accepts assignment before receiving services to avoid high out-of-pocket costs.
A doctor or clinician may be “non-participating” but can still agree to accept Medicare assignment for some services.
If you visit a doctor or clinician who has opted out (doesn’t accept Medicare), you may have to pay for your entire visit cost unless it’s a medical emergency.
Medigap Supplemental insurance (Medigap) plans won’t pay for service costs from doctors who don’t accept assignment.
One of the things that Original Medicare beneficiaries often enjoy about their coverage is that they can use it anywhere in the country. Unlike plans with provider networks, they can visit doctors either at home or on the road; both are covered the same.
But do all doctors accept Medicare patients?
Truth is, this wide-ranging coverage area only applies to doctors who accept Medicare assignment. Fortunately, most do. If you’re eligible for Medicare, it’s important to visit doctors and clinicians who accept Medicare assignment. This will help keep your out-of-pocket costs within your control. Doctors who agree to accept Medicare assignment sign an agreement that they’re willing to accept payment from Medicare for their services.
If you’re a current beneficiary or nearing enrollment, you may have other questions. Do all doctors accept Medicare Advantage plans? What about Medicare Supplement insurance (Medigap)? Read on to learn how to find doctors that accept Medicare assignment and how this keeps your healthcare costs down.
Let’s find your ideal Medicare Advantage plan.
What Is Medicare Assignment of Benefits?
When you’re eligible for Medicare, you have the option to visit doctors and clinicians who accept assignment. This means they are Medicare-approved providers who agree to receive Medicare reimbursement rates for covered services. This helps save you money.
If you have Original Medicare (Part A and B), your doctor visits are covered by your Part B plan. Inpatient services such as hospital stays and some skilled nursing care are covered by Part A .
In order for a participating doctor (or facility) to bill Medicare and be reimbursed, you must authorize Medicare to reimburse your doctor directly for your covered services. This is called the Medicare assignment of benefits. You transfer your right to receive Medicare payment for a covered service to your doctor or other provider.
Note: If you have a Medicare Supplement insurance ( Medigap ) plan to pay for out-of-pocket costs, you may also need to sign a separate assignment of benefits form for Medigap reimbursement. More on Medigap below.
How Can I Find Doctors Near Me That Accept Medicare?
There are several ways to find doctors and other clinicians who accept Medicare assignment close to you.
First, let’s take a look at the different types of Medicare providers.
They include:
Participating providers: Medicare-participating doctors and providers sign a participation agreement stating they will accept Medicare reimbursement rates for their services.
Non-participating providers: Doctors or providers who are non-participating providers are eligible to accept Medicare assignment but haven’t signed a Medicare agreement. They may choose to accept assignment on a case-by-case basis. If you visit a non-participating provider, make sure to ask if they accept assignment for your particular service. Also get a copy of their fees. They will need to select “yes” on Centers for Medicare & Medicaid Services CMS Form 1500 to accept assignment for the service.
Opt-out providers: Some doctors and other providers choose not to accept Medicare. If they choose to opt out, the period is two years (based on Medicare guidelines). The opt-out automatically renews if the provider doesn’t request a change in their status. You would be responsible for paying all costs for services received from an opt-out provider. You cannot bill Medicare for reimbursement unless the service was an urgent or emergency medical need. According to a report from KFF , roughly 1% of non-pediatric physicians opted out of Medicare in 2023.
Visiting a doctor who doesn’t accept assignment may cost you more. These providers can charge you up to 15% more than the Medicare-approved rate for a given service. This 15% charge is called the limiting charge. Some states limit this extra charge to a certain percent. This may also be called the Part B excess charge.
Here are some tips for finding doctors and providers who accept Medicare assignment:
- The easiest way to find a doctor who accepts Medicare assignment is to contact their office and ask them directly.
- If you’re looking for a new doctor, you can use the Medicare search tool to find clinicians and doctors that accept Medicare assignment.
- You can also ask a state health insurance assistance program (SHIP) representative for help in locating a doctor that accepts Medicare assignment.
- Don’t assume that having a longstanding relationship with your doctor means nothing will ever change. Check in with them to make sure they still accept Medicare assignment and whether they’re planning to opt out.
Note: Your doctor can choose to become a non-participating provider or opt out of participating in Medicare. It’s important to verify they accept Medicare assignment before receiving any services.
Ready for a new Medicare Advantage plan?
Do Doctors Who Accept Medicare Have to Accept Supplement Plans?
If your doctor accepts Medicare assignment and you have Original Medicare (Medicare Part A and Part B) with a Medicare Supplement (Medigap) plan, they will accept the supplemental insurance. Depending on your Medigap plan coverage , it may pay all or part of your out-of-pocket costs such as deductibles, copayments and coinsurance.
However, if you have a Medicare Advantage plan (Part C), you may have a network of covered doctors under the plan. If you visit an out-of-network doctor, you may need to pay all or part of the cost for your services.
Keep in mind that you can’t have a Medigap supplemental plan if you have a Medicare Advantage plan.
If you have questions or want to learn more about different Medicare plans like Original Medicare with Medigap versus Medicare Advantage, GoHealth has licensed insurance agents ready to help. They can shop your different options and offer impartial guidance where you need it.
Do Most Doctors Accept Medicare Advantage Plans?
Many doctors accept Medicare Advantage (Part C) plans, but these plans often use provider networks. These networks are groups of doctors and providers in an area that have agreed to treat an insurance company’s customers. If you have a Part C plan, you may be required to see in-network doctors with few exceptions. However, these types of plans are popular options for all-in-one coverage for your health needs. Plans must offer Part A and B coverage, plus a majority also include Part D , or prescription drug coverage. But whether a doctor accepts a Medicare Advantage plan may depend on where you live and the type of Medicare Advantage plan you have.
There are several types of Medicare Advantage plans including:
- Health Maintenance Organization (HMO): These plans have a network of covered providers, as well as a primary care physician to manage your care. If you visit a doctor outside your plan network, you may have to pay the full cost of your visit.
- Preferred Provider Organization (PPO): You’ll probably still have a primary care physician, but these are more flexible plans that allow you to go out of network in some cases. But you may have to pay more.
- Private Fee for Service (PFFS): You may be able to visit any doctor or provider with these plans, but your costs may be higher.
- Special Needs Plan (SNP): This type of plan is only for certain qualified individuals who either have a specific health condition ( C-SNP ) or who qualify for both Medicaid and Medicare insurance ( D-SNP ).
Have questions about your Medicare coverage?
What Are Medicare Assignment Codes?
Medicare assignment codes help Medicare pay for covered services. If your doctor or other provider accepts assignment and is a participating provider, they will file for reimbursement for services with a CMS-1500 form and the code will be “assigned.”
But non-participating providers can select “not assigned.” This means they are not accepting Medicare-assigned rates for a given service. They can charge up to 15% over the full Medicare rate for the service.
If you go to a doctor or provider who accepts assignment, you don’t need to file your own claim. Your doctor’s office will directly file with Medicare. Always check to make sure your doctor accepts assignment to avoid excess charges from your visit.
Health Insurance Claim Form . CMS.gov.
Lower costs with assignment . Medicare.gov.
How Many Physicians Have Opted-Out of the Medicare Program? KFF.org.
Joining a plan . Medicare.gov.
This website is operated by GoHealth, LLC., a licensed health insurance company. The website and its contents are for informational and educational purposes; helping people understand Medicare in a simple way. The purpose of this website is the solicitation of insurance. Contact will be made by a licensed insurance agent/producer or insurance company. Medicare Supplement insurance plans are not connected with or endorsed by the U.S. government or the federal Medicare program. Our mission is to help every American get better health insurance and save money. Any information we provide is limited to those plans we do offer in your area. Please contact Medicare.gov or 1-800-MEDICARE to get information on all of your options.
Let's see if you're missing out on Medicare savings.
We just need a few details.
Related Articles

What Is Medicare IRMAA?
What Is an IRMAA in Medicare?

How to Report Medicare Fraud
Medicare Fraud Examples & How to Report Abuse

How to Change Your Address with Medicare
Reporting a Change of Address to Medicare

Can I Get Medicare if I’ve Never Worked?
Can You Get Medicare if You've Never Worked?

Why Are Some Medicare Advantage Plans Free?
Why Are Some Medicare Advantage Plans Free? $0 Premium Plans Explained

What Is Medicare Assignment?

Am I Enrolled in Medicare?

When and How Do I Enroll?
When and How Do I Enroll in Medicare?

Medicare Frequently Asked Questions
Let’s see if you qualify for Medicare savings today!
Medicare Assignment: Understanding How It Works

Medicare assignment is a term used to describe how a healthcare provider agrees to accept the Medicare-approved amount. Depending on how you get your Medicare coverage, it could be essential to understand what it means and how it can affect you.
What is Medicare assignment?
Medicare sets a fixed cost to pay for every benefit they cover. This amount is called Medicare assignment.
You have the largest healthcare provider network with over 800,000 providers nationwide on Original Medicare . You can see any doctor nationwide that accepts Medicare.
Understanding the differences between your cost and the difference between accepting Medicare and accepting Medicare assignment could be worth thousands of dollars.
Doctors that accept Medicare
Your healthcare provider can fall into one of three categories:
Medicare participating provider and Medicare assignment
Medicare participating providers not accepting medicare assignment, medicare non-participating provider.
More than 97% of healthcare providers nationwide accept Medicare. Because of this, you can see almost any provider throughout the United States without needing referrals.
Let’s discuss the three categories the healthcare providers fall into.
Participating providers are doctors or healthcare providers who accept assignment. This means they will never charge more than the Medicare-approved amount.
Some non-participating providers accept Medicare but not Medicare assignment. This means you can see them the same way a provider accepts assignment.
You need to understand that since they don’t take the assigned amount, they can charge up to 15% more than the Medicare-approved amount.
Since Medicare will only pay the Medicare-approved amount, you’ll be responsible for these charges. The 15% overcharge is called an excess charge. A few states don’t allow or limit the amount or services of the excess charges. Only about 5% of providers charge excess charges.
Opt-out providers don’t accept Original Medicare, and these healthcare providers are in the minority in the United States. If healthcare providers don’t accept Medicare, they won’t be paid by Medicare.
This means choosing to see a provider that doesn’t accept Medicare will leave you responsible for 100% of what they charge you. These providers may be in-network for a Medicare Advantage plan in some cases.
Avoiding excess charges
Excess charges could be large or small depending on the service and the Medicare-approved amount. Avoiding these is easy. The simplest way is to ask your provider if they accept assignment before service.
If they say yes, they don’t issue excess charges. Or, on Medicare.gov , a provider search tool will allow you to look up your healthcare provider and show if they accept Medicare assignment or not.
Medicare Supplement and Medicare assignment
Medigap plans are additional insurance that helps cover your Medicare cost-share . If you are on specific plans, they’ll pay any extra costs from healthcare providers that accept Medicare but not Medicare assigned amount. Most Medicare Supplement plans don’t cover the excess charges.
The top three Medicare Supplement plans cover excess charges if you use a provider that accepts Medicare but not Medicare assignment.
Medicare Advantage and Medicare assignment
Medicare assignment does not affect Medicare Advantage plans since Medicare Advantage is just another way to receive your Medicare benefits. Since your Medicare Advantage plan handles your healthcare benefits, they set the terms.
Most Medicare Advantage plans require you to use network providers. If you go out of the network, you may pay more. If you’re on an HMO, you’d be responsible for the entire charge of the provider not being in the network.
Do all doctors accept Medicare Supplement plans?
All doctors that accept Original Medicare accept Medicare Supplement plans. Some doctors don’t accept Medicare. In this case, those doctors won’t accept Medicare Supplements.
Where can I find doctors who accept Medicare assignment?
Medicare has a physician finder tool that will show if a healthcare provider participates in Medicare and accepts Medicare assignments. Most doctors nationwide do accept assignment and therefore don’t charge the Part B excess charges.
Why do some doctors not accept Medicare?
Some doctors are called concierge doctors. These doctors don’t accept any insurance and require cash payments.
What is a Medicare assignment?
Accepting Medicare assignment means that the healthcare provider has agreed only to charge the approved amount for procedures and services.
What does it mean if a doctor does not accept Medicare assignment?
The doctor can change more than the Medicare-approved amount for procedures and services. You could be responsible for up to a 15% excess charge.
How many doctors accept Medicare assignment?
About 97% of doctors agree to accept assignment nationwide.
Is accepting Medicare the same as accepting Medicare assignment?
No. If a doctor accepts Medicare and accepts Medicare assigned amount, they’ll take what Medicare approves as payment in full.
If they accept Medicare but not Medicare assignment, they can charge an excess charge of up to 15% above the Medicare-approved amount. You could be responsible for this excess charge.
What is the Medicare-approved amount?
The Medicare-approved amount is Medicare’s charge as the maximum for any given medical service or procedure. Medicare has set forth an approved amount for every covered item or service.
Can doctors balance bill patients?
Yes, if that doctor is a Medicare participating provider not accepting Medicare assigned amount. The provider may bill up to 15% more than the Medicare-approved amount.
What happens if a doctor does not accept Medicare?
Doctors that don’t accept Medicare will require you to pay their full cost when using their services. Since these providers are non-participating, Medicare will not pay or reimburse for any services rendered.
Get help avoiding Medicare Part B excess charges
Whether it’s Medicare assignment, or anything related to Medicare, we have licensed agents that specialize in this field standing by to assist.
Give us a call, or fill out our online request form . We are happy to help answer questions, review options, and guide you through the process.
Related Articles
- What are Medicare Part B Excess Charges?
- How to File a Medicare Reimbursement Claim?
- Medicare Defined Coinsurance: How it Works?
- Welcome to Medicare Visit
- Guide to the Medicare Program

CALL NOW (833) 972-1339

Medicare Provider Enrollment Print

What’s Changed?
- Updated the enrollment application fee amount for 2024
- Added marriage and family therapists, mental health counselors, and certain dental specialties to the Part B suppliers list
- Merged Form CMS-855R into the CMS-855I paper enrollment application
- Added new provider specialty code information for dentists
Substantive content changes are in dark red.
Application Fee
Physicians, non-physician practitioners, physician organizations, non-physician organizations, and Medicare Diabetes Prevention Program suppliers don’t pay a Medicare enrollment application fee.
Generally, institutional providers and suppliers like DMEPOS suppliers and opioid treatment programs pay an application fee when enrolling, re-enrolling, revalidating, or adding a new practice location.
Enrollment Application Fee
The 2024 enrollment application fee is $709.
Whether you apply for Medicare enrollment online or use the paper application, you can pay the Medicare application fee online through:
- PECOS: During the application process, PECOS prompts you to pay the application fee
- CMS Paper Application: Go to PECOS Application Fee Information to submit the application fee
A hardship exception exempts you from paying a current application’s fee. If you request a hardship exception, submit a written request and supporting documentation describing the hardship and justifying an exception to paying the application fee with your PECOS or CMS paper application. We grant exceptions on a case-by-case basis.
Medicare Administrative Contractors (MACs) will only process applications with the proper application fee payment or an approved hardship exception.
If you don’t pay the fee or submit a hardship exception request, your MAC will send a letter allowing you 30 days to pay the fee. If you don’t pay the fee on time, the MAC may reject or deny your application or revoke your existing billing privileges, as appropriate.

Providers must enroll in the Medicare Program to get paid for providing covered services to Medicare patients. Determine if you’re eligible to enroll and how to complete enrollment.
We list institutional providers on the Medicare Enrollment Application: Institutional Providers (CMS-855A) , which include:
- Community mental health centers
- Comprehensive outpatient rehabilitation facilities
- Critical access hospitals
- ESRD facilities
- Federally Qualified Health Centers
- Histocompatibility labs
- Home health agencies
- Hospice organizations
- Indian Health Service facilities
- Organ procurement organizations
- Opioid treatment programs
- Outpatient physical therapy, occupational therapy, speech pathology services
- Religious nonmedical health care institutions
- Rural emergency hospitals
- Rural health clinics
- Skilled nursing facilities (SNFs)
Physicians, non-physician practitioners (NPPs), clinics or group practices, and specific suppliers who can enroll as Medicare Part B providers are defined in enrollment forms Medicare Enrollment Application: Physicians and Non-Physician Practitioners (CMS-855I) and Medicare Enrollment Application: Clinics/Group Practices and Other Suppliers (CMS-855B) .
Who’s an NPP?
NPPs include nurse practitioners, clinical nurse specialists, and physician assistants who practice with or under a physician’s supervision.
Physicians, NPPs, & Suppliers (CMS-855I)
- Anesthesiology assistants
- Audiologists
- Certified nurse-midwives
- Certified registered nurse anesthetists
- Clinical nurse specialists
- Clinical psychologists
- Clinical social workers
- Marriage and family therapists
- Mass immunization roster billers (individuals)
- Mental health counselors
- Nurse practitioners
- Occupational or physical therapists in private practice
- Dental anesthesiology
- Dental public health
- Endodontics
- Oral and maxillofacial surgery
- Oral and maxillofacial pathology
- Oral and maxillofacial radiology
- Oral medicine
- Orofacial pain
- Orthodontics and dentofacial orthopedics
- Pediatric dentistry
- Periodontics
- Prosthodontics
- Physician assistants
- Psychologists billing independently
- Registered dietitians or nutrition professionals
- Speech-language pathologists
Clinics, Group Practices, & Specific Suppliers (CMS-855B)
- Ambulatory surgical centers (ASCs)
- Clinics and group practices
- Home infusion therapy suppliers
- Hospital departments
- Independent clinical labs
- Independent diagnostic testing facilities
- Intensive cardiac rehabilitation suppliers
- Mammography centers
- Mass immunization roster billers (entities)
- Physical or occupational therapy groups in private practice
- Portable X-ray suppliers
- Radiation therapy centers
Medicare Diabetes Prevention Program Suppliers
Potential suppliers must use Medicare Enrollment Application: Medicare Diabetes Prevention Program (MDPP) Suppliers (CMS-20134) to enroll in the Medicare Program.
Beginning January 1, 2024, we established new provider specialty codes for dentists.
If you don’t see your provider type listed, contact your MAC’s provider enrollment center before submitting a Medicare enrollment application.
Medicare provider and supplier organizations have business structures, like corporations, partnerships, professional associations, or limited liability companies, which meet the provider and supplier definitions. Provider and supplier organizations don’t include organizations the IRS defines as sole proprietorships.
Provider and supplier organizations include:
- Medical group practices and clinics
You must have a provider or supplier employer identification number (EIN) to enroll in Medicare. An EIN is the same as the provider or supplier organization’s IRS-issued tax identification number (TIN).
Sole Proprietorships & Disregarded Entities
Sections 10.6.4 and 10.6.7.1(D)(5) of Medicare Program Integrity Manual, Chapter 10 have more information about sole proprietorships and disregarded entities.
Medicare participation means you agree to accept claims assignment for all covered patient services. By accepting assignment, you agree to accept Medicare-allowed amounts as payment in full. You can’t collect more from the patient than the deductible and coinsurance or copayment . The Social Security Act says you must submit patient Medicare claims whether or not you participate.
You have 90 days after we send your initial enrollment approval letter to decide if you want to be a participating provider or supplier. To participate as a Medicare Program provider or supplier, submit the Medicare Participating Physician or Supplier Agreement (CMS-460) upon initial enrollment. The only other time you may change your participation status is during the open enrollment period, generally from mid-November–December 31 each year.
Participating Provider or Supplier
- We pay 5% more to participating physicians and other suppliers
- Because these are assigned claims, we pay you directly
- We forward claim information to Medigap (Medicare supplement coverage) insurers
Non-Participating Provider or Supplier
- We pay 5% less to non-participating physicians and other suppliers
- You can’t charge patients more than the limiting charge, 115% of the Medicare Physician Fee Schedule amount
- You may accept assignment on a case-by-case basis
- You have limited appeal rights
Medicare Claims Processing Manual, Chapter 12 has more information.
Step 1: Get an NPI
To enroll in the Medicare Program, get an NPI through:
- Online Application: Get an Identity & Access Management (I&A) System user account. Then apply for an NPI in NPPES .
- Call 1-800-465-3203 (TTY 1-800-692-2326)
- Email [email protected]
- Bulk Enumeration: Apply for Electronic File Interchange access and upload your own CSV or XML files.
Not Sure If You Have an NPI?
Search for your NPI on the NPPES NPI Registry .
CMS Provider Enrollment Systems:
- I&A System
- Electronic Health Record (EHR) Incentive Payments
Multi-Factor Authentication
To better protect your information, we implemented I&A System multi-factor authentication for the provider enrollment systems listed above.

Step 2: Complete Proper Medicare Enrollment Application
After you get an NPI, you can complete Medicare Program enrollment, revalidate your enrollment, or change your enrollment information. Before applying, get the necessary enrollment information , and complete the actions using PECOS or the paper enrollment form.
A. Online PECOS Application
After we approve your I&A System registration, submit your PECOS application.
PECOS offers a scenario-driven application, asking questions to recover the information for your specific enrollment scenario. You can use PECOS to submit all supporting documentation. Follow these instructions:
- Log in to PECOS .
- Continue with an existing enrollment or create a new application.
- When PECOS determines your enrollment scenario and you confirm it’s correct, you’ll see the topics for submitting your application. To complete each topic, enter the necessary information.
- Confirms you entered all necessary data
- Lists MAC documents to submit for review
- Gives the option to electronically sign and certify
- Shows your MAC’s name and mailing address
- Lets you print your enrollment application for your records (don’t submit a paper copy to your MAC)
- Sends the application electronically to your MAC
- Emails you to confirm your MAC got the application
PECOS 2.0 Enhancements
PECOS will have enhanced features to better meet your needs. Watch this 2-minute video or read these FAQs to learn more about:
- A single application for multiple enrollments
- Data pre-population and an application that’s tailored to you
- Enhanced capability to add or delete group members
- Real-time processing checks and status updates
- Revalidation reminders
Visit Introducing PECOS 2.0 for more information.
PECOS Scroll Functionality
PECOS validates that you’ve read and acknowledged certification terms and conditions before you electronically submit your Medicare enrollment application. Review and scroll through each text box with certification requirements before you can select accept on these pages:
- Remote E-sign
Enrolling physicians, NPPs, or other Part B suppliers must choose 1 of the application descriptions below.
- You’re the only owner of a business, set up as a corporation, where you provide health care services
- Your business is legally separate from your personal assets
- You provide all health care services from a facility you own, lease, or rent
- You’re the only owner of a business that provides health care services
- You and your business are legally 1 and the same
- You’re personally responsible for the business’ financial obligations, and you report business income and losses on your personal tax return
- You provide all health care services as an employee of a group practice or clinic
- You arrange with your employer to submit claims and get paid for your services
- Choose Group Member Only if you’re reassigning all your benefits to a group practice or clinic
- You provide health care services as a group practice or clinic employee
- You agree with your employer to submit claims and get paid for your services
- You also provide health care services from a facility that you own, lease, or rent
- Your income through self-employment is part of your personal assets
- Your corporation doesn’t file taxes; instead, you file corporate taxes on your personal tax filing
B. Paper Medicare Enrollment Applications
Submit the appropriate paper enrollment application if you’re unable to use PECOS. Carefully review the paper application instructions to decide which form is right for your practice. The paper enrollment application collects your information, including documentation verifying your Medicare Program enrollment eligibility.
If you submit a paper application, your MAC processes your application and creates a Medicare enrollment record by entering the data into PECOS.
Medicare Enrollment Application: Institutional Providers (CMS-855A) : Institutional providers use this form to begin the Medicare enrollment or revalidation process or to change enrollment information.
Most physicians and NPPs complete the CMS-855I to begin the enrollment process. You can also use the CMS-855I if you reassign your benefits to another entity, like a medical group or group practice that gets paid for your services. We’ve merged the CMS-855R into the CMS-855I paper enrollment application.
- Medicare Enrollment Application: Clinics/Group Practices and Other Suppliers (CMS-855B) : Group practices and other organizational suppliers, except DMEPOS suppliers, use this form to begin the Medicare enrollment or revalidation process or to change enrollment information.
- Medicare Enrollment Application: Enrollment for Eligible Ordering/Certifying Physicians and Other Eligible Professionals (CMS-855O) : Physicians and other eligible NPPs use this form to enroll in Medicare solely to order or certify items or services for Medicare patients. This includes those physicians and other eligible NPPs who don’t send billed services claims to a MAC.
- Medicare Enrollment Application: Durable Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS) Suppliers (CMS-855S) : DMEPOS suppliers use this form to begin the Medicare enrollment or revalidation process or to change enrollment information.
- Medicare Enrollment Application: Medicare Diabetes Prevention Program (MDPP) Suppliers (CMS-20134) : MDPP suppliers use this form to begin the Medicare enrollment or revalidation process or to change enrollment information.
After you submit an enrollment application and all required supporting documentation to your MAC, they’ll send their recommendations to the State Survey Agency . The State Survey Agency then decides if specific providers meet Medicare enrollment conditions.
After a MAC makes a recommendation, the State Survey Agency or a CMS-recognized accrediting organization conducts a survey. Based on the survey results, the agency or organization recommends that we approve or deny the enrollment (certification of compliance or non-compliance).
Certain institutional provider types may elect voluntary accreditation by a CMS-recognized accrediting organization instead of a State Survey Agency. The accrediting organization will notify the State Survey Agency of their decision.
The State Survey Agency forwards us the survey results. We assign the CMS Certification Number and effective date, sign the provider agreement, and update the certification database. Your MAC will issue your final approval or denial letter.
If approved, you’ll get a fully executed provider agreement.
Electronic Funds Transfer
If enrolling in Medicare, revalidating, or making certain changes to your enrollment, we require you to set up an electronic funds transfer (EFT). Enroll in EFT by completing the PECOS EFT information section. When submitting a PECOS application:
- Complete the EFT information for your organization (if appropriate) or yourself
- Include a copy of a voided check or bank letter that has your individual or business legal name and applicable account and routing numbers
Step 3: Respond to Requests for More Information
MACs pre-screen and verify enrollment applications for completeness. If the MAC needs more information, respond to information requests within 30 days. If you don’t, the MAC may reject your enrollment .
Your MAC won’t fully process your PECOS enrollment application without your electronic or uploaded signature, application fee (if applicable), and necessary supporting documentation. The enrollment application filing date is when the MAC gets your enrollment application.
You can check your PECOS enrollment application status 2 ways:
- Log in to PECOS and select the View Enrollments link. In the Existing Enrollments section, find the application. The system shows the application status.
- To see your enrollment status without logging in, go to PECOS and, under Helpful Links , select Application Status.
When your MAC approves your application, it switches the PECOS record to an approved status and sends you an approval letter.
Provider Enrollment Site Visits
We conduct a site visit verification process using National Site Visit Contractors (NSVCs). A site visit helps prevent questionable providers and suppliers from enrolling or staying enrolled in the Medicare Program.
The NSVCs conduct unannounced site visits for all Medicare Part A and B providers and suppliers, including DMEPOS suppliers. The NSVCs may conduct an observational site visit or a detailed review to verify enrollment-related information and collect other details based on pre-defined CMS checklists and procedures.
During an observational visit, the inspector has minimal contact with the provider or supplier and doesn’t hinder the facility’s daily activities. The inspector will take facility photos as part of the site visit. During a detailed review, the inspector enters the facility, speaks with staff, and collects information to confirm the provider’s or supplier’s compliance with our standards.
Inspectors performing site visits will carry a photo ID and a CMS-issued, signed authorization letter the provider or supplier may review. If the provider or its staff want to verify we ordered a site visit, contact your MAC .
Make your office staff aware of the site visit verification process. An inspector’s inability to perform a site visit may result in denial of your Medicare enrollment application or revocation of your Medicare billing privileges.
Step 4: Use PECOS to Keep Enrollment Information Current
Report a Medicare enrollment change using PECOS. Physicians, NPPs, and physician and NPP organizations must report a change of ownership or control (including a change in authorized or delegated official), a change in practice location, and any final adverse legal actions (like a felony or suspension of a federal or state license) within 30 days of the change and report all other changes within 90 days of the change.
DMEPOS suppliers must report changes in their enrollment application information within 30 days of the change.
Independent diagnostic testing facilities must report changes in ownership, location, general supervision, and adverse legal actions within 30 days of the change and report all other changes within 90 days of the change.
Medicare Diabetes Prevention Program suppliers must report changes in ownership, including AO or Access Manager; location; coach roster; and adverse legal actions within 30 days of the change and report all other changes within 90 days of the change.
PECOS Users
We allow various organizations and users to work in our systems. The type of user depends on their relationship with you and the duties they perform in your practice.
You may choose other users to act for your organization to manage connections and staff, including appointing and approving other system-authorized users. Depending on your professional relationships with other providers, the CMS External User Services Help Desk may ask you for additional validation information.
One Account, Multiple Systems
We use several provider enrollment systems. Organizational providers and suppliers must use the Identity & Access Management (I&A) System to name an AO to work in CMS systems. The I&A System allows you to:
- Use NPPES to apply for and manage NPIs
- Use PECOS to enroll in Medicare or update or revalidate your current enrollment information
- Register to get electronic health record (EHR) incentive payments for eligible professionals and hospitals that adopt, use and upgrade, or show meaningful use of EHR technology
Authorized Officials, Access Managers, Staff End Users, & Surrogates
Organizational providers or suppliers must appoint and authenticate an Authorized Official (AO) through the I&A System to work in PECOS for them. That person must meet the AO regulatory definition. For example, an AO is a chief executive officer, chief financial officer, general partner, chair of the board, or direct owner who can legally enroll in the Medicare Program.
Respond to your employer’s AO invitation or initiate the request yourself. After you’re the confirmed AO, use PECOS for your provider or supplier organization. As an AO, you’re responsible for approving PECOS user system requests to work on behalf of the provider or supplier organization. Regularly check your email and take the requested actions.
AOs may delegate their responsibilities to an Access Manager who can also initiate or accept connections and manage staff for their organizations.
AOs or Access Managers may invite a Staff End User (SEU) or Surrogate to access PECOS for their organization. Once registered, an SEU or Surrogate may log in to access, view, and modify CMS system information, but they can’t represent the practice, manage staff, sign enrollment applications, or initiate or accept connections.
We recommend using the same I&A System-appointed AO and PECOS Access Managers. The assigned AO and Access Managers must have the right to legally bind the company and be responsible for approving the system staff and be CMS-approved in the I&A System.
Only AOs can sign an initial organization enrollment application. An Access Manager can sign changes, updates, and revalidations.
The I&A System Quick Reference Guide has detailed instructions on managing system users.
PECOS Technical Help
Using PECOS may require technical support. The first step toward a solution is knowing which CMS contractor to contact.
Common Problems & Who to Contact
You experience system-generated error messages, have trouble navigating through or accessing PECOS screens, encounter printing problems, or your valid I&A System user ID and password won’t allow PECOS access because of a malfunction (for example, the website operates slowly or not at all or a system-generated error message prevents you from entering data).
A system-generated error message doesn’t include messages created when you enter data incorrectly or ignore system prompts.
Solution: Contact the CMS External User Services Help Desk
The External User Services website has information on common problems and allows you to ask questions, chat live with a support team member, or look up previous support history.
Phone: 1-866-484-8049 (TTY 1-866-523-4759)
Email: [email protected]
EUS Hours of Operation:
- Monday–Friday: 6 am–6 pm CT
- Saturday–Sunday: Closed
Before you log in to PECOS, you need a valid I&A System user ID and password.
Passwords expire every 60 days. The I&A System tells you the number of days until your password expires. If you attempt to log in to PECOS with an expired password, the system redirects you to the I&A System to reset it.
Solution: Access I&A System or Contact I&A System Help
The I&A System website lets you create an I&A System user ID and password, change your password, and recover forgotten login information. You can also access several resources:
- The I&A FAQs helps you resolve common I&A System problems
- The I&A System Quick Reference Guide provides step-by-step instructions, including screenshots, and information about I&A System features and tools
On the I&A System website, select the Help button in the upper right corner of any webpage for more information on that webpage’s topic.
While using PECOS, you may have questions, experience problems enrolling, or need help completing specific PECOS enrollment application sections.
Solution: Contact Your Medicare Enrollment Contractor
Find detailed enrollment contact information in the Medicare Provider Enrollment Contact List . If you have questions, find your MAC’s website .
Solution: Refer to the CMS Provider Enrollment Assistance Guide
If you don’t know who to call for help, refer to the “Who should I call?” CMS Provider Enrollment Assistance Guide .
Find detailed enrollment contact information in the Medicare Provider Enrollment Contact List .
Organizational providers and suppliers must designate a provider enrollment AO to work in CMS systems, including the I&A System , NPPES , and PECOS . The AO may also authorize Access Managers, Surrogates, and SEUs to use PECOS. Individual providers and suppliers don’t require an AO but can authorize Surrogates and SEUs to work in PECOS. Refer to the I&A System Quick Reference Guide and I&A FAQs for more information on registering for an I&A System account or enrolling as an AO.
We use several provider enrollment systems. Specifically, the I&A System allows you to:
- Use PECOS to enroll in Medicare or to update or revalidate your current enrollment information
- Register to get EHR incentive payments for eligible professionals and hospitals that adopt, use and upgrade, or show meaningful use of certified EHR technology
Before completing PECOS enrollment, create an I&A System account. Organizational providers and suppliers must designate an AO to work in these systems.
Use the same information to enroll in Medicare using PECOS as you would for a paper enrollment application.
- If you don’t have an I&A System account, create your username and password
- Use your username and password to log in to NPPES to register for an NPI
- All Medicare provider enrollees must have an active NPI
Based on your provider type, you may also need this information:
- Personal identifying information, including your legal name on file with the Social Security Administration, date of birth, and SSN
- Legal business name of the provider or supplier organization
- Provider or supplier organization’s TIN; if any person or organization has 5% or more partnership interest or ownership (direct or indirect), you must list them on all enrollment records under your TIN
- Professional license information
- School degrees
- Certificates
- W-2 employees and contracted individuals and organizations with managerial control of the provider or supplier
- Accreditation information
- Surety bond information
- Providers self-designate their Medicare specialty on the Medicare enrollment application (CMS 855-I or CMS 855-O) or PECOS when they enroll in the Medicare Program
- Beginning January 1, 2024, we established new provider specialty codes for dentists
- Current medical practice location
- Federal, state, and local (city or county) business and professional licenses, certificates, and registrations specifically required to operate as a health care facility
- Medical record storage information
- Special payment information
- Bank account information
- Suspension, termination, or revocation of a license to provide health care by a state licensing authority or the Medicaid Program
- Conviction of a federal or state felony within 10 years before enrollment, revalidation, or re-enrollment
- Exclusion or debarment from federal or state health care program participation by the Office of Inspector General (OIG) or other federal or state offices with authority to exclude or sanction a provider (or those listed above)
An application is the paper or electronic form you submit for Medicare Program enrollment approval. After the MAC processes the application, PECOS keeps the enrollment record, which includes all your enrollment application data.
You can’t use PECOS to:
- Change your SSN
- Change a provider’s or supplier’s TIN
- Solely owned PA, PC, or LLC can’t be changed to a sole proprietorship
- Sole proprietorship can’t be changed to a PA, a PC, or an LLC
Submit changes noted above using the appropriate paper Medicare enrollment application .
No. All Fee-for-Service (FFS) providers can apply in PECOS.
PECOS is available 24 hours a day, Monday–Saturday, with scheduled downtime on Sunday. We offer technical support daily, 5 am–8 pm CT.
We encourage you to submit your enrollment application through PECOS because it’s faster and easier, but you may complete and mail the appropriate paper Medicare enrollment application to the address on the Medicare Fee-for-Service Provider Enrollment Contact List :
- Parts A and B Providers: Send forms to your Part A or Part B MAC.
- Home Health and Hospice Providers: Send forms to the Home Health and Hospice Contractor.
- DMEPOS Suppliers Send forms to the National Provider Enrollment (NPE) DMEPOS contractor in your region. Find your NPE contractor .
Even if you submit your application on a paper form, your MAC creates an enrollment record in PECOS.
When you electronically submit your Medicare enrollment application, you’ll get a Submission Confirmation page, which will remind you that the individual provider, or the provider or supplier organization AO or Access Manager must electronically sign the application or upload their signature. You’ll be able to see which MAC is processing your application, your unique application tracking number, and real-time information about your application.
PECOS emails the web tracking ID for the submitted application to each address in the Contact Person section of the application. Remember to verify all your completed signatures with either an electronic signature or uploading certification. Mail any required supporting documentation you didn’t upload during submission to the MAC, and include the PECOS tracking ID.
Create a new enrollment:
- If you change your services, like changing specialties
- If you change your location, causing your MAC to need new state surveys and other documentation (your MAC can determine this)
- If you have a change of ownership
- If a provider is creating a new TIN because of a change of ownership
- If you have provider-based vs. freestanding requirements (find your MAC’s website for more information)
Application Fee & Supporting Documentation
Generally, institutional providers and suppliers, like DMEPOS suppliers and opioid treatment programs, pay an application fee when enrolling, re-enrolling, revalidating, or adding a new practice location.
MACs will only process applications with the proper application fee payment or an approved hardship exception.
If you pay the fee during the 30-day period, the MAC processes the application in the usual manner.
No. When you electronically submit the Medicare enrollment application, a page appears that lists the supporting documentation to complete the enrollment. You can submit all this documentation electronically through PECOS.
Yes, either is acceptable. You must send this information electronically (as supporting documentation uploaded into PECOS).
During the PECOS application process, the Penalties for Falsifying Information page has the same text as the paper Medicare enrollment application and lists the consequences for providing false information. These consequences include criminal and civil penalties, fines, civil monetary penalties, exclusion from federal health care programs, and imprisonment, among others. You must acknowledge this page by selecting the Next Page button before continuing the PECOS submission process.
Enrollment Application Issues
First, make sure you entered your correct SSN, legal name, and date of birth. If you believe you entered the correct information but PECOS doesn’t accept this information, contact the Social Security Administration .
You must report an SSN to enroll in Medicare. If you don’t want to report your SSN over the web, use the appropriate paper Medicare enrollment application .
An Invalid Address error indicates the address entered doesn’t comply with the U.S. Postal Service address standards. This page lets you continue by either saving the address you entered or selecting the address PECOS displays.
As a security feature, PECOS will time out if you’re inactive (you don’t hit any keys on your computer keyboard) for 15 minutes. The system warns you of inactivity after 10 minutes. If it gets no response after 5 additional minutes, the system automatically times you out. Save your work if you anticipate inactivity while applying in PECOS. If you don’t save your work and the system times out, you must start from the beginning.
Submitting Reportable Events
No. If you report a change to existing information, check Change , include the effective date of change, and complete the appropriate fields in the impacted sections.
Yes. Following your initial enrollment, report certain changes (reportable events) to your MAC within 30 calendar days of the change. Report all other changes to your MAC within 90 days.
Report a Medicare enrollment change using PECOS. Physicians and NPPs must report a change of ownership or control (including a change in authorized or delegated official), a change in practice location, and any final adverse legal actions (like a felony or suspension of a federal or state license) within 30 days of the change and report all other changes within 90 days of the change.
Since Medicare pays claims by EFT, the Special Payments address should indicate where all other payment information must go (for example, paper remittance notices or special payments).
Providers and suppliers should report most changes using PECOS or the applicable paper Medicare enrollment application .
No. If you have a new business location, complete a new PECOS or paper application. Each DMEPOS enrollment record can only have 1 current business location.
Revalidations
Revalidation means resubmitting and recertifying your enrollment information.
DMEPOS suppliers must revalidate every 3 years, while all other providers and suppliers generally revalidate every 5 years. We can also conduct off-cycle revalidations . You can revalidate using PECOS or by submitting the appropriate paper Medicare enrollment application .
If you’re currently enrolled, check the Medicare Revalidation List to find your revalidation due date. If you see a due date, submit your revalidation before that date. Your MAC will also send you a revalidation notice.
Due dates are:
- Updated in the Medicare Revalidation List every 60 days at the beginning of the month
- Listed up to 7 months in advance or listed as to be determined (TBD) if the due date is more than 7 months away
Yes. Your MAC will send a revalidation notice 90–120 days before your revalidation due date.
If there’s no due date listed on the Medicare Revalidation List or you didn’t get a MAC letter requesting revalidation, don’t submit your revalidation application. Your MAC will return it to you.
However, if you’re within 2 months of the due date listed on the Medicare Revalidation List and didn’t get a MAC notice to revalidate, submit your revalidation application.
Yes. PECOS lets you review information on file and update and electronically submit your revalidation. If you use PECOS, you need to update only changed information.
If you submit your revalidation after its due date, your MAC may place a hold on your Medicare payments or deactivate your Medicare billing privileges. If the MAC requests additional documentation, respond within 30 days. If you don’t, they may deactivate your Medicare billing privileges.
Revalidation ensures all provider enrollment records are accurate and current. Generally, we don’t take administrative action against a provider or supplier for updating their records even though it wasn’t timely. However, we could take administrative actions, including recovering previous Medicare payments, when a provider or supplier that fails to report the change causes their Medicare enrollment to become ineligible.
PECOS users can’t mail documents that require a signature. When submitting your application, be prepared to send an e-signature or upload your signed documents.
Protect Your Identity & Privacy
You can help protect your professional medical identifiers from identity thieves attempting to defraud the Medicare Program.
Keep PECOS Enrollment Information Current
Log in to PECOS and review your Medicare enrollment information several times a year to ensure no unauthorized changes were made.
PECOS Provides Security
Only you, authorized surrogates, authorized CMS officials, and MACs may enter and view your Medicare PECOS enrollment information. CMS officials and MACs get security standards training and must protect your information. We don’t disclose your Medicare enrollment information to anyone, except when authorized or required by law.
Review & Protect Enrollment Information
Review your Medicare enrollment information in PECOS frequently to ensure it’s accurate, current, and unaltered.
Use your I&A System user ID and password to access PECOS. Keep your ID and password secure.
Protect Yourself & CMS Programs from Fraud
Your NPI and TIN are publicly available information. Use extra caution to monitor and protect your professional and personal information to help prevent fraud and abuse. Also ensure your patients’ personal health information is secure. Refer to these resources:
- Medicare Fraud & Abuse: Prevent, Detect, Report
- Office of Inspector General
- Reporting Medicare fraud & abuse
Take these steps to verify your Medicare enrollment information:

If you suspect your PECOS profile is incorrect due to unauthorized account access, contact your MAC, law enforcement authorities, and your bank. Your MAC and bank can flag your respective accounts for possible fraudulent activity, and law enforcement can begin investigating if and how your accounts were compromised.
Additional Privacy Tips
Take these additional actions to protect your Medicare enrollment information:
- Change your password in the I&A System before accessing PECOS the first time. You can’t change your user ID, but you must change your password every 60 days.
- Review your Medicare enrollment information several times a year to ensure no one changed information without your knowledge. Immediately report changes you didn’t submit.
- Maintain your Medicare enrollment record. Report Medicare enrollment changes known as reportable events, including change of ownership or control , change in practice location, banking arrangements, and any final adverse legal actions.
- Store PECOS copies or paper enrollment applications in a secure location. Don’t allow others access to this information as it contains your personal information, including your date of birth and SSN. Don’t leave copies in a public workspace.
- Enroll in electronic Medicare payments, and ensure they deposit directly into your bank account. We require all providers to use electronic funds transfer (EFT) when enrolling in Medicare, revalidating, or making changes to their enrollment. The most efficient way to enroll in EFT is to complete the EFT information section in PECOS and provide the required supporting documentation. Using EFT allows us to send payments directly to your bank account.
DMEPOS Supplier Requirements
Dmepos supplier standards, accreditation, & surety bond.
To enroll or keep your Medicare billing privileges, all DMEPOS suppliers (except certain exempted professionals) must meet supplier and DMEPOS Quality Standards to become accredited. Certain DMEPOS suppliers must also submit a surety bond .
DMEPOS suppliers (except those exempted eligible professionals and other persons) must be accredited by a CMS-approved accrediting organization before submitting a Medicare enrollment application to the National Provider Enrollment (NPE) DMEPOS contractors .
Each enrolled DMEPOS supplier covered under the Health Insurance Portability and Accountability Act (HIPAA) must name each practice location (if it has more than 1) as a sub-part and make sure each sub-part gets its own NPI.
Individual DMEPOS Suppliers (for example, sole proprietorships)
Physicians, NPPs, and DMEPOS suppliers may use their I&A System user ID and password to access PECOS . If you don’t already have an I&A System account, refer to the I&A System User Registration page and enter the information to open an account. For help, refer to the How to Setup Your Account if you are a Sole Owner section in the I&A System Quick Reference Guide .
As an individual DMEPOS supplier, you don’t need an AO or another authorized user.
Organizational DMEPOS Suppliers System Users
A DMEPOS supplier organization must appoint an AO to manage connections and staff, including appointing and approving other authorized PECOS users. The organization must identify the AO in the enrollment application. The AO must have ownership or managing control in the DMEPOS supplier organization.
Providers Who Solely Order or Certify
Physicians and other eligible professionals must enroll in the Medicare Program or have a valid opt-out affidavit on file to solely order or certify Medicare patient items or services.
Those physicians and other eligible professionals enrolled solely as ordering/certifying providers don’t send billed service claims to a MAC.
Ordering/Certifying Terms
Part B claims use the term ordering/certifying provider to identify the professional who orders or certifies an item or service reported in a claim. These are technically correct terms:
- Providers order non-physician patient items or services, like DMEPOS, clinical lab services, or imaging services
- Providers certify patient home health services
The health care industry uses the terms ordered , referred , and certified interchangeably .
Who Are Eligible Ordering/Certifying Providers?
Physicians or eligible professionals who order or certify Part A or Part B services but don’t want to submit Medicare claims are eligible ordering/certifying providers.
A person already enrolled as a Part B provider may submit claims listing themselves as the ordering/certifying provider without re-enrolling using Medicare Enrollment Application: Enrollment for Eligible Ordering/Certifying Physicians and Other Eligible Professionals (CMS-855O) .
Note: Those who enroll as eligible providers using CMS-855O can’t bill Medicare, and we can’t pay for their services because they have no Medicare billing privileges.
Organizational NPIs don’t qualify, and you can’t use them to order or certify.
Eligible providers must meet these basic conditions:
- Have an individual NPI
- Be enrolled in Medicare in either an approved or opt-out status
- Be an eligible specialty type to order or certify
Denial of Ordering/Certifying Claims
If claims lack a valid individual NPI, MACs deny them if they’re from:
- Clinical labs for ordered tests
- Imaging centers for ordered imaging procedures
- DMEPOS suppliers for ordered DMEPOS
- Part A home health agencies that aren’t ordered or certified by a Doctor of Medicine, Osteopathy, or Podiatric Medicine
If you bill a service that needs an eligible provider and they aren’t on the claim, the MAC will deny the claim. The claim must have a valid NPI and the eligible provider’s name as it appears in PECOS.
If a provider who’s on the Preclusion List prescribes a Medicare Part D drug, drug plans will deny it.
Requirement 1: Get an Individual NPI
The 2 types of NPIs are: Type 1 (individual) and Type 2 (organizational). Medicare allows only Type 1 NPIs to solely order items or certify services. Apply for an NPI through:
- Online Application: Get an I&A System user account. Then apply for an NPI in NPPES .
Requirement 2: Enroll in Medicare in an Approved or Opt-Out Status
Once you have an NPI, use PECOS to verify current Medicare enrollment record information, including your NPI and that you’re approved, or go to the Opt Out Affidavits list to check your status. To opt out of Medicare, submit an affidavit expressing your decision to opt out of the program.
Part C and Part D providers don’t have to enroll in Medicare in an approved or opt-out status.
*We deny certain power mobility device claims if the ordering provider isn’t on our eligible providers list.
Requirement 3: Be Eligible to Order or Certify
The physicians and eligible professionals who may enroll in Medicare solely for ordering or certifying include, but aren’t limited to, physicians and eligible professionals who are:
- Department of Veterans Affairs employees
- Public Health Service employees
- Department of Defense or TRICARE employees
- Indian Health Service or Tribal Organization employees
- Federally Qualified Health Center, Rural Health Clinic, or Critical Access Hospital employees
- Licensed Residents in an approved medical residency program defined in 42 CFR 413.75(b)
- Dentists, including oral surgeons
- Pediatricians
- Retired, licensed physicians
If you’re unsure whether your specific provider specialty qualifies to enroll as an ordering/certifying provider, refer to Section 4 of CMS-855O or find your MAC’s website before submitting a Medicare enrollment application.
Interns & Residents
Claims for items or services ordered or certified by licensed or unlicensed interns and residents must specify a teaching physician’s NPI and name. State-licensed residents may enroll to order or certify and can be listed on claims. If states offer provisional licenses or otherwise permit residents to order/certify, we allow interns and residents to enroll consistent with state law.
Requirement 4: Respond to Requests for More Information
- To see your enrollment status without logging in, go to PECOS and, under Helpful Links , select Application Status .
Requirement 5: Use PECOS to Keep Enrollment Information Current
Report a Medicare enrollment change using PECOS. Providers and suppliers must report a change of ownership or control (including a change in authorized or delegated official), a change in practice location, and any final adverse legal actions (like revocation or suspension of a federal or state license) within 30 days of the change and must report all other changes within 90 days of the change.
Revalidation
Revalidation, or re-submitting and recertifying your enrollment information accuracy, is an important anti-fraud tool. All Medicare-enrolled providers and suppliers must periodically revalidate their enrollment information .
Generally, physicians, including physician organizations, opioid treatment programs, Medicare Diabetes Prevention Program suppliers, and institutional providers, revalidate enrollment every 5 years or when we request it. DMEPOS suppliers must revalidate their enrollment information every 3 years.
PECOS is the most efficient way to revalidate information.
If you’re actively enrolled, go to the Medicare Revalidation List to find your revalidation due date. If you see a due date, submit your revalidation before that date. Your MAC notifies you when it’s time to revalidate. If you submit your revalidation application after the due date, your MAC may hold your Medicare payments or deactivate your billing privileges.
Rebuttal Process
MACs issue Medicare billing privilege deactivations. We permit providers and suppliers to file a rebuttal .
Get more information:
- 42 CFR 424.515
- Provider Enrollment Revalidation Cycle 2 FAQs
- Revalidations (Renewing Your Enrollment)
Large Group Coordination
Groups with more than 200 members can use the Medicare Revalidation List and search by their organization’s name to download group information. Their MAC will send them a letter and spreadsheet that lists the providers linked to their group who must revalidate within 6 months. Large groups should work together to ensure they submit only 1 application from each provider or supplier.
Use these resources to learn how to enroll in the Medicare Program, revalidate your enrollment, or change your enrollment information. Enroll in the Medicare Program to get paid for providing covered patient services. Enroll if you solely order items or certify services.
You can enroll online by using PECOS or the appropriate paper enrollment application you submit to your MAC.
- Get an I&A System user account
- Apply for your NPI in the NPPES
- Enroll in PECOS
Enrollment Forms
If you enroll using a paper application instead of PECOS , search the CMS Forms List to find the form you need and read on page 1, Who Should Submit This Application .
Commonly Used Terms
View the Medicare Learning Network® Content Disclaimer and Department of Health & Human Services Disclosure .
The Medicare Learning Network®, MLN Connects®, and MLN Matters® are registered trademarks of the U.S. Department of Health & Human Services (HHS).

Physician Acceptance of Medicare Assignment

- Medicare assignment pertains to an agreement between Medicare and participating doctors. Learn more about the physicians that accept Medicare assignment.
Medicare assignment, or Medicare assignment of benefits, is the process in which a Medicare beneficiary authorizes Medicare to directly reimburse health care providers for services. To ensure all services are charged at Medicare-determined rates, recipients should verify whether their primary physicians fall under the accept assignment definition prior to scheduling services.
What Is the Medicare Accept Assignment Definition?
The Medicare accept assignment definition pertains to physicians, medical suppliers and medical providers that agree to accept Medicare-approved charges as total and full payment for all covered services without adding extra charges. These providers also agree to charge only the allowed Medicare deductible and coinsurance charges to patients. Medicare-approved providers who accept Medicare assignment are referred to as participating providers.
Non-participating providers may accept Medicare and provide Medicare-covered services. However, as non-participating providers, they are not required to accept Medicare's pre-determined costs for procedures and office visits. Additionally, non-participating providers are legally allowed to charge up to 15% above Medicare-approved amounts. That extra amount is billed to the patient.
In addition to participating and non-participating providers, some providers choose not to accept Medicare in any capacity. These providers are referred to as opt-out providers. Only a small percentage (under 2%) of providers choose to completely opt out.
What Are Some Benefits of Medicare Assignment?
Medicare recipients who receive primary care through Medicare assignment providers may have lower out-of-pocket costs than recipients who utilize the services of non-participating providers. Providers who accept Medicare assignment must submit all claims directly to Medicare, so recipients can't be charged anything for claim submission. In most cases, Medicare assignment providers wait to charge recipients for their share in costs (when applicable) until after Medicare pays its share, which may help make medical expenses more manageable.
What May Happen When a Provider Doesn't Accept Assignment?
In addition to possibly being charged up to an additional 15% for procedures and services, individuals who use non-participating providers may be required to pay full costs for services upfront. Recipients may also need to submit their own insurance claims to Medicare to receive reimbursements. Medicare recipients who receive services through providers who are completely opted out are generally required to pay for all services and procedures, even if they would normally be covered by Medicare. Recipients who prefer to use opt-out providers may be able to set up payment plans through private contracts.
What Is Part B Medicare Assignment?
Medicare assignment Part B pertains to outpatient services. Recipients who work with participating providers are generally required to pay 20% of allowed amounts out of pocket. Those who choose providers defined as non-participating may be required to pay excess charges of up to 15%. Recipients with health care providers who are completely opted out may be responsible for 100% of costs for services and procedures.

Christian Worstell is a senior Medicare and health insurance writer with HelpAdivsor.com. He is also a licensed health insurance agent. Christian is well-known in the insurance industry for the thousands of educational articles he’s written, helping Americans better understand their health insurance and Medicare coverage.
Christian’s work as a Medicare expert has appeared in several top-tier and trade news outlets including Forbes, MarketWatch, WebMD and Yahoo! Finance.
While at HelpAdvisor, Christian has written hundreds of articles that teach Medicare beneficiaries the best practices for navigating Medicare. His articles are read by thousands of older Americans each month. By better understanding their health care coverage, readers may hopefully learn how to limit their out-of-pocket Medicare spending and access quality medical care.
Christian’s passion for his role stems from his desire to make a difference in the senior community. He strongly believes that the more beneficiaries know about their Medicare coverage, the better their overall health and wellness is as a result.
A current resident of Raleigh, Christian is a graduate of Shippensburg University with a bachelor’s degree in journalism. You can find Christian’s most recent articles in our blog .
If you’re a member of the media looking to connect with Christian, please don’t hesitate to email our public relations team at [email protected] .
- Does Medicare Cover Physical Therapy?
- What is the Medicare Wellness Exam?
- What Is the Welcome to Medicare Visit?
- Does Medicaid Cover Physical Therapy?
- Medicare Part B Medical Insurance: Costs, Coverage and Benefits

Medicare Interactive Medicare answers at your fingertips -->
Participating, non-participating, and opt-out providers, outpatient provider services.
You must be logged in to bookmark pages.
Email Address * Required
Password * Required
Lost your password?
If you have Original Medicare , your Part B costs once you have met your deductible can vary depending on the type of provider you see. For cost purposes, there are three types of provider, meaning three different relationships a provider can have with Medicare . A provider’s type determines how much you will pay for Part B -covered services.
- These providers are required to submit a bill (file a claim ) to Medicare for care you receive. Medicare will process the bill and pay your provider directly for your care. If your provider does not file a claim for your care, there are troubleshooting steps to help resolve the problem .
- If you see a participating provider , you are responsible for paying a 20% coinsurance for Medicare-covered services.
- Certain providers, such as clinical social workers and physician assistants, must always take assignment if they accept Medicare.
- Non-participating providers can charge up to 15% more than Medicare’s approved amount for the cost of services you receive (known as the limiting charge ). This means you are responsible for up to 35% (20% coinsurance + 15% limiting charge) of Medicare’s approved amount for covered services.
- Some states may restrict the limiting charge when you see non-participating providers. For example, New York State’s limiting charge is set at 5%, instead of 15%, for most services. For more information, contact your State Health Insurance Assistance Program (SHIP) .
- If you pay the full cost of your care up front, your provider should still submit a bill to Medicare. Afterward, you should receive from Medicare a Medicare Summary Notice (MSN) and reimbursement for 80% of the Medicare-approved amount .
- The limiting charge rules do not apply to durable medical equipment (DME) suppliers . Be sure to learn about the different rules that apply when receiving services from a DME supplier .
- Medicare will not pay for care you receive from an opt-out provider (except in emergencies). You are responsible for the entire cost of your care.
- The provider must give you a private contract describing their charges and confirming that you understand you are responsible for the full cost of your care and that Medicare will not reimburse you.
- Opt-out providers do not bill Medicare for services you receive.
- Many psychiatrists opt out of Medicare.
Providers who take assignment should submit a bill to a Medicare Administrative Contractor (MAC) within one calendar year of the date you received care. If your provider misses the filing deadline, they cannot bill Medicare for the care they provided to you. However, they can still charge you a 20% coinsurance and any applicable deductible amount.
Be sure to ask your provider if they are participating, non-participating, or opt-out. You can also check by using Medicare’s Physician Compare tool .
Update your browser to view this website correctly. Update my browser now

- Entertainment
- Investigations
- Latest Headlines
- Tropicana Closure
- What Are They Hiding?
- 2024 Election
- Clark County
- Nation and World
- Science and Technology
- Road Warrior
- Las Vegas Weather
- East Valley
- North Las Vegas
- Summerlin/Centennial Hills
- Remembering Oct. 1, 2017
- Deborah Wall
- Natalie Burt
- Remembering Jeff German
- Police Accountability
- Alpine Fire
- 100 Years of Growth
- Dangerous Driving
- Raiders News
- Golden Knights
- UNLV Football
- UNLV Basketball
- Nevada Preps
- Sports Betting 101
- Las Vegas Sportsbooks
- National Finals Rodeo
- Where Are They Now?
- On TV/Radio
- MMA and UFC
- Casinos & Gaming
- Conventions
- Inside Gaming
- Entrepreneurs
- Real Estate News
- Business Press
- Sheldon Adelson (1933-2021)
- Debra J. Saunders
- Michael Ramirez cartoons
- Victor Joecks
- Richard A. Epstein
- Victor Davis Hanson
- Drawing Board
- Homicide Tracker
- Faces of Death Row
- Kats’ Cool Hangs
- Arts & Culture
- Home and Garden
- Las Vegas Hiking Guide
- RJ Magazine
- Today’s Obituaries
- Submit an obit
- Dealer News
- Classifieds
- Place a Classified Ad
- Provided Content
- Real Estate Millions
- Internships
- Service Directory
- Transportation
- Merchandise
- Legal Information
- Real Estate Classifieds
- Garage Sales
- Contests and Promotions
- Best of Las Vegas
- Nevada State Bank
- Verizon Business
- P3 Health Partners
- Adult Health
- Star Nursery
- Partner Articles
- Ignite Funding
- Supplements
- Travel Nevada
- Subscriptions
- Newsletters
- Advertise with Us
- >> Live Well
How do you qualify for premium-free Medicare Part A?
Many Americans are not aware that they must work a certain amount of time and pay employment taxes to receive premium-free Part A.

Dear Toni: I made a mistake enrolling in Medicare. My husband, Sonny, was laid off in February and lost his employer health insurance, which I was on. He is a veteran and is receiving his health care from the VA, so he did not have to enroll in Medicare.
I have enrolled in Medicare since I am turning 65 in April. But I am not sure if I enrolled properly, because my Medicare is costing me an extra $505 for Part A and $174.70 for Part B. Isn’t Part A free?
I have not worked very much since Sonny and I married 40 years ago, and Social Security said that is my issue. Please explain what I should do to correct my Medicare mistake. — Terry, Laredo, Texas
Dear Terry: No, Medicare Part A is not free. Many Americans are not aware that they must work a certain amount of time and pay employment taxes to receive premium-free Part A. This is most likely the cause of your problem.
To qualify for Part A at no cost, you must have worked and paid Social Security and Medicare taxes from your payroll check for 10 years, or 40 quarters. For 2024, if you paid Medicare taxes for 30 to 39 quarters, then the standard Part A premium is $278 each month. If you paid Medicare taxes for less than 30 quarters, the premium for Part A is $505 each month.
However, those who do not qualify for premium-free Part A but who have been married for at least 10 years to an individual who has met the 10 years/40 quarters requirement should apply for Medicare under their spouse’s Social Security number. Terry, you should have applied for Medicare under Sonny’s account.
My advice would be to contact your local Social Security office. Ask for help to appeal your Part A premium of $505, because you have been a stay-at-home spouse but your husband has worked enough quarters to qualify for premium-free Part A.
Social Security will look over your husband’s Social Security accounts and verify with the IRS that he has enough quarters to qualify. Be prepared to provide a certified marriage license (not a copy) to Social Security.
Toni King is an author and columnist on Medicare and health insurance issues. If you have a Medicare question, email [email protected] or call 832-519-8664.


If you want to eat to lower blood pressure, bring this registered dietitian-approved list with you next time you go grocery shopping.

The year-old monument south of Las Vegas helps to preserve a wildlife corridor that stretches from Mojave National Preserve to the Colorado Plateau.

A new study found that Medicare patients spend about three weeks a year getting medical care in an American system that has grown “overwhelmingly complex.”

“The longer you are on the mat the more you will learn about yourself and the better you will feel,” Dray Gardner says.

On the first day of rehab, a doctor asked her goal from the program. Without hesitating, Channing Muller said: “I want to run again.”

Avoiding a Part B penalty when enrolling after 65 can be overwhelming. But initial enrollment is not the only stressful issue.

Here’s a rundown of which vaccines are recommended by the Centers for Disease Control and Prevention and how Medicare covers them.

“I’ve never done period, genre work, so I wanted to see how I looked in tights,” the 79-year-old Oscar winner jokes about portraying a Founding Father.

“Most of us have much more control than we realize when it comes to memory retention and brain health,” Dr. Gary Small says.

The question of whether these chatbots are delivering a mental health service is critical to the emerging digital health industry — and its survival.

- IC gets chief AI officer
- Schedule F blocked for good?
- Burnout causing turnover, low morale
- Sports Schedule
Hubbard Radio Washington DC, LLC. All rights reserved. This website is not intended for users located within the European Economic Area.
Medicare Part B special enrollment period for USPS annuitants begins today
USPS retirees who are eligible for Medicare Part B, but do not have it, can sign up between now and September 1 without having to pay a penalty.

- Open Season is not until this fall, but some feds may want to start looking at their health care early. A special enrollment period starts today for Postal Service annuitants. USPS retirees who are eligible for Medicare Part B, but do not have it, can sign up between now and September 1 without having to pay a penalty. The USPS is covering the cost of the penalty for any annuitants who do choose to sign up. The special enrollment period comes ahead of the launch of the brand-new Postal Service Health Benefits program for plan year 2025. And for everyone else, Open Season will run Nov. 11 to Dec. 9. ( Postal Service Health Benefits program - Office of Personnel Management)
- Nearly a two-year effort has concluded with agencies receiving their first update to the standards for collecting federal data on race and ethnicity in more than 25 years. The Office of Management and Budget's Chief Statistician Karin Orvis said the interagency working group made several significant changes to the standards, including adding Middle Eastern or North African as a new minimum category. Agencies are to begin updating their surveys and administrative forms as quickly as possible and must submit an agency action plan for complete compliance within 18 months. Orvis said the working group reviewed 20,000 comments and held almost 100 listening sessions as part of its effort to finalize the new standards. ( OMB updates standards to collect federal data on race, ethnicity - White House)
- The Defense Department has established the Office of the Assistant Secretary of Defense for Cyber Policy. The new office, officially launched on March 20, will oversee all cyber-related policy issues at the Pentagon. That includes certifying the department's cyber operations budget and overlooking cyber workforce development programs. Ashley Manning will serve as the official performing the duties of the assistant secretary until the Senate confirms an official for the position. President Joe Biden nominated Michael Sulmeyer, who is currently serving as the principal cyber adviser to the Army Secretary, to serve in the new role. ( Establishment of the Office of the Assistant Secretary of Defense for Cyber Policy - DoD)
- There is a new section to the FAR and it may be the most important change in decades. Get used to hearing about FAR Part 40. It's the new consolidated section of the Federal Acquisition Regulations for all things cybersecurity and supply chain security. The FAR Council issued the final rule today establishing this new section, bringing together clauses and regulations covering broad security requirements for most acquisitions. The new FAR part will provide contracting officers with a single, consolidated location to find these requirements. While the new FAR section does not create any new requirements or contract clauses, the council currently is reviewing three rules that would be added to Part 40 when finalized. ( FAR Council formally established new cybersecurity section - Federal Register)
We want to hear from federal technology leaders about how you are addressing current cyber demands and how your agency is making the most of its resources to improve its cyber posture. | Take our quick survey
- Senate lawmakers are pushing to bring federal record-keeping practices into the 21st century. Agencies would need to make sure employees back up their texts and other digital chats used for official business under the Strengthening Federal Records Act of 2024. Sens. Gary Peters (D-Mich.) and John Cornyn (R-Texas) are co-sponsoring the bill. They say the Federal Records Act needs to keep with rapidly changing technology. The bill would also strengthen the role of the National Archives and Records Administration in holding agencies accountable to record-keeping rules. ( Senate bill aims to bring federal records law into the age of ‘WhatsApp’ - Federal News Network)
- The Navy has created a sort of one-stop-shop of efficiency when it comes to Navy Culture. A new initiative dubbed Culture of Excellence 2.0 aligns several Navy programs and concepts, allowing the leadership to better understand the needs of its sailors. New materials released as part of the initiative include a playbook on mental health and a suicide-related behavior response guide. The women’s initiatives team and the new policy for the assignment of pregnant sailors also fall under the umbrella of Culture of Excellence 2.0. And there will be a new tool for commanders to better understand the risk of destructive behaviors within their commands. ( Navy updates its culture campaign - U.S. Navy)
- A new leader has taken the reins at the National Security Agency’s Cybersecurity Directorate (CSD). Dave Luber formally took over as CSD Director on Friday, replacing Rob Joyce, who had led the directorate since 2021. Luber previously served as CSD’s deputy director. He is a longtime veteran of the intelligence community, having also served as executive director at U.S. Cyber Command and in various positions throughout the NSA. The Cybersecurity Directorate is responsible for helping to secure defense industrial base networks and issuing public advisories on cyber threats. ( New NSA CSD director - X)
- When candidates go online to apply for a federal job, they will see a brand new look. USA jobs.gov has updated its homepage design and some key features of the website. There is now a "search tips" option for anyone who might need help narrowing down a search. A link at the top of the homepage will take users to a list of upcoming hiring events and information sessions. And there is info about what career fields are hiring right now, and how the federal hiring process works. ( Website homepage update - USAJobs.gov)
Copyright © 2024 Federal News Network. All rights reserved. This website is not intended for users located within the European Economic Area.
- Go Apple's Website to download the APP
- Go Google's Website to download the APP
Peter Musurlian is a producer at Federal News Network.
Follow @PMusurlianWFED
Related Stories

‘We are on the front line:’ USPS letter carriers recognized for heroic acts

Alpha-1, DoD’s portfolio of services, will accelerate AI adoption

Will that bridge collapse in Maryland affect federal supply chains?

- ‘We are on the front line:’ USPS letter carriers recognized for heroic acts Workforce
- Alpha-1, DoD’s portfolio of services, will accelerate AI adoption Defense
- Will that bridge collapse in Maryland affect federal supply chains? Management
Top Stories
- State Dept workforce in ‘tough position’ with 13% staffing gap, says deputy secretary Top Story
- OPM outlines how agencies, unions can recreate labor-management forums UNIONS
- Air Force seeks to override existing law, move Guard units to Space Force AIR FORCE
- OMB’s new guidance, RFI boost grant modernization efforts MANAGEMENT
- DoD Cloud Exchange 2024: Navy Reserve tech leaders on cloud-enabled access anywhere, anytime CLOUD COMPUTING
The Federal Register
The daily journal of the united states government, request access.
Due to aggressive automated scraping of FederalRegister.gov and eCFR.gov, programmatic access to these sites is limited to access to our extensive developer APIs.
If you are human user receiving this message, we can add your IP address to a set of IPs that can access FederalRegister.gov & eCFR.gov; complete the CAPTCHA (bot test) below and click "Request Access". This process will be necessary for each IP address you wish to access the site from, requests are valid for approximately one quarter (three months) after which the process may need to be repeated.
An official website of the United States government.
If you want to request a wider IP range, first request access for your current IP, and then use the "Site Feedback" button found in the lower left-hand side to make the request.
What Part B covers
If you're in a Medicare Advantage Plan or other Medicare plan, your plan may have different rules. But, your plan must give you at least the same coverage as Original Medicare. Some services may only be covered in certain facilities or for patients with certain conditions.
What's covered?
NEW INSULIN BENEFIT! If you use an insulin pump that's covered under Part B's durable medical equipment benefit, or you get your covered insulin through a Medicare Advantage Plan, your cost for a month's supply of Part B-covered insulin for your pump can't be more than $35. The Part B deductible won't apply. If you get a 3-month supply of Part B-covered insulin, your costs can't be more than $35 for each month's supply. This means you'll generally pay no more than $105 for a 3-month supply of covered insulin. If you have Part B and Medicare Supplement Insurance ( Medigap ) that pays your Part B coinsurance, you plan should cover the $35 (or less) cost for insulin.
Part B covers 2 types of services
- Medically necessary services: Services or supplies that are needed to diagnose or treat your medical condition and that meet accepted standards of medical practice.
- Preventive services : Health care to prevent illness (like the flu) or detect it at an early stage, when treatment is most likely to work best.
You pay nothing for most preventive services if you get the services from a health care provider who accepts assignment .
Part B covers things like:
- Clinical research
- Ambulance services
- Durable medical equipment (DME)
- Partial hospitalization
- Intensive outpatient program services (starting January 1, 2024)
- Limited outpatient prescription drugs
2 ways to find out if Medicare covers what you need
- Talk to your doctor or other health care provider about why you need certain services or supplies. Ask if Medicare will cover them. You may need something that's usually covered but your provider thinks that Medicare won't cover it in your situation. If so, you'll have to read and sign a notice . The notice says that you may have to pay for the item, service, or supply.
- Find out if Medicare covers your item, service, or supply .
Medicare coverage is based on 3 main factors
- Federal and state laws.
- National coverage decisions made by Medicare about whether something is covered.
- Local coverage decisions made by companies in each state that process claims for Medicare. These companies decide whether something is medically necessary and should be covered in their area.

IMAGES
VIDEO
COMMENTS
You can get the lowest cost if your doctor or other health care provider accepts the Medicare-approved amount as full payment for a covered service. This is called "accepting assignment." If a provider accepts assignment, it's for all Medicare-covered Part A and Part B services.
Here's how it works: Medicare will pay the provider 95% of the amount they would pay if the provider accepted assignment. The provider can charge the person receiving care more than the Medicare-approved amount, but only up to 15% more (some states limit this further). This extra amount, which the patient has to pay out-of-pocket, is known as ...
Medicare assignment is a fee schedule agreement between the federal government's Medicare program and a doctor or facility. When Medicare assignment is accepted, it means your doctor agrees to the payment terms of Medicare. Doctors that accept Medicare assignment fall under one of three designations: a participating doctor, a non ...
Because Medicare Part B covers doctor and outpatient services, your $240 deductible for Part B in 2024 applies before most coverage begins. All providers who accept assignment must submit claims directly to Medicare, which pays 80 percent of the approved cost for the service and will bill you the remaining 20 percent.
Summary: Medicare Assignment is an agreement between healthcare providers and Medicare, where providers accept the Medicare-approved amount as full payment, preventing them from charging beneficiaries extra. This benefits Medicare beneficiaries by controlling their costs and ensuring they only pay deductibles and copayments.
What is Medicare Assignment. Medicare assignment is an agreement by your doctor or other healthcare providers to accept the Medicare-approved amount as the full cost for a covered service. Providers who "accept assignment" bill Medicare directly for Part B-covered services and cannot charge you more than the applicable deductible and ...
Doctors that take Medicare can sign a contract to accept assignment for all Medicare services, or be a non-participating provider that accepts assignment for some services but not all. A medical provider that accepts Medicare assignment must submit claims directly to Medicare on your behalf. They will be paid the agreed upon amount by Medicare ...
If the therapist accepts the Medicare assignment, they will charge you $100 and bill Medicare. After Medicare pays $100, you'll owe 20%, or $20 for coinsurance. That's if you have already met your Part B deductible. If not, Medicare may not pay anything, up to the amount of the deductible, and you may be responsible for the entire bill.
Medicare assignment codes help Medicare pay for covered services. If your doctor or other provider accepts assignment and is a participating provider, they will file for reimbursement for services with a CMS-1500 form and the code will be "assigned.". But non-participating providers can select "not assigned.".
Medicare "participation" means you agree to accept claims assignment for all Medicare-covered services to your patients. By accepting assignment, you agree to accept Medicare-allowed amounts as payment in full. You may not collect more from the patient than the Medicare deductible and coinsurance or copayment. Participating Provider or ...
1. Participating providers, or those who accept Medicare assignment. These providers have an agreement with Medicare to accept the Medicare-approved amount as full payment for their services. You don't have to pay anything other than a copay or coinsurance (depending on your plan) at the time of your visit.
Medicare sets a fixed cost to pay for every benefit they cover. This amount is called Medicare assignment. You have the largest healthcare provider network with over 800,000 providers nationwide on Original Medicare. You can see any doctor nationwide that accepts Medicare. Understanding the differences between your cost and the difference ...
Medicare participation means you agree to accept claims assignment for all covered patient services. By accepting assignment, you agree to accept Medicare-allowed amounts as payment in full. You can't collect more from the patient than the deductible and coinsurance or copayment.The Social Security Act says you must submit patient Medicare claims whether or not you participate.
Medicare assignment Part B pertains to outpatient services. Recipients who work with participating providers are generally required to pay 20% of allowed amounts out of pocket. Those who choose providers defined as non-participating may be required to pay excess charges of up to 15%.
Participating providers accept Medicare and always take assignment. Taking assignment means that the provider accepts Medicare's approved amount for health care services as full payment. These providers are required to submit a bill (file a claim) to Medicare for care you receive. Medicare will process the bill and pay your provider directly ...
For Medicare Part B, this comes to 20%. ... Participating health providers have an agreement with Medicare to accept assignment for all Medicare-covered services. If the doctor accepts assignment:
Find doctors & clinicians near me. Find general information about doctors, clinicians and groups enrolled in Medicare. Find Medicare-approved providers near you & compare care quality for nursing homes, doctors, hospitals, hospice centers, more. Official Medicare site.
For 2024, if you paid Medicare taxes for 30 to 39 quarters, then the standard Part A premium is $278 each month. If you paid Medicare taxes for less than 30 quarters, the premium for Part A is ...
This benefit only covers your immunosuppressive drugs and no other items or services. It isn't a substitute for full health coverage. If you qualify, you can sign up for this benefit any time after your Part A coverage ends. To sign up, call Social Security at 1-877-465-0355. TTY users can call 1-800-325-0788.
If you have Original Medicare, see providers who accept Medicare assignment. ... For example, Part B would cover an EKG or chest x-ray for medical reasons, like an abnormal heart rhythm or severe ...
New materials released as part of the initiative include a playbook on mental health and a suicide-related behavior response guide. The women's initiatives team and the new policy for the assignment of pregnant sailors also fall under the umbrella of Culture of Excellence 2.0.
experienced with performance-based risk Medicare ACO initiatives. 42 CFR part 425, subpart B . 42 CFR part 425, subpart B . 42 CFR § 425.630\(b\) 42 CFR § 425.630\(b\) 42 CFR § 425.630\(b\) ... providers/suppliers in ACO-MS does not impact beneficiary assignment or Medicare FFS billing rules. If an ACO submits timely notice to CMS, the ...
After you meet the Part B deductible you pay 20% of the Medicare-approved amount (if your supplier accepts assignment). Medicare pays for different kinds of DME in different ways. Depending on the type of equipment: You may need to rent the equipment. You may need to buy the equipment. You may be able to choose whether to rent or buy the equipment.
Since these drug costs were attributable to the entire SNF and not limited to Medicare-allowable services, we propose to adjust the drug costs by the ratio of Medicare-allowable pharmacy total costs (Worksheet B, part I, column 11, for lines 30, 40 through 49, 51, 52, and 71) to total pharmacy costs from Worksheet B, part I, column 11, line 11.
You can only join, switch, or drop a Medicare Advantage Plan (Part C) or Medicare drug plan (Part D) during certain times, called enrollment periods. You need . both. Medicare Part A (Hospital Insurance) and Part B (Medical Insurance) to join a Medicare Advantage Plan. You need either Part A or Part B to join a Medicare drug plan.
Part B covers 2 types of services. Medically necessary services: Services or supplies that are needed to diagnose or treat your medical condition and that meet accepted standards of medical practice. Preventive services: Health care to prevent illness (like the flu) or detect it at an early stage, when treatment is most likely to work best.