An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Psychiatry

Mental Health Prevention and Promotion—A Narrative Review
Associated data.
Extant literature has established the effectiveness of various mental health promotion and prevention strategies, including novel interventions. However, comprehensive literature encompassing all these aspects and challenges and opportunities in implementing such interventions in different settings is still lacking. Therefore, in the current review, we aimed to synthesize existing literature on various mental health promotion and prevention interventions and their effectiveness. Additionally, we intend to highlight various novel approaches to mental health care and their implications across different resource settings and provide future directions. The review highlights the (1) concept of preventive psychiatry, including various mental health promotions and prevention approaches, (2) current level of evidence of various mental health preventive interventions, including the novel interventions, and (3) challenges and opportunities in implementing concepts of preventive psychiatry and related interventions across the settings. Although preventive psychiatry is a well-known concept, it is a poorly utilized public health strategy to address the population's mental health needs. It has wide-ranging implications for the wellbeing of society and individuals, including those suffering from chronic medical problems. The researchers and policymakers are increasingly realizing the potential of preventive psychiatry; however, its implementation is poor in low-resource settings. Utilizing novel interventions, such as mobile-and-internet-based interventions and blended and stepped-care models of care can address the vast mental health need of the population. Additionally, it provides mental health services in a less-stigmatizing and easily accessible, and flexible manner. Furthermore, employing decision support systems/algorithms for patient management and personalized care and utilizing the digital platform for the non-specialists' training in mental health care are valuable additions to the existing mental health support system. However, more research concerning this is required worldwide, especially in the low-and-middle-income countries.
Introduction
Mental disorder has been recognized as a significant public health concern and one of the leading causes of disability worldwide, particularly with the loss of productive years of the sufferer's life ( 1 ). The Global Burden of Disease report (2019) highlights an increase, from around 80 million to over 125 million, in the worldwide number of Disability-Adjusted Life Years (DALYs) attributable to mental disorders. With this surge, mental disorders have moved into the top 10 significant causes of DALYs worldwide over the last three decades ( 2 ). Furthermore, this data does not include substance use disorders (SUDs), which, if included, would increase the estimated burden manifolds. Moreover, if the caregiver-related burden is accounted for, this figure would be much higher. Individual, social, cultural, political, and economic issues are critical mental wellbeing determinants. An increasing burden of mental diseases can, in turn, contribute to deterioration in physical health and poorer social and economic growth of a country ( 3 ). Mental health expenditure is roughly 3–4% of their Gross Domestic Products (GDPs) in developed regions of the world; however, the figure is abysmally low in low-and-middle-income countries (LMICs) ( 4 ). Untreated mental health and behavioral problems in childhood and adolescents, in particular, have profound long-term social and economic adverse consequences, including increased contact with the criminal justice system, lower employment rate and lesser wages among those employed, and interpersonal difficulties ( 5 – 8 ).
Need for Mental Health (MH) Prevention
Longitudinal studies suggest that individuals with a lower level of positive wellbeing are more likely to acquire mental illness ( 9 ). Conversely, factors that promote positive wellbeing and resilience among individuals are critical in preventing mental illnesses and better outcomes among those with mental illness ( 10 , 11 ). For example, in patients with depressive disorders, higher premorbid resilience is associated with earlier responses ( 12 ). On the contrary, patients with bipolar affective- and recurrent depressive disorders who have a lower premorbid quality of life are at higher risk of relapses ( 13 ).
Recently there has been an increased emphasis on the need to promote wellbeing and positive mental health in preventing the development of mental disorders, for poor mental health has significant social and economic implications ( 14 – 16 ). Research also suggests that mental health promotion and preventative measures are cost-effective in preventing or reducing mental illness-related morbidity, both at the society and individual level ( 17 ).
Although the World Health Organization (WHO) defines health as “a state of complete physical, mental, and social wellbeing and not merely an absence of disease or infirmity,” there has been little effort at the global level or stagnation in implementing effective mental health services ( 18 ). Moreover, when it comes to the research on mental health (vis-a-viz physical health), promotive and preventive mental health aspects have received less attention vis-a-viz physical health. Instead, greater emphasis has been given to the illness aspect, such as research on psychopathology, mental disorders, and treatment ( 19 , 20 ). Often, physicians and psychiatrists are unfamiliar with various concepts, approaches, and interventions directed toward mental health promotion and prevention ( 11 , 21 ).
Prevention and promotion of mental health are essential, notably in reducing the growing magnitude of mental illnesses. However, while health promotion and disease prevention are universally regarded concepts in public health, their strategic application for mental health promotion and prevention are often elusive. Furthermore, given the evidence of substantial links between psychological and physical health, the non-incorporation of preventive mental health services is deplorable and has serious ramifications. Therefore, policymakers and health practitioners must be sensitized about linkages between mental- and physical health to effectively implement various mental health promotive and preventive interventions, including in individuals with chronic physical illnesses ( 18 ).
The magnitude of the mental health problems can be gauged by the fact that about 10–20% of young individuals worldwide experience depression ( 22 ). As described above, poor mental health during childhood is associated with adverse health (e.g., substance use and abuse), social (e.g., delinquency), academic (e.g., school failure), and economic (high risk of poverty) adverse outcomes in adulthood ( 23 ). Childhood and adolescence are critical periods for setting the ground for physical growth and mental wellbeing ( 22 ). Therefore, interventions promoting positive psychology empower youth with the life skills and opportunities to reach their full potential and cope with life's challenges. Comprehensive mental health interventions involving families, schools, and communities have resulted in positive physical and psychological health outcomes. However, the data is limited to high-income countries (HICs) ( 24 – 28 ).
In contrast, in low and middle-income countries (LMICs) that bear the greatest brunt of mental health problems, including massive, coupled with a high treatment gap, such interventions remained neglected in public health ( 29 , 30 ). This issue warrants prompt attention, particularly when global development strategies such as Millennium Development Goals (MDGs) realize the importance of mental health ( 31 ). Furthermore, studies have consistently reported that people with socioeconomic disadvantages are at a higher risk of mental illness and associated adverse outcomes; partly, it is attributed to the inequitable distribution of mental health services ( 32 – 35 ).
Scope of Mental Health Promotion and Prevention in the Current Situation
Literature provides considerable evidence on the effectiveness of various preventive mental health interventions targeting risk and protective factors for various mental illnesses ( 18 , 36 – 42 ). There is also modest evidence of the effectiveness of programs focusing on early identification and intervention for severe mental diseases (e.g., schizophrenia and psychotic illness, and bipolar affective disorders) as well as common mental disorders (e.g., anxiety, depression, stress-related disorders) ( 43 – 46 ). These preventive measures have also been evaluated for their cost-effectiveness with promising findings. In addition, novel interventions such as digital-based interventions and novel therapies (e.g., adventure therapy, community pharmacy program, and Home-based Nurse family partnership program) to address the mental health problems have yielded positive results. Likewise, data is emerging from LMICs, showing at least moderate evidence of mental health promotion intervention effectiveness. However, most of the available literature and intervention is restricted mainly to the HICs ( 47 ). Therefore, their replicability in LMICs needs to be established and, also, there is a need to develop locally suited interventions.
Fortunately, there has been considerable progress in preventive psychiatry over recent decades, including research on it. In the light of these advances, there is an accelerated interest among researchers, clinicians, governments, and policymakers to harness the potentialities of the preventive strategies to improve the availability, accessibility, and utility of such services for the community.
The Concept of Preventive Psychiatry
Origins of preventive psychiatry.
The history of preventive psychiatry can be traced back to the early 1900's with the foundation of the national mental health association (erstwhile mental health association), the committee on mental hygiene in New York, and the mental health hygiene movement ( 48 ). The latter emphasized the need for physicians to develop empathy and recognize and treat mental illness early, leading to greater awareness about mental health prevention ( 49 ). Despite that, preventive psychiatry remained an alien concept for many, including mental health professionals, particularly when the etiology of most psychiatric disorders was either unknown or poorly understood. However, recent advances in our understanding of the phenomena underlying psychiatric disorders and availability of the neuroimaging and electrophysiological techniques concerning mental illness and its prognosis has again brought the preventive psychiatry in the forefront ( 1 ).
Levels of Prevention
The literal meaning of “prevention” is “the act of preventing something from happening” ( 50 ); the entity being prevented can range from the risk factors of the development of the illness, the onset of illness, or the recurrence of the illness or associated disability. The concept of prevention emerged primarily from infectious diseases; measures like mass vaccination and sanitation promotion have helped prevent the development of the diseases and subsequent fatalities. The original preventive model proposed by the Commission on Chronic Illness in 1957 included primary, secondary, and tertiary preventions ( 48 ).
The Concept of Primary, Secondary, and Tertiary Prevention
The stages of prevention target distinct aspects of the illness's natural course; the primary prevention acts at the stage of pre-pathogenesis, that is, when the disease is yet to occur, whereas the secondary and tertiary prevention target the phase after the onset of the disease ( 51 ). Primary prevention includes health promotion and specific protection, while secondary and tertairy preventions include early diagnosis and treatment and measures to decrease disability and rehabilitation, respectively ( 51 ) ( Figure 1 ).

The concept of primary and secondary prevention [adopted from prevention: Primary, Secondary, Tertiary by Bauman et al. ( 51 )].
The primary prevention targets those individuals vulnerable to developing mental disorders and their consequences because of their bio-psycho-social attributes. Therefore, it can be viewed as an intervention to prevent an illness, thereby preventing mental health morbidity and potential social and economic adversities. The preventive strategies under it usually target the general population or individuals at risk. Secondary and tertiary prevention targets those who have already developed the illness, aiming to reduce impairment and morbidity as soon as possible. However, these measures usually occur in a person who has already developed an illness, therefore facing related suffering, hence may not always be successful in curing or managing the illness. Thus, secondary and tertiary prevention measures target the already exposed or diagnosed individuals.
The Concept of Universal, Selective, and Indicated Prevention
The classification of health prevention based on primary/secondary/tertiary prevention is limited in being highly centered on the etiology of the illness; it does not consider the interaction between underlying etiology and risk factors of an illness. Gordon proposed another model of prevention that focuses on the degree of risk an individual is at, and accordingly, the intensity of intervention is determined. He has classified it into universal, selective, and indicated prevention. A universal preventive strategy targets the whole population irrespective of individual risk (e.g., maintaining healthy, psychoactive substance-free lifestyles); selective prevention is targeted to those at a higher risk than the general population (socio-economically disadvantaged population, e.g., migrants, a victim of a disaster, destitute, etc.). The indicated prevention aims at those who have established risk factors and are at a high risk of getting the disease (e.g., family history of psychiatric illness, history of substance use, certain personality types, etc.). Nevertheless, on the other hand, these two classifications (the primary, secondary, and tertiary prevention; and universal, selective, and indicated prevention) have been intended for and are more appropriate for physical illnesses with a clear etiology or risk factors ( 48 ).
In 1994, the Institute of Medicine (IOM) Committee on Prevention of Mental Disorders proposed a new paradigm that classified primary preventive measures for mental illnesses into three categories. These are indicated, selected, and universal preventive interventions (refer Figure 2 ). According to this paradigm, primary prevention was limited to interventions done before the onset of the mental illness ( 48 ). In contrast, secondary and tertiary prevention encompasses treatment and maintenance measures ( Figure 2 ).

The interventions for mental illness as classified by the Institute of Medicine (IOM) Committee on Prevention of Mental Disorders [adopted from Mrazek and Haggerty ( 48 )].
Although the boundaries between prevention and treatment are often more overlapping than being exclusive, the new paradigm can be used to avoid confusion stemming from the common belief that prevention can take place at all parts of mental health management ( 48 ). The onset of mental illnesses can be prevented by risk reduction interventions, which can involve reducing risk factors in an individual and strengthening protective elements in them. It aims to target modifiable factors, both risk, and protective factors, associated with the development of the illness through various general and specific interventions. These interventions can work across the lifespan. The benefits are not restricted to reduction or delay in the onset of illness but also in terms of severity or duration of illness ( 48 ).On the spectrum of mental health interventions, universal preventive interventions are directed at the whole population without identifiable risk factors. The interventions are beneficial for the general population or sub-groups. Prenatal care and childhood vaccination are examples of preventative measures that have benefited both physical and mental health. Selective preventive mental health interventions are directed at people or a subgroup with a significantly higher risk of developing mental disorders than the general population. Risk groups are those who, because of their vulnerabilities, are at higher risk of developing mental illnesses, e.g., infants with low-birth-weight (LBW), vulnerable children with learning difficulties or victims of maltreatment, elderlies, etc. Specific interventions are home visits and new-born day care facilities for LBW infants, preschool programs for all children living in resource-deprived areas, support groups for vulnerable elderlies, etc. Indicated preventive interventions focus on high-risk individuals who have developed minor but observable signs or symptoms of mental disorder or genetic risk factors for mental illness. However, they have not fulfilled the criteria of a diagnosable mental disorder. For instance, the parent-child interaction training program is an indicated prevention strategy that offers support to children whose parents have recognized them as having behavioral difficulties.
The overall objective of mental health promotion and prevention is to reduce the incidence of new cases, additionally delaying the emergence of mental illness. However, promotion and prevention in mental health complement each other rather than being mutually exclusive. Moreover, combining these two within the overall public health framework reduces stigma, increases cost-effectiveness, and provides multiple positive outcomes ( 18 ).
How Prevention in Psychiatry Differs From Other Medical Disorders
Compared to physical illnesses, diagnosing a mental illness is more challenging, particularly when there is still a lack of objective assessment methods, including diagnostic tools and biomarkers. Therefore, the diagnosis of mental disorders is heavily influenced by the assessors' theoretical perspectives and subjectivity. Moreover, mental illnesses can still be considered despite an individual not fulfilling the proper diagnostic criteria led down in classificatory systems, but there is detectable dysfunction. Furthermore, the precise timing of disorder initiation or transition from subclinical to clinical condition is often uncertain and inconclusive ( 48 ). Therefore, prevention strategies are well-delineated and clear in the case of physical disorders while it's still less prevalent in mental health parlance.
Terms, Definitions, and Concepts
The terms mental health, health promotion, and prevention have been differently defined and interpreted. It is further complicated by overlapping boundaries of the concept of promotion and prevention. Some commonly used terms in mental health prevention have been tabulated ( Table 1 ) ( 18 ).
Commonly used terms in mental health prevention.
Mental Health Promotion and Protection
The term “mental health promotion” also has definitional challenges as it signifies different things to different individuals. For some, it means the treatment of mental illness; for others, it means preventing the occurrence of mental illness; while for others, it means increasing the ability to manage frustration, stress, and difficulties by strengthening one's resilience and coping abilities ( 54 ). It involves promoting the value of mental health and improving the coping capacities of individuals rather than amelioration of symptoms and deficits.
Mental health promotion is a broad concept that encompasses the entire population, and it advocates for a strengths-based approach and tries to address the broader determinants of mental health. The objective is to eliminate health inequalities via empowerment, collaboration, and participation. There is mounting evidence that mental health promotion interventions improve mental health, lower the risk of developing mental disorders ( 48 , 55 , 56 ) and have socioeconomic benefits ( 24 ). In addition, it strives to increase an individual's capacity for psychosocial wellbeing and adversity adaptation ( 11 ).
However, the concepts of mental health promotion, protection, and prevention are intrinsically linked and intertwined. Furthermore, most mental diseases result from complex interaction risk and protective factors instead of a definite etiology. Facilitating the development and timely attainment of developmental milestones across an individual's lifespan is critical for positive mental health ( 57 ). Although mental health promotion and prevention are essential aspects of public health with wide-ranging benefits, their feasibility and implementation are marred by financial and resource constraints. The lack of cost-effectiveness studies, particularly from the LMICs, further restricts its full realization ( 47 , 58 , 59 ).
Despite the significance of the topic and a considerable amount of literature on it, a comprehensive review is still lacking that would cover the concept of mental health promotion and prevention and simultaneously discusses various interventions, including the novel techniques delivered across the lifespan, in different settings, and level of prevention. Therefore, this review aims to analyze the existing literature on various mental health promotion and prevention-based interventions and their effectiveness. Furthermore, its attempts to highlight the implications of such intervention in low-resource settings and provides future directions. Such literature would add to the existing literature on mental health promotion and prevention research and provide key insights into the effectiveness of such interventions and their feasibility and replicability in various settings.
Methodology
For the current review, key terms like “mental health promotion,” OR “protection,” OR “prevention,” OR “mitigation” were used to search relevant literature on Google Scholar, PubMed, and Cochrane library databases, considering a time period between 2000 to 2019 ( Supplementary Material 1 ). However, we have restricted our search till 2019 for non-original articles (reviews, commentaries, viewpoints, etc.), assuming that it would also cover most of the original articles published until then. Additionally, we included original papers from the last 5 years (2016–2021) so that they do not get missed out if not covered under any published review. The time restriction of 2019 for non-original articles was applied to exclude papers published during the Coronavirus disease (COVID-19) pandemic as the latter was a significant event, bringing about substantial change and hence, it warranted a different approach to cater to the MH needs of the population, including MH prevention measures. Moreover, the COVID-19 pandemic resulted in the flooding of novel interventions for mental health prevention and promotion, specifically targeting the pandemic and its consequences, which, if included, could have biased the findings of the current review on various MH promotion and prevention interventions.
A time frame of about 20 years was taken to see the effectiveness of various MH promotion and protection interventions as it would take substantial time to be appreciated in real-world situations. Therefore, the current paper has put greater reliance on the review articles published during the last two decades, assuming that it would cover most of the original articles published until then.
The above search yielded 320 records: 225 articles from Google scholar, 59 articles from PubMed, and 36 articles from the Cochrane database flow-diagram of records screening. All the records were title/abstract screened by all the authors to establish the suitability of those records for the current review; a bibliographic- and gray literature search was also performed. In case of any doubts or differences in opinion, it was resolved by mutual discussion. Only those articles directly related to mental health promotion, primary prevention, and related interventions were included in the current review. In contrast, records that discussed any specific conditions/disorders (post-traumatic stress disorders, suicide, depression, etc.), specific intervention (e.g., specific suicide prevention intervention) that too for a particular population (e.g., disaster victims) lack generalizability in terms of mental health promotion or prevention, those not available in the English language, and whose full text was unavailable were excluded. The findings of the review were described narratively.
Interventions for Mental Health Promotion and Prevention and Their Evidence
Various interventions have been designed for mental health promotion and prevention. They are delivered and evaluated across the regions (high-income countries to low-resource settings, including disaster-affiliated regions of the world), settings (community-based, school-based, family-based, or individualized); utilized different psychological constructs and therapies (cognitive behavioral therapy, behavioral interventions, coping skills training, interpersonal therapies, general health education, etc.); and delivered by different professionals/facilitators (school-teachers, mental health professionals or paraprofessionals, peers, etc.). The details of the studies, interventions used, and outcomes have been provided in Supplementary Table 1 . Below we provide the synthesized findings of the available research.
The majority of the available studies were quantitative and experimental. Randomized controlled trials comprised a sizeable proportion of the studies; others were quasi-experimental studies and, a few, qualitative studies. The studies primarily focussed on school students or the younger population, while others were explicitly concerned with the mental health of young females ( 60 ). Newer data is emerging on mental health promotion and prevention interventions for elderlies (e.g., dementia) ( 61 ). The majority of the research had taken a broad approach to mental health promotion ( 62 ). However, some studies have focused on universal prevention ( 63 , 64 ) or selective prevention ( 65 – 68 ). For instance, the Resourceful Adolescent Program (RAPA) was implemented across the schools and has utilized cognitive-behavioral and interpersonal therapies and reported a significant improvement in depressive symptoms. Some of the interventions were directed at enhancing an individual's characteristics like resilience, behavior regulation, and coping skills (ZIPPY's Friends) ( 69 ), while others have focused on the promotion of social and emotional competencies among the school children and attempted to reduce the gap in such competencies across the socio-economic classes (“Up” program) ( 70 ) or utilized expressive abilities of the war-affected children (Writing for Recover (WfR) intervention) ( 71 ) to bring about an improvement in their psychological problems (a type of selective prevention) ( 62 ) or harnessing the potential of Art, in the community-based intervention, to improve self-efficacy, thus preventing mental disorders (MAD about Art program) ( 72 ). Yet, others have focused on strengthening family ( 60 , 73 ), community relationships ( 62 ), and targeting modifiable risk factors across the life course to prevent dementia among the elderlies and also to support the carers of such patients ( 61 ).
Furthermore, more of the studies were conducted and evaluated in the developed parts of the world, while emerging economies, as anticipated, far lagged in such interventions or related research. The interventions that are specifically adapted for local resources, such as school-based programs involving paraprofessionals and teachers in the delivery of mental health interventions, were shown to be more effective ( 62 , 74 ). Likewise, tailored approaches for low-resource settings such as LMICs may also be more effective ( 63 ). Some of these studies also highlight the beneficial role of a multi-dimensional approach ( 68 , 75 ) and interventions targeting early lifespan ( 76 , 77 ).
Newer Insights: How to Harness Digital Technology and Novel Methods of MH Promotion and Protection
With the advent of digital technology and simultaneous traction on mental health promotion and prevention interventions, preventive psychiatrists and public health experts have developed novel techniques to deliver mental health promotive and preventive interventions. These encompass different settings (e.g., school, home, workplace, the community at large, etc.) and levels of prevention (universal, selective, indicated) ( 78 – 80 ).
The advanced technologies and novel interventions have broadened the scope of MH promotion and prevention, such as addressing the mental health issues of individuals with chronic medical illness ( 81 , 82 ), severe mental disorders ( 83 ), children and adolescents with mental health problems, and geriatric population ( 78 ). Further, it has increased the accessibility and acceptability of such interventions in a non-stigmatizing and tailored manner. Moreover, they can be integrated into the routine life of the individuals.
For instance, Internet-and Mobile-based interventions (IMIs) have been utilized to monitor health behavior as a form of MH prevention and a stand-alone self-help intervention. Moreover, the blended approach has expanded the scope of MH promotive and preventive interventions such as face-to-face interventions coupled with remote therapies. Simultaneously, it has given way to the stepped-care (step down or step-up care) approach of treatment and its continuation ( 79 ). Also, being more interactive and engaging is particularly useful for the youth.
The blended model of care has utilized IMIs to a varying degree and at various stages of the psychological interventions. This includes IMIs as a supplementary approach to the face-to-face-interventions (FTFI), FTFI augmented by behavior intervention technologies (BITs), BITs augmented by remote human support, and fully automated BITs ( 84 ).
The stepped care model of mental health promotion and prevention strategies includes a stepped-up approach, wherein BITs are utilized to manage the prodromal symptoms, thereby preventing the onset of the full-blown episode. In the Stepped-down approach, the more intensive treatments (in-patient or out-patient based interventions) are followed and supplemented with the BITs to prevent relapse of the mental illness, such as for previously admitted patients with depression or substance use disorders ( 85 , 86 ).
Similarly, the latest research has developed newer interventions for strengthening the psychological resilience of the public or at-risk individuals, which can be delivered at the level of the home, such as, e.g., nurse family partnership program (to provide support to the young and vulnerable mothers and prevent childhood maltreatment) ( 87 ); family healing together program aimed at improving the mental health of the family members living with persons with mental illness (PwMI) ( 88 ). In addition, various novel interventions for MH promotion and prevention have been highlighted in the Table 2 .
Depiction of various novel mental health promotion and prevention strategies.
a/w, associated with; A-V, audio-visual; b/w, between; CBT, Cognitive Behavioral Therapy; CES-Dep., Center for Epidemiologic Studies-Depression scale; CG, control group; FU, follow-up; GAD, generalized anxiety disorders-7; IA, intervention arm; HCWs, Health Care Workers; LMIC, low and middle-income countries; MDD, major depressive disorders; mgt, management; MH, mental health; MHP, mental health professional; MINI, mini neuropsychiatric interview; NNT, number needed to treat; PHQ-9, patient health questionnaire; TAU, treatment as usual .
Furthermore, school/educational institutes-based interventions such as school-Mental Health Magazines to increase mental health literacy among the teachers and students have been developed ( 80 ). In addition, workplace mental health promotional activities have targeted the administrators, e.g., guided “e-learning” for the managers that have shown to decrease the mental health problems of the employees ( 102 ).
Likewise, digital technologies have also been harnessed in strengthening community mental health promotive/preventive services, such as the mental health first aid (MHFA) Books on Prescription initiative in New Zealand provided information and self-help tools through library networks and trained book “prescribers,” particularly in rural and remote areas ( 103 ).
Apart from the common mental disorders such as depression, anxiety, and behavioral disorders in the childhood/adolescents, novel interventions have been utilized to prevent the development of or management of medical, including preventing premature mortality and psychological issues among the individuals with severe mental illnesses (SMIs), e.g., Lets' talk about tobacco-web based intervention and motivational interviewing to prevent tobacco use, weight reduction measures, and promotion of healthy lifestyles (exercise, sleep, and balanced diets) through individualized devices, thereby reducing the risk of cardiovascular disorders ( 83 ). Similarly, efforts have been made to improve such individuals' coping skills and employment chances through the WorkingWell mobile application in the US ( 104 ).
Apart from the digital-based interventions, newer, non-digital-based interventions have also been utilized to promote mental health and prevent mental disorders among individuals with chronic medical conditions. One such approach in adventure therapy aims to support and strengthen the multi-dimensional aspects of self. It includes the physical, emotional or cognitive, social, spiritual, psychological, or developmental rehabilitation of the children and adolescents with cancer. Moreover, it is delivered in the natural environment outside the hospital premises, shifting the focus from the illness model to the wellness model ( 81 ). Another strength of this intervention is it can be delivered by the nurses and facilitate peer support and teamwork.
Another novel approach to MH prevention is gut-microbiota and dietary interventions. Such interventions have been explored with promising results for the early developmental disorders (Attention deficit hyperactive disorder, Autism spectrum disorders, etc.) ( 105 ). It works under the framework of the shared vulnerability model for common mental disorders and other non-communicable diseases and harnesses the neuroplasticity potential of the developing brain. Dietary and lifestyle modifications have been recommended for major depressive disorders by the Clinical Practice Guidelines in Australia ( 106 ). As most childhood mental and physical disorders are determined at the level of the in-utero and early after the birth period, targeting maternal nutrition is another vital strategy. The utility has been expanded from maternal nutrition to women of childbearing age. The various novel mental health promotion and prevention strategies are shown in Table 2 .
Newer research is emerging that has utilized the digital platform for training non-specialists in diagnosis and managing individuals with mental health problems, such as Atmiyata Intervention and The SMART MH Project in India, and The Allillanchu Project in Peru, to name a few ( 99 ). Such frameworks facilitate task-sharing by the non-specialist and help in reducing the treatment gap in these countries. Likewise, digital algorithms or decision support systems have been developed to make mental health services more transparent, personalized, outcome-driven, collaborative, and integrative; one such example is DocuMental, a clinical decision support system (DSS). Similarly, frameworks like i-PROACH, a cloud-based intelligent platform for research outcome assessment and care in mental health, have expanded the scope of the mental health support system, including promoting research in mental health ( 100 ). In addition, COVID-19 pandemic has resulted in wider dissemination of the applications based on the evidence-based psycho-social interventions such as National Health Service's (NHS's) Mind app and Headspace (teaching meditation via a website or a phone application) that have utilized mindfulness-based practices to address the psychological problems of the population ( 101 ).
Challenges in Implementing Novel MH Promotion and Prevention Strategies
Although novel interventions, particularly internet and mobile-based interventions (IMIs), are effective models for MH promotion and prevention, their cost-effectiveness requires further exploration. Moreover, their feasibility and acceptability in LMICs could be challenging. Some of these could be attributed to poor digital literacy, digital/network-related limitations, privacy issues, and society's preparedness to implement these interventions.
These interventions need to be customized and adapted according to local needs and context, for which implementation and evaluative research are warranted. In addition, the infusion of more human and financial resources for such activities is required. Some reports highlight that many of these interventions do not align with the preferences and use the pattern of the service utilizers. For instance, one explorative research on mental health app-based interventions targeting youth found that despite the burgeoning applications, they are not aligned with the youth's media preferences and learning patterns. They are less interactive, have fewer audio-visual displays, are not youth-specific, are less dynamic, and are a single touch app ( 107 ).
Furthermore, such novel interventions usually come with high costs. In low-resource settings where service utilizers have limited finances, their willingness to use such services may be doubtful. Moreover, insurance companies, including those in high-income countries (HICs), may not be willing to fund such novel interventions, which restricts the accessibility and availability of interventions.
Research points to the feasibility and effectiveness of incorporating such novel interventions in routine services such as school, community, primary care, or settings, e.g., in low-resource settings, the resource persons like teachers, community health workers, and primary care physicians are already overburdened. Therefore, their willingness to take up additional tasks may raise skepticism. Moreover, the attitudinal barrier to moving from the traditional service delivery model to the novel methods may also impede.
Considering the low MH budget and less priority on the MH prevention and promotion activities in most low-resource settings, the uptake of such interventions in the public health framework may be lesser despite the latter's proven high cost-effectiveness. In contrast, policymakers may be more inclined to invest in the therapeutic aspects of MH.
Such interventions open avenues for personalized and precision medicine/health care vs. the traditional model of MH promotion and preventive interventions ( 108 , 109 ). For instance, multivariate prediction algorithms with methods of machine learning and incorporating biological research, such as genetics, may help in devising tailored, particularly for selected and indicated prevention, interventions for depression, suicide, relapse prevention, etc. ( 79 ). Therefore, more research in this area is warranted.
To be more clinically relevant, greater biological research in MH prevention is required to identify those at higher risk of developing given mental disorders due to the existing risk factors/prominent stress ( 110 ). For instance, researchers have utilized the transcriptional approach to identify a biological fingerprint for susceptibility (denoting abnormal early stress response) to develop post-traumatic stress disorders among the psychological trauma survivors by analyzing the expression of the Peripheral blood mononuclear cell gene expression profiles ( 111 ). Identifying such biological markers would help target at-risk individuals through tailored and intensive interventions as a form of selected prevention.
Similarly, such novel interventions can help in targeting the underlying risk such as substance use, poor stress management, family history, personality traits, etc. and protective factors, e.g., positive coping techniques, social support, resilience, etc., that influences the given MH outcome ( 79 ). Therefore, again, it opens the scope of tailored interventions rather than a one-size-fits-all model of selective and indicated prevention for various MH conditions.
Furthermore, such interventions can be more accessible for the hard-to-reach populations and those with significant mental health stigma. Finally, they play a huge role in ensuring the continuity of care, particularly when community-based MH services are either limited or not available. For instance, IMIs can maintain the improvement of symptoms among individuals previously managed in-patient, such as for suicide, SUDs, etc., or receive intensive treatment like cognitive behavior therapy (CBT) for depression or anxiety, thereby helping relapse prevention ( 86 , 112 ). Hence, such modules need to be developed and tested in low-resource settings.
IMIs (and other novel interventions) being less stigmatizing and easily accessible, provide a platform to engage individuals with chronic medical problems, e.g., epilepsy, cancer, cardiovascular diseases, etc., and non-mental health professionals, thereby making it more relevant and appealing for them.
Lastly, research on prevention-interventions needs to be more robust to adjust for the pre-intervention matching, high attrition rate, studying the characteristics of treatment completers vs. dropouts, and utilizing the intention-to-treat analysis to gauge the effect of such novel interventions ( 78 ).
Recommendations for Low-and-Middle-Income Countries
Although there is growing research on the effectiveness and utility of mental health promotion/prevention interventions across the lifespan and settings, low-resource settings suffer from specific limitations that restrict the full realization of such public health strategies, including implementing the novel intervention. To overcome these challenges, some of the potential solutions/recommendations are as follows:
- The mental health literacy of the population should be enhanced through information, education, and communication (IEC) activities. In addition, these activities should reduce stigma related to mental problems, early identification, and help-seeking for mental health-related issues.
- Involving teachers, workplace managers, community leaders, non-mental health professionals, and allied health staff in mental health promotion and prevention is crucial.
- Mental health concepts and related promotion and prevention should be incorporated into the education curriculum, particularly at the medical undergraduate level.
- Training non-specialists such as community health workers on mental health-related issues across an individual's life course and intervening would be an effective strategy.
- Collaborating with specialists from other disciplines, including complementary and alternative medicines, would be crucial. A provision of an integrated health system would help in increasing awareness, early identification, and prompt intervention for at-risk individuals.
- Low-resource settings need to develop mental health promotion interventions such as community-and school-based interventions, as these would be more culturally relevant, acceptable, and scalable.
- Utilizing a digital platform for scaling mental health services (e.g., telepsychiatry services to at-risk populations) and training the key individuals in the community would be a cost-effective framework that must be explored.
- Infusion of higher financial and human resources in this area would be a critical step, as, without adequate resources, research, service development, and implementation would be challenging.
- It would also be helpful to identify vulnerable populations and intervene in them to prevent the development of clinical psychiatric disorders.
- Lastly, involving individuals with lived experiences at the level of mental health planning, intervention development, and delivery would be cost-effective.
Clinicians, researchers, public health experts, and policymakers have increasingly realized mental health promotion and prevention. Investment in Preventive psychiatry appears to be essential considering the substantial burden of mental and neurological disorders and the significant treatment gap. Literature suggests that MH promotive and preventive interventions are feasible and effective across the lifespan and settings. Moreover, various novel interventions (e.g., internet-and mobile-based interventions, new therapies) have been developed worldwide and proven effective for mental health promotion and prevention; such interventions are limited mainly to HICs.
Despite the significance of preventive psychiatry in the current world and having a wide-ranging implication for the wellbeing of society and individuals, including those suffering from chronic medical problems, it is a poorly utilized public health field to address the population's mental health needs. Lately, researchers and policymakers have realized the untapped potentialities of preventive psychiatry. However, its implementation in low-resource settings is still in infancy and marred by several challenges. The utilization of novel interventions, such as digital-based interventions, and blended and stepped-care models of care, can address the enormous mental health need of the population. Additionally, it provides mental health services in a less-stigmatizing and easily accessible, and flexible manner. More research concerning this is required from the LMICs.
Author Contributions
VS, AK, and SG: methodology, literature search, manuscript preparation, and manuscript review. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.898009/full#supplementary-material
Read our research on: Gun Policy | International Conflict | Election 2024
Regions & Countries
Mental health and the pandemic: what u.s. surveys have found.
The coronavirus pandemic has been associated with worsening mental health among people in the United States and around the world . In the U.S, the COVID-19 outbreak in early 2020 caused widespread lockdowns and disruptions in daily life while triggering a short but severe economic recession that resulted in widespread unemployment. Three years later, Americans have largely returned to normal activities, but challenges with mental health remain.
Here’s a look at what surveys by Pew Research Center and other organizations have found about Americans’ mental health during the pandemic. These findings reflect a snapshot in time, and it’s possible that attitudes and experiences may have changed since these surveys were fielded. It’s also important to note that concerns about mental health were common in the U.S. long before the arrival of COVID-19 .
Three years into the COVID-19 outbreak in the United States , Pew Research Center published this collection of survey findings about Americans’ challenges with mental health during the pandemic. All findings are previously published. Methodological information about each survey cited here, including the sample sizes and field dates, can be found by following the links in the text.
The research behind the first item in this analysis, examining Americans’ experiences with psychological distress, benefited from the advice and counsel of the COVID-19 and mental health measurement group at Johns Hopkins Bloomberg School of Public Health.
At least four-in-ten U.S. adults (41%) have experienced high levels of psychological distress at some point during the pandemic, according to four Pew Research Center surveys conducted between March 2020 and September 2022.
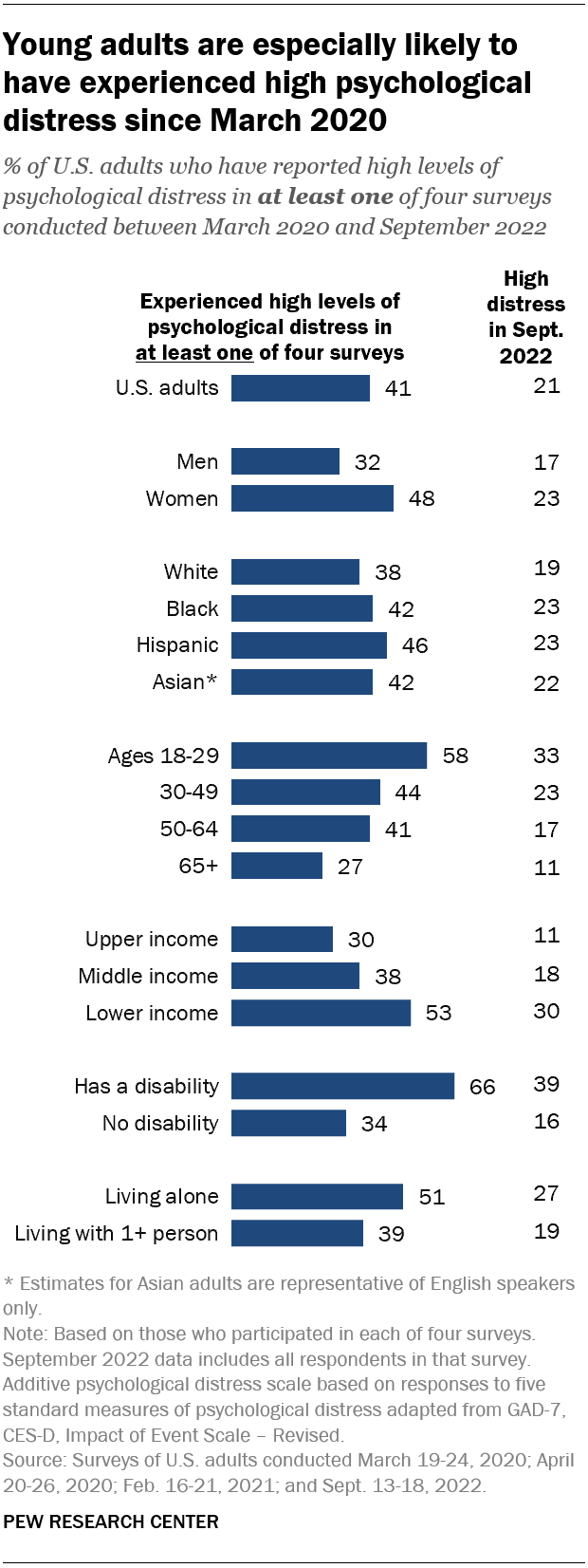
Young adults are especially likely to have faced high levels of psychological distress since the COVID-19 outbreak began: 58% of Americans ages 18 to 29 fall into this category, based on their answers in at least one of these four surveys.
Women are much more likely than men to have experienced high psychological distress (48% vs. 32%), as are people in lower-income households (53%) when compared with those in middle-income (38%) or upper-income (30%) households.
In addition, roughly two-thirds (66%) of adults who have a disability or health condition that prevents them from participating fully in work, school, housework or other activities have experienced a high level of distress during the pandemic.
The Center measured Americans’ psychological distress by asking them a series of five questions on subjects including loneliness, anxiety and trouble sleeping in the past week. The questions are not a clinical measure, nor a diagnostic tool. Instead, they describe people’s emotional experiences during the week before being surveyed.
While these questions did not ask specifically about the pandemic, a sixth question did, inquiring whether respondents had “had physical reactions, such as sweating, trouble breathing, nausea, or a pounding heart” when thinking about their experience with the coronavirus outbreak. In September 2022, the most recent time this question was asked, 14% of Americans said they’d experienced this at least some or a little of the time in the past seven days.
More than a third of high school students have reported mental health challenges during the pandemic. In a survey conducted by the Centers for Disease Control and Prevention from January to June 2021, 37% of students at public and private high schools said their mental health was not good most or all of the time during the pandemic. That included roughly half of girls (49%) and about a quarter of boys (24%).
In the same survey, an even larger share of high school students (44%) said that at some point during the previous 12 months, they had felt sad or hopeless almost every day for two or more weeks in a row – to the point where they had stopped doing some usual activities. Roughly six-in-ten high school girls (57%) said this, as did 31% of boys.
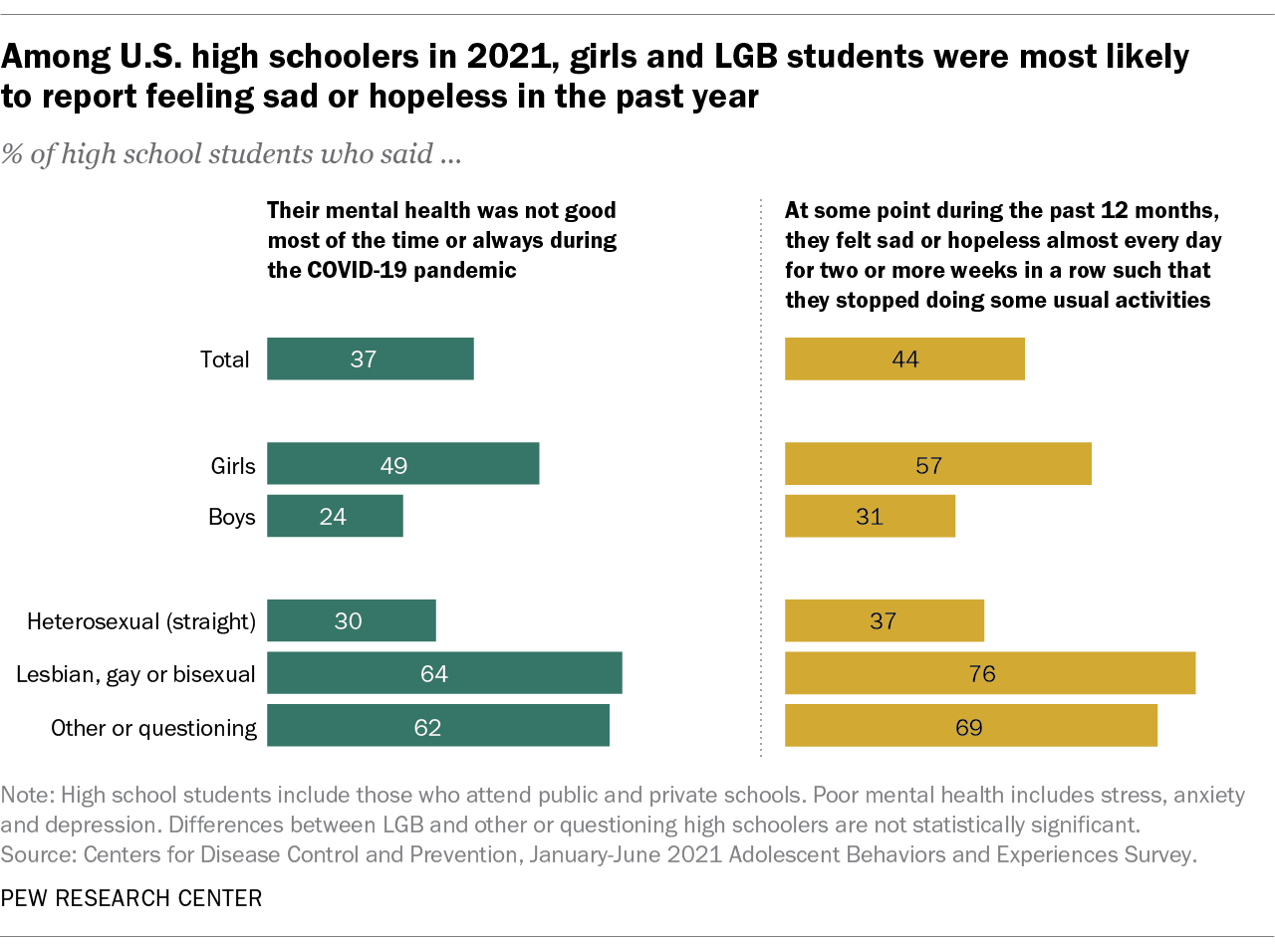
On both questions, high school students who identify as lesbian, gay, bisexual, other or questioning were far more likely than heterosexual students to report negative experiences related to their mental health.
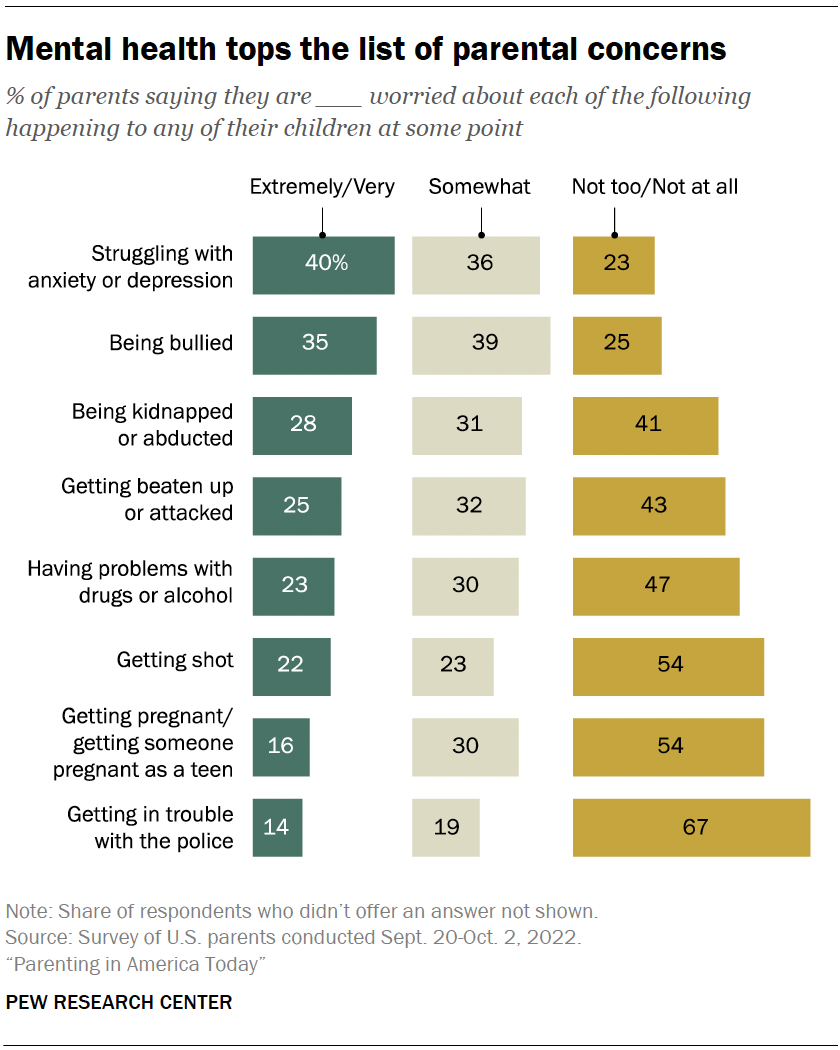
Mental health tops the list of worries that U.S. parents express about their kids’ well-being, according to a fall 2022 Pew Research Center survey of parents with children younger than 18. In that survey, four-in-ten U.S. parents said they’re extremely or very worried about their children struggling with anxiety or depression. That was greater than the share of parents who expressed high levels of concern over seven other dangers asked about.
While the fall 2022 survey was fielded amid the coronavirus outbreak, it did not ask about parental worries in the specific context of the pandemic. It’s also important to note that parental concerns about their kids struggling with anxiety and depression were common long before the pandemic, too . (Due to changes in question wording, the results from the fall 2022 survey of parents are not directly comparable with those from an earlier Center survey of parents, conducted in 2015.)
Among parents of teenagers, roughly three-in-ten (28%) are extremely or very worried that their teen’s use of social media could lead to problems with anxiety or depression, according to a spring 2022 survey of parents with children ages 13 to 17 . Parents of teen girls were more likely than parents of teen boys to be extremely or very worried on this front (32% vs. 24%). And Hispanic parents (37%) were more likely than those who are Black or White (26% each) to express a great deal of concern about this. (There were not enough Asian American parents in the sample to analyze separately. This survey also did not ask about parental concerns specifically in the context of the pandemic.)
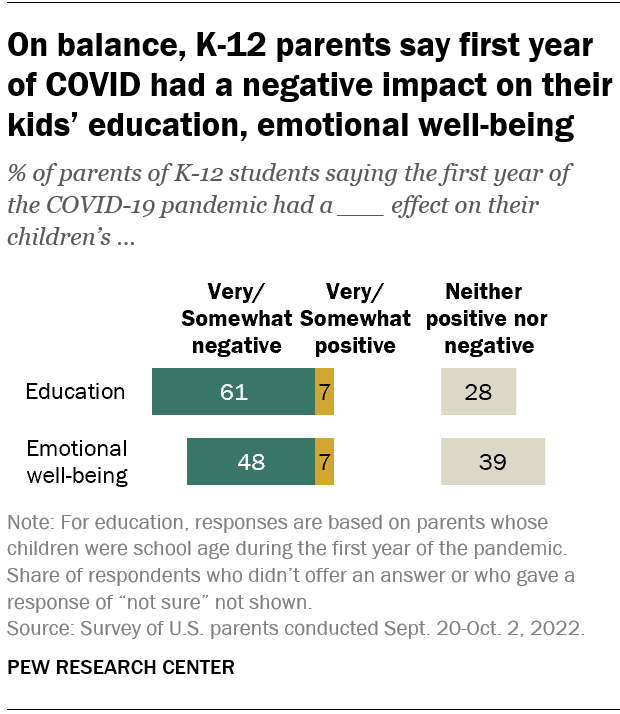
Looking back, many K-12 parents say the first year of the coronavirus pandemic had a negative effect on their children’s emotional health. In a fall 2022 survey of parents with K-12 children , 48% said the first year of the pandemic had a very or somewhat negative impact on their children’s emotional well-being, while 39% said it had neither a positive nor negative effect. A small share of parents (7%) said the first year of the pandemic had a very or somewhat positive effect in this regard.
White parents and those from upper-income households were especially likely to say the first year of the pandemic had a negative emotional impact on their K-12 children.
While around half of K-12 parents said the first year of the pandemic had a negative emotional impact on their kids, a larger share (61%) said it had a negative effect on their children’s education.

Sign up for our weekly newsletter
Fresh data delivered Saturday mornings
What federal education data shows about students with disabilities in the U.S.
Most americans who go to religious services say they would trust their clergy’s advice on covid-19 vaccines, what we know about online learning and the homework gap amid the pandemic, unvaccinated americans are at higher risk from covid-19 but express less concern than vaccinated adults, americans who relied most on trump for covid-19 news among least likely to be vaccinated, most popular.
About Pew Research Center Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
Editor's Choice: COVID-19 and Risk of New Mental Disorders

Vincent Paquin, MD; Manuela Ferrari, PhD; Soham Rej, MD, MSc; et al
Original Investigation | April 10, 2024
Just Published
- Adolescent Media Use and Psychotic Experiences Vincent Paquin, MD; et al. Original Investigation online first has multimedia Vincent Paquin, MD; et al.
- Trends in Deaths of Despair by Race and Ethnicity From 1999 to 2022 Joseph Friedman, PhD, MPH; et al. Research Letter online first Joseph Friedman, PhD, MPH; et al.
- Susceptibility to Treatment-Resistant Depression Within Families Chih-Ming Cheng, MD; et al. Original Investigation online first Chih-Ming Cheng, MD; et al.
- Heritability of Clinically Diagnosed Obsessive-Compulsive Disorder Among Twins David Mataix-Cols, PhD; et al. Research Letter online first open access David Mataix-Cols, PhD; et al.
- Genetic and Phenotypic Features of Schizophrenia in the UK Biobank Sophie E. Legge, PhD; et al. Original Investigation online first open access Sophie E. Legge, PhD; et al.
- Informed Consent to Psychedelic Treatment—A Work in Progress Paul S. Appelbaum, MD Editorial online first Paul S. Appelbaum, MD
- Medicaid Reentry Section 1115 Demonstration Opportunity William C. Lieber; et al. Viewpoint online first William C. Lieber; et al.
- JAMA Psychiatry —The Year in Review, 2023 Dost Öngür, MD, PhD Editorial online first free access Dost Öngür, MD, PhD
- Biological Aging and Mental Illness—A Vicious Cycle? Anthony S. Zannas, MD, MSc, PhD Viewpoint online first Anthony S. Zannas, MD, MSc, PhD
- Are Psychiatric Disorders Brain Diseases?—A New Look at an Old Question Kenneth S. Kendler, MD Viewpoint Kenneth S. Kendler, MD
- Essentials of Informed Consent to Psychedelic Medicine Mason Marks, MD, JD; et al. Special Communication online first has active quiz Mason Marks, MD, JD; et al. Editorial
- A Dynamical Systems View of Psychiatric Disorders—Practical Implications Marten Scheffer, PhD; et al. Review online first has active quiz Marten Scheffer, PhD; et al.
- A Dynamical Systems View of Psychiatric Disorders—Theory Marten Scheffer, PhD; et al. Review online first has active quiz has multimedia Marten Scheffer, PhD; et al.
- Prioritizing Maternal Mental Health in Addressing Morbidity and Mortality Katherine L. Wisner, MD, MS; et al. Special Communication online first has active quiz Katherine L. Wisner, MD, MS; et al.
- Parameter Space and Potential for Biomarker Development in 25 Years of fMRI Drug Cue Reactivity Addiction Cue-Reactivity Initiative (ACRI) Network Review has active quiz Addiction Cue-Reactivity Initiative (ACRI) Network
- 14,374 Views Suicide Decedent Profiles and Signs of Suicidal Intent
- 13,464 Views Adverse Childhood Experiences and Adult Mental Health Outcomes
- 10,414 Views ADHD Medications and Long-Term Risk of Cardiovascular Diseases
- 10,233 Views Adolescent Psychedelic Use and Psychotic or Manic Symptoms
- 8,341 Views Associations Between Social Media Time and Internalizing and Externalizing Problems Among US Youth
- 7,487 Views Effects of Psilocybin-Assisted Therapy on Major Depressive Disorder
- 6,244 Views Are Psychiatric Disorders Brain Diseases?—A New Look at an Old Question
- 6,125 Views Effect of Pain Reprocessing Therapy vs Placebo and Usual Care for Patients With Chronic Back Pain
- 6,118 Views A Dynamical Systems View of Psychiatric Disorders—Theory
- 5,924 Views Mindfulness-Based Stress Reduction vs Escitalopram for the Treatment of Anxiety Disorders
- 543 Citations Effects of Psilocybin-Assisted Therapy on Major Depressive Disorder
- 236 Citations Perturbations in Gut Microbiota Composition in Psychiatric Disorders
- 224 Citations How COVID-19 Affects the Brain
- 215 Citations Association Between Physical Activity and Risk of Depression
- 176 Citations Effectiveness, Core Elements, and Moderators of Response of Cognitive Remediation for Schizophrenia
- 149 Citations Psilocybin-Assisted Psychotherapy vs Placebo in the Treatment of Adult Patients With Alcohol Use Disorder
- 130 Citations Association Between Mood Disorders and Risk of COVID-19 Infection, Hospitalization, and Death
- 128 Citations Posttraumatic Stress Disorder in Patients After Severe COVID-19 Infection
- 127 Citations Association Between Mental Health Disorders and Mortality Among Patients With COVID-19 in 7 Countries
- 127 Citations US Drug Overdose Mortality Rates by Race and Ethnicity Before and During the COVID-19 Pandemic
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- Search by keyword
- Search by citation
Page 1 of 18
Support or justice: a triangulated multi-focal view of sexual assault victim support in a UK sexual assault referral centre (SARC)
Despite vast levels of underreporting, sexual assault remains an issue at scale in the UK, necessitating the presence of statutory and voluntary organisations in the support of victims. Understanding the exper...
- View Full Text
Delayed discharge in inpatient psychiatric care: a systematic review
Delayed discharge is problematic. It is financially costly and can create barriers to delivering best patient care, by preventing return to usual functioning and delaying admissions of others in need. This sys...
Community-based rehabilitation for people with psychosocial disabilities in low- and middle-income countries: a systematic review of the grey literature
Community based rehabilitation (CBR) aims to promote the inclusion and participation of people with disabilities, particularly in low- and middle-income countries (LMICs). Yet people with psychosocial disabili...
Can computer simulation support strategic service planning? Modelling a large integrated mental health system on recovery from COVID-19
COVID-19 has had a significant impact on people’s mental health and mental health services. During the first year of the pandemic, existing demand was not fully met while new demand was generated, resulting in...
Factors associated with satisfaction and perceived helpfulness of mental healthcare: a World Mental Health Surveys report
Mental health service providers are increasingly interested in patient perspectives. We examined rates and predictors of patient-reported satisfaction and perceived helpfulness in a cross-national general popu...
Mapping awareness-raising and capacity-building materials on developmental disabilities for non-specialists: a review of the academic and grey literature
Most children with developmental disabilities (DD), such as intellectual disabilities and autism, live in low- and middle-income countries (LMICs), where services are usually limited. Various governmental, non...
Mapping mental health care services for children and youth population in Colombia’s Pacific: potential for boundary spanning between community and formal services
Conflict and violence can impact on the mental health of children and young people, who are in a crucial stage of their personal growth. Not much is known about the provision of mental health care to young peo...
Assessing support for mental health policies among policy influencers and the general public in Alberta and Manitoba, Canada
There is a need to improve mental health policy in Canada to address the growing population burden of mental illness. Understanding support for policy options is critical for advocacy efforts to improve mental...
A roadmap for sustainable implementation of vocational rehabilitation for people with mental disorders and its outcomes: a qualitative evaluation
People suffering from mental health disorders have lower work participation compared to people without mental challenges. To increase work participation within this group vocational rehabilitation intervention...
Evaluation of a flexible assertive community treatment (FACT) program for patients with severe mental illness: an observational study in Salzburg, Austria
Inpatient treatment of severe mentally ill patients binds substantial resources and creates the dilemma of “revolving-door hospitalizations”. Evidence suggests that these patients benefit more from an assertiv...
Mental health integrated care models in primary care and factors that contribute to their effective implementation: a scoping review
In the state of Victoria, Australia, the 111-day lockdown due to the COVID-19 pandemic exacerbated the population’s prevailing state of poor mental health. Of the 87% of Australians who visit their GP annually...
Trends in mental health before and after the onset of the COVID-19 pandemic: a longitudinal survey of a conflict-affected population in Colombia
Focusing on the Meta region in Colombia, we investigated the relationship between mental health, the COVID-19 pandemic, and social determinants of health influenced by over five decades of civil conflict. We s...
An exploration of the Indonesian lay mental health workers’ (cadres) experiences in performing their roles in community mental health services: a qualitative study
Volunteers trained to support community mental health programs in Indonesia are known as ‘mental health cadres.’ These are lay people trained to provide basic support for people with mental illness in their lo...
Prescriptive factors for intensive home treatment in acute psychiatry: a secondary analysis of a randomised controlled trial
Intensive home treatment (IHT) aims to prevent psychiatric hospitalisation. Although this intervention is well tested, it is still unknown for whom this intervention works best. Therefore, this study aims to e...
Social skills interventions for Thai adolescents with Autism Spectrum Disorder (ASD): a qualitative study of the perceptions and experiences of Thai adolescents, their caregivers and healthcare professionals
Social skills interventions (SSIs) are effective for enhancing social skills and decreasing mental health problems in adolescents with autism spectrum disorder (ASD). However, these interventions have been des...
Family UNited: piloting of a new universal UNODC family skills programme to improve child mental health, resilience and parenting skills in Indonesia and Bangladesh
Family is one of the most influential social institutions and caregivers act as the main protective factors for children’s mental health and resilience skills. Family skills programmes support caregivers to be...
Predictors of time until return to work and duration of sickness absence in sick-listed precarious workers with common mental disorders: a secondary data-analysis of two trials and one cohort study
Common mental disorders (CMD) are highly prevalent among sick-listed precarious workers and often lead to long-term sickness-absence, work disability and unemployment. This study aimed to identify predictors o...
Impact of the COVID-19 pandemic on mental health care and people with mental health conditions in Ethiopia: the MASC mixed-methods study
The COVID-19 pandemic has had far-reaching effects on the mental health of populations around the world, but there has been limited focus on the impact on people with existing mental health conditions in low-i...
A quantitative analysis of human rights-related attitude changes towards people with mental health conditions and psychosocial, intellectual, or cognitive disabilities following completion of the WHO QualityRights e-training in Ghana
Despite growing recognition of essential human rights, people with mental health conditions and psychosocial, intellectual, or cognitive disabilities’ rights are known to be frequently violated in mental healt...
Experience of traumatic events in people with severe mental illness in a low-income country: a qualitative study
This study describes the trauma experiences of people with severe mental illness (SMI) in Ethiopia and presents a model of how SMI and trauma exposure interact to reduce functioning and quality of life in this...
Clinical and sociodemographic predictors of inpatient admission after presentation in a psychiatric emergency room: an observational study
The admission decision after presentation in the psychiatric emergency room (PER) has potentially far-reaching consequences for the patient and the community. In a short amount of time, information must be col...
Would you choose to be a psychiatrist again? A large-sample nationwide survey of psychiatrists and psychiatry residents in China
The mental health workforce sustainability in China suffers high rates of attrition and the intention to leave. Among current professionals, the intention to choose the same career is an interesting way to gau...
Validation and psychometric testing of the Arabic version of the mental health literacy scale among the Saudi Arabian general population
This study aimed to validate the Arabic Version of the Mental Health Literacy Scale (Arabic-MHLS) among the Saudi Arabian general population, assessing its internal consistency, test-retest reliability, and st...
Cascade training for scaling up care for perinatal depression in primary care in Nigeria
Task-shared care is a demonstrated approach for integrating mental health into maternal and child healthcare (MCH) services. Training and continued support for frontline providers is key to the success of task...
Provider perceptions of the anticipated benefits, barriers, and facilitators associated with implementing a stepped care model for the delivery of addiction and mental health services in New Brunswick: a mixed-methods observational implementation study
Providers who work within addiction and mental health (A&MH) services in New Brunswick (NB), Canada completed training in Stepped Care 2.0 and One-at-a-Time (OAAT) therapy as part of a provincial practice chan...
Detection of traumatic stress in the presence of traumatic experiences: the role of resilience factors in foster care children five years or younger
Children less than five years of age comprised approximately 30% in 2020 of foster care entries in the United States, and they are consistently the largest foster care entry group. Very young children can resp...
Treatment rates and barriers to mental health service utilisation among university students in South Africa
Mental health problems are common and impairing among university students, yet only a minority of students with psychological disorders access treatment. Understanding barriers to treatment is integral to plan...
Cost structure in specialist mental healthcare: what are the main drivers of the most expensive episodes?
Mental disorders are one of the costliest conditions to treat in Norway, and research into the costs of specialist mental healthcare are needed. The purpose of this article is to present a cost structure and t...
Shifting drug markets in North America - a global crisis in the making?
Understanding drug market dynamics and their underlying driving factors is paramount to developing effective responses to the overdose crisis in North America. This paper summarises the distinct drug market tr...
Piloting a community-based psychosocial group intervention designed to reduce distress among conflict-affected adults in Colombia: a mixed-method study of remote, hybrid, and in-person modalities during the COVID-19 pandemic
Community members in Quibdó (Choco, Colombia) are highly vulnerable to psychosocial problems associated with the internal armed conflict, poverty, and insufficient public services, and exacerbated by the COVID...
“You can create a little bit more closure in your own story when someone really connects with it”: exploring how involvement in youth peer support work can promote peer development
Peer support relates to the provision of social/emotional support that is delivered by individuals with lived experience of a key characteristic that is shared with clients. Although the main objective of peer...
A systematic review of measures of the personal recovery orientation of mental health services and staff
This review aimed to update and extend the Williams and colleagues 2012 systematic review of measures of recovery-orientation of mental health services by examining whether any of the specific knowledge gaps i...
A randomized controlled trial of mindfulness: effects on university students’ mental health
The development of mental health disorders is common in the university population, and mindfulness-based interventions (MBIs) seem to be effective in addressing them in different contexts. Thus, this study inv...
Assessing the quality of the care offer for people with personality disorders in Italy: the QUADIM project. A multicentre research based on the database of use of Mental Health services
Italy can be viewed as a laboratory to assess the quality of mental healthcare delivered in a community-oriented system, especially for severe mental disorders, such as personality disorders. Although initiati...
Mental health treatment programs for children and young people in secure settings: A systematic review
While there are mental health treatment programs for children and young people in secure settings (i.e., secure treatment programs) in many countries, there is a lack of transparency and consistency across the...
Implementing digital mental health interventions at scale: one-year evaluation of a national digital CBT service in Ireland
In recent years, exponential growth in digital innovations and internet access has provided opportunities to deliver health services at a much greater scale than previously possible. Evidence-based technology-...
The battle for mental well-being in Ukraine: mental health crisis and economic aspects of mental health services in wartime
The ongoing war in Ukraine is having profound impacts on both the local and global economy, as well as the infrastructure and overall well-being of the people. The prolonged duration of the conflict, coupled w...
Progress towards universal health coverage in the context of mental disorders in India: evidence from national sample survey data
Universal health coverage (UHC) has emerged as one of the important health policy discourses under the current sustainable development goals in the world. UHC in individual disease conditions is a must for att...
Attitude of mental healthcare providers toward tele-psychiatry services and associated factors at public referral hospitals in Addis Ababa city, Ethiopia
Health systems around the world are struggling with the massive numbers of people with mental disorders who require professional care. The treatment gap for mental disorders is high all over the world, with be...
Co-producing research on psychosis: a scoping review on barriers, facilitators and outcomes
Co-production is a collaborative approach to service user involvement in which users and researchers share power and responsibility in the research process. Although previous reviews have investigated co-produ...
“I decided to participate….because I saw it as benefiting our community and families” : a qualitative study of lay providers’ experiences with delivering an evidence-based mental health intervention for families in Uganda
Children and adolescents who live in resource-limited communities in sub-Saharan Africa (SSA) experience significant mental health problems, including behavioral problems. In SSA, one of the most significant i...
Using the National Mental Health Service Planning Framework to inform integrated regional planning: a case study in Tasmania, Australia
The aim of this study was to demonstrate the application of a needs-based mental health service planning model in Tasmania, Australia to identify indicative directions for future service development that ensur...
The mental health toll of COVID-19: significant increase in admissions to ICU for voluntary self-inflicted injuries after the beginning of the pandemic
COVID-19 outbreak deeply impacted on mental health, with high rate of psychological distress in healthcare professionals, patients and general population. Current literature on trauma showed no increase in ICU...
A framework for precision “dosing” of mental healthcare services: algorithm development and clinical pilot
One in five adults in the US experience mental illness and over half of these adults do not receive treatment. In addition to the access gap, few innovations have been reported for ensuring the right level of ...
Dynamics of hospitalizations and staffing of Ukraine’s mental health services during the Russian invasion
Since February 2022, the people of Ukraine have experienced devastating losses due to the Russian invasion, increasing the demand for mental healthcare across the nation. Using longitudinal data on mental heal...
Towards measuring effective coverage: critical bottlenecks in quality- and user-adjusted coverage for major depressive disorder in São Paulo metropolitan area, Brazil
Major depressive disorder (MDD) contributes to a significant proportion of disease burden, disability, economic losses, and impact on need of treatment and health care in Brazil, but systematic information abo...
Impact of COVID-19 on the lives of people with severe mental illness—front-line community psychiatry workers observation from a provincial survey of assertive community treatment teams in Ontario, Canada
Using an online survey distributed to members of the provincial organization that represents the 88 Assertive Community Treatment (ACT) and Flexible ACT teams in Ontario, Canada, this descriptive study relied ...
Managers as peer workers’ allies: A qualitative study of managers’ perceptions and actions to involve peer workers in Norwegian mental health and substance use services
Citizens with experience and knowledge about what it is like to use mental health and substance use services are increasingly employed within similar services as peer workers. Peer workers are portrayed as ach...
What does receiving autism diagnosis in adulthood look like? Stakeholders’ experiences and inputs
The age of diagnosis is crucial for optimal health outcomes; however, some individuals with Autism Spectrum Disorder (ASD) may not be diagnosed until adulthood. Limited information is available about the lived...
Translation of the mental health literacy questionnaire for young adults into Chichewa for use in Malawi: preliminary validation and reliability results
Mental Health Literacy (MHL) is the ability to recognise mental disorders, have knowledge of professional help available, effective self-help strategies, skills to give support to others, and knowledge of how ...
- Editorial Board
- Manuscript editing services
- Instructions for Editors
- Sign up for article alerts and news from this journal
Annual Journal Metrics
2022 Citation Impact 3.6 - 2-year Impact Factor 3.9 - 5-year Impact Factor 1.582 - SNIP (Source Normalized Impact per Paper) 1.138 - SJR (SCImago Journal Rank)
2023 Speed 44 days submission to first editorial decision for all manuscripts (Median) 290 days submission to accept (Median)
2023 Usage 1,612,135 downloads 428 Altmetric mentions
- More about our metrics
International Journal of Mental Health Systems
ISSN: 1752-4458
- Submission enquiries: [email protected]
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 5, Issue 6
- What is mental health? Evidence towards a new definition from a mixed methods multidisciplinary international survey
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Laurie A Manwell 1 , 2 ,
- Skye P Barbic 1 , 3 ,
- Karen Roberts 1 ,
- Zachary Durisko 1 ,
- Cheolsoon Lee 1 , 4 ,
- Emma Ware 1 ,
- Kwame McKenzie 1
- 1 Social Aetiology of Mental Illness Training Program , Centre for Addiction and Mental Health, University of Toronto , Toronto, Ontario , Canada
- 2 Department of Anatomy and Cell Biology , Schulich School of Medicine & Dentistry, University of Western , London, Ontario , Canada
- 3 Department of Psychiatry , University of British Columbia , Vancouver, British Columbia , Canada
- 4 Department of Psychiatry , Gyeongsang National University Hospital, School of Medicine, Gyeongsang National University , Jinju , Republic of Korea
- Correspondence to Dr Laurie A Manwell; lauriemanwell{at}gmail.com
Objective Lack of consensus on the definition of mental health has implications for research, policy and practice. This study aims to start an international, interdisciplinary and inclusive dialogue to answer the question: What are the core concepts of mental health?
Design and participants 50 people with expertise in the field of mental health from 8 countries completed an online survey. They identified the extent to which 4 current definitions were adequate and what the core concepts of mental health were. A qualitative thematic analysis was conducted of their responses. The results were validated at a consensus meeting of 58 clinicians, researchers and people with lived experience.
Results 46% of respondents rated the Public Health Agency of Canada (PHAC, 2006) definition as the most preferred, 30% stated that none of the 4 definitions were satisfactory and only 20% said the WHO (2001) definition was their preferred choice. The least preferred definition of mental health was the general definition of health adapted from Huber et al (2011). The core concepts of mental health were highly varied and reflected different processes people used to answer the question. These processes included the overarching perspective or point of reference of respondents (positionality), the frameworks used to describe the core concepts (paradigms, theories and models), and the way social and environmental factors were considered to act . The core concepts of mental health identified were mainly individual and functional, in that they related to the ability or capacity of a person to effectively deal with or change his/her environment. A preliminary model for the processes used to conceptualise mental health is presented.
Conclusions Answers to the question, ‘ What are the core concepts of mental health ?’ are highly dependent on the empirical frame used. Understanding these empirical frames is key to developing a useful consensus definition for diverse populations.
- MENTAL HEALTH
- mental illness
- social determinants of health
- human rights
- primary health care
This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
https://doi.org/10.1136/bmjopen-2014-007079
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Strengths and limitations of this study
Our study identifies a major obstacle for integrating mental health initiatives into global health programmes and health service delivery, which is a lack of consensus on a definition, and initiates a global, interdisciplinary and inclusive dialogue towards a consensus definition of mental health .
Despite the limitations of a small sample size and response saturation, our sample of global experts was able to demonstrate dissatisfaction with current definitions of mental health and significant agreement among subcomponents, specifically factors beyond the ‘ability to adapt and self-manage’, such as ‘diversity and community identity’ and creating distinct definitions, ‘one for individual and a parallel for community and society’.
This research demonstrates how experts in the field of mental health determine the core concepts of mental health, presenting a model of how empirical discourses shape definitions of mental health.
We propose a transdomain model of health to inform the development of a comprehensive definition capturing all of the subcomponents of health: physical, mental and social health.
Our study discusses the implications of the findings for research, policy and practice in meeting the needs of diverse populations.
Introduction
A major obstacle for integrating mental health initiatives into global health programmes and primary healthcare services is lack of consensus on a definition of mental health. 1–3 There is little agreement on a general definition of ‘mental health’ 4 and currently there is widespread use of the term ‘mental health’ as a euphemism for ‘mental illness’. 5 Mental health can be defined as the absence of mental disease or it can be defined as a state of being that also includes the biological, psychological or social factors which contribute to an individual’s mental state and ability to function within the environment. 4 , 6–11 For example, the WHO 12 includes realising one's potential, the ability to cope with normal life stresses and community contributions as core components of mental health. Other definitions extend beyond this to also include intellectual, emotional and spiritual development, 13 positive self-perception, feelings of self-worth and physical health, 11 , 14 and intrapersonal harmony. 8 Prevention strategies may aim to decrease the rates of mental illness but promotion strategies aim at improving mental health. The possible scope of promotion initiatives depends on the definition of mental health.
The purpose of this paper is to begin a global, interdisciplinary, interactive and inclusive series of dialogues leading to a consensus definition of mental health. It has been stimulated and informed by a recent debate about the need to redefine the term health . Huber et al 15 emphasised that health should encompass an individual's “ability to adapt and to self-manage” in response to challenges, rather than achieving “a state of complete wellbeing” as stated in current WHO 6 , 12 definitions. They also argued that a new definition must consider the demographics of stakeholders involved and future advances in science. 15 Responses to the article suggested the process of reconceptualising health be extended “beyond the esoteric world of academia and the pragmatic world of policy” 16 to include a “much wider lens to the aetiology of health” 17 along with patients and lay members of the public. Huber et al's 15 definition of health could include mental health but it is not clear that this would be satisfactory to patients, practitioners or researchers. We aimed to compare the satisfaction of mental health specialists, patients and the public with Huber et al ’s definition and other currently used definitions of mental health. We also asked them what they considered to be the core components of mental health.
Participants and procedures
A pool of 25 researchers in mental health was identified through literature/internet searches to capture expertise in (1) ‘community mental health’ and ‘public mental health’, (2) ‘human rights’ and ‘global mental health’, (3) ‘positive mental health’ and ‘resilience’, (4) ‘recovery’ and ‘mental health’, and (5) ‘natural selection’ and ‘evolutionary origins’ of ‘mental health’. Each of these five areas was assigned to an author with expertise in that area who then conducted a series of literature/internet searches using the key terms listed above. Proposed participants were identified based on their expert contributions, such as published papers, presentations, community outreach, and other evidence of work in their field that had implications for mental health. Each author presented their list to the research team which then narrowed the number to 5 per category for a total of 25 initial participants. An additional 31 individuals were added, which included people with lived experience of mental illness as well as the mentors of the Social Aetiology of Mental Illness (SAMI) Training Programme (funded by the Canadian Institutes of Health Research and includes a multidisciplinary group of experts with diverse interests, including biological, social and psychological sciences); all of these participants were identified through the SAMI/Centre for Addiction and Mental Health network. Fifty-six participants were sent the survey in the first round. Two subsequent rounds were completed using a snowballing technique: each person in round 1 was asked to indicate up to three other people they thought should receive the survey, which was then distributed to those identified individuals. This was repeated in round 2.
The ‘What is Mental Health?’ survey was created and distributed electronically using the SurveyMonkey platform. Respondents were asked to describe their areas of expertise, and list or describe the core concepts of mental health. Respondents ranked four definitions (without citations) of mental health 12 , 15 , 18 (McKenzie K. Community definition of Mental Health. What Is Mental Health Survey. Centre for Addiction and Mental Health, personal communication, 15 January 2014) and a fifth choice of ‘None of the existing definitions are satisfactory’ in order of preference (1=most preferred, 5=least preferred), and could rate multiple definitions as most and/or least preferred (see table 1 ). Respondents were asked to state, ‘What was missing and why?’ from these definitions.
- View inline
Current definitions of mental health and participant rank ordering from most to least preferred
Data analysis
Thematic analysis 19 was used to evaluate the core concepts of mental health, followed by triangulation (ie, multiple methods, analysts or theory/perspectives) to verify and validate the qualitative data analysis. 20
First, multiple analysts with knowledge from different disciplines reviewed the data. 20 Our collective areas of expertise encompass the following: animal models of human behaviour; arts; clinical, cognitive, political and social psychology; ecology; education; epidemiology; evolutionary theory; humanities; knowledge translation; measurement; molecular biology; neuroscience; occupational therapy; psychiatry; qualitative and quantitative research; social aetiology of mental illness; toxicology and transcultural health. All transcripts were reviewed by each coder first independently, then collectively, to become familiar with the data and create a mutually agreed on code book using NVivo 10. Codes were organised into themes, and compared and contrasted manually and through NVivo10 coding queries within each major theme and across response items. Initial models derived from the data were created and validated by the multidisciplinary research team.
Second, method triangulation was used to assess the consistency of our findings. 20 Preliminary results from the survey were presented and discussed at the 4th Annual Social Aetiology of Mental Illness Conference (20 May 2014) at the Centre for Addiction and Mental Health, University of Toronto (Toronto, Ontario, Canada). Attendees were divided into five focus groups of 10–12 people facilitated by a project leader and 2 trained note takers. The two consecutive 1 h focused discussions used the ORID method (Objective, Reflective, Interpretive and Decisional) 21 in order to elicit feedback on the methods and results of the survey. All responses from each of the five groups were transcribed by two recorders and disseminated to the research team for individual and collaborative review.
A second round of data analysis was conducted to validate the results according to key areas of interest and critique reported by the conference participants.
Survey respondents
Fifty-six surveys were distributed in the first round, 28 in the second and 38 in the third. Fifty people completed the survey (rounds 1, 2 and 3 had 32, 12 and 6 respondents, respectively) with a total response rate of 41%. Two-thirds of respondents (66%) were male and one-third were female (34%). Respondents’ current country of residence/employment included Canada (52%), UK (20%), USA (14%), Australia (6%), New Zealand (2%), Brazil (2%), South Africa (2%) and Togo (2%). The majority of respondents (72%) held academic positions at postsecondary institutions and were conducting research in the broad field of mental health. Sixty per cent were also involved in giving advice to mental health services or managing them. Thirty-four per cent of respondents were clinicians.
Survey items
Respondents had diverse expertise (see table 2 ). Forty-six per cent of respondents rated the Public Health Agency of Canada (PHAC) 18 definition as their most preferred. However, 30% stated that none were satisfactory. The WHO definition 12 was preferred by 20%. The least preferred definition of mental health was the general definition of health adapted from Huber et al 15 (see table 1 ).
Self-reported areas of expertise
Analysis of the three open-ended items established four major themes— Positionality, Social/Environmental Factors, Paradigms/Theories/Models and the Core Concepts of Mental Health —and five-directional relationships between them ( figure 1 ). Positionality represented the overarching perspective or point-of-reference from which the Core Concepts were derived; whereas Paradigms/Theories/Models represented the theoretical framework within which the Core Concepts were described. Core Concepts represented factors related to the individual; these were distinguishable from the Social/Environmental Factors related to society. Five significant relationships between these themes were established ( figure 1 ). First, respondents’ theoretical framework (Direction A) influenced the overarching point-of-reference they used to describe the core concepts and vice versa (Direction B). Positionality and Paradigms/Theories/Models significantly influenced the core concepts respondents provided and the corresponding descriptions (Direction C). Respondents described how social and environmental factors impacted the core concepts (Direction D) and reciprocally, how the core concepts could influence society (Direction E) ( tables 3 and 4 ). Feedback from the conference focus groups showed support for these five-directional relationships but questioned whether there was evidence for other direct relationships, specifically the impact of Social/Environmental Factors on both Paradigms/Theories/Models and Positionality . A second round of data analysis confirmed these relationships were not explicitly reported by respondents in the survey. Respondents did not discuss how social factors (ie, education or employment) would impact the adoption of a particular paradigm, theory or model (ie, quality of life, evolutionary theory or biomedical model).
Theme—Positionality
Theme—Core Concepts
- Download figure
- Open in new tab
- Download powerpoint
Themes of Positionality, Core Concepts, Social/Environmental Factors, and Paradigms/Theories/Models. *Indicates answers specifically from the third open-ended question asking respondents to state “what is missing” from the definitions provided for ranking.
The theme of Positionality demonstrated how respondents positioned their conceptualisations of mental health within an explicit or implicit framework of understanding ( table 3 , figures 2 and 3 ). Several respondents described the core concepts in terms of binary or conflicting dynamics or as categorical or continuous . Some respondents pointed to the mutual exclusivity of ‘mental health’ and ‘mental illness’ while others described these concepts as distinct points separated on a continuum or as overlapping. Respondents specified the complexity of mental health, for example, positioning mental health explicitly outside of, and specifically in between, the individual and society. Several respondents framed the core concepts of mental health as descriptive versus prescriptive , arguing that these must be empirically determined and defined (ie, describing what is ) rather than prescribed according to values and morals (ie, describing what should be ). In accordance with Hume's Law (ie, an ‘ought’ cannot be derived from an ‘is’), 22 several respondents cautioned that problems of living, such as ‘poverty, vices, social injustices and stupidity’, should not be defined ‘as medical problems’. Many respondents described mental health in relation to hierarchical levels , and/or temporal trajectories , and/or context ( table 3 , figure 3 ). Respondents articulated the multiple levels at which mental health can be understood (ie, from the basic unit of the gene, through the individual and up to the globe) and how meaning changes across time (ie, mental health described as functioning in line with our evolutionary ancestors, to current developmental mechanisms and including expectations of a peaceful death and spiritual existence) and across context (ie, from region, to race, to culture, to epistemology). In the second round of data analysis, we searched for bias in participants’ reporting of evidence-based models and bias against other sources of information; there was support for objective and subjective sources in conceptualising mental health.
Positionality. The overarching perspective or point-of-reference used to describe the constructs of mental health and illness.
Complexity. Descriptions of mental health in relation to hierarchical levels, and/or spatial directions, and/or temporal trajectories.
A second theme of Paradigms/Theories/Models developed as respondents discussed the need to perceive health through various frameworks (eg, recovery, resilience, human flourishing, quality of life, developmental and evolutionary theories, cultural psychiatry and ecology). Some respondents noted that current definitions of mental health treat problems of living as medical problems, rather than adaptive responses to the conditions that people experience, and that alternative explanations should be considered: “An evolutionary approach to these conditions suggests that anxiety and depression (as responses to social stressors) evolved to help the individual take corrective action that could ameliorate the negative effects of these stressors”. Some respondents emphasised that ‘low’ mental health did not equate to mental illness, but rather a state of hopelessness and lack of personal autonomy, whereas ‘high’ mental health was demonstrated by ‘meaningful participation, community citizenship, and life satisfaction’. Others referenced Westerhof and Keyes's 23 two-continuum model describing mental illness and mental health as related by two distinct dimensions.
The Core Concepts of mental health ( figure 1 , table 4 ) largely described factors relating to the individual—as opposed to society—that are observed in correlation with mental health and which are necessary, to some degree or another, but not normally sufficient on their own to achieve mental health. Concepts related to agency, autonomy and control appeared frequently in relation to an individual's ability or capacity to effectively deal with and/or create change in his or her environment (Directions D–E). Agency/autonomy/control reappeared as an essential component of other core concepts: agency may be required in order to engage in meaningful participation (eg, ‘sense of being part of a vibrant society, with agency to make change for you and others, and supportive relationships and governance’) and in dignity (eg, ‘a state of mind that allows one to lead one's life knowing that one’s dignity and integrity as a human being is respected by others’). A cluster of concepts describing the self signified (1) the subjective experience of the individual as fundamental to well-being and (2) the importance of one's ability, confidence and desire to live in accordance with one's own values and beliefs in moving towards the fulfilment of one's goals and ambitions ( figure 1 ).
Social and Environmental Factors reflected the societal factors external to the individual that affect mental health. Although many respondents listed the basic necessities for general health/mental health (eg, housing, food security, access to health services, equitable access to public resources, childcare, education, transportation, support for families, respect for diversity, opportunities for building resilience, self-esteem, personal and social efficacy, growth, meaning and purpose, and sense of safety and belonging, and employment), some also recommended approaches to achieving social equity (eg, “mental health needs to be protected by applying antiracism, antioppression, antidiscrimination lens to prevention and treatment”) ( figure 1 , Direction D). A distinct category of human rights developed from responses to the third open-ended question (eg, “What is missing?”) ( figure 1 ). Several respondents suggested that a basic standard, analogous to a legal definition, is required ( table 3 ) and/or that “a human rights, political, economic and ecosystem perspective” should be included.
The international exploratory ‘What is Mental Health?’ survey sought the opinions of individuals, across multiple modes of inquiry, on what they perceived to be the core concepts of mental health. The survey found dissatisfaction with current definitions of mental health. There was no consensus among this group on a common definition. However, there was significant agreement among subcomponents of the definitions, specifically factors beyond the ‘ability to adapt and self-manage’, such as ‘diversity and community identity’ and creating distinct definitions, “one for individual and a parallel for community and society.” The Core Concepts of mental health that participants identified were predominantly centred on factors relating to the individual, and one's capacity and ability for choice in interacting with society. The concepts of agency, autonomy and control were commonly mentioned throughout the responses, specifically in regard to the individual's ability or capacity to effectively deal with and/or create change in his or her environment. Similarly, respondents pointed to the self as an essential component of mental health, signifying the subjective experience of the individual as fundamental to well-being, particularly in relationship to achieving one's valued goals. Respondents suggested that mentally healthy individuals are socially connected through meaningful participation in valued roles (ie, in family, work, worship, etc), but that mental health may involve being able to disconnect by choice, as opposed to being excluded (eg, having the capacity and ability to reject social, legal and theological practices). In contrast, Social and Environmental Factors reflected respondents’ emphasis on factors that are external to the individual and which can influence the core concepts of mental health. Many respondents reiterated the basic necessities for general health/mental health, similar to the foundations of Maslow's hierarchy of needs, 24 and their recommendations for achieving social equity.
Descriptions of the core concepts of mental health were highly influenced by respondents’ Positionality and Paradigms/Theories/Models of reference, which often propelled the discourse of “What is mental health?” in opposing directions. The debate as to whether mental health and illness are distinct constructs, or points of reference on a continuum of being, was a common theme. Respondents were either, adamant in asserting the distinction between the descriptive or prescriptive nature of the core concepts, or, ardent in integrating them, producing ideas such as describing mental health as a life free of poverty, discrimination, oppression, human rights violations and war. Respondents’ made repeated references to human rights, suggesting that a basic standard, analogous to a legal definition, is required, and that ‘a human rights, political, economic and ecosystem perspective’ should be included. Again, in the tradition of Hume's ‘ought–is’ distinction, several respondents cautioned that problems of living, such as ‘poverty, vices and social injustices…’ should not be defined ‘as medical problems’. The significance of this issue cannot be understated: while we asked respondents what the core concepts of mental health are , overwhelmingly they answered in terms of what they should be. This finding is similar to other issues in public health policy that address instances of ‘conflating scientific evidence with moral argument’. 15 , 22 Indeed, a primary criticism of the WHO definition of health is that its declaration of “complete physical, mental, and social wellbeing” 6 is prescriptive rather than descriptive. 15 Such a definition “contributes to the medicalization of society” and excludes most people, most of the time, and has little practical value “because ‘complete’ is neither operational nor measurable.” 15
Accordingly, we propose a transdomain model of health ( figure 4 ) to inform the development of a comprehensive definition for all aspects of health. This model builds on the three domains of health as described by WHO 6 , 12 and Huber et al, 15 and expands these definitions to include four specific overlapping areas and the empirical, moral and legal considerations discussed in the current study. First, all three domains of health should have a basic legal standard of functioning and adaptation. Our findings suggest that for physical health, a standard level of biological functioning and adaptation would include allostasis (ie, homeostatic maintenance in response to stress), whereas for mental health, a standard level of cognitive–emotional functioning and adaptation would include sense of coherence (ie, subjective experience of understanding and managing stressors), similar to Huber et al 's 15 proposal. However, for social health, a standard level of interpersonal functioning and adaptation would include interdependence (ie, mutual reliance on, and responsibility to, others within society), rather than Huber et al 's 15 focus on social participation (ie, balancing social and environmental challenges). Our results provide further insight into how these domains interact to affect overall quality of life. Integration of mental and physical health can be defined by level of autonomy (ie, the capacity for control over one's self), whereas integration of mental and social health can be defined by a sense of ‘us’ (ie, capacity for relating to others); the integration of mental and physical health can be defined by control (ie, capacity for navigating social spaces). The highest degree of integration would be defined by agency , the ability to choose one's level of social participation (eg, to accept, reject or change social, legal or theological practices). Such a transdomain model of health could be useful in developing cross-cultural definitions of physical, social and mental health that are both inclusive and empirically valid. For example, Valliant's 25 seven models for conceptualizing mental health across cultures are all represented, to varying degrees, within the proposed transdomain model of health . The basic standard of functioning across domains which is proposed here is congruent with Valliant's 25 criteria for mental health to be ‘conceptualised as above normal’ and defined in terms of ‘multiple human strengths rather than the absence of weaknesses’, including maturity, resilience, positive emotionality and subjective well-being. In addition, Valliant's 25 conceptualisation of mental health as ‘high socio-emotional intelligence’ is also represented in the transdomain model's highest level of integration of the three areas for full individual autonomy. Finally, Valliant's 25 cautions for defining positive mental health—being culturally sensitive, recognising that population averages do not equate to individual normalcy and that state and trait functioning may overlap, and contextualising mental health in terms of overall health—are all addressed within the transdomain model .
Transdomain Model of Health. This model builds on the three domains of health as described by WHO 6 , 12 and Huber et al 15 and expands these definitions to include four specific overlapping areas and the empirical, moral, and legal considerations discussed in the current study. There are three domains of health (ie, physical, mental, and social), each of which would be defined in terms of a basic (human rights) standard of functioning and adaptation . There are four dynamic areas of integration or synergy between domains and examples of how the core concepts of mental health could be used to define them.
Strengths and limitations of the current study
We are unaware of any study to date that has asked this research question to a group of international experts in the broad field of mental health. Although our survey sample was small (N=50), it was diverse with regard to place of origin and expertise; it was also further validated by participants (N=58) at a day-long conference on mental health through discussion, debate and written responses. The current study included global experts who dedicate their research and professional lives to advancing the standards of mental health. Of particular note was that little to no consensus among the selected group of experts on any particular definition was found. In fact, this was simultaneously a limitation and strength of the study: the small sample size limited the scope of the core concepts of mental health, but indicated that it was sufficient to demonstrate that there are highly divergent definitions that are largely dependent on the respondents’ frame of reference. It is possible that saturation was not achieved in regards to the diversity of responses. Further, more than half of the survey respondents were from Canada, which may have influenced the preference towards the PHAC definition of mental health. Although there were advantages to using a snowball sampling method, another type of sampling method (eg, cluster sampling, stratified sampling) may have resulted in more varied responses to the survey items. The next logical step would be to survey experts in countries currently not represented and then ultimately survey members of the general public with regard to their conceptual and pragmatic understanding of mental health. One of the a priori objectives for the survey was to eventually create a consensus definition of mental health that could be used in public policy; this objective was not communicated in the survey, nor did we actually ask this question. Our results indicate that finding consensus on a definition of mental health will require much more convergence in the frame of reference and common language describing components of mental health. Even we, as authors, have been challenged by consensus. For example, some of us wish to emphasise that future work should focus on developing an operational definition that can be applied across disciplines and cultures. Others among us suggest further exploring what purpose a definition of mental health would or should serve, and why. In contrast, others among us wish to emphasise the process of conceptualising mental health versus the outcome or application of such a definition. What we hoped would be a straightforward, simple question, designed to create consensus for a definition of mental health, ultimately demonstrated the nuanced but crucial epistemological and empirical influences on the understanding of mental health. Based on the results of the survey and conference, we present a preliminary model for conceptualising mental health. Our study provides evidence that if we are to try to come to a common consensus on a definition of mental health, we will need to understand the frame of reference of those involved and try to parse out the paradigms, positionality and the social/environmental factors that are offered from the core concepts we make seek to describe. Future work may also need to distinguish between the scientific evidence of mental health and the arguments for mental health . Similar debates in bioethics 22 , 26–28 demonstrate the theoretical and practical limitations of science for proscribing human behaviour, especially with regard to individual freedom and social justice.
Conclusions
Our results suggest that any practical use of a definition of health will depend on the epistemological and moral framework through which it was developed, and that the mental and social domains may be differentially influenced than the physical domain. A definition of health, grounded solely in biology, may be more applicable across diverse populations. A definition of health encompassing the mental and social domains may vary more in application, particularly across systems, cultures or clinical practices that differ in values (eg, spiritual, religious) and ways of understanding and being (eg, epistemology). A universal (global) definition based on the physical domain could be parsed out separately from several unique (local) definitions based on the mental and social domains. Understanding the history and evolution of the concept of mental health is essential to understanding the problems it was intended to solve, and what it may be used for in the future.
Acknowledgments
The authors wish to extend their gratitude to their colleagues for their generous feedback, constructive critiques and recommendations for the project, and to the many volunteers who organised the conference. Special thanks to Nina Flora, Helen Thang, Andrew Tuck, Athena Madan, David Wiljer, Alex Jadad, Sean Kidd, Andrea Cortinois, Heather Bullock, Mehek Chaudhry and Anika Maraj.
- Whiteford HA ,
- Degenhardt L ,
- Rehn J , et al
- Belkin GS ,
- Chockalingham A , et al
- ↵ WHO . 2008 Policies and practices for mental health in Europe—meeting the challenges. http://www.euro.who.int/__data/assets/pdf_file/0006/96450/E91732.pdf .
- Carter JW ,
- Hidreth HM ,
- Knutson AL , et al
- ↵ WHO . 1948 Constitution of the World Health Organization , 2006 http://www.who.int/governance/eb/who_constitution_en.pdf
- ↵ WHO . Prevention of mental disorders . Geneva : 2004 . http://www.who.int/mental_health/evidence/en/prevention_of_mental_disorders_sr.pdf
- Sartorius N
- ↵ WHO . Mental health: strengthening mental health promotion, 2001 ; Fact Sheet No. 220 Geneva, Switzerland , 2001 . Updated August 2014: http://www.who.int/mediacentre/factsheets/fs220/en/
- ↵ Health Education Authority (HEA) . Mental health promotion: a quality framework. London : HEA , 1997 .
- ↵ Mental Health Foundation (MHF) . What works for you? London : MHF, 2008 .
- Knottnerus JA ,
- Green L , et al
- Macaulay AC
- ↵ Public Health Agency of Canada (PHAC) . The human face of mental health and mental illness in Canada 2006 . Ottawa, ON : Minister of Public Works and Government Services Canada , 2006 .
- Stanfield RB
- Westerhof GJ ,
- Valliant GE
Contributors All the authors contributed to the conceptualisation of the project. LAM wrote the manuscript. SB, KR, ZD, CL and KM contributed to the content and editing of the manuscript. LAM, SB, KR, ZD, CL and EW created the survey and conducted data analyses. SB, KR and LAM presented findings at the conference. LAM, SB, KR, ZD and EW led the focused discussion groups. KM supervised the project. LM is the guarantor.
Funding This work was performed with grants from the Canadian Institutes of Health Research (CIHR) for the Social Aetiology of Mental Illness Training Program at the Centre for Addiction and Mental Health.
Competing interests None declared.
Provenance and peer review Not commissioned; externally peer reviewed.
Data sharing statement No additional are data available.
Read the full text or download the PDF:
Mental Health Research News
Top headlines, latest headlines.
- Heart Disease, Depression Linked by Inflammation
- Feeding the Lonely Brain
- Detecting and Evaluating ADHD
- Ketogenic Diet for Severe Mental Illness
- Younger Women: Mental Health, Heart Health
- Premenstrual Disorders and Perinatal Depression
- Measures the Severity of Depression
- Brain pH Changes and Cognitive Issues
- Antipsychotics Use in Pregnancy
- Heart Disease: Treating Anxiety, Depression
Earlier Headlines
Thursday, march 14, 2024.
- How Fear Unfolds Inside Our Brains
Wednesday, March 13, 2024
- Researchers Identify Brain Connections Associated With ADHD in Youth
Monday, March 11, 2024
- 'Study Drugs' Set the Stage for Other Drug Use and Mental Health Decline
Wednesday, March 6, 2024
- New Study May Broaden the Picture of the Consequences of Childhood Adversity
Monday, March 4, 2024
- It's Not Just You: Young People Look, Feel Older When They're Stressed
Friday, March 1, 2024
- Link Between Adversity, Psychiatric and Cognitive Decline
- Study Paves the Way for Better Diagnosis and Treatment of Endocrine Diseases
Tuesday, February 27, 2024
- Teens Benefit from 'forest Bathing' -- Even in Cities
Monday, February 26, 2024
- Gut-Brain Communication Turned on Its Axis
- Intervention Reduces Likelihood of Developing Postpartum Anxiety and Depression by More Than 70%
- Yoga Provides Unique Cognitive Benefits to Older Women at Risk of Alzheimer's Disease
Wednesday, February 21, 2024
- Maternal Mental Conditions Drive Climbing Death Rate in U.S., Evidence Review Finds
Tuesday, February 20, 2024
- Wildfires Linked to Surge in Mental Health-Related Emergency Department Visits
- Stress During Pregnancy Can Lead to Early Maturation of First-Born Daughters
Monday, February 19, 2024
- Understanding the Relationship Between Our Sleep, Body Clock and Mental Health
Thursday, February 15, 2024
- Burnout: Identifying People at Risk
Tuesday, February 13, 2024
- A Closer Look at Cannabis Use and Binge Eating
Thursday, February 8, 2024
- Benefits of Resistance Exercise Training in Treatment of Anxiety and Depression
- Ketamine's Promise for Severe Depression Grows, but Major Questions Remain
Wednesday, February 7, 2024
- Researchers Make Progress Toward Developing Blood Tests for Psychiatric and Neurological Disorders
- Stress Influences Brain and Psyche Via Immune System
Tuesday, February 6, 2024
- Bullied Teens' Brains Show Chemical Change Associated With Psychosis
Monday, February 5, 2024
- Are Body Temperature and Depression Linked? Science Says, Yes
Thursday, February 1, 2024
- Psychological Care Delivered Over the Phone Is an Effective Way to Combat Loneliness and Depression, According to a Major New Study
Wednesday, January 31, 2024
- Potential Link Between High Maternal Cortisol, Unpredicted Birth Complications
Tuesday, January 30, 2024
- Researchers Find Early Symptoms of Psychosis Spectrum Disorder in Youth Higher Than Expected
Wednesday, January 24, 2024
- Mood Interventions May Reduce Inflammation in Crohn's and Colitis
Thursday, January 18, 2024
- Relationships With Caring Adults Provide a Buffer Against Depression, Anxiety, Regardless of Adverse Childhood Experiences
Wednesday, January 17, 2024
- Therapy Versus Medication: Comparing Treatments for Depression in Heart Disease
Friday, January 12, 2024
- Psychotherapy Effective in Treating Post-Traumatic Stress Disorder Following Multiple Traumatic Events, Meta-Study Finds
- Stress, Via Inflammation, Is Linked to Metabolic Syndrome
Wednesday, January 10, 2024
- Feeling Depressed Linked to Short-Term Increase in Bodyweight
- Newly Identified Genes for Depression May Lead to New Treatments
- Reduced Drug Use Is a Meaningful Treatment Outcome for People With Stimulant Use Disorders, Study Shows
Monday, January 8, 2024
- Clear Link Between Autoimmune Disease and Perinatal Depression
Thursday, January 4, 2024
- Bipolar Disorder Linked to Early Death
Thursday, December 21, 2023
- Psychologist Publishes Most Thorough Compilation of Sleep and Emotion Research to Date
- Connection Between Light Levels and Mental Health -- Climate Change Could Also Have an Impact in the Future
Thursday, December 14, 2023
- Genetic 'protection' Against Depression Was No Match for Pandemic Stress
Wednesday, December 13, 2023
- Unravelling the Association Between Neonatal Proteins and Adult Health
- Body Dissatisfaction Linked With Depression Risk in Children

Tuesday, December 12, 2023
- Caregiving Can Be Stressful, but It Could Also Lower Risk of Depression
Thursday, December 7, 2023
- Discrimination During Pregnancy May Alter Circuits in Infants' Brains
Tuesday, December 5, 2023
- Depression, Constipation, and Urinary Tract Infections May Precede MS Diagnosis
Monday, December 4, 2023
- New Study Maps Ketamine's Effects on Brain
Wednesday, November 29, 2023
- AI May Aid in Diagnosing Adolescents With ADHD
- Mindfulness-Based Intervention Shows Promise for PTSD in Cardiac Arrest Survivors
Tuesday, November 28, 2023
- Understanding Subjective Beliefs Could Be Vital to Tailoring More Effective Treatments for Depression and ADHD
Monday, November 27, 2023
- Discrimination During Pregnancy Can Affect Infant's Brain Circuitry
Thursday, November 16, 2023
- A Small Molecule Blocks Aversive Memory Formation, Providing a Potential Treatment Target for Depression
- High Levels of Maternal Stress During Pregnancy Linked to Children's Behavior Problems
- New Studies of Brain Activity Explain Benefits of Electroconvulsive Therapy
Tuesday, November 14, 2023
- US Men Die 6 Years Before Women, as Life Expectancy Gap Widens
- Genetic Testing Could Greatly Benefit Patients With Depression, Save Health System Millions
- Reducing 'vivid Imagery' That Fuels Addiction Cravings
Monday, November 13, 2023
- Early-Life Stress Changes More Genes in Brain Than a Head Injury
Thursday, November 9, 2023
- Brain Imaging Identifies Biomarkers of Mental Illness
- Study Shows Link Between Mental and Physical Health
Monday, November 6, 2023
- Location of Strong Sense of Discomfort in Brain Found
Friday, November 3, 2023
- Paid Family Leave Boosted Postpartum Wellbeing, Breastfeeding Rates
Thursday, November 2, 2023
- New Clues to the Mechanism Behind Treatment-Resistant Depression
Wednesday, November 1, 2023
- Contraceptive Pill Users Less Likely to Report Depression
Monday, October 30, 2023
- The Genetic Heritage of the Denisovans May Have Left Its Mark on Our Mental Health
Thursday, October 26, 2023
- Youngest Children in Class With ADHD as Likely to Keep Diagnosis in Adulthood as Older Pupils, Find Scientists
Wednesday, October 25, 2023
- New Distractibility 'd Factor' May Be Linked With ADHD
Monday, October 23, 2023
- Researchers Use Pioneering New Method to Unlock Brain's Noradrenaline System
- Heated Yoga May Reduce Depression Symptoms, According to Recent Clinical Trial
Friday, October 20, 2023
- Pupil Response May Shed Light on Who Responds Best to Transcranial Magnetic Stimulation for Depression
- Consistent Lack of Sleep Is Related to Future Depressive Symptoms
Thursday, October 19, 2023
- Researchers Confirm Postpartum Depression Heritability, Home in on Treatment Mechanism
- Ketamine's Effect on Depression May Hinge on Hope
- Study Finds Men's Antidepressant Use Did Not Negatively Impact IVF Success
Tuesday, October 17, 2023
- Adults With ADHD Are at Increased Risk for Developing Dementia
- Study Reveals Health Impact of Eating Disorders
- Depression, Anxiety Common Among College Students
Thursday, October 5, 2023
- Psychedelics Improve Mental Health, Cognition in Special Ops Veterans
Wednesday, October 4, 2023
- Strong Link Between ADHD and Car Crashes in Older Adult Drivers
- Should Fathers Be Screened for Postpartum Depression? Pilot Study
Monday, October 2, 2023
- Study Indicates Possible Link Between Chronic Stress and Alzheimer's Disease
Friday, September 29, 2023
- Increased Risk of Depression and Anxiety When in Higher Education, Study Finds
Thursday, September 28, 2023
- Grandparent Childcare May Not Help the Wellbeing of Mums or Reduce Mother-Child Conflict, Study Suggests
Monday, September 25, 2023
- Depression, Anxiety May Be Among Early Signs of MS
Friday, September 22, 2023
- Study Shows Millions of People Live With Co-Occuring Chronic Pain and Mental Health Symptoms
Thursday, September 21, 2023
- Posttraumatic Brain Activity Predicts Resilience to PTSD
Monday, September 18, 2023
- Study Shows Nearly 300% Increase in ADHD Medication Errors
Wednesday, September 13, 2023
- Inflammatory Signs for Adolescent Depression Differ Between Boys and Girls
Tuesday, September 12, 2023
- Older Adults With Digestive Diseases Experience Higher Rates of Loneliness, Depression
- Your Body's Own Cannabinoid Molecules Calm You During Stress
Monday, September 11, 2023
- Healthy Lifestyle Can Help Prevent Depression -- And New Research May Explain Why
- Antidepressants May Reduce Negative Memories While Improving Overall Memory
Friday, September 8, 2023
- Sleep-Wake Therapy Gives New Hope for Teens With Depression
Thursday, September 7, 2023
- Antidepressant Use in People With Both Physical Health Problems and Depression
Tuesday, September 5, 2023
- Active Children Are More Resilient
Wednesday, August 30, 2023
- Stress and Insomnia Linked to Irregular Heart Rhythms After Menopause
Tuesday, August 29, 2023
- Your Genes Influence Whether Depression Leads to Other Diseases
- More Sleep Could Reduce Impulsive Behavior in Children
Monday, August 21, 2023
- Formerly Depressed Patients Continue to Focus on Negative
Monday, August 14, 2023
- New Maps Reveal the Individual Brain Changes Linked to Different Mental Illness
Wednesday, August 9, 2023
- Brain Cells of Males and Females Respond Differently to Chronic Stress
Tuesday, August 8, 2023
- Mothers Experiencing Depression Can Still Thrive as Parents
- LATEST NEWS
- Health & Medicine
- Diseases & Conditions
- Alzheimer's Research
- Amyotrophic Lateral Sclerosis
- Attention Deficit Disorder
- Back and Neck Pain
- Birth Defects
- Bladder Disorders
- Blood Clots
- COVID and SARS
- Cervical Cancer
- Bladder Cancer
- Multiple Myeloma
- Pancreatic Cancer
- Brain Tumor
- Colon Cancer
- Breast Cancer
- Ovarian Cancer
- Lung Cancer
- Mesothelioma
- Skin Cancer
- Prostate Cancer
- Cerebral Palsy
- Chikungunya
- Chronic Fatigue Syndrome
- Cold and Flu
- Crohn's Disease
- Cystic Fibrosis
- Dengue Fever
- Down Syndrome
- Eating Disorder Research
- Encephalitis
- Epilepsy Research
- Erectile Dysfunction
- Fibromyalgia
- Gastrointestinal Problems
- HIV and AIDS
- Headache Research
- Hearing Loss
- Heart Health
- Cholesterol
- Stroke Prevention
- Heart Disease
- Hormone Disorders
- Hypertension
- Infectious Diseases
- Insomnia Research
- Irritable Bowel Syndrome
- Kidney Disease
- Liver Disease
- Lung Disease
- Lyme Disease
- Mental Health Research
- Multiple Sclerosis Research
- Mumps, Measles, Rubella
- Muscular Dystrophy
- Osteoporosis
- Parkinson's Research
- Prostate Health
- Restless Leg Syndrome
- Sickle Cell Anemia
- Sleep Disorder Research
- Thyroid Disease
- Triglycerides
- Tuberculosis
- Medical Topics
- Accident and Trauma
- Alternative Medicine
- Birth Control
- Bone and Spine
- Chronic Illness
- Controlled Substances
- Dietary Supplements and Minerals
- Epigenetics
- Food Additives
- Foodborne Illness
- Foot Health
- Gene Therapy
- Health Policy
- Human Biology
- Immune System
- Joint Health
- Medical Imaging
- Nervous System
- Pain Control
- Personalized Medicine
- Pharmacology
- Psychology Research
- Wounds and Healing
- PHYSICAL/TECH
- ENVIRONMENT
- SOCIETY & EDUCATION
- 3D Mouth of an Ancient Jawless Fish
- Connecting Lab-Grown Brain Cells
- Device: Self-Healing Materials, Drug Delivery
- How We Perceive Bitter Taste
- Next-Generation Digital Displays
- Feeling Insulted? How to Rid Yourself of Anger
- Pregnancy Accelerates Biological Aging
- Tiny Plastic Particles Are Found Everywhere
- What's Quieter Than a Fish? A School of Them
- Do Odd Bones Belong to Gigantic Ichthyosaurs?
Trending Topics
Strange & offbeat.
- Open access
- Published: 12 December 2023
Examining the role of community resilience and social capital on mental health in public health emergency and disaster response: a scoping review
- C. E. Hall 1 , 2 ,
- H. Wehling 1 ,
- J. Stansfield 3 ,
- J. South 3 ,
- S. K. Brooks 2 ,
- N. Greenberg 2 , 4 ,
- R. Amlôt 1 &
- D. Weston 1
BMC Public Health volume 23 , Article number: 2482 ( 2023 ) Cite this article
1849 Accesses
21 Altmetric
Metrics details
The ability of the public to remain psychologically resilient in the face of public health emergencies and disasters (such as the COVID-19 pandemic) is a key factor in the effectiveness of a national response to such events. Community resilience and social capital are often perceived as beneficial and ensuring that a community is socially and psychologically resilient may aid emergency response and recovery. This review presents a synthesis of literature which answers the following research questions: How are community resilience and social capital quantified in research?; What is the impact of community resilience on mental wellbeing?; What is the impact of infectious disease outbreaks, disasters and emergencies on community resilience and social capital?; and, What types of interventions enhance community resilience and social capital?
A scoping review procedure was followed. Searches were run across Medline, PsycInfo, and EMBASE, with search terms covering both community resilience and social capital, public health emergencies, and mental health. 26 papers met the inclusion criteria.
The majority of retained papers originated in the USA, used a survey methodology to collect data, and involved a natural disaster. There was no common method for measuring community resilience or social capital. The association between community resilience and social capital with mental health was regarded as positive in most cases. However, we found that community resilience, and social capital, were initially negatively impacted by public health emergencies and enhanced by social group activities.
Several key recommendations are proposed based on the outcomes from the review, which include: the need for a standardised and validated approach to measuring both community resilience and social capital; that there should be enhanced effort to improve preparedness to public health emergencies in communities by gauging current levels of community resilience and social capital; that community resilience and social capital should be bolstered if areas are at risk of disasters or public health emergencies; the need to ensure that suitable short-term support is provided to communities with high resilience in the immediate aftermath of a public health emergency or disaster; the importance of conducting robust evaluation of community resilience initiatives deployed during the COVID-19 pandemic.
Peer Review reports
For the general population, public health emergencies and disasters (e.g., natural disasters; infectious disease outbreaks; Chemical, Biological, Radiological or Nuclear incidents) can give rise to a plethora of negative outcomes relating to both health (e.g. increased mental health problems [ 1 , 2 , 3 , 4 ]) and the economy (e.g., increased unemployment and decreased levels of tourism [ 4 , 5 , 6 ]). COVID-19 is a current, and ongoing, example of a public health emergency which has affected over 421 million individuals worldwide [ 7 ]. The long term implications of COVID-19 are not yet known, but there are likely to be repercussions for physical health, mental health, and other non-health related outcomes for a substantial time to come [ 8 , 9 ]. As a result, it is critical to establish methods which may inform approaches to alleviate the longer-term negative consequences that are likely to emerge in the aftermath of both COVID-19 and any future public health emergency.
The definition of resilience often differs within the literature, but ultimately resilience is considered a dynamic process of adaptation. It is related to processes and capabilities at the individual, community and system level that result in good health and social outcomes, in spite of negative events, serious threats and hazards [ 10 ]. Furthermore, Ziglio [ 10 ] refers to four key types of resilience capacity: adaptive, the ability to withstand and adjust to unfavourable conditions and shocks; absorptive, the ability to withstand but also to recover and manage using available assets and skills; anticipatory, the ability to predict and minimize vulnerability; and transformative, transformative change so that systems better cope with new conditions.
There is no one settled definition of community resilience (CR). However, it generally relates to the ability of a community to withstand, adapt and permit growth in adverse circumstances due to social structures, networks and interdependencies within the community [ 11 ]. Social capital (SC) is considered a major determinant of CR [ 12 , 13 ], and reflects strength of a social network, community reciprocity, and trust in people and institutions [ 14 ]. These aspects of community are usually conceptualised primarily as protective factors that enable communities to cope and adapt collectively to threats. SC is often broken down into further categories [ 15 ], for example: cognitive SC (i.e. perceptions of community relations, such as trust, mutual help and attachment) and structural SC (i.e. what actually happens within the community, such as participation, socialising) [ 16 ]; or, bonding SC (i.e. connections among individuals who are emotionally close, and result in bonds to a particular group [ 17 ]) and bridging SC (i.e. acquaintances or individuals loosely connected that span different social groups [ 18 ]). Generally, CR is perceived to be primarily beneficial for multiple reasons (e.g. increased social support [ 18 , 19 ], protection of mental health [ 20 , 21 ]), and strengthening community resilience is a stated health goal of the World Health Organisation [ 22 ] when aiming to alleviate health inequalities and protect wellbeing. This is also reflected by organisations such as Public Health England (now split into the UK Health Security Agency and the Office for Health Improvement and Disparities) [ 23 ] and more recently, CR has been targeted through the endorsement of Community Champions (who are volunteers trained to support and to help improve health and wellbeing. Community Champions also reflect their local communities in terms of population demographics for example age, ethnicity and gender) as part of the COVID-19 response in the UK (e.g. [ 24 , 25 ]).
Despite the vested interest in bolstering communities, the research base establishing: how to understand and measure CR and SC; the effect of CR and SC, both during and following a public health emergency (such as the COVID-19 pandemic); and which types of CR or SC are the most effective to engage, is relatively small. Given the importance of ensuring resilience against, and swift recovery from, public health emergencies, it is critically important to establish and understand the evidence base for these approaches. As a result, the current review sought to answer the following research questions: (1) How are CR and SC quantified in research?; (2) What is the impact of community resilience on mental wellbeing?; (3) What is the impact of infectious disease outbreaks, disasters and emergencies on community resilience and social capital?; and, (4) What types of interventions enhance community resilience and social capital?
By collating research in order to answer these research questions, the authors have been able to propose several key recommendations that could be used to both enhance and evaluate CR and SC effectively to facilitate the long-term recovery from COVID-19, and also to inform the use of CR and SC in any future public health disasters and emergencies.
A scoping review methodology was followed due to the ease of summarising literature on a given topic for policy makers and practitioners [ 26 ], and is detailed in the following sections.
Identification of relevant studies
An initial search strategy was developed by authors CH and DW and included terms which related to: CR and SC, given the absence of a consistent definition of CR, and the link between CR and SC, the review focuses on both CR and SC to identify as much relevant literature as possible (adapted for purpose from Annex 1: [ 27 ], as well as through consultation with review commissioners); public health emergencies and disasters [ 28 , 29 , 30 , 31 ], and psychological wellbeing and recovery (derived a priori from literature). To ensure a focus on both public health and psychological research, the final search was carried across Medline, PsycInfo, and EMBASE using OVID. The final search took place on the 18th of May 2020, the search strategy used for all three databases can be found in Supplementary file 1 .
Selection criteria
The inclusion and exclusion criteria were developed alongside the search strategy. Initially the criteria were relatively inclusive and were subject to iterative development to reflect the authors’ familiarisation with the literature. For example, the decision was taken to exclude research which focused exclusively on social support and did not mention communities as an initial title/abstract search suggested that the majority of this literature did not meet the requirements of our research question.
The full and final inclusion and exclusion criteria used can be found in Supplementary file 2 . In summary, authors decided to focus on the general population (i.e., non-specialist, e.g. non-healthcare worker or government official) to allow the review to remain community focused. The research must also have assessed the impact of CR and/or SC on mental health and wellbeing, resilience, and recovery during and following public health emergencies and infectious disease outbreaks which affect communities (to ensure the research is relevant to the review aims), have conducted primary research, and have a full text available or provided by the first author when contacted.
Charting the data
All papers were first title and abstract screened by CH or DW. Papers then were full text reviewed by CH to ensure each paper met the required eligibility criteria, if unsure about a paper it was also full text reviewed by DW. All papers that were retained post full-text review were subjected to a standardised data extraction procedure. A table was made for the purpose of extracting the following data: title, authors, origin, year of publication, study design, aim, disaster type, sample size and characteristics, variables examined, results, restrictions/limitations, and recommendations. Supplementary file 3 details the charting the data process.
Analytical method
Data was synthesised using a Framework approach [ 32 ], a common method for analysing qualitative research. This method was chosen as it was originally used for large-scale social policy research [ 33 ] as it seeks to identify: what works, for whom, in what conditions, and why [ 34 ]. This approach is also useful for identifying commonalities and differences in qualitative data and potential relationships between different parts of the data [ 33 ]. An a priori framework was established by CH and DW. Extracted data was synthesised in relation to each research question, and the process was iterative to ensure maximum saturation using the available data.
Study selection
The final search strategy yielded 3584 records. Following the removal of duplicates, 2191 records remained and were included in title and abstract screening. A PRISMA flow diagram is presented in Fig. 1 .
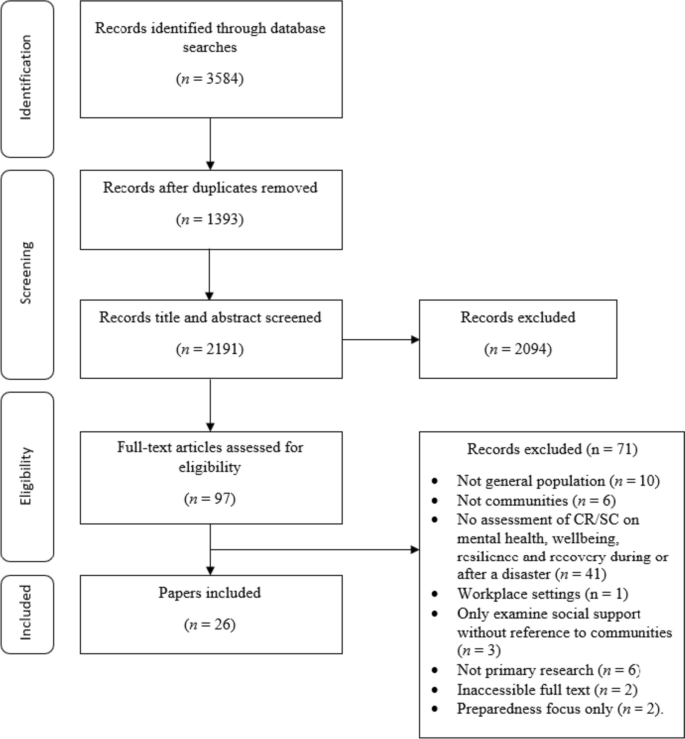
PRISMA flow diagram
At the title and abstract screening stage, the process became more iterative as the inclusion criteria were developed and refined. For the first iteration of screening, CH or DW sorted all records into ‘include,’ ‘exclude,’ and ‘unsure’. All ‘unsure’ papers were re-assessed by CH, and a random selection of ~ 20% of these were also assessed by DW. Where there was disagreement between authors the records were retained, and full text screened. The remaining papers were reviewed by CH, and all records were categorised into ‘include’ and ‘exclude’. Following full-text screening, 26 papers were retained for use in the review.
Study characteristics
This section of the review addresses study characteristics of those which met the inclusion criteria, which comprises: date of publication, country of origin, study design, study location, disaster, and variables examined.
Date of publication
Publication dates across the 26 papers spanned from 2008 to 2020 (see Fig. 2 ). The number of papers published was relatively low and consistent across this timescale (i.e. 1–2 per year, except 2010 and 2013 when none were published) up until 2017 where the number of papers peaked at 5. From 2017 to 2020 there were 15 papers published in total. The amount of papers published in recent years suggests a shift in research and interest towards CR and SC in a disaster/ public health emergency context.
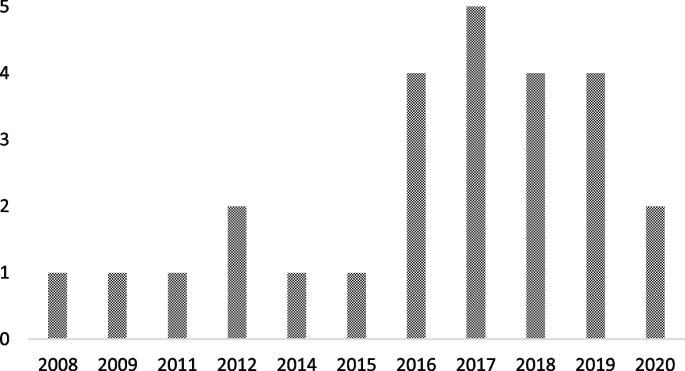
Graph to show retained papers date of publication
Country of origin
The locations of the first authors’ institutes at the time of publication were extracted to provide a geographical spread of the retained papers. The majority originated from the USA [ 35 , 36 , 37 , 38 , 39 , 40 , 41 ], followed by China [ 42 , 43 , 44 , 45 , 46 ], Japan [ 47 , 48 , 49 , 50 ], Australia [ 51 , 52 , 53 ], The Netherlands [ 54 , 55 ], New Zealand [ 56 ], Peru [ 57 ], Iran [ 58 ], Austria [ 59 ], and Croatia [ 60 ].
There were multiple methodological approaches carried out across retained papers. The most common formats included surveys or questionnaires [ 36 , 37 , 38 , 42 , 46 , 47 , 48 , 49 , 50 , 53 , 54 , 55 , 57 , 59 ], followed by interviews [ 39 , 40 , 43 , 51 , 52 , 60 ]. Four papers used both surveys and interviews [ 35 , 41 , 45 , 58 ], and two papers conducted data analysis (one using open access data from a Social Survey [ 44 ] and one using a Primary Health Organisations Register [ 56 ]).
Study location
The majority of the studies were carried out in Japan [ 36 , 42 , 44 , 47 , 48 , 49 , 50 ], followed by the USA [ 35 , 37 , 38 , 39 , 40 , 41 ], China [ 43 , 45 , 46 , 53 ], Australia [ 51 , 52 ], and the UK [ 54 , 55 ]. The remaining studies were carried out in Croatia [ 60 ], Peru [ 57 ], Austria [ 59 ], New Zealand [ 56 ] and Iran [ 58 ].
Multiple different types of disaster were researched across the retained papers. Earthquakes were the most common type of disaster examined [ 45 , 47 , 49 , 50 , 53 , 56 , 57 , 58 ], followed by research which assessed the impact of two disastrous events which had happened in the same area (e.g. Hurricane Katrina and the Deepwater Horizon oil spill in Mississippi, and the Great East Japan earthquake and Tsunami; [ 36 , 37 , 38 , 42 , 44 , 48 ]). Other disaster types included: flooding [ 51 , 54 , 55 , 59 , 60 ], hurricanes [ 35 , 39 , 41 ], infectious disease outbreaks [ 43 , 46 ], oil spillage [ 40 ], and drought [ 52 ].
Variables of interest examined
Across the 26 retained papers: eight referred to examining the impact of SC [ 35 , 37 , 39 , 41 , 46 , 49 , 55 , 60 ]; eight examined the impact of cognitive and structural SC as separate entities [ 40 , 42 , 45 , 48 , 50 , 54 , 57 , 59 ]; one examined bridging and bonding SC as separate entities [ 58 ]; two examined the impact of CR [ 38 , 56 ]; and two employed a qualitative methodology but drew findings in relation to bonding and bridging SC, and SC generally [ 51 , 52 ]. Additionally, five papers examined the impact of the following variables: ‘community social cohesion’ [ 36 ], ‘neighbourhood connectedness’ [ 44 ], ‘social support at the community level’ [ 47 ], ‘community connectedness’ [ 43 ] and ‘sense of community’ [ 53 ]. Table 1 provides additional details on this.
How is CR and SC measured or quantified in research?
The measures used to examine CR and SC are presented Table 1 . It is apparent that there is no uniformity in how SC or CR is measured across the research. Multiple measures are used throughout the retained studies, and nearly all are unique. Additionally, SC was examined at multiple different levels (e.g. cognitive and structural, bonding and bridging), and in multiple different forms (e.g. community connectedness, community cohesion).
What is the association between CR and SC on mental wellbeing?
To best compare research, the following section reports on CR, and facets of SC separately. Please see Supplementary file 4 for additional information on retained papers methods of measuring mental wellbeing.
- Community resilience
CR relates to the ability of a community to withstand, adapt and permit growth in adverse circumstances due to social structures, networks and interdependencies within the community [ 11 ].
The impact of CR on mental wellbeing was consistently positive. For example, research indicated that there was a positive association between CR and number of common mental health (i.e. anxiety and mood) treatments post-disaster [ 56 ]. Similarly, other research suggests that CR is positively related to psychological resilience, which is inversely related to depressive symptoms) [ 37 ]. The same research also concluded that CR is protective of psychological resilience and is therefore protective of depressive symptoms [ 37 ].
- Social capital
SC reflects the strength of a social network, community reciprocity, and trust in people and institutions [ 14 ]. These aspects of community are usually conceptualised primarily as protective factors that enable communities to cope and adapt collectively to threats.
There were inconsistencies across research which examined the impact of abstract SC (i.e. not refined into bonding/bridging or structural/cognitive) on mental wellbeing. However, for the majority of cases, research deems SC to be beneficial. For example, research has concluded that, SC is protective against post-traumatic stress disorder [ 55 ], anxiety [ 46 ], psychological distress [ 50 ], and stress [ 46 ]. Additionally, SC has been found to facilitate post-traumatic growth [ 38 ], and also to be useful to be drawn upon in times of stress [ 52 ], both of which could be protective of mental health. Similarly, research has also found that emotional recovery following a disaster is more difficult for those who report to have low levels of SC [ 51 ].
Conversely, however, research has also concluded that when other situational factors (e.g. personal resources) were controlled for, a positive relationship between community resources and life satisfaction was no longer significant [ 60 ]. Furthermore, some research has concluded that a high level of SC can result in a community facing greater stress immediately post disaster. Indeed, one retained paper found that high levels of SC correlate with higher levels of post-traumatic stress immediately following a disaster [ 39 ]. However, in the later stages following a disaster, this relationship can reverse, with SC subsequently providing an aid to recovery [ 41 ]. By way of explanation, some researchers have suggested that communities with stronger SC carry the greatest load in terms of helping others (i.e. family, friends and neighbours) as well as themselves immediately following the disaster, but then as time passes the communities recover at a faster rate as they are able to rely on their social networks for support [ 41 ].
Cognitive and structural social capital
Cognitive SC refers to perceptions of community relations, such as trust, mutual help and attachment, and structural SC refers to what actually happens within the community, such as participation, socialising [ 16 ].
Cognitive SC has been found to be protective [ 49 ] against PTSD [ 54 , 57 ], depression [ 40 , 54 ]) mild mood disorder; [ 48 ]), anxiety [ 48 , 54 ] and increase self-efficacy [ 59 ].
For structural SC, research is again inconsistent. On the one hand, structural SC has been found to: increase perceived self-efficacy, be protective of depression [ 40 ], buffer the impact of housing damage on cognitive decline [ 42 ] and provide support during disasters and over the recovery period [ 59 ]. However, on the other hand, it has been found to have no association with PTSD [ 54 , 57 ] or depression, and is also associated with a higher prevalence of anxiety [ 54 ]. Similarly, it is also suggested by additional research that structural SC can harm women’s mental health, either due to the pressure of expectations to help and support others or feelings of isolation [ 49 ].
Bonding and bridging social capital
Bonding SC refers to connections among individuals who are emotionally close, and result in bonds to a particular group [ 17 ], and bridging SC refers to acquaintances or individuals loosely connected that span different social groups [ 18 ].
One research study concluded that both bonding and bridging SC were protective against post-traumatic stress disorder symptoms [ 58 ]. Bridging capital was deemed to be around twice as effective in buffering against post-traumatic stress disorder than bonding SC [ 58 ].
Other community variables
Community social cohesion was significantly associated with a lower risk of post-traumatic stress disorder symptom development [ 35 ], and this was apparent even whilst controlling for depressive symptoms at baseline and disaster impact variables (e.g. loss of family member or housing damage) [ 36 ]. Similarly, sense of community, community connectedness, social support at the community level and neighbourhood connectedness all provided protective benefits for a range of mental health, wellbeing and recovery variables, including: depression [ 53 ], subjective wellbeing (in older adults only) [ 43 ], psychological distress [ 47 ], happiness [ 44 ] and life satisfaction [ 53 ].
Research has also concluded that community level social support is protective against mild mood and anxiety disorder, but only for individuals who have had no previous disaster experience [ 48 ]. Additionally, a study which separated SC into social cohesion and social participation concluded that at a community level, social cohesion is protective against depression [ 49 ] whereas social participation at community level is associated with an increased risk of depression amongst women [ 49 ].
What is the impact of Infectious disease outbreaks / disasters and emergencies on community resilience?
From a cross-sectional perspective, research has indicated that disasters and emergencies can have a negative effect on certain types of SC. Specifically, cognitive SC has been found to be impacted by disaster impact, whereas structural SC has gone unaffected [ 45 ]. Disaster impact has also been shown to have a negative effect on community relationships more generally [ 52 ].
Additionally, of the eight studies which collected data at multiple time points [ 35 , 36 , 41 , 42 , 47 , 49 , 56 , 60 ], three reported the effect of a disaster on the level of SC within a community [ 40 , 42 , 49 ]. All three of these studies concluded that disasters may have a negative impact on the levels of SC within a community. The first study found that the Deepwater Horizon oil spill had a negative effect on SC and social support, and this in turn explained an overall increase in the levels of depression within the community [ 40 ]. A possible explanation for the negative effect lays in ‘corrosive communities’, known for increased social conflict and reduced social support, that are sometimes created following oil spills [ 40 ]. It is proposed that corrosive communities often emerge due to a loss of natural resources that bring social groups together (e.g., for recreational activities), as well as social disparity (e.g., due to unequal distribution of economic impact) becoming apparent in the community following disaster [ 40 ]. The second study found that SC (in the form of social cohesion, informal socialising and social participation) decreased after the 2011 earthquake and tsunami in Japan; it was suggested that this change correlated with incidence of cognitive decline [ 42 ]. However, the third study reported more mixed effects based on physical circumstances of the communities’ natural environment: Following an earthquake, those who lived in mountainous areas with an initial high level of pre-community SC saw a decrease in SC post disaster [ 49 ]. However, communities in flat areas (which were home to younger residents and had a higher population density) saw an increase in SC [ 49 ]. It was proposed that this difference could be due to the need for those who lived in mountainous areas to seek prolonged refuge due to subsequent landslides [ 49 ].
What types of intervention enhance CR and SC and protect survivors?
There were mixed effects across the 26 retained papers when examining the effect of CR and SC on mental wellbeing. However, there is evidence that an increase in SC [ 56 , 57 ], with a focus on cognitive SC [ 57 ], namely by: building social networks [ 45 , 51 , 53 ], enhancing feelings of social cohesion [ 35 , 36 ] and promoting a sense of community [ 53 ], can result in an increase in CR and potentially protect survivors’ wellbeing and mental health following a disaster. An increase in SC may also aid in decreasing the need for individual psychological interventions in the aftermath of a disaster [ 55 ]. As a result, recommendations and suggested methods to bolster CR and SC from the retained papers have been extracted and separated into general methods, preparedness and policy level implementation.
General methods
Suggested methods to build SC included organising recreational activity-based groups [ 44 ] to broaden [ 51 , 53 ] and preserve current social networks [ 42 ], introducing initiatives to increase social cohesion and trust [ 51 ], and volunteering to increase the number of social ties between residents [ 59 ]. Research also notes that it is important to take a ‘no one left behind approach’ when organising recreational and social community events, as failure to do so could induce feelings of isolation for some members of the community [ 49 ]. Furthermore, gender differences should also be considered as research indicates that males and females may react differently to community level SC (as evidence suggests males are instead more impacted by individual level SC; in comparison to women who have larger and more diverse social networks [ 49 ]). Therefore, interventions which aim to raise community level social participation, with the aim of expanding social connections and gaining support, may be beneficial [ 42 , 47 ].
Preparedness
In order to prepare for disasters, it may be beneficial to introduce community-targeted methods or interventions to increase levels of SC and CR as these may aid in ameliorating the consequences of a public health emergency or disaster [ 57 ]. To indicate which communities have low levels of SC, one study suggests implementing a 3-item scale of social cohesion to map areas and target interventions [ 42 ].
It is important to consider that communities with a high level of SC may have a lower level of risk perception, due to the established connections and supportive network they have with those around them [ 61 ]. However, for the purpose of preparedness, this is not ideal as perception of risk is a key factor when seeking to encourage behavioural adherence. This could be overcome by introducing communication strategies which emphasise the necessity of social support, but also highlights the need for additional measures to reduce residual risk [ 59 ]. Furthermore, support in the form of financial assistance to foster current community initiatives may prove beneficial to rural areas, for example through the use of an asset-based community development framework [ 52 ].
Policy level
At a policy level, the included papers suggest a range of ways that CR and SC could be bolstered and used. These include: providing financial support for community initiatives and collective coping strategies, (e.g. using asset-based community development [ 52 ]); ensuring policies for long-term recovery focus on community sustainable development (e.g. community festival and community centre activities) [ 44 ]; and development of a network amongst cooperative corporations formed for reconstruction and to organise self-help recovery sessions among residents of adjacent areas [ 58 ].
This scoping review sought to synthesise literature concerning the role of SC and CR during public health emergencies and disasters. Specifically, in this review we have examined: the methods used to measure CR and SC; the impact of CR and SC on mental wellbeing during disasters and emergencies; the impact of disasters and emergencies on CR and SC; and the types of interventions which can be used to enhance CR. To do this, data was extracted from 26 peer-reviewed journal articles. From this synthesis, several key themes have been identified, which can be used to develop guidelines and recommendations for deploying CR and SC in a public health emergency or disaster context. These key themes and resulting recommendations are summarised below.
Firstly, this review established that there is no consistent or standardised approach to measuring CR or SC within the general population. This finding is consistent with a review conducted by the World Health Organization which concludes that despite there being a number of frameworks that contain indicators across different determinants of health, there is a lack of consensus on priority areas for measurement and no widely accepted indicator [ 27 ]. As a result, there are many measures of CR and SC apparent within the literature (e.g., [ 62 , 63 ]), an example of a developed and validated measure is provided by Sherrieb, Norris and Galea [ 64 ]. Similarly, the definitions of CR and SC differ widely between researchers, which created a barrier to comparing and summarising information. Therefore, future research could seek to compare various interpretations of CR and to identify any overlapping concepts. However, a previous systemic review conducted by Patel et al. (2017) concludes that there are nine core elements of CR (local knowledge, community networks and relationships, communication, health, governance and leadership, resources, economic investment, preparedness, and mental outlook), with 19 further sub-elements therein [ 30 ]. Therefore, as CR is a multi-dimensional construct, the implications from the findings are that multiple aspects of social infrastructure may need to be considered.
Secondly, our synthesis of research concerning the role of CR and SC for ensuring mental health and wellbeing during, or following, a public health emergency or disaster revealed mixed effects. Much of the research indicates either a generally protective effect on mental health and wellbeing, or no effect; however, the literature demonstrates some potential for a high level of CR/SC to backfire and result in a negative effect for populations during, or following, a public health emergency or disaster. Considered together, our synthesis indicates that cognitive SC is the only facet of SC which was perceived as universally protective across all retained papers. This is consistent with a systematic review which also concludes that: (a) community level cognitive SC is associated with a lower risk of common mental disorders, while; (b) community level structural SC had inconsistent effects [ 65 ].
Further examination of additional data extracted from studies which found that CR/SC had a negative effect on mental health and wellbeing revealed no commonalities that might explain these effects (Please see Supplementary file 5 for additional information)
One potential explanation may come from a retained paper which found that high levels of SC result in an increase in stress level immediately post disaster [ 41 ]. This was suggested to be due to individuals having greater burdens due to wishing to help and support their wide networks as well as themselves. However, as time passes the levels of SC allow the community to come together and recover at a faster rate [ 41 ]. As this was the only retained paper which produced this finding, it would be beneficial for future research to examine boundary conditions for the positive effects of CR/SC; that is, to explore circumstances under which CR/SC may be more likely to put communities at greater risk. This further research should also include additional longitudinal research to validate the conclusions drawn by [ 41 ] as resilience is a dynamic process of adaption.
Thirdly, disasters and emergencies were generally found to have a negative effect on levels of SC. One retained paper found a mixed effect of SC in relation to an earthquake, however this paper separated participants by area in which they lived (i.e., mountainous vs. flat), which explains this inconsistent effect [ 49 ]. Dangerous areas (i.e. mountainous) saw a decrease in community SC in comparison to safer areas following the earthquake (an effect the authors attributed to the need to seek prolonged refuge), whereas participants from the safer areas (which are home to younger residents with a higher population density) saw an increase in SC [ 49 ]. This is consistent with the idea that being able to participate socially is a key element of SC [ 12 ]. Overall, however, this was the only retained paper which produced a variable finding in relation to the effect of disaster on levels of CR/SC.
Finally, research identified through our synthesis promotes the idea of bolstering SC (particularly cognitive SC) and cohesion in communities likely to be affected by disaster to improve levels of CR. This finding provides further understanding of the relationship between CR and SC; an association that has been reported in various articles seeking to provide conceptual frameworks (e.g., [ 66 , 67 ]) as well as indicator/measurement frameworks [ 27 ]. Therefore, this could be done by creating and promoting initiatives which foster SC and create bonds within the community. Papers included in the current review suggest that recreational-based activity groups and volunteering are potential methods for fostering SC and creating community bonds [ 44 , 51 , 59 ]. Similarly, further research demonstrates that feelings of social cohesion are enhanced by general social activities (e.g. fairs and parades [ 18 ]). Also, actively encouraging activities, programs and interventions which enhance connectedness and SC have been reported to be desirable to increase CR [ 68 ]. This suggestion is supported by a recent scoping review of literature [ 67 ] examined community champion approaches for the COVID-19 pandemic response and recovery and established that creating and promoting SC focused initiatives within the community during pandemic response is highly beneficial [ 67 ]. In terms of preparedness, research states that it may be beneficial for levels of SC and CR in communities at risk to be assessed, to allow targeted interventions where the population may be at most risk following an incident [ 42 , 44 ]. Additionally, from a more critical perspective, we acknowledge that ‘resilience’ can often be perceived as a focus on individual capacity to adapt to adversity rather than changing or mitigating the causes of adverse conditions [ 69 , 70 ]. Therefore, CR requires an integrated system approach across individual, community and structural levels [ 17 ]. Also, it is important that community members are engaged in defining and agreeing how community resilience is measured [ 27 ] rather than it being imposed by system leads or decision-makers.
In the aftermath of the pandemic, is it expected that there will be long-term repercussions both from an economic [ 8 ] and a mental health perspective [ 71 ]. Furthermore, the findings from this review suggest that although those in areas with high levels of SC may be negatively affected in the acute stage, as time passes, they have potential to rebound at a faster rate than those with lower levels of SC. Ongoing evaluation of the effectiveness of current initiatives as the COVID-19 pandemic progresses into a recovery phase will be invaluable for supplementing the evidence base identified through this review.
- Recommendations
As a result of this review, a number of recommendations are suggested for policy and practice during public health emergencies and recovery.
Future research should seek to establish a standardised and validated approach to measuring and defining CR and SC within communities. There are ongoing efforts in this area, for example [ 72 ]. Additionally, community members should be involved in the process of defining how CR is measured.
There should be an enhanced effort to improve preparedness for public health emergencies and disasters in local communities by gauging current levels of SC and CR within communities using a standardised measure. This approach could support specific targeting of populations with low levels of CR/SC in case of a disaster or public health emergency, whilst also allowing for consideration of support for those with high levels of CR (as these populations can be heavily impacted initially following a disaster). By distinguishing levels of SC and CR, tailored community-centred approaches could be implemented, such as those listed in a guide released by PHE in 2015 [ 73 ].
CR and SC (specifically cognitive SC) should be bolstered if communities are at risk of experiencing a disaster or public health emergency. This can be achieved by using interventions which aim to increase a sense of community and create new social ties (e.g., recreational group activities, volunteering). Additionally, when aiming to achieve this, it is important to be mindful of the risk of increased levels of CR/SC to backfire, as well as seeking to advocate an integrated system approach across individual, community and structural levels.
It is necessary to be aware that although communities with high existing levels of resilience / SC may experience short-term negative consequences following a disaster, over time these communities might be able to recover at a faster rate. It is therefore important to ensure that suitable short-term support is provided to these communities in the immediate aftermath of a public health emergency or disaster.
Robust evaluation of the community resilience initiatives deployed during the COVID-19 pandemic response is essential to inform the evidence base concerning the effectiveness of CR/ SC. These evaluations should continue through the response phase and into the recovery phase to help develop our understanding of the long-term consequences of such interventions.
Limitations
Despite this review being the first in this specific topic area, there are limitations that must be considered. Firstly, it is necessary to note that communities are generally highly diverse and the term ‘community’ in academic literature is a subject of much debate (see: [ 74 ]), therefore this must be considered when comparing and collating research involving communities. Additionally, the measures of CR and SC differ substantially across research, including across the 26 retained papers used in the current review. This makes the act of comparing and collating research findings very difficult. This issue is highlighted as a key outcome from this review, and suggestions for how to overcome this in future research are provided. Additionally, we acknowledge that there will be a relationship between CR & SC even where studies measure only at individual or community level. A review [ 75 ] on articulating a hypothesis of the link to health inequalities suggests that wider structural determinants of health need to be accounted for. Secondly, despite the final search strategy encompassing terms for both CR and SC, only one retained paper directly measured CR; thus, making the research findings more relevant to SC. Future research could seek to focus on CR to allow for a comparison of findings. Thirdly, the review was conducted early in the COVID-19 pandemic and so does not include more recent publications focusing on resilience specifically in the context of COVID-19. Regardless of this fact, the synthesis of, and recommendations drawn from, the reviewed studies are agnostic to time and specific incident and contain critical elements necessary to address as the pandemic moves from response to recovery. Further research should review the effectiveness of specific interventions during the COVID-19 pandemic for collation in a subsequent update to this current paper. Fourthly, the current review synthesises findings from countries with individualistic and collectivistic cultures, which may account for some variation in the findings. Lastly, despite choosing a scoping review method for ease of synthesising a wide literature base for use by public health emergency researchers in a relatively tight timeframe, there are disadvantages of a scoping review approach to consider: (1) quality appraisal of retained studies was not carried out; (2) due to the broad nature of a scoping review, more refined and targeted reviews of literature (e.g., systematic reviews) may be able to provide more detailed research outcomes. Therefore, future research should seek to use alternative methods (e.g., empirical research, systematic reviews of literature) to add to the evidence base on CR and SC impact and use in public health practice.
This review sought to establish: (1) How CR and SC are quantified in research?; (2) The impact of community resilience on mental wellbeing?; (3) The impact of infectious disease outbreaks, disasters and emergencies on community resilience and social capital?; and, (4) What types of interventions enhance community resilience and social capital?. The chosen search strategy yielded 26 relevant papers from which we were able extract information relating to the aims of this review.
Results from the review revealed that CR and SC are not measured consistently across research. The impact of CR / SC on mental health and wellbeing during emergencies and disasters is mixed (with some potential for backlash), however the literature does identify cognitive SC as particularly protective. Although only a small number of papers compared CR or SC before and after a disaster, the findings were relatively consistent: SC or CR is negatively impacted by a disaster. Methods suggested to bolster SC in communities were centred around social activities, such as recreational group activities and volunteering. Recommendations for both research and practice (with a particular focus on the ongoing COVID-19 pandemic) are also presented.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Social Capital
Zortea TC, Brenna CT, Joyce M, McClelland H, Tippett M, Tran MM, et al. The impact of infectious disease-related public health emergencies on suicide, suicidal behavior, and suicidal thoughts. Crisis. 2020;42(6):474–87.
Article PubMed PubMed Central Google Scholar
Davis JR, Wilson S, Brock-Martin A, Glover S, Svendsen ER. The impact of disasters on populations with health and health care disparities. Disaster Med Pub Health Prep. 2010;4(1):30.
Article Google Scholar
Francescutti LH, Sauve M, Prasad AS. Natural disasters and healthcare: lessons to be learned. Healthc Manage Forum. 2017;30(1):53–5.
Article PubMed Google Scholar
Jones L, Palumbo D, Brown D. Coronavirus: How the pandemic has changed the world economy. BBC News; 2021. Accessible at: https://www.bbc.co.uk/news/business-51706225 .
Below R, Wallemacq P. Annual disaster statistical review 2017. Brussels: CRED, Centre for Research on the Epidemiology of Disasters; 2018.
Google Scholar
Qiu W, Chu C, Mao A, Wu J. The impacts on health, society, and economy of SARS and H7N9 outbreaks in China: a case comparison study. J Environ Public Health. 2018;2018:2710185.
Worldometer. COVID-19 coronavirus pandemic. 2021.
Harari D, Keep M. Coronavirus: economic impact house of commons library. Briefing Paper (Number 8866); 2021. Accessible at: https://commonslibrary.parliament.uk/research-briefings/cbp-8866/ .
Nabavi N. Covid-19: pandemic will cast a long shadow on mental health, warns England’s CMO. BMJ. 2021;373:n1655.
Ziglio E. Strengthening resilience: a priority shared by health 2020 and the sustainable development goals. No. WHO/EURO: 2017-6509-46275-66939. World Health Organization; Regional Office for Europe; 2017.
Asadzadeh A, Kotter T, Salehi P, Birkmann J. Operationalizing a concept: the systematic review of composite indicator building for measuring community disaster resilience. Int J Disaster Risk Reduct. 2017;25:147.
Sherrieb K, Norris F, Galea S. Measuring capacities for community resilience. Soc Indicators Res. 2010;99(2):227.
Poortinga W. Community resilience and health: the role of bonding, bridging, and linking aspects of social capital. Health Place. 2011;18(2):286–95.
Ferlander S. The importance of different forms of social capital for health. Acta Sociol. 2007;50(2):115–28.
Nakagawa Y, Shaw R. Social capital: a missing link to disaster recovery. Int J Mass Emerge Disasters. 2004;22(1):5–34.
Grootaert C, Narayan D, Jones VN, Woolcock M. Measuring social capital: an integrated questionnaire. Washington, DC: World Bank Working Paper, No. 18; 2004.
Adler PS, Kwon SW. Social capital: prospects for a new concept. Acad Manage Rev. 2002;27(1):17–40.
Aldrich DP, Meyer MA. Social capital and community resilience. Am Behav Sci. 2015;59(2):254–69.
Rodriguez-Llanes JM, Vos F, Guha-Sapir D. Measuring psychological resilience to disasters: are evidence-based indicators an achievable goal? Environ Health. 2013;12(1):115.
De Silva MJ, McKenzie K, Harpham T, Huttly SR. Social capital and mental Illness: a systematic review. J Epidemiol Community Health. 2005;59(8):619–27.
Bonanno GA, Galea S, Bucciarelli A, Vlahov D. Psychological resilience after disaster: New York City in the aftermath of the september 11th terrorist attack. Psychol Sci. 2006;17(3):181.
World Health Organization. Health 2020: a European policy framework and strategy for the 21st century. World Health Organization. Regional Office for Europe; 2013.
Public Health England. Community-Centred Public Health: Taking a Whole System Approach. 2020.
SPI-B. The role of Community Champion networks to increase engagement in the context of COVID19: Evidence and best practice. 2021.
Public Health England. Community champions: A rapid scoping review of community champion approaches for the pandemic response and recovery. 2021.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
World Health Organisation. WHO health evidence network synthesis report: what quantitative and qualitative methods have been developed to measure health-related community resilience at a national and local level. 2018.
Hall C, Williams N, Gauntlett L, Carter H, Amlôt R, Peterson L et al. Findings from systematic review of public perceptions and responses. PROACTIVE EU. Deliverable 1.1. 2019. Accessible at: https://proactive-h2020.eu/wp-content/uploads/2021/04/PROACTIVE_20210312_D1.1_V5_PHE_Systematic-Review-of-Public-Perceptions-and-Responses_revised.pdf .
Weston D, Ip A, Amlôt R. Examining the application of behaviour change theories in the context of Infectious disease outbreaks and emergency response: a review of reviews. BMC Public Health. 2020;20(1):1483.
Article PubMed PubMed Central CAS Google Scholar
Patel SS, Rogers MB, Amlôt R, Rubin GJ. What do we mean by ‘community resilience’? A systematic literature review of how it is defined in the literature. PLoS Curr. 2017;9:ecurrents.dis.db775aff25efc5ac4f0660ad9c9f7db2.
PubMed PubMed Central Google Scholar
Brooks SK, Weston D, Wessely S, Greenberg N. Effectiveness and acceptability of brief psychoeducational interventions after potentially traumatic events: a systematic review. Eur J Psychotraumatology. 2021;12(1):1923110.
Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review-a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy. 2005;10(1_suppl):21–34.
Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13:1–8.
Bearman M, Dawson P. Qualitative synthesis and systematic review in health professions education. Med Educ. 2013;47(3):252–60.
Heid AR, Pruchno R, Cartwright FP, Wilson-Genderson M. Exposure to Hurricane Sandy, neighborhood collective efficacy, and post-traumatic stress symptoms in older adults. Aging Ment Health. 2017;21(7):742–50.
Hikichi H, Aida J, Tsuboya T, Kondo K, Kawachi I. Can community social cohesion prevent posttraumatic stress disorder in the aftermath of a disaster? A natural experiment from the 2011 Tohoku Earthquake and tsunami. Am J Epidemiol. 2016;183(10):902–10.
Lee J, Blackmon BJ, Cochran DM, Kar B, Rehner TA, Gunnell MS. Community resilience, psychological resilience, and depressive symptoms: an examination of the Mississippi Gulf Coast 10 years after Hurricane Katrina and 5 years after the Deepwater Horizon oil spill. Disaster med. 2018;12(2):241–8.
Lee J, Blackmon BJ, Lee JY, Cochran DM Jr, Rehner TA. An exploration of posttraumatic growth, loneliness, depression, resilience, and social capital among survivors of Hurricane Katrina and the deepwater Horizon oil spill. J Community Psychol. 2019;47(2):356–70.
Lowe SR, Sampson L, Gruebner O, Galea S. Psychological resilience after Hurricane Sandy: the influence of individual- and community-level factors on mental health after a large-scale natural disaster. PLoS One. 2015;10(5):e0125761.
Rung AL, Gaston S, Robinson WT, Trapido EJ, Peters ES. Untangling the disaster-depression knot: the role of social ties after deepwater Horizon. Soc Sci Med. 2017;177:19–26.
Weil F, Lee MR, Shihadeh ES. The burdens of social capital: how socially-involved people dealt with stress after Hurricane Katrina. Soc Sci Res. 2012;41(1):110–9.
Hikichi H, Aida J, Matsuyama Y, Tsuboya T, Kondo K, Kawachi I. Community-level social capital and cognitive decline after a Natural Disaster: a natural experiment from the 2011 Great East Japan Earthquake and Tsunami. Soc Sci Med. 2018;257:111981.
Lau AL, Chi I, Cummins RA, Lee TM, Chou KL, Chung LW. The SARS (severe acute respiratory syndrome) pandemic in Hong Kong: effects on the subjective wellbeing of elderly and younger people. Aging Ment Health. 2008;12(6):746–60.
Sun Y, Yan T. The use of public health indicators to assess individual happiness in post-disaster recovery. Int J Environ Res Public Health. 2019;16(21):4101.
Wong H, Huang Y, Fu Y, Zhang Y. Impacts of structural social capital and cognitive social capital on the psychological status of survivors of the yaan Earthquake. Appl Res Qual Life. 2018;14:1411–33.
Xiao H, Zhang Y, Kong D, Li S, Yang N. Social capital and sleep quality in individuals who self-isolated for 14 days during the coronavirus disease 2019 (COVID-19) outbreak in January 2020 in China. Med Sci Monit. 2020;26:e923921.
PubMed PubMed Central CAS Google Scholar
Matsuyama Y, Aida J, Hase A, Sato Y, Koyama S, Tsuboya T, et al. Do community- and individual-level social relationships contribute to the mental health of disaster survivors? A multilevel prospective study after the great East Japan earthquake. Soc Sci Med. 2016;151:187–95.
Ozaki A, Horiuchi S, Kobayashi Y, Inoue M, Aida J, Leppold C, Yamaoka K. Beneficial roles of social support for mental health vary in the Japanese population depending on disaster experience: a nationwide cross-sectional study. Tohoku J Exp Med. 2018;246(4):213–23.
Sato K, Amemiya A, Haseda M, Takagi D, Kanamori M, Kondo K, et al. Post-disaster changes in Social Capital and Mental Health: a natural experiment from the 2016 Kumamoto Earthquake. Am J Epidemiol. 2020;189(9):910–21.
Tsuchiya N, Nakaya N, Nakamura T, Narita A, Kogure M, Aida J, Tsuji I, Hozawa A, Tomita H. Impact of social capital on psychological distress and interaction with house destruction and displacement after the great East Japan earthquake of 2011. J Neuropsychiatry Clin Neurosci. 2017;71(1):52–60.
Brockie L, Miller E. Understanding older adults’ resilience during the Brisbane floods: social capital, life experience, and optimism. Disaster Med Pub Health Prep. 2017;11(1):72–9.
Caldwell K, Boyd CP. Coping and resilience in farming families affected by drought. Rural Remote Health. 2009;9(2):1088.
PubMed Google Scholar
Huang Y, Tan NT, Liu J. Support, sense of community, and psychological status in the survivors of the Yaan earthquake. J Community Psychol. 2016;44(7):919–36.
Wind T, Fordham M, Komproe H. Social capital and post-disaster mental health. Glob Health Action. 2011;4(1):6351.
Wind T, Komproe IH. The mechanisms that associate community social capital with post-disaster mental health: a multilevel model. Soc Sci Med. 2012;75(9):1715–20.
Hogg D, Kingham S, Wilson TM, Ardagh M. The effects of spatially varying earthquake impacts on mood and anxiety symptom treatments among long-term Christchurch residents following the 2010/11 Canterbury Earthquakes, New Zealand. Health Place. 2016;41:78–88.
Flores EC, Carnero AM, Bayer AM. Social capital and chronic post-traumatic stress disorder among survivors of the 2007 earthquake in Pisco, Peru. Soc Sci Med. 2014;101:9–17.
Rafiey H, Alipour F, LeBeau R, Salimi Y, Ahmadi S. Exploring the buffering role of social capital in the development of posttraumatic stress symptoms among Iranian earthquake survivors. Psychol Trauma. 2019;14(6):1040–6.
Babcicky P, Seebauer S. The two faces of social capital in private Flood mitigation: opposing effects on risk perception, self-efficacy and coping capacity. J Risk Res. 2017;20(8):1017–37.
Bakic H, Ajdukovic D. Stability and change post-disaster: dynamic relations between individual, interpersonal and community resources and psychosocial functioning. Eur J Psychotraumatol. 2019;10(1):1614821.
Rogers RW. A protection motivation theory of fear appeals and attitude change. J Psychol. 1975;91(1):93–114.
Lindberg K, Swearingen T. A reflective thrive-oriented community resilience scale. Am J Community Psychol. 2020;65(3–4):467–78.
Leykin D, Lahad M, Cohen O, Goldberg A, Aharonson-Daniel L. Conjoint community resiliency assessment measure-28/10 items (CCRAM28 and CCRAM10): a self-report tool for assessing community resilience. Am J Community Psychol. 2013;52:313–23.
Sherrieb K, Norris FH, Galea S. Measuring capacities for community resilience. Soc Indic Res. 2010;99:227–47.
Ehsan AM, De Silva MJ. Social capital and common mental disorder: a systematic review. J Epidemiol Community Health. 2015;69(10):1021–8.
Pfefferbaum B, Van Horn RL, Pfefferbaum RL. A conceptual framework to enhance community resilience using social capital. Clin Soc Work J. 2017;45(2):102–10.
Carmen E, Fazey I, Ross H, Bedinger M, Smith FM, Prager K, et al. Building community resilience in a context of climate change: the role of social capital. Ambio. 2022;51(6):1371–87.
Humbert C, Joseph J. Introduction: the politics of resilience: problematising current approaches. Resilience. 2019;7(3):215–23.
Tanner T, Bahadur A, Moench M. Challenges for resilience policy and practice. Working paper: 519. 2017.
Vadivel R, Shoib S, El Halabi S, El Hayek S, Essam L, Bytyçi DG. Mental health in the post-COVID-19 era: challenges and the way forward. Gen Psychiatry. 2021;34(1):e100424.
Article CAS Google Scholar
Pryor M. Social Capital Harmonised Standard. London: Government Statistical Service. 2021. Accessible at: https://gss.civilservice.gov.uk/policystore/social-capital/ .
Public Health England NE. A guide to community-centred approaches for health and wellbeing. 2015.
Hawe P. Capturing the meaning of ‘community’ in community intervention evaluation: some contributions from community psychology. Health Promot Int. 1994;9(3):199–210.
Uphoff EP, Pickett KE, Cabieses B, Small N, Wright J. A systematic review of the relationships between social capital and socioeconomic inequalities in health: a contribution to understanding the psychosocial pathway of health inequalities. Int J Equity Health. 2013;12:1–12.
Download references
Acknowledgements
Not applicable.
This study was supported by the National Institute for Health Research Research Unit (NIHR HPRU) in Emergency Preparedness and Response, a partnership between Public Health England, King’s College London and the University of East Anglia. The views expressed are those of the author(s) and not necessarily those of the NIHR, Public Health England, the UK Health Security Agency or the Department of Health and Social Care [Grant number: NIHR20008900]. Part of this work has been funded by the Office for Health Improvement and Disparities, Department of Health and Social Care, as part of a Collaborative Agreement with Leeds Beckett University.
Author information
Authors and affiliations.
Behavioural Science and Insights Unit, Evaluation & Translation Directorate, Science Group, UK Health Security Agency, Porton Down, Salisbury, SP4 0JG, UK
C. E. Hall, H. Wehling, R. Amlôt & D. Weston
Health Protection Research Unit, Institute of Psychology, Psychiatry and Neuroscience, King’s College London, 10 Cutcombe Road, London, SE5 9RJ, UK
C. E. Hall, S. K. Brooks & N. Greenberg
School of Health and Community Studies, Leeds Beckett University, Portland Building, PD519, Portland Place, Leeds, LS1 3HE, UK
J. Stansfield & J. South
King’s Centre for Military Health Research, Institute of Psychology, Psychiatry and Neuroscience, King’s College London, 10 Cutcombe Road, London, SE5 9RJ, UK
N. Greenberg
You can also search for this author in PubMed Google Scholar
Contributions
DW, JSo and JSt had the main idea for the review. The search strategy and eligibility criteria were devised by CH, DW, JSo and JSt. CH conducted the database searches. CH and DW conducted duplicate, title and abstract and full text screening in accordance with inclusion criteria. CH conducted data extraction, CH and DW carried out the analysis and drafted the initial manuscript. All authors provided critical revision of intellectual content. All authors approved the final manuscript.
Authors’ information
Corresponding author.
Correspondence to D. Weston .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1., additional file 2., additional file 3., additional file 4., additional file 5., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Hall, C.E., Wehling, H., Stansfield, J. et al. Examining the role of community resilience and social capital on mental health in public health emergency and disaster response: a scoping review. BMC Public Health 23 , 2482 (2023). https://doi.org/10.1186/s12889-023-17242-x
Download citation
Received : 04 April 2022
Accepted : 16 November 2023
Published : 12 December 2023
DOI : https://doi.org/10.1186/s12889-023-17242-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health
- Community cohesion
- Public health emergency
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- COVID-19 and your mental health
Worries and anxiety about COVID-19 can be overwhelming. Learn ways to cope as COVID-19 spreads.
At the start of the COVID-19 pandemic, life for many people changed very quickly. Worry and concern were natural partners of all that change — getting used to new routines, loneliness and financial pressure, among other issues. Information overload, rumor and misinformation didn't help.
Worldwide surveys done in 2020 and 2021 found higher than typical levels of stress, insomnia, anxiety and depression. By 2022, levels had lowered but were still higher than before 2020.
Though feelings of distress about COVID-19 may come and go, they are still an issue for many people. You aren't alone if you feel distress due to COVID-19. And you're not alone if you've coped with the stress in less than healthy ways, such as substance use.
But healthier self-care choices can help you cope with COVID-19 or any other challenge you may face.
And knowing when to get help can be the most essential self-care action of all.
Recognize what's typical and what's not
Stress and worry are common during a crisis. But something like the COVID-19 pandemic can push people beyond their ability to cope.
In surveys, the most common symptoms reported were trouble sleeping and feeling anxiety or nervous. The number of people noting those symptoms went up and down in surveys given over time. Depression and loneliness were less common than nervousness or sleep problems, but more consistent across surveys given over time. Among adults, use of drugs, alcohol and other intoxicating substances has increased over time as well.
The first step is to notice how often you feel helpless, sad, angry, irritable, hopeless, anxious or afraid. Some people may feel numb.
Keep track of how often you have trouble focusing on daily tasks or doing routine chores. Are there things that you used to enjoy doing that you stopped doing because of how you feel? Note any big changes in appetite, any substance use, body aches and pains, and problems with sleep.
These feelings may come and go over time. But if these feelings don't go away or make it hard to do your daily tasks, it's time to ask for help.
Get help when you need it
If you're feeling suicidal or thinking of hurting yourself, seek help.
- Contact your healthcare professional or a mental health professional.
- Contact a suicide hotline. In the U.S., call or text 988 to reach the 988 Suicide & Crisis Lifeline , available 24 hours a day, seven days a week. Or use the Lifeline Chat . Services are free and confidential.
If you are worried about yourself or someone else, contact your healthcare professional or mental health professional. Some may be able to see you in person or talk over the phone or online.
You also can reach out to a friend or loved one. Someone in your faith community also could help.
And you may be able to get counseling or a mental health appointment through an employer's employee assistance program.
Another option is information and treatment options from groups such as:
- National Alliance on Mental Illness (NAMI).
- Substance Abuse and Mental Health Services Administration (SAMHSA).
- Anxiety and Depression Association of America.
Self-care tips
Some people may use unhealthy ways to cope with anxiety around COVID-19. These unhealthy choices may include things such as misuse of medicines or legal drugs and use of illegal drugs. Unhealthy coping choices also can be things such as sleeping too much or too little, or overeating. It also can include avoiding other people and focusing on only one soothing thing, such as work, television or gaming.
Unhealthy coping methods can worsen mental and physical health. And that is particularly true if you're trying to manage or recover from COVID-19.
Self-care actions can help you restore a healthy balance in your life. They can lessen everyday stress or significant anxiety linked to events such as the COVID-19 pandemic. Self-care actions give your body and mind a chance to heal from the problems long-term stress can cause.
Take care of your body
Healthy self-care tips start with the basics. Give your body what it needs and avoid what it doesn't need. Some tips are:
- Get the right amount of sleep for you. A regular sleep schedule, when you go to bed and get up at similar times each day, can help avoid sleep problems.
- Move your body. Regular physical activity and exercise can help reduce anxiety and improve mood. Any activity you can do regularly is a good choice. That may be a scheduled workout, a walk or even dancing to your favorite music.
- Choose healthy food and drinks. Foods that are high in nutrients, such as protein, vitamins and minerals are healthy choices. Avoid food or drink with added sugar, fat or salt.
- Avoid tobacco, alcohol and drugs. If you smoke tobacco or if you vape, you're already at higher risk of lung disease. Because COVID-19 affects the lungs, your risk increases even more. Using alcohol to manage how you feel can make matters worse and reduce your coping skills. Avoid taking illegal drugs or misusing prescriptions to manage your feelings.
Take care of your mind
Healthy coping actions for your brain start with deciding how much news and social media is right for you. Staying informed, especially during a pandemic, helps you make the best choices but do it carefully.
Set aside a specific amount of time to find information in the news or on social media, stay limited to that time, and choose reliable sources. For example, give yourself up to 20 or 30 minutes a day of news and social media. That amount keeps people informed but not overwhelmed.
For COVID-19, consider reliable health sources. Examples are the U.S. Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO).
Other healthy self-care tips are:
- Relax and recharge. Many people benefit from relaxation exercises such as mindfulness, deep breathing, meditation and yoga. Find an activity that helps you relax and try to do it every day at least for a short time. Fitting time in for hobbies or activities you enjoy can help manage feelings of stress too.
- Stick to your health routine. If you see a healthcare professional for mental health services, keep up with your appointments. And stay up to date with all your wellness tests and screenings.
- Stay in touch and connect with others. Family, friends and your community are part of a healthy mental outlook. Together, you form a healthy support network for concerns or challenges. Social interactions, over time, are linked to a healthier and longer life.
Avoid stigma and discrimination
Stigma can make people feel isolated and even abandoned. They may feel sad, hurt and angry when people in their community avoid them for fear of getting COVID-19. People who have experienced stigma related to COVID-19 include people of Asian descent, health care workers and people with COVID-19.
Treating people differently because of their medical condition, called medical discrimination, isn't new to the COVID-19 pandemic. Stigma has long been a problem for people with various conditions such as Hansen's disease (leprosy), HIV, diabetes and many mental illnesses.
People who experience stigma may be left out or shunned, treated differently, or denied job and school options. They also may be targets of verbal, emotional and physical abuse.
Communication can help end stigma or discrimination. You can address stigma when you:
- Get to know people as more than just an illness. Using respectful language can go a long way toward making people comfortable talking about a health issue.
- Get the facts about COVID-19 or other medical issues from reputable sources such as the CDC and WHO.
- Speak up if you hear or see myths about an illness or people with an illness.
COVID-19 and health
The virus that causes COVID-19 is still a concern for many people. By recognizing when to get help and taking time for your health, life challenges such as COVID-19 can be managed.
- Mental health during the COVID-19 pandemic. National Institutes of Health. https://covid19.nih.gov/covid-19-topics/mental-health. Accessed March 12, 2024.
- Mental Health and COVID-19: Early evidence of the pandemic's impact: Scientific brief, 2 March 2022. World Health Organization. https://www.who.int/publications/i/item/WHO-2019-nCoV-Sci_Brief-Mental_health-2022.1. Accessed March 12, 2024.
- Mental health and the pandemic: What U.S. surveys have found. Pew Research Center. https://www.pewresearch.org/short-reads/2023/03/02/mental-health-and-the-pandemic-what-u-s-surveys-have-found/. Accessed March 12, 2024.
- Taking care of your emotional health. Centers for Disease Control and Prevention. https://emergency.cdc.gov/coping/selfcare.asp. Accessed March 12, 2024.
- #HealthyAtHome—Mental health. World Health Organization. www.who.int/campaigns/connecting-the-world-to-combat-coronavirus/healthyathome/healthyathome---mental-health. Accessed March 12, 2024.
- Coping with stress. Centers for Disease Control and Prevention. www.cdc.gov/mentalhealth/stress-coping/cope-with-stress/. Accessed March 12, 2024.
- Manage stress. U.S. Department of Health and Human Services. https://health.gov/myhealthfinder/topics/health-conditions/heart-health/manage-stress. Accessed March 20, 2020.
- COVID-19 and substance abuse. National Institute on Drug Abuse. https://nida.nih.gov/research-topics/covid-19-substance-use#health-outcomes. Accessed March 12, 2024.
- COVID-19 resource and information guide. National Alliance on Mental Illness. https://www.nami.org/Support-Education/NAMI-HelpLine/COVID-19-Information-and-Resources/COVID-19-Resource-and-Information-Guide. Accessed March 15, 2024.
- Negative coping and PTSD. U.S. Department of Veterans Affairs. https://www.ptsd.va.gov/gethelp/negative_coping.asp. Accessed March 15, 2024.
- Health effects of cigarette smoking. Centers for Disease Control and Prevention. https://www.cdc.gov/tobacco/data_statistics/fact_sheets/health_effects/effects_cig_smoking/index.htm#respiratory. Accessed March 15, 2024.
- People with certain medical conditions. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. Accessed March 15, 2024.
- Your healthiest self: Emotional wellness toolkit. National Institutes of Health. https://www.nih.gov/health-information/emotional-wellness-toolkit. Accessed March 15, 2024.
- World leprosy day: Bust the myths, learn the facts. Centers for Disease Control and Prevention. https://www.cdc.gov/leprosy/world-leprosy-day/. Accessed March 15, 2024.
- HIV stigma and discrimination. Centers for Disease Control and Prevention. https://www.cdc.gov/hiv/basics/hiv-stigma/. Accessed March 15, 2024.
- Diabetes stigma: Learn about it, recognize it, reduce it. Centers for Disease Control and Prevention. https://www.cdc.gov/diabetes/library/features/diabetes_stigma.html. Accessed March 15, 2024.
- Phelan SM, et al. Patient and health care professional perspectives on stigma in integrated behavioral health: Barriers and recommendations. Annals of Family Medicine. 2023; doi:10.1370/afm.2924.
- Stigma reduction. Centers for Disease Control and Prevention. https://www.cdc.gov/drugoverdose/od2a/case-studies/stigma-reduction.html. Accessed March 15, 2024.
- Nyblade L, et al. Stigma in health facilities: Why it matters and how we can change it. BMC Medicine. 2019; doi:10.1186/s12916-019-1256-2.
- Combating bias and stigma related to COVID-19. American Psychological Association. https://www.apa.org/topics/covid-19-bias. Accessed March 15, 2024.
- Yashadhana A, et al. Pandemic-related racial discrimination and its health impact among non-Indigenous racially minoritized peoples in high-income contexts: A systematic review. Health Promotion International. 2021; doi:10.1093/heapro/daab144.
- Sawchuk CN (expert opinion). Mayo Clinic. March 25, 2024.
Products and Services
- A Book: Endemic - A Post-Pandemic Playbook
- Begin Exploring Women's Health Solutions at Mayo Clinic Store
- A Book: Future Care
- Antibiotics: Are you misusing them?
- COVID-19 and vitamin D
- Convalescent plasma therapy
- Coronavirus disease 2019 (COVID-19)
- COVID-19: How can I protect myself?
- Herd immunity and coronavirus
- COVID-19 and pets
- COVID-19 antibody testing
- COVID-19, cold, allergies and the flu
- COVID-19 drugs: Are there any that work?
- Long-term effects of COVID-19
- COVID-19 tests
- COVID-19 in babies and children
- Coronavirus infection by race
- COVID-19 travel advice
- COVID-19 vaccine: Should I reschedule my mammogram?
- COVID-19 vaccines for kids: What you need to know
- COVID-19 vaccines
- COVID-19 variant
- COVID-19 vs. flu: Similarities and differences
- COVID-19: Who's at higher risk of serious symptoms?
- Debunking coronavirus myths
- Different COVID-19 vaccines
- Extracorporeal membrane oxygenation (ECMO)
- Fever: First aid
- Fever treatment: Quick guide to treating a fever
- Fight coronavirus (COVID-19) transmission at home
- Honey: An effective cough remedy?
- How do COVID-19 antibody tests differ from diagnostic tests?
- How to take your pulse
- How to measure your respiratory rate
- How to take your temperature
- How well do face masks protect against COVID-19?
- Is hydroxychloroquine a treatment for COVID-19?
- Loss of smell
- Mayo Clinic Minute: You're washing your hands all wrong
- Mayo Clinic Minute: How dirty are common surfaces?
- Multisystem inflammatory syndrome in children (MIS-C)
- Nausea and vomiting
- Pregnancy and COVID-19
- Safe outdoor activities during the COVID-19 pandemic
- Safety tips for attending school during COVID-19
- Sex and COVID-19
- Shortness of breath
- Thermometers: Understand the options
- Treating COVID-19 at home
- Unusual symptoms of coronavirus
- Vaccine guidance from Mayo Clinic
- Watery eyes
Related information
- Mental health: What's normal, what's not - Related information Mental health: What's normal, what's not
- Mental illness - Related information Mental illness
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
- Skip to main content
- Keyboard shortcuts for audio player
- Your Health
- Treatments & Tests
- Health Inc.
- Public Health
Mental health care is hard to find, especially for people with Medicare or Medicaid
Rhitu Chatterjee

With rates of suicide and opioid deaths rising in the past decade and children's mental health declared a national emergency , the United States faces an unprecedented mental health crisis. But access to mental health care for a significant portion of Americans — including some of the most vulnerable populations — is extremely limited, according to a new government report released Wednesday.
The report, from the Department of Health and Human Services' Office of Inspector General, finds that Medicare and Medicaid have a dire shortage of mental health care providers.
The report looked at 20 counties with people on Medicaid, traditional Medicare and Medicare Advantage plans, which together serve more than 130 million enrollees — more than 40% of the U.S. population, says Meridith Seife , the deputy regional inspector general and the lead author of the report.
Medicaid serves people on low incomes, and Medicare is mainly for people 65 years or older and those who are younger with chronic disabilities.
The report found fewer than five active mental health care providers for every 1,000 enrollees. On average, Medicare Advantage has 4.7 providers per 1,000 enrollees, whereas traditional Medicare has 2.9 providers and Medicaid has 3.1 providers for the same number of enrollees. Some counties fare even worse, with not even a single provider for every 1,000 enrollees.
"When you have so few providers available to see this many enrollees, patients start running into significant problems finding care," says Seife.
The findings are especially troubling given the level of need for mental health care in this population, she says.
"On Medicare, you have 1 in 4 Medicare enrollees who are living with a mental illness," she says. "Yet less than half of those people are receiving treatment."
Among people on Medicaid, 1 in 3 have a mental illness, and 1 in 5 have a substance use disorder. "So the need is tremendous."
The results are "scary" but "not very surprising," says Deborah Steinberg , senior health policy attorney at the nonprofit Legal Action Center. "We know that people in Medicare and Medicaid are often underserved populations, and this is especially true for mental health and substance use disorder care."
Among those individuals able to find and connect with a provider, many see their provider several times a year, according to the report. And many have to drive a long way for their appointments.
"We have roughly 1 in 4 patients that had to travel more than an hour to their appointments, and 1 in 10 had to travel more than an hour and a half each way," notes Seife. Some patients traveled two hours each way for mental health care, she says.
Mental illnesses and substance use disorders are chronic conditions that people need ongoing care for, says Steinberg. "And when they have to travel an hour, more than an hour, for an appointment throughout the year, that becomes unreasonable. It becomes untenable."
"We know that behavioral health workforce shortages are widespread," says Heather Saunders , a senior research manager on the Medicaid team at KFF, the health policy research organization. "This is across all payers, all populations, with about half of the U.S. population living in a workforce shortage."
But as the report found, that's not the whole story for Medicare and Medicaid. Only about a third of mental health care providers in the counties studied see Medicare and Medicaid patients. That means a majority of the workforce doesn't participate in these programs.
This has been well documented in Medicaid, notes Saunders. "Only a fraction" of providers in provider directories see Medicaid patients, she says. "And when they do see Medicaid patients, they often only see a few."
Lower reimbursement rates and a high administrative burden prevent more providers from participating in Medicaid and Medicare, the report notes.
"In the Medicare program, they set a physician fee rate," explains Steinberg. "Then for certain providers, which includes clinical social workers, mental health counselors and marriage and family therapists, they get reimbursed at 75% of that rate."
Medicaid reimbursements for psychiatric services are even lower when compared with Medicare , says Ellen Weber , senior vice president for health initiatives at the Legal Action Center.
"They're baking in those discriminatory standards when they are setting those rates," says Steinberg.
The new report recommends that the Centers for Medicare & Medicaid Services (CMS) take steps to increase payments to providers and lower administrative requirements. In a statement, CMS said it has responded to those recommendations within the report.
According to research by Saunders and her colleagues at KFF, many states have already started to take action on these fronts to improve participation in Medicaid.
Several have upped their payments to mental health providers. "But the scale of those increases ranged widely across states," says Saunders, "with some states limiting the increase to one provider type or one type of service, but other states having rate increases that were more across the board."
Some states have also tried to simplify and streamline paperwork, she adds. "Making it less complex, making it easier to understand," says Saunders.
But it's too soon to know whether those efforts have made a significant impact on improving access to providers.
CMS has also taken steps to address provider shortages, says Steinberg.
"CMS has tried to increase some of the reimbursement rates without actually fixing that structural problem," says Steinberg. "Trying to add a little bit here and there, but it's not enough, especially when they're only adding a percent to the total rate. It's a really small increase."
The agency has also started covering treatments and providers it didn't use to cover before.
"In 2020, Medicare started covering opioid treatment programs, which is where a lot of folks can go to get medications for their substance use disorder," says Steinberg.
And starting this year, Medicare also covers "mental health counselors, which includes addiction counselors, as well as marriage and family therapists," she adds.
While noteworthy and important, a lot more needs to be done, says Steinberg. "For example, in the substance use disorder space, a lot of addiction counselors do not have a master's degree. And that's one of their requirements to be a counselor in the Medicare program right now."
Removing those stringent requirements and adding other kinds of providers, like peer support specialists, is key to improving access. And the cost of not accessing care is high, she adds.
"Over the past two decades, [in] the older adult population, the number of overdose deaths has increased fourfold — quadrupled," says Steinberg. "So this is affecting people. It is causing deaths. It is causing people to go to the hospital. It increases [health care] costs."
- Centers for Medicare & Medicaid Services
- mental health
ORIGINAL RESEARCH article
Challenges and support needs in psychological and physical health among pilots: a qualitative study.

- 1 School of Medicine, Shanghai Jiao Tong University, Shanghai, China
- 2 Other, Shanghai, China
- 3 National Center For Global Health and Medicine, Shinjuku, Tokyo, Japan
- 4 School of Public Health, School of Medicine, Shanghai Jiao Tong University, Shanghai, China
- 5 School of Nursing, Shanghai Jiao Tong University, Shanghai, Shanghai, China
- 6 International Peace Maternity and Child Health Hospital, Shanghai, Shanghai Municipality, China
The final, formatted version of the article will be published soon.
Select one of your emails
You have multiple emails registered with Frontiers:
Notify me on publication
Please enter your email address:
If you already have an account, please login
You don't have a Frontiers account ? You can register here
Abstract Introduction Physical and mental health problems among pilots affect their working state and impact flight safety. Although pilots’ physical and mental health problems have become increasingly prominent, their health has not been taken seriously. This study aimed to clarify challenges and support needs related to psychological and physical health among pilots to inform development of a more scientific and comprehensive physical and mental health system for civil aviation pilots. Methods This qualitative study recruited pilots from nine civil aviation companies. Focus group interviews via an online conference platform were conducted in August 2022. Colaizzi analysis was used to derive themes from the data and explore pilots’ experiences, challenges, and support needs. Results The main sub-themes capturing pilots’ psychological and physical health challenges were: 1) imbalance between family life and work; 2) pressure from assessment and physical examination eligibility requirements; 3) pressure from worries about being infected with COVID-19; 4) nutrition deficiency during working hours; 5) changes in eating habits because of the COVID-19 pandemic; 6) sleep deprivation; 7) occupational diseases; 8) lack of support from the company in coping with stress; 9) pilots’ yearly examination standards; 10) support with sports equipment; 11) respecting planned rest time; and 12) isolation periods. Discussion The interviewed pilots experienced major psychological pressure from various sources, and their physical health condition was concerning. We offer several suggestions that could be addressed to improve pilots’ physical and mental health. However, more research is needed to compare standard health measures for pilots around the world in order to improve their physical and mental health and contribute to overall aviation safety.
Keywords: Occupational Health, Mental Health, physical health, qualitative study, Pilots and cabin crew, COVID-19
Received: 06 Dec 2023; Accepted: 05 Apr 2024.
Copyright: © 2024 Xu, Bao, Zhang, Li, Zhang, Li, Jin, Chen, Duan, Shi, Wang, Lu, Chen, Gao, Han, Ren, Su and Xiang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Yuyan Bao, School of Medicine, Shanghai Jiao Tong University, Shanghai, China Lin Zhang, Other, Shanghai, China Qingqing Jin, Other, Shanghai, China Yan Chen, Other, Shanghai, China Qingqing Duan, Other, Shanghai, China Feng Shi, Other, Shanghai, China Linlin Wang, Other, Shanghai, China Ziyang Lu, School of Medicine, Shanghai Jiao Tong University, Shanghai, China Xuhua Chen, School of Medicine, Shanghai Jiao Tong University, Shanghai, China Qijing Gao, School of Medicine, Shanghai Jiao Tong University, Shanghai, China Bin Ren, Other, Shanghai, China Ya Su, School of Nursing, Shanghai Jiao Tong University, Shanghai, Shanghai, China Mi Xiang, School of Public Health, School of Medicine, Shanghai Jiao Tong University, Shanghai, 200240, China
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
This paper is in the following e-collection/theme issue:
Published on 10.4.2024 in Vol 26 (2024)
Effectiveness of a Web-Based Individual Coping and Alcohol Intervention Program for Children of Parents With Alcohol Use Problems: Randomized Controlled Trial
Authors of this article:

Original Paper
- Håkan Wall 1 , PhD ;
- Helena Hansson 2 , PhD ;
- Ulla Zetterlind 3 , PhD ;
- Pia Kvillemo 1 , PhD ;
- Tobias H Elgán 1 , PhD
1 Stockholm Prevents Alcohol and Drug Problems, Centre for Psychiatry Research, Department of Clinical Neuroscience, Karolinska Institutet, & Stockholm Health Care Services, Stockholm, Sweden
2 School of Social Work, Faculty of Social Sciences, Lund University, Lund, Sweden
3 Clinical Health Promotion Centre, Department of Health Sciences, Lund University, Lund, Sweden
Corresponding Author:
Tobias H Elgán, PhD
Stockholm Prevents Alcohol and Drug Problems, Centre for Psychiatry Research
Department of Clinical Neuroscience
Karolinska Institutet, & Stockholm Health Care Services
Norra Stationsgatan 69
Stockholm, 11364
Phone: 46 700011003
Email: [email protected]
Background: Children whose parents have alcohol use problems are at an increased risk of several negative consequences, such as poor school performance, an earlier onset of substance use, and poor mental health. Many would benefit from support programs, but the figures reveal that only a small proportion is reached by existing support. Digital interventions can provide readily accessible support and potentially reach a large number of children. Research on digital interventions aimed at this target group is scarce. We have developed a novel digital therapist-assisted self-management intervention targeting adolescents whose parents had alcohol use problems. This program aims to strengthen coping behaviors, improve mental health, and decrease alcohol consumption in adolescents.
Objective: This study aims to examine the effectiveness of a novel web-based therapist-assisted self-management intervention for adolescents whose parents have alcohol use problems.
Methods: Participants were recruited on the internet from social media and websites containing health-related information about adolescents. Possible participants were screened using the short version of the Children of Alcoholics Screening Test-6. Eligible participants were randomly allocated to either the intervention group (n=101) or the waitlist control group (n=103), and they were unblinded to the condition. The assessments, all self-assessed, consisted of a baseline and 2 follow-ups after 2 and 6 months. The primary outcome was the Coping With Parents Abuse Questionnaire (CPAQ), and secondary outcomes were the Center for Epidemiological Studies Depression Scale, Alcohol Use Disorders Identification Test (AUDIT-C), and Ladder of Life (LoL).
Results: For the primary outcome, CPAQ, a small but inconclusive treatment effect was observed (Cohen d =–0.05 at both follow-up time points). The intervention group scored 38% and 46% lower than the control group on the continuous part of the AUDIT-C at the 2- and 6-month follow-up, respectively. All other between-group comparisons were inconclusive at either follow-up time point. Adherence was low, as only 24% (24/101) of the participants in the intervention group completed the intervention.
Conclusions: The findings were inconclusive for the primary outcome but demonstrate that a digital therapist-assisted self-management intervention may contribute to a reduction in alcohol consumption. These results highlight the potential for digital interventions to reach a vulnerable, hard-to-reach group of adolescents but underscore the need to develop more engaging support interventions to increase adherence.
Trial Registration: ISRCTN Registry ISRCTN41545712; https://www.isrctn.com/ISRCTN41545712?q=ISRCTN41545712
International Registered Report Identifier (IRRID): RR2-10.1186/1471-2458-12-35
Introduction
Children who grow up with parents who have substance use problems or disorders face extraordinary challenges. Approximately 20% of all children have parents with alcohol problems [ 1 - 5 ], while approximately 5% have parents with alcohol use disorders [ 4 , 6 , 7 ]. Children growing up with parental substance abuse are at an increased risk of several negative outcomes, such as psychiatric morbidity [ 8 - 12 ]; poor intellectual, cognitive, and academic achievement [ 13 - 15 ]; domestic physical abuse [ 16 ]; and early drinking onset and the development of substance use problems [ 9 , 17 , 18 ]. Thus, children exposed to parental substance abuse comprise a target group for selective interventions and prevention strategies [ 19 - 22 ].
In Sweden, municipalities account for most of the support offered to these children. An annual survey by the junior association of the Swedish branch of Movendi International (ie, an international temperance movement) reported that 97% of all municipalities provided support resources [ 23 ]. However, estimates from the same survey showed that approximately 2% of the children in the target group received support. Hence, an overwhelming majority never receives support, mainly because of difficulties in identifying and attracting them to intervention programs [ 22 , 24 ].
The internet has become an appealing way to reach and support a large number of people [ 25 , 26 ]. Web-based interventions seem particularly attractive to adolescents, as they generally use digital technology and social media. Furthermore, research has shown that adolescents regard the internet as inviting because it is a readily accessible, anonymous way of seeking help [ 27 ]. Web-based interventions can reduce the stigma associated with face-to-face consultations in health care settings [ 28 ], and young people appreciate the flexibility of completing web-based sessions to fit their own schedules [ 29 ]. The positive effects of web-based interventions have been detected across a broad range of conditions. A recent review by Hedman-Lagerlöf et al [ 30 ] concluded that therapist-supported internet-based cognitive behavioral therapy for adults yielded similar effects as face-to-face therapy. To date, most web-based interventions have been designed for adults. Although the number of web-based interventions targeting children or adolescents is increasing [ 25 , 31 - 33 ], the number of digital interventions aimed at children of substance-abusing parents is still scarce [ 22 , 34 - 38 ]. Those described in the literature, however, all have in common that they are quite extensive, with a duration over several weeks, and a brief digital intervention could complement these more extended interventions. For instance, our research group initiated a study on a web-based group chat for 15- to 25-year-old individuals who have parents with mental illness or substance use problems [ 35 ]. The duration of the program is 8 weeks, and it is a translated version of a program from the Netherlands [ 34 ], which has been shown to have inconclusive treatment effects [ 39 ]. In Sweden, 2 other programs with inconclusive treatment effects have been tested that target significant others and their children [ 37 , 38 ]. Finally, a digital intervention developed in Australia for 18- to 25-year-old individuals with parents with mental illness or substance use disorder [ 36 ] was tested in a pilot study demonstrating positive findings [ 40 ].
To meet the need for a brief, web-based intervention that targets adolescents having parents with alcohol problems and build on the evidence base of digital interventions targeting this vulnerable group, we developed a novel internet-delivered therapist-assisted self-management intervention called “Alcohol and Coping.” Our program originated from a manual-based face-to-face intervention called the “Individual Coping and Alcohol Intervention Program” (ICAIP) [ 41 , 42 ]. Previous studies on both the ICAIP, which aimed at college students having parents with alcohol problems, and a coping skills intervention program, which aimed at spouses of partners with alcohol dependency [ 43 ], have demonstrated positive effects regarding decreased alcohol consumption and improved mental health and coping behaviors [ 41 - 44 ]. Furthermore, the results from these studies underscore the importance of improving coping skills [ 42 , 44 ]. Among college students, those who received a combination of coping skills and an alcohol intervention program had better long-term outcomes [ 42 ].
The aim of this study was to test the effectiveness of Alcohol and Coping among a sample of adolescents aged 15-19 years with at least 1 parent with alcohol use problems. We hypothesized that the intervention group would be superior to the control group in improving coping skills. Secondary research questions concerned the participants’ improvement in (1) depression, (2) alcohol consumption, and (3) quality of life.
This study was a parallel-group randomized controlled trial in which participants were randomized to either the intervention or waitlist control group in a 1:1 allocation ratio. The trial design is illustrated in Figure 1 .

Recruitment and Screening
The participants were recruited from August 2012 to December 2013 through advertisements on social media (Facebook). The advertisements targeted individuals aged 15-19 years with Facebook accounts. Participants were recruited on the internet through advertisements on websites containing health-related information about adolescents. The advertisements included the text, “Do your parents drink too much? Participate in a study.” The advertisement contained an invitation to perform a web-based, self-assessed screening procedure. In addition to questions about age and sex, participants were screened for having parents with alcohol problems using the short version of the Children of Alcoholics Screening Test-6 (CAST-6), developed from a 30-item original version [ 45 ]. The CAST-6 is a 6-item true-false measure designed to assess whether participants perceive their parents’ alcohol consumption to be problematic. The CAST-6 has demonstrated high internal consistency ( r =0.92-0.94), test-retest reliability ( r =0.94), and high validity as compared to the 30-item version ( r =0.93) using the recommended threshold score of 3 or higher [ 45 , 46 ]. We previously translated the CAST-6 into Swedish and validated the translated version among 1450 adolescents, showing good internal consistency (α=.88), excellent test-retest reliability (intraclass correlation coefficient=0.93), and loading into 1 latent factor [ 47 ]. Additional inclusion criteria included having access to a computer and the internet and being sufficiently fluent in Swedish. Participants were excluded from the study and were referred to appropriate care if there were indications of either suicidal or self-inflicted harmful behaviors. Individuals eligible for inclusion received further information about the study and were asked to provide consent to participate by providing an email address.
Data Collection and Measures
All assessments were administered through email invitations containing a hyperlink to the web-based self-reported assessments. Up to 3 reminders were sent through email at 5, 10, and 15 days after the first invitation. A baseline assessment (t 0 ) was collected before randomization, and follow-up assessments were conducted at 2 and 6 months (t 1 and t 2 , respectively) after the initial assessment.
Participants were asked for age, sex, whether they lived with a parent (mother and father, mother or father, mother or father and stepparent, or alternate between mother and father), where their parents were born (Sweden or a Nordic country excluding Sweden or outside of the Nordic countries), parental status (employed, student, on parental leave, or unemployed), and any previous or present participation in support activities for children having parents with alcohol use problems. The primary outcome was coping, measured using the Coping With Parents Abuse Questionnaire (CPAQ) based on the Coping Behavior Scale developed by Orford et al [ 48 ]. Secondary outcomes were the Center for Epidemiological Studies Depression Scale (CES-DC) [ 49 ], the 3-question Alcohol Use Disorders Identification Test (AUDIT-C) [ 50 ], and the Ladder of Life (LoL), which measures the overall quality of life by asking about the participants’ past, present, and future ratings of their overall life satisfaction [ 50 ]. CPAQ has been shown to be reliable [ 41 , 42 ]. For this study, this scale was factor-analyzed to reduce the number of questions from 37 to 20. The resulting scale measures 6 coping typologies (discord, emotion, control, relationship, avoidance, and taking specific action) using a 4-point Likert scale, with a threshold score above 50 points (out of 80) indicating dysfunctional coping behavior. The CES-DC measures depressive symptoms during the past week using a 4-point Likert scale, where a higher total score indicates more depressive symptoms [ 49 ]. A cutoff score of ≥16 indicates symptoms of moderate depression, while a score of ≥30 indicates symptoms of severe depression [ 51 , 52 ]. The scale measures 4 dimensions of depression: depressed mood, tiredness, inability to concentrate, and feelings of being outside and lonely, and has positively stated items [ 52 ]. Additionally, this scale is a general measure of childhood psychopathology [ 53 ] and has been demonstrated to be reliable and valid among Swedish adolescents [ 52 ]. Alcohol consumption was measured using a modified AUDIT-C, which assesses the frequency of drinking, quantity consumed on a typical occasion, and frequency of heavy episodic drinking (ie, binge drinking) [ 50 ] using a 30-day perspective (as opposed to the original 12-month perspective). These questions have previously been translated into Swedish [ 54 ], and a score of ≥4 and ≥5 points for women and men, respectively, was used as a cutoff for risky drinking. This scale has been demonstrated to be reliable and valid for Swedish adolescents [ 55 ]. Furthermore, 2 questions were added concerning whether the participants had ever consumed alcohol to the point of intoxication and their age at the onset of drinking and intoxication. The original version of the LoL was designed for adults and asked the respondents to reflect on their, present, and future life status from a 5-year perspective on a 10-point Visual Analogue Scale representing life status from “worst” to “best” possible life imaginable [ 56 ]. A modified version for children, using a time frame of 1 year, has been used previously in Sweden [ 57 ] and was used in this study.
Randomization
After completing the baseline assessment, each participant was allocated to either the intervention or the control group. An external researcher generated an unrestricted random allocation sequence using random allocation software [ 58 ]. Neither the participants nor the researchers involved in the study were blinded to group allocation.
Based on the order in which participants were included in the study, they were allocated to 1 of the 2 study groups and informed of their allocation by email. Additionally, those who were randomized to the intervention group received a hyperlink to the Alcohol and Coping program, whereas the control group participants received information that they would gain access to Alcohol and Coping after the last follow-up assessment (ie, the waitlist control group). All participants were informed about other information and support available through web pages, notably drugsmart [ 59 ], which contains general information and facts about alcohol and drugs, in addition to more specific information about having substance-abusing parents. Telephone numbers and contact information for other organizations and primary health care facilities were also provided.
The Intervention
As noted previously, Alcohol and Coping is derived from the aforementioned manual-based face-to-face ICAIP intervention program [ 41 , 42 ]. The ICAIP consists of a combination of an alcohol intervention program, which is based on the short version of the Brief Alcohol Screening and Intervention for College Students program [ 60 ], and a coping intervention program developed for the purpose of the ICAIP [ 41 , 42 ]. Like the original ICAIP intervention, Alcohol and Coping builds on psychoeducational principles and includes components such as film-based lectures, various exercises, and both automated and therapist-assisted feedback. Briefly, once the participants logged into the Alcohol and Coping platform, they were introduced to the program, which followed the pattern of a board game ( Figure 2 ). Following the introduction, participants took part in 3 film-based lectures (between 8 and 15 minutes each, Figure 3 ) concerning alcohol problems within the family. The respective lectures included information about (1) dependency in general as well as the genetic and environmental risks for developing dependency, (2) family patterns and how the family adapts to the one having alcohol problems, and (3) attitudes toward alcohol and how they influence drinking and the physiological effects of alcohol. After completing the lectures, the participants were asked to answer 2 questions about their own alcohol consumption (ie, how often they drink and how often they drink to intoxication), followed by an automatic feedback message that depended on their answers. It was then suggested that the participants log out of the intervention for a 1- to 2-day break. The reason for this break was to give the participants a chance to digest all information and impressions. When they logged back into the intervention, they were asked to answer 20 questions about their coping strategies, which were also followed by automatic feedback. This feedback comprised a library covering all the prewritten feedback messages, each of which was tailored to the participants’ specific answers. The participants then participated in a 5-minute–long film-based lecture on emotion and problem-focused coping in relation to family alcohol problems ( Figure 3 ). This was followed by 4 exercises where the participants read through vignette-like stories from 4 fictional persons describing their everyday lives related to coping and alcohol problems in the family. The stories are presented by film-based introductions that are each 1-2 minutes long. Participants were then requested to respond to each story by describing how the fictive person could have coped with their situation. As a final exercise, participants were asked to reflect on their own family situation and how they cope with situations. The participants then had to take a break for a few days.
During the break, a therapist composed individual feedback that covered reflections and confirmation of the participant’s exercises and answers to questions and included suggestions on well-suited coping strategies. Additionally, the therapist encouraged the participants to talk to others in their surroundings, such as friends, teachers, or coaches, and seek further support elsewhere, such as from municipal social services, youth health care centers, or other organizations. Finally, the therapist reflected on the participants’ alcohol consumption patterns and reminded them of increased genetic and environmental risks. Those who revealed patterns of risky alcohol use were encouraged to look at 2 additional film-based lectures with more information about alcohol and intoxication (4 minutes) and alcohol use and dependency (5 minutes). Participants received this feedback once they logged back into the program, but they also had the opportunity to receive feedback through email. The total estimated effective time for completing the program was about 1 hour, but as described above, there was 1 required break when the individualized feedback was written. To keep track of the dose each participant received, each of the 15 components in the program ( Figure 1 ) is equal to completing 6.7% (1/15) of the program in total.

Sample Size
The trial was designed to detect a medium or large effect size corresponding to a standardized mean difference (Cohen d >0.5) [ 61 ]. An a priori calculation of the estimated sample size, using the software G*Power (G*Power Team) [ 62 ], revealed that a total of 128 participants (64 in each group) were required to enroll in the trial (power=0.80; α=.05; 2-tailed). However, to account for an estimated attrition rate of approximately 30% [ 34 ], it was necessary to enroll a minimum of 128/(1 – 0.3) = 183 participants in the trial. After a total of 204 individuals had been recruited and randomized into 2 study arms, recruitment was ended.
Statistical Analysis
Data were analyzed according to the intention-to-treat (ITT) principle, and all randomized participants were included, irrespective of whether they participated in the trial. The 4 research variables were depression (CES-DC), coping (CPAQ), alcohol use (AUDIT-C), and life status (LoL).
Data analysis consisted of comparing outcome measurements at t 1 and t 2 . The baseline measurement t 0 value was added as an adjustment variable in all models. The resulting data from CPAQ, CES-DC, and LoL were normally distributed and analyzed using linear mixed models. The resulting AUDIT-C scores were nonnormally distributed, with an excess of 0 values, and were analyzed using a 2-part model for longitudinal data. This model is sufficiently flexible to account for numerous 0 reports. This was achieved by combining a logistic generalized linear mixed model (GLMM) for the 0 parts and a skewed continuous GLMM for the non-0 alcohol consumption parts. R-package brms (Bayesian regression models using Stan; R Foundation for Statistical Computing) [ 63 ], a higher-level interface for the probabilistic programming language Stan [ 64 ], and a custom brms family for a marginalized 2-part lognormal distribution were used to fit the model [ 65 ]. The logistic part of the model represents the subject-specific effects on the odds of reporting no drinking. The continuous part was modeled using a gamma GLMM with a log link. The exponentiated treatment effect represents the subject-specific ratio of the total AUDIT-C scores between the treatment and waitlist control groups for those who reported drinking during the specific follow-up period.
Handling of Missing Data
GLMMs include all available data and provide unbiased ITT estimates under the assumption that data are missing at random, meaning that the missing data can be explained by existing data. However, it is impossible to determine whether the data are missing at random or whether the missing data are due to unobserved factors [ 66 ]. Therefore, we also assumed that data were not missing at random, and subsequent sensitivity analyses were performed [ 66 ]. We used the pattern mixture method, which assumes not missing at random, to compare those who completed the follow-up at 6 months (t 2 ) with those who did not (but completed the 2-month follow-up). The overall effect of this model is a combination of the effects of each subgroup. We also tested the robustness of the results by performing ANCOVAs at the 2-month follow-up, both using complete cases and with missing values imputed using multilevel multiple imputation.
The effect of the program was estimated using Cohen d , where a value of approximately 0.2 indicates a small effect size and values of approximately 0.5 and 0.8 indicate medium and large effect sizes, respectively [ 61 ].
Ethical Considerations
All procedures were performed in accordance with the ethical standards of the institutional or national research committees, the 1964 Helsinki Declaration and its later amendments, and comparable ethical standards. Informed consent was obtained from all the participants included in the study. This study was approved by the Swedish Ethical Review Authority (formerly the Regional Ethical Review Board in Stockholm, No. 2011/1648-31/5).
To enhance the response rates, participants received a cinema gift certificate corresponding to approximately EUR 11 (US $12) as compensation for completing each assessment. If a participant completed all assessments, an additional gift certificate was provided. The participants could subsequently receive 4 cinema gift certificates totaling EUR 44 (US $48).
The trial profile is depicted in Figure 1 and reveals that 2722 individuals who were aged between 15 and 19 years performed the screening procedure. A total of 1448 individuals did not fulfill the inclusion criteria and were excluded, leaving 1274 eligible participants. Another 1070 individuals were excluded because they did not provide informed consent or complete the baseline assessment, leaving 204 participants who were allocated to 1 of the 2 study groups. A total of 140 (69%) and 131 (64%) participants completed t 1 and t 2 assessments, respectively. Of the participants in the intervention group (n=101), 63% (n=64) registered an account on the Alcohol and Coping website, 35% (n=35) completed the alcohol intervention section, and 24% (n=24) completed both the alcohol and coping intervention sections.
Sample Characteristics
The mean age of the sample was 17.0 (SD 1.23) years, and the vast majority were female, with both parents born in Sweden and currently working ( Table 1 ). Approximately one-third of the participants reported living with both parents. The mean score on the CAST-6 was 5.33 (SD 0.87) out of a total of 6, and the majority of the sample (147/204, 72.1%) perceived their father to have alcohol problems. Approximately 12% (25/204) had never consumed alcohol, whereas approximately 70% (144/204) had consumed alcohol at a level of intoxication. The mean age at onset was 13.7 (SD 2.07) years and the age at first intoxication was 14.8 (SD 1.56) years. The proportion of participants with symptoms of at least moderate depression was 77.5% (158/204), of whom 55.1% (87/158) had symptoms of severe depression and 42.6% (87/204) had symptoms of dysfunctional coping behaviors. The percentage of participants who consumed alcohol at a risky level was 39.7% (81/204). Table 1 provides complete information regarding the study sample.
a Significance levels calculated by Pearson chi-square statistics for categorical variables and 2-tailed t tests for continuous variables.
Treatment Effects
For the primary outcome, coping behavior (CPAQ), we found a small but inconclusive treatment effect in favor of treatment at both 2 (t 1 ) and 6 (t 2 ) months (Cohen d =–0.05 at both t 1 and t 2 ). For the secondary outcome, alcohol use (AUDIT-C), we found a treatment effect in that the intervention group scored 38% less than the control group on the continuous part (ie, drinking when it occurred) at t 1 and 46% less at t 2 . Regarding depression (CES-DC) and life status (LoL), all between-group comparisons of treatment effects were inconclusive at both follow-up time points ( Table 2 ).
a CPAQ: Coping With Parents Abuse Questionnaire.
b CES-DC: Center for Epidemiological Studies Depression Scale.
c LoL: Ladder of Life.
d AUDIT-C: Alcohol Use Disorders Identification Test.
e N/A: not applicable.
Missing Data
In contrast to the ITT analyses, the sensitivity analyses showed that the treatment group, averaged over the levels of dropout, scored higher (ie, a negative effect) on the main outcome, coping behavior (CPAQ), at t 1 (2.44; P =.20). However, the results remain inconclusive.
Dose-Response Effects
We did not find any evidence for greater involvement in the program being linked to improved outcomes with regard to coping behavior.
We did not find any support for the primary hypothesis: the intervention was not superior to the control condition with regard to coping behavior. Inconclusive results with small effect sizes were observed at both follow-up time points. However, for the secondary outcomes, we found that those in the intervention group who drank alcohol drank approximately 40%-50% less than those in the control group at both follow-ups. These results corroborate previous findings on the precursor face-to-face ICAIP intervention program, demonstrating that participants who received a combined alcohol and coping intervention reported superior outcomes with regard to alcohol-related outcomes compared to participants in the other 2 study arms, who received only a coping or alcohol intervention [ 41 , 42 ]. In contrast to this study, Hansson et al [ 42 ] found that all groups improved their coping skills, although the between-group comparisons were inconclusive and the improvements were maintained over time. These differences could be explained by the different settings in which the precursor program was provided (ie, face-to-face to young adults in a university setting), whereas this study targeted young people (15-19 years of age) through a web-based digital intervention. Additionally, the poor adherence in this study may explain the absence of primary results favoring the intervention group. In a recent study, parents without alcohol problems were recruited to participate in a randomized trial evaluating the web-based SPARE (Supportive Parenting and Reinforcement) program to improve children’s mental health and reduce coparents’ alcohol use. In line with our study, the authors did not find the primary outcome of the SPARE program to be superior to that of the active control group (which received written psychoeducation); however, both groups reported decreased coparental alcohol consumption [ 38 ].
Considering that approximately 3600 children in 2022 participated in various forms of support provided by Swedish municipalities [ 23 ], our recruitment activities reached a large number of eligible individuals, pointing to the potential of finding these children on these platforms. There were unexpectedly high levels of depression among the participants in this study. Although the intervention did not target depressive symptoms per se , there was a trend for the intervention group to have decreased depression levels compared to the control group. A large proportion of participants had symptoms of severe depression, which may have aggravated their capacity for improvement at follow-up [ 28 , 67 ]. Targeting dysfunctional coping patterns could affect an individual’s perceived mental health, and studies have shown that healthy coping strategies positively affect depression and anxiety in a positive way [ 68 ]. Using dysfunctional coping strategies, such as negative self-talk and alcohol consumption, can lead to depressive symptoms [ 69 ]. Targeting these symptoms in the context of healthy and unhealthy coping strategies may be a viable route to fostering appropriate coping strategies that work in the long run. Given that the young people who were reached by the intervention in this study displayed high levels of depression, future interventions for this group should include programs targeting depressive symptoms.
Almost 37% (37/101) of the intervention group did not log into the intervention at all, and only 24% (24/101) of the intervention group participants completed all parts of the program. The fact that a high proportion of the participants had symptoms of severe depression could explain the low adherence. Another reason could be that the initial film-based lectures were too long to maintain the participants’ attention, as the lectures ranged from 8-15 minutes. Yet a final reason could be that we had a 1- to 2-day break built into the intervention, and for unknown reasons, some participants did not log back into the intervention. However, we did not find a dose-response relationship indicating favorable outcomes for those who completed more of the program content. High levels of attrition are not uncommon in self-directed programs such as the one in this study; for example, in a study on a smoking cessation intervention, 37% of the participants never logged into the platform [ 70 ], and in a self-directed intervention for problem gamblers, a majority dropped out after 1 week and none completed the entire program [ 71 ]. Increased intervention adherence is a priority when developing new digital interventions, particularly for young people. One method is to use more persuasive technologies, such as primary tasks, dialogue, and social support [ 72 ]. Considering children whose parents have mental disorders, Grové and Reupert [ 73 ] suggested that digital interventions should include components such as providing information about parental mental illness, access to health care, genetic risk, and suggestions for how children might initiate conversations with parents who have the illness. These suggestions should be considered in future studies on interventions for youths whose parents have substance use problems. Representatives of the target group and other relevant stakeholders should also be involved in coproducing new interventions to increase the probability of developing more engaging programs [ 74 ]. Moreover, one cannot expect study participants to return to the program more than once, and for the sake of adherence, briefer interventions should not encourage participants to log-out for a break. To keep adherence at an acceptable level, similar future interventions for this target group should also consider having symptoms of severe depression as an exclusion criterion [ 28 , 67 ]. Further, to improve adherence, strategies of coproduction could be used where all stakeholders, including the target group, are involved in intervention development [ 75 ]. Other important factors identified to improve adherence to digital interventions are to make the content relatable, useful, and even more interactive [ 76 ]. Those participants who have symptoms of severe depression should be referred to other appropriate health care. Finally, it is probably beneficial to develop shorter psychoeducative film-based lectures than ours, lasting up to 15 minutes. Future self-directed digital interventions targeting this population should, therefore, focus on a very brief and focused intervention, which, based on theory, has the potential to foster healthy coping behaviors that can lead to an increased quality of life and improved mental health for this group of young people.
Another concern for future projects would be to use a data-driven approach during the program development phase, where A/B testing can be used to test different setups of the program to highlight which setup works best. Another aspect that must be considered is the fast-changing world of technology, where young people are exposed to an infinite number of different apps that grab their attention, which also calls for interventions to be short and to the point. Furthermore, if the program is to spread and become generally available, one must consider that keeping the program alive for a longer period will require funding and staffing for both product management and technical support.
Strengths and Limitations
This study had several strengths. First, Alcohol and Coping is a web-based intervention program, and it appears as if the internet is a particularly promising way to provide support to adolescents growing up with parents with alcohol problems because it offers an anonymous means of communicating and makes intervention programs readily accessible [ 25 ]. Our recruitment strategies reached a considerable number of interested and eligible individuals, demonstrating the potential for recruiting through social media and other web platforms. Additionally, this program is one of the first brief web-based interventions aimed at adolescents with parents with alcohol-related problems. We used the CAST-6, which has been validated among Swedish adolescents [ 47 ], to screen eligible participants. Another strength is that the intervention program involved personalized, tailored feedback in the form of prewritten automatic messages and therapist-written personalized feedback, both of which have proven to be important components of web-based interventions aimed at adolescents [ 77 , 78 ]. Finally, this study evaluated the effectiveness of the Alcohol and Coping program using a randomized controlled trial design, which is considered the strongest experimental design with regard to allocation bias.
This study had some limitations. First, the design with a passive waitlist control group and an active intervention group, both unblinded to study allocation, may have resulted in biased estimates of treatment effects. Intervention adherence was low, and most of the study participants had symptoms of depression, where 55% (87/158) had symptoms of severe depression. This may have contributed to the small and overall inconclusive effects on the primary outcomes of this study. Many digital interventions have problems with low adherence, and in a review by Välimäki et al [ 79 ], some studies reported adherence rates as low as 10%. A vast proportion of the study participants were women, making the findings difficult to generalize to men. However, another limitation concerns selection bias and external validity. We recruited study participants through social media and other relevant websites containing health-related information, including information about parents with alcohol-related problems. It is, therefore, possible that the study population can be classified as “information-seeking” adolescents, who may have different personality traits relative to other adolescents in the same home situation. Additionally, as an inclusion criterion was having ready access to computers and the internet, it is possible that participants belonging to a lower socioeconomic class were underrepresented in the study. It should also be noted that the data presented here were collected approximately 10 years ago. However, we believe our findings make an important contribution to the field since, like our intervention, many recent web-based interventions use strategies of psychoeducation, films, exercises, questions, and feedback. Further, the number of web-based interventions for this target group remains scarce in the literature, which underscores the need for future research. Finally, the study was powered to detect a medium effect size. However, given the small effect sizes detected in this study, it is plausible that too few participants were recruited to detect differences between the groups.
Implications for Practice
Although growing up with parents who have alcohol problems per se is not sufficient for developing psychosocial disorders, many children need support to manage their situation. Therefore, it is difficult to recruit children to support these groups. In Sweden, not even 2% of all children growing up with parental alcohol problems attend face-to-face support groups provided by municipalities.
Offering support through web-based intervention programs seems particularly attractive to adolescents whose parents have alcohol-related problems. To date, evidence for such programs is scarce, and there is an urgent need to develop and evaluate digital interventions targeting this group of adolescents. This study makes important contributions to this novel field of research. The results provide insight into effective strategies for delivering intervention programs to children of parents with substance abuse issues, highlighting the potential for digital interventions to reach a vulnerable, hard-to-reach group of adolescents. Our findings underscore the need to develop more engaging interventions in coproduction with the target group.
Conclusions
We found that a digital therapist-assisted self-management intervention for adolescents whose parents have alcohol use problems contributed to a reduction in the adolescents’ own alcohol consumption. This result highlights the potential for digital interventions to reach a large, vulnerable, and hard-to-reach group of adolescents with support efforts. Findings were inconclusive for all other outcomes, which may be attributable to low adherence. This points to the need for future research on developing more engaging digital interventions to increase adherence among adolescents.
Acknowledgments
This work was undertaken on behalf of the Swedish Council for Information on Alcohol and Other Drugs (CAN) and was supported by grants from the Swedish National Institute of Public Health and the Swedish Council for Working Life and Social Research.
Conflicts of Interest
HH and UZ developed the study interventions. However, the parties did not derive direct financial income from these interventions. HW, PK, and THE declare no conflicts of interest.
CONSORT-eHEALTH checklist (V 1.6.1).
- Haugland SH, Elgán TH. Prevalence of parental alcohol problems among a general population sample of 28,047 Norwegian adults: evidence for a socioeconomic gradient. Int J Environ Res Public Health. 2021;18(10):5412. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Elgán TH, Leifman H. Prevalence of adolescents who perceive their parents to have alcohol problems: a Swedish national survey using a web panel. Scand J Public Health. 2013;41(7):680-683. [ CrossRef ] [ Medline ]
- Laslett AM, Ferris J, Dietze P, Room R. Social demography of alcohol-related harm to children in Australia. Addiction. 2012;107(6):1082-1089. [ CrossRef ] [ Medline ]
- Manning V, Best DW, Faulkner N, Titherington E. New estimates of the number of children living with substance misusing parents: results from UK national household surveys. BMC Public Health. 2009;9:377. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Grant BF. Estimates of US children exposed to alcohol abuse and dependence in the family. Am J Public Health. 2000;90(1):112-115. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Raninen J, Elgán TH, Sundin E, Ramstedt M. Prevalence of children whose parents have a substance use disorder: findings from a Swedish general population survey. Scand J Public Health. 2016;44(1):14-17. [ CrossRef ] [ Medline ]
- Christoffersen MN, Soothill K. The long-term consequences of parental alcohol abuse: a cohort study of children in Denmark. J Subst Abuse Treat. 2003;25(2):107-116. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Martikainen PN, Korhonen K, Moustgaard H, Aaltonen M, Remes H. Substance abuse in parents and subsequent risk of offspring psychiatric morbidity in late adolescence and early adulthood: a longitudinal analysis of siblings and their parents. Soc Sci Med. 2018;217:106-111. [ CrossRef ] [ Medline ]
- Jääskeläinen M, Holmila M, Notkola IL, Raitasalo K. Mental disorders and harmful substance use in children of substance abusing parents: a longitudinal register-based study on a complete birth cohort born in 1991. Drug Alcohol Rev. 2016;35(6):728-740. [ CrossRef ] [ Medline ]
- Velleman R, Templeton LJ. Impact of parents' substance misuse on children: an update. BJPsych Adv. Apr 11, 2018;22(2):108-117. [ FREE Full text ] [ CrossRef ]
- Ohannessian CM, Hesselbrock VM, Kramer J, Bucholz KK, Schuckit MA, Kuperman S, et al. Parental substance use consequences and adolescent psychopathology. J Stud Alcohol. 2004;65(6):725-730. [ CrossRef ] [ Medline ]
- Johnson JL, Leff M. Children of substance abusers: overview of research findings. Pediatrics. 1999;103(5 Pt 2):1085-1099. [ CrossRef ] [ Medline ]
- Berg L, Bäck K, Vinnerljung B, Hjern A. Parental alcohol-related disorders and school performance in 16-year-olds-a Swedish national cohort study. Addiction. 2016;111(10):1795-1803. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Casas-Gil MJ, Navarro-Guzman JI. School characteristics among children of alcoholic parents. Psychol Rep. 2002;90(1):341-348. [ CrossRef ] [ Medline ]
- McGrath CE, Watson AL, Chassin L. Academic achievement in adolescent children of alcoholics. J Stud Alcohol. 1999;60(1):18-26. [ CrossRef ] [ Medline ]
- Velleman R, Templeton L, Reuber D, Klein M, Moesgen D. Domestic abuse experienced by young people living in families with alcohol problems: results from a cross‐european study. Child Abuse Rev. Nov 24, 2008;17(6):387-409. [ CrossRef ]
- Rothman EF, Edwards EM, Heeren T, Hingson RW. Adverse childhood experiences predict earlier age of drinking onset: results from a representative US sample of current or former drinkers. Pediatrics. 2008;122(2):e298-e304. [ CrossRef ] [ Medline ]
- Anda RF, Whitfield CL, Felitti VJ, Chapman D, Edwards VJ, Dube SR, et al. Adverse childhood experiences, alcoholic parents, and later risk of alcoholism and depression. Psychiatr Serv. 2002;53(8):1001-1009. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Straussner SLA, Fewell CH. A review of recent literature on the impact of parental substance use disorders on children and the provision of effective services. Curr Opin Psychiatry. 2018;31(4):363-367. [ CrossRef ] [ Medline ]
- Calhoun S, Conner E, Miller M, Messina N. Improving the outcomes of children affected by parental substance abuse: a review of randomized controlled trials. Subst Abuse Rehabil. 2015;6:15-24. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Emshoff JG, Price AW. Prevention and intervention strategies with children of alcoholics. Pediatrics. 1999;103(5 Pt 2):1112-1121. [ CrossRef ] [ Medline ]
- Cuijpers P. Prevention programmes for children of problem drinkers: a review. Drugs Educ Prev Policy. 2009;12(6):465-475. [ CrossRef ]
- Wannberg H. Plats för barnen—Om kommunernas stöd till barn som växer upp med missbrukande föräldrar [Make room for the children—municipalities and their support for children who grow up with parents with substance abuse]. Stockholm, Sweden. Junis, IOGT-NTO's ungdomsförbund; 2023.
- Elgán TH, Leifman H. Children of substance abusing parents: a national survey on policy and practice in Swedish schools. Health Policy. 2011;101(1):29-36. [ CrossRef ] [ Medline ]
- de Sousa D, Fogel A, Azevedo J, Padrão P. The effectiveness of web-based interventions to promote health behaviour change in adolescents: a systematic review. Nutrients. 2022;14(6):1258. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Andersson G. Internet-delivered psychological treatments. Annu Rev Clin Psychol. 2016;12:157-179. [ FREE Full text ] [ CrossRef ] [ Medline ]
- King R, Bambling M, Lloyd C, Gomurra R, Smith S, Reid W, et al. Online counselling: the motives and experiences of young people who choose the internet instead of face to face or telephone counselling. Couns Psychother Res. 2007;6(3):169-174. [ CrossRef ]
- Borghouts J, Eikey E, Mark G, De Leon C, Schueller SM, Schneider M, et al. Barriers to and facilitators of user engagement with digital mental health interventions: systematic review. J Med Internet Res. 2021;23(3):e24387. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Boggs JM, Beck A, Felder JN, Dimidjian S, Metcalf CA, Segal ZV. Web-based intervention in mindfulness meditation for reducing residual depressive symptoms and relapse prophylaxis: a qualitative study. J Med Internet Res. 2014;16(3):e87. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hedman-Lagerlöf E, Carlbring P, Svärdman F, Riper H, Cuijpers P, Andersson G. Therapist-supported internet-based cognitive behaviour therapy yields similar effects as face-to-face therapy for psychiatric and somatic disorders: an updated systematic review and meta-analysis. World Psychiatry. 2023;22(2):305-314. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lehtimaki S, Martic J, Wahl B, Foster KT, Schwalbe N. Evidence on digital mental health interventions for adolescents and young people: systematic overview. JMIR Ment Health. 2021;8(4):e25847. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Li J, Theng YL, Foo S. Game-based digital interventions for depression therapy: a systematic review and meta-analysis. Cyberpsychol Behav Soc Netw. 2014;17(8):519-527. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Pennant ME, Loucas CE, Whittington C, Creswell C, Fonagy P, Fuggle P, et al. Computerised therapies for anxiety and depression in children and young people: a systematic review and meta-analysis. Behav Res Ther. 2015;67:1-18. [ CrossRef ] [ Medline ]
- Woolderink M, Smit F, van der Zanden R, Beecham J, Knapp M, Paulus A, et al. Design of an internet-based health economic evaluation of a preventive group-intervention for children of parents with mental illness or substance use disorders. BMC Public Health. 2010;10:470. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Elgán TH, Kartengren N, Strandberg AK, Ingemarson M, Hansson H, Zetterlind U, et al. A web-based group course intervention for 15-25-year-olds whose parents have substance use problems or mental illness: study protocol for a randomized controlled trial. BMC Public Health. 2016;16(1):1011. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Maybery D, Reupert A, Bartholomew C, Cuff R, Duncan Z, Foster K, et al. A web-based intervention for young adults whose parents have a mental illness or substance use concern: protocol for a randomized controlled trial. JMIR Res Protoc. 2020;9(6):e15626. [ FREE Full text ] [ CrossRef ] [ Medline ]
- EÉk N, Romberg K, Siljeholm O, Johansson M, Andreasson S, Lundgren T, et al. Efficacy of an internet-based community reinforcement and family training program to increase treatment engagement for AUD and to improve psychiatric health for CSOs: a randomized controlled trial. Alcohol Alcohol. 2020;55(2):187-195. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Siljeholm O, Lindner P, Johansson M, Hammarberg A. An online self-directed program combining Community Reinforcement Approach and Family Training and parenting training for concerned significant others sharing a child with a person with problematic alcohol consumption: a randomized controlled trial. Addict Sci Clin Pract. 2022;17(1):49. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Woolderink M. Mind the gap: evaluation of an online preventive programme for adolescents with mentally ill or addicted parents. Maastricht University. 2016. URL: https://cris.maastrichtuniversity.nl/ws/portalfiles/portal/7281149/c5531.pdf [accessed 2024-03-14]
- Maybery D, Reupert A, Bartholomew C, Cuff R, Duncan Z, McAuliffe C, et al. An online intervention for 18-25-year-old youth whose parents have a mental illness and/or substance use disorder: a pilot randomized controlled trial. Early Interv Psychiatry. 2022;16(11):1249-1258. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hansson H, Rundberg J, Zetterlind U, Johnsson KO, Berglund M. An intervention program for university students who have parents with alcohol problems: a randomized controlled trial. Alcohol Alcohol. 2006;41(6):655-663. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hansson H, Rundberg J, Zetterlind U, Johnsson KO, Berglund M. Two-year outcome of an intervention program for university students who have parents with alcohol problems: a randomized controlled trial. Alcohol Clin Exp Res. 2007;31(11):1927-1933. [ CrossRef ] [ Medline ]
- Zetterlind U, Hansson H, Aberg-Orbeck K, Berglund M. Effects of coping skills training, group support, and information for spouses of alcoholics: a controlled randomized study. Nord J Psychiatry. 2001;55(4):257-262. [ CrossRef ] [ Medline ]
- Hansson H, Zetterlind U, Aberg-Orbeck K, Berglund M. Two-year outcome of coping skills training, group support and information for spouses of alcoholics: a randomized controlled trial. Alcohol Alcohol. 2004;39(2):135-140. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hodgins DC, Maticka-Tyndale E, El-Guebaly N, West M. The CAST-6: development of a short-form of the Children of Alcoholics Screening Test. Addict Behav. 1993;18(3):337-345. [ CrossRef ] [ Medline ]
- Hodgins DC, Shimp L. Identifying adult children of alcoholics: methodological review and a comparison of the CAST-6 with other methods. Addiction. 1995;90(2):255-267. [ Medline ]
- Elgán TH, Berman AH, Jayaram-Lindström N, Hammarberg A, Jalling C, Källmén H. Psychometric properties of the short version of the children of alcoholics screening test (CAST-6) among Swedish adolescents. Nord J Psychiatry. 2021;75(2):155-158. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Orford J, Guthrie S, Nicholls P, Oppenheimer E, Egert S, Hensman C. Self-reported coping behavior of wives of alcoholics and its association with drinking outcome. J Stud Alcohol. 1975;36(9):1254-1267. [ CrossRef ] [ Medline ]
- Schoenbach VJ, Kaplan BH, Grimson RC, Wagner EH. Use of a symptom scale to study the prevalence of a depressive syndrome in young adolescents. Am J Epidemiol. 1982;116(5):791-800. [ CrossRef ] [ Medline ]
- Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med. 1998;158(16):1789-1795. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Myers JK, Weissman MM. Use of a self-report symptom scale to detect depression in a community sample. Am J Psychiatry. 1980;137(9):1081-1084. [ CrossRef ] [ Medline ]
- Olsson G, von Knorring AL. Depression among Swedish adolescents measured by the self-rating scale Center for Epidemiology Studies-Depression Child (CES-DC). Eur Child Adolesc Psychiatry. 1997;6(2):81-87. [ CrossRef ] [ Medline ]
- Fendrich M, Weissman MM, Warner V. Screening for depressive disorder in children and adolescents: validating the Center for Epidemiologic Studies Depression Scale for Children. Am J Epidemiol. 1990;131(3):538-551. [ CrossRef ] [ Medline ]
- Bergman H, Källmen H, Rydberg U, Sandahl C. Tio frågor om alkohol identifierar beroendeproblem. Psykometrisk prövning på psykiatrisk akutmottagning [Ten questions about alcohol as identifier of addiction problems. Psychometric tests at an emergency psychiatric department]. Läkartidningen. 1998;95(43):4731-4735. [ FREE Full text ]
- Källmén H, Berman AH, Jayaram-Lindström N, Hammarberg A, Elgán TH. Psychometric properties of the AUDIT, AUDIT-C, CRAFFT and ASSIST-Y among Swedish adolescents. Eur Addict Res. 2019;25(2):68-77. [ CrossRef ] [ Medline ]
- Andrews FM, Withey SB. Developing measures of perceived life quality: results from several national surveys. Soc Indic Res. 1974;1(1):1-26. [ CrossRef ]
- Nagy E. Barns känsla av sammanhang—En valideringsstudie av BarnKASAM i årskurserna 1-6 (ålder 7-12 år) [Children's sense of coherence—a study validating SOC for children in grades 1-6 (7-12 years old)]. Lunds Universitet [Lund University]. 2004. URL: https://lup.lub.lu.se/luur/download?func=downloadFile&recordOId=1358959&fileOId=1358960 [accessed 2024-03-14]
- Saghaei M. Random allocation software for parallel group randomized trials. BMC Med Res Methodol. 2004;4:26. [ FREE Full text ] [ CrossRef ] [ Medline ]
- drugsmart. URL: https://www.drugsmart.se/ [accessed 2024-03-19]
- Dimeff LA, Baer JS, Kivlahan DR, Marlatt GA. Brief Alcohol Screening and Intervention for College Students: A Harm Reduction Approach. New York. The Guilford Press; 1999.
- Cohen J. A power primer. Psychol Bull. 1992;112(1):155-159. [ CrossRef ] [ Medline ]
- Faul F, Erdfelder E, Lang A, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175-191. [ CrossRef ] [ Medline ]
- Bürkner PC. brms: an R package for bayesian multilevel models using stan. J Stat Soft. 2017;80(1):1-28. [ FREE Full text ] [ CrossRef ]
- Carpenter B, Gelman A, Hoffman MD, Lee D, Goodrich B, Betancourt M, et al. Stan: a probabilistic programming language. J Stat Softw. 2017;76(1):1-32. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Magnusson K, Nilsson A, Carlbring P. Modeling longitudinal gambling data: challenges and opportunities. PsyArxiv. Preprint posted online on September 12, 2019. [ FREE Full text ] [ CrossRef ]
- Coertjens L, Donche V, De Maeyer S, Vanthournout G, Van Petegem P. To what degree does the missing-data technique influence the estimated growth in learning strategies over time? A tutorial example of sensitivity analysis for longitudinal data. PLoS One. 2017;12(9):e0182615. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kunas SL, Lautenbacher LM, Lueken PU, Hilbert K. Psychological predictors of cognitive-behavioral therapy outcomes for anxiety and depressive disorders in children and adolescents: a systematic review and meta-analysis. J Affect Disord. 2021;278:614-626. [ CrossRef ] [ Medline ]
- Stallman HM, Lipson SK, Zhou S, Eisenberg D. How do university students cope? An exploration of the health theory of coping in a US sample. J Am Coll Health. 2022;70(4):1179-1185. [ CrossRef ] [ Medline ]
- Stallman HM, Beaudequin D, Hermens DF, Eisenberg D. Modelling the relationship between healthy and unhealthy coping strategies to understand overwhelming distress: a Bayesian network approach. J Affect Disord Rep. 2021;3:100054. [ FREE Full text ] [ CrossRef ]
- McClure JB, Shortreed SM, Bogart A, Derry H, Riggs K, St John J, et al. The effect of program design on engagement with an internet-based smoking intervention: randomized factorial trial. J Med Internet Res. 2013;15(3):e69. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Humphrey G, Bullen C. Smartphone-based problem gambling evaluation and technology testing initiative ('SPGeTTI'): final report reference 354913/00 for the Ministry of Health. National Institute for Health Innovation (NIHI), Auckland UniServices Ltd, The Univerisy of Auckland. 2019. URL: https://www.health.govt.nz/system/files/documents/publications/20190424-spgetti-354913-00-final-report.pdf [accessed 2024-03-14]
- Kelders SM, Kok RN, Ossebaard HC, Van Gemert-Pijnen JEWC. Persuasive system design does matter: a systematic review of adherence to web-based interventions. J Med Internet Res. 2012;14(6):e152. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Grové C, Reupert A. Moving the field forward: developing online interventions for children of parents with a mental illness. Child Youth Serv Rev. 2017;82:354-358. [ CrossRef ]
- Moffat BM, Haines-Saah RJ, Johnson JL. From didactic to dialogue: assessing the use of an innovative classroom resource to support decision-making about cannabis use. Drugs Educ Prev Policy. 2016;24(1):85-95. [ FREE Full text ] [ CrossRef ]
- Bevan Jones R, Stallard P, Agha SS, Rice S, Werner-Seidler A, Stasiak K, et al. Practitioner review: co-design of digital mental health technologies with children and young people. J Child Psychol Psychiatry. 2020;61(8):928-940. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Garrido S, Millington C, Cheers D, Boydell K, Schubert E, Meade T, et al. What works and what doesn't work? A systematic review of digital mental health interventions for depression and anxiety in young people. Front Psychiatry. 2019;10:759. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Crutzen R, de Nooijer J, Brouwer W, Oenema A, Brug J, de Vries NK. Strategies to facilitate exposure to internet-delivered health behavior change interventions aimed at adolescents or young adults: a systematic review. Health Educ Behav. 2011;38(1):49-62. [ CrossRef ] [ Medline ]
- Milward J, Drummond C, Fincham-Campbell S, Deluca P. What makes online substance-use interventions engaging? A systematic review and narrative synthesis. Digit Health. 2018;4:2055207617743354. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Välimäki M, Anttila K, Anttila M, Lahti M. Web-based interventions supporting adolescents and young people with depressive symptoms: systematic review and meta-analysis. JMIR Mhealth Uhealth. 2017;5(12):e180. [ FREE Full text ] [ CrossRef ] [ Medline ]
Abbreviations
Edited by YH Lin; submitted 24.08.23; peer-reviewed by X Zhang, C Asuzu, D Liu; comments to author 28.01.24; revised version received 08.02.24; accepted 27.02.24; published 10.04.24.
©Håkan Wall, Helena Hansson, Ulla Zetterlind, Pia Kvillemo, Tobias H Elgán. Originally published in the Journal of Medical Internet Research (https://www.jmir.org), 10.04.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the Journal of Medical Internet Research, is properly cited. The complete bibliographic information, a link to the original publication on https://www.jmir.org/, as well as this copyright and license information must be included.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 10 May 2023
Mental health awareness: uniting advocacy and research
Nature Mental Health volume 1 , pages 295–296 ( 2023 ) Cite this article
3242 Accesses
6 Altmetric
Metrics details
Mental Health Month has been observed to reduce the stigma that is associated with mental illness and to educate the public and encourage individuals to make their mental health and wellbeing a priority. It is an important moment to bring the strengths of advocacy groups and researchers together to promote mental health awareness and to improve equity.
Observances have become a popular tool to garner media and notice for topics deserving attention, from medical conditions to public health concerns, commemoration of notable events, or celebration of cultural groups. Codifying the scope and needs connected to an issue or illness through awareness campaigns can provide opportunities for imparting useful information, reducing stigma and marshalling support for policy change. The impact of awareness campaigns can be difficult to measure beyond tallying social media mentions or news stories. Effective advocacy, however, extends beyond traffic and paves the way for the creation of knowledge and partnerships among allies and with those whose interests are being represented. When the magnitude of an issue and the potential for improvement are great and are matched by broad involvement and recognition by stakeholders, the possibility for impact is also great.

Held annually in May, Mental Health Month , also called Mental Health Awareness Month, is an observance with such reach, resonating with many people. Nearly everyone has experience with the challenges that are associated with mental health, either first-hand or through loved ones or in their community. There is a need for education, support and initiative to improve our understanding of the causes of mental health disorders and to increase the availability of resources for prevention and treatment. Mental Health Month also offers the possibility of bringing together groups who often work in parallel, such as mental health advocates and mental health research organizations, that can mutually benefit from each other’s functions and expertise.
Mental Health Month was first established in the US in 1949 by the National Mental Health Association, now known as Mental Health America . At a time more often associated with the outset of the Cold War and Marshall Plan than setting an agenda for domestic mental health and wellbeing advocacy, in the more than 70 years since, Mental Health Month has grown into an international event designed to reduce exclusion, stigma and discrimination against people with mental health conditions or disorders. Mental Health America are joined by other prominent mental health advocacy groups to sponsor related observances: Mental Health Awareness Week Canada (1–7 May, 2023) and Europe (22–28 May, 2023); and federal agencies such as the Substance Use Abuse and Mental Health Services Administration ( SAMSHA ) in the US, promoting related public education platforms, including National Prevention Week (7–13 May, 2023).
Observances and awareness campaigns also provide occasions to put mental health in context. Increasing acknowledgment of the role of social determinants, for example, as mechanisms that can increase vulnerability for developing disorders and that drive disparities in mental health are an important framework to underscore as part of promoting mental health awareness. Given the complex and broad scope of people, disorders, conditions and issues under the umbrella of mental health, observances also give us the chance to focus more closely on specific problems or experiences. The theme for Mental Health Month in 2023 is ‘Look Around, Look Within’, which emphasizes the interdependence of mental health and wellness with an individual’s internal and external experiences and environments.
“The ‘Look Around, Look Within’ theme builds on the growing recognition that all humans have mental health needs and that our available resources to build resilience and heal come in many forms — including in the natural world,” explains Jennifer Bright, Mental Health America Board Chair and President of Momentum Health Strategies. “Mental Health America’s strategic plan, focused on NextGen Prevention, carries a similar theme — that the social factors supporting mental health are essential building blocks. These encompass basic needs like healthy food, stable housing, and access to treatment and supports, but they also include spirituality, connection with peers with lived experience, and safe and natural spaces.”
Overlapping with Mental Health Month, Mental Health Foundation sponsors Mental Health Week in the UK (15–21 May, 2023), dedicating this year to raising awareness around anxiety. It shares an individual-centered approach to advocacy. In addition to providing toolkits and resources that point to how prevalent stress and anxiety can be to reduce stigma, it also promotes the accessibility of coping strategies for managing anxiety. As part of the Mental Health Awareness Week campaign, Mental Health Foundation and others use the international symbol of wearing a green ribbon or clothing to physically raise awareness around mental health. Nature Mental Health also incorporates the symbol of the green ribbon on the cover of this month’s issue and as our journal theme color. Green evokes the ideas of vitality, growth, new beginnings and hope — powerful imagery in mental health awareness.
Alongside stories, sponsorships and social media resources, mental health advocacy toolkits and strategy documents include fact sheets and messaging that are shaped and informed by research. Yet, there is often a perception that a divide exists between the mental health advocacy and research spaces, but observances such as Mental Health Month can bridge the two.
According to Lea Milligan, Chief Executive Officer of MQ: Transforming Mental Health , an international mental health research organization, there are complementary approaches and priorities in advocacy and research: “Mental health research can be used to bolster awareness by providing evidence-based information and resources that can help individuals and communities better understand mental health and the factors that contribute to mental health problems. This can include information on risk factors, prevention strategies, and available treatments.”
In addition, increased efforts to involve people with lived experience of mental illness in the research enterprise is a goal that is well-served through connection with advocacy. “While MQ is primarily focused on promoting mental health research, it also recognizes the importance of advocacy in advancing the mental health agenda” suggests Milligan. “MQ advocates for increased funding and support for mental health research, as well as policies that promote mental health and wellbeing. Additionally, MQ seeks to empower individuals with lived experience of mental health conditions to be involved in research and advocacy efforts, and to have their voices heard in the development of policies and programs that affect their lives. MQ provides resources and support for individuals with lived experience who wish to be involved in research or advocacy efforts, including training programs, research grants, and opportunities to participate in research studies.”
Involvement or engagement is certainly one of the most important metrics of advocacy. By strengthening collaboration between advocacy and research organizations and identifying the mutual areas of benefit, such as engagement and increased funding, we may find new ways to green light mental health awareness and action toward mental health equity.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Mental health awareness: uniting advocacy and research. Nat. Mental Health 1 , 295–296 (2023). https://doi.org/10.1038/s44220-023-00072-6
Download citation
Published : 10 May 2023
Issue Date : May 2023
DOI : https://doi.org/10.1038/s44220-023-00072-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

COMMENTS
Scope of Mental Health Promotion and Prevention in the Current Situation. Literature provides considerable evidence on the effectiveness of various preventive mental health interventions targeting risk and protective factors for various mental illnesses (18, 36-42).There is also modest evidence of the effectiveness of programs focusing on early identification and intervention for severe ...
Although most mental-health disorders arise during adolescence, UNICEF says that only one-third of investment in mental-health research is targeted towards young people. Moreover, the research ...
Mental health professionals can help craft messages to be delivered by trusted leaders. 4. The Covid-19 pandemic has alarming implications for individual and collective health and emotional and ...
Three years into the COVID-19 outbreak in the United States, Pew Research Center published this collection of survey findings about Americans' challenges with mental health during the pandemic.All findings are previously published. Methodological information about each survey cited here, including the sample sizes and field dates, can be found by following the links in the text.
D2/D3 dopamine supports the precision of mental state inferences and self-relevance of joint social outcomes. In this article, the authors demonstrate that haloperidol D2/D3 dopamine antagonism ...
To provide a contemporary global prevalence of mental health issues among the general population amid the coronavirus disease-2019 (COVID-19) pandemic. We searched electronic databases, preprint ...
Mindfulness-Based Stress Reduction vs Escitalopram for the Treatment of Anxiety Disorders. 5,841. Formerly Archives of General Psychiatry. Explore the latest science of anxiety, autism, depression, OCD, psychosis, psychotherapy, schizophrenia, and more.
Mental Health Literacy (MHL) is the ability to recognise mental disorders, have knowledge of professional help available, effective self-help strategies, skills to give support to others, and knowledge of how ... Sandra Jumbe, Joel Nyali and Chris Newby. International Journal of Mental Health Systems 2023 17 :14.
Objective Lack of consensus on the definition of mental health has implications for research, policy and practice. This study aims to start an international, interdisciplinary and inclusive dialogue to answer the question: What are the core concepts of mental health? Design and participants 50 people with expertise in the field of mental health from 8 countries completed an online survey.
Read the latest research as well as in-depth information on clinical depression, schizophrenia, bipolar disorder, ADHD and other mental health disorders in adults, teens, and children.
Published March 1, 2024. Forgiveness is defined by replacing ill will toward an offender with goodwill. A 2023 study suggests forgiveness boosts mental health by reducing depression and anxiety levels. Other evidence suggests physical benefits as well. Studies indicate forgiveness also eases stress, improves sleep, and lowers blood pressure and ...
On a global scale and based on imputations and modeling from survey data of self-reported mental health problems, the Global Burden of Disease (GBD) study 29 estimated that the COVID-19 pandemic ...
The World Health Organization today released its largest review of world mental health since the turn of the century. The detailed work provides a blueprint for governments, academics, health professionals, civil society and others with an ambition to support the world in transforming mental health. In 2019, nearly a billion people - including 14% of the world's adolescents - were living ...
For the general population, public health emergencies and disasters (e.g., natural disasters; infectious disease outbreaks; Chemical, Biological, Radiological or Nuclear incidents) can give rise to a plethora of negative outcomes relating to both health (e.g. increased mental health problems [1,2,3,4]) and the economy (e.g., increased unemployment and decreased levels of tourism [4,5,6]).
Worldwide surveys done in 2020 and 2021 found higher than typical levels of stress, insomnia, anxiety and depression. By 2022, levels had lowered but were still higher than before 2020. Though feelings of distress about COVID-19 may come and go, they are still an issue for many people. You aren't alone if you feel distress due to COVID-19.
It can arm researchers and mental health advocates in their call for a larger focus and innovation in the prevention of mental illness to reduce the burden on mental healthcare systems 36,37,38.
A report from the Department of Health and Human Services' inspector general finds a dire shortage of mental health care providers in Medicaid and Medicare, which together serve some 40% of Americans.
Depression is one of the most common mental health disorders in the US. About 18% of American adults - more than 1 in 6 - say they are depressed or receiving treatment for depression, a 2023 ...
ABSTRACT. Background: Research indicates refugees from the Democratic Republic of Congo (DRC), particularly females, have a higher incidence of mental health problems compared to the global norm for conflict-affected populations. Objective: This study aimed to unpack gender differences in the mental health of Congolese refugees by examining specific risk (trauma exposure, adaptation challenges ...
41%. Percentage of teens with the highest social media use who rate their overall mental health as poor or very poor, compared with 23% of those with the lowest use. For example, 10% of the highest use group expressed suicidal intent or self-harm in the past 12 months compared with 5% of the lowest use group, and 17% of the highest users expressed poor body image compared with 6% of the lowest ...
We offer several suggestions that could be addressed to improve pilots' physical and mental health. However, more research is needed to compare standard health measures for pilots around the world in order to improve their physical and mental health and contribute to overall aviation safety. Keywords: Occupational Health, Mental Health, ...
Using the Department of Health and Human Services regulations found at 45 CFR 46.101(b)(4), the Biomedical Research Alliance of New York LLC Institutional Review Board (IRB) determined that this ...
Background: Children whose parents have alcohol use problems are at an increased risk of several negative consequences, such as poor school performance, an earlier onset of substance use, and poor mental health. Many would benefit from support programs, but the figures reveal that only a small proportion is reached by existing support. Digital interventions can provide readily accessible ...
Mental health awareness: uniting advocacy and research. Nature Mental Health 1 , 295-296 ( 2023) Cite this article. Mental Health Month has been observed to reduce the stigma that is associated ...