Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character

Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- April 01, 2024 | VOL. 181, NO. 4 CURRENT ISSUE pp.255-346
- March 01, 2024 | VOL. 181, NO. 3 pp.171-254
- February 01, 2024 | VOL. 181, NO. 2 pp.83-170
- January 01, 2024 | VOL. 181, NO. 1 pp.1-82
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Substance Use Disorders and Addiction: Mechanisms, Trends, and Treatment Implications
- Ned H. Kalin , M.D.
Search for more papers by this author
The numbers for substance use disorders are large, and we need to pay attention to them. Data from the 2018 National Survey on Drug Use and Health ( 1 ) suggest that, over the preceding year, 20.3 million people age 12 or older had substance use disorders, and 14.8 million of these cases were attributed to alcohol. When considering other substances, the report estimated that 4.4 million individuals had a marijuana use disorder and that 2 million people suffered from an opiate use disorder. It is well known that stress is associated with an increase in the use of alcohol and other substances, and this is particularly relevant today in relation to the chronic uncertainty and distress associated with the COVID-19 pandemic along with the traumatic effects of racism and social injustice. In part related to stress, substance use disorders are highly comorbid with other psychiatric illnesses: 9.2 million adults were estimated to have a 1-year prevalence of both a mental illness and at least one substance use disorder. Although they may not necessarily meet criteria for a substance use disorder, it is well known that psychiatric patients have increased usage of alcohol, cigarettes, and other illicit substances. As an example, the survey estimated that over the preceding month, 37.2% of individuals with serious mental illnesses were cigarette smokers, compared with 16.3% of individuals without mental illnesses. Substance use frequently accompanies suicide and suicide attempts, and substance use disorders are associated with a long-term increased risk of suicide.
Addiction is the key process that underlies substance use disorders, and research using animal models and humans has revealed important insights into the neural circuits and molecules that mediate addiction. More specifically, research has shed light onto mechanisms underlying the critical components of addiction and relapse: reinforcement and reward, tolerance, withdrawal, negative affect, craving, and stress sensitization. In addition, clinical research has been instrumental in developing an evidence base for the use of pharmacological agents in the treatment of substance use disorders, which, in combination with psychosocial approaches, can provide effective treatments. However, despite the existence of therapeutic tools, relapse is common, and substance use disorders remain grossly undertreated. For example, whether at an inpatient hospital treatment facility or at a drug or alcohol rehabilitation program, it was estimated that only 11% of individuals needing treatment for substance use received appropriate care in 2018. Additionally, it is worth emphasizing that current practice frequently does not effectively integrate dual diagnosis treatment approaches, which is important because psychiatric and substance use disorders are highly comorbid. The barriers to receiving treatment are numerous and directly interact with existing health care inequities. It is imperative that as a field we overcome the obstacles to treatment, including the lack of resources at the individual level, a dearth of trained providers and appropriate treatment facilities, racial biases, and the marked stigmatization that is focused on individuals with addictions.
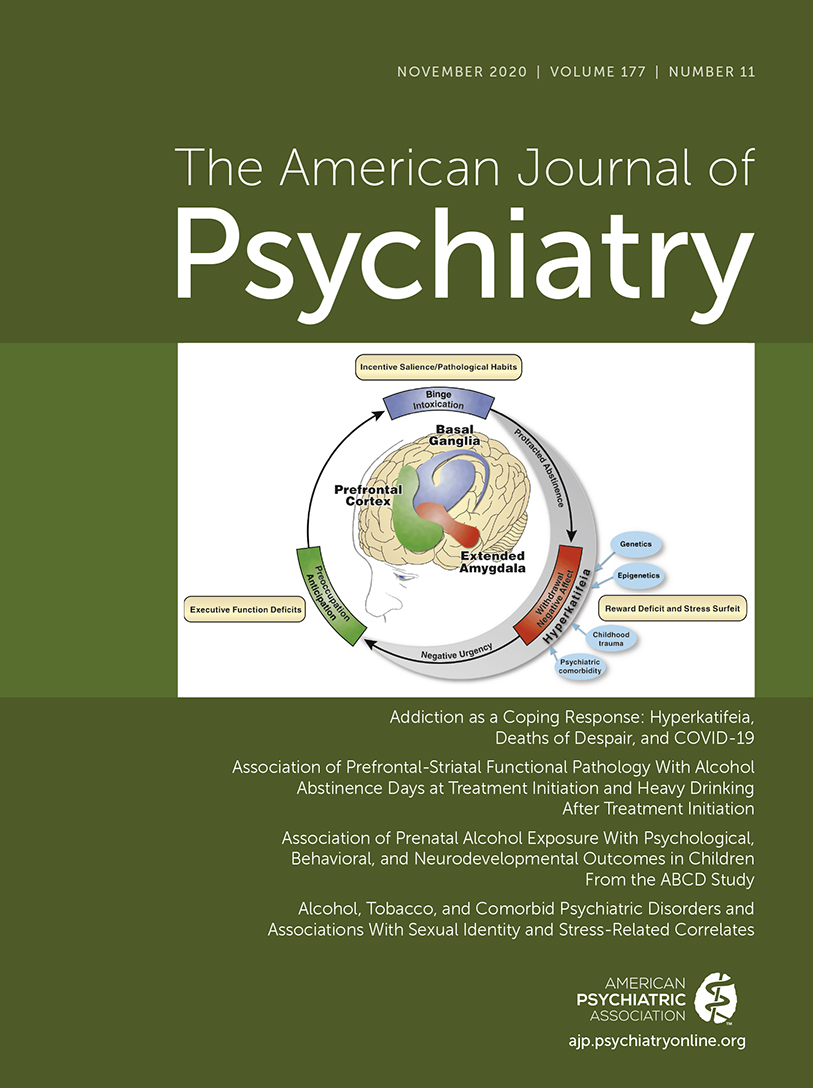
This issue of the Journal is focused on understanding factors contributing to substance use disorders and their comorbidity with psychiatric disorders, the effects of prenatal alcohol use on preadolescents, and brain mechanisms that are associated with addiction and relapse. An important theme that emerges from this issue is the necessity for understanding maladaptive substance use and its treatment in relation to health care inequities. This highlights the imperative to focus resources and treatment efforts on underprivileged and marginalized populations. The centerpiece of this issue is an overview on addiction written by Dr. George Koob, the director of the National Institute on Alcohol Abuse and Alcoholism (NIAAA), and coauthors Drs. Patricia Powell (NIAAA deputy director) and Aaron White ( 2 ). This outstanding article will serve as a foundational knowledge base for those interested in understanding the complex factors that mediate drug addiction. Of particular interest to the practice of psychiatry is the emphasis on the negative affect state “hyperkatifeia” as a major driver of addictive behavior and relapse. This places the dysphoria and psychological distress that are associated with prolonged withdrawal at the heart of treatment and underscores the importance of treating not only maladaptive drug-related behaviors but also the prolonged dysphoria and negative affect associated with addiction. It also speaks to why it is crucial to concurrently treat psychiatric comorbidities that commonly accompany substance use disorders.
Insights Into Mechanisms Related to Cocaine Addiction Using a Novel Imaging Method for Dopamine Neurons
Cassidy et al. ( 3 ) introduce a relatively new imaging technique that allows for an estimation of dopamine integrity and function in the substantia nigra, the site of origin of dopamine neurons that project to the striatum. Capitalizing on the high levels of neuromelanin that are found in substantia nigra dopamine neurons and the interaction between neuromelanin and intracellular iron, this MRI technique, termed neuromelanin-sensitive MRI (NM-MRI), shows promise in studying the involvement of substantia nigra dopamine neurons in neurodegenerative diseases and psychiatric illnesses. The authors used this technique to assess dopamine function in active cocaine users with the aim of exploring the hypothesis that cocaine use disorder is associated with blunted presynaptic striatal dopamine function that would be reflected in decreased “integrity” of the substantia nigra dopamine system. Surprisingly, NM-MRI revealed evidence for increased dopamine in the substantia nigra of individuals using cocaine. The authors suggest that this finding, in conjunction with prior work suggesting a blunted dopamine response, points to the possibility that cocaine use is associated with an altered intracellular distribution of dopamine. Specifically, the idea is that dopamine is shifted from being concentrated in releasable, functional vesicles at the synapse to a nonreleasable cytosolic pool. In addition to providing an intriguing alternative hypothesis underlying the cocaine-related alterations observed in substantia nigra dopamine function, this article highlights an innovative imaging method that can be used in further investigations involving the role of substantia nigra dopamine systems in neuropsychiatric disorders. Dr. Charles Bradberry, chief of the Preclinical Pharmacology Section at the National Institute on Drug Abuse, contributes an editorial that further explains the use of NM-MRI and discusses the theoretical implications of these unexpected findings in relation to cocaine use ( 4 ).
Treatment Implications of Understanding Brain Function During Early Abstinence in Patients With Alcohol Use Disorder
Developing a better understanding of the neural processes that are associated with substance use disorders is critical for conceptualizing improved treatment approaches. Blaine et al. ( 5 ) present neuroimaging data collected during early abstinence in patients with alcohol use disorder and link these data to relapses occurring during treatment. Of note, the findings from this study dovetail with the neural circuit schema Koob et al. provide in this issue’s overview on addiction ( 2 ). The first study in the Blaine et al. article uses 44 patients and 43 control subjects to demonstrate that patients with alcohol use disorder have a blunted neural response to the presentation of stress- and alcohol-related cues. This blunting was observed mainly in the ventromedial prefrontal cortex, a key prefrontal regulatory region, as well as in subcortical regions associated with reward processing, specifically the ventral striatum. Importantly, this finding was replicated in a second study in which 69 patients were studied in relation to their length of abstinence prior to treatment and treatment outcomes. The results demonstrated that individuals with the shortest abstinence times had greater alterations in neural responses to stress and alcohol cues. The authors also found that an individual’s length of abstinence prior to treatment, independent of the number of days of abstinence, was a predictor of relapse and that the magnitude of an individual’s neural alterations predicted the amount of heavy drinking occurring early in treatment. Although relapse is an all too common outcome in patients with substance use disorders, this study highlights an approach that has the potential to refine and develop new treatments that are based on addiction- and abstinence-related brain changes. In her thoughtful editorial, Dr. Edith Sullivan from Stanford University comments on the details of the study, the value of studying patients during early abstinence, and the implications of these findings for new treatment development ( 6 ).
Relatively Low Amounts of Alcohol Intake During Pregnancy Are Associated With Subtle Neurodevelopmental Effects in Preadolescent Offspring
Excessive substance use not only affects the user and their immediate family but also has transgenerational effects that can be mediated in utero. Lees et al. ( 7 ) present data suggesting that even the consumption of relatively low amounts of alcohol by expectant mothers can affect brain development, cognition, and emotion in their offspring. The researchers used data from the Adolescent Brain Cognitive Development Study, a large national community-based study, which allowed them to assess brain structure and function as well as behavioral, cognitive, and psychological outcomes in 9,719 preadolescents. The mothers of 2,518 of the subjects in this study reported some alcohol use during pregnancy, albeit at relatively low levels (0 to 80 drinks throughout pregnancy). Interestingly, and opposite of that expected in relation to data from individuals with fetal alcohol spectrum disorders, increases in brain volume and surface area were found in offspring of mothers who consumed the relatively low amounts of alcohol. Notably, any prenatal alcohol exposure was associated with small but significant increases in psychological problems that included increases in separation anxiety disorder and oppositional defiant disorder. Additionally, a dose-response effect was found for internalizing psychopathology, somatic complaints, and attentional deficits. While subtle, these findings point to neurodevelopmental alterations that may be mediated by even small amounts of prenatal alcohol consumption. Drs. Clare McCormack and Catherine Monk from Columbia University contribute an editorial that provides an in-depth assessment of these findings in relation to other studies, including those assessing severe deficits in individuals with fetal alcohol syndrome ( 8 ). McCormack and Monk emphasize that the behavioral and psychological effects reported in the Lees et al. article would not be clinically meaningful. However, it is feasible that the influences of these low amounts of alcohol could interact with other predisposing factors that might lead to more substantial negative outcomes.
Increased Comorbidity Between Substance Use and Psychiatric Disorders in Sexual Identity Minorities
There is no question that victims of societal marginalization experience disproportionate adversity and stress. Evans-Polce et al. ( 9 ) focus on this concern in relation to individuals who identify as sexual minorities by comparing their incidence of comorbid substance use and psychiatric disorders with that of individuals who identify as heterosexual. By using 2012−2013 data from 36,309 participants in the National Epidemiologic Study on Alcohol and Related Conditions–III, the authors examine the incidence of comorbid alcohol and tobacco use disorders with anxiety, mood disorders, and posttraumatic stress disorder (PTSD). The findings demonstrate increased incidences of substance use and psychiatric disorders in individuals who identified as bisexual or as gay or lesbian compared with those who identified as heterosexual. For example, a fourfold increase in the prevalence of PTSD was found in bisexual individuals compared with heterosexual individuals. In addition, the authors found an increased prevalence of substance use and psychiatric comorbidities in individuals who identified as bisexual and as gay or lesbian compared with individuals who identified as heterosexual. This was most prominent in women who identified as bisexual. For example, of the bisexual women who had an alcohol use disorder, 60.5% also had a psychiatric comorbidity, compared with 44.6% of heterosexual women. Additionally, the amount of reported sexual orientation discrimination and number of lifetime stressful events were associated with a greater likelihood of having comorbid substance use and psychiatric disorders. These findings are important but not surprising, as sexual minority individuals have a history of increased early-life trauma and throughout their lives may experience the painful and unwarranted consequences of bias and denigration. Nonetheless, these findings underscore the strong negative societal impacts experienced by minority groups and should sensitize providers to the additional needs of these individuals.
Trends in Nicotine Use and Dependence From 2001–2002 to 2012–2013
Although considerable efforts over earlier years have curbed the use of tobacco and nicotine, the use of these substances continues to be a significant public health problem. As noted above, individuals with psychiatric disorders are particularly vulnerable. Grant et al. ( 10 ) use data from the National Epidemiologic Survey on Alcohol and Related Conditions collected from a very large cohort to characterize trends in nicotine use and dependence over time. Results from their analysis support the so-called hardening hypothesis, which posits that although intervention-related reductions in nicotine use may have occurred over time, the impact of these interventions is less potent in individuals with more severe addictive behavior (i.e., nicotine dependence). When adjusted for sociodemographic factors, the results demonstrated a small but significant increase in nicotine use from 2001–2002 to 2012–2013. However, a much greater increase in nicotine dependence (46.1% to 52%) was observed over this time frame in individuals who had used nicotine during the preceding 12 months. The increases in nicotine use and dependence were associated with factors related to socioeconomic status, such as lower income and lower educational attainment. The authors interpret these findings as evidence for the hardening hypothesis, suggesting that despite the impression that nicotine use has plateaued, there is a growing number of highly dependent nicotine users who would benefit from nicotine dependence intervention programs. Dr. Kathleen Brady, from the Medical University of South Carolina, provides an editorial ( 11 ) that reviews the consequences of tobacco use and the history of the public measures that were initially taken to combat its use. Importantly, her editorial emphasizes the need to address health care inequity issues that affect individuals of lower socioeconomic status by devoting resources to develop and deploy effective smoking cessation interventions for at-risk and underresourced populations.
Conclusions
Maladaptive substance use and substance use disorders are highly prevalent and are among the most significant public health problems. Substance use is commonly comorbid with psychiatric disorders, and treatment efforts need to concurrently address both. The papers in this issue highlight new findings that are directly relevant to understanding, treating, and developing policies to better serve those afflicted with addictions. While treatments exist, the need for more effective treatments is clear, especially those focused on decreasing relapse rates. The negative affective state, hyperkatifeia, that accompanies longer-term abstinence is an important treatment target that should be emphasized in current practice as well as in new treatment development. In addition to developing a better understanding of the neurobiology of addictions and abstinence, it is necessary to ensure that there is equitable access to currently available treatments and treatment programs. Additional resources must be allocated to this cause. This depends on the recognition that health care inequities and societal barriers are major contributors to the continued high prevalence of substance use disorders, the individual suffering they inflict, and the huge toll that they incur at a societal level.
Disclosures of Editors’ financial relationships appear in the April 2020 issue of the Journal .
1 US Department of Health and Human Services: Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality: National Survey on Drug Use and Health 2018. Rockville, Md, SAMHSA, 2019 ( https://www.samhsa.gov/data/nsduh/reports-detailed-tables-2018-NSDUH ) Google Scholar
2 Koob GF, Powell P, White A : Addiction as a coping response: hyperkatifeia, deaths of despair, and COVID-19 . Am J Psychiatry 2020 ; 177:1031–1037 Link , Google Scholar
3 Cassidy CM, Carpenter KM, Konova AB, et al. : Evidence for dopamine abnormalities in the substantia nigra in cocaine addiction revealed by neuromelanin-sensitive MRI . Am J Psychiatry 2020 ; 177:1038–1047 Link , Google Scholar
4 Bradberry CW : Neuromelanin MRI: dark substance shines a light on dopamine dysfunction and cocaine use (editorial). Am J Psychiatry 2020 ; 177:1019–1021 Abstract , Google Scholar
5 Blaine SK, Wemm S, Fogelman N, et al. : Association of prefrontal-striatal functional pathology with alcohol abstinence days at treatment initiation and heavy drinking after treatment initiation . Am J Psychiatry 2020 ; 177:1048–1059 Abstract , Google Scholar
6 Sullivan EV : Why timing matters in alcohol use disorder recovery (editorial). Am J Psychiatry 2020 ; 177:1022–1024 Abstract , Google Scholar
7 Lees B, Mewton L, Jacobus J, et al. : Association of prenatal alcohol exposure with psychological, behavioral, and neurodevelopmental outcomes in children from the Adolescent Brain Cognitive Development Study . Am J Psychiatry 2020 ; 177:1060–1072 Link , Google Scholar
8 McCormack C, Monk C : Considering prenatal alcohol exposure in a developmental origins of health and disease framework (editorial). Am J Psychiatry 2020 ; 177:1025–1028 Abstract , Google Scholar
9 Evans-Polce RJ, Kcomt L, Veliz PT, et al. : Alcohol, tobacco, and comorbid psychiatric disorders and associations with sexual identity and stress-related correlates . Am J Psychiatry 2020 ; 177:1073–1081 Abstract , Google Scholar
10 Grant BF, Shmulewitz D, Compton WM : Nicotine use and DSM-IV nicotine dependence in the United States, 2001–2002 and 2012–2013 . Am J Psychiatry 2020 ; 177:1082–1090 Link , Google Scholar
11 Brady KT : Social determinants of health and smoking cessation: a challenge (editorial). Am J Psychiatry 2020 ; 177:1029–1030 Abstract , Google Scholar
- Cited by None
- Substance-Related and Addictive Disorders
- Addiction Psychiatry
- Transgender (LGBT) Issues
- Search Menu
- Advance Articles
- Editor's Choice
- Author Guidelines
- Submission Site
- Open Access
- About Health Education Research
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Dispatch Dates
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Introduction.
- < Previous
Understanding reasons for drug use amongst young people: a functional perspective
- Article contents
- Figures & tables
- Supplementary Data
Annabel Boys, John Marsden, John Strang, Understanding reasons for drug use amongst young people: a functional perspective, Health Education Research , Volume 16, Issue 4, August 2001, Pages 457–469, https://doi.org/10.1093/her/16.4.457
- Permissions Icon Permissions
This study uses a functional perspective to examine the reasons young people cite for using psychoactive substances. The study sample comprised 364 young poly-drug users recruited using snowball-sampling methods. Data on lifetime and recent frequency and intensity of use for alcohol, cannabis, amphetamines, ecstasy, LSD and cocaine are presented. A majority of the participants had used at least one of these six drugs to fulfil 11 of 18 measured substance use functions. The most popular functions for use were using to: relax (96.7%), become intoxicated (96.4%), keep awake at night while socializing (95.9%), enhance an activity (88.5%) and alleviate depressed mood (86.8%). Substance use functions were found to differ by age and gender. Recognition of the functions fulfilled by substance use should help health educators and prevention strategists to make health messages about drugs more relevant and appropriate to general and specific audiences. Targeting substances that are perceived to fulfil similar functions and addressing issues concerning the substitution of one substance for another may also strengthen education and prevention efforts.
The use of illicit psychoactive substances is not a minority activity amongst young people in the UK. Results from the most recent British Crime Survey show that some 50% of young people between the ages of 16 and 24 years have used an illicit drug on at least one occasion in their lives (lifetime prevalence) ( Ramsay and Partridge, 1999 ). Amongst 16–19 and 20–24 year olds the most prevalent drug is cannabis (used by 40% of 16–19 year olds and 47% of 20–24 year olds), followed by amphetamine sulphate (18 and 24% of the two age groups respectively), LSD (10 and 13%) and ecstasy (8 and 12%). The lifetime prevalence for cocaine hydrochloride (powder cocaine) use amongst the two age groups is 3 and 9%, respectively. Collectively, these estimates are generally comparable with other European countries ( European Monitoring Centre for Drugs and Drug Addiction, 1998 ) and the US ( Johnston et al ., 1997 , 2000 ).
The widespread concern about the use of illicit drugs is reflected by its high status on health, educational and political agendas in many countries. The UK Government's 10-year national strategy on drug misuse identifies young people as a critical priority group for prevention and treatment interventions ( Tackling Drugs to Build a Better Britain 1998 ). If strategies to reduce the use of drugs and associated harms amongst the younger population are to be developed, particularly within the health education arena, it is vital that we improve our understanding of the roles that both licit and illicit substances play in the lives of young people. The tendency for educators, practitioners and policy makers to address licit drugs (such as alcohol) separately from illegal drugs may be unhelpful. This is partly because young illicit drug users frequently drink alcohol, and may have little regard for the illicit and licit distinction established by the law. To understand the roles that drug and alcohol use play in contemporary youth culture, it is necessary to examine the most frequently used psychoactive substances as a set.
It is commonplace for young drug users to use several different psychoactive substances. The terms `poly-drug' or `multiple drug' use have been used to describe this behaviour although their exact definitions vary. The term `poly-drug use' is often used to describe the use of two or more drugs during a particular time period (e.g. over the last month or year). This is the definition used within the current paper. However, poly-drug use could also characterize the use of two or more psychoactive substances so that their effects are experienced simultaneously. We have used the term `concurrent drug use' to denote this pattern of potentially more risky and harmful drug use ( Boys et al. 2000a ). Previous studies have reported that users often use drugs concurrently to improve the effects of another drug or to help manage its negative effects [e.g. ( Power et al ., 1996 ; Boys et al. 2000a ; Wibberley and Price, 2000 )].
The most recent British Crime Survey found that 5% of 16–29 year olds had used more than one drug in the last month ( Ramsay and Partridge, 1999 ). Given that 16% of this age band reported drug use in the month prior to interview, this suggests that just under a third of these individuals had used more than one illicit substance during this time period. With alcohol included, the prevalence of poly-drug use is likely to be much higher.
There is a substantial body of literature on the reasons or motivations that people cite for using alcohol, particularly amongst adult populations. For example, research on heavy drinkers suggested that alcohol use is related to multiple functions for use ( Edwards et al ., 1972 ; Sadava, 1975 ). Similarly, research with a focus on young people has sought to identify motives for illicit drug use. There is evidence that for many young people, the decision to use a drug is based on a rational appraisal process, rather than a passive reaction to the context in which a substance is available ( Boys et al. 2000a ; Wibberley and Price, 2000 ). Reported reasons vary from quite broad statements (e.g. to feel better) to more specific functions for use (e.g. to increase self-confidence). However, much of this literature focuses on `drugs' as a generic concept and makes little distinction between different types of illicit substances [e.g. ( Carman, 1979 ; Butler et al ., 1981 ; Newcomb et al ., 1988 ; Cato, 1992 ; McKay et al ., 1992 )]. Given the diverse effects that different drugs have on the user, it might be proposed that reasons for use will closely mirror these differences. Thus stimulant drugs (such as amphetamines, ecstasy or cocaine) will be used for reasons relating to increased nervous system arousal and drugs with sedative effects (such as alcohol or cannabis), with nervous system depression. The present study therefore selected a range of drugs commonly used by young people with stimulant, sedative or hallucinogenic effects to examine this issue further.
The phrase `instrumental drug use' has been used to denote drug use for reasons specifically linked to a drug's effects ( WHO, 1997 ). Examples of the instrumental use of amphetamine-type stimulants include vehicle drivers who report using to improve concentration and relieve tiredness, and people who want to lose weight (particularly young women), using these drugs to curb their appetite. However, the term `instrumental substance use' seems to be used when specific physical effects of a drug are exploited and does not encompass use for more subtle social or psychological purposes which may also be cited by users. In recent reports we have described a `drug use functions' model to help understand poly-substance use phenomenology amongst young people and how decisions are made about patterns of consumption ( Boys et al ., 1999a , b , 2000a ). The term `function' is intended to characterize the primary or multiple reasons for, or purpose served by, the use of a particular substance in terms of the actual gains that the user perceives that they will attain. In the early, 1970s Sadava suggested that functions were a useful means of understanding how personality and environmental variables impacted on patterns of drug use ( Sadava, 1975 ). This work was confined to functions for cannabis and `psychedelic drugs' amongst a sample of college students. To date there has been little research that has examined the different functions associated with the range of psychoactive substances commonly used by young poly-drug users. It is unclear if all drugs with similar physical effects are used for similar purposes, or if other more subtle social or psychological dimensions to use are influential. Work in this area will help to increase understanding of the different roles played by psychoactive substances in the lives of young people, and thus facilitate health, educational and policy responses to this issue.
Previous work has suggested that the perceived functions served by the use of a drug predict the likelihood of future consumption ( Boys et al ., 1999a ). The present study aims to develop this work further by examining the functional profiles of six substances commonly used by young people in the UK.
Patterns of cannabis, amphetamine, ecstasy, LSD, cocaine hydrochloride and alcohol use were examined amongst a sample of young poly-drug users. Tobacco use was not addressed in the present research.
Sampling and recruitment
A snowball-sampling approach was employed for recruitment of participants. Snowball sampling is an effective way of generating a large sample from a hidden population where no formal sampling frame is available ( Van Meter, 1990 ). A team of peer interviewers was trained to recruit and interview participants for the study. We have described this procedure in detail elsewhere and only essential features are described here ( Boys et al. 2000b ). Using current or ex-drug users to gather data from hidden populations of drug using adults has been found to be successful ( Griffiths et al ., 1993 ; Power, 1995 ).
Study participants
Study participants were current poly-substance users with no history of treatment for substance-related disorders. We excluded people with a treatment history on the assumption that young people who have had substance-related problems requiring treatment represent a different group from the general population of young drug users. Inclusion criteria were: aged 16–22 years and having used two or more illegal substances during the past 90 days. During data collection, the age, gender and current occupation of participants were recorded and monitored to ensure that sufficient individuals were recruited to the groups to permit subgroup analyses. If an imbalance was observed in one of these variables, the interviewers were instructed to target participants with specific characteristics (e.g. females under the age of 18) to redress this imbalance.
Study measures
Data were collected using a structured interviewer-administered questionnaire developed specifically for the study. In addition to recording lifetime substance use, questions profiled consumption patterns of six substances in detail. Data were collected between August and November 1998. Interviews were audiotaped with the interviewee's consent. This enabled research staff to verify that answers had been accurately recorded on the questionnaire and that the interview had been conducted in accordance with the research protocol. Research staff also checked for consistency across different question items (e.g. the total number of days of drug use in the past 90 days should equal or exceed the number of days of cannabis use during the same time period). On the few occasions where inconsistencies were identified that could not be corrected from the tape, the interviewer was asked to re-contact the interviewee to verify the data.
Measures of lifetime use, consumption in the past year and past 90 days were based on procedures developed by Marsden et al . ( Marsden et al ., 1998 ). Estimated intensity of consumption (amount used on a typical using day) was recorded verbatim and then translated into standardized units at the data entry stage.
Functions for substance use scale
The questionnaire included a 17-item scale designed to measure perceived functions for substance use. This scale consisted of items developed in previous work ( Boys et al ., 1999a ) in addition to functions derived from qualitative interviews ( Boys et al ., 1999b ), new literature and informal discussions with young drug users. Items were drawn from five domains (Table I ).
Participants were asked if they had ever used a particular drug in order to fulfil each specific function. Those who endorsed the item were then invited to rate how frequently they had used it for this purpose over the past year, using a five-point Likert-type scale (`never' to `always'; coded 0–4). One item differed between the function scales used for the stimulant drugs and for alcohol and cannabis. For the stimulant drugs (amphetamines, cocaine and ecstasy) the item `have you ever used [named drug] to help you to lose weight' was used, for cannabis and alcohol this item was replaced with `have you ever used [drug] to help you to sleep?'. (The items written in full as they appeared in the questionnaire are shown in Table III , together with abbreviations used in this paper.)
Statistical procedures
The internal reliability of the substance use functions scales for each of the six substances was judged using Chronbach's α coefficient. Chronbach's α is a statistic that reflects the extent to which each item in a measurement scale is associated with other items. Technically it is the average of correlations between all possible comparisons of the scale items that are divided into two halves. An α coefficient for a scale can range from 0 (no internal reliability) to 1 (complete reliability). Analyses of categorical variables were performed using χ 2 statistic. Differences in scale means were assessed using t -tests.
The sample consisted of 364 young poly-substance users (205 males; 56.3%) with a mean age of 19.3 years; 69.8% described their ethnic group as White-European, 12.6% as Black and 10.1% were Asian. Just over a quarter (27.5%) were unemployed at the time of interview; a third were in education, 28.8% were in full-time work and the remainder had part-time employment. Estimates of monthly disposable income (any money that was spare after paying for rent, bills and food) ranged from 0 to over £1000 (median = £250).
Substance use history
The drug with the highest lifetime prevalence was cannabis (96.2%). This was followed by amphetamine sulphate (51.6%), cocaine hydrochloride (50.5%) (referred to as cocaine hereafter) and ecstasy (48.6%). Twenty-five percent of the sample had used LSD and this was more common amongst male participants (χ 2 [1] = 9.68, P < 0.01). Other drugs used included crack cocaine (25.5%), heroin (12.6%), tranquillizers (21.7%) and hallucinogenic mushrooms (8.0%). On average, participants had used a total of 5.2 different psychoactive substances in their lives (out of a possible 14) (median = 4.0, mode = 3.0, range 2–14). There was no gender difference in the number of different drugs ever used.
Table II profiles use of the six target drugs over the past year, and the frequency and intensity of use in the 90 days prior to interview.
There were no gender differences in drug use over the past year or in the past 90 days with the exception of amphetamines. For this substance, females who had ever used this drug were more likely to have done so during the past 90 days than males (χ 2 [1] = 4.14, P < 0.05). The mean number of target drugs used over the past 90 days was 3.2 (median = 3.0, mode = 3.0, range 2–6). No gender differences were observed. Few differences were also observed in the frequency and intensity of use. Males reported drinking alcohol more frequently during the three months prior to interview ( t [307] = 2.48, P < 0.05) and using cannabis more intensively on a `typical using day' ( t [337] = 3.56, P < 0.001).
Perceived functions for substance use
There were few differences between the functions endorsed for use of each drug `ever' and those endorsed for use during `the year prior to interview'. This section therefore concentrates on data for the year prior to interview. We considered that in order to use a drug for a specific function, the user must have first hand knowledge of the drug's effects before making this decision. Consequently, functions reported by individuals who had only used a particular substance on one occasion in their lives (i.e. with no prior experience of the drug at the time they made the decision to take it) were excluded from the analyses. Table III summarizes the proportion of the sample who endorsed each of the functions for drugs used in the past year. Roman numerals have been used to indicate the functions with the top five average scores. Table III also shows means for the total number of different items endorsed by individual users and the internal reliability of the function scales for each substance using Chronbach's α coefficients. There were no significant gender differences in the total number of functions endorsed for any of the six substances.
The following sections summarize the top five most popular functions drug-by-drug together with any age or gender differences observed in the items endorsed.
Cannabis use ( n = 345)
Overall the most popular functions for cannabis use were to `RELAX' (endorsed by 96.8% of people who had used the drug in the last year), to become `INTOXICATED' (90.7%) and to `ENHANCE ACTIVITY' (72.8%). Cannabis was also commonly used to `DECREASE BOREDOM' (70.1%) and to `SLEEP' (69.6%) [this item was closely followed by using to help `FEEL BETTER' (69.0%)]. Nine of the 17 function items were endorsed by over half of those who had used cannabis on more than one occasion in the past year. There were no significant gender differences observed, with the exception of using to `KEEP GOING', where male participants were significantly more likely to say that they had used cannabis to fulfil this function in the past year (χ 2 [1] = 6.10, P < 0.05).
There were statistically significant age differences on four of the function variables: cannabis users who reported using this drug in the past year to help feel `ELATED/EUPHORIC' or to help `SLEEP' were significantly older than those who had not used cannabis for these purposes (19.6 versus 19.0; t [343] = 3.32, P < 0.001; 19.4 versus 19.0; t [343] = 2.01, P < 0.05). In contrast, those who had used cannabis to `INCREASE CONFIDENCE' and to `STOP WORRYING' tended to be younger than those who did not (19.0 versus 19.4; t [343] = –2.26, P < 0.05; 19.1 versus 19.5; t [343] = –1.99, P < 0.05).
Amphetamines ( n = 160)
Common functions for amphetamine use were to `KEEP GOING' (95.6%), to `STAY AWAKE' (91.3%) or to `ENHANCE ACTIVITY' (66.2%). Using to help feel `ELATED/EUPHORIC' (60.6%) and to `ENJOY COMPANY' (58.1%) were also frequently mentioned. Seven of the 17 function items were endorsed by over half of participants who had used amphetamines in the past year. As with cannabis, gender differences were uncommon: females were more likely to use amphetamines to help `LOSE WEIGHT' than male participants (χ 2 [1] = 21.67, P < 0.001).
Significant age differences were found on four function variables. Individuals who reported using amphetamines in the past year to feel `ELATED/EUPHORIC' were significantly older than those who did not (19.9 versus 19.0; t [158] = 2.87, P < 0.01). In contrast, participants who used amphetamines to `STOP WORRYING' (18.8 versus 19.8; t [158] = –2.77, P < 0.01), to `DECREASE BOREDOM' (19.2 versus 19.9; t [158] = –2.39, P < 0.05) or to `ENHANCE ACTIVITY' (19.3 versus 20.1; t [158] = –2.88, P < 0.01) were younger than those who had not.
Ecstasy ( n = 157)
The most popular five functions for using ecstasy were similar to those for amphetamines. The drug was used to `KEEP GOING' (91.1%), to `ENHANCE ACTIVITY' (79.6%), to feel `ELATED/EUPHORIC' (77.7%), to `STAY AWAKE' (72.0%) and to get `INTOXICATED' (68.2%). Seven of the 17 function items were endorsed by over half of those who had used ecstasy in the past year. Female users were more likely to use ecstasy to help `LOSE WEIGHT' than male participants (Fishers exact test, P < 0.001).
As with the other drugs discussed above, participants who reported using ecstasy to feel `ELATED/EUPHORIC' were significantly older than those who did not (19.8 versus 18.9; t [155] = 2.61, P < 0.01). In contrast, those who had used ecstasy to `FEEL BETTER' (19.3 versus 20.0; t [155] = –2.29, P < 0.05), to `INCREASE CONFIDENCE' (19.2 versus 19.9; t [155] = –2.22, P < 0.05) and to `STOP WORRYING' (19.0 versus 19.9; t [155] = –2.96, P < 0.01) tended to be younger.
LSD ( n = 58)
Of the six target substances examined in this study, LSD was associated with the least diverse range of functions for use. All but two of the function statements were endorsed by at least some users, but only five were reported by more than 50%. The most common purpose for consuming LSD was to get `INTOXICATED' (77.6%). Other popular functions included to feel `ELATED/EUPHORIC' and to `ENHANCE ACTIVITY' (both endorsed by 72.4%), and to `KEEP GOING' and to `ENJOY COMPANY' (both endorsed by 58.6%). Unlike the other substances examined, no gender or age differences were observed.
Cocaine ( n = 168)
In common with ecstasy and amphetamines, the most widely endorsed functions for cocaine use were to help `KEEP GOING' (84.5%) and to help `STAY AWAKE' (69.0%). Consuming cocaine to `INCREASE CONFIDENCE' and to get `INTOXICATED' (both endorsed by 66.1%) were also popular. However, unlike the other stimulant drugs, 61.9% of the cocaine users reported using to `FEEL BETTER'. Ten of the 17 function items were endorsed by over half of those who had used cocaine in the past year.
Gender differences were more common amongst functions for cocaine use than the other substances surveyed. More males reported using cocaine to `IMPROVE EFFECTS' of other drugs (χ 2 [1] = 4.00, P < 0.05); more females used the drug to help `STAY AWAKE' (χ 2 [1] = 12.21, P < 0.001), to `LOSE INHIBITIONS' (χ 2 [1] = 9.01, P < 0.01), to `STOP WORRYING' (χ 2 [1] = 8.11, P < 0.01) or to `ENJOY COMPANY' of friends (χ 2 [1] = 4.34, P < 0.05). All participants who endorsed using cocaine to help `LOSE WEIGHT' were female.
Those who had used cocaine to `FEEL BETTER' (18.9 versus 19.8; t [166] = –3.06, P < 0.01), to `STOP WORRYING' (18.6 versus 19.7; t [166] = –3.86, P < 0.001) or to `DECREASE BOREDOM' (18.9 versus 19.6; t [166] = –2.52, P < 0.05) were significantly younger than those who did not endorse these functions. Similar to the other drugs, participants who had used cocaine to feel `ELATED/EUPHORIC' in the past year tended to be older than those who had not (19.6 versus 18.7; t [166] = 3.16, P < 0.01).
Alcohol ( n = 312)
The functions for alcohol use were the most diverse of the six substances examined. Like LSD, the most commonly endorsed purpose for drinking was to get `INTOXICATED' (89.1%). Many used alcohol to `RELAX' (82.7%), to `ENJOY COMPANY' (74.0%), to `INCREASE CONFIDENCE' (70.2%) and to `FEEL BETTER' (69.9%). Overall, 11 of the 17 function items were endorsed by over 50% of those who had drunk alcohol in the past year. Male participants were more likely to report using alcohol in combination with other drugs either to `IMPROVE EFFECTS' of other drugs (χ 2 [1] = 4.56, P < 0.05) or to ease the `AFTER EFFECTS' of other substances (χ 2 [1] = 7.07, P < 0.01). More females than males reported that they used alcohol to `DECREASE BOREDOM' (χ 2 [1] = 4.42, P < 0.05).
T -tests revealed significant age differences on four of the function variables: those who drank to feel `ELATED/EUPHORIC' were significantly older (19.7 versus 19.0; t [310] = 3.67, P < 0.001) as were individuals who drank to help them to `LOSE INHIBITIONS' (19.6 versus 19.0; t [310] = 2.36, P < 0.05). In contrast, participants who reported using alcohol just to get `INTOXICATED' (19.2 versus 20.3; t [310] = –3.31, P < 0.001) or to `DECREASE BOREDOM' (19.2 versus 19.6; t [310] = –2.25, P < 0.05) were significantly younger than those who did not.
Combined functional drug use
The substances used by the greatest proportion of participants to `IMPROVE EFFECTS' from other drugs were cannabis (44.3%), alcohol (41.0%) and amphetamines (37.5%). It was also common to use cannabis (64.6%) and to a lesser extent alcohol (35.9%) in combination with other drugs in order to help manage `AFTER EFFECTS'. Amphetamines, ecstasy, LSD and cocaine were also used for these purposes, although to a lesser extent. Participants who endorsed the combination drug use items were asked to list the three main drugs with which they had combined the target substance for these purposes. Table IV summarizes these responses.
Overall functions for drug use
In order to examine which functions were most popular overall, a dichotomous variable was created for each different item to indicate if one or more of the six target substances had been used to fulfil this purpose during the year prior to interview. For example, if an individual reported that they had used cannabis to relax, but their use of ecstasy, amphetamines and alcohol had not fulfilled this function, then the variable for `RELAX' was scored `1'. Similarly if they had used all four of these substances to help them to relax in the past year, the variable would again be scored as `1'. A score of `0' indicates that none of the target substances had been used to fulfil a particular function. Table V summarizes the data from these new variables.
Over three-quarters of the sample had used at least one target substance in the past year for 11 out of the 18 functions listed. The five most common functions for substance use overall were to `RELAX' (96.7%); `INTOXICATED' (96.4%); `KEEP GOING' (95.9%); `ENHANCE ACTIVITY' (88.5%) and `FEEL BETTER' (86.8%). Despite the fact that `SLEEP' was only relevant to two substances (alcohol and cannabis), it was still endorsed by over 70% of the total sample. Using to `LOSE WEIGHT' was only relevant to the stimulant drugs (amphetamines, ecstasy and cocaine), yet was endorsed by 17.3% of the total sample (almost a third of all female participants). Overall, this was the least popular function for recent substance use, followed by `WORK' (32.1%). All other items were endorsed by over 60% of all participants.
Gender differences were identified in six items. Females were significantly more likely to have endorsed the following: using to `INCREASE CONFIDENCE' (χ 2 [1] = 4.41, P < 0.05); `STAY AWAKE' (χ 2 [1] = 5.36, P < 0.05), `LOSE INHIBITIONS' (χ 2 [1] = 4.48, P < 0.05), `ENHANCE SEX' (χ 2 [1] = 5.17, P < 0.05) and `LOSE WEIGHT' (χ 2 [1] = 29.6, P < 0.001). In contrast, males were more likely to use a substance to `IMPROVE EFFECTS' of another drug (χ 2 [1] = 11.18, P < 0.001).
Statistically significant age differences were identified in three of the items. Those who had used at least one of the six target substances in the last year to feel `ELATED/EUPHORIC' (19.5 versus 18.6; t [362] = 4.07, P < 0.001) or to `SLEEP' (19.4 versus 18.9; t [362] = 2.19, P < 0.05) were significantly older than those who had not used for this function. In contrast, participants who had used in order to `STOP WORRYING' tended to be younger (19.1 versus 19.7; t [362] = –2.88, P < 0.01).
This paper has examined psychoactive substance use amongst a sample of young people and focused on the perceived functions for use using a 17-item scale. In terms of the characteristics of the sample, the reported lifetime and recent substance use was directly comparable with other samples of poly-drug users recruited in the UK [e.g. ( Release, 1997 )].
Previous studies which have asked users to give reasons for their `drug use' overall instead of breaking it down by drug type [e.g. ( Carman, 1979 ; Butler et al ., 1981 ; Newcomb et al ., 1988 ; Cato, 1992 ; McKay et al ., 1992 )] may have overlooked the dynamic nature of drug-related decision making. A key finding from the study is that that with the exception of two of the functions for use scale items (using to help sleep or lose weight), all of the six drugs had been used to fulfil all of the functions measured, despite differences in their pharmacological effects. The total number of functions endorsed by individuals for use of a particular drug varied from 0 to 15 for LSD, and up to 17 for cannabis, alcohol and cocaine. The average number ranged from 5.9 (for LSD) to 9.0 (for cannabis). This indicates that substance use served multiple purposes for this sample, but that the functional profiles differed between the six target drugs.
We have previously reported ( Boys et al. 2000b ) that high scores on a cocaine functions scale are strongly predictive of high scores on a cocaine-related problems scale. The current findings support the use of similar function scales for cannabis, amphetamines, LSD and ecstasy. It remains to be seen whether similar associations with problem scores exist. Future developmental work in this area should ensure that respondents are given the opportunity to cite additional functions to those included here so that the scales can be further extended and refined.
Recent campaigns that have targeted young people have tended to assume that hallucinogen and stimulant use is primarily associated with dance events, and so motives for use will relate to this context. Our results support assumptions that these drugs are used to enhance social interactions, but other functions are also evident. For example, about a third of female interviewees had used a stimulant drug to help them to lose weight. Future education and prevention efforts should take this diversity into account when planning interventions for different target groups.
The finding that the same functions are fulfilled by use of different drugs suggests that at least some could be interchangeable. Evidence for substituting alternative drugs to fulfil a function when a preferred drug is unavailable has been found in other studies [e.g. ( Boys et al. 2000a )]. Prevention efforts should perhaps focus on the general motivations behind use rather than trying to discourage use of specific drug types in isolation. For example, it is possible that the focus over the last decade on ecstasy prevention may have contributed inadvertently to the rise in cocaine use amongst young people in the UK ( Boys et al ., 1999c ). It is important that health educators do not overlook this possibility when developing education and prevention initiatives. Considering functions that substance use can fulfil for young people could help us to understand which drugs are likely to be interchangeable. If prevention programmes were designed to target a range of substances that commonly fulfil similar functions, then perhaps this could address the likelihood that some young people will substitute other drugs if deterred from their preferred substance.
There has been considerable concern about the perceived increase in the number of young people who are using cocaine in the UK ( Tackling Drugs to Build a Better Britain 1998 ; Ramsay and Partridge, 1999 ; Boys et al. 2000b ). It has been suggested that, for a number of reasons, cocaine may be replacing ecstasy and amphetamines as the stimulant of choice for some young people ( Boys et al ., 1999c ). The results from this study suggest that motives for cocaine use are indeed similar to those for ecstasy and amphetamine use, e.g. using to `keep going' on a night out with friends, to `enhance an activity', `to help to feel elated or euphoric' or to help `stay awake'. However, in addition to these functions which were shared by all three stimulants, over 60% of cocaine users reported that they had used this drug to `help to feel more confident' in a social situation and to `feel better when down or depressed'. Another finding that sets cocaine aside from ecstasy and amphetamines was the relatively common existence of gender differences in the function items endorsed. Female cocaine users were more likely to use to help `stay awake', `lose inhibitions', `stop worrying', `enjoy company of friends' or to help `lose weight'. This could indicate that women are more inclined to admit to certain functions than their male counterparts. However, the fact that similar gender differences were not observed in the same items for the other five substances, suggests this interpretation is unlikely. Similarly, the lack of gender differences in patterns of cocaine use (both frequency and intensity) suggests that these differences are not due to heavier cocaine use amongst females. If these findings are subsequently confirmed, this could point towards an inclination for young women to use cocaine as a social support, particularly to help feel less inhibited in social situations. If so, young female cocaine users may be more vulnerable to longer-term cocaine-related problems.
Many respondents reported using alcohol or cannabis to help manage effects experienced from another drug. This has implications for the choice of health messages communicated to young people regarding the use of two or more different substances concurrently. Much of the literature aimed at young people warns them to avoid mixing drugs because the interactive effects may be dangerous [e.g. ( HIT, 1996 )]. This `Just say No' type of approach does not take into consideration the motives behind mixing drugs. In most areas, drug education and prevention work has moved on from this form of communication. A more sophisticated approach is required, which considers the functions that concurrent drug use is likely to have for young people and tries to amend messages to make them more relevant and acceptable to this population. Further research is needed to explore the motivations for mixing different combinations of drugs together.
Over three-quarters of the sample reported using at least one of the six target substances to fulfil 11 out of the 18 functions. These findings provide strong evidence that young people use psychoactive drugs for a range of distinct purposes, not purely dependent on the drug's specific effects. Overall, the top five functions were to `help relax', `get intoxicated', `keep going', `enhance activity' and `feel better'. Each of these was endorsed by over 85% of the sample. Whilst all six substances were associated to a greater or lesser degree with each of these items, there were certain drugs that were more commonly associated with each. For example, cannabis and alcohol were popular choices for relaxation or to get intoxicated. In contrast, over 90% of the amphetamine and ecstasy users reported using these drugs within the last year to `keep going'. Using to enhance an activity was a common function amongst users of all six substances, endorsed by over 70% of ecstasy, cannabis and LSD users. Finally, it was mainly alcohol and cannabis (and to a lesser extent cocaine) that were used to `feel better'.
Several gender differences were observed in the combined functions for recent substance use. These findings indicate that young females use other drugs as well as cocaine as social supports. Using for specific physical effects (weight loss, sex or wakefulness) was also more common amongst young women. In contrast, male users were significantly more likely to report using at least one of the target substances to try to improve the effects of another substance. This indicates a greater tendency for young males in this sample to mix drugs than their female counterparts. Age differences were also observed on several function items: participants who had used a drug to `feel elated or euphoric' or to `help sleep' tended to be older and those who used to `stop worrying about a problem' were younger. If future studies confirm these differences, education programmes and interventions might benefit from tailoring their strategies for specific age groups and genders. For example, a focus on stress management strategies and coping skills with a younger target audience might be appropriate.
Some limitations of the study need to be acknowledged. The sample for this study was recruited using a snowball-sampling methodology. Although it does not yield a random sample of research participants, this method has been successfully used to access hidden samples of drug users [e.g. ( Biernacki, 1986 ; Lenton et al ., 1997 )]. Amongst the distinct advantages of this approach are that it allows theories and models to be tested quantitatively on sizeable numbers of subjects who have engaged in a relatively rare behaviour.
Further research is now required to determine whether our observations may be generalized to other populations (such as dependent drug users) and drug types (such as heroin, tranquillizers or tobacco) or if additional function items need to be developed. Future studies should also examine if functions can be categorized into primary and subsidiary reasons and how these relate to changes in patterns of use and drug dependence. Recognition of the functions fulfilled by substance use could help inform education and prevention strategies and make them more relevant and acceptable to the target audiences.
Structure of functions scales
Profile of substance use over the past year and past 90 days ( n = 364)
Proportion (%) of those who have used [substance] more than once, who endorsed each functional statement for their use in the past year
Combined functional substance use reported by the sample over the past year
Percentage of participants who reported having used at least one of the target substances to fulfil each of the different functions over the past year ( n = 364)
We gratefully acknowledge research support from the Health Education Authority (HEA). The views expressed in this paper are those of the authors and do not necessarily reflect those of the HEA. We would also like to thank the anonymous referees for helpful comments and suggestions on an earlier draft of this paper.
Biernacki, P. (1986) Pathways from Heroin Addiction: Recovery without Treatment . Temple University Press, Philadelphia, PA.
Boys, A., Marsden, J., Griffiths, P., Fountain, J., Stillwell, G. and Strang, J. ( 1999 ) Substance use among young people: the relationship between perceived functions and behavioural intentions. Addiction , 94 , 1043 –1050.
Boys, A., Marsden, J., Fountain, J., Griffiths, P., Stillwell, G. and Strang, J. ( 1999 ) What influences young people's use of drugs? A qualitative study of decision-making. Drugs: Education, Prevention and Policy , 6 , 373 –389.
Boys, A., Marsden, J. and Griffiths. P. ( 1999 ) Reading between the lines: is cocaine becoming the stimulant of choice for urban youth? Druglink , 14 , 20 –23.
Boys, A., Fountain, J., Marsden, J., Griffiths, P., Stillwell, G. and Strang, J. (2000a) Drug Decisions: A Qualitative Study of Young People , Drugs and Alcohol . Health Education Authority, London.
Boys, A., Marsden, J., Griffiths, P. and Strang, J. ( 2000 ) Drug use functions predict cocaine-related problems. Drug and Alcohol Review , 19 , 181 –190.
Butler, M. C., Gunderson, E. K. E. and Bruni, J. R. ( 1981 ) Motivational determinants of illicit drug use: an assessment of underlying dimensions and their relationship to behaviour. International Journal of the Addictions , 16 , 243 –252.
Carman, R. S. ( 1979 ) Motivations for drug use and problematic outcomes among rural junior high school students. Addictive Behaviors , 4 , 91 –93.
Cato, B. M. ( 1992 ) Youth's recreation and drug sensations: is there a relationship? Journal of Drug Education , 22 , 293 –301.
Edwards, G., Chandler, J. and Peto, J. ( 1972 ) Motivation for drinking among men in a London suburb, Psychological Medicine , 2 , 260 –271.
European Monitoring Centre for Drugs and Drug Addiction (1998) Annual Report on the State of the Drugs Problem in the European Union . EMCDDA, Lisbon.
Griffiths, P., Gossop, M., Powis, B. and Strang, J. ( 1993 ) Reaching hidden populations of drug users by privileged access interviewers: methodological and practical issues. Addiction , 88 , 1617 –1626.
HIT (1996) Chill Out: A Clubber's Guide—The Second Coming . HIT, Liverpool.
Johnston, L. D., O'Malley, P. M. and Bachman J. G. (1997) National Survey Results on Drug Use from the Monitoring the Future Study , 1975–1996: Secondary School Students . US DHHS, National Institute on Drug Abuse, Rockville, MD.
Johnston, L. D., O'Malley, P. M. and Bachman J. G. (2000) The Monitoring the Future National Results on Adolescent Drug Use: Overview of Key Findings 1999 . US DHHS, National Institute on Drug Abuse, Rockville, MD.
Lenton, S., Boys, A. and Norcross, K. ( 1997 ) Raves, drugs and experience: drug use by a sample of people who attend raves in Western Australia. Addiction , 92 , 1327 –1337.
Marsden, J., Gossop, M., Stewart, D., Best, D., Farrell, M., Edwards, C., Lehmann, P. and Strang, J. ( 1998 ) The Maudsley Addiction Profile (MAP): a brief instrument for assessing treatment outcome. Addiction , 93 , 1857 –1867.
McKay, J. R., Murphy, R. T., McGuire, J., Rivinus, T. R. and Maisto, S. A. ( 1992 ) Incarcerated adolescents' attributions for drug and alcohol use. Addictive Behaviors , 17 , 227 –235.
Newcomb. M. D., Chou, C.-P., Bentler, P. M. and Huba, G. J. ( 1988 ) Cognitive motivations for drug use among adolescents: longitudinal tests of gender differences and predictors of change in drug use. Journal of Counselling Psychology , 35 , 426 –438.
Power, R. ( 1995 ) A model for qualitative action research amongst illicit drug users. Addiction Research , 3 , 165 –181.
Power, R., Power, T. and Gibson, N. ( 1996 ) Attitudes and experience of drug use amongst a group of London teenagers. Drugs: Education, Prevention and Policy , 3 , 71 –80.
Ramsay, M. and Partridge, S. (1999) Drug Misuse Declared in 1998: Results from the British Crime Survey . Home Office, London.
Release (1997) Release Drugs and Dance Survey: An Insight into the Culture . Release, London.
Sadava, S. ( 1975 ) Research approaches in illicit drug use: a critical review. Genetic Psychology Monographs , 91 , 3 –59.
Tackling Drugs to Build a Better Britain (1998) The Government's 10-year Strategy on Drug Misuse. Central Drugs Co-ordinating Unit, London.
Van Meter, K. M. (1990) Methodological and design issues: techniques for assessing the representatives of snowball samples. In Lambert, E. Y. (ed.), The Collection and Interpretation of Data from Hidden Populations . US DHHS, National Institute on Drug Abuse, Rockville, MD, pp. 31–33.
Wibberley, C. and Price, J. ( 2000 ) Patterns of psycho-stimulant drug use amongst `social/operational users': implications for services. Addiction Research , 8 , 95 –111.
WHO (1997) Amphetamine-type Stimulants: A Report from the WHO Meeting on Amphetamines , MDMA and other Psychostimulants , Geneva, 12–15 November 1996. Programme on Substance Abuse, Division of Mental Health and Prevention of Substance Abuse, WHO, Geneva.
Email alerts
Citing articles via.
- Recommend to your Library
Affiliations
- Online ISSN 1465-3648
- Print ISSN 0268-1153
- Copyright © 2024 Oxford University Press
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Research Reports

Cannabis (Marijuana) Research Report
Common comorbidities with substance use disorders research report.

Heroin Research Report

Inhalants Research Report
MDMA (Ecstasy) Abuse Research Report

Medications to Treat Opioid Use Disorder Research Report

Methamphetamine Research Report

Misuse of Prescription Drugs Research Report

Prescription Opioids and Heroin Research Report

Substance Use in Women Research Report

Tobacco, Nicotine, and E-Cigarettes Research Report
- Research article
- Open access
- Published: 30 October 2020
“College fields of study and substance use”
- Wei-Lin Chen 1 &
- Jen-Hao Chen 2
BMC Public Health volume 20 , Article number: 1631 ( 2020 ) Cite this article
7433 Accesses
3 Citations
1 Altmetric
Metrics details
Numerous studies have documented factors that are associated with substance use behaviors among college-aged individuals. However, relatively few studies have considered the heterogeneity of the college experience by field of study (i.e., college major) and how that educational context might affect students’ health behaviors differently. Drawing from theories and prior research, this study investigates whether college majors are associated with different substance use behaviors, both during college and upon graduation.
The study analyzed longitudinal data from the National Longitudinal Survey of Youth 97 ( N = 1031), specifically data on individuals who obtained a bachelor’s degree, to examine the associations between college fields of study and trajectories of three substance use behaviors: smoking, heavy alcohol use, and marijuana use.
The results indicate that social science and business majors were associated with more substance use behaviors than arts and humanities and STEM majors. However, social science majors were associated with a faster decrease in substance use behaviors over time. Importantly, the differences we found in mean levels of substance use behaviors and trajectories were not explained by demographic characteristics, family SES background, childhood health conditions, and employment experience. Further analysis that examined college major and each substance use behavior individually suggests that the associations were stronger for heavy alcohol use and marijuana use. Moreover, we found the associations were more pronounced in men than women.
Conclusions
The study finds that not all college majors show the same level of engagement in substance use behaviors over time, and that the associations also vary by (1) the specific substance use behavior examined and (2) by gender. These findings suggest it is important to consider that the different learning and educational contexts that college majors provide may also be more or less supportive of certain health behaviors, such as substance use. Practical implications are discussed.
Peer Review reports
Introduction
Substance use is an important public health concern in the United States. National surveys consistently show that substance use peaks during emerging adulthood [ 1 ]. Although college students may show less substance use than non-students in the same age range [ 2 ], it remains true that smoking, heavy alcohol use, and illicit drug use are not uncommon [ 3 , 4 , 5 ] among college students and are considered pressing health issues [ 6 ]. O’Mally and Johnston’s [ 7 ] influential study shows a high prevalence of heavy alcohol use and smoking among college students, with only a slight improvement from 1980 to late 1990. Even the most recent national survey data suggest that substance use remains a pressing health concern of the college-age population. The national Monitoring the Future 2018 survey indicates that among full-time college students in the United States, 15.3% have used cigarette, 29% are heavy alcohol users, and 24.7% have used marijuana during the past 30 days [ 4 ].
Moreover, research makes clear that substance use during the college years has significant consequences for learning and health. College students who are heavy alcohol users are more likely to get injured [ 8 ], have lower academic performance and drop out of college at higher rates [ 9 ], and demonstrate poor working memory [ 10 ]. Marijuana can impair neuropsychological functioning and thus affect individuals’ learning and work performance [ 11 ]. Smoking is associated with lower cognitive function among college students, including a lower level of verbal or auditory competence [ 12 ]. Because so many college students use substances and their negative impact on physical health and learning can be significant, it is critical to investigate and understand the factors that relate to students’ substance use behaviors.
There are many prior studies that contribute to our understanding of the risk and protective factors that may promote or deter substance use among college students [ 13 , 14 , 15 , 16 ]. While a full review of the extant studies of substance use among college studies is beyond the scope of this research, it is useful to briefly summarize factors that have been shown to relate to college students’ substance use. Furthermore, studies using large-samples suggest that substance use behaviors (such as heavy alcohol use, smoking, marijuana use) among college students tend to co-occur [ 17 , 18 ], suggesting the need to investigate substance use behaviors simultaneously. Following Ham and Hope’s [ 19 ] approach in their influential systematic review of problematic drinking among college students, we classify previously identified risk and protective factors of substance use at three levels: individual, interpersonal, and contextual. First, substance use varies by individual demographic characteristics and personality factors. For example, studies consistently find that men have a higher likelihood of substance use than women [ 13 , 20 ] and that African American and Hispanic students have lower rates of substance use [ 13 , 20 , 21 ] than white students. Other studies find that certain personality traits appear to be associated with substance use among college students. For example, sensation seeking is related to heavy alcohol use [ 22 , 23 ].
However, individual factors offer little help in prevention and intervention. Therefore, in recent years, research has moved to investigate the role of interpersonal and contextual factors on college students’ substance use. For example, living with parents during college is associated with lower levels of substance use [ 2 ]. In contrast, two systematic literature reviews of problematic drinking and smoking suggest that living on campus appear to correlate with increased alcohol consumption and smoking [ 24 , 25 ]. In contrast, low academic performance, often measured by GPA, is associated with alcohol or illicit drug use. Heavy alcohol or drug use may impact cognitive functioning, which contributes to poorer grades. Evidence also shows that working part-time during college is associated with more substance use [ 26 , 27 ]. Membership in fraternities and sororities is found to be associated with substance use [ 28 , 29 ]. Finally, several studies start to pay attention to the educational context. In a systematic literature review by Carter and colleagues [ 25 ], they conclude that full-time college students, especially for those in 4-year college, display a greater engagement in heavy alcohol use. Cranford and colleagues [ 30 ] analyze a probability sample of students and find that undergraduates are associated with a higher likelihood of heavy alcohol use and marijuana use (but not smoking) than graduate students.
Although prior studies have investigated a wide range of individual, interpersonal, and contextual factors that relate to substance use among college students, the role of college major has received relatively little attention. This is a curious oversight because college education, by nature, is more heterogeneous than secondary education. Even within the same college, majors vary on curricula, expectations, learning environment, and level of professionalization. In addition, majors differ on whether and how much they expect students to learn specialized knowledge, gain hands-on experience, and collaborate on group projects [ 31 , 32 ]. Because a student’s academic experience differs so much by major and is so central to life during the college years, it is reasonable to believe that college major may affect students’ likelihood of engaging in substance use behaviors as they emerge into adulthood. In other words, some of the differences that exist across majors may be more or less protective against, or supportive of, students’ substance use. This study aims to addresses this key, relatively unexplored question: Does a student’s college major predict his/her likelihood of substance use during and after college?
Based on prior studies, there are strong empirical and theoretical reasons to believe that engaging in a health risk behavior, such as substance use, may vary by college major. First, only some majors expose students to knowledge of human health and physiology, which may produce differences in health literacy by major [ 33 ]. Differences in health literacy may, in turn, lead to differences in health behaviors. Second, the undergraduate socialization model conceptualizes college as the primary socialization field for young adults’ development [ 34 , 35 ]. Students are socialized into the norms of their major and participate in activities and social interactions that promote their success in related professional fields. Social learning theory posits that individuals learn from various forms of interaction with peers and colleagues, which highlights the importance of how students’ interactions in their major may affect how they learn health behaviors, such as substance use [ 36 , 37 , 38 ]. For example, health-related majors may be trained to avoid smoking and drug use because they will likely work in smoke-free and drug-free workplaces when they graduate. In contrast, business majors might be socialized to be more tolerant toward smoking and heavy alcohol use because those behaviors occur in the social interactions that graduates have with their clients. In these and other ways, college majors provide a different environment and socialization that may affect health behaviors.
Despite these reasons to believe that a student’s choice of college major may affect their substance use, there is limited empirical evidence on this research question. Of the studies that do exist on the substance use behaviors of college students, many rely on surveys at a single college or university (e.g.), [ 39 , 40 , 41 ]. Even fewer studies exist that consider college major as an influential factor in substance use behaviors over time. Finally, to our knowledge, it appears that no study exists that examines this question with the benefit of a large-scale, national sample with longitudinal data. This study aims to address these limitations by using a large-scale, longitudinal dataset to investigate whether and how engagement in substance use behaviors (i.e., smoking, heavy alcohol use, and marijuana use) varies by college major.
National Longitudinal Survey of youth 1997
This study used data from the National Longitudinal Survey of Youth 1997 (NLSY97), a nationally representative sample of youths who were born between 1980 and 1984. The NLSY97 began by interviewing 8984 respondents who were 12 to 18 years old in 1997–1998 (round 1). Respondents were followed every year until 2013–2014 (round 16). After that, respondents were followed every 2 years [ 42 ]. The NLSY97 aims to understand U.S. youths’ transition from school to work and into adulthood [ 43 ]. The NLSY97’s detailed information on college education, together with the large-scale, longitudinal national sample, provide a rare opportunity to examine college majors and substance use over time.
We used transcript data in the NLSY97 to identify when a respondent started college and when s/he received a college degree. College transcripts provide the most accurate information on when individuals started college and whether they received a bachelor’s degree. We limited the study to respondents who obtained a bachelor’s degree between 2001 and 2011 because no college transcript data was collected after 2011. After excluding any individual whose college major could not be identified or was missing, we were left with a sample of 1099 youths who completed college, obtained their degree between 2001 and 2011, and whose college major was known. A small proportion of youth in our sample had missing values on the variables of interest for health behaviors (i.e., smoking, heavy alcohol use, and marijuana use). For each youth, three rounds of data were used in the analysis: the wave when the respondent entered college, the wave when the respondent finished college, and the wave after college completion. The final sample for longitudinal analysis included 1031 youth.

Classification of college major
In each round of data collection in the NLSY97, respondents who enrolled in college were asked about their major(s); we used this self-reported information to identify the field of the college degree. We chose to rely on self-reports, rather than college transcript data, to identify college majors because the college transcript data from the NLSY97 did not provide raw data on specific majors. Instead, the NLSY97 raw data grouped college majors into categories, such as liberal arts, sciences, general studies, and humanities. Thus, it was unclear what a student’s exact college major was or how the NLSY97 defined its college major categories. Second, we chose to structure our data with self-reported college major rather than NLSY97-defined categories because it would allow future researchers to reclassify majors according to different definitions and research needs. We matched self-reported college major to the college transcript data for the year when respondents received a bachelor’s degree.
We followed the National Science Foundation’s (NSF) classification to group college majors into eight categories [ 44 ]. If a major appeared that was not on the NSF list, we followed the definitions of Liu, Sun, & Winters [ 45 ] because they expanded the NSF classification to include as many majors as possible in their study. If a respondent reported more than one major and the two majors were in the same field, we placed that respondent in the corresponding category (e.g., social sciences or STEM). If a respondent reported more than one major and the two majors were in different fields, we placed the respondent in the “multiple fields” category. Detailed definitions of each group are presented in Table 1 .
Measures of substance use behaviors
The NLSY97 asked respondents to report substance use behaviors during the past month for smoking, healthy alcohol use, and marijuana use. The questions were: “During the past 30 days, on how many days did you smoke a cigarette?”; “On how many days did you have five or more drinks on the same occasion during the past 30 days?”; and “On how many days have you used marijuana in the last 30 days?” We first converted respondents’ answers to binary variables, coding a response ‘one’ if a respondent’s answer indicated his or her engagement of the substance use behavior during the past 30 days, and ‘zero’ if otherwise. Next, because substance use behaviors sometimes cluster together, we generated a new variable for ‘degree of engagement in substance use behaviors.’ For this variable, we summed the three binary indicators to create an indicator of numbers of substance use behaviors (ranging from 0 to 3) in the past month.
The statistical analysis in this study controlled for potential confounders of substance use behaviors. The confounders included race/ethnicity, gender, highest level of parental education, age, childhood health problems (i.e., physical conditions, learning problems, and other chronic conditions), years of degree completion, self-rated general health, number of weeks working at a job during the year, and an income-to-poverty ratio for each year. In the baseline survey, parents were asked if the respondent had the following three childhood health problems that may potentially limit school in early life: (1) a physical condition, (2) a learning problem, and (3) any chronic condition.
Empirical strategy
The first step in the empirical analysis was to use negative binomial regressions to estimate whether receiving a bachelor’s degree was associated with degree of engagement in substance use behaviors in 2011. After completing this cross-sectional analysis, we applied multilevel negative binomial models to estimate the associations between college major and degree of engagement in substance use behaviors over time. We used the multilevel model approach to account for the nested nature of individual longitudinal data because one’s substance use at different time periods is nested within the invariant characteristics of the person [ 46 ]. Specifically, in our statistical model, level 1 represents individual substance use behaviors over time and level 2 represents personal characteristics. Furthermore, we used negative binomial regression in conjunction with the multilevel model approach. The negative binomial regression is widely used to model count data [ 47 ] and has been widely applied in substance use research (e.g.), [ 48 , 49 , 50 ]. More specifically, negative binomial regression can be used for over-dispersed count data, that is when the conditional variance exceeds the conditional mean. As such, it can be considered as a more generalized version of Poisson regression and becomes more efficient than Poisson when the outcome variable is over-dispersed [ 47 ]. In the longitudinal analysis, we also included interaction terms between college major and age to investigate whether substance use behaviors change over time by different majors. All regressions controlled for potential confounders.
For all regressions, we selected arts & humanities majors as the reference group. In addition, we did pair-wise comparisons across college majors using the same model and controlling for the full set of confounders. As such, we were able to fully test whether the association was statistically significant between each major. All analyses were done using Stata 16. This study is exempt from IRB review because it uses a survey dataset that is publicly available.
Table 2 presents sample characteristics for all respondents who obtained a bachelor’s degree between 2001 and 2011, as well as respondents’ substance use behaviors at the time of entering college and at the time of graduation, by college major. At the time of entering college, we observe substantial variations in substance use behavior by college major. For example, students who major in STEM, health sciences, and education showed a lower degree of engagement in substance use behaviors. In contrast, students who major in business, on average, showed a higher degree of engagement in substance use behaviors. A closer look at Table 2 also reveals a trend over time of increased substance use behaviors for individuals in nearly all majors. In other words, for students in nearly all majors, substance use at graduation was more prevalent than it was at college entry.
Table 3 presents the results of regression analyses that examined the association between level of education and substance use behaviors. The first column shows results for the full sample; the second and third columns show results for men and women separately. For the full sample, Model 1 found that individuals with a bachelor’s degree were less likely to engage in substance use behaviors, compared to individuals without a bachelor’s degree. Model 2 found that individuals with a STEM or education major were less likely to engage in substance use behaviors than individuals without a bachelor’s degree. While the coefficients of other majors were in the expected direction, they were not statistically significant. In addition, some gender differences were observed.
Table 4 presents the results from the multilevel negative binomial models that estimated the associations between college major and substance use behaviors over time. Again, the first column shows results for the full sample and the second and third columns show results for men and women separately. Results from the full sample suggest that the main effect of college major showed some variation in substance use behaviors. In addition, interaction terms showed that changes in substance use behaviors with age also differed by major. For example, individuals who majored in social sciences and business (marginally significant) were associated with decreased substance use with age, compared to individuals in arts and humanities majors. Importantly, the results in this table also show that differences between these college majors in substance use and changes over time cannot be explained by the covariates, including demographic characteristics, family SES background, childhood health, and employment. We also performed additional statistical tests that did pair-wise comparisons across majors; these analyses indicated some interesting patterns (results are in the Appendix: Table 6). For example, individuals with a social science major were also less likely to engage in substance use over time than individuals in a STEM major.
Moving to the second and third columns, results from the subsample of men and the subsample of women show remarkable differences. Men who majored in STEM, social sciences, or business were associated with decreased substance use with age, compared to men in arts and humanities majors. However, for women, the rates of changes in substance use behaviors did not vary significantly by majors.
Finally, because it is possible that each substance use behavior may correlate with college major differently, we analyzed each substance use behavior separately (i.e., smoking, heavy alcohol use, and marijuana use). Table 5 shows the regression results from the multilevel models that estimated associations between college majors and each substance use behavior over time. We found that trends in heavy alcohol use and marijuana use were more likely to vary by college major than trends in smoking, which did not vary across college majors. For example, individuals who majored in the social sciences or business were associated with decreased heavy alcohol use with age, compared to individuals in arts and humanities majors. Additionally, individuals in social sciences or health majors were associated with decreased marijuana use as they aged.
We also conducted a number of sensitivity analyses to check the robustness of the results. These analyses included: (1) investigating whether college major is associated with engaging in a substance use behavior in the past year (instead of the past 30 days) and (2) using multiple imputation instead of listwise deletion to recover missing values. The results from both sensitivity analyses were similar to the results in the main analysis. The results of all sensitivity analyses are available upon request.
The college years are a critical point in the life course when individuals build the foundation for a healthy and successful future. Whether college students develop healthy lifestyles and abstain from unhealthy substance use, particularly during the transition to adulthood, is thus a critical issue for public policy and practice. A student’s college experience is strongly shaped by his/her choice of major, with academic and social experiences differing greatly across majors. Nevertheless, the literature that seeks to understand college students’ health behaviors, including substance use, largely overlooks the role of college major. This question has gone unasked: Do all college degrees affect health behaviors in the same way, regardless of the field of study? This study sought to answer to this question by focusing on college major and substance use behaviors. Using longitudinal data from a national sample, the results revealed some interesting patterns between certain aspects of college education and substance use.
Consistent with prior studies, having a college degree was associated with a decreased likelihood of engaging in substance use behaviors (e.g., [ 2 ]). This study found some more specific variations in substance use by college major, particularly in terms of substance use prevalence and trajectories over time. Our analysis found that social science and business majors, on average, show higher rates of substance use than arts and humanities and STEM majors. Yet, social science and business majors also decreased their substance use more quickly over time than other majors did. When examining specific substance use behaviors, we found that college major is a significant predictor of heavy alcohol use and marijuana use, but not smoking. In addition, we observed strong gender differences: The associations we found between college major and substance use were more salient for men than women. Taken together, these findings lend some support to our hypothesis that college majors are heterogeneous and may potentially affect health behaviors, particularly substance use, differently.
The findings from this study are important because they inform the literature on college students’ health and substance use in several key ways. First, studies of substance use have traditionally focused only on the “social” and interpersonal” contexts. Indeed, the literature on adolescent health has long recognized the crucial role that peers and social context play in whether students engage in risky and unhealthy behaviors [ 51 , 52 ], and some recent studies suggest that college students are no exception [ 53 , 54 ]. However, particularly in college when the individual experience differs so much by major, it is also imperative to focus on a student’s ‘educational context’ and how it might relate to substance use and other health behaviors. By focusing on college major and substance use, this study demonstrates that important heterogeneity exists: Not all majors are associated equally with substance use behaviors and the patterns cannot be fully explained by standard social and interpersonal contexts, such as demographics, SES, employment, etc. Future studies can build on this research by digging deeper into college majors to elucidate the mechanisms through which they affect substance use behaviors or other health outcomes.
Second, the findings inform the literature by suggesting that business and social sciences majors may be less ‘healthy’, that is, that students in these majors have a higher likelihood of engaging in substance use behaviors than students in other majors. This finding deserves further discussion and, ultimately, further research. At first glance, the variations in substance use across majors may be assumed to be due to differences in health literacy, i.e., students in health-related majors are more aware of the health implications of their behaviors than other students. However, it is important to note that we found observable differences between students in arts and humanities and other, non-health fields of study; such differences cannot reasonably be explained by differences health literacy. For example, it is difficult to believe that arts and humanities majors would have better health knowledge than social science majors, such as political science, sociology, or pre-law [ 33 , 55 ]. Also, the assumption that the differences are due to what a student’s major teaches about health literacy is of limited explanatory value when one considers that recent, widespread public health campaigns have given all young adults a more similar baseline of health literacy. In fact, a recent study finds no difference in terms of health literacy by college majors [ 56 ]. Unfortunately, the NLSY97 does not include questions about students’ health literacy during the college years, so the aforementioned hypothesis cannot be tested. We argue that the higher likelihood we observe among business and social science majors to engage in substance use behaviors is an empirical finding that must be explained, and that it is likely that factors such as the learning experiences and opportunities in the student’s major may help explain the differences. Lipson, et al. [ 57 ] provides support for this idea, suggesting that a highly competitive environment surrounded by peers and faculty in the arts and humanities may help explain the prevalence of students’ mental health problems. Mental health challenges, in turn, are often associated with an increase in risky and unhealthy behaviors. Future studies that specifically investigate the peer influence and substance use culture for heavy alcohol use, smoking, or marijuana use initiation across learning contexts by college major will yield valuable insights that refine our hypothesis.
Finally, and more broadly, the findings from this study suggest a conceptual reconsideration of the role of education in social epidemiology theory and research. Most social epidemiological research focuses on the health benefits of education, which have been largely understood to mean only educational attainment. Indeed, it has been well documented that college graduates are healthier and exhibit more healthy behaviors than those with less education [ 58 , 59 , 60 , 61 , 62 ]. But, the import of education is not limited to achievement, per se. College graduates differ from non-graduates because they have spent a substantial amount of time in educational settings. Yet, the literature has less to say about what experiences in that educational setting make a difference for later health behaviors. Our understanding of how a college student’s field of study (college major) impacts individual health remains very limited. Findings from this study demonstrate the heterogeneity of college majors with respect to substance use, and in so doing, suggest the need to expand the concept of education in social epidemiology research.
Despite the strength of this study, we recognize a few limitations. First, since students do not randomly select into their major, the results are not causal. There are factors related to students and their lives that affect the choice of major and the choice to engage in risky health behaviors. As such, even though we used longitudinal data and controlled for a wide range of potential confounders, our findings remain associational. In particular, there is some evidence that heavy drinkers appear to gravitate toward business majors, which makes the causal relationship even more complicated [ 63 , 64 ]. Readers should be cautious and refrain from making causal interpretations of the associations reported in this study. Second, because the NLSY97 did not include measures of mental health in every wave of the survey, we could not control for mental health during the college years and thus test whether mental health mediates the associations we found. We hope that future research will shed light on this issue by examining mental health as it relates to college students’ field of study and substance use. Third, the definition of ‘heavy alcohol use’ used in the study differs slightly from the most-up-to-date definition of binge drinking, only because the NLSY97 survey question followed the earlier classification of binge drinking that was used in the National Survey on Drug Use and Health. As such, caution should be used when comparing our results on heavy alcohol use to other studies of binge drinking. Finally, despite the large sample size and detailed information on respondents’ college years, our findings might not be generalizable to current college students. The NLSY97 data is approximately a decade old, and college students today face a different policy context for substance use [ 65 ]. Future research that uses newer data may inform the generalizability of the NLSY97 data.
Limitations notwithstanding, this study demonstrates that even among people who have all completed college, there are significant variations in engaging in substance use, an important health risk behavior. The associations cannot be explained by demographic characteristics, familial SES background, and respondents’ employment and economic well-being. This robust conclusion has three practical implications. First, college health centers need to work with deans and department chairs in fields with a higher risk of substance use (i.e., business, social sciences) to increase awareness of the issue. Going further, our results should encourage deans and department chairs to consider not just the academic preparation of their majors for career success in terms of job placement and salary [ 66 ], but also the preparation of their majors for life success in terms of health behaviors. Our study suggests some majors come with a higher lifelong price, i.e., higher health risk. Increasing awareness of this issue is the very first step. Second, college health centers need to play a more active role in building a healthy culture among faculty members and students in fields that are more vulnerable to substance use. The idea that college major may affect substance use behaviors can be used to promote more collaboration between school health centers and leaders in academic divisions and departments. Finally, our findings call for deans and department chairs to pay greater attention to how the distinct learning and professionalization environment that their major provides might impact future health behaviors. In short, health should become a consideration in future curriculum design.
This study used a large-scale, longitudinal dataset to investigate whether and how engagement in substance use behaviors varies by college major. We find that not all college majors show the same level of engagement in substance use behaviors over time, and that the associations also vary by the specific substance use behavior examined and by gender. These findings suggest it is important to consider that the different learning and educational contexts that college majors provide may also be more or less supportive of substance use behaviors. Going further, our findings should higher education administrators to consider not just the academic preparation of different college majors for career success in terms of job placement and salary, but also the preparation of different majors for life success in terms of health behaviors. Ultimately, findings of this study may promote a more comprehensive understanding of the educational context of college, and how it affects not only students’ learning but also their substance use, will help us better prepare college students for career and life success.
Availability of data and materials
The authors have full access to the NLSY97 public-use dataset. Data can be downloaded from the following link: https://www.nlsinfo.org/investigator . The analytical sample and codes used and/or analyzed during the current study are available from the corresponding author, on reasonable request.
Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future: National Survey Results on Drug Use, 1975–2008. Volume II, College Students and Adults Ages 19–50. NIH Publication No. 09–7403. Natl Inst Drug Abuse (NIDA). 2009..
Gfroerer JC, Greenblatt JC, Wright DA. Substance use in the US college-age population: differences according to educational status and living arrangement. Am J Public Health. 1997;87(1):62–5..
Article CAS Google Scholar
Rigotti NA, Lee JE, Wechsler H. US college students' use of tobacco products: results of a national survey. JAMA. 2000;284:699–705.
Wechsler H, Kuo M. College students define binge drinking and estimate its prevalence: results of a national survey. J Am Coll Heal. 2000;49:57–64..
Schulenberg J, Johnston L, O'Malley P, Bachman J, Miech R, Patrick M. Monitoring the Future national survey results on drug use, 1975-2018: Volume II, college students and adults ages 19–60. Available at: http://www.monitoringthefuture.org//pubs/monographs/mtf-vol2_2018.pdf . Accessed August 9, 2019.
Patrick K, Grace TW, Lovato CY. Health issues for college students. Annu Rev Public Health. 1992;13:253–68..
O'Malley PM, Johnston LD. Epidemiology of alcohol and other drug use among American college students. J Stud Alcohol Suppl. 2002;63(2):23–40.
Article Google Scholar
Wechsler H, Davenport A, Dowdall G, Moeykens B, Castillo S. Health and behavioral consequences of binge drinking in college: a national survey of students at 140 campuses. JAMA. 1994;272:1672–7.
Jennison KM. The short-term effects and unintended long-term consequences of binge drinking in college: a 10-year follow-up study. Am J Drug Alcohol Abuse. 2004;30:659–84.
Crego A, Holguín SR, Parada M, Mota N, Corral M, Cadaveira F. Binge drinking affects attentional and visual working memory processing in young university students. Alcohol Clin Exp Res. 2009;33:1870–9.
Pope HG, Yurgelun-Todd D. The residual cognitive effects of heavy marijuana use in college students. JAMA. 1996;275:521–7.
Fried PA, Watkinson B, Gray R. Neurocognitive consequences of cigarette smoking in young adults—a comparison with pre-drug performance. Neurotoxicol Teratol. 2006;28:517–25.
McCabe SE, Knight JR, Teter CJ, Wechsler H. Non-medical use of prescription stimulants among US college students: prevalence and correlates from a national survey. Addiction. 2005;100(1):96–106.
White HR, Labouvie EW, Papadaratsakis V. Changes in substance use during the transition to adulthood: a comparison of college students and their noncollege age peers. J Drug Issues. 2005;35(2):281–306.
Stone AL, Becker LG, Huber AM, Catalano RF. Review of risk and protective factors of substance use and problem use in emerging adulthood. Addict Behav. 2012;37(7):747–75.
Welsh JW, Shentu Y, Sarvey DB. Substance use among college students. FOCUS A J Am Psychiatr Assoc. 2019;17(2):117–27.
Google Scholar
Bell R, Wechsler H, Johnston LD. Correlates of college student marijuana use: results of a US national survey. Addiction. 1997;92(5):571–81.
Weitzman ER, Chen YY. The co-occurrence of smoking and drinking among young adults in college: national survey results from the United States. Drug Alcohol Depend. 2005;80(3):377–86.
Ham LS, Hope DA. College students and problematic drinking: a review of the literature. Clin Psychol Rev. 2003;23(5):719–59.
Prendergast ML. Substance use and abuse among college students: a review of recent literature. J Am Coll Heal. 1994;43(3):99–113.
Martins SS, Kim JH, Chen LY, Levin D, Keyes KM, Cerdá M, Storr CL. Nonmedical prescription drug use among US young adults by educational attainment. Soc Psychiatry Psychiatr Epidemiol. 2015;50(5):713–24.
Kaynak Ö, Meyers K, Caldeira KM, Vincent KB, Winters KC, Arria AM. Relationships among parental monitoring and sensation seeking on the development of substance use disorder among college students. Addict Behav. 2013;38(1):1457–63.
Ravert RD, Schwartz SJ, Zamboanga BL, Kim SY, Weisskirch RS, Bersamin M. Sensation seeking and danger invulnerability: paths to college student risk-taking. Personal Individ Differ. 2009;47(7):763–8.
Patterson F, Lerman C, Kaufmann VG, Neuner GA, Audrain-McGovern J. Cigarette smoking practices among American college students: review and future directions. J Am Coll Heal. 2004;52(5):203–12.
Carter AC, Brandon KO, Goldman MS. The college and noncollege experience: a review of the factors that influence drinking behavior in young adulthood. J Stud Alcohol Drugs. 2010;71(5):742–50.
Safron DJ, Schulenberg JE, Bachman JG. Part-time work and hurried adolescence: the links among work intensity, social activities, health behaviors, and substance use. J Health Soc Behav. 2001:425–49.
Johnson MK. Further evidence on adolescent employment and substance use: differences by race and ethnicity. J Health Soc Behav. 2004;45(2):187–97.
Scott-Sheldon LA, Carey KB, Carey MP. Health behavior and college students: does Greek affiliation matter? J Behav Med. 2008;31(1):61–70.
Cheney MK, Harris LW, Gowin MJ, Huber J. Smoking and membership in a fraternity or sorority: a systematic review of the literature. J Am Coll Heal. 2014;62(4):264–76.
Cranford JA, Eisenberg D, Serras AM. Substance use behaviors, mental health problems, and use of mental health services in a probability sample of college students. Addict Behav. 2009;34(2):134–45.
Warren D. Curriculum design in a context of widening participation in higher education. Arts Humanit High Educ. 2002;1(1):85–99.
Carracedo FS, Soler A, Martín C, López D, Ageno A, Cabré J, Garcia J, Aranda J, Gibert K. Competency maps: an effective model to integrate professional competencies across a STEM curriculum. J Sci Educ Technol. 2018;27(5):448–68.
Joseph R, Fernandes S, Hyers L, O'Brien K. Health literacy: a cross-disciplinary study in American undergraduate college students. J Inf Lit. 2016;10.
Weidman J. Undergraduate socialization: A conceptual approach. High Educ. 1989;5:289–322.
Weidman J. Conceptualizing student socialization in higher education: an intellectual journey. In: Socialization in higher education and the early career. Cham: Springer; 2020. p. 11–28.
Chapter Google Scholar
Akers RL, Krohn MD, Lanza-Kaduce L, Radosevich M. Social learning and deviant behavior: A specific test of a general theory. In: Contemporary Masters in Criminology. Boston: Springer; 1995. p. 187–214.
Higgins GE, Makin DA. Does social learning theory condition the effects of low self-control on college students’ software piracy. J Econ Crime Manag. 2004;2:1–22.
Ward BW, Gryczynski J. Social learning theory and the effects of living arrangement on heavy alcohol use: results from a national study of college students. J Stud Alcohol Drugs. 2009;70:364–72.
Clements R. Prevalence of alcohol-use disorders and alcohol-related problems in a college student sample. J Am Coll Heal. 1999;48(3):111–8.
Yusko DA, Buckman JF, White HR, Pandina RJ. Alcohol, tobacco, illicit drugs, and performance enhancers: a comparison of use by college student athletes and nonathletes. J Am Coll Heal. 2008;57(3):281–90.
Kenne DR, Fischbein RL, Tan AS, Banks M. The use of substances other than nicotine in electronic cigarettes among college students. Subst Abus. 2017;11:1178221817733736.
Hagerty H. Round 16 of the National Longitudinal Survey of Youth, 1997 Cohort (NLSY97). Available at: http://www.norc.org/PDFs/NLSY97/Round%2016%20of%20the%20National%20Longitudinal%20Survey%20of%20Youth%20-%201997%20Cohort.pdf . Accessed August 9, 2019.
Moore W, Pedlow S, Krishnamurty P, Wolter, K. Technical Sampling Report. https://www.nlsinfo.org/sites/nlsinfo.org/files/attachments/121221/TechnicalSamplingReport.pdf . Published November 2000. Accessed August 9, 2019.
National Science Foundation (n.d.) Scientists and engineers statistical data system (SESTAT). Available at: https://wwwnsfgov/statistics/sestat/#sestat-faq Accessed September 2, 2020.
Liu S, Sun W, Winters JV. Up in STEM, down in business: changing college major decisions with the great recession. Contemp Econ Policy. 2019;37:476–91.
Steele F. Multilevel models for longitudinal data. J R Stat Soc. 2008;171(1):5–19.
Hilbe JM. Negative Binomial Regression: Cambridge University Press; 2011.
Guo J, Chung IJ, Hill KG, Hawkins JD, Catalano RF, Abbott RD. Developmental relationships between adolescent substance use and risky sexual behavior in young adulthood. J Adolesc Health. 2002;31(4):354–62.
Kaiser AJ, Milich R, Lynam DR, Charnigo RJ. Negative urgency, distress tolerance, and substance abuse among college students. Addict Behav. 2012;37(10):1075–83.
Forster M, Grigsby TJ, Rogers CJ, Benjamin SM. The relationship between family-based adverse childhood experiences and substance use behaviors among a diverse sample of college students. Addict Behav. 2018;76:298–304.
Maxwell KA. Friends: the role of peer influence across adolescent risk behaviors. J Youth Adolesc. 2002;31:267–77.
Gardner M, Steinberg L. Peer influence on risk taking, risk preference, and risky decision making in adolescence and adulthood: an experimental study. Dev Psychol. 2005;41:625.
Pinchevsky GM, Arria AM, Caldeira KM, Garnier-Dykstra LM, Vincent KB, O’Grady KE. Marijuana exposure opportunity and initiation during college: parent and peer influences. Prev Sci. 2012;13:43–54.
Beck KH, Caldeira KM, Vincent KB, Arria AM. Social contexts of drinking and subsequent alcohol use disorder among college students. Am J Drug Alcohol Abuse. 2013;39:38–43.
Rababah JA, Al-Hammouri MM, Drew BL, Aldalaykeh M. Health literacy: exploring disparities among college students. BMC Public Health. 2019;19:1401.
Dolezel D, Shanmugam R, Morrison EE. Are college students health literate? J Am Coll Heal. 2018:1–8.
Lipson SK, Zhou S, Wagner B III, Beck K, Eisenberg D. Major differences: variations in undergraduate and graduate student mental health and treatment utilization across academic disciplines. J Coll Stud Psychother. 2016;30:23–41.
Ross CE, Wu CL. The links between education and health. Am Sociol Rev. 1995:719–45.
Miech RA, Shanahan MJ. Socioeconomic status and depression over the life course. J Health Soc Behav. 2000:162–76.
Cutler DM, Lleras-Muney A. Education and health: evaluating theories and evidence. Natl Bur Econ Res. 2006.
Miech R, Pampel F, Kim J, Rogers RG. The enduring association between education and mortality: the role of widening and narrowing disparities. Am Sociol Rev. 2011;76:913–34.
Lawrence EM. Why do college graduates behave more healthfully than those who are less educated? J Health Soc Behav. 2017;58:291–306.
Gliksman L, Newton-Taylor B, Adlaf E, Giesbrecht N. Alcohol and other drug use by Ontario university students: the roles of gender, age, year of study, academic grades, place of residence and programme of study [1]. Drugs. 1997;4(2):117–29.
Wolaver AM. Effects of heavy drinking in college on study effort, grade point average, and major choice. Contemp Econ Policy. 2002;20(4):415–28.
Alley ZM, Kerr DC, Bae H. Trends in college students’ alcohol, nicotine, prescription opioid and other drug use after recreational marijuana legalization: 2008–2018. Addict Behav. 2020;102:106212.
Thomas SL, Zhang L. Post-baccalaureate wage growth within four years of graduation: the effects of college quality and college major. Res High Educ. 2005;46(4):437–59.
Download references
Acknowledgements
Not applicable.
Author information
Authors and affiliations.
Center for Teacher Education, National Sun Yat-sen University, Kaohsiung City, Taiwan
Wei-Lin Chen
Department of Sociology and Department of Psychology, National Chengchi University, 64, Section 2, Zhinan Rd., Taipei City, Taiwan
Jen-Hao Chen
You can also search for this author in PubMed Google Scholar
Contributions
WC analyzed and interpreted the data and was the major contributor in writing the Methods, Results, and Conclusions sections of the manuscript. JC designed the study and was a major contributor in writing the Introduction and Conclusions sections of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Jen-Hao Chen .
Ethics declarations
Ethics approval and consent to participate.
No ethics approval is waived for this study because it relies on a publicly-available dataset.
Consent for publication
Competing interests, additional information, publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Chen, WL., Chen, JH. “College fields of study and substance use”. BMC Public Health 20 , 1631 (2020). https://doi.org/10.1186/s12889-020-09722-1
Download citation
Received : 24 June 2020
Accepted : 16 October 2020
Published : 30 October 2020
DOI : https://doi.org/10.1186/s12889-020-09722-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- College major
- Health behaviors
- Health disparities
- Substance use
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]

- MJC Library & Learning Center
- Research Guides
Drug Abuse, Addiction, Substance Use Disorder
- Research Drug Abuse
Start Learning About Your Topic
Create research questions to focus your topic, find books in the library catalog, find articles in library databases, find web resources, cite your sources, key search words.
Use the words below to search for useful information in books and articles .
- substance use disorder
- substance abuse
- drug addiction
- substance addiction
- chemical dependency
- war on drugs
- names of specific drugs such as methamphetamine, cocaine, heroin
- opioid crisis
Background Reading:
It's important to begin your research learning something about your subject; in fact, you won't be able to create a focused, manageable thesis unless you already know something about your topic.
This step is important so that you will:
- Begin building your core knowledge about your topic
- Be able to put your topic in context
- Create research questions that drive your search for information
- Create a list of search terms that will help you find relevant information
- Know if the information you’re finding is relevant and useful
If you're working from off campus , you'll be prompted to log in just like you do for your MJC email or Canvas courses.
All of these resources are free for MJC students, faculty, & staff.
- Gale eBooks This link opens in a new window Use this database for preliminary reading as you start your research. Try searching these terms: addiction, substance abuse
Other eBooks from the MJC Library collection:
Use some of the questions below to help you narrow this broad topic. See "substance abuse" in our Developing Research Questions guide for an example of research questions on a focused study of drug abuse.
- In what ways is drug abuse a serious problem?
- What drugs are abused?
- Who abuses drugs?
- What causes people to abuse drugs?
- How do drug abusers' actions affect themselves, their families, and their communities?
- What resources and treatment are available to drug abusers?
- What are the laws pertaining to drug use?
- What are the arguments for legalizing drugs?
- What are the arguments against legalizing drugs?
- Is drug abuse best handled on a personal, local, state or federal level?
- Based on what I have learned from my research what do I think about the issue of drug abuse?
Why Use Books:
Use books to read broad overviews and detailed discussions of your topic. You can also use books to find primary sources , which are often published together in collections.
Where Do I Find Books?
You'll use the library catalog to search for books, ebooks, articles, and more.
What if MJC Doesn't Have What I Need?
If you need materials (books, articles, recordings, videos, etc.) that you cannot find in the library catalog , use our interlibrary loan service .
All of these resources are free for MJC students, faculty, & staff.
- EBSCOhost Databases This link opens in a new window Search 22 databases simultaneously that cover almost any topic you need to research at MJC. EBSCO databases include articles previously published in journals, magazines, newspapers, books, and other media outlets.
- Gale Databases This link opens in a new window Search over 35 databases simultaneously that cover almost any topic you need to research at MJC. Gale databases include articles previously published in journals, magazines, newspapers, books, and other media outlets.
- Psychology and Behavioral Sciences Collection This link opens in a new window Contains articles from nearly 560 scholarly journals, some dating as far back as 1965
- Access World News This link opens in a new window Search the full-text of editions of record for local, regional, and national U.S. newspapers as well as full-text content of key international sources. This is your source for The Modesto Bee from January 1989 to the present. Also includes in-depth special reports and hot topics from around the country. To access The Modesto Bee , limit your search to that publication. more... less... Watch this short video to learn how to find The Modesto Bee .
Use Google Scholar to find scholarly literature on the Web:

Browse Featured Web Sites:
- National Institute on Drug Abuse NIDA's mission is to lead the nation in bringing the power of science to bear on drug abuse and addiction. This charge has two critical components. The first is the strategic support and conduct of research across a broad range of disciplines. The second is ensuring the rapid and effective dissemination and use of the results of that research to significantly improve prevention and treatment and to inform policy as it relates to drug abuse and addiction.
- Drug Free America Foundation Drug Free America Foundation, Inc. is a drug prevention and policy organization committed to developing, promoting and sustaining national and international policies and laws that will reduce illegal drug use and drug addiction.
- Office of National Drug Control Policy A component of the Executive Office of the President, ONDCP was created by the Anti-Drug Abuse Act of 1988. ONDCP advises the President on drug-control issues, coordinates drug-control activities and related funding across the Federal government, and produces the annual National Drug Control Strategy, which outlines Administration efforts to reduce illicit drug use, manufacturing and trafficking, drug-related crime and violence, and drug-related health consequences.
- Drug Policy Alliance The Drug Policy Alliance (DPA) is the nation's leading organization promoting alternatives to current drug policy that are grounded in science, compassion, health and human rights.
Your instructor should tell you which citation style they want you to use. Click on the appropriate link below to learn how to format your paper and cite your sources according to a particular style.
- Chicago Style
- ASA & Other Citation Styles
- Last Updated: Apr 18, 2024 12:03 PM
- URL: https://libguides.mjc.edu/drugabuse
Except where otherwise noted, this work is licensed under CC BY-SA 4.0 and CC BY-NC 4.0 Licenses .
- Share full article
Advertisement
Supported by
A Conversation With …
Teen Drug Use Habits Are Changing, For the Good. With Caveats.
Dr. Nora Volkow, who leads the National Institutes of Drug Abuse, would like the public to know things are getting better. Mostly.

By Matt Richtel
Historically speaking, it’s not a bad time to be the liver of a teenager. Or the lungs.
Regular use of alcohol, tobacco and drugs among high school students has been on a long downward trend.
In 2023, 46 percent of seniors said that they’d had a drink in the year before being interviewed; that is a precipitous drop from 88 percent in 1979, when the behavior peaked, according to the annual Monitoring the Future survey, a closely watched national poll of youth substance use. A similar downward trend was observed among eighth and 10th graders, and for those three age groups when it came to cigarette smoking. In 2023, just 15 percent of seniors said that they had smoked a cigarette in their life, down from a peak of 76 percent in 1977 .
Illicit drug use among teens has remained low and fairly steady for the past three decades, with some notable declines during the Covid-19 pandemic.
In 2023, 29 percent of high school seniors reported using marijuana in the previous year — down from 37 percent in 2017, and from a peak of 51 percent in 1979.
There are some sobering caveats to the good news. One is that teen overdose deaths have sharply risen, with fentanyl-involved deaths among adolescents doubling from 2019 to 2020 and remaining at that level in the subsequent years.
Dr. Nora Volkow has devoted her career to studying use of drugs and alcohol. She has been the director of the National Institute on Drug Abuse since 2003. She sat down with The New York Times to discuss changing patterns and the reasons behind shifting drug-use trends.
What’s the big picture on teens and drug use?
People don’t really realize that among young people, particularly teenagers, the rate of drug use is at the lowest risk that we have seen in decades. And that’s worth saying, too, for legal alcohol and tobacco.
What do you credit for the change?
One major factor is education and prevention campaigns. Certainly, the prevention campaign for cigarette smoking has been one of the most effective we’ve ever seen.
Some of the policies that were implemented also significantly helped, not just making the legal age for alcohol and tobacco 21 years, but enforcing those laws. Then you stop the progression from drugs that are more accessible, like tobacco and alcohol, to the illicit ones. And teenagers don’t get exposed to advertisements of legal drugs like they did in the past. All of these policies and interventions have had a downstream impact on the use of illicit drugs.
Does social media use among teens play a role?
Absolutely. Social media has shifted the opportunity of being in the physical space with other teenagers. That reduces the likelihood that they will take drugs. And this became dramatically evident when they closed schools because of Covid-19. You saw a big jump downward in the prevalence of use of many substances during the pandemic. That might be because teenagers could not be with one another.
The issue that’s interesting is that despite the fact schools are back, the prevalence of substance use has not gone up to the prepandemic period. It has remained stable or continued to go down. It was a big jump downward, a shift, and some drug use trends continue to slowly go down.
Is there any thought that the stimulation that comes from using a digital device may satisfy some of the same neurochemical experiences of drugs, or provide some of the escapism?
Yes, that’s possible. There has been a shift in the types of reinforcers available to teenagers. It’s not just social media, it’s video gaming, for example. Video gaming can be very reinforcing, and you can produce patterns of compulsive use. So, you are shifting one reinforcer, one way of escaping, with another one. That may be another factor.
Is it too simplistic to see the decline in drug use as a good news story?
If you look at it in an objective way, yes, it’s very good news. Why? Because we know that the earlier you are using these drugs, the greater the risk of becoming addicted to them. It lowers the risk these drugs will interfere with your mental health, your general health, your ability to complete an education and your future job opportunities. That is absolutely good news.
But we don’t want to become complacent.
The supply of drugs is more dangerous, leading to an increase in overdose deaths. We’re not exaggerating. I mean, taking one of these drugs can kill you.
What about vaping? It has been falling, but use is still considerably higher than for cigarettes: In 2021, about a quarter of high school seniors said that they had vaped nicotine in the preceding year . Why would teens resist cigarettes and flock to vaping?
Most of the toxicity associated with tobacco has been ascribed to the burning of the leaf. The burning of that tobacco was responsible for cancer and for most of the other adverse effects, even though nicotine is the addictive element.
What we’ve come to understand is that nicotine vaping has harms of its own, but this has not been as well understood as was the case with tobacco. The other aspect that made vaping so appealing to teenagers was that it was associated with all sorts of flavors — candy flavors. It was not until the F.D.A. made those flavors illegal that vaping became less accessible.
My argument would be there’s no reason we should be exposing teenagers to nicotine. Because nicotine is very, very addictive.
Anything else you want to add?
We also have all of this interest in cannabis and psychedelic drugs. And there’s a lot of interest in the idea that psychedelic drugs may have therapeutic benefits. To prevent these new trends in drug use among teens requires different strategies than those we’ve used for alcohol or nicotine.
For example, we can say that if you take drugs like alcohol or nicotine, that can lead to addiction. That’s supported by extensive research. But warning about addiction for drugs like cannabis and psychedelics may not be as effective.
While cannabis can also be addictive, it’s perhaps less so than nicotine or alcohol, and more research is needed in this area, especially on newer, higher-potency products. Psychedelics don’t usually lead to addiction, but they can produce adverse mental experiences that can put you at risk of psychosis.
Matt Richtel is a health and science reporter for The Times, based in Boulder, Colo. More about Matt Richtel

Pathways of Addiction: Opportunities in Drug Abuse Research (1996)
Chapter: 1. introduction, 1 introduction.
Drug abuse research became a subject of sustained scientific interest by a small number of investigators in the late nineteenth and early twentieth centuries. Despite their creative efforts to understand drug abuse in terms of general advances in biomedical science, the medical literature of the early twentieth century is littered with now-discarded theories of drug dependence, such as autointoxication and antibody toxins, and with failed approaches to treatment. Eventually, escalating social concern about the use of addictive drugs and the emergence of the biobehavioral sciences during the post-World War II era led to a substantial investment in drug abuse research by the federal government (see Appendix B ). That investment has yielded substantial advances in scientific understanding about all facets of drug abuse and has also resulted in important discoveries in basic neurobiology, psychiatry, pain research, and other related fields of inquiry. In light of how little was understood about drug abuse such a short time ago, the advances of the past 25 years represent a remarkable scientific accomplishment. Yet there remains a disconnect between what is now known scientifically about drug abuse and addiction, the public's understanding of and beliefs about abuse and addiction, and the extent to which what is known is actually applied in public health settings.
During its brief history, drug abuse research has been supported mainly by the federal government, with occasional investments by major private foundations. At the federal level, the lead agency for drug abuse research is the National Institute on Drug Abuse (NIDA), which supports
85 percent of the world's research on drug abuse and addiction. Other sponsoring agencies include the National Institute of Mental Health (NIMH), the National Institute on Alcohol Abuse and Alcoholism (NIAAA), and the Substance Abuse and Mental Health Services Administration (SAMHSA), all in the Department of Health and Human Services; as well as the Office of Justice Programs (OJP) in the Department of Justice. Throughout the federal government, the FY 1995 investment in drug abuse research and development was $542.2 million, which represents 4 percent of the $13.3 billion spent by the federal government on drug abuse (ONDCP, 1996). By comparison, $8.5 billion (64 percent of the FY 1995 budget) was spent on criminal justice programs, 1 $2.7 billion (20 percent) on treatment of drug abuse, and $1.6 billion (12 percent) on prevention efforts.
In 1992, the General Accounting Office (GAO) released a report Drug Abuse Research: Federal Funding and Future Needs, which recommended that Congress review the place of research in drug control policy and its modest 4 percent share of the drug control budget. The report questioned whether the federal commitment to research was adequate, given the enormity of research needs (GAO, 1992), and whether adequate evaluation research was being conducted to determine the efficacy of various drug control programs. In FY 1995, drug abuse research was still little more than 4 percent of the entire drug control budget.
In January 1995, NIDA requested the Institute of Medicine (IOM) to examine accomplishments in drug abuse research and provide guidance for future research opportunities. This report by the IOM Committee on Opportunities in Drug Abuse Research focuses broadly on opportunities and priorities for future scientific research in drug abuse. After a brief review of major accomplishments in drug abuse research, the remainder of this chapter discusses the vocabulary and basic concepts used in the report, highlights the importance of the nation's investment in drug abuse research, and explores some of the factors that could improve the yield from that investment.
MAJOR ACHIEVEMENTS IN DRUG ABUSE RESEARCH
There have been remarkable achievements in drug abuse research over the past quarter of a century as researchers have learned more about the biological and psychosocial aspects of drug use, abuse, and dependence. Behavioral researchers have developed animal and human mod-
els of drug-seeking behavior, that have, for example, yielded objective measures of initiation and repeated administration of drugs, thereby providing the scientific foundation for assessments of "abuse liability" (i.e., the potential for abuse) of specific drugs (see Chapter 2 ). This information is an essential predicate for informed regulatory decisions under the Food, Drug and Cosmetic Act and the Controlled Substances Act. Taking advantage of technological advances in molecular biology, neuroscientists have identified receptors or receptor types in the brain for opioids, cocaine, benzodiazepines, and marijuana and have described the ways in which the brain adapts to, and changes after, exposure to drugs. Those alterations, which may persist long after the termination of drug use, appear to involve changes in gene expression. They may explain enhanced susceptibility to future drug exposure, thereby shedding light on the enigmas of withdrawal and relapse at the molecular level (see Chapter 3 ). Epidemiologists have designed and implemented epidemiological surveillance systems that enable policymakers to monitor patterns of drug use in the population ( Chapter 4 ) and that enable researchers to investigate the causes and consequences of drug use and abuse (Chapters 5 and 7 , respectively). Paralleling broader trends in health promotion and disease prevention in the past 20 years, the field of drug abuse prevention has made significant progress in evaluating the effectiveness of interventions implemented in a range of settings including communities, schools, and families (see Chapter 6 ).
Marked gains have also been made in treatment research, including improvements in diagnostic criteria; development of a wide range of treatment interventions and sophisticated methods to assess treatment outcome; and development and approval of Leo-alpha-acetylmethadol (LAAM), a medication for the treatment of opioid dependence. Pharmacological and psychosocial treatments, alone or in combination, have been shown to be effective for drug dependencies, and treatment has been shown to reduce drug use, HIV (human immunodeficiency virus) infection rates, health care costs, and criminal activity (see Chapter 8 ).
Drug abuse researchers have also made major contributions to knowledge in adjacent fields of scientific inquiry. For example, NIDA-sponsored research was the driving force in the identification of morphine-like substances that serve as neurotransmitters in specific neurons located throughout the central and peripheral nervous systems (Orson et al., 1994). Identification of these substances represents a dramatic breakthrough in understanding the mechanisms of pain, reinforcement, and stress. Additionally, the discovery of opioid peptides as neurotransmitters played a key role in the identification of numerous other peptide neurotransmitters (Cooper et al., 1991; Goldstein, 1994; Hokfelt et al., 1995). These discoveries have broadened the understanding of brain function and now
form the basis of many current strategies in the design of new drug treatments for neuropsychiatric disorders. Additionally, drug abuse research has contributed to the development of brain imaging techniques.
Drug abuse research has also provided a major impetus for neuropharmacological research in psychiatry since the late 1950s, when it was discovered that LSD (lysergic acid diethylamide; a hallucinogen that produces psychotic symptoms) affected the brain's serotonin systems (Cooper et al., 1991). That seminal discovery stimulated decades of research in the neuropharmacological basis of behavior and psychiatric disorders. The impact on antipsychotic research has been dramatic. In addition, stimulants (e.g., cocaine and amphetamine) were found to produce a state of paranoid psychosis, resembling schizophrenia, in some people. The actions of stimulants on the brain's dopamine pathways continue to inform researchers of the potential role of those pathways in the treatment, and perhaps the pathophysiology, of schizophrenia (Kahn and Davis, 1995). Drug abuse research also has had an impact on antidepressant research (e.g., the actions of drugs of abuse on the brain's serotonin systems have provided useful models with which to investigate the role of those systems in depression and mania). Depression is a risk factor for treatment failure in smoking cessation (Glassman et al., 1993) and depression-like symptoms are dominant during cocaine withdrawal (DiGregorio, 1990). Consequently, treatment of depression in nicotine and cocaine-dependent individuals has been an area of interest for drug abuse research.
Some drugs that are abused, most notably the opioid analgesics, have essential medical uses. Since its founding, NIDA has been the major supporter of research into brain mechanisms of pain and analgesia, analgesic tolerance, and analgesic pharmacology. The resulting discoveries have led to an understanding of which brain circuits are required to generate pain and pain relief (Wall and Melzack, 1994), have revolutionized the treatment of postoperative and cancer pain (Folly and Interesse, 1986; Car et al., 1992; Jacob et al., 1994), and have led to improved treatments for many other conditions that result in chronic pain (see Chapter 3 ).
VOCABULARY OF DRUG ABUSE
Ordinarily, scientific vocabulary evolves toward greater clarity and precision in response to new empirical discoveries and reconceptualizations. That creative process is evident within each of the disciplines of drug abuse research covered in various chapters of this report. Interestingly, however, the words describing the field as a whole, and connecting each chapter to the next, seem to defy the search for clarity and precision. Does "drug" include alcohol and tobacco? What is "abuse"? Are use and
abuse mutually exclusive categories? Are abuse and dependence mutually exclusive categories? Does use of illicit drugs per se amount to abuse? Does abuse include underage use of nicotine? Is addiction synonymous with dependence?
These ambiguities have persisted for decades because the vocabulary of drug abuse is inevitably influenced by peoples' attitudes and values. If the task were solely a scientific one, precise terminology would have emerged long before now. However, because the choice of words in this field always carries a nonscientific message, scientists themselves cannot always agree on a common vocabulary.
Consider the case of nicotine; from a pharmacological standpoint, nicotine is functionally similar to other psychoactive drugs. However, many researchers and policymakers choose to exclude nicotine from the category of drug. The same is true of alcohol; for example, other terms, such as ''chemical dependency" or "substance abuse," are often used as generic terms encompassing the abuse of nicotine and alcohol as well as abuse of illicit drugs. This semantic strategy is chosen to signify the difference in legal status among alcohol, nicotine, and illicit drugs. In recent years, however, a growing number of researchers have adopted a more inclusive use of the term drug. In the case of nicotine, this move tends to reflect a policy judgment that nicotine should be classified as a drug under the federal Food, Drug and Cosmetic Act.
In the committee's view, the term drug should be understood, in its generic sense, to encompass alcohol and nicotine as well as illicit drugs. It is very important for the general public to recognize that alcohol and nicotine constitute, by far, the nation's two largest drug problems, whether measured in terms of morbidity, mortality, or social cost. Abuse of and dependence on those drugs have serious individual and societal consequences. Continued separation of alcohol, nicotine, and illicit drugs in everyday speech is an impediment to public education, prevention, and therapeutic progress.
Although the committee uses the term drug, in its generic sense, to encompass alcohol and nicotine, the report focuses, at NIDA's request, on research opportunities relating to illicit drugs; research on alcohol and nicotine is discussed only when the scientific inquiries are intertwined. Because the report sometimes ranges more broadly than illicit drugs, however, the committee has adopted several semantic conventions to promote clarity and avoid redundancy. First, the term drug, unmodified, refers to all psychoactive drugs, including alcohol and nicotine. When reference is intended solely to illicit drugs such as heroin, cocaine, and other drugs regulated by the Controlled Substances Act, the committee says so explicitly. Occasionally, to ensure that the intended meaning is clear, the report refers to "illicit drugs and nicotine" or to "illicit drugs
and alcohol," as the case may be. Additionally, the words opiate and opioid are used interchangeably, although opiates are derivative of morphine and opioids are all compounds with morphine-like properties (they may be synthetic and not resemble morphine chemically).
The report employs the standard three-stage conceptualization of drug-taking behavior that applies to all psychoactive drugs, whether licit or illicit. Each stage—use, abuse, dependence—is marked by higher levels of use and increasingly serious consequences. Thus, when the report refers to the "use" of drugs, the term is usually employed in a narrow sense to distinguish it from intensified patterns of use. Conversely, the term "abuse" is used to refer to any harmful use, irrespective of whether the behavior constitutes a "disorder'' in the DSM-IV diagnostic nomenclature (see Appendix C ). When the intent is to emphasize the clinical categories of abuse and dependence, that is made clear.
The committee also draws a clear distinction between patterns of drug-taking behavior, however described, and the harmful consequences of that behavior for the individual and for society. These consequences include the direct, acute effects of drug taking such as a drug-induced toxic psychosis or impaired driving, the effects of repeated drug taking on the user's health and social functioning, and the effects of drug-seeking behavior on the individual and society. It bears emphasizing that adverse consequences can be associated with patterns of drug use that do not amount to abuse or dependence in a clinical sense, although the focus of this report and the committee's recommendations is on the more intensified patterns of use (i.e., abuse and dependence) since they cause the majority of the serious consequences.
DEFINITIONS AND BASIC CONCEPTS
Drug use may be defined as occasional use strongly influenced by environmental factors. Drug use is not a medical disorder and is not listed as such in either of the two most important diagnostic manuals—the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSMIV; APA, 1994); or the International Classification of Diseases (ICD-10; WHO, 1992). (See Appendix C for DSM-IV and ICD-10 diagnostic criteria.) Drug use implies intake for nonmedical purposes; it may or may not be accompanied by clinically significant impairment or distress on a given occasion.
Drug abuse is characterized in DSM-IV as including regular, sporadic, or intensive use of higher doses of drugs leading to social, legal, or interpersonal problems. Like DSM-IV, ICD-10 identifies a nondependent but problematic syndrome of drug use but calls it "harmful use" instead
of abuse. This syndrome is defined by ICD-10 as use resulting in actual physical or psychological harm.
Drug dependence (or addiction) is characterized in both DSM-IV and ICD-10 as drug-seeking behavior involving compulsive use of high doses of one or more drugs, either licit or illicit, for no clear medical indication, resulting in substantial impairment of health and social functioning. Dependence is usually accompanied by tolerance and withdrawal 2 and (like abuse) is generally associated with a wide range of social, legal, psychiatric, and medical problems. Unlike patients with chronic pain or persistent anxiety, who take medication over long periods of time to obtain relief from a specific medical or psychiatric disorder (often with resulting tolerance and withdrawal), persons with dependence seek out the drug and take it compulsively for nonmedical effects.
Tolerance occurs when certain medications are taken repeatedly. With opiates for example, it can be detected after only a few days of use for medical purposes such as the treatment of pain. If the patient suddenly stops taking the drug, a withdrawal syndrome may ensue. Physicians often confuse this phenomenon, referred to as physical dependence, with true addiction. That can lead to withholding adequate medication for the treatment of pain because of the very small risk that addiction with drug-seeking behavior may occur.
As a consequence of its compulsive nature involving the loss of control over drug use, dependence (or addiction) is typically a chronically relapsing disorder (IOM, 1990, 1995; Meter, 1996; O'Brien and McLennan, 1996; McLennan et al., in press). Although individuals with drug dependence can often complete detoxification and achieve temporary abstinence, they find it very difficult to sustain that condition and avoid relapse over time. Most persons who achieve sustained remission do so only after a number of cycles of detoxification and relapse (Dally and Marital, 1992). Relapse is caused by a constellation of biological, family, social, psychological, and treatment factors and is demonstrated by the fact that at least half of former cigarette smokers quit three or more times before they successfully achieve stable remission from nicotine addiction (Schilling, 1992). Similarly, within one year of treatment, relapse occurs in 30-50 percent of those treated for drug dependence, although the level
of drug use may not be as high as before treatment (Daley and Marlatt, 1992; McLellan et al., in press). Unlike those who use (or even abuse) drugs, individuals with addiction have a substantially diminished ability to control drug consumption, a factor that contributes to their tendency to relapse.
Another terminological issue arises in relation to the terms addiction and dependence. For some scientists, the proper terms for compulsive drug seeking is addiction, rather than dependence. In their view, addiction more clearly signifies the essential behavioral differences between compulsive use of drugs for their nonmedical effects and the syndrome of "physical dependence" that can develop in connection with repeated medical use. In response, many scientists argue that dependence has been defined in both ICD-10 and DSM-IV to encompass the behavioral features of the disorder and has become the generally accepted term in the diagnostic nomenclature. Moreover, some scientists object to the term addiction on the grounds that it is associated with stigmatizing social images and that a less pejorative term would help to promote public understanding of the medical nature of the condition. The committee has not attempted to resolve this controversy. For purposes of this report, the terms addiction and dependence are used interchangeably.
An inherent aspect of drug addiction is the propensity to relapse. Relapse should not be viewed as treatment failure; addiction itself should be considered a brain disease similar to other chronic and relapsing conditions such as hypertension, diabetes, and asthma (IOM, 1995; O'Brien and McLellan, 1996). In the latter, significant improvement is considered successful treatment even though complete remission or cure is not achieved. In the area of drug abuse, however, many individuals (both lay and professional) expect treatment programs to perform like vaccine programs, where one episode of treatment offers lifetime immunity. Not surprisingly, because of that expectation, people are inevitably disappointed in the relatively high relapse rates associated with most treatments. If, however, addiction is understood as a chronically relapsing brain disease, then—for any one treatment episode—evidence of treatment efficacy would include reduced consumption, longer abstention periods, reduced psychiatric symptoms, improved health, continued employment, and improved family relations. Most of those results are demonstrated regularly in treatment outcome studies.
The idea that drug addiction is a chronic relapsing condition, requiring long-term attention, has been resisted in the United States and in some other countries (Brewley, 1995). Many lay people view drug addiction as a character defect requiring punishment or incarceration. Proponents of the medical model, however, point to the fact that addiction is a distinct morbid process that has characteristics and identifiable signs and
symptoms that affect organ systems (Miller, 1991; Meter, 1996). Characterization of addiction as a brain disease is bolstered by evidence of genetic vulnerability to addiction, physical correlates of its clinical course, physiological changes as a result of repeated drug use, and fundamental changes in brain chemistry as evidenced by brain imaging (Volkow et al., 1993). This is not to say that behavioral, social, and environmental factors are immaterial—they all play a role in onset and outcome, just as they do in heart disease, kidney disease, tuberculosis, or other infectious diseases. Thus, the contemporary understanding of disease fully incorporates the voluntary behavioral elements that lead many people to be skeptical about the applicability of the medical model to drug addiction. In any case, the committee embraces the disease concept, not because it is indisputable but because this paradigm facilitates scientific investigation in many important areas of knowledge, without inhibiting or distorting scientific inquiry in other parts of the field.
IMPORTANCE OF DRUG ABUSE RESEARCH
The widespread prevalence of illicit drug use in the United States is well documented in surveys of households, students, and prison and jail inmates ( Chapter 4 ). Based on the National Household Survey on Drug Abuse (NHSDA), an annual survey presently sponsored by SAMHSA, it was estimated that in 1994, 12.6 million people had used illicit drugs (primarily marijuana) in the past month (SAMHSA, 1995). That figure represents 6 percent of the population 12 years of age or older. 3 The number of heavy drug users, using drugs at least once a week, is difficult to determine. It has been estimated that in 1993 there were 2.1 million heavy cocaine users and 444,000-600,000 heavy heroin users (Rhodes et al., 1995). This population represents a significant burden to society, not only in terms of federal expenditures but also in terms of costs related to the multiple consequences of drug abuse (see Chapter 7 ).
The ultimate aim of the nation's investment in drug abuse research is to enable society to take effective measures to prevent drug use, abuse, and dependence, and thereby reduce its adverse individual and social consequences and associated costs. The adverse consequences of drug abuse are numerous and profound and affect the individual's physical health and psychological and social functioning. Consequences of drug abuse include increased rates of HIV infection and tuberculosis (TB); education and vocational impairment; developmental harms to children of
drug-using parents associated with fetal exposure or maltreatment and neglect; and increased violence (see Chapter 7 ). It now appears that injection drug use is the leading risk factor for new HIV infection in the United States (Holmberg, 1996). Most (80 percent) HIV-infected heterosexual men and women who do not use injection drugs have been infected through sexual contact with HIV-infected injection drug users (IUDs). Thus, it is not surprising that the geographic distribution of heterosexual AIDS cases has been essentially the same as the distribution of male injection drug users' AIDS cases (Holmberg, 1996) Further, the IUDs-associated HIV epidemic in men is reflected in the heterosexual epidemic in women, which is reflected in HIV infection in children (CDC, 1995). Nearly all children who acquire HIV infection do so prenatal (see Chapter 7 ).
The extent of the impact of drug use and abuse on society is evidenced by its enormous economic burden. In 1990, illicit drug abuse is estimated to have cost the United States more than $66 billion. When the cost of illicit drug use and abuse is tallied with that of alcohol and nicotine ( Table 1.1 ), the collective cost of drug use and abuse exceeds the estimated annual $117 billion cost of heart disease and the estimated annual $104 billion cost of cancer (AHA, 1992; ACS, 1993; D. Rice, University of California at San Francisco, personal communication, 1995).
As noted above, the federal government accounts for a large segment of the societal expenditure on illicit drug abuse control—spending more than $13.3 billion in FY 1995 (ONDCP, 1996). About two-thirds was devoted to interdiction, intelligence, incarceration, and other law enforcement activities. Research, however, accounts for only 4 percent of federal outlays, a percentage that has remained virtually unchanged since 1981 (ONDCP, 1996) ( Figure 1.1 ). Given the social costs of illicit drug abuse and the enormity of the federal investment in prevention and control, research into the causes, consequences, treatment, and prevention of drug abuse should have a higher priority. Enhanced support for drug abuse research would be a socially sound investment, because scientific research can be expected to generate new and improved treatments, as well as prevention and control strategies that can help reduce the enormous social burden associated with drug abuse.
THE CONTEXT OF DRUG ABUSE RESEARCH
In the chapters that follow, the committee identifies research initiatives that seem most promising and most likely to lead to successful efforts to reduce drug abuse and its associated social costs. Although the yield from these initiatives will depend largely on the creativity and skill of scientists, the many contextual factors that will also have a major bear-
TABLE 1.1 Estimated Economic Costs (million dollars) of Drug Abuse, 1990

FIGURE 1.1 Federal drug control budget trends (1981-1995). NOTE: Figures are in current dollars. SOURCE: ONDCP (1996).
ing on the payoff from scientific inquiry cannot be ignored. The committee has identified six major factors that, if successfully addressed, could optimize the gains made in each area of drug abuse research: stable funding; use of a comprehensive public health framework; wider acceptance of a medical model of drug dependence; better translation of research findings into practice; raising the status of drug abuse research; and facilitating interdisciplinary research.
Stable Funding
A stable level of funding in any area of biomedical research is needed to sustain and build on research accomplishments, to retain a cadre of experts in a field, and to attract young investigators. Drug abuse research, in comparison with many other research venues, has not enjoyed consistent federal support (IOM, 1990, 1995; see also Appendix B ). The field has suffered from difficulties in recruiting and retaining young researchers and clinicians and in maintaining a stable research infrastructure (IOM, 1995). Society's capacity to contain and manage drug abuse
depends upon a stable, long-term investment in research. The vicissitudes in federal research funding often reflect changing currents in public opinion toward drugs and drug users ( Appendix B ). However, drug abuse will not disappear; it is an endemic social and public health problem. The nation must commit itself to a sustained effort. The social investment in research is an investment in "human capital" that must be sustained over the long term in order to reap the expected gains. An investment in this field is squandered if researchers who have been recruited and trained in drug abuse research are drawn to other fields because of uncertainty about the stability of future funding.
Adoption of a Comprehensive Public Health Framework
The social impact of drug abuse research can be enhanced significantly by conceptualizing goals and priorities within a comprehensive public health framework (Goldstein, 1994). All too often, public discourse about drug abuse is characterized by such unnecessary and fruitless disputes as whether drug abuse should be viewed as a social and moral problem or a health problem, whether the drug problem can best be solved by law enforcement or by medicine, whether priority should be placed on reducing supply or reducing demand, and so on. The truth is that these dichotomies oversimplify a brain disease impacted by a complex set of behaviors and a diverse array of potentially useful social responses. Forced choices of this nature also tend to inhibit or foreclose potentially useful research strategies. Confusion about social goals can lead to confusion about research priorities and can obscure the links between investigations viewing the subject through different lenses.
Some issues tend to recur. A prominent dispute centers on whether preventing drug use is important in itself or whether society should be more concerned with abuse or with the harmful consequences of use. The answer, of course, is that such a forced choice obscures, rather than clarifies, the issues. From a public health standpoint, drug use is a risk factor; the significance of use (whether of alcohol, nicotine, or illicit drugs) lies in the risk of harm associated with it (e.g., fires from smoking, impaired driving from alcohol or illicit drugs, or developmental setbacks) and in the risk that use will intensify, escalating to abuse or dependence. Those risks vary widely in relation to drug, user characteristics, social context, etc. Attention to the consequences of use and to the risk of escalation helps to set priorities (for research and policy) and provides a framework for assessing the impact of different interventions.
From a public policy standpoint, arguments about goals and priorities are fraught with controversy. From the standpoint of research strategy, however, the key lies in asking the right questions (e.g., What influ-
ences the pathways from use, to abuse, to dependence? What are the effects of needle exchange programs on illicit drug use and on HIV disease?) and in generating the knowledge required to facilitate informed policy debate. The main virtues of a comprehensive public health approach are that it helps to disentangle scientific questions from policy questions and that it encompasses all of the pertinent empirical questions, including the causes and consequences of use, abuse, and dependence, as well as the efficacy and cost of all types of interventions. In sum, the social payoff from drug abuse research can be enhanced substantially by integrating diverse strands of inquiry within a public health framework.
Acceptance of a Medical Model of Drug Dependence
Drug dependence is a chronic, relapsing brain disease that, like other diseases, can be evaluated and treated with the standard tools of medicine, including efforts in prevention, diagnosis, and treatment with medications and behavioral or psychosocial therapies. Unfortunately, the medical model of dependence is not universally accepted by health professionals and others in the treatment community; it is widely rejected within the law enforcement community and often by the public at large, which tends to view the complex and varied patterns of use, abuse, and dependence as an undifferentiated behavior rather than a medical problem.
Resistance to the medical model takes many forms. One is resistance to pharmacotherapies, such as methadone, that are seen as substituting licit drugs for illicit drugs without changing drug-taking behavior. Conversely, treatment approaches that adopt a rigid drug-free strategy preclude the use of medications for patients with other psychiatric disorders that are easily treated by pharmacotherapeutic approaches. On a subtler level, resistance to the use of pharmacotherapies is evidenced by the routine use of inadequate doses of methadone (D'Aunno and Vaughn, 1992). Finally, for others, all forms of drug abuse signify a failure of willpower or a moral weakness requiring punishment, incarceration, or moral education rather than treatment (Anglin and Hser, 1992).
Resistance to the medical model of drug dependence presents numerous barriers to research. Clinical researchers experience difficulty in soliciting participation by both treatment program administrators and patients, who are sometimes mistrustful of researchers' motives. If research involves a medication that is itself prone to abuse, there are additional regulatory requirements for drug scheduling, storage, and record keeping that act to discourage investigation (see Chapter 10 ; IOM, 1995). The ever-present threat of inappropriate intrusion by law enforcement agents has a chilling effect on treatment research (McDuff et al., 1993). All barri-
ers to inquiry, irrespective of whether they are legal or social in origin, raise the cost of research and discourage researchers from entering the field. Additionally, those barriers diminish the likelihood that a pharmaceutical company will invest in the development of antiaddiction medications (IOM, 1995). 4 Broader acceptance of the medical model of drug dependence would provide an incentive for researchers and clinicians to enter this field of research. Over time, a developing consensus in support of the medical model could facilitate common discourse, help to shape a shared research agenda within a public health framework, and diminish tensions between the research and treatment communities and the criminal justice system.
Better Translation of Research Findings into Practice and Policy
To benefit society, new research findings must be disseminated adequately to treatment providers, educators, law enforcement officials, and community leaders. In the case of prevention practices, it is often difficult for communities to change entrenched policies, particularly when combined with political imperatives for action to counteract drug abuse. In the case of treatment, technology transfer is impeded by the heterogeneity of providers and their marginalization at the outskirts of the medical community (see IOM, 1990, 1995; see also Chapter 8 ). Physicians and psychiatrists are seldom employed by specialized drug treatment facilities (approximately one-quarter employ medical doctors), and treatment is delivered by counselors whose training and supervision vary greatly and who have little access to and understanding of research results (Ball and Ross, 1991; Batten et al., 1993). These factors not only impede the transfer of research findings to the field but also impede communication from the field to the laboratory so that research designs can be modified in response to clinical realities (Pentz, 1994). Thus, there is a real need for bidirectional communication, from bench to bedside and back to the basic scientist (IOM, 1994).
The committee is aware, however, of recent technology transfer efforts in the field such as the Treatment Improvement Protocol Series, an initiative to establish guidelines for drug abuse treatment with an emphasis on incorporating research findings (SAMHSA, 1993), and the Prevention Enhancement Protocol System, a process implemented by the Center
for Substance Abuse Prevention in which scientists and practitioners develop protocols to identify and evaluate the strength of evidence on topics related to prevention interventions. Similar efforts will be invaluable for communicating and integrating research results to the treatment community.
Research frequently results in product development leading to changes in operations and an overall enhancement of the value of the enterprise. For example, in the pharmaceutical industry research often leads to the development of new medications or devices. In the public sector, however, research is often divorced from the implementation of findings and development. Research is often more basic than applied, and the fruits of research are not realized by the government, but by the private sector. Although that approach may be appropriate, it is unfortunately not always the most productive strategy for advancing research, knowledge, and product development. That is particularly true in the development of medications for opiate and cocaine addictions, where there is a great need for commitment from the private sector. However, many obstacles prevent active involvement of the pharmaceutical industry in this area of research and development (IOM, 1995).
A similar problem arises in relation to policymaking. Because debates about drug policy tend to be so highly polarized and politicized, research findings are often distorted, or selectively deployed, for rhetorical purposes. Researchers cannot prevent this practice, which is a common feature of political debate in a democratic society. However, researchers and their sponsors should not be indifferent to the disconnect between policy discourse and science. Researchers should establish and support institutional mechanisms for communicating an important message to policymakers and to the general public. Scientific research has produced a solid, and growing, body of knowledge about drug abuse and about the efficacy of various interventions that aim to prevent and control it. As long as drug abuse remains a poorly understood social problem, policy will be based mainly on wish and supposition; steps should be taken to educate policymakers about the scientific and technological advances in addiction research. Only then will it be possible for policymaking to support legislation that adequately funds new research and applies research findings. To some extent, persisting failure to reap the fruits of drug abuse research is attributable to the low visibility of the field—a problem to which the discussion now turns.
Raising the Status of Drug Abuse Research
Drug abuse research is often an undervalued area of inquiry, and most scientists and clinicians choose other disciplines in which to develop
their careers. Compared with other fields of research, investigators in drug abuse are often paid less, have less prestige among their peers, and must contend with the unique complexities of performing research in this area (e.g., regulations on controlled substances) (see IOM, 1995). The overall result is an insufficient number of basic and clinical researchers. IOM has recently begun a study, funded by the W. M. Keck Foundation of Los Angeles, to develop strategies to raise the status of drug abuse research. 5
Weak public support for this field of study is evident in unstable federal funding (see above), a lack of pharmaceutical industry investment in the development of antiaddiction medications (IOM, 1995), and inadequate funding for research training (IOM, 1995). NIDA's FY 1994 training budget, which is crucial to the flow of young researchers into the field, was about 2 percent of its extramural research budget, a percentage substantially lower than the overall National Institutes of Health (NIH) training budget, which averages 4.8 percent of its extramural research budget.
Beyond funding problems, investigators face a host of barriers to research: research subjects may pose health risks (e.g., TB, HIV/AIDS, and other infectious diseases), may be noncompliant, may deny their drug abuse problems, and may be involved in the criminal justice system. Even when research is successful and points to improvements in service delivery, the positive outcome may not be translated into practice or policy. For example, more than a year after the Food and Drug Administration's (FDA's) approval of levo-alpha-acetylmethadol (LAAM) as the first new medication for the treatment of opiate dependence in over 20 years, fewer than 1,000 patients nationwide actually had received the medication (IOM, 1995). More recently, scientific evidence regarding the beneficial effects of needle exchange programs (NRC, 1995) has received inadequate attention. Continuing indifference to scientific progress in drug abuse research inevitably depresses the status of the field, leading in turn to difficulties in recruiting new investigators.
Increasing Interdisciplinary Research
The breadth of expertise needed in drug abuse research spans many disciplines, including the behavioral sciences, pharmacology, medicine, and the neurosciences, and many fields of inquiry, including etiology, epidemiology, prevention, treatment, and health services research. Aspects of research relating to drug use tend to draw on developmental perspectives and to focus on general population samples in community settings, especially schools. Aspects of research relating to abuse and de-
pendence tend to be more clinical in nature, drawing on psychopathological perspectives. Additionally, a full account of any aspect of drug-taking behavior must also reflect an understanding of social context. The rich interplay between neuroscience and behavioral research and between basic and clinical research poses distinct challenges and opportunities.
Unfortunately, research tends to be fragmented within disciplinary boundaries. The difficulties in conducting successful interdisciplinary research are well known. Funds for research come from many separate agencies, such as the NIDA, NIMH, and SAMHSA. These agencies all have different programmatic emphases as they attempt to shape the direction of research in their respective fields. In times of funding constraints, agencies may be less inclined to fund projects at the periphery of their interests.
Additionally, NIH study sections, which rank grant proposals, are discipline specific, making it difficult for interdisciplinary proposals to ''qualify" (i.e., receive a high rank) for funding. Another problem is that the most advanced scientific literature tends to be compartmentalized within discipline or subject matter categories, making it difficult for scientists to see the whole field. The problem is exacerbated by what Tonry (1990) has called "fugitive literatures," studies carried out by private sector research firms or independent research agencies and available only in reports submitted to the sponsoring agency.
In light of lost opportunities for collaboration and interdisciplinary research, IOM (1995) previously recommended the creation and expansion of comprehensive drug abuse centers to coordinate all aspects of drug abuse research, training, and treatment. The field of drug abuse research presents a real opportunity to bridge the intellectual divide between the behavioral and neuroscience communities and to overcome the logistical impediments to interdisciplinary research.
INVESTING WISELY IN DRUG ABUSE RESEARCH
This report sets forth drug abuse research initiatives for the next decade based on a thorough assessment of what is now known and a calculated judgment about what initiatives are most likely to advance our knowledge in useful ways. This report is not meant to be a road map or tactical battle plan, but is best regarded as a strategic outline. Within each discipline of drug abuse research, the committee has highlighted priorities for future research. However, the committee did not make any attempt to prioritize recommendations across varied disciplines and fields of research. Prudent research planning must respond to newly emerging opportunities and needs while maintaining a steady commitment to the
achievement of long-term objectives. The ability to respond to new goals and needs may be the real challenge for the field of drug abuse research.
Drug abuse research is an important public investment. The ultimate aim of that investment is to reduce the enormous social costs attributable to drug abuse and dependence. Of course, drug abuse research must also compete for funding with research in other fields of public health, research in other scientific domains, and other pressing public needs. Recognizing the scarcity of resources, the committee has also considered ways in which the research effort can be harnessed most effectively to increase the yield per dollar invested. These include stable funding, use of a comprehensive public health framework, wider acceptance of a medical model of drug dependence, better translation of research findings into practice and policy, raising the status of drug abuse research, and facilitating interdisciplinary research.
The committee notes that there have been major accomplishments in drug abuse research over the past 25 years and commends NIDA for leading that effort. The committee is convinced that the field is on the threshold of significant advances, and that a sustained research effort will strengthen society's capacity to reduce drug abuse and to ameliorate its adverse consequences.
ORGANIZATION OF THE REPORT
This report sets forth a series of initiatives in drug abuse research. 6 Each chapter of the report covers a segment of the field, describes selected accomplishments, and highlights areas that seem ripe for future research. As noted, the committee has not prioritized areas for future research but, instead, has identified those areas that most warrant further exploration.
Chapter 2 describes behavioral models of drug abuse and demonstrates how the use of behavioral procedures has given researchers the ability to measure drug-taking objectively and to study the development, maintenance, and consequences of that behavior. Chapter 3 discusses drug abuse within the context of neurotransmission; it describes neurobiological advances in drug abuse research and provides the foundation for the current understanding of addiction as a brain disease. The epidemiological information systems designed to gather information on drug use in the United States are identified in Chapter 4 . The data collected from the systems provide an essential foundation for systematic study of
the etiology and consequences of drug abuse, which are addressed, respectively, in Chapters 5 and 7 . Chapter 6 addresses the efficacy of interventions designed to prevent drug abuse. The effectiveness of drug abuse treatment and the difficulties in treating special populations of drug users are discussed in Chapter 8 , while the impact of managed care on access, costs, utilization, and outcomes of treatment is addressed in Chapter 9 . Finally, Chapter 10 discusses the effects of drug control on public health and identifies areas for policy-relevant research.
Specific recommendations appear in each chapter. Although these recommendations reflect the committee's best judgment regarding priorities within the specific domains of research, the committee did not identify priorities or rank recommendations for the entire field of drug abuse research. Opportunities for advancing knowledge exist in all domains. It would be a mistake to invest too narrowly in a few fields of inquiry. At the present time, soundly conceived research should be pursued in all domains along the lines outlined in this report.
ACS (American Cancer Society). 1993. Cancer Facts and Figures, 1993 . Washington, DC: ACS.
AHA (American Heart Association). 1992. 1993 Heart and Stroke Fact Statistics . Dallas, TX: AHA.
Anglin MD, Hser Y. 1992. Treatment of drug abuse. In: Watson RR, ed. Drug Abuse Treatment. Vol. 3, Drug and Alcohol Abuse Reviews . New York: Humana Press.
APA (American Psychiatric Association). 1994. Diagnostic and Statistical Manual of Mental Disorders . 4th ed. Washington, DC: APA.
Ball JC, Ross A. 1991. The Effectiveness of Methadone Maintenance Treatment . New York: Springer-Verlag.
Batten H, Horgan CM, Prottas J, Simon LJ, Larson MJ, Elliott EA, Bowden ML, Lee M. 1993. Drug Services Research Survey Final Report: Phase I . Contract number 271-90-8319/1. Submitted to the National Institute of Drug Abuse. Waltham, MA: Bigel Institute for Health Policy, Brandeis University.
Brewley T. 1995. Conversation with Thomas Brewley. Addiction 90:883-892.
Carr DB, Jacox AK, Chapman CR, et al. 1992. Acute Pain Management: Operative or Medical Procedures and Trauma. Clinical Practice Guidelines . AHCPR Publication No. 92-0032. Rockville, MD: U.S. Public Health Service, Agency for Health Care Policy and Research.
CDC (Centers for Disease Control and Prevention). 1995. HIV/AIDS Surveillance Report 7(2).
Cooper JR, Bloom FE, Roth RH. 1991. The Biochemical Basis of Neuropharmacology . 6th ed. New York: Oxford University Press.
Daley DC, Marlatt GA. 1992. Relapse prevention: Cognitive and behavioral interventions. In: Lowinson JH, Ruiz P, Millman RB, Langrod JG, eds. Substance Abuse: A Comprehensive Textbook . Baltimore: Williams and Wilkins.
D'Aunno T, Vaughn TE. 1992. Variation in methadone treatment practices. Journal of the American Medical Association 267:253-258.
DiGregorio GJ. 1990. Cocaine update: Abuse and therapy. American Family Physician 41(1):247-250.
Foley KM, Inturrisi CE, eds. 1986. Opioid Analgesics in the Management of Clinical Pain. Advances in Pain Research and Therapy. Vol. 8. New York: Raven Press.
GAO (General Accounting Office). 1992. Drug Abuse Research: Federal Funding and Future Needs . GAO/PEMD-92-5. Washington, DC: GAO.
Glassman AH, Covey LS, Dalack GW, Stetner F, Rivelli SK, Fleiss J, Cooper TB. 1993. Smoking cessation, clonidine, and vulnerability to nicotine among dependent smokers. Clinical Pharmacology and Therapeutics 54(6):670-679.
Goldstein A. 1994. Addiction: From Biology to Drug Policy . New York: W.H. Freeman.
Hokfelt TGM, Castel MN, Morino P, Zhang X, Dagerlind A. 1995. General overview of neuropeptides. In: Bloom FE, Kupfer DJ, eds. Psychopharmacology: Fourth Generation of Progress . New York: Raven Press. Pp. 483-492.
Holmberg SD. 1996 . The estimated prevalence and incidence of HIV in 96 large U.S. metropolitan areas . American Journal of Public Health 86(5):642-654.
IOM (Institute of Medicine). 1990. Treating Drug Problems . Washington, DC: National Academy Press.
IOM (Institute of Medicine). 1994. AIDS and Behavior: An Integrated Approach . Washington, DC: National Academy Press.
IOM (Institute of Medicine). 1995. The Development of Medications for the Treatment of Opiate and Cocaine Addictions. Washington, DC: National Academy Press.
Jacox A, Carr DB, Payne R, et al. 1994. Management of Cancer Pain. Clinical Practice Guideline . AHCPR Publication No. 94-0592. Rockville, MD: U.S. Public Health Service, Agency for Health Care Policy and Research.
Kahn RS, Davis KL. 1995. New developments in dopamine and schizophrenia. In: Bloom FE, Kupfer DJ, eds. Psychopharmacology: Fourth Generation of Progress . New York: Raven Press. Pp. 1193-1204.
McDuff DR, Schwartz RP, Tommasello A, Tiegel S, Donovan T, Johnson JL. 1993. Outpatient benzodiazepine detoxification procedure for methadone patients. Journal of Substance Abuse Treatment 10:297-302.
McLellan AT, Metzger DS, Alterman Al, Woody GE, Durell J, O'Brien CP. In press. Is addiction treatment "worth it"? Public health expectations, policy-based comparisons. Milbank Quarterly .
Meyer R. 1996. The disease called addiction: Emerging evidence in a 200-year debate. Lancet 347:162-166.
Miller NS. 1991. Drug and alcohol addiction as a disease. In: Miller NS, ed. Comprehensive Handbook of Drug and Alcohol Addiction . New York: Marcel Dekker.
MMWR (Morbidity and Mortality Weekly Report). 1994. Medical care expenditures attributable to cigarette smoking, United States, 1993. Morbidity and Mortality Weekly Report 43(26):469-472.
NRC (National Research Council). 1995. Preventing HIV Transmission: The Role of Sterile Needles and Bleach . Washington, DC: National Academy Press.
O'Brien CP, McLellan AT. 1996. Myths about the treatment of addiction. Lancet 347:237-240.
Olson GA, Olson RD, Kastin AJ. 1994. Endogenous opiates, 1993. Peptides 15:1513-1556.
ONDCP (Office of National Drug Control Policy). 1996. National Drug Control Strategy . Washington, DC: ONDCP.
Pentz M. 1994. Directions for future research in drug abuse prevention. Preventive Medicine 23:646-652.
Rhodes W, Scheiman P, Pittayathikhun T, Collins L, Tsarfaty V. 1995. What America's Users Spend on Illegal Drugs, 1988-1993 . Prepared for the Office of National Drug Control Policy, Washington, DC.
Rice DP, Kelman S, Miller LS, Dunmeyer S. 1990. The Economic Costs of Alcohol and Drug Abuse and Mental Illness: 1985 . DHHS Publication No. (ADM) 90-1694. San Francisco: University of California, Institute for Health and Aging.
Rice DP, Max W, Novotny T, Shultz J, Hodgson T. 1992. The Cost of Smoking Revisited: Preliminary Estimates . Paper presented at the American Public Health Association Annual Meeting, November 23, 1992. Washington, DC.
SAMHSA (Substance Abuse and Mental Health Services Administration). 1993. Improving Treatment for Drug-Exposed Infants: Treatment Improvement Protocol (TIP) Series . Washington, DC: U.S. Department of Health and Human Services.
SAMHSA (Substance Abuse and Mental Health Services Administration). 1995. National Household Survey on Drug Abuse: Population Estimates 1994 . Washington, DC: U.S. Department of Health and Human Services.
Schelling TC. 1992 . Addictive drugs: The cigarette experience. Science 255:431-433.
Tonry M. 1990. Research on drugs and crime. In: Morris N, Tonry M, eds. Drugs and Crime . Vol. 13 . Chicago: University of Chicago Press.
Volkow ND, Fowler JS, Wang G-J, Hitzemann R, Logan J, Schlyer DJ, Dewey SI, Wolf AD. 1993. Decreased dopamine D2 receptor availability is associated with reduced frontal metabolism in cocaine abusers. Synapse 14:169-177.
Wall PD, Melzack R. 1994. Textbook of Pain . 3rd ed. Edinburg: Churchill-Livingstone.
WHO (World Health Organization). 1992. International Statistical Classification of Diseases and Related Health Problems . Tenth Revision. Geneva: WHO.
Drug abuse persists as one of the most costly and contentious problems on the nation's agenda. Pathways of Addiction meets the need for a clear and thoughtful national research agenda that will yield the greatest benefit from today's limited resources.
The committee makes its recommendations within the public health framework and incorporates diverse fields of inquiry and a range of policy positions. It examines both the demand and supply aspects of drug abuse.
Pathways of Addiction offers a fact-filled, highly readable examination of drug abuse issues in the United States, describing findings and outlining research needs in the areas of behavioral and neurobiological foundations of drug abuse. The book covers the epidemiology and etiology of drug abuse and discusses several of its most troubling health and social consequences, including HIV, violence, and harm to children.
Pathways of Addiction looks at the efficacy of different prevention interventions and the many advances that have been made in treatment research in the past 20 years. The book also examines drug treatment in the criminal justice setting and the effectiveness of drug treatment under managed care.
The committee advocates systematic study of the laws by which the nation attempts to control drug use and identifies the research questions most germane to public policy. Pathways of Addiction provides a strategic outline for wise investment of the nation's research resources in drug abuse. This comprehensive and accessible volume will have widespread relevance—to policymakers, researchers, research administrators, foundation decisionmakers, healthcare professionals, faculty and students, and concerned individuals.
READ FREE ONLINE
Welcome to OpenBook!
You're looking at OpenBook, NAP.edu's online reading room since 1999. Based on feedback from you, our users, we've made some improvements that make it easier than ever to read thousands of publications on our website.
Do you want to take a quick tour of the OpenBook's features?
Show this book's table of contents , where you can jump to any chapter by name.
...or use these buttons to go back to the previous chapter or skip to the next one.
Jump up to the previous page or down to the next one. Also, you can type in a page number and press Enter to go directly to that page in the book.
Switch between the Original Pages , where you can read the report as it appeared in print, and Text Pages for the web version, where you can highlight and search the text.
To search the entire text of this book, type in your search term here and press Enter .
Share a link to this book page on your preferred social network or via email.
View our suggested citation for this chapter.
Ready to take your reading offline? Click here to buy this book in print or download it as a free PDF, if available.
Get Email Updates
Do you enjoy reading reports from the Academies online for free ? Sign up for email notifications and we'll let you know about new publications in your areas of interest when they're released.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Research Review: What Have We Learned About Adolescent Substance Use?
Adolescence is a critical biological, psychological, and social developmental stage involving heightened risk for substance use and associated adverse consequences. This review, synthesizing emerging findings on this complex topic, is intended to inform research and clinical care focused on adolescents.
Literature searches were conducted using PubMed, yielding a cross-section of observational and interventional studies focused on adolescent substance use. Findings were organized and categorized to cover key areas of epidemiology, neurobiology, prevention, and treatment.
Adolescent substance-related attitudes and use patterns have evolved over time, informed by adult and peer behaviors, public policy, media messaging, substance availability, and other variables. A number of risk and resiliency factors contribute to individual differences in substance use and related consequences. Advances in observational techniques have provided enhanced understanding of adolescent brain development, and its implications for substance use. Prevention efforts have yielded mixed results, and while a number of adolescent-targeted evidence-based treatments for substance use disorders have been developed, effect sizes are generally modest, indicating the need for further research to enhance prevention and treatment outcomes.
Conclusions
Substance use in adolescence is heterogeneous, ranging from normative to pathological, and can lead to significant acute and long-term morbidity and mortality. Understanding risk and resiliency factors, underlying neurobiology, and optimal developmentally-sensitive interventions is critical in addressing substance-associated problems in adolescence.
Introduction
Adolescence is a critical developmental phase involving significant physical, cognitive, emotional, social, and behavioral changes. The neurobiological alterations underlying these complex developmental processes may predispose adolescents to initiate substance use, to develop substance use disorders, and to experience potentially serious and long-lasting substance-related adverse consequences. Given the high prevalence of problematic substance use in this age range, and given the unique biopsychosocial context, research has increasingly focused on characterizing adolescent substance use disorders, with particular focus on optimizing and disseminating evidence-based prevention, assessment, and treatment interventions. The present review was conducted to provide an overview of recent clinically relevant advances in the field.
Literature searches were conducted via PubMed, and information was compiled to yield an overview of clinically relevant advances in knowledge regarding adolescent substance use, spanning epidemiology, neurobiology, assessment, and interventions.
Epidemiology
Prevalence of use.
Substance use is typically initiated during adolescence. Alcohol is the most commonly used substance among adolescents, with 64% of 18 year olds endorsing lifetime alcohol use, followed by marijuana (45%) and cigarette use (31%) ( Johnston et al., 2017 ). Overall, rates of adolescent substance use have remained relatively stable over the past several years, with a few notable exceptions. Cigarette use has declined dramatically over the past several decades, while e-cigarette use has become more prevalent in recent years. Thirteen percent of teens report using e-cigarettes in the past month, compared to 3% reporting cigarette use, with a concerning increase in the number of never-smoking youth reporting e-cigarette use ( Bunnell et al., 2015 ). Another recent trend includes increased frequency of marijuana use, with 6% of 18 year olds reporting using marijuana daily ( Johnston et al., 2017 ). Attitudes about marijuana use continue to move toward greater acceptance; the perception of risk about using marijuana is at the lowest point ever recorded, with a third of 18 year olds reporting that regular marijuana use is harmful. While overall rates of marijuana use have remained relatively stable over the past several years, decreased perception of harm typically corresponds with increased use. Other drug use is relatively uncommon, with less than 6% of adolescents reporting past month use of other illicit drugs ( Johnston et al., 2017 ). A brief summary of rates of current substance use, by substance and by grade level, among adolescents in the United States is presented in Table 1 ( Johnston et al., 2017 ).
Rates (%) of current (30-day) substance use among adolescents in the United States, by substance and grade level ( Johnston et al., 2017 ).
NR=Not Reported
Prevalence of Substance Use Disorders
Adolescent substance use is heterogeneous, ranging from normative early experimentation with substance use to heavier and higher-risk patterns of use. Most youth who use substances do not become addicted; however, the prevalence of substance use disorders is still quite high, with 15% of youth meeting diagnostic criteria for alcohol abuse and 16% for drug abuse by age 18 ( Swendsen et al. 2012 ). Tobacco, alcohol, and marijuana are typically the first addictive substances that youth try. The likelihood of developing a substance use disorder increases significantly when individuals initiate alcohol and drug use during adolescence. Youth who begin drinking before age 15 have four to six times the rate of lifetime alcohol dependence than those who remain abstinent from alcohol use until age 21 ( Grant & Dawson, 1997 ; SAMHSA, 2014 ). The majority of adults who have a substance use disorder started using before age 18 and develop their disorder by age 20, highlighting the need to delay initiation of substance use for as long as possible ( Dennis et al., 2002 ).
Neurobiology
The brain undergoes significant neurodevelopment between childhood and young adulthood, with maturation continuing until around age 25 ( Pfefferbaum et al., 1994 ; Giedd 2004 ). Brain gray matter, which includes mostly nerve cell bodies and dendrites, tends to decrease during adolescence via synaptic pruning and changes in the extracellular matrix ( Gogtay et al., 2004 ; Paus, 2005 ; Petjanek et al., 2011; Raznahan et al., 2014 ; Sowell et al., 1999 ; Stiles & Jernigan, 2010 ). Concurrently, white-matter volume and white matter integrity increases over this time, which allows for more efficient and rapid communication between brain regions ( Giedd, 2004 ; Lebel et al., 2011 ; 2012 ). Brain regions have time-varying developmental trajectories, with lower-order sensorimotor regions maturing first, and regions associated with higher-order cognitive functioning (e.g., frontal and subcortical brain regions) developing later in adolescence and young adulthood ( Sowell et al., 1999 , 2004 ; Shaw et al., 2008 ; Giedd and Rapoport, 2010 ; Stiles & Jernigan, 2010 ). Healthy brain development throughout adolescence is imperative, with even minor changes in neurodevelopmental trajectories affecting a range of cognitive, emotional, and social functioning ( Nagy et al., 2004 ; Casey et al., 2008 ). Altered brain development due to exposure of neurotoxins during adolescence, particularly alcohol and other drug use, could set the stage for cognitive problems into adulthood, conferring functional consequences throughout life.
Adolescents are known to be particularly vulnerable, compared to children and adults, to initiation of substance use and progression to problematic use. Dopaminergic systems are significantly reorganized in the adolescent brain, with decreases in dopamine in striatal structures such as the nucleus accumbens, in the context of limited inhibitory control, potentially precipitating high-risk behaviors to compensate for dopaminergic void ( Chambers et al., 2003 ; Spear, 2002 ). Theories have suggested an “imbalance” in brain development underlying a propensity for risk behavior, including substance use, during adolescence, with emotion and reward systems (e.g., amygdala, nucleus accumbens) developing before cognitive control systems (e.g., prefrontal cortex) ( Casey et al., 2008 ; Somerville et al., 2010 ). Within the window of this imbalance, adolescents’ decisions may be based on brain processes favoring immediate reward over consideration of longer-term consequences ( Casey & Jones, 2010 ). This theoretical model has been supported by a number of recent experimental studies ( Baker et al., 2015 ; Mills et al., 2014 ; van Duijvenvoorde et al., 2016 ).
In the past 10 years, there has been a proliferation of neuroimaging and neurocognitive studies that have attempted to understand neural risk factors that predate adolescent substance use, as well as determine the effect of substance use on the developing brain. Because alcohol and marijuana are the two most commonly used substances, most existing research has focused on these substances. Several large-scale, multisite longitudinal studies are currently underway to help further understand the consequences of alcohol and marijuana use on cognitive functioning, as well as determine the effects of tobacco and other less frequently used drugs on adolescent brain development. These studies include the National Consortium on Alcohol and Neurodevelopment in Adolescence (NCANDA) which is following >800 youth across 5 different sites in the US for at least 10 years ( Brown et al., 2015 ); the IMAGEN study which has followed 2,000 youth from England, Ireland, Germany, and France for the past 8 years ( https://imagen-europe.com/ ); and the recently launched Adolescent Brain Cognitive Development (ABCD; http://abcdstudy.org/ ), which will follow 11,500 youth across 21 US sites for at least 10 years. Existing studies have relatively small, homogeneous samples; therefore, these large scale studies will allow for a more complex understanding how demographic, social, genetic, and environmental factors play a role in the impact of substance use on brain development.
Several neurocognitive features have been identified as risk factors for initiation of alcohol and other drug use during adolescence ( Squeglia & Gray, 2016 ; Squeglia & Cservenka, 2017 ). Findings suggest poorer performance on tasks of inhibition and working memory ( Heitzeg et al., 2015 ; Khurana et al., 2013 ; López-Caneda et al., 2014; Squeglia et al., 2014a , 2017 ), smaller brain volumes in reward and cognitive control regions ( Cheetham et al., 2012 , 2014 ; Squeglia et al., 2014a ; Urošević et al., 2015 ; Weiland et al., 2014 ; Whelan et al., 2014 ), less brain activation during executive functioning tasks, and heightened reward responsivity are important predictors of adolescent substance use ( Dager et al., 2014 ; Heitzeg et al., 2014 ; Mahmood et al., 2013 ; Norman et al., 2011 ; Ramage et al., 2015 ; Squeglia et al., 2012 , 2017 ; Wetherill et al., 2013a ; Whelan et al., 2014 ).
Alcohol and marijuana use during adolescence has been associated with poorer performance on a range of cognitive domains. In a sample of 234 healthy adolescents, greater alcohol and marijuana use between approximately ages 13 to 17 was associated with poorer verbal memory, visuospatial functioning, and psychomotor speed ( Nguyen-Louie et al., 2015 ). Gender specific effects have also been found, with heavy-drinking girls showing worsening performance on tests of visuospatial functioning compared to non-using girls, and alcohol-using boys showing poorer attention compared to alcohol-naïve boys ( Squeglia et al., 2009 ). In a 10-year longitudinal study, treatment-seeking youth who continued to use alcohol and other substances showed poorer verbal learning and memory, visuospatial functioning, and working memory and attention by age 25 ( Hanson et al., 2011a , 2011b ). A dose-dependent relationship was found, with heavier use patterns and greater hangover and withdrawal symptoms relating to poorer cognitive functioning. Youth who were in remission from alcohol and drug use performed similarly to those who continued to meet criteria for a substance use disorder, suggesting substance use during adolescence could have persisting effects into adulthood ( Hanson et al., 2011b ).
There is some suggestion that cognitive domains are differentially impacted by marijuana use in adolescence, with attention, declarative memory, and cognitive control particularly affected ( Randolph et al., 2013 ). In a longitudinal study of marijuana and alcohol-using youth, substance use was related to worsening performance on several cognitive domains when compared to non-using youth, including worse performance on tests of complex attention, memory, processing speed, and visuospatial functioning, with early use (before age 16) relating to worse performance ( Jacobus et al., 2015 ). A large longitudinal birth cohort study from New Zealand (N=1,037) found that persistent adolescent-onset marijuana use was associated with an IQ decline of more than 5 points in the most persistent marijuana-use group, with deficits persisting into adulthood ( Meier et al., 2012 ). However, a recent longitudinal twin study found that IQ deficits observed in marijuana users may be attributable to confounding factors like familial and environmental influences rather than the direct neurotoxic effect of marijuana ( Jackson et al., 2016 ). The follow-up assessment periods for these studies differed, with the Meier study ending at age 38 and the Jackson study following youth until age ~20; regular use over a prolonged period may result in more deleterious effects.
Adolescent alcohol and marijuana use has also been associated with a range of structural and functional brain changes. In the largest prospective study to date on this topic ( N =134), alcohol-using adolescents showed abnormal neurodevelopmental trajectories when compared to continuously non-using controls, including accelerated decreases in gray matter volume (particularly in frontal and temporal regions) and attenuated increases in white matter volume over the ~5 year follow-up ( Squeglia et al., 2015 ), replicating earlier studies with smaller sample sizes ( Luciana et al., 2013 ; Squeglia et al., 2014b ). These findings suggest potentially non-beneficial pruning or, alternatively, premature cortical gray matter decline in alcohol-using youth. In a study examining white matter development, adolescents with extensive marijuana- and alcohol-use histories showed worsening white matter integrity over an 18 month (Baba et al., 2013) and 3-year follow-up ( Jacobus et al., 2013a , 2013b ) in a number of important white matter tracts when compared to non-using youth, as well as poorer performance on tests of neurocognitive functioning. In conjunction with structural changes, adolescent alcohol and marijuana use appears to also affect brain functioning. On several functional MRI studies, youth who initiated heavy alcohol use during adolescence have shown increasing brain activation over time on tests of visual working memory ( Squeglia et al., 2012 ) and inhibition ( Wetherill et al., 2013a , 2013b ), when compared to non-using peers.
Risk Factors
Several factors increase the likelihood of an individual developing a substance use problem, including familial, social, and individual risk factors ( Whitesell et al., 2013 ). Vulnerability for developing substance-related problems is especially heightened among individuals with a family history of substance use disorder ( Cservenka, 2016 ). A recent meta-analysis of twin and adoption studies found that alcohol use disorder is approximately 50% heritable ( Verhulst, Neale, & Kendler, 2015 ); however, identifying specific genes has been challenging, highlighting the complexity and heterogeneity of the disorder ( Hart & Kranzler, 2015 ; Tawa, Hall, & Lohoff, 2016 ). Findings suggest there are a number of genes, each with relatively small effects, that interact with each other and with the environment ( Enoch, 2012 ) to make an individual more or less susceptible to having a substance use disorder ( Meyers & Dick, 2010 ). While specific genes have not been consistently identified, youth with a family history of alcohol use disorder are 3–5 times more likely to develop an alcohol use disorder than youth without a family history of alcoholism ( Cotton, 1979 ).
Males tend to have higher rates of substance use than females ( SAMSHA, 2014 ). Other important risk factors for adolescent substance use include environmental factors such as early exposure to traumatic life events ( Dube et al., 2006 ), prenatal exposure to alcohol and other drugs ( Enoch et al., 2011 ), lack of parental supervision and monitoring ( Nash et al., 2005 ), sleep problems (Shibely et al., 2008), being involved in romantic relationships ( Squeglia et al., 2017 ; Whelan et al., 2014 ), and peer substance use ( Leung et al., 2014 ). Co-occurring psychopathology, including ADHD and depression have been shown to significantly increase the risk of adolescent alcohol use ( Charach et al, 2011 ; Lee et al., 2011 ; Libby et al., 2005 ; Rao et al., 1999 ; Taylor, 2011 ; Wu et al., 2008 ). Additionally, childhood depression and conduct disorder symptoms predict persistence of substance dependence in adulthood ( Meier et al., 2016 ). Other research suggests that externalizing, but not internalizing, mental health problems in childhood predict later substance use in males and females, while among females adolescent substance use predicts internalizing disorders in adulthood ( Miettunen et al., 2014 ).
Prevention science is grounded in the premise that modulation of risk and protective factors may affect the probability of later problems ( Coie et al., 1993 ). Applied to adolescent substance use, this has been implemented across a number of modalities and settings, with the goal of reducing modifiable risk factors and enhancing/reinforcing modifiable protective factors ( Harrop & Catalano, 2016 ). Most commonly, programs have been developed and evaluated in school, family, and community settings. Evidence is mixed amid heterogeneity of methodology and outcomes between studies, but there is some support for parenting-focused ( Allen et al., 2016 ), school-based teacher-led ( Lize et al., 2017 ), and peer-led prevention programs ( MacArthur et al., 2016 ).
Screening and Assessment
Despite the serious implications of adolescent substance use, many clinical providers do not conduct routine screening, and most that do fail to utilize a validated screening method ( Harris et al., 2012 ). In light of this, considerable recent effort has focused on developing and disseminating efficient and reliable screening methods for adolescent substance use ( Levy et al., 2016 ). Screening tools can potentially be used across a number of settings where adolescents are present, though to date most research in this area has focused on primary care practice. The ideal tool would be both sensitive and specific to substance use and related problems, and would guide subsequent in-depth assessment and intervention when appropriate. This must be balanced with the need for time efficiency amid busy clinical practice in which a wide variety of health screening assessments are indicated.
Two brief screeners have strong evidence of achieving the balance of the aforementioned goals, and can be delivered via interview or electronic administration. The Screening to Brief Intervention (S2BI), which queries the adolescent regarding frequency of using 8 types of drugs in the past year, yields high sensitivity and specificity for identifying use and substance use disorders ( Levy et al., 2014 ). Similarly, the Brief Screener for Tobacco, Alcohol, and Other Drugs (BSTAD) queries frequency of use in the past year, with optimal cutoff points for identifying substance use disorders as ≥6 days of tobacco use, ≥2 days of alcohol use, and ≥2 days of marijuana use ( Kelly et al., 2014 ). Both screeners can be delivered electronically, which is a preferred method for adolescents. In practice, adolescent patients can complete the screener via mobile electronic device in the waiting area, and the results can be delivered to the provider in anticipation of the visit and interview.
Initial screeners such as the S2BI and BSTAD can be complemented with subsequent brief assessments to evaluate level of substance involvement and severity of substance-related problems. These assessments can help determine the level and modality of treatment that may be needed, spanning from psychoeducation and/or brief intervention in the primary care office to more intensive service referrals. The CRAFFT (Car, Relax, Alone, Friends/Family, Forget, Trouble), ASSIST (Alcohol, Smoking and Substance Involvement Screening Test) and GAIN (Global Appraisal of Individual Needs) are all validated for this purpose. The CRAFFT and ASSIST serve as adolescent-validated analogues to the adult screener CAGE, the latter of which is not developmentally appropriate for adolescents ( Gryczynski et al., 2015 ; Knight et al., 1999 ). The GAIN assesses for both substance use disorders and potentially associated mental health disorders, including four subscales assessing substance use, internalizing disorders, externalizing disorders, and crime/violence ( Dennis et al., 2006 ).
When more thorough and formal evaluation is indicated (i.e., when brief screening is highly suggestive of substance-related problems requiring intervention), diagnostic evaluation via the Diagnostic and Statistical Manual of Mental Disorders, 5 th Edition (DSM-5), may be undertaken ( American Psychiatric Association, 2013 ). Within this framework, problematic substance use may be diagnostically categorized as a substance use disorder (e.g., Cannabis Use Disorder), with severity of mild, moderate, or severe, depending on the number of substance use disorder symptoms endorsed for a given substance. Diagnostic evaluation should be complemented by functional behavioral analysis, in which substance use is evaluated as a problem behavior with antecedents and consequences which may be unique to a given adolescent’s substance use. The functional analysis framework is used to determine what antecedents and consequences are potentially modifiable to reduce the likelihood of ongoing problem behavior ( Randall et al., 2001 ).
Laboratory testing, most commonly urine drug testing, is often used to complement self-report when evaluating adolescent substance use; it is, however, not generally supported as a standalone screening or assessment for substance use ( Hadland & Levy, 2016 ). Particularly in situations when trust has been eroded within a family and the veracity of an adolescent’s self-report is in doubt, urine testing may serve as a useful, though imperfect, method for objective assessment. With some exceptions, most studies have shown reasonable agreement between adolescent self-report and urine drug test results ( Gignac et al., 2005 ). Parental report is comparatively less consistent with urine testing, reflecting that parents may not often be aware of the adolescent’s day-to-day substance use patterns. Variations in detection times due to substance, dose, chronicity of use, cutoff used, and metabolism of user, should be noted as potential limits of urine testing. Additionally, some “designer” and synthetic substances may not be included among commonly available urine drug testing panels. Home drug testing kits are widely available, but often lack informational guidance to inform parents/guardians of empirically supported strategies to incorporate them as a part of treatment and monitoring, indicating that clear guidance by the provider is critical when considering drug testing at home rather than in clinic ( Washio et al., 2014 ).
Treatment development for adolescent substance use disorders has focused primarily on psychosocial interventions, spanning individual, group, and family modalities. The intensity and duration of investigated treatments has varied from brief (even single-session) interventions to extended multimodal strategies. The majority of studies have evaluated office-based outpatient interventions, many of which were developmentally adapted from established adult-targeted treatments.
Despite the considerable appeal of brief interventions as part of the Screening, Brief Intervention, and Referral to Treatment (SBIRT) model, standalone brief interventions have demonstrated very limited effects when provided to adolescents with substance use disorders ( Young et al., 2014 ). This is similarly the case with brief school-based interventions ( Carney et al., 2016 ) and brief standalone motivational interviewing approaches ( Li et al., 2016 ). These strategies appear more useful when provided as a component of multimodal intervention with increased overall intensity and duration.
A recent comprehensive review indicated that the most well established efficacious treatments include ecological family-based treatment, group cognitive-behavioral therapy (CBT), and individual CBT, while fair evidence supports behavioral family therapy and motivational enhancement therapy (MET) ( Hogue et al., 2014 ). Substantial evidence supports combined treatment approaches, incorporating elements from the aforementioned modalities and others to enhance outcomes. Given that adolescent substance use disorders are heterogeneous and multidetermined, treatment approaches that address multiple biopsychosocial targets are often indicated. Among combined treatments, strong evidence supports combined MET and CBT, as well as combined MET, CBT, and behavioral family-based treatment ( Hogue et al., 2014 ). Outcomes are further enhanced by complementing the aforementioned treatments with contingency management (CM), a behavioral treatment based on operant conditioning principles, in which tangible rewards are provided for objectively confirmed desired behaviors (e.g., token provided for negative urine drug test) ( Stanger et al., 2015 , 2016 ). In general, evaluated treatments in large-scale trials have demonstrated short-term substance reduction and/or cessation, but adolescents with substance use disorders, even with the best evidence-based care, rarely achieve long-term abstinence ( Dennis et al., 2004 ; Hogue et al., 2014 ; Waldron & Turner, 2008 ).
Pharmacotherapy is an established complement to psychosocial treatment for adults with substance use disorders, with several medications receiving United States Food and Drug Administration (FDA) approval for treatment of alcohol, tobacco, and opioid use disorders. While the neuropathology of adolescent substance use disorders is increasingly recognized, relatively little work has focused on developing pharmacotherapies for this age group. To date, only buprenorphine-naloxone possesses FDA approval for opioid use disorder in youth ages 16 and older. Other medications have been studied at least preliminarily for youth alcohol, tobacco, cannabis, and opioid use disorders, yielding mixed results ( Hammond & Gray, 2016 ). Findings from randomized controlled trials, though not yet exhaustive, indicate that select pharmacotherapies may be considered as adjunctive treatments to psychosocial interventions: buprenorphine-naloxone maintenance to improve treatment retention and outcomes for opioid use disorder ( Marsch et al., 2005 ; Woody et al., 2008 ), N -acetylycysteine as an adjunct to cessation counseling and contingency management for cannabis use disorder ( Gray et al., 2012 ), and nicotine patch or bupropion SR to improve tobacco cessation rates ( Gray et al., 2011 , Moolchan et al., 2005 ; Muramoto et al., 2007 ).
Given the ubiquity of mobile technology among adolescents, and the considerable logistical barriers to office-based care (e.g., transportation, accessibility), recent research has focused on translating evidence-based care for delivery via electronic platforms. A meta-analysis revealed a small positive effect size for text messaging interventions for youth with substance use problems ( Mason et al., 2015 ), and a pilot study demonstrated the feasibility of using smartphones to provide recovery support for adolescents after discharge from residential treatment ( Dennis et al., 2015 ). Ongoing work is focused on combining ecological momentary assessment and smartphone application intervention in adolescents with substance use and co-occurring psychiatric disorders ( Benarous et al., 2016 ).
Limitations
This review provides a general overview of a broad, complex topic area, with multiple lines of ongoing research. The methodology of the review was by design not structured or meta-analytic, but rather a general cross-section of recent advances and findings. Additionally, the review focused largely, but not exclusively, on data derived from United States samples. As such, caution should be taken in interpreting findings, acknowledging the potential for limitations in generalizability across populations, policies, and cultural and environmental factors.
Recent research has significantly advanced the understanding of substance use in adolescence. Survey-based epidemiological studies have identified trends in substance-related attitudes and rates of use of various substances, while emerging longitudinal neuroimaging studies have elucidated the neurobiology underlying adolescents’ propensity for substance initiation and progression to substance use disorders, with potentially lasting substance-related adverse consequences. A variety of prevention programs have been implemented across settings with varying degrees of success. Novel screening and assessment instruments have been developed to efficiently identify youth with particular risk for serious substance-related problems, and a number of evidence-based treatment approaches have been shown to be effective in reducing substance use and substance-related problems. Unfortunately, adolescents with substance use disorders rarely achieve long-term abstinence even with the most robust evidence-based treatments, indicating that further work is needed to optimize methods to understand and address this important public health issue.
- ▪ Adolescents, amid rapid biopsychosocial development, are more prone than children or adults to initiating substance use and suffering lasting substance-related adverse consequences
- ▪ Recent research has elucidated the neurobiological processes underlying substance use risk in adolescents, as well as substance-related neuropathology among adolescents with substance use disorders
- ▪ Advances in prevention, screening, assessment, and treatment research have yielded evidence-based interventions to address adolescent substance use disorders
- ▪ Further research is needed to enhance outcomes and reduce the considerable public health burden of adolescent substance use disorders
Acknowledgments
Dr. Gray has received research support (medication only) from Pfizer.
Dr. Squeglia reports no competing interests.
- Allen ML, Garcia-Huidobro D, Porta C, Curran D, Patel R, Miller J, Borowsky I. Effective parenting interventions to reduce youth substance use: A systematic review. Pediatrics. 2016; 138 (2):e20154425. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Washington, DC: Author; 2013. [ Google Scholar ]
- Baker ST, Lubman DI, Yücel M, Allen NB, Whittle S, Fulcher BD, Zalesky A, Fornito A. Developmental changes in brain network hub connectivity in late adolescence. Journal of Neuroscience. 2015; 35 (24):9078–9087. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bava S, Jacobus J, Thayer RE, Tapert SF. Longitudinal changes in white matter integrity among adolescent substance users. Alcoholism: Clinical and Experimental Research. 2013; 37 (Suppl 1):E181–189. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Benarous X, Edel Y, Consoli A, Brunelle J, Etter JF, Cohen D, Khazaal Y. Ecological momentary assessment and smartphone application intervention in adolescents with substance use and comorbid severe psychiatric disorders: Study protocol. Frontiers in Psychiatry. 2016; 7 :157. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Brown SA, Brumback T, Tomlinson K, Cummins K, Thompson WK, Nagel BJ, De Bellis MD, Hooper SR, Clark DB, Chung T, Hasler BP, Colrain IM, Baker FB, Prouty D, Pfefferbaum A, Sullivan EV, Pohl KM, Rohlfing T, Nichols BN, Chu W, Tapert SF. The National Consortium on Alcohol and NeuroDevelopment in Adolescence (NCANDA): A multi-site study of adolescent development and substance use. Journal of Studies on Alcohol and Drugs. 2015; 76 :895–908. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bunnell R, Agaku IT, Arrazola RA, Apelberg BJ, Caraballo RS, Corey CG, Coleman BN, Dube SR, King BA. Intentions to smoke cigarettes among never-smoking US middle and high school electronic cigarette users: National Youth Tobacco Survey, 2011–2013. Nicotine & Tobacco Research. 2015; 17 (2):228–235. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Carney T, Myers BJ, Louw J, Okwundu CI. Brief school-based interventions and behavioural outcomes for substance-using adolescents. Cochrane Database of Systematic Reviews. 2016:CD008969. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Casey BJ, Jones RM. Neurobiology of the adolescent brain and behavior: Implications for substance use disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2010; 49 (12):1189–1201. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Casey BJ, Jones RM, Hare TA. The adolescent brain. Annals of the New York Academy of Sciences. 2008; 1124 :111–126. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Chambers RA, Taylor JR, Potenza MN. Developmental neurocircuitry of motivation in adolescence: A critical period of addiction vulnerability. American Journal of Psychiatry. 2003; 160 (6):1041–1052. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Charach A, Yeung E, Climans T, Lillie E. Childhood attention-deficit/hyperactivity disorder and future substance use disorders: Comparative meta-analyses. Journal of the American Academy of Child and Adolescent Psychiatry. 2011; 50 (1):9–21. [ PubMed ] [ Google Scholar ]
- Cheetham A, Allen NB, Whittle S, Simmons J, Yücel M, Lubman DI. Volumetric differences in the anterior cingulate cortex prospectively predict alcohol-related problems in adolescence. Psychopharmacology. 2014; 231 :1731–1742. [ PubMed ] [ Google Scholar ]
- Cheetham A, Allen NB, Whittle S, Simmons JG, Yücel M, Lubman DI. Orbitofrontal volumes in early adolescence predict initiation of cannabis use: A 4-year longitudinal and prospective study. Biological Psychiatry. 2012; 71 :684–692. [ PubMed ] [ Google Scholar ]
- Coie JD, Watt NF, West SG, Hawkins JD, Asarnow JR, Markman HJ, Ramey SL, Shure MB, Long B. The science of prevention: A conceptual framework and some directions for a national research program. American Psychologist. 1993; 48 (10):1013–1022. [ PubMed ] [ Google Scholar ]
- Cotton NS. The familial incidence of alcoholism: A review. Journal of Studies on Alcohol. 1979; 40 :89–116. [ PubMed ] [ Google Scholar ]
- Cservenka A. Neurobiological phenotypes associated with a family history of alcoholism. Drug and Alcohol Dependence. 2016; 158 :8–21. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Dager AD, Anderson BM, Rosen R, Khadka S, Sawyer B, Jiantonio-Kelly RE, Austad CS, Raskin SA, Tennen H, Wood RM, Fallahi CR, Pearlson GD. Functional magnetic resonance imaging (fMRI) response to alcohol pictures predicts subsequent transition to heavy drinking in college students. Addiction. 2014; 109 :585–595. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Dennis M, Babor TF, Roebuck C, Donaldson J. Changing the focus: The case for recognizing and treating cannabis use disorders. Addiction. 2002; 97 (s1):4–15. [ PubMed ] [ Google Scholar ]
- Dennis ML, Chan YF, Funk RR. Development and validation of the GAIN Short Screener (GSS) for internalizing, externalizing and substance use disorders and crime/violence problems among adolescents and adults. American Journal on Addiction. 2006; 15 (suppl 1):80–91. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Dennis M, Godley SH, Diamond G, Tims FM, Babor T, Donaldson J, Liddle H, Titus JC, Kaminer Y, Webb C, Hamilton N, Funk R. The Cannabis Youth Treatment (CYT) Study: Main findings from two randomized trials. Journal of Substance Abuse Treatment. 2004; 27 (3):197–213. [ PubMed ] [ Google Scholar ]
- Dennis ML, Scott CK, Funk RR, Nicholson L. A pilot study to examine the feasibility of potential effectiveness of using smartphones to provide recovery support for adolescents. Substance Abuse. 2015; 36 (4):486–492. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Meyers JL, Dick DM. Genetic and environmental risk factors for adolescent-onset substance use disorders. Child & Adolescent Psychiatric Clinics of North America. 2010; 19 (3):465–477. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Dube SR, Miller JW, Brown DW, Giles WH, Felitti VJ, Dong M, Anda RF. Adverse childhood experiences and the association with ever using alcohol and initiating alcohol use during adolescence. Journal of Adolescent Health. 2006; 38 (4):444.e1–10. [ PubMed ] [ Google Scholar ]
- Enoch MA. The role of early life stress as a predictor for alcohol and drug dependence. Psychopharmacology (Berl) 2011; 214 (1):17–31. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Enoch MA. The influence of gene-environment interactions on the development of alcoholism and drug dependence. Current Psychiatry Reports. 2012; 14 (2):150–158. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Giedd JN. Structural magnetic resonance imaging of the adolescent brain. Annals of the New York Academy of Sciences. 2004; 1021 :77–85. [ PubMed ] [ Google Scholar ]
- Giedd JN, Rapoport JL. Structural MRI of pediatric brain development: what have we learned and where are we going? Neuron. 2010; 67 :728–734. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gignac M, Wilens TE, Biederman J, Kwon A, Mick E, Swezey A. Assessing cannabis use in adolescents and young adults: What do urine screen and parental report tell you? Journal of Child and Adolescent Psychopharmacology. 2005; 15 :742–750. [ PubMed ] [ Google Scholar ]
- Gogtay N, Giedd JN, Lusk L, Hayashi KM, Greenstein D, Vaituzis AC, Nugent TF, 3rd, Herman DH, Clasen LS, Toga AW, Rapaport JL, Thompson PM. Dynamic mapping of human cortical development during childhood through early adulthood. Proceedings of the National Academy of Sciences of the United States of America. 2004; 101 (21):8174–8179. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Grant BF, Dawson DA. Age at onset of alcohol use and its association with DSM-IV alcohol abuse and dependence: Results from the National Longitudinal Alcohol Epidemiologic Survey. Journal of Substance Abuse. 1997; 9 :103–110. [ PubMed ] [ Google Scholar ]
- Gray KM, Carpenter MJ, Baker NL, Hartwell KJ, Lewis AL, Hiott DW, Deas D, Upadhyaya HP. Bupropion SR and contingency management for adolescent smoking cessation. Journal of Substance Abuse Treatment. 2011; 40 :77–86. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gray KM, Carpenter MJ, Baker NL, DeSantis SM, Kryway E, Hartwell KJ, McRae-Clark AL, Brady KT. A double-blind randomized controlled trial of N -acetylcysteine in cannabis-dependent adolescents. American Journal of Psychiatry. 2012; 169 :805–812. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gryczynski J, Kelly SM, Mitchell SG, Kirk A, O’Grady KE, Schwartz RP. Validation and performance of the Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) among adolescent primary care patients. Addiction. 2015; 110 (2):240–247. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hadland SE, Levy S. Objective testing: urine and other drug tests. Child and Adolescent Psychiatric Clinics of North America. 2016; 25 (3):549–565. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hammond CJ, Gray KM. Pharmacotherapy for substance use disorders in youths. Journal of Child and Adolescent Substance Abuse. 2016; 25 (4):292–316. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hanson KL, Cummins K, Tapert SF, Brown SA. Changes in neuropsychological functioning over 10 years following adolescent substance abuse treatment. Psychology of Addictive Behaviors. 2011a; 25 (1):127–142. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hanson KL, Medina KL, Padula CB, Tapert SF, Brown SA. Impact of adolescent alcohol and drug use on neuropsychological functioning in young adulthood: 10-year outcomes. Journal of Child and Adolescent Substance Abuse. 2011b; 20 (2):135–154. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Harris SK, Herr-Zaya K, Weinstein Z, Whelton K, Perfas F, Jr, Castro-Donlan C, Straus J, Schoneman K, Botticelli M, Levy S. Results of a statewide survey of adolescent substance use screening rates and practices in primary care. Substance Abuse. 2012; 33 :321–326. [ PubMed ] [ Google Scholar ]
- Harrop E, Catalano RF. Evidence-based prevention for adolescent substance use. Child and Adolescent Psychiatric Clinics of North America. 2016; 25 :387–410. [ PubMed ] [ Google Scholar ]
- Hart AB, Kranzler HR. Alcohol dependence genetics: Lessons learned from genome-wide association studies (GWAS) and post-GWAS analyses. Alcoholism: Clinical and Experimental Research. 2015; 39 (8):1312–1327. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Heitzeg MM, Cope LM, Martz ME, Hardee JE. Neuroimaging risk markers for substance abuse: Recent findings on inhibitory control and reward system functioning. Current Addiction Reports. 2015; 2 :91–103. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Heitzeg MM, Nigg JT, Hardee JE, Soules M, Steinberg D, Zubieta JK, Zucker RA. Left middle frontal gyrus response to inhibitory errors in children prospectively predicts early problem substance use. Drug and Alcohol Dependence. 2014; 141 :51–57. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hogue A, Henderson CE, Ozechowski TJ, Robbins MS. Evidence base on outpatient behavioral treatments for adolescent substance use: Updates and recommendations 2007–2013. Journal of Clinical Child & Adolescent Psychology. 2014; 43 (5):695–720. [ PubMed ] [ Google Scholar ]
- Jacobus J, Squeglia LM, Infante MA, Castro N, Brumback T, Meruelo AD, Tapert SF. Neuropsychological performance in adolescent marijuana users with co-occurring alcohol use: A three-year longitudinal study. Neuropsychology. 2015; 29 (6):829–843. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Khurana A, Romer D, Betancourt LM, Brodsky NL, Giannetta JM, Hurt H. Working memory ability predicts trajectories of early alcohol use in adolescents: The mediational role of impulsivity. Addiction. 2013; 108 :506–515. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Jackson NJ, Isen JD, Khoddam R, Irons D, Tuvblad C, Iacono WG, McGue M, Raine A, Baker LA. Impact of adolescent marijuana use on intelligence: Results from two longitudinal twin studies. Proceedings of the National Academy of Sciences of the United States of America. 2016; 113 (5):E500–E508. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Jacobus J, Squeglia LM, Bava S, Tapert SF. White matter characterization of adolescent binge drinking with and without co-occurring marijuana use: A 3-year investigation. Psychiatry Research. 2013a; 214 (3):374–381. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Jacobus J, Squeglia LM, Infante MA, Bava S, Tapert SF. White matter integrity pre- and post marijuana and alcohol initiation in adolescence. Brain Sciences. 2013b; 3 (1):396–414. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Johnston LD, O’Malley PM, Miech RA, Bachman JG, Schulenberg JE. Monitoring the Future national survey results on drug use, 1975–2016: Overview, key findings on adolescent drug use. Ann Arbor: Institute for Social Research, The University of Michigan; 2017. [ Google Scholar ]
- Kelly SM, Gryczynski J, Mitchell SG, Kirk A, O’Grady KE, Schwartz RP. Validity of brief screening instrument for adolescent tobacco, alcohol, and drug use. Pediatrics. 2014; 133 (5):819–826. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Knight JR, Shrier LA, Bravender TD, Farrell M, Vander Bilt J, Shaffer HJ. A new brief screen for adolescent substance abuse. Archives of Pediatrics and Adolescent Medicine. 1999; 153 (6):591–596. [ PubMed ] [ Google Scholar ]
- Lebel C, Beaulieu C. Longitudinal development of human brain wiring continues from childhood into adulthood. Journal of Neuroscience. 2011; 31 :10937–10947. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lebel C, Gee M, Camicioli R, Wieler M, Martin W, Beaulieu C. Diffusion tensor imaging of white matter tract evolution over the lifespan. Neuroimage. 2012; 60 :340–352. [ PubMed ] [ Google Scholar ]
- Lee SS, Humphreys KL, Flory K, Liu R, Glass K. Prospective association of childhood attention-deficit/hyperactivity disorder (ADHD) and substance use and abuse/dependence: A meta-analytic review. Clinical Psychology Review. 2011; 31 (3):328–341. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Leung RK, Toumbourou JW, Hemphill SA. The effect of peer influence and selection processes on adolescent alcohol use: A systematic review of longitudinal studies. Health Psychology Review. 2014; 8 (4):426–457. [ PubMed ] [ Google Scholar ]
- Levy S, Weiss R, Sherritt L, Ziemnik R, Spalding A, Van Hook S, Shrier LA. An electronic screen for triaging adolescent substance use by risk levels. JAMA Pediatrics. 2014; 168 (9):822–828. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Levy SJ, Williams JF AAP Committee on Substance Use and Prevention. Substance use screening, brief intervention, and referral to treatment. Pediatrics. 2016; 138 (1):e20161211. [ PubMed ] [ Google Scholar ]
- Li L, Zhu S, Tse N, Tse S, Wong P. Effectiveness of motivational interviewing to reduce illicit drug use in adolescents: A systematic review and meta-analysis. Addiction. 2016; 111 :795–805. [ PubMed ] [ Google Scholar ]
- Libby AM, Orton HD, Stover SK, Riggs PD. What came first, major depression or substance use disorder? Clinical characteristics and substance use comparing teens in a treatment cohort. Addictive Behaviors. 2005; 30 (9):1649–1662. [ PubMed ] [ Google Scholar ]
- Lize SE, Iachini AL, Tang W, Tucker J, Seay KD, Clone S, DeHart D, Browne T. A meta-analysis of the effectiveness of interactive middle school cannabis prevention programs. Prevention Science. 2017; 18 :50–60. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- López-Caneda E, Rodríguez Holguín S, Cadaveira F, Corral M, Doallo S. Impact of alcohol use on inhibitory control (and vice versa) during adolescence and young adulthood: A review. Alcohol and Alcoholism. 2015; 49 :173–181. [ PubMed ] [ Google Scholar ]
- Luciana M, Collins PF, Muetzel RL, Lim KO. Effects of alcohol use initiation on brain structure in typically developing adolescents. American Journal of Drug and Alcohol Abuse. 2013; 39 (6):345–355. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- MacArthur GJ, Harrison S, Caldwell DM, Hickman M, Campbell R. Peer-led interventions to prevent tobacco, alcohol and/or drug use among young people aged 11–21 years: A systematic review and meta-analysis. Addiction. 2016; 111 :391–407. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Mahmood OM, Goldenberg D, Thayer R, Migliorini R, Simmons AN, Tapert SF. Adolescents’ fMRI activation to a response inhibition task predicts future substance use. Addictive Behaviors. 2013; 38 :1435–1441. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Marsch LA, Bickel WK, Badger GJ, Stothart ME, Quesnel KJ, Stanger C, Brooklyn J. Comparison of pharmacological treatments for opioid-dependent adolescents. Archives of General Psychiatry. 2005; 62 :1157–1164. [ PubMed ] [ Google Scholar ]
- Mason M, Ola B, Zaharakis N, Zhang J. Text messaging interventions for adolescent and young adult substance use: A meta-analysis. Prevention Science. 2015; 16 :181–188. [ PubMed ] [ Google Scholar ]
- Meier MH, Caspi A, Ambler A, Harrington H, Houts R, Keefe RS, McDonald K, Ward A, Poulton R, Moffitt TE. Persistent cannabis users show neuropsychological decline from childhood to midlife. Proceedings of the National Academ of Sciences of the United States of America. 2012; 109 :E2657–E2664. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Meier MH, Hall W, Caspi A, Belsky DW, Cerdá M, Harrington HL, Houts R, Poulton R, Moffitt TE. Which adolescents develop persistent substance dependence in adulthood? Using population-representative longitudinal data to inform universal risk assessment. Psychological Medicine. 2016; 46 :877–889. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Miettunen J, Murray GK, Jones PB, Mäki P, Ebeling H, Taanila A, Joukamaa M, Savolainen J, Törmänsen S, Järvelin MR, Veijola J, Moilanen I. Longitudinal associations between childhood and adulthood externalizing and internalizing psychopathology and adolescent substance use. Psychological Medicine. 2014; 44 (8):1727–1738. [ PubMed ] [ Google Scholar ]
- Mills KL, Goddings AL, Clasen LS, Giedd JN, Blakemore SJ. The developmental mismatch in structural brain maturation during adolescence. Developmental Neuroscience. 2014; 36 (3–4):147–160. [ PubMed ] [ Google Scholar ]
- Moolchan ET, Robinson ML, Ernst M, Cadet JL, Pickworth WB, Heishman SJ, Schroeder JR. Safety and efficacy of the nicotine patch and gum for the treatment of adolescent tobacco addiction. Pediatrics. 2005; 115 :e407–e414. [ PubMed ] [ Google Scholar ]
- Muramoto ML, Leischow SJ, Sherrill D, Matthews E, Strayer LJ. Randomized, double-blind, placebo-controlled trial of 2 dosages of sustained-release bupropion for adolescent smoking cessation. Archives of Pediatrics and Adolescent Medicine. 2007; 161 :1068–1074. [ PubMed ] [ Google Scholar ]
- Nagy Z, Westerberg H, Klingberg T. Maturation of white matter is associated with the development of cognitive functions during childhood. Journal of Cognitive Neuroscience. 2004; 16 :1227–1233. [ PubMed ] [ Google Scholar ]
- Nash SG, McQueen A, Bray JH. Pathways to adolescent alcohol use: Family environment, peer influence, and parental expectations. Journal of Adolescent Health. 2005; 37 (1):19–28. [ PubMed ] [ Google Scholar ]
- Nguyen-Louie TT, Castro N, Matt GE, Squeglia LM, Brumback T, Tapert SF. Effects of emerging alcohol and marijuana use behaviors on adolescents’ neuropsychological functioning over four years. Journal of Studies on Alcohol and Drugs. 2015; 76 (5):738–748. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Norman AL, Pulido C, Squeglia LM, Spadoni AD, Paulus MP, Tapert SF. Neural activation during inhibition predicts initiation of substance use in adolescence. Drug and Alcohol Dependence. 2011; 119 :216–223. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Paus T. Mapping brain maturation and cognitive development during adolescence. Trends in Cognitive Science. 2005; 9 (2):60–68. [ PubMed ] [ Google Scholar ]
- Petanjek Z, Judas M, Simic G, Rasin MR, Uylings HB, Rakic P, Kostovic I. Extraordinary neoteny of synaptic spines in the human prefrontal cortex. Proceedings of the National Academy of Sciences of the United States of America. 2011; 108 (32):13281–13286. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pfefferbaum A, Mathalon DH, Sullivan EV, Rawles JM, Zipursky RB, Lim KO. A quantitative magnetic resonance imaging study of changes in brain morphology from infancy to late adulthood. Archives of Neurology. 1994; 51 :874–887. [ PubMed ] [ Google Scholar ]
- Ramage AE, Lin AL, Olvera RL, Fox PT, Williamson DE. Resting- state regional cerebral blood flow during adolescence: associations with initiation of substance use and prediction of future use disorders. Drug and Alcohol Dependence. 2015; 149 :40–48. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Randall J, Henggeler SW, Cunningham PB, Rowland MD, Swenson CC. Adapting multisystemic therapy to treat adolescent substance abuse more effectively. Cognitive and Behavioral Practice. 2001; 8 (4):359–366. [ Google Scholar ]
- Randolph K, Turull P, Margolis A, Tau G. Cannabis and cognitive systems in adolescents. Adolescent Psychiatry. 2013; 3 (2):135–147. [ Google Scholar ]
- Rao U, Ryan ND, Dahl RE, Birmaher B, Williamson DE, Perel JM. Factors associated with the development of substance use disorder in depressed adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 1999; 38 (9):1109–1117. [ PubMed ] [ Google Scholar ]
- Raznahan A, Shaw PW, Lerch JP, Clasen LS, Greenstein D, Berman R, Pipitone J, Chakravarty MM, Giedd JN. Longitudinal four-dimensional mapping of subcortical anatomy in human development. Proceedings of the National Academy of Sciences of the United States of America. 2014; 111 (4):1592–1597. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Shaw P, Kabani NJ, Lerch JP, Eckstrand K, Lenroot R, Gogtay N, Greenstein D, Clasen L, Evans A, Rapaport JL, Giedd JN, Wise SP. Neurodevelopmental trajectories of the human cerebral cortex. Journal of Neuroscience. 2008; 28 :3586–3594. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Shibley HL, Malcolm RJ, Veatch LM. Adolescents with insomnia and substance abuse: Consequences and comorbidities. Journal of Psychiatric Practice. 2008; 14 :146–153. [ PubMed ] [ Google Scholar ]
- Somerville LH, Jones RM, Casey BJ. A time of change: Behavioral and neural correlates of adolescent sensitivity to appetitive and aversive emotional cues. Brain and Cognition. 2010; 72 (1):124–133. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sowell ER, Thompson PM, Holmes CJ, Jernigan TL, Toga AW. In vivo evidence for post-adolescent brain maturation in frontal and striatal regions. Nature Neuroscience. 1999; 2 (10):859–861. [ PubMed ] [ Google Scholar ]
- Sowell ER, Thompson PM, Holmes CJ, Jernigan TL, Toga AW. In vivo evidence for post adolescent brain maturation in frontal and striatal regions. Nature Neuroscience. 1999; 2 :859–861. [ PubMed ] [ Google Scholar ]
- Sowell ER, Thompson PM, Leonard CM, Welcome SE, Kan E, Toga AW. Longitudinal mapping of cortical thickness and brain growth in normal children. Journal of Neuroscience. 2004; 24 :8223–8231. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Spear LP. The adolescent brain and the college drinker: Biological basis of propensity to use and misuse alcohol. Journal of Studies on Alcohol Supplement. 2002; 14 :71–81. [ PubMed ] [ Google Scholar ]
- Squeglia LM, Ball TM, Jacobus J, Brumback T, McKenna BS, Nguyen-Louie TT, Sorg SF, Paulus MP, Tapert SF. Neural predictors of alcohol use initiation during adolescence. American Journal of Psychiatry. 2017; 174 (2):172–185. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Squeglia LM, Cservenka A. Adolescence and drug use vulnerability: Findings from neuroimaging. Current Opinion in Behavioral Sciences. 2017; 13 :164–170. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Squeglia LM, Gray KM. Alcohol and drug use and the developing brain. Current Psychiatry Reports. 2016; 18 (5):46. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Squeglia LM, Jacobus J, Nguyen-Louie TT, Tapert SF. Inhibition during early adolescence predicts alcohol and marijuana use by late adolescence. Neuropsychology. 2014; 28 :782–790. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Squeglia LM, Pulido C, Wetherill RR, Jacobus J, Brown GG, Tapert SF. Brain response to working memory over three years of adolescence: influence of initiating heavy drinking. Journal of Studies on Alcohol and Drugs. 2012; 73 :749–760. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Squeglia LM, Rinker DA, Bartsch H, Castro N, Chung Y, Dale AM, Jernigan TL, Tapert SF. Brain volume reductions in adolescent heavy drinkers. Developmental Cognitive Neuroscience. 2014b; 9 :117–125. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Squeglia LM, Spadoni AD, Infante MA, Myers MG, Tapert SF. Initiating moderate to heavy alcohol use predicts changes in neuropsychological functioning for adolescent girls and boys. Psychology of Addictive Behaviors. 2009; 23 (4):715–722. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Squeglia LM, Tapert SF, Sullivan EV, Jacobus J, Meloy MJ, Rohlfing T, Pfefferbaum A. Brain development in heavy-drinking adolescents. American Journal of Psychiatry. 2015; 172 (6):531–542. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Stanger C, Lansing AH, Budney AJ. Advances in research on contingency management for adolescent substance use. Child and Adolescent Psychiatric Clinics of North America. 2016; 25 (4):645–659. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Stanger C, Ryan SR, Scherer EA, Norton GE, Budney AJ. Clinic- and home-based contingency management plus parent training for adolescent cannabis use disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2015; 54 (6):445–453. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Stiles J, Jernigan TL. The basics of brain development. Neuropsychology Review. 2010; 20 (4):327–348. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Substance Abuse and Mental Health Services Administration. Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings [PDF-3.2MB]NSDUH Series H-48, HHS Publication No(SMA) 14-4863. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014. [ Google Scholar ]
- Swendsen J, Burstein M, Case B, Conway KP, Dierker L, He J, Merikangas KR. Use and abuse of alcohol and illicit drugs in US adolescents: Results of the National Comorbidity Survey-Adolescent Supplement. Archives of General Psychiatry. 2012; 69 (4):390–398. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Tawa EA, Hall SD, Lohoff FW. Overview of the genetics of alcohol use disorder. Alcohol and Alcoholism. 2016; 51 (50):507–514. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Taylor OD. Adolescent depression as a contributing factor to the development of substance use disorders. Journal of Human Behavior in the Social Environment. 2011; 21 (6):696–710. [ Google Scholar ]
- Urošević S, Collins P, Muetzel R, Schissel A, Lim K, Luciana M. Effects of reward sensitivity and regional brain volumes on substance use initiation in adolescence. Social Cognitive and Affective Neuroscience. 2015; 10 :106–113. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Van Duijvenvoorde AC, Achterberg M, Braams BR, Peters S, Crone EA. Testing a dual-systems model of adolescent brain development using resting-state connectivity analysis. Neuroimage. 2016; 124 :409–420. [ PubMed ] [ Google Scholar ]
- Verhulst B, Neale MC, Kendler KS. The heritability of alcohol use disorders: A meta-analysis of twin and adoption studies. Psychological Medicine. 2015; 45 (5):1061–1072. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Waldron HB, Turner CW. Evidence-based psychosocial treatments for adolescent substance abuse. Journal of Clinical Child and Adolescent Psychology. 2008; 37 (1):238–261. [ PubMed ] [ Google Scholar ]
- Washio Y, Fairfax-Columbo J, Ball E, Cassey H, Arria AM, Bresani E, Curtis BL, Kirby KC. A review of guidelines on home drug testing web sites for parents. Journal of Addiction Medicine. 2014; 8 (4):258–263. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Weiland BJ, Korycinski ST, Soules M, Zubieta JK, Zucker RA, Heitzeg MM. Substance abuse risk in emerging adults associated with smaller frontal gray matter volumes and higher externalizing behaviors. Drug and Alcohol Dependence. 2014; 137 :68–75. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wetherill RR, Castro N, Squeglia LM, Tapert SF. Atypical neural activity during inhibitory processing in substance-naïve youth who later experience alcohol-induced blackouts. Drug and Alcohol Dependence. 2013; 128 :243–249. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wetherill RR, Squeglia LM, Yang TT, Tapert SF. A longitudinal examination of adolescent response inhibition: neural differences before and after the initiation of heavy drinking. Psychopharmacology (Berl) 2013; 230 (4):663–671. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Whelan R, Watts R, Orr CA, Althoff RR, Artiges E, Banaschewski T, Barker GJ, Bokde AL, Büchel C, Carvalho FM, Conrod PJ, Flor H, Fauth-Bühler M, Frouin V, Gallinat J, Gan G, Gowland P, Heinz A, Ittermann B, Lawrence C, Mann K, Martinot JL, Nees F, Ortiz N, Paillère-Martinot ML, Paus T, Pausova Z, Rietschel M, Robbins TW, Smolka MN, Ströhle A, Schumann G, Garavan H IMAGEN Consortium. Neuropsychosocial profiles of current and future adolescent alcohol misusers. Nature. 2014; 512 :185–189. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Whitesell M, Bachand A, Brown M. Familial, social, and individual factors contributing to risk for adolescent substance use. Journal of Addiction. 2013; 2013 :579310. doi: 10.1155/2013/579310. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Woody GE, Poole SA, Subramaniam G, Duosh K, Bogenschu M, Abbott P, Patkar A, Publicker M, McCain K, Potter JS, Forman R, Vetter V, McNicholas L, Blaine J, Lynch KG, Fudala P. Extended versus short-term buprenorphine-naloxone for treatment of opioid-addicted youth. Journal of the American Medical Association. 2008; 300 (17):2003–2011. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wu P, Hoven CW, Okezie N, Fuller CJ, Cohen P. Alcohol abuse and depression in children and adolescents. Journal of Child and Adolescent Substance Abuse. 2008; 17 (2):51–69. [ Google Scholar ]
- Young MM, Stevens A, Galipeau J, Pirie T, Garritty C, Singh K, Yazdi F, Golfam M, Pratt M, Turner L, Porath-Waller A, Arratoon C, Haley N, Leslie K, Reardon R, Sproule B, Grimshaw J, Moher D. Effectiveness of brief interventions as part of the Screening, Brief Intervention and Referral to Treatment (SBIRT) model for reducing the nonmedical use of psychoactive substances: A systematic Review. Systematic Reviews. 2014; 3 :50. [ PMC free article ] [ PubMed ] [ Google Scholar ]

COMMENTS
The numbers for substance use disorders are large, and we need to pay attention to them. Data from the 2018 National Survey on Drug Use and Health suggest that, over the preceding year, 20.3 million people age 12 or older had substance use disorders, and 14.8 million of these cases were attributed to alcohol.When considering other substances, the report estimated that 4.4 million individuals ...
The term `poly-drug use' is often used to describe the use of two or more drugs during a particular time period (e.g. over the last month or year). This is the definition used within the current paper. However, poly-drug use could also characterize the use of two or more psychoactive substances so that their effects are experienced simultaneously.
Introduction. Globally, substance use is associated with significant morbidity and mortality. In the 2017 Global Burden of Disease (GBD) study, substance use disorders (SUDs) were the second leading cause of disability among the mental disorders with 31,052,000 (25%) Years Lived with Disability (YLD) attributed to them [].In 2016, harmful alcohol use resulted in 3 million deaths (5.3% of all ...
Drug abuse is detrimental, and excessive drug usage is a worldwide problem. Drug usage typically begins during adolescence. Factors for drug abuse include a variety of protective and risk factors. Hence, this systematic review aimed to determine the risk and protective factors of drug abuse among adolescents worldwide. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA ...
This paper first introduces important conceptual and practical distinctions among three key terms: substance "use," "misuse," and "disorders" (including addiction), and goes on to describe and quantify the important health and social problems associated with these terms. National survey data are presented to summarize the prevalence ...
2. Substance Abuse and Different Social Groups. When researching substance abuse and its harmful effects, researchers predominantly focus on certain social groups with a higher tendency towards substance taking and misuse, such as adolescents and male adults [13,14,15,16,17,18].This is valid, as they may encounter various demanding life and social challenges, expectations, interpersonal ...
Abstract. The current opioid epidemic is one of the most severe public health crisis in US history. Responding to it has been difficult due to its rapidly changing nature and the severity of its associated outcomes. This review examines the origin and evolution of the crisis, the pharmacological properties of opioids, the neurobiology of opioid ...
Data on alcohol and drug use in the United States come from 3 major sources: the National Survey of Drug Use and Health, 1 the National Epidemiologic Survey on Alcohol and Related Conditions, 4 and the Monitoring the Future Study. 5 Since 1971, the Substance Abuse and Mental Health Services Administration has prepared an annual report that ...
Substance abuse during adolescence. The use of substances by youth is described primarily as intermittent or intensive (binge) drinking and characterized by experimentation and expediency (Degenhardt et al., Citation 2016; Morojele & Ramsoomar, Citation 2016; Romo-Avilés et al., Citation 2016).Intermittent or intensive substance use is linked to the adolescent's need for activities that ...
A litany of statistics attests to the unhealth of the United States with regard to mental illness and substance use disorders. The 2016 National Survey on Drug Use and Health (NSDUH) of 67,500 Americans indicates that mental illness affects a large number of adults and, tragically, young adults in areas such as serious mental illness (SMI), major depressive episode (MDE), and suicidal thoughts.
Fatal drug overdoses, now primarily driven by illicit opioids like fentanyl, continue to increase in the United States, reflecting a growing need for prevention and treatment strategies. Preventive interventions have primarily focused on curbing opioid prescribing, and treatment strategies target individuals. However, little is known about the broader social context surrounding these individuals.
Research Topics. En español. The National Institute on Drug Abuse (NIDA) is the largest supporter of the world's research on substance use and addiction. Part of the National Institutes of Health, NIDA conducts and supports biomedical research to advance the science on substance use and addiction and improve individual and public health.
These methods are drawn from the medical, psychological and substance use disorder treatment research fields. Next, the authors provide a very brief description and overview of specific pharmacological and behavioral therapies for alcohol and drug use disorders that have a documented evidence basis.
z Early Use. Although taking drugs at any age can lead to addiction, research shows that the earlier a person begins to use drugs, the more likely he or she is to develop serious problems.8This may reflect the harmful effect that drugs can have on the developing brain; it also may result from a mix of early social and biological
Misuse of Prescription Drugs Research Report | En español. June 2020 | Offers the latest research findings on prescription drug misuse ... Examines women and substance use and sex and gender differences in drug addiction treatment. Image. Research Report. Tobacco, Nicotine, and E-Cigarettes Research Report ...
The latter approach is frequently used to transform highly skewed frequency of drug use measures encountered with relatively young samples prior to drug use debut. 6 Other possible methodological challenges include the effects of reporting bias, sample selection bias, participation bias, recall effects, survey methodology (ACASI vs. paper and ...
Background Numerous studies have documented factors that are associated with substance use behaviors among college-aged individuals. However, relatively few studies have considered the heterogeneity of the college experience by field of study (i.e., college major) and how that educational context might affect students' health behaviors differently. Drawing from theories and prior research ...
II. DRUG REWARD. Dopamine (DA) lies at the center of drug reward (85, 182).Every drug with addiction potential increases DA, either through direct or indirect effects on DA neurons in the ventral tegmental area (VTA) with the consequent release of DA in the nucleus accumbens (NAc) ().Drugs of abuse increase DA through their initial action on different molecular targets and, depending on their ...
smoking of cigarettes and gradually drowns the person into the trap of drug abuse. Stress, anxiety, peer pressure, poverty are some of the main causes of drug abuse.As is well said -"it is ...
The Canadian Drug Laws project was a cross-jurisdictional qualitative study conducted in BC, Canada, to gather perspectives on current drug laws and alternatives from people who use drugs themselves. This paper uses the qualitative data collected from interviews with 24 people who use drugs between July and September 2020.
results on drug use, 1975-2014: volume 2, college students and adults ages 19-55. Ann Arbor (MI): Institute for Social Research; The University of Michigan; 2015.
Introduction. Illicit drug use remains a major global health problem. In 2017, an estimated 271 million people worldwide reported drug use in the previous year, a 30% increase since 2009 (UNODC, 2019), and 31.8 million (1.3%) of disability-adjusted life years globally were attributed to drug use (Degenhardt et al., 2018).In low- and middle-income countries (LMICs), substance use problems are ...
ONDCP advises the President on drug-control issues, coordinates drug-control activities and related funding across the Federal government, and produces the annual National Drug Control Strategy, which outlines Administration efforts to reduce illicit drug use, manufacturing and trafficking, drug-related crime and violence, and drug-related ...
Substance or Drug abuse is a serious public health problem affecting usually adolescents and young adults. It affects both males and females and it is. the major source of crimes in youth and ...
Illicit drug use among teens has remained low and fairly steady for the past three decades, with some notable declines during the Covid-19 pandemic. In 2023, 29 percent of high school seniors ...
The committee advocates systematic study of the laws by which the nation attempts to control drug use and identifies the research questions most germane to public policy. Pathways of Addiction provides a strategic outline for wise investment of the nation's research resources in drug abuse. This comprehensive and accessible volume will have ...
Alcohol is the most commonly used substance among adolescents, with 64% of 18 year olds endorsing lifetime alcohol use, followed by marijuana (45%) and cigarette use (31%) ( Johnston et al., 2017 ). Overall, rates of adolescent substance use have remained relatively stable over the past several years, with a few notable exceptions.