Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 13 May 2021

Global prevalence of mental health issues among the general population during the coronavirus disease-2019 pandemic: a systematic review and meta-analysis
- Surapon Nochaiwong ORCID: orcid.org/0000-0003-1100-7171 1 , 2 ,
- Chidchanok Ruengorn ORCID: orcid.org/0000-0001-7927-1425 1 , 2 ,
- Kednapa Thavorn ORCID: orcid.org/0000-0003-4738-8447 2 , 3 , 4 , 5 ,
- Brian Hutton ORCID: orcid.org/0000-0001-5662-8647 3 , 4 , 5 ,
- Ratanaporn Awiphan ORCID: orcid.org/0000-0003-3628-0596 1 , 2 ,
- Chabaphai Phosuya 1 ,
- Yongyuth Ruanta ORCID: orcid.org/0000-0003-4184-0308 1 , 2 ,
- Nahathai Wongpakaran ORCID: orcid.org/0000-0001-8365-2474 6 &
- Tinakon Wongpakaran ORCID: orcid.org/0000-0002-9062-3468 6
Scientific Reports volume 11 , Article number: 10173 ( 2021 ) Cite this article
54k Accesses
298 Citations
117 Altmetric
Metrics details
- Post-traumatic stress disorder
To provide a contemporary global prevalence of mental health issues among the general population amid the coronavirus disease-2019 (COVID-19) pandemic. We searched electronic databases, preprint databases, grey literature, and unpublished studies from January 1, 2020, to June 16, 2020 (updated on July 11, 2020), with no language restrictions. Observational studies using validated measurement tools and reporting data on mental health issues among the general population were screened to identify all relevant studies. We have included information from 32 different countries and 398,771 participants. The pooled prevalence of mental health issues amid the COVID-19 pandemic varied widely across countries and regions and was higher than previous reports before the COVID-19 outbreak began. The global prevalence estimate was 28.0% for depression; 26.9% for anxiety; 24.1% for post-traumatic stress symptoms; 36.5% for stress; 50.0% for psychological distress; and 27.6% for sleep problems. Data are limited for other aspects of mental health issues. Our findings highlight the disparities between countries in terms of the poverty impacts of COVID-19, preparedness of countries to respond, and economic vulnerabilities that impact the prevalence of mental health problems. Research on the social and economic burden is needed to better manage mental health problems during and after epidemics or pandemics. Systematic review registration : PROSPERO CRD 42020177120.
Similar content being viewed by others
Public mental health problems during COVID-19 pandemic: a large-scale meta-analysis of the evidence
Xuerong Liu, Mengyin Zhu, … Zhiyi Chen
Mental disorders following COVID-19 and other epidemics: a systematic review and meta-analysis
Candi M. C. Leung, Margaret K. Ho, … Michael Y. Ni

Prevalence of posttraumatic stress disorder after infectious disease pandemics in the twenty-first century, including COVID-19: a meta-analysis and systematic review
Kai Yuan, Yi-Miao Gong, … Lin Lu
Introduction
After the World Health Organisation (WHO) declared the rapid worldwide spread of coronavirus disease-2019 (COVID-19) to be a pandemic, there has been a dramatic rise in the prevalence of mental health problems both nationally and globally 1 , 2 , 3 . Early international evidence and reviews have reported the psychological effects of the COVID-19 outbreak on patients and healthcare workers, particularly those in direct contact with affected patients 4 , 5 , 6 , 7 , 8 . Besides patients with COVID-19, negative emotions and psychosocial distress may occur among the general population due to the wider social impact and public health and governmental response, including strict infection control, quarantine, physical distancing, and national lockdowns 2 , 9 , 10 .
Amid the COVID-19 pandemic, several mental health and psychosocial problems, for instance, depressive symptoms, anxiety, stress, post-traumatic stress symptoms (PTSS), sleep problems, and other psychological conditions are of increasing concern and likely to be significant 5 , 10 , 11 . Public psychological consequences can arise through direct effects of the COVID-19 pandemic that are sequelae related to fear of contagion and perception of danger 2 . However, financial and economic issues also contribute to mental health problems among the general population in terms of indirect effects 12 , 13 . Indeed, economic shutdowns have disrupted economies worldwide, particularly in countries with larger domestic outbreaks, low health system preparedness, and high economic vulnerability 14 , 15 , 16 .
The COVID-19 pandemic may affect the mental health of the general population differently based on national health and governmental policies implemented and the public resilience and social norms of each country. Unfortunately, little is known about the global prevalence of mental health problems in the general population during the COVID-19 pandemic. Previous systematic reviews have been limited by the number of participants included, and attention has been focussed on particular conditions and countries, with the majority of studies being conducted in mainland China 5 , 8 , 11 , 17 , 18 . To the best of our knowledge, evidence on mental health problems among the general population worldwide has not been comprehensively documented in the current COVID-19 pandemic. Therefore, a systematic review and meta-analysis at a global level is needed to provide robust and contemporary evidence to inform public health policies and long-term responses to the COVID-19 pandemic.
As such, we have performed a rigorous systematic review and meta-analysis of all available observational studies to shed light on the effects of the global COVID-19 pandemic on mental health problems among the general population. We aimed to: (1) summarise the prevalence of mental health problems nationally and globally, and (2) describe the prevalence of mental health problems by each WHO region, World Bank income group, and the global index and economic indices responses to the COVID-19 pandemic.
This systematic review and meta-analysis was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines 19 and reported in line with the Meta-analysis of Observational Studies in Epidemiology statement (Appendix, Table S1 ) 20 . The pre-specified protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO: CRD42020177120).
Search strategy
We searched electronic databases in collaboration with an experienced medical librarian using an iterative process. PubMed, Medline, Embase, PsycINFO, Web of Science, Scopus, CINAHL, and the Cochrane Library were used to identify all relevant abstracts. As the WHO declared the COVID-19 outbreak to be a public health emergency of international concern on January 30, 2020, we limited the search from January 1, 2020, to June 16, 2020, without any language restrictions. The main keywords used in the search strategy included “coronavirus” or “COVID-19” or “SARS-CoV-2”, AND “mental health” or “psychosocial problems” or “depression” or “anxiety” or “stress” or “distress” or “post-traumatic stress symptoms” or “suicide” or “insomnia” or “sleep problems” (search strategy for each database is provided in the Appendix, Table S2 ). Relevant articles were also identified from the reference lists of the included studies and previous systematic reviews. To updated and provide comprehensive, evidence-based data during the COVID-19 pandemic, grey literature from Google Scholar and the preprint reports from medRxiv, bioRxiv, and PsyArXiv were supplemented to the bibliographic database searches. A targeted manual search of grey literature and unpublished studies was performed through to July 11, 2020.
Study selection and data screening
We included observational studies (cross-sectional, case–control, or cohort) that (1) reported the occurrence or provided sufficient data to estimate the prevalence of mental health problems among the general population, and (2) used validated measurement tools for mental health assessment. The pre-specified protocol was amended to permit the inclusion of studies the recruited participants aged 12 years or older and college students as many colleges and universities were closed due to national lockdowns. We excluded studies that (1) were case series/case reports, reviews, or studies with small sample sizes (less than 50 participants); (2) included participants who had currently confirmed with the COVID-19 infection; and (3) surveyed individuals under hospital-based settings. If studies had overlapping participants and survey periods, then the study with the most detailed and relevant information was used.
Eligible titles and abstracts of articles identified by the literature search were screened independently by two reviewers (SN and CR). Then, potentially relevant full-text articles were assessed against the selection criteria for the final set of included studies. Potentially eligible articles that were not written in English were translated before the full-text appraisal. Any disagreement was resolved by discussion.
The primary outcomes were key parameters that reflect the global mental health status during the COVID-19 pandemic, including depression, anxiety, PTSS, stress, psychological distress, and sleep problems (insomnia or poor sleep). To deliver more evidence regarding the psychological consequences, secondary outcomes of interest included psychological symptoms, suicidal ideation, suicide attempts, loneliness, somatic symptoms, wellbeing, alcohol drinking problems, obsessive–compulsive symptoms, panic disorder, phobia anxiety, and adjustment disorder.
Data extraction and risk of bias assessment
Two reviewers (SN and YR) independently extracted the pre-specified data using a standardised approach to gather information on the study characteristics (the first author’s name, study design [cross-sectional survey, longitudinal survey, case–control, or cohort], study country, article type [published article, short report/letters/correspondence, or preprint reporting data], the data collection period), participant characteristics (mean or median age of the study population, the proportion of females, proportion of unemployment, history of mental illness, financial problems, and quarantine status [never, past, or current]), and predefined outcomes of interest (including assessment outcome definitions, measurement tool, and diagnostic cut-off criteria). For international studies, data were extracted based on the estimates within each country. For studies that had incomplete data or unclear information, the corresponding author was contacted by email for further clarification. The final set of data was cross-checked by the two reviewers (RA and CP), and discrepancies were addressed through a discussion.
Two reviewers (SN and CR) independently assessed and appraised the methodological quality of the included studies using the Hoy and colleagues Risk of Bias Tool-10 items 21 . A score of 1 (no) or 0 (yes) was assigned to each item. The higher the score, the greater the overall risk of bias of the study, with scores ranging from 0 to 10. The included studies were then categorised as having a low (0–3 points), moderate (4–6 points), or high (7 or 10 points) risk of bias. A pair of reviewers (RA and CP) assessed the risk of bias of each study. Any disagreements were resolved by discussion.
Data synthesis and statistical methods
A two-tailed P value of less than 0.05 was considered statistically significant. We used Stata software version 16.0 (StataCorp, College Station, TX, USA) for all analyses and generated forest plots of the summary pooled prevalence. Inter-rater agreements between reviewers for the study selection and risk of bias assessment were tested using the kappa (κ) coefficient of agreement 22 . Based on the crude information data, we recalculated and estimated the unadjusted prevalence of mental health and psychological problems using the crude numerators and denominators reported by each of the included studies. Unadjusted pooled prevalence with corresponding 95% confidence intervals (CIs) was reported for each WHO regions (Africa, America, South-East Asia, Europe, Eastern Mediterranean, and Western Pacific) and World Bank income group (low-, lower-middle-, upper-middle-, and high-income).
We employed the variance of the study-specific prevalence using the Freeman–Tukey double arcsine methods for transforming the crude data before pooling the effect estimates with a random-effect model to account for the effects of studies with extreme (small or large) prevalence estimates 23 . Heterogeneity was evaluated using the Cochran’s Q test, with a p value of less than 0.10 24 . The degree of inconsistency was quantified using I 2 values, in which a value greater than 60–70% indicated the presence of substantial heterogeneity 25 .
Pre-planned subgroup analyses were performed based on the participant (i.e., age, the proportion of female sex, the proportion of unemployment, history of mental illness, financial problems, and quarantine status) and study characteristics (article type, study design, data collection, and sample size). To explore the inequality and poverty impacts across countries, subgroup analyses based on the global index and economic indices responses to the COVID-19 pandemic were performed, including (1) human development index (HDI) 2018 (low, medium, high, and very high) 26 ; (2) gender inequality index 2018 (below vs above world average [0.439]) 27 ; (3) the COVID-19-government response stringency index during the survey (less- [less than 75%], moderate- [75–85%], and very stringent [more than 85%]) according to the Oxford COVID-19 Government Response Tracker reports 28 ; (4) the preparedness of countries in terms of hospital beds per 10,000 people, 2010–2018 (low, medium–low, medium, medium–high, and high) 15 ; (5) the preparedness of countries in terms of current health expenditure (% of gross domestic product [GDP] 2016; low, medium–low, medium, medium–high, and high) 15 ; (6) estimated percent change of real GDP growth based on the International Monetary Fund, April 2020 (below vs above world average [− 3.0]) 29 ; (7) the resilience of countries’ business environment based on the 2020 global resilience index reports (first-, second-, third-, and fourth-quartile) 30 ; and (8) immediate economic vulnerability in terms of inbound tourism expenditure (% of GDP 2016–2018; low, medium–low, medium, medium–high, and high) 15 .
To address the robustness of our findings, we conducted a sensitivity analysis by restricting the analysis to studies with a low risk of bias (Hoy and Colleagues-Tool, 0–3 points). Furthermore, a random-effects univariate meta-regression analysis was used to explore the effect of participant and study characteristics, and the global index and economic indices responses to the COVID-19 pandemic as described above on the prevalence estimates.
The visual inspection of funnel plots was performed when there was sufficient data and tested for asymmetry using the Begg’s and Egger’s tests for each specific. A P value of less than 0.10 was considered to indicate statistical publication bias 31 , 32 . If the publication bias was detected by the Begg’s and Egger’s regression test, the trim and fill method was then performed to calibrate for publication bias 33 .
Initially, the search strategy retrieved 4642 records. From these, 2682 duplicate records were removed, and 1960 records remained. Based on the title and abstract screening, we identified 498 articles that seemed to be relevant to the study question (the κ statistic for agreement between reviewers was 0.81). Of these, 107 studies fulfilled the study selection criteria and were included in the meta-analysis (Appendix, Figure S1 ). The inter-rater agreement between reviewers on the study selection and data extraction was 0.86 and 0.75, respectively. The reference list of all included studies in this review is provided in the Appendix, Table S3 .
Characteristics of included studies
In total, 398,771 participants from 32 different countries were included. The mean age was 33.5 ± 9.5 years, and the proportion of female sex was 60.9% (range, 16.0–51.6%). Table 1 summarises the characteristics of all the included studies according to World Bank income group, the global index of COVID-19 pandemic preparedness, and economic vulnerability indices. The included studies were conducted in the Africa (2 studies 34 , 35 [1.9%], n = 723), America (12 studies 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 [11.2%], n = 18,440), South-East Asia (10 studies 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 [9.4%], n = 11,953), Europe (27 studies 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 [25.2%], n = 148,430), Eastern Mediterranean (12 studies 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 [11.2%], n = 23,396), and Western Pacific WHO regions (44 studies 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 , 107 , 108 , 109 , 110 , 111 , 112 , 113 , 114 , 115 , 116 , 117 , 118 , 119 , 120 , 121 , 122 , 123 , 124 , 125 , 126 , 127 , 128 , 129 , 130 , 131 , 132 , 133 , 134 , 135 , 136 , 137 , 138 , 139 , 140 [41.1%], n = 195,829). Most of the included studies were cross-sectional (96 studies, 89.7%), used an online-based survey (101 studies, 95.3%), conducted in mainland China (34 studies, 31.8%), and were conducted in countries with upper-middle (49 studies, 45.8%) and high-incomes (44 studies, 41.1%). Detailed characteristics of the 107 included studies, measurement tools for evaluating the mental health status and psychological consequences, and the diagnostic cut-off criteria are described in Appendix, Table S4 . Of the 107 included studies, 76 (71.0%) had a low risk, 31 (29.0%) had a moderate risk, and no studies had a high risk of bias (Appendix, Table S5 ).
Global prevalence of mental health issues among the general population amid the COVID-19 pandemic
Table 2 presents a summary of the results of the prevalence of mental health problems among the general population amid the COVID-19 pandemic by WHO region and World Bank country groups. With substantial heterogeneity, the global prevalence was 28.0% (95% CI 25.0–31.2) for depression (75 studies 34 , 35 , 36 , 37 , 38 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 57 , 58 , 60 , 61 , 64 , 66 , 67 , 68 , 69 , 70 , 71 , 73 , 74 , 75 , 76 , 77 , 80 , 81 , 82 , 83 , 87 , 88 , 91 , 93 , 96 , 97 , 99 , 101 , 104 , 105 , 106 , 107 , 108 , 109 , 112 , 113 , 114 , 116 , 117 , 119 , 120 , 122 , 124 , 125 , 126 , 127 , 129 , 130 , 131 , 132 , 133 , 134 , 136 , 138 , 139 , 140 , n = 280,607, Fig. 1 ); 26.9% (95% CI 24.0–30.0) for anxiety (75 studies 35 , 37 , 38 , 40 , 42 , 43 , 44 , 46 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 57 , 58 , 60 , 61 , 64 , 66 , 67 , 68 , 69 , 71 , 73 , 74 , 75 , 76 , 77 , 80 , 81 , 82 , 83 , 87 , 88 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 104 , 105 , 107 , 108 , 109 , 112 , 113 , 114 , 115 , 116 , 117 , 119 , 120 , 122 , 124 , 125 , 126 , 129 , 130 , 131 , 132 , 133 , 134 , 136 , 138 , 139 , 140 , n = 284,813, Fig. 2 ); 24.1% (95% CI 17.0–32.0) for PTSS (28 studies 35 , 44 , 56 , 59 , 62 , 64 , 66 , 69 , 75 , 78 , 80 , 81 , 82 , 89 , 90 , 91 , 106 , 109 , 110 , 111 , 119 , 123 , 124 , 125 , 127 , 131 , 135 , 138 , n = 56,447, Fig. 3 ); 36.5% (95% CI 30.0–43.3) for stress (22 studies 37 , 50 , 51 , 52 , 53 , 54 , 57 , 58 , 71 , 73 , 75 , 76 , 80 , 114 , 117 , 119 , 120 , 122 , 125 , 129 , 131 , 136 , n = 110,849, Fig. 4 ); 50.0% (95% CI 41.8–58.2) for psychological distress (18 studies 39 , 47 , 52 , 59 , 63 , 65 , 70 , 72 , 78 , 79 , 85 , 86 , 88 , 102 , 110 , 118 , 121 , 128 , n = 81,815, Fig. 5 ); and 27.6% (95% CI 19.8–36.1) for sleep problems (15 studies 35 , 53 , 58 , 80 , 84 , 103 , 106 , 107 , 109 , 119 , 120 , 125 , 134 , 136 , 137 , n = 99,534, Fig. 6 ). The prevalence of mental health problems based on different countries varied (Appendix, Table S6 ), from 14.5% (South Africa) to 63.3% (Brazil) for depressive symptoms; from 7.7% (Vietnam) to 49.9% (Mexico) for anxiety; from 10.5% (United Kingdom) to 52.0% (Egypt) for PTSS; from 19.7% (Portugal) to 72.8% (Thailand) for stress; from 23.9% (China) to Jordan (92.9%) for psychological distress; from 9.2% (Italy) to 53.9% (Thailand) for sleep problems.
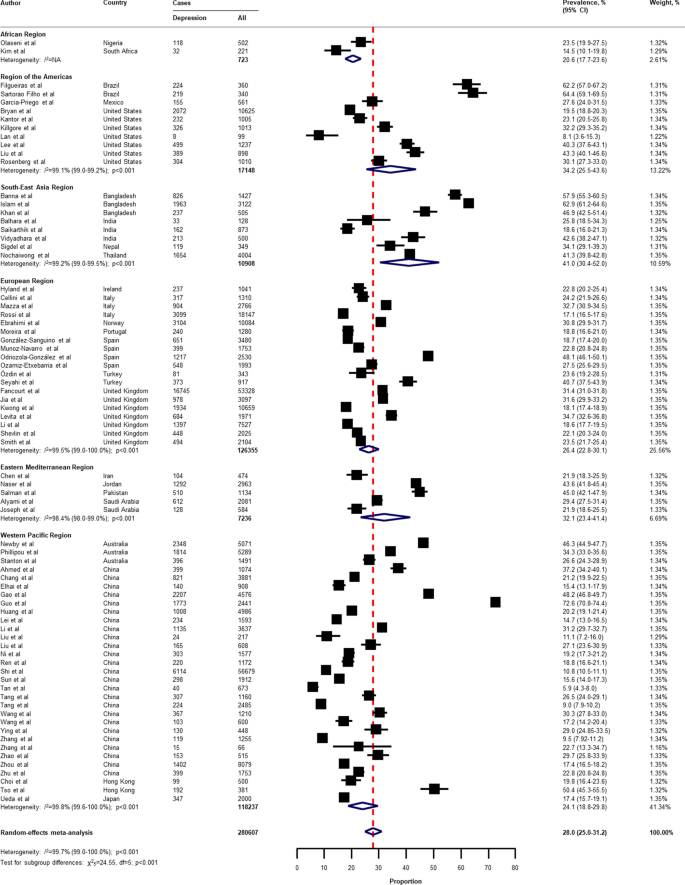
Pooled prevalence of depression among the general population amid the COVID-19 pandemic. COVID-19 coronavirus disease 2019, CI confidence interval, df degree of freedom, NA not applicable. References are listed according to WHO region in the appendix, Table S3 .
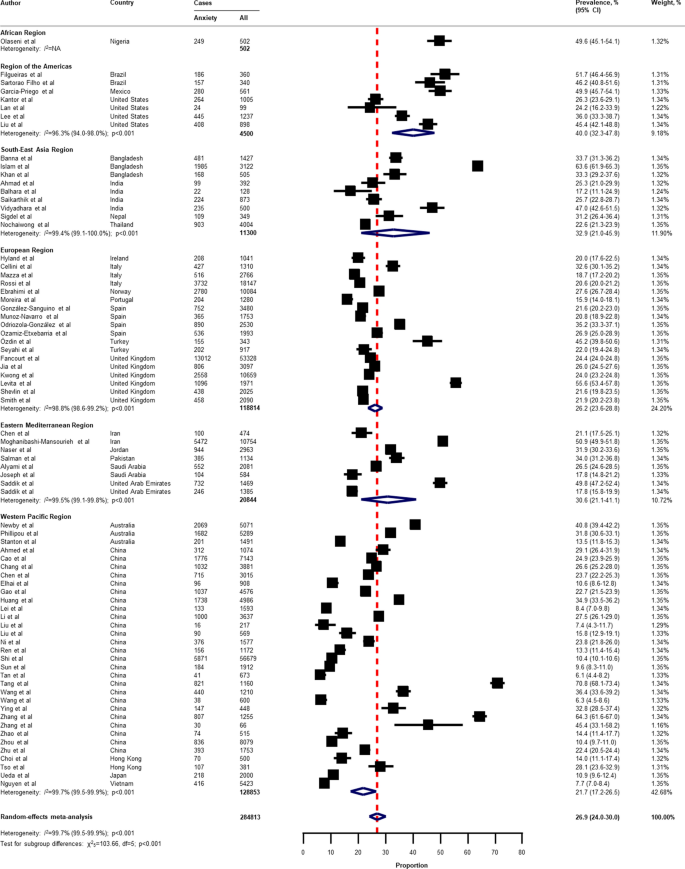
Pooled prevalence of anxiety among the general population amid the COVID-19 pandemic. COVID-19 coronavirus disease 2019, CI confidence interval, df degree of freedom, NA not applicable. References are listed according to WHO region in the appendix, Table S3 .
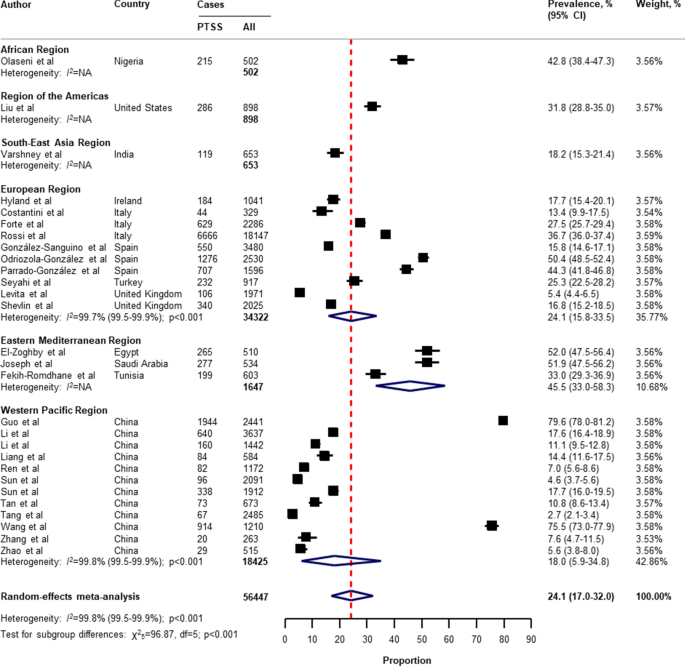
Pooled prevalence of PTSS among the general population amid the COVID-19 pandemic. COVID-19 coronavirus disease 2019, CI confidence interval, df degree of freedom, NA not applicable, PTSS post-traumatic stress symptoms. References are listed according to WHO region in the appendix, Table S3 .
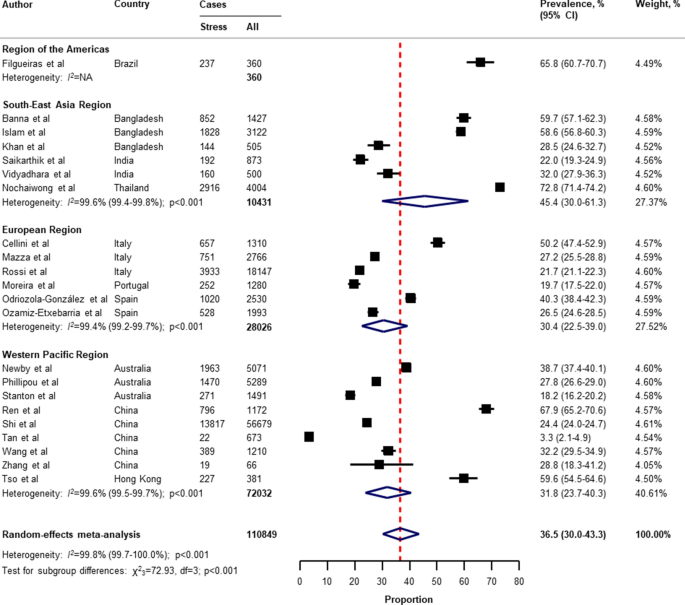
Pooled prevalence of stress among the general population amid the COVID-19 pandemic. COVID-19 coronavirus disease 2019, CI confidence interval, df degree of freedom, NA not applicable. References are listed according to WHO region in the appendix, Table S3 .
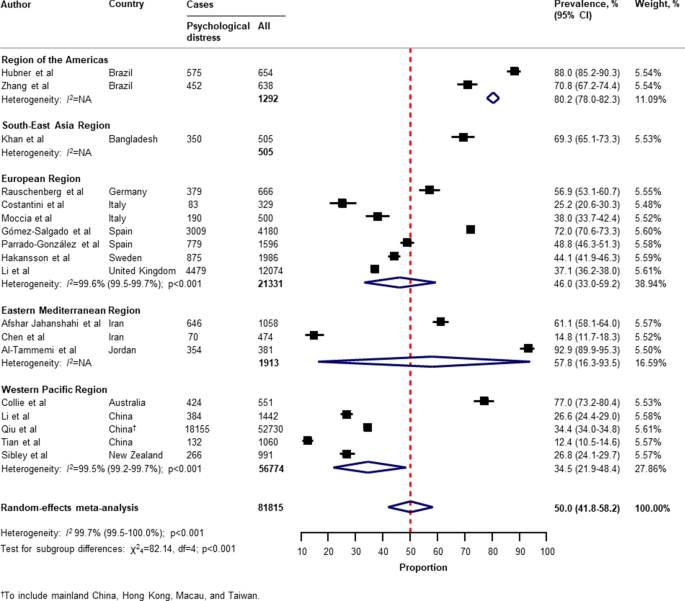
Pooled prevalence of psychological distress among the general population amid the COVID-19 pandemic. COVID-19 coronavirus disease 2019, CI confidence interval, df degree of freedom, NA not applicable. References are listed according to WHO region in the appendix, Table S3 .
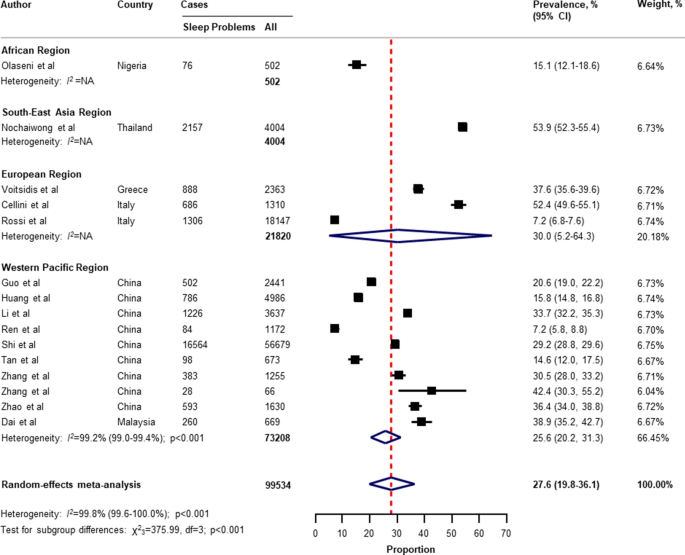
Pooled prevalence of sleep problems among the general population amid the COVID-19 pandemic. COVID-19 coronavirus disease 2019, CI confidence interval, df degree of freedom, NA not applicable. References are listed according to WHO region in the appendix, Table S3 .
With respect to the small number of included studies and high degree of heterogeneity, the pooled secondary outcome prevalence estimates are presented in Appendix, Table S7 . The global prevalence was 16.4% (95% CI 4.8–33.1) for suicide ideation (4 studies 36 , 41 , 53 , 124 , n = 17,554); 53.8% (95% CI 42.4–63.2) for loneliness (3 studies 41 , 44 , 45 , n = 2921); 30.7% (95% CI 2.1–73.3) for somatic symptoms (3 studies 53 , 69 , 134 , n = 7230); 28.6% (95% CI 9.2–53.6) for low wellbeing (3 studies 53 , 68 , 97 , n = 15,737); 50.5% (95% CI 49.2–51.7) for alcohol drinking problems (2 studies 97 , 114 , n = 6145); 6.4% (95% CI 5.5–7.4) for obsessive–compulsive symptoms (2 studies 73 , 134 , n = 2535); 25.7% (95% CI 23.7–27.8) for panic disorder (1 study 74 , n = 1753); 2.4% (95% CI 1.6–3.4) for phobia anxiety (1 study 134 , n = 1255); 22.8% (95% CI 22.1–23.4) for adjustment disorder (1 study 80 , n = 18,147); and 1.2% (95% CI 1.0–1.4) for suicide attempts (1 study 36 , n = 10,625).
Subgroup analyses, sensitivity analyses, meta-regression analyses, and publication bias
In the subgroup analyses (Appendix, Table S8 , Table S9 , Table S10 , Table S1 , Table S12 ), the prevalence of mental health problems was higher in countries with a low to medium HDI (for depression, anxiety, PTSS, and psychological distress), high HDI (for sleep problems), high gender inequality index (for depression and PTSS), very stringent government response index (for PTSS and stress), less stringent government response index (for sleep problems), low to medium hospital beds per 10,000 people (for depression, anxiety, PTSS, stress, psychological distress, and sleep problems), low to medium current health expenditure (for depression, PTSS, and psychological distress), estimated percent change of real GDP growth 2020 below − 3.0 (for psychological distress), low resilience (fourth-quartile) of business environment (for depression, anxiety, and PTSS), medium resilience (second-quartile) of business environment (for psychological distress, and sleep problems), high economic vulnerability-inbound tourism expenditure (for psychological distress, sleep problems), article type-short communication/letter/correspondence (for stress), cross-sectional survey (for PTSS and psychological distress), longitudinal survey (for anxiety and stress), non-mainland China (for depression, anxiety, and psychological distress), sample size of less than 1000 (for psychological distress), sample size of more than 5000 (for PTSS), proportion of females more than 60% (for stress and sleep problems), and measurement tools (for depression, anxiety, stress, and sleep problems). However, several pre-planned subgroup analyses based on participant characteristics and secondary outcomes reported could not be performed due to limited data in the included studies.
Findings from the sensitivity analysis were almost identical to the main analysis (Appendix, Table S14 ). The pooled prevalence by restricting the analysis to studies with a low risk of bias was 28.6% (95% CI 25.1–32.3) for depression, 27.4% (95% CI 24.1–30.8) for anxiety, 30.2% (95% CI 20.3–41.1) for PTSS, 40.1% (95% CI 32.5–47.9) for stress, 45.4% (95% CI 32.0–59.2) for psychological distress, and 27.7% (95% CI 19.4–36.9) for sleep problems.
On the basis of univariate meta-regression, the analysis was suitable for the primary outcomes (Appendix, Table S15 ). The increased prevalence of mental health problems was associated with the WHO region (for depression, anxiety, and psychological distress), female gender inequality index (for depression and anxiety), the COVID-19-government response stringency index during the survey (for sleep problems), hospital beds per 10,000 people (for depression and anxiety), immediate economic vulnerability-inbound tourism expenditure (for sleep problems), study design (cross-sectional vs longitudinal survey; for stress), surveyed country (mainland China vs non-mainland China; for depression and psychological distress), and risk of bias (for PTSS).
The visual inspection of the funnel plots, and the p values tested for asymmetry using the Begg’s and Egger’s tests for each prevalence outcome, indicated no evidence of publication bias related to the sample size (Appendix, Table S16 , and Figure S2 ).
This study is, to the best of our knowledge, the first systematic review and meta-analysis on the overall global prevalence of mental health problems and psychosocial consequences among the general population amid the COVID-19 pandemic. Overall, our findings indicate wide variability in the prevalence of mental health problems and psychosocial consequences across countries, particularly in relation to different regions, the global index of COVID-19 pandemic preparedness, inequalities, and economic vulnerabilities indices.
Two reports examined the global prevalence of common mental health disorders among adults prior to the COVID-19 outbreak. The first study was based on 174 surveys across 63 countries from 1980 to 2013. The estimated lifetime prevalence was 29.1% for all mental disorders, 9.6% for mood disorders, 12.9% for anxiety disorders, and 3.4% for substance use disorder 141 . Another report which was conducted as part of the Global Health Estimates by WHO in 2015, showed that the global estimates of depression and anxiety were 4.4% and 3.6% (more common among females than males), respectively 142 . Despite the different methodological methods used, our findings show that the pooled prevalence of mental health problems during the COVID-19 pandemic is higher than before the outbreak.
Previous studies on the prevalence of mental health problems during the COVID-19 pandemic have had substantial heterogeneity. Three systematic reviews reported the prevalence of depression, anxiety, and stress among the general population (mainly in mainland China). The first of these by Salari et al. 11 , was based on 17 included studies (from ten different countries in Asia, Europe, and the Middle East), the pooled prevalence of depression, anxiety, and stress were 33.7% (95% CI 27.5–40.6), 31.9% (95% CI 27.5–36.7), and 29.6% (95% CI 24.3–35.4), respectively. A review by Luo et al. 8 , which included 36 studies from seven different countries, reported a similar overall prevalence of 27% (95% CI 22–33) for depression and 32% (95% CI 25–39) for anxiety. However, a review by Ren et al. 17 , which focussed on only the Chinese population (8 included studies), found that the pooled prevalence was 29% (95% CI 16–42) and 24% (95% CI 16–32), respectively. Nevertheless, previous systematic reviews have been mainly on investigating the prevalence of PTSS, psychological distress, and sleep problems among the patients or healthcare workers that are limited to the general population during the COVID-19 pandemic. With regard to the general population, a review by Cénat et al. 143 , found that the pooled prevalence of PTSS, psychological distress, and insomnia were 22.4% (95% CI 7.6–50.3; 9 included studies), 10.2% (95% CI 4.6–21.0; 10 included studies), and 16.5% (95% CI 8.4–29.7; 8 included studies), respectively.
In this systematic review and meta-analysis, we updated and summarised the global prevalence of mental health problems and psychosocial consequences during the COVID-19 pandemic using information from 32 different countries, and 398,771 participants. A range of problems, including depression, anxiety, PTSS, stress, psychological distress, and sleep problems were reported. The global prevalence of our findings was in line with the previous reviews mentioned above in terms of depression (28.0%; 95% CI 25.0–31.2), anxiety (26.9%; 95% CI 24.0–30.0), and stress (36.5%; 95% CI 30.0–43.3). Interestingly, our findings highlight the poverty impacts of COVID-19 in terms of inequalities, the preparedness of countries to respond, and economic vulnerabilities on the prevalence of mental health problems across countries. For instance, our results suggest that countries with a low or medium HDI had a higher prevalence of depression and anxiety compared to countries with a high or very high HDI (Appendix, Table S8 , and Table S9 ). The prevalence of depression was higher among countries with a gender inequality index of 0.439 or greater (39.6% [95% CI 30.3–49.3] vs 26.2% [95% CI 23.1–29.3]; P = 0.020; Appendix, Table S8 ). Likewise, the prevalence of depression and anxiety was higher among countries with low hospital beds per 10,000 people (Appendix, Table S8 , and Table S9 ). Our findings suggest that the poverty impacts of COVID-19 are likely to be quite significant and related to the subsequent risk of mental health problems and psychosocial consequences. Although we performed a comprehensive review by incorporating articles published together with preprint reports, there was only limited data available on Africa, low-income groups, and secondary outcomes of interest (psychological distress, suicide ideation, suicide attempts, loneliness, somatic symptoms, wellbeing, alcohol drinking problems, obsessive–compulsive symptoms, panic disorder, phobia anxiety, and adjustment disorder).
Strengths and limitations of this review
From a methodological point of view, we used a rigorous and comprehensive approach to establish an up-to-date overview of the evidence-based information on the global prevalence of mental health problems amid the COVID-19 pandemic, with no language restrictions. The systematic literature search was extensive, comprising published peer-reviewed articles and preprints reporting data to present all relevant literature, minimise bias, and up to date evidence. Our findings expanded and addressed the limitations of the previous systematic reviews, such as having a small sample size and number of included studies, considered more aspects of mental health circumstance, and the generalisability of evidence at a global level 5 , 6 , 11 , 17 , 18 . To address biases from different measurement tools of assessment and the cultural norms across countries, we summarised the prevalence of mental health problems and psychosocial consequences using a random-effects model to estimate the pooled data with a more conservative approach. Lastly, the sensitivity analyses were consistent with the main findings, suggesting the robustness of our findings. As such, our data can be generalised to individuals in the countries where the included studies were conducted.
There were several limitations to this systematic review and meta-analysis. First, despite an advanced comprehensive search approach, data for some geographical regions according to the WHO regions and World Bank income groups, for instance, the Africa region, as well as the countries in the low-income group, were limited. Moreover, the reporting of key specific outcomes, such as suicide attempts and ideation, alcohol drinking or drug-dependence problems, and stigma towards COVID-19 infection were also limited. Second, a subgroup analysis based on participant characteristics (that is, age, sex, unemployment, history of mental illness, financial problems, and quarantine status), could not be performed as not all of the included studies reported this data. Therefore, the global prevalence of mental health problems and psychosocial consequences amid the COVID-19 pandemic cannot be established. Third, it should be noted that different methods, for example, face-to-face interviews or paper-based questionnaires, may lead to different prevalence estimates across the general population. Due to physical distancing, the included studies in this review mostly used online surveys, which can be prone to information bias and might affect the prevalence estimates of our findings. Fourth, a high degree of heterogeneity between the included studies was found in all outcomes of interest. Even though we performed a set of subgroup analyses concerning the participant characteristics, study characteristics, the global index, and economic indices responses to the COVID-19 pandemic, substantial heterogeneity persisted. However, the univariate meta-regression analysis suggested that the WHO region, gender inequality index, COVID-19-government response stringency index during the survey, hospital beds, immediate economic vulnerability (inbound tourism expenditure), study design, surveyed country (mainland China vs non-mainland China), and risk of bias were associated with an increased prevalence of mental health problems and psychosocial consequences amid the COVID-19 pandemic. Finally, we underline that the diagnostic cut-off criteria used were not uniform across the measurement tools in this review, and misclassification remains possible. The genuine variation in global mental health circumstances across countries cannot be explained by our analyses. Indeed, such variation might be predisposed by social and cultural norms, public resilience, education, ethnic differences, and environmental differences among individual study populations.
Implications for public health and research
Despite the limitations of our findings, this review provides the best available evidence that can inform the epidemiology of public mental health, implement targeted initiatives, improving screening, and reduce the long-term consequences of the COVID-19 pandemic, particularly among low-income countries, or those with high inequalities, low preparedness, and high economic vulnerability. Our findings could be improved by further standardised methods and measurement tools of assessment. There is a need for individual country-level data on the mental health problems and psychosocial consequences after the COVID-19 pandemic to track and monitor public health responses. There are a number network longitudinal surveys being conducted in different countries that aim to improve our understanding of the long-term effects of the COVID-19 pandemic 144 . To promote mental wellbeing, such initiatives could also be advocated for by public health officials and governments to increase awareness and provide timely proactive interventions in routine practice.
Conclusions
In conclusion, this systematic review and meta-analysis provides a more comprehensive global overview and evidence of the prevalence of mental health problems among the general population amid the COVID-19 pandemic. The results of this study reveal that the mental health problems and psychosocial consequences amid the COVID-19 pandemic are a global burden, with differences between countries and regions observed. Moreover, equality and poverty impacts were found to be factors in the prevalence of mental health problems. Studies on the long-term effects of the COVID-19 pandemic on the mental health status among the general population at a global level is needed. Given the high burden of mental health problems during the COVID-19 pandemic, an improvement of screening systems and prevention, prompt multidisciplinary management, and research on the social and economic burden of the pandemic, are crucial.
Data sharing
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Mahase, E. Covid-19: WHO declares pandemic because of “alarming levels” of spread, severity, and inaction. BMJ 368 , m1036 (2020).
Article PubMed Google Scholar
Pfefferbaum, B. & North, C. S. Mental health and the Covid-19 pandemic. N. Engl. J. Med. 383 , 510–512 (2020).
Article CAS PubMed Google Scholar
Burki, T. K. Coronavirus in China. Lancet Respir. Med. 8 , 238 (2020).
Article CAS PubMed PubMed Central Google Scholar
Chen, Q. et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry 7 , e15–e16 (2020).
Article PubMed PubMed Central Google Scholar
Vindegaard, N. & Benros, M. E. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav. Immun. 89 , 531–542. https://doi.org/10.1016/j.bbi.2020.05.048 (2020).
Pappa, S. et al. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav. Immun. 88 , 901–907 (2020).
Salazar de Pablo, G. et al. Impact of coronavirus syndromes on physical and mental health of health care workers: systematic review and meta-analysis. J. Affect. Disord. 275 , 48–57 (2020).
Luo, M., Guo, L., Yu, M., Jiang, W. & Wang, H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public: a systematic review and meta-analysis. Psychiatry Res. 291 , 113190 (2020).
Brooks, S. K. et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 395 , 912–920 (2020).
Kaufman, K. R., Petkova, E., Bhui, K. S. & Schulze, T. G. A global needs assessment in times of a global crisis: world psychiatry response to the COVID-19 pandemic. BJPsych Open 6 , e48 (2020).
Article PubMed CAS Google Scholar
Salari, N. et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Glob. Health 16 , 57 (2020).
Article Google Scholar
Kawohl, W. & Nordt, C. COVID-19, unemployment, and suicide. Lancet Psychiatry 7 , 389–390 (2020).
Frasquilho, D. et al. Mental health outcomes in times of economic recession: a systematic literature review. BMC Public Health 16 , 115 (2016).
World Bank. Global Economic Prospects, June 2020 (World Bank, 2020).
Book Google Scholar
Kovacevic, M. & Jahic, A. COVID-19 and Human Development: Exploring Global Preparedness and Vulnerability (Human Development Report Office, UNDP, 2020).
Google Scholar
Conceicao, P. et al. COVID-19 and Human Development: Assessing the Crisis, Envisioning the Recovery (Human Development Report Office, UNDP, 2020).
Ren, X. et al. Mental health during the Covid-19 outbreak in China: a meta-analysis. Psychiatr. Q. 91 (4), 1033–1045. https://doi.org/10.1007/s11126-020-09796-5 (2020).
Rogers, J. P. et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry 7 , 611–627 (2020).
Moher, D., Liberati, A., Tetzlaff, J. & Altman, D. G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339 , b2535 (2009).
Stroup, D. F. et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA 283 , 2008–2012 (2000).
Hoy, D. et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J. Clin. Epidemiol. 65 , 934–939 (2012).
Viera, A. J. & Garrett, J. M. Understanding interobserver agreement: the kappa statistic. Fam. Med. 37 , 360–363 (2005).
PubMed Google Scholar
Nyaga, V. N., Arbyn, M. & Aerts, M. Metaprop: a Stata command to perform meta-analysis of binomial data. Arch Public Health 72 , 39 (2014).
Cochran, W. G. The combination of estimates from different experiments. Biometrics 10 , 101–129 (1954).
Higgins, J. P. & Thompson, S. G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 21 , 1539–1558 (2002).
Human Development Report Office. Human Development Report 2019–Beyond Income, Beyond Averages, Beyond Today: Inequalities in Human DEVELOPMENT in the 21st century (United Nations Development Programme (UNDP), 2019).
Human Development Report Office. 2020 Human Development Persepctives: Tackling Social Norms–A game changer for gender inequalities (United National Development Programme (UNDP), 2020).
Hale, T. et al. Variation in government responses to COVID-19. Version 6.0. Blavatnik School of Government Working Paper. https://www.bsg.ox.ac.uk/covidtracker (2020).
International Monetary Fund (IMF). World Economic Outlook (April 2020), Real GDP growth Annual percent change . Accessed 29 July 2020. https://www.imf.org/external/datamapper/NGDP_RPCH@WEO/OEMDC/ADVEC/WEOWORLD (2020).
FM Global. 2020 FM Global Resilience Index: Make a Resilient Decision . Accessed 30 July 2020. https://www.fmglobal.com/research-and-resources/tools-and-resources/resilienceindex (2020).
Begg, C. B. & Mazumdar, M. Operating characteristics of a rank correlation test for publication bias. Biometrics 50 , 1088–1101 (1994).
Article CAS PubMed MATH Google Scholar
Egger, M., Davey Smith, G., Schneider, M. & Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 315 , 629–634 (1997).
Duval, S. & Tweedie, R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 56 , 455–463 (2000).
Kim, A. W., Nyengerai, T. & Mendenhall, E. Evaluating the mental health impacts of the COVID-19 pandemic in urban South Africa: perceived risk of COVID-19 infection and childhood trauma predict adult depressive symptoms. medRxiv. 2020.2006.2013.20130120 (2020).
Olaseni, A., Akinsola, O., Agberotimi, S. & Oguntayo, R. Psychological distress experiences of Nigerians amid COVID-19 pandemic. PsyArXiv May 6. 1031234/osfio/9v78y (2020).
Bryan, C., Bryan, A. O. & Baker, J. C. Associations among state-level physical distancing measures and suicidal thoughts and behaviors among U.S. adults during the early COVID-19 pandemic. PsyArXiv May 29 . 1031234/osfio/9bpr4 (2020).
Filgueiras, A. & Stults-Kolehmainen, M. Factors linked to changes in mental health outcomes among Brazilians in quarantine due to COVID-19. medRxiv. 2020.2005.2012.20099374 (2020).
Garcia-Priego, B. A. et al. Anxiety, depression, attitudes, and internet addiction during the initial phase of the 2019 coronavirus disease (COVID-19) epidemic: a cross-sectional study in Mexico. medRxiv. 2020.2005.2010.20095844 (2020).
Hubner, C. v. K., Bruscatto, M. L. & Lima, R. D. Distress among Brazilian university students due to the Covid-19 pandemic: survey results and reflections. medRxiv. 2020.2006.2019.20135251 (2020).
Kantor, B. N. & Kantor, J. Mental health outcomes and associations during the coronavirus disease 2019 pandemic: a cross-sectional survey of the US general population. medRxiv. 2020.2005.2026.20114140 (2020).
Killgore, W. D. S., Cloonan, S. A., Taylor, E. C. & Dailey, N. S. Loneliness: a signature mental health concern in the era of COVID-19. Psychiatry Res. 290 , 113117 (2020).
Lan, F.-Y., Suharlim, C., Kales, S. N. & Yang, J. Association between SARS-CoV-2 infection, exposure risk and mental health among a cohort of essential retail workers in the United States. medRxiv. 2020.2006.2008.20125120 (2020).
Lee, S. A., Jobe, M. C. & Mathis, A. A. Mental health characteristics associated with dysfunctional coronavirus anxiety. Psychol. Med. 1–2. https://doi.org/10.1017/S003329172000121X (2020).
Liu, C. H., Zhang, E., Wong, G. T. F., Hyun, S. & Hahm, H. C. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: clinical implications for U.S. young adult mental health. Psychiatry Res. 290 , 113172 (2020).
Rosenberg, M., Luetke, M., Hensel, D., Kianersi, S. & Herbenick, D. Depression and loneliness during COVID-19 restrictions in the United States, and their associations with frequency of social and sexual connections. medRxiv. 2020.2005.2018.20101840 (2020).
Sartorao Filho, C. I. et al. Impact of COVID-19 pandemic on mental health of medical students: a cross-sectional study using GAD-7 and PHQ-9 questionnaires. medRxiv. 2020.2006.2024.20138925 (2020).
Zhang, S. X., Wang, Y., Afshar Jahanshahi, A., Li, J. & Haensel Schmitt, V. G. Mental distress of adults in Brazil during the COVID-19 crisis. medRxiv. 2020.2004.2018.20070896 (2020).
Ahmad, A., Rahman, I. & Agarwal, M. Factors influencing mental health during COVID-19 outbreak: an exploratory survey among Indian population. medRxiv. 2020.2005.2003.20081380 (2020).
Balhara, Y. P. S., Kattula, D., Singh, S., Chukkali, S. & Bhargava, R. Impact of lockdown following COVID-19 on the gaming behavior of college students. Indian J. Public Health. 64 , S172-176 (2020).
Banna, H. A. et al. The impact of the COVID-19 pandemic on the mental health of the adult population in Bangladesh: a nationwide cross-sectional study. PsyArXiv May 24 . 1031234/osfio/chw5d. (2020).
Islam, M. S. et al. Psychological eesponses during the COVID-19 outbreak among university students in Bangladesh. PsyArXiv June 2 . 1031234/osfio/cndz7. (2020).
Khan, A. H. et al. The impact of COVID-19 pandemic on mental health & wellbeing among home-quarantined Bangladeshi students: a cross-sectional pilot study. PsyArXiv May 15 . 1031234/osfio/97s5r. (2020).
Nochaiwong, S. et al. Mental health circumstances among health care workers and general public under the pandemic situation of COVID-19 (HOME-COVID-19). Medicine (Baltimore) 99 , e20751 (2020).
Article CAS Google Scholar
Saikarthik, J., Saraswathi, I. & Siva, T. Assessment of impact of COVID-19 outbreak & lockdown on mental health status & its associated risk and protective factors in adult Indian population. medRxiv. 2020.2006.2013.20130153 (2020).
Sigdel, A. et al. Depression, anxiety and depression-anxiety comorbidity amid COVID-19 pandemic: an online survey conducted during lockdown in Nepal. medRxiv. 2020.2004.2030.20086926 (2020).
Varshney, M., Parel, J. T., Raizada, N. & Sarin, S. K. Initial psychological impact of COVID-19 and its correlates in Indian Community: an online (FEEL-COVID) survey. PLoS ONE 15 , e0233874 (2020).
Vidyadhara, S., Chakravarthy, A., Pramod Kumar, A., Sri Harsha, C. & Rahul, R. Mental health status among the South Indian pharmacy students during Covid-19 pandemic quarantine period: a cross-sectional study. medRxiv. 2020.2005.2008.20093708 (2020).
Cellini, N., Canale, N., Mioni, G. & Costa, S. Changes in sleep pattern sense of time and digital media use during COVID-19 lockdown in Italy. J. Sleep Res. 29 , e13074 (2020).
Costantini, A. & Mazzotti, E. Italian validation of CoViD-19 Peritraumatic Distress Index and preliminary data in a sample of general population. Riv. Psichiatr. 55 , 145–151 (2020).
Ebrahimi, O., Hoffart, A. & Johnson, S. U. The mental health impact of non-pharmacological interventions aimed at impeding viral transmission during the COVID-19 pandemic in a general adult population and the factors associated with adherence to these mitigation strategies. PsyArXiv May 9 . 1031234/osfio/kjzsp. (2020).
Fancourt, D., Steptoe, A. & Bu, F. Trajectories of depression and anxiety during enforced isolation due to COVID-19: longitudinal analyses of 59,318 adults in the UK with and without diagnosed mental illness. medRxiv. 2020.2006.2003.20120923 (2020).
Forte, G., Favieri, F., Tambelli, R. & Casagrande, M. COVID-19 pandemic in the Italian population: validation of a post-traumatic stress disorder questionnaire and prevalence of PTSD symptomatology. Int. J. Environ. Res. Public Health 17 , 4151 (2020).
Article CAS PubMed Central Google Scholar
Gómez-Salgado, J., Andrés-Villas, M., Domínguez-Salas, S., Díaz-Milanés, D. & Ruiz-Frutos, C. Related health factors of psychological distress during the COVID-19 pandemic in Spain. Int. J. Environ. Res. Public Health 17 , 3947 (2020).
Article PubMed Central CAS Google Scholar
González-Sanguino, C. et al. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav. Immun. 87 , 172–176 (2020).
Article PubMed PubMed Central CAS Google Scholar
Håkansson, A. Changes in gambling behavior during the COVID-19 pandemic: a web survey study in Sweden. Int. J. Environ. Res. Public Health 17 , 4013 (2020).
Hyland, P. et al. Anxiety and depression in the Republic of Ireland during the COVID-19 pandemic. PsyArXiv April 22. 1031234/osfio/8yqxr. (2020).
Jia, R. et al. Mental health in the UK during the COVID-19 pandemic: early observations. medRxiv. 2020.2005.2014.20102012 (2020).
Kwong, A. S. F. et al. Mental health during the COVID-19 pandemic in two longitudinal UK population cohorts. medRxiv. 2020.2006.2016.20133116 (2020).
Levita, L. et al. Impact of Covid-19 on young people aged 13–24 in the UK- preliminary findings. PsyArXiv June 30. 1031234/osfio/uq4rn. (2020).
Li, L. Z. & Wang, S. Prevalence and predictors of general psychiatric disorders and loneliness during COVID-19 in the United Kingdom: results from the Understanding Society UKHLS. medRxiv. 2020.2006.2009.20120139 (2020).
Mazza, C. et al. A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: immediate psychological responses and associated factors. Int. J. Environ. Res. Public Health 17 , 3165 (2020).
Moccia, L. et al. Affective temperament, attachment style, and the psychological impact of the COVID-19 outbreak: an early report on the Italian general population. Brain Behav. Immun. 87 , 75–79 (2020).
Moreira, P. S. et al. Protective elements of mental health status during the COVID-19 outbreak in the Portuguese population. medRxiv. 2020.2004.2028.20080671 (2020).
Munoz-Navarro, R., Cano-Vindel, A., Schmitz, F., Cabello, R. & Fernandez-Berrocal, P. Emotional distress and associated sociodemographic risk factors during the COVID-19 outbreak in Spain. medRxiv. 2020.2005.2030.20117457 (2020).
Odriozola-González, P., Planchuelo-Gómez, Á., Irurtia, M. J. & de Luis-García, R. Psychological effects of the COVID-19 outbreak and lockdown among students and workers of a Spanish university. Psychiatry Res. 290 , 113108 (2020).
Ozamiz-Etxebarria, N., Idoiaga Mondragon, N., Dosil Santamaría, M. & Picaza Gorrotxategi, M. Psychological symptoms during the two stages of lockdown in response to the COVID-19 outbreak: an investigation in a sample of citizens in Northern Spain. Front. Psychol. 11 , 1491 (2020).
Özdin, S. & Bayrak Özdin, Ş. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: the importance of gender. Int. J. Soc. Psychiatry 66 , 504–511 (2020).
Parrado-González, A. & León-Jariego, J. C. Covid-19: factors associated with emotional distress and psychological morbidity in Spanish population. Rev. Esp. Salud Publica 94 , e202006058 (2020).
Rauschenberg, C. et al. Social isolation, mental health and use of digital interventions in youth during the COVID-19 pandemic: a nationally representative survey. PsyArXiv June 29 . 1031234/osfio/v64hf (2020).
Rossi, R. et al. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. An N = 18147 web-based survey. medRxiv. 2020.2004.2009.20057802 (2020).
Seyahi, E., Poyraz, B. C., Sut, N., Akdogan, S. & Hamuryudan, V. The psychological state and changes in the routine of the patients with rheumatic diseases during the coronavirus disease (COVID-19) outbreak in Turkey: a web-based cross-sectional survey. Rheumatol. Int. 40 , 1229–1238 (2020).
Shevlin, M. et al. Anxiety, depression, traumatic stress, and COVID-19 related anxiety in the UK general population during the COVID-19 pandemic. PsyArXiv April 18. 1031234/osfio/hb6nq (2020).
Smith, L. E. et al. Factors associated with self-reported anxiety, depression, and general health during the UK lockdown; a cross-sectional survey. medRxiv. 2020.2006.2023.20137901 (2020).
Voitsidis, P. et al. Insomnia during the COVID-19 pandemic in a Greek population. Psychiatry Res. 289 , 113076 (2020).
Afshar Jahanshahi, A., Mokhtari Dinani, M., Nazarian Madavani, A., Li, J. & Zhang, S. X. The distress of Iranian adults during the Covid-19 pandemic: more distressed than the Chinese and with different predictors. medRxiv. 2020.2004.2003.20052571 (2020).
Al-Tammemi, A. a. B., Akour, A. & Alfalah, L. Is it just about physical health? An internet-based cross-sectional study exploring the psychological impacts of COVID-19 pandemic on university students in Jordan using Kessler psychological distress scale. medRxiv. 2020.2005.2014.20102343 (2020).
Alyami, H. S. et al. Depression and anxiety during 2019 coronavirus disease pandemic in Saudi Arabia: a cross-sectional study. medRxiv. 2020.2005.2009.20096677 (2020).
Chen, J. et al. The curvilinear relationship between the age of adults and their mental health in Iran after its peak of COVID-19 cases. medRxiv. 2020.2006.2011.20128132 (2020).
El-Zoghby, S. M., Soltan, E. M. & Salama, H. M. Impact of the COVID-19 pandemic on mental health and social support among adult Egyptians. J. Community Health 45 , 689–695 (2020).
Fekih-Romdhane, F., Ghrissi, F., Abbassi, B., Cherif, W. & Cheour, M. Prevalence and predictors of PTSD during the COVID-19 pandemic: findings from a Tunisian community sample. Psychiatry Res. 290 , 113131 (2020).
Joseph, R., Alshayban, D., Lucca, J. M. & Alshehry, Y. A. The immediate psychological response of the general population in Saudi Arabia during COVID-19 pandemic: a cross-sectional study. medRxiv. 2020.2006.2019.20135533 (2020).
Moghanibashi-Mansourieh, A. Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian J. Psychiatr. 51 , 102076 (2020).
Naser, A. Y. et al. Mental health status of the general population, healthcare professionals, and university students during 2019 coronavirus disease outbreak in Jordan: a cross-sectional study. Brain Behav. 10 (8), e01730. https://doi.org/10.1002/brb3.1730 (2020).
Saddik, B. et al. Assessing the influence of parental anxiety on childhood anxiety during the COVID-19 pandemic in the United Arab Emirates. medRxiv. 2020.2006.2011.20128371 (2020).
Saddik, B. et al. Increased levels of anxiety among medical and non-medical university students during the COVID-19 pandemic in the United Arab Emirates. medRxiv. 2020.2005.2010.20096933 (2020).
Salman, M. et al. Psychological impact of COVID-19 on Pakistani university students and how they are coping. medRxiv. 2020.2005.2021.20108647 (2020).
Ahmed, M. Z. et al. Epidemic of COVID-19 in China and associated psychological problems. Asian J. Psychiatr. 51 , 102092 (2020).
Cao, W. et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 287 , 112934 (2020).
Chang, J., Yuan, Y. & Wang, D. Mental health status and its influencing factors among college students during the epidemic of COVID-19. Nan Fang Yi Ke Da Xue Xue Bao 40 , 171–176 (2020).
Chen, S. H. et al. Public anxiety and its influencing factors in the initial outbreak of COVID-19. Fudan Univ. J. Med. Sci. 47 , 385–391 (2020).
Choi, E. P. H., Hui, B. P. H. & Wan, E. Y. F. Depression and anxiety in Hong Kong during COVID-19. Int. J. Environ. Res. Public Health 17 , 3740 (2020).
Collie, A. et al. Psychological distress among people losing work during the COVID-19 pandemic in Australia. medRxiv. 2020.2005.2006.20093773 (2020).
Dai, H., Zhang, S. X., Looi, K. H., Su, R. & Li, J. Health condition and test availability as predictors of adults' mental health during the COVID-19 pandemic. medRxiv. 2020.2006.2021.20137000 (2020).
Elhai, J. D., Yang, H., McKay, D. & Asmundson, G. J. G. COVID-19 anxiety symptoms associated with problematic smartphone use severity in Chinese adults. J. Affect. Disord. 274 , 576–582 (2020).
Gao, J. et al. Mental health problems and social media exposure during COVID-19 outbreak. PLoS ONE 15 , e0231924 (2020).
Guo, J., Feng, X. L., Wang, X. H. & van IJzendoorn, M. H. Coping with COVID-19: exposure to COVID-19 and negative impact on livelihood predict elevated mental health problems in Chinese adults. Int. J. Environ. Res. Public Health 17 , 3857 (2020).
Huang, Y. & Zhao, N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 288 , 112954 (2020).
Lei, L. et al. Comparison of prevalence and associated factors of anxiety and depression among people affected by versus people unaffected by quarantine during the COVID-19 epidemic in Southwestern China. Med. Sci. Monit. 26 , e924609 (2020).
Li, Y. et al. Insomnia and psychological reactions during the COVID-19 outbreak in China. J Clin. Sleep Med. https://doi.org/10.5664/jcsm.8524 (2020).
Li, Y. et al. Psychological distress among health professional students during the COVID-19 outbreak. Psychol. Med. 1–3. https://doi.org/10.1017/S0033291720001555 (2020).
Liang, L. et al. The effect of COVID-19 on youth mental health. Psychiatr. Q. 91 (3), 841–852. https://doi.org/10.1007/s11126-020-09744-3 (2020).
Liu, J. et al. Online mental health survey in a medical college in China during the COVID-19 outbreak. Front. Psychiatry 11 , 459 (2020).
Liu, X. et al. Psychological status and behavior changes of the public during the COVID-19 epidemic in China. Infect. Dis. Poverty 9 , 58 (2020).
Newby, J., O'Moore, K., Tang, S., Christensen, H. & Faasse, K. Acute mental health responses during the COVID-19 pandemic in Australia. medRxiv. 2020.2005.2003.20089961 (2020).
Nguyen, H. T. et al. Fear of COVID-19 scale-associations of its scores with health literacy and health-related behaviors among medical students. Int. J. Environ. Res. Public Health 17 , 4164 (2020).
Ni, M. Y. et al. Mental health, risk factors, and social media use during the COVID-19 epidemic and cordon sanitaire among the community and health professionals in Wuhan, China: cross-sectional survey. JMIR Ment. Health 7 , e19009 (2020).
Phillipou, A. et al. Eating and exercise behaviors in eating disorders and the general population during the COVID-19 pandemic in Australia: initial results from the COLLATE project. Int. J. Eat. Disord. 53 , 1158–1165 (2020).
Qiu, J. et al. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr. 33 , e100213 (2020).
Ren, Y. et al. Letter to the Editor “A longitudinal study on the mental health of general population during the COVID-19 epidemic in China”. Brain Behav. Immun. 87 , 132–133 (2020).
Shi, L. et al. Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA Netw. Open 3 , e2014053 (2020).
Sibley, C. G. et al. Effects of the COVID-19 pandemic and nationwide lockdown on trust, attitudes toward government, and well-being. Am. Psychol. 75 , 618–630 (2020).
Stanton, R. et al. Depression, anxiety and stress during COVID-19: associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int. J. Environ. Res. Public Health 17 , 4065 (2020).
Sun, L. et al. Prevalence and risk factors of acute posttraumatic stress symptoms during the COVID-19 outbreak in Wuhan, China. medRxiv. 2020.2003.2006.20032425 (2020).
Sun, S., Goldberg, S. B., Lin, D., Qiao, S. & Operario, D. Psychiatric symptoms, risk, and protective factors among university students in quarantine during the COVID-19 pandemic in China. medRxiv. 2020.2007.2003.20144931 (2020).
Tan, W. et al. Is returning to work during the COVID-19 pandemic stressful? A study on immediate mental health status and psychoneuroimmunity prevention measures of Chinese workforce. Brain Behav. Immun. 87 , 84–92 (2020).
Tang, F. et al. COVID-19 related depression and anxiety among quarantined respondents. Psychol. Health 36 (2), 164–178. https://doi.org/10.1080/08870446.2020.1782410 (2020).
Tang, W. et al. Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. J. Affect. Disord. 274 , 1–7 (2020).
Tian, F. et al. Psychological symptoms of ordinary Chinese citizens based on SCL-90 during the level I emergency response to COVID-19. Psychiatry Res. 288 , 112992 (2020).
Tso, I. F. & Sohee, P. Alarming levels of psychiatric symptoms and the role of loneliness during the COVID-19 epidemic: a case study of Hong Kong. PsyArXiv published online June 27. 1031234/osfio/wv9y2 (2020).
Ueda, M., Stickley, A., Sueki, H. & Matsubayashi, T. Mental health status of the general population during the COVID-19 pandemic: a cross-sectional national survey in Japan. medRxiv. 2020.2004.2028.20082453 (2020).
Wang, C. et al. Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus Disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health 17 , 1729 (2020).
Wang, Y., Di, Y., Ye, J. & Wei, W. Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychol. Health Med. 26 (1), 13–22. https://doi.org/10.1080/13548506.2020.1746817 (2020).
Ying, Y. et al. Mental health status among family members of health care workers in Ningbo, China during the Coronavirus Disease 2019 (COVID-19) outbreak: a Cross-sectional Study. medRxiv. 2020.2003.2013.20033290 (2020).
Zhang, W. R. et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother. Psychosom. 89 , 242–250 (2020).
Zhang, Y. & Ma, Z. F. Impact of the COVID-19 pandemic on mental health and quality of life among local residents in Liaoning Province, China: a cross-sectional study. Int. J. Environ. Res. Public Health 17 , 2381 (2020).
Zhang, Y., Zhang, H., Ma, X. & Di, Q. Mental health problems during the COVID-19 pandemics and the mitigation effects of exercise: a longitudinal study of college students in China. Int. J. Environ. Res. Public Health 17 , 3722 (2020).
Zhao, X., Lan, M., Li, H. & Yang, J. Perceived stress and sleep quality among the non-diseased general public in China during the 2019 coronavirus disease: a moderated mediation model. Sleep Med. S1389–9457 (1320), 30224–30220. https://doi.org/10.1016/j.sleep.2020.05.021 (2020).
Zhao, Y., An, Y., Tan, X. & Li, X. Mental health and its influencing factors among self-isolating ordinary citizens during the beginning epidemic of COVID-19. J. Loss Trauma https://doi.org/10.1080/15325024.15322020.11761592 (2020).
Zhou, S. J. et al. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur. Child Adolesc. Psychiatry 29 , 749–758 (2020).
Zhu, S. et al. The immediate mental health impacts of the COVID-19 pandemic among people with or without quarantine managements. Brain Behav.. Immun. 87 , 56–58 (2020).
Steel, Z. et al. The global prevalence of common mental disorders: a systematic review and meta-analysis 1980–2013. Int. J. Epidemiol. 43 , 476–493 (2014).
World Health Organization. Depression and Other Common Mental Disorders: Global Health Estimates (World Health Organization, 2017).
Cénat, J. M. et al. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 295 , 113599 (2021).
COVID-MINDS Network. COVID-MINDS network: global mental health in the COVID-19 pandemic , https://www.covidminds.org/ (2020).
Download references
Acknowledgements
The authors thank the research assistances and all staff of Pharmacoepidemiology and Statistics Research Center (PESRC), Chiang Mai, Thailand. This work reported in this manuscript was partially supported by a grant by the Chiang Mai University, Thailand. The funder of the study had no role in the study design collection, analysis, or interpretation of the data, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit it for publication.
Author information
Authors and affiliations.
Department of Pharmaceutical Care, Faculty of Pharmacy, Chiang Mai University, Chiang Mai, 50200, Thailand
Surapon Nochaiwong, Chidchanok Ruengorn, Ratanaporn Awiphan, Chabaphai Phosuya & Yongyuth Ruanta
Pharmacoepidemiology and Statistics Research Center (PESRC), Faculty of Pharmacy, Chiang Mai University, Chiang Mai, 50200, Thailand
Surapon Nochaiwong, Chidchanok Ruengorn, Kednapa Thavorn, Ratanaporn Awiphan & Yongyuth Ruanta
Ottawa Hospital Research Institute, Ottawa Hospital, Ottawa, ON, K1H 8L6, Canada
Kednapa Thavorn & Brian Hutton
Institute of Clinical and Evaluative Sciences, ICES uOttawa, Ottawa, ON, K1Y 4E9, Canada
School of Epidemiology and Public Health, Faculty of Medicine, University of Ottawa, Ottawa, ON, K1G 5Z3, Canada
Department of Psychiatry, Faculty of Medicine, Chiang Mai University, Chiang Mai, 50200, Thailand
Nahathai Wongpakaran & Tinakon Wongpakaran
You can also search for this author in PubMed Google Scholar
Contributions
S.N. conceived the study and, together with C.R., K.T., R.A., C.P., and Y.R. developed the protocol. S.N. and C.R. did the literature search, selected the studies. S.N. and Y.R. extracted the relevant information. S.N. synthesised the data. S.N. wrote the first draft of the paper. K.T., B.H., N.W., and T.W. critically revised successive drafts of the paper. All authors approved the final draft of the manuscript. SN is the guarantor of the study.
Corresponding author
Correspondence to Surapon Nochaiwong .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary figures and tables., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions

About this article
Cite this article.
Nochaiwong, S., Ruengorn, C., Thavorn, K. et al. Global prevalence of mental health issues among the general population during the coronavirus disease-2019 pandemic: a systematic review and meta-analysis. Sci Rep 11 , 10173 (2021). https://doi.org/10.1038/s41598-021-89700-8
Download citation
Received : 11 January 2021
Accepted : 29 April 2021
Published : 13 May 2021
DOI : https://doi.org/10.1038/s41598-021-89700-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Enhancing mental wellbeing by changing mindsets results from two randomized controlled trials.
- Carina Schreiber
- Marijke Schotanus-Dijkstra
BMC Psychology (2024)
Protocol for a pilot cluster randomised controlled trial of a multicomponent sustainable return to work IGLOo intervention
- Oliver Davis
- Jeremy Dawson
- Fehmidah Munir
Pilot and Feasibility Studies (2024)
The global prevalence of depression, anxiety, and sleep disorder among patients coping with Post COVID-19 syndrome (long COVID): a systematic review and meta-analysis
- Niloofar Seighali
- Abolfazl Abdollahi
- Mahmood Bakhtiyari
BMC Psychiatry (2024)
Effectiveness of gamified digital interventions in mental health prevention and health promotion among adults: a scoping review
- Leona Aschentrup
- Pia Anna Steimer
- Kamil J. Wrona
BMC Public Health (2024)
The relationships between perceived mental illness prevalence, mental illness stigma, and attitudes toward help-seeking
- Alexander Chang
- Paul Handal
Current Psychology (2024)
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Disclaimer » Advertising
- HealthyChildren.org
Selection Criteria
Search strategy, data extraction, risk of bias and applicability, data synthesis and analysis, parent ratings, teacher ratings, youth self-reports, combined rating scales, additional clinician tools, neuropsychological tests, biospecimen, neuroimaging, variation in diagnostic accuracy with clinical setting or patient subgroup, measures for diagnostic performance, available tools, importance of the comparator sample, clinical implications, future research, conclusions, acknowledgments, tools for the diagnosis of adhd in children and adolescents: a systematic review.
FUNDING: The work is based on research conducted by the Southern California Evidence-based Practice Center under contract to the Agency for Healthcare Research and Quality (AHRQ), Rockville, MD (Contract 75Q80120D00009). The Patient-Centered Outcomes Research Institute (PCORI) funded the research (PCORI Publication No. 2023-SR-03). The findings and conclusions in this manuscript are those of the authors, who are responsible for its contents; the findings and conclusions do not necessarily represent the views of AHRQ or PCORI, its Board of Governors, or Methodology Committee. Therefore, no statement in this report should be construed as an official position of PCORI, AHRQ or of the US Department of Health and Human Services.
CONFLICT OF INTEREST DISCLOSURES: The authors have indicated they have no conflicts of interest to disclose.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- CME Quiz Close Quiz
- Open the PDF for in another window
- Get Permissions
- Cite Icon Cite
- Search Site
Bradley S. Peterson , Joey Trampush , Morah Brown , Margaret Maglione , Maria Bolshakova , Mary Rozelle , Jeremy Miles , Sheila Pakdaman , Sachi Yagyu , Aneesa Motala , Susanne Hempel; Tools for the Diagnosis of ADHD in Children and Adolescents: A Systematic Review. Pediatrics 2024; e2024065854. 10.1542/peds.2024-065854
Download citation file:
- Ris (Zotero)
- Reference Manager
Correct diagnosis is essential for the appropriate clinical management of attention-deficit/hyperactivity disorder (ADHD) in children and adolescents.
This systematic review provides an overview of the available diagnostic tools.
We identified diagnostic accuracy studies in 12 databases published from 1980 through June 2023.
Any ADHD tool evaluation for the diagnosis of ADHD, requiring a reference standard of a clinical diagnosis by a mental health specialist.
Data were abstracted and critically appraised by 1 reviewer and checked by a methodologist. Strength of evidence and applicability assessments followed Evidence-based Practice Center standards.
In total, 231 studies met eligibility criteria. Studies evaluated parental ratings, teacher ratings, youth self-reports, clinician tools, neuropsychological tests, biospecimen, EEG, and neuroimaging. Multiple tools showed promising diagnostic performance, but estimates varied considerably across studies, with a generally low strength of evidence. Performance depended on whether ADHD youth were being differentiated from neurotypically developing children or from clinically referred children.
Studies used different components of available tools and did not report sufficient data for meta-analytic models.
A valid and reliable diagnosis of ADHD requires the judgment of a clinician who is experienced in the evaluation of youth with and without ADHD, along with the aid of standardized rating scales and input from multiple informants across multiple settings, including parents, teachers, and youth themselves.
Attention-deficit/hyperactivity disorder (ADHD) is one of the most prevalent neurodevelopmental conditions in youth. Its prevalence has remained constant at ∼5.3% worldwide over the years, and diagnostic criteria have remained constant when based on rigorous diagnostic procedures. 1 Clinical diagnoses, however, have increased steadily over time, 2 and currently, ∼10% of US children receive an ADHD diagnosis. 3 Higher rates of clinical compared with research-based diagnoses are because of an increasing clinician recognition of youth who have ADHD symptoms that are functionally impairing but do not fully meet formal diagnostic criteria. 4 The higher diagnostic rates over time in clinical samples also results from youth receiving a diagnosis incorrectly. Some youth, for example, are misdiagnosed as having ADHD when they have symptoms of other disorders that overlap with ADHD symptoms, such as difficulty concentrating, which occurs in many other conditions. 5 Moreover, ADHD is more than twice as likely to be diagnosed in boys than in girls, 3 in lower-income families, 6 and in white compared with nonwhite youth 7 ; differences that derive at least in part from diagnostic and cultural biases. 8 , – 11
Improving clinical diagnostic accuracy is essential to ensure that youth who truly have ADHD benefit from receiving treatment without delay. Similarly, youth who do not have ADHD should not be diagnosed since an incorrect diagnosis risks exposing them to unbeneficial treatments. 12 , 13 Clinician judgement alone, however, especially by nonspecialist clinicians, is poor in diagnosing ADHD 14 compared with expert, research-grade diagnoses made by mental health clinicians. 15 Accurately diagnosing ADHD is difficult because diagnoses are often made using subjective clinical impressions, and putative diagnostic tools have a confusing, diverse, and poorly described evidence base that is not widely accessible. The availability of valid diagnostic tools would especially help to reduce misdiagnoses from cultural biases and symptom overlap with ADHD. 12 , 16 , – 19
This review summarizes evidence for the performance of tools for children and adolescents with ADHD. We did not restrict to a set of known diagnostic tools but instead explored the range of available diagnostic tools, including machine-learning assisted and virtual reality-based tools. The review aimed to assess how diagnostic performance varies by clinical setting and patient characteristics.
The review aims were developed in consultation with the Agency for Healthcare Research and Quality (AHRQ), the Patient-Centered Outcomes Research Institute, the topic nominator American Academy of Pediatrics, key informants, a technical expert panel (TEP), and public input. The TEP reviewed the protocol and advised on key outcomes. Subgroup analyses and key outcomes were prespecified. The review is registered in PROSPERO (CRD42022312656) and the protocol is available on the AHRQ Web site as part of a larger evidence report on ADHD. The systematic review followed Methods of the (AHRQ) Evidence-based Practice Center Program. 20
Population: age <18 years.
Interventions: any ADHD tool for the diagnosis of ADHD.
Comparators: diagnosis by a mental health specialist, such as a psychologist, psychiatrist, or other provider, who often used published scales or semistructured diagnostic interviews to ensure a reliable DSM-based diagnosis of ADHD.
Key outcomes: diagnostic accuracy (eg, sensitivity, specificity, area under the curve).
Setting: any.
Study design: diagnostic accuracy studies.
Other: English language, published from 1980 to June 2023.
We searched PubMed, Embase, PsycINFO, ERIC, and ClinicalTrials.gov. We identified reviews for reference-mining through PubMed, Cochrane Database of Systematic Reviews, Campbell Collaboration, What Works in Education, PROSPERO, ECRI Guidelines Trust, G-I-N, and ClinicalKey. The peer reviewed strategy is in the Supplemental Appendix . All citations were screened by trained literature reviewers supported by machine learning ( Fig 1 ). Two independent reviewers assessed full text studies for eligibility. The TEP reviewed studies to ensure all were captured. Publications reporting on the same participants were consolidated into 1 record.

Literature flow diagram.
The data abstraction form included extensive guidance to aid reproducibility and standardization in recording study details, results, risk of bias, and applicability. One reviewer abstracted data and a methodologist checked accuracy and completeness. Data are publicly available in the Systematic Review Data Repository.
We assessed characteristics pertaining to patient selection, index test, reference standard, flow and timing that may have introduced bias, and evaluated applicability of study results, such as whether the test, its conduct, or interpretation differed from how the test is used in clinical practice. 21 , 22
We differentiated parent, teacher, and youth self-report ratings; tools for clinicians; neuropsychological tests; biospecimens; EEG; and neuroimaging. We organized analyses according to prespecified outcome measures. A narrative overview summarized the range of diagnostic performance for key outcomes. Because lack of reported detail in many individual studies hindered use of meta-analytic models, we created summary figures to document the diagnostic performance reported in each study. We used meta-regressions across studies to assess the effects of age, comorbidities, racial and ethnic composition, and diagnostic setting (differentiating primary care, specialty care, school settings, mixed settings, and not reported) on diagnostic performance. One researcher with experience in use of specified standardized criteria 23 initially assessed the overall strength of evidence (SoE) (see Supplemental Appendix ) for each study, then discussed it with the study team to communicate our confidence in each finding.
We screened 23 139 citations and 7534 publications retrieved as full text against the eligibility criteria. In total, 231 studies reported in 290 publications met the eligibility criteria (see Fig 1 ).
Methodological quality of the studies varied. Selection bias was likely in two-thirds of studies; several were determined to be problematic in terms of reported study flow and timing of assessments (eg, not stating whether diagnosis was known before the results of the index test); and several lacked details on diagnosticians or diagnostic procedures ( Supplemental Fig 1 ). Applicability concerns limited the generalizability of findings ( Supplemental Fig 2 ), usually because youth with comorbidities were excluded. Many different tools were assessed within the broader categories (eg, within neuropsychological tests), and even when reporting on the same diagnostic tool, studies often used different components of the tool (eg, different subscales of rating scales), or they combined components in a variety of ways (eg, across different neuropsychological test parameters).
The evidence table ( Supplemental Table 10 , Supplemental Appendix ) shows each study’s finding. The following highlights key findings across studies.
Fifty-nine studies used parent ratings to diagnose ADHD ( Fig 2 ). The most frequently evaluated tool was the CBCL (Child Behavior Checklist), alone or in combination with other tools, often using different score cutoffs for diagnosis, and evaluating different subscales (most frequently the attention deficit/hyperactivity problems subscale). Sensitivities ranged from 38% (corresponding specificity = 96%) to 100% (specificity = 4% to 92%). 24 , 25

Diagnostic performance parent and teacher ratings. For a complete list of scales see Supplemental Appendix .
Area under the curve (AUC) for receiver operator characteristic curves ranged widely from 0.55 to 0.95 but 3 CBCL studies reported AUCs of 0.83 to 0.84. 26 , – 28 Few studies reported measurement of reliability. SoE was downgraded for study limitation (lack of detailed reporting), imprecision (large performance variability), and inconsistent findings ( Supplemental Table 1 ).
Twenty-three studies used teacher ratings to diagnose ADHD ( Fig 2 ). No 2 studies reported on rater agreement, internal consistency, or test-retest reliability for the same teacher rating scale. The highest sensitivity was 97% (specificity = 26%). 25 The Teacher Report Form, alone or in combination with Conners teacher rating scales, yielded sensitivities of 72% to 79% 29 and specificities of 64% to 76%. 30 , 32 reported AUCs ranged from 0.65 to 0.84. 32 SoE was downgraded to low for imprecision (large performance variability) and inconsistency (results for specific tools not replicated), see Supplemental Table 2 .
Six studies used youth self-reports to diagnose ADHD. No 2 studies used the same instrument. Sensitivities ranged from 53% (specificity = 98%) to 86% (specificity = 70%). 35 AUCs ranged from 0.56 to 0.85. 36 We downgraded SoE for domain inconsistency (only 1 study reported on a given tool and outcome), see Supplemental Table 3 .
Thirteen studies assessed diagnostic performance of ratings combined across informants, often using machine learning for variable selection. Only 1 study compared performance of combined data to performance from single informants, finding negligible improvement (AUC youth = 0.71; parent = 0.85; combined = 0.86). 37 Other studies reported on limited outcome measures and used ad hoc methods to combine information from multiple informants. The best AUC was reported by a machine learning supported study combining parent and teacher ratings (AUC = 0.98). 38
Twenty-four studies assessed additional tools, such as interview guides, that can be used by clinicians to aid diagnosis of ADHD. Sensitivities varied, ranging from 67% (specificity = 65%) to 98% (specificity = 100%); specificities ranged from 36% (sensitivity = 89%) to 100% (sensitivity = 98%). 39 Some of the tools measured activity levels objectively using an actometer or commercially available activity tracker, either alone or as part of a diagnostic test battery. Reported performance was variable (sensitivity range 25% to 100%, 40 specificity range 66% to 100%, 40 AUCs range 0.75–0.9996 41 ). SoE was downgraded for imprecision (large performance variability) and inconsistency (outcomes and results not replicated), see Supplemental Table 4 .
Seventy-four studies used measures from various neuropsychological tests, including continuous performance tests (CPTs). Four of these included 3- and 4-year-old children. 42 , – 44 A large majority used a CPT, which assessed omission errors (reflecting inattention), commission errors (impulsivity), and reaction time SD (response time variability). Studies varied in use of traditional visual CPTs, such as the Test of Variables of Attention, more novel, multifaceted “hybrid” CPT paradigms, and virtual reality CPTs built upon environments designed to emulate real-world classroom distractibility. Studies used idiosyncratic combinations of individual cognitive measures to achieve the best performance, though many reported on CPT attention and impulsivity measures.
Sensitivity for all neuropsychological tests ranged from 22% (specificity = 96%) to 100% (specificity = 100%) 45 ( Fig 3 ), though the latter study reported performance for unique composite measures without replication. Specificities ranged from 22% (sensitivity = 91%) 46 to 100% (sensitivity = 100% to 75%). 45 , 47 AUCs ranged from 0.59 to 0.93. 48 Sensitivity for all CPT studies ranged from 22% ( specificity = 96) to 100% (specificity = 75%). 49 Specificities for CPTs ranged from 22% (sensitivity = 91%) to 100% (sensitivity = 89%) 47 ( Fig 3 ). AUCs ranged from 0.59 to 0.93. 50 , 51 SoE was deemed low for imprecise studies (large performance variability), see Supplemental Table 5.

Diagnostic performance neuropsychological tests, CPTs, activity monitors, biospecimen, EEG.
Seven studies assessed blood or urine biomarkers to diagnose ADHD. These measured erythropoietin or erythropoietin receptor, membrane potential ratio, micro RNA levels, or urine metabolites. Sensitivities ranged from 56% (specificity = 95%) to 100% (specificity = 100% for erythropoietin and erythropoietin receptors levels). 52 Specificities ranged from 25% (sensitivity = 79%) to 100% (sensitivity = 100%). 52 AUCs ranged from 0.68 to 1.00. 52 Little information was provided on reliability of markers or their combinations. SoE was downgraded for inconsistent and imprecise studies ( Supplemental Table 6 ).
Forty-five studies used EEG markers to diagnose ADHD. EEG signals were obtained in a variety of patient states, even during neuropsychological test performance. Two-thirds used machine learning algorithms to select classification parameters. Several combined EEG with demographic variables or rating scales. Sensitivity ranged widely from 46% to 100% (corresponding specificities 74 and 71%). 53 , 54 One study that combined EEG with demographics data supported by machine learning reported perfect sensitivity and specificity. 54 Specificity was also variable and ranged from 38% (sensitivity = 95%) to 100% (specificities = 71% or 100%). 53 , – 56 Reported AUCs ranged from 0.63 to 1.0. 57 , 58 SoE was downgraded for study imprecision (large performance variability) and limitations (diagnostic approaches poorly described), see Supplemental Table 7 .
Nineteen studies used neuroimaging for diagnosis. One public data set (ADHD-200) produced several analyses. All but 2 used MRI: some functional MRI (fMRI), some structural, and some in combination, with or without magnetic resonance spectroscopy (2 used near-infrared spectroscopy). Most employed machine learning to detect markers that optimized diagnostic classifications. Some combined imaging measures with demographic or other clinical data in the prediction model. Sensitivities ranged from 42% (specificity = 95%) to 99% (specificity = 100%) using resting state fMRI and a complex machine learning algorithm 56 to differentiate ADHD from neurotypical youth. Specificities ranged from 55% (sensitivity = 95%) to 100% 56 using resting state fMRI data. AUCs ranged from 0.58 to over 0.99, 57 SoE was downgraded for imprecision (large performance variability) and study limitations (diagnostic models are often not well described, and the number and type of predictor variables entering the model were unclear). Studies generally did not validate diagnostic algorithms or assess performance measures in an independent sample ( Supplemental Table 8 ).
Regression analyses indicated that setting was associated with both sensitivity ( P = .03) and accuracy ( P = .006) but not specificity ( P = .68) or AUC ( P = .28), with sensitivities lowest in primary care ( Fig 4 ). Sensitivity, specificity, and accuracy were also lower when differentiating youth with ADHD from a clinical sample than from typically developing youth (sensitivity P = .04, specificity P < .001, AUC P < .001) ( Fig 4 ), suggesting that clinical population is a source of heterogeneity in diagnostic performance. Findings should be interpreted with caution, however, as they were not obtained in meta-analytic models and, consequently, do not take into account study size or quality.

Diagnostic performance by setting and population.
Supplemental Figs 3–5 in the Supplemental Appendix document effects by age and gender. We did not detect statistically significant associations of age with sensitivity ( P = .54) or specificity ( P = .37), or associations of the proportion of girls with sensitivity ( P = .63), specificity ( P = .80), accuracy ( P = .34), or AUC ( P = .90).
We identified a large number of publications reporting on ADHD diagnostic tools. To our knowledge, no prior review of ADHD diagnostic tools has been as comprehensive in the range of tools, outcomes, participant ages, and publication years. Despite the large number of studies, we deemed the strength of evidence for the reported performance measures across all categories of diagnostic tools to be low because of large performance variability across studies and various limitations within and across studies.
We required that studies report diagnoses when using the tool compared with diagnoses made by expert mental health clinicians. Studies most commonly reported sensitivity (true-positive rate) and specificity (true-negative rate) when a study-specific diagnostic threshold was applied to measures from the tool being assessed. Sensitivity and specificity depend critically on that study-specific threshold, and their values are inherently a trade-off, such that varying the threshold to increase either sensitivity or specificity reduces the other. Interpreting diagnostic performance in terms of sensitivity and specificity, and comparing those performance measures across studies, is therefore challenging. Consequently, researchers more recently often report performance for sensitivity and specificity in terms of receiver operating characteristics (ROC) curves, a plot of sensitivity versus specificity across the entire range of possible diagnostic thresholds. The area under this ROC curve (AUC) provides an overall, single index of performance that ranges from 0.5 (indicating that the tool provides no information above chance for classification) to 1.0 (indicating a perfect test that can correctly classify all participants as having ADHD and all non-ADHD participants as not having it). AUC values of 90 to 100 are commonly classified as excellent performance; 80 to 90 as good; 70 to 80 as fair; 60 to 70 as poor; and 50 to 60 failed performance.
Most research is available on parental ratings. Overall, AUCs for parent rating scales ranged widely from “poor” 58 to “excellent.” 59 Analyses restricted to the CBCL, the most commonly evaluated scale, yielded more consistent “good” AUCs for differentiating youth with ADHD from others in clinical samples, but the number of studies contributing data were small. Internal consistency for rating scale items was generally high across most rating scales. Test-retest reliability was good, though only 2 studies reported it. One study reported moderate rater agreement between mothers and fathers for inattention, hyperactivity, and impulsivity symptoms. Few studies included youth under 7 years of age.
AUCs for teacher rating scales ranged from “failed” 33 to “good.” 34 Internal consistency for scale items was generally high. Teacher ratings demonstrated very low rater agreement with corresponding parent scales, suggesting either a problem with the instruments or a large variability in symptom presentation with environmental context (home or school).
Though data were limited, self-reports from youth seemed to perform less well than corresponding parent and teacher reports, with AUCs ranging from “failed” for CBCL or ASEBA when distinguishing ADHD from other patients 33 to “good” for the SWAN in distinguishing ADHD from neurotypical controls. 36 , 37
Studies evaluating neuropsychological tests yielded AUCs ranging from “poor” 60 , 61 to “excellent.” 50 Many used idiosyncratic combinations of cognitive measures, which complicates interpretation of the results across studies. Nevertheless, extracting specific, comparable measures of inattention and impulsivity from CPTs yielded diagnostic performance ranging from “poor” to “excellent” in differentiating ADHD youth from neurotypical controls and “fair” in differentiating ADHD youth from other patients. 42 , 60 , 62 No studies provided an independent replication of diagnosis using the same measure.
Blood biomarkers yielded AUCs ranging from “poor” (serum miRNAs) 63 to “excellent” (erythropoietin and erythropoietin receptors levels) 52 in differentiating ADHD from neurotypical youth. None have been independently replicated, and test-retest reliability was not reported. Most EEG studies used machine learning for diagnostic classification. AUCs ranged from “poor” 64 to “excellent” when differentiating ADHD youth from neurotypical controls. 65 Diagnostic performance was not prospectively replicated in any independent samples.
Most neuroimaging studies relied on machine learning to develop diagnostic algorithms. AUCs ranged from “poor” 66 to “excellent” for distinguishing ADHD youth from neurotypically developing controls. 57 Most studies used pre-existing data sets or repositories to retrospectively discriminate youths with ADHD from neurotypical controls, not from other clinical populations and not prospectively, and none assessed test-retest reliability or the independent reproducibility of findings. Reporting of final mathematical models or algorithms for diagnosis was limited. Activity monitors have the advantage of providing inexpensive, objective, easily obtained, and quantified measures that can potentially be widely disseminated and scaled.
Studies of combined approaches, such as integrating diagnostic tools with clinician impressions, were limited. One study reported increased sensitivity and specificity when an initial clinician diagnosis combined EEG indicators (the reference standard was a consensus diagnosis from a panel of ADHD experts). 67 These findings were not independently replicated, however, and no test-retest reliability was reported.
Many studies aimed to distinguish ADHD youth from neurotypical controls, which is a distinction of limited clinical relevance. In clinically referred youth, most parents, teachers, and clinicians are reasonably confident that something is wrong, even if they are unsure whether the cause of their concern is ADHD. To be informed by a tool that the child is not typically developing is not particularly helpful. Moreover, we cannot know whether diagnostic performance for tools that discriminate ADHD youth only from neurotypical controls is determined by the presence of ADHD or by the presence of any other characteristics that accompany clinical “caseness,” such as the presence of comorbid illnesses or symptoms shared or easily confused with those of other conditions, or the effects of chronic stress or current or past treatment. The clinically more relevant and difficult question is, therefore, how well the tool distinguishes youth with ADHD from those who have other emotional and behavioral problems. Consistent with these conceptual considerations that argue for assessing diagnostic performance in differentiating youth with ADHD from those with other clinical conditions, we found significant evidence that, across all studies, sensitivity, specificity, and AUC were all lower when differentiating youth with ADHD from a clinical sample than when differentiating them from neurotypical youth. These findings also suggest that the comparison population was a significant source of heterogeneity in diagnostic performance.
Despite the large number of studies on diagnostic tools, a valid and reliable diagnosis of ADHD ultimately still requires the judgement of a clinician who is experienced in the evaluation of youth with and without ADHD, along with the aid of standardized rating scales and input from multiple informants across multiple settings, including parents, teachers, and youth themselves. Diagnostic tools perform best when the clinical question is whether a youth has ADHD or is healthy and typically developing, rather than when the clinical question is whether a youth has ADHD or another mental health or behavioral problem. Diagnostic tools yield more false-positive and false-negative diagnoses of ADHD when differentiating youth with ADHD from youth with another mental health problem than when differentiating them from neurotypically developing youth.
Scores for rating scales tended to correlate poorly across raters, and ADHD symptoms in the same child varied across settings, indicating that no single informant in a single setting is a gold-standard for diagnosis. Therefore, diagnosis using rating scales will likely benefit from a more complete representation of symptom expression across multiple informants (parents, school personnel, clinicians, and youth) across more than 1 setting (home, school, and clinic) to inform clinical judgement when making a diagnosis, thus, consistent with current guidelines. 68 , – 70 Unfortunately, methods for combining scores across raters and settings that improve diagnosis compared with scores from single raters have not been developed or prospectively replicated.
Despite the widespread use of neuropsychological testing to “diagnose” youth with ADHD, often at considerable expense, indirect comparisons of AUCs suggest that performance of neuropsychological test measures in diagnosing ADHD is comparable to the diagnostic performance of ADHD rating scales from a single informant. Moreover, the diagnostic accuracy of parent rating scales is typically better than neuropsychological test measures in head-to-head comparisons. 44 , 71 Furthermore, the overall SoE for estimates of diagnostic performance with neuropsychological testing is low. Use of neuropsychological test measures of executive functioning, such as the CPT, may help inform a clinical diagnosis, but they are not definitive either in ruling in or ruling out a diagnosis of ADHD. The sole use of CPTs and other neuropsychological tests to diagnose ADHD, therefore, cannot be recommended. We note that this conclusion regarding diagnostic value is not relevant to any other clinical utility that testing may have.
No independent replication studies have been conducted to validate EEG, neuroimaging, or biospecimen to diagnose ADHD, and no clinical effectiveness studies have been conducted using these tools to diagnose ADHD in the real world. Thus, these tools do not seem remotely close to being ready for clinical application to aid diagnosis, despite US Food and Drug Administration approval of 1 EEG measure as a purported diagnostic aid. 67 , 72
All studies of diagnostic tools should report data in more detail (ie, clearly report false-positive and -negative rates, the diagnostic thresholds used, and any data manipulation undertaken to achieve the result) to support meta-analytic methods. Studies should include ROC analyses to support comparisons of test performance across studies that are independent of the diagnostic threshold applied to measures from the tool. They should also include assessment of test-retest reliability to help discern whether variability in measures and test performance is a function of setting or of measurement variability over time. Future studies should address the influence of co-occurring disorders on diagnostic performance and how well the tools distinguish youth with ADHD from youth with other emotional and behavioral problems, not simply from healthy controls. More studies should compare the diagnostic accuracy of different test modalities, head-to-head. Independent, prospective replication of performance measures of diagnostic tools in real-world settings is essential before US Food and Drug Administration approval and before recommendations for widespread clinical use.
Research is needed to identify consensus algorithms that combine rating scale data from multiple informants to improve the clinical diagnosis of ADHD, which at present is often unguided, ad hoc, and suboptimal. Diagnostic studies using EEG, neuroimaging, and neuropsychological tests should report precise operational definitions and measurements of the variable(s) used for diagnosis, any diagnostic algorithm employed, the selected statistical cut-offs, and the number of false-positives and false-negatives the diagnostic tool yields to support future efforts at synthetic analyses.
Objective, quantitative neuropsychological test measures of executive functioning correlate only weakly with the clinical symptoms that define ADHD. 73 Thus, many youth with ADHD have normal executive functioning profiles on neuropsychological testing, and many who have impaired executive functioning on testing do not have ADHD. 74 Future research is needed to understand how test measures of executive functioning and the real-world functional problems that define ADHD map on to one another and how that mapping can be improved.
One of the most important potential uses of systematic reviews and meta-analyses in improving the clinical diagnosis of ADHD and treatment planning would be identification of effect modifiers for the performance of diagnostic tools: determining, for example, whether tools perform better in patients who are younger or older, in ethnic minorities, or those experiencing material hardship, or who have a comorbid illness or specific ADHD presentation. Future studies of ADHD should more systematically address the modifier effects of these patient characteristics. They should make available in public repositories the raw, individual-level data and the algorithms or computer code that will aid future efforts at replication, synthesis, and new discovery for diagnostic tools across data sets and studies.
Finally, no studies meeting our inclusion criteria assessed the consequences of being misdiagnosed or labeled as either having or not having ADHD, the diagnosis of ADHD specifically in preschool-aged children, or the potential adverse consequences of youth being incorrectly diagnosed with or without ADHD. This work is urgently needed.
We thank Cynthia Ramirez, Erin Tokutomi, Jennifer Rivera, Coleman Schaefer, Jerusalem Belay, Anne Onyekwuluje, and Mario Gastelum for help with data acquisition. We thank Kymika Okechukwu, Lauren Pilcher, Joanna King, and Robyn Wheatley from the American Academy of Pediatrics (AAP), Jennie Dalton and Paula Eguino Medina from PCORI, Christine Chang and Kim Wittenberg from AHRQ, and Mary Butler from the Minnesota Evidence-based Practice Center. We thank Glendy Burnett, Eugenia Chan, MD, MPH, Matthew J. Gormley, PhD, Laurence Greenhill, MD, Joseph Hagan, Jr, MD, Cecil Reynolds, PhD, Le'Ann Solmonson, PhD, LPC-S, CSC, and Peter Ziemkowski, MD, FAAFP who served as key informants. We thank Angelika Claussen, PhD, Alysa Doyle, PhD, Tiffany Farchione, MD, Matthew J. Gormley, PhD, Laurence Greenhill, MD, Jeffrey M. Halperin, PhD, Marisa Perez-Martin, MS, LMFT, Russell Schachar, MD, Le'Ann Solmonson, PhD, LPC-S, CSC, and James Swanson, PhD who served as a technical expert panel. Finally, we thank Joel Nigg, PhD, and Peter S. Jensen, MD for their peer review of the data.
Drs Peterson and Hempel conceptualized and designed the study, collected data, conducted the analyses, drafted the initial manuscript, and critically reviewed and revised the manuscript; Dr Trampush conducted the critical appraisal; Ms Brown, Ms Maglione, Drs Bolshakova and Padkaman, and Ms Rozelle screened citations and abstracted the data; Dr Miles conducted the analyses; Ms Yagyu designed and executed the search strategy; Ms Motala served as data manager; and all authors provided critical input for the manuscript, approved the final manuscript as submitted, and agree to be accountable for all aspects of the work.
This trial has been registered at PROSPERO (identifier CRD42022312656).
COMPANION PAPER: A companion to this article can be found online at https://www.pediatrics.org/cgi/doi/10.1542/peds.2024-065787 .
Data sharing statement: Data are available in SRDRPlus.
attention-deficit/hyperactivity disorder
area under the curve
Child Behavior Checklist
continuous performance test
functional magnetic resonance imaging
receiver operating characteristics
strength of evidence
technical expert panel
Competing Interests
Supplementary data.
Advertising Disclaimer »
Citing articles via
Email alerts.
Affiliations
- Editorial Board
- Editorial Policies
- Journal Blogs
- Pediatrics On Call
- Online ISSN 1098-4275
- Print ISSN 0031-4005
- Pediatrics Open Science
- Hospital Pediatrics
- Pediatrics in Review
- AAP Grand Rounds
- Latest News
- Pediatric Care Online
- Red Book Online
- Pediatric Patient Education
- AAP Toolkits
- AAP Pediatric Coding Newsletter
First 1,000 Days Knowledge Center
Institutions/librarians, group practices, licensing/permissions, integrations, advertising.
- Privacy Statement | Accessibility Statement | Terms of Use | Support Center | Contact Us
- © Copyright American Academy of Pediatrics
This Feature Is Available To Subscribers Only
Sign In or Create an Account

Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years! Learn More >>
- Science News
- Meetings and Events
- Social Media
- Press Resources
- Email Updates
- Innovation Speaker Series
Revolutionizing the Study of Mental Disorders
March 27, 2024 • Feature Story • 75th Anniversary
At a Glance:
- The Research Domain Criteria framework (RDoC) was created in 2010 by the National Institute of Mental Health.
- The framework encourages researchers to examine functional processes that are implemented by the brain on a continuum from normal to abnormal.
- This way of researching mental disorders can help overcome inherent limitations in using all-or-nothing diagnostic systems for research.
- Researchers worldwide have taken up the principles of RDoC.
- The framework continues to evolve and update as new information becomes available.
President George H. W. Bush proclaimed the 1990s “ The Decade of the Brain ,” urging the National Institutes of Health, the National Institute of Mental Health (NIMH), and others to raise awareness about the benefits of brain research.
“Over the years, our understanding of the brain—how it works, what goes wrong when it is injured or diseased—has increased dramatically. However, we still have much more to learn,” read the president’s proclamation. “The need for continued study of the brain is compelling: millions of Americans are affected each year by disorders of the brain…Today, these individuals and their families are justifiably hopeful, for a new era of discovery is dawning in brain research.”

Still, despite the explosion of new techniques and tools for studying the brain, such as functional magnetic resonance imaging (fMRI), many mental health researchers were growing frustrated that their field was not progressing as quickly as they had hoped.
For decades, researchers have studied mental disorders using diagnoses based on the Diagnostic and Statistical Manual of Mental Disorders (DSM)—a handbook that lists the symptoms of mental disorders and the criteria for diagnosing a person with a disorder. But, among many researchers, suspicion was growing that the system used to diagnose mental disorders may not be the best way to study them.
“There are many benefits to using the DSM in medical settings—it provides reliability and ease of diagnosis. It also provides a clear-cut diagnosis for patients, which can be necessary to request insurance-based coverage of healthcare or job- or school-based accommodations,” said Bruce Cuthbert, Ph.D., who headed the workgroup that developed NIMH’s Research Domain Criteria Initiative. “However, when used in research, this approach is not always ideal.”
Researchers would often test people with a specific diagnosed DSM disorder against those with a different disorder or with no disorder and see how the groups differed. However, different mental disorders can have similar symptoms, and people can be diagnosed with several different disorders simultaneously. In addition, a diagnosis using the DSM is all or none—patients either qualify for the disorder based on their number of symptoms, or they don’t. This black-and-white approach means there may be people who experience symptoms of a mental disorder but just miss the cutoff for diagnosis.
Dr. Cuthbert, who is now the senior member of the RDoC Unit which orchestrates RDoC work, stated that “Diagnostic systems are based on clinical signs and symptoms, but signs and symptoms can’t really tell us much about what is going on in the brain or the underlying causes of a disorder. With modern neuroscience, we were seeing that information on genetic, pathophysiological, and psychological causes of mental disorders did not line up well with the current diagnostic disorder categories, suggesting that there were central processes that relate to mental disorders that were not being reflected in DMS-based research.”
Road to evolution
Concerned about the limits of using the DSM for research, Dr. Cuthbert, a professor of clinical psychology at the University of Minnesota at the time, approached Dr. Thomas Insel (then NIMH director) during a conference in the autumn of 2008. Dr. Cuthbert recalled saying, “I think it’s really important that we start looking at dimensions of functions related to mental disorders such as fear, working memory, and reward systems because we know that these dimensions cut across various disorders. I think NIMH really needs to think about mental disorders in this new way.”
Dr. Cuthbert didn’t know it then, but he was suggesting something similar to ideas that NIMH was considering. Just months earlier, Dr. Insel had spearheaded the inclusion of a goal in NIMH’s 2008 Strategic Plan for Research to “develop, for research purposes, new ways of classifying mental disorders based on dimensions of observable behavior and neurobiological measures.”
Unaware of the new strategic goal, Dr. Cuthbert was surprised when Dr. Insel's senior advisor, Marlene Guzman, called a few weeks later to ask if he’d be interested in taking a sabbatical to help lead this new effort. Dr. Cuthbert soon transitioned into a full-time NIMH employee, joining the Institute at an exciting time to lead the development of what became known as the Research Domain Criteria (RDoC) Framework. The effort began in 2009 with the creation of an internal working group of interdisciplinary NIMH staff who identified core functional areas that could be used as examples of what research using this new conceptual framework looked like.
The workgroup members conceived a bold change in how investigators studied mental disorders.
“We wanted researchers to transition from looking at mental disorders as all or none diagnoses based on groups of symptoms. Instead, we wanted to encourage researchers to understand how basic core functions of the brain—like fear processing and reward processing—work at a biological and behavioral level and how these core functions contribute to mental disorders,” said Dr. Cuthbert.
This approach would incorporate biological and behavioral measures of mental disorders and examine processes that cut across and apply to all mental disorders. From Dr. Cuthbert’s standpoint, this could help remedy some of the frustrations mental health researchers were experiencing.
Around the same time the workgroup was sharing its plans and organizing the first steps, Sarah Morris, Ph.D., was a researcher focusing on schizophrenia at the University of Maryland School of Medicine in Baltimore. When she first read these papers, she wondered what this new approach would mean for her research, her grants, and her lab.
She also remembered feeling that this new approach reflected what she was seeing in her data.
“When I grouped my participants by those with and without schizophrenia, there was a lot of overlap, and there was a lot of variability across the board, and so it felt like RDoC provided the pathway forward to dissect that and sort it out,” said Dr. Morris.
Later that year, Dr. Morris joined NIMH and the RDoC workgroup, saying, “I was bumping up against a wall every day in my own work and in the data in front of me. And the idea that someone would give the field permission to try something new—that was super exciting.”
The five original RDoC domains of functioning were introduced to the broader scientific community in a series of articles published in 2010 .
To establish the new framework, the RDoC workgroup (including Drs. Cuthbert and Morris) began a series of workshops in 2011 to collect feedback from experts in various areas from the larger scientific community. Five workshops were held over the next two years, each with a different broad domain of functioning based upon prior basic behavioral neuroscience. The five domains were called:
- Negative valence (which included processes related to things like fear, threat, and loss)
- Positive valence (which included processes related to working for rewards and appreciating rewards)
- Cognitive processes
- Social processes
- Arousal and regulation processes (including arousal systems for the body and sleep).
At each workshop, experts defined several specific functions, termed constructs, that fell within the domain of interest. For instance, constructs in the cognitive processes domain included attention, memory, cognitive control, and others.
The result of these feedback sessions was a framework that described mental disorders as the interaction between different functional processes—processes that could occur on a continuum from normal to abnormal. Researchers could measure these functional processes in a variety of complementary ways—for example, by looking at genes associated with these processes, the brain circuits that implement these processes, tests or observations of behaviors that represent these functional processes, and what patients report about their concerns. Also included in the framework was an understanding that functional processes associated with mental disorders are impacted and altered by the environment and a person’s developmental stage.
Preserving momentum
Over time, the Framework continued evolving and adapting to the changing science. In 2018, a sixth functional area called sensorimotor processes was added to the Framework, and in 2019, a workshop was held to better incorporate developmental and environmental processes into the framework.;
Since its creation, the use of RDoC principles in mental health research has spread across the U.S. and the rest of the world. For example, the Psychiatric Ratings using Intermediate Stratified Markers project (PRISM) , which receives funding from the European Union’s Innovative Medicines Initiative, is seeking to link biological markers of social withdrawal with clinical diagnoses using RDoC-style principles. Similarly, the Roadmap for Mental Health Research in Europe (ROAMER) project by the European Commission sought to integrate mental health research across Europe using principles similar to those in the RDoC Framework.;
Dr. Morris, who has acceded to the Head of the RDoC Unit, commented: “The fact that investigators and science funders outside the United States are also pursuing similar approaches gives me confidence that we’ve been on the right pathway. I just think that this has got to be how nature works and that we are in better alignment with the basic fundamental processes that are of interest to understanding mental disorders.”
The RDoC framework will continue to adapt and change with emerging science to remain relevant as a resource for researchers now and in the future. For instance, NIMH continues to work toward the development and optimization of tools to assess RDoC constructs and supports data-driven efforts to measure function within and across domains.
“For the millions of people impacted by mental disorders, research means hope. The RDoC framework helps us study mental disorders in a different way and has already driven considerable change in the field over the past decade,” said Joshua A. Gordon, M.D., Ph.D., director of NIMH. “We hope this and other innovative approaches will continue to accelerate research progress, paving the way for prevention, recovery, and cure.”
Publications
Cuthbert, B. N., & Insel, T. R. (2013). Toward the future of psychiatric diagnosis: The seven pillars of RDoC. BMC Medicine , 11 , 126. https://doi.org/10.1186/1741-7015-11-126
Cuthbert B. N. (2014). Translating intermediate phenotypes to psychopathology: The NIMH Research Domain Criteria. Psychophysiology , 51 (12), 1205–1206. https://doi.org/10.1111/psyp.12342
Cuthbert, B., & Insel, T. (2010). The data of diagnosis: New approaches to psychiatric classification. Psychiatry , 73 (4), 311–314. https://doi.org/10.1521/psyc.2010.73.4.311
Cuthbert, B. N., & Kozak, M. J. (2013). Constructing constructs for psychopathology: The NIMH research domain criteria. Journal of Abnormal Psychology , 122 (3), 928–937. https://doi.org/10.1037/a0034028
Garvey, M. A., & Cuthbert, B. N. (2017). Developing a motor systems domain for the NIMH RDoC program. Schizophrenia Bulletin , 43 (5), 935–936. https://doi.org/10.1093/schbul/sbx095
Insel, T. (2013). Transforming diagnosis . http://www.nimh.nih.gov/about/director/2013/transforming-diagnosis.shtml
Kozak, M. J., & Cuthbert, B. N. (2016). The NIMH Research Domain Criteria initiative: Background, issues, and pragmatics. Psychophysiology , 53 (3), 286–297. https://doi.org/10.1111/psyp.12518
Morris, S. E., & Cuthbert, B. N. (2012). Research Domain Criteria: Cognitive systems, neural circuits, and dimensions of behavior. Dialogues in Clinical Neuroscience , 14 (1), 29–37. https://doi.org/10.31887/DCNS.2012.14.1/smorris
Sanislow, C. A., Pine, D. S., Quinn, K. J., Kozak, M. J., Garvey, M. A., Heinssen, R. K., Wang, P. S., & Cuthbert, B. N. (2010). Developing constructs for psychopathology research: Research domain criteria. Journal of Abnormal Psychology , 119 (4), 631–639. https://doi.org/10.1037/a0020909
- Presidential Proclamation 6158 (The Decade of the Brain)
- Research Domain Criteria Initiative website
- Psychiatric Ratings using Intermediate Stratified Markers (PRISM)
- Roadmap for Mental Health Research in Europe (ROAMER)
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.12(6); 2020 Jun

Social Media Use and Its Connection to Mental Health: A Systematic Review
Fazida karim.
1 Psychology, California Institute of Behavioral Neurosciences and Psychology, Fairfield, USA
2 Business & Management, University Sultan Zainal Abidin, Terengganu, MYS
Azeezat A Oyewande
3 Family Medicine, California Institute of Behavioral Neurosciences and Psychology, Fairfield, USA
4 Family Medicine, Lagos State Health Service Commission/Alimosho General Hospital, Lagos, NGA
Lamis F Abdalla
5 Internal Medicine, California Institute of Behavioral Neurosciences and Psychology, Fairfield, USA
Reem Chaudhry Ehsanullah
Safeera khan.
Social media are responsible for aggravating mental health problems. This systematic study summarizes the effects of social network usage on mental health. Fifty papers were shortlisted from google scholar databases, and after the application of various inclusion and exclusion criteria, 16 papers were chosen and all papers were evaluated for quality. Eight papers were cross-sectional studies, three were longitudinal studies, two were qualitative studies, and others were systematic reviews. Findings were classified into two outcomes of mental health: anxiety and depression. Social media activity such as time spent to have a positive effect on the mental health domain. However, due to the cross-sectional design and methodological limitations of sampling, there are considerable differences. The structure of social media influences on mental health needs to be further analyzed through qualitative research and vertical cohort studies.
Introduction and background
Human beings are social creatures that require the companionship of others to make progress in life. Thus, being socially connected with other people can relieve stress, anxiety, and sadness, but lack of social connection can pose serious risks to mental health [ 1 ].
Social media
Social media has recently become part of people's daily activities; many of them spend hours each day on Messenger, Instagram, Facebook, and other popular social media. Thus, many researchers and scholars study the impact of social media and applications on various aspects of people’s lives [ 2 ]. Moreover, the number of social media users worldwide in 2019 is 3.484 billion, up 9% year-on-year [ 3 - 5 ]. A statistic in Figure 1 shows the gender distribution of social media audiences worldwide as of January 2020, sorted by platform. It was found that only 38% of Twitter users were male but 61% were using Snapchat. In contrast, females were more likely to use LinkedIn and Facebook. There is no denying that social media has now become an important part of many people's lives. Social media has many positive and enjoyable benefits, but it can also lead to mental health problems. Previous research found that age did not have an effect but gender did; females were much more likely to experience mental health than males [ 6 , 7 ].

Impact on mental health
Mental health is defined as a state of well-being in which people understand their abilities, solve everyday life problems, work well, and make a significant contribution to the lives of their communities [ 8 ]. There is debated presently going on regarding the benefits and negative impacts of social media on mental health [ 9 , 10 ]. Social networking is a crucial element in protecting our mental health. Both the quantity and quality of social relationships affect mental health, health behavior, physical health, and mortality risk [ 9 ]. The Displaced Behavior Theory may help explain why social media shows a connection with mental health. According to the theory, people who spend more time in sedentary behaviors such as social media use have less time for face-to-face social interaction, both of which have been proven to be protective against mental disorders [ 11 , 12 ]. On the other hand, social theories found how social media use affects mental health by influencing how people view, maintain, and interact with their social network [ 13 ]. A number of studies have been conducted on the impacts of social media, and it has been indicated that the prolonged use of social media platforms such as Facebook may be related to negative signs and symptoms of depression, anxiety, and stress [ 10 - 15 ]. Furthermore, social media can create a lot of pressure to create the stereotype that others want to see and also being as popular as others.
The need for a systematic review
Systematic studies can quantitatively and qualitatively identify, aggregate, and evaluate all accessible data to generate a warm and accurate response to the research questions involved [ 4 ]. In addition, many existing systematic studies related to mental health studies have been conducted worldwide. However, only a limited number of studies are integrated with social media and conducted in the context of social science because the available literature heavily focused on medical science [ 6 ]. Because social media is a relatively new phenomenon, the potential links between their use and mental health have not been widely investigated.
This paper attempt to systematically review all the relevant literature with the aim of filling the gap by examining social media impact on mental health, which is sedentary behavior, which, if in excess, raises the risk of health problems [ 7 , 9 , 12 ]. This study is important because it provides information on the extent of the focus of peer review literature, which can assist the researchers in delivering a prospect with the aim of understanding the future attention related to climate change strategies that require scholarly attention. This study is very useful because it provides information on the extent to which peer review literature can assist researchers in presenting prospects with a view to understanding future concerns related to mental health strategies that require scientific attention. The development of the current systematic review is based on the main research question: how does social media affect mental health?
Research strategy
The research was conducted to identify studies analyzing the role of social media on mental health. Google Scholar was used as our main database to find the relevant articles. Keywords that were used for the search were: (1) “social media”, (2) “mental health”, (3) “social media” AND “mental health”, (4) “social networking” AND “mental health”, and (5) “social networking” OR “social media” AND “mental health” (Table 1 ).
Out of the results in Table 1 , a total of 50 articles relevant to the research question were selected. After applying the inclusion and exclusion criteria, duplicate papers were removed, and, finally, a total of 28 articles were selected for review (Figure 2 ).

PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Inclusion and exclusion criteria
Peer-reviewed, full-text research papers from the past five years were included in the review. All selected articles were in English language and any non-peer-reviewed and duplicate papers were excluded from finally selected articles.
Of the 16 selected research papers, there were a research focus on adults, gender, and preadolescents [ 10 - 19 ]. In the design, there were qualitative and quantitative studies [ 15 , 16 ]. There were three systematic reviews and one thematic analysis that explored the better or worse of using social media among adolescents [ 20 - 23 ]. In addition, eight were cross-sectional studies and only three were longitudinal studies [ 24 - 29 ].The meta-analyses included studies published beyond the last five years in this population. Table 2 presents a selection of studies from the review.
IGU, internet gaming disorder; PSMU, problematic social media use
This study has attempted to systematically analyze the existing literature on the effect of social media use on mental health. Although the results of the study were not completely consistent, this review found a general association between social media use and mental health issues. Although there is positive evidence for a link between social media and mental health, the opposite has been reported.
For example, a previous study found no relationship between the amount of time spent on social media and depression or between social media-related activities, such as the number of online friends and the number of “selfies”, and depression [ 29 ]. Similarly, Neira and Barber found that while higher investment in social media (e.g. active social media use) predicted adolescents’ depressive symptoms, no relationship was found between the frequency of social media use and depressed mood [ 28 ].
In the 16 studies, anxiety and depression were the most commonly measured outcome. The prominent risk factors for anxiety and depression emerging from this study comprised time spent, activity, and addiction to social media. In today's world, anxiety is one of the basic mental health problems. People liked and commented on their uploaded photos and videos. In today's age, everyone is immune to the social media context. Some teens experience anxiety from social media related to fear of loss, which causes teens to try to respond and check all their friends' messages and messages on a regular basis.
On the contrary, depression is one of the unintended significances of unnecessary use of social media. In detail, depression is limited not only to Facebooks but also to other social networking sites, which causes psychological problems. A new study found that individuals who are involved in social media, games, texts, mobile phones, etc. are more likely to experience depression.
The previous study found a 70% increase in self-reported depressive symptoms among the group using social media. The other social media influence that causes depression is sexual fun [ 12 ]. The intimacy fun happens when social media promotes putting on a facade that highlights the fun and excitement but does not tell us much about where we are struggling in our daily lives at a deeper level [ 28 ]. Another study revealed that depression and time spent on Facebook by adolescents are positively correlated [ 22 ]. More importantly, symptoms of major depression have been found among the individuals who spent most of their time in online activities and performing image management on social networking sites [ 14 ].
Another study assessed gender differences in associations between social media use and mental health. Females were found to be more addicted to social media as compared with males [ 26 ]. Passive activity in social media use such as reading posts is more strongly associated with depression than doing active use like making posts [ 23 ]. Other important findings of this review suggest that other factors such as interpersonal trust and family functioning may have a greater influence on the symptoms of depression than the frequency of social media use [ 28 , 29 ].
Limitation and suggestion
The limitations and suggestions were identified by the evidence involved in the study and review process. Previously, 7 of the 16 studies were cross-sectional and slightly failed to determine the causal relationship between the variables of interest. Given the evidence from cross-sectional studies, it is not possible to conclude that the use of social networks causes mental health problems. Only three longitudinal studies examined the causal relationship between social media and mental health, which is hard to examine if the mental health problem appeared more pronounced in those who use social media more compared with those who use it less or do not use at all [ 19 , 20 , 24 ]. Next, despite the fact that the proposed relationship between social media and mental health is complex, a few studies investigated mediating factors that may contribute or exacerbate this relationship. Further investigations are required to clarify the underlying factors that help examine why social media has a negative impact on some peoples’ mental health, whereas it has no or positive effect on others’ mental health.
Conclusions
Social media is a new study that is rapidly growing and gaining popularity. Thus, there are many unexplored and unexpected constructive answers associated with it. Lately, studies have found that using social media platforms can have a detrimental effect on the psychological health of its users. However, the extent to which the use of social media impacts the public is yet to be determined. This systematic review has found that social media envy can affect the level of anxiety and depression in individuals. In addition, other potential causes of anxiety and depression have been identified, which require further exploration.
The importance of such findings is to facilitate further research on social media and mental health. In addition, the information obtained from this study can be helpful not only to medical professionals but also to social science research. The findings of this study suggest that potential causal factors from social media can be considered when cooperating with patients who have been diagnosed with anxiety or depression. Also, if the results from this study were used to explore more relationships with another construct, this could potentially enhance the findings to reduce anxiety and depression rates and prevent suicide rates from occurring.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.

IMAGES
COMMENTS
Ironically, referring to mental illness in terms of. mental health originated in the 1960s in an attempt to reduce stigma (Rowling et al. 2002). There is no widely agreed consensus on the meaning ...
Overview of the theoretical framework Effective school mental health programs mainly target the promotion of social and emotional learning (SEL) and resilience as well as the prevention of social, emotional, and behavioural difficulties, including risk behaviours (Browne et al., 2004; Cefai et al., 2018a; O'Reilly et al., 2018; Weare, 2010).
diseases or health conditions is a key ingredient of effective health policy, planning and evaluation. This booklet provides latest available estimates of the prevalence of depression and other common mental disorders at the global and regional level, together with data concerning the consequences of these disorders in terms of lost health.
found mental health concerns can cause a student to have difficulty in school. with poor academic performance, even chronic absenteeism, and disciplinary. concerns. Weist (2005) notes that in the prior two decades, "school mental health. programs have increased due to the recognition of the crisis in children's mental.
Scope of Mental Health Promotion and Prevention in the Current Situation. Literature provides considerable evidence on the effectiveness of various preventive mental health interventions targeting risk and protective factors for various mental illnesses (18, 36-42).There is also modest evidence of the effectiveness of programs focusing on early identification and intervention for severe ...
0hqwdo +hdowk dqg 6wxghqw /hduqlqj_ iru phqwdo khdowk frqfhuqv ehwzhhq wkh dqg dfdghplf \hduv 7kh\ dovr irxqg dq lqfuhdvh dfurvv uhsruwhg vhoi
The wide reach and near ubiquitous use of social media platforms may afford novel opportunities to. John A. Naslund [email protected]. Department of Global Health and Social Medicine, Harvard Medical School, 641 Huntington Avenue, Boston, MA 02115, USA. Digital Mental Health Research Consultant, Mumbai, India.
To provide a contemporary global prevalence of mental health issues among the general population amid the coronavirus disease-2019 (COVID-19) pandemic. We searched electronic databases, preprint ...
A determinant that has received much attention in mental health research concerns rumination. Rumination has been presented as a mediator but also as a risk factor for depression [ 57 , 210 , 259 ]. When studied as a risk factor, it appears that the relationship of rumination with depression is mediated by variables that include limited problem ...
A de nition of health encom-. fi. passing the mental and social domains may vary more in application, particularly across systems, cultures or clin-ical practices that differ in values (eg, spiritual, religious) and ways of understanding and being (eg, epistemol-ogy). A universal (global) de nition based on the phys-.
genetics, epigenetics, Indigenous mental health, and others, Canadian researchers are responsible for over a third of international research. Canadian research has strength in sub-specialities within the field of research on suicide and its prevention. Both the factors that contribute to suicide and suicidal behaviour, as well as potential
The COVID-19 pandemic has profoundly influenced the world. In wave after wave, many countries suffered from the pandemic, which caused social instability, hindered global growth, and harmed mental health. Although research has been published on various mental health issues during the pandemic, some profound effects on mental health are ...
tion has created the Mental Health Global Action Programme (mhGAP) as part of a major effort to implement the rec-ommendations of the World Health Report 2001 on mental health. The programme is based on strategies aimed at improving the mental health of populations. To implement those strategies, WHO is undertaking different projects and
Koehler, Sarah Nichole and Parrell, Bobbie Rose, "THE IMPACT OF SOCIAL MEDIA ON MENTAL HEALTH: A MIXED-METHODS RESEARCH OF SERVICE PROVIDERS' AWARENESS" (2020). Electronic Theses, Projects, ... I would like to dedicate this research paper to my family, friends, and loved ones. A special acknowledgment to my significant other, Donnie, for
1. Introduction. Young people's mental health is a major public health issue. Mental health problems among young people contribute to impaired physical and mental health extending into adulthood [1,2,3].Promoting young people's mental health is an integral component in ensuring their development and improving health and social wellbeing across their lifespan [].
research on mental health conditions that have been exacerbated by the COVID-19 pandemic, are associated with social stigma, and/or disparately affect or persist in certain populations due to
FUNDING: The work is based on research conducted by the Southern California Evidence-based Practice Center under contract to the Agency for Healthcare Research and Quality (AHRQ), Rockville, MD (Contract 75Q80120D00009). The Patient-Centered Outcomes Research Institute (PCORI) funded the research (PCORI Publication No. 2023-SR-03). The findings and conclusions in this manuscript are those of ...
President George H. W. Bush proclaimed the 1990s "The Decade of the Brain ," urging the National Institutes of Health, the National Institute of Mental Health (NIMH), and others to raise awareness about the benefits of brain research. "Over the years, our understanding of the brain—how it works, what goes wrong when it is injured or diseased—has increased dramatically.
Abstract. Social media are responsible for aggravating mental health problems. This systematic study summarizes the effects of social network usage on mental health. Fifty papers were shortlisted from google scholar databases, and after the application of various inclusion and exclusion criteria, 16 papers were chosen and all papers were ...
Research Paper on Mental Illness - Free download as PDF File (.pdf), Text File (.txt) or read online for free. research paper on mental illness