Critical Thinking in Critical Care: Five Strategies to Improve Teaching and Learning in the Intensive Care Unit
Affiliations.
- 1 1 Division of Pulmonary, Critical Care and Sleep Medicine, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, Massachusetts.
- 2 2 Shapiro Institute for Education and Research at Beth Israel Deaconess Medical Center and Harvard Medical School, Boston, Massachusetts; and.
- 3 3 Critical Care Medicine Department, Clinical Center, National Institutes of Health, Bethesda, Massachusetts.
- PMID: 28157389
- PMCID: PMC5461985
- DOI: 10.1513/AnnalsATS.201612-1009AS
Critical thinking, the capacity to be deliberate about thinking, is increasingly the focus of undergraduate medical education, but is not commonly addressed in graduate medical education. Without critical thinking, physicians, and particularly residents, are prone to cognitive errors, which can lead to diagnostic errors, especially in a high-stakes environment such as the intensive care unit. Although challenging, critical thinking skills can be taught. At this time, there is a paucity of data to support an educational gold standard for teaching critical thinking, but we believe that five strategies, routed in cognitive theory and our personal teaching experiences, provide an effective framework to teach critical thinking in the intensive care unit. The five strategies are: make the thinking process explicit by helping learners understand that the brain uses two cognitive processes: type 1, an intuitive pattern-recognizing process, and type 2, an analytic process; discuss cognitive biases, such as premature closure, and teach residents to minimize biases by expressing uncertainty and keeping differentials broad; model and teach inductive reasoning by utilizing concept and mechanism maps and explicitly teach how this reasoning differs from the more commonly used hypothetico-deductive reasoning; use questions to stimulate critical thinking: "how" or "why" questions can be used to coach trainees and to uncover their thought processes; and assess and provide feedback on learner's critical thinking. We believe these five strategies provide practical approaches for teaching critical thinking in the intensive care unit.
Keywords: cognitive errors; critical care; critical thinking; medical education.
- Clinical Competence*
- Critical Care*
- Education, Medical, Graduate / methods*
- Intensive Care Units
- Quality Improvement
- Unravelling the Mystery of Breast Cancer...
- Navigating Connectivity Challenges in Hospita

Molecular Phenotypes to Advance Precision...
- FAST TRACK CABG - First Successful Human...
- Microwave Ablation Offers New Treatment Optio

Early Systemic Insults Following Traumatic...

Modification in ICU Design May Affect Deliriu

Guidelines: Antibiotic Prophylaxis in Trauma
Strategies to improve critical thinking in critical care.
- Thu, 4 May 2017

- Making the thinking process explicit. This can be achieved by helping learners understand two primary cognitive processes - Type 1 which is an intuitive pattern-recognising process and Type 2 which is an analytic process.
- Discussing cognitive biases which could include premature closure and minimising biases by expressing uncertainty and keeping differentials broad.
- Modeling and teaching inductive reasoning. This can be done by utilising concept and mechanism maps and teaching learners how this differs from hypothetico-deductive reasoning.
- Stimulating critical thinking by asking How or Why questions which can help trainees uncover their thought processes.
- Assessing and providing feedback on the learner's critical thinking.
«« Sepsis Survivors Experience Lingering Effects
Expert Statements: Treatment of Critically Ill aHUS Patients »»
References:
Latest articles, pharmacist in the icu.
- ICU Journal Article
Pharmacists play a crucial role in the ICU, where patients often require complex medication regimens, including multiple medications and intravenous therapies. The role of a critical care pharmacist is multifaceted and vital to ensuring optimal patient care in the critical care setting. Cr
Defining Medicines Optimisation in the Intensive Care Unit
Complex polypharmacy and pathophysiology are common in the intensive care unit (ICU). Medicines optimisation is essential to deliver safe, effective, and individualised pharmacotherapy. This is ideally performed by a specialised ICU pharmacist. Introduction Medicines ar
Critical Care Pharmacists Save Lives
The purpose of this review is to discuss the role of critical care pharmacists on the interprofessional healthcare team in the care of critically ill patients and explore current gaps in the provision of comprehensive medication management. Introduction “The patient’s
Related Articles

#ESAGeneva: Frailer Patients at Greater Risk...

Critical Care at the End of Life: A Study...

5-Year Trends of Critical Care Practice and...

Is exercise good for elderly septic patients?
Latest news.

Ventilator-Associated Brain Injury - A Priority for Research in Mechanical Ventilation
Mechanical ventilation can lead to complications like ventilator-induced lung injury and ventilator-induced diaphragm dysfunction. However, there may be other forms of ventilator-

Evidence-Based Medicine and the Practice of Personalised Medicine
Sharon Einav-Bromiker from Tel Aviv, Israel, delivered a thought-provoking session @ISICEM, exploring the conflict between evidence-based medicine and personalised medicine. She...

Going Green in the ICU
The environmental impact of ICUs was in focus at ISICEM 2024. Nicole Hunfeld, a hospital pharmacist at Erasmus Medical Center in the Netherlands, emphasised the need for

Sex - A Biological Variable in the ICU
Dr Marlies Ostermann from Guy’s and St Thomas’ NHS Foundation Trust in London presented a tutorial at ISICEM 2024, highlighting the historical disparities and inequalitie

- Movers & Shakers

Former KPMG Chairman and CEO Lynne Doughtie...

Fresenius Medical Care Appoints Jörg Häring...

Abionic Appoints Patrick Pestalozzi as New...

Intensive Care Consultant to Lead NIHR's...

Radiology International 2024

AMGA Annual Conference 2024

ASBrS 2024 - The American Society of Breast...

13th World Congress on Design and Health...
- Advertising
- Submit Article
- Author Guide
- Privacy Policy
- Cookie Policy
- Terms and conditions
- Copyright and permissions
- Editorial Board
- White Papers & Case Studies
- IMAGING Highlights
- ICU Highlights
- EXEC Highlights
- IT Highlights
- CARDIO Highlights
- HealthManagement
- ICU Management
- (E)Hospital
- Imaging Management
- Imaging Management French
- Healthcare IT
- Cardiology Management
- IQ - Interventional Quarter
- List your event
- Past Events
- International Association
- National Association
- Universities - Institutions
- Paid Guest Posts
- I-I-I DigiFlash
Communities
- Decision Support
- Women's Health
- Enterprise Imaging
- Artificial Intelligence
- Finance Management
- Cybersecurity
- Sustainability
- Digital Transformation

Rue Villain XIV 53-55
B-1050 brussels, belgium, tel: +357 86 870 007, e-mail: [email protected], emea & row office, 166, agias filaxeos, cy-3083, limassol, cyprus, headquarters, kosta ourani, 5, petoussis court, 5th floor, cy-3085 limassol, cyprus.
The Value of Critical Thinking in Nursing

- How Nurses Use Critical Thinking
- How to Improve Critical Thinking
- Common Mistakes

Some experts describe a person’s ability to question belief systems, test previously held assumptions, and recognize ambiguity as evidence of critical thinking. Others identify specific skills that demonstrate critical thinking, such as the ability to identify problems and biases, infer and draw conclusions, and determine the relevance of information to a situation.
Nicholas McGowan, BSN, RN, CCRN, has been a critical care nurse for 10 years in neurological trauma nursing and cardiovascular and surgical intensive care. He defines critical thinking as “necessary for problem-solving and decision-making by healthcare providers. It is a process where people use a logical process to gather information and take purposeful action based on their evaluation.”
“This cognitive process is vital for excellent patient outcomes because it requires that nurses make clinical decisions utilizing a variety of different lenses, such as fairness, ethics, and evidence-based practice,” he says.
How Do Nurses Use Critical Thinking?
Successful nurses think beyond their assigned tasks to deliver excellent care for their patients. For example, a nurse might be tasked with changing a wound dressing, delivering medications, and monitoring vital signs during a shift. However, it requires critical thinking skills to understand how a difference in the wound may affect blood pressure and temperature and when those changes may require immediate medical intervention.
Nurses care for many patients during their shifts. Strong critical thinking skills are crucial when juggling various tasks so patient safety and care are not compromised.
Jenna Liphart Rhoads, Ph.D., RN, is a nurse educator with a clinical background in surgical-trauma adult critical care, where critical thinking and action were essential to the safety of her patients. She talks about examples of critical thinking in a healthcare environment, saying:
“Nurses must also critically think to determine which patient to see first, which medications to pass first, and the order in which to organize their day caring for patients. Patient conditions and environments are continually in flux, therefore nurses must constantly be evaluating and re-evaluating information they gather (assess) to keep their patients safe.”
The COVID-19 pandemic created hospital care situations where critical thinking was essential. It was expected of the nurses on the general floor and in intensive care units. Crystal Slaughter is an advanced practice nurse in the intensive care unit (ICU) and a nurse educator. She observed critical thinking throughout the pandemic as she watched intensive care nurses test the boundaries of previously held beliefs and master providing excellent care while preserving resources.
“Nurses are at the patient’s bedside and are often the first ones to detect issues. Then, the nurse needs to gather the appropriate subjective and objective data from the patient in order to frame a concise problem statement or question for the physician or advanced practice provider,” she explains.
Top 5 Ways Nurses Can Improve Critical Thinking Skills
We asked our experts for the top five strategies nurses can use to purposefully improve their critical thinking skills.
Case-Based Approach
Slaughter is a fan of the case-based approach to learning critical thinking skills.
In much the same way a detective would approach a mystery, she mentors her students to ask questions about the situation that help determine the information they have and the information they need. “What is going on? What information am I missing? Can I get that information? What does that information mean for the patient? How quickly do I need to act?”
Consider forming a group and working with a mentor who can guide you through case studies. This provides you with a learner-centered environment in which you can analyze data to reach conclusions and develop communication, analytical, and collaborative skills with your colleagues.
Practice Self-Reflection
Rhoads is an advocate for self-reflection. “Nurses should reflect upon what went well or did not go well in their workday and identify areas of improvement or situations in which they should have reached out for help.” Self-reflection is a form of personal analysis to observe and evaluate situations and how you responded.
This gives you the opportunity to discover mistakes you may have made and to establish new behavior patterns that may help you make better decisions. You likely already do this. For example, after a disagreement or contentious meeting, you may go over the conversation in your head and think about ways you could have responded.
It’s important to go through the decisions you made during your day and determine if you should have gotten more information before acting or if you could have asked better questions.
During self-reflection, you may try thinking about the problem in reverse. This may not give you an immediate answer, but can help you see the situation with fresh eyes and a new perspective. How would the outcome of the day be different if you planned the dressing change in reverse with the assumption you would find a wound infection? How does this information change your plan for the next dressing change?
Develop a Questioning Mind
McGowan has learned that “critical thinking is a self-driven process. It isn’t something that can simply be taught. Rather, it is something that you practice and cultivate with experience. To develop critical thinking skills, you have to be curious and inquisitive.”
To gain critical thinking skills, you must undergo a purposeful process of learning strategies and using them consistently so they become a habit. One of those strategies is developing a questioning mind. Meaningful questions lead to useful answers and are at the core of critical thinking .
However, learning to ask insightful questions is a skill you must develop. Faced with staff and nursing shortages , declining patient conditions, and a rising number of tasks to be completed, it may be difficult to do more than finish the task in front of you. Yet, questions drive active learning and train your brain to see the world differently and take nothing for granted.
It is easier to practice questioning in a non-stressful, quiet environment until it becomes a habit. Then, in the moment when your patient’s care depends on your ability to ask the right questions, you can be ready to rise to the occasion.
Practice Self-Awareness in the Moment
Critical thinking in nursing requires self-awareness and being present in the moment. During a hectic shift, it is easy to lose focus as you struggle to finish every task needed for your patients. Passing medication, changing dressings, and hanging intravenous lines all while trying to assess your patient’s mental and emotional status can affect your focus and how you manage stress as a nurse .
Staying present helps you to be proactive in your thinking and anticipate what might happen, such as bringing extra lubricant for a catheterization or extra gloves for a dressing change.
By staying present, you are also better able to practice active listening. This raises your assessment skills and gives you more information as a basis for your interventions and decisions.
Use a Process
As you are developing critical thinking skills, it can be helpful to use a process. For example:
- Ask questions.
- Gather information.
- Implement a strategy.
- Evaluate the results.
- Consider another point of view.
These are the fundamental steps of the nursing process (assess, diagnose, plan, implement, evaluate). The last step will help you overcome one of the common problems of critical thinking in nursing — personal bias.
Common Critical Thinking Pitfalls in Nursing
Your brain uses a set of processes to make inferences about what’s happening around you. In some cases, your unreliable biases can lead you down the wrong path. McGowan places personal biases at the top of his list of common pitfalls to critical thinking in nursing.
“We all form biases based on our own experiences. However, nurses have to learn to separate their own biases from each patient encounter to avoid making false assumptions that may interfere with their care,” he says. Successful critical thinkers accept they have personal biases and learn to look out for them. Awareness of your biases is the first step to understanding if your personal bias is contributing to the wrong decision.
New nurses may be overwhelmed by the transition from academics to clinical practice, leading to a task-oriented mindset and a common new nurse mistake ; this conflicts with critical thinking skills.
“Consider a patient whose blood pressure is low but who also needs to take a blood pressure medication at a scheduled time. A task-oriented nurse may provide the medication without regard for the patient’s blood pressure because medication administration is a task that must be completed,” Slaughter says. “A nurse employing critical thinking skills would address the low blood pressure, review the patient’s blood pressure history and trends, and potentially call the physician to discuss whether medication should be withheld.”
Fear and pride may also stand in the way of developing critical thinking skills. Your belief system and worldview provide comfort and guidance, but this can impede your judgment when you are faced with an individual whose belief system or cultural practices are not the same as yours. Fear or pride may prevent you from pursuing a line of questioning that would benefit the patient. Nurses with strong critical thinking skills exhibit:
- Learn from their mistakes and the mistakes of other nurses
- Look forward to integrating changes that improve patient care
- Treat each patient interaction as a part of a whole
- Evaluate new events based on past knowledge and adjust decision-making as needed
- Solve problems with their colleagues
- Are self-confident
- Acknowledge biases and seek to ensure these do not impact patient care
An Essential Skill for All Nurses
Critical thinking in nursing protects patient health and contributes to professional development and career advancement. Administrative and clinical nursing leaders are required to have strong critical thinking skills to be successful in their positions.
By using the strategies in this guide during your daily life and in your nursing role, you can intentionally improve your critical thinking abilities and be rewarded with better patient outcomes and potential career advancement.
Frequently Asked Questions About Critical Thinking in Nursing
How are critical thinking skills utilized in nursing practice.
Nursing practice utilizes critical thinking skills to provide the best care for patients. Often, the patient’s cause of pain or health issue is not immediately clear. Nursing professionals need to use their knowledge to determine what might be causing distress, collect vital information, and make quick decisions on how best to handle the situation.
How does nursing school develop critical thinking skills?
Nursing school gives students the knowledge professional nurses use to make important healthcare decisions for their patients. Students learn about diseases, anatomy, and physiology, and how to improve the patient’s overall well-being. Learners also participate in supervised clinical experiences, where they practice using their critical thinking skills to make decisions in professional settings.
Do only nurse managers use critical thinking?
Nurse managers certainly use critical thinking skills in their daily duties. But when working in a health setting, anyone giving care to patients uses their critical thinking skills. Everyone — including licensed practical nurses, registered nurses, and advanced nurse practitioners —needs to flex their critical thinking skills to make potentially life-saving decisions.
Meet Our Contributors

Crystal Slaughter, DNP, APRN, ACNS-BC, CNE
Crystal Slaughter is a core faculty member in Walden University’s RN-to-BSN program. She has worked as an advanced practice registered nurse with an intensivist/pulmonary service to provide care to hospitalized ICU patients and in inpatient palliative care. Slaughter’s clinical interests lie in nursing education and evidence-based practice initiatives to promote improving patient care.

Jenna Liphart Rhoads, Ph.D., RN
Jenna Liphart Rhoads is a nurse educator and freelance author and editor. She earned a BSN from Saint Francis Medical Center College of Nursing and an MS in nursing education from Northern Illinois University. Rhoads earned a Ph.D. in education with a concentration in nursing education from Capella University where she researched the moderation effects of emotional intelligence on the relationship of stress and GPA in military veteran nursing students. Her clinical background includes surgical-trauma adult critical care, interventional radiology procedures, and conscious sedation in adult and pediatric populations.

Nicholas McGowan, BSN, RN, CCRN
Nicholas McGowan is a critical care nurse with 10 years of experience in cardiovascular, surgical intensive care, and neurological trauma nursing. McGowan also has a background in education, leadership, and public speaking. He is an online learner who builds on his foundation of critical care nursing, which he uses directly at the bedside where he still practices. In addition, McGowan hosts an online course at Critical Care Academy where he helps nurses achieve critical care (CCRN) certification.
Medical Education in Pulmonary, Critical Care, and Sleep Medicine pp 177–193 Cite as
Teaching in the ICU
- William Graham Carlos III 6 &
- Emily Cochard 6
- First Online: 15 May 2019
804 Accesses
Part of the book series: Respiratory Medicine ((RM))
The complexity of the intensive care unit (ICU) environment provides ample opportunity for teaching learners. The challenge lies in tailoring different teaching methods to an audience with a varying knowledge base. This chapter aims to address teaching learners throughout their ICU experience. The reader will discover how to set the stage with an orientation, to find teaching moments at and away from the bedside, and to give individual as well as team feedback.
This is a preview of subscription content, log in via an institution .
Buying options
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Durable hardcover edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Oriol MD. Crew resource management: applications in healthcare organizations. JONA. 2006;36(9):402–6.
Article Google Scholar
Schull MJ, Ferris LE, Tu JV, Hux JE, Redelmeier DA. Problems for clinical judgment: 3. Thinking clearly in an emergency. CMAJ. 2001;164(8):1170–5.
CAS PubMed PubMed Central Google Scholar
Reader TW, Cuthbertson BH. Teamwork and team training in the ICU: where do the similarities with aviation end? Crit Care. 2011;15:313.
Nedrow A, Steckler NA, Hardman J. Physician resilience and burnout: can you make the switch. Fam Pract Manag. 2013;20:25–30. www.aafp.org/fpm .
PubMed Google Scholar
Moss M, Good VS, Gozal D, Kleinpell R, Sessler CN. A critical care societies collaborative statement: burnout syndrome in critical care health-care professionals. A call for action. Am J Respir Crit Care Med. 2016;194(1):106–13.
Eisendrath SJ, Link N, Matthay M. Intensive care unit: how stressful for physicians? Crit Care Med. 1986;14(2):95–6.
Article CAS Google Scholar
Wolfe KK, Unti SM. Critical care rotation impact on pediatric resident mental health and burnout. BMC Med Educ. 2017;17:181.
Fargen KM, Spiotta AM, Turner RD, Patel S. The importance of exercise in the well-rounded physician: dialogue for the inclusion of a physical fitness program in neurosurgery resident training. World Neurosurg. 2016;90:380–4.
Lebensohn P, Dodds S, Benn R, Brooks AJ, Birch M, Cook P, Schneider C, Sroka S, Waxman D, Maizes V. Resident wellness behaviors: relationship to stress, depression, and burnout. Fam Med. 2013;45(8):541–9.
Davidson JE. Family presence on rounds in neonatal, pediatric, and adult intensive care units. Ann Am Thorac Soc. 2013;10(2):152–6.
Jacobowski NL, Girard TD, Mulder JA, Ely EW. Communication in critical care: family rounds in the intensive care unit. Am J Crit Care. 2010;19:421–30.
Carlos WG, Kritek PA, Clay AS, Luks AM, Thomson CC. Teaching at the bedside: maximal impact in minimal time. Ann Am Thorac Soc. 2016;13(4):545–8.
Google Scholar
Piquette D, Moulton C, LeBlanc VR. Model of interactive clinical supervision in acute care environments: balancing patient care and teaching. Ann ATS. 2015;12(4):498–504.
Hayes MM, Chatterjee S, Schwartzstein RM. Critical thinking in critical care: five strategies to improve teaching and learning in the intensive care unit. Ann Am Thorac Soc. 2017;14(4):569–75.
Verghese A, Brady E, Kapur CC, Horwitz RI. The bedside evaluation: ritual and reason. Ann Intern Med. 2011;155:550–3.
Chi J, Verghese A. Clinical education and the electronic health record: the flipped patient. JAMA. 2014;312:2331–2.
Block L, Habicht R, Wu AW, et al. In the wake of the 2003 and 2011 duty hours regulations, how do internal medicine interns spend their time? J Gen Intern Med. 2013;28:1042–7.
Chi J, Artandi M, Kugler J, Ozdalga E, Hosamani P, Koehler E, Osterberg L, Zaman J, Thadaney S, Elder A, Verghese A. The five-minute moment. Am J Med. 2016;129(8):792–5.
Narasimhan M, Koenig SJ, Mayo PH. A whole-body approach to point of care ultrasound. Chest. 2016;150(4):772–6.
Frankel HL, Kirkpatrick AW, Elbarbary M, Blaivas M, Desai H, Evans D, Summerfield DT, Slonim A, Breitkreutz R, Price S, Marik PE, Talmor D, Levitov A. Guidelines for the appropriate use of bedside general and cardiac ultrasonography in the evaluation of critically ill patients-part I: general ultrasonography. Crit Care Med. 2015;43(11):2479–502.
Levitov A, Frankel HL, Blaivas M, Kirkpatrick AW, Su E, Evans D, Summerfield DT, Slonim A, Breitkreutz R, Price S, McLaughlin M, Marik PE, Elbarbary M. Guidelines for the appropriate use of bedside general and cardiac ultrasonography in the evaluation of critically ill patients-part II: cardiac ultrasonography. Crit Care Med. 2016;44(6):1206–27.
So S, Patel RM, Orebaugh SL. Ultrasound imaging in medical student education: impact on learning anatomy and physical diagnosis. Anat Sci Educ. 2016;10(2):176–89.
Hoppmann RA, Rao VV, Poston MB, Howe DB, Hunt PS, Fowler SD, Paulman LE, Wells JR, Richeson NA, Catalana PV, Thomas LK, Wilson LB, Cook T, Riffle S, Neuffer FH, McCallum JB, Keisler BD, Brown RS, Gregg AR, Sims KM, Powell CK, Garber MD, Morrison JE, Owens WB, Carnevale KA, Jennings WR, Fletcher S. An integrated ultrasound curriculum (iUSC) for medical students: 4-year experience. Crit Ultrasound J. 2011;3:52.
Wilson SP, Mefford JM, Lahham S, Lotfipour S, Subeh M, Maldonado G, Spann S, Fox JC. Implementation of a 4-year point-of-care ultrasound curriculum in a liaison committee on medical education-accredited US medical school. J Ultrasound Med. 2017;36(2):321–5.
Torre DM, Simpson D, Sebastian JL, Elnicki DM. Learning/feedback activities and high-quality teaching: perceptions of third year medical students during an inpatient rotation. Acad Med. 2005;80:950–4.
Wayne DB, Butter J, Siddall VJ, Fudala MJ, Linquist LA, Feinglass J, Wade LD, McGaghie WC. Simulation-based training of internal medicine residents in advanced cardiac life support protocols: a randomized trial. Teach Learn Med. 2005;17(3):202–8.
Wayne DB, Butter J, Siddall VJ, Fudala MJ, Wade LD, Feinglass J, McGaghie WC. Master learning of advanced cardiac life support skills by internal medicine residents using simulation technology and deliberate practice. J Gen Intern Med. 2006;21:251–6.
Wayne DB, Didwania A, Feinglass J, Fudala MJ, Barsuk JF, McGaghie WC. Simulation-based education improves quality of care during cardiac arrest team responses at an academic teaching hospital: a case-control study. Chest. 2008;133:56–61.
Barsuk JH, McGaghie WC, Cohen ER, O’Leary KJ, Wayne DB. Simulation-based mastery learning reduces complications during central venous catheter insertion in a medical intensive care unit. Crit Care Med. 2009;37:2697–701.
Sekiguchi H, Tokita JE, Minami T, Eisen LA, Mayo PH, Narasimhan M. A prerotational, simulation-based workshop improves the safety of central venous catheter insertion: results of a successful internal medicine house staff training program. Chest. 2011;140(3):652–8.
Mayo PH, Hackney JE, Mueck JT, Ribaudo V, Schneider RF. Achieving house staff competence in emergency airway management: results of a teaching program using a computer patient simulator. Crit Care Med. 2004;32(12):2422–7.
Rosenthal ME, Adachi M, Ribaudo V, Mueck JT, Schneider RF, Mayo PH. Achieving house staff competence in emergency airway management using scenario based simulation training. Chest. 2006;129:1453–8.
Cheng A, Hunt EA, Donoghue A. Examining pediatric resuscitation education using simulation and scripted debriefing: a multicenter randomized trial. JAMA Pediatr. 2013;167(6):528–36.
Barsuk JH, Cohen ER, Potts S, Demo H, Gupta S, Feinglass J, McGaghie WC, Wayne DB. Dissemination of a simulation-based mastery learning intervention reduces central line-associated bloodstream infections. BMJ Qual Saf. 2014;23:749–56.
Schroedl CJ, Corbridge TC, Cohen ER, Fakhran SS, Schimmel D, McGaghie WC, Wayne DB. Use of simulation-based education to improve resident learning and patient care in the medical intensive care unit: a randomized trial. J Crit Care. 2012;27:219.e7–219.e13.
Kleinpell R, Ely EW, Williams G, Liolios A, Ward N, Tisherman SA. Web-based resources for critical care education. Crit Care Med. 2011;39(3):541–53.
Carlos WG, Goss K, Morad M. YouTube-based critical care videos go viral. Academic Medicine; Really Good Stuff Section. Med Educ. 2014;48:522–8.
About TeamSTEPPS®. Content last reviewed April 2017. Rockville: Agency for Healthcare Research and Quality. http://www.ahrq.gov/teamstepps/about-teamstepps/index.html .
Horsley TL, Reed T, Muccino K, Quinones D, Siddall VJ, McCarthy J. Developing a foundation for interprofessional education within nursing and medical curricula. Nurse Educ. 2016;41(5):234–8.
Mayer CM, Cluff L, Lin WT, Willis TS, Stafford RE, Williams C, Saunders R, Short KA, Lenfestey N, Kane HL, Amoozegar JB. Evaluating efforts to optimize TeamSTEPPS implementation in surgical and pediatric intensive care units. Jt Comm J Qual Patient Saf. 2011;37(8):365–74.
Clay AS, Que L, Petrusa ER, Sebastian M, Govert J. Debriefing in the intensive care unit: a feedback tool to facilitate bedside teaching. Crit Care Med. 2007;35(3):738–54.
Thistlethwaite J, Dallest K, Moran M, Dunston R, Roberts C, Eley D, Bogossian F, Forman D, Bainbridge L, Drynan D, Fyfe S. Introducing the individual Teamwork Observation and Feedback Tool (iTOFT): development and description of a new interprofessional teamwork measure. J Interprof Care. 2016;30(4):526–8.
Download references
Author information
Authors and affiliations.
Indiana University School of Medicine, Indianapolis, IN, USA
William Graham Carlos III & Emily Cochard
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to William Graham Carlos III .
Editor information
Editors and affiliations.
University of Washington, Seattle, WA, USA
Patricia A. Kritek
Harvard University, Boston, MA, USA
Jeremy B. Richards
Rights and permissions
Reprints and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter.
Carlos, W.G., Cochard, E. (2019). Teaching in the ICU. In: Kritek, P., Richards, J. (eds) Medical Education in Pulmonary, Critical Care, and Sleep Medicine. Respiratory Medicine. Humana, Cham. https://doi.org/10.1007/978-3-030-10680-5_10
Download citation
DOI : https://doi.org/10.1007/978-3-030-10680-5_10
Published : 15 May 2019
Publisher Name : Humana, Cham
Print ISBN : 978-3-030-10679-9
Online ISBN : 978-3-030-10680-5
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
LOGIN
Annual Report
- Board of Directors
- Nomination Process
- Organizational Structure
- ATS Policies
- ATS Website
- MyATS Tutorial
- ATS Experts
- Press Releases
Member Newsletters
- ATS in the News
- ATS Conference News
- Embargo Policy
ATS Social Media
Breathe easy podcasts, ethics & coi, health equity, industry resources.
- Value of Collaboration
- Corporate Members
- Advertising Opportunities
- Clinical Trials
- Financial Disclosure
In Memoriam
Global health.
- International Trainee Scholarships (ITS)
- MECOR Program
- Forum of International Respiratory Societies (FIRS)
- 2019 Latin American Critical Care Conference
Peer Organizations
Careers at ats, affordable care act, ats comments and testimony, forum of international respiratory societies, tobacco control, tuberculosis, washington letter, clinical resources.
- ATS Quick Hits
- Asthma Center
Best of ATS Video Lecture Series
- Coronavirus
- Critical Care
- Disaster Related Resources
- Disease Related Resources
- Resources for Patients
- Resources for Practices
- Vaccine Resource Center
Career Development
- Resident & Medical Students
- Junior Faculty
- Training Program Directors
- ATS Reading List
- ATS Scholarships
- ATS Virtual Network
ATS Podcasts
Ats webinars, professional accreditation, pulmonary function testing (pft), calendar of events, patient resources.
- Asthma Today
- Breathing in America
- Fact Sheets: A-Z
- Fact Sheets: Topic Specific
- Patient Videos
- Other Patient Resources

Lung Disease Week
Public advisory roundtable.
- PAR Publications
- PAR at the ATS Conference
Assemblies & Sections
- Abstract Scholarships
- ATS Mentoring Programs
- ATS Official Documents
- ATS Interest Groups
- Genetics and Genomics
- Medical Education
- Terrorism and Inhalation Disasters
- Allergy, Immunology & Inflammation
- Behavioral Science and Health Services Research
- Clinical Problems
- Environmental, Occupational & Population Health
- Pulmonary Circulation
- Pulmonary Infections and Tuberculosis
- Pulmonary Rehabilitation
- Respiratory Cell & Molecular Biology
- Respiratory Structure & Function
- Sleep & Respiratory Neurobiology
- Thoracic Oncology
- Joint ATS/CHEST Clinical Practice Committee
- Clinicians Advisory
- Council of Chapter Representatives
- Documents Development and Implementation
- Drug/Device Discovery and Development
- Environmental Health Policy
- Ethics and Conflict of Interest
- Health Equity and Diversity Committee
- Health Policy
- International Conference Committee
- International Health
- Members In Transition and Training
- View more...
- Membership Benefits
- Categories & Fees
- Special Membership Programs
- Renew Your Membership
- Update Your Profile
- ATS DocMatter Community
- Respiratory Medicine Book Series
- Elizabeth A. Rich, MD Award
- Member Directory
- ATS Career Center
- Welcome Trainees
- ATS Wellness
- Thoracic Society Chapters
- Chapter Publications
- CME Sponsorship
Corporate Membership
- Assemblies and Sections
Webinar Date: March 7, 2023
This webinar is focused on providing our perspective on the importance of macro cognition and team cognition in the decision-making process in healthcare settings, most notably the intensive care unit (ICU). The webinar includes live presentations by experts in the field followed by an interactive session from attendees. This webinar features renowned experts: Abdullah Alismail, PhD, RRT, FCCP, FAARC Associate Professor of Cardiopulmonary Sciences & Medicine Department of Cardiopulmonary Sciences, School of Allied Health Professions, Loma Linda University Health, Loma Linda, CA Lauren Blackwell, MD Assistant Professor of Medicine Division of Pulmonary, Critical Care, and Sleep Medicine, Icahn School of Medicine, Mount Sinai Beth Israel, New York, NY Sugeet K. Jagpal, MD Assistant Professor Division of Pulmonary, Critical Care and Sleep Medicine, Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ May Lee, MD, ATSF, FCCP, FACP Clinical Associate Professor of Medicine Director, Pulmonary and Critical Care Fellowship Program Keck Medical Center of USC, Division of Pulmonary and Critical Care, Los Angeles, CA Erica Lin, MD Assistant Professor Division of Pulmonary, Critical Care and Sleep Medicine, University of California San Diego, La Jolla, CA
Jared Chiarchiaro, MD MS Associate Professor of Medicine Clinical Chief, Division of Pulmonary, Allergy, & Critical Care Medicine Oregon Health & Science University, Portland, OR
Nayla Ahmed, M.B.B.S Pulmonary & Critical Care medicine fellow at Mayo Clinic We invite your participation in this session and look forward to an insightful discussion. If you have questions about this session or have suggestions for future sessions, please contact: Avraham Cooper ATS Section on Medical Education [email protected]

The American Thoracic Society improves global health by advancing research, patient care, and public health in pulmonary disease, critical illness, and sleep disorders. Founded in 1905 to combat TB, the ATS has grown to tackle asthma, COPD, lung cancer, sepsis, acute respiratory distress, and sleep apnea, among other diseases.
AMERICAN THORACIC SOCIETY 25 Broadway New York, NY 10004 United States of America Phone: +1 (212) 315-8600 Fax: +1 (212) 315-6498 Email: [email protected]
Privacy Statement | Term of Use | COI Conference Code of Conduct


- Publisher Home
- Editorial Board
- Submit Manuscript
RESEARCH ARTICLE
Application of evidence-based practice in intensive and critical care nursing, article information.

Identifiers and Pagination:
Article history:, article metrics, crossref citations:, total statistics:, unique statistics:.

Background:
Evidence-based solutions are the main point of high-quality and patient-centered care. Studies analyzing the implementation of evidence-based nursing are an integral part of quality improvement. The study aims to analyze the application of evidence-based practice in intensive and critical care nursing.
This research was performed in the Hospital of Lithuanian University of Health Sciences Kaunas Clinics in intensive care units (ICU) departments in 2019. 202 critical care nurses participated in this survey (response rate 94.3%)—method of research – anonymous questionnaire. Research object – implementing evidence-based nursing practice among nurses working in intensive care units. Research instrument – questionnaire composed by McEvoy et al. (2010) [1]. Statistical analysis was performed with SPSS 24.0 and MS Excel 2016 software. Descriptive statistics were used to analyse our sample and presented in percentages. Quantitive data are presented as mean with standard deviation (m±SD). Among exploratory groups, a p-value <0.05 was considered statistically significant.
Nurses with higher university education claim to know evidence-based nursing terminology better with a statistical significance (p= 0.001) and to have higher self-confidence in evidence application (p= 0.001) compared to nurses with professional or higher non-university education. It has been determined that age directly correlates with the implementation of evidence-based nursing: compared to their older colleagues, younger nurses have statistically significantly more knowledge (p= 0.001), skills (p= 0.012) and self-confidence when applying evidence (p= 0.001) as well as a more positive approach to evidence-based nursing (p= 0.041). Nurses whose total work experience exceeds 20 years have statistically significantly less knowledge of evidence-based practice terminology than nurses whose work experience is 10 years or less (p= 0.001). It has been determined that Intensive and Critical Care Nurses (ICU Nurses) with 10 years or less experience under their belt know the terms related to evidence-based nursing statistically significantly better (p= 0.001) and applies evidence-based knowledge in clinical practice more often, compared to nurses who have worked in the ICU for longer, e.g. , 11-20 years or more than 20 years (p= 0.006). Compared to the nurses working in the ICU for 11-20 years, 10 years or less, those working for more than 20 years encounter statistically significantly more problems when applying an evidence-based approach in clinical practice (p=0.017).
Conclusion:
Younger nurses with higher education and less general work experience tend to have more knowledge and a more positive approach to evidence-based nursing. Problems with an evidence-based approach in clinical practice more often occur in nurses who have worked in the ICU for more than 20 years. Most of the nurses who participated in the study claimed that the lack of time was one of the key problems when practicing evidence-based nursing.
1. INTRODUCTION
In light of the changes in the health care system and the increasing expectations of society, the attitude towards nursing science and the limits of nursing competencies also change, increasing autonomy and advancement of the science of nursing [ 2 ]. Scientists return to the holistic approach to human health, evidence-based clinical solutions and treatment and nursing methods more and more often [ 3 ]. Evidence-based nursing is a fair application of an evidence-based approach in clinical practice and making decisions that ensure the highest quality of patient care [ 4 ]. Evidence-based practice forms a system of clinical solutions to problems and allows nurses to improve continuously and seek only the best professional results [ 5 , 6 ]. Efficient and high-quality care and patient safety are the most important aspects that are ensured by applying evidence-based nursing practice [ 7 ].
ICU Nurses make many clinical decisions in their work. According to the researchers, ICU nurses must make clinical decisions every five seconds [ 8 ]. Thus, it is especially important to base those decisions on scientific evidence. Systematic application of evidence in intensive and critical care has undisputable benefits both to the nurses and to the patients. Nurses get a boost in work satisfaction, gain autonomy and have higher self-confidence in making decisions directly related to their patients' health conditions [ 9 ]. Meanwhile, the patients and their relatives know that all performed manipulations are safe and efficient, as proven by scientific studies, their hospitalization is shorter, mistakes are avoided, and the individual wishes and needs of patients are taken into account [ 10 , 11 ]. Evidence-based nursing practice significantly contributes to avoiding common complications in ICU, such as respiratory tract infection and sepsis [ 12 - 14 ].
When introducing evidence-based nursing in an institution, the preparedness and attitude of employees are very important. Studies analyzing the knowledge, predisposition and skills of nurses and the obstacles they face in implementing advanced nursing practice are an important and integral part of the healthcare service improvement chain [ 15 , 16 ]. Analysis of organizational barriers to applying evidence-based practice is also important [ 17 ]. Courses, simulations and seminars initiated by the workplace notably contribute to nurses' capability to apply evidence-based practice [ 18 ]. However, not all healthcare professionals apply the evidence-based practice. There are various reasons for that. For example, nurses are not interested in scientific innovations; they value work experience based more on traditions due to tight working schedules, willingness to learn, lack of knowledge or other factors [ 19 ]. Timely correction of obstacles to applying evidence-based practice may significantly improve the quality of healthcare services [ 20 ]. Aspects related to evidence-based nursing are not widely researched in Lithuania, unlike in other countries worldwide. This is why a study was carried out to analyze the application of evidence-based practice in intensive and critical care nursing.
2. MATERIALS AND METHODS
The study was carried out at the ICU of Kaunas Clinics of the Lithuanian University of Health Sciences Hospital in 2019. The Center of Bioethics of the Lithuanian University of Health Sciences issued a permit to carry out the study after the presentation of the annotation and the research instrument. Targeted sampling was applied. The respondents were the nurses working at the ICU of Kaunas Clinics of the Lithuanian University of Health Sciences Hospital. A total of 202 nurses were questioned, with a response rate of 94.3%. Research method: an anonymous questionnaire-based survey. Research object: applying the evidence-based practice in intensive and critical care nursing. A total of 20 questionnaire examples were given to the ICU Nurses before the study. The pilot study results revealed that the questions given in the questionnaire were understandable. The nurses gave no comments, and thus no corrections were made. The research instrument was the questionnaire prepared by McEvoy et al. (2010) [ 1 ]. Cronbach’s alpha of the questionnaire is 0,954. It shows reliability and high internal consistency. The questionnaire was used with the permission of the authors. The questions could be categorized as follows:
1. Demographic questions determined the respondents' age, gender, education, professional experience, work experience at the current institution and work positions.
2. The respondents had to rate evidence-based nursing-related statements and terms from 1 to 5 based on the Likert scale, where 1 meant total disagreement and 5 meant total agreement. Factor analysis helped to sort the 58 statements into 5 areas: importance, obstacles, terminology, practice and self-confidence.
2.1. Statistical Data Analysis
Statistical data analysis was conducted using the SPSS 24.0 (Statistical Package for the Social Sciences) software and MC Excel 2016. Descriptive statistics, i.e. , absolute (n) and percentage (%) values, were applied to assess the distribution of the analyzed aspects in the sample. The quantitative data were presented as arithmetic means (m) with standard deviation (SD). The normalcy of the probability distribution of quantitative variables was assessed using the Kolmogorov–Smirnov test. The ANOVA test was used, the Fisher criterion (F) was calculated, and the Bonferroni adjustment was employed to compare the mean values of parametric variables of more than two independent samples. Tables of related aspects were made to assess the connections between aspects. The dependence of aspects was determined using the chi-square (χ2) test, and the pair comparisons were carried out via the z-test and Bonferroni adjustment. The Pearson correlation coefficient (r) was calculated to assess the strength of the aspect connection satisfying the normalcy assumption (r). In the case of 0<|r|≤0.3, the values were slightly dependent, in the case of 0.3<|r|≤0.8, the values were averagely dependent, and in the case of 0.8<|r|≤1, the values were strongly dependent [ 21 ]. The correlation coefficient was positive when a value increased with another value and negative when a value decreased with another value. Linear regression was used to assess variable dependence when the significance level was p<0.05, the difference of aspects in respondent groups was deemed statistically significant and when p<0.001, it was deemed highly statistically significant.
3.1. Knowledge and Attitude of Icu Nurses in Terms of Evidence-based Nursing
The study included comparing evidence-based nursing application areas based on the respondents' education. Nurses with higher university education claimed to know evidence-based nursing terminology better with a statistical significance than nurses with professional or higher non-university education. The research data also showed that nurses with higher university education had statistically significantly more self-confidence when applying scientific evidence than nurses with professional or higher non-university education. Detailed scores of evidence-based nursing application areas with standard deviations and their comparison are given in Table 1 below.
Linear regression was done to analyze the dependency of evidence-based nursing application areas on the age of the respondents. The results showed that all areas of evidence-based nursing application were statistically significantly dependent on the age of the respondents. Negative β coefficients in all four areas meant that as the age of the respondents increased, their agreement with the statements reflecting the analyzed areas decreased. Older nurses deemed evidence-based nursing to be less important than the younger ones. The terminology knowledge of older respondents was also poorer than that of their younger colleagues. Also, older nurses exhibited less evidence-based nursing-related practice and lower self-confidence (Table 2 ).
The application of evidence-based nursing in the ICU based on the work experience of the respondents was analyzed. The way the nurses with work experience in the ICU assessed evidence-based nursing areas was compared. It was determined that nurses who have worked in the ICU for 10 years or less knew the terminology related to evidence-based nursing statistically significantly better. Also, these nurses statistically significantly more often based their decisions in clinical practice on scientific evidence, compared to nurses who have worked in the ICU for longer, e.g. , 11-20 years or over 20 years. Compared to respondents with over 20 years of work experience in the ICU, nurses with 10 years or less experience had statistically significantly high self-confidence in their knowledge and skills to apply evidence-based practice in nursing. Detailed information on the evidence-based nursing application area scores and standard deviations and their comparison with the work experience of the ICU Nurses are presented in Table 3 .
3.2. Obstacles That ICU Nurses Face When Applying Evidence-based Nursing
The comparison of the obstacles to evidence-based nursing based on the work experience of the nurses in the ICU was carried out. The maximum available score was 35. A statistically significant difference was found: compared to respondents who have worked for 11-20 years, 10 years or less, ICU Nurses with over 20 years of experience faced many obstacles when applying an evidence-based nursing approach. Thus, the longer the nurses work in the ICU, the more obstacles they face when applying an evidence-based nursing approach. Detailed information about the mean values of the scores and their comparison based on the work experience of the respondents in their current workplace is presented in Fig. ( 1 ).
3.3. Peculiarities Of Evidence-based Practice In Intensive And Critical Care Units Of Different Medical Fields
The study analyzed the peculiarities of applying the evidence-based practice in intensive and critical care units of different medical fields. It was determined that the ICU Nurses at the Department of Obstetrics and Gynecology considered evidence-based nursing to be less important than the Nurses working at the Central Resuscitation Department and the Neurosurgery Department. The difference was statistically significant. The importance of applying evidence in their work was rated highest by the ICU Nurses at the Neurosurgery Department and lowest by the ICU Nurses at the Department of Obstetrics and Gynecology. Detailed information about the importance of evidence-based nursing scores by the respondents from various departments and their comparison are presented in Fig. ( 2 ).
The study assessed the self-confidence of nurses when applying the evidence-based nursing approach and compared it among different departments. Self-confidence in evidence-based nursing and making evidence-based clinical decisions revealed statistically significant differences among the ICUs of the Obstetrics and Gynecology Department, Cardiology Department, Neurosurgery Department and Central Resuscitation Department. Compared to the nurses in other departments, the ICU Nurses in the Obstetrics and Gynecology Department had lower self-confidence when applying the evidence-based nursing approach (Fig. 3 ).
The study revealed that nurses applying the evidence-based approach faced certain barriers. The obstacles encountered in evidence-based nursing in the ICU of different medical fields were compared. The results revealed that the majority of problems in evidence-based nursing were experienced by the ICU Nurses of the Obstetrics and Gynecology Department. The Newborn ICU Nurses encountered the least problems. The difference was deemed statistically significant. Detailed information about the comparison of problems in evidence-based nursing based on the ICU profile is presented in Fig. ( 4 ).
4. DISCUSSION
The study analyzed the implementation of evidence-based nursing by the ICU Nurses at Kaunas Clinics in different aspects. The comparison of evidence-based nursing-related knowledge and attitude, the implementation of the evidence-based approach and self-confidence in its implementation was carried out in terms of the education of the respondents. The results revealed that nurses with higher university education had more knowledge and self-confidence when applying scientific evidence in clinical practice. Bovino et al. presented similar findings: according to their research of 2017, nurses with higher university education (bachelor’s or master’s degree) used evidence in their clinical practice more often and had higher self-confidence in their actions, compared to nurses with a lower level of education [ 22 ]. According to the study of Balakas et al. (2016), the implementation of evidence-based nursing was directly related to the education of the nurses, i.e. , those with master’s or doctor’s degrees showed better results in formulating clinical questions, searching for the most reliable evidence and applying it in clinical practice [ 23 ]. Majid et al. research showed that nurses with higher education and participating in evidence-based training had fewer barriers to applying evidence-based practice [ 19 ]. According to Li et al. , nurses with higher education and positions were more competent in applying evidence-based practice [ 24 ].
The age of the nurses also influenced the application of the evidence-based nursing approach. The study revealed that older nurses faced more obstacles when implementing evidence-based nursing. They had less knowledge and skills related to applying evidence in nursing. According to the study of Warren et al. (2016), younger nurses (22-29 years old) were statistically significantly better prepared to base their actions on evidence in clinical practice. Also, a statistically significantly higher number of younger nurses had a positive attitude toward evidence-based nursing and supported its importance [ 25 ].
Based on the opinion of many researchers, critical thinking is a key skill for ICU Nurses in making urgent clinical decisions, and the latter is integral to evidence-based practice. Ludin (2018) carried out a study with 113 ICU Nurses. It was determined that age and work experience in the ICU greatly affected the nurses' critical thinking and decision-making based on scientific evidence, e.g. , older nurses with higher work experience had statistically significantly better skills in critical thinking and making clinical decisions [ 8 ]. Meanwhile, the results of this study were the opposite: the clinical decisions made by younger nurses with less work experience were more often based on scientific evidence. The research conducted by Alqahtani and co-authors (2022) showed that nurses working in the intensive care unit and emergency department have more knowledge about evidence-based practice than nurses from general units. Their research also concluded that nurses who participated in evidence-based practice courses had better attitudes, knowledge, and leadership skills than nurses who did not participate [ 26 ].
The attitude of the nurses is very important in an evidence-based approach in clinical practice. This study revealed that older nurses deemed evidence-based nursing less important than younger nurses. Nurses with higher education showed a more positive attitude to the application of scientific evidence in nursing: the statement ‘I have had enough of evidence-based nursing’ gained the agreement of 34.2% of nurses with professional education, 11.5% of nurses with higher non-university education, and 14.9% of nurses with higher university education. The difference is statistically significant. Based on the study by Swiss researchers Pereira et al. (2018), nurses with a more positive attitude towards evidence-based nursing usually base their clinical decisions on evidence statistically significantly more often [ 27 ]. The same trend was seen in this study: younger nurses, who, as mentioned previously, deemed evidence-based practice more important than older nurses, based their clinical decisions on scientific evidence statistically significantly more often. 507 nurses participated in a study by Degu and co-authors (2022). 55% of participants had a positive attitude toward evidence-based practice. Research showed that higher-education nurses had more knowledge about evidence-based practice, which led to a more positive attitude to evidence-based practice [ 28 ].
The research data revealed that certain barriers existed when implementing evidence-based nursing. Stavor et al. (2017) indicated that the main obstacles to applying an evidence-based approach in nursing were the avoidance of change, negative attitude and lack of time [ 29 ]. According to a study by Chinese scientists (2020), the lack of knowledge was the main problem in applying evidence-based nursing [ 30 ]. O’Connell et al. (2018) distinguished the two barriers: insufficient knowledge and the lack of cooperation between the nurses and the doctors [ 31 ]. In this study, more than half of the respondents (55.4%) said that the lack of time was one of the largest obstacles to implementing evidence-based nursing in clinical practice. The study also revealed that compared to younger nurses and nurses with less experience in intensive and critical care, older nurses and nurses with more work experience in the ICU encountered more problems when applying the evidence-based approach in nursing. Al-Lenjawi et al. conducted a study with 278 nurses from ICU. The research revealed that the main barriers to applying evidence-based practice are lack of time and support from colleagues, inability to understand statistics, and negative attitude to evidence-based practice [ 32 ]. The mentorship program is one method to encourage nurses to use evidence-based practice. Nurses gained more knowledge and a more positive attitude; there were fewer obstacles to applying evidence-based practice after the mentorship program [ 33 ]. Following Patelarou et al. , evidence-based practice training strongly contributes to more effective healthcare and should be the priority in establishing nursing education programs [ 34 ]. The benefits of evidence-based practice training were emphasized by Ruppel et al. based on the data of their study – nurses with a positive attitude towards evidence-based practice still indicated that training is necessary due to a lack of knowledge [ 35 ].
Thus, critical thinking, a holistic approach to a patient’s health condition, and the ability to work and plan patient care in a multidisciplinary team based on the most trustworthy scientific evidence for each individual case should be the daily duties and responsibilities of each nurse. Studies analyzing the implementation of evidence-based practice are important in attaining the best results in nursing and its practice [ 36 ]. Most of this study's results comply with the studies of foreign researchers. Younger nurses with higher education have better knowledge of applying evidence-based practice in nursing and have a more positive attitude toward it. Nurses with a lower level of education, and in this study, older nurses encounter more problems when applying evidence in clinical practice. The main obstacles to implementing evidence-based nursing are the lack of time, resources and knowledge.
1. The knowledge and attitude of the ICU Nurses related to evidence-based nursing and the implementation of this approach depend on such factors as education, age and work experience. Younger nurses with higher education and less work experience in the ICU tend to have more knowledge of evidence-based nursing and a more positive attitude toward it.
2. Older nurses and nurses whose work experience in the ICU is over 20 years encounter problems when applying scientific evidence in clinical practice more often. Most of the respondents believe the lack of time is one of the major obstacles to implementing evidence-based nursing in clinical practice.
3. The comparison of the peculiarities of employing evidence-based nursing in the ICUs of different medical fields revealed that the ICU Nurses of the Obstetrics and Gynecology Department deemed evidence-based nursing to be less important and thus had lower self-confidence and encountered more problems when applying an evidence-based approach in nursing.
LIST OF ABBREVIATIONS
Ethics approval and consent to participate.
The Center of Bioethics of the Lithuanian University of Health Sciences issued a permit to carry out the study after the presentation of the annotation and the research instrument (the approval number BEC-ISP(M)-14). Participants submitted informed consent.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were per the ethical standards of institutional and/or research committees and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from all participants.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
This study was funded by Lithuanian University of Health Sciences Kaunas Clinics Department of Cardiac, Thoracic and Vascular Surgery.
CONFLICT OF INTEREST
The authors declare no conflicts of interest, financial or otherwise.
ACKNOWLEDGEMENTS
We would like to thank the ICU Nurses of Kaunas Clinics of the Lithuanian University of Health Sciences Hospital, who have consented to participate in the study.
Track Your Manuscript
Published contents, about the editor, journal metrics, readership statistics:, total views/downloads: 1,048,554, unique views/downloads: 254,962, about the journal, table of contents.
- INTRODUCTION
- Statistical Data Analysis
- Knowledge and Attitude of Icu Nurses in Terms of Evidence-based Nursing
- Obstacles That ICU Nurses Face When Applying Evidence-based Nursing
- Peculiarities Of Evidence-based Practice In Intensive And Critical Care Units Of Different Medical Fields
Press Release
The open nursing journal, published by bentham open, has been accepted for inclusion in the directory of nursing journals.
The Directory of Nursing Journals is a joint service of Nurse, Author & Editor and the International Academy of Nursing Editors (INANE) . Their primary goal in maintaining this list is to help nurse authors find suitable and reputable journals in which to publish their work. The directory informs readers and consumers of nursing literature about the credibility of literature sources used to guide practice, research, policy and education. The two committees follow the COPE Principles of Transparency and Best Practice in Scholarly Publishing to vet journals.
The Open Nursing Journal is an Open Access online journal, which publishes research articles, reviews, letters and guest edited thematic issues in all areas of nursing. The Journal is an important and reliable source of current information on developments in nursing research and practice. The journal publishes quality papers that are freely accessible to readers worldwide.
For more information about the journal, please visit: https://opennursingjournal.com/index.php
Bentham Open Welcomes Sultan Idris University of Education (UPSI) as Institutional Member
Bentham Open is pleased to welcome Sultan Idris University of Education (UPSI), Malaysia as Institutional Member. The partnership allows the researchers from the university to publish their research under an Open Access license with specified fee discounts. Bentham Open welcomes institutions and organizations from world over to join as Institutional Member and avail a host of benefits for their researchers.
Sultan Idris University of Education (UPSI) was established in 1922 and was known as the first Teacher Training College of Malaya. It is known as one of the oldest universities in Malaysia. UPSI was later upgraded to a full university institution on 1 May, 1997, an upgrade from their previous college status. Their aim to provide exceptional leadership in the field of education continues until today and has produced quality graduates to act as future educators to students in the primary and secondary level.
Bentham Open publishes a number of peer-reviewed, open access journals. These free-to-view online journals cover all major disciplines of science, medicine, technology and social sciences. Bentham Open provides researchers a platform to rapidly publish their research in a good-quality peer-reviewed journal. All peer-reviewed accepted submissions meeting high research and ethical standards are published with free access to all.
Ministry Of Health, Jordan joins Bentham Open as Institutional Member
Bentham Open is pleased to announce an Institutional Member partnership with the Ministry of Health, Jordan . The partnership provides the opportunity to the researchers, from the university, to publish their research under an Open Access license with specified fee concessions. Bentham Open welcomes institutions and organizations from the world over to join as Institutional Member and avail a host of benefits for their researchers.
The first Ministry of Health in Jordan was established in 1950. The Ministry began its duties in 1951, the beginning of the health development boom in Jordan. The first accomplishment was the establishment of six departments in the districts headed by a physician and under the central administration of the Ministry. The Ministry of Health undertakes all health affairs in the Kingdom and its accredited hospitals include AL-Basheer Hospital, Zarqa Governmental Hospital, University of Jordan Hospital, Prince Hashem Military Hospital and Karak Governmental Hospital.
Bentham Open publishes a number of peer-reviewed, open access journals. These free-to-view online journals cover all major disciplines of science, medicine, technology and social sciences. Bentham Open provides researchers a platform to rapidly publish their research in a good-quality peer-reviewed journal. All peer-reviewed, accepted submissions meeting high research and ethical standards are published with free access to all.
Porto University joins Bentham Open as Institutional Member
Bentham Open is pleased to announce an Institutional Member partnership with the Porto University, Faculty of Dental Medicine (FMDUP) . The partnership provides the opportunity to the researchers, from the university, to publish their research under an Open Access license with specified fee concessions. Bentham Open welcomes institutions and organizations from world over to join as Institutional Member and avail a host of benefits for their researchers.
The Porto University was founded in 1911. Porto University create scientific, cultural and artistic knowledge, higher education training strongly anchored in research, the social and economic valorization of knowledge and active participation in the progress of the communities in which it operates.
Join Our Editorial Board
The Open Nursing Journal is an Open Access online journal, which publishes research articles, reviews, letters, case reports and guest-edited single topic issues in all areas of nursing. Bentham Open ensures speedy peer review process and accepted papers are published within 2 weeks of final acceptance.
The Open Nursing Journal is committed to ensuring high quality of research published. We believe that a dedicated and committed team of editors and reviewers make it possible to ensure the quality of the research papers. The overall standing of a journal is in a way, reflective of the quality of its Editor(s) and Editorial Board and its members.
The Open Nursing Journal is seeking energetic and qualified researchers to join its editorial board team as Editorial Board Members or reviewers.
- Experience in nursing with an academic degree.
- At least 20 publication records of articles and /or books related to the field of nursing or in a specific research field.
- Proficiency in English language.
- Offer advice on journals’ policy and scope.
- Submit or solicit at least one article for the journal annually.
- Contribute and/or solicit Guest Edited thematic issues to the journal in a hot area (at least one thematic issue every two years).
- Peer-review of articles for the journal, which are in the area of expertise (2 to 3 times per year).
If you are interested in becoming our Editorial Board member, please submit the following information to [email protected] . We will respond to your inquiry shortly.
- Email address
- City, State, Country
- Name of your institution
- Department or Division
- Website of institution
- Your title or position
- Your highest degree
- Complete list of publications and h-index
- Interested field(s)
Testimonials
"Open access will revolutionize 21 st century knowledge work and accelerate the diffusion of ideas and evidence that support just in time learning and the evolution of thinking in a number of disciplines."
"It is important that students and researchers from all over the world can have easy access to relevant, high-standard and timely scientific information. This is exactly what Open Access Journals provide and this is the reason why I support this endeavor."
"Publishing research articles is the key for future scientific progress. Open Access publishing is therefore of utmost importance for wider dissemination of information, and will help serving the best interest of the scientific community."
"Open access journals are a novel concept in the medical literature. They offer accessible information to a wide variety of individuals, including physicians, medical students, clinical investigators, and the general public. They are an outstanding source of medical and scientific information."
"Open access journals are extremely useful for graduate students, investigators and all other interested persons to read important scientific articles and subscribe scientific journals. Indeed, the research articles span a wide range of area and of high quality. This is specially a must for researchers belonging to institutions with limited library facility and funding to subscribe scientific journals."
"Open access journals represent a major break-through in publishing. They provide easy access to the latest research on a wide variety of issues. Relevant and timely articles are made available in a fraction of the time taken by more conventional publishers. Articles are of uniformly high quality and written by the world's leading authorities."
"Open access journals have transformed the way scientific data is published and disseminated: particularly, whilst ensuring a high quality standard and transparency in the editorial process, they have increased the access to the scientific literature by those researchers that have limited library support or that are working on small budgets."
"Not only do open access journals greatly improve the access to high quality information for scientists in the developing world, it also provides extra exposure for our papers."
"Open Access 'Chemistry' Journals allow the dissemination of knowledge at your finger tips without paying for the scientific content."
"In principle, all scientific journals should have open access, as should be science itself. Open access journals are very helpful for students, researchers and the general public including people from institutions which do not have library or cannot afford to subscribe scientific journals. The articles are high standard and cover a wide area."
"The widest possible diffusion of information is critical for the advancement of science. In this perspective, open access journals are instrumental in fostering researches and achievements."
"Open access journals are very useful for all scientists as they can have quick information in the different fields of science."
"There are many scientists who can not afford the rather expensive subscriptions to scientific journals. Open access journals offer a good alternative for free access to good quality scientific information."
"Open access journals have become a fundamental tool for students, researchers, patients and the general public. Many people from institutions which do not have library or cannot afford to subscribe scientific journals benefit of them on a daily basis. The articles are among the best and cover most scientific areas."
"These journals provide researchers with a platform for rapid, open access scientific communication. The articles are of high quality and broad scope."
"Open access journals are probably one of the most important contributions to promote and diffuse science worldwide."
"Open access journals make up a new and rather revolutionary way to scientific publication. This option opens several quite interesting possibilities to disseminate openly and freely new knowledge and even to facilitate interpersonal communication among scientists."
"Open access journals are freely available online throughout the world, for you to read, download, copy, distribute, and use. The articles published in the open access journals are high quality and cover a wide range of fields."
"Open Access journals offer an innovative and efficient way of publication for academics and professionals in a wide range of disciplines. The papers published are of high quality after rigorous peer review and they are Indexed in: major international databases. I read Open Access journals to keep abreast of the recent development in my field of study."
"It is a modern trend for publishers to establish open access journals. Researchers, faculty members, and students will be greatly benefited by the new journals of Bentham Science Publishers Ltd. in this category."
This website uses cookies. By using the website you agree to our cookie policy. You can change your cookie settings in your browser. Find out more
A Breath Ahead - Free Respiratory CEUs

An Introduction from Winnie Sywulak
“At Dräger, we continue to support our customers with clinical solutions that add value. Our complimentary education series from leading key opinion leaders supports this sustained effort.”

10+ Years of A Breath Ahead
A Breath Ahead is an interactive community for leaders and practitioners in respiratory care. Find the newest webinars on featured topics and earn free continuing respiratory care education (CRCE) credits. Download our infographic to see how A Breath Ahead has supported the respiratory care community for the last 10+ years.
Continuing Respiratory Care Education (CRCE) Courses
Earn complimentary CRCE credits by successfully completing our online webinars and presentations for respiratory professionals. You can take tests by selecting "Take your test" after watching one of our webinars. After successfully completing a test and course evaluation, you'll receive an email with your CRCE certificate.
Choose from our list of accredited webinars and presentations and start earning CRCE credits now!
*Each program has been approved for 1.0 contact hour Continuing Respiratory Care Education (CRCE) credit by the American Association for Respiratory Care, 9425 N. MacArthur Blvd., Suite 100, Irving, TX 75063
Adult Courses
Featured Course - Implementing New Strategies in Respiratory Care
Despite all the pressures in the respiratory world with staffing shortages, workload and continuous implementation of new equipment - how can Respiratory Therapists find time for performance improvement and proper implementation of new strategies and modalities? Join Mr. John Emberger as he presents performance improvement concepts and change management strategies for real world respiratory care scenarios.
Take your test
Critical Thinking in the ICU
Dr. Aaron Light will discuss unique situations encountered in the ICU that require the clinician to critically think. In addition, he will present patient cases with pertinent and distracting information for you to determine what is the best course of action for the patient. After which a review of each will offer a better understanding and discuss the associated pathology, physiology and assessment components.
Lung Protection Using APRV/TCAV
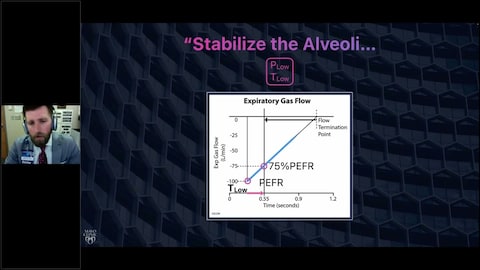
APRV following a TCAV protocol is infrequently used by most clinicians and understood by even fewer. But when applied appropriately, APRV-TCAV has tremendous potential to restore lung architecture, recruit physiologic lung volumes, and promote safety, comfort, and ultimately liberation from the ventilator. In this presentation, Dr. Ben Daxon will review the literature that details how this is done and answer some of the most common questions when using the mode.
Ventilator-Induced Diaphragm Dysfunction
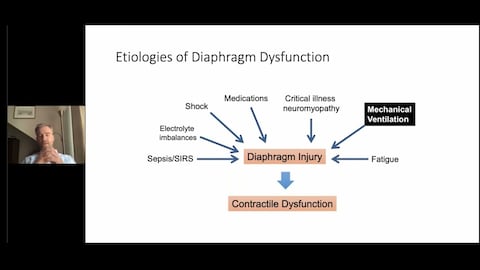
The diaphragm is the primary muscle of respiration and its function is critical to recovery from respiratory failure. Diaphragm function is impaired in many mechanically ventilated patients, in part because of injury to the muscle related to mechanical ventilation. Dr. Ewan Goligher will review the mechanisms and impact of ventilator-induced diaphragm dysfunction and identifies potential therapeutic strategies.
Dr. Goligher is Assistant Professor of Medicine and Physiology at the University of Toronto, and clinician-scientist at University Health Network. His program of research is aimed at developing and testing lung- and diaphragm-protective strategies for patients with acute respiratory failure.
Weaning Strategies in the ICU for Ventilated Patients

When mechanical ventilation is initiated, the near-, and long-term goal is ventilator liberation. How and when that goal is achieved is of the utmost importance. Spontaneous breathing trials are one aspect of ventilator liberation; support of the patient's respiratory status post-mechanical ventilation must also be guided by current evidence. This lecture will review evidenced based practice that lead to successful ventilator liberation.
Value-Based Respiratory Care
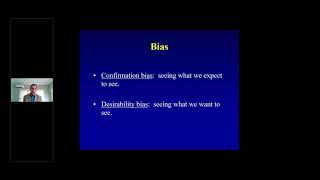
The days of obtaining reimbursement for every procedure, test, and intervention are only distant memories. Counting procedures and billable service units are examples of ‘counting what we can count’ and must be replaced with ‘doing what counts’. Garry W. Kauffman will address the changing health care system, with attention to the current and forecasted demands on health care professionals and professional opportunities within the evolving health care system.
TU-BE or not TU-BE, That Really is the Question!
The current healthcare environment has emphasized the critical role the Respiratory Therapist plays in the treatment paradigm, including the use of non-invasive modes of ventilation like Heated High Flow Nasal Cannula (HHFNC) and BiPAP. From a transport perspective, this has also added a challenging level of caring for these sick patients and trying to avoid mechanical ventilation and avoiding other pitfalls that can be presented. This lecture will discuss and identify these patients at risk and examine some case studies as they relate to these decisions.
Proportional Pressure Support – PPS
In conventional ventilation we tend to look at the delivered volume and see how much pressure that is required to meet the desired volume. Proportional ventilation has been around for 30 years and Maria Madden will share how to best use this mode of ventilation and how to set to meet your patient’s lung resistance and elastance. Ms. Madden will review the current literature on the use of proportional ventilation and the benefits it provides the patient. Finally, you will be able to learn how to sculpt that sinusoidal waveform through clear examples of patients being ventilated by PPS.
Management of the COVID-19 Patient with Acute Hypoxemia
Mr. Emberger will discuss patients who present with acute hypoxemia due to COVID-19. Guidelines and literature for this population along with a few cases will be discussed to underscore the management techniques for COVID-19 patients with acute hypoxemia.
Navigating Non-Invasive Respiratory Support and COVID-19
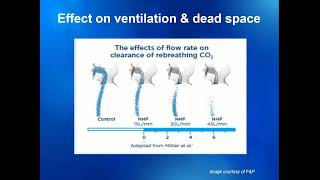
Speaker: Tracey Roberts BS, RRT, RRT-NPS, Clinical Respiratory Care Educator, University of North Carolina Medical Center, Children’s Hospital, Chapel Hill, NC
Ms. Roberts will present on noninvasive respiratory support when treating COVID-19 Patient in the constantly changing environment. Reviewing lessons learned from previous outbreaks as well as what is known as of today September 2020.
Transitioning Your NIV Patient from Acute Care
Transitioning non-invasive ventilation patient from the acute care environment can be challenging. Laura Marchiano shares her experiences from initiation of NIV in the acute care setting to successful transition into the long term care or even the home environments. Ms. Marchiano will focus on topics such as chronic hypoventilation, CO2 monitoring, ventilator titration, patient interfaces, and ultimately continued monitoring once the patient has left the acute care setting.
APRV using the TCAV Method: Science, Research, and Application - AARC 2020 Symposia (Part 1 of 2)
Airway Pressure Release Ventilation (APRV) has been available in a mechanical ventilator since 1987, there are many clinicians that have never used the mode in clinical practice. In this video, learn about the science and research behind APRV using the TCAV method from Mr. Gary Nieman and Dr. Nader Habashi.
*The button below will take you directly to the AARC University website where you can take the course.
APRV using the TCAV Method: Science, Research, and Application - AARC 2020 Symposia (Part 2 of 2)
Airway Pressure Release Ventilation (APRV) has been available in a mechanical ventilator since 1987, there are many clinicians that have never used the mode in clinical practice. In this video, Ms. Penny Andrews and Ms. Maria Madden will provide clinical application and cases studies using APRV with the Time Controlled Adaptive Ventilation (TCAV) method.
Early Mobilization and the ICU Patient
The idea of moving patients early after surgery is not a new concept and Mr. Piraino will discuss the early mobility in the intensive care unit including the safety, feasibility, and the areas for further study.
Mechanical Breath Magic: Gas Exchange Without Tissue Damage in the ARDS Lung. Does It Work for Covid-19 Induced ARDS?

Speaker: Gary Nieman, Professor and Senior Research Scientist in the Department of Surgery, Director, Cardiopulmonary and Critical Care Laboratory, Upstate Medical University Syracuse, NY
Mr. Nieman is the director of the Cardiopulmonary and Critical Care Laboratory which is a large animal translation laboratory investigating that pathophysiology and treatment of septic and traumatic shock. Specifically, Gary’s group studies the pathogenesis and treatment of ARDS and VILI. Mr. Nieman will provide an overview of the pathophysiology of the lung with ARDS. Identify and review literature regarding the current standard of care and hypothesize alternatives to improve patient outcomes. Ultimately could these approaches help treat the COVID 19 induced ARDS and what is said in literature today.
Mechanical Ventilation: Historical Perspective
Dr. Arthur Slutsky is a critical care physician whose research, teaching and patient care has touched broad sectors of the health care community. His research interests span the fields of acute respiratory failure, non-conventional ventilation, classic respiratory mechanics, asthma pathophysiology, lung transplantation, myocardial preservation during cardiac surgery, and recently, the primary role mechanical ventilation plays in the development of subsequent lung injury and multiple organ failure. In this presentation, Dr. Slutsky will present the early beginnings of respiratory care and how mechanical ventilation has grown from the "early days" of the iron lung and polio epidemic, the "birth of the ICU" and how technology has grown from the 1800s to today.
Lung Recruitment: Techniques
In this presentation, Mr Emberger will provide an overview of current options and methods to safely and effectively recruit the collapsed lung.
Neonatal Courses
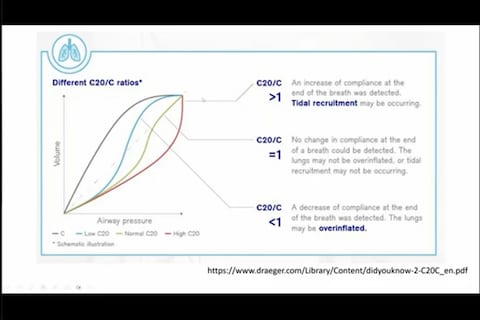
Featured Course - Concepts in Neonatal Ventilation
This lecture will describe the indications for neonatal ventilation and emphasize the practical and useful modes of the ventilation. In particular, the talk will highlight the advantages of volume guarantee mode over traditional SIMV and present a working algorithm for when AC/VG and SIMV/VG with or without PS should be used. Dr. Mitchel Goldstein will present the importance of ventilator graphics and the usefulness of available pulmonary function parameters in making these selections.
Take Your Test
Using Neonatal Airway Graphics to Optimize Care in Neonatal Patients
Airway graphical waveform analysis is one form of monitoring that can provide real-time assessment on underlying pathophysiologic changes in mechanical ventilated patients. Improvements in flow sensor design and ventilator technology now allow clinicians to accurately monitor graphics at the airway in neonatal patients. This interactive discussion will focus on airway graphics monitoring in the neonatal intensive care unit setting using novel modes of ventilation and different disease types.
Overview of Updates for Neonatal Resuscitation, NRP 8th Edition
Maria Rog is a registered nurse and Neonatal Senior Clinical Application Specialist. This presentation will not provide a certification but an overview and review of those updates that have been made to the Neonatal Resuscitation Program, NRP.
Evolution of Respiratory Care in the NICU to Reduce the Use of Invasive Ventilation
John Emberger will discuss the history of newborn respiratory care. He will help us better understand those key drivers that push forward the care of this patient population. Over the years, alternative therapies and management strategies for the newborn patient have improved patient outcomes through the reduction in the need of invasive mechanical ventilation to our smallest patients. Mr. Emberger will share important insights and best practices in neonatal respiratory support.
Mandatory Minute Ventilation in Neonates

Respiratory insufficiency remains one of the major causes of neonatal mortality. Providing adequate respiratory support for spontaneous breathing and promoting the weaning process while preventing events of inadequate oxygenation and CO2-removal due to irregular breathing efforts are the goals. Professor Jane Pillow will help you become familiar with the theory, the clinical application and operating principle of MMV.
Caring for the BPD Patient; Current Updates and Outcomes
Ms. Napolitano will present what’s new when caring for severe bronchopulmonary dysplasia (BPD) patients based on the most recent literature to include optimization of mechanical ventilation as well as therapeutic aerosolized treatments for this patient population.
Volume-Targeted Ventilation in Neonatal Care
In this webinar, Dr. Martin Keszler, Director of Respiratory Care at the Women and Infants’ Hospital in Providence, RI, discusses how to treat neonatal pediatric patients. Among the topics Dr. Keszler discusses:
- How to select appropriate inspiratory times, pressures and tidal volumes
- Clinical applications of Volume Guarantee
About Martin Keszler
Name: Dr. Martin Keszler Position: Associate Professor of Pediatrics Place of employment: Women and Infants’ Hospital, Providence, RI
Neonatal Pulmonary Disorders
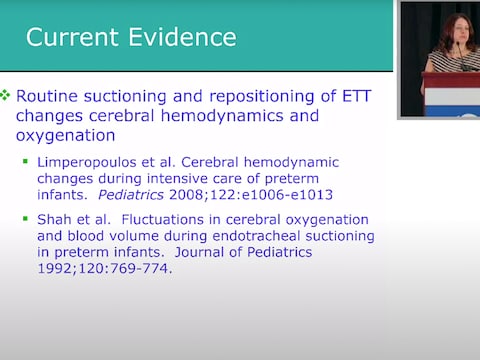
Natalie Napolitano, MPH, RRT-NPS, FAARC is a Research Clinical Specialist at the Children's Hospital of Philadelphia. In this presentation she will discuss challenges in neonatal resuscitation including what the literature tells us, and challenges implementing the recommendations.
Get in Touch With Your Specialist

Draeger, Inc. – Medical
3135 Quarry Road Telford, PA 18969

A Crash Course in Critical Thinking
What you need to know—and read—about one of the essential skills needed today..
Posted April 8, 2024 | Reviewed by Michelle Quirk
- In research for "A More Beautiful Question," I did a deep dive into the current crisis in critical thinking.
- Many people may think of themselves as critical thinkers, but they actually are not.
- Here is a series of questions you can ask yourself to try to ensure that you are thinking critically.
Conspiracy theories. Inability to distinguish facts from falsehoods. Widespread confusion about who and what to believe.
These are some of the hallmarks of the current crisis in critical thinking—which just might be the issue of our times. Because if people aren’t willing or able to think critically as they choose potential leaders, they’re apt to choose bad ones. And if they can’t judge whether the information they’re receiving is sound, they may follow faulty advice while ignoring recommendations that are science-based and solid (and perhaps life-saving).
Moreover, as a society, if we can’t think critically about the many serious challenges we face, it becomes more difficult to agree on what those challenges are—much less solve them.
On a personal level, critical thinking can enable you to make better everyday decisions. It can help you make sense of an increasingly complex and confusing world.
In the new expanded edition of my book A More Beautiful Question ( AMBQ ), I took a deep dive into critical thinking. Here are a few key things I learned.
First off, before you can get better at critical thinking, you should understand what it is. It’s not just about being a skeptic. When thinking critically, we are thoughtfully reasoning, evaluating, and making decisions based on evidence and logic. And—perhaps most important—while doing this, a critical thinker always strives to be open-minded and fair-minded . That’s not easy: It demands that you constantly question your assumptions and biases and that you always remain open to considering opposing views.
In today’s polarized environment, many people think of themselves as critical thinkers simply because they ask skeptical questions—often directed at, say, certain government policies or ideas espoused by those on the “other side” of the political divide. The problem is, they may not be asking these questions with an open mind or a willingness to fairly consider opposing views.
When people do this, they’re engaging in “weak-sense critical thinking”—a term popularized by the late Richard Paul, a co-founder of The Foundation for Critical Thinking . “Weak-sense critical thinking” means applying the tools and practices of critical thinking—questioning, investigating, evaluating—but with the sole purpose of confirming one’s own bias or serving an agenda.
In AMBQ , I lay out a series of questions you can ask yourself to try to ensure that you’re thinking critically. Here are some of the questions to consider:
- Why do I believe what I believe?
- Are my views based on evidence?
- Have I fairly and thoughtfully considered differing viewpoints?
- Am I truly open to changing my mind?
Of course, becoming a better critical thinker is not as simple as just asking yourself a few questions. Critical thinking is a habit of mind that must be developed and strengthened over time. In effect, you must train yourself to think in a manner that is more effortful, aware, grounded, and balanced.
For those interested in giving themselves a crash course in critical thinking—something I did myself, as I was working on my book—I thought it might be helpful to share a list of some of the books that have shaped my own thinking on this subject. As a self-interested author, I naturally would suggest that you start with the new 10th-anniversary edition of A More Beautiful Question , but beyond that, here are the top eight critical-thinking books I’d recommend.
The Demon-Haunted World: Science as a Candle in the Dark , by Carl Sagan
This book simply must top the list, because the late scientist and author Carl Sagan continues to be such a bright shining light in the critical thinking universe. Chapter 12 includes the details on Sagan’s famous “baloney detection kit,” a collection of lessons and tips on how to deal with bogus arguments and logical fallacies.

Clear Thinking: Turning Ordinary Moments Into Extraordinary Results , by Shane Parrish
The creator of the Farnham Street website and host of the “Knowledge Project” podcast explains how to contend with biases and unconscious reactions so you can make better everyday decisions. It contains insights from many of the brilliant thinkers Shane has studied.
Good Thinking: Why Flawed Logic Puts Us All at Risk and How Critical Thinking Can Save the World , by David Robert Grimes
A brilliant, comprehensive 2021 book on critical thinking that, to my mind, hasn’t received nearly enough attention . The scientist Grimes dissects bad thinking, shows why it persists, and offers the tools to defeat it.
Think Again: The Power of Knowing What You Don't Know , by Adam Grant
Intellectual humility—being willing to admit that you might be wrong—is what this book is primarily about. But Adam, the renowned Wharton psychology professor and bestselling author, takes the reader on a mind-opening journey with colorful stories and characters.
Think Like a Detective: A Kid's Guide to Critical Thinking , by David Pakman
The popular YouTuber and podcast host Pakman—normally known for talking politics —has written a terrific primer on critical thinking for children. The illustrated book presents critical thinking as a “superpower” that enables kids to unlock mysteries and dig for truth. (I also recommend Pakman’s second kids’ book called Think Like a Scientist .)
Rationality: What It Is, Why It Seems Scarce, Why It Matters , by Steven Pinker
The Harvard psychology professor Pinker tackles conspiracy theories head-on but also explores concepts involving risk/reward, probability and randomness, and correlation/causation. And if that strikes you as daunting, be assured that Pinker makes it lively and accessible.
How Minds Change: The Surprising Science of Belief, Opinion and Persuasion , by David McRaney
David is a science writer who hosts the popular podcast “You Are Not So Smart” (and his ideas are featured in A More Beautiful Question ). His well-written book looks at ways you can actually get through to people who see the world very differently than you (hint: bludgeoning them with facts definitely won’t work).
A Healthy Democracy's Best Hope: Building the Critical Thinking Habit , by M Neil Browne and Chelsea Kulhanek
Neil Browne, author of the seminal Asking the Right Questions: A Guide to Critical Thinking, has been a pioneer in presenting critical thinking as a question-based approach to making sense of the world around us. His newest book, co-authored with Chelsea Kulhanek, breaks down critical thinking into “11 explosive questions”—including the “priors question” (which challenges us to question assumptions), the “evidence question” (focusing on how to evaluate and weigh evidence), and the “humility question” (which reminds us that a critical thinker must be humble enough to consider the possibility of being wrong).

Warren Berger is a longtime journalist and author of A More Beautiful Question .
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Teletherapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience

IMAGES
VIDEO
COMMENTS
Promoting Critical Thinking in Your Intensive Care Unit Team. 2022 Jan;38 (1):113-127. doi: 10.1016/j.ccc.2021.08.002. Jeremy B Richards Richard M Schwartzstein. 34794626. 10.1016/j.ccc.2021.08.002. Effective and efficient critical thinking skills are necessary to engage in accurate clinical reasoning and to make appropriate clinical decisions.
The ICU environment is conducive to teaching critical thinking skills and demonstrating key communication skills such as empathy. For bedside teaching to remain valuable, we encourage educators to pay attention to details throughout the rounding process (prior to, during, and following rounds).
Effective and efficient critical thinking skills are necessary to engage in accurate clinical reasoning and to make appropriate clinical decisions. Teaching and promoting critical thinking skills in the intensive care unit is challenging because of the volume of data and the constant distractions of competing obligations. Understanding and acknowledging cognitive biases and their impact on ...
Without critical thinking, physicians, and particularly residents, are prone to cognitive errors, which can lead to diagnostic errors, especially in a high-stakes environment such as the intensive care unit. Although challenging, critical thinking skills can be taught.
Critical thinking is defined as efficiently and effectively analyzing or evaluating medical in-formation to make decisions that are precise, logical, accurate, and appropriate. The intensive care unit is a dynamic and challenging environment where volume and complexity of data increases the risk of cognitive errors, morbidity, and mortality.
Teaching clinical reasoning is challenging, particularly in the time-pressured and complicated environment of the ICU. Clinical reasoning is a complex process in which one identifies and prioritizes pertinent clinical data to develop a hypothesis and a plan to confirm or refute that hypothesis. Clinical reasoning is related to and dependent on critical thinking skills, which are defined as one ...
Fig. 3 Framework for critical thinking in the ICU. (Adapted from Hayes MM, Chatterjee S, Schwartzstein RM. Critical Thinking in Critical Care: Five Strategies to Improve Teaching and Learning in the Intensive Care Unit. Ann Am Thorac Soc. 2017;14(4):569 to 575.
The intensive care unit (ICU) can be a place of considerable stress for frontline nurses. ... ICU nurses employ analytical-driven thinking - an information seeking-method of interpreting and managing data. ... Literature published in the English language were retrieved using the following key search words: nurs*, ICU, intensive care, critical ...
Schwartztein, Richard M. (2017) Critical Thinking in Critical Care: Five Strategies to Improve Teaching and Learning in the Intensive Care Unit. Annals of American Thoracic Society; Apr;14 (4):569-575. doi: 10.1513/AnnalsATS.201612-1009AS. Critical thinking is basically the capacity to be deliberate about thinking.
Critical thinking skills are necessary to engage in effective patient care in the ICU, and clinicians and educators can help learners develop their reasoning skills by emphasizing the role of inductive reasoning in clinical practice, asking effective questions (using "how" and "why'), acknowledging the impact of cognitive biases in ...
The COVID-19 pandemic created hospital care situations where critical thinking was essential. It was expected of the nurses on the general floor and in intensive care units. Crystal Slaughter is an advanced practice nurse in the intensive care unit (ICU) and a nurse educator.
The intensive care unit (ICU) is an incredibly rich environment for teaching the pathophysiology behind many diseases. The pace, acuity, and complexity provide unique challenges for teachers and learners alike. Faculty are challenged to practice quality critical care in an academic environment where learners require varying levels of guidance ...
A Multidisciplinary Model for Critical Thinking in the Intensive Care Unit. Webinar Date: March 7, 2023. This webinar is focused on providing our perspective on the importance of macro cognition and team cognition in the decision-making process in healthcare settings, most notably the intensive care unit (ICU).
Critical thinking helps the nurse to navigate the complex and stressful environment of the ICU. Critical thinking includes more than just nursing knowledge. It includes the ability to think through complex, multifaceted problems to anticipate needs, recognize potential and actual complications, and to expertly communicate with the team.
Based on the opinion of many researchers, critical thinking is a key skill for ICU Nurses in making urgent clinical decisions, and the latter is integral to evidence-based practice. Ludin (2018) carried out a study with 113 ICU Nurses. ... Thus, critical thinking, a holistic approach to a patient's health condition, and the ability to work ...
The journey to self-satisfaction is a large section at the centre of the pyramid, representing a significant period of self-reflection and developing critical thinking skills. ICU commitment is a slender portion at the top, where the NQN accepts themselves as an 'ICU nurse' and expresses a desire to stay.
Critical Thinking in the ICU. Play video. Dr. Aaron Light will discuss unique situations encountered in the ICU that require the clinician to critically think. In addition, he will present patient cases with pertinent and distracting information for you to determine what is the best course of action for the patient. After which a review of each ...
In light of these data and the Institute of Medicine's 2015 recommendation to "enhance health care professional education and training in the diagnostic process ," we present this framework as a practical approach to teaching critical thinking skills in the intensive care unit (ICU). The process of critical thinking can be taught ...
Here is a series of questions you can ask yourself to try to ensure that you are thinking critically. Conspiracy theories. Inability to distinguish facts from falsehoods. Widespread confusion ...