- Study protocol
- Open access
- Published: 21 July 2018

Targeted prevention in primary care aimed at lifestyle-related diseases: a study protocol for a non-randomised pilot study
- Lars Bruun Larsen ORCID: orcid.org/0000-0001-9120-4751 1 ,
- Anders Larrabee Sonderlund 1 ,
- Jens Sondergaard 1 ,
- Janus Laust Thomsen 1 ,
- Anders Halling 2 ,
- Niels Christian Hvidt 1 ,
- Elisabeth Assing Hvidt 1 ,
- Troels Mønsted 3 ,
- Line Bjornskov Pedersen 1 , 4 ,
- Ewa M. Roos 5 ,
- Pia Vivian Pedersen 6 &
- Trine Thilsing 1
BMC Family Practice volume 19 , Article number: 124 ( 2018 ) Cite this article
11k Accesses
19 Citations
4 Altmetric
Metrics details
The consequences of lifestyle-related disease represent a major burden for the individual as well as for society at large. Individual preventive health checks to the general population have been suggested as a mean to reduce the burden of lifestyle-related diseases, though with mixed evidence on effectiveness. Several systematic reviews, on the other hand, suggest that health checks targeting people at high risk of chronic lifestyle-related diseases may be more effective. The evidence is however very limited. To effectively target people at high risk of lifestyle-related disease, there is a substantial need to advance and implement evidence-based health strategies and interventions that facilitate the identification and management of people at high risk. This paper reports on a non-randomized pilot study carried out to test the acceptability, feasibility and short-term effects of a healthcare intervention in primary care designed to systematically identify persons at risk of developing lifestyle-related disease or who engage in health-risk behavior, and provide targeted and coherent preventive services to these individuals.
The intervention took place over a three-month period from September 2016 to December 2016. Taking a two-pronged approach, the design included both a joint and a targeted intervention. The former was directed at the entire population, while the latter specifically focused on patients at high risk of a lifestyle-related disease and/or who engage in health-risk behavior. The intervention was facilitated by a digital support system. The evaluation of the pilot will comprise both quantitative and qualitative research methods. All outcome measures are based on validated instruments and aim to provide results pertaining to intervention acceptability, feasibility, and short-term effects.
This pilot study will provide a solid empirical base from which to plan and implement a full-scale randomized study with the central aim of determining the efficacy of a preventive health intervention.
Trial registration
Registered at Clinical Trial Gov (Unique Protocol ID: TOFpilot2016 ). Registered 29 April 2016. The study adheres to the SPIRIT guidelines.
Peer Review reports
In this paper we report on a non-randomized pilot study examining the efficacy of a preventive healthcare intervention. The intervention has been designed to systematically identify patients at high risk of developing lifestyle-related disease, and provide targeted and coherent preventive services to these individuals [ 1 ].
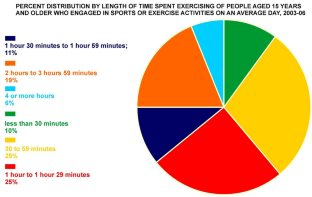
Lifestyle-related disease refers to health conditions that are predominantly caused by health-risk behaviors, such as poor diet, smoking, high consumption of alcohol, or lack of exercise. The consequences of lifestyle-related disease represent a major challenge for the individual as well as for society at large [ 2 ]. In Denmark, people who smoke tobacco, consume excessive amounts of alcohol, and have a sedentary lifestyle are nearly seven times as likely to die from lifestyle-related diseases than physically active non-smokers with a moderate intake of alcohol [ 3 ]. It is estimated that 80% of cardio-vascular disease (CVD), type 2-diabetes mellitus (T2DM), and chronic obstructive pulmonary disease (COPD), and 40% of all cancers may be averted by maintaining healthy dietary habits, regularly exercising, and refraining from smoking [ 4 ]. Indeed, preventable lifestyle-related diseases account for approximately 50 to 60% of all hospital admissions [ 5 ]. It is expected that increasing rates of obesity and physical inactivity will lead to a surge in the number of patients with lifestyle-related diseases in the decades to come [ 6 , 7 , 8 ]. In light of these trends, there is a substantial need to advance and implement evidence-based health strategies and interventions that facilitate the identification and management of people at risk of developing these diseases [ 9 ].
Disease prevention is a central task in general practice in Denmark and the Nordic countries [ 10 ]. Two recent systematic reviews of general practice health checks suggest that people at high risk of chronic disease may benefit from targeted preventive health checks [ 11 , 12 ]. Indeed, targeted, or selective, preventive healthcare is a generally accepted and well-integrated part of healthcare systems worldwide (e.g. treatment of hypertension and hyperlipidemia). Other studies, however, suggest that systematic screening of the general population does not improve clinical endpoints above and beyond those associated with opportunistic screening. These studies indicate that, at a population level, systematic screening of the general population does more harm than good [ 13 , 14 , 15 ]. Overall, however, the evidence on targeted and systematic screening of chronic disease is very limited, possibly providing an explanation for the apparent contradictions in the literature. To this end, projects in the Netherlands and Great Britain are currently underway, testing different approaches to targeted and systematic intervention in general practice [ 16 , 17 ].
There is an even greater lack of evidence when it comes to targeted preventive interventions that comprise both general practice and community health services. In such an approach the general practitioner (GP) targets patients at high risk for lifestyle-related diseases and engages in risk-management of biomarkers and disease with behavior change and pharmaceutical interventions when needed. Community health services, on the other hand, focus primarily on the prevention of health-risk behaviors - including tobacco use, poor diet, excessive alcohol consumption, and sedentary lifestyles - and provide behavior-change interventions such as smoking cessation assistance and dietary advice. Danish studies suggest a potential to enhance the collaboration and cohesiveness of the various components that comprise the preventive healthcare services in the Danish primary care system – especially between GPs and community health services [ 18 , 19 ]. Outside of the Danish context, the benefits of a more unified and coherent healthcare service have also been advanced in peer-reviewed studies [ 20 , 21 ]. However, effectiveness studies of a unified approach, such as that described above, seem to be lacking.
In 2012, we carried out a feasibility study, testing a novel approach to population-based risk stratification at four Danish GP clinics [ 22 ]. The intervention combined lifestyle survey data with health record information in order to identify presumably healthy individuals who nonetheless were at high risk of developing lifestyle-related diseases. These individuals were then offered a health check at their GP for a more definitive assessment of their general health as well as their risk of developing lifestyle-related diseases. Results indicated that this approach to preventive action was indeed feasible, and thus ultimately inspired the development of a large randomized study, the present TOF-project (TOF is a Danish acronym for Early Detection and Prevention). The principal aim of the upcoming TOF-project is to examine the efficacy of a preventive healthcare intervention that systematically identifies individuals at high risk of lifestyle-related disease, and provides targeted and coherent preventive services. We expect that significant changes in the targeting and systematization of disease prevention in the Danish primary care sector, including earlier detection and more coherent preventive services, will diminish the individual and societal burden of chronic disease. Due to the complexity of the TOF intervention, and the relatively high number of stakeholders, a pilot study needs to be conducted before full-scale implementation and evaluation [ 23 ]. The aim of the pilot study is to test the acceptability, feasibility, and short-term effects of a selective preventive program, designed to systematically help patients evaluate their individual risk of lifestyle-related disease. The program also offers targeted and coordinated preventive services in the primary healthcare sector.
The pilot study was designed as a population based non-randomized study in the Region of Southern Denmark, comprising 22 municipalities, 787 GPs, and a general population of 1,2 million. The Danish health care system is a tax-based system comprising three levels: A national level responsible for, among other things, public health, planning, and patient safety; a regional level responsible for the hospitals and the primary care sector; and a municipal level responsible for primary prevention, rehabilitation, and patient education. General practice and the municipalities have shared responsibility for preventive services aimed at the individual. Specifically, GPs assess patient health and implement disease-specific secondary prevention. The municipalities, however, are tasked with primary prevention such as smoking cessation, alcohol treatment, and other lifestyle related services. GPs are organized in clinics with an average of two GPs per clinic. While most clinics comprise a single GP, some have up to ten. Almost all Danish citizens (98%) are registered with a GP [ 24 , 25 ]. Each GP has an average of 1600 registered patients.
Recruitment
The pilot study targets adults born between year 1957 and 1986. All 22 municipalities in the Region of Southern Denmark were invited to participate in TOF. Ten municipalities (Esbjerg, Haderslev, Varde, Sønderborg, Aabenraa, Middelfart, Kerteminde, Nyborg, Svendborg, Langeland) submitted expressions of interest to participate in the study, and were approved for participation by the Regional Council. Two of the municipalities (Haderslev and Varde) volunteered to participate in the pilot study.
The municipalities of Haderslev and Varde comprise 55,971 and 50,110 citizens, and 37 and 29 GPs, respectively. All GPs from each municipality were invited to an information meeting before being formally invited to participate in the pilot study. The invitation was followed up with telephone calls to the individual GP clinics. All patients were invited at baseline, and the intervention was taken up by the patients at their own convenience during the intervention period. See Additional file 1 for a more detailed project flow showing the recruitment, intervention and evaluation phases.
Organization and development of the intervention
The intervention was planned during a two-year combined effort involving all stakeholders. End users were involved in the design of the intervention, including patients, GPs, and municipal health professionals. A group of seven GPs developed the targeted intervention at a general practice level during five workshops. Similarly, a group of 10 municipal health workers, one from each of the participating municipalities, developed the targeted intervention at a municipal level during 10 workshops. The workshops lasted between 2 h and 2 days. A digital support system was created and tested by user populations, including patients, non-government patient organizations, GPs, and municipal health professionals.
A steering committee was established at the start of the project, consisting of managers or board members from the Region of Southern Denmark (project owner), The Organization of General Practitioners in Denmark (PLO), the 10 participating municipalities, the Research Unit for General Practice at the University of Southern Denmark (FEA), and the Danish Quality Unit for General Practice (DAK-E). The chair of the committee is the health director from the Region of Southern Denmark. A research committee with participation from the steering committee chair and the primary investigator has been established. A mission statement has been approved by the steering committee and an agreement of co-operation has been signed between the Region of Southern Denmark and the University of Southern Denmark. The agreement states that the University of Southern Denmark holds all rights, intellectual as well as judicial, to the research data, and that the Region of Southern Denmark has no right to oppose publication of results. The research committee approves all access to research data from affiliated researchers.
Prior to study commencement, all enrolled GPs, practice nurses (PN), and health professionals from the municipalities were invited to a joint three-hour training course (August 2016). The course focused on the assigned intervention activities and tasks both within the GP clinics and the municipality respectively, and between GPs and the municipality.
Invitation and consent
The source population received an invitation to participate, sent on behalf of the GP and the municipality to the individual’s digital mailbox. All permanent residents in Denmark are obligated to have a digital mailbox, which is essentially a digital mail-system provided by the government for secure and direct communication between individuals and public authorities and other trusted organizations (e.g. banks and insurance companies) [ 26 ]. People may opt out of the digital mail system, citing low IT-literacy (usually elderly persons), cognitive impairment, or other complicating factors. To enroll in the study, individuals were asked to follow a link in the invitation to a digital support system protected by a two-phased NemID password [ 27 ]. NemID is a password system providing an exact identification of the user. This system is utilized by Danish public and non-public institutions to provide secure access to personal information, such as health and financial data. Through digital mail and NemID, we were able to reach and identify 97% of the target population. In April 2016, participants received an invitation with an embedded hyperlink to a digital consent form on a secure webpage in their digital mailbox. The consent form outlined study participation and disclosure of data from the GPs electronic patient record (EPR) and was supplemented with short videos describing the purpose of the study and the intervention. Participants were asked to read the information and electronically sign the consent form. Two reminders were sent after one and 2 weeks if participants failed to sign the form. Enrollment closed after 6 weeks. At this time, information on relevant diagnosis (International Classification of Primary Care (ICPC-2) codes) and prescribed medicine (Anatomical Therapeutic Chemical Classification (ATC) codes incl. Text fields with indication for treatment) were collected from the GPs EPR system (See Table 1 for the ICPC-2 codes and ATC codes that were accessed based on the consent). Five months after consent (September 2016), participants received another digital invitation in the digital mailbox, this time to fill in a questionnaire and access a personal health profile. Participants could opt-out at any time during the intervention period by clicking an “opt-out” button on the digital support system.
Intervention
The duration of the intervention was 3 months and took place between September 2016 and December 2016. The intervention comprised a two-pronged approach: [ 1 ] a joint intervention applied to the entire sample, regardless of whether the participants were healthy, at risk, or already in treatment for T2DM, COPD, CVD, hypercholesterolemia or hypertension [ 2 ] a targeted intervention that was offered only to participants who presumably would benefit from either further examinations at the GP (high risk), or from receiving community health services, such as smoking cessation, dietary advice, or physical activity (health-risk behavior).
The joint intervention consisted of:
Stratification to one of four risk groups. Stratification to a specific risk group was determined by use of risk algorithms and EPR information
A digital support system with user interfaces for all users, including the patient, the GP, and the municipal health professional
An individual health profile
The targeted intervention consisted of:
A focused clinical examination and a subsequent health dialogue with a GP (targeting patients at high risk), and / or
A short telephone-based health dialogue with a municipal health professional. For patients with limited capability to care for their own health, this initial talk could be followed up with a subsequent face-to-face health dialogue (targeting patients with health-risk behavior)
For all present intents and purposes, the term health dialogue refers to a consultation that includes the elements of the 5As model (see Table 1 ) and the techniques used in motivational interviewing [ 28 , 29 ].
The joint intervention
All participants gained access to the digital support system and were invited to fill in a questionnaire. The participant questionnaire contained 15 items on height, weight, self-perceived health status, family history of lifestyle-related diseases, COPD related symptoms, smoking status, leisure activity level, alcohol consumption, diet, and osteoarthritis risk factors. Questions about family history of diabetes and leisure activity level were taken from the Danish Diabetes Risk model [ 30 ]. Similarly, questions on COPD-related symptoms and smoking status were derived from the COPD-PS screener [ 31 ] and the Heartscore BMI score [ 32 ]. Items tapping dietary habits were from the Swedish National Guidelines on Disease Prevention [ 33 ]. The questionnaire took approximately 5 min to complete.
Based on the questionnaire and information from the individual EPR, participants were stratified into four distinct risk groups:
Group 1 – Participants with a pre-existing diagnosis and/or in current treatment for a lifestyle-related disease.
Group 2 – Participants at high risk of developing lifestyle-related disease, and thus eligible for the offer of a targeted intervention at the GP.
Group 3 – Participants engaging in health-risk behavior, and thus eligible for the offer of a targeted intervention at the municipality.
Group 4 – Participants with a healthy lifestyle and no need for further intervention.
Stratification to group 1
EPR data was collected via certified EPR-suppliers. We used International Classification of Primary Care-2 codes (ICPC-2) registered by the GP and/or Anatomical Therapeutic Chemical Classification ( ATC) codes for prescribed medicine within the past 2 years, together with the indication for prescribing the medicine, to identify Group 1 participants (see Table 2 ).
Given the pre-existing diagnosis and/or treatment, Group 1 was excluded from the subsequent risk estimation and stratification into Group 2, 3, and 4.
Stratification to group 2
Next, participants at risk of lifestyle-related disease were identified using three validated risk scores: the Chronic Obstructive Pulmonary Disease Population Screener (COPD-PS), the Danish Diabetes Risk model, and a modified Heartscore BMI score [ 30 , 31 , 32 ]. The COPD-PS uses an algorithm accounting for age, lifetime use of cigarettes, and smoking-related symptoms to identify at-risk patients who may benefit from a spirometry to test for COPD (Table 3 ) [ 31 ]. The Danish Diabetes Risk score is based on an algorithm that incorporates age, sex, BMI, known hypertension, leisure activity level, and family history of diabetes (Table 4 ) [ 30 ]. The modified Heartscore BMI score accounts for age, sex, body mass index (BMI), and smoking status (Table 5 ) [ 32 ].
Consistent with the criteria of the four distinct stratification groups defined above, participants were categorized into Group 2 when one or more of the risk assessment algorithms indicated high likelihood of developing lifestyle-related disease (see Tables 3 , 4 and 5 ).
Stratification to group 3 and 4
Finally, participants engaging in health-risk behavior with one or more risk factors were categorized in Group 3 (Group 3). Health-risk behavior was defined by the presence of at least one of the following behaviors: smoking tobacco on a daily basis, consuming more than 14/21 (male/female) standard units of alcohol per week, sustaining an unhealthy diet (diet score ≤ 4 on a 12-point score drawn from the Swedish National Guidelines on Disease Prevention) [ 4 ], maintaining a BMI ≥ 35, and/or engaging in a generally sedentary lifestyle. Lastly, participants with no lifestyle-related disease or risk thereof were stratified into Group 4.
Digital support system
All users had access to a digital support system in the form of a web page with a common database and specific user interfaces for the GP, the municipality health professionals, and the patient. No apps were developed. The system design drew inspiration from the work by Krist and colleagues’ research on preventive EPRs, and was further inspired by the results of a Delphi process carried out to identify factors for optimal development of health-related websites [ 34 , 35 , 36 ]. Due to challenges in terms of interoperability between the eight suppliers of EPR systems used by GPs, and at least three suppliers of electronic care records (ECR) in the municipalities, it was not feasible to develop a support system that completely integrated the EPR and ECR systems. Instead, the digital support system was developed as a parallel system with an additional functionality facilitating the transfer of information (e.g. relating to lifestyle and/or prevention plans) to the EPR and ECR systems using Electronic Data Interchange (EDIfact) messages [ 22 ]. The patient controlled access to personal health information on the system, such that the GP and municipal health professional were only able to access this information with the explicit consent of the patient.
The digital support system was developed iteratively in collaboration with the users during the before mentioned workshops with municipality health professionals and GPs and in the form of usability tests with patients. The user interface for the patient was responsive and compatible with most devices, including mobile phones, tablets, laptops and stationary computers. Due to technical constraints in the secure log-in provided by NemID, the user interface for health professionals was only developed for laptops and stationary computers. In order to make the user interface for the patient as intuitive and user-friendly as possible, the digital support system made extensive use of simple visualizations, icons, and short information videos (Fig. 1 ). The primary text-based messages were kept short and concise with the provided possibility of accessing secondary in-depth information, retrieved from the Danish Health Portal, sundhed.dk [ 37 ].
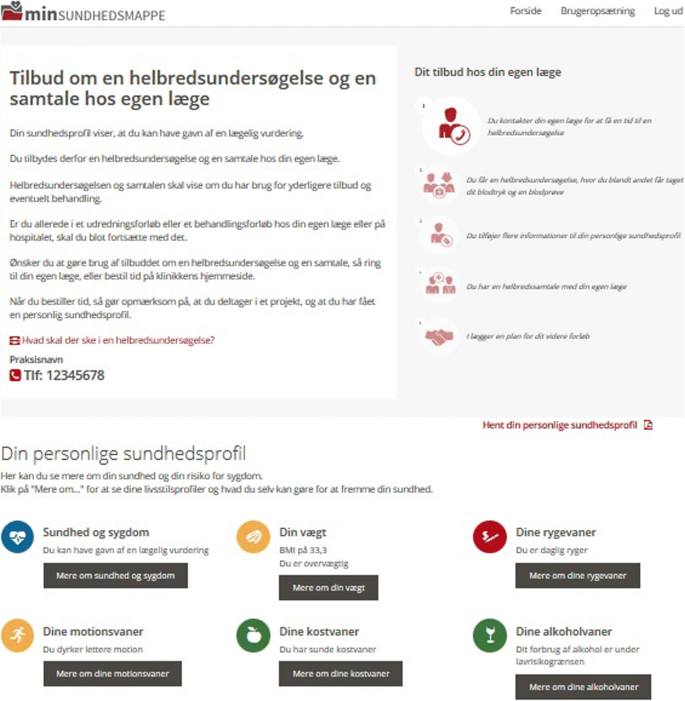
Screen dump from digital support system (in Danish)
Beyond facilitating the intervention, the digital support system also enabled data collection for research purposes. A number of questionnaires were sent from the digital support system to the participants at specific time-points, including immediately after consent, after receiving the personal health profile, following the health dialogue at the GP, and at the end of the implementation period. Questionnaire reminders were sent by e-mail with a link to the digital support system. The GPs and municipal health professionals received audits in the form of short questionnaires immediately after each consultation as well as before and after the study period (GPs only).
Personal health profile
Based on results of the stratification process, each patient received a personal health profile on the digital support system. The purpose of the health profile was to encourage patients to change their health-risk behavior and follow the tailored advice provided by the system. Patients who were at increased risk of developing a lifestyle-related disease (Group 2) were advised to consult their GP for further examination and advice. Similarly, patients engaging in health-risk behavior (Group 3) were offered lifestyle counseling, or lifestyle courses from the municipality health services. By definition, Group 4 patients lead a relatively healthy life with no need for health-risk behavior change. Group 1 patients were advised to continue their treatment and use the information provided to change health-risk behavior.
The personal health profile included individualized information on current health-risk behavior and risk of disease. The information was tailored based on the questionnaire, the information from the EPR, and the risk scores on COPD, T2DM, and CVD. It also included general health information and information about preventive health services concerning smoking, diet, exercise, and alcohol consumption. This information was provided by the municipality, the Region of Southern Denmark, or national health services, and targeted the individual (e.g. via links to apps and webpages) based on his/her specific health-risk behavior.
The targeted intervention
The intervention at the gp.
The intervention at the general practice level consisted of a focused clinical examination and a subsequent health dialogue and was offered to patients who were at increased risk of developing a lifestyle-related disease (Group 2). Group 2 patients accepted the offer of the intervention by scheduling an appointment at the GP (either by phone or the GP’s webpage). Whether the patient participated in the intervention or not was thus determined by their motivation and capabilities as well as the extent to which the content of the personal health profile motivated the patient to take action. The intervention was applied within the framework of the 5As model (see Table 1 ) [ 28 ]. The content of the focused clinical examination was based on the patient’s health profile, and might include measurements of blood glucose (HbA1c) and cholesterol levels, as well as height, weight, blood pressure, and lung function measurements and Electrocardiogram (ECG). Results from the examinations were registered in the digital support system where both the patient and the GP could access them at any time. After the focused clinical examination all patients were given the opportunity to prepare for the subsequent health dialogue by answering a questionnaire inspired by three systematic reviews on the determinants of behavior change [ 38 , 39 , 40 ]. These included questions about motivation, resources, former experiences with behavior change, social network, mental health (WHO-5 for stress and Major Depression Inventory (MDI) for depression) [ 41 , 42 ], and a scheme to qualitatively self-report on facilitators and barriers to behavior change (a so-called balance-sheet). The questionnaire results were shared with the GP on the digital support system. Based on the health dialogue, the GP and the patient developed a prevention plan that included a goal, a time frame, and identification of the appropriate means to fulfill the plan (e.g. reference to a smoking cessation course, or follow-up at the GP). The prevention plan was registered on the digital support system by the GP and was accessible to both the GP and the patient.
The intervention at the municipal level
The intervention at the municipal level was offered to patients exhibiting health-risk behavior (Group 3) and consisted of a short telephone consultation with a health professional – for example a nurse, a dietician, or a physiotherapist. A subsequent face-to-face health dialogue was offered to patients who were deemed to potentially benefit from more extensive support. Group 3 patients requested the intervention on the digital support system by filling in a short form and sending it by e-mail to the municipality. A municipal health professional would then call the patient within the following week. Similar to the GP intervention, the intervention at the municipal level was thus also determined by patient motivation and capabilities as well as the extent to which the content of the personal health profile motivated the patient to take action. Immediately after the intervention, a participation form was sent to the municipality. Patients could prepare for the upcoming call from a municipal health professional in the same way as Group 2 patients prepared for the health dialogue – that is, by answering a short questionnaire. Ultimately, a prevention plan, including concrete details on its execution, was developed based on the telephone consultation and the face-to-face health dialogue. The prevention plan was registered by the municipal health professional and presented on the user interfaces of both the municipality and the patient.
Sample size calculation
While aiming to test the acceptability, feasibility, and short-term effects of the pilot, we estimated a sample size for each GP that would allow the GP to familiarize him/herself with the intervention without unnecessary increases in workload during the intervention period. In agreement with the GP representative in the Region of Southern Denmark, we set a target of four health checks for each GP. From the feasibility study, we estimated that 60% would consent to the study, and that 75% of these participants would receive a personal digital health profile [ 22 ]. Also based on the feasibility study, we estimated that 12% of the study population would be recommended to consult their GP (Group 2). From results obtained in similar Dutch studies, we finally estimated that 35% of the these patients (Group 2) would eventually consult the GP [ 43 ]. Given these figures, we calculated that a total sample of approximately 200 patients from each GP would be required to reach the target of four completed health checks per GP.
Data collection and analysis
Evaluation outcomes.
Evaluation of the study will be carried out using quantitative as well as qualitative research methods (Table 6 ). All outcome measures are based on validated instruments and aim to provide results pertaining to intervention acceptability, feasibility, and short-term effects. In addition, outcomes related to other associated topics will be included. The specific instruments used will be described in detail in later publications.
Qualitative data
Qualitative data will be derived from interviews (individual and focus groups comprising GPs, practice staff members, municipality staff members, patients from group 2 and 3, stakeholders, project leaders and researchers) and participant observations (during the health dialogues at the GP). The estimated number of participants is shown in Table 6 .
Quantitative data
Quantitative data will be derived from questionnaires as well as Danish National registers (see section below). Table 7 shows the content of the questionnaires applied while a diagram, attached as Additional file 1 , shows a flow of the entire intervention and the timing of the questionnaires during the intervention.
Register based data
Data from the Danish national registers concerning demographic information, prescriptions, and health care usage of the target population ( n = 9.400) will be obtained from Statistics Denmark ( https://www.dst.dk/da ) [ 44 ]. Information from the different registers will be linked by the patients’ Danish Personal Identification Number.
Socio-demographic variables
Information on socio-demography encompassed educational level, occupation, income, cohabitation status, ethnicity, and residency.
Education is defined as the highest formal educational attainment obtained on the first of October in each calendar year.
Occupation is defined as the occupational status on the first of November in each calendar year.
OECD-adjusted income level is defined as the individual’s/family’s disposable income, adjusted for family size and categorized in relative terms (low/middle/high income) [ 45 ].
Cohabitation status is defined as cohabitating or living alone.
Ethnicity is based on country of origin and descendance.
Information on health/disease status (hypertension, hypercholesterolemia, type-2 diabetes, cardio-vascular disease) is defined in terms of ICD-10 diagnosis codes and medical usage. The ‘National Patient Registry’ will provide information on ICD-10 diagnostic codes. The ‘Register of Medicinal Product Statistics’ provide information on medical usage [ 46 , 47 ].
Contextual variables
Contextual variables include information on study site and neighborhood social deprivation. Neighborhood social deprivation will be derived on a census district level and is principally defined in terms of the following three variables: educational attainment, employment status (employed/social welfare), and income (mean family disposable income). Educational, employment, and income deprivation thus specifically refer to the proportion of citizens within each census district who has access to basic education (up to high school), who is unemployed (e.g. students, unemployed workers), and who belongs to the lowest income quartile, respectively. Each variable is ranked, grouped in quartiles, and given a value between 0 and 3 (3 = high deprivation). This results in an aggregated ranking system ranging from 0 (low deprivation) to 9 (high deprivation). The aggregated rank is then grouped in quartiles. A neighborhood social deprivation score will be calculated for all census districts in Denmark in order to obtain local deprivation scores that mirror the relative social deprivation of the individual census district [ 48 ].
This pilot study will provide a solid empirical base from which to plan and implement a full-scale randomized study with the central aim of determining the efficacy of a preventive health intervention. The intervention was designed to systematically identify persons at risk of developing lifestyle-related disease or who engage in health-risk behavior, and provide targeted and coherent preventive services to these individuals.
Strengths and limitations
Much effort has been made to define the specific nature and objective of pilot and/or feasibility studies. In a scoping review of optimization strategies for complex interventions prior to randomized trials, Levati asserts the notion that different frameworks for intervention development, such as intervention mapping and the MRC framework for complex intervention, call for different approaches to pilot and feasibility studies [ 49 ]. As a common feature when developing complex randomized trials, the authors suggest “that the acceptability of the intervention to those directly involved in the delivery and receipt of the final intervention, together with the anticipated effect of the intervention, are important elements to take into account as early as possible in the pre-trial stage.” [ 49 ].
Eldridge et al. used a Delphi survey to arrive at distinct definitions of feasibility and pilot studies [ 1 ]. They suggest that “feasibility study” is an overarching term with “pilot study” representing a subset of feasibility studies. Generally, feasibility studies ask whether something can be done, should we proceed with it, and if so, how? Pilot studies ask the same questions, but with a specific design feature of a larger study, conducted on a smaller scale. According to the authors, pilot studies can be separated in two distinct types: non-randomized and randomized. Non-randomized pilot studies do not include a control group and are usually external to the subsequent randomized controlled trial (RCT), that is, the participants are not included in the effect analysis of the RCT. Randomized pilot studies, on the other hand, randomize participants to an intervention or control group and can be internal to the subsequent RCT. Bowen et al. complement the work of Eldridge et al. and propose eight foci (design features) of feasibility studies: Acceptability, demand, implementation, practicality, adaptation, integration, expansion, and limited efficacy [ 50 ].
According to Eldridge et al., the study presented in this paper is a non-randomized pilot study. We chose a non-randomized design in order to examine the specific design features of a stepped wedge cluster randomized design for the full-scale randomized study. A stepped-wedge design is a type of cluster randomized design that meets the specific ethical and logistical demands of a delayed intervention performed in routine care where all participants will be offered the intervention [ 51 ]. The pilot resembles one cluster in a stepped wedge cluster randomized study, and will thus allow us to ascertain whether the intervention can be delivered during a three-month period, or if longer time is required to avoid carry-over effects [ 51 ]. In the event that more time is necessary to deliver the intervention, it will be difficult, if not impossible, to accurately determine the optimal duration of a cluster. This will likewise complicate the stepped wedge design. One way to compensate for incomplete knowledge on the optimal timeframe for the intervention may be to include a “wash out” period after every cluster allowing for any delay or lag in implementation before the next cluster is commenced [ 52 ]. The length of the “wash out” period can be estimated from the results of the pilot study.
We have randomly sampled 200 patients from each GP in order to have a source population that is representative of the target population. We have chosen to target people born between 1957 and 1986 to assess the risk of lifestyle-related disease and health-risk behavior at an age interval where changes in lifestyle will provide significant health effects and be cost-effective. To this end, we have chosen to assess variation in the proportion of patients at increased risk of lifestyle-related disease between baseline and the 12-week follow up as our primary health-related outcome. Further, given the fact that complex interventions, such as the one described here, usually have concurrent endpoints [ 23 ], we also collect data on a variety of other variables – both questionnaire- and register-based – related to both lifestyle and disease. We have yet to determine which of these endpoints to include in the full-scale randomized study.
We have planned the intervention in collaboration with the stakeholders, patients, and service providers in order to run a pilot study that is both acceptable and relevant for all user groups. We use quantitative as well as qualitative research methods to assess the acceptability, demand, implementation, and practicality of the pilot, from the viewpoint of both users and service-providers. In addition to evaluating the intervention, we assess the organizational challenges of planning and implementing IT-supported pilot studies [ 53 ]. At the same time we test different methods of data collection, including electronic collection of data from the digital support system and participant observations at the GP clinics. We also test various types of questionnaires, including ones that involve simple items with binary outcomes as well as others in more complex discrete choice format. The pilot will hence enable us to assess whether the intervention can be executed, and whether the organizational approach taken, fit the purpose. We will further be able to make an informed decision about how we can collect data during the full-scale study in the most efficient and cost-effective way that is also acceptable to both users and service-providers.
From pilot to full-scale randomized study
Another issue raised by Levati et al. and Eldridge et al. concerns pinpointing the appropriate time to move from piloting to full-scale RCT. That is, should we proceed with the project, and if so, how? [ 1 , 49 ]. Proceeding from pilot to a full-scale randomized study is probably the most under-researched part of the implementation of complex interventions. Bugge et al. suggest a three step process to establish the best possible foundation on which to make a decision to advance a full-scale randomized study [ 54 ]. First, any problems should be categorized into three distinct types: Issues that are likely to complicate the full-scale study, issues that are likely to complicate both trial and real-world situations, and issues that are likely to complicate real-world situations only. Next, potential solutions should be identified for the expected issues, ideally with lay participation. Finally, the best of these solutions should be selected to determine the best way to proceed. With this strategy in mind, we will do a thorough assessment of the problems encountered in the pilot before advancing the full-scale study. We will thus identify solutions in collaboration with the service providers (GPs and municipal health professionals) who participated in the pilot study, as well as with those who took part in the design of the intervention. We will also seek patient-feedback on the technical and communicative properties of the digital support system before defining its final specifications. The final assessment is presented to the steering committee that will take the decision on the way forward.
Abbreviations
Anatomical Therapeutic Chemical Classification
Body mass index
Chronic Obstructive Pulmonary Disease
Chronic Obstructive Pulmonary Disease Population Screener
Cardio vascular disease
Electronic Data Interchange messages
Electronic patient record
General practitioner
International classification of diseases
International classification of primary care
Randomized controlled trial
Type 2 diabetes mellitus
Eldridge SM, Lancaster GA, Campbell MJ, Thabane L, Hopewell S, Coleman CL, et al. Defining Feasibility and Pilot Studies in Preparation for Randomised Controlled Trials: Development of a Conceptual Framework. PLoS ONE. 2016;11(3). Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4792418/ . [cited 2016 Nov 10].
WHO. Global Status on Noncommunicable diseases. Geneva: WHO; 2010.
Google Scholar
Juel K, Sørensen J, Brønnum-Hansen H. Supplement: risk factors and public health in Denmark. Scand J Public Health. 2008;36(1 suppl):1–227.
Article Google Scholar
WHO TRS 916. Diet, Nutrition, and the Prevention of Chronic Diseases. 2003.
Glümer C, Hilding-Nørkjær H, Jensen H, Jørgensen T, Andreasen A, Ladelund S. Sundhedsprofil for region og kommuner 2008. Region Hovedstaden: Glostrup; 2008.
Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87(1):4–14.
Article PubMed CAS Google Scholar
Yusuf S, Reddy S, Ounpuu S, Anand S. Global burden of cardiovascular diseases: part I: general considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation. 2001;104(22):2746–53.
NCD Risk Factor Collaboration (NCD-RisC). Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants. Lancet 2016;387(10026):1377–1396.
Beaglehole R, Bonita R, Horton R, Adams C, Alleyne G, Asaria P, et al. Priority actions for the non-communicable disease crisis. Lancet. 2011;377(9775):1438–47.
Article PubMed Google Scholar
The Role of General Practitioners in Preventing disease and promoting health in the Nordic countries [Internet]. Nordic Federation of General Practice; 2013. Available from: http://www.nfgp.org/files/8/policypaper_preventing_2.pdf . [cited 2016 Nov 6]
Si S, Moss JR, Sullivan TR, Newton SS, Stocks NP. Effectiveness of general practice-based health checks: a systematic review and meta-analysis. Br J Gen Pract. 2014;64(618):e47–53.
den Engelsen C, Koekkoek PS, Godefrooij MB, Spigt MG, Rutten GE. Screening for increased cardiometabolic risk in primary care: a systematic review. Br J Gen Pract. 2014;64(627):e616–26.
Jørgensen T, Jacobsen RK, Toft U, Aadahl M, Glümer C, Pisinger C. Effect of screening and lifestyle counselling on incidence of ischaemic heart disease in general population: Inter99 randomised trial. BMJ. 2014;348:g3617.
Article PubMed PubMed Central CAS Google Scholar
Krogsbøll LT, Jørgensen KJ, Grønhøj Larsen C, Gøtzsche PC. General health checks in adults for reducing morbidity and mortality from disease: Cochrane systematic review and meta-analysis. BMJ. 2012;345:e7191.
Article PubMed PubMed Central Google Scholar
Dyakova M, Shantikumar S, Colquitt JL, Drew CM, Sime M, MacIver J, et al. Systematic versus opportunistic risk assessment for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2016;1:CD010411.
Badenbroek IF, Stol DM, Nielen MM, Hollander M, Kraaijenhagen RA, de Wit GA, et al. Design of the INTEGRATE study: effectiveness and cost-effectiveness of a cardiometabolic risk assessment and treatment program integrated in primary care. BMC Fam Pract. 2014;15:90.
Marshall T, Caley M, Hemming K, Gill P, Gale N, Jolly K. Mixed methods evaluation of targeted case finding for cardiovascular disease prevention using a stepped wedged cluster RCT. BMC Public Health. 2012;12:908.
Andersen JH, Thorsen T, Kousgaard MB. Samarbejde mellem kommuner og almen praksis om henvisning til kommunale sundhedstilbud for patienter med kroniske sygdomme [Internet]. København: Forskningsenheden for almen praksis; 2014. Available from: http://patientuddannelse.info/media/95449/samarbejde_mellem_almen_praksis_og_kommuner.pdf . [cited 2016 Oct 20]
Helbech hansen B. Omfanget af henvisninger fra alment praktiserende læger til kommunale sundheds- og forebyggelsestilbud [Internet]. København: Kommunernes Landsforening; 2015. Available from: http://www.kl.dk/ImageVaultFiles/id_74921/cf_202/Henvisninger_fra_almen_praktiserende_l-ger_til_kom.PDF . [cited 2016 Oct 20]
Porterfield DS, Hinnant LW, Kane H, Horne J, McAleer K, Roussel A. Linkages between clinical practices and community organizations for prevention: a literature review and environmental scan. Am J Public Health. 2012 Jun;102(Suppl 3):S375–82.
Krist AH, Shenson D, Woolf SH, Bradley C, Liaw WR, Rothemich SF, et al. Clinical and community delivery Systems for Preventive Care. Am J Prev Med. 2013 Oct 1;45(4):508–16.
Bruun Larsen L, Soendergaard J, Halling A, Thilsing T, Thomsen JL. A novel approach to population-based risk stratification, comprising individualized lifestyle intervention in Danish general practice to prevent chronic diseases: Results from a feasibility study. Health Informatics J. 2017;23(4):249–59. https://doi-org.proxy1-bib.sdu.dk/10.1177/146045821664514 .
Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ. 2008;337. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2769032/ . [cited 2014 Jan 16].
Pedersen KM, Andersen JS, Søndergaard J. General practice and primary health Care in Denmark. J Am Board Fam Med. 2012;25(Suppl 1):S34–8.
Pedersen KM, Søndergaard J. Det samarbejdende hospital: Almen praksis og kommuner. In: Fremtidens Hospital. København: Munksgaard; 2014. p. 115–26.
e-boks webpage. URL: http://www.e-boks.dk/default.aspx . Accessed: 2016 Oct 19. (Archived by WebCite® at http://www.webcitation.org/6lN8fheQf ).
NemID webpage. The Danish Agence for Digitisation. URL: https://www.nemid.nu/dk-en/ . Accessed: 2016 Oct 19. (Archived by WebCite® at http://www.webcitation.org/6lN81XyxY ).
Whitlock E. Evaluating primary care behavioral counseling interventions an evidence-based approach. Am J Prev Med. 2002 May;22(4):267–84.
Den motiverende samtale [Internet]. Dansk selskab for almen medicin; 1999 . Available from: http://www.dsam.dk/files/9/den_motiverende_samtale_1999.pdf . [cited 2014 Nov 16].
Christensen JO, Sandbaek A, Lauritzen T, Borch-Johnsen K. Population-based stepwise screening for unrecognised type 2 diabetes is ineffective in general practice despite reliable algorithms. Diabetologia. 2004;47(9):1566–73.
Martinez FJ, Raczek AE, Seifer FD, Conoscenti CS, Curtice TG, D’Eletto T, et al. Development and initial validation of a self-scored COPD population screener questionnaire (COPD-PS). COPD. 2008;5(2):85–95.
European Society of Cardiology. Heartscore webpage. URL: http://www.heartscore.org/en_GB/ . Accessed: 2016 Oct 19. (Archived by WebCite® at http://www.webcitation.org/6lN9ncXMD ).
Svenska Socialstyrelsen. Sjukdomsförebyggande metoder. Vetenskabeligt underlag för nationella riktlinjer. Svenska Socialstyrelsen; 2011.
Schneider F, van Osch L, de Vries H. Identifying factors for optimal development of health-related websites: a Delphi study among experts and potential future users. J Med Internet Res. 2012;14(1):e18.
Krist AH, Woolf SH. A vision for patient-centered health information systems. JAMA. 2011;305(3):300–1.
Krist AH, Beasley JW, Crosson JC, Kibbe DC, Klinkman MS, Lehmann CU, et al. Electronic health record functionality needed to better support primary care. J Am Med Inform Assoc. 2014;21(5):764–71.
sundhed.dk webpage. URL: https://www.sundhed.dk /. Accessed: 2016 Oct 19. (Archived by WebCite® at http://www.webcitation.org/710tT6aOg ).
Murray J, Craigs CL, Hill KM, Honey S, House A. A systematic review of patient reported factors associated with uptake and completion of cardiovascular lifestyle behaviour change. BMC Cardiovasc Disord. 2012;12:120.
Murray J, Honey S, Hill K, Craigs C, House A. Individual influences on lifestyle change to reduce vascular risk: a qualitative literature review. Br J Gen Pract J R Coll Gen Pract. 2012;62(599):e403–10.
Murray J, Fenton G, Honey S, Bara AC, Hill KM, House A. A qualitative synthesis of factors influencing maintenance of lifestyle behaviour change in individuals with high cardiovascular risk. BMC Cardiovasc Disord. 2013;13:48.
Olsen LR, Jensen DV, Noerholm V, Martiny K, Bech P. The internal and external validity of the major depression inventory in measuring severity of depressive states. Psychol Med. 2003;33(2):351–6.
Topp CW, Østergaard SD, Søndergaard S, Bech P. The WHO-5 well-being index: a systematic review of the literature. Psychother Psychosom. 2015;84(3):167–76.
Van der Meer V, Nielen MM, Drenthen AJ, Van Vliet M, Assendelft WJ, Schellevis FG. Cardiometabolic prevention consultation in the Netherlands: screening uptake and detection of cardiometabolic risk factors and diseases - a pilot study. BMC Fam Pract. 2013;14:29.
Thygesen LC, Daasnes C, Thaulow I, Brønnum-Hansen H. Introduction to Danish (nationwide) registers on health and social issues: structure, access, legislation, and archiving. Scand J Public Health. 2011;39(7 suppl):12–6.
What are the equivalence scales [Internet]. OECD Project on Income Distribution and Poverty. Available from: http://www.oecd.org/els/soc/OECD-Note-EquivalenceScales.pdf . [cited 2016 Mar 23].
Schmidt M, Schmidt SAJ, Sandegaard JL, Ehrenstein V, Pedersen L, Sørensen HT. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol. 2015;7:449–90.
Pottegård A, Schmidt SAJ, Wallach-Kildemoes H, Sørensen HT, Hallas J, Schmidt M. Data resource profile: the Danish National Prescription Registry. Int J Epidemiol. 2017;46(3):798–798f. https://doi.org/10.1093/ije/dyw213 .
Bender AM, Kawachi I, Jørgensen T, Pisinger C. Neighborhood deprivation is strongly associated with participation in a population-based health check. PLoS One. 2015;10(6):e0129819.
Levati S, Campbell P, Frost R, Dougall N, Wells M, Donaldson C, et al. Optimisation of complex health interventions prior to a randomised controlled trial: a scoping review of strategies used. Pilot Feasibility Stud. 2016;2:17.
Bowen DJ, Kreuter M, Spring B, Cofta-Woerpel L, Linnan L, Weiner D, et al. How we design feasibility studies. Am J Prev Med. 2009;36(5):452–7.
Hargreaves JR, Copas AJ, Beard E, Osrin D, Lewis JJ, Davey C, et al. Five questions to consider before conducting a stepped wedge trial. Trials. 2015;16:350.
Copas AJ, Lewis JJ, Thompson JA, Davey C, Baio G, Hargreaves JR. Designing a stepped wedge trial: three main designs, carry-over effects and randomisation approaches. Trials. 2015;16:352.
Hertzum M, Bansler JP, Havn EC, Simonsen J. Pilot implementation: learning from field tests in IS development. Commun Assoc Inf Syst. 2012;30. Article 20. Available at: http://aisel.aisnet.org/cais/vol30/iss1/20 .
Bugge C, Williams B, Hagen S, Logan J, Glazener C, Pringle S, et al. A process for decision-making after pilot and feasibility trials (ADePT): development following a feasibility study of a complex intervention for pelvic organ prolapse. Trials. 2013;14:353.
Ingham SL, Moody A, Abhishek A, Doherty SA, Zhang W, Doherty M. Development and validation of self-reported line drawings for assessment of knee malalignment and foot rotation: a cross-sectional comparative study. BMC Med Res Methodol. 2010;10:57.
Download references
Acknowledgements
Thanks to all the patients, GPs and municipal health professionals who provided valuable input to the development of the intervention. Also thanks to the steering committee members whose contribution to the realisation of the study was significant.
The project has received funding from the Region of Southern Denmark for secretarial support, participatory processes, digital support system and remuneration of the participating GPs; The joint Quality and educational committee (KEU) of the Region of Southern Denmark and the The Organization of general practitioners in Denmark for funding of research work-packages; And The Ministry of Health for testing and evaluation of the digital support system. The funders of the project have no role in the analysis, or interpretation of the data, writing of research papers, or the decision to submit a paper for publication.
Availability of data and materials
The data that support the findings of this study will be available from Statistics Denmark but restrictions apply to the availability of these data, which will be used under license for the current study, and so are not publicly available. Data will however be available from the authors upon reasonable request and with permission of Statistics Denmark.
Author information
Authors and affiliations.
Department of Public Health, Research Unit of General Practice, University of Southern Denmark, Odense, Denmark
Lars Bruun Larsen, Anders Larrabee Sonderlund, Jens Sondergaard, Janus Laust Thomsen, Niels Christian Hvidt, Elisabeth Assing Hvidt, Line Bjornskov Pedersen & Trine Thilsing
Department of Clinical Sciences, Center for Primary Health Care Research, Lund University, Lund, Sweden
Anders Halling
Department of Informatics, University of Oslo, Oslo, Norway
Troels Mønsted
Department of Business and Economics, COHERE, University of Southern Denmark, Odense, Denmark
Line Bjornskov Pedersen
Department of Sports Science and Clinical Biomechanics, Research Unit for Musculoskeletal Function and Physiotherapy, University of Southern Denmark, Odense, Denmark
Ewa M. Roos
National Institute of Public Health, University of Southern Denmark, Copenhagen, Denmark
Pia Vivian Pedersen
You can also search for this author in PubMed Google Scholar
Contributions
All authors participate in the design and evaluation of the study. LBL, TT, JLT, AH and JS wrote the study proposal. NCH, TSM, LBP, PVP, EAH, LBL, TT and EMR supplied the study with research protocols and conduct the research. LBL, TT and ALS conduct the study and coordinate the evaluation. The manuscript for the study protocol was edited and revised by all authors. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Lars Bruun Larsen .
Ethics declarations
Ethics approval and consent to participate.
The study adheres to the SPIRIT guidelines and has been approved by the Danish Data Protection Agency (J.nr 2015–57-0008) and registered at Clinical Trial Gov (Unique Protocol ID: TOFpilot2016). According to Danish regulations (Act on Research Ethics Review of Health Research Projects (section 14,2)) this study does not need approval from a health research ethics committee as no research on human tissue or other biological material is performed. The study complies with the Helsinki declaration with informed consent to study participation and to disclosure of data from the GPs EPR obtained from all participants before enrolment. Participants were asked to read the information and electronically sign the consent form that was supplemented with short videos of the principal investigator and a GP describing the purpose of the study and the intervention. Before linking project data and national registers from Statistics Denmark participants will be pseudomized. Data management and data analysis of quantitative data will be performed on secure servers at Statistics Denmark.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:.
Detailed project flow showing the recruitment, intervention and evaluation phases. Detailed project flow from recruitment to intervention and evaluation. It shows how participants will be recruited, how they will be stratified using algorithms and what intervention elements the participant will receive. Furthermore, it shows when quantitative data will be collected for evaluative purposes. (TIF 1491 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Larsen, L.B., Sonderlund, A.L., Sondergaard, J. et al. Targeted prevention in primary care aimed at lifestyle-related diseases: a study protocol for a non-randomised pilot study. BMC Fam Pract 19 , 124 (2018). https://doi.org/10.1186/s12875-018-0820-8
Download citation
Received : 23 December 2016
Accepted : 15 July 2018
Published : 21 July 2018
DOI : https://doi.org/10.1186/s12875-018-0820-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Targeted health checks
- Primary care
- Intersectoral collaboration
BMC Primary Care
ISSN: 2731-4553
- General enquiries: [email protected]
Advertisement
Lifestyle modifications for preventing and managing cardiovascular diseases
- Published: 22 August 2023
- Volume 20 , pages 23–36, ( 2024 )
Cite this article

- Princess Oghenekeno Samuel 1 ,
- Great Iruoghene Edo 1 , 2 ,
- Oghenerume Lucky Emakpor 3 ,
- Gift Onyinyechi Oloni 1 ,
- Gracious Okeoghene Ezekiel 4 ,
- Arthur Efeoghene Athan Essaghah 5 ,
- Endurance Agoh 6 &
- Joy Johnson Agbo 7
461 Accesses
Explore all metrics
Cardiovascular diseases (CVDs) are a prominent cause of death and disability across the globe, and this article provides a comprehensive review of the many risk factors for their onset and progression. It investigates how changes in food and exercise might help prevent and treat cardiovascular diseases. It explores the role of eating plans like the Mediterranean diet and plant-based diets in lowering cardiovascular disease risk. The positive benefits of exercise on lowering and controlling CVD risk are also discussed. As an added bonus, the essay delves into the intricate relationship between healthy eating and physical activity as it relates to the prevention and treatment of cardiovascular diseases. Overall, this research article is helpful in that it sheds light on the most important elements that contribute to CVDs and stresses the need of leading a healthy lifestyle to lower the chance of developing CVDs.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others

The Role of Nutrition and Lifestyle in the Prevention and Treatment of Cardiovascular Disease

Lifestyle Strategies for Cardiovascular Risk Reduction

Physical Activity and Cardiovascular Health
Data availability.
Not applicable.
Code availability
Kyrou I, Tsigos C, Mavrogianni C et al (2020) Sociodemographic and lifestyle-related risk factors for identifying vulnerable groups for type 2 diabetes: a narrative review with emphasis on data from Europe. BMC Endocr Disord 20:134. https://doi.org/10.1186/s12902-019-0463-3
Article PubMed PubMed Central Google Scholar
Brinks J, Fowler A, Franklin BA, Dulai J (2017) Lifestyle modification in secondary prevention. Am J Lifestyle Med 11:137–152. https://doi.org/10.1177/1559827616651402
Article PubMed Google Scholar
Stewart J, Manmathan G, Wilkinson P (2017) Primary prevention of cardiovascular disease: a review of contemporary guidance and literature. JRSM Cardiovasc Dis 6:204800401668721. https://doi.org/10.1177/2048004016687211
Article Google Scholar
Franklin BA, Eijsvogels TMH, Pandey A et al (2022) Physical activity, cardiorespiratory fitness, and cardiovascular health: a clinical practice statement of the American Society for Preventive Cardiology Part I: Bioenergetics, contemporary physical activity recommendations, benefits, risks, extreme exerci. Am J Prev Cardiol 12:100424. https://doi.org/10.1016/j.ajpc.2022.100424
Nguyen V, Kim E, Lee S-R et al (2018) Evaluation of strain-rate sensitivity of selective laser melted H13 tool steel using nanoindentation tests. Metals (Basel) 8:589. https://doi.org/10.3390/met8080589
Article CAS Google Scholar
Sharman JE, La Gerche A, Coombes JS (2015) Exercise and cardiovascular risk in patients with hypertension. Am J Hypertens 28:147–158. https://doi.org/10.1093/ajh/hpu191
Joseph P, Leong D, McKee M et al (2017) Reducing the global burden of cardiovascular disease, part 1. Circ Res 121:677–694. https://doi.org/10.1161/CIRCRESAHA.117.308903
Article CAS PubMed Google Scholar
Mertens E, Markey O, Geleijnse JM et al (2018) Adherence to a healthy diet in relation to cardiovascular incidence and risk markers: evidence from the Caerphilly Prospective Study. Eur J Nutr 57:1245–1258. https://doi.org/10.1007/s00394-017-1408-0
Tuttolomondo A, Simonetta I, Daidone M et al (2019) Metabolic and vascular effect of the mediterranean diet. Int J Mol Sci 20:4716. https://doi.org/10.3390/ijms20194716
Article CAS PubMed PubMed Central Google Scholar
Engeda JC, Lhachimi SK, Rosamond WD et al (2020) Projections of incident atherosclerotic cardiovascular disease and incident type 2 diabetes across evolving statin treatment guidelines and recommendations: A modelling study. PLOS Med 17:e1003280. https://doi.org/10.1371/journal.pmed.1003280
Fairchild G, Tasseff B, Khalsa H et al (2018) Epidemiological data challenges: planning for a more robust future through data standards. Front Public Heal. https://doi.org/10.3389/fpubh.2018.00336
Schwingshackl L, Morze J, Hoffmann G (2020) Mediterranean diet and health status: active ingredients and pharmacological mechanisms. Br J Pharmacol 177:1241–1257. https://doi.org/10.1111/bph.14778
Mills KT, Stefanescu A, He J (2020) The global epidemiology of hypertension. Nat Rev Nephrol 16:223–237. https://doi.org/10.1038/s41581-019-0244-2
Drewnowski A, Rehm C (2013) Sodium intakes of US children and adults from foods and beverages by location of origin and by specific food source. Nutrients 5:1840–1855. https://doi.org/10.3390/nu5061840
Maillot M, Vieux F, Rehm CD et al (2019) Consumption patterns of milk and 100% juice in relation to diet quality and body weight among United States children: analyses of NHANES 2011–16 data. Front Nutr. https://doi.org/10.3389/fnut.2019.00117
Aspri M, Papademas P, Tsaltas D (2020) Review on non-dairy probiotics and their use in non-dairy based products. Fermentation 6:30. https://doi.org/10.3390/fermentation6010030
Bertoluci MC, Rocha VZ (2017) Cardiovascular risk assessment in patients with diabetes. Diabetol Metab Syndr 9:25. https://doi.org/10.1186/s13098-017-0225-1
Raghavan S, Vassy JL, Ho Y et al (2019) Diabetes mellitus-related all-cause and cardiovascular mortality in a national cohort of adults. J Am Heart Assoc. https://doi.org/10.1161/JAHA.118.011295
Holt-Lunstad J, Smith TB, Layton JB (2010) Social relationships and mortality risk: a meta-analytic review. PLoS Med 7:e1000316. https://doi.org/10.1371/journal.pmed.1000316
Gallucci G, Tartarone A, Lerose R et al (2020) Cardiovascular risk of smoking and benefits of smoking cessation. J Thorac Dis 12:3866–3876. https://doi.org/10.21037/jtd.2020.02.47
Kotb A, Hsieh S, Wells GA (2014) The effect of telephone support interventions on coronary artery disease (CAD) patient outcomes during cardiac rehabilitation: a systematic review and meta-analysis. PLoS ONE 9:e96581. https://doi.org/10.1371/journal.pone.0096581
Article ADS CAS PubMed PubMed Central Google Scholar
Ali FMH, Nikoloski Z, Reka H et al (2014) The diabetes-obesity-hypertension nexus in Qatar: evidence from the World Health Survey. Popul Health Metr 12:18. https://doi.org/10.1186/1478-7954-12-18
Franklin BA, Thompson PD, Al-Zaiti SS et al (2020) Exercise-related acute cardiovascular events and potential deleterious adaptations following long-term exercise training: placing the risks into perspective–an update: a scientific statement from the American Heart Association. Circulation. https://doi.org/10.1161/CIR.0000000000000749
Nuttall FQ (2015) Body mass index. Nutr Today 50:117–128. https://doi.org/10.1097/NT.0000000000000092
Herforth A, Arimond M, Álvarez-Sánchez C et al (2019) A global review of food-based dietary guidelines. Adv Nutr 10:590–605. https://doi.org/10.1093/advances/nmy130
Arnett DK, Blumenthal RS, Albert MA et al (2019) 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Circulation. https://doi.org/10.1161/CIR.0000000000000678
Cercato C, Fonseca FA (2019) Cardiovascular risk and obesity. Diabetol Metab Syndr 11:74. https://doi.org/10.1186/s13098-019-0468-0
Csige I, Ujvárosy D, Szabó Z et al (2018) The impact of obesity on the cardiovascular system. J Diabetes Res 2018:1–12. https://doi.org/10.1155/2018/3407306
Sacks FM, Lichtenstein AH, Wu JHY et al (2017) Dietary fats and cardiovascular disease: a presidential advisory from the American Heart Association. Circulation. https://doi.org/10.1161/CIR.0000000000000510
Fioranelli M, Bottaccioli AG, Bottaccioli F et al (2018) Stress and inflammation in coronary artery disease: a review psychoneuroendocrineimmunology-based. Front Immunol. https://doi.org/10.3389/fimmu.2018.02031
Dhaka V, Gulia N, Ahlawat KS, Khatkar BS (2011) Trans fats—sources, health risks and alternative approach—a review. J Food Sci Technol 48:534–541. https://doi.org/10.1007/s13197-010-0225-8
Parziale A, Ooms G (2019) The global fight against trans-fat: the potential role of international trade and law. Global Health 15:46. https://doi.org/10.1186/s12992-019-0488-4
Ouimet M, Barrett TJ, Fisher EA (2019) HDL and reverse cholesterol transport. Circ Res 124:1505–1518. https://doi.org/10.1161/CIRCRESAHA.119.312617
Xie Y, Wu Z, Sun L et al (2021) The effects and mechanisms of exercise on the treatment of depression. Front Psychiatry. https://doi.org/10.3389/fpsyt.2021.705559
Herbert C, Meixner F, Wiebking C, Gilg V (2020) Regular physical activity, short-term exercise, mental health, and well-being among university students: the results of an online and a laboratory study. Front Psychol. https://doi.org/10.3389/fpsyg.2020.00509
Klionsky DJ, Abdelmohsen K, Abe A et al (2016) Guidelines for the use and interpretation of assays for monitoring autophagy (3rd edition). Autophagy 12:1–222. https://doi.org/10.1080/15548627.2015.1100356
Chatenet M, Pollet BG, Dekel DR et al (2022) Water electrolysis: from textbook knowledge to the latest scientific strategies and industrial developments. Chem Soc Rev 51:4583–4762. https://doi.org/10.1039/D0CS01079K
Cappelletti S, Daria P, Sani G, Aromatario M (2015) Caffeine: Cognitive and physical performance enhancer or psychoactive drug? Curr Neuropharmacol 13:71–88. https://doi.org/10.2174/1570159X13666141210215655
Romieu I, Dossus L, Barquera S et al (2017) Energy balance and obesity: What are the main drivers? Cancer Causes Control 28:247–258. https://doi.org/10.1007/s10552-017-0869-z
Mozaffarian D, Angell SY, Lang T, Rivera JA (2018) Role of government policy in nutrition—barriers to and opportunities for healthier eating. BMJ. https://doi.org/10.1136/bmj.k2426
Dhingra D, Michael M, Rajput H, Patil RT (2012) Dietary fibre in foods: a review. J Food Sci Technol 49:255–266. https://doi.org/10.1007/s13197-011-0365-5
Ijarotimi OS (2013) Determinants of childhood malnutrition and consequences in developing countries. Curr Nutr Rep 2:129–133. https://doi.org/10.1007/s13668-013-0051-5
Kearney J (2010) Food consumption trends and drivers. Philos Trans R Soc B Biol Sci 365:2793–2807. https://doi.org/10.1098/rstb.2010.0149
Tardy A-L, Pouteau E, Marquez D et al (2020) Vitamins and minerals for energy, fatigue and cognition: a narrative review of the biochemical and clinical evidence. Nutrients 12:228. https://doi.org/10.3390/nu12010228
Pinckard K, Baskin KK, Stanford KI (2019) Effects of exercise to improve cardiovascular health. Front Cardiovasc Med. https://doi.org/10.3389/fcvm.2019.00069
Jiménez SL, Díaz-Lara J, Pareja-Galeano H, Del Coso J (2021) Caffeinated drinks and physical performance in sport: a systematic review. Nutrients 13:2944. https://doi.org/10.3390/nu13092944
Haas TL, Lloyd PG, Yang H, Terjung RL (2012) Exercise training and peripheral arterial disease. In: Comprehensive physiology. Wiley, London, pp 2933–3017
Hasler G (2010) Pathophysiology of depression: Do we have any solid evidence of interest to clinicians? World Psychiatry 9:155–161. https://doi.org/10.1002/j.2051-5545.2010.tb00298.x
Rudrapal M, Khairnar SJ, Khan J et al (2022) Dietary polyphenols and their role in oxidative stress-induced human diseases: insights into protective effects, antioxidant potentials and mechanism(s) of action. Front Pharmacol. https://doi.org/10.3389/fphar.2022.806470
Al-Jawaldeh A, Abbass MMS (2022) Unhealthy dietary habits and obesity: the major risk factors beyond non-communicable diseases in the eastern Mediterranean region. Front Nutr. https://doi.org/10.3389/fnut.2022.817808
Galaviz KI, Narayan KMV, Lobelo F, Weber MB (2018) Lifestyle and the prevention of type 2 diabetes: a status report. Am J Lifestyle Med 12:4–20. https://doi.org/10.1177/1559827615619159
Wiers CE, Vendruscolo LF, van der Veen J-W et al (2021) Ketogenic diet reduces alcohol withdrawal symptoms in humans and alcohol intake in rodents. Sci Adv 7:eabf6780. https://doi.org/10.1126/sciadv.abf6780
Guo N, Zhu Y, Tian D et al (2022) Role of diet in stroke incidence: an umbrella review of meta-analyses of prospective observational studies. BMC Med 20:194. https://doi.org/10.1186/s12916-022-02381-6
Martins GL, Guilherme JPLF, Ferreira LHB et al (2020) Caffeine and exercise performance: possible directions for definitive findings. Front Sport Act Liv. https://doi.org/10.3389/fspor.2020.574854
Malm C, Jakobsson J, Isaksson A (2019) Physical activity and sports—real health benefits: a review with insight into the public health of Sweden. Sports 7:127. https://doi.org/10.3390/sports7050127
Anderson E, Durstine JL (2019) Physical activity, exercise, and chronic diseases: a brief review. Sport Med Heal Sci 1:3–10. https://doi.org/10.1016/j.smhs.2019.08.006
Jung AY, Behrens S, Schmidt M et al (2019) Pre- to postdiagnosis leisure-time physical activity and prognosis in postmenopausal breast cancer survivors. Breast Cancer Res 21:117. https://doi.org/10.1186/s13058-019-1206-0
Willis LH, Slentz CA, Bateman LA et al (2012) Effects of aerobic and/or resistance training on body mass and fat mass in overweight or obese adults. J Appl Physiol 113:1831–1837. https://doi.org/10.1152/japplphysiol.01370.2011
Janssen I, LeBlanc AG (2010) Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int J Behav Nutr Phys Act 7:40. https://doi.org/10.1186/1479-5868-7-40
Download references
Acknowledgements
The authors wish to thank Mr. Joseph Sani Sahjury (Department of Information Technology) for SPSS training during this research.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and affiliations.
Department of Petroleum Chemistry, Faculty of Science, Delta State University of Science and Technology, Ozoro, Nigeria
Princess Oghenekeno Samuel, Great Iruoghene Edo & Gift Onyinyechi Oloni
Department of Chemical Science, Faculty of Science, Delta State University of Science and Technology, Ozoro, Nigeria
Great Iruoghene Edo
Department of Agronomy, Faculty of Agriculture, Delta State University, Abraka, Delta State, Nigeria
Oghenerume Lucky Emakpor
Department of Biotechnology, Faculty of Science, Delta State University, Abraka, Nigeria
Gracious Okeoghene Ezekiel
Department of Urban and Regional Planning, Faculty of Environmental Sciences, Delta State University, Abraka, Nigeria
Arthur Efeoghene Athan Essaghah
Department of Nursing Science, Basic Medical Sciences, Delta State University, Abraka, Nigeria
Endurance Agoh
Department of Nursing, Faculty of Health Sciences, Cyprus International University, Nicosia, Turkey
Joy Johnson Agbo
You can also search for this author in PubMed Google Scholar
Contributions
GE, PS, OE, EA, JA, GO, GE, AE were responsible for the conception and design of the study. GE, PS, OE, EA, JA performed data collection. GE, PS performed data analysis and drafted the article. GE supervised the study, contributed to data analysis, interpretation, and critical revisions. All authors approved the final manuscript.
Corresponding author
Correspondence to Great Iruoghene Edo .
Ethics declarations
Conflict of interest.
The authors declare no conflict of interest.
Consent to participate
Consent for publication.
All authors have read and agreed to the published version of the manuscript.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Samuel, P.O., Edo, G.I., Emakpor, O.L. et al. Lifestyle modifications for preventing and managing cardiovascular diseases. Sport Sci Health 20 , 23–36 (2024). https://doi.org/10.1007/s11332-023-01118-z
Download citation
Received : 22 February 2023
Accepted : 14 August 2023
Published : 22 August 2023
Issue Date : March 2024
DOI : https://doi.org/10.1007/s11332-023-01118-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Cardiovascular diseases
- Find a journal
- Publish with us
- Track your research
Disease Prevention

Chronic diseases —including heart disease , stroke , diabetes , and cancer — account for some of the most common health problems in the United States, according to statistics from the Centers for Disease Control and Prevention (CDC). Yet many of these chronic diseases are preventable, as they’re linked to poor diet and lifestyle choices including tobacco use, excessive alcohol consumption, and inadequate physical activity.
The CDC reports some sobering statistics about Americans:
- Chronic diseases are the leading causes of death and disability.
- 70% of annual deaths are due to chronic diseases.
- These preventable conditions not only compromise quality of life, they add to rising health care costs—75% of our health care dollars are devoted to treat these diseases.
- Among adults ages 20 to 74, diabetes remains the leading cause of kidney failure, blindness, and non-traumatic lower-extremity amputations.
The good news is that you have the power to help prevent chronic disease, as making positive diet and lifestyle changes can help reduce risk. Eating healthy foods , getting enough exercise , and refraining from tobacco and excessive alcohol use confer numerous health benefits—including possibly preventing the onset of chronic diseases.
Terms of Use
The contents of this website are for educational purposes and are not intended to offer personal medical advice. You should seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The Nutrition Source does not recommend or endorse any products.
- Reference Manager
- Simple TEXT file
People also looked at
Review article, prioritized research for the prevention, treatment, and reversal of chronic disease: recommendations from the lifestyle medicine research summit.

- 1 Department of Surgery, University of Pittsburgh, Pittsburgh, PA, United States
- 2 Department of Medicine, George Washington University School of Medicine, Washington, DC, United States
- 3 Department of Nutrition, Harvard T.H. Chan School of Public Health, Boston, MA, United States
- 4 School of Education, University of Pittsburgh, Pittsburgh, PA, United States
- 5 American College of Lifestyle Medicine, Chesterfield, MO, United States
- 6 Community Care, Pittsburgh, PA, United States
- 7 Department of Psychiatry, University of Pittsburgh, Pittsburgh, PA, United States
- 8 Department of Medicine, University of Pittsburgh, Pittsburgh, PA, United States
- 9 Department of Physical Medicine and Rehabilitation, University of Pittsburgh, Pittsburgh, PA, United States
- 10 Institute for Bioengineering of Catalunya, Barcelona Institute of Science and Technology, Catalan Institute of Advanced Studies, Barcelona, Spain
- 11 Department of Internal Medicine, Rush University Medical Center, Chicago, IL, United States
- 12 American Heart Association, Dallas, TX, United States
- 13 Lifestyle Medical, Riverside, CA, United States
- 14 Department of Internal Medicine, University of Arizona, Tucson, AZ, United States
- 15 United States Air Force, Washington, DC, United States
- 16 Department of Physical Medicine and Rehabilitation, Veterans Administration Boston Healthcare System, Boston, MA, United States
- 17 True Health Initiative, Derby, CT, United States
- 18 Department of Pediatrics, University of Pittsburgh, Pittsburgh, PA, United States
- 19 Department of Environmental Health Sciences, University of California, Los Angeles, Los Angeles, CA, United States
- 20 Department of Pediatrics and Environmental Medicine, New York University, New York, NY, United States
- 21 Department of Family Medicine and Population Health, Virginia Commonwealth University, Richmond, VA, United States
- 22 Division of Geriatrics and Clinical Gerontology, National Institute on Aging, Bethesda, MD, United States
- 23 Department of Family Medicine, University of Pittsburgh, Pittsburgh, PA, United States
- 24 Phipps Conservatory and Botanical Gardens, Pittsburgh, PA, United States
- 25 Department of Medicine, Preventive Medicine and Public Health, Loma Linda University, Loma Linda, CA, United States
- 26 Ardmore Institute of Health, Ardmore, OK, United States
- 27 University of Pittsburgh Medical Center Health Plan/WorkPartners, Pittsburgh, PA, United States
Declining life expectancy and increasing all-cause mortality in the United States have been associated with unhealthy behaviors, socioecological factors, and preventable disease. A growing body of basic science, clinical research, and population health evidence points to the benefits of healthy behaviors, environments and policies to maintain health and prevent, treat, and reverse the root causes of common chronic diseases. Similarly, innovations in research methodologies, standards of evidence, emergence of unique study cohorts, and breakthroughs in data analytics and modeling create new possibilities for producing biomedical knowledge and clinical translation. To understand these advances and inform future directions research, The Lifestyle Medicine Research Summit was convened at the University of Pittsburgh on December 4–5, 2019. The Summit's goal was to review current status and define research priorities in the six core areas of lifestyle medicine: plant-predominant nutrition, physical activity, sleep, stress, addictive behaviors, and positive psychology/social connection. Forty invited subject matter experts (1) reviewed existing knowledge and gaps relating lifestyle behaviors to common chronic diseases, such as cardiovascular disease, diabetes, many cancers, inflammatory- and immune-related disorders and other conditions; and (2) discussed the potential for applying cutting-edge molecular, cellular, epigenetic and emerging science knowledge and computational methodologies, research designs, and study cohorts to accelerate clinical applications across all six domains of lifestyle medicine. Notably, federal health agencies, such as the Department of Defense and Veterans Administration have begun to adopt “whole-person health and performance” models that address these lifestyle and environmental root causes of chronic disease and associated morbidity, mortality, and cost. Recommendations strongly support leveraging emerging research methodologies, systems biology, and computational modeling in order to accelerate effective clinical and population solutions to improve health and reduce societal costs. New and alternative hierarchies of evidence are also be needed in order to assess the quality of evidence and develop evidence-based guidelines on lifestyle medicine. Children and underserved populations were identified as prioritized groups to study. The COVID-19 pandemic, which disproportionately impacts people with chronic diseases that are amenable to effective lifestyle medicine interventions, makes the Summit's findings and recommendations for future research particularly timely and relevant.
Introduction
A recent 60-years review of mortality in the United States, with special focus on the past two decades, revealed declining life expectancy that is particularly pronounced in ages 25–44, typically Americans' most productive years. The primary causes of this increase in midlife mortality were unhealthy behaviors, such as drug and alcohol use, suicides, hypertensive diseases, diabetes, and obesity which collectively have taken a (largely preventable) toll on both the length and quality of life of Americans relative to peers in other high-income countries ( 1 ).
The disparity between leading causes of death and federal research spending was recently highlighted in a review of the U.S National Institutes of Health (NIH) Prevention Research Portfolio for the period 2012–2017 ( 2 ). Eleven-thousand studies characterized as primary or secondary research studies, comprising 17% of total NIH research spending, were identified for analysis. Only 26% of those studies addressed a leading cause of death as the outcome of interest (e.g., heart disease, cancer, injury, etc.). One third of the studies addressed one of the leading risk factors for death, such as diet, tobacco use, high blood pressure, weight, elevated blood sugar, and high cholesterol. A third addressed the leading causes of disability. Randomized, placebo-controlled interventional trials, the highest level of evidence for clinical interventions, comprised 25% of spending. Only 3% of the studies addressed multiple risk factors or behaviors (as they typically co-occur in a population); 20% involved youth; 10% studied elderly, urban populations or women, particularly pregnant women; 5% or fewer of the studies focused on low income, rural, sexual and gender, underrepresented race/ethnicity groups, institutionalized, or the disabled populations. Essentially no studies evaluated the use of lifestyle interventions to treat and reverse the major chronic diseases that increasingly are the primary root causes of premature mortality and costly morbidity. This disparity is especially glaring given the major advances across a host of basic and translational science methodologies that have received extensive NIH funding and have helped set the stage for Precision Medicine application across a wide range of diseases.
Lifestyle Medicine addresses the use of a whole-food, plant-predominant diet, regular physical activity, restorative sleep, stress management, avoidance of risky substances and positive emotions/social connection as a primary therapeutic modality for treatment and reversal of chronic disease ( 3 ). Given the aforementioned paucity of studies focused on lifestyle medicine and the rapid methodological advances impacting numerous aspects of the biomedical enterprise, leading national experts were invited to review existing knowledge and gaps relating lifestyle behaviors to common chronic diseases, such as cardiovascular disease, diabetes, cancer, inflammatory- and immune-related disorders and other conditions. The 2-days Lifestyle Medicine Research Summit ( 4 ) prioritized major research questions from basic science to population health. This intentionally broad but interrelated perspective included lifestyle-induced or -associated inflammation; immune dysfunction; cellular dysbiosis; microbiome alterations; neuroplasticity; genomics, epigenetics, proteomics, metabolomics, and computational and systems approaches for assessing health and disease. Innovative research methodologies considered included new approaches to clinical trials design, in silico (computer) modeling, and opportunities for population-based and/or banked serological/specimen investigations using existing cohorts. The foundational and synergistic roles of sociocultural influences, built environment, and environmental exposures as well as the need to focus on underserved and understudied populations were also emphasized. Notably, the Summit was the first lifestyle medicine meeting with so wide-ranging an interdisciplinary scope.
The potential clinical impact of applying lifestyle medicine practices to the leading causes of disease begins by understanding their biological impact, especially on the common, inflammation-mediated pathways leading to multi-organ and -system disease ( 5 , 6 ) [ Figure 1 ; adapted from Figure 3, Bodai et al. ( 5 ) with permission from The Permanente Press]. The health effects of diet, sedentary lifestyle, chronic stress, medications (often used to treat lifestyle-determined conditions), and other aspects of lifestyle (sleep, substance use, emotions and attitudes, positive psychology and social connection) are mediated through common subcellular, epigenetic, and other mechanisms and to create dysbiosis (a state in which gastrointestinal flora become unbalanced or perturbed), cellular stress and injury (often in the form of oxidative stress). These biological pathways often culminate in the inflammatory response, which then feeds back to drive further cellular stress, dysbiosis, and related epigenetic changes to create a self-sustaining state of chronic inflammation. In turn, chronic systemic inflammation is an early precursor for heart disease; Type 1 and 2 diabetes and depression; and a variety of other endocrine, autoimmune, rheumatologic, and neurological disorders ( Figure 1 ). A multitude of computational and systems biology approaches are elucidating the interconnections among these processes in the context of specific diseases and distinct sub-populations. While this emerging knowledge has been helpful in elucidating biological mechanisms, it has not made a major impact on clinical practice or lifestyle medicine research.
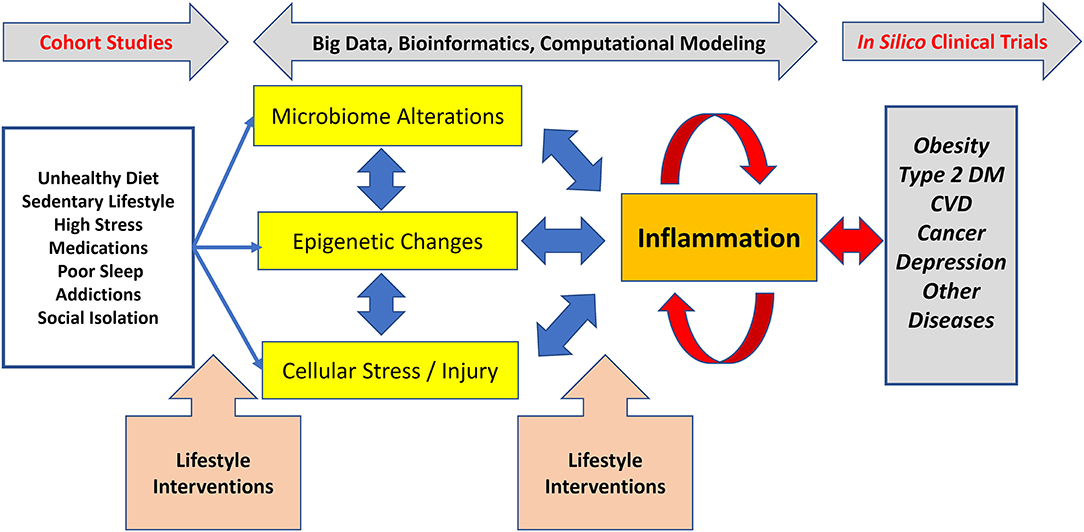
Figure 1 . Lifestyle-associated pathogenesis, interventions, and emerging methods for lifestyle medicine research. Unhealthy lifestyles cause dysregulation in the microbiome, epigenetic changes, and various types of cellular stress and injury which, together, drive inflammation. In turn, inflammation can drive further derangements in the microbiome, can cause distinct epigenetic changes, and can drive further cellular stress and injury. This positive feedback leads to a process wherein inflammation becomes chronic and self-sustaining, ultimately resulting in chronic diseases, such as Type 2 diabetes. The non-linear nature of these processes means that simple reductionist approaches to understanding the connections between lifestyle mismanagement and chronic disease are likely to fail. Effective lifestyle interventions prevent, treat, and reverse common chronic diseases. To accelerate the adoption and dissemination of clinical lifestyle medicine interventions, there is a need for cutting edge biological and computational approaches decipher this complexity. Adapted from Figure 3, Bodai et al. ( 5 ) with permission from The Permanente Press.
The Summit convened cross-disciplinary subject matter experts to address these knowledge gaps by exploring the synergy among emerging sciences, innovative research methodologies and populations, and the major domains of lifestyle medicine. We hypothesized that this multi-dimensional and multi-disciplinary intersection of perspectives ( Figure 1 ) has the potential to create new insights and cross-sectoral strategies to articulate and explore potential breakthrough research priorities for scientists, clinicians, and funding agencies who are seeking more effective means to address health, medical care, and population health challenges. The overarching goal of the Summit was to inform the research community as well as public and private funding agencies. It sought to “close the gap” between what is known and what needs to be discovered to accelerate the further development and deployment of lifestyle medicine practices primarily but not exclusively in the clinical setting.
Foundational Understanding of Common Pathways: Inflammation, Epigenomics, the Microbiome, and Neuroplasticity
Inflammation, a prototypical complex system with positive and negative feedbacks ( 7 ), plays a key role in linking lifestyle (mis)management to downstream pathobiology ( 8 ) ( Figure 1 ). Inflammation is an adaptive response to stress that regulates multiple physiological processes, including the immune response, both positively and negatively ( 8 ). In turn, inflammation is itself regulated at multiple levels, including a newly appreciated role with metabolites such as glucose and lactate ( 9 ) and for related epigenetic changes ( 10 ) that are affected by lifestyle (e.g. diet) ( 11 ) ( Figure 1 ). Furthermore, inflammation regulates – and is regulated by – changes in the microbiome ( Figure 1 ) and, ultimately, by neural circuits that also regulate the microbiome and vice versa ( 12 ). This “neuroplasticity,” or the changeability of brain processes and pathways formerly presumed to be “fixed,” which is increasingly understood as a significant component of the “mind-body” mechanism ( 13 ). Microbiome changes occur with diet, sleep, exercise, stress, addiction, and the built as well as natural environment ( 14 ).
The conceptual framework for aging have also changed, from focusing only at the terminal stages of life to thinking across the entire lifespan, including the construct of “healthspan” (i.e., the length of time that the person is healthy, not merely alive) ( 15 ). Understanding how the body brings itself into balance (homeostasis) and the beneficial effects of stress below a certain level (hormesis) are also areas of increasing research interest related to healthspan. How much one exercises (type, frequency, duration, timing, intensity, etc.) and how much (and what) one eats (pattern, timing, quality, etc.) are clearly linked to potentially persistent epigenetic changes ( 11 ). We expand on these concepts below.
Inflammation, a common end pathway for multiple diseases promoted by lifestyle behaviors and “mismanagement,” is often assessed using relatively non-specific biomarkers, such as C-reactive protein and the erythrocyte sedimentation rate. When studying the impact of lifestyle on specific inflammatory mediators it is important to note that correlation does not imply causality. Accordingly, there is a major need to combine targeted inflammation biomarkers (e.g., interleukin-6 or tumor necrosis factor-α) with an unbiased approach involving systems and computational biology that takes into consideration state-of-the-art ‘omics methodology and concepts in order to define the impact of lifestyle (mis)management on inflammation-associated chronic diseases ( Figure 1 ). As discussed in the following sections, this need introduces the intertwined discussions of emerging computational methodology and appropriate study cohorts.
Current and Future Research Models: Roles for Big Data, Artificial Intelligence, and in silico Modeling
In parallel with the growing application of computational methods to biomedicine in general, machine learning (the method by which computers interpret data, also lumped together with “Big Data” (which refers to the increasingly large amount of data of multiple types obtained from multiple sources that are the starting point for machine learning) or “Artificial Intelligence” (involving a computer's ability to make decisions based on data analysis that would otherwise require human intervention) ( 16 ) have found increasing use in lifestyle medicine, predominantly in the area of epidemiology ( Figure 1 ; see below). Collectively, these approaches are based on the use of computer algorithms to generate statistically grounded models based on various correlations within data, with the goal of discovering hidden or non-intuitive (and often non-linear) associations or predictive features; there has been much discussion of the application of machine learning approaches in medicine, though this is still an emerging field ( 17 ). Epidemiology is advancing in many directions, building upon a longstanding track record of successful application of traditional epidemiological methods. The past 10–15 years have brought a major paradigm shift known as “Systems Epidemiology,” based on nutritional genomics, nutritional metabolomics, the nutritional microbiome, and metagenomic analysis ( 12 , 18 ). These “omics”-based methods have been facilitated by the rapid improvements in technology and concomitant drop in cost, especially for genomic sequencing. The Big Data approach has also improved dramatically in the past 10–20 years, with initial primary focus on traditional risk factor analysis now expanded to high-dimensional data analysis, network analysis, and pathway analysis ( 12 , 18 ). One key pitfall to these statistically based approaches is that many identified associations do not necessarily reflect causal relationships, though well-performed studies address key confounders and incorporate biological pathways. Another, related pitfall to these approaches, the so-called “curse of dimensionality,” is that in a very real sense the data generated are actually “Small Data,” wherein very large amounts of data (e.g., 400,000 DNA methylation sites) are generated from a relatively small number of subjects (e.g., 400 patients, often sampled at only one or two time points), which can lead to highly over-fit statistical models without external validation ( 19 ). Thus, it is difficult to try to use purely data-centered approaches to get a comprehensive understanding of the dynamic impact of lifestyle on biology and vice versa . For example, network diagrams are static representations of data that can help suggest connections and formulate hypotheses (including in highly complex settings, such as the brain connectome or acute inflammation). However, even when derived from data obtained at multiple time points, these static models cannot be played backward to understand where the changes came from or to discover emergent phenomena ( 20 ). An alternative approach, “mechanistic computational modeling,” involves encoding key interactions and mechanisms as differential equations or “agents” in agent-based models. Mechanistic modeling is dynamic modeling, meaning that the models are meant to be played forward and tested against data obtained over time, and can also be played backward to gain insights as to why a given phenomenon might have occurred. This modeling approach can be used to generate “digital twins” (by calibrating these mechanistic models to data in individuals) and virtual population—or virtual ( in silico ) clinical trials. Notably, these methods were pioneered in studying inflammation ( 20 ). Importantly, data-driven and mechanistic modeling approaches can and should be used in tandem to leverage their respective strengths while minimizing their weaknesses ( 20 ).
Lifestyle medicine would be a key domain wherein in silico clinical trials and other forms of “Network Medicine” could prove invaluable ( Figure 1 ), since it is often neither possible to carry out true randomized controlled trials of dietary or other lifestyle modifications ( 21 ) nor to reduce symptoms to single underlying mechanistic causes ( 20 ) (see also below). The use of computational models to capture the multi-factor and multi-scale organization of pathologies introduces a paradigm in which theory-driven biology can lead to theory-driven, rather than largely empirical, clinical interventions ( 20 ). Examples include work in stroke rehabilitation, where neuroscience theory has been used to develop technology-driven, patient-centered solutions shifting interventions from peripheral manipulation to central functional re-organization using AI techniques combined with virtual reality content delivery ( 22 ). Ultimately, however, computational models are by definition hypotheses ( 20 ). Both mechanistic models and some classes of machine learning models (e.g., a network depiction of the data), are forms of hypotheses about relationships, and so there should not be a tension between these in silico approaches and the “pure” hypothesis-driven approaches ( 23 , 24 ).
The foregoing discussion emphasizes the crucial need to define the populations that should be studied and the types of data to be collected to facilitate in silico approaches. Populations exist within communities, defined either geographically or by shared demographic, cultural, behavioral or disease characteristics. The data typically used in Systems Epidemiology analyses are derived from the subjects of cohort studies, observational cohorts, and dietary intervention studies, as well as from electronic health records ( 25 ). For example, these include large and well-established cohorts, such as the Framingham Heart Study ( 26 ), the Nurses' Health Study ( 27 ), the UK Biobank ( 28 ), etc. In the past several decades, these studies have collected extensive data on diet, lifestyle, genetics, biomarkers, and health outcomes, which now also incorporates technology-derived elements, such as geographic information systems (GIS) data and other “digital phenotyping” data using multiple personal devices. The Adventist Health Studies conducted by Loma Linda University have involved nearly 100,000 participants for more than six decades ( 29 ). This long-term epidemiologic research has assessed the long-term relationship between lifestyle, diet, disease, and mortality among Seventh-day Adventists. The Department of Defense (DoD) Serum Repository, in existence since 1985, collects 2 million serum specimens per year from active duty military members for surveillance of operationally-relevant conditions ( 30 ). The DoD also conducts the Millennium Cohort Study, initiated in 1999 to understand military service members' health longitudinally both during and after a military career ( 31 ). Innovative, birth-to-high school age, community-based cohorts, such as the newly launched Pittsburgh Study ( 32 ) create new partnerships and opportunities to understand the complex interactions among individual, family, community, and environmental factors that contribute to disease, educational and social outcomes that are amenable to evidence-based interventions. The NIH “All of Us” Cohort study creates another unique opportunity to combine “Big Data” analytics and with state-of-the-art in silico modeling capabilities to examine the complex interactions between genomics and the environment on health and disease outcomes ( 33 ).
A major focus of any lifestyle medicine study—whether observational or interventional—is data quality. This is particularly important because most lifestyle data are self-reported. Keys to improving the quality of self-reported data include the use of validated and standardized questionnaires, the repeated measures of diet and lifestyle, high follow-up rates, and the complementary use of objective biomarkers. When the field moves into the “omics” era, although the genotyping data are highly accurate, the “noise” existing in other types of “omics” data (especially epigenomics and meta-genomics data) are substantial, and thus quality control and careful data analyses and interpretation are critical. An important element in understanding the biologic impact of lifestyle is the dynamics of molecular and cellular processes, which dovetails with the use of dynamic computational modeling methods ( Figure 1 ). Intertwined with the need to obtain data at multiple time points is the need for retention of subjects in the study cohort for years or decades, which is a major challenge. Another major challenge is the use of appropriate methodology to synthesize the vast amount of data through systematic reviews and meta-analyses, which should be conducted with caution and interpreted in light of the broader context of the field ( 25 ).
Patients exist within communities, embedded in complex interactions with their environment—the social, cultural, political, pharmacological, and economic environment—which is intrinsically connected to their lifestyle and their health. This complex collection and integration of multiple personal and potentially sensitive data sources will require intensive efforts, and new approaches to ensure the understanding, trust, and consent of studied populations. This may be particularly challenging when partnering with groups and communities that have been underserved or understudied and discriminated against, and/or are often the most susceptible to poor health outcomes associated with lifestyle behaviors and unhealthy environments.
Lifestyle Medicine Domain-Specific Findings and Recommendations
Subject matter experts for each of the lifestyle medicine domains provided an overview of the current scientific knowledge and made recommendations for prioritized research to accelerate the understanding and use of clinical application to prevent, treat and reverse those diseases.
Nutrition Overview and Prioritized Research
Cardiovascular disease.
The etiology of cardiovascular disease (CVD) has been elucidated through the definition of risk factors in epidemiologic studies, notably the Framingham Study, initiated in 1948 ( 34 ). Interventional trials using relatively simple diet changes demonstrated rapid reduction of these risk factors and clinical benefits ( 35 , 36 ). Interventional trials have demonstrated how a Mediterranean eating pattern significantly reduced cardiovascular events ( 37 ). More comprehensive interventions using a variety of lifestyle factors including diet have not only reduced but actually reversed existing coronary disease ( 38 , 39 ), but these studies were small and of short-duration. In contrast to the notion that CVD occurs largely as a direct function of aging, research on the roles of dyslipidemia and inflammation creates new research opportunities for clinical and population-based interventions. Cardiovascular disease begins in childhood or even in utero , as demonstrated when mothers who have obesity give birth to children with thickened vasculature ( 40 ), perhaps even with early loss of lumbar arteries ( 41 ). Lifestyle medicine research should therefore prioritize children, as adult behaviors often begin in childhood.
There is emerging evidence to support the benefits of plant-based dietary patterns in primary prevention of CVD. Long-term epidemiologic studies have found that a healthful plant-based diet (that does not necessarily exclude all animal products) was associated with a significantly lower risk of type 2 diabetes and CVD ( 42 ). Small intervention studies have shown that a shift from a typical western diet to a vegan diet substantially lowered a atherogenic gut flora metabolite called trimethylamine-N-oxide (TMAO) which is induced by higher consumption of animal products especially red meat ( 43 ). Similarly, circulating lipoprotein (a) (Lp(a)), an established CVD risk factor that was previously thought to be genetically determined, has been shown to improve with plant-based diets ( 44 ). These observed health benefits of plant-based dietary patterns suggest other areas of inquiry that integrate basic, clinical, and translational research, especially when conducted within the cultural context of high-risk communities. Larger-scale, community-based interventional trials using adapted plant-based diets which are culturally sensitive to dietary traditions focusing on the African-American populations are underway ( 45 ).
The World Cancer Research Fund and American Institute Cancer Research Fund have summarized evidence on cancer risk factors ( 46 ). The cancers most affected by diet and lifestyle behaviors are those of the gastrointestinal tract (e.g., colorectal) and hormonal cancers (e.g., breast and prostate). The Women's Health Initiative study (WHI) ( 47 ) was conducted to study cancer prevention and, while well-designed, utilized a weak dietary intervention. Thus, WHI yielded only a small difference in outcomes between the intervention and control arms and did not find significant benefits of the low-fat interventions on breast cancer incidence. However, a secondary analysis of WHI found that the low-fat pattern significantly improved overall survival among post-menopausal breast cancer patients ( 48 ). On the other hand, a clinical trial of breast cancer patients that dramatically increased consumption of fruits, vegetables, and fiber had no appreciable effect on breast cancer recurrence or mortality ( 49 , 50 ).
Type 1 diabetes (“insulin-dependent diabetes” as the pancreas is unable to produce insulin) and Type 2 diabetes (“insulin-resistant diabetes” in which the body produces insulin but tissues are not able to respond to it) are both strongly linked to nutrition.
Excess adiposity is the strongest determinant of type 2 diabetes. The association of type 2 diabetes with dietary patterns is well-established, most notably the dramatic difference in type 2 diabetes prevalence in daily meat eaters when compared to vegans ( 51 ). At the tissue level, studies using magnetic resonance imaging have demonstrated lipid deposition in muscle and liver cells, leading to insulin resistance ( 52 ). Interventional trials using plant-based diets suggest that these diets can improve and potentially even reverse the course of diabetes ( 53 ).
The dietary etiology of type 1 diabetes needs to be explored further to test the various dietary factors that have been hypothesized to trigger the production of antibodies to insulin-producing cells including cow's milk ( 54 ), gluten, preservatives, such as nitrosamines, and low vitamin D levels. Clinical trials have not yet explored the role of plant-based diets for type 1 diabetes prevention and management. The association of prolonged breastfeeding with low rates of type 1 diabetes also needs to be explored further.
Autoimmune Diseases
Several studies have shown substantial benefits of plant-based diets for controlling rheumatoid arthritis, suggesting a role for dietary interventions not only for rheumatoid arthritis but also for auto-immune diseases more broadly ( 55 ).
Hormonal Conditions
Studies in the 1990's demonstrated that estrogen levels increase with high fat consumption and decrease with fiber intake, which is of particular relevance for breast cancer, dysmenorrhea, endometriosis, fibroids, and infertility ( 56 ).

Brain Health and Neurological Conditions
Observational studies ( 57 ) have demonstrated that a lower intake of saturated and trans fats is associated with greatly reduced risk of developing Alzheimer's disease. These findings are now being studied with the MIND Trial ( 58 ), among other studies using largely plant-based diets. Short-term dietary interventions have been shown to improve depression scores in both normal individuals ( 59 ) and those with depressive symptoms, the latter finding in both young ( 60 ) and general ( 61 ) populations. The dietary interventions typically reduce saturated fat and increase consumption of plant-based foods. Randomized trials have also supported a role for aerobic exercise in the treatment of depression in a dose-related manner ( 62 ). More clinical trials are needed both for cognitive and mood disorders.
Renal Disease
The beneficial role of plant-based diets in treating and potentially reversing chronic kidney disease is being explored. Kidney disease is particularly common among African-Americans and is mediated through diet and the APOL-1 gene ( 63 – 65 ). The Adventist Health Studies have shown significant inverse associations between plant-based dietary patterns and risk of type 2 diabetes and total mortality among African-Americans ( 66 ), suggesting the possibility of benefit for reducing renal failure in this population.
In summary, strong, well-designed and -powered intervention studies using appropriate comparator groups are needed to advance the understanding of plant-predominant eating on the prevention and treatment of a wide array of diseases. High priority populations include children ( 41 ) and understudied, underserved, and disadvantaged populations with highest incidence of multiple diet-impacted disease. Emphasis should be placed on human rather than animal studies.
Studies should also focus on our current understanding of diet quality ( 52 , 67 ) considering the quality of fats, carbohydrates, and protein not merely their relative proportions. Sources of animal- vs. plant-based proteins and high quality low or high fat, low or high carbohydrate consumption, and quality of overall diet need to be specified more precisely in study designs. Large cohort studies have shown that long-term consumption of plant-based (as compared to animal-based) protein is associated with lower all-cause and cardiovascular disease mortality ( 68 , 69 ). The associations of low-carbohydrate diets (LCDs) and low-fat diets (LFDs) with mortality may depend on the quality and food sources of macronutrients rather than the carbohydrate or fat proportionate content alone ( 70 ).
Plant-predominant nutrition research priorities appear in Table 1 .
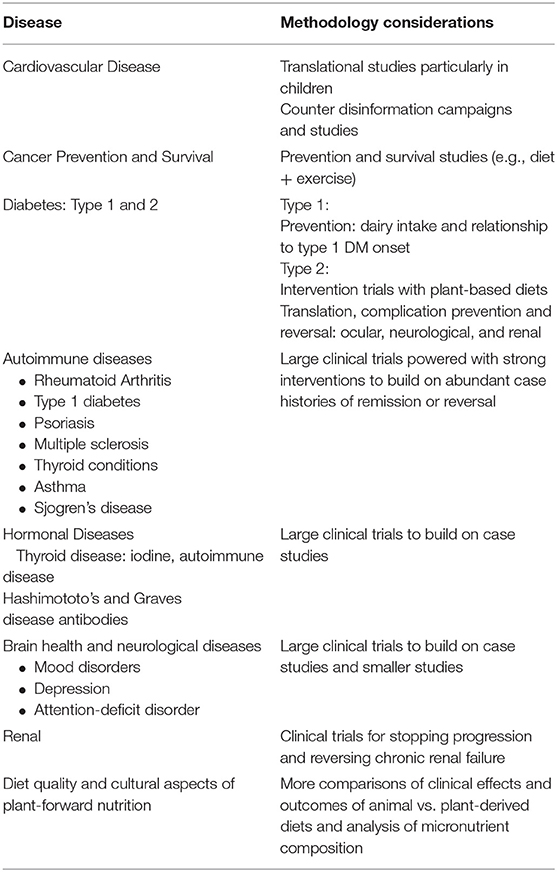
Table 1 . Nutrition research priorities.
Physical Activity Overview and Prioritized Research
Physical activity is recognized as a key behavior related to the prevention and treatment of many chronic diseases and other health-related conditions. Exercise is associated with mitigation of stress and depression ( 71 ). The evidence to support the health benefits of physical activity have been accumulating for decades. Some of the early research to support the health benefits of physical activity came from observational studies, such as studies of transit employees or other types of occupations ( 72 ). These studies showed that individuals with more occupational physical activity had lower risk of mortality and some morbidities than those individuals in more sedentary occupations. These observations provide a foundation of scientific study to support the importance of physical activity as a key lifestyle behavior to promote health and well-being.
There have been key publications and reports over the past few decades that summarize the evolving list of health benefits of physical activity along with key contemporary considerations for the promotion of a physically active lifestyle ( 73 – 75 ). For example, the initial Surgeon General's Report and the 2008 Physical Activity Guidelines stated that physical activity should be accumulated in bouts of at least 10 min to achieve an average of 30 min per day of moderate-to-vigorous physical activity ( 73 – 75 ). In addition to common recommendations for the amount of physical activity that may be needed to improve health, guidance on how to achieve this amount has evolved over time. The 2018 Physical Activity Guidelines Advisory Committee suggested that all moderate-to-vigorous physical activity, regardless of the length of bout in which it was accumulated, contributed to the potential health benefits ( 75 ).
Another important area of study involves sedentary behavior, mostly in the form of sitting, and how it contributes to poor health. Research now suggests that sedentary behavior may have negative influences on health that are independent of participation in moderate-to-vigorous physical activity. This has resulted in new recommendations that persons should sit less and move more to improve health ( 75 ).
Molecular, Cellular, and Aging Mechanisms
Understanding physical activity-induced effects on molecular, sub-cellular, cellular, tissue, organ systems, and intra-systems (e.g., cardiovascular and central nervous system) can now be pursued ( 76 ) ( Figure 1 ). The cellular and molecular mechanisms of physical activity-induced health benefits are becoming better understood ( 77 ). Comprehensive models are being created that include both inherent (genetic and epigenetic) and acquired factors (age, disease state, environment, fitness, and nutrition), which together determine individual differences in how physical activity impacts health and disease ( Figure 1 ).
Why we age and the rate at which we age, i.e., chronological age vs. biological age or lifespan vs. healthspan—are determined by multiple molecular processes. Exercise stimulates stem cell self-renewal in brain, muscle, and other tissues ( 78 ). Telomere shortening, bioenergetics, mitochondrial function, and a variety of pleiotropic effects affect biological aging and the development of age-related conditions. The exploration of “exerkines” and epigenetic mechanisms may yield insights into the signaling pathways that connect exercise and cognitive function as well as other observed improvements ( 79 , 80 ) ( Figure 1 ).
Better understanding of the factors that promote adopting and sustaining health behaviors generally, and regular physical activity specifically, is needed. Exercise and physical activity are more likely to be incorporated into daily living when tied to one's personal life goals, mission, aspiration, and purpose. Health coaching ( 81 ) and the use of digital or other trackers, feedback and social support either in person or through virtual groups have been shown to improve initiation and reinforcement of activity and healthier behaviors. Long-term healthy habit improvement and adoption are most likely when incremental small steps are introduced, achieved, and reinforced ( 82 ). Other important factors to increase successful engagement include clinician modeling of desired behaviors and a clinical systems approach using multi-disciplinary teams, the “prescription” of lifestyle behaviors, and support which elevates the importance of their therapeutic use and impact as embodied in “exercise as medicine” ( 81 , 83 ).
Physical activity research priorities appear in Table 2 .
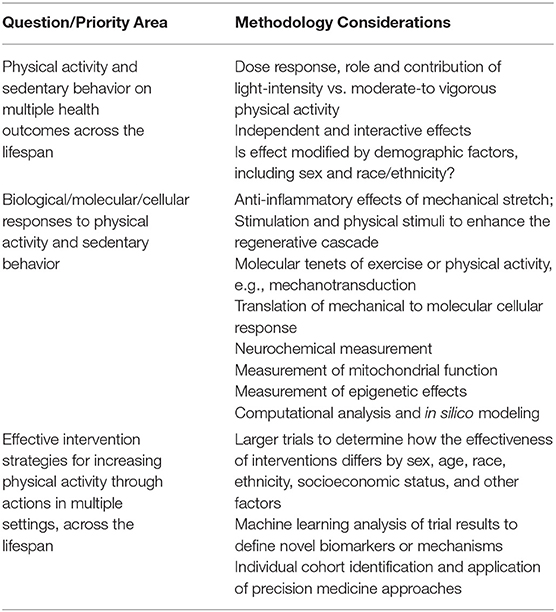
Table 2 . Physical activity research priorities.
Sleep Overview and Prioritized Research
The sleep/wake cycle is the most enduring and obvious manifestation of the circadian timing system which can influence inflammation, immune dysfunction, oxidative stress, and epigenetic modification, all associated or causally related with the onset and disease ( Figure 1 ). Sleep is defined as a recurring, reversible, neuro-behavioral state of relative perceptual disengagement from and unresponsiveness to the environment. Sleep optimizes adaptation and function at every level of biological organization: molecular energy function, cellular, tissue, circuit organ, organ system, systemic physiology cognition and affect. Sleep and wakefulness exist within the 24-h rhythms that organize almost every aspect of our physiology. Every cell has a circadian clock that rests on a transcription-translation feedback pathway involving nine core clock genes which regulate their own transcription every 24 h ( 84 ). The “master pacemaker,” the suprachiasmatic nucleus of the hypothalamus located above the optic chiasm, receives light-dark inputs ( 85 ). Endogenous rhythmicity occurs within cells determining such functions as core body temperature and cortisol production which vary over 24-h periods. Performance, which varies during the course of each day and among individuals, can be expressed as “chronotype” viz the preference for evening or morning hours. Sleep can be measured by self-report, actigraphy, electrophysiologic sleep studies ( 86 ), brain imaging, and even in cultured tissue outside the body ( 87 ). Circadian variation of gene expression is not only important for disease but also for therapeutics of those diseases ( 88 ). The circadian timing system impacts, is impacted by, and receives feedback regulation from health behaviors, such as physical activity, sleep, eating, and light-dark cycles ( 89 ). These clocks in the brain and cells regulate brain and body function that determines physiology, behavior, and performance.
Behaviors change the timing of the clock, and in turn the clock affects all of the health behaviors that lead to disease. Sleep ultimately optimizes function at every level of biological organization from molecules to entire organisms. Sleep provides protection from oxidative stress ( 90 ) and clears the brain of waste and breakdown materials that accumulate during wakefulness. The so-called “glymphatic system,” a lymphatic system for the brain, helps clear beta-amyloid and other proteins in the cerebrospinal fluid interstitial spaces ( 91 , 92 ). Aging reduces glymphatic clearance, which is associated with the accumulation of beta amyloid protein and other proteins associated with Alzheimer's disease, which is also marked by severe sleep-wake and circadian dysregulation ( 71 , 93 ). Food consumption patterns and timing entrain circadian rhythms and metabolism and can be tied to weight gain and obesity ( 94 , 95 ). Sleep restriction increases appetite and reduces insulin sensitivity ( 96 ). Time-restricted feeding may help prevent obesity and promote weight loss ( 77 , 97 – 99 ).
Sleep health is characterized by regularity, efficiency, duration, timing, alertness, and satisfaction. Regular sleep of sufficient duration, efficiency, timing, and quality is related to health and disease. Sleep disorders, such as insomnia, sleep-related movement conditions, parasomnias, and central nervous system-mediated and breathing-related abnormalities, such as obstructive sleep apnea have been shown to be associated with health risks. Obstructive sleep apnea has been most notably associated with cardiovascular risk (hypertension, coronary artery disease, stroke, and atrial fibrillation), cardiometabolic risk (obesity and diabetes) ( 100 ), and neuropsychiatric risk (sleepiness, inattention, impaired cognition, and depression). Furthermore, a meta-analysis suggests a positive association between insomnia and future depression ( 101 ), and other studies suggest that sleep duration is inversely correlated with adolescent suicidal behaviors ( 102 ).
Circadian rhythms and sleep patterns (amount, regularity, timing) should be proactively leveraged and promoted to improve health and mitigate diseases which can be exacerbated by sleep disturbances and the metabolic changes they produce. Use of a broader socio-ecological model which incorporates environmental changes, policies and practices to improve recognition of circadian rhythm, essential nature of sleep, and health ( 103 – 105 ) is important and likely to be clinically impactful.
Sleep research priorities appear in Table 3 .
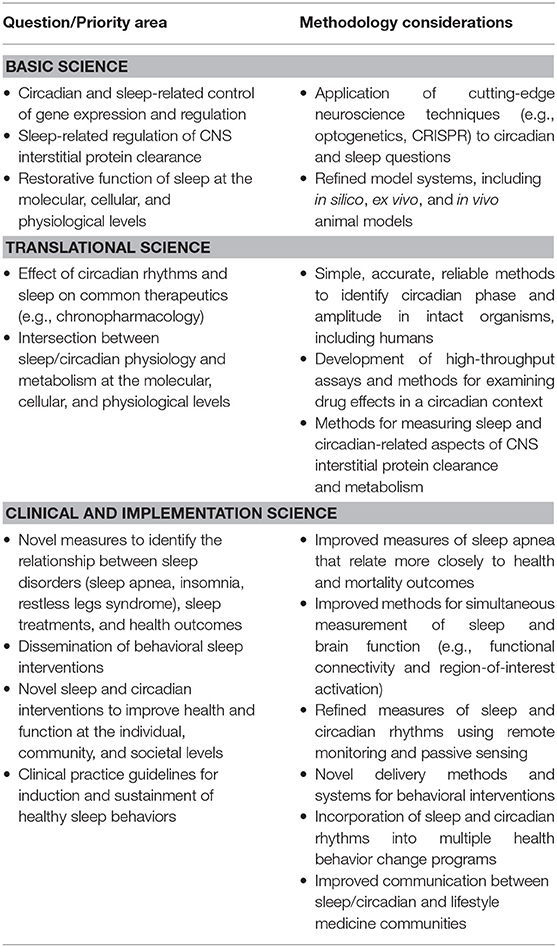
Table 3 . Sleep research priorities.
Stress Overview and Prioritized Research
The acute stress response is adaptive and helps activate the cascade of biological and physiological responses to actual or perceived threats. This response is triggered autonomically to help remove people from danger and enhance survival. With prolonged or extreme stress, brain and body responses can become overwhelmed, and physiological changes due to chronic stress increase the risk of physical and mental conditions, such as cardiovascular disease, irritable bowel disease, obesity, and depression ( 106 – 108 ) ( Figure 1 ).
Depression is a multi-determined disease with rates of the disorder and related disability and costs on the rise worldwide. Biological (e.g., genetic, biochemical, hormonal, inflammatory) and environmental (e.g., psychosocial adversity) have been implicated as predisposing, precipitating, and perpetuating factors ( 109 ). Depressive disorders have shown increased prevalence and in turn increased the incidence of many chronic physical diseases including asthma, arthritis, autoimmune diseases, cardiovascular disease, cancer, diabetes, neurological disorders, and obesity ( 110 – 112 ). The biological underpinnings, such as autonomic dysregulation and inflammation shared across depression and many of these conditions, serve as targets for stress reduction strategies with antidepressant effects.
One's ability to reset the stress response to a homeostatic resting state is called allostasis and the toll of maintaining this adaptive capacity over a lifetime is the allostatic load ( 113 ). Resilience is the degree to which people can cultivate adaptive responses by reducing negative effects of stress and returning to a state of healthy well-being ( 114 , 115 ). One of the most powerful mechanisms to reduce stress and enhance resilience is by eliciting a relaxation response ( 116 ). Mind-body therapies (MBT, such as mindfulness meditation, breathing exercises, yoga, etc.) and cognitive behavioral therapy (CBT) can elicit relaxation and improve negative brain-body effects of chronic stress while maintaining reactivity to acute stress ( 117 ). Mindfulness training fosters attention and acceptance toward one's present moment experience. CBT teaches adaptive coping by reappraisal of (negative) thinking and changing maladaptive behaviors. Cognitive appraisal can be a powerful mediator of perceived stress ( 71 ). With regular practice, these types of MBTs enhance both reactive and anticipatory resilience and have been associated with improved immune function and reductions in chronic pain, cardiovascular disease, anxiety and depression ( 118 – 121 ). The growing availability of these behavioral interventions by digital technology has greatly increased their accessibility and reach worldwide ( 122 ).
Notably, it is important to create better understanding, definition and dissemination of a framework for understanding, research, and practice that distinguishes “stress” from the “stress response” ( 113 , 123 – 125 ). In this regard, there are emerging molecular studies in the MBT field that tie into the lifestyle medicine research priorities described above ( Figure 1 ). For example, recent epigenetic research ( 126 ) on the positive role of meditation in rapid, epigenetically driven protein expression to reduce IL-6 ( 127 ) suggest the need to study the link between MBT's and inflammation ( Figure 1 ).
The current COVID-19 pandemic has occurred in the context of stress associated with issues of political, socioeconomic, and racial divisions that is unusual in both scope and intensity ( 125 ). Perhaps at no time in recent memory has the ability of individuals, families, and communities to recognize and proactively address mental, physical, and emotional adverse effects from these “acute” catastrophes (COVID-19 illness, mortality, social and economic effects) and “chronic” life-shortening institutional biases (racism, poverty, social disparities) been more needed.
Stress research priorities appear at Table 4 .
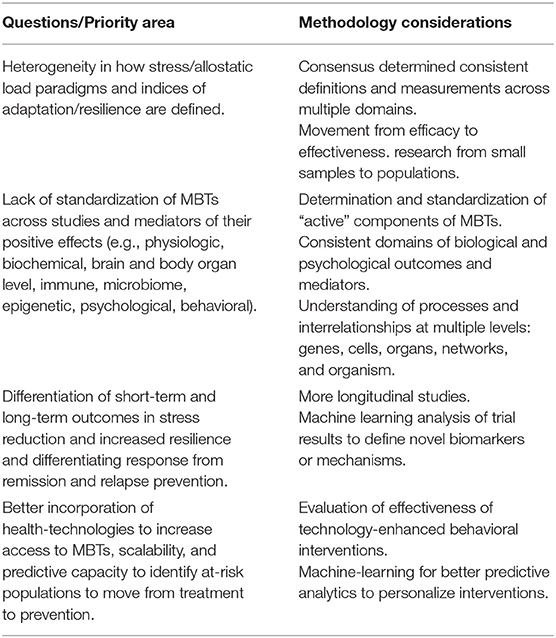
Table 4 . Stress research priorities.
Substance Abuse and Addiction Overview and Prioritized Research
Tobacco use remains the leading cause of U.S. preventable deaths. Despite decades of successful public policy and clinical efforts, thirty-four (34) million Americans still smoke and two-thirds report a desire to quit. Our collective challenge remains to deploy proven effective policy, environmental health and clinical solutions to reduce smoking and undertake targeted emerging basic science and behavioral research to better understand nicotine addiction and accelerate our progress to date ( 128 ).
Recent social, economic, and environmental factors have fueled the national rise in substance abuse generally and the opioid epidemic, specifically. Misuse of alcohol and other substances are common in the U.S. with ~7% of the population meeting criteria for a substance use disorder (SUD), 19% using illicit substances, 6% misusing prescription medications, and 6% consuming unhealthy amounts of alcohol ( 126 ). Despite the prevalence, those with a SUD have traditionally been excluded from the healthcare system and relegated to a disconnected collection of acute care specialty treatment providers, with limited access to either medical care or medications for SUD. The opioid epidemic has revealed the limitations of the disconnected SUD treatment system, as many people with an opioid use disorder (OUD) have died while cycling between hospitals, jails, or emergency medical service (EMS) contacts and without access to evidence-based treatment, including lifesaving medications ( 129 ).
Integrating people with an OUD as well as other SUDs into the healthcare system is the solution to reducing mortality and morbidity associated with this population. Individuals with an OUD are like other patients with chronic health disorders; they need ongoing care within a primary care patient-centered medical home (PCMH) as well as easy access to the array of specialty treatments and services to address the sequelae of infections, organ damage, and socioeconomic loss that result from their chronic illness. The rapid application of agonist medications, including methadone and buprenorphine, could reduce the OUD mortality rate by 50%, which translates to over 25,000 lives saved each year ( 129 ).
A four-stage cascade model of care has been recommended as a framework for engaging and retaining people with an OUD, based on the protocol used to identify and rapidly treat individuals infected with HIV ( 130 ). Individuals can be identified in hospitals, emergency departments, jails, EMS, needle exchange centers or homeless shelters (stage 1), where rapid access to buprenorphine can lead to 70% or more patients engaging in treatment, upon discharge ( 131 – 133 ). Effective treatment (stage 2) includes rapid access to medication-based treatment and other psychosocial services ( 134 ). Providing a community-based recovery coach or case manager can improve the transfer rate from crisis to medication-based treatment ( 135 , 136 ). Stepped care procedures, such as the hub and spoke or collaborative care models (stage 3), are used to modify a person's OUD medications, medical care and psychosocial needs over 6 or more months, using the same approach that primary care practices (PCPs) apply to chronic diseases. Innovations in primary care, such as value-based payments for improved outcomes, expansion of telemedicine technology ( 137 ), embedding recovery coaches in PCPs ( 138 ), and measurement-based care ( 139 ) have all been found to improve long-term outcomes for people with an OUD (stage 4).
Finally, it is important to leverage existing innovative and integrative research funding programs, such as the NIH OppNet, which seeks to foster collaboration across NIH to accelerate discoveries in basic behavioral and social sciences research (including addictions) ( 140 ).
Substance abuse and addiction research priorities appear in Table 5 .
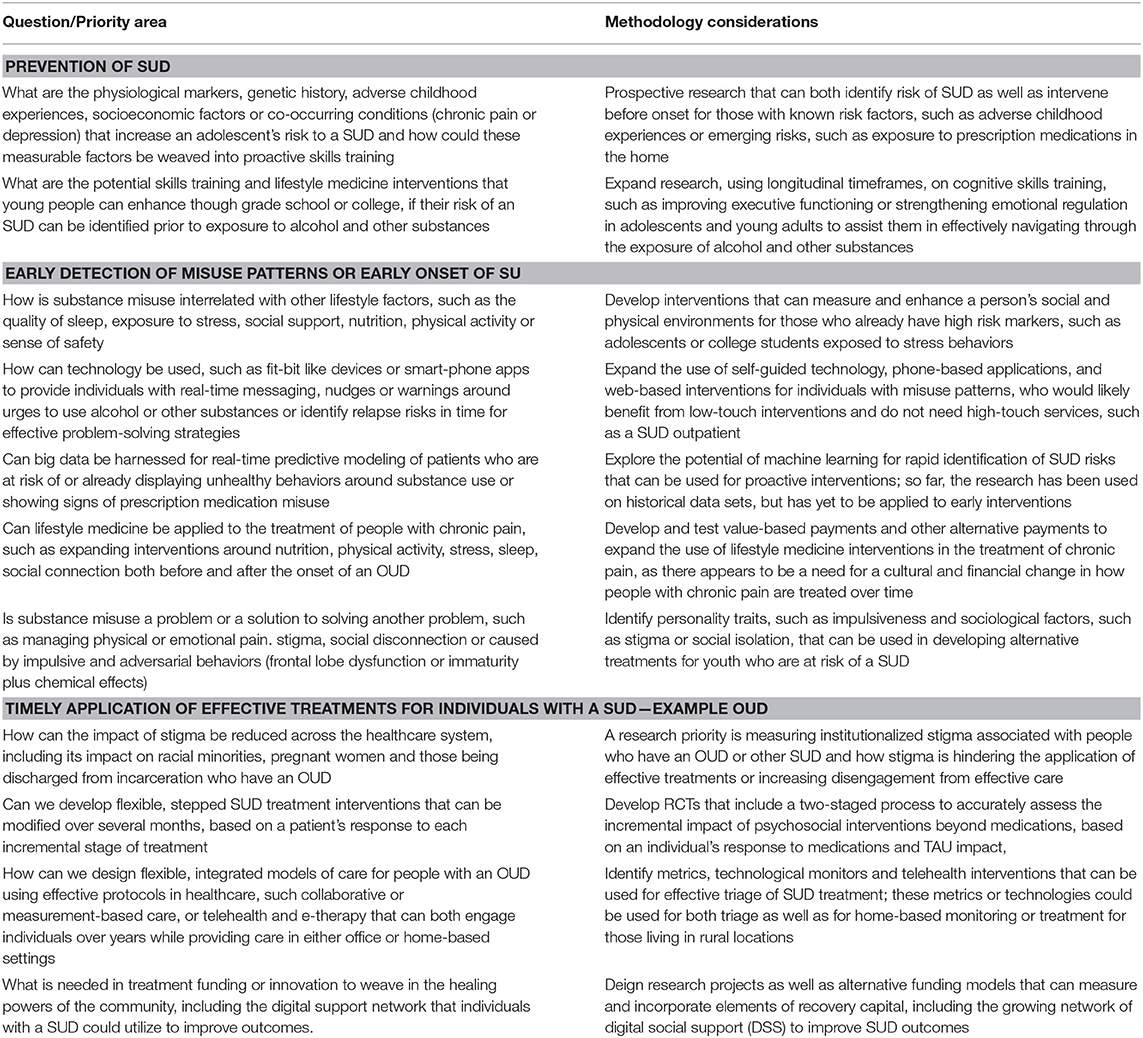
Table 5 . Addiction research priorities.
Positive Psychology and Social Connectivity Overview and Prioritized Research
Positive psychology interventions have been shown to improve subjective well-being, which is associated with improved health behaviors, health outcomes, and longevity. The upward spiral theory of lifestyle change suggests positive emotion promotes healthy lifestyle choices ( 141 ). A meta-analysis of a spectrum of positive psychology interventions, such as the practice of gratitude, forgiveness, and savoring shows a small, but statistically significant, impact on psychological and subjective well-being, which can, in turn, be associated with physical health benefits ( 142 ). Other studies have shown an association between having a sense of life purpose and meaning and higher use of preventive services, as well as lower CVD mortality in those who already have the disease ( 143 ) ( Figure 1 ).
Of the positive psychology pillars (positive emotion, engagement, relationships, meaning, and accomplishment), social connectivity has the most powerful health benefits in long term cohort studies. These include the ongoing, eight-decade cohort in the Harvard Study on Adult Development, which has conducted analyses controlling for many confounding variables ( 144 , 145 ). Groups with close social ties tend to live longer than those with similar risk conditions but lacking social ties. Conversely, social isolation (such as living alone, having a small social network, participating in few social activities, feeling lack of social support and loneliness) is associated with greater all-cause mortality, increased morbidity, lower immune system function (likely linked to chronic inflammation), depression, and cognitive decline ( 146 – 148 ) ( Figure 1 ). Interestingly, recent research on micro-moments of connectivity during human interactions with strangers, as well as friends, demonstrates a boost in the parasympathetic nervous system, the “tend and befriend” response, with correlated physiologic benefits ( 149 , 150 ).
What is the “active ingredient” of effective positive psychology interventions? Further study is needed to uncover the biological and physiological mechanisms of action and nuanced effects of these types of interventions, including social connectivity, in populations of different demographics and cultures at both the individual and community level. Also, the impact of in-person vs. digital technology delivery channels, optimal “dosing,” “person-activity fit,” and the nuanced effects of high arousal vs. low arousal emotional states require careful study. These studies of proximal outcomes should be incorporated and tested in non-mental health care settings (e.g., lifestyle medicine and primary care), as well as mental health care settings, to develop a robust evidence-base of effective interventions for medical practitioners and health teams. The field of lifestyle medicine that aims to treat and reverse, as well as prevent, lifestyle-related diseases through comprehensive lifestyle interventions is in a prime position to help build the evidence-base for applying positive psychology and social connectivity interventions in health care.
Positive psychology and social connection research priorities appear in Table 6 .
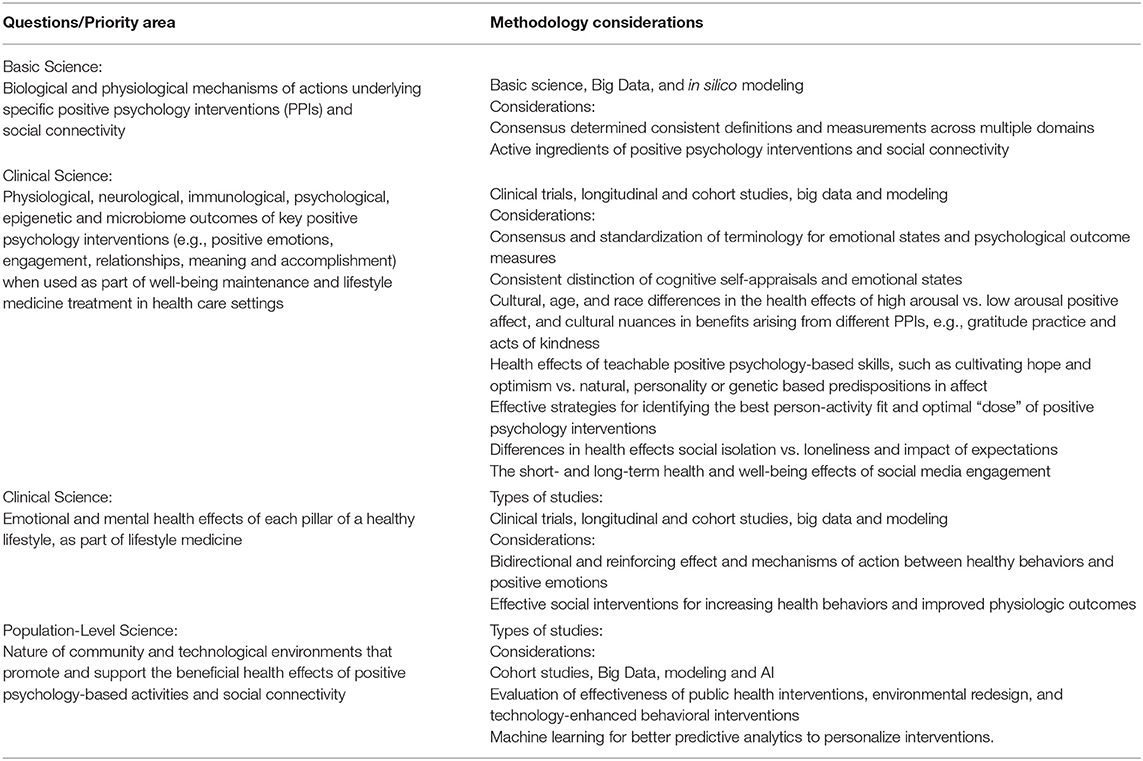
Table 6 . Positive psychology and social connectivity research priorities.
Socioecological Influences, Environment, and Exposures
There is a need to move beyond framing individual lifestyle behaviors as only personal “choices” toward using an integrated model of socioecological influences on health, within which clinical application of lifestyle medicine is a foundational best practice component. The term “lifestyle medicine” could, if taken in isolation, imply that an individual clinical approach could singularly or adequately treat and reverse chronic diseases which are strongly influenced by a variety of socioecological factors ( 151 ). Many are beyond the control of individuals and are subject to public policies, economic trends, social inequities, and other macrostructural influences.
Every patient and family exists within, and is supported (or constrained) by, specific and different environments that are increasingly defined by culture, location, employment, education, housing, air, water and community. Not surprisingly, then, human health, well-being, performance, and environmental health are closely connected. Built and natural environments (sidewalks, parks) are needed to support safe physical activities which become part of regular, easy-to-do routines at home, in schools, at worksites and in neighborhoods ( 152 ). There is growing evidence that social and environmental inequities experienced by some racial and ethnic groups and underserved populations contribute to increased rates of a variety of diseases ( 153 ). Inequities in the social determinants of health (many operating across generations), contribute to health behaviors and outcomes across population groups and geographies. We suggest that the imperative to address not only the social but also the ethical determinants of health should underlie all initiatives to improve health, increase access to medical care, and create better outcomes ( 154 ).
Environmental conditions, both indoor and outdoor, have been linked to objective measures of the stress and relaxation response, such as heart rate variability and cortisol levels. In striking recent studies, environmental conditions have been associated with epigenetic changes in children living in disadvantaged neighborhoods ( 155 , 156 ). As most Americans currently spend over 90% of their time indoors, the critical role of building design and environmental conditions on cognitive function, sleep, stress and productivity is increasingly being realized ( 157 , 158 ). This role has become especially apparent during the recent period of enforced, long-term lockdowns due to the COVID-19 pandemic. Improved indoor air quality utilizing frequent ventilation changes which lower CO 2 and volatile organic compound (VOC) levels are among the measures outlined in the Living Building Challenge certification ( 159 ). Additionally, sustainable sourcing of building materials, natural light access, and energy efficient heating/cooling systems are required. These measures often invoke the concept of “Biophilia” ( 160 )—humans' innate connection to nature- and biophilic design ( 161 ). This, a deliberate design paradigm intended to foster an affinity in the built environment produces measurable improvements in health, healing and pain management ( 162 , 163 ). It may ultimately produce healthier, happier, and more productive individuals and populations in the home, school, workplace, and neighborhood. Green building certification, such as the WELL building certification ( 164 ) measures even more directly how the indoor environment affects human health and provides guidelines for improving occupant health outcomes.
Growing scientific and medical evidence of the health impact of environmental chemicals builds on the troubling legacy of dichlorodiphenyltrichloroethane (DDT) and diethylstilbestrol (DES). Research over the past two decades has consistently identified that minute levels of a broad suite of synthetic chemicals can disrupt endocrine pathways and thereby contribute to disease and disability, including at low levels of exposure in susceptible windows of vulnerability.
The accumulating evidence is strongest for four categories of chemicals: flame retardants used in furniture and electronics; pesticides used in agriculture; phthalates used in food packaging, cosmetics, and personal care products; and bisphenols used in aluminum can linings and thermal paper receipts ( 165 ). In addition, at least 1,000 synthetic chemicals can disrupt endocrine (including insulin and thyroid hormones) and reproductive functions (testosterone, sperm count, polycystic ovary syndrome, endometriosis and fibroids), increase the risk of obesity and impact human development (e.g., IQ). Better understanding of risk and exposure relationships is fundamental to advancing prevention and intervention strategies. Of particular concern are agricultural workers exposed to the highest levels of pesticides and children most impacted by exposure to environmental lead and pesticides in local drinking water. Population-based policy solutions, akin to removing lead from gasoline must be applied more often and broadly. The EAT-Lancet Commission report “Eat, Food, Planet” related greater adoption of plant-based dietary patterns and improved agricultural practices to enhanced environmental sustainability ( 166 ). Finally, while beyond the scope of the Summit, we note that lifestyle practices are clearly affected by the most glaring, overarching environmental concern leading to multiple adverse health effects, namely climate change.
Underserved and Understudied Populations and Perspectives
Women, children, and marginalized populations have been excluded from much research. Most common chronic diseases occur later in life and thus research has largely focused on older adults. However, the foundations of lifestyle behaviors are set early in life providing an opportunity to create an integrated approach to the full continuum of women's and children's health. A lifecourse approach can encompass pre-conception, pregnancy, infancy, childhood, and adolescence in ways that will influence health later in life. Preparation for pregnancy and pregnancy itself ( 167 ) represent the ideal “teachable moment” for assisting women and families to understand the foundation of healthy living and to develop and adopt life skills to promote optimal growth and development which can span multiple generations. Pre-conception health “primes” not only maternal health (e.g., avoiding excessive weight gain and pregnancy complications) but also affects embryonic development and growth that are key drivers for the development of congenital malformations and intrauterine growth restriction. During pregnancy and the perinatal period, inadequate plant-based nutrition, lack of folic acid supplementation, stress, environmental toxins, smoking, alcohol, and endocrine disrupters can adversely affect pregnancy outcomes and subsequent children's disorders. Alterations to the epigenome and germ cells mediate these health and transgenerational effects ( 168 ) ( Figure 1 ). Maternal exposure to environmental chemicals and their transmission in breast milk to the infant are beginning to be studied ( 169 ). Plant-based nutrition, providing a diet rich in micronutrients, as well as regular physical activity are now seen as essential for producing healthy pregnancies and babies.
“Toxic stress” in early childhood from psychological trauma, physical abuse or adverse child experiences is now known to affect neurological development at the molecular level and increase the risk for future medical and psychological chronic disease ( 170 , 171 ). Poor childhood lifestyle behaviors often become manifest in preventable conditions involving multiple organ systems. These behaviors drive overuse of the medical system and numerous specialty consultations when root causes are either overlooked or unaddressed. Lifestyle change is more likely to occur and be impactful during younger childhood when family dynamics can be leveraged, as opposed to during adolescence, which is often characterized by rebellion. Methodological challenges to conducting pediatric obesity studies have been described ( 172 ). Additionally, treatment of children with serious medical conditions must concurrently address psychosocial and lifestyle-related needs and behaviors of the patient and their family as their traumatic experiences can negatively affect medical compliance and long-term outcomes.
Racial, ethnic, and cultural groups have specific strengths, challenges, and beliefs that should be recognized, leveraged, and addressed. Foundational to a whole person- and family-centric approach is acknowledgment of the chronic stress and physiological effects which accompany the sense of discrimination and bias.
We need to better understand and leverage the sociocultural aspects of purpose, spirituality and religion which are powerful forces aligned with healthy behaviors and have not been well-studied. Many religions, for example, in addition to providing stress relief, emotional and spiritual comfort, have emphasized healthy living through eating plants rather than animals. However, the study of how to leverage these specific values and messages in the context of religious and spiritual belief systems and cultures is lacking.
Optimizing the economic value of health and productivity ( 173 , 174 )—particularly among large, self-insured employers—represents an important route to demonstrate the “business case” for lifestyle medicine. Extending beyond clinical and health outcomes to include safety, absenteeism and productivity, the Total Worker Health framework created and promoted by the National Institute of Occupational Safety and Health (NIOSH) ( 175 ) represents research opportunities to assess the impact of chronic disease treatment and reversal through clinical practice, particularly through the use of on-site clinics and lifestyle medicine ( 176 ). The occupational productivity impact of sleep quality and insomnia was recently reviewed and summarized ( 177 ). A recent national health and economic analysis of limiting BPA in foods demonstrated a significant reduction in childhood obesity, heart disease, and cost savings ( 174 ). Similarly, recent large, US-based population analyses which model the national economic impact of adoption of healthy, plant-based eating can be shared and extended to other lifestyle domains as the basic and clinical science continues to emerge ( 178 ).
Applying Appropriate Strength of Evidence Methodologies to Lifestyle Medicine Interventions
The Summit reviewed strength of evidence methodologies and discussed whether a new framework would be more appropriate to measure the impact of applying clinical lifestyle treatment and reversal interventions to reduce disease and improve healthy aging ( Figure 1 ). Current methods for assessing strength of evidence (SOE) prioritize the contributions of randomized, placebo-controlled trials (RCTs). However, RCT's may not always be suitable to study lifestyle interventions for improved longevity, vitality, or successful aging. Assessment of evidence relevant to lifestyle medicine requires adaptation of SOE approaches when outcomes and/or exposures obviate exclusive or preferential reliance on RCT designs. SOE tools, such as the Hierarchies of Evidence Applied to Lifestyle Medicine ( 21 ) are needed to accelerate and prioritize impactful lifestyle-based clinical research and practice deployment.
Moving Forward: Focusing and Accelerating Public and Private Sector Research to Treat Root Causes of Chronic Disease
In the coming years, federal biomedical funding priorities via the NIH are likely to be targeted to precision medicine, genome editing, the brain, and cancer immunotherapy (with foundational emphasis on immunology and inflammation). The recently announced 2020–2030 Strategic Plan for NIH Nutrition Research ( 179 ) highlights the systems approach to addressing molecular, behavioral, and societal factors in the prevention and management of diet-related diseases.
Non-federal research-supporting organizations, such as the American Heart Association (AHA) will also have a significant role in supporting new knowledge generation around lifestyle and chronic disease prevention, treatment, and reversal. The AHA's “Life's Simple 7”: not smoking, healthy eating, physical activity, healthy weight, blood pressure, cholesterol, and blood glucose are already emphasized ( 180 ). Adding healthy sleep would create a “Life's Essential 8.” The AHA's promotion of Big Data and Precision Medicine as well as accelerating progress and breakthroughs through using interdisciplinary consortia (e.g., the Strategic Focus Research Networks) to focus on specific conditions, issues and populations can be re-visited given progress in basic, clinical and population sciences.
The U.S. military has focused on eight interrelated components in the DoD Total Force Fitness framework ( 181 ), which mirrors lifestyle medicine domains and informs the Department's research priorities. The U.S. Special Operations Command Preservation of the Force and Family program, one of the first lifestyle medicine-focused initiatives in DoD emphasizes service and family member health, well-being and performance ( 182 ). Importantly, the military understands that care providers must be embedded in military units which may include physical therapists, occupational therapists, and potentially also human performance coaches. The U.S. Veterans Health Administration, also prioritizes the broad spectrum of well-being by including a focus on spirit and soul in caring for veterans, as encompassed in the Whole Health aspirational framework ( 183 ). This approach has had a favorable impact not only on patients but also on doctors, who report a much lower sense of burnout.
The COVID-19 pandemic has exhibited increased severity and mortality among those who are socioeconomically disadvantaged, including African-American, Hispanic/Latino, Native Americans, and those with multiple co-morbidities ( 184 , 185 ). The increased risk for both transmission and severity once infected is multifactorial including the inability to shelter at home, need to work in service jobs with heightened exposure to the virus, and living with socioeconomic disadvantages often caused by a history of systemic marginalization and exclusion. Living or working in overcrowded conditions without access to COVID testing or health care also are factors. Higher prevalence of chronic diseases further increases immune susceptibility and inflammation leading to greater COVID-19 morbidity and mortality ( 186 ). The need to accelerate efforts to promote health and to prevent, treat and reverse chronic diseases must be grounded in a commitment to greater equity for marginalized populations and reduction of exclusionary policies that block access to healthy behaviors. Leveraging emerging science, new application of research methods and technologies, and more appropriate evidence-grading systems to inform clinical care to deploy effective lifestyle medicine practices must become a significant emerging strategy to improve the lifespan and healthspan.
Finally, we believe that this Summit, its interdisciplinary framework, and recommendations are groundbreaking not only in the context of lifestyle medicine, but also potentially for application to other fields of medicine as well.
Author Contributions
YV and MP wrote the manuscript. All authors participated in editing of the manuscript.
The Lifestyle Medicine Research Summit was supported by a grant from the Ardmore Institute of Health. Summit information, videos, and slides are available at https://www.ardmoreinstituteofhealth.org/lmrsummit .
The participation and opinions expressed herein of MS, EP, and CJ should not be interpreted as representing the official viewpoint of the U.S. Department of Health and Human Services, the National Institutes of Health or the National Institute on Aging; the Veterans Health Administration; and the Department of Defense or its components; respectively.
Conflict of Interest
YV Co-founder of, and stakeholder in, Immunetrics, Inc. PV is the founder and interim CEO of Eodyne S L, which aims at bringing scientifically validated neurorehabilitation technologies to society. JJ Serves on the Scientific Advisory Board for WW International, Inc. and also serves on the Scientific Advisory Board for Spark360. TF is the Founder and Chief Scientific Officer of Generian Pharmaceuticals. DB has served as a paid consultant to Bayer, BeHealth Solutions, Cereve/Ebb Therapeutics, Emmi Solutions, National Cancer Institute, Pear Therapeutics, Philips Respironics, Sleep Number, and Weight Watchers International. He has served as a paid consultant for professional educational programs developed by the American Academy of Physician Assistants and CME Institute, and received payment for a professional education program sponsored by Eisai (content developed exclusively by Dr. Buysse). He is an author of the Pittsburgh Sleep Quality Index, Pittsburgh Sleep Quality Index Addendum for PTSD (PSQI-A), Brief Pittsburgh Sleep Quality Index (B-PSQI), Daytime Insomnia Symptoms Scale, Pittsburgh Sleep Diary, Insomnia Symptom Questionnaire, and RU_SATED (copyright held by University of Pittsburgh). These instruments have been licensed to commercial entities for fees. He is also co-author of the Consensus Sleep Diary (copyright held by Ryerson University), which is licensed to commercial entities for a fee. NB serves without compensation as president of the Physicians Committee for Responsible Medicine and Barnard Medical Center in Washington, DC, nonprofit organizations providing educational, research, and medical services related to nutrition. He writes books and articles and gives lectures related to nutrition and health and has received royalties and honoraria from these sources.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Woolf SH, Schoomaker H. Life expectancy and mortality rates in the United States, 1959-2017. JAMA . (2019) 322:1996–2016. doi: 10.1001/jama.2019.16932
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Vargas AJ, Schully SD, Villani J, Ganoza Caballero L, Murray DM. Assessment of prevention research measuring leading risk factors and causes of mortality and disability supported by the US National Institutes of Health. JAMA Netw Open. (2019) 2:e1914718. doi: 10.1001/jamanetworkopen.2019.14718
3. American College of Lifestyle Medicine. Available online at: https://lifestylemedicine.org/What-is-Lifestyle-Medicine
4. Lifestyle Medicine Research Summit. Available online at: https://www.ardmoreinstituteofhealth.org/lmrsummit
5. Bodai BI, Nakata TE, Wong WT, Clark DR, Lawenda S, Tsou C, et al. Lifestyle medicine: a brief review of its dramatic impact on health and survival. Perm J. (2018) 22:17–25. doi: 10.7812/TPP/17-025
6. Furman D, Campisi J, Verdin E, Carrera-Bastos P, Targ S, Franceschi C, et al. Chronic inflammation in the etiology of disease across the life span. Nat Med. (2019) 25:1822–32. doi: 10.1038/s41591-019-0675-0
7. An G, Vodovotz Y. Complex Systems and Computational Biology Approaches to Acute Inflammation . New York, NY: Springer (2013).
Google Scholar
8. Kotas ME, Medzhitov R. Homeostasis, inflammation, and disease susceptibility. Cell. (2015) 160:816–27. doi: 10.1016/j.cell.2015.02.010
9. Gaber T, Strehl C, Buttgereit F. Metabolic regulation of inflammation. Nat Rev Rheumatol. (2017) 13:267–79. doi: 10.1038/nrrheum.2017.37
10. Placek K, Schultze JL, Aschenbrenner AC. Epigenetic reprogramming of immune cells in injury, repair, and resolution. J Clin Invest. (2019) 129:2994–3005. doi: 10.1172/JCI124619
11. Hernández-Saavedra D, Moody L, Xu GB, Chen H, Pan YX. Epigenetic regulation of metabolism and inflammation by calorie restriction. Adv Nutr. (2019) 10:520–36. doi: 10.1093/advances/nmy129
12. Cryan JF, Dinan TG. Mind-altering microorganisms: the impact of the gut microbiota on brain and behaviour. Nat Rev Neurosci. (2012) 13:701–12. doi: 10.1038/nrn3346
13. Gulyaeva NV. Molecular mechanisms of neuroplasticity: an expanding universe. Biochemistry. (2017) 82:237–42. doi: 10.1134/S0006297917030014
14. Hills RD Jr., Pontefract BA, Mishcon HR, Black CA, Sutton SC, et al. Gut microbiome: profound implications for diet and disease. Nutrients . (2019) 11:1613. doi: 10.3390/nu11071613
15. Partridge L, Deelen J, Slagboom PE. Facing up to the global challenges of ageing. Nature. (2018) 561:45–56. doi: 10.1038/s41586-018-0457-8
16. Chandra H. Artificial Intelligence (AI) vs Machine Learning (ML) vs Big Data . (2019). Available online at: https://heartbeat.fritz.ai/artificial-intelligence-ai-vs-machine-learning-ml-vs-big-data-909906eb6a92
17. Topol EJ. Deep Medicine: How Artificial Intelligence Can Make Healthcare Human Again . New York, NY: Basic Books (2019).
PubMed Abstract | Google Scholar
18. Cornelis MC, Hu FB. Systems epidemiology: a new direction in nutrition and metabolic disease research. Curr Nutr Rep. (2013) 2:10.1007/s13668-013-0052-4. doi: 10.1007/s13668-013-0052-4
19. Mirza B, Wang W, Wang J, Choi H, Chung NC, Ping P. Machine learning and integrative analysis of biomedical big data. Genes (Basel). (2019) 10:87. doi: 10.3390/genes10020087
20. An G, Vodovotz Y. Translational Systems Biology: Concepts and Practice for the Future of Biomedical Research . New York, NY: Elsevier (2014).
21. Katz DL, Karlsen MC, Chung M, Shams-White MM, Green LW, Fielding J, et al. Hierarchies of evidence applied to lifestyle Medicine (HEALM): introduction of a strength-of-evidence approach based on a methodological systematic review. BMC Med Res Methodol. (2019) 19:178. doi: 10.1186/s12874-019-0811-z
22. Maier M, Ballester BR, Verschure P. Principles of neurorehabilitation after stroke based on motor learning and brain plasticity mechanisms. Front Syst Neurosci. (2019) 13:74. doi: 10.3389/fnsys.2019.00074
23. Azhar N, Mi Q, Ziraldo C, Buliga M, Constantine G, Vodovotz Y. Integrating data driven and mechanistic models of the inflammatory response in sepsis and trauma. In: Vodovotz Y, An G, editors. Complex Systems and Computational Biology Approaches to Acute Inflammation . New York, NY: Springer (2013). p.143–57. doi: 10.1007/978-1-4614-8008-2_8
CrossRef Full Text | Google Scholar
24. Alber M, Buganza Tepole A, Cannon WR, De S, Dura-Bernal S, Garikipati K, et al. Integrating machine learning and multiscale modeling-perspectives, challenges, and opportunities in the biological, biomedical, and behavioral sciences. NPJ Digit Med. (2019) 2:115. doi: 10.1038/s41746-019-0193-y
PubMed Abstract | CrossRef Full Text
25. Satija A, Yu E, Willett WC, Hu FB. Understanding nutritional epidemiology and its role in policy. Adv Nutr. (2015) 6:5–18. doi: 10.3945/an.114.007492
26. Andersson C, Johnson AD, Benjamin EJ, Levy D, Vasan RS. 70-year legacy of the Framingham Heart Study. Nat Rev Cardiol. (2019) 16:687–98. doi: 10.1038/s41569-019-0202-5
27. Bao Y, Bertoia ML, Lenart EB, Stampfer MJ, Willett WC, Speizer FE, et al. Origin, methods, and evolution of the three Nurses' Health Studies. Am J Public Health. (2016) 106:1573–81. doi: 10.2105/AJPH.2016.303338
28. The UK Biobank. Available online at: https://www.ukbiobank.ac.uk/
29. Loma Linda University. Available online at: https://adventisthealthstudy.org/?rsource=publichealth.llu.edu/adventist-health-studies .
30. Perdue CL, Eick-Cost AA, Rubertone MV. A brief description of the operation of the DoD Serum Repository. Mil Med. (2015) 180:10–2. doi: 10.7205/MILMED-D-14-00739
31. Smith TC. The US Department of Defense Millennium Cohort Study: career span and beyond longitudinal follow-up. J Occup Environ Med. (2009) 51:1193–201. doi: 10.1097/JOM.0b013e3181b73146
32. Children's Hospital Pittsburgh. Available online at: https://www.chp.edu/research/pittsburgh-study
33. National Institutes of Health. Available online at: https://allofus.nih.gov/about
34. Boston University and the National Institutes of Health. Available online at: https://framinghamheartstudy.org/
35. Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med. (1997) 336:1117–24. doi: 10.1056/NEJM199704173361601
36. Yokoyama Y, Nishimura K, Barnard ND, Takegami M, Watanabe M, Sekikawa A, et al. Vegetarian diets and blood pressure: a meta-analysis. JAMA Intern Med. (2014) 174:577–87. doi: 10.1001/jamainternmed.2013.14547
37. Martínez-González MA, Ros E, Estruch R. Primary prevention of cardiovascular disease with a mediterranean diet supplemented with extra-virgin olive oil or nuts. N Engl J Med. (2018) 379:1388–9. doi: 10.1056/NEJMc1809971
38. Ornish D, Scherwitz LW, Billings JH, Brown SE, Gould KL, Merritt TA, et al. Intensive lifestyle changes for reversal of coronary heart disease. JAMA. (1998) 280:2001–7. doi: 10.1001/jama.280.23.2001
39. Esselstyn CB Jr., Gendy G, Doyle J, Golubic M, Roizen MF. A way to reverse CAD? J Fam Pract . (2014) 63:356–64.
40. Skilton MR, Celermajer DS, Cosmi E, Crispi F, Gidding SS, Raitakari OT, et al. Natural history of atherosclerosis and abdominal aortic intima-media thickness: rationale, evidence, and best practice for detection of atherosclerosis in the young. J Clin Med. (2019) 8:1201. doi: 10.3390/jcm8081201
41. Ryder JR, Northrop E, Rudser KD, Kelly AS, Gao Z, Khoury PR, et al. Accelerated early vascular aging among adolescents with obesity and/or Type 2 diabetes mellitus. J Am Heart Assoc. (2020) 9:e014891. doi: 10.1161/JAHA.119.014891
42. Hemler EC, Hu FB. Plant-based diets for personal, population, and planetary health. Adv Nutr. (2019) 10:S275–s283. doi: 10.1093/advances/nmy117
43. Smits LP, Kootte RS, Levin E, Prodan A, Fuentes S, Zoetendal EG, et al. Effect of vegan fecal microbiota transplantation on carnitine- and choline-derived trimethylamine-N-oxide production and vascular inflammation in patients with metabolic syndrome. J Am Heart Assoc. (2018) 7:e008342. doi: 10.1161/JAHA.117.008342
44. Garcia-Rios A, Leon-Acuna A, Lopez-Miranda J, Perez-Martinez P. Lipoprotein (a) management: lifestyle and hormones. Curr Med Chem. (2017) 24:979–88. doi: 10.2174/0929867324666170124144427
45. Turner-Mcgrievy G, Wilcox S, Frongillo EA, Murphy A, Hutto B, Williams K, et al. The Nutritious Eating with Soul (NEW Soul) study: study design and methods of a two-year randomized trial comparing culturally adapted soul food vegan vs. omnivorous diets among African American adults at risk for heart disease. Contemp Clin Trials. (2020) 88:105897. doi: 10.1016/j.cct.2019.105897
46. Clinton SK, Giovannucci EL, Hursting SD. The World Cancer Research Fund/American Institute for Cancer Research third expert report on diet, nutrition, physical activity, and cancer: impact and future directions. J Nutr. (2020) 150:663–71. doi: 10.1093/jn/nxz268
47. Prentice RL, Caan B, Chlebowski RT, Patterson R, Kuller LH, Ockene JK, et al. Low-fat dietary pattern and risk of invasive breast cancer: the Women's Health Initiative randomized controlled dietary modification trial. JAMA. (2006) 295:629–42. doi: 10.1001/jama.295.6.629
48. Chlebowski RT, Aragaki AK, Anderson GL, Simon MS, Manson JE, Neuhouser ML, et al. Association of low-fat dietary pattern with breast cancer overall survival: a secondary analysis of the Women's Health Initiative randomized clinical tsrial. JAMA Oncol. (2018) 4:e181212. doi: 10.1001/jamaoncol.2018.1212
49. Pierce JP, Natarajan L, Caan BJ, Parker BA, Greenberg ER, Flatt SW, et al. Influence of a diet very high in vegetables, fruit, and fiber and low in fat on prognosis following treatment for breast cancer: the Women's Healthy Eating and Living (WHEL) randomized trial. JAMA. (2007) 298:289–98. doi: 10.1001/jama.298.3.289
50. Ornish D, Weidner G, Fair WR, Marlin R, Pettengill EB, Raisin CJ, et al. Intensive lifestyle changes may affect the progression of prostate cancer. J Urol . (2005) 174:1065–1069; discussion 1069–70. doi: 10.1097/01.ju.0000169487.49018.73
51. Tonstad S, Butler T, Yan R, Fraser GE. Type of vegetarian diet, body weight, and prevalence of type 2 diabetes. Diabetes Care. (2009) 32:791–6. doi: 10.2337/dc08-1886
52. Razak F, Anand SS. Impaired mitochondrial activity in the insulin-resistant offspring of patients with type 2 diabetes. N Engl J Med . (2004) 350:664–71. doi: 10.1056/NEJMoa031314
53. Kelly J, Karlsen M, Steinke G. Type 2 diabetes remission and lifestyle medicine: a position statement from the American College of Lifestyle Medicine. Am J Lifestyle Med. (2020) 14:1559827620930962. doi: 10.1177/1559827620930962
54. Karjalainen J, Martin JM, Knip M, Ilonen J, Robinson BH, Savilahti E, et al. A bovine albumin peptide as a possible trigger of insulin-dependent diabetes mellitus. N Engl J Med. (1992) 327:302–7. doi: 10.1056/NEJM199207303270502
55. Alwarith J, Kahleova H, Rembert E, Yonas W, Dort S, Calcagno M, et al. Nutrition interventions in rheumatoid arthritis: the potential use of plant-based diets. A review. Front Nutr. (2019) 6:141. doi: 10.3389/fnut.2019.00141
56. Goldin BR, Woods MN, Spiegelman DL, Longcope C, Morrill-Labrode A, Dwyer JT, et al. The effect of dietary fat and fiber on serum estrogen concentrations in premenopausal women under controlled dietary conditions. Cancer. (1994) 74:1125–31. doi: 10.1002/1097-0142(19940801)74:3+<1125::AID-CNCR2820741521>3.0.CO;2-5
57. Morris MC, Evans DA, Bienias JL, Tangney CC, Bennett DA, Aggarwal N, et al. Dietary fats and the risk of incident Alzheimer disease. Arch Neurol. (2003) 60:194–200. doi: 10.1001/archneur.60.2.194
58. The MIND Diet Intervention to Prevent Alzheimer's Disease. Available online at: https://mind-diet-trial.org/
59. Agarwal U, Mishra S, Xu J, Levin S, Gonzales J, Barnard ND. A multicenter randomized controlled trial of a nutrition intervention program in a multiethnic adult population in the corporate setting reduces depression and anxiety and improves quality of life: the GEICO study. Am J Health Promot. (2015) 29:245–54. doi: 10.4278/ajhp.130218-QUAN-72
60. Francis HM, Stevenson RJ, Chambers JR, Gupta D, Newey B, Lim CK. A brief diet intervention can reduce symptoms of depression in young adults–a randomised controlled trial. PLoS ONE. (2019) 14:e0222768. doi: 10.1371/journal.pone.0222768
61. Firth J, Marx W, Dash S, Carney R, Teasdale SB, Solmi M, et al. The Effects of dietary improvement on symptoms of depression and anxiety: a meta-analysis of randomized controlled trials. Psychosom Med. (2019) 81:265–80. doi: 10.1097/PSY.0000000000000673
62. Dunn AL, Trivedi MH, Kampert JB, Clark CG, Chambliss HO. Exercise treatment for depression: efficacy and dose response. Am J Prev Med. (2005) 28:1–8. doi: 10.1016/j.amepre.2004.09.003
63. Clegg DJ, Hill Gallant KM. Plant-based diets in CKD. Clin J Am Soc Nephrol. (2019) 14:141–3. doi: 10.2215/CJN.08960718
64. Kim H, Caulfield LE, Garcia-Larsen V, Steffen LM, Grams ME, Coresh J, et al. Plant-based diets and incident CKD and kidney function. Clin J Am Soc Nephrol. (2019) 14:682–91. doi: 10.2215/CJN.12391018
65. Lan X, Wen H, Lederman R, Malhotra A, Mikulak J, Popik W, et al. Protein domains of APOL1 and its risk variants. Exp Mol Pathol. (2015) 99:139–44. doi: 10.1016/j.yexmp.2015.06.003
66. Tonstad S, Stewart K, Oda K, Batech M, Herring RP, Fraser GE. Vegetarian diets and incidence of diabetes in the Adventist Health Study-2. Nutr Metab Cardiovasc Dis. (2013) 23:292–9. doi: 10.1016/j.numecd.2011.07.004
67. Shan Z, Li Y, Baden MY, Bhupathiraju SN, Wang DD, Sun Q, et al. Association between healthy eating patterns and risk of cardiovascular disease. JAMA Intern Med. (2020) 180:1090–100. doi: 10.1001/jamainternmed.2020.2176
68. Budhathoki S, Sawada N, Iwasaki M, Yamaji T, Goto A, Kotemori A, et al. Association of animal and plant protein intake with all-cause and cause-specific mortality in a Japanese cohort. JAMA Intern Med. (2019) 179:1509–18. doi: 10.1001/jamainternmed.2019.2806
69. Huang J, Liao LM, Weinstein SJ, Sinha R, Graubard BI, Albanes D. Association between plant and animal protein intake and overall and cause-specific mortality. JAMA Intern Med. (2020) 180:1173–84. doi: 10.1001/jamainternmed.2020.2790
70. Shan Z, Guo Y, Hu FB, Liu L, Qi Q. Association of low-carbohydrate and low-fat diets with mortality among US adults. JAMA Intern Med. (2020) 180:513–23. doi: 10.1001/jamainternmed.2019.6980
71. Boespflug EL, Iliff JJ. The emerging relationship between interstitial fluid-cerebrospinal fluid exchange, Amyloid-β, and Sleep. Biol Psychiatry. (2018) 83:328–36. doi: 10.1016/j.biopsych.2017.11.031
72. Morris JN, Heady JA, Raffle PA, Roberts CG, Parks JW. Coronary heart disease and physical activity of work. Lancet. (1953) 265:1053–7. doi: 10.1016/S0140-6736(53)90665-5
73. US Department of Health and Human Services. Physical Activity and Health: A Report of the Surgeon General . Atlanta, GA: US Department of Health and Human Services (1996).
74. US Department of Health and Human Services. Physical Activity Guidelines Advisory Committee Report 2008 . Washington, DC: US Department of Health and Human Services (2008). Available online at: http://www.health.gov/paguidelines/committeereport.aspx (accessed January 19, 2009).
75. US Department of Health and Human Services. Physical Activity Guidelines Advisory Committee Report 2018 . Washington, DC: US Department of Health and Human Services (2018).
76. Neufer PD, Bamman MM, Muoio DM, Bouchard C, Cooper DM, Goodpaster BH, et al. Understanding the cellular and molecular mechanisms of physical activity-induced health benefits. Cell Metab. (2015) 22:4–11. doi: 10.1016/j.cmet.2015.05.011
77. Gill S, Panda S. A smartphone app reveals erratic diurnal eating patterns in humans that can be modulated for health benefits. Cell Metab. (2015) 22:789–98. doi: 10.1016/j.cmet.2015.09.005
78. Boppart MD, De Lisio M, Witkowski S. Exercise and stem cells. Prog Mol Biol Transl Sci. (2015) 135:423–56. doi: 10.1016/bs.pmbts.2015.07.005
79. Safdar A, Tarnopolsky MA. Exosomes as mediators of the systemic adaptations to endurance exercise. Cold Spring Harb Perspect Med. (2018) 8:a029827. doi: 10.1101/cshperspect.a029827
80. Lee TH, Formolo DA, Kong T, Lau SW, Ho CS, Leung RYH, et al. Potential exerkines for physical exercise-elicited pro-cognitive effects: insight from clinical and animal research. Int Rev Neurobiol. (2019) 147:361–95. doi: 10.1016/bs.irn.2019.06.002
81. Budzowski AR, Parkinson MD, Silfee VJ. An evaluation of lifestyle health coaching programs using trained health coaches and evidence-based curricula at 6 months over 6 years. Am J Health Promot. (2019) 33:912–5. doi: 10.1177/0890117118824252
82. Fogg BJ. Tiny Habits: The Small Changes That Change Everything . Boston, MA: Houghton Mifflin Harcourt (2020).
83. Parkinson MD, Hammonds T, Keyser DJ, Wheeler JR, Peele PB. Impact of physician referral to health coaching on patient engagement and health risks: an observational study of UPMC's prescription for wellness. Am J Health Promot. (2020) 34:366–75. doi: 10.1177/0890117119900588
84. Mohawk JA, Green CB, Takahashi JS. Central and peripheral circadian clocks in mammals. Annu Rev Neurosci. (2012) 35:445–62. doi: 10.1146/annurev-neuro-060909-153128
85. Dibner C, Schibler U, Albrecht U. The mammalian circadian timing system: organization and coordination of central and peripheral clocks. Annu Rev Physiol. (2010) 72:517–49. doi: 10.1146/annurev-physiol-021909-135821
86. Cajochen C, Kräuchi K, Wirz-Justice A. Role of melatonin in the regulation of human circadian rhythms and sleep. J Neuroendocrinol. (2003) 15:432–7. doi: 10.1046/j.1365-2826.2003.00989.x
87. Guenthner CJ, Luitje ME, Pyle LA, Molyneux PC, Yu JK, Li AS, et al. Circadian rhythms of Per2::Luc in individual primary mouse hepatocytes and cultures. PLoS ONE. (2014) 9:e87573. doi: 10.1371/journal.pone.0087573
88. Zhang R, Lahens NF, Ballance HI, Hughes ME, Hogenesch JB. A circadian gene expression atlas in mammals: implications for biology and medicine. Proc Natl Acad Sci U.S.A. (2014) 111:16219–24. doi: 10.1073/pnas.1408886111
89. Videnovic A, Lazar AS, Barker RA, Overeem S. ‘The clocks that time US'–circadian rhythms in neurodegenerative disorders. Nat Rev Neurol. (2014) 10:683–93. doi: 10.1038/nrneurol.2014.206
90. Hill VM, O'connor RM, Sissoko GB, Irobunda IS, Leong S, Canman JC, et al. A bidirectional relationship between sleep and oxidative stress in Drosophila. PLoS Biol . (2018) 16:e2005206. doi: 10.1371/journal.pbio.2005206
91. Xie L, Kang H, Xu Q, Chen MJ, Liao Y, Thiyagarajan M, et al. Sleep drives metabolite clearance from the adult brain. Science. (2013) 342:373–7. doi: 10.1126/science.1241224
92. Jessen NA, Munk AS, Lundgaard I, Nedergaard M. The glymphatic system: a beginner's guide. Neurochem Res. (2015) 40:2583–99. doi: 10.1007/s11064-015-1581-6
93. Kress BT, Iliff JJ, Xia M, Wang M, Wei HS, Zeppenfeld D, et al. Impairment of paravascular clearance pathways in the aging brain. Ann Neurol. (2014) 76:845–61. doi: 10.1002/ana.24271
94. Masri S, Sassone-Corsi P. The circadian clock: a framework linking metabolism, epigenetics and neuronal function. Nat Rev Neurosci. (2013) 14:69–75. doi: 10.1038/nrn3393
95. Baron KG, Reid KJ, Kern AS, Zee PC. Role of sleep timing in caloric intake and BMI. Obesity (Silver Spring). (2011) 19:1374–81. doi: 10.1038/oby.2011.100
96. Van Cauter E, Spiegel K, Tasali E, Leproult R. Metabolic consequences of sleep and sleep loss. Sleep Med. (2008) 9:S23–8. doi: 10.1016/S1389-9457(08)70013-3
97. Chaix A, Zarrinpar A, Miu P, Panda S. Time-restricted feeding is a preventative and therapeutic intervention against diverse nutritional challenges. Cell Metab. (2014) 20:991–1005. doi: 10.1016/j.cmet.2014.11.001
98. Hatori M, Vollmers C, Zarrinpar A, Ditacchio L, Bushong EA, Gill S, et al. Time-restricted feeding without reducing caloric intake prevents metabolic diseases in mice fed a high-fat diet. Cell Metab. (2012) 15:848–60. doi: 10.1016/j.cmet.2012.04.019
99. Mcclung CA. Mind your rhythms: an important role for circadian genes in neuroprotection. J Clin Invest. (2013) 123:4994–6. doi: 10.1172/JCI73059
100. Buysse DJ. Sleep health: can we define it? Does it matter? Sleep. (2014) 37:9–17. doi: 10.5665/sleep.3298
101. Baglioni C, Battagliese G, Feige B, Spiegelhalder K, Nissen C, Voderholzer U, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. (2011) 135:10–9. doi: 10.1016/j.jad.2011.01.011
102. Fitzgerald CT, Messias E, Buysse DJ. Teen sleep and suicidality: results from the youth risk behavior surveys of 2007 and 2009. J Clin Sleep Med. (2011) 7:351–6. doi: 10.5664/JCSM.1188
103. Jackson CL, Redline S, Emmons KM. Sleep as a potential fundamental contributor to disparities in cardiovascular health. Annu Rev Public Health. (2015) 36:417–40. doi: 10.1146/annurev-publhealth-031914-122838
104. Stokols D. Translating social ecological theory into guidelines for community health promotion. Am J Health Promot. (1996) 10:282–98. doi: 10.4278/0890-1171-10.4.282
105. Mcleroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. (1988) 15:351–77. doi: 10.1177/109019818801500401
106. Miller GE, Blackwell E. Turning up the heat: inflammation as a mechanism linking chronic stress, depression, and heart disease. Curr Direct Psychol Sci. (2006) 15:269–72. doi: 10.1111/j.1467-8721.2006.00450.x
107. Moloney RD, Johnson AC, O'mahony SM, Dinan TG, Greenwood-Van Meerveld B, Cryan JF. Stress and the microbiota-gut-brain axis in visceral pain: relevance to irritable bowel syndrome. CNS Neurosci Ther . (2016) 22:102–17. doi: 10.1111/cns.12490
108. Razzoli M, Bartolomucci A. The dichotomous effect of chronic stress on obesity. Trends Endocrinol Metab. (2016) 27:504–15. doi: 10.1016/j.tem.2016.04.007
109. Slavich GM, Irwin MR. From stress to inflammation and major depressive disorder: a social signal transduction theory of depression. Psychol Bull. (2014) 140:774–815. doi: 10.1037/a0035302
110. Chapman DP, Perry GS, Strine TW. The vital link between chronic disease and depressive disorders. Prev Chronic Dis. (2005) 2:A14.
111. Patten SB, Williams JV, Lavorato DH, Modgill G, Jetté N, Eliasziw M. Major depression as a risk factor for chronic disease incidence: longitudinal analyses in a general population cohort. Gen Hosp Psychiatry. (2008) 30:407–13. doi: 10.1016/j.genhosppsych.2008.05.001
112. Marrie RA, Walld R, Bolton JM, Sareen J, Walker JR, Patten SB, et al. Increased incidence of psychiatric disorders in immune-mediated inflammatory disease. J Psychosom Res. (2017) 101:17–23. doi: 10.1016/j.jpsychores.2017.07.015
113. Del Giudice M, Buck CL, Chaby LE, Gormally BM, Taff CC, Thawley CJ, et al. What is stress? A systems perspective. Integr Comp Biol. (2018) 58:1019–32. doi: 10.1093/icb/icy114
114. Mcewen BS. Protective and damaging effects of stress mediators. N Engl J Med. (1998) 338:171–9. doi: 10.1056/NEJM199801153380307
115. Dusek JA, Benson H. Mind-body medicine: a model of the comparative clinical impact of the acute stress and relaxation responses. Minn Med. (2009) 92:47–50.
116. Dossett ML, Fricchione GL, Benson H. A new era for mind-body medicine. N Engl J Med. (2020) 382:1390–1. doi: 10.1056/NEJMp1917461
117. Loiselle E, Proszynski J. Behavioral approaches to manage stress. In: Rippe J, editor. Lifestyle Medicine , 3rd ed. Boca Raton, FL: CRC Press (2019). p. 281–98. doi: 10.1201/9781315201108-23
118. Khoury B, Sharma M, Rush SE, Fournier C. Mindfulness-based stress reduction for healthy individuals: a meta-analysis. J Psychosom Res. (2015) 78:519–28. doi: 10.1016/j.jpsychores.2015.03.009
119. Cherkin DC, Herman PM. Cognitive and mind-body therapies for chronic low back pain and neck pain: effectiveness and value. JAMA Intern Med. (2018) 178:556–7. doi: 10.1001/jamainternmed.2018.0113
120. Khoo EL, Small R, Cheng W, Hatchard T, Glynn B, Rice DB, et al. Comparative evaluation of group-based mindfulness-based stress reduction and cognitive behavioural therapy for the treatment and management of chronic pain: a systematic review and network meta-analysis. Evid Based Ment Health. (2019) 22:26–35. doi: 10.1136/ebmental-2018-300062
121. Chin B, Lindsay EK, Greco CM, Brown KW, Smyth JM, Wright AGC, et al. Psychological mechanisms driving stress resilience in mindfulness training: a randomized controlled trial. Health Psychol. (2019) 38:759–68. doi: 10.1037/hea0000763
122. Oser M, Wallace ML, Solano F, Szigethy EM. Guided digital cognitive behavioral program for anxiety in primary care: propensity-matched controlled trial. JMIR Ment Health. (2019) 6:e11981. doi: 10.2196/11981
123. Kranner I, Minibayeva FV, Beckett RP, Seal CE. What is stress? Concepts, definitions and applications in seed science. New Phytol. (2010) 188:655–73. doi: 10.1111/j.1469-8137.2010.03461.x
124. Harkness KL, Monroe SM. The assessment and measurement of adult life stress: basic premises, operational principles, and design requirements. J Abnorm Psychol. (2016) 125:727–45. doi: 10.1037/abn0000178
125. Dewilde C, Carrington J, Abbate A, Burton CW, Bearman G, Salyer J. Structural stress and otherness: how do they influence psychological stress? J Transcult Nurs. (2019) 30:478–91. doi: 10.1177/1043659618823915
126. Kaliman P. Epigenetics and meditation. Curr Opin Psychol. (2019) 28:76–80. doi: 10.1016/j.copsyc.2018.11.010
127. Chaix R, Fagny M, Cosin-Tomás M, Alvarez-López M, Lemee L, Regnault B, et al. Differential DNA methylation in experienced meditators after an intensive day of mindfulness-based practice: implications for immune-related pathways. Brain Behav Immun. (2020) 84:36–44. doi: 10.1016/j.bbi.2019.11.003
128. US Department of Health and Human Services. Smoking Cessation: A Report of the Surgeon General–Executive Summary . Atlanta, GA: US Department of Health and Human Services (2020). Available online at: https://www.hhs.gov/sites/default/files/2020-cessation-sgr-full-report.pdf
129. National Academies of Sciences, Medicine, Health, Medicine, Board on Health Sciences, Committee on Medication-Assisted Treatment for Opioid Use. The National Academies collection: reports funded by National Institutes of Health. In: Mancher M, Leshner AI, editors. Medications for Opioid Use Disorder Save Lives . Washington, DC: National Academies Press (US) (2019). p.1–156.
130. Williams AR, Nunes EV, Bisaga A, Levin FR, Olfson M. Development of a cascade of care for responding to the opioid epidemic. Am J Drug Alcohol Abuse. (2019) 45:1–10. doi: 10.1080/00952990.2018.1546862
131. Cushman PA, Liebschutz JM, Anderson BJ, Moreau MR, Stein MD. Buprenorphine initiation and linkage to outpatient buprenorphine do not reduce frequency of injection opiate use following hospitalization. J Subst Abuse Treat. (2016) 68:68–73. doi: 10.1016/j.jsat.2016.06.003
132. D'Onofrio G, Chawarski MC, O'connor PG, Pantalon MV, Busch SH, Owens PH, et al. Emergency department-Iiitiated buprenorphine for opioid dependence with continuation in primary care: outcomes during and after intervention. J Gen Intern Med . (2017) 32:660–6. doi: 10.1007/s11606-017-3993-2
133. Srivastava A, Kahan M, Njoroge I, Sommer LZ. Buprenorphine in the emergency department: randomized clinical controlled trial of clonidine versus buprenorphine for the treatment of opioid withdrawal. Can Fam Physician. (2019) 65:e214–20.
134. Winograd RP, Wood CA, Stringfellow EJ, Presnall N, Duello A, Horn P, et al. Implementation and evaluation of Missouri's Medication First treatment approach for opioid use disorder in publicly-funded substance use treatment programs. J Subst Abuse Treat. (2020) 108:55–64. doi: 10.1016/j.jsat.2019.06.015
135. Mcguire AB, Powell KG, Treitler PC, Wagner KD, Smith KP, Cooperman N, et al. Emergency department-based peer support for opioid use disorder: emergent functions and forms. J Subst Abuse Treat. (2020) 108:82–7. doi: 10.1016/j.jsat.2019.06.013
136. Scott CK, Dennis ML, Grella CE, Nicholson L, Sumpter J, Kurz R, et al. Findings from the recovery initiation and management after overdose (RIMO) pilot study experiment. J Subst Abuse Treat. (2020) 108:65–74. doi: 10.1016/j.jsat.2019.08.004
137. Shi JM, Henry SP, Dwy SL, Orazietti SA, Carroll KM. Randomized pilot trial of Web-based cognitive-behavioral therapy adapted for use in office-based buprenorphine maintenance. Subst Abuse. (2019) 40:132–5. doi: 10.1080/08897077.2019.1569192
138. Snow RL, Simon RE, Jack HE, Oller D, Kehoe L, Wakeman SE. Patient experiences with a transitional, low-threshold clinic for the treatment of substance use disorder: a qualitative study of a bridge clinic. J Subst Abuse Treat. (2019) 107:1–7. doi: 10.1016/j.jsat.2019.09.003
139. Labelle CT, Han SC, Bergeron A, Samet JH. Office-based opioid treatment with buprenorphine (OBOT-B): statewide implementation of the Massachusetts Collaborative Care Model in community health centers. J Subst Abuse Treat. (2016) 60:6–13. doi: 10.1016/j.jsat.2015.06.010
140. Basic Behavioral and Social Science Opportunity Network (OppNet). Available online at: https://oppnet.nih.gov/ .
141. Fredrickson BL, Cohn MA, Coffey KA, Pek J, Finkel SM. Open hearts build lives: positive emotions, induced through loving-kindness meditation, build consequential personal resources. J Pers Soc Psychol. (2008) 95:1045–62. doi: 10.1037/a0013262
142. Hendriks T, Schotanus-Dijkstra M, Hassankhan A, De Jong J, Bohlmeijer E. The efficacy of multi-component positive psychology interventions: a systematic review and meta-analysis of randomized controlled trials. J Happ Stud. (2020) 21:357–90. doi: 10.1007/s10902-019-00082-1
143. Kim ES, Sun JK, Park N, Kubzansky LD, Peterson C. Purpose in life and reduced risk of myocardial infarction among older U.S. adults with coronary heart disease: a two-year follow-up. J Behav Med . (2013) 36:124–33. doi: 10.1007/s10865-012-9406-4
144. Vaillant GE. Surprising Guideposts to a Happier Life From the Landmark Study of Adult Development . New York, NY: Little, Brown and Spark, Hatchette Book Group (2002).
145. Vaillant GE. Triumphs of Experience: The Men of the Harvard Grant Study . Cambridge, MA: Belknap Press (2012).
146. Uchino BN, Cacioppo JT, Kiecolt-Glaser JK. The relationship between social support and physiological processes: a review with emphasis on underlying mechanisms and implications for health. Psychol Bull. (1996) 119:488–531. doi: 10.1037/0033-2909.119.3.488
147. Barnes LL, Mendes De Leon CF, Wilson RS, Bienias JL, Evans DA. Social resources and cognitive decline in a population of older African Americans and whites. Neurology. (2004) 63:2322–6. doi: 10.1212/01.WNL.0000147473.04043.B3
148. Tanskanen J, Anttila T. A prospective study of social isolation, loneliness, and mortality in Finland. Am J Public Health. (2016) 106:2042–8. doi: 10.2105/AJPH.2016.303431
149. Kok BE, Fredrickson BL. Upward spirals of the heart: autonomic flexibility, as indexed by vagal tone, reciprocally and prospectively predicts positive emotions and social connectedness. Biol Psychol. (2010) 85:432–6. doi: 10.1016/j.biopsycho.2010.09.005
150. Sandstrom GM, Dunn EW. Social interactions and well-being: the surprising power of weak ties. Pers Soc Psychol Bull. (2014) 40:910–22. doi: 10.1177/0146167214529799
151. Woolf SH, Braveman P. Where health disparities begin: the role of social and economic determinants–and why current policies may make matters worse. Health Aff. (2011) 30:1852–9. doi: 10.1377/hlthaff.2011.0685
152. Jackson RJ. Designing Healthy Communities . Hoboken, NJ: Jossey-Bass (2011).
153. Fabisiak JP, Jackson EM, Brink LL, Presto AA. A risk-based model to assess environmental justice and coronary heart disease burden from traffic-related air pollutants. Environ Health. (2020) 19:34. doi: 10.1186/s12940-020-00584-z
154. Berwick DM. The moral determinants of health. JAMA. (2020) 324:225–6. doi: 10.1001/jama.2020.11129
155. Smith JA, Zhao W, Wang X, Ratliff SM, Mukherjee B, Kardia SLR, et al. Neighborhood characteristics influence DNA methylation of genes involved in stress response and inflammation: the multi-ethnic study of atherosclerosis. Epigenetics. (2017) 12:662–73. doi: 10.1080/15592294.2017.1341026
156. Reuben A, Sugden K, Arseneault L, Corcoran DL, Danese A, Fisher HL, et al. Association of neighborhood disadvantage in childhood with DNA methylation in young adulthood. JAMA Netw Open. (2020) 3:e206095–e206095. doi: 10.1001/jamanetworkopen.2020.6095
157. Allen JG, Macnaughton P, Satish U, Santanam S, Vallarino J, Spengler JD. Associations of cognitive function scores with carbon dioxide, ventilation, and volatile organic compound exposures in office workers: a controlled exposure study of green and conventional office environments. Environ Health Perspect. (2016) 124:805–12. doi: 10.1289/ehp.1510037
158. Macnaughton P, Satish U, Laurent JGC, Flanigan S, Vallarino J, Coull B, et al. The impact of working in a green certified building on cognitive function and health. Build Environ. (2017) 114:178–86. doi: 10.1016/j.buildenv.2016.11.041
159. International Living Future Institute. Living Building Challenge . Available online at: https://living-future.org/lbc/
160. Wilson EO. Biophilia, The Human Bond With Other Species . Cambridge, MA: Harvard University Press (1984).
161. Kellert SR, Wilson EO. The Biophilia Hypothesis . Washington, DC: Island Press (1993).
162. Ulrich RS, Zimring C, Zhu X, Dubose J, Seo HB, Choi YS, et al. A review of the research literature on evidence-based healthcare design. Herditiy. (2008) 1:61–125. doi: 10.1177/193758670800100306
163. James P, Banay RF, Hart JE, Laden F. A review of the health benefits of greenness. Curr Epidemiol Rep. (2015) 2:131–42. doi: 10.1007/s40471-015-0043-7
164. Zeller JM, Rothberg L, Landay AL. Evaluation of human monocyte oxidative metabolism utilizing a flow cytometric assay. Clin Exp Immunol . (1989) 78:91–6.
165. Trasande L. Sicker, Fatter, Poorer: The Urgent Threat of Hormone-Disrupting Chemicals to Our Health and Future and What We Can Do About It . New York, NY: Houghton Mifflin Harcourt (2019).
166. Willett W, Rockström J, Loken B, Springmann M, Lang T, Vermeulen S, et al. Food in the anthropocene: the EAT-Lancet Commission on healthy diets from sustainable food systems. Lancet . (2019) 393:447–92. doi: 10.1016/S0140-6736(18)31788-4
167. Maizes V, Weil A. Be Fruitful: The Essential Guide to Maximizing Fertility and Giving Birth to a Healthy Child. New York, NY: Scribner (2013).
168. Feil R, Fraga MF. Epigenetics and the environment: emerging patterns and implications. Nat Rev Genet. (2012) 13:97–109. doi: 10.1038/nrg3142
169. Mead MN. Contaminants in human milk: weighing the risks against the benefits of breastfeeding. Environ. Health Perspect. (2008) 116:A427–34. doi: 10.1289/ehp.116-a426
170. Shonkoff JP, Boyce WT, Mcewen BS. Neuroscience, molecular biology, and the childhood roots of health disparities: building a new framework for health promotion and disease prevention. JAMA. (2009) 301:2252–9. doi: 10.1001/jama.2009.754
171. Lippard ETC, Nemeroff CB. The devastating clinical consequences of child abuse and neglect: increased disease vulnerability and poor treatment response in mood disorders. Am J Psychiatry. (2020) 177:20–36. doi: 10.1176/appi.ajp.2019.19010020
172. Parikh Y, Mason M, Williams K. Researchers' perspectives on pediatric obesity research participant recruitment. Clin Transl Med. (2016) 5:20. doi: 10.1186/s40169-016-0099-0
173. Parkinson MD. Employer health and productivity roadmap™ strategy. J Occup Environ Med. (2013) 55:S46–51. doi: 10.1097/JOM.0000000000000049
174. Trasande L. Further limiting bisphenol a in food uses could provide health and economic benefits. Health Aff. (2014) 33:316–23. doi: 10.1377/hlthaff.2013.0686
175. Centers for Disease Control National Institute of Occupational Safety and Health. Total Worker Health . Available online at: https://www.cdc.gov/niosh/twh/default.html
176. Mishra S, Xu J, Agarwal U, Gonzales J, Levin S, Barnard ND. A multicenter randomized controlled trial of a plant-based nutrition program to reduce body weight and cardiovascular risk in the corporate setting: the GEICO study. Eur J Clin Nutr. (2013) 67:718–24. doi: 10.1038/ejcn.2013.92
177. Kucharczyk ER, Morgan K, Hall AP. The occupational impact of sleep quality and insomnia symptoms. Sleep Med Rev. (2012) 16:547–59. doi: 10.1016/j.smrv.2012.01.005
178. Scrafford CG, Bi X, Multani JK, Murphy MM, Schmier JK, Barraj LM. Health economic evaluation modeling shows potential health care cost savings with increased conformance with healthy dietary patterns among adults in the United States. J Acad Nutr Diet. (2019) 119:599–616. doi: 10.1016/j.jand.2018.10.002
179. https://www.niddk.nih.gov/about-niddk/strategic-plans-reports/strategic-plan-nih-nutrition-research
180. American Heart Association Lifes Simple 7. Available online at: https://www.heart.org/en/professional/workplace-health/lifes-simple-7
181. Department of Defense. DOD Total Force Fitness. Available online at: https://www.health.mil/News/Articles/2020/01/07/Joint-Chiefs-say-mind-body-spirit-all-part-of-Total-Force-Fitness
PubMed Abstract
182. US Special Operations Command (USSOCOM). Preservation of the Force and Family Program . Available online at: https://www.socom.mil/POTFF/Pages/About-POTFF.aspx
183. Veterans Administration. Whole Health Program . Available online at: https://www.va.gov/wholehealth/
184. Richardson S, Hirsch JS, Narasimhan M, Crawford JM, Mcginn T, Davidson KW, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. (2020) 323:2052–9. doi: 10.1001/jama.2020.6775
185. Stokes EK, Zambrano LD, Anderson KN, Merder EP, Raz KM, El Burai Felix S, et al. Coronavirus disease 2019 case surveillance–United States, January 22-May 30, 2020. MMWR Morb Mortal Wkly Rep. (2020) 69:759–65. doi: 10.15585/mmwr.mm6924e2
186. Tay MZ, Poh CM, Rénia L, Macary PA, Ng LFP. The trinity of COVID-19: immunity, inflammation and intervention. Nat Rev Immunol. (2020) 20:363–74. doi: 10.1038/s41577-020-0311-8
Keywords: lifestyle medicine, chronic disease, inflammation, epigenetics, research methodologies, in silico modeling, nutrition, physical activity
Citation: Vodovotz Y, Barnard N, Hu FB, Jakicic J, Lianov L, Loveland D, Buysse D, Szigethy E, Finkel T, Sowa G, Verschure P, Williams K, Sanchez E, Dysinger W, Maizes V, Junker C, Phillips E, Katz D, Drant S, Jackson RJ, Trasande L, Woolf S, Salive M, South-Paul J, States SL, Roth L, Fraser G, Stout R and Parkinson MD (2020) Prioritized Research for the Prevention, Treatment, and Reversal of Chronic Disease: Recommendations From the Lifestyle Medicine Research Summit. Front. Med. 7:585744. doi: 10.3389/fmed.2020.585744
Received: 21 July 2020; Accepted: 20 November 2020; Published: 22 December 2020.
Reviewed by:
Copyright © 2020 Vodovotz, Barnard, Hu, Jakicic, Lianov, Loveland, Buysse, Szigethy, Finkel, Sowa, Verschure, Williams, Sanchez, Dysinger, Maizes, Junker, Phillips, Katz, Drant, Jackson, Trasande, Woolf, Salive, South-Paul, States, Roth, Fraser, Stout and Parkinson. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Michael D. Parkinson, parkinsonmd@upmc.edu
- Share full article
Advertisement
Supported by
Why Are Younger Adults Developing This Common Heart Condition?
New research suggests that A-fib may be more prevalent, and more dangerous, in people under 65 than previously thought.

By Dani Blum
Atrial fibrillation, a common cardiac condition that raises the risk of stroke, is increasingly affecting the health of people under the age of 65.
For years, experts thought that A-fib, a type of irregular heartbeat, primarily occurred in people age 65 and older, and that younger people with the condition most likely wouldn’t develop other cardiac issues, said Dr. Aditya Bhonsale, a cardiac electrophysiologist at the University of Pittsburgh Medical Center. But in new research published Monday, Dr. Bhonsale and his colleagues examined data on more than 67,000 patients with A-fib who were treated at the center, nearly one-quarter of whom were under the age of 65. Those patients had an increased risk of death, compared to people without the condition. They also often had risk factors for A-fib like high blood pressure, obesity and sleep apnea, which could make cardiovascular health issues worse.
What is A-fib?
In A-fib, the upper and lower chambers of the heart are not coordinated as they should be, which makes the heart beat chaotically — sometimes too slow, sometimes too fast, often just irregularly. People with the condition can experience a fluttering heartbeat and palpitations.
Dr. Geoffrey Barnes, a cardiologist and vascular medicine specialist at University of Michigan Health, said that he frequently saw patients who say “I felt like my heart was racing away” or “I felt like it was skipping beats.” People with A-fib can also experience shortness of breath and chest discomfort. Some people have occasional episodes; others will continuously experience an irregular heartbeat. People often have no symptoms and don’t even realize they have the condition, Dr. Barnes said.
Increasingly, doctors said, patients are seeking care because their smart watches have detected an irregular heartbeat. That might help explain why more younger people are being diagnosed, said Dr. Hugh Calkins, a professor of cardiology at Johns Hopkins Medicine. “The more you screen, the more you’re going to find,” he said.
Doctors typically diagnose atrial fibrillation with an electrocardiogram while factoring in your medical and family history. They will sometimes give patients a portable monitor to wear for up to a month to look for an irregular heartbeat.
A-fib can cause clots to form in the heart that can travel to the brain and lead to strokes, even in younger patients, Dr. Bhonsale said. The condition may also raise the risk of cognitive decline and dementia , as well as heart failure. In the study, researchers found that people with A-fib under the age of 65 were at a significantly higher risk of hospitalization for heart failure, stroke and heart attack, compared to people without A-fib.
What’s driving the increase in younger adults?
Atrial fibrillation may also be increasing among younger adults because many of the risk factors for the condition — including pre-existing heart disease and diabetes — are on the rise in that age group, too, Dr. Bhonsale said.
Nearly one in five people in the study who had A-fib also had obstructive sleep apnea , which is a significant risk factor for the condition. People with sleep apnea stop and restart breathing in the night; they struggle to get sufficient rest. The condition, which often goes undiagnosed , is tied to a range of cardiovascular issues .
There is also a correlation between how much alcohol people consume and the likelihood they will develop A-fib, said Dr. Bradley Knight, the medical director of electrophysiology at the Northwestern Medicine Bluhm Cardiovascular Institute. Smoking cigarettes and vaping are also linked with a greater risk of A-fib, Dr. Barnes said.
While exercise in general is associated with a lower risk of cardiac conditions, extreme endurance exercise, like marathons and triathlons, are linked with a higher risk of A-fib, Dr. Calkins said.
How is A-fib treated?
Doctors work with patients to address factors that make A-fib more likely to occur, such as by making sure someone with sleep apnea is using a CPAP machine or by helping patients quit smoking. Sometimes, particularly for younger patients, physicians will recommend a procedure called catheter ablation , which doctors use to get rid of tissue in the heart that may be causing an irregular heartbeat.
Doctors may also prescribe blood thinners, to reduce stroke risk, as well as other medications to manage symptoms. These include drugs that can help regulate heart rate and rhythm , Dr. Knight said. While medications can help reduce the frequency and duration of A-fib episodes, “they rarely eliminate the A-fib,” he added. He tells patients that the disease is like high blood pressure: It must be continuously managed.
“If you are diagnosed with A-fib at any age, but in particular at a younger age, you have been given a great opportunity to now say, OK, what things can I do to help better manage my health and reduce the chance of having a problem later in life?” Dr. Barnes said. “I almost think of it like a wake-up call.”
Dani Blum is a health reporter for The Times. More about Dani Blum
Tips for Better Sleep
Tired of tossing and turning there are some strategies you could try to maximize your hours in bed..
Four out of five people say that they suffer from sleep problems at least once a week and wake up feeling exhausted. Use our guide for a better night’s sleep .
Poor sleep can make anxiety, depression and other mental health issues worse. Here’s what to do about it .
Sleep deprivation doesn’t just feel terrible — it can also hamper your ability to form and recall memories .
The “sleepy girl mocktail” has gone viral on TikTok, where wellness influencers are touting it as a must-have to help you sleep. But is it effective ?
Do sleeping pills work? We asked experts about the different types of medications for treating insomnia .
Sharing a bed with a restless partner doesn’t have to be torture. Try these tips .
Turn Your Bedroom Into a Sleep Sanctuary With Wirecutter’s Recommendations
Good rest starts with a great mattress. These tips can help you pick the right one for you out of the countless options available .
Next, you’ll need a good pillow. These customizable models offer the comfort you need — whether you sleep on your stomach, side or back.
Looking for a more luxe experience? The right sheets can make a big difference. Here is a selection to choose from .
White noise machines have the power to mask yapping dogs, clanky radiators and late-night parties. Consider buying one .
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
Latest science news, discoveries and analysis

Bird flu in US cows: is the milk supply safe?

Judge dismisses superconductivity physicist’s lawsuit against university

NIH pay raise for postdocs and PhD students could have US ripple effect

Hello puffins, goodbye belugas: changing Arctic fjord hints at our climate future
China's moon atlas is the most detailed ever made, ‘shut up and calculate’: how einstein lost the battle to explain quantum reality, rat neurons repair mouse brains — and restore sense of smell, mini-colon and brain 'organoids' shed light on cancer and other diseases, ecologists: don’t lose touch with the joy of fieldwork chris mantegna.

Should the Maldives be creating new land?

Lethal AI weapons are here: how can we control them?

Algorithm ranks peer reviewers by reputation — but critics warn of bias

How gliding marsupials got their ‘wings’
Future of humanity institute shuts: what's next for ‘deep future’ research, nato is boosting ai and climate research as scientific diplomacy remains on ice, plastic pollution: three numbers that support a crackdown, the maldives is racing to create new land. why are so many people concerned.
Retractions are part of science, but misconduct isn’t — lessons from a superconductivity lab

Any plan to make smoking obsolete is the right step

Citizenship privilege harms science
European ruling linking climate change to human rights could be a game changer — here’s how charlotte e. blattner, will ai accelerate or delay the race to net-zero emissions, current issue.

Surprise hybrid origins of a butterfly species
Stripped-envelope supernova light curves argue for central engine activity, optical clocks at sea, research analysis.

Ancient DNA traces family lines and political shifts in the Avar empire
A chemical method for selective labelling of the key amino acid tryptophan

Robust optical clocks promise stable timing in a portable package
Targeting RNA opens therapeutic avenues for Timothy syndrome
Bioengineered ‘mini-colons’ shed light on cancer progression, galaxy found napping in the primordial universe, tumours form without genetic mutations, marsupial genomes reveal how a skin membrane for gliding evolved.

Scientists urged to collect royalties from the ‘magic money tree’

Breaking ice, and helicopter drops: winning photos of working scientists

Shrouded in secrecy: how science is harmed by the bullying and harassment rumour mill
How ground glass might save crops from drought on a caribbean island, londoners see what a scientist looks like up close in 50 photographs, books & culture.

How volcanoes shaped our planet — and why we need to be ready for the next big eruption
Dogwhistles, drilling and the roots of Western civilization: Books in brief

Cosmic rentals
Las borinqueñas remembers the forgotten puerto rican women who tested the first pill, dad always mows on summer saturday mornings, nature podcast.

Latest videos
Nature briefing.
An essential round-up of science news, opinion and analysis, delivered to your inbox every weekday.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Volume 30, Number 5—May 2024
Cross-sectional study of q fever seroprevalence among blood donors, israel, 2021.
Main Article
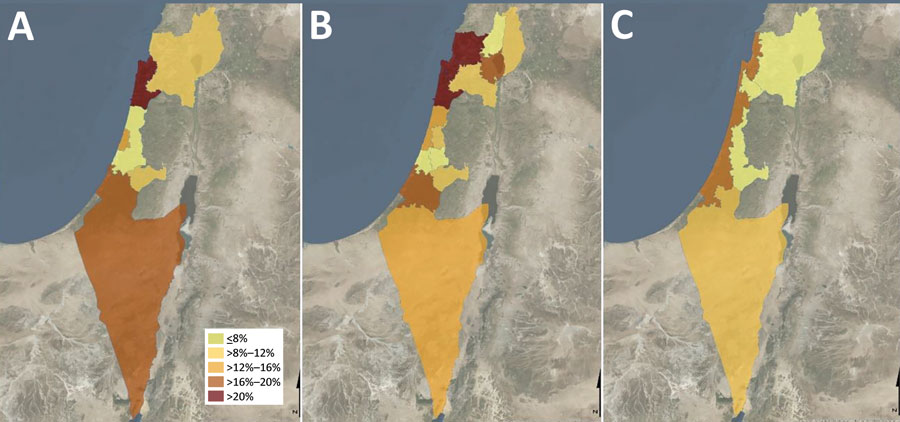
Figure . Q fever prevalence by district, subdistrict, and natural region in cross-sectional study of seroprevalence among blood donors, Israel, 2021. Spatial distribution of Q fever seroprevalence uses different geographic classifications. A) Seroprevalence rates by district; the highest rate was in Haifa district. B) Seroprevalence rates by subdistrict; the highest rate was in Hadera subdistrict. C) Seroprevalence rates by 4 natural region clusters; the highest rate was in the coastal plain area.
1 These authors contributed equally to this article.
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
What is ADHD?
Signs and symptoms.
- Managing Symptoms
ADHD in Adults
More information.
ADHD is one of the most common neurodevelopmental disorders of childhood. It is usually first diagnosed in childhood and often lasts into adulthood. Children with ADHD may have trouble paying attention, controlling impulsive behaviors (may act without thinking about what the result will be), or be overly active.
It is normal for children to have trouble focusing and behaving at one time or another. However, children with ADHD do not just grow out of these behaviors. The symptoms continue, can be severe, and can cause difficulty at school, at home, or with friends.
A child with ADHD might:
- daydream a lot
- forget or lose things a lot
- squirm or fidget
- talk too much
- make careless mistakes or take unnecessary risks
- have a hard time resisting temptation
- have trouble taking turns
- have difficulty getting along with others
Learn more about signs and symptoms

Get information and support from the National Resource Center on ADHD
There are three different ways ADHD presents itself, depending on which types of symptoms are strongest in the individual:
- Predominantly Inattentive Presentation: It is hard for the individual to organize or finish a task, to pay attention to details, or to follow instructions or conversations. The person is easily distracted or forgets details of daily routines.
- Predominantly Hyperactive-Impulsive Presentation: The person fidgets and talks a lot. It is hard to sit still for long (e.g., for a meal or while doing homework). Smaller children may run, jump or climb constantly. The individual feels restless and has trouble with impulsivity. Someone who is impulsive may interrupt others a lot, grab things from people, or speak at inappropriate times. It is hard for the person to wait their turn or listen to directions. A person with impulsiveness may have more accidents and injuries than others.
- Combined Presentation: Symptoms of the above two types are equally present in the person.
Because symptoms can change over time, the presentation may change over time as well.
Learn about symptoms of ADHD, how ADHD is diagnosed, and treatment recommendations including behavior therapy, medication, and school support.
Causes of ADHD
Scientists are studying cause(s) and risk factors in an effort to find better ways to manage and reduce the chances of a person having ADHD. The cause(s) and risk factors for ADHD are unknown, but current research shows that genetics plays an important role. Recent studies link genetic factors with ADHD. 1
In addition to genetics, scientists are studying other possible causes and risk factors including:
- Brain injury
- Exposure to environmental risks (e.g., lead) during pregnancy or at a young age
- Alcohol and tobacco use during pregnancy
- Premature delivery
- Low birth weight
Research does not support the popularly held views that ADHD is caused by eating too much sugar, watching too much television, parenting, or social and environmental factors such as poverty or family chaos. Of course, many things, including these, might make symptoms worse, especially in certain people. But the evidence is not strong enough to conclude that they are the main causes of ADHD.

Download and Print this fact sheet [PDF – 473 KB]
Deciding if a child has ADHD is a process with several steps. There is no single test to diagnose ADHD, and many other problems, like anxiety, depression, sleep problems, and certain types of learning disabilities, can have similar symptoms. One step of the process involves having a medical exam, including hearing and vision tests , to rule out other problems with symptoms like ADHD. Diagnosing ADHD usually includes a checklist for rating ADHD symptoms and taking a history of the child from parents, teachers, and sometimes, the child.
Learn more about the criteria for diagnosing ADHD

In most cases, ADHD is best treated with a combination of behavior therapy and medication. For preschool-aged children (4-5 years of age) with ADHD, behavior therapy, particularly training for parents, is recommended as the first line of treatment before medication is tried. What works best can depend on the child and family. Good treatment plans will include close monitoring, follow-ups, and making changes, if needed, along the way.
Learn more about treatments
Managing Symptoms: Staying Healthy
Being healthy is important for all children and can be especially important for children with ADHD. In addition to behavioral therapy and medication, having a healthy lifestyle can make it easier for your child to deal with ADHD symptoms. Here are some healthy behaviors that may help:
- Developing healthy eating habits such as eating plenty of fruits, vegetables, and whole grains and choosing lean protein sources
- Participating in daily physical activity based on age
- Limiting the amount of daily screen time from TVs, computers, phones, and other electronics
- Getting the recommended amount of sleep each night based on age
If you or your doctor has concerns about ADHD, you can take your child to a specialist such as a child psychologist, child psychiatrist, or developmental pediatrician, or you can contact your local early intervention agency (for children under 3) or public school (for children 3 and older).
The Centers for Disease Control and Prevention (CDC) funds the National Resource Center on ADHD , a program of CHADD – Children and Adults with Attention-Deficit/Hyperactivity Disorder. Their website has links to information for people with ADHD and their families. The National Resource Center operates a call center (1-866-200-8098) with trained staff to answer questions about ADHD.
For more information on services for children with special needs, visit the Center for Parent Information and Resources. To find the Parent Center near you, you can visit this website.
ADHD can last into adulthood. Some adults have ADHD but have never been diagnosed. The symptoms can cause difficulty at work, at home, or with relationships. Symptoms may look different at older ages, for example, hyperactivity may appear as extreme restlessness. Symptoms can become more severe when the demands of adulthood increase. For more information about diagnosis and treatment throughout the lifespan, please visit the websites of the National Resource Center on ADHD and the National Institutes of Mental Health .
- National Resource Center on ADHD
- National Institute of Mental Health (NIMH)
- Faraone, S. V., Banaschewski, T., Coghill, D., Zheng, Y., Biederman, J., Bellgrove, M. A., . . . Wang, Y. (2021). The World Federation of ADHD International Consensus Statement: 208 evidence-based conclusions about the disorder. Neuroscience & Biobehavioral Reviews. doi:10.1016/j.neubiorev.2021.01.022
To receive email updates about this topic, enter your email address:
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
2024 NIOSH Science and Service Awards

Exemplary science is the foundation for all National Institute for Occupational Safety and Health (NIOSH) research and prevention activities. Each year, NIOSH recognizes outstanding science and service from our employees. This year’s Science and Service Awards took place on April 25, 2024. The awards booklet contains the finalists, awardees, and honorable mentions as well as information on the occupational safety and health pioneers whom many of the awards are named after. The winners in each category and a brief description of their work are included below.
James P. Keogh Award for Outstanding Service in Occupational Safety and Health
This award recognizes a current or former NIOSH employee for exceptional service in the field of occupational safety and health.

Dr. Morata is a prolific scientist holding many leadership positions and serving as a Founding Associate Editor for the International Journal of Audiology and Founding Editorial Board Member for the prestigious Cochrane Systematic Reviews on Occupational Safety and Health. She is also responsible for creating the Safe-in-Sound Excellence in Hearing Loss Prevention Award Program . Her forward-thinking vision led to many collaborations with Wikipedia, Wikimedia, and the Wiki Education Foundation to train students and expand the reach of safety and health information and working towards one of her goals to provide NIOSH resources in multiple languages to reach a larger global audience.
Read more about Dr. Morata’s accomplishments in the 2024 awards booklet.
Alice Hamilton Award for Occupational Safety and Health
This award recognizes the scientific excellence of NIOSH technical and instructional materials. Categories include Behavioral and Social Science, Communication and Guidance, Engineering and Control, Epidemiology and Surveillance, Exposure and Risk Assessment, Methods and Laboratory Science, and Research Service. The annual award honors Dr. Alice Hamilton (1869– 1970), a pioneering researcher and occupational physician. Read more about the award winners, honorable mentions, finalists, and Alice Hamilton in the 2024 Awards Booklet.
Behavioral and Social Science Awardee
Hope M. Tiesman, Scott A. Hendricks, Douglas M. Wiegand, Barbara Lopes-Cardozo, Carol Y. Rao, Libby Horter, Charles E. Rose, and Ramona Byrkit
Workplace Violence and the Mental Health of Public Health Workers During COVID-19 is the first to document the prevalence and impact of violence directed towards the public health workforce during an ongoing public health emergency. The findings revealed that nearly 1 out of 3 public health workers experienced workplace violence increasing the impact on their mental health.
Communication and Guidance Awardee
Eric J. Esswein, David Caruso, Kyla Hagan-Haynes, John E. Snawder, Laura Styles, Robert Harrison, Jordon Plotsky, and Jeff Knight
The video, You’ve Got This: Understanding Hazards, Risks, and Controls for Safer Fluid Transfers in Oil and Gas Extraction , addresses a critical need in the oil and gas extraction industry for increased awareness about how to safely transfer all fluids from tanks to tanker trucks, and how workers can protect themselves from exposures when doing so.
Engineering and Control Awardee
Drew Thompson and Chaolong Qi
Characterization of the Emissions and Crystalline Silica Content of Airborne Dust Generated from Grinding Natural and Engineered Stones used a standard measurement method to characterize dust generation rates during grinding of engineered and natural stone products in a laboratory testing system.
Epidemiology and Surveillance Awardee
Alysha R. Meyers, Steven J. Wurzelbacher, Edward F. Krieg, Jessica G. Ramsey, Kenneth Crombie, Annette L. Christianson, Lian Luo, and Susan Burt
Work-Related Risk Factors for Rotator Cuff Syndrome in a Prospective Study of Manufacturing and Healthcare Workers highlights the importance of assessing combinations of exposure to forceful repetition and upper arm elevation when developing interventions for preventing rotator cuff syndrome.
Exposure & Risk Assessment Awardee
David B . Richardson, Klervi Leuraud, Dominique Laurier, Michael Gillies, Richard Haylock, Kaitlin Kelly-Reif, Stephen Bertke, Robert D . Daniels, Isabelle Thierry-Chef, Monika Moissonnier, Ausrele Kesminiene, and Mary K . Schubauer-Berigan
Cancer mortality after low dose exposure to ionizing radiation in workers in France, the United Kingdom, and the United States (INWORKS): cohort study reports that workers in nuclear facilities who are persistently exposed to low doses of ionizing radiation experience an increase in deaths due to cancer.
Methods & Laboratory Science Awardee
Cornelius Rimayi and Ju-Hyenong Park
Adjustment of Matrix Effects in Analysis of 36 Secondary Metabolites of Microbial and Plant Origin in Indoor Floor Dust Using Liquid Chromatography-Tandem Mass Spectrometry documents a method to accurately estimate the concentration of microbial secondary metabolites, which are biochemical products of indoor mold and bacteria, in damp indoor environments.
Research Service Category Awardee
Jessica F. Li, Dallas S. Shi, Dylan T. Neu, Sophia Chiu, and Melissa Charles
In the Health Hazard Evaluation, Evaluation of Occupational Exposures to Illicit Drugs in Forensic Laboratories, investigators found detectable levels of methamphetamine, cocaine, fentanyl, and heroin on surfaces of a toxicology lab and provided recommendations to improve the safety and health of the workplace.
Bullard-Sherwood Research to Practice
This award recognizes outstanding efforts by NIOSH scientists and their partners in applying occupational safety and health research to prevent work-related injury, illness, and death. It highlights efforts that demonstrate noteworthy impact through partnerships. The award is named in honor of two distinguished inventors who made significant improvements in workplace injury and illness prevention. Edward W. Bullard designed the first “hard hat” as protective headgear for miners. R. Jeremy (Jerry) Sherwood merged research and industrial hygiene by inventing the first practical personal sampling pump in the late 1950s. Read more about this year’s winner and the inventors who inspired the award in the awards booklet.
The Bullard Sherwood Knowledge Award is given for research resulting in the development and transfer of new knowledge into practice.
Gavin P. Horn, Kenneth W. Fent, Steve Kerber, Dennis L. Smith, Alex Mayer, Angela Bennett, Leeanne Poist, Doug Mansen, and Peter Couste
An article and a free online training course were developed to help communicate the importance of exposure controls, policies, and procedures to protect firefighters from carcinogens.
Plain Language Awardees
The Plain Writing Act of 2010 requires that federal agencies provide clear communication that the public can understand and use. NIOSH encourages plain language in all communication products. Awards are given in two categories: Before and After and Original products.
Before and After Category Awardee
Asha Brogan, Amy Mobley, Jennifer Tyrawski, David Byrne, Wei Gong, Pamela Graydon, Elizabeth Masterson, Thais Morata, Christi Themann, and Ed Zechmann
Original Category Awardee
James Couch, Jessica Rinsky, Reed Grimes, Krystin Carlson, Laura Reynolds, Garrett Burnett, Rebecca Tsai, and Susan Afanuh
The infographic fact sheet Leave Lead at Work highlights the importance of take-home lead, defines the problem, conveys the health effects, and walks workers through steps to reduce potential lead exposures outside of work.
Service Excellence Awardees
These awards focus on both the management and operations side of the Institute and recognize NIOSH staff who provide excellent administrative and managerial support to the Institute’s mission and projects.
Excellence in Administration
Peter Grandillo , Office of Extramural Coordination and Special Projects, for his proactive and continuous improvement approach which has led to the development of sustainable systems and tools that contribute to efficient and effective grant administration.
Excellence in Leadership
Susan Moore , PhD, National Personal Protective Technology Laboratory, for proactively addressing challenges faced by NPPTL staff including the development of a guidance document and standard operating procedures to reduce the workload of NPPTL staff.
Aaron Reeder , National Personal Protective Technology Laboratory, for his exceptional leadership to help ensure NPPTL remains a world leader and innovator in respirator testing.
Dan Farwick , Division of Field Studies and Engineering, for his innovative use of technology resulting in an accelerated pace of research and significant government savings.
Excellence in Workforce Development
The NPPTL Workplace Satisfaction Committee’s Workforce Development Team for the development and execution of a multifaceted plan to assist employees in maximizing their workforce development and increasing workplace morale.
Team members: Christian Coby, Maryann D’Alessandro, Patrick Dempsey, Mihili Edirisooriya, Barbara Ginsburg, Lacy Hannon, Colleen Miller, Frank Palya, Jeff Peterson, Jonisha Pollard, Heather Reed, Adam Smith, Jonathan Szalajda, Brooke Vollmer, Justin Wehring, and Dawn Zubasic.
Excellence in Workforce Diversity
The NPPTL Recruitment Excellence and Diversity Team : Susan Moore, Nora Payne, and Hom Sharma for the development of an NPPTL Candidate Recruitment and Selection standard operating procedure to help achieve a diverse workforce.
Director’s Intramural Award for Extraordinary Science Awardees
The Director’s Intramural Awards for Extraordinary Science recognize outstanding contributions to scientific excellence at NIOSH by scientists and support staff.
Emily Haas, PhD, received the Lew Wade Distinguished Career Scientist Award for her work in merging engineering and behavioral research to reduce worker risks. She has led efforts to conduct safety climate assessments in hazardous workplaces; tailor leadership, communication, and engagement practices using a workplace health safety management system; integrate personal protective technology to minimize exposure; and coordinate high-visibility surveillance efforts.
Jennie Cox, PhD , received the Early Career Scientist Award for her work generating and obtaining funding for a new line of research into illicit drug exposures, publishing a collaborative review on the evaluation of SARS-CoV-2 sampling methods, and promoting diversity and inclusiveness within and outside of NIOSH.
Donnie Booher received the Scientific Support Award for his technical expertise and support of the Health Hazard Evaluation program as a Biomedical Engineering Technician for over 30 years. His highly sought after expertise ranges from how to procure the right PPE to the most technical details of putting a direct-reading instrument into a hostile environment. The countless HHE staff and NIOSH first responders are truly grateful for his contributions and support.
Congratulations to the NIOSH researchers and staff on their important work to protect America’s workforce!
The winners described here are only the tip of the iceberg. The awards booklet contains the honorable mentions and finalists in each category which further demonstrates the breadth of the Institute’s research. For more examples of NIOSH research see our website , e-News , blog , and social media accounts .
John Howard, MD , NIOSH Director
Marie de Perio, MD, MPH, Associate Director for Science
Kelley A. Durst, MPA, Deputy Director for Management
Christina Spring, MA , Associate Director, Communication and Research to Practice
Post a Comment
Cancel reply.
Your email address will not be published. Required fields are marked *
- 50th Anniversary Blog Series
- Additive Manufacturing
- Aging Workers
- Agriculture
- Animal/Livestock hazards
- Artificial Intelligence
- Back Injury
- Bloodborne pathogens
- Cardiovascular Disease
- cold stress
- commercial fishing
- Communication
- Construction
- Cross Cultural Communication
- Dermal Exposure
- Education and Research Centers
- Electrical Safety
- Emergency Response/Public Sector
- Engineering Control
- Environment/Green Jobs
- Epidemiology
- Fire Fighting
- Food Service
- Future of Work and OSH
- Healthy Work Design
- Hearing Loss
- Heat Stress
- Holiday Themes
- Hydraulic Fracturing
- Infectious Disease Resources
- International
- Landscaping
- Law Enforcement
- Manufacturing
- Manufacturing Mondays Series
- Mental Health
- Motor Vehicle Safety
- Musculoskeletal Disorders
- Nanotechnology
- National Occupational Research Agenda
- Needlestick Prevention
- NIOSH-funded Research
- Nonstandard Work Arrangements
- Observances
- Occupational Health Equity
- Oil and Gas
- Outdoor Work
- Partnership
- Personal Protective Equipment
- Physical activity
- Policy and Programs
- Prevention Through Design
- Prioritizing Research
- Reproductive Health
- Research to practice r2p
- Researcher Spotlights
- Respirators
- Respiratory Health
- Risk Assessment
- Safety and Health Data
- Service Sector
- Small Business
- Social Determinants of Health
- Spanish translations
- Sports and Entertainment
- Strategic Foresight
- Struck-by injuries
- Student Training
- Substance Use Disorder
- Surveillance
- Synthetic Biology
- Systematic review
- Take Home Exposures
- Teachers/School Workers
- Temporary/Contingent Workers
- Total Worker Health
- Translations (other than Spanish)
- Transportation
- Uncategorized
- Veterinarians
- Wearable Technologies
- Wholesale and Retail Trade
- Work Schedules
- Workers' Compensation
- Workplace Medical Mystery
- Workplace Supported Recovery
- World Trade Center Health Program
- Young Workers
To receive email updates about this page, enter your email address:
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Prev Chronic Dis
Non–Peer Reviewed
Global perspectives on improving chronic disease prevention and management in diverse settings, collins o. airhihenbuwa.
1 Health Policy and Behavioral Sciences, School of Public Health, Georgia State University, Atlanta, Georgia
Tung-Sung Tseng
2 Behavioral and Community Health Sciences Department, School of Public Health, Louisiana State University Health Sciences Center, New Orleans, Louisiana
Victor D. Sutton
3 Office of Preventive Health and Health Equity, Mississippi State Department of Health, Jackson, Mississippi
LeShawndra Price
4 Office of Research Training and Special Programs, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Bethesda, Maryland
The Centers for Disease Control and Prevention (CDC) define chronic diseases as conditions that last 1 year or more and that require ongoing medical attention or limit activities of daily living, or both ( 1 ). Chronic diseases may be influenced by a combination of genetics, lifestyle and social behaviors, health care system factors, community influences, and environmental determinants of health ( 2 ). These risk factors often coexist and interact with each other. Therefore, a better understanding of determinants of chronic diseases such as tobacco use, unhealthy eating, and physical inactivity stands to benefit from effective strategies for improving primary, secondary, and tertiary disease prevention and management in diverse global settings ( 3 ). Strategies to prevent and manage chronic disease outcomes such as diabetes and cardiovascular diseases (CVDs) have global commonalities ( 4 – 7 ). The impact of chronic diseases is disproportionately evident in Black and Brown communities ( 8 , 9 ). Chronic disease prevention and management typically focus on behavioral interventions such as healthy eating, increased physical activity, and cessation of unhealthy practices such as tobacco and alcohol use ( 10 – 15 ). In 2020, the COVID-19 pandemic added to the fact that chronic diseases disproportionately affect low-resource communities, where many Black and Brown populations live ( 16 , 17 ). COVID-19 demonstrated that chronic disease disparities actually present as preexisting conditions in Black and Brown communities, who are disproportionately affected by COVID-19 outcomes. Although most of the articles in this Preventing Chronic Disease (PCD) collection were published before the pandemic, the insights they present, combined with the racial and ethnic data on the burden of COVID-19 thus far, support this reality. Many researchers and public health practitioners often consider the need to sufficiently address the relationships between chronic diseases and social, behavioral, and community factors ( 18 ). Global lessons in the prevention and management of chronic diseases, therefore, can help researchers and practitioners benefit from the shared lessons and experience derived from research and interventions conducted in different parts of the world. There are more than 7 billion people worldwide, who speak diverse languages and who have different nationalities, identities, and health systems. Yet, if we share challenges and opportunities for chronic disease prevention and management, many of the global adversities to improving health and well-being can be ameliorated, which is the purpose of this collection. The authors in this collection share lessons that represent experiences in diverse contexts across countries and regions of the world.
Objective and Themes of the Collection
The goal of the collection is to assemble recently published articles that focus on innovative and effective strategies to improve chronic disease outcomes in diverse populations globally. As efforts to improve global health have accelerated in response to achieving sustainable development goals, chronic disease continues to be a major contributor to poor health outcomes, which often lead to reduction in quality of life, including associated increases in health care costs ( 19 , 20 ). Reducing the burden of chronic diseases remains a global challenge, requiring collaborations across academic disciplines and economic sectors. As discussed in the articles included in this collection, certain individual and societal factors are effective in interventions against chronic diseases. We considered articles that address numerous social and behavioral and risk factors for chronic diseases to offer readers an overview of the similarities and differences that may exist in chronic disease research in diverse global and domestic settings.
This collection consists of 15 articles published over 4 years, from March 2017 to December 2020. This global collection includes articles from North America (United States), South America (Brazil, Mexico, Guatemala), Europe (Spain, Denmark, UK global authors), Asia (Taiwan, Iran, South Korea), Africa (South Africa, Nigeria, Senegal), and Australia. For this collection, the 15 articles were grouped into 2 themes: 1) chronic disease outcomes such as diabetes and CVDs, as well as the impact of COVID-19; and 2) behaviors and strategies (such as healthy food, smoking cessation, breastfeeding, and physical activity) that either prevent or aid in chronic disease management.
To address chronic disease management and prevention, location matters and is a major factor in achieving research goals. In the United States, barbershops and beauty salons, for example, have been used as sites of health intervention to reach African American communities. Barbershops are considered important cultural venues with convenient community locations for addressing health and social issues that affect the Black community ( 21 ). The contribution by Smith et al ( 22 ) demonstrated the effectiveness of the Arkansas Minority Barber and Beauty Shop Health Initiative in improving CVD health outcomes of minority populations in the state through health screenings, health education, and disease management. This article describes chronic health conditions that presented during screening at a barber shop or beauty salon and the impact of a health education promotion campaign at this location. In addition, it showed how medical referrals and participant follow-ups can be integrated into screening initiatives based in barber shops and beauty salons. Specific chronic diseases included diabetes, CVD, and obesity.
Diabetes is associated with illness and premature death and affects an estimated 285 million people, which corresponds to 6.4% of the world’s adult population ( 23 ). Globally, type 2 diabetes is a growing public health challenge, and public health and health care systems play important roles in prevention and management of complications related to both type 1 and type 2 diabetes ( 23 ). Some programs, such as weight or diet management, physical activity, hemoglobin A 1c control, and diabetic retinopathy screening, are useful approaches for diabetes prevention and management. The article by Mendoza-Herrera et al ( 24 ) presents a low-cost and easy-to-apply new screening tool to detect people who are at high risk for diabetic retinopathy in low-income Mexican communities. This noninvasive screening tool for diabetic retinopathy could be used by nonspecialized health personnel in low-income communities. The screening tool requires the assessment of glycemia, blood pressure, and information related to diabetes and physical activity recommendations. From a clinical or health care perspective, many diabetes management programs provide short-term or long-term quality diabetes care. In a systematic review of the literature, pay-for-performance (P4P) or value-based purchasing programs were shown, across many countries, to contribute to the efficient delivery of long-term, multidisciplinary diabetes management behaviors ( 25 ). Hsieh et al ( 26 ) evaluated the effects of diabetes management on risks of cancer incidence and mortality among patients with type 2 diabetes through a diabetes P4P program in Taiwan. This study showed that diabetes P4P programs reduced risks of all-cause mortality and competing causes of death due to cancer-specific and diabetes-related mortality among patients with type 2 diabetes. Other studies focusing on chronic disease management programs (CDMPs) have incorporated health coaching into their programs, as was done at Royal North Shore Hospital in Sydney, Australia, in 2013 ( 27 ). This study assessed changes in patients’ general knowledge of diabetes, self-reported health status, diabetes distress, body mass index (BMI), and glycemic control after enrollment in a face-to-face CDMP group health coaching session (with telephone follow-up), compared with participation in telephone-only health coaching, during a 12-month period.
In addition to addressing chronic diseases like diabetes, some articles also addressed risk factors such as obesity. Obesity is not only a chronic disease but also a risk factor for other diseases, including heart disease, hypertension, and some cancers. According to CDC, from 1999–2000 through 2017–2018, the prevalence of obesity in the US increased from 30.5% to 42.4%, and the prevalence of severe obesity increased from 4.7% to 9.2% ( 28 ). The association between obesity and chronic disease risk factors is complex and may vary by population. Risk factors or risk situations include those addressed in this collection, including food swamps, poor eating, and physical inactivity. The article by Petersen et al ( 29 ) introduced efforts by CDC’s Division of Nutrition, Physical Activity, and Obesity (DNPAO) to address related racial and ethnic disparities. For example, DNPAO competitively funds 16 state health departments (or similar entities), 15 land grant colleges and universities, and 31 community-focused grantees to work with multiple sectors and coalitions to prioritize and implement best practices for increasing healthy eating and active living to prevent obesity and other chronic diseases. In addition, 2 public health practice programs, the Racial and Ethnic Approaches to Community Health program and the High Obesity Program, have had success in reducing risk factors for obesity in target populations with the highest disparities. For surveillance of obesity prevalence, DNPAO has published state-specific obesity maps using self-reported data of height and weight from the Behavioral Risk Factor Surveillance System since 1999. These maps have shown that obesity prevalence among adults remains high across the country, year by year. Many research efforts to prevent obesity and other chronic disease risks exist, as presented in the second theme of this collection.
Evidence shows that physical activity reliably protects against CVDs. In the article by Modesto et al ( 30 ), the team analyzed whether an individualized, prescribed intervention that consists of walking in the park would assist in improving cardiovascular health among participants. A total of 1,466 adults aged 40 to 80 were initially enrolled into the study, and 152 participants completed the full postintervention reevaluation and followed the prescribed regimens within 3 to 6 months. Among those who completed the full walk-in-park intervention, significant changes were found in BMI, waist circumference, and systolic blood pressure. Diastolic blood pressure, blood glucose, and total cholesterol remained unchanged. The article by López-Bueno and colleagues ( 31 ) describes a study designed to analyze whether levels of physical activity were associated with higher odds of common chronic conditions within the Spanish workforce. Using data from the Spanish National Health Survey 2017 (N = 9,695), López-Bueno examined differences in the 6 most prevalent chronic conditions among a workforce that engaged in physical activity. Results indicated that participants who performed less physical activity per week were significantly more likely to experience chronic conditions than those who performed more. In a related study on the benefits of leisure time physical activity, Sturm and Cohen ( 32 ) found that not having free time was not enough to explain physical inactivity in the study population. In reviewing data that covered a 3-year period (2014–2016) for more than 32,000 people aged 15 years or older, the authors examined activity types and levels in places where participants learned, prayed, or worked. They concluded that motivation to exercise was an important factor to consider even for those who have free time. As more Americans continue to be physically inactive, the authors suggested that making spaces for physical activity be more inviting and engaging is important to increasing the level of physical activities for adults.
Just as increasing physical activity is important, so too is healthy nutrition. Maxwell et al ( 33 ) adapted a British healthy eating intervention for elementary school children in an under-resourced setting in South Los Angeles to promote healthier eating and improve children’s long-term health outcomes. This intervention was developed in collaboration with YMCA with the goal of promoting eating vegetables among young people. This intervention, based on the British-developed Tiny Tastes program, was designed to expose young people to small portions of vegetables as a way of encouraging them to adopt the habit of eating vegetables. Fifty children aged 7 to 12 years who attended a summer camp were repeatedly exposed to initially disliked vegetables, daily, over a 2-week period. Follow-up assessments were conducted immediately after the last exposure (2 weeks) and after 14 additional days of nonexposure (4-weeks follow up). Findings showed a significant increase in children’s propensity toward initially disliked vegetables to which they were repeatedly exposed but not to vegetables to which they did not receive repeated exposure. Results of the study demonstrate that repeated vegetable tasting strategies offered in community settings may be a practical, low-cost, easy-to-implement strategy for health promotion, decreasing prevalence of chronic diseases, and subsequently improving population health in under-resourced communities.
Public health and medical researchers use body mass index (BMI) to measure risk for chronic diseases. However, questions remain as to whether the standard BMI measure accurately captures variance that may exist in different racial and ethnic populations. The contribution by Darbandi et al ( 34 ) is a systematic meta-analysis of studies that use BMI to predict CVD. The analysis included adults aged 18 or older in cross-sectional and prospective cohort studies. The studies were conducted between 1996 and 2019 in 15 countries. Of all the studied indexes, it appears that BMI, waist circumference, and waist-to-hip ratio all presented reliable predictive power for risk of CVD. However, waist-to-hip ratio indexes presented stronger predictive power. In another study on measurement of risks, Lee et al ( 35 ) proposed a cumulative social risk composite score that provides specificity in predicting CVD beyond the traditional Framingham risk score. Their analysis used a nationally representative group of South Korean adults aged 19 or older with CVD, using the cumulative social risk measure (which includes income, education, and marital status).
Collective multidisciplinary approaches are needed to address risk behaviors as a life course determinant of chronic diseases. For example, the need to continue to address healthy diet at an early age is a strategy to reduce obesity in childhood. Still, early age healthy eating can produce positive health benefits over one’s lifespan. The article by Garvin et al ( 36 ) showed, through an evaluation project of the National Early Childhood and Education Learning Collaborative (ECELC) programs, that 10 states were successful in increasing healthy eating habits of young people. The ECELC programs demonstrated the benefits and merits of a multidisciplinary approach to implementation and evaluation of a public health intervention program. The authors evaluated a multidisciplinary and multisectoral partnership strategy to promote healthy eating and increased physical activity in early childhood. They concluded that this type of collective approach offers an opportunity for an early intervention to prevent chronic diseases. Another article assessed the nutritional challenges of an unhealthy food environment in Guatemala, particularly in locations where schools are swamped with unhealthy foods. Food swamps, as opposed to food deserts, have mostly been reported in the Global North as a result of the proliferation of fast foods in low-income communities. The article by Chew et al ( 37 ) is one of the few that have reported on food swamps in the Global South as evidence of the high concentration of fast food outlets in low-income locations around schools. The article demonstrates how food swamps are a global health problem and pose a particular threat of adopting unhealthy food practices in communities. As we address unhealthy behaviors, it is important to learn from those who have changed their behaviors from unhealthy to healthy behaviors. The article by Murphy-Hoefer et al ( 38 ) reported lessons learned from people who have been successful in discontinuing smoking. The lessons of former smokers may hold promise for smoking cessation efforts globally, particularly as we begin to address the epidemic of vaping.
In this collection, 1 article shows the intersection of chronic diseases and infectious diseases such as COVID-19. Black and Brown populations are disproportionately affected by both chronic diseases and COVID-19. The article by Airhihenbuwa et al ( 39 ) makes the point that for historically disempowered communities to benefit from public health interventions, both individual and structural factors must be equally valued in communicating about risks and mitigation. The article addresses the fact that COVID-19 messaging that focuses on individual risk behaviors, such as hand washing and physical distancing, may not fully account for contexts in which congested housing and public-facing jobs structurally make individually focused messages untenable. Equally addressing individual and collective risks allows us to address the structural and social determinants (eg, food access, job availability, housing conditions) that influence risks and vulnerability for COVID-19 and chronic diseases. To address the contexts, the PEN-3 cultural model was presented as an example.
The Future of Global Chronic Disease Research and Action
The articles in this collection reflect a common problem and solution for chronic diseases globally. The strategies offered in one context hold promise for others. The articles demonstrate the need to balance individual-based prevention and management efforts (like healthy eating and increased physical activity) with environmentally based strategies like food swamps or food deserts. If we are going to be successful in improving health globally, voices from the global community must be heard and incorporated into the interventions to have relevant, appropriate, and optimal outcomes for different regions of the world ( 40 ). Environmental and systemic risks should be considered as ways of providing contexts for individual risks. For example, COVID-19’s disproportionate impact on those with chronic diseases in Black and Brown communities is well documented. In PCD in 2020, these articles shed light on the tasks ahead, which is to address the historical contexts of racial inequities and to promote social justice as global health.
At the global level, chronic disease is commonly referred to as, or used interchangeably with, noncommunicable disease (NCD). NCD has gained increased attention as its burden has outstripped that of infectious/communicable diseases in the Global South. The rate of increase in the burden of NCDs is unprecedented and precipitated the 2018 United Nations high-level commission to frame a global response to NCDs ( 41 ). The focus of the 2018 meeting was not only to address risk behaviors but also to highlight structural levers of change, therefore highlighting the urgency for countries to prioritize NCD reduction goals and objectives to have both health and economic benefits. Prioritizing NCDs should be considered an investment with economic gains that can be calculated in dollars saved, productivity increased, and overall economic growth ( 42 ). A global urgency exists for chronic disease and other health intervention strategies to advance health equity for Black and Brown populations, which can be done only when we collectively address structures and systems, such as place and group status, rather than focusing only on individuals ( 43 ). For example, there is a renewed call to decolonize global health ( 44 ). The renewed demand for decolonization has been led mostly by public health students, notably at Harvard and Duke Universities. The demand to decolonize global health has been further reignited in large part by the Black Lives Matter movement, whose goal to address structural and systemic racism became a global movement following the killing of George Floyd, Breonna Taylor, and others. The future of reducing chronic diseases globally must therefore be connected with collective efforts to address global health inequities.
The articles presented in this collection suggest that innovation in evidence-based approaches is essential to improving population-based health strategies for chronic disease prevention and management. Collective sharing and learning across countries and regions is needed. Our approaches should be anchored in community-engaged, multidisciplinary, and multisectoral relationships to prevent and manage chronic diseases globally. Committing to this global North/South sharing and learning must be strengthened and expanded to inform policy, transform systems, and contextualize strategies so that interventions are responsive to both individual and structural changes and sustainability.
Global health begins with local health. Each article in this collection reflects chronic disease issues in local settings with global relevance and lessons. These articles clearly show that the local is part of the global. Preventing and managing chronic diseases reinforce the value that individual experiences hold lessons in both promise and challenges that can be shared globally. Important and timely as the articles included in this collection are, global health should help advance strategies that address structural and systemic determinants of chronic diseases so that individual behavior change can be sustainable. Although we have learned much from these articles, what is needed for the future is research to address more of the structural levers to preventing and managing chronic diseases to improve quality of life where people work, live, play, pray, and learn. Thus, helping to change individual behaviors relative to eating, physical activity, and sleep are important but should be better understood within the contexts of the condition in the same: where people live (housing conditions), work (if they have jobs), play (if they have space), pray (to develop resilience), and learn (if they have access to quality education).
Acknowledgments
The authors have no conflicts of interest to declare and no copyrighted material was used in this editorial.
The opinions expressed by authors contributing to this journal do not necessarily reflect the opinions of the U.S. Department of Health and Human Services, the Public Health Service, the Centers for Disease Control and Prevention, or the authors' affiliated institutions.
Suggested citation for this article: Airhihenbuwa CO, Tseng T, Sutton VD, Price L. Global Perspectives on Improving Chronic Disease Prevention and Management in Diverse Settings. Prev Chronic Dis 2021;18:210055. DOI: https://doi.org/10.5888/pcd18.210055 .

IMAGES
VIDEO
COMMENTS
This concept is supported by literally thousands of research articles and incorporated in multiple evidence-based guidelines for the prevention and/or treatment of chronic metabolic diseases. The study of how habits and actions affect both prevention and treatment of diseases has coalesced around the concept of "lifestyle medicine."
Dr Rippe's research organization, Rippe Lifestyle Institute, has conducted numerous research studies in various aspects of lifestyle medicine, including physical activity, proper nutrition, and weight management and their impact on short- and long-term health and quality of life. ... Centers for Disease Control and Prevention. Current ...
Abstract. Cardiovascular diseases (CVDs) remain a leading cause of morbidity and mortality worldwide. Lifestyle modifications have gained increasing recognition as key interventions in preventing and managing CVDs. This narrative review aims to provide a thorough assessment of the impact of lifestyle modifications on cardiovascular health.
Lifestyle Medicine encompasses research, prevention, diagnosis and treatment of dysfunctions caused by a non-physiological lifestyle (lifestyle-related diseases, LRDs) and morbidogenic environments conducive to promoting such lifestyles. ... We must improve education and training in the treatment and prevention of lifestyle-related diseases 30.
The consequences of lifestyle-related disease represent a major burden for the individual as well as for society at large. Individual preventive health checks to the general population have been suggested as a mean to reduce the burden of lifestyle-related diseases, though with mixed evidence on effectiveness. Several systematic reviews, on the other hand, suggest that health checks targeting ...
In this Review, we provide a summary of the epidemiological research supporting the preventive and antihypertensive effects of major lifestyle interventions (regular physical exercise, body weight ...
Lifestyle medicine is an approach that focuses on modifying unhealthy behaviors and promoting healthy ones to prevent and manage chronic diseases. This modality addresses multiple risk factors such as physical inactivity, unhealthy diet, tobacco use, and stress. Evidence shows that adopting a healthy lifestyle can significantly reduce the ...
System dynamics models can help us establish a holistic concept and analyze the prevention of chronic diseases as a whole. The steps for establishing system dynamics models are 1) problem definition, 2) development of a conceptual model, 3) development of a quantitative model, 4) validation and testing, and 5) policy simulation. In the process ...
Cardiovascular diseases (CVDs) are a prominent cause of death and disability across the globe, and this article provides a comprehensive review of the many risk factors for their onset and progression. It investigates how changes in food and exercise might help prevent and treat cardiovascular diseases. It explores the role of eating plans like the Mediterranean diet and plant-based diets in ...
Chronic diseases —including heart disease, stroke, diabetes, and cancer— account for some of the most common health problems in the United States, according to statistics from the Centers for Disease Control and Prevention (CDC). Yet many of these chronic diseases are preventable, as they're linked to poor diet and lifestyle choices including tobacco use, excessive alcohol consumption ...
Get Regular Physical Activity. Regular physical activity can help you prevent, delay, or manage chronic diseases. Aim for moderate intensity physical activity (like brisk walking or gardening) for at least 150 minutes a week, with muscle-strengthening activities 2 days a week. Physical Activity and Health. Adding Physical Activity to Your Life.
Declining life expectancy and increasing all-cause mortality in the United States have been associated with unhealthy behaviors, socioecological factors, and preventable disease. A growing body of basic science, clinical research, and population health evidence points to the benefits of healthy behaviors, environments and policies to maintain health and prevent, treat, and reverse the root ...
Abstract. Abstract Personalized care, which includes personalized medicine, personalized nutrition, and even personalized exercise, is a useful and a more effective method for the treatment and ...
Disease prevention is a procedure through which individuals, particularly those with risk factors for a disease, are treated in order to prevent a disease from occurring. Treatment normally begins ...
The Tracking Network hosts the following lifestyle risk factor data. Data sources include CDC's Behavioral Risk Factor Surveillance System, CDC's Population Level Analysis and Community Estimates (PLACES) Project, and the U.S. Census Bureau. These data are available at the state, county, or census tract level for all 50 states.
A lifestyle disease is linked to the way a person lives. Lifestyle diseases are ailments that are primarily based on the day to day habits of people. Habits that detract people from activity and ...
The diagnosis of incident diabetes was based on an oral glucose tolerance test (OGTT). The overall risk reduction of T2D by the lifestyle interventions was 0.53 (95% CI 0.41; 0.67). Most of the trials aimed to reduce weight, increase physical activity, and apply a diet relatively low in saturated fat and high in fiber.
Adverse lifestyles have a major impact on the burden of coronary heart disease (CHD). Physical inactivity, 1 smoking, 2 obesity, 3 and several aspects of diet are the underlying causative factors for CHD and its risk factors. Blood pressure (BP), a major risk factor for CHD, 4 is strongly associated with obesity, 5 physical inactivity, 6 sodium ...
Lifestyle diseases are ailments that are primarily based on the. day to day habits of people. Habits that detract people from activity. and push them towards a sedentary routine can cause a number ...
Lifestyle diseases encompass a wide range of health conditions that are directly linked to unhealthy lifestyle choices. These diseases can affect various organ systems in the body and include ...
The conclusions, findings, and opinions expressed by authors contributing to this journal do not necessarily reflect the official position of the U.S. Department of Health and Human Services, the Public Health Service, the Centers for Disease Control and Prevention, or the authors' affiliated institutions.
New research suggests that A-fib may be more prevalent, and more dangerous, in people under 65 than previously thought. By Dani Blum Atrial fibrillation, a common cardiac condition that raises the ...
Ferdinand Cacho, MD, pediatric pulmonology fellow, Center for Asthma Research, VUMC. The Centers for Disease Control & Prevention recommends early immunization with nirsevimab for all infants, but ...
NCDs majorly refers to cancers, diabetes, hypertension, cardiovascular diseases, mental health and others. They are together governed by a cluster of risk factors and their determinants, like tobacco and alcohol use, unhealthy diet, lack of physical activity, overweight & obesity, pollution (air, water and soil) and stress.
Find breaking science news and analysis from the world's leading research journal.
The conclusions, findings, and opinions expressed by authors contributing to this journal do not necessarily reflect the official position of the U.S. Department of Health and Human Services, the Public Health Service, the Centers for Disease Control and Prevention, or the authors' affiliated institutions.
Preliminary research presented at the American Heart Association's Epidemiology and Prevention -- Lifestyle and Cardiometabolic Scientific Sessions 2024, indicates that when boys have one sugary ...
ADHD is one of the most common neurobehavioral disorders of childhood. It is usually first diagnosed in childhood and often lasts into adulthood. Children with ADHD have trouble paying attention, controlling impulsive behaviors (may act without thinking about what the result will be), and in some cases, are overly active.
Exemplary science is the foundation for all National Institute for Occupational Safety and Health (NIOSH) research and prevention activities. Each year, NIOSH recognizes outstanding science and service from our employees. This year's Science and Service Awards took place on April 25, 2024.
The Centers for Disease Control and Prevention (CDC) define chronic diseases as conditions that last 1 year or more and that require ongoing medical attention or limit activities of daily living, or both ().Chronic diseases may be influenced by a combination of genetics, lifestyle and social behaviors, health care system factors, community influences, and environmental determinants of health ().