

Mental Health Case Study: Understanding Depression through a Real-life Example
Imagine feeling an unrelenting heaviness weighing down on your chest. Every breath becomes a struggle as a cloud of sadness engulfs your every thought. Your energy levels plummet, leaving you physically and emotionally drained. This is the reality for millions of people worldwide who suffer from depression, a complex and debilitating mental health condition.
Understanding depression is crucial in order to provide effective support and treatment for those affected. While textbooks and research papers provide valuable insights, sometimes the best way to truly comprehend the depths of this condition is through real-life case studies. These stories bring depression to life, shedding light on its impact on individuals and society as a whole.
In this article, we will delve into the world of mental health case studies, using a real-life example to explore the intricacies of depression. We will examine the symptoms, prevalence, and consequences of this all-encompassing condition. Furthermore, we will discuss the significance of case studies in mental health research, including their ability to provide detailed information about individual experiences and contribute to the development of treatment strategies.
Through an in-depth analysis of a selected case study, we will gain insight into the journey of an individual facing depression. We will explore their background, symptoms, and initial diagnosis. Additionally, we will examine the various treatment options available and assess the effectiveness of the chosen approach.
By delving into this real-life example, we will not only gain a better understanding of depression as a mental health condition, but we will also uncover valuable lessons that can aid in the treatment and support of those who are affected. So, let us embark on this enlightening journey, using the power of case studies to bring understanding and empathy to those who need it most.
Understanding Depression
Depression is a complex and multifaceted mental health condition that affects millions of people worldwide. To comprehend the impact of depression, it is essential to explore its defining characteristics, prevalence, and consequences on individuals and society as a whole.
Defining depression and its symptoms
Depression is more than just feeling sad or experiencing a low mood. It is a serious mental health disorder characterized by persistent feelings of sadness, hopelessness, and a loss of interest in activities that were once enjoyable. Individuals with depression often experience a range of symptoms that can significantly impact their daily lives. These symptoms include:
1. Persistent feelings of sadness or emptiness. 2. Fatigue and decreased energy levels. 3. Significant changes in appetite and weight. 4. Difficulty concentrating or making decisions. 5. Insomnia or excessive sleep. 6. feelings of guilt, worthlessness, or hopelessness. 7. Loss of interest or pleasure in activities.
Exploring the prevalence of depression worldwide
Depression knows no boundaries and affects individuals from all walks of life. According to the World Health Organization (WHO), an estimated 264 million people globally suffer from depression. This makes depression one of the most common mental health conditions worldwide. Additionally, the WHO highlights that depression is more prevalent among females than males.
The impact of depression is not limited to individuals alone. It also has significant social and economic consequences. Depression can lead to impaired productivity, increased healthcare costs, and strain on relationships, contributing to a significant burden on families, communities, and society at large.
The impact of depression on individuals and society
Depression can have a profound and debilitating impact on individuals’ lives, affecting their physical, emotional, and social well-being. The persistent sadness and loss of interest can lead to difficulties in maintaining relationships, pursuing education or careers, and engaging in daily activities. Furthermore, depression increases the risk of developing other mental health conditions, such as anxiety disorders or substance abuse.
On a societal level, depression poses numerous challenges. The economic burden of depression is significant, with costs associated with treatment, reduced productivity, and premature death. Moreover, the social stigma surrounding mental health can impede individuals from seeking help and accessing appropriate support systems.
Understanding the prevalence and consequences of depression is crucial for policymakers, healthcare professionals, and individuals alike. By recognizing the significant impact depression has on individuals and society, appropriate resources and interventions can be developed to mitigate its effects and improve the overall well-being of those affected.
The Significance of Case Studies in Mental Health Research
Case studies play a vital role in mental health research, providing valuable insights into individual experiences and contributing to the development of effective treatment strategies. Let us explore why case studies are considered invaluable in understanding and addressing mental health conditions.
Why case studies are valuable in mental health research
Case studies offer a unique opportunity to examine mental health conditions within the real-life context of individuals. Unlike large-scale studies that focus on statistical data, case studies provide a detailed examination of specific cases, allowing researchers to delve into the complexities of a particular condition or treatment approach. This micro-level analysis helps researchers gain a deeper understanding of the nuances and intricacies involved.
The role of case studies in providing detailed information about individual experiences
Through case studies, researchers can capture rich narratives and delve into the lived experiences of individuals facing mental health challenges. These stories help to humanize the condition and provide valuable insights that go beyond a list of symptoms or diagnostic criteria. By understanding the unique experiences, thoughts, and emotions of individuals, researchers can develop a more comprehensive understanding of mental health conditions and tailor interventions accordingly.
How case studies contribute to the development of treatment strategies
Case studies form a vital foundation for the development of effective treatment strategies. By examining a specific case in detail, researchers can identify patterns, factors influencing treatment outcomes, and areas where intervention may be particularly effective. Moreover, case studies foster an iterative approach to treatment development—an ongoing cycle of using data and experience to refine and improve interventions.
By examining multiple case studies, researchers can identify common themes and trends, leading to the development of evidence-based guidelines and best practices. This allows healthcare professionals to provide more targeted and personalized support to individuals facing mental health conditions.
Furthermore, case studies can shed light on potential limitations or challenges in existing treatment approaches. By thoroughly analyzing different cases, researchers can identify gaps in current treatments and focus on areas that require further exploration and innovation.
In summary, case studies are a vital component of mental health research, offering detailed insights into the lived experiences of individuals with mental health conditions. They provide a rich understanding of the complexities of these conditions and contribute to the development of effective treatment strategies. By leveraging the power of case studies, researchers can move closer to improving the lives of individuals facing mental health challenges.
Examining a Real-life Case Study of Depression
In order to gain a deeper understanding of depression, let us now turn our attention to a real-life case study. By exploring the journey of an individual navigating through depression, we can gain valuable insights into the complexities and challenges associated with this mental health condition.
Introduction to the selected case study
In this case study, we will focus on Jane, a 32-year-old woman who has been struggling with depression for the past two years. Jane’s case offers a compelling narrative that highlights the various aspects of depression, including its onset, symptoms, and the treatment journey.
Background information on the individual facing depression
Before the onset of depression, Jane led a fulfilling and successful life. She had a promising career, a supportive network of friends and family, and engaged in hobbies that brought her joy. However, a series of life stressors, including a demanding job, a breakup, and the loss of a loved one, began to take a toll on her mental well-being.
Jane’s background highlights a common phenomenon – depression can affect individuals from all walks of life, irrespective of their socio-economic status, age, or external circumstances. It serves as a reminder that no one is immune to mental health challenges.
Presentation of symptoms and initial diagnosis
Jane began noticing a shift in her mood, characterized by persistent feelings of sadness and a lack of interest in activities she once enjoyed. She experienced disruptions in her sleep patterns, appetite changes, and a general sense of hopelessness. Recognizing the severity of her symptoms, Jane sought help from a mental health professional who diagnosed her with major depressive disorder.
Jane’s case exemplifies the varied and complex symptoms associated with depression. While individuals may exhibit overlapping symptoms, the intensity and manifestation of those symptoms can vary greatly, underscoring the importance of personalized and tailored treatment approaches.
By examining this real-life case study of depression, we can gain an empathetic understanding of the challenges faced by individuals experiencing this mental health condition. Through Jane’s journey, we will uncover the treatment options available for depression and analyze the effectiveness of the chosen approach. The case study will allow us to explore the nuances of depression and provide valuable insights into the treatment landscape for this prevalent mental health condition.
The Treatment Journey
When it comes to treating depression, there are various options available, ranging from therapy to medication. In this section, we will provide an overview of the treatment options for depression and analyze the treatment plan implemented in the real-life case study.
Overview of the treatment options available for depression
Treatment for depression typically involves a combination of approaches tailored to the individual’s needs. The two primary treatment modalities for depression are psychotherapy (talk therapy) and medication. Psychotherapy aims to help individuals explore their thoughts, emotions, and behaviors, while medication can help alleviate symptoms by restoring chemical imbalances in the brain.
Common forms of psychotherapy used in the treatment of depression include cognitive-behavioral therapy (CBT), interpersonal therapy (IPT), and psychodynamic therapy. These therapeutic approaches focus on addressing negative thought patterns, improving relationship dynamics, and gaining insight into underlying psychological factors contributing to depression.
In cases where medication is utilized, selective serotonin reuptake inhibitors (SSRIs) are commonly prescribed. These medications help rebalance serotonin levels in the brain, which are often disrupted in individuals with depression. Other classes of antidepressant medications, such as serotonin-norepinephrine reuptake inhibitors (SNRIs) or tricyclic antidepressants (TCAs), may be considered in specific cases.
Exploring the treatment plan implemented in the case study
In Jane’s case, a comprehensive treatment plan was developed with the intention of addressing her specific needs and symptoms. Recognizing the severity of her depression, Jane’s healthcare team recommended a combination of talk therapy and medication.
Jane began attending weekly sessions of cognitive-behavioral therapy (CBT) with a licensed therapist. This form of therapy aimed to help Jane identify and challenge negative thought patterns, develop coping strategies, and cultivate more adaptive behaviors. The therapeutic relationship provided Jane with a safe space to explore and process her emotions, ultimately helping her regain a sense of control over her life.
In conjunction with therapy, Jane’s healthcare provider prescribed an SSRI medication to assist in managing her symptoms. The medication was carefully selected based on Jane’s specific symptoms and medical history, and regular follow-up appointments were scheduled to monitor her response to the medication and adjust the dosage if necessary.
Analyzing the effectiveness of the treatment approach
The effectiveness of treatment for depression varies from person to person, and it often requires a period of trial and adjustment to find the most suitable intervention. In Jane’s case, the combination of cognitive-behavioral therapy and medication proved to be beneficial. Over time, she reported a reduction in her depressive symptoms, an improvement in her overall mood, and increased ability to engage in activities she once enjoyed.
It is important to note that the treatment journey for depression is not always linear, and setbacks and challenges may occur along the way. Each individual responds differently to treatment, and adjustments might be necessary to optimize outcomes. Continuous communication between the individual and their healthcare team is crucial to addressing any concerns, monitoring progress, and adapting the treatment plan as needed.
By analyzing the treatment approach in the real-life case study, we gain insights into the various treatment options available for depression and how they can be tailored to meet individual needs. The combination of psychotherapy and medication offers a holistic approach, addressing both psychological and biological aspects of depression.
The Outcome and Lessons Learned
After undergoing treatment for depression, it is essential to assess the outcome and draw valuable lessons from the case study. In this section, we will discuss the progress made by the individual in the case study, examine the challenges faced during the treatment process, and identify key lessons learned.
Discussing the progress made by the individual in the case study
Throughout the treatment process, Jane experienced significant progress in managing her depression. She reported a reduction in depressive symptoms, improved mood, and a renewed sense of hope and purpose in her life. Jane’s active participation in therapy, combined with the appropriate use of medication, played a crucial role in her progress.
Furthermore, Jane’s support network of family and friends played a significant role in her recovery. Their understanding, empathy, and support provided a solid foundation for her journey towards improved mental well-being. This highlights the importance of social support in the treatment and management of depression.
Examining the challenges faced during the treatment process
Despite the progress made, Jane faced several challenges during her treatment journey. Adhering to the treatment plan consistently proved to be difficult at times, as she encountered setbacks and moments of self-doubt. Additionally, managing the side effects of the medication required careful monitoring and adjustments to find the right balance.
Moreover, the stigma associated with mental health continued to be a challenge for Jane. Overcoming societal misconceptions and seeking help required courage and resilience. The case study underscores the need for increased awareness, education, and advocacy to address the stigma surrounding mental health conditions.
Identifying the key lessons learned from the case study
The case study offers valuable lessons that can inform the treatment and support of individuals with depression:
1. Holistic Approach: The combination of psychotherapy and medication proved to be effective in addressing the psychological and biological aspects of depression. This highlights the need for a holistic and personalized treatment approach.
2. Importance of Support: Having a strong support system can significantly impact an individual’s ability to navigate through depression. Family, friends, and healthcare professionals play a vital role in providing empathy, understanding, and encouragement.
3. Individualized Treatment: Depression manifests differently in each individual, emphasizing the importance of tailoring treatment plans to meet individual needs. Personalized interventions are more likely to lead to positive outcomes.
4. Overcoming Stigma: Addressing the stigma associated with mental health conditions is crucial for individuals to seek timely help and access the support they need. Educating society about mental health is essential to create a more supportive and inclusive environment.
By drawing lessons from this real-life case study, we gain insights that can improve the understanding and treatment of depression. Recognizing the progress made, understanding the challenges faced, and implementing the lessons learned can contribute to more effective interventions and support systems for individuals facing depression.In conclusion, this article has explored the significance of mental health case studies in understanding and addressing depression, focusing on a real-life example. By delving into case studies, we gain a deeper appreciation for the complexities of depression and the profound impact it has on individuals and society.
Through our examination of the selected case study, we have learned valuable lessons about the nature of depression and its treatment. We have seen how the combination of psychotherapy and medication can provide a holistic approach, addressing both psychological and biological factors. Furthermore, the importance of social support and the role of a strong network in an individual’s recovery journey cannot be overstated.
Additionally, we have identified challenges faced during the treatment process, such as adherence to the treatment plan and managing medication side effects. These challenges highlight the need for ongoing monitoring, adjustments, and open communication between individuals and their healthcare providers.
The case study has also emphasized the impact of stigma on individuals seeking help for depression. Addressing societal misconceptions and promoting mental health awareness is essential to create a more supportive environment for those affected by depression and other mental health conditions.
Overall, this article reinforces the significance of case studies in advancing our understanding of mental health conditions and developing effective treatment strategies. Through real-life examples, we gain a more comprehensive and empathetic perspective on depression, enabling us to provide better support and care for individuals facing this mental health challenge.
As we conclude, it is crucial to emphasize the importance of continued research and exploration of mental health case studies. The more we learn from individual experiences, the better equipped we become to address the diverse needs of those affected by mental health conditions. By fostering a culture of understanding, support, and advocacy, we can strive towards a future where individuals with depression receive the care and compassion they deserve.
Similar Posts

Exploring the World of Bipolar Bingo: Understanding the Game and Its Connection to Bipolar Disorder
Imagine a world where a game of chance holds the power to bring solace and support to individuals affected by bipolar disorder. A seemingly unlikely connection, but one that exists nonetheless. Welcome to the world of…

Can Anxiety Disorders be Genetic? Exploring the Hereditary Aspects of Anxiety Disorders
Introduction to Genetic Factors in Anxiety Disorders Understanding anxiety disorders Anxiety disorders are a common mental health condition that affect millions of individuals worldwide. People with anxiety disorders experience overwhelming feelings of fear, worry, and unease…

Understanding the Abbreviations and Acronyms for Bipolar Disorder
Living with bipolar disorder can be a challenging journey. The constant rollercoaster of emotions, the highs and lows, can take a toll on a person’s mental and emotional well-being. But what if there was a way…

The Connection Between Ice Cream and Depression: Can Ice Cream Really Help?
Ice cream has long been hailed as a delightful treat, bringing joy to people of all ages. It is often associated with carefree summer days, laughter, and moments of pure bliss. But what if I told…

Understanding the Relationship Between Bipolar Disorder and PTSD
Imagine living with extreme mood swings that can range from feeling on top of the world one day to plunging into the depths of despair the next. Now add the haunting memories of a traumatic event…

The Connection Between Meth and Bipolar: Understanding the Link and Seeking Treatment
It’s a tangled web of interconnectedness – the world of mental health and substance abuse. One doesn’t often think of them as intertwined, but for those battling bipolar disorder, the link becomes all too clear. And…
Ohio State nav bar
The Ohio State University
- BuckeyeLink
- Find People
- Search Ohio State
Patient Case Presentation

Figure 1. Blue and silver stethoscope (Pixabay, N.D.)
Ms. S.W. is a 48-year-old white female who presented to an outpatient community mental health agency for evaluation of depressive symptoms. Over the past eight weeks she has experienced sad mood every day, which she describes as a feeling of hopelessness and emptiness. She also noticed other changes about herself, including decreased appetite, insomnia, fatigue, and poor ability to concentrate. The things that used to bring Ms. S.W. joy, such as gardening and listening to podcasts, are no longer bringing her the same happiness they used to. She became especially concerned as within the past two weeks she also started experiencing feelings of worthlessness, the perception that she is a burden to others, and fleeting thoughts of death/suicide.
Ms. S.W. acknowledges that she has numerous stressors in her life. She reports that her daughter’s grades have been steadily declining over the past two semesters and she is unsure if her daughter will be attending college anymore. Her relationship with her son is somewhat strained as she and his father are not on good terms and her son feels Ms. S.W. is at fault for this. She feels her career has been unfulfilling and though she’d like to go back to school, this isn’t possible given the family’s tight finances/the patient raising a family on a single income.
Ms. S.W. has experienced symptoms of depression previously, but she does not think the symptoms have ever been as severe as they are currently. She has taken antidepressants in the past and was generally adherent to them, but she believes that therapy was more helpful than the medications. She denies ever having history of manic or hypomanic episodes. She has been unable to connect to a mental health agency in several years due to lack of time and feeling that she could manage the symptoms on her own. She now feels that this is her last option and is looking for ongoing outpatient mental health treatment.
Past Medical History
- Hypertension, diagnosed at age 41
Past Surgical History
- Wisdom teeth extraction, age 22
Pertinent Family History
- Mother with history of Major Depressive Disorder, treated with antidepressants
- Maternal grandmother with history of Major Depressive Disorder, Generalized Anxiety Disorder
- Brother with history of suicide attempt and subsequent inpatient psychiatric hospitalization,
- Brother with history of Alcohol Use Disorder
- Father died from lung cancer (2012)
Pertinent Social History
- Works full-time as an enrollment specialist for Columbus City Schools since 2006
- Has two children, a daughter age 17 and a son age 14
- Divorced in 2015, currently single
- History of some emotional abuse and neglect from mother during childhood, otherwise denies history of trauma, including physical and sexual abuse
- Smoking 1/2 PPD of cigarettes
- Occasional alcohol use (approximately 1-2 glasses of wine 1-2 times weekly; patient had not had any alcohol consumption for the past year until two weeks ago)

Antidepressants: A Research Update and a Case Example
What experiences do people have if they take antidepressants.
Posted December 20, 2018
- Find a therapist to overcome depression or anxiety

This post briefly reviews what researchers have been finding about the effectiveness and also the downsides of antidepressant medications — Zoloft, Prozac, and the like. The post then adds a fascinating case example, a self-description submitted to me by a reader who has experienced both the ups and the downs of antidepressant drugs. First, though, a word about my personal bias : Antidepressant pills definitely do help some people. At the same time, I regard them as vastly over-prescribed for mild to moderate depression and also for anxiety . Other treatment strategies for these situations can be equally or more effective, and without the downsides. In my TEDx talk on lifting depression , for instance, I demonstrate an antidepressant visualization exercise that I have used effectively in my clinical practice for decades. See also the techniques here .
What does the latest research suggest about whether you should take antidepressant medications?
For a particularly comprehensive review of the established medical risks of antidepressants , this article from Harvard Medical School is especially informative. You can find many similar articles with a web search of antidepressant risks.
In addition, a recent comprehensive review article of 522 trials and more than 116,000 patients — a meta-analysis combining the findings of all the available studies — reported on findings regarding 21 antidepressant drugs. This review was described as the most comprehensive analysis of the evidence ever undertaken. The Lancet Psychiatry , which reported the study, also then published a further analysis by the study’s authors. Here are their conclusions:
- Antidepressants can be, on average, an effective treatment for adults with moderate-to-severe major depression in the acute phase of illness.
- Effective as defined in this study means that there was a 50 percent or more reduction of depressive symptoms over an eight-week period. “Effective” did not imply complete remission (removal) of the depression.
- Some patients experienced great benefit from the medication ; others gained little or no benefit. In general, the more severe the depression, the more benefits from the antidepressant.
- The average response to a placebo (a sugar pill disguised as medication) was 35 percent. The average response to antidepressants ranged between 42 percent (reboxetine) and 53 percent (amitriptyline).
- For between 47 and 58 percent of subjects, depending on the specific drug, the medication was not effective. That is, they did not experience at least a 50 percent reduction in their depression symptoms.
Note that the depressed clients who did receive relief from taking an antidepressant medication definitely felt better — and yet not necessarily fully healed. Again, "effective" is defined as a 50 percent improvement in symptoms. This definition raises a number of questions:
- What about the remaining effects of depression, if only 50 percent of the symptoms have been relieved by the medication?
- Are antidepressant drugs appropriate to prescribe for milder depression? Or are non-medication therapy techniques just as or more effective? The research deals with only moderate to severe depression. Yet most prescriptions for antidepressants are given for milder to moderate depressive reactions.
- Earlier studies have concluded that the combination of both drugs and psychotherapy has the highest response rate. Both show about equal effectiveness on their own, except that psychotherapy has longer-lasting positive impacts, because it teaches skills and understandings that have long-term benefits. And what about the European research which has found that after people have taken an antidepressant, they become more likely to have subsequent depressive episodes?
- Because of the addictive potential of anti-anxiety drugs, like Xanax and Librium (xxx), antidepressants with sedating side-effect profiles now are prescribed to keep anxiety at bay. What are the effectiveness rates of antidepressants for treating anxiety?
- What about the negative side effects of antidepressants? The Lancet Psychiatry summary article says nothing about these, the most significant of which is drug dependency. Drug dependency means that once people have taken an antidepressant over a significant time period, their body begins to depend on it. The result is that when they try to discontinue taking the medication, their body has a rebound reaction of depression. That depression does not mean that they needed the antidepressant all along. It just means that the drug has caused their body to no longer produce the chemistry of well-being on its own.
A Medications Case Example: Despair, Delight, Disaster, and More
Many thanks to LC, for sharing her antidepressant experiences.
LC: It all started one late afternoon. I was in my car with my toddler-aged son, driving home through typical late afternoon traffic.
Suddenly I smelled the distinct scent of burning. Ahead of me, just five cars away, a plume of neon orange fire was climbing higher and higher. It was so out of place and so sudden that I didn't feel panicked or scared, I just stared for a few seconds, mouth wide open, my brain calibrating a fire on the highway.
Then I saw the people starting to run. And the panic set in. People all around me were jumping out of their cars and running down the highway, away from the gas truck that was literally on fire in front of us. The truck was still mostly intact, and it dawned on me all at once that a larger explosion might be imminent.
I jumped out of the car, pried open the car-seat straps, and then, flinging my son over my shoulder, ran to get as far away from the gasoline truck as possible. There was a BOOM sound, but I didn't look back. I just kept running and saying, "It's OK. We just need to move away from the fire," both to my son, and to myself.
The sirens started. Police and fire-trucks and ambulances somehow made their way through the maze of stopped cars.
A tragic gas leak had killed the driver of the truck. I texted my husband. I called and apologized profusely to my one-year-old's sitter for being so late.
Three hours later, I was on my way home. I had to run to the grocery store, pick up my 4-year-old from preschool, and make dinner. With three young children, I didn't have time to panic, process, or recover. I had to just keep going.

It was only later that night, after 11:00 p.m., that I felt the effects of that experience. My husband tried to calm me down. I was inconsolable. I wanted to scream or cry or run, but I was paralyzed and terrified.
The next day, I couldn't do anything. My anxiety was telling me that I was in danger. I wasn't, but the panic was still there. I was dreading trying to sleep again.
My sister told me to go immediately to a psychiatrist. I did. The psychiatrist talked to me for about 1 minute and then handed me a Xanax (an anti-anxiety pill) and a cup of water: "You are having a panic attack, and you've been in it for almost 24 hours. We need to get you calmed down."
Having a doctor hand me something I could swallow immediately soothed me. I was able finally to speak enough to tell the psychiatrist that I had seen a terrifying accident, and that I had never really suffered from anxiety or panic attacks before. I begged her to please make the anxiety stop.
The psychiatrist prescribed Xanax for a couple of weeks and then Cipralex, a commonly-used SSRI antidepressant that treats both depression and anxiety, to take long-term. She also said that it was imperative that I find a therapist and explore what was going on in my mind. I guess she assumed the trigger was deeper than just seeing a gasoline truck in flames.
Dr. Heitler: Traumatic events can trigger intense panic either during or at some point after the dangerous event has concluded. Eventually, especially with a chance to talk about what happened, the anxiety calms down. In LC’s case however, the parasympathetic nervous system , whose job it is to calm feelings of fear , was not functioning.
Fortunately, the anti-anxiety pill, Xanax, is fast-acting and effective.
Fortunately also, the psychiatrist had suggested that Lia speak with a talk therapist. Talking about the thoughts that were barraging her would enable Lia to digest her thoughts and feelings, both from the recent trauma and from prior events that had troubled her for some time.
Unfortunately, the psychiatrist did not offer non-pill options to calm the intense anxiety reaction. As the saying goes, to a man with a hammer, the world is a nail.
In this case, the hammer was in fact effective. Xanax brought Lia immediate relief. There are, however, non-pill options that can produce the same immediate calming effect. Both acupoint tapping and a visualization called the spinning technique would probably have done the job equally well. In addition, Lia easily could learn to do these techniques on her own at home should the anxiety return.
LC: The thing is . . . I knew that I needed therapy. It had been a long time coming. An unspoken trauma from the past was finding its way out, visiting me in dreams , and violating random moments in my life. I had been doing my best to silence it, shushing it desperately, hoping that it would just go away. So I started therapy. And I started the antidepressant drugs. And I was able to breathe. For a while.
Therapy opened my mind to myself. I had closed it years before. Re-opening it was as if a door had been kicked down. The halls and rooms of my mind were inviting me to explore, to wander, and to get reacquainted with my inner-world.
The SSRI seemed to be working too. I was more calm. I was more at ease. I wasn't barking at my husband about crumbs on the counter or scrubbing toys with bleach every night. I was laughing a little more, yelling a little less, more balanced.
What was from therapy, and what was from the SSRI? I didn’t care. I was just relieved to be breathing normally.
Dr. Heitler: Multiple studies of the treatment of serious emotional distress conclude that the combination of medication and psychotherapy is more potent than either alone. Lia’s case exemplifies this principle. Pills and talk therapy can potentiate each other, that is, cause each other to be more effective than either treatment alone could be.
At the same time, newer therapy techniques, such as the Body Code and Emotion Code, enable a therapist to radically shorten the time and intensity of talk therapy. Within one session or several, an Emotion Code therapist can pinpoint the earlier problem and immediately release trapped negative emotions so that they cease to have impact. With the underground spring that had been feeding anxious, angry and/or depressed feelings turned off, the feelings of vitality and well-being that we call mental health can emerge.
Marriage therapy also might well have helped Lia. My policy is when anyone who is married seeks therapy with me, I encourage them to bring their spouse. In almost all cases, underlying marital issues have been fanning the flames of negative emotions.
The spouse also can have a significant role in fostering a return to mental health. For instance, an anxious or depressed person may have an impulse to spend his evenings isolating and ruminating, saying troubling thoughts over and over to himself. Rumination exacerbates anxiety and depression. If husband and wife enjoy activities together in the evening, they are likely to be able to replace the rumination with pleasant interactions.
LC: I don't regret starting the antidepressant, the Cipralex. I truly feel like that drug saved my mind. It also probably held my marriage together for several more years. But by a year later, I knew that something was off. I knew that it was the medication.
Dr. Heitler: An antidepressant, especially in combination with good talk therapy, can work miracles in enabling people to get back to functioning in a normal emotional zone. The difficulties tend to come with the duration of use.
By prescribing an antidepressant medication and then keeping her on it for more than an initial several months, LC’s psychiatrist had inadvertently invited increasingly negative side effects. The negative side effects which had begun while Lia was taking the pills became even worse when she tried to get off the pills.
LC: At about a year, I started feeling fuzzy, numb, and detached. I would have several-minute episodes of not knowing what I was doing or how I got there. Then the confusion would dissipate, and I would be left thinking that I was just imagining it. But it would happen again. Fleeting, but tangible. Almost leaving a taste in my mouth.
I shared this with my husband, but he was worried about the anxiety returning if I messed with my medication. I waited.
Dr. Heitler: LC’s husband’s concerns had some genuine validity. The difficulty is that after a year of taking antidepressants, anyone who attempts to stop taking them must end their use very slowly. Otherwise, removal of the drugs can precipitate serious depression and/or anxiety.
It’s not that these emotions had been lurking there all along. Rather, antidepressants create drug dependency. The body forgets how to produce the chemicals that sustain well-being when they are being provided artificially by pills.
LC: The side effects worsened. I had no sex drive. I stopped feeling motivated to hang out with friends. I stopped caring about how I looked or what I was wearing. I was sinking. I had been saved from anxiety, and was now slipping into depression.
I made a unilateral decision to go off my meds. It wasn't a wise one. Looking back, I see that it was very much a desperate stand against the many factors in my life that I wasn't in control of — my devastation over my marriage that was quietly but quickly ending, my loss of focus on my passions and hobbies, my overweight and exhausted body, too strict in my religious life . . . the list goes on.
To simply argue that the SSRIs were ruining my life would be short-sighted and most likely wrong. I was ruining my life. But I was absolutely clear that the drug I was putting into my body every day was dragging me down and making it much harder to move forward. I felt very much alone — and for the first time in a while, very clear in my mission.
Dr. Heitler: In addition to creating drug dependency when used for more than several months at a stretch, antidepressants can produce a number of further negative side effects. Weight gain, loss of sexual feelings, emotional numbness, and "brain zapping" are among the most common. LC experienced these, and more.
LC: Going off SSRIs cold-turkey is nothing short of a ride through hell. The physical and emotional effects of suddenly depriving your brain of serotonin is horrific.
I was tormented by anxiety. I experienced electric pulses starting in my head and traveling down my entire body. I found myself in tears over everything. I had so much guilt over the decision. But I couldn't put that pill back in my mouth.
I pushed. It was raw without the drug. My husband and I separated. I said goodbye to God on a park bench and said hello to myself. I sabotaged a friendship — not something I'm proud of. I lost 35 pounds. I started singing out loud. I started running.
I told the psychiatrist what I had done. Even though so many things were better, I was on the verge of another breakdown, and I didn't know what to do.
The psychiatrist prescribed a different drug, this time an SNRI (two chemicals for the brain's "happy" place instead of one). She explained that since I was in the middle of a divorce — a major life-crisis for anyone — it probably wasn't the best time to go off psychiatric drugs.
That night I sat with the new pill in my hand. It took a serious pep talk to swallow it, but I did. I felt like I needed all the help I could get. I had three young children depending on me to keep it together, and I couldn't afford to let emotions destroy me. I had delved extensively into my past and had finally put to rest the lurking earlier trauma. I told myself I would take the drug, and when life settled down, I would get off.
Fast-forward a year and a half. A very similar cycle ensued. At first the SNRI filled me with renewed calm. It was like a rosy tint on life was just a pill away. And then . . . the fog set in. Again, about a year in, I felt that familiar detachment. I stopped caring about the little things. I started to feel like I was being numbed. Like I was underwater. Watching the world from below, too slow to stay actively involved in my own life. My sex drive started dying, and with it, my drive for life deteriorated.
With this new and more powerful drug, I again started feeling physical side effects. If I took the pill a few hours later than usual, I would get extremely nauseous. But if I took it in the morning, I would also get nausea and throw up. On the drug, I was more prone to migraines , I fainted several times that year, and I started gaining weight quite rapidly — despite my strictly healthy lifestyle.
This time around, I was determined to get off the drug safely. I checked in with a doctor. I started by taking off just one-quarter of the dose and did so every four weeks, allowing my brain to adapt each time.
Nonetheless, again it was hard, even painful. Each time I weaned down a dose, I had a week of horrible brain zaps. Even worse, I was much more reactive and impatient with my children. The weaning process took four months.
At the same time, I truly feel like this time around I experienced a beautiful and inspiring rebirth of myself. My senses feel heightened. My experiences are fully my own again.
Dr. Heitler: Paradoxically, ending her use of antidepressants turned out for LC to be the ultimate cure. With the pills no longer compromising her body’s chemistry, LC’s natural vitality eventually returned. So did her sexual feelings, ability to lose weight, eventual loss of the brain zapping, and a return of her former good-humored self.
LC’s conclusions: I'm still forming an objective opinion on the use of SSRIs. The power of these drugs, for better and for worse, is something that shouldn't be taken lightly. Off them now though, for me, heading away from antidepressants is heading in the right direction.
Dr. Heitler’s conclusions: Again, as I said at the outset, for a severe or suicidal depressive episode, antidepressant medications can relieve the intensity of dark thoughts and desperate feelings.
At the same time, Lia’s case illustrates well that antidepressants may:
- Have limited or no effectiveness for almost half of users
- Help somewhat, while many aspects of the depression remain
- Produce problematic side effects, like weight gain, decreased sexual feelings, brain zapping, nausea, clouded thinking, and numbing of feelings of joy as well as of negative emotions
- Create drug dependence when used for longer than a few months, and therefore difficult withdrawal symptoms, including withdrawal-induced depression
- Be prescribed for usages for which they are not intended (i.e., mild depressive reactions and anxiety) and for which non-drug options may be equally effective
- Be prescribed at length, for years rather than months, increasing the difficulties of eventual withdrawal

Susan Heitler, Ph.D ., is the author of many books, including From Conflict to Resolution and The Power of Two . She is a graduate of Harvard University and New York University.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

At any moment, someone’s aggravating behavior or our own bad luck can set us off on an emotional spiral that threatens to derail our entire day. Here’s how we can face our triggers with less reactivity so that we can get on with our lives.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
Case Study Research Method in Psychology
Saul Mcleod, PhD
Editor-in-Chief for Simply Psychology
BSc (Hons) Psychology, MRes, PhD, University of Manchester
Saul Mcleod, PhD., is a qualified psychology teacher with over 18 years of experience in further and higher education. He has been published in peer-reviewed journals, including the Journal of Clinical Psychology.
Learn about our Editorial Process
Olivia Guy-Evans, MSc
Associate Editor for Simply Psychology
BSc (Hons) Psychology, MSc Psychology of Education
Olivia Guy-Evans is a writer and associate editor for Simply Psychology. She has previously worked in healthcare and educational sectors.
On This Page:
Case studies are in-depth investigations of a person, group, event, or community. Typically, data is gathered from various sources using several methods (e.g., observations & interviews).
The case study research method originated in clinical medicine (the case history, i.e., the patient’s personal history). In psychology, case studies are often confined to the study of a particular individual.
The information is mainly biographical and relates to events in the individual’s past (i.e., retrospective), as well as to significant events that are currently occurring in his or her everyday life.
The case study is not a research method, but researchers select methods of data collection and analysis that will generate material suitable for case studies.
Freud (1909a, 1909b) conducted very detailed investigations into the private lives of his patients in an attempt to both understand and help them overcome their illnesses.
This makes it clear that the case study is a method that should only be used by a psychologist, therapist, or psychiatrist, i.e., someone with a professional qualification.
There is an ethical issue of competence. Only someone qualified to diagnose and treat a person can conduct a formal case study relating to atypical (i.e., abnormal) behavior or atypical development.
Famous Case Studies
- Anna O – One of the most famous case studies, documenting psychoanalyst Josef Breuer’s treatment of “Anna O” (real name Bertha Pappenheim) for hysteria in the late 1800s using early psychoanalytic theory.
- Little Hans – A child psychoanalysis case study published by Sigmund Freud in 1909 analyzing his five-year-old patient Herbert Graf’s house phobia as related to the Oedipus complex.
- Bruce/Brenda – Gender identity case of the boy (Bruce) whose botched circumcision led psychologist John Money to advise gender reassignment and raise him as a girl (Brenda) in the 1960s.
- Genie Wiley – Linguistics/psychological development case of the victim of extreme isolation abuse who was studied in 1970s California for effects of early language deprivation on acquiring speech later in life.
- Phineas Gage – One of the most famous neuropsychology case studies analyzes personality changes in railroad worker Phineas Gage after an 1848 brain injury involving a tamping iron piercing his skull.
Clinical Case Studies
- Studying the effectiveness of psychotherapy approaches with an individual patient
- Assessing and treating mental illnesses like depression, anxiety disorders, PTSD
- Neuropsychological cases investigating brain injuries or disorders
Child Psychology Case Studies
- Studying psychological development from birth through adolescence
- Cases of learning disabilities, autism spectrum disorders, ADHD
- Effects of trauma, abuse, deprivation on development
Types of Case Studies
- Explanatory case studies : Used to explore causation in order to find underlying principles. Helpful for doing qualitative analysis to explain presumed causal links.
- Exploratory case studies : Used to explore situations where an intervention being evaluated has no clear set of outcomes. It helps define questions and hypotheses for future research.
- Descriptive case studies : Describe an intervention or phenomenon and the real-life context in which it occurred. It is helpful for illustrating certain topics within an evaluation.
- Multiple-case studies : Used to explore differences between cases and replicate findings across cases. Helpful for comparing and contrasting specific cases.
- Intrinsic : Used to gain a better understanding of a particular case. Helpful for capturing the complexity of a single case.
- Collective : Used to explore a general phenomenon using multiple case studies. Helpful for jointly studying a group of cases in order to inquire into the phenomenon.
Where Do You Find Data for a Case Study?
There are several places to find data for a case study. The key is to gather data from multiple sources to get a complete picture of the case and corroborate facts or findings through triangulation of evidence. Most of this information is likely qualitative (i.e., verbal description rather than measurement), but the psychologist might also collect numerical data.
1. Primary sources
- Interviews – Interviewing key people related to the case to get their perspectives and insights. The interview is an extremely effective procedure for obtaining information about an individual, and it may be used to collect comments from the person’s friends, parents, employer, workmates, and others who have a good knowledge of the person, as well as to obtain facts from the person him or herself.
- Observations – Observing behaviors, interactions, processes, etc., related to the case as they unfold in real-time.
- Documents & Records – Reviewing private documents, diaries, public records, correspondence, meeting minutes, etc., relevant to the case.
2. Secondary sources
- News/Media – News coverage of events related to the case study.
- Academic articles – Journal articles, dissertations etc. that discuss the case.
- Government reports – Official data and records related to the case context.
- Books/films – Books, documentaries or films discussing the case.
3. Archival records
Searching historical archives, museum collections and databases to find relevant documents, visual/audio records related to the case history and context.
Public archives like newspapers, organizational records, photographic collections could all include potentially relevant pieces of information to shed light on attitudes, cultural perspectives, common practices and historical contexts related to psychology.
4. Organizational records
Organizational records offer the advantage of often having large datasets collected over time that can reveal or confirm psychological insights.
Of course, privacy and ethical concerns regarding confidential data must be navigated carefully.
However, with proper protocols, organizational records can provide invaluable context and empirical depth to qualitative case studies exploring the intersection of psychology and organizations.
- Organizational/industrial psychology research : Organizational records like employee surveys, turnover/retention data, policies, incident reports etc. may provide insight into topics like job satisfaction, workplace culture and dynamics, leadership issues, employee behaviors etc.
- Clinical psychology : Therapists/hospitals may grant access to anonymized medical records to study aspects like assessments, diagnoses, treatment plans etc. This could shed light on clinical practices.
- School psychology : Studies could utilize anonymized student records like test scores, grades, disciplinary issues, and counseling referrals to study child development, learning barriers, effectiveness of support programs, and more.
How do I Write a Case Study in Psychology?
Follow specified case study guidelines provided by a journal or your psychology tutor. General components of clinical case studies include: background, symptoms, assessments, diagnosis, treatment, and outcomes. Interpreting the information means the researcher decides what to include or leave out. A good case study should always clarify which information is the factual description and which is an inference or the researcher’s opinion.
1. Introduction
- Provide background on the case context and why it is of interest, presenting background information like demographics, relevant history, and presenting problem.
- Compare briefly to similar published cases if applicable. Clearly state the focus/importance of the case.
2. Case Presentation
- Describe the presenting problem in detail, including symptoms, duration,and impact on daily life.
- Include client demographics like age and gender, information about social relationships, and mental health history.
- Describe all physical, emotional, and/or sensory symptoms reported by the client.
- Use patient quotes to describe the initial complaint verbatim. Follow with full-sentence summaries of relevant history details gathered, including key components that led to a working diagnosis.
- Summarize clinical exam results, namely orthopedic/neurological tests, imaging, lab tests, etc. Note actual results rather than subjective conclusions. Provide images if clearly reproducible/anonymized.
- Clearly state the working diagnosis or clinical impression before transitioning to management.
3. Management and Outcome
- Indicate the total duration of care and number of treatments given over what timeframe. Use specific names/descriptions for any therapies/interventions applied.
- Present the results of the intervention,including any quantitative or qualitative data collected.
- For outcomes, utilize visual analog scales for pain, medication usage logs, etc., if possible. Include patient self-reports of improvement/worsening of symptoms. Note the reason for discharge/end of care.
4. Discussion
- Analyze the case, exploring contributing factors, limitations of the study, and connections to existing research.
- Analyze the effectiveness of the intervention,considering factors like participant adherence, limitations of the study, and potential alternative explanations for the results.
- Identify any questions raised in the case analysis and relate insights to established theories and current research if applicable. Avoid definitive claims about physiological explanations.
- Offer clinical implications, and suggest future research directions.
5. Additional Items
- Thank specific assistants for writing support only. No patient acknowledgments.
- References should directly support any key claims or quotes included.
- Use tables/figures/images only if substantially informative. Include permissions and legends/explanatory notes.
- Provides detailed (rich qualitative) information.
- Provides insight for further research.
- Permitting investigation of otherwise impractical (or unethical) situations.
Case studies allow a researcher to investigate a topic in far more detail than might be possible if they were trying to deal with a large number of research participants (nomothetic approach) with the aim of ‘averaging’.
Because of their in-depth, multi-sided approach, case studies often shed light on aspects of human thinking and behavior that would be unethical or impractical to study in other ways.
Research that only looks into the measurable aspects of human behavior is not likely to give us insights into the subjective dimension of experience, which is important to psychoanalytic and humanistic psychologists.
Case studies are often used in exploratory research. They can help us generate new ideas (that might be tested by other methods). They are an important way of illustrating theories and can help show how different aspects of a person’s life are related to each other.
The method is, therefore, important for psychologists who adopt a holistic point of view (i.e., humanistic psychologists ).
Limitations
- Lacking scientific rigor and providing little basis for generalization of results to the wider population.
- Researchers’ own subjective feelings may influence the case study (researcher bias).
- Difficult to replicate.
- Time-consuming and expensive.
- The volume of data, together with the time restrictions in place, impacted the depth of analysis that was possible within the available resources.
Because a case study deals with only one person/event/group, we can never be sure if the case study investigated is representative of the wider body of “similar” instances. This means the conclusions drawn from a particular case may not be transferable to other settings.
Because case studies are based on the analysis of qualitative (i.e., descriptive) data , a lot depends on the psychologist’s interpretation of the information she has acquired.
This means that there is a lot of scope for Anna O , and it could be that the subjective opinions of the psychologist intrude in the assessment of what the data means.
For example, Freud has been criticized for producing case studies in which the information was sometimes distorted to fit particular behavioral theories (e.g., Little Hans ).
This is also true of Money’s interpretation of the Bruce/Brenda case study (Diamond, 1997) when he ignored evidence that went against his theory.
Breuer, J., & Freud, S. (1895). Studies on hysteria . Standard Edition 2: London.
Curtiss, S. (1981). Genie: The case of a modern wild child .
Diamond, M., & Sigmundson, K. (1997). Sex Reassignment at Birth: Long-term Review and Clinical Implications. Archives of Pediatrics & Adolescent Medicine , 151(3), 298-304
Freud, S. (1909a). Analysis of a phobia of a five year old boy. In The Pelican Freud Library (1977), Vol 8, Case Histories 1, pages 169-306
Freud, S. (1909b). Bemerkungen über einen Fall von Zwangsneurose (Der “Rattenmann”). Jb. psychoanal. psychopathol. Forsch ., I, p. 357-421; GW, VII, p. 379-463; Notes upon a case of obsessional neurosis, SE , 10: 151-318.
Harlow J. M. (1848). Passage of an iron rod through the head. Boston Medical and Surgical Journal, 39 , 389–393.
Harlow, J. M. (1868). Recovery from the Passage of an Iron Bar through the Head . Publications of the Massachusetts Medical Society. 2 (3), 327-347.
Money, J., & Ehrhardt, A. A. (1972). Man & Woman, Boy & Girl : The Differentiation and Dimorphism of Gender Identity from Conception to Maturity. Baltimore, Maryland: Johns Hopkins University Press.
Money, J., & Tucker, P. (1975). Sexual signatures: On being a man or a woman.
Further Information
- Case Study Approach
- Case Study Method
- Enhancing the Quality of Case Studies in Health Services Research
- “We do things together” A case study of “couplehood” in dementia
- Using mixed methods for evaluating an integrative approach to cancer care: a case study
Related Articles
Research Methodology
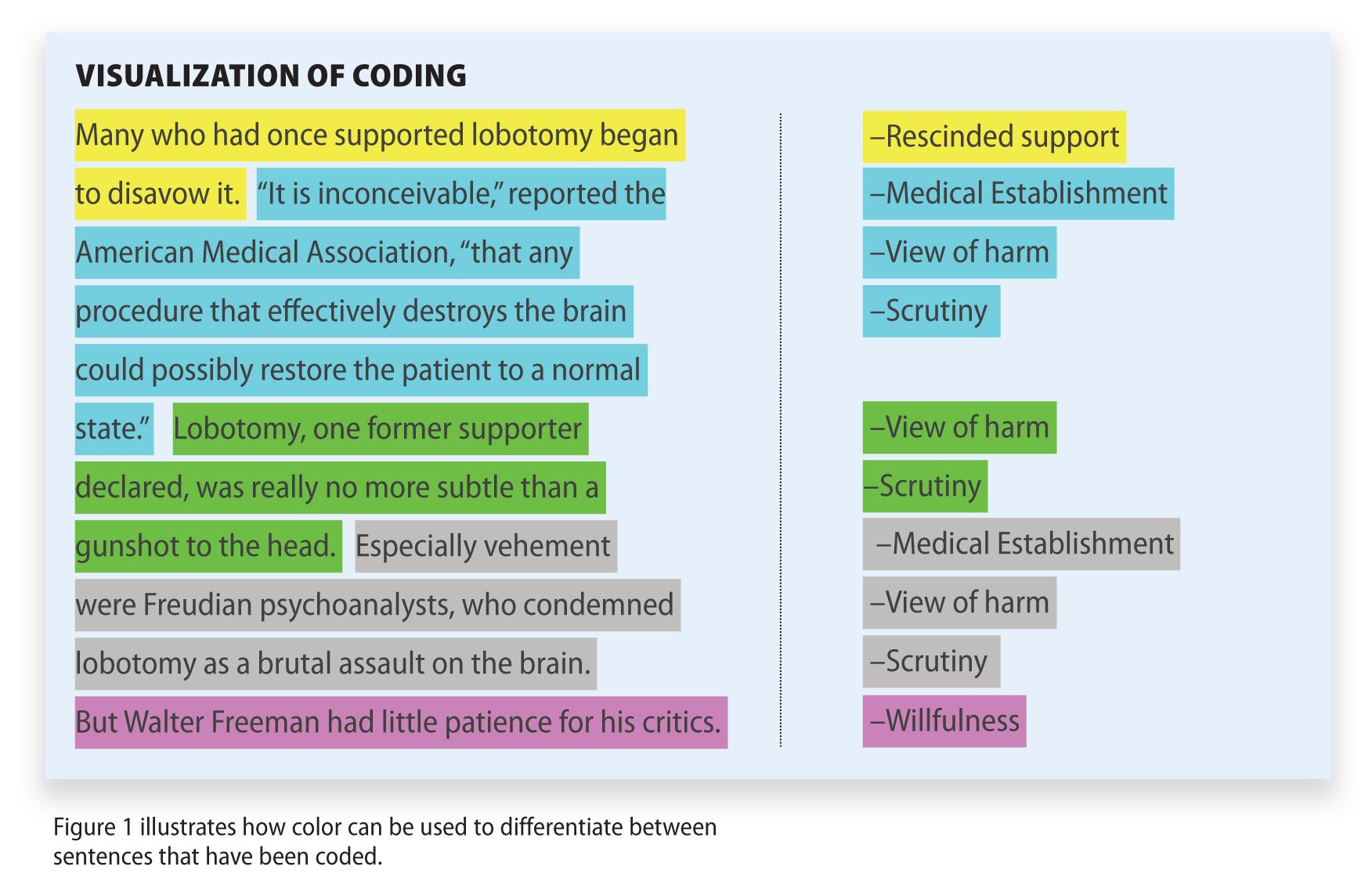
Qualitative Data Coding

What Is a Focus Group?
Cross-Cultural Research Methodology In Psychology

What Is Internal Validity In Research?

Research Methodology , Statistics
What Is Face Validity In Research? Importance & How To Measure

Criterion Validity: Definition & Examples
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 30 May 2024
ProMENDA: an updated resource for proteomic and metabolomic characterization in depression
- Juncai Pu 1 , 2 na1 ,
- Yue Yu 3 na1 ,
- Yiyun Liu 2 ,
- Dongfang Wang ORCID: orcid.org/0000-0002-7517-3972 2 ,
- Siwen Gui 2 ,
- Xiaogang Zhong 2 ,
- Weiyi Chen ORCID: orcid.org/0000-0002-2520-1082 1 , 2 ,
- Xiaopeng Chen 1 , 2 ,
- Yue Chen 1 , 2 ,
- Xiang Chen 1 , 2 ,
- Renjie Qiao 1 , 2 ,
- Yanyi Jiang 1 , 2 ,
- Hanping Zhang 1 , 2 ,
- Li Fan 1 , 2 ,
- Yi Ren 1 , 2 ,
- Xiangyu Chen 1 , 2 ,
- Haiyang Wang 2 &
- Peng Xie ORCID: orcid.org/0000-0002-0081-6048 1 , 2 , 4 , 5
Translational Psychiatry volume 14 , Article number: 229 ( 2024 ) Cite this article
Metrics details
- Molecular neuroscience
Depression is a prevalent mental disorder with a complex biological mechanism. Following the rapid development of systems biology technology, a growing number of studies have applied proteomics and metabolomics to explore the molecular profiles of depression. However, a standardized resource facilitating the identification and annotation of the available knowledge from these scattered studies associated with depression is currently lacking. This study presents ProMENDA, an upgraded resource that provides a platform for manual annotation of candidate proteins and metabolites linked to depression. Following the establishment of the protein dataset and the update of the metabolite dataset, the ProMENDA database was developed as a major extension of its initial release. A multi-faceted annotation scheme was employed to provide comprehensive knowledge of the molecules and studies. A new web interface was also developed to improve the user experience. The ProMENDA database now contains 43,366 molecular entries, comprising 20,847 protein entries and 22,519 metabolite entries, which were manually curated from 1370 human, rat, mouse, and non-human primate studies. This represents a significant increase (more than 7-fold) in molecular entries compared to the initial release. To demonstrate the usage of ProMENDA, a case study identifying consistently reported proteins and metabolites in the brains of animal models of depression was presented. Overall, ProMENDA is a comprehensive resource that offers a panoramic view of proteomic and metabolomic knowledge in depression. ProMENDA is freely available at https://menda.cqmu.edu.cn .
Similar content being viewed by others

Analysis of gene expression in the postmortem brain of neurotypical Black Americans reveals contributions of genetic ancestry


Integrating human endogenous retroviruses into transcriptome-wide association studies highlights novel risk factors for major psychiatric conditions

The serotonin theory of depression: a systematic umbrella review of the evidence
Introduction.
Depression is a prevalent mental disorder characterized by low mood and loss of pleasure, with a lifetime prevalence of 11.1%–14.6% [ 1 , 2 ]. The condition leads to severe functional impairment and was reported as one of the top three leading causes of burden in 2019 [ 3 ]. Unlike other somatic diseases, the clinical diagnosis of depression relies entirely on the clinical symptoms of patients, while reliable biomarkers are still lacking [ 4 , 5 ]. Moreover, the clinical efficacy of antidepressants is limited, with more than one-third of patients demonstrating inadequate treatment responses [ 6 ]. Furthermore, the long-term use of antidepressants may lead to various side effects and treatment discontinuation [ 7 ]. Therefore, the screening of biomarkers and new drug targets is expected to improve the diagnosis and treatment of depression [ 8 ]. Despite substantial research efforts, the precise mechanism underlying the onset of depression remains incompletely defined, and a systematic molecular profile of depression is still lacking.
The rapid development of systems biology technology has led to the emergence of multi-omics approaches as powerful methods enabling the determination of molecular profiles of diseases with complex biological mechanisms [ 9 , 10 ]. In the field of depression, omics methods, such as metabolomics and proteomics, have been widely applied to study the brain and peripheral samples of patients and animal models. The results have identified numerous differential metabolites and proteins between depressed and normal states [ 11 , 12 , 13 ]. Recent developments and applications in omics research have highlighted the need for comprehensive resources that integrate the available knowledge from scattered studies and provide a panoramic view of molecular characterization in depression [ 14 ]. Therefore, MENDA was developed to present the manually curated metabolic characterization (with 5,600 metabolite entries) in the context of depression [ 15 ]. Since its first release in 2019, multiple integrated studies have employed MENDA to generate meaningful biological insights [ 16 , 17 , 18 , 19 ]. However, the number of metabolomics studies has doubled since the first release, and the core dataset warrants an update. Moreover, molecular data at the protein level is required to capture the multi-level biochemical dysregulation of depression, which could provide information on specific enzymes in the metabolic pathways and networks [ 20 , 21 ]. A growing body of proteomics studies have identified alterations in protein abundances in depression [ 22 , 23 , 24 ], providing an important resource of proteomic information. To date, a platform facilitating the systematic curation of proteomic changes in depression is still lacking. Adding protein information to the MENDA will contribute to a deeper understanding of molecular alterations in depression.
This study aimed to create a standardized resource for all available knowledge in the growing area of proteomic and metabolomic research in depression. Therefore, this study presents Protein and Metabolite Network of Depression Database (ProMENDA), an upgraded resource that provides a platform for the manual annotation of candidate proteins and metabolites linked to depression. The data set now contains 43,366 molecular entries from 1370 studies that investigated differential proteins and metabolites in both patients and animal models of depression. This update represents a significant increase (more than 7-fold) in molecular entries compared to the initial release of MENDA. Additionally, the web interface was redesigned to enhance the ease of use. The design and implementation of these updates and changes are described below. To demonstrate the usage of ProMENDA, a case study analyzing the molecular changes in the brains of animal models is presented. ProMENDA is expected to contribute to the investigation of the molecular profile of depression.
Materials and methods
Overview of promenda framework.
The schematic overview of ProMENDA is illustrated in Fig. 1 . In brief, information on study design and candidate molecules from proteomics and metabolomics studies of depression was manually collected using standardized data extraction tables. These tables were then integrated into annotated datasets based on a multi-faceted annotation scheme. In addition, a brand-new web interface was developed in this update to enhance user experience.
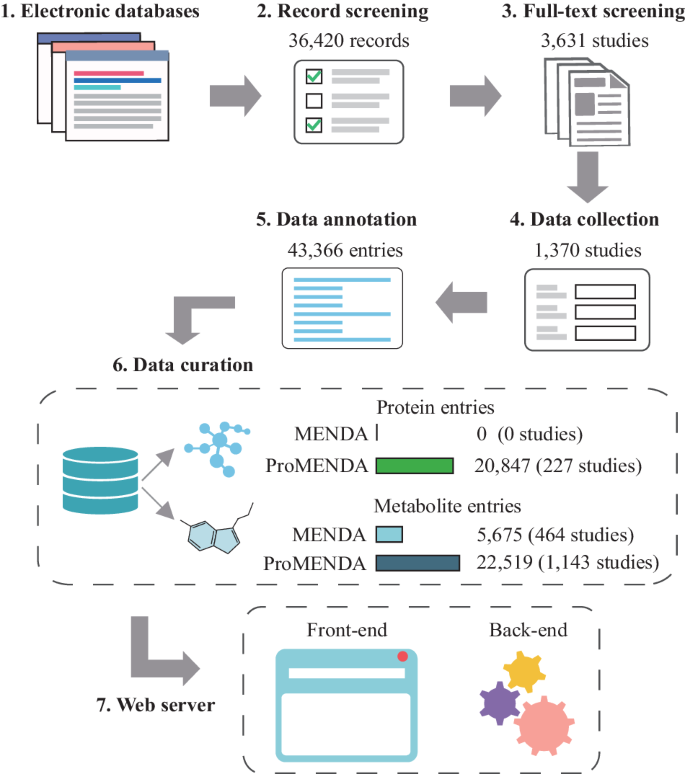
The flowchart of the construction process for the ProMENDA.
Creation of the proteomic dataset
Data from proteomic studies of depression were incorporated to expand the scope of MENDA. Relevant proteomic studies were searched from PubMed, Embase, Web of Science, and PsychInfo (Table S1 ), resulting in a cumulative total of 13,742 literature records retrieved as of May 18, 2023 (Table S2 ). Studies that investigated proteomic changes associated with depression and its treatment in both human and animal models were screened based on titles and abstracts, yielding 436 potential studies. After checking the full text of these studies, 227 studies were finally included. The exclusion reasons are summarized in Table S3 .
Subsequently, a proteomic dataset was created by manually selecting the study information and differentially expressed proteins from the full texts and supplementary materials of these studies using a standardized data abstraction spreadsheet (Table S4 ). To present experimental information on each protein, the proteomic data were annotated based on a multi-faceted annotation scheme as described in MENDA [ 15 ], with minor modifications. The annotation scheme involved manual annotation of information of interest at both the study and protein levels, including experimental design, types of organisms, categories of depression, categories of tissues, experimental techniques, citations, etc.
Moreover, protein information was annotated to ensure standardization, including UniProt accessions, UniProt entry names, protein names, and gene symbols based on the UniProtKB database (version 2023_03) [ 25 ]. This step was necessary as proteins were presented in different formats in the original reports, such as protein names, Uniprot accession, or gene symbols. A total of 20,847 protein entries were finally curated.
Update for metabolomic dataset
In this update, MENDA was expanded to include more comprehensive and up-to-date metabolite entries. The initial release of MENDA included 5675 metabolite entries from 464 metabolomics and magnetic resonance spectroscopy studies as of March 20, 2018. To ensure that the ProMENDA remains current, literature databases were re-screened as of May 18, 2023, resulting in a cumulative total of 22,678 records. After screening the full text of 3195 studies, a total of 1143 eligible studies were included in ProMENDA. The reasons for the exclusion of the ineligible studies are summarized in Table S3 . Using a similar data extraction and annotation process to the proteomic dataset, a total of 22,519 differential metabolite entries were curated in this update. The expansion of the metabolite dataset will provide researchers with a more comprehensive overview of metabolic changes associated with depression.
Web interface implementation
The front end of the ProMENDA website has been implemented using HTML, JavaScript, and CSS. The web interface was designed using Bootstrap ( https://getbootstrap.com/ ) and jQuery ( https://jquery.com/ ) libraries, and the interactive tables were constructed using the DataTables library ( https://datatables.net/ ). In addition, the website is hosted on an Apache server ( https://httpd.apache.org ).
Case study for applications of ProMENDA
In addition to data browsing, users can download data from ProMENDA to conduct data mining studies. To illustrate the potential applications of ProMENDA, a case study involving an integrated analysis was conducted based on protein and metabolite entries in the brains of animal models of depression. Metabolite and protein entries were selected based on the following criteria: (1) differential molecules between depressed vs. healthy states; (2) all types of animal models; (3) all brain tissues; and (4) all analytical platforms. Semi-quantitative analyses were performed based on selected data. Considering the possibility of inconsistencies in the up- and down-regulation of certain molecules (with unique gene symbols or metabolite names) across different studies, a vote-counting method was utilized for semi-quantitative analysis. This approach effectively identifies the molecules exhibiting consistent up- or down-regulation under specific conditions, indicating their high reproducibility and potential as biomarkers [ 26 ]. Furthermore, the binom.test function in R (version 4.3.0, https://www.rproject.org/ ) was used based on the downloaded data of interest to identify consistently differentially expressed molecules [ 27 ]. Candidate molecules with one-tailed P < 0.05 across different studies were considered as consistently altered. ImageGP was used to create plots [ 28 ].
Data summary
The initial release of MENDA comprised 5675 metabolite entries. In ProMENDA, significant efforts have been made to expand the molecular entries. A cumulative total of 36,420 records were screened from electronic databases, and after checking the full texts of 3631 studies, 1370 studies that investigated the levels of proteins and metabolites in depression and its treatment were included. A standardized data extraction and annotation process was adopted, and 43,366 molecular entries were curated, including 20,847 protein entries (Supplementary Data 1 ) and 22,519 metabolite entries (Supplementary Data 2 ). This has resulted in a significant increase (more than 7-fold) in molecular entries compared to the previous version of MENDA (Fig. 1 ). Moreover, our laboratory provided 3173 metabolites entries and 3927 protein entries in ProMENDA, accounting for 16.4% of all molecular entries.
The number of studies that explored molecular alterations in each organism and each tissue is shown in Fig. S1 . In ProMENDA, 7490 molecular entries were curated from human tissues, 1487 from non-human primate tissues, 19,925 from rat tissues, and 14,464 from mice (Fig. 2A ). The numbers of unique proteins and metabolites in humans, non-human primates, rats, and mice are shown in Fig. 2B . Specifically, in humans, 3161 protein entries (from 1877 unique proteins) and 4329 metabolite entries (from 2991 unique metabolites) were curated from 8 types of tissues (Fig. 2C ). In non-human primates, 143 protein entries (from 131 unique proteins) and 1344 metabolite entries (from 1100 unique metabolites) were curated from 8 types of tissues (Fig. 2D ). In rats, 10,302 protein entries (from 4563 unique proteins) and 9623 metabolite entries (from 2180 unique metabolites) were collected from 14 types of tissues (Fig. 2E ). In mice, 7241 protein entries (from 4165 unique proteins) and 7223 metabolite entries (from 3046 unique metabolites) were obtained from 11 types of tissues (Fig. 2F ). The most frequently reported proteins and metabolites in each organism are displayed in Fig. S2 . Among these molecular entries, 72.7% of protein entries and 63.8% of metabolite entries were collected from studies that compared molecular levels between depressed and healthy states; the remaining entries were collected from studies that investigated molecular changes resulting from antidepressant treatments.
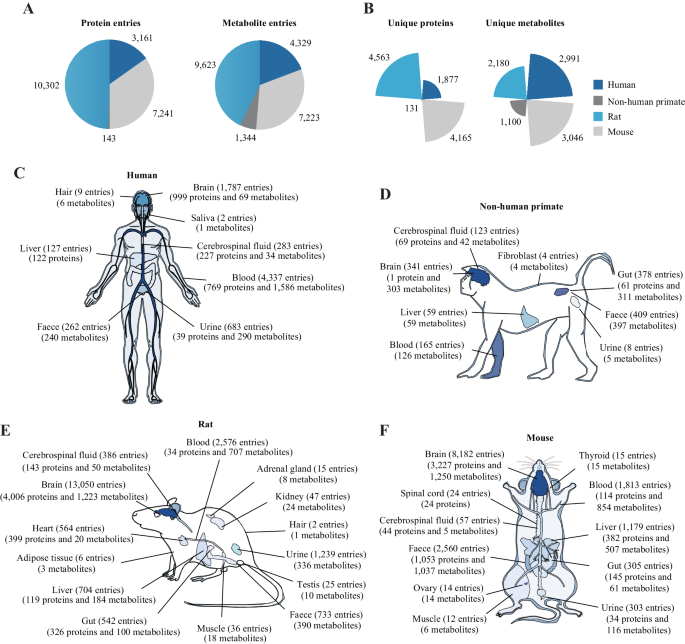
A The number of molecular entries from each organism. B The number of unique proteins and metabolites from each organism. C The number of molecular entries and unique molecules in 8 human tissues. D The number of molecular entries and unique molecules in 8 non-human primate tissues. E The number of molecular entries and unique molecules in 14 rat tissues. F The numbers of molecular entries and unique molecules in 11 mouse tissues.
Web interface of ProMENDA
To facilitate the storage and access of study-level and molecular-level datasets, a new web interface was developed for ProMENDA. This interface comprises three main web pages, including Browse, Search, and Download.
Browse page: The Browse page features interactive tables that present molecular and study information, providing web links for each study and molecule (Fig. 3 ). Users can easily search these tables by using search columns and applying filters based on study type, organism, categories of depression, tissue, platform, and up/down-regulation. Users are also allowed to select and download data of interest. Basic information about the molecule is provided on the web page of each molecule and the related data entries are summarized. On the web page of each study, its experimental design and candidate molecules are listed.
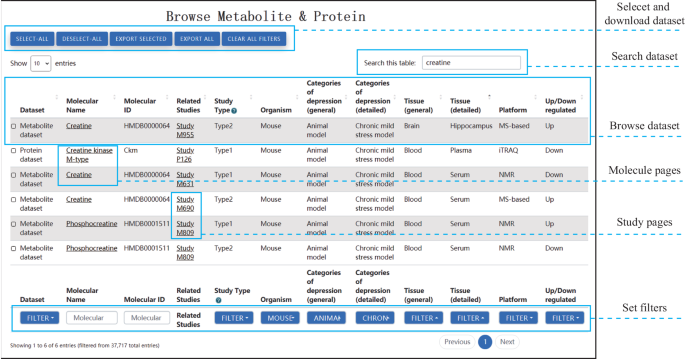
The web interface allows users to easily browse, search, filter, and download molecular entries of interest. The browse page displays molecular entries in an interactive table format, enabling users to quickly access relevant information.
(ii) Search page: On the Search page, users can search for protein or metabolite entries using molecular names or IDs. Each query generates hyperlinks for relevant molecules and their links to other databases, including UniProt, HMDB, KEGG, and PubChem [ 25 , 29 , 30 , 31 ].
(iii) Download page: The Download page provides free access to the core datasets of ProMENDA, with additional information available in the Excel documents.
(iv) Others: In addition to the pages mentioned above, ProMENDA also offers other pages in its web interface, including Home, Introduction, News, Tutorial, and Contact pages. These pages enhance the user experience and provide users with a complete understanding of ProMENDA and its features.
Use case: investigating molecular changes in the brains of animal models of depression
To illustrate the usage of ProMENDA, a case study was conducted to investigate the molecular changes of candidate proteins and metabolites in the brains of animal models of depression (Fig. 4A ). Based on the inclusion criteria, 9458 protein entries and 4132 metabolite entries were initially included from the ProMENDA database. From these molecular entries, 317 candidate proteins and 127 candidate metabolites (or metabolite ratios) were identified from more than four studies. The results of the vote-counting strategy showed that the levels of 28 proteins and 32 metabolites were consistently dysregulated in the brain ( P < 0.05; Fig. 4B and Table S5 ).
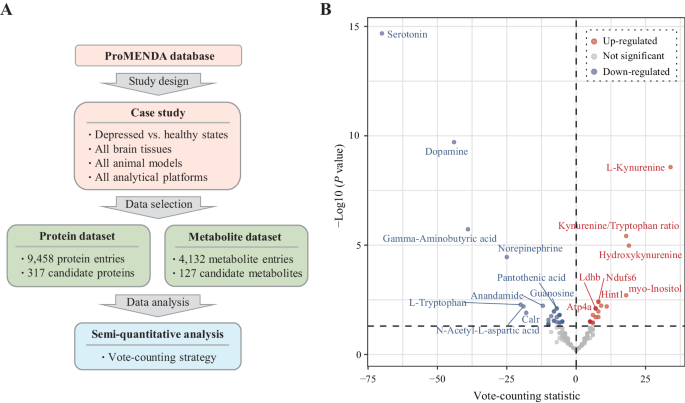
A Overview of the study design for the case study. B Volcano plot showing consistently dysregulated molecules in the vote-counting procedure.
Depression is a prevalent disease with complex molecular alterations, and exploring potential molecular changes presents an opportunity to unravel the neurobiology and treatment targets of depression [ 32 ]. In recent years, numerous clinical and preclinical studies with various designs have employed high-throughput assays to study the molecular changes associated with depression. However, collecting and integrating this massive amount of data from a systems biology perspective remains challenging. Therefore, MENDA was previously developed, containing over 5000 metabolite entries associated with depression. Building on this foundation, ProMENDA was created, presenting a significant extension of the initial release of MENDA, which includes both a new protein dataset and an updated metabolite dataset.
The prime objective of this study was to create a comprehensive knowledge base for proteomic and metabolomic characterization in depression, which may serve as a valuable resource for researchers in the field of depression. To complement the initial release of MENDA, the molecular entries were expanded in ProMENDA by adding a proteomic dataset. While metabolic disturbance only covers a small portion of all biological processes in depression, a platform facilitating the systematic curation of molecules other than metabolites is required. Proteins are major macromolecules that are involved in complex biological functions and regulate metabolic processes; hence, proteomics is a powerful technology enabling a comprehensive understanding of human biology [ 33 , 34 , 35 ]. To provide a deeper understanding of candidate protein alterations in depression, 20,847 protein entries were manually curated from 227 studies, which significantly expanded our knowledge base of proteomic alterations in depression. ProMENDA demonstrates the molecular landscape of depression at both the protein and metabolite levels. Compared to Pharos, which contains about 1318 candidate proteins associated with depression based on evidence from proteins, genes, or transcriptions [ 36 ], ProMENDA provides a significantly wider selection of protein entries and rich annotation information.
In addition to expanding the proteomic dataset, the metabolite dataset was also updated in ProMENDA. Currently, 22,519 metabolite entries are provided, which is more than three times the number of entries since the initial release of MENDA. The metabolite entries in ProMENDA were compared with other knowledge bases such as MetSigDis, which provides a comprehensive resource of metabolite alterations in 129 diseases [ 37 ]. Compared to MetSigDis, ProMENDA provided a 3.2-fold higher number of metabolite entries for pan-diseases and a 600-fold higher number of metabolite entries for depression. This significantly higher number of metabolite entries in ProMENDA will provide researchers with a more comprehensive understanding of the metabolomic landscape of depression. Additionally, a new web interface was implemented in this update, integrating data browsing, searching, selecting, filtering, and downloading functions, improving user access to data analysis.
The efficient usage of ProMENDA was demonstrated in a case study investigating molecular alterations in the brains of animal models of depression. Compared to the initial release of MENDA, which only contained metabolite data, the integrated analysis based on changes in both protein expression and metabolite concentrations provided a more comprehensive insight due to the chemical and functional diversities between proteins and metabolites, as well as their interactions [ 38 ]. The results of the vote-counting strategy in the case study revealed that 60 molecules were consistently up-regulated or down-regulated across animal studies. Expectedly, this case study found significantly decreased levels of several neurotransmitters, including serotonin, dopamine, gamma-aminobutyric acid, and norepinephrine, which further support the role of monoamines and gamma-aminobutyric acid in depression [ 39 , 40 ]. In addition to the analysis methods mentioned in the case study, users are also encouraged to perform further analysis using other analytical strategies and analysis tools. In a previous study, Fu et al. constructed a comprehensive knowledge graph focusing on food, gut microbiota, and mental diseases, which incorporated metabolite-disease associations from our database [ 41 ]. Moreover, Gao et al. performed a comprehensive analysis of metabolites in the hippocampus of depression models based on our database. They employed pathway analysis and experiment validation and found that disturbances in the neurotransmitter pathways of the hippocampus were associated with depression [ 42 ]. However, users should take data heterogeneity into account during study design, such as differences between human and animal studies, the subtypes of depression, and the type of tissues.
Limitations
Despite the significant improvements made in ProMENDA compared to MENDA, the platform still has some limitations. Only data from omics studies was included, so molecular entries from traditional experimental methods such as Western blotting have not been included. The slow manual curation process poses a major challenge for researchers who wish to collect and annotate molecular entries from all relevant publications [ 43 ]. However, the continuous progress of biomedical text mining techniques might facilitate the curation of large-scale molecular data from scattered literature [ 44 , 45 ]. Another limitation of ProMENDA is the need for additional omics data, such as genomic and transcriptomic data, reflecting the multifactorial molecular changes that occur in depression. Data curation for the ProMENDA database will be an ongoing process. ProMENDA provides a more comprehensive understanding of the molecular landscape of depression; subsequent updates will facilitate the development of new therapeutic strategies.
Conclusions
In summary, ProMENDA is a valuable resource for depression research, offering a significant expansion of the core dataset compared to the initial release of MENDA. The current version of ProMENDA includes 43,366 molecular entries, comprising 20,847 protein entries and 22,519 metabolite entries, which were manually curated from 1370 human, rat, mouse, and non-human primate studies. This represents a more than seven-fold increase in molecular entries compared to the previous version of MENDA. ProMENDA is freely accessible to the public at https://menda.cqmu.edu.cn and provides a new user-friendly web interface that allows users to browse, search, select, filter, and download data.
Data availability
The datasets generated in the current study are available in Supplementary Data 1 and Supplementary Data 2 , or on the ProMENDA website ( https://menda.cqmu.edu.cn ).
Kessler RC, Bromet EJ. The epidemiology of depression across cultures. Annu Rev Public Health. 2013;34:119–38.
Article PubMed PubMed Central Google Scholar
Lu J, Xu X, Huang Y, Li T, Ma C, Xu G, et al. Prevalence of depressive disorders and treatment in China: a cross-sectional epidemiological study. Lancet Psychiatry. 2021;8:981–90.
Article PubMed Google Scholar
GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry. 2022;9:137–50.
Article PubMed Central Google Scholar
Kim YK, Park SC. An alternative approach to future diagnostic standards for major depressive disorder. Prog Neuropsychopharmacol Biol Psychiatry. 2021;105:110133.
Gadad BS, Jha MK, Czysz A, Furman JL, Mayes TL, Emslie MP, et al. Peripheral biomarkers of major depression and antidepressant treatment response: current knowledge and future outlooks. J Affect Disord. 2018;233:3–14.
Article CAS PubMed Google Scholar
Fava M, Rush AJ, Alpert JE, Balasubramani GK, Wisniewski SR, Carmin CN, et al. Difference in treatment outcome in outpatients with anxious versus nonanxious depression: a STAR*D report. Am J Psychiatry. 2008;165:342–51.
Carvalho AF, Sharma MS, Brunoni AR, Vieta E, Fava GA. The safety, tolerability and risks associated with the use of newer generation antidepressant drugs: a critical review of the literature. Psychother Psychosom. 2016;85:270–88.
Abi-Dargham A, Moeller SJ, Ali F, DeLorenzo C, Domschke K, Horga G, et al. Candidate biomarkers in psychiatric disorders: state of the field. World Psychiatry. 2023;22:236–62.
Wörheide MA, Krumsiek J, Kastenmüller G, Arnold M. Multi-omics integration in biomedical research - a metabolomics-centric review. Anal Chim Acta. 2021;1141:144–62.
Hu C, Jia W. Multi-omics profiling: the way towards precision medicine in metabolic diseases. J Mol Cell Biol. 2021;13:576–93.
CAS PubMed PubMed Central Google Scholar
Bot M, Milaneschi Y, Al-Shehri T, Amin N, Garmaeva S, Onderwater GLJ, et al. Metabolomics profile in depression: a pooled analysis of 230 metabolic markers in 5283 cases with depression and 10,145 controls. Biol Psychiatry. 2020;87:409–18.
Pu J, Liu Y, Zhang H, Tian L, Gui S, Yu Y, et al. An integrated meta-analysis of peripheral blood metabolites and biological functions in major depressive disorder. Mol Psychiatry. 2021;26:4265–76.
Li S, Luo H, Lou R, Tian C, Miao C, Xia L, et al. Multiregional profiling of the brain transmembrane proteome uncovers novel regulators of depression. Sci Adv. 2021;7:eabf0634.
Article CAS PubMed PubMed Central Google Scholar
Brookes AJ, Robinson PN. Human genotype-phenotype databases: aims, challenges and opportunities. Nat Rev Genet. 2015;16:702–15.
Pu J, Yu Y, Liu Y, Tian L, Gui S, Zhong X, et al. MENDA: a comprehensive curated resource of metabolic characterization in depression. Brief Bioinform. 2020;21:1455–64.
Gao Y, Li X, Zhao HL, Ling-Hu T, Zhou YZ, Tian JS, et al. Comprehensive analysis strategy of nervous-endocrine-immune-related metabolites to evaluate arachidonic acid as a novel diagnostic biomarker in depression. J Proteome Res. 2021;20:2477–86.
Lei X, Tie J, Pan Y. Inferring metabolite-disease association using graph convolutional networks. IEEE/ACM Trans Comput Biol Bioinform. 2022;19:688–98.
PubMed Google Scholar
Pu J, Liu Y, Gui S, Tian L, Yu Y, Song X, et al. Metabolomic changes in animal models of depression: a systematic analysis. Mol Psychiatry. 2021;26:7328–36.
Tian L, Pu J, Liu Y, Gui S, Zhong X, Song X, et al. Metabolomic analysis of animal models of depression. Metab Brain Dis. 2020;35:979–90.
Karczewski KJ, Snyder MP. Integrative omics for health and disease. Nat Rev Genet. 2018;19:299–310.
Tolani P, Gupta S, Yadav K, Aggarwal S, Yadav AK. Big data, integrative omics and network biology. Adv Protein Chem Struct Biol. 2021;127:127–60.
Choi JE, Lee JJ, Kang W, Kim HJ, Cho JH, Han PL, et al. Proteomic analysis of hippocampus in a mouse model of depression reveals neuroprotective function of ubiquitin C-terminal hydrolase L1 (UCH-L1) via stress-induced cysteine oxidative modifications. Mol Cell Proteomics. 2018;17:1803–23.
Qi YJ, Lu YR, Shi LG, Demmers JAA, Bezstarosti K, Rijkers E, et al. Distinct proteomic profiles in prefrontal subareas of elderly major depressive disorder and bipolar disorder patients. Transl Psychiatry. 2022;12:275.
Liu Y, Wang H, Gui S, Zeng B, Pu J, Zheng P, et al. Proteomics analysis of the gut-brain axis in a gut microbiota-dysbiosis model of depression. Transl Psychiatry. 2021;11:568.
UniProt Consortium. UniProt: the universal protein knowledgebase in 2021. Nucleic Acids Res. 2021;49:D480–9.
Article Google Scholar
Rikke BA, Wynes MW, Rozeboom LM, Barón AE, Hirsch FR. Independent validation test of the vote-counting strategy used to rank biomarkers from published studies. Biomark Med. 2015;9:751–61.
Pu J, Liu Y, Gui S, Tian L, Yu Y, Wang D, et al. Effects of pharmacological treatment on metabolomic alterations in animal models of depression. Transl Psychiatry. 2022;12:175.
Chen T, Liu Y, Huang L. ImageGP: an easy-to-use data visualization web server for scientific researchers. iMeta. 2022;1:e5.
Wishart DS, Guo A, Oler E, Wang F, Anjum A, Peters H, et al. HMDB 5.0: the Human Metabolome Database for 2022. Nucleic Acids Res. 2022;50:D622–31.
Kanehisa M, Furumichi M, Sato Y, Ishiguro-Watanabe M, Tanabe M. KEGG: integrating viruses and cellular organisms. Nucleic Acids Res. 2021;49:D545–51.
Kim S, Chen J, Cheng T, Gindulyte A, He J, He S, et al. PubChem in 2021: new data content and improved web interfaces. Nucleic Acids Res. 2021;49:D1388–95.
Cui L, Li S, Wang S, Wu X, Liu Y, Yu W, et al. Major depressive disorder: hypothesis, mechanism, prevention and treatment. Signal Transduct Target Ther. 2024;9:30.
Müller JB, Geyer PE, Colaço AR, Treit PV, Strauss MT, Oroshi M, et al. The proteome landscape of the kingdoms of life. Nature. 2020;582:592–6.
Bludau I, Aebersold R. Proteomic and interactomic insights into the molecular basis of cell functional diversity. Nat Rev Mol Cell Biol. 2020;21:327–40.
Noor Z, Ahn SB, Baker MS, Ranganathan S, Mohamedali A. Mass spectrometry-based protein identification in proteomics-a review. Brief Bioinform. 2021;22:1620–38.
Kelleher KJ, Sheils TK, Mathias SL, Yang JJ, Metzger VT, Siramshetty VB, et al. Pharos 2023: an integrated resource for the understudied human proteome. Nucleic Acids Res. 2023;51:D1405–16.
Cheng L, Yang H, Zhao H, Pei X, Shi H, Sun J, et al. MetSigDis: a manually curated resource for the metabolic signatures of diseases. Brief Bioinform. 2019;20:203–9.
Piazza I, Kochanowski K, Cappelletti V, Fuhrer T, Noor E, Sauer U, et al. A map of protein-metabolite interactions reveals principles of chemical communication. Cell. 2018;172:358–72.e323.
Krishnan V, Nestler EJ. The molecular neurobiology of depression. Nature. 2008;455:894–902.
Duman RS, Sanacora G, Krystal JH. Altered connectivity in depression: GABA and glutamate neurotransmitter deficits and reversal by novel treatments. Neuron. 2019;102:75–90.
Fu C, Huang Z, van Harmelen F, He T, Jiang X. Food4healthKG: Knowledge graphs for food recommendations based on gut microbiota and mental health. Artif Intell Med. 2023;145:102677.
Gao Y, Mu J, Xu T, Linghu T, Zhao H, Tian J, et al. Metabolomic analysis of the hippocampus in a rat model of chronic mild unpredictable stress-induced depression based on a pathway crosstalk and network module approach. J Pharm Biomed Anal. 2021;193:113755.
Saqi M, Lysenko A, Guo YK, Tsunoda T, Auffray C. Navigating the disease landscape: knowledge representations for contextualizing molecular signatures. Brief Bioinform. 2019;20:609–23.
Karatzas E, Baltoumas FA, Kasionis I, Sanoudou D, Eliopoulos AG, Theodosiou T, et al. Darling: a web application for detecting disease-related biomedical entity associations with literature mining. Biomolecules. 2022;12:520.
Singhal A, Leaman R, Catlett N, Lemberger T, McEntyre J, Polson S, et al. Pressing needs of biomedical text mining in biocuration and beyond: opportunities and challenges. Database. 2016;2016:baw161.
Download references
Acknowledgements
This work was supported by the Natural Science Foundation Project of China (Grant no. 82101596, 82371526, and 81820108015), the Joint project of Chongqing Municipal Science and Technology Bureau and Chongqing Health Commission (Grant no. 2023CCXM003), the National Key Research and Development Program of China (Grant no. 2017YFA0505700), the Young Elite Scientists Sponsorship Program by CAST (Grant no. 2021QNRC001), the China Postdoctoral Science Foundation (Grant no. 2022MD723735), the Natural Science Foundation of Chongqing (Grant no. cstc2022ycjh-bgzxm0033), and the Chongqing Postdoctoral Science Foundation (Grant no. 2022NSCQ-BHX1283). We thank Home for Researchers editorial team ( www.home-for-researchers.com ) for language editing service.
Author information
These authors contributed equally: Juncai Pu, Yue Yu.
Authors and Affiliations
Department of Neurology, The First Affiliated Hospital of Chongqing Medical University, Chongqing, 400016, China
Juncai Pu, Weiyi Chen, Xiaopeng Chen, Yue Chen, Xiang Chen, Renjie Qiao, Yanyi Jiang, Hanping Zhang, Li Fan, Yi Ren, Xiangyu Chen & Peng Xie
NHC Key Laboratory of Diagnosis and Treatment on Brain Functional Diseases, The First Affiliated Hospital of Chongqing Medical University, Chongqing, 400016, China
Juncai Pu, Yiyun Liu, Dongfang Wang, Siwen Gui, Xiaogang Zhong, Weiyi Chen, Xiaopeng Chen, Yue Chen, Xiang Chen, Renjie Qiao, Yanyi Jiang, Hanping Zhang, Li Fan, Yi Ren, Xiangyu Chen, Haiyang Wang & Peng Xie
Department of Health Sciences Research, Mayo Clinic, MN, 55901, USA
The Jinfeng Laboratory, Chongqing, 401336, China
Chongqing Institute for Brain and Intelligence, Chongqing, 400072, China
You can also search for this author in PubMed Google Scholar
Contributions
Concept, design, and supervision of the study: Juncai Pu, Yue Yu and Peng Xie. Data collection: Juncai Pu, Yiyun Liu, Dongfang Wang, Siwen Gui, Xiaogang Zhong, Weiyi Chen, Xiaopeng Chen, Yue Chen, Xiang Chen, Renjie Qiao, Yanyi Jiang, Hanping Zhang, Li Fan, Yi Ren, Xiangyu Chen and Haiyang Wang. Drafting display items: Juncai Pu, Yue Yu and Siwen Gui. Drafting manuscript: Juncai Pu and Peng Xie. All authors read and approved the final version of the manuscript.
Corresponding author
Correspondence to Peng Xie .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Ethics approval and consent to participate
The study was approved by The Ethics Committee of Chongqing Medical University (2017013). The datasets generated in the current study were collected from publicly available literature or reports, therefore informed consent forms are not applicable.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Pu, J., Yu, Y., Liu, Y. et al. ProMENDA: an updated resource for proteomic and metabolomic characterization in depression. Transl Psychiatry 14 , 229 (2024). https://doi.org/10.1038/s41398-024-02948-2
Download citation
Received : 24 December 2023
Revised : 15 May 2024
Accepted : 17 May 2024
Published : 30 May 2024
DOI : https://doi.org/10.1038/s41398-024-02948-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Online bullying and playground taunts can lead to teen mental health issues. Here's how the experts recommend handling a bully
Matt Purcell was just six years old when a group of older boys stuffed him in a council bin and left him to stew in the juices.
It was the final act following months of daily school bus bullying that the Korean-Australian had been keeping to himself.
"I was an adoptee from South Korea and my parents were nothing like me, and that was targeted by bullies at my school," he said.
When his adopted parents learned about the behaviour they called the school and the boys were punished.
The physical assaults stopped, but the school bus taunts continued.
"What bullying does, it dehumanises you," Mr Purcell said.
"Being bullied at the age of six right through to high school made me feel like not a human. I struggled with my identity for years.
"My life was pretty sad for a long time."
His father enrolled him in Kung Fu classes, but that also caused problems when Mr Purcell responded to the bullies with his own violence.
"If it wasn't for mentors in my life who pursued me, I wouldn't be here today."
This week an international study found Australia's teens experience bullying at the second highest rate among developed countries.
The Australian Council for Educational Research analysed data from the OECD's Program for International Student Assessment (PISA) test which surveyed more than 13,437 Australian students in 2022.
It found Australia ranked number two for bullying, with 17 per cent of students reporting that "other students made fun of me" but the overall trend was down compared to 2018.
Students in Tasmania reported the highest levels of bullying with the lowest in Victoria, NSW and the ACT.
The study found teen girls were reporting anxiety, fear and panic at twice the rate of boys, but boys appeared more resilient to stress than girls.
Bullying can send some teens to the brink
Bullying is a type of trauma that falls under the banner of Adverse Childhood Experiences (ACE) and it may be contributing to the current surge in youth mental health problems.
"These mental health issues that appear in adolescence, they don't just happen overnight. Usually there's been precursors through the early childhood years," Children's Commissioner Anne Hollonds said.
Numerous studies have found bullying, including cyberbullying, is widespread and more than two-thirds of children aged 12 to 13 have experienced at least one bullying-like behaviour in a 12-month period.
Online, approximately one in four Australians aged between 14 and 17 have been the victim of cyberbullying in the past year.
A major 2021 Australian review found that of all the Adverse Childhood Experiences, bullying — including cyberbullying — was associated with double the risk of suicide in later life.
Teens who were victims of cyberbullying were more likely to report elevated symptoms of depression or anxiety, and the use of social media in particular, was also associated with a high risk of depression and anxiety.
The impact of being left out
Dr Deirdre Gartland leads the Resilience and Mental Health research program at Murdoch Children's Research Institute and says long term bullying could impact how children regulate their emotions, causing them to miss school or disengage at home.
"Ongoing stresses that are persistent and significant for a young person are going to affect how the pathways in the brain develop," she said.
Commissioner Hollonds said greater focus was needed on what she called "the middle years" — ages 8 to 14.
"What we now know is that in those years children are really looking for a sense of belonging," she said.
"If they're not able to build that sense of belonging at school, then that will lead to them starting to disengage from school or to behave in ways that causes them actually to be pushed out."
In a bid to address the impacts of bullying, funding of $4.2 million for school resources and programs such as the Anti-Bullying Collective and the National Day of Action against Bullying and Violence, was allocated in last week's federal budget.
What can parents do?
Dr Gartland said there were facets of life that proved to have a protective effect when it came to resilience and coping with traumatic events like bullying.
These include:
- Fostering a positive sense of self-identity
- Maintaining a good connection to family and friends
- Maintaining a strong connection to culture
- Ensuring teens are enjoying hobbies or activities outside of school hours
- Family guidance
- Ensuring there's a positive engagement with the school and the teachers there
- Fostering a sense of optimism for the future; and
- Helping teens build the capacity to identify and regulate their emotions
She said parents could facilitate some of these by having family traditions like birthdays or family holidays or enrol children in language courses to help them connect to their culture as well as extra-curricular activities such as sport, music or art.
"Connecting in with something that your child or young person really enjoys doing is a really wonderful way to build their resilience," she said.
Parents also needed to be role models and help children understand their emotions during turbulent times.
"Parents can be helping children and young people to both name and recognise their feelings," she said.
Commissioner Hollonds said parents should try to find creative ways to stay connected with teens — whether it be watching trashy television together or cooking a meal.
"Don't think that just because they don't seem to want to spend time with you that that means they don't want you around. Teenagers want you around. That's a fact," she said.
"The more time you spend with them and have those incidental conversations, the more you get a sense of what that child's well-being is over time."
Resilience isn't about 'bouncing back'
Dr Gartland said it was important to remember that resilience did not mean "bouncing back".
"Resilience is about a child or a young person drawing on their internal strengths and drawing on the strengths and resources that sit around them," she said.
"When children do have access to these resources, they are much more likely to have positive mental health and well-being irrespective of what's happening to them in their lives."
Mr Purcell urged parents to become detectives in their teens' lives and use "I statements" such as, "I noticed you've not being going to basketball" to try to draw out what was wrong while sitting shoulder to shoulder with their teen.
"So you've got to get the information out — who's doing what and is this a pattern?" he said.
"Make a decision. Do I need to make my kid move school? Do I need to have a conversation?"
He suggested parents relate their own school experiences to help connect with their teen and even use themselves as a soft target to role play ways to deal with bullies.
"It's a verbal dojo. We practice questioning back to each other. How could I come back to that? Is that actually true?" he explained.
And what not to do…
A key message from the experts to parents is to avoid common cliches like "just ignore them" or "well, just hit them back".
Dr Gartland said those kinds of messages could be damaging.
"It's really important to acknowledge the challenges that young people and children may be going through."
Years after his own bullying experience Mr Purcell became a youth worker and noticed other young people also didn't have the skills to combat verbal abuse.
As a result, he created Social Kung Fu, a program designed to give young people the words and phrases to combat schoolyard and online bullying.
Teens are given mock scripts and taught to use questions like, "what do you mean by that?" and "how do you know it's true?" as verbal blocks to put those spreading rumours and making accusations on the back foot.
Mr Purcell said responding with violence escalated the situation instead of resolving it, and while ignoring bullies may work for one-off incidents, he believed it was less effective for ongoing targeting.
"By being passive you're teaching the bully it's okay," he said.
Mr Purcell said the answer lay in teaching young people that their words could have tremendous impact.
"If we can help people use their words to defend themselves and to give value, then I believe that [good] mental health will increase," he said.
Mental health disorders among young people have soared by nearly 50 per cent in 15 years. The ABC is talking to youth, parents, and researchers about what's driving this pattern, and what can be done to turn things around.
- X (formerly Twitter)
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Psychiatry
Fecal Microbiota Transplantation (FMT) as an Adjunctive Therapy for Depression—Case Report
Jessica p. k. doll.
1 Department of Psychiatry (UPK), University of Basel, Basel, Switzerland
Jorge F. Vázquez-Castellanos
2 Department of Microbiology and Immunology, Rega Institute for Medical Research, KU Leuven-University of Leuven, Leuven, Belgium
Anna-Chiara Schaub
Nina schweinfurth, cedric kettelhack, else schneider, gulnara yamanbaeva, laura mählmann, serge brand.
3 Center for Affective, Stress- and Sleep Disorders (ZASS), Psychiatric Clinics (UPK), University of Basel, Basel, Switzerland
4 Sleep Disorders Research Center, Kermanshah University of Medical Sciences, Kermanshah, Iran
5 Substance Abuse Prevention Research Center, Kermanshah University of Medical Sciences, Kermanshah, Iran
6 Division of Sport Science and Psychosocial Health, Department of Sport, Exercise, and Health, University of Basel, Basel, Switzerland
7 Department of Psychiatry, School of Medicine, Tehran University of Medical Sciences, Tehran, Iran
Christoph Beglinger
8 Department of Research, St. Clara Hospital, Basel, Switzerland
Stefan Borgwardt
9 Department of Psychiatry and Psychotherapy, University of Lübeck, Lübeck, Germany
Jeroen Raes
André schmidt, undine e. lang, associated data.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Depression is a debilitating disorder, and at least one third of patients do not respond to therapy. Associations between gut microbiota and depression have been observed in recent years, opening novel treatment avenues. Here, we present the first two patients with major depressive disorder ever treated with fecal microbiota transplantation as add-on therapy. Both improved their depressive symptoms 4 weeks after the transplantation. Effects lasted up to 8 weeks in one patient. Gastrointestinal symptoms, constipation in particular, were reflected in microbiome changes and improved in one patient. This report suggests further FMT studies in depression could be worth pursuing and adds to awareness as well as safety assurance, both crucial in determining the potential of FMT in depression treatment.
Introduction
Major depressive disorder (MDD) is an illness affecting more than 264 million people worldwide ( 1 ) and influencing functioning and quality of life (QoL) ( 2 ). Despite advancements in the development of therapeutics, current treatments have not reached optimal efficacy and approximately one third of patients do not respond to treatment after two or more trials of antidepressant medication ( 3 , 4 ). Therefore, the identification of new treatment options is crucial.
Recently, interest has been drawn toward the importance of the biochemical signaling between the gastrointestinal (GI) and the central nervous system, also known as the microbiome-gut-brain axis (MGBA) ( 5 – 9 ). Several studies have linked the gut microbiome to depression ( 6 , 8 – 11 ). The gut microbiota composition appears to be altered in depressed people ( 12 – 15 ), presenting predominance of potentially harmful bacterial groups and/or reduction in beneficial bacterial groups ( 12 ). Such dysbiosis could be related to depressive symptoms ( 16 , 17 ), as the MGBA is a bi-directional pathway, which involves multiple communication modalities, including metabolites, the immune system or the vagus nerve ( 8 , 10 , 18 , 19 ). Together, these studies feed the hypothesis that modification of the gut microbiome could decrease MDD symptoms. There are various ways to manipulate the gut microbiome, such as administration of prebiotics ( 20 – 22 ), probiotics ( 21 , 22 ), postbiotics ( 22 ), or fecal microbiome transplantation (FMT) ( 23 ). Preclinical evidence showed that adult germ-free rodents receiving fecal samples from MDD-patients showed increased depressive-like behavior compared to controls ( 17 , 23 ). Therefore, transplanting healthy fecal microbiome to MDD-patients could potentially ameliorate depressive symptoms. The intention of FMT is to introduce a beneficial microbial gut community by transferring intestinal microbiota from a healthy donor to a patient.
FMT has proven to be an effective treatment for recurrent Clostridium difficile infection ( rCDI ) ( 24 , 25 ). To our best knowledge, in MDD only one case treated with FMT has been reported so far ( 26 ).
Therefore, we initiated a randomized controlled trial (RCT), testing the efficacy of oral frozen FMT-capsules as adjuvant therapy in patients with moderate/severe MDD at the University Psychiatric Clinics Basel (UPK). While our RCT was running, the Food and Drug Administration released a safety alert regarding FMT (see Supplementary Methods for details) and we decided to cease the study for safety reasons after including a total of four patients. In the present article, we report clinical and safety results from two cases that had already received the active product.
Case Descriptions
Both patients were women and between 50 and 60 years old ( Table 1 ). Before starting the intervention, both received treatment as usual (TAU), which included pharmacological treatment, psychotherapy and additional medical-therapeutical treatments ( Figure 1 and Supplementary Tables 1, 2 . Changes in their treatment took place based on medical indication and patients' preferences.
Sociodemographic information.

Timeline with relevant timepoints from the episode of study and care.
Patient 1 had a diagnosis of MDD and chronic constipation. According to the patient, her first depressive episode started in adolescence, with a suicide attempt later in life. She was diagnosed with MDD in 2006 and had been hospitalized twice in her life. Depression is common in her family, with two male second-degree relatives having suffered from it, one deceased by suicide. At the time of baseline assessment, the patient had been in therapy as an inpatient for almost 3 months and treated for depression and constipation with persevering symptoms (see Supplementary Table 1 ).
Patient 2 had a diagnosis of MDD. She was diagnosed with depression in 1980 and has been hospitalized twice since then. A family history of depression is unknown. After more than 2 months of inpatient treatment, the patient's symptoms persevered. She was medicated with antidepressants and benzodiazepines ( Supplementary Table 2 ). At time of FMT intervention, the patient was suffering from negative emotions and GI symptoms, such as flatulence and constipation. For a more detailed description of the patients (see Supplementary Case Description ).
Diagnostic Assessment and Study Design
The RCT was approved by the local ethics committee (Ethikkommission Nordwest- und Zentralschweiz) and was conducted in accordance with the principles of the Declaration of Helsinki and the International Conference on Harmonization Tripartite Guideline on Good Clinical Practice. Eligible patients were informed about the study and provided written informed consent. The study was registered at ClinicalTrials.gov prior to study start (NCT03281004). MDD-patients were recruited from the UPK (Switzerland). At baseline, we assessed depressive symptoms [Hamilton Depression Rating Scale; HAMD ( 27 ) and Beck Depression Inventory-II; BDI II ( 28 )], GI-symptoms [Gastrointestinal Rating Scale; GSRS ( 29 )] and collected anthropometric and demographic data. Then the intake of oral frozen FMT-capsules followed. After the treatment, participants were observed and assessed on a weekly basis over a period of 4 weeks. After 4 weeks, post-intervention measurements were conducted. Additionally, an 8-week follow-up was performed. Stool samples were collected at baseline and 4 weeks after the intervention. For one of the patients, stool samples were available 8 weeks after the intervention ( Supplementary Material ).
Intervention
Patients were administered 30 oral frozen FMT-capsules within 90 min under the observation of a physician. Each active 30-capsule-dose consisted of 8.25 g donor stool, originating from a single donor, which was a different donor for each patient. For a detailed description of the methods (see Supplementary Methods ).
Both patients adhered to the intervention. They tolerated the oral frozen FMT-capsules well and did not report any serious adverse events (SAEs).
Depressive Symptoms
For patient 1, symptoms of depression improved, indicated by a decreased HAMD-score from 21 points at baseline to nine points 4 weeks post-intervention. At 8-week follow-up, the HAMD-score increased to 19 points ( Figure 2A ). For patient 2, the HAMD-score decreased from 31 to 10 points after 4 weeks and increased by two points after 8 weeks ( Figure 2A ). Thus, the FMT intervention resulted in a 4-week change score of 12 and 21 HAMD-points for patient 1 and 2, respectively, and an 8-week change score of 2 and 19 points, respectively ( Figure 2B ). As the present results come from two cases and do not allow for statistical comparison, we mapped our HAMD change scores together with meta-analysis results from Kirsch et al. ( 30 ) ( Supplementary Figures 1 , 2 ); methods and results can be found in the Supplementary Material . Additionally, we explored the depressive symptoms from two patients, who had received placebo. Both placebo-patients tolerated the placebo-capsules well. HAMD-scores from both placebo-patients only improved within the first 2 weeks after placebo-intake and increased back to baseline scores, which is visible in Supplementary Figures 3A,B (placebo 1: baseline 16, post-intervention 16, follow-up 9; placebo 2: baseline 22, post-intervention 22, follow-up not available).

(A) HAMD-scores for patient 1 and 2 over time, including cut-offs for depressive symptom severity. (B) Change scores of HAMD rating for both patients at 4-weeks compared to baseline and 8-weeks compared to baseline. A higher (and positive) change score indicates improvement of depressive symptoms as the change score was calculated by subtracting the score at post-intervention from the score at baseline (e.g., baseline score: 21, post-intervention score: 9, equals 21–9 = 12). (C) GSRS-scores for both patients over time; without cut-off for GI-symptom severity as different clusters of symptoms are defined by the GSRS (e.g., constipation) and classification of severity would be only possible for each symptom, not for the overall score. (D) GSRS change scores for both patients at 4-weeks compared to baseline and 8-weeks compared to baseline. (E) BDI-II-scores for both patients over time. (F) BDI-II change scores for both patients at 4-weeks compared to baseline and 8-weeks compared to baseline.
The BDI-II-scores dropped for both FMT-patients 4 weeks after FMT; from 50 to 31 points for patient 1 and from 24 to 12 points for patient 2, which results in change scores of 19 and 12, respectively. At 8-week follow-up, patient 1 reported a BDI-II-score of 34 and patient 2 a score of 9, resulting in change scores from baseline to follow-up of 16 and 15, respectively ( Figures 2E,F ).
Gastrointestinal Symptoms
Gastrointestinal symptoms improved in both patients ( Figure 2C ). Patient 1 benefitted by 56 points after 4 weeks, which worsened by only three points after 8 weeks. At baseline, she suffered from stomach pains, sickness, bloating, burping, and constipation. All symptoms improved over time. Patient 2 reported only a slight improvement of three points 4-week post-FMT and continued reporting constipation and bloating. The patient slightly improved by three more points at 8-week follow-up ( Figures 2C,D ).
Microbiome Composition and Diversity
In both patients, moisture decreased over time [ Supplementary Figure 6A ; Mixed-effects model (MEM) ANOVA p adjusted < 0.05]. Our patients showed lower moisture levels than the ones reported in a healthy population ( 31 ) (Wilcoxon test: W = 50, p = 0.025, Supplementary Figure 7 ). The bacterial load reflected in the cell counts was constant among the three time points for both patients (MEM ANOVA p adjuste d = 1). Diversity analysis was done to measure the taxonomic evenness (Pielou index), the richness (the number of observed species) and the diversity (inversed Simpson and Shannon indices) after FMT. Both patients showed an increase in the Pielou index after FMT, suggesting an evolution toward a more even distribution of species ( Figure 3A ). The species richness was generally reduced upon intervention ( Figure 3B ) and sustained until week eight in patient 1 ( Figure 3B ). We found that patient 1 showed increased inversed Simpson and Shannon diversity ( Figures 3C,D ), whereas patient 2 showed decreased diversity ( Figures 3C,D ).

Patients' microbiome diversity. Mixed-effects models (MEM) of the genus level (A) Pielou evenness, (B) observed species, (C) inverse simpson, and (D) Shannon index, the alpha diversity estimators were modeled into a discrete manner and represent its results as boxplot and into a continuous way, representing the MEM slope into line-plots. The gray area into the continuous MEM represents the 95% confidence level. Patient 1 is displayed in purple, patient 2 in orange. (E) Mixed-effects models (MEM) of the ASV after the FMT intervention. The columns remarked in blue indicates the increase in the abundance of the ASV of patient 1, patient 2, and when the increase is congruent between both. Similarly, the columns remarked in blue indicates the decrease of the ASV in time. The blue scale represents the MEM positive coefficient; in red, the negative. The ASV was set as a putative biomarker if both the continuous and discrete mixed-effect-model time coefficients were significant (ANOVA < 0.05).
The FMT intervention revealed a different effect on the bacterial composition of the two patients. Patient 1 maintained the Ruminococcus enterotype over all time points; while patient 2 switched from the Ruminococcus to the Bacteroides-2-enterotype 4 weeks post-intervention ( Supplementary Figure 8 ), indicating a dysbiotic microbial composition previously linked to fast transit and inflammation ( 31 , 32 ). The switch in the bacterial composition was also associated with an increase of the fecal calprotectin levels, which was higher than the ones reported in healthy subjects ( Supplementary Figure 9A ) ( 31 ). However, the bacterial load increased in patient 2 4 weeks post-intervention; the cell counts increased to a level between the 75 and 95 quantile ( Supplementary Figure 9B ) ( 31 ).
The FMT intervention displayed different effects on the taxa abundance between the patients ( Figure 3E ). Patient 1 showed an increase of 13 amplicon sequence variants (ASV) of the genera Alistipes, Oscillibacter, Coprococcus, Clostridium IV , and the families Ruminococcaceae and Lachnospiraceae, the order Clostridiales, and the Firmicutes phylum ( Figure 3E ). Contrary, nine ASV from the genera Victivallis, Alistipes, Roseburia, Prevotella, Ruminococcus, Blautia , and Faecalibacterium and two ASV of the family Lachnospiraceae decreased after FMT ( Figure 3E ). Patient 2 showed an increase of ASV of the Ruminococcaceae family, including Ruminococcus E , and one ASV of the species Flavonifractor plautii ( Figure 3E ), which has been reported to be increased in MDD-patients ( 16 ). Patient 2 showed a decrease of five ASV of the genera Ruminococcus, Alistipes, Bifidobacterium, Oscillibacter , and the family Lachnospiraceae ( Figure 3E ). Further results are documented in the Supplementary Results .
Four weeks after the intake of oral frozen FMT-capsules, depressive symptoms improved in both patients, objectively graded from severe/moderate to mild depression ( 33 ); this is in line with previous results implicating that FMT reduced depressive symptoms in patients with irritable bowel syndrome (IBS) 4 weeks after treatment ( 34 ). Intriguingly, in the study by Kurokawa et al. ( 34 ), the clinical improvement after FMT was accompanied by increased gut bacteria diversity and decreased GI-symptoms. The relationship between IBS and depression seems to be bi-directional ( 34 , 35 ). Both of our patients were not formally diagnosed with IBS, but experienced GI-symptoms at baseline. While patient 1 was able to defecate regularly even 8 weeks after FMT, patient 2 was initially relieved, but after 4 weeks, again afflicted by constipation.
At baseline, both subjects showed a Ruminoccus enterotype bacterial composition and low fecal moisture, a proxy of slow transit time, and congruent with the prevalence of constipation in mood disorders ( 36 – 38 ). Patient 1 increased in diversity and maintained the Ruminococcus enterotype, indicating a better microbial response to FMT. However, the improvement of constipation in patient 1 is not reflected by the enterotype, since Ruminococcus is associated with slow transit time ( 36 , 37 ).
Compared to patient 2, patient 1 showed a higher abundance of short-chain fatty acid (SCFA) producers such as Butyrivibrio and Faecalibacterium that, along with Dialister , seem to be depleted in depressed people ( 16 ). Additionally, patient 1 showed an increase of species related to other healthy commensal species from the genera Methanobrevibacter and Sporobacter . Such species are related to low transit time and a healthy microbial establishment indicating the good recovery of the microbial community after oral frozen FMT-capsules. Moreover, patient 1 showed an increase and decrease of different ASV of the Alistipes genera after FMT. It is reasonable to assume that different Alistipes species may have different roles in host health; it has been reported that the decrease in Alistipes exerts an immunoregulatory effect and contributes to the decrease in SCFA which are suggested to have anti-depressant effects ( 39 , 40 ). Simultaneously, Alistipes are increased in depressed subjects ( 41 ).
Patient 2 still experienced constipation after the oral frozen FMT-capsules. It has been reported that prolonged constipation leads to a dysbiotic microbial configuration ( 42 , 43 ); indeed, patient 2 showed increased fecal calprotectin and switched to the Bacteroides-2-enterotype. Although until now this enterotype has mostly been linked to fast transit, constipated Bacteroides-2-individuals do exist (Raes, unpublished results). This patient's bacterial community showed an increase of species of the Flavonifractor genus, which is related to depression ( 16 , 31 , 44 ), and an increase of species of the Streptococcus genus, which is associated with high calprotectin and pro-inflammatory conditions ( 31 ). We assume that prolonged constipation in depressed people may have compromised the effectiveness of the oral frozen FMT-capsules by preventing the engraftment of the healthy microbial commensal species. A previous case report of FMT, as mono-treatment for depression and introduced via colonoscopy, reported a MDD-patient who also suffered from constipation ( 26 ). Interestingly, 4 days after FMT, the patient's GI- and depressive symptoms improved and persevered until 6 months after FMT ( 26 ).
The positive depression outcome did not persevere for both of our patients. Objective rating of the first patient's depressive condition, who improved GI conditions, indicated moderate depression at 8-week follow-up. Contrary, patient 2, who did not improve greatly on GI conditions, remained within the range of mild depression with a tendency to increase depressive symptoms. A study recently reported significant improvement of QoL and fatigue in IBS-patients 3 months after receiving FMT ( 45 ), which implicates a long-lasting positive effect of FMT compared to our results. They also found dose-dependent effects and that improvement in QoL and fatigue was not entirely in line with improvement of GI symptoms. FMT results on depressive and GI symptoms are conflicting, and RCTs investigating FMT in depressed patients are lacking. While some studies found improvement in depressive symptoms and QoL after FMT ( 34 , 45 ), there is also evidence of QoL and depressive symptoms not being affected by FMT ( 46 ).
One important factor for such mixed results is the general heterogeneity of illness presentation in MDD and IBS populations. As FMT success might depend on the recipient's microbial composition before FMT or on the microbial resemblance of the donor and the recipient, identifying subgroups of depressed patients might be crucial ( 47 ). Another reason could be the differing methodology between studies, such as choosing one (super)donor ( 45 ) or several donors ( 46 ), the FMT administration (e.g., oral capsule or colonoscopy) ( 48 , 49 ), or the formulation (e.g., frozen or fresh) ( 24 , 50 ). Other arising questions regard the optimal dose and durability of FMT ( 45 ). Barbara and Ianiro ( 50 ) discuss such issues of FMT methodology.
Notably, although the small participant number precludes statistical group comparison, the HAMD-scores of the two FMT and the two placebo-patients present interesting descriptive results. We would expect an improvement in depressive symptoms over time as the patients received TAU. Nonetheless, the two placebo participants presented only a 2-week improvement after placebo-capsule intake, which then relapsed to baseline scores. This might be attributed to the placebo effect, especially as one of the placebo participants thought she had received the active product. The other placebo patient reported increased depressive symptoms, which even restrained her from coming to the post-intervention assessment. Combined with the results from the FMT-patients, these results indicate that frozen oral FMT-capsules as add-on therapy might have the potential to improve depressive symptoms.
Critically, the report of cases suffering from SAEs after FMT raises the importance of extensive donor screening and cautious selection of FMT-patients ( 50 ). To overcome these issues, more large-scale controlled clinical studies are needed, investigating gut microbiota modulation in depression, gaining knowledge of its underlying mechanisms, neuroactive potential and beneficial, and harmful microbes and eventually, reconstituting microbes in the laboratory. This would make safety control, retraceability, and substantial FMT production possible ( 50 ). The resulting clinical trials could greatly improve our knowledge and eventually lead to the translation of controlled and specific FMT to clinical practice, and finally, improve depressed people's wellbeing.
Limitations
The current study reports some limitations, starting with the limited sample size. Second, both patients also had comorbidities, such as obesity and constipation, which both might be confounding factors as overweight and constipation seem to be associated with altered gut microbiota composition ( 51 , 52 ). They received FMT additionally to TAU which makes attribution of effects solely to FMT impossible; the outcome could be influenced by other pathologies or be the result of FMT and antidepressants working in synergy as antidepressants may influence the gut microbiota ( 53 ). Additionally, our patients were constipated at baseline, which might be due to medication as some of the medication might modify the transit time ( Supplementary Table 4 ). Third, we did not include any information about the patients' diets. However, diet has been found to be associated with depression ( 54 ) and is one of the most significant modulators of gut microbial community ( 55 ). A fourth limitation is the comparably low amount of donor stool (8.25 g). As the dose may play a crucial role in the effects, future research should also include dose-finding strategies. Further, although a previous study revealed that oral FMT-capsules are non-inferior to colonoscopy in efficacy in CDI -patients ( 25 ), the most efficient delivery mode in patients with depression needs to be established.
Lastly, the microbial resemblance of the donor and recipient may play an important role. As we do not have information on the donors' microbial composition, such comparison was impossible in this report. Future studies should include information on the donors' microbiome and compare it to the recipients' microbiome to identify subgroups for better treatment options.
Patients' Perspectives
Both patients were positive toward the intervention and had a feeling that they had received the active product. They felt better regarding their depressive symptoms, which is visible by the subjective measurement with the BDI-II ( Figures 2E,F ). In 2021 we contacted the patients via telephone, which was ~2.5 and 1.5 years after the intervention for patient 1 and 2, respectively. At that time, both were going on in their daily lives. One participant emphasized that one of her major treatment milestones was FMT.
Data Availability Statement
Ethics statement.
The studies involving human participants were reviewed and approved by Ethikkommission Nordwest- und Zentralschweiz. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author Contributions
AS: had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis and study supervision. LM, CB, SBo, AS, and UL: study concept and design. JD, JV-C, ACS, NS, CK, ES, GY, JR, and AS: acquisition, analysis, or interpretation of data. JD, JV-C, and AS: drafting the manuscript. All authors: critical revision of the manuscript for important intellectual content. JD and JV-C: statistical analysis. SBo, AS, and UL: obtained funding. LM, SBr, SBo, JR, AS, and UL: administrative, technical, or material support. All authors contributed to the article and approved the submitted version.
This work was supported by the Gertrud Thalmann-Fonds (SBo, UL), Seerave Foundation (UL), Kämpf-Bötschi Stiftung (UL), and Research Fund Junior Researchers of the University of Basel (Appln 3MS1041, AS). JV-C was supported by the postdoctoral fellowships fromthe Research Fund–Flanders (FWO 1236321N). The Raes lab was supported by VIB, KU Leuven, and the Rega Foundation.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank Jan Klaproth for information gathering and support in preparing the present case report.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.815422/full#supplementary-material

IMAGES
VIDEO
COMMENTS
Learn how different interventions are applied to treat depression across the lifespan, from children to older adults. See case examples of cognitive-behavioral, interpersonal, behavioral, and other therapies, with references and links.
In a study of 239 outpatients diagnosed with major depressive disorder in a NIMH. 16-week multi-center clinical trial, participants were assigned to interpersonal therapy, CBT, imipramine with clinical management, or placebo with clinical management. One. hundred sixty-two patients completed the trial.
Dr. SooJeong Youn: This case highlights the importance of attending to the intricate, multilevel, systemic factors that affect the mental health experience and clinical presentation of patients ...
When a patient with depression is feeling sleepy, be aware of sleep apnoea. A 67-year-old man was referred to an outpatient clinic of geriatric psychiatry because of persistent symptoms of depression and anxiety, accompanied by sleepiness. The latter had been evaluated multiple times in the general practice over several years; each time it was ...
Introduction to the selected case study. In this case study, we will focus on Jane, a 32-year-old woman who has been struggling with depression for the past two years. Jane's case offers a compelling narrative that highlights the various aspects of depression, including its onset, symptoms, and the treatment journey.
The severity of depressive episodes was measured using the Hamilton Depression Scale (HAM-D). Themes of guilt and shame were measured by using the State of Guilt and Shame Scale (SSGS). This case study was presented as a poster abstract at the 'RCPsych Faculty of General Adult Psychiatry Annual Conference 2021.'
the case study had a therapist who was a doctoral level graduate student in clinical psychology trained in CBT who received weekly supervision from a licensed clinical psychologist with a Ph.D. Qualitative data for this case study were analyzed by reviewing progress notes and video recordings of therapy sessions. SESSIONS 1-4
Diagnosis of depression can be made using the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) or the 10th revision of the International Statistical Classification of Disease and Related Health Problems (ICD-10). 5 (Refer to Appendix 3 and 4, pages 73-76 in CPG.) 6,7
The European "Group for the Study of Resistant Depression" (GSRD) multi-site study found that age at first treatment (i.e., early-onset and early treatment), age, timespan between first and ...
Patient Case Presentation. Figure 1. Blue and silver stethoscope (Pixabay, N.D.) Ms. S.W. is a 48-year-old white female who presented to an outpatient community mental health agency for evaluation of depressive symptoms. Over the past eight weeks she has experienced sad mood every day, which she describes as a feeling of hopelessness and emptiness.
The current study is a small-scale, exploratory study, in which we carried out semi-structured interviews with six adolescents with depression entering outpatient psychotherapy in Germany. In addition to the experience of depression, we studied the expectations of therapy that will be published elsewhere ( Weitkamp, Klein, Wiegand-Grefe ...
Antidepressants can be, on average, an effective treatment for adults with moderate-to-severe major depression in the acute phase of illness. Effective as defined in this study means that there ...
current issue. current issue; browse recently published; browse full issue index; learning/cme
We present here a case study of a complex 14 years old girl, with adolescence onset dysthymia, anorexia nervosa and obsessive-compulsive disorder and its management issues. ... Depression and ...
A case study of a person with depression using cognitive behavioural therapy (CBT) by a psychiatric social worker. The study assessed psychosocial problems, provided intervention and measured outcomes using various instruments.
Abstract. Depression is a complex mental health condition influenced by biological, psychological, and social factors. Psychiatric social workers play a crucial role in conducting comprehensive assessments and implementing interventions to address the multi-dimensional nature of depression. This case study seeks to evaluate the psychosocial ...
What does depression look like in adolescents? According to the Diagnostic and statistical manual of mental disorders, fourth edition, 5 an adolescent must have five out of nine characteristic symptoms most of the time for at least 2 weeks for a diagnosis of major depressive disorder. At least one of these symptoms must be either depressed or irritable mood or a pervasive loss of pleasure or ...
Study with Quizlet and memorize flashcards containing terms like the nurse completes a physical assessment. when asked what brought her to the hospital, Bethany replies, "Things just aren't right" and begins to cry. After further conversation, Bethany describes her mood as very sad now. She rarely goes out or invites friends to visit. She admits that she feels like strangers are saying bad ...
Case studies are in-depth investigations of a person, group, event, or community. Typically, data is gathered from various sources using several methods (e.g., observations & interviews). The case study research method originated in clinical medicine (the case history, i.e., the patient's personal history). In psychology, case studies are ...
Intranasal esketamine is an approved drug for treatment-resistant depression (TRD); however, it is costly and may result in specific adverse effects. In this single case study, we explored if oral esketamine can be a suitable alternative. Methods
Associations Between Vitamin K and Suicide Attempts in Patients with Depression: A Case-Control Study. Shao-Ting Wang Department of Clinical Laboratory, Institute of ... via its anti-inflammatory properties, Citation 8 which may link vitamin K deficiency to depression. Previous studies have reported that vitamin K deficiency was involved in ...
Depression from an evolutionary perspective. Because of the universality and prevalence of mental illness, attempts have been made in Evolutionary Psychology to explain the possible functions of utility of some symptoms 23-25.From this perspective, some mental disorders are seen as having present or past fitness advantages 26 and therefore might have been naturally selected (e.g., mild and ...
Depression is a prevalent mental disorder with a complex biological mechanism. Following the rapid development of systems biology technology, a growing number of studies have applied proteomics ...
The study found teen girls were reporting anxiety, fear and panic at twice the rate of boys, but boys appeared more resilient to stress than girls. Bullying can send some teens to the brink
A Case Study on Polypharmacy and Depression in a 75-Year-Old Woman with Visual Deficits and Charles Bonnet Syndrome. ... Depression is one of the most prevalent pathologies in older adults. Its diagnosis and treatment are complex due to different factors that intervene in its development and progression, including intercurrent organic diseases ...
The study evaluates whether the spread of the coronavirus disease 2019 (COVID-19) worsened the onset of post-surgical distress and symptoms of anxiety and depression in a population undergoing hysterectomy for benign disease during the pandemic era, comparing it with a population with the same characteristics but recruited before COVID-19.
a. A data charting form was created to capture the data elements of interest, including the authors, titles, determinants (biological, psychological, social), and the type of depression assessed by the research (e.g., major depression, depressive symptoms, depressive behaviour). b.
The paper entitled "Characteristics, preservation mechanisms, and significance of aragonite in lacustrine shale: A case study from the Jiyang Depression, Bohai Bay Basin", which we wish to be considered for publication in "Petroleum Science". The data involved in the manuscript has no conflict of interest and has been authorized by all ...
Associations between gut microbiota and depression have been observed in recent years, opening novel treatment avenues. Here, we present the first two patients with major depressive disorder ever treated with fecal microbiota transplantation as add-on therapy. Both improved their depressive symptoms 4 weeks after the transplantation.