- Search by keyword
- Search by citation
Page 1 of 8

Longitudinal studies of bipolar patients and their families: translating findings to advance individualized risk prediction, treatment and research
Bipolar disorder is a broad diagnostic construct associated with significant phenotypic and genetic heterogeneity challenging progress in clinical practice and discovery research. Prospective studies of well-c...
- View Full Text
Sociodemographic, clinical and treatment characteristics of current rapid-cycling bipolar disorder: a multicenter Chinese study
Rapid cycling bipolar disorder (RCBD), characterized by four or more episodes per year, is a complex subtype of bipolar disorder (BD) with poorly understood characteristics.
Type of cycle, temperament and childhood trauma are associated with lithium response in patients with bipolar disorders
Lithium stands as the gold standard in treating bipolar disorders (BD). Despite numerous clinical factors being associated with a favorable response to lithium, comprehensive studies examining the collective i...
How effective are mood stabilizers in treating bipolar patients comorbid with cPTSD? Results from an observational study
Multiple traumatic experiences, particularly in childhood, may predict and be a risk factor for the development of complex post-traumatic stress disorder (cPTSD). Unfortunately, individuals with bipolar disord...
Perceived loneliness and social support in bipolar disorder: relation to suicidal ideation and attempts
The suicide rate in bipolar disorder (BD) is among the highest across all psychiatric disorders. Identifying modifiable variables that relate to suicidal thoughts and behaviors (STBs) in BD may inform preventi...
Effectiveness of ultra-long-term lithium treatment: relevant factors and case series
The phenomenon of preventing the recurrences of mood disorders by the long-term lithium administration was discovered sixty years ago. Such a property of lithium has been unequivocally confirmed in subsequent ...
Prevention of suicidal behavior with lithium treatment in patients with recurrent mood disorders
Suicidal behavior is more prevalent in bipolar disorders than in other psychiatric illnesses. In the last thirty years evidence has emerged to indicate that long-term treatment of bipolar disorder patients wit...
Correlations between multimodal neuroimaging and peripheral inflammation in different subtypes and mood states of bipolar disorder: a systematic review
Systemic inflammation-immune dysregulation and brain abnormalities are believed to contribute to the pathogenesis of bipolar disorder (BD). However, the connections between peripheral inflammation and the brai...
Lithium: how low can you go?
Why is lithium [not] the drug of choice for bipolar disorder a controversy between science and clinical practice.
During over half a century, science has shown that lithium is the most efficacious treatment for bipolar disorder but despite this, its prescription has consistently declined internationally during recent deca...
Biomarkers for neurodegeneration impact cognitive function: a longitudinal 1-year case–control study of patients with bipolar disorder and healthy control individuals
Abnormalities in cerebrospinal fluid (CSF)-amyloid-beta (Aβ)42, CSF-Aβ40, CSF-Aβ38, CSF-soluble amyloid precursor proteins α and β, CSF-total-tau, CSF-phosphorylated-tau, CSF-neurofilament light protein (NF-L)...
Cognitive behavioural therapy for social anxiety disorder in people with bipolar disorder: a case series
Social anxiety disorder increases the likelihood of unfavourable outcomes in people with bipolar disorder. Cognitive behavioural therapy (CBT) is the first-line treatment for social anxiety disorder. However, ...
Lithium prescription trends in psychiatric inpatient care 2014 to 2021: data from a Bavarian drug surveillance project
Lithium (Li) remains one of the most valuable treatment options for mood disorders. However, current knowledge about prescription practices in Germany is limited. The objective of this study is to estimate the...
Lifetime risk of severe kidney disease in lithium-treated patients: a retrospective study
Lithium is an essential psychopharmaceutical, yet side effects and concerns about severe renal function impairment limit its usage.
Factors associated with suicide attempts in the antecedent illness trajectory of bipolar disorder and schizophrenia
Factors associated with suicide attempts during the antecedent illness trajectory of bipolar disorder (BD) and schizophrenia (SZ) are poorly understood.
Behavioral lateralization in bipolar disorders: a systematic review
Bipolar disorder (BD) is often seen as a bridge between schizophrenia and depression in terms of symptomatology and etiology. Interestingly, hemispheric asymmetries as well as behavioral lateralization are shi...
High lithium concentration at delivery is a potential risk factor for adverse outcomes in breastfed infants: a retrospective cohort study
Neonatal effects of late intrauterine and early postpartum exposure to lithium through mother’s own milk are scarcely studied. It is unclear whether described symptoms in breastfed neonates are caused by place...
Key questions on the long term renal effects of lithium: a review of pertinent data
For over half a century, it has been widely known that lithium is the most efficacious maintenance treatment for bipolar disorder. Despite thorough research on the long-term effects of lithium on renal functio...
Controversies regarding lithium-associated weight gain: case–control study of real-world drug safety data
The impact of long-term lithium treatment on weight gain has been a controversial topic with conflicting evidence. We aim to assess reporting of weight gain associated with lithium and other mood stabilizers c...
Differential diagnosis of unipolar versus bipolar depression by GSK3 levels in peripheral blood: a pilot experimental study
The differential diagnosis of patients presenting for the first time with a depressive episode into unipolar disorder versus bipolar disorder is crucial to establish the correct pharmacological therapy (antide...
Supra-second interval timing in bipolar disorder: examining the role of disorder sub-type, mood, and medication status
Widely reported by bipolar disorder (BD) patients, cognitive symptoms, including deficits in executive function, memory, attention, and timing are under-studied. Work suggests that individuals with BD show imp...
Association between childhood trauma, cognition, and psychosocial function in a large sample of partially or fully remitted patients with bipolar disorder and healthy participants
Childhood trauma (CT) are frequently reported by patients with bipolar disorder (BD), but it is unclear whether and how CT contribute to patients’ cognitive and psychosocial impairments. We aimed to examine th...
Countering the declining use of lithium therapy: a call to arms
For over half a century, it has been widely known that lithium is the most efficacious treatment for bipolar disorder. Yet, despite this, its prescription has consistently declined over this same period of tim...
Paediatric bipolar disorder: an age-old problem
Nrx-101 (d-cycloserine plus lurasidone) vs. lurasidone for the maintenance of initial stabilization after ketamine in patients with severe bipolar depression with acute suicidal ideation and behavior: a randomized prospective phase 2 trial.
We tested the hypothesis that, after initial improvement with intravenous ketamine in patients with bipolar disorder (BD) with severe depression and acute suicidal thinking or behavior, a fixed-dose combinatio...
The IBER study: a feasibility randomised controlled trial of imagery based emotion regulation for the treatment of anxiety in bipolar disorder
Intrusive mental imagery is associated with anxiety and mood instability within bipolar disorder and therefore represents a novel treatment target. Imagery Based Emotion Regulation (IBER) is a brief structured...
Mitochondrial genetic variants associated with bipolar disorder and Schizophrenia in a Japanese population
Bipolar disorder (BD) and schizophrenia (SZ) are complex psychotic disorders (PSY), with both environmental and genetic factors including possible maternal inheritance playing a role. Some studies have investi...
Differential characteristics of bipolar I and II disorders: a retrospective, cross-sectional evaluation of clinical features, illness course, and response to treatment
The distinction between bipolar I and bipolar II disorder and its treatment implications have been a matter of ongoing debate. The aim of this study was to examine differences between patients with bipolar I a...
Neonatal admission after lithium use in pregnant women with bipolar disorders: a retrospective cohort study
Lithium is the preferred treatment for pregnant women with bipolar disorders (BD), as it is most effective in preventing postpartum relapse. Although it has been prescribed during pregnancy for decades, the sa...
Rates and associations of relapse over 5 years of 2649 people with bipolar disorder: a retrospective UK cohort study
Evidence regarding the rate of relapse in people with bipolar disorder (BD), particularly from the UK, is lacking. This study aimed to evaluate the rate and associations of clinician-defined relapse over 5 yea...
Exploratory study of ultraviolet B (UVB) radiation and age of onset of bipolar disorder
Sunlight contains ultraviolet B (UVB) radiation that triggers the production of vitamin D by skin. Vitamin D has widespread effects on brain function in both developing and adult brains. However, many people l...
Characteristics of rapid cycling in 1261 bipolar disorder patients
Rapid-cycling (RC; ≥ 4 episodes/year) in bipolar disorder (BD) has been recognized since the 1970s and associated with inferior treatment response. However, associations of single years of RC with overall cycl...
Clinicians’ preferences and attitudes towards the use of lithium in the maintenance treatment of bipolar disorders around the world: a survey from the ISBD Lithium task force
Lithium has long been considered the gold-standard pharmacological treatment for the maintenance treatment of bipolar disorders (BD) which is supported by a wide body of evidence. Prior research has shown a st...
Phenotype fingerprinting of bipolar disorder prodrome
Detecting prodromal symptoms of bipolar disorder (BD) has garnered significant attention in recent research, as early intervention could potentially improve therapeutic efficacy and improve patient outcomes. T...
Predictors of adherence to electronic self-monitoring in patients with bipolar disorder: a contactless study using Growth Mixture Models
Several studies have reported on the feasibility of electronic (e-)monitoring using computers or smartphones in patients with mental disorders, including bipolar disorder (BD). While studies on e-monitoring ha...
Racial differences in the major clinical symptom domains of bipolar disorder
Across clinical settings, black individuals are disproportionately less likely to be diagnosed with bipolar disorder compared to schizophrenia, a traditionally more severe and chronic disorder with lower expec...
Methylomic biomarkers of lithium response in bipolar disorder: a clinical utility study
Response to lithium (Li) is highly variable in bipolar disorders (BD). Despite decades of research, no clinical predictor(s) of response to Li prophylaxis have been consistently identified. Recently, we develo...
A compelling need to empirically validate bipolar depression
Structured physical exercise for bipolar depression: an open-label, proof-of concept study.
Physical exercise (PE) is a recommended lifestyle intervention for different mental disorders and has shown specific positive therapeutic effects in unipolar depressive disorder. Considering the similar sympto...
Experiences that matter in bipolar disorder: a qualitative study using the capability, comfort and calm framework
When assessing the value of an intervention in bipolar disorder, researchers and clinicians often focus on metrics that quantify improvements to core diagnostic symptoms (e.g., mania). Providers often overlook...
Emotion regulation in bipolar disorder type-I: multivariate analysis of fMRI data
Bipolar disorder type-I (BD-I) patients are known to show emotion regulation abnormalities. In a previous fMRI study using an explicit emotion regulation paradigm, we compared responses from 19 BD-I patients a...
Lithium levels and lifestyle in patients with bipolar disorder: a new tool for self-management
Patients should get actively involved in the management of their illness. The aim of this study was to assess the influence of lifestyle factors, including sleep, diet, and physical activity, on lithium levels...
Reduced parenting stress following a prevention program decreases internalizing and externalizing symptoms in the offspring of parents with bipolar disorder
Offspring of parents with bipolar disorder (OBD) are at risk for developing mental disorders, and the literature suggests that parenting stress may represent an important risk factor linking parental psychopat...
Stigma in people living with bipolar disorder and their families: a systematic review
Stigma affects different life aspects in people living with bipolar disorder and their families. This study aimed to examining the experience of stigma and evaluating predictors, consequences and strategies to...
Lithium use in childhood and adolescence, peripartum, and old age: an umbrella review
Lithium is one of the most consistently effective treatment for mood disorders. However, patients may show a high level of heterogeneity in treatment response across the lifespan. In particular, the benefits o...
Risk of childhood trauma exposure and severity of bipolar disorder in Colombia
Bipolar disorder (BD) is higher in developing countries. Childhood trauma exposure is a common environmental risk factor in Colombia and might be associated with a more severe course of bipolar disorder in Low...
A systematic review on the effectiveness of dialectical behavior therapy for improving mood symptoms in bipolar disorders
Evidence-based psychotherapies available to treat patients with bipolar disorders (BD) are limited. Dialectical behavior therapy (DBT) may target several common symptoms of BD. We conducted a systematic review...
Bipolar disorder and sexuality: a preliminary qualitative pilot study
Individuals with mental health disorders have a higher risk of sexual problems impacting intimate relations and quality of life. For individuals with bipolar disorder (BD) the mood shifts might to a particular...
Long-term lithium therapy and risk of chronic kidney disease, hyperparathyroidism and hypercalcemia: a cohort study
Lithium is well recognized as the first-line maintenance treatment for bipolar disorder (BD). However, besides therapeutic benefits attributed to lithium therapy, the associated side effects including endocrin...
The association of genetic variation in CACNA1C with resting-state functional connectivity in youth bipolar disorder
CACNA1C rs1006737 A allele, identified as a genetic risk variant for bipolar disorder (BD), is associated with anomalous functional connectivity in adults with and without BD. Studies have yet to investigate the ...
- Editorial Board
- Sign up for article alerts and news from this journal
- ISSN: 2194-7511 (electronic)
Bipolar disorders
Affiliations.
- 1 Mood Disorders Psychopharmacology Unit, University Health Network, Toronto, ON, Canada; Department of Psychiatry, University of Toronto, Toronto, ON, Canada; Department of Pharmacology, University of Toronto, Toronto, ON, Canada; Brain and Cognition Discovery Foundation, Toronto, ON, Canada. Electronic address: [email protected].
- 2 Institute for Mental and Physical Health and Clinical Translation Strategic Research Centre, School of Medicine, Deakin University, Melbourne, VIC, Australia; Mental Health Drug and Alcohol Services, Barwon Health, Geelong, VIC, Australia; Orygen, The National Centre of Excellence in Youth Mental Health, Melbourne, VIC, Australia; Centre for Youth Mental Health, Florey Institute for Neuroscience and Mental Health, Melbourne, VIC, Australia; Department of Psychiatry, The University of Melbourne, Melbourne, VIC, Australia.
- 3 Department of Psychiatry, Adult Division, Kingston General Hospital, Kingston, ON, Canada; Department of Psychiatry, Queen's University School of Medicine, Queen's University, Kingston, ON, Canada; Centre for Neuroscience Studies, Queen's University, Kingston, ON, Canada.
- 4 Department of Psychiatry, University of Toronto, Toronto, ON, Canada; Centre for Youth Bipolar Disorder, Sunnybrook Health Sciences Centre, Toronto, ON, Canada.
- 5 Department of Psychiatry, Faculty of Medicine, University of Antioquia, Medellín, Colombia; Mood Disorders Program, Hospital Universitario San Vicente Fundación, Medellín, Colombia.
- 6 Copenhagen Affective Disorders Research Centre, Psychiatric Center Copenhagen, Rigshospitalet, Copenhagen, Denmark; Department of Psychiatry, Faculty of Health and Medical Sciences, University of Copenhagen, Copenhagen, Denmark.
- 7 Discipline of Psychiatry, Northern Clinical School, University of Sydney, Sydney, NSW, Australia; Department of Academic Psychiatry, Northern Sydney Local Health District, Sydney, Australia.
- 8 Department of Psychiatry, University of Toronto, Toronto, ON, Canada.
- 9 Mood Disorders Psychopharmacology Unit, University Health Network, Toronto, ON, Canada; Department of Psychiatry, University of Toronto, Toronto, ON, Canada; Dauten Family Center for Bipolar Treatment Innovation, Massachusetts General Hospital, Harvard Medical School, Boston, MA, USA.
- 10 Mood Disorders Psychopharmacology Unit, University Health Network, Toronto, ON, Canada.
- 11 Hospital Clinic, Institute of Neuroscience, University of Barcelona, IDIBAPS, CIBERSAM, Barcelona, Spain.
- 12 Department of Psychiatry, Faculty of Health and Medical Sciences, University of Copenhagen, Copenhagen, Denmark; Psychiatric Research Unit, Psychiatric Centre North Zealand, Hillerød, Denmark.
- 13 Department of Psychological Medicine, Institute of Psychiatry, Psychology and Neuroscience, King's College London and South London and Maudsley National Health Service Foundation Trust, Bethlem Royal Hospital, London, UK.
- 14 Mood Disorders Psychopharmacology Unit, University Health Network, Toronto, ON, Canada; Department of Psychiatry, University of Toronto, Toronto, ON, Canada.
- PMID: 33278937
- DOI: 10.1016/S0140-6736(20)31544-0
Bipolar disorders are a complex group of severe and chronic disorders that includes bipolar I disorder, defined by the presence of a syndromal, manic episode, and bipolar II disorder, defined by the presence of a syndromal, hypomanic episode and a major depressive episode. Bipolar disorders substantially reduce psychosocial functioning and are associated with a loss of approximately 10-20 potential years of life. The mortality gap between populations with bipolar disorders and the general population is principally a result of excess deaths from cardiovascular disease and suicide. Bipolar disorder has a high heritability (approximately 70%). Bipolar disorders share genetic risk alleles with other mental and medical disorders. Bipolar I has a closer genetic association with schizophrenia relative to bipolar II, which has a closer genetic association with major depressive disorder. Although the pathogenesis of bipolar disorders is unknown, implicated processes include disturbances in neuronal-glial plasticity, monoaminergic signalling, inflammatory homoeostasis, cellular metabolic pathways, and mitochondrial function. The high prevalence of childhood maltreatment in people with bipolar disorders and the association between childhood maltreatment and a more complex presentation of bipolar disorder (eg, one including suicidality) highlight the role of adverse environmental exposures on the presentation of bipolar disorders. Although mania defines bipolar I disorder, depressive episodes and symptoms dominate the longitudinal course of, and disproportionately account for morbidity and mortality in, bipolar disorders. Lithium is the gold standard mood-stabilising agent for the treatment of people with bipolar disorders, and has antimanic, antidepressant, and anti-suicide effects. Although antipsychotics are effective in treating mania, few antipsychotics have proven to be effective in bipolar depression. Divalproex and carbamazepine are effective in the treatment of acute mania and lamotrigine is effective at treating and preventing bipolar depression. Antidepressants are widely prescribed for bipolar disorders despite a paucity of compelling evidence for their short-term or long-term efficacy. Moreover, antidepressant prescription in bipolar disorder is associated, in many cases, with mood destabilisation, especially during maintenance treatment. Unfortunately, effective pharmacological treatments for bipolar disorders are not universally available, particularly in low-income and middle-income countries. Targeting medical and psychiatric comorbidity, integrating adjunctive psychosocial treatments, and involving caregivers have been shown to improve health outcomes for people with bipolar disorders. The aim of this Seminar, which is intended mainly for primary care physicians, is to provide an overview of diagnostic, pathogenetic, and treatment considerations in bipolar disorders. Towards the foregoing aim, we review and synthesise evidence on the epidemiology, mechanisms, screening, and treatment of bipolar disorders.
Copyright © 2020 Elsevier Ltd. All rights reserved.
Publication types
- Research Support, Non-U.S. Gov't
- Anticonvulsants / therapeutic use
- Antidepressive Agents / therapeutic use
- Antimanic Agents / therapeutic use
- Antipsychotic Agents / therapeutic use
- Bipolar Disorder / classification*
- Bipolar Disorder / drug therapy*
- Bipolar Disorder / genetics
- Bipolar Disorder / psychology
- Carbamazepine / therapeutic use
- Cardiovascular Diseases / complications
- Cardiovascular Diseases / mortality
- Child Abuse / psychology
- Comorbidity
- Depressive Disorder, Major / drug therapy*
- Depressive Disorder, Major / genetics
- Depressive Disorder, Major / psychology
- Environmental Exposure / adverse effects
- Lamotrigine / therapeutic use
- Lithium / therapeutic use
- Mania / drug therapy
- Mania / psychology
- Suicide / psychology
- Suicide Prevention*
- Valproic Acid / therapeutic use
- Young Adult
- Anticonvulsants
- Antidepressive Agents
- Antimanic Agents
- Antipsychotic Agents
- Carbamazepine
- Valproic Acid
- Lamotrigine
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Special Report: Bipolar Disorder II—Frequently Neglected, Misdiagnosed
- Trisha Suppes , M.D., Ph.D. ,
- Holly A. Swartz , M.D. ,
- Sara Schley
Search for more papers by this author
Unlike its cousin, bipolar I disorder, which has been extensively studied and depicted in popular literature and on screen, bipolar II disorder is poorly understood, underdiagnosed, and insufficiently treated. This has often resulted in an over 10-year delay in diagnosis.

Even experienced clinicians know surprisingly little about bipolar II disorder (BD II), despite its inclusion as a distinct entity in DSM since 1994. An abundance of studies supports conceptualization of BD II as a unique phenotype within the bipolar illness spectrum, although many fail to recognize it as distinct disorder apart from bipolar I disorder (BD I).
Alternatively, BD II is considered a “lesser form” of BD I, despite numerous studies showing comparable illness severity and risk of suicide in these two BD subtypes. Perhaps because of its under-recognition, treatment studies of BD II are limited, and too often results from studies of patients with BD I are simply applied to those with BD II with no direct evidence supporting this practice. BD II is an understudied and unmet treatment challenge in psychiatry.
In this review, we will provide a broad overview of BD II including differential diagnosis, course of illness, comorbidities, and suicide risk. We will summarize treatment studies specific to BD II, identifying gaps in the literature. This review will reveal similarities between BD I and II, including suicide risk and predominance of depression over the course of illness, but also differences between the phenotypes in treatment response, for example to antidepressants.
We highlight the perspective of an expert by experience who discusses her lived experiences of BD II in an accompanying interview ( Interview With an Expert by Lived Experience ).
Diagnosis History
Alternating states of mania and melancholia are among the earliest described human diseases, first noted by ancient Greek physicians, philosophers, and poets. Hippocrates (460-337 B.C.E.), who formulated the first known classification of mental disorders, systematically described bipolar mood states: melancholia, mania, and paranoia. More than two millennia later, Emil Kraepelin, recognized as one of the founders of modern psychiatry, described manic-depressive illness as a singular disease characterized by alternating cycles of mania or melancholia. However, Kraepelin was more focused on mood changes and cycling than the polarity of episodes per se. Thus, his concept included what we now term recurrent major depressive disorder (MDD) . Nevertheless, his and other formulations from this period provide background for our modern concepts of bipolar disorder, differentiating it from unipolar depression (MDD and related disorders).
The hiding in plain sight of patients with BD II was brought to awareness by David L. Dunner, M.D., in the 1960s. When examining a cohort of individuals with mood disorders in a study by the National Institute of Mental Health (NIMH), he identified a subgroup of patients with recurrent episodes of depression who also had a history of at least one period of hypomania and a strong family history of bipolar disorder. This subgroup was found to have a different course of illness compared with those with recurrent depression and a history of mania (BD I). Thanks to this work, BD II was recognized as a distinct disorder, separate from BD I. It finally entered the DSM lexicon in 1994 in DSM-IV and was added to ICD-10 even more recently.
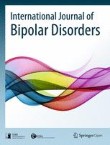
Conceptualization of bipolar disorders continues to evolve as the field learns more; for example, changes were made to the DSM-5 diagnostic criteria for BD such that Criteria A for both mania and hypomania now include increased energy as well as elevated or irritable mood (see Table 1). Thus, BD II is now recognized as a disorder of energy as well as mood.
DSM focuses on categorial diagnoses—that is, thresholds for absence or presence of disease. In parallel to this framework, many have argued for considering bipolar disorders along a continuous spectrum of illness. Thus, the term bipolar spectrum is used to describe both the spectrum of severity across BD symptoms as well as combinations of mood symptoms with manic/hypomanic and depressive components. Some refer to BD II as a part of the bipolar spectrum. These concepts reflect a growing awareness that dimensional descriptions of mood disorders may better map onto continuous biological markers of disease, compared with DSM ’s categorical approach, but the debate about diagnostic boundaries and disease etiology continues. Importantly, conceptualizations of BD as a spectrum condition versus discrete diagnostic categories (that is, BD I or BD II) are not mutually exclusive but rather speak to ongoing efforts to understand and best describe the phenomenology of BD.
Differential Diagnosis
The validity of BD II as a separate disorder has been reified through multiple empirical studies. The clinical diagnosis is reliably separable from BD I, as seen in APA clinical trials preparing for DSM-5 and in careful clinical interviews. In DSM-5 field trials to assess reliability of diagnoses, BD I was among the most recognizable, but BD II fell in the acceptable range and well above MDD as a reliable diagnostic entity. Family studies also support the diagnosis of BD II as an independent entity with distinct familial heritability, according to a 1976 study by Dunner et al. and a 1990 study by J. Raymond DePaulo, M.D., et al., and the authors of this report. Finally, genetic studies have found correlations suggesting the heterogeneity between BD I and BD II is “nonrandom,” supporting the concept of distinct conditions.
BD II diagnosis requires at least one lifetime hypomanic episode and one major depressive episode. Despite clarity of BD II diagnostic criteria, clinicians struggle to accurately identify it in practice. BD II is often either missed or incorrectly diagnosed, resulting in an over 10-year delay in diagnosis. Difficulties in accurate diagnosis arise from several sources. First, DSM-5 criteria for the depressive phase of BD II are identical to those required for a major depressive episode, which make BD II and MDD cross-sectionally indistinguishable. This is particularly notable as MDD diagnoses make up a substantial percent of the incorrect diagnoses for patients with BD II. Second, hypomania, which by definition is a less severe form of mania, may be difficult for patients to distinguish from a “normal” mood state when accompanied by extra energy and good mood. Third, mixed hypomanic mood states are very common in BD II, and in fact more common than euphoric hypomanic states. Mixed mood states are characterized by the presence of symptoms of opposite polarity during a depressive or hypomanic episode. In a mixed hypomania, patients might believe they are simply irritable and angry in the context of depression rather than recognizing the additional hypomanic symptoms warranting a diagnosis of mixed hypomanic state. Finally, patients rarely present for treatment in the midst of a hypomanic episode, a mood state that is either perceived as ego-syntonic or simply not identified as part of their illness during mixed hypomania.
The primary reason patients with BD II seek care is depression. Depression dominates the course of BD II, both in the early and late stages. However, retrospectively identifying episodes of hypomania during a depressive episode can be challenging. Further, many individuals see hypomania (either the euphoric or mixed variant) as part of “normal” mood rather than part of a bipolar spectrum, contributing to misreporting of mood episodes. Especially after unrelenting episodes of depression, it is understandable that many would perceive hypomania as a return to baseline. However, under-recognition of hypomania contributes to incorrect diagnoses. In sum, many individuals with BD II fail to recall, recognize, or report histories of hypomania, leading to an MDD (mis)diagnosis.
In psychiatry, all diagnoses are a one-way road. Individuals who have ever met criteria for a manic episode will continue to carry the diagnosis of BD I—even without further manic episodes. Similarly, patients who have a distant episode of hypomania and at least one prior major depressive episode would be considered to have BD II disorder, even in the absence of additional hypomanic episodes that meet symptom and duration criteria. Thus, accurate diagnosis of BD II relies on careful history taking. To improve diagnostic acumen, it is essential that clinicians systematically screen all patients with MDD for BD and ask careful questions about prior episodes of hypomania.
Course of Illness and Comorbidity
Kraepelin noted before the medication era that the course of illness for patients with BD generally progresses into more persistent and severe depression with aging. While he was primarily referring to manic-depressive illness, which we would call BD I today, the same principle applies to patients with BD II. In the NIMH collaborative study by Lewis Judd, M.D., et al., which included long-term follow-up of up to 20 years, patients with BD II experienced a course of illness characterized by more depressive episodes and fewer well intervals over time.
There is a longstanding debate in the literature whether patients with BD II suffer the same impairments and risks as those with BD I. BD II was previously—and incorrectly—labeled a “less severe” version of BD I. In fact, studies consistently show comparable disease burden in BD I and II. A recent Swedish study by Alina Karanti, M.D., et al. reported higher rates of depressive episodes, illness onset at a younger age, and significantly higher rates of psychiatric comorbidity (anxiety disorders, eating disorders, and ADHD) among patients with BD II compared with those with BD I. In this Swedish sample, (n>8,700) no differences were noted in substance abuse between BD I and BD II. Interestingly, individuals with BD II generally obtained more education and achieved a higher level of independence than those with BD I.
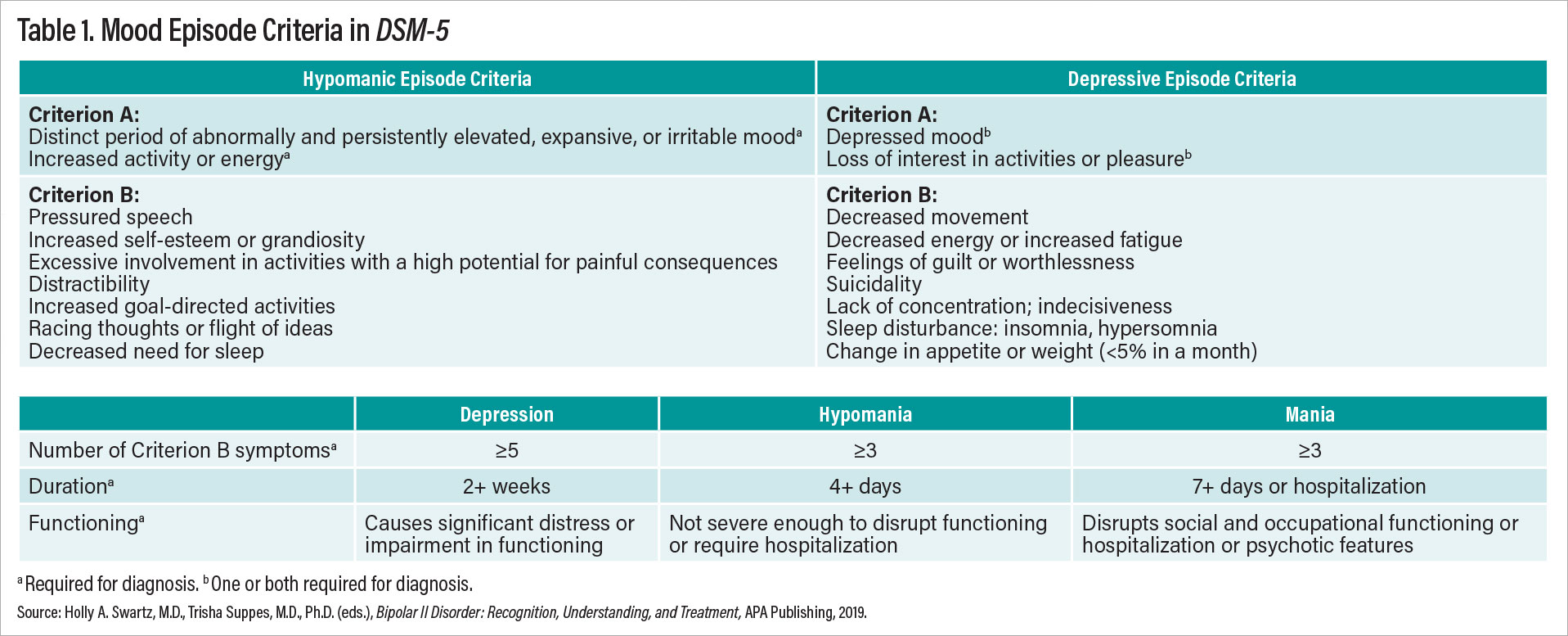
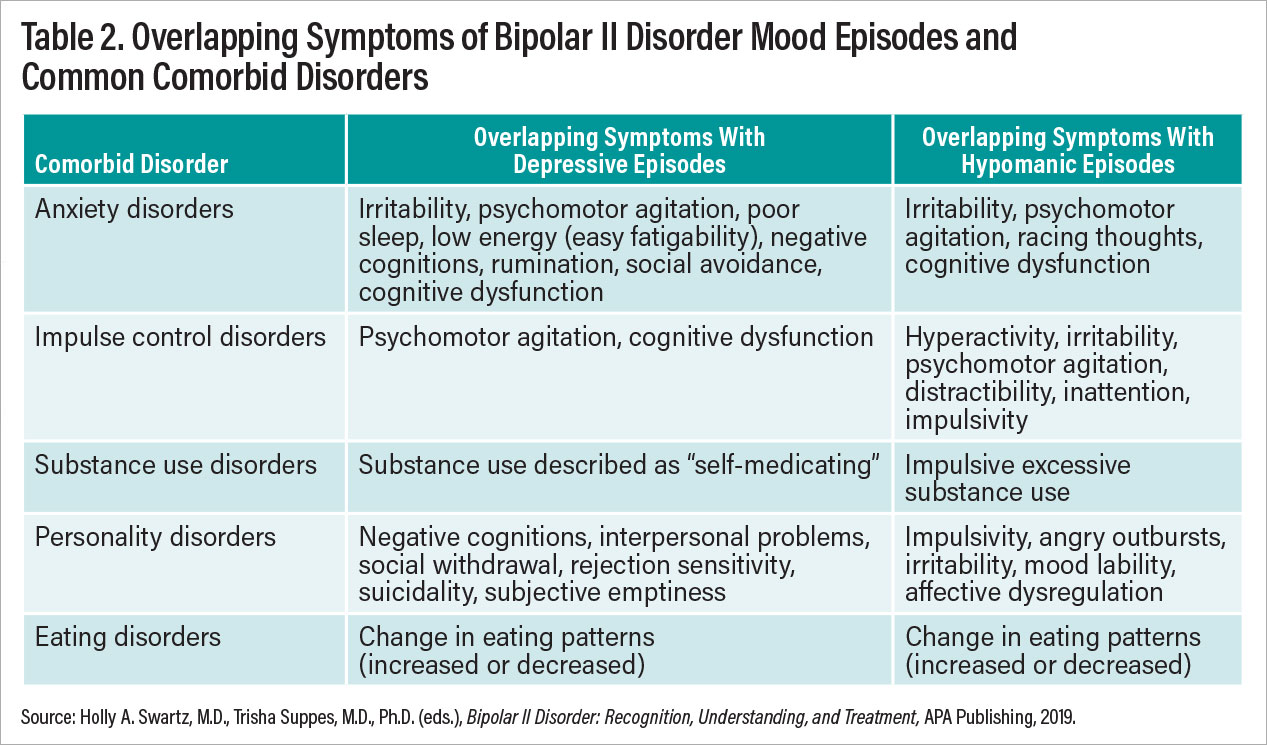
High rates of psychiatric comorbidity in patients with BD II further compound the challenge of differential diagnosis. There is considerable overlap between BD II and anxiety disorders. Attention-deficit/hyperactivity disorder also frequently co-occurs. Approximately 20% of individuals with BD II also meet criteria for borderline personality disorder (BPD), and up to 40% of those with BPD are incorrectly diagnosed as having BD I or II. Tables 2 and 3 show estimated co-occurring psychiatric illnesses for patients with BD II. The diagnosis of BD II requires a careful clinical interview of both past and current symptomatology.
Suicide is a significant risk for all patients with BD, and historically patients with BD I were viewed as having a higher risk than BD II due to the extremities of mania. However, data from a number of sources support that suicide risk is high across all patients with BD, and relatively little difference is found in risk for patients with BD I versus BD II. Older studies have suggested this risk may be higher for patients with BD II than BD I, and, indeed, the Swedish bipolar registry database study recently indicated that the rate of suicide attempts was significantly higher in patients with BD II though no data on completed suicides were provided. Overall, the reports from the International Society for Bipolar Disorders Task Force on Suicide found that the risk for suicide was estimated at 164 of 100,000 per year in patients with BD versus 10 of 100,000 per year in the general population (see the reference by Ayal Schaffer, M.D., at the end of this report).
Treatment of BD II
Treatment guidelines for bipolar disorder often give only a passing nod to distinguishing appropriate treatments for BD I versus BD II. The combined guidelines by the Canadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) were unusual in making a point of distinguishing the evidence base for BD I versus BD II. They are reported in a 2018 paper by Lakshmi N. Yatham, M.D., et al. (see reference at end of article).
These guidelines have a separate section devoted to BD II, and they clearly state that one cannot directly apply studies on patients with BD I to management of patients with BD II. The conclusion of these guidelines is that there are too few controlled studies in patients with BD II to make detailed evidence-based recommendations or develop evidence-based treatment algorithms. Below is a brief overview of our current knowledge of treatments for patients with BD II with medication and/or psychotherapy.
Antidepressants
It is worth highlighting that, while monotherapy antidepressants would be viewed as an inappropriate practice for patients with BD I depression, studies suggest that the risks and benefits may be different for those with BD I and BD II. In at least one study, risk of switching to hypomania was no greater with lithium than with sertraline monotherapy. Other studies have shown antidepressant monotherapy to be an efficacious monotherapy for BD II. Meta-analyses on risk of antidepressant-induced switches are inconclusive, though the risk of treatment-emergent (hypo)mania due to medication appears to be less in patients with BD II than in patients with BD I depression receiving monotherapy antidepressants. Absent conclusive data on antidepressant switch rates, without a past record of good response to antidepressant monotherapy, current treatment guidelines suggest starting with lithium or a mood stabilizer before adding or switching to antidepressant monotherapy. Additionally, it is important to note that antidepressants in some patients may worsen the overall course of illness and may not be efficacious in some patients with BD II. Any patient who experiences hypomania or mania (which must be distinguished from transient activation symptoms) while on antidepressant medication should be presumed to be on the bipolar spectrum.
Antipsychotics
Most atypical antipsychotics have not been studied for the treatment of both BD I and BD II depression, with two notable exceptions. Quetiapine registration trials included individuals with BD II, with post-hoc analyses demonstrating efficacy of quetiapine monotherapy for BD II depression. Lumateperone is the first antipsychotic formally studied for depression response in patients with BD II since quetiapine trials in the early 2000s. Lumateperone, in randomized, controlled trials, performed as well or better for BD II than BD I, according to a 2021 study by Joseph R. Calabrese, M.D., et al. Cariprazine and lurasidone, while both FDA approved to treat bipolar depression, were never formally studied in patients with BD II. There have been case series supporting their use in BD II depression, but no randomized, controlled trials have been carried out. FDA approval to treat patients with BD II depression with lumateperone came in 2021, 15 years after quetiapine was approved. This glacial rate of accruing new FDA-approved compounds for BD II speaks to the need for more studies in this population.
Lithium and Anticonvulsants
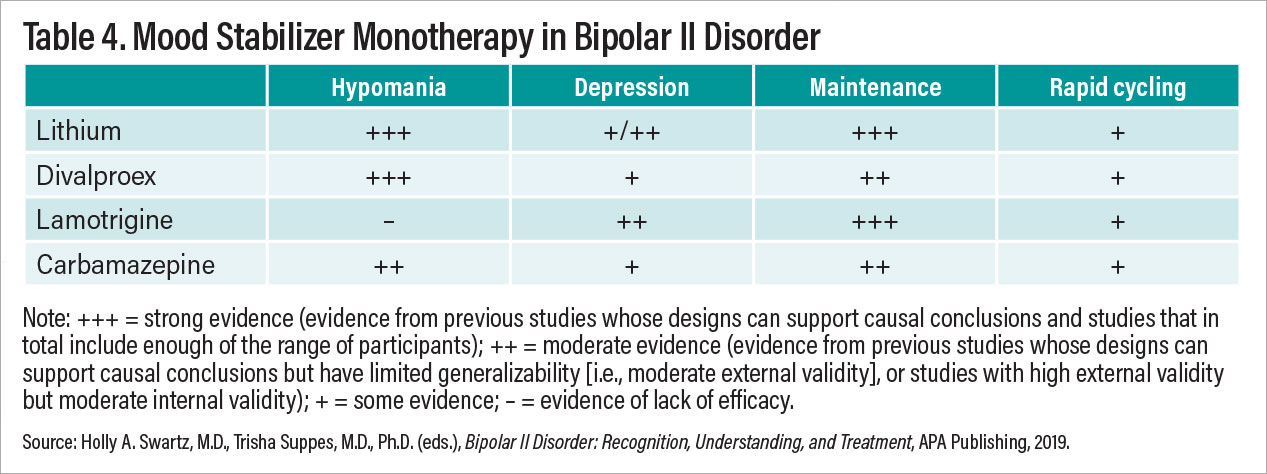
While we might expect lithium to be the frontrunner treatment for managing BD II, study results are varied. Certainly, for hypomania and maintenance treatment of patients with BD II, lithium is a top choice. Lithium has a disappointingly poor track record for treating BD II depression with little indication that response rates are superior to those of antidepressants and atypical antipsychotics. Lamotrigine has good evidence for preventing new depression episodes in the context of BD (both BD II and I). The evidence, however, is less robust for treating acute depression in patients with BD II. In clinical practice, many clinicians prescribe lamotrigine, especially as an adjunctive treatment, for BD II depression, but our ability to make firm recommendations with confidence about lamotrigine is limited.
Other Therapies
Rapid-acting therapies are on the rise across all treatments for depression. There has been a recent surge of clinical work and research examining transcranial magnetic stimulation (TMS), ketamine, and psychedelics and related compounds. More work is needed specifically focused on BD II depression before firm conclusions may be drawn.
There is limited evidence supporting the use of TMS for BD II depression. This evidence base is developing, and more information is forthcoming on the utility of TMS for BD II depression.
Ketamine and Psychedelic Studies
Racemic ketamine has been in use for many years as an anesthetic and more recently was approved by the FDA as intranasal esketamine (the s-enantiomer of racemic ketamine) as a treatment for MDD. Three small studies of racemic ketamine suggest that it is effective for BD II depression. A 2022 observational study by Farhan Fancy et al. assessing patients with BD I versus BD II treated with racemic ketamine included more than 60 patients (n=35 BD II). In this largest open observational study to date involving ketamine and BD, patients with BD II demonstrated a more robust response than those with BD I. More studies are in development exploring this new use of an old drug; to date, there is no information on the role of esketamine for bipolar depression, let alone BD II.
Recently, it’s been difficult to pick up a journal or look at other media without seeing something about psychedelics and related compounds. There is a surge of interest in psychedelics for MDD, although evidence about their effectiveness is still early and with rare exceptions involves small samples. There is one report on treatment of depression with psilocybin in patients with BD II. In this pilot study, 15 patients with BD II were given a one-time dose of psilocybin (25 mg) and provided preparatory, dosing, and integration therapy consistent with psilocybin studies in MDD. In this small open study by Scott Aaronson, M.D., et al., the rate of response at 3 and 12 weeks was more robust than has been observed in MDD studies. An ongoing study is assessing the durability of patients’ response to psilocybin administered one time for patients with BD II depression. While no notable adverse events or increased mood lability were noted in this small sample to date, further study is needed to assess benefits and harms.
Psychotherapy
Most information about psychotherapy for BD II is derived from trials of interventions for BD in general that also included a subset of individuals with BD II. A recent systematic review of psychotherapies for BD II identified over 1,000 individuals with BD II who participated in randomized, controlled trials testing psychosocial interventions to treat depression or prevent recurrence of mood symptoms. However, relatively few of these trials—only eight of 27—examined outcomes in those with BD II separately. From this review, we concluded that there is preliminary evidence supporting the efficacy of several evidence-based psychotherapies for BD II: cognitive-behavioral therapy, psychoeducation, family focused therapy, interpersonal and social rhythm therapy (IPSRT), and functional remediation. None of these psychotherapies have undergone rigorous testing in randomized, controlled trials focused specifically on BD II depression, with the exception of IPSRT, pointing to the need for additional research in this area. To our knowledge, no meta-analysis of psychotherapy for BD II has been published.
IPSRT, the only psychosocial intervention to be tested in a randomized, controlled trial consisting of participants with BD II only (rather than a mixed patient population of BD I and II), focuses on helping individuals develop more regular routines to stabilize underlying disturbances in circadian rhythms. Because abnormalities in circadian biology have been implicated in the genesis of bipolar disorders, including BD II, a chronobiologic behavioral approach may be especially helpful to mitigate BD II symptoms.
Conclusions
BD II is a relatively common disorder affecting approximately 0.4% of the population. Its prevalence, morbidity, and mortality are comparable to that of BD I. Evidence supports conceptualizing BD II as a distinct phenotype, separable from both BD I and MDD. Compared with BD I and MDD, far less is known about BD II and how to treat it. Further, despite being reliably diagnosed in DSM-5 field trials, BD II is frequently misdiagnosed in practice, resulting in a decade-long lag between onset of symptoms and appropriate diagnosis. A neglected condition, BD II causes unnecessary suffering in those who are misdiagnosed or for whom appropriate treatments are unclear. More research is urgently needed to improve identification and treatments for BD II. ■
David L. Dunner, M.D., et al. “ Heritable Factors in the Severity of Affective Illness ,” Biological Psychiatry , February 1976.
J. Raymond DePaulo, M.D., et al. “ Bipolar II Disorder in Six Sisters ,” Journal of Affective Disorders , August 1990.
Lewis Judd, M.D., et al. “ Long-Term Symptomatic Status of Bipolar I vs. Bipolar II Disorders ,” International Journal of Neuropsychopharmacology, June 2003.
Alina Karanti, Ph.D., et al. “ Characteristics of Bipolar I and II Disorder: A Study of 8766 Individuals ,” Bipolar Disorders , June 2020.
Ayal Schaffer, M.D., et al. “ A Review of Factors Associated With Greater Likelihood of Suicide Attempts and Suicide Deaths in Bipolar Disorder: Part II of a Report of the International Society for Bipolar Disorders Task Force on Suicide in Bipolar Disorder ,” Australian & New Zealand Journal of Psychiatry , November 2015.
Lakshmi N. Yatham, M.D., et al. “ Canadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) 2018 Guidelines for the Management of Patients With Bipolar Disorder ,” Bipolar Disorders , March 2018.
Joseph R. Calabrese, M.D., et al. “ Efficacy and Safety of Lumateperone for Major Depressive Episodes Associated With Bipolar I or Bipolar II Disorder: A Phase 3 Randomized Placebo-Controlled Trial ,” American Journal of Psychiatry , December 2021.
Farhan Fancy, et al. “ Real-World Effectiveness of Repeated Ketamine Infusions for Treatment-Resistant Bipolar Depression ,” Bipolar Disorders , December 14, 2022.
Scott Aaronson, M.D., et al. “ COMP360 Psilocybin Therapy Shows Potential in Open-Label Study in Type II Bipolar Disorder ,” Global Newswire, December 8, 2022.

Trisha Suppes, M.D., Ph.D., is a professor of psychiatry, staff psychiatrist at the VA Palo Alto, and director of the Exploratory Therapeutics Laboratory at Stanford University.
Holly A. Swartz, M.D., is a professor of psychiatry at the University of Pittsburgh School of Medicine and director of the Center for Advanced Psychotherapy at Western Psychiatric Hospital.
They are co-editors of Bipolar II Disorder: Recognition, Understanding, and Treatment from APA Publishing. APA members may purchase the book at a discount.
Sara Schley is the author of Brainstorm: From Broken to Blessed on the Bipolar Spectrum (Seed Systems, 2022). She is the founder of a consulting business and has worked with hundreds of renowned companies worldwide.


Innovations in the treatment of bipolar disorder Stanford University School of Medicine
Servings our Nation's Veterans Stanford University School of Medicine in Collaboration with VA Palo Alto Healthcare System
The bipolar and depression research program.
The Bipolar and Depression Research Program is a clinical research program focused on treatment of individuals with bipolar and major depressive disorders directed by Drs. Trisha Suppes and Michael Ostacher . It is located on the campus of the VA Palo Alto Health Care System and affiliated with the VA and the Stanford School of Medicine. All studies are open to the general public as well as veterans and active duty military personnel. Our research focuses on Bipolar Disorder, including Bipolar Disorder that occurs with Generalized Anxiety Disorder or Life Time Panic Disorder, Major Depressive Disorder and Post Traumatic Stress Disorder (PTSD). We have several current studies underway. A new division of our research efforts is addressing moods disorders using exploratory therapeutics. Compounds under consideration for depressed individuals: Psilocybin and Pramipexole.
Learn more about our current studies
- Research article
- Open access
- Published: 08 February 2021
Bipolar I disorder: a qualitative study of the viewpoints of the family members of patients on the nature of the disorder and pharmacological treatment non-adherence
- Nasim Mousavi 1 ,
- Marzieh Norozpour ORCID: orcid.org/0000-0002-8894-9178 1 ,
- Zahra Taherifar 2 ,
- Morteza Naserbakht 3 &
- Amir Shabani 3
BMC Psychiatry volume 21 , Article number: 83 ( 2021 ) Cite this article
18k Accesses
4 Citations
4 Altmetric
Metrics details
Bipolar disorder is a common psychiatric disorder with a massive psychological and social burden. Research indicates that treatment adherence is not good in these patients. The families’ knowledge about the disorder is fundamental for managing their patients’ disorder. The purpose of the present study was to investigate the knowledge of the family members of a sample of Iranian patients with bipolar I disorder (BD-I) and to explore the potential reasons for treatment non-adherence.
This study was conducted by qualitative content analysis. In-depth interviews were held and open-coding inductive analysis was performed. A thematic content analysis was used for the qualitative data analysis.
The viewpoints of the family members of the patients were categorized in five themes, including knowledge about the disorder, information about the medications, information about the treatment and the respective role of the family, reasons for pharmacological treatment non-adherence, and strategies applied by families to enhance treatment adherence in the patients. The research findings showed that the family members did not have enough information about the nature of BD-I, which they attributed to their lack of training on the disorder. The families did not know what caused the recurrence of the disorder and did not have sufficient knowledge about its prescribed medications and treatments. Also, most families did not know about the etiology of the disorder.
The lack of knowledge among the family members of patients with BD-I can have a significant impact on relapse and treatment non-adherence. These issues need to be further emphasized in the training of patients’ families. The present findings can be used to re-design the guidelines and protocols in a way to improve treatment adherence and avoid the relapse of BD-I symptoms.
Peer Review reports
Bipolar I disorder (BD-I) is a chronic and recurrent psychiatric disorder in which a person has a manic episode for 1 week, which may present before or after hypomanic or major depressive episodes [ 1 ].
BD-I is accompanied by chronic stress, disability, increased risk of sudden mood swings, higher rates of comorbid disorders and moral, financial, and legal problems. The disorder is ranked the sixth debilitating disease according to the World Health Organization (WHO). BD-I is considered the most expensive mental disorder in terms of the health and behavioral care required by the patients and the burden on governmental institutions and insurance companies [ 2 , 3 , 4 ]. According to a report by the Central Bank of the Islamic Republic of Iran, the average annual income of an Iranian household in 2012 was 209,050,000 Rials. The direct annual cost of one BD-I patient consists of 10% of this average family income [ 5 ].
BD-I affects the patient’s life and has long-term consequences that are visible in the patient’s social performance and quality of life [ 6 , 7 ]. Severe impairment in job performance is observed in about 30% of the patients with BD-I. In such cases, functional improvement falls substantially behind symptom improvement [ 1 ].
Pharmacological treatment is the first-line treatment for BD-I. Evidence shows that about 40% of patients with BD-I do not have good medication adherence, which translates into a higher probability of symptom relapse, hospitalization, and increased suicide risk [ 8 ]. In a study in Tehran, Iran, poor treatment adherence was noticed in about 30% of BD-I patients [ 9 ]. Another study from Iran [ 10 ] also reported the prevalence of poor compliance in BD-I patients after the first episode of mania as 38.1% during a 17-month follow-up period. Therefore, it is of great importance to better understand and investigate the underlying reasons for treatment non-adherence in BD-I patients.
Given the changes implemented in health care systems over the last two decades and the resultant focus on community-based services, the role of families in caring for BD-I patients has become more prominent [ 6 ]. The insufficient knowledge of families about the disorder, its symptoms, and medications has made the management of BD-I more difficult and eventually imposes additional costs on them [ 6 ]. The higher is the cost imposed on the family, the more likely is it for the family members to show adverse reactions to the BD-I patients, which itself leads to a higher chance of disorder relapse [ 3 ].
In Iran, the general public is acquainted with various types of psychiatric illnesses through mass media and public educational websites such as the website of the Iranian Psychiatric Association ( https://iranmentalhealth.com ) and other Persian public written sources. Patients with BD-I and their families become familiar with the treatment process after consulting a general practitioner, a psychiatrist, or a psychologist, and, if necessary, the patients are admitted to the hospital through a psychiatrist. In addition to medical treatment, they receive the necessary training and information about their treatment process in the hospital. Furthermore, an association called ABR (Association of Mental Health Promotion), with an active website ( http://abrcharity.ir ), independently monitors patients, including those with bipolar disorder, after discharge.
Many studies have examined the views and roles of patients with BD-I and their caregivers and also the importance of family awareness and its impact on medication adherence. Tacchi & Scott [ 11 ] and Veligan et al. [ 12 ] suggest that the family members’ beliefs about the nature of BD-I and the information they have about the disorder affect the patient’s medication adherence. The review of literature showed no precise studies conducted to explore the knowledge, information, and opinions of family members of BD-I patients about the disorder and the causes of their medication non-adherence.
In a previous study in Iran [ 13 ], the authors held qualitative interviews with the family members of patients with BD-I and reported that treatment non-adherence is a major problem in these patients. They also reported that the patients and their families did not have sufficient knowledge about the nature of this disorder. Considering these findings about the insufficient knowledge of the family members of BD-I patients and the high rate of treatment non-adherence, it is necessary to conduct more studies to investigate the possible causes of treatment non-adherence and families’ knowledge and beliefs about this disorder in Iran. This study was thus carried out to explore the viewpoints of the family members of BD-I patients about the nature of this disorder and the potential causes of treatment non-adherence. The results can be used for revising the psychoeducation guidelines for BD-I patients, as clinical guidelines mandate the inclusion of psychoeducation in the treatment plan adopted for these patients. The results can also be used to design a protocol to address the disorder relapse, which can have substantial consequences in terms of reducing healthcare costs.
The findings of this study are reported according to the Consolidated Criteria for Reporting Qualitative Research (COREQ) checklist [ 14 ].
Study samples’ characteristics
The participants were the family members of patients diagnosed with BD-I. The patients had been admitted to Iran Psychiatry Hospital in Tehran, Iran, and were receiving pharmacological treatments.
This study used purposive sampling to select the participants. From November 2017 to April 2018, 12 patients were interviewed by two psychiatrists based on the DSM-5 criteria [ 1 ] and received the diagnosis of BD-I. Then these diagnoses were confirmed by A.SH. and their families were invited to participate in the study.
None of the family members refused to participate in the study and they all completed the entire course of the study. The mean age of the participants was 50.83 years. There were three male (25%) and nine female (75%) participants (Table 1 ). Table 2 shows further details on patients’ characteristics.
Data collection
After diagnosing patients with BD-I, and obtaining the written consent of the family members of patients to participate in this study, data were collected by in-depth interviews from family members of patients, conducted at the hospital’s conference hall. No one else was present at the time of the interviews except for the interviewer and the participant. Each interview lasted approximately 20 min and was digitally recorded for subsequent analyses. Two female PhD candidates (N. M. and M. N.) in clinical psychology at the University of Social Welfare and Rehabilitation Sciences, Tehran, Iran, who had already received training on the implementation of qualitative studies, held the interviews. They did not know any of the participants. The interviewers introduced themselves to the participants before the beginning of each interview. The interview questions were provided by the authors. The interviews were held only once and were not repeated. Data saturation was reached with 12 participants, and no further participants were interviewed after reaching this number. Data saturation occurs when no new information is obtained by conducting further interviews [ 15 ].
Data analysis
Thematic analysis was used for the qualitative data analysis [ 16 , 17 ]. To this end, the six steps proposed by Clark and Brown [ 17 ] were used.
The raw data derived from the interviews were used for the analysis. The content of the interviews were transcribed verbatim immediately after each interview. Field notes were made during the interviews and were reviewed in this stage. Three authors (M. N., N. M., and Z. T.) read the interviews several times for immersing in the data and getting familiar with it. Line-by-line coding was then applied to generate the initial codes. These steps were performed manually by the three authors without using any computer programs. One author encoded each interview and the interview was then read by another author and encoded again. The individually-extracted codes were then integrated and modified, if necessary.
In the next step, by linking the codes together, their common patterns and concepts were extracted and potential themes and subthemes were identified, keeping the research questions in mind. The data related to the themes were then collected and examined to verify the accuracy of the themes and subthemes, which resulted in five final themes.
Several statements were selected from the interviews as examples and are reported in the results section. To preserve participants’ anonymity, their names and ages are not mentioned in the results; instead, they are represented by random numbers.
Taking into account comprehensiveness, homogeneity, and overlap, the components of the family members’ viewpoints on the nature of the disorder and the reasons for pharmacological treatment non-adherence were categorized into five themes, including knowledge about the disorder, information about the medications, information about the treatment and the respective role of the family, reasons for pharmacological treatment non-adherence, and strategies applied by families to enhance treatment adherence in the patients.
Each of the themes contained several subthemes, which were themselves made up of some open codes. These subthemes contained recurrent codes and concepts that shared a common meaning.
Table 3 presents the themes, subthemes and examples of some of the codes.
Theme one: knowledge about the disorder
Most interviewees did not have sufficient or accurate knowledge about the nature of BD-I, the signs and symptoms of depression and mania cycles, and the outcome of the disorder. They mentioned the lack of training or inadequate training (especially by healthcare providers) as the main cause of insufficient knowledge about BD-I. Additionally, most families did not have a good understanding of the etiology of BD-I.
Some of them considered BD-I as a genetic abnormality, while others considered factors such as adolescent maltreatment, parents’ unusual conditions during sexual intercourse, and the lack of proper training before parenthood as potential causes of BD-I.
Participant No. 5 (a patient’s wife): “I was told that he has a nervous problem.” Participant No. 3 (a patient‘s mother): "I have a theory about having babies. I think that not everyone should have children. The husband and wife should be screened and monitored for two years to see if they understand the matter clearly. Do you see these anomalies now? ... These shameful movies they watch … The person is not feeling well when raising their kid … From an Islamic point of view, from a human’s point of view, both the husband and wife need to be monitored. Their food and other things should also be monitored to see if they can have a healthy baby.”
Participant No. 7 (a patient’s mother): "Because this boy is always impressed by me, sometimes I tell myself, maybe I didn’t fully understand him during his puberty. Sometimes I blame myself, as he has said this many times. I always blame myself … . Sometimes he says, ‘You did this to me, that’s why I’m sick now and take drugs’. For example, when hitting puberty, in the first or second year of high school, he used to get up late and so he got to school very late. Then the school’s principal complained to me, ‘Why is he late again?’ And he says, ‘Why did you wake me up early in the morning? You did this to me.” Participant No. 10 (a patient’s mother), referring to her son's divorce: "That's why he's so broken.” Participant No. 11 (a patient’s sister): "Bipolar disorder has a genetic background. I think there would be no one out there who suffered from the disorder unless they got the genes. It is a genetic disorder, but it emerges when a patient experiences a series of shocking events. Well, some have higher potentials, such as those who get very angry. I mean, the anger itself is not part of the disorder, but in angry people, shocking events affect the patient more rapidly.”
Theme two: information about the medications
Many family members had a misconception about the treatment of the disorder and the effects of psychotropic medications on the patients. In other words, they were unable to accurately identify the therapeutic effects of the administered medications and the time it took for the patients to show signs of improvement. Also, some participants were unaware of the side-effects of the prescribed medications. Some mentioned side-effects like memory loss and drug addiction; however, almost all the participants believed that pharmacological treatment is necessary for the patients despite the side-effects.
Participant No. 1 (a patient’s mother): "The problem of her running away from home with her boyfriend was a big burden for us, but as the prescribed meds began to show their effectiveness, this problem was gradually solved and we finally managed to put up with her aggressiveness and other problems. That is, we were saying to ourselves, ‘This is a period of angriness; we had better not said this, not done that’... We thought the medication was working. But now they’ve told me, ‘No, your patient has not recovered at all, has not been cured.”
Participant No. 1 (a patient's mother): "Her first psychiatrist, who has been visiting her for eight years, was frequently asking if she studies, watches TV or goes to work at all. ‘Whenever she goes back to these routines, then she has recovered,’ the therapist would say. Recently, she’s always been saying, ‘I would love to go to work’ and so on. Once, her employer told her to do some cleaning, and she had responded, ‘I’m not your servant.’ She suddenly broke it off and said, ‘I won’t go to work anymore.’ She didn’t sleep at all, saying, ‘I work so much, but I don’t feel exhausted at all.’ We were also excited and thought ‘Yeah, so this doctor's meds have been good; she’s getting back to normal, she’s working,’ She was frequently organizing her closet, like an obsession.”
Participant No. 3 (a patient’s mother): “I can’t remember the side-effects but I’ve heard about them in classes. My daughter is taking lithium now but she gets these chills. Her stomach is not well. Its side-effects are such that they affect her memory. However, when we compare the pros and cons, we have to take it. "
Theme three: information about the treatment
The regular intake of medications, stress control, work, exercise, regular visits to a psychiatrist or psychologist, and the need to provide insight into the patient’s illness through education were noted by the families in this part. Some participants believed that psychotherapy sessions cannot help treat this disorder while some had completely false or superstitious beliefs about treatment of the disorder.
Participant No. 4 (a patient's son): "Our patient doesn’t accept justifications. When you bring them to classes and convince them that ‘You are sick, and you have to take this medication because of this and that, and we have evidence that you have this disorder,’ and then we show it to them, prove it like in the movies, say that this disorder is serious because of so and so reasons, I think, it would be much easier.”
Participant No. 1 (a patient’s mother): "They sent us to get counseling. Of course, my daughter did not cooperate and didn’t come with. So, I got an appointment under my name to get information and find out how to deal with this disorder. Then the psychologist said, 'No, your daughter is diagnosed with bipolar disorder; this is an acute illness. Counseling does not work for her. She should take medications –a lot of them. And since the doc said those words, we withdrew from counseling altogether.”
Participant No. 5 (a patient’s wife): "My mother-in-law says, ‘If God gives him a baby, he’ll be fine.’ Because his ex-wife also failed to bear a child for him.”
Theme four: information about the role of the family in the treatment
Most families defined their role as helping the patient recover and adhere to their treatment, reminding them to take the medications, encouraging them to go to the doctor, not leaving them alone, and doing whatever they wanted to do so that things went as the patient wished. The patients also appeared to feel guilty when their families tried to comfort them, and this pattern was observed in several of the participants in this study.
Participant No. 6 (a patient’s husband): "We should put up with her, love her, not argue about what she says, listen to her, get her to do exercise to keep busy. I'm here now and I brought her with me too instead of leaving her alone to think about stuff.”
Participant No. 2 (a patient’s mother): "You should be good to them, listen to them, make home a peaceful environment, and not argue.”
Participant No. 8 (a patient’s wife): “I don't know. If he just thinks that everything is okay, all will be okay; but such feelings don’t last forever.”
Participant No. 2 (a patient’s mother): "I tell him to take his meds on time … Say, ‘Let's go to the park to take a look around ... Don't stay at home too much. God is merciful; it won’t be that bad’ … I talk to him, I comfort him sometimes, tell him that I’m ill too because I feel your pain.’ I really do. I’ve been crying alone at home many times. God, what will happen at the end?"(She cries).
Theme five: reasons for pharmacological treatment non-adherence
As for this theme, the participants noted issues that were mostly about the comments made by other people, including relatives or care-providers, such as doctors or specialists in other disciplines. An interesting observation was made by a participant who mentioned a celebrity talking on TV about the inefficiency of medications; following these comments, the patient had stopped taking his medications. Another issue was that the families’ constant changing of the patient’s physician contributed to their medication non-adherence. Another reason noted for non-adherence was that the patients did not suffer from mania symptoms and found that it was not so crucial for them to take the medications. Additionally, some patients reported the physical discomfort and weakness (e.g., impotence) experienced as side-effects of the prescribed medications a reason for their medication non-adherence.
Participant No. 2 (a patient’s mother): "She didn't take the meds for seven to eight months. Her friend had told her ‘Your eyes look different. When you take the medicine, your eyes turn into a strange shape. Get rid of them.’ After seven months, her disease relapsed.”
Participant No. 6 (a patient’s husband): "If we go to a party somewhere and someone asks her, ‘Oh, you take drugs?’ … But that person is not aware of the matter, cause she might look all well, and that person doesn’t know what’s actually happening in my wife’s mind, who then has to admit that she is alright."
Participant No. 7 (a patient’s mother): "At one point at work, some colleagues told him, ‘You will become addicted to the medicines, you will get sick.’ Then, he put the medicines aside and became pessimistic about his work. ‘This job has made me sick,’ so he said and left his job all of a sudden. He had a great job, not a difficult one. He could manage it by himself very easily.”
Participant No. 3 (a patient’s mother): “My son had gone to a doctor to remove the corn on his feet. The doctor had checked his medicine prescriptions and asked, ‘What are these you’re taking? You won’t be able to conceive a baby in the future. It’ll affect you poorly’ and so on. My son keeps repeating what the doctor told him.”
Participant No. 1 (a patient’s mother): "That emergency nurse who came to our house told us to change her doctor. Since then, she has kept repeating this sentence. She threw out all her medicines.”
Participant No. 3 (a patient’s mother): “Since the beginning of the new year, he’s began to no longer take his medications. In Khandevaneh, Footnote 1 Mr. Mehran Ghafourian (a famous Iranian actor) said, ‘I was in a bad mood ... I had depression. I put the medications aside and started exercising.’ My son stopped taking his medicines on hearing those words. I asked him many times to go see a doctor but he said no. He continued to not take his medicines and then his disorder worsened. He was frequently beating us up until we took him to the hospital with the help of the police.”
Participant No. 3 (a patient’s mother): “There was a child psychiatrist on a TV talk. We took our son to her office. We used to visit a counselor as well. The psychiatrist prescribed him some medications. We didn’t know what the medications were. He was taking his medicines. In the middle of therapy, we stopped it. Then, my son-in-law, who is a doctor, said ‘Dr. A -his professor- is a very good doctor.’ My son used to go to Dr. A. earlier when he was a college student. He was taking medicines and he believed in him so much. Then again, my eldest daughter, who is a physician, said ‘Dr. B. is a very helpful therapist. All the doctors, engineers, and educated people go to visit him.’ Then he went there ... And two years ago, I took him to Dr. S. too, to help him get rid of his substance abuse." (This participant named seven different doctors).
Participant No. 4 (a patient’s son) discussed the reasons for the patient’s refusal to take the medications and said: "Well, he doesn't actually believe in the disorder being a real one (in the manic episode). Maybe now he takes the pill in front of you, but you know that it is not something that bothers him. You take pills more easily if you have actual pain, but when you don’t, you ask yourself ‘Why do I have to take all these pills?”
Participant No. 11 (a patient’s sister): “We can note the poor behaviors of those around him. He considers any weaknesses he experiences (e.g., sexual problems) a side-effect of the medicines he’s taking. And he’s linking everything to the medicines and thinking they’re going to make him different from the others.”
The findings of this study regarding the viewpoints of the family members of patients with BD-I were categorized into five themes. Although qualitative studies do not allow for the identification of the extent and relative importance of every condition, recurrent themes and concepts stated by the participants at different individual and social levels were extracted.
Research suggests that there is a relationship between families’ knowledge and beliefs about the disorder and the patients’ medication adherence [ 12 ]. The attitudes and knowledge of the family members have a significant influence on the patient’s own beliefs and attitudes and affect the patient’s decision about treatment compliance [ 18 ]. In agreement with previous studies [ 19 , 20 ], the family caretakers in this study were shown to lack sufficient information and knowledge about the nature of BD-I. In addition, many participants had inaccurate or false information and insisted on these false beliefs. A review study on treatment acceptance found that brief interventions focused on relapse prevention and psychoeducation-based interventions have the greatest impact on relapse prevention [ 21 ]. Maintaining the patients’ circadian rhythms (especially sleep rhythm), controlling activity levels, verifying and controlling initial symptoms of mania and depressive episodes, and not using narcotics or stimulants have been recommended in approved psychotherapy protocols for bipolar patients [ 22 ]. Nonetheless, the participants in this study did not discuss any of these important factors. The lack of knowledge about these important issues among families can have a significant impact on relapse and treatment non-adherence in the patients. These points need to be further emphasized in training patients’ families.
In a qualitative study on bipolar patients and their families, Peters, Pontin, Lobban, and Morriss [ 23 ] found that the viewpoints of patients and their families play an important role in managing the disorder; however, the families usually get despondent about participating in this process, and their perception was that some mental health workers believe that family involvement makes their work more complicated. Meanwhile, the present study showed that, in Iran, families do not have enough information about their role in preventing disorder relapse and attribute their patient’s relapse only to factors such as medication withdrawal, unemployment, lack of community support, and financial problems. Most of them believed that if everything goes as the patient wishes, the disorder will not relapse.
Furthermore, the participants did not have adequate information about the non-pharmacological treatment options available for this disorder and the role that psychologists can play in helping the patients enhance their medication adherence and prevent the symptoms of relapse. A variety of behavioral, cognitive, and emotion-focused interventions are used in the management of bipolar disorders [ 22 ]. Nevertheless, the participants did not have sufficient knowledge about these treatments. The observation that many psychologists in Iran appear unwilling to participate in the treatment of bipolar disorder patients seems to play a role in this lack of knowledge. According to Farhoudian et al. [ 24 ], only about 1.5% of all the studies on psychiatric disorders conducted in Iran between 1973 and 2003 involved bipolar and cyclothymic patients. In a qualitative study on bipolar-II patients and their families, Fisher et al. [ 25 ] found that the number of resources available to patients for deciding about their treatment has increased and their priorities have been given increasing attention; yet, the patients’ and their families’ preferences are not fully considered.
Similar to the studies carried out by Jönsson, Wijk, Skärsäter & Danielson [ 26 ] and Shamsaei, Mohamad Khan Kermanshahi, and Vanaki [ 27 ], in the present study, the patients and their families were struggling with the acceptance, understanding, and management of the disorder. According to the participants, the families’ lack of insight into the patients’ disorder contributed significantly to their medication non-adherence. This finding is in line with Scott and Pope’s [ 28 ] research, but Delmas, Proudfoot, Parker, and Manicavasagar [ 29 ] stated that the rejection of treatment is a complex issue that depends on various factors.
Some of the results of this study are consistent with the findings reported by Clatworthy, Bowskill, Rank, Parham, and Horne [ 8 ], who noted that deliberate treatment non-adherence is associated with factors such as patients’ concerns about the prescribed medications and their side-effects in the case of continuous consumption. Proudfoot et al. [ 30 ] stated that the side-effects of medications, coping with unpleasant symptoms, the extent of awareness about the nature of the disorder, and the reactions to it as well as the stigma associated with the disorder affect the patient’s life path. Besides, these symptoms have a permanent impact on the disorder relapse [ 31 ]. The findings showed that the interaction of the disorder, patient, medications, psychiatric attitude, and cultural attitude with non-compliance is very complex [ 32 ].
In addition to the themes mentioned, there were some interesting results concerning the response process in all the interviews. For example, the majority of the participants only reported symptoms of the manic episode, while two major studies [ 33 , 34 ] have shown that people with bipolar I and II (especially type II) disorders spend most of their symptomatic days with depression. Patients suffer greatly during the depressive episodes but have elevated or irritable moods during the manic episode; in contrast, families find the mania symptoms more annoying and disruptive to themselves. This duality can negatively impact reaching a common understanding with the patient about visiting the doctor and taking medications. Moreover, the fact that some families do not have enough information about the depressive episode can eventuate in neglecting the patient’s need to take medications during this phase, which can then adversely affect medication adherence. These results are somewhat contradictory to the results of a previous study [ 29 ], which reported that both patients and their family members report symptoms of mania and hypomania to their physicians less often, as some of them enjoy the manic symptoms. Family members feel relieved when they see that their patient is happy and shows mania symptoms. A major cause of this discrepancy in findings may be the differences in the study populations. While Delmas et al. [ 29 ] studied patients with bipolar I and II, the present study examined only patients with BD-I. The discrepancy may also partially originate from cultural differences. It seems that when there is a pattern of greater attention to objective and apparent symptoms, very important mental symptoms such as suicidal thoughts, whether during the mania or depressive episode, are neglected by families.
This study showed that families with a higher educational and socioeconomic status tend to seek psychiatric care from different psychiatrists. Frequently changing the treating psychiatrist can cause treatment non-adherence in the patients. Furthermore, as the family members of such patients falsely think that they have greater medical information, they are more likely to encourage the patient to stop taking their prescribed medications.
A major limitation of this study was that most participants were the mothers of the patients, as it was hard to find other family members of the patients to participate in the study. For example, only one child of a patient and one sister were among the participants. Also, all the participants were from Tehran and were selected from one hospital; therefore, the generalization of the results to other cities in Iran should be pursued with caution.
The authors suggest using the findings of this qualitative study regarding the knowledge of the family members of patients with bipolar I disorder (BD-I) as well as the dominating cultural beliefs to design further quantitative studies. The quantitative assessment of individual, familial, and social reasons for treatment non-adherence is also a recommendation for future research. Conducting similar studies on the family members of patients with other types of bipolar disorder with an attention to the different processes and outcomes involved is also recommended. Since there are different ethnicities and subcultures in Iran, the results obtained by examining the residents of the country’s capital city cannot be generalized to the population of other cities and towns, and it is necessary to repeat the study in other populations in order to get familiar with other viewpoints in Iran.
Overall, the results of this study contribute to the emerging qualitative research on bipolar disorder and provide the readers with an insight into the viewpoints of the family members of patients with BD-I. Some inaccurate information might have been observed in participants’ statements due to some deeply-rooted cultural attitudes and beliefs and their correction may require extensive interventions.
The results of this study can be used to compile educational content for patients with bipolar disorder and their families as well as for psychologists, psychiatrists, psychiatry assistants, and hospital health workers.

Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
A popular comedy show on Iranian television
Diagnostic and statistical manual of mental disorders. Fifth edition (DSM-5). Arlington: American Psychiatric Association; 2013.
Kaushik P, Bhatia M. Burden and quality of life in spouses of patients with schizophrenia and bipolar disorder. Delhi Psychiatry J. 2013;16(1):83-9.
Maji KR SMSRKS, Maji KR, Sood M, Sagar R, Khandelwal SK. No Title. 2012 Mar 18 [cited 2020 mar 16];58(2). Available from: http://www.ncbi.nlm.nih.gov/pubmed/21421638 .
Zergew A, Hailemariam D, Alem A, Kebede D. A longitudinal comparative analysis of economic and family caregiver burden due to bipolar disorder. Afr J Psychiatry. 2008;11(3):191–8.
Article Google Scholar
Shirkhoda SA. The investigation of the amount of cost for bipolar disorder type I and its related factors during the 1-year follow-up for the hospitalized patients in Iran educational-therapeutic psychiatric center [dissertaion]. Iran University of Medical Sciences ;2014.
Jönsson PD, Skärsäter I, Wijk H, Danielson E. Experience of living with a family member with bipolar disorder. Int J Ment Health Nurs. 2011;20(1):29–37.
Shabani A, Ahmadzad-Asl M, Zangeneh K, Teimurinejad S, Kokar S, Taban M, et al. Quality of life in patients with bipolar I disorder: is it related to disorder outcome? Acta Med Iran 2013:51(6):386-93.
Clatworthy J, Bowskill R, Rank T, Parham R, Horne R. Adherence to medication in bipolar disorder: a qualitative study exploring the role of patients’ beliefs about the condition and its treatment. Bipolar Disord 2007;9(6):656-64.
Sharifi A, Shabani A, Ahmadzadasl M. The pattern of adherence in patients with bipolar I disorder; an eight weeks study: Iranian Journal of Psychiatry and Behav Sci 2009;3(2):39-43.
Shabani A, Eftekhar M. Non Compliance After First Episode of Manic or Mixed Mood State: A 17-Month Follow-up. 2007;1(2):46-49.
Tacchi M-J, Scott J. Improving adherence in schizophrenia and bipolar disorders: Wiley; 2005;7:24-31.
Velligan D, Weiden P, Sajatovic M, Scott J, Carpenter D, Ross R, et al. Expert Consensus Panel on Adherence Problems in Serious and Persistent Mental Illness. The expert consensus guideline series: adherence problems in patients with serious and persistent mental illness. J Clin Psychiatry 2009;70(suppl 4):1-46.
Shabani A, Sobhani S, Tahmasebi N, Ghahramani S, Dejman M: How family caregivers of patients with bipolar disorder conceptualize caring problems: a qualitative study, unpublished.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007;19(6):349-57.
Fusch PI, Ness LR. Are we there yet? Data saturation in qualitative research. Qual Rep. 2015;20(9):1408.
Clarke V, Braun V. Using thematic analysis in counselling and psychotherapy research: A critical reflection. Couns Psychother Res 2018;18(2):107-10.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3(2):77-101.
Chakrabarti S. Treatment-adherence in bipolar disorder: a patient-centred approach. World J Psychiatry 2016;6(4):399.
Shamsaei F, Mohammadkhan Kermanshahi S, Vanaki Z. Survey of Family Caregiver Needs of Patients with Bipolar Disorder. Avicenna J Clin Med 2010;17(3):57-63.
Rahmani F, Ebrahimi H, Ranjbar F, Asghari E. The effect of group psychoeducational program on attitude toward mental illness in family caregivers of patients with bipolar disorder. Hayat. 2016;21(4):65-79.
MacDonald L, Chapman S, Syrett M, Bowskill R, Horne R. Improving medication adherence in bipolar disorder: A systematic review and meta-analysis of 30 years of intervention trials. J Affect Disord 2016;194:202-21.
Wright JH. Cognitive-behavior therapy for severe mental illness: An illustrated guide: American Psychiatric Pub; 2009.
Peters S, Pontin E, Lobban F, Morriss R. Involving relatives in relapse prevention for bipolar disorder: a multi-perspective qualitative study of value and barriers. BMC Psychiatry 2011;11(1):172.
Farhoudian A, Rad Goodarzi R, Rahimi Movaghar A, Sharifi V, Mohammadi MR, Sahimi Izadian E, et al. Trend of Researches in the Field of Psychiatric Disorders in Iran. Iran J Psychiatry Clin Psychol 2007;12(4):327-36.
Fisher A, Manicavasagar V, Sharpe L, Laidsaar-Powell R, Juraskova I. A qualitative exploration of patient and family views and experiences of treatment decision-making in bipolar II disorder. J Ment Health 2018;27(1):66-79.
Jönsson PD, Wijk H, Skärsäter I, Danielson E. Persons living with bipolar disorder—their view of the illness and the future. Issues Mental Health Nurs 2008;29(11):1217-36.27.
Shamsaei F, Mohamad khan Kermanshahi S, Vanaki Z. Meaning of Health from the Perspective of Family Member Caregiving to Patients with Bipolar Disorder. Journal of Mazandaran University of Medical Sciences. 2012;22(90):52-65.
Scott J, Pope M. Nonadherence with mood stabilizers: prevalence and predictors. J Clin Psychiatry 2002;63(5):384-390.
Delmas K, Proudfoot J, Parker G, Manicavasagar V. Recoding past experiences: A qualitative study of how patients and family members adjust to the diagnosis of bipolar disorder. J Nerv Ment Dis 2011;199(2):136-9.
Proudfoot JG, Parker GB, Benoit M, Manicavasagar V, Smith M, Gayed A. What happens after diagnosis? Understanding the experiences of patients with newly-diagnosed bipolar disorder. Health Expect 2009;12(2):120-9.
Crowe M, Inder M, Carlyle D, Wilson L, Whitehead L, Panckhurst A, et al. Feeling out of control: a qualitative analysis of the impact of bipolar disorder. J Psychiatr Ment Health Nurs 2012;19(4):294-302.
Weiss RD, Greenfield SF, Najavits LM, Soto JA, Wyner D, Tohen M, et al. Medication compliance among patients with bipolar disorder and substance use disorder. J Clin Psychiatry 1998;59(4):172-4.
Judd LL, Akiskal HS, Schettler PJ, Endicott J, Maser J, Solomon DA, et al. The long-term natural history of the weekly symptomatic status of bipolar I disorder. Arch Gen Psychiatry 2002;59(6):530-7.
Judd LL, Schettler PJ, Akiskal HS, Maser J, Coryell W, Solomon D, et al. Long-term symptomatic status of bipolar I vs. bipolar II disorders. Int J Neuropsychopharmacol 2003;6(2):127-37.
Download references
Acknowledgements
The authors express their gratitude to all the staff of Iran Psychiatry Hospital for their generous cooperation in the study.
This research is funded by the Mental Health Research Center of Iran University of Medical Sciences (grant number 95–01–121-27963).
The views expressed are those of the authors and not necessarily those of the Mental Health Research Center of Iran University of Medical Sciences. The funders had no role in the study design, data collection and analysis, interpretation, decision to publish or the writing and preparation of the manuscript.
Author information
Authors and affiliations.
Department of Clinical Psychology, University of Social Welfare and Rehabilitation Sciences, Tehran, Islamic Republic of Iran
Nasim Mousavi & Marzieh Norozpour
Department of Psychology, Faculty of Psychology and Educational Sciences, University of Tehran, Tehran, Islamic Republic of Iran
Zahra Taherifar
Faculty of Behavioral Sciences and Mental Health, Tehran Psychiatry Institute, Iran University of Medical Sciences, Tehran, Islamic Republic of Iran
Morteza Naserbakht & Amir Shabani
You can also search for this author in PubMed Google Scholar
Contributions
NM, MN and ASH conceived the study idea and design. NM, and MN conducted the interviews. NM, MN and ZT conducted transcription and data analysis. NM, MNA and ZT interpreted and presented the results, and contributed to the manuscript. ASH supervised the research activities and contributed to the interpretation of results. NM, MN and ZT wrote the manuscript. All authors have read, edited and approved the final manuscript for submission.
Corresponding author
Correspondence to Marzieh Norozpour .
Ethics declarations
Ethics approval and consent to participate.
This research has been approved by the Research Ethics Committee of Iran University of Medical Sciences (Code of Ethics: IR.IUMS.REC 1395.95–01–121-27963). Written informed consent was obtained from all the research participants prior to participating in the study.
Consent for publication
Not applicable as no personal information is provided in the manuscript.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Mousavi, N., Norozpour, M., Taherifar, Z. et al. Bipolar I disorder: a qualitative study of the viewpoints of the family members of patients on the nature of the disorder and pharmacological treatment non-adherence. BMC Psychiatry 21 , 83 (2021). https://doi.org/10.1186/s12888-020-03008-x
Download citation
Received : 20 March 2020
Accepted : 08 December 2020
Published : 08 February 2021
DOI : https://doi.org/10.1186/s12888-020-03008-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Bipolar I disorder
- Treatment non-adherence
- Family psychological education
- Qualitative study
BMC Psychiatry
ISSN: 1471-244X
- Submission enquiries: [email protected]
- General enquiries: [email protected]

Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years! Learn More >>
- Health Topics
- Brochures and Fact Sheets
- Help for Mental Illnesses
- Clinical Trials
Bipolar Disorder
What is bipolar disorder.
Bipolar disorder (formerly called manic-depressive illness or manic depression) is a mental illness that causes unusual shifts in a person’s mood, energy, activity levels, and concentration. These shifts can make it difficult to carry out day-to-day tasks.
There are three types of bipolar disorder. All three types involve clear changes in mood, energy, and activity levels. These moods range from periods of extremely “up,” elated, irritable, or energized behavior (known as manic episodes) to very “down,” sad, indifferent, or hopeless periods (known as depressive episodes). Less severe manic periods are known as hypomanic episodes.
- Bipolar I disorder is defined by manic episodes that last for at least 7 days (nearly every day for most of the day) or by manic symptoms that are so severe that the person needs immediate medical care. Usually, depressive episodes occur as well, typically lasting at least 2 weeks. Episodes of depression with mixed features (having depressive symptoms and manic symptoms at the same time) are also possible. Experiencing four or more episodes of mania or depression within 1 year is called “rapid cycling.”
- Bipolar II disorder is defined by a pattern of depressive episodes and hypomanic episodes. The hypomanic episodes are less severe than the manic episodes in bipolar I disorder.
- Cyclothymic disorder (also called cyclothymia) is defined by recurring hypomanic and depressive symptoms that are not intense enough or do not last long enough to qualify as hypomanic or depressive episodes.
Sometimes a person might experience symptoms of bipolar disorder that do not match the three categories listed above, and this is referred to as “other specified and unspecified bipolar and related disorders.”
Bipolar disorder is often diagnosed during late adolescence (teen years) or early adulthood. Sometimes, bipolar symptoms can appear in children. Although the symptoms may vary over time, bipolar disorder usually requires lifelong treatment. Following a prescribed treatment plan can help people manage their symptoms and improve their quality of life.
What are the signs and symptoms of bipolar disorder?
People with bipolar disorder experience periods of unusually intense emotion and changes in sleep patterns and activity levels, and engage in behaviors that are out of character for them—often without recognizing their likely harmful or undesirable effects. These distinct periods are called mood episodes. Mood episodes are very different from the person’s usual moods and behaviors. During an episode, the symptoms last every day for most of the day. Episodes may also last for longer periods, such as several days or weeks.
Sometimes people have both manic and depressive symptoms in the same episode, and this is called an episode with mixed features. During an episode with mixed features, people may feel very sad, empty, or hopeless while at the same time feeling extremely energized.
A person may have bipolar disorder even if their symptoms are less extreme. For example, some people with bipolar II disorder experience hypomania, a less severe form of mania. During a hypomanic episode, a person may feel very good, be able to get things done, and keep up with day-to-day life. The person may not feel that anything is wrong, but family and friends may recognize changes in mood or activity levels as possible symptoms of bipolar disorder. Without proper treatment, people with hypomania can develop severe mania or depression.
Receiving the right diagnosis and treatment can help people with bipolar disorder lead healthy and active lives. Talking with a health care provider is the first step. The health care provider can complete a physical exam and other necessary medical tests to rule out other possible causes. The health care provider may then conduct a mental health evaluation or provide a referral to a trained mental health care provider, such as a psychiatrist, psychologist, or clinical social worker who has experience in diagnosing and treating bipolar disorder.
Mental health care providers usually diagnose bipolar disorder based on a person’s symptoms, lifetime history, experiences, and, in some cases, family history. Accurate diagnosis in youth is particularly important.
Find tips to help prepare for and get the most out of your visit with your health care provider.
Bipolar disorder and other conditions
Many people with bipolar disorder also have other mental disorders or conditions such as anxiety disorders , attention-deficit/hyperactivity disorder (ADHD) , misuse of drugs or alcohol , or eating disorders. Sometimes people who have severe manic or depressive episodes also have symptoms of psychosis , which may include hallucinations or delusions. The psychotic symptoms tend to match the person’s extreme mood. For example, someone having psychotic symptoms during a depressive episode may falsely believe they are financially ruined, while someone having psychotic symptoms during a manic episode may falsely believe they are famous or have special powers.
Looking at a person’s symptoms over the course of the illness and examining their family history can help a health care provider determine whether the person has bipolar disorder along with another disorder.
What are the risk factors for bipolar disorder?
Researchers are studying possible causes of bipolar disorder. Most agree that there are many factors that are likely to contribute to a person’s chance of having the disorder.
Brain structure and functioning: Some studies show that the brains of people with bipolar disorder differ in certain ways from the brains of people who do not have bipolar disorder or any other mental disorder. Learning more about these brain differences may help scientists understand bipolar disorder and determine which treatments will work best. At this time, health care providers base the diagnosis and treatment plan on a person’s symptoms and history, rather than brain imaging or other diagnostic tests.
Genetics: Some research suggests that people with certain genes are more likely to develop bipolar disorder. Research also shows that people who have a parent or sibling with bipolar disorder have an increased chance of having the disorder themselves. Many genes are involved, and no one gene causes the disorder. Learning more about how genes play a role in bipolar disorder may help researchers develop new treatments.
How is bipolar disorder treated?
Treatment can help many people, including those with the most severe forms of bipolar disorder. An effective treatment plan usually includes a combination of medication and psychotherapy, also called talk therapy.
Bipolar disorder is a lifelong illness. Episodes of mania and depression typically come back over time. Between episodes, many people with bipolar disorder are free of mood changes, but some people may have lingering symptoms. Long-term, continuous treatment can help people manage these symptoms.
Certain medications can help manage symptoms of bipolar disorder. Some people may need to try different medications and work with their health care provider to find the medications that work best.
The most common types of medications that health care providers prescribe include mood stabilizers and atypical antipsychotics. Mood stabilizers such as lithium or valproate can help prevent mood episodes or reduce their severity. Lithium also can decrease the risk of suicide. Health care providers may include medications that target sleep or anxiety as part of the treatment plan.
Although bipolar depression is often treated with antidepressant medication, a mood stabilizer must be taken as well—taking an antidepressant without a mood stabilizer can trigger a manic episode or rapid cycling in a person with bipolar disorder.
Because people with bipolar disorder are more likely to seek help when they are depressed than when they are experiencing mania or hypomania, it is important for health care providers to take a careful medical history to ensure that bipolar disorder is not mistaken for depression.
People taking medication should:
- Talk with their health care provider to understand the risks and benefits of the medication.
- Tell their health care provider about any prescription drugs, over-the-counter medications, or supplements they are already taking.
- Report any concerns about side effects to a health care provider right away. The health care provider may need to change the dose or try a different medication.
- Remember that medication for bipolar disorder must be taken consistently, as prescribed, even when one is feeling well.
It is important to talk to a health care provider before stopping a prescribed medication. Stopping a medication suddenly may lead symptoms to worsen or come back. You can find basic information about medications on NIMH's medications webpage . Read the latest medication warnings, patient medication guides, and information on newly approved medications on the Food and Drug Administration (FDA) website.
Psychotherapy
Psychotherapy, also called talk therapy, can be an effective part of treatment for people with bipolar disorder. Psychotherapy is a term for treatment techniques that aim to help people identify and change troubling emotions, thoughts, and behaviors. This type of therapy can provide support, education, and guidance to people with bipolar disorder and their families.
Cognitive behavioral therapy (CBT) is an important treatment for depression, and CBT adapted for the treatment of insomnia can be especially helpful as part of treatment for bipolar depression.
Treatment may also include newer therapies designed specifically for the treatment of bipolar disorder, including interpersonal and social rhythm therapy (IPSRT) and family-focused therapy.
Learn more about the various types of psychotherapies .
Other treatment options
Some people may find other treatments helpful in managing their bipolar symptoms:
- Electroconvulsive therapy (ECT) is a brain stimulation procedure that can help relieve severe symptoms of bipolar disorder. Health care providers may consider ECT when a person’s illness has not improved after other treatments, or in cases that require rapid response, such as with people who have a high suicide risk or catatonia (a state of unresponsiveness).
- Repetitive transcranial magnetic stimulation (rTMS) is a type of brain stimulation that uses magnetic waves to relieve depression over a series of treatment sessions. Although not as powerful as ECT, rTMS does not require general anesthesia and has a low risk of negative effects on memory and thinking.
- Light therapy is the best evidence-based treatment for seasonal affective disorder (SAD) , and many people with bipolar disorder experience seasonal worsening of depression or SAD in the winter. Light therapy may also be used to treat lesser forms of seasonal worsening of bipolar depression.
Unlike specific psychotherapy and medication treatments that are scientifically proven to improve bipolar disorder symptoms, complementary health approaches for bipolar disorder, such as natural products, are not based on current knowledge or evidence. Learn more on the National Center for Complementary and Integrative Health website .
Finding treatment
- A family health care provider is a good resource and can be the first stop in searching for help. Find tips to help prepare for and get the most out of your visit .
- To find mental health treatment services in your area, call the Substance Abuse and Mental Health Services Administration (SAMHSA) National Helpline at 1-800-662-HELP (4357), visit the SAMHSA online treatment locator , or text your ZIP code to 435748.
- Learn more about finding help on the NIMH website.
If you or someone you know is struggling or having thoughts of suicide, call or text the 988 Suicide & Crisis Lifeline at 988 or chat at 988lifeline.org . In life-threatening situations, call 911.
Coping with bipolar disorder
Living with bipolar disorder can be challenging, but there are ways to help make it easier.
- Work with a health care provider to develop a treatment plan and stick with it. Treatment is the best way to start feeling better.
- Follow the treatment plan as directed. Work with a health care provider to adjust the plan, as needed.
- Structure your activities. Try to have a routine for eating, sleeping, and exercising.
- Try regular, vigorous exercise like jogging, swimming, or bicycling, which can help with depression and anxiety, promote better sleep, and support your heart and brain health.
- Track your moods, activities, and overall health and well-being to help recognize your mood swings.
- Ask trusted friends and family members for help in keeping up with your treatment plan.
- Be patient. Improvement takes time. Staying connected with sources of social support can help.
Long-term, ongoing treatment can help control symptoms and enable you to live a healthy life.
How can I find a clinical trial for bipolar disorder?
Clinical trials are research studies that look at new ways to prevent, detect, or treat diseases and conditions. The goal of clinical trials is to determine if a new test or treatment works and is safe. Although individuals may benefit from being part of a clinical trial, participants should be aware that the primary purpose of a clinical trial is to gain new scientific knowledge so that others may be better helped in the future.
Researchers at NIMH and around the country conduct many studies with patients and healthy volunteers. We have new and better treatment options today because of what clinical trials uncovered years ago. Be part of tomorrow’s medical breakthroughs. Talk to your health care provider about clinical trials, their benefits and risks, and whether one is right for you.
To learn more or find a study, visit:
- NIMH’s Clinical Trials webpage : Information about participating in clinical trials
- Clinicaltrials.gov: Current Studies on Bipolar Disorder : List of clinical trials funded by the National Institutes of Health (NIH) being conducted across the country
- Join a Study: Bipolar Disorder – Adults : List of studies being conducted on the NIH Campus in Bethesda, MD
Where can I learn more about bipolar disorder?
Free brochures and shareable resources.
- Bipolar Disorder : A brochure on bipolar disorder that offers basic information on signs and symptoms, treatment, and finding help. Also available en español .
- Bipolar Disorder in Children and Teens : A brochure on bipolar disorder in children and teens that offers basic information on signs and symptoms, treatment, and finding help. Also available en español .
- Bipolar Disorder in Teens and Young Adults: Know the Signs : An infographic presenting common signs and symptoms of bipolar disorder in teens and young adults. Also available en español .
- Shareable Resources on Bipolar Disorder : Digital resources, including graphics and messages, to help support bipolar disorder awareness and education.
- NIMH Experts Discuss Bipolar Disorder in Adults : Learn the signs and symptoms, risk factors, treatments of bipolar disorder, and the latest NIMH-supported research in this area.
- Mental Health Minute: Bipolar Disorder in Adults : A minute-long video to learn about bipolar disorder in adults.
- NIMH Expert Discusses Bipolar Disorder in Adolescents and Young Adults : A video with an expert who explains the signs, symptoms, and treatments of bipolar disorder.
Research and Statistics
- Journal Articles : This webpage provides information on references and abstracts from MEDLINE/PubMed (National Library of Medicine).
- Bipolar Disorder Statistics : An NIMH webpage that provides information on the prevalence of bipolar disorder among adults and adolescents.
Last Reviewed: February 2024
Unless otherwise specified, the information on our website and in our publications is in the public domain and may be reused or copied without permission. However, you may not reuse or copy images. Please cite the National Institute of Mental Health as the source. Read our copyright policy to learn more about our guidelines for reusing NIMH content.
- Open access
- Published: 06 December 2023
Facts and myths about the use of lithium for bipolar disorder in routine clinical practice: an expert consensus paper
- Andrea Fiorillo 1 ,
- Gaia Sampogna 1 ,
- Umberto Albert 2 ,
- Giuseppe Maina 3 , 4 ,
- Giulio Perugi 5 ,
- Maurizio Pompili 6 ,
- Gianluca Rosso 3 , 4 ,
- Gabriele Sani 7 , 8 &
- Alfonso Tortorella 9
Annals of General Psychiatry volume 22 , Article number: 50 ( 2023 ) Cite this article
4556 Accesses
25 Altmetric
Metrics details
Bipolar disorder is one of the most burdensome severe mental disorders, characterized by high levels of personal and social disability. Patients often need an integrated pharmacological and non-pharmacological approach. Lithium is one of the most effective treatments available not only in psychiatry, but in the whole medicine, and its clinical efficacy is superior to that of other mood stabilizers. However, a declining trend on lithium prescriptions has been observed worldwide in the last 20 years, supporting the notion that lithium is a ‘forgotten drug’ and highlighting that the majority of patients with bipolar disorder are missing out the best available pharmacological option.
Based on such premises, a narrative review has been carried out on the most common “misconceptions” and “stereotypes” associated with lithium treatment; we also provide a list of “good reasons” for using lithium in ordinary clinical practice to overcome those false myths.
A narrative search of the available literature has been performed entering the following keywords: “bipolar disorder”, “lithium”, “myth”, “mythology”, “pharmacological treatment”, and “misunderstanding”. The most common false myths have been critically revised and the following statements have been proposed: (1) Lithium should represent the first choice for the treatment of patients with bipolar disorder; (2) lithium treatment is effective in different patients’ groups suffering from bipolar disorder; (3) Drug–drug interaction risk can be easily managed during lithium treatment; (4) The optimal management of lithium treatment includes periodical laboratory tests; (5) Slow-release lithium formulation has advantages compared to immediate release formulation; (6) Lithium treatment has antisuicidal properties; (7) Lithium can be carefully managed during pregnancy.
Conclusions
In recent years, a discrepancy between evidence-based recommendations and clinical practice in using lithium treatment for patients with bipolar disorder has been highlighted.
It is time to disseminate clear and unbiased information on the clinical efficacy, effectiveness, tolerability and easiness to use of lithium treatment in patients with bipolar disorder. It is necessary to reinvigorate the clinical and academic discussion about the efficacy of lithium, to counteract the decreasing prescription trend of one of the most effective drugs available in the whole medicine.
Bipolar disorder is one of the most burdensome severe mental disorders, characterized by high levels of personal and social disability [ 1 ]. Patients often need an integrated [ 2 , 3 , 4 ] and personalized [ 5 , 6 ] pharmacological and non-pharmacological approach [ 7 , 8 ]. In particular, when an acute depressive, manic or mixed episode occurs, a pharmacological treatment is usually needed; however, the majority of bipolar patients need long-term treatments, to prolong the free interval, to prevent recurrences, to lessen subthreshold symptoms, to improve relational, social, and occupational functioning [ 6 , 9 ]. Treatment may be complicated by the presence of comorbid physical illnesses, such as cardiovascular diseases, metabolic syndromes (i.e., type 2 diabetes and obesity) [ 10 , 11 , 12 ], and other mental disorders, such as alcohol or substance disorder, anxiety disorders and personality disorders [ 13 , 14 , 15 , 16 , 17 , 18 , 19 ].
Several pharmacological treatments are indicated as first-line treatment for the management of patients with bipolar disorder, with lithium being the gold standard due to its established mood-stabilizing properties, its effectiveness in preventing recurrences, and its anti-suicidal effects [ 20 , 21 ]. Since its introduction more than 70 years ago [ 22 ], lithium has been successfully used to treat bipolar disorder, and it is now unanimously considered the first line option for acute and long-term treatment [ 23 , 24 ]. Lithium is also highly effective in other serious mental disorders characterized by internalizing and externalizing behaviours, due to its anti-impulsivity and anti-suicidality effects.
Lithium is one of the most effective treatments available not only in psychiatry, but in the whole medicine [ 25 ], and its clinical efficacy is superior to that of other mood stabilizers. However, a declining trend on lithium prescriptions has been observed worldwide in the last 20 years, supporting the notion that lithium is a ‘forgotten drug’ [ 26 ] and highlighting that the majority of BD patients are missing out the best available pharmacological option [ 27 ].
This decreasing trend in the use of lithium in clinical practice can be due to several factors, including its narrow therapeutic index, the side-effect/tolerability profile, the need for regular blood checking [ 28 ], the preference of many psychiatrists—particularly the less experienced ones—to use other mood stabilizers which are commonly considered more manageable, safer and less toxic [ 29 ]. However, this reflects an important incongruity between evidence-based recommendations and psychiatric clinical practice, and is probably due to the presence of several “false myths” about lithium use among physicians [ 21 , 28 ], patients and their family members. Providing appropriate education might reverse this concerning trend. Thus, efforts in improving training on lithium should represent a priority for postgraduates and residents around the world in the next years [ 30 ].
Based on such premises, we carried out a narrative review of the available literature on the most common “misconceptions” and “stereotypes” associated with lithium treatment; for each false myth, we provide a list of “good reasons” for using lithium in ordinary clinical practice.
The keywords “bipolar disorder”, “lithium”, “myth”, “mythology”, “pharmacological treatment”, and “misunderstanding” were entered in PubMed, ISI Web of Knowledge, Scopus and Medline. Terms and databases were combined using the Boolean search technique, which consists of a logical information retrieval system (two or more terms combined to make searches more restrictive or detailed).
All selected papers were evaluated by two authors (GS and AF); main findings of included papers are summarized in Fig. 1 and in Table 1 .
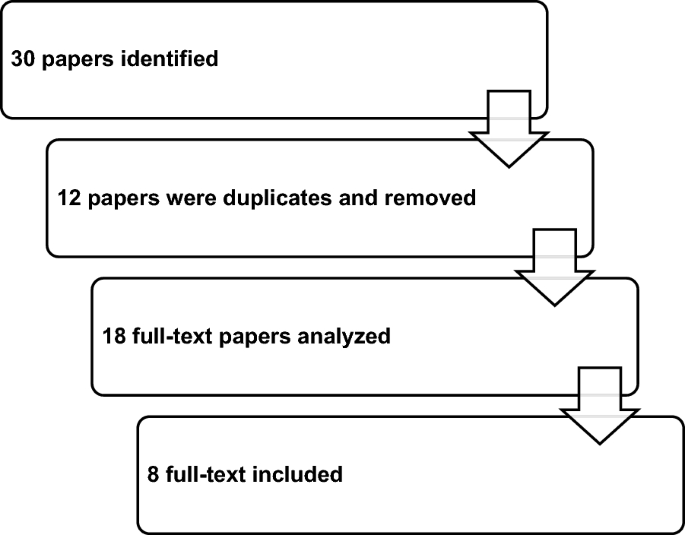
Selection process of included papers in the narrative review
Results from the narrative clinical review
Based on the search strategy, 30 papers were identified; 12 papers were removed because duplicates; 18 full-text papers were fully analyzed, and eight papers were finally included in the review (Fig. 1 ).
The majority of studies were carried out in the US [ 31 , 32 , 33 , 34 , 35 , 36 , 37 ] in the period 1968–2021 and published in peer-reviewed international scientific journals, such as the American Journal of Psychiatry or Bipolar Disorder (Table 1 ).
The most common false myths, which have been critically revised, are the following: (1) lithium is not the first choice for treating patients with bipolar disorder; (2) lithium should be avoided in adolescents or elderly patients due to its side effects; (3) the risk of drug–drug interactions is one of the most common limitations in lithium treatment; (4) weekly lab tests are required during treatment with lithium; (5) different lithium formulations do not modify its tolerability profile; (6) no drug has antisuicidal effects; (7) lithium should be avoided during pregnancy (Table 2 ). The following statements, based upon the most recent evidence on lithium treatment, are proposed: (1) lithium should represent the first choice for the treatment of patients with bipolar disorder; (2) lithium treatment is effective in different patients’ groups, including young and elderly patients; (3) the risk of drug–drug interaction during lithium treatment can be easily managed; (4) the optimal management of lithium treatment includes periodical laboratory tests; (5) slow-release lithium formulation has advantages compared to immediate release formulation; (6) lithium has an antisuicidal effect; (7) lithium can be carefully managed during pregnancy.
Myth 1: lithium is not the first choice for treating patients with bipolar disorder
Fact 1: lithium should represent the first choice for the treatment of patients with bipolar disorder.
Lithium plays a relevant role in acute and long-term management of bipolar disorder and must considered as first-line treatment [ 38 ]. In fact, lithium increases the duration of free intervals, minimizes the risk of recurrences and improves inter-episodic symptomatology. Nowadays, lithium is still the gold standard in studies evaluating the efficacy of various medications in the long-term treatment of recurrent mood disorders [ 39 ].
Available evidence strongly indicates that patients suffering from bipolar disorder should be primarily treated with lithium, using other mood stabilizers as add-on in case of partial response [ 40 ]. Moreover, lithium treatment should be started as early as possible, since response rates for mania and for long-term treatments decrease in individuals with more than three episodes [ 41 ]. Maintenance treatment with lithium should be started after two hypomanic episodes or even after one severe psychotic, manic or mixed episode [ 42 ].
Patients should be educated about the many benefits of a long-term treatment with lithium, in terms of prophylaxis of mood episodes, reduction of suicidal risk, and neuroprotective effects, with a probable reduction of the risk of dementia and a potential protection against cognitive impairment that is a long-term consequence of multiple mood episodes [ 43 ].
Myth 2: lithium should be avoided in adolescents or elderly patients due to its side effects
Fact 2: lithium treatment is effective in different patients’ groups, including young and elderly patients.
Lithium represents the gold standard for the treatment of adult with bipolar disorder, but its role in treating bipolar disorder in childhood or adolescence is still debated.
Amerio et al. [ 44 ] concluded that lithium monotherapy is safe and effective for acute mania and for the prevention of affective episodes in children and adolescents. A recent umbrella review highlighted that lithium is reasonably safe and effective in children and adolescents, with adverse events similar to those observed in adults; however, the authors underlined that available evidence is limited, and further studies are needed [ 45 ].
Optimal dosing strategies have been extensively studied in the pediatric literature. In children weighing > 30 kg, due to the shorter half-life elimination and the greater creatinine clearance, the dosing strategy with lithium begins at a dose of 300 mg daily, followed by a 300 mg weekly increase, until it reaches serum lithium levels ranging from 0.8 to 1.2 mmol/l, similar to those of adults [ 46 ]. This strategy yielded mean total daily doses of 1500 mg (SD = 400.9 mg) and a mean weight-adjusted total daily dose of 29.1 mg/kg/day.
According to the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) study, lithium is prescribed more frequently to adult (37.8%) than to elderly bipolar patients (29.5%) [ 47 ]. However, because elderly subjects are often excluded from randomized clinical trials, studies focused on the treatment of bipolar disorder in older age are lacking and the information is mainly based on data derived from mixed age populations [ 48 , 49 ]. A growing attention is being given to a subset of patients with bipolar disorder, defined “older age bipolar disorder” (OABD), i.e., bipolar patients aged 50 years and over with prevalent cognitive deficits, increased risk of dementia, impaired psychosocial functioning, frequent physical comorbidities, and premature death [ 50 , 51 ]. In a double-blind, randomized, controlled trial in elderly patients with bipolar disorder, lithium was more effective than valproate in reducing manic symptoms during a 9 week follow-up and both drugs were similarly well tolerated [ 52 ].
Recently, it has been proposed that optimal serum levels of lithium in elderly patients between 60 and 79 years should be 0.4–0.8 mmol/l, while in patients aged 80 or more lithium levels should be between 0.4 and 0.7 mmol/l [ 53 ]. In the case of physical comorbidities, polypharmacy, cerebrovascular diseases, parkinsonism and dementia, a serum lithium concentration equal to or lower than 0.5 mmol/l (measured after 12 h) is recommended [ 54 ].
A dose reduction of lithium of about 20% is often required in elderly patients compared to younger patients. However, for maintenance monotherapy in OABD lithium is effective and well tolerated and it still represents the preferred choice, if correctly used. However, special caution is required to prevent nephropathy and intoxication.
In the elderly, lithium seems to be used more frequently as add-on to antidepressants in the treatment of resistant depression than in bipolar disorder [ 55 ]. Long-term treatment with lithium in the elderly is effective and relatively well tolerated both in patients with bipolar disorder and in those suffering from resistant depression. Morlet et al. [ 56 ] found that patients with depressive and bipolar disorder who had taken lithium in previous years (12.5 years on average) had less severe psychiatric symptoms, less severe depressive symptoms, and less use of benzodiazepines compared to those who had not received lithium therapy. Except for hypothyroidism, patients taking lithium have no more side effects compared to those not taking lithium.
Myth 3: the risk of drug–drug interactions represents one of the most common limitations in lithium treatment
Fact 3: drug–drug interaction risk can be easily managed during lithium treatment.
Drug–drug interactions with lithium can be pharmacokinetic or pharmacodynamic in nature.
As regards pharmacokinetic interactions, lithium has a narrow therapeutic index and changes in plasma concentrations can have significant clinical consequences. The ion is extensively absorbed in the gastrointestinal tract, is not metabolized and is almost entirely eliminated by the kidneys [ 57 ]. Serum lithium levels are sensitive to physiological factors that affect renal function, including age, dehydration, sodium balance; the most important drug interactions occur when co-administered drugs alter renal function, specifically modifying glomerular filtration and tubular reabsorption.
The most commonly prescribed drugs that have the potential to interact with lithium are ACE inhibitors, angiotensin-II receptor antagonists (sartans), diuretics, and non-steroidal anti-inflammatory drugs (NSAIDs) [ 58 ] (Table 3 ).
Case reports and hospital admission studies have shown that ACE inhibitors and angiotensin-II receptor antagonists can increase lithium serum concentrations, thus increasing the risk of toxicity [ 59 ]. Closer monitoring of lithium concentrations is needed when people start either of these drugs, and lithium dose probably needs to be reduced until a stable therapeutic concentration has been achieved. Closer monitoring for several days is also required when those drugs are stopped.
Lithium concentrations must be carefully monitored when a diuretic drug is prescribed. Thiazide and thiazide-like diuretics increase sodium reabsorption, which decreases the clearance of lithium and significantly elevates its serum concentrations [ 60 ]. Amiloride is recommended as a diuretic because of its mechanism of action that reduces lithium accumulation and improves kidney function in long-term treatment [ 61 ].
Patients taking lithium should be advised not to use regularly nonsteroidal anti-inflammatory drugs (NSAIDs) that can alter lithium concentrations through multiple mechanisms [ 62 ]. If NSAIDs are indicated, they should be used under medical guidance with a close monitoring of lithium concentrations; in these cases, lower lithium doses may be required.
Accelerating lithium elimination can be obtained through decreasing lithium reabsorption in the proximal tubule by osmotic diuresis (e.g., mannitol), carbonic anhydrase inhibitor, acetazolamide, and sodium bicarbonate [ 63 ]. Some calcium-channel blockers, such as nifedipine or nimodipine, can increase lithium clearance by producing afferent arteriolar vasodilatation. A similar effect is produced by xanthines, such as aminophylline, theophylline, and caffeine. Abrupt withdrawal from excessive drinking of coffee or tea may decrease lithium clearance, which may result in intoxication [ 57 ].
When combining lithium with other mood stabilizers, such as carbamazepine, valproate or lamotrigine, there is no significant influence on the levels of each drug; furthermore, combinations with tricyclic antidepressants are pretty safe [ 64 ].
Increased lithium neurotoxicity can be caused by the interaction with many drugs, particularly if they are administered at high doses and in elderly patients. These drugs include first (chlorpromazine and other phenothiazines, haloperidol) and second-generation antipsychotics (clozapine, olanzapine, quetiapine, risperidone, paliperidone, aripiprazole, and brexpiprazole). Lithium and antidopaminergic drugs can induce a profound dopamine hypofunctionality as a causative mechanism for neurotoxicity, resulting in increased risk of extrapyramidal symptoms, neuroleptic malignant syndrome and tardive dyskinesia [ 65 ].
Other interactions include the enhancement and prolongation of the action of competitive (e.g., pancuronium) and depolarizing (succinylcholine) muscle relaxants which, in rare cases, can trigger attacks of congenital muscle fatigue [ 66 ].
Patients with bipolar disorder often receive specific medications for treating comorbid physical conditions, such as obesity, hypertension and cardiovascular disorders. Therefore, interactions between lithium and those medications are frequent.
In patients with high blood pressure treated with certain diuretics, i.e., thiazide diuretics, ACE-inhibitors, and angiotensin-II receptor antagonists, or undergoing low sodium diet, serum levels of lithium might increase up to toxic concentrations. Therefore, different therapeutic options, i.e., loop diuretics, should be considered in these patients [ 67 ].
Although caution is required when prescribing lithium to subjects with cardiovascular diseases, such as arrythmias and QT prolongation, especially with concomitant electrolyte imbalances [ 53 ], Ponzer et al. [ 51 ] found a lower risk for cardiovascular and cerebrovascular diseases in BD patients receiving lithium.
Since lithium pharmacokinetics and body distribution change with body weight, larger maintenance doses may be required in obese patients. Therefore, a strict monitoring of the onset of potential side effects of lithium [ 68 ] is recommended.
According to the most recent recommendations, a target serum lithium concentration range of 0.5–0.8 mmol/L (varying upon clinical indication, age, and concurrent physical status) seems most appropriate for most patients. Lower end levels of the therapeutic range (0.5–0.6 mmol/L) are generally recommended for older patients (50 years and over) and for those taking interacting concomitant medications for other risk factors such as heart disease, renal impairment, diabetes insipidus, thyroid dysfunction [ 67 ].
Lithium should be prescribed with caution in patients receiving drugs that can slow its renal elimination and increase the risk of toxic effects (e.g., thiazide diuretics, ACE-inhibitors, angiotensin converting enzyme inhibitors, NSAIDs, when assumed more than occasionally and for extended periods), and if a low-sodium diet is required for medical reasons [ 53 ].
Kuramochi et al. [ 69 ] investigated the administration rates of NSAIDs, loop/thiazide diuretics, angiotensin-converting enzyme inhibitors, and/or angiotensin-II receptor blockers between lithium users and age- and sex-matched non-lithium users. They also investigated the number of patients in the two groups with a diagnosis of somatic conditions who were receiving those medications. Results show that prescriptions of the above medications are less frequent in lithium users compared to non-users (18.3 vs. 31.9%), with subsequent suboptimal treatment of medical comorbidities and impact on physical health.
The presence of alcohol use disorders (AUD) and substances use disorders (SUD) should always be considered when initiating a treatment with lithium [ 70 , 71 ]. Lithium is still considered the first-line treatment in comorbid BD-AUD/SUD patients who show good adherence. Also, medications for AUD can be safely used in BD given the lack of significant pharmacological interactions [ 72 ]. However, in these patients the combination of more drugs is often the rule for improving patients’ outcome. For example, in patients affected by bipolar disorder with AUD/SUD, adding an anticonvulsant drug to lithium is preferable to lithium monotherapy for their effects on substance consumption and craving [ 73 ]; the combination of lithium and valproate is effective for affective symptoms and reduces substance use, possibly through an indirect effect on mood stability [ 74 ]. Nevertheless, studies are still scarce, findings are often inconsistent and with no difference according to the main substance of use [ 70 ]. Further studies are needed before evidence-based guidelines can be delivered for clinician's use.
Myth 4: lithium treatment requires weekly lab tests
Fact 4: the optimal management of lithium treatment includes periodical laboratory tests.
Lithium treatment can be easily implemented in ordinary clinical practice, both at inpatient and outpatient settings. Before starting treatment with lithium, it is recommended to assess blood concentrations of creatinine and urea-nitrogen (to check renal functioning), the levels of electrolytes (sodium, potassium, calcium), and the levels of thyroid and parathyroid hormones, as well as obtaining an electrocardiogram. Lithium blood concentration should be checked 5 days after the targeted dose is achieved. The evaluation of lithium blood concentration levels can be repeated until lithium reaches its therapeutic levels. Afterwards, lithium, creatinine, and TSH levels should be checked every one to 2 months in the first 6 months, and then every 6–12 months, or as clinically indicated.
The most common early side effects of lithium include reduced urinary concentrating ability (by 15% of normal maximum) with possible polyuria/polydipsia, tremor, and gastrointestinal symptoms. Clinical hypothyroidism and/or increased thyroid stimulating hormone (TSH), parathyroid abnormalities (usually normocalcemic hyperparathyroidism), impaired glomerular filtration rate and chronic kidney disease usually occur after a long-term exposure to lithium [ 75 , 76 , 77 ].
Some of lithium acute side effects can be reduced simply by ensuring that the lowest needed plasma levels are maintained and using prolonged-release formulations that are associated with lower plasma peaks.
In the long term, lithium is associated with a higher risk of impaired glomerular rate filtration and chronic kidney disease stage 3 (GFR < 60 mL/min/1.73 m 2 ) as compared to valproate, olanzapine and quetiapine (but not CKD stage 4—GFR < 30 mL/min/1.73 m 2 ); but lithium is significantly less associated with weight gain and hypertension than other mood stabilizers (e.g., valproate, olanzapine and quetiapine) [ 78 ]. Long-term antipsychotic exposure, especially some of the most used atypical antipsychotics such as olanzapine or quetiapine, is indeed associated with increased rates of obesity, metabolic syndrome and cardiovascular diseases, with an excess of mortality due to cardiovascular events [ 79 ]. Moreover, long-term exposure to dopamine-blocking agents may have an impact on brain’s reward system and on the extrapyramidal system.
In a small group of patients, lithium is associated with hypercalcemia or normocalcemic hyperparathyroidism (risk of reduced mineral density, osteoporosis and increased fracture risk over the long-term), but their clinical significance remains doubtful. In fact, opposite findings have been found recently, with decreased risk of osteoporosis (HRR, 0.62; 95% CI 0.53–0.72) in bipolar patients treated with lithium compared to those not receiving lithium. Treatment with antipsychotics, valproate, and lamotrigine was not associated with reduced risk of osteoporosis [ 80 ]. Concerning clinical hypothyroidism, annual TSH measurements may be sufficient to prevent overt hypothyroidism; in any case, thyroid function abnormalities should not constitute an outright contraindication to lithium treatment, as well as lithium should not be stopped if a responsive patient develops thyroid abnormalities [ 81 , 82 ].
No studies have been performed to date evaluating the long-term effect of exposure to prolonged-release lithium versus immediate-release lithium on thyroid and renal function; however, one can expect that the lower peak plasma levels and the smaller peak-to-through plasma differences of the prolonged-release formulations are associated with a preserved thyroid and renal function.
Concerning adverse effects associated with lithium treatment, some clarifications need to be made. First, severe adverse renal and endocrine outcomes are very rare (although the absolute risk is higher and significant, the absolute number is low). According to a study in two regions of Sweden with 2.7 million inhabitants [ 83 ], renal replacement therapy in patients exposed to lithium occurs in 0.53% as compared to 0.08% in the general population (1.2% in those on lithium for more than 15 years), while a more recent study found that chronic kidney disease occurs in 0.6% of patients (median treatment time 19 months) [ 84 ]. Moreover, adverse renal consequences are associated with higher mean plasma levels (greater than 0.60–0.70 mEq/L) [ 85 , 86 ], indicating that a regular monitoring of plasma levels can minimize or even neutralize the risk. Practical guidelines for prevention and management of renal side effects of lithium therapy advise to use a once-daily dosing schedule, which allow an effective treatment while preventing lithium intoxication [ 87 ].
Myth 5: different formulations of lithium do not modify its tolerability profile
Fact 5: slow-release lithium formulation has advantages compared to immediate release formulation.
Conventional slow-release (SR) lithium preparations provide a modulated release of the active ingredient, that is obtained for the reduced solubility of the saline compound used (lithium sulphate), or with the inclusion of lithium in a less easily absorbable matrix. In both cases, lithium is absorbed more slowly, and the peak plasma concentration, which is lower than the immediate-release (IR) formulations, occurs within 4–12 h; the pharmacokinetics, therefore, follow a plateau.
The slower increase in serum lithium concentrations and the lower Cmax (maximum concentration of drug detected in the blood) with SR formulations compared to IR lithium formulations translate into a reduced rate or less severity for some lithium-related adverse events, including tremors, upper gastrointestinal cramps, nausea, rash, cognitive obtundation, polyuria; a close relationship between changes in blood lithium levels and frequency and severity of side effects has been recently highlighted. Pompili et al. [ 88 ] found that SR lithium salts offer clinical advantages over IR formulations in terms of more stable circulating concentrations of lithium, less adverse impact on renal function, low incidence of adverse neurological effects (including cognitive impairment and tremor), low subjectively unpleasant adverse effects such as fatigue and weight-gain, and greater treatment adherence.
Slow-release formulations reduce the post-absorption peaks of plasma levels, which is beneficial for patients with gastric upset or transient side effects (e.g., tremors) secondary to temporary increases in blood levels.
Long-term treatment with SR lithium is associated with less impairment of the kidney's function to concentrate urine compared with IR lithium. A drug delivery system designed to achieve prolonged therapeutic effects by continuously releasing the medication over an extended time after the administration of a single dose reduces daily peaks in plasma lithium concentrations, thus preserving the functionality of the kidney.
A worsening of lower gastrointestinal disorders (e.g., diarrhea) has been occasionally reported with SR formulations of lithium compared to IR formulations [ 89 ].
A single daily administration of lithium can produce benefits compared to repeated daily administrations regarding adherence to therapy and reduction of renal and thyroid side effects. Double administration of lithium during the same day could produce renal impairment and a higher risk of polyuria [ 90 ]. A single evening dosage is recommended, allowing greater treatment adherence [ 38 ].
The overall decrease in adverse events with SR formulations compared to lithium IR formulations may reduce drug discontinuation, although this factor has not been evaluated in controlled clinical studies [ 90 , 91 , 92 , 93 ].
Prolonged-release lithium sulphate represents a therapeutic option of great advantage for the clinician, as it allows for constant plasma concentrations of lithium while minimizing the undesirable effects associated with concentration peaks of standard-release formulations [ 94 ]. Furthermore, in the event of an overdose of slow-release preparations, the chances of survival increase [ 95 ].
According to Bowden [ 89 ], adverse effects of lithium can be resolved by dose reduction, extended-release lithium, or combination therapy.
Barbuti et al. [ 96 ] investigated differences between patients receiving IR (lithium carbonate) vs. SR (lithium sulphate) lithium formulations in a prospective naturalistic study. Both lithium formulations significantly improved severity (CGI-BP scale) and functioning (FAST scale). These authors found a similar effect of lithium sulfate and lithium carbonate, but a lower incidence of tremors and gastrointestinal disturbances, as well as higher levels of adherence with lithium sulfate compared to lithium carbonate. Both formulations significantly improved both BD episode severity and functioning comparably to each other.
In a randomized clinical trial investigating the switch from IR to SR lithium formulation in poorly tolerant IR lithium-treated patients, Pelacchi et al. [ 97 ] found a significantly higher percentage of patients randomized to lithium sulfate (SR) vs. patients randomized to lithium carbonate (IR) who showed an improvement in tremor after the 1st week of treatment; and a persistence of tremor improvement after 12 weeks of treatment. Furthermore, a higher score for the «convenience» item (e.g., route of administration, dosing frequency) of the Treatment Satisfaction Questionnaire for Medication (TSQM scale) was reported by patients randomized to lithium sulfate vs. those randomized to lithium carbonate.
These benefits have led to a frequent use of the extended-release formulation of lithium in many European countries. Still, maybe due to the minimal publicity of these benefits, relatively less use has occurred in other parts of the world.
Myth 6: no drug has an antisuicidal effect
Fact 6: lithium treatment has antisuicidal properties.
Lithium is recommended for the reduction of suicide risk among patients with bipolar disorder [ 98 ]. The first evidence of lithium’s antisuicidal properties date back to the seminal studies by Barraclough [ 99 ], pointing out that lithium was effective in preventing “recurrent affective illness”. Jamison [ 100 ] postulated that lithium would demonstrate its role in preventing suicide in bipolar disorders in the next 10 years. Several studies reported strong evidence of the role of lithium in suicide risk protection among patients suffering from mood disorders. The fatality rate was 8.7 times lower during versus after discontinuing lithium and gradual vs. rapid discontinuation of lithium could limit the risk of suicidal behavior [ 101 ].
A significant reduction in suicidal risks (attempts > suicides) with lithium maintenance therapy in unipolar ≥ bipolar II ≥ bipolar I disorder to overall levels close to general population rates was found in people treated with lithium. Patients who did not receive lithium had alarming rates of both suicides and suicide attempts in all types of the above-mentioned mood disorders [ 102 ].
Patients suffering from bipolar disorder or any other major affective disorder treated with lithium reported a risk of completed and attempted suicides lower than 80% compared with patients treated with other drugs (risk ratio = 4.91, CI 3.82–6.31; P < 0.0001) [ 103 ].
A potentially important new observation is a strong association of lithium treatment with the ratio of attempted to completed suicides, which was proposed as an index of the lethality of suicidal acts. In the available literature, the attempted suicide/completed suicide ratio (A/S) is 2.5 times greater among lithium-treated subjects than in those not treated with lithium, and nearly three times higher among bipolar disorder cases, suggesting a reduction in lethality attributable to lithium treatment with fewer fatalities per attempt.
Lithium can have an independent antisuicidal effect because of suicidal behavior in a selected group of high-risk mood disorder patients. Evidence supports the notion of a significantly decreased rate of suicide attempts compared to pre-lithium figures, not only in patients with excellent treatment outcomes, but also in those with moderate or poor response to lithium prophylaxis [ 104 ]. These findings highlight a specific antisuicidal action of lithium on the suicide risk dimension, independent from the clinical mood disorder picture [ 105 ]. Cipriani et al. [ 106 ] found that lithium effectively prevents suicide, deliberate self-harm, and death from all causes in patients with mood disorders. The anti-suicidal properties of lithium in mood disorders have been more recently confirmed [ 107 , 108 ].
However, some studies did not find consistent antisuicidal action of lithium salts. For example, a randomized controlled trial did not find differences between lithium and valproate in preventing suicide attempts and suicide events in bipolar disorder patients [ 109 ]. Another randomized placebo-controlled clinical trial found that adding lithium to treatment does not reduce the incidence of suicide-related events in veterans with major depressive disorder or bipolar disorder who experienced a recent suicide event. In addition, they observed that adding lithium to existing medication regimens does not prevent a broad range of suicide-related events in patients who were being treated for mood disorders and previously engaged in suicidal behavior [ 110 ]. However, such exceptions seem irrelevant when considering that nearly three dozen observational trials have found fewer suicides or attempts in patients treated with lithium than without; that there are similar effects in several randomized clinical trials in which suicidal behaviors were considered adverse events rather than an explicit outcome, and that there is marked, temporary increases in suicidal behavior soon after discontinuing lithium treatment [ 111 ].
Furthermore, the use of lithium as a lethal mean for suicide has not received support, as data indicate that mortality from an overdose of lithium is similar to that associated with other psychotropic drugs, or even less, as well as suicidal gestures with lithium are uncommon, or even absent, during long-term lithium treatment [ 98 ]. The availability of slow-release formulation may reduce side effects and improve adherence [ 88 , 97 ].
Lithium has the potential to act trans-diagnostically, given evidence emerging from studies of lithium in drinking water and the rates of suicide risk in selective areas with higher concentrations [ 112 ]. Despite the controversy, drinking lithium-rich water may protect general populations from suicide. As hospitalizations are a critical time for mood disorders patients, especially at discharge for the increased suicide risk, it is noteworthy to mention a recent study [ 113 ] that demonstrates a marked overall reduction in hospitalization during lithium treatment compared to the year before starting lithium, both for bipolar disorder and major depressive disorder.
Myth 7: lithium treatment should be avoided during pregnancy
Fact 7: lithium can be carefully managed during pregnancy.
The decision to treat mood disorders during the peripartum period should be carefully considered, balancing the risk of prenatal and neonatal exposure to the medication versus the potentially deleterious effects of untreated affective episodes on the maternal and neonatal health. Accumulating evidence shows that the continuation of prophylactic medication with mood stabilizers (particularly lithium) during the perinatal period may prevent affective recurrences.
Lithium should be considered the first-choice treatment for bipolar disorder in the peripartum period, especially in women already treated and stabilized with lithium before pregnancy.
Stevens and colleagues [ 114 ] demonstrated that the rates of peripartum mood relapses in bipolar disorder are significantly higher if stabilizing therapy is discontinued before or during pregnancy (68%) compared to its continuation (23%). The recurrence risk is much increased if the cessation of the mood stabilizer is rapid and abrupt (within 14 days): about half of women who suspended suddenly or quickly lithium experienced a mood recurrence within 2 weeks [ 115 ]. Instead, the maintenance of therapy with lithium reduces the relative risk of relapse by 66% [ 114 ].
The efficacy/safety ratio seems to be in favour of lithium in respect to other mood stabilizers in the prophylactic treatment of pregnant women with bipolar disorder. The use of lithium during pregnancy is very effective in preventing depressive and (hypo)manic episodes and associated with few side effects on fetal and newborn health [ 116 ]. During pregnancy, the administration of lithium may be correlated with an increased risk of cardiac malformations (2.1% among lithium-exposed pregnancies vs 1.6% among non-exposed), but the difference is not significant [ 117 ]. Especially, lithium exposure may induce the development of Ebstein’s anomaly, affecting 5–7 infants per 1.000 live births (instead of 1 per 20.000 live births in general population) [ 118 ]. The risk of developing heart defects is associated with the time of lithium intake (higher in the first-trimester of pregnancy) and dosage exposure (lower if serum lithium levels < 0.64 mEq/L and dosages < 600–900 mg/day) [ 118 , 119 ]. Lithium exposure during the first trimester of pregnancy seems to be associated with higher rates of spontaneous abortion compared with those in general population; however, the risk of miscarriage appears similar when comparing with lithium-unexposed patients with affective disorders [ 119 ].
The administration of lithium treatment does not contraindicate breastfeeding because of the absence of severe adverse events reported in infants exposed through maternal milk [ 120 ]. Few studies show rare and transient lithium toxicity (e.g., hypotonia, weight loss in the first week, thyroid and renal parameter alterations) in breastfed infants, which recovers after discontinuation of lactation [ 121 ]. Lithium salts can be taken during breastfeeding, but a frequent evaluation of infant serum levels and a strict paediatric monitoring are mandatory [ 122 ]. However, the decision to breastfeed should also be evaluated in relation to the risk of affective relapses correlated to sleep dysregulation [ 123 ].
Some caution must be used in the stabilizing treatment of pregnant women. Preferentially, lithium should be prescribed as monotherapy, in fractionated doses or in slow-release formulations, to avoid plasma peak concentrations and within the lowest therapeutic range throughout pregnancy, particularly during the first trimester. Furthermore, lithium dosages can be reduced immediately before delivery to reduce the risk of postnatal adaptation syndrome [ 124 ]. Because of changes in the mother's plasma volume and renal clearance through pregnancy, a close monitoring of lithium blood levels is recommended: lithium blood levels decrease in the first trimester, remains stable in the second trimester, increase in the third trimester and are still slightly increased after delivery [ 125 ]. In addition, supplementation with folic acid (5 mg/day) in pregnancy reduces the risk of foetal and neonatal negative outcomes [ 122 ].
Personalized and integrated treatment, including pharmacological and non-pharmacological interventions, should be used in patients with bipolar disorder. Although several pharmacological treatments are indicated as first-line treatment for the management of patients with bipolar disorder, lithium is the gold standard due to its established mood-stabilizing properties [ 23 , 24 , 126 ].
Lithium is one of the most effective treatments available in psychiatry [ 25 ], and psychiatrists should be aware of the great applicability of lithium use, considering its efficacy and good tolerability profile. However, the recent years have witnessed a decreasing trend in the use of lithium in clinical practice. Many early career psychiatrists or recently graduated physicians do not feel skilled enough to use lithium, which is considered a difficult-to-use agent, mainly for its subtleties, the need for periodical blood checking, and its side effects [ 29 ]. Moreover, several stereotypes related to the difficulties in managing lithium treatment exist, which further reduce the use of lithium in clinical practice. Thus, in this narrative review we aim to overcome some of these misconceptions regarding lithium, by counterarguing myths with facts.
Lithium is an excellent treatment for patients suffering from bipolar disorder. In particular, lithium is a valid treatment option in the different phases of bipolar disorder, including treatment of current manic/hypomanic episodes, especially in combination with second-generation antipsychotics. A recent review of all clinical practice guidelines for the treatment of patients with bipolar disorder highlights that lithium is recognized as a key pharmacotherapeutic agent in the treatment of bipolar disorder [ 127 ].
Lithium has also been found to have an outstanding efficacy in the maintenance or prophylactic treatment of bipolar disorder [ 128 , 129 ], representing the gold standard treatment for the long-term prevention of affective relapses in patients with bipolar disorder [ 130 ]. In both controlled clinical trials and in observational studies, lithium has shown its efficacy and superiority in the prophylaxis of any type of affective episode [ 39 , 131 , 132 , 133 , 134 , 135 ].
One important misconception regarding lithium is that it should be avoided in adolescents or elderly patients due to its side effects. This notion has been counteracted by several clinical studies, which have highlighted that lithium is well-tolerated and effective both in adolescents and in elderly patients with bipolar disorder [ 46 , 136 ]. In particular, the recent umbrella review by Janiri et al. [ 45 ] found that lithium is superior to placebo in pediatric and adolescent patients with bipolar disorder. All studies specified that lithium was generally well tolerated in this group of patients, with common side effects (e.g., gastrointestinal, polyuria or headache) similar to those reported in adults. As regards the use of lithium treatment in elderly patients with bipolar disorder, De Fazio et al. [ 136 ] found that lithium was superior to placebo and to other mood stabilizers in treating mania. The efficacy of lithium in geriatric patients with resistant major depressive disorder is supported also by Ross [ 137 ] and by Cooper et al. [ 138 ]. Regarding lithium tolerability in elderly patients, the clear evidence is that lithium may be relatively well-tolerated, but low doses should be used in the elderly, since the risk of adverse events increases according to a dose-dependent pattern.
Many early career psychiatrists frequently report to not prescribe lithium treatment since they feel not enough skilled in detecting and managing the potential drug–drug interactions and their impact on patients. This misconception highlights the need for an adequate training of prescribers on the potential pharmacodynamic and pharmacokinetic interactions of lithium. Improving knowledge and confidence with lithium monitoring can significantly contribute to improve patient outcomes and increase lithium use in ordinary clinical practice. The risk of potential drug–drug interactions can be easily monitored in patients treated with lithium, also considering that the risk increases when patient gets older because of declining renal function and accumulation of medical comorbidities [ 139 ]. Other conditions requiring a careful evaluation of lithium treatment are those causing haemodynamic and volume alterations such as dehydration, fever, gastrointestinal loss, perioperative management and surgery. Prescribers should be aware that the most common (potential) interactions occur with ACE inhibitors, angiotensin II receptor antagonists (sartans), diuretics, and NSAIDs. Combinations of these drugs are frequent, so clinicians—being aware of their additive effects—should regularly check lithium concentration, not excluding lithium treatment. As suggested by Malhi et al. [ 140 ], “lithiumeter”, which is a visual and practical guide for determining lithium levels in the management of bipolar disorder, is a useful tool for supporting the use of lithium treatment in ordinary clinical practice. Furthermore, providing patients with correct information on the benefits of lithium treatment is essential to improve their adherence to the prescribed therapy [ 141 , 142 , 143 ].
Another common stereotype is that using different lithium formulations does not modify lithium tolerability. On the contrary, the availability of prolonged-release lithium formulation represents an important strength of lithium treatment choice since it reduces some of the most common side effects of lithium, such as tremor and gastrointestinal symptoms, and also has a positive effect on adherence [ 96 , 97 ].
A relevant statement clearly emerging by our review is that lithium has antisuicidal properties, which might be unrelated to its mood-stabilizing effects, considering that suicidality is a complex phenomenon, with multifactorial causes [ 144 , 145 , 146 , 147 , 148 ]. In fact, there is a significant reduction in the number of suicide attempts among individuals who take lithium, even among those who do not respond well to the prophylaxis of mood symptoms with lithium. The anti-suicidal properties of lithium appear to be as effective at low concentrations as at therapeutic levels. Sustained low doses of lithium intake have shown to decrease suicidality. Suicide prevention in patients taking lithium occurs when the serum concentrations are within a therapeutic range of 0.5–1.0 mmol/L. The lowest efficacious lithium level in the long-term treatment of patients with bipolar disorder has been shown to be 0.4 mmol/L, with optimal response achieved at concentrations between 0.6 and 0.75 mmol/L. Those with manic symptoms might benefit from higher levels of lithium concentration. The duration of lithium treatment is also important for suicide prevention. Even among patients with only poor-to-moderate clinical response, a decrease in the number of suicide attempts has been observed when patients take lithium compared to those who do not take it. Research supports the recommendation that lithium treatment should be considered for anyone at high risk for suicide, even if mood-stabilization is not achieved [ 149 , 150 ].
Finally, a very controversial issue is the use of lithium in pregnancy. The review by Poels et al. [ 151 ] reported lower risk estimates of the association between first trimester lithium exposure and risk of congenital malformations than previously reported. Moreover, no association between lithium use and pregnancy or delivery-related outcomes were found, although studies are needed. Therefore, lithium is effective and relatively safe in pregnancy and postpartum for the prevention of relapse in bipolar disorder; during the first trimester, tapering of lithium treatment should be considered weighing benefits against relapse risks. Accumulating evidence shows that the continuation of prophylactic medication with mood stabilizers (particularly lithium) during the perinatal period may prevent affective recurrences. In particular, Stevens et al. [ 114 ] demonstrated that the rates of peripartum mood relapses in bipolar disorder are significantly higher if stabilizing therapy is discontinued before or during pregnancy. When lithium is prescribed during pregnancy, some caution must be used, and lithium blood levels should be monitored more frequently, preferably weekly in the third trimester.
Finally, given its neuroprotective and neurotrophic properties, lithium improves cognition, either associated or not to an acute affective episode [ 152 , 153 ]. Increasing evidence indicates lithium efficacy in neuroprotection, since it restores both neurotransmission and brain structure [ 154 ]. The recognition of lithium as neuroprotective agent is explained by the discoveries of several key cell signaling-related enzymes activated by lithium treatment. These include glycogen synthase kinase-3, inositol monophosphatase, phosphoadenosylphosphate phosphatase, and Akt/beta-arrestin 2. Processes associated with these enzymes include autophagy, BDNF cellular signaling, neuroinflammation, mitochondrial function, and apoptosis. The involvement of these processes in a variety of brain disorders beyond bipolar disorders, such as stroke, Huntington’s disease, Alzheimer’s disease, Parkinson’s disease, fragile X syndrome, amyotrophic lateral sclerosis, and multiple sclerosis raised the interest in exploring lithium’s potential neuroprotective property in these neurodegenerative and neurodevelopmental disorders [ 155 ].
The present study has some limitations which must be acknowledged. Firstly, the consensus paper is based on a narrative review of the available literature on efficacy, tolerability and use of lithium in ordinary clinical practice. The search has not adopted a rigorous methodology, analyzing all available databases and sources of information. Moreover, a specific focus on myths/facts related to lithium treatment with a specific focus on adolescent/young patients is missing, since other recent papers have already assessed the use of lithium in such target group.
It is time to disseminate clear and unbiased information on the clinical efficacy, effectiveness, tolerability and easiness to use of lithium treatment in patients with bipolar disorder. The availability of different formulations of lithium represents a further strength of this therapeutic choice, since the treatment can be more easily adapted to patients’ needs.
It is necessary to reinvigorate the clinical and academic discussion about the efficacy of lithium, to counteract the decreasing prescription trend one of the most effective drugs available in the whole medicine.
Availability of data and materials
Upon request to corresponding author.
McIntyre RS, Alda M, Baldessarini RJ, Bauer M, Berk M, Correll CU, et al. The clinical characterization of the adult patient with bipolar disorder aimed at personalization of management. World Psychiatry. 2022;21(3):364–87. https://doi.org/10.1002/wps.20997 .
Article PubMed PubMed Central Google Scholar
Yatham LN, Kennedy SH, Parikh SV, Schaffer A, Bond DJ, Frey BN, et al. Canadian network for mood and anxiety treatments (CANMAT) and international society for bipolar disorders (ISBD) 2018 guidelines for the management of patients with bipolar disorder. Bipolar Disord. 2018;20(2):97–170. https://doi.org/10.1111/bdi.12609 .
Kendler KS. Incremental advances in psychiatric molecular genetics and nosology. World Psychiatry. 2022;21(3):415–6. https://doi.org/10.1002/wps.20999 .
Krueger RF. Incremental integration of nosological innovations is improving psychiatric diagnosis and treatment. World Psychiatry. 2022;21(3):416–7. https://doi.org/10.1002/wps.21001 .
Perugi G, De Rossi P, Fagiolini A, Girardi P, Maina G, Sani G, et al. Personalized and precision medicine as informants for treatment management of bipolar disorder. Int Clin Psychopharmacol. 2019;34(4):189–205. https://doi.org/10.1097/YIC.0000000000000260 .
Article PubMed Google Scholar
Linden M. Twelve rather than three waves of cognitive behavior therapy allow a personalized treatment. World Psychiatry. 2022;21(2):316–8. https://doi.org/10.1002/wps.20985 .
Flückiger C, Paul J, Hilpert P, Vîslă A, Gómez Penedo JM, Probst GH, et al. Estimating the reproducibility of psychotherapy effects in mood and anxiety disorders: the possible utility of multicenter trials. World Psychiatry. 2021;20(3):445–6. https://doi.org/10.1002/wps.20901 .
Leichsenring F, Steinert C, Rabung S, Ioannidis JPA. The efficacy of psychotherapies and pharmacotherapies for mental disorders in adults: an umbrella review and meta-analytic evaluation of recent meta-analyses. World Psychiatry. 2022;21(1):133–45. https://doi.org/10.1002/wps.20941 .
Volkmann C, Bschor T, Köhler S. Lithium treatment over the lifespan in bipolar disorders. Front Psychiatry. 2020;11:377. https://doi.org/10.3389/fpsyt.2020.00377 .
Bai YM, Li CT, Tsai SJ, Tu PC, Chen MH, Su TP. Metabolic syndrome and adverse clinical outcomes in patients with bipolar disorder. BMC Psychiatry. 2016;16(1):448. https://doi.org/10.1186/s12888-016-1143-8 .
Kim H, Turiano NA, Forbes MK, Kotov R, Krueger RF, Eaton NR, et al. Internalizing psychopathology and all-cause mortality: a comparison of transdiagnostic vs. diagnosis-based risk prediction. World Psychiatry. 2021;20(2):276–82. https://doi.org/10.1002/wps.20859 .
Warner A, Holland C, Lobban F, Tyler E, Harvey D, Newens C, et al. Physical health comorbidities in older adults with bipolar disorder: a systematic review. J Affect Disord. 2023;326:232–42. https://doi.org/10.1016/j.jad.2023.01.083 .
Price AL, Marzani-Nissen GR. Bipolar disorders: a review. Am Fam Physician. 2012;85(5):483–93.
PubMed Google Scholar
Forte A, Baldessarini RJ, Tondo L, Vázquez GH, Pompili M, Girardi P. Long-term morbidity in bipolar-I, bipolar-II, and unipolar major depressive disorders. J Affect Disord. 2015;178:71–8. https://doi.org/10.1016/j.jad.2015.02.011 .
Arango C, Dragioti E, Solmi M, Cortese S, Domschke K, Murray RM, et al. Risk and protective factors for mental disorders beyond genetics: an evidence-based atlas. World Psychiatry. 2021;20(3):417–36. https://doi.org/10.1002/wps.20894 .
Mulder R. The evolving nosology of personality disorder and its clinical utility. World Psychiatry. 2021;20(3):361–2. https://doi.org/10.1002/wps.20915 .
Correll CU, Solmi M, Croatto G, Schneider LK, Rohani-Montez SC, Fairley L, et al. Mortality in people with schizophrenia: a systematic review and meta-analysis of relative risk and aggravating or attenuating factors. World Psychiatry. 2022;21(2):248–71. https://doi.org/10.1002/wps.20994 .
Klingberg T, Judd N, Sauce B. Assessing the impact of environmental factors on the adolescent brain: the importance of regional analyses and genetic controls. World Psychiatry. 2022;21(1):146–7. https://doi.org/10.1002/wps.20934 .
Sengupta G, Jena S. Psychiatric comorbidity and quality of life in patients with bipolar disorder. Ind Psychiatry J. 2022;31(2):318–24. https://doi.org/10.4103/ipj.ipj_24_21 .
Sampogna G, Janiri D, Albert U, Caraci F, Martinotti G, Serafini G, et al. Why lithium should be used in patients with bipolar disorder? A scoping review and an expert opinion paper. Expert Rev Neurother. 2022;22(11–12):923–34. https://doi.org/10.1080/14737175.2022.2161895 .
Article CAS PubMed Google Scholar
Hidalgo-Mazzei D, Mantingh T, Pérez de Mendiola X, Samalin L, Undurraga J, Strejilevich S, et al. Clinicians’ preferences and attitudes towards the use of lithium in the maintenance treatment of bipolar disorders around the world: a survey from the ISBD lithium task force. Int J Bipolar Disord. 2023;11(1):20. https://doi.org/10.1186/s40345-023-00301-y .
Cade JF. Lithium salts in the treatment of psychotic excitement. Med J Aust. 1949;2(10):349–52. https://doi.org/10.1080/j.1440-1614.1999.06241.x .
Malhi GS, Tanious M, Das P, Berk M. The science and practice of lithium therapy. Aust N Z J Psychiatry. 2012;46(3):192–211. https://doi.org/10.1177/0004867412437346 .
Geddes JR, Miklowitz DJ. Treatment of bipolar disorder. Lancet. 2013;381(9878):1672–82. https://doi.org/10.1016/S0140-6736(13)60857-0 .
Leucht S, Hierl S, Kissling W, Dold M, Davis JM. Putting the efficacy of psychiatric and general medicine medication into perspective: review of meta-analyses. Br J Psychiatry. 2012;200(2):97–106. https://doi.org/10.1192/bjp.bp.111.096594 .
Maj M. Lithium, the forgotten drug. In: McDonald C, Schulze K, Murray R, Wright P, editors. Bipolar Disorder. The Upswing in Research and Treatment. 1st Edition- London: CRC Press; 2005
Poranen J, Koistinaho A, Tanskanen A, Tiihonen J, Taipale H, Lähteenvuo M. Twenty-year medication use trends in first-episode bipolar disorder. Acta Psychiatr Scand. 2022;146(6):583–93. https://doi.org/10.1111/acps.13504 .
Malhi GS, Bell E, Jadidi M, Gitlin M, Bauer M. Countering the declining use of lithium therapy: a call to arms. Int J Bipolar Disord. 2023;11(1):30. https://doi.org/10.1186/s40345-023-00310-x .
Rhee TG, Olfson M, Nierenberg AA, Wilkinson ST. 20-Year trends in the pharmacologic treatment of bipolar disorder by psychiatrists in outpatient care settings. Am J Psychiatry. 2020;177(8):706–15. https://doi.org/10.1176/appi.ajp.2020.19091000 .
Bartoli F. The lithium paradox: declining prescription of the gold standard treatment for bipolar disorder. Acta Psychiatr Scand. 2023;147(3):314–5. https://doi.org/10.1111/acps.13525 .
Malhi GS, Bell E, Hamilton A, Morris G, Gitlin M. Lithium mythology. Bipolar Disord. 2021;23(1):7–10. https://doi.org/10.1111/bdi.13043 .
Fawcett J. Some provocative thoughts about continuation and maintenance treatment. Psychiatr Ann. 2013;24(6):279–80.
Article Google Scholar
Schou M. Lithium prophylaxis: myths and realities. Focus. 2003;1(1):53–7. https://doi.org/10.1176/foc.1.1.53 .
Sachs GS, Lafer B, Truman CJ, Noeth M, Thibault AB. Lithium monotherapy: miracle, myth and misunderstanding. Psychiatr Ann. 1994;24(6):299–306. https://doi.org/10.3928/0048-5713-19940601-09 .
Schou M. Lithium prophylaxis: myths and realities. Am J Psychiatry. 1989;146(5):573–6. https://doi.org/10.1176/ajp.146.5.573 .
Shepherd M. A prophylactic myth. Int J Psychiatry. 1989;9:423–5.
Google Scholar
Blackwell B, Shepherd M. Prophylactic lithium: another therapeutic myth? An examination of the evidence to date. Lancet. 1968;1(7549):968–71. https://doi.org/10.1016/s0140-6736(68)90917-3 .
Goodwin GM, Haddad PM, Ferrier IN, Aronson JK, Barnes T, Cipriani A, et al. Evidence-based guidelines for treating bipolar disorder: revised third edition recommendations from the British association for psychopharmacology. J Psychopharmacol. 2016;30(6):495–553. https://doi.org/10.1177/0269881116636545 .
Article CAS PubMed PubMed Central Google Scholar
Miura T, Noma H, Furukawa TA, Mitsuyasu H, Tanaka S, Stockton S, et al. Comparative efficacy and tolerability of pharmacological treatments in the maintenance treatment of bipolar disorder: a systematic review and network meta-analysis. Lancet Psychiatry. 2014;1(5):351–9. https://doi.org/10.1016/S2215-0366(14)70314-1 .
Fountoulakis KN, Tohen M, Zarate CA Jr. Lithium treatment of bipolar disorder in adults: a systematic review of randomized trials and meta-analyses. Eur Neuropsychopharmacol. 2022;54:100–15.
Berk M, Brnabic A, Dodd S, Kelin K, Tohen M, Malhi GS, et al. Does stage of illness impact treatment response in bipolar disorder? Empirical treatment data and their implication for the staging model and early intervention. Bipolar Disord. 2011;13(1):87–98. https://doi.org/10.1111/j.1399-5618.2011.00889.x .
Yatham LN, Kennedy SH, Parikh SV, Schaffer A, Beaulieu S, Alda M, et al. Canadian network for mood and anxiety treatments (CANMAT) and international society for bipolar disorders (ISBD) collaborative update of CANMAT guidelines for the management of patients with bipolar disorder: update 2013. Bipolar Disord. 2013;15(1):1–44. https://doi.org/10.1111/bdi.12025 .
Kessing LV, Forman JL, Andersen PK. Does lithium protect against dementia? Bipolar Disord. 2010;12(1):87–94. https://doi.org/10.1111/j.1399-5618.2009.00788.x .
Amerio A, Ossola P, Scagnelli F, Odone A, Allinovi M, Cavalli A, et al. Safety and efficacy of lithium in children and adolescents: a systematic review in bipolar illness. Eur Psychiatry. 2018;54:85–97. https://doi.org/10.1016/j.eurpsy.2018.07.012 .
Janiri D, Sampogna G, Albert U, Caraci F, Martinotti G, Serafini G, et al. Lithium use in childhood and adolescence, peripartum, and old age: an umbrella review. Int J Bipolar Disord. 2023;11(1):8. https://doi.org/10.1186/s40345-023-00287-7 .
Findling RL, Kafantaris V, Pavuluri M, McNamara NK, McClellan J, Frazier JA, et al. Dosing strategies for lithium monotherapy in children and adolescents with bipolar I disorder. J Child Adolesc Psychopharmacol. 2011;21(3):195–205. https://doi.org/10.1089/cap.2010.0084 .
Al Jurdi RK, Marangell LB, Petersen NJ, Martinez M, Gyulai L, Sajatovic M. Prescription patterns of psychotropic medications in elderly compared with younger participants who achieved a “recovered” status in the systematic treatment enhancement program for bipolar disorder. Am J Geriatr Psychiatry. 2008;16(11):922–33. https://doi.org/10.1097/JGP.0b013e318187135f .
Depp CA, Jeste DV. Bipolar disorder in older adults: a critical review. Bipolar Disord. 2004;6(5):343–67. https://doi.org/10.1111/j.1399-5618.2004.00139.x .
Ljubic N, Ueberberg B, Grunze H, Assion HJ. Treatment of bipolar disorders in older adults: a review. Ann Gen Psychiatry. 2021;20(1):45. https://doi.org/10.1186/s12991-021-00367-x . (PMID: 34548077; PMCID: PMC8456640).
Beunders AJM, Orhan M, Dols A. Older age bipolar disorder. Curr Opin Psychiatry. 2023;36(5):397–404. https://doi.org/10.1097/YCO.0000000000000883 .
Ponzer K, Millischer V, Schalling M, Gissler M, Lavebratt C, Backlund L. Lithium and risk of cardiovascular disease, dementia and venous thromboembolism. Bipolar Disord. 2023. https://doi.org/10.1111/bdi.13300 .
Young RC, Mulsant BH, Sajatovic M, Gildengers AG, Gyulai L, Al Jurdi RK, et al. GERI-BD: a randomized double-blind controlled trial of lithium and divalproex in the treatment of mania in older patients with bipolar disorder. Am J Psychiatry. 2017;174(11):1086–93. https://doi.org/10.1176/appi.ajp.2017.15050657 .
Tondo L, Alda M, Bauer M, Bergink V, Grof P, Hajek T, et al. Clinical use of lithium salts: guide for users and prescribers. Int J Bipolar Disord. 2019;7(1):16. https://doi.org/10.1186/s40345-019-0151-2 .
Shulman KI, Almeida OP, Herrmann N, Schaffer A, Strejilevich SA, Paternoster C, et al. Delphi survey of maintenance lithium treatment in older adults with bipolar disorder: an ISBD task force report. Bipolar Disord. 2019;21(2):117–23. https://doi.org/10.1111/bdi.12714 .
Paton C, Barnes TR, Shingleton-Smith A, McAllister-Williams RH, Kirkbride J, Jones PB, et al. Lithium in bipolar and other affective disorders: prescribing practice in the UK. J Psychopharmacol. 2010;24(12):1739–46. https://doi.org/10.1177/0269881110367728 .
Morlet E, Costemale-Lacoste JF, Poulet E, McMahon K, Hoertel N, Limosin F, et al. Psychiatric and physical outcomes of long-term use of lithium in older adults with bipolar disorder and major depressive disorder: a cross-sectional multicenter study. J Affect Disord. 2019;259:210–7. https://doi.org/10.1016/j.jad.2019.08.056 .
Finley PR. Drug interactions with lithium: an update. Clin Pharmacokinet. 2016;55(8):925–41. https://doi.org/10.1007/s40262-016-0370-y .
Scherf-Clavel M, Treiber S, Deckert J, Unterecker S, Hommers L. Drug-drug interactions between lithium and cardiovascular as well as anti-inflammatory drugs. Pharmacopsychiatry. 2020;53(5):229–34. https://doi.org/10.1055/a-1157-9433 .
Hommers L, Fischer M, Reif-Leonhard C, Pfuhlmann B, Deckert J, Unterecker S. The combination of lithium and ACE inhibitors: hazardous, critical, possible? Clin Drug Investig. 2019;39(5):485–9. https://doi.org/10.1007/s40261-019-00768-7 .
Ferensztajn-Rochowiak E, Rybakowski JK. Long-term lithium therapy: side effects and interactions. Pharmaceuticals. 2023;16(1):74. https://doi.org/10.3390/ph16010074 .
Kortenoeven ML, Li Y, Shaw S, Gaeggeler HP, Rossier BC, Wetzels JF, et al. Amiloride blocks lithium entry through the sodium channel thereby attenuating the resultant nephrogenic diabetes insipidus. Kidney Int. 2009;76(1):44–53. https://doi.org/10.1038/ki.2009.91 .
Nunes RP. Lithium interactions with non-steroidal anti-inflammatory drugs and diuretics–a review. Arch Clin Psychiatry. 2018;45:38–40.
Schou M, Kampf D. Lithium and the kidneys. In: Bauer M, Grof P, Müller-Oerlinghausen B, editors. Lithium in neuropsychiatry. Boca Raton: Taylor & Francis; 2006.
de Montigny C, Cournoyer G, Morissette R, Langlois R, Caillé G. Lithium carbonate addition in tricyclic antidepressant-resistant unipolar depression. Correlations with the neurobiologic actions of tricyclic antidepressant drugs and lithium ion on the serotonin system. Arch Gen Psychiatry. 1983;40(12):1327–34. https://doi.org/10.1001/archpsyc.1983.01790110069012 .
Boeker H, Seidl A, Schopper C. Neurotoxicitiy related to combined treatment with lithium, antidepressants and atpyical neuroleptics: a series of cases. Schweizer Archiv für Neurologie und Psychiatrie. 2022;162(2):72–6.
Hill GE, Wong KC, Hodges MR. Lithium carbonate and neuromuscular blocking agents. Anesthesiology. 1977;46(2):122–6. https://doi.org/10.1097/00000542-197702000-00008 .
Wijeratne C, Draper B. Reformulation of current recommendations for target serum lithium concentration according to clinical indication, age and physical comorbidity. Aust N Z J Psychiatry. 2011;45(12):1026–32. https://doi.org/10.3109/00048674.2011.610296 .
Kemp DE, Gao K, Chan PK, Ganocy SJ, Findling RL, Calabrese JR. Medical comorbidity in bipolar disorder: relationship between illnesses of the endocrine/metabolic system and treatment outcome. Bipolar Disord. 2010;12(4):404–13. https://doi.org/10.1111/j.1399-5618.2010.00823.x .
Kuramochi S, Yatomi T, Uchida T, Takeuchi H, Mimura M, Uchida H. Drug combinations for mood disorders and physical comorbidities that need attention: a cross-sectional national database survey. Pharmacopsychiatry. 2022;55(3):157–62. https://doi.org/10.1055/a-1744-6582 .
Kitanaka N, Hall FS, Uhl GR, Kitanaka J. Lithium pharmacology and a potential role of lithium on methamphetamine abuse and dependence. Curr Drug Res Rev. 2019;11(2):85–91. https://doi.org/10.2174/2589977511666190620141824 .
Preuss UW, Schaefer M, Born C, Grunze H. Bipolar disorder and comorbid use of illicit substances. Medicina. 2021;57(11):1256. https://doi.org/10.3390/medicina57111256 .
Grunze H, Soyka M. The pharmacotherapeutic management of comorbid bipolar disorder and alcohol use disorder. Expert Opin Pharmacother. 2022;23(10):1181–93. https://doi.org/10.1080/14656566.2022.2083500 .
Janiri D, Di Nicola M, Martinotti G, Janiri L. Who’s the leader, mania or depression? predominant polarity and alcohol/polysubstance use in bipolar disorders. Curr Neuropharmacol. 2017;15(3):409–16. https://doi.org/10.2174/1570159X14666160607101400 .
Coles AS, Sasiadek J, George TP. Pharmacotherapies for co-occurring substance use and bipolar disorders: a systematic review. Bipolar Disord. 2019;21(7):595–610. https://doi.org/10.1111/bdi.12794 .
McKnight RF, Adida M, Budge K, Stockton S, Goodwin GM, Geddes JR. Lithium toxicity profile: a systematic review and meta-analysis. Lancet. 2012;379(9817):721–8. https://doi.org/10.1016/S0140-6736(11)61516-X .
Albert U, De Cori D, Aguglia A, Barbaro F, Lanfranco F, Bogetto F, et al. Lithium-associated hyperparathyroidism and hypercalcaemia: a case-control cross-sectional study. J Affect Disord. 2013;151(2):786–90. https://doi.org/10.1016/j.jad.2013.06.046 .
Albert U, De Cori D, Aguglia A, Barbaro F, Lanfranco F, Bogetto F, et al. Effects of maintenance lithium treatment on serum parathyroid hormone and calcium levels: a retrospective longitudinal naturalistic study. Neuropsychiatr Dis Treat. 2015;11:1785–91. https://doi.org/10.2147/NDT.S86103 .
Hayes JF, Marston L, Walters K, Geddes JR, King M, Osborn DP. Adverse renal, endocrine, hepatic, and metabolic events during maintenance mood stabilizer treatment for bipolar disorder: a population-based cohort study. PLoS Med. 2016;13(8):e1002058. https://doi.org/10.1371/journal.pmed.1002058 .
Vancampfort D, Stubbs B, Mitchell AJ, De Hert M, Wampers M, Ward PB, et al. Risk of metabolic syndrome and its components in people with schizophrenia and related psychotic disorders, bipolar disorder and major depressive disorder: a systematic review and meta-analysis. World Psychiatry. 2015;14(3):339–47. https://doi.org/10.1002/wps.20252 .
Köhler-Forsberg O, Rohde C, Nierenberg AA, Østergaard SD. Association of lithium treatment with the risk of osteoporosis in patients with bipolar disorder. JAMA Psychiat. 2022;79(5):454–63. https://doi.org/10.1001/jamapsychiatry.2022.0337 .
Bocchetta A, Loviselli A. Lithium treatment and thyroid abnormalities. Clin Pract Epidemiol Ment Health. 2006;2:23. https://doi.org/10.1186/1745-0179-2-23 .
Haissaguerre M, Vantyghem MC. What an endocrinologist should know for patients receiving lithium therapy. Ann Endocrinol (Paris). 2022;83(4):219–25. https://doi.org/10.1016/j.ando.2022.01.001 .
Bendz H, Schön S, Attman PO, Aurell M. Renal failure occurs in chronic lithium treatment but is uncommon. Kidney Int. 2010;77(3):219–24. https://doi.org/10.1038/ki.2009.433 .
Wiuff AC, Rohde C, Jensen BD, Nierenberg AA, Østergaard SD, Köhler-Forsberg O. Association between lithium treatment and renal, thyroid and parathyroid function: a cohort study of 6659 patients with bipolar disorder. Bipolar Disord. 2023. https://doi.org/10.1111/bdi.13356 .
Shine B, McKnight RF, Leaver L, Geddes JR. Long-term effects of lithium on renal, thyroid, and parathyroid function: a retrospective analysis of laboratory data. Lancet. 2015;386(9992):461–8. https://doi.org/10.1016/S0140-6736(14)61842-0 .
Rej S, Herrmann N, Gruneir A, McArthur E, Jeyakumar N, Muanda FT, et al. Association of lithium use and a higher serum concentration of lithium with the risk of declining renal function in older adults: a population-based cohort study. J Clin Psychiatry. 2020;81(5):1913045. https://doi.org/10.4088/JCP.19m13045 .
Schoot TS, Molmans THJ, Grootens KP, Kerckhoffs APM. Systematic review and practical guideline for the prevention and management of the renal side effects of lithium therapy. Eur Neuropsychopharmacol. 2020;31:16–32. https://doi.org/10.1016/j.euroneuro.2019.11.006 .
Pompili M, Magistri C, Mellini C, Sarli G, Baldessarini RJ. Comparison of immediate and sustained release formulations of lithium salts. Int Rev Psychiatry. 2022;34(7–8):753–9. https://doi.org/10.1080/09540261.2022.2122706 .
Bowden CL. Key treatment studies of lithium in manic-depressive illness: efficacy and side effects. J Clin Psychiatry. 1998;59(6):13–9.
CAS PubMed Google Scholar
Carter L, Zolezzi M, Lewczyk A. An updated review of the optimal lithium dosage regimen for renal protection. Can J Psychiatry. 2013;58(10):595–600. https://doi.org/10.1177/070674371305801009 .
Durbano F, Mencacci C, Dorigo D, Riva M, Buffa G. The long-term efficacy and tolerability of carbolithium once a day: an interim analysis at 6 months. Clin Ter. 2002;153(3):161–6.
Girardi P, Brugnoli R, Manfredi G, Sani G. Lithium in bipolar disorder: optimizing therapy using prolonged-release formulations. Drugs R D. 2016;16(4):293–302. https://doi.org/10.1007/s40268-016-0139-7 .
Wallin L, Alling C. Effect of sustained-release lithium tablets on renal function. Br Med J. 1979;2(6201):1332. https://doi.org/10.1136/bmj.2.6201.1332 .
Cooper TB, Simpson GM, Lee JH, Bergner PE. Evaluation of a slow-release lithium carbonate formulation. Am J Psychiatry. 1978;135(8):917–22. https://doi.org/10.1176/ajp.135.8.917 .
Grof P. Some practical aspects of lithium treatment: blood levels, dosage prediction, and slow-release preparations. Arch Gen Psychiatry. 1979;36(8):891–3. https://doi.org/10.1001/archpsyc.1979.01780080065015 .
Barbuti M, Colombini P, Ricciardulli S, Amadori S, Gemmellaro T, De Dominicis F, et al. Treatment adherence and tolerability of immediate- and prolonged-release lithium formulations in a sample of bipolar patients: a prospective naturalistic study. Int Clin Psychopharmacol. 2021;36(5):230–7. https://doi.org/10.1097/YIC.0000000000000373 .
Pelacchi F, Dell’Osso L, Bondi E, Amore M, Fagiolini A, Iazzetta P, et al. Clinical evaluation of switching from immediate-release to prolonged-release lithium in bipolar patients, poorly tolerant to lithium immediate-release treatment: a randomized clinical trial. Brain Behav. 2022;12(3):e2485. https://doi.org/10.1002/brb3.2485 .
Tondo L, Baldessarini RJ. Reduction of suicidal behavior in bipolar disorder patients during long-term treatment with lithium. In: Koslow SH, Ruitz P, Nemeroff CB, editors. A concise guide to understanding suicide. Cambridge: Cambridge University Press; 2014. p. 217–28.
Barraclough B. Suicide prevention, recurrent affective disorder and lithium. Br J Psychiatry. 1972;121(563):391–2. https://doi.org/10.1192/bjp.121.4.391 .
Jamison KR. Suicide and bipolar disorders. Ann N Y Acad Sci. 1986;487:301–15. https://doi.org/10.1111/j.1749-6632.1986.tb27909.x .
Tondo L, Baldessarini RJ, Hennen J, Floris G, Silvetti F, Tohen M. Lithium treatment and risk of suicidal behavior in bipolar disorder patients. J Clin Psychiatry. 1998;59(8):405–14. https://doi.org/10.4088/jcp.v59n0802 .
Baldessarini RJ, Tondo L, Hennen J. Lithium treatment and suicide risk in major affective disorders: update and new findings. J Clin Psychiatry. 2003;64(Suppl 5):44–52.
Baldessarini RJ, Tondo L, Davis P, Pompili M, Goodwin FK, Hennen J. Decreased risk of suicides and attempts during long-term lithium treatment: a meta-analytic review. Bipolar Disord. 2006;8(5 Pt 2):625–39. https://doi.org/10.1111/j.1399-5618.2006.00344.x .
Ahrens B, Müller-Oerlinghausen B. Does lithium exert an independent antisuicidal effect? Pharmacopsychiatry. 2001;34(4):132–6. https://doi.org/10.1055/s-2001-15878 .
Pompili M, Berardelli I, Sarubbi S, Rogante E, Germano L, Sarli G, Erbuto D, Baldessarini RJ. Lithium treatment versus hospitalization in bipolar disorder and major depression patients. J Affect Disord. 2023;1(340):245–9. https://doi.org/10.1016/j.jad.2023.08.028 .
Cipriani A, Pretty H, Hawton K, Geddes JR. Lithium in the prevention of suicidal behavior and all-cause mortality in patients with mood disorders: a systematic review of randomized trials. Am J Psychiatry. 2005;162(10):1805–19. https://doi.org/10.1176/appi.ajp.162.10.1805 .
Cipriani A, Hawton K, Stockton S, Geddes JR. Lithium in the prevention of suicide in mood disorders: updated systematic review and meta-analysis. BMJ. 2013;346:f3646. https://doi.org/10.1136/bmj.f3646 .
Smith KA, Cipriani A. Lithium and suicide in mood disorders: updated meta-review of the scientific literature. Bipolar Disord. 2017;19(7):575–86. https://doi.org/10.1111/bdi.12543 .
Oquendo MA, Galfalvy HC, Currier D, Grunebaum MF, Sher L, Sullivan GM, et al. Treatment of suicide attempters with bipolar disorder: a randomized clinical trial comparing lithium and valproate in the prevention of suicidal behavior. Am J Psychiatry. 2011;168(10):1050–6. https://doi.org/10.1176/appi.ajp.2011.11010163 .
Katz IR, Rogers MP, Lew R, Thwin SS, Doros G, Ahearn E, et al. Lithium treatment in the prevention of repeat suicide-related outcomes in veterans with major depression or bipolar disorder: a randomized clinical trial. JAMA Psychiat. 2022;79(1):24–32. https://doi.org/10.1001/jamapsychiatry.2021.3170 .
Baldessarini RJ, Tondo L. Testing for antisuicidal effects of lithium treatment. JAMA Psychiat. 2022;79(1):9–10. https://doi.org/10.1001/jamapsychiatry.2021.2992 .
Pompili M, Vichi M, Dinelli E, Pycha R, Valera P, Albanese S, Lima A, De Vivo B, Cicchella D, Fiorillo A, Amore M, Girardi P, Baldessarini RJ. Relationships of local lithium concentrations in drinking water to regional suicide rates in Italy. World J Biol Psychiatry. 2015;16(8):567–74. https://doi.org/10.3109/15622975.2015.1062551 .
Pompili M, Berardelli I, Sarubbi S, Rogante E, Germano L, Sarli G, et al. Lithium treatment versus hospitalization in bipolar disorder and major depression patients. J Affect Disord. 2023. https://doi.org/10.1016/j.jad.2023.08.028 .
Stevens AWMM, Goossens PJJ, Knoppert-van der Klein EAM, Draisma S, Honig A, Kupka RW. Risk of recurrence of mood disorders during pregnancy and the impact of medication: a systematic review. J Affect Disord. 2019;249:96–103. https://doi.org/10.1016/j.jad.2019.02.018 .
Viguera AC, Whitfield T, Baldessarini RJ, Newport DJ, Stowe Z, Reminick A, et al. Risk of recurrence in women with bipolar disorder during pregnancy: prospective study of mood stabilizer discontinuation. Am J Psychiatry. 2007;164(12):1817–24. https://doi.org/10.1176/appi.ajp.2007.06101639 .
Rosso G, Albert U, Di Salvo G, Scatà M, Todros T, Maina G. Lithium prophylaxis during pregnancy and the postpartum period in women with lithium-responsive bipolar I disorder. Arch Womens Ment Health. 2016;19(2):429–32. https://doi.org/10.1007/s00737-016-0601-0 .
Munk-Olsen T, Liu X, Viktorin A, Brown HK, Di Florio A, D’Onofrio BM, et al. Maternal and infant outcomes associated with lithium use in pregnancy: an international collaborative meta-analysis of six cohort studies. Lancet Psychiatry. 2018;5(8):644–52. https://doi.org/10.1016/S2215-0366(18)30180-9 .
Patorno E, Huybrechts KF, Bateman BT, Cohen JM, Desai RJ, Mogun H, et al. Lithium use in pregnancy and the risk of cardiac malformations. N Engl J Med. 2017;376(23):2245–54. https://doi.org/10.1056/NEJMoa1612222 .
Fornaro M, Maritan E, Ferranti R, Zaninotto L, Miola A, Anastasia A, et al. Lithium exposure during pregnancy and the postpartum period: a systematic review and meta-analysis of safety and efficacy outcomes. Am J Psychiatry. 2020;177(1):76–92. https://doi.org/10.1176/appi.ajp.2019.19030228 .
Gentile S. Prophylactic treatment of bipolar disorder in pregnancy and breastfeeding: focus on emerging mood stabilizers. Bipolar Disord. 2006;8(3):207–20. https://doi.org/10.1111/j.1399-5618.2006.00295.x .
Imaz ML, Torra M, Soy D, García-Esteve L, Martin-Santos R. Clinical lactation studies of lithium: a systematic review. Front Pharmacol. 2019;10:1005. https://doi.org/10.3389/fphar.2019.01005 .
Gentile S. Lithium in pregnancy: the need to treat, the duty to ensure safety. Expert Opin Drug Saf. 2012;11(3):425–37. https://doi.org/10.1517/14740338.2012.670419 .
Nordon C, Sutter AL, Verdoux H. Prise en charge des femmes souffrant d’un trouble bipolaire de la conception au post-partum. Presse Med. 2007;36(12):1913–8. https://doi.org/10.1016/j.lpm.2007.03.042 .
Hermann A, Gorun A, Benudis A. Lithium use and non-use for pregnant and postpartum women with bipolar disorder. Curr Psychiatry Rep. 2019;21(11):114. https://doi.org/10.1007/s11920-019-1103-3 .
Wesseloo R, Wierdsma AI, van Kamp IL, Munk-Olsen T, Hoogendijk WJG, Kushner SA, et al. Lithium dosing strategies during pregnancy and the postpartum period. Br J Psychiatry. 2017;211(1):31–6. https://doi.org/10.1192/bjp.bp.116.192799 .
Heinz A, Liu S. Challenges and chances for mental health care in the 21st century. World Psychiatry. 2022;21(3):423–4. https://doi.org/10.1002/wps.21006 .
Malhi GS, Gessler D, Outhred T. The use of lithium for the treatment of bipolar disorder: Recommendations from clinical practice guidelines. J Affect Disord. 2017;217:266–80. https://doi.org/10.1016/j.jad.2017.03.052 .
Jauhar S, Young AH. Controversies in bipolar disorder; role of second-generation antipsychotic for maintenance therapy. Int J Bipolar Disord. 2019;7(1):10. https://doi.org/10.1186/s40345-019-0145-0 .
Severus E, Bauer M, Geddes J. Efficacy and effectiveness of lithium in the long-term treatment of bipolar disorders: an update 2018. Pharmacopsychiatry. 2018;51(5):173–6. https://doi.org/10.1055/a-0627-7489 .
Carvalho AF, Firth J, Vieta E. Bipolar disorder. N Engl J Med. 2020;383(1):58–66. https://doi.org/10.1056/NEJMra1906193 .
Severus E, Taylor MJ, Sauer C, Pfennig A, Ritter P, Bauer M, et al. Lithium for prevention of mood episodes in bipolar disorders: systematic review and meta-analysis. Int J Bipolar Disord. 2014;2:15. https://doi.org/10.1186/s40345-014-0015-8 .
Berk M, Cowdery S, Williams L, Malhi GS. Recalibrating the risks and benefits of lithium therapy. Br J Psychiatry. 2017;211(1):1–2. https://doi.org/10.1192/bjp.bp.116.193789 .
González-Pinto A, López-Peña P, Bermúdez-Ampudia C, Vieta E, Martinez-Cengotitabengoa M. Can lithium salts prevent depressive episodes in the real world? Eur Neuropsychopharmacol. 2018;28(12):1351–9. https://doi.org/10.1016/j.euroneuro.2018.09.008 .
Kessing LV, Bauer M, Nolen WA, Severus E, Goodwin GM, Geddes J. Effectiveness of maintenance therapy of lithium vs other mood stabilizers in monotherapy and in combinations: a systematic review of evidence from observational studies. Bipolar Disord. 2018. https://doi.org/10.1111/bdi.12623 .
Lähteenvuo M, Tanskanen A, Taipale H, Hoti F, Vattulainen P, Vieta E, et al. Real-world effectiveness of pharmacologic treatments for the prevention of rehospitalization in a finnish nationwide cohort of patients with bipolar disorder. JAMA Psychiat. 2018;75(4):347–55. https://doi.org/10.1001/jamapsychiatry.2017.4711 .
De Fazio P, Gaetano R, Caroleo M, Pavia M, De Sarro G, Fagiolini A, et al. Lithium in late-life mania: a systematic review. Neuropsychiatr Dis Treat. 2017;13:755–66. https://doi.org/10.2147/NDT.S126708 .
Ross J. Discontinuation of lithium augmentation in geriatric patients with unipolar depression: a systematic review. Can J Psychiatry. 2008;53(2):117–20. https://doi.org/10.1177/070674370805300207 .
Cooper C, Katona C, Lyketsos K, Blazer D, Brodaty H, Rabins P, et al. A systematic review of treatments for refractory depression in older people. Am J Psychiatry. 2011;168(7):681–8. https://doi.org/10.1176/appi.ajp.2011.10081165 .
Reynolds CF 3rd, Jeste DV, Sachdev PS, Blazer DG. Mental health care for older adults: recent advances and new directions in clinical practice and research. World Psychiatry. 2022;21(3):336–63. https://doi.org/10.1002/wps.20996 .
Malhi GS, Bell E, Outhred T, Berk M. Lithium therapy and its interactions. Aust Prescr. 2020;43(3):91–3. https://doi.org/10.1877/austprescr.2020.024 .
Samalin L, Honciuc M, Boyer L, de Chazeron I, Blanc O, Abbar M, et al. Efficacy of shared decision-making on treatment adherence of patients with bipolar disorder: a cluster randomized trial (ShareD-BD). BMC Psychiatry. 2018;18(1):103. https://doi.org/10.1186/s12888-018-1686-y .
Fulford KWM, Handa A. New resources for understanding patients’ values in the context of shared clinical decision-making. World Psychiatry. 2021;20(3):446–7. https://doi.org/10.1002/wps.20902 .
Swift JK, Mullins RH, Penix EA, Roth KL, Trusty WT. The importance of listening to patient preferences when making mental health care decisions. World Psychiatry. 2021;20(3):316–7. https://doi.org/10.1002/wps.20912 .
Pompili M. Epidemiology of suicide: from population to single cases. Epidemiol Psychiatr Sci. 2019;29:e68. https://doi.org/10.1017/S2045796019000647 .
Armstrong G, Haregu T, Arya V, Vijayakumar L, Sinyor M, Niederkrotenthaler T, et al. Suicide-related Internet search queries in India following media reports of a celebrity suicide: an interrupted time series analysis. World Psychiatry. 2021;20(1):143–4. https://doi.org/10.1002/wps.20832 .
Hawton K, Pirkis J. Suicide is a complex problem that requires a range of prevention initiatives and methods of evaluation. Br J Psychiatry. 2017;210(6):381–3. https://doi.org/10.1192/bjp.bp.116.197459 .
Keyes KM, Whitley R, Fink D, Santaella J, Pirkis J. The global impact of celebrity suicides: implications for prevention. World Psychiatry. 2021;20(1):144–5. https://doi.org/10.1002/wps.20761 .
Laugesen K, Farkas DK, Vestergaard M, Jørgensen JOL, Petersen I, Sørensen HT. Glucocorticoid use and risk of suicide: a Danish population-based case-control study. World Psychiatry. 2021;20(1):142–3. https://doi.org/10.1002/wps.20831 .
Klonsky ED, Dixon-Luinenburg T, May AM. The critical distinction between suicidal ideation and suicide attempts. World Psychiatry. 2021;20(3):439–41. https://doi.org/10.1002/wps.20909 .
Ehring T. Thinking too much: rumination and psychopathology. World Psychiatry. 2021;20(3):441–2. https://doi.org/10.1002/wps.20910 .
Poels EMP, Bijma HH, Galbally M, Bergink V. Lithium during pregnancy and after delivery: a review. Int J Bipolar Disord. 2018;6(1):26. https://doi.org/10.1186/s40345-018-0135-7 .
Haussmann R, Noppes F, Brandt MD, Bauer M, Donix M. Lithium: a therapeutic option in Alzheimer’s disease and its prodromal stages? Neurosci Lett. 2021;760:136044. https://doi.org/10.1016/j.neulet.2021.136044 .
Simonetti A, Sani G, Dacquino C, Piras F, De Rossi P, Caltagirone C, et al. Hippocampal subfield volumes in short- and long-term lithium-treated patients with bipolar I disorder. Bipolar Disord. 2016;18(4):352–62. https://doi.org/10.1111/bdi.12394 .
Puglisi-Allegra S, Ruggieri S, Fornai F. Translational evidence for lithium-induced brain plasticity and neuroprotection in the treatment of neuropsychiatric disorders. Transl Psychiatry. 2021;11(1):366. https://doi.org/10.1038/s41398-021-01492-7 .
Agam G, Levine J. Neuroprotective effects of lithium in neuropsychiatric disorders. In: Gozes I, Levine J, editors. Neuroprotection in Autism, Schizophrenia and Alzheimer’s disease. Cambridge: Academic Press; 2020. p. 209–41.
Chapter Google Scholar
Zivanovic O. Lithium: a classic drug-Frequently discussed, but, sadly, seldom prescribed! Aust N Z J Psychiatry. 2017;51(9):886–96. https://doi.org/10.1177/0004867417695889 .
Download references
Acknowledgements
The publication of the present manuscript has been supported by an unrestricted grant by Angelini Pharma.
Author information
Authors and affiliations.
Department of Psychiatry, University of Campania “L. Vanvitelli”, Largo Madonna delle Grazie, Naples, Italy
Andrea Fiorillo & Gaia Sampogna
Department of Medicine, Surgery and Health Sciences, University of Trieste, Trieste, Italy
Umberto Albert
San Luigi Gonzaga Hospital, University of Turin, Turin, Italy
Giuseppe Maina & Gianluca Rosso
Department of Neurosciences “Rita Levi Montalcini”, University of Turin, Turin, Italy
Department of Clinical and Experimental Medicine, University of Pisa, Pisa, Italy
Giulio Perugi
Department of Neurosciences, Mental Health and Sensory Organs, Suicide Prevention Center, Sant’Andrea Hospital - Sapienza University of Rome, Rome, Italy
Maurizio Pompili
Department of Neuroscience, Section of Psychiatry, Università Cattolica del Sacro Cuore, Largo Francesco Vito 1, 00168, Rome, Italy
Gabriele Sani
Department of Psychiatry, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Largo Agostino Gemelli 8, 00168, Rome, Italy
Department of Psychiatry, University of Perugia, Perugia, Italy
Alfonso Tortorella
You can also search for this author in PubMed Google Scholar
Contributions
All authors approved the final version of the manuscript.
Corresponding author
Correspondence to Gaia Sampogna .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
All authors agreed to the final version of the manuscript.
Competing interests
Additional information, publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Fiorillo, A., Sampogna, G., Albert, U. et al. Facts and myths about the use of lithium for bipolar disorder in routine clinical practice: an expert consensus paper. Ann Gen Psychiatry 22 , 50 (2023). https://doi.org/10.1186/s12991-023-00481-y
Download citation
Received : 17 October 2023
Accepted : 20 November 2023
Published : 06 December 2023
DOI : https://doi.org/10.1186/s12991-023-00481-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Bipolar disorder
- Pharmacological treatment
- Side effect
- Neuroprotection
Annals of General Psychiatry
ISSN: 1744-859X
- Submission enquiries: [email protected]
Dsm 5 Autism Spectrum Disorder
This essay about the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), discusses the significant changes in the classification of Autism Spectrum Disorder (ASD). The shift from multiple distinct categories to a unified spectrum approach reflects a more accurate representation of the diverse manifestations of autism. It highlights how the DSM-5 emphasizes two primary diagnostic criteria: challenges in social communication and repetitive behavioral patterns, including sensory sensitivities. The essay also addresses the implications of these changes for personalized treatment and the broader acceptance of neurodiversity. Concerns about the consistency of diagnoses under the new criteria are discussed, underscoring the need for ongoing adjustments in the diagnostic process to better encompass the full range of autistic experiences. Overall, the essay evaluates how the updated DSM-5 criteria lead to a deeper understanding and improved support for individuals with ASD.
How it works
The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) marks a notable advancement in the way mental health professionals understand and approach Autism Spectrum Disorder (ASD). This latest edition has redefined the framework for diagnosing autism, broadening our perspective and enhancing the way support is provided to individuals across the spectrum.
In earlier iterations like the DSM-IV, autism was fragmented into several distinct categories, such as Asperger’s Syndrome and pervasive developmental disorder-not otherwise specified (PDD-NOS). However, the DSM-5 consolidates these into a single category: ASD.
This consolidation is based on the realization that autism manifests through a continuum of symptoms rather than discrete blocks, making a spectrum approach more reflective of the true nature of these experiences.
The criteria for diagnosing ASD in DSM-5 focus heavily on two primary areas: persistent challenges in social communication and interaction across multiple contexts, and patterns of behavior that are restricted and repetitive. This framework acknowledges that while some may face significant challenges in social situations, others might be more affected by sensory sensitivities or inflexible adherence to routines. Including these varied experiences under one category allows for a more nuanced understanding of each individual’s needs.
One significant addition in DSM-5 is the greater emphasis on sensory sensitivities. This new diagnostic element recognizes that sensory experiences—how individuals perceive touch, sound, and light, for example—can greatly impact their social and emotional lives. By considering these factors, the DSM-5 addresses aspects of ASD that were previously underappreciated, allowing for a more comprehensive approach to care.
The adoption of a spectrum-based classification also influences how treatments are designed and implemented. It paves the way for customized support plans that are more closely aligned with the diverse strengths and challenges of individuals with ASD. This tailored approach not only optimizes developmental outcomes but also enhances quality of life, promoting a higher level of inclusion and participation in society.
Despite these improvements, the transition to the DSM-5 criteria has sparked discussions and concerns, particularly regarding the consistency of diagnoses. Some argue that the broader framework might exclude individuals who would have been diagnosed under the more segmented DSM-IV approach. These debates underscore the importance of continued refinement in diagnostic processes, ensuring they capture the full range of autism experiences without narrowing the scope of who receives support.
Reflecting on the changes brought about by the DSM-5, it’s clear that the updated diagnostic criteria represent more than just medical terminology adjustments—they signify a deeper understanding of autism as a diverse and complex experience. This evolution in thought and practice not only helps medical professionals and educators provide better support but also aligns more closely with the advocacy community’s push for recognition and acceptance of neurodiversity.
In sum, the shift to a spectrum-based view in DSM-5 enhances our approach to understanding and supporting individuals with autism. It brings us closer to a society that values and integrates the unique perspectives and abilities of all its members, acknowledging that diversity in human experience enriches us all.
Cite this page
Dsm 5 Autism Spectrum Disorder. (2024, Apr 14). Retrieved from https://papersowl.com/examples/dsm-5-autism-spectrum-disorder/
"Dsm 5 Autism Spectrum Disorder." PapersOwl.com , 14 Apr 2024, https://papersowl.com/examples/dsm-5-autism-spectrum-disorder/
PapersOwl.com. (2024). Dsm 5 Autism Spectrum Disorder . [Online]. Available at: https://papersowl.com/examples/dsm-5-autism-spectrum-disorder/ [Accessed: 15 Apr. 2024]
"Dsm 5 Autism Spectrum Disorder." PapersOwl.com, Apr 14, 2024. Accessed April 15, 2024. https://papersowl.com/examples/dsm-5-autism-spectrum-disorder/
"Dsm 5 Autism Spectrum Disorder," PapersOwl.com , 14-Apr-2024. [Online]. Available: https://papersowl.com/examples/dsm-5-autism-spectrum-disorder/. [Accessed: 15-Apr-2024]
PapersOwl.com. (2024). Dsm 5 Autism Spectrum Disorder . [Online]. Available at: https://papersowl.com/examples/dsm-5-autism-spectrum-disorder/ [Accessed: 15-Apr-2024]
Don't let plagiarism ruin your grade
Hire a writer to get a unique paper crafted to your needs.

Our writers will help you fix any mistakes and get an A+!
Please check your inbox.
You can order an original essay written according to your instructions.
Trusted by over 1 million students worldwide
1. Tell Us Your Requirements
2. Pick your perfect writer
3. Get Your Paper and Pay
Hi! I'm Amy, your personal assistant!
Don't know where to start? Give me your paper requirements and I connect you to an academic expert.
short deadlines
100% Plagiarism-Free
Certified writers
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Dialogues Clin Neurosci
- v.10(2); 2008 Jun
Language: English | Spanish | French
Current research in child and adolescent bipolar disorder
Investigación actual en el trastorno bipolar en niños y adolescentes, travaux actuels sur les troubles bipolaires de l'enfant et de l'adolescent, christine a. demeter.
Department of Psychiatry, University Hospitals Case Medical Center/Case Western Reserve University, Cleveland, Ohio, USA
Lisa D. Townsend
The Mandel School of Applied Social Sciences at Case Western Reserve University, Cleveland Ohio, USA
Michael Wilson
Robert l. findling.
Although recently more research has considered children with bipolar disorder than in the past, much controversy still surrounds the validity of the diagnosis. Furthermore, questions remain as to whether or not childhood expressions of bipolarity are continuous with adult manifestations of the illness. In order to advance current knowledge of bipolar disorders in children, researchers have begun to conduct phenomenological, longitudinal, treatment, and neuroimaging studies in youths who exhibit symptoms of bipolar illness, as well as offspring of parents with bipolar disorders. Regardless of the differences between research groups regarding how bipolar disorder in children is defined, it is agreed that pediatric bipolarity is a serious and pernicious illness. With early intervention during the period of time in which youths are exhibiting subsyndromal symptoms of pediatric bipolarity, it appears that the progression of the illness to the more malignant manifestation of the disorder may be avoided. This paper will review what is currently known and what still is left to learn about clinically salient topics that pertain to bipolar disorder in children and adolescents.
Aunque en la actualidad hay más investigatión que ha incluido niños con trastorno bipolar que en el pasado, todavía existe mucha controversia alrededor de la validez del diagnóstico. Además persisten preguntas si acaso las expresiones de bipolaridad en la niñez constituyen un continuo con las manifestaciones de la enfermedad en el adulto. Para avanzar en el conocimiento actual de los trastornos bipolares en los niños los investigadores han comenzado a realizar estudios fenomenológicos, longitudinales, terapéuticos y de neuroimágenes en jóvenes que presentan síntomas de enfermedad bipolar, como también en hijos de padres con trastornos bipolares. A pesar de las diferencias entre grupos de investigatión respecto a cómo está definido el trastorno bipolar en niños, hay acuerdo en que la bipolaridad pediátrica es una enfermedad seria y dañina. Con una intervención precoz durante el período de tiempo en el cual los jóvenes presentan síntomas subsindromáticos de bipolaridad pediátrica, parece que la progresión de la enfermedad hacia la manifestación más maligna del trastorno se puede evitar. Este artículo revisará el conocimiento actual y lo que todavía falta por aprender acerca de tópicos clínicamente destacados que pertenecen al trastorno bipolar en niños y adolescentes.
La valeur du diagnostic des troubles bipolaires reste encore très controversée chez les enfants, bien que des travaux récents s'y intéressent plus que par le passé. Un certain nombre de questions demeurent, comme celle de savoir si la bipolarité dans l'enfance est en continuité avec les manifestations pathologiques de l'âge adulte. Les chercheurs ont entrepris des études longitudinales phénoménologiques et thérapeutiques ainsi que des études de neuro-imagerie chez les jeunes qui présentent des symptômes de troubles bipolaires, mais également chez les descendants de parents bipolaires, afin de faire avancer l'état actuel des connaissances sur les troubles bipolaires de l'enfant. La bipolarité pédiatrique est reconnue pour être une pathologie sérieuse et pernicieuse, quelles que soient les différences de définition entre les équipes de recherche. Si les jeunes sont traités précocement, dès l'apparition des symptômes subsyndromaux de la maladie bipolaire pédiatrique, la progression vers les formes les plus sévères pourrait être évitée. Cet article passe en revue les connaissances actuelles et ce qu'il reste à apprendre à propos de sujets cliniquement pertinents liés aux troubles bipolaires chez l'enfant et l'adolescent.
Children and adolescents diagnosed with a bipolar (BP) disorder face substantial obstacles. Besides the human suffering associated with the mood symptomatology which they experience, greater academic problems, difficulties with peers, and high levels of family dysfunction are often found in youths with bipolar disorder. 1 , 2 Furthermore, children and adolescents with bipolar disorder have an increased risk of substance use, suicidal ideation, suicide attempts, and completed suicide. 3 , 4 In fact, Goldstein et al 5 found that approximately 32% of 405 youths under the age of 18 with a bipolar spectrum disorder reported having a previous serious suicide attempt. In the hope of reducing the substantive sequelae associated with this condition, research has begun to examine how best to recognize early-onset bipolar disorder in children and effectively treat these patients earlier in their course of illness.
Prevalence of bipolar disorder
The lifetime prevalence of a bipolar spectrum disorder in adults has been estimated to be approximately 4.5%, with subsyndromal bipolar disorders being more prevalent (2.4%) than Bipolar I Disorder (BP-I) or Bipolar II Disorder (BP-II). 6 Epidemiological studies have found bipolar spectrum disorders to be present in approximately 0.1% to 1% of children and adolescents (sec ref 7 for review). Recently it has been noted that the number of office visits for youth with bipolar disorder has increased 40-fold over the past 10 years, indicating that either this syndrome was under-recognized in the past, or that children arc now being diagnosed incorrectly. 8 As will be discussed later, there is substantial symptom overlap that exists between bipolar spectrum disorders and other psychiatric conditions. In fact, it is possible that it is this symptom overlap that may account for the differences between the past and present rates at which the diagnosis of bipolarity is given to children and adolescents.
Phenomenology
Phenomenology studies have begun to explore the symptom presentation of bipolar disorder throughout early childhood, adolescence, and into adulthood. 9 - 12 As a result of current research, there is a growing body of evidence to support the assertion that elevated mood may be a key symptom in pediatric BP spectrum disorders, which distinguishes this condition from other psychiatric illnesses. 13 For example, Axelson et al 4 found that approximately 82% of youths with bipolar disorder not otherwise specified (BP-NOS) and 92% of children and adolescents with BP-I reported elevated mood. Furthermore, Findling et al 14 found that elevated mood was the best predictor of BP-NOS or cyclothymic disorder in offspring of a parent with bipolar disorder.
Although elevated mood is a distinguishing symptom in pediatric bipolarity, youths with bipolar disorders have been shown to exhibit substantive rates of aggression and irritability. 13 , 15 , 16 For instance, Danielyan et al 9 found that 88.5% of their sample reported aggression and 84.6% reported irritability. However, it should be noted that symptoms of aggression and irritability, although prominent in pediatric bipolarity, are symptoms of many other childhood psychiatric disorders such as disruptive behavior disorders and depression. Therefore, due to their lack of diagnostic specificity, irritability and aggression may not be the best means by which to differentiate pediatric bipolar illness from other psychiatric conditions in the young.
Other common symptoms observed in children and adolescents with bipolar illness across multiple pediatric studies include other diagnostic symptom criteria for mania described in the DSM-IV 17 : increased energy, distractibility, pressured speech, grandiosity, and racing thoughts (see ref 13 for review).
Notably, it appears that most children and adolescents meet DSM-IV criteria for BP-NOS rather than the symptomatic manifestations of BP-I or BP-II. 12 Additionally, it appears that the most common reason that children and adolescents meet DSM-IV criteria for BP-NOS but do not meet criteria for BP-I or BP-II is not due to lack of meeting an adequate number of symptom criteria, but rather failing to meet episode duration criteria. 4 However, despite the fact that subjects do not meet full DSM-IV criteria for BPI or BP-II, patients with BP-NOS and cyclothymic disorder also suffer from impairing mood symptoms. 4 , 14 In short, although the rates at which symptoms are reported in pediatric bipolar illness appear to vary somewhat across research sites, it is clear that there is a group of children and adolescents who present with symptoms of bipolar spectrum disorders as defined by DSM.-IV criteria. 17
Comorbidity
In addition to mood episodes and their associated symptoms, adults and children with bipolar disorder also have been reported to experience high rates of comorbid psychiatric diagnoses. In a nationally representative sample of adults, over 90% of respondents with a bipolar spectrum disorder reported at least one comorbid diagnosis. 6 The most frequent comorbid diagnoses found in adults with bipolar disorder in this study were anxiety disorders. Similarly to adults, high rates of comorbid diagnoses have been found in children and adolescents with bipolar disorders. For example, Tillman et al 18 found that almost 98% of 91 children and adolescents with a bipolar spectrum disorder examined also suffered from a comorbid psychiatric disorder. Kowatch et al 13 reported in a metaanalysis that attention deficit-hyperactivity disorder (ADHD) was the most frequent comorbid diagnosis in children and adolescents with bipolar disorder. Other common comorbid diagnoses in youth with bipolar disorder include oppositional defiant disorder (ODD), anxiety disorders, conduct disorder (CD), and substance use disorders. 13 Rates of comorbid psychiatric diagnoses reported in youth with bipolar disorders vary from 11% to 90% presenting with ADHD, 46% to 75% with ODD, 5% to 37% with CD, 12% to 77% with anxiety disorders, and up to 40% of adolescents with a substance use disorder. 4 , 10 , 12 , 19 - 24 One possible explanation for the varying and high rates of reported comorbid diagnoses in youths with a bipolar spectrum disorder may be the result of overlapping symptoms across diagnoses that may be attributable to other disorders. For example, inattention, distractibility, impulsivity, psychomotor agitation, and sleep disturbances can be characteristic of both children and adolescents with bipolar disorder as well as ADHD. 25 As noted above, irritability and aggression are common symptoms observed in adolescents with bipolar disorder. However, these symptoms are also characteristic of a disruptive behavior disorder (DBD).
As might be expected, children and adolescents diagnosed with a bipolar disorder and a comorbid psychiatric diagnosis have a more complicated clinical presentation, and often have confounding issues that need to be addressed in treatment. For instance, in those youths with bipolar disorder and other comorbid conditions, both the youths and parents reported more family conflict and lower family cohesion in comparison with youths with bipolar disorder only. 2 In both the pharmacological and therapeutic treatment of bipolar disorder, comorbid diagnoses further complicate the treatment plan by necessitating intervention for multiple psychiatric conditions.
Longitudinal course
Age of onset.
Most patients experience their first mood episode between the ages of 17 and 42 years, with a median age of onset of 25 years. 26 However, there is evidence to suggest that children do in fact experience the onset of symptoms of bipolar disorder prior to the age of 17 years. 19 , 27 In addition, retrospective studies examining adults with bipolar disorder have reported childhood onset of symptoms in a substantive number of subjects. For instance, Perlis et al 28 found when patients recalled their first mood episode, approximately 65% of adults experienced onset of symptoms prior to the age of 18. Moreover, 27.7% of adults reported that they experienced their first mood episode before the age of 13 years. 28
Age of onset appears to impact the course of illness. 29 For example, in a retrospective study of adults, patients with childhood or adolescent onset of bipolar symptoms experienced a greater number of mood episodes and were more likely to have comorbid psychiatric conditions and higher rates of rapid cycling. 30 In this same study, adults with an onset of symptoms at 12 years of age or younger had the greatest incidence of bipolar and unipolar disorders in their parents. This younger age at onset subgroup experienced a higher incidence of dysphoric mania, and a higher prevalence of a lifetime diagnosis of an anxiety disorder and drug abuse compared with adults who reported an age of onset of 13 years or greater. 30
Additionally, the age of onset of a parent's bipolar disorder has been found to have implications in their offspring. For example, Tsuang and Faraone 31 found in adults that there was a higher risk of developing a mood disorder if a subject had relatives with an earlier age of onset of a mood disorder in comparison with subjects whose relatives had a later age of onset.
Rather than relying on retrospective studies conducted in adults, researchers have begun to examine the impact of age of onset in children and adolescents with bipolar disorder. Youths with early onset of bipolar disorder prior to the age of 12 have been found to have more firstdegree relatives with a family history of ADHD, conduct disorder, anxiety disorders, substance dependence, suicidal behavior, and suicide attempt and completion in comparison with those subjects with a later onset of bipolar symptoms at 12 years or later. 32 In addition, it has been reported that children and adolescents with childhood onset of bipolar disorder were more likely to have suffered from ADHD than those with onset during adolescence. 33
Symptom course
It appears that after illness onset, children and adolescents with bipolar disorder spend the majority of time fluctuating between syndromal and subsyndromal mood episodes, with short periods of euthymia interspersed. 19 For instance, Birmaher et al 34 found that in 263 youths with a bipolar spectrum disorder, subjects were symptomatic during approximately 60% of the 2-year follow-up period. Furthermore, DelBello et al 35 found that adolescents that had been hospitalized with a BP-I diagnosis, during the year following their index inpatient stay, spent a predominant amount of their lives symptomatic. More specifically, these adolescents spent 84% of the year experiencing at least subsyndromal symptoms following their hospitalization. In addition, Geller et al 21 reported that in youths experiencing mania, manic episodes lasted approximately an average of 80 weeks in duration. Similarly, in a pediatric cohort with bipolar disorder followed for 2 years, only 68% of the cohort experienced minimal or no symptoms for 8 consecutive weeks after their index episode. 34 Furthermore, in those subjects that recovered from their index episode, a median of 78 weeks elapsed from the onset of the presenting mood episode until symptom remission. 34
The polarity of mood episodes that occur during the course of bipolarity appear to change as patients with bipolar disorder age. In adults with bipolar disorder, evidence suggests that depression is the predominant mood state, with patients spending approximately three times as much time depressed as manic or hypomanic. 36 However, in children and adolescents, researchers have reported that hypomanic and manic symptoms dominate, with depressive episodes being less frequent. 19
Moreover, the mood state of the initial mood episode has been found to influence time until symptom remission. For instance, Strober et al 37 reported that adolescent patients who presented initially in a manic or mixed episode had a shorter time until mood stabilization in comparison with patients who experienced a depressive mood episode initially. Additionally, the longitudinal outcome appears to be worse in children and adolescents who have an earlier age of onset of diagnosis, with lower social economic status, rapid mood fluctuations, psychosis, mixed episodes, more comorbid diagnoses, and family psychopathology being reported. 38
Evolution of symptoms
There is evidence to suggest that mood and symptoms of other psychiatric diagnoses in patients may evolve over time. For instance, mood symptomatology in adults appears to become more severe with increased number of mood episodes. In addition, adults appear to experience fewer periods of euthymia throughout their lifetime. 39 Moreover, with time, mood episodes that occurred as a result of a psychological stressor may begin to occur spontaneously without a precipitant. 39
There is also some evidence to suggest that an evolution of mood symptoms may occur across the diagnostic categories of the bipolar spectrum disorders over time. For instance, it appears that patients may experience symptoms that meet diagnostic symptom criteria for BP-NOS and cyclothymia prior to meeting diagnostic symptom criteria for more syndromal diagnoses of BP-I and BPII. 3 , 40 Birmaher et al 34 found that approximately 20% of patients initially diagnosed with BP-II converted to BPI, and 25% of patients initially diagnosed with BP-NOS converted to BP-I or BP-II over a mean of 2 years of follow-up monitoring.
ADHD and anxiety symptoms have also been observed to precede mood symptoms in patients later diagnosed with bipolar disorder. 24 , 40 , 41 It has been suggested that the high rates of DBDs and ADHD in children of parents with bipolar disorder may be indicative that DBD and ADHD symptoms may be prodromal manifestations of bipolar disorder. 42 By examining children and adolescents at high risk of developing a bipolar disorder prospectively, this endeavor offers an opportunity to better investigate early symptoms and biological markers of bipolar disorders.
High risk studies
It has been suggested that if children are treated soon after the initial onset of mood symptoms, the developmental impact of the psychiatric illness may be minimized. 39 Furthermore, it appears that bipolar disorders are highly heritable conditions. 43 - 45 High rates of affective disorders in first-degree relatives have been reported in children with bipolar disorder. For instance, Faedda et al 20 found that 90% of patients with bipolar disorder had a family history of bipolar disorder. Additionally, it has been well documented that children and adolescents with parents diagnosed with a bipolar disorder are at high risk of developing bipolar disorder themselves. 14 , 46 , 47 Therefore, in an attempt to better study the course of bipolar disorder and treat patients as soon as possible after symptom onset, patients who are at risk for developing pediatric bipolarity are now being examined.
Children of parents with a mood disorder (depression and/or bipolar disorders) not only have an increased risk for developing bipolar disorder, but also other psychiatric disorders. For instance, offspring of parents with a mood disorder were found to be at risk for depression, anxiety, ADHD, DBD diagnoses, and more impaired psychosocial functioning. 14 , 42 , 47 - 49 Furthermore, independent of diagnosis, children and adolescents of parents with bipolar disorder have been shown to exhibit higher rates of hostility and irritability in comparison with offspring of parents without a psychiatric disorder. 50
Moreover, having only one parent versus both parents being afflicted with bipolar disorder appears to have additional implications for the youth's course of illness. For instance, offspring of two parents with bipolar disorder have been found to experience more severe depression and irritability, lack of mood reactivity, and rejection sensitivity in comparison with children with only one parent with bipolar disorder. 47 Therefore, a patient's family history may offer insight into the probability of a child presenting with or eventually developing bipolar disorder.
Biological underpinnings
Genetic predispositions.
Due to the observed high heritability of bipolar disorders, several genetic etiologies of bipolar spectrum disorders have been explored. Multiple genomic regions have been associated with bipolar disorder and the age of onset of mood symptoms. 51 - 54 For instance, regions on chromosomes 2, 4, 6, 8, 11, 12, 13, 16, 18, 21, 22, and X have been found to be possibly linked to bipolar disorder (see ref 55 for review). 43 , 55 , 57 Furthermore, several functional candidate genes have been identified to be possibly linked to bipolar disorder including catechol-Omcthyl transferase (COMT), brain-derived neurotropic factor, tyrosine hydroxylase, D-amino acid oxidase activator, and neuregulin (see ref 57 for review). 52 , 57 In addition, earlier age of onset and increased severity of illness in subsequent generations of family members have led to genetic anticipation being hypothesized in bipolar disorder (see ref 58 for review). More specifically, it has been suggested that trinucleotide repeats may be involved in the genetic predisposition to eventual development of a bipolar disorder. 58
Structural brain differences
With advances in imaging techniques, researchers have begun to investigate whether or not structural differences in individuals afflicted with bipolar disorder exist when compared with individuals without a psychiatric illness. Examinations of neuroanatomical structure differences of children with bipolar disorder compared with children without psychiatric disorders have reported conflicting results. However, it has been found that youths with bipolar disorder may have structural brain differences when compared with children and adolescents with other psychiatric conditions and youths without psychiatric diagnoses. These differences include smaller hippocampal volumes, smaller cerebral volumes (bilateral parietal and left temporal lobes), and smaller cingulate volumes. 59 - 62 Recently, in one of the largest samples of youths with bipolar disorder who underwent a magnetic resonance imaging (MRI) study, larger right nucleus accumbens of the basal ganglia were found in this patient population in comparison with children and adolescents with no psychiatric diagnoses. 63 Additionally, a significant inverse relationship was found between the right nucleus accumbens volume and the number of medications the youth was currently receiving. 63
Due to the involvement of the amgydalac in emotion processing, this area of the brain has also been examined. For instance, Chang et al 64 found that youths with at least one parent with bipolar disorder and a bipolar disorder I diagnosis had significantly smaller left and right amgydalar volumes in comparison with healthy offspring of parents with no psychiatric disorders. In addition, Blumberg et al 65 found adults and adolescents with bipolar disorder have decreased volumes of the medial temporal lobe structures, especially in the amygdala in comparison with subjects without a psychiatric diagnosis. Moreover, abnormalities in the amygdala-striatal-ventral prefrontal cortex circuit, which is involved with mood regulation, have been found in pediatric bipolar disorder (review in ref 66).
In a review of adult and youth research, subjects with a recent onset of bipolar disorder were found to have ventricular, white matter, caudate, putamen, amygdala, hippocampus, and subgenual prefrontal cortex volume differences (see ref 67 for a review). Furthermore, relatives of individuals with bipolar disorder showed a reduction of the subgenual prefrontal cortex in several studies, suggesting a possible neuroanatomical marker for youth at risk for developing bipolar disorder. 67
There has been some evidence to suggest a possible change of brain structures over time in adults with bipolar disorder. For instance, over a 4-year period, adults with bipolar disorder showed a greater decline in hippocampal, fusiform, and cerebellar gray matter density than adults without a psychiatric disorder. 68 Moreover, in one longitudinal examination of children prior to and after the development of bipolar disorder, an increase in left temporal cortex gray matter volume and decreased bilateral anterior cingulate cortex gray matter volume was found in comparison with children without a psychiatric diagnosis or other psychotic disorder over the course of 4 to 8 years. 69
Functional neuroimaging
Differences in areas of brain activation during ncurocognitive tasks in patients with bipolar disorder have also been examined in an attempt to provide insights into the pathophysiology of this condition. For instance, during mood episodes, adults with bipolar disorder have been found to exhibit attentional, memory, and executive functioning impairments during mood episodes, which are sustained to a lesser degree during euthymic periods. 70 It has been suggested that these continued cognitive impairments during euthymic periods may be a result of underlying dysfunctional neurophysiology. 71 More specifically, using functional MRI (fMRI), euthymic adults with bipolar disorder were found to perform similarly in completion of an attentional task to healthy controls. However, the euthymic bipolar group showed greater activation in the anterior limbic region in compared with healthy controls. 72 Furthermore, Strakowski et al 71 found that in adults with bipolar disorder who were euthymic, the same pattern of activation in an fMRI during the Stroop interference condition was not found in the healthy controls, suggesting possible deficits in impulse control in the patient group. In comparison with children without a psychiatric disorder or a first-degree relative with a psychiatric disorder, youths with bipolar disorder showed deficits in engaging striatal structures and the right ventral prefrontal cortex using fMRI during unsuccessful motor inhibition. 73 Additionally, Chang et al 74 found that children and adolescents with bipolar disorder who also had at least one parent with a bipolar disorder showed increased activation in the prefrontal areas including the bilateral anterior cingulate cortex, bilateral caudate, putamen, thalamus, dorsolateral prefrontal cortex, and inferior frontal gyrus while performing cognitive and affective tasks in comparison with normal controls. This increased cerebral activation may suggest that children with bipolar disorder may require increased activation of prefrontal areas of the brain during periods of euthymia in order to counteract a hyperactive limbic system. 74 By researchers examining and characterizing putative biological markers of early onset bipolar disorder, neuroimaging may eventually be able to provide clinically salient information early in the course of illness.
Neuropsychological and social-cognitive factors
Emotional and cognitive processing has been examined in youth with bipolar disorder. Evidence suggests that children and adolescents may misperceive emotions during social interactions with others. McClure et al 75 found that sad, happy, and fearful peer facial expressions were misinterpreted more often by children with bipolar disorder in comparison with children with anxiety disorders or subjects with no psychiatric diagnosis. In addition, when viewing neutral faces, youth with bipolar disorder perceived more hostility and experienced more anxiety in comparison with youth without a psychiatric disorder. 76 In another study, children and adolescents with bipolar disorder were more likely to mistakenly characterize facial emotions than youths without a psychiatric disorder. 77 Moreover, the pediatric patients with bipolar disorder were less likely to choose appropriate responses when presented with interpersonal situation vignettes when compared with a healthy control group. 77 These emotional and social interpretation deficits may be due to neural circuitry differences. For example, Rich et al 78 found that youths with bipolar disorder have less functional connectivity in areas that may be involved in processing facial expressions and emotional stimuli. These areas include the neural circuitry between the left amygdala and areas bordering the right posterior cingulate/precuncus and the right fusiform gyrus/parahippocampal gyrus.
Other studies have found that youths with bipolar disorder exhibit less cognitive flexibility in adapting to changing contingencies in cognitive testing. 77 , 79 Pavuluri et al 80 found evidence to suggest that activation patterns in brain regions are different in pediatric bipolar patients in comparison with healthy controls when subjects observed angry and happy faces. These activation differences implicate a disturbance in affect neurocircuitry which may contribute to emotional dysregulation and social cognitive deficits in youths with bipolar disorder. 80 An understanding of these emotional and cognitive processing findings may have clinical relevance, as they might allow clinicians to direct a portion of their psychotherapy to address interpersonal skills and allow educators to modify lesson plans in order to accommodate the possible cognitive deficits.
Neurochemical differences
Similarly to serotonergic dysfunction observed in depressive conditions, using positron emission tomography (PET), a lower serotonin transporter binding potential (proportional to serotonin transporter number) was found in adults with bipolar disorder in comparison with adults with no psychiatric conditions. 81 In addition, using magnetic resonance spectroscopy (MRS), elevated gray matter lactate and y-aminobutyric acid levels have been found in adults with bipolar disorder in comparison with adults without a psychiatric diagnosis. 82 Furthermore, unmedicated youth with bipolar disorder were found to have significantly lower glutamine levels in the anterior cingulate cortex compared with subjects with a bipolar disorder who were currently receiving medications and subjects without a psychiatric diagnosis, using MRS. 83 By determining neurochemical differences in youth with bipolar disorder in comparison with normal controls, pharmacotherapies could eventually be developed that could target the neurochemical underpinnings of pediatric bipolarity.
Advances in the treatment of bipolarity in children
Psychopharmacology.
Unfortunately, historically there have been limited studies of methodological rigor in children and adolescents with bipolar disorder. Current recommended treatments in pediatric bipolar disorder include mood stabilizers and antipsychotic medications that may be coprescribed with adjunctive treatments administered for the treatment of comorbid psychiatric conditions. 84
Acute treatments
There have been a limited number of placebo-controlled trials that have been performed to investigate efficacy in the acute treatment of pediatric bipolar illness. Psychotropics that have been found to be superior to placebo in the acute treatment of children and adolescents with bipolar disorder presenting with manic or mixed episodes include olanzapine, 85 risperidone, 86 quetiapine, 87 and aripiprazole. 88
Several studies have examined the efficacy of treatment with divalproex (DVPX) in children with BP-I presenting in a mixed or manic episode. Using DVPX extendedrelease in a double-blind trial, there was not a significant improvement of manic symptoms after 4 weeks compared with placebo. 89 However, DVPX was found to be efficacious in a double-blind study that compared 8 weeks of treatment with DVPX, lithium, and placebo. 90 Furthermore, although the decrease in manic symptoms in the lithium group did not reach statistical significance in comparison with the placebo group, there was a decrease of greater magnitude in manic symptoms in the lithium group when compared with the placebo. 90 Notably, this trend for lithium to be efficacious may become more definitively substantiated in subsequent studies in which higher lithium doses or a larger sample size is employed.
Failed placebo-controlled trials in the acute treatment of pediatric bipolar disorder include topiramate 91 and oxcarbazepine. 92 It should be noted that the trial examining the efficacy of topiramate was underpowered due to cessation of the study after results of the compound in adults failed to show efficacy. However, when comparing the mean decrease in total Young Mania Rating Scale (YM.RS) scores over time, statistical significance was almost reached, with the topiramate group showing a greater change from baseline scores. Therefore, due to sample size considerations, whether or not topiramate truly docs or does not have efficacy in this patient population remains to be seen. 91
Open-label trials examining the effectiveness and safety of additional agents and medications mentioned above when administered to younger cohorts have also shown positive preliminary results. For example, in youths with bipolar disorder presenting currently with manic or mixed states, ziprasidone 93 - 95 and lithium 96 , 97 may be effective in reducing manic symptoms. Moreover, in studies of patients too young to be included in the aforestated placebo-controlled trials, olanzapine and risperidone were found to be effective in children as young as 4 years of age. 98 , 99 Open-label treatment with carbamazepine has also been reported to provide amelioration of manic symptoms in youths with bipolar disorder. 100
When examining the treatment of youths with bipolar disorder presenting with depression, open-label trials have noted that lithium monotherapy, 101 lamotrigine monotherapy, and lamotrigine adjunctive treatment 102 may be effective in alleviating mood symptoms. Finally, treatment with open-label clozapine has described as being effective in youths who were treatment-resistant. 103 , 104 Although ziprasidone, carbamazepine, lithium, lamotrigine, and clozapine have shown positive effects in open-label trials, randomized placebo-controlled trials are needed to produce more definitive conclusions.
While some salutary effects have been found in drug monotherapy studies, it appears that most children and adolescents do not experience complete symptom remission with thymoleptic monotherapy. Therefore, in an attempt to more completely address mood symptoms, combination pharmacotherapy has been examined in several clinical trials. In fact, in open-label studies, combination psychotropic treatments appear to be more successful than monotherapy treatments in pediatric bipolar disorder. For example, after 6 weeks of treatment with lithium, DVPX sodium, or carbamazepine, only 38% to 53% of subjects experienced symptom recovery, with those patients in the carbamazepine group experiencing the least symptom recovery. 100 However, a proportion of subjects who did not originally respond to lithium, DVPX sodium, or carbamazepine monotherapy responded to combination treatment with two of the abovementioned mood stabilizers and adjunctive stimulants, antipsychotic agents, or an antidepressant medication. 105
In addition, DelBello et al 106 found in a double-blind study that treatment with quetiapine plus valproate was more effective than treatment with quetiapine monotherapy in youths with bipolar disorder. Furthermore, combination treatment with both risperidone and lithium or risperidone and DVPX was found to be effective and safe in the treatment of children and adolescents with bipolar I disorder over a 6-month period. 107 Combination treatment with lithium and DVPX has been found to ameliorate mood symptoms in several studies. 105 , 108 , 109 Finally, positive results were found with combination treatment with lithium plus cither risperidone or a neuroleptic. 97 , 107
Recently, other treatment options have been explored in pediatric bipolarity. For instance, Wozniak et al 110 found open-label treatment with omega-3 fatty acids to improve manic symptoms in youth with bipolar disorder. Although the results of the abovementioned open-label trials are promising, randomized, placebo-controlled trials in children and adolescents are needed to provide more definitive results. Table I includes the dosing and most frequently reported adverse events in the abovementioned studies.
Maintenance treatments
While bipolar disorder is a chronic condition, little attention has focused on long-term maintenance treatments in youth. In one of the few maintenance trials, Kafantaris et al 111 randomized adolescents who had been stabilized on lithium monotherapy for a minimum of 4 weeks to either lithium or placebo for 2 subsequent weeks of treatment. Results showed that there was not a significant difference between treatment groups in rates of symptom exacerbation. Although this study provides preliminary insights regarding the continued use of lithium in adolescents with mania, definitive conclusions about lithium as a maintenance treatment cannot be determined from these data. Although this was an important trial, methodological limitations included a small sample size, the study's brevity, and the fact that there was a relatively abrupt discontinuation of lithium over 3 days in those subjects randomized to receive placebo in the discontinuation phase. In another maintenance double -blind trial, the efficacy of lithium or DVPX monotherapy for up to 76 weeks in youths who had been stabilized on combination lithium and DVPX treatment was examined. 112 In this study, no difference in length of study enrollment was found between the lithium and DVPX sodium treatment groups, with both groups ending the study after a mean of approximately 20 weeks. 112 These results appear to indicate that once a patient responds to a combination treatment, discontinuation of one of the agents used in combination therapy may lead to symptom relapse.
Psychosocial treatments
Favorable results in the treatment of bipolar disorder are not limited to medication trials. Several psychosocial treatments have shown positive results in the treatment of youth with bipolar disorder. For example, dialectal behavior therapy has been reported to significantly improve suicidally, self-injurious behavior, emotional dysrcgulation, and depressive symptoms after 1 year of sessions in adolescents diagnosed with a bipolar spectrum disorder currently receiving psychotropic medications. 113 In addition, a 21-session adjunctive familyfocused treatment (FFT) that included psychocducation, communication enhancement training, and problem-solving skills training was found to decrease depressive symptoms, maniac symptoms, and behavior problems in adolescents with bipolar disorder. 114 Moreover, individual family treatment (IFP) and multifamily psychoeducation groups (MFPG) were developed to provide support, psychoeducation, and increase problem-solving and communication skills in families with a child with a mood disorder. 115 Both IFP and MFPG have been shown to increase the understanding of mood disorders, ameliorate mood symptoms, improve the family environment, and increase mental health service utilization. 115
Additionally, cognitive behavior therapy (CBT) was found to reduce manic and depressive symptoms in youth diagnosed with a bipolar disorder spectrum disorder after 12 sessions. 116 CBT supplemented with familyfocused therapy has also shown to ameliorate bipolar symptoms and increase global functioning scores in patients with bipolar disorder. 117 Furthermore, the childand family-focused CBT program was effective in maintaining long-term management of mood symptoms over 3 years in youths with bipolar disorder. 118
Interpersonal and social rhythm therapy (IPSRT) is another treatment that uses some of CBT's behavioral interventions to address mood symptoms. However, IPSRT also focuses both on the youth's expectations in their own interpersonal life, and attempts to help the patient maintain stable social and sleep routines. 119 In adults, IPSRT has been found to be effective in prolonging the time until patients experience a new mood episode. 120 Based on these adult data, IPSRT may be an effective treatment for adolescents with bipolar disorder. 119 However, due to difficulties in extrapolating adult based behavioral interventions in préadolescents, IPSRT has not been studied in younger children. In short, multiple psychosocial treatments have been reported to be effective and are becoming more refined to address issues specific to youth with bipolar disorder. These treatments may prove to be useful in increasing medication treatment adherence and providing the additional assistance needed where medication is not able to fully treat all aspects of pediatric bipolarity.
Future areas of research
Although recent research has broadened the knowledge about bipolar disorder in youth, there are many unanswered questions that remain. More phenomenology studies may provide insights into whether or not the comorbid symptoms of additional psychiatric disorders that are seen in this population are distinct, separate entities, or simply part of this mood disorder when it presents during childhood. Furthermore, as children appear to experience more elevated mood and irritability in comparison with adults who report more depressive symptoms, future longitudinal examinations may provide answers to the question of whether or not symptoms of childhood bipolarity evolve into more adult-like presentations over time.
Examining youths who are at high risk for developing bipolar disorder, such as offspring of parents with mood disorders, provides a unique opportunity in carefully characterizing the evolution of mood symptomatology. By exploring high-risk cohorts and identifying prodromal symptoms, effective treatments can be used earlier in the course of pediatric bipolarity. 121 Furthermore, treating children and adolescents with subsyndromal expressions of bipolar disorders soon after the onset of symptoms may prevent illness progression to the more severe and prototypic presentations of the disorder.
Although technological advances have begun to allow investigators to examine the biological underpinnings of pediatric bipolarity, larger sample sizes and replication studies are needed in order to confirm or refute whether or not the genetic, anatomical, and neurochemical differences reported thus far are not chance findings. Ideally, genetic and neuroimaging methodologies could eventually be used as a diagnostic tools that could facilitate the psychiatric assessment, and treatment processes. Although there is a growing body of evidence that pertains to the acute monotherapy pharmacological treatment of pediatric bipolar illness, future studies are also needed to investigate various combination psychotropic treatments and adjunctive psychosocial therapies. In addition, longer term safety and maintenance efficacy studies with medications are still few in number and are clearly needed.
In conclusion, with earlier, accurate identification and diagnosis of bipolar disorders, psychotropic and psychosocial treatment can be initiated earlier in the course of the illness. It is hoped that with the development, of safe and effective interventions, the probability that the child suffering from bipolar illness will develop into a well-adjusted adult with high academic, family, and social functioning will be better than it. is at present.
Selected abbreviations and acronyms
Dr Findling receives or has received research support, acted as a consultant and/or served on a speaker's bureau for Abbott, AstraZeneca, Bristol-Myers Squibb, Cypress Biosciences, Forest, GlaxoSmithKline, Johnson & Johnson, Lilly, Neuropharm, New River, Novartis, Organon, Otsuka, Pfizer, SanofiAventis, Sepracore, Shire, Solvay, Supernus Pharmaceuticals, and Wyeth. Dr Wilson, Christine Demeter, and Lisa Townsend have no financial ties to disclose.

IMAGES
VIDEO
COMMENTS
Bipolar disorder is a broad diagnostic construct associated with significant phenotypic and genetic heterogeneity challenging progress in clinical practice and discovery research. Prospective studies of well-c... Anne Duffy and Paul Grof. International Journal of Bipolar Disorders 2024 12 :12.
Bipolar disorders (BDs) are recurrent and sometimes chronic disorders of mood that affect around 2% of the world's population and encompass a spectrum between severe elevated and excitable mood states (mania) to the dysphoria, low energy, and despondency of depressive episodes. The illness commonly starts in young adults and is a leading cause of disability and premature mortality. The ...
Bipolar disorders are a complex group of severe and chronic disorders that includes bipolar I disorder, defined by the presence of a syndromal, manic episode, and bipolar II disorder, defined by the presence of a syndromal, hypomanic episode and a major depressive episode. Bipolar disorders substantially reduce psychosocial functioning and are ...
Introduction. Bipolar disorder (BD) is a chronic illness associated with severely debilitating symptoms that can have profound effects on both patients and their caregivers (Miller, 2006).BD typically begins in adolescence or early adulthood and can have life‐long adverse effects on the patient's mental and physical health, educational and occupational functioning, and interpersonal ...
Bipolar disorders are a complex group of severe and chronic disorders that includes bipolar I disorder, defined by the presence of a syndromal, manic episode, and bipolar II disorder, defined by the presence of a syndromal, hypomanic episode and a major depressive episode. Bipolar disorders substantially reduce psychosocial functioning and are associated with a loss of approximately 10-20 ...
Overview of bipolar disorder. Bipolar disorder is a chronic and complex mood disorder that is characterized by an admixture of manic (bipolar mania), hypomanic and depressive (bipolar depression) episodes, with significant subsyndromal symptoms that commonly present between major mood episodes Citation 1.Ranked among the leading causes of worldwide disability Citation 2, bipolar I disorder has ...
Bipolar I disorder is defined by the presence of overt manic episodes with a range of manifestations, including overconfidence, grandi-osity, talkativeness, extreme disinhibition, irritability ...
Abstract. Bipolar disorder is a severe, complicated, and often misunderstood disorder that can have serious impacts on a person's quality of life, sense of self-worth, and overall health. This ...
Bipolar disorder (BD) is a severe psychiatric illness with an increasing prevalence worldwide. Although the pathological mechanism of and pharmacological interventions for BD have been extensively investigated in preclinical and clinical studies, a scientometric analysis of the developmental trends, interdisciplinary frontiers, and research hotspots in this field has not yet been conducted.
Bipolar disorder, also known as bipolar affective disorder, is one of the top 10 leading causes of disability worldwide. Bipolar disorder is characterized by chronically occurring episodes of mania or hypomania alternating with depression and is often misdiagnosed initially. Treatment involves pharmacotherapy and psychosocial interventions, but ...
Conceptualization of bipolar disorders continues to evolve as the field learns more; for example, changes were made to the DSM-5 diagnostic criteria for BD such that Criteria A for both mania and hypomania now include increased energy as well as elevated or irritable mood (see Table 1). Thus, BD II is now recognized as a disorder of energy as well as mood.
The reclassification of paediatric bipolar disorder into 'adolescent bipolar disorder', with its emergence clearly anchored to the post-pubertal phase, will allow firstly, greater homogeneity of patient samples for research and more age-appropriate assessment tools and treatment interventions (see Figure 2). Secondly, it will draw attention ...
Research paper. Impact of bipolar disorder on health-related quality of life and work productivity: Estimates from the national health and wellness survey in Japan ... Bipolar disorder (BD) manifests as both manic and depressive episodes that is recurrent in an individual's life following onset, usually in early adulthood.
The Bipolar and Depression Research Program is a clinical research program focused on treatment of individuals with bipolar and major depressive disorders directed by Drs. Trisha Suppes and Michael Ostacher. It is located on the campus of the VA Palo Alto Health Care System and affiliated with the VA and the Stanford School of Medicine. All ...
Bipolar disorder is a common psychiatric disorder with a massive psychological and social burden. Research indicates that treatment adherence is not good in these patients. The families' knowledge about the disorder is fundamental for managing their patients' disorder. The purpose of the present study was to investigate the knowledge of the family members of a sample of Iranian patients ...
Introduction. Bipolar spectrum disorders are a major public health problem, with estimates of lifetime prevalence in the general population of the United States at 3.9 percent, 1 with a range from 1.5 to 6.0 percent. 2 Bipolar disorder is also associated with significant mortality risk, with approximately 25 percent of patients attempting suicide and 11 percent of patients completing. 3 ...
Bipolar disorder (formerly called manic-depressive illness or manic depression) is a mental illness that causes unusual shifts in a person's mood, energy, activity levels, and concentration. These shifts can make it difficult to carry out day-to-day tasks. There are three types of bipolar disorder. All three types involve clear changes in ...
Bipolar disorder is one of the most burdensome severe mental disorders, characterized by high levels of personal and social disability [].Patients often need an integrated [2,3,4] and personalized [5, 6] pharmacological and non-pharmacological approach [7, 8].In particular, when an acute depressive, manic or mixed episode occurs, a pharmacological treatment is usually needed; however, the ...
While several studies have explored this topic, there remains a scarcity of research comparing internalized stigma across both these illnesses. We investigated and compared how internalized stigma is associated with different socio-demographic factors among individuals diagnosed with schizophrenia and bipolar affective disorder in remission.
Background. Bipolar disorder (BD) is a major mood disorder characterized by recurrent episodes of depression and (hypo)mania (Goodwin and Jamison 2007).According to the Diagnostic and Statistical Manual 5 (DSM-5), the two main subtypes are BD-I (manic episodes, often combined with depression) and BD-II (hypomanic episodes, combined with depression) (APA 2014).
In 2023, the Heinz C. Prechter Bipolar Research Program was named as one of six institutions that is part of the BD² Integrated Network with BD²: Breakthrough Discoveries for Thriving with Bipolar Disorder.. Along with Brigham and Women's Hospital-McLean Hospital, University of California Los Angeles, Johns Hopkins University, Mayo Clinic, UTHealth Houston, the Prechter Program at the ...
Abstract. Bipolar disorder (BD) is a leading cause of global disability. Its biological basis is unknown, and its treatment unsatisfactory. Here, we review two recent areas of progress. First, the discovery of risk genes and their implications, with a focus on voltage-gated calcium channels as part of the disease process and as a drug target.
Induced pluripotent stem cell (iPSC) derived hippocampal dentate granule cell-like neurons from individuals with bipolar disorder (BD) are hyperexcitable and more spontaneously active relative to healthy control (HC) neurons. These abnormalities are normalised after the application of lithium in neurons derived from lithium responders (LR) only. How these abnormalities impact hippocampal ...
DOI: 10.1145/3644116.3644220 Corpus ID: 268984447; Research on the application of Artificial Intelligence in Bipolar Disorder @inproceedings{Yuan2023ResearchOT, title={Research on the application of Artificial Intelligence in Bipolar Disorder}, author={Yiwen Yuan and Yafen Wu and Huajie Sui and Rubin Deng}, booktitle={International Symposium on Artificial Intelligence in Medical Sciences ...
PMO is a rare, often misdiagnosed, visual disorder in which human faces appear distorted in shape, texture, position, or color. Most patients with PMO see these distorted facial features all the ...
Systematic review. 16 studies. Despite heterogeneity in methods, findings across studies were consistent; clinical risk factors of bipolar were early-onset panic attacks and disorder, separation anxiety and generalized anxiety disorders, conduct symptoms and disorder, ADHD, impulsivity and criminal behaviour.
Abstract. Bipolar disorders (BDs) are recurrent and sometimes chronic disorders of mood that afect around 2% of the world's population and encompass a spectrum between severe elevated and excitable mood states (mania) to the dysphoria, low energy, and despondency of depressive episodes. The illness commonly starts in young adults and is a ...
This essay about the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), discusses the significant changes in the classification of Autism Spectrum Disorder (ASD). The shift from multiple distinct categories to a unified spectrum approach reflects a more accurate representation of the diverse manifestations of autism.
This paper will review what is currently known and what still is left to learn about clinically salient topics that pertain to bipolar disorder in children and adolescents. Keywords: bipolar disorder, child, adolescent, phenomenology, treatment. Children and adolescents diagnosed with a bipolar (BP) disorder face substantial obstacles.