An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List


Treatment Guidelines for PTSD: A Systematic Review
Alicia martin.
1 Discipline of Pharmacy, Faculty of Health, University of Canberra, Canberra, ACT 2617, Australia; [email protected] (M.N.); [email protected] (S.K.); [email protected] (G.P.); [email protected] (J.T.); [email protected] (J.K.C.)
Mark Naunton
Gregory peterson.
2 School of Pharmacy and Pharmacology, University of Tasmania, Hobart, TAS 7001, Australia
Jackson Thomas
Julia k. christenson, associated data.
The data presented in this study are available within the article.
Background: The aim of this review was to assess the quality of international treatment guidelines for post-traumatic stress disorder (PTSD), and identify differences between guideline recommendations, with a focus on the treatment of nightmares. Methods: Guidelines were identified through electronic searches of MEDLINE, CINAHL, PubMed, Embase and Science Direct, as well as web-based searches of international guideline repositories, websites of psychiatric organisations and targeted web-searches for guidelines from the three most populous English-speaking countries in each continent. Data in relation to recommendations were extracted and the AGREE II criteria were applied to assess for quality. Results: Fourteen guidelines, published between 2004–2020, were identified for inclusion in this review. Only five were less than 5 years old. Three guidelines scored highly across all AGREE II domains, while others varied between domains. Most guidelines consider both psychological and pharmacological therapies as first-line in PTSD. All but one guideline recommended cognitive behavioural therapy (CBT) as first-line psychological treatment, and selective serotonin reuptake inhibitors (SSRIs) as first-line pharmacological treatment. Most guidelines do not mention the targeted treatment of nightmares as a symptom of PTSD. Prazosin is discussed in several guidelines for the treatment of nightmares, but recommendations vary widely. Most PTSD guidelines were deemed to be of good quality; however, many could be considered out of date. Recommendations for core PTSD symptoms do not differ greatly between guidelines. However, despite the availability of targeted treatments for nightmares, most guidelines do not adequately address this. Conclusions: Guidelines need to be kept current to maintain clinical utility. Improvements are most needed in the AGREE II key domains of ‘applicability’, ‘rigour of development’ and ‘stakeholder involvement’. Due to the treatment-resistant nature of nightmares, guideline development groups should consider producing more detailed recommendations for their targeted treatment. More high-quality trials are also required to provide a solid foundation for making these clinical recommendations for the management of nightmares in PTSD.
1. Introduction
Post-traumatic stress disorder (PTSD) is a debilitating mental condition that can significantly impact the sufferer’s quality of life [ 1 , 2 , 3 ]. A study by Rapaport et al. found that 59% of patients suffering from PTSD had severely impaired overall quality of life based on the Quality of Life Enjoyment and Satisfaction Questionnaire [ 4 ]. Stein et al. found that 38.9% of patients with PTSD had missed at least one work day in the last month due to emotional problems, compared to only 5.4% of people who did not suffer from a mental health condition, and Kessler reported that a PTSD diagnosis increases the likelihood of being homeless by 150% [ 5 , 6 ]. PTSD is also commonly associated with comorbidities of depression and substance use disorders, and a significantly increased risk of suicide [ 7 ].
PTSD comprises four symptom clusters: ‘avoidance’, ‘numbing’, ‘hyper-arousal’ and the hallmark ‘re-experiencing’ or ‘intrusive symptoms’, which include unwanted thoughts, flashbacks and nightmares [ 8 ]. Nightmares are often resistant to general PTSD treatment and have been linked with a five-fold increase in suicidality [ 9 ]. Nightmares should therefore be considered one of the most important symptoms to treat, yet they are often overlooked as a secondary symptom of PTSD [ 10 , 11 , 12 ]. In addition, there appears to be few recommendations for the treatment of nightmares in guidelines, even though there are targeted treatments available, such as image rehearsal therapy (IRT) and pharmacotherapies including prazosin, terazosin and some atypical antipsychotics [ 13 , 14 ].
PTSD can be treated using psychological therapies, pharmacotherapy or a combination of the two. The recommended psychological therapies in Australia include trauma-focused cognitive behavioural therapy (CBT) and eye movement desensitisation reprocessing (EMDR) [ 15 , 16 ]. For pharmacotherapy in PTSD, the selective serotonin reuptake inhibitor (SSRI) antidepressants are recommended [ 15 , 16 ].
Evidence-based guidelines for the diagnosis and treatment of PTSD are valuable resources for psychiatrists and other health professionals to aid in the development of appropriate individual treatment plans for their patients, whilst also deterring the implementation of potentially ineffective or harmful treatments [ 17 , 18 ]. It can be difficult for healthcare professionals to keep up with and critically appraise the enormous volume of newly-published research in their field [ 19 , 20 , 21 ]. Evidence indicates that clinical psychiatric practice is often not in line with current guideline recommendations and hence may not reflect the best available evidence [ 22 , 23 ]. There are many barriers to implementing guidelines into practice. These include a perceived lack of time to review lengthy guidelines, an oversupply of guidelines (often with conflicting recommendations), a lack of usefulness in patients with significant comorbidities, a belief that current practice is best care based on past clinical experience, and an aversion to the perceived “rigidity” of guideline recommendations [ 19 , 21 , 22 ]. Every guideline is developed using different methodologies which can influence the quality of recommendations.
This review aimed to assess the quality of international treatment guidelines for PTSD, as well as identify differences between guideline recommendations, with a focus on the treatment of nightmares.
2. Materials and Methods
The Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement was followed to report the results of this review [ 24 ]. The review was registered with PROSPERO on the 21st of December 2017, registration number: CRD42017084122 [ 25 ].
2.1. Search Strategy
Relevant guidelines were identified via an electronic search of databases MEDLINE, CINAHL, PubMed, Embase and Science Direct, conducted in October 2017 using the search terms in Table 1 . There were no date restrictions imposed; however, searches were restricted to the English language. A secondary search following the same methods was completed in September 2020 to identify any guidelines published after the initial search. Database searching was supplemented by web-based searches of guideline repositories ( www.guidelines.gov , clinicalguidelines.gov.au and https://www.g-i-n.net/ (accessed date: 5 October 2017 and 21 September 2020), websites of international psychiatric organisations and targeted web-searches for guidelines from the three most populous English-speaking countries in each continent using combinations of the country names and search terms in Table 1 . The latter was an additional step in an attempt to systematically capture any country-specific guidelines that were not listed in a guideline repository and may have otherwise been missed due to the search engine’s algorithm preferencing already identified guidelines. Reference lists of relevant guidelines were also searched manually for further relevant guidelines.
Search Terms.
2.2. Selection Criteria
All treatment guidelines for PTSD or nightmares were considered for inclusion. Guidelines were excluded if they were specific to children or adolescents, were based entirely on other guidelines, did not make clear recommendations for treatments or were specific to complex PTSD. Complex PTSD is caused by exposure to an extreme or prolonged stressor from which escape is difficult or impossible (such as childhood abuse), presenting with a range of symptoms in addition to core PTSD symptoms, and for which there is a lack of available evidence for diagnosis and treatment [ 26 ].
Titles/abstracts of all identified records were reviewed and assessed for relevance by one researcher (AM). Full-text documents of relevant records were then obtained and reassessed against the inclusion criteria by the same researcher. Any concerns were rectified by consensus with two additional researchers (MN and SK).
2.3. Data Collection and Analysis
Data from relevant guidelines were independently extracted into a table by one researcher (AM). The following data were extracted: guideline title, author/institution, country, publication date, methodology for development of recommendations, first-line treatment recommendations and recommendations for the targeted treatment of PTSD-associated nightmares. No statistical analyses were completed.
2.4. Evaluation of Guideline Quality
The AGREE II instrument is a validated tool for the appraisal of health-related guidelines [ 27 ]. It consists of a checklist of 23 items grouped into six domains: scope and purpose; stakeholder involvement; rigour of development; clarity and presentation; applicability; and editorial independence. Each item is given a score from 1–7, with a score of 7 indicating that reporting of that item is exceptional and all criteria for the item have been met and a score of 1 indicating reporting of the item is absent or reporting criteria were not met. A quality score is then calculated for each of the 6 domains. This score is reported as a percentage of the maximum possible score for that domain and can then be used to interpret the strengths and limitations of the guideline, noting that there is no accepted cut-off score to define a ‘good’ guideline. The ‘Recommended for use?’ assessment (with options of Yes, No or Yes with modifications) is based on whether the guideline scored reasonably across all domains, the overall readability and usability of the guideline, and if the content is current. On completion of the AGREE II online tutorial, three reviewers (AM, JC & KM) independently assessed each guideline against the AGREE II criteria. They later met and agreed by consensus on the final averaged scores.
The search strategy identified a total of 133 records, of which, 14 guidelines matched the criteria for inclusion in this review. The secondary search in September 2020 identified updated versions of three previously identified guidelines. Reasons for exclusion of records are summarised in Figure 1 . The general characteristics of each guideline are summarised in Table 2 .

PRISMA Flow Diagram.
Characteristics of included guidelines.
CBT = cognitive behaviour therapy, CPT = cognitive processing therapy, CT = cognitive therapy, EMDR = eye movement desensitisation and reprocessing, IRT = image rehearsal therapy, PE = prolonged exposure, SNRI = serotonin-norepinephrine reuptake inhibitor, SSRI = selective serotonin reuptake inhibitor, TCA = tricyclic antidepressant. * This guideline has not been reviewed since its publication in 2006. It is the policy of the Canadian Psychiatric Association to review clinical practice guidelines every 5 years, and any document that does not explicitly state that it has been reviewed should be considered as a historical document only. It is included in this review for interest, but we acknowledge that it is not considered current guidance.
3.1. Guideline Characteristics
The fourteen guidelines identified in this review were published between 2004 and 2020, with only five less than 5 years old. There were four guidelines from the US, three from international organisations (the International Society for Traumatic Stress Studies, the World Federation of Societies of Biological Psychiatry and the World Health Organisation) two each from Australia, Canada and the UK, and one from South Africa. Their recommendations were based on evidence from conducting a systematic review, a consensus process, or a combination of the two.
3.2. Assessment of Guideline Quality
Domain scores and guideline abbreviations are presented in Table 3 . All guidelines scored well in domain 1 ‘scope and purpose’. It had the second highest median score of 87% (range: 68–100%) and two guidelines (Phoenix & VA) scored 100% in this domain.
AGREE II assessment scores * for each guideline.
Y/M = Yes with modifications. * Domain 1. Scope and Purpose is concerned with the overall aim of the guideline, the specific health questions, and the target population (items 1–3). Domain 2. Stakeholder Involvement focuses on the extent to which the guideline was developed by appropriate stakeholders and represents the views of its intended users (items 4–6). Domain 3. Rigour of Development relates to the process used to gather and synthesise the evidence, the methods to formulate the recommendations, and to update them (items 7–14). Domain 4. Clarity of Presentation deals with the language, structure, and format of the guideline (items 15–17). Domain 5. Applicability pertains to the likely barriers and facilitators to implementation, strategies to improve uptake, and resource implications of applying the guideline (items 18–21). Domain 6. Editorial Independence is concerned with the formulation of recommendations not being unduly biased with competing interests (items 22–23). ** The ISTSS guidelines are published as a book for purchase. The Methodology and Recommendations document is available publicly on the internet, but the Evidence Summary documents, and reference lists are available for members only. These documents were requested but not supplied, so it is likely the ISTSS guideline would have scored higher in certain categories if these documents were available.
Scores in domain 2 ‘stakeholder involvement’ were more varied, with two guidelines scoring below 50% (AASM & WFSBP) yet four scoring above 90% (Phoenix, VA, APoA & NICE) (range 30–100%). Scores in domain 3 ‘rigour of development’ varied similarly to domain 2, with one guideline scoring below 50% (SASOP) and two above 90% (APoA & WHO) (Range: 44–92%). The highest scores were seen in domain 4 ‘clarity of presentation’, with a median score of 90% (range 71–100%). This is in contrast with domain 5 ‘applicability’, which saw high variability and a median score of just 49% (range 30–74%). Finally, domain 6 ‘editorial independence’ had the greatest variability between guidelines, with four scores of 90% or more (AASM, Phoenix, eTG and APoA) and four scores of 50% or less (CPA, WFSBP, ISTSS & SASOP) (range: 26–100%). Overall, the PTSD guidelines were of reasonably high quality; six are recommended for use, six are recommended with modifications, and two are not recommended for use after quality assessment ( Table 3 ).
3.3. Recommendations in Guidelines
Five guidelines (36%) recommended that pharmacological interventions should be second-line to psychological interventions, while the others made no specific recommendation for one over the other. All fourteen guidelines (100%) recommended CBT (in various forms) as a first-line psychological treatment for PTSD. EMDR was also included as a first-line psychological option in 43%of the guidelines (Phoenix, BAP, WHO, eTG, NICE and ISTSS). All guidelines except one (93%), AASM, which was specific to treating nightmares, recommended an SSRI as first-line pharmacological treatment for PTSD if pharmacological treatment was indicated. Some recommended SSRIs broadly, while others specifically recommended only paroxetine, fluoxetine or sertraline. Most guidelines (71%) also included the serotonin-noradrenaline reuptake inhibitor (SNRI) venlafaxine as a first-line pharmacological treatment option. The WHO guideline also included tricyclic antidepressants (TCAs) as a first-line pharmacological recommendation.
Eight guidelines (57%) did not mention the targeted treatment of nightmares as a symptom of PTSD. Of the six guidelines (43%) that did mention targeted treatment, all mentioned prazosin as a potential option; although the strength of recommendations varied from no recommendation to first-line. Two guidelines (14%) also recommended IRT for targeted treatment of nightmares (AASM and APiA).
4. Discussion
To our knowledge, this review is the first study comparing international treatment guidelines for PTSD using a validated tool.
4.1. Quality of Guidelines
The AGREE II domains needing most attention were the critical ones of ‘applicability’, ‘rigour of development’ and ‘stakeholder involvement’. The Phoenix, APoA, WHO, NICE and VA guidelines received the highest scores across all domains (all >50%), while the ADAC and WFSBP guidelines received the lowest scores across all domains and were not recommended for use. Overall, guidelines scored well in the ‘scope and purpose’ and ‘clarity of presentation’ domains, consistently and clearly describing the guideline objectives and target populations. Scores in the stakeholder involvement domain varied. Low scores were generally due to a lack of information provided about the guideline development group members and/or a lack of consultation with patient representatives for their views and preferences.
No guidelines achieved a perfect score in the ‘rigour of development’ domain. While some guidelines scored highly, generally the external review process was missing entirely or lacked rigour. The SASOP guidelines scored particularly low in this domain, as the development process was not systematic. Each chapter was written by an expert or group of experts in the field, but there was no systematic evidence search described. However, this guideline was designed to be specific to a South African population, in which there is a lack of published evidence to review. Hence, a guideline based on experts’ clinical knowledge could be highly relevant, and still recommended for use despite low scores in some domains. All guidelines generally had lower scores in the applicability domain, while the editorial independence domain saw the greatest variance, with scores between 26–100%. Low scores in applicability were generally due to failure to identify barriers to implementation of the guidelines, as well as a lack of tools provided to aid implementation. In addition, very few guidelines performed economic evaluations to assess the potential resource implications of the application of their recommendations. While many guidelines scored highly in the ‘editorial independence’ domain, low scores were generally due to a lack of acknowledgement of the funding body or failure to state that no funding was received, highlighting a potential risk of bias in some guidelines.
The ‘rigour of development’ domain requires guideline developers to describe a procedure for updating the guideline. Seven guidelines (50%) described an intention for updates to occur. Some described a specific time interval (most commonly 5 years), while others stated updates were due only when new information becomes available. Interestingly, three of the remaining seven guidelines (50%) that did not describe an intention to update (BAP, ISTSS, VA) were updated versions of previous guidelines. While one could assume that one update means regular updates are planned, even updated guidelines should describe a procedure to be updated again, to remain valid. Of the seven guidelines (50%) that did describe an intention to be updated, two (eTG, WHO) are due for update based on the time interval they described. In addition, some guidelines that did not describe a time interval were likely to be due for update, although the ideal frequency of updates for clinical guidelines is unclear. A study by Shakelle et al. investigating how quickly clinical guidelines become outdated found that after 5.8 years, 50% of guidelines were no longer valid [ 40 ]. They concluded that all guidelines should generally be reassessed for validity at 3-year intervals [ 40 ]. However, a strict time interval recommendation is impractical in many cases, so the authors acknowledged that a 3-year interval will not always be suitable [ 40 ]. The evidence in certain fields is unlikely to change in 3 years, or even 10 years, while other rapidly evolving fields may require updates more frequently [ 40 , 41 , 42 ]. However, when making the recommendation to update a guideline “when new information becomes available” there must be a robust procedure in place to ensure new information is found and included in a timely manner to maintain the validity of the guideline [ 42 ].
4.2. Recommendations in Guidelines
SSRIs are universally accepted as first-line pharmacological treatment of PTSD in clinical guidelines. The evidence is strongest for paroxetine and fluoxetine, as well as the SNRI venlafaxine which is also commonly recommended as a first-line pharmacological treatment for PTSD [ 43 ]. A 2015 systematic review and meta-analysis of pharmacological treatment for PTSD found statistically significant improvements in PTSD symptom severity with paroxetine, fluoxetine and venlafaxine, when compared to placebo, with effect sizes similar to those seen for antidepressants in depression, although it should be noted these effect sizes are relatively small [ 43 ]. When all SSRIs were grouped together and compared to placebo, a small positive effect size was seen; however, based on current evidence it seems that greater benefit would be seen using either paroxetine or fluoxetine over other SSRIs [ 43 ].
TCAs were also recommended as a first-line pharmacological option in the WHO guideline, although it should be noted that pharmacological options were not recommended first-line unless CBT and EMDR are unavailable, have failed or there is severe comorbid depression. The evidence for TCAs is considered inferior to SSRIs and venlafaxine in most guidelines, and adverse effects are of greater concern. However, a recent systematic review of pharmacotherapy for combat-related PTSD found TCAs to have similar efficacy to SSRIs and, as such, more research in this area may be warranted [ 44 ].
Around one third of guidelines recommended psychotherapy over pharmacotherapy for first-line treatment of PTSD. This recommendation is supported by a recent meta-analysis comparing the two treatment approaches head to head, which found significantly greater effect sizes for trauma-focused psychotherapies compared to medications for treating PTSD [ 45 ]. However, this recommendation will not be appropriate for all patients; for example, cost of treatment may be a crucial factor for the patient, appropriate psychotherapy may not be readily available to patients in rural areas, patients may have comorbidities such as depression which could benefit from medications, or they may simply prefer medication over psychotherapy. In these situations, clinicians must use clinical judgement to determine the most appropriate course of action for the patient.
All guidelines included in this review described CBT as the first-line psychological treatment for PTSD. CBT is a broad term that can encompass several specific therapies, such as cognitive processing therapy (CPT), prolonged exposure therapy (PE) and image rehearsal therapy (IRT), which have a focus on cognitive, behavioural and emotional processing techniques [ 46 ]. Several guidelines use the term ‘trauma-focused CBT’, which tends to encompass CBT as well as trauma-focused psychotherapies, such as EMDR. However, some guidelines recommended EMDR as a separate therapy, which can be confusing when comparing recommendations [ 45 ]. A recent meta-analysis comparing CBT to EMDR found that EMDR was slightly superior to CBT for intrusive and arousal symptoms, but found no significant difference between groups for avoidance symptoms [ 47 ]. In addition, a systematic review of CBT for PTSD found that specific trauma-focused therapies were all superior to supportive, non-trauma-focused therapies [ 46 ]. Based on these findings, it is reasonable for guidelines to use the broad term “trauma-focused psychotherapies”, which includes CBT, CPT, PE and EMDR, as they all have comparable evidence for safety and efficacy, and the use of this term may reduce confusion while allowing for flexibility in treatment selection.
Eight (57%) of the guidelines (APoA, CPA, eTG, ISTSS, NICE, Phoneix and WFSBP, WHO) did not address the targeted treatment of nightmares, despite the fact that nightmares are often resistant to treatment and are associated with a significantly increased suicide risk [ 9 , 11 , 12 ]. Prazosin is recommended as first-line treatment for nightmares in PTSD in two guidelines (ADAC and AASM) while others recommended it as third-line therapy or included no specific recommendation but discussed potential for its use. In addition, the guidelines that did address targeted treatment often lacked significant depth and detail in both the evidence search and clarity of recommendations when compared to their recommendations for core PTSD symptoms. Three recently published meta-analyses investigating the efficacy of prazosin for PTSD nightmares found prazosin to be significantly more effective than placebo in reducing trauma-related nightmares [ 3 , 10 , 48 ]. These findings were based on improvements in the clinician-administered PTSD scale (CAPS) “distressing dreams item”, which is a measure of both the frequency and intensity of nightmares. Improvements were statistically significant and of large magnitude based on Cohen’s convention [ 3 , 10 , 48 ]. They did, however, highlight some important limitations, namely, small sample sizes and a lack of variability in both the research groups and participants, who were overwhelmingly male, combat veterans. Additionally, two more recent RCTs [ 49 , 50 ], not included in these meta-analyses, with relatively larger sample sizes, found no significant difference between prazosin and placebo in improving the CAPS distressing dreams item, or for any other primary outcome measures. While earlier positive trials for prazosin did not exclude participants with psychosocial instability, both negative studies excluded these patients. It is postulated that prazosin may only be effective in a sub-group of patients experiencing more severe adrenergic dysfunction, who may have been excluded from the negative studies [ 50 , 51 ]. While further research in this area is required, it remains important that guidelines consider the targeted treatment of nightmares in PTSD. Two guidelines also recommended IRT for targeted treatment of nightmares in PTSD. A recent systematic review and meta-analysis comparing IRT to prazosin found IRT to be equally effective as prazosin in treating nightmares in PTSD [ 14 ]. The most effective treatment, however, was IRT in combination with CBT for insomnia, which showed significant improvement in sleep quality when compared to prazosin or IRT alone ( p = 0.03] [ 14 ]. It should be noted that there were significantly more trials investigating IRT than prazosin, and these included larger and more variable cohorts of participants, suggesting that the evidence for IRT is more robust than that for prazosin, yet IRT is recommended less frequently in treatment guidelines [ 14 ].
4.3. Strengths and Limitations
Strengths of this review include the use of the AGREE II criteria to assess the quality of each identified guideline, the development of a systematic method to search grey literature for guidelines, and a focus on the targeted treatment of nightmares. The AGREE II criteria is a validated assessment tool, which has been used in several similar systematic reviews of treatment guidelines in the area of mental health treatment [ 52 , 53 , 54 ]. It is also acknowledged that assessment using the AGREE II criteria can be relatively subjective, with no pre-defined cut-off scores.
Many systematic reviews of treatment guidelines do not clearly describe the method by which grey literature was searched to locate guidelines, or do not describe a systematic method that could be repeated by other researchers. Often, guidelines are not published in journals, and instead are posted on the webpages of the author organisation, or in guideline repositories, meaning that grey literature searches should form a major part of the search process [ 55 ]. Our grey literature search method was unique, transparent and systematic, and could be repeated by other researchers for future systematic reviews of treatment guidelines in any area of health care. This review also had a strong focus on the treatment of nightmares in PTSD, which are often resistant to general PTSD treatments [ 9 ]. Critical appraisal of the guidelines highlighted a lack of information about the targeted treatment of nightmares, despite the availability and importance of such treatments. A limitation of this review is the restriction to guidelines written in the English language, and although our method for searching the grey literature was highly systematic, it remains possible that eligible guidelines could have been missed.
5. Conclusions
There are a plethora of treatment guidelines being produced world-wide to aid health professionals in clinical decision making. However, it is important for health professionals to be able to identify which guidelines can be the most trusted. This review assessed the quality of international treatment guidelines for PTSD. We identified that many PTSD guidelines could be considered out of date require improvement in the AGREE II key domains of ‘applicability’, ‘rigour of development’ and ‘stakeholder involvement’. We have also highlighted a significant lack of information regarding the targeted treatment of nightmares, despite the availability of both psychological and pharmacological treatments. Due to the treatment-resistant nature of nightmares in PTSD and significantly increased risk of suicide, guideline development groups should consider producing more detailed recommendations for their treatment. In part, this is dependent on the availability of a solid evidence base if making specific treatment suggestions. Therefore, there is a need for more well-designed RCTs to establish the true clinical efficacy of targeted treatments for nightmares in PTSD.
Author Contributions
Conceptualization, M.N., S.K., J.T., A.M.; methodology, M.N., S.K., J.T. and A.M.; formal analysis, A.M.; investigation, A.M., J.K.C.; writing—original draft preparation, A.M.; writing—review and editing, M.N., S.K., G.P., J.T. and J.K.C.; supervision, M.N., S.K.; All authors have read and agreed to the published version of the manuscript.
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Data availability statement, conflicts of interest.
The authors declare no conflict of interest.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
- Open access
- Published: 28 September 2018
Posttraumatic stress disorder: from diagnosis to prevention
- Xue-Rong Miao ORCID: orcid.org/0000-0002-0665-8271 1 ,
- Qian-Bo Chen 1 ,
- Kai Wei 1 ,
- Kun-Ming Tao 1 &
- Zhi-Jie Lu 1
Military Medical Research volume 5 , Article number: 32 ( 2018 ) Cite this article
54k Accesses
43 Citations
18 Altmetric
Metrics details
Posttraumatic stress disorder (PTSD) is a chronic impairment disorder that occurs after exposure to traumatic events. This disorder can result in a disturbance to individual and family functioning, causing significant medical, financial, and social problems. This study is a selective review of literature aiming to provide a general outlook of the current understanding of PTSD. There are several diagnostic guidelines for PTSD, with the most recent editions of the DSM-5 and ICD-11 being best accepted. Generally, PTSD is diagnosed according to several clusters of symptoms occurring after exposure to extreme stressors. Its pathogenesis is multifactorial, including the activation of the hypothalamic–pituitary–adrenal (HPA) axis, immune response, or even genetic discrepancy. The morphological alternation of subcortical brain structures may also correlate with PTSD symptoms. Prevention and treatment methods for PTSD vary from psychological interventions to pharmacological medications. Overall, the findings of pertinent studies are difficult to generalize because of heterogeneous patient groups, different traumatic events, diagnostic criteria, and study designs. Future investigations are needed to determine which guideline or inspection method is the best for early diagnosis and which strategies might prevent the development of PTSD.
Posttraumatic stress disorder (PTSD) is a recognized clinical phenomenon that often occurs as a result of exposure to severe stressors, such as combat, natural disaster, or other events [ 1 ]. The diagnosis of PTSD was first introduced in the 3rd edition of the Diagnostic and Statistical Manual (DSM) (American Psychiatric Association) in 1980 [ 2 ].
PTSD is a potentially chronic impairing disorder that is characterized by re-experience and avoidance symptoms as well as negative alternations in cognition and arousal. This disease first raised public concerns during and after the military operations of the United States in Afghanistan and Iraq, and to date, a large number of research studies report progress in this field. However, both the underlying mechanism and specific treatment for the disease remain unclear. Considering the significant medical, social and financial problems, PTSD represents both to nations and to individuals, all persons caring for patients suffering from this disease or under traumatic exposure should know about the risks of PTSD.
The aim of this review article is to present the current understanding of PTSD related to military injury to foster interdisciplinary dialog. This article is a selective review of pertinent literature retrieved by a search in PubMed, using the following keywords: “PTSD[Mesh] AND military personnel”. The search yielded 3000 publications. The ones cited here are those that, in the authors’ view, make a substantial contribution to the interdisciplinary understanding of PTSD.
Definition and differential diagnosis
Posttraumatic stress disorder is a prevalent and typically debilitating psychiatric syndrome with a significant functional disturbance in various domains. Both the manifestation and etiology of it are complex, which has caused difficulty in defining and diagnosing the condition. The 3rd edition of the DSM introduced the diagnosis of PTSD with 17 symptoms divided into three clusters in 1980. After several decades of research, this diagnosis was refined and improved several times. In the most recent version of the DSM-5 [ 3 ], PTSD is classified into 20 symptoms within four clusters: intrusion, active avoidance, negative alterations in cognitions and mood as well as marked alterations in arousal and reactivity. The diagnosis requirement can be summarized as an exposure to a stressor that is accompanied by at least one intrusion symptom, one avoidance symptom, two negative alterations in cognitions and mood symptoms, and two arousal and reactivity turbulence symptoms, persisting for at least one month, with functional impairment. Interestingly, in the DSM-5, PTSD has been moved from the anxiety disorder group to a new category of ‘trauma- and stressor-related disorders’, which reflects the cognizance alternation of PTSD. In contrast to the DSM versions, the World Health Organization’s (WHO) International Classification of Diseases (ICD) has proposed a substantially different approach to diagnosing PTSD in the most recent ICD-11 version [ 4 ], which simplified the symptoms into six under three clusters, including constant re-experiencing of the traumatic event, avoidance of traumatic reminders and a sense of threat. The diagnosis requires at least one symptom from each cluster which persists for several weeks after exposure to extreme stressors. Both diagnostic guidelines emphasize the exposure to traumatic events and time of duration, which differentiate PTSD from some diseases with similar symptoms, including adjustment disorder, anxiety disorder, obsessive-compulsive disorder, and personality disorder. Patients with the major depressive disorder (MDD) may or may not have experienced traumatic events, but generally do not have the invasive symptoms or other typical symptoms that PTSD presents. In terms of traumatic brain injury (TBI), neurocognitive responses such as persistent disorientation and confusion are more specific symptoms. It is worth mentioning that some dissociative reactions in PTSD (e.g., flashback symptoms) should be recognized separately from the delusions, hallucinations, and other perceptual impairments that appear in psychotic disorders since they are based on actual experiences. The ICD-11 also recognizes a sibling disorder, complex PTSD (CPTSD), composed of symptoms including dysregulation, negative self-concept, and difficulties in relationships based on the diagnosis of PTSD. The core CPTSD symptom is PTSD with disturbances in self-organization (DSO).
In consideration of the practical applicability of the PTSD diagnosis, Brewin et al. conducted a study to investigate the requirement differences, prevalence, comorbidity, and validity of the DSM-5 and ICD-11 for PTSD criteria. According to their study, diagnostic standards for symptoms of re-experiencing are higher in the ICD-11 than the DSM, whereas the standards for avoidance are less strict in the ICD-11 than in the DSM-IV [ 5 ]. It seems that in adult subjects, the prevalence of PTSD using the ICD-11 is considerably lower compared to the DSM-5. Notably, evidence suggested that patients identified with the ICD-11 and DSM-5 were quite different with only partially overlapping cases; this means each diagnostic system appears to find cases that would not be diagnosed using the other. In consideration of comorbidity, research comparing these two criteria show diverse outcomes, as well as equal severity and quality of life. In terms of children, only very preliminary evidence exists suggesting no significant difference between the two. Notably, the diagnosis of young children (age ≤ 6 years) depends more on the situation in consideration of their physical and psychological development according to the DSM-5.
Despite numerous investigations and multiple revisions of the diagnostic criteria for PTSD, it remains unclear which type and what extent of stress are capable of inducing PTSD. Fear responses, especially those related to combat injury, are considered to be sufficient enough to trigger symptoms of PTSD. However, a number of other types of stressors were found to correlate with PTSD, including shame and guilt, which represent moral injury resulting from transgressions during a war in military personnel with deeply held moral and ethical beliefs. In addition, military spouses and children may be as vulnerable to moral injury as military service members [ 6 ]. A research study on Canadian Armed Forces personnel showed that exposure to moral injury during deployments is common among military personnel and represents an independent risk factor for past-year PTSD and MDD [ 7 ]. Unfortunately, it seems that pre- and post-deployment mental health education was insufficient to moderate the relationship between exposure to moral injury and adverse mental health outcomes.
In general, a large number of studies are focusing on the definition and diagnostic criteria of PTSD and provide considerable indicators for understanding and verifying the disease. However, some possible limitations or discrepancies continue to exist in current research studies. One is that although the diagnostic criteria for a thorough examination of the symptoms were explicit and accessible, the formal diagnosis of PTSD using structured clinical interviews was relatively rare. In contrast, self-rating scales, such as the Posttraumatic Diagnostic Scale (PDS) [ 8 ] and the Impact of Events Scale (IES) [ 9 ], were used frequently. It is also noteworthy that focusing on PTSD explicitly could be a limitation as well. The complexity of traumatic experiences and the responses to them urge comprehensive investigations covering all aspects of physical and psychological maladaptive changes.
Prevalence and importance
Posttraumatic stress disorder generally results in poor individual-level outcomes, including co-occurring disorders such as depression and substance use, and physical health problems. According to the DSM-5 reporting, more than 80% of PTSD patients share one or more comorbidities; for instance, the morbidity of PTSD with concurrent mild TBI is 48% [ 8 ]. Moreover, cognitive impairment has been identified frequently in PTSD. The reported incidence rate for PTSD ranges from 5.4 to 16.8% in military service members and veterans [ 10 , 11 , 12 , 13 , 14 ], which is almost double those in the general population. The estimated prevalence of PTSD varies depending on the group of patients studied, the traumatic events occurred, and the measurement method used (Table 1 ). However, it still reflects the profound effect of this mental disease, especially with the rise in global terrorism and military conflict in recent years. While PTSD can arise at any life stage in any population, most research in recent decades has focused on returned veterans; this means most knowledge regarding PTSD has come from the military population. Meanwhile, the impact of this disease on children has received scant attention.
The discrepancy of PTSD prevalence in males and females is controversial. In a large study of OEF/OIF veterans, the prevalence of PTSD in males and females was similar, although statistically more prevalent in men versus women (13% vs. 11%) [ 15 ]. Another study on the Navy and Marine Corps showed a slightly higher incidence for PTSD in the women compared to men (6.6% vs. 5.3%) [ 12 ]. However, the importance of combat exposure is unclear. Despite a lower level of combat exposure than male military personnel, females generally have considerably higher rates of military sexual trauma, which is significantly associated with the development of PTSD [ 16 ].
It is reported that 44–72% of veterans suffer high levels of stress after returning to civilian life. Many returned veterans with PTSD show emotion regulation problems, including emotion identification, expression troubles and self-control issues. Nevertheless, a meta-analytic investigation of 34 studies consistently found that the severity of PTSD symptoms was significantly associated with anger, especially in military samples [ 17 ]. Not surprisingly, high levels of PTSD and emotional regulation troubles frequently lead to poor family functioning or even domestic violence in veterans. According to some reports, parenting difficulties in veteran families were associated with three PTSD symptom clusters. Evans et al. [ 18 ] conducted a survey to evaluate the impact of PTSD symptom clusters on family functioning. According to their analysis, avoidance symptoms directly affected family functioning, whereas hyperarousal symptoms had an indirect association with family functioning. Re-experience symptoms were not found to impact family functioning. Notably, recent epidemiologic studies using data from the Veterans Health Administration (VHA) reported that veterans with PTSD were linked to suicide ideations and behaviors [ 19 ] (e.g., non-suicidal self-injury, NSSI), in which depression as well as other mood disruptions, often serve as mediating factors.
Previously, there was a controversial attitude toward the vulnerability of young children to PTSD. However, growing evidence suggests that severe and persistent trauma could result in stress responses worse than expected as well as other mental and physical sequelae in child development. The most prevalent traumatic exposures for young children above the age of 1 year were interpersonal trauma, mostly related to or derived from their caregivers, including witnessing intimate partner violence (IPV) and maltreatment [ 20 ]. Unfortunately, because of the crucial role that caregivers play in early child development, these types of traumatic events are especially harmful and have been associated with developmental maladaptation in early childhood. Maladaptation commonly represents a departure from normal development and has even been linked to more severe effects and psychopathology. In addition, the presence of psychopathology may interfere with the developmental competence of young children. Research studies have also broadened the investigation to sequelae of PTSD on family relationships. It is proposed that the children of parents with symptoms of PTSD are easily deregulated or distressed and appear to face more difficulties in their psychosocial development in later times compared to children of parents without. Meanwhile, PTSD veterans described both emotional (e.g., hurt, confusion, frustration, fear) and behavioral (e.g., withdrawal, mimicking parents’ behavior) disruption in their children [ 21 ]. Despite the increasing emphasis on the effects of PTSD on young children, only a limited number of studies examined the dominant factors that influence responses to early trauma exposures, and only a few prospective research studies have observed the internal relations between early PTSD and developmental competence. Moreover, whether exposure to both trauma types in early life is associated with more severe PTSD symptoms than exposure to one type remains an outstanding question.
Molecular mechanism and predictive factors
The mechanisms leading to posttraumatic stress disorder have not yet been fully elucidated. Recent literature suggests that both the neuroendocrine and immune systems are involved in the formulation and development of PTSD [ 22 , 23 ]. After traumatic exposures, the stress response pathways of the hypothalamic–pituitary–adrenal (HPA) axis and sympathetic nervous system are activated and lead to the abnormal release of glucocorticoids (GC) and catecholamines. GCs have downstream effects on immunosuppression, metabolism enhancement, and negative feedback inhibition of the HPA axis by binding to the GC receptor (GR), thus connecting the neuroendocrine modulation with immune disturbance and inflammatory response. A recent meta-analysis of 20 studies found increased plasma levels of proinflammatory cytokines tumor necrosis factor-alpha (TNF-a), interleukin-1beta (IL-1b), and interleukin-6 (IL-6) in individuals with PTSD compared to healthy controls [ 24 ]. In addition, some other studies speculate that there is a prospective association of C-reactive protein (CRP) and mitogen with the development of PTSD [ 25 ]. These findings suggest that neuroendocrine and inflammatory changes, rather than being a consequence of PTSD, may in fact act as a biological basis and preexisting vulnerability for developing PTSD after trauma. In addition, it is reported that elevated levels of terminally differentiated T cells and an altered Th1/Th2 balance may also predispose an individual to PTSD.
Evidence indicates that the development of PTSD is also affected by genetic factors. Research has found that genetic and epigenetic factors account for up to 70% of the individual differences in PTSD development, with PTSD heritability estimated at 30% [ 26 ]. While aiming to integrate genetic studies for PTSD and build a PTSD gene database, Zhang et al. [ 27 ] summarized the landscape and new perspective of PTSD genetic studies and increased the overall candidate genes for future investigations. Generally, the polymorphisms moderating HPA-axis reactivity and catecholamines have been extensively studied, such as FKBP5 and catechol-O-methyl-transferase (COMT). Other potential candidates for PTSD such as AKT, a critical mediator of growth factor-induced neuronal survival, were also explored. Genetic research has also made progress in other fields. For example, researchers have found that DNA methylation in multiple genes is highly correlated with PTSD development. Additional studies have found that stress exposure may even affect gene expression in offspring by epigenetic mechanisms, thus causing lasting risks. However, some existing problems in the current research of this field should be noted. In PTSD genetic studies, variations in population or gender difference, a wide range of traumatic events and diversity of diagnostic criteria all may attribute to inconsistency, thus leading to a low replication rate among similar studies. Furthermore, PTSD genes may overlap with other mental disorders such as depression, schizophrenia, and bipolar disorder. All of these factors indicate an urgent need for a large-scale genome-wide study of PTSD and its underlying epidemiologic mechanisms.
It is generally acknowledged that some mental diseases, such as major depressive disorder (MDD), bipolar disorder, and schizophrenia, are associated with massive subcortical volume change. Recently, numerous studies have examined the relationship between the morphology changes of subcortical structures and PTSD. One corrected analysis revealed that patients with PTSD show a pattern of lower white matter integrity in their brains [ 28 ]. Prior studies typically found that a reduced volume of the hippocampus, amygdala, rostral ventromedial prefrontal cortex (rvPFC), dorsal anterior cingulate cortex (dACC), and the caudate nucleus may have a relationship with PTSD patients. Logue et al. [ 29 ] conducted a large neuroimaging study of PTSD that compared eight subcortical structure volumes (nucleus accumbens, amygdala, caudate, hippocampus, pallidum, putamen, thalamus, and lateral ventricle) between PTSD patients and controls. They found that smaller hippocampi were particularly associated with PTSD, while smaller amygdalae did not show a significant correlation. Overall, rigorous and longitudinal research using new technologies, such as magnetoencephalography, functional MRI, and susceptibility-weighted imaging, are needed for further investigation and identification of morphological changes in the brain after a traumatic exposure.
Psychological and pharmacological strategies for prevention and treatment
Current approaches to PTSD prevention span a variety of psychological and pharmacological categories, which can be divided into three subgroups: primary prevention (before the traumatic event, including prevention of the event itself), secondary prevention (between the traumatic event and the development of PTSD), and tertiary prevention (after the first symptoms of PTSD become apparent). The secondary and tertiary prevention of PTSD has abundant methods, including different forms of debriefing, treatments for Acute Stress Disorder (ASD) or acute PTSD, and targeted intervention strategies. Meanwhile, the process of primary prevention is still in its infancy and faces several challenges.
Based on current research on the primary prevention of post-trauma pathology, psychological and pharmacological interventions for particular groups or individuals (e.g., military personnel, firefighters, etc.) with a high risk of traumatic event exposure were applicable and acceptable for PTSD sufferers. Of the studies that reported possible psychological prevention effects, training generally included a psychoeducational component and a skills-based component relating to stress responses, anxiety reducing and relaxation techniques, coping strategies and identifying thoughts, emotion and body tension, choosing how to act, attentional control, emotion control and regulation [ 30 , 31 , 32 ]. However, efficiency for these training has not been evaluated yet due to a lack of high-level evidence-based studies. Pharmacological options have targeted the influence of stress on memory formation, including drugs relating to the hypothalamic-pituitary-adrenal (HPA) axis, the autonomic nerve system (especially the sympathetic nerve system), and opiates. Evidence has suggested that pharmacological prevention is most effective when started before and early after the traumatic event, and it seems that sympatholytic drugs (alpha and beta-blockers) have the highest potential for primary prevention of PTSD [ 33 ]. However, one main difficulty limiting the exploration in this field is related to rigorous and complex ethical issues, as the application of pre-medication for special populations and the study of such options in hazardous circumstances possibly touches upon questions of life and death. Significantly, those drugs may have potential side effects.
There are several treatment guidelines for patients with PTSD produced by different organizations, including the American Psychiatric Association (APA), the United Kingdom’s National Institute for Health and Clinical Excellence (NICE), the International Society for Traumatic Stress Studies (ISTSS), the Institute of Medicine (IOM), the Australian National Health and Medical Research Council, and the Department of Veterans Affairs and Department of Defense (VA, DoD) [ 34 , 35 , 36 , 37 , 38 ]. Additionally, a large number of research studies are aiming to evaluate an effective treatment method for PTSD. According to these guidelines and research, treatment approaches can be classified as psychological interventions and pharmacological treatments (Fig. 1 ); most of the studies provide varying degrees of improvement in individual outcomes after standard interventions, including PTSD symptom reduction or remission, loss of diagnosis, release or reduction of comorbid medical or psychiatric conditions, quality of life, disability or functional impairment, return to work or to active duty, and adverse events.
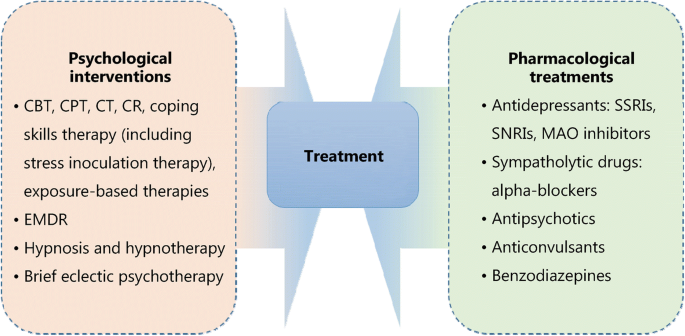
Psychological and pharmacological strategies for treatment of PTSD. CBT. Cognitive behavioral therapy; CPT. Cognitive processing therapy; CT. Cognitive therapy; CR. Cognitive restructuring; EMDR. Eye movement desensitization and reprocessing; SSRIs. Selective serotonin reuptake inhibitors; SNRIs. Serotonin and norepinephrine reuptake inhibitors; MAO. Monoamine oxidase
Most guidelines identify trauma-focused psychological interventions as first-line treatment options [ 39 ], including cognitive behavioral therapy (CBT), cognitive processing therapy (CPT), cognitive therapy (CT), cognitive restructuring (CR), coping skills therapy (including stress inoculation therapy), exposure-based therapies, eye movement desensitization and reprocessing (EMDR), hypnosis and hypnotherapy, and brief eclectic psychotherapy. These treatments are delivered predominantly to individuals, but some can also be conducted in family or group settings. However, the recommendation of current guidelines seems to be projected empirically as research on the comparison of outcomes of different treatments is limited. Jonas et al. [ 40 ] performed a systematic review and network meta-analysis of the evidence for treatment of PTSD. The study suggested that all psychological treatments showed efficacy for improving PTSD symptoms and achieving the loss of PTSD diagnosis in the acute phase, and exposure-based treatments exhibited the strongest evidence of efficacy with high strength of evidence (SOE). Furthermore, Kline et al. [ 41 ] conducted a meta-analysis evaluating the long-term effects of in-person psychotherapy for PTSD in 32 randomized controlled trials (RCTs) including 2935 patients with long-term follow-ups of at least 6 months. The data suggested that all studied treatments led to lasting improvements in individual outcomes, and exposure therapies demonstrated a significant therapeutic effect as well with larger effect sizes compared to other treatments.
Pharmacological treatments for PTSD include antidepressants such as selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors (SNRIs), and monoamine oxidase (MAO) inhibitors, sympatholytic drugs such as alpha-blockers, antipsychotics, anticonvulsants, and benzodiazepines. Among these medications, fluoxetine, paroxetine, sertraline, topiramate, risperidone, and venlafaxine have been identified as efficacious in treatment. Moreover, in the Jonas network meta-analysis of 28 trials (4817 subjects), they found paroxetine and topiramate to be more effective for reducing PTSD symptoms than most other medications, whereas evidence was insufficient for some other medications as research was limited [ 40 ]. It is worth mentioning that in these studies, efficacy for the outcomes, unlike the studies of psychological treatments, was mostly reported as a remission in PTSD or depression symptoms; other outcomes, including loss of PTSD diagnosis, were rarely reported in studies.
As for the comparative evidence of psychological with pharmacological treatments or combinations of psychological treatments and pharmacological treatments with other treatments, evidence was insufficient to draw any firm conclusions [ 40 ]. Additionally, reports on adverse events such as mortality, suicidal behaviors, self-harmful behaviors, and withdrawal of treatment were relatively rare.
PTSD is a high-profile clinical phenomenon with a complicated psychological and physical basis. The development of PTSD is associated with various factors, such as traumatic events and their severity, gender, genetic and epigenetic factors. Pertinent studies have shown that PTSD is a chronic impairing disorder harmful to individuals both psychologically and physically. It brings individual suffering, family functioning disorders, and social hazards. The definition and diagnostic criteria for PTSD remain complex and ambiguous to some extent, which may be attributed to the complicated nature of PTSD and insufficient research on it. The underlying mechanisms of PTSD involve changes in different levels of psychological and molecular modulations. Thus, research targeting the basic mechanisms of PTSD using standard clinical guidelines and controlled interference factors is needed. In terms of treatment, psychological and pharmacological interventions could relief PTSD symptoms to different degrees. However, it is necessary to develop systemic treatment as well as symptom-specific therapeutic methods. Future research could focus on predictive factors and physiological indicators to determine effective prevention methods for PTSD, thereby reducing its prevalence and preventing more individuals and families from struggling with this disorder.
Abbreviations
American Psychiatric Association
Acute stress disorder
Cognitive behavioral therapy
Catechol-O-methyl-transferase
Cognitive processing therapy
Complex posttraumatic stress disorder
Cognitive restructuring
C-reactive protein
Cognitive therapy
Dorsal anterior cingulate cortex
Diagnostic and Statistical Manual
Disturbances in self-organization
Eye movement desensitization and reprocessing
Glucocorticoids
Glucocorticoids receptor
Hypothalamic–pituitary–adrenal axis
International classification of diseases
Impact of events scale
Interleukin-1beta
Interleukin-6
Institute of Medicine
Intimate partner violence
International Society for Traumatic Stress Studies
Monoamine oxidase
Major depressive disorder
United Kingdom’s National Institute for Health and Clinical Excellence
Non-suicidal self-injury
Posttraumatic diagnostic scale
Posttraumatic stress disorder
Randomized controlled trials
Rostral ventromedial prefrontal cortex
Serotonin and norepinephrine reuptake inhibitors;
Strength of evidence
Selective serotonin reuptake inhibitors
Tumor necrosis factor-alpha
DoD Department of Veterans Affairs and Department of Defense
Veterans Health Administration
World Health Organization
White J, Pearce J, Morrison S, Dunstan F, Bisson JI, Fone DL. Risk of post-traumatic stress disorder following traumatic events in a community sample. Epidemiol Psychiatr Sci. 2015;24(3):1–9.
Article Google Scholar
Kendell RE. Diagnostic and statistical manual of mental disorders, 3rd ed., revised (DSM-III-R). America J Psychiatry. 1980;145(10):1301–2.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders : DSM-5. America J Psychiatry. 2013. doi: https://doi.org/10.1176/appi.books.9780890425596.744053 .
Maercker A, Brewin CR, Bryant RA, Cloitre M, Reed GM, Van OM, et al. Proposals for mental disorders specifically associated with stress in the international classification of Diseases-11. Lancet. 2013;381(9878):1683–5.
Brewin CR, Cloitre M, Hyland P, Shevlin M, Maercker A, Bryant RA, et al. A review of current evidence regarding the ICD-11 proposals for diagnosing PTSD and complex PTSD. Clin Psychol Rev. 2017;58(1): 1–15.
Google Scholar
Nash WP, Litz BT. Moral injury: a mechanism for war-related psychological trauma in military family members. Clin Child Fam Psychol Rev. 2013;16(4):365–75.
Nazarov A, Fikretoglu D, Liu A, Thompson M, Zamorski MA. Greater prevalence of post-traumatic stress disorder and depression in deployed Canadian Armed Forces personnel at risk for moral injury. Acta Psychiatr Scand. 2018;137(4):342–54.
Article CAS Google Scholar
Foa EB, Cashman L, Jaycox L, Perry K. The validation of a self-report measure of posttraumatic stress disorder: the posttraumatic diagnostic scale. Psychol Assess. 1997;9(9):445–51.
Gnanavel S, Robert RS. Diagnostic and statistical manual of mental disorders (5th edit) and the impact of events scale-revised. Chest. 2013;144(6):1974–5.
Reijnen A, Rademaker AR, Vermetten E, Geuze E. Prevalence of mental health symptoms in Dutch military personnel returning from deployment to Afghanistan: a 2-year longitudinal analysis. Eur Psychiatry. 2015;30(2):341–6.
Sundin J, Herrell RK, Hoge CW, Fear NT, Adler AB, Greenberg N, et al. Mental health outcomes in US and UK military personnel returning from Iraq. Br J Psychiatry. 2014;204(3):200–7.
Macera CA, Aralis HJ, Highfill-McRoy R, Rauh MJ. Posttraumatic stress disorder after combat zone deployment among navy and marine corps men and women. J Women's Health (Larchmt). 2014;23(6):499–505.
Macgregor AJ, Tang JJ, Dougherty AL, Galarneau MR. Deployment-related injury and posttraumatic stress disorder in US military personnel. Injury. 2013;44(11):1458–64.
Sandweiss DA, Slymen DJ, Leardmann CA, Smith B, White MR, Boyko EJ, et al. Preinjury psychiatric status, injury severity, and postdeployment posttraumatic stress disorder. Arch Gen Psychiatry. 2011;68(5):496–504.
Seal KH, Bertenthal D, Maguen S, Gima K, Chu A, Marmar CR. Getting beyond "Don't ask; don't tell": an evaluation of US veterans administration postdeployment mental health screening of veterans returning from Iraq and Afghanistan. Am J Public Health. 2008;98(4):714–20.
Street AE, Rosellini AJ, Ursano RJ, Heeringa SG, Hill ED, Monahan J, et al. Developing a risk model to target high-risk preventive interventions for sexual assault victimization among female U.S. army soldiers. Clin Psychol Sci. 2016;4(6):939–56.
Olatunji BO, Ciesielski BG, Tolin DF. Fear and loathing: a meta-analytic review of the specificity of anger in PTSD. Behav Ther. 2010;41(1):93–105.
Evans L, Cowlishaw S, Hopwood M. Family functioning predicts outcomes for veterans in treatment for chronic posttraumatic stress disorder. J Fam Psychol. 2009;23(4):531–9.
Mckinney JM, Hirsch JK, Britton PC. PTSD symptoms and suicide risk in veterans: serial indirect effects via depression and anger. J Affect Disord. 2017;214(1):100–7.
Briggsgowan MJ, Carter AS, Ford JD. Parsing the effects violence exposure in early childhood: modeling developmental pathways. J Pediatric Psychol. 2012;37(1):11–22.
Enlow MB, Blood E, Egeland B. Sociodemographic risk, developmental competence, and PTSD symptoms in young children exposed to interpersonal trauma in early life. J Trauma Stress. 2013;26(6):686–94.
Newport DJ, Nemeroff CB. Neurobiology of posttraumatic stress disorder. Curr Opin eurobiol. 2009;14(1 Suppl 1):13.
Neigh GN, Ali FF. Co-morbidity of PTSD and immune system dysfunction: opportunities for treatment. Curr Opin Pharmacol. 2016;29:104–10.
Passos IC, Vasconcelos-Moreno MP, Costa LG, Kunz M, Brietzke E, Quevedo J, et al. Inflammatory markers in post-traumatic stress disorder: a systematic review, meta-analysis, and meta-regression. Lancet Psychiatry. 2015;2(11):1002.
Eraly SA, Nievergelt CM, Maihofer AX, Barkauskas DA, Biswas N, Agorastos A, et al. Assessment of plasma C-reactive protein as a biomarker of posttraumatic stress disorder risk. JAMA Psychiatry. 2014;71(4):423.
Lebois LA, Wolff JD, Ressler KJ. Neuroimaging genetic approaches to posttraumatic stress disorder. Exp Neurol. 2016;284(Pt B):141–52.
Zhang K, Qu S, Chang S, Li G, Cao C, Fang K, et al. An overview of posttraumatic stress disorder genetic studies by analyzing and integrating genetic data into genetic database PTSD gene. Neurosci Biobehav Rev. 2017;83(1):647–56.
Bolzenius JD, Velez CS, Lewis JD, Bigler ED, Wade BSC, Cooper DB, et al. Diffusion imaging findings in US service members with mild traumatic brain injury and posttraumatic stress disorder. J Head Trauma Rehabil. 2018. https://doi.org/10.1097/HTR.0000000000000378 [Epub ahead of print].
Logue MW, Rooij SJHV, Dennis EL, Davis SL, Hayes JP, Stevens JS, et al. Smaller hippocampal volume in posttraumatic stress disorder: a multi-site ENIGMA-PGC study. Biol. Psychiatry . 2018;83(3):244–53.
Sijaric-Voloder S, Capin D. Application of cognitive behavior therapeutic techniques for prevention of psychological disorders in police officers. Health Med. 2008;2(4):288–92.
Deahl M, Srinivasan M, Jones N, Thomas J, Neblett C, Jolly A. Preventing psychological trauma in soldiers: the role of operational stress training and psychological debriefing. Brit J Med Psychol. 2000;73(1):77–85.
Wolmer L, Hamiel D, Laor N. Preventing children's posttraumatic stress after disaster with teacher-based intervention: a controlled study. J Am Acad Child Adolesc Psychiatry. 2011;50(4):340–8 348.e1–2.
Skeffington PM, Rees CS, Kane R. The primary prevention of PTSD: a systematic review. J Trauma Dissociation. 2013;14(4):404–22.
Jaques H. Introducing the national institute for health and clinical excellence. Eur Heart J. 2012;33(17):2111–2.
PubMed Google Scholar
Schnyder U. International Society for Traumatic Stress Studies (ISTSS). Psychosomatik Und Konsiliarpsychiatrie. 2008;2(4):261.
Bulger RE. The institute of medicine. Kennedy Inst Ethics J. 1992;2(1):73–7.
Anderle R, Brown DC, Cyran E. Department of Defense[C]. African Studies Association. 2011;2011:340–2.
Feussner JR, Maklan CW. Department of Veterans Affairs[J]. Med Care. 1998;36(3):254–6.
Sripada RK, Rauch SA, Liberzon I. Psychological mechanisms of PTSD and its treatment. Curr Psychiatry Rep. 2016;18(11):99.
Jonas DE, Cusack K, Forneris CA, Wilkins TM, Sonis J, Middleton JC, et al. Psychological and pharmacological treatments for adults with posttraumatic stress disorder (PTSD). Agency Healthcare Res Quality (AHRQ). 2013;4(1):1–760.
Kline AC, Cooper AA, Rytwinksi NK, Feeny NC. Long-term efficacy of psychotherapy for posttraumatic stress disorder: a meta-analysis of randomized controlled trials. Clin Psychol Rev. 2018;59:30–40.
Download references

Acknowledgments
We thank Jamie Bono for providing professional writing suggestions.
This work was supported by the National Natural Science Foundation of China (31371084 and 31171013 by ZJL), and the National Natural Science Foundation of China (81100276 by XRM).
Author information
Authors and affiliations.
Department of Anesthesiology and Intensive Care, Third Affiliated Hospital of Second Military Medical University, Shanghai, China
Xue-Rong Miao, Qian-Bo Chen, Kai Wei, Kun-Ming Tao & Zhi-Jie Lu
You can also search for this author in PubMed Google Scholar
Contributions
ZJL and XRM conceived the project. QBC, KW and KMT conducted the article search and acquisition. XRM and QBC analyzed the data. XRM wrote the manuscript. All the authors read and discussed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Xue-Rong Miao .
Ethics declarations
Ethics approval and consent to participate.
Not Applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Miao, XR., Chen, QB., Wei, K. et al. Posttraumatic stress disorder: from diagnosis to prevention. Military Med Res 5 , 32 (2018). https://doi.org/10.1186/s40779-018-0179-0
Download citation
Received : 20 March 2018
Accepted : 10 September 2018
Published : 28 September 2018
DOI : https://doi.org/10.1186/s40779-018-0179-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Cognitive impairment
- Psychological interventions
- Neuroendocrine
Military Medical Research
ISSN: 2054-9369
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Breakthrough Study on Post-Traumatic Stress Disorder
A collaboration of researchers, institutions and databases makes advances on the understanding of the genetic component of ptsd.
- Joseph McClain - [email protected]
Media contact:
- Miles Martin - [email protected]
Published Date
Share this:, article content.
The Psychiatric Genetics Consortium (PGC), a consortium of researchers led by scientists at University of California San Diego School of Medicine has made significant advancements in the understanding of the neurobiology of post-traumatic stress disorder (PTSD), a condition the World Health Organization says affects some 250 million people around the world.
The group recently announced their findings from a genome-wide association study of 1,222,822 people in a paper recently published in the journal Nature Genetics .
Caroline M. Nievergelt, Ph.D., professor of psychiatry at UC San Diego School of Medicine, is the co-first author on the paper, together with Adam X. Maihofer, PhD., an assistant project scientist in Nievergelt’s lab. PGC-PTSD co-chair Murray B. Stein M.D., M.P.H., professor of psychiatry and public health at UC San Diego is also a co-author of the study.
Nievergelt explained that the work confirmed previous neurobiological studies of PTSD and built upon them, identifying 95 loci — positions of genes on a chromosome — significant to PTSD, including 80 new loci.
“As the number of samples has increased, we have gained a better understanding of the genetic factors that contribute to PTSD risk,” Stein said.
The paper underscores the importance of heritability in PTSD risk and notes that the identified genes influence processes related to PTSD symptoms such as stress, fear and threat responses. She said their findings also point to possible associations among PTSD and other mental and physical disorders.
The PGC was formed in 2007, dedicated to finding genes that predispose an individual to psychiatric disorders, such as bipolar disorder or schizophrenia, Nievergelt said. She added that each disorder is addressed by one of 11 working groups, one of which is the PGC for PTSD, which she chairs.
Nievergelt explained that the benefits of research by a consortium extend beyond the hive-mind input of numerous collaborators working toward a common goal. A genome-wide association study (GWAS) examines and compares genomes of a large number of people in a search for genetic markers associated with a specific condition. A GWAS for polygenic disorders such as PTSD necessarily requires an enormous sample size, she noted.
“And no one PI (principal investigator) is able to get nearly enough subjects for a genome-wide association study, so through the consortium we have a large number of collaborators combining data from all over the world,” Nievergelt said.
The PCG for PTSD consortium includes researchers from a wide number of research institutions and universities worldwide. Notable participants include co-chairs Karestan Koenen, Ph.D., from the Harvard Chan School of Public Health and the Broad Institute of MIT, and Kerry Ressler, M.D., Ph.D., of Harvard Medical School and McLean Hospital.
{/exp:typographee}
The brain, DNA, and a fractured glass effect as a PTSD metaphor. Photo by Adobe AI.
The consortium’s database was assembled from various sources, representing a variety of causes and levels of trauma. Nievergelt said the sources included the Marine Resiliency Study, in which U.S. Marine Corps members were assessed before and after going to war, and Army STARRS, a longitudinal study of U.S. Army soldiers. Another is the Grady Trauma Project that includes victims of violent crime, mostly African American individuals from inner cities. Other datasets incorporated into the PGC for PTSD megadata list came from Electronic Health Records (EHRs) and the VA Million Veterans Program. The consortium also incorporated data from Europe and Latin America.
At an appropriate stage, the consortium members agree on a data freeze and begin their examination, seeking to identify specific genes likely to be associated with PTSD. The paper represents “a milestone” in the understanding of the genetic component of PTSD, Nievergelt said.
“It’s the first time that we actually have a very strong genetic signal,” said Maihofer, who analyzed the data. The genetic signal — essentially a mapping of RNA or DNA activity relevant to PTSD — allowed the consortium to pinpoint specific genes and analyze pathways of gene expression for future research or even for eventual treatment strategies, Maihofer explained.
Nievergelt says there are several directions the consortium wants to take in terms of next steps. One is to increase and diversify the sample size. She said the group has received funding from the National Institute of Mental Health to go to Africa and enroll African people in the genetics study, an effort lead by co-chair Koenen. “That will help us improve risk prediction for other people of African ancestry, a group that has been relatively neglected in earlier studies,” Nievergelt noted.
UC San Diego co-authors
Authors affiliated with the University of California San Diego School of Medicine Department of Psychiatry, in addition to first authors Caroline M. Nievergelt and Adam X. Maihofer, are: Dewleen G. Baker, Carol E. Franz, William S. Kremen, Elizabeth A. Mikita, Sonya B. Norman, Matthew S. Panizzon and Murray B. Stein, also affiliated with the UCSD Herbert Wertheim School of Public Health and Human Longevity Science. Other UC San Diego authors are Anders M. Dale, of the Department of Radiology, Department of Neurosciences, and Wesley K. Thompson, of the Herbert Wertheim School of Public Health and Human Longevity Science.
Other noteworthy participants in the study
PGC-PTSD co-chairs:
Kerry J. Ressler, of the Department of Psychiatry at Harvard Medical School; McLean Hospital, and Department of Medicine (Biomedical Genetics), Boston University Chobanian & Avedisian School of Medicine; as well as Karestan C. Koenen, of the Department of Epidemiology at the Harvard T.H. Chan School of Public Health, the Broad Institute of MIT and Harvard, the Stanley Center for Psychiatric Research; and McLean Hospital Developmental Biopsychiatry Research Program.
Writing group members are:
Elizabeth G. Atkinson, Department of Molecular and Human Genetics, Baylor College of Medicine; Chia-Yen Chen, Biogen Inc.,Translational Sciences; Karmel W. Choi, Department of Epidemiology, Harvard T.H. Chan School of Public Health, and the Department of Psychiatry at Massachusetts General Hospital; Jonathan R. I. Coleman, King’s College London, National Institute for Health and Care Research Maudsley Biomedical Research Centre, and King’s College London, Social, Genetic and Developmental Psychiatry Centre, Institute of Psychiatry, Psychology and Neuroscience; Nikolaos P. Daskalakis, Broad Institute of MIT and Harvard, and the Stanley Center for Psychiatric Research in the Department of Psychiatry of Harvard Medical School, and the McLean Hospital, Center of Excellence in Depression and Anxiety Disorders; Laramie E. Duncan, Department of Psychiatry and Behavioral Sciences, Stanford University; Renato Polimanti, VA Connecticut Healthcare Center, and the Department of Psychiatry of Yale University School of Medicine.
Competing interest
Murray B. Stein has in the past three years received consulting income from Aptinyx, atai Life Sciences, BigHealth, Biogen, Bionomics, Boehringer Ingelheim, Delix Therapeutics, EmpowerPharm, Engrail Therapeutics, Janssen, Jazz Pharmaceuticals, Karuna Therapeutics, NeuroTrauma Sciences, Otsuka US, PureTech Health, Sage Therapeutics, and Roche/Genentech. He also has stock options in Oxeia Biopharmaceuticals and EpiVario. Anders M. Dale holds equity in CorTechs Labs and serves on the Scientific Advisory Board of Human Longevity and the Mohn Medical Imaging and Visualization Center, and also receives funding through research grants with General Electric Healthcare. Other authors associated with UCSD declare no competing interests.
Support and funding
Major financial support for the PGC-PTSD was provided by the National Institute of Mental Health (NIMH) grants R01MH106595 and R01MH124847, by the Cohen Veterans Bioscience and by the Stanley Center for Psychiatric Research at the Broad Institute.
Full lists of authors and their affiliations and competing interests, funding/support sources are available on the paper.
"No one PI (principal investigator) is able to get together nearly enough subjects for a genome-wide association study, so through the consortium we have a large number of collaborators combining data from all over the world."
You May Also Like
A flexible microdisplay can monitor and visualize brain activity in real-time during brain surgery, materials scientist awarded schmidt science fellowship, study finds x’s community notes provides accurate responses to vaccine misinformation, innovative microscopy demystifies metabolism of alzheimer’s, stay in the know.
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.
You have been successfully subscribed to the UC San Diego Today Newsletter.
Campus & Community
Arts & culture, visual storytelling.
- Media Resources & Contacts
Signup to get the latest UC San Diego newsletters delivered to your inbox.
Award-winning publication highlighting the distinction, prestige and global impact of UC San Diego.
Popular Searches: Covid-19 Ukraine Campus & Community Arts & Culture Voices
PTSD Research Paper

This sample PTSD research paper features: 6100 words (approx. 20 pages), an outline, and a bibliography with 13 sources. Browse other research paper examples for more inspiration. If you need a thorough research paper written according to all the academic standards, you can always turn to our experienced writers for help. This is how your paper can get an A! Feel free to contact our writing service for professional assistance. We offer high-quality assignments for reasonable rates.

Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% off with 24start discount code, i. reactions to traumatic events, a. acute reactions, b. posttraumatic stress disorder, c. course of ptsd, ii. measures of ptsd, a. interviews, b. self-report measures, iii. prevalence of ptsd, iv. vulnerability and resiliency factors in ptsd, v. concomitant problems following trauma, vi. theories on the development and maintenance of ptsd, a. psychoanalytic theories, b. cognitive and behavioral theories, c. psychobiological approaches, vii. psychological and pharmacological interventions in ptsd, a. early interventions, b. cognitive-behavioral therapies, 1. prolonged exposure (pe), 2. stress inoculation training (sit), 3. cognitive therapy, 4. cognitive processing therapy (cpt), 5. eye movement desensitization and reprocessing (emdr), c. pharmacotherapy, d. hypnotherapy and psychodynamic psychotherapy.
VIII. Bibliography
Psychologists and physicians have long been interested in vulnerability and resilience factors in reaction to extreme stress. Earlier accounts of posttrauma reactions focused on descriptions of cases. Spurred by inclusion of Post-traumatic Stress Disorder (PTSD) in the psychiatric diagnosis nomenclature in 1980, experimental research has examined many facets of the phenomenon.
In the Diagnostic and Statistical Manual (DSM-IV) published by the American Psychiatric Association in 1994, a trauma is defined as an experienced or witnessed event that involves threat of death or serious injury, and which evokes feelings of terror, horror, or helplessness. Thus, events such as anticipated death of a loved one, job loss, or divorce would not qualify as a trauma in this formulation. The International Classification of Diseases (ICD-10), published by the World Health Organization in 1992, describes a traumatic event as having an exceptionally threatening or catastrophic nature, which would be likely to cause pervasive distress in almost anyone.
The most common traumas studied are combat, sexual assault, sexual abuse in childhood, criminal victimization, torture, accidents, and natural disasters. Larger-scale traumas, such as mass migration, refugee camp experiences, and holocausts, have not yet been thoroughly researched. Clearly, such mass traumas would be expected to have considerable impact on those individuals directly affected as well as on their children, communities, and cultures.
A number of physical and psychological symptoms are considered common reactions immediately after a traumatic experience. Many trauma victims report being disoriented and anxious after a trauma and have difficulty sleeping and concentrating. Victims are often reluctant to talk about the trauma or deliberately contemplate it; nevertheless the traumatic memory intrudes on their thoughts quite frequently. In recognition of the severe distress and psychological dysfunction that often occur immediately after a trauma, a new diagnostic classification called Acute Stress Disorder (ASD) was adopted in the DSM-IV in 1994. The focus of this disorder is on dissociative features, and, consequently, the symptom criteria include at least three of the following: a sense of numbing, detachment, or lack of emotional responsiveness, a reduction in awareness of surroundings (e.g., being in a daze), derealization, depersonalization, and dissociative amnesia. Reexperiencing of the trauma, avoidance, and arousal, as defined in the criteria for PTSD, must also exist. A diagnosis of Acute Stress Disorder is warranted when such symptoms last between 2 days and 1 month, occur within 1 month of the trauma, and interfere significantly with daily functioning.
Posttraumatic Stress Disorder, as described in DSM-IV, is a set of symptoms that begins after a trauma and persists for at least 1 month. The symptoms fall into three clusters. First, the individual must reexperience the trauma in one of the following ways: nightmares, flashbacks, or intrusive and distressing thoughts about the event; or intense emotional distress or physiological reactivity when reminded of the event. Second, the individual must have three of the following avoidance symptoms: avoidance of thoughts or feelings related to the trauma, avoidance of trauma reminders, psychogenic amnesia, emotional numbing, detachment or estrangement from others, decreased interest in leisure activities, or a sense of foreshortened future. Third, the individual must experience two of the following arousal symptoms: difficulty falling or staying asleep, difficulty concentrating, irritability or outbursts of anger, hypervigilance, or an exaggerated startle response. To meet diagnostic criteria for PTSD, the symptoms must cause significant impairment in daily functioning. These criteria provide a good operational definition of PTSD, as they describe the symptoms seen in most cases. However, the three categories of symptoms are not empirically validated as distinct symptom clusters. For instance, it is not clear that the symptoms of behavioral avoidance and emotional numbing are similar and belong in the same category.
The ICD-IO criteria for PTSD also include some reexperiencing symptoms (nightmares, flashbacks, distress on exposure to reminders), actual or preferred avoidance of trauma reminders, and either an inability to recall important aspects of the trauma or sustained psychological sensitivity and arousal (sleep disturbance, hypervigilance, difficulty concentrating). These three criteria must all be met within 6 months of the traumatic event for a diagnosis to be given.
Several differences between the two definitions can be identified. First, the DSM-IV specifies a minimal number of symptoms that need to be observed to receive the diagnosis, whereas the ICD-IO leaves more freedom for clinical judgment. The advantage of the former approach is its utility in clearly operationalizing the concept of PTSD. The disadvantage is its rigidity and the possibility that one symptom can determine diagnostic membership. Second, the ICD-IO does not recognize the numbing symptoms, which together with flashbacks and nightmares are thought to be cardinal features of PTSD. Third, arousal symptoms are optional in the ICD-IO but are required in the DSM-IE Clinical observation and theoretical accounts of PTSD support the importance of these symptoms and render the ICD-IO diagnostic criteria less satisfactory.
The course of PTSD is variable. For the majority of individuals, symptoms begin immediately after the trauma, although some appear to have a delayed reaction. During the first 3 months after the trauma, the individual is said to have acute PTSD, whereas chronic PTSD is defined as symptoms persisting beyond 3 months. Symptoms can fluctuate over time between diagnosis of PTSD, subthreshold symptoms, and few or no symptoms. Recovery is affected by a number of factors, including perception of oneself and one’s surroundings, actual social support, life stress, coping style, and personality.
A number of measures have been developed to assess PTSD, including clinical interviews and self-report instruments. These measures vary widely in terms of the target symptoms, administration time, and the samples used for ascertaining psychometric properties. Adult assessment tools are reviewed in the next section. Although some measures have also been developed for children, they are outside the scope of this paper.
The Structured Clinical Interview for DSM (SCID) is believed to be the most widely used diagnostic interview. Its major disadvantage, however, is that it does not provide a measure of symptom severity. Several other interviews that provide information of both diagnostic status and symptom severity are available. Two interviews are becoming quite widely used in PTSD research. The first is the Clinician-Administered PTSD Scale (CAPS) that yields separate scores for frequency and intensity for each symptom. Disadvantages of this interview include a long administration time and validation on military veterans only. The second interview, the PTSD Symptom Scale Interview (PSS-I), includes a combined frequency/severity rating for each of the 17 PTSD symptoms in the DSM-IV and thus yields both a diagnosis and a continuous severity rating. Unlike the CAPS, the PSS-I takes only about 15 to 20 minutes to administer and was validated on female assault victims.
Several self-report scales have been developed to assess symptoms of PTSD. The first was the Revised Impact of Events Scale (RIES), which yields two factors: intrusion and avoidance. A revised version of the RIES added hyperarousal items, but has shown mixed results in reliability studies and, like its predecessor, does not correspond fully to the DSM-IV PTSD symptoms. Two scales, the Mississippi Scale and the Penn Inventory, have excellent psychometric properties in veteran samples but do not provide information about diagnostic status because they do not fully correspond to the DSM-IV defining symptoms.
The PTSD Symptom Scale-Self-Report (PSS-SR) and its successor, the PTSD Diagnostic Scale (PDS), provide information about each of the 17 DSM-IV symptoms, yielding both diagnostic and severity information. The PDS is the only self-report instrument that assesses all DSM-IV criteria, including information about the nature of the traumatic event and the level of functional interference, in addition to information about PTSD diagnosis and symptom severity. It was validated in a sample of victims of a wide range of traumas and evidenced sound psychometric properties, and thus can be used in studies of various trauma populations.
Lifetime prevalence of PTSD in the general population is estimated at 9%, with up to a third of these cases having chronic PTSD. Among trauma victims, the rate is much higher, estimated at 24 %. However, the rates of PTSD tend to vary considerably among different types of trauma. For instance, estimates of the lifetime prevalence of PTSD in Vietnam War veterans range from 27 to 65%; in civilian populations exposed to terrorism and torture, prevalence ranges from 33 to 54%. Between 35% and 94% of victims of violent assaults manifest PTSD. In contrast, accidents and natural disasters appear to produce lower rates of PTSD, 4.6 to 59%, depending on the event studied and the degree of exposure. Even individuals with little or no direct exposure to the trauma can develop PTSD; this phenomenon has been referred to as the “ripples outward” effect. Importantly, certain occupations are at risk for PTSD by virtue of increased probability of repeated direct exposure to trauma; between 9% and 26% of professionals such as police, nurses, and firefighters develop PTSD in reaction to stressors experienced on the job.
Prevalence in certain vulnerable populations is much higher than in the general population, presumably because individuals in these groups have been exposed to more traumatic experiences. These include populations seeking outpatient psychotherapy and those in substance abuse clinics. Women appear to be somewhat more likely than men to develop PTSD after trauma, 10.4 % versus 5 %, respectively. As noted earlier, the prevalence of emotional difficulties after mass traumas, such as refugee camp experiences or holocausts, has not been systematically studied.
Factors implicated in posttrauma reactions can be divided into three categories: pretrauma variables, variables related to the trauma itself, and posttrauma variables.
Research on pretrauma demographic variables has not identified reliable predictors of who will develop chronic PTSD with one exception: women are somewhat more likely to manifest PTSD than men after experiencing a similar trauma. In contrast, it appears that poor psychological and social functioning prior to the trauma renders the individual vulnerable to developing chronic symptoms. For instance, prior hospitalization and a history of drug abuse were found to be associated with a more severe posttrauma reaction. Also, a history of traumatic events in childhood or adulthood predicts a more severe response to a new trauma.
The nature of the trauma itself also appears to affect recovery. First, traumas differ in their likelihood of producing PTSD; rape, for example, is more likely to produce persistent symptoms than a natural disaster. Second, given a specific trauma (e.g., rape), injury and perceived threat of death produce more severe and persistent reactions.
Several posttrauma factors have been found to exacerbate symptoms. It appears that dissociation (emotional numbing, amnesia, depersonalization) shortly after a trauma hinders recovery. Also, on average, assault victims who exhibit more severe initial reactions to the trauma also show more symptoms later on. Thus, individuals seem to differ in how strongly they are affected by a similar trauma, and their initial reaction is associated with later psychopathology.
Evidence on the role of social support as facilitating or hindering recovery is equivocal. It seems that negative reactions from others, such as blame, increase posttrauma psychopathology, but, unfortunately, positive reactions do not show the expected positive effects. Excessive anger or guilt after the trauma also appears to block readjustment. Additional longitudinal research on the factors that promote resilience to trauma are clearly needed.
Traumatized individuals not only exhibit ASD or PTSD symptoms, but also depression, substance abuse, anxiety, dissociation, and physical health problems.
The rate of use and abuse of drugs and alcohol, including nicotine, in traumatized individuals is higher than in the general population. There are at least two explanations for this finding. First, traumatized individuals may choose to cope with their symptoms by increasing substance use. Second, substance abuse may increase the risk of being exposed to a traumatic experience.
Many individuals report symptoms of depression after a traumatic event, such as sadness, lack of energy, diminished interest in leisure activities, hopelessness, sleeplessness, and eating disturbances. Although some of these symptoms overlap with the defining symptoms of PTSD (e.g., markedly diminished interest in activities), the two disorders are separate entities and both can develop independently as a response to a traumatic experience.
The incidence of comorbid anxiety disorders is also elevated among individuals with PTSD. For example, lifetime comorbidity of panic disorder in Vietnam veterans with PTSD was 21% in females and 8% in males, versus 1.5 to 3.5% in the general population. The lifetime prevalence of obsessive-compulsive disorder was found to be 13% in females and 10% in males, as compared with 2.5 % in the general population.
There is a greater frequency of physical health problems among trauma victims than in the general population, especially among those who develop chronic PTSD. Trauma victims have higher rates of gastrointestinal disorders and pelvic or abdominal pain, and visit the doctor more often than the general population. In the aftermath of rape and child sexual abuse, gynecological and psychosexual problems such as vaginal discharge, dysmennorhea, dyspareunia, vaginismus, and pelvic pain have also been noted.
Reactions to trauma have long captured the interest of theorists of psychopathology. Janet’s 1889 theory of reactions to trauma has influenced both early and contemporary conceptualizations. Janet proposed that when confronted with a traumatic event that besieges the victim with an overabundance of intense thoughts and feelings, too numerous or intense to integrate, some individuals selectively attend away from the trauma to trauma-irrelevant thoughts and feelings. Thus, ideas related to the trauma remain split off or dissociated from normal consciousness and become “fixed.” Although out of consciousness, these “fixed ideas” remain part of the victim’s ideational content, and therefore continue to exert influence over his or her thought, mood, and behavior in the form of fragmented reliving of the trauma such as visual images, somatic states, emotional conditions, or behavioral reenactment.
Freud wrestled with understanding the influence of traumatic experiences on the individual’s psyche. In early writings, he was influenced by Janet’s theory on the strength of the emotional reactions that are produced by a traumatic experience and that force the victim to become fixated on the trauma. Later, Freud abandoned the dissociation view and proposed that the persistence of trauma reactions reflects an association between the traumatic event and childhood repressed conflicts, ideas, or impulses, and the efforts to prevent conscious awareness of them. He also coined the concept of “repetition compulsion” to explain trauma reexperiencing, proposing that because of the need to keep it away from consciousness, the individual is forced to repeat aspects of the trauma as a contemporary experience rather than as a memory of it. Influenced by World War I experiences, Freud refocused on the external reality, and, in the spirit of Janet, viewed the emotional upheaval generated by the trauma as the source of traumatic neurosis. He suggested that the intensity of the trauma, the inability to find conscious expressions for it, and the unpreparedness of the individual cause a breach to the stimulus barrier and overwhelm the defense mechanisms. More recent theorists have proposed that the developmental level and ego resources available to the victim are central to the manner in which the trauma is experienced and to the production of symptoms. For instance, a young child, easily overwhelmed and flooded with emotion, may experience complete helplessness in the face of trauma, whereas a mature adult would be more likely to respond through emotional numbing and cognitive constriction. Psychoanalytic theorists and practitioners focus on the need to help the victim acknowledge and bear the trauma and the resulting psychic damage, and develop coping mechanisms such that the memories of the trauma are incorporated into his or her current experience.
Several schools of thought inspired cognitive-behavioral theories of PTSD. The first is learning theory, which explains PTSD symptoms in terms of instrumental and classical conditioning. The learning model that most directly influenced cognitive-behavioral treatments (CBT) aimed at anxiety reduction was Mowrer’s two-factor theory. First, Mowrer proposed that fear is acquired through classical conditioning, where a neutral stimulus comes to evoke fear through its pairing with an aversive stimulus. Applying this theory to explain PTSD symptoms, neutral stimuli (e.g., supermarket) that were present during the trauma are presumed to acquire the ability to elicit fear through their associations with the danger stimuli (e.g., gun). Through the processes of generalization and second-order conditioning, stimuli similar to those present during the trauma also come to evoke fear. For instance, the stimuli all men, being alone, and the word rape can all acquire the capacity to cause anxiety. In Mowrer’s second stage, avoidance behavior is established through the process of operant conditioning. That is, an individual learns to reduce trauma-related anxiety through avoidance of, or escape from, the feared stimuli. Escape and avoidance behaviors are negatively reinforced because avoidance diminishes the aversive fear state.
Cognitive-behavioral therapy of PTSD has also been influenced by cognitive theory. Cognitive theory assumes that the interpretation of events, rather than events themselves, underlies emotional reactions. Accordingly, an event can be interpreted in different ways and consequently can evoke different emotions. Aaron Beck and colleagues suggest that trauma victims who manifest chronic persistent anxiety are unable to discriminate between safe and unsafe signals, and consequently their thinking is dominated by the perception of danger. They also suggest that traumatic fear can be maintained through a sense of incompetence to handle stressful events.
Other cognitive theorists have postulated that cognitive schemas are disrupted after victimization. A schema is a meaning structure that guides the perception, organization, and interpretation of incoming information. Common to these theories is the supposition that a traumatic experience requires cognitive modification and that such modification is accomplished by assimilation and accommodation. Accordingly, the victim must either assimilate the traumatic experience into preexisting schemas, or, more often, change schemas to accommodate the traumatic experience. In her 1992 book, Janoff-Bulman took the position that people in general hold the assumptions: “the world is benevolent, the world is meaningful, and self is worthy,” and these assumptions are incompatible with a traumatic experience. Building on Janoff-Bulman’s ideas, other theorists suggest that the following areas are of particular relevance: safety, dependency/trust of self and others, power, esteem, intimacy, and independence.
Coming from the psychoanalytic tradition, Horowitz integrated psychoanalytical and information processing notions in his 1986 book, suggesting that people have a basic need to match trauma-related information with their “inner models based on old information.” The process of recovery entails the repeated revision of both trauma-related information and the inner models until they agree, which Horowitz referred to as the “completion tendency.”
Foa and Kozak integrated cognitive and learning theories to explain the development and maintenance of pathological anxiety in what they called emotional processing theory. In their 1986 paper, fear is conceived as a cognitive structure or a program for escaping danger which includes representations of fear stimuli, fear responses, and their meaning. Pathological fear, they suggested, is distinguished from normal fear in that it includes erroneous associations and evaluations. Emotional processing theory views anxiety disorders as representing distinctive fear structures in memory, and the persistence of anxiety symptoms is conceived as reflecting impairment in emotional processing. Accordingly, PTSD is construed as reflecting a fear memory that contains erroneous associations and evaluations, whereas a normal trauma memory reflects associations and evaluations that better match reality. First, a pathological PTSD structure contains excessive response representations that are reflected in the PTSD symptoms. Second, this structure includes erroneous stimulus-stimulus associations that do not accurately represent the world. For example, the pathological fear structure of a woman who was raped at gunpoint by a bald man would contain an association between “bald men” and “gun.” In reality, however, bald men are not more likely to carry guns or to rape than men with a full head of hair. Third, the structure also includes erroneous associations between harmless stimuli such as “bald,” “home, …. suburbs,” and the meaning of “dangerous.” Being raped one time while at home in the suburbs does not tangibly increase the chance of encountering violence in that environment. Fourth, the structure includes erroneous associations between harmless stimuli and escape or avoidance responses. For example, the victim who was raped by the bald man would tend to run away from such men. In reality, however, running away from “bald men” is not likely to enhance safety. These erroneous associations would lead to mistakenly interpreting the world as entirely dangerous.
Another set of erroneous associations and evaluations is the interpretation of the victim’s response representations. It is thought that the victim’s responses during and after the trauma, and in particular the PTSD symptoms, are interpreted to mean self-incompetence. In summary, emotional processing theory hypothesizes that two major pathological concepts underlie PTSD: the world as entirely dangerous, and the self as entirely inept.
Psychophysiological, neurohormonal, neuroanatomical, and immunological changes have been observed in animals exposed to extreme stress and in trauma victims who developed PTSD (van der Kolk, McFarlane, & Weisaeth, 1996). These changes have been hypothesized to disregulate responses to incoming information and to inhibit successful processing of traumatic memories.
The normal stress response upon exposure to a high-magnitude stressor is a complex neurohormonal response, including the release of catecholamines (e.g., epinephrine and norepinephrine), serotonin, endogenous opioids, and hormones of the hypothalamus, pituitary, or adrenal gland (e.g., cortisol, vasopressin, oxytocin). Normally, the introduction of a stressor produces intense and rapid stress responses, and these dissipate quickly after the removal of the stressor. However, after prolonged exposure to stress, the stress responses become disregulated.
Theorists propose that PTSD reflects a failure to regulate autonomic reactions to stimuli such that the individual either experiences hyperreactivity or “shutting down” and emotional numbing. Individuals with PTSD show hyperreactivity, as measured by heart rate, skin conductance, and blood pressure, in reaction to reminders of traumatic events. This disregulation of the emotional and physiological responsiveness occurs with specific reminders of the trauma as well as in reaction to intense but neutral stimuli, signifying a loss of stimulus discrimination. In addition, the individual may come to fear his or her emotional reactions because of being able to do little to control them.
Neurohormonal changes in individuals with PTSD have also been found. First, prolonged stress causes depletion of the noradrenergic system, such that receptors become hypersensitive to any new release of norepinephrine. This noradrenergic hyperreactivity is linked to the increased arousal and startle of PTSD. The high levels of norepinephrine are proposed to inhibit the release of corticotrophin-releasing hormone and thereby inhibit the entire hypothalamic-pituitaryadrenocortical axis. This inhibition, in turn, produces a deficiency in endogenous opioids. Some theories postulate that the reexperiencing symptoms of PTSD cause a burst in the release of endogenous opioids and therefore make up for this deficiency. These endogenous opioids are thought to produce an artificial numbing or calmness, another hallmark of PTSD. Additional theories propose that cortisol responses are lowered in retraumatized individuals and that serotonin levels may decrease in response to prolonged inescapable stress.
In addition to psychophysiological and neurohormonal factors, specific brain abnormalities have recently been detected in individuals with PTSD. One system that is implicated in the disorder is the limbic system, which is thought to function in memory and in emotional reactions to incoming stimuli. One area in the limbic system, the hippocampus, is presumed to record spatial and temporal aspects of experiences in memory. Researchers have noted decreased hippocampal volume in trauma victims with PTSD compared with those without PTSD. One possible explanation for this finding is that individuals with smaller hippocampuses are more likely to develop PTSD; a more likely interpretation of these results is that increased cortisol activity causes shrinkage, because cortisol is toxic to the hippocampus.
A second area in the limbic system, the amygdala, also appears to be altered in individuals with PTSD. The amygdala is thought to assign meaning to incoming stimulation by integrating memory images with emotional experiences associated with those memories, guiding emotional behavior. A single intense stimulation of the amygdala appears to alter the limbic physiology such that a “kindling” effect occurs. That is, the behavior that follows may be predominantly either “fight” or “flight,” and a pattern of conditioned behavior is set up such that there is limited processing of incoming information before the response is initiated.
Several psychological interventions have been used with trauma victims, including supportive counseling individually or in groups, brief dynamic psychotherapy, hypnotherapy, pharmacotherapy, and cognitivebehavioral therapy. As recently reviewed by Foa and Meadows, although a variety of psychological interventions are used routinely with trauma victims, controlled outcome studies have tended to focus on cognitive-behavioral treatments such as systematic desensitization, exposure, and anxiety management. Nevertheless, hypnotherapy and psychodynamic therapy have also shown promise in the few studies examining their efficacy.
The popular supposition among trauma theories is that for recovery to occur after a traumatic experience, special processing efforts should take place. This view has prompted the development of early intervention programs. These programs have focused on education, debriefing after trauma, and training professionals at risk (e.g., police). Usually, “critical incident stress debriefing” is conducted in groups, such as emergency workers, and focuses on education about common reactions to traumatic experiences, encouraging trauma victims to process their experiences in a group setting. Although such programs have become routine in many places, little is known about their efficacy. In fact, some experts have raised concerns that such programs could interfere with rather than facilitate the natural recovery process.
The recognition that victims who exhibit severe reactions immediately after the trauma are more likely to develop chronic dysfunction has prompted researchers to implement interventions that aim to prevent chronic PTSD. Foa and colleagues conducted a study to compare PTSD severity of female assault victims, who received a brief prevention program (four individual therapy sessions), to that of victims who underwent an assessment procedure. Victims who received the brief prevention program had less severe PTSD and depressive symptoms 2 months after the assault. Clearly, more studies of this type are needed before confidence in prevention efforts can be established.
Currently, five cognitive-behavioral interventions are in use for PTSD: Prolonged Exposure, cognitive therapy, Stress Inoculation Training, Cognitive Processing Therapy, and Eye Movement Desensitization and Reprocessing.
This is a set of procedures that involves confrontation with feared stimuli, either in vivo or in imagination. With PTSD, exposure therapy typically includes repeated reliving of the traumatic event in imagination and actual confrontation with feared situations and objects that have been avoided because they are reminders of the trauma but are not intrinsically dangerous.
As discussed earlier, the theoretical basis of PE lies in learning and emotional-processing theories. Foa and Kozak have proposed that successful therapy involves correcting the pathological elements of the fear structure, and that this corrective process is the essence of emotional processing. They further suggest that regardless of the type of therapeutic intervention used, two conditions are required for fear reduction. First, the fear structure must be activated through introduction of fear-relevant information. If the fear structure is not activated (fear is not evoked), the structure would not be available for modification. Second, during exposure, information that is incompatible with the existing pathological elements (e.g., fear reduction) must be provided so that the pathological fear structure can be corrected. Specifically, exposure researchers hypothesize that repeated reliving promotes several cognitive changes. First, it promotes habituation of anxiety associated with the trauma memory, and this habituation disconfirms the victim’s erroneous belief that anxiety will stay forever and therefore lead to disastrous consequences. Second, reliving promotes discrimination between “remembering” the trauma and “encountering” it again, thus reinforcing the realization that remembering itself is not dangerous. Third, repeated exposure promotes differentiation between the trauma and similar but safe situations, disconfirming the idea that the world is extremely dangerous. Fourth, it promotes the association between PTSD symptoms and a sense of mastery, rather than incompetence. Finally, repeated recounting of the trauma narrative helps to organize the narrative and thereby to facilitate the integration of the trauma memory.
Several controlled studies on exposure have shown their usefulness in treating PTSD. Whereas studies on veterans showed only modest improvement, two studies with female rape victims showed more improvement. Foa and colleagues found that exposure (imaginal and in vivo) was effective in eliminating PTSD in 55% of rape victims with chronic PTSD compared with 45% of those who received supportive counseling. Superior results were found in a second study: about 70% of victims who received Prolonged Exposure lost their PTSD diagnosis, and none of the women in a wait-list group lost their diagnosis. These treatment effects were maintained at 6-month follow-up.
This intervention consists of training victims to handle anxiety with several skills for anxiety management: relaxation, thought stopping, assertiveness, cognitive therapy, coping self-statements, and guided imagery. Although the direct goal of anxiety management techniques is to teach patients techniques to manage their anxiety, the successful acquisition of such techniques can have indirect effects on the victim’s schemas of self and the world. Specifically, the victim’s experience of being able to control the anxiety fosters a more positive self-image and thereby modifies the perception of the world as overwhelmingly dangerous. Several studies point to the efficacy of this program used alone or in combination with other techniques. For example, the two studies on rape victims reported earlier found that SIT significantly reduced PTSD, to a degree comparable to that of exposure.
Researchers believed that if PE and SIT are quite, but not completely, successful in ameliorating PTSD symptoms, a program that combined these two treatments would yield superior results. However, research does not support this view: combined programs were helpful for female assault victims, but not more than exposure or stress inoculation alone.
Cognitive techniques are often incorporated into anxiety management programs that teach patients to examine and change systematically maladaptive thoughts that can lead to negative responses. Cognitive therapy involves the use of discourse, in which the patient is taught to identify the beliefs underlying the fear, to examine whether they are distorted or accurately reflect reality, and to replace mistaken or dysfunctional beliefs with more realistic, functional ideas about the ability of the patient to cope with stress and the dangerousness of the world. One possible benefit of cognitive restructuring is that it addresses directly beliefs underlying emotions other than fear, such as anger and guilt. Early investigations of this technique revealed some promise in the use of this therapy to reduce symptoms of PTSD in rape victims.
Another cognitive-behavioral program called Cognitive Processing Therapy is described in Resick and Schnicke’s 1992 book. It involves cognitive restructuring and exposure through writing about the trauma. The cognitive therapy is geared toward correcting maladaptive cognitions associated with rape, such as power, safety, and esteem. In one study, on the average, victims who received CPT reported 40% symptom reduction, and these gains were maintained over time. More studies are needed to establish the efficacy of this relatively new treatment.
This therapy, described by Shapiro in 1995, is a form of exposure with a cognitive emphasis, accompanied by guided eye movements. The studies that have evaluated the efficacy of this treatment produced equivocal results. Some show good results, but others show no improvement. Because these studies have many methodological problems, it is difficult to determine the validity of the findings. Further well-controlled studies are needed before a definite conclusion about the value of EMDR can be made.
Many medications have been used for the treatment of PTSD, but only a few have been systematically studied. Most of these have used male combat veterans, and thus the efficacy of pharmacotherapy for other traumatized populations is largely unknown. Tricyclic antidepressants have been used in an attempt to reduce locus coeruleus overactivity and noradrenergic disregulation found in PTSD, with equivocal results. Amitriptyline and imipramine have shown modest reductions in PTSD symptoms in comparison with placebo in double-blind studies with male veterans. In contrast, desipramine failed to show efficacy. One study of fluoxetine, a selective serotonin reuptake inhibitor used to regulate serotonergic dysfunction in individuals with PTSD, found it to be effective in reducing symptoms of PTSD, especially in trauma victims other than Vietnam veterans.
Other medications that have been tested include anticonvulsants such as carbamazepine and valproic acid; but no double-blind studies have been conducted to date. Beta-adrenergic blockers such as propanolol have shown promise in reducing aggressivity and arousal symptoms in open studies, and alpha2-adrenergic agonists, such as clonidine, appear to be effective through their suppression of locus coeruleus activity.
Finally, benzodiazepines have been widely used to suppress anxiety and are believed to reduce PTSD symptoms by reducing limbic system kindling and reversing neurochemical changes in the locus coeruleus and hypothalamus. However, the rebound anxiety and withdrawal symptoms associated with benzodiazepines can be problematic.
In summary, most of our knowledge about efficacy of pharmacotherapy for PTSD is confounded by the restricted samples used in existing studies. Most were conducted on Vietnam veterans, whose symptoms are particularly resistant to all types of treatments, and therefore the present results may underestimate the efficacy of this treatment.
Hypnotherapy uses heightened concentration and focused attention to facilitate treatment related to trauma. It is based on the supposition that individuals with PTSD are unknowingly entering trance states when they reexperience the trauma and that hypnotherapy can help them learn how to control their trance states and digest the dissociated traumatic experience in a controlled manner. One study found hypnosis to be as effective as psychodynamic psychotherapy and a type of exposure called systematic desensitization. More studies of this technique are needed before conclusions can be drawn about the usefulness of hypnotherapy.
Psychodynamic psychotherapy has also been used to help individuals recover from trauma. It focuses on intrapsychic conflict about the trauma rather than on resolution of specific symptoms of PTSD. The methods used are in some respects similar to those used in cognitive-behavioral therapy, as these interventions focus on helping the victims process the traumatic experience and on teaching them how to tolerate anxiety. Both individual and group therapies have been used, and some preliminary studies suggest the utility of these interventions.
Bibliography:
- American Psychiatric Association. (1994). Diagnostic and statistical manual (4th ed.). Washington, DC: American Psychiatric Press.
- Davidson, J. R. T., & Foa, E. B. (Eds.). (1993). Post-traumatic stress disorder: DSM-IV and beyond. Washington, DC: American Psychiatric Press.
- Foa, E. B., & Kozak, M. J. (1986). Emotional processing of fear: Exposure to corrective information. Psychological Bulletin, 99, 20-35.
- Foa, E. B., & Meadows, E. A. (1997). Psychosocial treatments for post-traumatic stress disorder: A critical review. In J. Spence (Ed.), Annual review of psychology. Palo Alto, CA: Annual Reviews, Inc.
- Foa, E. B., & Riggs, D. S. (1993). Post-traumatic stress disorder in rape victims. In J. Oldham, M. B. Riba, & A. Tasman (Eds.), American psychiatric press review of psychiatry (Vol. 12, pp. 273-303). Washington, DC: American Psychiatric Press.
- Horowitz, M. J. (1986). Stress response syndromes (2nd edition). Northvale, NJ: Jason Aronson, Inc.
- Janet, P. (1889). L’Automatisme psychologique. Paris: Felix Alcan. (Reprinted 1973, Paris, Societe Pierre Janet.)
- Janoff-Bulman, R. (1992). Shattered assumptions: Towards a new psychology of trauma. New York: Free Press.
- Kessler, R. C., Sonnega, A., Bromet, E., Hughes, M., & Nelson, C. B. (1995). Post-traumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry, 52, 1048-1060.
- Resick, P. A., & Schnicke, M. K. (1992). Cognitive processing therapy for sexual assault survivors: A treatment manual. Newbury Park, CA: Sage.
- Shapiro, F. (1995). Eye movement desensitization and reprocessing: Basic principles, protocols, and procedures. New York: Guilford Press.
- van der Kolk, B. A., McFarlane, A. C., & Weisaeth, L. (Eds.). (1996). Traumatic stress: The effect of overwhelming experience on mind, body, and society. New York: Guilford Press.
- World Health Organization. (1993). ICD- I O: The ICD- IO classification of mental and behavioural disorders: Diagnostic criteria for research. Geneva, Switzerland: Author.
ORDER HIGH QUALITY CUSTOM PAPER

Purdue Online Writing Lab Purdue OWL® College of Liberal Arts
Reference List: Textual Sources

Welcome to the Purdue OWL
This page is brought to you by the OWL at Purdue University. When printing this page, you must include the entire legal notice.
Copyright ©1995-2018 by The Writing Lab & The OWL at Purdue and Purdue University. All rights reserved. This material may not be published, reproduced, broadcast, rewritten, or redistributed without permission. Use of this site constitutes acceptance of our terms and conditions of fair use.
Basic Format for Books
Edited book, no author, edited book with an author or authors, a translation.
Note : When you cite a republished work, like the one above, in your text, it should appear with both dates: Plato (385-378/1989)
Edition Other Than the First
Article or chapter in an edited book.
Note : When you list the pages of the chapter or essay in parentheses after the book title, use "pp." before the numbers: (pp. 1-21). This abbreviation, however, does not appear before the page numbers in periodical references, except for newspapers. List any edition number in the same set of parentheses as the page numbers, separated by a comma: (2nd ed., pp. 66-72).
Multivolume Work
Articles in periodicals.
APA style dictates that authors are named with their last name followed by their initials; publication year goes between parentheses, followed by a period. The title of the article is in sentence-case, meaning only the first word and proper nouns in the title are capitalized. The periodical title is run in title case, and is followed by the volume number which, with the title, is also italicized. If a DOI has been assigned to the article that you are using, you should include this after the page numbers for the article. If no DOI has been assigned and you are accessing the periodical online, use the URL of the website from which you are retrieving the periodical.
Article in Print Journal
Note: APA 7 advises writers to include a DOI (if available), even when using the print source. The example above assumes no DOI is available.
Article in Electronic Journal
Note : This content also appears on Reference List: Online Media .
As noted above, when citing an article in an electronic journal, include a DOI if one is associated with the article.
DOIs may not always be available. In these cases, use a URL. Many academic journals provide stable URLs that function similarly to DOIs. These are preferable to ordinary URLs copied and pasted from the browser's address bar.
Article in a Magazine
Article in a newspaper.

IMAGES
VIDEO
COMMENTS
Posttraumatic stress disorder. Posttraumatic stress disorder (PTSD) may develop when someone lives through or witnesses an event in which they believe that there is a threat to life or physical integrity and safety and experiences fear, terror, or helplessness. People with PTSD may relive the trauma in painful recollections, flashbacks, or ...
CPT is considered a first-line treatment for PTSD by APA and international treatment guidelines (APA, 2017; ISTSS, 2018; NICE, 2018; The Management of Posttraumatic Stress Disorder Work Group, 2017). Overall, research has found treatment effect sizes around 1.5 and loss of PTSD diagnosis in about 50% of individuals in RCTs, comparable to PE ...
Posttraumatic Stress Disorder (PTSD) is an anxiety problem that develops in some people after extremely traumatic events, such as combat, crime, an accident, or natural disaster. This page showcases content from APA Publishing about PTSD. For more resources from APA, visit our Clinical Practice Guideline for the Treatment of Posttraumatic ...
Posttraumatic Stress Disorder (PTSD)) conducted by the Research Triangle Institute-University of North Carolina Evidence-based Practice Center as its primary evidence base (Jonas, Cusack, Forneris, Wilkins, Sonis, Middleton, et al., 2013). ... How the APA PTSD Guideline Recommendations Are Similar To or Different From Other PTSD
The American Psychological Association (APA) developed a clinical practice guideline (CPG) to provide recommendations on psychological and pharmacological treatments for posttraumatic stress disorder (PTSD) in adults. This paper is a summary of the CPG, including the development process. Members of the guideline development panel (GDP) used a comprehensive systematic review conducted by the ...
The PTSD treatment guideline was the first to be completed (American Psychological Association, 2017).It generated considerable critical response among clinicians working with traumatized people, a controversy discussed in more detail in the articles that make up the special issue of Psychotherapy. In general, the critiques had to do with the fact that the most highly recommended treatments ...
Background: Many people will experience a potentially traumatic event in their lifetime and a minority will go on to develop post-traumatic stress disorder (PTSD). A wealth of literature explores different trajectories of PTSD, focusing mostly on resilient, chronic, recovered and delayed-onset trajectories. Less is known about other potential trajectories such as recurring episodes of PTSD ...
Note: In 2021 the APA Board of Directors appointed a multidisciplinary panel to update the 2017 Clinical Practice Guideline for the Treatment of PTSD in Adults. Reports on the panel's progress and requests for input will be made periodically to the APA Council of Representatives, APA boards and committees, APA members, and the broader public.
This APA Clinical Practice Guideline for the Treatment of Post Traumatic Stress Disorder in Adults was approved as APA policy by the Council of Representatives on February 24, 2017. ... This APA Clinical Practice Guideline for the Treatment of Post Traumatic Stress Disorder in Adults was approved as APA policy by the Council of Representatives ...
This special issue of Psychotherapy, published jointly with a companion issue in Practice Innovations (Volume 4, Issue 3), features the APA Clinical Practice Guideline for the Treatment of Posttraumatic Stress Disorder (PTSD). Readers of these special issues are encouraged to review the full clinical practice guideline and accompanying resources.
Future research will contribute to our knowledge about commonly used and newly emerging interventions over time. TABLE 1.1. Summary of Recommendations of the APA Guideline Development Panel for the Treatment of Posttraumatic Stress Disorder (PTSD) Strength of recommendation Psychotherapy For adult patients with PTSD, the panel strongly recommends
Individuals with elevated symptoms of posttraumatic stress disorder (PTSD) or a PTSD diagnosis are at increased risk of thinking about, attempting, and dying by suicide. Yet, there remain key gaps in the field's understanding of the relation between PTSD and suicidal thoughts and behaviors. In response, Psychological Trauma: Theory, Research, Practice, and Policy organized this Special ...
Post-traumatic stress disorder (PTSD) is a psychiatric disorder that results from the experience or witnessing of traumatic or life-threatening events. PTSD has profound psychobiological correlates, which can impair the person's daily life and be life threatening. In light of current events (e.g. extended combat, terrorism, exposure to certain ...
Current treatment strategies for control of trauma-associated symptoms of Post Traumatic Stress Disorder (PTSD) have recently been updated by the Veterans Affairs (VA) and the Department of Defense (DoD, after over a decade of dedicated research. The most recent evidence is compelling that its use of trauma-focused therapies such as Cognitive ...
Post-traumatic stress disorder (PTSD) is a chronic mental disorder resulting in a reduced quality of life and increased economic burden. Exposure to a traumatic stressor is the trigger for PTSD development . For that, a distinction between ordinary and traumatic stressors (those that have the potential to result in PTSD) is necessary.
pandemic ways of coping (Holmes et al., 2020). Posttraumatic stress disorder (PTSD) is a mental health problem that develops following exposure to a traumatic life event (i.e., an experience of actual or threatened death, injury or sexual violence). People who meet criteria for a PTSD diagnosis as de ned by the.
Posttraumatic stress disorder (PTSD) is a chronic, often debilitating mental health disorder that may develop after a traumatic life event. Fortunately, effective psychological treatments for PTSD exist. In 2017, the Veterans Health Administration and Department of Defense (VA/DoD) and the American Psychological Association (APA) each published ...
The paper provides a concise review of the evolution of PTSD diagnosis in the Diagnostic and Statistical Manual of Mental Disorders, impact of PTSD in the community, an overview of the established risk factors for developing PTSD, and assessment and treatment. Throughout the paper, controversies and clinical implications are discussed.
Although traumatic stress has been known for over 100 years by a number of terms, including "shell shock", "battle fatigue", or "soldier's heart" 1, it was only in the 1980s that persistent stress reactions were recognized in psychiatric nosology.In the wake of the mental health problems evident in many troops returning from deployment in Vietnam, the DSM-III introduced the ...
1. Introduction. Post-traumatic stress disorder (PTSD) is a debilitating mental condition that can significantly impact the sufferer's quality of life [1,2,3].A study by Rapaport et al. found that 59% of patients suffering from PTSD had severely impaired overall quality of life based on the Quality of Life Enjoyment and Satisfaction Questionnaire [].
APA is currently updating its 2017 Clinical Practice Guideline for the Treatment of Posttraumatic Stress Disorder (PTSD) in Adults, which is based on systematic reviews of the scientific evidence, an assessment of the benefits, harms/burdens, balance of benefits to harms/burdens, patient values and preferences, and applicability.The updated guideline will include treatment recommendations and ...
Posttraumatic stress disorder (PTSD) is a recognized clinical phenomenon that often occurs as a result of exposure to severe stressors, such as combat, natural disaster, or other events [].The diagnosis of PTSD was first introduced in the 3rd edition of the Diagnostic and Statistical Manual (DSM) (American Psychiatric Association) in 1980 [].PTSD is a potentially chronic impairing disorder ...
The ICD-11 di-agnosis of PTSD consists of only six symptoms, substantially fewer than the 20 PTSD symptoms in the fth edition of the Diag-fi nostic and Statistical Manual of Mental Disorders (DSM5; - American Psychiatric Association [APA], 2013). The six PTSD. This article was published Online First December 30, 2021.
Drawing from PTSD best practices, the APA-initiated Center for Deployment Psychology includes exposure therapy in the training of psychologists ... the National Center for PTSD's Keane believes that much more research is needed on treating PTSD and psychiatric co-morbidities such as depression, anxiety, substance abuse, personality disorders ...
Spirituality/religion is clinically relevant to patients experiencing posttraumatic stress disorder (PTSD) and/or alcohol use disorder (AUD). Despite the comorbidity of PTSD and AUD among first responders (i.e., firefighters, law enforcement, paramedics, corrections officers), relatively little research has investigated the lived experience of first responders with PTSD and AUD as it related ...
PGC-PTSD co-chair Murray B. Stein M.D., M.P.H., professor of psychiatry and public health at UC San Diego is also a co-author of the study. Nievergelt explained that the work confirmed previous neurobiological studies of PTSD and built upon them, identifying 95 loci — positions of genes on a chromosome — significant to PTSD, including 80 ...
PTSD Research Paper. This sample PTSD research paper features: 6100 words (approx. 20 pages), an outline, and a bibliography with 13 sources. Browse other research paper examples for more inspiration. If you need a thorough research paper written according to all the academic standards, you can always turn to our experienced writers for help.
Title of chapter. In E. E. Editor & F. F. Editor (Eds.), Title of work: Capital letter also for subtitle (pp. pages of chapter). Publisher. Note: When you list the pages of the chapter or essay in parentheses after the book title, use "pp." before the numbers: (pp. 1-21). This abbreviation, however, does not appear before the page numbers in ...
Almost a year after APA issued its health advisory on social media use in adolescence, society continues to wrestle with ways to maximize the benefits of these platforms while protecting youth from the potential harms associated with them. 1. By early 2024, few meaningful changes to social media platforms had been enacted by industry, and no federal policies had been adopted.