Healthy Eating Learning Opportunities and Nutrition Education

Healthy eating learning opportunities includes nutrition education and other activities integrated into the school day that can give children knowledge and skills to help choose and consume healthy foods and beverages. 1 Nutrition education is a vital part of a comprehensive health education program and empowers children with knowledge and skills to make healthy food and beverage choices. 2-8
US students receive less than 8 hours of required nutrition education each school year, 9 far below the 40 to 50 hours that are needed to affect behavior change. 10,11 Additionally, the percentage of schools providing required instruction on nutrition and dietary behaviors decreased from 84.6% to 74.1% between 2000 and 2014. 9
Given the important role that diet plays in preventing chronic diseases and supporting good health, schools would ideally provide students with more hours of nutrition education instruction and engage teachers and parents in nutrition education activities. 5, 12 Research shows that nutrition education can teach students to recognize how healthy diet influences emotional well-being and how emotions may influence eating habits. However, because schools face many demands, school staff can consider ways to add nutrition education into the existing schedule. 11
Nutrition education can be incorporated throughout the school day and in various locations within a school. This provides flexibility allowing schools to use strategies that work with their settings, daily schedule, and resources.
In the Classroom
Nutrition education can take place in the classroom, either through a stand-alone health education class or combined into other subjects including 2,5 :
- Counting with pictures of fruits and vegetables.
- Learning fractions by measuring ingredients for a recipe.
- Examining how plants grow.
- Learning about cultural food traditions.
Nutrition education should align with the National Health Education Standards and incorporate the characteristics of an effective health education curriculum .

Farm to School
Farm-to-school programs vary in each school or district, but often include one or more of the following strategies:
- Purchasing and serving local or regionally produced foods in the school meal programs.
- Educating students about agriculture, food, health, and nutrition.
- Engaging students in hands-on learning opportunities through gardening, cooking lessons, or farm field trips.
Students who participate in farm-to-school activities have increased knowledge about nutrition and agriculture, are more willing to try new foods, and consume more fruits and vegetables. 14-17

School Gardens
School garden programs can increase students’ nutrition knowledge, willingness to try fruit and vegetables, and positive attitudes about fruits and vegetables. 18-22 School gardens vary in size and purpose. Schools may have window sill gardens, raised beds, greenhouses, or planted fields.
Students can prepare the soil for the garden, plant seeds, harvest the fruits and vegetables, and taste the food from the garden. Produce from school gardens can be incorporated into school meals or taste tests. Classroom teachers can teach lessons in math, science, history, and language arts using the school garden.

In the Cafeteria
Cafeterias are learning labs where students are exposed to new foods through the school meal program, see what balanced meals look like, and may be encouraged to try new foods through verbal prompts from school nutrition staff, 23 or taste tests. 24-25 Cafeterias may also be decorated with nutrition promotion posters or student artwork promoting healthy eating. 24
Other Opportunities
Schools can add messages about nutrition and healthy eating into the following:
- Morning announcements.
- School assemblies.
- Materials sent home to parents and guardians. 24
- Staff meetings.
- Parent-teacher group meetings.
These strategies can help reinforce messages about good nutrition and help ensure that students see and hear consistent information about healthy eating across the school campus and at home. 2
Shared use agreements can extend healthy eating learning opportunities. As an example, an after-school STEM club could gain access to school gardens as learning labs.
CDC Parents for Healthy Schools: Ideas for Parents
Nutrition: Gardening Interventions | The Community Guide
Dietary Guidelines for Americans, 2020–2025
Introduction to School Gardens
Learning Through the Garden
National Farm-to-School Network
National Farm to School Network Resource Database
National Health Education Standards
Team Nutrition Curricula
USDA Farm to School
USDA Team Nutrition
- Centers for Disease Control and Prevention. School health guidelines to promote healthy eating and physical activity. MMWR Morb Mortal Wkly Rep . 2011;60(RR-5):1–76.
- Joint Committee on National Health Education Standards. National Health Education Standards: Achieving Excellence. 2nd ed. Atlanta, GA: American Cancer Society; 2007.
- Centers for Disease Control and Prevention. Health Education Curriculum Analysis Tool, 2012, Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services; 2012. Available at http://www.cdc.gov/healthyyouth/hecat/index.htm. Accessed April 9, 2019.
- Price C, Cohen D, Pribis P, Cerami J. Nutrition education and body mass index in grades K–12: a systematic review. J Sch Health. 2017;87:715–720.
- Meiklejohn S, Ryan L, Palermo C. A systematic review of the impact of multi-strategy nutrition education programs on health and nutrition of adolescents. J Nutr Educ Behav . 2016;48:631–646.
- Silveira JA, Taddei JA, Guerra PH, Nobre MR. The effect of participation in school-based nutrition education interventions on body mass index: A meta-analysis of randomized controlled community trials. Prev Med . 2013;56:237–243.
- County Health Rankings and Roadmaps. School-based Nutrition Education Programs website. http://www.countyhealthrankings.org/take-action-to-improve-health/what-works-for-health/policies/school-based-nutrition-education-programs . Accessed on April 9, 2019.
- Results from the School Health Policies and Practices Study 2014 . Atlanta, GA: Centers for Disease Control and Prevention; 2014.
- Connell DB, Turner RR, Mason EF. Results of the school health education evaluation: health promotion effectiveness, implementation, and costs . J Sch Health . 1985;55(8):316–321.
- Institute of Medicine. Nutrition Education in the K–12 Curriculum: The Role of National Standards: Workshop Summary. Washington, DC: The National Academies Press; 2014.
- Murimi MW, Moyeda-Carabaza AF, Nguyen B, Saha S, Amin R, Njike V. Factors that contribute to effective nutrition education interventions in children: a systematic review. Nutr Rev . 2018;76(8):553–580.
- Hayes D, Contento IR, Weekly C. Position of the American Dietetic Association, School Nutrition Association, and Society for Nutrition Education: comprehensive school nutrition services. J Acad Nutr Diet . 2018; 118:913–919.
- Joshi A, Misako Azuma A, Feenstra G. Do farm-to-school programs make a difference? Findings and future research needs . J Hunger Environ Nutr . 2008;3:229–246.
- Moss A, Smith S, Null D, Long Roth S, Tragoudas U. Farm to school and nutrition education: Positively affecting elementary school-aged children’s nutrition knowledge and consumption behavior. Child Obes . 2013;9(1):51–6.
- Bontrager Yoder AB, Liebhart JL, McCarty DJ, Meinen A, Schoeller D, Vargas C, LaRowe T. Farm to elementary school programming increases access to fruits and vegetables and increases their consumption among those with low intake . J Nutr Educ Behav . 2014;46(5):341–9.
- The National Farm to School Network. The Benefits of Farm to School website. http://www.farmtoschool.org/Resources/BenefitsFactSheet.pdf . Accessed on June 14, 2019.
- Berezowitz CK, Bontrager Yoder AB, Schoeller DA. School gardens enhance academic performance and dietary outcomes in children. J Sch Health . 2015;85:508–518.
- Davis JN, Spaniol MR, Somerset S. Sustenance and sustainability: maximizing the impact of school gardens on health outcomes. Public Health Nutr . 2014;18(13):2358–2367.
- Langellotto GA, Gupta A. Gardening increases vegetable consumption in school-aged children: A meta-analytical synthesis. Horttechnology . 2012;22(4):430–445.
- Community Preventative Services Task Force. Nutrition: Gardening Interventions to Increase Fruit and Vegetable Consumption Among Children. Finding and Rationale Statement .. https://www.thecommunityguide.org/sites/default/files/assets/Nutrition-Gardening-Fruit-Vegetable-Consumption-Children-508.pdf . Accessed on May 16, 2019.
- Savoie-Roskos MR, Wengreen H, Durward C. Increasing Fruit and Vegetable Intake among Children and Youth through Gardening-Based Interventions: A Systematic Review. Journal of the Academy of Nutrition and Dietetics 2017;11(2):240–50.
- Schwartz M. The influence of a verbal prompt on school lunch fruit consumption: a pilot study. Int J Behav Nutr Phys Act. 2007;4:6.
- Fulkerson JA, French SA, Story M, Nelson H, Hannan PJ. Promotions to increase lower-fat food choices among students in secondary schools: description and outcomes of TACOS (Trying Alternative Cafeteria Options in Schools). Public Health Nutr. 2003 ;7(5):665–674.
- Action for Healthy Kids. Tips for Hosting a Successful Taste Test website. http://www.actionforhealthykids.org/tools-for-schools/find-challenges/classroom-challenges/701-tips-for-hosting-a-successful-taste-test . Accessed on May 19, 2019.

Healthy Youth
To receive email updates about this page, enter your email address:

Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Appointments at Mayo Clinic
- Nutrition and healthy eating
- Nutrition basics
- Healthy diets
- Healthy cooking
- Healthy menus and shopping strategies
- Nutritional supplements
Do you feel like you can't keep up with the latest nutrition news because it's always changing? It's true that knowledge about nutrition and diet evolves over time. But there are some nutrition basics that can help you sort through the latest research and advice.
Nutrition basics come down to eating wholesome foods that support your health.
Want to go beyond the basics? Talk to a healthcare professional, such as a dietitian. You can ask for diet advice that takes into account your health, lifestyle and food preferences.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- 2020-2025 Dietary Guidelines for Americans. U.S. Department of Health and Human Services and U.S. Department of Agriculture. https://www.dietaryguidelines.gov. Accessed June 13, 2023.
- Zeratsky KA (expert opinion). Mayo Clinic. June 21, 2023.
- Hensrud DD, ed. Add 5 habits. In: The Mayo Clinic Diet. 3rd ed. Mayo Clinic Press; 2023.
- Dietary supplements: What you need to know. Office of Dietary Supplements. https://ods.od.nih.gov/factsheets/WYNTK-Consumer/ Accessed June 13, 2023.
- Vitamins, minerals and supplements: Do you need to take them? Academy of Nutrition and Dietetics. https://www.eatright.org/health/essential-nutrients/supplements/vitamins-minerals-and-supplements-do-you-need-to-take-them. Accessed June 22, 2023.
Products and Services
- Available Health Products from Mayo Clinic Store
- A Book: Cook Smart, Eat Well
- Nutritional Supplements at Mayo Clinic Store
- A Book: The Mayo Clinic Diet Bundle
- The Mayo Clinic Diet Online
- A Book: Mayo Clinic on High Blood Pressure
- A Book: Live Younger Longer
- Newsletter: Mayo Clinic Health Letter — Digital Edition
- A Book: Mayo Clinic Book of Home Remedies
- A Book: Mayo Clinic Family Health Book, 5th Edition
- A Book: Mayo Clinic on Digestive Health
- Health foods
- Antioxidants
- Alcohol use
- Alkaline water
- Artificial sweeteners and other sugar substitutes
- Autism spectrum disorder and digestive symptoms
- Breastfeeding nutrition: Tips for moms
- Butter vs. margarine
- Caffeine content
- Caffeine: How much is too much?
- Is caffeine dehydrating?
- Timing calcium supplements
- Calorie calculator
- COVID-19 and vitamin D
- Can vitamins help prevent a heart attack?
- Can whole-grain foods lower blood pressure?
- Can zinc supplements help treat hidradenitis suppurativa?
- Carbohydrates
- Chart of high-fiber foods
- Cholesterol: Top foods to improve your numbers
- Clear liquid diet
- Coconut water: Is it super hydrating?
- Coffee and health
- Cuts of beef
- DASH diet: Recommended servings
- Sample DASH menus
- Diet soda: How much is too much?
- Dietary fats
- Dietary fiber
- Diverticulitis attack triggers
- Diverticulitis diet
- Vitamin C and mood
- Prickly pear cactus
- Does soy really affect breast cancer risk?
- Don't get tricked by these 3 heart-health myths
- Eggs and cholesterol
- Enlarged prostate: Does diet play a role?
- Fasting diet: Can it improve my heart health?
- Fiber supplements
- Ground flaxseed
- Food safety
- Foodborne illness
- Gluten sensitivity and psoriasis: What's the connection?
- Gluten-free diet
- Gout diet: What's allowed, what's not
- Grass-fed beef
- Guide to herbs and spices
- Healthy meals start with planning
- Heartburn medicines and B-12 deficiency
- High-protein diets
- How to track saturated fat
- Intermittent fasting
- Is there a special diet for Crohn's disease?
- Low-fiber diet
- Low-glycemic index diet
- Meatless meals
- Mediterranean diet
- Menus for heart-healthy eating
- Moldy cheese
- Monosodium glutamate (MSG)
- Multivitamins for kids
- Nuts and your heart: Eating nuts for heart health
- Omega-3 in fish
- Omega-6 fatty acids
- Organic foods
- Phenylalanine
- Picnic Problems: High Sodium
- Portion control
- Prenatal vitamins
- Probiotics and prebiotics
- Safely reheat leftovers
- Sea salt vs. table salt
- Taurine in energy drinks
- Nutrition and pain
- Vitamin C megadoses
- Underweight: Add pounds healthfully
- Vegetarian diet
- Vitamin D and MS: Any connection?
- Vitamin D deficiency
- Can a lack of vitamin D cause high blood pressure?
- Vitamin D for babies
- Vitamin D toxicity
- Vitamins for MS: Do supplements make a difference?
- Water after meals
- Daily water requirement
- What is BPA?
- Whole grains
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.

Healthy Food Choices in Schools
3 Ways Nutrition Influences Student Learning Potential and School Performance

Advocates of child health have experimented with students’ diets in the United States for more than twenty years. Initial studies focused on benefits of improving the health of students are apparent. Likewise, improved nutrition has the potential to positively influence students’ academic performance and behavior.
Though researchers are still working to definitively prove the link, existing data suggests that with better nutrition students are better able to learn, students have fewer absences, and students’ behavior improves, causing fewer disruptions in the classroom. [1]
Improve Nutrition to Increase Brain Function
Several studies show that nutritional status can directly affect mental capacity among school-aged children. For example, iron deficiency, even in early stages, can decrease dopamine transmission, thus negatively impacting cognition. [2] Deficiencies in other vitamins and minerals, specifically thiamine, vitamin E, vitamin B, iodine, and zinc, are shown to inhibit cognitive abilities and mental concentration. [3] Additionally, amino acid and carbohydrate supplementation can improve perception, intuition, and reasoning. [4] There are also a number of studies showing that improvements in nutrient intake can influence the cognitive ability and intelligence levels of school-aged children. [5]
Provide a Balanced Diet for Better Behaviors and Learning Environments
Good Nutrition helps students show up at school prepared to learn. Because improvements in nutrition make students healthier, students are likely to have fewer absences and attend class more frequently. Studies show that malnutrition leads to behavior problems [6] , and that sugar has a negative impact on child behavior. [7] However, these effects can be counteracted when children consume a balanced diet that includes protein, fat, complex carbohydrates, and fiber. Thus students will have more time in class, and students will have fewer interruptions in learning over the course of the school year. Additionally, students’ behavior may improve and cause fewer disruptions in the classroom, creating a better learning environment for each student in the class.
Promote Diet Quality for Positive School Outcomes
Sociologists and economists have looked more closely at the impact of a student’s diet and nutrition on academic and behavioral outcomes. Researchers generally find that a higher quality diet is associated with better performance on exams, [8] and that programs focused on increasing students’ health also show modest improvements in students’ academic test scores. [9] Other studies find that improving the quality of students’ diets leads to students being on task more often, increases math test scores, possibly increases reading test scores, and increases attendance. [10] Additionally, eliminating the sale of soft drinks in vending machines in schools and replacing them with other drinks had a positive effect on behavioral outcomes such as tardiness and disciplinary referrals. [11]
Every student has the potential to do well in school. Failing to provide good nutrition puts them at risk for missing out on meeting that potential. However, taking action today to provide healthier choices in schools can help to set students up for a successful future full of possibilities.
Contributor
David Just Phd- Cornell Center for Behavioral Economics in Child Nutrition Programs
[1] Sorhaindo, A., & Feinstein, L. (2006). What is the relationship between child nutrition and school outcomes. Wider Benefits of Learning Research Report No.18. Centre for Research on the Wider Benefits of Learning
[2] Pollitt E. (1993). Iron deficiency and cognitive function. Annual Review of Nutrition, 13, 521–537.
[3] Chenoweth, W. (2007). Vitamin B complex deficiency and excess. In R. Kliegman, H. Jenson, R. Behrman, & B. Stanton (Eds.), Nelson Textbook of Pediatrics, 18 th edition . Philadelphia: Saunders.
Greenbaum, L. (2007a). Vitamin E deficiency. In R. Kliegman, H. Jenson, R. Behrman, & B. Stanton (Eds.), Nelson Textbook of Pediatrics, 18 th Edition . Philadelphia: Saunders.
Greenbaum, L. (2007b). Micronutrient mineral deficiencies. In R. Kliegman, H. Jenson, R. Behrman, & B. Stanton (Eds.), Nelson Textbook of Pediatrics, 18 th Edition . Philadelphia: Saunders.
Bryan, J., Osendarp, S., Hughes, D., Calvaresi, E., Baghurst, K. & van Klinken, J. (2004). Nutrients for cognitive development in school-aged children. Nutrition Reviews, 62 (8), 295–306.
Delange, F. (2000) The role of iodine in brain development. Proceedings of the Nutrition Society, 59 , 75–79. Sandstead, H. (2000). Causes of iron and zinc deficiencies and their effects on brain. Journal of Nutrition, 130 , 347–349.
[4] Lieberman, H. (2003). Nutrition, brain function, and cognitive performance. Appetite, 40, 245–254.
Frisvold, D. (2012). Nutrition and cognitive achievement: An evaluation of the school breakfast program. Working Paper, Emory University.
[5] Benton, D. & Roberts, G. (1988). Effect of vitamin and mineral supplementation on intelligence in a sample of schoolchildren. The Lancet, 1, 140–143.
Schoenthaler, S., Amos, S., Doraz, W., Kelly, M., & Wakefield, J. (1991). Controlled trial of vitamin – mineral supplementation on intelligence and brain function. Personality and Individual Differences, 12, 343–350.
Benton, D. & Buts, J. (1990). Vitamins/mineral supplementation and intelligence. The Lancet, 335, 1158–1160.
Nelson, M. (1992) Vitamin and mineral supplementation and academic performance in schoolchildren. Proceedings of the Nutrition Society, 51, 303–313.
Eysenck, H., & Schoenthaler, S. (1997). Raising IQ level by vitamin and mineral supplementation. In R. Sternberg and E. Grigorenko (Eds.), Intelligence, heredity and environment (pp. 363 – 392). Cambridge: Cambridge University Press.
[6] Kleinman, R., Murphy, J., Little, M., Pagano, M., Wehler, C., Regal, K., & Jellinek, M. (1998) Hunger in children in the United States: Potential behavioral and emotional correlates. Pediatrics, 101(1), e3.
[7] Jones, T., Borg, W., Boulware, S., McCarthy, G., Sherwin, R., Tamborlane, W. (1995). Enhanced adrenomedullary response and increased susceptibility to neuroglygopenia: Mechanisms underlying the adverse effect of sugar ingestion in children. Journal of Pediatrics, 126, 171–177.
[8] Florence, M., Asbridge, M., & Veugelers, P. (2008). Diet quality and academic performance. Journal of School Health, 78, 209–215.
[9] Meyers, A., Sampson, A., Wietzman, M., Rogers, B., & Kayne, H. (1989). School breakfast program and school performance. American Journal of Diseases of Children, 143, 1234–1239.
Kleinman, R., Murphy, J., Little, M., Pagano, M., Wehler, C., Regal, K., & Jellinek, M. (1998) Hunger in children in the United States: Potential behavioral and emotional correlates. Pediatrics, 101(1), e3.
[10] Powell, C., Walker, S., Chang, S., & Grantham-McGregor, S. (1998). Nutrition and education: A randomized trial of the effects of breakfast in rural primary school children. American Journal of Clinical Nutrition, 68, 873–879.
Cueto, S. (2001). Breakfast and dietary balance: The enKid study. Public Health Nutrition, 4, 1429–1431.
Storey, H., Pearce, J., Ashfield-Watt, P., Wood, L., Baines, E., & Nelson, M. (2011). A randomized controlled trial of the effect of school food and dining room modifications on classroom behaviour in secondary school children. European Journal of Clinical Nutrition, 65, 32–38.
Hollar, D., Messiah, S., Lopez-Mitnik, G., Hollar, T., Almon, M., & Agatston, A. (2010). Effect of a two-year obesity prevention intervention on percentile changes in body mass index and academic performance in low income elementary school children. American Journal of Public Health, 100(4), 646–653.
[11] Price, J. (2012). De-fizzing schools: The effect on student behavior of having vending machines in schools. Agricultural and Resource Economics Review, 41(1), 92–99.
What you need to know about education for health and well-being
Why focus on education for health and well-being.
Children and young people who receive a good quality education are more likely to be healthy, and likewise those who are healthy are better able to learn.
Globally, learners face a range of challenges that stand in the way of their education, their schooling and their futures. A few of these are related to their health and well-being. Estimates show that some 246 million learners experience violence in and around school every year and 73 million children live in extreme poverty, food insecurity and hunger. Pregnancy related complications are the leading cause of death among girls aged 15-19, and the COVID-19 pandemic has vividly highlighted the unmet needs of learners and their mental health.
UNESCO works to promote the physical and mental health and well-being of learners. By reducing health-related barriers to learning, such as gender inequality, HIV and other sexually transmitted infections (STIs), early and unintended pregnancy, violence and discrimination, and malnutrition, UNESCO, governments and school systems can pose serious threats to the well-being of learners, and to the completion of all learners’ education.
Why is health and well-being key for learners?
The link between education to health and well-being is clear. Education develops the skills, values and attitudes that enable learners to lead healthy and fulfilled lives, make informed decisions, and engage in positive relationships with everyone around them. Poor health can have a detrimental effect on school attendance and academic performance. Health-promoting schools that are safe and inclusive for all children and young people are essential for learning.
Statistics show that higher levels of education among mothers improve children’s nutrition and vaccination rates, while reducing preventable child deaths, maternal mortality and HIV infections. Maternal deaths would be reduced by two thirds, saving 98,000 lives, if all girls completed primary education. There would be two‑thirds fewer child marriages, and an increase in modern contraceptive use, if all girls completed secondary education.
At UNESCO, education for health and well-being refers to resilient, health-promoting education systems that integrate school health and well-being as a fundamental part of their daily mission. Only then will our learners be prepared to thrive, to learn and to build healthy, peaceful and sustainable futures for all.
- The relevance and contributions of education for health and well-being to the advancement of human rights, sustainable development & peace: thematic paper , UNESCO, 2022
How is UNESCO advancing learners’ health and well-being for school and life?
UNESCO has a long-standing commitment to improve health and education outcomes for learners. Guided by the UNESCO Strategy on Education for Health and Well-Being, UNESCO envisions a world where learners thrive and works across three priority areas to ensure all learners are empowered through:
- school systems that promote their physical and mental health and well-being
- quality, gender-transformative comprehensive sexuality education that includes HIV, life skills, family and rights
- safe and inclusive learning environments free from all forms of violence, bullying, stigma and discrimination
Through its unique expertise, wide network and a range of strategic partnerships, UNESCO supports tailored interventions in formal educational settings at regional and country levels, with a focus on adolescents. Key areas of actions include: technical guidance at global levels, and targeted and holistic action at national levels such as the Our Rights, Our Lives, Our Future (O3) programme; joint efforts through the Global Partnership Forum for comprehensive sexuality education and the School-related gender-based violence working group ; guidance on school health and nutrition; advocacy around the International Day against violence and bullying at school ; capacity-building and knowledge generation such as the Health and education resource centre .
UNESCO aims to make health education appropriate and relevant for different age groups including young learners and adolescents, thus working closely with young people and youth networks. It identifies adolescence (ages 10-19) as ‘a critical window of opportunity to invest in education, skills and competencies; with benefits for well-being now, into future adult life, and for the next generation’ and a time when schools should impart healthy habits that will empower adolescents to become healthy citizens. Young People Today is an initiative aiming to improve the health and well-being of young people in the Eastern and Southern Africa region.
Why is comprehensive sexuality education key for learners’ health and well-being?
Comprehensive sexuality education (CSE) is widely recognised as a key intervention to advance gender equality, healthy relationships and sexual and reproductive health, all of which have been shown to positively improve education and health outcomes.
At UNESCO, CSE is a curriculum-based process of teaching and learning about the cognitive, emotional, physical and social aspects of sexuality. It offers life-saving knowledge and develops the values, skills and behaviours young people need to make informed choices for their health and well-being while promoting respect for human rights, gender equality and diversity. CSE empowers learners to realize their health, well-being and dignity, develop respectful relationships and understand their sexual and health rights throughout their lives. Effective CSE is delivered in an age-appropriate manner.
Without correct knowledge on sexual and reproductive health, learners face risks directly impacting their education and future. For example, early and unintended pregnancy increases the risk of absenteeism, poor academic attainment and early drop-out from school for girls, while also having educational implications for young fathers.
Through its O3 flagship programme, UNESCO contributes to the health and well-being of young people in Africa with a view to reducing new HIV infections, early and unintended pregnancy, gender-based violence, and child and early marriage. The O3 programme has benefitted over 28 million learners so far and has introduced ‘O3Plus’, focusing on actions in favour of young people in tertiary education.
UNESCO’s Foundation for Life and Love campaign (#CSEandMe) aims to highlight the benefits of good quality CSE for all young people. Because CSE is about relationships, gender, puberty, consent, and sexual and reproductive health, for all young people.
Why is UNESCO building back healthy and resilient schools?
As the education of 1.6 billion learners came to a halt as a result of the unprecedented COVID-19 global health pandemic, the world became witness to the crucial importance of schools as lifelines for learners’ health and well-being. Schools are a social safety net providing essential health education and services including meals, identifying signs of mistreatment or violence, establishing links to health services, fostering social connections and promoting physical activity. And without this safety net, millions of learners were at risk.
For example, early and forced marriage and unintended adolescent pregnancy rose during the pandemic and lockdown periods. This resulted in more dropouts from school, leaving learners and girls in particular out of school. The pandemic vividly illustrated the interlinkages between education and health, and the urgent need to work across sectors to advance the interests of future generations, building back resilient education systems to prevent, prepare for and respond to health crises. It also highlighted learners’ unmet need for support around their mental health.
Learner mental health and well-being is an integral part of UNESCO’s work on health education and the promotion of safe and inclusive learning environments. UNESCO joined with UNICEF and the WHO to launch a Technical Advisory Group of experts to advise educational institutions on ensuring schools respond appropriately to crises like the COVID-19 pandemic.
Related items
- Health education
- Nutrition education
- Topics: hea
- See more add

- Submit Member Login
Login to your account
If you don't remember your password, you can reset it by entering your email address and clicking the Reset Password button. You will then receive an email that contains a secure link for resetting your password
If the address matches a valid account an email will be sent to __email__ with instructions for resetting your password
Current Issue Links
- Articles in Press
- Past Issues
- Supplement: SNEB 2023 International Conference Proceedings
Submit Mobile
- Submit article Opens in new window
- Call For Papers
- Article Collections
- Submit Article Opens in new window
- Aims and Scope
- For Authors
- Supports Open Access Opens in new window
- Society Membership Opens in new window
- Journal Club Opens in new window
- Facebook Opens in new window
- YouTube Opens in new window
- LinkedIn Opens in new window
Featured This Month

SNAP Student Rules Are Not So Snappy: Lessons Learned From a Qualitative Study of California County Agency Workers

The Influence of the School Neighborhood Food Retail Environment on Unhealthy Food Purchasing Behaviors Among Adolescents: A Systematic Review

Call for Papers: Learn more about our current calls for papers

Professional benefits of being a Reviewer
- Current Issue
Participant Insights From a Family-based Meal Kit Delivery Intervention
A Qualitative Study of Breastfeeding Experiences Among Mothers Who Used Galactagogues to Increase Their Milk Supply
Learning What Works: A Mixed-Methods Study of American Self-identified Food Conservers
Associations between subjective social status and health behaviors among college students, in the news, press release.
Confusing Assistance Requirements Contribute to Food Insecurity Among College Students

Suzanna M. Martinez, PhD, MS, University of California San Francisco, highlights a new study that illustrates how challenging SNAP rules are for college students and those involved in their implementation. The research supports simplifying the student SNAP process to increase participation for eligible students, especially for historically minoritized racial and ethnic groups and low-income students for whom equitable access to SNAP benefits is critical.
Read the Article
Household Food Waste Reduced Through Whole-Family Food Literacy Intervention

How can parents and kids work together to reduce household food waste? Amar Laila, PhD, University of Guelph, discusses the feasibility, acceptability, and effectiveness of a new pilot study of Weeknight Supper Savers, a whole-family food literacy intervention that teaches how to prepare, store, and eat leftovers. The tool successfully encouraged families to prepare meals together and reduced food waste.
Participants in School-Based Gardening and Food Programs Benefit From Lasting Impacts on Dietary Behaviors

Christine St. Pierre, MPH, RD, presents the results of a new study to determine the impact on dietary behaviors on current and former elementary school students who participated in FRESHFARM FoodPrints’ school-based gardening and food education classes over the past 15 years. Analysis revealed how this early learning positively influenced food decisions as children grew older, extending into adulthood.
Poor Diet Quality During Adolescence Is Linked to Serious Health Risks

- New Resources

Volume 55, Issue 1 – Slow Cooked: An Unexpected Life in Food Politics by Marion Nestle reviewed by Dr. Jennifer Wilkins, Cornell University. For the full review see this issue .

Volume 54, Issue 12 – Quick recap of the review of The Vitamins: Fundamental Aspects in Nutrition and Health by Dr. Kritika Gupta, Center for Research Evaluation, the University of Mississippi, reviews. For the full review see this issue .

Volume 54, Issue 11 – Quick recap of the review of Motivational Interviewing in Nutrition and Fitness with Dr. Mateja R. Savoie-Roskos. For the full review see this issue .
Online First
Perceived impacts of urban gardens and peer nutritional counseling for people living with hiv in the dominican republic.
School Nutrition Stakeholders Find Utility in MealSim : An Agent-Based Model
A qualitative study of the meaning of food and religious identity.
NEFPAT Plus: A Valid and Reliable Tool for Assessing the Nutrition Environment in Food Pantries
Journal of nutrition education and behavior.
The Journal of Nutrition Education and Behavior ( JNEB ), the official peer-reviewed journal of the Society for Nutrition Education and Behavior Opens in new window , since 1969, serves as a global resource to advance nutrition education and behavior related research, practice, and policy. JNEB publishes original research, as well as papers focused on emerging issues, policies and practices broadly related to nutrition education and behavior. These topics include, but are not limited to, nutrition education interventions; theoretical interpretation of behavior; epidemiology of nutrition and health; food systems; food assistance programs; nutrition and behavior assessment; and public health nutrition.

The Society for Nutrition Education and Behavior (SNEB) Opens in new window represents the unique professional interests of nutrition educators in the United States and worldwide. SNEB is dedicated to promoting effective nutrition education and communication to support and improve healthful behaviors and has a vision of healthy communities through nutrition education and advocacy. SNEB provides forums for sharing innovative strategies for nutrition education, expressing a range of views on important issues, and disseminating research findings. Members of SNEB educate individuals, families, fellow professionals, and students, and influence policy makers about nutrition, food, and health.
- More Journal Metrics Opens in new window
- Submit a Manuscript Opens in new window
- Top Social Media Articles
- Time to Online Publication Opens in new window
Most Read (Last 30 Days)
Hierarchy of Food Needs
- Ellyn Satter
Participant Perspectives on the Impact of a School-Based, Experiential Food Education Program Across Childhood, Adolescence, and Young Adulthood
Most cited (previous 3 years).
- Access for Developing Countries
- Articles & Issues
- Articles In Press
- List of Issues
- Supplements
- Author Guidelines
- Submit Your Manuscript
- Statistical Methods
- Guidelines for Authors of Educational Material Reviews
- Permission to Reuse
- About Open Access
- Researcher Academy
- For Reviewers
- General Guidelines
- Methods Paper Guidelines
- Qualitative Guidelines
- Quantitative Guidelines
- Questionnaire Methods Guidelines
- Statistical Methods Guidelines
- Systematic Review Guidelines
- Perspective Guidelines
- GEM Reviewing Guidelines
- Journal Info
- About the Journal
- Disclosures
- Abstracting/Indexing
- Impact/Metrics
- Contact Information
- Editorial Staff and Board
- Info for Advertisers
- Member Access Instructions
- New Content Alerts
- Sponsored Supplements
- Statistical Reviewers
- Reviewer Appreciation
- New Resources for Nutrition Educators
- Submit New Resources for Review
- Guidelines for Writing Reviews of New Resources for Nutrition Educators
- Podcast/Webinars
- New Resources Podcasts
- Press Release & Other Podcasts
- Collections
- Society News
The content on this site is intended for healthcare professionals.
- Privacy Policy
- Terms and Conditions
- Accessibility
- Help & Contact

Nutrition and Healthy Eating
Goal: improve health by promoting healthy eating and making nutritious foods available..

Many people in the United States don’t eat a healthy diet. Healthy People 2030 focuses on helping people get the recommended amounts of healthy foods — like fruits, vegetables, and whole grains — to reduce their risk for chronic diseases and improve their health. 1 The Nutrition and Healthy Eating objectives also aim to help people get recommended amounts of key nutrients, like calcium and potassium.
People who eat too many unhealthy foods — like foods high in saturated fat and added sugars — are at increased risk for obesity, heart disease, type 2 diabetes, and other health problems. Strategies and interventions to help people choose healthy foods can help reduce their risk of chronic diseases and improve their overall health.
Some people don’t have the information they need to choose healthy foods. Other people don’t have access to healthy foods or can’t afford to buy enough food. Public health interventions that focus on helping everyone get healthy foods are key to reducing food insecurity and hunger and improving health.
Objective Status
Learn more about objective types
Related Objectives
The following is a sample of objectives related to this topic. Some objectives may include population data.
Nutrition and Healthy Eating — General
Adolescents.
- Heart Disease and Stroke
Overweight and Obesity
Other topics you may be interested in.
U.S. Department of Health and Human Services and U.S. Department of Agriculture. (2015). 2015-2020 Dietary Guidelines for Americans. Retrieved from https://health.gov/our-work/food-nutrition/2015-2020-dietary-guidelines/guidelines/
The Office of Disease Prevention and Health Promotion (ODPHP) cannot attest to the accuracy of a non-federal website.
Linking to a non-federal website does not constitute an endorsement by ODPHP or any of its employees of the sponsors or the information and products presented on the website.
You will be subject to the destination website's privacy policy when you follow the link.

Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Basic Nutrition
Printable Materials and Handouts
Find printable handouts and fact sheets that can be used for health fairs, classes, and other food or nutrition-related events.
Cook up something new in your kitchen with these healthy, delicious recipes.
View four tips to help you save money when food shopping and help the environment.
View printable brochures and handouts with healthy eating tips based on the Dietary Guidelines for Americans, 2020-2025 , including:
- Build a Healthy Eating Routine
- Cut Down on Added Sugars
Browse the MyPlate collection of printable tip sheets and resources. These materials are in the public domain.
Want your kids to learn how to build a healthy meal? Use these clever activity sheets to find ideas and tips!
View this fact sheet with nutrition tips for breastfeeding moms.
View printable materials about food safety, including guides, activity books, and tip sheets.
View lessons, workshops, activities, and curricula for teachers. Topics include food, nutrition, physical activity, and food safety.
Use this checklist to track healthy eating and exercise habits throughout your day!
View tips for building healthy eating habits in infants, toddlers, and preschoolers. This fact sheet is available in 13 languages.
Printable fact sheets for living with and managing diabetes.
FDA’s Center for Food Safety and Applied Nutrition developed “Everyday Food Safety” resources to increase food safety awareness among young adults ages 18 – 29. Check out the materials available to use in your classroom, health expo, waiting room, or website.
The U.S. Food and Drug Administration (FDA) has updated the Nutrition Facts label on packaged foods and beverages with a new design, making it easier to make informed choices towards healthy eating habits.
This one-page handout highlights the key changes being made to the new Nutrition Facts Label.
Share these tips to reduce food waste, save money, and protect the environment.
Browse handouts and recipes for the Dietary Approaches to Stop Hypertension (DASH) Diet. Topics include getting more potassium, staying on track, and meal tracking for different calorie levels.
Looking for materials about healthy aging for older adults? Download or order these free handouts and booklets on exercise, nutrition, and other health topics.
View science-based fact sheets and handouts for health fairs and community events.
The Sisters Together program encourages Black women ages 18 and older to reach and maintain a healthy weight. Learn how to bring the program to your community.
Download, print,or order a free copy of this brochure on eating disorders. Also available in Spanish.
Access vitamin and mineral supplement fact sheets for the consumer or health professional. Available in PDF format, and in Spanish.
Find handouts that teach how to build a healthy eating routine, cut down on added sugars, cut down on sodium, and cut down on saturated fat.
Print and share these fact sheets and posters to help people learn key recommendations from the Physical Activity Guidelines. Find materials for adults, older adults, parents and kids, and during and after pregnancy.
Browse by health topic or resource type to find 1-page printable fact sheets written at the 6th- to 8th-grade reading level in English or Spanish.
Challenge yourself to eating fruits and vegetables in new ways by following along to this 30-day calendar.
What are healthy cooking methods, and what equipment do you need for each method? Read this handout to find out.
Use this 31-day calendar to challenge yourself to one choice for a healthy weight each day.
View a table of spices to learn about their flavors and uses.
Use this handout to measure your hunger level on a scale of 1 to 10.
Find handouts to help you manage your weight with healthy eating and physical activity.
Use this handout to plan weekly meals and create a grocery list.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

The relationship between education and health: reducing disparities through a contextual approach
Anna zajacova.
Western University
Elizabeth M. Lawrence
University of North Carolina
Adults with higher educational attainment live healthier and longer lives compared to their less educated peers. The disparities are large and widening. We posit that understanding the educational and macro-level contexts in which this association occurs is key to reducing health disparities and improving population health. In this paper, we briefly review and critically assess the current state of research on the relationship between education and health in the United States. We then outline three directions for further research: We extend the conceptualization of education beyond attainment and demonstrate the centrality of the schooling process to health; We highlight the dual role of education a driver of opportunity but also a reproducer of inequality; We explain the central role of specific historical socio-political contexts in which the education-health association is embedded. This research agenda can inform policies and effective interventions to reduce health disparities and improve health of all Americans.
URGENT NEED FOR NEW DIRECTIONS IN EDUCATION-HEALTH RESEARCH
Americans have worse health than people in other high-income countries, and have been falling further behind in recent decades ( 137 ). This is partially due to the large health inequalities and poor health of adults with low education ( 84 ). Understanding the health benefits of education is thus integral to reducing health disparities and improving the well-being of 21 st century populations. Despite tremendous prior research, critical questions about the education-health relationship remain unanswered, in part because education and health are intertwined over the lifespans within and across generations and are inextricably embedded in the broader social context.
We posit that to effectively inform future educational and heath policy, we need to capture education ‘in action’ as it generates and constrains opportunity during the early lifespans of today’s cohorts. First, we need to expand our operationalization of education beyond attainment to consider the long-term educational process that precedes the attainment and its effect on health. Second, we need to re-conceptualize education as not only a vehicle for social success, valuable resources, and good health, but also as an institution that reproduces inequality across generations. And third, we argue that investigators need to bring historical, social and policy contexts into the heart of analyses: how does the education-health association vary across place and time, and how do political forces influence that variation?
During the past several generations, education has become the principal pathway to financial security, stable employment, and social success ( 8 ). At the same time, American youth have experienced increasingly unequal educational opportunities that depend on the schools they attend, the neighborhoods they live in, the color of their skin, and the financial resources of their family. The decline in manufacturing and rise of globalization have eroded the middle class, while the increasing returns to higher education magnified the economic gaps among working adults and families ( 107 ). In addition to these dramatic structural changes, policies that protected the welfare of vulnerable groups have been gradually eroded or dismantled ( 129 ). Together, these changes triggered a precipitous growth of economic and social inequalities in the American society ( 17 ; 106 ).
Unsurprisingly, health disparities grew hand in hand with the socio-economic inequalities. Although the average health of the US population improved over the past decades ( 67 ; 85 ), the gains largely went to the most educated groups. Inequalities in health ( 53 ; 77 ; 99 ) and mortality ( 86 ; 115 ) increased steadily, to a point where we now see an unprecedented pattern: health and longevity are deteriorating among those with less education ( 92 ; 99 ; 121 ; 143 ). With the current focus of the media, policymakers, and the public on the worrisome health patterns among less-educated Americans ( 28 ; 29 ), as well as the growing recognition of the importance of education for health ( 84 ), research on the health returns to education is at a critical juncture. A comprehensive research program is needed to understand how education and health are related, in order to identify effective points of intervention to improve population health and reduce disparities.
The article is organized in two parts. First, we review the current state of research on the relationship between education and health. In broad strokes, we summarize the theoretical and empirical foundations of the education-health relationship and critically assess the literature on the mechanisms and causal influence of education on health. In the second part, we highlight gaps in extant research and propose new directions for innovative research that will fill these gaps. The enormous breadth of the literature on education and health necessarily limits the scope of the review in terms of place and time; we focus on the United States and on findings generated during the rapid expansion of the education-health research in the past 10–15 years. The terms “education” and “schooling” are used interchangeably. Unless we state otherwise, both refer to attained education, whether measured in completed years or credentials. For references, we include prior review articles where available, seminal papers, and recent studies as the best starting points for further reading.
THE ASSOCIATION BETWEEN EDUCATION AND HEALTH
Conceptual toolbox for examining the association.
Researchers have generally drawn from three broad theoretical perspectives to hypothesize the relationship between education and health. Much of the education-health research over the past two decades has been grounded in the Fundamental Cause Theory ( 75 ). The FCT posits that social factors such as education are ‘fundamental’ causes of health and disease because they determine access to a multitude of material and non-material resources such as income, safe neighborhoods, or healthier lifestyles, all of which protect or enhance health. The multiplicity of pathways means that even as some mechanisms change or become less important, other mechanisms will continue to channel the fundamental dis/advantages into differential health ( 48 ). The Human Capital Theory (HCT), borrowed from econometrics, conceptualizes education as an investment that yields returns via increased productivity ( 12 ). Education improves individuals’ knowledge, skills, reasoning, effectiveness, and a broad range of other abilities, which can be utilized to produce health ( 93 ). The third approach, the Signaling or Credentialing perspective ( 34 ; 125 ) has been used to explain the observed large discontinuities in health at 12 or 16 years of schooling, typically associated with the receipt of a high school and college degrees, respectively. This perspective views earned credentials as a potent signal about one’s skills and abilities, and emphasizes the economic and social returns to such signals. Thus all three perspectives postulate a causal relationship between education and health and identify numerous mechanisms through which education influences health. The HCT specifies the mechanisms as embodied skills and abilities, FCT emphasizes the dynamism and flexibility of mechanisms, and credentialism identifies social responses to educational attainment. All three theoretical approaches, however, operationalize the complex process of schooling solely in terms of attainment and thus do not focus on differences in educational quality, type, or other institutional factors that might independently influence health. They also focus on individual-level factors: individual attainment, attainment effects, and mechanisms, and leave out the social context in which the education and health processes are embedded.
Observed associations between education and health
Empirically, hundreds of studies have documented “the gradient” whereby more schooling is linked with better health and longer life. A seminal 1973 book by Kitagawa and Hauser powerfully described large differences in mortality by education in the United States ( 71 ), a finding that has since been corroborated in numerous studies ( 31 ; 42 ; 46 ; 109 ; 124 ). In the following decades, nearly all health outcomes were also found strongly patterned by education. Less educated adults report worse general health ( 94 ; 141 ), more chronic conditions ( 68 ; 108 ), and more functional limitations and disability ( 118 ; 119 ; 130 ; 143 ). Objective measures of health, such as biological risk levels, are similarly correlated with educational attainment ( 35 ; 90 ; 140 ), showing that the gradient is not a function of differential reporting or knowledge.
The gradient is evident in men and women ( 139 ) and among all race/ethnic groups ( 36 ). However, meaningful group differences exist ( 60 ; 62 ; 91 ). In particular, education appears to have stronger health effects for women than men ( 111 ) and stronger effects for non-Hispanic whites than minority adults ( 134 ; 135 ) even if the differences are modest for some health outcomes ( 36 ). The observed variations may reflect systematic social differences in the educational process such as quality of schooling, content, or institutional type, as well as different returns to educational attainment in the labor market across population groups ( 26 ). At the same time, the groups share a common macro-level social context, which may underlie the gradient observed for all.
To illustrate the gradient, we analyzed 2002–2016 waves of the National Health Interview Survey (NHIS) data from adults aged 25–64. Figure 1 shows the levels of three health outcomes across educational attainment levels in six major demographic groups predicted at age 45. Three observations are noteworthy. First, the gradient is evident for all outcomes and in all race/ethnic/gender groups. Self-rated health exemplifies the staggering magnitude of the inequalities: White men and women without a high school diploma have about 57% chance of reporting fair or poor health, compared to just 9% for college graduates. Second, there are major group differences as well, both in the predicted levels of health problems, as well as in the education effects. The latter are not necessarily visible in the figures but the education effects are stronger for women and weaker for non-white adults as prior studies showed (table with regression model results underlying the prior statement is available from the authors). Third, an intriguing exception pertains to adults with “some college,” whose health is similar to high school graduates’ in health outcomes other than general health, despite their investment in and exposure to postsecondary education. We discuss this anomaly below.

Predicted Probability of Health Problems
Source: 2002–2016 NHIS Survey, Adults Age 25–64
Pathways through which education impacts health
What explains the improved health and longevity of more educated adults? The most prominent mediating mechanisms can be grouped into four categories: economic, health-behavioral, social-psychological, and access to health care. Education leads to better, more stable jobs that pay higher income and allow families to accumulate wealth that can be used to improve health ( 93 ). The economic factors are an important link between schooling and health, estimated to account for about 30% of the correlation ( 36 ). Health behaviors are undoubtedly an important proximal determinant of health but they only explain a part of the effect of schooling on health: adults with less education are more likely to smoke, have an unhealthy diet, and lack exercise ( 37 ; 73 ; 105 ; 117 ). Social-psychological pathways include successful long-term marriages and other sources of social support to help cope with stressors and daily hassles ( 128 ; 131 ). Interestingly, access to health care, while important to individual and population health overall, has a modest role in explaining health inequalities by education ( 61 ; 112 ; 133 ), highlighting the need to look upstream beyond the health care system toward social factors that underlie social disparities in health. Beyond these four groups of mechanisms that have received the most attention by investigators, many others have been examined, such as stress, cognitive and noncognitive skills, or environmental exposures ( 11 ; 43 ). Several excellent reviews further discuss mechanisms ( 2 ; 36 ; 66 ; 70 ; 93 ).
Causal interpretation of the education-health association
A burgeoning number of studies used innovative approaches such as natural experiments and twin design to test whether and how education causally affects health. These analyses are essential because recommendations for educational policies, programs, and interventions seeking to improve population health hinge on the causal impact of schooling on health outcomes. Overall, this literature shows that attainment, measured mostly in completed years of schooling, has a causal impact on health across numerous (though not all) contexts and outcomes.
Natural experiments take advantage of external changes that affect attainment but are unrelated to health, such as compulsory education reforms that raise the minimum years of schooling within a given population. A seminal 2005 study focused on increases in compulsory education between 1915 and 1939 across US states and found that a year of schooling reduced mortality by 3.6% ( 78 ). A re-analysis of the data indicated that taking into account state-level mortality trends rendered the mortality effects null but it also identified a significant and large causal effect on general health ( 88 ). A recent study of a large sample of older Americans reported a similar pattern: a substantial causal effect of education for self-rated health but not for mortality ( 47 ). School reform studies outside the US have reported compelling ( 122 ) or modest but significant ( 32 ) effects of schooling on health, although some studies have found nonsignificant ( 4 ), or even negative effects ( 7 ) for a range of health outcomes.
Twin design studies compare the health of twins with different levels of education. This design minimizes the influence of family resources and genetic differences in skills and health, especially for monozygotic twins, and thus serves to isolate the effect of schooling. In the US, studies using this design generated robust evidence of a causal effect of education on self-rated health ( 79 ), although some research has identified only modest ( 49 ) or not significant ( 3 ; 55 ) effects for other physical and mental health outcomes. Studies drawing on the large twin samples outside of the US have similarly found strong causal effects for mortality ( 80 ) and health ( 14 ; 16 ; 51 ) but again some analyses yielded no causal effects on health ( 13 ; 83 ) or health behaviors ( 14 ). Beyond our brief overview, readers may wish consult additional comprehensive reviews of the causal studies ( 40 ; 45 ; 89 ).
The causal studies add valuable evidence that educational attainment impacts adult health and mortality, even considering some limitations to their internal validity ( 15 ; 88 ). To improve population health and reduce health disparities, however, they should be viewed as a starting point to further research. First, the findings do not show how to improve the quality of schooling or its quantity for in the aggregate population, or how to overcome systematic intergenerational and social differences in educational opportunities. Second, their findings do take into account contexts and conditions in which educational attainment might be particularly important for health. In fact, the variability in the findings may be attributable to the stark differences in contexts across the studies, which include countries characterized by different political systems, different population groups, and birth cohorts ranging from the late 19 th to late 20 th centuries that were exposed to education at very different stages of the educational expansion process ( 9 ).
TOWARD A SOCIALLY-EMBEDDED UNDERSTANDING OF THE EDUCATION-HEALTH RELATIONSHIP
To date, the extensive research we briefly reviewed above has identified substantial health benefits of educational attainment in most contexts in today’s high-income countries. Still, many important questions remain unanswered. We outline three critical directions to gain a deeper understanding of the education-health relationship with particular relevance for policy development. All three directions shift the education-health paradigm to consider how education and health are embedded in life course and social contexts.
First, nearly universally, the education-health literature conceptualizes and operationalizes education in terms of attainment, as years of schooling or completed credentials. However, attainment is only the endpoint, although undoubtedly important, of an extended and extensive process of formal schooling, where institutional quality, type, content, peers, teachers, and many other individual, institutional, and interpersonal factors shape lifecourse trajectories of schooling and health. Understanding the role of the schooling process in health outcome is relevant for policy because it can show whether interventions should be aimed at increasing attainment, or whether it is more important to increase quality, change content, or otherwise improve the educational process at earlier stages for maximum health returns. Second, most studies have implicitly or explicitly treated educational attainment as an exogenous starting point, a driver of opportunities in adulthood. However, education also functions to reproduce inequality across generations. The explicit recognition of the dual function of education is critical to developing education policies that would avoid unintended consequence of increasing inequalities. And third, the review above indicates substantial variation in the education-health association across different historical and social contexts. Education and health are inextricably embedded in these contexts and analyses should therefore include them as fundamental influences on the education-health association. Research on contextual variation has the potential to identify contextual characteristics and even specific policies that exacerbate or reduce educational disparities in health.
We illustrate the key conceptual components of future research into the education-health relationship in Figure 2 . Important intergenerational and individual socio-demographic factors shape educational opportunities and educational trajectories, which are directly related to and captured in measures of educational attainment. This longitudinal and life course process culminates in educational disparities in adult health and mortality. Importantly, the macro-level context underlies every step of this process, shaping each of the concepts and their relationships.

Enriching the conceptualization of educational attainment
In most studies of the education-health associations, educational attainment is modeled using years of schooling, typically specified as a continuous covariate, effectively constraining each additional year to have the same impact. A growing body of research has substituted earned credentials for years. Few studies, however, have considered how the impact of additional schooling is likely to differ across the educational attainment spectrum. For example, one additional year of education compared to zero years may be life-changing by imparting basic literacy and numeracy skills. The completion of 14 rather than 13 years (without the completion of associated degree) could be associated with better health through the accumulation of additional knowledge and skills as well, or perhaps could be without health returns, if it is associated with poor grades, stigma linked to dropping out of college, or accumulated debt ( 63 ; 76 ). Examining the functional form of the education-health association can shed light on how and why education is beneficial for health ( 70 ). For instance, studies found that mortality gradually declines with years of schooling at low levels of educational attainment, with large discontinuities at high school and college degree attainment ( 56 ; 98 ). Such findings can point to the importance of completing a degree, not just increasing the quantity (years) of education. Examining mortality, however, implicitly focused on cohorts who went to school 50–60 years ago, within very different educational and social contexts. For findings relevant to current education policies, we need to focus on examining more recent birth cohorts.
A particularly provocative and noteworthy aspect of the functional form is the attainment group often identified as “some college:” adults who attended college but did not graduate with a four-year degree. Postsecondary educational experiences are increasingly central to the lives of American adults ( 27 ) and college completion has become the minimum requirement for entry into middle class ( 65 ; 87 ). Among high school graduates, over 70% enroll in college ( 22 ) but the majority never earn a four-year degree ( 113 ). In fact,, the largest education-attainment group among non-elderly US adults comprises the 54 million adults (29% of total) with some college or associate’s degree ( 113 ). However, as in Figure 1 , this group often defies the standard gradient in health. Several recent studies have found that the health returns to their postsecondary investments are marginal at best ( 110 ; 123 ; 142 ; 144 ). This finding should spur new research to understand the outcomes of this large population group, and to glean insights into the health returns to the postsecondary schooling process. For instance, in the absence of earning a degree, is greater exposure to college education in terms of semesters or earned credits associated with better health or not? How do the returns to postsecondary schooling differ across the heterogeneous institutions ranging from selective 4-year to for-profit community colleges? How does accumulated college debt influence both dropout and later health? Can we identify circumstances under which some college education is beneficial for health? Understanding the health outcomes for this attainment group can shed light on the aspects of education that are most important for improving health.
A related point pertains to the reliability and validity of self-reported educational attainment. If a respondent reports 16 completed years of education, for example, are they carefully counting the number of years of enrollment, or is 16 shorthand for “completed college”? And, is 16 years the best indicator of college completion in the current context when the median time to earn a four-year degree exceeds 5 years ( 30 )? And, is longer time in college given a degree beneficial for health or does it signify delayed or disrupted educational pathways linked to weaker health benefits ( 132 )? How should we measure part-time enrollment? As studies begin to adjudicate between the health effects of years versus credentials ( 74 ) in the changing landscape of increasingly ‘nontraditional’ pathways through college ( 132 ), this measurement work will be necessary for unbiased and meaningful analyses. An in-depth understanding may necessitate primary data collection and qualitative studies. A feasible direction available with existing data such as the National Longitudinal Survey of Youth 1997 (NLSY97) is to assess earned college credits and grades rather than years of education beyond high school.
As indicated in Figure 2 , beyond a more in-depth usage of the attainment information, we argue that more effective conceptualization of the education-health relationship as a developmental life course process will lead to important findings. For instance, two studies published in 2016 used the NLSY97 data to model how gradual increases in education predict within-individual changes in health ( 39 ; 81 ). Both research teams found that gradual accumulation of schooling quantity over time was not associated with gradual improvements in health. The investigators interpreted the null findings as an absence of causal effects of education on health, especially once they included important confounders (defined as cognitive and noncognitive skills and social background). Alternatively, perhaps the within-individual models did not register health because education is a long-term, developing trajectory that cannot be reduced to point-in-time changes in exposure. Criticisms about the technical aspects of theses studies notwithstanding ( 59 ), we believe that these studies and others like them, which wrestle with the question of how to capture education as a long-term process grounded in the broader social context, and how this process is linked to adult health, are desirable and necessary.
Education as (re)producer of inequality
The predominant theoretical framework for studying education and health focuses on how education increases skills, improves problem-solving, enhances employment prospects, and thus opens access to other resources. In sociology, however, education is viewed not (only) as increasing human capital but as a “sieve more than a ladder” ( 126 ), an institution that reproduces inequality across generations ( 54 ; 65 ; 103 ; 114 ). The mechanisms of the reproduction of inequality are multifarious, encompassing systematic differences in school resources, quality of instruction, academic opportunities, peer influences, or teacher expectations ( 54 ; 114 ; 132 ). The dual role of education, both engendering and constraining social opportunities, has been recognized from the discipline’s inception ( 52 ) and has remained the dominant perspective in sociology of education ( 18 ; 126 ). Health disparities research, which has largely dismissed the this perspective as “specious” ( 93 ), could benefit from pivoting toward this complex sociological paradigm.
As demonstrated in Figure 2 , parental SES and other background characteristics are key social determinants that set the stage for one’s educational experiences ( 20 ; 120 ). These characteristics, however, shape not just attainment, but the entire educational and social trajectories that drive and result in particular attainment ( 21 ; 69 ). Their effects range from the differential quality and experiences in daycare or preschool settings ( 6 ), K-12 education ( 24 ; 136 ), as well as postsecondary schooling ( 5 ; 127 ). As a result of systematically different experiences of schooling over the early life course stratified by parental SES, children of low educated parents are unlikely to complete higher education: over half of individuals with college degrees by age 24 came from families in the top quartile of family income compared to just 10% in the bottom quartile ( 23 ).
Unfortunately, prior research has generally operationalized the differences in educational opportunities as confounders of the education-health association or as “selection bias” to be statistically controlled, or best as a moderating influence ( 10 ; 19 ). Rather than remove the important life course effects from the equation, studies that seek to understand how educational and health differences unfold over the life course, and even across generations could yield greater insight ( 50 ; 70 ). A life course, multigenerational approach can provide important recommendations for interventions seeking to avoid the unintended consequence of increasing disparities. Insofar as socially advantaged individuals are generally better positioned to take advantage of interventions, research findings can be used to ensure that policies and programs result in decreasing, rather than unintentionally widening, educational and health disparities.
Education and health in social context
Finally, perhaps the most important and policy-relevant emerging direction to improving our understanding of the education-health relationship is to view both as inextricably embedded within the broad social context. As we highlight in Figure 2 , this context underlies every feature of the development of educational disparities in health. In contrast to the voluminous literature focusing on individual-level schooling and health, there has been a “startling lack of attention to the social/political/economic context” in which the relationships are grounded ( 33 ). By context, we mean the structure of a society that varies across time and place, encompassing all major institutions, policy environments, as well as gender, race/ethnicity, age, and socioeconomic stratification. Under what circumstances, conditions, and policies are the associations between education and health stronger or weaker?
Within the United States, the most relevant units of geo-political boundaries generating distinct policy contexts are states, although smaller geographic units are also pertinent ( 44 ; 100 ). Since the 1980s, the federal government has devolved an increasing range of key socioeconomic, political, and health-care decisions to states. This decentralization has resulted in increasing diversity across states in conditions for a healthy life ( 96 ; 101 ). A recent study demonstrates how different environments across US states yield vastly different health returns to education ( 100 ). State-level characteristics had little impact on adults with high education, whose disability levels were similarly low regardless of their state of residence. In contrast, disability levels of low-educated adults were not only high but also varied substantially across states: disability was particularly high in states that have invested less in the social welfare of its residents, such as Mississippi, Kentucky, and West Virginia. Highly-educated adults, particularly white adults and men who can convert education into other resources most readily, use personal resources to protect their health like a ‘personal firewall’ ( 97 ). Their less-educated peers, meanwhile, are vulnerable without social safety nets. Demonstrating the potential for informing policy in this area, the findings directly identify state policies that influence the extent to which educational attainment matters for health and longevity. These include economic policies including state income tax structures and education expenditures per capita, as well as policies influencing social cohesion in a state, such as income inequality and unemployment rates. Beyond the US, investigators can leverage differences in political systems across countries to assess the impact of different welfare regimes on the education-health associations, as some European researchers began generating ( 41 ; 82 ).
Similar to variation across geo-political boundaries, research on variation across time can highlight policies and conditions that mitigate or inflate health disparities. How has the education-health association changed over time? In recent decades, the association has become increasingly strong, with widening disparities in health outcomes across education ( 53 ; 77 ; 86 ; 116 ; 143 ). These increases started in the 1980s ( 17 ) at the same time that social inequality began rising with the political embrace of pro-market neoliberal policies ( 33 ). Since then, the United States has been increasingly marked by plummeting economic wellbeing (except for the wealthiest Americans), growing economic segregation, emerging mass incarceration, downward social mobility, and despair in many working-class communities ( 17 ; 95 ; 129 ). Conversely, in the two decades prior (1960s and 70s), social disparities in health were decreasing ( 1 ; 72 ). During those decades, many pro-social policies such as Civil rights legislation, War on Poverty programs, and racial desegregation were improving social inequalities. Macro-level political forces, clearly, can influence not only social but also health inequalities ( 104 ). Two facts follow: growing disparities are not inevitable and changes in the education-health relationship may be strongly linked to social policies. While some of the growth in educational inequalities may be attributable to changes in educational composition of the population with increasingly negatively select groups of adults at the lowest levels of schooling, these compositional changes likely play only a minor role in the overall trends ( 38 ; 58 ). Linking education and health to the broader social context brings to the forefront the ways in which we, as individuals and a collective society, produce and maintain health disparities.
Implications for Policy and Practice
Reducing macro-level inequalities in health will require macro-level interventions. Technological progress and educational expansion over the past several decades have not decreased disparities; on the contrary, educational disparities in health and mortality have grown in the US. Moreover, the consistent, durable relationship between education and health and the multitude of mechanisms linking them suggests that programs targeting individual behaviors will have limited impact to counteract disparities. Thus, we argue that future findings from the new research directions proposed here can be used to intervene at the level of social contexts to alter educational trajectories from an early age, with the ultimate goal of reducing health disparities. We note two promising avenues for policy development.
One potential solution may focus on universal federal and state-level investment in the education and well-being of children early in the life course to disrupt the reproduction of social inequalities and change subsequent educational trajectories. Several experimental early-education programs such as the Perry Preschool Project and Carolina Abecedarian Project have demonstrated substantial, lasting, and wide-ranging benefits, including improved adult health ( 25 ; 57 ; 102 ). These programs provided intensive, exceptionally high-quality, and diverse services to children, and it is these characteristics that appear central to their success ( 138 ). Further research on the qualitative and social dimensions of education and their effects on health can inform future model educational programs and interventions across all ages.
Another important issue for both researchers and policymakers pertains to postsecondary enrollment and attrition, and their effects on health. Educational expansion in the college-for-all era has yielded high post-secondary enrollment, but also unacceptable dropout rates with multiple detrimental consequences, including high rates of student debt ( 64 ) and stigma ( 76 ), which may negatively affect health. Emerging studies found that college dropouts fail to benefit from their postsecondary investments. Next we need to understand under what circumstances college goers do reap health benefits, or how their postsecondary experience can be modified to improve their health.
For both of these avenues, effective implementation will need further research on the specific institutional characteristics and social contexts that shape the schooling effects. However, in designing interventions and policies, we need to be aware of the dual role of education as a drive and reproducer of inequality. Individuals from advantaged backgrounds may be better positioned to take advantage of new educational opportunities, and thus any interventions and programs need to ensure that marginalized populations have equal or greater access in order to avoid the unintended consequence of further intensifying disparities. Finally, researchers and policymakers should engage in a dialogue such that researchers effectively communicate their insights and recommendations to policymakers, and policymakers convey the needs and challenges of their practices to researchers.
Education and health are central to individual and population well-being. They are also inextricably embedded in the social context and structure. Future research needs to expand beyond the individual-focused analyses and hypothesize upstream ( 96 ), taking a contextual approach to understanding education and health. Such an approach will require interdisciplinary collaborations, innovations in conceptual models, and rich data sources. The three directions for further research on health returns to education we outlined above can help generate findings that will inform effective educational and health policies and interventions to reduce disparities. During this critical time when health differences are widening and less educated Americans are experiencing social and health declines, research and policy has the opportunity to make a difference and improve the health and well-being of our population.
Contributor Information
Anna Zajacova, Western University.
Elizabeth M. Lawrence, University of North Carolina.
- Skip to main content
- Skip to FDA Search
- Skip to in this section menu
- Skip to footer links

The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
U.S. Food and Drug Administration
- Search
- Menu
- Food Labeling & Nutrition
Nutrition Education Resources & Materials
Resources on the importance of good nutrition.
The Nutrition Facts Label

The Nutrition Facts label reflects current scientific information, including the link between diet and chronic diseases such as obesity and heart disease. The label makes it easier for you and your audience to make more informed food choices.
Learn about What’s on the Nutrition Facts Label , including details on: Calories, Serving Sizes, Added Sugars, and Percent Daily Value.
Industry members, read more about the changes to the Nutrition Facts label requirements .
More on the Nutrition Facts Label
How to Understand and Use the Nutrition Facts Label Learn how to use this information more effectively and easily.

Interactive Nutrition Facts Label An interactive way to learn about the Nutrition Facts label and discover the wealth of information it contains.
For Educators
Health Educator’s Nutrition Toolkit Teach your audience how to use the Nutrition Facts label and to make informed choices.

"Behind the Label” with FDA Information for Educators View this video for health educators that explains the changes to the Nutrition Facts label.
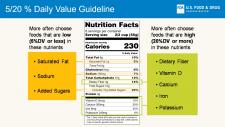
For Youth & Youth Educators
Read the Label Use these hands-on materials to challenge kids and families to look for and use the Nutrition Facts label.
Science and Our Food Supply | Curriculum for Middle/High School Teachers Introduce students to the fundamentals of informed food choices with this nutrition-based curriculum.

Whyville Snack Shack Games Kids can play two fun games that test their knowledge about using the Nutrition Facts label to make healthy snack choices.

For Older Adults
A How-To Guide for Older Adults Good nutrition can help older adults feel their best and stay strong. It can also help lower the risk of developing some health conditions that are common among older adults.

For Physicians & Healthcare Professionals
Physicians' Continuing Medical Education Program Resources for talking to patients about using the Nutrition Facts label to make healthy food choices.

Pediatricians' Continuing Medical Education Program Resources for talking to parents and patients about using the Nutrition Facts label to make healthy food choices.

More on Labeling
Gluten-Free Labeling Learn how gluten-free labeling can help your audience manage health and dietary intake — especially those with celiac disease.

Calories on the Menu | Menu Labeling Information Find out how calorie labeling on menus can help your community make informed and healthful decisions about meals and snacks.

Sodium | Look at the Label Learn the basics on sodium’s health effects, how-to’s for using the Nutrition Facts label to reduce sodium intake, and more.

Using the Nutrition Facts Label to Choose Milk and Plant-Based Beverages Use the Nutrition Facts Label to compare the nutrient content of different products to help you make the best choices for you and your family when choosing milk and plant-based beverages.

CFSAN Education Resource Library
FDA's Center for Food Safety and Applied Nutrition (CFSAN) has a wealth of nutrition education materials.
Consumers, educators, teachers, dietitians, and health professionals are invited to explore CFSAN’s Education Resource Library – a catalog of downloadable and printable materials and videos on nutrition (including labeling and dietary supplements), food safety, and cosmetics.
Education Newsletter
Get regular FDA email updates delivered on this topic to your inbox.

WIC is changing in 2024. Here's what to expect

Serhii - stock.adobe.com
WIC provides nutritious foods, nutrition education, and health care referrals to more than 6 million women, infants, and children who are at nutritional risk. The program’s latest revisions will strengthen WIC food packages to better align with the science-based recommendations of the latest Dietary Guidelines for Americans and the National Academies of Sciences, Engineering, and Medicine.
What is WIC?
The Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) is a federal nutrition program that currently provides food, nutrition education, and healthcare referrals for millions of families in the US.
WIC is one of the most effective programs for improving access to nutritious foods with over 6 million women, infants, and children participating in the program.
“WIC has a half-century track record of caring for young families. USDA and the Biden-Harris Administration are committed to ensuring that moms, babies, and young children continue to thrive through WIC,” said Secretary of Agriculture Tom Vilsack in a press release.
How is WIC changing?
On April 9, 2024, the USDA finalized a rule that will update and strengthen WIC food packages to better align with the latest science-based recommendations of both the 2020-2025 Dietary Guidelines for Americans and the National Academies of Sciences, Engineering, and Medicine.
More fruits and vegetables
WIC participants will see a permanent increase in the overall benefits value that will allow more purchases of fruits and vegetables, and an expanded variety available for purchase. The revisions will make permanent the widely praised $15-$36 increase in fruits and vegetables allowance (depending on package type) that have been temporarily available to participants since October 2021.
Higher fruit and vegetable issuance to WIC participants is critical for improving health outcomes and closing nutrition gaps. Nationwide, nearly 90 percent of toddlers consume less than the recommended intake of vegetables, and about 40 percent consume less than the recommended intake of fruit. Pregnant and lactating people, on average, consume less than the recommended intake of total fruits and vegetables. When analyzing WIC-eligible populations, NASEM found that 100 percent of postpartum women, 99 percent of children, and 99 percent of pregnant women fall short of DGA-recommended vegetable intake.
More whole grains
Now, 75 percent of approved cereals will list a whole grain as the first ingredient; for reference, the DGA recommends that at least half of the grains consumed in a day are whole grains . Participants will soon be able to choose from a wider variety of grains, including quinoa, wild rice, millet, triticale, amaranth, kamut, sorghum, wheat berries, tortillas with folic acid-fortified corn masa flour, corn meal (including blue), teff, buckwheat, and whole wheat pita, English muffins, bagels, and naan, allowing for culturally relevant choices and increased options for those with food sensitivities (like wheat allergy or celiac disease) that were not previously available.
Introducing whole grains during childhood is critical as whole grain consumption boosts intake of priority nutrients like fiber and iron and is associated with reduced risk of cardiovascular disease, type 2 diabetes, and other chronic diseases.
Changes to dairy options
The new USDA rule allows only unflavored milk, and will, for the first time, set added sugars limits for yogurt and soy beverages. Participants will also have access to lactose-free options, and the new revision will allow flexibility on package sizes and non-dairy substitution options (like plant-based yogurt and cheese).
Wider variety of proteins
Canned fish will now be included in some WIC packages without a reduction in other proteins, like legumes or peanut butter.
Seafood is an important source of protein and other nutrients like iron, choline, omega-3 fatty acids, calcium, and vitamin D that are a priority for the WIC population. The 2020 DGAs emphasized the benefits of seafood consumption for pregnant and breastfeeding women, noting the potential benefits to a child’s cognitive development. Women who are pregnant generally eat less than the recommended amount of seafood , while lactating women are generally in the lower range of recommendations. The USDA’s new rule will greatly expand access to seafood.
Flexibility for cultural or dietary preferences
Canned beans will also be made available to WIC participants, who were previously offered only dried beans and legumes. Beans, lentils, chickpeas, and other pulses are high in protein, fiber, minerals, and vitamins and low in fat. Eating beans and lentils as part of a healthy diet can help prevent chronic diseases , and expanded options make more plant-based proteins available to meet participants’ cultural or dietary preferences.
This will help millions of women, infants, and children participating in the program get the nutrition they need while maintaining participant choice honoring cultural food preferences, and helping address barriers like limited cooking facilities, storage, and transportation.
CSPI supports healthy kids and nutrition security
The Center for Science in the Public Interest is a leading voice in healthy kids’ policies and programs, including healthier school foods , expanded healthy meal access , improvements to SNAP and WIC , safety reforms for infant formula and children’s foods, better restaurant meals for children , better enforcement of laws about marketing food products to children , and expanded fresh food options at common retailers like Dollar General .
“Unlike other nutrition programs, WIC has a very specific charge to supplement the diets of women, infants, and children who are at nutritional risk. These changes to the food packages will make it easier for moms to get the nutrition they need and build healthy habits for life for their babies and children participating in WIC. We applaud the USDA today for doing right by moms and kids,” says CSPI Campaign Manager of Federal Child Nutrition Programs Meghan Maroney.

How you can help
“Nutrition security,” or access to nutritious foods, does not yet have a standardized definition or measurement. Developing a way to track nutrition security and report on access to nutritious food in the Supplemental Nutrition Assistance Program (SNAP) can strengthen support for programs that provide fruit and vegetable incentives to people who shop with SNAP benefits and help us understand how to improve health and food access for people participating in the program.
Support our effort to define and improve nutrition security:
Tell Congress to support nutrition for people with low incomes
- Healthy Kids
- Healthy Eating

Stirring the Pot
Join the fight for safer, healthier food
Sign up to receive action alerts and opportunities to support our work in Stirring the Pot, our monthly newsletter roundup.
- Open access
- Published: 11 April 2024
Perception of faculty in the community health sciences colleges towards simulation-based education in clinical nutrition undergraduate practical courses
- Iman Abdullah Bindayel ORCID: orcid.org/0000-0001-5452-115X 1 &
- Shahad Ahmed Alahmad ORCID: orcid.org/0009-0006-9339-2518 1
BMC Medical Education volume 24 , Article number: 402 ( 2024 ) Cite this article
Metrics details
Simulation now is widely used for training and education in different fields including healthcare education. Medicine and healthcare students can be trained in a secure, efficient, and engaging setting by Simulation-based Education (SBE). Therefore, this study aimed to assess the perception of faculty members in the community health departments towards SBE to be used in practical subjects for clinical nutrition undergraduate courses.
This cross-sectional survey was conducted among community health sciences faculty members. The perception was assessed using a self-administered questionnaire that included three sections.
This questionnaire was completed by 125 faculty members, of whom 36 (28.8%) were male and 89 (71.2%) were female. Overall, faculty members had positive perceptions, with a mean score of 3.86 ± 0.74, but a high level of anxiety toward SBE, with a mean score of 3.42 ± 0.75. There was a statistically significant difference between the responses of the faculty members based on the training they received in simulation ( P = 0.001).
The study results indicate that community health sciences faculty members’ perception of SBE in Saudi Arabia is generally positive. However, the results show high levels of anxiety among faculty members toward SBE.
Peer Review reports
Medicine and healthcare students can be trained in a secure, efficient, and engaging setting thanks to Simulation-based Education (SBE) [ 1 ]. A training or educational technique known as SBE uses guided experiences to supplement or replace real-world experience [ 2 ]. It is defined as an educational strategy based on learning theories rather than technology [ 1 ]. Simulation aims to interactively recreate elements of the real world so that learners can fully immerse themselves in the learning environment [ 2 , 3 ]. Simulators have long been used in aviation and the military to train employees in technical skills and safety-related attitudes (such as teamwork and communication) [ 4 ]. There are various simulation techniques available [ 5 ]. The most prevalent techniques are role-playing, standardized or simulated patients, computerized mannequins, and virtual simulations [ 5 ]. SBE has been the subject of extensive study and research for over two decades [ 5 ]. A significant portion of the undergraduate curriculum now includes simulation in the healthcare sciences as an evidence-based, efficient learning tool [ 5 ].
Simulation in medical healthcare practice and education has been applied since the early twentieth century [ 6 , 7 ]. Unlike simulation in medicine, nursing, and other healthcare sectors, simulation in nutrition and dietetics began to see the light in the late 70s [ 8 ]. Most of the research was conducted in the United States. In 1979, The University of Connecticut used simulation exercises for interview training in dietetics to develop counseling and interviewing skills for the students [ 8 ]. In the same year, Syracuse University applied a course in the first semester of the junior year, which involved a simulated team conference for nursing and dietetics students to educate them about the healthcare team [ 9 ]. In 1981, at The University of Pennsylvania, the students watched videotaped simulated interviews to learn counseling and communication skills in the nutrition course [ 10 ]. In the mid-80s, The University of Pittsburgh used simulation interviews to evaluate students` clinical skills for nutrition counseling [ 11 ]. This evaluation aimed to assess graduate students` clinical skills to resolve issues with dietary adherence [ 11 ]. During the same period, The University of Kentucky developed a learning technique for senior dietetics students to prepare them for the future [ 12 ]. This learning activity included scenarios and simulation games where the students selected a career choice and discussed the options created by the scenarios [ 12 ]. In the late 80s, The University of Nebraska provided a nutrition workshop for 30 managers of government-sponsored nutrition centers for the elderly in different areas of the country [ 13 ]. The workshop involved videotaped simulations of typical nutritional issues experienced by older adults in these centers [ 13 ]. As an outcome, the knowledge increased, and 75% of the managers benefited and applied the ideas from the workshop [ 13 ]. In the 1990s, the research surrounding simulation in nutrition and dietetics began to appear and continued to increase until today [ 14 ]. Furthermore, the interest and demand for simulation in medical education have increased due to its advantages, including providing safe and effective patient care, reducing medical errors, experiential learning, deliberate practice, transformative learning, and debriefing techniques [ 15 ]. Despite that, simulation application in nutrition and dietetics is underexplored compared with other medical fields where simulation has been practiced for decades [ 14 ].
A systematic review published in 2019 and included fourteen studies about simulation in dietetics demonstrated that using simulated patients was essential for building and developing counseling skills and readiness for practice [ 16 ]. Moreover, simulated patients could be used to assess counseling skills in Objective Structured Clinical Examination (OSCE) exams [ 16 ]. Since the decision-making in dietetics depends on evidence-based practice, the development and application of evaluation methods are needed to support the evidence base for simulation skill acquisition in dietetics education [ 16 ]. Eventually, further research about simulation in dietetics and nutrition is needed to determine the skills likely to be developed and enhanced by simulation [ 16 ].
There are only a few studies in the last five years that were published about the use of simulation in nutrition and dietetics training or education worldwide [ 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 ]. As is the case worldwide, to the best of our knowledge, only a few studies were done in Saudi Arabia about the perception towards simulation in education, either among faculty members or students in health colleges [ 1 , 26 ]. Consequently, as far as we know, this is the first study in Saudi Arabia that assessed faculty perception towards SBE in the community health sciences departments. It is suggested that the use of simulation in education will improve students` self-esteem, skills, critical thinking, teamwork, essential procedural skills, and decision-making, likewise increasing patients` safety and reducing medical errors [ 15 ]. Based on the MedTeams study, simulation practice decreased medical errors by 26.5% [ 27 ]. Moreover, most studies about simulation and nutrition published in the last ten years were conducted among students, athletes, and the general population. Thus, this study aimed to assess faculty members` perception in the community health departments towards SBE to be used in practical subjects for clinical nutrition undergraduate courses, to identify faculty members’ perceived barriers toward the integration of SBE, and to fill the gap regarding SBE in nutrition.
Study setting
This is a cross-sectional survey in which Saudi universities that provided a Clinical Nutrition program in Saudi Arabia were targeted during the last semester of the academic year 2022–2023. The study surveyed faculty members from the Colleges of Applied Medical Sciences (CAMS) in 16 universities. Universities that are included in this study are King Saud University, King Saud bin Abdulaziz University for Health Sciences, Princess Nourah bint Abdulrahman University, Umm Al-Qura University, King Abdulaziz University, King Faisal University, Qassim University, Taibah University, University of Hail, Jazan University, Al Baha University, Northern Borders University, Imam Abdulrahman Bin Faisal University, University of Hafr al Batin, University of Tabuk, and Shaqra University.
Faculty were invited via university email to fill out a self-administered questionnaire. Social media platforms such as LinkedIn, WhatsApp, and Twitter were used to distribute the questionnaire among faculty using a snowball sampling technique. The study will identify the universities by pseudonym, as well as, the anonymity of the participants to ensure confidentiality.
In this cross-sectional survey, faculty members from different universities in Saudi Arabia were approached. Faculty members from both genders who have taught clinical nutrition practical subjects and who have had at least two years of experience in their academic work were included. Faculty members who had never taught clinical nutrition practical subjects were excluded. Furthermore, the exclusion criteria included newly employed faculty members.
G*Power 3 [ 28 ] was used to determine the sample size that will allow for the assessment of meaningful associations and the detection of effect sizes (small, medium, or large). Using the one-way ANOVA test and an alpha value of 0.05, the results indicated that with a power of 0.95, sample sizes of 1865, 305, and 125 were needed to detect effect sizes of 0.10 (small), 0.25 (medium), and 0.40 (large), respectively. Reaching the study’s sample size of 125 meant that large effect sizes could be detected in the statistical analyses.
Data collection
The questionnaire used for this study was developed by Ahmed et al. [ 26 ], which was inspired by literature [ 2 , 28 , 29 , 30 ] and resulted from discussions with medical teachers. The questionnaire was subjected to a pilot sample of 35 faculty members before being distributed in its final form. The data was initially treated to verify the psychometric characteristics of the questionnaire, so the reliability coefficient of Cronbach’s alpha was extracted for the questionnaire dimensions separately. Then, the overall reliability of the questionnaire was calculated. The reliability coefficient of Cronbach’s alpha showed that the questionnaire has good reliability coefficients ranging from the value (0.86) to (0.90), that have located in the range of excellent reliability coefficients (0.80–1) identified by [ 32 ], which makes it valid to achieve the objectives of the study. In general, the result showed that the reliability of the overall questionnaire is (0.88), which means that it is possible to obtain identical results by (88%) between this application and re-application of this questionnaire, and this implicitly means that the items are clear and explicit and carry accurate ideas for which the respondent’s understanding of it does not vary with time. Pearson correlation coefficients were calculated to examine the correlation of the questionnaire’s items with the dimensions to which they belong to ensure the structural validity of the questionnaire. The result showed that the correlation coefficients of the items with their affiliated dimensions are significant correlations at the level of significance (0.01), which indicates a high internal validity of the dimensions of the questionnaire. The items associated with the total average of the responses of the dimensions are considered valid expressions that measure what they were set for.
The questionnaire, in its final form, consisted of [ 27 ] items, which were divided into four main dimensions: 1st faculty members’ perceptions toward simulation-based education, 2nd determine anxiety of faculty members toward simulation-based education, 3rd faculty members’ perception toward the integration of simulation in education, and 4th faculty members’ perceived barriers to simulation-based education in undergraduate curricula.
At the beginning of the questionnaire form, a brief paragraph about the study and the study’s aim helped introduce the respondents to the study. To obtain consent, the respondents agreed to participate by clicking a button for participation agreement before answering the questionnaire. The survey was distributed in English, and it involved three parts. The first part included socio-demographic data of respondents such as gender, age, education, occupation, level of experience, teaching university, formal training for SBE, and exposure to SBE during teachers’ clinical nutrition education. The second part included some questions to assess teachers’ perceptions of SBE and integrate it into their teaching. Answers from the respondents were read on a five-point Likert-type scale. In the last part, an open-ended question was asked to explore faculty members’ perceived barriers toward SBE. Faculty were invited via university email to fill out a self-administered questionnaire. Social media platforms such as LinkedIn, WhatsApp, and Twitter were used to distribute the questionnaire among faculty using a snowball sampling technique. The study will identify the universities by pseudonym, as well as the anonymity of the participants to ensure confidentiality.
Statistical analysis
After the data collection, data were organized, checked, and analyzed with the Statistical Package for the Social Sciences (SPSS) version 25. Frequencies and percentages expressed the number of participants in the socio-demographic variables. Descriptive statistics, t-test, one-way ANOVA, chi-square test, means, and standard deviation were used for data analysis. A P-value < 0.05 will be considered to be statistically significant.
Likert’s scale intervals
The length of the intervals in the five-point Likert scale was determined by calculating the range (5 − 1 = 4) and then dividing it by the most significant value in the scale to get the length of the interval (4 ÷ 5 = 0.8), then this value was added to the lowest value in the scale (the beginning of the scale, which is an integer one), to determine the upper limit of this interval. Table 1 . shows Likert’s scale intervals.
Socio-demographic data of the sample
A total of 125 faculty members filled out the questionnaire. Table 2 . shows the distribution of the participants according to the study variables. The majority were females (71.2%), and (93.6%) aged less than 60 years. Most participants held either a Master’s degree (45.6%) or followed by Doctorate (43.2%) and none of the respondents had postgraduate diplomas. Most of the participants had more than five years of experience. 68% of participants did not receive formal simulation training ( P = 0.001), and 62.4% were not exposed to SBE during their education.
As shown in Table 3 . there was a statistically significant difference in age between received training for simulation or not ( P = 0.016); 62.5% of those who received formal training for simulation were aged 40–59 years, whereas 57.6% of those who did not were 20–39 years. As well as for training for simulation and educational level ( P = 0.012), 50.6% of those who did not receive formal training for simulation were with a Doctorate, and 65% of those who received formal training for simulation were with a Master’s degree. Furthermore, a statistically significant difference between received training for simulation and occupation was observed ( P = 0.015). Associate Professors and Professors were the occupations that received the most formal training for simulation (50%).
As shown in Table 4 . there was a statistically significant difference between the exposure to simulation during education and educational level (P = < 0.001), ); 68.1% of participants with a Master’s degree were exposed to simulation during schooling. No differences were observed between the exposure to simulation during education and other socio-demographic variables.
Faculty members’ perceptions toward simulation-based education
Table 5 demonstrates faculty members` perceptions toward SBE in percentages and numbers, which will be shown in detail in the following sections with means and standard deviation.
First dimension: faculty members’ perceptions toward simulation-based education
Table 6 shows the arithmetic means and standard deviations of the sample responses sorted in descending order for each item of the first dimension. The general perception toward SBE was positive, with a mean score of 3.86 ± 0.74.
Second dimension: determine the anxiety of faculty members toward simulation-based education
Table 7 shows the arithmetic means and standard deviations of the sample responses sorted in descending order for each item of the second dimension. The general anxiety toward SBE was high, with a mean score of 3.42 ± 0.75.
Third dimension: faculty members’ perception toward the integration of simulation in education
Table 8 shows the arithmetic means and standard deviations of the sample responses sorted in descending order for each item of the third dimension. The general perception toward the integration of simulation was positive, with a mean score of 3.54 ± 0.79.
Fourth dimension: faculty members’ perceived barriers towards the integration of simulation in education
Faculty members answered an open-ended question regarding perceived barriers they face towards SBE. The most frequent answers were the lack of time, training, facilities, resources, access, simulation labs, or simulation classrooms. The less frequent answers were the lack of cooperation, quick technical support, and motivation.
The answers only mentioned once were: the lack of training on implementation of the tool and the criteria for assessing, the lack of experience as they did not use the simulation at all, the difficulty in applying simulation/challenging to apply, the simulation was not integrated in the curriculum, and cultural barriers. One of the faculty mentioned that ‘there is always room for error, no matter how accurate the learning simulation is, there is always some scope for error and doubt when it comes to the re-creation of real-life scenarios, and the biggest drawback of using simulation is maintenance and updates can be costly. Besides these barriers, lack of time, labs, and enough training, particularly during COVID-19, were also mentioned.
Barriers related to the institution/university itself were reported, such as space, university environment, funding, lack of tools/materials, poor facilities, and support. The too busy schedule of the simulation center, insufficiently equipped laboratory, and the number of students per faculty; it is hard for one faculty to manage the students in simulation education, and lack of cooperation of leaders and other faculty members as it requires a lot of work early on and possibly a committee on its own to establish the rubrics for each subject and make the necessary refinement as needed. In addition, some community health departments are not using simulation as mentioned by the faculty, ‘it is unavailable in the department to be applied or used for the students.
Some of the faculties answered that no barriers were observed, but simulated education is not an original component of the curriculum and is only used as a backup.
Presented herein is the general perception and attitude of 125 faculty members about SBE application in the Colleges of Applied Medical Sciences in the Kingdom of Saudi Arabia. The general perception toward SBE was positive. The main findings of this study are that faculty members in the CAMS perceive SBE as an enjoyable way to teach, it increases students` interest and is considered an effective assessment tool to evaluate students` learning, improving learning outcomes, gives more freedom compared with actual wards and clinics, the best way for teaching communication skills, and improving patient safety. With a mean score of 3.86 ± 0.90. With this regard, the perception of faculty members toward SBE in this study is similar to students` perception in health colleges reported in other studies [ 1 , 33 , 34 ]. The students responded positively and believed that the simulations helped them better understand concepts, were a valuable learning experience, helped to stimulate critical thinking, and were realistic. The students also found that the knowledge gained from simulations can be transferred to real-life and clinical practice and that the simulations must be included in the undergraduate curriculum [ 33 ]. Many studies have demonstrated the importance of simulation as a teaching tool for healthy college students [ 33 , 34 , 35 , 37 ]. The literature highlighted that students perceive SBE promotes learning outcomes [ 31 , 32 ].
However, our results demonstrate that most CAMS faculty members have high levels of anxiety toward SBE. Faculty members agree and strongly agree with the statement that they need extra support to function effectively in simulation-based teaching and need more time to plan teaching with simulation tools compared with real patients. Unlike another study done in Saudi Arabia to evaluate the perception of medical teachers, their findings demonstrated that medical teachers have low levels of anxiety toward SBE [ 26 ]. The study compared the results for medical teachers in basic/clinical sciences, and they found that (59%/57.9%) disagree and strongly disagree with the statement that they avoid integrating simulation in their teaching [ 26 ]. Moreover, (42.3%/40.5%) of basic/clinical sciences medical teachers strongly agree that interaction with standardized patients will make the students interact artificially with actual patients.
Additionally, the results highlight that faculty members` perception was positive toward the integration of simulation in education. Faculty members agree and strongly agree with the statement that simulation should be a part of the medical curriculum and not a stand-alone activity, simulation-based activities should be introduced in the undergraduate curriculum from year 1, and simulation tools are the best choice for teaching their subject area. It has been demonstrated that the early introduction of SBE for basic clinical skills may simplify the integration of clinical and basic science knowledge, which may also increase student motivation and self-esteem [ 36 , 38 , 39 ].
Our findings also show that there was a statistically significant difference between the responses of the faculty members based on the training they received in simulation based on age, education level, and occupation. The rate of participants who received formal training for simulation was higher in 40–59 years (62.5%), holding a Master’s degree (65%) and working as Associate Professors and Professors (50%). Compared with the study that was done in Saudi Arabia to assess medical teachers` perception, the demographic factors of age, gender, received training, and perception of SBE, its anxiety, and integration were not statistically different [ 26 ].
Our study also identifies faculty members’ perceived barriers toward the integration of SBE, and the most frequently mentioned barriers were time, training, facilities, resources, access, and simulation labs/simulation classrooms. Compared to the other studies, curriculum design was one of the major barriers to the integration of SBE [ 26 ]. Another study aimed to assess the perceived barriers in applying simulation classes and reported the lack of interest to participate, lack of timely and effective feedback, and the high number of students in each class as perceived barriers to SBE [ 34 ].
This study has some strengths. First, this is a multicenter study; the population of participants was drawn from multiple institutions/universities in Saudi Arabia with different histories of curricular SBE. Thus, the findings can represent and generalize the perception of other institutions. Second, external validity and lower systematic bias compared to a single institution dataset. Third, to the best of our knowledge, this is the first study in Saudi Arabia that assessed faculty perception towards SBE in the community health sciences departments. Fourth, this study includes diverse faculty with various levels of experience and educational levels. Fifth, the second objective was to identify faculty members’ perceived barriers toward the integration of SBE, so this study offers the chance to identify the barriers and offer some solutions.
This study also has its limitations. Since data collection depended on a self-administered questionnaire, low response rates were the biggest challenges we faced. Other limitations related to self-administered questionnaires include misunderstanding, over/underestimation, and low monitoring ability. There is a possibility of selection and response bias even with anonymity since the faculty doesn’t have the same access or engagement with social media. The results can’t be generalized and may not be representative of the entire population of faculty members in Saudi Arabia to other programs because of the study design (cross-sectional). The interview was the best choice to take the expert opinion, but due to the lack of time and resources, we chose social media platforms and university emails to take the responses. As well, the sampling method we chose (snowball sampling) limited the ability to calculate the response rate. However, further observational and experimental studies are needed to assess the effect of SBE on learning and healthcare outcomes among students and healthcare practitioners.
The study’s key results demonstrate the positive perception and attitude of medical teachers towards the SBE to be used for clinical nutrition undergraduate practical courses. However, the results show high levels of anxiety among faculty members toward SBE. For the effective use of simulation in practical courses, the study identifies the need for training, support, and evaluation of faculty members in SBE. Our findings highlight the barriers that CAMS administrations must address to support the integration of SBE in undergraduate practical courses, develop a faculty training program, and assess its impact. Further research is needed to be done in Saudi Arabia to demonstrate the SBE outcomes in the level of education and healthcare practice.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
Colleges of Applied Medical Sciences
Institutional Review Board
Objective Structured Clinical Examination
Simulation-based Education
AlBalawi I, Alqahtani JS, Al Ghamdi SS, Aldhahir AM, Alnasser M, Alqahtani AS et al. Health Sciences Students’ Attitude, Perception, and Experience of Using Educational Simulation in Saudi Arabia: A Cross-Sectional Study. Nurs Reports [Internet]. 2022 Sep 1 [cited 2023 Feb 11];12(3):620. Available from: /pmc/articles/PMC9501630/.
Gaba DM. The future vision of simulation in health care. Qual Saf Health Care [Internet]. 2004 Oct 1 [cited 2023 Feb 4];13 Suppl 1(Suppl 1):i2–10. Available from: https://pubmed.ncbi.nlm.nih.gov/15465951/ .
Jeffries PR, Rodgers B, Adamson K. NLN Jeffries Simulation Theory: Brief Narrative Description. Nurs Educ Perspect [Internet]. 2015 [cited 2023 Feb 11];36(5):292–3. Available from: https://pubmed.ncbi.nlm.nih.gov/26521496/ .
Aebersold M. The History of Simulation and Its Impact on the Future. AACN Adv Crit Care [Internet]. 2016 [cited 2023 Feb 11];27(1):56–61. Available from: https://pubmed.ncbi.nlm.nih.gov/26909454/ .
Aebersold M. Simulation-based learning: No longer a novelty in undergraduate education. Online J Issues Nurs [Internet]. 2018 May 1 [cited 2023 Feb 11];23(2):1–1. Available from: https://www.researchgate.net/publication/328628589_Simulation-Based_Learning_No_Longer_a_Novelty_in_Undergraduate_Education .
Nestel D, Scerbo MW, Kardong-Edgren SE, A Contemporary History of Healthcare Simulation Research. Healthc Simul Res [Internet]. 2019 [cited 2022 Dec 14];9–14. Available from: https://link.springer.com/chapter/10.1007/978-3-030-26837-4_2 .
Rosen KR. The history of medical simulation. J Crit Care. 2008;23(2):157–66.
Article Google Scholar
Adams CH, Fitz PA. Simulation exercises for interview training in dietetics: a module on listening skills. J Am Diet Assoc. 1979;74(1):50–2.
Caliendo MA, Pulaski FR. Teaching the health care team concept to dietetic and nursing students: Simulated team conferences. J Am Diet Assoc. 1979;74(5):571–3.
Sutnick MR, Carroll JG. Using patient simulators to teach clinical interviewing skills. J Am Diet Assoc. 1981;78(6):614–6.
Russell ML, Caggiula AW, Gloninger MF. Evaluation of clinical skills for nutrition counseling. J Am Coll Nutr [Internet]. 1985 Jan 1 [cited 2023 Jan 21];4(5):521–9. Available from: https://pubmed.ncbi.nlm.nih.gov/4056236/ .
Sayers SL. Creating images of the future: a simulation game for dietetics students. J Am Diet Assoc. 1986;86(8):1052–4.
Stanek KL, Fox HM. A nutrition education workshop for managers of nutrition centers for the elderly utilizing videotaped simulations for assessment. J Nutr Elder [Internet]. 1989 Jul 31 [cited 2023 Jan 21];8(3–4):101–6. Available from: https://pubmed.ncbi.nlm.nih.gov/2769575/ .
Hampl JS, Herbold NH, Schneider MA, Sheeley AE. Using standardized patients to train and evaluate dietetics students. J Am Diet Assoc [Internet]. 1999 [cited 2022 Dec 25];99(9):1094–7. Available from: https://pubmed.ncbi.nlm.nih.gov/10491679/ .
Boonmak P, Suraseranivongse S, Pattaravit N, Boonmak S, Jirativanont T, Lertbunnaphong T et al. Simulation-based medical education in Thailand: a cross-sectional online national survey. BMC Med Educ [Internet]. 2022 Dec 1 [cited 2022 Dec 26];22(1):1–9. Available from: https://bmcmededuc.biomedcentral.com/articles/ https://doi.org/10.1186/s12909-022-03369-9 .
O’Shea MC, Palermo C, Rogers GD, Williams LT. Simulation-based Learning experiences in Dietetics Programs: a systematic review. J Nutr Educ Behav. 2020;52(4):429–38.
Gaba A, Costa SA, Schnoll R, Dorfman ME, Cordova S, Jakuboski S et al. Development and Evaluation of an Online Simulated Hospital Unit for Nutrition Assessment Training. Top Clin Nutr [Internet]. 2023 Apr 1 [cited 2023 May 21];38(2):133–43. Available from: https://journals.lww.com/topicsinclinicalnutrition/Fulltext/2023/04000/Development_and_Evaluation_of_an_Online_Simulated.6.aspx .
Espinoza V, Marileo L, Viscardi S, Espinoza V, Marileo L, Viscardi S. Clinical simulation with dramatization, a teaching-learning strategy for undergraduate students of nutrition and dietetics. Arch Latinoam Nutr [Internet]. 2022 Jun 1 [cited 2023 Feb 11];72(2):93–9. Available from: http://ve.scielo.org/scielo.php?script=sci_arttext&pid=S0004-06222022000200093&lng=es&nrm=iso&tlng=en
Moullet C, Depeyre J, Kehl C. [Diabetes simulation learning method for nutrition and dietetics students]. Rev Med Suisse [Internet]. 2021 Dec 1 [cited 2023 Feb 12];17(763):2209–12. Available from: https://europepmc.org/article/med/34910409 .
O’brien L, Collins K, Webb R, Davies I, Doran D, Amirabdollahian F. The Effects of Pre-Game Carbohydrate Intake on Running Performance and Substrate Utilisation during Simulated Gaelic Football Match Play. Nutr 2021, Vol 13, Page 1392 [Internet]. 2021 Apr 21 [cited 2023 Feb 12];13(5):1392. Available from: https://www.mdpi.com /2072-6643/13/5/1392/htm.
Alkhaldy AA, Mosli RH. High-Fidelity Patient Simulation Increases Saudi Dietetics Students’ Self-efficacy in Applying the Nutrition Care Process. Top Clin Nutr [Internet]. 2020 Apr 1 [cited 2023 Jun 5];35(2):93–103. Available from: https://journals.lww.com/topicsinclinicalnutrition/Fulltext/2020/04000/High_Fidelity_Patient_Simulation_Increases_Saudi.2.aspx .
BUCHHOLZ AC, Hendrickson M, Giroux I, CORREA JA, Hanning R, Eisenbraun C et al. Simulation in Learning and Using the Nutrition Care Process/Terminology: Experiences and Perceptions of Dietitians in Canada. Can J Diet Pract Res [Internet]. 2020 Sep 1 [cited 2023 Feb 12];81(3):150–3. Available from: https://pubmed.ncbi.nlm.nih.gov/32495644/ .
Tyler C, Alnaim L, Diekemper J, Hamilton-Reeves J, Goetz J, Sullivan DK et al. Simulations for Teaching and Evaluating Nutrition-Focused Physical Exam Skills. J Nutr Educ Behav [Internet]. 2020 Sep 1 [cited 2023 Feb 12];52(9):882–9. Available from: https://pubmed.ncbi.nlm.nih.gov/32446847/ .
Buchholz AC, Vanderleest K, MacMartin C, Prescod A, Wilson A. Patient Simulations Improve Dietetics Students’ and Interns’ Communication and Nutrition-Care Competence. J Nutr Educ Behav [Internet]. 2020 Apr 1 [cited 2023 Feb 12];52(4):377–84. Available from: https://pubmed.ncbi.nlm.nih.gov/31699616/ .
Steinhauser J, Janssen M, Hamm U. Who Buys Products with Nutrition and Health Claims? A Purchase Simulation with Eye Tracking on the Influence of Consumers’ Nutrition Knowledge and Health Motivation. Nutr 2019, Vol 11, Page 2199 [Internet]. 2019 Sep 12 [cited 2023 Feb 12];11(9):2199. Available from: https://www.mdpi.com /2072-6643/11/9/2199/htm.
Ahmed S, Al-Mously N, Al-Senani F, Zafar M, Ahmed M. Medical teachers’ perception towards simulation-based medical education: A multicenter study in Saudi Arabia. Med Teach [Internet]. 2016 Mar 25 [cited 2023 Feb 2];38 Suppl 1:S37–44. Available from: https://pubmed.ncbi.nlm.nih.gov/26984032/ .
Morey JC, Simon R, Jay GD, Wears RL, Salisbury M, Dukes KA et al. Error Reduction and Performance Improvement in the Emergency Department through Formal Teamwork Training: Evaluation Results of the MedTeams Project. Health Serv Res [Internet]. 2002 [cited 2023 Jan 22];37(6):1553. Available from: /pmc/articles/PMC1464040/.
Erdfelder E, FAul F, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods [Internet]. 2009 [cited 2023 Jun 12];41(4):1149–60. Available from: https://pubmed.ncbi.nlm.nih.gov/19897823/ .
Ziv A, Root Wolpe P, Small SD, Glick S. Simulation-based medical education: an ethical imperative. Acad Med [Internet]. 2003 Aug 1 [cited 2023 Feb 4];78(8):783–8. Available from: https://pubmed.ncbi.nlm.nih.gov/12915366/ .
Issenberg SB, McGaghie WC, Petrusa ER, Gordon DL, Scalese RJ. Features and uses of high-fidelity medical simulations that lead to effective learning: a BEME systematic review. Med Teach [Internet]. 2005 Jan [cited 2023 Feb 4];27(1):10–28. Available from: https://pubmed.ncbi.nlm.nih.gov/16147767/ .
McGaghie WC, Issenberg SB, Petrusa ER, Scalese RJ. A critical review of simulation-based medical education research: 2003–2009. Med Educ [Internet]. 2010 Jan [cited 2023 Feb 4];44(1):50–63. Available from: https://pubmed.ncbi.nlm.nih.gov/20078756/ .
Taber KS, The Use of Cronbach’s Alpha When Developing and Reporting Research Instruments in Science Education. Res Sci Educ [Internet]. 2018 Dec 1 [cited 2023 Jun 9];48(6):1273–96. Available from: https://link.springer.com/article/10.1007/s11165-016-9602-2 .
Howard VM, Englert N, Kameg K, Perozzi K. Integration of Simulation across the undergraduate curriculum: Student and Faculty perspectives. Clin Simul Nurs. 2011;7(1):e1–10.
Nuzhat A, Salem RO, Al Shehri FN, Al Hamdan N. Role and challenges of simulation in undergraduate curriculum. Med Teach [Internet]. 2014 [cited 2023 Jun 9];36 Suppl 1(SUPPL.1). Available from: https://pubmed.ncbi.nlm.nih.gov/24617788/ .
Issenberg SB. The scope of simulation-based healthcare education. Simul Healthc [Internet]. 2006 [cited 2023 Jun 9];1(4):203–8. Available from: https://journals.lww.com/simulationinhealthcare/Fulltext/2006/00140/The_Scope_of_Simulation_based_Healthcare_Education.1.aspx .
McGaghie WC. Research opportunities in simulation-based medical education using deliberate practice. Acad Emerg Med [Internet]. 2008 Nov [cited 2023 Jun 9];15(11):995–1001. Available from: https://pubmed.ncbi.nlm.nih.gov/18811635/ .
AlMously N, Baalash A, Salem R, Mukaddam S. The proper timing to introduce simulation-based education in internal medicine clerkship. J Contemp Med Educ [Internet]. 2014 [cited 2023 Jun 9];2(3):180. Available from: https://www.researchgate.net/publication/287537558_The_proper_timing_to_introduce_simulation-based_education_in_internal_medicine_clerkship .
Valler-Jones T, Meechan R, Jones H. Simulated practice–a panacea for health education? Br J Nurs [Internet]. 2011 May 26 [cited 2023 Jun 9];20(10):628–31. Available from: https://pubmed.ncbi.nlm.nih.gov/21646995/ .
K AD, Kadir SY, Viswanathan N. Early introduction of clinical skills in the pre-clinical phase of an integrated medical curriculum. J Contemp Med Educ [Internet]. 2013 Jul 10 [cited 2023 Jun 9];1(3):142–4. Available from: https://www.jcmedu.org/abstract/early-introduction-of-clinical-skills-in-the-preclinical-phase-of-an-integrated-medical-curriculum-48446.html .
Download references
Acknowledgements
We would like to thank faculty members who participated in this study and anyone who aided in this project. We are also grateful to King Saud University for their valuable contributions and to all other universities included in this study for their collaborations.
Not applicable.
Author information
Authors and affiliations.
Department of Community Health Sciences, College of Applied Medical Sciences, King Saud University, Riyadh, Saudi Arabia
Iman Abdullah Bindayel & Shahad Ahmed Alahmad
You can also search for this author in PubMed Google Scholar
Contributions
Both authors contributed equally to this work, and reviewed the manuscript.
Corresponding author
Correspondence to Iman Abdullah Bindayel .
Ethics declarations
Ethics approval and consent to participate.
The study was reviewed and approved by the Institutional Review Board (IRB) of King Saud University, Riyadh (IRB No. 23–353). Permission to conduct the study was also obtained from the deans of the CAMS. The participants were informed about the study at the beginning of the questionnaire, and no identifying data was collected. Informed consent has been obtained from all the participants.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Bindayel, I.A., Alahmad, S.A. Perception of faculty in the community health sciences colleges towards simulation-based education in clinical nutrition undergraduate practical courses. BMC Med Educ 24 , 402 (2024). https://doi.org/10.1186/s12909-024-05338-w
Download citation
Received : 11 October 2023
Accepted : 21 March 2024
Published : 11 April 2024
DOI : https://doi.org/10.1186/s12909-024-05338-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Simulation-based education
- Undergraduate
- Faculty members
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Entire Site
- Research & Funding
- Health Information
- About NIDDK
- Diabetes Overview
Healthy Living with Diabetes
- Español
On this page:
How can I plan what to eat or drink when I have diabetes?
How can physical activity help manage my diabetes, what can i do to reach or maintain a healthy weight, should i quit smoking, how can i take care of my mental health, clinical trials for healthy living with diabetes.
Healthy living is a way to manage diabetes . To have a healthy lifestyle, take steps now to plan healthy meals and snacks, do physical activities, get enough sleep, and quit smoking or using tobacco products.
Healthy living may help keep your body’s blood pressure , cholesterol , and blood glucose level, also called blood sugar level, in the range your primary health care professional recommends. Your primary health care professional may be a doctor, a physician assistant, or a nurse practitioner. Healthy living may also help prevent or delay health problems from diabetes that can affect your heart, kidneys, eyes, brain, and other parts of your body.
Making lifestyle changes can be hard, but starting with small changes and building from there may benefit your health. You may want to get help from family, loved ones, friends, and other trusted people in your community. You can also get information from your health care professionals.
What you choose to eat, how much you eat, and when you eat are parts of a meal plan. Having healthy foods and drinks can help keep your blood glucose, blood pressure, and cholesterol levels in the ranges your health care professional recommends. If you have overweight or obesity, a healthy meal plan—along with regular physical activity, getting enough sleep, and other healthy behaviors—may help you reach and maintain a healthy weight. In some cases, health care professionals may also recommend diabetes medicines that may help you lose weight, or weight-loss surgery, also called metabolic and bariatric surgery.
Choose healthy foods and drinks
There is no right or wrong way to choose healthy foods and drinks that may help manage your diabetes. Healthy meal plans for people who have diabetes may include
- dairy or plant-based dairy products
- nonstarchy vegetables
- protein foods
- whole grains
Try to choose foods that include nutrients such as vitamins, calcium , fiber , and healthy fats . Also try to choose drinks with little or no added sugar , such as tap or bottled water, low-fat or non-fat milk, and unsweetened tea, coffee, or sparkling water.
Try to plan meals and snacks that have fewer
- foods high in saturated fat
- foods high in sodium, a mineral found in salt
- sugary foods , such as cookies and cakes, and sweet drinks, such as soda, juice, flavored coffee, and sports drinks
Your body turns carbohydrates , or carbs, from food into glucose, which can raise your blood glucose level. Some fruits, beans, and starchy vegetables—such as potatoes and corn—have more carbs than other foods. Keep carbs in mind when planning your meals.
You should also limit how much alcohol you drink. If you take insulin or certain diabetes medicines , drinking alcohol can make your blood glucose level drop too low, which is called hypoglycemia . If you do drink alcohol, be sure to eat food when you drink and remember to check your blood glucose level after drinking. Talk with your health care team about your alcohol-drinking habits.

Find the best times to eat or drink
Talk with your health care professional or health care team about when you should eat or drink. The best time to have meals and snacks may depend on
- what medicines you take for diabetes
- what your level of physical activity or your work schedule is
- whether you have other health conditions or diseases
Ask your health care team if you should eat before, during, or after physical activity. Some diabetes medicines, such as sulfonylureas or insulin, may make your blood glucose level drop too low during exercise or if you skip or delay a meal.
Plan how much to eat or drink
You may worry that having diabetes means giving up foods and drinks you enjoy. The good news is you can still have your favorite foods and drinks, but you might need to have them in smaller portions or enjoy them less often.
For people who have diabetes, carb counting and the plate method are two common ways to plan how much to eat or drink. Talk with your health care professional or health care team to find a method that works for you.
Carb counting
Carbohydrate counting , or carb counting, means planning and keeping track of the amount of carbs you eat and drink in each meal or snack. Not all people with diabetes need to count carbs. However, if you take insulin, counting carbs can help you know how much insulin to take.
Plate method
The plate method helps you control portion sizes without counting and measuring. This method divides a 9-inch plate into the following three sections to help you choose the types and amounts of foods to eat for each meal.
- Nonstarchy vegetables—such as leafy greens, peppers, carrots, or green beans—should make up half of your plate.
- Carb foods that are high in fiber—such as brown rice, whole grains, beans, or fruits—should make up one-quarter of your plate.
- Protein foods—such as lean meats, fish, dairy, or tofu or other soy products—should make up one quarter of your plate.
If you are not taking insulin, you may not need to count carbs when using the plate method.

Work with your health care team to create a meal plan that works for you. You may want to have a diabetes educator or a registered dietitian on your team. A registered dietitian can provide medical nutrition therapy , which includes counseling to help you create and follow a meal plan. Your health care team may be able to recommend other resources, such as a healthy lifestyle coach, to help you with making changes. Ask your health care team or your insurance company if your benefits include medical nutrition therapy or other diabetes care resources.
Talk with your health care professional before taking dietary supplements
There is no clear proof that specific foods, herbs, spices, or dietary supplements —such as vitamins or minerals—can help manage diabetes. Your health care professional may ask you to take vitamins or minerals if you can’t get enough from foods. Talk with your health care professional before you take any supplements, because some may cause side effects or affect how well your diabetes medicines work.
Research shows that regular physical activity helps people manage their diabetes and stay healthy. Benefits of physical activity may include
- lower blood glucose, blood pressure, and cholesterol levels
- better heart health
- healthier weight
- better mood and sleep
- better balance and memory
Talk with your health care professional before starting a new physical activity or changing how much physical activity you do. They may suggest types of activities based on your ability, schedule, meal plan, interests, and diabetes medicines. Your health care professional may also tell you the best times of day to be active or what to do if your blood glucose level goes out of the range recommended for you.

Do different types of physical activity
People with diabetes can be active, even if they take insulin or use technology such as insulin pumps .
Try to do different kinds of activities . While being more active may have more health benefits, any physical activity is better than none. Start slowly with activities you enjoy. You may be able to change your level of effort and try other activities over time. Having a friend or family member join you may help you stick to your routine.
The physical activities you do may need to be different if you are age 65 or older , are pregnant , or have a disability or health condition . Physical activities may also need to be different for children and teens . Ask your health care professional or health care team about activities that are safe for you.
Aerobic activities
Aerobic activities make you breathe harder and make your heart beat faster. You can try walking, dancing, wheelchair rolling, or swimming. Most adults should try to get at least 150 minutes of moderate-intensity physical activity each week. Aim to do 30 minutes a day on most days of the week. You don’t have to do all 30 minutes at one time. You can break up physical activity into small amounts during your day and still get the benefit. 1
Strength training or resistance training
Strength training or resistance training may make your muscles and bones stronger. You can try lifting weights or doing other exercises such as wall pushups or arm raises. Try to do this kind of training two times a week. 1
Balance and stretching activities
Balance and stretching activities may help you move better and have stronger muscles and bones. You may want to try standing on one leg or stretching your legs when sitting on the floor. Try to do these kinds of activities two or three times a week. 1
Some activities that need balance may be unsafe for people with nerve damage or vision problems caused by diabetes. Ask your health care professional or health care team about activities that are safe for you.

Stay safe during physical activity
Staying safe during physical activity is important. Here are some tips to keep in mind.
Drink liquids
Drinking liquids helps prevent dehydration , or the loss of too much water in your body. Drinking water is a way to stay hydrated. Sports drinks often have a lot of sugar and calories , and you don’t need them for most moderate physical activities.
Avoid low blood glucose
Check your blood glucose level before, during, and right after physical activity. Physical activity often lowers the level of glucose in your blood. Low blood glucose levels may last for hours or days after physical activity. You are most likely to have low blood glucose if you take insulin or some other diabetes medicines, such as sulfonylureas.
Ask your health care professional if you should take less insulin or eat carbs before, during, or after physical activity. Low blood glucose can be a serious medical emergency that must be treated right away. Take steps to protect yourself. You can learn how to treat low blood glucose , let other people know what to do if you need help, and use a medical alert bracelet.
Avoid high blood glucose and ketoacidosis
Taking less insulin before physical activity may help prevent low blood glucose, but it may also make you more likely to have high blood glucose. If your body does not have enough insulin, it can’t use glucose as a source of energy and will use fat instead. When your body uses fat for energy, your body makes chemicals called ketones .
High levels of ketones in your blood can lead to a condition called diabetic ketoacidosis (DKA) . DKA is a medical emergency that should be treated right away. DKA is most common in people with type 1 diabetes . Occasionally, DKA may affect people with type 2 diabetes who have lost their ability to produce insulin. Ask your health care professional how much insulin you should take before physical activity, whether you need to test your urine for ketones, and what level of ketones is dangerous for you.
Take care of your feet
People with diabetes may have problems with their feet because high blood glucose levels can damage blood vessels and nerves. To help prevent foot problems, wear comfortable and supportive shoes and take care of your feet before, during, and after physical activity.

If you have diabetes, managing your weight may bring you several health benefits. Ask your health care professional or health care team if you are at a healthy weight or if you should try to lose weight.
If you are an adult with overweight or obesity, work with your health care team to create a weight-loss plan. Losing 5% to 7% of your current weight may help you prevent or improve some health problems and manage your blood glucose, cholesterol, and blood pressure levels. 2 If you are worried about your child’s weight and they have diabetes, talk with their health care professional before your child starts a new weight-loss plan.
You may be able to reach and maintain a healthy weight by
- following a healthy meal plan
- consuming fewer calories
- being physically active
- getting 7 to 8 hours of sleep each night 3
If you have type 2 diabetes, your health care professional may recommend diabetes medicines that may help you lose weight.
Online tools such as the Body Weight Planner may help you create eating and physical activity plans. You may want to talk with your health care professional about other options for managing your weight, including joining a weight-loss program that can provide helpful information, support, and behavioral or lifestyle counseling. These options may have a cost, so make sure to check the details of the programs.
Your health care professional may recommend weight-loss surgery if you aren’t able to reach a healthy weight with meal planning, physical activity, and taking diabetes medicines that help with weight loss.
If you are pregnant , trying to lose weight may not be healthy. However, you should ask your health care professional whether it makes sense to monitor or limit your weight gain during pregnancy.
Both diabetes and smoking —including using tobacco products and e-cigarettes—cause your blood vessels to narrow. Both diabetes and smoking increase your risk of having a heart attack or stroke , nerve damage , kidney disease , eye disease , or amputation . Secondhand smoke can also affect the health of your family or others who live with you.
If you smoke or use other tobacco products, stop. Ask for help . You don’t have to do it alone.
Feeling stressed, sad, or angry can be common for people with diabetes. Managing diabetes or learning to cope with new information about your health can be hard. People with chronic illnesses such as diabetes may develop anxiety or other mental health conditions .
Learn healthy ways to lower your stress , and ask for help from your health care team or a mental health professional. While it may be uncomfortable to talk about your feelings, finding a health care professional whom you trust and want to talk with may help you
- lower your feelings of stress, depression, or anxiety
- manage problems sleeping or remembering things
- see how diabetes affects your family, school, work, or financial situation
Ask your health care team for mental health resources for people with diabetes.
Sleeping too much or too little may raise your blood glucose levels. Your sleep habits may also affect your mental health and vice versa. People with diabetes and overweight or obesity can also have other health conditions that affect sleep, such as sleep apnea , which can raise your blood pressure and risk of heart disease.

NIDDK conducts and supports clinical trials in many diseases and conditions, including diabetes. The trials look to find new ways to prevent, detect, or treat disease and improve quality of life.
What are clinical trials for healthy living with diabetes?
Clinical trials—and other types of clinical studies —are part of medical research and involve people like you. When you volunteer to take part in a clinical study, you help health care professionals and researchers learn more about disease and improve health care for people in the future.
Researchers are studying many aspects of healthy living for people with diabetes, such as
- how changing when you eat may affect body weight and metabolism
- how less access to healthy foods may affect diabetes management, other health problems, and risk of dying
- whether low-carbohydrate meal plans can help lower blood glucose levels
- which diabetes medicines are more likely to help people lose weight
Find out if clinical trials are right for you .
Watch a video of NIDDK Director Dr. Griffin P. Rodgers explaining the importance of participating in clinical trials.
What clinical trials for healthy living with diabetes are looking for participants?
You can view a filtered list of clinical studies on healthy living with diabetes that are federally funded, open, and recruiting at www.ClinicalTrials.gov . You can expand or narrow the list to include clinical studies from industry, universities, and individuals; however, the National Institutes of Health does not review these studies and cannot ensure they are safe for you. Always talk with your primary health care professional before you participate in a clinical study.
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts.
NIDDK would like to thank: Elizabeth M. Venditti, Ph.D., University of Pittsburgh School of Medicine.
More Produce, Less Dairy for Low-Income Families Under US Nutrition Program Changes

FILE PHOTO: A person shops in a supermarket selling fruit and vegetables in Manhattan, New York City, U.S., March 28, 2022. REUTERS/Andrew Kelly/File Photo
By Leah Douglas
(Reuters) -Nearly 7 million low-income women and children will be able to purchase more fruits and vegetables but less dairy after the U.S. Department of Agriculture finalized changes to a key federal nutrition program on Tuesday.
The updates to the Special Supplemental Nutrition Program for Women, Infants and Children (WIC), the first since 2014, were made to better align the program's food packages with the best dietary science, USDA said.
"These participant-centered changes will strengthen WIC by ensuring the foods participants receive reflect the latest nutrition science to support healthy eating and the brightest futures," Agriculture Secretary Tom Vilsack said in a statement.
WIC participants receive benefits to purchase certain food items depending on age and dietary needs. The USDA proposed changes to the program in November 2022 and received over 17,000 comments, it said.
The final provision increases allowances for fruits, vegetables, and seafood, and decreases the amounts of juice, dairy and cheese. It also adds more non-dairy options like plant-based and lactose-free milk.
"The National WIC Association applauds USDA for adhering to an independent, science-based review process that led to these stronger standards, and we urge swift implementation," said Georgia Machell, interim president and CEO of the group, in a statement.
The changes were criticized by dairy promotion groups.
"(The National Milk Producers Federation) is disturbed by the decision to reduce access to the essential nutrients dairy adds to the diet," said Gregg Doud, president and CEO of the group, in a statement.
A USDA spokesperson said that the agency expects dairy purchases through WIC to rise by as much as $400 million by 2025 due to projected increased participation, and that WIC participants were typically not redeeming the full volume of milk provided under the earlier allowances.
WIC is administered by the USDA and serves 6.6 million pregnant, breastfeeding and postpartum women and children up to age 5.
Congress recently expanded the amount of money for WIC after the White House and nutrition advocates warned a budget shortfall put millions of eligible families at risk of being turned away.
(Reporting by Leah Douglas; Editing by Marguerita Choy and Andrea Ricci)
Copyright 2024 Thomson Reuters .
Join the Conversation
Tags: United States
America 2024

Health News Bulletin
Stay informed on the latest news on health and COVID-19 from the editors at U.S. News & World Report.
Sign in to manage your newsletters »
Sign up to receive the latest updates from U.S News & World Report and our trusted partners and sponsors. By clicking submit, you are agreeing to our Terms and Conditions & Privacy Policy .
You May Also Like
The 10 worst presidents.
U.S. News Staff Feb. 23, 2024

Cartoons on President Donald Trump
Feb. 1, 2017, at 1:24 p.m.

Photos: Obama Behind the Scenes
April 8, 2022

Photos: Who Supports Joe Biden?
March 11, 2020

Johnson Turns to Trump Amid GOP Dissent
Aneeta Mathur-Ashton April 11, 2024

A Reprieve for Inflation?
Tim Smart April 11, 2024

Embattled Johnson Bruised Again
Aneeta Mathur-Ashton April 10, 2024

What to Know About Biden's State Dinner
Laura Mannweiler April 10, 2024

Fed: Inflation Path ‘Somewhat Uneven’
Tim Smart April 10, 2024

No Letup From Inflation in March

- Government Offices
- Health Departments
North Central Health District - Latah County in Moscow, Idaho
Contact information, about north central health district - latah county.
Public Health - Idaho North Central District (PH-INCD) is a public health agency serving Latah County, Idaho. Located in Moscow, Idaho, PH-INCD provides disease prevention, health promotion, and environmental health services to the community. The agency works in partnership with Gritman Medical Center and the University of Idaho to promote the health and well-being of the region's residents.
Public Health - Idaho North Central District (PH-INCD)
- Moscow, ID 83843
Hours of Operation:
- Monday - Friday, 8:00 a.m. - 5:00 p.m. (excluding holidays)
- Disease prevention
- Health promotion
- Environmental health
- Gritman Medical Center
- University of Idaho
North Central Health District - Latah County Services
Helpful resources.
Idaho Public Health District 2 https://idahopublichealth.com/ Information on public health services, including home visitation and parent education programs, for Clearwater, Idaho, Latah, Lewis, and Nez Perce counties.
District 2 on the Idaho Public Health Website https://idahopublichealth.com/district-2 Information about the activities and services of the Public Health - Idaho North Central District.
Office Locations - Idaho Public Health District 2 https://idahopublichealth.com/district-2/aboutidahopublichealth/officelocations Contact information and addresses for offices in Kamiah, Lewiston, Moscow, and Orofino, Idaho.
Other Health Departments Nearby
North Central Health District 10th Street, Lewiston, ID - 20.6 miles
Lewiston Health Department 16th Avenue, Lewiston, ID - 21.6 miles
North Central Health District - Clearwater County 115th Street, Orofino, ID - 36.4 miles Provides WIC services, nutrition support, and education to eligible families and individuals in Clearwater County, Idaho.
Orofino Health Department 115th Street, Orofino, ID - 36.4 miles Provides WIC services, nutrition support, and education to eligible families and individuals in Clearwater County, Idaho.
Panhandle Health District 1 - Benewah County North 8th Street, St. Maries, ID - 46.2 miles The Panhandle Health District provides environmental health, public health nursing, and WIC services to residents of Benewah, Bonner, Boundary, Kootenai, and Shoshone counties in Idaho.
Map of North Central Health District - Latah County in Moscow, Idaho
Related Latah County Public Records
- Birth Records
- Death Records
- Genealogy Records
- Professional Licenses
- Vital Records
- All Latah County Public Records
Related Moscow Government Offices
- Coroners & Medical Examiners
- Social Services Departments
- Veterans Affairs Departments
- Water Departments
- All Moscow Government Offices
Health Departments in Nearby Cities
- Pullman, WA
- Clarkston, WA
- Lewiston, ID
- Pomeroy, WA
- Orofino, ID
- St. Maries, ID
Health Departments in Nearby Counties
- Benewah County, ID
- Clearwater County, ID
- Nez Perce County, ID
- Whitman County, WA
- Shoshone County, ID
- All Health Departments in Idaho

Takeda Announces New U.S. Corporate Social Responsibility Program Partners to Build Equity through STEM Education and Access to Nutritional Food
- FY23 Investment Brings Program Total to Nearly $55 Million, Welcoming Eight New Grant Partners
- Company Continues to Advance Equity in Under-Resourced Communities with a Focus on Nutrition and STEM Education
- Takeda Publishes its Annual U.S. Community Impact Report Highlighting Program Progress
CAMBRIDGE, Massachusetts, April 8, 2024 – Takeda (TSE:4502/NYSE:TAK) today announced the selection of eight new U.S. non-profit organizations as grant recipients, as part of its $14.6 million commitment to its FY2023 U.S. Corporate Social Responsibility (CSR) program. To create greater impact and foster equity in under-resourced communities, the company is focusing its philanthropic efforts on the two areas of Food is Health and Building STEM (Science, Technology, Engineering and Math) Foundations and providing larger, multi-year grants to select nonprofits. Combined with previous investments since 2021, Takeda’s total contribution to these initiatives now amounts to $54.1 million.
“By focusing our efforts on Food is Health and Building STEM Foundations, we are evolving our program to address two areas of significant need that will help build up communities and narrow disparities that can prevent people from realizing their full potential," said Julie Kim, president of Takeda’s U.S. Business Unit and U.S. Country Head. "We are excited to continue this important work with our new partners, collectively striving to drive long-term impact within our local communities and more broadly.”
Takeda reviews grant applications for its U.S. CSR program twice a year. The company partners with local and national organizations that align with its philanthropic focus areas, actively listening and valuing their insights and expertise to understand the areas of greatest need within communities. By leveraging this collaborative approach, Takeda provides support to address these critical needs and make a positive impact on people's lives.
Takeda’s FY2023 U.S. CSR Grantees
Strengthening the Connection Between Food and Health for vulnerable and underserved communities around the country:
- Community Servings:
Medically tailored nutrition program and advancement of policies that prioritize food’s role in public health
- West End House:
Health, nutrition, food access and education programs
- Open Hand Atlanta:
Medically tailored meals for socially vulnerable individuals
- Project Angel Food:
Home delivered medically tailored meals program for critically ill people
- Northern Illinois Food Bank:
Build healthy communities program
- Greater Chicago Food Depository:
Prepared meals program
Building STEM Foundations to promote educational equity from kindergarten through college:
- Project Scientist:
Phased national expansion of STEAM programming and gender- and race-equitable teacher training through the Project Scientist Teaching Institute
- Thrive Scholars:
STEM pathways (Technology, Engineering and Life Sciences) support and Boston expansion
Takeda recently published Caring for Tomorrow: 2023 U.S. Community Impact Report , an annual report that provides a comprehensive overview of the initiatives and partnerships that are making a difference in the lives of communities across the country. Further details on the company’s U.S. CSR, health equity and diversity, equity and inclusion programs can be found in the report.
Learn more about Takeda’s U.S. CSR Program and its philanthropic strategy here . You can find more details about Takeda’s Global CSR Program here .
About Takeda
Takeda is focused on creating better health for people and a brighter future for the world. We aim to discover and deliver life-transforming treatments in our core therapeutic and business areas, including gastrointestinal and inflammation, rare diseases, plasma-derived therapies, oncology, neuroscience and vaccines. Together with our partners, we aim to improve the patient experience and advance a new frontier of treatment options through our dynamic and diverse pipeline. As a leading values-based, R&D-driven biopharmaceutical company headquartered in Japan, we are guided by our commitment to patients, our people and the planet. Our employees in approximately 80 countries and regions are driven by our purpose and are grounded in the values that have defined us for more than two centuries. For more information, visit www.takeda.com .
Media Contacts:
U.S. and International Media
Megan Ostrower [email protected]
Forward-Looking Statements
This press release and any materials distributed in connection with this press release may contain forward-looking statements, beliefs or opinions regarding Takeda’s future business, future position and results of operations, including estimates, forecasts, targets and plans for Takeda. Without limitation, forward-looking statements often include words such as “targets”, “plans”, “believes”, “hopes”, “continues”, “expects”, “aims”, “intends”, “ensures”, “will”, “may”, “should”, “would”, “could” “anticipates”, “estimates”, “projects” or similar expressions or the negative thereof. These forward-looking statements are based on assumptions about many important factors, including the following, which could cause actual results to differ materially from those expressed or implied by the forward-looking statements: the economic circumstances surrounding Takeda’s global business, including general economic conditions in Japan and the United States; competitive pressures and developments; changes to applicable laws and regulations, including global health care reforms; challenges inherent in new product development, including uncertainty of clinical success and decisions of regulatory authorities and the timing thereof; uncertainty of commercial success for new and existing products; manufacturing difficulties or delays; fluctuations in interest and currency exchange rates; claims or concerns regarding the safety or efficacy of marketed products or product candidates; the impact of health crises, like the novel coronavirus pandemic, on Takeda and its customers and suppliers, including foreign governments in countries in which Takeda operates, or on other facets of its business; the timing and impact of post-merger integration efforts with acquired companies; the ability to divest assets that are not core to Takeda’s operations and the timing of any such divestment(s); and other factors identified in Takeda’s most recent Annual Report on Form 20-F and Takeda’s other reports filed with the U.S. Securities and Exchange Commission, available on Takeda’s website at: https://www.takeda.com/investors/sec-filings-and-security-reports/ or at www.sec.gov . Takeda does not undertake to update any of the forward-looking statements contained in this press release or any other forward-looking statements it may make, except as required by law or stock exchange rule. Past performance is not an indicator of future results and the results or statements of Takeda in this press release may not be indicative of, and are not an estimate, forecast, guarantee or projection of Takeda’s future results.

Current Openings
APPLICANT LOGIN

LEAD HEALTH AND NUTRITION SERVICES SPECIALIST
- DEPT OF EDUCATION
- Closing at: Apr 14 2024 at 23:55 MST
Arizona Department of Education
The arizona department of education is a service organization committed to raising academic outcomes and empowering parents..
Health and Nutrition Services Division
Phoenix Location
Salary: $73,000
Closing date: 04/14/2024.
This position will be the lead specialist responsible for providing guidance and support for data-related reporting of Summer Electric Benefit Transfer (S-EBT) and data needs as it relates to Health and Nutrition Services (HNS). Consumers of this data includes Local Education Agencies, other divisions within ADE, other State Agencies, United States Department of Agriculture (USDA), and the general public. Occasional in-state and rare out-of-state travel is required for this position. The Arizona Department of Education currently utilizes a hybrid work environment, with up to two days of remote work (contingent upon business needs). Candidates should apply with an ability and willingness to work in-office up to five days per week as business needs necessitate.
This position: • As a team lead, provides support to the S-EBT team in their actioning of day-to-day tasks and general understanding of S-EBT; • Serves as a content expert of State and Federal guidance, department platforms, and initiatives; • Creates and delivers training, contributes S-EBT related content for meetings. Resolves issues elevated from S-EBT staff; • Aids in the development of processes and procedures that ensures the S-EBT team efficiently and effectively meets strategic goals; • Proactively works with directors to minimize barriers staff may face in completing required job duties; • Serves as content expert on S-EBT technology systems, data and program requirements; • Creates and validates data sets for USDA federal reporting related to S-EBT and reporting Arizona Department of Economic Security (DES) ensuring eligible participants are issued valid payments; • Serves as S-EBT liaison between partnering agency, Arizona Department of Economic Security (DES) and Health and Nutrition Services; and • Represents HNS during appeal hearings requested by parents/guardians of denied household income applications
Knowledge in: • Data gathering and cleaning techniques • Federal Nutrition Assistance Programs such as Supplemental Nutrition Assistance Program (SNAP), Temporary Assistance for Needy Families (TANF), Child Nutrition Programs, and Food Distribution Program on Indian Reservations (FDPIR) • Federal regulations, state laws, and policies pertaining to all Child Nutrition Programs • National and local legislative and health and nutrition program issues • A Bachelor's and/or Master's degree with emphasis in data management and/or statistics, or equivalent experience to substitute for the degree, is required. Skills in: • Analysis • Problem solving • Public speaking • Written and oral communication • Technical writing • Organization • Time management • Multiple project/task management • Expertise in training adult learners • Meeting and group discussion facilitation • Self-initiative for project development, implementation, and oversight • Decision making • Intermediate skill in using Microsoft Word, Excel, Access, and Outlook Ability to: • Provide exceptional customer service • Set and meet deadlines • Work with and understand large data sets • Communicate effectively both verbally and in writing • Research regulatory guidance • Research, review, and draw interpretations from public laws and rules • Establish and maintain interpersonal relationships • Perform multiple tasks • Think critically and make objective determinations • Express ideas and information clearly and concisely, both orally and writing
Preference will be given to those applicants with: • Customer service experience and/or employment with a government agency, school district or charter school • Experience with Federal Nutrition Assistance Programs (Child Nutrition Programs, SNAP, TANF, FDPIR) • Multi-lingual speaking skills
• Offers are contingent upon successful completion of all background and reference checks, required documents and, if applicable, a post-offer medical/physical evaluation.
If this position requires driving or the use of a vehicle as an essential function of the job to conduct State business, then the following requirements apply: Driver’s License Requirements.
All newly hired State employees are subject to and must successfully complete the Electronic Employment Eligibility Verification Program (E-Verify).
The State of Arizona provides an excellent comprehensive benefits package including: • Affordable medical, dental, life, and short-term disability insurance plans • Top-ranked retirement and long-term disability plans • Ten paid holidays per year • Vacation time accrued at 4.00 hours bi-weekly for the first 3 years • Sick time accrued at 3.70 hours bi-weekly • Paid Parental Leave-Up to 12 weeks per year paid leave for newborn or newly-placed foster/adopted child (pilot program). • Deferred compensation plan • Wellness plans
Learn more about the Paid Parental Leave pilot program here . For a complete list of benefits provided by The State of Arizona, please visit our benefits page
You will be required to participate in the Arizona State Retirement System (ASRS) upon your 27th week of employment, subject to waiting period. On or shortly after, your first day of employment you will be provided with enrollment instructions and effective date.
The State of Arizona is an Equal Opportunity/Reasonable Accommodation Employer. Persons with a disability may request a reasonable accommodation such as a sign language interpreter or an alternative format by calling (602) 542-3186 or emailing [email protected]. Requests should be made as early as possible to allow sufficient time to arrange the accommodation.
ARIZONA MANAGEMENT SYSTEM (AMS)
All Arizona state employees operate within the Arizona Management System (AMS), an intentional, results-driven approach for doing the work of state government whereby every employee reflects on performance, reduces waste, and commits to continuous improvement with sustainable progress. Through AMS, every state employee seeks to understand customer needs, identify problems, improve processes, and measure results. State employees are highly engaged, collaborative and embrace a culture of public service.
The State of Arizona is an Equal Opportunity/Reasonable Accommodation Employer.
If this position requires driving or the use of a vehicle as an essential function of the job to conduct State business, then the following requirements apply: Driver’s License Requirements

This website uses cookies.
We use cookies to personalize content such as job recommendations, and to analyze our traffic. You consent to our cookies if you click "I Accept". If you click on "I Do Not Accept", then we will not use cookies but you may have a deteriorated user experience. You can change your settings by clicking on the Settings link on the top right of the device.

IMAGES
VIDEO
COMMENTS
Healthy eating learning opportunities includes nutrition education and other activities integrated into the school day that can give children knowledge and skills to help choose and consume healthy foods and beverages. 1 Nutrition education is a vital part of a comprehensive health education program and empowers children with knowledge and skills to make healthy food and beverage choices. 2-8
School health and nutrition is about investing both in learners' education and their health, with benefits extending to homes and communities.Ensuring the health and well-being of learners is one of the most transformative ways to improve education outcomes, promote inclusion and equity and to rebuild the education system, especially following the COVID-19 pandemic.
It's true that knowledge about nutrition and diet evolves over time. But there are some nutrition basics that can help you sort through the latest research and advice. Nutrition basics come down to eating wholesome foods that support your health.
The Health Educator's Nutrition Toolkit is designed to help health educators, dietitians, physicians, other health care and nutrition professionals, social workers, youth counselors, and program ...
Nutrition. Nutrition is a critical part of health and development. Better nutrition is related to improved infant, child and maternal health, stronger immune systems, safer pregnancy and childbirth, lower risk of non-communicable diseases (such as diabetes and cardiovascular disease), and longevity. Healthy children learn better.
Advocates of child health have experimented with students' diets in the United States for more than twenty years. ... Nutrition and education: A randomized trial of the effects of breakfast in rural primary school children. American Journal of Clinical Nutrition, 68, 873-879. Cueto, S. (2001). Breakfast and dietary balance: The enKid study ...
The link between education to health and well-being is clear. Education develops the skills, values and attitudes that enable learners to lead healthy and fulfilled lives, make informed decisions, and engage in positive relationships with everyone around them. Poor health can have a detrimental effect on school attendance and academic performance.
Nutrition education is the process of teaching the science of nutrition to an individual or group. Health professionals have a different role in educating an individual in the clinic, community, or long-term health-care facility. In these settings, the dietician, nutritionist, or nurse serves to assist or enable individuals to incorporate ...
Discover nutrient content for over 20,000 carrot products and variations in the USDA's FoodData Central. Follow Nutrition.gov on Twitter to stay up to date on new resources and seasonal recipes. Nutrition.gov is powered by USDA Science and offers credible information to help you make healthful eating choices.
The aim of the Nutrients Special Issue "Implications of Nutrition Education, for Health, Behavior, and Lifestyle" is to publish original research articles and reviews that report the design and implementation of nutrition education intervention programs and their effectiveness in terms of lifestyle, health, and wellbeing. The importance of exploring this field in depth is highlighted in ...
The Journal of Nutrition Education and Behavior ( JNEB ), the official peer-reviewed journal of the Society for Nutrition Education and Behavior Opens in new window , since 1969, serves as a global resource to advance nutrition education and behavior related research, practice, and policy. JNEB publishes original research, as well as papers ...
Many people in the United States don't eat a healthy diet. Healthy People 2030 focuses on helping people get the recommended amounts of healthy foods — like fruits, vegetables, and whole grains — to reduce their risk for chronic diseases and improve their health. 1 The Nutrition and Healthy Eating objectives also aim to help people get recommended amounts of key nutrients, like calcium ...
Education as a Social Determinant of Health. January 27, 2021. Eating healthy, getting regular medical check-ups, exercising and sleeping sufficiently are all behaviors well-known to influence health quality. However, studies suggest one unexpected factor that can predict how long people will live: education.
USDA, HHS. View printable brochures and handouts with healthy eating tips based on the Dietary Guidelines for Americans, 2020-2025, including: Build a Healthy Eating Routine. Cut Down on Added Sugars. MyPlate Print Materials. USDA, Food and Nutrition Service, Center for Nutrition Policy and Promotion.
Nutrition - Public health nutrition information from the CDC. USDA Food and Nutrition - This federal department works to increase food security and reduce hunger by providing children and low-income people better access to a healthful diet and nutrition education. Related Health Topics. Aloe Vera; Arsenic; Gene and Environment Interaction ...
Nutrition Education & Food Safety. FNS programs deliver science-based nutrition education to people at every stage of life from birth through adulthood. Nutrition education complements USDA nutrition assistance programs and supports the health and well-being of individuals, families, and communities. Team Nutrition.
URGENT NEED FOR NEW DIRECTIONS IN EDUCATION-HEALTH RESEARCH. Americans have worse health than people in other high-income countries, and have been falling further behind in recent decades ().This is partially due to the large health inequalities and poor health of adults with low education ().Understanding the health benefits of education is thus integral to reducing health disparities and ...
CFSAN Education Resource Library. FDA's Center for Food Safety and Applied Nutrition (CFSAN) has a wealth of nutrition education materials. Consumers, educators, teachers, dietitians, and health ...
This recognition is evident in the first goal of the EFA which is to expand and improve comprehensive early childhood care and education, especially for the most vulnerable and disadvantaged children, and in five of the MDG goals which relate to the health, nutrition and education of children. 1 Other high-ranked solutions were: number 2 ...
The George Mason College of Public Health has achieved major advancements in the latest U.S. News & World Report rankings, marking a moment of recognition for its commitment to academic excellence and innovation in health education. The institution proudly announces that five of its programs are now ranked among the top 100 in their respective fields, with two distinguished graduate degrees ...
WIC provides nutritious foods, nutrition education, and health care referrals to more than 6 million women, infants, and children who are at nutritional risk. The program's latest revisions will strengthen WIC food packages to better align with the science-based recommendations of the latest Dietary Guidelines for Americans and the National ...
Simulation now is widely used for training and education in different fields including healthcare education. Medicine and healthcare students can be trained in a secure, efficient, and engaging setting by Simulation-based Education (SBE). Therefore, this study aimed to assess the perception of faculty members in the community health departments towards SBE to be used in practical subjects for ...
Healthy living is a way to manage diabetes. To have a healthy lifestyle, take steps now to plan healthy meals and snacks, do physical activities, get enough sleep, and quit smoking or using tobacco products. Healthy living may help keep your body's blood pressure, cholesterol, and blood glucose level, also called blood sugar level, in the ...
The USDA proposed changes to the program in November 2022 and received over 17,000 comments, the agency said. The final provision increases allowances for fruits, vegetables, and seafood, and ...
Who Gets WIC and How to Apply. WIC Eligibility Requirements. Benefits and Services. DOD - WIC Overseas Program. WIC Fact Sheet. WIC FMNP. Links to Other Services. Use the links below to learn more about WIC benefits and services.
Lewiston Health Department 16th Avenue, Lewiston, ID - 21.6 miles. North Central Health District - Clearwater County 115th Street, Orofino, ID - 36.4 miles Provides WIC services, nutrition support, and education to eligible families and individuals in Clearwater County, Idaho. Orofino Health Department 115th Street, Orofino, ID - 36.4 miles
The number of mental health professionals has reduced in recent years. According to the World Health Organization, there are currently 8.5 psychiatrists and 4.6 psychologists per 100,000 of the population. If you need mental health treatment in Russia, you can visit your GP who will refer you for necessary treatment.
Takeda Announces New U.S. Corporate Social Responsibility Program Partners to Build Equity through STEM Education and Access to Nutritional Food. CAMBRIDGE, Massachusetts, April 8, 2024 - Takeda (TSE:4502/NYSE:TAK) today announced the selection of eight new U.S. non-profit organizations as grant recipients, as part of its $14.6 million ...
Arizona Department of Education The Arizona Department of Education is a service organization committed to raising academic outcomes and empowering parents. LEAD HEALTH AND NUTRITION SERVICES SPECIALIST Job Location: Health and Nutrition Services Division Phoenix Location Posting Details: Salary: $73,000 Grade: 21 Closing Date: 04/14/2024 Job Summary: This position will be the lead specialist ...