- See us on facebook
- See us on twitter
- See us on youtube
- See us on linkedin
- See us on instagram

Experimental depression treatment is nearly 80% effective in controlled study
In a double-blind controlled study, high doses of magnetic brain stimulation, given on an accelerated timeline and individually targeted, caused remission in 79% of trial participants with severe depression.
October 28, 2021 - By Mandy Erickson

Since receiving an experimental depression treatment at Stanford, Tommy Van Brocklin has been walking Scout for "the sheer joy of it." Nellie Van Brocklin
A new type of magnetic brain stimulation brought rapid remission to almost 80% of participants with severe depression in a study conducted at the Stanford University School of Medicine .
The treatment, known as Stanford accelerated intelligent neuromodulation therapy (SAINT) or simply Stanford neuromodulation therapy, is an intensive, individualized form of transcranial magnetic stimulation. In the study, remission typically occurred within days and lasted months. The only side effects were temporary fatigue and headaches.
“It works well, it works quickly and it’s noninvasive,” said Nolan Williams , MD, an assistant professor of psychiatry and behavioral sciences. “It could be a game changer.” Williams is the senior author of the study, which was published Oct. 29 in the American Journal of Psychiatry .
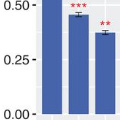
Twenty-nine people with treatment-resistant depression participated in the study: About half received SAINT, and the rest underwent a placebo procedure that mimicked the real treatment. After five days of treatment, 78.6% of the participants in the treatment group were no longer depressed, according to several standard methods of evaluation. “It’s quite a dramatic effect, and it’s quite sustained,” said Alan Schatzberg , MD, the Kenneth T. Norris, Jr. Professor in Psychiatry and Behavioral Sciences, who was a co-author of the study.
A lifetime of depression
Tommy Van Brocklin, 60, has suffered from depression since he was 15. “In 1975, they didn’t have the medication and understanding they do now,” he said. “I was told I wasn’t trying hard enough.”
“I’ve functioned all these years, but it’s been very difficult at times,” the civil engineer added. Talk therapy helped “for about half a day after an appointment.” When selective serotonin reuptake inhibitors became available in the 1990s, he started on paroxetine, commonly sold under the brand name Paxil.
“It worked like a miracle drug,” he said, but after 10 or 15 years it started to lose its effect. After 25 years, it stopped working entirely. He tried other medications, but none helped; one even made him suicidal.
His sister, who lives near Stanford, connected him with the researchers studying SAINT. He flew from his home in Memphis, Tennessee, and underwent the treatment in September. He felt nothing the first day; on day two, he began feeling emotional — “I felt the struggle of what I’d been through all these years.”
“The next day, all of a sudden, it broke through,” he said. “I felt so much better, and it’s stuck with me.”
Specialized magnetic stimulation
The transcranial magnetic stimulation treatment currently approved by the Food and Drug Administration requires six weeks of once-daily sessions. Only about half of patients who undergo the treatment improve, and only about a third experience remission from depression.
SAINT advances that treatment by targeting the magnetic pulses according to each patient’s neurocircuitry and providing a greater number of pulses at a faster pace.
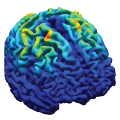
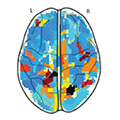
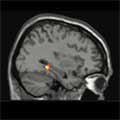
In the study, the researchers first used MRI to locate the best location to target within each participant’s dorsolateral prefrontal cortex, which regulates executive functions, such as problem solving and inhibiting unwanted responses. They applied the stimulation in a subregion that has the strongest relationship with the subgenual cingulate, a part of the brain that is overactive in people experiencing depression. The transcranial magnetic stimulation strengthens the connection between the two regions, facilitating dorsolateral prefrontal cortex control of the activity in the subgenual cingulate.
The researchers also used 1,800 pulses per session instead of 600. (The larger amount has been used safely in other forms of brain stimulation for neurological disorders such as Parkinson’s disease.) And instead of providing one treatment a day, they gave participants 10 10-minute treatments, with 50-minute breaks in between.
For the control group, the researchers disguised the treatment with a magnetic coil that mimicked the experience of the magnetic pulse; both the control and active treatment groups wore noise-canceling earphones and received a topical ointment to dull sensation. Neither the researcher administering the procedure nor the participant knew whether the participant was receiving real treatment.
A hard-to-treat group
The trial participants ranged in age from 22 to 80; on average, they had suffered depression for nine years. They had tried medications, but either they had had no effect or they had stopped working. During the trial, participants who were on medication maintained their regular dosage; participants who weren’t taking medications did not start any.

Nolan Williams demonstrates SAINT, the magnetic brain stimulation therapy he and his colleagues developed, on Deirdre Lehman, a participant in a previous study of the treatment. Steve Fisch
Within four weeks after treatment, 12 of the 14 participants who had received the treatment improved, and 11 of them met FDA criteria for remission. In contrast, only two of the 15 participants who had received the placebo met the criteria for remission.
Because the study participants typically felt better within days of starting SAINT, the researchers are hoping it can be used to quickly treat patients who are at a crisis point. Patients who start taking medication for depression typically don’t experience any reduction of symptoms for a month.
“We want to get this into emergency departments and psychiatric wards where we can treat people who are in a psychiatric emergency,” Williams said. “The period right after hospitalization is when there’s the highest risk of suicide.”
Van Brocklin said that since he returned home following treatment, he’s made some radical changes. “I have a really strong desire to get my life together,” he said.
“I don’t procrastinate anymore,” he added. “I’m sleeping better. I completely quit alcohol. I’m walking my dog and playing the guitar again, for nothing more than the sheer joy of it.”
Most importantly, he said, “I’m remaining positive and being respectful of others. These are big changes in my life.”
Other Stanford scientists who contributed to the study are former postdoctoral scholars Eleanor Cole, PhD, and Angela Phillips, PhD; Brandon Bentzley, MD, PhD, David Carreon, MD, Jennifer Keller, PhD, Kristin Raj, MD, and Flint Espil, PhD, all clinical assistant professors of psychiatry and behavioral sciences; clinical research coordinators Katy Stimpson, Romina Nejad, Clive Veerapal, Nicole Odenwald and Maureen Chang; former clinical research coordinators Fahim Barmak, MD, Naushaba Khan and Rachel Rapier; postdoctoral scholars Kirsten Cherian, PhD, James Bishop, PhD, Azeezat Azeez, PhD, and John Coetzee, PhD; life science research professional Heather Pankow; clinical research manager Jessica Hawkins; Charles DeBattista, MD, professor of psychiatry and behavioral sciences; and Booil Jo, PhD, associate professor of psychiatry and behavioral sciences.
Scientists from the U.S. Department of Veterans Affairs; Palo Alto University; the Centre for Neuroimaging and Cognitive Genomics at the National University of Ireland; and the School of Medicine at Southern Illinois University, Carbondale, contributed to the research.
The research was funded by a Brain and Behavior Research Foundation Young Investigator Award, Charles R. Schwab, the David and Amanda Chao Fund II, the Amy Roth PhD Fund, the Neuromodulation Research Fund, the Lehman Family, the Still Charitable Trust, the Marshall and Dee Ann Payne Fund, and the Gordie Brookstone Fund.
Stanford’s Department of Psychiatry and Behavioral Sciences also contributed to the work.
If you're interested in participating in a study, please email [email protected] .

About Stanford Medicine
Stanford Medicine is an integrated academic health system comprising the Stanford School of Medicine and adult and pediatric health care delivery systems. Together, they harness the full potential of biomedicine through collaborative research, education and clinical care for patients. For more information, please visit med.stanford.edu .
Artificial intelligence
Exploring ways AI is applied to health care


Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years! Learn More >>
- Science News
- Meetings and Events
- Social Media
- Press Resources
- Email Updates
- Innovation Speaker Series
Science News About Depression

February 27, 2024 • Press Release
Results from a large clinical trial funded by the National Institutes of Health show that an intervention for anxiety provided to pregnant women living in Pakistan significantly reduced the likelihood of the women developing moderate-to-severe anxiety, depression, or both six weeks after birth.
December 18, 2023 • Research Highlight
This clinical trial found that MST is equally effective at reducing depression symptoms as ECT, but with fewer side effects.

October 27, 2023 • Feature Story • 75th Anniversary
NIMH supported science and NIMH researchers helped pave the way for the development of ketamine—a groundbreaking treatment that has improved the lives of those who are impacted by treatment-resistant depression.

June 16, 2023 • Research Highlight
In this NIMH-funded study, researchers examined how trauma gets passed from one generation to the next.

May 15, 2023 • Research Highlight
New NIMH-funded research tracked population-level rates of postpartum depression among new mothers before, during, and after pregnancy.

January 9, 2023 • Research Highlight
An NIMH-supported study suggests that a brief self-association training program can extend the effects of a single ketamine infusion by shifting people’s negative self-beliefs.

September 29, 2022 • Research Highlight
In a recent study supported by the National Institute of Mental Health, researchers examined the impact of a family-based intervention on suicide risk in youth and found risk-reduction benefits up to 10 years later.

May 9, 2022 • Research Highlight
NIMH-supported researchers have found an online mindfulness-based cognitive behavioral therapy—called Mindful Mood Balance—is effective at reducing residual depressive symptoms and at reducing suicidal ideation in those who experience these symptoms.

March 25, 2022 • Research Highlight
TMS can only directly stimulate the outermost layer of the brain, but NIMH researchers have found that mapping a person’s brain architecture may make it possible to guide TMS to deep brain targets.

February 28, 2022 • Research Highlight
A recent NIMH-supported study investigated whether deep brain stimulation could be personalized for individuals with treatment-resistant depression.

May 26, 2021 • Research Highlight
NIMH-supported researchers investigated suicide risk among women in the year before and year after giving birth.

April 15, 2021 • Research Highlight
NIMH is working to meet the urgent need for rapid-acting suicide prevention interventions by supporting research investigating the feasibility and safety of treatment protocols that have the potential to quickly reduce severe suicide risk in youth and adults.

February 9, 2021 • Press Release
A new study conducted by researchers at NIMH suggests that differences in the expression of gene transcripts – readouts copied from DNA that help maintain and build our cells – may hold the key to understanding how mental disorders with shared genetic risk factors result in different patterns of onset, symptoms, course of illness, and treatment responses.

October 29, 2020 • Research Highlight
In a project funded by the NIMH Small Business Technology Transfer program, researchers are investigating whether mobile technology can be used to create a passive monitoring system that can predict teens’ depressive symptoms and improve the quality of their care.

October 22, 2020 • Institute Update
Carlos Zarate Jr., M.D., chief of the Experimental Therapeutics and Pathophysiology Branch within the NIMH Intramural Research Program, has been elected to the National Academy of Medicine.

April 20, 2020 • Press Release
Researchers investigating how temperament shapes adult life-course outcomes have found that behavioral inhibition in infancy predicts a reserved, introverted personality at age 26 and for some, a risk of internalizing psychopathology such as anxiety and depression.

March 30, 2020 • Press Release
An innovative NIMH-funded trial shows that a receptor involved in the brain’s reward system may be a viable target for treating anhedonia (or lack of pleasure), a key symptom of several mood and anxiety disorders.

February 25, 2020 • Research Highlight
The use of right unilateral ultrabrief pulse (RUL-UB) electroconvulsive therapy (ECT) in combination with the antidepressant venlafaxine to treat depression in elderly patients is well tolerated and results in minimal neurocognitive side effects, according to a new NIH-funded study published in the American Journal of Geriatric Psychiatry.

For many adults who have a mental disorder, symptoms were present—but often not recognized or addressed—in childhood and adolescence. Early treatment can help prevent more severe, lasting impairment or disability as a child grows up.

February 10, 2020 • Press Release
NIH-funded research uses machine learning algorithm to predict individual response to a commonly-prescribed antidepressant.

November 18, 2019 • Press Release
A single, low-dose ketamine infusion was relatively free of side effects for patients with treatment-resistant depression.

October 2, 2019 • Press Release
Researchers have uncovered sex-based differences in the development of the hippocampus and amygdala—brain areas that have been implicated in the biology of several mental disorders that impact males and females differently.

September 3, 2019 • Institute Update
Mental health research center directors emerged from a recent meeting with a renewed commitment to help each other achieve their common mission – to transform care of children, adolescents and adults with severe psychiatric disorders.

April 29, 2019 • Press Release
A study conducted by researchers at several universities, hospitals, and the National Institute of Mental Health (NIMH) found that the Netflix show “13 Reasons Why” was associated with a 28.9% increase in suicide rates among U.S. youth ages 10-17 in the month (April 2017) following the shows release, after accounting for ongoing trends in suicide rates.

The National Institutes of Health invites students ages 16 to 18 years old to participate in the “Speaking Up About Mental Health!” essay contest to explore ways to address the stigma and social barriers that adolescents from racial and ethnic minority populations may face when seeking mental health treatment.

April 11, 2019 • Press Release
Researchers have identified ketamine-induced brain-related changes that are responsible for maintaining the remission of behaviors related to depression in mice — findings that may help researchers develop interventions that promote lasting remission of depression in humans.

March 19, 2019 • Media Advisory
FDA approval of the postpartum depression treatment brexanolone represents the final phase of a bench-to-bedside journey for this drug — a journey that began in the NIMH Intramural Research Program. NIMH experts are available to provide information on postpartum depression and the importance of, and the science underlying, this new drug.
March 13, 2019 • Press Release
Researchers have identified changes in brain connectivity and brain activity during rest and reward anticipation in children with anhedonia, a condition where people lose interest and pleasure in activities they used to enjoy.

March 11, 2019 • Press Release
A research team found nearly one-third of youth ages 10 to 12 years screened positive for suicide risk in emergency department settings, including those seeking help for physical concerns only.

December 13, 2018 • Science Update
A new study looking at interactions among sleep, energy, activity level, and mood suggests that instability in activity and sleep systems could lead to mood changes. The findings suggest new targets for depression treatment.

June 20, 2018 • Press Release
Researchers funded by the National Institutes of Health have shown that a therapy-based treatment for disruptive behavioral disorders can be adapted and used as an effective treatment option for early childhood depression.

April 16, 2018 • Institute Update
On May 3, 2018, join NIMH for a Twitter chat on teen depression with experts Dr. Argyris Stringaris and Dr. Ken Towbin.
March 1, 2018 • Science Update
Depression, schizophrenia and autism spectrum disorder share some of the same patterns of suspect gene expression – molecular signatures.
February 13, 2018 • Science Update
On February 20, 2018, join NIMH for a Twitter chat on Seasonal Affective Disorder with expert Dr. Matthew Rudorfer.
November 2, 2017 • Press Release
Using a molecular method likely to become widely adopted by the field, researchers have discovered brain circuitry essential for alertness – and for brain states more generally.
August 28, 2017 • Science Update
Brain gene expression associated with depression differed markedly between men and women. Such divergent “transcriptional signatures” may signal divergent underlying illness processes requiring sex-specific treatments.

July 20, 2017 • Institute Update
This November 2016 RDoC webinar highlights the role of fear and anxiety in disorders such as phobias and depression.
May 31, 2017 • Science Update
NIMH grantee Karl Deisseroth, M.D., Ph.D., of Stanford University, has been awarded one of science’s most generous prizes. A German foundation presented the inventor of technologies that are transforming neuroscience with its 4 million euros Fresenius Prize.

A streamlined behavioral therapy delivered in a pediatrics practice offered much greater benefit to youth with anxiety and depression than a more standard referral to mental health care with follow-up in a clinical trial comparing the two approaches.
April 19, 2017 • Science Update
Brain scans reveal that fluctuations in estrogen can trigger atypical functioning in a key brain memory circuit in women with a common version of a gene. Since working memory function is often disturbed in mental disorders, such gene-hormone interactions are suspect mechanisms that may confer risk.

August 1, 2016 • Press Release
Scientists have discovered 15 genome sites – the first ever – linked to depression in people of European ancestry. But – in a twist – the researchers didn’t have to sequence anyone’s genes! Instead, they analyzed data already shared by people who had purchased their own genetic profiles via an online service and elected to participate in its research option.
July 18, 2016 • Science Update
An individualized program of follow-up treatment with electroconvulsive therapy (ECT) combined with an antidepressant was effective in preventing relapse in patients 60 years and older who had had a successful initial course of treatment for severe depression.
June 16, 2016 • Live Chat
A live Twitter chat discussing African American men’s mental health.
May 4, 2016 • Press Release
A chemical byproduct, or metabolite, created as the body breaks down likely holds the secret to its rapid antidepressant action .

March 17, 2016 • Science Update
On March 17, 2016, NIMH hosts a Facebook Q&A on electroconvulsive therapy with expert Dr. Sarah Lisanby.

February 19, 2016 • Science Update
Is mobile mental health research the next frontier for smartphones? Based on Dr. Patricia Areán’s pioneering BRIGHTEN study, research via smartphone app is already a reality.

August 12, 2015 • Science Update
View the archived webinars with NIMH experts and grantees, which focus on training, research, and methodology

July 16, 2015 • Science Update
A new video about postpartum depression marks the launch of a mental health education collaboration by two NIH Institutes and one of the nation’s largest African-American women’s organizations.

July 14, 2015 • Live Chat
NIMH and NCI host a Twitter chat on how patients and caregivers, across all ages, can deal with the psychological impact of cancer.

January 29, 2015 • Science Update
Risk genes for different mental disorders work through same pathways

November 5, 2014 • Live Chat
NIMH Twitter Chat on Men and Depression
October 17, 2014 • Press Release
A drug being studied as a fast-acting mood-lifter restored pleasure-seeking behavior independent of – and ahead of – its other antidepressant effects.
October 2, 2014 • Science Update
NIMH Twitter Chat on Depression and the Development of Novel Medications
July 29, 2014 • Science Update
NIMH Twitter Chat on Premenstrual Dysphoric Disorder
June 10, 2014 • Science Update
May 5, 2014 • Science Update
NIMH Twitter Chat on Postpartum Depression

April 17, 2014 • Press Release
Scientists have traced vulnerability to depression-like behaviors to out-of-balance neuronal electrical activity and made mice resilient by reversing it.

March 11, 2014 • Science Update
Girls in public housing benefited emotionally from a move to a better neighborhood while boys fared worse than if they’d stayed in the poor neighborhood. Rates of depression and conduct disorder markedly increased in boys and decreased in girls. Boys also experienced significantly increased rates of post-traumatic stress disorder (PTSD), complicating housing policy decision-making.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- World J Clin Cases
- v.9(31); 2021 Nov 6
Major depressive disorder: Validated treatments and future challenges
Rabie karrouri.
Department of Psychiatry, Moulay Ismaïl Military Hospital, Faculty of Medicine and Pharmacy, Sidi Mohamed Ben Abdellah University, Fez 30070, Morocco
Zakaria Hammani
Roukaya benjelloun.
Department of Psychiatry, Faculty of Medicine, Mohammed VI University of Health Sciences, Casablanca 20000, Morocco
Yassine Otheman
Department of Psychiatry, Moulay Ismaïl Military Hospital, Faculty of Medicine and Pharmacy, Sidi Mohamed Ben Abdellah University, Fez 30070, Morocco. [email protected]
Corresponding author: Yassine Otheman, MD, Associate Professor, Chief Doctor, Department of Psychiatry, Moulay Ismaïl Military Hospital, Faculty of Medicine and Pharmacy, Sidi Mohamed Ben Abdellah University, 1893, Km 2.2 road of Sidi Hrazem, Fez 30070, Morocco. [email protected]
Depression is a prevalent psychiatric disorder that often leads to poor quality of life and impaired functioning. Treatment during the acute phase of a major depressive episode aims to help the patient reach a remission state and eventually return to their baseline level of functioning. Pharmacotherapy, especially selective serotonin reuptake inhibitors antidepressants, remains the most frequent option for treating depression during the acute phase, while other promising pharmacological options are still competing for the attention of practitioners. Depression-focused psychotherapy is the second most common option for helping patients overcome the acute phase, maintain remission, and prevent relapses. Electroconvulsive therapy is the most effective somatic therapy for depression in some specific situations; meanwhile, other methods have limits, and their specific indications are still being studied. Combining medications, psychotherapy, and somatic therapies remains the most effective way to manage resistant forms of depression.
Core Tip: Depression is a persistent public health problem for which treatments must be codified and simplified to enhance current practice. Several therapies have been suggested worldwide, with varying levels of validity. This article explores effective and valid therapies for treating depression by addressing current and future research topics for different treatment categories.
INTRODUCTION
Depression is a common psychiatric disorder and a major contributor to the global burden of diseases. According to the World Health Organization, depression is the second-leading cause of disability in the world and is projected to rank first by 2030[ 1 ]. Depression is also associated with high rates of suicidal behavior and mortality[ 2 ].
Treatments administered during the acute phase of a major depressive episode aim to help the patient reach a remission state and eventually return to their baseline level of functioning[ 3 ]. Acute-phase treatment options include pharmacotherapy, depression-focused psychotherapy, combinations of medications and psychotherapy, and somatic therapies such as electroconvulsive therapy (ECT). Nevertheless, managing the acute phase of depression is only the first step in a long therapy process that aims to maintain remission and prevent relapses. In this article, we discuss various treatment options implemented by clinicians, highlighting the role that each option plays in actual psychiatric practice.
PHARMACOTHERAPY
While selective serotonin reuptake inhibitors (SSRIs) remain the gold-standard treatment for depression, new antidepressants are always being developed and tested. The ultimate goal is to discover a molecule that exhibits quick effectiveness with as few side effects as possible.
Daniel Bovet studied the structure of histamine (the causative agent in allergic responses) to find an antagonist, which was finally synthesized in 1937[ 4 ]. Since then, many researchers have studied the link between the structures and activities of different antihistaminic agents, contributing to the discovery of almost all antidepressants[ 5 ].
In the following subsections, we list the main classes of antidepressants in chronological order of apparition, highlighting the most widely used molecules in daily psychiatric practice.
Monoamine oxidase inhibitors
Iproniazid was the first drug defined as an antidepressant; it was later classified as a monoamine oxidase inhibitor (MAOI)[ 6 , 7 ]. Several other MAOIs have been introduced since 1957[ 8 ]. Due to their irreversible inhibition of monoamine oxidase, MOAIs have numerous side effects, such as hepatotoxicity and hypertensive crises, that can lead to lethal intracranial hemorrhages. Consequently, MAOIs have become less commonly used over time[ 9 ].
Trials have demonstrated that MAOIs’ efficacy is comparable to that of tricyclic antidepressants (TCAs)[ 10 , 11 ]. However, considering MAOIs’ drug interactions, dietary restrictions, and potentially dangerous side effects, they are now almost exclusively prescribed for patients who have not responded to several other pharmacotherapies, including TCAs[ 9 ]. Furthermore, MAOIs have demonstrated specific efficacy in treating depression with atypical features, such as reactive moods, reverse neuro-vegetative symptoms, and sensitivity to rejection[ 12 ].
MAOIs are also a potential therapeutic option when ECT is contraindicated[ 13 ]. MAOIs’ effectiveness is still unclear for treating depression in patients who are resistant to multiple sequential trials with SSRIs and serotonin-norepinephrine reuptake inhibitors (SNRIs)[ 14 ]. Nevertheless, psychiatrists’ use of MAOIs has declined over the years[ 15 , 16 ]. The use of MAOIs is generally restricted to patients who do not respond to other treatments.
The first TCA was discovered and released for clinical use in 1957 under the brand name Tofranil[ 5 , 17 ]. Since then, TCAs have remained among the most frequently prescribed drugs worldwide[ 9 ]. TCAs-such as amitriptyline, nortriptyline, protriptyline, imipramine, desipramine, doxepin, and trimipramine-are about as effective as other classes of antidepressants-including SSRIs, SNRIs, and MAOIs-in treating major depression[ 18 , 19 ].
However, some TCAs can be more effective than SSRIs when used to treat hospitalized patients[ 20 ]. This efficacy can be explained by the superiority of TCAs over SSRIs for patients with severe major depressive disorder (MDD) symptoms who require hospitalization[ 21 - 24 ]. However, no differences have been detected in outpatients who are considered less severely ill[ 18 , 20 ]. In most cases, TCAs should generally be reserved for situations when first-line drug treatments have failed[ 25 ].
In December 1987, a series of clinical studies confirmed that an SSRI called fluoxetine was as effective as TCAs for treating depression while causing fewer adverse effects[ 26 ]. After being released onto the market, its use expanded more quickly than that of any other psychotropic in history. In 1994, it was the second-best-selling drug in the world[ 7 ].
Currently available SSRIs include fluoxetine, sertraline, paroxetine, fluvoxamine, citalopram, and escitalopram. They have elicited different tolerance rates and side effects-mostly sexual and digestive (nausea and loss of appetite), as well as irritability, anxiety, insomnia, and headaches[ 27 ]. Nevertheless, SSRIs have a good tolerability profile[ 28 ].
In most systematic reviews and meta-analyses, SSRIs have demonstrated comparable efficacy to TCAs[ 18 , 19 , 29 ], and there is no significant evidence indicating the superiority of any other class or agent over SSRIs[ 29 - 31 ]. Furthermore, studies show no differences in efficacy among individual SSRIs[ 29 , 31 - 34 ]. Therefore, most guidelines currently recommend SSRIs as the first-line treatment for patients with major depression[ 25 ].
Norepinephrine reuptake inhibitors
Other monoamine (norepinephrine, serotonin, and dopamine) neurotransmitter reuptake inhibitors called SNRIs emerged during the 1990s to protect patients against the adverse effects of SSRIs[ 35 ]. Currently available SNRIs are venlafaxine, desvenlafaxine (the principal metabolite of venlafaxine), and duloxetine. The extended-release form of venlafaxine is the most commonly used drug in this class. Clinical guidelines commonly recommend prescribing SNRI to patients who do not respond to SSRIs[ 25 ].
In individual studies, venlafaxine and duloxetine are generally considered effective as SSRIs[ 36 ]. Also, venlafaxine’s efficacy is comparable to that of TCAs[ 37 , 38 ].
According to some meta-analyses, reboxetine (a selective noradrenaline reuptake inhibitor) seems less efficacious than SSRIs[ 39 ]. However, these findings could be due to the relatively poor tolerance of reboxetine[ 40 ].
Other antidepressants
Trazodone is the oldest medication of the so-called “other antidepressants” group that is still in wide use[ 41 , 42 ]. It has been shown to be an effective antidepressant in placebo-controlled research. However, in contemporary practice, it is much more likely to be used in low doses as a sedative-hypnotic than as an antidepressant[ 41 , 42 ].
Nefazodone’s structure is analogous to that of trazodone, though it has different pharmacological properties[ 43 ]. Its efficacy and overall tolerability are comparable to those of SSRIs, as indicated by comparative trials[ 43 ]. However, its use is associated with rare (but fatal) cases of clinical idiosyncratic hepatotoxicity[ 44 ].
Bupropion’s mechanism of action remains unclear, though it is classified as a norepinephrine and dopamine reuptake inhibitor[ 45 ]. It appears to have a more activating profile than SSRIs that are modestly superior to bupropion in patients with MDD[ 46 ]. However, for individuals with low to moderate levels of anxiety, the efficacy of bupropion in treating MDD is comparable to that of SSRIs[ 46 ]. Moreover, bupropion has a better tolerability profile than SSRIs, with minimal weight gain (or even leading to weight loss)[ 46 ]. In addition, bupropion is more likely than some SSRIs to improve symptoms of fatigue and sleepiness[ 47 ].
Mirtazapine and mianserin are tetracyclic compounds believed to increase the availability of serotonin or norepinephrine (or both), at least initially. Mirtazapine’s ability to antagonize serotoninergic subtypes receptors, <5-HT2A> and <5-HT2C>, could also increase norepinephrine and dopamine release in cortical regions[ 25 ]. Mirtazapine is about as effective as SSRIs[ 48 ].
Recently, drugs have been developed that block serotonin reuptake while affecting a variety of 5-HT receptor subtypes. The advantages of these agents ( e.g. , vilazodone and vortioxetine) over SSRIs are not fully clear. However, they appear to produce less sexual dysfunction and, in the specific case of vortioxetine, have particular benefits in depression-related cognitive impairment[ 49 ]. Indeed, vortioxetine is a very recent antidepressant with a multimodal mechanism that is thought to have a high affinity for serotonin transporters and 5-HT3, 5HT1A, 5HT7 receptors. Such a specific profile seems to indicate a level of efficacy to other antidepressants with a specific action on cognitive impairments[ 50 , 51 ].
In conclusion, no significant differences have been found between different classes of antidepressants in terms of their efficacy[ 52 ], though some drugs show some weak-to-moderate evidence indicating they are more effective than some other drugs[ 53 ]. Concerning the acceptability of these drugs, citalopram, escitalopram, fluoxetine, sertraline, and vortioxetine have been deemed more tolerable than other antidepressants, whereas amitriptyline, clomipramine, duloxetine, fluvoxamine, trazodone, and venlafaxine had the highest dropout rates[ 53 ] because of their more frequent and severe side effects. Nausea and vomiting were the most common reasons for treatment discontinuation; sexual dysfunction, sedation, priapism, and cardiotoxicity were also reported[ 31 , 41 ].
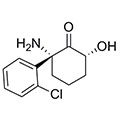
Ketamine and related molecules
In intravenous sub-anesthetic doses, ketamine has very quick effects on resistant unipolar (and, possibly, bipolar) depression and acute suicidal ideation[ 54 , 55 ]. The antidepressant effect of ketamine can persist for several days but eventually wanes. A few reports are have cited oral and intranasal formulations of ketamine for treatment-resistant depression[ 56 , 57 ], but there is still no data about the potential link between the onset of action and the route of administration.
Common adverse effects of ketamine include dizziness, neurotoxicity, cognitive dysfunction, blurred vision, psychosis, dissociation, urological dysfunction, restlessness, headache, nausea, vomiting, and cardiovascular symptoms[ 58 ]. Such adverse effects tend to be brief in acute, low-dose treatments[ 36 ], whereas prolonged exposure may predispose patients to neurotoxicity and drug dependence[ 56 ]. Lastly, since ketamine is associated with a higher risk of drug abuse and addiction, it cannot be recommended in daily clinical practice[ 59 , 60 ].
Ketamine is not a miracle drug, and many important factors still need to be defined, such as the most effective dose and the optimal administration route[ 61 , 62 ]. The current lack of guidelines about the therapeutic monitoring of ketamine treatment for depression further complicates the expanding use of this treatment[ 56 ]. Even though ketamine might never reach the market, it has stimulated research in the neurobiology of depression, including studies on potential fast and long-lasting antidepressants.
Ketamine has an active metabolite (hydroxynorketamine) that can produce rapid and sustained glutamatergic stimulation. It also seems to be free of many of the safety problems associated with ketamine and, thus, should be studied.
Research on the S-enantiomer of ketamine (S-ketamine, or esketamine, especially intranasal) could also be valuable, as it has a 3 to 4 times greater affinity than ketamine for the N-methyl-D-aspartate (NMDA) receptor[ 40 ]. It was approved by the United States Food and Drug Administration in March 2019 for treatment-resistant depression. However, current knowledge about the effects of prolonged esketamine therapy is still preliminary. In addition, regarding the potential risk of abuse, esketamine use must be carefully monitored[ 63 - 65 ].
Other glutamate receptor modulators have been evaluated in small studies as monotherapy agents or as adjuncts to other antidepressants. Examples include noncompetitive NMDA receptor antagonists (memantine, dextromethorphan/quinidi-ne, dextromethorphan/bupropion, and lanicemine), NR2B subunit-specific NMDA receptor antagonists (traxoprodil), NMDA receptor glycine site partial agonists (D-cycloserine, rapastinel), and metabotropic glutamate receptor antagonists (basimglurant, declogurant)[ 66 - 68 ] (Table (Table1). 1 ).
Main classes of antidepressants with their date of approval, contributions, and disadvantages
NMDA: N-methyl-D-aspartate; SSRI: DSelective serotonin reuptake inhibitors; MDD: Major depressive disorder; MAOI: Monoamine oxidase inhibitor.
Perspectives
A purely neurotransmitter-based explanation for antidepressant drug action-especially serotonin-inhibiting drugs-is challenged by the significant percentage of patients who never achieve full remission[ 6 ] and the delayed clinical onset, which varies from two to four weeks. Moreover, studies show an acute increase in monoamines in the synaptic cleft immediately following treatment[ 69 ], even when the depletion of tryptophan (serotonin’s precursor) does not induce depressive-like behavior in healthy humans[ 70 , 71 ].
This finding shows that research on the pharmacological options for treating depression must go beyond monoaminergic neurotransmission systems. Research on the development of new antidepressants should explore several mechanisms of action on several types of receptors: Antagonism, inhibition of the reuptake of neurotransmitters, and modulators of glutamate receptors, as well as interactions with α-amino-3-acid receptors, hydroxy-5-methyl-4-isoxazolepropionic, brain-derived neurotrophic factor, tyrosine kinase B receptor (the mechanistic target of rapamycin), and glycogen synthase kinase-3[ 72 ].
Identifying the cellular targets of rapid-acting agents like ketamine could help practitioners develop more effective antidepressant molecules by revealing other receptors involved in gamma-aminobutyric acid regulation and glutamate transmission[ 73 ].
PSYCHOTHERAPY
Psychotherapeutic interventions are widely used to treat and prevent most psychiatric disorders. Such interventions are common in cases of depression, psychosocial difficulties, interpersonal problems, and intra-psychic conflicts. The specific psychotherapy approach chosen for any given case depends on the patient’s preference, as well as on the clinician’s background and availability[ 74 ] . Psychotherapy for patients with depression strengthens the therapeutic alliance and enables the patient to monitor their mood, improve their functioning, understand their symptoms better, and master the practical tools they need to cope with stressful events[ 75 ]. The following subsections briefly describe psychotherapeutic interventions that have been designed specifically for patients with depression.
Overview of psychotherapy in depression
Depression-focused psychotherapy is typically considered the initial treatment method for mild to moderate MDD. Based on significant clinical evidence, two specific psychotherapeutic methods are recommended: Cognitive-behavioral therapy (CBT) and interpersonal therapy (IPT). Supportive therapy (ST) and psychoeducational intervention (PEI) have also been recommended, those the evidence supporting these methods s not as strong. In more cases of severe depression, ST and PEI are used only to augment pharmacological treatments.
After remission, CBT, PEI, and mindfulness-based cognitive therapy (MBCT) are proposed to maintain and prevent depression. However, when psychotherapy has been effective during the initial phases of a depressive episode, it should be continued to maintain remission and prevent relapses while reducing the frequency of sessions[ 25 , 75 , 76 ].
Specific and intensive psychotherapeutic support is recommended for patients with chronic depression because of high rates of comorbidity with personality disorders, early trauma, and attachment deficits. The European Psychiatric Association recommends using the Cognitive Behavioral Analysis System of Psychotherapy (CBASP) for treating chronic depression and utilizing specific approaches suited to each patient’s preferences[ 77 ]. All these therapeutic options are summarized in Figure Figure1 1 .

Overview of psychotherapy in different clinical situations of depression. MDD: Major depressive disorder; CBT: Cognitive-behavioral therapy; IPT: Interpersonal therapy; ST: Supportive therapy; PEI: Psycho-educational intervention; MBCT: Mindfulness based cognitive therapy; SIPS: Specific and intensive psychotherapeutic support; CBASP: Cognitive Behavioral Analysis System of Psychotherapy.
Structured psychotherapies
Cognitive and behavioral therapies: Based on robust evidence, CBT is one of the most well-documented and validated psychotherapeutic methods available. Interventional strategies are based on modifying dysfunctional behaviors and cognitions[ 77 ]. CBT targets depressed patients’ irrational beliefs and distorted cognitions that perpetuate depressive symptoms by challenging and reversing them[ 3 ]. Thus, CBT is a well-known effective treatment method for MDD[ 78 ] and has been recommended in most guidelines as a first-line treatment[ 79 - 81 ].
However, the effectiveness of CBT depends on patient’s capacity to observe and change their own beliefs and behaviors. Some simple techniques were developed to overcome this issue, especially in primary care management. Behavioral activation is one such technique, consisting of integrating pleasant activities into daily life to increase the number and intensity of the positive interactions that the patient has with their environment[ 82 , 83 ].
Acceptance and commitment therapy is another form of CBT. This type of therapy, which is based on functional contextualism, can help patients accept and adjusting to persistent problems. It appears to be effective in reducing depressive symptoms and preventing relapses[ 77 , 84 ].
Another form of CBT is computerized CBT (CCBT), implemented via a computer with a CD-ROM, DVD, or online CCBT, allowing patients to benefit from this therapy under conditions of reduced mobility, remoteness, confinement, or quarantine[ 79 ] .
CCBT and guided bibliotherapy based on CBT could be considered for self-motivated patients with mild to moderate major depression or as a complementary treatment to pharmacotherapy[ 25 ]. CBT is also recommended for patients with resistant depression in combination with antidepressants[ 85 ].
Schema therapy is another CBT-derived therapy that can be used in patients who have failed classical CBT, like patients with personality disorder comorbidity. Schema therapy is about as effective as CBT for treating depression[ 86 ]. In adolescent patients with depression, CBT is also a recommended option with plenty of evidence from multiple trials. Meanwhile, it remains the first-line treatment in children despite mixed findings across trials[ 87 ] . CBT is also a promising option for elderly depressed patients, though substantial evidence is still lacking because of the limited data on the subject[ 88 ] .
IPT: The goal of IPT is to identify the triggers of depressive symptoms or episodes. These triggers may include losses, social isolation, or difficulties in social interactions. The role of the intervention is to facilitate mourning (in the case of bereavement), help the patient recognize their own affect, and resolve social interaction dysfunction by building their social skills and social supports[ 89 ]. IPT, like CBT, is a first-line treatment for mild to moderate major depressive episodes in adults; it is also a well-established intervention for adolescents with depression[ 25 ] .
Problem-solving therapy: The problem-solving therapy (PST) approach combines cognitive and interpersonal elements, focusing on negative assessments of situations and problem-solving strategies. PST has been used in different clinical situations, like preventing depression among the elderly and treating patients with mild depressive symptoms, especially in primary care. Despite its small effect sizes, PST is comparable to other psychotherapeutic methods used to treat depression[ 88 , 90 ].
Marital and family therapy: Marital and family therapy (MFT) is effective in treating some aspects of depression. Family therapy has also been used to treat severe forms of depression associated with medications and hospitalization[ 91 ]. Marital and family problems can make people more vulnerable to depression, and MFT addresses these issues[ 92 ]. Marital therapy includes both members of the couple, as depression is considered in an interpersonal context in such cases. Some of the goals of this therapy are to facilitate communication and resolve different types of marital conflict. Family therapy uses similar principles as other forms of therapy while involving all family members and considering depression within the context of pathological family dynamics[ 93 ].
ST: Although ST is not as well-structured or well-evaluated as CBT or IPT, it is still commonly used to support depressed patients. In addition to sympathetic listening and expressing concern for the patient’s problems, ST requires emotionally attuned listening, empathic paraphrasing, explaining the nature of the patient’s suffering, and reassuring and encouraging them. These practices allow the patient to ventilate and accept their feelings, increase their self-esteem, and enhance their adaptive coping skills[ 94 ].
Psychodynamic therapy: Psychodynamic therapy encompasses a range of brief to long-term psychological interventions derived from psychoanalytic theories. This type of therapy focuses on intrapsychic conflicts related to shame, repressed impulses, problems in early childhood with one’s emotional caretakers that lead to low self-esteem and poor emotional self-regulation[ 93 , 95 ]. Psychodynamic therapy’s efficacy in the acute phase of MDD is well-established compared to other forms of psychotherapy.
Group therapy: The application of group therapy (GT) to MDD remains limited. Some data support the efficacy of specific types of GT inspired by CBT and IPT[ 96 - 98 ]. Group CBT for patients with subthreshold depression is an effective post-depressive-symptomatology treatment but not during the follow-up period[ 99 ]. Supportive GT and group CBT reduce depressive symptoms[ 96 ], especially in patients with common comorbid conditions[ 100 ]. However, studies are still lacking in this domain.
MBCT: MBCT is a relatively recent technique that combines elements of CBT with mindfulness-based stress reduction[ 101 ]. Studies have shown that eight weeks of MBCT treatment during remission reduces relapse. Thus, it is a potential alternative to reduce, or even stop, antidepressant treatment without increasing the risk of depressive recurrence, especially for patients at a high risk of relapse ( i.e. , patients with more than two previous episodes and patients who have experienced childhood abuse or trauma)[ 102 ].
Other psycho-interventions
Psycho-education: This type of intervention educates depressed patients and (with their permission) family members involved in the patient’s life about depression symptoms and management. This education should be provided in a language that the patient understands. Issues such as misperceptions about medication, treatment duration, the risk of relapse, and prodromes of depression should be addressed. Moreover, patients should be encouraged to maintain healthy lifestyles and enhance their social skills to prevent depression and boost their overall mental health. Many studies have highlighted the role of psycho-education in improving the clinical course, treatment adherence, and psychosocial functioning in patients with depression[ 103 ].
Physical exercise: Most guidelines for treating depression, including the National Institute for Health and Care Excellence, the American Psychiatric Association, and the Royal Australian and New Zealand College of Psychiatrists, recommend that depressed patients perform regular physical activity to alleviate symptoms and prevent relapses[ 104 ] . Exercise also promotes improvements in one’s quality of life in general[ 105 ] . However, exercise is considered an adjunct to other anti-depressive treatments[ 25 ] .
Although psychotherapy is effective for treating depression and improving patients’ quality of life, its direct actions against depressive symptoms are not fully understood[ 106 ]. Identifying factors ( e.g. , interpersonal variables) linked to treatment responses can help therapists choose the right therapeutic strategy for each patient and guide research to modify existing therapies and develop new ones[ 107 ].
Since depression is a primary care problematic, simplifying psychotherapy procedures will increase the use of psychological interventions for depression, especially in general practice. Brief forms (six to eight sessions) of CBT and PST have already shown their effectiveness for treating depression[ 108 ]. Nevertheless, simpler solutions must be made available to practitioners to help them manage and prevent depression.
SOMATIC TREATMENTS
In many situations, depression can also be managed via somatic treatments. ECT is the most well-known treatment for resistant depression, and solid evidence supports its effectiveness and safety. In recent decades, various innovative techniques have been proposed, such as repetitive transcranial magnetic stimulation (rTMS), transcranial direct current stimulation (tDCS), vagus nerve stimulation (VNS), deep brain stimulation (DBS), and magnetic seizure therapy, with varying efficiency levels[ 109 ].
ECT is arguably the most effective treatment modality in psychiatry, and its superiority over pharmacotherapy for major unipolar depression is widely supported[ 110 ]. ECT reduces the number of hospital readmissions and lightens the burden of depression, leading to a better quality of life[ 111 , 112 ].
Moreover, ECT is considered safe[ 113 ]. Advances in anesthesia and ECT techniques have decreased complications related to ECT while also improving cognitive outcomes and patient satisfaction.
However, the stigma surrounding ECT limits its use. Most misconceptions date back to early ECT techniques (when it was performed without muscle relaxants or anesthesia). Nevertheless, some people still consider ECT as the last option for treating depression, even though most studies indicate that ECT is more beneficial in patients with fewer pharmacological treatments[ 114 - 116 ].
ECT is typically recommended for patients with severe and psychotic depression, a high risk of suicide, or Parkinson’s disease, as well as pregnant patients[ 117 - 119 ]. The maintenance ECT also appears to prevent relapses[ 120 ]. The current practice of ECT continues to improve as protocols become more advanced, mainly owing to bioinformatics, and as more research is carried out in this domain[ 121 - 125 ].
This method, which is a type of biological stimulation that affects brain metabolism and neuronal electrical activity, has been widely used in research on depression[ 126 ]. Recent literature shows a significant difference between rTMS and fictitious stimulation regarding its improvements in depressive symptoms[ 127 ]. Preliminary research has revealed synergistic ( e.g. , rTMS/quetiapine) and antagonizing ( e.g. , rTMS/cannabinoid receptor (CB1) antagonist) interactions between neuro-modulation and pharmacotherapy[ 128 ]. Treatments combining rTMS and antidepressants are significantly more effective than placebo conditions, with mild side effects and good acceptability[ 129 ]. Although these results are encouraging, they remain inconsistent due to differences in rTMS treatment frequencies, parameters, and stimulation sites[ 129 ]. Therefore, clinical trials with large sample sizes are needed to specify which factors promote favorable therapeutic responses. Also, additional preclinical research should investigate the synergistic effects of other pharmacological molecules and guide integrated approaches (rTMS plus pharmacotherapy).
This technique delivers weak currents to the brain via electrodes placed on the scalp[ 130 ]. It is easy to use, safe, and tolerable[ 131 ]. The tDCS technique significantly outperforms the simulator in terms of the rate of response and remission[ 132 ]. However, its effect remains lower than that of antidepressants[ 133 ] and rTMS[ 134 ]. It can be used as a complementary intervention or as monotherapy to reduce depressive symptoms in unipolar or bipolar depression patients[ 135 ]. The antidepressant effects of tDCS may involve long-term neuroplastic changes that continue to occur even after the acute phase of treatment, which explains its delayed efficacy[ 135 ].
Recently, neurophysiological studies have shown that the clinical effects of tDCS do not have a direct linear relationship with the dose of stimulation[ 136 ]. tDCS, as a relatively simple and portable technology, is well-suited for remote supervised treatment and assessment at home, thus facilitating long treatment durations[ 136 ].
Since the optimal clinical effects of tDCS are delayed, future clinical trials should use longer evaluation periods and aim to identify responsive patients using algorithms[ 137 ].
VNS is a therapeutic method that has been used for the last sixteen years to treat resistant unilateral or bipolar depression. However, despite several clinical studies attesting to its favorable benefit-risk ratio and its approval by the Food Drug Administration in 2005, it is not used very often[ 138 ].
VNS involves the implantation of a pacemaker under the collarbone that is connected to an electrode surrounding the left vagus nerve. The left vagus nerve is preferred because it exposes the patient to fewer potential adverse cardiac effects. Indeed, most cardiac afferent fibers originate from the right vagus nerve[ 139 ]. Since the turn of the century, numerous studies have demonstrated the efficacy of VNS in resistant depression[ 140 - 142 ].
However, only one randomized, double-blind, controlled trial comparing VNS with usual medical treatment has been conducted over a short period of 10 wk[ 141 ]. Moreover, the results of this study did not indicate that the combination of VNS with typical medical treatments was better than the typical medical treatment on its own.
However, VNS has demonstrated progressively increasing improvements in depressive symptoms, with significant positive outcomes observed after six to 12 mo; these benefits can last for up to two years[ 143 ].
More long-term studies are needed to fully determine the predictors of the correct response.
According to the literature, DBS of the subgenual cingulate white matter (Brodmann area = BA 25) elicited a clinical response in 60% of resistant depression patients after six months and clinical remission in 35% of patients, with benefits maintained for over 12 mo[ 144 ]. The stimulation of other targets, in particular the nucleus accumbens, to treat resistant depression has gained interest recently. Behavioral effects indicate the quick and favorable impact of stimulation on anhedonia, with significant effects on mood appearing as early as week one after treatment begins[ 145 ].
Magnetic seizure therapy
Magnetic seizure therapy involves inducing a therapeutic seizure by applying magnetic stimulation to the brain while the patient is under anesthesia. This technique is still being investigated as a viable alternative to ECT to treat many psychiatric disorders. Evidence supporting its effectiveness on depressive symptoms continues to grow, and it appears to induce fewer neurocognitive effects than ECT[ 146 , 147 ].
Luxtherapy (phototherapy)
The first description of reduced depression symptoms due to intense light exposure was presented in 1984[ 148 ]. Optimal improvements were obtained with bright light exposure of 2500 Lux for two hours per day, with morning exposure shown to be superior to evening exposure[ 149 ].
A review and meta-analysis[ 150 ] showed that more intense (but shorter) exposures (10000 Lux for half an hour per day or 6000 Lux for 1.5 h per day) have the same efficacy. Importantly, this treatment method is effective both for those with seasonal and non-seasonal depression. Benefits of phototherapy related to sleep deprivation and drug treatments have also been reported[ 151 ].
Neuro-modulation treatments offer a range of treatment options for patients with depression. ECT remains the most documented and effective method in this category[ 151 ]. rTMS is an interesting technique as well, as it offers a well-tolerated profile[ 85 ], while tDCS offers encouraging but varying results that depend on the study’s design and the techniques used[ 130 ].
More investigations are needed to specify which indications are the best for each method according to the clinical and biological profiles of patients. The uses of such methods are expanding, probably, with their efficiency increasing when they are tailored to the patient. Furthermore, somatic interventions for depression need to be regularly assessed and integrated into psychiatrists’ therapeutic arsenals.
Treating depression is still a significant challenge. Finding the best option for each patient is the best way to obtaining short- and long-term effectiveness. The three principal methods available to caregivers are antidepressants, specifically structured psychotherapies, and somatic approaches. Research on depression pharmacotherapy continues to examine new molecules implicated in gamma-aminobutyric acid regulation and glutamate transmission. Also, efforts to personalize and simplify psychotherapeutic interventions are ongoing. Protocols using somatic interventions need to be studied in more depth, and their indications must be specified. ECT is the only somatic treatment with confirmed indications for certain forms of depression. Combinations of medications, psychotherapy, and somatic therapies remain the most effective ways to manage resistant forms of depression.
Conflict-of-interest statement: All authors declare that they have no conflict of interest related to this article.
Manuscript source: Invited manuscript
Peer-review started: March 31, 2021
First decision: June 5, 2021
Article in press: October 11, 2021
Specialty type: Medicine, research and experimental
Country/Territory of origin: Morocco
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Narumiya K S-Editor: Fan JR L-Editor: A P-Editor: Fan JR
Contributor Information
Rabie Karrouri, Department of Psychiatry, Moulay Ismaïl Military Hospital, Faculty of Medicine and Pharmacy, Sidi Mohamed Ben Abdellah University, Fez 30070, Morocco.
Zakaria Hammani, Department of Psychiatry, Moulay Ismaïl Military Hospital, Faculty of Medicine and Pharmacy, Sidi Mohamed Ben Abdellah University, Fez 30070, Morocco.
Roukaya Benjelloun, Department of Psychiatry, Faculty of Medicine, Mohammed VI University of Health Sciences, Casablanca 20000, Morocco.
Yassine Otheman, Department of Psychiatry, Moulay Ismaïl Military Hospital, Faculty of Medicine and Pharmacy, Sidi Mohamed Ben Abdellah University, Fez 30070, Morocco. [email protected] .

- Latest news
- UCL in the media
- Services for media
- Student news
- Tell us your story

No evidence that depression is caused by low serotonin levels, finds comprehensive review
20 July 2022
After decades of study, there remains no clear evidence that serotonin levels or serotonin activity are responsible for depression, according to a major review of prior research led by UCL scientists.

The new umbrella review – an overview of existing meta-analyses and systematic reviews – published in Molecular Psychiatry , suggests that depression is not likely caused by a chemical imbalance, and calls into question what antidepressants do. Most antidepressants are selective serotonin reuptake inhibitors (SSRIs), which were originally said to work by correcting abnormally low serotonin levels. There is no other accepted pharmacological mechanism by which antidepressants affect the symptoms of depression.
Lead author Professor Joanna Moncrieff, a Professor of Psychiatry at UCL and a consultant psychiatrist at North East London NHS Foundation Trust (NELFT), said: “It is always difficult to prove a negative, but I think we can safely say that after a vast amount of research conducted over several decades, there is no convincing evidence that depression is caused by serotonin abnormalities, particularly by lower levels or reduced activity of serotonin.
“The popularity of the ‘chemical imbalance’ theory of depression has coincided with a huge increase in the use of antidepressants. Prescriptions for antidepressants have risen dramatically since the 1990s, with one in six adults in England and 2% of teenagers now being prescribed an antidepressant in a given year.
“Many people take antidepressants because they have been led to believe their depression has a biochemical cause, but this new research suggests this belief is not grounded in evidence.”
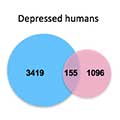
The umbrella review aimed to capture all relevant studies that have been published in the most important fields of research on serotonin and depression. The studies included in the review involved tens of thousands of participants.
Research that compared levels of serotonin and its breakdown products in the blood or brain fluids did not find a difference between people diagnosed with depression and healthy control (comparison) participants.
Research on serotonin receptors and the serotonin transporter, the protein targeted by most antidepressants, found weak and inconsistent evidence suggestive of higher levels of serotonin activity in people with depression. However, the researchers say the findings are likely explained by the use of antidepressants among people diagnosed with depression, since such effects were not reliably ruled out.
The authors also looked at studies where serotonin levels were artificially lowered in hundreds of people by depriving their diets of the amino acid required to make serotonin. These studies have been cited as demonstrating that a serotonin deficiency is linked to depression. A meta-analysis conducted in 2007 and a sample of recent studies found that lowering serotonin in this way did not produce depression in hundreds of healthy volunteers, however. There was very weak evidence in a small subgroup of people with a family history of depression, but this only involved 75 participants, and more recent evidence was inconclusive.
Very large studies involving tens of thousands of patients looked at gene variation, including the gene for the serotonin transporter. They found no difference in these genes between people with depression and healthy controls. These studies also looked at the effects of stressful life events and found that these exerted a strong effect on people’s risk of becoming depressed – the more stressful life events a person had experienced, the more likely they were to be depressed. A famous early study found a relationship between stressful events, the type of serotonin transporter gene a person had and the chance of depression. But larger, more comprehensive studies suggest this was a false finding.
These findings together led the authors to conclude that there is “no support for the hypothesis that depression is caused by lowered serotonin activity or concentrations.”
The researchers say their findings are important as studies show that as many as 85-90% of the public believes that depression is caused by low serotonin or a chemical imbalance. A growing number of scientists and professional bodies are recognising the chemical imbalance framing as an over-simplification.* There is also evidence that believing that low mood is caused by a chemical imbalance leads people to have a pessimistic outlook on the likelihood of recovery, and the possibility of managing moods without medical help. This is important because most people will meet criteria for anxiety or depression at some point in their lives.
The authors also found evidence from a large meta-analysis that people who used antidepressants had lower levels of serotonin in their blood. They concluded that some evidence was consistent with the possibility that long-term antidepressant use reduces serotonin concentrations. The researchers say this may imply that the increase in serotonin that some antidepressants produce in the short term could lead to compensatory changes in the brain that produce the opposite effect in the long term.
While the study did not review the efficacy of antidepressants, the authors encourage further research and advice into treatments that might focus instead on managing stressful or traumatic events in people’s lives, such as with psychotherapy, alongside other practices such as exercise or mindfulness, or addressing underlying contributors such as poverty, stress and loneliness.
Professor Moncrieff said: “Our view is that patients should not be told that depression is caused by low serotonin or by a chemical imbalance, and they should not be led to believe that antidepressants work by targeting these unproven abnormalities. We do not understand what antidepressants are doing to the brain exactly, and giving people this sort of misinformation prevents them from making an informed decision about whether to take antidepressants or not.”
Co-author Dr Mark Horowitz, a training psychiatrist and Clinical Research Fellow in Psychiatry at UCL and NELFT, said: “I had been taught that depression was caused by low serotonin in my psychiatry training and had even taught this to students in my own lectures. Being involved in this research was eye-opening and feels like everything I thought I knew has been flipped upside down.
“One interesting aspect in the studies we examined was how strong an effect adverse life events played in depression, suggesting low mood is a response to people’s lives and cannot be boiled down to a simple chemical equation.”
Professor Moncrieff added: “Thousands of people suffer from side effects of antidepressants, including the severe withdrawal effects that can occur when people try to stop them, yet prescription rates continue to rise. We believe this situation has been driven partly by the false belief that depression is due to a chemical imbalance. It is high time to inform the public that this belief is not grounded in science.”
The researchers caution that anyone considering withdrawing from antidepressants should seek the advice of a health professional, given the risk of adverse effects following withdrawal. Professor Moncrieff and Dr Horowitz are conducting ongoing research into how best to gradually stop taking antidepressants .
- Research paper in Molecular Psychiatry
- Professor Joanna Moncrieff’s academic profile
- UCL Psychiatry
- * For example, the Royal College of Psychiatrists removed all reference to ‘chemical imbalances’ from their website in recent years. They now say in official statements that “the original idea that antidepressants ‘correct a chemical imbalance in the brain’ is an over-simplification.”
- Media coverage
- Source: iLexx on iStock
Media contact
tel: +44 20 7679 9222
E: chris.lane [at] ucl.ac.uk

Depression and Serotonin: What the New Review Actually Says
Using but not overusing the evidence presented in this controversial study..
Posted July 26, 2022 | Reviewed by Abigail Fagan
- What Is Depression?
- Find a therapist to overcome depression
- A new published review finds no evidence that low serotonin levels cause depression.
- The authors use their data to refute the "chemical imbalance" hypothesis of depression, which is an old and imprecise term.
- Despite the claims of some, the study does not disprove that biological factors are irrelevant to depression.
- The dominant model of depression for decades has been one that recognizes the importance of biological, psychological, and social factors.
Some quite strong feelings and very broad conclusions have come following the recent publication of a review study published in the reputable journal Molecular Psychiatry that found little evidence that low levels of the brain neurotransmitter serotonin are related to the development of depression . The study has received strong media coverage and has spurred intense exchanges on social media . Some see the study as a scientific earthquake and total vindication for those who have been skeptical of the “biological” theory of depression from the start, while others view it as the penultimate dead horse beating that has absolutely no bearing on current practices for understanding or treating depression, now the world’s #1 cause for disability.
The study is what is called an “umbrella” review, which means that no new data are presented and the authors are reviewing and summarizing studies that themselves reviewed and summarized individual research studies. They focus on studies that have used various lines of investigation to link depression with low serotonin levels. This includes research (in people only) that compare levels of serotonin in the blood or cerebrospinal fluid between people who are depressed and not-depressed, studies of how well certain protein receptors are able to bind serotonin when depressed, and studies examining the role of a single but very famous gene , the serotonin transporter. The bottom line is that they find little to no evidence from the types of studies they examined that low serotonin levels or activity play a significant role in the development of depression.
These kinds of studies often put people to sleep, but in this case the reaction has been intense and personal. Much of this has to do with the authors pulling in the term “chemical imbalance” as implications of their work. This poorly-chosen term is actually one of psychiatry’s creation and now it’s being thrown back in our face imbued with even broader meaning.
While originally employed as a shortcut term for the monoamine hypothesis (briefly, the idea that some kind of deficiency in a few brain neurotransmitters, including serotonin, was a key contributor to depression), it was quickly incorporated by the pharmaceutical industry as a catch phrase for marketing purposes to depict depression as a biological illness requiring biological treatments.
The monoamine hypothesis faded as a dominant model with further research and was supplanted decades ago by the “biopsychosocial” model of psychiatric disorders which continues to prevail today. Nevertheless, the old chemical imbalance lingo remains a lightening rod to critics of psychiatry. More recently, the term has begun to be the punching bag for people who don’t believe that biological factors (also a squishy term) of any sort play a role in causing depression.
Unfortunately, the current review makes little distinction between the narrower serotonin deficit theory of depression they actually address and this ever expanding but still ill-defined “chemical imbalance” view of mental illness. This has predictably pushed the door wide open for those who want to take this review as proof that neurobiology doesn’t matter at all when it comes to depression, a claim which isn’t supported by this review or wider research whatsoever.
There is some middle ground here. While many of us in psychiatry are a little embarrassed by what now looks like some over simplistic and naïve ideas about the development of depression, there’s no denying that many of these individual studies supporting a straightforward role of serotonin and depression created quite a lot of enthusiasm in their day among the psychiatric community when first published.
These notions were then imparted to students and patients in an attempt to explain what depression was. I remember some of my own Powerpoint slides I previously used in teaching related to a very influential study that the onset of depression was related to the combination of having a particular version of the serotonin transporter gene combined with the presence of an adverse environment. There’s also no denying that selected studies supporting serotonin’s role were heavily leveraged by the pharmaceutical industry to market more antidepressants . For most of us, however, the attractiveness of these simple theories wasn’t in their advertising value but in their ability to help patients see their struggles as something that wasn’t their fault at a time when feelings of guilt and worthlessness were already sky high. Overall, then, this study is an uncomfortable reminder that we did indeed learn and repeat ideas that today look a little foolish.
At the same time, it is important not to let people take this extremely limited study to wild and sweeping conclusions and to prevent the portrayal of the psychiatric community in archaic and stereotypical forms. Depression experts have well moved on from the low serotonin theory years if not decades ago, and although they could have announced this shift better, there certainly is no organized effort to suppress this information. Over two years ago I published a post here on Psychology Today called The Rise and Fall of the Depression Gene which cited some of the same research as this review. Personally, I don’t think I’ve used the term “chemical imbalance” to explain depression in 20 years and current textbooks and information sources provide much more nuance and balance (and vagueness) when describing the origin of depression. Yes, you can still hear people occasionally drop the chemical imbalance term when trying to turn complicated processes into quick soundbites, but that’s a long way from it being an organized and accepted theory promoted by the proverbial psychiatry establishment.

The review also has a number of real problems, which is a little ironic for a study which is one of the few not to have a “limitations” section as part of the manuscript. I’ll blame the editorial staff of the journal for that one, as well as for letting the authors use studies that examine simple depression versus controls differences in serotonin levels to conclude that serotonin, let alone all biological factors, have no role in depression at all.
Reading this study, one would never know that there are animal studies, neuroimaging studies, twin and adoption studies, inflammation research, and many other lines of evidence suggesting that depression is a very complex condition that people can arrive at from multiple pathways. Interestingly, if you look directly at some of the source studies for this review, you will see some of this evidence. For example, the meta-analysis by Ogawa cited in the review did indeed find no evidence of a link between serotonin and depression but did find evidence of a link between dopamine and depression. This statement should not be interpreted as a pitch to trade one overly simplistic view of depression for another but to point out the hazards of making conclusions that far overstep your data.
Another poor choice in this review is that while the authors don’t quite tell readers to stop taking antidepressants, they walk right up to that edge with their claim that the old chemical imbalance theory is one of the primary justifications for why people take them (rather than something like wanting to feel better). This, in my view, is careless and problematic for people who take antidepressants and for those who care for them. Just as many rightly point out that the fact that antidepressants' help shouldn’t be used as evidence of a serotonin deficit in depression, the lack of a clear serotonin deficit in depression shouldn’t be used as evidence to abandon the use of these important medications, any more than (as been said previously) a lack of an “acetaminophen deficit” should be used as evidence not to use Tylenol when you have a headache. Admittedly, we don’t know very well how antidepressants work, but for millions of people, they do.
In the end, it seems best to welcome this study for what it does say while being quite clear about what it doesn’t. Depression is complicated. Different people get there from different paths and find their way out through different means. Ascribing all depression as due to low serotonin, or poor diet , or trauma , or smartphones, or poverty will just end with a study like this.
Moncrieff J, Cooper RE, Stockmann T, et al. The serotonin theory of depression: A systematic umbrella review of the evidence. Mol Psychiatry. 2022; Jul 20. doi: 10.1038/s41380-022-01661-0. Online ahead of print.
Ogawa S, Tsuchimine S, Kunugi H. Cerebrospinal fluid monoamine metabolite concentrations in depressive disorder: A meta-analysis of historic evidence. J Psychiatr Res. 2018; 105:137–46.

David Rettew, M.D. , is a child and adolescent psychiatrist and faculty at the Oregon Health and Science University.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Teletherapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience
- Latest Latest
- The West The West
- Sports Sports
- Opinion Opinion
- Magazine Magazine
Study says depression not caused by chemical imbalance, raising questions about antidepressants
University college london research says depression is not a serotonin imbalance and drugs that target it may not be the answer.

By Lois M. Collins
Millions of Americans take antidepressants, but a new study suggests the theory underpinning their use may be entirely wrong. Research from the University College London raises doubt that chemical imbalance in the brain is responsible for depression .
A major review of previous studies on serotonin’s role in depression, just published in the journal Molecular Psychiatry, concluded that serotonin level — the target of antidepressants — is not responsible for depression.
The researchers found “no support for the hypothesis that depression is caused by lowered serotonin activity or concentrations.”
They found stronger evidence that stressful life events can lead to depression.
The question is, do antidepressants help, and if so, how? If not, could they be doing harm?
Experts are divided and the study has drawn some pushback.
“Some of the studies in our overview that included people who were taking or had previously taken antidepressants showed evidence that antidepressants may actually lower the concentration or activity of serotonin,” according to an article in The Conversation by the study’s authors, Joanna Moncrieff, professor of psychiatry, and Mark Horowitz, clinical research fellow in psychiatry, both of University College London.
“Most antidepressants are selective serotonin reuptake inhibitors, which were originally said to work by correcting abnormally low serotonin levels. There is no other accepted pharmacological mechanism by which antidepressants affect the symptoms of depression,” the researchers said in a news release .
The research suggests depression is not biochemical and questions how, given that, a biochemical solution would work. Horowitz and Moncrieff also question whether that kind of treatment, which acts on brain chemistry, does more harm than good.
“Our view is that patients should not be told that depression is caused by low serotonin or by a chemical imbalance, and they should not be led to believe that antidepressants work by targeting these unproven abnormalities. We do not understand what antidepressants are doing to the brain exactly, and giving people this sort of misinformation prevents them from making an informed decision about whether to take antidepressants or not,” Moncrieff said.
Targeting serotonin
The “chemical imbalance” theory has dominated the thinking about depression for several decades, according to the researchers.
“It is always difficult to prove a negative, but I think we can safely say that after a vast amount of research conducted over several decades, there is no convincing evidence that depression is caused by serotonin abnormalities, particularly by lower levels or reduced activity of serotonin,” Moncrieff said.
In the United States between 2015 and 2018, 13.9% of adults took antidepressants for depression, according to the National Center for Health Statistics in the Centers for Disease Control and Prevention.
As many as 1 in 6 adults in England are now prescribed antidepressants every year, according to the study.
“I had been taught that depression was caused by low serotonin in my psychiatry training and had even taught this to students in my own lectures. Being involved in this research was eye-opening and feels like everything I thought I knew has been flipped upside down,” said Horowitz in background material.
As Mike McRae wrote for ScienceAlert , “This doesn’t necessarily mean serotonin-based treatments aren’t working on some other mechanism we don’t yet understand. And no one should consider ditching their meds without consulting their doctors. But given so many people are relying on these drugs, it is important to figure out what’s really going on.”
Study nuts and bolts
In all, studies in the review included tens of thousands of participants. Among the serotonin mechanisms studied and the findings:
- No difference was seen between people with depression and healthy control subjects in levels of serotonin and breakdown products in the blood or brain fluids.
- In studies of serotonin receptors and the serotonin transporter protein most antidepressants target, they found “weak and inconsistent evidence” suggesting higher levels of serotonin activity in those who are depressed. They believe that was caused by use of antidepressants.
- Studies that lowered serotonin levels in hundreds of healthy volunteers did not produce depression. The researchers saw “very weak evidence” in a small 75-person subgroup of people with a family history of depression. A study after that was inconclusive.
- No evidence of variation in the serotonin transporter gene was found between those with depression and healthy control subjects.
On the other hand, stressful life events had a “strong effect” on the risk of becoming depressed. And the more one experienced stress or trauma, the greater the likelihood of depression.
“A famous early study found a relationship between stressful events, the type of serotonin transporter gene a person had and the chance of depression. But larger, more comprehensive studies suggest this was a false finding,” the release said.
In the piece from The Conversation , Moncrieff and Horowitz wrote, “It is important that people know that the idea that depression results from a ‘chemical imbalance’ is hypothetical. And we do not understand what temporarily elevating serotonin or other biochemical changes produced by antidepressants do to the brain. We conclude that it is impossible to say that taking SSRI antidepressants is worthwhile, or even completely safe.”
Public perception
Surveys suggest as many as 90% of people believe depression is caused by low serotonin or chemical imbalance. There’s evidence believing that creates a “pessimistic outlook on the likelihood of recovery” and the hope of managing depression without medical help, the study said.
Doubts about brain chemistry’s role in depression have been around a while.
“If you’re among those who are hearing all of this for the first time, the hypothesis has been on shaky ground practically since it took off in the 1990s, with study after study failing to support the idea,” wrote ScienceAlert’s McRae . He noted the Moncrieff and Horowitz limited their research to high-quality, peer-evaluated studies.
“Just 17 studies made the cut, which included a genetic association study, another umbrella review, and a dozen systematic reviews and meta-analyses,” he wrote.
The impact is huge, given most people will have diagnosable levels of anxiety or depression at some point, the researchers said.
The researchers also said one large meta-analysis found people using antidepressants had less serotonin in their blood, which could mean that antidepressants designed to raise levels of serotonin may do the opposite over time.
The researchers note they didn’t look at the efficacy of antidepressants. Their hope, they said, is that more research and treatment will focus on helping people manage stressful or traumatic events, “such as with psychotherapy, alongside other practices such as exercise or mindfulness, or addressing underlying contributors such as poverty, stress and loneliness.”
Some experts disagree
The research has attracted some pushback.
The Guardian quoted Dr. Michael Bloomfield, a consultant psychiatrist and principal clinical research fellow at University College London, who was not involved in the study: “Many of us know that taking paracetamol can be helpful for headaches, and I don’t think anyone believes that headaches are caused by not enough paracetamol in the brain. The same logic applies to depression and medicines used to treat depression.”
He added, “There is consistent evidence that antidepressant medicines can be helpful in the treatment of depression and can be life-saving.”
Johan Lundberg at the Karolinska Institute in Sweden told New Scientist that one limitation of the study is failure to distinguish between those with long-term depression and those having episodes of depression, because their state during the study could be different in terms of serotonin. “It is key to separately analyze data from studies that examine the same patients when ill and when in remission, to have optimal conditions to examine the hypothesis,” he said.
The same article quoted a spokesperson for the Royal College of Psychiatrists who was talking about treatment guidelines from public health officials in England, who said antidepressants are an effective treatment for depression and some other physical and mental health conditions.
The spokesperson noted that “antidepressants will vary in effectiveness for different people, and the reasons for this are complex. We would not recommend for anyone to stop taking their antidepressants based on this review, and encourage anyone with concerns about their medication to contact their (family doctor).”
‘Boys are disappearing’ from mental health care as signs of depression go undetected

Teenage boys are drowning in just as much of the depression and anxiety that’s been well documented in girls . Experts warn that many young men struggling with their mental health are left undetected and without the help they need.
“We are right to be concerned about girls,” said Kathleen Ethier, director of the Division of Adolescent and School Health at the Centers for Disease Control and Prevention. “But I don’t ever want us to lose sight of the fact that boys aren’t doing well, either.”
Depression in boys may go unnoticed, Ethier and other experts said, because boys usually don’t show it through signs of melancholy typically found in girls.
“We have this very classic understanding of depression as being sad, being tearful, crying more, not eating as much and losing weight,” said Dr. Lauren Teverbaugh, pediatrician and child psychiatrist at Tulane University in New Orleans. “That’s just not how it looks for a lot of young boys.”
‘Boys are disappearing’
A recent study published in the journal Pediatrics found that while antidepressant prescriptions have risen dramatically for teenage girls and women in their 20s, the rate of such prescriptions for young men “declined abruptly during March 2020 and did not recover.”
Dr. Kao-Ping Chua, a pediatrician at the Susan B. Meister Child Health Evaluation and Research Center at the University of Michigan, led the study. He said that his finding that boys weren’t accessing antidepressant medications once the pandemic hit has been “perplexing.”
“In males, it’s theoretically possible that this reflects improved mental health, but I’m struggling with that explanation,” Chua said. “Given that everybody’s mental health got worse, I would have expected that boys’ antidepressant dispensing would have at least remained stable, not decrease.”
The more likely explanation in Chua’s experience as a pediatrician, he said, was that boys stopped engaging with the health care system overall during the pandemic, leading to an underdetection and, consequently, an undertreatment of mental health problems in young men.
“There was something happening to make male adolescents not come in for mental health,” Chua said. “They didn’t go to their doctors. They skipped physicals.”
“Boys are disappearing,” he said.
What does depression look like in boys?
Boys struggling with their mental health tend to show it with a shorter fuse: They’re easily irritated, frustrated or aggressive.
“A lot of times, parents who have boys with depression say that they’re walking on eggshells around them because they don’t know what would set them off,” said Dr. Mai Uchida, a pediatric psychiatrist and director of the Child Depression Program at Massachusetts General Hospital.
Parents, pediatricians and even psychiatrists may not pick up on mental health problems in boys, Uchida said, because “they don’t fit the stereotypical image of depression.”
Women have long been much more likely to be diagnosed with depression than men. But a 2013 study found that when “irritability” is considered a main symptom, the rate of depression actually equalized between the sexes: 30.6% of men and 33.3% of women.
In addition to irritability, depression symptoms in boys can include impulsivity, risk-taking behavior and being more argumentative than usual.
Dr. Willough Jenkins, a psychiatrist and the medical director of emergency and consultation liaison psychiatry at Rady Children’s Hospital in San Diego, blamed, in part, a societal normalization of teenage angst and irritability.
“There’s a myth that teenagers are supposed to be irritable, that they’re supposed to be cranky,” she said. “I think too many parents have heard that and think it’s normal behavior, when it’s really indicating that there could be a struggle.”
Evidence of mental health distress among teens — especially young girls — has been mounting for years. Covid-19 lockdowns worsened the situation.
In 2023, a sobering report from the CDC revealed that girls experienced unprecedented levels of sadness and hopelessness early in the pandemic.
The research might indicate that boys don’t require the same level of mental health care as girls. That’s not true, experts insist.
“Both boys and girls are struggling,” Jenkins said. “None of our young people are doing well in terms of their mental health.”
‘Anger caused by sadness’
Eighteen-year-old Noah Power, who lives in Yukon, Canada, said his struggles with anxiety and depression began when he was about 12 years old.

His mental health symptoms first took the form of headaches and crushing pressure in his chest. Over time, those symptoms developed into a “rush of anger that I couldn’t explain,” he said. “It was like anger caused by sadness.”
Power said that expressing himself through anger and irritability felt like a natural, healthy outlet.
“It can be a bit much, but for us, we feel like we’re doing something good for our own brain,” he said.
In addition to long-term psychotherapy and medication, Power has relied on physical outlets for his anxiety and depression. Running, he said, is key.
“Being able to run and run and run and get all of my energy out has been the most helpful thing for me,” Power said. “You sweat out all of your energy.”
Lockdowns led to fewer referrals
Teachers, coaches and other caregivers outside of the home are on the front lines of monitoring teen mental health, Tulane’s Teverbaugh said.
“Not only do they see that child, but they see other children their same age also experiencing some of the same environmental factors,” she said. “They’re a really good measure for being able to pick up on something that is beyond the norm.” Teverbaugh and other experts said that many referrals for boys seeking mental health treatment stem from behavioral issues in school.
When schools went remote and sports and other activities were canceled in 2020, those referrals decreased.
“We’re often not seeing [boys] in the office, because it’s just not being picked up as much in the community,” she said.
Advice for parents
Mass General’s Uchida — a mother of three young boys — encourages parents to permit sons to express their sadness and frustrations.
“We have to really allow them to feel that and hold their hand and appreciate that they are expressing that kind of emotion,” she said. “They’re going through a lot. We often forget to empathize with them.”
Power said that having a parent or caregiver calmly listen, even during verbal outbursts, is helpful. “What we really, really appreciate is the listening and being able to just vent,” he said. “Just getting it all out is a huge relief.”
And if teenage boys can’t find the words to express themselves, allow them other outlets.
“They may not use emotional language like, ‘I feel sad,’” Teverbaugh said. “But when they’re playing their video games together, or they’re on the basketball court just goofing around, that’s engagement. That’s social interaction. That’s them being able to feel connected.”
Power also credits online gaming as a coping skill. “It’s an easy way to talk to your friends and have a good time,” he said. “Face-to-face social pressure can be a lot, especially when you’re going through something and you don’t want to break down in front of the person.”
Erika Edwards is a health and medical news writer and reporter for NBC News and "TODAY."
Positive associations between premenstrual disorders and perinatal depression
Researchers utilize data from swedish nationwide registers of over 900,000 women.
Women affected by premenstrual disorders have a higher risk of perinatal depression compared with those who do not, according to research published March 28 in the open access journal PLOS Medicine . The relationship works both ways: those with perinatal depression are also more likely to develop premenstrual disorders after pregnancy and childbirth. This study suggests that a common mechanism might contribute to the two conditions.
Menstruating women experience cyclical hormone fluctuations through puberty, menstrual cycle, pregnancy and menopause. Some women have difficult to manage symptoms of low mood and depression during these fluctuations. Between a fifth and a third of women are reportedly affected by premenstrual disorders and 11% of mothers suffer perinatal depression -- depressive symptoms during pregnancy and up to 12 months after delivery.
Qian Yang and colleagues at the Karolinska Institutet, Sweden and University of Iceland used the Swedish nationwide registers from 2001 to 2018 and identified 84,949 women with perinatal depression and 849,482 unaffected women. The researchers matched the women on age and calendar year, and further controlled for demographic factors, smoking, BMI, parity and history of psychiatric disorders. Among women with perinatal depression, almost 3% had premenstrual disorders before pregnancy compared with 0.6% of matched unaffected women. Women with perinatal depression were also twice as likely to report premenstrual disorders when the menstruation resumed after childbirth, compared to those unaffected by perinatal depression.
The research sheds light on the association between the two conditions and supports a theory that they may share underlying biological mechanisms and/or risk factors. Understanding this association could help healthcare providers to better target support to women most likely to be affected.
The authors add, "This study reveals a strong bidirectional relationship between perinatal depression and premenstrual disorders, using data from over 900,000 pregnancies. The findings suggest that both disorders may exist on a continuum, and emphasize the importance of recognizing these susceptibilities in clinical practice."
- Mental Health Research
- Pregnancy and Childbirth
- Mental Health
- Gender Difference
- Postpartum depression
- Bipolar disorder
- Nutrition and pregnancy
- Mental illness
- Psychopathology
- Clinical depression
Story Source:
Materials provided by PLOS . Note: Content may be edited for style and length.
Journal Reference :
- Qian Yang, Emma Bränn, Elizabeth R. Bertone- Johnson, Arvid Sjölander, Fang Fang, Anna Sara Oberg, Unnur A. Valdimarsdóttir, Donghao Lu. The bidirectional association between premenstrual disorders and perinatal depression: A nationwide register-based study from Sweden . PLOS Medicine , 2024; 21 (3): e1004363 DOI: 10.1371/journal.pmed.1004363
Cite This Page :

Explore More
- Heart Disease Risk: More Than One Drink a Day
- Unlocking Supernova Stardust Secrets
- Why Do Some Memories Become Longterm?
- What Controls Sun's Differential Rotation?
- Robot, Can You Say 'Cheese'?
- Researchers Turn Back the Clock On Cancer Cells
- Making Long-Term Memories: Nerve-Cell Damage
- A Solar Cell You Can Bend and Soak in Water
- 'Cosmic Cannibals': Fast-Moving Jets in Space
- Risk Factors for Faster Brain Aging
Trending Topics
Strange & offbeat.
Study Tracks Shifts in Student Mental Health During College
Dartmouth study followed 200 students all four years, including through the pandemic.

Phone App Uses AI to Detect Depression From Facial Cues
A four-year study by Dartmouth researchers captures the most in-depth data yet on how college students’ self-esteem and mental health fluctuates during their four years in academia, identifying key populations and stressors that the researchers say administrators could target to improve student well-being.
The study also provides among the first real-time accounts of how the coronavirus pandemic affected students’ behavior and mental health. The stress and uncertainty of COVID-19 resulted in long-lasting behavioral changes that persisted as a “new normal” even as the pandemic diminished, including students feeling more stressed, less socially engaged, and sleeping more.
The researchers tracked more than 200 Dartmouth undergraduates in the classes of 2021 and 2022 for all four years of college. Students volunteered to let a specially developed app called StudentLife tap into the sensors that are built into smartphones. The app cataloged their daily physical and social activity, how long they slept, their location and travel, the time they spent on their phone, and how often they listened to music or watched videos. Students also filled out weekly behavioral surveys, and selected students gave post-study interviews.
The study—which is the longest mobile-sensing study ever conducted—is published in the Proceedings of the ACM on Interactive, Mobile, Wearable and Ubiquitous Technologies .
The researchers will present it at the Association of Computing Machinery’s UbiComp/ISWC 2024 conference in Melbourne, Australia, in October.
These sorts of tools will have a tremendous impact on projecting forward and developing much more data-driven ways to intervene and respond exactly when students need it most.
The team made their anonymized data set publicly available —including self-reports, surveys, and phone-sensing and brain-imaging data—to help advance research into the mental health of students during their college years.
Andrew Campbell , the paper’s senior author and Dartmouth’s Albert Bradley 1915 Third Century Professor of Computer Science, says that the study’s extensive data reinforces the importance of college and university administrators across the country being more attuned to how and when students’ mental well-being changes during the school year.
“For the first time, we’ve produced granular data about the ebb and flow of student mental health. It’s incredibly dynamic—there’s nothing that’s steady state through the term, let alone through the year,” he says. “These sorts of tools will have a tremendous impact on projecting forward and developing much more data-driven ways to intervene and respond exactly when students need it most.”
First-year and female students are especially at risk for high anxiety and low self-esteem, the study finds. Among first-year students, self-esteem dropped to its lowest point in the first weeks of their transition from high school to college but rose steadily every semester until it was about 10% higher by graduation.
“We can see that students came out of high school with a certain level of self-esteem that dropped off to the lowest point of the four years. Some said they started to experience ‘imposter syndrome’ from being around other high-performing students,” Campbell says. “As the years progress, though, we can draw a straight line from low to high as their self-esteem improves. I think we would see a similar trend class over class. To me, that’s a very positive thing.”
Female students—who made up 60% of study participants—experienced on average 5% greater stress levels and 10% lower self-esteem than male students. More significantly, the data show that female students tended to be less active, with male students walking 37% more often.
Sophomores were 40% more socially active compared to their first year, the researchers report. But these students also reported feeling 13% more stressed during their second year than during their first year as their workload increased, they felt pressure to socialize, or as first-year social groups dispersed.
One student in a sorority recalled that having pre-arranged activities “kind of adds stress as I feel like I should be having fun because everyone tells me that it is fun.” Another student noted that after the first year, “students have more access to the whole campus and that is when you start feeling excluded from things.”
In a novel finding, the researchers identify an “anticipatory stress spike” of 17% experienced in the last two weeks of summer break. While still lower than mid-academic year stress, the spike was consistent across different summers.
In post-study interviews, some students pointed to returning to campus early for team sports as a source of stress. Others specified reconnecting with family and high school friends during their first summer home, saying they felt “a sense of leaving behind the comfort and familiarity of these long-standing friendships” as the break ended, the researchers report.
“This is a foundational study,” says Subigya Nepal , first author of the study and a PhD candidate in Campbell’s research group. “It has more real-time granular data than anything we or anyone else has provided before. We don’t know yet how it will translate to campuses nationwide, but it can be a template for getting the conversation going.”
The depth and accuracy of the study data suggest that mobile-sensing software could eventually give universities the ability to create proactive mental-health policies specific to certain student populations and times of year, Campbell says.
For example, a paper Campbell’s research group published in 2022 based on StudentLife data showed that first-generation students experienced lower self-esteem and higher levels of depression than other students throughout their four years of college.
“We will be able to look at campus in much more nuanced ways than waiting for the results of an annual mental health study and then developing policy,” Campbell says. “We know that Dartmouth is a small and very tight-knit campus community. But if we applied these same methods to a college with similar attributes, I believe we would find very similar trends.”
Weathering the pandemic
When students returned home at the start of the coronavirus pandemic, the researchers found that self-esteem actually increased during the pandemic by 5% overall and by another 6% afterward when life returned closer to what it was before. One student suggested in their interview that getting older came with more confidence. Others indicated that being home led to them spending more time with friends talking on the phone, on social media, or streaming movies together.
The data show that phone usage—measured by the duration a phone was unlocked—indeed increased by nearly 33 minutes, or 19%, during the pandemic, while time spent in physical activity dropped by 52 minutes, or 27%. By 2022, phone usage fell from its pandemic peak to just above pre-pandemic levels, while engagement in physical activity had recovered to exceed the pre-pandemic period by three minutes.
Despite reporting higher self-esteem, students’ feelings of stress increased by more than 10% during the pandemic. By the end of the study in June 2022, stress had fallen by less than 2% of its pandemic peak, indicating that the experience had a lasting impact on student well-being, the researchers report.
In early 2021, as students returned to campus, their reunion with friends and community was tempered by an overwhelming concern about the still-rampant coronavirus. “There was the first outbreak in winter 2021 and that was terrifying,” one student recalls. Another student adds: “You could be put into isolation for a long time even if you did not have COVID. Everyone was afraid to contact-trace anyone else in case they got mad at each other.”
Female students were especially concerned about the coronavirus, on average 13% more than male students. “Even though the girls might have been hanging out with each other more, they are more aware of the impact,” one female student reported. “I actually had COVID and exposed some friends of mine. All the girls that I told tested as they were worried. They were continually checking up to make sure that they did not have it and take it home to their family.”
Students still learning remotely had social levels 16% higher than students on campus, who engaged in activity an average of 10% less often than when they were learning from home. However, on-campus students used their phones 47% more often. When interviewed after the study, these students reported spending extended periods of time video-calling or streaming movies with friends and family.
Social activity and engagement had not yet returned to pre-pandemic levels by the end of the study in June 2022, recovering by a little less than 3% after a nearly 10% drop during the pandemic. Similarly, the pandemic correlates with students sticking closer to home, with their distance traveled nearly cut in half during the pandemic and holding at that level since then.
Campbell and several of his fellow researchers are now developing a smartphone app known as MoodCapture that uses artificial intelligence paired with facial-image processing software to reliably detect the onset of depression before the user even knows something is wrong.
Morgan Kelly can be reached at [email protected] .
- Mental Health and Wellness
- Innovation and Impact
- Arts and Sciences
- Class of 2021
- Class of 2022
- Department of Computer Science
- Guarini School of Graduate and Advanced Studies
- Mental Health
Class of 2028 Draws Record Number of Applicants

Writing about important events in our lives, not just ‘I had a coffee today,’ but ‘I had this deep discussion with my mom,’ generally provides more benefit therapeutically.

4 Scents That Can Reduce Depression, New Research Shows
Posted: March 15, 2024 | Last updated: March 15, 2024

For centuries, people have used aromatherapy for its therapeutic benefits, including emotional regulation. Now, research is exploring how it could be used to combat specific mental health problems, such as depression and anxiety.
For instance, a 2022 study published in the medical journal Frontiers in Neuroscience looked at the relationship between one's sense of smell and their likelihood of developing depressive traits. They note that people who lost their senses of smell were more likely than those who did not to develop clinical depression within five to 10 years, and that the severity of one's sensory loss could actually predict the severity of their eventual depression.
Based on these findings, the team proposed that enhancing your sense of smell may help improve your symptoms of depression. Olfactory enrichment in the form of aromatherapy "modifies brain structures and improves cognitive and emotional status," the researchers wrote.
If you're looking to improve your own mental wellbeing with aromatherapy, these are the four specific scents that researchers recommend for reducing symptoms of depression.
RELATED: 8 Houseplants That Improve Your Mental Health, Science Says .

New research published last month in JAMA Open Network suggests that familiar scents can improve symptoms in people with depressive disorders. That's because individuals who suffer from depression are known to have more difficulty recalling specific autobiographical memories. However, smelling familiar scents helped the study subjects recall more memories. Kymberly Young , an associate professor of psychiatry at the University of Pittsburgh and a co-author on the study, suggested while speaking to NBC News that with a little training, those with depression might be able to lessen their symptoms by using scents to conjure positive memories.
And, it seems any scent you have a personal memory of will do. The scents used in the study included orange, vanilla extract, cumin, whiskey, red wine, cough syrup, disinfectant, shoe polish, and more.

Many of us associate lavender with calm, and in keeping with the findings of the last study, that association likely enhances its ability to improve depression and anxiety. However, studies show that there also appear to be other mechanisms behind lavender's antidepressant and anxiolytic (anti-anxiety) effects.
RELATED: Taking a "Smell Walk" Slashes Stress and Boosts Your Mood—Here's How to Do It .

Bergamot orange is a citrus fruit that's too bitter to eat on its own. However, Bergamot oil is commonly used in perfumes and aromatherapy—and touted for its mood-boosting benefits.
"Fifteen minutes of Bergamot essential oil exposure improved participants' positive feelings compared with the control group (17 percent higher)," says a 2017 study published in the journal Phytotherapy Research . The study authors note that Bergamot is characterized by a high content of limonene, linalool, and linalyl acetate—three compounds associated with antidepressant and anxiolytic benefits.
Ultimately, they concluded, "that bergamot essential oil aromatherapy can be an effective adjunct treatment to improve individuals' mental health and well‐being."

A 2021 study published in the International Journal of Molecular Sciences found that chamomile was yet another scent that could improve mental well-being when used as aromatherapy. The study noted that inhaling chamomile oil helped to decrease levels of depression, anxiety, and stress in older adults.
"It was suggested that the anxiolytic and antidepressant effects could be associated with the suppression of the activity of the sympathetic nervous system," the researchers note.
RELATED:For more up-to-date information, sign up for our daily newsletter.
Read the original article on Best Life .
More for You
The 10 movies everyone's watching on Netflix right now
Have a Bunch of Old Pillows? Here Are 7 Things You Can Do With Them
Jerry Seinfeld's Star-Studded “Unfrosted” Trailer Presents a Silly Pop-Tarts Origin Story
Chinese Spy Plane Detected Flying Into Pacific
Judge Throws Cold Water on Hunter Biden’s Political-Prosecution Claim: ‘No Evidence’
3 Expenses You Should Never Put on a Credit Card
17 Most Stolen Items in the US – What You Should Know
I quit sugar for 6 months and this is what it did to my face and body
‘World’s largest small town’ offering $10,000 for workers to move there
Injured Allied Navy Sailors Given Combat Medals After China Clash
WuMo by Wulff & Morgenthaler
Jeremy Renner Makes His Comeback in ‘Mayor of Kingstown' Season 3 Trailer
KFC rolls out new menu item to challenge McDonald’s, Burger King
MyPillow faces eviction from warehouse, but Mike Lindell says firm's in 'great shape'
Kevin O'Leary says an annual salary is a ‘drug' that employers feed you to forget your dreams — claims it's very easy to stay at a comfy job with low risk. 3 ways to gain some upside
20 facts you may not know about 'The Mummy'
Bluebird museum tells restorers to stop harassment
Putin Issues F-16 Warning
A Data Broker Reportedly Tracked Visitors to Jeffrey Epstein’s Island
Heart of the City by Steenz
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- NATURE BRIEFING
- 30 August 2022
Daily briefing: New treatments offer fresh hope for depression
- Flora Graham
You can also search for this author in PubMed Google Scholar
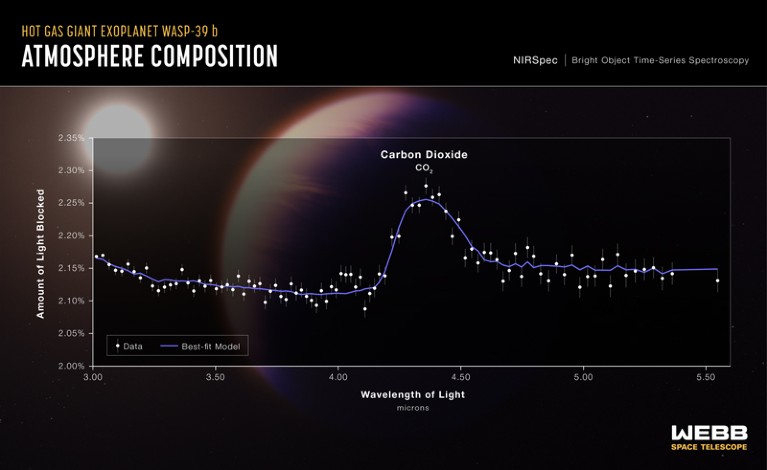
Researchers detected carbon dioxide in WASP-39b’s atmosphere when the exoplanet crossed in front of its star. The data plot shows a telltale blip where infrared wavelengths from the star’s light were absorbed by carbon dioxide on the exoplanet. Credit: NASA, ESA, CSA, Leah Hustak (STScI), Joseph Olmsted (STScI)
First CO 2 seen on exoplanet
The James Webb Space Telescope has captured the first unambiguous evidence of carbon dioxide in the atmosphere of a planet outside the Solar System . The telescope gleaned information about the composition of the gas giant WASP-39b as it moved across the face of its star. Starlight shone through the planet’s atmosphere, where various molecules absorbed specific wavelengths of infrared light, creating the telltale absorption spectrum in the image above. “We’ve had hints of it before, but this is the first time it’s really been a ‘punch in the face’ kind of detection,” says astronomer Jessie Christiansen. The result has bolstered confidence that Webb is going to be revolutionary for exoplanet research.
Nature | 5 min read
Reference: arXiv preprint
US reveals big changes to open-access policy
US research agencies will have to make the results of all federally funded research free to read in public repositories as soon as they are published . The policy change — to be implemented by the end of 2025, if not sooner — is a shift from current regulations that apply to only the largest funding agencies and permit a delay of up to a year before papers must be posted outside paywalls. The policy does not insist that federally funded papers be free to read in scientific journals. But it’s still “a game changer for scholarly publishing”, says Johan Rooryck, the executive director of cOAlition S, the group of funders behind Plan S, a similar move in Europe. “This will help accelerate the momentum toward flipping the system to where journals are fully open access,” says Lisa Hinchliffe, a librarian at the University of Illinois at Urbana–Champaign.
Nature | 6 min read
Vaccines slash risk of spreading Omicron
People infected with the Omicron variant are less likely to spread the virus if they have been vaccinated or have had a prior SARS-CoV-2 infection . A study in US prisons, which has not yet been peer reviewed, found that vaccination and previous infection both reduced the likelihood of a person infecting their close contacts — in this case, cellmates. Having had both was best: among individuals with COVID-19, those who had been both vaccinated and previously infected were 41% less likely to pass on the virus than unvaccinated individuals without a previous infection.
Nature | 4 min read
Reference: medRxiv preprint
Array catches split-second astronomy
An array of 38 small telescopes will soon capture second-by-second changes in the stars above the Appalachian Mountains — creating movies, in real time, of transient events in a patch of the sky 1,700 times the size of the Moon. The developers of the Argus Array Pathfinder hope it will lead the way for an even larger array of 900 telescopes. They could monitor the entire visible night sky for short-lived or quickly changing events, such as exploding stars, mergers of neutron stars, or even the brief blinking out of stars as the mysterious Planet 9 — a hypothetical planet at the edge of our Solar System — passes in front of them.
Science | 5 min read
Features & opinion
Political savvy is key to us climate efforts.
One reason why the United States historically failed to make climate change a political priority is because its effects mostly made the weather nicer there, says Megan Mullin, who has studied US climate politics for more than a decade. Political acumen, not public pressure, drove the success of a milestone climate bill signed into law in August, she argues. Now a period of extreme wildfires, drought, flooding and heatwaves means that “people in the United States are just waking up to the severity of the problem they helped to create”. As the US faces the challenge of climate adaptation, understanding political feasibility and political behaviour will be key , she writes.
Reference: Nature paper (from 2016) & the related News & Views article (Nature paywall)

Depression: new treatments, new hope
Biological factors that might contribute to clinical depression are coming into light. One increasingly supported theory is that depression is linked to a slowing of nerve growth — so measures that encourage neuron formation could help to stave off the condition. Obesity is both a cause and a consequence of depression , creating a vicious cycle. And the disruptions of ancient sleep patterns by electric lighting, smartphones and modern conveniences wreak havoc on mental health. Researchers around the world are finding links between depression and COVID-19, heart health, exercise and the use of social media .
Depression rates are rising fastest in young people . The condition is also disproportionately experienced by women , because the ebb and flow of hormones during menstruation, during pregnancy, after childbirth and during menopause can trigger biochemical cascades that result in the condition. These hormonal effects are very common around the time of menopause — yet the link is still ignored by many health-care professionals .
Antidepressant drugs are commonly prescribed as a treatment, but none is universally helpful. Other types of therapy are beginning to enter the scene, from psychedelic compounds such as psilocybin to implanted devices that zap the brain with pulses of electricity .
Where I work

Abdulrahman Bamerni is a geologist at the University of Duhok in Iraq. Credit: Alice Martins for Nature
In this photo, taken in the mountains of Duhok in Iraqi Kurdistan, geologist Abdulrahman Bamerni is extracting rock samples that can help us to understand what life looked like there just after the dinosaurs went extinct, more than 65 million years ago. “For me, this is more than just research: it’s also a way to defy the Islamist terrorist group ISIS, whose members tried to kill me,” says Bamerni. He was targeted by ISIS in 2008, while he was studying at the University of Mosul in Iraq . “The attack made me more determined than ever to carry on with science,” he says. ( Nature | 3 min read )
QUOTE OF THE DAY
“‘you can’t harm this,’ i wrote in an early poem, about the ocean. oh how wrong.”.
Poet and essayist Kathleen Jamie mourns the Scottish sea birds that are being devastated by avian influenza H5N1, the escalation of ecological wounds and the damage to nature as a source of solace. ( The London Review of Books | 8 min read )
doi: https://doi.org/10.1038/d41586-022-02783-9
Apologies for promising, on Friday, that Leif Penguinson’s hiding place would be revealed on Monday. It was a holiday here in the United Kingdom and there was no Briefing. Sorry to keep you waiting!
On Friday, our peripatetic penguin wass relaxing on a lush riverside in Guadeloupe National Park . Did you find Leif Penguinson ? When you're ready, here's the answer .
Thanks for reading,
Flora Graham, senior editor, Nature Briefing
With contributions by Smriti Mallapaty
Related Articles
Daily briefing: What these scientists learnt from a year of saying no
Daily briefing: Spectacular Jupiter image from James Webb Space Telescope
Daily briefing: Do tiny blood clots cause long COVID?
Postdoctoral Fellowships at West China Hospital/West China School of Medicine of Sichuan University
Open to PhD students, PhD, Post-Doc and residents.
Chengdu, Sichuan, China
West China School of Medicine/West China Hospital
Welcome Global Talents to West China Hospital/West China School of Medicine of Sichuan University
Top Talents; Leading Talents; Excellent Overseas Young Talents on National level; Overseas Young Talents
Faculty Positions& Postdoctoral Research Fellow, School of Optical and Electronic Information, HUST
Job Opportunities: Leading talents, young talents, overseas outstanding young scholars, postdoctoral researchers.
Wuhan, Hubei, China
School of Optical and Electronic Information, Huazhong University of Science and Technology
Professor/Associate Professor/Assistant Professor/Senior Lecturer/Lecturer
The School of Science and Engineering (SSE) at The Chinese University of Hong Kong, Shenzhen (CUHK-Shenzhen) sincerely invites applications for mul...
Shenzhen, China
The Chinese University of Hong Kong, Shenzhen (CUHK Shenzhen)
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Elon Musk says ketamine can get you out of a 'negative frame of mind'. What does the research say?
Analysis Elon Musk says ketamine can get you out of a 'negative frame of mind'. What does the research say?
Elon Musk recently described using small amounts of ketamine "once every other week" to manage the "chemical tides" that cause his depression. He says it's helpful to get out of a "negative frame of mind".
This has caused a range of reactions in the media, including on Musk-owned X (formerly Twitter), from strong support for Musk's choice of treatment, to allegations he has a drug problem.
But what exactly is ketamine? And what is its role in the treatment of depression?
It was first used as an anaesthetic
Ketamine is a dissociative anaesthetic used in surgery and to relieve pain.
At certain doses, people are awake but are disconnected from their bodies. This makes it useful for paramedics, for example, who can continue to talk to injured patients while the drug blocks pain but without affecting the person's breathing or blood flow.
Ketamine is also used to sedate animals in veterinary practice.
Ketamine is a mixture of two molecules, usually referred to a S-Ketamine and R-Ketamine.
S-Ketamine, or esketamine, is stronger than R-Ketamine and was approved in 2019 in the United States under the drug name Spravato for serious and long-term depression that has not responded to at least two other types of treatments.
Ketamine is thought to change chemicals in the brain that affect mood. While the exact way ketamine works on the brain is not known, scientists think it changes the amount of the neurotransmitter glutamate and therefore changes symptoms of depression .
How was it developed?
Ketamine was first synthesised by chemists at the Parke Davis pharmaceutical company in Michigan in the United States as an anaesthetic. It was tested on a group of prisoners at Jackson Prison in Michigan in 1964 and found to be fast acting with few side effects .
The US Food and Drug Administration approved ketamine as a general anaesthetic in 1970. It is now on the World Health Organization's core list of essential medicines for health systems worldwide as an anaesthetic drug .
In 1994, following patient reports of improved depression symptoms after surgery where ketamine was used as the anaesthetic, researchers began studying the effects of low doses of ketamine on depression .
The first clinical trial results were published in 2000 . In the trial, seven people were given either intravenous ketamine or a salt solution over two days. Like the earlier case studies, ketamine was found to reduce symptoms of depression quickly, often within hours and the effects lasted up to seven days.
Over the past 20 years, researchers have studied the effects of ketamine on treatment resistant depression, bipolar disorder , post-traumatic sress disorder obsessive-compulsive disorder, eating disorders and for reducing substance use , with generally positive results.
One study in a community clinic providing ketamine intravenous therapy for depression and anxiety found the majority of patients reported improved depression symptoms eight weeks after starting regular treatment.
While this might sound like a lot of research, it's not. A recent review of ketamine research conducted in the past 30 years found only 22 ketamine studies involving a total of 2,336 patients worldwide. In comparison, in 2021 alone, there were 1,489 studies being conducted on cancer drugs .
Is ketamine prescribed in Australia?
Even though the research results on ketamine's effectiveness are encouraging, scientists still don't really know how it works. That's why it's not readily available from GPs in Australia as a standard depression treatment. Instead, ketamine is mostly used in specialised clinics and research centres.
However, the clinical use of ketamine is increasing. Spravato nasal spray was approved by the Australian Therapuetic Goods Administration (TGA) in 2021. It must be administered under the direct supervision of a health-care professional, usually a psychiatrist.
Spravato dosage and frequency varies for each person. People usually start with three to six doses over several weeks to see how it works, moving to fortnightly treatment as a maintenance dose. The nasal spray costs between $600 and $900 per dose, which will significantly limit many people's access to the drug.
Ketamine can be prescribed "off-label" by GPs in Australia who can prescribe schedule 8 drugs. This means it is up to the GP to assess the person and their medication needs. But experts in the drug recommend caution because of the lack of research into negative side-effects and longer-term effects.
What about its illicit use?
Concern about use and misuse of ketamine is heightened by highly publicised deaths connected to the drug .
Ketamine has been used as a recreational drug since the 1970s. People report it makes them feel euphoric, trance-like, floating and dreamy. However, the amounts used recreationally are typically higher than those used to treat depression .
Information about deaths due to ketamine is limited. Those that are reported are due to accidents or ketamine combined with other drugs . No deaths have been reported in treatment settings .
Reducing stigma
Depression is the third leading cause of disability worldwide and effective treatments are needed.
Seeking medical advice about treatment for depression is wiser than taking Musk's advice on which drugs to use .
However, Musk's public discussion of his mental health challenges and experiences of treatment has the potential to reduce stigma around depression and help-seeking for mental health conditions.
Julaine Allan is an associate professor of mental health and addiction at the Rural Health Research Institute at Charles Sturt University. This piece first appeared on The Conversation .
- X (formerly Twitter)
Related Stories
Thousands sign up for ketamine trial to wipe out chronic surgical pain.
One-in-five people with severe depression see results from ketamine in landmark Australia-NZ study
If you buy this popular party drug, you're likely to get something entirely different
- Drug Education
- Medical Research
- Mental Health
- Mental Wellbeing
AI Fails to Detect Depression Signs in Social Media Posts by Black Americans, Study Finds

FILE PHOTO: Figurines with computers and smartphones are seen in front of the words "Artificial Intelligence AI" in this illustration taken, February 19, 2024. REUTERS/Dado Ruvic/Illustration/File Photo
By Nancy Lapid
(Reuters) - Analyzing social media using artificial intelligence may pick up signals of depression in white Americans but not in Black counterparts, according to a study that highlights the risk of training AI models for healthcare-related tasks without data from diverse racial and ethnic groups.
The AI model used for the study was more than three times less predictive for depression when applied to Black people who use Meta Platforms' Facebook than for white people, the researchers reported.
"Race seems to have been especially neglected in work on language-based assessment of mental illness," the authors of the U.S. study wrote in a report published in PNAS, the Proceedings of the National Academy of Sciences.
Previous research on social media posts had indicated that people who frequently use first-person pronouns, such as I, me or mine, and certain categories of words, such as self-deprecating terms, are at higher risk for depression.
For the new study, researchers used an "off the shelf" AI tool to analyze language in posts from 868 volunteers, including equal numbers of Black and white adults who shared other characteristics such as age and gender.
All participants also completed a validated questionnaire used by healthcare providers to screen for depression.
The use of "I-talk" or self-focused attention, and self-deprecation, self-criticism and feeling like an outsider were related to depression exclusively for white individuals, said study co-author Sharath Chandra Guntuku of the Center for Insights to Outcomes at Penn Medicine.
"We were surprised that these language associations found in numerous prior studies didn't apply across the board," Guntuku said.
Social media data cannot be used to diagnose a patient with depression, Guntuku acknowledged, but it could be used for risk assessment of an individual or group.
An earlier study by his team analyzed language in social media posts to evaluate communities’ mental health during the COVID-19 pandemic.
In patients with substance abuse disorders, language on social media indicating depression has been shown to provide insight into the likelihood of treatment dropout and relapse, said Brenda Curtis of the U.S. National Institute on Drug Abuse at the National Institutes of Health, who also worked on the study.
(Reporting by Nancy Lapid; Editing by Michele Gershberg and Bill Berkrot)
Copyright 2024 Thomson Reuters .
Join the Conversation
Tags: artificial intelligence , United States , depression
America 2024

Health News Bulletin
Stay informed on the latest news on health and COVID-19 from the editors at U.S. News & World Report.
Sign in to manage your newsletters »
Sign up to receive the latest updates from U.S News & World Report and our trusted partners and sponsors. By clicking submit, you are agreeing to our Terms and Conditions & Privacy Policy .
You May Also Like
The 10 worst presidents.
U.S. News Staff Feb. 23, 2024

Cartoons on President Donald Trump
Feb. 1, 2017, at 1:24 p.m.

Photos: Obama Behind the Scenes
April 8, 2022

Photos: Who Supports Joe Biden?
March 11, 2020

Who is ISIS-K?
Trevor Bach March 28, 2024

Consumers Steady as Economy Hums Along
Tim Smart March 28, 2024

The Baltimore Bridge Collapse, Explained
Elliott Davis Jr. March 28, 2024

'Very Active' 2024 Hurricane Season
Cecelia Smith-Schoenwalder March 27, 2024

EXPLAINER: The Total Solar Eclipse

Trump’s Checkered Biblical Past
Lauren Camera March 27, 2024


IMAGES
VIDEO
COMMENTS
A new type of magnetic brain stimulation brought rapid remission to almost 80% of participants with severe depression in a study conducted at the Stanford University School of Medicine. The treatment, known as Stanford accelerated intelligent neuromodulation therapy (SAINT) or simply Stanford neuromodulation therapy, is an intensive, individualized form of transcranial magnetic stimulation.
Newly discovered trigger for major depression opens new possibilities for treatments. ScienceDaily . Retrieved March 25, 2024 from www.sciencedaily.com / releases / 2023 / 03 / 230330172127.htm
Depression is one of them, according to the latest research. In the largest-ever study of depression and inflammation, published in 2021 in the American Journal of Psychiatry , scientists ...
Research Open Access 26 Mar 2024 Molecular Psychiatry P: 1-11 Oral esketamine in patients with treatment-resistant depression: a double-blind, randomized, placebo-controlled trial with open-label ...
Depression is common, costly, debilitating, and associated with increased risk of suicide. It is one of the leading global public health problems. Although existing available pharmacological treatments can be effective, their onset of action can take up to 6 weeks, side-effects are common, and recovery can require treatment with multiple different agents. Although psychosocial interventions ...
The idea that depression is the result of abnormalities in brain chemicals, particularly serotonin (5-hydroxytryptamine or 5-HT), has been influential for decades, and provides an important ...
The current speed of progress in depression research is simply remarkable. We have therefore been able to create a second special issue of Molecular Psychiatry, 2020, focused on depression, with ...
Analysis of published papers around the world from 2009 to 2019 in depressive disorder. A The total number of papers [from a search of the Web of Science database (search strategy: TI = (depression$) or ts = ("major depressive disorder$")) and py = (2009-2019), Articles)].B The top 10 countries publishing on the topic.C Comparison of papers in China and the USA.
Read the latest research findings and in-depth information on clinical depression and stress in adults, teens, and children. Expand your understanding of the symptoms and available treatment for ...
FDA approval of the postpartum depression treatment brexanolone represents the final phase of a bench-to-bedside journey for this drug — a journey that began in the NIMH Intramural Research Program. NIMH experts are available to provide information on postpartum depression and the importance of, and the science underlying, this new drug.
Overall, this research did not show a difference between people with depression and those without depression. Another area of research has focused on serotonin receptors, which are proteins on the ends of the nerves that serotonin links up with and which can transmit or inhibit serotonin's effects.
Research on the development of new antidepressants should explore several mechanisms of action on several types of receptors: ... and somatic approaches. Research on depression pharmacotherapy continues to examine new molecules implicated in gamma-aminobutyric acid regulation and glutamate transmission. Also, efforts to personalize and simplify ...
D.C. Steffens. N Engl J Med 2024;390:630-639. Treatment-resistant depression in older adults is common and can be difficult to manage. Strategies include ensuring adequate antidepressant therapy ...
The new umbrella review - an overview of existing meta-analyses and systematic reviews - published in Molecular Psychiatry, ... The umbrella review aimed to capture all relevant studies that have been published in the most important fields of research on serotonin and depression. The studies included in the review involved tens of thousands ...
Source: vdnhieu/Pixabay. The idea that depression is caused by chemical imbalance in the brain—specifically lower serotonin levels—and can therefore be treated effectively with drugs that ...
Key points. There has been no direct evidence that serotonin plays a key role in depression until now. New research reported here uses a radioactive tracer and PET scans to show that serotonin ...
A new published review finds no evidence that low serotonin levels cause depression. The authors use their data to refute the "chemical imbalance" hypothesis of depression, which is an old and ...
Research round-up: depression Why depression in women is so misunderstood ... An essential round-up of science news, opinion and analysis, delivered to your inbox every weekday. Email address. Yes!
Depressive disorder (also known as depression) is a common mental disorder. It involves a depressed mood or loss of pleasure or interest in activities for long periods of time. Depression is different from regular mood changes and feelings about everyday life. It can affect all aspects of life, including relationships with family, friends and ...
Millions of Americans take antidepressants, but a new study suggests the theory underpinning their use may be entirely wrong. Research from the University College London raises doubt that chemical imbalance in the brain is responsible for depression.. A major review of previous studies on serotonin's role in depression, just published in the journal Molecular Psychiatry, concluded that ...
March 17, 2024, 3:00 AM PDT. By Erika Edwards. Teenage boys are drowning in just as much of the depression and anxiety that's been well documented in girls. Experts warn that many young men ...
Date: March 28, 2024. Source: PLOS. Summary: Women affected by premenstrual disorders have a higher risk of perinatal depression compared with those who do not, according to new research. The ...
The team made their anonymized data set publicly available—including self-reports, surveys, and phone-sensing and brain-imaging data—to help advance research into the mental health of students during their college years.. Andrew Campbell, the paper's senior author and Dartmouth's Albert Bradley 1915 Third Century Professor of Computer Science, says that the study's extensive data ...
New research published last month in JAMA Open Network suggests that familiar scents can improve symptoms in people with depressive disorders. That's because individuals who suffer from depression ...
As scientists uncover the biological factors that contribute to clinical depression, new forms of treatment are emerging. Plus, the Webb telescope spots CO2 on an exoplanet for the first time, and ...
In 1994, following patient reports of improved depression symptoms after surgery where ketamine was used as the anaesthetic, researchers began studying the effects of low doses of ketamine on ...
US News is a recognized leader in college, grad school, hospital, mutual fund, and car rankings. Track elected officials, research health conditions, and find news you can use in politics ...
Biased AI. The analyses found that while artificial intelligence (AI) can detect signs of depression in white Americans through social media use, it may not be as effective for Black individuals. In fact, it was three times less predictive when applied to Facebook posts by Black people, as compared to those by White people.