Home — Essay Samples — Nursing & Health — Anxiety — Anxiety and Depression Among College Students: A Critical Analysis

Anxiety and Depression Among College Students: a Critical Analysis
- Categories: Anxiety
About this sample

Words: 496 |
Published: Mar 6, 2024
Words: 496 | Page: 1 | 3 min read
Table of contents
Factors contributing to anxiety and depression, strategies for prevention and support.

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Dr. Heisenberg
Verified writer
- Expert in: Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
6 pages / 2718 words
3 pages / 1288 words
5 pages / 2122 words
3 pages / 1305 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Anxiety
Defensive pessimism is a unique psychological strategy that involves anticipating the worst possible outcome in a given situation. While it may sound counterintuitive, defensive pessimism is not about pessimism for its own sake [...]
Have you ever felt the insidious grip of anxiety slowly tightening around you, squeezing the breath from your lungs and clouding your thoughts? Anxiety, a common mental health issue affecting millions of people worldwide, can [...]
Social anxiety, also known as social phobia, is a prevalent mental health condition that affects numerous individuals worldwide. This debilitating disorder manifests as an intense fear and discomfort in social situations and can [...]
Understanding anxiety disorders is vital for addressing the impacts they have on individuals and communities. By continuing to conduct research and advocating for mental health awareness, we can work towards destigmatizing [...]
There is definitely nothing incorrect in being anxious. When confronted with a circumstance or an issue, people experience stress and anxiety. Most people have the propensity to worry when trying to end up a due date that seems [...]
“Eat your vegetables! Exercise! Get a good night's sleep!” We’ve all known to take care of our bodies since grade school P. E. class. But what about our mental health, isn’t mental health just as important as physical health? [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
Anxiety Disorders and Depression Essay (Critical Writing)
Introduction, description section, feelings section, action plan, reference list.
Human beings become anxious in different situations that are uncertain to them. Depression and anxiety occur at a similar time. Anxiety is caused due to an overwhelming fear of an expected occurrence of an event that is unclear to a person. More than 25 million people globally are affected by anxiety disorders. People feel anxious in moments such as when making important decisions, before facing an interview panel, and before taking tests. Anxiety disorders are normally brained reactions to stress as they alert a person of impending danger. Most people feel sad and low due to disappointments. Feelings normally overwhelm a person leading to depression, especially during sad moments such as losing a loved one or divorce. When people are depressed, they engage in reckless behaviors such as drug abuse that affect them physically and emotionally. However, depression manifests in different forms in both men and women. Research shows that more women are depressed compared to men. This essay reflects on anxiety disorders and depression regarding from a real-life experience extracted from a publication.
“Every year almost 20% of the general population suffers from a common mental disorder, such as depression or an anxiety disorder” (Cuijpers et al. 2016, p.245). I came across a publication by Madison Jo Sieminski available who was diagnosed with depression and anxiety disorders (Madison 2020). She explains how she was first diagnosed with anxiety disorders and depression and how it felt unreal at first. She further says that she developed the need to get a distraction that would keep her busy so that she won’t embrace her situation. In her case, anxiety made her feel that she needed to do more, and everything needed to be perfect.
Madison further said that the struggle with anxiety is that it never seemed to happen, but it happened eventually. She always felt a feeling of darkness and loneliness. She could barely stay awake for more than 30 minutes for many days. Anxiety and depression made her question herself if she was good enough, and this resulted in tears in her eyes due to the burning sensation and overwhelmed emotions. In her own words, she said, “Do I deserve to be here? What is my purpose?” (Madison 2020). Anxiety made her lose confidence in herself and lowered her self-esteem. She could lay in bed most of the time and could not take any meal most of the days.
Madison said that since the sophomore year of high school, all was not well, and she suddenly felt someone in her head telling her to constantly worry and hold back from everything. She could wake up days when she could try a marathon to keep her mind busy. However, she sought help on 1 January 2020, since she felt her mental health was important, and she needed to be strong. She was relieved from her biggest worries, and what she thought was failure turned into a biggest achievement. She realized that her health needed to be her priority. Even after being diagnosed with depression disorders, she wanted to feel normal and have a normal lifestyle like other people.
Madison was happy with her decision to seek medical help even though she had her doubts. She was happy that she finally took that step to see a doctor since she was suffering in silence. She noted that the background of her depression and anxiety disorders was her family. It was kind of genetic since her mom also struggled with depression and anxiety disorders. Her mom was always upset, and this broke her heart. She said it took her years to better herself, but she still had bad days. Madison decided to take the challenge regarding her mother’s experience. Also, Madison said she was struggling to get over depression since her childhood friends committed suicide, and it affected her deeply. She also told the doctor how she often thought of harming herself. The doctor advised her on the different ways she could overcome her situation after discovering she had severe depression and anxiety disorders.
After going through Madison’s story, I was hurt by the fact that he had to go through that for a long time, and something tragic could have happened if she had not resorted to medical help. I felt emotional by the fact that she constantly blamed herself due to her friends who committed suicide, and she decided to accumulate all the pain and worries. The fact that I have heard stories of how people commit suicide due to depression and anxiety disorders made me have a somber mood considering her case. In this case, you will never know what people are going through in their private lives until they decide to open up. We normally assume every person is okay, yet they fight their demons and struggle to look okay. Hence, it won’t cost any person to check up on other people, especially if they suddenly change their social characters.
Madison’s story stood out for me since she had struggled since childhood to deal with depression and anxiety disorders. In her case, she was unable to seek help first even when she knew that she was suffering in silence (Madison 2020). However, most people find it hard to admit they need help regardless of what they are going through, like Madison. People who are depressed cannot work as they lack the motivation to do anything. In my knowledge, depression affects people close to you, including your family and friends. Depression also hurts those who love someone suffering from it. Hence, it is complex to deal with. Madison’s situation stood out for me since her childhood friends committed suicide, and she wished silently she could be with them. Hence, this leads to her constant thoughts of harming herself. Childhood friends at one point can become your family even though you are not related by blood due to the memories you share.
Depression and Anxiety disorders have been common mental health concerns globally for a long time. Depression and anxiety disorders create the impression that social interactions are vague with no meaning. It is argued by Cuijpers (2016, p.245) that people who are depressed normally have personality difficulties as they find it hard to trust people around them, including themselves. In this case, Madison spent most of her time alone, sleeping, and could not find it necessary to hang around other people. Negativity is the order of the day as people depressed find everything around them not interesting.
People who are depressed find it easy to induce negativity in others. Hence, they end up being rejected. Besides, if someone is depressed and is in a relationship, he/she may be the reason for ending the relationship since they would constantly find everything offensive. Research shows that people who are clinically depressed, such as Madison, prefer sad facial expressions to happy facial expressions. Besides, most teenagers in the 21 st century are depressed, and few parents tend to notice that. Also, most teenagers lack parental love and care since their parents are busy with their job routines and have no time to engage their children. Research has shown that suicide is the second cause of death among teenagers aged between 15-24 years due to mental disorders such as suicide and anxiety disorders.
Despite depression being a major concern globally, it can be controlled and contained if specific actions are taken. Any person needs to prioritize their mental health to avoid occurrences of depression and anxiety orders. Emotional responses can be used to gauge if a person is undergoing anxiety and depression. The best efficient way to deal with depression and anxiety is to sensitize people about depression through different media platforms (Cuijpers et al. 2016). A day in a month should be set aside where students in colleges are sensitized on the symptoms of depression and how to cope up with the situation. Some of the basic things to do to avoid anxiety and depression include; talking to someone when you are low, welcoming humor, learning the cause of your anxiety, maintaining a positive attitude, exercising daily, and having enough sleep.
Depression and anxiety disorders are different forms among people, such as irritability and nervousness. Most people are diagnosed with depression as a psychiatric disorder. Technology has been a major catalyst in enabling depression among people as they are exposed to many negative experiences online. Besides, some people are always motivated by actions of other people who seem to have given up due to depression. Many people who develop depression normally have a history of anxiety disorders. Therefore, people with depression need to seek medical attention before they harm themselves or even commit suicide. Also, people need to speak out about what they are going through to either their friends or people they trust. Speaking out enables people to relieve their burden and hence it enhances peace.
Cuijpers, P., Cristea, I.A., Karyotaki, E., Reijnders, M. and Huibers, M.J., 2016. How effective are cognitive behavior therapies for major depression and anxiety disorders? A meta‐analytic update of the evidence . World Psychiatry 15(3), pp. 245-258.
Madison, J. 2020. Open Doors .
- Concept Care Plan Mapping: Eva Madison
- The United States Supreme Court: Marbury vs. Madison
- Federalist Paper Number 10
- Cerebral Palsy: Epidemiology and Etiology
- Neurological System Disorder of Falling Asleep
- Migraine Headache and Tension Headache Compared
- Neurodevelopmentally at‐Risk Infants
- Migraine Without Aura Treatment Plan
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2022, June 16). Anxiety Disorders and Depression. https://ivypanda.com/essays/anxiety-disorders-and-depression/
"Anxiety Disorders and Depression." IvyPanda , 16 June 2022, ivypanda.com/essays/anxiety-disorders-and-depression/.
IvyPanda . (2022) 'Anxiety Disorders and Depression'. 16 June.
IvyPanda . 2022. "Anxiety Disorders and Depression." June 16, 2022. https://ivypanda.com/essays/anxiety-disorders-and-depression/.
1. IvyPanda . "Anxiety Disorders and Depression." June 16, 2022. https://ivypanda.com/essays/anxiety-disorders-and-depression/.
Bibliography
IvyPanda . "Anxiety Disorders and Depression." June 16, 2022. https://ivypanda.com/essays/anxiety-disorders-and-depression/.
Mental Health Matters: Anxiety and Depression
Anxiety the most common mental health diagnosis in college students
Special Report Mental Health Matters
Anxiety and depression.
Mental Health has become a critical issue on college campuses. Here at BU, Behavioral Medicine clinicians report that the number of students in crisis coming in for help has increased sharply—from 647 in the 2014–2015 academic year to 906 last year. And the number of students needing medical transports for psychiatric evaluation has also risen, from 120 in the 2014–2015 academic year to 134 last year.
In light of this alarming trend, this week BU Today is republishing a special three-part series, “ Mental Health Matters ,” that was originally published last October. We have updated the series to include new statistics and information.
When it was announced in spring 2014 that a Penn State study had found that anxiety had surpassed depression as the leading mental health issue facing college students, the story made national headlines . According to the study of more than 100,000 students by Penn’s Center for Collegiate Mental Health , more than half of the students visiting campus health clinics listed anxiety as a concern. That finding was borne out by the American College Health Association (ACHA) 2015 National College Health Assessment survey , which reported that nearly one in six college students (15.8 percent) had been diagnosed with, or treated for, anxiety.
The same survey found that 21.9 percent of students said that within the last 12 months, anxiety had affected their academic performance, defined as receiving a lower grade on an exam or important project, receiving an incomplete, or dropping a course. That’s up from 18.2 percent in the ACHA’s 2008 survey. Meanwhile, 13.8 percent reported that in the last 12 months, depression had affected their academic performance, up from 11.2 percent in 2008.
These findings don’t surprise mental health clinicians at BU.
“We have all become less able to tolerate ambiguity and the unknown due to the incredible technological advances we have seen,” says Carrie Landa, director of Behavioral Medicine at Student Health Services . “Immediacy is sometimes the antidote to anxiety: having to wait for anything—a text, an exam grade, ‘How am I going to do?’—all create anticipatory anxiety. Unfortunately, there are many things in life that aren’t quickly resolved and waiting is necessary.”
In the 2015 Healthy Minds study , an annual web-based survey examining mental health on college campuses, the number of BU students who score positive on a measure of depression was larger, at 23 percent, than the number who scored positive on a measure of anxiety, 17 percent. In fact, depression and anxiety are two sides of the same coin, says Dori Hutchinson (SAR’85,’96), director of services at BU’s Center for Psychiatric Rehabilitation and a Sargent College clinical associate professor. Both are treatable with therapy, lifestyle changes, and medication when indicated—and sometimes a combination of all three.
What’s normal and when to seek help
Every student feels stressed out at one time or another, especially during midterms and finals. And it’s normal for students to feel blue on occasion, too. So when do those feelings become reason for more concern?
“When your mood state interferes with your ability to function at school,” Hutchinson says, “like when you’re finding you can’t get to class, and you don’t want to hang out with your friends or teammates, and you’re having difficulty concentrating because you’re feeling so distressed—that’s when we want to reach out and help you.”
“ Often it is more important to manage your emotional reaction to stress than to try to change the stressful situation, which may not be fully under your control.” —Lisa Smith
Other warning signs are prolonged feelings of sadness or despair, excessive anxiety or panic, isolation or withdrawal from typical daily activities, thoughts of self-harm or suicide, giving away possessions, changes in personal hygiene, and excessive use of alcohol or other drugs, which are often used by students experiencing social anxiety to self-medicate.
“When any emotions or behaviors are a big change from your regular, day-to-day functioning, it’s important to stop and ask yourself what’s going on,” says Landa. “We see normal anxiety morph into distress when a student is having panic attacks, can’t sleep or slow themselves down, persistently worries or obsesses about what’s next, or is having other physical symptoms consistent with anxiety. When day-to-day functioning is affected, but before it’s impaired, that’s when to get help. Similarly, with depression, everyone experiences a low mood day or a disappointment they just can’t shake off, whether that’s because of a bad grade, a relationship ending, or a fight with a friend. But when feelings of sadness, loneliness, or low self-worth become the norm, reaching out is really important.”
“We know that stress can be a trigger of psychological conditions, especially in the context of unpredictability and uncontrollability. This seems to be inherent in the transition to college,” says Lisa Smith, director of BU’s Center for Anxiety & Related Disorders and a College of Arts & Sciences clinical associate professor of psychological and brain sciences. “At the point where your emotions are interfering with your life or are causing significant distress is when you would want to take action to adjust your emotional functioning in response to stress.
“Often it is more important to manage your emotional reaction to stress than to try to change the stressful situation, which may not be fully under your control,” she says. “I often think that if students were given an Emotions 101 course in high school or college, they would be much better equipped to know how emotions work well versus what emotional coping strategies only serve to heighten anxiety and depression. It’s often surprisingly counterintuitive.”
For many students, Smith says, a brief program of cognitive-behavioral treatment can help them shift to more effective emotion management.
STUDENT STRESS AND ANXIETY NATIONALLY, BY THE NUMBERS
Despite the fact that depression and anxiety are treatable, many students are reluctant to admit they have a problem and to seek help.
Case in point: Victoria Pae (CAS’16). During freshman year, she says, she felt overwhelmed by stress and anxiety, but she was afraid to seek help. “Everyone was doing so much, everyone was so on top of their games, it seemed like they had it all together,” says Pae, a double major in neuroscience and psychology, who as a high school student had done very well academically and in extracurricular activities. “You’re seeing everyone excelling above you. And even though you have the ability to excel too, you’re too scared of making a fool of yourself to actually try to do it.”
Pae found it hard to admit she had a problem. She kept her feelings of anxiety and being overwhelmed to herself. “I didn’t want to tell myself that I needed to get help, so I didn’t,” she says. “I just told myself, it’s all in my head, get over it.”
“A colleague of mine has started calling it the ‘game face’ that students put on, that tells everybody else in the world, ‘I’m just fine, I’m handling it, look at me juggling school, extracurricular activities, and work,’” says Katharine Mooney (SPH’12), director of Wellness & Prevention Services at Student Health Services. “But that’s not how they’re feeling…they feel really alone, isolated, that no one else feels like they do. And that’s just not the case.”
Rather than confront her feelings, Pae says, she would party with friends. Her grades began to suffer as well. But at the beginning of her sophomore year, she started working with the BU chapter of the student mental-health group Active Minds , which works to make people more aware of mental health issues, reduce prejudice against those with mental health challenges, and direct students to behavioral health resources on campus.
“I was teaching students that it’s OK to receive support, but here I was with a mental health disorder and not seeking help. I thought that was very hypocritical,” Pae says. The spring after she joined Active Minds, she began to see an off-campus therapist to help treat her anxiety.
“I won’t say I’m 100 percent OK now, as I still have my moments of self-doubt and of neglecting self-care,” Pae says, “but I’m definitely doing better than I was a couple of years ago.”
A chance for everyone to be screened
Tomorrow, October 5, all students, as well as faculty and staff, can receive free, confidential screenings for depression and anxiety as part of National Depression Screening Day .
The screenings, brief anonymous questionnaires with multiple choice answers, are being offered on both the Charles River and Medical Campuses and take only two to three minutes to complete. The questionnaire asks about eating and sleeping habits and having feelings of hopelessness, suicidal thoughts, or an inability to stop worrying. The results can help determine if someone is experiencing depression, anxiety, a mood disorder, or even post-traumatic stress.
A clinician will review the answers on site and discuss what the proper next steps might be and provide referral cards directing students to Behavioral Medicine, the Center for Anxiety & Related Disorders, or the Center for Psychiatric Rehabilitation. Everyone who is screened receives information about counseling and other services, regardless of whether they show symptoms of anxiety and depression. No appointment is needed.
“ Sometimes a screening can be lifesaving, while other times it helps facilitate the small change that allows someone to go from feeling okay to feeling good.” —Carrie Landa
“If your score is high, we say, ‘What can we do to help?’ and direct them toward resources on campus,” Hutchinson says.
The screenings will be held at three locations on the Charles River Campus: at both the George Sherman Union Link and the Yawkey Center for Student Services dining room, from noon to 3 p.m. and in the FitRec lobby, from 3:30 to 6:30 p.m. Screenings on the Medical Campus will be in the School of Medicine L-Instructional Building lobby, from 4 to 6:30 p.m. At each site, clinicians will be on hand for confidential feedback and there free chocolate will be given out.
During last year’s National Depression Screening Day event at BU, 445 people came for checkups, Hutchinson says, and 19 percent were referred to Behavioral Medicine for appointments or other follow-ups. Six students received urgent care after noting that they were in extreme distress. The first year BU held the screenings, in 2008, one person was hospitalized after the questionnaire revealed suicidal impulses.
“That may have helped save his life and put him on the path to wellness,” says Hutchinson.
The screenings coincide with the semester kicking into high gear. “The honeymoon is over, the schoolwork is hard—it might be growing,” Hutchinson says. “Midterms are right around the corner, and if someone is living with depression, it can worsen. The screenings are really a way for our community to say, we care about you.”
Landa urges everyone to avail themselves of the opportunity to be screened Wednesday. “National Depression Screening Day is a great opportunity to check in with yourself, be able to quickly look at some key behaviors and feelings that are markers for wellness. Sometimes a screening can be lifesaving, while other times it helps facilitate the small change that allows someone to go from feeling okay to feeling good.”
Pae says her experience with anxiety made her realize the benefits of getting help. “I think a lot of students…are scared to admit that they’re stressed and worried their life might be crumbling before their eyes,” she says. The former president of BU’s Active Minds chapter, Pae says the group emphasizes that “whether the difficulties you’re going through are major or minor, it’s OK to seek help.”
Those seeking free, confidential mental health counseling can contact Student Health Services Behavioral Medicine (617-353-3569) (available 24 hours for psychiatric emergencies), the Center for Psychiatric Rehabilitation (617-353-3549), the Danielsen Institute (617-353-3047), and the Center for Anxiety & Related Disorders (617-353-9610). Faculty and staff with mental health issues can contact BU’s Faculty & Staff Assistance office (617-353-5381). The Samaritans of Boston suicide prevention hotline is 877-870-4673. The Active Minds student support group is best reached through its Facebook page . For crises related to crime and interpersonal or sexual violence, BU’s Sexual Assault Response & Prevention Center crisis counselors are available 24 hours a day, 7 days a week (617-353-SARP) (7277). If you, or someone you know, have questions about their drug or alcohol use, Wellness & Prevention Services can help (617-358-0485). Students who require academic or other accommodations for a psychological disability can also consult BU’s Disability Services (617-353-3658). Accommodations and services could include testing modifications, reduced course load, developing skills in self-advocating with faculty, executive functioning coaching, and more. Services are free and confidential.
Next, in the final installment of our series “Mental Health Matters,” we’ll look at healthy ways of coping with stress and where to seek help at BU.
This Series

Mental Health Matters: Getting Help, Helping Yourself
Mental health matters.
October 1, 2016
Mental Health Matters: A Growing Challenge
Series home
- Share this story
- 10 Comments Add
Staff Writer

Joel Brown is a staff writer at BU Today and Bostonia magazine. He’s written more than 700 stories for the Boston Globe and has also written for the Boston Herald and the Greenfield Recorder . Profile
Comments & Discussion
Boston University moderates comments to facilitate an informed, substantive, civil conversation. Abusive, profane, self-promotional, misleading, incoherent or off-topic comments will be rejected. Moderators are staffed during regular business hours (EST) and can only accept comments written in English. Statistics or facts must include a citation or a link to the citation.
There are 10 comments on Mental Health Matters: Anxiety and Depression
Maybe the screening should be done before the potential student registers! Alas, then the University could be held at fault?
Books are a great resource as well. I read the books by mark hyman, and i read the book Presence and Positivity the new energy sources of the 21st century by victor hagen . it solved So much for me, not only anxiety but also gave me a lot of new energy
What desperately needs to be done is to overhaul our entire mental health education and practice and the “Bible of filth” needs to be seriously looked at. How stupid can these mental health workers be anyway? Take suicide for instance the rates kept going up and up and yet they refused to even consider that what they were doing was not working instead they blame everything else but their own failures.
Hi there, Just read your post. I’m currently struggling with my own Mental health issues. Would you be willing to tell me more about what path one should take in such a situation ? I am also under the impression the way Doctors prescribe meds etc, is the wrong way to go
I would have to agree that I have seen this myself being a current college student. It is very unfortunate that so many students struggle with this issue.
I am a current college student, in my junior year. This is completely relevant and accurate. I myself was diagnosed with anxiety and depression, which before college, I never had an issue with. And looking back on myself the last few years, I can see it in other students around me.
Our society has always been so hush hush about mental illness and this country has more mental illness cases than any other country in the world. People need to be able to talk about mental illness without being afraid or ashamed because it is really a common thing. I have a son that struggles with mental illness and he also goes in and out of denial is afraid to talk about it. It can be a very scary thing for young people who don’t know why things are happening to them mentally.
I struggled to find work in my field after finishing my post-grad work, so I panicked and fell into commercial research work. Within a couple of years I’d been promoted up and away from all scientific and technical aspects of the business to become Spreadsheet Commander. Eight years later, I’ve got a ‘good’ career but I hate it and all my scientific skills are eight years out of date, so moving into something else would be very hard even if I could afford it.
My message to anyone leaving Higher Ed would be: Don’t panic, you’ve got plenty of time. Don’t lose sight of what you really want to do because you’re worried about getting a mortgage or keeping up with the Joneses.
It is important for all to know the difference between an anxiety and an anxiety disorder that requires medical attention.
In general, anxiety is a normal reaction to stress feelings of tension, worried thoughts. In fact, it can be a good thing. Anxiety motivates you to accomplish your assignments, to study harder for a test and it can warn you when you’re in a dangerous situation. An anxiety disorder, however, involves intense and excessive anxiety, along with other debilitating symptoms. Physical symptoms, such as increased blood pressure and nausea, may also become evident. These responses move beyond anxiety into an anxiety disorder. http://everydayscience.blog/anxiety-disorder/
In summary, mental health problems are common among college students. Academic pressure together with stressors typical of starting and attending college may precipitate the first onset of mental health and substance use problems or an exacerbation of symptoms. Often the nature of psychopathology is chronic due to low rate of treatment seeking and low adherence to treatment. Thus, it is critical to employ outreach programs and implement strategies to ensure treatment retention. Given that many traditional students continue to depend on their family while in college, parental involvement in treatment is important. Finally, given the effect that the academic calendar may have on continuity of care, it is critical for clinicians to ensure that college students receive treatment throughout the year and to coordinate with other clinicians that may be involved in the students’ care. Thus, expertise in developmental psychopathology, family dynamics, specific college issues, and systems of care is critical to conduct clinical treatment to college students.
Post a comment. Cancel reply
Your email address will not be published. Required fields are marked *
Latest from BU Today
Pov: remembering charlie pohonich, did you win the free furiosa: a mad max saga tickets for tonight, karen antman stepping down as bu’s medical school dean and medical campus provost, a bu class tackles the massachusetts housing crisis, zesty potato salad, my reflections on the last four years of college: why small life events matter, exploring bu’s vibrant asian student communities for aapi heritage month, photo essay: behind the scenes at a bu commencement, how three class of 2024 grads landed jobs before graduating, protests unfold in and around nickerson field during bu’s 151st commencement, quotes, comments, and cheers from bu’s 151st commencement, sights and sounds from boston university’s 151st commencement, “i’m excited to embark on this journey we call life”, bu celebrates 7,600 graduates at buoyant 151st commencement, “we are called, my friends, to be peacemakers,” rev. walter e. fluker tells boston university’s baccalaureate audience, class of 2024 chobanian & avedisian school of medicine graduates urged to become changemakers, bu’s commencement student speaker is proud of being a changemaker, anthony hollenberg named new president of boston medical center, three inspiring bu master’s and professional graduates who plan to give back to their communities, from masks to mortarboards: class of 2024 reflects on a unique four years.
1 in 5 college students have anxiety or depression. Here’s why
Professor of Psychiatry and Neuroscience, Wayne State University
Disclosure statement
David Rosenberg receives funding from the Children’s Hospital of Michigan Foundation, Detroit, MI, and a grant from the National Institute of Mental Health (R01MH59299).
Wayne State University provides funding as a member of The Conversation US.
View all partners

Many of us think of college as a wondrous time of new experiences and great freedom to explore new ideas and find one’s true self.
In recent years, however, depression and anxiety have afflicted college students at alarming rates. As noted in the latest Center for Collegiate Mental Health report , anxiety and depression are the top reasons that college students seek counseling.
Research shows that nearly 1 in 5 university students are affected with anxiety or depression .
So why are these disorders so prevalent in our college students? As a professor of psychiatry and a practicing psychiatrist who has experience with mental health problems among college students, I see a number of factors.
Dangers in technology
Social media and technology are among the most dangerous of these factors. Excessive use of each tends to engender impaired social interactions and an increased sense of isolation .
Excessive social media use also fosters a certain competition between one’s real life and one’s virtual life . That is, a tug of war between being engrossed in posting experiences on social media, sending texts and taking selfies instead of enjoying the moment for what it’s worth.
Many college students are living dual virtual and real lives, and the virtual life is competing and at times becomes more important than real life. This is not only something that those of us in the trenches see clinically but it has been well- documented in research studies.
Several other studies have found that mobile phone addiction , as well as excess smartphone use, is also associated with increased sleep disturbance , depression , anxiety and overall stress.
For example, one study found that almost 50 percent of college students indicated they woke up at night to answer text messages. The same study found that the more people use technology during their sleeping hours, the poorer the quality of their sleep and the higher their rates of depression and anxiety.
Seeking out drugs
But there are other culprits, such as the desire to get into a good college – and stay in college with good grades. To attain these goals, it is not uncommon for students and their parents to seek chemical assistance.
In the past five years, the number of requests I receive from high school and college students and their parents for stimulants such as Ritalin and Adderall has skyrocketed. A decade ago, I rarely, if ever, got such a request. Now, I get several per month. These requests are often made prior to taking major exams, such as finals, the MCAT or the LSAT. For those who are curious, I never acquiesce to these requests and instead recommend a comprehensive psychiatric assessment to make an accurate diagnosis and determine the most appropriate treatment, if one is necessary. The conversation often stops there.

While these medicines can be very effective and safely prescribed in patients with attention deficit hyperactivity disorder, there is considerable risk when they are used for other reasons. It is well-known that side effects from Ritalin and Adderall include anxiety and depression. This risk is even higher in people taking the medicine for an unapproved reason or who do not take the medicine as prescribed.
Another factor at play is that rates of depression in our society have increased significantly over the past 20 years. This means more parents of college students have higher rates of depression. And since depression has a significant genetic component , the risk for depression in the children of a depressed parent is much higher than in the general population.
College students who reported being victims of cyberbullying in high school — which has nearly doubled in the past decade — also had significantly higher rates of anxiety and depression.
Cigarette smoking has been associated with significantly more sleep problems in college students and increased risk for depression and anxiety. Fortunately, the rate of cigarette smoking and e-cigarette use continues to decline with the rate of past-month use declining to around 16 percent of college students in 2016.
College students with a history of attention deficit hyperactivity disorder also have much higher rates of anxiety and depression. It is estimated that between 2 to 8 percent of college students struggle with symptoms of this disorder.
Other stressors
Moreover, while going to college can be exciting for many, for some the adjustment is hard with profound homesickness and separation anxiety. These students are at very high risk for depression and anxiety.
Financial stresses brought about by the rising cost of college , including the dread of debt and fear of not getting a job after college and having to move back in with mom and dad after graduation, are associated with increased risk for depression and anxiety in college students.
In the past, it was taken for granted that our children would surpass their parents. Now that is not so. Many college students believe that they will not be able to accomplish as much as their parents did. There is a sense of frustration and that there are no “good” jobs out there anymore.
Parents are also more involved in their children’s college and work experience. It is not uncommon for parents to call college counselors, bosses and work managers. Once that would have been absolutely off-limits. Now, this is commonplace .
Such parental overinvolvement can foster dependence, anxiety and depression, and thwart creativity. I do not mean to blame parents who are concerned and who want the best for their children. However, sometimes failing or not getting an A on a test can be more instructive and instill a sense of resilience and the ability to “bounce back.”
So what do we do to curtail anxiety and depression among college students?
Help, hotlines and hope
Tough problems do not always yield simple, easy solutions. Having an insurance card, 24-hour helplines and hotlines can provide a false sense of security and belief that excellent care is available. However, one study that looked at mental health service use in university students found that even when universal access to mental health care is provided, most students with mental disorders do not get treatment.
The good news is that if we are proactive there is a solution that is cost-effective and that can work, but only if there is buy-in at every level of the particular university and society.
And, ironically, while technology can be a source of anxiety and depression, technology can also be used to treat depression. That is, computers, iPads and smartphones can be used to virtually bring a mental health professional to the student where he or she is, be that in their dorm room or off campus.
The key is recognizing those at highest risk and who are most vulnerable early. Colleges have to respond on day one and confront the stigma that still follows those with mental illness. Training peer support groups is vital. This is not something to be done in isolation but under the guidance, supervision, and training of experienced psychiatrists, psychologists and psychiatric social workers.
Most of all, students and parents need to know from the very beginning of the college experience that the physical and mental well-being of students matters. Colleges should let parents and students know that there are trained and qualified people who can help students at risk discreetly and confidentially.
- Mental health
- Student depression
- Student counselling

Clinical Education Strategy & Risk Project Officer

Senior Research Fellow - Women's Health Services

Lecturer / Senior Lecturer - Marketing

Assistant Editor - 1 year cadetship

Executive Dean, Faculty of Health

How to Handle Stress and Anxiety in College
Practical advice beyond the all-too-commonly-prescribed meditation and exercise..
Posted July 31, 2021 | Reviewed by Tyler Woods
- What Is Stress?
- Find a therapist to overcome stress
- Stress and anxiety is a reality in college and psychology courses are no exception.
- There are a number of practical ways to handle the stress and anxiety that college can provoke.
- The solutions may not be what you expect.

With college comes anxiety . Deadlines, grades, performance pressure…if you’re not feeling it, are you even in college?
I know there is a lot out there about how unfair it is for classes to cause stress. Test time limits are stressful and unfair, due dates are anxiety-provoking and unjust, rules are oppression.
We can continue having those debates, but in the meantime, how do we deal with the reality?
Introductory psychology students, for example, are usually getting used to the expectations of college, a transition from dependent to independent learning, while learning a new formal writing style, learning how to find and understand research, practicing critical thinking skills, and studying the approximately 5 million topics that come in an introductory course.
So, what are some practical ways to handle the stress and anxiety college can invoke?
Assume Good Intent
The student is there to earn points. The professor is not there to take them away. That small shift in perspective can do wonders. Professors want students to learn and tend to do everything they can to make that happen, but understand that professors are not free agents.

I stole that line directly from my colleague, Janet Carney-Clarke. As she reminds her students, instructors are beholden to government regulations, school policies, and rules of the department. In other words, professors can’t just “do whatever they want.” There are rules we have to follow, too.
Tragically, the professor-student relationship is too often framed as one of enemy combatants. No, no, no! Students are there to learn and professors are there to facilitate learning. We are each partners in the learning process; each role has responsibilities and expectations.
Check Expectations
“I didn’t do the assignment because you didn’t remind me to do it.” –former student
“I got some questions wrong and didn’t get all of my points. I deserve all of my points!” –former student
“I can’t come to class this semester due to my schedule, so I need you to repeat your lectures in office hours.” –former student
Where do I begin? Students who do best in college understand the expectations at that level, even if they don’t agree with them. This becomes an equity issue when some students are exposed to them far in advance and some never are. In fact, I can’t tell you how many high school sophomores and juniors take my introductory psychology courses.
Learning college-level expectations, let alone taking college-level coursework, in high school is quite a privilege. Almost every college and university, however, now offers preparatory courses for students who have not had that advantage. Take them!

Take Advantage of Office Hours
I was scared of some of my professors. With courage, I got myself through that office door and into drop-in hours. Doing so was truly giving a gift to myself. Frankly, office hours are what single-handedly pulled my grade up from a D to an A in Psychology of the Law.
Professors (and teaching assistants) get paid for office hours. Trust me, they are often sitting there waiting, just waiting, for a student to come in. Be that student!
Utilize School Resources
Schools have resources to help students. There are so many! And they often go under-utilized. Student health services usually offer support to students experiencing anxiety and stress and, in my experience, students tell me that they benefitted greatly. The point is, there are free resources available to students that really help. Ask professors, search online, they’re there and they are waiting to be used.
One thing to keep in mind, especially if you’re a psychology (or related discipline) student: Your instructor is not your therapist. They can’t be. The person in charge of your grade should never provide you clinical guidance. Sure, professors can give you resources and suggestions, but students should never seek therapy from an instructor…even if that instructor is a therapist in another life.

Use Other Free Resources
In the age of, “Take care of yourself!” there are approximately one billion apps and free meditation /relaxation tools out there, beyond resources provided by schools. One I love to share with students is U.C. Berkeley’s Greater Good Science Center. Specifically, they have an action center that offers science-backed activities that help with relaxation, stress, happiness , optimism , and so much more. I particularly appreciate that each activity provides a study backing why it works.
In psychology, we know that a sense of accomplishment has great benefits for confidence , self-esteem , and the like. So, take that scary test. Draft that frightening paper. Do it! Experience matters. Not only will accomplishing the anxiety-provoking task literally end that anticipatory stress, but it will also tell your brain that you can do this again in the future, thus reducing your stress. You succeeded!
Not What You Expected?
Meditation, exercise, taking breaks: Those are the expected solutions in a “take care of yourself” world, and for good reason—they work. But in an environment of prolonged stress and anxiety like college, the above solutions just may help go beyond the Band-Aid and provide healing deeper into the wound.

Ashley Maier teaches psychology at Los Angeles Valley College.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

At any moment, someone’s aggravating behavior or our own bad luck can set us off on an emotional spiral that threatens to derail our entire day. Here’s how we can face our triggers with less reactivity so that we can get on with our lives.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
- Companies & Schools
Should you discuss mental health issues in your college essay?
by Erica L. Meltzer | Oct 20, 2018 | Blog , College Essays | 6 comments
Image ©Nickshot, Adobe Stock
Note, January 2022: This post was written in 2018, before the start of the Covid-19 pandemic. Obviously, many things have changed since then, not least the amount of psychological pressure that many high school students have experienced. Clearly, some of the boundaries and expectations surrounding acceptable/advisable topics for admissions essays have shifted, and applicants undoubtedly have more leeway in discussing mental-health issues than they did in the past. That said, I would still caution against making this subject the exclusive focus of your essay(s). If it happens to be relevant—and it very well might be, given the events of the last couple of years— then you should focus on discussing it in a mature way that conveys qualities such as empathy and resilience, and that demonstrates your ability to reflect insightfully on what may have been very difficult situations.
As regular readers of my blog may know, I periodically trawl the forums over at College Confidential to see what’s trending. Recently, I’ve noticed a concerning uptick in the number of students asking whether it’s appropriate for them to write about mental health issues, most frequently ADD and/or anxiety, in their college applications.
So the short answer: don’t do it.
The slightly longer version:
If you’re concerned about a drop in grades or an inconsistent transcript, talk to your guidance counselor. If these types of issues are addressed, the GC’s letter is the most appropriate place for them. If, for any reason, the GC is unable/unwilling to discuss them and the issues had a significant impact on your performance in school that unequivocally requires explanation, you can put a brief, matter of fact note in the “is there any additional information you’d like us to know?” section, but think very carefully about how you present it. Do not write your main essay about the issue.
The full version:
To understand why these topics should generally be avoided, you need to understand what information colleges are actually seeking to gain from the personal statement. Although it is technically a personal narrative, it is, in a sense, also a persuasive essay: its purpose is to convey what sets you apart from the thousands of others with equally good grades and scores, and to suggest whether you have qualities that make you more likely to thrive at university x than the other 10 or 15 or even 20 applicants clamoring for that spot.
Now, whether such thing can actually be determined from 650 words (with which some students receive significant help) is of course questionable; however, the bottom line is that, adcoms are looking for students who will be successful in college. Discussing one’s inability to focus or intense aversion to social situations does not exactly inspire confidence, even if a student insists those problems have been overcome. Leaving home, dealing with professors and roommates and more challenging classes… Those are all major stressors. There is a tacit understanding that of course some students will flame out, have breakdowns, etc., but adcoms are understandably hesitant to admit anyone who is already at a higher risk for those issues. You want them to be excited about the prospect of admitting you, not debate whether you’ll really be able to handle college. (In fact, I had multiple students with various issues who were not truly ready for college and who did flame out — colleges have good reason to take these things seriously.)
This concern goes beyond any particular student’s well-being: graduation rates get factored into rankings, and every student who doesn’t make it through drags that statistic just a little bit lower. If a student does develop serious problems while on campus, there are also potential legal/liability issues involved, and no school wants to deliberately court those.
Besides, if your grades are iffy, it is extremely difficult not to sound as if you are making excuses. You are much better off talking about an experience or interest that will make them look past the transcript and think, “Hey, I really like this kid.” And the reality is that if your grades are that iffy, you’re probably not a competitive candidate at super-selective colleges anyway. These schools are looking for applicants who are on the way to fulfilling their potential, not for ones who need to explain away chronic underachievement.
In addition, one thing applicants — and sometimes their parents — have difficulty wrapping their heads around is the sheer number of applications the average admissions officer has encountered. Situations that may seem extreme and dramatic to adolescents who have recently confronted them may in fact have already been experienced — and written about — by thousands of other applicants. A 17-year old may believe that describing their anxiety in morbid detail will make them seem complex and introspective, but more likely it will only come off as overwrought and trite.
I know that might sound harsh, but please remember that admissions officers are coming at this process with no pre-existing knowledge of you as a person, only a few minutes to spend on your essay, and hundreds of other applications to get through. They are also under intense pressure to ensure that the appropriate demographics targets are being met and all the various institutional constituencies (coaches, development office, orchestra conductor) are being satisfied. They’re not ogres, and they’ll try to give you the benefit of the doubt, but if yours is the fifth essay about overcoming anxiety they’ve seen in the last 48 hours, they will look at it and reflexively think, “oh, another one of these.” That is not a first impression you want to make.
Now, are there exceptions? Yes, of course, but they are rare. In all the time I did college admissions work, I had exactly one student successfully discuss anxiety in an essay. It was, however, introduced in the context of a family tragedy that had profoundly shaped the student’s life; given that background, the discussion seemed natural and matter of fact rather than overdramatized. Even so, I made the student take a good week to think about whether that topic was truly the one they wanted to write about.
Ultimately, of course, the decision is yours, and the choice depends on the larger story you want to tell as well as your ability as a writer, but these topics are so difficult to pull off well that you are best off avoiding them if you can (particularly if you don’t have access to someone with a lot of admissions experience who can review your essay). Find another topic/ experience that you enjoy writing about (and that others are likely to enjoy reading about); that presents you as someone interesting and thoughtful; and that suggest you are ready to thrive in college.
If you really are concerned about your ability to function in college, most schools have plenty of resources for you to take advantage of (academic support, counseling center, etc.). But those are things to investigate after you get admitted. Before that, don’t go out of your way to fly red flags where none are warranted.
Why is Dyslexia ok to mention on an essay, but overcoming selective mutism is not?
Dyslexia is a learning disability that lends itself to proof that it has been overcome through excellent scores in reading and writing. It’s not easy to overcome or cope with dyslexia so an essay showing how a student did it demonstrates their tenacity and resourcefulness. Grades and scores are proof that the dyslexia will not be a problem in college, while the essay can highlight the characteristics that led to the student’s success and which will serve them well in college.
I wrote about how my dog helped me overcome me ending my life/depression and moving to another school is that too common
Thanks for the tips and perspective. It seems like common sense to me as a parent and tutor, but now I have an “established author” to cite!
I want to write about how depression had change me. But my grades and statistics are all great. Is this okay to write? My bad mental health somehow didn’t manage to get to the others parts of my life.
Is it okay to write about how despite psychosis I could manage to get good grades?
Submit a Comment Cancel reply
Your email address will not be published. Required fields are marked *
Currently you have JavaScript disabled. In order to post comments, please make sure JavaScript and Cookies are enabled, and reload the page. Click here for instructions on how to enable JavaScript in your browser.
Yes, add me to your mailing list.
Sign up for the Question of the Day
Question of the Day
Complete SAT/ACT Grammar Rules
Complete GMAT Sentence Correction Rules
AP English Comp Terms, Condensed
10 Tips for Acing SAT Reading
Commas With Names and Titles, Simplified
Why You Won’t Go to Harvard on a National Merit Scholarship
Recent Posts
- Why are SAT and ACT English benchmarks so low?
- “However” vs. “though”: similar, but not the same
- Statement regarding the recent website outage
- Digital SAT math timing, Common Core, and the “deep understanding” trap
- “SAT® Vocabulary: A New Approach” for the Digital SAT is now available!
Posts by Category
- ACT English/SAT Writing (36)
- ACT Essay (8)
- ACT Reading (22)
- College Admissions (44)
- College Essays (2)
- English Proficiency Exams (1)
- Financial Aid (2)
- General Tips (35)
- Grammar (SAT & ACT) (27)
- Issues in Education (69)
- Parents (13)
- Phonics (26)
- Questions (1)
- Reading (SAT & ACT) (20)
- Reading Wars (7)
- SAT Critical Reading (Old Test) (52)
- SAT Essay (13)
- SAT Grammar (Old Test) (30)
- SAT Reading (12)
- SAT vs. ACT (5)
- Students (10)
- Test Optional (1)
- The Digital SAT (12)
- The Mental Game (18)
- The New SAT (59)
- The Science of Reading (9)
- Time Management (7)
- Tutor Interviews (9)
- Tutoring (27)
- Tutors (16)
- Uncategorized (10)
- Vocabulary (17)
Favorite Links
Barry Garelick on Common Core Math
Cogito Zero Sum
Hannah Arendt on The Crisis in Education
Critical Thinking: Why is it So Hard to Teach?
A Don’s Life (Mary Beard’s Blog)
Educational Jargon Generator
EduBabble Bingo
English is Not Normal
Everybody is Stupid Except You
The Fluency Factory
Gary Saul Morson on Anna Karenina
How I Rewired My Brain to Become Fluent in Math
Letter Against Learning Styles
Mercedes Schneider’s EduBlog
MIT Admissions Blog
Reflections on Liberal Education
The Revenge of K-12 Education
Seven Myths About Education
Silent StopWatch (for standardized tests)
The Usefulness of Brief Instruction in Reading Comprehension Strategies
What David Coleman Doesn’t Know About Literature
Why a Great Individual is Better than a Good Team
Depression and Anxiety in College Students
- First Online: 05 December 2020
Cite this chapter

- Ayesha K. Chaudhary 3 , 4
517 Accesses
College health clinicians are often first line in detecting the presence of, and providing intervention for, depressive and anxiety disorders in young adult students. Caring for mental health conditions in the primary care setting can be complex, requiring a nuanced and comprehensive approach. The importance of diagnostic accuracy and differentiation of clinical pathology from developmental, nonpathological states, along with carefully defining any underlying comorbidities, are determinants of intervention options and the successful resolution of symptoms. While symptom remission is in itself a primary outcome, other important outcomes include suicide risk reduction, treatment adherence, sustained remission, improved quality of life, and development of positive attitudes toward mental health care. This chapter provides a review of the epidemiology of depression and anxiety in college students, guidance for providers regarding the clinical diagnostic process, strategies to engage students in treatment planning, and an overview of pharmacologic and nonpharmacologic interventions.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as EPUB and PDF
- Read on any device
- Instant download
- Own it forever
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Statistics NC for E. College navigator. National Center for Education Statistics, U.S. Department of Education. 2008.
Google Scholar
National Center for Education Statistics. College enrollment rates. Cond Educ 2018. 2017.
Redford J, Mulvaney Hoyer K. First-generation and continuing-generation college students: a comparison of high school and postsecondary experiences. National Center for Education Statistics; 2017.
Beiter R, Nash R, McCrady M, Rhoades D, Linscomb M, Clarahan M, et al. The prevalence and correlates of depression, anxiety, and stress in a sample of college students. J Affect Disord. 2015.
Turner JC, Leno EV, Keller A. Causes of mortality among American college students: a pilot study. J Coll Stud Psychother. 2013;27(1):31–42.
Article Google Scholar
Bernstein L. U.S. life expectancy declines again, a dismal trend not seen since World War I – The Washington Post. The Washington Post; 2018.
Eisenberg D, Speer N, Hunt JB. Attitudes and beliefs about treatment among college students with untreated mental health problems. Psychiatr Serv. 2012.
Arnett JJ. Emerging adulthood: a theory of development from the late teens through the twenties. Am Psychol. 2000.
Arnett JJ. Emerging adulthood: understanding the new way of coming of age. In: Emerging adults in America: coming of age in the 21st century; American Psychologica Assoc. 2007.
Zald DH, Cowan RL, Riccardi P, Baldwin RM, Ansari MS, Li R, et al. Midbrain dopamine receptor availability is inversely associated with novelty-seeking traits in humans. J Neurosci. 2008.
Kessler RC, Angermeyer M, Anthony JC, de Graaf R, Demyttenaere K, Gasquet I, et al. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry. 2007.
Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of. Arch Gen Psychiatry. 2005.
Pedrelli P, Nyer M, Yeung A, Zulauf C, Wilens T. College students: mental health problems and treatment considerations. Acad Psychiatry. 2015.
Lipson SK, Kern A, Eisenberg D, Breland-Noble AM. Mental health disparities among college students of color. J Adolesc Health. 2018.
Viruell-Fuentes EA, Miranda PY, Abdulrahim S. More than culture: structural racism, intersectionality theory, and immigrant health. Soc Sci Med. 2012.
Heyman JC, Kelly PL, Reback GM, Blumenstock KH. Social determinants of health. In: Health and social work: practice, policy, and research; Springer Publ. 2018.
Hunt JB, Eisenberg D, Lu L, Gathright M. Racial/ethnic disparities in mental health care utilization among U.S. college students: applying the institution of medicine definition of health care disparities. Acad Psychiatry. 2015.
Sturdy S. William Osler: a life in medicine. BMJ. 2000;321(7268):1087.
Downey MM, Jackson K, Fernandez T. Free, brief, and validated: Standardized instruments for low-resources mental health settings. Resour Ment Health Settings. 2016;22(1):5–19.
Hirschfeld RM. Differential diagnosis of bipolar disorder and major depressive disorder. J Affect Disord. 2014.
Bowden CL. A different depression: clinical distinctions between bipolar and unipolar depression. J Affect Disord. 2005;84(2–3):117–25.
Hirschfeld RMA, Williams JBW, Spitzer RL, Calabrese JR, Flynn L, Keck J, et al. Development and validation of a screening instrument for bipolar spectrum disorder: the mood disorder questionnaire. Am J Psychiatry. 2000.
Kline E, Wilson C, Ereshefsky S, Denenny D, Thompson E, Pitts SC, et al. Psychosis risk screening in youth: a validation study of three self-report measures of attenuated psychosis symptoms. Schizophr Res. 2012.
Cranford JA, Eisenberg D, Serras AM. Substance use behaviors, mental health problems, and use of mental health services in a probability sample of college students. Addict Behav. 2009.
Massey SH, Lieberman DZ, Reiss D, Leve LD, Shaw DS, Neiderhiser JM. Association of clinical characteristics and cessation of tobacco, alcohol, and illicit drug use during pregnancy. Am J Addict. 2011.
Köhler S, Gaus S, Bschor T. The challenge of treatment in bipolar depression: evidence from clinical guidelines, treatment recommendations and complex treatment situations. Pharmacopsychiatry. 2014;47(2):53–9.
Fela-Thomas AL, Olotu OS, Esan O. Risk of manic switch with antidepressants use in patients with bipolar disorder in a Nigerian neuropsychiatric hospital. South Afr J Psychiatry. 2018;24:1–6.
Lamis DA, Ballard ED, May AM, Dvorak RD. Depressive symptoms and suicidal ideation in college students: the mediating and moderating roles of hopelessness, alcohol problems, and social support. J Clin Psychol. 2016;72(9):919–32.
Beesdo-Baum K, Knappe S. Developmental epidemiology of anxiety disorders. Child Adolesc Psychiatr Clin N Am. 2012.
Bandelow B, Michaelis S. Epidemiology of anxiety disorders in the 21st century. Dialogues Clin Neurosci. 2015.
Kizilbash AH, Vanderploeg RD, Curtiss G. The effects of depression and anxiety on memory performance. Arch Clin Neuropsychol. 2002.
Singh RL, Schommer JC, Worley MM, Peden-McAlpine C. Antidepressant use amongst college students: findings of a phenomenological study. Inov Pharm. 2012;3(2):1–13.
McGorry PD, Hickie IB, Yung AR, Pantelis C, Jackson HJ. Clinical staging of psychiatric disorders: a heuristic framework for choosing earlier, safer and more effective interventions. Aust N Z J Psychiatry. 2006.
Lynch D, Tamburrino M, Nagel R, Smith MK. Telephone-based treatment for family practice patients with mild depression. Psychol Rep. 2004;94(3 I):785–92.
Khan A, Faucett J, Lichtenberg P, Kirsch I, Brown WA. A systematic review of comparative efficacy of treatments and controls for depression. PLoS One. 2012.
Ströhle A. Physical activity, exercise, depression and anxiety disorders. J Neural Transm. 2009;116(6):777–84.
Nasrin F. A randomized controlled trial of mindfulness versus yoga [Internet]. J Am Psychiatric Nurses Assoc. 2016;22:483–97. Available from https://doi.org/10.1177/1078390316663307
Cuijpers P, van Straten A, Warmerdam L. Behavioral activation treatments of depression: a meta-analysis. Clin Psychol Rev. 2007.
Bersani FS, Iannitelli A, Pacitti F, Bersani G. Sleep and biorhythm disturbances in schizophrenia, mood and anxiety disorders: a review. Riv Psichiatr. 2012.
Shephard RJ. Sleep, biorhythms and human performance. Sports Med Int J Appl Med Sci Sport Exerc. 1984.
Tuma JM, Pratt JM. Clinical child psychology practice and training: a survey. J Clin Child Adolesc Psychol. 1982;137:37–41. https://doi.org/10.1037/a0022390 , Gobry F. {T}his is a title. {M}y Journal. 1999;1:120–30., Osment SE (1980). TA of R 1250–1550. … and RH of LM and R…. R from http://scholar.google.com/scholar?hl=en&btnG=Search&q=intitle:THE+AGE+OF+REFORM+125.-1550#2%5Cnhttp://scholar.google.com/scholar?hl=en&btnG=S., Caprara G, Fida R. Longitudinal analysis of the role of perceived self-efficacy for self-regulated learning in academic continuance and achievement. … of Educational …, 2008;100(3):525–34. https://doi.org/10.1037/0022-0663.100.3.525 , Shanker S. Philosophy of science logic and mathematics in the twentieth century. … PL and NYR. 2003. https://doi.org/10.4324/978020302947 ., Marenbon J. RH of PI… PL and NYR. 1998. https://doi.org/10.4324/978020306227 ., et al. Sleep disturbance in heavy marijuana users. Sleep. 2008.
Deykin EY, Levy JC, Wells V. Adolescent depression, alcohol and drug abuse. Am J Public Health. 1987.
Benjamin AB, Dooley TP. Anxiolytic benefits of compounded Atenolol–Scopolamine in eight patients in psychiatry. Pers Med Psychiatry [Internet]. 2020;19–20:100051. Available from https://doi.org/10.1016/j.pmip.2019.10.001
Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: a meta-analytic review. J Consult Clin Psychol. 2010.
Carek PJ, Laibstain SE, Carek SM. Exercise for the treatment of depression and anxiety. Int J Psychiatry Med. 2011.
Cooney G, Dwan K, Mead G. Exercise for depression. JAMA J Am Med Assoc. 2014.
Smits JAJ, Berry AC, Rosenfield D, Powers MB, Behar E, Otto MW. Reducing anxiety sensitivity with exercise. Depress Anxiety. 2008.
Vital-Lopez FG, Ramakrishnan S, Doty TJ, Balkin TJ, Reifman J. Caffeine dosing strategies to optimize alertness during sleep loss. J Sleep Res. 2018.
Furukawa TA, Cipriani A, Cowen PJ, Leucht S, Egger M, Salanti G. Optimal dose of selective serotonin reuptake inhibitors, venlafaxine, and mirtazapine in major depression: a systematic review and dose-response meta-analysis. Lancet Psychiatry [Internet]. 2019;6(7):601–9. Available from https://doi.org/10.1016/S2215-0366(19)30217-2
Parris M, Marver J, Chaudhury S, Ellis S, Metts K, Allison, Burke A, Oquendo M, Mann J, Grunebaum M. Effects of anxiety on suicidal ideation: exploratory analysis of paroxetine versus bupropion randomized trial. Int Clin Psychopharmacol. 2018;33(1):139–48.
Duhoux A, Fournier L, Menear M. Quality indicators for depression treatment in primary care: a systematic literature review. Curr Psychiatr Rev. 2011.
Gaynes BN, Rush AJ, Trivedi MH, Wisniewski SR, Balasubramani GK, McGrath PJ, et al. Primary versus specialty care outcomes for depressed outpatients managed with measurement-based care: results from STAR*D. J Gen Intern Med. 2008.
Eisenberg D, Chung H. Adequacy of depression treatment among college students in the United States. Gen Hosp Psychiatry. 2012.
Kirsch I, Deacon BJ, Huedo-Medina TB, Scoboria A, Moore TJ, Johnson BT. Initial severity and antidepressant benefits: a meta-analysis of data submitted to the food and drug administration. PLoS Med. 2008.
Kovich H, Dejong A. Common questions about the pharmacologic management of depression in adults. Am Fam Physician. 2015;92(2):94–100.
PubMed Google Scholar
Warden D, Rush AJ, Trivedi MH, Fava M, Wisniewski SR. The STAR*D project results: a comprehensive review of findings. Curr Psychiatry Rep. 2007.
Paykel ES. Partial remission, residual symptoms, and relapse in depression. Dialogues Clin Neurosci. 2008.
Abraham G, Milev R, Stuart Lawson J. T3 augmentation of SSRI resistant depression. J Affect Disord. 2006.
Cipriani A, Hawton K, Stockton S, Geddes JR. Lithium in the prevention of suicide in mood disorders: updated systematic review and meta-analysis. BMJ. 2013.
Ketter TA, Wang PW, Chandler RA, Alarcon AM, Becker OV, Nowakowska C, et al. Dermatology precautions and slower titration yield low incidence of lamotrigine treatment-emergent rash. J Clin Psychiatry. 2005.
Cipriani A, Furukawa TA, Salanti G, Chaimani A, Atkinson LZ, Ogawa Y, et al. Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: a systematic review and network meta-analysis. Lancet [Internet]. 2018;391(10128):1357–66. Available from https://doi.org/10.1016/S0140-6736(17)32802-7
Article CAS Google Scholar
Faquih AE, Memon RI, Hafeez H, Zeshan M, Naveed S. A review of novel antidepressants: a guide for clinicians. Cureus. 2019;11(3):e4185.
PubMed PubMed Central Google Scholar
Thase ME, Greenhouse JB, Frank E, Reynolds CF 3rd, Pilkonis PA, Hurley K, et al. Treatment of major depression with psychotherapy or psychotherapy-pharmacotherapy combinations. Arch Gen Psychiatry. 1997;54(11):1009–15.
Burlingame GM, Fuhriman A, Mosier J. The differential effectiveness of group psychotherapy: a meta-analytic perspective. Group Dyn. 2003.
Bamber MD, Kraenzle Schneider J. Mindfulness-based meditation to decrease stress and anxiety in college students: a narrative synthesis of the research. Educ Res Rev. 2016.
Li AW, Goldsmith CAW. The effects of yoga on anxiety and stress. Altern Med Rev. 2012.
Swiecicki L. Seasonal affective disorder and phototherapy. Psychiatr Pol. 1990.
Kasper S, Rogers SLB, Yancey A, Schulz PM, Skwerer RG, Rosenthal NE. Phototherapy in individuals with and without subsyndromal seasonal affective disorder. Arch Gen Psychiatry. 1989.
Download references
Author information
Authors and affiliations.
Department of Psychiatry, Duke University, Durham, NC, USA
Ayesha K. Chaudhary
Womens Health Center, Durham Veterans Affairs Medical Center, Durham, NC, USA
You can also search for this author in PubMed Google Scholar
Editor information
Editors and affiliations.
Director, Student Health Services, Associate Professor, Family Medicine and Community Health, Duke University, Durham, NC, USA
John A. Vaughn
Professor and Chair, Department of Family Medicine and Community Health, Duke University, Durham, NC, USA
Anthony J. Viera
Rights and permissions
Reprints and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Chaudhary, A.K. (2021). Depression and Anxiety in College Students. In: Vaughn, J.A., Viera, A.J. (eds) Principles and Practice of College Health. Springer, Cham. https://doi.org/10.1007/978-3-030-56309-7_4
Download citation
DOI : https://doi.org/10.1007/978-3-030-56309-7_4
Published : 05 December 2020
Publisher Name : Springer, Cham
Print ISBN : 978-3-030-56308-0
Online ISBN : 978-3-030-56309-7
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Are you seeking one-on-one college counseling and/or essay support? Limited spots are now available. Click here to learn more.
Mental Health in College Students – From Application to Enrollment
August 16, 2022

Sometimes it takes unspeakably tragic events to bring the existence of a widespread problem into the national conversation. In the past decade, highly-publicized suicides at Penn, Hamilton College, MIT, NYU, and Cornell, among others, have moved the discussion of mental health in college students right to the forefront of the higher education discourse.
Thankfully, these are, of course, extreme cases of mental health challenges. However, the shift in focus could benefit the massive numbers of students who enter college each year with depression/anxiety. According to a survey by the CDC in 2022, 44% of American adolescents report feeling persistent feelings of sadness and hopelessness; 28% said that they had thoughts of self-harm at some point in their lives. Perhaps even more startling is the fact that only an estimated 40% of those suffering actually receive any form of treatment (the National Institute of Mental Health). According to just about every survey in the world conducted after March 2020, the pandemic has had a profoundly determinantal impact on teens’ (and everybody’s) mental health.
In this piece, we will offer recommendations for dealing with depression/anxiety on your college application. But perhaps more importantly, we will share what mental health experts and current research says are important considerations for managing your illness on campus.
*Disclaimer: Mind you, we are college planning experts, not mental health experts. We are merely summarizing mental health considerations as related to college admissions and attendance. Your mental health provider may offer additional advice based on the specifics of your situation .
Impact on your high school career
For many, dealing with a mental health condition will negatively impact their high school career in some way, potentially impacting areas such as academic performance, school attendance, teacher relationships, and extracurricular involvement. There is ample statistical evidence to support this. For example, students with social phobia are twice as likely to fail a grade as those without. Students with a depression diagnosis have been found to earn significantly lower grades than their similarly-abled peers.
Given the impact of mental illness on a teen’s academics, a significant number of high school seniors are faced with a difficult choice each year—do I reveal my condition on my college application? There is no blanket answer that will guide every applicant. Ultimately, the decision to reveal your condition is an entirely personal one.
Did your academic performance suffer?
Perhaps your mental health issues were managed successfully and never impacted your grades. If this is the case, we advise that there is no reason to reveal your condition on an application. You should, however, still check out our recommendations on how to check out a college’s mental health services (below).
If your academic performance did suffer as a result of your condition and you do choose to share your challenges with prospective colleges in an essay and/or interview, we recommend that you consider framing your experience in one of the following ways:
The “overcoming obstacles” angle
Overcoming challenges and citing evidence of personal growth can be a winning story arc. If a bout of depression during your sophomore year contributed toward failing grades but you received treatment and rebounded academically the following year, then revealing that journey may be extremely helpful to your admissions chances. Knowing that you faced a significant challenge in your life and successfully emerged from it speaks volumes about your resilience, maturity, and grit, traits that are greatly valued by admissions officers.
Weakness as strength
Another approach is highlighting the strength that you draw from what others call an “illness.” An associate of Abraham Lincoln said of our 16th president that the “melancholy dripped from him as he walked.” Yet, many historians feel that Lincoln’s lifelong depression helped sparked his legendary wisdom, insight, and brilliant strategic thinking. Lincoln was hardly alone. Many of the greatest, most creative minds throughout history were, at least in part, driven by mental conditions. Darwin, Michelangelo, and Einstein were all likely sufferers of Obsessive Compulsive Disorder. If we were to list all of all the great writers, artists, comedians, actors, and directors who were influenced by depression and anxiety, this blog post would be longer than the 1,017 page novel, Bleak House, penned by Charles Dickens, who was himself a lifelong victim of severe depression.

The semantic shift
Cautious applicants might consider simply substituting the term “medical condition” for “mental illness.” After all, mental health issues are treatable medical conditions in the same vein as mono or a broken bone. Simply stating that you were afflicted by a “serious medical condition” which caused a temporary academic decline and led to you quitting the school newspaper and the baseball team will suffice.
Check out a college’s services ahead of time
In a recent survey of college students with a diagnosed mental health condition, 45% rated their respective college as being somewhere between supportive and very supportive. The other 55% felt that mental health care on campus was less than ideal. Factors that were rated as being most important by students included: access to a psychiatrist for medication management, a 24-hour crisis hotline, community connections to additional mental healthcare, and the school’s overall culture of understanding that college can be stress-inducing and that mental health is paramount.
It is essential that parents and students research the mental health services on campus ahead of time. Check out each prospective college’s counseling office online to get a sense of what is available to students. If a college does not offer long-term therapy on campus, then parents should take the reins and find a good private therapist located near campus who accepts their insurance. Do this well before school starts.
Colleges are expanding mental health services
Many state universities, despite budget crunches, are recognizing the need to expand their mental health offerings. For example, in the fall of 2017, UCLA began offering free online screenings for depression; 2,700 students took advantage. Ohio State opened a dozen new mental health clinics in 2016. Penn State has increased their spending on mental health significantly in the last few years. The University of Michigan and Virginia Tech, in an attempt to make mental health more accessible, have embedded counselors in buildings around campus, rather than at one centralized location. Many schools operate prevention/wellness programs that assist students before they enter a crisis. These schools include Harvard, Georgia Tech, UVA, and Bowdoin College.
Amherst, Skidmore, Princeton, Drexel, and Carnegie Mellon are just a handful of schools that now offer access to 24-hour crisis hotlines manned by either peers or professional counselors. Unfortunately, excessively long wait times for a counseling appointment at many schools persist. At schools like Northwestern, Carleton College, and WashU, wait times to see a counselor range from one-to-three weeks.
Relevant statistics on mental health at college
Just to highlight some other meaningful stats on the subject:
- Only 50% of college students report disclosing their mental health issue to their school
- Of those with a diagnosed mental illness who dropped out of college, 64% directly attribute this event to their condition/disorder.
- Only 36% of college students with a mental illness are sure that their university includes mental health information on their website.
- 39% of students reported a wait time of 5+ to obtain an appointment for clinical services and supports.
- 73% of those entering college with previous mental health concerns have experienced a “mental health crisis” while on campus.
- Half of students believe that their peers will think less of anyone receiving treatment for mental health.
- The percentage of college students seriously considering suicide has doubled in the last decade.
- More than 1,000 suicides occur on college campuses each year.
College Transitions bottom line
If you are going to discuss your depression, anxiety, or other mental condition in your application, do so in a strategic manner for the purpose of illuminating otherwise unexplained inconsistencies in your academic record. A well-conceived and well-delivered narrative about your struggles with mental illness can be beneficial to your admissions chances. Contrarily, a poorly crafted disclosure may have the opposite effect.
Of even greater importance is that you do your research on the mental health services offered at each prospective college. Ensuring that the necessary supports at your disposal is critical to your overall well-being. It is also likely critical to your academic performance over the next four years.
To view hundreds of free and easy-to-sort tables of higher education data, visit our DATAVERSE .
- Application Strategies

Andrew Belasco
A licensed counselor and published researcher, Andrew's experience in the field of college admissions and transition spans two decades. He has previously served as a high school counselor, consultant and author for Kaplan Test Prep, and advisor to U.S. Congress, reporting on issues related to college admissions and financial aid.
- 2-Year Colleges
- Best Colleges by Major
- Best Colleges by State
- Big Picture
- Career & Personality Assessment
- College Essay
- College Search/Knowledge
- College Success
- Costs & Financial Aid
- Data Visualizations
- Dental School Admissions
- Extracurricular Activities
- Graduate School Admissions
- High School Success
- High Schools
- Law School Admissions
- Medical School Admissions
- Navigating the Admissions Process
- Online Learning
- Private High School Spotlight
- Summer Program Spotlight
- Summer Programs
- Teacher Tools
- Test Prep Provider Spotlight

“Innovative and invaluable…use this book as your college lifeline.”
— Lynn O'Shaughnessy
Nationally Recognized College Expert
College Planning in Your Inbox
Join our information-packed monthly newsletter.
I am a... Student Student Parent Counselor Educator Other First Name Last Name Email Address Zip Code Area of Interest Business Computer Science Engineering Fine/Performing Arts Humanities Mathematics STEM Pre-Med Psychology Social Studies/Sciences Submit
Loyola University > Center for Digital Ethics & Policy > Research & Initiatives > Essays > Archive > 2018 > The Role of Social Media in Adolescent/Teen Depression and Anxiety
The role of social media in adolescent/teen depression and anxiety, april 3, 2018.
The adolescent and teen years have always been a challenging time. Peer pressure, insecurity and hormones are just some of the issues facing those in these age groups. But does social media exacerbate these problems?
For example, researchers from the Alberta Teachers’ Association, the University of Alberta, Boston Children’s Hospital and Harvard Medical School released a study that found significant changes in students at every grade level as a result of digital technology. In the past three to five years, 90 percent of teachers at the University of Alberta saw increases in emotional challenges, 85 percent saw social challenges and 77 percent observed cognitive challenges. Also, 56 percent of teachers report an increase in the number of kids sharing stories about online harassment and/or cyberbullying. There are increases in other areas as well. The majority of teachers say there has been an increase in students diagnosed with the following conditions: anxiety disorders (85 percent), ADD and ADHD (75 percent), and such mood disorders as depression (73 percent).
Also, a recent study by researchers at the Royal Society for Public Health and Young Health Movement found that 91 percent of those between the ages of 16 and 24 said Instagram was the worst social media platform as it relates to mental health. Instagram was most likely to cause negative effects such as poor body image, fear of missing out and sleep deprivation. Snapchat came in second place, followed by Facebook, Twitter and YouTube. The researchers theorize that Instagram and Snapchat are image-focused platforms and users compare themselves to others.
A review of 36 social media studies, published in JAMA Pediatrics, found that 23 percent of kids are victims of cyberbullying. The review also found that cyberbullying results in low self-esteem, depression, self-harm and behavioral problems — in both the victims and the bullies. In addition, cyberbullying was more likely to produce suicidal thoughts than traditional bullying.
Another study , conducted by researchers at Glasgow University found that kids (some of whom were pre-teens) were on social media until the wee morning hours, and some were on more than one device (for example, a phone and a tablet) so they could simultaneously view multiple sites. These individuals reported lower sleep quality rates in addition to higher levels of depression and anxiety.
In a survey by the National Campaign to Support Teen and Unplanned Pregnancy, almost 20 percent of teens admitted to participating in "sexting" or sending nude photos.
The pressure these adolescents and teens feel can be intensified by the time they get to college. Stanford University coined the phrase “ Duck syndrome ” to describe the erroneous attitude of incoming freshmen that they’re struggling while everyone else is gliding along smoothly — but in reality, the gliders are also “paddling furiously under the water just to keep up.” Adolescents and teens become accustomed to creating the impression that everything is perfect to match the equally perfect posts of their friends. But it becomes too difficult to maintain this façade, resulting in suicide among college students who appear to be well-adjusted, but are actually experiencing mental and emotional problems.
Another report , published in the American Journal of Preventive Medicine, reveals that among young adults between the ages of 19 and 32, those with high social media usage (those logging on for more than 2 hours a day and checking their accounts 58 times a week) were more likely to deal with feelings of isolation than those with low social media use (they logged on for 30 minutes and checked their accounts 9 times a week).
In light of these studies, who is responsible for the role of social media in adolescent/teen depression and anxiety?
Many tech leaders seem to understand the unhealthy, addictive nature of technology in general and social media in particular. As far back as 2010, New York Times reporter Nick Bilton interviewed the late Steve Jobs of Apple. Jobs told Bilton that he limited the amount of technology that his kids use. Bill Gates shared that he didn’t let his kids have mobile devices until they were 14 years old, and he sets a time for them to turn off the devices at night.
Evan Williams, one of the founders of Twitter, Medium and Blogger, told Bilton that his kids read physical books instead of using iPads. Dick Costolo, former CEO of Twitter, told Bilton that his teenagers had to be in the living room when they used their tech devices.
But, perhaps the most shocking revelation came from Sean Parker, former president of Facebook, in an interview with Axios. Referring to Facebook, Parker said, “God only knows what it’s doing to our children’s brains.”
But there’s more. Parker also said, “ . . . How do we consume as much of your time and conscious attention as possible? . . . And that means that we need to sort of give you a little dopamine hit every once in a while, because someone liked or commented on a photo or a post or whatever . . . And that's going to get you to contribute more content, and that's going to get you ... more likes and comments . . . It's a social-validation feedback loop ... exactly the kind of thing that a hacker like myself would come up with, because you're exploiting a vulnerability in human psychology . . . The inventors, creators — it's me, it's Mark [Zuckerberg], it's Kevin Systrom on Instagram, it's all of these people — understood this consciously . . . And we did it anyway.”
So, if Parker confessed that social media was designed to be addictive, should social media companies be responsible for depression, anxiety, bullying and other issues among adolescents and teens?
Donna Shea, director of The Peter Pan Center for Social and Emotional Growth, and Nadine Briggs, director of Simply Social Kids , are passionate about helping kids make and keep friends, and together have formed How to Make and Keep Friends, LLC. Shea and Briggs both lead community-based social groups at their centers in Massachusetts and have also formed the Social Success in School initiative. The two have also written several books for kids and teens, including, “Tips for Teens on Life and Social Success” .
Both Shea and Briggs believe that it is the job of parents to monitor their kid’s social media activity. “You wouldn’t allow your teen to put a lock on their bedroom door, but your teen is not only now interacting with peers at school or in your neighborhood, they are interacting with the entire world,” Shea said. “It is a parent’s job to be as involved in their teen’s online life as they are in their offline life.”
In fact, she is not in favor of giving adolescents and teens a phone as a gift. “Mobile devices belong to the parent and the teen is being allowed to use it,” Shea said. “A contract can be a useful tool before putting a device in the hands of your teen which would allow parents to have access to the phone.”
She believes that parents should monitor their adolescent/teen’s activity — and teens should know this is being done. “Parents do not need to be sneaky about that — tell your child to hand over the phone,” she said. Shea also recommends that parents use subscription services to view all of their teens’ activities. “Teens should be prepared to be monitored until they are of legal adult age,” she said.
However, Briggs admits that apps change so quickly that it’s almost impossible to keep up with them. “Other than doing your best to monitor your teen’s activity — and it won’t be 100% effective - it’s important from the very beginning that you teach your child and teen to be good consumers of what is available to them,” Briggs said. “This is the new norm, and we think it’s the parent’s responsibility to be involved in their teen’s online life.”
She compares giving kids a phone or device to putting them behind the wheel of a car. “Both can be dangerous in their own way, but teens can learn the responsibilities that go along with these more adult activities.”
But, do parents bear sole responsibility? For example, everyone knows that tobacco is bad for your health, and people consume it willingly; however, they continue to sue and win lawsuits against tobacco companies. In 2014, one plaintiff was awarded $23.6 billion when her husband died of lung cancer as a result of smoking up to three packs of cigarettes a day. He started smoking at the age of 13 and died at the age of 36. The plaintiff (his widow) argued that the tobacco company willfully deceived consumers with addictive products.
How is this scenario different from what social media companies are doing? And speaking of willful deception, what about companies that make secretive apps that allow teens to hide their sexting?
If someone trips and falls on your property, you could be sued. If someone gets harmed at your nightclub, you could be held liable for not having “adequate security.” If one of your employees sexually harasses a colleague, you would be held responsible — even if you didn’t know about it. If you sell alcohol, you’re responsible for making sure it doesn’t get into the hands of a minor. In fact, according to the Dram Shop Law, if you let an adult have too many drinks and this individual is involved in an accident, you could be responsible.
However, if kids become addicted to a communication platform that was designed to be addictive, if they’re bullied online, if there are no safeguards to stop them from utilizing the types of secretive apps that encourage risky behavior, shouldn’t these companies be held responsible?
I think they should be, but this is not likely to happen until society holds them responsible. Since most adults are also addicted to social media — and some of them are internet bullies and engage in sexting, it seems unlikely that they would advocate for changes.
In the aforementioned study by the Royal Society for Public Health and Young Health Movement, researchers offered several ways to reduce some of the problems adolescents and teens face online. For example, one of the reasons kids feel so much pressure to look perfect is because of the doctored photos they see. The researchers recommend that social media companies include some sort of notification, such as a watermark, when photos have been digitally manipulated (68 percent of surveyed students support this action).
Another suggestion is to create a social media cap. Users would be logged out if they went over a pre-determined usage level (30 percent of surveyed students agree with this suggestion).
The majority of surveyed students (84 percent) approve of schools having classes on safe social media.
Another suggestion by the researchers (which did not include student responses) was to use social media posts to identify kids and teens who might be at risk for mental health problems. However, problems have already been identified with using Facebook to identity potential problem drinkers .
In addition, it was suggested that youth workers be trained in digital media.
These are nice Band-Aid solutions. But they don’t address the addictive nature of social media and the incredible amount of peer pressure that it involves. Parents can provide guidance, but history has shown that their values rarely outweigh the pressure of peers.
Albert Einstein once said, “We can’t solve our problems with the same thinking we used to create them.” But in this situation, the social media giants can solve these problems with the exact same thinking they used to create them. Just as they figured out what it would take to make these platforms addictive, they can figure out what it would take to make the platforms less addictive. But don’t hold your breath because the person who creates the problem and profits from the problem has no incentive to solve the problem.
Terri Williams writes for a variety of clients including USA Today , Yahoo , U.S. News & World Report , The Houston Chronicle , Investopedia , and Robert Half . She has a Bachelor of Arts in English from the University of Alabama at Birmingham. Follow her on Twitter @Territoryone .
Research & Initiatives
Return to top.
- Support LUC
- Directories
- Symposia Archive
- Upcoming Events
- Past Events
- Publications
- CDEP in the News
© Copyright & Disclaimer 2024
Search form
How to fight anxiety and depression in college students.
By Jane Hurst with the assistance of Dr. Carlo Carandang
As a college student, you experience a number of stressors, such as living independently from your parents, keeping up with the rigors of your college courses compared to your high school courses, managing your time adequately, managing a budget, balancing your checkbook, figuring out what you want to do for the rest of your life, deciding on a major, worrying about getting a job after graduation, and managing your intimate relationships. When you are not able to cope with all these stressors, you begin to feel burnt-out (or stressed-out) and wonder if you will be able to continue with your studies in college. Eventually, if you do not handle these stressors adequately, you may go on to develop anxiety and/or depression. So having stress is part of college life…if you are resilient, then you will do just fine and may even benefit from all the stressors to push you to higher achievements. However, for those with maladaptive coping skills, the stressors can trigger you to develop anxiety and/or depression.
What is Anxiety?
Anxiety is characterized by worry, nervousness, or fear when you are exposed to a feared situation, person, or object. Anxiety disorders develop when you become fearful, worried, or nervous:
- out of proportion to the feared stimulus;
- in anticipation of being exposed to the feared stimulus; or
- when the feared stimulus is no longer present.
In addition, anxiety triggers the fight or flight response, which results in the release of adrenaline and is responsible for the physical symptoms of anxiety:
- muscle tension
- increased heart rate
- increased breathing
- butterflies in the stomach
- lump in the throat
There are 6 major anxiety disorders, and each has characteristic symptoms:
- Generalized anxiety disorder (GAD) – GAD is characterized by generalized worry about everyday events.
- Social phobia – It is also known as social anxiety disorder (SAD). SAD is characterized by fear of social scrutiny, or fear of being embarrassed when in front of people or when performing. Performance anxiety, such as stage fright, is a type of social phobia.
- Specific phobia – This is characterized by extreme fear of an object, person, or situation, such as fear of heights, flying, spiders, snakes, etc.
- Panic disorder – This is characterized by panic attacks, and you anticipate having the next panic attack.
- Obsessive compulsive disorder (OCD) – OCD is characterized by having recurrent, intrusive thoughts (obsessions) with compensatory actions/behaviors (compulsions) that decrease the anxiety associated with the obsessions.
- Post traumatic stress disorder (PTSD) – PTSD occurs after a life-threatening trauma, and it is characterized by re-experiencing the traumatic event through flashbacks and nightmares. In addition, you have hypervigilance and you are on guard all the time for any further danger in the environment. Finally, you try to avoid any reminders of the traumatic event.
What is Depression?
Depression is characterized by:
- loss of pleasure in things
- sleep disturbance
- feelings of guilt or hopelessness
- low energy level
- poor concentration
- poor appetite
- being slowed down or revved up
- suicidal ideations
When triggered by stressors, a depressive disorder can develop, known as major depressive disorder (MDD). MDD, like anxiety disorders, will cause significant impairment to your functioning in college and your relationships. Additionally, MDD and anxiety disorders can co-exist at the same time.
Treating Anxiety and Depression
Fortunately, there are effective treatments for anxiety and depression. The treatments for anxiety and depression are similar:
- Psychotherapy – First line treatment for anxiety and depression is psychotherapy, or talk therapy. The most studied form of psychotherapy shown to be effective for anxiety and depression is cognitive behavioral therapy (CBT). CBT works on the premise that your thoughts about a situation cause you to be anxious or depressed, and it is not the situation that makes you sad or anxious. Also, your anxiety or depression can be made worse by your avoidant behaviors. CBT helps you to become less anxious and depressed by changing to more adaptive ways of thinking about a situation, and by addressing the avoidant and safety behaviors.
- Medication – Prescription medication treatment is last resort treatment for anxiety and depression. Prescription medication should only be prescribed when you do not response to CBT, or if you have a severe case of anxiety or depression. Contrary to what the drug companies advertise, their products should only be used as a last resort- when more benign and conservative treatments have been tried first.
- Self-help – You can also help yourself to get over anxiety and depression. There are many things you can do, including yoga, exercise, reading AnxietyBoss by Dr. Carlo Carandang, following a balanced diet, and getting plenty of sleep. You should also avoid too much caffeine and alcohol. Identify your stressors, and keep track of them by writing things down in a journal. Join a club or find a hobby to take your mind of things, and finally, find someone to talk to.
The article was written by Jane Hurst and revised by Dr. Carlo Carandang, MD, an anxiety expert. Dr. Carandang is a Fellow of the American Psychiatric Association, and he has a medical license from Washington State.
One comment on “How to Fight Anxiety and Depression in College Students”
Thank you for sharing this article! The insight provided, especially the first paragraph, is extremely helpful for both parents and students. We are parents of a Junior in college who has has experienced terrible anxiety this year which led to a depressed state. We thought the adjustment predominately happened during freshman year but not for our daughter. As studies got harder and social relationships changed, finding her way at a large university 8 hours from home became overwhelming. She did not share her struggles with us until Christmas break when she came home so “broken”. It is heart breaking for parents. She was diagnosed with depression and started on medication alone with little therapy support. I believe what is needed more is addressing the anxiety and developing coping skills. We are hoping that utilizing the Counseling Services on campus will be helpful (first appointment next week). I don’t think this problem is uncommon.
Leave a comment
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- Stanford Home
- Maps & Directions
- Search Stanford
- Emergency Info
- Terms of Use
- Non-Discrimination
- Accessibility
© Stanford University , Stanford , California 94305 .
- Open access
- Published: 16 May 2024
Procrastination, depression and anxiety symptoms in university students: a three-wave longitudinal study on the mediating role of perceived stress
- Anna Jochmann 1 ,
- Burkhard Gusy 1 ,
- Tino Lesener 1 &
- Christine Wolter 1
BMC Psychology volume 12 , Article number: 276 ( 2024 ) Cite this article
563 Accesses
Metrics details
It is generally assumed that procrastination leads to negative consequences. However, evidence for negative consequences of procrastination is still limited and it is also unclear by which mechanisms they are mediated. Therefore, the aim of our study was to examine the harmful consequences of procrastination on students’ stress and mental health. We selected the procrastination-health model as our theoretical foundation and tried to evaluate the model’s assumption that trait procrastination leads to (chronic) disease via (chronic) stress in a temporal perspective. We chose depression and anxiety symptoms as indicators for (chronic) disease and hypothesized that procrastination leads to perceived stress over time, that perceived stress leads to depression and anxiety symptoms over time, and that procrastination leads to depression and anxiety symptoms over time, mediated by perceived stress.
To examine these relationships properly, we collected longitudinal data from 392 university students at three occasions over a one-year period and analyzed the data using autoregressive time-lagged panel models.
Procrastination did lead to depression and anxiety symptoms over time. However, perceived stress was not a mediator of this effect. Procrastination did not lead to perceived stress over time, nor did perceived stress lead to depression and anxiety symptoms over time.
Conclusions
We could not confirm that trait procrastination leads to (chronic) disease via (chronic) stress, as assumed in the procrastination-health model. Nonetheless, our study demonstrated that procrastination can have a detrimental effect on mental health. Further health outcomes and possible mediators should be explored in future studies.
Peer Review reports
Introduction
“Due tomorrow? Do tomorrow.”, might be said by someone who has a tendency to postpone tasks until the last minute. But can we enjoy today knowing about the unfinished task and tomorrow’s deadline? Or do we feel guilty for postponing a task yet again? Do we get stressed out because we have little time left to complete it? Almost everyone has procrastinated at some point when it came to completing unpleasant tasks, such as mowing the lawn, doing the taxes, or preparing for exams. Some tend to procrastinate more frequently and in all areas of life, while others are less inclined to do so. Procrastination is common across a wide range of nationalities, as well as socioeconomic and educational backgrounds [ 1 ]. Over the last fifteen years, there has been a massive increase in research on procrastination [ 2 ]. Oftentimes, research focuses on better understanding the phenomenon of procrastination and finding out why someone procrastinates in order to be able to intervene. Similarly, the internet is filled with self-help guides that promise a way to overcome procrastination. But why do people seek help for their procrastination? Until now, not much research has been conducted on the negative consequences procrastination could have on health and well-being. Therefore, in the following article we examine the effect of procrastination on mental health over time and stress as a possible facilitator of this relationship on the basis of the procrastination-health model by Sirois et al. [ 3 ].
Procrastination and its negative consequences
Procrastination can be defined as the tendency to voluntarily and irrationally delay intended activities despite expecting negative consequences as a result of the delay [ 4 , 5 ]. It has been observed in a variety of groups across the lifespan, such as students, teachers, and workers [ 1 ]. For example, some students tend to regularly delay preparing for exams and writing essays until the last minute, even if this results in time pressure or lower grades. Procrastination must be distinguished from strategic delay [ 4 , 6 ]. Delaying a task is considered strategic when other tasks are more important or when more resources are needed before the task can be completed. While strategic delay is viewed as functional and adaptive, procrastination is classified as dysfunctional. Procrastination is predominantly viewed as the result of a self-regulatory failure [ 7 ]. It can be understood as a trait, that is, as a cross-situational and time-stable behavioral disposition [ 8 ]. Thus, it is assumed that procrastinators chronically delay tasks that they experience as unpleasant or difficult [ 9 ]. Approximately 20 to 30% of adults have been found to procrastinate chronically [ 10 , 11 , 12 ]. Prevalence estimates for students are similar [ 13 ]. It is believed that students do not procrastinate more often than other groups. However, it is easy to examine procrastination in students because working on study tasks requires a high degree of self-organization and time management [ 14 ].
It is generally assumed that procrastination leads to negative consequences [ 4 ]. Negative consequences are even part of the definition of procrastination. Research indicates that procrastination is linked to lower academic performance [ 15 ], health impairment (e.g., stress [ 16 ], physical symptoms [ 17 ], depression and anxiety symptoms [ 18 ]), and poor health-related behavior (e.g., heavier alcohol consumption [ 19 ]). However, most studies targeting consequences of procrastination are cross-sectional [ 4 ]. For that reason, it often remains unclear whether an examined outcome is a consequence or an antecedent of procrastination, or whether a reciprocal relationship between procrastination and the examined outcome can be assumed. Additionally, regarding negative consequences of procrastination on health, it is still largely unknown by which mechanisms they are mediated. Uncovering such mediators would be helpful in developing interventions that can prevent negative health consequences of procrastination.
The procrastination-health model
The first and only model that exclusively focuses on the effect of procrastination on health and the mediators of this effect is the procrastination-health model [ 3 , 9 , 17 ]. Sirois [ 9 ] postulates three pathways: An immediate effect of trait procrastination on (chronic) disease and two mediated pathways (see Fig. 1 ).
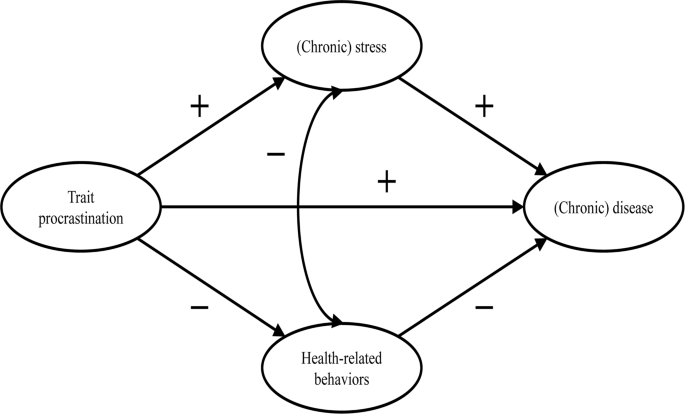
Adopted from the procrastination-health model by Sirois [ 9 ]
The immediate effect is not further explained. Research suggests that procrastination creates negative feelings, such as shame, guilt, regret, and anger [ 20 , 21 , 22 ]. The described feelings could have a detrimental effect on mental health [ 23 , 24 , 25 ].
The first mediated pathway leads from trait procrastination to (chronic) disease via (chronic) stress. Sirois [ 9 ] assumes that procrastination creates stress because procrastinators are constantly aware of the fact that they still have many tasks to complete. Stress activates the hypothalamic-pituitary-adrenocortical (HPA) system, increases autonomic nervous system arousal, and weakens the immune system, which in turn contributes to the development of diseases. Sirois [ 9 ] distinguishes between short-term and long-term effects of procrastination on health mediated by stress. She believes that, in the short term, single incidents of procrastination cause acute stress, which leads to acute health problems, such as infections or headaches. In the long term, chronic procrastination, as you would expect with trait procrastination, causes chronic stress, which leads to chronic diseases over time. There is some evidence in support of the stress-related pathway, particularly regarding short-term effects [ 3 , 17 , 26 , 27 , 28 ]. However, as we mentioned above, most of these studies are cross-sectional. Therefore, the causal direction of these effects remains unclear. To our knowledge, long-term effects of trait procrastination on (chronic) disease mediated by (chronic) stress have not yet been investigated.
The second mediated pathway leads from trait procrastination to (chronic) disease via poor health-related behavior. According to Sirois [ 9 ], procrastinators form lower intentions to carry out health-promoting behavior or to refrain from health-damaging behavior because they have a low self-efficacy of being able to care for their own health. In addition, they lack the far-sighted view that the effects of health-related behavior only become apparent in the long term. For the same reason, Sirois [ 9 ] believes that there are no short-term, but only long-term effects of procrastination on health mediated by poor health-related behavior. For example, an unhealthy diet leads to diabetes over time. The findings of studies examining the behavioral pathway are inconclusive [ 3 , 17 , 26 , 28 ]. Furthermore, since most of these studies are cross-sectional, they are not suitable for uncovering long-term effects of trait procrastination on (chronic) disease mediated by poor health-related behavior.
In summary, previous research on the two mediated pathways of the procrastination-health model mainly found support for the role of (chronic) stress in the relationship between trait procrastination and (chronic) disease. However, only short-term effects have been investigated so far. Moreover, longitudinal studies are needed to be able to assess the causal direction of the relationship between trait procrastination, (chronic) stress, and (chronic) disease. Consequently, our study is the first to examine long-term effects of trait procrastination on (chronic) disease mediated by (chronic) stress, using a longitudinal design. (Chronic) disease could be measured by a variety of different indicators (e.g., physical symptoms, diabetes, or coronary heart disease). We choose depression and anxiety symptoms as indicators for (chronic) disease because they signal mental health complaints before they manifest as (chronic) diseases. Additionally, depression and anxiety symptoms are two of the most common mental health complaints among students [ 29 , 30 ] and procrastination has been shown to be a significant predictor of depression and anxiety symptoms [ 18 , 31 , 32 , 33 , 34 ]. Until now, the stress-related pathway of the procrastination-health model with depression and anxiety symptoms as the health outcome has only been analyzed in one cross-sectional study that confirmed the predictions of the model [ 35 ].
The aim of our study is to evaluate some of the key assumptions of the procrastination-health model, particularly the relationships between trait procrastination, (chronic) stress, and (chronic) disease over time, surveyed in the following analysis using depression and anxiety symptoms.
In line with the key assumptions of the procrastination-health model, we postulate (see Fig. 2 ):
Procrastination leads to perceived stress over time.
Perceived stress leads to depression and anxiety symptoms over time.
Procrastination leads to depression and anxiety symptoms over time, mediated by perceived stress.
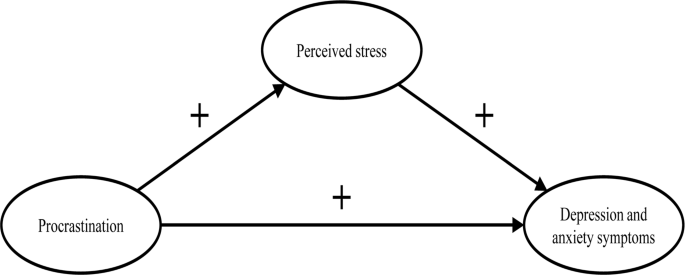
The section of the procrastination-health model we examined
Materials and methods
Our study was part of a health monitoring at a large German university Footnote 1 . Ethical approval for our study was granted by the Ethics Committee of the university’s Department of Education and Psychology. We collected the initial data in 2019. Two occasions followed, each at an interval of six months. In January 2019, we sent out 33,267 invitations to student e-mail addresses. Before beginning the survey, students provided their written informed consent to participate in our study. 3,420 students took part at the first occasion (T1; 10% response rate). Of these, 862 participated at the second (T2) and 392 at the third occasion (T3). In order to test whether dropout was selective, we compared sociodemographic and study specific characteristics (age, gender, academic semester, number of assessments/exams) as well as behavior and health-related variables (procrastination, perceived stress, depression and anxiety symptoms) between the participants of the first wave ( n = 3,420) and those who participated three times ( n = 392). Results from independent-samples t-tests and chi-square analysis showed no significant differences regarding sociodemographic and study specific characteristics (see Additional file 1: Table S1 and S2 ). Regarding behavior and health-related variables, independent-samples t-tests revealed a significant difference in procrastination between the two groups ( t (3,409) = 2.08, p < .05). The mean score of procrastination was lower in the group that participated in all three waves.
The mean age of the longitudinal respondents was 24.1 years ( SD = 5.5 years), the youngest participants were 17 years old, the oldest one was 59 years old. The majority of participants was female (74.0%), 7 participants identified neither as male nor as female (1.8%). The respondents were on average enrolled in the third year of studying ( M = 3.9; SD = 2.3). On average, the students worked about 31.2 h ( SD = 14.1) per week for their studies, and an additional 8.5 h ( SD = 8.5) for their (part-time) jobs. The average income was €851 ( SD = 406), and 4.9% of the students had at least one child. The students were mostly enrolled in philosophy and humanities (16.5%), education and psychology (15.8%), biology, chemistry, and pharmacy (12.5%), political and social sciences (10.6%), veterinary medicine (8.9%), and mathematics and computer science (7.7%).
We only used established and well evaluated instruments for our analyses.
- Procrastination
We adopted the short form of the Procrastination Questionnaire for Students (PFS-4) [ 36 ] to measure procrastination. The PFS-4 assesses procrastination at university as a largely stable behavioral disposition across situations, that is, as a trait. The questionnaire consists of four items (e.g., I put off starting tasks until the last moment.). Each item was rated on a 5-point scale ((almost) never = 1 to (almost) always = 5) for the last two weeks. All items were averaged, with higher scores indicating a greater tendency to procrastinate. The PFS-4 has been proven to be reliable and valid, showing very high correlations with other established trait procrastination scales, for example, with the German short form of the General Procrastination Scale [ 37 , 38 ]. We also proved the scale to be one-dimensional in a factor analysis, with a Cronbach’s alpha of 0.90.
Perceived stress
The Heidelberger Stress Index (HEI-STRESS) [ 39 ] is a three-item measure of current perceived stress due to studying as well as in life in general. For the first item, respondents enter a number between 0 (not stressed at all) and 100 (completely stressed) to indicate how stressed their studies have made them feel over the last four weeks. For the second and third item, respondents rate on a 5-point scale how often they feel “stressed and tense” and as how stressful they would describe their life at the moment. We transformed the second and third item to match the range of the first item before we averaged all items into a single score with higher values indicating greater perceived stress. We proved the scale to be one-dimensional and Cronbach’s alpha for our study was 0.86.
Depression and anxiety symptoms
We used the Patient Health Questionnaire-4 (PHQ-4) [ 40 ], a short form of the Patient Health Questionnaire [ 41 ] with four items, to measure depression and anxiety symptoms. The PHQ-4 contains two items from the Patient Health Questionnaire-2 (PHQ-2) [ 42 ] and the Generalized Anxiety Disorder Scale-2 (GAD-2) [ 43 ], respectively. It is a well-established screening scale designed to assess the core criteria of major depressive disorder (PHQ-2) and generalized anxiety disorder (GAD-2) according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). However, it was shown that the GAD-2 is also appropriate for screening other anxiety disorders. According to Kroenke et al. [ 40 ], the PHQ-4 can be used to assess a person’s symptom burden and impairment. We asked the participants to rate how often they have been bothered over the last two weeks by problems, such as “Little interest or pleasure in doing things”. Response options were 0 = not at all, 1 = several days, 2 = more than half the days, and 3 = nearly every day. Calculated as the sum of the four items, the total scores range from 0 to 12 with higher scores indicating more frequent depression and anxiety symptoms. The total scores can be categorized as none-to-minimal (0–2), mild (3–5), moderate (6–8), and severe (9–12) depression and anxiety symptoms. The PHQ-4 was shown to be reliable and valid [ 40 , 44 , 45 ]. We also proved the scale to be one-dimensional in a factor analysis, with a Cronbach’s alpha of 0.86.
Data analysis
To test our hypotheses, we performed structural equation modelling (SEM) using R (Version 4.1.1) with the package lavaan. All items were standardized ( M = 0, SD = 1). Due to the non-normality of some study variables and a sufficiently large sample size of N near to 400 [ 46 ], we used robust maximum likelihood estimation (MLR) for all model estimations. As recommended by Hu and Bentler [ 47 ], we assessed the models’ goodness of fit by chi-square test statistic, root mean square error of approximation (RMSEA), standardized root mean square residual (SRMR), Tucker-Lewis index (TLI), and comparative fit index (CFI). A non-significant chi-square indicates good model fit. Since chi-square is sensitive to sample size, we also evaluated fit indices less sensitive to the number of observations. RMSEA and SRMR values of 0.05 or lower as well as TLI and CFI values of 0.97 or higher indicate good model fit. RMSEA values of 0.08 or lower, SRMR values of 0.10 or lower, as well as TLI and CFI values of 0.95 or higher indicate acceptable model fit [ 48 , 49 ]. First, we conducted confirmatory factor analysis for the first occasion, defining three factors that correspond to the measures of procrastination, perceived stress, and depression and anxiety symptoms. Next, we tested for measurements invariance over time and specified the measurement model, before testing our hypotheses.
Measurement invariance over time
To test for measurement invariance over time, we defined one latent variable for each of the three occasions, corresponding to the measures of procrastination, perceived stress, and depression and anxiety symptoms, respectively. As recommended by Geiser and colleagues [ 50 ], the links between indicators and factors (i.e., factor loadings and intercepts) should be equal over measurement occasions; therefore, we added indicator specific factors. A first and least stringent step of testing measurement invariance is configural invariance (M CI ). It was examined whether the included constructs (procrastination, perceived stress, depression and anxiety symptoms) have the same pattern of free and fixed loadings over time. This means that the assignment of the indicators to the three latent factors over time is supported by the underlying data. If configural invariance was supported, restrictions for the next step of testing measurement invariance (metric or weak invariance; M MI ) were added. This means that each item contributes to the latent construct to a similar degree over time. Metric invariance was tested by constraining the factor loadings of the constructs over time. The next step of testing measurement invariance (scalar or strong invariance; M SI ) consisted of checking whether mean differences in the latent construct capture all mean differences in the shared variance of the items. Scalar invariance was tested by constraining the item intercepts over time. The constraints applied in the metric invariance model were retained [ 51 ]. For the last step of testing measurement invariance (residual or strict invariance; M RI ), the residual variables were also set equal over time. If residual invariance is supported, differences in the observed variables can exclusively be attributed to differences in the variances of the latent variables.
We used the Satorra-Bentler chi-square difference test to evaluate the superiority of a more stringent model [ 52 ]. We assumed the model with the largest number of invariance restrictions – which still has an acceptable fit and no substantial deterioration of the chi-square value – to be the final model [ 53 ]. Following previous recommendations, we considered a decrease in CFI of 0.01 and an increase in RMSEA of 0.015 as unacceptable to establish measurement invariance [ 54 ]. If a more stringent model had a significant worse chi-square value, but the model fit was still acceptable and the deterioration in model fit fell within the change criteria recommended for CFI and RMSEA values, we still considered the more stringent model to be superior.
Hypotheses testing
As recommended by Dormann et al. [ 55 ], we applied autoregressive time-lagged panel models to test our hypotheses. In the first step, we specified a model (M 0 ) that only included the stabilities of the three variables (procrastination, perceived stress, depression and anxiety symptoms) over time. In the next step (M 1 ), we added the time-lagged effects from procrastination (T1) to perceived stress (T2) and from procrastination (T2) to perceived stress (T3) as well as from perceived stress (T1) to depression and anxiety symptoms (T2) and from perceived stress (T2) to depression and anxiety symptoms (T3). Additionally, we included a direct path from procrastination (T1) to depression and anxiety symptoms (T3). If this path becomes significant, we can assume a partial mediation [ 55 ]. Otherwise, we can assume a full mediation. We compared these nested models using the Satorra-Bentler chi-square difference test and the Akaike information criterion (AIC). The chi-square difference value should either be non-significant, indicating that the proposed model including our hypotheses (M 1 ) does not have a significant worse model fit than the model including only stabilities (M 0 ), or, if significant, it should be in the direction that M 1 fits the data better than M 0 . Regarding the AIC, M 1 should have a lower value than M 0 .
Table 1 displays the means, standard deviations, internal consistencies (Cronbach’s alpha), and stabilities (correlations) of all study variables. The alpha values of procrastination, perceived stress, and depression and anxiety symptoms are classified as good (> 0.80) [ 56 ]. The correlation matrix of the manifest variables used for the analyses can be found in the Additional file 1: Table S3 .
We observed the highest test-retest reliabilities for procrastination ( r ≥ .74). The test-retest reliabilities for depression and anxiety symptoms ( r ≥ .64) and for perceived stress ( r ≥ .54) were a bit lower (see Table 1 ). The pattern of correlations shows a medium to large but positive relationship between procrastination and depression and anxiety symptoms [ 57 , 58 ]. The association between procrastination and perceived stress was small, the one between perceived stress and depression and anxiety symptoms very large (see Table 1 ).
Confirmatory factor analysis showed an acceptable to good fit (x 2 (41) = 118.618, p < .001; SRMR = 0.042; RMSEA = 0.071; TLI = 0.95; CFI = 0.97). When testing for measurement invariance over time for each construct, the residual invariance models with indicator specific factors provided good fit to the data (M RI ; see Table 2 ), suggesting that differences in the observed variables can exclusively be attributed to differences of the latent variables. We then specified and tested the measurement model of the latent constructs prior to model testing based on the items of procrastination, perceived stress, and depression and anxiety symptoms. The measurement model fitted the data well (M M ; see Table 3 ). All items loaded solidly on their respective factors (0.791 ≤ β ≤ 0.987; p < .001).
To test our hypotheses, we analyzed the two models described in the methods section.
The fit of the stability model (M 0 ) was acceptable (see Table 3 ). Procrastination was stable over time, with stabilities above 0.82. The stabilities of perceived stress as well as depression and anxiety symptoms were somewhat lower, ranging from 0.559 (T1 -> T2) to 0.696 (T2 -> T3) for perceived stress and from 0.713 (T2 -> T3) to 0.770 (T1 -> T2) for depression and anxiety symptoms, respectively.
The autoregressive mediation model (M 1 ) fitted the data significantly better than M 0 . The direct path from procrastination (T1) to depression and anxiety symptoms (T3) was significant (β = 0.16; p < .001), however, none of the mediated paths (from procrastination (T1) to perceived stress (T2) and from perceived stress (T2) to depression and anxiety symptoms (T3)) proved to be substantial. Also, the time-lagged paths from perceived stress (T1) to depression and anxiety symptoms (T2) and from procrastination (T2) to perceived stress (T3) were not substantial either (see Fig. 3 ).
To examine whether the hypothesized effects would occur over a one-year period rather than a six-months period, we specified an additional model with paths from procrastination (T1) to perceived stress (T3) and from perceived stress (T1) to depression and anxiety symptoms (T3), also including the stabilities of the three constructs as in the stability model M 0 . The model showed an acceptable fit (χ 2 (486) = 831.281, p < .001; RMSEA = 0.048; SRMR = 0.091; TLI = 0.95; CFI = 0.95), but neither of the two paths were significant.
Therefore, our hypotheses, that procrastination leads to perceived stress over time (H1) and that perceived stress leads to depression and anxiety symptoms over time (H2) must be rejected. We could only partially confirm our third hypothesis, that procrastination leads to depression and anxiety over time, mediated by perceived stress (H3), since procrastination did lead to depression and anxiety symptoms over time. However, this effect was not mediated by perceived stress.
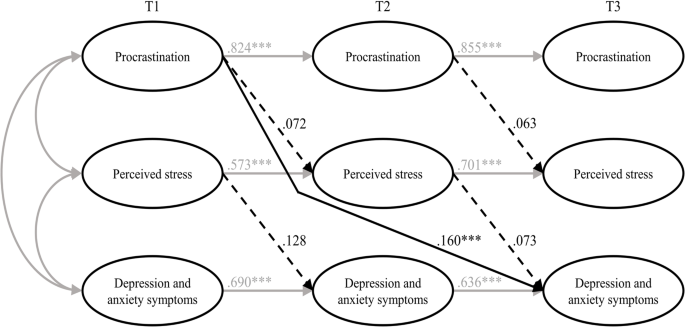
Results of the estimated model including all hypotheses (M 1 ). Note Non-significant paths are dotted. T1 = time 1; T2 = time 2; T3 = time 3. *** p < .001
To sum up, we tried to examine the harmful consequences of procrastination on students’ stress and mental health. Hence, we selected the procrastination-health model by Sirois [ 9 ] as a theoretical foundation and tried to evaluate some of its key assumptions in a temporal perspective. The author assumes that trait procrastination leads to (chronic) disease via (chronic) stress. We chose depression and anxiety symptoms as indicators for (chronic) disease and postulated, in line with the key assumptions of the procrastination-health model, that procrastination leads to perceived stress over time (H1), that perceived stress leads to depression and anxiety symptoms over time (H2), and that procrastination leads to depression and anxiety symptoms over time, mediated by perceived stress (H3). To examine these relationships properly, we collected longitudinal data from students at three occasions over a one-year period and analyzed the data using autoregressive time-lagged panel models. Our first and second hypotheses had to be rejected: Procrastination did not lead to perceived stress over time, and perceived stress did not lead to depression and anxiety symptoms over time. However, procrastination did lead to depression and anxiety symptoms over time – which is in line with our third hypothesis – but perceived stress was not a mediator of this effect. Therefore, we could only partially confirm our third hypothesis.
Our results contradict previous studies on the stress-related pathway of the procrastination-health model, which consistently found support for the role of (chronic) stress in the relationship between trait procrastination and (chronic) disease. Since most of these studies were cross-sectional, though, the causal direction of these effects remained uncertain. There are two longitudinal studies that confirm the stress-related pathway of the procrastination-health model [ 27 , 28 ], but both studies examined short-term effects (≤ 3 months), whereas we focused on more long-term effects. Therefore, the divergent findings may indicate that there are short-term, but no long-term effects of trait procrastination on (chronic) disease mediated by (chronic) stress.
Our results especially raise the question whether trait procrastination leads to (chronic) stress in the long term. Looking at previous longitudinal studies on the effect of procrastination on stress, the following stands out: At shorter study periods of two weeks [ 27 ] and four weeks [ 28 ], the effect of procrastination on stress appears to be present. At longer study periods of seven weeks [ 59 ], three months [ 28 ], six months, and twelve months, as in our study, the effect of procrastination on stress does not appear to be present. There is one longitudinal study in which procrastination was a significant predictor of stress symptoms nine months later [ 34 ]. The results of this study should be interpreted with caution, though, because the outbreak of the COVID-19 pandemic fell within the study period, which could have contributed to increased stress symptoms [ 60 ]. Unfortunately, Johansson et al. [ 34 ] did not report whether average stress symptoms increased during their study. In one of the two studies conducted by Fincham and May [ 59 ], the COVID-19 pandemic outbreak also fell within their seven-week study period. However, they reported that in their study, average stress symptoms did not increase from baseline to follow-up. Taken together, the findings suggest that procrastination can cause acute stress in the short term, for example during times when many tasks need to be completed, such as at the end of a semester, but that procrastination does not lead to chronic stress over time. It seems possible that students are able to recover during the semester from the stress their procrastination caused at the end of the previous semester. Because of their procrastination, they may also have more time to engage in relaxing activities, which could further mitigate the effect of procrastination on stress. Our conclusions are supported by an early and well-known longitudinal study by Tice and Baumeister [ 61 ], which compared procrastinating and non-procrastinating students with regard to their health. They found that procrastinators experienced less stress than their non-procrastinating peers at the beginning of the semester, but more at the end of the semester. Additionally, our conclusions are in line with an interview study in which university students were asked about the consequences of their procrastination [ 62 ]. The students reported that, due to their procrastination, they experience high levels of stress during periods with heavy workloads (e.g., before deadlines or exams). However, the stress does not last, instead, it is relieved immediately after these periods.
Even though research indicates, in line with the assumptions of the procrastination-health model, that stress is a risk factor for physical and mental disorders [ 63 , 64 , 65 , 66 ], perceived stress did not have a significant effect on depression and anxiety symptoms in our study. The relationship between stress and mental health is complex, as people respond to stress in many different ways. While some develop stress-related mental disorders, others experience mild psychological symptoms or no symptoms at all [ 67 ]. This can be explained with the help of vulnerability-stress models. According to vulnerability-stress models, mental illnesses emerge from an interaction of vulnerabilities (e.g., genetic factors, difficult family backgrounds, or weak coping abilities) and stress (e.g., minor or major life events or daily hassles) [ 68 , 69 ]. The stress perceived by the students in our sample may not be sufficient enough on its own, without the presence of other risk factors, to cause depression and anxiety symptoms. However, since we did not assess individual vulnerability and stress factors in our study, these considerations are mere speculation.
In our study, procrastination led to depression and anxiety symptoms over time, which is consistent with the procrastination-health model as well as previous cross-sectional and longitudinal evidence [ 18 , 21 , 31 , 32 , 33 , 34 ]. However, it is still unclear by which mechanisms this effect is mediated, as perceived stress did not prove to be a substantial mediator in our study. One possible mechanism would be that procrastination impairs affective well-being [ 70 ] and creates negative feelings, such as shame, guilt, regret, and anger [ 20 , 21 , 22 , 62 , 71 ], which in turn could lead to depression and anxiety symptoms [ 23 , 24 , 25 ]. Other potential mediators of the relationship between procrastination and depression and anxiety symptoms emerge from the behavioral pathway of the procrastination-health model, suggesting that poor health-related behaviors mediate the effect of trait procrastination on (chronic) disease. Although evidence for this is still scarce, the results of one cross-sectional study, for example, indicate that poor sleep quality might mediate the effect of procrastination on depression and anxiety symptoms [ 35 ].
In summary, we found that procrastination leads to depression and anxiety symptoms over time and that perceived stress is not a mediator of this effect. We could not show that procrastination leads to perceived stress over time, nor that perceived stress leads to depression and anxiety symptoms over time. For the most part, the relationships between procrastination, perceived stress, and depression and anxiety symptoms did not match the relationships between trait procrastination, (chronic) stress, and (chronic) disease as assumed in the procrastination-health model. Explanations for this could be that procrastination might only lead to perceived stress in the short term, for example, during preparations for end-of-semester exams, and that perceived stress may not be sufficient enough on its own, without the presence of other risk factors, to cause depression and anxiety symptoms. In conclusion, we could not confirm long-term effects of trait procrastination on (chronic) disease mediated by (chronic) stress, as assumed for the stress-related pathway of the procrastination-health model.
Limitations and suggestions for future research
In our study, we tried to draw causal conclusions about the harmful consequences of procrastination on students’ stress and mental health. However, since procrastination is a trait that cannot be manipulated experimentally, we have conducted an observational rather than an experimental study, which makes causal inferences more difficult. Nonetheless, a major strength of our study is that we used a longitudinal design with three waves. This made it possible to draw conclusions about the causal direction of the effects, as in hardly any other study targeting consequences of procrastination on health before [ 4 , 28 , 55 ]. Therefore, we strongly recommend using a similar longitudinal design in future studies on the procrastination-health model or on consequences of procrastination on health in general.
We chose a time lag of six months between each of the three measurement occasions to examine long-term effects of procrastination on depression and anxiety symptoms mediated by perceived stress. However, more than six months may be necessary for the hypothesized effects to occur [ 72 ]. The fact that the temporal stabilities of the examined constructs were moderate or high (0.559 ≤ β ≤ 0.854) [ 73 , 74 ] also suggests that the time lags may have been too short. The larger the time lag, the lower the temporal stabilities, as shown for depression and anxiety symptoms, for example [ 75 ]. High temporal stabilities make it more difficult to detect an effect that actually exists [ 76 ]. Nonetheless, Dormann and Griffin [ 77 ] recommend using shorter time lags of less than one year, even with high stabilities, because of other influential factors, such as unmeasured third variables. Therefore, our time lags of six months seem appropriate.
It should be discussed, though, whether it is possible to detect long-term effects of the stress-related pathway of the procrastination-health model within a total study period of one year. Sirois [ 9 ] distinguishes between short-term and long-term effects of procrastination on health mediated by stress, but does not address how long it might take for long-term effects to occur or when effects can be considered long-term instead of short-term. The fact that an effect of procrastination on stress is evident at shorter study periods of four weeks or less but in most cases not at longer study periods of seven weeks or more, as we mentioned earlier, could indicate that short-term effects occur within the time frame of one to three months, considering the entire stress-related pathway. Hence, it seems appropriate to assume that we have examined rather long-term effects, given our study period of six and twelve months. Nevertheless, it would be beneficial to use varying study periods in future studies, in order to be able to determine when effects can be considered long-term.
Concerning long-term effects of the stress-related pathway, Sirois [ 9 ] assumes that chronic procrastination causes chronic stress, which leads to chronic diseases over time. The term “chronic stress” refers to prolonged stress episodes associated with permanent tension. The instrument we used captures perceived stress over the last four weeks. Even though the perceived stress of the students in our sample was relatively stable (0.559 ≤ β ≤ 0.696), we do not know how much fluctuation occurred between each of the three occasions. However, there is some evidence suggesting that perceived stress is strongly associated with chronic stress [ 78 ]. Thus, it seems acceptable that we used perceived stress as an indicator for chronic stress in our study. For future studies, we still suggest the use of an instrument that can more accurately reflect chronic stress, for example, the Trier Inventory for Chronic Stress (TICS) [ 79 ].
It is also possible that the occasions were inconveniently chosen, as they all took place in a critical academic period near the end of the semester, just before the examination period began. We chose a similar period in the semester for each occasion for the sake of comparability. However, it is possible that, during this preparation periods, stress levels peaked and procrastinators procrastinated less because they had to catch up after delaying their work. This could have introduced bias to the data. Therefore, in future studies, investigation periods should be chosen that are closer to the beginning or in the middle of a semester.
Furthermore, Sirois [ 9 ] did not really explain her understanding of “chronic disease”. However, it seems clear that physical illnesses, such as diabetes or cardiovascular diseases, are meant. Depression and anxiety symptoms, which we chose as indicators for chronic disease, represent mental health complaints that do not have to be at the level of a major depressive disorder or an anxiety disorder, in terms of their quantity, intensity, or duration [ 40 ]. But they can be viewed as precursors to a major depressive disorder or an anxiety disorder. Therefore, given our study period of one year, it seems appropriate to use depression and anxiety symptoms as indicators for chronic disease. At longer study periods, we would expect these mental health complaints to manifest as mental disorders. Moreover, the procrastination-health model was originally designed to be applied to physical diseases [ 3 ]. Perhaps, the model assumptions are more applicable to physical diseases than to mental disorders. By applying parts of the model to mental health complaints, we have taken an important step towards finding out whether the model is applicable to mental disorders as well. Future studies should examine additional long-term health outcomes, both physical and psychological. This would help to determine whether trait procrastination has varying effects on different diseases over time. Furthermore, we suggest including individual vulnerability and stress factors in future studies in order to be able to analyze the effect of (chronic) stress on (chronic) diseases in a more differentiated way.
Regarding our sample, 3,420 students took part at the first occasion, but only 392 participated three times, which results in a dropout rate of 88.5%. At the second and third occasion, invitation e-mails were only sent to participants who had indicated at the previous occasion that they would be willing to participate in a repeat survey and provided their e-mail address. This is probably one of the main reasons for our high dropout rate. Other reasons could be that the students did not receive any incentives for participating in our study and that some may have graduated between the occasions. Selective dropout analysis revealed that the mean score of procrastination was lower in the group that participated in all three waves ( n = 392) compared to the group that participated in the first wave ( n = 3,420). One reason for this could be that those who have a higher tendency to procrastinate were more likely to procrastinate on filling out our survey at the second and third occasion. The findings of our dropout analysis should be kept in mind when interpreting our results, as lower levels of procrastination may have eliminated an effect on perceived stress or on depression and anxiety symptoms. Additionally, across all age groups in population-representative samples, the student age group reports having the best subjective health [ 80 ]. Therefore, it is possible that they are more resilient to stress and experience less impairment of well-being than other age groups. Hence, we recommend that future studies focus on other age groups as well.
It is generally assumed that procrastination leads to lower academic performance, health impairment, and poor health-related behavior. However, evidence for negative consequences of procrastination is still limited and it is also unclear by which mechanisms they are mediated. In consequence, the aim of our study was to examine the effect of procrastination on mental health over time and stress as a possible facilitator of this relationship. We selected the procrastination-health model as a theoretical foundation and used the stress-related pathway of the model, assuming that trait procrastination leads to (chronic) disease via (chronic) stress. We chose depression and anxiety symptoms as indicators for (chronic) disease and collected longitudinal data from students at three occasions over a one-year period. This allowed us to draw conclusions about the causal direction of the effects, as in hardly any other study examining consequences of procrastination on (mental) health before. Our results indicate that procrastination leads to depression and anxiety symptoms over time and that perceived stress is not a mediator of this effect. We could not show that procrastination leads to perceived stress over time, nor that perceived stress leads to depression and anxiety symptoms over time. Explanations for this could be that procrastination might only lead to perceived stress in the short term, for example, during preparations for end-of-semester exams, and that perceived stress may not be sufficient on its own, that is, without the presence of other risk factors, to cause depression and anxiety symptoms. Overall, we could not confirm long-term effects of trait procrastination on (chronic) disease mediated by (chronic) stress, as assumed for the stress-related pathway of the procrastination-health model. Our study emphasizes the importance of identifying the consequences procrastination can have on health and well-being and determining by which mechanisms they are mediated. Only then will it be possible to develop interventions that can prevent negative health consequences of procrastination. Further health outcomes and possible mediators should be explored in future studies, using a similar longitudinal design.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
University Health Report at Freie Universität Berlin.
Abbreviations
Comparative fit index
Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition
Generalized Anxiety Disorder Scale-2
Heidelberger Stress Index
Hypothalamic-pituitary-adrenocortical
Robust maximum likelihood estimation
Short form of the Procrastination Questionnaire for Students
Patient Health Questionnaire-2
Patient Health Questionnaire-4
Root mean square error of approximation
Structural equation modeling
Standardized root mean square residual
Tucker-Lewis index
Lu D, He Y, Tan Y, Gender S, Status. Cultural differences, Education, family size and procrastination: a sociodemographic Meta-analysis. Front Psychol. 2021. https://doi.org/10.3389/fpsyg.2021.719425 .
Article PubMed PubMed Central Google Scholar
Yan B, Zhang X. What research has been conducted on Procrastination? Evidence from a systematical bibliometric analysis. Front Psychol. 2022. https://doi.org/10.3389/fpsyg.2022.809044 .
Sirois FM, Melia-Gordon ML, Pychyl TA. I’ll look after my health, later: an investigation of procrastination and health. Pers Individ Dif. 2003;35:1167–84. https://doi.org/10.1016/S0191-8869(02)00326-4 .
Article Google Scholar
Grunschel C. Akademische Prokrastination: Eine qualitative und quantitative Untersuchung von Gründen und Konsequenzen [Unpublished doctoral dissertation]: Universität Bielefeld; 2013.
Steel P. The Nature of Procrastination: a Meta-Analytic and Theoretical Review of Quintessential Self-Regulatory failure. Psychol Bull. 2007;133:65–94. https://doi.org/10.1037/0033-2909.133.1.65 .
Article PubMed Google Scholar
Corkin DM, Yu SL, Lindt SF. Comparing active delay and procrastination from a self-regulated learning perspective. Learn Individ Differ. 2011;21:602–6. https://doi.org/10.1016/j.lindif.2011.07.005 .
Balkis M, Duru E. Procrastination, self-regulation failure, academic life satisfaction, and affective well-being: underregulation or misregulation form. Eur J Psychol Educ. 2016;31:439–59. https://doi.org/10.1007/s10212-015-0266-5 .
Schulz N. Procrastination und Planung – Eine Untersuchung zum Einfluss von Aufschiebeverhalten und Depressivität auf unterschiedliche Planungskompetenzen [Doctoral dissertation]: Westfälische Wilhelms-Universität Münster; 2007.
Sirois FM. Procrastination, stress, and Chronic Health conditions: a temporal perspective. In: Sirois FM, Pychyl TA, editors. Procrastination, Health, and well-being. London: Academic; 2016. pp. 67–92. https://doi.org/10.1016/B978-0-12-802862-9.00004-9 .
Harriott J, Ferrari JR. Prevalence of procrastination among samples of adults. Psychol Rep. 1996;78:611–6. https://doi.org/10.2466/pr0.1996.78.2.611 .
Ferrari JR, O’Callaghan J, Newbegin I. Prevalence of Procrastination in the United States, United Kingdom, and Australia: Arousal and Avoidance delays among adults. N Am J Psychol. 2005;7:1–6.
Google Scholar
Ferrari JR, Díaz-Morales JF, O’Callaghan J, Díaz K, Argumedo D. Frequent behavioral Delay tendencies by adults. J Cross Cult Psychol. 2007;38:458–64. https://doi.org/10.1177/0022022107302314 .
Day V, Mensink D, O’Sullivan M. Patterns of academic procrastination. JCRL. 2000;30:120–34. https://doi.org/10.1080/10790195.2000.10850090 .
Höcker A, Engberding M, Rist F, Prokrastination. Ein Manual Zur Behandlung Des Pathologischen Aufschiebens. 2nd ed. Göttingen: Hogrefe; 2017.
Kim KR, Seo EH. The relationship between procrastination and academic performance: a meta-analysis. Pers Individ Dif. 2015;82:26–33. https://doi.org/10.1016/j.paid.2015.02.038 .
Khalid A, Zhang Q, Wang W, Ghaffari AS, Pan F. The relationship between procrastination, perceived stress, saliva alpha-amylase level and parenting styles in Chinese first year medical students. Psychol Res Behav Manag. 2019;12:489–98. https://doi.org/10.2147/PRBM.S207430 .
Sirois FM. I’ll look after my health, later: a replication and extension of the procrastination–health model with community-dwelling adults. Pers Individ Dif. 2007;43:15–26. https://doi.org/10.1016/j.paid.2006.11.003 .
Reinecke L, Meier A, Aufenanger S, Beutel ME, Dreier M, Quiring O, et al. Permanently online and permanently procrastinating? The mediating role of internet use for the effects of trait procrastination on psychological health and well-being. New Media Soc. 2018;20:862–80. https://doi.org/10.1177/1461444816675437 .
Westgate EC, Wormington SV, Oleson KC, Lindgren KP. Productive procrastination: academic procrastination style predicts academic and alcohol outcomes. J Appl Soc Psychol. 2017;47:124–35. https://doi.org/10.1111/jasp.12417 .
Feyzi Behnagh R, Ferrari JR. Exploring 40 years on affective correlates to procrastination: a literature review of situational and dispositional types. Curr Psychol. 2022;41:1097–111. https://doi.org/10.1007/s12144-021-02653-z .
Rahimi S, Hall NC, Sticca F. Understanding academic procrastination: a longitudinal analysis of procrastination and emotions in undergraduate and graduate students. Motiv Emot. 2023. https://doi.org/10.1007/s11031-023-10010-9 .
Patrzek J, Grunschel C, Fries S. Academic procrastination: the perspective of University counsellors. Int J Adv Counselling. 2012;34:185–201. https://doi.org/10.1007/s10447-012-9150-z .
Watson D, Clark LA, Carey G. Positive and negative affectivity and their relation to anxiety and depressive disorders. J Abnorm Psychol. 1988;97:346–53. https://doi.org/10.1037//0021-843x.97.3.346 .
Cândea D-M, Szentagotai-Tătar A. Shame-proneness, guilt-proneness and anxiety symptoms: a meta-analysis. J Anxiety Disord. 2018;58:78–106. https://doi.org/10.1016/j.janxdis.2018.07.005 .
Young CM, Neighbors C, DiBello AM, Traylor ZK, Tomkins M. Shame and guilt-proneness as mediators of associations between General Causality orientations and depressive symptoms. J Soc Clin Psychol. 2016;35:357–70. https://doi.org/10.1521/jscp.2016.35.5.357 .
Stead R, Shanahan MJ, Neufeld RW. I’ll go to therapy, eventually: Procrastination, stress and mental health. Pers Individ Dif. 2010;49:175–80. https://doi.org/10.1016/j.paid.2010.03.028 .
Dow NM. Procrastination, stress, and sleep in tertiary students [Master’s thesis]: University of Canterbury; 2018.
Sirois FM, Stride CB, Pychyl TA. Procrastination and health: a longitudinal test of the roles of stress and health behaviours. Br J Health Psychol. 2023. https://doi.org/10.1111/bjhp.12658 .
Hofmann F-H, Sperth M, Holm-Hadulla RM. Psychische Belastungen Und Probleme Studierender. Psychotherapeut. 2017;62:395–402. https://doi.org/10.1007/s00278-017-0224-6 .
Liu CH, Stevens C, Wong SHM, Yasui M, Chen JA. The prevalence and predictors of mental health diagnoses and suicide among U.S. college students: implications for addressing disparities in service use. Depress Anxiety. 2019;36:8–17. https://doi.org/10.1002/da.22830 .
Aftab S, Klibert J, Holtzman N, Qadeer K, Aftab S. Schemas mediate the Link between Procrastination and Depression: results from the United States and Pakistan. J Rat-Emo Cognitive-Behav Ther. 2017;35:329–45. https://doi.org/10.1007/s10942-017-0263-5 .
Flett AL, Haghbin M, Pychyl TA. Procrastination and depression from a cognitive perspective: an exploration of the associations among Procrastinatory Automatic thoughts, rumination, and Mindfulness. J Rat-Emo Cognitive-Behav Ther. 2016;34:169–86. https://doi.org/10.1007/s10942-016-0235-1 .
Saddler CD, Sacks LA. Multidimensional perfectionism and academic procrastination: relationships with Depression in University students. Psychol Rep. 1993;73:863–71. https://doi.org/10.1177/00332941930733pt123 .
Johansson F, Rozental A, Edlund K, Côté P, Sundberg T, Onell C, et al. Associations between procrastination and subsequent Health outcomes among University students in Sweden. JAMA Netw Open. 2023. https://doi.org/10.1001/jamanetworkopen.2022.49346 .
Gusy B, Jochmann A, Lesener T, Wolter C, Blaszcyk W. „Get it done – schadet Aufschieben Der Gesundheit? Präv Gesundheitsf. 2023;18:228–33. https://doi.org/10.1007/s11553-022-00950-4 .
Glöckner-Rist A, Engberding M, Höcker A, Rist F. Prokrastinationsfragebogen für Studierende (PFS): Zusammenstellung sozialwissenschaftlicher items und Skalen. ZIS - GESIS Leibniz Institute for the Social Sciences; 2014.
Klingsieck KB, Fries S. Allgemeine Prokrastination: Entwicklung Und Validierung Einer Deutschsprachigen Kurzskala Der General Procrastination Scale (Lay, 1986). Diagnostica. 2012;58:182–93. https://doi.org/10.1026/0012-1924/a000060 .
Lay CH. At last, my research article on procrastination. J Res Pers. 1986;20:474–95. https://doi.org/10.1016/0092-6566(86)90127-3 .
Schmidt LI, Obergfell J. Zwangsjacke Bachelor?! Stressempfinden Und Gesundheit Studierender: Der Einfluss Von Anforderungen Und Entscheidungsfreiräumen Bei Bachelor- Und Diplomstudierenden Nach Karaseks Demand-Control-Modell. Saarbrücken: VDM Verlag Dr. Müller; 2011.
Kroenke K, Spitzer RL, Williams JB, Löwe B. An Ultra-brief Screening Scale for anxiety and depression: the PHQ-4. Psychosomatics. 2009;50:613–21. https://doi.org/10.1016/S0033-3182(09)70864-3 .
Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ Primary Care Study. JAMA. 1999;282:1737–44. https://doi.org/10.1001/jama.282.18.1737 .
Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item Depression Screener. Med Care. 2003;41:1284–92.
Kroenke K, Spitzer RL, Williams JB, Monahan PO, Löwe B. Anxiety disorders in Primary Care: prevalence, impairment, Comorbidity, and detection. Ann Intern Med. 2007;146:317–25. https://doi.org/10.7326/0003-4819-146-5-200703060-00004 .
Khubchandani J, Brey R, Kotecki J, Kleinfelder J, Anderson J. The Psychometric properties of PHQ-4 depression and anxiety screening scale among College Students. Arch Psychiatr Nurs. 2016;30:457–62. https://doi.org/10.1016/j.apnu.2016.01.014 .
Löwe B, Wahl I, Rose M, Spitzer C, Glaesmer H, Wingenfeld K, et al. A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J Affect Disorders. 2010;122:86–95. https://doi.org/10.1016/j.jad.2009.06.019 .
Boomsma A, Hoogland JJ. The robustness of LISREL modeling revisited. In: Cudeck R, Du Toit S, Sörbom D, editors. Structural equation modeling: Present and Future: a festschrift in honor of Karl Jöreskog. Lincolnwood: Scientific Software International; 2001. pp. 139–68.
Hu L, Bentler PM. Fit indices in Covariance structure modeling: sensitivity to Underparameterized Model Misspecification. Psychol Methods. 1998;3:424–53. https://doi.org/10.1037/1082-989X.3.4.424 .
Schermelleh-Engel K, Moosbrugger H, Müller H. Evaluating the fit of structural equation models: test of significance and descriptive goodness-of-fit measures. MPR. 2003;8:23–74.
Hu L, Bentler PM. Cutoff criteria for fit indexes in Covariance structure analysis: conventional criteria Versus New Alternatives. Struct Equ Model. 1999;6:1–55. https://doi.org/10.1080/10705519909540118 .
Geiser C, Eid M, Nussbeck FW, Courvoisier DS, Cole DA. Analyzing true change in Longitudinal Multitrait-Multimethod studies: application of a Multimethod Change Model to Depression and anxiety in children. Dev Psychol. 2010;46:29–45. https://doi.org/10.1037/a0017888 .
Putnick DL, Bornstein MH. Measurement invariance conventions and reporting: the state of the art and future directions for psychological research. Dev Rev. 2016;41:71–90. https://doi.org/10.1016/j.dr.2016.06.004 .
Satorra A, Bentler PM. A scaled difference chi-square test statistic for moment structure analysis. Psychometrika. 2001;66:507–14. https://doi.org/10.1007/BF02296192 .
Geiser C. Datenanalyse Mit Mplus: Eine Anwendungsorientierte Einführung. Wiesbaden: VS Verlag für Sozialwissenschaften; 2010.
Book Google Scholar
Chen F, Curran PJ, Bollen KA, Kirby J, Paxton P. An empirical evaluation of the use of fixed cutoff points in RMSEA Test Statistic in Structural equation models. Sociol Methods Res. 2008;36:462–94. https://doi.org/10.1177/0049124108314720 .
Dormann C, Zapf D, Perels F. Quer- und Längsschnittstudien in der Arbeitspsychologie [Cross-sectional and longitudinal studies in occupational psychology.]. In: Kleinbeck U, Schmidt K-H,Enzyklopädie der Psychologie [Encyclopedia of psychology]:, Themenbereich D, Serie III, Band 1, Arbeitspsychologie [Subject Area, Series D. III, Volume 1, Industrial Psychology]. Göttingen: Hogrefe Verlag; 2010. pp. 923–1001.
Nunnally JC, Bernstein IH. Psychometric theory. 3rd ed. New York: McGraw-Hill; 1994.
Gignac GE, Szodorai ET. Effect size guidelines for individual differences researchers. Pers Indiv Differ. 2016;102:74–8. https://doi.org/10.1016/j.paid.2016.06.069 .
Funder DC, Ozer DJ. Evaluating effect size in Psychological Research: sense and nonsense. Adv Methods Practices Psychol Sci. 2019;2:156–68. https://doi.org/10.1177/2515245919847202 .
Fincham FD, May RW. My stress led me to procrastinate: temporal relations between perceived stress and academic procrastination. Coll Stud J. 2021;55:413–21.
Daniali H, Martinussen M, Flaten MA. A Global Meta-Analysis of Depression, anxiety, and stress before and during COVID-19. Health Psychol. 2023;42:124–38. https://doi.org/10.1037/hea0001259 .
Tice DM, Baumeister RF. Longitudinal study of procrastination, performance, stress, and Health: the costs and benefits of Dawdling. Psychol Sci. 1997;8:454–8. https://doi.org/10.1111/j.1467-9280.1997.tb00460.x .
Schraw G, Wadkins T, Olafson L. Doing the things we do: a grounded theory of academic procrastination. J Educ Psychol. 2007;99:12–25. https://doi.org/10.1037/0022-0663.99.1.12 .
Slavich GM. Life Stress and Health: a review of conceptual issues and recent findings. Teach Psychol. 2016;43:346–55. https://doi.org/10.1177/0098628316662768 .
Phillips AC, Carroll D, Der G. Negative life events and symptoms of depression and anxiety: stress causation and/or stress generation. Anxiety Stress Coping. 2015;28:357–71. https://doi.org/10.1080/10615806.2015.1005078 .
Hammen C. Stress and depression. Annu Rev Clin Psychol. 2005;1:293–319. https://doi.org/10.1146/annurev.clinpsy.1.102803.143938 .
Blazer D, Hughes D, George LK. Stressful life events and the onset of a generalized anxiety syndrome. Am J Psychiatry. 1987;144:1178–83. https://doi.org/10.1176/ajp.144.9.1178 .
Southwick SM, Charney DS. The Science of Resilience: implications for the Prevention and Treatment of Depression. Science. 2012;338:79–82. https://doi.org/10.1126/science.1222942 .
Ingram RE, Luxton DD. Vulnerability-stress models. In: Hankin BL, Abela JR, editors. Development of psychopathology: a vulnerability-stress perspective. Thousand Oaks: Sage; 2005. pp. 32–46.
Chapter Google Scholar
Maercker A. Modelle Der Klinischen Psychologie. In: Petermann F, Maercker A, Lutz W, Stangier U, editors. Klinische psychologie – Grundlagen. Göttingen: Hogrefe; 2018. pp. 13–31.
Krause K, Freund AM. Delay or procrastination – a comparison of self-report and behavioral measures of procrastination and their impact on affective well-being. Pers Individ Dif. 2014;63:75–80. https://doi.org/10.1016/j.paid.2014.01.050 .
Grunschel C, Patrzek J, Fries S. Exploring reasons and consequences of academic procrastination: an interview study. Eur J Psychol Educ. 2013;28:841–61. https://doi.org/10.1007/s10212-012-0143-4 .
Dwyer JH. Statistical models for the social and behavioral sciences. New York: Oxford University Press; 1983.
Cohen JA, Power Primer. Psychol Bull. 1992;112:155–9. https://doi.org/10.1037//0033-2909.112.1.155 .
Ferguson CJ. An effect size primer: a Guide for clinicians and Researchers. Prof Psychol Res Pr. 2009;40:532–8. https://doi.org/10.1037/a0015808 .
Hinz A, Berth H, Kittel J, Singer S. Die zeitliche Stabilität (Test-Retest-Reliabilität) Von Angst Und Depressivität Bei Patienten Und in Der Allgemeinbevölkerung. Z Med Psychol. 2011;20:24–31. https://doi.org/10.3233/ZMP-2010-2012 .
Adachi P, Willoughby T. Interpreting effect sizes when controlling for stability effects in longitudinal autoregressive models: implications for psychological science. Eur J Dev Psychol. 2015;12:116–28. https://doi.org/10.1080/17405629.2014.963549 .
Dormann C, Griffin M. Optimal time lags in Panel studies. Psychol Methods. 2015;20:489–505. https://doi.org/10.1037/met0000041 .
Weckesser LJ, Dietz F, Schmidt K, Grass J, Kirschbaum C, Miller R. The psychometric properties and temporal dynamics of subjective stress, retrospectively assessed by different informants and questionnaires, and hair cortisol concentrations. Sci Rep. 2019. https://doi.org/10.1038/s41598-018-37526-2 .
Schulz P, Schlotz W, Becker P. TICS: Trierer Inventar Zum chronischen stress. Göttingen: Hogrefe; 2004.
Heidemann C, Scheidt-Nave C, Beyer A-K, Baumert J, Thamm R, Maier B, et al. Health situation of adults in Germany - results for selected indicators from GEDA 2019/2020-EHIS. J Health Monit. 2021;6:3–25. https://doi.org/10.25646/8459 .
Download references
Acknowledgements
Not applicable.
Open Access Funding provided by Freie Universität Berlin.
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and affiliations.
Division of Prevention and Psychosocial Health Research, Department of Education and Psychology, Freie Universität Berlin, Habelschwerdter Allee 45, 14195, Berlin, Germany
Anna Jochmann, Burkhard Gusy, Tino Lesener & Christine Wolter
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization: A.J., B.G., T.L.; methodology: B.G., A.J.; validation: B.G.; formal analysis: A.J., B.G.; investigation: C.W., T.L., B.G.; data curation: C.W., T.L., B.G.; writing–original draft preparation: A.J., B.G.; writing–review and editing: A.J., T.L., B.G., C.W.; visualization: A.J., B.G.; supervision: B.G., T.L.; project administration: C.W., T.L., B.G.; All authors contributed to the article and approved the submitted version.
Corresponding authors
Correspondence to Anna Jochmann or Burkhard Gusy .
Ethics declarations
Ethics approval and consent to participate.
This study was performed in line with the principles of the Declaration of Helsinki. Ethical approval was obtained from the Ethics Committee of the Department of Education and Psychology, Freie Universität Berlin. All methods were carried out in accordance with relevant guidelines and regulations. The participants provided their written informed consent to participate in this study.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Selective dropout analysis and correlation matrix of the manifest variables
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Jochmann, A., Gusy, B., Lesener, T. et al. Procrastination, depression and anxiety symptoms in university students: a three-wave longitudinal study on the mediating role of perceived stress. BMC Psychol 12 , 276 (2024). https://doi.org/10.1186/s40359-024-01761-2
Download citation
Received : 25 May 2023
Accepted : 02 May 2024
Published : 16 May 2024
DOI : https://doi.org/10.1186/s40359-024-01761-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Student health
- Longitudinal study
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Anxiety vs. Depression: Having One or Both Disorders
- Why They Co-Occur
Generalized anxiety disorder (GAD) and major depressive disorder (MDD) are mental health conditions that can affect your emotions, state of mind, and behavior. Many people refer to these conditions as "anxiety" and "depression."
Depression can make you feel sad, empty, hopeless, and sluggish. Anxiety, on the other hand, can make you feel excessive worry, fear, and restlessness. It's possible to have both anxiety and depression; in fact, they frequently occur together.
In this article, learn more about the characteristics of anxiety and depression and how to cope with one or both conditions.
Galina Zhigalova / Getty Images
Anxiety Attacks vs. Depression Episodes
Some anxiety and depression symptoms overlap, whereas others are different. Below is a comparison of the official symptoms of anxiety versus depression, according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), which is the handbook that providers in the United States use to diagnose mental health conditions.
Excessive anxiety or worry
Being easily fatigued
Sleep disturbance
Difficulty concentrating or mind going blank
Restlessness or feeling on edge
Irritability
Muscle tension
Difficulty controlling worry
Problems in daily life stemming from anxiety
Depressed mood
Fatigue or low energy
Difficulty concentrating or thinking
Decreased efficiency
Loss of interest in previously enjoyed activities
Changes in appetite
Weight loss or gain
Psychomotor changes (slower- or faster-than-usual movement)
Feelings of worthlessness and guilt
Recurrent thoughts of dying
Similarities
As noted above, some shared symptoms of anxiety and depression include:
- Changes in sleep patterns, such as sleeping too much or too little
- Challenges with concentration and thinking. In anxiety, this may also manifest as your mind "going blank," and in depression, you may struggle with decision-making
- Having low energy and being easily fatigued
Both anxiety and depression can affect your moods, thoughts, how you see yourself, and how you interact with others and the world around you.
There are similar changes in the brain that lead to anxiety and depression. Research shows that among people with anxiety and depression, there are shared brain changes in the areas that manage cognitive control, executive functioning, and emotional regulation.
Differences
There are also differences between anxiety and depression. At its core, depression brings feelings of despair and sadness, whereas anxiety is associated with worry, fear, and dread that is disproportionate to the situation.
While both conditions affect you physically, they do so in different ways. People with anxiety are more likely to be restless, tense, sweaty, have heart palpitations, or fidget. Those with depression are more likely to have slowed-down movement and speech, appetite changes, and weight loss or gain.
Why Anxiety and Depression Occur Together
You can have anxiety and depression at the same time. Among people with depression, 45.7% also have an anxiety disorder at some point in their life. For people with anxiety disorders, between 20% and 70% will also have depression in their lifetime, with rates varying based on different types of anxiety disorder.
The reasons for this co-occurrence are complex, but there are multiple theories about shared causes and risk factors, such as:
- Chronic disease and pain : People with chronic illness or chronic pain are also more prone to both anxiety and depression due to the effects of these conditions on their quality of life.
- Genetics : There is a high level of shared genetic risk factors between anxiety and depression, but there is a lot that scientists have yet to understand about this connection. The ongoing Genetic Links to Anxiety and Depression (GLAD) study is the most extensive genetic study on this subject, with over 40,000 participants.
- Nongenetic risk factors : There are other characteristics that anxiety and depression have in common, which could explain the overlap between the two conditions. These include childhood trauma or neglect, parenting style, and stressful events.
- Personality traits : Studies have identified the personality trait of neuroticism as linked to a higher risk of both anxiety and depression.
Can Anxiety Cause Depression?
Older longitudinal research shows that having an anxiety disorder significantly increases your of developing secondary depression.
The symptoms of anxiety can be very limiting. You may constantly feel worried and afraid, leading you to avoid socializing or feeling restricted in where you can go and what you can do. Over time, this can lead to feelings of depression.
Anxiety affects the brain in ways that can contribute to depression. In people with anxiety disorders, the amygdala (the brain structure involved in the fight-or-flight response) processes become exaggerated, leading to a greater perception of danger and difficulty regulating other parts of the brain, like the prefrontal cortex and hippocampus .
These changes can lead to depression. Some studies have found an enlarged amygdala in people who have both anxiety and depression.
Do You Need a Diagnosis Before Treatment?
You don't need an official anxiety or depression diagnosis to make lifestyle changes to help you feel better. However, effective treatment for these conditions often includes medications and therapy, which are typically only accessible with a diagnosis.
That's why it's in your best interest to seek professional help for a proper diagnosis if your symptoms impact your daily life.
For Anxiety
There are several different anxiety disorders, such as generalized anxiety disorder , obsessive-compulsive disorder (OCD), and social anxiety . Treatment can vary among conditions, which is one reason getting an official diagnosis is essential.
If symptoms like worry, fear, difficulty concentrating, feeling on edge, and more affect your daily life, then it's time to seek professional help.
For Depression
Similar to anxiety, there are different types of depressive disorder. These include major depressive disorder , seasonal affective disorder (SAD), perinatal depression , and bipolar disorder .
Treatment is different for each condition. For example, someone with SAD would greatly benefit from a light box, whereas overexposure to this type of therapy may trigger someone with bipolar disorder. That is why a diagnosis is needed to get the most effective treatment.
How to Cope Through Anxiety vs. Depression
Whether you have anxiety, depression, or both, it can be challenging to cope in day-to-day life. You may feel that your symptoms are controlling you and making it difficult to do the things you need to do, such as going to work or school, socializing with friends, or even engaging in hobbies that you used to enjoy.
Healthcare providers often treat anxiety and depression with a combination of medication, therapy, and lifestyle changes. Because everyone is unique, treatment should reflect each individual's symptoms, values, and preferences.
An Integrated Approach to Treatment
If you have both anxiety and depression, your healthcare providers will create an integrated approach to treatment since many of the treatments for these two conditions overlap.
For example, antidepressant medication is also effective at treating anxiety. Cognitive behavioral therapy (CBT) is a highly effective form of talk therapy shown to improve symptoms of both anxiety and depression. Various lifestyle changes benefit people with both depression and anxiety. Examples include exercise, mindfulness, sticking to a routine, and sleep hygiene.
Reminders to Offset Anxiety vs. Depression
Do not blame yourself if you have anxiety or depression. There are ways to help manage your mental health, particularly if you know that you are prone to anxiety or depression.
These strategies include:
- Eat a healthy, balanced diet.
- Get 2.5 to 5 hours of exercise per week or 30 minutes daily.
- Keep up with regular healthcare appointments.
- Learn your triggers.
- Limit your intake of alcohol, caffeine, smoking, or drugs.
- Practice mindfulness.
- Practice sleep hygiene, including sticking to a sleep schedule.
- Take any medication as prescribed.
While these strategies won't completely cure or prevent anxiety and depression, they can help you limit symptoms, identify anxious or depressive episodes, and seek the care you need.
Anxiety and depression are two separate disorders that often occur together due to shared risk factors, heritability, and overlapping brain changes associated with each condition. In simple terms, people who are depressed experience sadness, hopelessness, and despair, whereas people who are anxious experience excessive worry and fear. Treatment is available for both conditions.
Kalin NH. The critical relationship between anxiety and depression . AJP . 2020;177(5):365-367. doi:10.1176/appi.ajp.2020.20030305
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition . American Psychiatric Association ; 2013. doi:10.1176/appi.books.9780890425596
Hwang Y, Oh J. Relationship between depression, anxiety, stress, and health-related quality of life in adults with and without chronic diseases: A cross-sectional study . Medicine (Baltimore) . 2024;103(2):e36967. doi: 10.1097%2FMD.0000000000036967
Davies MR, Kalsi G, Armour C, et al. The Genetic Links to Anxiety and Depression (Glad) Study: Online recruitment into the largest recontactable study of depression and anxiety . Behaviour Research and Therapy . 2019;123:103503. doi: 10.1016%2Fj.brat.2019.103503
Zinbarg RE, Mineka S, Bobova L, et al. Testing a hierarchical model of neuroticism and its cognitive facets: latent structure and prospective prediction of first onsets of anxiety and unipolar mood disorders during 3 years in late adolescence . Clinical Psychological Science . 2016;4(5):805-824. doi:10.1177/2167702615618162
Yang T, Guo Z, Zhu X, Liu X, Guo Y. The interplay of personality traits, anxiety, and depression in Chinese college students: a network analysis. Front Public Health . 2023;11:1204285. doi: https://doi.org/10.3389%2Ffpubh.2023.1204285
Wittchen HU, Kessler RC, Pfister H, Lieb M. Why do people with anxiety disorders become depressed? A prospective-longitudinal community study . Acta Psychiatr Scand Suppl . 2000;(406):14-23. PMID: 11131466
Mah L, Szabuniewicz C, Fiocco AJ. Can anxiety damage the brain? Curr Opin Psychiatry . 2016;29(1):56-63. doi:10.1097/yco.0000000000000223
Espinoza Oyarce DA, Shaw ME, Alateeq K, Cherbuin N. Volumetric brain differences in clinical depression in association with anxiety: a systematic review with meta-analysis. Journal of Psychiatry & Neuroscience . 2020;45(6):406-429. doi: 10.1503/jpn.190156
Sit DK, Terman M, Wisner KL. Light therapy and risk of hypomania, mania, or mixed state emergence: response to benedetti et al. AJP . 2018;175(9):906-906. doi: 10.1176/appi.ajp.2018.18020231r
National Institute of Mental Health. Mental health medications . December 2023.
Coffey SF, Banducci AN, Vinci C. Common questions about cognitive behavior therapy for psychiatric disorders . Am Fam Physician . 2015;92(9):807-812. PMID: 26554473.
Anxiety and Depression Association of America. Tips and strategies to manage anxiety and stress. December 4, 2023.
By Sarah Bence, OTR/L Bence is an occupational therapist with a range of work experience in mental healthcare settings. She is living with celiac disease and endometriosis.
Your Best College Essay
Maybe you love to write, or maybe you don’t. Either way, there’s a chance that the thought of writing your college essay is making you sweat. No need for nerves! We’re here to give you the important details on how to make the process as anxiety-free as possible.

What's the College Essay?
When we say “The College Essay” (capitalization for emphasis – say it out loud with the capitals and you’ll know what we mean) we’re talking about the 550-650 word essay required by most colleges and universities. Prompts for this essay can be found on the college’s website, the Common Application, or the Coalition Application. We’re not talking about the many smaller supplemental essays you might need to write in order to apply to college. Not all institutions require the essay, but most colleges and universities that are at least semi-selective do.
How do I get started?
Look for the prompts on whatever application you’re using to apply to schools (almost all of the time – with a few notable exceptions – this is the Common Application). If one of them calls out to you, awesome! You can jump right in and start to brainstorm. If none of them are giving you the right vibes, don’t worry. They’re so broad that almost anything you write can fit into one of the prompts after you’re done. Working backwards like this is totally fine and can be really useful!
What if I have writer's block?
You aren’t alone. Staring at a blank Google Doc and thinking about how this is the one chance to tell an admissions officer your story can make you freeze. Thinking about some of these questions might help you find the right topic:
- What is something about you that people have pointed out as distinctive?
- If you had to pick three words to describe yourself, what would they be? What are things you’ve done that demonstrate these qualities?
- What’s something about you that has changed over your years in high school? How or why did it change?
- What’s something you like most about yourself?
- What’s something you love so much that you lose track of the rest of the world while you do it?
If you’re still stuck on a topic, ask your family members, friends, or other trusted adults: what’s something they always think about when they think about you? What’s something they think you should be proud of? They might help you find something about yourself that you wouldn’t have surfaced on your own.
How do I grab my reader's attention?
It’s no secret that admissions officers are reading dozens – and sometimes hundreds – of essays every day. That can feel like a lot of pressure to stand out. But if you try to write the most unique essay in the world, it might end up seeming forced if it’s not genuinely you. So, what’s there to do? Our advice: start your essay with a story. Tell the reader about something you’ve done, complete with sensory details, and maybe even dialogue. Then, in the second paragraph, back up and tell us why this story is important and what it tells them about you and the theme of the essay.
THE WORD LIMIT IS SO LIMITING. HOW DO I TELL A COLLEGE MY WHOLE LIFE STORY IN 650 WORDS?
Don’t! Don’t try to tell an admissions officer about everything you’ve loved and done since you were a child. Instead, pick one or two things about yourself that you’re hoping to get across and stick to those. They’ll see the rest on the activities section of your application.
I'M STUCK ON THE CONCLUSION. HELP?
If you can’t think of another way to end the essay, talk about how the qualities you’ve discussed in your essays have prepared you for college. Try to wrap up with a sentence that refers back to the story you told in your first paragraph, if you took that route.
SHOULD I PROOFREAD MY ESSAY?
YES, proofread the essay, and have a trusted adult proofread it as well. Know that any suggestions they give you are coming from a good place, but make sure they aren’t writing your essay for you or putting it into their own voice. Admissions officers want to hear the voice of you, the applicant. Before you submit your essay anywhere, our number one advice is to read it out loud to yourself. When you read out loud you’ll catch small errors you may not have noticed before, and hear sentences that aren’t quite right.
ANY OTHER ADVICE?
Be yourself. If you’re not a naturally serious person, don’t force formality. If you’re the comedian in your friend group, go ahead and be funny. But ultimately, write as your authentic (and grammatically correct) self and trust the process.
And remember, thousands of other students your age are faced with this same essay writing task, right now. You can do it!
- Share full article
Advertisement
Supported by
Guest Essay
The Happiness Gap Between Left and Right Isn’t Closing

By Thomas B. Edsall
Mr. Edsall contributes a weekly column from Washington, D.C., on politics, demographics and inequality.
Why is it that a substantial body of social science research finds that conservatives are happier than liberals?
A partial answer: Those on the right are less likely to be angered or upset by social and economic inequities, believing that the system rewards those who work hard, that hierarchies are part of the natural order of things and that market outcomes are fundamentally fair.
Those on the left stand in opposition to each of these assessments of the social order, prompting frustration and discontent with the world around them.
The happiness gap has been with us for at least 50 years, and most research seeking to explain it has focused on conservatives. More recently, however, psychologists and other social scientists have begun to dig deeper into the underpinnings of liberal discontent — not only unhappiness but also depression and other measures of dissatisfaction.
One of the findings emerging from this research is that the decline in happiness and in a sense of agency is concentrated among those on the left who stress matters of identity, social justice and the oppression of marginalized groups.
There is, in addition, a parallel phenomenon taking place on the right as Donald Trump and his MAGA loyalists angrily complain of oppression by liberals who engage in a relentless vendetta to keep Trump out of the White House.
There is a difference in the way the left and right react to frustration and grievance. Instead of despair, the contemporary right has responded with mounting anger, rejecting democratic institutions and norms.
In a 2021 Vox article, “ Trump and the Republican Revolt Against Democracy ,” Zack Beauchamp described in detail the emergence of destructive and aggressive discontent among conservatives.
Citing a wide range of polling data and academic studies, Beauchamp found:
More than twice as many Republicans (39 percent) as Democrats (17 percent) believed that “if elected leaders won’t protect America, the people must act — even if that means violence.”
Fifty-seven percent of Republicans considered Democrats to be “enemies,” compared with 41 percent of Democrats who viewed Republicans as “enemies.”
Among Republicans, support for “the use of force to defend our way of life,” as well as for the belief that “strong leaders bend rules” and that “sometimes you have to take the law in your own hands,” grows stronger in direct correlation with racial and ethnic hostility.
Trump has repeatedly warned of the potential for political violence. In January he predicted bedlam if the criminal charges filed in federal and state courts against him damaged his presidential campaign:
I think they feel this is the way they’re going to try and win, and that’s not the way it goes. It’ll be bedlam in the country. It’s a very bad thing. It’s a very bad precedent. As we said, it’s the opening of a Pandora’s box.
Before he was indicted in New York, Trump claimed there would be “potential death and destruction” if he was charged.
At an Ohio campaign rally in March, Trump declared, “If I don’t get elected, it’s going to be a blood bath for the whole country.”
In other words, Trump and his allies respond to adversity and what they see as attacks from the left with threats and anger, while a segment of the left often but not always responds to adversity and social inequity with dejection and sorrow.
There are significant consequences for this internalization.
Jamin Halberstadt , a professor of psychology at the University of Otago in New Zealand and a co-author of “ Outgroup Threat and the Emergence of Cohesive Groups : A Cross-Cultural Examination,” argued in his emailed reply to my inquiry that because “a focus on injustice and victimhood is, by definition, disempowering (isn’t that why we talk of ‘survivors’ rather than ‘victims’?), loss of control is not good for self-esteem or happiness.”
But, he pointed out:
this focus, while no doubt a part of the most visible and influential side of progressive ideology, is still just a part. Liberalism is a big construct, and I’m reluctant to reduce it to a focus on social justice issues. Some liberals have this view, but I suspect their influence is outsized because (a) they have the social media megaphone and (b) we are in a climate in which freedom of expression and, in particular, challenges to the worldview you characterize have been curtailed.
Expanding on this line of argument, Halberstadt wrote:
I’m sure some self-described liberals have views that are counterproductive to their own happiness. One sub-ideology associated with liberalism is, as you describe, a sense of victimhood and grievance. But there is more than one way to respond to structural barriers. Within that group of the aggrieved, some probably see systemic problems that cannot be overcome, and that’s naturally demoralizing and depressing. But others see systemic problems as a challenge to overcome.
Taking Halberstadt’s assessment of the effects of grievance and victimhood a step farther, Timothy A. Judge , the chairman of the department of management and human resources at Notre Dame, wrote in a 2009 paper, “ Core Self-Evaluations and Work Success ”:
Core self-evaluations (C.S.E.) is a broad, integrative trait indicated by self-esteem, locus of control, generalized self-efficacy and (low) neuroticism (high emotional stability). Individuals with high levels of C.S.E. perform better on their jobs, are more successful in their careers, are more satisfied with their jobs and lives, report lower levels of stress and conflict, cope more effectively with setbacks and better capitalize on advantages and opportunities.
I asked Judge and other scholars a question: Have liberal pessimists fostered an outlook that spawns unhappiness as its adherents believe they face seemingly insurmountable structural barriers?
Judge replied by email:
I do share the perspective that a focus on status, hierarchies and institutions that reinforce privilege contributes to an external locus of control. And the reason is fairly straightforward. We can only change these things through collective and, often, policy initiatives — which tend to be complex, slow, often conflictual and outside our individual control. On the other hand, if I view “life’s chances” (Virginia Woolf’s term) to be mostly dependent on my own agency, this reflects an internal focus, which will often depend on enacting initiatives largely within my control.
Judge elaborated on his argument:
If our predominant focus in how we view the world is social inequities, status hierarchies, societal unfairness conferred by privilege, then everyone would agree that these things are not easy to fix, which means, in a sense, we must accept some unhappy premises: Life isn’t fair; outcomes are outside my control, often at the hands of bad, powerful actors; social change depends on collective action that may be conflictual; an individual may have limited power to control their own destiny, etc. These are not happy thoughts because they cause me to view the world as inherently unfair, oppressive, conflictual, etc. It may or may not be right, but I would argue that these are in fact viewpoints of how we view the world, and our place in it, that would undermine our happiness.
Last year, George Yancey , a professor of sociology at Baylor University, published “ Identity Politics, Political Ideology, and Well-Being : Is Identity Politics Good for Our Well-Being?”
Yancey argued that recent events “suggest that identity politics may correlate to a decrease in well-being, particularly among young progressives, and offer an explanation tied to internal elements within political progressiveness.”
By focusing on “political progressives, rather than political conservatives,” Yancey wrote, “a nuanced approach to understanding the relationship between political ideology and well-being begins to emerge.”
Identity politics, he continued, focuses “on external institutional forces that one cannot immediately alleviate.” It results in what scholars call the externalization of one’s locus of control, or viewing the inequities of society as a result of powerful if not insurmountable outside forces, including structural racism, patriarchy and capitalism, as opposed to believing that individuals can overcome such obstacles through hard work and collective effort.
As a result, Yancey wrote, “identity politics may be an important mechanism by which progressive political ideology can lead to lower levels of well-being.”
Conversely, Yancey pointed out, “a class-based progressive cognitive emphasis may focus less on the group identity, generating less of a need to rely on emotional narratives and dichotomous thinking and may be less likely to be detrimental to the well-being of a political progressive.”
Yancey tested this theory using data collected in the 2021 Baylor Religion Survey of 1,232 respondents.
“Certain types of political progressive ideology can have contrasting effects on well-being,” Yancey wrote. “It is plausible that identity politics may explain the recent increase well-being gap between conservatives and progressives.”
Oskari Lahtinen , a senior researcher in psychology at the University of Turku in Finland, published a study in March, “ Construction and Validation of a Scale for Assessing Critical Social Justice Attitudes ,” that reinforces Yancey’s argument.
Lahtinen conducted two surveys of a total of 5,878 men and women to determine the share of Finnish citizens who held “critical social justice attitudes” and how those who held such views differed from those who did not.
Critical social justice proponents, on Lahtinen’s scale,
point out varieties of oppression that cause privileged people (e.g., male, white, heterosexual, cisgender) to benefit over marginalized people (e.g., woman, Black, gay, transgender). In critical race theory, some of the core tenets include that (1) white supremacy and racism are omnipresent and colorblind policies are not enough to tackle them, (2) people of color have their own unique standpoint and (3) races are social constructs.
What did Lahtinen find?
The critical social justice propositions encountered
strong rejection from men. Women expressed more than twice as much support for the propositions. In both studies, critical social justice was correlated modestly with depression, anxiety, and (lack of) happiness, but not more so than being on the political left was.
In an email responding to my inquiries about his paper, Lahtinen wrote that one of the key findings in his research was that “there were large differences between genders in critical social justice advocacy: Three out of five women but only one out of seven men expressed support for the critical social justice claims.”
In addition, he pointed out, “there was one variable in the study that closely corresponded to external locus of control: ‘Other people or structures are more responsible for my well-being than I myself am.’”
The correlation between agreement with this statement and unhappiness was among the strongest in the survey:
People on the left endorsed this item (around 2 on a scale of 0 to 4) far more than people on the right (around 0.5). Endorsing the belief was determined by political party preference much more than by gender, for instance.
Such measures as locus of control, self-esteem, a belief in personal agency and optimism all play major roles in daily life.
In a December 2022 paper, “ The Politics of Depression : Diverging Trends in Internalizing Symptoms Among U.S. Adolescents by Political Beliefs,” Catherine Gimbrone , Lisa M. Bates , Seth Prins and Katherine M. Keyes , all at Columbia’s Mailman School of Public Health, noted that “trends in adolescent internalizing symptoms diverged by political beliefs, sex and parental education over time, with female liberal adolescents experiencing the largest increases in depressive symptoms, especially in the context of demographic risk factors, including parental education.”
“These findings,” they added, “indicate a growing mental health disparity between adolescents who identify with certain political beliefs. It is therefore possible that the ideological lenses through which adolescents view the political climate differentially affect their mental well-being.”
Gimbrone and her co-authors based their work on studies of 85,000 teenagers from 2005 to 2018. They found that
while internalizing symptom scores worsened over time for all adolescents, they deteriorated most quickly for female liberal adolescents. Beginning in approximately 2010 and continuing through 2018, female liberal adolescents reported the largest changes in depressive affect, self-esteem, self-derogation and loneliness.
In conclusion, the authors wrote, “socially underprivileged liberals reported the worst internalizing symptom scores over time, likely indicating that the experiences and beliefs that inform a liberal political identity are ultimately less protective against poor mental health than those that inform a conservative political identity.”
From another vantage point, Nick Haslam , a professor of psychology at the University of Melbourne, argued in his 2020 paper “ Harm Inflation: Making Sense of Concept Creep ” that recent years have seen “a rising sensitivity to harm within at least some Western cultures, such that previously innocuous or unremarked phenomena were increasingly identified as harmful and that this rising sensitivity reflected a politically liberal moral agenda.”
As examples, Haslam wrote that the definition of “trauma” has been
progressively broadened to include adverse life events of decreasing severity and those experienced vicariously rather than directly. “Mental disorder” came to include a wider range of conditions, so that new forms of psychopathology were added in each revision of diagnostic manuals and the threshold for diagnosing some existing forms was lowered. “Abuse” extended from physical acts to verbal and emotional slights and incorporated forms of passive neglect in addition to active aggression.
Haslam described this process as concept creep and argued that “some examples of concept creep are surely the work of deliberate actors who might be called expansion entrepreneurs.”
Concept expansion, Haslam wrote, “can be used as a tactic to amplify the perceived seriousness of a movement’s chosen social problem.” In addition, “such expansion can be effective means of enhancing the perceived seriousness of a social problem or threat by increasing the perceived prevalence of both ‘victims’ and ‘perpetrators.’”
Haslam cited studies showing that strong “correlates of holding expansive concepts of harm were compassion-related trait values, left-liberal political attitudes and forms of morality associated with both.” Holding expansive concepts of harm was also “associated with affective and cognitive empathy orientation and most strongly of all with endorsement of harm- and fairness-based morality.” Many of these characteristics are associated with the political left.
“The expansion of harm-related concepts has implications for acceptable self-expression and free speech,” Haslam wrote. “Creeping concepts enlarge the range of expressions judged to be unacceptably harmful, thereby increasing calls for speech restrictions. Expansion of the harm-related concepts of hate and hate speech exemplifies this possibility.”
While much of the commentary on the progressive left has been critical, Haslam takes a more ambivalent position: “Sometimes concept creep is presented in an exclusively negative frame,” he wrote, but that fails to address the “positive implications. To that end, we offer three positive consequences of the phenomenon.”
The first is that expansionary definitions of harm “can be useful in drawing attention to harms previously overlooked. Consider the vertical expansion of abuse to include emotional abuse.”
Second, “concept creep can prevent harmful practices by modifying social norms.” For example, “changing definitions of bullying that include social exclusion and antagonistic acts expressed horizontally rather than only downward in organizational hierarchies may also entrench norms against the commission of destructive behavior.”
And finally:
The expansion of psychology’s negative concepts can motivate interventions aimed at preventing or reducing the harms associated with the newly categorized behaviors. For instance, the conceptual expansion of addiction to include behavioral addictions (e.g., gambling and internet addictions) has prompted a flurry of research into treatment options, which has found that a range of psychosocial treatments can be successfully used to treat gambling, internet and sexual addictions.
Judge suggested an approach to this line of inquiry that he believed might offer a way for liberalism to regain its footing:
I would like to think that there is a version of modern progressivism that accepts many of the premises of the problem and causes of inequality but does so in a way that also celebrates the power of individualism, of consensus and of common cause. I know this is perhaps naïve. But if we give in to cynicism (that consensus can’t be found), that’s self-reinforcing, isn’t it? I think about the progress on how society now views sexual orientation and the success stories. The change was too slow, painful for many, but was there any other way?
The Times is committed to publishing a diversity of letters to the editor. We’d like to hear what you think about this or any of our articles. Here are some tips . And here's our email: [email protected] .
Follow the New York Times Opinion section on Facebook , Instagram , TikTok , WhatsApp , X and Threads .
Thomas B. Edsall has been a contributor to the Times Opinion section since 2011. His column on strategic and demographic trends in American politics appears every Wednesday. He previously covered politics for The Washington Post. @ edsall
- Inside SMCM
- Tips & Tricks
- Academic Calendar
- Contact Directory
- H.C.L. Library
- Student Portal
Four Psychology Students Present Research at External Conferences in April 2024
Four psychology majors presented research to outside audiences in April 2024. Alongside former SMCM Visiting Assistant Professor of Psychology Amie Severino ‘11 (now at Mount Saint Mary’s University), Briana Corbin ’24 presented at the Anxiety and Depression Association of America conference in Boston, MA. Gabrielle Blew ’24, Angelie Roche ’24 and Katya Scott ’24 presented their individual St. Mary’s Projects (all conducted under the mentorship of Professor of Psychology Libby Nutt Williams) at the L. Starling Reid Undergraduate Psychology Conference held at the University of Virginia in Charlottesville, VA on April 26.
Corbin’s poster, “Risk Factors Associated with the Etiology of Adolescent Mood Disorders,” was based on work conducted as part of her 2023 Summer Undergraduate Research Fellowship (SURF) project with Severino. Abstract: Risk factors in a young person’s environment can lead to the expression of mood disorders such as anxiety and depression in adolescence. These mental health disorders often lead to detrimental psychosocial and academic impacts during adolescence and may persist throughout adulthood. It is important to identify the risk factors of adolescent mood disorders to allow for the implementation of early interventions. We implemented a rigorous methodological strategy to synthesize the existing evidence of environmental risk factors for anxiety and depression of adolescents in the United States (age 13-19) from quantitative, empirical sources that were published in the last 10 years (2013-2023) in peer-reviewed journals. After reviewing 29 articles from an initial search query of 16,363 articles, we identified common themes of risk factors associated with the development of anxiety and depression in adolescence. These themes were trauma, factors relating to the neighborhood and community the youth resided in, negative life events, victimization, peer rejection, factors related to the income level of the youths' environment, discrimination, family factors, and substance use. Only one of the 29 studies examined puberty as an indication of adolescence. Additionally, a few studies indicated the interaction of mood disorders with biological implications, such as anxiety being associated with sleep disturbances. Understanding how to effectively address these identified risk factors is essential to clinical interventions for adolescent mood disorders and the potential life-long biological consequences.
Blew presented a poster entitled “To Gift or Not to Gift: Examining the Impact of Telehealth on Client Gift Giving.” Abstract: Gift-giving is an ethical dilemma in psychotherapy, often discussed by many psychotherapists. There is no clear answer on how therapists should respond when they are presented with a gift by a client, which is likely due to the controversy of gift-giving within psychotherapy more broadly. There is a lack of understanding of how other morally gray areas of psychology, such as the introduction of telehealth, have impacted the overall issue of client gift-giving. Zoom interviews were conducted to better understand therapists’ views and experiences with client gift-giving, and how their experiences differed between in-person and telehealth settings. Eight therapists who had been practicing for a minimum of five years, have provided telehealth services and who have been offered at least one gift by a client were interviewed. These interviews were analyzed using Consensual Qualitative Research methods (Hill, Thompson, & Williams, 1997; Hill et al., 2005). Major findings include that only four of the eight therapists had received gifts while seeing clients via telehealth, with these gifts usually being delivered through electronic means. Additionally, most of these therapists had only one experience where a telehealth client had attempted to give them a gift. Typically, the therapists felt like gift-giving is less prevalent via telehealth, which may be related to how it fosters a less personal relationship. Overall, these results suggest that telehealth may have minimized the ethical dilemma of gift-giving within the realm of psychotherapy.
Roche presented a poster entitled “Summer Camp Counselor Experiences: The Influence of Training, Self-Efficacy, and Organizational Cohesion.” Abstract: Many overnight camps use Counselor-in-Training (CIT) programs to prepare adolescent campers for the counselor role. Although research has investigated the efficacy of individual CIT programs, studies have not compared the experiences of previous CITs to the experiences of new, non-CIT counselors across camp types. We recruited 314 camp counselors (130 previous CITs and 185 non-CITs) from camps across the US and Canada for an online survey assessing their self-efficacy and organizational cohesion (Chen et al., 2001; Ruga, 2014) and other items related to their experiences as first-year counselors. The majority of the sample reported positive experiences. Although CIT completion did not correlate significantly with any variable, individual and camp factors such as job fit, satisfaction with training and comfort talking to administrators correlated with self-efficacy and organizational cohesion. More between-camps research is needed to examine training, overall climate and the true efficacy of CIT programs.
Scott presented a talk entitled “Art Therapy with Ukrainian Refugees: A Pilot Program”. Abstract: There is little empirical research available that explores art therapy with adult refugees. Refugees face increased risk for mental health conditions such as depression, anxiety, and post-traumatic stress disorder; post-migration, they also often face challenges such as cultural isolation and a loss of community. As the number of refugees worldwide increases at an alarming rate, well-researched, culturally sensitive systems of mental health support must be made available to anyone who requires them. Group art therapy may be a particularly helpful intervention due to a focus on social connections and a de-emphasis on verbal processing, which might help lessen the impact of language barriers and support those with difficulty expressing painful experiences in words. To ensure programs are culturally sensitive, adopting the Multicultural Orientation (MCO) framework is an ideal approach. Current research on art therapy with refugees is extremely limited, particularly with adults. However, incorporating culturally significant materials into art therapy programs may be a promising route for future work. To address this gap in research, we conducted a mixed-methods study of a five-week group art therapy program incorporating culturally significant materials with adult Ukrainian refugees. Via pre- and post-intervention surveys, we analyzed the program’s potential influence on anxiety, resilience, and connection to community. We also conducted brief interviews with participants about their experiences in the program and analyzed these using Consensual Qualitative Research (CQR). The results offer potential directions for research in this area that should be further explored in future studies.
For her SMP work, Katya Scott was presented with the Myron G. Marlay Award for Science at this year's Awards Convocation. Angelie Roche was selected as one of two winners of the 2024 Department of Psychology's SMP Award.


IMAGES
VIDEO
COMMENTS
The central hypothesis for this study is that college students have a higher rate of anxiety and depression. The study will integrate various methodologies to prove the hypothesis of nullifying it. High rates of anxiety and depression can lead to substance misuse, behavioral challenges, and suicide (Lipson et al., 2018).
By nearly every metric, student mental health is worsening. During the 2020-2021 school year, more than 60% of college students met the criteria for at least one mental health problem, according to the Healthy Minds Study, which collects data from 373 campuses nationwide (Lipson, S. K., et al., Journal of Affective Disorders, Vol. 306, 2022).In another national survey, almost three quarters ...
The Healthy Minds Study 2018-2019, which collected data from 62,171 college students across the country, reports that 57% of students with positive anxiety or depression screens have not used counseling or therapy, and 64% of them have not taken any psychotropic medications within the past 12 months (Healthy Minds, 2019).
Research consistently shows that anxiety and depression are among the most common mental health disorders experienced by college students. According to a study conducted by the American College Health Association, about 60% of college students reported experiencing overwhelming anxiety in the past year, while 40% reported feeling so depressed that it was difficult to function.
For instance, in Asia, a follow-up survey and analysis based on 1401 undergraduates in China over four consecutive years showed that approximately 20% to 40% of undergraduates suffered from depression, anxiety and stress to different degrees, and approximately 35% of them had higher depression levels than the normal population.
Anxiety disorders are normally brained reactions to stress as they alert a person of impending danger. Most people feel sad and low due to disappointments. Feelings normally overwhelm a person leading to depression, especially during sad moments such as losing a loved one or divorce. When people are depressed, they engage in reckless behaviors ...
The distress that comes with anxiety and depression can impact many aspects of a student's life. Research from 2021 revealed that untreated mental health is linked to alcohol and substance ...
February 17, 2021. 25. Kat J. McAlpine. A survey by a Boston University researcher of nearly 33,000 college students across the country reveals the prevalence of depression and anxiety in young people continues to increase, now reaching its highest levels, a sign of the mounting stress factors due to the coronavirus pandemic, political unrest ...
When it was announced in spring 2014 that a Penn State study had found that anxiety had surpassed depression as the leading mental health issue facing college students, the story made national headlines.According to the study of more than 100,000 students by Penn's Center for Collegiate Mental Health, more than half of the students visiting campus health clinics listed anxiety as a concern.
Anxiety and depression are the top reasons that college students seek counseling. Many of us think of college as a wondrous time of new experiences and great freedom to explore new ideas and find ...
Abstract. Objective: Psychiatric disorders, such as depression and anxiety, can hinder academic performance among college-age individuals.Participants: Mental health among college students is a growing public health concern, with some scholars describing collegiate mental health as a crisis (Chen et al., Psychiatr Serv. 2019;70(6):442-449).Methods: This study analyzes data from four annual ...
In recent years, however, depression and anxiety have afflicted college students at alarming rates. As noted in the latest Center for Collegiate Mental Health report, anxiety and depression are ...
All authors contributed to conceptualization, formal analysis, investigation, methodology, writing and editing of the original draft, and read and agreed to the published version of the manuscript. ... The Effect of anxiety and depression on college students' academic performance: exploring social support as a moderator. Electron Theses Diss ...
Draft that frightening paper. Do it! Experience matters. Not only will accomplishing the anxiety-provoking task literally end that anticipatory stress, but it will also tell your brain that you ...
More than 60 percent of college students said they had experienced "overwhelming anxiety" in the past year. Over 40 percent said they felt so depressed they had difficulty functioning.
Yes, of course, but they are rare. In all the time I did college admissions work, I had exactly one student successfully discuss anxiety in an essay. It was, however, introduced in the context of a family tragedy that had profoundly shaped the student's life; given that background, the discussion seemed natural and matter of fact rather than ...
Abstract. College health clinicians are often first line in detecting the presence of, and providing intervention for, depressive and anxiety disorders in young adult students. Caring for mental health conditions in the primary care setting can be complex, requiring a nuanced and comprehensive approach. The importance of diagnostic accuracy and ...
However, the shift in focus could benefit the massive numbers of students who enter college each year with depression/anxiety. According to a survey by the CDC in 2022, 44% of American adolescents report feeling persistent feelings of sadness and hopelessness; 28% said that they had thoughts of self-harm at some point in their lives.
These individuals reported lower sleep quality rates in addition to higher levels of depression and anxiety. In a survey by the National Campaign to Support Teen and Unplanned Pregnancy, almost 20 percent of teens admitted to participating in "sexting" or sending nude photos.
Self-help - You can also help yourself to get over anxiety and depression. There are many things you can do, including yoga, exercise, reading AnxietyBoss by Dr. Carlo Carandang, following a balanced diet, and getting plenty of sleep. You should also avoid too much caffeine and alcohol.
At least half (50%) of mental health issues begin by age 14 and 75% of those same issues begin by age 24. 1. This generation may seem more open to discussing mental health and breaking stigmas, but 67% of people aged 18-24 with anxiety or depression still do not seek treatment. 1. ADAA provides effective resources and education to ensure that ...
Background It is generally assumed that procrastination leads to negative consequences. However, evidence for negative consequences of procrastination is still limited and it is also unclear by which mechanisms they are mediated. Therefore, the aim of our study was to examine the harmful consequences of procrastination on students' stress and mental health. We selected the procrastination ...
At its core, depression brings feelings of despair and sadness, whereas anxiety is associated with worry, fear, and dread that is disproportionate to the situation. While both conditions affect you physically, they do so in different ways. People with anxiety are more likely to be restless, tense, sweaty, have heart palpitations, or fidget.
College students are at risk of experiencing stress, anxiety and depression, which cause psychological distress and may impact on their academic performance . Worldwide, it is estimated that 12-50% of college students present at least one diagnostic criterion for one or more mental disorders [ 14 ].
At the same time, writing poetry helps me cope with anxiety and depression. In other words, because I'm the kind of person who loves to write poetry, I also may be the kind of person who's ...
When we say "The College Essay" (capitalization for emphasis - say it out loud with the capitals and you'll know what we mean) we're talking about the 550-650 word essay required by most colleges and universities. Prompts for this essay can be found on the college's website, the Common Application, or the Coalition Application.
While there's been significant attention and worry regarding the mental health of school-aged children, perhaps we should be even more worried about the mental health of college-aged (and just beyond) adults.. A report through the Harvard Graduate School of Education and Making Caring Common project, published in late 2023 found that the rates of anxiety and depression among those 18 to 25 ...
The happiness gap has been with us for at least 50 years, and most research seeking to explain it has focused on conservatives. More recently, however, psychologists and other social scientists ...
Social anxiety disorder (SAD) is a common psychiatric disorder characterized by intense fear or anxiety in social scenarios. The onset of SAD typically occurs early in life (childhood or adolescence), and it frequently has a lifelong impact being associated with considerable functional disability and reduced quality of life (1-4).Current pharmacological treatment options for SAD are limited ...
Four psychology majors presented research to outside audiences in April 2024. Alongside former SMCM Visiting Assistant Professor of Psychology Amie Severino '11 (now at Mount Saint Mary's University), Briana Corbin '24 presented at the Anxiety and Depression Association of America conference in Boston, MA. Gabrielle Blew '24, Angelie Roche '24 and Katya Scott '24 presented their ...