Jump to content

American College of Surgeons | Online Learning
Bookmark/search this post.

You are here
Ten hot topics in general surgery.

Accreditation
- Register/Take course
Session Description
This rapid-fire/quick-shot session will cover ten currently popular issues in general surgery.
Moderator: Kenneth W. Sharp, MD, FACS, Nashville, TN
Co-Moderator: E. Christopher Ellison, MD, FACS, Powell, OH
Presentations
Bullet Removal: Pros and Cons John A. Weigelt, MD, DVM, FACS, Lead, SD
Nipple-Sparing Mastectomy: Use and Indications Raeshell S. Sweeting, MD, Nashville, TN
Troubleshooting Surgical Staple Failure and Malfunction Jon C. Gould, MD, FACS, Milwaukee, WI
Laparoscopic Common Duct Exploration Dana A. Telem, MD, MPH, FACS, Ann Arbor, MI
Extremity Lumps and Bumps Valerie P. Grignol, MD, FACS, Columbus, OH
Update on Tranverse Abdominus Release for Ventral Hernia Bruce Ramshaw, MD, FACS, Knoxville, TN
Recurrent Rectal Prolapse: What to Do? Alexander T. Hawkins, MD, MPH, Nashville, TN
The Case for Robotics in Rural Surgery Jared M. Slater, MD, FACS, Victoria, MN
Optimal Surgical Treatment or Type II Diabetes: Gastric Sleeve or Bypass? Jonathan Carter, MD, San Francisco, CA
Transoral Thyroidectomy: Ready for Prime Time Gustavo G. Fernandez Ranvier, MD, PhD, FACS, Long Island City, NY
Sponsored by the Advisory Council for General Surgery
Learning Objectives
- Apply new knowledge and ideas to improve their surgical practice
- Adapt concepts and quality measures in support of research advancements
- Enhance the quality of patient care
For questions about the course, please contact [email protected] .
- 1.50 AMA PRA Category 1 Credit™
- 1.50 Certificate of Completion
- 1.50 Self Assessment Credit
Disclosure Information
In accordance with the ACCME Accreditation Criteria, the American College of Surgeons must ensure that anyone in a position to control the content of the educational activity (planners and speakers/authors/discussants/moderators) has disclosed all relevant financial relationships with any commercial interest. For additional information, please visit the ACCME website .
The ACCME also requires that ACS manage any reported conflict and eliminate the potential for bias during the educational activity. Any conflicts noted below have been managed to our satisfaction. The disclosure information is intended to identify any commercial relationships and allow learners to form their own judgments. However, if you perceive a bias during a activity, please report it on the evaluation.
(Download the full list of disclosures ).
Faculty and Disclosures
Alexander T. Hawkins MD, MPH - Nothing to Disclose Bruce Ramshaw, MD, FACS - Atrium: Consulting Fee: Consultant; Ethicon (J & J): Honoraria: Consultant; ConMed: Honoraria: Consultant; Medtronic: Honoraria: Speaker; Pacira Pharmaceutical: Honoraria: Consultant, Speaker; WL Gore: Honoraria: Consultant, Speaker E. Christopher Ellison, MD, FACS - McGraw Hill Medical: Royalty: Author; Wolters Kluwer: Royalty: Associate Editor Eric M. Pauli MD, FACS, FASGE - Nothing to Disclose Gustavo G. Fernandez-Ranvier MD, PhD, FACS - Nothing to Disclose Jared M. Slater MD, FACS - Nothing to Disclose John A. Weigelt MD, DVM, FACS - Nothing to Disclose Jon C. Gould, MD, FACS - Gore: Honorarium: Speaker; Torax/Ethicon: Consulting Fee: Consultant and preceptor for LINX Jonathan Carter, MD - VERB Surgical: Consulting Fee: Consultant Kenneth W. Sharp MD, FACS - Nothing to Disclose Raeshell S. Sweeting MD - Nothing to Disclose Valerie P. Grignol MD, FACS - Nothing to Disclose
Program Committee and Disclosures
CHAIR: Henri R. Ford, MD, MHA, FACS, FAAP, FRCSEng(Hon), Miami, FL - Nothing to Disclosure VICE-CHAIR: David T. Cooke, MD, FACS, Sacramento, CA - Nothing to Disclosure
David C. Borgstrom, MD, FACS, Morgantown, WV - Nothing to Disclosure Daniel L. Dent, MD, FACS, San Antonio, TX - Nothing to Disclosure Roger R. Dmochowski, MD, FACS, Nashville, TN - Allergen: Honoraria: Consultant Cynthia D. Downard, MD, FACS, Louisville, KY - Nothing to Disclosure Audra A. Duncan, MD, FACS, London, ON - Nothing to Disclosure Mariam F. Eskander, MD, Boston, MA - Nothing to Disclosure Paula Ferrada, MD, FACS, Richmond, VA - Nothing to Disclosure Neil H. Hyman, MD, FACS, Chicago, IL - Nothing to Disclosure Martin S. Karpeh, Jr., MD, FACS, New York, NY - Nothing to Disclosure Dennis H. Kraus, MD, FACS, New York, NY - Nothing to Disclosure Kenneth W. Sharp, MD, FACS, Nashville, TN - Nothing to Disclosure
Ex-Officios
Daniel M. Herron, MD, FACS, FASBMS, New York, NY - Nothing to Disclosure Edith Tzeng, MD, FACS, Pittsburgh, PA - Nothing to Disclosure
Consultants
Barbara Lee Bass, MD, FACS, FRCSEng(Hon), FRCSI(Hon), FCOSECSA(Hon), Houston, TX - Nothing to Disclosure Quan-Yang Duh, MD, FACS, San Francisco, CA - Nothing to Disclosure B. J. Hancock, MD, FACS, FRCSC, Winnipeg, MB - Nothing to Disclosure Ronald V. Maier, MD, FACS, FRCSEd(Hon), Seattle, WA - Nothing to Disclosure
Continuing Medical Education Credit Information
The American College of Surgeons is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians.
AMA PRA Category 1 Credits™
The American College of Surgeons designates this enduring activity for a maximum of 1.5 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Of the AMA PRA Category 1 Credits™ listed above, a maximum of 1.5 credits meets the requirements for Self-Assessment.

Note: Residents will receive a Certificate of Completion.
Available Credit
This course is available as part of the Clinical Congress 2019 Webcast Packages
Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
- Find in topic
RELATED TOPICS
Contributor Disclosures
Please read the Disclaimer at the end of this page.
The following represent additions to UpToDate from the past six months that were considered by the editors and authors to be of particular interest. The most recent What's New entries are at the top of each subsection.
ABDOMINAL WALL AND HERNIA SURGERY
Updated analysis on the risks and benefits of paraesophageal hernia repair (March 2024)
Paraesophageal hernia repair has not been advised for asymptomatic patients due to a high perioperative mortality relative to the risk of developing symptoms. However, in an updated Markov analysis of surgery versus expectant management for such patients, the mortality of elective laparoscopic repair was reduced to <0.5 percent, while the mortality of emergency repair remained high at 10 percent on average [ 1 ]. The annual probabilities of developing symptoms that would necessitate elective and emergency surgery were estimated to be 5.8 and 1.7 percent, respectively. Based on this new analysis, patients with a paraesophageal hernia should be referred for surgical consultation regardless of symptoms to determine if they are an appropriate candidate for hernia repair. In particular, older patients have a higher incidence of paraesophageal hernia and should not be denied surgical consultation. (See "Surgical management of paraesophageal hernia", section on 'Indications for surgical repair' .)
COLORECTAL SURGERY
Duration of antibiotic therapy following appendectomy for perforated appendicitis (February 2024)
The duration of antibiotic therapy following appendectomy for perforated appendicitis is debated. In a trial of 104 patients with complicated appendicitis (defined as gangrenous or perforated) who received 24 hours of intravenous or oral amoxicillin-clavulanate , the 30-day complication rate was not different (15 percent in both groups) [ 2 ]. Because the study population was dominated by patients with gangrenous appendicitis (75 percent) and 67 percent of organ/space infections occurred in patients with perforated appendicitis, these findings may not be generalizable to the latter group. Thus, until further data are available, we continue to suggest two to four days of intravenous antibiotics after appendectomy for those with perforated appendicitis, based on data from previous trials. (See "Management of acute appendicitis in adults", section on 'Antibiotics for perforated appendicitis' .)
Timing of appendectomy for uncomplicated appendicitis (November 2023)
Appendectomy is traditionally performed urgently to reduce the risk of perforation. However, a large randomized trial showed that patients with uncomplicated appendicitis (including those with appendicolith on computed tomography) who had an in-hospital delay of up to 24 hours before surgery had no increased risk of perforation or other complications compared with those who underwent surgery within 8 hours [ 3 ]. Given these data and general acceptance of antibiotic management of these patients, we suggest performing appendectomy within 24 hours of presentation in patients with uncomplicated appendicitis who elect to undergo surgery. (See "Management of acute appendicitis in adults", section on 'Timing of appendectomy' .)
BREAST SURGERY
Regional nodal radiation in early breast cancer (November 2023)
Studies are evaluating the impact of adjuvant regional nodal radiotherapy (RT) in patients with early breast cancer. In a meta-analysis including over 12,000 patients, absolute improvements in breast cancer recurrence and mortality from regional nodal RT in trials from the 1990s through 2000s were greatest for patients at highest risk for recurrence; absolute reductions in 15-year breast cancer mortality were 1 to 2 percent among those with no positive axillary lymph nodes, 2 to 3 percent among those with one to three positive nodes, and 4 to 5 percent for those with four or more positive nodes [ 4 ]. However, no benefits were observed in earlier trials of nodal RT. The discrepancy is likely due to refinements in radiation techniques. For patients with node-positive or high-risk node-negative breast cancer, we offer adjuvant regional nodal RT. (See "Adjuvant radiation therapy for women with newly diagnosed, non-metastatic breast cancer", section on 'Approach' .)
Peritumoral lidocaine injection before incision for breast cancer surgery (September 2023)
In a multicenter, randomized trial of over 1000 patients with early breast cancer undergoing mastectomy or breast-conserving surgery, peritumoral injection of 0.5% lidocaine prior to incision improved five-year disease-free survival (87 versus 83 percent) and five-year overall survival (90 versus 86 percent) [ 5 ]. The mechanism is unknown but thought to involve blocking voltage-gated sodium channels and thereby preventing activation of prometastatic pathways. The trial protocol for surgical management of breast cancer deviated from what may be considered standard treatment in many clinical practices, so further validation is necessary; however, peritumoral injection of lidocaine may be a reasonable intervention given its simplicity and minimal cost. (See "Breast-conserving therapy", section on 'Incision' .)
ENDOCRINE SURGERY
Risk of autoimmune disease after surgical cure of Cushing disease (February 2024)
In patients with a corticotropin (ACTH)-secreting pituitary tumor (Cushing disease), transsphenoidal surgery with adenomectomy provides a high rate of initial cure. Surgical cure of Cushing disease improves skeletal and cardiometabolic health, but it also may contribute to increased risk of autoimmune disorders. In a retrospective study in predominantly female adults (mean age approximately 44 years) with pituitary adenoma who underwent successful surgical management, patients with Cushing disease (n = 194) had a higher rate of new-onset autoimmune disease following surgery compared with patients with a nonfunctioning adenoma (n = 92; cumulative three-year incidence 10.4 versus 1.6 percent, respectively) [ 6 ]. Autoimmune thyroid disease was most common, and family history of autoimmune disease was associated with higher risk of developing an autoimmune disorder. These findings support the need for long-term monitoring of patients with Cushing disease, even after curative surgical treatment. (See "Primary therapy of Cushing disease: Transsphenoidal surgery and pituitary irradiation", section on 'Long-term health risks' .)
Cardiometabolic features of adrenal incidentaloma with mild autonomous cortisol secretion (December 2023)
In some individuals with adrenal incidentaloma, mild autonomous cortisol secretion (MACS) is evident in the absence of clinical features of Cushing syndrome. The long-term risks of MACS and optimal management strategies are not well defined. In a meta-analysis of 47 observational studies in 17,156 patients with adrenal incidentaloma, individuals with MACS (defined as serum cortisol >1.8 mcg/dL after a 1 mg overnight dexamethasone suppression test) exhibited a higher prevalence of diabetes, hypertension, and dyslipidemia compared with individuals with nonfunctioning adrenal adenomas [ 7 ]. Further, patients with MACS who underwent adrenalectomy showed greater improvement in cardiometabolic parameters than those who did not undergo surgery. These findings demonstrate the potential cardiometabolic risks of MACS and support our preference for adrenalectomy in patients with MACS and younger age or evidence of cardiometabolic dysregulation. (See "Evaluation and management of the adrenal incidentaloma", section on 'Clinical manifestations' .)
PERIOPERATIVE CARE
Postoperative noninvasive ventilation or high-flow nasal oxygen for patients with obesity (November 2023)
The optimal postoperative ventilatory strategy for patients with severe obesity has been unclear. In a 2023 network meta-analysis of randomized trials that compared various postoperative noninvasive ventilatory strategies in these patients, high-flow nasal oxygen (HFNO) or bilevel positive airway pressure (BiPAP) reduced atelectasis; HFNO, BiPAP, or continuous positive airway pressure (CPAP) reduced postoperative pneumonia; and HFNO reduced length of stay compared with conventional oxygen therapy [ 8 ]. For patients with obesity who are hypoxic in the post-anesthesia care unit despite oxygen supplementation and incentive spirometry, we suggest a trial of HFNO, BiPAP, or CPAP prior to considering intubation. (See "Anesthesia for the patient with obesity", section on 'Post-anesthesia care unit management' .)
Negative pressure wound therapy for contaminated surgical wounds (November 2023)
Prophylactic negative pressure wound therapy (NPWT) is used on clean surgical wounds, but it may also be useful for contaminated surgical wounds. In a randomized trial that compared NPWT with standard wound care in 69 patients who underwent surgery for gastrointestinal perforation and had fascial closure, NPWT reduced rates of surgical site infection (18 versus 61 percent) and fascial dehiscence (9 versus 48 percent), increased the rate of delayed primary skin closure (91 versus 48 percent), and decreased median time to wound healing (19 versus 26 days) [ 9 ]. The results of this small trial are encouraging, and, in the absence of contraindications, we use NPWT over intact fascia to expedite closure of contaminated surgical wounds. (See "Negative pressure wound therapy", section on 'Prophylactic use' .)
SKIN AND SOFT TISSUE SURGERY
Lymphatic venous bypass reduces cellulitis frequency in patients with lower extremity lymphedema (March 2024)
Observational studies suggest lymphatic venous bypass procedures provide benefits beyond limb volume reduction. In a trial comparing lymphatic venous anastomosis (LVA) plus complex decongestive therapy (CDT) versus CDT alone in patients with lower extremity lymphedema, LVA resulted in a greater reduction in cellulitis frequency from baseline (0.57 versus 0.21 fewer episodes over six months) [ 10 ]. LVA also reduced thigh area hardness; however, limb circumference and pain were similar. All patients had undergone at least three months of CDT before randomization. The outcomes of this trial support our practice of offering LVA for patients with lymphedema and recurrent cellulitis. (See "Surgical treatment of primary and secondary lymphedema", section on 'Lymphatic bypass outcomes' .)
TRANSPLANTATION
Lung transplant outcomes for COVID-19 end-stage lung disease (September 2023)
COVID-19 end-stage lung disease is a new indication for lung transplantation with limited outcome data. Two groups have recently analyzed overlapping cohorts of approximately 400 patients who underwent lung transplantation in the United States for COVID-19-associated end-stage lung disease between March 2020 and August 2022 and who comprised almost 9 percent of all lung transplants performed during this time period [ 11,12 ]. Compared with other lung transplant recipients, these patients were generally younger and more likely to need mechanical ventilation or extracorporeal membrane oxygenation support before transplantation. Despite longer hospital stays, overall survival over the first 12 months was similar to that seen in patients who received lung transplantation for other causes (86 to 87 percent). Lung transplantation provides effective treatment for carefully selected patients with irreversible end-stage lung disease caused by COVID-19. (See "Lung transplantation: General guidelines for recipient selection", section on 'Lung disease due to COVID-19' .)
TRAUMA AND BURN SURGERY
Skin preparation prior to fracture repair (March 2024)
The optimal preparation of contaminated or dirty wounds and whether any skin preparation can influence surgical site infection (SSI) independent of other factors (eg, prophylactic systemic antibiotics) are unknown. In a multiple-period, cluster-randomized, crossover trial comparing skin preparation with iodine povacrylex in alcohol versus chlorhexidine gluconate in alcohol in 1700 open fracture repairs, the incidence of superficial or deep SSI was similar for both approaches [ 13 ]. Based on these findings, which are consistent with those from a previous trial, either chlorhexidine- or iodine-based skin preparations can be used prior to surgery for open, traumatic lower extremity wounds. (See "Surgical management of severe lower extremity injury", section on 'Limb preparation and skin antisepsis' .
Whole blood transfusion for severe traumatic hemorrhage (January 2024)
For severe traumatic hemorrhage, whole blood transfusion is an alternative to balanced component transfusion (1:1:1 ratio of packed red blood cells/plasma/platelets). In an observational study comparing these two approaches, low titer group O whole blood transfusion was associated with lower 24-hour mortality (8 versus 19 percent) and lower volume of blood products received at 72 hours (48 versus 82 mL/kg) [ 14 ]. The survival benefit was greatest in patients with shock or coagulopathy. While this study suggests improved outcomes for whole blood transfusion, randomized trials are needed to determine which transfusion strategy might be superior and which patients would benefit the most. (See "Ongoing assessment, monitoring, and resuscitation of the severely injured patient", section on 'Whole blood transfusion' .)
Tranexamic acid for burn wound excision (November 2023)
Randomized trials have established that tranexamic acid (TXA) reduces blood loss and transfusion requirements in various surgical settings, but data in burn surgery are limited. In a meta-analysis of observational studies evaluating intravenous and topical TXA in burn surgery, use of TXA was associated with reductions in blood loss, use of intraoperative transfusion, and number of units transfused but no change in venous thromboembolism or mortality rates [ 15 ]. Based on this review and data from other surgical settings, we routinely administer intravenous TXA for burn wound excisions over 20 percent of total body surface area. (See "Overview of the management of the severely burned patient", section on 'Coagulopathy' .)
No benefit of Cryoprecipitate in massive transfusion protocol for trauma (October 2023)
Cryoprecipitate is a source of fibrinogen; some institutions may include it in their massive transfusion protocols for trauma patients. In a new trial, 1604 trauma patients were randomly assigned to receive or not receive Cryoprecipitate in addition to a standard massive transfusion protocol [ 16 ]. Mortality at 28 days was comparable between the no Cryoprecipitate controls and the Cryoprecipitate group (26 versus 25 percent). This finding supports the practice of reserving Cryoprecipitate for patients with low fibrinogen levels. Transfusion medicine personnel and/or individuals with hemostasis expertise can help to determine the value for specific patients. (See "Cryoprecipitate and fibrinogen concentrate", section on 'Trauma' .)
VASCULAR AND ENDOVASCULAR SURGERY
Phosphodiesterase type 5 inhibition for Raynaud phenomenon (January 2024)
Phosphodiesterase type 5 (PDE5) inhibitors such as sildenafil and tadalafil are widely used to treat digital ischemia from Raynaud phenomenon. In an updated meta-analysis of nine randomized trials comprising 411 patients with Raynaud phenomenon (most of whom had scleroderma), treatment with PDE5 inhibition resulted in three fewer attacks weekly and a reduction in the average duration of the attacks by five minutes [ 17 ]. However, PDE5 inhibition led to minimal to no reduction in the pain associated with Raynaud phenomenon. This study implies that while PDE5 inhibition has a modest impact on the duration and frequency of Raynaud attacks, it might not be adequate to address all symptoms experienced by patients with severe disease. (See "Treatment of Raynaud phenomenon: Initial management", section on 'Phosphodiesterase type 5 inhibitor' .)
Genes associated with an increased risk for Raynaud phenomenon (October 2023)
A genetic basis for Raynaud phenomenon (RP) is supported by family and twin studies, but robust evidence for specific causal genes has been lacking. A genome-wide association study has identified two candidate genes associated with an increased risk for RP: ADRA2A and IRX1 [ 18 ]. The potential role of these genes in the pathogenesis of RP requires further study. (See "Pathogenesis and pathophysiology of Raynaud phenomenon", section on 'Genetic factors' .)
OTHER SURGICAL SPECIALTIES
Moderate hypothermia during aortic arch surgery with antegrade cerebral perfusion (March 2024)
Observational data have supported a shift from deep to moderate hypothermia during circulatory arrest for aortic arch surgery, particularly with adjunctive antegrade cerebral perfusion (ACP). A recent trial has now compared outcomes for 251 patients undergoing aortic arch surgery with ACP and randomly assigned to deep (≤20.0°C), low-moderate (20.1 to 24.0°C), or high-moderate (24.1 to 28.0°C) circulatory arrest temperature [ 19 ]. At one-month follow-up, the three groups had similar neurocognitive and neuroimaging outcomes and similar mortality, major morbidity, and quality of life. The volume of transfused blood products was higher in the deep group, but transfusion-related complications were not different. Based on this trial, moderate (20.1 to 28.0°C) rather than deep hypothermia is reasonable during aortic arch surgery when ACP is also used. Whether a low-moderate or high-moderate temperature is selected depends on the anticipated duration of hypothermia. (See "Overview of open surgical repair of the thoracic aorta", section on 'Basic principles' .)
Complications of transrectal versus transperineal prostate biopsy (February 2024)
The merit of transrectal versus transperineal prostate biopsy has been vigoroulsy debated. In the first randomized trial comparing these procedures in over 760 patients undergoing biopsies in the office setting, the two approaches had similar rates of both infectious (2.6 versus 2.7 percent) and non-infectious (1.7 versus 2.2 percent) complications [ 20 ]. This suggests that both approaches can be performed with a low risk of complications. Antibiotic prophylaxis was given to all patients prior to transrectal biopsy but omitted in most patients undergoing transperineal biopsy. (See "Prostate biopsy", section on 'Transrectal versus transperineal biopsy' .)
Pregnancy and childbirth after urinary incontinence surgery (January 2024)
Patients with stress urinary incontinence (SUI) have historically been advised to delay midurethral sling (MUS) surgery until after childbearing because of concerns for worsening SUI symptoms following delivery. In a meta-analysis of patients with MUS surgery who were followed for a mean of nearly 10 years, similar low SUI recurrence and reoperation rates were reported for the 381 patients with and the 860 patients without subsequent childbirth [ 21 ]. Birth route did not affect the findings. Although the total number of recurrences and reoperations was small, this study adds to the body of evidence suggesting that subsequent childbirth does not worsen SUI outcomes for patients who have undergone MUS. (See "Surgical management of stress urinary incontinence in females: Retropubic midurethral slings", section on 'Subsequent pregnancy' .)
Tranexamic acid to reduce bleeding after percutaneous nephrolithotomy (December 2023)
Postoperative bleeding can occur after percutaneous nephrolithotomy (PNL) for kidney stone removal; most bleeding is venous in origin and can be managed with conservative measures. A recent meta-analysis of 10 randomized trials found that use of tranexamic acid (TXA), an antifibrinolytic agent used to reduce bleeding in other clinical settings, may reduce the risk of blood transfusion after PNL [ 22 ]. Most trials were conducted in low- to middle-income settings in populations that were younger than those in higher-income settings; whether these findings are generalizable to practice in higher-income settings is uncertain. Pending additional data, we do not routinely use TXA after PNL. (See "Kidney stones in adults: Surgical management of kidney and ureteral stones", section on 'Bleeding' .)
Choice of intervention for aortic stenosis with low surgical risk (November 2023)
The choice of intervention for severe aortic stenosis (AS) is based upon an individualized assessment by a multidisciplinary heart valve team. Two randomized trials reported outcomes for transcatheter aortic valve implantation (TAVI) and surgical aortic valve replacement (SAVR) in selected low surgical risk patients with severe AS [ 23,24 ]:
● In one trial in which nearly 1500 patients were randomly assigned to TAVI with a self-expanding valve or SAVR, rates of mortality, disabling stroke, and aortic valve rehospitalization at four years were similar in the two groups.
● In another trial in which 1000 patients were randomly assigned to TAVI with a balloon-expanding valve or SAVR, rates of mortality, stroke, and rehospitalization at five years were similar in the two groups.
These trials indicate generally favorable results for TAVI up to four and five years for selected low surgical risk patients with severe AS and anatomical suitability for TAVI; additional data, including longer-term outcomes, will further inform the choice of intervention in this clinical setting. (See "Choice of intervention for severe calcific aortic stenosis", section on 'In low-risk symptomatic patients' .)
No benefit to routinely adding vancomycin for prophylaxis before joint replacement (November 2023)
For preoperative antibiotic prophylaxis in patients undergoing joint replacement, vancomycin is sometimes added to cefazolin to empirically cover methicillin-resistant staphylococci. In a randomized trial of over 4000 patients undergoing joint replacement, the rate of surgical site infection was similar following prophylaxis with cefazolin plus vancomycin compared with cefazolin plus placebo (4.5 versus 3.5 percent) [ 25 ]. There were no differences in rates of infection due to methicillin-resistant Staphylococcus aureus (MRSA) or Staphylococcus epidermidis. We use cefazolin alone for prophylaxis in patients undergoing joint replacement who are not known to have MRSA colonization or infection. (See "Prevention of prosthetic joint and other types of orthopedic hardware infection", section on 'Antimicrobial prophylaxis' .)
Timing of prophylactic aortic surgery for patients with bicuspid aortic valve (October 2023)
The optimal timing for prophylactic aortic surgery for patients with a bicuspid valve (BAV) and ascending aorta diameters of 5.0 to 5.4 cm is uncertain. In a retrospective multicenter study including nearly 500 patients with BAV and aortic diameters in this range who were followed for a median of seven years, over one-half of the patients underwent elective aortic surgery, with an operative mortality rate of 1.9 percent [ 26 ]. Aortic dissection occurred during surveillance in 1.8 percent of the nearly 500 patients. These findings illustrate the risk trade-offs for early surgery versus surveillance for patients with BAV; a randomized trial is underway to compare these approaches in patients with ascending aorta diameters of 5.0 to 5.4 cm, including patients with BAV. (See "Bicuspid aortic valve: Intervention for valve disease or aortopathy in adults", section on 'Without high-risk features' .)
High-dose dual-antibiotic loaded cement does not reduce infection compared with low-dose single-antibiotic loaded cement in hip arthroplasty (September 2023)
The optimal dosing and effectiveness of antibiotic-loaded cement for hip arthroplasty is uncertain. In a randomized trial, high-dose dual-antibiotic-loaded cement did not reduce the incidence of deep surgical site infection after hip arthroplasty compared with low-dose single-antibiotic-loaded cement [ 27 ]. Based on this trial, when antibiotic cement fixation is selected for hip arthroplasty, available cement preparations that use a low-dose single antibiotic are adequate for reducing the risk of surgical site infection and also minimize the risk of fixation weakening associated with high-dose dual-antibiotic-loaded cement. (See "Total hip arthroplasty", section on 'Total hip arthroplasty implant design' .)
- DeMeester SR, Bernard L, Schoppmann SF, et al. Elective Laparoscopic Paraesophageal Hernia Repair Leads to an Increase in Life Expectancy Over Watchful Waiting in Asymptomatic Patients: An Updated Markov Analysis. Ann Surg 2024; 279:267.
- Lipping E, Saar S, Reinsoo A, et al. Short Postoperative Intravenous Versus Oral Antibacterial Therapy in Complicated Acute Appendicitis: A Pilot Noninferiority Randomized Trial. Ann Surg 2024; 279:191.
- Jalava K, Sallinen V, Lampela H, et al. Role of preoperative in-hospital delay on appendiceal perforation while awaiting appendicectomy (PERFECT): a Nordic, pragmatic, open-label, multicentre, non-inferiority, randomised controlled trial. Lancet 2023; 402:1552.
- Early Breast Cancer Trialists' Collaborative Group (EBCTCG). Radiotherapy to regional nodes in early breast cancer: an individual patient data meta-analysis of 14 324 women in 16 trials. Lancet 2023; 402:1991.
- Badwe RA, Parmar V, Nair N, et al. Effect of Peritumoral Infiltration of Local Anesthetic Before Surgery on Survival in Early Breast Cancer. J Clin Oncol 2023; 41:3318.
- Nyanyo DD, Mikamoto M, Galbiati F, et al. Autoimmune Disorders Associated With Surgical Remission of Cushing's Disease : A Cohort Study. Ann Intern Med 2024.
- Pelsma ICM, Fassnacht M, Tsagarakis S, et al. Comorbidities in mild autonomous cortisol secretion and the effect of treatment: systematic review and meta-analysis. Eur J Endocrinol 2023; 189:S88.
- Li R, Liu L, Wei K, et al. Effect of noninvasive respiratory support after extubation on postoperative pulmonary complications in obese patients: A systematic review and network meta-analysis. J Clin Anesth 2023; 91:111280.
- Singh H, Avudaiappan M, Kharel J, et al. Negative pressure wound therapy versus standard care for incisional laparotomy subcutaneous wounds in gastrointestinal perforations: A randomized controlled study. Surgery 2023; 174:291.
- Mihara M, Hara H, Kawasaki Y, et al. Lymphatic venous anastomosis and complex decongestive therapy for lymphoedema: randomized clinical trial. Br J Surg 2024; 111.
- Okumura K, Jyothula S, Kaleekal T, Dhand A. 1-Year Outcomes of Lung Transplantation for Coronavirus Disease 2019-Associated End-Stage Lung Disease in the United States. Clin Infect Dis 2023; 76:2140.
- Tasoudis P, Lobo LJ, Coakley RD, et al. Outcomes Following Lung Transplant for COVID-19-Related Complications in the US. JAMA Surg 2023; 158:1159.
- PREP-IT Investigators, Sprague S, Slobogean G, et al. Skin Antisepsis before Surgical Fixation of Extremity Fractures. N Engl J Med 2024; 390:409.
- Shea SM, Mihalko EP, Lu L, et al. Doing more with less: low-titer group O whole blood resulted in less total transfusions and an independent association with survival in adults with severe traumatic hemorrhage. J Thromb Haemost 2024; 22:140.
- Fijany AJ, Givechian KB, Zago I, et al. Tranexamic acid in burn surgery: A systematic review and meta-analysis. Burns 2023; 49:1249.
- Davenport R, Curry N, Fox EE, et al. Early and Empirical High-Dose Cryoprecipitate for Hemorrhage After Traumatic Injury: The CRYOSTAT-2 Randomized Clinical Trial. JAMA 2023; 330:1882.
- Maltez N, Maxwell LJ, Rirash F, et al. Phosphodiesterase 5 inhibitors (PDE5i) for the treatment of Raynaud's phenomenon. Cochrane Database Syst Rev 2023; 11:CD014089.
- Hartmann S, Yasmeen S, Jacobs BM, et al. ADRA2A and IRX1 are putative risk genes for Raynaud's phenomenon. Nat Commun 2023; 14:6156.
- Hughes GC, Chen EP, Browndyke JN, et al. Cognitive Effects of Body Temperature During Hypothermic Circulatory Arrest Trial (GOT ICE): A Randomized Clinical Trial Comparing Outcomes After Aortic Arch Surgery. Circulation 2024; 149:658.
- Mian BM, Feustel PJ, Aziz A, et al. Complications Following Transrectal and Transperineal Prostate Biopsy: Results of the ProBE-PC Randomized Clinical Trial. J Urol 2024; 211:205.
- Nahshon C, Abramov Y, Kugelman N, et al. The effect of subsequent pregnancy and childbirth on stress urinary incontinence recurrence following midurethral sling procedure: a meta-analysis. Am J Obstet Gynecol 2024; 230:308.
- Cleveland B, Norling B, Wang H, et al. Tranexamic acid for percutaneous nephrolithotomy. Cochrane Database Syst Rev 2023; 10:CD015122.
- Mack MJ, Leon MB, Thourani VH, et al. Transcatheter Aortic-Valve Replacement in Low-Risk Patients at Five Years. N Engl J Med 2023; 389:1949.
- Forrest JK, Deeb GM, Yakubov SJ, et al. 4-Year Outcomes of Patients With Aortic Stenosis in the Evolut Low Risk Trial. J Am Coll Cardiol 2023; 82:2163.
- Peel TN, Astbury S, Cheng AC, et al. Trial of Vancomycin and Cefazolin as Surgical Prophylaxis in Arthroplasty. N Engl J Med 2023; 389:1488.
- Ye Z, Lane CE, Beachey JD, et al. Clinical outcomes in patients with bicuspid aortic valves and ascending aorta ≥50 mm under surveillance. JACC Adv 2023; 2:100626.
- Agni NR, Costa ML, Achten J, et al. High-dose dual-antibiotic loaded cement for hip hemiarthroplasty in the UK (WHiTE 8): a randomised controlled trial. Lancet 2023; 402:196.
- ACS Foundation
- Diversity, Equity, and Inclusion
- ACS Archives
- Careers at ACS
- Federal Legislation
- State Legislation
- Regulatory Issues
- Get Involved
- SurgeonsPAC
- About ACS Quality Programs
- Accreditation & Verification Programs
- Data & Registries
- Standards & Staging
- Membership & Community
- Practice Management
- Professional Growth
- News & Publications
- Information for Patients and Family
- Preparing for Your Surgery
- Recovering from Your Surgery
- Jobs for Surgeons
- Become a Member
- Media Center
Our top priority is providing value to members. Your Member Services team is here to ensure you maximize your ACS member benefits, participate in College activities, and engage with your ACS colleagues. It's all here.
- Membership Benefits
- Find a Surgeon
- Find a Hospital or Facility
- Quality Programs
- Education Programs
- Member Benefits
- Clinical Congress 2023
- Clinical Congress News
- Quick-Fire Session Spotlig...
Quick-Fire Session Spotlights 10 Hot Topics in General Surgery
September 20, 2023
In this popular 90-minute session, distinguished panelists will explore compelling topics that are fueling discussions throughout general surgery, selected from the ACS Communities, scientific conferences, and current research literature.
For the 12th time at Clinical Congress, ACS President E. Christopher Ellison, MD, FACS, and ACS Regent Kenneth W. Sharp, MD, FACS, have paired up to co-moderate Ten Hot Topics in General Surgery, which takes place on Wednesday, October 25, from 12:45 pm to 2:15 pm in Ballroom East.
“We’re going prime time this year,” said Dr. Christopher Ellison.
“We’re going prime time this year,” said Dr. Ellison, referring to the new day and afternoon time slot for this year’s session. (Clinical Congress 2023 ends on Wednesday instead of Thursday as it has in previous years.)
In this rapid-fire style session, a panel featuring experts in general surgery will present a series of 6-minute presentations on topics that are cutting edge and controversial.
“Honestly, with these fast-paced presentations, we have to depend a little bit on the skill of the speaker,” explained Dr. Sharp. “Between Dr. Ellison and me, we know 95% of these speakers personally, and we know that they can give a very focused talk in just a few minutes.”
"We really believe every attendee will come away with information that will be useful in their own practices," said Dr. Kenneth Sharp
Each presentation will be immediately followed by a 3-minute, unscripted discussion with the audience, representing a variety of thoughts and perspectives, and providing attendees with takeaway information for future reflection.
“We know that all ten topics will not suit every surgeon,” said Dr. Sharp. “But we really believe every attendee will come away with information that will be useful in their own practices—or that will stimulate them to look at two or three new areas that they don’t know much about.”
This year’s session will cover a wide scope of topics, each representing new and emerging areas of interest in general surgery, including a presentation by Patricia Sylla, MD, FACS, on transanal mesorectal excision for rectal cancer.
“This is a very advanced surgical technique that not everyone will adopt or use—but they should be aware of it because it enhances recovery and gives patients a better quality outcome than some of the standard techniques,” Dr. Ellison said.
Dr. Sharp added that while this cutting-edge technique likely will be limited to high-volume colorectal surgeons, “if you don't know about some of the new advances, you can't take advantage of them.”
The full agenda for this year’s session includes:
Repair of Paraesophesophageal Hiatal Hernias—Add a Fundoplication or Not? Kelly Haisley, MD, FACS, Columbus, OH
Peritoneal Dialysis Catheters—Tips and Tricks M. T. Nelson, MD, FACS, Tulsa, OK
Transanal Mesorectal Excision for Rectal Cancer Patricia Sylla, MD, FACS, New York, NY
Glucagon-like Peptide-1 (GLP-1) Agonists—The End of Bariatric Surgery? Matthew D. Spann, MD, FACS, Nashville, TN
Perforated Duodenal Ulcers: Close or Patch—And How? Jon C. Gould, MD, FACS, Milwaukee, WI
Biliary Dyskinesia—Why Are We Still Debating This? Bryan K. Richmond, MD, MBA, FACS, Charleston, WV
Appendiceal Carcinoma: Decision-Making for the General Surgeon Matthew F. Kalady, MD, FACS, Columbus, OH
Transoral Thyroidectomy William B. Inabnet III, MD, MHA, FACS, Lexington, KY
Surgical Rib Fixation in Trauma—Who and When? Brian J. Daley, MD, FACS, Knoxville, TN
Choosing Wisely—Management of the Axilla in Women over 70 with Breast Cancer Kelly C. Hewitt, MD, FACS, Nashville, TN
This session also will be available for on-demand viewing.
About Clinical Congress
Access the virtual platform for on-demand content and credit claiming until May 1, 2024. Haven't registered yet? Register for virtual access.

- Theatre Etiquette
- Hand Washing
- Scrubbing, Gowning, and Gloving
- Assisting in Theatre
- The Operation Note
- Surgical Safety
- Suture Materials
- Surgical Instruments
- Infiltration of Local Anaesthetic
- Drain Insertion
- Abscess Drainage
- Skin Lesion Excision
- Damage to Local Structures
- Acute Inflammation
- Chronic Inflammation
- Wound Healing
- Basic Wound Management
- Venepuncture
- Cannulation
- Blood Cultures
- Intravenous Infusions
- Female Catheterisation
- Male Catheterisation
- Pre-Op Assessment
- Pre-Op Management
- Fluid Management
- Blood Products
- Perioperative Nutrition
- Enhanced Recovery
- Day Case Surgery
- Haemorrhage
- Nausea & Vomiting
- Atelectasis
- Fat Embolism
- Anastomotic Leak
- Post-Op Ileus
- Bowel Adhesions
- Incisional Hernia
- Constipation
- Acute Kidney Injury
- Urinary Retention
- Urinary Tract Infection
- Hypoglycaemia
- Hyperkalaemia
- Hypokalaemia
- Hypernatremia
- Hyponatraemia
- Surgical Site Infection
- Wound Dehiscence
- Initial Assessment
- The General Approach
- A-E Assessment
- Referring a Patient
- IV Fluid Management
- Post-Op Fever
- Post-Op Pain
- Cardiovascular
- Respiratory
- Cardiothoracic Incisions
- Digital Rectal
- Abdominal Incisions
- Peripheral Vascular
- Peripheral Venous
- Cranial Nerves
- Peripheral Neurological
- Diabetic Foot
- Thyroid Gland
- Foot & Ankle
- Oral Cavity
- Certifying Death
- Acute Abdomen
- Haematemesis
- Gastric Outlet Obstruction
- Bowel Obstruction
- Bowel Perforation
- Rectal Bleeding
- Oesophageal Cancer
- Oesophageal Tears
- Motility Disorders
- Hiatus Hernia
- Peptic Ulcer Disease
- Gastric Cancer
- Inguinal Hernia
- Femoral Hernia
- Abdominal Wall Hernia
- Gastroenteritis
- Angiodysplasia
- Small Bowel Tumours
- Neuroendocrine Tumours
- Acute Appendicitis
- Colorectal Cancer
- Diverticular Disease
- Crohn’s Disease
- Ulcerative Colitis
- Pseudo-Obstruction
- Haemorrhoids
- Pilonidal Sinus
- Fistula-in-Ano
- Anorectal Abscess
- Anal Fissure
- Rectal Prolapse
- Anal Cancer
- Colic & Cholecystitis
- Cholangitis
- Cholangiocarcinoma
- Hepatocellular Carcinoma
- Liver Cysts
- Liver Abscess
- Acute Pancreatitis
- Chronic Pancreatitis
- Pancreatic Cancer
- Cystic Neoplasms of the Pancreas
- Splenic Infarct
- Splenic Rupture
- Acutely Painful Limb
- Lower Limb Ulcers
- Carotid Artery Disease
- Abdominal Aortic Aneurysm
- Aortic Dissection
- Thoracic Aortic Aneurysm
- Acute Limb Ischaemia
- Chronic Limb Ischaemia
- Acute Mesenteric Ischaemia
- Chronic Mesenteric Ischaemia
- Pseudoaneurysm
- Peripheral & Visceral Aneurysms
- Varicose Veins
- Venous Insufficiency
- Thoracic Outlet Syndrome
- Subclavian Steal Syndrome
- Hyperhidrosis
- Scrotal Pain
- Acute Urinary Retention
- Chronic Urinary Retention
- Lower Urinary Tract Symptoms
- Scrotal Lumps
- Renal Tract Calculi
- Pyelonephritis
- Renal Cancer
- Renal Cysts
- Urinary Incontinence
- Bladder Cancer
- Benign Prostatic Hyperplasia
- Prostate Cancer
- Prostatitis
- Epididymitis
- Testicular Torsion
- Testicular Cancer
- Fournier’s Gangrene
- Paraphimosis
- Penile Fracture
- Penile Cancer
- Peyronie’s Disease
- Hypospadias
- Cryptorchidism
- Balanitis Xerotica Obliterans
- Osteoarthritis
- Fracture Management
- Acutely Swollen Joint
- Open Fracture
- Compartment Syndrome
- Septic Arthritis
- Osteomyelitis
- Bone Tumours
- Clavicle Fracture
- Rotator Cuff Tear
- Shoulder Fracture
- Shoulder Dislocation
- Humeral Shaft Fracture
- Biceps Tendinopathy
- Adhesive Capsulitis
- Subacromial Impingement Syndrome
- Supracondylar Fracture
- Olecranon Fracture
- Radial Head Fracture
- Elbow Dislocation
- Olecranon Bursitis
- Epicondylitis
- Distal Radius Fracture
- Scaphoid Fracture
- Carpal Tunnel Syndrome
- Dupuytren’s Contracture
- De Quervain’s Tenosynovitis
- Ganglionic Cysts
- Trigger Finger
- Radiculopathy
- Degenerative Disc Disease
- Cervical Fracture
- Thoracolumbar Fracture
- Neck of Femur Fracture
- Hip Osteoarthritis
- Femoral Shaft Fracture
- Quadriceps Tendon Rupture
- Distal Femur Fracture
- Pelvic Fracture
- Acetabular Fracture
- Knee Osteoarthritis
- Meniscal Tear
- Patella Fracture
- Tibial Shaft Fracture
- Tibial Plateau Fracture
- Iliotibial Band Syndrome
- Ankle Fracture
- Calcaneal Fracture
- Achilles Tendonitis
- Talar Fracture
- Tibial Pilon Fracture
- Lisfranc injury
- Hallux Valgus
- Plantar Fasciitis
- The Limping Child
- Growth Plate Fracture
- Triple Assessment
- Galactorrhoea
- Inflammatory Disease
- Benign Tumours
- Gynaecomastia
- Carcinoma in Situ
- Invasive Cancer
- Surgical Treatments
- Non-Surgical Treatments
- Hoarse Voice
- Facial Palsy
- Hearing Loss
- Otitis Externa
- Acute Otitis Media
- Otitis Media with Effusion
- Chronic Mucosal Otitis Media
- Chronic Squamous Otitis Media
- Acute Rhinosinusitis
- Chronic Rhinosinusitis
- Periorbital Cellulitis
- Nasal Trauma
- Obstructive Sleep Apnoea
- Tonsillitis
- Deep Neck Space Infections
- Foreign Bodies
- Sialolithiasis
- Sialadenitis
- Salivary Gland Tumours
- Thyroid Cancer
- Head & Neck Cancer
- Assessment of Head Injury
- Extradural Haematoma
- Subdural Haematoma
- Diffuse Axonal Injury
- Traumatic Spinal Cord Injury
- Monro-Kellie Doctrine
- Intracranial Pressure Monitoring
- Hydrocephalus
- Subarachnoid Haemorrhage
- Intracranial Aneurysms
- Intracerebral Haemorrhage
- Arteriovenous Malformation
- Intracranial Infections
- Pituitary Tumours
- Spinal Tumours
- Deep Brain Stimulation
- Epilepsy Surgery
- Cauda Equina Syndrome
- Spinal Cord Compression
- Spinal Infections
- Principles of Wound Management
- Burns Assessment
- Burns Reconstruction
- Skin Grafts and Flaps
- Basal Cell Carcinoma
- Squamous Cell Carcinoma
- Flexor Tendon Injuries
- Extensor Tendon Injuries
- Metacarpal Fractures
- Phalangeal Fractures
- Nail Bed Injuries
- Finger Replantation
- Skin Abscess
- Necrotising Fasciitis
- Bite Injuries
- Hand Infections
- Cardiopulmonary Bypass
- Bridge to Transplantation
- Foetal & Adult Circulation
- Coronary Artery Disease
- Valvular Disease
- Cardiac Tumours
- Lung Cancer
- Airway Disorders
- Chest Wall Disorders
- Mediastinal Tumours
- Diaphragmatic Hernia
- Pneumothorax
- Haemothorax
- Principles of Transplantation
- Concepts of Brain Death
- Organ Retrieval
- Immunosuppression in Transplantation
- Renal Transplantation
- Liver Transplantation
- Pancreas Transplantation
- Heart Transplantation
- Lung Transplantation
- I&D Abscess
- Diagnostic Laparoscopy
- Appendicectomy
- Small Bowel Resection
- Hartmann’s Procedure
- Gastroscopy
- Colonoscopy
- Excision of a Lump
- Open Inguinal Hernia Repair
- Laparoscopic Inguinal Hernia Repair
- Open Umbilical Hernia Repair
- Laparoscopic Cholecystectomy
- Nissen Fundoplication
- Oesophagectomy
- Gastric Band
- Gastric Bypass
- Sleeve Gastrectomy
- Lay Open Fistula
- Haemorrhoidectomy
- Pilonidal Sinus Repair
- Reversal of a Stoma
- Right Hemicolectomy
- Left Hemicolectomy
- Anterior Resection
- Abdominoperineal Resection
- Carotid Endarterectomy
- Open AAA Repair
- Lower Limb Amputation
- Angioplasty and Stenting
- Embolectomy
- Femoral Endarterectomy
- Arterial Bypass
- Axillofemoral Bypass
- Lower Limb Bypass
- Fem-Fem Crossover
- Endovenous Ablation
- Varicose Veins Stripping
- Foam Sclerotherapy
- AV Fistula Formation
- Cervical Rib Excision
- Flexible Cystoscopy
- Rigid Cystoscopy
- Suprapubic Catheterisation
- Scrotal Exploration
- Inguinal Orchidectomy
- Hydrocoele Excision
- Epididymal Cyst Excision
- Circumcision
- Dorsal Slit Procedure
- Ureteric Stent Insertion
- Percutaneous Nephrolithotomy
- Nephrectomy
- Flexible Nasal Endoscopy
- Microlaryngoscopy
- Grommet Insertion
- Myringoplasty
- Adenoidectomy
- Septoplasty
- Functional Endoscopic Sinus Surgery
- Parotidectomy
Presentations
Within general surgery, there are a wide range of clinical presentations that patients can present with, and the underlying pathologies are even wider.
The most common of these is acute abdominal pain, often termed the “acute abdomen” and is essential to know how to approach this presentation and potential investigations required. Various abdominal incisions may be present as well for several patients you see, therefore knowing what the various scars mean is useful to know.
Bowel obstruction and bowel perforation are serious disease presentations and should be investigated and managed promptly.
Haematemesis, melena, and haematochezia can also suggest slightly different pathologies present, yet all can lead to potential surgical intervention being required if severe or untreated, therefore are essential presentations to learn how to approach.
Found an error? Is our article missing some key information? Make the changes yourself here!
Once you've finished editing, click 'Submit for Review', and your changes will be reviewed by our team before publishing on the site.
We use cookies to improve your experience on our site and to show you relevant advertising. To find out more, read our privacy policy .
Privacy Overview
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
Current Topics in Surgical Research
This article is only available in the PDF format. Download the PDF to view the article, as well as its associated figures and tables.
This is the third volume of papers from the Association for Academic Surgery. The presentations which are included in the current book were delivered at the fourth annual meeting of the Association which was held in Denver in November 1970. This surgical society is composed of young, fulltime academic surgeons, less than 40 years of age when elected. The editors selected for publication 46 of the 64 papers that were delivered at the 1970 meeting.
The papers are primarily reports of clinical and laboratory research studies. The contents have been divided into sections, so that papers are grouped, approximately equally, into the following categories: I: Cardiovascular; II: Wound Healing and Shock; III: Neurosurgery; IV: Genitourinary; V: Transplantation; VI: Oncology; VII: Gastrointestinal and Biliary. The authors of the papers represent 39 teaching institutions in the United States and Canada and include most of the surgical specialties.
The quality of the presentations
Beal JM. Current Topics in Surgical Research. Arch Surg. 1972;104(2):229. doi:10.1001/archsurg.1972.04180020107028
Manage citations:
© 2024
Artificial Intelligence Resource Center
Surgery in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- General surgery...
General surgery resources for students
- Related content
- Peer review
- Matas Morkevicius , fifth year medical student 1
- 1 Vilnius University Medical School, Lithuania
Medical students spend lots of money on textbooks. But now the internet contains lots of resources including several surgical textbooks that are available free of charge.
Surgical Treatment: Evidence Based and Problem-Oriented ( www.ncbi.nlm.nih.gov/books/bv.fcgi?call=bv.View..ShowTOC&rid=surg.TOC ) is probably one of the best online texts which covers the various topics in general surgery. The contents follow the usual format of paper surgery textbooks and classify the chapters according to the diseased organ. At the end of each section, a reference section links to Pubmed.
An extensive list of relevant surgical topics is covered at Emedicine ( www.emedicine.com/med/GENERAL_SURGERY.htm ). You can find review and tutorial articles, written by experts in surgery. The text is aimed at students, so even the basic science part of each surgical condition is described in detail. At the bottom of each article are references which help you to find more detailed information.
The University of Chicago Medical School's website holds lecture notes for students on most common surgical topics ( http://surgery.uchicago.edu/ed/readings.cfm?section=General ). Visitors to this website are supposed to have some basic knowledge of normal anatomy since only information about clinically oriented anatomy is given. At the end of each lecture are self assessment questions. Although “acute appendicitis” is not covered, the site is still a good resource for most common surgical diseases.
The University of Iowa offers a few books in general surgery. The first one is the Emergency War Surgery Handbook ( www.vnh.org/EWSurg/EWSTOC.html ) which covers the pathologic basis and management of wounds. The second one, the General Surgery University of Iowa Family Practice Handbook ( www.vh.org/adult/provider/familymedicine/FPHandbook/15.html ), is a good resource for those who need just a brief guide. Here you can find really concise guidelines on urgent surgical conditions.
Few websites contain colour atlases, but one of them is Westcott Atlas of Surgery ( www.bgsm.edu/surg-sci/atlas/atlas.html ), which contains the schemes and pictures of different laparoscopic surgeries. Another site ( www.laparoscopy.com ) has a collection of pictures and videos of the most common laparoscopic procedures in the different branches of surgery. These websites are particularly useful for making presentations.
Advanced level medical students might refer to peer reviewed surgery journals with free access to full text articles. There are quite a few, including BMC Surgery ( www.biomedcentral.com/1471-2482 ), the Canadian Journal of Surgery ( www.cma.ca/cjs/index.htm ), and Contemporary Surgery ( www.contemporarysurgery.com ).
Originally published as: Student BMJ 2004;12:391
- Open access
- Published: 06 October 2023
Enhanced perioperative care in emergency general surgery: the WSES position paper
- Marco Ceresoli 1 , 2 ,
- Marco Braga 1 , 2 ,
- Nicola Zanini 3 ,
- Fikri M. Abu-Zidan 4 ,
- Dario Parini 5 ,
- Thomas Langer 1 , 6 ,
- Massimo Sartelli 7 ,
- Dimitrios Damaskos 8 ,
- Walter L. Biffl 9 ,
- Francesco Amico 10 ,
- Luca Ansaloni 11 ,
- Zsolt J. Balogh 12 ,
- Luigi Bonavina 13 ,
- Ian Civil 14 ,
- Enrico Cicuttin 11 ,
- Mircea Chirica 15 ,
- Yunfeng Cui 16 ,
- Belinda De Simone 17 ,
- Isidoro Di Carlo 18 ,
- Andreas Fette 19 ,
- Giuseppe Foti 1 , 20 ,
- Michele Fogliata 1 , 2 ,
- Gustavo P. Fraga 21 ,
- Paola Fugazzola 11 ,
- Joseph M. Galante 22 ,
- Solomon Gurmu Beka 23 ,
- Andreas Hecker 24 ,
- Johannes Jeekel 25 ,
- Andrew W. Kirkpatrick 26 ,
- Kaoru Koike 27 ,
- Ari Leppäniemi 28 , 29 ,
- Ingo Marzi 30 ,
- Ernest E. Moore 31 ,
- Edoardo Picetti 32 ,
- Emmanouil Pikoulis 33 ,
- Michele Pisano 34 ,
- Mauro Podda 35 ,
- Boris E. Sakakushev 36 ,
- Vishal G. Shelat 37 , 38 ,
- Edward Tan 39 ,
- Giovanni D. Tebala 40 ,
- George Velmahos 41 ,
- Dieter G. Weber 42 ,
- Vanni Agnoletti 43 ,
- Yoram Kluger 44 ,
- Gianluca Baiocchi 45 ,
- Fausto Catena 3 &
- Federico Coccolini 46
World Journal of Emergency Surgery volume 18 , Article number: 47 ( 2023 ) Cite this article
4329 Accesses
1 Citations
Metrics details
This article has been updated
Enhanced perioperative care protocols become the standard of care in elective surgery with a significant improvement in patients’ outcome. The key element of the enhanced perioperative care protocol is the multimodal and interdisciplinary approach targeted to the patient, focused on a holistic approach to reduce surgical stress and improve perioperative recovery. Enhanced perioperative care in emergency general surgery is still a debated topic with little evidence available. The present position paper illustrates the existing evidence about perioperative care in emergency surgery patients with a focus on each perioperative intervention in the preoperative, intraoperative and postoperative phase. For each item was proposed and approved a statement by the WSES collaborative group.
Introduction
Enhanced recovery after surgery (ERAS®) protocol refers to a standardized multimodal approach based on the application of structured protocols in perioperative patients' management. The main goal of these interventions is patient management optimization during the perioperative period under all aspects of perioperative care, not only about the surgical technique, by reducing surgical stress, minimizing the physiological response to surgery, and improving postoperative recovery. The key element of the ERAS protocol is the multimodal and interdisciplinary approach targeted to the patient, focused on a holistic approach [ 1 ].
Perioperative care protocols are structured as a bundle of interventions to be applied during the preoperative, intraoperative and postoperative periods. Each intervention is linked to the others and shares the common goal of reducing the burden of perioperative patient stress (Fig. 1 ). For this reason, it is very difficult to evaluate the efficacy of a single item without considering the effect of all the others, applied as a bundle. Designing studies to evaluate and demonstrate the effect of every single intervention is therefore a major challenge, markedly limiting the available scientific evidence.

Enhanced perioperative care items and interventions
The effectiveness and safety of ERAS protocols in elective surgery are now widely established. Several meta-analyses comparing standard care and fast-track approach show that ERAS protocols in elective surgery lead to a reduction in length of stay and in the rate of postoperative non-surgical complications [ 2 , 3 , 4 , 5 ]. Most of the available studies focused on the postoperative phase, considering the main “surgical” items as study outcomes, with relatively small attention being devoted to preoperative and intraoperative interventions. However, main postoperative items such as oral feeding, urinary drain removal and mobilization should also be considered as compliance indicators rather than only interventions to be implemented [ 6 ]. From a methodological standpoint, there is a clear difference between adherence and compliance to an enhanced recovery protocol. Adherence should identify the percentage of items applied throughout the perioperative care process, while postoperative compliance also reflects how the patient follows the enhanced recovery process. For example, patients’ compliance to a postoperative pathway including early oral feeding and mobilization can be obtained easier if there is good adherence to a preoperative and an intraoperative enhanced pathway (and not only for a medical decision).
Based on the beneficial effect of enhanced perioperative care protocols in elective surgery, the implementation of structured protocols for emergency general surgery patients has also been advocated after the promising results of some studies [ 7 , 8 ]. However, enhanced perioperative care in emergency general surgery remains a “grey area” with little evidence available and great debate.
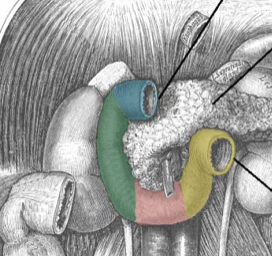
Patients undergoing elective surgery should be normothermic, euvolemic, clean, and “healthy”, and surgery per se represents their main stressful factor. Emergency surgery represents a more complex scenario where surgery is at the same time a stressful factor but also the key-intervention to solve the pre-existing physiologic imbalance secondary to the acute underlying disease (Fig. 2 ).
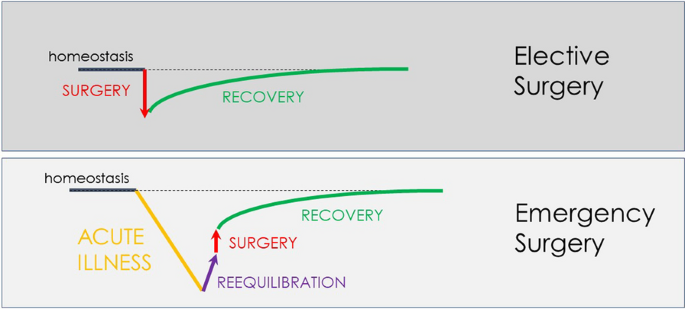
Perioperative diagram of patient’s homeostasis in elective and emergency general surgery
The diagram (Fig. 2 ) shows the impact of the pre-existing acute disorder causing a marked decline of the physiological reserve. The importance of the preoperative phase (re-equilibration) seems intuitive. Despite emergency surgery by definition does not allow schedulable interventions, some preoperative optimization is still possible in the emergency setting, though with much reduced time. The time available between patient presentation and surgery should be optimized to improve the patient’s physiological status to promote post-surgical recovery. In this complex scenario, also the timing of surgery should be carefully evaluated. One of the most intriguing and difficult challenges is to identify the right balance between hastening surgery to directly "face" the acute disease and delaying surgery in trying to improve the patient's condition.
Evidence supporting enhanced perioperative care in emergency general surgery.
Currently, available studies about enhanced perioperative care in emergency general surgery are few, sparse and very heterogeneous. In addition, the perioperative care protocol derived from the elective ERAS protocol but with several and substantial differences [ 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 ]. Tables 1 and 2 show in detail the protocols adopted in the evaluated studies. A single perioperative care protocol cannot be identified through the existing literature, and each study applied different interventions.
Huddart et al. demonstrated that the introduction of a bundle evidence care protocol decreased mortality among patients undergoing emergency laparotomy, with a reduction in delayed diagnosis, increased implementation of goal-directed fluid therapy, and improved restoration of biochemical homeostasis [ 29 ]. The bundle protocol consisted in an accurate preoperative assessment with early warning score, early broad-spectrum antibiotics, prompt resuscitation using goal-directed techniques and postoperative ICU admission for all high-risk patients.
Tandberg and colleagues introduced a standardized perioperative care protocol in patients undergoing high-risk emergency abdominal surgery [ 9 ]. The study protocol included consultant-led attention and care, early resuscitation and high-dose antibiotics, surgery within 6 h, perioperative stroke volume-guided volume status optimization, standardized analgesic treatment, early mobilization and early oral feeding. Compared with a historical cohort from the same department, the introduction of the protocol lead to a significant reduction in mortality from 21.8 to 15.5%.
An Italian observational multicentric study demonstrated that adherence to the intraoperative protocol items was low. Major determinants of postoperative compliance were minimally invasive surgery and low intraoperative fluid infusions [ 22 ].
Several other studies investigated the introduction of enhanced perioperative care protocols in emergency general surgery [ 10 , 12 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 22 , 23 , 27 ]. Each study applied a different protocol in different subsets of patients with contrasting results. Some studies adopted a modified ERAS protocol in patients with obstructive colorectal cancer [ 13 , 14 , 16 , 19 ], others on patients with perforated peptic ulcer [ 10 , 15 , 17 ], others on major emergency laparotomy and trauma [ 12 , 18 , 20 , 22 ]. Most of the published enhanced recovery programs in emergency surgery focus on the intra- and postoperative phases of the program, reporting no substantial differences in the preoperative care of patients enrolled in ERAS protocols versus standard “not-ERAS” patients. The majority of the existing studies did not report results on adherence to the protocol items; moreover, also data on compliance to the postoperative pathway were lacking.
The results of some of these studies were included in a meta-analysis published by Hajibandeh et al. published in 2020 [ 30 ]. Despite the great heterogeneity and the poor quality of the evidence, the results showed a reduction in length of stay, pulmonary complications, postoperative ileus and wound infections. No differences were observed in 30-day rehospitalization and 30-day mortality rates.
Despite the promising results, the implementation of an enhanced perioperative care protocol in emergency general surgery may encounter several obstacles. Patients receiving urgent care typically present to medical teams with a complex situation: their conditions at the time of admission are not optimal and they have extremely heterogeneous characteristics [ 31 , 32 ]. The acute illness often leads to several physiological derangements secondary to fasting, vomiting, dehydration, augmented capillary permeability, and metabolic imbalance.
Columbus et al. [ 33 ] have identified two main critical issues concerning the urgent care field: the diversification of patients and the wide range of possible settings and operative contexts (including the hospital organization and the medical team management). Therefore, efforts should focus on improving the structural and organizational aspects. Dedicated medical personnel training and a widespread standardization of the diagnostic and therapeutic process may improve medical performance and, ultimately, the clinical outcome. A recent study demonstrated that the familiarity between surgeon and anesthetist used to work together improve patients’ outcome [ 34 ]. Unfortunately, emergency general surgery is rarely managed by a dedicated staff. Emergency care requires a higher number of specialists and personnel turnover and, therefore, it would lead to wider cross-collaborations and variability in staff composition. In addition, patients undergoing emergency surgery are rarely managed by enhanced recovery-trained anesthetists, surgeons and nurses (working in abdominal surgery), making the development of new treatment protocols very difficult.
The availability of resources is another central tenant to the safe and optimal delivery of surgical care in the emergency setting. For example, laparoscopic facilities or advanced hemodynamic monitoring systems are not universally available, and reported unavailable by some authors, due to logistical issues, timing of surgical interventions (e.g., in office hours vs. after hours), and higher costs [ 18 , 35 ].
The WSES panel promoted the development of this position paper. The work process consisted of two different phases. The first phase was a review of the existing literature about enhanced recovery protocol in emergency general surgery. The second phase was the identification of enhanced recovery protocol items and the development of position statements for each perioperative intervention. This position paper was written according to the WSES methodology [ 36 ]. All the statements contained the level of evidence (LoE) available about the topic, graded according to the GRADE methodology. The consensus on the position paper statements was assessed through a web survey (by Google Form) open to all the members of the steering committee and the experts’ panel, as well as the board of governor members of the WSES. The consensus was reached if a statement was associated with ≥ 70% of the agreement. Otherwise, the statement was re-discussed by email or videoconference, modified, and resubmitted to the experts’ vote until consensus was reached. Table 3 summarizes approved statements.
Preoperative interventions
Education and counseling, patient counseling and education should be encouraged and implemented to explain perioperative risks and post-operative pathway (loe d).
Relieving patient anxiety through preoperative counseling is of utmost importance, especially in an emergent situation. Full preoperative counseling, which is known to reduce post-operative stress, pain and anxiety, may not be possible in the emergency setting. Nevertheless, information such as details of the procedure, possible perioperative complications, the need for the creation of a stoma and length of hospitalization should be communicated with patients and their families before the procedure [ 30 , 37 ]. A recent meta-analysis focusing on the implementation of enhanced recovery protocols in emergency abdominal surgery reported that adapted preoperative counseling was carried out in all of the six included studies. No data about adherence to this counseling were reported [ 30 ]. Depending on the urgency of surgery, preoperative education/counseling may not be possible. However, a recently published multidisciplinary experience reported very high compliance (more than 90% 1 year after implementation) with items such as standardized preoperative patient information and bilateral ostomy marking in patients undergoing emergency general surgery [ 11 , 38 ]. In the case of stoma creation, the implementation of patient education reduced stoma complications and improved postoperative quality of life, reducing the average hospital stay [ 39 ]. However, although it seems feasible and of some utility to appropriately counsel patients before emergency procedures, evidence in support of this hypothesis has not been produced yet and the degree of benefit in terms of postoperative recovery has not been measured.
Fluid balance and volemic status
Volemic status should be evaluated and corrected with goal-directed fluid therapy as soon as possible in the pre-operative phase (loe b).
The majority of emergency general surgery patients present with fluid derangements, mostly related to acute illness, underlying sepsis, prolonged fasting and vomiting. In this setting, preoperative evaluation of the patient should focus on the volemic assessment to rapidly correct alterations in patients' homeostasis, including stress response, gut dysfunction, insulin resistance, electrolyte imbalances, fluid shifts, SIRS and sepsis with varying degrees of organ dysfunction. Although complete optimization of medical conditions cannot be fully achieved in the emergency setting, adequate intravenous fluid resuscitation in emergency general surgery is crucial and feasible, and it should be attempted in all patients. A prospective randomized trial demonstrated better postoperative outcomes when patients were preoperatively managed with a fixed protocol to reach homeostasis [ 40 ]. The adopted protocol defined three targets for the goal-directed crystalloid resuscitation: central venous pressure of 8–12 cmH 2 O, mean arterial pressure > 65 mmHg and urinary output > 0.5 mL/Kg/h. The initial resuscitation should be titrated to the clinical response, such as fluid responsiveness, and not solely guided by a predetermined protocol, with particular attention to the underlying disease. Despite restoring homeostasis should be considered a goal, surgical treatment should not be delayed. According to the indications from the 2016 Surviving Sepsis Guidelines, resuscitation from sepsis-induced hypoperfusion should require at least 30 ml/kg of intravenous crystalloid fluids within the first 3 h [ 41 ]. However, in the updated 2021 version of the Guidelines, the strength of this recommendation was downgraded from “strong” to “weak” (quality of evidence: low) and the recommendation was modified in a suggestion [ 42 ]. Massive fluid therapy has been challenged in the enhanced recovery approach [ 9 ]. Fluid overload should be avoided since it is associated with higher rates of respiratory complications ( i.e., pneumonia, pleural effusion, and respiratory failure) and secondary anastomotic leaks. Early, i.e., preoperative, goal-directed fluid therapy in sepsis was the treatment of the experimental arm in a randomized clinical trial enrolling septic patients published in 2001 [ 43 ]. Excluding patients who needed immediate surgery from the trial, in-hospital mortality was 30.5% in the group assigned to early goal-directed therapy, as compared with 46.5% in the group assigned to standard therapy ( P = 0.009). Tendberg et al. developed a perioperative protocol for emergency high-risk abdominal surgery in which stroke volume-guided hemodynamic optimization before surgery was a key element. The study has shown a significant reduction in mortality as well as postoperative length of ICU stay after the introduction of the standardized protocol [ 9 ]. Therefore, patients should be carefully evaluated and goal-directed fluid resuscitation should be implemented as soon as possible.
Metabolic balance
Glycemic control should be implemented in all emergency surgery patients to prevent both hypo- and hyperglycemia (loe c).
Perioperative hyperglycemia has been demonstrated to be associated with adverse clinical outcomes [ 44 ]. The correction of hyperglycemia with insulin administration and the management of glycemia with the implementation of glycaemic control protocols have been shown to reduce hospital complications and decreases mortality in elective general surgery patients [ 45 ]. Pre-existing diabetes mellitus, acute illness and physiologic changes accompanying a surgical procedure contribute to the worsening of glycemic control. The resulting hyperglycemia due to an abnormal glucose balance is a risk factor for postoperative complications that include poor wound healing and postoperative infections as well as an increase in morbidity, mortality, intensive care unit admission, and hospital length of stay [ 46 ]. Preoperative hyperglycemia has been demonstrated to have a role in postoperative compliance to an enhanced recovery pathway also in emergency surgery patients [ 22 ]. However, in emergency general surgery and in critically ill patients the role of hyperglycemia is more debated and less certain. Hyperglycemia could be considered a marker of organ failure and disease severity. A recent network meta-analysis comparing four different target blood glucose concentrations (< 110, 110–144, 144–180, and > 180 mg/dL) in terms of the benefit and risk of insulin therapy found no significant difference in the risk of mortality and infection among four target blood glucose ranges in critically ill patients, but indicated that target blood glucose levels of below 144 mg/dL were associated with a higher risk of hypoglycemia [ 47 ]. Although a proactive approach to avoid both hyper- and hypoglycemia should be suggested in emergency patients, close glycemic control is advisable and Institutions should develop their own protocols to treat both hyper and hypoglycemia in critically ill patients.
Intraoperative interventions
Postoperative nausea and vomiting (ponv) prevention, ponv prevention with a multimodal approach in an emergency setting should be implemented (loe d).
Prevention of PONV in elective general surgery has become a key element of enhanced recovery protocols [ 48 ]. PONV is very common after general anesthesia and it may negatively impact recovery and short-term outcomes [ 49 ]. Several factors are linked to the occurrence of PONV; however, its exact pathophysiology is still unclear [ 50 ]. Some risk factors are patient-related such as advanced age, female gender, non-smoking status, pain, and anxiety. Other risk factors are related to the type of operative gastro-intestinal manipulation and vagal stimulation, anesthetics, and opioids [ 50 , 51 , 52 ]. Few data are available on emergency patients who frequently complain of nausea and vomiting before surgery in association with anxiety and pain. Several studies investigated the role of different drugs to prevent PONV. The commonest antiemetic drugs are dopamine and serotonin antagonists (e.g., ondansetron) and corticosteroids (e.g., dexamethasone) [ 53 , 54 , 55 , 56 ]. Pre-emptive anesthesia was associated with better pain control and reduction in PONV [ 57 , 58 ].
Other suggested interventions are opioid-sparing anesthesia and avoidance of volatile anesthetics. Unfortunately, the vast majority of evidence is based on elective surgery and very few data are available on emergency general surgery. The emergency setting is associated with more fear, anxiety, pain and, probably, nausea even before surgery. Nevertheless, prevention of PONV should be implemented also in emergency general surgery. Among the interventions suggested, there are opioid-sparing anesthesia, avoidance of volatile anesthetics and a multimodal approach to pharmacological prevention.
Anesthesia and analgesia
General anesthesia warrants proper analgesia, amnesia and muscle relaxation. The ideal general anesthesia protocol should target all these goals, but it should also reduce the need for intraoperative fluids, reduce post-operative residual effects, such as PONV and delirium and it should permit rapid awakening. Several interventions have been implemented to optimize the intraoperative management of the patient. Whether anesthesia should be maintained by a totally intravenous approach or with inhalation drugs still remains uncertain and no recommendations can be made [ 59 ]
Benzodiazepines
Benzodiazepines should be avoided in the emergency anesthetic protocol, in particular in older patients, to reduce delirium risk in the postoperative period (loe c).
The incidence of delirium in the postoperative period has an important impact on clinical outcomes including higher mortality, functional decline, prolonged hospitalizations and risk for institutionalization [ 60 ]. Upon the several risk factors for development, that include acute illness and pain management, medications adopted also for general anesthesia play an important role [ 61 ]. For these reasons, anesthetic protocols should focus on reducing the use of these medications. Benzodiazepines have been linked with the development of delirium in the postoperative period, with a marked effect in elderly and frail patients [ 62 , 63 ]. Despite the potential beneficial effects in treating preoperative anxiety, these drugs should be avoided.
Opioid use should be limited to short-acting drugs in the perioperative period (LoE D)
Opioids are related to several adverse effects such as nausea, vomiting, respiratory depression, sedation and postoperative ileus. Despite their important role in pain management, the undesired effects may impact negatively on patients' recovery. Some experiences exist about opioid-free anesthesia, with the claim of more patient safety [ 64 ]. For this reason, opioids use should be limited to short-acting drugs avoiding morphine to minimize residual effects and to warrant rapid recovery [ 65 ].
Anesthesia depth monitoring
Anesthesia depth monitoring should be implemented in the emergency setting, to minimize anesthesia side effects such intra-operative hypotension, increased need for fluids and postoperative delirium (loe c).
To reduce all the detrimental effects of general anesthetics, such as cognitive effects and vasoactive depressing activity, titrating the minimal needed drug dose guided by the depth of anesthesia monitoring has been recommended. Monitoring of anesthesia depth could be guided by the bispectral index (BIS) or other techniques based on electrical brain activity (EEG). Anesthesia depth monitoring has been demonstrated to be associated with a lower incidence of postoperative delirium and with decreased morbidity [ 66 , 67 , 68 ]. Moreover, depth monitoring has been demonstrated to be associated also with a higher intraoperative mean arterial pressure, possibly reducing the need for fluid administration to maintain adequate systemic perfusion [ 69 ].
Neuromuscular blockade monitoring
Neuromuscular blockade monitoring should be implemented to reduce post-operative morbidity (loe c).
Neuromuscular blockade is needed during abdominal surgery to improve surgical exposure. A post-operative residual neuromuscular block is a risk factor for morbidity and mortality, conditioning weakness of airway muscles, airway obstruction and aspiration with consequent increased postoperative pulmonary complications [ 70 ]. Residual neuromuscular block has been reported in up to 40% of patients treated with neuromuscular blocking agents [ 71 ]. Adopting strategies such as the qualitative monitoring of the peripheral muscular blockade as the train of four (TOF) has been demonstrated to significantly reduce the residual blockade at the end of anesthesia [ 72 ]. Monitoring of the neuromuscular blockade is therefore recommended to avoid potential side effects.
Multimodal pain control
Multimodal analgesia, with a combination of systemic and loco-regional approaches, should be encouraged in the emergency setting to improve pain control and reduce the need for analgesics and opioids (loe c).
Pain is one of the limitations to patient recovery after surgery. Standard general anesthesia warrants analgesia during surgery, but has no effect on pain control after surgery, requiring drug administration with possible detrimental effects such as opioids. Multimodal analgesia has been proposed to manage pain with several different treatments reducing the need for systemic opioids and avoiding their potential side effects [ 73 ]. The association of general and locoregional analgesia has been demonstrated also to reduce the incidence of postoperative delirium [ 74 ].
Thoracic epidural analgesia (TEA) has been demonstrated to be superior to systemic opioids in pain management in open elective abdominal surgery [ 75 ]. A recent Scandinavian population study reported that epidural analgesia was adopted in emergency general surgery in less than one third of patients; epidural analgesia was associated with lower 90-day mortality probably due to a reduction in paralytic ileus and pain that most likely allowed an early mobilization and coughing [ 76 ]. TEA was included in an emergency general surgery enhanced recovery protocol that demonstrated a significant reduction in mortality, despite the adherence to this specific item was not reported [ 9 ]. Spinal analgesia has been proposed as an alternative to epidural analgesia in patients treated with minimally invasive colorectal surgery: the administration of long-acting local anesthetics and opioids warrant pain control in the first postoperative hours allowing early mobilization. Moreover, it has been associated with a lower risk of hypotension and fluid overload [ 77 ]. However, spinal and epidural anesthesia should be considered with caution in septic patients.
Surgical incision is one of the main responsible of postoperative pain. To manage this pain, abdominal wall blockade such as the Transversus abdominis plane (TAP) block has been proposed. The adjunct of abdominal wall blocks to general anesthesia has been demonstrated to have beneficial effects on pain control during the first 24 h and to allow faster recovery and better hemodynamic control in elective abdominal surgery [ 78 , 79 , 80 , 81 ]. Of note, the TAP block can be performed both ultrasound-guided and laparoscopy-guided [ 82 ]. Currently, no studies focus on the performance of the TAP block in emergency general surgery. However, abdominal wall blocks should be considered in a multimodal analgesic approach.
Active warming
Active warming and body temperature monitoring should be encouraged in the emergency setting to reduce postoperative morbidity (loe c).
Body temperature plays an important role in several pathophysiologic mechanisms Hypothermia typically occurs during general and locoregional anesthesia due to vasodilatation and a rapid redistribution of heat from the core to peripheral districts. Moreover, several anesthetic drugs impair thermoregulatory control, further contributing to the maintenance of hypothermia. Finally, the development of hypothermia is facilitated by direct heat loss deriving from the surgical exposure of the abdominal cavity and by the low operating theater temperature. Importantly, perioperative hypothermia implicates an increased risk of surgical site infection, morbidity and mortality. Moreover, hypothermia may alter drug metabolism and it is also associated with an increased risk for coagulopathy and a consequent increased blood loss [ 83 ]. Body temperature monitoring is therefore mandatory and allows temperature correction with active warming. Active warming, ideally starting before the entrance to the operating room, has been recognized as one of the core items of the enhanced recovery pathway and its implementation significantly reduced postoperative morbidity [ 84 , 85 ].
Fluid management
Fluids should be managed within a goal-directed fluid therapy strategy to target the amount of given fluids on patient needs (loe c).
General anesthetics lead to dose-depend myocardial depression and systemic vasodilatation. The associated increased venous capacitance leads to a relative hypovolemia that, along with myocardial depression, might lead to hypotension, and organ hypoperfusion with the related consequences. Therefore, during surgery, fluids are frequently administered to maintain an adequate intravascular volume status and systemic perfusion. However, both hypovolemia and hypervolemia are associated with postoperative morbidity and several studies demonstrated the J-shaped relation between intraoperative fluids administered and postoperative morbidity [ 86 , 87 , 88 ]. Intraoperative fluid management should therefore be balanced, giving the needed amounts of fluids to warrant euvolemia and systemic perfusion, but avoiding fluid overload [ 89 , 90 ]. Fluid overload is associated with several detrimental effects related to tissue edema. Increased interstitial fluids might impair gas exchange with consequent respiratory failure and foster the development of pneumonia. Moreover, fluid overload is associated with bowel edema and postoperative ileus, conditioning a delayed recovery of GI function [ 91 ]. For these reasons in elective surgery, a restrictive fluid strategy has been proposed, with the target of a near-zero fluid balance during surgery and a limited amount of fluids given (generally around 3 mL/Kg/h) [ 92 ]. This approach is valid under the condition that patients arrive at the surgery in perfect homeostasis without fluid derangements.
Several factors may worsen and make fluid management in emergency surgery patients more difficult. Increased vascular permeability related to acute illness, preoperative fasting, preoperative dehydration and blood loss may dramatically increase the need for intraoperative fluids compared to elective surgical patients. In this complex scenario, goal-directed fluid therapy has been proposed to titrate and balance the amount of fluids. Fluid therapy should be guided by hemodynamic monitoring systems, ideally capable of monitoring dynamic parameters, such as cardiac output, stroke volume variation, pulse pressure variation and stroke volume variation [ 93 , 94 ]. The implementation of an intraoperative goal-directed fluid strategy, associated with restrictive fluid regimens and the early adoption of vasopressors to maintain adequate circulating volumes has been demonstrated to significantly reduce perioperative morbidity [ 94 ]. While only few studies exist on fluid management during general emergency surgery, available evidence derived from elective surgery and current pathophysiological understanding strongly underlines the importance of reasoned fluid management during emergency surgery. In the emergency setting, a recent study highlighted the importance of fluid therapy, with a negative correlation between increasing intraoperative fluids given and patients' recovery [ 22 ].
Minimally invasive surgery
Minimally invasive surgery approach in emergency surgery should be encouraged whenever possible and needed skills are available (loe c).
Reducing surgical stress is the cornerstone of an enhanced perioperative care protocol. The use of minimally invasive surgery in elective major surgery has been demonstrated to reduce inflammation, improve pulmonary function, and facilitate GI function with a consequent reduction in morbidity and length of stay [ 95 , 96 , 97 ]. Minimally invasive surgery, even within an enhanced recovery pathway, has been associated with a faster recovery when compared with open surgery [ 98 ]. In emergency major abdominal surgery, such as repair for perforated peptic ulcer and colorectal surgery invasive minimally techniques have been associated with better clinical outcomes with a lower mortality and length of stay [ 99 , 100 , 101 ]. A population study on the commonest abdominal surgical emergencies in the USA demonstrated an increasing trend of a laparoscopic approach. Minimally invasive surgery was associated with lower mortality, surgical site infection rate and length of stay. However, minimally invasive surgery in major interventions such as peptic ulcer repair and small bowel obstruction was adopted in less than 40% and 10%, respectively [ 102 ]. Data from the national emergency laparotomy audit (NELA) from the U.K. demonstrated that laparoscopy is adopted in less than 20% of major surgeries [ 99 ]. Existing data demonstrated the beneficial effect of minimally invasive surgery but also its poor diffusion among surgeons with several difficulties [ 103 ]. A recent prospective study identified minimally invasive surgery as the major determinant of postoperative compliance to an enhanced recovery protocol [ 22 ]. Efforts should be made to implement laparoscopy in emergency general surgery daily practice.
Abdominal drains should be placed for limited indications, including in the presence of gross bacterial contamination and inadequate source control (LoE D)
The routine positioning of a peritoneal drain after elective major colorectal surgery has been demonstrated to be ineffective in preventing surgical complications and is not recommended [ 104 ]. Moreover, the presence of a drain has been identified as one of the main failure predictors of an enhanced recovery pathway, both in elective and emergency surgery [ 22 , 105 ]. Drain in emergency general surgery is justified by a clear rationale, in case of contaminated surgical field and intra-abdominal infections. Few experiences exist about avoiding drains in emergency general surgery: some studies focused on the introduction of enhanced perioperative care protocol on colorectal emergencies (obstructions) demonstrated better results avoiding the drain (along with other interventions) [ 13 , 14 , 16 ]; other studies demonstrated the safety of an early removal in perforated peptic ulcer and trauma [ 15 , 20 ]. Evidence quality is very low to recommend avoiding abdominal drains, but we believe drains should be placed only in case of gross abdominal contamination and high risk for collection and abdominal abscess.
Postoperative care
Multimodal analgesia, using different classes of analgesics and avoiding long-acting opioids, should be recommended in the postoperative phase (loe c).
Proper analgesia and pain control are key elements of a patient’s recovery after surgery. The control of pain in the postoperative period is the result of many several factors related to patients' characteristics, invasiveness of surgical intervention, the underlying diagnosis and adopted intra- and post-operative analgesia techniques. Perioperative management should be focused on maximizing the effect of pain control and avoiding the side effects of drugs. The use of long-acting opioids, such as morphine, should be ideally avoided also in the postoperative period. Indeed, avoiding opioids has been demonstrated to facilitate mobilization and to fasten GI function recovery [ 65 ]. The treatment of pain should be multimodal and tailored to patients’ conditions, according to available skills [ 106 ].
Early nasogastric tube removal
The nasogastric tube should be removed as soon as possible, even at the end of surgery (loe d).
According to a reactive policy, the nasogastric tube (NGT) was traditionally removed after GI function recovery to prevent PONV and inhalation. Enhanced recovery protocols recommend the removal of NGT at the end of elective surgery. This practice reduced pulmonary complications and promoted GI function recovery [ 107 ]. Preliminary studies carried out in patients with obstructive colorectal cancer or perforated peptic ulcer reported a high patient compliance to NGT removal at the end of surgery [ 17 , 19 , 108 ]. Other studies suggested removing the NGT when the output was less than 300 ml [ 15 , 18 ]. When patients are managed according to enhanced recovery protocols, the early removal of NGT is safe and should be implemented in clinical practice.
Early mobilization
Early mobilization should be encouraged and stimulated as soon as possible to reduce post-operative morbidity (loe c).
Prolonged immobilization is associated with insulin resistance, thromboembolic events and respiratory complications [ 109 ]. Several studies reported that early mobilization after surgery reduced overall morbidity and shortened the length of hospital stay [ 110 , 111 , 112 , 113 ]. Several factors can negatively impact on patient’s mobilization such as abdominal drain, urinary catheter, suboptimal pain control, prolonged i.v fluids, and patient's motivation. In emergency surgery, different protocols have been proposed targeting mobilization the same day of surgery [ 15 , 18 ] or on postoperative day 1 [ 14 , 16 , 19 ]. According to existing evidence, patient mobilization should be encouraged as early as possible, along with all the interventions that could facilitate it, such as proper pain control, and the early removal of urinary catheter and drains.
Nutrition and early oral feeding
Early oral feeding should be encouraged and promoted as soon as tolerated by patients (loe c).
The close relationship between preoperative nutritional status and surgical outcomes has been extensively reported in elective surgery, where tailored nutritional and prehabilitation programs can be planned before the operation [ 114 ]. Postoperative fasting has been demonstrated to be harmful in elective surgery with delayed recovery and increased complications[ 2 , 115 , 116 ]. Oral feeding can be resumed early after surgery regardless of bowel canalization, whether removal of the nasogastric tube, PONV prophylaxis, near zero fluid balance, early mobilization, and pain control have been carried out according to enhanced recovery protocol. Patients undergoing emergency surgery often have an altered metabolic status, with dehydration and several derangements such as prolonged fasting, vomiting, impairment of GI function, and fluid loss related to the acute illness. The great condition's heterogeneity in emergency surgery patients makes quite impossible to standardize the timing of oral feeding recovery. However, studies carried out in patients with perforated peptic ulcer or obstructive colorectal cancer demonstrated both feasibility and safety of early oral feeding [ 19 , 20 , 117 ]. Perioperative nutritional intervention should be therefore tailored to the patient's conditions adopting as the target the earliest possible recovery.
Urinary catheter removal
Urinary catheter should be removed as soon as possible when urinary output no longer needs to be monitored (loe c).
Urinary output monitoring is a key element to assess patients' volemic status and to guide goal-directed fluid therapy. In emergency surgery patients, the urine output target should be 0.5 ml/Kg/h. Different policies about the timing of catheter removal have been proposed: immediately after surgery in a randomized study on perforated peptic ulcer patients [ 17 ], on postoperative day 1 [ 19 , 20 ] or according to urinary output (> 1 ml/Kg/h) [ 15 , 18 ]. Regardless, the urinary catheter should be removed as early as possible after reaching the minimum urinary output target to facilitate mobilization and reduce infections.

Postoperative fluids
Postoperative intravenous fluids should be minimized and maintained until oral fluid intake is adequate (loe c).
Fluid therapy should be targeted to restore the euvolemic status and to maintain adequate hydration and tissue perfusion until the oral intake can be restarted. As reported for operative management, fluid therapy can be harmful if too many or too few fluids are given [ 86 , 87 , 88 ]. Following elective colorectal surgery i.v. fluids should be stopped on postoperative day one. Studies performed on emergency surgery patients did not report on timing to stop i.v fluids; however, infusions should be tailored to patient conditions, giving the minimum fluid amount to restore and maintain euvolemia and to obtain adequate perfusion.
Antibiotic therapy
Antibiotic therapy should not be continued in case of non-complicated intra-abdominal infections, while a short course antibiotic therapy is indicated in case of complicated infection (LoE A).
A large part of emergency patients undergo surgery for intra-abdominal infections; therefore, antibiotic therapy is a cornerstone of treatment along with surgical source control . The need for antibiotics during the postoperative period may contribute to delaying patient recovery, as an obstacle to active mobilization and i.v. infusions suspension; moreover, prolonged antibiotic therapies may have a role in delaying home return. Postoperative antibiotic therapy should be reserved for patients with complicated intra-abdominal infections. In these patients, a short therapy (3–5 days) after adequate surgical source control is not inferior when compared to longer therapy [ 118 , 119 , 120 ]. In non-complicated infections, antibiotic therapy should be stopped at the end of surgery if the source control is adequate.
The majority of patients presenting with a severe infection who initially require IV therapy can be switched to oral therapy after 24–48 h provided that they are improving clinically and can tolerate an oral formulation. The switch from IV to oral route should be encouraged.
Research agenda
The present position paper highlights the great heterogeneity of protocols adopted and the lack of good-quality evidence supporting the implementation of enhanced recovery pathway in emergency general surgery. Further studies on this topic should address:
The definition of the safety, feasibility and effectiveness of each perioperative intervention.
The definition of a standardized enhanced recovery protocol for emergency general surgery procedures
The selection of patients who may benefit from an enhanced recovery pathway and the clinical scenarios in which enhanced recovery pathway could be applied.
Conclusions
Enhanced perioperative care, similar to elective surgery, should be implemented in emergency general surgery. One of the key elements for the success of the enhanced pathways is the multimodal approach involving surgeons, anesthetists, ICU physicians, nurses, patients and patient families. Available evidence suggests future required research on the implementation of enhanced recovery pathways in clinical practice.
Availability of data and materials
Data are available under request to the corresponding author.
Change history
15 october 2023.
The CRUE CSIC TA funding note has been removed
Ljungqvist O, Scott M, Fearon KC. Enhanced recovery after surgery: a review. JAMA Surg [Internet]. 2017;152:292–8.
PubMed Google Scholar
Greco M, Capretti G, Beretta L, Gemma M, Pecorelli N, Braga M. Enhanced recovery program in colorectal surgery: a meta-analysis of randomized controlled trials. World J Surg [Internet]. 2014;38:1531–41.
Lee Y, Yu J, Doumouras AG, Li J, Hong D. Enhanced recovery after surgery (ERAS) versus standard recovery for elective gastric cancer surgery: a meta-analysis of randomized controlled trials. Surg Oncol. 2020;32:75–87.
Ni X, Jia D, Chen Y, Wang L, Suo J. Is the enhanced recovery after surgery (ERAS) program effective and safe in laparoscopic colorectal cancer surgery? A meta-analysis of randomized controlled trials. J Gastrointest Surg [Internet]. 2019;23:1502–12.
Ni X, Jia D, Guo Y, Sun X, Suo J. The efficacy and safety of enhanced recovery after surgery (ERAS) program in laparoscopic digestive system surgery: a meta-analysis of randomized controlled trials. Int J Surg. 2019;69:108–15.
Ceresoli M, Braga M. Reply to: Early non compliance to enhanced recovery pathway might be an alert for underlying complications following colon surgery. Eur J Surg Oncol. 2023;49:526.
Quiney N, Aggarwal G, Scott M, Dickinson M. Survival after emergency general surgery: what can we learn from enhanced recovery programmes? World J Surg [Internet]. 2016;40:1283–7. https://doi.org/10.1007/s00268-016-3418-0 .
Article CAS PubMed Google Scholar
Aggarwal G, Peden CJ, Mohammed MA, Pullyblank A, Williams B, Stephens T, et al. Evaluation of the collaborative use of an evidence-based care bundle in emergency laparotomy. JAMA Surg [Internet]. 2019;154:e190145.
Tengberg LT, Bay-Nielsen M, Bisgaard T, Cihoric M, Lauritsen ML, Foss NB, et al. Multidisciplinary perioperative protocol in patients undergoing acute high-risk abdominal surgery. Br J Surg [Internet]. 2017;104:463–71.
CAS PubMed Google Scholar
Møller MH, Adamsen S, Thomsen RW, Møller AM. Multicentre trial of a perioperative protocol to reduce mortality in patients with peptic ulcer perforation. Br J Surg. 2011;98:802–10.
Burcharth J, Falkenberg A, Oreskov JO, Ekeloef S, Gögenur I. Patients’ perceptions of barriers to enhanced recovery after emergency abdominal surgery. Langenbecks Arch Surg. 2021;406:405–12.
Wisely JC, Barclay KL. Effects of an Enhanced Recovery After Surgery programme on emergency surgical patients. ANZ J Surg. 2016;86:883–8.
Lohsiriwat V. Enhanced recovery after surgery for emergency colorectal surgery: Are there any differences between intra-abdominal infection and other indications? J Visc Surg [Internet]. 2019;156:489–96.
Lohsiriwat V. Enhanced recovery after surgery vs conventional care in emergency colorectal surgery. World J Gastroenterol [Internet]. 2014;20:13950.
Mohsina S, Shanmugam D, Sureshkumar S, Kundra P, Mahalakshmy T, Kate V. Adapted ERAS pathway vs. standard care in patients with perforated duodenal ulcer—a randomized controlled trial. J Gastrointest Surg [Internet]. 2018;22:107–16. https://doi.org/10.1007/s11605-017-3474-2 .
Article PubMed Google Scholar
Shang Y, Guo C, Zhang D. Modified enhanced recovery after surgery protocols are beneficial for postoperative recovery for patients undergoing emergency surgery for obstructive colorectal cancer. Medicine [Internet]. 2018;97:e12348. Available from: https://journals.lww.com/00005792-201809280-00034 .
Gonenc M, Dural AC, Celik F, Akarsu C, Kocatas A, Kalayci MU, et al. Enhanced postoperative recovery pathways in emergency surgery: a randomised controlled clinical trial. Am J Surg [Internet]. 2014;207:807–14. https://doi.org/10.1016/j.amjsurg.2013.07.025 .
Pranavi AR, Sureshkumar S, Mahalakshmy T, Kundra P, Kate V. Adapted ERAS pathway versus standard care in patients undergoing emergency surgery for perforation peritonitis—a randomized controlled trial. J Gastrointest Surg [Internet]. 2022;26:39–49. https://doi.org/10.1007/s11605-021-05184-x .
Roulin D, Blanc C, Muradbegovic M, Hahnloser D, Demartines N, Hübner M. Enhanced recovery pathway for urgent colectomy. World J Surg [Internet]. 2014;38:2153–9. https://doi.org/10.1007/s00268-014-2518-y .
Purushothaman V, Priyadarshini P, Bagaria D, Joshi M, Choudhary N, Kumar A, et al. Enhanced recovery after surgery (ERAS) in patients undergoing emergency laparotomy after trauma: a prospective, randomized controlled trial. Trauma Surg Acute Care Open [Internet]. 2021;6:e000698.
Nechay T, Titkova S, Tyagunov A, Anurov M, Sazhin A. Modified enhanced recovery after surgery protocol in patients with acute cholecystitis: efficacy, safety and feasibility. Multicenter randomized control study. Updates Surg. 2021;73:1407–17.
Ceresoli M, Biloslavo A, Bisagni P, Ciuffa C, Fortuna L, La Greca A, et al. Implementing enhanced perioperative care in emergency general surgery: a prospective multicenter observational study. World J Surg [Internet]. 2023. https://doi.org/10.1007/s00268-023-06984-9 .
Sharma J, Kumar N, Huda F, Payal YS. Enhanced recovery after surgery protocol in emergency laparotomy: a randomized control study. Surg J. 2021;07:e92–9.
Google Scholar
Masood A, Viqar S, Zia N, Ghani M usman. Early oral feeding compared with traditional postoperative care in patients undergoing emergency abdominal surgery for perforated duodenal ulcer. Cureus. 2021.
Chndan MN, Khakholia M, Bhuyan K. Enhanced recovery after surgery (ERAS) versus standard care in patients undergoing emergency surgery for perforated peptic ulcer. Indian J Surg. 2020;82:1044–9.
Ruiz-Tovar J, Llavero C, Perez-Lopez M, Garcia-Marin A. Implementation of an enhanced recovery after surgery (ERAS) protocol for acute complicated and uncomplicated appendicitis. Tech Coloproctol. 2021;25:1073–8.
Saurabh K, Sureshkumar S, Mohsina S, Mahalakshmy T, Kundra P, Kate V. Adapted ERAS pathway versus standard care in patients undergoing emergency small bowel surgery: a randomized controlled trial. J Gastrointest Surg [Internet]. 2020;24:2077–87.
Pathrikar SG, Jadhav GS, Adhikari GR. The application of enhanced recovery after surgery protocols in patients with perforated duodenal ulcer. Cureus. 2023.
Huddart S, Peden CJ, Swart M, McCormick B, Dickinson M, Mohammed MA, et al. Use of a pathway quality improvement care bundle to reduce mortality after emergency laparotomy. Br J Surg [Internet]. 2015;102:57–66.
Hajibandeh S, Hajibandeh S, Bill V, Satyadas T. Meta-analysis of enhanced recovery after surgery (ERAS) protocols in emergency abdominal surgery. World J Surg [Internet]. 2020;44:1336–48. https://doi.org/10.1007/s00268-019-05357-5 .
Lee KC, Sturgeon D, Lipsitz S, Weissman JS, Mitchell S, Cooper Z. Mortality and health care utilization among medicare patients undergoing emergency general surgery vs those with acute medical conditions. JAMA Surg. 2020;155:216.
Quiney N, Aggarwal G, Scott M, Dickinson M. Survival after emergency general surgery: what can we learn from enhanced recovery programmes? World J Surg. 2016;40:1283–7.
Columbus AB, Morris MA, Lilley EJ, Harlow AF, Haider AH, Salim A, et al. Critical differences between elective and emergency surgery: identifying domains for quality improvement in emergency general surgery. Surgery [Internet]. 2018;163:832–8.
Hallet J, Sutradhar R, Jerath A, Perez D’empaire P, Carrier F, Turgeon A, et al. Association between familiarity of the surgeon-anesthesiologist dyad and postoperative patient outcomes for complex gastrointestinal cancer surgery. JAMA Surg [Internet]. 2023.
Puccetti F, Elmore U, Rosati R. Application of ERAS protocols in esophagogastric emergency surgery: is it feasible and does it make sense? Updates Surg. 2023;75:383–7.
Bala M, Kashuk J, Moore EE, Catena F, Leppaniemi A, Ansaloni L, et al. Establishing position papers by the WSES. World J Emerg Surg. 2018;13:1.
CAS PubMed PubMed Central Google Scholar
Shuldham C. A review of the impact of pre-operative education on recovery from surgery. Int J Nurs Stud. 1999;36:171–7.
Burcharth J, Abdulhady L, Danker J, Ekeloef S, Jørgensen T, Lauridsen H, et al. Implementation of a multidisciplinary perioperative protocol in major emergency abdominal surgery. Eur J Trauma Emerg Surg [Internet]. 2021;47:467–77. https://doi.org/10.1007/s00068-019-01238-7 .
Ferrara F, Parini D, Bondurri A, Veltri M, Barbierato M, Pata F, et al. Italian guidelines for the surgical management of enteral stomas in adults. Tech Coloproctol. 2019;23:1037–56.
Sethi A, Debbarma M, Narang N, Saxena A, Mahobia M, Tomar GS. Impact of targeted preoperative optimization on clinical outcome in emergency abdominal surgeries: a prospective randomized trial. Anesth Essays Res [Internet]. 2018;12:149.
Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, et al. Surviving sepsis campaign. Crit Care Med. 2017;45:486–552.
Evans L, Rhodes A, Alhazzani W, Antonelli M, Coopersmith CM, French C, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Crit Care Med. 2021;49:e1063–143.
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med [Internet]. 2001;345:1368–77. https://doi.org/10.1056/NEJMoa010307 .
Duggan EW, Carlson K, Umpierrez GE. Perioperative hyperglycemia management. Anesthesiology. 2017;126:547–60.
Umpierrez GE, Smiley D, Jacobs S, Peng L, Temponi A, Mulligan P, et al. Randomized study of basal-bolus insulin therapy in the inpatient management of patients with type 2 diabetes undergoing general surgery (RABBIT 2 Surgery). Diabetes Care. 2011;34:256–61.
Jehan F, Joseph B. Perioperative glycemic control and postoperative complications in patients undergoing emergency general surgery: what is the role of HbA1c? J Trauma Acute Care Surg. 2019;86:379–379.
Yatabe T, Inoue S, Sakaguchi M, Egi M. The optimal target for acute glycemic control in critically ill patients: a network meta-analysis. Intensive Care Med. 2017;43:16–28.
Gustafsson UO, Scott MJ, Hubner M, Nygren J, Demartines N, Francis N, et al. Guidelines for perioperative care in elective colorectal surgery: enhanced recovery after surgery (ERAS®) society recommendations: 2018. World J Surg [Internet]. 2019;43:659–95.
Koivuranta M, Läärä E, Snåre L, Alahuhta S. A survey of postoperative nausea and vomiting. Anaesthesia [Internet]. 1997;52:443–9.
Horn CC, Wallisch WJ, Homanics GE, Williams JP. Pathophysiological and neurochemical mechanisms of postoperative nausea and vomiting. Eur J Pharmacol [Internet]. 2014;722:55–66.
Veiga-Gil L, Pueyo J, López-Olaondo L. Postoperative nausea and vomiting: physiopathology, risk factors, prophylaxis and treatment. Rev Esp Anestesiol Reanim [Internet]. 2017;64:223–32.
Cozza V, Barberis L, Altieri G, Donatelli M, Sganga G, Greca A la. Prediction of postoperative nausea and vomiting by point-of-care gastric ultrasound: can we improve complications and length of stay in emergency surgery? A cohort study. 2021. https://doi.org/10.1186/s12871-021-01428-0 .
de Oliveira GS, Castro-Alves LJS, Ahmad S, Kendall MC, McCarthy RJ. Dexamethasone to prevent postoperative nausea and vomiting: an updated meta-analysis of randomized controlled trials. Anesth Analg [Internet]. 2013;116:58–74.
Eberhart LHJ, Mauch M, Morin AM, Wulf H, Geldner G. Impact of a multimodal anti-emetic prophylaxis on patient satisfaction in high-risk patients for postoperative nausea and vomiting. Anaesthesia [Internet]. 2002;57:1022–7.
Apfel CC, Bacher A, Biedler A, Danner K, Danzeisen O, Eberhart LHJ, et al. A factorial trial of six interventions for the prevention of postoperative nausea and vomiting. Anaesthesist [Internet]. 2005;54:201–9.
Polderman JA, Farhang-Razi V, van Dieren S, Kranke P, DeVries JH, Hollmann MW, et al. Adverse side effects of dexamethasone in surgical patients. Cochrane Database Syst Rev [Internet] 2018;11.
Doleman B, Leonardi-Bee J, Heinink TP, Boyd-Carson H, Carrick L, Mandalia R, et al. Pre-emptive and preventive NSAIDs for postoperative pain in adults undergoing all types of surgery. Cochrane Database Syst Rev [Internet] 2021;6.
Apfel CC, Turan A, Souza K, Pergolizzi J, Hornuss C. Intravenous acetaminophen reduces postoperative nausea and vomiting: a systematic review and meta-analysis. Pain [Internet]. 2013;154:677–89.
Miller D, Lewis SR, Pritchard MW, Schofield-Robinson OJ, Shelton CL, Alderson P, et al. Intravenous versus inhalational maintenance of anaesthesia for postoperative cognitive outcomes in elderly people undergoing non-cardiac surgery. Cochrane Database Syst Rev [Internet] 2018;8.
Saljuqi AT, Hanna K, Asmar S, Tang A, Zeeshan M, Gries L, et al. Prospective evaluation of delirium in geriatric patients undergoing emergency general surgery. J Am Coll Surg [Internet]. 2020;230:758–65.
Moller JT, Cluitmans P, Rasmussen LS, Houx P, Rasmussen H, Canet J, et al. Long-term postoperative cognitive dysfunction in the elderly: ISPOCD1 study. Lancet [Internet]. 1998;351:857–61.
Clegg A, Young JB. Which medications to avoid in people at risk of delirium: a systematic review. Age Ageing [Internet]. 2011;40:23–9.
Duprey MS, Devlin JW, Griffith JL, Travison TG, Briesacher BA, Jones R, et al. Association between perioperative medication use and postoperative delirium and cognition in older adults undergoing elective noncardiac surgery. Anesth Analg [Internet]. 2022;134:1154–63.
McLott J, Stahel PF. Opioid-free anesthesia: the next frontier in surgical patient safety. Patient Saf Surg. BioMed Central Ltd; 2022.
Wick EC, Grant MC, Wu CL. Postoperative multimodal analgesia pain management with nonopioid analgesics and techniques: a review. JAMA Surg [Internet]. 2017;152:691–7.
Chan MTV, Cheng BCP, Lee TMC, Gin T. BIS-guided anesthesia decreases postoperative delirium and cognitive decline. J Neurosurg Anesthesiol [Internet]. 2013;25:33–42.
Zorrilla-Vaca A, Healy RJ, Wu CL, Grant MC. Relation between bispectral index measurements of anesthetic depth and postoperative mortality: a meta-analysis of observational studies. Can J Anaesth [Internet]. 2017;64:597–607.
Evered LA, Chan MTV, Han R, Chu MHM, Cheng BP, Scott DA, et al. Anaesthetic depth and delirium after major surgery: a randomised clinical trial. Br J Anaesth [Internet]. 2021;127:704–12.
Short TG, Campbell D, Frampton C, Chan MTV, Myles PS, Corcoran TB, et al. Anaesthetic depth and complications after major surgery: an international, randomised controlled trial. Lancet [Internet]. 2019;394:1907–14.
Berg H, Viby-Mogensen J, Roed J, Mortensen CR, Engbæk J, Skovgaard LT, et al. Residual neuromuscular block is a risk factor for postoperative pulmonary complications. A prospective, randomised, and blinded study of postoperative pulmonary complications after atracurium, vecuronium and pancuronium. Acta Anaesthesiol Scand [Internet]. 1997;41:1095–103.
Naguib M, Kopman AF, Ensor JE. Neuromuscular monitoring and postoperative residual curarisation: a meta-analysis. Br J Anaesth [Internet]. 2007;98:302–16.
Carvalho H, Verdonck M, Cools W, Geerts L, Forget P, Poelaert J. Forty years of neuromuscular monitoring and postoperative residual curarisation: a meta-analysis and evaluation of confidence in network meta-analysis. Br J Anaesth [Internet]. 2020;125:466–82.
Carli F, Kehlet H, Baldini G, Steel A, McRae K, Slinger P, et al. Evidence basis for regional anesthesia in multidisciplinary fast-track surgical care pathways. Reg Anesth Pain Med [Internet]. 2011;36:63–72.
Li YW, Li HJ, Li HJ, Zhao BJ, Guo XY, Feng Y, et al. Delirium in older patients after combined epidural-general anesthesia or general anesthesia for major surgery: a randomized trial. Anesthesiology [Internet]. 2021;135:218–32.
Werawatganon T, Charuluxananan S. Patient controlled intravenous opioid analgesia versus continuous epidural analgesia for pain after intra-abdominal surgery. Cochrane Database Syst Rev [Internet]. 2013. https://doi.org/10.1002/14651858.CD004088.pub3/full .
Vester-Andersen M, Lundstrøm LH, Møller MH. The association between epidural analgesia and mortality in emergency abdominal surgery: a population-based cohort study. Acta Anaesthesiol Scand [Internet]. 2020;64:104–11.
Hübner M, Blanc C, Roulin D, Winiker M, Gander S, Demartines N. Randomized clinical trial on epidural versus patient-controlled analgesia for laparoscopic colorectal surgery within an enhanced recovery pathway. Ann Surg [Internet]. 2015;261:648–53.
Tsuchiya M, Takahashi R, Furukawa A, Suehiro K, Mizutani K, Nishikawa K. Transversus abdominis plane block in combination with general anesthesia provides better intraoperative hemodynamic control and quicker recovery than general anesthesia alone in high-risk abdominal surgery patients. Minerva Anestesiol [Internet]. 2012;78:1241–7.
McDonnell JG, O’Donnell B, Curley G, Heffernan A, Power C, Laffey JG. The analgesic efficacy of transversus abdominis plane block after abdominal surgery: A prospective randomized controlled trial. Anesth Analg [Internet]. 2007;104:193–7.
Walter CJ, Maxwell-Armstrong C, Pinkney TD, Conaghan PJ, Bedforth N, Gornall CB, et al. A randomised controlled trial of the efficacy of ultrasound-guided transversus abdominis plane (TAP) block in laparoscopic colorectal surgery. Surg Endosc [Internet]. 2013;27:2366–72.
Tikuisis R, Miliauskas P, Lukoseviciene V, Samalavicius N, Dulskas A, Zabuliene L, et al. Transversus abdominis plane block for postoperative pain relief after hand-assisted laparoscopic colon surgery: a randomized, placebo-controlled clinical trial. Tech Coloproctol [Internet]. 2016;20:835–44.
Hamid HK, Emile SH, Saber AA, Ruiz-Tovar J, Minas V, Cataldo TE. Laparoscopic-guided transversus abdominis plane block for postoperative pain management in minimally invasive surgery: systematic review and meta-analysis. J Am Coll Surg [Internet]. 2020;231:376-386.e15.
Billeter AT, Hohmann SF, Druen D, Cannon R, Polk HC. Unintentional perioperative hypothermia is associated with severe complications and high mortality in elective operations. Surgery [Internet]. 2014;156:1245–52.
Braga M, Scatizzi M, Borghi F, Missana G, Radrizzani D, Gemma M, et al. Identification of core items in the enhanced recovery pathway. Clin Nutr ESPEN. 2018;25:139–44.
Balki I, Khan JS, Staibano P, Duceppe E, Bessissow A, Sloan EN, et al. Effect of perioperative active body surface warming systems on analgesic and clinical outcomes: a systematic review and meta-analysis of randomized controlled trials. Anesth Analg. 2020;131:1430–43.
Bellamy MC. Wet, dry or something else? Br J Anaesth [Internet]. 2006;97:755–7.
Shin CH, Long DR, McLean D, Grabitz SD, Ladha K, Timm FP, et al. Effects of intraoperative fluid management on postoperative outcomes: a hospital registry study. Ann Surg [Internet]. 2018;267:1084–92.
Thacker JKM, Mountford WK, Ernst FR, Krukas MR, Mythen MG. Perioperative fluid utilization variability and association with outcomes: considerations for enhanced recovery efforts in sample US surgical populations. Ann Surg [Internet]. 2016;263:502–10.
Lowell JA, Schifferdecker C, Driscoll DF, Benotti PN, Bistrian BR. Postoperative fluid overload: not a benign problem. Crit Care Med [Internet]. 1990;18:728–33.
Nisanevich V. Effect of intraoperative fluid management on outcome after intraabdominal surgery. Anesthesiology [Internet]. 2005;103:25–32.
Holte K, Sharrock NE, Kehlet H. Pathophysiology and clinical implications of perioperative fluid excess. Br J Anaesth [Internet]. 2002;89:622–32.
Brandstrup B. Fluid therapy for the surgical patient. Best Pract Res Clin Anaesthesiol [Internet]. 2006;20:265–83.
Bundgaard-Nielsen M, Holte K, Secher NH, Kehlet H. Monitoring of peri-operative fluid administration by individualized goal-directed therapy. Acta Anaesthesiol Scand [Internet]. 2007;51:331–40.
Jessen MK, Vallentin MF, Holmberg MJ, Bolther M, Hansen FB, Holst JM, et al. Goal-directed haemodynamic therapy during general anaesthesia for noncardiac surgery: a systematic review and meta-analysis. Br J Anaesth. 2022;128:416–33.
Mamidanna R, Burns EM, Bottle A, Aylin P, Stonell C, Hanna GB, et al. Reduced risk of medical morbidity and mortality in patients selected for laparoscopic colorectal resection in England: a population-based study. Arch Surg [Internet]. 2012;147:219–27.
Kehlet H. Surgical stress response: does endoscopic surgery confer an advantage? World J Surg [Internet]. 1999;23:801–7.
Novitsky YW, Litwin DEM, Callery MP. The net immunologic advantage of laparoscopic surgery. Surg Endosc [Internet]. 2004;18:1411–9.
Braga M, Borghi F, Scatizzi M, Missana G, Guicciardi MA, Bona S, et al. Impact of laparoscopy on adherence to an enhanced recovery pathway and readiness for discharge in elective colorectal surgery: results from the PeriOperative Italian Society registry. Surg Endosc [Internet]. 2017;31:4393–9. https://doi.org/10.1007/s00464-017-5486-0 .
Pucher PH, Mackenzie H, Tucker V, Mercer SJ. A national propensity score-matched analysis of emergency laparoscopic versus open abdominal surgery. Br J Surg [Internet]. 2021;108:934–40.
Tan S, Wu G, Zhuang Q, Xi Q, Meng Q, Jiang Y, et al. Laparoscopic versus open repair for perforated peptic ulcer: a meta analysis of randomized controlled trials. Int J Surg. 2016;33:124–32.
Warps A-LK, Zwanenburg ES, Dekker JWT, Tollenaar RAEM, Bemelman WA, Hompes R, et al. Laparoscopic versus open colorectal surgery in the emergency setting. Ann Surg Open. 2021;2:e097.
PubMed PubMed Central Google Scholar
Arnold M, Elhage S, Schiffern L, Lauren Paton B, Ross SW, Matthews BD, et al. Use of minimally invasive surgery in emergency general surgery procedures. Surg Endosc [Internet]. 2020;34:2258–65. https://doi.org/10.1007/s00464-019-07016-1 .
Ceresoli M, Pisano M, Abu-Zidan F, Allievi N, Gurusamy K, Biffl WL, et al. Minimally invasive surgery in emergency surgery: a WSES survey. World J Emerg Surg. 2022;17:18.
Zhang HY, Zhao CL, Xie J, Ye YW, Sun JF, Ding ZH, et al. To drain or not to drain in colorectal anastomosis: a meta-analysis. Int J Colorectal Dis [Internet]. 2016;31:951–60.
Chen JS, da Sun S, Wang ZS, Cai TH, Huang LK, Sun WX, et al. The factors related to failure of Enhanced Recovery after Surgery (ERAS) in colon cancer surgery. Langenbecks Arch Surg [Internet]. 2020;405:1025–30.
Coccolini F, Corradi F, Sartelli M, Coimbra R, Kryvoruchko IA, Leppaniemi A, et al. Postoperative pain management in non-traumatic emergency general surgery: WSES-GAIS-SIAARTI-AAST guidelines. World J Emerg Surg [Internet]. 2022;17:1–15.
Nelson R, Edwards S, Tse B. Prophylactic nasogastric decompression after abdominal surgery. Cochrane Database Syst Rev [Internet]. 2007;10:50. https://doi.org/10.1002/14651858.CD004929.pub3/full .
Article Google Scholar
Shang Y, Guo C, Zhang D. Modified enhanced recovery after surgery protocols are beneficial for postoperative recovery for patients undergoing emergency surgery for obstructive colorectal cancer. Medicine [Internet]. 2018;97:e12348.
Brower RG. Consequences of bed rest. Crit Care Med. 2009;37:S422–8.
Wren SM, Martin M, Yoon JK, Bech F. Postoperative pneumonia-prevention program for the inpatient surgical ward. J Am Coll Surg. 2010;210:491–5.
Haines KJ, Skinner EH, Berney S. Association of postoperative pulmonary complications with delayed mobilisation following major abdominal surgery: an observational cohort study. Physiotherapy. 2013;99:119–25.
Castelino T, Fiore JF, Niculiseanu P, Landry T, Augustin B, Feldman LS. The effect of early mobilization protocols on postoperative outcomes following abdominal and thoracic surgery: a systematic review. Surgery. 2016;159:991–1003.
Rosowicz A, Brody JS, Lazar DJ, Bangla VG, Panahi A, Nobel TB, et al. Early ambulation is associated with improved outcomes following colorectal surgery. Am Surg. 2022. https://doi.org/10.1177/00031348221142 .
Gillis C, Carli F. Promoting perioperative metabolic and nutritional care. Anesthesiology. 2015;123:1455–72.
Zhuang C-L, Ye X-Z, Zhang C-J, Dong Q-T, Chen B-C, Yu Z. Early versus traditional postoperative oral feeding in patients undergoing elective colorectal surgery: a meta-analysis of randomized clinical trials. Dig Surg. 2013;30:225–32.
Andersen HK, Lewis SJ, Thomas S. Early enteral nutrition within 24h of colorectal surgery versus later commencement of feeding for postoperative complications. Cochrane Database Syst Rev. 2006.
Gonenc M, Gemici E, Kalayci MU, Karabulut M, Turhan AN, Alis H. Intracorporeal knotting versus metal endoclip application for the closure of the appendiceal stump during laparoscopic appendectomy in uncomplicated appendicitis. J Laparoendosc Adv Surg Tech. 2011;22:231–5.
Sawyer RG, Claridge JA, Nathens AB, Rotstein OD, Duane TM, Evans HL, et al. Trial of short-course antimicrobial therapy for intraabdominal infection. N Engl J Med [Internet]. 2015;372:1996–2005.
Sartelli M, Catena F, Ansaloni L, Coccolini F, di Saverio S, Griffiths EA. Duration of antimicrobial therapy in treating complicated intra-abdominal infections: a comprehensive review. Surg Infect. 2016;17:9–12. https://doi.org/10.1089/sur.2015.130 .
Sartelli M, Coccolini F, Kluger Y, Agastra E, Abu-Zidan FM, Abbas AES, et al. WSES/GAIS/SIS-E/WSIS/AAST global clinical pathways for patients with intra-abdominal infections. World J Emerg Surg. 2021;16:1–48. https://doi.org/10.1186/s13017-021-00387-8 .
Download references
No fundings were received for this paper.
Author information
Authors and affiliations.
School of Medicine and Surgery, Milano-Bicocca University, Monza, Italy
Marco Ceresoli, Marco Braga, Thomas Langer, Giuseppe Foti & Michele Fogliata
General and Emergency Surgery Department, Fondazione IRCCS San Gerardo dei Tintori, Via Pergolesi 33, 20900, Monza, Italy
Marco Ceresoli, Marco Braga & Michele Fogliata
General Surgery Department, Bufalini Hospital, Cesena, Italy
Nicola Zanini & Fausto Catena
The Research Office, College of Medicine and Health Sciences, United Arab Emirates University, Al Ain, UAE
Fikri M. Abu-Zidan
General Surgery Department - Santa Maria Della Misericordia Hospital, Rovigo, Italy
Dario Parini
Department of Anesthesia and Critical Care, ASST Grande Ospedale Metropolitano Niguarda, Milan, Italy
Thomas Langer
General Surgery, Macerata Hospital, Macerata, Italy
Massimo Sartelli
Department of General Surgery, Royal Infirmary of Edinburgh, Edinburgh, UK
Dimitrios Damaskos
Scripps Memorial Hospital La Jolla, La Jolla, CA, USA
Walter L. Biffl
John Hunter Hospital Trauma Service and School of Medicine and Public Health, The University of Newcastle, Newcastle, AU, Australia
Francesco Amico
General Surgery, Fondazione IRCCS San Matteo, Pavia, Italy
Luca Ansaloni, Enrico Cicuttin & Paola Fugazzola
Department of Traumatology, John Hunter Hospital and University of Newcastle, Hunter Medical Research Institute, Newcastle, NSW, Australia
Zsolt J. Balogh
Division of General and Foregut Surgery, Department of Biomedical Sciences for Health, IRCCS Policlinico San Donato, University of Milan, Milan, Italy
Luigi Bonavina
University of Auckland, Auckland, New Zealand
Department of Digestive Surgery, CHU Grenoble Alpes, Grenoble, France
Mircea Chirica
Department of Surgery, Tianjin Nankai Hospital, Nankai Clinical School of Medicine, Tianjin Medical University, Tianjin, China
Yunfeng Cui
Unit of Emergency and Trauma Surgery, Villeneuve St Georges Academic Hospital, Villeneuve St Georges, France
Belinda De Simone
Department of Surgical Sciences and Advanced Technologies, General Surgery Cannizzaro Hospital, University of Catania, Catania, Italy
Isidoro Di Carlo
PS_SS Weissach im Tal, Weissach im Tal, Germany
Andreas Fette
Department of Critical Care and Anesthesia, Fondazione IRCCS San Gerardo Dei Tintori, Monza, Italy
Giuseppe Foti
Division of Trauma Surgery, School of Medical Sciences (FCM), University of Campinas (Unicamp), Campinas, Brazil
Gustavo P. Fraga
University of California, Davis, Sacramento, CA, USA
Joseph M. Galante
University of Otago, Dunebin, New Zealand
Solomon Gurmu Beka
Department of General and Thoracic Surgery, University Hospital of Giessen, Gießen, Germany
Andreas Hecker
Erasmus MC University, Rotterdam, The Netherlands
Johannes Jeekel
General, Acute Care, Abdominal Wall Reconstruction, and Trauma Surgery, Foothills Medical Centre, Calgary, AB, Canada
Andrew W. Kirkpatrick
Department of Primary Care and Emergency Medicine, Kyoto University Graduate School of Medicine, Kyoto, Japan
Kaoru Koike
Helsinki University Hospital and University of Helsinki, Helsinki, Finland
Ari Leppäniemi
Andrei Litvin, CEO AI Medica Hospital Center, Kaliningrad, Russia
Department of Trauma, Hand, and Reconstructive Surgery, Goethe University, Frankfurt University Hospital, Frankfurt am Main, Germany
Director of Surgery Research, Ernest E. Moore Shock Trauma Center, Distinguished Professor of Surgery, University of Colorado, Denver, CO, USA
Ernest E. Moore
Department of Anesthesia and Intensive Care, Parma University Hospital, Parma, Italy
Edoardo Picetti
Third Department of Surgery, Attikon University Hospital, Athene, Greece
Emmanouil Pikoulis
General Surgery, ASST Papa Giovanni XXIII, Bergamo, Italy
Michele Pisano
Department of Surgical Science, University of Cagliari, Cagliari, Italy
Mauro Podda
RIMU Plovdiv/UMHAT St George Plovdiv, Plovdiv, Bulgaria
Boris E. Sakakushev
Department of General Surgery, Tan Tock Seng Hospital, Singapore, Singapore
Vishal G. Shelat
Department of Surgery, Brody School of Medicine, East Carolina University, Greenville, NC, USA
Former Chair Department of Emergency Medicine, HEMS Physician, Radboud University Medical Center, Nijmegen, The Netherlands
Digestive and Emergency Surgery Department, Azienda Ospedaliera S.Maria, Terni, Italy
Giovanni D. Tebala
Harvard Medical School - Massachusetts General Hospital, Boston, USA
George Velmahos
Department of General Surgery, Royal Perth Hospital, Head of Service and Director of Trauma, Royal Perth Hospital, The University of Western Australia, Perth, Australia
Dieter G. Weber
Anesthesia and Critical Care Department, Bufalini Hospital, Cesena, Italy
Vanni Agnoletti
Department of General Surgery, The Rambam Academic Hospital, Haifa, Israel
Yoram Kluger
General Surgery, University of Brescia, ASST Cremona, Cremona, Italy
Gianluca Baiocchi
Emergency Surgery, University of Pisa, Pisa, Italy
Federico Coccolini
You can also search for this author in PubMed Google Scholar
Contributions
All the authors contributed to the conception, writing, discussion and approval of the present manuscript.
Corresponding author
Correspondence to Marco Ceresoli .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was not required for this review and position paper.
Competing interests
All the authors have no conflict of interest to declare.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ceresoli, M., Braga, M., Zanini, N. et al. Enhanced perioperative care in emergency general surgery: the WSES position paper. World J Emerg Surg 18 , 47 (2023). https://doi.org/10.1186/s13017-023-00519-2
Download citation
Received : 13 September 2023
Accepted : 30 September 2023
Published : 06 October 2023
DOI : https://doi.org/10.1186/s13017-023-00519-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
World Journal of Emergency Surgery
ISSN: 1749-7922
- Submission enquiries: [email protected]
- Harvard Library
- Research Guides
- Countway Library – Health Sciences
Surgery Clerkship
- Finding Classic Papers
- Finding Information
- Online Books
- Visuals/Video
- Board/Exam Info
- Anatomy/Physiology
- Procedures/Instruments/the OR
- Core Journals
How to find a "classic" or "watershed" paper
Here are some suggestions on finding "watershed" or classic papers for your presentation:
- Check the list of Surgical Milestone Papers on to see if it includes your topic. The times an article has been cited is noted when available. Citation indexing became available with the publication of Science Citation Index in 1964. A number of these articles are too early to be included in the SCI database that goes back to 1900 and some of the journals are not indexed in SCI.
- Look at relevant sections of the text Surgery: Basic Science and Clinical Evidence - online and on reserve at Call# WO 100 S9613 2008 . This book is a gold mine. Each chapter gives a summary of the history of surgery for a particular indication including historical vignettes, and an excellent bibliography!
- Other books:
Sabiston's Textbook of Surgery (online) Find the chapter on your topic; some include a brief section on history, look especially at the Selected References at the end of each chapter. As a bonus, these are annotated to explain their value and importance to surgery in this field.
Landmark papers in general surgery (Online) / edited by Graham J. MacKay, Richard G. Molloy, Patrick J. O'Dwyer. Oxford : Oxford University Press, 2013.
Great Ideas in the History of Surgery. Countway WO11 Z5q There is a bibliography is on page 548, but you will need to read the related section of text on your topic for background on the significance of entry. Use the Index.
Operations that Made History Countway WO11.1 E470 This slim volume covers only 18 surgical procedures but if your topic is there you will find a very concise bibliographies after each.
Surgical Case Histories from the Past. Countway WO11.1 E47s Each case history describes a case which leads to a surgical breakthrough. If you topic is in here the 3-4 references of your section will be valuable.
Surgical oncology : fundamentals, evidence-based approaches, and new technology Countway QZ 268 S961 2012 - superb for oncology topics includes list of "landmark papers" and tables of evidence.
- You can consult other authoritative textbooks on your topic and look at the references to the most relevant chapter . If the authors have done a good job writing the background section of the chapter they should reference the "watershed" papers. Try searching the HOLLIS catalog and/or ask a librarian for help identifying books . It's good to give the "big names" (Schwartz or Sabiston), but also think about texts on the specific topic. For example, Principles and practice of surgical oncology : multidisciplinary approach to difficult problems . OR 50 Studies Every Plastic Surgeon Should Know .
- Search in Science Citation Index (aka Web of Science) which allows you to search on a topic and then rank articles by the most cited. Be sure to search multiple synonyms since this database has no indexing. It is computer generated so the keywords the author used are what is found. For example if you topic is gastric cancer, I would suggest entering "gastric cancer" OR "stomach neoplasms" OR "stomach cancer" OR "gastric neoplasms" as a start. Be sure to put the phrases in quotes so it will be searched as a unit and to change the field searched to topic.
When you have the search results, on the right hand side of the screen change the "Sort by" option to "Times Cited" on the drop down menu. This will bring the most cited studies to the top of the list. - Search HOLLIS for works that end with "collected works" OR look for "classic papers" in the title. You might search for "gastrointestinal surgery-collected works to find collections of papers.
Stuck? Not finding what you need? Ask a Librarian for help!
Tips for Specific Presentation Topics
In addition to the broad strategies listed above, here are some suggested sources to consult in your search for classic papers for your presentations. Definitely try the broad strategies in addition to looking at these titles. The suggestions are not comprehensive but they should give you a good start. Please, if you find other valuable sources, let me know so we can expand these lists.
- Acute Abdomen - Sources for classic paper references
- Bariatric Surgery - Finding Important Papers
- Cholangiocarcinoma and Hepatocellular Carcinoma
- ClassisPapersBreastCancerSurgery Tips to help surgery clerkship students find classic papers for Dr. Osteen's presentations
- Gastric Cancer Classic Articles
- Soft Tissue Sarcomas - Suggested sources for classic papers
- Pancreatic Cancer
- Surgical Treatment for Peripheral Artery Disease
- Thyroid Cancer- Sources for Classic Paper
Using PubMed to Find Historical Stuff
PubMed doesn't have any tools to help you find specific landmark papers, but there are specific tools to help you find historical works:
Use the History subset . You can access this search limit by choosing "Show Additional Filters" from the column to the left of your PubMed results. Choose "Subjects" then at the bottom of the new Subjects box, choose customize. Here you can select History to limit your search to historical articles.
With less fuss, you can just append AND history[sb] to your search. For example
cholecystectomy AND history[sb]
If that returns to much stuff, you can use the history subheading , either on its own or appended to a MeSH term:
cholecystectomy AND history[subheading]
"Cholecystectomy/history"[Majr]
Need more help? Check the PubMed User Guide .
- << Previous: Finding Information
- Next: Online Books >>
- Last Updated: Dec 15, 2020 1:53 PM
- URL: https://guides.library.harvard.edu/surgery
- Paper Presentations
Presented paper on on comparative study between 0.5 % Ropivacaine with Fentanyl and 0.5 % bupivacaine with fentanyl in USG guided supraclavicular Block in Upper Limb Surgeeries
Presented e-paper on the effect of ketamine in lowering the incidence and severity of post op sore throat after endotrttacheal in patients receiving GA on 19 DEC 2020 at TNISA PG Conclave
Ashish , Logeshwari P
Presented an e-poster on’A randomised control study comparing effect of intravenous dexmedetomidine vs IV esmolol omn attenuation of pressor response to laryngoscopy and endotracheal intubatiion’ and e-paper on ‘the effectiven3ess of dexmedetomidine as an additive to Ropivacaine in supraclavicular brachial plexus block.
Presented e-paper on MAHAYUVAISACON 21 on 20 th Feb 2021 titled as “the effect of nebulised ketamine in decreasing the incidence and severity of post operative sore throat after endotracheal intubation in patients receiving general anaesthesia.
Biochemistry
Made presentation on scientists and clinicians preceptorship for translational research in Webinar 'Biology to Omics' organized by TMS-ACTREC, Navi Mumbai during March 10-12, 2021
Community Medicine
Sero Surveillance in the Wardha District of central India to monitor
SARS Cov 2 infection status among asymptomatic General population
International conference Conquering COVID-19 , at Kasibai Navle
Medical College, Pune.18-19 December 2020
Participated in 5th National IAPSM postgraduate quiz Competition 48th Annual National Conference of Indian Association of Preventive and Social Medicine (IAPSMCON),PGIMER, Chandigarh,19-21 March 2021
Kolhe R , Gupta SS
Relationship of Father's engagement in responsive caregiving with child development a cohort study - presented at IAPSMCON 2021, PGIMER, Chandigarh, 19-21 March,21(poster presentation)
48th Annual National Conference of Indian Association of Preventive and Social Medicine (IAPSMCON),PGIMER, Chandigarh,19-21 March 2021 - Participated in (WAR OF VIDEO COMPETITION) “MAHASANGAM”
2nd IAPSM Young Leaders National Conclave,26-27 March 2021 Participated in (Worth A Thousand Word: Public Health Photography Competition)
Forensic Medicine
Moderate a session topic- crime scene examination-role of doctor in state conference of MLAM“forensicon 2020 on 10 th april 2021 Organized by Department of Forensic Medicine &Toxicology, TNMC & BYL charitable , hospital, Mumbai
Khandekar I L
Chaired a session in 42 nd Annual National conference of IAFM “FORENSIC MEDICON 2021” organized at SCB medical college cuttack, odisha from 23 rd - 24 th Jan 2021,
Moderate a session topic- Non uniformity of medical & medicolegal certificates in state. in state conference of MLAM“ forensicon 2020 on 10 th april 2021 Organized by Department of Forensic Medicine &Toxicology, TNMC & BYL charitable , hospital, Mumbai
Politics of Science in a Pandemic: Impact of Evidence Based Medicine (Guest Speaker)
8 th National Bioethics Conference, 12 December 2020
SP Kalantri
Predictors of Mortality in Venomous Snakebites: Sevagram Story (Guest Speaker)
Amrita Institute of Medical Science (AIMS) Kochi. Amrita National Conference on Snakebite. 22 November 2020
How Covid Vaccines Are Being Developed: Clinical Trials in India (Guest Speaker)
BOOM, 6 August 2020
Aarupadai Veedu Medical College & Hospital. AVMC Webinar Series – ‘Forefront of Future Frontiers’ (Guest Speaker)
Clinical Trials in COVID -19: The Science and Ethics’, 31 July 2020
The Need for Evidence Based Medicine in Treating Covid19 (Guest Speaker)
20 July 2020
14th National Cancer Grid webinar on COVID19 Preparedness (Guest Speaker)
Research Priorities for COVID-19, 18 July 2020
Can Alternative Medicine Be Subject To Modern Rigour? (Guest Speaker)
The Hindu Podcast by Jacob Koshy,3 July 2020
Webinar: Ethical Challenges of Research in a Pandemic (Guest Speaker)
Sunoindia podcast, 27 June 2020
The Why, How & What of Research during COVID era (Guest Speaker)
11 th National Cancer Grid webinar on COVID-19 preparedness, 20 June 2020
Covid and Rural India: Wardha Story (Guest Speaker)
Podcast: SoundCloud by Rukmini S, 10 June 2020
Hydroxychloroquine: More Questions than Answers (Guest Speaker)
BOOM, 5 June 2020
TheEvidence and/or Lack of Evidence for the Effectiveness of Hydroxychloroquinein Treating COVID-19
BBC (British Broadcasting Corporation) Talk , 20 May 2020
Dr. Amrish Saxena
Poster Presentation on Magnitude and determinants of depression in chronic kidney disease patients on maintenance hemodialysis in rural tertiary care hospital at ISN-WZ 2020, 36 th Annual ISN West Zone Conference, Nagpur, 19 th & 20 th September, 26 th & 27 th September 2020.
Microbiology
Presented a paper (Oral Presentation) on “Co infection of pneumocystis
carinii and cryptococcus neoformans” in the 2 nd Annual Conference of
Vidarbha Association of Medical Microbiology VAMMCON-2021 (online) held at Akola on 20 th and 21 st February, 2021
Maraskolhe D
Presented a paper (Oral Presentation) on “Are tuberculosis patients at greater risk of acquiring COVID-19 MGIMS data and Review of literature” in the 2 nd Annual Conference of Vidarbha Association of Medical Microbiology VAMMCON-2021 (online) held at Akola on 20 th and 21 st February, 2021 and received Dr. Ashok Pathak Junior Best Oral Paper Award
Obstetrics and Gynaecology
Presentation on Elderly Girls and How can we keep the rural work force we have ?” Unwanted pregnancies in adolescent girls – Global Challenges
Virtual 17 th WONCA World Health Rural Conference (Speaker)
Primary Care and Rural Health Bangladesh (PCRHB), Bangladesh, 15 th -18 th April, 2020
Critical Obstetric Care (Transfusion protocol, use of anticoagulants, Labour and Delivery in ICU training Webcast conference ( Panelist)
FOGSI 26 th April, 2020
4 th Global Virtual summit featuring wizard of endoscopy
Indian association of Gynaecology Endoscopist 21 st June, 2020
Mid Life Health Issue (Panelist)
Mid life Health committee Online conference (Chairperson nominee) Amravati Obstetrics and Gynaecology Society, Amravati, 12 th August, 2020
Management of worst Obstetric emergencies, PPH Online workshop on “ PPH Management” ( Panelist)
Ghaziabad Obstetrics and Gynaecological Society 13 th August, 2020
Hypertensive DS of Pregnancy Online Conference on “Hypertensive Pregnancy” (Panelist)
Nagpur Obstetrics and Gynaecological Society, Nagpur, 18 th August, 2020
USG in Infertility E-conference on “USG in Infertility “The Third Eye” ( Guest lecture)
Revari Obstetrics and Gynaecological Society, Rewari, Haryana, 4 th Sept, 2020
Classic For Clinician - RH Incompatibility in Obstetrics
Classic for Clinician Webinar Series 2, 25th November, 2020
NHM-UNICEF-NQOCN Webinar on Management of Post Partum Haemorrhage With Bundle Approach -Management Of Mother And Newborn In Labour Room
NQOCN with support of UNICEF, 28th November, 2020
Family Integrated Care
NQOCN 14 th December, 2020
Gestational Diabetes – Early intervention key to best Outcome
Rewari Obst & Gynaec Society, 11th January, 2021
Virtual conference on High risk pregnancy, infertility and Gynaecologic
Pune Obstetric and Gynaecology Society, 5 th -7 th March, 2021
Appropriate Blood and Blood Product Transfusion Guidelines PPH- Prevent the Catastrophe Part -5
Association of Madhya Pradesh Obst & Gynae Society and Raipur Obst & Gynae society 9th March, 2021
Amenorrhoea - Clinician's Perspective 29 th Annual POGS Conference “REEDIFY 2021” (Panelist)
Organised by Pune Obstetrics and Gynaecological Society, Pune, 5 th -7 th March, 2021
Maternal Health Care Bundles Classic for Clinician Webinar Series
25th March, 2021
Case Presentation & Table Viva Orator- Respectful Maternity Care (Late Dr. Leela Dube Oration) Virtual PG Force-2021 Nagpur Obstetrics and Gynaecology (Faculty)
Organized by Dept of OBGY, NKP Salve Institute of Medical Sciences & Research Centre & Lata Mangeshkar Hospital, Nagpur in Association with Nagpur Obstetrics and Gynaecology Society, Nagpur 16 th -21 st March, 2021
PMNCH Call to action on COVID 19 Webinar on PMNCH Stratergry outline
WHO 30th March, 2021
Infertility E-conference on “Roll of USG in Pregnancy” ( Chief Guest) Rewari Obst & Gynaec Society Rewari, Haryana 4 th September, 2020
Unwanted Pregnancies in Adolescent Girl, Global Challenges For Safe Baby, Safe Childhood, Safe Motherhood, Safe Womenhood, Maternity Violence must stop. How?
Rural Tribal Elderly Women’s suffering in a low resource region
Workshop-How Can We Keep the Rural Workforce We Have?”: A
Workshop on Rural Workforce Retention
TUFH Network : Primary Health Care: A Path towards Social Justice-
System and Community Based response to Covid-19,
Mexico, 23 rd -25 th September,2020
"Partograph and its interpretation: Risk for mother and Newborn"
NQOCN for Madhya Pradesh 15 th September, 2020
Developing prospective authors from QI teams across India for preparing QI reports for publication in peer reviewed journals
NQOCN 27 th October, 2020
Checklist For Immediate Postpartum Vigilence- For Mother And Newborn
Nqocn 10 th December, 2020
The Nuances of Infertility Webinar on The Nuances of Infertility ( Chaired the Session)
Nagpur Obstetrics and Gynaecology Society, Nagpur, 23 rd December, 2020
Triaging and Emergency Management in Obstetrics emergency (Guest Speaker) Topic of Webinar- Respectful Maternity Care in Covid/ Non-Covid era: Pregnant Women deserves the Quality Care in any Situation
13th February, 2021
Post natal care – recent advances (Guest speaker) Topic of Webinar- Respectful Maternity Care in Covid/ Non-Covid era: Pregnant Women deserves the Quality Care in any Situation - Day 4
27th February, 2021
Infection Prevention Practices- Covid/ Non Covid Topic of Webinar- Respectful Maternity Care in Covid/ Non-Covid era:
Pregnant Women deserves the Quality Care in any Situation
31st March, 2021
Ophthalmology
Diabetic Retinopathy Screening by Teleophthalmology (Guest Speaker)
Annual Delhi Ophthalmic Society International Hybrid Conference of 19 th December, 2020
Enhancing Clincal Skills in Ophthalmology using OSCE’s (Guest Speaker)
Annual Delhi Ophthalmic Society International Hybrid Conference of 18 th December, 2020
Lens Induced Glaucoma
Annual Delhi Ophthalmic Society International Hybrid Conference of
19 th December, 2020
Tayde D , Shukla A K, Singh S, Sheikh A, Lilhare K
Correlation between ablation depth and change in corneal curvature after
LASIK surgery”
45 th Virtual Annual Conference VOS-VRCON 2020 of the Vidarbha Ophthalmic Society from 26 th & 27 th December, 2020
More A , Shukla A K, Singh S, Sheikh A, Bhosale N
Management of Diabetic Patients with Vision Threatening Diabetic
Retinopathy in Rural Vidarbha region”
Peddawad S , Shukla A K, Singh S, Sheikh A, Bhosale N
Screening for vitamin A deficiency in tribal Maharashtra (Melghat)”
Bhosale N , Shukla A K, Singh S, More A
Visual outcome after small incision cataract surgery (SICS) in diabetic and non-diabetic patients”
Rathi N , Singh S, Shukla A K, Tayde D
Corneal topographic patterns in myopic eyes”
Taneshwari S , Dhabarde A, Shukla A K, Pednekar N, Sarode K
Analysis of Causes of Protposis in a Rural Based Tertiary Care Hospital
Tejashree B , Shukla A K, Singh S, Bang P, Peddawad S
An Insight into the Burden of Concomitant Strabismus among Primary School Children in Central India”
Yadav V , Shukla A K, Singh S, Tayde D, Malwe G
A case of lid ptosis and total ophthalmoplegia Annual Delhi Ophthalmic
Society International Hybrid Conference of 18 th December, 2020
Study of change in contrast sensitivity and corneal aberration in eyes
undergoing LASIK (Laser in situ Keratomileusis)
Bhosale N , Shukla A K, Singh S, More A, Malwe G
Bilateral Optic neuropathy: a rare presentation of Systemic lupus erythematosus ( e Poster)
Rosai Dorfmann Disease of Orbit” ( e Poster)
A case of optic nerve head drusens mimicking optic disc oedema” ( e Poster)
Yadav V , Shukla A K, Singh S, Tayde D, Chauragade S
An unusual presentation of mucormycosis in a known diabetic 45 th Virtual
Annual Conference VOS-VRCON 2020 of the Vidarbha Ophthalmic Society from 26 th & 27 th December, 2020
CISP II Workshop (Convener and Resource Person)
28—29 August 2020 at MGIMS, Sevagram
Graduate Medical Education Regulation (2019) on 28 th August 2020
Alignment & Integration on 29 th August 2020
Skills training on 29 th August 2020
Panel discussion on the impact of the corona pandemic on medical
education in the country. ( Panelist )
The Indian Medical Association- Indian Medical Students Network and the Medical Students Association of India, 14 Jun 2020
Enhancing learner engagement in online sessions. (Guest speaker)
Medical Education Unit, NKP Salve Institute of Medical Sciences and Lata Mangeshkar Hospital, Nagpur, 27 May 2020
Case based learning in Pathology . (Resource person)
E-course on Competency based learning in Pathology. 6 May 2020
Online teaching learning: Modalities for student engagement. (Guest speaker)
Webinar by Indian Association of Public Health Dentistry, 16 May 2020
Anshu Attention please: Tips for enhancing learner engagement online. (Guest speaker)
Webinar organized by Academy of Health Professions Educators, 19 April 2020
MGIMS Sevagram's Village Adoption Scheme and Social Service Camp for medical students. (Guest speaker)
Organized by the Network Towards Unity for Health (TUFH) Social Accountability Institute. 14 Apr 2020
Enhancing student engagement in online teaching. (Guest speaker)
Medical Education Unit, MGIMS, Sevagram, 17 Aug 2020
Enhancing student engagement in online teaching: Tips and tools (Guest speaker)
Centre for Continuing Education and Inter professional Development (CCEID), Manipal Academy of Higher Education, 25 Jul 2020.
Effective strategies for online learning. (Resource person)
Personal and Professional Development Group of Melaka Manipal Medical College for Malaysian students of I MBBS, 11 Jul 2020
Should a pathologist be a jack of all trades or a master of one? (Debate,
Invited speaker)
Vidarbha Association of Pathologists and Microbiologists, Nagpur, 20 Dec 2020
Pharmacology
National Level e-poster competition
Dr. P.R. Pote Patil College of Pharmacy, Amravati, June 2020
Gorjelwar P
Transfusion-Related Adverse Reactions in patients admitted in medicine department at Tertiary Care Teaching Hospital of Central India
Virtually Online, IPCON 2021 Date: 25 Feb 2021
Gorjelwar P & Kale R
Poster presentation in National Level e poster competition on Proposed
treatment of Covid 19
PR Pote Patil College of Pharmacy, Amravati, 31 st May 2020
Singh Rajput A
To study the effect of wound healing activity of Musa Balbisiana Sp.peel as anti-inflamatory activity on wistar Rats
2 nd World Congress on infectious Disease & Antibiotics 2020
J.N. Tata Auditorium, Indian institute of Science, Bengluru, 17 th Oct 2020
Knowledge attitude and practice towards covid 19 among medical students: a questionnaire based study (Poster Presentation)
Asian ACPCON 2021 organised by American college of physician- india chapter supported by acp chapters, 6 th 7 th feb 2021
International Webinar on Cardiovascular & VO 2 Max Assessment”
AD Instruments, South East Asia, 9 Sep 2020
Webinar : IPS community psychiatry seminar “Healthy eating, under nutrition and obesity among Indian children and adolescent (Guest Speaker)
Organized by : Dr.KS Shubrata, 2 nd May 2020
Annual National CME of industrial Psychiatry of India “Mental Health Issues in IT Industry” Theme - Current and emerging mental health issues in different industries, on 12/12/2020 (Guest Speaker)
KK Mishra, Ahmed
Title – ‘Absenteeism in Health Care Industries’ (Award Paper)
18 th ANCAIPI” held at DY Patil, Pune on 4 th to 6 th March 2021.
“IK Mujawar Award Poster”
Annual Conference IPS West Zone 2 nd & 4 th Oct. 2020.(Webinar)
Radiotherapy
Palliative radiotherapy to triage patients for radical treatment in locally
advanced oral cavity cancer during COVID CRISIS’ Annual Conference of
Association of Radiation Oncologist of Maharashtra, 19 Dec 2020
Clinical outcomes of reirradiation of brain metastasis with erlotinib in
metastatic adenocarcinoma lung’ 10 th Annual Conference of Indian Society
for study of lung cancer, Association of Radiation Oncologist, 26 Sept 2020
Covid 19 a double edge sword for cancer patients’
The Federation of Obstetric & Gynecological Societies of India and POGS international Conference of Indian society for study of lung cancer, Association of Radiation Oncologist, 11 Dec 2020
Efficacy and outcomes of hypofractionation in locally advanced head and neck cancer’
Annual Conference of Association of Radiation Oncologist of India North zone, 2 Oct 2020
Evaluation of nasogastric tube feeding during radiotherapy in head and neck cancer patients’
Annual Conference of Association of Oncologist of North East India, 19 Jan 2021
Left Coronary Artery Dose Exposure Predicts Major Adverse Cardiac Events in Coronary Heart Disease Negative Lung Cancer Patients’
Best of ASTRO 2020, 15 Aug 2020
The Dutch Lung Cancer Audit-Radiotherapy (DLCA-R): Real-World Data on
Elderly Stage III Non-Small Cell Lung Cancer Treated with Definitive
Chemoradiation
Best of ASTRO 2020 16 Aug 2020
Changing Paradigm in Radiotherapy of Postmastectomy Breast Cancer patients A comparative study of 3DCRT vs IMRT : Dosimetry,Toxicity and Outcome at the end of 4 years’
Annual Conference of Indian Society of Medical and Paediatric Oncology, 6 Nov 2020
How to optimally utilize the waiting time/area of patients while they are in
waiting hall before their RT commences for the purpose of patient education 43rd Indian Cooperative Oncology Network Virtual Conference, 9 Oct 2020
Role of prophylactic nasogastric feeding tube to maintain nutrition during
radiotherapy in head and neck cancer patients” Virtual Symposium on
Nutrition in Cancer Care & Management of Mucositis to be held on Friday,
26th February 2021
Kale P, Kalbande P , Rangari P , Datta NR
An evaluation of cost-effective nutrition supplement using homemade recipes vs commercially available formulations in cancer patients on liquid diet from low-middle-income group countries”
Virtual Symposium on Nutrition in Cancer Care & Management of Mucositis to be held on Friday, 26th February 2021
Skin & VD
Puzzling papules on the neck: Cutaneous metastasis from the breast ( e-Poster)
49th National Conference of IADVL, 5th to 7th February, 2021
Patrick S , Kar S, Gangane N, Deshmukh A
Lepromatous Hansen’s disease simulating Still’s Disease: a parodying case
report with diagnostic conundrum (e-Poster)
Manwar P , Kar S, Sawant A, Patrick S, Nandwani S
Blaschkolinear Atrophoderma of Pasini and Pierni with shortening of foot –A
Rare Entity ( e-Poster)
Nandwani S , Kar S, Sawant A, Patrick S, Manwar P
Leprosy presenting as a diagnostic challenge in a case of HIV with Pulmonary Tuberculosis at a rural tertiary care hospital (e-Poster)
Approach to obstructive Jaundice (Guest Lecture)
ASICON-2020 (virtual) from 14 - 19 th Dec. 2020
- Departments
- NAAC Cycle 3
- Courses Attended
- Academic Activities Conducted
- CME Attended
- Conference Attended
- Students Activities
- Student Awards
- Academy of Medical Sciences
- Medical Education Unit
- Institutional Ethics Committee
- Internal Quality Assurance Cell
- Dr Sushila Nayar School of Public Health
- UG Students
- PG Students
- Teaching Staff
- Non-Teaching Staff
- Senior Residents
- Non PG Junior Residents
- Outpatient Services
- Inpatient Services
- Accident and Emergency
- Investigation Facilities
- Information Technology
- Hospital in Numbers
- Hospital Charges
- Life Saving Equipment
- Bio Medical Waste
- Institutional Research
- Student Research
- In-house Publication
- Journal of MGIMS
- Publications
- Community Activities
- Community Based Medical Education
- Social Impact
- Government Approval
- History and Heritage
- Our Founder
- Administration
- Citizen Charter
- Life at Sevagram
- Anti-Ragging
- Right to Information
- Women's Complaints Committee
- Annual Report
- Employe's Information
- Audited Statements
- Foreign Contributions
- Human Rights Complaints
- Mandatory Disclosure
- Getting Here
- NMC Disclosure
- MUHS Mandate
- See us on twitter
- See us on facebook
- See us on youtube
- See us on instagram
General Surgery Research
Faculty in the division are involved in health service, education, technology, clinical trials, and translational and basic research projects. These research areas are focused on a variety topics including healthcare delivery, health policy and disease-specific gaps in knowledge. The goal of the research being conducted in the division is to ultimately impact patient care and optimize health care delivery that results in improved patient outcome based on cost-effective strategies. While contributing to the research mission is germane to any academic division, we believe our faculty at Stanford University are uniquely positioned to make transformative research contributions through their diverse research interest in an unparalleled environment and community of thought leaders. Please enjoy learning about our faculty research interests and contributions and engaging with them.
General Surgery: Clinical Resources
- Clinical Resources
- Other eBooks
- Plastic Surgery
- Pharmacology
- Patient Education
Point of Care
- Quick Answers Surgery | Access Surgery
- Topics General Surgery | UpToDate
Calculators
- GuidelineCentral Surgery, General
- UpToDate General Surgery
- ClinicalKey Surgery
- UpToDate Society Guidelines General Surgery
Research Tools
Core ebooks.
Search eBooks
Clinical Trials
Please let us know if you have any suggestions , questions, or find broken links
Mayo Clinic Libraries
Mayo Clinic Libraries Services
Mayo clinic resources.
- Procedural Videos | ClinicalKey Surgery
- Videos | AccessSurgery
https://libraryguides.mayo.edu/generalsurgery
- Next: Other eBooks >>
- Last Updated: Apr 2, 2024 10:01 AM
- URL: https://libraryguides.mayo.edu/generalsurgery
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Dent J (Basel)
Hot Topics in Clinical Oral Implants Research: Recent Trends in Literature Coverage
Vesela valkova.
1 Medical University of Vienna, Bernhard Gottlieb School of Dentistry, Sensengasse 2a, A-1090 Vienna, Austria; [email protected] (V.V.); moc.oohay@aneeneec (C.U.M.)
Ceeneena Ubaidha Maheen
Bernhard pommer.
2 Academy for Oral Implantology, Lazarettgasse 19/DG, A-1090 Vienna, Austria
Xiaohui Rausch-Fan
3 Medical University of Vienna, Rausch-Fan Laboratory, Sensengasse 2a, A-1090 Vienna, Austria; [email protected]
Rudolf Seemann
4 Medical University of Vienna, Department of Oral and Maxillofacial Surgery, Währinger Gürtel 18-20, A-1090 Vienna, Austria; [email protected]
This systematic review looks at thematic trends in clinical research publications on dental implants. For this purpose, MEDLINE electronic searches as well as additional hand searches of six main journals in the field were conducted. A total of 2875 clinical studies published between 2001 and 2012 met the inclusion criteria and were subjected to statistical analysis. Hot topics in dental implant literature included immediate loading (14.3%), bone substitutes (11.6%), cross-arch full bridges (8.0%), and immediate implant placement (7.5%). A significant increase in scientific interest for immediate loading (+6.3%, p = 0.001), platform switching (+2.9%, p = 0.001), guided implant surgery (+1.9%, p = 0.011), growth factors ( p = 0.014, +1.4%), piezoelectric surgery (+1.3%, p = 0.015), and restorative materials (+0.7%, p = 0.011) was found. A declining scientific interest in onlay grafting (−0.3%, p = 0.042) was recorded. The findings regarding current clinical oral implants research tie in with better-informed consumers and increased patient demands. Our results demonstrate an increasing interest in techniques that avoid complicated procedures such as bone grafting and that reduce treatment duration.
1. Introduction
The present special issue of Dentistry Journal deals with “Advances in Implant Dentistry,” and the following keywords denote hot topics in this field: template-guided implant placement, minimally invasive techniques, short lengths and reduced implant diameters, novel bone grafting techniques, medically compromised patients, peri-implantitis treatment, immediate placement and restoration, transition from a failing dentition, CAD/CAM prosthetics, and optical intraoral impressions. As the first paper in this special issue, the following review aims to provide the background to recent trends and “hot topics” in advanced and minimally invasive oral implant treatment [ 1 ].
The concept of osseointegration of oral implants was introduced by Branemark 40 years ago and set the precedent for new knowledge in oral medicine. Since then, oral implantology has become one of the most investigated topics in dental medicine, with exponential growth in the use of implant products [ 2 ]. Data shows that the number of implants used for oral rehabilitation in the USA increased ten-fold between 1983 and 2002 and also ten-fold from 2000 to 2010 [ 3 ]. While previously the primary aim of research on oral implantology was to find ways to rehabilitate function [ 4 ], many efforts nowadays are focused on the shortening of treatment procedures, simplifying surgical techniques, and esthetic improvement [ 5 ]. It is well known that oral implantology is a prosthetically driven field with a major surgical component [ 6 ]. Therefore, the current state of the art in implant dentistry represents advances in both surgical and prosthodontic techniques [ 5 ].
Keeping pace with research development, the aim of this systematic review was to investigate contemporary issues in oral implantology research and to perform a topical trend analysis of clinical studies published in the time period from 2001 to 2012.
2. Material and Methods
2.1. search strategy.
A MEDLINE electronic literature search was conducted, limited to clinical studies on dental implants published between 2001 and 2012. The search term “dental implant,” sorted by “year of publication” was used in order to capture all relevant articles [ 7 ]. Additional hand searching was performed to examine six main journals in the field: The International Journal of Maxillofacial Implants , Journal of Oral Implantology , Clinical Oral Implant Related Research , Implant Dentistry , European Journal of Oral Implantology , and Clinical Oral Implant Research . Two reviewers independently identified all trials [ 8 ]. The PubMed search initially identified 15,695 publications, and 5048 additional results were identified by hand search. These studies were screened for their relevance based upon a threshold set [ 9 ]:
- inclusion criteria: prospective and retrospective studies, cross-sectional studies, case-control studies, case reports with at least 10 patients
- exclusion criteria: non-English publications, statistical studies, animal studies, finite element analyses, in vitro studies, review articles, and case series with fewer than 10 patients.
A total number of 3695 articles were subjected to abstract review. Where the abstract provided little information, a full text analysis was performed. Authors of potentially relevant publications, which were not available or lacked data, were contacted and asked for cooperation. Ultimately, 2875 clinical studies were identified as meeting the inclusion criteria. Our goal was to investigate how trends change over time as regards the topics examined in modern implant dentistry research. In this respect, we have determined that 31 topics were appropriate: 23 of them concerned surgical issues and 8 dealt with prosthodontic issues ( Table 1 ). First, all relevant publications were screened for the topics listed in Table 1 independently by two reviewers. Thereafter, the results were verified, and all doubtful publications were discussed before the final decision was taken.
Topics sorted by literature coverage. Absolute numbers of publications per year as well as the total percentage of all clinical papers 2001–2012 (* indicates prosthodontic topics).
2.2. Statistical Analysis
As mentioned above, 2875 publications were analyzed. In order to find statistical trends in respect to the relevant topics between 2001 and 2012, Poisson regression analysis was performed, taking the level of significance as p ≤ 0.05, using R-project statistical software version 3.1.0. This statistical test was used to model count data, which in this case was the number of publications. p -values were calculated for every topic, taking into account the relative number publications per topic from the total number of publications.
The surgical and prosthodontic topics of interest were computed as percentages of the total number of publications ( Table 1 ). Among the most covered surgical topics in the literature were immediate loading (14.3%), bone substitutes (11.6%), immediate implant placement (7.5%), simultaneous implant placement with bone augmentation (6.4%), onlay grafting (4.3%), medically compromised patients (4.0%), healing modality (3.7%), transcrestal sinus floor elevation (3.0%), flapless surgery (2.7%), socket grafting (2.6%), and guided surgery (2.4%). Immediate loading (14.3%), cross-arch implant bridges (8.0%), early loading (4.5%), and platform switching (1.7%) were ranked as the most prevalent prosthodontic issues in current oral implant research.
The surgical issues were the more prevalent topics, demonstrating an increasing rate of publications over the time in terms of mean coverage (0.53 ± 0.01) per publication ( Figure 1 ), as compared to prosthodontic issues (0.33 ± 0.05 hits). The mean coverage values were estimated based on yearly ratios: the number of prosthodontic/surgical publications per year in relation to the total number of publications per year. The significant increase in publications on surgical issues over the years was demonstrated by Poisson regression analysis ( p = 0.002).

Literature coverage of surgical (s) versus prosthodontic (p) issues: x-axis indicates year of publication, y-axis indicates the ratio of numbers of publications (surgical/prosthodontic) to the total number of publications per year.
A total of eight topics showed significant trends ( p < 0.05) over the years 2001 to 2012 ( Table 2 ). Immediate loading demonstrated the highest increase with a positive change of +6.3% and p = 0.001 ( Figure 2 a). Platform switching (+2.9%, p = 0.001) was the second topic showing a significant increase; however, only one relevant article was detected between 2001 and 2006 ( Figure 2 b). These topics were followed by guided implant surgery (+1.9%, p = 0.011), growth factors (+1.4%, p = 0.014), piezoelectric surgery (+1.3%, p = 0.015), and restorative materials (+0.7%, p = 0.011). The green line represents the percentage of the total number of publications for every year. The black trend line reveals the relationship between the year of publication (x-variable) and the percentage of the total number of publications (y-variable). Since there were no publications on platform switching between 2002 and 2005, there is a negative trend line intercept starting from 2001 ( Figure 2 b). Decreasing scientific interest and a corresponding downward trend were recorded for the topic onlay grafting (−0.3%, p = 0.042).

Trend curves (percentage out of the total number of publications per year) for ( a ) immediate loading; ( b ) platform switching; ( c ) flapless implant surgery; ( d ) guided implant surgery; ( e ) growth factors; ( f ) piezoelectric surgery; ( g )restorative materials; and ( h ) onlay grafting.
Topics demonstrating a significant increase (positive) or decrease (negative change) of scientific interest in the years 2001–2012.
4. Discussion
Comparisons of published clinical trials per year revealed a trend of increasing interest in conducting clinical trials, starting with 137 relevant articles in the year 2001 and reaching the number of 446 publications in the year 2012. However, even the total number of 3695 articles is smaller than the total number of 4655 clinical studies published between 1989 and 1999 reported by Russo et al. [ 10 ]. Given that the number of publications increased with every year, it was considered more appropriate to perform Poisson regression analysis related to percentage-based values rather than related to absolute values for all topics.
Immediate loading proved to be the most studied topic in the last decade ( Figure 2 a). This avid scientific interest can be explained by several advantages it offers, such as shortened treatment protocols, immediate rehabilitation of the function, and high patient satisfaction. Meta-analyses on single-tooth implant placement have shown encouraging results for the immediate loading protocol as a promising alternative to conventional loading, as it may be equally successful and may not significantly affect marginal bone resorption and implant success rates [ 11 , 12 , 13 ]. Another meta-analysis by Papaspyridakos et al. [ 14 ] reported that there was no significant difference between immediate, early, and conventional loading in edentulous patients with fixed prostheses, and all three protocols showed a high level of success. However, other reviewers disagree with this assessment of the unimpaired success of the immediate loading protocol. A meta-analysis of clinical studies comparing the immediate and conventional loading of single tooth implants discovered that immediate loading has a significantly higher risk of implant failure [ 15 ]. Schimmel and coworkers [ 16 ] concluded that, despite the high implant survival rates, the conventional and early loading protocols are superior to immediate loading as better documented protocols, providing better results in the first year of loading. A survey among implantologists from 16 countries all over the world stated that immediate loading was the treatment protocol most accepted by dentists in Australia and Europe [ 17 ]. Based on these controversial statements in the literature, it can be concluded that there is still a lack of well-designed RCTs concerning loading protocol [ 18 ] and immediate loading may well retain its place as a hot topic of discussion over the coming years.
The platform-switching concept arose in 1980 with the introduction of the wide diameter implants. Due to the lack of commercially available matching components for wide diameter implants, the standard-diameter abutments were used. Later, it was found that “platform-switched” implants demonstrated osseointegration with less initial crestal bone loss and were thus superior to the “platform-matched implants” [ 19 ]. However, the first introduction of this concept appeared in 2005 [ 20 ]. Radiographic observation over a period of 13 years demonstrated that platform switching resulted in little or no crestal bone loss as compared to the conventional implants, whereas marginal bone resorption of 1.5 mm on average was accepted as one of the criteria for success of the dental implant [ 21 ]. Our study shows that the increasing publication rate of clinical studies happened to coincide with the first official introduction of this concept, with a positive linear trend for this topic starting in 2005 ( Figure 2 b). Since guided surgery is performed in combination with the flapless procedure in most cases, [ 22 ] the similarity in literature coverage, illustrated in both scatter plots, does not come as a surprise ( Figure 2 c,d).
In contrast to the last decade of the 20th century, when the main progress in the field of oral implant research was made in alveolar bone resorption management to refine the different graft techniques [ 23 ], our findings show that in the 21st century there has been increasing interest in methods developed to overcome the grafting procedures and even a loss of interest in one of the most used augmentation techniques, i.e. , onlay bone grafting. It seems that dental implant scientific work is inspired more by the patient’s appraisals [ 24 ], seeking to improve minimally invasive surgical techniques [ 25 ], diminish patient morbidity, and shorten the treatment time. However, the role of industrial funding for conducting clinical studies should be taken into consideration. 32.4% of the clinical trials are supported by industry as a source of funding, which is a suitable way for companies not only to comply with safety and efficacy standards, but also to introduce their new products to the market [ 26 ]. This industry sponsorship may lead to biased reporting and pro-industry conclusions [ 27 ]. This does have the potential to reflect on ongoing trends in clinical research. In this connection for instance, the relatively innovative technique of guided implant surgery provides less painful and invasive treatment but at the same time is a more difficult and expensive procedure than conventional implant placement, demonstrating the same survival rate. However, a survey by Hof and coworkers [ 28 ] showed that the main priority for the patients when it comes to implant therapy remains the predictability of treatment success. The achievements brought about by ongoing clinical research, such as improved quality, ease of use of implant systems, as well as shorter treatment duration [ 29 ] may provide grounds for future researchers to face the challenge of preserving the perspectives of clinical implant research, and specifically, to enhance the relationship between private practice and science without involving marketing.
In order to adhere to ethical rules on explicit reporting, including also the disadvantages of any study, the researchers are obligated to report their study’s limitations. Undoubtedly, meta-analysis is the “gold standard” for performing any systematic review aiming at assessing treatment effects. Given that the variable investigated in the present study was the number of publications, the Poisson regression was selected as a statistical tool. The Poisson regression is used to model count data (in the present case this is the number of publications) and is an appropriate statistical method for predicting trends. Therefore, no methods estimating risk of bias, quality design, or heterogeneity of the studies provided by the meta-analysis were applied in this study.
A further limitation is presented by the use of only one database source. The findings in the present work are based on analysis, including studies from MEDLINE, and an additional hand search of six journals. However, the search strategy did not consider other databases such as EMBASE and the Cochrane Central Register of Controlled Trials.
In conclusion, the analysis of scientific literature on dental implants revealed several hot topics in the time period between 2001 and 2012. The most frequently covered surgical issues were bone substitutes (11.6%) and immediate implant placement, (7.5%), while the most prevalent prosthodontic topics involved immediate loading (14.3%) and cross-arch full bridges (8.0%). Given that the topics demonstrating the highest increase in interest were prosthodontic topics, i.e. , immediate loading (+6.3%) and platform switching (+2.9%), the interest in researching prosthodontic topics will most likely continue to increase.
Acknowledgments
No funding was received to support the study.
Author Contributions
Bernhard Pommer conceived and designed the experiments; Vesela Valkova and Ceeneena Ubaidha Maheen performed the experiments; Rudolf Seemann analyzed the data; Xiaohui Rausch-Fan contributed analysis tools; Vesela Valkova wrote the paper.
Conflicts of Interest
The authors declare no conflict of interest.

IMAGES
VIDEO
COMMENTS
General Surgery articles covering presentation, surgical treatment, prognosis, and follow-up. Peer reviewed and up-to-date recommendations written by leading experts.
In this popular session, the panelists review 10 of the hottest topics in general surgery selected from the ACS General Surgery Communities, recent surgery meetings, and the literature. Course Outline. Approaches to Femoral Hernia Benjamin K. Poulose, MD, MPH, FACS, Nashville, TN; Pure Tissue Repair of Inguinal Hernia: Resurrection of a Lost Art
Ten Hot Topics in General Surgery. This popular annual session provides brief presentations by experts in general surgery who discuss a specific topic in a rapid-fire format. ACS Immediate Past-President E. Christopher Ellison, MD, FACS, and Regent Kenneth W. Sharp, MD, FACS, moderated the wide-ranging session, which included presentations on:
Ten Hot Topics in General Surgery. Ten Hot Topics in General Surgery ... This rapid-fire/quick-shot session will cover ten currently popular issues in general surgery. Moderator: Kenneth W. Sharp, MD, FACS, Nashville, TN. Co-Moderator: E. Christopher Ellison, MD, FACS, Powell, OH. Presentations. Bullet Removal: Pros and Cons John A. Weigelt, MD ...
Given these data and general acceptance of antibiotic management of these patients, we suggest performing appendectomy within 24 hours of presentation in patients with uncomplicated appendicitis who elect to undergo surgery. (See "Management of acute appendicitis in adults", section on 'Timing of appendectomy'.) BREAST SURGERY
For the 12th time at Clinical Congress, ACS President E. Christopher Ellison, MD, FACS, and ACS Regent Kenneth W. Sharp, MD, FACS, have paired up to co-moderate Ten Hot Topics in General Surgery, which takes place on Wednesday, October 25, from 12:45 pm to 2:15 pm in Ballroom East. "We're going prime time this year," said Dr. Christopher ...
Within general surgery, there are a wide range of clinical presentations that patients can present with, and the underlying pathologies are even wider. The most common of these is acute abdominal pain, often termed the "acute abdomen" and is essential to know how to approach this presentation and potential investigations required.
General Surgery - Science topic A specialty in which manual or operative procedures are used in the treatment of disease, injuries, or deformities. Questions (105)
A potential reviewer may not be an expert in the exact topic that the manuscript covers, but they should have some familiarity with the general field and type of research. For example, if a reviewer is a surgical oncologist, it is probably appropriate to review manuscripts for general surgery and oncology topics, whereas vascular surgery topics ...
This is the third volume of papers from the Association for Academic Surgery. The presentations which are included in the current book were delivered at the fourth annual meeting of the Association which was held in Denver in November 1970. This surgical society is composed of young, fulltime academic surgeons, less than 40 years of age when ...
Topics include "the acute abdomen," "management of AAA's," "approaches to hernia repairs," "assessing the need for lower extremity revascularization," "management of small bowel obstruction," etc. You get the idea. Remember that the shelf is all about management, so you may as well kill 2 birds with one stone and learn about a bread-and-butter ...
The contents follow the usual format of paper surgery textbooks and classify the chapters according to the diseased organ. At the end of each section, a … General surgery resources for students | The BMJ
The effectiveness and safety of ERAS protocols in elective surgery are now widely established. Several meta-analyses comparing standard care and fast-track approach show that ERAS protocols in elective surgery lead to a reduction in length of stay and in the rate of postoperative non-surgical complications [2,3,4,5].Most of the available studies focused on the postoperative phase, considering ...
Here are some suggestions on finding "watershed" or classic papers for your presentation: - Check the list of Surgical Milestone Papers on to see if it includes your topic. The times an article has been cited is noted when available. ... Landmark papers in general surgery (Online) / edited by Graham J. MacKay, Richard G. Molloy, Patrick J. O ...
Presented a paper (Oral Presentation) on "Co infection of pneumocystis. carinii and cryptococcus neoformans" in the 2 nd Annual Conference of. Vidarbha Association of Medical Microbiology VAMMCON-2021 (online) held at Akola on 20 th and 21 st February, 2021. Maraskolhe D.
General Surgery Research. Faculty in the division are involved in health service, education, technology, clinical trials, and translational and basic research projects. These research areas are focused on a variety topics including healthcare delivery, health policy and disease-specific gaps in knowledge. The goal of the research being ...
1 2 3. A collection of articles relating to general surgery, including abdominal incision types, common general surgical presentations and more.
Operative Techniques in Surgery, 2nd ed. by Mary T. Hawn, 2023. Textbook of Emergency General Surgery by Federico Coccolini andFausto Catena, 2024. Current Diagnosis and Treatment Surgery, 15th Edition by Gerard M. Doherty, 2020. Current Surgical Therapy, 14th ed. by John L. Cameron; Andrew M. Cameron, 2023.
General Surgery topics Specialty topics. MS General Surgery Page 6 Basic sciences include anatomy, physiology, biochemistry, ... Prospective data collection/ writing case reports and clinical papers Giving presentation / Computer presentation Preoperative work up-concept of fitness for surgery; basic medical workup; workup in
Key Topics in General Surgery . DOI link for Key Topics in General Surgery. Key Topics in General Surgery. Edited By N. R. F. Lagattolla, C. R. Lattimer, N. M. Wilson. Edition 2nd Edition. First Published 2002. eBook Published 22 April 2013. Pub. Location London. Imprint CRC Press.
As the first paper in this special issue, the following review aims to provide the background to recent trends and "hot topics" in advanced and minimally invasive oral implant treatment . The concept of osseointegration of oral implants was introduced by Branemark 40 years ago and set the precedent for new knowledge in oral medicine.