Attention Deficit Hyperactivity Disorder (ADHD): A Case Study and Exploration of Causes and Interventions
- First Online: 02 March 2019

Cite this chapter

- Bijal Chheda-Varma 5
3200 Accesses
The male to female ratio of ADHD is 4:1. This chapter on ADHD provides a wide perspective on understanding, diagnosis and treatment for ADHD. It relies on a neurodevelopmental perspective of ADHD. Signs and symptoms of ADHD are described through the DSM-V criteria. A case example (K, a patient of mine) is illustrated throughout the chapter to provide context and illustrations, and demonstrates the relative merits of “doing” (i.e. behavioural interventions) compared to cognitive insight, or medication alone. Finally, a discussion of the Cognitive Behavioral Modification Model (CBM) for the treatment of ADHD provides a snapshot of interventions used by clinicians providing psychological help.
- Neuro-developmental disorders
- Behaviour modification
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Durable hardcover edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Alderson, R. M., Hudec, K. L., Patros, C. H. G., & Kasper, L. J. (2013). Working memory deficits in adults with attention-deficit/hyperactivity disorder (ADHD): An examination of central executive and storage/rehearsal processes. Journal of Abnormal Psychology, 122 (2), 532–541. http://dx.doi.org/10.1037/a0031742 .
Arcia, E., & Conners, C. K. (1998). Gender differences in ADHD? Journal of Developmental and Behavioral Pediatrics, 19 (2), 77–83. http://dx.doi.org/10.1097/00004703-199804000-00002 .
Barkley, R. A. (1990). Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment . New York: Guildford.
Google Scholar
Barkley, R. A. (1997). ADHD and the nature of self-control . New York: Guilford Press.
Barkley, R. A. (2000). Commentary on the multimodal treatment study of children with ADHD. Journal of Abnormal Child Psychology, 28 (6), 595–599. https://doi.org/10.1023/A:1005139300209 .
Article Google Scholar
Barkley, R., Knouse, L., & Murphy, K. Correction to Barkley et al. (2011). Psychological Assessment [serial online]. June 2011; 23 (2), 446. Available from: PsycINFO, Ipswich, MA. Accessed December 11, 2014.
Beck, A. T. (1976). Cognitive therapy and the emotional disorders . New York, NY: International Universities Press.
Brown, T. E. (2005). Attention deficit disorder: The unfocused mind in children and adults . New Haven, CT: Yale University Press.
Brown, T. (2013). A new understanding of ADHD in children and adults . New York: Routledge.
Chacko, A., Kofler, M., & Jarrett, M. (2014). Improving outcomes for youth with ADHD: A conceptual framework for combined neurocognitive and skill-based treatment approaches. Clinical Child and Family Psychology Review . https://doi.org/10.1007/s10567-014-0171-5 .
Chronis, A., Jones, H. A., Raggi, V. L. (2006, August). Evidence-based psychosocial treatments for children and adolescents with attention-deficit/hyperactivity disorder. Clinical Psychology Review, 26 (4), 486–502. ISSN 0272-7358. http://dx.doi.org/10.1016/j.cpr.2006.01.002 .
Curatolo, P., D’Agati, E., & Moavero, R. (2010). The neurobiological basis of ADHD. Italian Journal of Pediatrics, 36 , 79. http://doi.org/10.1186/1824-7288-36-79 . http://www.sciencedirect.com/science/article/pii/S0272735806000031 .
Curtis, D. (2010). ADHD symptom severity following participation in a pilot, 10-week, manualized, family-based behavioral intervention. Child & Family Behavior Therapy, 32 , 231–241. https://doi.org/10.1080/07317107.2010.500526 .
De Young, R. (2014). Using the Stroop effect to test our capacity to direct attention: A tool for navigating urgent transitions. http://www.snre.umich.edu/eplab/demos/st0/stroopdesc.html .
Depue, B. E., Orr, J. M., Smolker, H. R., Naaz, F., & Banich, M. T. (2015). The organization of right prefrontal networks reveals common mechanisms of inhibitory regulation across cognitive, emotional, and motor processes. Cerebral Cortex (New York, NY: 1991), 26 (4), 1634–1646.
D’Onofrio, B. M., Van Hulle, C. A., Waldman, I. D., Rodgers, J. L., Rathouz, P. J., & Lahey, B. B. (2007). Causal inferences regarding prenatal alcohol exposure and childhood externalizing problems. Archives of General Psychiatry, 64, 1296–1304 [PubMed].
DSM-V. (2013). Diagnostic and statistical manual of mental disorders . American Psychological Association.
Eisenberg, D., & Campbell, B. (2009). Social context matters. The evolution of ADHD . http://evolution.binghamton.edu/evos/wp-content/uploads/2012/02/eisenberg-and-campbell-2011-the-evolution-of-ADHD-artice-in-SF-Medicine.pdf .
Gizer, I. R., Ficks, C., & Waldman, I. D. (2009). Hum Genet, 126 , 51. https://doi.org/10.1007/s00439-009-0694-x .
Hinshaw, S. P., & Scheffler, R. M. (2014). The ADHD explosion: Myths, medication, money, and today’s push for performance . New York: Oxford University Press.
Kapalka, G. M. (2008). Efficacy of behavioral contracting with students with ADHD . Boston: American Psychological Association.
Kapalka, G. (2010). Counselling boys and men with ADHD . New York: Routledge, Taylor & Francis Group.
Book Google Scholar
Knouse, L. E., et al. (2008, October). Recent developments in psychosocial treatments for adult ADHD. National Institute of Health, 8 (10), 1537–1548. https://doi.org/10.1586/14737175.8.10.1537 .
Laufer, M., Denhoff, E., & Solomons, G. (1957). Hyperkinetic impulse disorder in children’s behaviour problem. Psychosomatic Medicine, 19, 38–49.
Raggi, V. L., & Chronis, A. M. (2006). Interventions to address the academic impairment of children and adolescents with ADHD. Clinical Child and Family Psychology Review, 9 (2), 85–111. https://doi.org/10.1007/s10567-006-0006-0 .
Ramsay, J. R. (2011). Cognitive behavioural therapy for adult ADHD. Journal of Clinical Outcomes Management, 18 (11), 526–536.
Retz, W., & Retz-Junginger, P. (2014). Prediction of methylphenidate treatment outcome in adults with attention deficit/hyperactivity disorder (ADHD). European Archives of Psychiatry and Clinical Neuroscience . https://doi.org/10.1007/s00406-014-0542-4 .
Safren, S. A., Otto, M. W., Sprich, S., Winett, C. L., Wilens, T. E., & Biederman, J. (2005, July). Cognitive-behavioral therapy for ADHD in medication-treated adults with continued symptoms. Behaviour Research and Therapy, 43 (7), 831–842. ISSN 0005-7967. http://dx.doi.org/10.1016/j.brat.2004.07.001 . http://www.sciencedirect.com/science/article/pii/S0005796704001366 .
Sibley, M. H., Kuriyan, A. B., Evans, S. W., Waxmonsky, J. G., & Smith, B. H. (2014). Pharmacological and psychosocial treatments for adolescents with ADHD: An updated systematic review of the literature. Clinical Psychology Review, 34 (3), 218–232. https://doi.org/10.1016/j.cpr.2014.02.001 .
Simchon, Y., Weizman, A., & Rehavi, M. (2010). The effect of chronic methylphenidate administration on presynaptic dopaminergic parameters in a rat model for ADHD. European Neuropsychopharmacology, 20 (10), 714–720. ISSN 0924-977X. https://doi.org/10.1016/j.euroneuro.2010.04.007 . http://www.sciencedirect.com/science/article/pii/S0924977X10000891 .
Swanson, J. M., & Castellanos, F. X. (2002). Biological bases of ADHD: Neuroanatomy, genetics, and pathophysiology. In P. S. Jensen & J. R. Cooper (Eds.), Attention deficit hyperactivity disorder: State if the science, best practices (pp. 7-1–7-20). Kingston, NJ: Civic Research Institute.
Toplak, M. E., Connors, L., Shuster, J., Knezevic, B., & Parks, S. (2008, June). Review of cognitive, cognitive-behavioral, and neural-based interventions for attention-deficit/hyperactivity disorder (ADHD). Clinical Psychology Review, 28 (5), 801–823. ISSN 0272-7358. http://dx.doi.org/10.1016/j.cpr.2007.10.008 . http://www.sciencedirect.com/science/article/pii/S0272735807001870 .
Wu, J., Xiao, H., Sun, H., Zou, L., & Zhu, L.-Q. (2012). Role of dopamine receptors in ADHD: A systematic meta-analysis. Molecular Neurobiology, 45 , 605–620. https://doi.org/10.1007/s12035-012-8278-5 .
Download references
Author information
Authors and affiliations.
Foundation for Clinical Interventions, London, UK
Bijal Chheda-Varma
You can also search for this author in PubMed Google Scholar
Editor information
Editors and affiliations.
UCL, London, UK
John A. Barry
Norfolk and Suffolk NHS Foundation Trust, Wymondham, UK
Roger Kingerlee
Change, Grow, Live, Dagenham/Southend, Essex, UK
Martin Seager
Community Interest Company, Men’s Minds Matter, London, UK
Luke Sullivan
Rights and permissions
Reprints and permissions
Copyright information
© 2019 The Author(s)
About this chapter
Chheda-Varma, B. (2019). Attention Deficit Hyperactivity Disorder (ADHD): A Case Study and Exploration of Causes and Interventions. In: Barry, J.A., Kingerlee, R., Seager, M., Sullivan, L. (eds) The Palgrave Handbook of Male Psychology and Mental Health. Palgrave Macmillan, Cham. https://doi.org/10.1007/978-3-030-04384-1_15
Download citation
DOI : https://doi.org/10.1007/978-3-030-04384-1_15
Published : 02 March 2019
Publisher Name : Palgrave Macmillan, Cham
Print ISBN : 978-3-030-04383-4
Online ISBN : 978-3-030-04384-1
eBook Packages : Behavioral Science and Psychology Behavioral Science and Psychology (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Volume 14 Supplement 11
Current situation and challenges for mental health focused on treatment and care in Japan and the Philippines - highlights of the training program by the National Center for Global Health and Medicine
- Meeting report
- Open access
- Published: 03 August 2020
- Crystal Amiel Estrada 1 ,
- Masahide Usami 2 ,
- Naoko Satake 3 ,
- Ernesto Gregorio Jr 4 ,
- Cynthia Leynes 5 ,
- Norieta Balderrama 5 ,
- Japhet Fernandez de Leon 6 ,
- Rhodora Andrea Concepcion 7 ,
- Cecile Tuazon Timbalopez 8 ,
- Noa Tsujii 9 ,
- Ikuhiro Harada 10 ,
- Jiro Masuya 11 ,
- Hiroaki Kihara 12 ,
- Kazuhiro Kawahara 13 ,
- Yuta Yoshimura 2 ,
- Yuuki Hakoshima 2 &
- Jun Kobayashi 14
BMC Proceedings volume 14 , Article number: 11 ( 2020 ) Cite this article
194k Accesses
7 Citations
4 Altmetric
Metrics details
Background and purpose
Mental health has emerged as an important public health concern in recent years. With a high proportion of children and adolescents affected by mental disorders, it is important to ensure that they are provided with proper care and treatment. With the goal of sharing the activities and good practices on child and adolescent mental health promotion, care, and treatment in Japan and the Philippines, the National Center for Global Health and Medicine conducted a training program on the promotion of mental health focused on treatment and care in Japan and the Philippines in September and November 2019.
Key highlights
The training program comprised of a series of lectures, site visits, and round table discussions in Japan and the Philippines. The lectures and site visits focused on the current situation of child and adolescent psychiatry, diagnosis of childhood mental disorders, abuse, health financing for mental disorders, pharmacotherapy, psychotherapy, and disaster child psychiatry in both countries. Round table discussions provided an opportunity to explore the similarities and differences between the two countries in terms of the themes discussed during the lectures.
The training program identified the need to collaborate with other professionals to improve the diagnosis of mental disorders in children and adolescents and to increase the workforce capable of addressing mental health issues among children and adolescents. It also emphasized the importance of cooperation between government efforts during and after disasters to ensure that affected children and their families are provided with the care and support that they need.
Introduction
Current situation of mental health in the western pacific region.
Globally, an estimated 10 to 20% of children and adolescents are affected by mental health problems [ 1 ], with more than half occurring before the age of 14 [ 2 ]. In the Western Pacific Region, mental disorders rank third in the leading causes of disability-adjusted life years (DALY) among children [ 3 ] and the prevalence of suicide attempts is high [ 4 ]. Nevertheless, despite these alarming statistics, the figures may still be underreported due to stigma and taboo which affect help seeking and reporting of mental health problems.
The Mental Health Action Plan of the World Health Organization highlighted the importance of mental health promotion especially in the early stages of life [ 5 ]. Association of South East Asian Countries (ASEAN) countries have reported that mental health education towards students was focused on coping skills whereas teacher training focused on mental illness knowledge and how to provide support to students. Despite these mental health education thrusts, there is limited medical and psychological care available in schools, thus leading to an increased interest in creating an environment that can provide mental health support to students [ 6 ].
Background and aim of the training program
Mental health has emerged as an important public health concern in recent years. In the Philippines, the Philippine Mental Health Act came into force in 2019, and it is expected that the general public will be more concerned about mental health services and rights of patients and their families. However, there are only five government hospitals with psychiatric facilities for children, 84 general hospitals with psychiatric units, 46 outpatient facilities, and only 2.0 mental health professionals per 100,000 people [ 7 ].
The population of the Philippines is estimated to be at 100,981,437 [ 8 ]. Over the past 20 years, infant mortality has decreased [ 9 ] and about a third of the entire population are under 14 years old [ 10 ]. About 27% of children under 5 years are malnourished.
Children with mental health problems are also a cause of concern in the Philippines [ 11 ]. An assessment of the Philippine mental health system reported a 16% prevalence of mental disorders among children [ 12 ]. In addition, the latest Global School-based Student Health Survey found that 16.8% of students aged 13 to 17 attempted suicide one or more times during the 12 months before the survey [ 13 ]. More recent initiatives on establishing the landscape of mental health problems include a nationwide mental health survey being conducted by the Department of Health. This is the first nationwide baseline study that will establish the prevalence of mental disorders in the Philippines. The study is ongoing and the results will be made available by the end of the year.
Despite mental health problems being a cause of concern among children and adolescents in the Philippines, health facilities and human resources for mental health remain limited. Currently, there are only 60 child psychiatrists in the Philippines, with the majority practicing in urban areas such as the National Capital Region. In addition, there are only 11 inpatient and 11 outpatient facilities for children and adolescents, while only 0.28 beds in the mental hospitals are allocated for children and adolescents [ 7 ]. With the focus on mental health increasing in the Philippines, it is expected that the medical treatment and mental health promotion needs of children and adolescents in the Philippines will increase in the future.
In Japan, the National Center for Global Health and Medicine (NCGM) shares the Japanese experience in promoting public health practices and medical technology advancement to developing countries. In conjunction with this, the Department of Psychiatry and Child and Adolescent Psychiatry of Kohnodai Hospital conducts training programs focusing on child and adolescent health. In 2017, Kohnodai Hospital co-created a training program for children’s mental health in disaster-affected areas in the Philippines [ 14 ]. Continuing its thrust on improving child and adolescent mental health, Kohnodai Hospital conducted another training program in partnership with the Philippine Society for Child and Adolescent Psychiatry. This training focused on identifying the current situation and challenges for the promotion of mental health focused on treatment and care in Japan and the Philippines.
The objective of this training was to share the activities and good practices on child and adolescent mental health promotion, care, and treatment in Japan and the Philippines through a series of field visits and discussions. In addition, the training aimed to create a multi-institutional network for childcare such as medical care, health, education, as well as a network of medical staff of various types of occupations between the two countries.
Outline of the training program
Training content.
The current program was composed of a training in the Philippines and in Japan. The first training was conducted in Manila, Philippines from September 11 to 13, 2019 (Table 1 ). Seven Japanese mental health professionals, one social worker, and one public health researcher were dispatched to the Philippines as part of the program. The Japanese experts, engaged in providing mental health promotion, care, and management to children and adolescents, discussed with Philippine experts common mental health issues, diagnostic techniques, and practices and protocols. In addition, site visits to mental health facilities in the Philippines were conducted as part of the program.
The second training was held in Ichikawa, Japan from November 5 to 7, 2019 (Table 2 ). The participants from the Philippines - composed of four child psychiatrists and a researcher - visited government institutions providing mental health services to children and adolescents. The activities of government institutions that provide assistance related to mental health care to children and their families, including its relationship to the community, were also presented during the training.
Participants
Nine health experts from Kohnodai Hospital, National Center of Neurology and Psychiatry, and University of the Ryukyus and 31 participants coming from different Philippine health, academic, government, and non-government institutions attended the first training in the Philippines. The second training was attended by five Philippine health experts from the University of the Philippines Manila College of Medicine, College of Public Health, National Center for Mental Health, and the Lung Center of the Philippines. Table 3 summarizes the profile of the participants in both training programs.
Training outcome: field observations and round table discussion
Diagnosis and prevalence of mental health problems.
In Japan, increasing cases of Attention Deficit Hyperactivity Disorder (ADHD) and Autism Spectrum Disorder (ASD), futoukou (school refusal), and child abuse are issues of major concern. In the Philippines, child abuse, ADHD, and adjustment disorder were the top primary mental health diagnoses.
Similarities were identified in both countries in terms of trend, screening, and diagnosis of neurodevelopmental disorders. In Japan, a significant increase in cases of ADHD and ASD has been noted in recent years. In 1975, the rate of autism was recorded at 1 in 5000 but it was found to be at 1 in 100 in a more recent survey [ 15 ]. Likewise, the Philippines has reported an increase in cases of ASD, from 500,000 cases in 2008 to 1,000,000 in 2018 [ 16 ]. In both countries, initial identification of neurodevelopmental disorders is conducted in schools. When cases are identified, the schools refer the children to hospitals for diagnosis. However, the limited number of available CAPs poses a constraint.
Japan and the Philippines also identified suicide and gaming disorders as major social issues. In the Philippines, common circumstances which are correlated with mental health issues among youth are: too much academic pressure with great difficulty balancing time and excessive use of digital devices engaging in network gaming and social media. Excessive digital device and social media use can lead to depression, breakdown of personal connectedness, and cyberbullying. The Philippines, being one of the most active users of social media sites [ 17 ], is at risk of adolescent addiction and depression. In Japan, First Person Shooting (FPS) games are popular and may pose a dangerous threat to young children.
Psychological abuse in younger children is the most common type of abuse in Japan. Younger children experience higher rates of abuse, with most deaths due to abuse perpetrated by mothers. Neighbors were found to be the most frequent to report cases of child abuse to child counseling centers. Child abuse cases in Japan can be reported to a hotline which is available 24 h a day, 7 days a week and cases are mainly handled by the child counseling center. Currently, child counseling centers are facing difficulties in coping with rapidly increasing cases of child abuse. The number of staff in child counseling centers has increased, but the addition of child counseling centers is an urgent issue since there are few specialized hospitals that can treat children’s mental health problems such as post-traumatic stress disorder (PTSD) due to child abuse.
There are more cases of online child sexual exploitation and substance abuse in the Philippines when compared to Japan. The Philippines has been identified as one of the top sources of child pornography material [ 18 ]. While cases of antisocial behavior have been decreasing recently in Japan, the Philippines has reported that it is an emerging social issue in the country. In the Philippines, an increasing trend in sexual abuse has been observed [ 18 ]. Physical abuse is likely to be underreported because corporal punishment is a commonly accepted method of disciplining Filipino children. Psychological abuse is the least recognized and reported, even though a national baseline study found that 3 of 5 children experience it [ 19 ].
The Women and Child Protection Unit (WCPUs) provide medical and psychosocial care to abused women and children in the Philippines. Trauma-informed psychosocial processing which is based on the principle of cognitive behavioral therapy (CBT) and other therapies are utilized to treat the children brought to the CPU. There are 106 WCPUs distributed in 55 provinces across the country providing 24 h a day, 7 days a week consultation, but there is a lack of mental health professionals in all these WCPUs. Not all WCPUs have a psychiatrist, but it has been proposed to have at least one psychiatrist or psychologist for each CPU. In the meantime, social workers are being trained to process cases being handled by the CPU to address the effects of trauma. More severe cases are referred to the psychologist or psychiatrist of the unit or other government hospitals. For example, the WCPU of the National Center for Mental Health (NCMH), established in 2010, is currently headed by a general psychiatrist with two to three psychiatry residents rotating every 3 months. Most of the cases the WCPU of the NCMH cater to are victims of sexual and physical abuse.
Both countries have identified key strategies in addressing child abuse. In Japan, the national policy focused on service-oriented strategies with three key points: 1) preventing child abuse by conducting home visits; 2) early detection through a regional council for child abuse and child consultation center; and 3) by protection and independent support for abused children. Meanwhile, the Philippine Plan of Action to End Violence Against Children (PPAEVAC) focused on strengthening the administrative aspect of child abuse prevention through the following strategies: development of a national database on child abuse; conduct and utilization of relevant researches on violence against children in all settings; advocacy for laws and policies relevant to violence against children; and strengthening the capacity of Local Councils for the Protection of Children (LPCs).
Schools also play a role in preventing child abuse. The Department of Education of the Philippines has issued DepEd Order no. 40 s. 2012, also known as the Child Protection Policy. This department order describes the policy and guidelines on protecting children in school from bullying, violence, exploitation, discrimination, and abuse [ 20 ]. In Japan, when cases of abuse are discovered, the school principal handles the case.
Human resources for mental health
The lack of child psychiatrists is common in both countries. In Japan, there are 361 accredited doctors by the Japan Child and Adolescent Psychiatric Association as of June 2019. The number of child and adolescent psychiatrists in Japan are fewer when compared with the US and Europe. As of this writing, there are only 60 child psychiatrists and eight fellows in training in the Philippines, with most of the child psychiatrists practicing in Manila. Compounding the severe lack of child psychiatrists in the Philippines is the decision of some child psychiatrists to practice their profession overseas. As a response to the inadequate number of child psychiatrists in both countries, pediatricians are being trained on how to deal with patients with depression or suicidal ideation or behaviors.
Child and adolescent psychiatrists in both countries also need to go through general psychiatry for three to 4 years before they can proceed to child and adolescent psychiatry (CAP). In Japan, there is no curriculum for CAP but the certification to practice as a CAP is being administered by the Japanese Child and Adolescent Psychiatry Society (JSCAP). The curriculum for the subspecialization of CAP in the Philippines is developed and administered by the Philippine Psychiatric Association (PAP) through the Philippine Society of Child and Adolescent Psychiatry (PSCAP). In order to be a recognized fellow, psychiatrists must pass a written and oral examination. However, the two countries differ in terms of training programs for child and adolescent psychiatry. In Japan, there is no national training program for CAPs, while there are three training programs for CAPs in the Philippines.
There is also a lack of psychologists in both countries. There are no child psychologists in Japan but there are many adult psychologists working in the field of child psychology. The Philippines also faces the challenge of having very few child psychologists in the country.
In addition to the lack of child psychiatrists and psychologists in both countries, Japan and the Philippines also lack teachers who can teach children with special needs (SPED teachers). Japan also faces increasing cases of futoukou , or children who refuse to go to school. School refusal is a complex problem and is possibly caused by several factors such as school bullying, trauma, and relationship issues. Meanwhile, in the Philippines, teachers who encounter children with behavioral problems conduct home visits to determine what kind of support, e.g. referral, the children and their family need. Some children drop out of school due to conduct problems.
Some differences in terms of the availability of mental health workers in the school setting were also noted. In Japan, all schools have a school nurse, majority have a school counselor, and some schools even have a social worker. The guidance counselors and teachers play a major role in detecting mental health problems among students and are trained to deal with mental health issues. In contrast, most of the public schools in the Philippines have nurses assigned at the division level (i.e. one nurse provides school health services for several schools). In addition, due to a lack of guidance counselors in public schools, some schools assign a school guidance teacher. However, private schools have their own school nurse and guidance counselor.
Health financing
In Japan, the national health insurance provides 100% subsidy for inpatient and outpatient medical expenses of children below junior high school age (i.e. below 15 years old) care. After junior high school, medical expenses are partially subsidized by the government (70%) and the remaining costs will be out-of-pocket (30%). However, children sometimes need to wait for 3 months to a year to see a specialist due to the overcrowding of hospital CAP units. Financial resources from the welfare section of local governments are also available to provide support to families.
In the Philippines, majority of individuals with mental health disorders pay mostly or entirely out-of-pocket for services and medicines. However, inpatient care at government hospitals is free since the care and treatment of individuals with major mental disorders such as bipolar disorder, depression, and psychosis are covered by the national health insurance [ 7 ]. Nevertheless, the Philippine Health Insurance only reimburses the first week of confinement and it is selective about the diseases it covers. Moreover, it does not cover child mental health. Upon discharge from an inpatient facility, patients can avail of free medicines from the Department of Health’s Medicine Access Program. Patients can also apply to the Philippine Charity Sweepstakes Office (PCSO) which can cover at least 3 months’ worth of free medication provided that the medical doctor will give the medical abstract. Discounts can also be applied for persons with disability (PWDs) when they purchase medicines. Outpatient cases are not subsidized by the government and patients need to pay 100% of the cost from their own pocket.
Pharmacotherapy
The same medications for ADHD, depression, and childhood depression are available in both Japan and the Philippines. Drugs for ADHD such as methylphenidate (MPH) and atomoxetine (ATX) and drugs for ASD such as risperidone (RSP) and aripiprazole (APZ) are being used in both countries. However, more medicines are available in Japan. For example, drugs such as amphetamine, guanfacine (GXR) and lisdexamfetamine (LDX) for the treatment of ADHD and pimozide for ASD are available in Japan but not in the Philippines. Unlike Japan, the Philippines does not use psychostimulants as first line drugs for ADHD treatment.
The Philippines follows the UK National Institute for Health and Care Guidelines (NICE) Clinical Guideline for Autism management for pharmacological treatment. It also emphasizes that treatment requires multidisciplinary action. The environment may play a role why children are exhibiting challenging behaviors hence it is recommended to address environmental factors prior to recommending medication.
In contrast with the Philippines, where off-label use of medicines is not commonly practiced, the off-label use of psychotropic drugs among children in Japan is common. Almost all Pharmaceuticals and Medical Devices Agency (PMDA)-approved drugs are authorized for use among children in Japan. The off-label use of antipsychotics is not associated with patient refusal of the prescription; rather, the most common factor for patient refusal of medications was the belief that antidepressant use causes more harm than good. Glucose and prolactin monitoring are infrequent in children initiated with antipsychotic therapy [ 21 ]. Concern in the use of antipsychotics in pediatric patients in Japan is also limited but there is a need for psychiatrists to routinely monitor the metabolic condition of patients. Additionally, standard educational programs and practice guidelines that provide evidence-based support to psychiatrists for prescription of psychotropic drugs are needed in Japan.
Both countries reported that a special license is needed by psychiatrists to prescribe certain stimulants such as methylphenidate. However, the prescription rate of MPH in Japan is lower than that in other countries, which may be associated with the restriction policy for prescribing stimulants in Japan.
Psychosocial intervention
Both countries employed multidisciplinary teams to manage cases. The team is composed of child psychiatrists, social workers, nurses, and occupational therapists. For child abuse cases in both Japan and the Philippines, social workers serve as case managers.
Japanese CAPs are trained on different forms of psychotherapy during their training. Trauma-focused Cognitive Behavioral Therapy (TF-CBT), adapted from Cognitive Behavioral Therapy (CBT), is widely used for abused children in Japan. In the Philippines, some social workers are trained to conduct CBT-based therapy for child abuse cases.
Charging fees for psychotherapy are unclear for both countries. Psychotherapy provided by public Japanese facilities are free. In the Philippines, government hospitals with psychiatric facilities do not charge consultation fee. In some of these hospitals, there is an initial expense for the payment of a hospital ID. Expenses for laboratory examinations are paid for by the patient.
Disaster child psychiatry
In times of disasters, children experience a wide range of mental and behavioral disturbances such as sleeplessness, fear, anxiety, depression, and post-traumatic stress disorder [ 22 ]. In Japan, children who were affected by the GEJE experienced long-term sleep disruption [ 23 ], with children from the affected Fukushima area exhibiting increasing numbers of suicide, child abuse, bullying, and absenteeism. Suicide risk and psychological symptoms were also observed among junior high school students 5 years after the GEJE. Children with evacuation experience and living in temporary housing had externalization symptoms. Economic disparities, the parents’ mental state and less social support may affect the children. In the Japanese experts’ experience, care for disabled children after disasters is also a challenge; children with ASD have difficulty adjusting to the crowded evacuation centers.
Evacuation centers in the Philippines are usually crowded after a disaster and this in turn, affect the mental health of the children and their family. Adding to this problem is the lack of mental health services for children in the Philippines after disasters. Due to the small number of practicing child psychiatrists in the country, adult psychiatrists have also been trained on how to deal with trauma of children after disasters and they examine child patients in some cases. Psychologists also help out during disasters. The Philippine Psychiatric Association also train people to process the trauma that children have experienced.
In the Philippines, where more than 90% of the total population identify as Christians, religion plays a major role in the social fabric and has become an important pathway for psychosocial support. Faith-based organizations have established mental health and psychosocial support services (MHPSS) especially during times of disasters, such as when Typhoon Haiyan struck in 2013 [ 24 ].
Mental health problems can impact children long after the disaster [ 25 ], hence providing mental health support is vital [ 26 ]. Following traumatic experiences such as disasters, schools, especially teachers, can play a key role in maintaining the well-being of children and adolescents [ 27 , 28 ]. Psychological first aid is described as a “ humane, supportive response to a fellow human being who is suffering and who may need support ” [ 29 ]. In Japan and the Philippines, teachers undergo training on psychological first aid (PFA) and are being trained to identify children who are traumatized. Teachers are also trained on some play sessions and storytelling they can use with the children to help them deal with their trauma. In terms of psychological preparedness, Japan does not have psychological preparedness in schools. In the Philippines, while psychological preparedness is not integrated in the curriculum, some schools conduct trainings on psychological preparedness for teachers and students alike.
Differences were also observed in terms of government response to disasters. Concerted efforts by the Japanese government facilitated an efficient response to the needs of the population affected by the disaster. The Great Hanshin-Awaji Earthquake, which occurred in 1995, was the first disaster that focused on the need for mental health care for affected individuals. Interest in volunteer activities spiked in the aftermath of this disaster. In 2011, Kokoronokea (mental healthcare in Japanese) team provided medical support specializing psychiatry during the Great East Japan Earthquake (GEJE) and in 2013 the Disaster Psychiatric Assistance Team (DPAT) was established from this experience. The importance of providing support for carers or supporters and collaborating with educational institutions and school counselors were also vital lessons that Japan learned from the 2016 Kumamoto earthquake. In contrast, the Philippine experience during the aftermath of Typhoon Haiyan in 2013 highlighted the need for better coordination among non- government organizations as well as between these organizations and the government.
The activities of the training program held in Japan and the Philippines successfully provided an opportunity to share the current situation on the care, diagnosis, and management of mental disorders in children and adolescents in the Philippines and Japan. In addition, the training program enabled Japanese and Philippine experts to identify similarities and differences and sharing of best practices between the two countries. The importance of creating partnerships with the religious sector was also highlighted. The training program is expected to create more opportunities for exchanging best practices on child and adolescent mental health promotion and care among countries in the future.
Clinical implication and recommendation
Based on the outcome of the roundtable discussions, it is recommended to collaborate with the societies of other practitioners such as pediatricians, psychologists, teachers, and social workers to improve the identification and diagnosis of mental disorders. In addition, training other practitioners in identifying cases of mental disorders among children and adolescents can help ease the lack of child and adolescent psychiatrists in both countries.
Further studies on pharmacotherapy dosages specific to Asian setting needs to be done. In addition, developing clinical guidelines and protocols at the country or regional levels for treating children with mental disorders is also recommended. A standard system for availing of psychotherapy including its payment schemes will also be beneficial to children and families who avail of these services.
Cooperation between government efforts pre, during and post disasters is necessary to ensure that affected children and their families are provided with the needed and appropriate care and support. It is also important to provide long-term support to ensure the well-being of children and adolescents. Likewise, psychosocial preparedness needs to be integrated into school and community activities to equip the population with the knowledge and skills that are needed before, during, and after a disaster.
Availability of data and materials
Not applicable.
Abbreviations
Attention deficit hyperactivity disorder
Aripiprazole
Autism spectrum disorder
Association of South East Asian Nations
Atomoxetine
Child and adolescent psychiatry
Cognitive behavioral therapy
Disability-adjusted life years
Disaster Psychiatric Assistance Team
First Person Shooting
Great East Japan Earthquake
Japanese Child and Adolescent Psychiatry Society
Lisdexamfetamine
Local Councils for the Protection of Children
Mental Health Gap
Mental Health and Psychosocial Support Services
Methylphenidate
National Center for Global Health and Medicine
Philippine Psychiatric Association
Philippine Charity Sweepstakes Office
Psychological first aid
Philippine Plan of Action to End Violence Against Children
Philippine Society of Child and Adolescent Psychiatry
Post-traumatic stress disorder
Persons with disability
Risperidone
Trauma-focused cognitive behavioral therapy
Women and Child Protection Unit
Child and adolescent mental health [Internet]. World Health Organization. [cited 2020 Mar 06.]. Available from: https://www.who.int/mental_health/maternal-child/child_adolescent/en/ .
Kessler RC, Angermeyer M, Anthony JC, et al. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization’s world mental health survey initiative. World Psychiatry. 2007;6:168–76.
PubMed PubMed Central Google Scholar
Baranne ML, Falissard B. Global burden of mental disorders among children aged 5–14 years. Child Adolesc Psychiatry Ment Health. 2018;12(1):19.
Article PubMed PubMed Central Google Scholar
Uddin R, Burton NW, Maple M, Khan SR, Khan A. Suicidal ideation, suicide planning, and suicide attempts among adolescents in 59 low-income and middle-income countries: a population-based study. Lancet Child Adolesc Health. 2019;3(4):223–33.
Article PubMed Google Scholar
World Health Organization. Mental Health Action Plan 2013–2020 [Internet]. World Health Organization; 2013 [cited 2020 Mar 10]. Available from https://apps.who.int/iris/bitstream/handle/10665/89966/9789241506021_eng.pdf;jsessionid=3E09FA457C31F4CAF837E14AD6FD2B18?sequence=1 .
Nishio A, Kakimoto M, Bernardo TM, Kobayashi J. Current situation and comparison of school mental health in ASEAN countries. Pediatr Int. 2020;62(4):438–43.
Mental Health Atlas 2017 Member State Profile Philippines [Internet]. World Health Organization; 2017 [cited 2020 Jan 24]. Available from https://www.who.int/mental_health/evidence/atlas/profiles-2017/PHL.pdf?ua=1 .
Philippine Statistics Authority. Highlights of the Philippine Population 2015 Census of Population [Internet]. Philippine Statistics Authority. 2016 [cited 2020 Mar 10]. Available from: https://psa.gov.ph/content/highlights-philippine-population-2015-census-population .
2017 National Demographic and Health Survey Key Findings [Internet]. Philippine Statistics Authority; 2017 [cited 2020 Jan 24]. Available from: http://www.psa.gov.ph/sites/default/files/2017%20PHILIPPINES%20NDHS%20KEY%20FINDINGS_092518.pdf .
The World Factbook: Philippines [Internet]. Central Intelligence Agency. Central Intelligence Agency; 2018 [cited 2020 Jan 24]. Available from: https://www.cia.gov/library/publications/the-world-factbook/geos/rp.html#field-anchor-people-and-society-population-distribution .
Cagande C. Child Mental Health in the Philippines. Adolesc Psychiatry. 2013;3(1). https://doi.org/10.2174/2210676611303010003 .
WHO-AIMS Report on Mental Health System in the Philippines [Internet]. World Health Organization; 2007 [cited 2020 Jan 24]. Available from: https://www.who.int/mental_health/evidence/philippines_who_aims_report.pdf .
NCDs | Global school-based student health survey (GSHS) [Internet]. World Health Organization. World Health Organization; 2019 [cited 2020 Jan 24]. Available from: https://www.who.int/ncds/surveillance/gshs/PIH2015_fact_sheet.pdf .
Usami M, Lomboy MF, Satake N, Estrada CA, Kodama M, Gregorio ER Jr, Suzuki Y, Uytico RB, Molon MP, Harada I, Yamamoto K. Addressing challenges in children’s mental health in disaster-affected areas in Japan and the Philippines–highlights of the training program by the National Center for Global Health and Medicine. In: BMC proceedings; 2018. (Vol. 12, No. 14, pp. 1-8). BioMed Central.
Google Scholar
Weintraub K. Autism counts. Nature. 2011;479(7371):22.
Article CAS PubMed Google Scholar
Lambatin LO. DOH6: Persons with autism rising [Internet]. PIA News. Philippine Information Agency; 2018 [cited 2020 Mar 09]. Available from: https://pia.gov.ph/news/articles/1006481 .
Pond R, Leeding G, Ryan Dubras W-DD. Digital 2020: 3.8 billion people use social media [Internet]. We Are Social. 2020 [cited 2020 Mar 10]. Available from: https://wearesocial.com/blog/2020/01/digital-2020-3-8-billion-people-use-social-media .
UNICEF Philippines. A Systematic Literature Review of the Drivers of Violence Affecting Children in the Philippines [Internet]. UNICEF Philippines; 2016 [cited 23 March 2020]. Available from: https://www.unicef.org/philippines/media/506/file/National%20Baseline%20Study%20on%20Violence%20Against%20Children%20in%20the%20Philippines:%20Systematic%20literature%20review%20of%20drivers%20of%20violence%20affecting%20children%20(executive%20summary).pdf .
Council for the Welfare of Children, UNICEF Philippines. National Baseline Study on Violence Against Children: Philippines Executive Summary [Internet]. 2016 [cited 23 March 2020]. Available from: https://www.unicef.org/philippines/media/491/file/National%20Baseline%20Study%20on%20Violence%20Against%20Children%20in%20the%20Philippines:%20Results%20(executive%20summary).pdf .
Department of Education. DepEd Order No. 40 s. 2012 Child Protection Policy [Internet]. Department of Education [cited 10 Mar 2020]. Available from https://www.deped.gov.ph/wp-content/uploads/2012/05/DO_s2012_40.pdf .
Okumura Y, Usami M, Okada T, Saito T, Negoro H, Tsujii N, Fujita J, Iida J. Glucose and prolactin monitoring in children and adolescents initiating antipsychotic therapy. J Child Adolesc Psychopharmacology. 2018;28(7):454–62.
Article CAS Google Scholar
Kar N. Psychological impact of disasters on children: review of assessment and interventions. World J Pediatr. 2009;5(1):5–11.
Usami M, Iwadare Y, Ushijima H, Inazaki K, Tanaka T, Kodaira M, Watanabe K, Kawahara K, Morikawa M, Kontani K, Murakami K. Did kindergarteners who experienced the great East Japan earthquake as infants develop traumatic symptoms? Series of questionnaire-based cross-sectional surveys: a concise and informative title: traumatic symptoms of kindergarteners who experienced disasters as infants. Asian J Psychiatr. 2019;44:38–44.
Psychosocial Support and Children’s Rights Resource Center (PSTCRRC) and Mental Health and Psychosocial Support Network (MHPSSN). Mental Health and Psychosocial Support in Philippines: Minimal Response Matrix and Mapping: Final Report [Internet]. July 2014 [cited 2020 Jun 23]. Available from: https://www.alnap.org/system/files/content/resource/files/main/mhpss-philippines-mapping-final-version.pdf .
Kar N. Psychosocial issues following a natural disaster in a developing country: a qualitative longitudinal observational study. Int J Disaster Med. 2006;4(4):169–76.
Article Google Scholar
Centers for Disease Control and Prevention. Children's Mental Health & Disasters [Internet]. Centers for Disease Control and Prevention; 2020 [cited 2020 Mar 09]. Available from: https://www.cdc.gov/childrenindisasters/features/disasters-mental-health.html .
Pfefferbaum B, Shaw JA. Practice parameter on disaster preparedness. J Am Acad Child Adolesc Psychiatry. 2013;52(11):1224–38.
Mutch C. The role of schools in disaster preparedness, response and recovery: what can we learn from the literature? Pastoral Care Educ. 2014;32(1):5–22.
Psychological first aid: Guide for field workers [Internet]. World Health Organization. World Health Organization; 2011 [cited 2020 Mar 09]. Available from: https://apps.who.int/iris/bitstream/handle/10665/44615/9789241548205_eng.pdf?sequence=1 .
Download references
Acknowledgments
We would like to express our deepest appreciation to the Philippine Society of Child and Adolescent Psychiatry, National Center for Mental Health, Philippine General Hospital, Department of Education in the Philippines, Ichikawa City Education Center, Ichikawa City Child Care Support Section, and Ichikawa Child Consultation Center in Japan.
This program was funded by the International Promotion of Japan’s Healthcare Technologies and Services in 2019 conducted by the National Center for Global Health and Medicine under the Ministry of Health, Labor and Welfare, Japan. Publication of this article was sponsored by the National Center for Global Health and Medicine grant (30–3).
Author information
Authors and affiliations.
Department of Environmental and Occupational Health, College of Public Health University of the Philippines Manila SEAMEO TROPMED Philippines Regional Centre for Public Health, Hospital Administration, Environmental and Occupational Health, Manila, Philippines
Crystal Amiel Estrada
Department of Child and Adolescent Psychiatry, Kohnodai Hospital, National Center for Global Health and Medicine, Ichikawa, Japan
Masahide Usami, Yuta Yoshimura & Yuuki Hakoshima
Department of Psychiatry, National Center Hospital of Neurology and Psychiatry, Kodaira, Japan
Naoko Satake
Department of Health Promotion and Education, College of Public Health University of the Philippines Manila, SEAMEO TROPMED Philippines Regional Centre for Public Health, Hospital Administration, Environmental and Occupational Health, Manila, Philippines
Ernesto Gregorio Jr
College of Medicine, University of the Philippines Manila, Manila, Philippines
Cynthia Leynes & Norieta Balderrama
West Visayas State University Medical Center, Iloilo, Philippines
Japhet Fernandez de Leon
Lung Center of the Philippines, Quezon City, Philippines
Rhodora Andrea Concepcion
National Center for Mental Health, Mandaluyong City, Philippines
Cecile Tuazon Timbalopez
Department of Neuropsychiatry, Kindai University Faculty of Medicine, Osakasayama, Osaka, Japan
Office of Social Work Service, Kohnodai Hospital, National Center for Global Health and Medicine, Ichikawa, Japan
Ikuhiro Harada
Department of Psychiatry, Tokyo Medical University, Tokyo, Japan
Jiro Masuya
Department of Neuropsychiatry, Kanazawa Medical, Ishikawa, Japan
Hiroaki Kihara
Department of Neuropsychiatry, Faculty of Life Sciences, Kumamoto University, Kumamoto, Japan
Kazuhiro Kawahara
Department of Global Health, Graduate School of Health Sciences, Faculty of Medicine, University of the Ryukyus, Okinawa, Japan
Jun Kobayashi
You can also search for this author in PubMed Google Scholar
Contributions
MU, NS, YH, JK, ERG, and CL planned the training program. MU, NS, YH, IH, NT, HK, KK, NB, RAC, JFDL, and CL delivered presentations as part of the training program. All authors (CAE, MU, NS, ERG, CL, NB, JFDL, RAC, CT, NT, IH, JM, HK, KK, YY, YH, JK) participated in the field visits and roundtable discussions. CAE, UM, NS, NB, ERG, NT, RAC, CT, JFDL, NB, and CL contributed to the manuscript. All the authors had read and approved the final version of the manuscript.
Corresponding author
Correspondence to Masahide Usami .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Estrada, C.A., Usami, M., Satake, N. et al. Current situation and challenges for mental health focused on treatment and care in Japan and the Philippines - highlights of the training program by the National Center for Global Health and Medicine. BMC Proc 14 (Suppl 11), 11 (2020). https://doi.org/10.1186/s12919-020-00194-0
Download citation
Published : 03 August 2020
DOI : https://doi.org/10.1186/s12919-020-00194-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health
- Training programs
- Health promotion
- Philippines
BMC Proceedings
ISSN: 1753-6561
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Philippine E-Journals
Home ⇛ leaps: miriam college faculty research journal ⇛ vol. 25 no. 1 (2005), the education of children with adhd.
Ma. Paz A. Manaligod
Discipline: Education , Child Development , Cognitive Learning
Research studies have found that the prevalence of Attention Deficit Hyperactivity Disorder (ADHD) ADHD ranges from 3% -- 5% of the school-age population. Children with ADHD are more likely to develop depression or anxiety, exhibit disruptive behavior, and have poorer school performance, and more learning disabilities than do unaffected children of the same age. However, when ADHD is effectively managed, the characteristics may be used to the person’s advantage, creating a significant contrast. The design of this study, involves a descriptive survey to determine the relevant policies; existing institutional programs; and existing intervention strategies of teachers and parents. On the basis of existing educational programs, the study intends to surface an emerging model in the education of children with ADHD.
The study shows that concrete steps have been undertaken by the different educational institutions to respond to the needs of students with ADHD. These measures have been classified into four (4) models of intervention, consisting of 10 institutional programs.
The study proposes a model program that include significant elements that will ensure the educational success of students with ADHD. The emerging model emphasizes, among others an inclusive environment and an individualized educational program.
Nonetheless, the success of any educational program is anchored on the strong partnership between the school and the family. This partnership in the education of children with ADHD is a complex and continuing process that comes in different forms. Despite the modest role it presently plays in the Philippine setting, the fact remains that this partnership is very crucial in the educational success of students with ADHD.
Note: Kindly Login or Register to gain access to this article.
Share Article:

ISSN 0116-7235 (Print)
- Citation Generator
- ">Indexing metadata
- Print version
Copyright © 2024 KITE E-Learning Solutions | Exclusively distributed by CE-Logic | Terms and Conditions
- [email protected]
How Increased ADHD Awareness Benefits Filipino Society
In the pursuit of a more understanding and inclusive society, acknowledging and addressing the needs and challenges of individuals with Attention-Deficit/Hyperactivity Disorder (ADHD) is crucial. The quest for increased ADHD awareness in Filipino society is not just about fostering empathy, but about dismantling misconceptions that have long shadowed the true essence of this neurodevelopmental disorder.
ADHD, characterized by a persistent pattern of inattention and/or hyperactivity-impulsivity, transcends more than just an inability to sit still or a proclivity for distraction. It’s a complex disorder that significantly impacts the lives of individuals, their families, and the communities they interact with.
As per recent data, the prevalence of ADHD among Filipino children is around 7.7% , although the exact figure might be higher due to under-diagnosis. The significance of ADHD awareness extends from the corridors of educational institutions to the broader spectrum of social interactions and professional life.
Understanding ADHD is the first step towards creating a supportive environment for individuals to thrive despite the challenges they face due to their neurodivergence.
Understanding ADHD
What Does ADHD Entail?
Delving deeper into ADHD, the symptoms can be broadly categorized into two types: inattentiveness and hyperactivity/impulsivity. Individuals may experience challenges like difficulty in maintaining focus, being easily distracted, forgetfulness, fidgeting, restlessness, and impulsiveness. These symptoms often manifest before the age of 12 and can continue into adulthood, affecting daily functioning and quality of life.
Misconceptions and Challenges in the Philippines
The road towards understanding ADHD in the Philippines is frequently met with bumps of misconceptions. Common myths surrounding ADHD include beliefs that it’s a result of poor parenting, lack of discipline, or merely a phase that a child will outgrow.
These misconceptions, often rooted in a lack of awareness and understanding, contribute to the stigma and discrimination that individuals with ADHD might face in various facets of their lives.
In the educational sphere, children with ADHD may typically be wrongly labeled as lazy, naughty, or unintelligent. In reality, with the right support, individuals with ADHD can excel academically and in other areas of life.
Moreover, the lack of trained professionals and resources for accurate diagnosis and management of ADHD poses a significant challenge.
The ripple effect of these misconceptions and challenges underscores the dire need for increased ADHD awareness in Filipino society.
By shedding light on what ADHD truly is and debunking the myths surrounding it, a more empathetic and inclusive society can be fostered where individuals with ADHD are recognized for their potential and not defined by their disorder.
The Path to Early Diagnosis and Intervention
The journey towards understanding and supporting individuals with ADHD begins with awareness. The increased ADHD awareness in Filipino society is a stepping stone towards early diagnosis and intervention.
When ADHD is identified early , appropriate strategies and interventions can be initiated, which are instrumental in helping individuals manage their symptoms and improve their quality of life.
Fostering a Supportive Society
Awareness morphs into understanding, which in turn, cultivates a supportive environment. When society is well-informed about ADHD, the misconceptions fade away, giving rise to empathy and support.
This change in societal attitude is essential for creating conducive learning and working environments for individuals with ADHD. It also helps in alleviating the self-stigma that individuals with ADHD might experience, enabling them to seek help and thrive.
Historical Stigma Surrounding ADHD in the Philippines
The historical perspective on ADHD in the Philippines is tinted with misconceptions and lack of understanding.
Traditionally, behaviors associated with ADHD were often misattributed to lack of discipline, defiance, or merely a phase of childhood. This misinterpretation frequently led to a culture of blame, where parents or the individuals themselves were blamed for the symptoms of ADHD.
Real-life Encounters with Stigma
Let’s consider the story of Jose, a bright young boy with ADHD, who was often reprimanded by teachers for his inability to sit still or pay attention in class. His parents faced criticism from relatives and friends, who believed that stricter parenting would ‘cure’ his behaviors. These attitudes exacerbated Jose’s challenges and discouraged him from seeking help.
The Spiral of Misconceptions
The lack of ADHD awareness in the Philippines has historically perpetuated a cycle of stigma and misinformation. When society is uninformed about the true nature of ADHD, the stereotypes continue to thrive, pushing individuals with ADHD further into the shadows.
This lack of awareness not only hampers the accurate identification and management of ADHD, but also fosters a hostile environment where individuals with ADHD are misunderstood and unsupported.
Campaigns Breeding Awareness
The tide of change is gradually sweeping across the archipelago with various initiatives and campaigns aimed at increasing ADHD awareness in the Philippines . Schools, healthcare institutions, and community centers are now becoming platforms for disseminating accurate information about ADHD and its management.
Champions of Change: Organizations and Advocates
Numerous organizations and dedicated advocates are leading the charge in promoting increased ADHD awareness in Filipino society. Their relentless efforts are educating the masses and combating the prevailing stigma around ADHD.
By providing resources, organizing awareness campaigns, and fostering supportive communities, these advocates are making significant strides in transforming societal attitudes towards ADHD.
Unlocking Doors: Academic and Employment Accommodations
With the augmenting ADHD awareness, the landscape of academic and employment accommodations for individuals with ADHD is evolving. Schools are now more equipped with the knowledge and tools to support students with ADHD.
Similarly, employers are becoming more understanding and providing conducive work environments that cater to the diverse needs of their employees, including those with ADHD.
Building Bridges: Familial and Societal Understanding
The ripple effect of increased ADHD awareness in Filipino society is also felt within the familial circles. Families are now more understanding and equipped to support their loved ones with ADHD.
This enhanced understanding is the cornerstone for building a more inclusive and supportive society where individuals with ADHD can thrive without prejudice.
The Unending Journey: Sustaining ADHD Awareness
The journey towards a society that fully understands and supports individuals with ADHD is unending. The gains achieved through increased ADHD awareness need to be sustained and built upon.
Continuous efforts from all stakeholders, including government bodies, educational institutions , and the general public, are crucial for this cause.
Your Role in the Larger Picture
You, as a reader, also have a significant role to play. By participating in ADHD awareness campaigns, sharing accurate information, and supporting individuals with ADHD, you contribute to a more empathetic and understanding society.
Together, we can work towards a future where ADHD is understood, accepted, and supported in every facet of Filipino society.
Conclusion: Reflecting on the Journey
The journey through the facets of ADHD awareness in the Philippines reveals a significant narrative. The narrative of evolving societal understanding, support mechanisms, and the collective effort to foster a conducive environment for individuals with ADHD.
The key takeaway resonates with the critical role of increased ADHD awareness in Filipino society in bridging gaps and nurturing a more inclusive and supportive milieu.

A Call to Action: Be the Change
The dialogue on ADHD doesn’t end here. It continues with you, the reader. By sharing this blog and spreading the word, you become part of a larger movement.
A movement aimed at vanquishing stigma, fostering understanding, and creating a Filipino society that not only acknowledges ADHD but supports and empowers individuals affected by it.
The time to act is now. Share this blog, talk about ADHD, and let’s collectively contribute to a more informed and inclusive society.
Resources and Additional Reading
For those seeking to delve deeper into the realm of ADHD awareness and support, numerous resources are available. Here are some organizations and campaigns that are pivotal in promoting ADHD awareness in the Philippines:
- ADHD Society of the Philippines
- ADHD Awareness Month : Observed every October, it’s a concerted campaign to raise awareness, provide resources and support for individuals with ADHD and their families.
Engage with these resources, expand your understanding, and be a beacon of support and awareness in your community. Together, we can make a significant difference in the lives of individuals with ADHD in the Philippines.
Your Support is Our Strength: Join Us Today!
Our community thrives on the support and involvement of people like you. Don’t miss the chance to be part of something meaningful.
Maria Redillas
Maria is an accomplished digital marketing professional, specializing in content marketing and SEO. Her commitment to staying ahead in the industry is evidenced by her multiple certifications. She is always eager for new opportunities where she can apply her expertise and drive further growth and engagement.
No Comment! Be the first one.
Leave a reply cancel reply.
You must be logged in to post a comment.
This site uses Akismet to reduce spam. Learn how your comment data is processed .
You Might Also Like

Meet Reclaim AI: The AI Assistant Protecting Your Time & Sanity
Beginner’s Guide to Figma: Master the Essentials for Efficient Design

Mangools for Beginners: Simplifying SEO

Beyond Brainstorms: Creative Applications for FigJam
Our site uses cookies. By using this site, you agree to the Privacy Policy and Terms of Use .
Cathleen Rui Lin Lau Case Manager, Twinkle Intervention Center , Singapore
Guo Hui Xie EdD, Board-Certified Educational Therapist Special Needs Consultancy & Services, Singapore
..................................................
Education Journals
European Journal of Education Studies
European Journal Of Physical Education and Sport Science
European Journal of F oreign Language Teaching
European Journal of English Language Teaching
European Journal of Alternative Education Studies
European Journal of Open Education and E-learning Studies
European Journal of Literary Studies
European Journal of Applied Linguistics Studies
..................................................
Public Health Journals
European Journal of Public Health Studies
European Journal of Fitness, Nutrition and Sport Medicine Studies
European Journal of Physiotherapy and Rehabilitation Studies
Social Sciences Journals
European Journal of Social Sciences Studies
European Journal of Economic and Financial Research
European Journal of Management and Marketing Studies
European Journal of Human Resource Management Studies
European Journal of Political Science Studies
Literature, Language and Linguistics Journals
European Journal of Literature, Language and Linguistics Studies
European Journal of Multilingualism and Translation Studies
- Other Journals
- ##Editorial Board##
- ##Indexing and Abstracting##
- ##Author's guidelines##
- ##Covered Research Areas##
- ##Announcements##
- ##Related Journals##
- ##Manuscript Submission##
A CASE STUDY OF A CHILD WITH ATTENTION DEFICIT/HYPERACIVITY DISORDER (ADHD) AND MATHEMATICS LEARNING DIFFICULTY (MLD)
This is a case study of a male child, EE, aged 8+ years, who was described as rather disruptive in class during lesson. For past years, his parents, preschool and primary school teachers noted his challenging behavior and also complained that the child showed a strong dislike for mathematics and Chinese language – both are examinable academic subjects. As a result of the disturbing condition, EE was referred to an educational therapist at a private intervention center for a diagnostic assessment. The child was identified with Attention Deficit-Hyperactivity Disorder (ADHD)-Combined subtype. This aim of this paper is to discuss about the effects of ADHD on mathematics learning and how to avoid misdiagnosis or over-diagnosis of a behavioral-cum-learning disorder.
Article visualizations:
Aiken, L.R. (1972). Research on attitudes toward mathematics. Arithmetic Teacher, 19, 229-234.
American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (DSM-5®). Washington, DC: American Psychiatric Association.
Anastopulos, A.D., Spisto, M.A., & Maher, M.C. (1994). The WISC-III freedom from distractibility factor: Its utility in identifying children with attention deficit/hyperactivity disorder. Psychological Assessment, 6(4), 368-371.
Brown, V.L., Cronin, M.E., & McEntire, E. (1994). Test of Mathematical Abilities (2nd ed.): Examiner’s manual. Austin, TX: Pro-Ed.
Brown, V.L., & McEntire, E. (1984). Test of Mathematical Abilities (TOMA): A method for assessing mathematical aptitudes and attitudes. Austin, TX: Pro-Ed.
Brummitt-Yale, J. (2017). What is diagnostic assessment? - Definition & examples. Retrieved on 15 February, 2020, from: https://study.com/academy/lesson/what-is-diagnostic-assessment-definition-examples.html.
Chia, K.H. (2008). Educating the whole child in a child with special needs: What we know and understand and what we can do. ASCD Review, 14, 25-31.
Chia, K.H. (2012). Psychogogy. Singapore: Pearson Education.
Code, W., Merchant, S., Maciejewski, W., Thomas, M., & Lo, J. (2016). The Mathematics Attitudes and Perceptions Survey: An instrument to assess expert-like views and dispositions among undergraduate mathematics students. International Journal of Mathematical Education in Science and Technology (21 pages). Retrieved on 14 February, 2020, from: http://dx.doi.org/10.1080/0020739X.2015.1133854.
Cooijmans, P. (n.d.). IQ and real-life functioning. Retrieved 15 February, 2020, from: https://paulcooijmans.com/intelligence/iq_ranges.html.
DB.net (2018) Difference between ability and skill. Retrieved on 29 December, 2019, from: http://www.differencebetween.net/language/difference-between-ability-and-skill/#ixzz5WS3m4ldH.
Dunn, W. (1999). Sensory Profile. San Antonio, CA: The Psychological Corporation.
DuPaul, G.J., Power, T.J., Anastopoulos, A.D., & Reid, R. (1998). ADHD Rating Scale IV: Checklists, norms, and clinical interpretation. New York, NY: Guilford Press.
Flanagan, D.P., & McGrew, K.S. (1997). A cross-battery approach to assessing and interpreting cognitive abilities: Narrowing the gap between practice and cognitive science. In D.P. Flanagan, J. Genshaft, and P.L. Harrison (Eds.), Contemporary intellectual assessment: theories, tests, and issues (Chapter 8). New York, NY: Guilford press.
Flanagan, D.P., Ortiz, S.O., & Alfonso, V.C. (2007). Use of the cross-battery approach in the assessment of diverse individuals. In A.S. Kaufman and N.L. Kaufman (Series Eds.), Essentials of cross-battery assessment second edition (pp.146-205). Hoboken, NJ: John Wiley & Sons.
Gilliam, J.E. (2006). Gilliam Autism Rating Scale (2nd Edition). Austin, TX: Pro-Ed.
Harrier, L.K., & DeOrnellas, K. (2005). Performance of children diagnosed with attention deficit/hyperactivity disorder on selected planning and reconstitution tests. Applied Neuropsychology, 12 (2), 106-119.
Julita (2011) Difference Between ability and skill. DifferenceBetween.net. Retrieved on 23 December, 2019, from: http://www.differencebetween.net/language/difference-between-ability-and-skill/.
Kaufman, A.S. (1994). Intelligence testing with the WISC-III. New York, NY: John Wiley & Sons.
Kennedy, D. (2019). The ADHD symptoms that complicate and exacerbate a math learning disability. Retrieved on 28 December, 2019, from: https://www.additudemag.com/math-learning-disabilities-dyscalculia-adhd/?utm_source=eletter&utm_medium=email&utm_campaign=treatment_january_2020&utm_content=010220&goal=0_d9446392d6-793865f9f5-297687009.
Kulm, G. (1980). Research on mathematics attitude. In J. Shumway (Ed.), Research in mathematics education (pp.356-387). Reston, VA: The National Council of Teachers of Mathematics, Inc.
Low, K. (2016). The challenges of building math skills with ADHD. Retrieved on 12 February, 2020, from: https://www.verywellmind.com/adhd-and-math-skills-20804.
Newman, R.M. (1998). Gifted and math learning disabled. Retrieved on 16 December, 2019, from: http://www.dyscalculia.org/EDu561.html.
Newman, R.M. (1999). The dyscalculia syndrome. Retrieved on 16 December, 2019, from: http://www.dyscalculia.org/thesis.html.
Pearson, N.A., Patton, J.R., & Mruzek, D.W. (2006). Adaptive Behavior Diagnostic Scale. Austin, TX: Pro-Ed.
Renfrew, C. (2019). Renfrew Language Scales (5th Ed.). London, UK: Routledge (Taylor & Francis).
Riccio, C.A., Cohen, M.J., Hall, J., & Ross, C.M. (1997). The third and fourth factors of the WISC-III: What they don’t measure. Journal of Psychoeducational Assessment, 15, 27-39.
Rosenfeld, C. (2019). ADHD and math: 3 struggles for students with ADHD (and how to help). Retrieved 14 December, 2019, from: https://www.ectutoring.com/adhd-and-math.
Sandhu, I.K. (2019). The Wechsler Intelligence Scale for Children-Fourth Edition (WISC–IV). Retrieved on 19 December, 2019, from: http://www.brainy-child.com/expert/WISC_IV.shtml.
Sattler, J.M. (1982). Assessment of children's intelligence and special abilities (2nd ed.). Boston, MA: Allyn & Bacon.
Watkins, M.W., Kush, J.C., & Glutting, J.J. (1997). Discriminant and predictive validity of the WISC-III ACID profile among children with learning disabilities. Psychology in the Schools, 34, 309-319.
Wechsler, D. (2003). The Wechsler Intelligence Scale for Children (4th ed.): Examiner’s manual, San Antonio, TX: The Psychological Corporation.
Copyright © 2015 - 2023. European Journal of Special Education Research (ISSN 2501 - 2428) is a registered trademark of Open Access Publishing Group . All rights reserved.
This journal is a serial publication uniquely identified by an International Standard Serial Number ( ISSN ) serial number certificate issued by Romanian National Library ( Biblioteca Nationala a Romaniei ). All the research works are uniquely identified by a CrossRef DOI digital object identifier supplied by indexing and repository platforms.
All the research works published on this journal are meeting the Open Access Publishing requirements and can be freely accessed, shared, modified, distributed and used in educational, commercial and non-commercial purposes under a Creative Commons Attribution 4.0 International License (CC BY 4.0) .

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Qual Stud Health Well-being
- v.12(sup1); 2017
ADHD: a critical update for educational professionals
Sanne te meerman.
a Department of Special Needs Education and Child Care , University of Groningen , Groningen, the Netherlands
Laura Batstra
Hans grietens, allen frances.
b Department of Psychiatry , School of Medicine, Duke University , NC, USA
A medical approach towards behavioural problems could make professionals without a medical background, like teachers and other educational professionals feel inapt. In this article, we raise six scientifically grounded considerations regarding ADHD, currently the most prevalent childhood psychiatric diagnosis. These “need to knows” show just how misguided and potentially stigmatizing current conceptualizations of unruly behaviour have become. Some examples are given of how teachers are misinformed, and alternative ways of reporting about neuropsychological research are suggested. A reinvigorated conceptual understanding of ADHD could help educational institutions to avoid the expensive outsourcing of behavioural problems that could also—and justifiably better—be framed as part of education’s primary mission of professionalized socialization.
Introduction
Attention deficit hyperactivity disorder (ADHD) is one of the syndromes defined in the Diagnostic and Statistical Manual of Mental Disorders (DSM). In the DSM-5 (American Psychiatric Association, 2013 ) it is described as a neuro-developmental disorder with a persistent behavioural pattern of severe inattention and/or hyperactivity/impulsivity. The behaviours must be uncharacteristic for the developmental age of the child, be manifest in different settings (for example at home and at school), have started before the age of 12, be present for at least 6 months, and interfere with social and academic performance.
ADHD is currently the most prevalent parent-reported diagnosis among children in the USA (Visser et al., 2014 ). When DSM-IV was published in 1994 (American Psychiatric Association, 1994 ) the prevalence of ADHD was an estimated 3% (Goldman, Genel, Bezman, & Slanetz, 1998 ). Since then, the percentage of children with a parent-reported ADHD diagnosis increased substantially, from 7.8% in 2003 to 9.5% in 2007 to 11.0% in 2011. In 2011, nearly one in five high school boys had been diagnosed with ADHD and about 13.3% of all 11-year-old boys were medicated for ADHD (Visser et al., 2014 ).
In the USA, the total number of children on ADHD medication skyrocketed from 1.5 million in 1995 (Safer & Zito, 1996 ) to 3.5 million in 2011 (Visser et al., 2014 ). Sales of prescription stimulants have quintupled in the last decade (Schwarz, 2013 ), to well over 11 billion in 2015 ( www.jsonline.com, accessed 23 September 2016).
Co-author Allen Frances, who was chair of the DSM-IV, as well as the chair of the DSM-5, David Kupfer, have called the rise in childhood ADHD an “unreal epidemic” (Frances, 2011 ; Verhoeff, 2010 ). In an interview in the New York Times (Schwarz, 2013 ), Keith Conners, a professor emeritus at Duke University who spent much of his career in legitimizing the diagnosis of ADHD, named the rising rates of the ADHD diagnosis in the USA “a national disaster of dangerous proportions”.
Teachers and other school personnel are often the first to suggest the diagnosis of ADHD in a child (Phillips, 2006 ; Sax & Kautz, 2003 ). Previous research suggests that teachers tend to feel insecure about dealing with behavioural problems (Walter, Gouze, & Lim, 2006 ) and hesitant to accept responsibility for students with special needs (Pijl, 2010 ). In this article, we present six scientifically grounded “need to knows” that unravel misconceptions about ADHD. These topics are selected from a wide array of issues surrounding ADHD because we believe they are the most effective in revealing the catch-all (Singh, 2011 ) nature of the ADHD classification, and/or the most exemplary of the adverse effects related to the misunderstandings regarding ADHD. We draw mostly from research and practices in the USA, as the epicenter of ADHD (Lloyd, Stead, & Cohen, 2006 , p. 3). However, we concur with Richards ( 2013 ) that in general “Europe has followed the USA’s lead” by using the DSM-IV and its successor and will also refer to European studies if deemed appropriate. The topics we address are meaningful to teachers and other educational professionals, but certainly also to others such as policy makers who decide on society’s investments in schools.
1. Birth month matters
Several studies (Elder, 2010 ; Evans, Morrill, & Parente, 2010 ; Halldner et al., 2014 ; Morrow et al., 2012 ; Zoëga, Valdimarsdóttir, & Hernández-Díaz, 2012 ) showed that relative age is a significant determinant of ADHD diagnosis and treatment. Overall, the youngest children in class are twice as likely as their classmates to receive a diagnosis of ADHD and medication. Apparently, health care professionals and teachers tend to classify relative immaturity as ADHD. Additional research has indicated that the majority of general practitioners and teachers are unaware of this association between relative age, ADHD-diagnoses and prescribed medicine (Krabbe, Thoutenhoofd, Conradi, Pijl, & Batstra, 2014 ). When a child is more restless and less focused than its classmates, teachers should take the child’s relative age into account when judging his/her behaviour. Furthermore, teachers should be aware of the many potential causes of a child’s unruly behaviour. Seeing ADHD as the cause of inattention and hyperactivity is in fact a logical fallacy as it is circular (Erlandsson, Lundin, & Punzi, 2016 ).
2. There is no single cause of ADHD
ADHD is a behavioural description based on criteria that are sensitive to subjectivity and cognitive biases (Gambrill, 2014 ; Stolzer, 2007 ). There are no measurable biological markers or objective tests to establish the presence or absence of ADHD (or any other given DSM syndrome). As heuristics, the disorders in the DSM have proven useful in clinical practice and research, especially by creating a common language. Unfortunately, the disorders within these classifications are not generally treated as “heuristic, but (…) have become reified (…) [and] are often treated as if they were natural kinds” (Hyman, 2010 ). Such “reification” results in circular claims that the behaviour we call ADHD, is caused by ADHD, and that the criteria for “diagnosing” someone are “symptoms” of an underlying mental illness.
Unfortunately, confusing naming and explaining is a common error with regard to behavioural problems (Batstra, Nieweg, & Hadders-Algra, 2014 ). Seeing ADHD as a brain defect causing problematic behaviour may be tempting: one cause, one solution. However, many factors have been associated with ADHD. These factors may interact and do not always imply causality. They range from divorce (Allen, 2010 ), poverty (Russell, Ford, Rosenberg, & Kelly, 2013 ), parenting styles (Johnston, Mash, Miller, & Ninowski, 2012 ), low maternal education, lone parenthood and reception of social welfare ((Hjern, Weitoft, & Lindblad, 2010 ), sexual abuse (Weinstein, Staffelbach, & Biaggio, 2000 ), lack of sleep (Thakkar, 2013 ), heritability (Larsson, Chang, D’Onofrio, & Lichtenstein, 2013 ) and perinatal issues (Schmitt & Romanos, 2012 ) to eczema (Schmitt, Buske-Kirschbaum, & Roessner, 2010 ), artificial food additives (McCann et al., 2007 ), mobile phone use (Byun et al., 2013 ) and growing up in areas with low solar intensity (Arns, van der Heijden, Arnold, & Kenemans, 2013 ). All these factors and more may play a role when a particular child exhibits impairing hyperactive and inattentive behaviours, and there is no conclusive cause of ADHD.
3. Most children with ADHD behaviour have “normal” brains
The classification provided by the DSM, and even the phenomenon of reification can be useful for research purposes (Cromwell, 2010 ), for example because the categories may facilitate the quest for biological origins of behaviour. And indeed, “case-control” studies -comparing groups of children with and without a diagnosis of ADHD show small group differences in terms of brain anatomy (Sowell et al., 2003 ) and, in some studies, dopaminergic function (Swanson et al., 2007 ). However, these differences do not apply to all children diagnosed with ADHD: within-group variation is large, but between-group differences are small and can be demonstrated at group level only (Batstra et al., 2014 ). In the case of anatomic studies, for example, this means that many with a diagnosis actually have a larger brain than average, while many without a diagnosis have a smaller brain than average. An ADHD diagnosis is a poor predictor of brain size, and brain size is a poor predictor of an ADHD diagnosis.
Furthermore, such individual differences do not refer to a fixed state but to slower anatomical development that mostly catches up later in life (Shaw, Gogtay, & Rapoport, 2010 ). They are only “abnormal” in the sense that they are less common. They do not reveal any innate defect as is illustrated by the fact that many people with an unusual anatomy or physiology do not experience ADHD related problems.
In addition, one should bear in mind that the groups tested in many brain related studies are rigorously screened and not representative of all those diagnosed with ADHD. These individuals with a so called “refined phenotype” (see also e.g. Horga, Kaur, & Peterson, 2014 ) are then compared with “supernormal” or “well controls” with no mental disorder and often privileged in other areas of life as well (Schwartz & Susser, 2011 ; Uher & Rutter, 2012 ). Although such selection in both patient and control groups might help the search for biological markers, these research findings should not be generalized to children diagnosed in everyday society. The samples do not comprise an accurate representation of their respective populations, meaning an average child with a diagnosis of ADHD and an average “normal” child. This problem is particularly urgent since the DSM 5 has lowered the age of onset criterion, as well as the impairment criterion compared to the previous version, the DSM-IV (Thomas, Mitchell, & Batstra, 2013 ). Alongside the lowered threshold, the potential to generalize earlier research findings has lowered as well.
The excerpts in Table 1 illustrate that websites with information about ADHD addressed to teachers might not mention the aforementioned limitations of case-control studies. The examples are taken from the top 10 websites for teachers using the search engine Google. Our alternatives, as well as the last example suggest more thoughtful descriptions.
Online information addressed at teachers.
Note that the research by Castellanos, cited by websites 2–4, uses both refined phenotypes as well as supernormal controls. This means that the average findings are probably not representative for all children with the diagnosis. “ADHD information for teachers” (September, 2016).
4. The genetic origins of ADHD may be overestimated
Claims of ADHD heritability are sometimes as high and seemingly accurate as 0.77 (Banerjee, Middleton, & Faraone, 2007 ). Although activity level might have a substantial genetic basis according to twin studies, “this doesn’t have anything to do with disease” according to Judith Rapoport, researcher at the National Institute of Mental Health (NIMH) ( https://www.dnalc.org/view/2198-ADHD-as-a-Genetic-Disorder, accessed 20 December 2016). Furthermore, these heritability claims vary strongly and are subject to debate because of methodological issues of twin, familial and adoption studies that are used for calculating the heritability coefficient. For example, the higher co-occurrence of ADHD between monozygotic twins (who share 100% of their genes) compared to their dizygotic counterparts (who share 50% of their genes) cannot rule out the influence of environment, as homozygote twins are often treated more similarly and more often have a physical and psychological closeness than their heterozygotic counterparts (Furman, 2008 ). Moreover, these studies still depend on observational tools to assess both parent and child behaviour, and the more sophisticated these tools are (and less prone to rater bias), the lower the estimated genetic effect (Freitag, Rohde, Lempp, & Romanos, 2010 ). Research into the co-occurrence of ADHD in families suffers from extreme difficulty to separate genetic influences from environmental factors (Furman, 2008 ) that typically run in families such as poverty, parenting style and divorce (Hjern et al., 2010 ). Finally, the heritability estimate subsumes the effect of the interplay of genes and environment (Taylor & Sonuga-Barke, 2008 ).
In genetic association studies that really analyse genetic material and that are more powerful when separating the influence of genetics from other etiologic sources, associated genes show only very small effects (Dillon & Craven, 2014 ). Combined, they explain less than 10% of variance (Franke, Neale, & Faraone, 2009 ). This means they occur only slightly more often in diagnosed individuals than in controls, and they do not explain nor predict ADHD behaviours. For educational professionals, this is important to consider as an ADHD label might give a false sense of security with regard to the alleged (genetic) cause of a child’s behaviour and the preferred cure (medication).
5. Medication does not benefit most children in the long run
ADHD-related information addressed at teachers, on the internet and in study books, often depicts ADHD as a highly heritable disorder with visible anatomic and neurochemical differences in children diagnosed. (Erlandsson et al., 2016 ; (Freedman, 2015 ; Mitchell & Read, 2012 ). This may have contributed to the rising use of medication over the years. Initially, the widely publicized results of the first MTA (Multimodal Treatment of Attention Deficity Hyperactivity Disorder) study, the largest study in child psychiatry ever, seemed to confirm this biomedical view and the merits of medication. The study suggested that intensive medication management was superior to behavioural therapy as well as combined treatment (MTA cooperative group, 1999 ). However, follow-up studies of the long-term effects 3 years (Jensen et al., 2007 ) and 8 years later (Molina et al., 2009 ) showed that the outcomes between the different experimental groups converged over time, until, on average, no significant difference between medicated and non-medicated children remained after 8 years. Interestingly, the results of the follow-up studies did not nearly draw the amount of attention and publicity as the previous findings did (Nieweg, 2010 ; Schwarz, 2013 ). Web of Science indicates that the first results were cited 1483 times while the results after 3 and 8 years were cited 203 and 307 times, respectively. A critical review of the MTA by one of the researchers involved, “Just say yes to drugs alone?” (Pelham, 1999 ), was cited 56 times only (Web of Science, consulted September, 2016).
Other longitudinal studies also report no long-term benefits (Riddle et al., 2013 ) or even worse outcomes and adverse effects (Smith, Jongeling, Hartmann, & Russel, 2010 ) of long-term stimulant use. Hence, while medication may help a small group of children in the long run, most will not benefit from long-term pharmaceutical treatment.
6. A diagnosis can be harmful for children
In several countries a confirmed DSM diagnosis opens the door to reimbursement for treatment and school services. This may have promoted “the search for pathology” (Ysseldyke, 2005 ) in relatively mild cases. US data show that 86% of children diagnosed with ADHD are described as having mild or moderate problems (Visser, Bitsko, Danielson, Perou, & Blumberg, 2010 ). The question is whether in these mild cases the merits of a confirmed diagnosis—such as acknowledgement of problems and access to help—outweigh possible demerits. Some known disadvantages of a diagnosis are: low teacher and parent expectations that become self-fulfilling prophecies (Pygmalion/Golem effect); prejudice and stigmatization of diagnosed children; children applying stereotypes to themselves, leading to self-stigma and low self-esteem; decline of self-efficacy; a less effective and potentially counter-effective focus on fixed traits instead of behaviours; a more passive role towards problems; difficulties getting life and disability insurances later on in life; and the risk of overlooking contextual, social and societal explanations, due to the specious explanation offered by labelling (Batstra et al., 2012 ; Cimpian, Arce, Markman, & Dweck, 2007 ; Heyman & Dweck, 1992 ; Kamins & Dweck, 1999 ; Mehta & Farina, 1997 ; O’Rourke, Haimovitz, Ballweber, Dweck, & Popović, 2014 ). For these reasons caution is advisable when considering psychiatric classifications for children.
Conclusion: children need our time, and money
We addressed six issues that educational professionals should be aware of when confronted with inattention and hyperactivity in the classroom. Often, such behaviours are merely the slightly less occurring variations at the poles of any bell-curved behavioural indicator. It is therefore understandable that they are often confused with normal “young” behaviours (paragraph 1). However, disputable yet pervasive claims of ADHD as a genetic neurodevelopmental disorder (paragraphs 3 and 4) could make teachers and other educational professionals feel inapt and might urge them to find solutions outside the realms of their own skills and facilities. Indeed, previous research indicates that teachers are hesitant to accept responsibility for students with special needs (Pijl, 2010 ). A particular vivid example comes from a teacher in Norway, clearly confusing naming and explaining (see paragraph 2) and expressing hope in the questionable merits of medication (paragraph 5). The teacher finally mentions the eventual marginalization of an unruly child into a separate group, potentially stigmatizing the child (paragraph 6), and effectively defeating the goal of inclusive education:
The diagnosis confirms Roar’s special problems. It’s not me that is wrong or bad or something (…). Now Roar has been given his medicine, and consequently I can expect him to behave properly (…) things are going to be normal again. If not, he’ll be moved to “the group for the badly behaved ones”. (Berg, 2013 ) cited by Reindal (Reindal, 2016 ).
For educational professionals, but also for medical and behavioural experts and policy makers, these issues have at least the following implications.
First, more caution is needed with regard to claims made about the etiology of ADHD in general, particularly information addressed at teachers. Generalizing, pathologizing views on the etiology of ADHD-related behaviours—widely dispersed on the internet and in books—do little justice to the different interacting causes of ADHD related behaviours.
Second, we hope that a reinvigorated understanding of ADHD makes us reconsider our own expectations of children. Research indicates that many young children, particularly those diagnosed with ADHD, thrive with more space for physical activity (Song, Lauseng, Lee, Nordstrom, & Katch, 2016 ), playful learning (Panksepp, 2007 ), and smaller classrooms (Biddle & Berliner, 2008 ). Although it might remain necessary to have medical professionals stand by to prevent medical problems being labelled as behavioural in some cases, it is often the other way around. In the absence of proof of ADHD as a clear-cut medical entity, we mostly need to prevent that behavioural problems are unjustly medicalized.
Third, we hope that a reinvigorated conceptual understanding will make teachers and other educational professionals more apprehensive with regard to requesting a diagnosis for a child. Many obtrusive children at risk of falling under the ADHD catch-all umbrella may simply display a difficult temperament. This may have a substantial genetic basis but it is not necessarily a disorder in itself, although it can become one in interaction with an environment that is not sufficiently adapted to the child’s needs. Other children’s unruly or distracted behaviour may be a sign of distress and adverse circumstances. In either case, focusing on these behaviours, and avoiding a disability narrative, is more helpful in teaching these children the behaviours we expect from them. For the tailored approach this entails, we need to provide sufficient (financial) space to the institution and its professionals we entrusted with the larger part of the socialization of our children.
Disclosure statement
Allen Frances was Chair of the DSM-IV Task Force.
- Allen D. M. (2010). How dysfunctional families spur mental disorders: A balanced approach to resolve problems and reconcile relationships . Santa Barbara, CA: Praeger. [ Google Scholar ]
- American Psychiatric Association (1994). Diagnostic and statistical manual of mental disorders (DSM-IV) . Arlington, VA: Author. [ Google Scholar ]
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders: DSM-5™ (5th ed.). Arlington, VA: Author. [ Google Scholar ]
- Arns M., van der Heijden K. B., Arnold L. E., & Kenemans J. L. (2013). Geographic variation in the prevalence of attention-deficit/hyperactivity disorder: The sunny perspective . Biological Psychiatry , 74 ( 8 ), 585–7. doi: 10.1016/j.biopsych.2013.02.010 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Banerjee T. D., Middleton F., & Faraone S. V. (2007). Environmental risk factors for attention-deficit hyperactivity disorder . Acta Paediatrica (Oslo, Norway: 1992) , 96 ( 9 ), 1269–1274. doi: 10.1111/j.1651-2227.2007.00430.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Batstra L., Hadders-Algra M., Nieweg E., Van Tol D., Pijl S. J., & Frances A. (2012). Childhood emotional and behavioral problems: Reducing overdiagnosis without risking undertreatment . Developmental Medicine & Child Neurology , 54 ( 6 ), 492–494. doi: 10.1111/j.1469-8749.2011.04176.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Batstra L., Nieweg E. H., & Hadders-Algra M. (2014). Exploring five common assumptions on attention deficit hyperactivity disorder . Acta Paediatrica , 103 ( 7 ), 696–700. doi: 10.1111/apa.12642 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Berg K. (2013). Teachers’ narratives on professional identities and inclusive education . Nordic Studies in Education , 33 ( 04 ), 269–283. [ Google Scholar ]
- Biddle B. J, & Berliner D. C. (2008). Small class size and its effects. schools and society . A Sociological Approach To Education , 3 , 86-95. [ Google Scholar ]
- Byun Y., Ha M., Kwon H., Hong Y., Leem J., Sakong J., … Scott J. G. (2013). Mobile phone use, blood lead levels, and attention deficit hyperactivity symptoms in children: A longitudinal study . Plos One , 8 ( 3 ), e59742. doi: 10.1371/journal.pone.0059742 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Castellanos F. X., Lee P. P., Sharp W., Jeffries N. O., Greenstein D. K., Clasen L. S., … Rapoport J. L. (2002). Developmental trajectories of brain volume abnormalities in children and adolescents with attention-deficit/hyperactivity disorder . JAMA: Journal of the American Medical Association , 288 ( 14 ), 1740–1748. doi: 10.1001/jama.288.14.1740 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cimpian A., Arce H. C., Markman E. M., & Dweck C. S. (2007). Subtle linguistic cues affect children’s motivation . Psychological Science , 18 ( 4 ), 314–316. doi: 10.1111/j.1467-9280.2007.01896.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cromwell R. L. (2010). Being human, human being: Manifesto for a new psychology . New York, NY: iUniverse. [ Google Scholar ]
- Dillon A., & Craven R. G. (2014). Examining the genetic contribution to ADHD . Ethical Human Psychology & Psychiatry , 16 ( 1 ), 20–28. doi: 10.1891/1559-4343.16.1.20 [ CrossRef ] [ Google Scholar ]
- Elder T. E. (2010). The importance of relative standards in ADHD diagnoses: Evidence based on exact birth dates . Journal of Health Economics , 29 ( 5 ), 641–656. doi: 10.1016/j.jhealeco.2010.06.003 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Erlandsson S., Lundin L., & Punzi E. (2016). A discursive analysis concerning information on “ADHD” presented to parents by the national institute of mental health (USA) . International Journal of Qualitative Studies on Health and Well-Being , 11 , 30938. doi: 10.3402/qhw.v11.30938 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Evans W. N., Morrill M. S., & Parente S. T. (2010). Measuring inappropriate medical diagnosis and treatment in survey data: The case of ADHD among school-age children . Journal of Health Economics , 29 ( 5 ), 657–673. doi: 10.1016/j.jhealeco.2010.07.005 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Frances A. (2011). The epidemic of attention deficit disorder: Real or fad? Retrieved from http://www.psychiatrictimes.com/display/article/10168/1864222
- Franke B., Neale B., & Faraone S. (2009). Genome-wide association studies in ADHD . Human Genetics , 126 ( 1 ), 13–50. doi: 10.1007/s00439-009-0663-4 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Freedman J. E. (2015). An analysis of the discourses on attention deficit hyperactivity disorder (ADHD) in US special education textbooks, with implications for inclusive education . International Journal of Inclusive Education , 20 ( 1 ), 32–51. doi: 10.1080/13603116.2015.1073375 [ CrossRef ] [ Google Scholar ]
- Freitag C. M., Rohde L. A., Lempp T., & Romanos M. (2010). Phenotypic and measurement influences on heritability estimates in childhood ADHD . European Child & Adolescent Psychiatry , 19 ( 3 ), 311–323. doi: 10.1007/s00787-010-0097-5 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Furman L. M. (2008). Attention-deficit hyperactivity disorder (ADHD): Does new research support old concepts? Journal of Child Neurology , 23 ( 7 ), 775–784. doi: 10.1177/0883073808318059 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gambrill E. (2014). The diagnostic and statistical manual of mental disorders as a major form of dehumanization in the modern world . Research on Social Work Practice , 24 ( 1 ), 13–36. doi: 10.1177/1049731513499411 [ CrossRef ] [ Google Scholar ]
- Goldman L. S., Genel M., Bezman R. J., & Slanetz P. J. (1998). Diagnosis and treatment of attention-deficit/hyperactivity disorder in children and adolescents. council on scientific affairs, american medical association . JAMA: The Journal of the American Medical Association , 279 ( 14 ), 1100–1107. doi: 10.1001/jama.279.14.1100 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Halldner L., Tillander A., Lundholm C., Boman M., Långström N., Larsson H., & Lichtenstein P. (2014). Relative immaturity and ADHD: Findings from nationwide registers, parent- and self-reports . Journal of Child Psychology and Psychiatry , 55 ( 8 ), 897–904. doi: 10.1111/jcpp.12229 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Heyman G. D., & Dweck C. S. (1992). Young children’s vulnerability to self-blame and helplessness: Relationship to beliefs about goodness . Child Development , 63 ( 2 ), 401. doi: 10.1111/1467-8624.ep9207061020 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hjern A., Weitoft G. R., & Lindblad F. (2010). Social adversity predicts ADHD-medication in school children–a national cohort study . Acta Paediatrica (Oslo, Norway: 1992) , 99 ( 6 ), 920–924. doi: 10.1111/j.1651-2227.2009.01638.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Horga G., Kaur T., & Peterson B. S. (2014). Annual research review: Current limitations and future directions in MRI studies of child- and adult-onset developmental psychopathologies . Journal of Child Psychology and Psychiatry , 55 ( 6 ), 659–680. doi: 10.1111/jcpp.12185 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hyman S. E. (2010). The diagnosis of mental disorders: The problem of reification . Annual Review of Clinical Psychology , 6 , 155–179. doi: 10.1146/annurev.clinpsy.3.022806.091532 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jensen P. S., Arnold L. E., Swanson J. M., Vitiello B., Abikoff H. B., Greenhill L. L., … Hur K. (2007). 3-year follow-up of the NIMH MTA study . Journal of the American Academy of Child & Adolescent Psychiatry , 46 ( 8 ), 989–1002. doi: 10.1097/CHI.0b013e3180686d48 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Johnston C., Mash E. J., Miller N., & Ninowski J. E. (2012). Parenting in adults with attention-deficit/hyperactivity disorder (ADHD) . Clinical Psychology Review , 32 ( 4 ), 215–228. doi: 10.1016/j.cpr.2012.01.007 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kamins M. L., & Dweck C. S. (1999). Person versus process praise and criticism: Implications for contingent self-worth and coping . Developmental Psychology , 35 ( 3 ), 835–847. doi: 10.1037/0012-1649.35.3.835 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Krabbe E. E., Thoutenhoofd E. D., Conradi M., Pijl S. J., & Batstra L. (2014). Birth month as predictor of ADHD medication use in Dutch school classes . European Journal of Special Needs Education , 29 ( 4 ), 571–578. doi: 10.1080/08856257.2014.943564 [ CrossRef ] [ Google Scholar ]
- Larsson H., Chang Z., D’Onofrio B. M., & Lichtenstein P. (2013). The heritability of clinically diagnosed attention deficit hyperactivity disorder across the lifespan . Psychological Medicine , 44 ( 10 ), 2223–2229. doi: 10.1017/S0033291713002493 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lloyd G., Stead J., & Cohen D. (2006). Critical new perspectives on ADHD . New York: Routledge. [ Google Scholar ]
- McCann D., Barrett A., Cooper A., Crumpler D., Dalen L., Grimshaw K., … Stevenson J. (2007). Food additives and hyperactive behaviour in 3-year-old and 8/9-year-old children in the community: A randomised, double-blinded, placebo-controlled trial . Lancet , 370 ( 9598 ), 1560–1567. doi: 10.1016/S0140-6736(07)61306-3 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mehta S., & Farina A. (1997). Is being ‘sick’ really better? effect of the disease view of mental disorder on stigma . Journal of Social and Clinical Psychology , 16 ( 4 ), 405–419. doi: 10.1521/jscp.1997.16.4.405 [ CrossRef ] [ Google Scholar ]
- Mitchell J., & Read J. (2012). Attention-deficit hyperactivity disorder, drug companies and the internet . Clinical Child Psychology and Psychiatry , 17 ( 1 ), 121–139. doi: 10.1177/1359104510396432 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Molina B. S. G., Hinshaw S. P., Swanson J. M., Arnold L. E., Vitiello B., Jensen P. S., & Cooperative Grp M. T. A. (2009). The MTA at 8 years: Prospective follow-up of children treated for combined-type ADHD in a multisite study . Journal of the American Academy of Child and Adolescent Psychiatry , 48 ( 5 ), 484–500. doi: 10.1097/CHI.0b013e31819c23d0 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Morrow R. L., Garland E. J., Wright J. M., Maclure M., Taylor S., & Dormuth C. R. (2012). Influence of relative age on diagnosis and treatment of attention-deficit/hyperactivity disorder in children . CMAJ: Canadian Medical Association Journal , 184 ( 7 ), 755–762. doi: 10.1503/cmaj.111619 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- MTA cooperative group, t (1999). A 14-month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorder. the MTA cooperative group. multimodal treatment study of children with ADHD . Archives of General Psychiatry , 56 ( 12 ), 1073–1086. [ PubMed ] [ Google Scholar ]
- Nieweg E. H. (2010). [Does ADHD medication stop working after 2-3 years? on the surprising, but little-known follow-up of the MTA study] . Tijdschrift Voor Psychiatrie , 52 ( 4 ), 245–254. [ PubMed ] [ Google Scholar ]
- O’Rourke E., Haimovitz K., Ballweber C., Dweck C., & Popović Z. (2014). Brain points: A growth mindset incentive structure boosts persistence in an educational game . In Proceedings of the 32nd Annual ACM Conference on Human Factors in Computing Systems (pp. 3339–3348.). ON, Canada: ACM. [ Google Scholar ]
- Panksepp J. (2007). Can PLAY diminish ADHD and facilitate the construction of the social brain? Journal of the Canadian Academy of Child and Adolescent Psychiatry , 16 ( 2 ), 57–66. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pelham W. (1999). The NIMH multimodal treatment study for attention-deficit hyperactivity disorder: Just say yes to drugs alone? Canadian Journal of Psychiatry , 44 ( 10 ), 981–990. doi: 10.1177/070674379904401004 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Phillips C. B. (2006). Medicine goes to school: Teachers as sickness brokers for ADHD . Plos Medicine , 3 ( 4 ), e182–e182. doi: 10.1371/journal.pmed.0030182 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pijl S. J. (2010). Preparing teachers for inclusive education: Some reflections from the netherlands . Journal of Research in Special Educational Needs , 10 ( 1 ), 197–201. doi: 10.1111/j.1471-3802.2010.01165.x [ CrossRef ] [ Google Scholar ]
- Reindal S. M. (2016). Discussing inclusive education: An inquiry into different interpretations and a search for ethical aspects of inclusion using the capabilities approach . European Journal of Special Needs Education , 31 ( 1 ), 1–12. doi: 10.1080/08856257.2015.1087123 [ CrossRef ] [ Google Scholar ]
- Richards L. M. (2013). It is time for a more integrated bio-psycho-social approach to ADHD . Clinical Child Psychology and Psychiatry , 18 ( 4 ), 483–503. doi: 10.1177/1359104512458228 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Riddle M. A., Yershova K., Lazzaretto D., Paykina N., Yenokyan G., Greenhill L., … Posner K. (2013). The preschool attention-deficit/hyperactivity disorder treatment study (PATS) 6-year follow-up . Journal of the American Academy of Child & Adolescent Psychiatry , 52 ( 3 ), 264–278.e2. doi: 10.1016/j.jaac.2012.12.007 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Russell G., Ford T., Rosenberg R., & Kelly S. (2013). The association of attention deficit hyperactivity disorder with socioeconomic disadvantage: Alternative explanations and evidence . Journal of Child Psychology and Psychiatry , 55 ( 5 ), 436–445. doi: 10.1111/jcpp.12170 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Safer D. J., & Zito J. M. (1996). Increased methylphenidate usage for attention deficit disorder in the 1990s . Pediatrics , 98 ( 6 ), 1084. [ PubMed ] [ Google Scholar ]
- Sax L., & Kautz K. J. (2003). Who first suggest the diagnosis of attention-deficit/hyperactivity disorder? Annals of Family Medicine , 1 ( 3 ), 171. doi: 10.1370/afm.3 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schmitt J., Buske-Kirschbaum A., & Roessner V. (2010). Is atopic disease a risk factor for attention-deficit/hyperactivity disorder? A systematic review . Allergy , 65 ( 12 ), 1506–1524. doi: 10.1111/j.1398-9995.2010.02449.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schmitt J., & Romanos M. (2012). Prenatal and perinatal risk factors for attention-deficit/hyperactivity disorder . Archives of Pediatrics & Adolescent Medicine , 166 ( 11 ), 1074–1075. doi: 10.1001/archpediatrics.2012.1078 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schwartz S., & Susser E. (2011). The use of well controls: An unhealthy practice in psychiatric research . Psychological Medicine , 41 ( 6 ), 1127–1131. doi: 10.1017/S0033291710001595 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schwarz A. (2013, December 15). The selling of attention deficit disorder . New York Times , pp. A1.
- Shaw P., Gogtay N., & Rapoport J. (2010). Childhood psychiatric disorders as anomalies in neurodevelopmental trajectories . Human Brain Mapping , 31 ( 6 ), 917–925. doi: 10.1002/hbm.21028 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Singh I. (2011). A disorder of anger and aggression: Children’s perspectives on attention deficit/hyperactivity disorder in the UK . Social Science & Medicine , 73 ( 6 ), 889–896. doi: 10.1016/j.socscimed.2011.03.049 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Smith G., Jongeling B., Hartmann P., & Russel C. (2010). Raine ADHD study: Long-term outcomes associated with stimulant medication in the treatment of ADHD in children Government of Western Australia . Department of Health. [ Google Scholar ]
- Song M., Lauseng D., Lee S., Nordstrom M., & Katch V. (2016). Enhanced physical activity improves selected outcomes in children with ADHD: Systematic review . Western Journal of Nursing Research , 38 ( 9 ), 1155–1184. doi: 10.1177/0193945916649954 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sowell E. R., Thompson P. M., Welcome S. E., Henkenius A. L., Toga A. W., & Peterson B. S. (2003). Cortical abnormalities in children and adolescents with attention-deficit hyperactivity disorder . Lancet , 362 ( 9397 ), 1699–1707. [ PubMed ] [ Google Scholar ]
- Stolzer J. M. (2007). The ADHD epidemic in America . Ethical Human Psychology and Psychiatry: an International Journal of Critical Inquiry , 9 ( 2 ), 109–116. doi: 10.1891/152315007782021204 [ CrossRef ] [ Google Scholar ]
- Swanson J., Kinsbourne M., Nigg J., Lanphear B., Stefanatos G., Volkow N., … Wadhwa P. (2007). Etiologic subtypes of attention-deficit/hyperactivity disorder: Brain imaging, molecular genetic and environmental factors and the dopamine hypothesis . Neuropsychology Review , 17 ( 1 ), 39–59. doi: 10.1007/s11065-007-9019-9 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Taylor E., & Sonuga-Barke E. J. S. (2008). Disorders of attention and activity In Rutter M., Bishop D., Pine D., Scott S., Stevenson J. S., Taylor E. A., & Thapar A. (Eds.), Rutter’s child and adolescent psychiatry (5th ed., pp. 521–522–542). West Sussex, UK: John Wiley & Sons. [ Google Scholar ]
- Thakkar V. G. (2013, April 28). Diagnosing the wrong deficit . The New York Times , pp. SR1.
- Thomas R., Mitchell G. K., & Batstra L. (2013). Attention-deficit/hyperactivity disorder: Are we helping or harming? BMJ (Clinical Research Ed.) , 347 , f6172–f6172. doi: 10.1136/bmj.f6172 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Uher R., & Rutter M. (2012). Basing psychiatric classification on scientific foundation: Problems and prospects . International Review of Psychiatry , 24 ( 6 ), 591–605. doi: 10.3109/09540261.2012.721346 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Verhoeff B. (2010). Drawing borders of mental disorders: An interview with David Kupfer . BioSocieties , 5 ( 4 ), 467–475. doi: 10.1057/biosoc.2010.24 [ CrossRef ] [ Google Scholar ]
- Visser S., Bitsko R., Danielson M., Perou R., & Blumberg S. (2010). Increasing prevalence of parent-reported attention-deficit/hyperactivity disorder among children—United States, 2003 and 2007 . Morbidity and Mortality Weekly Report , 59 ( 44 ), 1439–1443. [ PubMed ] [ Google Scholar ]
- Visser S., Danielson M., Bitsko R. H., Holbrook J., Kogan M., Ghandour R., … Blumberg S. (2014). Trends in the parent-report of health care provider-diagnosed and medicated attention-deficit/hyperactivity disorder: United States, 2003–2011 . Journal of the American Academy of Child & Adolescent Psychiatry , 53 ( 1 ), 34–46. doi: 10.1016/j.jaac.2013.09.001 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Walter H. J., Gouze K., & Lim K. G. (2006). Teachers’ beliefs about mental health needs in inner city elementary schools . Journal of the American Academy of Child & Adolescent Psychiatry , 45 ( 1 ), 61–68. doi: 10.1097/01.chi.0000187243.17824.6c [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Weinstein D., Staffelbach D., & Biaggio M. (2000). Attention-deficit hyperactivity disorder and posttraumatic stress disorder: Differential diagnosis in childhood sexual abuse . Clinical Psychology Review , 20 ( 3 ), 359–378. doi: 10.1016/S0272-7358(98)00107-X [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ysseldyke J. (2005). Assessment and decision making for students with learning disabilities: What if this is as good as it gets? Learning Disability Quarterly , 28 ( 2 ), 125. doi: 10.2307/1593610 [ CrossRef ] [ Google Scholar ]
- Zoëga H., Valdimarsdóttir U. A., & Hernández-Díaz S. (2012). Age, academic performance, and stimulant prescribing for ADHD: A nationwide cohort study . Pediatrics , 130 ( 6 ), 1012–1018. doi: 10.1542/peds.2012-0689 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Disclaimer » Advertising
- HealthyChildren.org

- Previous Article
- Next Article
Eligibility Criteria
Search strategy, data extraction, risk of bias, data synthesis and analysis, medications, youth-directed psychosocial treatments, parent support, school interventions, cognitive training, neurofeedback, nutrition and supplements, complementary, alternative, or integrative medicine, combined medication and behavioral treatments, moderation of treatment response, long-term outcomes, clinical implications, strengths and limitations, future research needs, acknowledgments, treatments for adhd in children and adolescents: a systematic review.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- CME Quiz Close Quiz
- Open the PDF for in another window
- Get Permissions
- Cite Icon Cite
- Search Site
Bradley S. Peterson , Joey Trampush , Margaret Maglione , Maria Bolshakova , Mary Rozelle , Jeremy Miles , Sheila Pakdaman , Morah Brown , Sachi Yagyu , Aneesa Motala , Susanne Hempel; Treatments for ADHD in Children and Adolescents: A Systematic Review. Pediatrics April 2024; 153 (4): e2024065787. 10.1542/peds.2024-065787
Download citation file:
- Ris (Zotero)
- Reference Manager
Effective treatment of attention-deficit/hyperactivity disorder (ADHD) is essential to improving youth outcomes.
This systematic review provides an overview of the available treatment options.
We identified controlled treatment evaluations in 12 databases published from 1980 to June 2023; treatments were not restricted by intervention content.
Studies in children and adolescents with clinically diagnosed ADHD, reporting patient health and psychosocial outcomes, were eligible. Publications were screened by trained reviewers, supported by machine learning.
Data were abstracted and critically appraised by 1 reviewer and checked by a methodologist. Data were pooled using random-effects models. Strength of evidence and applicability assessments followed Evidence-based Practice Center standards.
In total, 312 studies reported in 540 publications were included. We grouped evidence for medication, psychosocial interventions, parent support, nutrition and supplements, neurofeedback, neurostimulation, physical exercise, complementary medicine, school interventions, and provider approaches. Several treatments improved ADHD symptoms. Medications had the strongest evidence base for improving outcomes, including disruptive behaviors and broadband measures, but were associated with adverse events.
We found limited evidence of studies comparing alternative treatments directly and indirect analyses identified few systematic differences across stimulants and nonstimulants. Identified combination of medication with youth-directed psychosocial interventions did not systematically produce better results than monotherapy, though few combinations have been evaluated.
A growing number of treatments are available that improve ADHD symptoms and other outcomes, in particular for school-aged youth. Medication therapies remain important treatment options but are associated with adverse events.
Attention-deficit/hyperactivity disorder (ADHD) is a common mental health problem in youth, with a prevalence of ∼5.3%. 1 , 2 Youth with ADHD are prone to future risk-taking problems, including substance abuse, motor vehicle accidents, unprotected sex, criminal behavior, and suicide attempts. 3 Although stimulant medications are currently the mainstay of treatment of school-age youth with ADHD, other treatments have been developed for ADHD, including cognitive training, neurofeedback, neuromodulation, and dietary and nutritional interventions. 4 – 7
This systematic review summarizes evidence for treatments of ADHD in children and adolescents. The evidence review extends back to 1980, when contemporary diagnostic criteria for ADHD and long-acting stimulants were first introduced. Furthermore, we did not restrict to a set of prespecified known interventions for ADHD, and instead explored the range of available treatment options for children and adolescents, including novel treatments. Medication evaluations had to adhere to a randomized controlled trial (RCT) design, all other treatments could be evaluated in RCTs or nonrandomized controlled studies that are more common in the psychological literature, as long as the study reported on a concurrent comparator. Outcomes were selected with input from experts and stakeholders and were not restricted to ADHD symptoms. To our knowledge, no previous review for ADHD treatments has been as comprehensive in the range of interventions, clinical and psychosocial outcomes, participant ages, and publication years.
The review aims were developed in consultation with the Agency for Healthcare Research and Quality (AHRQ), the Patient-Centered Outcomes Research Institute, the topic nominator American Academy of Pediatrics (AAP), key informants, a technical expert panel (TEP), and public input. The TEP reviewed the protocol and advised on key outcomes. Subgroup analyses and key outcomes were prespecified. The review is registered in PROSPERO (#CRD42022312656) and the protocol is available on the AHRQ Web site as part of a larger evidence report on ADHD. The systematic review followed Methods of the (AHRQ) Evidence-based Practice Center Program. 8
Population: Children or adolescents with a clinical diagnosis of ADHD, age <18 years
Interventions: Any ADHD treatment, alone or in combination, and ≥4 weeks’ treatment
Comparators: No treatment, waitlist, placebo, passive comparators, or active comparators
Outcomes: Patient health and psychosocial outcomes
Setting: Any
Study designs: RCTs for medication; RCTs, controlled clinical trials without random assignment, or cohort studies comparing 1 or more treatment groups for nondrug treatments. Studies either had to be large or demonstrate that they could detect effects as a standalone study (operationalized as ≥100 participants or a power calculation)
Other limiters: English-language (to ensure transparency for a US guideline), published from 1980
We searched the databases PubMed, Embase, PsycINFO, ERIC, and ClinicalTrials.gov. We identified reviews for reference-mining through PubMed, Cochrane Database of Systematic Reviews, Campbell Collaboration, What Works in Education, PROSPERO, ECRI Guidelines Trust, G-I-N, and ClinicalKey. The search underwent peer review; the full strategy is in the Online Appendix. All citations were reviewed by trained literature reviewers supported by machine learning to ensure no studies were inadvertently missed. Two independent reviewers assessed full-text studies for eligibility. Publications reporting on the same participants were consolidated into 1 record so that no study entered the analyses more than once. The TEP reviewed studies to ensure all were captured.
The data abstraction form included extensive guidance to aid reproducibility and standardization in recording study details, outcomes, 9 – 12 study quality, and applicability. One reviewer abstracted data, and a methodologist checked its accuracy and completeness. Data are publicly available in the Systematic Review Data Repository.
We assessed 6 domains 13 : Selection, performance, attrition, detection, reporting, and study-specific biases ( Supplemental Figs 6 and 7 ).
We organized analyses by treatment and comparison type. We grouped treatments according to intervention content and target (eg, youth or parents). The intervention taxonomy differentiated medication, psychosocial interventions, parent support, nutrition and supplements, neurofeedback, neurostimulation, physical exercise, complementary medicine, school interventions, and provider approaches. We differentiated effects versus passive control groups (eg, placebo) and comparative effects (ie, comparing to an alternative treatment). The following outcomes were selected as key outcomes: (1) ADHD symptoms (eg, ADHD Rating Scale 14 , 15 ), (2) disruptive behavior (eg, conduct problems), (3) broadband measures (eg, Clinical Global Impression 16 ), (4) functional impairment (eg, Weiss Functional Impairment Rating Scale 17 , 18 ), (5) academic performance (eg, grade point average), (6) appetite suppression, and (7) number of participants reporting adverse events.
Studies reported on a large range of outcome measures as documented in the evidence table in the Online Appendix. To facilitate comparisons across studies, we converted outcomes to scale-independent standardized mean differences (SMDs) for continuous symptom outcome variables and relative risks (RRs) for categorical reports, presenting summary estimates and 95% confidence intervals (CIs) for all analyses. We used random-effects models performed in R with Metafor_v4.2-0 for statistical pooling, correcting for small numbers of studies when necessary, to synthesize available evidence. 19 We conducted sensitivity analyses for all analyses that included studies without random assignment. We also compared treatment effectiveness indirectly across studies in meta-regressions that added potential, prespecified effect modifiers to the meta-analytic model. In particular, we assessed whether ADHD presentation or cooccurring disorders modified intervention effects. We tested for heterogeneity using graphical displays, documented I 2 statistics (values >50% are highlighted in the text), and explored sources of heterogeneity in subgroup and sensitivity analyses. 20
We assessed publication bias with Begg and Egger tests 21 , 22 and used the trim-and-fill methods for alternative estimates where necessary. 23 Applicability of findings to real-world clinical practices in typical US settings was assessed qualitatively using AHRQ’s Methods Guide. An overall strength of evidence (SoE) assessment communicating our confidence in each finding was determined initially by 1 researcher with experience in use of specified standardized criteria 24 ( Supplemental Information ), then discussed with the study team. We downgraded SoE for study limitations, imprecision, inconsistency, and reporting bias, and we differentiated high, moderate, low, and insufficient SoE.
We screened 23 139 citations and retrieved 7534 publications as full text against the eligibility criteria. In total, 312 treatment studies, reported in 540 publications (see list of included studies in the Online Appendix), met eligibility criteria ( Fig 1 ).

Literature flow diagram.
Although studies from 1980 were eligible, the earliest study meeting all eligibility criteria was from 1995. All included studies are documented in the evidence table in the Supplemental Information . The following highlights key findings. Results for intervention groups and individual studies, subgroup and sensitivity analyses, characteristics of participants and interventions contributing to the analyses, and considerations that determined the SoE for results are documented in the Online Appendix.
As a class, traditional stimulants (methylphenidate, amphetamines) significantly improved ADHD symptom severity (SMD, −0.88; CI, −1.13 to −0.63; studies = 12; n = 1620) and broadband measures (RR, 0.38; CI, 0.30–0.48; studies = 12; n = 1582) (both high SoE), but not functional impairment (SMD, 1.00; CI, −0.25 to 2.26; studies = 4; n = 540) ( Fig 2 , Supplemental Fig 8 , Supplemental Table 1 ). Methylphenidate formulations significantly improved ADHD symptoms (SMD, −0.68; CI, −0.91 to −0.46; studies = 7; n = 863) ( Fig 2 , Supplemental Table 1 ) and broadband measures (SMD, 0.66; CI, 0.04–1.28; studies = 2; n = 302). Only 1 study assessed academic performance, reporting large improvements compared with a control group (SMD, −1.37; CI, −1.72 to −1.03; n = 156) ( Supplemental Fig 9 ). 25 Methylphenidate statistically significantly suppressed appetite (RR, 2.80; CI, 1.47–5.32; studies = 8; n = 1110) ( Fig 3 ), and more patients reported adverse events (RR, 1.32; CI, 1.25–1.40; studies = 6; n = 945). Amphetamine formulations significantly improved ADHD symptoms (SMD, −1.16; CI, −1.64 to −0.67; studies = 5; n = 757) ( Fig 2 , Supplemental Table 1 ) but not broadband measures (SMD, 0.68; CI, −0.72 to 2.08; studies = 3; n = 561) ( Supplemental Fig 9 ). Amphetamines significantly suppressed appetite (RR, 7.08; CI, 2.72–18.42; studies = 8; n = 1229) ( Fig 3 ), and more patients reported adverse events (RR, 1.41; CI, 1.25–1.58; studies = 8; n = 1151). Modafinil (US Food and Drug Administration [FDA]-approved to treat narcolepsy and sleep apnea but not ADHD) in each individual study significantly improved ADHD symptoms, but aggregated estimates were nonsignificant (SMD, −0.76; CI, −1.75 to 0.23; studies = 4; n = 667) ( Fig 2 , Supplemental Table 1 ) because of high heterogeneity (I 2 = 91%). It did not improve broadband measures (RR, 0.49; CI, −0.12 to 2.07; studies = 3; n = 539) ( Supplemental Fig 9 ), and it significantly suppressed appetite (RR, 4.44; CI, 2.27–8.69; studies = 5; n = 780) ( Fig 3 ).

Medication effects on ADHD symptom severity. S-AMPH-LDX, lisdexamfetamine; S-AMPH-MAS, mixed amphetamines salts; S-MPH-DEX, dexmethylphenidate; S-MPH-ER, extended-release methylphenidate; S-MPH-IR, immediate release methylphenidate; S-MPH-OROS, osmotic-release oral system methylphenidate; S-MPH-TP, dermal patch methylphenidate; NS-NRI-ATX, atomoxetine; NS-NRI-VLX, viloxazine; NS-ALA-CLON, clonidine; NS-ALA-GXR, guanfacine extended-release.

Medication effects on appetite suppression. Abbreviations as in legend for Fig 2 .
As a class, nonstimulants significantly improved ADHD symptoms (SMD, −0.52; CI, −0.59 to −0.46; studies = 37; n = 6065; high SoE) ( Fig 2 , Supplemental Table 1 ), broadband measures (RR, 0.66; CI, 0.58–0.76; studies = 12; n = 2312) ( Supplemental Fig 8 ), and disruptive behaviors (SMD, 0.66; CI, 0.22–1.10; studies = 4; n = 523), but not functional impairment (SMD, 0.20; CI, −0.05 to 0.44; studies = 6; n = 1163). Norepinephrine reuptake inhibitors (NRI) improved ADHD symptoms (SMD, −0.55; CI, −0.62 to −0.47; studies=28; n = 4493) ( Fig 2 , Supplemental Table 1 ) but suppressed appetite (RR, 3.23; CI, 2.40–4.34; studies = 27; n = 4176) ( Fig 3 ), and more patients reported adverse events (RR, 1.31; CI, 1.18–1.46; studies = 15; n = 2600). Alpha-agonists (guanfacine and clonidine) improved ADHD symptoms (SMD, −0.52; CI, −0.67 to −0.37; studies = 11; n = 1885) ( Fig 2 , Supplemental Table 1 ), without (guanfacine) significantly suppressing appetite (RR, 1.49; CI, 0.94–2.37; studies = 4; n = 919) ( Fig 3 ), but more patients reported adverse events (RR, 1.21; CI, 1.11–1.31; studies = 14, n = 2544).
One study compared amphetamine versus methylphenidate, head-to-head, finding more improvement in ADHD symptoms (SMD, −0.46; CI, −0.73 to −0.19; n = 222) and broadband measures (SMD, 0.29; CI, 0.02–0.56; n = 211), but not functional impairment (SMD, 0.16; CI, −0.11 to 0.43; n = 211), 26 with lisdexamfetamine (an amphetamine) than osmotic-release oral system methylphenidate. No difference was found in appetite suppression (RR, 1.01; CI, 0.72–1.42; studies = 2, n = 414) ( Fig 3 ) or adverse events (RR, 1.11; CI, 0.93–1.33; study = 1, n = 222). Indirect comparisons yielded significantly larger effects for amphetamine than methylphenidate in improving ADHD symptoms ( P = .02) but not broadband measures ( P = .97) or functional impairment ( P = .68). Stimulants did not differ in appetite suppression ( P = .08) or adverse events ( P = .35).
One study provided information on NRI versus alpha-agonists by directly comparing an alpha-agonist (guanfacine) with an NRI (atomoxetine), 27 finding significantly greater improvement in ADHD symptoms with guanfacine (SMD, −0.47; CI, −0.73 to −0.2; n = 226) but not a broadband measure (RR, 0.84; CI, 0.68–1.04; n = 226). It reported less appetite suppression for guanfacine (RR, 0.48; CI, 0.27–0.83; n = 226) but no difference in adverse events (RR, 1.14; CI, 0.97–1.34; n = 226). Indirect comparisons did not indicate significantly different effect sizes for ADHD symptoms ( P = .90), disruptive behaviors ( P = .31), broadband measures ( P = .41), functional impairment ( P = .46), or adverse events ( P = .06), but suggested NRIs more often suppressed appetite compared with guanfacine ( P = .01).
Studies directly comparing nonstimulants versus stimulants (all were the NRI atomoxetine and stimulants methylphenidate in all but 1) tended to favor stimulants but did not yield significance for ADHD symptom severity (SMD, 0.23; CI, −0.03 to 0.49; studies = 7; n = 1611) ( Fig 2 ). Atomoxetine slightly but statistically significantly produced greater improvements in disruptive behaviors (SMD, −0.08; CI, −0.14 to −0.03; studies = 4; n = 608) ( Supplemental Fig 10 ) but not broadband measures (SMD, −0.16; CI, −0.36 to 0.04; studies = 4; n = 1080) ( Supplemental Fig 9 ). They did not differ significantly in appetite suppression (RR, 0.82; CI, 0.53–1.26; studies = 8; n = 1463) ( Fig 3 ) or number with adverse events (RR, 1.11; CI, 0.90–1.37; studies = 4; n = 756). Indirect comparisons indicated significant differences favoring stimulants over nonstimulants in improving ADHD symptom severity ( P < .0001), broadband measures ( P = .0002), and functional impairment ( P = .04), but not appetite suppression ( P = .31) or number with adverse events ( P = .12).
Several studies assessed whether adding nonstimulant to stimulant medication (all were alpha-agonists added to different stimulants) improved outcomes compared with stimulant medication alone, yielding a small but significant additional improvement in ADHD symptoms (SMD, −0.36; CI, −0.52 to −0.19; studies = 5; n = 724) ( Fig 4 ).

Combination treatment. CLON, clonidine, GXR guanfacine.
We identified 32 studies evaluating psychosocial, psychological, or behavioral interventions targeting ADHD youth, either alone or combined with components for parents and teachers. Interventions were highly diverse, and most were complex with multiple components (see supplemental results in the Online Appendix). They significantly improved ADHD symptoms (SMD, −0.35; CI, −0.51 to −0.19; studies = 14; n = 1686; moderate SoE) ( Fig 4 ), even when restricting to RCTs only (SMD, −0.36; CI, −0.53 to −0.19; removing high-risk-of-bias studies left 7 with similar effects SMD, −0.38; CI, −0.69 to −0.07), with minimal heterogeneity (I 2 = 52%); but not disruptive behaviors (SMD, −0.18; CI, −0.48 to 0.12; studies = 8; n = 947) or academic performance (SMD, −0.07; CI, −0.49 to 0.62; studies = 3; n = 459) ( Supplemental Fig 11 ).
We identified 19 studies primarily targeting parents of youth aged 3 to 18 years, though only 3 included teenagers. Interventions were highly diverse (see Online Appendix), but significantly improved ADHD symptoms (SMD, −0.31; CI, −0.57 to −0.05; studies = 11; n = 1078; low SoE) ( Fig 4 ), even when restricting to RCTs only (SMD, −0.35; CI, −0.61 to −0.09; removing high-risk-of-bias studies yielded the same point estimate, but CIs were wider, and the effect was nonsignificant SMD, −0.31; CI, −0.76 to 0.14). There was some evidence of publication bias (Begg P = .16; Egger P = .02), but the trim and fill method to correct it found a similar effect (SMD, −0.43; CI, −0.63 to −0.22). Interventions improved broadband scores (SMD, 0.41; CI, 0.23–0.58; studies = 7; n = 613) and disruptive behaviors (SMD, −0.52; CI, −0.85 to −0.18; studies = 4; n = 357) but not functional impairment (SMD, 0.35; CI, −0.69 to 1.39; studies = 3; n = 252) (all low SoE) ( Supplemental Fig 12 ).
We identified 10 studies, mostly for elementary or middle schools (see Online Appendix). Interventions did not significantly improve ADHD symptoms (SMD, −0.50; CI, −1.05 to 0.06; studies = 5; n = 822; moderate SoE) ( Fig 4 ), but there was evidence of heterogeneity (I 2 = 87%). Although most studies reported improved academic performance, this was not statistically significant across studies (SMD, −0.19; CI, −0.48 to 0.09; studies = 5; n = 854) ( Supplemental Fig 13 ).
We identified 22 studies, for youth aged 6 to 17 years without intellectual disability (see Online Appendix). Cognitive training did improve ADHD symptoms (SMD, −0.37; CI, −0.65 to −0.06; studies = 12; n = 655; low SoE) ( Fig 4 ), with some heterogeneity (I 2 = 65%), but not functional impairment (SMD, 0.41; CI, −0.24 to 1.06; studies = 5; n = 387) ( Supplemental Fig 14 ) or disruptive behaviors (SMD, −0.29; CI, −0.84 to 0.27; studies [all RCTs] = 5; n = 337). It improved broadband measures (SMD, 0.50; CI, 0.12–0.88; studies = 6; n = 344; RCTs only: SMD, 0.43; CI, −0.06 to 0.93) (both low SoE). It did not increase adverse events (RR, 3.30; CI, 0.03–431.32; studies = 2; n = 402).
We identified 21 studies: Two-thirds involved θ/β EEG marker modulation, and one-third modulation of slow cortical potentials (see Online Appendix). Neurofeedback significantly improved ADHD symptoms (SMD, −0.44; CI, −0.65 to −0.22; studies = 12; n = 945; low SoE) ( Fig 4 ), with little heterogeneity (I 2 = 33%); restricting to the 10 RCTs yielded the same point estimate, also statistically significant (SMD, −0.44; CI, −0.71 to −0.16). Neurofeedback did not systematically improve disruptive behaviors (SMD, −0.33; CI, −1.33 to 0.66; studies = 4; n = 372), or functional impairment (SMD, 0.21; CI, −0.14 to 0.55; studies = 3; n = 332) ( Supplemental Fig 15 ).
We identified 39 studies with highly diverse nutrition interventions (see Online Appendix), including omega-3 (studies = 13), vitamins (studies = 3), or diets (studies = 3), and several evaluated supplements as augmentation to stimulants. Most were placebo-controlled. Across studies, interventions improved ADHD symptoms (SMD, −0.39; CI, −0.67 to −0.12; studies = 23; n = 2357) ( Fig 4 ), even when restricting to RCTs (SMD, −0.32; CI, −0.55 to −0.08), with high heterogeneity (I 2 = 89%) but no publication bias. The group of nutritional approaches also improved disruptive behaviors (SMD, −0.28; CI, −0.37 to −0.18; studies [all RCTs] = 5; n = 360) ( Supplemental Fig 16 , low SoE), without increasing the number reporting adverse events (RR, 0.77; CI, 0.47–1.27; studies = 8; n = 735). However, we did not identify any specific supplements that consistently improved outcomes, including omega-3 (eg, ADHD symptoms: SMD, −0.11; CI, −0.45, 0.24; studies = 7; n = 719; broadband measures: SMD, 0.04; CI, −0.24 to 0.32; studies = 7; n = 755, low SoE).
We identified 6 studies assessing acupuncture, homeopathy, and hippotherapy. They did not individually or as a group significantly improve ADHD symptoms (SMD, −0.15; CI, −1.84 to 1.53; studies = 3; n = 313) ( Fig 4 ) or improve other outcomes across studies (eg, broadband measures: SMD, 0.03; CI, −3.66 to 3.73; studies = 2; n = 218) ( Supplemental Fig 17 ).
Eleven identified studies evaluated a combination of medication- and youth-directed psychosocial treatments. Most allowed children to have common cooccurring conditions, but intellectual disability and severe neurodevelopmental conditions were exclusionary. Medication treatments were stimulant or atomoxetine. Psychosocial treatments included multimodal psychosocial treatment, cognitive behavioral therapy, solution-focused therapy, behavioral therapy, and a humanistic intervention. Studies mostly compared combinations of medication and psychosocial treatment to medication alone, rather than no treatment or placebo. Combined therapy did not statistically significantly improve ADHD symptoms across studies (SMD, −0.36; CI, −0.73 to 0.01; studies = 7; n = 841; low SoE; only 2 individual studies reported statistically significant effects) ( Fig 5 ) or broadband measures (SMD, 0.42; CI, −0.72 to 1.56; studies = 3; n = 171), but there was indication of heterogeneity (I 2 = 71% and 62%, respectively).

Nonmedication intervention effects on ADHD symptom severity.
We found little evidence that either ADHD presentation (inattentive, hyperactive, combined-type) or cooccurring psychiatric disorders modified treatment effects on any ADHD outcome, but few studies addressed this question systematically (see Online Appendix).
Only a very small number of studies (33 of 312) reported on outcomes at or beyond 12 months of follow-up (see Online Appendix). Many did not report on key outcomes of this review. Studies evaluating combined psychosocial and medication interventions, such as the multimodal treatment of ADHD study, 28 did not find sustained effects beyond 12 months. Analyses for medication, psychosocial, neurofeedback, parent support, school intervention, and provider-focused interventions did not find sustained effects for more than a single study reporting on the same outcome. No complementary medicine, neurostimulation, physical exercise, or cognitive training studies reported long-term outcomes.
We identified a large body of evidence contributing to knowledge of ADHD treatments. A substantial number of treatments have been evaluated in strong study designs that provide evidence statements regarding the effects of the treatments on children and adolescents with ADHD. The body of evidence shows that numerous intervention classes significantly improve ADHD symptom severity. This includes large but variable effects for amphetamines, moderate-sized effects for methylphenidate, NRIs, and alpha-agonists, and small effects for youth-directed psychosocial treatment, parent support, neurofeedback, and cognitive training. The SoE for effects on ADHD symptoms was high across FDA-approved medications (methylphenidate, amphetamines, NRIs, alpha-agonists); moderate for psychosocial interventions; and low for parent support, neurofeedback, and nutritional interventions. Augmentation of stimulant medication with non-stimulants produced small but significant additional improvement in ADHD symptoms over stimulant medication alone (low SoE).
We also summarized evidence for other outcomes beyond specific ADHD symptoms and found that broadband measures (ie, global clinical measures not restricted to assessing specific symptoms and documenting overall psychosocial adjustment), methylphenidate (low SoE), nonstimulant medications (moderate SoE), and cognitive training (low SoE) yielded significant, medium-sized effects, and parent support small effects (moderate SoE). For disruptive behaviors, nonstimulant medications (high SoE) and parent support (low SoE) produced significant improvement with medium effect. No treatment modality significantly improved functional impairment or academic performance, though the latter was rarely assessed as a treatment outcome.
The enormous variability in treatment components and delivery of youth-directed psychotherapies, parent support, neurofeedback, and nutrition and supplement therapies, and in ADHD outcomes they have targeted, complicates the synthesis and meta-analysis of their effects compared with the much more uniform interventions, delivery, and outcome assessments for medication therapies. Moreover, most psychosocial and parent support studies compared an active treatment against wait list controls or treatment as usual, which did not control well for the effects of parent or therapist attention or other nonspecific effects of therapy, and they have rarely been able to blind adequately either participants or study assessors to treatment assignment. 29 , 30 These design limitations weaken the SoE for these interventions.
The large number of studies, combined with their medium-to-large effect sizes, indicate collectively and with high SoE that FDA-approved medications improve ADHD symptom severity, broadband measures, functional impairment, and disruptive behaviors. Indirect comparison showed larger effect sizes for stimulants than for nonstimulants in improving ADHD symptoms and functional impairment. Results for amphetamines and methylphenidate varied, and we did not identify head-to-head comparisons of NRIs versus alpha-agonists that met eligibility criteria. Despite compelling evidence for their effectiveness, stimulants and nonstimulants produced more adverse events than did other interventions, with a high SoE. Stimulants and nonstimulant NRIs produced significantly more appetite suppression than placebo, with similar effect sizes for methylphenidate, amphetamine, and NRI, and much larger effects for modafinil. Nonstimulant alpha-agonists (specifically, guanfacine) did not suppress appetite. Rates of other adverse events were similar between NRIs and alpha-agonists.
Perhaps contrary to common belief, we found no evidence that youth-directed psychosocial and medication interventions are systematically better in improving ADHD outcomes when delivered as combination treatments 31 – 33 ; both were effective as monotherapies, but the combination did not signal additional statistically significant benefits (low SoE). However, it should be noted that few psychosocial and medication intervention combinations have been studied to date. We also found that treatment outcomes did not vary with ADHD presentation or the presence of cooccurring psychiatric disorders, but indirect analyses are limited in detecting these effect modifiers, and more research is needed. Furthermore, although children of all ages were eligible for inclusion in the review, we note that very few studies assessed treatments (especially medications) in children <6 years of age; evidence is primarily available for school-age children and adolescents. Finally, despite the research volume, we still know little about long-term effects of ADHD treatments. The limited available body of evidence suggests that most interventions, including combined medication and psychological treatment, yield few significant long-term improvements for most ADHD outcomes.
This review provides compelling evidence that numerous, diverse treatments are available and helpful for the treatment of ADHD. These include stimulant and nonstimulant medications, youth-targeted psychosocial treatments, parent support, neurofeedback, and cognitive training, though nonmedication interventions appear to have considerably weaker effects than medications on ADHD symptoms. Nonetheless, the body of evidence provides youth with ADHD, their parents, and health care providers with options.
The paucity of head-to-head studies comparing treatments precludes research-based recommendations regarding which is likely to be most helpful and which should be tried first, and decisions need to be based on clinical considerations and patient preferences. Stimulant and nonstimulant NRI medications, separately and in head-to-head comparisons, have shown similar effectiveness and rates of side effects, including appetite suppression, across identified studies. The moderate effect sizes for nonstimulant alpha-agonists, their low rate of appetite suppression, and their evidence for effectiveness in augmenting the effects of stimulant medications in reducing ADHD symptom severity provides additional treatment options. Furthermore, we found low SoE that neurofeedback and cognitive training improve ADHD symptoms. We also found that nutritional supplements and dietary interventions improve ADHD symptoms and disruptive behaviors. The SoE for nutritional interventions, however, is still low, and despite the research volume, we did not identify systematic benefits for specific supplements.
Clinical guidelines currently advise starting treatment of youth >6 years of age with FDA-approved medications, 33 which the findings of this review support. Furthermore, FDA-approved medications have been shown to significantly improve broadband measures, and nonstimulant medications have been shown to improve disruptive behaviors, suggesting their clinical benefits extend beyond improving only ADHD symptoms. Clinical guidelines for preschool children advise parent training and/or classroom behavioral interventions as the first line of treatment, if available. These recommendations remain supported by the present review, given the paucity of studies in preschool children in general, and because many existing studies, in particular medication and youth-directed psychosocial interventions, do not include young children. 31 – 33
This review incorporated publications dating from 1980, assessing diverse intervention targets (youth, parent, school) and ADHD outcomes across numerous functional domains. Limitations in its scope derive from eligibility criteria. Requiring treatment of 4 weeks ensured that interventions were intended as patient treatment rather than proof of concept experiments, but it also excluded some early studies contributing to the field and other brief but intense psychosocial interventions. Requiring studies to be sufficiently large to detect effects excluded smaller studies that contribute to the evidence base. We explicitly did not restrict to RCTs (ie, a traditional medical study design), but instead identified all studies with concurrent comparators so as not to bias against psychosocial research; nonetheless, the large majority of identified studies were RCTs. Our review aimed to provide an overview of the diverse treatment options and we abstracted findings regardless of the suitability of the study results for meta-analysis. Although many ADHD treatments are very different in nature and the clinical decision for 1 treatment approach over another is likely not made primarily on effect size estimates, future research could use the identified study pool and systematically analyze comparative effectiveness of functionally interchangeable treatments in a network meta-analysis, building on previous work on medication options. 34
Future studies of psychosocial, parent, school-based, neurofeedback, and nutritional treatments should employ more uniform interventions and study designs that provide a higher SoE for effectiveness, including active attention comparators and effective blinding of outcome assessments. Higher-quality studies are needed for exercise and neuromodulation interventions. More trials are needed that compare alternative interventions head-to-head or compare combination treatments with monotherapy. Clinical trials should assess patient-centered outcomes other than ADHD symptoms, including functional impairment and academic performance. Much more research is needed to assess long-term treatment effectiveness, compliance, and safety, including in preschool youth. Studies should assess patient characteristics as modifiers of treatment effects, to identify which treatments are most effective for which patients. To aid discovery and confirmation of these modifiers, studies should make publicly available all individual-level demographic, clinical, treatment, and outcome data.
We thank the following individuals providing expertise and helpful comments that contributed to the systematic review: Esther Lee, Becky Nguyen, Cynthia Ramirez, Erin Tokutomi, Ben Coughli, Jennifer Rivera, Coleman Schaefer, Cindy Pham, Jerusalem Belay, Anne Onyekwuluje, Mario Gastelum, Karin Celosse, Samantha Fleck, Janice Kang, and Sreya Molakalaplli for help with data acquisition. We thank Kymika Okechukwu, Lauren Pilcher, Joanna King, and Robyn Wheatley from the American Academy of Pediatrics; Jennie Dalton and Paula Eguino Medina from the Patient-Centered Outcomes Research Institute; Christine Chang and Kim Wittenberg from AHRQ; and Mary Butler from the Minnesota Evidence-based Practice Center. We thank Glendy Burnett, Eugenia Chan, MD, MPH; Matthew J. Gormley, PhD; Laurence Greenhill, MD; Joseph Hagan, Jr, MD; Cecil Reynolds, PhD; Le’Ann Solmonson, PhD, LPC-S, CSC; and Peter Ziemkowski, MD, FAAFP; who served as key informants. We thank Angelika Claussen, PhD; Alysa Doyle, PhD; Tiffany Farchione, MD; Matthew J. Gormley, PhD; Laurence Greenhill, MD; Jeffrey M. Halperin, PhD; Marisa Perez-Martin, MS, LMFT; Russell Schachar, MD; Le’Ann Solmonson, PhD, LPC-S, CSC; and James Swanson, PhD; who served as a technical expert panel. Finally, we thank Joel Nigg, PhD; and Peter S. Jensen, MD; for their peer review of the data.
Drs Peterson and Hempel conceptualized and designed the study, collected data, conducted the analyses, drafted the initial manuscript, and critically reviewed and revised the manuscript; Dr Trampush conducted the critical appraisal; Drs Bolshakova and Pakdaman, and Ms Rozelle, Ms Maglione, and Ms Brown screened citations and abstracted the data; Dr Miles conducted the analyses; Ms Yagyu designed and executed the search strategy; Ms Motala served as data manager; and all authors provided critical input for the manuscript, approved the final manuscript as submitted, and agree to be accountable for all aspects of the work.
This study is registered at PROSPERO, #CRD42022312656. Data are available in SRDRPlus.
COMPANION PAPER: A companion to this article can be found online at www.pediatrics.org/cgi/doi/10.1542/peds.2024-065854 .
FUNDING: The work is based on research conducted by the Southern California Evidence-based Practice Center under contract to the Agency for Healthcare Research and Quality (AHRQ), Rockville, MD (Contract No. 75Q80120D00009). The Patient-Centered Outcomes Research Institute funded the research (Publication No. 2023-SR-03). The findings and conclusions in this manuscript are those of the authors, who are responsible for its contents; the findings and conclusions do not necessarily represent the views of the AHRQ or the Patient-Centered Outcomes Research Institute, its board of governors or methodology committee. Therefore, no statement in this report should be construed as an official position of the Patient-Centered Outcomes Research Institute, the AHRQ, or the US Department of Health and Human Services.
CONFLICT OF INTEREST DISCLOSURES: The authors have indicated they have no conflicts of interest relevant to this article to disclose.
attention-deficit/hyperactivity disorder
Agency for Healthcare Research and Quality
US Food and Drug Administration
confidence interval
norepinephrine reuptake inhibitors
randomized controlled trial
relative risk
standardized mean difference
strength of evidence
technical expert panel
Supplementary data
Advertising Disclaimer »
Citing articles via
Email alerts.

Affiliations
- Editorial Board
- Editorial Policies
- Journal Blogs
- Pediatrics On Call
- Online ISSN 1098-4275
- Print ISSN 0031-4005
- Pediatrics Open Science
- Hospital Pediatrics
- Pediatrics in Review
- AAP Grand Rounds
- Latest News
- Pediatric Care Online
- Red Book Online
- Pediatric Patient Education
- AAP Toolkits
- AAP Pediatric Coding Newsletter
First 1,000 Days Knowledge Center
Institutions/librarians, group practices, licensing/permissions, integrations, advertising.
- Privacy Statement | Accessibility Statement | Terms of Use | Support Center | Contact Us
- © Copyright American Academy of Pediatrics
This Feature Is Available To Subscribers Only
Sign In or Create an Account
Copyright © 2024 OccupationalTherapy.com - All Rights Reserved
Pediatric Case Study: Child with ADHD
Nicole quint, dr.ot, otr/l.
- Early Intervention and School-Based
To earn CEUs for this article, become a member.
unlimit ed ceu access | $129/year
Attention deficit hyperactivity disorder (adhd).
Hello everyone. Today, we are going to be talking about attention deficit hyperactivity disorder. I consider this to be under the umbrella of "invisible diagnoses." This population has a special place in my heart because it is very easy to misconstrue some of the challenges that they have as intentional and behavior-based, and therefore, sometimes they get a bad rap. Thus, I am always happy to help kids with ADHD.
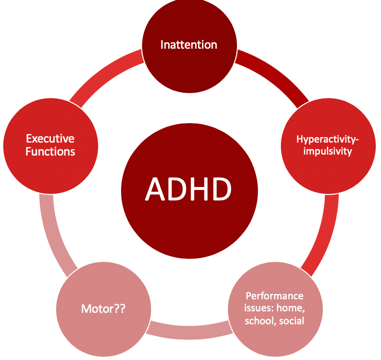
Figure 1. Overview of ADHD.
Individuals with ADHD have a lot of challenges that affect their occupational participation and performance. I think most of us are very comfortable with the idea that inattention, hyperactivity, and impulsivity are the hallmarks, but what sometimes can get lost is the idea that executive functions are very much affected by impulsivity. Motor issues are also often involved with kids with ADHD and are not always considered. In fact, there is a lot of evidence to support that the motor needs of these kids often go unaddressed. Typically, these kids come to us when parents or schools have major concerns about their behavior. Therefore, this tends to be where everyone focuses their attention. Oftentimes, the motor issues then fly under the radar and do not get addressed. The cool thing is that motor interventions can be the means to make some really significant changes for these kids, particularly in the area of executive function. There is a win-win situation when we address the motor issues. Lastly, they tend to also have performance issues not only in their home environment but also in their school and social environments as well.
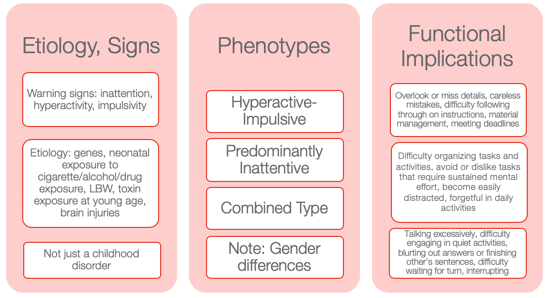
Figure 2. Other information from the NIMH Information Resource Center (2020).
I wanted to provide some information to help you to appreciate how diverse ADHD is. Many might still use ADD when we are talking about the children who have an inattentive type as it seems to make more sense. However, that is not how it is defined in the Diagnostic and Statistical Manual of Mental Disorders (DSM–5).
Etiology and Signs
The etiology and the signs are inattention, hyperactivity, and impulsivity. We also know there is a genetic predisposition to this. Neonatal exposure to cigarettes, alcohol, and drugs can also lead to ADHD. Low birth weight and toxin exposure are some of the environmental elements. ADHD can also be the result of a brain injury. This is not just a childhood disorder, and people do not grow out of it. In fact, the symptoms can actually get worse as life gets harder as one gets older. Adults who have ADHD can have some significant struggles, particularly if they do not know that they have ADHD or if it was never addressed.
There are three phenotypes: hyperactive-impulsive type, predominantly inattentive type, and a combination type. I think the hyperactive-impulsive type is the picture most people have when they think of ADHD. Then, we have the predominantly inattentive type. These are the daydreamers or the individuals that jump from one thought to the next. They have a really hard time staying focused for long. Lastly, there is the combined type. This is where we see both elements of inattention and hyperactivity and/or impulsivity. I think it is really important to also appreciate gender differences. You can see very different types of ADHD in girls versus boys. Boys obviously tend to be of the hyperactive-impulsive type, but even the inattentive type can be a little different. Girls, who have ADHD, tend to be talkative and a little more anxious. They definitely have a different predisposition as opposed to the boys. Thus, it might be the same diagnosis but look very different between the genders.
Functional Implications
Functional implications become extremely important. These are individuals who tend to overlook or miss details. They might make careless mistakes. They have difficulty following through with directions at school. Material management can become very challenging especially dealing with paperwork. They can miss deadlines and have a hard time keeping track of and prioritizing tasks. These are some of the higher-level executive functions. You might also see an avoidance or an expressed dislike of tasks that require a significant amount of sustained mental effort. They might tell you it is too hard, and they might feel very overwhelmed. They become very easily distracted by anything. The use of electronics adds to the issue. They can be forgetful in daily activities, talk excessively, have difficulty engaging in quiet activities, and tend to blurt out answers or finish others' sentences. Often, the perception is they are interrupting and being rude. They may have difficulty waiting for their turn or interrupt during someone else's turn. These are examples of impulsive behaviors. We will talk more about this when we get to executive functions.
Differential Diagnosis Between ADHD and SPD
- A high rate of comorbidity between SMD and ADHD
- ADHD and SMD
- Both at risk for limited participation in many aspects of daily life
- ADHD slightly worse attention scores than SMD
- Tactile, taste/smell, and movement sensitivity, visual-auditory sensitivity; behavioral manifestations of sensory systems
- Exaggerated electrodermal responses to sensory stimulation, thus increased risk of sympathetic “fight or flight” reactions
(Miller et al., 2012; Yochman et al., 2013)
Sometimes, kids who have ADHD also have some sensory issues. You may wonder, "Do they have just ADHD by itself?" This is probably one of the most common questions I get when working with kids with ADHD whether it is from teachers, other therapists, or from parents. Next, we are going to be talking about a child who has straight ADHD. However, for a few minutes, I want to talk about the whole idea of differential diagnosis between ADHD and SPD and how this all fits together. There is a very high comorbidity between sensory modulation disorder and ADHD. When I am referring to sensory modulation disorder, I am using the Lucy Jane Miller nosology. Sensory modulation disorder refers to the over-responsive, under-responsive, and/or craving of sensory input. For both ADHD and sensory modulation disorder, you will see that these diagnoses are both at risk for limited participation. These are kids who will not participate in certain activities because the sensory input is too much or overwhelming for them. ADHD will have slightly worse attention scores than SMD when you complete a formal attention test like the Test of Everyday Attention. However, you will see the same kind of impulsive behaviors.
Those with sensory modulation disorders tend to have difficulty with tactile, taste, smell, and movement sensitivities. You might also see some visual-auditory sensitivity so there are some behavioral manifestations that come of that. They might become stressed related to fears of vestibular or other movement input. They might also dislike certain noises or touch.
They found in the research that sensory modulation dysfunction, not ADHD , will have an exaggerated electrodermal response to sensory stimulation. This means that they have an increased risk of sympathetic activation which is the fight-or-flight, freeze/faint reactions, and meltdowns. When you have a child with meltdowns, you want to investigate if they have sensory modulation dysfunction right away. And, if you have a child with ADHD who does not have a history of meltdowns, that is a really good sign of your initial hypothesis. While this alone does not mean that they do not a sensory modulation dysfunction, chances are that they do not. Additionally, they might have dyspraxia or a discrimination disorder.
This is just a brief summary of how this all comes to play with an ADHD diagnosis and possible comorbidities.
Case Introduction: Jeremy (Age 9, ADHD, Combined Type)
- He lives with his mother and older sister in SFH and goes to his father’s house on the weekend (divorced)
- He is in the 4th grade and has an IEP for OHI
- Strengths: funny, good at math, helps the family to take care of pets, watches WWE with father, loves dogs, likes to play board games (Monopoly, Sorry)
- School concerns: material management, organization, completing tasks or losing work , impulsive, social difficulties (short-lived relationships, fights), “lacks self-control” and “messy”, underperforming and sometimes seems “lost”
- Family concerns: Fights with a sibling, sleep difficulties, messy room, messy notebooks, and backpack, loses things, avoids homework, resists bedtime, difficult to wake in the morning and slow with routine , poor hygiene
- Jeremy’s goal: make friends, be able to find his schoolwork, have good friends, be better at kickball and wrestling
Jeremy is nine, and his diagnosis is ADHD, combined type. I have a feeling Jeremy is probably similar to a lot of the kids you see. I know I have seen a lot of these types of kids. He lives with his mother and older sister in a single-family home and goes to his father's house on the weekend because of a divorce. He is in the fourth grade, is eligible for an IEP because of an OHI (other health impairment), and is eligible for special education services because of his diagnosis of ADHD.
I always like to start with strengths with all kids, especially ADHD because these kids can have a really hard time with confidence and self-esteem. They also get blamed for their behaviors. For his strengths, he is funny, good at math, and he likes to help take care of his pets at home. He likes to watch wrestling, World Wrestling Federation (WWF) with his father, loves dogs, and loves to play board games. He is really good at Monopoly and Sorry.
At school, he had challenges with material management, organization, completing tasks, and not losing work. These last two are highlighted as we are going to focus on that. He is impulsive, and he has social difficulties. His teacher described his relationships as short-lived. He would have a friend, and then all of a sudden, they were not friends anymore. She also reported that he lacked self-control, was messy, and thought he underperformed. And, she felt like he always seemed lost. When they were going through the instructions or going through something, he was always looking at his peer's work or looking confused while he was trying to figure out what was going on.
The family had some concerns about his fighting with a sibling, significant sleep difficulties, a messy room, messy notebooks and backpack, and that he would often lose things. He also avoided his homework and resisted bedtime. As a result, it was very difficult to wake him up in the morning, and he was slow with his AM routine. His mom said that he also had an impulsive way of performing hygiene tasks. For example, he would brush his teeth in two seconds and say he was done. Everything was quick and impulsive. This is very typical for boys with this type of ADHD.
His goals were to make friends and find his school work. He said it was very stressful to always feel like he was losing his school work. He was motivated to do well in school. He did not just want to make friends, but he wanted to have good friends. He also wanted to be better at kickball because that is what the kids played at recess and in PE. He also wanted to be better at wrestling as not only did he like to watch with his dad, but he also liked to wrestle with him.
I want to go back to the highlighted areas in my list: completing tasks, losing work, and difficulty waking in the morning. These are the areas we are going to focus on.
Assessments
Assessments are one of the most challenging things for people because they are often under a time crunch, and the reports are difficult to write up and are time-consuming. However, it is really important with these kids as it gives us a full perspective on where they are having challenges. Knowing that he has "ADHD combined type" does not really tell us about his occupational performance and participation. We want to really get all that information. I like to be pretty thorough, and I will scatter assessments throughout my time with them to try to get a good idea. Again, I really like to check out their motor skills. I have kids that are superstars in sports, but I will still find out that there are some motor problems.
Typically, the motor challenges with ADHD have to do with bilateral coordination, dexterity, and those kinds of things. They might be good at some things, like basketball or baseball, but this does not mean that they are good at fine manipulation. Thus, it is really important to find out where they are. Figure 3 shows a summary of the assessments I did with Jeremy.
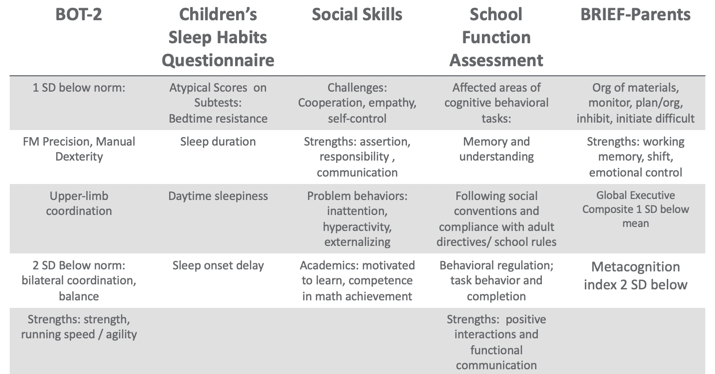
Figure 3. Assessment results.
Using the BOT, I found that Jeremy was one standard deviation below the norm in fine motor, precision, and manual dexterity, which was not surprising. He was two standard deviations below the norm in bilateral coordination and balance. However, his overall strength, running speed, and agility were fine.
There are many great tools out there for sleep including free ones. One of my favorites is the Sleep Habits Questionnaire. It is free online. It is great because it uncovers behaviors regarding going to bed, sleep duration, daytime sleepiness, and sleep onset delay. Many kids with ADHD have an overactive thinking process which then causes a sleep latency problem. It is hard for them to settle their brain and get to sleep. They also might have difficulty with sleep duration and not get enough sleep or good quality of sleep. If their arousal level is still high at night, it' is hard to get them to calm down and want to go to bed, especially if they are very disorganized in their thinking. This questionnaire gives you good information. Our results with Jeremy found that had bedtime resistance, sleep duration, daytime sleepiness, and sleep onset delays that were all atypical scores.
I also did a social skills assessment with him because his goal was to make friends, and school indicated that he had a hard time with solid friendships. I like to have a social-emotional learning perspective, and the more I know about a child's emotional intelligence, the better. We want these kids to be successful in their social interactions because that affects their whole life. With the Social Skills Improvement System (SSIS) Rating Scales, I found challenges with cooperation, empathy, and self-control. His strengths included assertion, responsibility, and communication. Under "problem behaviors", I found inattention, hyperactivity, and some externalizing behaviors. With his diagnosis, this all seems to fit. For academics, he was motivated to learn and had competence in math achievement. We already knew he had strengths in math.
I also did the School Function Assessment. I love this tool. There is one section that is a little dated as it talks about a floppy disk or something, but the other information on there is fantastic. This is especially true if you have kids who have a hard time following rules, social conventions, and material management. You can give it to the teacher, and they can score that. I found that Jeremy had some affected areas with memory and understanding, following social conventions, and compliance with adult directives and school rules. Additionally, he had some behavioral regulation issues, and task behavior and completion were difficult for him. His strengths included positive interactions and functional communication. Communication is strong for him,= which is a good thing.
The BRIEF (Behavior Rating Inventory of Executive Function) is an executive function tool that I did that with his parents. What we found was that the organization of materials, monitoring, planning and organization, inhibition, and initiation were difficult for him. His strengths were his working memory. Additionally, cognitive shifting and emotional control were also strong. However, his global executive composite was one standard deviation below the mean which means that he was low in everything. While it was not devastatingly low, he was below the average in everything. He struggled the most in metacognition, and that was two standard deviations below the norm. Thinking about his own thinking was a struggle for him.
From an observation standpoint, I also got a video from him mom of his AM routine so I could see what that looked like. He was in slow motion, very tired, not wanting to do the routine, and his performance was of low quality, I would put it, writing examples from school, because sometimes you'll see that the handwriting is indicative kind of the brain and the body not matching up, the brain going a little faster than the body. And so I also had a homework video watching him kind of resist homework. And then I did ocular motor testing, checked his tracking, convergence, divergence, and saccades and those kinds of things. Because there is a correlation between having some difficulties with that sometimes. But he actually was fine, and that wasn't a complaint from parents. So I just wanted to make sure it wasn't an issue that we were missing. So that gave me a lot of information.
Research Implications: Assessment
This is information about some of the research implications regarding the assessment process and kind of why I chose the tools that I chose and why I recommend a comprehensive one.
- Motor: Children with parent-reported motor issues received more PT than those with teacher-reported motor issues (risk)/undertreated motor problems in children with ADHD (due to behavioral factors in referral); HW difficulties; higher ADHD and lower motor proficiency scores reported more sleep problems (Papadopoulos et al., 2018)
- Sleep: Sleep deficits negatively affect inhibitory control (Cremone-Caira et al., 2019); Difficulties initiating and maintaining sleep 25-50% in ADHD (Corkum et al., 1998); Prevalence of sleep disorders 84.8 % affecting QoL (Yurumez & Gunay Kilic, 2013)
- EF: Motor skills and EF related (Pan et al., 2015); boys with ADHD have lower EF abilities than typical peers on both performance-based and parent report tools, thus combo is recommended (Sgunibu et al., 2012)
- Social: Children with ADHD 50% lower odds of sports participation than children with asthma with higher incidences of screen time (Tanden et al., 2019); childhood ADHD associated with obesity (Kim et al., 2011); underlying lack of interpersonal empathy (Cordier et al., 2010); Playfulness indicators: ADHD group “typical” with some difficult items but difficulty with basic skills (sharking) (Wilkes-Gillan et al., 2014); seek green outdoor settings at a higher rate (Taylor & Kuo, 2011)
For motor, Papadopoulos and his group (2018) found that there is some difficulty with handwriting. They also reported the higher ADHD and lower motor proficiency scores, the more sleep problems. The fact that Jeremy had sleep problems made me want to look at his motor skills for this reason. This is another interesting one. Children with parent-reported motor issues received more PT than those with teacher-reported motor issues. The fact that we listen to the parents more than the teachers about motor issues is important to consider. Under-treated motor problems in children with ADHD are really due to a behavioral focus so that is why it tends to get missed.
Sleep deficits negatively affect inhibitory control (Cremone-Caira et al., 2019). If we know that these kids have inhibition issues, we need to help them get some sleep. Poor sleep is only reinforcing their challenges and making it worse. They found that there were difficulties initiating and maintaining sleep at a rate of 20 to 50% of kids with ADHD (Corkum et al., 1998). Now, granted, that was 20 years ago, but they have replicated that since. And, if you have a sleep disorder, there is an 84.8% chance that it is negatively affecting your quality of life (Yurumez & Gunay Kilic, 2013).
Motor skills and executive functions are related. If you have some motor difficulties, it is going to influence your executive function ability (Pan et al., 2015). Boys with ADHD have lower executive function ability than typical peers on both performance-based and parent report tools, thus, it is really important that you use a combination of both performance and parent report tools (Sgunibu et al., 2012).
Children with ADHD are 50% less likely to participate in sports than children with asthma (Tanden et al., 2019). I find that amazing. Kids with ADHD also have a higher incidence of screen time usage, and we know that that is always a challenge (Tanden et al., 2019). Childhood ADHD is also associated with obesity. Hence, if you are not doing anything physical and you are sitting there watching your computer or playing video games, and you are impulsive, you are more likely to be obese (Kim et al., 2011). An underlying lack of interpersonal empathy can be something that you often see in ADHD. This affects social abilities and participation and success (Cordier et al., 2010). There are also playfulness indicators. An ADHD group might score as "typical" with some difficult play criteria, but then have more difficulty with basic items (Wilkes-Gillan et al., 2014). Their play may be developmentally out of whack. Again, they might be okay with some high-level types of behaviors, but then when it comes to something simple like taking turns or sharing, they cannot do it. Sometimes we have to go back and practice these rudimentary skills. This might be why they are struggling socially because they are having problems with age-inappropriate items. Lastly, these kids with ADHD really seek green outdoor settings at a higher rate (Taylor & Kuo, 2011). It would be interesting to monitor how outside time might influence their performance on assessments.
EF and Self-Regulation Connection
- Inhibitory control
- Cognitive/mental flexibility
- Working memory
Can these kids self-regulate? When they cannot, it does not work out well for them in school or at home, and it does not work out well in terms of social abilities. When they become adults, they have trouble keeping and maintaining a job. This is the definition of EF.
Some of you might be very familiar with this definition, but it is also quite complicated. This is how we remember information, filter distractions, resist impulses, and sustain attention during an activity that is also goal-directed. While we also adjust our plan as needed to avoid frustration in the process. That is a lot of working parts. Many times, you see people refer to executive functions like an air traffic controller of information and materials. These are the "big 3."
This is how we remember information, filter distractions, resist impulses, and sustain attention during an activity that is goal-directed while adjusting our plan as necessary and avoiding frustration!
Miyake, A., Friedman, N. P., Emerson, M. J., Witzki, A. H., Howerter, A., & Wager, T. D. (2000). The unity and diversity of executive functions and their contributions to complex "frontal lobe" tasks: A latent variable analysis, Cognitive Psychology, 41 , 49-100.
- Impulse Control
- socially acceptable (Olson, 2010)
- Ability to store, update and manipulate /process information over short periods of time (Best & Miller, 2010)
- “Limited-capacity information-processing system” (Roman et al., 2015)
- Verbal, visuospatial, and coordinating central executive
- Ability to think flexibly and shift perspective and approaches easily, critical to learning new ideas (different perspectives)
- Switching between two or more mental sets with each set containing several tasks rules
- Feedback related (unlike inhibition) (Best & Miller, 2010)
All these things are important, but the three basic dimensions are inhibitory control, which develops first around four years of age, cognitive and mental flexibility, and working memory. Mental flexibility is the result of inhibitory control and working memory working together. If you have a problem with inhibition or working memory, or both, you are going to have problems with cognitive flexibility. The flip side of that would be rigidity. It is also being able to shift your thinking in the moment back and forth. The flip side of that would be to be stuck. Working memory is the ability to use your memory functionally. It is very important to know that we only have a very limited amount of memory capacity, and it is all we have. I like to call my working memory my suitcase. You have to make sure you pack the right things in there for the trip that you are going on. If you pack your suitcase for Fiji and you are going to Alaska, you are going to be on the beach with boots and a parka and be miserable. It is really important that we pull in the information that we need. This takes sustained attention. If you cannot sustain your attention, you are not going to capture the right memories. And again, if there are problems with inhibitory control or impulse control, this is going to be challenging. Impulse control is controlling yourself in the moment. If I can string those together, now I have more self-regulation ability. Again, these are the big three: inhibition, working memory, and cognitive flexibility and shifting.
I already explained these, but I want you to appreciate what the research says. Inhibition requires an arbitrary rule to be held in your mind while you are inhibiting one response to produce an alternative response, which is typically the one that is more socially acceptable. Working memory is storing, updating, and manipulating information over short periods of time. It has a limited capacity, and it is verbal and visuospatial. Then, for cognitive shifting and flexibility, there are two pieces to it. It is being open and being able to shift. Here is what is interesting. Cognitive flexibility and shifting respond really well to internal feedback. You can actually start to observe things and gain some insight and make changes. Why that is important is because inhibition does not get better from internal feedback. It only gets better from external feedback. Think about someone you know who interrupts a lot because they are impulsive. They see that they do it and do not change because no one has said anything to them. It requires external feedback for them to say, "Oh, I'm doing it wrong." We do not have this internal mechanism to change our impulsivity. We cannot assume these kids will figure it out and fix it, because they will not. We have to be very stern and to the point and say, "You're doing it wrong. This is why it's wrong and here's what you need to do instead." This is the key. Figure 4 is an executive function cheat sheet.
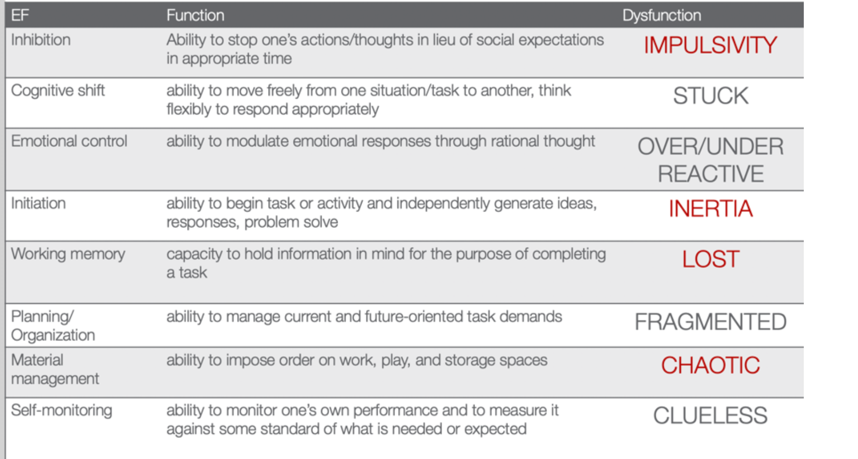
(Cooper-Kahn & Dietzel, 2008)
Figure 4. EF cheat sheet.
This is from Cooper-Kahn and Dietzel (2008). They tell you the executive function, what the function is, and then the end dysfunction. For inhibition, the dysfunction is impulsive. If you cannot cognitively shift, you can get stuck. If you do not have emotional control, you are going to be over or under-reactive. If you cannot initiate a task, you are stuck in inertia. If you do not have a good working memory, you are lost. If you cannot plan and organize, you are fragmented. If you cannot manage your materials, you are chaotic. And then, if you cannot self-monitor, you are clueless. The red ones are those that Jeremy struggled with. He was impulsive, had inertia, was lost, and chaotic. He was also a little fragmented and had a difficult time with organization. However, these four things were his biggest challenges.
Review of Evidence-based Interventions for Case
One of the objectives is to talk about evidence and how we are going to use the evidence to support our intervention. I focused on motor, social, executive functions, and sleep. These are the things that were assessed that also had evidence for different intervention strategies (see Figure 5).
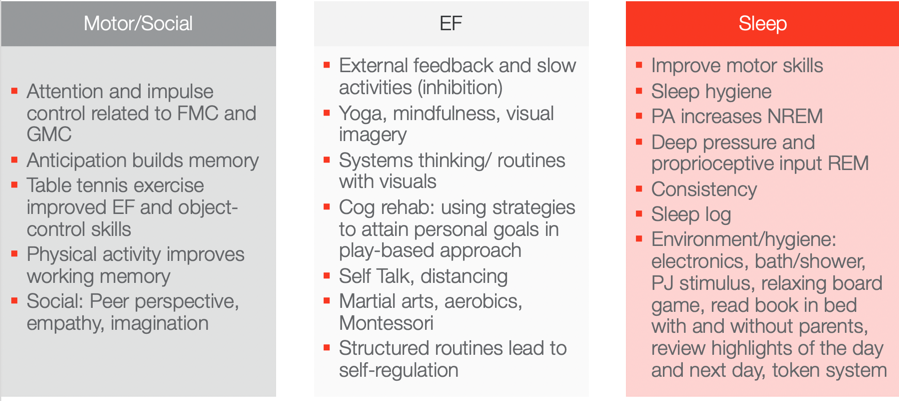
Figure 5. Evidence-based interventions ((Hui Tseng, et al., 2004; Hahn-Markowitz et al., 2016; Washington University, n.d.; Diamond & Lee, 2011; White & Carlson, 2016; Winsler et al., 2009; Marjorek et al., 2004; Kuhn & Floress, 2008; Frike et al, 2006; Keshavarzi et al., 2014).
Motor/Social Categories
Let's look at the motor and social categories. What is really interesting is that attention and impulse control are related to fine motor and gross motor coordination. If we can work on coordination, we can also increase attention and impulse control. This is killing two birds with one stone in Jeremy's case. I do not know who is familiar with Hebbian's law, but it says is that the (brain) cells that fire together wire together. One of the ways to do that is through the concept of anticipation. Anticipation builds memory capacity and will improve working memory. Anticipation is a context, and you can basically put anticipation in anything. With turn-taking, there is anticipation. If there is a competition, there is anticipation among the competitors. If you know you are going to be called on, there is anticipation. If you are playing a game where something might jump out, there is anticipation. These are just a few examples of where you can build in anticipation. If you can add that into your activities, you can build memory capacity. Another study looked at how table tennis exercises improved executive function and object control skills. Table tennis does not require a lot of heavy-duty cardio and it is not a tiring exercise, but it requires a lot of hand-eye coordination and sustained attention. I think this is a really good occupation-based strategy to improve executive function and object control. Physical activity also improves working memory. I have had tons of success with kids doing physical activity both in therapy and at home to improve their working memory. Some of the social strategies that work really for kids, and we will talk about a few in a little bit, is taking a peer's perspective and working on empathy and imagination. These things were really shown to be effective ways to change someone's social success.
Executive Function
For executive function, you have to give them external feedback. You have to tell them when they are being impulsive, and then you have to tell them how to fix it. These are kids who are on a very fast, impulsive temporal context. I talk to them about the hare versus the turtle. I tell them to be more like the turtle. Yoga, mindfulness, and visual imagery are other strategies. Yoga and mindfulness are occupations, and you can incorporate visual imagery into any occupation. They are so effective especially living in a very stressful, fast-paced society. There is self-distancing involved which we know also helps with the social skills for these kids. Systems thinking and routines with visuals are other options. The more visuals we use, the better for these kids. If we can give them visual imagery, it helps. Here is an example of systems thinking. You have family coming over for Thanksgiving dinner. There are 17 people coming and three courses. Each dish takes this long and I need these ingredients for each. Additionally, these dishes all cook at different times so they come out at the right time. This is systems thinking. As a strategy, I gather my recipes and my materials and then put them in order for which ones I have to cook first and for how long. I form a little assembly line of what I am going to do. We can use this type of strategy for kids who struggle with material management and organization. It can be a game-changer. Other ideas include self-talk, martial arts, aerobics, and Montessori. I do not know if anyone has any experience with a Montessori approach. One of the reasons why it is effective is because Montessori uses self-distancing activities. Telling the kids what you want them to do instead of what you do not want them to do really works. It also includes structured routines that lead to self-regulation.
The last section shows that motor skills, as well as sleep hygiene, can improve sleep. Physical activity actually increases non-REM sleep. Deep pressure and proprioceptive can increase REM sleep. A sleep log is actually evidence-based as well. Shortly, I am going to describe a routine that works with kids that is evidence-based. All of these things here you can use as your evidence-based toolkit to work with kids with ADHD.
Case Study Application- Improve ADLs
Top-down analysis.
Jeremy's goal is to have a timely morning routine which involves waking up, dressing, brushing teeth, and packing a backpack. This is a top-down analysis in Figure 6.
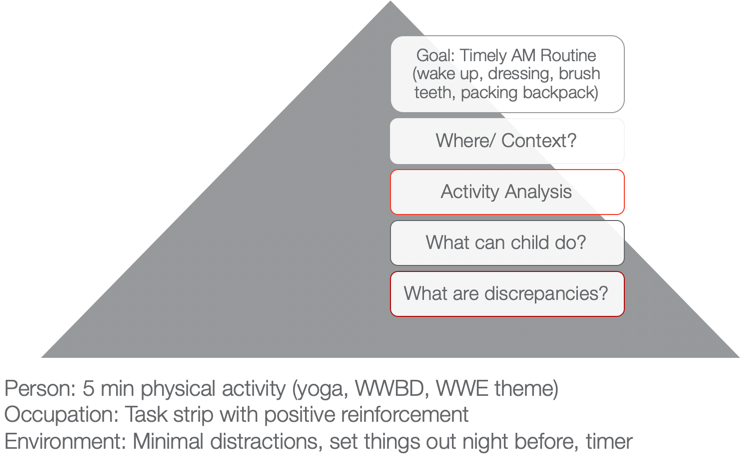
Figure 6. Example of a top-down analysis for ADL routine.
When we use a top-down approach, we are starting with the actual occupation and the goal is to look at where this happens and in what context. I want you to think about where that would happen. In Jeremy's case, it is his bedroom and bathroom. Activity analysis is the bread and butter of OTs. His routine consists of waking up, dressing, brushing his teeth, and packing a backpack. During this analysis, we want to see what he can do and what he cannot do. What are some of your thoughts? Here are some answers from our audience:
- Being aware of time during all tasks/Using a timer. You are seeing a discrepancy between time awareness, time estimation, time monitoring, and time management. I would agree with you that he probably has a hard time all of those.
- Packing the backpack. We know that he is sleepy in the morning and he has a difficult time staying organized. This is especially true if he is half asleep or stressed in the morning.
- Finding his folders. Folders can be elusive sometimes to these kids, so that is a great point. Folders can be found in very strange places.
- Hygiene/organization. Even in hygiene, it is important to make sure that they are organized.
I used a PEO or person-occupation-environment perspective here. We started with some physical activity in the morning to help him to wake up. We did yoga. I asked, "What would Batman do?" He was a big Batman guy. We did some self-distancing by him coming up with strategies for Batman. Or, we used a wresting theme. These activities helped him to be more alert and be able to increase his attention.
We also used a task strip with positive reinforcement to help him see what he needed to do. Visuals can be very helpful for these kids.
Then, we used minimal distractions. We set things out the night before and used that visual so he could match things. We also devised a place where his folders could go. This all might seem trivial, but it really matters for this type of kid. The timer helps as well. You can make it a game.
Activities to Improve ADLs
- Focus on physical activity, motor skills with automaticity and incorporate aspects of yoga to increase sustained attention and memory
- Visual supports and routine with structure
- Self-talk and self-distancing strategies
- Positively reward
To improve ADLs, the key is to focus on physical activity and motor skills with the goal of automaticity. For example, we can incorporate yoga to increase sustained attention and memory. As we talked about earlier, visual supports and structured routines are other great ideas. I cannot emphasize enough the idea of self-talk. This helps with self-regulation and impulsivity on a lower level. The ability to "self-talk" should be pretty solid for kids around the age of seven, but the kids that we are talking about lack this skill. Self-distancing, or having them give strategies to someone other than themselves, is also great. Let them problem-solve and talk it through for someone else, like Batman or John Cena. This way they do not feel like they are picking on themselves or feeling pressured to figure it out for themselves. They are figuring out for someone else, and this strategy is evidence-based. We often forget to positively reward these kids. I like to do something like time with mom and dad, I develop short-term and long-term rewards with mom and dad. For example, Jeremy wanted a wrestling figure for his long term reward. But on a daily basis, he got wrestling bucks and that bought time to wrestle with dad on the weekends.
Case Study Application- Finish a Task with Necessary Supplies
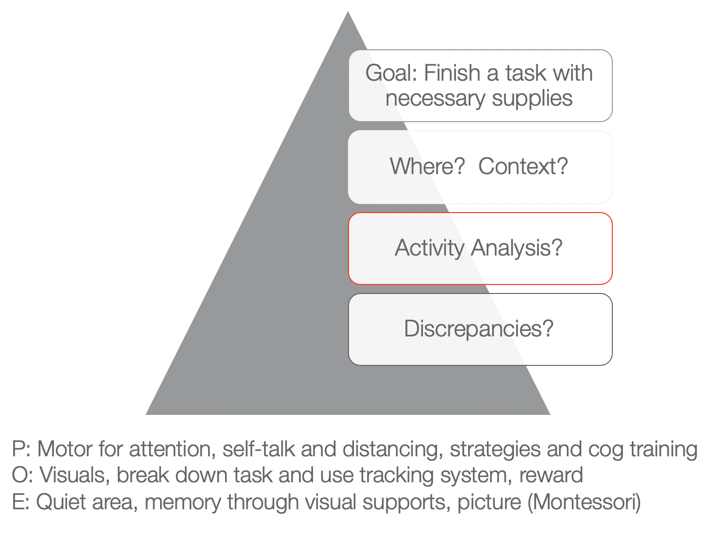
Figure 7. Example of a top-down analysis for finishing a task with necessary supplies.
The next goal is to finish a task with the necessary supplies. You can fill in whatever task that he needed to do like homework, hygiene, or whatever it was with the necessary supplies. Typically, he would start something and then not have all the supplies he needed. He would then run to go get something and then lose track of what he was doing. Activities would not get done and then there would be a mess. We want to know when this would happen and the context. What is required of that activity, and then what can he do versus what he cannot do? Those are the discrepancies.
As I stated a few moments ago, he tends to not have the needed materials. That is the first issue right out of the gate. And because he is impulsive, he starts doing something else. Eventually, he does not finish anything due to a lack of persistence and distractibility. From a personal standpoint, we could work on using motor tasks for increased attention. We know that fine motor and gross motor tasks are going to help. We could also look at using coordination tasks, self-talk, and distancing. Cognitive training is also evidence-based. Can they start to use a checklist or something to create a better strategy?
Then, from an occupation standpoint, again we can use visuals and break down the task. We can also use a tracking system that we are going to go over in just a second.
From an environmental aspect, we can encourage the use of quiet areas to help with sustained attention and better memory. Here we can also use some visual supports or a Montessori approach. "This is what the task is supposed to look like when I am finished." If we have a task, what does the end result look like so that the person knows? And even better, what are the supplies pictured so I know what I have to get first, and then I know what the end result should look like. That is super helpful for someone who is so disorganized when putting materials together.
Activities for Completing Tasks
- Inhibition: Self-talk, slowing down, self-distancing, external feedback
- WM: physical activity
- Attention: physical activity
- Using environmental strategies and visuals to support
- Behavioral: task breakdown, positive reinforcers
- Occupation-based is imperative!
We want to use occupation-based tasks, but we want them to be fun and let the child make a choice. When things are getting easier, we can then move toward less preferred tasks. For example, we do not want to start with homework.
Case Study Application: Social
- Involve a peer or sibling
- Play-based model:
- Capture intrinsic motivations (WWE)
- Empathy focus
- Arrange the environment to foster mutually enjoyable social interaction and imagination
- Teaching social play language and reading expressive body language (can use dogs and their behavior)
- Incorporate parents and coach them so they can coach outside of therapy
(Cordier et al., 2009; Wilkes-Gillan et al., 2016)
There is a play-based model that is evidence-based. They recommend involving a peer or sibling. This play-based model focuses on intrinsic motivation. With Jeremy, we could do wrestling. We could focus on empathy. It is important to arrange the environment so that it is mutually enjoyable. We need to teach social play language and reading expressive body language. The evidence was interesting as it said to use dogs because it could help the child start to read behaviors. Dogs are a little bit easier than people. Jeremy loves dogs so that would work. You could then incorporate parents in order to coach him outside of therapy. They found that to be very successful.
Case Study Application: Sleep
- Turn off electronics 2 hours prior
- Hot bath or shower
- PJs prepped
- Boardgame in room
- Read in bed (parents, then alone
- Highlights with organizer, feelings
- Token reward system
- Flexibility on weekends
- Sleep logs are evidence-based
- Physical activity during day imperative
(Kuhn & Floress, 2008; Fricke et al., 2006)
For sleep, this is the protocol that is highly recommended for these kids. You should turn electronics off two hours prior. Do not shoot the messenger. I know that is really easier said than done. Another protocol is to have the child take a hot bath or shower. They need to have their pajamas prepared. It is a stimulus that can help them progress through the routine. They can do a board game in the room. Another activity is reading in bed. It can start out with the parents reading and then progress to the child reading alone. They can also organize their thoughts and feelings throughout the day. It will help the brain calm down. A token reward system is another great strategy. Make sure to incorporate flexibility on the weekends. It is ok. Sleep logs are evidence-based. And again, physical activity during the day really works.
Systems and Organization
This information is what we already talked about, but I wanted to give you a good resource as well in Figure 8.
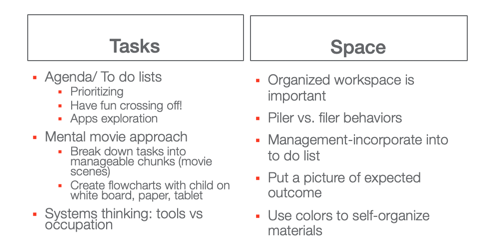
Great resource: https://www.understood.org/~/media/040bfb1894284d019bf78ac01a5f1513.pdf
Figure 8. Systems and organization examples.
I like the idea of a mental movie approach. If they are piler and not a filer, we have to appreciate that and try to use things that can help them. This may be an accordion folder or something like that.
Self-Monitoring: GOAL Attainment Scaling
This is the idea of a Goal Attainment Scale (see Figure 9). It is a strategy to identify changes in academic and social behavior. It creates habits and routines.
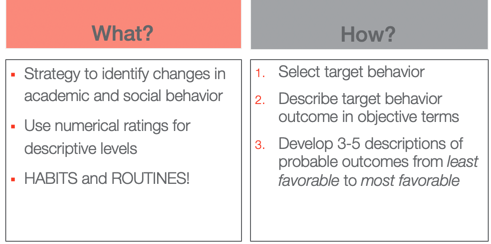
Figure 9. Goal Attainment Scale overview.
The way that you do it is you select the target behavior. You describe that behavior outcome in objective terms and then you develop three to five (I typically use five) descriptions of probable outcomes from least favorable to most favorable.
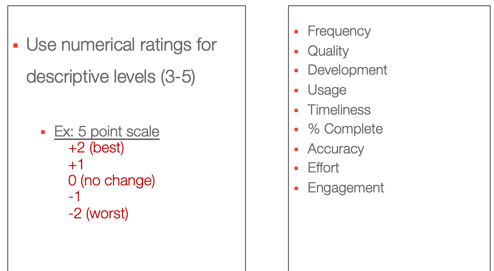
Figure 10. Numerical ratings for the Goal Attainment Scale.
These are some options that you can use, frequency, quality, usage, percent complete.
- Frequency (Never–Sometimes–Very Often–Almost Always–Always)·
- Quality (Poor–Fair–Good–Excellent)·
- Development (Not Present–Emerging–Developing–Accomplished–Exceeding)·
- Usage (Unused–Inappropriate Use–Appropriate Use–Exceptional Use)·
- Timeliness (Late–On-Time–Early)·
- Percent complete (0%–25%–50%–75%–100%)·
- Accuracy (Totally Incorrect–Partially Correct–Totally Correct)·
- Effort (Not Attempted–Minimal Effort–Acceptable Effort–Outstanding Effort)·
- Amount of Support Needed (Totally Dependent–-Extensive Assistance–Some Assistance–Limited Assistance–Independent)·
- Engagement (None–Limited–Acceptable–Exceptional)
This is what the five looks like. You have two choices. You can do a baseline here at zero or the baseline at minus two where that is the worst with no change. Or, you can start at their baseline here at two and only go up. If they cannot handle seeing that they went down, you might choose that option instead. We do not want any negative things causing them anxiety. I have also listed the actual ratings. Here is the example for our friend Jeremy in Figure 11.
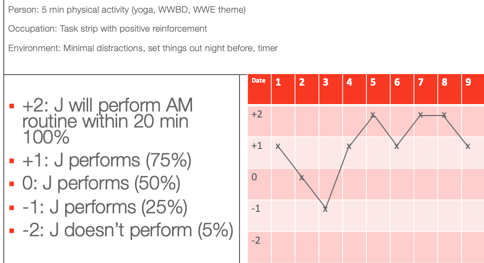
Figure 11. GAS scale example for Jeremy.
He wanted to perform his AM routine within 20 minutes according to his mom. On the first date, he was a +1, which is he did only 75% within 20 minutes. On Day 2, he had 50% of his stuff done within 20 minutes. Day three, he had only 25% done. On four, he was back up to 75%. Day five, he did everything in 20 minutes. Day six, he was back to 75%. And then you see on days seven and eight, he actually met his goal. And on day nine, he almost met his goal. Once you plot the dates you have a graph. This shows change over time and whether or not things are working. You can also do this at home to capture the change in a more specific and sensitive way. On that note, we focused on time.
Thanks for joining me today. I hope you find the information helpful. Feel free to reach out to me if you have any questions.
Best, J. R., & Miller, P. H. (2010). A developmental perspective on executive function. Child Development, 81 (6), 1641-1660.
Cremone-Caira, A., Root, H., Harvey, E. A., McDermott, J. M., & Spencer, R. M. (2019). Effects of sleep extension on inhibitory control in children with ADHD: A pilot study. Journal of Attention Disorders , 1087054719851575.
Corkum, P., Tannock, R., & Moldofsky, H. (1998). Sleep disturbances in children with attention-deficit/hyperactivity disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 37 , 637-646.
Cordier, R., Bundy, A., Hocking, C., & Einfeld, S. (2010). Empathy in the play of children with attention deficit hyperactivity disorder. OTJR: Occupation, Participation, and Health, 30 (3), 122-132.
Diamond, A. (2012). Activities and programs that improve children’s executive functions. Current Directions in Psychological Science, 21 (5), 335-341.
Levanon-Erez, N., Cohen, M., Traub Bar-Ilan, R., & Maeir, A. (2017). Occupational identity of adolescents with ADHD: A mixed methods study. Scandinavian journal of occupational therapy, 24 (1), 32-40.
Hahn-Markowitz, J., Berger, I., Manor, I., & Maeir, A. (2016). Efficacy of cognitive-functional (Cog-Fun) occupational therapy intervention among children with ADHD: An RCT. Journal of Attention Disorders , 1087054716666955.
Faber Taylor, A., & Kuo, F. E. (2011). Could exposure to everyday green spaces help treat ADHD? Evidence from children's play settings. Applied Psychology: Health and Well‐Being, 3 (3), 281-303.
Fricke L, Mitschke A, Wiater A, Lehmkuhl G. 2006. A new treatment program for children with sleep disorders – concept, practicability, and first empirical results. Prax Kinderpsychol Kinderpsychiatr 55 :141–154.
Keshavarzi, Z., Bajoghli, H., Mohamadi, M. R., Salmanian, M., Kirov, R., Gerber, M., ... & Brand, S. (2014). In a randomized case–control trial with 10-years olds suffering from attention deficit/hyperactivity disorder (ADHD) sleep and psychological functioning improved during a 12-week sleep-training program. The World Journal of Biological Psychiatry, 15 (8), 609-619.
Kuhn BR, Floress MT. (2008). Nonpharmacological interventions for sleep disorders in children. In Ivanenko A, ed. Sleep and psychiatric disorders in children and adolescents . New York, NY: Informa Healthcare USA Inc. pp 261–278.
Majored, M., Tüchelmann, T., & Heusser, P. (2004). Therapeutic Eurythmy—movement therapy for children with attention deficit hyperactivity disorder (ADHD): a pilot study. Complementary therapies in Nursing and Midwifery, 10 (1), 46-53.
Pan, C. Y., Tsai, C. L., Chu, C. H., Sung, M. C., Huang, C. Y., & Ma, W. Y. (2019). Effects of physical exercise intervention on motor skills and executive functions in children with ADHD: A pilot study. Journal of Attention Disorders, 23 (4), 384-397.
Papadopoulos, N., Stavropoulos, V., McGinley, J., Bellgrove, M., Tonge, B., Murphy, A., ... & Rinehart, N. (2019). Moderating effect of motor proficiency on the relationship between ADHD symptoms and sleep problems in children with attention deficit hyperactivity disorder–combined type. Behavioral Sleep Medicine, 17 (5), 646-656.
Tandon, P. S., Sasser, T., Gonzalez, E. S., Whitlock, K. B., Christakis, D. A., & Stein, M. A. (2019). Physical activity, screen time, and sleep in children with ADHD. Journal of Physical Activity and Health, 16 (6), 416-422.
Toplak, M. E., West, R. F., & Stanovich, K. E. (2017). The assessment of executive functions in attention-deficit/hyperactivity disorder: Performance-based measures versus ratings of behavior.
Tseng, M. H., Henderson, A., Chow, S. M., & Yao, G. (2004). Relationship between motor proficiency, attention, impulse, and activity in children with ADHD. Developmental Medicine and Child Neurology, 46 (6), 381-388.
Wilkes-Gillan, S., Bundy, A., Cordier, R., Lincoln, M., & Chen, Y. W. (2016). A randomised controlled trial of a play-based intervention to improve the social play skills of children with attention deficit hyperactivity disorder (ADHD). PLOS one, 11 (8), e0160558
Yürümez, E., & Kılıç, B. G. (2016). Relationship between sleep problems and quality of life in children with ADHD. Journal of Attention Disorders, 20 (1), 34-40.
Quint, N. (2020). Pediatric case study: Child with ADHD. OccupationalTherapy.com, Article 5145 . Retrieved from http://OccupationalTherapy.com

Nicole Quint has been an occupational therapist for over 15 years, currently serving as an Associate Professor in the Occupational Therapy Department at Nova Southeastern University, teaching in both the Masters and Doctoral programs. She provides outpatient pediatric OT services, specializing in children and adolescents with Sensory Processing Disorder and concomitant disorders. She also provides consultation services for schools, professional development, and special education services. She provides continuing education on topics related to SPD, pediatric considerations on the occupation of sleep, occupational therapy and vision, reflective therapist, executive functions, leadership in occupational therapy and social emotional learning.
Related Courses
Evidence-based approaches: a pediatric perspective of the occupation of sleep, course: #6204 level: intermediate 2 hours, pediatric case study: child with oculomotor and perceptual challenges, course: #4536 level: intermediate 1 hour, from meltdowns to an occupation-centered approach for self-regulation and management, course: #6106 level: intermediate 2 hours, course: #4577 level: intermediate 1 hour, motor skill acquisition for optimal occupational performance, course: #3747 level: introductory 1 hour.
Our site uses cookies to improve your experience. By using our site, you agree to our Privacy Policy .
A CASE STUDY
Observations of a student with ADHD over a 3-week time span.
Student X is a 14 year-old male in a 9 th Grade English class. He is average height and build. He has no physical disabilities, but suffers from a mental disorder – ADHD. He often makes careless mistakes in schoolwork. He does not pay attention to detail. He has trouble staying focused while reading long texts. He also has difficulty staying still during a lecture. He fidgets and shakes his legs uncontrollably when seemingly annoyed or anxious. He has trouble turning in homework on time and meeting deadlines in general. He frequently does not respond when spoken to directly and appears to be distracted even though he is performing no obvious task. He lets his mind wander and appears to daydream often. When he does respond and participate, he is usually off topic. Overall, he appears uninterested and aloof. One might say that the behavior is defiant – a consciously overt reluctance to participate in school. However, this student has been diagnosed by a physician as being ADHD. He has an involuntary learning disability which requires support, therapy, social skills training and/or medication.
Ready to Make a Change?
Educating children with ADHD is no easy task. Know that you are not alone. Please enlist the help of our school to find the right plan and solution for your child.

IMAGES
VIDEO
COMMENTS
The case of a child with Attention Deficit Hyperactivity Disorder, a Case Study. October 2020. DOI: 10.13140/RG.2.2.23809.48480. Authors: Rodrigo Vasquez Lopiga. Polytechnic University of the ...
CASE STUDY 10-year-old boy diagnosed with ADHD. Referral Concerns. When the client first came to HANDLE he was a ten-year-old fifth grader with a history of prob- lems in school. Teachers reported his "approach to class work is very chaotic," and he rarely could focus on one task for longer than two to three minutes.
1.1. Evaluation of ADHD. The current diagnostic criteria for ADHD can be found in the DSM-5 [] and in the International Statistical Classification of Diseases and Related Health Problems, eleventh revision, from the World Health Organization [].Various evaluation instruments are used to identify ADHD, from general assessments via broad scales such as the Wechsler scale, to more specific tests ...
Social Stories for Children with ADHD Melina Sy1, Thelma Rabago-Mingoa, PhD 2 1De La Salle University -Manila 2De La Salle University -Manila *[email protected] Abstract: This action research used social story as a sole intervention to help decrease disruptive classroom behaviours of children with ADHD. It showed students
Case K described in this chapter was diagnosed as a child with ADHD Combined type; this is a typical presentation for a male child. Inattention: Six or more symptoms of inattention for children up to age 16, or five or more for adolescents 17 and older and adults; symptoms of inattention have been present for at least 6 months, and they are ...
Outcomes in children with ADHD compared to children without ADHD Quality of the study; Parent-reported: 1: Bai et al. (2017) Cross-sectional ... (n = 20), with one cohort study, one case-control study, and one secondary analysis of a randomized controlled trial. Ten studies were from Europe, seven from the Middle East-North Africa region, five ...
the child with ADHD. The purpose ~f an examination of this nature was to create a greater understanding of the disorder and through this understanding, create a learning environment which will allow the child with ADHD to achieve to hisher full potential. 1 . 1 4 ---- An examination _ of ADHD begirW by looking at the questions surrounding
This is the first nationwide baseline study that will establish the prevalence of mental disorders in the Philippines. The study is ongoing and the results will be made available by the end of the year. ... (school refusal), and child abuse are issues of major concern. In the Philippines, child abuse, ADHD, and adjustment disorder were the top ...
concluded that children with ADHD exhibit higher levels of theta waves and lower levels. ... fact may be related to the ADHD profile, in our case study, with 75 neurofeedback sessions,
The design of this study, involves a descriptive survey to determine the relevant policies; existing institutional programs; and existing intervention strategies of teachers and parents. On the basis of existing educational programs, the study intends to surface an emerging model in the education of children with ADHD. The study shows that ...
ABSTRACT. This study investigates parents' lived experiences of having a child diagnosed with Attention Deficit Hyperactivity Disorder (ADHD). The aim was to explore parents' meaning-making processes in relation to their children's ADHD with a focus on understanding the impact that receiving a diagnosis had on the parents' perceptions of, and ways of managing, their children's ...
The quest for increased ADHD awareness in Filipino society is not just about fostering empathy, but about dismantling misconceptions that have long shadowed the true essence of this neurodevelopmental disorder. ADHD, characterized by a persistent pattern of inattention and/or hyperactivity-impulsivity, transcends more than just an inability to ...
Case Study 1 - Jack Jack is a 7 year old male Grade 1 student who lives in Toronto with his parents. He is the only child to two parents, both of whom have completed post-graduate education. There is an extended family history of Attention Deficit/Hyperactivity Disorder (ADHD), mental health concerns as well as academic excellence.
Status of mental health system for children in the Philippines. According to the National Statistics Office (NSO), mental health illnesses rank as the third most common form of morbidity among Filipinos. 8 In the assessment conducted on the Philippine mental health system, a prevalence of 16% of mental disorders among children was reported. 9 With this alarming number of cases, it is ...
Welcome to the video section of the ADHD Society of the Philippines (ADHDSocPhils) website, your one-stop resource for all things related to ADHD. ADHD Story: Xandrino. Discover how the adult ADHD support group transformed the life of Xandrino Mangunay, our dynamic co-Director of Public Relations.
This is a case study of a male child, EE, aged 8+ years, who was described as rather disruptive in class during lesson. For past years, his parents, preschool and primary school teachers noted his challenging behavior and also complained that the child showed a strong dislike for mathematics and Chinese language - both are examinable academic subjects.
3. Most children with ADHD behaviour have "normal" brains. The classification provided by the DSM, and even the phenomenon of reification can be useful for research purposes (Cromwell, 2010), for example because the categories may facilitate the quest for biological origins of behaviour.And indeed, "case-control" studies -comparing groups of children with and without a diagnosis of ...
Abstract. The debate about diagnoses and treatment of attention deficit hyperactive disorder (ADHD) in children continue to range on between the developmental and biological perspectives. While ...
examine the cognitive, affective, and behavioral experiences of parents of children with ADHD are few in the Philippines. Hence, this study, was conceptualized to investigate this occurrence. This study contributes to the literature by describing the parenting experiences of mothers with a child diagnosed with ADHD.
The use of neurofeedback in interventions for ADHD began in 1973, although the first study with positive results was published in 1976 [17]. Since then, various studies have reported benefits from using neurofeedback in infants, with improvements in behavior, attention, and impulsivity control (e.g., [18-22]).
Modafinil (US Food and Drug Administration [FDA]-approved to treat narcolepsy and sleep apnea but not ADHD) in each individual study significantly improved ADHD symptoms, but aggregated estimates were nonsignificant (SMD, −0.76; CI, −1.75 to 0.23; studies = 4; n = 667) (Fig 2, Supplemental Table 1) because of high heterogeneity (I 2 = 91%
Children with ADHD are 50% less likely to participate in sports than children with asthma (Tanden et al., 2019). I find that amazing. Kids with ADHD also have a higher incidence of screen time usage, and we know that that is always a challenge (Tanden et al., 2019). Childhood ADHD is also associated with obesity.
Among those with a history of ADHD diagnosis, 83% were reported as currently having ADHD (8.8%); 69% of children with current ADHD were taking medication for ADHD (6.1%, 3.5 million children).
He has no physical disabilities, but suffers from a mental disorder - ADHD. He often makes careless mistakes in schoolwork. He does not pay attention to detail. He has trouble staying focused while reading long texts. He also has difficulty staying still during a lecture. He fidgets and shakes his legs uncontrollably when seemingly annoyed or ...