

On The Site
Harvard educational review.
Edited by Maya Alkateb-Chami, Jane Choi, Jeannette Garcia Coppersmith, Ron Grady, Phoebe A. Grant-Robinson, Pennie M. Gregory, Jennifer Ha, Woohee Kim, Catherine E. Pitcher, Elizabeth Salinas, Caroline Tucker, Kemeyawi Q. Wahpepah

Individuals
Institutions.
- Read the journal here
Journal Information
- ISSN: 0017-8055
- eISSN: 1943-5045
- Keywords: scholarly journal, education research
- First Issue: 1930
- Frequency: Quarterly
Description
The Harvard Educational Review (HER) is a scholarly journal of opinion and research in education. The Editorial Board aims to publish pieces from interdisciplinary and wide-ranging fields that advance our understanding of educational theory, equity, and practice. HER encourages submissions from established and emerging scholars, as well as from practitioners working in the field of education. Since its founding in 1930, HER has been central to elevating pieces and debates that tackle various dimensions of educational justice, with circulation to researchers, policymakers, teachers, and administrators.
Our Editorial Board is composed entirely of doctoral students from the Harvard Graduate School of Education who review all manuscripts considered for publication. For more information on the current Editorial Board, please see here.
A subscription to the Review includes access to the full-text electronic archives at our Subscribers-Only-Website .
Editorial Board
2023-2024 Harvard Educational Review Editorial Board Members
Maya Alkateb-Chami Development and Partnerships Editor, 2023-2024 Editor, 2022-2024 [email protected]
Maya Alkateb-Chami is a PhD student at the Harvard Graduate School of Education. Her research focuses on the role of schooling in fostering just futures—specifically in relation to language of instruction policies in multilingual contexts and with a focus on epistemic injustice. Prior to starting doctoral studies, she was the Managing Director of Columbia University’s Human Rights Institute, where she supported and co-led a team of lawyers working to advance human rights through research, education, and advocacy. Prior to that, she was the Executive Director of Jusoor, a nonprofit organization that helps conflict-affected Syrian youth and children pursue their education in four countries. Alkateb-Chami is a Fulbright Scholar and UNESCO cultural heritage expert. She holds an MEd in Language and Literacy from Harvard University; an MSc in Education from Indiana University, Bloomington; and a BA in Political Science from Damascus University, and her research on arts-based youth empowerment won the annual Master’s Thesis Award of the U.S. Society for Education Through Art.
Jane Choi Editor, 2023-2025
Jane Choi is a second-year PhD student in Sociology with broad interests in culture, education, and inequality. Her research examines intra-racial and interracial boundaries in US educational contexts. She has researched legacy and first-generation students at Ivy League colleges, families served by Head Start and Early Head Start programs, and parents of pre-K and kindergarten-age children in the New York City School District. Previously, Jane worked as a Research Assistant in the Family Well-Being and Children’s Development policy area at MDRC and received a BA in Sociology from Columbia University.
Jeannette Garcia Coppersmith Content Editor, 2023-2024 Editor, 2022-2024 [email protected]
Jeannette Garcia Coppersmith is a fourth-year Education PhD student in the Human Development, Learning and Teaching concentration at the Harvard Graduate School of Education. A former public middle and high school mathematics teacher and department chair, she is interested in understanding the mechanisms that contribute to disparities in secondary mathematics education, particularly how teacher beliefs and biases intersect with the social-psychological processes and pedagogical choices involved in math teaching. Jeannette holds an EdM in Learning and Teaching from the Harvard Graduate School of Education where she studied as an Urban Scholar and a BA in Environmental Sciences from the University of California, Berkeley.
Ron Grady Editor, 2023-2025
Ron Grady is a second-year doctoral student in the Human Development, Learning, and Teaching concentration at the Harvard Graduate School of Education. His central curiosities involve the social worlds and peer cultures of young children, wondering how lived experience is both constructed within and revealed throughout play, the creation of art and narrative, and through interaction with/production of visual artifacts such as photography and film. Ron also works extensively with educators interested in developing and deepening practices rooted in reflection on, inquiry into, and translation of the social, emotional, and aesthetic aspects of their classroom ecosystems. Prior to his doctoral studies, Ron worked as a preschool teacher in New Orleans. He holds a MS in Early Childhood Education from the Erikson Institute and a BA in Psychology with Honors in Education from Stanford University.
Phoebe A. Grant-Robinson Editor, 2023-2024
Phoebe A. Grant-Robinson is a first year student in the Doctor of Education Leadership(EdLD) program at the Harvard Graduate School of Education. Her ultimate quest is to position all students as drivers of their destiny. Phoebe is passionate about early learning and literacy. She is committed to ensuring that districts and school leaders, have the necessary tools to create equitable learning organizations that facilitate the academic and social well-being of all students. Phoebe is particularly interested in the intersection of homeless students and literacy. Prior to her doctoral studies, Phoebe was a Special Education Instructional Specialist. Supporting a portfolio of more than thirty schools, she facilitated the rollout of New York City’s Special Education Reform. Phoebe also served as an elementary school principal. She holds a BS in Inclusive Education from Syracuse University, and an MS in Curriculum and Instruction from Pace University.
Pennie M. Gregory Editor, 2023-2024
Pennie M. Gregory is a second-year student in the Doctor of Education Leadership (EdLD) program at the Harvard Graduate School of Education. Pennie was born in Incheon, South Korea and raised in Gary, Indiana. She has decades of experience leading efforts to improve outcomes for students with disabilities first as a special education teacher and then as a school district special education administrator. Prior to her doctoral studies, Pennie helped to create Indiana’s first Aspiring Special Education Leadership Institute (ASELI) and served as its Director. She was also the Capacity Events Director for MelanatED Leaders, an organization created to support educational leaders of color in Indianapolis. Pennie has a unique perspective, having worked with members of the school community, with advocacy organizations, and supporting state special education leaders. Pennie holds an EdM in Education Leadership from Marian University.
Jennifer Ha Editor, 2023-2025
Jen Ha is a second-year PhD student in the Culture, Institutions, and Society concentration at the Harvard Graduate School of Education. Her research explores how high school students learn to write personal narratives for school applications, scholarships, and professional opportunities amidst changing landscapes in college access and admissions. Prior to doctoral studies, Jen served as the Coordinator of Public Humanities at Bard Graduate Center and worked in several roles organizing academic enrichment opportunities and supporting postsecondary planning for students in New Haven and New York City. Jen holds a BA in Humanities from Yale University, where she was an Education Studies Scholar.
Woohee Kim Editor, 2023-2025
Woohee Kim is a PhD student studying youth activists’ civic and pedagogical practices. She is a scholar-activist dedicated to creating spaces for pedagogies of resistance and transformative possibilities. Shaped by her activism and research across South Korea, the US, and the UK, Woohee seeks to interrogate how educational spaces are shaped as cultural and political sites and reshaped by activists as sites of struggle. She hopes to continue exploring the intersections of education, knowledge, power, and resistance.
Catherine E. Pitcher Editor, 2023-2025
Catherine is a second-year doctoral student at Harvard Graduate School of Education in the Culture, Institutions, and Society program. She has over 10 years of experience in education in the US in roles that range from special education teacher to instructional coach to department head to educational game designer. She started working in Palestine in 2017, first teaching, and then designing and implementing educational programming. Currently, she is working on research to understand how Palestinian youth think about and build their futures and continues to lead programming in the West Bank, Gaza, and East Jerusalem. She holds an EdM from Harvard in International Education Policy.
Elizabeth Salinas Editor, 2023-2025
Elizabeth Salinas is a doctoral student in the Education Policy and Program Evaluation concentration at HGSE. She is interested in the intersection of higher education and the social safety net and hopes to examine policies that address basic needs insecurity among college students. Before her doctoral studies, Liz was a research director at a public policy consulting firm. There, she supported government, education, and philanthropy leaders by conducting and translating research into clear and actionable information. Previously, Liz served as a high school physics teacher in her hometown in Texas and as a STEM outreach program director at her alma mater. She currently sits on the Board of Directors at Leadership Enterprise for a Diverse America, a nonprofit organization working to diversify the leadership pipeline in the United States. Liz holds a bachelor’s degree in civil engineering from the Massachusetts Institute of Technology and a master’s degree in higher education from the Harvard Graduate School of Education.
Caroline Tucker Co-Chair, 2023-2024 Editor, 2022-2024 [email protected]
Caroline Tucker is a fourth-year doctoral student in the Culture, Institutions, and Society concentration at the Harvard Graduate School of Education. Her research focuses on the history and organizational dynamics of women’s colleges as women gained entry into the professions and coeducation took root in the United States. She is also a research assistant for the Harvard and the Legacy of Slavery Initiative’s Subcommittee on Curriculum and the editorial assistant for Into Practice, the pedagogy newsletter distributed by Harvard University’s Office of the Vice Provost for Advances in Learning. Prior to her doctoral studies, Caroline served as an American politics and English teaching fellow in London and worked in college advising. Caroline holds a BA in History from Princeton University, an MA in the Social Sciences from the University of Chicago, and an EdM in Higher Education from the Harvard Graduate School of Education.
Kemeyawi Q. Wahpepah Co-Chair, 2023-2024 Editor, 2022-2024 [email protected]
Kemeyawi Q. Wahpepah (Kickapoo, Sac & Fox) is a fourth-year doctoral student in the Culture, Institutions, and Society concentration at the Harvard Graduate School of Education. Their research explores how settler colonialism is addressed in K-12 history and social studies classrooms in the United States. Prior to their doctoral studies, Kemeyawi taught middle and high school English and history for eleven years in Boston and New York City. They hold an MS in Middle Childhood Education from Hunter College and an AB in Social Studies from Harvard University.
Submission Information
Click here to view submission guidelines .
Contact Information
Click here to view contact information for the editorial board and customer service .
Subscriber Support
Individual subscriptions must have an individual name in the given address for shipment. Individual copies are not for multiple readers or libraries. Individual accounts come with a personal username and password for access to online archives. Online access instructions will be attached to your order confirmation e-mail.
Institutional rates apply to libraries and organizations with multiple readers. Institutions receive digital access to content on Meridian from IP addresses via theIPregistry.org (by sending HER your PSI Org ID).
Online access instructions will be attached to your order confirmation e-mail. If you have questions about using theIPregistry.org you may find the answers in their FAQs. Otherwise please let us know at [email protected] .
How to Subscribe
To order online via credit card, please use the subscribe button at the top of this page.
To order by phone, please call 888-437-1437.
Checks can be mailed to Harvard Educational Review C/O Fulco, 30 Broad Street, Suite 6, Denville, NJ 07834. (Please include reference to your subscriber number if you are renewing. Institutions must include their PSI Org ID or follow up with this information via email to [email protected] .)
Permissions
Click here to view permissions information.
Article Submission FAQ
Closing the open call, question: “i have already submitted an article to her and i am awaiting a decision, what can i expect”.
Answer: First, any manuscripts already submitted through the open call and acknowledged by HER, as well as all invited manuscripts, R&R’d manuscripts, and manuscripts currently in production are NOT affected in any way by our pause in open calls. Editors are working to move through all current submissions and you can expect to receive any updates or decisions as we move through each step of our production process. If you have any questions, please contact the Co-Chairs, Caroline Tucker and Kemeyawi Wahpepah at [email protected] .
Question: “Can you share more about why you are closing the open call?”
Answer: As a graduate student run journal, we perform our editorial tasks in addition to our daily lives as doctoral students. We have been (and continue to be) incredibly grateful for the authors who share their work with us. In closing the open call, we hope to give ourselves time to review each manuscript in the best manner possible.
Submissions
Question: “what manuscripts are a good fit for her ”.
Answer: As a generalist scholarly journal, HER publishes on a wide range of topics within the field of education and related disciplines. We receive many articles that deserve publication, but due to the restrictions of print publication, we are only able to publish very few in the journal. The originality and import of the findings, as well as the accessibility of a piece to HER’s interdisciplinary, international audience which includes education practitioners, are key criteria in determining if an article will be selected for publication.
We strongly recommend that prospective authors review the current and past issues of HER to see the types of articles we have published recently. If you are unsure whether your manuscript is a good fit, please reach out to the Content Editor at [email protected] .
Question: “What makes HER a developmental journal?”
Answer: Supporting the development of high-quality education research is a key tenet of HER’s mission. HER promotes this development through offering comprehensive feedback to authors. All manuscripts that pass the first stage of our review process (see below) receive detailed feedback. For accepted manuscripts, HER also has a unique feedback process called casting whereby two editors carefully read a manuscript and offer overarching suggestions to strengthen and clarify the argument.
Question: “What is a Voices piece and how does it differ from an essay?”
Answer: Voices pieces are first-person reflections about an education-related topic rather than empirical or theoretical essays. Our strongest pieces have often come from educators and policy makers who draw on their personal experiences in the education field. Although they may not present data or generate theory, Voices pieces should still advance a cogent argument, drawing on appropriate literature to support any claims asserted. For examples of Voices pieces, please see Alvarez et al. (2021) and Snow (2021).
Question: “Does HER accept Book Note or book review submissions?”
Answer: No, all Book Notes are written internally by members of the Editorial Board.
Question: “If I want to submit a book for review consideration, who do I contact?”
Answer: Please send details about your book to the Content Editor at [email protected].
Manuscript Formatting
Question: “the submission guidelines state that manuscripts should be a maximum of 9,000 words – including abstract, appendices, and references. is this applicable only for research articles, or should the word count limit be followed for other manuscripts, such as essays”.
Answer: The 9,000-word limit is the same for all categories of manuscripts.
Question: “We are trying to figure out the best way to mask our names in the references. Is it OK if we do not cite any of our references in the reference list? Our names have been removed in the in-text citations. We just cite Author (date).”
Answer: Any references that identify the author/s in the text must be masked or made anonymous (e.g., instead of citing “Field & Bloom, 2007,” cite “Author/s, 2007”). For the reference list, place the citations alphabetically as “Author/s. (2007)” You can also indicate that details are omitted for blind review. Articles can also be blinded effectively by use of the third person in the manuscript. For example, rather than “in an earlier article, we showed that” substitute something like “as has been shown in Field & Bloom, 2007.” In this case, there is no need to mask the reference in the list. Please do not submit a title page as part of your manuscript. We will capture the contact information and any author statement about the fit and scope of the work in the submission form. Finally, please save the uploaded manuscript as the title of the manuscript and do not include the author/s name/s.
Invitations
Question: “can i be invited to submit a manuscript how”.
Answer: If you think your manuscript is a strong fit for HER, we welcome your request for invitation. Invited manuscripts receive one round of feedback from Editors before the piece enters the formal review process. To submit information about your manuscript for the Board to consider for invitation, please fill out the Invitation Request Form. Please provide as many details as possible. Whether we could invite your manuscript depends on the interest and availability of the current Board. Once you submit the form, we will give you an update in about 2–3 weeks on whether there are Editors who are interested in inviting your manuscript.
Review Timeline
Question: “who reviews manuscripts”.
Answer: All manuscripts are reviewed by the Editorial Board composed of doctoral students at Harvard University.
Question: “What is the HER evaluation process as a student-run journal?”
Answer: HER does not utilize the traditional external peer review process and instead has an internal, two-stage review procedure.
Upon submission, every manuscript receives a preliminary assessment by the Content Editor to confirm that the formatting requirements have been carefully followed in preparation of the manuscript, and that the manuscript is in accord with the scope and aim of the journal. The manuscript then formally enters the review process.
In the first stage of review, all manuscripts are read by a minimum of two Editorial Board members. During the second stage of review, manuscripts are read by the full Editorial Board at a weekly meeting.
Question: “How long after submission can I expect a decision on my manuscript?”
Answer: It usually takes 6 to 10 weeks for a manuscript to complete the first stage of review and an additional 12 weeks for a manuscript to complete the second stage. Due to time constraints and the large volume of manuscripts received, HER only provides detailed comments on manuscripts that complete the second stage of review.
Question: “How soon are accepted pieces published?”
Answer: The date of publication depends entirely on how many manuscripts are already in the queue for an issue. Typically, however, it takes about 6 months post-acceptance for a piece to be published.
Submission Process
Question: “how do i submit a manuscript for publication in her”.
Answer: Manuscripts are submitted through HER’s Submittable platform, accessible here. All first-time submitters must create an account to access the platform. You can find details on our submission guidelines on our Submissions page.

Impact Factor 1.7
ISSN: 0017-8055 eISSN: 1943-5045
Welcome to the Harvard Educational Review The Harvard Educational Review is a scholarly journal of opinion and research in education. It provides an interdisciplinary forum for discussion and debate about the field’s most vital issues. Since its founding in 1930, HER has become a prestigious education journal, with circulation to policymakers, researchers, administrators, and teachers.
Submit an Article

Features & Information

The Harvard Educational Review accepts contributions from researchers, scholars, policy makers, practitioners, teachers, students, and informed observers in education and related fields. We welcome original reports of research and theory as well as articles that reflect on teaching and practice in educational settings around the world.
More information is available here .

Voices in Education Blog
Harvard Education Publishing Group’s Voices in Education blog features a variety of perspectives on current education topics, such as race and equity, teacher preparation, and classroom practice.
Read the blog .

Coming Soon
Published four times per year, the Harvard Educational Review provides scholarly opinion and research articles on the most vital issues in education.
View a list of upcoming articles.
- ©2024 President and Fellows of Harvard College. All Rights Reserved
- Harvard Education Publishing Group
- 8 Story Street, Cambridge, Massachusetts 02138 | (617) 495-3432
- Editorial Board
- Technical Support
- Trademark Notice
- Digital Accessibility Policy
Affiliations
- eISSN 1943-5045
- ISSN 0017-8055
- Privacy Policy
- Get Adobe Acrobat Reader
This Feature Is Available To Subscribers Only
Sign In or Create an Account
Educational Review
Subject Area and Category
Publication type.
00131911, 14653397
Information
How to publish in this journal
The set of journals have been ranked according to their SJR and divided into four equal groups, four quartiles. Q1 (green) comprises the quarter of the journals with the highest values, Q2 (yellow) the second highest values, Q3 (orange) the third highest values and Q4 (red) the lowest values.
The SJR is a size-independent prestige indicator that ranks journals by their 'average prestige per article'. It is based on the idea that 'all citations are not created equal'. SJR is a measure of scientific influence of journals that accounts for both the number of citations received by a journal and the importance or prestige of the journals where such citations come from It measures the scientific influence of the average article in a journal, it expresses how central to the global scientific discussion an average article of the journal is.
Evolution of the number of published documents. All types of documents are considered, including citable and non citable documents.
This indicator counts the number of citations received by documents from a journal and divides them by the total number of documents published in that journal. The chart shows the evolution of the average number of times documents published in a journal in the past two, three and four years have been cited in the current year. The two years line is equivalent to journal impact factor ™ (Thomson Reuters) metric.
Evolution of the total number of citations and journal's self-citations received by a journal's published documents during the three previous years. Journal Self-citation is defined as the number of citation from a journal citing article to articles published by the same journal.
Evolution of the number of total citation per document and external citation per document (i.e. journal self-citations removed) received by a journal's published documents during the three previous years. External citations are calculated by subtracting the number of self-citations from the total number of citations received by the journal’s documents.
International Collaboration accounts for the articles that have been produced by researchers from several countries. The chart shows the ratio of a journal's documents signed by researchers from more than one country; that is including more than one country address.
Not every article in a journal is considered primary research and therefore "citable", this chart shows the ratio of a journal's articles including substantial research (research articles, conference papers and reviews) in three year windows vs. those documents other than research articles, reviews and conference papers.
Ratio of a journal's items, grouped in three years windows, that have been cited at least once vs. those not cited during the following year.
Leave a comment
Name * Required
Email (will not be published) * Required
* Required Cancel
The users of Scimago Journal & Country Rank have the possibility to dialogue through comments linked to a specific journal. The purpose is to have a forum in which general doubts about the processes of publication in the journal, experiences and other issues derived from the publication of papers are resolved. For topics on particular articles, maintain the dialogue through the usual channels with your editor.
Follow us on @ScimagoJR Scimago Lab , Copyright 2007-2024. Data Source: Scopus®
Cookie settings
Cookie Policy
Legal Notice
Privacy Policy
Education Review

About the Journal
Welcome! Education Review (ISSN: 1094-5296) publishes reviews of recent books in English, Spanish, and Portuguese spanning a wide range of education scholarship and practice across the globe. We also publish autobiographical essays highlighting the acquired wisdom and pedagogical legacies of esteemed educational researchers.
IMPORTANT NOTE: The journal will be selective regarding new requests to review English titles for the next few months as we restructure our journal offerings.
Announcements
Nova legados pedagógicos / new pedagogical legacies, current issue, pequenos grandes livros, resenha do livro a ilusão fecunda: a luta por educação nos movimentos populares.
- PDF (Português (Brasil))
Review of Teach truth to power: How to engage in education policy
Review of black male success in higher education: how the mathematical brotherhood empowers a collegiate community to thrive, review of culturally and socially responsible assessment: theory, research, and practice.
ISSN: 1094-5296
- Español (España)
- Português (Brasil)
Make a Submission
Anped books for review.
Pé no chão! Na construção e defesa da EJA pública e popular
Autor/Org: Marco Mello e César Rolim (Orgs.)

Mais informações e livros
Solicitar para revisão
Mais informações para chamada
Additional Information
Disclaimer: The views or opinions presented in book reviews are solely those of the author(s) and do not necessarily represent those of Education Review .

Education Review/Reseñas Educativas/Resenhas Educativas is supported by the Scholarly Communications Group at the Mary Lou Fulton Teachers College, Arizona State University.

- Open access
- Published: 15 April 2024
Correction: Role of AI chatbots in education: systematic literature review
- Lasha Labadze 1 ,
- Maya Grigolia 2 &
- Lela Machaidze 3
International Journal of Educational Technology in Higher Education volume 21 , Article number: 28 ( 2024 ) Cite this article
Metrics details
The Original Article was published on 31 October 2023
Correction: Int J Educ Technol High Educ 20, 56 (2023)
https://doi.org/10.1186/s41239-023-00426-1
After publication of the original article (Labadze et al., 2023 ), the authors became aware that the use of a Large Language Model (LLM) has not been sufficiently documented in accordance with our editorial policy.
In view of this, the authors would like to add the following sentence to the Methodology section of the article:
“To improve the clarity of the discussion section, we employed Large Language Model (LLM) for stylistic suggestions.”
The original article has been updated.
Labadze, L., Grigolia, M., & Machaidze, L. (2023). Role of AI chatbots in education: Systematic literature review. Int J Educ Technol High Educ , 20 , 56. https://doi.org/10.1186/s41239-023-00426-1 .
Article Google Scholar
Download references
Author information
Authors and affiliations.
Finance Department, American University of the Middle East, Block 6, Building 1, Egaila, Kuwait
Lasha Labadze
Statistics Department, American University of the Middle East, Block 6, Building 1, Egaila, Kuwait
Maya Grigolia
Caucasus School of Business, Caucasus University, 1 Paata Saakadze St, Tbilisi, 0102, Georgia
Lela Machaidze
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Lasha Labadze .
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The online version of the original article can be found at https://doi.org/10.1186/s41239-023-00426-1 .
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Labadze, L., Grigolia, M. & Machaidze, L. Correction: Role of AI chatbots in education: systematic literature review. Int J Educ Technol High Educ 21 , 28 (2024). https://doi.org/10.1186/s41239-024-00461-6
Download citation
Published : 15 April 2024
DOI : https://doi.org/10.1186/s41239-024-00461-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Open access
- Published: 14 October 2023
A scoping review of ‘Pacing’ for management of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS): lessons learned for the long COVID pandemic
- Nilihan E. M. Sanal-Hayes 1 , 7 ,
- Marie Mclaughlin 1 , 8 ,
- Lawrence D. Hayes 1 ,
- Jacqueline L. Mair ORCID: orcid.org/0000-0002-1466-8680 2 , 3 ,
- Jane Ormerod 4 ,
- David Carless 1 ,
- Natalie Hilliard 5 ,
- Rachel Meach 1 ,
- Joanne Ingram 6 &
- Nicholas F. Sculthorpe 1
Journal of Translational Medicine volume 21 , Article number: 720 ( 2023 ) Cite this article
3312 Accesses
5 Citations
21 Altmetric
Metrics details
Controversy over treatment for people with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is a barrier to appropriate treatment. Energy management or pacing is a prominent coping strategy for people with ME/CFS. Whilst a definitive definition of pacing is not unanimous within the literature or healthcare providers, it typically comprises regulating activity to avoid post exertional malaise (PEM), the worsening of symptoms after an activity. Until now, characteristics of pacing, and the effects on patients’ symptoms had not been systematically reviewed. This is problematic as the most common approach to pacing, pacing prescription, and the pooled efficacy of pacing was unknown. Collating evidence may help advise those suffering with similar symptoms, including long COVID, as practitioners would be better informed on methodological approaches to adopt, pacing implementation, and expected outcomes.
In this scoping review of the literature, we aggregated type of, and outcomes of, pacing in people with ME/CFS.
Eligibility criteria
Original investigations concerning pacing were considered in participants with ME/CFS.
Sources of evidence
Six electronic databases (PubMed, Scholar, ScienceDirect, Scopus, Web of Science and the Cochrane Central Register of Controlled Trials [CENTRAL]) were searched; and websites MEPedia, Action for ME, and ME Action were also searched for grey literature, to fully capture patient surveys not published in academic journals.
A scoping review was conducted. Review selection and characterisation was performed by two independent reviewers using pretested forms.
Authors reviewed 177 titles and abstracts, resulting in 17 included studies: three randomised control trials (RCTs); one uncontrolled trial; one interventional case series; one retrospective observational study; two prospective observational studies; four cross-sectional observational studies; and five cross-sectional analytical studies. Studies included variable designs, durations, and outcome measures. In terms of pacing administration, studies used educational sessions and diaries for activity monitoring. Eleven studies reported benefits of pacing, four studies reported no effect, and two studies reported a detrimental effect in comparison to the control group.
Conclusions
Highly variable study designs and outcome measures, allied to poor to fair methodological quality resulted in heterogenous findings and highlights the requirement for more research examining pacing. Looking to the long COVID pandemic, our results suggest future studies should be RCTs utilising objectively quantified digitised pacing, over a longer duration of examination (i.e. longitudinal studies), using the core outcome set for patient reported outcome measures. Until these are completed, the literature base is insufficient to inform treatment practises for people with ME/CFS and long COVID.
Introduction
Post-viral illness occurs when individuals experience an extended period of feeling unwell after a viral infection [ 1 , 2 , 3 , 4 , 5 , 6 ]. While post-viral illness is generally a non-specific condition with a constellation of symptoms that may be experienced, fatigue is amongst the most commonly reported [ 7 , 8 , 9 ]. For example, our recent systematic review found there was up to 94% prevalence of fatigue in people following acute COVID-19 infection [ 3 ]. The increasing prevalence of long COVID has generated renewed interest in symptomology and time-course of post-viral fatigue, with PubMed reporting 72 articles related to “post-viral fatigue” between 2020 and 2022, but less than five for every year since 1990.
As the coronavirus pandemic developed, it became clear that a significant proportion of the population experienced symptoms which persisted beyond the initial viral infection, meeting the definition of a post-viral illness. Current estimates suggest one in eight people develop long COVID [ 10 ] and its symptomatology has repeatedly been suggested to overlap with clinical demonstrations of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). In a study by Wong and Weitzer [ 11 ], long COVID symptoms from 21 studies were compared to a list of ME/CFS symptoms. Of the 29 known ME/CFS symptoms the authors reported that 25 (86%) were reported in at least one long COVID study suggesting significant similarities. Sukocheva et al. [ 12 ] reported that long COVID included changes in immune, cardiovascular, metabolic, gastrointestinal, nervous and autonomic systems. When observed from a pathological stance, this list of symptoms is shared with, or is similar to, the symptoms patients with ME/CFS describe [ 13 ]. In fact, a recent article reported 43% of people with long COVID are diagnosed with ME/CFS [ 13 ], evidencing the analogous symptom loads.
A striking commonality between long COVID and similar conditions such as ME/CFS is the worsening of symptoms including fatigue, pain, cognitive difficulties, sore throat, and/or swollen lymph nodes following exertion. Termed post exertional malaise (PEM) [ 14 , 15 , 16 , 17 ], lasting from hours to several days, it is arguably one of the most debilitating side effects experienced by those with ME/CFS [ 16 , 17 , 18 ]. PEM is associated with considerably reduced quality of life amongst those with ME/CFS, with reduced ability to perform activities of daily living, leading to restraints on social and family life, mental health comorbidities such as depression and anxiety, and devastating employment and financial consequences [ 19 , 20 , 21 , 22 ]. At present, there is no cure or pharmacological treatments for PEM, and therefore, effective symptom management strategies are required. This may be in part because the triggers of PEM are poorly understood, and there is little evidence for what causes PEM, beyond anecdotal evidence. The most common approach to manage PEM is to incorporate activity pacing into the day-to-day lives of those with ME/CFS with the intention of reducing the frequency of severity of bouts of PEM [ 23 ]. Pacing is defined as an approach where patients are encouraged to be as active as possible within the limits imposed by the illness [ 23 , 24 , 25 ]. In practice, pacing requires individuals to determine a level at which they can function, but which does not lead to a marked increase in fatigue and other symptoms [ 26 , 27 ].
Although long COVID is a new condition [ 3 , 14 ], the available evidence suggests substantial overlap with the symptoms of conditions such as ME/CFS and it is therefore pragmatic to consider the utility of management strategies (such as pacing) used in ME/CFS for people with long COVID. In fact, a recent Delphi study recommended that management of long COVID should incorporate careful pacing to avoid PEM relapse [ 28 ]. This position was enforced by a multidisciplinary consensus statement considering treatment of fatigue in long COVID, recommending energy conservation strategies (including pacing) for people with long COVID [ 29 ]. Given the estimated > 2 million individuals who have experienced long COVID in the UK alone [ 30 , 31 , 32 ], there is an urgent need for evidence-based public health strategies. In this context, it seems pragmatic to borrow from the ME/CFS literature.
From a historical perspective, the 2007 NICE guidelines for people with ME/CFS advised both cognitive behavioural therapy (CBT) and graded exercise therapy (GET) should be offered to people with ME/CFS [ 33 ]. As of the 2021 update, NICE guidelines for people with ME/CFS do not advise CBT or GET, and the only recommended management strategy is pacing [ 34 ]. In the years between changes to these guidelines, the landmark PACE trial [ 35 ] was published in 2011. This large, randomised control trial (RCT; n = 639) compared pacing with CBT and reported GET and CBT were more effective than pacing for improving symptoms. Yet, this study has come under considerable criticism from patient groups and clinicians alike [ 36 , 37 , 38 , 39 ]. This may partly explain why NICE do not advise CBT or GET as of 2021, and only recommend pacing for symptom management people with ME/CFS [ 34 ]. There has been some controversy over best treatment for people with ME/CFS in the literature and support groups, potentially amplified by the ambiguity of evidence for pacing efficacy and how pacing should be implemented. As such, before pacing can be advised for people with long COVID, it is imperative previous literature concerning pacing is systematically reviewed. This is because a consensus is needed within the literature for implementing pacing so practitioners treating people with ME/CFS or long COVID can do so effectively. A lack of agreement in pacing implementation is a barrier to adoption for both practitioners and patients. Despite several systematic reviews concerning pharmacological interventions or cognitive behavioural therapy in people with ME/CFS [ 36 , 40 , 41 ], to date, there are no systematic reviews concerning pacing.
Despite the widespread use of pacing, the literature base is limited and includes clinical commentaries, case studies, case series, and few randomised control trials. Consequently, while a comprehensive review of the effects of pacing in ME/CFS is an essential tool to guide symptom management advice, the available literature means that effective pooling of data is not feasible [ 42 ] and therefore, a traditional systematic review and meta-analysis, with a tightly focussed research question would be premature [ 43 ]. Consequently, we elected to undertake a scoping review. This approach retains the systematic approach to literature searching but aims to map out the current state of the research [ 43 ]. Using the framework of Arksey and O'Malley [ 44 ], a scoping review aims to use a broad set of search terms and include a wide range of study designs and methods (in contrast to a systematic review [ 44 ]). This approach, has the benefit of clarifying key concepts, surveying current data collection approaches, and identifying critical knowledge gaps.
We aimed to provide an overview of existing literature concerning pacing in ME/CFS. Our three specific objectives of this scoping review were to (1) conduct a systematic search of the published literature concerning ME/CFS and pacing, (2) map characteristics and methodologies used, and (3) provide recommendations for the advancement of the research area.
Protocol and registration
The review was conducted and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for scoping reviews (PRISMA-ScR) guidelines [ 45 ] and the five-stage framework outlined in Arksey and O’Malley [ 44 ]. Registration is not recommended for scoping reviews.
Studies that met the following criteria were included in this review: (1) published as a full-text manuscript; (2) not a review; (3) participants with ME/CFS; (4) studies employed a pacing intervention or retrospective analysis of pacing or a case study of pacing. Studies utilising sub-analysis of the pacing, graded activity, and cognitive behaviour therapy: a randomised evaluation (PACE) trial were included as these have different outcome measures and, as this is not a meta-analysis, this will not influence effect size estimates. Additionally, due to the paucity of evidence, grey literature has also been included in this review.
Search strategy
The search strategy consisted of a combination of free-text and MeSH terms relating to ME/CFS and pacing, which were developed through an examination of published original literature and review articles. Example search terms for PubMed included: ‘ME/CFS’ OR ‘ME’ OR ‘CFS’ OR ‘chronic fatigue syndrome’ OR ‘PEM’ OR ‘post exertional malaise’ OR ‘pene’ OR ‘post-exertion neurogenic exhaust’ AND ‘pacing’ OR ‘adaptive pacing’. The search was performed within title/abstract. Full search terms can be found in Additional file 1 .
Information sources
Six electronic databases [PubMed, Scholar, ScienceDirect, Scopus, Web of Science, and the Cochrane Central Register of Controlled Trials (CENTRAL)] were searched to identify original research articles published from the earliest available date up until 02/02/2022. Additional records were identified through reference lists of included studies. ‘Grey literature’ repositories including MEPedia, Action for ME, and ME Action were also searched with the same terms.
Study selection and data items
Once each database search was completed and manuscripts were sourced, all studies were downloaded into a single reference list (Zotero, version 6.0.23) and duplicates were removed. Titles and abstracts were screened for eligibility by two reviewers independently and discrepancies were resolved through discussion between reviewers. Subsequently, full text papers of potentially relevant studies were retrieved and assessed for eligibility by the same two reviewers independently. Any uncertainty by reviewers was discussed in consensus meetings and resolved by agreement. Data extracted from each study included sample size, participant characteristics, study design, trial registration details, study location, pacing description (type), intervention duration, intervention adherence, outcome variables, and main outcome data. Descriptions were extracted with as much detail as was provided by the authors. Study quality was assessed using the Physiotherapy Evidence Database (PEDro) scale [ 46 , 47 ].
Role of the funding source
The study sponsors had no role in study design, data collection, analysis, or interpretation, nor writing the report, nor submitting the paper for publication.
Study selection
After the initial database search, 281 records were identified (see Fig. 1 ). Once duplicates were removed, 177 titles and abstracts were screened for inclusion resulting in 22 studies being retrieved as full text and assessed for eligibility. Of those, five were excluded, and 17 articles remained and were used in the final qualitative synthesis.
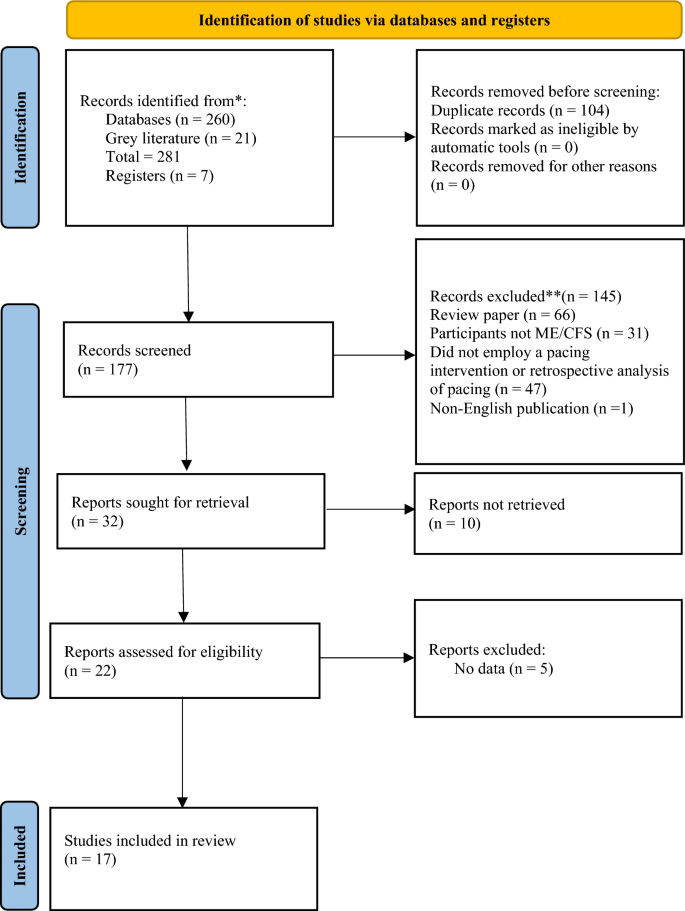
Schematic flow diagram describing exclusions of potential studies and final number of studies. RCT = randomized control trial. CT = controlled trial. UCT = uncontrolled trial
Study characteristics
Study characteristics are summarised in Table 1 . Of the 17 studies included, three were randomised control trials (RCTs [ 35 , 48 , 49 ]); one was an uncontrolled trial [ 50 ]; one was a case series [ 51 ]; one was a retrospective observational study [ 52 ], two were prospective observational studies [ 53 , 54 ]; four were cross-sectional observational studies [ 25 , 55 , 56 ]; and five were cross-sectional analytical studies [ 57 , 58 , 59 , 60 , 61 ] including sub-analysis of the PACE trial [ 35 , 56 , 59 , 61 ]. Seven of the studies were registered trials [ 35 , 48 , 49 , 50 , 56 , 57 , 58 ]. Diagnostic criteria for ME/CFS are summarised in Table 2 .
Types of pacing
Pacing interventions.
Of the 17 studies included, five implemented their own pacing interventions and will be discussed in this section. Sample sizes ranged from n = 7 in an interventional case series [ 51 ] to n = 641 participants in the largest RCT [ 35 ]. The first of these five studies considered an education session on pacing and self-management as the ‘pacing’ group, and a ‘pain physiology education’ group as the control group [ 49 ]. Two studies included educational sessions provided by a therapist plus activity monitoring via ActiGraph accelerometers [ 51 ] and diaries [ 48 ] at baseline and follow-up. In the first of these two studies, Nijs and colleagues [ 51 ] implemented a ‘self-management program’ which asked patients to estimate their current physical capabilities prior to commencing an activity and then complete 25–50% less than their perceived energy envelope. They[ 51 ] did not include a control group and had a sample size of only n = 7. Six years later, the same research group [ 48 ] conducted another pacing study which utilised relaxation as a comparator group (n = 12 and n = 14 in the pacing and relaxation groups, respectively). The pacing group underwent a pacing phase whereby participants again aimed to complete 25–50% less than their perceived energy envelope, followed by a gradual increase in exercise after the pacing phase (the total intervention spanned three weeks, and it is unclear how much was allocated to pacing, and how much to activity increase). Therefore, it could be argued that Kos et al. [ 48 ] really assessed pacing followed by a gradual exercise increase as outcome measures were assessed following the graded activity phase. Another pacing intervention delivered weekly educational sessions for six weeks and utilised a standardised rehabilitation programme using the ‘activity pacing framework’ [ 50 ] in a single-arm, no comparator group feasibility study. Finally, the PACE trial adopted an adaptive pacing therapy intervention consisting of occupational therapists helping patients to plan and pace activities utilising activity diaries to identify activities associated with fatigue and staying within their energy envelope [ 35 ]. This study incorporated standard medical care, cognitive behavioural therapy (CBT) and graded exercise therapy (GET) as comparator groups [ 35 ]. It is worth noting that the pacing group and the CBT group were both ‘encouraged’ to increase physical activity levels as long as participants did not exceed their energy envelope. Although not all five intervention studies explicitly mentioned the “Energy Envelope Theory”, which dictates that people with ME/CFS should not necessarily increase or decrease their activity levels, but moderate activity and practice energy conservation [ 62 ], all intervention studies used language analogous to this theory, such as participants staying within limits, within capacity, or similar.
The interventions included in this review were of varying durations, from a single 30-min education session [ 49 ], a 3-week (one session a week) educational programme [ 51 ], a 3-week (3 × 60–90 min sessions/week) educational programme [ 48 ], a 6-week rehabilitation programme [ 50 ], to a 24-week programme [ 35 ]. Intervention follow-up durations also varied across studies from immediately after [ 49 ], 1-week [ 51 ], 3-weeks [ 48 ], 3-months [ 50 ], and 1-year post-intervention [ 35 ].
Observational studies of pacing
Eight studies were observational and, therefore, included no intervention. Observational study sample sizes ranged from 16 in a cross-sectional interview study [ 25 ] to 1428 in a cross-sectional survey [ 52 ]. One study involved a retrospective analysis of participants’ own pacing strategies varying from self-guided pacing or pacing administered by a therapist compared with implementation of CBT and GET [ 52 ]. Five involved a cross-sectional analysis of participants own pacing strategies which varied from activity adjustment, planning and acceptance [ 50 , 55 ], and the Energy Envelope method [ 58 , 60 ]. Two studies were prospective observational studies investigating the Energy Envelope theory [ 53 , 54 ]. Four studies [ 56 , 57 , 59 , 61 ] included in this review involved sub-analysis of results of the PACE trial [ 35 ].
Outcome measures
Quantitative health outcomes.
ME/CFS severity and general health status were the most common outcome measures across studies (16/17) [ 35 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 63 ]. Studies utilised different instruments, including the Short-Form 36 (SF-36; 8/16) [ 35 , 51 , 53 , 54 , 56 , 57 , 58 , 60 ], SF-12 (2/16) [ 50 , 63 ], ME symptom and illness severity (2/16) [ 52 , 55 ], Patient health (PHQ-15; 1/16) [ 59 ], DePaul symptom questionnaire (DSQ; 1/16) [ 58 ], and the Patient health questionnaire-9 (1/16) [ 50 ]. Additionally, some studies used diagnostic criteria for ME/CFS as an outcome measure to determine recovery [ 57 , 59 , 61 ].
Pain was assessed by most included studies (11/17) [ 35 , 49 , 50 , 51 , 53 , 54 , 55 , 57 , 59 , 60 , 61 , 63 ]. Two studies [ 59 , 61 ] included the international CDC criteria for CFS which contain five painful symptoms central to a diagnosis of CFS: muscle pain and joint pain. Other methods of assessment included Brief Pain Inventory (1/11) [ 53 ], Chronic Pain Coping Inventory (CPCI; 1/11) [ 49 ], Pain Self Efficacy Questionnaire (PSEQ; 1/11) [ 50 ], Tampa Scale for Kinesiophobia–version CFS (1/11) [ 49 ], algometry (1/11) [ 49 ], Knowledge of Neurophysiology of Pain Test (1/12) [ 49 ], Pain Catastrophizing Scale (1/11) [ 49 ], Pain Anxiety Symptoms Scale short version (PASS-20; 1/11) [ 50 ], Pain Numerical Rating Scale (NRS; 1/11) [ 63 ].
Fatigue or post-exertional malaise was assessed by 11 of the 17 studies [ 35 , 48 , 50 , 51 , 53 , 54 , 56 , 57 , 60 , 61 , 63 ]. Again, measurement instruments were divergent between studies and included the Chalder Fatigue Questionnaire (CFQ; 4/11) [ 35 , 50 , 57 , 63 ], Fatigue Severity Scale (2/11) [ 53 , 60 ], the Chronic Fatigue Syndrome Medical Questionnaire (1/11) [ 60 ], and Checklist Individual Strength (CIS; 2/11) [ 48 , 51 ].
Anxiety and depression were also common outcome measures, utilised by four studies (4/17) [ 50 , 53 , 59 , 63 ]. These were also assessed using different instruments including Hospital Anxiety and Depression Scale (HADS; 2/4) [ 59 , 63 ], Generalised Anxiety Disorder Assessment (1/4 [ 50 ]), Beck Depression Inventory (BDI-II; 1/4) [ 53 ], Beck Anxiety Inventory (BAI; 1/4) [ 53 ], and Perceived Stress Scale (PSS; 1/4) [ 53 ].
Outcome measures also included sleep (2/17) [ 53 , 59 ], assessed by The Pittsburgh Sleep Quality Index (1/2) [ 53 ] and Jenkins sleep scale (1/2) [ 59 ]; and quality of life (2/17) [ 50 , 53 ] as assessed by the EuroQol five-dimensions, five-levels (EQ-5D-5L; 1/2) [ 50 ] and The Quality-of-Life Scale (1/2) [ 53 ]. Self-Efficacy was measured in four studies [ 50 , 53 , 59 , 60 ], assessed by the Brief Coping Orientation to Problems Experienced Scale (bCOPE; 1/4) [ 60 ] and the Chronic Disease Self-Efficacy measure (3/4) [ 50 , 53 , 59 ].
Quantitative evaluation of pacing
Some studies (4/17) [ 25 , 50 , 52 , 63 ] included assessments of the participants’ experiences of pacing, using the Activity Pacing Questionnaire (APQ-28; 1/4 [ 50 ], APQ-38 (2/4) [ 25 , 63 ]), a re-analysis of the 228 question survey regarding treatment (1/4) [ 52 ] originally produced by the ME Association [ 55 ], and qualitative semi-structured telephone interviews regarding appropriateness of courses in relation to individual patient needs (1/4) [ 25 ]. The APQ-28 and -38 have been previously validated, but the 228-question survey has not. When outcome measures included physical activity levels (4/17), the Canadian Occupational Performance Measure (COPM) was used in two studies [ 48 , 51 ], and two studies used accelerometers to record physical activity [ 51 , 54 ]. Of these two studies, Nijs [ 51 ] examined accelerometery after a 3-week intervention based on the Energy Envelope Theory and Brown et al. [ 54 ] evaluated the Energy Envelope Theory of pacing over 12 months.
Other outcomes
Two [ 53 , 59 ] of the 17 studies included structured clinical interviews for the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV) to assess psychiatric comorbidity and psychiatric exclusions. One study included a disability benefits questionnaire [ 55 ], and one study included employment and education questionnaire [ 55 ]. Additionally, satisfaction of primary care was also used as an outcome measure (2/17) [ 25 , 55 ] assessed using the Chronic Pain Coping Inventory (CPCI).
Efficacy of pacing interventions
The majority of studies (12/17) [ 25 , 48 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 58 , 60 , 63 ] highlighted improvements in at least one outcome following pacing (Fig. 2 ). When the effect of pacing was assessed by ME symptomology and general health outcomes, studies reported pacing to be beneficial [ 25 , 50 , 51 , 53 , 54 , 55 , 56 , 58 ]. It is worth noting however that pacing reportedly worsened ME symptoms in 14% of survey respondents, whilst improving symptoms in 44% of respondents [ 52 ]. Most studies using fatigue as an outcome measure reported pacing to be efficacious (7/10) [ 50 , 51 , 53 , 54 , 56 , 60 , 63 ]. However, one study reported no change in fatigue with a pacing intervention (1/10) [ 35 ], and 2/10 studies [ 53 , 63 ] reported a worsening of fatigue with pacing. Physical function was used to determine the efficacy of pacing in 11 studies [ 35 , 48 , 50 , 51 , 53 , 54 , 56 , 58 , 59 , 60 , 63 ]. Of these, the majority found pacing improved physical functioning (8/10) [ 48 , 50 , 51 , 53 , 54 , 56 , 58 , 60 ], with 1/10 [ 35 ] studies reporting no change in physical functioning, and 1/10 [ 59 ] reporting a worsening of physical functioning from pre- to post-pacing. Of the seven studies [ 35 , 49 , 50 , 51 , 53 , 54 , 60 ] which used pain to assess pacing efficacy, 4/7 [ 50 , 51 , 53 , 60 ] reported improvements in pain and 3/7 [ 35 , 51 , 53 ] reported no change in pain scores with pacing. All studies reporting quality of life (1/1) [ 53 ], self-efficacy (3/3) [ 50 , 53 , 59 ], sleep (2/2) [ 53 , 59 ], and depression and anxiety (4/4) [ 50 , 53 , 59 , 63 ], found pacing to be efficacious for ME/CFS participants.
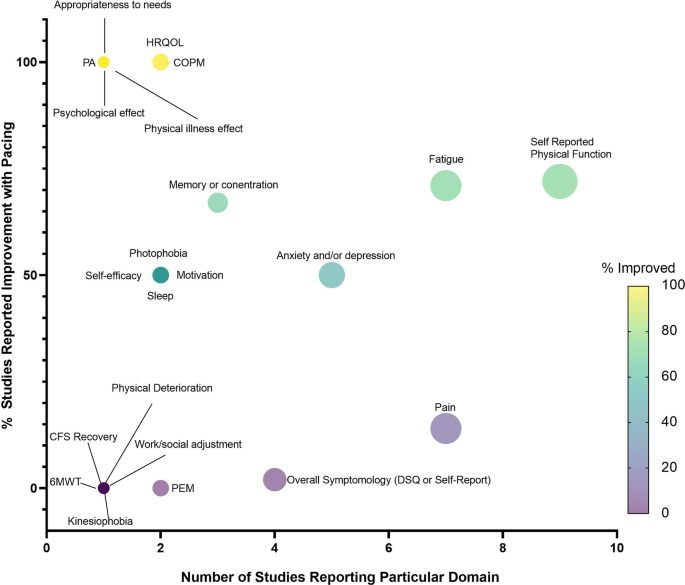
Bubble plot displaying number of studies reporting each domain (x-axis) and the percentage of studies reporting improvement with pacing (y-axis), including a coloured scale of improvement from 0–100%. PEM = post-exertional malaise, 6MWT = 6-min walk time, CFS = chronic fatigue syndrome, DSQ = DePaul Symptom Questionnaire, PA = Physical Activity, HRQOL = Health-related quality of life, COPM = The Canadian Occupational Performance Measure
Participant characteristics
The majority of studies (10/17) [ 25 , 50 , 52 , 53 , 54 , 58 , 59 , 60 , 61 , 63 ] did not report age of the participants. For those which did report age, this ranged from 32 ± 14 to 43 ± 13 years. Where studies reported sex (11/17) [ 35 , 48 , 49 , 50 , 51 , 54 , 55 , 56 , 57 , 58 , 60 ], this was predominantly female, ranging from 75 to 100% female. Only six studies [ 35 , 54 , 56 , 57 , 58 , 60 ] reported ethnicity, with cohorts predominantly Caucasian (94–98%). Time since diagnosis was mostly unreported (12/17) [ 25 , 48 , 49 , 50 , 52 , 53 , 54 , 58 , 59 , 60 , 61 , 63 ] but ranged from 32 to 96 months, with a cross-sectional survey reporting 2% of the participants were diagnosed 1–2 years previously; 6% 3–4 years since diagnosis; 13% 3–4 years since diagnosis; 12% 5–6 years since diagnosis; 20% 7–10 years since diagnosis; 29% 11–21 years since diagnosis; 13% 21–30 years since diagnosis; and 5% > 30 years since diagnosis. Of the studies which reported comorbidities of the participants (6/17) [ 25 , 35 , 50 , 56 , 57 , 63 ], the comorbidities were chronic pain, depressive disorder, psychiatric disorder.
Study location
Of the 17 studies, 14 were from Europe [ 25 , 35 , 48 , 49 , 50 , 51 , 52 , 55 , 56 , 57 , 58 , 59 , 61 , 63 ], and three from North America [ 53 , 54 , 60 ]. Of the 14 studies[ 25 , 35 , 48 , 49 , 50 , 51 , 52 , 55 , 56 , 57 , 58 , 59 , 61 , 63 ] from Europe, ten [ 25 , 35 , 50 , 52 , 55 , 56 , 57 , 58 , 59 , 61 , 63 ] were conducted in the United Kingdom, three in Belgium [ 48 , 49 , 51 ], and one was a multicentred study between the United Kingdom and Norway [ 58 ].
Recruitment strategy
Of the 17 studies, three [ 53 , 54 , 60 ] used announcements in a newspaper and physician referrals to recruit participants, two [ 50 , 63 ] recruited patients referred by a consultant from a National Health Service (NHS) Trust following a pain diagnosis, two [ 52 , 55 ] concerned online platforms on the web, two [ 59 , 61 ] recruited from secondary care clinics, and two used the PACE trial databases [ 56 , 57 ]. Moreover, one study recruited from the hospital [ 58 ], one from physiotherapist referrals [ 25 ], two from specialist clinic centres [ 35 , 64 ], one from waiting list of rehabilitation centre [ 48 ], and one from medical files [ 49 ].
Study settings
Ten studies were carried out in hospital and clinic setting [ 25 , 35 , 48 , 49 , 50 , 51 , 58 , 59 , 61 , 63 ]. Two studies were performed on online platforms [ 52 , 55 ]. Three studies did not report study setting [ 53 , 54 , 60 ]. Two studies generated output from PACE trial databases [ 56 , 57 ]
Adherence and feasibility
All five intervention studies reported adherence rates (which they defined as number of sessions attended), which ranged from 4–44% (4% [ 49 ], 8% [ 35 ], 25% [ 48 ], 29% [ 51 ], and 44% [ 50 ]). One study reported the median number of rehabilitation programme sessions attended was five out of six possible sessions, with 58.9% [ 50 ] participants attending ≥ 5 sessions; 83.2% participants attending at least one educational session on activity pacing and 56.1% attending both activity pacing sessions.
This scoping review summarises the existing literature, with a view to aid physicians and healthcare practitioners better summarise evidence for pacing in ME/CFS and use this knowledge for other post-viral fatiguing conditions. Overall, studies generally reported pacing to be beneficial for people with ME/CFS. The exception to this trend is the controversial PACE trial [ 36 , 37 , 38 , 39 ], which we will expand on in subsequent sections. We believe information generated within this review can facilitate discussion of research opportunities and issues that need to be addressed in future studies concerning pacing, particularly given the immediate public health issue of the long COVID pandemic. As mentioned, we found some preliminary evidence for improved symptoms following pacing interventions or strategies. However, we wish to caution the reader that the current evidence base is extremely limited and hampered by several limitations which preclude clear conclusions on the efficacy of pacing. Firstly, studies were of poor to fair methodological quality (indicated by the PEDro scores), often with small sample sizes, and therefore unknown power to detect change. Moreover, very few studies implemented pacing, with most studies merely consulting on people’s views on pacing. This may of course lead to multiple biases such as reporting, recruitment, survivorship, confirmation, availability heuristic, to name but a few. Thus, there is a pressing need for more high-quality intervention studies. Secondly, the reporting of pacing strategies used was inconsistent and lacked detail, making it difficult to describe current approaches, or implement them in future research or symptom management strategies. Furthermore, outcome evaluations varied greatly between studies. This prevents any appropriate synthesis of research findings.
The lack of evidence concerning pacing is concerning given pacing is the only NICE recommended management strategy for ME/CFS following the 2021 update [ 34 ]. Given the analogous nature of long COVID with ME/CFS, patients and practitioners will be looking to the ME/CFS literature for guidance for symptom management. There is an urgent need for high quality studies (such as RCTs) investigating the effectiveness of pacing and better reporting of pacing intervention strategies so that clear recommendations can be made to patients. If this does not happen soon, there will be serious healthcare and economic implications for years to come [ 65 , 66 ].
Efficacy of pacing
Most studies (12/17) highlighted improvements in at least one outcome measure following pacing. Pacing was self-reported to be the most efficacious, safe, acceptable, and preferred form of activity management for people with ME/CFS [ 55 ]. Pacing was reported to improve symptoms and improve general health outcomes [ 25 , 50 , 52 , 58 , 63 ], fatigue and PEM [ 48 , 50 , 51 , 53 , 54 , 55 , 56 , 60 , 63 ], physical functioning [ 48 , 50 , 51 , 53 , 56 , 58 , 60 , 63 ], pain [ 25 , 50 , 55 , 63 ], quality of life [ 50 ], self-efficacy [ 50 , 53 ], sleep [ 53 , 55 ], and depression and anxiety [ 50 , 53 , 63 ]. These positive findings provide hope for those with ME/CFS, and other chronic fatiguing conditions such as long COVID, to improve quality of life through symptom management.
Conversely, some studies reported no effects of pacing on ME/CFS symptoms [ 52 ], fatigue, physical functioning [ 35 ], or pain scores [ 49 , 61 ]. Some studies even found pacing to have detrimental effects in those with ME/CFS, including a worsening of symptoms in 14% of survey participants recalling previous pacing experiences [ 52 ]. Furthermore, a worsening of fatigue [ 35 , 59 ], and physical functioning from pre- to post-pacing [ 35 , 57 , 59 , 61 ] was reported by the PACE trial and sub-analysis of the PACE trial [ 56 , 57 , 61 ]. The PACE trial [ 35 ], a large RCT (n = 639) comparing pacing with CBT and GET, reported GET and CBT were more effective for reducing ME/CFS-related fatigue and improving physical functioning than pacing. However, the methodology and conclusions from the PACE trial have been heavily criticised, mainly due to the authors lowering the thresholds they used to determine improvement [ 36 , 37 , 38 , 67 ]. With this in mind, Sharpe et al. [ 56 ] surveyed 75% of the participants from the PACE trial 1-year post-intervention and reported pacing improved fatigue and physical functioning, with effects similar to CBT and GET.
Lessons for pacing implementation
All pacing intervention studies (5/5) implemented educational or coaching sessions. These educational components were poorly reported in terms of the specific content and how and where they had been developed, with unclear pedagogical approaches. Consequently, even where interventions reported reduction in PEM or improved symptoms, it would be impossible to transfer that research into practice, future studies, or clinical guidance, given the ambiguity of reporting. Sessions typically contained themes of pacing such as activity adjustment (decrease, break-up, and reschedule activities based on energy levels), activity consistency (maintaining a consistently low level of activity to prevent PEM), activity planning (planning activities and rest around available energy levels), and activity progression (slowly progressing activity once maintaining a steady baseline) [ 35 , 48 , 49 , 50 , 51 ]. We feel it is pertinent to note here that although activity progression has been incorporated as a pacing strategy in these included studies, some view activity progression as a form of GET. The NICE definition of GET is “first establishing an individual's baseline of achievable exercise or physical activity, then making fixed incremental increases in the time spent being physically active” [ 34 ]. Thus, this form of pacing can also be considered a type of ‘long-term GET’ in which physical activity progression is performed over weeks or months with fixed incremental increases in time spent being physically.
Intervention studies attempted to create behaviour change, through educational programmes to modify physical activity, and plan behaviours. However, none of these studies detailed integrating any evidence-based theories of behaviour change [ 68 ] or reported using any frameworks to support behaviour change objectives. This is unfortunate since there is good evidence that theory-driven behaviour change interventions result in greater intervention effects [ 69 ]. Indeed, there is a large body of work regarding methods of behaviour change covering public health messaging, education, and intervention design, which has largely been ignored by the pacing literature. Interventions relied on subjective pacing (5/5 studies), with strategies including keeping an activity diary (3/5 studies) to identify links between activity and fatigue [ 35 , 48 , 50 ]. Given the high prevalence of ‘brain fog’ within ME/CFS [ 70 , 71 , 72 , 73 ], recall may be extremely difficult and there is significant potential for under-reporting. Other strategies included simply asking participants to estimate energy levels available for daily activities (2/5 studies [ 48 , 51 ]). Again, this is subjective and relies on participants’ ability to recall previous consequences of the activity. Other methods of activity tracking and measuring energy availability, such as wearable technology [ 74 , 75 , 76 , 77 , 78 ] could provide a more objective measure of adherence and pacing strategy fidelity in future studies. Despite technology such as accelerometers being widely accessible since well-before the earliest interventional study included in this review (which was published in 2009), none of the interventional studies utilised objective activity tracking to track pacing and provide feedback to participants. One study considered accelerometery alongside an activity diary [ 51 ]. However, accelerometery was considered the outcome variable, to assess change in activity levels from pre- to post-intervention and was not part of the intervention itself (which was one pacing coaching sessions per week for 3 weeks). Moreover, most research-grade accelerometers cannot be used as part of the intervention since they have no ability to provide continuous feedback and must be retrieved by the research team in order to access any data. Consequently, their use is mostly limited to outcome assessments only. As pacing comprises a limit to physical activity to prevent push-crash cycles, it is an astonishing observation from this scoping review that only two studies objectively measured physical activity to quantify changes to activity as a result of pacing [ 51 , 54 ]. If the aim of pacing is to reduce physical activity, or reduce variations in physical activity (i.e., push-crash cycles), only two studies have objectively quantified the effect pacing had on physical activity, so it is unclear whether pacing was successfully implemented in any of the other studies.
By exploring the pacing strategies previously used, in both intervention studies and more exploratory studies, we can identify and recommend approaches to improve symptoms of ME/CFS. These approaches can be categorised as follows: activity planning, activity consistency, activity progression, activity adjustment and staying within the Energy Envelope [ 50 , 53 , 60 , 63 ]. Activity planning was identified as a particularly effective therapeutic strategy, resulting in improvement of mean scores of all symptoms included in the APQ-28, reducing current pain, improvement of physical fatigue, mental fatigue, self-efficacy, quality of life, and mental and physical functioning [ 50 ]. Activity planning aligns with the self-regulatory behaviour change technique ‘Action Planning’ [ 79 ] which is commonly used to increase physical activity behaviour. In the case of ME/CFS, activity planning is successfully used to minimise rather than increase physical activity bouts to prevent expending too much energy and avoid PEM. Activity consistency, meaning undertaking similar amounts of activity each day, was also associated with reduced levels of depression, exercise avoidance, and higher levels of physical function [ 63 ]. Activity progression was associated with higher levels of current pain. Activity adjustment associated with depression and avoidance, and lower levels of physical function [ 63 ]. Staying within the Energy Envelope was reported to reduce PEM severity [ 53 , 60 ], improve physical functioning [ 53 , 60 ] and ME/CFS symptom scores [ 53 ], and more hours engaged in activity than individuals with lower available energy [ 53 ]. These results suggest that effective pacing strategies would include activity planning, consistency, and energy management techniques while avoiding progression. This data is, of course, limited by the small number of mostly low-quality studies and should be interpreted with some caution. Nevertheless, these are considerations that repeatedly appear in the literature and, as such, warrant deeper investigation. In addition, and as outlined earlier, most studies are relatively old, and we urgently need better insight into how modern technologies, particularly longitudinal activity tracking and contemporaneous heart-rate feedback, might improve (or otherwise) adaptive pacing. Such longitudinal tracking would also enable activities and other behaviours (sleep, diet, stress) to be linked to bouts of PEM. Linking would enable a deeper insight into potential PEM triggers and mitigations that might be possible.
The PACE trial
We feel it would be remiss of us to not specifically address the PACE trial within this manuscript, as five of the 17 included studies resulted from the PACE trial [ 35 , 56 , 57 , 59 , 61 ]. There has been considerable discussion around the PACE trial, which has been particularly divisive and controversial [ 37 , 38 , 39 , 59 , 67 , 80 , 81 ]. In the PACE trial, GET and CBT were deemed superior to pacing by the authors. Despite its size and funding, the PACE trial has received several published criticisms and rebuttals. Notably, NICE's most recent ME/CFS guideline update removed GET and CBT as suggested treatment options, which hitherto had been underpinned by the PACE findings. While we will not restate the criticisms and rebuttals here, what is not in doubt, is that the PACE trial has dominated discussions of pacing, representing almost a third of all the studies in this review. However, the trial results were published over a decade ago, with the study protocol devised almost two decades ago [ 82 ]. The intervening time has seen a revolution in the development of mobile and wearable technology and an ability to remotely track activity and provide real-time feedback in a way which was not available at that time. Furthermore, there has been no substantive research since the PACE trial that has attempted such work. Indeed, possibly driven by the reported lack of effect of pacing in the PACE trial, this review has demonstrated the dearth of progress and innovation in pacing research since its publication. Therefore, regardless of its findings or criticisms, the pacing implementation in the PACE trial is dated, and there is an urgent need for more technologically informed approaches to pacing research.
Limitations of the current evidence
The first limitation to the literature included in this scoping review is that not all studies followed the minimum data set (MDS) of patient-reported outcome measures (PROMs) agreed upon by the British Association of CFS/ME Professionals (BACME) (fatigue, sleep quality, self-efficacy, pain/discomfort, anxiety/depression, mobility, activities of daily living, self-care, and illness severity) [ 83 , 84 ]. All but one study included in this review measured illness severity, most studies included fatigue and pain/discomfort, and some studies included assessments of anxiety/depression. There was a lack of quantitative assessment of sleep quality, self-efficacy, mobility, activities of daily living, and self-care. Therefore, studies did not consistently capture the diverse nature of the symptoms experienced, with crucial domains missing from the analyses. The MDS of PROMs were established in 2012 [ 83 , 84 ] and therefore, for studies published out prior to 2012, these are not applicable [ 35 , 49 , 51 , 53 , 54 ]. However, for the 12 studies carried out after this time, the MDS should have been considered elucidate the effects of pacing on ME/CFS. Importantly, despite PEM being a central characteristic of ME/CFS, only two studies included PEM as an outcome measure [ 55 , 60 ]. This may be because of the difficulty of accurately measuring fluctuating symptoms, as PEM occurs multiple times over a period of months, and therefore pre- to post- studies and cross-sectional designs cannot adequately capture PEM incidence. Therefore, it is likely studies opted for measuring general fatigue instead. More appropriate longitudinal study designs are required to track PEM over time to capture a more representative picture of PEM patterns. Secondly, reporting of participant characteristics was inadequate, but in the studies that did describe participants, characteristics were congruent with the epidemiological literature and reporting of ME/CFS populations (i.e., 60–65% female) [ 85 ]. Therefore, in this respect, studies included herein were representative samples. However, the lack of reporting of participant characteristics limits inferences we can draw concerning any population-related effects (i.e. whether older, or male, or European, or people referred by a national health service would be more or less likely to respond positively to pacing). Thirdly, comparison groups (where included) were not ideal, with CBT or GET sometimes used as comparators to pacing [ 35 ], and often no true control group included. Penultimately, there is a distinct lack of high-quality RCTs (as mentioned throughout this manuscript). Finally, in reference to the previous section, inferences from the literature are dated and do not reflect the technological capabilities of 2023.
Recommendations for advancement of the investigative area
It is clear from the studies included in this scoping review for the last decade or more, progress and innovation in pacing research have been limited. This is unfortunate for several reasons. People with ME/CFS or long COVID are, of course, invested in their recovery. From our patient and public involvement (PPI) group engagement, it is clear many are ahead of the research and are using wearable technology to track steps, heart rate, and, in some cases, heart rate variability to improve their own pacing practice. While the lack of progress in the research means this is an understandable response by patients, it is also problematic. Without underpinning research, patients may make decisions based on an individual report of trial-and-error approaches given the lack of evidence-based guidance.
A more technologically-informed pacing approach could be implemented by integrating wearable trackers [ 77 , 78 , 86 , 87 ] to provide participants with live updates on their activity and could be integrated with research-informed messaging aimed at supporting behaviour change, as has been trialled in other research areas [ 88 , 89 , 90 , 91 ]. However, more work is needed to evaluate how to incorporate wearable activity trackers and which metrics are most helpful.
A more technologically-informed approach could also be beneficial for longitudinal symptom tracking, particularly useful given the highly variable symptom loads of ME/CFS and episodic nature of PEM. This would overcome reliance on assessments at a single point in time (as the studies within this review conducted). Similarly, mobile health (mHealth) approaches also allow questionnaires to be digitised to make it easier for participants to complete if they find holding a pen or reading small font problematic [ 92 ]. Reminders and notifications can also be helpful for patients completing tasks [ 77 , 93 , 94 , 95 ]. This approach has the added advantage of allowing contemporaneous data collection rather than relying on pre- to post-intervention designs limited by recall bias. Future work must try to leverage these approaches, as unless we collect large data sets on symptoms and behaviours (i.e. activity, diet, sleep, and pharmacology) in people with conditions like ME/CFS we will not be able to leverage emerging technologies such as AI and machine learning to improve the support and care for people with these debilitating conditions. The key areas for research outline in the NICE guidelines (2021 update) speaks to this, with specific mention of improved self-monitoring strategies, sleep strategies, and dietary strategies, all of which can be measured using mHealth approaches, in a scalable and labour-inexpensive way.
The potential for existing pacing research to address the long COVID pandemic
There is now an urgent public health need to address long COVID, with over 200 million sufferers worldwide [ 30 ]. Given the analogous symptomology between ME/CFS and long COVID, and the lack of promising treatment and management strategies in ME/CFS, pacing remains the only strategy for managing long COVID symptoms. This is concerning as the quality of evidence to support pacing is lacking. Given long COVID has reached pandemic proportions, scalable solutions will be required. In this context, we propose that technology should be harnessed to a) deliver, but also b) evaluate, pacing. We recently reported on a just-in-time adaptive intervention to increase physical activity during the pandemic [ 78 ]. However, this method could be adapted to decrease or maintain physical activity levels (i.e., pacing) in long COVID. This method has the advantage of scalability and remote data collection, reducing resource commitments and participant burden, essential for addressing a condition with so many sufferers.
This review highlights the need for more studies concerning pacing in chronic fatiguing conditions. Future studies would benefit from examining pacing’s effect on symptomology and PEM with objectively quantified pacing, over a longer duration of examination, using the MDS. It is essential this is conducted as an RCT, given that in the case of long COVID, participants may improve their health over time, and it is necessary to determine whether pacing exerts an additional effect over time elapsing. Future studies would benefit from digitising pacing to support individuals with varying symptom severity and personalise support. This would improve accessibility and reduce selection bias, in addition to improving scalability of interventions. Finally, clinicians and practitioners should be cognisant of the strength of evidence reported in this review and should exert caution when promoting pacing in their patients, given the varying methods utilised herein.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Activity Pacing Questionnaire
Beck Anxiety Inventory
Beck Depression Inventory
Brief Coping Orientation to Problems Experienced Scale
Canadian Occupational Performance Measure
Centers for disease control and prevention
Chalder Fatigue Questionnaire
Checklist Individual Strength
Chronic Pain Coping Inventory
Cognitive behavioural therapy
Cochrane Central Register of Controlled Trials
DePaul symptom questionnaire
EuroQol five-dimensions, five-levels questionnaire
Graded exercise therapy
Hospital Anxiety and Depression Scale
Myalgic encephalomyelitis/chronic fatigue syndrome
Pain Self Efficacy Questionnaire
Pain Anxiety Symptoms Scale short version
Pain Numerical Rating Scale
Patient health questionnaire
Patient reported outcome measures
Physiotherapy Evidence Database
Perceived Stress Scale
Post exertional malaise
Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for scoping reviews
Randomised control trial
McMurray JC, May JW, Cunningham MW, Jones OY. Multisystem Inflammatory Syndrome in Children (MIS-C), a post-viral myocarditis and systemic vasculitis-a critical review of its pathogenesis and treatment. Front Pediatr. 2020;8: 626182.
Article PubMed PubMed Central Google Scholar
Perrin R, Riste L, Hann M, Walther A, Mukherjee A, Heald A. Into the looking glass: post-viral syndrome post COVID-19. Med Hypotheses. 2020;144: 110055.
Article PubMed PubMed Central CAS Google Scholar
Hayes LD, Ingram J, Sculthorpe NF. More than 100 persistent symptoms of SARS-CoV-2 (Long COVID): A scoping review. Front Med. 2021. https://doi.org/10.3389/fmed.2021.750378 .
Article Google Scholar
McLaughlin M, Cerexhe C, Macdonald E, Ingram J, Sanal-Hayes NEM, Hayes LD, et al. A Cross-sectional study of symptom prevalence, frequency, severity, and impact of long-COVID in Scotland: part I. Am J Med. 2023. https://doi.org/10.1016/j.amjmed.2023.07.009 .
Article PubMed Google Scholar
McLaughlin M, Cerexhe C, Macdonald E, Ingram J, Sanal-Hayes NEM, Hayes LD, et al. A cross-sectional study of symptom prevalence, frequency, severity, and impact of long-COVID in Scotland: part II. Am J Med. 2023. https://doi.org/10.1016/j.amjmed.2023.07.009 .
Hayes LD, Sanal-Hayes NEM, Mclaughlin M, Berry ECJ, Sculthorpe NF. People with long covid and ME/CFS exhibit similarly impaired balance and physical capacity: a case-case-control study. Am J Med. 2023;S0002–9343(23):00465–75.
Google Scholar
Jenkins R. Post-viral fatigue syndrome. Epidemiology: lessons from the past. Br Med Bull. 1991;47:952–65.
Article PubMed CAS Google Scholar
Sandler CX, Wyller VBB, Moss-Morris R, Buchwald D, Crawley E, Hautvast J, et al. Long COVID and post-infective fatigue syndrome: a review. Open Forum Infect Dis. 2021;8:440.
Carod-Artal FJ. Post-COVID-19 syndrome: epidemiology, diagnostic criteria and pathogenic mechanisms involved. Rev Neurol. 2021;72:384–96.
PubMed CAS Google Scholar
Ballering AV, van Zon SKR, Olde Hartman TC, Rosmalen JGM. Lifelines corona research initiative. Persistence of somatic symptoms after COVID-19 in the Netherlands: an observational cohort study. Lancet. 2022;400:452–61.
Wong TL, Weitzer DJ. Long COVID and Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)-a systemic review and comparison of clinical presentation and symptomatology. Medicina (Kaunas). 2021;57:418.
Sukocheva OA, Maksoud R, Beeraka NM, Madhunapantula SV, Sinelnikov M, Nikolenko VN, et al. Analysis of post COVID-19 condition and its overlap with myalgic encephalomyelitis/chronic fatigue syndrome. J Adv Res. 2021. https://doi.org/10.1016/j.jare.2021.11.013 .
Bonilla H, Quach TC, Tiwari A, Bonilla AE, Miglis M, Yang P, et al. Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) is common in post-acute sequelae of SARS-CoV-2 infection (PASC): results from a post-COVID-19 multidisciplinary clinic. medrxiv. 2022. https://doi.org/10.1101/2022.08.03.22278363v1 .
Twomey R, DeMars J, Franklin K, Culos-Reed SN, Weatherald J, Wrightson JG. Chronic fatigue and postexertional malaise in people living with long COVID: an observational study. Phys Ther. 2022;102:005.
Barhorst EE, Boruch AE, Cook DB, Lindheimer JB. Pain-related post-exertional malaise in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and fibromyalgia: a systematic review and three-level meta-analysis. Pain Med. 2022;23:1144–57.
Goudsmit EM. The psychological aspects and management of chronic fatigue syndrome [Internet] [Thesis]. Brunel University, School of Social Sciences; 1996 [cited 2022 Jan 20]. https://scholar.google.co.uk/scholar_url?url=https://bura.brunel.ac.uk/bitstream/2438/4283/1/FulltextThesis.pdf&hl=en&sa=X&ei=kNYjZdeuA4-8ywTAmKmADQ&scisig=AFWwaeZvdxcuHmzGL08L3jp-QwNn&oi=scholarr . Accessed 2 Aug 2022
Stussman B, Williams A, Snow J, Gavin A, Scott R, Nath A, et al. Characterization of post-exertional malaise in patients with myalgic encephalomyelitis/chronic fatigue syndrome. Front Neurol. 2020;11:1025.
Holtzman CS, Bhatia KP, Cotler J, La J. Assessment of Post-Exertional Malaise (PEM) in Patients with Myalgic Encephalomyelitis (ME) and Chronic Fatigue Syndrome (CFS): a patient-driven survey. Diagnostics. 2019. https://doi.org/10.3390/diagnostics9010026 .
Fukuda K, Straus SE, Hickie I, Sharpe MC, Dobbins JG, Komaroff A. The chronic fatigue syndrome: a comprehensive approach to its definition and study. International Chronic Fatigue Syndrome Study Group. Ann Intern Med. 1994;121:953–9.
Carruthers BM, van de Sande MI, De Meirleir KL, Klimas NG, Broderick G, Mitchell T, et al. Myalgic encephalomyelitis: international consensus criteria. J Intern Med. 2011;270:327–38.
Carruthers JD, Lowe NJ, Menter MA, Gibson J, Eadie N, Botox Glabellar Lines II Study Group. Double-blind, placebo-controlled study of the safety and efficacy of botulinum toxin type A for patients with glabellar lines. Plast Reconstr Surg. 2003;112:1089–98.
Jason LA, Jordan K, Miike T, Bell DS, Lapp C, Torres-Harding S, et al. A pediatric case definition for myalgic encephalomyelitis and chronic fatigue syndrome. J Chronic Fatigue Syndrome. 2006;13:1–44.
Goudsmit EM, Nijs J, Jason LA, Wallman KE. Pacing as a strategy to improve energy management in myalgic encephalomyelitis/chronic fatigue syndrome: a consensus document. Disabil Rehabil. 2012;34:1140–7.
Antcliff D, Keenan A-M, Keeley P, Woby S, McGowan L. Engaging stakeholders to refine an activity pacing framework for chronic pain/fatigue: a nominal group technique. Musculoskeletal Care. 2019;17:354–62.
Antcliff D, Keeley P, Campbell M, Woby S, McGowan L. Exploring patients’ opinions of activity pacing and a new activity pacing questionnaire for chronic pain and/or fatigue: a qualitative study. Physiotherapy. 2016;102:300–7.
Yoshiuchi K, Cook DB, Ohashi K, Kumano H, Kuboki T, Yamamoto Y, et al. A real-time assessment of the effect of exercise in chronic fatigue syndrome. Physiol Behav. 2007;92:963–8.
Davenport TE, Stevens SR, Baroni K, Van Ness M, Snell CR. Diagnostic accuracy of symptoms characterising chronic fatigue syndrome. Disabil Rehabil. 2011;33:1768–75.
Nurek M, Rayner C, Freyer A, Taylor S, Järte L, MacDermott N, Delaney BC, Panellists D, et al. Recommendations for the recognition, diagnosis, and management of long COVID: a Delphi study. Br J Gen Pract. 2021. https://doi.org/10.3399/BJGP.2021.0265 .
Herrera JE, Niehaus WN, Whiteson J, Azola A, Baratta JM, Fleming TK, Kim SY, Naqvi H, Sampsel S, Silver JK, Gutierrez MV, Maley J, Herman E, Abramoff Benjamin, et al. Multidisciplinary collaborative consensus guidance statement on the assessment and treatment of fatigue in postacute sequelae of SARS-CoV-2 infection (PASC) patients. PM & R. 2021. https://doi.org/10.1002/pmrj.12684 .
Chen C, Haupert SR, Zimmermann L, Shi X, Fritsche LG, Mukherjee B. Global prevalence of post COVID-19 condition or long COVID: a meta-analysis and systematic review. J Infect Dis. 2022. https://doi.org/10.1093/infdis/jiac136 .
Office for National Statistics. Prevalence of ongoing symptoms following coronavirus (COVID-19) infection in the UK [Internet]. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/prevalenceofongoingsymptomsfollowingcoronaviruscovid19infectionintheuk/7july2022 . Accessed 2 Aug 2022
Office for National Statistics. Prevalence of ongoing symptoms following coronavirus (COVID-19) infection in the UK [Internet]. [cited 2022 Apr 1]. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/prevalenceofongoingsymptomsfollowingcoronaviruscovid19infectionintheuk/3march2022
Baker R, Shaw EJ. Diagnosis and management of chronic fatigue syndrome or myalgic encephalomyelitis (or encephalopathy): summary of NICE guidance. BMJ. 2007;335:446–8.
NICE. Overview | Myalgic encephalomyelitis (or encephalopathy)/chronic fatigue syndrome: diagnosis and management | Guidance | NICE [Internet]. NICE; [cited 2022 Aug 22]. https://www.nice.org.uk/guidance/ng206 . Accessed 2 Aug 2022
White P, Goldsmith K, Johnson A, Potts L, Walwyn R, DeCesare J, et al. Comparison of adaptive pacing therapy, cognitive behaviour therapy, graded exercise therapy, and specialist medical care for chronic fatigue syndrome (PACE): a randomised trial. The Lancet. 2011;377:823–36.
Article CAS Google Scholar
Vink M. PACE trial authors continue to ignore their own null effect. J Health Psychol. 2017;22:1134–40.
Petrie K, Weinman J. The PACE trial: it’s time to broaden perceptions and move on. J Health Psychol. 2017;22:1198–200.
Stouten B. PACE-GATE: an alternative view on a study with a poor trial protocol. J Health Psychol. 2017;22:1192–7.
Agardy S. Chronic fatigue syndrome patients have no reason to accept the PACE trial results: response to Keith J Petrie and John Weinman. J Health Psychol. 2017;22:1206–8.
Kim D-Y, Lee J-S, Park S-Y, Kim S-J, Son C-G. Systematic review of randomized controlled trials for chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME). J Transl Med. 2020;18:7.
Twisk FNM, Maes M. A review on cognitive behavorial therapy (CBT) and graded exercise therapy (GET) in myalgic encephalomyelitis (ME) / chronic fatigue syndrome (CFS): CBT/GET is not only ineffective and not evidence-based, but also potentially harmful for many patients with ME/CFS. Neuro Endocrinol Lett. 2009;30:284–99.
PubMed Google Scholar
Mays N, Roberts E, Popay J. Synthesising research evidence. In: Fulop N, Allen P, Clarke A, Black N, editors. Studying the organisation and delivery of health services: research methods. London: Routledge; 2001. p. 188–220.
Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18:143.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169:467–73.
de Morton NA. The PEDro scale is a valid measure of the methodological quality of clinical trials: a demographic study. Aust J Physiother. 2009;55:129–33.
Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83:713–21.
Kos D, van Eupen I, Meirte J, Van Cauwenbergh D, Moorkens G, Meeus M, et al. Activity pacing self-management in chronic fatigue syndrome: a randomized controlled trial. Am J Occup Ther. 2015;69:6905290020.
Meeus M, Nijs J, Van Oosterwijck J, Van Alsenoy V, Truijen S. Pain physiology education improves pain beliefs in patients with chronic fatigue syndrome compared with pacing and self-management education: a double-blind randomized controlled trial. Arch Phys Med Rehabil. 2010;91:1153–9.
Antcliff D, Keenan A-M, Keeley P, Woby S, McGowan L. Testing a newly developed activity pacing framework for chronic pain/fatigue: a feasibility study. BMJ Open. 2021;11: e045398.
Nijs J, van Eupen I, Vandecauter J, Augustinus E, Bleyen G, Moorkens G, et al. Can pacing self-management alter physical behavior and symptom severity in chronic fatigue syndrome? A case series. J Rehabil Res Dev. 2009;46:985–96.
Geraghty K, Hann M, Kurtev S. Myalgic encephalomyelitis/chronic fatigue syndrome patients’ reports of symptom changes following cognitive behavioural therapy, graded exercise therapy and pacing treatments: Analysis of a primary survey compared with secondary surveys. J Health Psychol. 2019;24:1318–33.
Jason L, Muldowney K, Torres-Harding S. The energy envelope theory and myalgic encephalomyelitis/chronic fatigue syndrome. AAOHN J. 2008;56:189–95.
Brown M, Khorana N, Jason LA. The role of changes in activity as a function of perceived available and expended energy in non-pharmacological treatment outcomes for ME/CFS. J Clin Psychol. 2011;67:253.
Association ME. ME/CFS illness management survey results:‘“No decisions about me without me.” Part 1: Results and in-depth analysis of the 2012 ME association patient survey examining the acceptability, efficacy and safety of cognitive behavioural therapy, graded exercise therapy and pacing, as interventions used as management strategies for ME/CFS. 2015. https://www.meassociation.org.uk/wp-content/uploads/NO-DECISIONS-WITHOUT-ME-report.docx . Accessed 2 Feb 2022
Sharpe M, Goldsmith KA, Johnson AL, Chalder T, Walker J, White PD. Rehabilitative treatments for chronic fatigue syndrome: long-term follow-up from the PACE trial. The Lancet Psychiatry. 2015;2:1067–74.
White PD, Goldsmith K, Johnson AL, Chalder T, Sharpe M. Recovery from chronic fatigue syndrome after treatments given in the PACE trial. Psychol Med. 2013;43:2227–35.
O’connor K, Sunnquist M, Nicholson L, Jason LA, Newton JL, Strand EB. Energy envelope maintenance among patients with myalgic encephalomyelitis and chronic fatigue syndrome: Implications of limited energy reserves. Chronic Illn. 2019;15:51–60.
Dougall D, Johnson A, Goldsmith K, Sharpe M, Angus B, Chalder T, et al. Adverse events and deterioration reported by participants in the PACE trial of therapies for chronic fatigue syndrome. J Psychosom Res. 2014;77:20–6.
Brown AA, Evans MA, Jason LA. Examining the energy envelope and associated symptom patterns in chronic fatigue syndrome: does coping matter? Chronic Illn. 2013;9:302–11.
Bourke JH, Johnson AL, Sharpe M, Chalder T, White PD. Pain in chronic fatigue syndrome: response to rehabilitative treatments in the PACE trial. Psychol Med. 2014;44:1545–52.
Jason LA, Brown M, Brown A, Evans M, Flores S, Grant-Holler E, et al. Energy conservation/envelope theory interventions to help patients with myalgic encephalomyelitis/chronic fatigue syndrome. Fatigue. 2013;1:27–42.
Antcliff D, Campbell M, Woby S, Keeley P. Activity pacing is associated with better and worse symptoms for patients with long-term conditions. Clin J Pain. 2017;33:205–14.
Nijs T, Klein Y, Mousavi S, Ahsan A, Nowakowska S, Constable E, et al. The different faces of 4’-Pyrimidinyl-Functionalized 4,2’:6’,4"-Terpyridin es: metal-organic assemblies from solution and on Au(111) and Cu(111) surface platforms. J Am Chem Soc. 2018;140:2933–9.
Cutler DM, Summers LH. The COVID-19 pandemic and the $16 Trillion Virus. JAMA. 2020;324:1495–6.
Cutler DM. The costs of long COVID. JAMA Health Forum. 2022;3:e221809–e221809.
Geraghty K. ‘PACE-Gate’: when clinical trial evidence meets open data access. J Health Psychol. 2017;22:1106–12.
Davis R, Campbell R, Hildon Z, Hobbs L, Michie S. Theories of behaviour and behaviour change across the social and behavioural sciences: a scoping review. Health Psychol Rev. 2015;9:323–44.
Prestwich A, Sniehotta FF, Whittington C, Dombrowski SU, Rogers L, Michie S. Does theory influence the effectiveness of health behavior interventions? Meta-analysis Health Psychol. 2014;33:465–74.
Balinas C, Eaton-Fitch N, Maksoud R, Staines D, Marshall-Gradisnik S. Impact of life stressors on Myalgic encephalomyelitis/chronic fatigue syndrome symptoms: an Australian longitudinal study. Int J Environ Res Public Health. 2021;18:10614.
McGregor NR, Armstrong CW, Lewis DP, Gooley PR. Post-exertional malaise is associated with hypermetabolism, hypoacetylation and purine metabolism deregulation in ME/CFS cases. Diagnostics. 2019;9:70.
Nacul LC, Lacerda EM, Campion P, Pheby D, de Drachler M, Leite JC, et al. The functional status and well being of people with myalgic encephalomyelitis/chronic fatigue syndrome and their carers. BMC Public Health. 2011;11:402.
Deumer U-S, Varesi A, Floris V, Savioli G, Mantovani E, López-Carrasco P, et al. Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS): an overview. J Clin Med. 2021. https://doi.org/10.3390/jcm10204786 .
Düking P, Giessing L, Frenkel MO, Koehler K, Holmberg H-C, Sperlich B. Wrist-worn wearables for monitoring heart rate and energy expenditure while sitting or performing light-to-vigorous physical activity: validation study. JMIR Mhealth Uhealth. 2020;8: e16716.
Falter M, Budts W, Goetschalckx K, Cornelissen V, Buys R. Accuracy of apple watch measurements for heart rate and energy expenditure in patients with cardiovascular disease: cross-sectional study. JMIR Mhealth Uhealth. 2019;7: e11889.
Fuller D, Colwell E, Low J, Orychock K, Tobin MA, Simango B, et al. Reliability and validity of commercially available wearable devices for measuring steps, energy expenditure, and heart rate: systematic review. JMIR Mhealth Uhealth. 2020;8: e18694.
Mair JL, Hayes LD, Campbell AK, Sculthorpe N. Should we use activity tracker data from smartphones and wearables to understand population physical activity patterns? J Measur Phys Behav. 2022;1:1–5.
Mair JL, Hayes LD, Campbell AK, Buchan DS, Easton C, Sculthorpe N. A personalized smartphone-delivered just-in-time adaptive intervention (JitaBug) to increase physical activity in older adults: mixed methods feasibility study. JMIR Formative Res. 2022;6: e34662.
Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46:81–95.
Feehan SM. The PACE trial in chronic fatigue syndrome. The Lancet. 2011;377:1831–2.
Giakoumakis J. The PACE trial in chronic fatigue syndrome. The Lancet. 2011;377:1831.
White PD, Sharpe MC, Chalder T, DeCesare JC, Walwyn R, PACE trial group. Protocol for the PACE trial: a randomised controlled trial of adaptive pacing, cognitive behaviour therapy, and graded exercise, as supplements to standardised specialist medical care versus standardised specialist medical care alone for patients with the chronic fatigue syndrome/myalgic encephalomyelitis or encephalopathy. BMC Neurol. 2007;7:6.
Reuben DB, Tinetti ME. Goal-oriented patient care–an alternative health outcomes paradigm. N Engl J Med. 2012;366:777–9.
Roberts D. Chronic fatigue syndrome and quality of life. PROM. 2018;9:253–62.
Valdez AR, Hancock EE, Adebayo S, Kiernicki DJ, Proskauer D, Attewell JR, et al. Estimating prevalence, demographics, and costs of ME/CFS using large scale medical claims data and machine learning. Front Pediatr. 2019. https://doi.org/10.3389/fped.2018.00412 .
Greiwe J, Nyenhuis SM. Wearable technology and how this can be implemented into clinical practice. Curr Allergy Asthma Rep. 2020;20:36.
Sun S, Folarin AA, Ranjan Y, Rashid Z, Conde P, Stewart C, et al. Using smartphones and wearable devices to monitor behavioral changes during COVID-19. J Med Internet Res. 2020;22: e19992.
Hardeman W, Houghton J, Lane K, Jones A, Naughton F. A systematic review of just-in-time adaptive interventions (JITAIs) to promote physical activity. Int J Behav Nutr Phys Act. 2019;16:31.
Perski O, Hébert ET, Naughton F, Hekler EB, Brown J, Businelle MS. Technology-mediated just-in-time adaptive interventions (JITAIs) to reduce harmful substance use: a systematic review. Addiction. 2022;117:1220–41.
AhmedS A, van Luenen S, Aslam S, van Bodegom D, Chavannes NH. A systematic review on the use of mHealth to increase physical activity in older people. Clinical eHealth. 2020;3:31–9.
Valenzuela T, Okubo Y, Woodbury A, Lord SR, Delbaere K. Adherence to technology-based exercise programs in older adults: a systematic review. J Geriatric Phys Ther. 2018;41:49–61.
Bowling A. Mode of questionnaire administration can have serious effects on data quality. J Public Health. 2005;27:281–91.
Burns SP, Terblanche M, Perea J, Lillard H, DeLaPena C, Grinage N, et al. mHealth intervention applications for adults living with the effects of stroke: a scoping review. Arch Rehabil Res Clin Transl. 2021;3: 100095.
Vandelanotte C, Müller AM, Short CE, Hingle M, Nathan N, Williams SL, et al. Past, present, and future of eHealth and mHealth research to improve physical activity and dietary behaviors. J Nutr Educ Behav. 2016;48:219-228.e1.
Ludwig K, Arthur R, Sculthorpe N, Fountain H, Buchan DS. Text messaging interventions for improvement in physical activity and sedentary behavior in youth: systematic review. JMIR Mhealth Uhealth. 2018;6:e10799.
Download references
Acknowledgements
We have no acknowledgements to make.
Open access funding provided by Swiss Federal Institute of Technology Zurich. This work was supported by grants from the National Institute for Health and Care Research (COV-LT2-0010) and the funder had no role in the conceptualisation, design, data collection, analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and affiliations.
Sport and Physical Activity Research Institute, School of Health and Life Sciences, University of the West of Scotland, Glasgow, UK
Nilihan E. M. Sanal-Hayes, Marie Mclaughlin, Lawrence D. Hayes, David Carless, Rachel Meach & Nicholas F. Sculthorpe
Future Health Technologies, Singapore-ETH Centre, Campus for Research Excellence and Technological Enterprise (CREATE), Singapore, Singapore
Jacqueline L. Mair
Saw Swee Hock School of Public Health, National University of Singapore, Singapore, Singapore
Long COVID Scotland, 12 Kemnay Place, Aberdeen, UK
Jane Ormerod
Physios for ME, London, UK
Natalie Hilliard
School of Education and Social Sciences, University of the West of Scotland, Glasgow, UK
Joanne Ingram
School of Health and Society, University of Salford, Salford, UK
Nilihan E. M. Sanal-Hayes
School of Sport, Exercise & Rehabilitation Sciences, University of Hull, Hull, UK
Marie Mclaughlin
You can also search for this author in PubMed Google Scholar
Contributions
Authors’ contributions are given according to the CRediT taxonomy as follows: Conceptualization, N.E.M.S–H., M.M., L.D.H, and N.F.S.; methodology, N.E.M.S–H., M.M., L.D.H., and N.F.S.; software, N.E.M.S–H., M.M., L.D.H., and N.F.S.B.; validation, N.E.M.S–H., M.M., L.D.H, and N.F.S.; formal analysis, N.E.M.S–H., M.M., L.D.H., and N.F.S.; investigation, N.E.M.S–H., M.M., L.D.H., and N.F.S.; resources, L.D.H., J.O., D.C., N.H., J.L.M., and N.F.S.; data curation, N.E.M.S.-H., M.M., L.D.H., and N.F.S.; writing—original draft preparation, N.E.M.S.-H., M.M., L.D.H., and N.F.S.; writing—review and editing, N.E.M.S–H., M.M., L.D.H., J.O., D.C., N.H., R.M., J.L.M., J.I., and N.F.S.; visualisation, N.E.M.S–H. and M.M., supervision, N.F.S; project administration, N.E.M.S–H., M.M., L.D.H., and N.F.S.; funding acquisition, L.D.H., J.O., D.C., N.H., J.L.M., J.I., and N.F.S. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Correspondence to Jacqueline L. Mair .
Ethics declarations
Ethical approval and content to participate.
This manuscript did not involve human participants, data, or tissues, so did not require ethical approval.
Consent for publication
This paper does not contain any individual person’s data in any form.

Competing interests
We report no financial and non-financial competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Supplementary file 1. Full search string for databse searching.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Sanal-Hayes, N.E.M., Mclaughlin, M., Hayes, L.D. et al. A scoping review of ‘Pacing’ for management of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS): lessons learned for the long COVID pandemic. J Transl Med 21 , 720 (2023). https://doi.org/10.1186/s12967-023-04587-5
Download citation
Received : 30 June 2023
Accepted : 03 October 2023
Published : 14 October 2023
DOI : https://doi.org/10.1186/s12967-023-04587-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Myalgic encephalomyelitis
- Chronic fatigue syndrome
- Post-exertional malaise
Journal of Translational Medicine
ISSN: 1479-5876
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]

- Entertainment
- Investigations
- Latest Headlines
- Law Office Shooting
- What Are They Hiding?
- 2024 Election
- Clark County
- Nation and World
- Science and Technology
- Road Warrior
- Las Vegas Weather
- East Valley
- North Las Vegas
- Summerlin/Centennial Hills
- Remembering Oct. 1, 2017
- Deborah Wall
- Natalie Burt
- Remembering Jeff German
- Police Accountability
- Alpine Fire
- 100 Years of Growth
- Dangerous Driving
- Raiders News
- Golden Knights
- UNLV Football
- UNLV Basketball
- Nevada Preps
- Sports Betting 101
- Las Vegas Sportsbooks
- National Finals Rodeo
- Where Are They Now?
- On TV/Radio
- MMA and UFC
- Casinos & Gaming
- Conventions
- Inside Gaming
- Entrepreneurs
- Real Estate News
- Business Press
- Sheldon Adelson (1933-2021)
- Debra J. Saunders
- Michael Ramirez cartoons
- Victor Joecks
- Richard A. Epstein
- Victor Davis Hanson
- Drawing Board
- Homicide Tracker
- Faces of Death Row
- Kats’ Cool Hangs
- Arts & Culture
- Home and Garden
- Las Vegas Hiking Guide
- RJ Magazine
- Today’s Obituaries
- Submit an obit
- Dealer News
- Classifieds
- Place a Classified Ad
- Provided Content
- Real Estate Millions
- Internships
- Service Directory
- Transportation
- Merchandise
- Legal Information
- Real Estate Classifieds
- Garage Sales
- Contests and Promotions
- Best of Las Vegas
- Nevada State Bank
- Verizon Business
- P3 Health Partners
- Adult Health
- Star Nursery
- Partner Articles
- Ignite Funding
- Supplements
- Travel Nevada
- Subscriptions
- Newsletters
- Advertise with Us
- >> Local
- >> Education
CCSD approves $3.4B budget amid drop in student enrollment
The Clark County School Board approved a tentative $3.4 billion budget for the 2024-25 school year. The tentative budget now will be filed with the State of Nevada for review.

The Clark County School Board on Thursday approved the school district’s tentative $3.4 billion budget for the 2024-25 school year that is predicted to see a slight decline in student enrollment.
The district’s tentative budget now will be filed with the State of Nevada for review.
Under state law, the tentative budget must be available for public review before it comes back to the board later for formal approval, Jason Goudie, the school district’s chief financial officer, said in a presentation to the board.
Meanwhile, the district faces higher costs because of inflation and a decrease of less than 1 percent in enrollment, continuing a downward trend over the past several years, mostly during the COVID pandemic when students were learning remotely, Goudie said.
“We’re also a very large district so these small decreases in enrollment do not affect our financial stability,” he said.
Construction costs for the district “have gone up dramatically” because of rising inflation and will “require changes and additional costs to be incurred,” Goudie said.
Inflation over the past few years also has been the cause of “challenges” for the district’s employees, he said.
The number of students in classes within the district — the nation’s fifth largest — for 2024-25 is projected to be 287,352, a fall of 3,066 from the 2023-24 school year, according to figures in the tentative budget.
Per pupil spending up
The good news is that the state Legislature approved an increase in base per pupil funding to $9,497 for 2024-25, up substantially from $9,045 for 2023-24, Goudie said.
The tentative budget lists an unassigned ending fund balance of $156.6 million, according to district officials.
By far the largest portion of the estimated spending in the tentative spending plan is the 84 percent allocated to cover salaries and benefits for district employees, Goudie said.
The other 16 percent would be spent on books and supplies, technology, professional services, utilities and other district needs, he said.
The tentative budget, for funding purposes, also includes the new measure for defining “at risk” students, from those students in need of a free or reduced cost school lunch to students at risk of “not graduating with their cohorts,” Goudie said.
The money included in the tentative budget comes from “property taxes, sales taxes rolled up into the state education fund, and that is the primary source for K-12 education,” Goudie said.
Supplemental funding
In other action, the board sent a request to the state Interim Finance Committee for supplemental funding for district employees as allocated by Senate Bill 231 from the 2023 legislative session.
The bill approved $173.8 million in extra compensation, including $58 million to cover 3 percent retroactive pay for district support professionals and $4,250 extra pay for hard-to-fill positions; $114.7 million to cover 1.8 percent retroactive pay to licensed educators and extra pay of $5,000 for hard-to-fill and special education positions; and $1 million on a 4.1 percent salary increase for school police officers.
Contact Jeff Burbank at [email protected] or 702-383-0382. Follow him @JeffBurbank2 on X.


More than half of the 120-acre tech park in the southwest valley is still undeveloped but a film studio and more are in the works.

Bishop Gorman High School will soon have a new principal, according to a letter sent to the private school’s community.

Two K-9s from the Clark County School District Police Department have returned to work after being exposed to “dangerous drugs.”

Two K-9s with the Clark County School District Police Department are back with their handlers after being exposed to “some illegal and extremely dangerous drugs.”

The Clark County School Board voted unanimously to approve a request for proposals to select a firm to search for a new superintendent.

The lawsuit says the Clark County School District knew its schools, including Eldorado High, were beset by a “lack of safety and security” but failed to act.

The Southern Nevada Health District is investigating two cases of active tuberculosis (TB) at two separate schools in the Las Vegas Valley.

Former Clark County School District superintendent Jesus Jara was the highest-paid district employee, records show.

The university released more than 20 hours of video and audio from the Dec. 6 shooting which left three professors dead.

Magician legend David Copperfield, the late Shecky Greene and acclaimed composer Keith Thompason will be honored by the UNLV College of Fine Arts Hall of Fame.

This paper is in the following e-collection/theme issue:
Published on 12.4.2024 in Vol 26 (2024)
The Effectiveness of a Digital App for Reduction of Clinical Symptoms in Individuals With Panic Disorder: Randomized Controlled Trial
Authors of this article:

Original Paper
- KunJung Kim, MD ;
- Hyunchan Hwang, MD, PhD ;
- Sujin Bae, PhD ;
- Sun Mi Kim, MD, PhD ;
- Doug Hyun Han, MD, PhD
Chung Ang University Hospital, Seoul, Republic of Korea
Corresponding Author:
Doug Hyun Han, MD, PhD
Chung Ang University Hospital
102 Heucsock ro
Seoul, 06973
Republic of Korea
Phone: 82 2 6299 3132
Fax:82 2 6299 3100
Email: [email protected]
Background: Panic disorder is a common and important disease in clinical practice that decreases individual productivity and increases health care use. Treatments comprise medication and cognitive behavioral therapy. However, adverse medication effects and poor treatment compliance mean new therapeutic models are needed.
Objective: We hypothesized that digital therapy for panic disorder may improve panic disorder symptoms and that treatment response would be associated with brain activity changes assessed with functional near-infrared spectroscopy (fNIRS).
Methods: Individuals (n=50) with a history of panic attacks were recruited. Symptoms were assessed before and after the use of an app for panic disorder, which in this study was a smartphone-based app for treating the clinical symptoms of panic disorder, panic symptoms, depressive symptoms, and anxiety. The hemodynamics in the frontal cortex during the resting state were measured via fNIRS. The app had 4 parts: diary, education, quest, and serious games. The study trial was approved by the institutional review board of Chung-Ang University Hospital (1041078-202112-HR-349-01) and written informed consent was obtained from all participants.
Results: The number of participants with improved panic symptoms in the app use group (20/25, 80%) was greater than that in the control group (6/21, 29%; χ 2 1 =12.3; P =.005). During treatment, the improvement in the Panic Disorder Severity Scale (PDSS) score in the app use group was greater than that in the control group ( F 1,44 =7.03; P =.01). In the app use group, the total PDSS score declined by 42.5% (mean score 14.3, SD 6.5 at baseline and mean score 7.2, SD 3.6 after the intervention), whereas the PDSS score declined by 14.6% in the control group (mean score 12.4, SD 5.2 at baseline and mean score 9.8, SD 7.9 after the intervention). There were no significant differences in accumulated oxygenated hemoglobin (accHbO 2 ) at baseline between the app use and control groups. During treatment, the reduction in accHbO 2 in the right ventrolateral prefrontal cortex (VLPFC; F 1,44 =8.22; P =.006) and the right orbitofrontal cortex (OFC; F 1,44 =8.88; P =.005) was greater in the app use than the control group.
Conclusions: Apps for panic disorder should effectively reduce symptoms and VLPFC and OFC brain activity in patients with panic disorder. The improvement of panic disorder symptoms was positively correlated with decreased VLPFC and OFC brain activity in the resting state.
Trial Registration: Clinical Research Information Service KCT0007280; https://cris.nih.go.kr/cris/search/detailSearch.do?seq=21448
Introduction
Panic disorder is a common and important disease in clinical practice that leads to a reduction of individual productivity and increased use of health care [ 1 ]. The lifetime prevalence of panic disorder in the general population is 4.8%, and 22.7% of people experience panic attacks [ 2 ]. The most common symptoms of panic disorder include palpitations, shortness of breath, chest pain, numbness of the hands and feet, and cardiorespiratory-type symptoms, in addition to fear of dying, sweating, tremors, dizziness, nausea, and chills [ 3 ]. The US Food and Drug Administration has currently only approved selective serotonin reuptake inhibitors (SSRIs) for the treatment of panic disorder [ 4 ]. However, it is clinically difficult to expect an improvement in symptoms using SSRIs alone in the acute phase; thus we treat patients with benzodiazepine, which can lead to dependence and withdrawal symptoms [ 5 , 6 ]. The most common side effects of SSRIs reported by patients are reduced sexual function, drowsiness, and weight gain [ 7 ], and clinicians may hesitate to use benzodiazepines due to dependence and withdrawal symptoms [ 8 ]. Cognitive behavioral therapy (CBT) is the most widely used nonpharmaceutical treatment for anxiety disorders [ 9 ]. Additional nonpharmaceutical treatments, such as group therapy and supportive psychotherapy, are also available for patients with panic disorder [ 10 , 11 ]. However, these treatments have the disadvantage of requiring face-to-face contact; therefore, other therapeutic alternatives should be offered to patients during pandemics such as COVID-19.
The definition of a digital therapeutic (DTx) is a therapeutic that delivers evidence-based interventions to prevent, manage, or treat a medical disorder or disease; DTxs are currently used in many areas [ 12 ]. This kind of medical and public health use of smartphones and digital technologies is also known as mobile health (mHealth). DTxs related to mental health medicine are actively used in various psychiatric disorders, such as insomnia, substance abuse, attention-deficit/hyperactivity disorder, and anxiety and depression, among others [ 13 ]. In particular, the use of Freespira, a panic disorder DTx, reduced panic symptoms, avoidance behaviors, and treatment costs in patients with panic disorder [ 14 ].
As brain imaging technology advances, a great deal of functional mapping information on the human brain has been accumulated from positron emission tomography (PET), functional magnetic resonance imaging (fMRI), and functional near-infrared spectroscopy (fNIRS). Among these technologies, fNIRS can measure brain activity in a noninvasive and safe manner through measuring changes in the hemoglobin oxygenation state of the human brain [ 15 ]. Various studies have been conducted using fNIRS and fMRI to reveal correlations between panic disorder and brain regions. For example, patients with panic disorder show increased activity in the inferior frontal cortex, hippocampus, cingulate (both anterior and posterior), and orbitofrontal cortex (OFC) [ 16 ]. Previously, we confirmed that patients with panic disorder during rest periods showed increased activity in the OFC [ 17 ].
In this study, we determined whether an app for panic disorder would improve panic disorder symptoms. In addition, we used fNIRS to confirm the association between changes in panic disorder symptoms and changes in activity in specific brain regions.
Participants
Patients who had experiences of panic attacks were recruited between March 1 and July 30, 2022, through billboard advertisements at our hospital. The inclusion criteria for the study were as follows: (1) age between 20 and 65 years, (2) diagnosis of panic disorder based on the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition and (3) ability to use apps without problems. The exclusion criteria were as follows: (1) a history of other psychiatric disorders, except for anxiety disorder, or substance dependence, except for habitual alcohol and tobacco use; and (2) a history of head trauma and chronic medical conditions. The research clinician assessed whether patients fulfilled the inclusion or exclusion criteria. Written informed consent was acquired from all participants at the first visit. This study has been registered with the Clinical Research Information Service (KCT0007280).
Assessment Scales for Anxiety Symptoms
The severity of panic symptoms was assessed using the Panic Disorder Severity Scale (PDSS). The PDSS was developed by Shear et al [ 18 ] in 1997. It is a 7-item instrument used to rate the overall severity of panic disorder and was validated in Korea by Lim et al [ 19 ] in 2001.
The anxiety symptoms of all participants were assessed using the clinician-based Hamilton Anxiety Scale (HAM-A) questionnaire and the participant-based Generalized Anxiety Disorder-7 (GAD-7) questionnaire. The HAM-A was developed by Hamilton in 1969 [ 20 ]. The 14-item version remains the most used outcome measure in clinical trials of treatments for anxiety disorders and was validated in Korea by Kim [ 21 ] in 2001.
The GAD-7 questionnaire, developed by Spitzer et al [ 22 ], is a 7-item self-report anxiety questionnaire designed to assess the patient’s health status during the previous 2 weeks. The GAD-7 was translated into the Korean language and is freely downloadable on the Patient Health Questionnaire website [ 23 ].
Hemodynamic Response of the Prefrontal Cortex
The hemodynamics in the frontal cortex during the resting state were measured using the fNIRS device (NIRSIT; OBELAB Inc). The NIRSIT has 24 laser diodes (sources) emitting light at 2 wavelengths (780 nm and 850 nm) and 32 photodetectors with a sampling rate of 8.138 Hz [ 24 ]. The distance between the source and photodetector is 15 mm. Based on the suggested suitable sensor-detector separation distance for measuring cortical hemodynamic changes, only 30-mm channels were analyzed in this study [ 25 ].
For our study, we used the 48-channel configuration ( Figure 1 ). The detected light signals in each wavelength were filtered with a band-pass filter (0.00 Hz-0.1 Hz) to reduce the effect of environmental noise–related light and body movements. In addition, channels with low-quality information (signal-to-noise ratio <30 dB) were removed from the hemodynamic analysis. The accumulated oxygenated hemoglobin (accHbO 2 ) values in the resting state represent the activation of the prefrontal cortex. In accordance with the theory that oxygenated hemoglobin has superior sensitivity and signal-to-noise ratio compared to deoxygenated hemoglobin data, only oxygenated hemoglobin were used for this analysis [ 26 - 28 ].

The means and SDs for accHbO 2 were calculated from regions of interest (ROIs) in the right and left dorsolateral prefrontal cortices (DLPFCs), right and left ventrolateral prefrontal cortices (VLPFCs), right and left frontopolar cortices (FPCs), and right and left orbitofrontal cortices (OFCs), based on Brodmann area 46. The right and left DLPFCs comprise channels 1, 2, 3, 5, 6, 11, 17, and 18 and channels 19, 20, 33, 34, 35, 38, 39, and 43, respectively. The right and left VLPFCs comprise channels 4, 9, and 10 and channels 40, 44, and 45, respectively. The right and left FPCs comprise channels 7, 8, 12, 13, 21, 22, 25, and 26 and channels 23, 24, 27, 28, 36, 37, 41, and 42, respectively. The right and left OFCs comprise channels 14, 15, 16, 29, and 30 and channels 31, 32, 46, 47, and 48, respectively ( Figure 1 ).
Digital App for Panic Disorder
The app for panic disorder is a smartphone-based app for treatment of clinical symptoms of panic disorder. The mobile app has 4 categories: diary, education, quest, and serious games. The diary category has three items: (1) assessment of daily psychological status, including mood and anxiety; (2) assessment of panic symptoms, including frequency and severity; and (3) consumption of medication, including regular medication and pro re nata medications. The education category has three items: (1) knowledge about panic disorders, (2) knowledge about medications for panic disorder, and (3) knowledge about panic disorder treatment, including CBT, breathing therapy, and positive thinking therapy. The quests include two treatments: (1) eye movement desensitization and reprocessing therapy and (2) positive thinking therapy. The serious games include two games: (1) a breathing game and (2) an exposure therapy game.
The diary, education, and serious games (ie, the breathing game and exposure therapy game) are important parts of CBT for panic disorder [ 29 - 32 ]. The efficacy of CBT for panic disorder has been examined in various randomized controlled trials [ 33 , 34 ]. Eye movement desensitization and reprocessing therapy are also known to help reduce panic symptoms [ 35 , 36 ]. We confirmed that the replacement of worry with different forms of positive ideation shows beneficial effects [ 37 ], so a similar type of positive thinking therapy can also be expected to show benefits. Multimedia Appendix 1 provides additional information on the app.
Ethical Considerations
The study trial was approved by the institutional review board of Chung-Ang University Hospital (1041078-202112-HR-349-01) and written informed consent was obtained from all participants. Participants received an explanation from the researchers that included an overview of the study and a description of the methodology and purpose before deciding to participate. Additionally, they were informed that participation was voluntary, informed about our confidentiality measures, given the option to withdraw, and informed about potential side effects and compensation. Participants in this study received ₩100,000 (US $75.50) as transportation reimbursement. Additionally, the various scales and fNIRS assessments were offered at no cost to the participants. The participants received the results of the tests in the form of a report via postal mail or email after the conclusion of the study. They also receive an explanatory document and consent form from the researchers that included contact information for any inquiries. If the participant agreed to take part in the study after understanding the consent form, the research proceeded. The participants’ personal information was not collected. Instead, a unique identifier was assigned to the collected data for the sole purpose of research management.
Study Procedure
A randomized and treatment-as-usual–controlled design was applied in this study. After screening, all participants with panic disorder were randomly assigned to the app use group or the control group. The randomization sequence in our design was generated using SPSS (version 24.0; IBM Corp), with a 1:1 allocation between groups. At baseline and after intervention, all patients with panic disorder were assessed with the PDSS for panic symptoms, the HAM-A for objective anxiety symptoms, and the GAD-7 for subjective anxiety symptoms. At baseline and after intervention, the hemodynamic response in all patients with panic disorder was assessed using NIRSIT. The app use group was asked to use the app for panic disorder 20 minutes per day, 5 times per week, for 4 weeks. The control group was asked to read short educational letters that were delivered via a social network service 5 times per week for 4 weeks. The short letters contained information about panic disorder and its treatment.
Demographic and Clinical Characteristics
After recruitment, 56 patients underwent eligibility assessments. A total of 6 individuals were excluded because they did not meet the inclusion criteria. The remaining patients were divided into 2 groups: 25 were assigned to the app use group and 21 to the control group, as 4 patients were excluded; contact was suddenly lost with 1 patient contact and 1 dropped out for personal reasons. In addition, 2 patients in the control group quit the study after reporting poor benefits from the short educational letters. Therefore, 25 people in the app use group and 21 people in the control group were analyzed. Figure 2 shows the Consolidated Standards of Reporting Trials (CONSORT) flowchart for participant flow through the trial.

There were no significant differences in age, sex ratio, years of education, marital status, employment status, or substance habits, including smoking and alcohol use, between the app use group and the control group ( Table 1 ).
b Chi-square.
There were no significant differences in HAM-A score, GAD-7 score, or PDSS score at baseline between the app use group and control group ( Table 1 ).
Comparison of Changes in Clinical Scales Between App Use Group and Control Group
The number of participants with improved panic symptoms in the app use group (20/25, 80%) was greater than in the control group (6/21, 29%; χ 2 1 =12.3; P =.005).
During the treatment period, the app use group showed greater improvement in PDSS score than the control group ( F 1,44 =7.03; P =.01). In the app use group, the PDSS score decreased by 42.5% (mean score 14.3, SD 6.5 at baseline and mean score 7.2, SD 3.6 after the intervention), while the score decreased by 14.6% in the control group (mean score 12.4, SD 5.2 at baseline and mean score 9.8, SD 7.9 after intervention) ( Figure 3 ).

During the treatment period, there were no significant differences in the change in HAM-A scores ( F 1,44 =2.83; P =.09) and GAD-7 scores ( F 1,44 =0.22; P =.64) between the app use group and control group ( Figure 3 ).
Comparison of Changes in accHbO 2 Values Between App Use Group and Control Group
There were no significant differences in accHbO 2 in the right (t 45 =0.84; P =.40) or left (t 45 =0.73; P =.46) DLPFCs, right (t 45 =1.04; P =.31) or left (t 45 =0.88; P =.39) VLPFCs, right (t 45 =-0.18; P =.86) or left (t 45 =1.85; P =.07) FPCs, or right (t 45 =0.33; P =.74) or left (t 45 =1.89; P =.07) OFCs in the app use and control groups at baseline.
During the treatment period, the app use group showed a greater reduction in accHbO 2 in the right VLPFC ( F 1,44 =8.22; P =.006) and right OFC ( F 1,44 =8.88; P =.005) compared to the control group ( Figure 1 ). During the treatment period, there were no significant differences in the change in accHbO 2 in the other ROIs between the app use and control groups.
Correlations Between the Changes in PDSS Scores and the Changes in accHbO 2
In all participants (ie, the app use group plus the control group), there was a positive correlation between the change in PDSS score and the change in accHbO 2 in the right VLPFC ( r =0.44; P =.002). In the app use group, there was a positive correlation between the change in PDSS score and the changes in accHbO 2 in the right VLPFC ( r =0.42; P =.04). However, in the control group, there was no significant correlation between the change in PDSS score and the change in accHbO 2 in the right VLPFC ( r =0.22; P =.16).
In all participants, there was a positive correlation between the change in PDSS score and the change in accHbO 2 in the right OFC ( r =0.44; P =.002). In both the app use group ( r =0.34; P =.09) and control group ( r =0.33; P =.13), there was no significant correlation between the change in PDSS score and the change in accHbO 2 in the right OFC ( Figure 4 ).

Principal Findings
This study showed that a digital app was effective for symptom reduction, as well as decreasing brain activity in the VLPFCs and OFCs, in patients with panic disorder. In addition, the panic disorder symptom improvement was positively correlated with decreased brain activity in the VLPFCs and OFCs in the resting state.
The digital app used in this trial proved to be effective in reducing panic symptoms when compared to the control group, as demonstrated by the reduction in the PDSS score. We believe that this is due to the combined effect of the 4 parts of the program, namely the diary, education, quest, and serious games. The diary component helps identify and correct faulty perceptions and enables cognitive reconstruction. The education component provides information about the nature and physiology of panic disorder. The breathing game helps the participant return to a relaxed condition, while the exposure therapy game allows the participant to experience agoraphobic situations in a safe environment, which helps cognitive restructuring. These are the important parts of CBT for panic disorder and have shown efficacy, as reported earlier [ 29 - 32 ]. The control group also received educational data, including the importance of keeping a diary of one’s panic symptoms and how to do it, as well as self-guided direction on breathing exercises, but failed to show a significant reduction of symptoms compared to the app use group. We think this is due to lack of proper feedback in the control group. The app shows real-time feedback on breathing exercises using breathing sounds, and a message was sent if the user of the program failed to use the program for more than 2 days. We know that the therapeutic effect is better when immediate feedback is provided to patients undergoing CBT treatment [ 38 ]. Therefore, we think that the decrease in PDSS score was smaller because the control group did not receive feedback from the app.
The control group also received educational data on diary recording, panic disorder information, and how to execute breathing therapy and exposure therapy. We measured their reduction in the PDSS score, but we found it was less than in the app use group due to a lack of proper daily management.
However, the app failed to lead to a difference in the reduction in anxiety, as defined by the HAM-A and GAD-7 scales, between the 2 groups. This is most likely due to a lack of power, as the trial was conducted as a pilot study. Other studies using CBT techniques or serious games have demonstrated reductions in anxiety symptoms in patients with panic disorder [ 14 ]. Likewise, this study showed a trend toward a reduction in anxiety symptoms, although this was not statistically significant, and future research with more participants may show that these kinds of programs are also effective in controlling anxiety.
Two major changes in brain activity were noted in the app use group, namely reductions in VLPFC and OFC activation. The functions of the OFC are varied and include control of inappropriate behavior and emotional responses, decision-making, and solving problems [ 39 , 40 ]. Abnormalities in the function of the OFC can cause problems in dealing with anxiety and show that it is deeply involved in the increasing the sense of fear in the fear response [ 17 ]. The results of this study confirm that OFC activity decreases as treatment progresses. This reinforces the results of a previous study, which showed that patients with panic disorder had increased OFC activity and that when the panic disorder was treated, the activity of the OFC was reduced, as indicated by decreased cerebral glucose metabolic rates [ 17 , 41 ].
The VLPFC is known to be associated with the amygdala and to maintain flexible attention and responses to environmental threats [ 42 , 43 ]. The amygdala is the backbone of the fear network, and the VLPFC is also known to be deeply involved in the processing of fear [ 43 - 45 ]. Several studies have shown increased activity in patients with panic disorder in the inferior frontal gyrus, which envelops the VLPFC, and other related regions, including the prefrontal cortex, hippocampus, and OFC [ 16 , 46 , 47 ]. After panic disorder treatment, such as with CBT, decreased amygdala and inferior frontal gyrus activation in fear situations was confirmed [ 48 , 49 ]. Through panic disorder treatment, inferior frontal gyrus activation decreased to a normal level; this happened because the treatment reduced fear cognition related to harm expectancy or attention to threats [ 49 - 51 ]. We consider that VLPFC activation increases to modulate the amygdala and decreases with treatment for panic disorder.
We believe that these reductions of brain activity in the VLPFC and OFC reflect how the app affected the patients. We know that overprediction of fear or panic is an important feature of anxiety disorders [ 52 ]. The app for panic disorder, including diary, education, quest, and serious game components, allowed users to correct their faulty perceptions about fear. As mentioned earlier, the VLPFC and OFC are related to fear management, so we can expect that activity of the VLPFC and OFC will be reduced through repeated app use as users learn how to deal with fear.
Limitations
This study has the following limitations: Most of the patients were effectively treated with alprazolam or other anxiolytics, such as SSRIs. Thus, treatment with antianxiety drugs may have influenced our results. Moreover, this study assessed changes immediately after app use. A long-term follow-up to evaluate the sustainability of the observed improvements would provide valuable insights into the effectiveness of the intervention over time. App use time could be easily tracked for the app use group; however, it was challenging to independently monitor the time the control group spent reading educational materials. Due to the limitations of available research tools, no investigation has been conducted on deep brain structures such as the amygdala, which is most closely related to panic disorders.
Conclusions
We believe that this app for panic disorder effectively reduces symptoms and noticeably impacts brain activity in specific areas. We observed a positive link between improvement in panic symptoms and decreased brain activity in the VLPFCs and OFCs in a resting state. These findings support the use of targeted interventions to determine the brain’s contribution to symptom relief. Further research should explore the duration of these positive effects and make digital therapy accessible to more individuals, thus unlocking its full potential in mental health care.
Data Availability
The data sets generated and analyzed during this study are not publicly available as they contain information that could compromise the privacy and consent of the research participants. However, the transformed data are available upon reasonable request from the authors.
Conflicts of Interest
None declared.
Digital app for panic disorder.
CONSORT-eHEALTH checklist (V 1.6.1).
- Roy-Byrne PP, Craske MG, Stein MB. Panic disorder. Lancet. Sep 16, 2006;368(9540):1023-1032. [ CrossRef ] [ Medline ]
- Kessler RC, Chiu WT, Jin R, Ruscio AM, Shear K, Walters EE. The epidemiology of panic attacks, panic disorder, and agoraphobia in the National Comorbidity Survey Replication. Arch Gen Psychiatry. Apr 2006;63(4):415-424. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Meuret AE, White KS, Ritz T, Roth WT, Hofmann SG, Brown TA. Panic attack symptom dimensions and their relationship to illness characteristics in panic disorder. J Psychiatr Res. Sep 2006;40(6):520-527. [ CrossRef ] [ Medline ]
- Locke A, Kirst N, Shultz CG. Diagnosis and management of generalized anxiety disorder and panic disorder in adults. Am Fam Physician. May 01, 2015;91(9):617-624. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Bruce SE, Vasile RG, Goisman RM, Salzman C, Spencer M, Machan JT, et al. Are benzodiazepines still the medication of choice for patients with panic disorder with or without agoraphobia? Am J Psychiatry. Aug 2003;160(8):1432-1438. [ CrossRef ] [ Medline ]
- Owen R, Tyrer P. Benzodiazepine dependence. A review of the evidence. Drugs. Apr 1983;25(4):385-398. [ CrossRef ] [ Medline ]
- Cascade E, Kalali AH, Kennedy SH. Real-world data on SSRI antidepressant side effects. Psychiatry (Edgmont). Feb 2009;6(2):16-18. [ FREE Full text ] [ Medline ]
- Breilmann J, Girlanda F, Guaiana G, Barbui C, Cipriani A, Castellazzi M, et al. Benzodiazepines versus placebo for panic disorder in adults. Cochrane Database Syst Rev. Mar 28, 2019;3(3):CD010677. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Schuurmans J, Comijs H, Emmelkamp PMG, Weijnen IJC, van den Hout M, van Dyck R. Long-term effectiveness and prediction of treatment outcome in cognitive behavioral therapy and sertraline for late-life anxiety disorders. Int Psychogeriatr. Dec 2009;21(6):1148-1159. [ CrossRef ] [ Medline ]
- Rufer M, Albrecht R, Schmidt O, Zaum J, Schnyder U, Hand I, et al. Changes in quality of life following cognitive-behavioral group therapy for panic disorder. Eur Psychiatry. Jan 2010;25(1):8-14. [ CrossRef ] [ Medline ]
- Shear MK, Houck P, Greeno C, Masters S. Emotion-focused psychotherapy for patients with panic disorder. Am J Psychiatry. Dec 2001;158(12):1993-1998. [ CrossRef ] [ Medline ]
- Digital health, digital medicine, digital therapeutics (DTx): What’s the difference. HealthXL. Oct 23, 2023. URL: https://www.healthxl.com/blog/digital-health-digital-medicine-digital-therapeutics-dtx-whats-the-difference [accessed 2023-03-19]
- Cho C, Lee H. Could digital therapeutics be a game changer in psychiatry? Psychiatry Investig. Feb 2019;16(2):97-98. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kaplan A, Mannarino AP, Nickell PV. Evaluating the impact of Freespira on panic disorder patients' health outcomes and healthcare costs within the Allegheny Health Network. Appl Psychophysiol Biofeedback. Sep 2020;45(3):175-181. [ CrossRef ] [ Medline ]
- Hoshi Y. Functional near-infrared optical imaging: utility and limitations in human brain mapping. Psychophysiology. Jul 2003;40(4):511-520. [ CrossRef ] [ Medline ]
- Bystritsky A, Pontillo D, Powers M, Sabb FW, Craske MG, Bookheimer SY. Functional MRI changes during panic anticipation and imagery exposure. Neuroreport. Dec 21, 2001;12(18):3953-3957. [ CrossRef ] [ Medline ]
- Milad MR, Rauch SL. The role of the orbitofrontal cortex in anxiety disorders. Ann N Y Acad Sci. Dec 2007;1121(1):546-561. [ CrossRef ] [ Medline ]
- Shear MK, Brown TA, Barlow DH, Money R, Sholomskas DE, Woods SW, et al. Multicenter collaborative Panic Disorder Severity Scale. Am J Psychiatry. Nov 1997;154(11):1571-1575. [ CrossRef ] [ Medline ]
- Lim YJ, Yu BH, Kim JH. Korean Panic Disorder Severity Scale: construct validity by confirmatory factor analysis. Depress Anxiety. 2007;24(2):95-102. [ CrossRef ] [ Medline ]
- Maier W, Buller R, Philipp M, Heuser I. The Hamilton Anxiety Scale: reliability, validity and sensitivity to change in anxiety and depressive disorders. J Affect Disord. 1988;14(1):61-68. [ CrossRef ] [ Medline ]
- Kim CY. Psychiatric Assessment Instruments. Seoul, South Korea. Hana Psychiatric Publishing; 2001;99-101.
- Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. May 22, 2006;166(10):1092-1097. [ CrossRef ] [ Medline ]
- Screener overview. PHQ Screeners. URL: https://www.phqscreeners.com/select-screener [accessed 2024-03-27]
- Choi J, Kim J, Hwang G, Yang J, Choi M, Bae H. Time-divided spread-spectrum code-based 400 fw-detectable multichannel fNIRS IC for portable functional brain imaging. IEEE J Solid-State Circuits. Feb 2016;51(2):484-495. [ FREE Full text ] [ CrossRef ]
- Yamamoto T, Maki A, Kadoya T, Tanikawa Y, Yamad Y, Okada E, et al. Arranging optical fibres for the spatial resolution improvement of topographical images. Phys Med Biol. Sep 21, 2002;47(18):3429-3440. [ CrossRef ] [ Medline ]
- Cui X, Bray S, Bryant DM, Glover GH, Reiss AL. A quantitative comparison of NIRS and fMRI across multiple cognitive tasks. Neuroimage. Feb 14, 2011;54(4):2808-2821. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Miyai I, Tanabe HC, Sase I, Eda H, Oda I, Konishi I, et al. Cortical mapping of gait in humans: a near-infrared spectroscopic topography study. Neuroimage. Nov 2001;14(5):1186-1192. [ CrossRef ] [ Medline ]
- Strangman G, Culver JP, Thompson JH, Boas DA. A quantitative comparison of simultaneous BOLD fMRI and NIRS recordings during functional brain activation. Neuroimage. Oct 2002;17(2):719-731. [ Medline ]
- Barlow DH, Craske MG, Cerny JA, Klosko JS. Behavioral treatment of panic disorder. Behav Ther. 1989;20(2):261-282. [ CrossRef ]
- Clark D, Salkovskis PM, Hackmann A, Wells A, Ludgate J, Gelder M. Brief cognitive therapy for panic disorder: a randomized controlled trial. J Consult Clin Psychol. Aug 1999;67(4):583-589. [ CrossRef ] [ Medline ]
- Telch MJ, Lucas JA, Schmidt NB, Hanna HH, LaNae Jaimez T, Lucas RA. Group cognitive-behavioral treatment of panic disorder. Behav Res Ther. Mar 1993;31(3):279-287. [ CrossRef ] [ Medline ]
- Bouchard S, Gauthier J, Laberge B, French D, Pelletier M, Godbout C. Exposure versus cognitive restructuring in the treatment of panic disorder with agoraphobia. Behav Res Ther. Mar 1996;34(3):213-224. [ CrossRef ] [ Medline ]
- Barlow D, Gorman JM, Shear MK, Woods SW. Cognitive-behavioral therapy, imipramine, or their combination for panic disorder: A randomized controlled trial. JAMA. May 17, 2000;283(19):2529-2536. [ CrossRef ] [ Medline ]
- Gould RA, Ott MW, Pollack MH. A meta-analysis of treatment outcome for panic disorder. Clin Psychol Rev. Jan 1995;15(8):819-844. [ CrossRef ]
- Faretta E. EMDR and cognitive behavioral therapy in the treatment of panic disorder: a comparison. J EMDR Prac Res. Jan 01, 2013;7(3):121-133. [ CrossRef ]
- Goldstein AJ, Feske U. Eye movement desensitization and reprocessing for panic disorder: a case series. J Anxiety Disord. 1994;8(4):351-362. [ CrossRef ]
- Eagleson C, Hayes S, Mathews A, Perman G, Hirsch CR. The power of positive thinking: pathological worry is reduced by thought replacement in generalized anxiety disorder. Behav Res Ther. Mar 2016;78:13-18. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Shapiro JR, Bauer S. Use of short message service (SMS)-based interventions to enhance low intensity CBT. Oxford guide to low intensity CBT interventions. In: Bennett-Levy J, editor. Oxford Guide to Low Intensity CBT Interventions. Oxford, UK. Oxford University Press; 2010;281-286.
- Schoenbaum G, Roesch M. Orbitofrontal cortex, associative learning, and expectancies. Neuron. Sep 01, 2005;47(5):633-636. [ FREE Full text ] [ CrossRef ] [ Medline ]
- O'Doherty J. Can't learn without you: predictive value coding in orbitofrontal cortex requires the basolateral amygdala. Neuron. Aug 28, 2003;39(5):731-733. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Nordahl TE, Stein MB, Benkelfat C, Semple WE, Andreason P, Zametkin A, et al. Regional cerebral metabolic asymmetries replicated in an independent group of patients with panic disorders. Biol Psychiatry. Nov 15, 1998;44(10):998-1006. [ CrossRef ] [ Medline ]
- Monk CS, Nelson EE, McClure EB, Mogg K, Bradley BP, Leibenluft E, et al. Ventrolateral prefrontal cortex activation and attentional bias in response to angry faces in adolescents with generalized anxiety disorder. Am J Psychiatry. Jun 2006;163(6):1091-1097. [ CrossRef ] [ Medline ]
- Hariri AR, Mattay VS, Tessitore A, Fera F, Weinberger DR. Neocortical modulation of the amygdala response to fearful stimuli. Biol Psychiatry. Mar 15, 2003;53(6):494-501. [ CrossRef ] [ Medline ]
- Gorman J, Kent JM, Sullivan GM, Coplan JD. Neuroanatomical hypothesis of panic disorder, revised. Am J Psychiatry. Apr 2000;157(4):493-505. [ CrossRef ] [ Medline ]
- Tian S, Huang F, Gao J, Li P, Ouyang X, Zhou S, et al. Ventrolateral prefrontal cortex is required for fear extinction in a modified delay conditioning paradigm in rats. Neuroscience. Aug 25, 2011;189:258-268. [ CrossRef ] [ Medline ]
- Ball TM, Ramsawh HJ, Campbell-Sills L, Paulus MP, Stein MB. Prefrontal dysfunction during emotion regulation in generalized anxiety and panic disorders. Psychol Med. Jul 2013;43(7):1475-1486. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Dresler T, Hindi Attar C, Spitzer C, Löwe B, Deckert J, Büchel C, et al. Neural correlates of the emotional Stroop task in panic disorder patients: an event-related fMRI study. J Psychiatr Res. Dec 2012;46(12):1627-1634. [ CrossRef ] [ Medline ]
- Beutel M, Stark R, Pan H, Silbersweig D, Dietrich S. Changes of brain activation pre-post short-term psychodynamic inpatient psychotherapy: an fMRI study of panic disorder patients. Psychiatry Res. Nov 30, 2010;184(2):96-104. [ CrossRef ] [ Medline ]
- Kircher T, Arolt V, Jansen A, Pyka M, Reinhardt I, Kellermann T, et al. Effect of cognitive-behavioral therapy on neural correlates of fear conditioning in panic disorder. Biol Psychiatry. Jan 01, 2013;73(1):93-101. [ CrossRef ] [ Medline ]
- Hofmann S. Cognitive processes during fear acquisition and extinction in animals and humans: implications for exposure therapy of anxiety disorders. Clin Psychol Rev. Feb 2008;28(2):199-210. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Bishop SJ. Neural mechanisms underlying selective attention to threat. Ann N Y Acad Sci. 2008;1129(1):141-152. [ CrossRef ] [ Medline ]
- Rachman S. The overprediction of fear: a review. Behav Res Ther. Sep 1994;32(7):683-690. [ CrossRef ] [ Medline ]
Abbreviations
Edited by A Mavragani; submitted 03.08.23; peer-reviewed by M Aksoy; comments to author 01.09.23; revised version received 11.09.23; accepted 08.03.24; published 12.04.24.
©KunJung Kim, Hyunchan Hwang, Sujin Bae, Sun Mi Kim, Doug Hyun Han. Originally published in the Journal of Medical Internet Research (https://www.jmir.org), 12.04.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the Journal of Medical Internet Research, is properly cited. The complete bibliographic information, a link to the original publication on https://www.jmir.org/, as well as this copyright and license information must be included.
Some results uranium dioxide powder structure investigation
- Processes of Obtaining and Properties of Powders
- Published: 28 June 2009
- Volume 50 , pages 281–285, ( 2009 )
Cite this article
- E. I. Andreev 1 ,
- K. V. Glavin 2 ,
- A. V. Ivanov 3 ,
- V. V. Malovik 3 ,
- V. V. Martynov 3 &
- V. S. Panov 2
115 Accesses
7 Citations
Explore all metrics
Features of the macrostructure and microstructure of uranium dioxide powders are considered. Assumptions are made on the mechanisms of the behavior of powders of various natures during pelletizing. Experimental data that reflect the effect of these powders on the quality of fuel pellets, which is evaluated by modern procedures, are presented. To investigate the structure of the powders, modern methods of electron microscopy, helium pycnometry, etc., are used. The presented results indicate the disadvantages of wet methods for obtaining the starting UO 2 powders by the ammonium diuranate (ADU) flow sheet because strong agglomerates and conglomerates, which complicate the process of pelletizing, are formed. The main directions of investigation that can lead to understanding the regularities of formation of the structure of starting UO 2 powders, which will allow one to control the process of their fabrication and stabilize the properties of powders and pellets, are emphasized.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others

Investigation of the Properties of Uranium-Molybdenum Pellet Fuel for VVER
L. A. Karpyuk, V. V. Novikov, … O. A. Bakhteev

Investigation of the Influence of the Energy of Thermal Plasma on the Morphology and Phase Composition of Aluminosilicate Microspheres
V. V. Shekhovtsov
Evaluation of the Possibility of Fabricating Uranium-Molybdenum Fuel for VVER by Powder Metallurgy Methods
A. V. Lysikov, E. N. Mikheev, … D. S. Missorin
Patlazhan, S.A., Poristost’ i mikrostruktura sluchainykh upakovok tverdykh sharov raznykh razmerov (Porosity and Microstructure of Chaotic Packings of Solid Spheres of Different Sizes), Chernogolovka: IKhF RAN, 1993.
Google Scholar
Andreev, E.I., Bocharov, A.S., Ivanov, A.V., et al., Izv. Vyssh. Uchebn. Zaved., Tsvetn. Metall. , 2003, no. 1, p. 48.
Assmann, H., Dörr, W., and Peehs, M., “Control of HO 2 Microstructure by Oxidative Sintering,” J. Nucl. Mater. , 1986, vol. 140,issue 1, pp. 1–6.
Article ADS CAS Google Scholar
Download references
Author information
Authors and affiliations.
Elektrostal’ Polytechnical Institute (Branch), Moscow Institute of Steel and Alloys, ul. Pervomaiskaya 7, Elektrostal’, Moscow oblast, 144000, Russia
E. I. Andreev
Moscow Institute of Steel and Alloys (State Technical University), Leninskii pr. 4, Moscow, 119049, Russia
K. V. Glavin & V. S. Panov
JSC “Mashinostroitelny Zavod”, ul. K. Marksa 12, Elektrostal’, Moscow oblast, 144001, Russia
A. V. Ivanov, V. V. Malovik & V. V. Martynov
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to K. V. Glavin .
Additional information
Original Russian Text © E.I. Andreev, K.V. Glavin, A.V. Ivanov, V.V. Malovik, V.V. Martynov, V.S. Panov, 2009, published in Izvestiya VUZ. Poroshkovaya Metallurgiya i Funktsional’nye Pokrytiya, 2008, No. 4, pp. 19–24.
About this article
Andreev, E.I., Glavin, K.V., Ivanov, A.V. et al. Some results uranium dioxide powder structure investigation. Russ. J. Non-ferrous Metals 50 , 281–285 (2009). https://doi.org/10.3103/S1067821209030183
Download citation
Published : 28 June 2009
Issue Date : June 2009
DOI : https://doi.org/10.3103/S1067821209030183
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- nuclear fuel
- uranium dioxide
- uranium protoxide-oxide
- crystallite
- agglomerate
- conglomerate
- surface morphology
- ADU-ammonium diuranate
- Find a journal
- Publish with us
- Track your research

Turn Your Curiosity Into Discovery
Latest facts.
10 Facts About International Romani Day April 8th
9 Facts About National Cherish An Antique Day April 9th
40 facts about elektrostal.
Written by Lanette Mayes
Modified & Updated: 02 Mar 2024
Reviewed by Jessica Corbett

Elektrostal is a vibrant city located in the Moscow Oblast region of Russia. With a rich history, stunning architecture, and a thriving community, Elektrostal is a city that has much to offer. Whether you are a history buff, nature enthusiast, or simply curious about different cultures, Elektrostal is sure to captivate you.
This article will provide you with 40 fascinating facts about Elektrostal, giving you a better understanding of why this city is worth exploring. From its origins as an industrial hub to its modern-day charm, we will delve into the various aspects that make Elektrostal a unique and must-visit destination.
So, join us as we uncover the hidden treasures of Elektrostal and discover what makes this city a true gem in the heart of Russia.
Key Takeaways:
- Elektrostal, known as the “Motor City of Russia,” is a vibrant and growing city with a rich industrial history, offering diverse cultural experiences and a strong commitment to environmental sustainability.
- With its convenient location near Moscow, Elektrostal provides a picturesque landscape, vibrant nightlife, and a range of recreational activities, making it an ideal destination for residents and visitors alike.
Known as the “Motor City of Russia.”
Elektrostal, a city located in the Moscow Oblast region of Russia, earned the nickname “Motor City” due to its significant involvement in the automotive industry.
Home to the Elektrostal Metallurgical Plant.
Elektrostal is renowned for its metallurgical plant, which has been producing high-quality steel and alloys since its establishment in 1916.
Boasts a rich industrial heritage.
Elektrostal has a long history of industrial development, contributing to the growth and progress of the region.
Founded in 1916.
The city of Elektrostal was founded in 1916 as a result of the construction of the Elektrostal Metallurgical Plant.
Located approximately 50 kilometers east of Moscow.
Elektrostal is situated in close proximity to the Russian capital, making it easily accessible for both residents and visitors.
Known for its vibrant cultural scene.
Elektrostal is home to several cultural institutions, including museums, theaters, and art galleries that showcase the city’s rich artistic heritage.
A popular destination for nature lovers.
Surrounded by picturesque landscapes and forests, Elektrostal offers ample opportunities for outdoor activities such as hiking, camping, and birdwatching.
Hosts the annual Elektrostal City Day celebrations.
Every year, Elektrostal organizes festive events and activities to celebrate its founding, bringing together residents and visitors in a spirit of unity and joy.
Has a population of approximately 160,000 people.
Elektrostal is home to a diverse and vibrant community of around 160,000 residents, contributing to its dynamic atmosphere.
Boasts excellent education facilities.
The city is known for its well-established educational institutions, providing quality education to students of all ages.
A center for scientific research and innovation.
Elektrostal serves as an important hub for scientific research, particularly in the fields of metallurgy, materials science, and engineering.
Surrounded by picturesque lakes.
The city is blessed with numerous beautiful lakes, offering scenic views and recreational opportunities for locals and visitors alike.
Well-connected transportation system.
Elektrostal benefits from an efficient transportation network, including highways, railways, and public transportation options, ensuring convenient travel within and beyond the city.
Famous for its traditional Russian cuisine.
Food enthusiasts can indulge in authentic Russian dishes at numerous restaurants and cafes scattered throughout Elektrostal.
Home to notable architectural landmarks.
Elektrostal boasts impressive architecture, including the Church of the Transfiguration of the Lord and the Elektrostal Palace of Culture.
Offers a wide range of recreational facilities.
Residents and visitors can enjoy various recreational activities, such as sports complexes, swimming pools, and fitness centers, enhancing the overall quality of life.
Provides a high standard of healthcare.
Elektrostal is equipped with modern medical facilities, ensuring residents have access to quality healthcare services.
Home to the Elektrostal History Museum.
The Elektrostal History Museum showcases the city’s fascinating past through exhibitions and displays.
A hub for sports enthusiasts.
Elektrostal is passionate about sports, with numerous stadiums, arenas, and sports clubs offering opportunities for athletes and spectators.
Celebrates diverse cultural festivals.
Throughout the year, Elektrostal hosts a variety of cultural festivals, celebrating different ethnicities, traditions, and art forms.
Electric power played a significant role in its early development.
Elektrostal owes its name and initial growth to the establishment of electric power stations and the utilization of electricity in the industrial sector.
Boasts a thriving economy.
The city’s strong industrial base, coupled with its strategic location near Moscow, has contributed to Elektrostal’s prosperous economic status.
Houses the Elektrostal Drama Theater.
The Elektrostal Drama Theater is a cultural centerpiece, attracting theater enthusiasts from far and wide.
Popular destination for winter sports.
Elektrostal’s proximity to ski resorts and winter sport facilities makes it a favorite destination for skiing, snowboarding, and other winter activities.
Promotes environmental sustainability.
Elektrostal prioritizes environmental protection and sustainability, implementing initiatives to reduce pollution and preserve natural resources.
Home to renowned educational institutions.
Elektrostal is known for its prestigious schools and universities, offering a wide range of academic programs to students.
Committed to cultural preservation.
The city values its cultural heritage and takes active steps to preserve and promote traditional customs, crafts, and arts.
Hosts an annual International Film Festival.
The Elektrostal International Film Festival attracts filmmakers and cinema enthusiasts from around the world, showcasing a diverse range of films.
Encourages entrepreneurship and innovation.
Elektrostal supports aspiring entrepreneurs and fosters a culture of innovation, providing opportunities for startups and business development.
Offers a range of housing options.
Elektrostal provides diverse housing options, including apartments, houses, and residential complexes, catering to different lifestyles and budgets.
Home to notable sports teams.
Elektrostal is proud of its sports legacy, with several successful sports teams competing at regional and national levels.
Boasts a vibrant nightlife scene.
Residents and visitors can enjoy a lively nightlife in Elektrostal, with numerous bars, clubs, and entertainment venues.
Promotes cultural exchange and international relations.
Elektrostal actively engages in international partnerships, cultural exchanges, and diplomatic collaborations to foster global connections.
Surrounded by beautiful nature reserves.
Nearby nature reserves, such as the Barybino Forest and Luchinskoye Lake, offer opportunities for nature enthusiasts to explore and appreciate the region’s biodiversity.
Commemorates historical events.
The city pays tribute to significant historical events through memorials, monuments, and exhibitions, ensuring the preservation of collective memory.
Promotes sports and youth development.
Elektrostal invests in sports infrastructure and programs to encourage youth participation, health, and physical fitness.
Hosts annual cultural and artistic festivals.
Throughout the year, Elektrostal celebrates its cultural diversity through festivals dedicated to music, dance, art, and theater.
Provides a picturesque landscape for photography enthusiasts.
The city’s scenic beauty, architectural landmarks, and natural surroundings make it a paradise for photographers.
Connects to Moscow via a direct train line.
The convenient train connection between Elektrostal and Moscow makes commuting between the two cities effortless.
A city with a bright future.
Elektrostal continues to grow and develop, aiming to become a model city in terms of infrastructure, sustainability, and quality of life for its residents.
In conclusion, Elektrostal is a fascinating city with a rich history and a vibrant present. From its origins as a center of steel production to its modern-day status as a hub for education and industry, Elektrostal has plenty to offer both residents and visitors. With its beautiful parks, cultural attractions, and proximity to Moscow, there is no shortage of things to see and do in this dynamic city. Whether you’re interested in exploring its historical landmarks, enjoying outdoor activities, or immersing yourself in the local culture, Elektrostal has something for everyone. So, next time you find yourself in the Moscow region, don’t miss the opportunity to discover the hidden gems of Elektrostal.
Q: What is the population of Elektrostal?
A: As of the latest data, the population of Elektrostal is approximately XXXX.
Q: How far is Elektrostal from Moscow?
A: Elektrostal is located approximately XX kilometers away from Moscow.
Q: Are there any famous landmarks in Elektrostal?
A: Yes, Elektrostal is home to several notable landmarks, including XXXX and XXXX.
Q: What industries are prominent in Elektrostal?
A: Elektrostal is known for its steel production industry and is also a center for engineering and manufacturing.
Q: Are there any universities or educational institutions in Elektrostal?
A: Yes, Elektrostal is home to XXXX University and several other educational institutions.
Q: What are some popular outdoor activities in Elektrostal?
A: Elektrostal offers several outdoor activities, such as hiking, cycling, and picnicking in its beautiful parks.
Q: Is Elektrostal well-connected in terms of transportation?
A: Yes, Elektrostal has good transportation links, including trains and buses, making it easily accessible from nearby cities.
Q: Are there any annual events or festivals in Elektrostal?
A: Yes, Elektrostal hosts various events and festivals throughout the year, including XXXX and XXXX.
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
Share this Fact:

IMAGES
VIDEO
COMMENTS
Educational Review is a leading research journal for generic educational scholarship. For almost seventy-five years it has offered cutting-edge scholarly analyses of global issues in all phases of education, formal and informal, in order to rethink and shape the future of education. It publishes peer-reviewed papers from international ...
About this journal About. Journal metrics Aims & scope Journal information University information Editorial board News & calls for papers Advertising information; Browse all articles & issues Browse. Latest articles Current issue ... Educational Review, Volume 76, Issue 3 (2024)
The Journal of the European Association for Research on Learning and Instruction (EARLI) Educational Research Review is an international journal addressed to researchers and various agencies interested in the review of studies and theoretical papers in education at any level.The journal accepts high quality articles that are solving educational research problems by using a review approach.
The Review of Educational Research (RER) publishes critical, integrative reviews of research literature bearing on education, including conceptualizations, interpretations, and syntheses of literature and scholarly work in a field broadly relevant to education and educational research. View full journal description.
HER publishes opinion and research pieces from interdisciplinary and wide-ranging fields that advance educational theory, equity, and practice. It is edited by doctoral students from the Harvard Graduate School of Education and has been central to elevating educational justice since 1930.
Review of Education is the only journal outlet for publication of both major studies and substantial reviews in education, and comprehensive Research Syntheses (8,000 to 20,000 words). Review of Education publishes supplementary materials alongside articles, such as video abstracts and teaching resources, allowing you to maximize the impact of ...
The American Educational Research Journal (AERJ) is the flagship journal of AERA, with articles that advance the empirical, theoretical, and methodological understanding of education and learning. It publishes original peer-reviewed analyses spanning the field of education research across all subfields and disciplines and all levels of analysis, all levels of education throughout the life span ...
Review of Research in Education. Review of Research in Education (RRE), published annually, provides a forum for analytic research reviews on selected education topics of significance to the field. Each volume addresses a topic of broad relevance to education and learning, and … | View full journal description.
Review of Educational Research (RER) publishes critical, integrative reviews of research literature bearing on education. Such reviews should include conceptualizations, interpretations, and syntheses of literature and scholarly work in a field. ... For example, if the current year is 2008 and a journal has a 5 year moving wall, articles from ...
The Harvard Educational Review is a scholarly journal of opinion and research in education. It provides an interdisciplinary forum for discussion and debate about the field's most vital issues. Since its founding in 1930, HER has become a prestigious education journal, with circulation to policymakers, researchers, administrators, and teachers.
Educational Review is a leading journal for generic educational research and scholarship. For over seventy years it has offered scholarly analyses of global issues in all phases of education, formal and informal. It publishes peer-reviewed papers from international contributors across a range of education fields and or perspectives including ...
About the Journal. Welcome! Education Review (ISSN: 1094-5296) publishes reviews of recent books in English, Spanish, and Portuguese spanning a wide range of education scholarship and practice across the globe. We also publish autobiographical essays highlighting the acquired wisdom and pedagogical legacies of esteemed educational researchers.
ABOUT THE JOURNAL Frequency: 4 issues/year ISSN: 0010-4086 E-ISSN: 1545-701X 2022 CiteScore*: 2.7 Ranked #526 out of 1,469 "Education" journals. The Comparative Education Review (CER) is the flagship journal of the Comparative and International Education Society.Its editorial team pursues greater critical engagement, interrogation and innovation in the field of comparative and ...
This paper reports a systematic narrative synthesis review conducted on the educational effectiveness of genre theory/systemic functional linguistics pedagogies for improving reading and writing outcomes in K-10 education within mainstream classrooms in Australia, the UK, the USA, New Zealand, and Canada. This framework has significant influence on reading and writing curriculum, teacher ...
About this journal About. Journal metrics Aims & scope Journal information University information Editorial board News & calls for papers ... Browse the list of issues and latest articles from Educational Review. All issues Special issues Collections . Latest articles Partial Access; Volume 76 2024 Volume 75 2023 ...
Correction: Role of AI chatbots in education: systematic literature review. Lasha Labadze 1, Maya Grigolia 2 & Lela Machaidze 3 International Journal of Educational Technology in Higher Education volume 21, Article number: 28 (2024) Cite this article
Impact of the Article. The review should be seen as an important contribution and tool for the many different educators dealing with the educational problems and issues confronting society. 5. Advancement of the Field. The review should validate or inform the knowledge of researchers and guide and improve the quality of their research and ...
Rationale. Post-viral illness occurs when individuals experience an extended period of feeling unwell after a viral infection [1,2,3,4,5,6].While post-viral illness is generally a non-specific condition with a constellation of symptoms that may be experienced, fatigue is amongst the most commonly reported [7,8,9].For example, our recent systematic review found there was up to 94% prevalence of ...
The Clark County School Board approved a tentative $3.4 billion budget for the 2024-25 school year. The tentative budget now will be filed with the State of Nevada for review.
The hemodynamics in the frontal cortex during the resting state were measured via fNIRS. The app had 4 parts: diary, education, quest, and serious games. The study trial was approved by the institutional review board of Chung-Ang University Hospital (1041078-202112-HR-349-01) and written informed consent was obtained from all participants.
Educational Review is a leading research journal for generic educational scholarship. For almost seventy-five years it has offered cutting-edge scholarly analyses of global issues in all phases of education, formal and informal, in order to rethink and shape the future of education. It publishes peer-reviewed papers from international ...
Since the pandemic, which accelerated the shift to a virtual existence, people are moving less than ever, Gibbs said. Just 1 in 4 men and 1 in 5 women and adolescents currently get the recommended amount of aerobic and muscle-strengthening exercise, the federal guidelines say. "We have engineered physical activity out of our lives," Gibbs said.
All journal articles featured in Educational Review vol 76 issue 1. Log in | Register Cart. Home All Journals Educational Review List of Issues Volume 76, Issue 1 ... List of reviewers for Educational Review 2023. Pages: i-iii. Published online: 16 Jan 2024.
Features of the macrostructure and microstructure of uranium dioxide powders are considered. Assumptions are made on the mechanisms of the behavior of powders of various natures during pelletizing. Experimental data that reflect the effect of these powders on the quality of fuel pellets, which is evaluated by modern procedures, are presented. To investigate the structure of the powders, modern ...
Yale University's museum, which recently completed a four-year reconstruction, is now bigger and free to visit—and yet, caught up in the controversies of the field, it's evidently skeptical ...
40 Facts About Elektrostal. Elektrostal is a vibrant city located in the Moscow Oblast region of Russia. With a rich history, stunning architecture, and a thriving community, Elektrostal is a city that has much to offer. Whether you are a history buff, nature enthusiast, or simply curious about different cultures, Elektrostal is sure to ...
Zid Mancenido. Preview abstract. Restricted access Research article First published May 24, 2023 pp. 268-307. xml GET ACCESS. Table of contents for Review of Educational Research, 94, 2, Apr 01, 2024.
In this study, the possibility of sintering industrial pressed uranium dioxide pellets using microwave radiation for the production of nuclear fuel is shown. As a result, the conditions for sintering pellets in an experimental microwave oven (power 2.9 kW, frequency 2.45 GHz) were chosen to ensure that the characteristics of the resulting fuel pellets meet the regulatory requirements for ...
Journal metrics can be a useful tool for readers, as well as for authors who are deciding where to submit their next manuscript for publication. However, any one metric only tells a part of the story of a journal's quality and impact. Each metric has its limitations which means that it should never be considered in isolation, and metrics ...
Energies 2022, 15, 9193 4 of 8 350 to 1600 C at a rate of about 8.0 C/min had visible cracks.For this reason, the two modes shown in Figure2with heating rates of no more than 4.0-5.0 C/min were chosen as working modes. 1XVXXð1W[ð1_W_Y1 Z1 1 _1