Fastest Nurse Insight Engine
- MEDICAL ASSISSTANT
- Abdominal Key
- Anesthesia Key
- Basicmedical Key
- Otolaryngology & Ophthalmology
- Musculoskeletal Key
- Obstetric, Gynecology and Pediatric
- Oncology & Hematology
- Plastic Surgery & Dermatology
- Clinical Dentistry
- Radiology Key
- Thoracic Key
- Veterinary Medicine
- Gold Membership

Case study of a patient with tuberculosis
15 Case study of a patient with tuberculosis Maria Mercer Chapter aims • To provide you with a case study of a patient who has been diagnosed with pulmonary tuberculosis (TB) together with the rationale for care • To encourage you to research and deepen your knowledge of TB Introduction This chapter provides you with an example of the nursing care that a patient with pulmonary TB might require. The case study has been written by a TB nurse specialist and provides you with a patient profile to enable you to understand the context of the patient. The case study aims to guide you through the assessment, nursing action and evaluation of a patient with pulmonary TB together with the rationale for care. Activity In Chapter 1 you were asked to revise the normal anatomy and physiology of the respiratory system (see Montague et al 2005 ) and a brief definition of TB was given. Before reading the case study below, find out how pulmonary TB would affect the respiratory system and what symptoms a patient with TB might present with. The following article may help you: William VG (2006). Tuberculosis: clinical features, diagnosis and management. Nursing Standard 20(22):49–53. Online. Available at: http://nursingstandard.rcnpublishing.co.uk/archive/article-tuberculosis-clinical-features-diagnosis-and-management (accessed July 2011). Patient profile Mr Patel is a 21-year-old gentleman who lives in a shared flat with friends and studies English at a local college. He is a new arrival to the UK having arrived from Bangladesh in October 2009. There are six adults, including Mr Patel, who share a two-bedroom flat. They share three adults to a room. He was referred to accident and emergency (A&E) via his GP with a 2-month history of a productive cough (no episodes of haemoptysis), associated fevers, drenching night sweats, loss of appetite and a 5-kg weight loss. In the last 7 days his symptoms have worsened and warranted the admission via A&E. Assessment on admission Mr Patel has a pyrexia of 38.5°C, he is cachectic and has pleuritic chest pain. His respiratory rate is slightly raised at 18 per minute and he has a tachycardia of 114 beats per minute. Blood pressure is normal. Inflammatory markers – erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) – are raised at 72 mm/h and 65.4 mg/L. A chest X-ray has been reported as abnormal: ‘Patchy shadowing seen in left upper lobe? Pulmonary TB.’ Activity See Appendix 4 in Holland et al ( 2008 ) for possible questions to consider during the assessment stage of care planning. Mr Patel’s problems Based on your assessment of Mr Patel, the following problems should form the basis of your care plan: • Mr Patel has a potential diagnosis of pulmonary TB which can be an infectious disease and public health risk. • Mr Patel feels stigmatised because of respiratory isolation measures and the potential diagnosis of TB. • Mr Patel has a temperature, raised inflammatory markers, a slightly elevated respiratory rate and a tachycardia. • Mr Patel is nutritionally compromised because of a 5-kg weight loss due to anorexia. • Mr Patel has pleuritic chest pain associated with coughing and expectoration of sputum. Mr Patel’s nursing care plans 1. Problem: Mr Patel has an infection. Pulmonary TB is felt to be the primary diagnosis. Goal: To limit transmission of TB to other patients and staff and ensure prompt treatment is commenced. Nursing action Rationale Mr Patel to be isolated in a side room with bathroom facilities with respiratory isolation measures in place immediately The door to the side room must be shut at all times Appropriate face masks (FFP2 or FFP3, depending on risk assessment – refer to infection control/TB policy) should be worn when entering Mr Patel’s room and he should wear the appropriate face mask if he needs to leave the side room for investigations Gloves and aprons do not need to be worn unless handling bodily secretions Liaise with bed managers and infection control team to expedite bed availability as necessary To reduce the risk of TB transmission to other patients and staff Collect three consecutive sputum specimens for acid-fast bacilli (AFB) Send one sputum specimen urgently on day of admission To ascertain diagnosis and ensure the appropriate treatment is commenced promptly Ensure Mr Patel is aware that sputum specimens need to be collected consecutively. Label 3 sputum pots clearly and leave in side room. Instruct Mr Patel to inform the nurse caring for him when the sputum for each day is ready so it can be collected and sent to the Laboratory as soon as possible. To ascertain diagnosis and ensure the appropriate treatment is commenced promptly. Contact the TB nurses to perform a Mantoux test if prescribed by the medical staff. To facilitate prompt diagnosis and obtain specialist nursing advice and support Ensure effective communication with Mr Patel explaining why the above measures are necessary and providing reassurance and support To alleviate fear and anxiety Evaluation:
Share this:
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)
Related posts:
- Medical placements
- Revision and future learning
- The end of the journey
- Medicines management
Stay updated, free articles. Join our Telegram channel
Comments are closed for this page.

Full access? Get Clinical Tree

A case study of a patient with multidrug-resistant tuberculosis
Affiliation.
- 1 Community nurse working in South West England.
- PMID: 30048191
- DOI: 10.12968/bjon.2018.27.14.806
In this case study, a nurse presents her reflections on the challenges of supporting a patient through his treatment journey for multidrug-resistant tuberculosis. The patient has significant comorbidities and social issues, such as diabetes and homelessness. There was also a language barrier. All these aspects made the management of his treatment challenging. The medication side effects and his lifestyle were also a barrier to full engagement. The same multidisciplinary team was involved with the patient and, despite the obstacles, he seemed willing to engage with treatment and the team.
Keywords: Comorbidities; Language barrier; Multidisciplinary team; Multidrug-resistant tuberculosis; Pulmonary TB; Under-served population.
- Alcohol Drinking
- Antitubercular Agents / administration & dosage
- Antitubercular Agents / therapeutic use*
- Communication Barriers
- Diabetes Complications
- Drug Therapy, Combination
- Social Support
- Tuberculosis, Multidrug-Resistant / complications
- Tuberculosis, Multidrug-Resistant / drug therapy*
- Tuberculosis, Multidrug-Resistant / nursing*
- United Kingdom
- Antitubercular Agents
TB Personal Stories
TB is still a life-threatening problem in this country. TB knows no borders, and people here in the United States are suffering from TB. Anyone can get TB. These stories highlight the personal experiences of people who were diagnosed and treated for latent TB infection and TB disease, as well as the work of TB control professionals.
- TB Personal Stories from TB Free California external icon
To receive email updates about this page, enter your email address:
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
- Case report
- Open access
- Published: 19 November 2022
A case report of persistent drug-sensitive pulmonary tuberculosis after treatment completion
- Sergo A. Vashakidze 1 , 2 ,
- Abivarma Chandrakumaran 3 ,
- Merab Japaridze 1 ,
- Giorgi Gogishvili 1 ,
- Jeffrey M. Collins 4 ,
- Manana Rekhviashvili 1 &
- Russell R. Kempker 4
BMC Infectious Diseases volume 22 , Article number: 864 ( 2022 ) Cite this article
5225 Accesses
1 Citations
2 Altmetric
Metrics details
Mycobacterium tuberculosis (Mtb) has been found to persist within cavities in patients who have completed their anti-tuberculosis therapy. The clinical implications of Mtb persistence after therapy include recurrence of disease and destructive changes within the lungs. Data on residual changes in patients who completed anti-tuberculosis therapy are scarce. This case highlights the radiological and pathological changes that persist after anti-tuberculosis therapy completion and the importance of achieving sterilization of cavities in order to prevent these changes.
Case presentation
This is a case report of a 33 year old female with drug-sensitive pulmonary tuberculosis who despite successfully completing standard 6-month treatment had persistent changes in her lungs on radiological imaging. The patient underwent multiple adjunctive surgeries to resect cavitary lesions, which were culture positive for Mtb. After surgical treatment, the patient’s chest radiographies improved, symptoms subsided, and she was given a definition of cure.
Conclusions
Medical therapy alone, in the presence of severe cavitary lung lesions may not be able to achieve sterilizing cure in all cases. Cavities can not only cause reactivation but also drive inflammatory changes and subsequent lung damage leading to airflow obstruction, bronchiectasis, and fibrosis. Surgical removal of these foci of bacilli can be an effective adjunctive treatment necessary for a sterilizing cure and improved long term lung health.
Peer Review reports
Mycobacterium tuberculosis treatment has been evolving over the years, especially with the introduction of newer drugs and shorter regimens [ 1 , 2 ]. Apart from the cavitary nature of tuberculous disease, patients who have been treated with current regimens often are given the designation of cure without achieving proper sterilization. Patients who complete the tuberculous regimen are given the definition of cure after they achieve sputum negativity but many of these patients harbor bacilli within cavities that continue to exert their effects on the respiratory system [ 3 ]. The residual changes that occur in patients who have completed medical therapy have been poorly attended to in the literature. Patients that underwent surgical and medical sterilization have been reported to have better pulmonary health in the long term, especially after the removal of cavities [ 4 ].
Here, we report a patient who underwent a complete regimen of medical therapy for pulmonary tuberculosis and later had to have surgical resection of her cavities, which grew tuberculous bacilli even after achieving sputum negativity.
A 33-year-old female from the country of Georgia presented to a tuberculosis dispensary on July 10, 2020, with a temperature of 38° C and symptoms of malaise, productive cough, and night sweats. The patient had no known medical problems. She reported smoking ~ 10 cigarettes daily and denied alcohol or illicit drug use. She had 3 children and her husband was a prisoner being treated for pulmonary tuberculosis. Upon physical examination there were decreased breath sounds in the upper lobes of the lungs with dullness to percussion. The patient had a body mass index (BMI) of 16.3 kg/m 2 . A complete blood count revealed a moderate leukocytosis of 10.2 × 10 9 /L and an erythrocyte sedimentation rate (ESR) of 42 mm/h. Biochemical blood parameters were normal. Sputum testing found a negative acid-fast bacilli (AFB) microscopy, positive Xpert MTB/RIF test (no RIF resistance), and positive culture for Mycobacterium tuberculosis (Mtb). Additionally, drug susceptibility testing (DST) revealed sensitivity to rifampin, isoniazid, and ethambutol. Chest radiography revealed multiple small foci in the upper lobes of both lungs and a cavity in the right lung (Fig. 1 A). The patient was initiated on daily outpatient treatment with three pills of a fixed dosed combination pill containing isoniazid 75 mg, rifampin 150 mg, ethambutol 275 mg and pyrazinamide 400 mg. Treatment was given through directly observed therapy (DOT). She converted her sputum cultures to negative at 2 months and continued rifampin and isoniazid to finish 6 months of treatment. An end of treatment chest x-ray revealed fibrosis and honeycombing in the right upper lung, and fibrosis and dense focal shadows in the 1st and 2nd intercostal spaces of the left lung (Fig. 1 B). The complete treatment timeline is summarized in Fig. 2 .
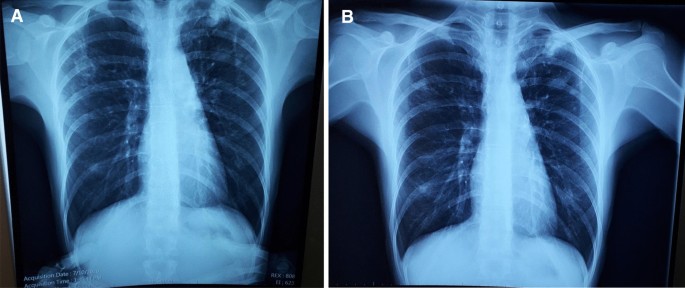
A (left): Baseline chest X-ray showing a cavity in the right lung and multiple foci in the upper lobes of both lungs. B (right): End of initial treatment chest X-ray, showing fibrosis, local honeycombing and dense focal shadows in both lungs
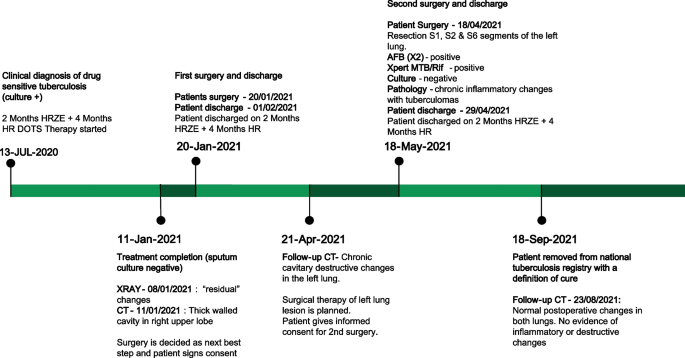
Patient treatment timeline ( HRZE isoniazid, rifampin, pyrazinamide, ethambutol; HR isoniazid & rifampin; DOTS directly observed therapy, short-course; CT computed tomography; AFB acid fast bacilli)
A follow up chest computed tomography (CT) scan demonstrated a cavity in the right upper lobe measuring 12 × 10 mm in size with a thick and heterogeneous wall and nodules and bronchiectasis in the left lung (Fig. 3 A–D). Based on CT findings and in accordance with National tuberculosis guidelines, the patient was offered surgical resection of the affected portion of the lung. It should be noted that the patient reported no symptoms, complaints, or functional disability before the surgery. Preoperative workup including pulmonary function testing, an echocardiogram, bronchoscopy, and blood chemistries were normal. The patient consented to surgery and underwent a surgical resection of the S1 and S2 segments of the right lung 2 weeks later. Intraoperatively, moderate adhesions were visualized in the S1 and S2 area with a palpable dense formation ~ 3.0 cm in diameter, in addition to a dense nodule. Gross pathology of the resected lesion showed a thick-walled fibrous cavity filled with caseous necrosis (Fig. 4 A) corresponding to the right preoperative CT lesion seen on Fig. 3 A, C.
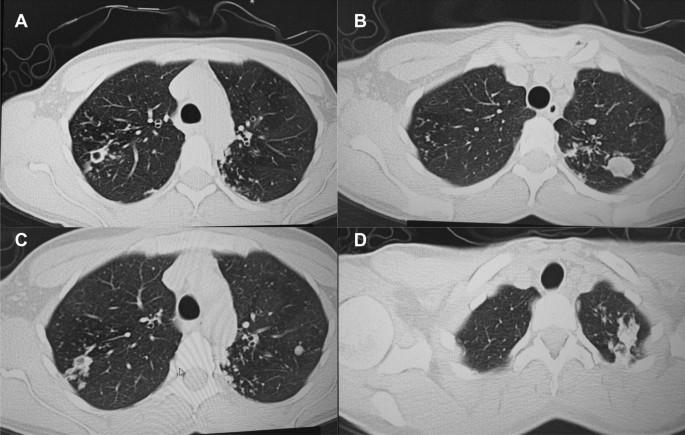
CT scan (January 11, 2021) showing, A a cavity in the upper lobe of the right lung with heterogeneous thick walls. B S1 and S2 segments of the left lung shows a 23 × 18 mm oval shaped calcified inclusions; C , D areas with calcified, compacted nodules 13 × 20 mm in size with additional traction bronchiectasis

A Gross pathological image of a resected cavity with caseous material from first surgery (S1 & S2 segment of right lung). B The gross pathology from the second surgery showed the presence of a blocked cavity measuring up to 2 cm in diameter filled with caseous material in the S1, S2 and C Tuberculoma in S6 segment
Microbiological analysis on the resected tissue revealed acid-fast bacilli on microscopy, and positive Xpert MTB/RIF and culture results. Mtb grew from the caseous center, inner and outer walls of the cavity and a resected foci located ~ 3 cm from the cavity. DST revealed sensitivity to isoniazid, rifampin, and ethambutol.
Pathological examination of the resected lesion showed findings consistent with fibrocavernous tuberculosis. No postoperative complications were experienced, and the patient reinitiated first-line therapy via DOT on the 2nd postoperative day and was discharged on postoperative day 11.
A follow up CT scan performed after 3 months showed postoperative changes in the right upper lobe, and an unchanged left lung (Fig. 5 A–C). Based on the persistent conglomerate of tuberculomas and multiple small tuberculous foci, growth of Mtb from the previous surgical specimen, and the patient’s social situation (mother of three young children) a second surgery to optimize the chance of cure was recommended. The patient reported no symptoms, complaints, or functional disability before the surgery. Preoperative sputum testing found negative AFB smear microscopy and culture. The patient underwent the second operation on May 18, 2021, in which the S1, S2 and part of the S6 segment of the left lung were resected. Intraoperatively, moderate adhesions seen along with a dense palpable ~ 3 cm mass in the S1 and S2 region and a dense focus in S6.
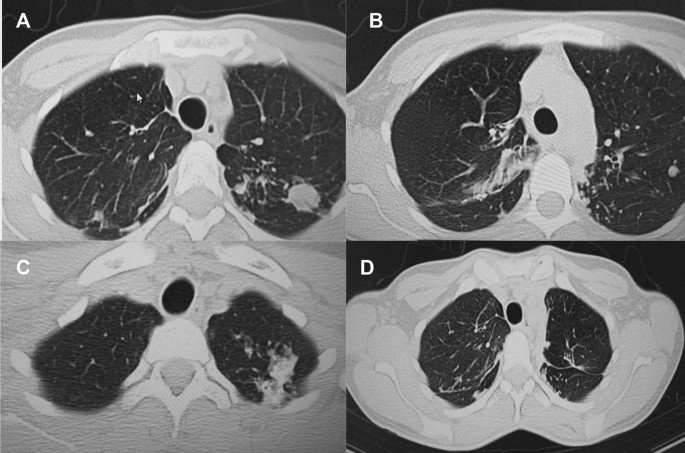
A – C Follow-up CT scan after first adjunctive surgery showing postoperative changes of the right lung and radiological changes in the left lung, that were unchanged compared to the initial CT. D Final CT scan showing normal postoperative changes with no cavities as previously seen
Microbiological examinations performed on resected tissue revealed positive AFB smear microscopy and Xpert MTB/RIF results and a negative AFB culture. The pathological examination of the surgical samples indicated a variety of destructive changes in addition to ongoing inflammation. The gross specimen of S1 and S2 segments of the left lung showed fibrocavernous tuberculosis shown in Fig. 4 B, which corresponds to the left lung lesion seen on the first preoperative CT in Figs. 3 B and 5 A in the second preoperative CT; the gross specimen of the S6 segment showed progressive tuberculoma seen in Fig. 4 C, which corresponds to the left lung lesion seen on the first preoperative CT in Figs. 3 D and 5 C in the second preoperative CT.
There were no postoperative complications, and tuberculosis (TB) treatment was reinitiated. The patient successfully completed treatment with normalization of clinical and laboratory parameters and a clinical outcome of cure in September 2021, ~ 14 months after beginning treatment. The patient had reported near complete resolution of her symptoms, having a much better ability to perform her daily activities. The patient appreciated the effects surgery had on her recovery and was happy to have gone through that treatment route. A post treatment CT scan demonstrated postoperative changes in the upper segments of both lungs (Fig. 5 D). Results from post treatment lung function testing were all within normal range.
Discussion and conclusions
We present this case to highlight the heterogeneous nature of pulmonary tuberculosis and need for an individualized treatment approach, especially for patients with cavitary disease. Over the last decade, novel diagnostics, drugs, and treatment regimens have revolutionized TB management including a recent landmark clinical trial demonstrating an effective 4-month regimen for drug-susceptible TB [ 1 ]. The move towards shorter regimens is critical to improve treatment completion rates and help meet TB elimination goals. However, during a transition to shorter treatment durations it is imperative that clinicians remain aware of complex and severe pulmonary TB cases that may require longer durations of treatment and adjunctive therapies such as surgery. Supporting evidence comes from a recent landmark study finding persistent inflammation on imaging associated with finding Mtb mRNA in sputum after successful treatment and a meta-analysis demonstrating a hard-to-treat TB phenotype not cured with the standard 6 months of treatment [ 2 , 5 ]. However, regarding recommendations for prolonging treatment beyond 6 months for drug-susceptible pulmonary tuberculosis, ATS/CDC/IDSA recommends (expert opinion) extended treatment for persons with cavitary disease and a positive 2 month culture (our patient would not have met this criteria); World Health Organization (WHO) does not recommend extended treatment for any persons with drug-susceptible TB [ 6 , 7 ]. Accumulating evidence demonstrates surgical resection may be an effective adjunctive treatment in cases with cavitary disease [ 8 , 9 , 10 , 11 , 12 ]. Ultimately, a precision medicine approach towards TB will be able to identify patients who would benefit from short course therapy and those who would benefit from longer therapy and adjunctive treatment including surgery [ 13 ].
Mtb has a unique ability and propensity to induce cavities in humans with various studies showing cavitary lesions in ~ 30 to 85% of patients with pulmonary tuberculosis [ 14 ]. Lung cavities are more common in certain groups including patients with diabetes mellitus and undernutrition such as our patient who had a baseline BMI of 16.3 kg/m 2 [ 15 , 16 ]. Their presence indicates more advanced and severe pulmonary disease as evidenced by their association with worse clinical outcomes. Cavitary disease has been associated with higher rates of treatment failure, disease relapse, acquired drug resistance, and long term-term pulmonary morbidity [ 2 , 17 , 18 , 19 ]. The impact of cavitary disease may be more pronounced in drug-resistant disease as shown in an observational study from our group which found a five times higher rate of acquired drug resistance and eight times higher rate of treatment failure among patients multidrug- or extensively drug-resistant cavitary disease compared to those without [ 20 ].
Mtb cavities are characterized by a fibrotic surface with variable vascularization, a lymphocytic cuff at the periphery followed by a cellular layer consisting of primarily macrophages and a necrotic center with foamy apoptotic macrophages and high concentrations of bacteria. Historically, each portion of the TB cavity has been conceptualized as concentric layers of a spherical structure due to its appearance on histologic cross-sections. However, recent studies using more detailed imaging techniques have shown most TB cavities exhibit complex structures with diverse, branching morphologies [ 21 ]. A dysregulated host immune response to Mtb is thought to contribute to the development of lung cavities, which may explain why cavitary lesions are seen less frequently among immunosuppressed patients including people living with Human Immunodeficiency Virus (HIV) [ 14 ]. The center of the TB cavity (caseum) is characterized by accumulation of pro-inflammatory lipid signaling molecules (eicosanoids) and reactive oxygen species, which result in ongoing tissue destruction, but do little to control Mtb replication [ 22 ]. Conversely, the cellular rim and lymphocytic cuff are characterized by a lower abundance of pro-inflammatory lipids and increases in immunosuppressive signals including elevated expression of TGF-beta and indoleamine-2,3-dioxygenase-1 [ 22 ]. The anti-inflammatory milieu within these TB cavity microenvironments impairs effector T cell responses, further limiting control of bacterial replication [ 23 , 24 , 25 ].
The combination of impaired cell-mediated immune responses with accumulation of inflammatory mediators at the rim of the caseum leads to ongoing tissue destruction with the potential for long-term pulmonary sequelae. Many with cavitary tuberculosis suffer chronic obstructive pulmonary disease after successful treatment and the risk may be greater in those with multidrug-resistant disease [ 3 , 4 ]. This has led to research into adjunctive treatment with immune modulator therapies with a goal of mitigating the over-exuberant inflammatory response at the interior edge of the cavity to limit tissue damage. In a recent randomized clinical trial, patients with radiographically severe pulmonary tuberculosis treated with adjunctive everolimus or CC-11050 (phosphodiesterase inhibitor with anti-inflammatory properties) achieved better long-term pulmonary outcomes versus those who received placebo [ 26 ]. Such results suggest the inflammatory response can be modified with appropriate host-directed therapies to improve pulmonary outcomes, particularly in those with cavitary tuberculosis.
Tuberculosis cavities not only hinder an effective immune response, but also prevent anti-tuberculosis drugs from achieving sterilizing concentrations throughout the lesion and especially in necrotic regions. The necrotic center of cavitary lesions is associated with extremely high rates of bacilli (up to 10 9 per milliliter), many of which enter a dormant state with reduced metabolic activity. Bacilli in this dormant state may be less responsive to the host immune response and exhibit phenotypic resistance to some anti-tuberculosis drugs thereby preventing sterilization and increasing chances of relapse [ 14 , 27 , 28 ]. The fact that the specimens from our patient’s second surgery were Xpert and AFB positive, but culture negative may indicate the presence of either dead bacilli or metabolically altered(dormant) bacilli that may be alive, but not culturable by standard techniques. Further, genomic sequencing studies have also found distinct strains of Mtb within different areas of the cavity that have varying drug-susceptibilities demonstrating cavities as a potential incubator for drug resistance [ 27 , 29 ].
Emerging literature has started to elucidate the varying abilities of drugs to penetrate into cavitary lesions and the importance of adequate target site concentrations. One notable study found that decreasing tissue concentrations within resected cavitary TB lesions were associated with increasing drug phenotypic MIC values [ 30 ]. Innovative studies using MALDI mass spectrometry imaging have further demonstrated varied spatiotemporal penetration of anti-TB drugs in human TB cavities [ 31 ]. This study found rifampin accumulated within caseum, moxifloxacin preferentially at the cellular rim, and pyrazinamide throughout the lesion, demonstrating the need to consider drug penetration when designing drug regimens in patients with cavitary TB. Computational modeling studies have further demonstrated the importance of complete lesion drug coverage to ensure relapse-free cure [ 32 ]. Furthermore, clinical trials are now incorporating these principles into study design by (1) using radiological characteristics to determine treatment length and (2) incorporating tissue penetration into drug selection and regimen design [ 33 , 34 ]. Beyond tissue penetration, varying drug levels and rapid INH acetylation status can also lead to suboptimal pharmacokinetics and poor clinical outcomes [ 35 , 36 ]. As highlighted in a recent expert document, clinical standards to optimize and individualize dosing need to be developed to improve outcomes [ 37 ].
Available literature points to a benefit of adjunctive surgical resection particularly among patients with drug resistant tuberculosis. A meta-analysis of 24 comparative studies found surgical intervention was associated with favorable treatment outcomes among patients with drug-resistant TB (odds ratio 2.24, 95% CI 1.68–2.97) [ 38 ]. Additionally, an individual patient data meta-analysis found that partial lung resection (adjusted OR 3.9, 95% CI 1.5–5.9) but not pneumectomy was associated with treatment success [ 39 ]. In two observational studies, we have also found that adjunctive surgical resection was associated with high and improved outcomes compared to patients with cavitary disease not undergoing surgery and was associated with less reentry into TB care. It should be noted that all studies of surgical resection for pulmonary TB were observational studies, which may be subject to selection bias, and no clinical trials (very difficult to implement in practice) were conducted to provide more conclusive evidence. Based on available evidence, the WHO has provided guidance to consider surgery among certain hard to treat cases of both drug-susceptible and resistant cavitary disease [ 40 ]. Criteria for surgical intervention included (1) failure of medical therapy (persistent sputum culture positive for M. tuberculosis ), (2) a high likelihood of treatment failure or disease relapse, (3) complications from the disease, (4) localized cavitary lesion, and (5) sufficient pulmonary function to tolerate surgery. For our patient, the severity of disease, lack of improvement of radiological imaging despite appropriate treatment, and high risk of relapse were the main indicators for surgery. Contraindications for surgery included a forced expiratory volume (FEV1) < 1000 mL, severe malnutrition, or patients at high risk for perioperative cardiovascular complications. With strict adherence to indications and contraindications for surgery, an acceptable level of postoperative complications are noted (5–17%) [ 4 , 38 ]. Our results also demonstrate the safety of adjunctive surgery, as our post-operative complication rate (8%) was low with the majority being minor complications [ 41 ].
As our case highlights, patients with persistent cavitary disease at the end of treatment require close clinical follow up and a tailored, individualized plan to determine the best approach for disease elimination and cure. In certain cases, including those with persistent cavitary disease and end of treatment, and where available, surgical resection is an effective adjunctive treatment option that can reduce disease burden and aid anti-tuberculosis agents in providing a sterilizing cure. As we enter an era of welcomed new shorter treatment options for tuberculosis it is imperative for clinicians to be able to identify and recognize complicated TB cases that require prolonged treatment and potentially adjunctive surgery.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Abbreviations
Acid fast bacilli
American Thoracic Society
Body mass index
Center for Disease Control
Computed tomography
Directly observed therapy
Drug sensitive tuberculosis
Erythrocyte sedimentation rate
Human Immunodeficiency Virus
Infectious Diseases Society of America
Mycobacterium tuberculosis
- Tuberculosis
World Health Organization
Dorman S, Nahid P, Kurbatova E, Phillips P, Bryant K, Dooley K, et al. Four-month rifapentine regimens with or without moxifloxacin for tuberculosis. N Engl J Med. 2021;384(18):1705–18.
Article PubMed PubMed Central CAS Google Scholar
Imperial M, Nahid P, Phillips P, Davies G, Fielding K, Hanna D, et al. A patient-level pooled analysis of treatment-shortening regimens for drug-susceptible pulmonary tuberculosis. Nat Med. 2018;24(11):1708–15.
Vashakidze S, Kempker J, Jakobia N, Gogishvili S, Nikolaishvili K, Goginashvili L, et al. Pulmonary function and respiratory health after successful treatment of drug-resistant tuberculosis. Int J Infect Dis. 2019;82:66–72.
Article PubMed PubMed Central Google Scholar
Harris RC, Khan MS, Martin LJ, et al. The effect of surgery on the outcome of treatment for multidrug-resistant tuberculosis: a systematic review and meta-analysis. BMC Infect Dis. 2016;16:262.
Malherbe S, Shenai S, Ronacher K, Loxton A, Dolganov G, Kriel M, et al. Persisting positron emission tomography lesion activity and Mycobacterium tuberculosis mRNA after tuberculosis cure. Nat Med. 2016;22(10):1094–100.
Nahid P, Dorman S, Alipanah N, Barry P, Brozek J, Cattamanchi A, et al. Official American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America clinical practice guidelines: treatment of drug-susceptible tuberculosis. Clin Infect Dis. 2016;63(7):e147–95.
World Health Organization. The WHO consolidated guidelines on tuberculosis, module 4: treatment—drug-susceptible tuberculosis treatment. Geneva: WHO; 2022.
Google Scholar
Kang M, Kim H, Choi Y, Kim K, Shim Y, Koh W, et al. Surgical treatment for multidrug-resistant and extensive drug-resistant tuberculosis. Ann Thorac Surg. 2010;89(5):1597–602.
Article PubMed Google Scholar
Pomerantz B, Cleveland J, Olson H, Pomerantz M. Pulmonary resection for multi-drug resistant tuberculosis. J Thorac Cardiovasc Surg. 2001;121(3):448–53.
Article PubMed CAS Google Scholar
Somocurcio J, Sotomayor A, Shin S, Portilla S, Valcarcel M, Guerra D, et al. Surgery for patients with drug-resistant tuberculosis: report of 121 cases receiving community-based treatment in Lima, Peru. Thorax. 2007;62(5):416–21.
Dravniece G, Cain K, Holtz T, Riekstina V, Leimane V, Zaleskis R. Adjunctive resectional lung surgery for extensively drug-resistant tuberculosis. Eur Respir J. 2009;34(1):180–3.
Wang H, Lin H, Jiang G. Pulmonary resection in the treatment of multidrug-resistant tuberculosis: a retrospective study of 56 cases. Ann Thorac Surg. 2008;86(5):1640–5.
Lange C, Aarnoutse R, Chesov D, van Crevel R, Gillespie S, Grobbel H, et al. Perspective for precision medicine for tuberculosis. Front Immunol. 2020. https://doi.org/10.3389/fimmu.2020.566608 .
Urbanowski M, Ordonez A, Ruiz-Bedoya C, Jain S, Bishai W. Cavitary tuberculosis: the gateway of disease transmission. Lancet Infect Dis. 2020;20(6):e117–28.
Zafar M, Chen L, Xiaofeng Y, Gao F. Impact of diabetes mellitus on radiological presentation of pulmonary tuberculosis in otherwise non-immunocompromised patients: a systematic review. Curr Med Imaging Rev. 2019;15(6):543–54.
Sinha P, Bhargava A, Carwile M, Cintron C, Cegielski J, Lönnroth K, et al. Undernutrition can no longer be an afterthought for global efforts to eliminate TB. Int J Tuberc Lung Dis. 2022;26(6):477–80.
Cegielski J, Dalton T, Yagui M, Wattanaamornkiet W, Volchenkov G, Via L, et al. Extensive drug resistance acquired during treatment of multidrug-resistant tuberculosis. Clin Infect Dis. 2014;59(8):1049–63.
Gao J, Ma Y, Du J, Zhu G, Tan S, Fu Y, et al. Later emergence of acquired drug resistance and its effect on treatment outcome in patients treated with Standard Short-Course Chemotherapy for tuberculosis. BMC Pulm Med. 2016. https://doi.org/10.1186/s12890-016-0187-3 .
Shin S, Keshavjee S, Gelmanova I, Atwood S, Franke M, Mishustin S, et al. Development of extensively drug-resistant tuberculosis during multidrug-resistant tuberculosis treatment. Am J Respir Crit Care Med. 2010;182(3):426–32.
Kempker R, Kipiani M, Mirtskhulava V, Tukvadze N, Magee M, Blumberg H. Acquired drug resistance in Mycobacterium tuberculosis and poor outcomes among patients with multidrug-resistant tuberculosis. Emerg Infect Dis. 2015;21(6):992–1001.
Wells G, Glasgow J, Nargan K, Lumamba K, Madansein R, Maharaj K, et al. Micro-computed tomography analysis of the human tuberculous lung reveals remarkable heterogeneity in three-dimensional granuloma morphology. Am J Respir Crit Care Med. 2021;204(5):583–95.
Marakalala M, Raju R, Sharma K, Zhang Y, Eugenin E, Prideaux B, et al. Inflammatory signaling in human tuberculosis granulomas is spatially organized. Nat Med. 2016;22(5):531–8.
McCaffrey E, Donato M, Keren L, Chen Z, Delmastro A, Fitzpatrick M, et al. The immunoregulatory landscape of human tuberculosis granulomas. Nat Immunol. 2022;23(2):318–29.
Gern B, Adams K, Plumlee C, Stoltzfus C, Shehata L, Moguche A, et al. TGFβ restricts expansion, survival, and function of T cells within the tuberculous granuloma. Cell Host Microbe. 2021;29(4):594-606.e6.
Gautam U, Foreman T, Bucsan A, Veatch A, Alvarez X, Adekambi T, et al. In vivo inhibition of tryptophan catabolism reorganizes the tuberculoma and augments immune-mediated control of Mycobacterium tuberculosis. Proc Natl Acad Sci USA. 2017. https://doi.org/10.1073/pnas.1711373114 .
Wallis R, Ginindza S, Beattie T, Arjun N, Likoti M, Edward V, et al. Adjunctive host-directed therapies for pulmonary tuberculosis: a prospective, open-label, phase 2, randomised controlled trial. Lancet Respir Med. 2021;9(8):897–908.
Kaplan G, Post F, Moreira A, Wainwright H, Kreiswirth B, Tanverdi M, et al. Mycobacterium tuberculosis growth at the cavity surface: a microenvironment with failed immunity. Infect Immun. 2003;71(12):7099–108.
Fattorini L, Piccaro G, Mustazzolu A, Giannoni F. Targeting dormant bacilli to fight tuberculosis. Mediterr J Hematol Infect Dis. 2013;5(1):e2013072.
Moreno-Molina M, Shubladze N, Khurtsilava I, Avaliani Z, Bablishvili N, Torres-Puente M, et al. Genomic analyses of Mycobacterium tuberculosis from human lung resections reveal a high frequency of polyclonal infections. Nat Commun. 2021;12(1):2716.
Dheda K, Lenders L, Magombedze G, Srivastava S, Raj P, Arning E, et al. Drug-penetration gradients associated with acquired drug resistance in patients with tuberculosis. Am J Respir Crit Care Med. 2018;198(9):1208–19.
Prideaux B, Via L, Zimmerman M, Eum S, Sarathy J, O’Brien P, et al. The association between sterilizing activity and drug distribution into tuberculosis lesions. Nat Med. 2015;21(10):1223–7.
Strydom N, Gupta S, Fox W, Via L, Bang H, Lee M, et al. Tuberculosis drugs’ distribution and emergence of resistance in patient’s lung lesions: a mechanistic model and tool for regimen and dose optimization. PLoS Med. 2019;16(4): e1002773.
Chen R, Via L, Dodd L, Walzl G, Malherbe S, Loxton A, et al. Using biomarkers to predict TB treatment duration (predict TB): a prospective, randomized, noninferiority, treatment shortening clinical trial. Gates Open Res. 2017;1:9.
Bartelink I, Zhang N, Keizer R, Strydom N, Converse P, Dooley K, et al. New paradigm for translational modeling to predict long-term tuberculosis treatment response. Clin Transl Sci. 2017;10(5):366–79.
Pasipanodya J, Srivastava S, Gumbo T. Meta-analysis of clinical studies supports the pharmacokinetic variability hypothesis for acquired drug resistance and failure of antituberculosis therapy. Clin Infect Dis. 2012;55(2):169–77.
Colangeli R, Jedrey H, Kim S, Connell R, Ma S, Chippada Venkata U, et al. Bacterial factors that predict relapse after tuberculosis therapy. N Engl J Med. 2018;379(9):823–33.
Alffenaar J, Stocker S, Forsman L, Garcia-Prats A, Heysell S, Aarnoutse R, et al. Clinical standards for the dosing and management of TB drugs. Int J Tuberc Lung Dis. 2022;26(6):483–99.
Marrone M, Venkataramanan V, Goodman M, Hill A, Jereb J, Mase S. Surgical interventions for drug-resistant tuberculosis: a systematic review and meta-analysis [review article]. Int J Tuberc Lung Dis. 2013;17(1):6–16.
Fox G, Mitnick C, Benedetti A, Chan E, Becerra M, Chiang C, et al. Surgery as an adjunctive treatment for multidrug-resistant tuberculosis: an individual patient data metaanalysis. Clin Infect Dis. 2016;62(7):887–95.
Word Health Organization Europe. The role of surgery in the treatment of pulmonary TB and multidrug and extensively drug-resistant TB. Copenhagen: WHO Regional Office for Europe; 2014.
Vashakidze SA, Gogishvili SG, Nikolaishvili KG, et al. Adjunctive surgery versus medical treatment among patients with cavitary multidrug-resistant tuberculosis. Eur J Cardiothorac Surg. 2021;60(6):1279–85. https://doi.org/10.1093/ejcts/ezab337 .
Download references
Acknowledgements
The authors thank the physicians, nurses, and staff at the NCTLD in Tbilisi, Georgia, who provided care for the patient described in this report. Additionally, the authors are thankful for the patient with pulmonary tuberculosis who was willing to have their course of illness presented and help contribute meaningful data that may help future patients with the same illness.
This study did not receive any specific funding.
Author information
Authors and affiliations.
Thoracic Surgery Department, National Center for Tuberculosis and Lung Diseases, 50 Maruashvili, 0101, Tbilisi, Georgia
Sergo A. Vashakidze, Merab Japaridze, Giorgi Gogishvili & Manana Rekhviashvili
The University of Georgia, Tbilisi, Georgia
Sergo A. Vashakidze
Tbilisi State Medical University, Tbilisi, Georgia
Abivarma Chandrakumaran
Division of Infectious Diseases, Department of Medicine, Emory University School of Medicine, Atlanta, GA, USA
Jeffrey M. Collins & Russell R. Kempker
You can also search for this author in PubMed Google Scholar
Contributions
SAV: Conceptualization; Data collection and interpretation; Scientific Writing including initial draft preparation and manuscript revision and editing. AC: Data interpretation; Table and Figure preparation; Literature review; Scientific Writing including initial draft preparation and manuscript revision and editing. MJ: Data collection; Scientific Writing including manuscript review and editing. GG: Data collection; Scientific Writing including manuscript review and editing. JMC: Data interpretation; Scientific Writing including manuscript review and editing. MR: Data interpretation; Scientific Writing including manuscript review and editing. RRK: Conceptualization; Literature review; Scientific Writing including manuscript review and editing. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Sergo A. Vashakidze .
Ethics declarations
Ethics approval and consent to participate.
The authors confirm that written informed consent has been obtained from the patient involved in the case report. Ethics approval is not needed for case reports according to our institutional (National Center for Tuberculosis and Lung Disease) review board.
Consent for publication
The authors confirm that written consent has been obtained from the patient for publication of images.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Vashakidze, S.A., Chandrakumaran, A., Japaridze, M. et al. A case report of persistent drug-sensitive pulmonary tuberculosis after treatment completion. BMC Infect Dis 22 , 864 (2022). https://doi.org/10.1186/s12879-022-07836-y
Download citation
Received : 08 August 2022
Accepted : 02 November 2022
Published : 19 November 2022
DOI : https://doi.org/10.1186/s12879-022-07836-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Thoracic surgery
BMC Infectious Diseases
ISSN: 1471-2334
- Submission enquiries: [email protected]
- General enquiries: [email protected]
We have a new app!
Take the Access library with you wherever you go—easy access to books, videos, images, podcasts, personalized features, and more.
Download the Access App here: iOS and Android . Learn more here!
- Remote Access
- Save figures into PowerPoint
- Download tables as PDFs

34: Tuberculosis
David Cluck
- Download Chapter PDF
Disclaimer: These citations have been automatically generated based on the information we have and it may not be 100% accurate. Please consult the latest official manual style if you have any questions regarding the format accuracy.
Download citation file:
- Search Book
Jump to a Section
Patient presentation.
- Full Chapter
- Supplementary Content
Chief Complaint
“I have a cough that won’t go away.”
History of Present Illness
A 63-year-old male presents to the emergency department with complaints of cough/shortness of breath which he attributes to a “nagging cold.” He states he fears this may be something worse after experiencing hemoptysis for the past 3 days. He also admits to waking up in the middle of the night “drenched in sweat” for the past few weeks. When asked, the patient denies ever having a positive PPD and was last screened “several years ago.” His chart indicates he was in the emergency department last week with similar symptoms and was diagnosed with community-acquired pneumonia and discharged with azithromycin.
Past Medical History
Hypertension, dyslipidemia, COPD, atrial fibrillation, generalized anxiety disorder
Surgical History
Appendectomy at age 18
Family History
Father passed away from a myocardial infarction 4 years ago; mother had type 2 DM and passed away from a ruptured abdominal aortic aneurysm
Social History
Retired geologist recently moved from India to live with his son who is currently in medical school in upstate New York. Smoked ½ ppd × 40 years and drinks 6 to 8 beers per day, recently admits to drinking ½ pint of vodka “every few days” since the passing of his wife 6 months ago.
Sulfa (hives); penicillin (nausea/vomiting); shellfish (itching)
Home Medications
Albuterol metered-dose-inhaler 2 puffs q4h PRN shortness of breath
Aspirin 81 mg PO daily
Atorvastatin 40 mg PO daily
Budesonide/formoterol 160 mcg/4.5 mcg 2 inhalations BID
Clonazepam 0.5 mg PO three times daily PRN anxiety
Lisinopril 20 mg PO daily
Metoprolol succinate 100 mg PO daily
Tiotropium 2 inhalations once daily
Venlafaxine 150 mg PO daily
Warfarin 7.5 mg PO daily
Physical Examination
Vital signs.
Temp 100.8°F, P 96, RR 24 breaths per minute, BP 150/84 mm Hg, pO 2 92%, Ht 5′10″, Wt 56.4 kg
Slightly disheveled male in mild-to-moderate distress
Normocephalic, atraumatic, PERRLA, EOMI, pale/dry mucous membranes and conjunctiva, poor dentition
Bronchial breath sounds in RUL
Cardiovascular
NSR, no m/r/g
Soft, non-distended, non-tender, (+) bowel sounds
Genitourinary
Sign in or create a free Access profile below to access even more exclusive content.
With an Access profile, you can save and manage favorites from your personal dashboard, complete case quizzes, review Q&A, and take these feature on the go with our Access app.
Pop-up div Successfully Displayed
This div only appears when the trigger link is hovered over. Otherwise it is hidden from view.
Please Wait
Case Report: Pulmonary tuberculosis and raised transaminases without pre-existing liver disease- Do we need to modify the antitubercular therapy?
Sanjeev Gautam Roles: Data Curation, Writing – Original Draft Preparation Keshav Raj Sigdel Roles: Conceptualization, Supervision, Writing – Review & Editing Sudeep Adhikari Roles: Writing – Original Draft Preparation, Writing – Review & Editing Buddha Basnyat Roles: Conceptualization, Supervision, Writing – Review & Editing Buddhi Paudyal Roles: Supervision, Writing – Review & Editing Jiwan Poudel Roles: Writing – Review & Editing Ujjwol Risal Roles: Writing – Review & Editing
This article is included in the Oxford University Clinical Research Unit (OUCRU) gateway.
tuberculosis, transaminitis, standard ATT, liver friendly regimen
Revised Amendments from Version 1
The changes have been made in the revised manuscript as suggested by the reviewers. The concerns of reviewers regarding limited workup of the patient for liver disease has been addressed in the manuscript. This is a single case report and further studies are required to make a firm recommendation for management of pulmonary tuberculosis with transaminitis without pre-existing liver disease. We have acknowledged the fact in the revised manuscript.
See the authors' detailed response to the review by Vivek Neelakantan See the authors' detailed response to the review by Neesha Rockwood See the authors' detailed response to the review by Prajowl Shrestha and Ashesh Dhungana
Tuberculosis is the biggest infectious disease killer in the world 1 , and is endemic in Nepal with the national prevalence at 416 cases per 100000 population 2 . Pulmonary tuberculosis is the most common form. In Nepal, tuberculosis prevalence is more in productive age group (25–64 years) and men. Poverty, malnutrition, overcrowding, immunocompromised state like HIV infection, alcohol, smoking, air pollution, diabetes and other comorbidities are important risk factors for acquiring the disease 3 . Though under-reported, involvement of liver with tuberculosis is encountered often in clinical practice in endemic areas like Nepal.Liver can be involved; a) diffusely as a part of disseminated miliary tuberculosis or as primary miliary tuberculosis of liver, or b) focal involvement as hepatic tuberculoma or abscess, as was classified by Reed in 1990 4 . The biochemical pattern of liver function abnormality in these forms of extrapulmonary tuberculosis is cholestatic (predominantly raised alkaline phosphatase and gamma-glutamyltranspeptidase) rather than hepatocellular (predominantly raised transaminases) 5 , 6 . The hepatocellular pattern of liver injury is seen in cases with pre-existing liver disease including hepatotoxic drug use, which are unrelated to tuberculosis 7 , 8 .
As per national protocol of Nepal, any patient with tuberculosis receives combination antitubercular therapy (ATT) including four drugs; Isoniazid (H), Rifampicin (R), Pyrazinamide (Z) and Ethambutol (E) for initial 2 months popularly known as HRZE. This is followed by 4 months of two drugs; HR. Treatment is given under Directly Observed Treatment Short- Course (DOTS) to improve the patient compliance which could otherwise be compromised owing to lower socioeconomic status of patients, longer duration of treatment and side effects 9 . Patients with extrapulmonary hepatic tuberculosis are treated with full dose of standard ATT 5 , 6 . But three out of the four drugs (H, R and Z) are hepatotoxic 7 . So the patients having pre-existing liver disease usually require liver-friendly modified regimens to protect the liver but they may be suboptimal for eradicating underlying tuberculosis 8 . The protocol of Nepal does not warrant baseline investigations except chest X-ray and sputum smear microscopy to be done routinely before prescribing ATT in programmatic setting 9 . However in hospital setting like our case, baseline blood investigations including liver function tests are usually done before starting treatment even in absence of features suggesting liver injury and therapy modified accordingly.
Here we present a case of pulmonary tuberculosis with predominant transaminitis but there was no feature of pre-existing liver disease nor a history of hepatotoxic drug use. The liver injury was attributed to the pulmonary tuberculosis itself, and treated with standard first line ATT which led to resolution of liver function abnormalities.
Case presentation
A 33 year old Newar housewife from Kathmandu, Nepal, with no known comorbidity, presented to Patan Hospital Emergency Department in November, 2019 with a history of cough with occasional sputum production over the previous 20 days and low grade fever for 10 days. There was no history of chest pain, difficulty breathing, headache, vomiting, altered mentation, abdominal pain, yellowish discoloration of eyes, burning urine, hair loss, photosensitivity, joint pain, or rash but she had decreased appetite and weight loss. There was no past history of tuberculosis or jaundice. She did not consume alcohol or any drugs including acetaminophen, aflatoxin or herbal products. Her father-in-law had been diagnosed with pulmonary tuberculosis five years earlier, but there was no family history of liver disease.
Initial examination showed temperature of 101 o F with pulse of 110 beats/minute and respiratory rate of 26 breaths/minute. There was diffuse fine crepitation on the left side on auscultation of the chest. There was no lymphadenopathy, icterus, peripheral edema or wheezes. Neck veins were not distended. Liver and spleen were not palpable, and abdomen examination was normal.
Laboratory parameters with normal ranges in parenthesis are as follow:
Complete blood count before transfusion: white cell count 7.8 (4–10) × 10 9 /L; neutrophils 80%; lymphocytes 16%; monocytes 4%; red blood cells 3.6 (4.2–5.4) × 10 12 /L; haemoglobin 10.6 (12–15) g/dL; platelets 410 (150–400) × 10 9 /L.
Biochemistry: random blood sugar 126 (65–110) mg/dL; urea 39 (17–45) mg/dL; creatinine 1.1 (0.8–1.3) mg/dL; sodium 138 (135–145) mmol/L and potassium 4 (3.5–5) mmol/L.
Chest X-ray ( Figure 1 ) showed thick walled cavitating lesions in the left upper lobe and patchy infiltrates in left middle and lower zones. There were hyperinflated lung fields with blunting of left costophrenic angle. Sputum smear examination showed 3+ acid fast bacilli. Sputum Gene Xpert was positive for Rifampicin sensitive tubercle bacilli. A diagnosis of pulmonary tuberculosis was made, and planned for starting ATT.
Figure 1. Chest X-ray showing thick walled cavitating lesions in the left upper lobe and patchy infiltrates in left middle and lower zones.
Liver function test was performed as baseline workup before starting treatment which showed the following results (with normal ranges in parenthesis): bilirubin total 1.1 (0.1–1.2) mg/dL and direct 0.5 (0–0.4) mg/dL; alanine transaminase 308 (5–30) units/L; aspartate transaminase 605 (5–30) units/L; alkaline phosphatase 149 (50–100) IU/L; gamma-glutamyltranspeptidase66 (9–48) units/L. The raised transaminases led us to perform further workup for liver disease. There was no clinical evidence of chronic liver disease or portal hypertension. Liver synthetic functions were as following;albumin 3.5 (3.5–5) g/dL; total protein 6.5 (6–8.3) g/dL; prothrombin time 14 (11–13.5) s. Serologies for HIV, HBsAg, Hepatitis C virus (HCV), Hepatitis A virus (HAV) and Hepatitis E virus (HEV) were nonreactive. Testing for other hepatotropic viruses was not done because of unavailability of the tests. Neurological examinations and the slit lamp examination of eye were normal. Ultrasound of the abdomen showed a normal sized liver with smooth outline and echotexture. However fibroscan, upper gastrointestinal endoscopy, abdominal CT scan and liver biopsy were not done due to financial constraints of the patient.
She was admitted to the respiratory isolation unit. At first there was some hesitation in starting the full treatment for her pulmonary tuberculosis because of her liver function tests. But taking into consideration her presentation and laboratory findings, we opted for the full treatment rather than a modified TB regimen. We started standard four drugs ATT based on her weight as per national TB guidelines which included three tablets of HRZE given once daily with each tablet containing 75 mg isoniazid (H), 150 mg rifampicin (R), 400 mg pyrazinamide (Z) and 275 mg ethambutol (E). This led to improvement in her clinical status. She was closely observed for possible worsening of her liver disease due to the hepatotoxic antitubercular drugs. Providentially, at 1 week after starting treatment, she was afebrile and continuing to improve and her liver function test showed a total bilirubin of 0.7 mg/dl, aspartate transaminase of 40 IU/L and alanine transaminase of 62 IU/L.
She was discharged with advice to follow up in 1 month. At 1 month follow up she had no symptoms and therefore no further tests were done. At 2 months, she was still asymptomatic and her sputum smear was negative for acid fast bacilli. Her liver function test showed a total bilirubin of 0.6 mg/dl, aspartate transaminase of 30 IU/L and alanine transaminase of 35 IU/L. She was switched to3 tablets of HR to be taken for 4 months.
Our patient with pulmonary tuberculosis had predominantly raised transaminases (hepatocellular pattern)during the initial presentation, with only modest elevation in alkaline phosphatase and gamma glutamyltranspeptidase. The workup for liver disease could not be performed completely because of resource limitation. Looking for clinical evidences by history and examination, and performing liver function tests, abdominal ultrasound and serology for common hepatotropic viruses are usually considered sufficient in our limited setup. We perform further tests only if the initial workup hints towards another etiology. There were no clinical features of chronic liver disease or portal hypertension. She had no risk factors for liver disease such as family history, alcohol, drugs, toxins, features suggesting autoimmune or metabolic liver diseases. Her viral hepatitis serologies were negative. Ultrasound also showed normal liver architecture and size.Though incomplete, the initial workup led us to believe that she had no pre-existing liver injury.
Patients with extrapulmonary hepatic tuberculosis as classified by Reed (diffuse or focal)usually present withnonspecific symptoms like abdominal pain, jaundice, fever, night sweats, fatigue, weight loss and hepatomegaly. They havecholestatic pattern of liver function abnormality with normal transaminases, increased protein- albumin gap owing to raised serum globulin. Hepatic imaging with ultrasound or CT scan reveal abnormalities in 76 and 88% cases respectively. Liver biopsy and demonstration of caseating granuloma and mycobacterial culture remain gold standard for diagnosing hepatic tuberculosis 4 – 6 . Following points in our patient precluded making the diagnosis of hepatic tuberculosis; a) absence of abdominal symptoms and hepatomegaly; b) predominantly raised transaminases (hepatocellular pattern) and normal protein- albumin gap; and c) normal ultrasound finding (though CT and biopsy were not done).
There is another classification schema, given by Levine in 1990 which has incorporated additional entity under hepatic tuberculosis which is ‘pulmonary tuberculosis withliver involvement’ 10 . In the absence of obvious pre-existing liver disease or drug and the presence of active cavitary tuberculosis in lungs, we attributed the transaminitisin our patient to the pulmonary tuberculosis itself. In our anecdotal experience, we have found many such patients though we do not have any formal data to back this up. They are often managed with modified liver-friendly antitubercular regimens for fear of increasing the hepatotoxicity and causing acute liver failure with the use of standard regimen. Few case reports are available in literature reporting the use of the modified regimens 11 , 12 . We believe such cases are underreported, and firm guidelines have not been established to guide clinicians in these cases. Given this, many clinicians in low-middle income countries, including Nepal, who have been treating tuberculosis patients tend to be skeptical in using full doses of first line ATT in such patients and tend to use a modified regimen. However, this practice may potentially lead to under-treatment and therefore increase fatality 13 . The use of modified regimen may also increase the risk of developing drug-resistant tuberculosis because of exclusion of more potent drugs 14 . Though there was some hesitation at first in our case, we soon started treatment with the standard ATT in our patient with close monitoring. This we believe led to the resolution of liver injury, evidenced by the normalization of transaminases.
However, acknowledging that the patient may develop drug induced liver injury (DILI) with the hepatotoxic antitubercular drugs, we should monitorsuch patients closely in an inpatient basis to look forclinical deterioration or any feature suggesting liver failureand liver function test repeated regularly. Though there is no firm recommendation for when to repeat the tests, patient should not be discharged till there is significant improvement in the transaminases level. The close monitoring is important in those with higher risks for developing DILI associated with ATT such as elderly, females, alcohol consumers, the malnourished and those with genetic susceptibility like slow acetylators 7 . Such monitoring is even more important in our setup because there are possibilities of missing occult hepatic diseases owing tolimited workup.Our patient had improving transaminases evidenced till 2 months follow up.
Though limited by incomplete investigations, we concluded pulmonary tuberculosis as the cause for transaminitis in our patient, and the normalization of transaminases after starting the standard dose of ATT further supports this conclusion. We believe pulmonary TB presenting with transaminitis is a common problem and that treatment may often be compromised because of decreased dosing of ATT.We further aim to perform case series study to explore the magnitude of problem and reach specific conclusions.
When treating a tuberculosis patient with transaminitis, it is important to look for any possibility of pre-existing liver disease or drug use. If none is found, then the use of standard ATT from the beginning with close inpatient monitoring of the patient may be essential for optimal management of tuberculosis, and this may help resolve any liver injury caused by the tuberculosis. This is a single case report, so further case series or cohort studies would be helpful to reach some conclusion and provide concrete recommendations.
Written informed consent for publication of their clinical details and clinical images was obtained from the patient.
Data availability
Underlying data.
All data underlying the results are available as part of the article and no additional source data are required.
- 1. https://www.who.int/news-room/fact-sheets/detail/tuberculosis . .
- 2. https://nepalntp.gov.np/wp-content/uploads/2020/03/NEPAL-NATIONAL-TB-PREVALENCE-SURVEY-BRIEF-March-24-2020.pdf . .
- 3. https://nepalntp.gov.np/wp-content/uploads/2020/04/NTP-Annual-Report-2075-76-2018-19.pdf .
- 4. Reed DH, Nash AF, Valabhji P: Radiological diagnosis and management of a solitary tuberculous hepatic abscess. Br J Radiol. 1990; 63 (755): 902–4. PubMed Abstract | Publisher Full Text
- 5. Hickey AJ, Gounder L, Moosa MY, et al. : A systematic review of hepatic tuberculosis with considerations in human immunodeficiency virus co-infection. BMC Infect Dis. 2015; 15 : 209. PubMed Abstract | Publisher Full Text | Free Full Text
- 6. Wu Z, Wang WL, Zhu Y, et al. : Diagnosis and treatment of hepatic tuberculosis: report of five cases and review of literature. Int J Clin Exp Med. 2013; 6 (9): 845–50. PubMed Abstract | Free Full Text
- 7. Ramappa V, Aithal GP: Hepatotoxicity related to anti-tuberculosis drugs: mechanisms and management. J Clin Exp Hepatol. 2013; 3 (1): 37–49. PubMed Abstract | Publisher Full Text | Free Full Text
- 8. Sonika U, Kar P: Tuberculosis and liver disease: management issues. Trop Gastroenterol. 2012; 33 (2): 102–6. PubMed Abstract | Publisher Full Text
- 9. https://nepalntp.gov.np/wp-content/uploads/2019/10/National-Tuberculosis-Management-Guidelines-2019_Nepal.pdf . .
- 10. Levine C: Primary macronodular hepatic tuberculosis: US and CT appearances. Gastrointest Radiol. 1990; 15 (4): 307–9. PubMed Abstract | Publisher Full Text
- 11. Sanchez-Codez M, Hunt WG, Watson J, et al. : Hepatitis in children with tuberculosis: a case report and review of the literature. BMC Pulm Med. 2020; 20 (1): 173. PubMed Abstract | Publisher Full Text | Free Full Text
- 12. Shastri M, Kausadikar S, Jariwala J, et al. : Isolated hepatic tuberculosis: An uncommon presentation of a common culprit. Australas Med J. 2014; 7 (6): 247–50. PubMed Abstract | Publisher Full Text | Free Full Text
- 13. Essop AR, Posen JA, Hodkinson JH, et al. : Tuberculosis hepatitis: a clinical review of 96 cases. Q J Med. 1984; 53 (212): 465–77. PubMed Abstract
- 14. Kumar N, Kedarisetty CK, Kumar S, et al. : Antitubercular therapy in patients with cirrhosis: challenges and options. World J Gastroenterol. 2014; 20 (19): 5760–72. PubMed Abstract | Publisher Full Text | Free Full Text
Comments on this article Comments (0)
Open peer review.
Competing Interests: No competing interests were disclosed.
Reviewer Expertise: Tuberculosis, Interventional Pulmonology, ILD
- Respond or Comment
- COMMENT ON THIS REPORT
Reviewer Expertise: History of Tuberculosis, Global Health, South and Southeast Asia, Medical Humanities
Is the background of the case’s history and progression described in sufficient detail?
Are enough details provided of any physical examination and diagnostic tests, treatment given and outcomes?
Is sufficient discussion included of the importance of the findings and their relevance to future understanding of disease processes, diagnosis or treatment?
Is the case presented with sufficient detail to be useful for other practitioners?
Reviewer Expertise: Management of HIV/tuberculosis; PK/PD for tuberculosis
- Author Response 16 Oct 2020 Sudeep Adhikari , Internal Medicine, Patan Academy of Health Sciences, Lalitpur, Nepal 16 Oct 2020 Author Response We would like to whole-heartedly thank you for spending so much time and effort to improve our manuscript. Here below is the point by point response. The title needs to convey that ... Continue reading We would like to whole-heartedly thank you for spending so much time and effort to improve our manuscript. Here below is the point by point response. The title needs to convey that this is new onset transaminitis attributed to tuberculosis prior to commencement of anti tubercular therapy Response: Title has been modified. Thank you Background Please outline the baseline work up for TB in programmatic setting in Nepal. Do all patients have baseline LFTs done? Response: Programmatic setting does not require any baseline workup except sputum smear and in chest Xray. But in hospital setting, we perform baseline blood investigations like blood counts, renal function, electrolytes and liver function tests before starting treatment, so that treatment can be modified accordingly. Changes have been made in the background section. Case presentation Has this patient had normal LFTs recorded prior to current TB presentation? Response: No prior LFT testing was done by the patient Mention drug history incl. paracetamol, aflatoxin exposure, family history of liver disease. Text has been modified to state the fact. Thank you The liver screen is incomplete - e.g. autoimmune and inherited liver disease, paracetamol levels, ferritin, occult hep B. Also liver fibrosis assessment. Baseline GGT and clotting needs to be given. Please give a table of ALT, AST, GGT, Alk phos, Albumin and clotting during first 2 weeks of treatment (and any further tests during 6 months of treatment) Of note, there is no clear evidence of disseminated miliary TB on CXR. Abdominal or liver CT was not done. Hence, no comment can be made regarding liver/splenic micronodular abscesses. It appears no mycobacterial blood cultures were taken to assess for bacteraemia. Nor was a liver biopsy done. All relevant negatives and limitations should be mentioned. Response: The liver disease screen is incomplete as the reviewer pointed out. However, because of resource limitation and financial constraints, it is not usually possible to perform full liver disease screening in Nepal. So we usually opt for limited screen, and rely more on history, physical examination and initial limited investigations. Then we perform further tests only if the initial workup hints towards another etiology. Text has been modified to include investigations and other limitations. When was she discharged? Response: She was discharged after 1 week after becoming afebrile and improvement in transaminases. Considering she was never symptomatic from the point of view of GI/hepatobiliary system, was there no further blood work to monitor LFTs since discharge? Response: LFT was repeated first at 1 week before discharge, then at 2 months follow up after discharge. Discussion: Briefly explain classifications of liver TB e.g. Reed, Alvarez, Levine. The authors do not clearly say what clinical, biochemical, radiological and histopathological presentation would be seen with disseminated TB involving liver. This case does not clearly illustrate steps to confirm a transaminitis secondary disseminated miliary TB. Response: Text has been modified to include further discussion. Thank you The implications of this case report would have greater impact and relevance for practitioners in the context of a case series or retrospective cohort and the authors should consider doing this. Response: Yes we hope further case reports and case series would be published in future, and we look forward to do case series and we have included this notion in the ms. Thank you. Further discussion is needed of considerations such as potentiated toxicity with pharmacogenomic factors e.g. slow acetylators, the need for individualized monitoring e.g. therapeutic drug monitoring. Response: Further discussion has been added. Unfortunately such therapeutic drug monitoring is not widely available in Nepal. How long should these patients have monitoring of their LFTs? Is there are risk of paradoxical reactions? Unlike Drug induced liver injury, there is no specific monitoring protocols for patients described in our case. The monitoring should be done till the deranged tests normalize and patient becomes clinically well. We have not encountered paradoxical reactions so far. We would like to whole-heartedly thank you for spending so much time and effort to improve our manuscript. Here below is the point by point response. The title needs to convey that this is new onset transaminitis attributed to tuberculosis prior to commencement of anti tubercular therapy Response: Title has been modified. Thank you Background Please outline the baseline work up for TB in programmatic setting in Nepal. Do all patients have baseline LFTs done? Response: Programmatic setting does not require any baseline workup except sputum smear and in chest Xray. But in hospital setting, we perform baseline blood investigations like blood counts, renal function, electrolytes and liver function tests before starting treatment, so that treatment can be modified accordingly. Changes have been made in the background section. Case presentation Has this patient had normal LFTs recorded prior to current TB presentation? Response: No prior LFT testing was done by the patient Mention drug history incl. paracetamol, aflatoxin exposure, family history of liver disease. Text has been modified to state the fact. Thank you The liver screen is incomplete - e.g. autoimmune and inherited liver disease, paracetamol levels, ferritin, occult hep B. Also liver fibrosis assessment. Baseline GGT and clotting needs to be given. Please give a table of ALT, AST, GGT, Alk phos, Albumin and clotting during first 2 weeks of treatment (and any further tests during 6 months of treatment) Of note, there is no clear evidence of disseminated miliary TB on CXR. Abdominal or liver CT was not done. Hence, no comment can be made regarding liver/splenic micronodular abscesses. It appears no mycobacterial blood cultures were taken to assess for bacteraemia. Nor was a liver biopsy done. All relevant negatives and limitations should be mentioned. Response: The liver disease screen is incomplete as the reviewer pointed out. However, because of resource limitation and financial constraints, it is not usually possible to perform full liver disease screening in Nepal. So we usually opt for limited screen, and rely more on history, physical examination and initial limited investigations. Then we perform further tests only if the initial workup hints towards another etiology. Text has been modified to include investigations and other limitations. When was she discharged? Response: She was discharged after 1 week after becoming afebrile and improvement in transaminases. Considering she was never symptomatic from the point of view of GI/hepatobiliary system, was there no further blood work to monitor LFTs since discharge? Response: LFT was repeated first at 1 week before discharge, then at 2 months follow up after discharge. Discussion: Briefly explain classifications of liver TB e.g. Reed, Alvarez, Levine. The authors do not clearly say what clinical, biochemical, radiological and histopathological presentation would be seen with disseminated TB involving liver. This case does not clearly illustrate steps to confirm a transaminitis secondary disseminated miliary TB. Response: Text has been modified to include further discussion. Thank you The implications of this case report would have greater impact and relevance for practitioners in the context of a case series or retrospective cohort and the authors should consider doing this. Response: Yes we hope further case reports and case series would be published in future, and we look forward to do case series and we have included this notion in the ms. Thank you. Further discussion is needed of considerations such as potentiated toxicity with pharmacogenomic factors e.g. slow acetylators, the need for individualized monitoring e.g. therapeutic drug monitoring. Response: Further discussion has been added. Unfortunately such therapeutic drug monitoring is not widely available in Nepal. How long should these patients have monitoring of their LFTs? Is there are risk of paradoxical reactions? Unlike Drug induced liver injury, there is no specific monitoring protocols for patients described in our case. The monitoring should be done till the deranged tests normalize and patient becomes clinically well. We have not encountered paradoxical reactions so far. Competing Interests: none Close Report a concern Reply -->
- The authors describe a patient with pulmonary tuberculosis and raised liver enzymes (Transaminases). They do mention that the patient did not have any preexisting liver disease or drug use, but do not mention how they systematically ruled out other causes of tansaminitis (other non A-E viral hepatitis like GBV, Hep G, EBV,TT virus and other tropical infections).
- “In this report, we gave full dose standard antitubercular drugs, and the liver injury resolved evidenced by normalization of transaminases”. The authors should make their message more clear to “presence of transamnitis with no obvious common underlying etiology may not warrant a modification of standard antitubercular regimen”
- Evaluation of patient: Diagnostic work-up is incomplete and should also include evaluation for degree of hepatocellular injury. Prothrombin time is not mentioned, GGT levels not mentioned, Serum globulin levels not mentioned (hepatic TB has inverted albumin to globulin ration), imaging was limited (only USG performed, CT not done), liver biopsy not performed. More investigations should have been performed to rule out underlying chronic liver diseases: Fibroscan, upper GI endoscopy for Portal HTN)
- Figure 1: The quality of the image is suboptimal. The entire bony cage is not visible. Right costophrenic angle is not visible. Finding of hyperinflated lung fields and blunting of left CP angle are not described. Did the patient have underlying obstructive airway disease? If so did she also have pulmonary hypertension?. Could hepatic congestion due to RHF explain the raised liver enzymes?
- Follow up: The patient improved significantly at 1 month follow up. It would be desirable to have a complete follow up of the patient with evaluation of liver enzymes at least once during treatment as patient initially also did not have any liver specific symptoms.
- The authors argue that the patient did not have underlying liver disease or liver involvement due to tuberculosis as there was no features of Granuloma and cholestatic pattern of liver enzyme elevation. To ascribe the transamnitis to be caused by TB would be an arbitrary statement especially in the absence of liver biopsy.
- The authors mention that they have found many patients of pulmonary TB to have predominant transamnitis and without any preexisting liver disease in their experience. Such statement is not backed by any formal data.
- The authors conclude that pulmonary TB was the cause of transamnitis in their patient, not hepatic TB or underlying liver disease. In the absence of complete workup, such strong conclusions should not be made.
- Author Response 16 Oct 2020 Sudeep Adhikari , Internal Medicine, Patan Academy of Health Sciences, Lalitpur, Nepal 16 Oct 2020 Author Response We would like to whole-heartedly thank you for spending so much time and effort to improve our manuscript. Here below is the point by point response. Title: The title ... Continue reading We would like to whole-heartedly thank you for spending so much time and effort to improve our manuscript. Here below is the point by point response. Title: The title is unclear as to whether the transaminitis in the index patient is caused by tuberculosis (as proposed by the authors in the subsequent report) or a consequence of other coexisting condition. The title needs to be rephrased as to impart a message that the authors want to convey Response: Title has been modified to make our message clearer. Thank you Abstract: The authors describe a patient with pulmonary tuberculosis and raised liver enzymes (Transaminases). They do mention that the patient did not have any preexisting liver disease or drug use, but do not mention how they systematically ruled out other causes of tansaminitis (other non A-E viral hepatitis like GBV, Hep G, EBV,TT virus and other tropical infections). ○ References: DOI: 10.5812/hepatmon.188651; Alter HJ, Bradley DW. Non-A, non-B hepatitis unrelated to the hepatitis C virus (non ABC) Semin Liver Dis 1995; 15:110-1202; Current Opinion in Infectious Diseases: October 2002 - Volume 15 - Issue 5 - p 529-5343. Testing of other viruses were not done due to unavailability.Since raised transaminases resolved after starting ATT we assumed tuberculosis was most likely explanation. “In this report, we gave full dose standard antitubercular drugs, and the liver injury resolved evidenced by normalization of transaminases”. The authors should make their message more clear to “presence of transaminitis with no obvious common underlying etiology may not warrant a modification of standard antitubercular regimen” Response: Text has been modified to make our message clearer. Thank you Case report Evaluation of patient: Diagnostic work-up is incomplete and should also include evaluation for degree of hepatocellular injury. Prothrombin time is not mentioned, GGT levels not mentioned, Serum globulin levels not mentioned (hepatic TB has inverted albumin to globulin ration), imaging was limited (only USG performed, CT not done), liver biopsy not performed. More investigations should have been performed to rule out underlying chronic liver diseases: Fibroscan, upper GI endoscopy for Portal HTN) Response: The liver disease screen is incomplete as the reviewers pointed out. However, because of resource limitation and financial constraints, it is not usually possible to perform full liver disease screening in Nepal. So we usually opt for limited screen, and rely more on history, physical examination and initial limited investigations. Then we perform further tests only if the initial workup hints towards another etiology. Text has been modified to include further lab reports. The limitations have been acknowledged. Figure 1: The quality of the image is suboptimal. The entire bony cage is not visible. Right costophrenic angle is not visible. Finding of hyperinflated lung fields and blunting of left CP angle are not described. Did the patient have underlying obstructive airway disease? If so did she also have pulmonary hypertension?. Could hepatic congestion due to RHF explain the raised liver enzymes? Response: There was no history of underlying lung disease. Although echocardiography was not done hepatic congestion due to RHF is unlikely as there was no suggestive history and examination findings and patient responded without any diuretics or fluid restrictions. Follow up: The patient improved significantly at 1 month follow up. It would be desirable to have a complete follow up of the patient with evaluation of liver enzymes at least once during treatment as patient initially also did not have any liver specific symptoms. Response: Text has been modified to include follow up reports. LFT was repeated first at 1 week before discharge, then at 2 months follow up after discharge. Discussion: The authors argue that the patient did not have underlying liver disease or liver involvement due to tuberculosis as there was no features of Granuloma and cholestatic pattern of liver enzyme elevation. To ascribe the transaminitis to be caused by TB would be an arbitrary statement especially in the absence of liver biopsy. Response: Imaging and further investigations were limited, so hepatic tuberculosis could not be ruled out with certainty especially without biopsy of liver. However this would not make much difference. Because even if the diagnosis of hepatic tuberculosis had been considered in our patient, the management would be the same, i.e. with standard ATT as we did in our patient. The point we wanted to make here is that modification in treatment may not be required in the absence of pre-existing liver disease. Text has been modified to include the limitations. Thank you The authors mention that they have found many patients of pulmonary TB to have predominant transaminitis and without any preexisting liver disease in their experience. Such statement is not backed by any formal data. Response: We need more data but unfortunately not much is being published from low middle income countries even for endemic diseases like tuberculosis. There is no formal data to back up our claim, and this has been acknowledged as limitation. The authors conclude that pulmonary TB was the cause of transaminitis in their patient, not hepatic TB or underlying liver disease. In the absence of complete workup, such strong conclusions should not be made. Response: Due to rapid resolution of raised transaminases after starting ATT, preexisting liver disease would be unlikely cause. Although hepatic tb is a possibility, it was our opinion that standard dose ATT can be safely started in the patient and further imaging would not be cost effective in terms of treatment. We agree with the reviewer that the strong conclusions are not justified due to incomplete workup and this section has been toned down and modified to highlight the limitations. Thank you Conclusion The authors recommend use of full dose standard ATT for patients with transaminitis and no underlying liver disease. This recommendation should not be made based on a single case report. Response: We agree. Text have been modified to include our limitations. Thank you. Opinion: The case report describes a common scenario especially in low income countries while treating patients with tuberculosis. The availability of resources limit the diagnostic workup of such patients in our settings. I opine that this case report is suitable for indexing with modifications. Response: Thank you We would like to whole-heartedly thank you for spending so much time and effort to improve our manuscript. Here below is the point by point response. Title: The title is unclear as to whether the transaminitis in the index patient is caused by tuberculosis (as proposed by the authors in the subsequent report) or a consequence of other coexisting condition. The title needs to be rephrased as to impart a message that the authors want to convey Response: Title has been modified to make our message clearer. Thank you Abstract: The authors describe a patient with pulmonary tuberculosis and raised liver enzymes (Transaminases). They do mention that the patient did not have any preexisting liver disease or drug use, but do not mention how they systematically ruled out other causes of tansaminitis (other non A-E viral hepatitis like GBV, Hep G, EBV,TT virus and other tropical infections). ○ References: DOI: 10.5812/hepatmon.188651; Alter HJ, Bradley DW. Non-A, non-B hepatitis unrelated to the hepatitis C virus (non ABC) Semin Liver Dis 1995; 15:110-1202; Current Opinion in Infectious Diseases: October 2002 - Volume 15 - Issue 5 - p 529-5343. Testing of other viruses were not done due to unavailability.Since raised transaminases resolved after starting ATT we assumed tuberculosis was most likely explanation. “In this report, we gave full dose standard antitubercular drugs, and the liver injury resolved evidenced by normalization of transaminases”. The authors should make their message more clear to “presence of transaminitis with no obvious common underlying etiology may not warrant a modification of standard antitubercular regimen” Response: Text has been modified to make our message clearer. Thank you Case report Evaluation of patient: Diagnostic work-up is incomplete and should also include evaluation for degree of hepatocellular injury. Prothrombin time is not mentioned, GGT levels not mentioned, Serum globulin levels not mentioned (hepatic TB has inverted albumin to globulin ration), imaging was limited (only USG performed, CT not done), liver biopsy not performed. More investigations should have been performed to rule out underlying chronic liver diseases: Fibroscan, upper GI endoscopy for Portal HTN) Response: The liver disease screen is incomplete as the reviewers pointed out. However, because of resource limitation and financial constraints, it is not usually possible to perform full liver disease screening in Nepal. So we usually opt for limited screen, and rely more on history, physical examination and initial limited investigations. Then we perform further tests only if the initial workup hints towards another etiology. Text has been modified to include further lab reports. The limitations have been acknowledged. Figure 1: The quality of the image is suboptimal. The entire bony cage is not visible. Right costophrenic angle is not visible. Finding of hyperinflated lung fields and blunting of left CP angle are not described. Did the patient have underlying obstructive airway disease? If so did she also have pulmonary hypertension?. Could hepatic congestion due to RHF explain the raised liver enzymes? Response: There was no history of underlying lung disease. Although echocardiography was not done hepatic congestion due to RHF is unlikely as there was no suggestive history and examination findings and patient responded without any diuretics or fluid restrictions. Follow up: The patient improved significantly at 1 month follow up. It would be desirable to have a complete follow up of the patient with evaluation of liver enzymes at least once during treatment as patient initially also did not have any liver specific symptoms. Response: Text has been modified to include follow up reports. LFT was repeated first at 1 week before discharge, then at 2 months follow up after discharge. Discussion: The authors argue that the patient did not have underlying liver disease or liver involvement due to tuberculosis as there was no features of Granuloma and cholestatic pattern of liver enzyme elevation. To ascribe the transaminitis to be caused by TB would be an arbitrary statement especially in the absence of liver biopsy. Response: Imaging and further investigations were limited, so hepatic tuberculosis could not be ruled out with certainty especially without biopsy of liver. However this would not make much difference. Because even if the diagnosis of hepatic tuberculosis had been considered in our patient, the management would be the same, i.e. with standard ATT as we did in our patient. The point we wanted to make here is that modification in treatment may not be required in the absence of pre-existing liver disease. Text has been modified to include the limitations. Thank you The authors mention that they have found many patients of pulmonary TB to have predominant transaminitis and without any preexisting liver disease in their experience. Such statement is not backed by any formal data. Response: We need more data but unfortunately not much is being published from low middle income countries even for endemic diseases like tuberculosis. There is no formal data to back up our claim, and this has been acknowledged as limitation. The authors conclude that pulmonary TB was the cause of transaminitis in their patient, not hepatic TB or underlying liver disease. In the absence of complete workup, such strong conclusions should not be made. Response: Due to rapid resolution of raised transaminases after starting ATT, preexisting liver disease would be unlikely cause. Although hepatic tb is a possibility, it was our opinion that standard dose ATT can be safely started in the patient and further imaging would not be cost effective in terms of treatment. We agree with the reviewer that the strong conclusions are not justified due to incomplete workup and this section has been toned down and modified to highlight the limitations. Thank you Conclusion The authors recommend use of full dose standard ATT for patients with transaminitis and no underlying liver disease. This recommendation should not be made based on a single case report. Response: We agree. Text have been modified to include our limitations. Thank you. Opinion: The case report describes a common scenario especially in low income countries while treating patients with tuberculosis. The availability of resources limit the diagnostic workup of such patients in our settings. I opine that this case report is suitable for indexing with modifications. Response: Thank you Competing Interests: none Close Report a concern Reply -->
- Author Response 16 Oct 2020 Sudeep Adhikari , Internal Medicine, Patan Academy of Health Sciences, Lalitpur, Nepal 16 Oct 2020 Author Response We would like to whole-heartedly thank you for spending so much time and effort to improve our manuscript. Here below is the point by point response. Title: ... Continue reading We would like to whole-heartedly thank you for spending so much time and effort to improve our manuscript. Here below is the point by point response. Title: Drug-resistant TB is a hot topic in medicine today. Research on TB treatment-associated transaminitis would further the existing scholarly understanding on drug-resistant TB. A close keyword search on PubMed revealed only 17 hit on TB AND transaminitis. For this reason, the case report is potentially publishable but suffers from several drawbacks in its current draft that must be remedied before the contribution is re-refereed. But the title itself is unclear. “With” is repeated twice. It is not clear to a medical historian what transaminitis is. A better framing of the title is urgently needed. A cogent argument can be organised around the title. What is four-drugs therapy? It is clear to medical practitioners but not clear to the larger scholarly community. Avoid jargons in the title. 1) What is transaminitis? Why not provide a brief explanation at the start so that the general reader can follow the rest of the article. 2) The two levels of transaminitis: (a) pre-existing liver disease leads to transaminitis. (b) Hepatoxicity of anti-TB drugs. This needs to be made explicit in the very beginning. The authors have not been explicit about the two levels of transaminitis and that is where the problem begins. “While encountering such patients, it is important to differentiate if the patient had pre-existing liver disease or if the present infection with tuberculosis has impacted on the liver, as the approach to management differs given the hepatotoxicity associated with first line drugs.” Rewrite this sentence. Make more explicit. Response: Title and text have been modified to make our message clearer. Thank you Summary and Abstract: The writers present a case of pulmonary TB with transaminitis without pre-existing liver damage. The therapeutic regimen of the authors included anti-TB drugs and liver injury resolved evidenced by normalization of transaminase. The abstract merits rewriting for clarity. Response: Abstract has been modified to make our message clearer Background: Needs to sketch out the larger socio-economic picture of TB patients in Nepal. Medicine for whom? Response: Background has been modified to make it clear. The socioeconomic picture of TB patients in Nepal has been highlighted. In Nepal, tuberculosis prevalence is more in productive age group (25-64 years) and men. Poverty, malnutrition, overcrowding, immunocompromised state like HIV infection, alcohol, smoking, air pollution, diabetes and other comorbidities are important risk factors for acquiring the disease. All patients diagnosed with TB receive treatment as per the national protocol which has been mentioned in the text. Case Presentation: How do you define compliance with TB treatment? How socio-economic factors militate against the successful completion of treatment? Response: To improve the treatment compliance, treatment of TB is done under DOTS program all over Nepal, which stands for ‘Directly Observed Treatment Short Course’. Otherwise the compliance would be compromised owing to the lower socioeconomic status of patients, longer duration of therapy and side effects of drugs. Specific quote from the report: “In our anecdotal experience, we have found many patients with pulmonary tuberculosis, similarly to subject of this case report, present with predominant transaminitis and without pre-existing liver disease or drugs-use. They are often managed with modified liver-friendly antitubercular regimens for fear of increasing the hepatotoxicity and causing acute liver failure with the use of standard regimen. Few case reports are available in literature reporting the use of the modified regimens. We believe such cases are underreported, and firm guidelines have not been established to guide clinicians in these cases. Given this, many clinicians in low-middle income countries, including Nepal, who have been treating tuberculosis patients tend to be skeptical in using full doses of first line ATT in such patients and tend to use a modified regimen. However, this practice may potentially lead to undertreatment and therefore increase fatality9. Though there was some hesitation at first in our case, we soon started treatment with the standard ATT in our patient with close monitoring. This we believe led to the resolution of liver injury, evidenced by the normalization of transaminases.” What is your sample size? Unclear. What guidelines can be established with the aid of the study?" Make explicit and elaborate Response: Our opinion is that there are cases of pulmonary tb with some hepatic involvement, which are sometimes being managed with modified regimen when it can be safely managed with standard regimen. Unfortunately very few published research is available from low middle income countries. Text has been edited to include limitation of evidence. This is a case report only and further research is needed. Conclusion: The report lacks an inevitable conclusion. The conclusion needs to point to the “so what” question? So, what are the implications of this study? What protocols could be devised? How does this case history further medical practitioners’ as well as policymakers’ understanding of drug-resistant TB? Response: Being a case report and paucity of previous research, we have toned down our previous strong conclusions, also as suggested above by another reviewer. We hope that further reports will be published. The use of modified drug regimen excluding more potent drugs, instead of standard regimen may promote drug resistance, and how far such practices are prevalent can be another area of further study. Other points: Please make sure that the manuscript is thoroughly copyedited for legibility of prose, clarity of argument, and grammar. The social context of TB in Nepal merits attention (alcoholism is a contributing factor). You need to compare transaminitis with case studies from other countries. Carefully refer to the PLoS Response: Text has been revised to correct errors. Social context of TB in Nepal has been mentioned in the text. Thank you Murphy, Richard A., Vincent C. Marconi, Rajesh T. Gandhi, Daniel R. Kuritzkes, and Henry Sunpath. "Coadministration of lopinavir/ritonavir and rifampicin in HIV and tuberculosis co-infected adults in South Africa." PLoS One 7, no. 9 (2012): e447931. Sarda, Pawan, S. K. Sharma, Alladi Mohan, Govind Makharia, Arvind Jayaswal, R. M. Pandey, and Sarman Singh. "Role of acute viral hepatitis as a confounding factor in antituberculosis treatment induced hepatotoxicity." Indian Journal of Medical Research 129, no. 1 (2009): 642. How does your case differ from the 2 references mentioned above? Response: As compared to first article our patient did not have HIV. As compared to second article, our patient did not have antituberculous drug induced hepatotoxicity but liver injury likely due to tuberculosis itself. Thank you We would like to whole-heartedly thank you for spending so much time and effort to improve our manuscript. Here below is the point by point response. Title: Drug-resistant TB is a hot topic in medicine today. Research on TB treatment-associated transaminitis would further the existing scholarly understanding on drug-resistant TB. A close keyword search on PubMed revealed only 17 hit on TB AND transaminitis. For this reason, the case report is potentially publishable but suffers from several drawbacks in its current draft that must be remedied before the contribution is re-refereed. But the title itself is unclear. “With” is repeated twice. It is not clear to a medical historian what transaminitis is. A better framing of the title is urgently needed. A cogent argument can be organised around the title. What is four-drugs therapy? It is clear to medical practitioners but not clear to the larger scholarly community. Avoid jargons in the title. 1) What is transaminitis? Why not provide a brief explanation at the start so that the general reader can follow the rest of the article. 2) The two levels of transaminitis: (a) pre-existing liver disease leads to transaminitis. (b) Hepatoxicity of anti-TB drugs. This needs to be made explicit in the very beginning. The authors have not been explicit about the two levels of transaminitis and that is where the problem begins. “While encountering such patients, it is important to differentiate if the patient had pre-existing liver disease or if the present infection with tuberculosis has impacted on the liver, as the approach to management differs given the hepatotoxicity associated with first line drugs.” Rewrite this sentence. Make more explicit. Response: Title and text have been modified to make our message clearer. Thank you Summary and Abstract: The writers present a case of pulmonary TB with transaminitis without pre-existing liver damage. The therapeutic regimen of the authors included anti-TB drugs and liver injury resolved evidenced by normalization of transaminase. The abstract merits rewriting for clarity. Response: Abstract has been modified to make our message clearer Background: Needs to sketch out the larger socio-economic picture of TB patients in Nepal. Medicine for whom? Response: Background has been modified to make it clear. The socioeconomic picture of TB patients in Nepal has been highlighted. In Nepal, tuberculosis prevalence is more in productive age group (25-64 years) and men. Poverty, malnutrition, overcrowding, immunocompromised state like HIV infection, alcohol, smoking, air pollution, diabetes and other comorbidities are important risk factors for acquiring the disease. All patients diagnosed with TB receive treatment as per the national protocol which has been mentioned in the text. Case Presentation: How do you define compliance with TB treatment? How socio-economic factors militate against the successful completion of treatment? Response: To improve the treatment compliance, treatment of TB is done under DOTS program all over Nepal, which stands for ‘Directly Observed Treatment Short Course’. Otherwise the compliance would be compromised owing to the lower socioeconomic status of patients, longer duration of therapy and side effects of drugs. Specific quote from the report: “In our anecdotal experience, we have found many patients with pulmonary tuberculosis, similarly to subject of this case report, present with predominant transaminitis and without pre-existing liver disease or drugs-use. They are often managed with modified liver-friendly antitubercular regimens for fear of increasing the hepatotoxicity and causing acute liver failure with the use of standard regimen. Few case reports are available in literature reporting the use of the modified regimens. We believe such cases are underreported, and firm guidelines have not been established to guide clinicians in these cases. Given this, many clinicians in low-middle income countries, including Nepal, who have been treating tuberculosis patients tend to be skeptical in using full doses of first line ATT in such patients and tend to use a modified regimen. However, this practice may potentially lead to undertreatment and therefore increase fatality9. Though there was some hesitation at first in our case, we soon started treatment with the standard ATT in our patient with close monitoring. This we believe led to the resolution of liver injury, evidenced by the normalization of transaminases.” What is your sample size? Unclear. What guidelines can be established with the aid of the study?" Make explicit and elaborate Response: Our opinion is that there are cases of pulmonary tb with some hepatic involvement, which are sometimes being managed with modified regimen when it can be safely managed with standard regimen. Unfortunately very few published research is available from low middle income countries. Text has been edited to include limitation of evidence. This is a case report only and further research is needed. Conclusion: The report lacks an inevitable conclusion. The conclusion needs to point to the “so what” question? So, what are the implications of this study? What protocols could be devised? How does this case history further medical practitioners’ as well as policymakers’ understanding of drug-resistant TB? Response: Being a case report and paucity of previous research, we have toned down our previous strong conclusions, also as suggested above by another reviewer. We hope that further reports will be published. The use of modified drug regimen excluding more potent drugs, instead of standard regimen may promote drug resistance, and how far such practices are prevalent can be another area of further study. Other points: Please make sure that the manuscript is thoroughly copyedited for legibility of prose, clarity of argument, and grammar. The social context of TB in Nepal merits attention (alcoholism is a contributing factor). You need to compare transaminitis with case studies from other countries. Carefully refer to the PLoS Response: Text has been revised to correct errors. Social context of TB in Nepal has been mentioned in the text. Thank you Murphy, Richard A., Vincent C. Marconi, Rajesh T. Gandhi, Daniel R. Kuritzkes, and Henry Sunpath. "Coadministration of lopinavir/ritonavir and rifampicin in HIV and tuberculosis co-infected adults in South Africa." PLoS One 7, no. 9 (2012): e447931. Sarda, Pawan, S. K. Sharma, Alladi Mohan, Govind Makharia, Arvind Jayaswal, R. M. Pandey, and Sarman Singh. "Role of acute viral hepatitis as a confounding factor in antituberculosis treatment induced hepatotoxicity." Indian Journal of Medical Research 129, no. 1 (2009): 642. How does your case differ from the 2 references mentioned above? Response: As compared to first article our patient did not have HIV. As compared to second article, our patient did not have antituberculous drug induced hepatotoxicity but liver injury likely due to tuberculosis itself. Thank you Competing Interests: none Close Report a concern Reply -->
Reviewer Status
Alongside their report, reviewers assign a status to the article:
Reviewer Reports
- Vivek Neelakantan , Independent Medical Historian, Mumbai, India
- Prajowl Shrestha , Bir Hospital, Kathmandu, Nepal Ashesh Dhungana , Bir Hospital, Kathmandu, Nepal
- Neesha Rockwood , University of Cape Town, London, UK; University of Cape Town, Cape Town, South Africa; University of Colombo, Colombu, Sri Lanka
Comments on this article
All Comments (0)
Competing Interests Policy
Provide sufficient details of any financial or non-financial competing interests to enable users to assess whether your comments might lead a reasonable person to question your impartiality. Consider the following examples, but note that this is not an exhaustive list:
- Within the past 4 years, you have held joint grants, published or collaborated with any of the authors of the selected paper.
- You have a close personal relationship (e.g. parent, spouse, sibling, or domestic partner) with any of the authors.
- You are a close professional associate of any of the authors (e.g. scientific mentor, recent student).
- You work at the same institute as any of the authors.
- You hope/expect to benefit (e.g. favour or employment) as a result of your submission.
- You are an Editor for the journal in which the article is published.
- You expect to receive, or in the past 4 years have received, any of the following from any commercial organisation that may gain financially from your submission: a salary, fees, funding, reimbursements.
- You expect to receive, or in the past 4 years have received, shared grant support or other funding with any of the authors.
- You hold, or are currently applying for, any patents or significant stocks/shares relating to the subject matter of the paper you are commenting on.
Stay Updated
Sign up for content alerts and receive a weekly or monthly email with all newly published articles
Register with Wellcome Open Research
Already registered? Sign in
Not now, thanks
Are you a Wellcome-funded researcher?
If you are a previous or current Wellcome grant holder, sign up for information about developments, publishing and publications from Wellcome Open Research.
We'll keep you updated on any major new updates to Wellcome Open Research
The email address should be the one you originally registered with F1000.
You registered with F1000 via Google, so we cannot reset your password.
To sign in, please click here .
If you still need help with your Google account password, please click here .
You registered with F1000 via Facebook, so we cannot reset your password.
If you still need help with your Facebook account password, please click here .
If your email address is registered with us, we will email you instructions to reset your password.
If you think you should have received this email but it has not arrived, please check your spam filters and/or contact for further assistance.
- Open access
- Published: 21 February 2023
Tuberculosis in older adults: case studies from four countries with rapidly ageing populations in the western pacific region
- Alvin Kuo Jing Teo 1 , 2 , 11 ,
- Kalpeshsinh Rahevar 3 ,
- Fukushi Morishita 3 ,
- Alicia Ang 15 ,
- Takashi Yoshiyama 5 ,
- Akihiro Ohkado 5 ,
- Lisa Kawatsu 5 ,
- Norio Yamada 5 ,
- Kazuhiro Uchimura 5 ,
- Youngeun Choi 6 ,
- Zi Chen 7 ,
- Siyan Yi 1 , 8 , 9 ,
- Manami Yanagawa 3 ,
- Kyung Hyun Oh 3 ,
- Kerri Viney 10 na1 ,
- Ben Marais 2 , 11 na1 ,
- Heejin Kim 6 na1 ,
- Seiya Kato 5 na1 ,
- Yuhong Liu 12 na1 ,
- Catherine W.M. Ong 4 , 13 , 14 na1 &
- Tauhid Islam 3 na1
BMC Public Health volume 23 , Article number: 370 ( 2023 ) Cite this article
3895 Accesses
3 Citations
1 Altmetric
Metrics details
A Correction to this article was published on 07 June 2023
This article has been updated
The Western Pacific Region has one of the fastest-growing populations of older adults (≥ 65 years) globally, among whom tuberculosis (TB) poses a particular concern. This study reports country case studies from China, Japan, the Republic of Korea, and Singapore reflecting on their experiences in managing TB among older adults.
Across all four countries, TB case notification and incidence rates were highest among older adults, but clinical and public health guidance focused on this population was limited. Individual country reports illustrated a range of practices and challenges. Passive case finding remains the norm, with limited active case finding (ACF) programs implemented in China, Japan, and the Republic of Korea. Different approaches have been trialled to assist older adults in securing an early diagnosis, as well as adhering to their TB treatment. All countries emphasised the need for person-centred approaches that include the creative application of new technology and tailored incentive programs, as well as reconceptualisation of how we provide treatment support. The use of traditional medicines was found to be culturally entrenched among older adults, with a need for careful consideration of their complementary use. TB infection testing and the provision of TB preventive treatment (TPT) were underutilised with highly variable practice.
Older adults require specific consideration in TB response policies, given the burgeoning aging population and their high TB risk. Policymakers, TB programs and funders must invest in and develop locally contextualised practice guidelines to inform evidence-based TB prevention and care practices for older adults.
Peer Review reports
Globally the number of older adults (aged ≥ 65 years) is expected to triple by 2100 [ 1 ]. Life expectancy at birth has gradually increased since the 1950s, [ 1 ] with the number of older adults projected to exceed children aged < 5, across all economies by 2020 [ 2 ]. The Western Pacific Region has one of the fastest-growing populations of older adults globally. In 2019, life expectancy at birth of the population was 4 years above the global estimate of 73.3 years [ 3 ]. Japan, for instance, is the most aged country in the world (average life expectancy 85 years) [ 4 ]. Several other countries in the region, particularly the People’s Republic of China (hereinafter referred to as China), the Republic of Korea, and the Republic of Singapore (hereinafter referred to as Singapore), were estimated to have an increase in the proportion of older adults globally between 2019 and 2050.
Japan has the highest proportion of older adults in the world, at 28% of the total population in 2020, [ 5 ] and the proportion is expected to rise to 38% by 2065 [ 6 ]. China is also undergoing a profound demographic transition. In 2021, the number of older adults reached 191 million, amounting to 13.5% of the total population. The number rose by 4.6% compared to the previous year, [ 7 ] and the increasing trend is likely to persist with the number of older adults expected to exceed 480 million (34.6% of the total population) by 2050 [ 8 ]. Similarly, the demographic transition in the Republic of Korea has seen rapid growth in the older adult population. In 2020, 16% of the total population was ≥ 65 years; this is expected to reach 37% by 2050 [ 9 ]. The older adult population made up 13% of the total population in Singapore in 2020 [ 5 ]. The proportion is projected to rise on the same trajectory as China, Japan, and the Republic of Korea in the next few decades [ 1 ].
Improvements in life expectancy have been attributed to better nutrition, political stability, risk factor reduction and improved healthcare access [ 10 ]. Globally, older adults contributed 26% of the total disease burden (measured in disability-adjusted life years [DALYs]); 38% of the burden in high and upper-middle-income, and 16% in low-and lower-middle-income regions in 2019 [ 11 ]. Non-communicable diseases such as cancer, cardiovascular disease and neurological disorders accounted for most of this burden, but respiratory infections, including tuberculosis (TB), are a major contributor as well [ 11 ]. In fact, TB case notifications and estimated disease incidence rates were highest among older adults in China, Japan, the Republic of Korea, and Singapore (Fig. 1 ) [ 12 ].
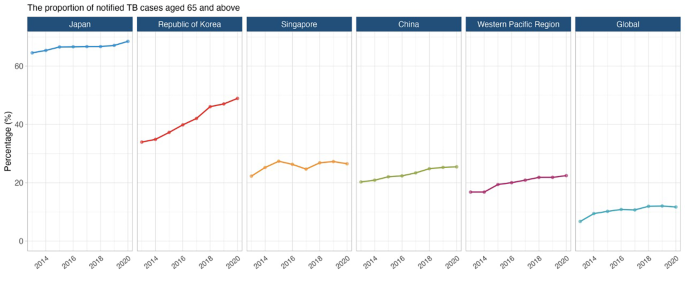
The proportion of notified TB cases aged ≥ 65 in Japan, the Republic of Korea, Singapore, China, the Western Pacific region, and globally 2013−2020
Data source: World Health Organization Global TB Programme 2021
With increasing age, progressive immune dysfunction (immunosenescence) increases the risk for TB disease development [ 13 , 14 ]. The convergence of co-morbidities such as diabetes, chronic respiratory disease and undernutrition, and lifestyle behaviour like tobacco smoking also increase TB risk [ 15 , 16 , 17 , 18 ]. Considering the burgeoning aging population in the Western Pacific Region and the limited guidance specific to this population, it is clear that the needs of older adults require greater recognition in TB response policies. This study reports country case studies from China, Japan, the Republic of Korea, and Singapore, reflecting on country-specific experiences in TB diagnosis and management among older adults. The case studies are a part of a broader endeavour, including a narrative review and analysis of epidemiological trends, to understand and document TB management among older adults in the region. The findings from the narrative review (see supplementary materials for methods) were used to support the country-specific experiences reported in the case studies.
TB epidemiology
China has the second-highest TB burden globally. In 2020, China had an estimated 842,000 people with TB (59 per 100,000 population per year), with older adults accounting for a quarter of all cases [ 12 ]. China notified 159,100 cases (19% of all notified cases) among older adults, [ 12 ] and a consistently increasing trend has been observed over the last two decades [ 19 ]. The fifth national TB epidemiological survey performed in 2010 recorded prevalence rates for clinical and bacteriologically confirmed TB as 482 and 138/100,000 population, respectively, among older adults [ 20 ]. The TB prevalence rate in the survey increased with age and peaked in the 75−79 year age group at 866/100,000 population (overall prevalence rate: 442/100,000 population [95% CI 417−469]) [ 20 ]. A subsequent prospective cohort study reported high TB incidence rates, [ 21 ] highlighting the need to prioritise older adults in the TB response. TB-related mortality was also more prevalent among older adults [ 19 ] concentrated in China’s Central and South-Eastern regions, [ 22 ] among lower-income residents from rural areas and in those with comorbidities [ 23 ].
Health system structure and TB services
The Government of China introduced directly observed treatment (DOT) (now known as treatment support), [ 24 ] as a strategy, in 13 provinces in 1991, with a nationwide scale-up by 2001 [ 25 , 26 ]. The National Center for Disease Control (CDC) is responsible for coordination, policymaking, standards and technical guidance, while provincial CDCs conduct TB programs and monitor disease trends at the prefecture and county level.
TB diagnosis and treatment are provided under the free-TB service policy in China [ 27 , 28 ]. The policy is implemented through an integrated model where designated hospitals (specialised centres for infectious diseases and general hospitals with TB departments) provide TB diagnosis and treatment services [ 29 ]. Persons with drug-resistant TB are treated at designated prefectural or provincial-level hospitals [ 29 ]. Primary healthcare providers are responsible for referring older adults presenting with TB symptoms to designated county-level hospitals for diagnostic investigation. They also conduct follow-up, case management and support, and health education activities at the community level [ 29 ]. The private sector is not involved in TB management. This free-TB service policy is supported by funds from the central and local governments [ 29 ]. Expenditures incurred beyond the free-TB service policy are generally covered by other government-linked insurance schemes [ 27 ]. However, the insurance and financial support schemes vary between provinces, resulting in different levels of financial reimbursement.
Despite this policy, catastrophic costs due to TB remain substantial. Studies report that more than 50% of TB patients incurred out-of-pocket payments exceeding 40% of the household’s ‘capacity to pay, [ 30 , 31 ] indicating a need for better financial support plans and packages to be considered. In addition to financial support, social support through better health education, supportive services, and community engagement is important to improve TB treatment adherence and outcomes [ 32 ].
TB case finding
Active case finding (ACF), a provider-initiated systematic screening and testing for TB disease, [ 33 ] has been deployed in conjunction with the annual physical assessments program for older adults since 2015. Such an integrated approach was feasible and effective for TB case detection among older adults, especially those with comorbidities such as diabetes [ 34 , 35 , 36 ]. TB management is carried out by community health service centres under the technical guidance of the National Tuberculosis Plan [ 37 , 38 ].
Institutionalised aged care is a booming sector in China. As of September 2021, more than 2.6 million older adults were living in retirement facilities [ 39 ]. The quality of services provided in these facilities provides is inconsistent, often resulting in over-crowding in poorly ventilated conditions. Consequently, disease outbreaks are common and in one TB outbreak, 40% of the residents were diagnosed with TB disease [ 40 ]. Therefore, amendments to existing legislation regarding infection prevention and control in such facilities should be considered, with relevant TB information provided to residents and staff. ACF should be prioritised with the expansion of the annual physical assessments program.
TB treatment, care and support have been decentralised using various enablers such as the community, family members, local primary healthcare providers, and technology (electronic medication monitor) for people with TB who were clinically stable and non-infectious [ 26 , 41 ]. However, given their advancing age, existing chronic health conditions, and weakened immunity, older adults are prone to stopping treatment (loss to follow-up) and death [ 42 ]. Currently, limited guidance is provided at the country and global levels to address issues encountered by older adults, such as adverse event monitoring and management, drug-drug interactions and treatment adherence.
Traditional Chinese herbal medicines have been used to treat TB and as adjuvants to improve the tolerability of TB treatment. Although not endorsed by the WHO, herbal medicines are widely used in China [ 43 ]. In 2020, a meta-analysis reported some potential benefits, [ 44 ] but unfortunately, the evaluated studies lacked methodological rigour. Given how widely herbal medicines are used in China, especially in older adults, practice guidelines should consider how best to advise and regulate health practitioners.

TB prevention
The ramp-up of TB response through nationwide expansion of treatment support (historically known as directly observed treatment [DOT]) and improvement of disease reporting and referral system saw a 28% and 65% reduction in the prevalence of pulmonary TB and smear-positive TB, respectively, between 1990 and 2010 in China [ 45 ]. As the risk of infection and transmission decreases, it is expected that reactivation will be the main driver of TB disease occurrence as the population ages in the coming decades [ 46 , 47 ]. China has around 350 million people with TB infection, [ 48 ] however, screening for TB infection and the uptake of TB preventive treatment (TPT) among at-risk groups is limited. Incorporation of TB infection screening into the annual health assessment could improve awareness regarding TB infection and uptake of TPT among at-risk groups but requires further evaluation for feasibility and safety [ 49 ].
The estimated TB incidence in Japan has declined from 36 to 12/100,000 population per year from 2000 to 2020 [ 12 ]. The treatment coverage (notification rate as a proportion of the estimated incidence) was approximately 85%, with 69% reported among older adults (43% among those ≥ 80 years) [ 12 , 50 ]. The median age of a person notified with TB in 2020 was 77 years [ 50 ]. While the number and rate of TB cases have decreased in the last decade, the proportion of older adults among new cases has increased from 48% to 2000 to 59% in 2010 and 69% in 2020 [ 50 ]. Although this is mainly driven by reactivation, multiple outbreaks with transmission in health and aged-care facilities have been reported [ 51 , 52 ]. Despite increased rates of disease, TB mortality among older adults has declined from > 10 to < 5 deaths per 100,000 population in recent years [ 53 ]. Nevertheless, the highest number of TB deaths occurred among older adults in Japan [ 53 ].
The Ministry of Health, Labour, and Welfare of Japan comprises 18 departments, bureaus, and offices that oversee public health, workplace safety and sanitation, medical services, and health insurance [ 54 ]. Access to healthcare in Japan is facilitated by a universal health insurance scheme with population-wide coverage. While approximately 80% of the health facilities are privately owned, they are regulated by the government, and payment for services is controlled by the ministry under the insurance scheme [ 54 ]. These facilities provide direct medical care for people with TB, including in-patient care during TB treatment. Meanwhile, the public health centres provide other aspects of TB response such as screening for TB disease and infection, contact investigation, surveillance, and community-based treatment support [ 55 ]. National TB surveillance data are managed by the Research Institute of Tuberculosis [ 55 ].
TB care is covered by national health insurance and public subsidies at about 70% and 25%, respectively. The remaining 5% is paid out-of-pocket, but a public assistance fund can be used to offset costs for those who cannot afford it [ 55 ]. Medical expenses incurred during hospitalisation are wholly covered by health insurance and public subsidies. Given the rising need for dedicated and specialised care for older adults, a long-term care insurance scheme was introduced in 2020 to support those in need, as well as their family members [ 54 ].
In Japan, TB among older adults has historically been detected passively at outpatient and inpatient health facilities [ 56 , 57 ]. TB case finding among older adults in the health facilities were facilitated by the presence of comorbidities and routine follow-up for other health conditions, thus increasing the likelihood of care-seeking at the onset of TB symptoms and, subsequently, screening for TB [ 58 ]. However, case finding in such settings hinge on a clinician’s awareness of the need to screen for TB. On presentation to health facilities, TB diagnosis among older adults has historically been difficult due to atypical presentation in older adults. For example, one study reported that > 40% of older adults with TB presented with atypical features of TB in Japan [ 59 ]. The non-specific symptoms and low awareness of TB [ 60 ], especially in intermediate TB burden settings such as Japan, could lead to delayed diagnosis.
In addition, community-based ACF programs targeting older adults have been recommended and implemented [ 61 ]. Currently, these programs prioritise older adults ≥ 80 years for TB screening using mobile chest x-rays in the community. For institutionalised older adults, those aged ≥ 65 are offered annual TB disease screening to prevent outbreaks in aged-care facilities. Before admission to an aged-care facility, TB screening using chest radiography has also been implemented to facilitate the early detection of TB disease [ 62 ]. This obligation is also extended to frontline workers in health and aged-care facilities and welfare facilities.
Treatment of drug-susceptible TB in Japan generally follows the standard 6-month regimen [ 55 ] . However, a 9-month regimen without pyrazinamide (2 months of isoniazid, rifampicin, and ethambutol, followed by isoniazid and rifampicin for 7 months) is widely prescribed for older adults, particularly those aged ≥ 80, and the national guidelines did not recommend pyrazinamide for older adults with TB until 2018 [ 63 ]. While recent studies have reported that the pyrazinamide-based regimens do not lead to significantly higher rates of treatment discontinuation, liver injuries, and death than regimens without pyrazinamide, [ 63 , 64 ] the proportion of those receiving the standard 6-month regimen with pyrazinamide declines with age, particularly for those aged ≥ 75 years [ 50 ].
The overall treatment success rate of drug-susceptible TB was 66% in Japan in 2019 [ 50 ] . The treatment success rate among people with TB < 65 years was 82%, and the rate decreased among the older age groups (65−74 years; 76%, 75−84 years; 65%, ≥85 years; 46%) [ 50 ]. The low treatment success rate among older adults has been ascribed to a high death rate during TB treatment. In 2019, 33% of older adults with TB died during treatment, and > 60% died of non-TB-related causes [ 50 ]. Japan has a comprehensive treatment support strategy for people with TB disease or TB infection (TPT). For those who require in-patient care, treatment support that comprises patient education is provided in the hospital. Upon discharge, an individual support plan for community-based treatment support is developed based on the person’s risk of non-adherence, and the frequency and means of medication support are determined. A treatment support conference is held to evaluate and review the plan. Through a patient-centred care approach, treatment support may be provided by health professionals in the local community, community health workers and volunteers, or family members.
Tuberculin skin tests (TST) and interferon-gamma release assays (IGRA) are used to diagnose TB infection in Japan; both tests are covered by national health insurance. TB infection has been a notifiable condition since 2006 [ 50 ]. While there are no policies to actively screen older adults as a priority group for TB infection, notification of TB infection among older adults ≥ 65 has gradually increased since 2010 [ 50 ]. In 2020, approximately 49% of older adults with TB infection were detected via contact investigation, [ 50 ] a national policy to facilitate early detection of TB disease and infection and prevent onward transmission. There was also an increasing number of older adults diagnosed with TB infection in the hospital due to TB infection testing carried out before treating other medical conditions such as rheumatoid arthritis [ 65 ]. Nevertheless, the lower sensitivity of IGRA among older adults remains a concern. A 2017 study in Japan reported discrepancies between IGRA positivity rates and the corresponding estimated prevalence of TB infection among older adults, highlighting the utility and applicability of IGRA in this population [ 66 ]. Furthermore, providing TPT for older adults remains controversial among clinicians due to the risk of adverse events.
- Republic of Korea
In 2020, in the Republic of Korea, there was an estimated TB incidence was 25,000 people with incident TB (49 per 100,000 population per year); 94% of these were notified to the national authorities, of which 49% were aged ≥ 65 [ 12 ]. [ 12 ] While the number of people with TB has steadily declined in the last decade, the proportion of older adults among new TB patients has risen (19.2% in 2001 and 49.1% in 2020) [ 67 ] . In 2020, the TB notification rate among older adults aged 65−69 was 58 per 100,000 population; the rate increased with age and peaked among those aged ≥ 80 years at 235 per 100,000 population [ 67 ]. TB mortality among older adults ≥ 65 was 13.8 per 100,000 population in 2020, the lowest rate recorded since 2001. However, of all TB-related deaths, 82.5% involved those aged ≥ 65, and the proportion has been above 80% since 2016 (2001; 58.0%, 2010; 72.1%). Despite the decline in overall TB burden and mortality rates, the course is predicted to reverse after 2032 (TB incidence) and 2026 (TB deaths) due to increasing trends among older adults, particularly those aged ≥ 80 69 .
The Ministry of Health and Welfare is the national policymaking and governing body for public health and medical services in the Republic of Korea [ 70 ]. The ministry also oversees the national health insurance scheme, a compulsory scheme that confers health care coverage and benefits for the entire population [ 70 ]. The Korean Disease Control and Prevention Agency (KDCA) is responsible for disease surveillance, public health response, disease prevention, and research and oversees the National TB Elimination Project [ 70 ]. While policies regarding TB prevention and care are established by the government, the private sector’s involvement in TB care began in the 1990s and was formalised in 2011 through the public-private mix model [ 71 ].
TB care in the public and private sectors is covered by national health insurance. A 10% co-payment scheme was in place until 2016 [ 71 ]. Since 2017, all expenses incurred during TB care, including hospitalisation, isolation orders (movement restriction to prevent further transmission), and an allowance for dependents, are included in the policy, thereby minimising out-of-pocket payments for people affected by TB. Interventions such as contact investigation and the screening of close contacts for TB disease and infection are also covered by health insurance. While there is specific funding for TB interventions targeted at older adults in the Republic of Korea, the budget only amounted to 1.8% of the total budget for the national TB control program in 2018 [ 71 ].
Since the inception of the national TB control program in the 1960s, early detection and treatment of TB has been a mainstay of TB policies, including for older adults [ 71 ]. In 2020, the TB incidence rate detected through TB screening among older adults ≥ 65 using mobile chest x-ray machines in 17 regions and provinces was 75 per 100,000, 1.9 times higher than the general population’s rate [ 72 ]. This high detection rate prompted KDCA to implement nationwide TB screening among older adults in the community and aged-care facilities as a key strategy to detect TB early in this group.
With an increasingly aging population and the growth in the proportion of women in the labour market, the number of older adults living in institutionalised settings has also increased proportionally, partly due to the introduction of long-term care insurance, which covers home and institutional care services, assistive equipment such as walker and wheelchair, and cash benefits [ 73 ]. In fact, the number of recipients of long-term care insurance increased three-fold between 2008 and 2019 [ 74 ]. Using mobile chest x-ray, TB screening among older adults ≥ 65 in long-term care facilities in 17 regions and provinces resulted in an incidence rate of 66 per 100,000 in 2020 [ 72 ].
Drug-susceptible TB in the Republic of Korea is treated using the standard 6-month regimen [ 75 ]. Partly due to concerns about potential pyrazinamide hepatotoxicity, there is ongoing work to optimise TB treatment among older adults through establishing an adverse events monitoring system, managing adverse events, and developing biomarkers that may predict diagnostic and therapeutic responses [ 76 ].
Overall, the TB treatment success rate has been sitting at approximately > 80% over the last two decades [ 12 ]. However, the treatment success rate among older adults was lower than the general population at approximately 70% between 2012 and 2015 [ 77 ]. Treatment support remains the main treatment administration option. Video-observed therapy and support through a comprehensive support centre for older adults living alone had been trialled with some success. Preliminary data showed higher treatment success rate among older adults enrolled in the programme [ 78 ]. Other incentives have been implemented, such as providing food, daily necessities, and medical accompaniment service for older adults who have trouble remaining on treatment. Furthermore, an approach to assess the vulnerability of people with TB, particularly older adults, with customised case management and linkage with social welfare services have also been implemented.
A comprehensive epidemiologic and contact investigations protocol is in place to screen at-risk populations for both TB disease and infection. TB disease and infection screening is mandatory for healthcare and nursery workers and teachers. Other at-risk groups, such as people living with HIV, those with silicosis, organ transplant recipients, and patients with kidney disease on dialysis, are recommended to be screened for TB infection. For household contacts of persons with TB, chest x-ray investigations and TB infection workups (TST/IGRA, but not mandatory) will be offered (covered by health insurance). TPT (3HP [isoniazid-rifapentine once-weekly for 3 months], 3RH [rifampicin-isoniazid daily for 3 months], or 4R [rifampicin daily for 4 months) is offered to those eligible for it. However, there is no policy to screen older adults for TB infection. In a 2016 study conducted across 11 regions, 40% of those aged ≥60 tested positive for TB infection using IGRA [ 79 ]. Considering the potentially high prevalence of TB infection and risk for reactivation among older adults, [ 80 ] a systematic approach to TB infection screening and TPT administration in this population is warranted.
An estimated 2700 people were affected by TB in 2020 (46 per 100,000 population per year); 89% of these (2400) were notified to the national authorities in 2020. [ 12 ] Of the 2400 people with TB, approximately 57% were Singapore citizens and permanent residents [ 81 ]. The TB incidence rate has been approximately 40 per 100,000 since the late 1990s and may be attributed to migration (about 30−50% of the cases were detected among short and long-term visitors, including work pass holders and students) and an aging population [ 82 , 83 ]. In 2020, older age groups (≥60) made up a significant proportion of the TB notifications both among Singaporean-born (58%) and foreign-born (46%) individuals [ 81 ]. While reactivation of past infections could sustain the TB epidemic among older residents, outbreaks in aged-care facilities have also been reported. Overall, TB mortality rates have remained < 1 per 100,000 population in the past few years [ 12 ]. However, the TB mortality rate among older adults ≥70 was higher at 5.1 per 100,000 population in 2018 [ 84 ].
The Ministry of Health (MOH) Singapore initiated the national TB program, named Singapore TB Elimination Program (STEP), to strengthen TB response efforts by detecting and treating TB disease and infection and preventing drug-resistance TB in 1997 [ 82 ]. STEP manages a notification registry and a treatment surveillance system to monitor TB notification and treatment outcomes. The TB Control Unit (TBCU) is the referral centre for TB management in Singapore, responsible for treatment support, contact investigation, and the administration of TPT. Both public and private hospitals can offer TB diagnosis and treatment. Referrals for TB diagnosis and treatment can be made by primary care physicians in public, private, and community-based organisations (such as the Singapore Anti-Tuberculosis Association).
Singapore’s health system is financed through subsidies, a national health savings account (MediSave), a basic national health insurance scheme (MediShield) for hospitalisation and treatment bills, and an endowment scheme for individuals who have exhausted other means of payment [ 85 ]. For citizens and permanent residents, TB diagnosis and treatment costs are covered by the health financing system. Non-residents, such as those holding long-term work visas, are not covered by these schemes and must rely on employer coverage, private health insurance, or out-of-pocket payment for TB screening and diagnosis costs. TB medications are provided to all at no cost.
TB is diagnosed by passive case finding when a person presents with symptoms or a chest x-ray for other medical conditions (yet suggestive of TB) [ 86 ]. TB screening is conducted for foreigners applying for work or long-term visas and during the visa renewal process using chest radiography [ 86 ]. The same approach applies to everyone regardless of age. There are currently no specific interventions targeting TB screening among older adults. Some aged-care facilities may enquire about the date and information of the last chest x-ray or require a chest x-ray to be conducted before admission. However, this policy is inconsistent.
Treatment of drug-susceptible TB in Singapore follows the standard 6-month regimen (2 months of isoniazid, rifampicin, ethambutol, and pyrazinamide followed by isoniazid and rifampicin for 4 months) [ 86 ]. However, for older adults who may be unlikely to tolerate pyrazinamide, a 9-month regimen comprising ethambutol, rifampicin, and isoniazid for 2 months (intensive phase), followed by rifampicin and isoniazid for 7 months (continuation phase) is used [ 86 ]. It is required by law under the Infectious Diseases Act for all clinicians to report treatment progress and the outcomes of people with TB to the MOH [ 86 ].
The treatment success rate was 79% in 2019, [ 12 ] and the treatment success rate among older adults was not known at the time of writing. Different forms of treatment support have been implemented to support treatment. Outpatient treatment support is implemented at all the 18 public polyclinics and the TBCU. People with TB disease can choose to have their treatment administered at the nearest public health facility. In a 2016 study among adults with TB in Singapore, 72% of respondents reported that they could accept the schedule of facility-based treatment support [ 87 ]. However, 45% perceived the arrangement to be disruptive to their work, school, and social activities [ 87 ]. The results were not age disaggregated. While not specific to older adults, incentive-based intervention to encourage treatment adherence among people with TB from the lower-income bracket has shown promise compared to the non-intervention group in Singapore [ 88 ]. Other forms of treatment support, such as administration in aged-care facilities and through outreach for recipients who have mobility issues or are frail, have been implemented [ 86 ]. Self-administered treatment is also used in Singapore, especially for those treated in the private sector. However, there are no data on self-administered treatment among older adults.
The STEP strategy includes contact investigation to identify close contacts of persons with bacteriologically confirmed TB [ 86 ]. Testing for TB infection is recommended for high-risk groups if there is an intention to treat with TPT [ 86 ]. IGRA is the preferred test for TB infection; variable TPT options are available, including 6 H (isoniazid daily for 6 months), or 4R (daily rifampicin for 4 months) [ 86 ]. Although TB infection has been estimated to affect up to 30% of older adults in Singapore, [ 81 ] there is no policy or specific guideline regarding TPT use for older adults. The risk of adverse events associated with TPT remains a concern, and further studies are needed.
Summary and conclusion
The four case studies presented exemplify the range of practices and challenges in managing TB among older adults in the Western Pacific Region. Here we summarise the key findings and action points based on country experiences:
While passive case finding remains the mainstay intervention contributing to TB case detection in older adults, routine ACF has been implemented in China, Japan, and the Republic of Korea. The optimal use of ACF requires further consideration and assessment in different contexts.
A person-centred approach to TB care was identified as a key theme in all four countries. Nevertheless, limited guidance is available at the country and global levels to address issues older adults encounter (e.g., adverse event monitoring and management, consideration of drug-drug interactions, and treatment adherence). Existing evidence (and evidence gaps) related to the optimal management of older adults with TB require systematic review and guideline development.
There is a lack of standardisation in the approach to TB infection testing and TPT provision. It is important to generate the necessary evidence to inform benefit-risk estimates for managing TB infection among older adults.
The use of traditional medicines is culturally deeply rooted among older adults in this region. Their complementary use in TB care should be explored and carefully considered.
A summary of the approaches implemented by the four countries is outlined in Fig. 2 .
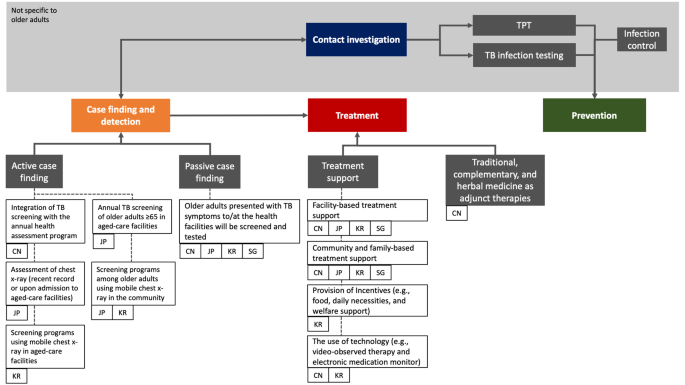
TB management among older adults in China, Japan, the Republic of Korea, and Singapore
TB management experiences were mapped based on three main domains: case finding and detection, treatment, and prevention. The relevant policies and interventions are tagged to the respective implementing countries. Areas shaded in grey represent cross-cutting interventions that extend beyond the older adult population. Treatment support was historically known as directly observed treatment (DOT)
Abbreviations: TB; tuberculosis, TPT; TB preventive treatment, CN; China, JP; Japan, KR; Republic of Korea, SG; Singapore
Cross-cutting challenges
The COVID-19 pandemic has severely disrupted access to TB care. with an 18% decrease in TB disease notifications globally [ 89 ]. Health services for older people were often more severely.
affected and TB services in South-East Asia and the Western Pacific Regions were highly impacted [ 12 ]. Of the four countries included in this study, TB notification data for 2020 and 2021 were lower than 2019 [ 12 , 90 ].
In addition to key risk factors for TB such as living in crowded and poorly ventilated conditions, indoor air pollution and tobacco smoking, [ 91 ] older adults also have age-associated immune dysfunction, financial resources constraints, and frequent comorbidities [ 92 ]. Caring for older adults with TB can be difficult and complex cases may require referral to appropriate specialty care. Service integration between relevant specialties should facilitate better care for older adults with TB. TB diagnosis in older adults is further complicated by challenges related to cognitive impairment, communication challenges and difficulties in obtaining quality sputum samples [ 93 , 94 ]. Dementia, which primarily affects older adults, has been associated with difficult TB diagnosis and poor adherence to TB treatment in the absence of tailored treatment support [ 95 ].
TB-related stigma (perceived and experienced) remains pervasive in many communities [ 96 ]. While systematic assessment of TB-related stigma among older adults has not been conducted, older adults in China have reported unwillingness to seek TB care due to fear of discrimination and self-isolation because of stigma [ 32 , 97 ]. Anecdotally, aged care facilities in Japan were reluctant to accept returning residents after hospital admission for TB care due to fear and stigma, while unwillingness to be screened for TB has also been ascribed to stigma.
The high standards of living and well-being may have shaped the notion that TB is not a significant concern, rendering a lower index of TB suspicion, including among healthcare workers [ 98 ]. A recent cross-sectional study conducted among older adults in Shenzhen, China, reported that > 70% of the respondents were aware of TB as a contagious disease, its symptoms, and preventive measures. Yet, less than half knew that TB was curable, and only one-third were willing to be screened for TB if they were to develop suspicious symptoms [ 99 ].
Considering that aging populations is a global phenomenon that implies a heightened TB risk, particularly in areas with historically high rates of TB, policymakers and funders must invest more to deliver and generate the evidence required to inform optimal TB prevention and care initiatives in older adults.
Data Availability
Data used for this case study comprised published literature, reports, and co-authors’ experience in managing TB among older adults in their respective settings.
Change history
07 june 2023.
A Correction to this paper has been published: https://doi.org/10.1186/s12889-023-15576-0
United Nations Population Division. World Population Prospects. 2019. New York: United Nations Department of Economic and Social Affairs, 2019 (accessed Sept 8, 2021). https://population.un.org/wpp/Graphs/DemographicProfiles/Line/900
World Bank. Population ages 65 and above, total. 2020. (accessed Sept 13, 2021). https://data.worldbank.org/indicator/SP.POP.65UP.TO
The Global Health Observatory. Life expectancy at birth (years). 2020. (accessed Sept 10, 2021). https://www.who.int/data/gho/data/indicators/indicator-details/GHO/life-expectancy-at-birth-(years)
World Bank. Life expectancy at birth, total (years) - Japan. 2020. (accessed Oct 27, 2022). https://data.worldbank.org/indicator/SP.DYN.LE00.IN?locations=JP
World Bank. Population ages 65 and above (% of total population). 2020. (accessed Sept 13, 2021). https://data.worldbank.org/indicator/SP.POP.65UP.TO.ZS?most_recent_value_desc=true
National Institute of Population and Social Security Research. Population projections for Japan (2016–2065). 2017. https://www.ipss.go.jp/pp-zenkoku/e/zenkoku_e2017/pp_zenkoku2017e_gaiyou.html
National Bureau of Statistics of China. The 7th national population census. 2021. (accessed April 1, 2022). http://www.stats.gov.cn/tjsj/tjgb/rkpcgb/qgrkpcgb/202106/t20210628_1818824.html
Department of Economic and Social Affairs, United Nations. World population prospects: population by age and sex (China). 2019. (accessed April 1, 2022). https://population.un.org/wpp/DataQuery/
Korean Statistical Information Service. Projected population by age (Korea). 2021. &tblId=DT_1BPA001&vw_cd=MT_ETITLE&list_id=A41_10&scrId=&language=en&seqNo=&lang_mode=en&obj_var_id=&itm_id=&conn_path=MT_ETITLE&path=%252Feng%252FstatisticsList%252FstatisticsListIndex.do.. https://kosis.kr/statHtml/statHtml.do?orgId=101
Mathers CD, Stevens GA, Boerma T, White RA, Tobias MI. Causes of international increases in older age life expectancy. The Lancet. 2015;385:540–8.
Article Google Scholar
Institute for Health Metrics and Evaluation (IHME). GBD compare data visualizations, Seattle. Washington: IHME, University of Washington, 2021 (accessed Sept 14, 2021). http://vizhub.healthdata.org/gbd-compare
World Health Organization. Global tuberculosis report 2021.Geneva, 2021 https://www.who.int/publications/i/item/9789240037021
Mori T, Leung CC. Tuberculosis in the Global Aging Population. Infect Dis Clin N Am. 2010;24:751–68.
Shaw AC, Joshi S, Greenwood H, Panda A, Lord JM. Aging of the Innate Immune System. Curr Opin Immunol. 2010;22:507–13.
Article CAS PubMed PubMed Central Google Scholar
Uchimura K, Ngamvithayapong-Yanai J, Kawatsu L, et al. Characteristics and treatment outcomes of tuberculosis cases by risk groups, Japan, 2007–2010. Western Pac Surveillance Response Journal: WPSAR. 2013;4:11–8.
Article PubMed PubMed Central Google Scholar
Byrne AL, Marais BJ, Mitnick CD, Lecca L, Marks GB. Tuberculosis and chronic respiratory disease: a systematic review. Int J Infect Dis. 2015;32:138–46.
Article PubMed Google Scholar
Donini LM, ScarDeLLa P, PioMbo L. Malnutrition in elderly: social and economic determinants. J Nutr Health Aging. 2013;17:7.
Bates MN, Khalakdina A, Pai M, Chang L, Lessa F, Smith KR. Risk of Tuberculosis from exposure to Tobacco smoke: a systematic review and Meta-analysis. Arch Intern Med. 2007;167:335–42.
Wang L, Wang W. Temporal Trends in notification and mortality of tuberculosis in China, 2004–2019: a joinpoint and age-period-cohort analysis. Int J Environ Res Public Health. 2021;18:5607.
The Office of the Fifth National TB Epidemiological Survey. The fifth national tuberculosis epidemiological survey 2010. China J Antituberc. 2012;34:485–508.
Google Scholar
Cheng J, Sun Y-N, Zhang C-Y, et al. Incidence and risk factors of tuberculosis among the elderly population in China: a prospective cohort study. Infect Dis Poverty. 2020;9:13.
Amsalu E, Liu M, Li Q, et al. Spatial-temporal analysis of tuberculosis in the geriatric population of China: an analysis based on the bayesian conditional autoregressive model. Arch Gerontol Geriatr. 2019;83:328–37.
Wang L, Xu C, Hu M, et al. Spatio-temporal variation in tuberculosis incidence and risk factors for the disease in a region of unbalanced socio-economic development. BMC Public Health. 2021;21:1817.
World Health Organization. WHO operational handbook on tuberculosis: module 4: treatment: drug-susceptible tuberculosis treatment. Geneva: World Health Organization., 2022 (accessed Jan 25, 2022). https://www.who.int/publications/i/item/9789240048126
Xianyi C, Fengzeng Z, Hongjin D, et al. The DOTS strategy in China: results and lessons after 10 years. Bull World Health Organ. 2002;80:430–6.
PubMed PubMed Central Google Scholar
Hou W-L, Song F-J, Zhang N-X, et al. Implementation and community involvement in DOTS strategy: a systematic review of studies in China [Review article]. Int J Tuberc Lung Dis. 2012;16:1433–40.
Chen S, Zhang H, Pan Y, et al. Are free anti-tuberculosis drugs enough? An empirical study from three cities in China. Infect Dis Poverty. 2015;4:47.
Wei X, Zou G, Walley J, et al. China Tuberculosis Policy at Crucial Crossroads: comparing the practice of different hospital and tuberculosis control collaboration models using Survey Data. PLoS ONE. 2014;9:e90596.
Long Q, Guo L, Jiang W, Huan S, Tang S. Ending tuberculosis in China: health system challenges. The Lancet Public Health. 2021;6:e948–53.
Zhou C, Long Q, Chen J, et al. Factors that determine catastrophic expenditure for tuberculosis care: a patient survey in China. Infect Dis Poverty. 2016;5:6.
Duan W, Zhang W, Wu C, et al. Extent and determinants of catastrophic health expenditure for tuberculosis care in Chongqing municipality, China: a cross-sectional study. BMJ Open. 2019;9:e026638.
Li X, Wang B, Tan D, et al. Effectiveness of comprehensive social support interventions among elderly patients with tuberculosis in communities in China: a community-based trial. J Epidemiol Commun Health. 2018;72:369–75.
Article CAS Google Scholar
World Health Organization. WHO consolidated guidelines on tuberculosis. Module 2: screrening - systematic screening for tuberculosis disease. Geneva: World Health Organization., 2021 (accessed March 9, 2022). https://www.who.int/publications/i/item/9789240001503
Zhang C, Xia L, Rainey JJ, et al. Findings from a pilot project to assess the feasibility of active tuberculosis case finding among seniors in rural Sichuan Province, China, 2017. PLoS ONE. 2019;14:e0214761.
Zhang X-L, Li S-G, Li H-T, et al. Integrating tuberculosis screening into annual health examinations for the rural elderly improves case detection. Int J Tuberculosis Lung Disease: Official J Int Union Against Tuberculosis Lung Disease. 2015;19:787–91.
Li J, Liu X-Q, Jiang S-W, et al. Improving tuberculosis case detection in underdeveloped multi-ethnic regions with high disease burden: a case study of integrated control program in China. Infect Dis Poverty. 2017;6:151.
Office of the State Council. People’s Republic of China. National tuberculosis plan for the 13th five-year plan period. Beijing: Office of the State Council, People’s Republic of China; 2017.
National Health Commission of China. Chinese tuberculosis control and prevention: technical work regulations. Beijing: National Health Commission of China; 2020. http://tb.chinacdc.cn/ggl/202004/P020200414515703939844.pdf
National Ministry of Civil Affairs. Third quarterly report of social welfare institutions 2021. Beijing: National Ministry of Civil Affairs; 2021. http://www.mca.gov.cn/article/sj/tjjb/2021/202103jgqk.html
Hu Y, Hu Y, Ye X. Epidemiological investigation of an outbreak of tuberculosis. Mod Prev Med. 2015;42:982–3.
Wang N, Shewade HD, Thekkur P, et al. Electronic medication monitor for people with tuberculosis: implementation experience from thirty counties in China. PLoS ONE. 2020;15:e0232337.
Abuaku B, Tan H, Li X, Chen M, Huang X. Treatment default and death among tuberculosis patients in Hunan, China. Scand J Infect Dis. 2010;42:281–7.
Tomioka H, Tatano Y, Shimizu T, Sano C. Clinical and basic studies on therapeutic efficacy of Herbal Medicines against Mycobacterial Infections. Med (Basel). 2019;6:E67.
Li X, Li X, Liu Q, et al. Traditional chinese medicine combined with western medicine for the treatment of secondary pulmonary tuberculosis: a PRISMA-compliant meta-analysis. Med (Baltim). 2020;99:e19567.
Wang L, Zhang H, Ruan Y, et al. Tuberculosis prevalence in China, 1990–2010; a longitudinal analysis of national survey data. The Lancet. 2014;383:2057–64.
Huynh GH, Klein DJ, Chin DP, et al. Tuberculosis control strategies to reach the 2035 global targets in China: the role of changing demographics and reactivation disease. BMC Med. 2015;13:88.
Cui X, Gao L, Cao B. Management of latent tuberculosis infection in China: exploring solutions suitable for high-burden countries. Int J Infect Dis. 2020;92:37–40.
Gao L, Bai L, Liu J, et al. Annual risk of tuberculosis infection in rural China: a population-based prospective study. Eur Respir J. 2016;48:168–78.
Article CAS PubMed Google Scholar
Gao L, Zhang H, Xin H, et al. Short-course regimens of rifapentine plus isoniazid to treat latent tuberculosis infection in older chinese patients: a randomised controlled study. Eur Respir J. 2018;52:1801470.
Tuberculosis Surveillance Center. Tuberculosis in Japan: annual report 2021. Tokyo: Department of Epidemiology and Clinical Research, Research Institute of Tuberculosis Japan., 2021 https://jata.or.jp/english/dl/pdf/TB_in_Japan_2021.pdf
Toyota M, Sasaki Y. [The issue of tuberculosis in the elderly in Japan]. Kekkaku. 2010;85:881–94.
PubMed Google Scholar
Seto J, Wada T, Suzuki Y, et al. Mycobacterium tuberculosis Transmission among Elderly Persons, Yamagata Prefecture, Japan, 2009–2015. Emerg Infect Dis. 2017;23:448–55.
Hagiya H, Koyama T, Zamami Y, et al. Trends in incidence and mortality of tuberculosis in Japan: a population-based study, 1997–2016. Epidemiol Infect. 2018;147:e38.
Sakamoto H, Rahman MdM, Nomura S et al. Japan health system review. New Delhi:World Health Organization, Regional Office forSouth-East Asia, 2018 https://apps.who.int/iris/handle/10665/259941
Katsuda N, Hirosawa T, Reyer JA, Hamajima N. Roles of public health centers (hokenjo) in tuberculosis control in Japan. Nagoya J Med Sci. 2015;77:19–28.
Hoshino H, Ohmori M, Uchimura K, Yamauchi Y. [TB epidemiology in an elderly group in Japan]. Kekkaku. 2008;83:423–9.
Kawatsu L, Yoshiyama T, Kato S. Tuberculosis in the Elderly. In: Migliori GB, Raviglione MC, editors. Essential tuberculosis. Cham: Springer International Publishing; 2021. pp. 253–8.
Chapter Google Scholar
Yoshikawa R, Kawatsu L, Uchimura K, Ohkado A. Delay in health-care-seeking treatment among tuberculosis patients in Japan: what are the implications for control in the era of universal health coverage? Western Pac Surveill Response J. 2020;11:37–47.
Hikone M, Ainoda Y, Sakamoto N, Ohnishi K. Clinical characteristics of elderly pulmonary tuberculosis in an acute-care general hospital in Tokyo, Japan: a 12-year retrospective study. J Infect Chemother. 2020;26:245–50.
Nakao M, Sone K, Kagawa Y, et al. Diagnostic delay of pulmonary tuberculosis in patients with acute respiratory distress syndrome associated with aspiration pneumonia: two case reports and a mini-review from Japan. Exp Ther Med. 2016;12:835–9.
Ghotbi N, Nishimura S, Takatsuka N. Japan’s national tuberculosis control strategies with economic considerations. Environ Health Prev Med. 2005;10:213–8.
Ohmori M, Wada M, Mitarai S, et al. [Tuberculosis control in health care facilities for the elderly, from the viewpoint of risk management]. Kekkaku: [Tuberculosis]. 2006;81:71–7.
Hagiwara E, Suido Y, Asaoka M, et al. Safety of pyrazinamide-including regimen in late elderly patients with pulmonary tuberculosis: a prospective randomized open-label study. J Infect Chemother. 2019;25:1026–30.
Takaku T, Saito T, Nemoto K, Oisihi S, Hayashihara K. Comparison of adverse effects in tuberculosis patients over 80 years of age with and without pyrazinamide treatment. Eur Respir J. 2017;50. https://doi.org/10.1183/1393003.congress-2017.PA3045
Kawatsu L, Uchimura K, Ohkado A. Trend and treatment outcomes of latent tuberculosis infection among migrant persons in Japan: retrospective analysis of Japan tuberculosis surveillance data. BMC Infect Dis. 2021;21:42.
Kato S, Ota M, Suenaga M, Hirayama T, Yoshiyama T. Estimation of positive rates of interferon-gamma release assay by age group in Japan. Kekkaku. 2017;92:365–70.
Korea Disease Control and Prevention Agency. Annual report on notified tuberculosis in Korea 2020. Seoul: Korea Disease Control and Prevention Agency, 2021.
Hyewon L, Jinsun K, Hye Kyung I, Youmi K. Characteristics and trends in deaths from tuberculosis in the Republic of Korea 2001–2020. Seoul: Division of Tuberculosis Prevention and Control, Korea Disease Control and Prevention Agency, 2021 &bid=0031&list_no=717657&act=view. https://kdca.go.kr/board/board.es?mid=a30501000000
Jang SY, Kim MJ, Cheong H-K, Oh I-H. Estimating disability-adjusted life years due to tuberculosis in Korea through to the Year 2040. Int J Environ Res Public Health. 2020;17:5960.
Sooman K, Tae-jin L, Chang-yup K. Republic of Korea health system review. Manila: World Health Organization Regional Office for the Western Pacific, 2015 (accessed April 9, 2022). https://apps.who.int/iris/handle/10665/208215
Cho KS. Tuberculosis control in the Republic of Korea. Epidemiol Health. 2018;40:e2018036.
HeeAe K, JeeYeon S, HyeKyung I, EunHye S, WeonJung J, YunSoo K. Results of the 2020 elderly tuberculosis screening in Republic of Korea. Seoul: Korea Disease Control and Prevention Agency; 2021. &bid=0031&list_no=713470&act=view. https://www.kdca.go.kr/board/board.es?mid=a30501000000
Chung Yu L, Euisook K. Long-term care in developing countries: ten case studies (Korea). Geneva: World Health Organization and WHO Collaborating Centre for Health and Long-Term Care Policy and Research; 2003. https://apps.who.int/iris/handle/10665/42769
Ga H. Long-term Care System in Korea. Ann Geriatr Med Res. 2020;24:181–6.
Joint Committee for the Revision of Korean Guidelines for Tuberculosis. Korean guidelines for tuberculosis. 4th ed. Seoul: Korea Disease Control and Prevention Agency; 2020. https://tbzero.kdca.go.kr/tbzero/contents.do
Min J. Study on the optimization of pulmonary TB treatment in elderly 2020–2022. Seoul: Catholic University and the Korean National Institute of Health, 2022 https://cris.nih.go.kr/cris/search/detailSearch.do/17218#step8
Son H, Mok J, Lee M, et al. Status and determinants of treatment outcomes among New Tuberculosis Patients in South Korea: a retrospective cohort study. Asia Pac J Public Health. 2021;33:907–13.
Kim HJ. Enhanced video observed therapy (VOT) to the elderly TB patients: case study of Korea [PowerPoint presentation]. 2021.
Hwang H-J, Park J-H, Nam S, et al. Characteristics of a large latent tuberculous infection screening programme using QuantiFERON®-TB gold in Korea. Int J Tuberc Lung Dis. 2018;22:504–9.
Rajagopalan S. Tuberculosis and aging: A Global Health Problem. Clin Infect Dis. 2001;33:1034–9.
Ministry of Health Singapore. Update on tuberculosis situation in Singapore. Singapore: Ministry of Health Singapore., 2021 https://www.moh.gov.sg/news-highlights/details/update-on-tuberculosis-situation-in-singapore-2022
Loh KS, Hsu LY. Tuberculosis in Singapore: past and future. Ann Acad Med Singap. 2019;48:72–4.
Tam G, Lai SW. Is Singapore on track to eliminate tuberculosis by 2030? A policy case study. SAGE Open Medicine. 2019;7. https://doi.org/10.1177/2050312119851331
Communicable Diseases Division, Ministry of Health Singapore. Communicable diseases surveillance Singapore 2018. Singapore: Ministry of Health Singapore, 2019 https://www.moh.gov.sg/docs/librariesprovider5/diseases-updates/communicable-diseases-surveillance-in-singapore-2018210c9a3beaa94db49299c2da53322dce.pdf
Lim J. Sustainable Health Care Financing: the Singapore experience. Global Policy. 2017;8:103–9.
Ministry of Health Singapore. Prevention, diagnosis, and management of tuberculosis: MOH clinical practice guidelines. Singapore: Ministry of Health Singapore., 2016 https://www.moh.gov.sg/hpp/doctors/guidelines/GuidelineDetails/cpgmed_prevention_diagnosis_management_tuberculosis
Lee HK, Teo SSH, Barbier S, Tang SC, Yeo GH, Tan NC. The impact of direct observed therapy on daily living activities, quality of life and socioeconomic burden on patients with tuberculosis in primary care in Singapore. Proceedings of Singapore Healthcare 2016; 25: 235–42.
Chua AP-G, Lim LK-Y, Ng H, Chee CB-E, Wang YT. Outcome of a grocery voucher incentive scheme for low-income tuberculosis patients on directly observed therapy in Singapore. Singap Med J. 2015;56:274–9.
Migliori GB, Thong PM, Alffenaar J-W, et al. Gauging the impact of the COVID-19 pandemic on tuberculosis services: a global study. Eur Respir J. 2021. 58. https://doi.org/10.1183/13993003.01786-2021
Morishita F. COVID-19 impact on TB notification in the Western Pacific Region. 2022.
Lönnroth K, Jaramillo E, Williams BG, Dye C, Raviglione M. Drivers of tuberculosis epidemics: the role of risk factors and social determinants. Soc Sci Med. 2009;68:2240–6.
Negin J, Abimbola S, Marais BJ. Tuberculosis among older adults–time to take notice. Int J Infect diseases: IJID: official publication Int Soc Infect Dis. 2015;32:135–7.
Sharma M, Onozaki I, Nunn P. TB in older people in Asia: why it is important. Int J Tuberc Lung Dis. 2021;25:521–4.
Hong JM, Lee H, Menon NV, Lim CT, Lee LP, Ong CWM. Point-of-care diagnostic tests for tuberculosis disease. Sci Transl Med. 2022. published online April 6. https://doi.org/10.1126/scitranslmed.abj4124
Bea S, Lee H, Kim JH, et al. Adherence and Associated factors of treatment regimen in drug-susceptible tuberculosis patients. Front Pharmacol. 2021;12:625078.
Courtwright A, Turner AN. Tuberculosis and stigmatization: pathways and interventions. Public Health Rep. 2010;125:34–42.
Wang Y, Feng J, Zhang J, et al. Willingness to seek medical care for tuberculosis and associated factors among the elderly population in Shenzhen: a cross-sectional study. BMJ Open. 2021;11:e051291.
Watts K. Is Australia neglecting the local Topography when it comes to Catastrophic costs and ending tuberculosis? Trop Med Infect Disease. 2018;3:126.
Wang Y, Gan Y, Zhang J, et al. Analysis of the current status and associated factors of tuberculosis knowledge, attitudes, and practices among elderly people in Shenzhen: a cross-sectional study. BMC Public Health. 2021;21:1163.
Download references
Acknowledgements
We would like to thank Jeffery Cutter, Jun Yang Tay, and Shera Tan of the Singapore TB Program for verifying the section on Singapore’s experience.
The author(s) received no specific funding for this work.
Author information
Kerri Viney, Ben Marais, Heejin Kim, Seiya Kato, Yuhong Liu, Catherine W.M. Ong and Tauhid Islam are joint senior authors.
Authors and Affiliations
Saw Swee Hock School of Public Health, National University of Singapore and National University Health System, Singapore, Singapore
Alvin Kuo Jing Teo & Siyan Yi
Faculty of Medicine and Health, University of Sydney, Sydney, NSW, Australia
Alvin Kuo Jing Teo & Ben Marais
World Health Organization, Regional Office for the Western Pacific, Manila, Philippines
Kalpeshsinh Rahevar, Fukushi Morishita, Manami Yanagawa, Kyung Hyun Oh & Tauhid Islam
Division of Infectious Diseases, Department of Medicine, National University Hospital, Singapore, Singapore
Catherine W.M. Ong
Research Institute of Tuberculosis, Anti-Tuberculosis Association, Tokyo, Japan
Takashi Yoshiyama, Akihiro Ohkado, Lisa Kawatsu, Norio Yamada, Kazuhiro Uchimura & Seiya Kato
Korean National Tuberculosis Association, Seoul, Republic of Korea
Youngeun Choi & Heejin Kim
Office of International Cooperation, Innovation Alliance on Tuberculosis Diagnosis and Treatment, Beijing, China
KHANA Center for Population Health Research, Phnom Penh, Cambodia
Center for Global Health Research, Public Health Program, Touro University California, Vallejo, CA, USA
Global Tuberculosis Programme, World Health Organization, Geneva, Switzerland
Kerri Viney
The University of Sydney Institute for Infectious Diseases (Sydney ID) and the Centre of Research Excellence in Tuberculosis (TB-CRE), Sydney, NSW, Australia
Beijing Chest Hospital, Capital Medical University, Beijing, China
Infectious Diseases Translational Research Programme, Department of Medicine, National University of Singapore, Singapore, Singapore
Institute of Health Innovation and Technology (iHealthtech), National University of Singapore, Singapore, Singapore
Division of Infectious Diseases, Department of Medicine, Woodlands Health, Singapore, Singapore
You can also search for this author in PubMed Google Scholar
Contributions
KR, FM, TI, and SY conceptualised the study. AA, TY, AO, LK, NY, KU, YC, ZC, SK, YL, and CWMO contributed to the country experiences reported in this study. AKJT collated the information. AKJT, BM, KV, KR, FM, MY, and KHO wrote the initial draft. All authors critically reviewed the manuscript and approved the final version.
Corresponding author
Correspondence to Kalpeshsinh Rahevar .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests. The authors alone are responsible for the views expressed in this article, and they do not necessarily represent the views, decisions, or policies of the institutions with which they are affiliated.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article has been updated to correct a typo and a missing disclaimer.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Teo, A., Rahevar, K., Morishita, F. et al. Tuberculosis in older adults: case studies from four countries with rapidly ageing populations in the western pacific region. BMC Public Health 23 , 370 (2023). https://doi.org/10.1186/s12889-023-15197-7
Download citation
Received : 28 October 2022
Accepted : 02 February 2023
Published : 21 February 2023
DOI : https://doi.org/10.1186/s12889-023-15197-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Best practices
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Case Report
- Open access
- Published: 01 April 2024
Unusual presentation of miliary tuberculosis in a 12-year-old girl: a case report
- Mahsa Kamali 1 ,
- Mohammad Reza Navaeifar 1 ,
- Ali Abbaskhanian 1 ,
- Azin Hajialibeig 1 ,
- Farnaz Godazandeh 2 ,
- Mahsa Salehpour 1 &
- Mohammad Sadegh Rezai 1
BMC Pediatrics volume 24 , Article number: 223 ( 2024 ) Cite this article
Metrics details
Miliary tuberculosis (TB) is a lethal hematogenous spread form of mycobacterium tuberculosis with approximately 15–20% mortality rate in children. The present report highlights the clinical manifestations of an unusual presentation of miliary tuberculosis in a 12-year-old girl.
Case presentation
In this case, extensive lung involvement was presented despite the absence of respiratory symptoms. Also, some central hypo-intense with hyper-intense rim nodules were detected in the brain’s pons, right cerebral peduncles and lentiform nucleus.
The results of this study showed that severe miliary TB may occur even in a person who received the Bacille Calmette-Guérin (BCG) vaccine.
Peer Review reports
Tuberculosis (TB), caused by mycobacteria, is a preventable and curable disease with 1.5 million mortality annually most of them live in low and middle-income countries [ 1 ]. Intracranial tuberculosis (ITB) is an unusual and rare presentation of extrapulmonary tuberculosis [ 2 ]. The incidence of ITB is 5–30% of all intracranial lesions [ 3 ]. Nevertheless, it often remains underestimated [ 4 ]. Disseminated TB and miliary TB had similar pathogenesis but the anatomical-pathological findings are different [ 5 ]. Disseminated TB is an important cause of mortality and morbidity in children under 15 years old especially in developing countries [ 6 ]. Disseminated TB describing as entering the bacteria into the systemic circulation, then they multiply and infect extrapulmonary organs [ 7 ]. They account for highly variable clinical manifestations including fever, weight loss, anorexia and nocturnal sweating [ 8 ]. Miliary TB is a lethal hematogenous spread form of mycobacterium tuberculosis to several organs, diagnosed by the presence of a diffuse miliary infiltrate on a chest X-ray, CT scan and pathological evidence [ 9 ]. Peripheral lymphadenopathy and hepatosplenomegaly are the most common childhood military TB signs. The mortality rate of childhood miliary TB is approximately 15–20% [ 10 , 11 ]. As a huge challenge, the nonspecific clinical features of miliary TB often result in delayed diagnosis followed by a poor prognosis condition [ 12 ]. Also, this clinically silent TB leads to inadequate treatment in young children [ 13 ]. So, in children, considering ITB as a differential diagnosis is important. The present case report highlights the clinical presentation of unusual miliary TB evidence in a 12 years old girl.
A 12-year-old girl was admitted to a general hospital, in one of the western cities of Mazandaran province, with chief complaints of muscle atonia, and foam coming from the mouth for 20 s following fever and transient left hemiparesis. Ten minutes later, she agitated and presented generalized tonic-clonic movements lasting for 15 min and decreased consciousness following urinary incontinence. During this episode, she didn’t have foam coming from her mouth. She was intubated immediately and transferred to the PICU (Pediatric intensive care unit) of a tertiary hospital, in Sari, Mazandaran province. She had been visited by a general physician due to fever (T = 38.5 o c), vomiting (digested food particles and non-bloody), diplopia and headache one week before hospitalization and received symptomatic treatment. With relative recovery, the signs and symptoms aggravated the night before hospital admission. Her family reported unintentional weight loss accompanying anorexia and weakness from two months ago, but additional imaging was not performed.
Medical history and physical examination were as follows: The initial vital signs were blood pressure: 105/70 mmHg, the pulse rate: 110 beats per minute, respiratory rate: 22 per minute, axillary temperature: 37.4 o c and SPO2: 98% (intubated). Skin: Negative in terms of petechia, purpura and ecchymosis. Eyes: pale conjunctiva. Extremities: 1 + deep tendon reflexes. The tone and power of muscle were normal and there were not any signs of cerebellar or basal ganglion involvement. Lymph node: No lymphadenopathy. Chest and lung: No chest deformity, she was intubated, and symmetric lung sounds. Abdomen: No distention and organomegaly. No sign and symptom of increased intracranial pressure. She had no history of contact with Coronavirus disease 2019 (COVID-19) patients, contaminated water, rice field and trauma. She had fainted in her childhood period following excessive activity (medical follow-up showed cardiac chamber defect) and improved spontaneously when she was 3 years old. She completed all doses of recommended childhood vaccines but did not receive the COVID-19 vaccine. She had a drug allergy to Cefixime and penicillin and a food allergy to eggplant. Initially, her family did not report a positive family history of TB, but after the final diagnosis, they declared that her uncle died following TB 3 years ago.
Para-clinical investigations: The result of COVID-19 Reverse transcription polymerase chain reaction (RT-PCR) and galactomannan level was negative. Also, the levels of HIV (human immunodeficiency virus) antibody, Venereal disease research laboratory (VDRL), CD4 (cluster of differentiation 4), CD19 and Complement hemolysis (CH50) were normal. The echocardiography showed mild Tricuspid valve regurgitation and mild pulmonary valve insufficiency. Also, there was no pulmonary hypertension. Based on the possible COVID-19 bilateral involvement in chest X-ray and lung CT scan, Pro-BNP, D-dimer and troponin levels were requested. Only the D-dimer level was high. It was 1710. The lumbar puncture (LP) was done on the first day of the PICU admission. The Cerebrospinal fluid (CSF) analysis results are presented in Table 1 . Although, the girl had no signs and symptoms of meningitis including Brudzinski’s and Kernig’s signs, there was CSF involvement. CSF analysis showed increased levels of protein and WBC. The patient had not the coughing or sputum, so the gastric aspirate culture PCR (three times) had been done and the result was positive for miliary TB. Findings of the chest X-ray (Fig. 1 ), lung CT scan (Figs. 2 and 3 ) and brain MRI (Fig. 4 ) were suggestive of caseating tuberculomas. Finally, the miliary TB was diagnosed based on brain MRI, positive gastric aspirate culture and also two organs involvement. AP chest x-ray demonstrates wide spread tiny nodular opacities distributed throughout both lungs. The PPD test were normal.
A pediatric infectious diseases specialist prescribed rifampin, ethambutol, pyrazinamide, isoniazid and vitamin B6 (For prevention of the side effect of isoniazid) based on the miliary TB evidence in MRI. The anti-tuberculosis medication dosage was adjusted due to elevated AST and ALT levels 10 days later. So, the rifampin and isoniazid were discontinued and in the follow-up due to the normal levels of AST and ALT, the rifampin and isoniazid were added to the medication regimen. At the time of discharge, approximately one month later, the gastric aspiration result was negative. She was discharged in stable condition with fixed-dose combination anti-TB medication (III), acid folic and vitamin B6 tablets daily. On her follow-up, AST and ALT levels were normal. Also, her medication changed to two-drug formulations. The girl had been follow-up for at least one year and the MRI finding and gastric aspirate on follow-up were normal.
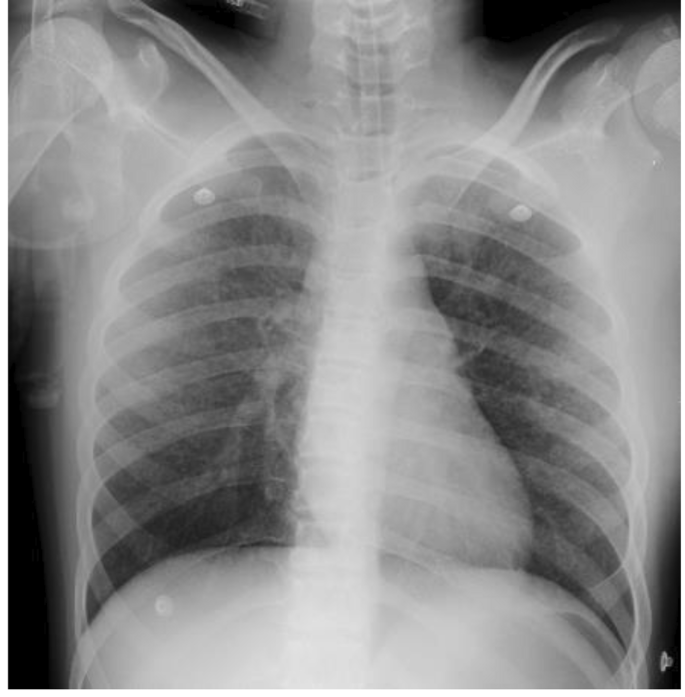
CXR. PICU admission: AP chest x-ray demonstrates wide spread tiny nodular opacities distributed throughout both lungs
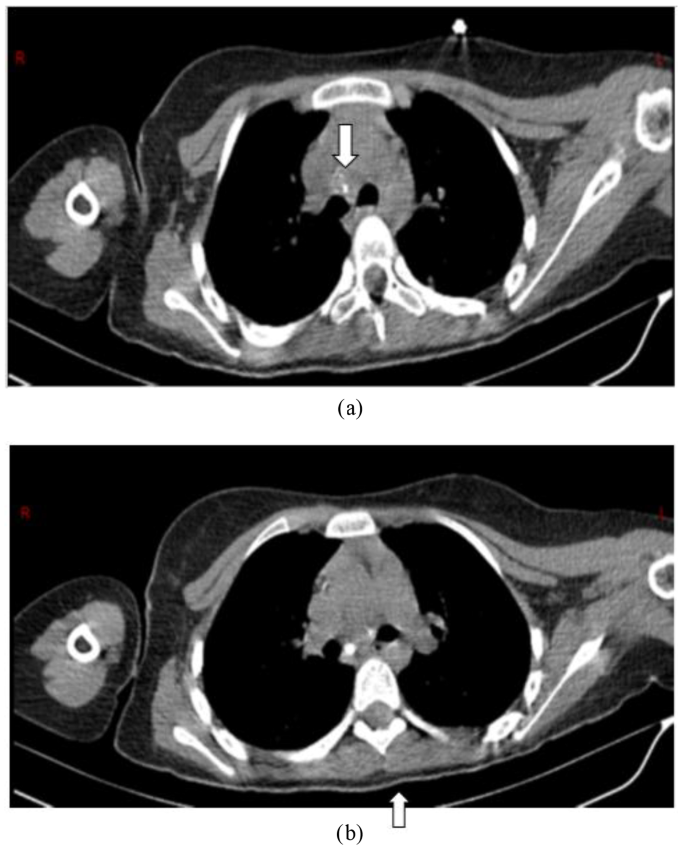
a, b ) Chest CT scan without contrast (mediastinal window): Some calcified lymphadenopathies in the right paratracheal and subcarinal space of the middle mediastinum (white arrows)
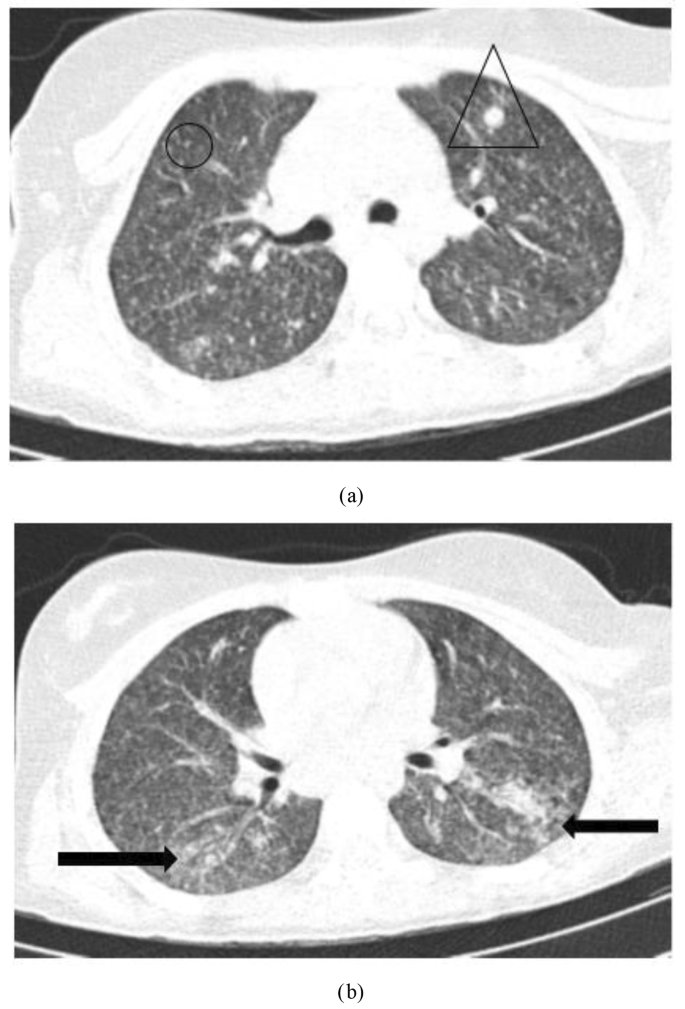
a, b ) Chest CT scan without contrast (Lung window): Diffuse multiple miliary nodules (black circle) and some scattered micronodules in a random distribution (black triangle) in both lungs associated with patchy consolidation (black arrows) in lower lobes, in favor of pulmonary TB
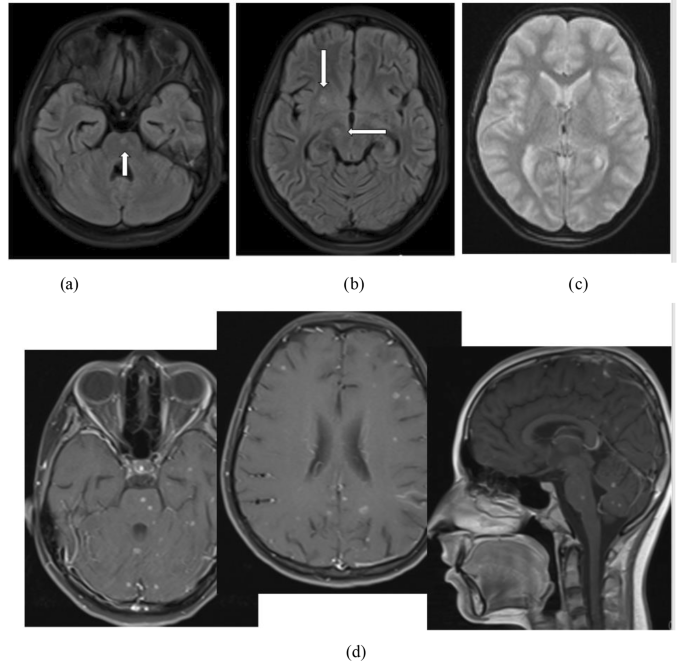
Brain MRI without contrast: 4- a & 4- b ) Flair sequence: some central hypo-intense with hyper-intense rim nodules in the pons, right cerebral peduncles and lentiform nucleus (white arrows). 4- c ) DWI/ADC: no restricted diffusion. 4- d ) Contrast–enhanced MRI: Diffuse Multiple rim-enhancing nodules in both cerebral, cerebellar hemispheres and brainstem. These findings are suggestive of caseating tuberculomas with tuberculous meningitis. DWI: Diffusion-weighted imaging – ADC: Apparent diffusion coefficient
In the present case report, the miliary TB evidence was presented in a 12 years old girl. Miliary TB has been more prevalent in middle age and older people than children [ 14 , 15 ]. Also, 60% of the cases are male with a mean age of 55 years in studies [ 16 , 17 , 18 ]. Although the mean age of miliary TB patients has increased, the rates remain relatively low in children [ 19 , 20 ]. In the present study, the unusual miliary TB pattern was seen in a 12 years old girl. The miliary TB in young patients is reported in TB-endemic countries [ 21 ]. Based on the results of a retrospective descriptive study in South Africa, 32.7% of children were TB meningitis. Also, the recent study reported 43.3% of children drug resistant was the main reason for hospitalization [ 22 ]. But, in our case, the girl had no drug resistance. Approximately 13% of the TB cases suffer from HIV infections [ 23 ]. TB becomes more generalized and affects more than one organ when progressive immunosuppression occurs [ 24 ]. However, the present case didn’t have HIV infection as co-infection or other immunodeficiency condition. Corticosteroid therapy can reactivate cryptic TB [ 25 ]. Song et al. reported a 36-year-old man who underwent corticosteroid therapy and two weeks later, he experienced an acute exacerbation of miliary TB [ 26 ]. But in our study, the patient had no history of recent corticosteroid therapy. Considering increased the number of BCG-vaccinated children and improving the diet status of children, we see the modified clinical profile of neurotuberculosis including TB meningitis nowadays with wide varieties of clinical manifestations according to the site of the brain lesion [ 27 ]. The clinical presentation of neurotuberculosis may be nonspecific leading to delayed treatment and poor clinical outcome [ 28 ]. The present case had diffuse multiple rim-enhancing nodules in both cerebral, cerebellar hemispheres and brainstem in the brain. The brain and central nervous systems are two target organs of mycobacterium tuberculosis that cause serious and dangerous forms of extrapulmonary tuberculosis [ 29 ]. The most obvious initial clinical symptoms of our case were fever, weight loss, anorexia and seizure. Other studies reported fever, cough, seizure, diarrhea, hepatomegaly, splenomegaly, jaundice, anorexia and weight loss as the most common clinical presentations in children [ 6 , 30 , 31 ]. A male three-months Brazilian infant was admitted with nocturnal fever, sweating and coughing 10 days before hospitalization and he was not responsive to antibiotic therapy. The results of the chest X-ray showed bilateral miliary TB and also CNS TB based on the CT-scan report [ 32 ]. Similar to our case, the recent case showed early diagnosis and treatment in endemic areas. Delayed diagnosis in miliary TB patients can cause serious complications including cranial nerve involvement, convulsions and death [ 16 ] as a seizure occurred in our case. Machida et al.’s report showed 1% of TB patients had CNS involvement which is about a high mortality rate and permanent neurological sequelae [ 33 ]. Fortunately, in the present case, follow-up interventions showed no neurological sequelae and she was in good general condition. Multiple diagnostic tests are provided to detect miliary TB, including PCR, sputum smear and acid-fast staining, in addition to histopathological findings but radiology plays a major role in this regard [ 34 ]. In this case, despite the absence of respiratory symptoms and non-significant lung involvement in chest X-ray, extensive lung involvement was seen including diffuse multiple miliary nodules. Also, a chest CT scan revealed some scattered micronodules in a random distribution in both lungs associated with patchy consolidation in lower lobes in favor of pulmonary TB. Additionally, in the brain, some central hypo-intense with hyper-intense rim nodules in the pons, right cerebral peduncles and lentiform nucleus, multiple diffuse rims enhancing nodules in both cerebral, cerebellar hemispheres and brainstem were obvious.
The COVID-19 pandemic has emerged new conditions, including neuro-COVID which has presented by lung involvement and seizure [ 35 ]. During the COVID-19 pandemic, miliary TB should be considered in TB endemic areas due to neuro-COVID diagnosis.
Our study showed that teenage patients might present extensive lung involvement in favor of miliary TB even in the absence of respiratory symptoms. Also, we found that severe miliary TB may occur even in a person who received the bacille Calmette-Guérin (BCG) vaccine. In an Iranian study, in 15 children aged under 72 months, disseminated BCG infection occurred after BCG vaccination [ 36 ]. Also, in patients with CNS symptoms including seizure especially in TB endemic areas, miliary TB should be considered as a differential diagnosis, to prevent delay in diagnosis and treatment. We live in the TB endemic area. So, when a patient is admitted with a decreased level of consciousness and there is no reasonable cause, we should consider TB as a differential diagnosis. In the current case report, due to early diagnosis and treatment, neurological sequelae were not observed.
Data Availability
Due to the privacy of the patients, the data generated during the current study are not publicly available but are available from the corresponding author upon reasonable request.
WHO. Health topics:Tuberculosis 2022 [updated 2020. Available from: https://www.who.int/health-topics/tuberculosis#tab=tab_1 .
Frioui S, Jemni S. Cerebral tuberculoma: an entity not to ignore. Pan Afr Med J. 2016;24(1).
Zahrou F, Elallouchi Y, Ghannane H, Benali SA, Aniba K. Diagnosis and management of intracranial tuberculomas: about 2 cases and a review of the literature. Pan Afr Med J. 2019;34.
Alharbi A, Khairy S, Al Sufiani F, Alkhani A. Intracranial tuberculomas: a case report of clinical, radiological, and pathological characteristics. Int J Surg Case Rep. 2021;88:106477.
Article PubMed PubMed Central Google Scholar
Buonsenso D, Mariani F, Morello R, Song R. State-of-the-art of miliary Tuberculosis in children: protocol for a scoping review of the literature. F1000Research. 2023;12(309):309.
Article Google Scholar
Khan FY. Review of literature on disseminated Tuberculosis with emphasis on the focused diagnostic workup. J Fam Commun Med. 2019;26(2):83.
Krishnan N, Robertson BD, Thwaites G. The mechanisms and consequences of the extra-pulmonary dissemination of Mycobacterium tuberculosis. Tuberculosis. 2010;90(6):361–6.
Article CAS PubMed Google Scholar
Khan FY, Dosa K, Fuad A, Ibrahim W, Alaini A, Osman L, et al. Disseminated Tuberculosis among adult patients admitted to Hamad general hospital, Qatar: a five year hospital based study. Mycobact Dis. 2016;6(212):104172.
Google Scholar
Sharma SK, Mohan A. Miliary tuberculosis. Tuberculosis and nontuberculous mycobacterial infections. 2021:415 – 35.
Starke JR. Tuberculosis in infants and children. Tuberculosis and nontuberculous mycobacterial infections. 2021:456 – 75.
Triasih R, Helmi R, Laksanawati IS. Clinical profile and outcome of extrapulmonary Tuberculosis in children in Indonesia. Pediatr Respirol Crit Care Med. 2018;2(3):51.
Letchuman V, Guillotte AR, Lundy PA, Dharia A, Lakis NS, Camarata PJ. Intracranial tuberculoma: a rare complication of extrapulmonary Tuberculosis. Illustrative case. J Neurosurgery: Case Lessons. 2022;4(1).
Abuhamed M, Bo X, Yan C. Central nervous system tuberculomas: a review article. Am J Infect Dis. 2008;4(2):168–73.
Lee J, Lim JK, Kim EJ, Lee DH, Kim YK, Yoo SS, et al. Comparison of clinical manifestations and treatment outcome according to age groups in adult patients with miliary Tuberculosis. J Thorac Disease. 2018;10(5):2881.
Munt PW. Miliary Tuberculosis in the chemotherapy era: with a clinical review in 69 American adults. Medicine. 1972;51(2):139–55.
Hosseini MJ, IMANI FA. Miliary tuberculosis with empyema, a case report. 2010.
Takahashi K, Akatsuka M, Yamamoto S. Miliary Tuberculosis complicated with acute respiratory distress syndrome and hemophagocytic syndrome. Oxf Med Case Rep. 2022;2022(1):omab142.
Arfaoui H, Aidou S, Bahma H, Jabri H, El Khattabi W, Afif H. Miliary Tuberculosis: Moroccan series of 101 cases. SAS J Med. 2022;2:100–5.
Sahn SA, Neff TA. Miliary Tuberculosis. Am J Med. 1974;56(4):495–505.
Kilgore J, Pelletier J, Becken B, Kenny S, Das S, Parnell L. Miliary Tuberculosis in a paediatric patient with psoriasis. BMJ Case Reports CP. 2021;14(3):e237580.
organization WH, Tuberculosis, WHO. ; 2021 [Available from: https://www.who.int/health-topics/tuberculosis#tab=tab_1 .
Musonda H, Rose P, Switala J, Schaaf H. Paediatric admissions to a TB hospital: reasons for admission, clinical profile and outcomes. Int J Tuberc Lung Dis. 2022;26(3):217–23.
Pinzon RT, Wijaya VO, Paramitha D. Encephalitis due to miliary Tuberculosis in a patient with human immunodeficiency virus: a case report. J Clin Tuberculosis Other Mycobact Dis. 2021;23:100230.
Article CAS Google Scholar
Letang E, Ellis J, Naidoo K, Casas EC, Sánchez P, Hassan-Moosa R, et al. Tuberculosis-HIV co-infection: progress and challenges after two decades of global antiretroviral treatment roll-out. Arch Bronconeumol. 2020;56(7):446–54.
Article PubMed Google Scholar
Sahn SA, Lakshminarayan S. Tuberculosis after corticosteroid therapy. Br J Dis Chest. 1976;70:195–205.
Song M, Kim SJ, Yoo JY. Corticosteroid-induced exacerbation of cryptic miliary Tuberculosis to acute respiratory distress syndrome: a case report. Medicine. 2020;99:46.
Yeredla VVR, Tammali S, Ravula CJ, Kalivela S. Changing trends in the clinical profile of childhood in Tuberculosis patients-at a tertiary centre. EUREKA: Health Sciences. 2023;2:24–32.
de Gusmão Filho FA, Marques HHdS, Marques-Dias MJ, Ramos SRS. Tuberculose do sistema nervoso central em crianças: 1. Apresentação clínica E Laboratorial. Arq Neuropsiquiatr. 2001;59:71–6.
Babamahmoodi F, Alikhani A, Yazdani Charati J, Ghovvati A, Ahangarkani F, Delavarian L et al. Clinical epidemiology and paraclinical findings in tuberculosis patients in north of Iran. BioMed research international. 2015;2015.
Tanrikulu C, Gürkan F, DAĞLI CE, Ayfer G, Süner A. A comparative review of pediatric and adult patients with miliary Tuberculosis. Eur J Gen Med. 2007;4(2).
Gurkan F, Bosnak M, Dikici B, Bosnak V, Yaramis A, Tas MA, et al. Miliary Tuberculosis in children: a clinical review. Scand J Infect Dis. 1998;30(4):359–62.
de Andrade MR, Lacerda CA, Vicente JFC, Lamounier JA. An infant with central nervous system tuberculosis and miliary tuberculosis.
Machida M, Toyoda K, Matsuda M, Sumida K, Yamamoto A, Sakurai K, et al. Extensive perivascular dissemination of cerebral miliary tuberculomas: a case report and review of the literature. Acta Radiol Open. 2018;7(12):2058460118817918.
PubMed PubMed Central Google Scholar
Mortazavi-Moghaddam SGR, Sharifzadeh GR, Rezvani MR. Status of exudative pleural effusion in adults of South Khorasan Province, northeast Iran: pleural Tuberculosis tending toward elderly. Iran J Med Sci. 2016;41(4):322.
PubMed Google Scholar
Frontera J, Mainali S, Fink EL, Robertson CL, Schober M, Ziai W, et al. Global consortium study of neurological dysfunction in COVID-19 (GCS-NeuroCOVID): study design and rationale. Neurocrit Care. 2020;33(1):25–34.
Article CAS PubMed PubMed Central Google Scholar
Rezai MS, Khotaei G, Mamishi S, Kheirkhah M, Parvaneh N. Disseminated bacillus Calmette–Guerin Infection after BCG vaccination. J Trop Pediatr. 2008;54(6):413–6.
Download references
Acknowledgements
The authors would like to extend their gratitude to all the healthcare providers who were involved in the treatment of the present case.
Author information
Authors and affiliations.
Pediatric Infectious Diseases Research Center, Communicable Diseases Institute, Mazandaran University of Medical Sciences, Sari, Iran
Mahsa Kamali, Mohammad Reza Navaeifar, Ali Abbaskhanian, Azin Hajialibeig, Mahsa Salehpour & Mohammad Sadegh Rezai
Department of Radiology, Faculty of Medicine, Mazandaran University of medical sciences, Sari, Iran
Farnaz Godazandeh
You can also search for this author in PubMed Google Scholar
Contributions
MR: critically edited the manuscript. MK: Drafting the manuscript. MN, AA, AH, MS, MR: Involved in treatment. FG: Interpreting the CXR, MRI and CT-scan. All authors approved final version of the manuscript.
Corresponding author
Correspondence to Mohammad Sadegh Rezai .
Ethics declarations
Ethics approval and consent to participate.
The research objectives were explained to the subjects, and they were ensured of confidentiality terms regarding their personal information.
Consent for publication
Informed consent for publication was obtained from patient’s legal guardian.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Kamali, M., Navaeifar, M.R., Abbaskhanian, A. et al. Unusual presentation of miliary tuberculosis in a 12-year-old girl: a case report. BMC Pediatr 24 , 223 (2024). https://doi.org/10.1186/s12887-023-04427-x
Download citation
Received : 18 February 2023
Accepted : 16 November 2023
Published : 01 April 2024
DOI : https://doi.org/10.1186/s12887-023-04427-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Tuberculosis
- Mycobacteria
BMC Pediatrics
ISSN: 1471-2431
- Submission enquiries: [email protected]
- General enquiries: [email protected]
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Case study: 33-year-old female presents with chronic sob and cough.
Sandeep Sharma ; Muhammad F. Hashmi ; Deepa Rawat .
Affiliations
Last Update: February 20, 2023 .
- Case Presentation
History of Present Illness: A 33-year-old white female presents after admission to the general medical/surgical hospital ward with a chief complaint of shortness of breath on exertion. She reports that she was seen for similar symptoms previously at her primary care physician’s office six months ago. At that time, she was diagnosed with acute bronchitis and treated with bronchodilators, empiric antibiotics, and a short course oral steroid taper. This management did not improve her symptoms, and she has gradually worsened over six months. She reports a 20-pound (9 kg) intentional weight loss over the past year. She denies camping, spelunking, or hunting activities. She denies any sick contacts. A brief review of systems is negative for fever, night sweats, palpitations, chest pain, nausea, vomiting, diarrhea, constipation, abdominal pain, neural sensation changes, muscular changes, and increased bruising or bleeding. She admits a cough, shortness of breath, and shortness of breath on exertion.
Social History: Her tobacco use is 33 pack-years; however, she quit smoking shortly prior to the onset of symptoms, six months ago. She denies alcohol and illicit drug use. She is in a married, monogamous relationship and has three children aged 15 months to 5 years. She is employed in a cookie bakery. She has two pet doves. She traveled to Mexico for a one-week vacation one year ago.
Allergies: No known medicine, food, or environmental allergies.
Past Medical History: Hypertension
Past Surgical History: Cholecystectomy
Medications: Lisinopril 10 mg by mouth every day
Physical Exam:
Vitals: Temperature, 97.8 F; heart rate 88; respiratory rate, 22; blood pressure 130/86; body mass index, 28
General: She is well appearing but anxious, a pleasant female lying on a hospital stretcher. She is conversing freely, with respiratory distress causing her to stop mid-sentence.
Respiratory: She has diffuse rales and mild wheezing; tachypneic.
Cardiovascular: She has a regular rate and rhythm with no murmurs, rubs, or gallops.
Gastrointestinal: Bowel sounds X4. No bruits or pulsatile mass.
- Initial Evaluation
Laboratory Studies: Initial work-up from the emergency department revealed pancytopenia with a platelet count of 74,000 per mm3; hemoglobin, 8.3 g per and mild transaminase elevation, AST 90 and ALT 112. Blood cultures were drawn and currently negative for bacterial growth or Gram staining.
Chest X-ray
Impression: Mild interstitial pneumonitis
- Differential Diagnosis
- Aspiration pneumonitis and pneumonia
- Bacterial pneumonia
- Immunodeficiency state and Pneumocystis jiroveci pneumonia
- Carcinoid lung tumors
- Tuberculosis
- Viral pneumonia
- Chlamydial pneumonia
- Coccidioidomycosis and valley fever
- Recurrent Legionella pneumonia
- Mediastinal cysts
- Mediastinal lymphoma
- Recurrent mycoplasma infection
- Pancoast syndrome
- Pneumococcal infection
- Sarcoidosis
- Small cell lung cancer
- Aspergillosis
- Blastomycosis
- Histoplasmosis
- Actinomycosis
- Confirmatory Evaluation
CT of the chest was performed to further the pulmonary diagnosis; it showed a diffuse centrilobular micronodular pattern without focal consolidation.
On finding pulmonary consolidation on the CT of the chest, a pulmonary consultation was obtained. Further history was taken, which revealed that she has two pet doves. As this was her third day of broad-spectrum antibiotics for a bacterial infection and she was not getting better, it was decided to perform diagnostic bronchoscopy of the lungs with bronchoalveolar lavage to look for any atypical or rare infections and to rule out malignancy (Image 1).
Bronchoalveolar lavage returned with a fluid that was cloudy and muddy in appearance. There was no bleeding. Cytology showed Histoplasma capsulatum .
Based on the bronchoscopic findings, a diagnosis of acute pulmonary histoplasmosis in an immunocompetent patient was made.
Pulmonary histoplasmosis in asymptomatic patients is self-resolving and requires no treatment. However, once symptoms develop, such as in our above patient, a decision to treat needs to be made. In mild, tolerable cases, no treatment other than close monitoring is necessary. However, once symptoms progress to moderate or severe, or if they are prolonged for greater than four weeks, treatment with itraconazole is indicated. The anticipated duration is 6 to 12 weeks total. The response should be monitored with a chest x-ray. Furthermore, observation for recurrence is necessary for several years following the diagnosis. If the illness is determined to be severe or does not respond to itraconazole, amphotericin B should be initiated for a minimum of 2 weeks, but up to 1 year. Cotreatment with methylprednisolone is indicated to improve pulmonary compliance and reduce inflammation, thus improving work of respiration. [1] [2] [3]
Histoplasmosis, also known as Darling disease, Ohio valley disease, reticuloendotheliosis, caver's disease, and spelunker's lung, is a disease caused by the dimorphic fungi Histoplasma capsulatum native to the Ohio, Missouri, and Mississippi River valleys of the United States. The two phases of Histoplasma are the mycelial phase and the yeast phase.
Etiology/Pathophysiology
Histoplasmosis is caused by inhaling the microconidia of Histoplasma spp. fungus into the lungs. The mycelial phase is present at ambient temperature in the environment, and upon exposure to 37 C, such as in a host’s lungs, it changes into budding yeast cells. This transition is an important determinant in the establishment of infection. Inhalation from soil is a major route of transmission leading to infection. Human-to-human transmission has not been reported. Infected individuals may harbor many yeast-forming colonies chronically, which remain viable for years after initial inoculation. The finding that individuals who have moved or traveled from endemic to non-endemic areas may exhibit a reactivated infection after many months to years supports this long-term viability. However, the precise mechanism of reactivation in chronic carriers remains unknown.
Infection ranges from an asymptomatic illness to a life-threatening disease, depending on the host’s immunological status, fungal inoculum size, and other factors. Histoplasma spp. have grown particularly well in organic matter enriched with bird or bat excrement, leading to the association that spelunking in bat-feces-rich caves increases the risk of infection. Likewise, ownership of pet birds increases the rate of inoculation. In our case, the patient did travel outside of Nebraska within the last year and owned two birds; these are her primary increased risk factors. [4]
Non-immunocompromised patients present with a self-limited respiratory infection. However, the infection in immunocompromised hosts disseminated histoplasmosis progresses very aggressively. Within a few days, histoplasmosis can reach a fatality rate of 100% if not treated aggressively and appropriately. Pulmonary histoplasmosis may progress to a systemic infection. Like its pulmonary counterpart, the disseminated infection is related to exposure to soil containing infectious yeast. The disseminated disease progresses more slowly in immunocompetent hosts compared to immunocompromised hosts. However, if the infection is not treated, fatality rates are similar. The pathophysiology for disseminated disease is that once inhaled, Histoplasma yeast are ingested by macrophages. The macrophages travel into the lymphatic system where the disease, if not contained, spreads to different organs in a linear fashion following the lymphatic system and ultimately into the systemic circulation. Once this occurs, a full spectrum of disease is possible. Inside the macrophage, this fungus is contained in a phagosome. It requires thiamine for continued development and growth and will consume systemic thiamine. In immunocompetent hosts, strong cellular immunity, including macrophages, epithelial, and lymphocytes, surround the yeast buds to keep infection localized. Eventually, it will become calcified as granulomatous tissue. In immunocompromised hosts, the organisms disseminate to the reticuloendothelial system, leading to progressive disseminated histoplasmosis. [5] [6]
Symptoms of infection typically begin to show within three to17 days. Immunocompetent individuals often have clinically silent manifestations with no apparent ill effects. The acute phase of infection presents as nonspecific respiratory symptoms, including cough and flu. A chest x-ray is read as normal in 40% to 70% of cases. Chronic infection can resemble tuberculosis with granulomatous changes or cavitation. The disseminated illness can lead to hepatosplenomegaly, adrenal enlargement, and lymphadenopathy. The infected sites usually calcify as they heal. Histoplasmosis is one of the most common causes of mediastinitis. Presentation of the disease may vary as any other organ in the body may be affected by the disseminated infection. [7]
The clinical presentation of the disease has a wide-spectrum presentation which makes diagnosis difficult. The mild pulmonary illness may appear as a flu-like illness. The severe form includes chronic pulmonary manifestation, which may occur in the presence of underlying lung disease. The disseminated form is characterized by the spread of the organism to extrapulmonary sites with proportional findings on imaging or laboratory studies. The Gold standard for establishing the diagnosis of histoplasmosis is through culturing the organism. However, diagnosis can be established by histological analysis of samples containing the organism taken from infected organs. It can be diagnosed by antigen detection in blood or urine, PCR, or enzyme-linked immunosorbent assay. The diagnosis also can be made by testing for antibodies again the fungus. [8]
Pulmonary histoplasmosis in asymptomatic patients is self-resolving and requires no treatment. However, once symptoms develop, such as in our above patient, a decision to treat needs to be made. In mild, tolerable cases, no treatment other than close monitoring is necessary. However, once symptoms progress to moderate or severe or if they are prolonged for greater than four weeks, treatment with itraconazole is indicated. The anticipated duration is 6 to 12 weeks. The patient's response should be monitored with a chest x-ray. Furthermore, observation for recurrence is necessary for several years following the diagnosis. If the illness is determined to be severe or does not respond to itraconazole, amphotericin B should be initiated for a minimum of 2 weeks, but up to 1 year. Cotreatment with methylprednisolone is indicated to improve pulmonary compliance and reduce inflammation, thus improving the work of respiration.
The disseminated disease requires similar systemic antifungal therapy to pulmonary infection. Additionally, procedural intervention may be necessary, depending on the site of dissemination, to include thoracentesis, pericardiocentesis, or abdominocentesis. Ocular involvement requires steroid treatment additions and necessitates ophthalmology consultation. In pericarditis patients, antifungals are contraindicated because the subsequent inflammatory reaction from therapy would worsen pericarditis.
Patients may necessitate intensive care unit placement dependent on their respiratory status, as they may pose a risk for rapid decompensation. Should this occur, respiratory support is necessary, including non-invasive BiPAP or invasive mechanical intubation. Surgical interventions are rarely warranted; however, bronchoscopy is useful as both a diagnostic measure to collect sputum samples from the lung and therapeutic to clear excess secretions from the alveoli. Patients are at risk for developing a coexistent bacterial infection, and appropriate antibiotics should be considered after 2 to 4 months of known infection if symptoms are still present. [9]
Prognosis
If not treated appropriately and in a timely fashion, the disease can be fatal, and complications will arise, such as recurrent pneumonia leading to respiratory failure, superior vena cava syndrome, fibrosing mediastinitis, pulmonary vessel obstruction leading to pulmonary hypertension and right-sided heart failure, and progressive fibrosis of lymph nodes. Acute pulmonary histoplasmosis usually has a good outcome on symptomatic therapy alone, with 90% of patients being asymptomatic. Disseminated histoplasmosis, if untreated, results in death within 2 to 24 months. Overall, there is a relapse rate of 50% in acute disseminated histoplasmosis. In chronic treatment, however, this relapse rate decreases to 10% to 20%. Death is imminent without treatment.
- Pearls of Wisdom
While illnesses such as pneumonia are more prevalent, it is important to keep in mind that more rare diseases are always possible. Keeping in mind that every infiltrates on a chest X-ray or chest CT is not guaranteed to be simple pneumonia. Key information to remember is that if the patient is not improving under optimal therapy for a condition, the working diagnosis is either wrong or the treatment modality chosen by the physician is wrong and should be adjusted. When this occurs, it is essential to collect a more detailed history and refer the patient for appropriate consultation with a pulmonologist or infectious disease specialist. Doing so, in this case, yielded workup with bronchoalveolar lavage and microscopic evaluation. Microscopy is invaluable for definitively diagnosing a pulmonary consolidation as exemplified here where the results showed small, budding, intracellular yeast in tissue sized 2 to 5 microns that were readily apparent on hematoxylin and eosin staining and minimal, normal flora bacterial growth.
- Enhancing Healthcare Team Outcomes
This case demonstrates how all interprofessional healthcare team members need to be involved in arriving at a correct diagnosis. Clinicians, specialists, nurses, pharmacists, laboratory technicians all bear responsibility for carrying out the duties pertaining to their particular discipline and sharing any findings with all team members. An incorrect diagnosis will almost inevitably lead to incorrect treatment, so coordinated activity, open communication, and empowerment to voice concerns are all part of the dynamic that needs to drive such cases so patients will attain the best possible outcomes.
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Histoplasma Contributed by Sandeep Sharma, MD
Disclosure: Sandeep Sharma declares no relevant financial relationships with ineligible companies.
Disclosure: Muhammad Hashmi declares no relevant financial relationships with ineligible companies.
Disclosure: Deepa Rawat declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Sharma S, Hashmi MF, Rawat D. Case Study: 33-Year-Old Female Presents with Chronic SOB and Cough. [Updated 2023 Feb 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Review Palliative Chemotherapy: Does It Only Provide False Hope? The Role of Palliative Care in a Young Patient With Newly Diagnosed Metastatic Adenocarcinoma. [J Adv Pract Oncol. 2017] Review Palliative Chemotherapy: Does It Only Provide False Hope? The Role of Palliative Care in a Young Patient With Newly Diagnosed Metastatic Adenocarcinoma. Doverspike L, Kurtz S, Selvaggi K. J Adv Pract Oncol. 2017 May-Jun; 8(4):382-386. Epub 2017 May 1.
- Review Breathlessness with pulmonary metastases: a multimodal approach. [J Adv Pract Oncol. 2013] Review Breathlessness with pulmonary metastases: a multimodal approach. Brant JM. J Adv Pract Oncol. 2013 Nov; 4(6):415-22.
- A 50-Year Old Woman With Recurrent Right-Sided Chest Pain. [Chest. 2022] A 50-Year Old Woman With Recurrent Right-Sided Chest Pain. Saha BK, Bonnier A, Chong WH, Chenna P. Chest. 2022 Feb; 161(2):e85-e89.
- Suicidal Ideation. [StatPearls. 2024] Suicidal Ideation. Harmer B, Lee S, Duong TVH, Saadabadi A. StatPearls. 2024 Jan
- Review Domperidone. [Drugs and Lactation Database (...] Review Domperidone. . Drugs and Lactation Database (LactMed®). 2006
Recent Activity
- Case Study: 33-Year-Old Female Presents with Chronic SOB and Cough - StatPearls Case Study: 33-Year-Old Female Presents with Chronic SOB and Cough - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
University of Notre Dame
Notre Dame News
- Home ›
- News ›
Cancer therapies show promise in combating tuberculosis
Published: March 25, 2024
Author: Brandi Wampler

What could cancer teach us about tuberculosis? That’s a question Meenal Datta has been chasing since she was a graduate student.
Once the body’s immune system is infected with tuberculosis, it forms granulomas — tight clusters of white blood cells — in an attempt to wall off the infection-causing bacteria in the lungs. But more often than not, granulomas do more harm than good.
Charged with analyzing the similarities between granulomas and tumors, Datta discovered that both are structurally and functionally abnormal. In 2015, she and other researchers looked at the vascular structures of granulomas and showed that they are compromised and leaky just like tumor blood vessels, which limits drug delivery and successful treatment in both diseases.
“It was the first time we showed definitively that there was this pathophysiological similarity between these two diseases that present with different causes and symptoms,” said Datta, assistant professor of aerospace and mechanical engineering at the University of Notre Dame. “Cancer doesn’t sound anything like an infectious disease. And yet, here are two different diseases with the same problem of dysfunctional blood vessels.”
Now a study from the same team at the University of Notre Dame, Massachusetts General Hospital and the National Institutes of Health has identified a combination of medications that may improve blood flow within granulomas, benefiting drug delivery. Published in the Proceedings of the National Academy of Sciences , the study leverages decades of cancer research to study tuberculosis-affected lung tissue and improve treatment.
“Much like in tumors, many of the blood vessels in granulomas are compressed or squeezed shut — just like if you stepped on your garden hose,” said Datta, the first author on the study. “In cancer, we know that happens because of the growing tumor mass and the supportive protein scaffolding it puts down, called matrix. We thought maybe the same thing was happening in tuberculosis.”
The study confirmed that a similar phenomenon is occurring in granulomas — too much cell mass and protein scaffolding. This impaired function makes blood flow through blood vessels nearly impossible, crippling the ability to get a medication to the tuberculosis disease site.
Datta and her collaborators used losartan, an affordable drug used to treat high blood pressure. However, it also has the beneficial side effect of reducing the amount of matrix being created inside a granuloma, thus opening the compressed blood vessels and restoring blood flow.
Researchers then combined losartan with bevacizumab, a drug used by cancer patients to stop the overproduction of poorly formed blood vessels. With this two-pronged medicinal approach, Datta and the team were able to make the granuloma blood vessels function and behave more normally.
When the researchers applied the host-directed therapies losartan and bevacizumab along with antibiotics, they showed improved drug delivery and antibiotic concentration within granulomas.
Additionally, Datta’s graduate student Maksym Zarodniuk analyzed genome sequencing data produced by the team, and found that even without antibiotics, there was a reduction in tuberculosis bacteria within the granulomas.
“When we gave just those host-directed therapies, we were getting good treatment benefit even without adding the antibiotics. Those therapies were promoting the body’s inflammatory response to fight against the bacteria, which we did not expect,” Datta said.
For Datta, this study caps off a stretch of tuberculosis research that started when she began her doctoral research at Massachusetts General Hospital and Harvard Medical School in 2011, and has spanned multiple phases of her career. Tuberculosis, although largely controlled in the U.S., is still considered one of the deadliest infectious diseases worldwide.
“The advantage of the host-directed therapies we selected is that these agents or very similar drugs of the same class are already approved by regulatory agencies around the globe, and they are affordable,” Datta said. “We hope that our preclinical results will be found compelling enough to start a clinical trial to benefit tuberculosis patients.”
Today, Datta’s lab at the University of Notre Dame primarily focuses its research on understanding glioblastoma , a rare treatment-resistant brain cancer. Datta said that being an engineer allows her to cross into other areas of research and with a different perspective, making an excellent case for the importance of multidisciplinary research.
“I do believe that really is an advantage of being an engineer. It’s easier for me to sometimes make connections between contexts that seem disparate,” Datta said. “We depend on our life science and clinical colleagues to walk through those details, but engineers are very good at approaching complex problems from a simplified systems approach.”
The study, “Normalizing granuloma vasculature and matrix improves drug delivery and reduces bacterial burden in tuberculosis-infected rabbits,” was funded by the Bill & Melinda Gates Foundation and the National Institutes of Health. Datta is an affiliated member of Notre Dame’s Berthiaume Institute for Precision Health , Eck Institute for Global Health , Harper Cancer Research Institute , Lucy Family Institute for Data and Society , NDnano and Warren Center for Drug Discovery . Datta is an assistant professor in the following doctorate programs: aerospace and mechanical engineering, bioengineering, and materials science and engineering.
Contact: Brandi Wampler, associate director of media relations, 574-631-2632, [email protected]
- Brief Communication
- Open access
- Published: 28 March 2024
Presence of tuberculosis symptoms among HIV-positive men who have sex with men (MSM) in Zimbabwe
- Munyaradzi Mapingure 1 ,
- Innocent Chingombe 1 ,
- Tafadzwa Dzinamarira 1 ,
- Brian Moyo 2 ,
- Chesterfield Samba 3 ,
- Delight Murigo 3 ,
- Owen Mugurungi 2 ,
- Elliot Mbunge 4 ,
- Rutendo Birri Makota 5 ,
- Grant Murewanhema 6 &
- Godfrey Musuka 7
AIDS Research and Therapy volume 21 , Article number: 18 ( 2024 ) Cite this article
63 Accesses
1 Altmetric
Metrics details
We conducted secondary data analysis using a biobehavioral survey dataset of 1538 MSM from Zimbabwe. Survey participants were screened for the four symptoms suggestive of tuberculosis infection using the WHO TB screening algorithm. Results: All participants experienced at least one symptom suggestive of tuberculosis. 40% of HIV-positive MSM reported having had a cough in the last month and 13% of them experienced unexpected weight loss. The prevalence of experiencing any of the four TB symptoms amongst HIV-positive MSM was 23%.
Contribution
There is an urgent need for active TB case finding and treatment amongst HIV-positive MSM in Zimbabwe. Clinicians will need to ensure that MSM who need TB testing receive it timeously.
Despite being both preventable and treatable, TB remains an important public health problem in all countries and age groups [ 1 ]. Globally and in sub-Saharan Africa, tuberculosis is a major cause of mortality and morbidity [ 2 , 3 ]. Being HIV-positive without viral load suppression is a predisposing factor for TB infection, amongst MSM. TB prevalence surveys in resource-poor countries consistently show a high burden of patients with TB disease who remain undiagnosed and are thus infectious to others [ 4 ]. Improving international case detection for TB also contributes to achieving health-related global goals [ 5 ]. HIV prevalence is declining in Zimbabwe but remains one of the highest in sub-Saharan Africa at 11.6% among the general population [ 6 ] and is higher at 23.4% among men who have sex with men (MSM) [ 7 ].
Eliciting of symptoms is an essential step in the diagnosis and care of presumptive MSM tuberculosis patients [ 8 ]. MSM are among the critical populations identified to be at higher risk of tuberculosis infection and disease [ 9 ]. However, there is limited TB data among MSM [ 10 , 11 ].
Data from our study on HIV and STI biobehavioral surveys (BBS) among MSM in Zimbabwe [ 7 ] was used to determine the prevalence of tuberculosis (TB) symptoms amongst HIV-positive MSM. Data were collected from 1538 individual MSM in the Zimbabwe cities of Harare and Bulawayo.
The study was a cross-sectional BBS using respondent-driven sampling (RDS). RDS is a peer-referral sampling methodology designed for data collection among hard-to-reach populations. Consenting participants completed a questionnaire on sociodemographics, sexual identity and history, sexual behaviour, mental health, alcohol and drug use, HIV testing services, stigma and violence, social cohesion, health services and TB. As part of the study, participants were screened for the four symptoms suggestive of tuberculosis infection using the WHO TB screening algorithm, and to our knowledge, this is the first and only BBS in Zimbabwe to have done so. After being tested for HIV, participants were also screened for tuberculosis (TB) symptoms. Participants who screened positive for TB symptoms were offered the option of being driven that day to a designated MSM-friendly referral healthcare facility that offers MSM-friendly HIV and other related services. Additionally, a peer escort to accompany them was provided. If the participant declined, they were given a referral card for the clinic that offers MSM-friendly HIV and related services. STATA statistical package version 17 was used for statistical analysis. The study received ethical clearance from the national institutional review board, the Medical Research Council of Zimbabwe # (MRCZ/A/2156).
In terms of demographics, the HIV-positive MSM were older than the negative, with Mean (Standard deviations) of 31.8 (9.2) and 26.4 (7.9) years respectively, p = 0.001. The majority (> 96%) were Black Africans, who had primarily attained (> 70%) secondary education. Close to 40% were unemployed, see Table 1 . All participants experienced at least one symptom suggestive of tuberculosis, with prevalences of 7%, 4%, 7%, and 1% for persistent cough, night sweats, unexpected weight loss and fever respectively. Having had a cough in the last month was higher among HIV-positive MSMs compared to those not affected with HIV, 40% vs. 5%, p = 0.001. The same was the case with experiencing unexpected weight loss, 13% vs. 6%, p = 0.001 and experiencing a fever in the last month, 3% vs. 1%, p = 0.037. The prevalence of experiencing any of the four TB symptoms was 13%, and this prevalence was higher among the HIV-positive MSM compared to those who are not infected with HIV, 23% vs. 11%, p = 0.001. Three per cent reported that they had been exposed to a person with TB in the last 12 months.
Discussions
A systematic review by Divala and others [ 8 ] shows that invariably, tuberculosis symptom screening is a critical entry point for the diagnosis of the disease [ 12 , 13 , 14 , 15 ]. Additionally, there is a need for more accurate screening tools, that remain accessible and low-cost for countries with high tuberculosis burden.
Some individuals wait for the spontaneous resolution of TB symptoms, and most do not seek healthcare help [ 15 ]. The biological and epidemiological interconnectedness of TB and HIV has generated a new form of stigma, TB–HIV stigma, which sometimes makes people afraid to go for TB symptoms as this would be perceived to be HIV-related TB.
We note that there is limited information on TB among critical populations such as MSM, and the findings in this letter are crucial for understanding TB symptoms among MSM. There is a need for ongoing campaigns to encourage people to seek healthcare help when experiencing TB symptoms so that we do not have infectious patients who remain undiagnosed and are thus contagious to others. Targeted TB screening is warranted, especially among key populations, resulting in a greater yield of identifying TB cases, which aligns with the International Standards for Tuberculosis Care.
Tuberculosis symptom screening has limitations. However, there is a need to increase the frequency of when it is offered to MSM to enhance the opportunity of identifying those individuals in need of further investigations and treatment. Additionally, in Zimbabwe MSM experience considerable amounts of stigma and discrimination at most health facilities due to cultural imperatives as noted in the formative survey which was part of the BBS survey [ 7 ]. For Zimbabwe to ensure its health for all targets are met timeously there is a need to ensure that no group is left behind, including MSM and other key populations. A key intervention by the Zimbabwe Ministry of Health will be to train its healthcare workers in the provision of key population-friendly services and non-discriminatory behaviour.
Non-governmental organisations in Zimbabwe provide principally HIV-related services to MSM in secluded locals to avoid harassment from the police and security forces [ 7 ]. It will be also key to provide tuberculosis-related screening to those MSM using such services. Those individuals who screen positive for tuberculosis should immediately be provided with tuberculosis diagnostic tests and those testing positive should be immediately linked to care.
Abbreviations
Biobehavioral Survey
Human Immunodeficiency Virus
Men who have Sex with Men
Respondent Driven Sampling
Tuberculosis
World Health Organization Global Tuberculosis Report. 2021. Geneva, Switzerland: WHO; 2021.
World Health Organization Global Health Estimates. 2016: deaths by cause, age, sex, by country and by region. Geneva, Switzerland: WHO; 2018.
Corbett EL, Marston B, Churchyard GJ, De Cock KM. Tuberculosis in sub-saharan Africa: opportunities, challenges and change in the era of antiretroviral treatment. Lancet. 2006;367:926–37.
Article PubMed Google Scholar
Borgdorff MW, Nagelkerke NJ, Dye C, Nunn P. Gender and tuberculosis: a comparison of prevalence surveys with notification data to explore sex differences in case detection. Int J Tuberculosis Lung Disease. 2000;4:123–32.
CAS Google Scholar
Kemp JR, Gillian M, Simwaka BN, Salaniponi FM, Squire BS. Can Malawi’s poor afford free tuberculosis services? Patient and household costs associated with a tuberculosis diagnosis in Lilongwe. Bull World Health Organ. 2007;85:580–5.
Article PubMed PubMed Central Google Scholar
Ministry of Health and Child Care (MoHCC). Zimbabwe Population-based HIV Impact Assessment (ZIMPHIA 2020): Final Report. Harare. 2021.
HIV and STI Biobehavioral Survey among Men Who Have Sex with Men. Transgender women, and Genderqueer individuals in Zimbabwe - Final Report. New York: ICAP at Columbia University; 2020.
Google Scholar
Divala TH, Lewis J, Bulterys MA, Lutje V, Corbett EL, Schumacher SG, MacPherson P. Missed opportunities for diagnosis and treatment in patients with TB symptoms: a systematic review. Public Health Action. 2022;12(1):10–7. https://doi.org/10.5588/pha.21.0022 .
Article CAS PubMed PubMed Central Google Scholar
UNAIDS. HIV prevention among key populations. 2016.
Xin HN, Li XW, Zhang L, Li Z, Zhang HR, Yang Y. Tuberculosis infection testing in HIV-positive men who have sex with men from Xi’an China. Epidemiol Infect. 2017;145(3):498–502.
Article CAS PubMed Google Scholar
WHO, UNAIDS CDC, FHI 360. Biobehavioral survey guidelines for populations at risk for HIV. Geneva: World Health Organisation; 2017.
Storla DG, Yimer S, Bjune GA. A systematic review of delay in the diagnosis and treatment of tuberculosis. BMC Public Health. 2008;8(1):15.
Kranzer K, Afnan-Holmes H, Tomlin K, Golub JE, Shapiro AE, Schaap A, Corbett EL, Lönnroth K, Glynn JR. The benefits to communities and individuals of screening for active tuberculosis disease: a systematic review. Int J Tuberc Lung Dis. 2013;17(4):432–46.
Yoon C, Dowdy DW, Esmail H, MacPherson P, Schumacher SG. Screening for tuberculosis: time to move beyond symptoms. Lancet Respir Med. 2019;7(3):202–4.
Willie B, Hakim AJ, Badman SG, Weikum D, Narokobi R, Coy K, Gabuzzi J, Pekon S, Gene S, Amos A, Kupul M, Hou P, Dala NM, Whiley DM, Wapling J, Kaldor KM, Vallely AJ, Kelly-Hanku A. High prevalence of pulmonary tuberculosis among female sex workers, men who have sex with men, and transgender women in Papua New Guinea. Trop Med Health. 2021;49:4. https://doi.org/10.1186/s41182-020-00293-w .
Download references
Acknowledgements
The authors would like to thank all individuals who took part in the survey.
The study was not funded.
Author information
Authors and affiliations.
ICAP in Zimbabwe, Harare, Zimbabwe
Munyaradzi Mapingure, Innocent Chingombe & Tafadzwa Dzinamarira
AIDS and TB Programmes, Ministry of Health and Child Care, Harare, Zimbabwe
Brian Moyo & Owen Mugurungi
GALZ, Harare, Zimbabwe
Chesterfield Samba & Delight Murigo
Department of Computer Science, Faculty of Science and Engineering, University of Eswatini, Kwaluseni, Eswatini
Elliot Mbunge
Department of Biological Sciences and Ecology, University of Zimbabwe, Harare, Zimbabwe
Rutendo Birri Makota
Unit of Obstetrics and Gynaecology, Faculty of Medicine and Health Sciences, University of Zimbabwe, Harare, Zimbabwe
Grant Murewanhema
International Initiative for Impact Evaluation, Harare, Zimbabwe
Godfrey Musuka
You can also search for this author in PubMed Google Scholar
Contributions
GMus conceived the brief communication. GMus & MM carried out the statistical analysis. GMus & MM wrote the first draft of the brief communication. All authors (MM, IC, TD, BM, CS, DM, OM, EM, RB, GM, and GMus) contributed to the writing of the brief communication. All authors (MM, IC, TD, BM, CS, DM, EM, RB, GM) read and approved the final brief communication.
Corresponding author
Correspondence to Godfrey Musuka .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Mapingure, M., Chingombe, I., Dzinamarira, T. et al. Presence of tuberculosis symptoms among HIV-positive men who have sex with men (MSM) in Zimbabwe. AIDS Res Ther 21 , 18 (2024). https://doi.org/10.1186/s12981-024-00605-8
Download citation
Received : 06 November 2023
Accepted : 14 March 2024
Published : 28 March 2024
DOI : https://doi.org/10.1186/s12981-024-00605-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Tuberculosis symptoms
- Case finding
AIDS Research and Therapy
ISSN: 1742-6405
- Submission enquiries: [email protected]
Opinion What Charles and Catherine’s diagnoses reveal about how we see cancer
Regarding the March 25 news article “ With two senior royals facing cancer, British monarchy must do more with less ”:
The announcements by King Charles III and Catherine, Princess of Wales, that they have each been diagnosed with cancer draw attention to two conundrums.
Not revealing their specific diagnoses feeds an obsolete narrative of cancer as a monolithic disease, one universally dreaded, given the perception that patients have only distant hopes of “a” cure. But cancer is a broad term that covers many diseases. Even within subcategories of cancer, patients’ outcomes may vary widely based on genomic characteristics that often require radically differing treatments.
Survival rates for pancreatic and liver cancers, for example, are still dire compared with outcomes associated with early detection and treatment of testicular or skin cancers. In just the past two decades, research on once uniformly deadly cancers such as multiple myeloma and chronic myelogenous leukemia has progressed such that those diseases have become chronic conditions able to be managed for majorities of patients.
On the other hand, there is an almost perverse anticipation among cancer patient interests throughout the world that Charles and Kate will make their specific diagnoses public. Doing so would raise awareness, direct research funds and activity to their cancers, and spur aggressive fundraising efforts for select advocacy organizations.
The ongoing speculation surrounding Charles and Catherine feeds an odd mix of concern, hope, fear and cynicism, underscoring a historical ignorance of how cancer is — or, to be more accurate, cancers are — perceived by the public.
Greg Brozeit , Fairlawn, Ohio
Tackling TB costs money and time
Regarding John Green’s March 24 Sunday Opinion column, “ My brother’s cancer care? First-rate. The world’s TB problem? Shocking. ”
While I am now retired from the Centers for Disease Control-President’s Emergency Plan for AIDS Relief team working on tuberculosis and HIV, I can attest to the fact that there are rigorous efforts underway to reduce the burden of TB in the countries Mr. Green mentioned in his Sunday Opinion column. The cost of the testing equipment is not the whole problem.
Getting physicians in some of those countries to order rapid tests and use them, instead of relying on culture tests that take weeks to get results, is incredibly frustrating. I have been to many countries where the rapid-testing equipment sits idle or the lab waits until there are enough specimens to run a batch, thinking it is more cost effective to wait. Some ministries of health tout their GeneXpert machines, but no one monitors their acceptance by physicians or the number of daily tests run. This test is not complicated — even a registered nurse or licensed practical nurse can be trained to do it in a day, as I have seen for myself in some teaching hospitals in South Africa. Missed opportunities in quality care because of poor implementation is killing millions of men, women and children. Getting the cost down should be easy. Implementation is the real challenge.
Virginia Lipke , Cincinnati
I am so moved by John Green and his brother Hank’s willingness to share Hank’s story and to contrast their experiences with those of millions of people suffering and dying from tuberculosis. As a family physician who has spent my 40-year career in under-resourced communities, I would add that the deadliest infectious disease isn’t merely a science problem. It’s a priorities problem.
John Green got me thinking about how our government sets priorities and spends our tax dollars. With roughly half of the federal government’s discretionary budget allocated to the military, Congress must bicker over how to split the remains among everything else. I recently learned about a backdoor, little-known source of additional military funding: the Unfunded Priorities Lists. Each branch of the military is required to submit these wish lists of items that didn’t make it into the budget to Congress, even though senior military leaders have criticized the process as a flawed way to flag key armed service needs. No other part of the federal government gets the opportunity to lobby for extra funding in this manner.
It’s time for Congress to end UPLs. I urge Senate Majority Leader Charles E. Schumer (D-N.Y.) and House Speaker Mike Johnson (R-La.) to support the bipartisan Streamline Pentagon Budgeting Act , which would repeal the requirement for the military to submit wish lists to Congress. Perhaps we could fund a global tuberculosis eradication program instead.
Nancy Bermon , Nyack, N.Y.
Come sit under the Apple tree
Regarding the March 22 front-page article “ DOJ swipes at Apple iPhone ”:
The antitrust lawsuit filed by the Justice Department against Apple reminded me of Queen Gertrude’s declaration in “Hamlet”: “The lady doth protest too much, methinks.” In this instance, the facts of the phone industry speak much more loudly than the government’s filings.
The Justice Department’s complaint points out that the original iPhone was priced at $299, which would be roughly $450 today, adjusting for inflation. But the premium price Apple charges for its latest iteration of the device is not de facto evidence that Apple is a monopolist. The iPhone 15 is a radically different device in size and technological complexity than the original released in 2008. Other models of the iPhone are available gratis through many mobile providers if one is willing to forgo the cachet of the hottest model.
Comparing Apple’s supposed dominance of the smartphone market with Microsoft’s command in the web browser field, which rose as high as 94 percent in 2002, also reveals the flaws in the government’s case. Apple had 24.7 percent of the global smartphone market in the fourth quarter of 2023, and Chinese smartphone makers Xiaomi and Transsion are growing at much faster year-over-year rates.
And Apple hardly seems to have made other products worse, as it popularized both the touch screen and the rubber banding effect when users reach the end of a web page or document.
The Justice Department accuses Apple of “making it harder or more expensive for its users and developers to leave …[rather than] making it more attractive for them to stay.” But Apple created a radically new product that consumers continue to love. That’s hardly the usurious technological “Hotel California” it’s portrayed to be.
Greg Boyd , Washington
The Justice Department’s antitrust suit against Apple feels like a mistake. By trying to bust open Apple’s smartphone ecosystem, they may end up destroying a good thing. To my mind, Apple’s “closed universe” benefits its customers. Their controlled environment protects users from many of the viruses and crashes users experienced when using Microsoft and Google. Apple made a choice to protect users by erecting some barriers and I’m just fine with that.
Before retiring, I enjoyed a great career managing technology policy issues in Washington. (Apple was never a client.) But I was not good at getting into the operations of my personal technologies. After retiring I knew I could not survive as my own tech support. So I ran away from Windows and Gmail, finding great ease and safety in Apple’s MacBook, iPhone, iPad and ApplePay. It all just worked.
Yes, we pay a little more for the products and there are a few things we can’t do. But why should we break up a tech ecosystem that works just to drag it down to a lower common denominator? Let the marketplace decide which way works best. Open vs. closed is a market choice, it’s not good versus evil. Personally, I’ll keep picking Apple.
William R. Moroney , Washington
Trump’s favorite book
Regarding the March 26 online analysis “ An all-American Bible — with a cut of the sales going to Trump ”:
Recently, Donald Trump claimed the Bible was his favorite book and endorsed a Bible he is attempting to sell to raise money for his personal gain. Because I was born and raised a Missouri Synod Lutheran and attended Lutheran school from elementary through high school, I am familiar with the teachings of the Bible. It is my favorite book as well. These teachings include the injunctions to “Love your neighbor as yourself” from the Book of Mark, to forgive those who have wronged you not just “Until seven times: but, Until seventy times seven,” and last but not least, to “Love your enemies and pray for those who persecute you,” both from the Book of Matthew.
You’d think that if someone had a favorite book, they would know it inside out, study it and follow its teachings. This doesn’t hold true for Mr. Trump, and that deeply offends me, especially because he is using the Bible for monetary gain. To capitalize on God’s word is blasphemy. The Bible makes this clear: When Jesus saw people using the temple for monetary gain, He drove them out, and He taught, “You cannot serve both God and money.”
If anything, Mr. Trump should be giving away Bibles to further the Gospel instead of putting his seal of approval on them, as if that even mattered to anyone, least of all God. God doesn’t need anyone’s stamp of approval because He is omnipotent, omniscient and omnipresent. He is the final authority, not Mr. Trump.
The real question is: How many more lies will the American people let Mr. Trump get away with? This one is too much for me.
Sarah Hayes , Lincoln, Neb.
- Opinion | How a four-day workweek could change Americans’ lives March 31, 2024 Opinion | How a four-day workweek could change Americans’ lives March 31, 2024
- Opinion | What Charles and Catherine’s diagnoses reveal about how we see cancer March 29, 2024 Opinion | What Charles and Catherine’s diagnoses reveal about how we see cancer March 29, 2024
- Opinion | Readers critique The Post: No more side-eye from Fani Willis March 29, 2024 Opinion | Readers critique The Post: No more side-eye from Fani Willis March 29, 2024


IMAGES
COMMENTS
The case study aims to guide you through the assessment, nursing action and evaluation of a patient with pulmonary TB together with the rationale for care. Activity. In Chapter 1 you were asked to revise the normal anatomy and physiology of the respiratory system (see Montague et al 2005) and a brief definition of TB was given.
Introduction. Tuberculosis (TB) is caused by strains of Mycobacterium tuberculosis (M. Tuberculosis). TB is a primarily pulmonary infection spread by airborne droplet transmission. The development and spread of drug-resistant strains of M. tuberculosis greatly jeopardize TB control efforts. In the US, 91 cases of MDR-TB were reported in 2014.
The present case can demonstrate the role of pharmacist and the need of patient counseling in a disease condition like Pulmonary tuberculosis. Discover the world's research 25+ million members
Abstract. In this case study, a nurse presents her reflections on the challenges of supporting a patient through his treatment journey for multidrug-resistant tuberculosis. The patient has significant comorbidities and social issues, such as diabetes and homelessness. There was also a language barrier. All these aspects made the management of ...
TB is still a life-threatening problem in this country. TB knows no borders, and people here in the United States are suffering from TB. Anyone can get TB. These stories highlight the personal experiences of people who were diagnosed and treated for latent TB infection and TB disease, as well as the work of TB control professionals. Personal ...
Clinical and radiological manifestations of tuberculosis (TB) are heterogeneous, and differential diagnosis can include both benign and malignant diseases (e.g., sarcoidosis, metastatic diseases, and lymphoma). Diagnostic dilemmas can delay appropriate therapy, favoring Mycobacterium tuberculosis transmission.We report on a case of TB in an immunocompetent, Somalian 22-year-old boy admitted in ...
Background Mycobacterium tuberculosis (Mtb) has been found to persist within cavities in patients who have completed their anti-tuberculosis therapy. The clinical implications of Mtb persistence after therapy include recurrence of disease and destructive changes within the lungs. Data on residual changes in patients who completed anti-tuberculosis therapy are scarce. This case highlights the ...
Case Study. A 44-year-old man presented to the TB Clinic with symptoms of progressive shortness of breath and cough with greenish sputum production. His sputum test results showed that he had atypical TB ( Mycobacterium Avium Complex MAC infection ). He was HIV negative at this time. Past history revealed that he was in good health till 1991 ...
Community-based active case-finding for tuberculosis might be effective in changing tuberculosis epidemiology and thereby improving population health if delivered with high coverage and intensity. If possible, active case-finding projects should incorporate a well designed, robust evaluation to contribute to the evidence base and help elucidate which delivery methods and diagnostic strategies ...
Background. Tuberculosis (TB) is a communicable infectious disease affecting around one quarter of the world's population [].The 'BRICS' countries of Brazil , Russia, India, China, and South Africa account for 47% of the total number of TB cases annually [1-3].Caused by the bacillus Mycobacterium tuberculosis, around 5-10% of those infected will develop active disease.
The Mycobacterium tuberculosis complex includes the following mycobacteria, which are characterized by a slow growing rate: M. tuberculosis, M. africanum, M. bovis, and M. microti ().In recently published reports of two cases of lymphatic node tuberculosis (TB), the strains were recognized as belonging to a new taxon of M. tuberculosis (2,3).These isolates were characterized by a highly ...
Understand the goals of a tuberculosis (TB) interview in a TB contact investigation . ¾. Be familiar with the criteria used to decide when a TB investigation should be initiated . ¾. Define an outbreak . ¾. Identify the steps you would take in investigating an outbreak . ¾. Create a line list . ¾. Distinguish between a case-control and a ...
Seldom does patient-care follow the relatively straight-forward path outlined in the CDC Self-Study Modules on TB. Due to this, the case studies in this book are designed to provide guidance and relevant reference material to gain insight into challenges faced in TB case management. Patients will often
Aspirin 81 mg PO daily. Atorvastatin 40 mg PO daily. Budesonide/formoterol 160 mcg/4.5 mcg 2 inhalations BID. Clonazepam 0.5 mg PO three times daily PRN anxiety. Lisinopril 20 mg PO daily. Metoprolol succinate 100 mg PO daily. Tiotropium 2 inhalations once daily. Venlafaxine 150 mg PO daily. Warfarin 7.5 mg PO daily.
improve adherence. A case study highlights patient-centered TB case management. Chapter 3: Tuberculosis Nurse Case Management in Special Situations and Circumstances This chapter provides information and case studies on TB in selected situations and circumstances, ranging from TB in people experiencing homelessness to those with TB and diabetes.
Personal Stories from TB Survivors - My Journey fighting TB. 3 June 2020. Tuberculosis (TB) is the world's top infectious killer today. It is airborne and can affect any one of us. Over 5 000 women, men and children still die each day from TB. The social and economic impacts are devastating, including poverty, stigma and discrimination.
Tuberculosis deaths have increased because of reduced access to care. 2 In 2020, there were roughly 1.5 million tuberculosis deaths worldwide, representing the first year-over-year increase in ...
The third case study on screening TB patients for DM had no such group . However, if the stakeholder committee had decided on two different screening methods, then a comparison study would have been needed. ... Fine P.E.M. Cotrimoxazole prophylaxis reduces mortality in human immunodeficiency virus-positive tuberculosis patients in Karonga ...
Tuberculosis is the biggest infectious disease killer in the world 1, and is endemic in Nepal with the national prevalence at 416 cases per 100000 population 2. Pulmonary tuberculosis is the most common form. In Nepal, tuberculosis prevalence is more in productive age group (25-64 years) and men. Poverty, malnutrition, overcrowding ...
Although tuberculosis (TB) is a curable disease, treatment is complex and prolonged, requiring considerable commitment from patients. This study aimed to understand the common perspectives of TB patients across Brazil, Russia, India, China, and South Africa throughout their disease journey, including the emotional, psychological, and practical challenges that patients and their families face.
The Western Pacific Region has one of the fastest-growing populations of older adults (≥ 65 years) globally, among whom tuberculosis (TB) poses a particular concern. This study reports country case studies from China, Japan, the Republic of Korea, and Singapore reflecting on their experiences in managing TB among older adults. Across all four countries, TB case notification and incidence ...
In the present case report, the miliary TB evidence was presented in a 12 years old girl. Miliary TB has been more prevalent in middle age and older people than children [14, 15].Also, 60% of the cases are male with a mean age of 55 years in studies [16,17,18].Although the mean age of miliary TB patients has increased, the rates remain relatively low in children [19, 20].
Patients with highly drug-resistant forms of tuberculosis have limited treatment options and historically have had poor outcomes. In an open-label, single-group study in which follow-up is ongoing ...
Clinical Case Reports aims to improve global health outcomes by sharing clinical knowledge through the use of medical case reports, clinical images & procedural videos. Key Clinical Message Tuberculosis (TB) pericarditis, while uncommon, should be considered in patients with pericardial masses and effusion.
Case Presentation. History of Present Illness: A 33-year-old white female presents after admission to the general medical/surgical hospital ward with a chief complaint of shortness of breath on exertion. She reports that she was seen for similar symptoms previously at her primary care physician's office six months ago.
We thought maybe the same thing was happening in tuberculosis." The study confirmed that a similar phenomenon is occurring in granulomas — too much cell mass and protein scaffolding. This impaired function makes blood flow through blood vessels nearly impossible, crippling the ability to get a medication to the tuberculosis disease site.
We conducted secondary data analysis using a biobehavioral survey dataset of 1538 MSM from Zimbabwe. Survey participants were screened for the four symptoms suggestive of tuberculosis infection using the WHO TB screening algorithm. Results: All participants experienced at least one symptom suggestive of tuberculosis. 40% of HIV-positive MSM reported having had a cough in the last month and 13% ...
Background and Objectives: Tuberculosis is caused by Mycobacterium tuberculosis (MTB), while nontuberculous mycobacteria (NTM) encompass a group of mycobacterial species that are distinct from the MTB complex and leprae. Spondyloarthritis (SpA) is a group of chronic inflammatory diseases with shared clinical characteristics and is treated with biological agents; however, their use may elevate ...
Plus, readers on diagnosing tuberculosis, lowering the cost of asthma inhalers and the risks of breaking up Apple. ... also reveals the flaws in the government's case. ... study it and follow ...